User login
Opt for redo root surgery, not TAVI, in young patients
CHICAGO – Whether to perform transcatheter aortic valve implantation in a 57-year-old patient with a severely calcified aortic homograft was the subject of a case report presented at Heart Valve Summit 2012.
"In our center, even though we do a huge number of TAVIs [transcatheter aortic valve implantations], we still believe TAVI should be left for the older patients and those with a restricted life expectancy, because the long-term results are not known," said Dr. Michael Borger, assistant director of the Leipzig (Germany) Heart Center.
The patient in this case was a 57 year-old woman who presented with increased shortness of breath and was found to have NYHA II-III heart failure. At age 40, she had received a homograft aortic root replacement for destructive endocarditis.
Her ejection fraction and left ventricular dimensions were preserved, her AV gradient was 86/52 mm Hg, and her effective orifice area (EOA) was 0.6 cm2. She had no other risk factors and was taking no medications. A coronary angiogram showed a severely calcified homograft and isolated proximal stenosis of the right coronary artery.
Dr. Borger discussed two options: redo root replacement surgery with a bypass to the right coronary artery or a transcatheter aortic valve replacement (TAVR) with a PCI to the right coronary artery.
The decision was to perform conventional surgery. "The patient underwent a redo Bentall operation with a mechanical valve, as well as a RIMA (right internal mammary artery) to RCA (right coronary artery) bypass. She did very well postoperatively without any complications," he said.
Aortic root replacements with aortic homografts are not without risk, and the literature shows relatively high mortality for homograft reoperations. Reoperation after stentless AVR also has been performed, but it often requires replacement of the aortic root and is associated with increased mortality (Ann. Thorac. Surg. 2007;84:737-43).
"Most of those [stentless] operations are difficult because of the inability to get a good plane of cleavage between the stentless valve and the native aortic root," said Dr. Borger. "The large majority of those patients end up leaving the OR with a full root replacement."
Dr. Borger’s fellow panelist, Dr. Michael Reardon, agreed. "I was a real fan of the Toronto SPV valve, and ... I’ve taken a couple out," said Dr. Reardon, professor and vice chair of the Methodist DeBakey Heart and Vascular Center in Houston. "They all end up in root replacements. By the time you’re finished you end up having these shards of tissue ... and porcine tissue incites a huge dermoplastic reaction. ... I personally found it very difficult."
Dr. Borger noted, "In Leipzig we have put in a large number of Toronto roots and, knock on wood, have not reoperated on one of them yet. However, they have not yet reached the period whereby you expect to observe structural valve dysfunction."
A study of valve-related events after aortic root replacement with cryopreserved aortic homografts examined risk after placement of a homograft and found that a heavily calcified homograft at the time of reoperation was a significant predictor of death (Ann. Thorac. Surg. 2005;79:1491-5).
"I’m not saying that TAVI is not an option for all young patients," said Dr. Borger. "If you’ve got a young patient who is at very high risk for conventional surgery with lots of comorbidities, whose life expectancy is 5 years or less, then sure, do a TAVI. But for this particular patient, if she survives the operation, you’re going to put her back on an almost normal survival curve."
Dr. Borger disclosed consultant fees and honoraria from Medtronic, St. Jude Medical, and Edwards Lifesciences.
CHICAGO – Whether to perform transcatheter aortic valve implantation in a 57-year-old patient with a severely calcified aortic homograft was the subject of a case report presented at Heart Valve Summit 2012.
"In our center, even though we do a huge number of TAVIs [transcatheter aortic valve implantations], we still believe TAVI should be left for the older patients and those with a restricted life expectancy, because the long-term results are not known," said Dr. Michael Borger, assistant director of the Leipzig (Germany) Heart Center.
The patient in this case was a 57 year-old woman who presented with increased shortness of breath and was found to have NYHA II-III heart failure. At age 40, she had received a homograft aortic root replacement for destructive endocarditis.
Her ejection fraction and left ventricular dimensions were preserved, her AV gradient was 86/52 mm Hg, and her effective orifice area (EOA) was 0.6 cm2. She had no other risk factors and was taking no medications. A coronary angiogram showed a severely calcified homograft and isolated proximal stenosis of the right coronary artery.
Dr. Borger discussed two options: redo root replacement surgery with a bypass to the right coronary artery or a transcatheter aortic valve replacement (TAVR) with a PCI to the right coronary artery.
The decision was to perform conventional surgery. "The patient underwent a redo Bentall operation with a mechanical valve, as well as a RIMA (right internal mammary artery) to RCA (right coronary artery) bypass. She did very well postoperatively without any complications," he said.
Aortic root replacements with aortic homografts are not without risk, and the literature shows relatively high mortality for homograft reoperations. Reoperation after stentless AVR also has been performed, but it often requires replacement of the aortic root and is associated with increased mortality (Ann. Thorac. Surg. 2007;84:737-43).
"Most of those [stentless] operations are difficult because of the inability to get a good plane of cleavage between the stentless valve and the native aortic root," said Dr. Borger. "The large majority of those patients end up leaving the OR with a full root replacement."
Dr. Borger’s fellow panelist, Dr. Michael Reardon, agreed. "I was a real fan of the Toronto SPV valve, and ... I’ve taken a couple out," said Dr. Reardon, professor and vice chair of the Methodist DeBakey Heart and Vascular Center in Houston. "They all end up in root replacements. By the time you’re finished you end up having these shards of tissue ... and porcine tissue incites a huge dermoplastic reaction. ... I personally found it very difficult."
Dr. Borger noted, "In Leipzig we have put in a large number of Toronto roots and, knock on wood, have not reoperated on one of them yet. However, they have not yet reached the period whereby you expect to observe structural valve dysfunction."
A study of valve-related events after aortic root replacement with cryopreserved aortic homografts examined risk after placement of a homograft and found that a heavily calcified homograft at the time of reoperation was a significant predictor of death (Ann. Thorac. Surg. 2005;79:1491-5).
"I’m not saying that TAVI is not an option for all young patients," said Dr. Borger. "If you’ve got a young patient who is at very high risk for conventional surgery with lots of comorbidities, whose life expectancy is 5 years or less, then sure, do a TAVI. But for this particular patient, if she survives the operation, you’re going to put her back on an almost normal survival curve."
Dr. Borger disclosed consultant fees and honoraria from Medtronic, St. Jude Medical, and Edwards Lifesciences.
CHICAGO – Whether to perform transcatheter aortic valve implantation in a 57-year-old patient with a severely calcified aortic homograft was the subject of a case report presented at Heart Valve Summit 2012.
"In our center, even though we do a huge number of TAVIs [transcatheter aortic valve implantations], we still believe TAVI should be left for the older patients and those with a restricted life expectancy, because the long-term results are not known," said Dr. Michael Borger, assistant director of the Leipzig (Germany) Heart Center.
The patient in this case was a 57 year-old woman who presented with increased shortness of breath and was found to have NYHA II-III heart failure. At age 40, she had received a homograft aortic root replacement for destructive endocarditis.
Her ejection fraction and left ventricular dimensions were preserved, her AV gradient was 86/52 mm Hg, and her effective orifice area (EOA) was 0.6 cm2. She had no other risk factors and was taking no medications. A coronary angiogram showed a severely calcified homograft and isolated proximal stenosis of the right coronary artery.
Dr. Borger discussed two options: redo root replacement surgery with a bypass to the right coronary artery or a transcatheter aortic valve replacement (TAVR) with a PCI to the right coronary artery.
The decision was to perform conventional surgery. "The patient underwent a redo Bentall operation with a mechanical valve, as well as a RIMA (right internal mammary artery) to RCA (right coronary artery) bypass. She did very well postoperatively without any complications," he said.
Aortic root replacements with aortic homografts are not without risk, and the literature shows relatively high mortality for homograft reoperations. Reoperation after stentless AVR also has been performed, but it often requires replacement of the aortic root and is associated with increased mortality (Ann. Thorac. Surg. 2007;84:737-43).
"Most of those [stentless] operations are difficult because of the inability to get a good plane of cleavage between the stentless valve and the native aortic root," said Dr. Borger. "The large majority of those patients end up leaving the OR with a full root replacement."
Dr. Borger’s fellow panelist, Dr. Michael Reardon, agreed. "I was a real fan of the Toronto SPV valve, and ... I’ve taken a couple out," said Dr. Reardon, professor and vice chair of the Methodist DeBakey Heart and Vascular Center in Houston. "They all end up in root replacements. By the time you’re finished you end up having these shards of tissue ... and porcine tissue incites a huge dermoplastic reaction. ... I personally found it very difficult."
Dr. Borger noted, "In Leipzig we have put in a large number of Toronto roots and, knock on wood, have not reoperated on one of them yet. However, they have not yet reached the period whereby you expect to observe structural valve dysfunction."
A study of valve-related events after aortic root replacement with cryopreserved aortic homografts examined risk after placement of a homograft and found that a heavily calcified homograft at the time of reoperation was a significant predictor of death (Ann. Thorac. Surg. 2005;79:1491-5).
"I’m not saying that TAVI is not an option for all young patients," said Dr. Borger. "If you’ve got a young patient who is at very high risk for conventional surgery with lots of comorbidities, whose life expectancy is 5 years or less, then sure, do a TAVI. But for this particular patient, if she survives the operation, you’re going to put her back on an almost normal survival curve."
Dr. Borger disclosed consultant fees and honoraria from Medtronic, St. Jude Medical, and Edwards Lifesciences.
EXPERT ANALYSIS FROM HEART VALVE SUMMIT 2012
Minimally invasive surgery with sutureless valves shows benefits
CHICAGO – European data suggest that minimally invasive aortic valve surgery has several benefits and few downsides when compared to conventional aortic valve replacement.
Bleeding is decreased, as is ICU and hospital length of stay. Cosmesis is improved. Sutureless valves may facilitate the performance of minimally invasive aortic valve replacement (AVR), and are associated with decreased ischemic times and lower transvalvular gradients – an advantage when concomitant procedures are performed or patients are high risk, according to a presentation at the 2012 Heart Valve summit.
Sutureless aortic valves facilitate minimal basic AVR and minimize myocardial ischemic time, said Dr. Michael Borger of Leipzig (Germany) Heart Center.
He described the evidence to date, as well as his personal experience, at this educational program of the American Association for Thoracic Surgery (AATS) and the American College of Cardiology Foundation (ACCF).
Leipzig Heart Center is one of Europe’s largest cardiac facilities, with 4,000 cardiac operations per year.
The number of patients who undergo minimally invasive aortic valve procedures is still very low, said Dr. Borger, and he urged the audience to consider this option in the future, especially when transcatheter aortic valve implantation (TAVI) becomes as widely accepted in America as it is in Europe. In Germany alone, 31% of isolated AVRs are now done by TAVI.
"Decreased myocardial ischemic time doesn’t matter for someone who needs an isolated aortic valve, [such as a] 70-year-old patient with no risk factors. It doesn’t matter if you shorten their ischemic time by 20 minutes. That’s not the point. The point is that a sutureless valve facilitates minimally invasive surgery by making it easier to do; and a marker for that is decreased ischemic time."
One subgroup of patients who do benefit from decreased ischemic times, however, are those requiring complex multivalve procedures. Patients who have a poor ejection fraction also benefit.
"We are applying lessons that we’ve learned from TAVI to these sutureless valves," said Dr. Borger. "TAVI has been in Europe – transfemoral for 10 years, transapical for 6 years – and what we know from TAVI is that a stent is able to hold an aortic valve in the left ventricular outflow tract and prevent it from embolizing afterwards. In addition, we now know that you do not need to fully decalcify the annulus. As a matter of fact, you’re better off leaving some calcification in the annulus when implanting sutureless valves ... to avoid the formation of annular tears or defects."
There are two approaches: the upper hemisternotomy approach, which is favored in Leipzig, and the upper right midlateral thoracotomy approach.
Three sutureless valves are currently in use in Europe: the Medtronic (formerly ATS) Enable sutureless valve, the Sorin Perceval S sutureless valve, and the Edwards Intuity valve.
The Medtronic Enable valve is equine pericardium and was the first sutureless valve to get CE mark approval in Europe. The literature is limited, but a study from Switzerland (J. Thorac. Cardiovasc. Surg. 2010;140:313-6) of the 3f Enable valve in 28 patients showed that the valve could be implanted safely and quickly with favorable early hemodynamics.
"Again, I just want to stress, the goal is not to go from 60 minutes down to 40 minutes of ischemia; the goal is to facilitate a minimally invasive approach," said Dr. Borger. He noted that the hemodynamics were excellent for all three sutureless valves.
The second valve to receive CE mark approval in Europe was the Sorin Perceval S, at the beginning of 2012. It has a bovine pericardial leaflet, also attached to a Nitinol stent, and is crimped at the bedside. This results in an advantage for implantation.
"You can see exactly that the valve is in the position where you want it to be before deploying it," said Dr. Borger. The long-term results of crimping the leaflets are not yet known.
This particular model is currently available in sizes of 21, 23, and 25 mm. Even a 25-mm valve can only be put in a relatively small annulus, making the Perceval valve most appropriate for the small, elderly patient.
Sorin has reported results from 186 patients who received the Perceval valve, and noted short cross-clamp times (mean cross-clamp time for isolated AVR, 28.6 minutes) and 2.8% mortality.
The third and final sutureless aortic prosthesis is the Edwards Intuity valve, whose top is a traditional design based on the Magna Ease valve, and whose bottom is stent technology borrowed from Edwards’ TAVI program. A recent study of 152 patents revealed an average cross-clamp time of 41 minutes for isolated AVR, with a perioperative mortality rate of 2.1% and a paravalvular leak rate of 1.4% (J. Thorac. Cardiovasc. Surg. 2012;145:110-16). In addition, hemodynamics were excellent, with a mean transvalvular gradient of 9.8 mm Hg.
Dr. Borger disclosed receiving speaking honoraria from Edwards Lifesciences, Medtronic, and St. Jude Medical. He was a researcher in the Edwards Intuity and Sorin Perceval studies.
Leipzig Heart Center,
CHICAGO – European data suggest that minimally invasive aortic valve surgery has several benefits and few downsides when compared to conventional aortic valve replacement.
Bleeding is decreased, as is ICU and hospital length of stay. Cosmesis is improved. Sutureless valves may facilitate the performance of minimally invasive aortic valve replacement (AVR), and are associated with decreased ischemic times and lower transvalvular gradients – an advantage when concomitant procedures are performed or patients are high risk, according to a presentation at the 2012 Heart Valve summit.
Sutureless aortic valves facilitate minimal basic AVR and minimize myocardial ischemic time, said Dr. Michael Borger of Leipzig (Germany) Heart Center.
He described the evidence to date, as well as his personal experience, at this educational program of the American Association for Thoracic Surgery (AATS) and the American College of Cardiology Foundation (ACCF).
Leipzig Heart Center is one of Europe’s largest cardiac facilities, with 4,000 cardiac operations per year.
The number of patients who undergo minimally invasive aortic valve procedures is still very low, said Dr. Borger, and he urged the audience to consider this option in the future, especially when transcatheter aortic valve implantation (TAVI) becomes as widely accepted in America as it is in Europe. In Germany alone, 31% of isolated AVRs are now done by TAVI.
"Decreased myocardial ischemic time doesn’t matter for someone who needs an isolated aortic valve, [such as a] 70-year-old patient with no risk factors. It doesn’t matter if you shorten their ischemic time by 20 minutes. That’s not the point. The point is that a sutureless valve facilitates minimally invasive surgery by making it easier to do; and a marker for that is decreased ischemic time."
One subgroup of patients who do benefit from decreased ischemic times, however, are those requiring complex multivalve procedures. Patients who have a poor ejection fraction also benefit.
"We are applying lessons that we’ve learned from TAVI to these sutureless valves," said Dr. Borger. "TAVI has been in Europe – transfemoral for 10 years, transapical for 6 years – and what we know from TAVI is that a stent is able to hold an aortic valve in the left ventricular outflow tract and prevent it from embolizing afterwards. In addition, we now know that you do not need to fully decalcify the annulus. As a matter of fact, you’re better off leaving some calcification in the annulus when implanting sutureless valves ... to avoid the formation of annular tears or defects."
There are two approaches: the upper hemisternotomy approach, which is favored in Leipzig, and the upper right midlateral thoracotomy approach.
Three sutureless valves are currently in use in Europe: the Medtronic (formerly ATS) Enable sutureless valve, the Sorin Perceval S sutureless valve, and the Edwards Intuity valve.
