User login
New recommendations for hyperglycemia management
This transcript has been edited for clarity.
I’m Dr. Neil Skolnik. Today we’re going to talk about the consensus report by the American Diabetes Association and the European Association for the Study of Diabetes on the management of hyperglycemia.
After lifestyle modifications, metformin is no longer the go-to drug for every patient in the management of hyperglycemia. It is recommended that we assess each patient’s personal characteristics in deciding what medication to prescribe. For patients at high cardiorenal risk, refer to the left side of the algorithm and to the right side for all other patients.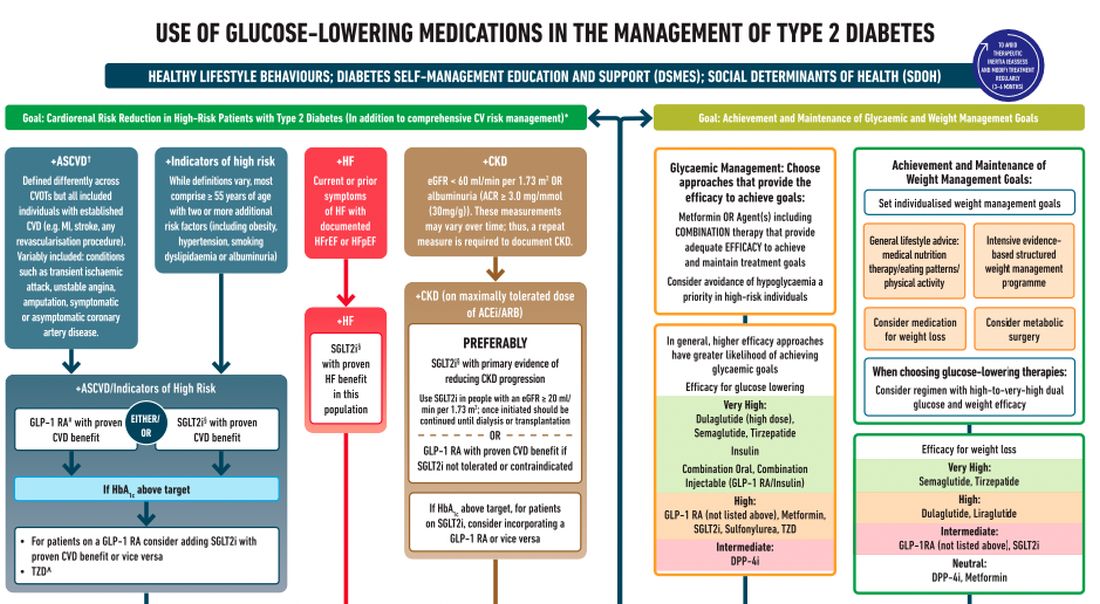
Cardiovascular disease. First, assess whether the patient is at high risk for atherosclerotic cardiovascular disease (ASCVD) or already has ASCVD. How is ASCVD defined? Either coronary artery disease (a history of a myocardial infarction [MI] or coronary disease), peripheral vascular disease, stroke, or transient ischemic attack.
What is high risk for ASCVD? Diabetes in someone older than 55 years with two or more additional risk factors. If the patient is at high risk for or has existing ASCVD then it is recommended to prescribe a glucagon-like peptide 1 (GLP-1) agonist with proven CVD benefit or an sodium-glucose cotransporter 2 (SGLT-2) inhibitor with proven CVD benefit.
For patients at very high risk for ASCVD, it might be reasonable to combine both agents. The recommendation to use these agents holds true whether the patients are at their A1c goals or not. The patient doesn’t need to be on metformin to benefit from these agents. The patient with reduced or preserved ejection fraction heart failure should be taking an SGLT-2 inhibitor.
Chronic kidney disease. Next up, chronic kidney disease (CKD). CKD is defined by an estimated glomerular filtration rate < 60 mL/min/1.73 m2 or a urine albumin to creatinine ratio > 30. In that case, the patient should be preferentially on an SGLT-2 inhibitor. Patients not able to take an SGLT-2 for some reason should be prescribed a GLP-1 receptor agonist.
If someone doesn’t fit into that high cardiorenal risk category, then we go to the right side of the algorithm. The goal then is achievement and maintenance of glycemic and weight management goals.
Glycemic management. In choosing medicine for glycemic management, metformin is a reasonable choice. You may need to add another agent to metformin to reach the patient’s glycemic goal. If the patient is far away from goal, then a medication with higher efficacy at lowering glucose might be chosen.
Efficacy is listed as:
- Very high efficacy for glucose lowering: dulaglutide at a high dose, semaglutide, tirzepatide, insulin, or combination injectable agents (GLP-1 receptor agonist/insulin combinations).
- High glucose-lowering efficacy: a GLP-1 receptor agonist not already mentioned, metformin, SGLT-2 inhibitors, sulfonylureas, thiazolidinediones.
- Intermediate glucose lowering efficacy: dipeptidyl peptidase 4 (DPP-4) inhibitors.
