User login
Case Study: Managing Opioid Addiction After a Back Injury
Has your patient’s opioid use escalated to opioid addiction? How can you tell, and what interventions can you take to help this patient in the context of a 15-minute appointment?
In this edition of Mental Health Consult, our panel discusses their recommendations for workup and next steps for managing a 45-year-old man who has no history of psychiatric disorders and appears to now be dependent on the opioid painkillers that he initially received after a back injury.
Join our panel of experts from George Washington University, Washington, including Daniel Lieberman, MD, professor of psychiatry and behavioral sciences clinical director; April Barbour, MD, MPH, director of the division of general internal medicine; and Lorenzo Norris, MD, medical director of psychiatric and behavioral services, as they discuss how to treat pain medication–related addiction, including when to refer to pain specialists and how various practice models drive treatment decisions and reimbursement.
Click here for a PDF of the case study.

Has your patient’s opioid use escalated to opioid addiction? How can you tell, and what interventions can you take to help this patient in the context of a 15-minute appointment?
In this edition of Mental Health Consult, our panel discusses their recommendations for workup and next steps for managing a 45-year-old man who has no history of psychiatric disorders and appears to now be dependent on the opioid painkillers that he initially received after a back injury.
Join our panel of experts from George Washington University, Washington, including Daniel Lieberman, MD, professor of psychiatry and behavioral sciences clinical director; April Barbour, MD, MPH, director of the division of general internal medicine; and Lorenzo Norris, MD, medical director of psychiatric and behavioral services, as they discuss how to treat pain medication–related addiction, including when to refer to pain specialists and how various practice models drive treatment decisions and reimbursement.
Click here for a PDF of the case study.

Has your patient’s opioid use escalated to opioid addiction? How can you tell, and what interventions can you take to help this patient in the context of a 15-minute appointment?
In this edition of Mental Health Consult, our panel discusses their recommendations for workup and next steps for managing a 45-year-old man who has no history of psychiatric disorders and appears to now be dependent on the opioid painkillers that he initially received after a back injury.
Join our panel of experts from George Washington University, Washington, including Daniel Lieberman, MD, professor of psychiatry and behavioral sciences clinical director; April Barbour, MD, MPH, director of the division of general internal medicine; and Lorenzo Norris, MD, medical director of psychiatric and behavioral services, as they discuss how to treat pain medication–related addiction, including when to refer to pain specialists and how various practice models drive treatment decisions and reimbursement.
Click here for a PDF of the case study.

VIDEO: A case study in managing opioid addiction after a back injury
Has your patient’s opioid use escalated to opioid addiction? How can you tell, and what interventions can you take to help this patient in the context of a 15-minute appointment?
In this edition of Mental Health Consult, our panel discusses their recommendations for workup and next steps for managing a 45-year-old man who has no history of psychiatric disorders and appears to now be dependent on the opioid painkillers that he initially received after a back injury.
Join our panel of experts from George Washington University, Washington, including Daniel Lieberman, MD, professor of psychiatry and behavioral sciences clinical director; April Barbour, MD, MPH, director of the division of general internal medicine; and Lorenzo Norris, MD, medical director of psychiatric and behavioral services, as they discuss how to treat pain medication–related addiction, including when to refer to pain specialists and how various practice models drive treatment decisions and reimbursement.
On Twitter @whitneymcknight
Has your patient’s opioid use escalated to opioid addiction? How can you tell, and what interventions can you take to help this patient in the context of a 15-minute appointment?
In this edition of Mental Health Consult, our panel discusses their recommendations for workup and next steps for managing a 45-year-old man who has no history of psychiatric disorders and appears to now be dependent on the opioid painkillers that he initially received after a back injury.
Join our panel of experts from George Washington University, Washington, including Daniel Lieberman, MD, professor of psychiatry and behavioral sciences clinical director; April Barbour, MD, MPH, director of the division of general internal medicine; and Lorenzo Norris, MD, medical director of psychiatric and behavioral services, as they discuss how to treat pain medication–related addiction, including when to refer to pain specialists and how various practice models drive treatment decisions and reimbursement.
On Twitter @whitneymcknight
Has your patient’s opioid use escalated to opioid addiction? How can you tell, and what interventions can you take to help this patient in the context of a 15-minute appointment?
In this edition of Mental Health Consult, our panel discusses their recommendations for workup and next steps for managing a 45-year-old man who has no history of psychiatric disorders and appears to now be dependent on the opioid painkillers that he initially received after a back injury.
Join our panel of experts from George Washington University, Washington, including Daniel Lieberman, MD, professor of psychiatry and behavioral sciences clinical director; April Barbour, MD, MPH, director of the division of general internal medicine; and Lorenzo Norris, MD, medical director of psychiatric and behavioral services, as they discuss how to treat pain medication–related addiction, including when to refer to pain specialists and how various practice models drive treatment decisions and reimbursement.
On Twitter @whitneymcknight
Maximize depression treatment efforts with measurement-based care
WASHINGTON – Challenging patients with depression to stay engaged in their recovery while rigorously monitoring and measuring their treatment response can mean the difference between remission or resistance, according to an expert.
“We all wish for better treatments, but we really don’t have any coming available to us in the near future, so our task is to do as well as we can with what we have,” Michael E. Thase, MD, professor of psychiatry at the University of Pennsylvania, Philadelphia, said at Summit in Neurology & Psychiatry.
“We know far too well that there is a large gap between what we might be able to accomplish and what actually happens in clinical practice,” Dr. Thase said.
To close that gap, start with evaluating what can be done to combat patient nonadherence. A 2007 study indicated that just under 20% of patients adhere to antidepressant medication guidelines (Prim Care Companion J Clin Psychiatry. 2007;9[2]:91-9.), and according to Dr. Thase, less than 10% of patients being seen for depression in primary care actually fill their prescriptions.
“Don’t delude yourself that these patients drop out of treatment because they no longer need it. They drop out mostly because they have gotten disgusted, disappointed, or discouraged,” said Dr. Thase, attributing the high rate of nonadherence to the nature of depression itself.
“Depression is a state of pessimism, low confidence, and of not really feeling capable.”
Helping patients overcome their reluctance to follow treatment guidelines begins with accurately assessing their symptom severity. Patients who rate 4 or less on the Patient Health Questionnaire–9 (PHQ-9), which is based on the DSM-IV, are considered in remission or not to have severe depression. Similarly, patients who score 5 or less on the Quick Inventory of Depressive Symptomatology (QIDS) are not considered in the danger zone.
The severity ratings included in the DSM-5 can help clinicians pinpoint the level of depression a patient is experiencing, as can a therapeutic relationship with the patient and the family, Dr. Thase said at the summit, held by Global Academy for Medical Education.
He urged clinicians to monitor adherence routinely by asking patients whether or not they have filled or refilled their prescriptions. It is helpful to ask patients about missing doses and whether they are feeling any improvement, he said.
“It’s a very simple process: You keep track of the patients. Chase after them if they don’t follow through. If you’re not keeping track, the patients think [what they do] doesn’t matter,” Dr. Thase said.
A 2010 study of chronic depression treatment in primary care practices showed that compared with regular care, aggressive monitoring of patient adherence and outcomes in 728 adults with depression resulted in better remission rates across 18 months of treatment. At 6 months 43.4% of patients who had been contacted regularly by nursing and social worker staff were in remission, compared with 33.3% of the 78 who had received regular care (P = .11). At 12 months, the results were 52% vs. 33.9% (P = .012), and at 18 months remission was reported in 49.2% vs. 27.3% (P = .004) (Ann Fam Med. 2010 Sep;8[5]:387-96).
By being alert to side effects, using a rating scale to measure symptom reduction, and not staying “locked” into the idea that all treatments require 6-8 weeks before patients see any improvement, clinicians can boost chances for adherence – and thus for remission – since patients who don’t improve in the first 2 weeks have just a 15% chance for improvement, Dr. Thase said. “You need 6-8 weeks to get to the maximum titration. That old 8-week rule applies mostly to patients who are showing improvement by week 2.”
If by week 2, the patient is not tolerating the medication’s side effects and has no symptom reduction, then move on to the next medication, Dr. Thase said, emphasizing the importance of seeing patients at least twice monthly. “If we’re only seeing a patient once a month, we’ve already fallen behind in the up-titration part, and we’ve missed the opportunity for early intervention if the patient is having side effects.”
Algorithms for choosing depression treatments should be a “fact of life,” he said. Start with the safest, easiest to tolerate, and least expensive of the available antidepressants, such as escitalopram and fluoxetine before working through the second- and third-line therapies and adjunctive therapies, all of which have greater risk profiles as you move through them. This algorithmic approach has been shown to result in patients scoring at least 10 points higher on a depression rating scale (JAMA Psychiatry. 2004;61:[7]669-80), which Dr. Thase said is equivalent to about a 30% higher chance of remission. “Don’t go over and over with the simple treatments that aren’t [evoking] a response. Move briskly on to the more complex treatments until patients respond.”
Treatment algorithms can include psychotherapies, either in combination with pharmacotherapy or as monotherapy. He encouraged clinicians to refer to the American Psychiatric Association (APA) practice guideline for depression for more details. The absence of depressive symptoms alone is not indicative of remission, according to the guideline, which Dr. Thase coauthored. The presence of positive emotions and resilience, along with a sense of control over emotions and hope for the future, indicates remission.
If after applying those methods a patient remains depressed and has been negatively screened for bipolar disorder, the use of tricyclics or monoamine oxidase inhibitors (MAOIs) may be appropriate. “MAOIs account for less than 1 in every 1,000 prescriptions for antidepressants, yet for people who don’t respond to modern antidepressants, they still can carry a 30%-40% response rate. So, if you don’t prescribe them yourself, please get access to someone who does,” Dr. Thase said.
The tenets of measurement-based care are essentially the lessons learned from the landmark Sequenced Treatment Alternatives to Relieve Depression (STAR*D) trial, which sought to address how pharmacologic care for depression could be delivered based on adequate dosing, attenuation of symptoms, fewer side effects, and other factors (Am J Psychiatry. 2006;163:1905-17).
Now,10 years later, measurement-based treatment is still finding its way into practice, Dr. Thase said in an interview. “But, there’s no reason to be unduly pessimistic. Ten years ago, depression screening was in the same position, and now it is both considered to be the standard of care and is widely done.”
Dr. Thase reported having extensive industry relationships, noting that he has been involved in the development of nearly every drug for the treatment of mood disorders. Global Academy and this news organization are owned by the same company.
On Twitter @whitneymcknight
Ten years ago, the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study highlighted the importance of close monitoring of patients with depression. This is best done with a team-based approach; it’s best suited to handle issues of compliance, side effects, efficacy, and close follow-up. The team may consist of a psychotherapist, nurse, and, possibly, a pharmacist – in addition to the internist, Nitin S. Damle, MD, said in an interview.
 |
| Courtesy American College of Physicians Dr. Nitin S. Damle |
Integrating behavioral health into primary care practices involves structure, which includes office visits – even every 2 weeks until stable – follow-up phone calls by the nurse to assess adherence and problems with medication, and a pharmacist to track refill rates and side effects, and to recommend changes to medication due to lack of efficacy or side effects, he said.
Treatment algorithms are an effective means to find the most effective and safest medication, and screening with PHQ-9 and even QIDS has become more common in the primary care office. Still, the adaption of measurement-based care has been slow, partly because of the absence of adequate funding for an integrated primary care team-based approach to mental illness. Now there is no mechanism to cover the costs of personnel and infrastructure to provide for the level of monitoring and treatment that measurement-based care requires, according to Dr. Damle.
Health plans need to review the evidence, such as that from the STAR*D and other studies, and create funding mechanisms so that their members stay healthy and avoid complications of mental illness.
Dr. Damle is president of the American College of Physicians and clinical associate professor of medicine at Brown University, Providence, R.I. He has no relevant disclosures.
Ten years ago, the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study highlighted the importance of close monitoring of patients with depression. This is best done with a team-based approach; it’s best suited to handle issues of compliance, side effects, efficacy, and close follow-up. The team may consist of a psychotherapist, nurse, and, possibly, a pharmacist – in addition to the internist, Nitin S. Damle, MD, said in an interview.
 |
| Courtesy American College of Physicians Dr. Nitin S. Damle |
Integrating behavioral health into primary care practices involves structure, which includes office visits – even every 2 weeks until stable – follow-up phone calls by the nurse to assess adherence and problems with medication, and a pharmacist to track refill rates and side effects, and to recommend changes to medication due to lack of efficacy or side effects, he said.
Treatment algorithms are an effective means to find the most effective and safest medication, and screening with PHQ-9 and even QIDS has become more common in the primary care office. Still, the adaption of measurement-based care has been slow, partly because of the absence of adequate funding for an integrated primary care team-based approach to mental illness. Now there is no mechanism to cover the costs of personnel and infrastructure to provide for the level of monitoring and treatment that measurement-based care requires, according to Dr. Damle.
Health plans need to review the evidence, such as that from the STAR*D and other studies, and create funding mechanisms so that their members stay healthy and avoid complications of mental illness.
Dr. Damle is president of the American College of Physicians and clinical associate professor of medicine at Brown University, Providence, R.I. He has no relevant disclosures.