The Medtronic Enable valve is equine pericardium and was the first sutureless valve to get CE mark approval in Europe. The literature is limited, but a study from Switzerland (J. Thorac. Cardiovasc. Surg. 2010;140:313-6) of the 3f Enable valve in 28 patients showed that the valve could be implanted safely and quickly with favorable early hemodynamics.
"Again, I just want to stress, the goal is not to go from 60 minutes down to 40 minutes of ischemia; the goal is to facilitate a minimally invasive approach," said Dr. Borger. He noted that the hemodynamics were excellent for all three sutureless valves.
The second valve to receive CE mark approval in Europe was the Sorin Perceval S, at the beginning of 2012. It has a bovine pericardial leaflet, also attached to a Nitinol stent, and is crimped at the bedside. This results in an advantage for implantation.
"You can see exactly that the valve is in the position where you want it to be before deploying it," said Dr. Borger. The long-term results of crimping the leaflets are not yet known.
This particular model is currently available in sizes of 21, 23, and 25 mm. Even a 25-mm valve can only be put in a relatively small annulus, making the Perceval valve most appropriate for the small, elderly patient.
Sorin has reported results from 186 patients who received the Perceval valve, and noted short cross-clamp times (mean cross-clamp time for isolated AVR, 28.6 minutes) and 2.8% mortality.
The third and final sutureless aortic prosthesis is the Edwards Intuity valve, whose top is a traditional design based on the Magna Ease valve, and whose bottom is stent technology borrowed from Edwards’ TAVI program. A recent study of 152 patents revealed an average cross-clamp time of 41 minutes for isolated AVR, with a perioperative mortality rate of 2.1% and a paravalvular leak rate of 1.4% (J. Thorac. Cardiovasc. Surg. 2012;145:110-16). In addition, hemodynamics were excellent, with a mean transvalvular gradient of 9.8 mm Hg.
Dr. Borger disclosed receiving speaking honoraria from Edwards Lifesciences, Medtronic, and St. Jude Medical. He was a researcher in the Edwards Intuity and Sorin Perceval studies.
CHICAGO – European data suggest that minimally invasive aortic valve surgery has several benefits and few downsides when compared to conventional aortic valve replacement.
Bleeding is decreased, as is ICU and hospital length of stay. Cosmesis is improved. Sutureless valves may facilitate the performance of minimally invasive aortic valve replacement (AVR), and are associated with decreased ischemic times and lower transvalvular gradients – an advantage when concomitant procedures are performed or patients are high risk, according to a presentation at the 2012 Heart Valve summit.
Sutureless aortic valves facilitate minimal basic AVR and minimize myocardial ischemic time, said Dr. Michael Borger of Leipzig (Germany) Heart Center.
He described the evidence to date, as well as his personal experience, at this educational program of the American Association for Thoracic Surgery (AATS) and the American College of Cardiology Foundation (ACCF).
Leipzig Heart Center is one of Europe’s largest cardiac facilities, with 4,000 cardiac operations per year.
The number of patients who undergo minimally invasive aortic valve procedures is still very low, said Dr. Borger, and he urged the audience to consider this option in the future, especially when transcatheter aortic valve implantation (TAVI) becomes as widely accepted in America as it is in Europe. In Germany alone, 31% of isolated AVRs are now done by TAVI.
"Decreased myocardial ischemic time doesn’t matter for someone who needs an isolated aortic valve, [such as a] 70-year-old patient with no risk factors. It doesn’t matter if you shorten their ischemic time by 20 minutes. That’s not the point. The point is that a sutureless valve facilitates minimally invasive surgery by making it easier to do; and a marker for that is decreased ischemic time."
One subgroup of patients who do benefit from decreased ischemic times, however, are those requiring complex multivalve procedures. Patients who have a poor ejection fraction also benefit.
"We are applying lessons that we’ve learned from TAVI to these sutureless valves," said Dr. Borger. "TAVI has been in Europe – transfemoral for 10 years, transapical for 6 years – and what we know from TAVI is that a stent is able to hold an aortic valve in the left ventricular outflow tract and prevent it from embolizing afterwards. In addition, we now know that you do not need to fully decalcify the annulus. As a matter of fact, you’re better off leaving some calcification in the annulus when implanting sutureless valves ... to avoid the formation of annular tears or defects."
There are two approaches: the upper hemisternotomy approach, which is favored in Leipzig, and the upper right midlateral thoracotomy approach.
Three sutureless valves are currently in use in Europe: the Medtronic (formerly ATS) Enable sutureless valve, the Sorin Perceval S sutureless valve, and the Edwards Intuity valve.
The Medtronic Enable valve is equine pericardium and was the first sutureless valve to get CE mark approval in Europe. The literature is limited, but a study from Switzerland (J. Thorac. Cardiovasc. Surg. 2010;140:313-6) of the 3f Enable valve in 28 patients showed that the valve could be implanted safely and quickly with favorable early hemodynamics.
"Again, I just want to stress, the goal is not to go from 60 minutes down to 40 minutes of ischemia; the goal is to facilitate a minimally invasive approach," said Dr. Borger. He noted that the hemodynamics were excellent for all three sutureless valves.
The second valve to receive CE mark approval in Europe was the Sorin Perceval S, at the beginning of 2012. It has a bovine pericardial leaflet, also attached to a Nitinol stent, and is crimped at the bedside. This results in an advantage for implantation.
"You can see exactly that the valve is in the position where you want it to be before deploying it," said Dr. Borger. The long-term results of crimping the leaflets are not yet known.
This particular model is currently available in sizes of 21, 23, and 25 mm. Even a 25-mm valve can only be put in a relatively small annulus, making the Perceval valve most appropriate for the small, elderly patient.
Sorin has reported results from 186 patients who received the Perceval valve, and noted short cross-clamp times (mean cross-clamp time for isolated AVR, 28.6 minutes) and 2.8% mortality.
The third and final sutureless aortic prosthesis is the Edwards Intuity valve, whose top is a traditional design based on the Magna Ease valve, and whose bottom is stent technology borrowed from Edwards’ TAVI program. A recent study of 152 patents revealed an average cross-clamp time of 41 minutes for isolated AVR, with a perioperative mortality rate of 2.1% and a paravalvular leak rate of 1.4% (J. Thorac. Cardiovasc. Surg. 2012;145:110-16). In addition, hemodynamics were excellent, with a mean transvalvular gradient of 9.8 mm Hg.
Dr. Borger disclosed receiving speaking honoraria from Edwards Lifesciences, Medtronic, and St. Jude Medical. He was a researcher in the Edwards Intuity and Sorin Perceval studies.
Leipzig Heart Center,
Leipzig Heart Center,
EXPERT ANALYSIS FROM HEART VALVE SUMMIT 2012
Progress Limited in Transcatheter Repair of Mitral Regurgitation
CHICAGO – Within narrow limits, transcatheter repair of mitral regurgitation can have outcomes meeting or even exceeding those of surgery.
"I believe that mitral regurgitation is mostly a surgical disease, but that interventional devices will, sooner or later, be able to manage some of the spectrum of mitral pathology," said Dr. Howard C. Herrmann at the Heart Valve Summit 2012. Dr. Herrmann is professor of medicine and director of interventional cardiology and cardiac catheterization at the University of Pennsylvania, Philadelphia.
"Transcatheter approaches are always going to be somewhat more limited than surgery," said Dr. Herrmann. The device that repairs a leaflet edge to edge is very different from the one that can be used to perform indirect annular dilatation via the coronary sinus, he noted.
Two devices relevant to those indications show promise, although neither is yet approved by the Food and Drug Administration (FDA), he said. These are Cardiac Dimensions’ Carillon for annular dilatation, and Abbott Vascular’s MitraClip for leaflet repair.
In the European TITAN clinical trial, 36 of 53 patients (68%) were implanted with the Carillon Mitral Contour System. The average baseline ejection fraction of all 53 patients was 28%, which Dr. Herrmann characterized as true functional mitral regurgitation (FMR). The prospective, nonrandomized, double-arm study compared results from the implanted group to results from a group without implants.
Implanted patients demonstrated significant reductions in FMR as assessed by multiple quantitative measures, including mean regurgitant volume, which decreased from 34.5 +/– 11.5 mL to 17.4 +/– 12.4 mL over 12 months (P less than .001) (Eur. J. Heart Fail. 2012;14:931-8).
These and other reductions correlated with symptomatic improvement, said Dr. Herrmann. However, the coronary sinus approach to percutaneous mitral annuloplasty is clearly limited by the variable anatomy between the coronary sinus and the posterior mitral annulus, as well as by the risk of coronary artery constriction, he said. Additionally, the long-term benefit of a surgical partial circumference ring is unknown (Circulation 2006;114:377-80).
The other device, the MitraClip, was evaluated in the EVEREST II trial for safety and efficacy in treatment of mitral valve regurgitation.
"Clearly, if you look at the primary effectiveness rate as defined by the trial, which is not a very high bar, surgery still beat the device," said Dr. Herrmann. However, he noted, the device clearly beat surgery in terms of morbidity and other safety end points.
"But when you look at it from an intent-to-treat analysis, those results are clearly inferior with MitraClip: At 2 years, 78.2% of percutaneous patients are free from mitral valve surgery, versus 96.1% of surgery patients (P less than .001).
"MitraClip should not and is not being used for low-risk patients with degenerative disease amenable to surgical repair. ... That said, in the patients who had good results with MitraClip, those results do appear to be fairly durable," he said. At 3 years, all-cause mortality was very similar between the two interventions. (J. Thorac. Cardiovasc. Surg. 2012;143:S60-3; J. Am. Coll. Cardiol. 2012;59:130-9).
Analysis of the high-surgical-risk cohort (n = 78) from EVEREST II revealed a 45% decrease in rehospitalizations (P = .02) at 12 months after intervention with MitraClip, said Dr. Herrmann. This finding led investigators to launch the COAPT trial, which has been approved by the FDA and is expected to start soon in the United States. Approximately 420 patients with significant FMR, thought to be at extremely high risk for surgery, will be randomized 1:1 to MitraClip (n = 210) or medical therapy (n = 210). The primary end point is a reduction in subsequent heart failure hospitalizations.
"This is truly a trial looking at palliative benefit, not mortality," he said.
He concluded by noting that several devices are under development, including others for leaflet repair, indirect annuloplasty, and direct annular or left ventricular remodeling; as well as direct LV shape-altering devices, transcatheter mitral valve replacement devices, and devices that mimic surgical ring annuloplasty.
The Heart Valve Summit was an educational program presented jointly by the American Association for Thoracic Surgery and the American College of Cardiology Foundation. Dr. Hermann has grant/research support from Abbott Vascular, Edwards Lifesciences, St. Jude Medical, Medtronic, and Gore, and has received consulting fees and honoraria from these and other device companies. His presentation was not sponsored.
CHICAGO – Within narrow limits, transcatheter repair of mitral regurgitation can have outcomes meeting or even exceeding those of surgery.
"I believe that mitral regurgitation is mostly a surgical disease, but that interventional devices will, sooner or later, be able to manage some of the spectrum of mitral pathology," said Dr. Howard C. Herrmann at the Heart Valve Summit 2012. Dr. Herrmann is professor of medicine and director of interventional cardiology and cardiac catheterization at the University of Pennsylvania, Philadelphia.
"Transcatheter approaches are always going to be somewhat more limited than surgery," said Dr. Herrmann. The device that repairs a leaflet edge to edge is very different from the one that can be used to perform indirect annular dilatation via the coronary sinus, he noted.
Two devices relevant to those indications show promise, although neither is yet approved by the Food and Drug Administration (FDA), he said. These are Cardiac Dimensions’ Carillon for annular dilatation, and Abbott Vascular’s MitraClip for leaflet repair.
In the European TITAN clinical trial, 36 of 53 patients (68%) were implanted with the Carillon Mitral Contour System. The average baseline ejection fraction of all 53 patients was 28%, which Dr. Herrmann characterized as true functional mitral regurgitation (FMR). The prospective, nonrandomized, double-arm study compared results from the implanted group to results from a group without implants.
Implanted patients demonstrated significant reductions in FMR as assessed by multiple quantitative measures, including mean regurgitant volume, which decreased from 34.5 +/– 11.5 mL to 17.4 +/– 12.4 mL over 12 months (P less than .001) (Eur. J. Heart Fail. 2012;14:931-8).
These and other reductions correlated with symptomatic improvement, said Dr. Herrmann. However, the coronary sinus approach to percutaneous mitral annuloplasty is clearly limited by the variable anatomy between the coronary sinus and the posterior mitral annulus, as well as by the risk of coronary artery constriction, he said. Additionally, the long-term benefit of a surgical partial circumference ring is unknown (Circulation 2006;114:377-80).
The other device, the MitraClip, was evaluated in the EVEREST II trial for safety and efficacy in treatment of mitral valve regurgitation.
"Clearly, if you look at the primary effectiveness rate as defined by the trial, which is not a very high bar, surgery still beat the device," said Dr. Herrmann. However, he noted, the device clearly beat surgery in terms of morbidity and other safety end points.
"But when you look at it from an intent-to-treat analysis, those results are clearly inferior with MitraClip: At 2 years, 78.2% of percutaneous patients are free from mitral valve surgery, versus 96.1% of surgery patients (P less than .001).
"MitraClip should not and is not being used for low-risk patients with degenerative disease amenable to surgical repair. ... That said, in the patients who had good results with MitraClip, those results do appear to be fairly durable," he said. At 3 years, all-cause mortality was very similar between the two interventions. (J. Thorac. Cardiovasc. Surg. 2012;143:S60-3; J. Am. Coll. Cardiol. 2012;59:130-9).
Analysis of the high-surgical-risk cohort (n = 78) from EVEREST II revealed a 45% decrease in rehospitalizations (P = .02) at 12 months after intervention with MitraClip, said Dr. Herrmann. This finding led investigators to launch the COAPT trial, which has been approved by the FDA and is expected to start soon in the United States. Approximately 420 patients with significant FMR, thought to be at extremely high risk for surgery, will be randomized 1:1 to MitraClip (n = 210) or medical therapy (n = 210). The primary end point is a reduction in subsequent heart failure hospitalizations.
"This is truly a trial looking at palliative benefit, not mortality," he said.
He concluded by noting that several devices are under development, including others for leaflet repair, indirect annuloplasty, and direct annular or left ventricular remodeling; as well as direct LV shape-altering devices, transcatheter mitral valve replacement devices, and devices that mimic surgical ring annuloplasty.
The Heart Valve Summit was an educational program presented jointly by the American Association for Thoracic Surgery and the American College of Cardiology Foundation. Dr. Hermann has grant/research support from Abbott Vascular, Edwards Lifesciences, St. Jude Medical, Medtronic, and Gore, and has received consulting fees and honoraria from these and other device companies. His presentation was not sponsored.
CHICAGO – Within narrow limits, transcatheter repair of mitral regurgitation can have outcomes meeting or even exceeding those of surgery.
"I believe that mitral regurgitation is mostly a surgical disease, but that interventional devices will, sooner or later, be able to manage some of the spectrum of mitral pathology," said Dr. Howard C. Herrmann at the Heart Valve Summit 2012. Dr. Herrmann is professor of medicine and director of interventional cardiology and cardiac catheterization at the University of Pennsylvania, Philadelphia.
"Transcatheter approaches are always going to be somewhat more limited than surgery," said Dr. Herrmann. The device that repairs a leaflet edge to edge is very different from the one that can be used to perform indirect annular dilatation via the coronary sinus, he noted.
Two devices relevant to those indications show promise, although neither is yet approved by the Food and Drug Administration (FDA), he said. These are Cardiac Dimensions’ Carillon for annular dilatation, and Abbott Vascular’s MitraClip for leaflet repair.
In the European TITAN clinical trial, 36 of 53 patients (68%) were implanted with the Carillon Mitral Contour System. The average baseline ejection fraction of all 53 patients was 28%, which Dr. Herrmann characterized as true functional mitral regurgitation (FMR). The prospective, nonrandomized, double-arm study compared results from the implanted group to results from a group without implants.
Implanted patients demonstrated significant reductions in FMR as assessed by multiple quantitative measures, including mean regurgitant volume, which decreased from 34.5 +/– 11.5 mL to 17.4 +/– 12.4 mL over 12 months (P less than .001) (Eur. J. Heart Fail. 2012;14:931-8).