Weight management. For weight management, lifestyle modification (diet and exercise) is important. If lifestyle modification alone is insufficient, consider either a medication that specifically helps with weight management or metabolic surgery.
We particularly want to focus on weight management in patients who have complications from obesity. What would those complications be? Sleep apnea, hip or knee pain from arthritis, back pain – that is, biomechanical complications of obesity or nonalcoholic fatty liver disease. Medications for weight loss are listed by degree of efficacy:
- Very high efficacy for weight loss: semaglutide, tirzepatide.
- High efficacy for weight loss: dulaglutide and liraglutide.
- Intermediate for weight loss: GLP-1 receptor agonist (not listed above), SGLT-2 inhibitor.
- Neutral for weight loss: DPP-4 inhibitors and metformin.
Where does insulin fit in? If patients present with a very high A1c, if they are on other medications and their A1c is still not to goal, or if they are catabolic and losing weight because of their diabetes, then insulin has an important place in management.
These are incredibly important guidelines that provide a clear algorithm for a personalized approach to diabetes management.
Dr. Skolnik is professor, department of family medicine, Sidney Kimmel Medical College, Philadelphia, and associate director, department of family medicine, Abington (Pa.) Jefferson Health. He reported conflicts of interest with AstraZeneca, Teva, Eli Lilly, Boehringer Ingelheim, Sanofi, Sanofi Pasteur, GlaxoSmithKline, Merck, and Bayer. A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
I’m Dr. Neil Skolnik. Today we’re going to talk about the consensus report by the American Diabetes Association and the European Association for the Study of Diabetes on the management of hyperglycemia.
After lifestyle modifications, metformin is no longer the go-to drug for every patient in the management of hyperglycemia. It is recommended that we assess each patient’s personal characteristics in deciding what medication to prescribe. For patients at high cardiorenal risk, refer to the left side of the algorithm and to the right side for all other patients.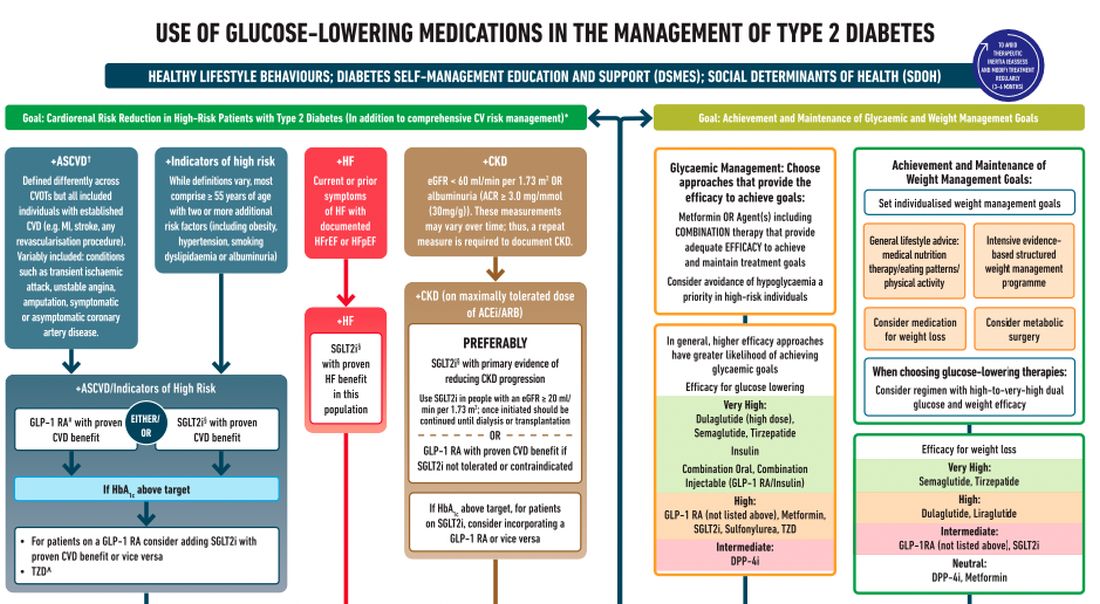
Cardiovascular disease. First, assess whether the patient is at high risk for atherosclerotic cardiovascular disease (ASCVD) or already has ASCVD. How is ASCVD defined? Either coronary artery disease (a history of a myocardial infarction [MI] or coronary disease), peripheral vascular disease, stroke, or transient ischemic attack.
What is high risk for ASCVD? Diabetes in someone older than 55 years with two or more additional risk factors. If the patient is at high risk for or has existing ASCVD then it is recommended to prescribe a glucagon-like peptide 1 (GLP-1) agonist with proven CVD benefit or an sodium-glucose cotransporter 2 (SGLT-2) inhibitor with proven CVD benefit.
For patients at very high risk for ASCVD, it might be reasonable to combine both agents. The recommendation to use these agents holds true whether the patients are at their A1c goals or not. The patient doesn’t need to be on metformin to benefit from these agents. The patient with reduced or preserved ejection fraction heart failure should be taking an SGLT-2 inhibitor.