Ten years ago, the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study highlighted the importance of close monitoring of patients with depression. This is best done with a team-based approach; it’s best suited to handle issues of compliance, side effects, efficacy, and close follow-up. The team may consist of a psychotherapist, nurse, and, possibly, a pharmacist – in addition to the internist, Nitin S. Damle, MD, said in an interview.
 |
| Courtesy American College of Physicians Dr. Nitin S. Damle |
Integrating behavioral health into primary care practices involves structure, which includes office visits – even every 2 weeks until stable – follow-up phone calls by the nurse to assess adherence and problems with medication, and a pharmacist to track refill rates and side effects, and to recommend changes to medication due to lack of efficacy or side effects, he said.
Treatment algorithms are an effective means to find the most effective and safest medication, and screening with PHQ-9 and even QIDS has become more common in the primary care office. Still, the adaption of measurement-based care has been slow, partly because of the absence of adequate funding for an integrated primary care team-based approach to mental illness. Now there is no mechanism to cover the costs of personnel and infrastructure to provide for the level of monitoring and treatment that measurement-based care requires, according to Dr. Damle.
Health plans need to review the evidence, such as that from the STAR*D and other studies, and create funding mechanisms so that their members stay healthy and avoid complications of mental illness.
Dr. Damle is president of the American College of Physicians and clinical associate professor of medicine at Brown University, Providence, R.I. He has no relevant disclosures.
WASHINGTON – Challenging patients with depression to stay engaged in their recovery while rigorously monitoring and measuring their treatment response can mean the difference between remission or resistance, according to an expert.
“We all wish for better treatments, but we really don’t have any coming available to us in the near future, so our task is to do as well as we can with what we have,” Michael E. Thase, MD, professor of psychiatry at the University of Pennsylvania, Philadelphia, said at Summit in Neurology & Psychiatry.
“We know far too well that there is a large gap between what we might be able to accomplish and what actually happens in clinical practice,” Dr. Thase said.
To close that gap, start with evaluating what can be done to combat patient nonadherence. A 2007 study indicated that just under 20% of patients adhere to antidepressant medication guidelines (Prim Care Companion J Clin Psychiatry. 2007;9[2]:91-9.), and according to Dr. Thase, less than 10% of patients being seen for depression in primary care actually fill their prescriptions.
“Don’t delude yourself that these patients drop out of treatment because they no longer need it. They drop out mostly because they have gotten disgusted, disappointed, or discouraged,” said Dr. Thase, attributing the high rate of nonadherence to the nature of depression itself.
“Depression is a state of pessimism, low confidence, and of not really feeling capable.”
Helping patients overcome their reluctance to follow treatment guidelines begins with accurately assessing their symptom severity. Patients who rate 4 or less on the Patient Health Questionnaire–9 (PHQ-9), which is based on the DSM-IV, are considered in remission or not to have severe depression. Similarly, patients who score 5 or less on the Quick Inventory of Depressive Symptomatology (QIDS) are not considered in the danger zone.
The severity ratings included in the DSM-5 can help clinicians pinpoint the level of depression a patient is experiencing, as can a therapeutic relationship with the patient and the family, Dr. Thase said at the summit, held by Global Academy for Medical Education.
He urged clinicians to monitor adherence routinely by asking patients whether or not they have filled or refilled their prescriptions. It is helpful to ask patients about missing doses and whether they are feeling any improvement, he said.
“It’s a very simple process: You keep track of the patients. Chase after them if they don’t follow through. If you’re not keeping track, the patients think [what they do] doesn’t matter,” Dr. Thase said.
A 2010 study of chronic depression treatment in primary care practices showed that compared with regular care, aggressive monitoring of patient adherence and outcomes in 728 adults with depression resulted in better remission rates across 18 months of treatment. At 6 months 43.4% of patients who had been contacted regularly by nursing and social worker staff were in remission, compared with 33.3% of the 78 who had received regular care (P = .11). At 12 months, the results were 52% vs. 33.9% (P = .012), and at 18 months remission was reported in 49.2% vs. 27.3% (P = .004) (Ann Fam Med. 2010 Sep;8[5]:387-96).
By being alert to side effects, using a rating scale to measure symptom reduction, and not staying “locked” into the idea that all treatments require 6-8 weeks before patients see any improvement, clinicians can boost chances for adherence – and thus for remission – since patients who don’t improve in the first 2 weeks have just a 15% chance for improvement, Dr. Thase said. “You need 6-8 weeks to get to the maximum titration. That old 8-week rule applies mostly to patients who are showing improvement by week 2.”
If by week 2, the patient is not tolerating the medication’s side effects and has no symptom reduction, then move on to the next medication, Dr. Thase said, emphasizing the importance of seeing patients at least twice monthly. “If we’re only seeing a patient once a month, we’ve already fallen behind in the up-titration part, and we’ve missed the opportunity for early intervention if the patient is having side effects.”
Algorithms for choosing depression treatments should be a “fact of life,” he said. Start with the safest, easiest to tolerate, and least expensive of the available antidepressants, such as escitalopram and fluoxetine before working through the second- and third-line therapies and adjunctive therapies, all of which have greater risk profiles as you move through them. This algorithmic approach has been shown to result in patients scoring at least 10 points higher on a depression rating scale (JAMA Psychiatry. 2004;61:[7]669-80), which Dr. Thase said is equivalent to about a 30% higher chance of remission. “Don’t go over and over with the simple treatments that aren’t [evoking] a response. Move briskly on to the more complex treatments until patients respond.”
Treatment algorithms can include psychotherapies, either in combination with pharmacotherapy or as monotherapy. He encouraged clinicians to refer to the American Psychiatric Association (APA) practice guideline for depression for more details. The absence of depressive symptoms alone is not indicative of remission, according to the guideline, which Dr. Thase coauthored. The presence of positive emotions and resilience, along with a sense of control over emotions and hope for the future, indicates remission.
If after applying those methods a patient remains depressed and has been negatively screened for bipolar disorder, the use of tricyclics or monoamine oxidase inhibitors (MAOIs) may be appropriate. “MAOIs account for less than 1 in every 1,000 prescriptions for antidepressants, yet for people who don’t respond to modern antidepressants, they still can carry a 30%-40% response rate. So, if you don’t prescribe them yourself, please get access to someone who does,” Dr. Thase said.
The tenets of measurement-based care are essentially the lessons learned from the landmark Sequenced Treatment Alternatives to Relieve Depression (STAR*D) trial, which sought to address how pharmacologic care for depression could be delivered based on adequate dosing, attenuation of symptoms, fewer side effects, and other factors (Am J Psychiatry. 2006;163:1905-17).
Now,10 years later, measurement-based treatment is still finding its way into practice, Dr. Thase said in an interview. “But, there’s no reason to be unduly pessimistic. Ten years ago, depression screening was in the same position, and now it is both considered to be the standard of care and is widely done.”
Dr. Thase reported having extensive industry relationships, noting that he has been involved in the development of nearly every drug for the treatment of mood disorders. Global Academy and this news organization are owned by the same company.
On Twitter @whitneymcknight
WASHINGTON – Challenging patients with depression to stay engaged in their recovery while rigorously monitoring and measuring their treatment response can mean the difference between remission or resistance, according to an expert.
“We all wish for better treatments, but we really don’t have any coming available to us in the near future, so our task is to do as well as we can with what we have,” Michael E. Thase, MD, professor of psychiatry at the University of Pennsylvania, Philadelphia, said at Summit in Neurology & Psychiatry.
“We know far too well that there is a large gap between what we might be able to accomplish and what actually happens in clinical practice,” Dr. Thase said.
To close that gap, start with evaluating what can be done to combat patient nonadherence. A 2007 study indicated that just under 20% of patients adhere to antidepressant medication guidelines (Prim Care Companion J Clin Psychiatry. 2007;9[2]:91-9.), and according to Dr. Thase, less than 10% of patients being seen for depression in primary care actually fill their prescriptions.
“Don’t delude yourself that these patients drop out of treatment because they no longer need it. They drop out mostly because they have gotten disgusted, disappointed, or discouraged,” said Dr. Thase, attributing the high rate of nonadherence to the nature of depression itself.
“Depression is a state of pessimism, low confidence, and of not really feeling capable.”
Helping patients overcome their reluctance to follow treatment guidelines begins with accurately assessing their symptom severity. Patients who rate 4 or less on the Patient Health Questionnaire–9 (PHQ-9), which is based on the DSM-IV, are considered in remission or not to have severe depression. Similarly, patients who score 5 or less on the Quick Inventory of Depressive Symptomatology (QIDS) are not considered in the danger zone.
The severity ratings included in the DSM-5 can help clinicians pinpoint the level of depression a patient is experiencing, as can a therapeutic relationship with the patient and the family, Dr. Thase said at the summit, held by Global Academy for Medical Education.
He urged clinicians to monitor adherence routinely by asking patients whether or not they have filled or refilled their prescriptions. It is helpful to ask patients about missing doses and whether they are feeling any improvement, he said.
“It’s a very simple process: You keep track of the patients. Chase after them if they don’t follow through. If you’re not keeping track, the patients think [what they do] doesn’t matter,” Dr. Thase said.
A 2010 study of chronic depression treatment in primary care practices showed that compared with regular care, aggressive monitoring of patient adherence and outcomes in 728 adults with depression resulted in better remission rates across 18 months of treatment. At 6 months 43.4% of patients who had been contacted regularly by nursing and social worker staff were in remission, compared with 33.3% of the 78 who had received regular care (P = .11). At 12 months, the results were 52% vs. 33.9% (P = .012), and at 18 months remission was reported in 49.2% vs. 27.3% (P = .004) (Ann Fam Med. 2010 Sep;8[5]:387-96).
By being alert to side effects, using a rating scale to measure symptom reduction, and not staying “locked” into the idea that all treatments require 6-8 weeks before patients see any improvement, clinicians can boost chances for adherence – and thus for remission – since patients who don’t improve in the first 2 weeks have just a 15% chance for improvement, Dr. Thase said. “You need 6-8 weeks to get to the maximum titration. That old 8-week rule applies mostly to patients who are showing improvement by week 2.”
If by week 2, the patient is not tolerating the medication’s side effects and has no symptom reduction, then move on to the next medication, Dr. Thase said, emphasizing the importance of seeing patients at least twice monthly. “If we’re only seeing a patient once a month, we’ve already fallen behind in the up-titration part, and we’ve missed the opportunity for early intervention if the patient is having side effects.”
Algorithms for choosing depression treatments should be a “fact of life,” he said. Start with the safest, easiest to tolerate, and least expensive of the available antidepressants, such as escitalopram and fluoxetine before working through the second- and third-line therapies and adjunctive therapies, all of which have greater risk profiles as you move through them. This algorithmic approach has been shown to result in patients scoring at least 10 points higher on a depression rating scale (JAMA Psychiatry. 2004;61:[7]669-80), which Dr. Thase said is equivalent to about a 30% higher chance of remission. “Don’t go over and over with the simple treatments that aren’t [evoking] a response. Move briskly on to the more complex treatments until patients respond.”
Treatment algorithms can include psychotherapies, either in combination with pharmacotherapy or as monotherapy. He encouraged clinicians to refer to the American Psychiatric Association (APA) practice guideline for depression for more details. The absence of depressive symptoms alone is not indicative of remission, according to the guideline, which Dr. Thase coauthored. The presence of positive emotions and resilience, along with a sense of control over emotions and hope for the future, indicates remission.
If after applying those methods a patient remains depressed and has been negatively screened for bipolar disorder, the use of tricyclics or monoamine oxidase inhibitors (MAOIs) may be appropriate. “MAOIs account for less than 1 in every 1,000 prescriptions for antidepressants, yet for people who don’t respond to modern antidepressants, they still can carry a 30%-40% response rate. So, if you don’t prescribe them yourself, please get access to someone who does,” Dr. Thase said.
The tenets of measurement-based care are essentially the lessons learned from the landmark Sequenced Treatment Alternatives to Relieve Depression (STAR*D) trial, which sought to address how pharmacologic care for depression could be delivered based on adequate dosing, attenuation of symptoms, fewer side effects, and other factors (Am J Psychiatry. 2006;163:1905-17).
Now,10 years later, measurement-based treatment is still finding its way into practice, Dr. Thase said in an interview. “But, there’s no reason to be unduly pessimistic. Ten years ago, depression screening was in the same position, and now it is both considered to be the standard of care and is widely done.”
Dr. Thase reported having extensive industry relationships, noting that he has been involved in the development of nearly every drug for the treatment of mood disorders. Global Academy and this news organization are owned by the same company.
On Twitter @whitneymcknight
EXPERT ANALYSIS FROM SUMMIT OF NEUROLOGY & PSYCHIATRY
AUDIO: New bipolar disorder algorithm changes ranking of first-line therapies
WASHINGTON – In 2015, the Florida Agency for Health Care Administration published clinical guidelines for numerous psychiatric conditions, including bipolar disorder, demoting several first-line therapies, and promoting others.
Because the authors of the Florida Best Practice Psychotherapeutic Medication Guidelines for Adults agreed that inflammation is a mechanism of action in bipolar disorder, they adopted an approach to care that seeks to avoid inflammation at all costs.
“Some medications create metabolic disturbances, which can be disruptive to the inflammatory milieu,” said Roger McIntyre, MD, a professor of psychiatry and pharmacology at the University of Toronto, and head of the Mood Disorders Psychopharmacology Unit at the University Health Network, Toronto. Dr. McIntyre, one of the coauthors of the guidelines, discussed why the combination of olanzapine and fluoxetine has been deferred in the algorithm, why other medications have moved further up, why antidepressants also are lower in the order of priority, and why psychoeducation, social rhythm therapy, and lifestyle changes have been emphasized more than ever before.