These and other reductions correlated with symptomatic improvement, said Dr. Herrmann. However, the coronary sinus approach to percutaneous mitral annuloplasty is clearly limited by the variable anatomy between the coronary sinus and the posterior mitral annulus, as well as by the risk of coronary artery constriction, he said. Additionally, the long-term benefit of a surgical partial circumference ring is unknown (Circulation 2006;114:377-80).
The other device, the MitraClip, was evaluated in the EVEREST II trial for safety and efficacy in treatment of mitral valve regurgitation.
"Clearly, if you look at the primary effectiveness rate as defined by the trial, which is not a very high bar, surgery still beat the device," said Dr. Herrmann. However, he noted, the device clearly beat surgery in terms of morbidity and other safety end points.
"But when you look at it from an intent-to-treat analysis, those results are clearly inferior with MitraClip: At 2 years, 78.2% of percutaneous patients are free from mitral valve surgery, versus 96.1% of surgery patients (P less than .001).
"MitraClip should not and is not being used for low-risk patients with degenerative disease amenable to surgical repair. ... That said, in the patients who had good results with MitraClip, those results do appear to be fairly durable," he said. At 3 years, all-cause mortality was very similar between the two interventions. (J. Thorac. Cardiovasc. Surg. 2012;143:S60-3; J. Am. Coll. Cardiol. 2012;59:130-9).
Analysis of the high-surgical-risk cohort (n = 78) from EVEREST II revealed a 45% decrease in rehospitalizations (P = .02) at 12 months after intervention with MitraClip, said Dr. Herrmann. This finding led investigators to launch the COAPT trial, which has been approved by the FDA and is expected to start soon in the United States. Approximately 420 patients with significant FMR, thought to be at extremely high risk for surgery, will be randomized 1:1 to MitraClip (n = 210) or medical therapy (n = 210). The primary end point is a reduction in subsequent heart failure hospitalizations.
"This is truly a trial looking at palliative benefit, not mortality," he said.
He concluded by noting that several devices are under development, including others for leaflet repair, indirect annuloplasty, and direct annular or left ventricular remodeling; as well as direct LV shape-altering devices, transcatheter mitral valve replacement devices, and devices that mimic surgical ring annuloplasty.
The Heart Valve Summit was an educational program presented jointly by the American Association for Thoracic Surgery and the American College of Cardiology Foundation. Dr. Hermann has grant/research support from Abbott Vascular, Edwards Lifesciences, St. Jude Medical, Medtronic, and Gore, and has received consulting fees and honoraria from these and other device companies. His presentation was not sponsored.
EXPERT ANALYSIS FROM THE HEART VALVE SUMMIT 2012
What's New? The Changing Landscape of Infective Endocarditis
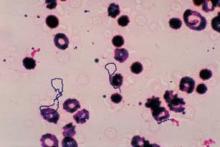
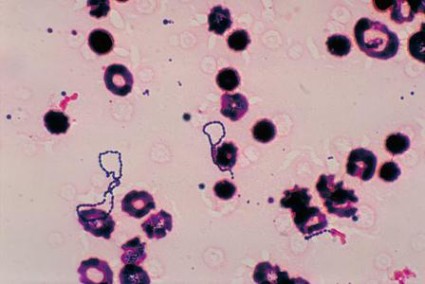
CHICAGO -- Mitral valve endocarditis is a medical-surgical problem that demands a team approach, and the landscape of the disease has changed significantly for the worst in the recent past, according to a presentation at Heart Valve Summit 2012.
"If you’re lucky enough to have a valve infection with the Strep viridans microorganism, you’re likely to do well," said Dr. Patrick T. O’Gara, director of clinical cardiology at Brigham and Women’s Hospital, Boston.
On the other hand, patients who’ve been infected with any other type of organism, particularly Staph aureus or its increasingly frequent relative methicillin-resistant Staph aureus, could be in real trouble.
"There’s no question that these organisms are smarter than we are and can lead to destruction of the valve and death of the patient, despite our best intentions," said Dr. O’Gara. He described the evolving epidemiology, natural history, and indications for surgery for this disease to this educational program of the American Association for Thoracic Surgery (AATS) and the American College of Cardiology Foundation (ACCF).
"Unfortunately, despite our best efforts, and worldwide, among centers with an interest in the care of patients with endocarditis, 6-month mortality rates still approach 25%," he said. This is close to the mortality rate of a type A aortic dissection, so it is by no means trivial. Early surgery is now performed on many who present with the disease in early stages, and perioperative mortality is 12%-20%.
It is a challenge to manage a patient who is asymptomatic with respect to heart failure but who has a large mobile vegetation involving the anterior mitral leaflet, said Dr. O’Gara. Vegetations in this location are the most prone to embolize.
"This is the common question now posed to consulting cardiologists: Does my patient require early surgery for prevention of embolic complications? We don’t really get asked too much any more: ‘Does my patient need early surgery because they’ve developed heart failure?’ I guess we’re much more confident in proceeding under those circumstances."
He discussed considerations for surgery, including the level of local surgical expertise. The intervention is complex and delicate. "This is not something for the faint of heart," said Dr. O’Gara.
In the early time frame following presentation, there is a relationship between the size of the vegetation and the risk of embolization.
The risk of stroke drops rapidly after initiation of antimicrobial therapy. Patients who develop stroke as a complication of endocarditis typically do so the day before, the day of, or the day after presentation, he said. Stroke risk continues to drop quickly in the first 2 weeks after initiation of antibiotics, and by week 5 it’s almost nil.
"If you’re thinking about intervention for prevention of stroke, it makes sense to do so in the first week, after identification of a patient at risk with a large mobile vegetation. It makes much less sense to do so in weeks 2 or 3."
The size of the vegetation alone may dictate mortality. A size of 1.5 cm or greater is associated with increased risk of death at 1 year in the setting of native valve endocarditis.
The good news is that event-free survival rates have been shown to be much better for those who undergo surgery in the first 7 days after presentation with high-risk native, left-sided endocarditis. In-hospital mortality as a function of early surgery appears to have declined over the course of time.
"So, in summary, I think for our management considerations, it’s early diagnosis, risk stratification, a heart team approach, consider early surgery, particularly if you have the operative expertise. The early risk of re-infection in implanted prosthetic material is very low," Dr. O’Gara said.
Dr. O’Gara disclosed ties with the Data Safety Monitoring Board and Lantheus Medical Imaging.
CHICAGO -- Mitral valve endocarditis is a medical-surgical problem that demands a team approach, and the landscape of the disease has changed significantly for the worst in the recent past, according to a presentation at Heart Valve Summit 2012.
"If you’re lucky enough to have a valve infection with the Strep viridans microorganism, you’re likely to do well," said Dr. Patrick T. O’Gara, director of clinical cardiology at Brigham and Women’s Hospital, Boston.
On the other hand, patients who’ve been infected with any other type of organism, particularly Staph aureus or its increasingly frequent relative methicillin-resistant Staph aureus, could be in real trouble.
"There’s no question that these organisms are smarter than we are and can lead to destruction of the valve and death of the patient, despite our best intentions," said Dr. O’Gara. He described the evolving epidemiology, natural history, and indications for surgery for this disease to this educational program of the American Association for Thoracic Surgery (AATS) and the American College of Cardiology Foundation (ACCF).
"Unfortunately, despite our best efforts, and worldwide, among centers with an interest in the care of patients with endocarditis, 6-month mortality rates still approach 25%," he said. This is close to the mortality rate of a type A aortic dissection, so it is by no means trivial. Early surgery is now performed on many who present with the disease in early stages, and perioperative mortality is 12%-20%.
It is a challenge to manage a patient who is asymptomatic with respect to heart failure but who has a large mobile vegetation involving the anterior mitral leaflet, said Dr. O’Gara. Vegetations in this location are the most prone to embolize.
"This is the common question now posed to consulting cardiologists: Does my patient require early surgery for prevention of embolic complications? We don’t really get asked too much any more: ‘Does my patient need early surgery because they’ve developed heart failure?’ I guess we’re much more confident in proceeding under those circumstances."
He discussed considerations for surgery, including the level of local surgical expertise. The intervention is complex and delicate. "This is not something for the faint of heart," said Dr. O’Gara.
In the early time frame following presentation, there is a relationship between the size of the vegetation and the risk of embolization.
The risk of stroke drops rapidly after initiation of antimicrobial therapy. Patients who develop stroke as a complication of endocarditis typically do so the day before, the day of, or the day after presentation, he said. Stroke risk continues to drop quickly in the first 2 weeks after initiation of antibiotics, and by week 5 it’s almost nil.
"If you’re thinking about intervention for prevention of stroke, it makes sense to do so in the first week, after identification of a patient at risk with a large mobile vegetation. It makes much less sense to do so in weeks 2 or 3."
The size of the vegetation alone may dictate mortality. A size of 1.5 cm or greater is associated with increased risk of death at 1 year in the setting of native valve endocarditis.
The good news is that event-free survival rates have been shown to be much better for those who undergo surgery in the first 7 days after presentation with high-risk native, left-sided endocarditis. In-hospital mortality as a function of early surgery appears to have declined over the course of time.
"So, in summary, I think for our management considerations, it’s early diagnosis, risk stratification, a heart team approach, consider early surgery, particularly if you have the operative expertise. The early risk of re-infection in implanted prosthetic material is very low," Dr. O’Gara said.
Dr. O’Gara disclosed ties with the Data Safety Monitoring Board and Lantheus Medical Imaging.
CHICAGO -- Mitral valve endocarditis is a medical-surgical problem that demands a team approach, and the landscape of the disease has changed significantly for the worst in the recent past, according to a presentation at Heart Valve Summit 2012.
"If you’re lucky enough to have a valve infection with the Strep viridans microorganism, you’re likely to do well," said Dr. Patrick T. O’Gara, director of clinical cardiology at Brigham and Women’s Hospital, Boston.
On the other hand, patients who’ve been infected with any other type of organism, particularly Staph aureus or its increasingly frequent relative methicillin-resistant Staph aureus, could be in real trouble.
"There’s no question that these organisms are smarter than we are and can lead to destruction of the valve and death of the patient, despite our best intentions," said Dr. O’Gara. He described the evolving epidemiology, natural history, and indications for surgery for this disease to this educational program of the American Association for Thoracic Surgery (AATS) and the American College of Cardiology Foundation (ACCF).
"Unfortunately, despite our best efforts, and worldwide, among centers with an interest in the care of patients with endocarditis, 6-month mortality rates still approach 25%," he said. This is close to the mortality rate of a type A aortic dissection, so it is by no means trivial. Early surgery is now performed on many who present with the disease in early stages, and perioperative mortality is 12%-20%.
It is a challenge to manage a patient who is asymptomatic with respect to heart failure but who has a large mobile vegetation involving the anterior mitral leaflet, said Dr. O’Gara. Vegetations in this location are the most prone to embolize.
"This is the common question now posed to consulting cardiologists: Does my patient require early surgery for prevention of embolic complications? We don’t really get asked too much any more: ‘Does my patient need early surgery because they’ve developed heart failure?’ I guess we’re much more confident in proceeding under those circumstances."
He discussed considerations for surgery, including the level of local surgical expertise. The intervention is complex and delicate. "This is not something for the faint of heart," said Dr. O’Gara.
In the early time frame following presentation, there is a relationship between the size of the vegetation and the risk of embolization.
The risk of stroke drops rapidly after initiation of antimicrobial therapy. Patients who develop stroke as a complication of endocarditis typically do so the day before, the day of, or the day after presentation, he said. Stroke risk continues to drop quickly in the first 2 weeks after initiation of antibiotics, and by week 5 it’s almost nil.
"If you’re thinking about intervention for prevention of stroke, it makes sense to do so in the first week, after identification of a patient at risk with a large mobile vegetation. It makes much less sense to do so in weeks 2 or 3."
The size of the vegetation alone may dictate mortality. A size of 1.5 cm or greater is associated with increased risk of death at 1 year in the setting of native valve endocarditis.
The good news is that event-free survival rates have been shown to be much better for those who undergo surgery in the first 7 days after presentation with high-risk native, left-sided endocarditis. In-hospital mortality as a function of early surgery appears to have declined over the course of time.
"So, in summary, I think for our management considerations, it’s early diagnosis, risk stratification, a heart team approach, consider early surgery, particularly if you have the operative expertise. The early risk of re-infection in implanted prosthetic material is very low," Dr. O’Gara said.
Dr. O’Gara disclosed ties with the Data Safety Monitoring Board and Lantheus Medical Imaging.
EXPERT ANALYSIS FROM HEART VALVE SUMMIT 2012
Retreatment With High-Dose Rituximab Reduced DAS28 Levels
CHICAGO – In patients with rheumatoid arthritis, initial treatment with two 500-mg infusions of rituximab or two 1,000-mg infusions led to comparable clinical outcomes.
But when the next course was given, only the rituximab regimen of two doses of 1,000 mg each was associated with further DAS28 reductions. This was the finding of an observational cohort study of 2,873 patients from the CERERRA collaboration.
"We know that the approved dose of rituximab in rheumatoid arthritis is 1,000 mg x 2, but some data from clinical trials have suggested similar clinical efficacy with 500 mg x 2. The purpose of this analysis was to compare the efficacy of the two dosages given as first or second treatment course," said principal investigator Dr. Katerina Chatzidionysiou of the Karolinska Institute in Stockholm.
Data for this study were collected from the 10 European registries of CERERRA (European Collaborative Registries for the Evaluation of Rituximab in Rheumatoid Arthritis). The data contained demographic, efficacy, and treatment information for patients who had started a course of rituximab. Efficacy of treatment and retreatment was assessed at 6 months for DAS28 reductions and EULAR responses, Dr. Chatzidionysiou said at the annual meeting of the American College of Rheumatology.
From a total of 3,266 patients, data on rituximab dosing were available for 2,873 (88%), of whom 2,625 (91.4%) received a regimen of two doses of 1,000 mg each and 248 (8.6%) received two doses of 500 mg each.
"Only the high dose, 1,000 mg, leads to significant improvements after retreatment."
There were significant differences between the groups in demographic and disease characteristics, said Dr. Chatzidionysiou. Patients treated with the lower dose were significantly older (55.2 plus or minus 15.8 years in the 500-mg group vs. 52.6 plus or minus 12.6 years in the 1,000-mg group, P = .002), had a longer duration of disease (13.6 plus or minus 11.9 years vs. 10.9 plus or minus 8.2 years, respectively, P less than .0001), and had used a lower number of prior biologics (0.7 vs. 1.0, P less than .0001). Patients in the lower-dose group were also more likely than those in the higher-dose group to have been treated with concomitant corticosteroids (65.7% vs. 59.3%, P = .03), and less likely to have been treated with concomitant disease-modifying antirheumatic drugs (72.6% vs. 83.1%, P less than .0001), with a majority using methotrexate (46.4% vs. 63.4%, P less than .0001). In the 500-mg group, 42% were identified as being anti–tumor necrosis factor (anti-TNF) agent naive, and the remaining 58% failed to respond to anti-TNF therapy. In the 1,000-mg group, 62.5% were anti-TNF naive and 37.5% failed to respond to anti-TNF therapy.
The two treatment groups started from different DAS28 baselines (5.7 plus or minus 1.3 in the 500-mg group vs. 5.9 plus or minus 1.3 in the 1,000-mg group, P = .02), and at 6 months, the DAS28 improvement was very similar (DAS28 score changed by 1.7 plus or minus 1.4 vs. 1.9 plus or minus 1.4, respectively, P = .5), said Dr. Chatzidionysiou.
No difference was observed in EULAR responses at 6 months, either, and no difference was noted according to whether the patients were anti-TNF naive or anti-TNF failures.
The study identified 622 patients who received a second cycle of rituximab: 579 were retreated with 1,000 mg and 26 with 500 mg. Seventeen patients who were retreated at different time points were eliminated from this count.
"We observed that when rituximab is given as a retreatment, the high dose leads to significantly better results at 6 months after therapy," said Dr. Chatzidionysiou.
"The DAS28 at 12 months was significantly lower in patients retreated with 1,000 mg," she said. EULAR responses and remission rates yielded similar results.
To compensate for the disparity in patient numbers between the two groups, a second, confirmatory analysis was performed using patients retreated only once during the first 12 months, at either 3, 6, or 9 months. This yielded 819 patients retreated with a high dose and 81 retreated with a lower dose.
"But again we came to a similar conclusion: Only the high dose, 1,000 mg, leads to significant improvements after retreatment," said Dr. Chatzidionysiou. Again, the EULAR responses and remission rates at 12 months were significantly higher with high-dose rituximab.