Chronic kidney disease. Next up, chronic kidney disease (CKD). CKD is defined by an estimated glomerular filtration rate < 60 mL/min/1.73 m2 or a urine albumin to creatinine ratio > 30. In that case, the patient should be preferentially on an SGLT-2 inhibitor. Patients not able to take an SGLT-2 for some reason should be prescribed a GLP-1 receptor agonist.
If someone doesn’t fit into that high cardiorenal risk category, then we go to the right side of the algorithm. The goal then is achievement and maintenance of glycemic and weight management goals.
Glycemic management. In choosing medicine for glycemic management, metformin is a reasonable choice. You may need to add another agent to metformin to reach the patient’s glycemic goal. If the patient is far away from goal, then a medication with higher efficacy at lowering glucose might be chosen.
Efficacy is listed as:
- Very high efficacy for glucose lowering: dulaglutide at a high dose, semaglutide, tirzepatide, insulin, or combination injectable agents (GLP-1 receptor agonist/insulin combinations).
- High glucose-lowering efficacy: a GLP-1 receptor agonist not already mentioned, metformin, SGLT-2 inhibitors, sulfonylureas, thiazolidinediones.
- Intermediate glucose lowering efficacy: dipeptidyl peptidase 4 (DPP-4) inhibitors.
Weight management. For weight management, lifestyle modification (diet and exercise) is important. If lifestyle modification alone is insufficient, consider either a medication that specifically helps with weight management or metabolic surgery.
We particularly want to focus on weight management in patients who have complications from obesity. What would those complications be? Sleep apnea, hip or knee pain from arthritis, back pain – that is, biomechanical complications of obesity or nonalcoholic fatty liver disease. Medications for weight loss are listed by degree of efficacy:
- Very high efficacy for weight loss: semaglutide, tirzepatide.
- High efficacy for weight loss: dulaglutide and liraglutide.
- Intermediate for weight loss: GLP-1 receptor agonist (not listed above), SGLT-2 inhibitor.
- Neutral for weight loss: DPP-4 inhibitors and metformin.
Where does insulin fit in? If patients present with a very high A1c, if they are on other medications and their A1c is still not to goal, or if they are catabolic and losing weight because of their diabetes, then insulin has an important place in management.
These are incredibly important guidelines that provide a clear algorithm for a personalized approach to diabetes management.
Dr. Skolnik is professor, department of family medicine, Sidney Kimmel Medical College, Philadelphia, and associate director, department of family medicine, Abington (Pa.) Jefferson Health. He reported conflicts of interest with AstraZeneca, Teva, Eli Lilly, Boehringer Ingelheim, Sanofi, Sanofi Pasteur, GlaxoSmithKline, Merck, and Bayer. A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
I’m Dr. Neil Skolnik. Today we’re going to talk about the consensus report by the American Diabetes Association and the European Association for the Study of Diabetes on the management of hyperglycemia.
After lifestyle modifications, metformin is no longer the go-to drug for every patient in the management of hyperglycemia. It is recommended that we assess each patient’s personal characteristics in deciding what medication to prescribe. For patients at high cardiorenal risk, refer to the left side of the algorithm and to the right side for all other patients.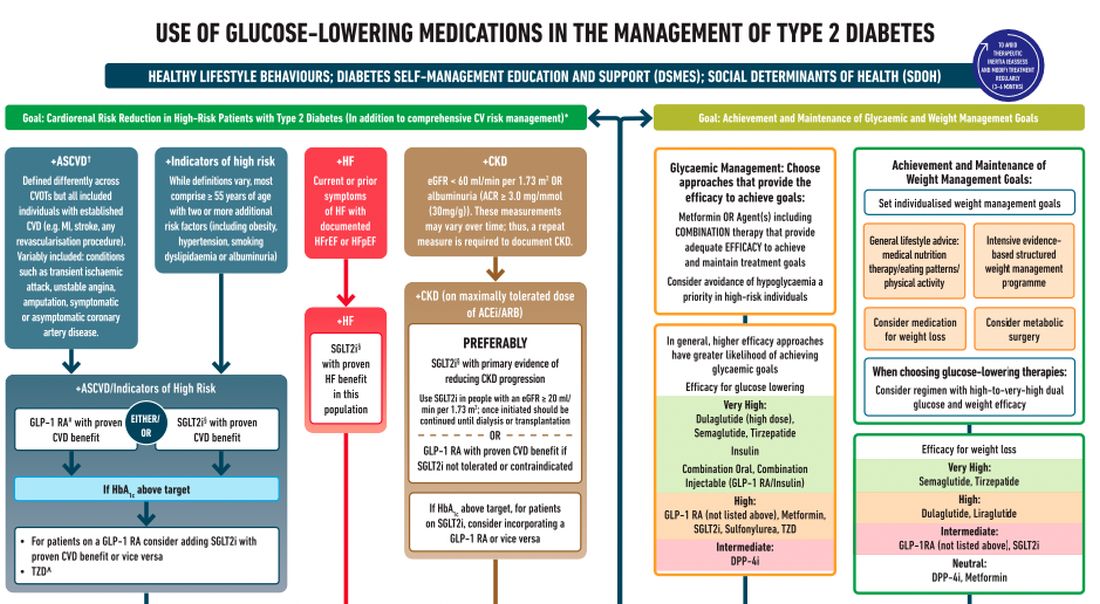
Cardiovascular disease. First, assess whether the patient is at high risk for atherosclerotic cardiovascular disease (ASCVD) or already has ASCVD. How is ASCVD defined? Either coronary artery disease (a history of a myocardial infarction [MI] or coronary disease), peripheral vascular disease, stroke, or transient ischemic attack.