“There is no way our bipolar patients are going to achieve their goals with medication alone,” Dr. McIntyre said at the meeting, held by the Global Academy for Medical Education. In addition, Dr. McIntyre outlined why adding bipolar screening in the primary care setting is critical in 2016, and called the new recommendations “the most up-to-date guidelines for treating bipolar disorder, and the new nosology of major depression disorder with mixed features.”
To access the Florida Best Practice Psychotherapeutic Medication Guidelines for Adults online, visit the Florida Medicaid Drug Therapy Management Program for Behavioral Health website.
Dr. McIntyre has numerous industry relationships, including research funding from Eli Lilly, Janssen-Ortho, Astra-Zeneca; Pfizer, and Lundbeck. Global Academy and this news organization are owned by the same company.
On Twitter @whitneymcknight
WASHINGTON – In 2015, the Florida Agency for Health Care Administration published clinical guidelines for numerous psychiatric conditions, including bipolar disorder, demoting several first-line therapies, and promoting others.
Because the authors of the Florida Best Practice Psychotherapeutic Medication Guidelines for Adults agreed that inflammation is a mechanism of action in bipolar disorder, they adopted an approach to care that seeks to avoid inflammation at all costs.
“Some medications create metabolic disturbances, which can be disruptive to the inflammatory milieu,” said Roger McIntyre, MD, a professor of psychiatry and pharmacology at the University of Toronto, and head of the Mood Disorders Psychopharmacology Unit at the University Health Network, Toronto. Dr. McIntyre, one of the coauthors of the guidelines, discussed why the combination of olanzapine and fluoxetine has been deferred in the algorithm, why other medications have moved further up, why antidepressants also are lower in the order of priority, and why psychoeducation, social rhythm therapy, and lifestyle changes have been emphasized more than ever before.
“There is no way our bipolar patients are going to achieve their goals with medication alone,” Dr. McIntyre said at the meeting, held by the Global Academy for Medical Education. In addition, Dr. McIntyre outlined why adding bipolar screening in the primary care setting is critical in 2016, and called the new recommendations “the most up-to-date guidelines for treating bipolar disorder, and the new nosology of major depression disorder with mixed features.”
To access the Florida Best Practice Psychotherapeutic Medication Guidelines for Adults online, visit the Florida Medicaid Drug Therapy Management Program for Behavioral Health website.
Dr. McIntyre has numerous industry relationships, including research funding from Eli Lilly, Janssen-Ortho, Astra-Zeneca; Pfizer, and Lundbeck. Global Academy and this news organization are owned by the same company.
On Twitter @whitneymcknight
WASHINGTON – In 2015, the Florida Agency for Health Care Administration published clinical guidelines for numerous psychiatric conditions, including bipolar disorder, demoting several first-line therapies, and promoting others.
Because the authors of the Florida Best Practice Psychotherapeutic Medication Guidelines for Adults agreed that inflammation is a mechanism of action in bipolar disorder, they adopted an approach to care that seeks to avoid inflammation at all costs.
“Some medications create metabolic disturbances, which can be disruptive to the inflammatory milieu,” said Roger McIntyre, MD, a professor of psychiatry and pharmacology at the University of Toronto, and head of the Mood Disorders Psychopharmacology Unit at the University Health Network, Toronto. Dr. McIntyre, one of the coauthors of the guidelines, discussed why the combination of olanzapine and fluoxetine has been deferred in the algorithm, why other medications have moved further up, why antidepressants also are lower in the order of priority, and why psychoeducation, social rhythm therapy, and lifestyle changes have been emphasized more than ever before.
“There is no way our bipolar patients are going to achieve their goals with medication alone,” Dr. McIntyre said at the meeting, held by the Global Academy for Medical Education. In addition, Dr. McIntyre outlined why adding bipolar screening in the primary care setting is critical in 2016, and called the new recommendations “the most up-to-date guidelines for treating bipolar disorder, and the new nosology of major depression disorder with mixed features.”
To access the Florida Best Practice Psychotherapeutic Medication Guidelines for Adults online, visit the Florida Medicaid Drug Therapy Management Program for Behavioral Health website.
Dr. McIntyre has numerous industry relationships, including research funding from Eli Lilly, Janssen-Ortho, Astra-Zeneca; Pfizer, and Lundbeck. Global Academy and this news organization are owned by the same company.
On Twitter @whitneymcknight
AT SUMMIT IN NEUROLOGY & PSYCHIATRY
July 2016: Click for Credit
Here are 4 articles in the July issue of Clinician Reviews (individual articles are valid for one year from date of publication—expiration dates below):
1. Pregnancy Alters Pharmacodynamics of Anti-TNF Agents in Women With IBD
To take the posttest, go to: http://bit.ly/1VQFIHf
Expires May 24, 2017
VITALS
Key clinical point: Blood levels of infliximab rose during pregnancy, while adalimumab levels remained stable, even after researchers accounted for changes in albumin, body mass index, and C-reactive protein levels.
Major finding: Median infliximab concentrations rose from 8.5 mcg/mL in the first trimester to a peak of 21 mcg/mL during the middle of the third trimester (P = .04). Median adalimumab levels ranged between 8.6 and 12.2 mcg/mL during pregnancy.
Data source: A prospective study of 25 pregnant women with ulcerative colitis or Crohn's disease.
Disclosures: Dr. Seow disclosed ties with Janssen, AbbVie, Takeda, Shire, and Actavis.
2. Vascular Disease Linked to Sight Loss in Giant Cell Arteritis
To take the posttest, go to: http://bit.ly/1UqLuu5
Expires May 10, 2017
VITALS
Key clinical point: Patients with vascular disease who develop giant cell arteritis may require careful monitoring for sight loss.
Major finding: Overall, 42.9% of patients had some visual disturbance at first clinic review; 7.9% were blind at 6 months.
Data source: Analysis of 433 patients newly diagnosed with GCA participating in the Diagnostic and Classification Criteria in Vasculitis Study (DCVAS).
Disclosures: The DCVAS study is supported by the American College of Rheumatology and is funded by the European League Against Rheumatism and the Vasculitis Foundation. Dr. Yates reported that he had no relevant disclosures.
3. Pediatric and Adolescent Mental Health
Part 1: Diagnoses, drug prescribing vary widely
To take the posttest, go to: http://bit.ly/24FHTxY
Expires April 1, 2017
VITALS
Key clinical point: A lack of psychiatrists only partially accounted for substantial variations in rates of mental illness diagnosis and prescriptions for psychotropic medications given in practices nationwide, a study has shown.
Major finding: Nationwide, 15% of pediatric patients received a mental health diagnosis, and 14% were prescribed psychotropic medications in primary care, regardless of colocated mental health services.
Data source: A retrospective study of electronic health records for 294,748 patients aged 4-18 years.
Disclosures: Dr. Alexander G. Fiks is an investigator for Pfizer; the other researchers said they had no relevant financial disclosures. This study was funded by the National Institutes of Health and the National Institute of Child Health and Human Development under the Best Pharmaceuticals for Children Act.
Part 2: Disorders prevalent in young transgender women
To take the posttest, go to: http://bit.ly/24FCDdq
Expires March 21, 2017
VITALS
Key clinical point: Young transgender women have a high prevalence of psychiatric disorders that is two to four times higher than that in the general population.
Major finding: 41.5% of the study participants had at least one psychiatric disorder, such as major depressive disorder, suicidality, generalized anxiety, PTSD, and alcohol or substance dependence.
Data source: An observational cohort study involving 298 transgender women aged 16-29 years residing in Chicago and Boston.
Disclosures: This study was supported by the National Institute of Mental Health. Dr. Reisner and his associates reported having no relevant financial disclosures.
Here are 4 articles in the July issue of Clinician Reviews (individual articles are valid for one year from date of publication—expiration dates below):
1. Pregnancy Alters Pharmacodynamics of Anti-TNF Agents in Women With IBD
To take the posttest, go to: http://bit.ly/1VQFIHf
Expires May 24, 2017
VITALS
Key clinical point: Blood levels of infliximab rose during pregnancy, while adalimumab levels remained stable, even after researchers accounted for changes in albumin, body mass index, and C-reactive protein levels.
Major finding: Median infliximab concentrations rose from 8.5 mcg/mL in the first trimester to a peak of 21 mcg/mL during the middle of the third trimester (P = .04). Median adalimumab levels ranged between 8.6 and 12.2 mcg/mL during pregnancy.
Data source: A prospective study of 25 pregnant women with ulcerative colitis or Crohn's disease.
Disclosures: Dr. Seow disclosed ties with Janssen, AbbVie, Takeda, Shire, and Actavis.
2. Vascular Disease Linked to Sight Loss in Giant Cell Arteritis
To take the posttest, go to: http://bit.ly/1UqLuu5
Expires May 10, 2017
VITALS
Key clinical point: Patients with vascular disease who develop giant cell arteritis may require careful monitoring for sight loss.
Major finding: Overall, 42.9% of patients had some visual disturbance at first clinic review; 7.9% were blind at 6 months.
Data source: Analysis of 433 patients newly diagnosed with GCA participating in the Diagnostic and Classification Criteria in Vasculitis Study (DCVAS).
Disclosures: The DCVAS study is supported by the American College of Rheumatology and is funded by the European League Against Rheumatism and the Vasculitis Foundation. Dr. Yates reported that he had no relevant disclosures.
3. Pediatric and Adolescent Mental Health
Part 1: Diagnoses, drug prescribing vary widely
To take the posttest, go to: http://bit.ly/24FHTxY
Expires April 1, 2017
VITALS
Key clinical point: A lack of psychiatrists only partially accounted for substantial variations in rates of mental illness diagnosis and prescriptions for psychotropic medications given in practices nationwide, a study has shown.
Major finding: Nationwide, 15% of pediatric patients received a mental health diagnosis, and 14% were prescribed psychotropic medications in primary care, regardless of colocated mental health services.
Data source: A retrospective study of electronic health records for 294,748 patients aged 4-18 years.
Disclosures: Dr. Alexander G. Fiks is an investigator for Pfizer; the other researchers said they had no relevant financial disclosures. This study was funded by the National Institutes of Health and the National Institute of Child Health and Human Development under the Best Pharmaceuticals for Children Act.
Part 2: Disorders prevalent in young transgender women
To take the posttest, go to: http://bit.ly/24FCDdq
Expires March 21, 2017
VITALS
Key clinical point: Young transgender women have a high prevalence of psychiatric disorders that is two to four times higher than that in the general population.
Major finding: 41.5% of the study participants had at least one psychiatric disorder, such as major depressive disorder, suicidality, generalized anxiety, PTSD, and alcohol or substance dependence.
Data source: An observational cohort study involving 298 transgender women aged 16-29 years residing in Chicago and Boston.
Disclosures: This study was supported by the National Institute of Mental Health. Dr. Reisner and his associates reported having no relevant financial disclosures.
Here are 4 articles in the July issue of Clinician Reviews (individual articles are valid for one year from date of publication—expiration dates below):
1. Pregnancy Alters Pharmacodynamics of Anti-TNF Agents in Women With IBD
To take the posttest, go to: http://bit.ly/1VQFIHf
Expires May 24, 2017
VITALS
Key clinical point: Blood levels of infliximab rose during pregnancy, while adalimumab levels remained stable, even after researchers accounted for changes in albumin, body mass index, and C-reactive protein levels.
Major finding: Median infliximab concentrations rose from 8.5 mcg/mL in the first trimester to a peak of 21 mcg/mL during the middle of the third trimester (P = .04). Median adalimumab levels ranged between 8.6 and 12.2 mcg/mL during pregnancy.
Data source: A prospective study of 25 pregnant women with ulcerative colitis or Crohn's disease.
Disclosures: Dr. Seow disclosed ties with Janssen, AbbVie, Takeda, Shire, and Actavis.
2. Vascular Disease Linked to Sight Loss in Giant Cell Arteritis
To take the posttest, go to: http://bit.ly/1UqLuu5
Expires May 10, 2017
VITALS
Key clinical point: Patients with vascular disease who develop giant cell arteritis may require careful monitoring for sight loss.
Major finding: Overall, 42.9% of patients had some visual disturbance at first clinic review; 7.9% were blind at 6 months.
Data source: Analysis of 433 patients newly diagnosed with GCA participating in the Diagnostic and Classification Criteria in Vasculitis Study (DCVAS).
Disclosures: The DCVAS study is supported by the American College of Rheumatology and is funded by the European League Against Rheumatism and the Vasculitis Foundation. Dr. Yates reported that he had no relevant disclosures.
3. Pediatric and Adolescent Mental Health
Part 1: Diagnoses, drug prescribing vary widely
To take the posttest, go to: http://bit.ly/24FHTxY
Expires April 1, 2017
VITALS
Key clinical point: A lack of psychiatrists only partially accounted for substantial variations in rates of mental illness diagnosis and prescriptions for psychotropic medications given in practices nationwide, a study has shown.
Major finding: Nationwide, 15% of pediatric patients received a mental health diagnosis, and 14% were prescribed psychotropic medications in primary care, regardless of colocated mental health services.
Data source: A retrospective study of electronic health records for 294,748 patients aged 4-18 years.