However, she noted, "it is difficult to interpret the results of the retreatment analysis because of the small number of patients and the differences between the two groups regarding baseline characteristics."
Dr. Chatzidionysiou disclosed being a consultant to Roche.
CHICAGO – In patients with rheumatoid arthritis, initial treatment with two 500-mg infusions of rituximab or two 1,000-mg infusions led to comparable clinical outcomes.
But when the next course was given, only the rituximab regimen of two doses of 1,000 mg each was associated with further DAS28 reductions. This was the finding of an observational cohort study of 2,873 patients from the CERERRA collaboration.
"We know that the approved dose of rituximab in rheumatoid arthritis is 1,000 mg x 2, but some data from clinical trials have suggested similar clinical efficacy with 500 mg x 2. The purpose of this analysis was to compare the efficacy of the two dosages given as first or second treatment course," said principal investigator Dr. Katerina Chatzidionysiou of the Karolinska Institute in Stockholm.
Data for this study were collected from the 10 European registries of CERERRA (European Collaborative Registries for the Evaluation of Rituximab in Rheumatoid Arthritis). The data contained demographic, efficacy, and treatment information for patients who had started a course of rituximab. Efficacy of treatment and retreatment was assessed at 6 months for DAS28 reductions and EULAR responses, Dr. Chatzidionysiou said at the annual meeting of the American College of Rheumatology.
From a total of 3,266 patients, data on rituximab dosing were available for 2,873 (88%), of whom 2,625 (91.4%) received a regimen of two doses of 1,000 mg each and 248 (8.6%) received two doses of 500 mg each.
"Only the high dose, 1,000 mg, leads to significant improvements after retreatment."
There were significant differences between the groups in demographic and disease characteristics, said Dr. Chatzidionysiou. Patients treated with the lower dose were significantly older (55.2 plus or minus 15.8 years in the 500-mg group vs. 52.6 plus or minus 12.6 years in the 1,000-mg group, P = .002), had a longer duration of disease (13.6 plus or minus 11.9 years vs. 10.9 plus or minus 8.2 years, respectively, P less than .0001), and had used a lower number of prior biologics (0.7 vs. 1.0, P less than .0001). Patients in the lower-dose group were also more likely than those in the higher-dose group to have been treated with concomitant corticosteroids (65.7% vs. 59.3%, P = .03), and less likely to have been treated with concomitant disease-modifying antirheumatic drugs (72.6% vs. 83.1%, P less than .0001), with a majority using methotrexate (46.4% vs. 63.4%, P less than .0001). In the 500-mg group, 42% were identified as being anti–tumor necrosis factor (anti-TNF) agent naive, and the remaining 58% failed to respond to anti-TNF therapy. In the 1,000-mg group, 62.5% were anti-TNF naive and 37.5% failed to respond to anti-TNF therapy.
The two treatment groups started from different DAS28 baselines (5.7 plus or minus 1.3 in the 500-mg group vs. 5.9 plus or minus 1.3 in the 1,000-mg group, P = .02), and at 6 months, the DAS28 improvement was very similar (DAS28 score changed by 1.7 plus or minus 1.4 vs. 1.9 plus or minus 1.4, respectively, P = .5), said Dr. Chatzidionysiou.
No difference was observed in EULAR responses at 6 months, either, and no difference was noted according to whether the patients were anti-TNF naive or anti-TNF failures.
The study identified 622 patients who received a second cycle of rituximab: 579 were retreated with 1,000 mg and 26 with 500 mg. Seventeen patients who were retreated at different time points were eliminated from this count.
"We observed that when rituximab is given as a retreatment, the high dose leads to significantly better results at 6 months after therapy," said Dr. Chatzidionysiou.
"The DAS28 at 12 months was significantly lower in patients retreated with 1,000 mg," she said. EULAR responses and remission rates yielded similar results.
To compensate for the disparity in patient numbers between the two groups, a second, confirmatory analysis was performed using patients retreated only once during the first 12 months, at either 3, 6, or 9 months. This yielded 819 patients retreated with a high dose and 81 retreated with a lower dose.
"But again we came to a similar conclusion: Only the high dose, 1,000 mg, leads to significant improvements after retreatment," said Dr. Chatzidionysiou. Again, the EULAR responses and remission rates at 12 months were significantly higher with high-dose rituximab.
However, she noted, "it is difficult to interpret the results of the retreatment analysis because of the small number of patients and the differences between the two groups regarding baseline characteristics."
Dr. Chatzidionysiou disclosed being a consultant to Roche.
CHICAGO – In patients with rheumatoid arthritis, initial treatment with two 500-mg infusions of rituximab or two 1,000-mg infusions led to comparable clinical outcomes.
But when the next course was given, only the rituximab regimen of two doses of 1,000 mg each was associated with further DAS28 reductions. This was the finding of an observational cohort study of 2,873 patients from the CERERRA collaboration.
"We know that the approved dose of rituximab in rheumatoid arthritis is 1,000 mg x 2, but some data from clinical trials have suggested similar clinical efficacy with 500 mg x 2. The purpose of this analysis was to compare the efficacy of the two dosages given as first or second treatment course," said principal investigator Dr. Katerina Chatzidionysiou of the Karolinska Institute in Stockholm.
Data for this study were collected from the 10 European registries of CERERRA (European Collaborative Registries for the Evaluation of Rituximab in Rheumatoid Arthritis). The data contained demographic, efficacy, and treatment information for patients who had started a course of rituximab. Efficacy of treatment and retreatment was assessed at 6 months for DAS28 reductions and EULAR responses, Dr. Chatzidionysiou said at the annual meeting of the American College of Rheumatology.
From a total of 3,266 patients, data on rituximab dosing were available for 2,873 (88%), of whom 2,625 (91.4%) received a regimen of two doses of 1,000 mg each and 248 (8.6%) received two doses of 500 mg each.
"Only the high dose, 1,000 mg, leads to significant improvements after retreatment."
There were significant differences between the groups in demographic and disease characteristics, said Dr. Chatzidionysiou. Patients treated with the lower dose were significantly older (55.2 plus or minus 15.8 years in the 500-mg group vs. 52.6 plus or minus 12.6 years in the 1,000-mg group, P = .002), had a longer duration of disease (13.6 plus or minus 11.9 years vs. 10.9 plus or minus 8.2 years, respectively, P less than .0001), and had used a lower number of prior biologics (0.7 vs. 1.0, P less than .0001). Patients in the lower-dose group were also more likely than those in the higher-dose group to have been treated with concomitant corticosteroids (65.7% vs. 59.3%, P = .03), and less likely to have been treated with concomitant disease-modifying antirheumatic drugs (72.6% vs. 83.1%, P less than .0001), with a majority using methotrexate (46.4% vs. 63.4%, P less than .0001). In the 500-mg group, 42% were identified as being anti–tumor necrosis factor (anti-TNF) agent naive, and the remaining 58% failed to respond to anti-TNF therapy. In the 1,000-mg group, 62.5% were anti-TNF naive and 37.5% failed to respond to anti-TNF therapy.
The two treatment groups started from different DAS28 baselines (5.7 plus or minus 1.3 in the 500-mg group vs. 5.9 plus or minus 1.3 in the 1,000-mg group, P = .02), and at 6 months, the DAS28 improvement was very similar (DAS28 score changed by 1.7 plus or minus 1.4 vs. 1.9 plus or minus 1.4, respectively, P = .5), said Dr. Chatzidionysiou.
No difference was observed in EULAR responses at 6 months, either, and no difference was noted according to whether the patients were anti-TNF naive or anti-TNF failures.
The study identified 622 patients who received a second cycle of rituximab: 579 were retreated with 1,000 mg and 26 with 500 mg. Seventeen patients who were retreated at different time points were eliminated from this count.
"We observed that when rituximab is given as a retreatment, the high dose leads to significantly better results at 6 months after therapy," said Dr. Chatzidionysiou.
"The DAS28 at 12 months was significantly lower in patients retreated with 1,000 mg," she said. EULAR responses and remission rates yielded similar results.
To compensate for the disparity in patient numbers between the two groups, a second, confirmatory analysis was performed using patients retreated only once during the first 12 months, at either 3, 6, or 9 months. This yielded 819 patients retreated with a high dose and 81 retreated with a lower dose.
"But again we came to a similar conclusion: Only the high dose, 1,000 mg, leads to significant improvements after retreatment," said Dr. Chatzidionysiou. Again, the EULAR responses and remission rates at 12 months were significantly higher with high-dose rituximab.
However, she noted, "it is difficult to interpret the results of the retreatment analysis because of the small number of patients and the differences between the two groups regarding baseline characteristics."
Dr. Chatzidionysiou disclosed being a consultant to Roche.
FROM THE ANNUAL MEETING OF THE AMERICAN COLLEGE OF RHEUMATOLOGY
Major Finding: In patients with rheumatoid arthritis, initial treatment with rituximab 500 mg x 2 or 1,000 mg x 2 led to comparable clinical outcomes, but in a following treatment course, only the higher dose (1,000 mg x 2) was associated with further DAS28 reductions.
Data Source: 2,873 of 3,266 patients from the CERERRA collaboration.
Disclosures: Dr. Chatzidionysiou disclosed being a consultant to Roche.
Two Biomarkers Predict Response to Rituximab in RA
CHICAGO – Early B-cell repopulation and rheumatoid factor positivity predict early relapse in patients with rheumatoid arthritis who are being treated with rituximab, according to an observational study of 104 patients.
"We’re interested in predicting duration of response to rituximab," said lead author Dr. Edward M. Vital of the University of Leeds (England). "[W]hilst the majority of patients do respond, virtually all will relapse at some point. ... [T]he time to relapse is very variable, so that means that we don’t know what the best retreatment regime is. Some advocate retreatment every 6 months, but this may be excessive for some patients, with implications for cost and possibly safety."
With the sensitive B-cell assay, 88% of patients had detectable B cells by 6 months. However, a small group of patients have persistent B-cell depletion at 6 months, and this group had a longer clinical response. In fact, their responses continued to improve from 6 to 9 months, said Dr. Vital. Maintaining a low B-cell number is likely to maintain a good clinical response, he said, although not all patients with B-cell return relapsed immediately. Dr. Vital presented his data at the annual meeting of the American College of Rheumatology.
The study’s objective was to examine whether known predictors of initial response to rituximab could be used after treatment to predict maintenance of response to 12 months.
All 104 patients were positive for either rheumatoid factor or anti–cyclic citrullinated peptide at baseline, prior to treatment with rituximab in a regimen involving infused doses of 1,000 mg with concomitant methotrexate or leflunomide. Of the original study population, 78 (75%) had a known EULAR (European League Against Rheumatism) response at 6 months, and these were investigated for time to relapse. All use of corticosteroids and NSAIDs was similarly controlled in this group, and outcomes were measured by EULAR response and DAS28 (Disease Activity Score including a 28-joint count) at 0, 6, 9, and 12 months by one of two joint-count assessors.
Highly sensitive flow cytometry with a limit of detection of 0.0001 cells x 109/L was used to measure naive, memory B, and plasmablast subsets. Conventional flow cytometry has a limit of detection of 0.01 cells x 109/L.
At 6 months, 44 (57%) of the 78 patients had a EULAR moderate response, and 34 (43%) had a EULAR good response. In patients with detectable B cells at 6 months, DAS28 worsened by a mean 0.45, whereas in patients with undetectable B cells, it improved by a mean 0.44.
At 12 months, 40 patients (51%) had no response, 22 patients (28%) had a EULAR moderate response, and 16 patients (21%) had a EULAR good response.
A binary logistic regression model was created to predict continued EULAR response at 12 months. It included B-cell detection, plasmablast count, rheumatoid factor, and DAS28, and produced a significant (P = .001) model with an overall accuracy of 72%.
"Since rheumatoid factor and DAS28 were the strongest predictors of these, this suggested that it might actually be possible to make a very simple prediction model that doesn’t require specialized techniques," said Dr. Vital.
The authors subsequently created a simplified, two-variable categorical model using a rheumatoid factor threshold of 108 IU/mL, and a DAS28 threshold of 3.7, to predict relapse. This simplified model’s overall accuracy was 69% (P = .001).
"As you can see, we still have a significant model with just a slight reduction in the overall accuracy. ... If at 6 months the DAS28 was less than 3.7 and the rheumatoid factor was less than 108, then 73% of those patients maintained their clinical response out to 12 months ... and if both [DAS28 and rheumatoid factor] were higher, then only 8% of patients responded out to 12 months," said Dr. Vital.
The study concluded that these findings – in particular, the levels used in the two-variable model – need to be validated in another population. When validated, they may allow for selection of retreatment regime based on B-cell biomarkers.
Dr. Vital is on the Roche speakers bureau, and Roche provided rituximab for the patients in this study. The study was funded by the U.K. National Institute for Health Research Doctoral Research Fellowship and sponsored by the NIHR and the University of Leeds.
CHICAGO – Early B-cell repopulation and rheumatoid factor positivity predict early relapse in patients with rheumatoid arthritis who are being treated with rituximab, according to an observational study of 104 patients.
"We’re interested in predicting duration of response to rituximab," said lead author Dr. Edward M. Vital of the University of Leeds (England). "[W]hilst the majority of patients do respond, virtually all will relapse at some point. ... [T]he time to relapse is very variable, so that means that we don’t know what the best retreatment regime is. Some advocate retreatment every 6 months, but this may be excessive for some patients, with implications for cost and possibly safety."
With the sensitive B-cell assay, 88% of patients had detectable B cells by 6 months. However, a small group of patients have persistent B-cell depletion at 6 months, and this group had a longer clinical response. In fact, their responses continued to improve from 6 to 9 months, said Dr. Vital. Maintaining a low B-cell number is likely to maintain a good clinical response, he said, although not all patients with B-cell return relapsed immediately. Dr. Vital presented his data at the annual meeting of the American College of Rheumatology.
The study’s objective was to examine whether known predictors of initial response to rituximab could be used after treatment to predict maintenance of response to 12 months.
All 104 patients were positive for either rheumatoid factor or anti–cyclic citrullinated peptide at baseline, prior to treatment with rituximab in a regimen involving infused doses of 1,000 mg with concomitant methotrexate or leflunomide. Of the original study population, 78 (75%) had a known EULAR (European League Against Rheumatism) response at 6 months, and these were investigated for time to relapse. All use of corticosteroids and NSAIDs was similarly controlled in this group, and outcomes were measured by EULAR response and DAS28 (Disease Activity Score including a 28-joint count) at 0, 6, 9, and 12 months by one of two joint-count assessors.
Highly sensitive flow cytometry with a limit of detection of 0.0001 cells x 109/L was used to measure naive, memory B, and plasmablast subsets. Conventional flow cytometry has a limit of detection of 0.01 cells x 109/L.
At 6 months, 44 (57%) of the 78 patients had a EULAR moderate response, and 34 (43%) had a EULAR good response. In patients with detectable B cells at 6 months, DAS28 worsened by a mean 0.45, whereas in patients with undetectable B cells, it improved by a mean 0.44.
At 12 months, 40 patients (51%) had no response, 22 patients (28%) had a EULAR moderate response, and 16 patients (21%) had a EULAR good response.
A binary logistic regression model was created to predict continued EULAR response at 12 months. It included B-cell detection, plasmablast count, rheumatoid factor, and DAS28, and produced a significant (P = .001) model with an overall accuracy of 72%.
"Since rheumatoid factor and DAS28 were the strongest predictors of these, this suggested that it might actually be possible to make a very simple prediction model that doesn’t require specialized techniques," said Dr. Vital.
The authors subsequently created a simplified, two-variable categorical model using a rheumatoid factor threshold of 108 IU/mL, and a DAS28 threshold of 3.7, to predict relapse. This simplified model’s overall accuracy was 69% (P = .001).
"As you can see, we still have a significant model with just a slight reduction in the overall accuracy. ... If at 6 months the DAS28 was less than 3.7 and the rheumatoid factor was less than 108, then 73% of those patients maintained their clinical response out to 12 months ... and if both [DAS28 and rheumatoid factor] were higher, then only 8% of patients responded out to 12 months," said Dr. Vital.
The study concluded that these findings – in particular, the levels used in the two-variable model – need to be validated in another population. When validated, they may allow for selection of retreatment regime based on B-cell biomarkers.