What is high risk for ASCVD? Diabetes in someone older than 55 years with two or more additional risk factors. If the patient is at high risk for or has existing ASCVD then it is recommended to prescribe a glucagon-like peptide 1 (GLP-1) agonist with proven CVD benefit or an sodium-glucose cotransporter 2 (SGLT-2) inhibitor with proven CVD benefit.
For patients at very high risk for ASCVD, it might be reasonable to combine both agents. The recommendation to use these agents holds true whether the patients are at their A1c goals or not. The patient doesn’t need to be on metformin to benefit from these agents. The patient with reduced or preserved ejection fraction heart failure should be taking an SGLT-2 inhibitor.
Chronic kidney disease. Next up, chronic kidney disease (CKD). CKD is defined by an estimated glomerular filtration rate < 60 mL/min/1.73 m2 or a urine albumin to creatinine ratio > 30. In that case, the patient should be preferentially on an SGLT-2 inhibitor. Patients not able to take an SGLT-2 for some reason should be prescribed a GLP-1 receptor agonist.
If someone doesn’t fit into that high cardiorenal risk category, then we go to the right side of the algorithm. The goal then is achievement and maintenance of glycemic and weight management goals.
Glycemic management. In choosing medicine for glycemic management, metformin is a reasonable choice. You may need to add another agent to metformin to reach the patient’s glycemic goal. If the patient is far away from goal, then a medication with higher efficacy at lowering glucose might be chosen.
Efficacy is listed as:
- Very high efficacy for glucose lowering: dulaglutide at a high dose, semaglutide, tirzepatide, insulin, or combination injectable agents (GLP-1 receptor agonist/insulin combinations).
- High glucose-lowering efficacy: a GLP-1 receptor agonist not already mentioned, metformin, SGLT-2 inhibitors, sulfonylureas, thiazolidinediones.
- Intermediate glucose lowering efficacy: dipeptidyl peptidase 4 (DPP-4) inhibitors.
Weight management. For weight management, lifestyle modification (diet and exercise) is important. If lifestyle modification alone is insufficient, consider either a medication that specifically helps with weight management or metabolic surgery.
We particularly want to focus on weight management in patients who have complications from obesity. What would those complications be? Sleep apnea, hip or knee pain from arthritis, back pain – that is, biomechanical complications of obesity or nonalcoholic fatty liver disease. Medications for weight loss are listed by degree of efficacy:
- Very high efficacy for weight loss: semaglutide, tirzepatide.
- High efficacy for weight loss: dulaglutide and liraglutide.
- Intermediate for weight loss: GLP-1 receptor agonist (not listed above), SGLT-2 inhibitor.
- Neutral for weight loss: DPP-4 inhibitors and metformin.
Where does insulin fit in? If patients present with a very high A1c, if they are on other medications and their A1c is still not to goal, or if they are catabolic and losing weight because of their diabetes, then insulin has an important place in management.
These are incredibly important guidelines that provide a clear algorithm for a personalized approach to diabetes management.
Dr. Skolnik is professor, department of family medicine, Sidney Kimmel Medical College, Philadelphia, and associate director, department of family medicine, Abington (Pa.) Jefferson Health. He reported conflicts of interest with AstraZeneca, Teva, Eli Lilly, Boehringer Ingelheim, Sanofi, Sanofi Pasteur, GlaxoSmithKline, Merck, and Bayer. A version of this article first appeared on Medscape.com.
Medical technology should keep patient in mind
Indeed, science and technology provide opportunities to improve outcomes in ways not even imagined 100 years ago, yet we must acknowledge that technology also threatens to erect barriers between us and our patients. We can be easily tempted to confuse new care delivery tools with the actual care itself.
Threats to the physician-patient relationship
Medical history provides many examples of how our zeal to innovate can have untoward consequences to the physician-patient relationship.
In the late 1800s, for example, to convey a sense of science, purity of intent, and trust, the medical community began wearing white coats. Those white coats have been discussed as creating emotional distance between physicians and their patients.1
Even when we in the medical community are slow and reluctant to change, the external forces propelling us forward often seem unstoppable; kinetic aspirations to innovate electronic information systems and new applications seem suddenly to revolutionize care delivery when we least expect it. The rapidity of change in technology can sometimes be dizzying but can at the same time can occur so swiftly we don’t even notice it.