Disclosures: Dr. Alexander G. Fiks is an investigator for Pfizer; the other researchers said they had no relevant financial disclosures. This study was funded by the National Institutes of Health and the National Institute of Child Health and Human Development under the Best Pharmaceuticals for Children Act.
Part 2: Disorders prevalent in young transgender women
To take the posttest, go to: http://bit.ly/24FCDdq
Expires March 21, 2017
VITALS
Key clinical point: Young transgender women have a high prevalence of psychiatric disorders that is two to four times higher than that in the general population.
Major finding: 41.5% of the study participants had at least one psychiatric disorder, such as major depressive disorder, suicidality, generalized anxiety, PTSD, and alcohol or substance dependence.
Data source: An observational cohort study involving 298 transgender women aged 16-29 years residing in Chicago and Boston.
Disclosures: This study was supported by the National Institute of Mental Health. Dr. Reisner and his associates reported having no relevant financial disclosures.
ACIP hints at move from three-dose to two-dose HPV vaccination schedule for youth
A work group for the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices is leaning toward recommending a change from three to two doses of the human papillomavirus (HPV) vaccine in boys and girls aged 11-12 years.
Members of the ACIP Human Papillomavirus Work Group told the entire committee at ACIP’s June meeting that a review of all available data showed that, regardless of whether the HPV vaccine were bivalent, quadrivalent, or nine-valent, two doses were found to be noninferior, compared with three doses. A two-dose schedule, therefore, could possibly be recommended at the next ACIP meeting later this year.
The work group said it also could recommend that HPV vaccine–naive women up to age 26 years and HPV vaccine-naive men up to age 21 years also receive the vaccine. For persons who initiated but did not complete vaccination before age 15 years, or for persons who initiate the schedule after their 15th birthday – the same schedule as is currently recommended for 11- and 12-year-olds – a similar schedule is likely to be recommended again.
The recommendation for immunocompromised persons of any age would be to receive the three-dose schedule.
If these recommendations are put forth officially, the question of whether families also should be given a three-dose option will need to be decided, work group members said.
Although studies are ongoing to determine antibody persistence and long-term effectiveness after two doses, existing data indicate that waning antibody responses to HPV18 in persons vaccinated with three doses of quadrivalent HPV were not associated with loss of protection. This could mean that protective levels are actually lower than the minimum levels detected by assays, or that antibodies against other epitopes also are protective.
Predictive modeling showed that, if a two-dose schedule can provide more than 20 years of protection, over $118,000 per quality adjusted life year could be realized without sacrificing population health benefits.
The current CDC vaccination schedule for HPV in adolescents is for a three-dose series of the vaccine on a schedule of 0, 1-2, and 6 months. The same vaccination schedule is recommended for “catch-up” of previously unvaccinated adolescents aged 13-18 years.
On Twitter @whitneymcknight
A work group for the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices is leaning toward recommending a change from three to two doses of the human papillomavirus (HPV) vaccine in boys and girls aged 11-12 years.
Members of the ACIP Human Papillomavirus Work Group told the entire committee at ACIP’s June meeting that a review of all available data showed that, regardless of whether the HPV vaccine were bivalent, quadrivalent, or nine-valent, two doses were found to be noninferior, compared with three doses. A two-dose schedule, therefore, could possibly be recommended at the next ACIP meeting later this year.
The work group said it also could recommend that HPV vaccine–naive women up to age 26 years and HPV vaccine-naive men up to age 21 years also receive the vaccine. For persons who initiated but did not complete vaccination before age 15 years, or for persons who initiate the schedule after their 15th birthday – the same schedule as is currently recommended for 11- and 12-year-olds – a similar schedule is likely to be recommended again.
The recommendation for immunocompromised persons of any age would be to receive the three-dose schedule.
If these recommendations are put forth officially, the question of whether families also should be given a three-dose option will need to be decided, work group members said.
Although studies are ongoing to determine antibody persistence and long-term effectiveness after two doses, existing data indicate that waning antibody responses to HPV18 in persons vaccinated with three doses of quadrivalent HPV were not associated with loss of protection. This could mean that protective levels are actually lower than the minimum levels detected by assays, or that antibodies against other epitopes also are protective.
Predictive modeling showed that, if a two-dose schedule can provide more than 20 years of protection, over $118,000 per quality adjusted life year could be realized without sacrificing population health benefits.
The current CDC vaccination schedule for HPV in adolescents is for a three-dose series of the vaccine on a schedule of 0, 1-2, and 6 months. The same vaccination schedule is recommended for “catch-up” of previously unvaccinated adolescents aged 13-18 years.
On Twitter @whitneymcknight
A work group for the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices is leaning toward recommending a change from three to two doses of the human papillomavirus (HPV) vaccine in boys and girls aged 11-12 years.
Members of the ACIP Human Papillomavirus Work Group told the entire committee at ACIP’s June meeting that a review of all available data showed that, regardless of whether the HPV vaccine were bivalent, quadrivalent, or nine-valent, two doses were found to be noninferior, compared with three doses. A two-dose schedule, therefore, could possibly be recommended at the next ACIP meeting later this year.
The work group said it also could recommend that HPV vaccine–naive women up to age 26 years and HPV vaccine-naive men up to age 21 years also receive the vaccine. For persons who initiated but did not complete vaccination before age 15 years, or for persons who initiate the schedule after their 15th birthday – the same schedule as is currently recommended for 11- and 12-year-olds – a similar schedule is likely to be recommended again.
The recommendation for immunocompromised persons of any age would be to receive the three-dose schedule.
If these recommendations are put forth officially, the question of whether families also should be given a three-dose option will need to be decided, work group members said.
Although studies are ongoing to determine antibody persistence and long-term effectiveness after two doses, existing data indicate that waning antibody responses to HPV18 in persons vaccinated with three doses of quadrivalent HPV were not associated with loss of protection. This could mean that protective levels are actually lower than the minimum levels detected by assays, or that antibodies against other epitopes also are protective.
Predictive modeling showed that, if a two-dose schedule can provide more than 20 years of protection, over $118,000 per quality adjusted life year could be realized without sacrificing population health benefits.
The current CDC vaccination schedule for HPV in adolescents is for a three-dose series of the vaccine on a schedule of 0, 1-2, and 6 months. The same vaccination schedule is recommended for “catch-up” of previously unvaccinated adolescents aged 13-18 years.
On Twitter @whitneymcknight
FROM AN ACIP MEETING
ACIP votes to scrap LAIV vaccine for 2016-2017 influenza season
The Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices has voted to scrap the use of the live attenuated influenza vaccine for the 2016-2017 flu season.
ACIP’s interim recommendation guidance to the CDC is that “no live attenuated influenza vaccines (LAIV) should be used in any setting,” after reviewing data showing that for three consecutive influenza seasons, LAIV’s vaccine effectiveness (VE) against any flu virus was 3% (95% confidence interval, -49%-37%) in children aged 2-17 years. Meanwhile, injectable inactivated influenza vaccine (IIV) had a VE estimate of 63% (95% CI, 52%-72%) against any flu virus in that age group. Findings were similar across age groups.
CDC epidemiologist Brendan Flannery, Ph.D., painted a damning picture of the intranasal LAIV, presenting preliminary data from the U.S. Flu Vaccine Effectiveness Network for 2015-2016 that showed quadrivalent LAIV offered children “no significant protection against influenza A(H1N1)pdm09.” He also presented 2015-2016 national cohort data from Finland showing that unadjusted vaccine effectiveness (VE) against the H1N1 strain for LAIV in 2-year-olds was 47%, compared with 78% for IIV. Dr. Flannery also cited a series of other U.S. and international studies that did not support the use of LAIV, including unpublished Department of Defense 2015-2016 influenza season data for military families indicating that VE for LAIV against the strain last season was “insignificant” in children aged 2-17 years.
Data from an industry study of the quadrivalent LAIV FluMist (MedImmune) also indicated that in this cohort, for the 2015-2016 influenza season, LAIV underperformed compared with IIV, 46% vs. 65%.
Still more bad news for LAIV came from an English study published online just as the ACIP meeting was getting underway. Those data showed that from October 2015 through May 2016, LAIV in children aged 2-17 years had a VE of 57.6% against influenza A and B.
Debate over whether to pull support for LAIV entirely or to allow the use of it in certain circumstances – such as when a person declined a flu shot – hinged on the projected upheaval pulling LAIV is likely to cause.
Concerns were raised around what would happen in the case of LAIV vaccine orders already placed, over whether pulling LAIV would mean a shortage of other vaccine alternatives, and how communicating contingencies might only confuse the public, but several committee members spoke forcefully in favor of what they said the data compelled them to do.
“The science simply shows that LAIV has not worked for the past 3 years, whereas IIV has,” American Academy of Pediatrics Infectious Disease Committee’s Red Book editor, and AAP liaison to ACIP, Dr. David Kimberlin said before the vote.
Restricting but not prohibiting LAIV also would have allowed for an easier transition back to LAIV if the vaccine were successfully reformulated, ACIP Influenza Work Group Chair Dr. Ruth Karron said while presenting potential policy recommendations.
During the debate over whether to pull or limit support for the inhaled vaccine, Dr. Karron reminded the committee that at the time the Food and Drug Administration approved LAIV, serum antibody responses to both the tri- and quadrivalent vaccine were modest, prompting the FDA to call for effectiveness studies. “So, my question to the FDA now is, ‘What are their plans?’ ”
“We’ve seen the studies, but we’ve not really reviewed all the data,” Dr. Wellington Sun, the FDA’s ACIP liaison responded. “I think we have to acknowledge that LAIV has offered advantages over IIV in the past. At this point, we’re not ready to undertake a program for changing the prescriber’s information. We want to continue to work with MedImmune to find out the root cause of this phenomenon.”
“We’ve increased our research into understanding the biology of the H1N1pdm09 LAIV strains so we can improve their effectiveness in future seasons,” Dr. Chris Ambrose, vice president of U.S. medical affairs for infectious disease at MedImmune’s parent company AstraZeneca, told the committee.
“I think this is a very sad day for the influenza vaccination program,” ACIP chair Dr. Nancy Bennett said before adjourning the meeting. “We all had great hopes. It’s not over. If you’ve seen 1 influenza year, you’ve seen 1 influenza year. We may be back here next year having a very different discussion.”
The CDC is not obligated to adopt ACIP recommendations, but typically does. The committee also accepted a resolution to update the Vaccines for Children program in accordance with the recommendation to deny support for LAIV this flu season.
Thirteen members of the committee voted in favor of the recommendation. Dr. Edward Belongia abstained citing a conflict of interest, and Ms. Cynthia Pelligrini voted no, citing “insufficient time to consider this information.” The ICICLE trial NCT01997450, was sponsored by MedImmune, a subsidiary of AstraZeneca where Dr. Ambrose is vice president of U.S. medical affairs for infectious disease.
On Twitter @whitneymcknight
The Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices has voted to scrap the use of the live attenuated influenza vaccine for the 2016-2017 flu season.
ACIP’s interim recommendation guidance to the CDC is that “no live attenuated influenza vaccines (LAIV) should be used in any setting,” after reviewing data showing that for three consecutive influenza seasons, LAIV’s vaccine effectiveness (VE) against any flu virus was 3% (95% confidence interval, -49%-37%) in children aged 2-17 years. Meanwhile, injectable inactivated influenza vaccine (IIV) had a VE estimate of 63% (95% CI, 52%-72%) against any flu virus in that age group. Findings were similar across age groups.
CDC epidemiologist Brendan Flannery, Ph.D., painted a damning picture of the intranasal LAIV, presenting preliminary data from the U.S. Flu Vaccine Effectiveness Network for 2015-2016 that showed quadrivalent LAIV offered children “no significant protection against influenza A(H1N1)pdm09.” He also presented 2015-2016 national cohort data from Finland showing that unadjusted vaccine effectiveness (VE) against the H1N1 strain for LAIV in 2-year-olds was 47%, compared with 78% for IIV. Dr. Flannery also cited a series of other U.S. and international studies that did not support the use of LAIV, including unpublished Department of Defense 2015-2016 influenza season data for military families indicating that VE for LAIV against the strain last season was “insignificant” in children aged 2-17 years.
Data from an industry study of the quadrivalent LAIV FluMist (MedImmune) also indicated that in this cohort, for the 2015-2016 influenza season, LAIV underperformed compared with IIV, 46% vs. 65%.
Still more bad news for LAIV came from an English study published online just as the ACIP meeting was getting underway. Those data showed that from October 2015 through May 2016, LAIV in children aged 2-17 years had a VE of 57.6% against influenza A and B.
Debate over whether to pull support for LAIV entirely or to allow the use of it in certain circumstances – such as when a person declined a flu shot – hinged on the projected upheaval pulling LAIV is likely to cause.
Concerns were raised around what would happen in the case of LAIV vaccine orders already placed, over whether pulling LAIV would mean a shortage of other vaccine alternatives, and how communicating contingencies might only confuse the public, but several committee members spoke forcefully in favor of what they said the data compelled them to do.
“The science simply shows that LAIV has not worked for the past 3 years, whereas IIV has,” American Academy of Pediatrics Infectious Disease Committee’s Red Book editor, and AAP liaison to ACIP, Dr. David Kimberlin said before the vote.
Restricting but not prohibiting LAIV also would have allowed for an easier transition back to LAIV if the vaccine were successfully reformulated, ACIP Influenza Work Group Chair Dr. Ruth Karron said while presenting potential policy recommendations.