Dr. Vital is on the Roche speakers bureau, and Roche provided rituximab for the patients in this study. The study was funded by the U.K. National Institute for Health Research Doctoral Research Fellowship and sponsored by the NIHR and the University of Leeds.
CHICAGO – Early B-cell repopulation and rheumatoid factor positivity predict early relapse in patients with rheumatoid arthritis who are being treated with rituximab, according to an observational study of 104 patients.
"We’re interested in predicting duration of response to rituximab," said lead author Dr. Edward M. Vital of the University of Leeds (England). "[W]hilst the majority of patients do respond, virtually all will relapse at some point. ... [T]he time to relapse is very variable, so that means that we don’t know what the best retreatment regime is. Some advocate retreatment every 6 months, but this may be excessive for some patients, with implications for cost and possibly safety."
With the sensitive B-cell assay, 88% of patients had detectable B cells by 6 months. However, a small group of patients have persistent B-cell depletion at 6 months, and this group had a longer clinical response. In fact, their responses continued to improve from 6 to 9 months, said Dr. Vital. Maintaining a low B-cell number is likely to maintain a good clinical response, he said, although not all patients with B-cell return relapsed immediately. Dr. Vital presented his data at the annual meeting of the American College of Rheumatology.
The study’s objective was to examine whether known predictors of initial response to rituximab could be used after treatment to predict maintenance of response to 12 months.
All 104 patients were positive for either rheumatoid factor or anti–cyclic citrullinated peptide at baseline, prior to treatment with rituximab in a regimen involving infused doses of 1,000 mg with concomitant methotrexate or leflunomide. Of the original study population, 78 (75%) had a known EULAR (European League Against Rheumatism) response at 6 months, and these were investigated for time to relapse. All use of corticosteroids and NSAIDs was similarly controlled in this group, and outcomes were measured by EULAR response and DAS28 (Disease Activity Score including a 28-joint count) at 0, 6, 9, and 12 months by one of two joint-count assessors.
Highly sensitive flow cytometry with a limit of detection of 0.0001 cells x 109/L was used to measure naive, memory B, and plasmablast subsets. Conventional flow cytometry has a limit of detection of 0.01 cells x 109/L.
At 6 months, 44 (57%) of the 78 patients had a EULAR moderate response, and 34 (43%) had a EULAR good response. In patients with detectable B cells at 6 months, DAS28 worsened by a mean 0.45, whereas in patients with undetectable B cells, it improved by a mean 0.44.
At 12 months, 40 patients (51%) had no response, 22 patients (28%) had a EULAR moderate response, and 16 patients (21%) had a EULAR good response.
A binary logistic regression model was created to predict continued EULAR response at 12 months. It included B-cell detection, plasmablast count, rheumatoid factor, and DAS28, and produced a significant (P = .001) model with an overall accuracy of 72%.
"Since rheumatoid factor and DAS28 were the strongest predictors of these, this suggested that it might actually be possible to make a very simple prediction model that doesn’t require specialized techniques," said Dr. Vital.
The authors subsequently created a simplified, two-variable categorical model using a rheumatoid factor threshold of 108 IU/mL, and a DAS28 threshold of 3.7, to predict relapse. This simplified model’s overall accuracy was 69% (P = .001).
"As you can see, we still have a significant model with just a slight reduction in the overall accuracy. ... If at 6 months the DAS28 was less than 3.7 and the rheumatoid factor was less than 108, then 73% of those patients maintained their clinical response out to 12 months ... and if both [DAS28 and rheumatoid factor] were higher, then only 8% of patients responded out to 12 months," said Dr. Vital.
The study concluded that these findings – in particular, the levels used in the two-variable model – need to be validated in another population. When validated, they may allow for selection of retreatment regime based on B-cell biomarkers.
Dr. Vital is on the Roche speakers bureau, and Roche provided rituximab for the patients in this study. The study was funded by the U.K. National Institute for Health Research Doctoral Research Fellowship and sponsored by the NIHR and the University of Leeds.
FROM THE ANNUAL MEETING OF THE AMERICAN COLLEGE OF RHEUMATOLOGY
Major Finding: Continued response to rituximab in patients with RA after 6 months of therapy can be predicted by B-cell repopulation and rheumatoid factor.
Data Source: A study of 104 patients with RA that was treated with rituximab, from which were culled 78 patients with EULAR responses at 6 months.
Disclosures: Dr. Vital is on the Roche speakers bureau, and Roche provided rituximab for the patients in this study. The study was funded by the U.K. National Institute for Health Research Doctoral Research Fellowship and sponsored by the NIHR and the University of Leeds.
Seropositivity Predicts Good Response to Rituximab in RA
CHICAGO – Patients with rheumatoid arthritis who are seropositive for rheumatoid factor and/or anti-citrullinated-protein antibody respond better to rituximab than do seronegative patients, according to an observational study of 3,266 patients from the CERERRA collaboration.
Patients who were seropositive for either biomarker achieved significantly greater reductions in DAS28 and more EULAR good responses at 6 months. Baseline anti-citrullinated-protein antibody (ACPA) positivity may be a better predictor of EULAR good response to rituximab therapy than rheumatoid factor positivity.
"The aim of the CERERRA collaboration is to try to answer some of the clinical questions about rituximab treatment that remain unclear today, and one of these things is to find prognostic factors of response," said principal investigator Dr. Katerina Chatzidionysiou of the Karolinska Institute in Stockholm. "We know from clinical trials and epidemiological studies that seropositivity is correlated with a good response to rituximab. And to examine this in real-life patients, in an observational cohort, was the purpose of this analysis."
The study was designed to assess 6-month response to the first rituximab course in rheumatoid arthritis (RA) according to rheumatoid factor and ACPA status. Data came from the 10 European registries of CERERRA, the European Collaborative Registries for the Evaluation of Rituximab in Rheumatoid Arthritis, Dr. Chatzidionysiou said at the annual meeting of the American College of Rheumatology.
Anonymous data sets of patients with RA who had started rituximab were pooled and analyzed. The chi-square test was used to compare categorical variables, and the t-test was used for continuous data. Predictors of response were identified by univariate and multivariate logistic regression analysis.
A majority of the 3,266 patients in the CERERRA cohort were rheumatoid factor positive and ACPA positive. Of 2,553 patients whose rheumatoid factor status was known, 2,041 (79.9%) were rheumatoid factor positive and 512 (20.1%) were rheumatoid factor negative.
Of 1,198 patients whose ACPA status was known, 877 (73.2%) were ACPA positive and 321 (26.8%) were ACPA negative.
The patients were well balanced for demographics and baseline disease characteristics (ACPA-positive 1.1 plus or minus 1.0 versus ACPA-negative 1.3 plus or minus 1.1, P = .006).
At 6 months, there were greater DAS28 reductions in the rheumatoid factor–positive and ACPA-positive cohorts. This led Dr. Chatzidionysiou to make three observations: that seropositive patients achieved significantly greater DAS28 improvements at 6 months; that the difference was more pronounced between ACPA-positive and ACPA-negative patients, compared to rheumatoid factor–positive and negative; and that rheumatoid factor–negative and ACPA-negative patients also achieved a significant improvement from baseline to 6 months, although moderate compared with seropositive patients.
As for EULAR responses at 6 months, the study showed a significantly higher percentage of good responders among ACPA-positive patients versus ACPA-negative (23.9% versus 14.9%, P = .009), but the difference was borderline significant between rheumatoid factor–positive and negative patients (21.5% versus 17.4%, P = .06).
In adjusted univariate analysis, "It was mainly the ACPA status, positive versus negative, which was significantly correlated with EULAR good response to therapy at 6 months with an OR of 2.03," said Dr. Chatzidionysiou (ACPA+ [vs.-]: coefficient 0.71, OR [95% CI] 2.03 [1.14-3.60], P = .02).
Multivariate logistic regression analysis found that ACPA-positive status remained predictive (odds ratio 1.8; 95% confidence interval, 1.1-3.3; P = .05), as did the lower number of prior biologics (OR 0.5; 95% CI, 0.3-0.8; P = .007).
"This was important to correct for the number of prior biologic DMARDs because we know from previous analyses that the lower number of prior TNF inhibitors is a significant predictor of good response," said Dr. Chatzidionysiou.
She said the study was limited in that it was observational and uncontrolled, in that there was a concern for missing data, and for the heterogeneity between countries.
This is an investigator led initiative, supported by Roche.
CHICAGO – Patients with rheumatoid arthritis who are seropositive for rheumatoid factor and/or anti-citrullinated-protein antibody respond better to rituximab than do seronegative patients, according to an observational study of 3,266 patients from the CERERRA collaboration.
Patients who were seropositive for either biomarker achieved significantly greater reductions in DAS28 and more EULAR good responses at 6 months. Baseline anti-citrullinated-protein antibody (ACPA) positivity may be a better predictor of EULAR good response to rituximab therapy than rheumatoid factor positivity.
"The aim of the CERERRA collaboration is to try to answer some of the clinical questions about rituximab treatment that remain unclear today, and one of these things is to find prognostic factors of response," said principal investigator Dr. Katerina Chatzidionysiou of the Karolinska Institute in Stockholm. "We know from clinical trials and epidemiological studies that seropositivity is correlated with a good response to rituximab. And to examine this in real-life patients, in an observational cohort, was the purpose of this analysis."
The study was designed to assess 6-month response to the first rituximab course in rheumatoid arthritis (RA) according to rheumatoid factor and ACPA status. Data came from the 10 European registries of CERERRA, the European Collaborative Registries for the Evaluation of Rituximab in Rheumatoid Arthritis, Dr. Chatzidionysiou said at the annual meeting of the American College of Rheumatology.
Anonymous data sets of patients with RA who had started rituximab were pooled and analyzed. The chi-square test was used to compare categorical variables, and the t-test was used for continuous data. Predictors of response were identified by univariate and multivariate logistic regression analysis.
A majority of the 3,266 patients in the CERERRA cohort were rheumatoid factor positive and ACPA positive. Of 2,553 patients whose rheumatoid factor status was known, 2,041 (79.9%) were rheumatoid factor positive and 512 (20.1%) were rheumatoid factor negative.
Of 1,198 patients whose ACPA status was known, 877 (73.2%) were ACPA positive and 321 (26.8%) were ACPA negative.
The patients were well balanced for demographics and baseline disease characteristics (ACPA-positive 1.1 plus or minus 1.0 versus ACPA-negative 1.3 plus or minus 1.1, P = .006).
At 6 months, there were greater DAS28 reductions in the rheumatoid factor–positive and ACPA-positive cohorts. This led Dr. Chatzidionysiou to make three observations: that seropositive patients achieved significantly greater DAS28 improvements at 6 months; that the difference was more pronounced between ACPA-positive and ACPA-negative patients, compared to rheumatoid factor–positive and negative; and that rheumatoid factor–negative and ACPA-negative patients also achieved a significant improvement from baseline to 6 months, although moderate compared with seropositive patients.
As for EULAR responses at 6 months, the study showed a significantly higher percentage of good responders among ACPA-positive patients versus ACPA-negative (23.9% versus 14.9%, P = .009), but the difference was borderline significant between rheumatoid factor–positive and negative patients (21.5% versus 17.4%, P = .06).
In adjusted univariate analysis, "It was mainly the ACPA status, positive versus negative, which was significantly correlated with EULAR good response to therapy at 6 months with an OR of 2.03," said Dr. Chatzidionysiou (ACPA+ [vs.-]: coefficient 0.71, OR [95% CI] 2.03 [1.14-3.60], P = .02).
Multivariate logistic regression analysis found that ACPA-positive status remained predictive (odds ratio 1.8; 95% confidence interval, 1.1-3.3; P = .05), as did the lower number of prior biologics (OR 0.5; 95% CI, 0.3-0.8; P = .007).
"This was important to correct for the number of prior biologic DMARDs because we know from previous analyses that the lower number of prior TNF inhibitors is a significant predictor of good response," said Dr. Chatzidionysiou.
She said the study was limited in that it was observational and uncontrolled, in that there was a concern for missing data, and for the heterogeneity between countries.
This is an investigator led initiative, supported by Roche.
CHICAGO – Patients with rheumatoid arthritis who are seropositive for rheumatoid factor and/or anti-citrullinated-protein antibody respond better to rituximab than do seronegative patients, according to an observational study of 3,266 patients from the CERERRA collaboration.
Patients who were seropositive for either biomarker achieved significantly greater reductions in DAS28 and more EULAR good responses at 6 months. Baseline anti-citrullinated-protein antibody (ACPA) positivity may be a better predictor of EULAR good response to rituximab therapy than rheumatoid factor positivity.
"The aim of the CERERRA collaboration is to try to answer some of the clinical questions about rituximab treatment that remain unclear today, and one of these things is to find prognostic factors of response," said principal investigator Dr. Katerina Chatzidionysiou of the Karolinska Institute in Stockholm. "We know from clinical trials and epidemiological studies that seropositivity is correlated with a good response to rituximab. And to examine this in real-life patients, in an observational cohort, was the purpose of this analysis."
The study was designed to assess 6-month response to the first rituximab course in rheumatoid arthritis (RA) according to rheumatoid factor and ACPA status. Data came from the 10 European registries of CERERRA, the European Collaborative Registries for the Evaluation of Rituximab in Rheumatoid Arthritis, Dr. Chatzidionysiou said at the annual meeting of the American College of Rheumatology.
Anonymous data sets of patients with RA who had started rituximab were pooled and analyzed. The chi-square test was used to compare categorical variables, and the t-test was used for continuous data. Predictors of response were identified by univariate and multivariate logistic regression analysis.
A majority of the 3,266 patients in the CERERRA cohort were rheumatoid factor positive and ACPA positive. Of 2,553 patients whose rheumatoid factor status was known, 2,041 (79.9%) were rheumatoid factor positive and 512 (20.1%) were rheumatoid factor negative.
Of 1,198 patients whose ACPA status was known, 877 (73.2%) were ACPA positive and 321 (26.8%) were ACPA negative.
The patients were well balanced for demographics and baseline disease characteristics (ACPA-positive 1.1 plus or minus 1.0 versus ACPA-negative 1.3 plus or minus 1.1, P = .006).
At 6 months, there were greater DAS28 reductions in the rheumatoid factor–positive and ACPA-positive cohorts. This led Dr. Chatzidionysiou to make three observations: that seropositive patients achieved significantly greater DAS28 improvements at 6 months; that the difference was more pronounced between ACPA-positive and ACPA-negative patients, compared to rheumatoid factor–positive and negative; and that rheumatoid factor–negative and ACPA-negative patients also achieved a significant improvement from baseline to 6 months, although moderate compared with seropositive patients.
As for EULAR responses at 6 months, the study showed a significantly higher percentage of good responders among ACPA-positive patients versus ACPA-negative (23.9% versus 14.9%, P = .009), but the difference was borderline significant between rheumatoid factor–positive and negative patients (21.5% versus 17.4%, P = .06).
In adjusted univariate analysis, "It was mainly the ACPA status, positive versus negative, which was significantly correlated with EULAR good response to therapy at 6 months with an OR of 2.03," said Dr. Chatzidionysiou (ACPA+ [vs.-]: coefficient 0.71, OR [95% CI] 2.03 [1.14-3.60], P = .02).
Multivariate logistic regression analysis found that ACPA-positive status remained predictive (odds ratio 1.8; 95% confidence interval, 1.1-3.3; P = .05), as did the lower number of prior biologics (OR 0.5; 95% CI, 0.3-0.8; P = .007).
"This was important to correct for the number of prior biologic DMARDs because we know from previous analyses that the lower number of prior TNF inhibitors is a significant predictor of good response," said Dr. Chatzidionysiou.
She said the study was limited in that it was observational and uncontrolled, in that there was a concern for missing data, and for the heterogeneity between countries.
This is an investigator led initiative, supported by Roche.
FROM THE ANNUAL MEETING OF THE AMERICAN COLLEGE OF RHEUMATOLOGY
Major Finding: Patients with rheumatoid arthritis who are seropositive achieve significantly greater reductions in DAS28 at 6 months than do those who are seronegative, and baseline ACPA positivity may be a better predictor of EULAR good response to rituximab therapy than rheumatoid factor positivity.
Data Source: Study of 3,266 patients from the CERERRA collaboration.
Disclosures: This is an investigator led initiative, supported by Roche.
Early Detection of Scleroderma-Associated PAH Enhanced Survival
CHICAGO – Early detection of incident systemic sclerosis–associated pulmonary arterial hypertension enhanced survival in a prospective cohort study of 131 patients from the multicenter PHAROS, according to data presented at the annual meeting of the American College of Rheumatology.