After René Laennec invented the stethoscope in the early 1800s, clinicians no longer needed to physically lean in and place an ear directly onto patients to hear their hearts beating. This created a distance from patients that was still lamented 50 years later, when a professor of medicine is reported to have said, “he that hath ears to hear, let him use his ears and not a stethoscope.” Still, while the stethoscope has literally distanced us from patients, it is such an important tool that we no longer think about this distancing. We have adapted over time to remain close to our patients, to sincerely listen to their thoughts and reassure them that we hear them without the need to feel our ears on their chests.
Francis Peabody, the eminent Harvard physician, wrote an essay in 1927 titled, “The Care of the Patient.” At the end of the first paragraph, he states: “The most common criticism made at present by older practitioners is that young graduates ... are too “scientific” and do not know how to take care of patients.” He goes on to say that “one of the essential qualities of the clinician is interest in humanity, for the secret of the care of the patient is in caring for the patient.”2
We agree with Dr. Peabody. As we embrace science and technology that can change health outcomes, our patients’ needs to feel understood and cared for will not diminish. Instead, that need will continue to be an important aspect of our struggle and joy in providing holistic, humane, competent care into the future.
Twenty-first century physicians have access to an ever-growing trove of data, yet our ability to truly know our patients seems somehow less accessible. Home health devices have begun to provide a flow of information about parameters, ranging from continuous glucose readings to home blood pressures, weights, and inspiratory flow readings. These data can provide much more accurate insight into patients than what we can glean from one point in time during an office visit. Yet we need to remember that behind the data are people with dreams and desires, not just table entries in an electronic health record.
In 1923, the German philosopher Martin Buber published the book for which he is best known, “I and Thou.” In that book, Mr. Buber says that there are two ways we can approach relationships: “I-Thou” or “I-It.” In I-It relationships, we view the other person as an “it” to be used to accomplish a purpose, or to be experienced without his or her full involvement. In an I-Thou relationship, we appreciate the other people for all their complexity, in their full humanness. We must consciously remind ourselves amid the rush of technology that there are real people behind those data. We must acknowledge and approach each person as a unique individual who has dreams, goals, fears, and wishes that may be different from ours but to which we can still relate.
‘From the Beating End of the Stethoscope’
John Ciardi, an American poet, said the following in a poem titled, “Lines From the Beating End of the Stethoscope”:
I speak, as I say, the patient’s point of view.
But, given time, doctors are patients, too.
And there’s our bond: beyond anatomy,
Or in it, through it, to the mystery
Medicine takes the pulse of and lets go
Forever unexplained. It’s art, we know,
Not science at the heart. Doctor be whole,
I won’t insist the patient is a soul,
But he’s a something, possibly laughable,
Or possibly sublime, but not quite graphable.
Not quite containable on a bed chart.
Where science touches man it turns to art.3
This poem is a reminder of the subtle needs of patients during their encounters with doctors, especially around many of the most important decisions and events in their lives. Patients’ needs are varied, complex, difficult to discern, and not able to be fully explained or understood through math and science.
Einstein warned us that the modern age would be characterized by a perfection of means and a confusion of goals.4 As clinicians, we should strive to clarify and align our goals with those of our patients, providing care that is real, compassionate, and personal, not just an optimized means to achieve standardized metrics. While technology can assist us in this pursuit, we’ll need be careful that our enchantment with innovation does not cloud our actual goal: truly caring for our patients.
Dr. Notte is a family physician and chief medical officer of Abington (Pa.) Hospital–Jefferson Health. Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington Hospital–Jefferson Health. They have no conflicts related to the content of this piece.
References
1. Jones VA. The white coat: Why not follow suit? JAMA. 1999;281(5):478. doi: 10.1001/jama.281.5.478-JMS0203-5-1
2. Peabody, Francis (1927). “The care of the patient.” JAMA. 88(12):877-82. doi: 10.1001/jama.1927.02680380001001.
3. Ciardi, John. Lines from the Beating End of the Stethoscope. Saturday Review, Nov. 18, 1968.
4. Albert Einstein, Out of My Later Years, 1950.
Indeed, science and technology provide opportunities to improve outcomes in ways not even imagined 100 years ago, yet we must acknowledge that technology also threatens to erect barriers between us and our patients. We can be easily tempted to confuse new care delivery tools with the actual care itself.
Threats to the physician-patient relationship
Medical history provides many examples of how our zeal to innovate can have untoward consequences to the physician-patient relationship.
In the late 1800s, for example, to convey a sense of science, purity of intent, and trust, the medical community began wearing white coats. Those white coats have been discussed as creating emotional distance between physicians and their patients.1
Even when we in the medical community are slow and reluctant to change, the external forces propelling us forward often seem unstoppable; kinetic aspirations to innovate electronic information systems and new applications seem suddenly to revolutionize care delivery when we least expect it. The rapidity of change in technology can sometimes be dizzying but can at the same time can occur so swiftly we don’t even notice it.