During the debate over whether to pull or limit support for the inhaled vaccine, Dr. Karron reminded the committee that at the time the Food and Drug Administration approved LAIV, serum antibody responses to both the tri- and quadrivalent vaccine were modest, prompting the FDA to call for effectiveness studies. “So, my question to the FDA now is, ‘What are their plans?’ ”
“We’ve seen the studies, but we’ve not really reviewed all the data,” Dr. Wellington Sun, the FDA’s ACIP liaison responded. “I think we have to acknowledge that LAIV has offered advantages over IIV in the past. At this point, we’re not ready to undertake a program for changing the prescriber’s information. We want to continue to work with MedImmune to find out the root cause of this phenomenon.”
“We’ve increased our research into understanding the biology of the H1N1pdm09 LAIV strains so we can improve their effectiveness in future seasons,” Dr. Chris Ambrose, vice president of U.S. medical affairs for infectious disease at MedImmune’s parent company AstraZeneca, told the committee.
“I think this is a very sad day for the influenza vaccination program,” ACIP chair Dr. Nancy Bennett said before adjourning the meeting. “We all had great hopes. It’s not over. If you’ve seen 1 influenza year, you’ve seen 1 influenza year. We may be back here next year having a very different discussion.”
The CDC is not obligated to adopt ACIP recommendations, but typically does. The committee also accepted a resolution to update the Vaccines for Children program in accordance with the recommendation to deny support for LAIV this flu season.
Thirteen members of the committee voted in favor of the recommendation. Dr. Edward Belongia abstained citing a conflict of interest, and Ms. Cynthia Pelligrini voted no, citing “insufficient time to consider this information.” The ICICLE trial NCT01997450, was sponsored by MedImmune, a subsidiary of AstraZeneca where Dr. Ambrose is vice president of U.S. medical affairs for infectious disease.
On Twitter @whitneymcknight
The Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices has voted to scrap the use of the live attenuated influenza vaccine for the 2016-2017 flu season.
ACIP’s interim recommendation guidance to the CDC is that “no live attenuated influenza vaccines (LAIV) should be used in any setting,” after reviewing data showing that for three consecutive influenza seasons, LAIV’s vaccine effectiveness (VE) against any flu virus was 3% (95% confidence interval, -49%-37%) in children aged 2-17 years. Meanwhile, injectable inactivated influenza vaccine (IIV) had a VE estimate of 63% (95% CI, 52%-72%) against any flu virus in that age group. Findings were similar across age groups.
CDC epidemiologist Brendan Flannery, Ph.D., painted a damning picture of the intranasal LAIV, presenting preliminary data from the U.S. Flu Vaccine Effectiveness Network for 2015-2016 that showed quadrivalent LAIV offered children “no significant protection against influenza A(H1N1)pdm09.” He also presented 2015-2016 national cohort data from Finland showing that unadjusted vaccine effectiveness (VE) against the H1N1 strain for LAIV in 2-year-olds was 47%, compared with 78% for IIV. Dr. Flannery also cited a series of other U.S. and international studies that did not support the use of LAIV, including unpublished Department of Defense 2015-2016 influenza season data for military families indicating that VE for LAIV against the strain last season was “insignificant” in children aged 2-17 years.
Data from an industry study of the quadrivalent LAIV FluMist (MedImmune) also indicated that in this cohort, for the 2015-2016 influenza season, LAIV underperformed compared with IIV, 46% vs. 65%.
Still more bad news for LAIV came from an English study published online just as the ACIP meeting was getting underway. Those data showed that from October 2015 through May 2016, LAIV in children aged 2-17 years had a VE of 57.6% against influenza A and B.
Debate over whether to pull support for LAIV entirely or to allow the use of it in certain circumstances – such as when a person declined a flu shot – hinged on the projected upheaval pulling LAIV is likely to cause.
Concerns were raised around what would happen in the case of LAIV vaccine orders already placed, over whether pulling LAIV would mean a shortage of other vaccine alternatives, and how communicating contingencies might only confuse the public, but several committee members spoke forcefully in favor of what they said the data compelled them to do.
“The science simply shows that LAIV has not worked for the past 3 years, whereas IIV has,” American Academy of Pediatrics Infectious Disease Committee’s Red Book editor, and AAP liaison to ACIP, Dr. David Kimberlin said before the vote.
Restricting but not prohibiting LAIV also would have allowed for an easier transition back to LAIV if the vaccine were successfully reformulated, ACIP Influenza Work Group Chair Dr. Ruth Karron said while presenting potential policy recommendations.
During the debate over whether to pull or limit support for the inhaled vaccine, Dr. Karron reminded the committee that at the time the Food and Drug Administration approved LAIV, serum antibody responses to both the tri- and quadrivalent vaccine were modest, prompting the FDA to call for effectiveness studies. “So, my question to the FDA now is, ‘What are their plans?’ ”
“We’ve seen the studies, but we’ve not really reviewed all the data,” Dr. Wellington Sun, the FDA’s ACIP liaison responded. “I think we have to acknowledge that LAIV has offered advantages over IIV in the past. At this point, we’re not ready to undertake a program for changing the prescriber’s information. We want to continue to work with MedImmune to find out the root cause of this phenomenon.”
“We’ve increased our research into understanding the biology of the H1N1pdm09 LAIV strains so we can improve their effectiveness in future seasons,” Dr. Chris Ambrose, vice president of U.S. medical affairs for infectious disease at MedImmune’s parent company AstraZeneca, told the committee.
“I think this is a very sad day for the influenza vaccination program,” ACIP chair Dr. Nancy Bennett said before adjourning the meeting. “We all had great hopes. It’s not over. If you’ve seen 1 influenza year, you’ve seen 1 influenza year. We may be back here next year having a very different discussion.”
The CDC is not obligated to adopt ACIP recommendations, but typically does. The committee also accepted a resolution to update the Vaccines for Children program in accordance with the recommendation to deny support for LAIV this flu season.
Thirteen members of the committee voted in favor of the recommendation. Dr. Edward Belongia abstained citing a conflict of interest, and Ms. Cynthia Pelligrini voted no, citing “insufficient time to consider this information.” The ICICLE trial NCT01997450, was sponsored by MedImmune, a subsidiary of AstraZeneca where Dr. Ambrose is vice president of U.S. medical affairs for infectious disease.
On Twitter @whitneymcknight
FROM AN ACIP MEETING
ACIP recommends MenACWY vaccine for HIV-infected persons 2 months and older
The Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices unanimously voted to recommend that all HIV-infected persons aged 2 months and older receive the meningococcal ACWY (MenACWY) vaccine.
Guidance for this recommendation states that persons 2 months and older with HIV who have not been vaccinated previously should receive a two-dose, primary series of MenACWY; and that HIV-infected persons who have been vaccinated previously with one dose of MenACWY should receive a second dose at the earliest opportunity, with an 8-week minimum interval between doses. After that, boosters are to be given at the appropriate intervals.
Committee members voted in favor of immunizing earlier rather than waiting until 11 years of age or older, in part because human complement (hSBA) antibody titers following up to two doses of MenACWY vaccine in HIV-infected children ages 2-10 years is higher than in those ages 11-24 years. Also, the agreed upon recommended policy for earlier immunization is in step with current ACIP recommendations for use of the vaccine in persons with functional/anatomic asplenia or complement component deficiencies.
Despite an overall decline in the risk of meningococcal disease in the United States, there was a 13-fold increased risk in HIV-infected persons aged 25-64 years between 2000 and 2008, according to surveillance data presented to ACIP by Ms. Jessica MacNeil, MPH, an epidemiologist at the National Center for Immunization and Respiratory Diseases at the CDC in Atlanta. A ten-fold increase in risk was recorded in New York City alone in this population between 2000 and 2011.
Although fatality data are mixed, the infections were due primarily to serogroups C, W, and Y, for which the immune response wanes rapidly, according to Ms. MacNeil.
There are no safety or immunogenicity data currently available for the use of serogroup B meningococcal vaccines in HIV-infected persons, she said.
ACIP members also unanimously recommended this vaccine be covered under the Vaccines for Children program.
No information about disclosures was available at press time.
On Twitter @whitneymcknight
The Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices unanimously voted to recommend that all HIV-infected persons aged 2 months and older receive the meningococcal ACWY (MenACWY) vaccine.
Guidance for this recommendation states that persons 2 months and older with HIV who have not been vaccinated previously should receive a two-dose, primary series of MenACWY; and that HIV-infected persons who have been vaccinated previously with one dose of MenACWY should receive a second dose at the earliest opportunity, with an 8-week minimum interval between doses. After that, boosters are to be given at the appropriate intervals.
Committee members voted in favor of immunizing earlier rather than waiting until 11 years of age or older, in part because human complement (hSBA) antibody titers following up to two doses of MenACWY vaccine in HIV-infected children ages 2-10 years is higher than in those ages 11-24 years. Also, the agreed upon recommended policy for earlier immunization is in step with current ACIP recommendations for use of the vaccine in persons with functional/anatomic asplenia or complement component deficiencies.
Despite an overall decline in the risk of meningococcal disease in the United States, there was a 13-fold increased risk in HIV-infected persons aged 25-64 years between 2000 and 2008, according to surveillance data presented to ACIP by Ms. Jessica MacNeil, MPH, an epidemiologist at the National Center for Immunization and Respiratory Diseases at the CDC in Atlanta. A ten-fold increase in risk was recorded in New York City alone in this population between 2000 and 2011.
Although fatality data are mixed, the infections were due primarily to serogroups C, W, and Y, for which the immune response wanes rapidly, according to Ms. MacNeil.
There are no safety or immunogenicity data currently available for the use of serogroup B meningococcal vaccines in HIV-infected persons, she said.
ACIP members also unanimously recommended this vaccine be covered under the Vaccines for Children program.
No information about disclosures was available at press time.
On Twitter @whitneymcknight
The Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices unanimously voted to recommend that all HIV-infected persons aged 2 months and older receive the meningococcal ACWY (MenACWY) vaccine.
Guidance for this recommendation states that persons 2 months and older with HIV who have not been vaccinated previously should receive a two-dose, primary series of MenACWY; and that HIV-infected persons who have been vaccinated previously with one dose of MenACWY should receive a second dose at the earliest opportunity, with an 8-week minimum interval between doses. After that, boosters are to be given at the appropriate intervals.
Committee members voted in favor of immunizing earlier rather than waiting until 11 years of age or older, in part because human complement (hSBA) antibody titers following up to two doses of MenACWY vaccine in HIV-infected children ages 2-10 years is higher than in those ages 11-24 years. Also, the agreed upon recommended policy for earlier immunization is in step with current ACIP recommendations for use of the vaccine in persons with functional/anatomic asplenia or complement component deficiencies.
Despite an overall decline in the risk of meningococcal disease in the United States, there was a 13-fold increased risk in HIV-infected persons aged 25-64 years between 2000 and 2008, according to surveillance data presented to ACIP by Ms. Jessica MacNeil, MPH, an epidemiologist at the National Center for Immunization and Respiratory Diseases at the CDC in Atlanta. A ten-fold increase in risk was recorded in New York City alone in this population between 2000 and 2011.
Although fatality data are mixed, the infections were due primarily to serogroups C, W, and Y, for which the immune response wanes rapidly, according to Ms. MacNeil.
There are no safety or immunogenicity data currently available for the use of serogroup B meningococcal vaccines in HIV-infected persons, she said.
ACIP members also unanimously recommended this vaccine be covered under the Vaccines for Children program.
No information about disclosures was available at press time.
On Twitter @whitneymcknight
FROM AN ACIP MEETING
AAP, NASPAG issue joint guidance on menstruation management in teens with disabilities
For the first time, the American Academy of Pediatrics is offering guidance on managing menstruation and sexuality education in adolescents with disabilities.
Written jointly with the North American Society for Pediatric and Adolescent Gynecology, the clinical report offers guidance on options for menstrual management, sexual education and expression, and protection from sexual abuse. The report gives guidance regarding the care of adolescents with physical and/or intellectual abilities, but not for those with psychiatric illnesses (Pediatrics. 2016 April. doi: 10.1542/peds.2016-0295).
“Taking care of teens with disabilities and figuring out what to do with menstrual management has been all over the map,” Dr. Cora Collette Breuner, chair of the AAP’s committee on adolescence, said in an interview. “So, we tried to clarify it and help clinicians know what to do and when.”
A particular concern for the two groups was the threat of adverse events. “We wanted to cover what’s safe and what’s not in menstruation management, especially around bone health and thromboembolic events,” said Dr. Breuner, a professor of pediatrics and adolescent medicine at the University of Washington, Seattle.
Some of the information will not surprise clinicians, but there are some data that will perhaps come as news, said Dr. Breuner, including the recommendation that long-acting reversible contraception (LARC), such as the levonorgestrel intrauterine device or the progesterone implant rod should be considered first-line management therapies. “We point out that a number of studies show that these are safe.”
The report emphasizes offering anticipatory guidance before menses begins, noting that most teens with disabilities mature at the same rate as teens without disabilities. The report does not recommend premenarchal suppression in these patients, because doing so can interfere with normal bone growth. Such suppression also prevents patients and their families and caregivers from discovering that coping with the onset of menses is perhaps not as difficult as they might fear, the report states.