The survival rates for patients with incident systemic sclerosis (SSc)–associated pulmonary arterial hypertension who were enrolled in PHAROS (Pulmonary Hypertension Assessment and Recognition of Outcomes in Scleroderma) "were better than for other recently described cohorts, with 1- and 3-year survival of 93% and 75%, respectively," said principal investigator Dr. Lorinda Chung of the department of immunology and rheumatology at Stanford (Calif.) University Medical Center.
"This may be due to the fact that we are screening our patients with [echocardiography and pulmonary function tests], and detecting their disease earlier, perhaps at a less severe stage," she said.
Furthermore, 17% of deaths in this cohort were not related to pulmonary arterial hypertension (PAH), suggesting that rheumatologists should remain involved in care even after patients are diagnosed with PAH, said Dr. Chung.
"Causes of death can be related to their underlying scleroderma or its complications," she said.
The independent predictors of death included functional class IV status, age greater than 60, male sex, and low (less than 39%) diffusion lung carbon monoxide, according to findings from a multivariate analysis.
PHAROS is a multicenter, U.S.-based prospective registry of SSc patients at high risk for PAH, or with definite pulmonary hypertension diagnosed by right heart catheterization within 6 months of enrollment. Of 434 patients enrolled in PHAROS, 131 had PAH.
Despite the availability of several therapies specific to pulmonary arterial hypertension, findings from recent studies of patients with incident scleroderma-associated PAH suggest that 1-year survival rates are as low as 72%-86% and 3-year survival rates are as low as 39%-67%.
This analysis included only patients with World Health Organization group I PAH, defined as mean pulmonary arterial pressure greater than 25 mm Hg and pulmonary capillary wedge pressure less than or equal to 15 mm Hg. Patients were excluded if they were found to have significant interstitial lung disease, defined as severe fibrosis on high-resolution CT or moderate fibrosis and a forced vital capacity less than 60% predicted.
Kaplan-Meier curves were used to estimate survival from the time of the diagnostic right heart catheterization, and Cox regression models were used to identify significant predictors of mortality.
The mean age of the 131 patients with PAH was 60.4±10.4 years, and most were female (84%) and white (82%). Fully 70% had limited cutaneous disease. Disease duration from the first Raynaud’s symptom was about 14.5 years and from the first non-Raynaud’s symptom was about 10 years.
"About a third of the patients had anticentromere antibodies and about a quarter had a nucleolar pattern on the ANA [antinuclear antibodies]," said Dr. Chung.
Over a mean follow-up period of 2.0 (1.4) years, 24 patients (18%) died. For the majority of those patients (20, or 83%), the cause of death was PAH or multiorgan failure, and the other four deaths were not related to PAH. In patients with incident SSc-associated PAH, 92.9 % survived at 1 year, 87.7 % at 2 years, and 74.8% at 3 years.
For the sake of comparison, Dr. Chung cited estimates from REVEAL (Registry to Evaluate Early and Long-Term Pulmonary Arterial Hypertension Disease Management), a U.S.-based prospective registry of patients with PAH, which includes a subgroup of patients with scleroderma. The majority of patients with incident SSc-associated PAH in the REVEAL registry were functional class III and IV at the time of PAH diagnosis, and their 3-year survival was only 54% – more than 20% less than patients in the PHAROS registry.
However, she said in the PHAROS cohort, "patients in functional class IV at enrollment had much poorer survival compared to those who were in functional classes I, II, or III." SSc-associated PAH patients with low diffusing capacity also had poorer survival. "The median value for the diffusion lung carbon monoxide was 39% predicted, and patients who had values below the median at enrollment experienced much poorer survival," she said.
Better survival was seen in systemic sclerosis–associated pulmonary arterial hypertension patients enrolled in the PHAROS registry.
PHAROS is an investigator-initiated study initially funded by Actelion, the Scleroderma Foundation, and the Sibley Foundation, with ongoing funding by Gilead. Dr. Chung reported financial relationships with Actelion, Gilead, Pfizer and United Therapeutics.
CHICAGO – Early detection of incident systemic sclerosis–associated pulmonary arterial hypertension enhanced survival in a prospective cohort study of 131 patients from the multicenter PHAROS, according to data presented at the annual meeting of the American College of Rheumatology.
The survival rates for patients with incident systemic sclerosis (SSc)–associated pulmonary arterial hypertension who were enrolled in PHAROS (Pulmonary Hypertension Assessment and Recognition of Outcomes in Scleroderma) "were better than for other recently described cohorts, with 1- and 3-year survival of 93% and 75%, respectively," said principal investigator Dr. Lorinda Chung of the department of immunology and rheumatology at Stanford (Calif.) University Medical Center.
"This may be due to the fact that we are screening our patients with [echocardiography and pulmonary function tests], and detecting their disease earlier, perhaps at a less severe stage," she said.
Furthermore, 17% of deaths in this cohort were not related to pulmonary arterial hypertension (PAH), suggesting that rheumatologists should remain involved in care even after patients are diagnosed with PAH, said Dr. Chung.
"Causes of death can be related to their underlying scleroderma or its complications," she said.
The independent predictors of death included functional class IV status, age greater than 60, male sex, and low (less than 39%) diffusion lung carbon monoxide, according to findings from a multivariate analysis.
PHAROS is a multicenter, U.S.-based prospective registry of SSc patients at high risk for PAH, or with definite pulmonary hypertension diagnosed by right heart catheterization within 6 months of enrollment. Of 434 patients enrolled in PHAROS, 131 had PAH.
Despite the availability of several therapies specific to pulmonary arterial hypertension, findings from recent studies of patients with incident scleroderma-associated PAH suggest that 1-year survival rates are as low as 72%-86% and 3-year survival rates are as low as 39%-67%.
This analysis included only patients with World Health Organization group I PAH, defined as mean pulmonary arterial pressure greater than 25 mm Hg and pulmonary capillary wedge pressure less than or equal to 15 mm Hg. Patients were excluded if they were found to have significant interstitial lung disease, defined as severe fibrosis on high-resolution CT or moderate fibrosis and a forced vital capacity less than 60% predicted.
Kaplan-Meier curves were used to estimate survival from the time of the diagnostic right heart catheterization, and Cox regression models were used to identify significant predictors of mortality.
The mean age of the 131 patients with PAH was 60.4±10.4 years, and most were female (84%) and white (82%). Fully 70% had limited cutaneous disease. Disease duration from the first Raynaud’s symptom was about 14.5 years and from the first non-Raynaud’s symptom was about 10 years.
"About a third of the patients had anticentromere antibodies and about a quarter had a nucleolar pattern on the ANA [antinuclear antibodies]," said Dr. Chung.
Over a mean follow-up period of 2.0 (1.4) years, 24 patients (18%) died. For the majority of those patients (20, or 83%), the cause of death was PAH or multiorgan failure, and the other four deaths were not related to PAH. In patients with incident SSc-associated PAH, 92.9 % survived at 1 year, 87.7 % at 2 years, and 74.8% at 3 years.
For the sake of comparison, Dr. Chung cited estimates from REVEAL (Registry to Evaluate Early and Long-Term Pulmonary Arterial Hypertension Disease Management), a U.S.-based prospective registry of patients with PAH, which includes a subgroup of patients with scleroderma. The majority of patients with incident SSc-associated PAH in the REVEAL registry were functional class III and IV at the time of PAH diagnosis, and their 3-year survival was only 54% – more than 20% less than patients in the PHAROS registry.
However, she said in the PHAROS cohort, "patients in functional class IV at enrollment had much poorer survival compared to those who were in functional classes I, II, or III." SSc-associated PAH patients with low diffusing capacity also had poorer survival. "The median value for the diffusion lung carbon monoxide was 39% predicted, and patients who had values below the median at enrollment experienced much poorer survival," she said.
Better survival was seen in systemic sclerosis–associated pulmonary arterial hypertension patients enrolled in the PHAROS registry.
PHAROS is an investigator-initiated study initially funded by Actelion, the Scleroderma Foundation, and the Sibley Foundation, with ongoing funding by Gilead. Dr. Chung reported financial relationships with Actelion, Gilead, Pfizer and United Therapeutics.
CHICAGO – Early detection of incident systemic sclerosis–associated pulmonary arterial hypertension enhanced survival in a prospective cohort study of 131 patients from the multicenter PHAROS, according to data presented at the annual meeting of the American College of Rheumatology.
The survival rates for patients with incident systemic sclerosis (SSc)–associated pulmonary arterial hypertension who were enrolled in PHAROS (Pulmonary Hypertension Assessment and Recognition of Outcomes in Scleroderma) "were better than for other recently described cohorts, with 1- and 3-year survival of 93% and 75%, respectively," said principal investigator Dr. Lorinda Chung of the department of immunology and rheumatology at Stanford (Calif.) University Medical Center.
"This may be due to the fact that we are screening our patients with [echocardiography and pulmonary function tests], and detecting their disease earlier, perhaps at a less severe stage," she said.
Furthermore, 17% of deaths in this cohort were not related to pulmonary arterial hypertension (PAH), suggesting that rheumatologists should remain involved in care even after patients are diagnosed with PAH, said Dr. Chung.
"Causes of death can be related to their underlying scleroderma or its complications," she said.
The independent predictors of death included functional class IV status, age greater than 60, male sex, and low (less than 39%) diffusion lung carbon monoxide, according to findings from a multivariate analysis.
PHAROS is a multicenter, U.S.-based prospective registry of SSc patients at high risk for PAH, or with definite pulmonary hypertension diagnosed by right heart catheterization within 6 months of enrollment. Of 434 patients enrolled in PHAROS, 131 had PAH.
Despite the availability of several therapies specific to pulmonary arterial hypertension, findings from recent studies of patients with incident scleroderma-associated PAH suggest that 1-year survival rates are as low as 72%-86% and 3-year survival rates are as low as 39%-67%.
This analysis included only patients with World Health Organization group I PAH, defined as mean pulmonary arterial pressure greater than 25 mm Hg and pulmonary capillary wedge pressure less than or equal to 15 mm Hg. Patients were excluded if they were found to have significant interstitial lung disease, defined as severe fibrosis on high-resolution CT or moderate fibrosis and a forced vital capacity less than 60% predicted.
Kaplan-Meier curves were used to estimate survival from the time of the diagnostic right heart catheterization, and Cox regression models were used to identify significant predictors of mortality.
The mean age of the 131 patients with PAH was 60.4±10.4 years, and most were female (84%) and white (82%). Fully 70% had limited cutaneous disease. Disease duration from the first Raynaud’s symptom was about 14.5 years and from the first non-Raynaud’s symptom was about 10 years.
"About a third of the patients had anticentromere antibodies and about a quarter had a nucleolar pattern on the ANA [antinuclear antibodies]," said Dr. Chung.
Over a mean follow-up period of 2.0 (1.4) years, 24 patients (18%) died. For the majority of those patients (20, or 83%), the cause of death was PAH or multiorgan failure, and the other four deaths were not related to PAH. In patients with incident SSc-associated PAH, 92.9 % survived at 1 year, 87.7 % at 2 years, and 74.8% at 3 years.
For the sake of comparison, Dr. Chung cited estimates from REVEAL (Registry to Evaluate Early and Long-Term Pulmonary Arterial Hypertension Disease Management), a U.S.-based prospective registry of patients with PAH, which includes a subgroup of patients with scleroderma. The majority of patients with incident SSc-associated PAH in the REVEAL registry were functional class III and IV at the time of PAH diagnosis, and their 3-year survival was only 54% – more than 20% less than patients in the PHAROS registry.
However, she said in the PHAROS cohort, "patients in functional class IV at enrollment had much poorer survival compared to those who were in functional classes I, II, or III." SSc-associated PAH patients with low diffusing capacity also had poorer survival. "The median value for the diffusion lung carbon monoxide was 39% predicted, and patients who had values below the median at enrollment experienced much poorer survival," she said.
Better survival was seen in systemic sclerosis–associated pulmonary arterial hypertension patients enrolled in the PHAROS registry.
PHAROS is an investigator-initiated study initially funded by Actelion, the Scleroderma Foundation, and the Sibley Foundation, with ongoing funding by Gilead. Dr. Chung reported financial relationships with Actelion, Gilead, Pfizer and United Therapeutics.
FROM THE ANNUAL MEETING OF THE AMERICAN COLLEGE OF RHEUMATOLOGY
Major Finding: Survival at 1 and 3 years was 93% and 75% in patients whose incident systemic sclerosis–associated pulmonary arterial hypertension was detected early.
Data Source: 131 patients with PAH of a total of 434 SSc patients in the PHAROS registry.
Disclosures: PHAROS is an investigator-initiated study initially funded by Actelion, the Scleroderma Foundation, and the Sibley Foundation, with ongoing funding by Gilead. Dr. Chung has received honoraria for consulting services from Gilead and Actelion, and research funding from Gilead, United Therapeutics, and Pfizer.
Calcium and Vitamin D Are No Longer Boring
CHICAGO – Physicians may want to be a bit more aggressive in their use of calcium and vitamin D supplementation in patients at high-risk for osteoporotic fracture than has been recommended by the Institute of Medicine, according to Dr. Kenneth G. Saag.
The IOM guidelines on calcium and vitamin D have introduced controversy to a once sleepy area of bone mineral density management, said Dr. Saag, professor of medicine at the University of Alabama at Birmingham.
"Calcium and vitamin D used to be the least controversial part of any lecture on osteoporosis," said Dr. Saag. But no more. The IOM recommends daily allowances of calcium of 1,200 mg/day for women older than age 51 years in a consensus report issued November 2010. "We’ve been thinking maybe 1,500 mg was a better target for certain older adults," said Dr. Saag. He said that IOM recommendations are population based and do not necessarily apply to patients with osteoporosis or low bone mass. "We believe it may be prudent to be a little bit more aggressive in patients with documented osteoporosis."
The IOM report raised questions about calcium safety. A meta-analysis of all large studies of calcium alone – even though calcium is rarely given alone – found trends toward negative cardiovascular effects in individuals taking excess calcium (BMJ 2010;341:c3691).
However, a more recent study of cardiovascular risk did not show increased risk from excess calcium (J. Bone Miner. Res. 2011;26:35-41).
"The controversy in treatment now is not whether we should initiate therapy in high-risk [fracture] patients, but how long should we treat?"
Vitamin D likewise has its share of controversies, including finding the optimal target level, choosing between D2 and D3, and assessing the risk of kidney stones. There is also the open question as to whether or not vitamin D increases fracture rates.
Pulse therapy of 50,000 U once or twice a week is not uncommon for patients who are deficient in vitamin D, said Dr. Saag. "Could that be a problem, in terms of long-term fracture risk?"
After the IOM recommendations were issued, the U.S. Preventive Services Task Force issued its own meta-analysis looking at falls, and suggested that vitamin D might be protective against falls (Ann. Intern. Med. 2010;153:815-25).
"We can’t really get the experts to fully concur on many of these different issues," said Dr. Saag.
Dr. Saag’s conclusion was that overzealous use of calcium and/or vitamin D supplements could be deleterious. He believes that vitamin D3 is a little better than vitamin D2. As for target level, the IOM report suggested 20 ng/mL as the target, rather than 32 ng/mL, which has been advocated for the past decade. "This is really a target at a population level," said Dr. Saag. Individual patients may differ.
He said that the World Health Organization’s FRAX fracture risk assessment tool can help make treatment decisions for an osteopenic patient. It’s also helpful for the patient who is at very low risk. However, the tool is only for treatment-naive patients, and can lead to underestimating the fracture risk because it does not account for multiple fractures, steroid dose, and other variables. FRAX can also lead to overestimating fracture risk, depending on the quality of data entered, he said. There are limited data on treating those with high absolute risk but reasonable BMD. For the patient on 7.5 mg/day of steroids, it is necessary to adjust the risk upward (J. Clin. Densitom. 2011;14:212-9).
"The controversy in treatment now is not whether we should initiate therapy in high-risk patients, people who have fractured and have low bone mass, but how long should we treat? Do we want to continue, in particular our bisphosphonates, for an extended period of time?" said Dr. Saag.
A study of long-term extensions to the FIT (Fracture Intervention Trial) and FLEX (Long-Term Extension of FIT), which measured lumbar spine and total hip BMD, found that the group continuing alendronate had a persistent rise in bone mineral density.
"But interestingly, the group that switched to placebo didn’t lose all that much bone," said Dr. Saag. "This is consistent with my practice."