After René Laennec invented the stethoscope in the early 1800s, clinicians no longer needed to physically lean in and place an ear directly onto patients to hear their hearts beating. This created a distance from patients that was still lamented 50 years later, when a professor of medicine is reported to have said, “he that hath ears to hear, let him use his ears and not a stethoscope.” Still, while the stethoscope has literally distanced us from patients, it is such an important tool that we no longer think about this distancing. We have adapted over time to remain close to our patients, to sincerely listen to their thoughts and reassure them that we hear them without the need to feel our ears on their chests.
Francis Peabody, the eminent Harvard physician, wrote an essay in 1927 titled, “The Care of the Patient.” At the end of the first paragraph, he states: “The most common criticism made at present by older practitioners is that young graduates ... are too “scientific” and do not know how to take care of patients.” He goes on to say that “one of the essential qualities of the clinician is interest in humanity, for the secret of the care of the patient is in caring for the patient.”2
We agree with Dr. Peabody. As we embrace science and technology that can change health outcomes, our patients’ needs to feel understood and cared for will not diminish. Instead, that need will continue to be an important aspect of our struggle and joy in providing holistic, humane, competent care into the future.
Twenty-first century physicians have access to an ever-growing trove of data, yet our ability to truly know our patients seems somehow less accessible. Home health devices have begun to provide a flow of information about parameters, ranging from continuous glucose readings to home blood pressures, weights, and inspiratory flow readings. These data can provide much more accurate insight into patients than what we can glean from one point in time during an office visit. Yet we need to remember that behind the data are people with dreams and desires, not just table entries in an electronic health record.
In 1923, the German philosopher Martin Buber published the book for which he is best known, “I and Thou.” In that book, Mr. Buber says that there are two ways we can approach relationships: “I-Thou” or “I-It.” In I-It relationships, we view the other person as an “it” to be used to accomplish a purpose, or to be experienced without his or her full involvement. In an I-Thou relationship, we appreciate the other people for all their complexity, in their full humanness. We must consciously remind ourselves amid the rush of technology that there are real people behind those data. We must acknowledge and approach each person as a unique individual who has dreams, goals, fears, and wishes that may be different from ours but to which we can still relate.
‘From the Beating End of the Stethoscope’
John Ciardi, an American poet, said the following in a poem titled, “Lines From the Beating End of the Stethoscope”:
I speak, as I say, the patient’s point of view.
But, given time, doctors are patients, too.
And there’s our bond: beyond anatomy,
Or in it, through it, to the mystery
Medicine takes the pulse of and lets go
Forever unexplained. It’s art, we know,
Not science at the heart. Doctor be whole,
I won’t insist the patient is a soul,
But he’s a something, possibly laughable,
Or possibly sublime, but not quite graphable.
Not quite containable on a bed chart.
Where science touches man it turns to art.3
This poem is a reminder of the subtle needs of patients during their encounters with doctors, especially around many of the most important decisions and events in their lives. Patients’ needs are varied, complex, difficult to discern, and not able to be fully explained or understood through math and science.
Einstein warned us that the modern age would be characterized by a perfection of means and a confusion of goals.4 As clinicians, we should strive to clarify and align our goals with those of our patients, providing care that is real, compassionate, and personal, not just an optimized means to achieve standardized metrics. While technology can assist us in this pursuit, we’ll need be careful that our enchantment with innovation does not cloud our actual goal: truly caring for our patients.
Dr. Notte is a family physician and chief medical officer of Abington (Pa.) Hospital–Jefferson Health. Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington Hospital–Jefferson Health. They have no conflicts related to the content of this piece.
References
1. Jones VA. The white coat: Why not follow suit? JAMA. 1999;281(5):478. doi: 10.1001/jama.281.5.478-JMS0203-5-1
2. Peabody, Francis (1927). “The care of the patient.” JAMA. 88(12):877-82. doi: 10.1001/jama.1927.02680380001001.
3. Ciardi, John. Lines from the Beating End of the Stethoscope. Saturday Review, Nov. 18, 1968.
4. Albert Einstein, Out of My Later Years, 1950.
Indeed, science and technology provide opportunities to improve outcomes in ways not even imagined 100 years ago, yet we must acknowledge that technology also threatens to erect barriers between us and our patients. We can be easily tempted to confuse new care delivery tools with the actual care itself.
Threats to the physician-patient relationship
Medical history provides many examples of how our zeal to innovate can have untoward consequences to the physician-patient relationship.
In the late 1800s, for example, to convey a sense of science, purity of intent, and trust, the medical community began wearing white coats. Those white coats have been discussed as creating emotional distance between physicians and their patients.1
Even when we in the medical community are slow and reluctant to change, the external forces propelling us forward often seem unstoppable; kinetic aspirations to innovate electronic information systems and new applications seem suddenly to revolutionize care delivery when we least expect it. The rapidity of change in technology can sometimes be dizzying but can at the same time can occur so swiftly we don’t even notice it.