Although combined oral contraceptives are not contraindicated in teens with mobility issues, to guard against the threat of thromboembolic events in teens who use wheelchairs, the report recommends taking a thorough family history to rule out inherited thrombophilia. Otherwise, the recommendation is to prescribe the lowest-dose estrogen with a first- or second-generation progestin, as these are associated with lower rates of venous thrombotic events.
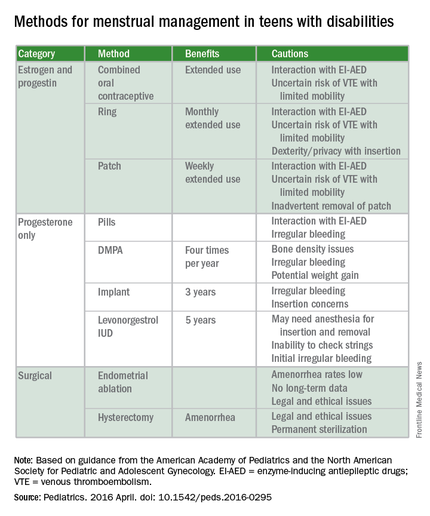
The guidance states that if cycles are creating difficulties in the patient’s life, “as determined by health care providers, patients, and families,” then menstrual management is appropriate. Even though it may take up to 3 years before a menstrual cycle becomes regular, the report cites irregularities caused by certain medications can be reason enough for menstrual management. Specific drugs noted include those affecting the dopaminergic system, valproic acid, and medications that elevate prolactin. Teens with obesity, seizure disorders, and polycystic ovary syndrome also can experience higher rates of irregularity.
The report also warns against the assumption that teens with disabilities are asexual or uninterested in sex. When appropriate, they should be offered the same confidential conversations about sexuality as are recommended for all teenagers by the AAP and the American College of Obstetricians and Gynecologists. “Teenagers with physical disabilities are just as likely to be sexually active as their peers and have a higher incidence of sexual abuse,” the report states. It is typically when a patient is cognitively impaired that consent to confidential services may require “discussion about legal guardianship or medical power of attorney status for families,” according to the report.
The report’s comprehensive review of four main menstrual management techniques – estrogen-containing, progestin-only, nonhormonal methods, and surgical requests and options – begins with the caveat that regardless of the method used, the threat of abuse or sexually transmitted infections remain. When a patient’s family or caregivers request suppression of menarche in a patient, stating fears of abuse or pregnancy, further investigation into the patient’s circumstances is warranted, the report states.
“It’s always worth reminding physicians that in this cohort, endometrial ablation can have legal implications, and it’s not recommended in this age group,” Dr. Breuner said.
On average, 1.5 hormonal methods are tried before achieving management goals, according to the report. Data cited in the study showed that at 42%, oral contraception is the preferred method of menstrual suppression, followed by the patch at 20%. Expectant management was third at 15%, followed by DMPA (depot medroxyprogesterone acetate) at 12%. The least utilized method was the levonorgestrel intrauterine device at 3%. No data were provided for the implantable contraceptive rod.
The clinical report is a companion document to another AAP clinical report, “Sexuality of Children and Adolescents with Developmental Disabilities” (Pediatrics. 2006. doi: 10.1542/peds.2006-1115).
AAP guidance on these matters in teens with psychiatric illnesses is expected to be issued within a few years, Dr. Breuner said.
There was no external funding and the authors have no relevant financial disclosures.
On Twitter @whitneymcknight
Although this guideline focuses on menstrual management and the guidance for you to help teens with disabilities through the pubertal transition, it’s very important to put this topic also into the context of sexuality. I think you have a great opportunity to do this because, often, you already have developed long-term relationships with these teenagers and their families, so the trust is already there. You should be the one to ensure all patients have appropriate sex education and help families with this.
 |
Dr. Elisabeth Quint |
For some of these teens who are cognitively impaired, the initial conversations about sex may focus more on safety and abuse prevention. For example, which parts of their body should not be touched by other people. You can help the families really be the educators. Parents can be the ones to teach their kids how to protect themselves by rehearsing the answers to questions like, “What do you do if someone touches you? Who do you tell? Where do you go? What if it happens at school?” As part of the safety aspects, you also can help families assess whether the patient will be able to have a consensual sexual relationship. It’s the teens who have mild cognitive impairment that I worry about most, because often they are friendly and open to people, and can be taken advantage of. You just want to make sure they have the right information at their appropriate level.
Adolescents with physical disabilities are going to be just as interested in sex as any other teens and should be helped with any potential issues that they may have around that issue. They will likely get sex education in schools, but are still often viewed as not interested in sex or sexually active, and they may not get the usual confidential teen questions or appropriate screenings. Menstrual management and sexuality education both are important aspects of reproductive health care for teens with disabilities.
Dr. Elisabeth Quint, lead author of the AAP clinical report “Menstrual Management for Adolescents,” is a clinical professor of obstetrics and gynecology at the University of Michigan, Ann Arbor. She is also a past president of the North American Society for Pediatric and Adolescent Gynecology.
Although this guideline focuses on menstrual management and the guidance for you to help teens with disabilities through the pubertal transition, it’s very important to put this topic also into the context of sexuality. I think you have a great opportunity to do this because, often, you already have developed long-term relationships with these teenagers and their families, so the trust is already there. You should be the one to ensure all patients have appropriate sex education and help families with this.
 |
Dr. Elisabeth Quint |
For some of these teens who are cognitively impaired, the initial conversations about sex may focus more on safety and abuse prevention. For example, which parts of their body should not be touched by other people. You can help the families really be the educators. Parents can be the ones to teach their kids how to protect themselves by rehearsing the answers to questions like, “What do you do if someone touches you? Who do you tell? Where do you go? What if it happens at school?” As part of the safety aspects, you also can help families assess whether the patient will be able to have a consensual sexual relationship. It’s the teens who have mild cognitive impairment that I worry about most, because often they are friendly and open to people, and can be taken advantage of. You just want to make sure they have the right information at their appropriate level.
Adolescents with physical disabilities are going to be just as interested in sex as any other teens and should be helped with any potential issues that they may have around that issue. They will likely get sex education in schools, but are still often viewed as not interested in sex or sexually active, and they may not get the usual confidential teen questions or appropriate screenings. Menstrual management and sexuality education both are important aspects of reproductive health care for teens with disabilities.
Dr. Elisabeth Quint, lead author of the AAP clinical report “Menstrual Management for Adolescents,” is a clinical professor of obstetrics and gynecology at the University of Michigan, Ann Arbor. She is also a past president of the North American Society for Pediatric and Adolescent Gynecology.
Although this guideline focuses on menstrual management and the guidance for you to help teens with disabilities through the pubertal transition, it’s very important to put this topic also into the context of sexuality. I think you have a great opportunity to do this because, often, you already have developed long-term relationships with these teenagers and their families, so the trust is already there. You should be the one to ensure all patients have appropriate sex education and help families with this.
 |
Dr. Elisabeth Quint |
For some of these teens who are cognitively impaired, the initial conversations about sex may focus more on safety and abuse prevention. For example, which parts of their body should not be touched by other people. You can help the families really be the educators. Parents can be the ones to teach their kids how to protect themselves by rehearsing the answers to questions like, “What do you do if someone touches you? Who do you tell? Where do you go? What if it happens at school?” As part of the safety aspects, you also can help families assess whether the patient will be able to have a consensual sexual relationship. It’s the teens who have mild cognitive impairment that I worry about most, because often they are friendly and open to people, and can be taken advantage of. You just want to make sure they have the right information at their appropriate level.
Adolescents with physical disabilities are going to be just as interested in sex as any other teens and should be helped with any potential issues that they may have around that issue. They will likely get sex education in schools, but are still often viewed as not interested in sex or sexually active, and they may not get the usual confidential teen questions or appropriate screenings. Menstrual management and sexuality education both are important aspects of reproductive health care for teens with disabilities.
Dr. Elisabeth Quint, lead author of the AAP clinical report “Menstrual Management for Adolescents,” is a clinical professor of obstetrics and gynecology at the University of Michigan, Ann Arbor. She is also a past president of the North American Society for Pediatric and Adolescent Gynecology.
For the first time, the American Academy of Pediatrics is offering guidance on managing menstruation and sexuality education in adolescents with disabilities.
Written jointly with the North American Society for Pediatric and Adolescent Gynecology, the clinical report offers guidance on options for menstrual management, sexual education and expression, and protection from sexual abuse. The report gives guidance regarding the care of adolescents with physical and/or intellectual abilities, but not for those with psychiatric illnesses (Pediatrics. 2016 April. doi: 10.1542/peds.2016-0295).
“Taking care of teens with disabilities and figuring out what to do with menstrual management has been all over the map,” Dr. Cora Collette Breuner, chair of the AAP’s committee on adolescence, said in an interview. “So, we tried to clarify it and help clinicians know what to do and when.”
A particular concern for the two groups was the threat of adverse events. “We wanted to cover what’s safe and what’s not in menstruation management, especially around bone health and thromboembolic events,” said Dr. Breuner, a professor of pediatrics and adolescent medicine at the University of Washington, Seattle.
Some of the information will not surprise clinicians, but there are some data that will perhaps come as news, said Dr. Breuner, including the recommendation that long-acting reversible contraception (LARC), such as the levonorgestrel intrauterine device or the progesterone implant rod should be considered first-line management therapies. “We point out that a number of studies show that these are safe.”
The report emphasizes offering anticipatory guidance before menses begins, noting that most teens with disabilities mature at the same rate as teens without disabilities. The report does not recommend premenarchal suppression in these patients, because doing so can interfere with normal bone growth. Such suppression also prevents patients and their families and caregivers from discovering that coping with the onset of menses is perhaps not as difficult as they might fear, the report states.
Although combined oral contraceptives are not contraindicated in teens with mobility issues, to guard against the threat of thromboembolic events in teens who use wheelchairs, the report recommends taking a thorough family history to rule out inherited thrombophilia. Otherwise, the recommendation is to prescribe the lowest-dose estrogen with a first- or second-generation progestin, as these are associated with lower rates of venous thrombotic events.
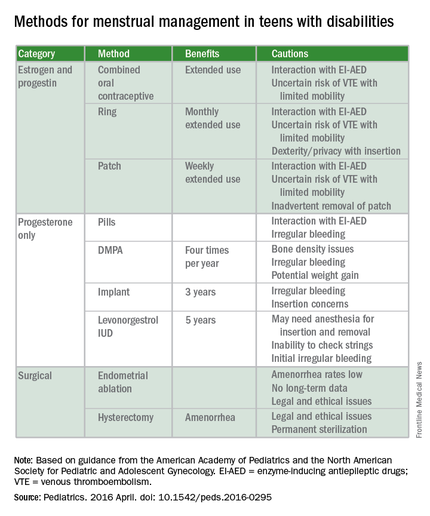
The guidance states that if cycles are creating difficulties in the patient’s life, “as determined by health care providers, patients, and families,” then menstrual management is appropriate. Even though it may take up to 3 years before a menstrual cycle becomes regular, the report cites irregularities caused by certain medications can be reason enough for menstrual management. Specific drugs noted include those affecting the dopaminergic system, valproic acid, and medications that elevate prolactin. Teens with obesity, seizure disorders, and polycystic ovary syndrome also can experience higher rates of irregularity.
The report also warns against the assumption that teens with disabilities are asexual or uninterested in sex. When appropriate, they should be offered the same confidential conversations about sexuality as are recommended for all teenagers by the AAP and the American College of Obstetricians and Gynecologists. “Teenagers with physical disabilities are just as likely to be sexually active as their peers and have a higher incidence of sexual abuse,” the report states. It is typically when a patient is cognitively impaired that consent to confidential services may require “discussion about legal guardianship or medical power of attorney status for families,” according to the report.
The report’s comprehensive review of four main menstrual management techniques – estrogen-containing, progestin-only, nonhormonal methods, and surgical requests and options – begins with the caveat that regardless of the method used, the threat of abuse or sexually transmitted infections remain. When a patient’s family or caregivers request suppression of menarche in a patient, stating fears of abuse or pregnancy, further investigation into the patient’s circumstances is warranted, the report states.
“It’s always worth reminding physicians that in this cohort, endometrial ablation can have legal implications, and it’s not recommended in this age group,” Dr. Breuner said.
On average, 1.5 hormonal methods are tried before achieving management goals, according to the report. Data cited in the study showed that at 42%, oral contraception is the preferred method of menstrual suppression, followed by the patch at 20%. Expectant management was third at 15%, followed by DMPA (depot medroxyprogesterone acetate) at 12%. The least utilized method was the levonorgestrel intrauterine device at 3%. No data were provided for the implantable contraceptive rod.
The clinical report is a companion document to another AAP clinical report, “Sexuality of Children and Adolescents with Developmental Disabilities” (Pediatrics. 2006. doi: 10.1542/peds.2006-1115).
AAP guidance on these matters in teens with psychiatric illnesses is expected to be issued within a few years, Dr. Breuner said.
There was no external funding and the authors have no relevant financial disclosures.
On Twitter @whitneymcknight
For the first time, the American Academy of Pediatrics is offering guidance on managing menstruation and sexuality education in adolescents with disabilities.
Written jointly with the North American Society for Pediatric and Adolescent Gynecology, the clinical report offers guidance on options for menstrual management, sexual education and expression, and protection from sexual abuse. The report gives guidance regarding the care of adolescents with physical and/or intellectual abilities, but not for those with psychiatric illnesses (Pediatrics. 2016 April. doi: 10.1542/peds.2016-0295).