The trials’ results suggested that for many women, discontinuing alendronate for up to 5 years did not appear to increase fracture risk significantly at all sites (JAMA 2006;296:2927-38).
No loss of benefit was observed with continued use of bisphosphonates. There were small losses of bone mineral density and heightened fracture risk with discontinuation, but not at all sites.
"There is a persistent fracture risk after discontinuation, if the BMD remains low," said Dr. Saag. The trials have not yet yielded the optimal duration of therapy, but there were no long-term safety concerns, at least in clinical trials.
Oral bisphosphonates were another story. Potential safety issues with them include osteonecrosis of the jaw (ONJ), atypical fractures, and esophageal cancer. However, Dr. Saag did not think that was "that big a concern."
"We know from the oncology literature that it’s maybe [1%-10% of patients who] get these monthly infusions of the potent IV bisphosphonates" who may go on to develop ONJ, he said. But in the setting of osteoporosis, the rough incidence is more likely to be between 1 per 10,000 and 1 per 100,000, he said.
"Calcium and vitamin D used to be the least controversial part of any lecture on osteoporosis."
Atypical femoral fractures have been associated with bisphosphonates, but Dr. Saag said that the past evidence has been circumstantial. However, a recent observational study from Scandinavia found a significant association between bisphosphonate use and the risk of subtrochanteric and femoral shaft fractures in older women (JAMA 2011;305:783-9).
Moving on to denosumab, Dr. Saag praised the drug as highly potent antiresorptive with a well-defined mechanism of action. However, he cited evidence of serious infectious adverse events in four randomized, controlled trials: DEFEND (J. Clin. Endocrinol. Metab. 2008;93:2149-57), DECIDE (J. Bone Miner. Res. 2009;24:153-61), STAND (ASBMR 2008, poster M395), and FREEDOM (N. Engl. J. Med. 2009;361:756-65).
"There appears to be a signal of cellulitis," he said.
A study of the combination of zoledronate and teriparatide and their effect on lumbar spine BMD yielded an interesting point about sequencing (J. Bone Miner. Res. 2011;26:503-11).
"When you give bisphosphonate in a pulsatile way, in contrast to a continuous exposure with the weekly therapy, it actually seems to have less suppressive effects on osteoblasts. And that may be why we see [that] the combination of the two results in more increase in bone mineral density than [does] either agent alone," said Dr. Saag. "We don’t know whether that equates to fracture risk reduction."
Support for this meeting came from Abbott, Amgen, Centocor, Genentech, Human Genome Science, and UCB. Dr. Saag disclosed research funding from the National Institutes of Health, the Agency for Healthcare Research and Quality, the American College of Rheumatology (ACR), Amgen, Lilly, and Merck. He is a member of the board of trustees of the National Osteoporosis Foundation and is chair of the quality of care committee of the ACR; he serves on advisory boards at Amgen, Lilly, Merck, and Novartis.
CHICAGO – Physicians may want to be a bit more aggressive in their use of calcium and vitamin D supplementation in patients at high-risk for osteoporotic fracture than has been recommended by the Institute of Medicine, according to Dr. Kenneth G. Saag.
The IOM guidelines on calcium and vitamin D have introduced controversy to a once sleepy area of bone mineral density management, said Dr. Saag, professor of medicine at the University of Alabama at Birmingham.
"Calcium and vitamin D used to be the least controversial part of any lecture on osteoporosis," said Dr. Saag. But no more. The IOM recommends daily allowances of calcium of 1,200 mg/day for women older than age 51 years in a consensus report issued November 2010. "We’ve been thinking maybe 1,500 mg was a better target for certain older adults," said Dr. Saag. He said that IOM recommendations are population based and do not necessarily apply to patients with osteoporosis or low bone mass. "We believe it may be prudent to be a little bit more aggressive in patients with documented osteoporosis."
The IOM report raised questions about calcium safety. A meta-analysis of all large studies of calcium alone – even though calcium is rarely given alone – found trends toward negative cardiovascular effects in individuals taking excess calcium (BMJ 2010;341:c3691).
However, a more recent study of cardiovascular risk did not show increased risk from excess calcium (J. Bone Miner. Res. 2011;26:35-41).
"The controversy in treatment now is not whether we should initiate therapy in high-risk [fracture] patients, but how long should we treat?"
Vitamin D likewise has its share of controversies, including finding the optimal target level, choosing between D2 and D3, and assessing the risk of kidney stones. There is also the open question as to whether or not vitamin D increases fracture rates.
Pulse therapy of 50,000 U once or twice a week is not uncommon for patients who are deficient in vitamin D, said Dr. Saag. "Could that be a problem, in terms of long-term fracture risk?"
After the IOM recommendations were issued, the U.S. Preventive Services Task Force issued its own meta-analysis looking at falls, and suggested that vitamin D might be protective against falls (Ann. Intern. Med. 2010;153:815-25).
"We can’t really get the experts to fully concur on many of these different issues," said Dr. Saag.
Dr. Saag’s conclusion was that overzealous use of calcium and/or vitamin D supplements could be deleterious. He believes that vitamin D3 is a little better than vitamin D2. As for target level, the IOM report suggested 20 ng/mL as the target, rather than 32 ng/mL, which has been advocated for the past decade. "This is really a target at a population level," said Dr. Saag. Individual patients may differ.
He said that the World Health Organization’s FRAX fracture risk assessment tool can help make treatment decisions for an osteopenic patient. It’s also helpful for the patient who is at very low risk. However, the tool is only for treatment-naive patients, and can lead to underestimating the fracture risk because it does not account for multiple fractures, steroid dose, and other variables. FRAX can also lead to overestimating fracture risk, depending on the quality of data entered, he said. There are limited data on treating those with high absolute risk but reasonable BMD. For the patient on 7.5 mg/day of steroids, it is necessary to adjust the risk upward (J. Clin. Densitom. 2011;14:212-9).
"The controversy in treatment now is not whether we should initiate therapy in high-risk patients, people who have fractured and have low bone mass, but how long should we treat? Do we want to continue, in particular our bisphosphonates, for an extended period of time?" said Dr. Saag.
A study of long-term extensions to the FIT (Fracture Intervention Trial) and FLEX (Long-Term Extension of FIT), which measured lumbar spine and total hip BMD, found that the group continuing alendronate had a persistent rise in bone mineral density.
"But interestingly, the group that switched to placebo didn’t lose all that much bone," said Dr. Saag. "This is consistent with my practice."
The trials’ results suggested that for many women, discontinuing alendronate for up to 5 years did not appear to increase fracture risk significantly at all sites (JAMA 2006;296:2927-38).
No loss of benefit was observed with continued use of bisphosphonates. There were small losses of bone mineral density and heightened fracture risk with discontinuation, but not at all sites.
"There is a persistent fracture risk after discontinuation, if the BMD remains low," said Dr. Saag. The trials have not yet yielded the optimal duration of therapy, but there were no long-term safety concerns, at least in clinical trials.
Oral bisphosphonates were another story. Potential safety issues with them include osteonecrosis of the jaw (ONJ), atypical fractures, and esophageal cancer. However, Dr. Saag did not think that was "that big a concern."
"We know from the oncology literature that it’s maybe [1%-10% of patients who] get these monthly infusions of the potent IV bisphosphonates" who may go on to develop ONJ, he said. But in the setting of osteoporosis, the rough incidence is more likely to be between 1 per 10,000 and 1 per 100,000, he said.
"Calcium and vitamin D used to be the least controversial part of any lecture on osteoporosis."
Atypical femoral fractures have been associated with bisphosphonates, but Dr. Saag said that the past evidence has been circumstantial. However, a recent observational study from Scandinavia found a significant association between bisphosphonate use and the risk of subtrochanteric and femoral shaft fractures in older women (JAMA 2011;305:783-9).
Moving on to denosumab, Dr. Saag praised the drug as highly potent antiresorptive with a well-defined mechanism of action. However, he cited evidence of serious infectious adverse events in four randomized, controlled trials: DEFEND (J. Clin. Endocrinol. Metab. 2008;93:2149-57), DECIDE (J. Bone Miner. Res. 2009;24:153-61), STAND (ASBMR 2008, poster M395), and FREEDOM (N. Engl. J. Med. 2009;361:756-65).
"There appears to be a signal of cellulitis," he said.
A study of the combination of zoledronate and teriparatide and their effect on lumbar spine BMD yielded an interesting point about sequencing (J. Bone Miner. Res. 2011;26:503-11).
"When you give bisphosphonate in a pulsatile way, in contrast to a continuous exposure with the weekly therapy, it actually seems to have less suppressive effects on osteoblasts. And that may be why we see [that] the combination of the two results in more increase in bone mineral density than [does] either agent alone," said Dr. Saag. "We don’t know whether that equates to fracture risk reduction."
Support for this meeting came from Abbott, Amgen, Centocor, Genentech, Human Genome Science, and UCB. Dr. Saag disclosed research funding from the National Institutes of Health, the Agency for Healthcare Research and Quality, the American College of Rheumatology (ACR), Amgen, Lilly, and Merck. He is a member of the board of trustees of the National Osteoporosis Foundation and is chair of the quality of care committee of the ACR; he serves on advisory boards at Amgen, Lilly, Merck, and Novartis.
CHICAGO – Physicians may want to be a bit more aggressive in their use of calcium and vitamin D supplementation in patients at high-risk for osteoporotic fracture than has been recommended by the Institute of Medicine, according to Dr. Kenneth G. Saag.
The IOM guidelines on calcium and vitamin D have introduced controversy to a once sleepy area of bone mineral density management, said Dr. Saag, professor of medicine at the University of Alabama at Birmingham.
"Calcium and vitamin D used to be the least controversial part of any lecture on osteoporosis," said Dr. Saag. But no more. The IOM recommends daily allowances of calcium of 1,200 mg/day for women older than age 51 years in a consensus report issued November 2010. "We’ve been thinking maybe 1,500 mg was a better target for certain older adults," said Dr. Saag. He said that IOM recommendations are population based and do not necessarily apply to patients with osteoporosis or low bone mass. "We believe it may be prudent to be a little bit more aggressive in patients with documented osteoporosis."
The IOM report raised questions about calcium safety. A meta-analysis of all large studies of calcium alone – even though calcium is rarely given alone – found trends toward negative cardiovascular effects in individuals taking excess calcium (BMJ 2010;341:c3691).
However, a more recent study of cardiovascular risk did not show increased risk from excess calcium (J. Bone Miner. Res. 2011;26:35-41).
"The controversy in treatment now is not whether we should initiate therapy in high-risk [fracture] patients, but how long should we treat?"
Vitamin D likewise has its share of controversies, including finding the optimal target level, choosing between D2 and D3, and assessing the risk of kidney stones. There is also the open question as to whether or not vitamin D increases fracture rates.
Pulse therapy of 50,000 U once or twice a week is not uncommon for patients who are deficient in vitamin D, said Dr. Saag. "Could that be a problem, in terms of long-term fracture risk?"
After the IOM recommendations were issued, the U.S. Preventive Services Task Force issued its own meta-analysis looking at falls, and suggested that vitamin D might be protective against falls (Ann. Intern. Med. 2010;153:815-25).
"We can’t really get the experts to fully concur on many of these different issues," said Dr. Saag.
Dr. Saag’s conclusion was that overzealous use of calcium and/or vitamin D supplements could be deleterious. He believes that vitamin D3 is a little better than vitamin D2. As for target level, the IOM report suggested 20 ng/mL as the target, rather than 32 ng/mL, which has been advocated for the past decade. "This is really a target at a population level," said Dr. Saag. Individual patients may differ.
He said that the World Health Organization’s FRAX fracture risk assessment tool can help make treatment decisions for an osteopenic patient. It’s also helpful for the patient who is at very low risk. However, the tool is only for treatment-naive patients, and can lead to underestimating the fracture risk because it does not account for multiple fractures, steroid dose, and other variables. FRAX can also lead to overestimating fracture risk, depending on the quality of data entered, he said. There are limited data on treating those with high absolute risk but reasonable BMD. For the patient on 7.5 mg/day of steroids, it is necessary to adjust the risk upward (J. Clin. Densitom. 2011;14:212-9).
"The controversy in treatment now is not whether we should initiate therapy in high-risk patients, people who have fractured and have low bone mass, but how long should we treat? Do we want to continue, in particular our bisphosphonates, for an extended period of time?" said Dr. Saag.
A study of long-term extensions to the FIT (Fracture Intervention Trial) and FLEX (Long-Term Extension of FIT), which measured lumbar spine and total hip BMD, found that the group continuing alendronate had a persistent rise in bone mineral density.
"But interestingly, the group that switched to placebo didn’t lose all that much bone," said Dr. Saag. "This is consistent with my practice."
The trials’ results suggested that for many women, discontinuing alendronate for up to 5 years did not appear to increase fracture risk significantly at all sites (JAMA 2006;296:2927-38).
No loss of benefit was observed with continued use of bisphosphonates. There were small losses of bone mineral density and heightened fracture risk with discontinuation, but not at all sites.
"There is a persistent fracture risk after discontinuation, if the BMD remains low," said Dr. Saag. The trials have not yet yielded the optimal duration of therapy, but there were no long-term safety concerns, at least in clinical trials.
Oral bisphosphonates were another story. Potential safety issues with them include osteonecrosis of the jaw (ONJ), atypical fractures, and esophageal cancer. However, Dr. Saag did not think that was "that big a concern."
"We know from the oncology literature that it’s maybe [1%-10% of patients who] get these monthly infusions of the potent IV bisphosphonates" who may go on to develop ONJ, he said. But in the setting of osteoporosis, the rough incidence is more likely to be between 1 per 10,000 and 1 per 100,000, he said.
"Calcium and vitamin D used to be the least controversial part of any lecture on osteoporosis."
Atypical femoral fractures have been associated with bisphosphonates, but Dr. Saag said that the past evidence has been circumstantial. However, a recent observational study from Scandinavia found a significant association between bisphosphonate use and the risk of subtrochanteric and femoral shaft fractures in older women (JAMA 2011;305:783-9).
Moving on to denosumab, Dr. Saag praised the drug as highly potent antiresorptive with a well-defined mechanism of action. However, he cited evidence of serious infectious adverse events in four randomized, controlled trials: DEFEND (J. Clin. Endocrinol. Metab. 2008;93:2149-57), DECIDE (J. Bone Miner. Res. 2009;24:153-61), STAND (ASBMR 2008, poster M395), and FREEDOM (N. Engl. J. Med. 2009;361:756-65).
"There appears to be a signal of cellulitis," he said.
A study of the combination of zoledronate and teriparatide and their effect on lumbar spine BMD yielded an interesting point about sequencing (J. Bone Miner. Res. 2011;26:503-11).
"When you give bisphosphonate in a pulsatile way, in contrast to a continuous exposure with the weekly therapy, it actually seems to have less suppressive effects on osteoblasts. And that may be why we see [that] the combination of the two results in more increase in bone mineral density than [does] either agent alone," said Dr. Saag. "We don’t know whether that equates to fracture risk reduction."
Support for this meeting came from Abbott, Amgen, Centocor, Genentech, Human Genome Science, and UCB. Dr. Saag disclosed research funding from the National Institutes of Health, the Agency for Healthcare Research and Quality, the American College of Rheumatology (ACR), Amgen, Lilly, and Merck. He is a member of the board of trustees of the National Osteoporosis Foundation and is chair of the quality of care committee of the ACR; he serves on advisory boards at Amgen, Lilly, Merck, and Novartis.
EXPERT ANALYSIS FROM THE MIDWEST RHEUMATOLOGY SUMMIT
Measures of RA Progression Remain Flawed Predictors of Outcomes
CHICAGO – The disease activity score outcome in rheumatoid arthritis should be used with caution as a treatment target when the clinical aim is to prevent radiographic progression. The DAS may show that a patient is in remission when in fact the disease is still active.
The van der Heijde/Sharp score is also flawed in that the total mean change is less meaningful than is the probability of progression of rheumatoid arthritis (RA) and may be misleading, said Dr. Edward Keystone.
"The change in the mean Sharp score point is of some importance, but not nearly as important as the proportion of people who are progressing, or those particularly rapid progressors," said Dr. Keystone, professor of medicine at the University of Toronto. In general, a large change in Sharp score points is needed to reduce physical function, noting that a change in 2 points per year will be significant over a decade, he said.
"If you change by 3 [points] a year, in 10 years you’re going to have disability."