After René Laennec invented the stethoscope in the early 1800s, clinicians no longer needed to physically lean in and place an ear directly onto patients to hear their hearts beating. This created a distance from patients that was still lamented 50 years later, when a professor of medicine is reported to have said, “he that hath ears to hear, let him use his ears and not a stethoscope.” Still, while the stethoscope has literally distanced us from patients, it is such an important tool that we no longer think about this distancing. We have adapted over time to remain close to our patients, to sincerely listen to their thoughts and reassure them that we hear them without the need to feel our ears on their chests.
Francis Peabody, the eminent Harvard physician, wrote an essay in 1927 titled, “The Care of the Patient.” At the end of the first paragraph, he states: “The most common criticism made at present by older practitioners is that young graduates ... are too “scientific” and do not know how to take care of patients.” He goes on to say that “one of the essential qualities of the clinician is interest in humanity, for the secret of the care of the patient is in caring for the patient.”2
We agree with Dr. Peabody. As we embrace science and technology that can change health outcomes, our patients’ needs to feel understood and cared for will not diminish. Instead, that need will continue to be an important aspect of our struggle and joy in providing holistic, humane, competent care into the future.
Twenty-first century physicians have access to an ever-growing trove of data, yet our ability to truly know our patients seems somehow less accessible. Home health devices have begun to provide a flow of information about parameters, ranging from continuous glucose readings to home blood pressures, weights, and inspiratory flow readings. These data can provide much more accurate insight into patients than what we can glean from one point in time during an office visit. Yet we need to remember that behind the data are people with dreams and desires, not just table entries in an electronic health record.
In 1923, the German philosopher Martin Buber published the book for which he is best known, “I and Thou.” In that book, Mr. Buber says that there are two ways we can approach relationships: “I-Thou” or “I-It.” In I-It relationships, we view the other person as an “it” to be used to accomplish a purpose, or to be experienced without his or her full involvement. In an I-Thou relationship, we appreciate the other people for all their complexity, in their full humanness. We must consciously remind ourselves amid the rush of technology that there are real people behind those data. We must acknowledge and approach each person as a unique individual who has dreams, goals, fears, and wishes that may be different from ours but to which we can still relate.
‘From the Beating End of the Stethoscope’
John Ciardi, an American poet, said the following in a poem titled, “Lines From the Beating End of the Stethoscope”:
I speak, as I say, the patient’s point of view.
But, given time, doctors are patients, too.
And there’s our bond: beyond anatomy,
Or in it, through it, to the mystery
Medicine takes the pulse of and lets go
Forever unexplained. It’s art, we know,
Not science at the heart. Doctor be whole,
I won’t insist the patient is a soul,
But he’s a something, possibly laughable,
Or possibly sublime, but not quite graphable.
Not quite containable on a bed chart.
Where science touches man it turns to art.3
This poem is a reminder of the subtle needs of patients during their encounters with doctors, especially around many of the most important decisions and events in their lives. Patients’ needs are varied, complex, difficult to discern, and not able to be fully explained or understood through math and science.
Einstein warned us that the modern age would be characterized by a perfection of means and a confusion of goals.4 As clinicians, we should strive to clarify and align our goals with those of our patients, providing care that is real, compassionate, and personal, not just an optimized means to achieve standardized metrics. While technology can assist us in this pursuit, we’ll need be careful that our enchantment with innovation does not cloud our actual goal: truly caring for our patients.
Dr. Notte is a family physician and chief medical officer of Abington (Pa.) Hospital–Jefferson Health. Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington Hospital–Jefferson Health. They have no conflicts related to the content of this piece.
References
1. Jones VA. The white coat: Why not follow suit? JAMA. 1999;281(5):478. doi: 10.1001/jama.281.5.478-JMS0203-5-1
2. Peabody, Francis (1927). “The care of the patient.” JAMA. 88(12):877-82. doi: 10.1001/jama.1927.02680380001001.
3. Ciardi, John. Lines from the Beating End of the Stethoscope. Saturday Review, Nov. 18, 1968.
4. Albert Einstein, Out of My Later Years, 1950.
Smart watch glucose monitoring on the horizon
Earlier this year, technology news sites reported that the Apple Watch Series 7 and the Samsung Galaxy Watch 4 were going to have integrated optical sensors for checking interstitial fluid glucose levels with no blood sampling needed. By the summer, new articles indicated that the glucose sensing watches would not be released this year for either Apple or Samsung.
For now, the newest technology available for monitoring glucose is continuous glucose monitoring (CGM), which involves a tiny sensor being inserted under the skin. The sensor tests glucose every few minutes, and a transmitter wirelessly sends the information to a monitor, which may be part of an insulin pump or a separate device. Some CGMs send information directly to a smartphone or tablet, according to the National Institutes of Health.
In 1999 the Food and Drug Administration approved the first CGM, which was only approved for downloading 3 days of data at a doctor’s office. Interestingly, the first real-time CGM device for patients to use on their own was a watch, the Glucowatch Biographer. Because of irritation and other issues, that watch never caught on. In 2006 and 2008, Dexcom and then Abbott released the first real-time CGMs that allowed patients to frequently check their own blood sugars.1,2
How CGM has advanced diabetes management
The advent of CGM has advanced the field of diabetes management in many ways.