“Taking care of teens with disabilities and figuring out what to do with menstrual management has been all over the map,” Dr. Cora Collette Breuner, chair of the AAP’s committee on adolescence, said in an interview. “So, we tried to clarify it and help clinicians know what to do and when.”
A particular concern for the two groups was the threat of adverse events. “We wanted to cover what’s safe and what’s not in menstruation management, especially around bone health and thromboembolic events,” said Dr. Breuner, a professor of pediatrics and adolescent medicine at the University of Washington, Seattle.
Some of the information will not surprise clinicians, but there are some data that will perhaps come as news, said Dr. Breuner, including the recommendation that long-acting reversible contraception (LARC), such as the levonorgestrel intrauterine device or the progesterone implant rod should be considered first-line management therapies. “We point out that a number of studies show that these are safe.”
The report emphasizes offering anticipatory guidance before menses begins, noting that most teens with disabilities mature at the same rate as teens without disabilities. The report does not recommend premenarchal suppression in these patients, because doing so can interfere with normal bone growth. Such suppression also prevents patients and their families and caregivers from discovering that coping with the onset of menses is perhaps not as difficult as they might fear, the report states.
Although combined oral contraceptives are not contraindicated in teens with mobility issues, to guard against the threat of thromboembolic events in teens who use wheelchairs, the report recommends taking a thorough family history to rule out inherited thrombophilia. Otherwise, the recommendation is to prescribe the lowest-dose estrogen with a first- or second-generation progestin, as these are associated with lower rates of venous thrombotic events.
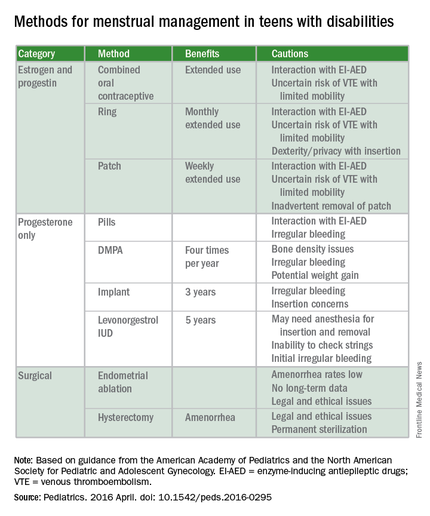
The guidance states that if cycles are creating difficulties in the patient’s life, “as determined by health care providers, patients, and families,” then menstrual management is appropriate. Even though it may take up to 3 years before a menstrual cycle becomes regular, the report cites irregularities caused by certain medications can be reason enough for menstrual management. Specific drugs noted include those affecting the dopaminergic system, valproic acid, and medications that elevate prolactin. Teens with obesity, seizure disorders, and polycystic ovary syndrome also can experience higher rates of irregularity.
The report also warns against the assumption that teens with disabilities are asexual or uninterested in sex. When appropriate, they should be offered the same confidential conversations about sexuality as are recommended for all teenagers by the AAP and the American College of Obstetricians and Gynecologists. “Teenagers with physical disabilities are just as likely to be sexually active as their peers and have a higher incidence of sexual abuse,” the report states. It is typically when a patient is cognitively impaired that consent to confidential services may require “discussion about legal guardianship or medical power of attorney status for families,” according to the report.
The report’s comprehensive review of four main menstrual management techniques – estrogen-containing, progestin-only, nonhormonal methods, and surgical requests and options – begins with the caveat that regardless of the method used, the threat of abuse or sexually transmitted infections remain. When a patient’s family or caregivers request suppression of menarche in a patient, stating fears of abuse or pregnancy, further investigation into the patient’s circumstances is warranted, the report states.
“It’s always worth reminding physicians that in this cohort, endometrial ablation can have legal implications, and it’s not recommended in this age group,” Dr. Breuner said.
On average, 1.5 hormonal methods are tried before achieving management goals, according to the report. Data cited in the study showed that at 42%, oral contraception is the preferred method of menstrual suppression, followed by the patch at 20%. Expectant management was third at 15%, followed by DMPA (depot medroxyprogesterone acetate) at 12%. The least utilized method was the levonorgestrel intrauterine device at 3%. No data were provided for the implantable contraceptive rod.
The clinical report is a companion document to another AAP clinical report, “Sexuality of Children and Adolescents with Developmental Disabilities” (Pediatrics. 2006. doi: 10.1542/peds.2006-1115).
AAP guidance on these matters in teens with psychiatric illnesses is expected to be issued within a few years, Dr. Breuner said.
There was no external funding and the authors have no relevant financial disclosures.
On Twitter @whitneymcknight
FROM PEDIATRICS
Psychiatry’s role rising in hospital care
BALTIMORE – A team of physicians and mental health experts at Johns Hopkins Hospital is trying something new: combining mental health services with medical ones. Hospital leadership hopes the experiment will pay off in shorter lengths of stay, lower readmission rates, and better overall patient care.
“We’re still collecting that data,” Melissa Richardson, the hospital’s director of care coordination, said in an interview. “We also will look at the impact on staffing ratios on the units. For example, has the number of patient observers gone down? Has the overall severity of certain cases on the unit been reduced by embedding mental health workers there?”
The medical-surgical mental health team debuted in April, and is separate from the hospital’s other psychiatric services. Comprised of a social worker, a nurse practitioner, a nurse care coordinator, and an attending psychiatrist, the team typically works a regular day shift, beginning each morning with patient chart reviews prepared by medical-surgical personnel. They discuss which patients will be seen by whom, since all team members are trained to do psychiatric evaluations.
Not all medical patients require psychiatric care, but according to the program’s clinical director and attending psychiatrist, Dr. Patrick T. Triplett, up to 38% of all medical admissions have a psychiatric comorbidity. Addressing those comorbidities while patients are in the hospital often leads to improved outcomes.
The team’s social worker connects patients with the appropriate outpatient mental health services in the community, and the team’s nurse care coordinator arranges any necessary transfers from the medical-surgical units to the inpatient psychiatric unit. Dr. Triplett and the psychiatric nurse practitioner are the only two team members who can diagnose and prescribe. Dr. Triplett’s time is billed as consultation services, and the hospital absorbs the cost of the rest of the team, according to Ms. Richardson.
‘Complex medically ill’ patients
As some procedures and medical treatments have shifted to the outpatient setting in recent years, and joint replacements or acute conditions such as myocardial infarctions can be managed successfully in shorter stays, more complicated patients, such as joint replacement patients who develop delirium, have been left on the medical-surgical unit, said Dr. Constantine G. Lyketsos, the Elizabeth Plank Althouse Professor at Johns Hopkins Bayview, Baltimore.
“Also, these days, up to 20% of our admissions are linked to opioids. Then, there are the chronically mentally ill. They tend to be a population with high rates of obesity, smoking, and diabetes, so they end up in the hospital with higher-level, more complicated conditions, that because of the disintegration of the mental health system, receive neither good psychiatric nor outpatient medical care,” Dr. Lyketsos, also chief of psychiatry at Johns Hopkins Bayview, said in an interview.
This surge in the number of complex medically ill patients has led to a growing number of hospitals nationwide calling upon psychiatrists for help in improving overall care. Hopkins is only the latest to join the ranks of other institutions such as Massachusetts General Hospital in Boston, State University of New York Downstate Medical Center in Brooklyn (N.Y.), Dartmouth-Hitchcock Medical Center in Lebanon, N.H., and New York–Presbyterian/Columbia University Medical Center in New York City.
The progenitor of this collaborative inpatient care model is Yale New Haven (Conn.) Hospital. The behavioral intervention team (BIT) at Yale New Haven includes nurses, social workers, and psychiatrists who proactively screen for and address behavioral barriers to care for medical patients with a co-occurring mental illness, said Dr. Hochang B. Lee, one of the psychiatrists who helped created the model in 2008. Dr. Lee is Yale’s psychological medicine section chief and director of the school’s Psychological Medicine Research Center. He also is an associate professor of psychiatry and an associate clinical professor of nursing.
“The goal was to create a proactive model of care, not the reactive one that is traditional consultation-liaison psychiatry,” Dr. Lee said in an interview. “Before the BIT model, medical teams often missed behavioral issues or made consultation requests too late in the course of hospitalization to avoid psychiatric crisis.”
LOS, costs reduced
A study
“The hospital is not making money off of us, but they’re losing less money because of us. That’s good!” Dr. Philip R. Muskin, chief of consultation-liaison psychiatry at New York–Presbyterian/Columbia, said in an interview.
Patients at New York Presbyterian have been comanaged since 2004 when, according to Dr. Muskin, a donor gift specifically intended for such a purpose was matched by the hospital’s department of medicine. The unspent money was enough to cover the cost of a consultation-liaison psychiatrist to round full time as an attending with the medical team.
“We were lucky at NYPCH, because someone gave us the gift to hire a full-time psychiatrist we could embed into the medical team,” Dr. Muskin said. “But there is no one right way to deliver collaborative care in the inpatient setting.”
The NYPCH program has grown to include a second full-time and one part-time psychiatrist, serving about half of all medical services at the campus, with plans to hire more. There is also a social worker to assist with outplacement services. Dr. Muskin said he is currently looking to hire a psychiatric nurse practitioner.
‘Nurses love us’
Restoration of staff morale is another benefit to this kind of practice, according to Maureen Lewis, an accredited psychiatric nurse practitioner who is part of the Hopkins integrated team.
“Med-surge nurses love us. Patients who come in with an overdose or who have any psychiatric conditions but need to have their medical comorbidities dealt with first, they are at their sickest with their psychiatric illnesses when they first arrive,” Ms. Lewis said. “It’s the med-surge nurses who have to care for them, but it’s not their comfort zone or their skill set. They like that we are helping them manage the patient.”
A decline in the number of assaults on the nursing staff also has been recorded since the Hopkins program began, Dr. Lyketsos said.
The psychiatrists themselves tend to be happier, too. “Knowing the cases before you even walk up on the unit is a huge benefit,” Dr. Triplett said. “To have to dive into an emergency all the time is just exhausting. It changes your relationship with the patient. When you’re not in that crisis mode, the patient isn’t a ‘problem’ anymore.”
A formal assessment of the entire medical-surgical staff satisfaction involved in the Hopkins program also is underway, said Ms. Richardson, the director of care coordination.
Having psychiatrists at the fore of this evolution in care provides more opportunities for training, too.
The comanagement model gives medical staff a chance to learn more not just about the direct care of complex behaviorally disordered patients, but also to understand their own emotions and states of mind as they interact with these patients. The teaching happens naturally as the team discusses patients while making rounds, Dr. Muskin said. “That’s really an integral part of what consult-liaison psychiatry is supposed to be about, anyway.”
By helping the medical staff reflect on their experiences, Dr. Muskin said, psychiatrists are helping to change the culture of inpatient medicine. “Once you change the culture, if you keep the things that brought it about in place, it doesn’t change back.”
Creating bridge services
A problem with this kind of inpatient collaborative care model is that hospitals that run them aren’t able to control all the variables associated with the cost of providing them.
The hope is that by spending more up front to identify and treat high-risk behavioral health patients, they won’t need readmission; but if the appropriate follow-up care can’t be found on the outpatient side, they could still end up back in the hospital, driving up readmission rates and possibly lengths of stay.
To address such contingencies, Hopkins has participated in state-sponsored partnerships for improving community care and is using monies from accountable care organization funding to create bridge services. The hospital system also has 14 primary care practices that have embedded psychiatric services, and the plan is to create a team to care for more complicated patients who need care 60-90 days after discharge.
For Dr. Lyketsos, however, fixing what he says is a broken mental health system isn’t up to the hospital alone. “We’re not going to be able to bring about real change without working with our legislators and our payers. It’s a complex problem that needs a complex solution. But there is a commonality of mind that we need to fix things, that patients need better care – and that this is a good place to start.”
On Twitter @whitneymcknight
CORRECTION, 6/28/16: A previous version of this article misstated Dr. Hochang B. Lee's name.
BALTIMORE – A team of physicians and mental health experts at Johns Hopkins Hospital is trying something new: combining mental health services with medical ones. Hospital leadership hopes the experiment will pay off in shorter lengths of stay, lower readmission rates, and better overall patient care.
“We’re still collecting that data,” Melissa Richardson, the hospital’s director of care coordination, said in an interview. “We also will look at the impact on staffing ratios on the units. For example, has the number of patient observers gone down? Has the overall severity of certain cases on the unit been reduced by embedding mental health workers there?”
The medical-surgical mental health team debuted in April, and is separate from the hospital’s other psychiatric services. Comprised of a social worker, a nurse practitioner, a nurse care coordinator, and an attending psychiatrist, the team typically works a regular day shift, beginning each morning with patient chart reviews prepared by medical-surgical personnel. They discuss which patients will be seen by whom, since all team members are trained to do psychiatric evaluations.
Not all medical patients require psychiatric care, but according to the program’s clinical director and attending psychiatrist, Dr. Patrick T. Triplett, up to 38% of all medical admissions have a psychiatric comorbidity. Addressing those comorbidities while patients are in the hospital often leads to improved outcomes.