Joint space narrowing may be more predictive than are erosions of radiographic progression. "Most methotrexate-inadequate responders, despite the fact that they’re clinically active, may still have less radiographic progression," Dr. Keystone said at the Midwest Rheumatology Summit.
"So how good is methotrexate, in patients failing methotrexate?" he said. "That’s the question."
Remission is the clinical target in RA, but its measurement is complex. True remission is a state of low-disease activity in patients who are not progressing, said Dr. Keystone. Unfortunately, there is dissociation between clinical and radiographic outcomes, and radiographic progression may occur in patients in clinical remission. Patients with active disease may likewise not progress radiographically.
The composite indices defining remission allow for a significant degree of clinical synovitis, and residual synovitis detected with sensitive imaging might explain the progression in structural damage, even in clinical remission (Arthritis Rheum. 2006;4:3761-73).
Joint space narrowing is more predictive of disability than erosion, as demonstrated by the 5-year HAQ.
As for patients with clinical disease activity who do not progress radiographically, Dr. Keystone said that the concept comes from the ACR 20 nonresponders.
"People who do not make an ACR 20 are still responders," said Dr. Keystone. It’s the difference in patient-derived vs. physician-derived outcomes, he said. In established disease, ACR 20 nonresponders to biologics do not seem to progress radiographically but may still improve.
"Why do most people not achieve an ACR 20? It’s not the swollen and tender joint. It’s usually the patient-derived outcome. ... That’s the problem: The patient says ‘I’m not better.’ Therefore when you look at the ACR 20 data, he’s a nonresponder."
Early disease can present conundrums as well.
In the PREMIER study, methotrexate was clinically identical to monotherapy adalimumab. Nevertheless, a 10-point Sharp score change was observed with methotrexate alone, vs. a 5-point Sharp score change with adalimumab monotherapy (Arthritis Rheum. 2006;54:26-37).
"Clinically, they looked alike, but radiographically, adalimumab monotherapy was much better in reducing the Sharp score." However, he said, the mean change in total Sharp score reflects the Total Sharp Score change only of those patients progressing. "And rheumatologists make decisions on the basis of probability, not mean change in [total Sharp score]," he said. The mean change in total Sharp score means less than the probability of progression, and may lead you astray, he said.
The 52-week results from the JESMR (Efficacy and Safety of Etanercept on Active Rheumatoid Arthritis Despite Methotrexate Therapy in Japan) study found that combination therapy of etanercept plus methotrexate resulted in better clinical and radiographic outcomes than etanercept monotherapy, even in patients with active rheumatoid arthritis and despite methotrexate treatment. (Rheumatology 2011;38:1585-92). This led to the conclusion that methotrexate should be continued at the commencement of etanercept therapy even in patients with rheumatoid arthritis who showed an inappropriate response to methotrexate as demonstrated by changes in radiographic progression.
However, only four patients were rapid progressors, said Dr. Keystone, leading him to conclude that it may not be so bad to stop methotrexate, because the probability of being a rapid progressor is not very high.
In early rheumatoid arthritis, radiographic progression influences disability in a short time, according to results of TEMPO (Trial of Etanercept and Methotrexate with Radiographic Patient Outcomes) (Ann. Rheum. Dis. 2008;67:1267-70).
The PREMIER study found a relationship between structural damage, as reflected in the total Sharp score and disability, as measured by the Health Assessment Questionnaire (HAQ) (J. Rheumatol. 2010;37:2237-46). The trial quantified the meaning of progression of joint damage to physical function in early rheumatoid arthritis as a noticeable change in physical function would occur with an approximate 100-unit change in total Sharp score.
Radiographic progression results in disability early in disease, said Dr. Keystone, but a substantial change in total Sharp score is needed to have a noticeable change in physical function in both early and established disease.
Furthermore, joint space narrowing is more predictive of disability than erosion, as demonstrated by the 5-year HAQ (Rheumatology 2004;43:79-84).
"Joint space narrowing determines unemployment," said Dr. Keystone. It has a greater effect than do erosions on disability.
Finally, he said that timing of response is predictive of long-term outcome. The disease state achieved at 12 weeks is a predictor of long-term outcome. The U.S. is the last country in the world to adopt Treat to Target, as described in the EULAR treatment recommendations (Ann. Rheum. Dis. 2010;69:964-75).
It is not just the target achieved, it\'s the time to reach the target that’s important, said Dr. Keystone.
"People who have a lot of pain, a lot of disability at baseline, they often take longer than people who are in the lower disease state. And it’s patient-derived outcomes that made the difference," said Dr. Keystone. "The sicker you are, the worse you are in terms of what the difference or the cost of delay is."
The Foundation for Osteoporosis Research and Education, a CME accredited provider, acknowledged commercial support for this meeting from Abbott, Amgen, Centocor, Genentech, Human Genome Science, and UCB. Dr. Keystone disclosed financial relationships with Abbott, Amgen, AstraZeneca, Biotest, BMS, Centocor, Genentech, Genzyme, Merck, Novartis, Nycomed, Pfizer, Roche, and UCB.
CHICAGO – The disease activity score outcome in rheumatoid arthritis should be used with caution as a treatment target when the clinical aim is to prevent radiographic progression. The DAS may show that a patient is in remission when in fact the disease is still active.
The van der Heijde/Sharp score is also flawed in that the total mean change is less meaningful than is the probability of progression of rheumatoid arthritis (RA) and may be misleading, said Dr. Edward Keystone.
"The change in the mean Sharp score point is of some importance, but not nearly as important as the proportion of people who are progressing, or those particularly rapid progressors," said Dr. Keystone, professor of medicine at the University of Toronto. In general, a large change in Sharp score points is needed to reduce physical function, noting that a change in 2 points per year will be significant over a decade, he said.
"If you change by 3 [points] a year, in 10 years you’re going to have disability."
Joint space narrowing may be more predictive than are erosions of radiographic progression. "Most methotrexate-inadequate responders, despite the fact that they’re clinically active, may still have less radiographic progression," Dr. Keystone said at the Midwest Rheumatology Summit.
"So how good is methotrexate, in patients failing methotrexate?" he said. "That’s the question."
Remission is the clinical target in RA, but its measurement is complex. True remission is a state of low-disease activity in patients who are not progressing, said Dr. Keystone. Unfortunately, there is dissociation between clinical and radiographic outcomes, and radiographic progression may occur in patients in clinical remission. Patients with active disease may likewise not progress radiographically.
The composite indices defining remission allow for a significant degree of clinical synovitis, and residual synovitis detected with sensitive imaging might explain the progression in structural damage, even in clinical remission (Arthritis Rheum. 2006;4:3761-73).
Joint space narrowing is more predictive of disability than erosion, as demonstrated by the 5-year HAQ.
As for patients with clinical disease activity who do not progress radiographically, Dr. Keystone said that the concept comes from the ACR 20 nonresponders.
"People who do not make an ACR 20 are still responders," said Dr. Keystone. It’s the difference in patient-derived vs. physician-derived outcomes, he said. In established disease, ACR 20 nonresponders to biologics do not seem to progress radiographically but may still improve.
"Why do most people not achieve an ACR 20? It’s not the swollen and tender joint. It’s usually the patient-derived outcome. ... That’s the problem: The patient says ‘I’m not better.’ Therefore when you look at the ACR 20 data, he’s a nonresponder."
Early disease can present conundrums as well.
In the PREMIER study, methotrexate was clinically identical to monotherapy adalimumab. Nevertheless, a 10-point Sharp score change was observed with methotrexate alone, vs. a 5-point Sharp score change with adalimumab monotherapy (Arthritis Rheum. 2006;54:26-37).
"Clinically, they looked alike, but radiographically, adalimumab monotherapy was much better in reducing the Sharp score." However, he said, the mean change in total Sharp score reflects the Total Sharp Score change only of those patients progressing. "And rheumatologists make decisions on the basis of probability, not mean change in [total Sharp score]," he said. The mean change in total Sharp score means less than the probability of progression, and may lead you astray, he said.
The 52-week results from the JESMR (Efficacy and Safety of Etanercept on Active Rheumatoid Arthritis Despite Methotrexate Therapy in Japan) study found that combination therapy of etanercept plus methotrexate resulted in better clinical and radiographic outcomes than etanercept monotherapy, even in patients with active rheumatoid arthritis and despite methotrexate treatment. (Rheumatology 2011;38:1585-92). This led to the conclusion that methotrexate should be continued at the commencement of etanercept therapy even in patients with rheumatoid arthritis who showed an inappropriate response to methotrexate as demonstrated by changes in radiographic progression.
However, only four patients were rapid progressors, said Dr. Keystone, leading him to conclude that it may not be so bad to stop methotrexate, because the probability of being a rapid progressor is not very high.
In early rheumatoid arthritis, radiographic progression influences disability in a short time, according to results of TEMPO (Trial of Etanercept and Methotrexate with Radiographic Patient Outcomes) (Ann. Rheum. Dis. 2008;67:1267-70).
The PREMIER study found a relationship between structural damage, as reflected in the total Sharp score and disability, as measured by the Health Assessment Questionnaire (HAQ) (J. Rheumatol. 2010;37:2237-46). The trial quantified the meaning of progression of joint damage to physical function in early rheumatoid arthritis as a noticeable change in physical function would occur with an approximate 100-unit change in total Sharp score.
Radiographic progression results in disability early in disease, said Dr. Keystone, but a substantial change in total Sharp score is needed to have a noticeable change in physical function in both early and established disease.
Furthermore, joint space narrowing is more predictive of disability than erosion, as demonstrated by the 5-year HAQ (Rheumatology 2004;43:79-84).
"Joint space narrowing determines unemployment," said Dr. Keystone. It has a greater effect than do erosions on disability.
Finally, he said that timing of response is predictive of long-term outcome. The disease state achieved at 12 weeks is a predictor of long-term outcome. The U.S. is the last country in the world to adopt Treat to Target, as described in the EULAR treatment recommendations (Ann. Rheum. Dis. 2010;69:964-75).
It is not just the target achieved, it\'s the time to reach the target that’s important, said Dr. Keystone.
"People who have a lot of pain, a lot of disability at baseline, they often take longer than people who are in the lower disease state. And it’s patient-derived outcomes that made the difference," said Dr. Keystone. "The sicker you are, the worse you are in terms of what the difference or the cost of delay is."
The Foundation for Osteoporosis Research and Education, a CME accredited provider, acknowledged commercial support for this meeting from Abbott, Amgen, Centocor, Genentech, Human Genome Science, and UCB. Dr. Keystone disclosed financial relationships with Abbott, Amgen, AstraZeneca, Biotest, BMS, Centocor, Genentech, Genzyme, Merck, Novartis, Nycomed, Pfizer, Roche, and UCB.
CHICAGO – The disease activity score outcome in rheumatoid arthritis should be used with caution as a treatment target when the clinical aim is to prevent radiographic progression. The DAS may show that a patient is in remission when in fact the disease is still active.
The van der Heijde/Sharp score is also flawed in that the total mean change is less meaningful than is the probability of progression of rheumatoid arthritis (RA) and may be misleading, said Dr. Edward Keystone.
"The change in the mean Sharp score point is of some importance, but not nearly as important as the proportion of people who are progressing, or those particularly rapid progressors," said Dr. Keystone, professor of medicine at the University of Toronto. In general, a large change in Sharp score points is needed to reduce physical function, noting that a change in 2 points per year will be significant over a decade, he said.
"If you change by 3 [points] a year, in 10 years you’re going to have disability."
Joint space narrowing may be more predictive than are erosions of radiographic progression. "Most methotrexate-inadequate responders, despite the fact that they’re clinically active, may still have less radiographic progression," Dr. Keystone said at the Midwest Rheumatology Summit.
"So how good is methotrexate, in patients failing methotrexate?" he said. "That’s the question."
Remission is the clinical target in RA, but its measurement is complex. True remission is a state of low-disease activity in patients who are not progressing, said Dr. Keystone. Unfortunately, there is dissociation between clinical and radiographic outcomes, and radiographic progression may occur in patients in clinical remission. Patients with active disease may likewise not progress radiographically.
The composite indices defining remission allow for a significant degree of clinical synovitis, and residual synovitis detected with sensitive imaging might explain the progression in structural damage, even in clinical remission (Arthritis Rheum. 2006;4:3761-73).
Joint space narrowing is more predictive of disability than erosion, as demonstrated by the 5-year HAQ.
As for patients with clinical disease activity who do not progress radiographically, Dr. Keystone said that the concept comes from the ACR 20 nonresponders.
"People who do not make an ACR 20 are still responders," said Dr. Keystone. It’s the difference in patient-derived vs. physician-derived outcomes, he said. In established disease, ACR 20 nonresponders to biologics do not seem to progress radiographically but may still improve.
"Why do most people not achieve an ACR 20? It’s not the swollen and tender joint. It’s usually the patient-derived outcome. ... That’s the problem: The patient says ‘I’m not better.’ Therefore when you look at the ACR 20 data, he’s a nonresponder."
Early disease can present conundrums as well.
In the PREMIER study, methotrexate was clinically identical to monotherapy adalimumab. Nevertheless, a 10-point Sharp score change was observed with methotrexate alone, vs. a 5-point Sharp score change with adalimumab monotherapy (Arthritis Rheum. 2006;54:26-37).
"Clinically, they looked alike, but radiographically, adalimumab monotherapy was much better in reducing the Sharp score." However, he said, the mean change in total Sharp score reflects the Total Sharp Score change only of those patients progressing. "And rheumatologists make decisions on the basis of probability, not mean change in [total Sharp score]," he said. The mean change in total Sharp score means less than the probability of progression, and may lead you astray, he said.
The 52-week results from the JESMR (Efficacy and Safety of Etanercept on Active Rheumatoid Arthritis Despite Methotrexate Therapy in Japan) study found that combination therapy of etanercept plus methotrexate resulted in better clinical and radiographic outcomes than etanercept monotherapy, even in patients with active rheumatoid arthritis and despite methotrexate treatment. (Rheumatology 2011;38:1585-92). This led to the conclusion that methotrexate should be continued at the commencement of etanercept therapy even in patients with rheumatoid arthritis who showed an inappropriate response to methotrexate as demonstrated by changes in radiographic progression.
However, only four patients were rapid progressors, said Dr. Keystone, leading him to conclude that it may not be so bad to stop methotrexate, because the probability of being a rapid progressor is not very high.
In early rheumatoid arthritis, radiographic progression influences disability in a short time, according to results of TEMPO (Trial of Etanercept and Methotrexate with Radiographic Patient Outcomes) (Ann. Rheum. Dis. 2008;67:1267-70).
The PREMIER study found a relationship between structural damage, as reflected in the total Sharp score and disability, as measured by the Health Assessment Questionnaire (HAQ) (J. Rheumatol. 2010;37:2237-46). The trial quantified the meaning of progression of joint damage to physical function in early rheumatoid arthritis as a noticeable change in physical function would occur with an approximate 100-unit change in total Sharp score.
Radiographic progression results in disability early in disease, said Dr. Keystone, but a substantial change in total Sharp score is needed to have a noticeable change in physical function in both early and established disease.
Furthermore, joint space narrowing is more predictive of disability than erosion, as demonstrated by the 5-year HAQ (Rheumatology 2004;43:79-84).
"Joint space narrowing determines unemployment," said Dr. Keystone. It has a greater effect than do erosions on disability.
Finally, he said that timing of response is predictive of long-term outcome. The disease state achieved at 12 weeks is a predictor of long-term outcome. The U.S. is the last country in the world to adopt Treat to Target, as described in the EULAR treatment recommendations (Ann. Rheum. Dis. 2010;69:964-75).
It is not just the target achieved, it\'s the time to reach the target that’s important, said Dr. Keystone.
"People who have a lot of pain, a lot of disability at baseline, they often take longer than people who are in the lower disease state. And it’s patient-derived outcomes that made the difference," said Dr. Keystone. "The sicker you are, the worse you are in terms of what the difference or the cost of delay is."
The Foundation for Osteoporosis Research and Education, a CME accredited provider, acknowledged commercial support for this meeting from Abbott, Amgen, Centocor, Genentech, Human Genome Science, and UCB. Dr. Keystone disclosed financial relationships with Abbott, Amgen, AstraZeneca, Biotest, BMS, Centocor, Genentech, Genzyme, Merck, Novartis, Nycomed, Pfizer, Roche, and UCB.
EXPERT ANALYSIS FROM THE MIDWEST RHEUMATOLOGY SUMMIT