The team’s social worker connects patients with the appropriate outpatient mental health services in the community, and the team’s nurse care coordinator arranges any necessary transfers from the medical-surgical units to the inpatient psychiatric unit. Dr. Triplett and the psychiatric nurse practitioner are the only two team members who can diagnose and prescribe. Dr. Triplett’s time is billed as consultation services, and the hospital absorbs the cost of the rest of the team, according to Ms. Richardson.
‘Complex medically ill’ patients
As some procedures and medical treatments have shifted to the outpatient setting in recent years, and joint replacements or acute conditions such as myocardial infarctions can be managed successfully in shorter stays, more complicated patients, such as joint replacement patients who develop delirium, have been left on the medical-surgical unit, said Dr. Constantine G. Lyketsos, the Elizabeth Plank Althouse Professor at Johns Hopkins Bayview, Baltimore.
“Also, these days, up to 20% of our admissions are linked to opioids. Then, there are the chronically mentally ill. They tend to be a population with high rates of obesity, smoking, and diabetes, so they end up in the hospital with higher-level, more complicated conditions, that because of the disintegration of the mental health system, receive neither good psychiatric nor outpatient medical care,” Dr. Lyketsos, also chief of psychiatry at Johns Hopkins Bayview, said in an interview.
This surge in the number of complex medically ill patients has led to a growing number of hospitals nationwide calling upon psychiatrists for help in improving overall care. Hopkins is only the latest to join the ranks of other institutions such as Massachusetts General Hospital in Boston, State University of New York Downstate Medical Center in Brooklyn (N.Y.), Dartmouth-Hitchcock Medical Center in Lebanon, N.H., and New York–Presbyterian/Columbia University Medical Center in New York City.
The progenitor of this collaborative inpatient care model is Yale New Haven (Conn.) Hospital. The behavioral intervention team (BIT) at Yale New Haven includes nurses, social workers, and psychiatrists who proactively screen for and address behavioral barriers to care for medical patients with a co-occurring mental illness, said Dr. Hochang B. Lee, one of the psychiatrists who helped created the model in 2008. Dr. Lee is Yale’s psychological medicine section chief and director of the school’s Psychological Medicine Research Center. He also is an associate professor of psychiatry and an associate clinical professor of nursing.
“The goal was to create a proactive model of care, not the reactive one that is traditional consultation-liaison psychiatry,” Dr. Lee said in an interview. “Before the BIT model, medical teams often missed behavioral issues or made consultation requests too late in the course of hospitalization to avoid psychiatric crisis.”
LOS, costs reduced
A study
“The hospital is not making money off of us, but they’re losing less money because of us. That’s good!” Dr. Philip R. Muskin, chief of consultation-liaison psychiatry at New York–Presbyterian/Columbia, said in an interview.
Patients at New York Presbyterian have been comanaged since 2004 when, according to Dr. Muskin, a donor gift specifically intended for such a purpose was matched by the hospital’s department of medicine. The unspent money was enough to cover the cost of a consultation-liaison psychiatrist to round full time as an attending with the medical team.
“We were lucky at NYPCH, because someone gave us the gift to hire a full-time psychiatrist we could embed into the medical team,” Dr. Muskin said. “But there is no one right way to deliver collaborative care in the inpatient setting.”
The NYPCH program has grown to include a second full-time and one part-time psychiatrist, serving about half of all medical services at the campus, with plans to hire more. There is also a social worker to assist with outplacement services. Dr. Muskin said he is currently looking to hire a psychiatric nurse practitioner.
‘Nurses love us’
Restoration of staff morale is another benefit to this kind of practice, according to Maureen Lewis, an accredited psychiatric nurse practitioner who is part of the Hopkins integrated team.
“Med-surge nurses love us. Patients who come in with an overdose or who have any psychiatric conditions but need to have their medical comorbidities dealt with first, they are at their sickest with their psychiatric illnesses when they first arrive,” Ms. Lewis said. “It’s the med-surge nurses who have to care for them, but it’s not their comfort zone or their skill set. They like that we are helping them manage the patient.”
A decline in the number of assaults on the nursing staff also has been recorded since the Hopkins program began, Dr. Lyketsos said.
The psychiatrists themselves tend to be happier, too. “Knowing the cases before you even walk up on the unit is a huge benefit,” Dr. Triplett said. “To have to dive into an emergency all the time is just exhausting. It changes your relationship with the patient. When you’re not in that crisis mode, the patient isn’t a ‘problem’ anymore.”
A formal assessment of the entire medical-surgical staff satisfaction involved in the Hopkins program also is underway, said Ms. Richardson, the director of care coordination.
Having psychiatrists at the fore of this evolution in care provides more opportunities for training, too.
The comanagement model gives medical staff a chance to learn more not just about the direct care of complex behaviorally disordered patients, but also to understand their own emotions and states of mind as they interact with these patients. The teaching happens naturally as the team discusses patients while making rounds, Dr. Muskin said. “That’s really an integral part of what consult-liaison psychiatry is supposed to be about, anyway.”
By helping the medical staff reflect on their experiences, Dr. Muskin said, psychiatrists are helping to change the culture of inpatient medicine. “Once you change the culture, if you keep the things that brought it about in place, it doesn’t change back.”
Creating bridge services
A problem with this kind of inpatient collaborative care model is that hospitals that run them aren’t able to control all the variables associated with the cost of providing them.
The hope is that by spending more up front to identify and treat high-risk behavioral health patients, they won’t need readmission; but if the appropriate follow-up care can’t be found on the outpatient side, they could still end up back in the hospital, driving up readmission rates and possibly lengths of stay.
To address such contingencies, Hopkins has participated in state-sponsored partnerships for improving community care and is using monies from accountable care organization funding to create bridge services. The hospital system also has 14 primary care practices that have embedded psychiatric services, and the plan is to create a team to care for more complicated patients who need care 60-90 days after discharge.
For Dr. Lyketsos, however, fixing what he says is a broken mental health system isn’t up to the hospital alone. “We’re not going to be able to bring about real change without working with our legislators and our payers. It’s a complex problem that needs a complex solution. But there is a commonality of mind that we need to fix things, that patients need better care – and that this is a good place to start.”
On Twitter @whitneymcknight
CORRECTION, 6/28/16: A previous version of this article misstated Dr. Hochang B. Lee's name.
BALTIMORE – A team of physicians and mental health experts at Johns Hopkins Hospital is trying something new: combining mental health services with medical ones. Hospital leadership hopes the experiment will pay off in shorter lengths of stay, lower readmission rates, and better overall patient care.
“We’re still collecting that data,” Melissa Richardson, the hospital’s director of care coordination, said in an interview. “We also will look at the impact on staffing ratios on the units. For example, has the number of patient observers gone down? Has the overall severity of certain cases on the unit been reduced by embedding mental health workers there?”
The medical-surgical mental health team debuted in April, and is separate from the hospital’s other psychiatric services. Comprised of a social worker, a nurse practitioner, a nurse care coordinator, and an attending psychiatrist, the team typically works a regular day shift, beginning each morning with patient chart reviews prepared by medical-surgical personnel. They discuss which patients will be seen by whom, since all team members are trained to do psychiatric evaluations.
Not all medical patients require psychiatric care, but according to the program’s clinical director and attending psychiatrist, Dr. Patrick T. Triplett, up to 38% of all medical admissions have a psychiatric comorbidity. Addressing those comorbidities while patients are in the hospital often leads to improved outcomes.
The team’s social worker connects patients with the appropriate outpatient mental health services in the community, and the team’s nurse care coordinator arranges any necessary transfers from the medical-surgical units to the inpatient psychiatric unit. Dr. Triplett and the psychiatric nurse practitioner are the only two team members who can diagnose and prescribe. Dr. Triplett’s time is billed as consultation services, and the hospital absorbs the cost of the rest of the team, according to Ms. Richardson.
‘Complex medically ill’ patients
As some procedures and medical treatments have shifted to the outpatient setting in recent years, and joint replacements or acute conditions such as myocardial infarctions can be managed successfully in shorter stays, more complicated patients, such as joint replacement patients who develop delirium, have been left on the medical-surgical unit, said Dr. Constantine G. Lyketsos, the Elizabeth Plank Althouse Professor at Johns Hopkins Bayview, Baltimore.
“Also, these days, up to 20% of our admissions are linked to opioids. Then, there are the chronically mentally ill. They tend to be a population with high rates of obesity, smoking, and diabetes, so they end up in the hospital with higher-level, more complicated conditions, that because of the disintegration of the mental health system, receive neither good psychiatric nor outpatient medical care,” Dr. Lyketsos, also chief of psychiatry at Johns Hopkins Bayview, said in an interview.
This surge in the number of complex medically ill patients has led to a growing number of hospitals nationwide calling upon psychiatrists for help in improving overall care. Hopkins is only the latest to join the ranks of other institutions such as Massachusetts General Hospital in Boston, State University of New York Downstate Medical Center in Brooklyn (N.Y.), Dartmouth-Hitchcock Medical Center in Lebanon, N.H., and New York–Presbyterian/Columbia University Medical Center in New York City.
The progenitor of this collaborative inpatient care model is Yale New Haven (Conn.) Hospital. The behavioral intervention team (BIT) at Yale New Haven includes nurses, social workers, and psychiatrists who proactively screen for and address behavioral barriers to care for medical patients with a co-occurring mental illness, said Dr. Hochang B. Lee, one of the psychiatrists who helped created the model in 2008. Dr. Lee is Yale’s psychological medicine section chief and director of the school’s Psychological Medicine Research Center. He also is an associate professor of psychiatry and an associate clinical professor of nursing.
“The goal was to create a proactive model of care, not the reactive one that is traditional consultation-liaison psychiatry,” Dr. Lee said in an interview. “Before the BIT model, medical teams often missed behavioral issues or made consultation requests too late in the course of hospitalization to avoid psychiatric crisis.”
LOS, costs reduced
A study
“The hospital is not making money off of us, but they’re losing less money because of us. That’s good!” Dr. Philip R. Muskin, chief of consultation-liaison psychiatry at New York–Presbyterian/Columbia, said in an interview.
Patients at New York Presbyterian have been comanaged since 2004 when, according to Dr. Muskin, a donor gift specifically intended for such a purpose was matched by the hospital’s department of medicine. The unspent money was enough to cover the cost of a consultation-liaison psychiatrist to round full time as an attending with the medical team.
“We were lucky at NYPCH, because someone gave us the gift to hire a full-time psychiatrist we could embed into the medical team,” Dr. Muskin said. “But there is no one right way to deliver collaborative care in the inpatient setting.”
The NYPCH program has grown to include a second full-time and one part-time psychiatrist, serving about half of all medical services at the campus, with plans to hire more. There is also a social worker to assist with outplacement services. Dr. Muskin said he is currently looking to hire a psychiatric nurse practitioner.
‘Nurses love us’
Restoration of staff morale is another benefit to this kind of practice, according to Maureen Lewis, an accredited psychiatric nurse practitioner who is part of the Hopkins integrated team.
“Med-surge nurses love us. Patients who come in with an overdose or who have any psychiatric conditions but need to have their medical comorbidities dealt with first, they are at their sickest with their psychiatric illnesses when they first arrive,” Ms. Lewis said. “It’s the med-surge nurses who have to care for them, but it’s not their comfort zone or their skill set. They like that we are helping them manage the patient.”
A decline in the number of assaults on the nursing staff also has been recorded since the Hopkins program began, Dr. Lyketsos said.
The psychiatrists themselves tend to be happier, too. “Knowing the cases before you even walk up on the unit is a huge benefit,” Dr. Triplett said. “To have to dive into an emergency all the time is just exhausting. It changes your relationship with the patient. When you’re not in that crisis mode, the patient isn’t a ‘problem’ anymore.”
A formal assessment of the entire medical-surgical staff satisfaction involved in the Hopkins program also is underway, said Ms. Richardson, the director of care coordination.
Having psychiatrists at the fore of this evolution in care provides more opportunities for training, too.
The comanagement model gives medical staff a chance to learn more not just about the direct care of complex behaviorally disordered patients, but also to understand their own emotions and states of mind as they interact with these patients. The teaching happens naturally as the team discusses patients while making rounds, Dr. Muskin said. “That’s really an integral part of what consult-liaison psychiatry is supposed to be about, anyway.”
By helping the medical staff reflect on their experiences, Dr. Muskin said, psychiatrists are helping to change the culture of inpatient medicine. “Once you change the culture, if you keep the things that brought it about in place, it doesn’t change back.”
Creating bridge services
A problem with this kind of inpatient collaborative care model is that hospitals that run them aren’t able to control all the variables associated with the cost of providing them.
The hope is that by spending more up front to identify and treat high-risk behavioral health patients, they won’t need readmission; but if the appropriate follow-up care can’t be found on the outpatient side, they could still end up back in the hospital, driving up readmission rates and possibly lengths of stay.
To address such contingencies, Hopkins has participated in state-sponsored partnerships for improving community care and is using monies from accountable care organization funding to create bridge services. The hospital system also has 14 primary care practices that have embedded psychiatric services, and the plan is to create a team to care for more complicated patients who need care 60-90 days after discharge.
For Dr. Lyketsos, however, fixing what he says is a broken mental health system isn’t up to the hospital alone. “We’re not going to be able to bring about real change without working with our legislators and our payers. It’s a complex problem that needs a complex solution. But there is a commonality of mind that we need to fix things, that patients need better care – and that this is a good place to start.”
On Twitter @whitneymcknight
CORRECTION, 6/28/16: A previous version of this article misstated Dr. Hochang B. Lee's name.