It has allowed patients to get real time feedback on how their behavior affects their blood sugar. The use of CGM along with the ensuing behavioral changes actually leads to a decrease in hemoglobin A1c, along with a lower risk of hypoglycemia. CGM has also resulted in patients having a better understanding of several aspects of glucose control, including glucose variability and nocturnal hypoglycemia.
Affordable, readily accessible CGM monitors that allow patients to intermittently use CGM have become available over the last 3 years.
In the United States alone, 34.2 million people have diabetes – nearly 1 in every 10 people. Many do not do self-monitoring of blood glucose and most do not use CGM. The current alternative to CGM – self monitoring of blood glucose – is cumbersome, and, since it requires regular finger sticks, is painful. Also, there is significant cost to each test strip that is used to self-monitor, and most insurance limits the number of times a day a patient can check their blood sugar. CGM used to be reserved only for patients who use multiple doses of insulin daily, and only began being approved for use for patients on basal insulin alone in June 2021.3
Most primary care doctors are just beginning to learn how to interpret CGM data.
Smart watch glucose monitoring predictions
When smart watch glucose monitoring arrives, it will suddenly change the playing field for patients with diabetes and their doctors alike.
We expect it to bring down the price of CGM and make it readily available to any patient who owns a smart watch with that function.
For doctors, the new technology will result in them suddenly being asked to advise their patients on how to use the data generated by watch-based CGM.
Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington (Pa.) Hospital–Jefferson Health. They have no conflicts related to the content of this piece. Dr. Persampiere is a second-year resident in the family medicine residency program at Abington Jefferson Health. You can contact them at fpnews@mdedge.com.
References
1. Hirsh I. Introduction: History of Glucose Monitoring, in “Role of Continuous Glucose Monitoring in Diabetes Treatment.” American Diabetes Association. 2018.
2. Peters A. The Evidence Base for Continuous Glucose Monitoring, in “Role of Continuous Glucose Monitoring in Diabetes Treatment.” American Diabetes Association 2018.
3. “Medicare Loosening Restrictions for Continuous Glucose Monitor (CGM) Coverage,” Healthline. 2021 Jul 13.
Earlier this year, technology news sites reported that the Apple Watch Series 7 and the Samsung Galaxy Watch 4 were going to have integrated optical sensors for checking interstitial fluid glucose levels with no blood sampling needed. By the summer, new articles indicated that the glucose sensing watches would not be released this year for either Apple or Samsung.
For now, the newest technology available for monitoring glucose is continuous glucose monitoring (CGM), which involves a tiny sensor being inserted under the skin. The sensor tests glucose every few minutes, and a transmitter wirelessly sends the information to a monitor, which may be part of an insulin pump or a separate device. Some CGMs send information directly to a smartphone or tablet, according to the National Institutes of Health.
In 1999 the Food and Drug Administration approved the first CGM, which was only approved for downloading 3 days of data at a doctor’s office. Interestingly, the first real-time CGM device for patients to use on their own was a watch, the Glucowatch Biographer. Because of irritation and other issues, that watch never caught on. In 2006 and 2008, Dexcom and then Abbott released the first real-time CGMs that allowed patients to frequently check their own blood sugars.1,2
How CGM has advanced diabetes management
The advent of CGM has advanced the field of diabetes management in many ways.
It has allowed patients to get real time feedback on how their behavior affects their blood sugar. The use of CGM along with the ensuing behavioral changes actually leads to a decrease in hemoglobin A1c, along with a lower risk of hypoglycemia. CGM has also resulted in patients having a better understanding of several aspects of glucose control, including glucose variability and nocturnal hypoglycemia.
Affordable, readily accessible CGM monitors that allow patients to intermittently use CGM have become available over the last 3 years.
In the United States alone, 34.2 million people have diabetes – nearly 1 in every 10 people. Many do not do self-monitoring of blood glucose and most do not use CGM. The current alternative to CGM – self monitoring of blood glucose – is cumbersome, and, since it requires regular finger sticks, is painful. Also, there is significant cost to each test strip that is used to self-monitor, and most insurance limits the number of times a day a patient can check their blood sugar. CGM used to be reserved only for patients who use multiple doses of insulin daily, and only began being approved for use for patients on basal insulin alone in June 2021.3
Most primary care doctors are just beginning to learn how to interpret CGM data.
Smart watch glucose monitoring predictions
When smart watch glucose monitoring arrives, it will suddenly change the playing field for patients with diabetes and their doctors alike.
We expect it to bring down the price of CGM and make it readily available to any patient who owns a smart watch with that function.
For doctors, the new technology will result in them suddenly being asked to advise their patients on how to use the data generated by watch-based CGM.
Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington (Pa.) Hospital–Jefferson Health. They have no conflicts related to the content of this piece. Dr. Persampiere is a second-year resident in the family medicine residency program at Abington Jefferson Health. You can contact them at fpnews@mdedge.com.
References
1. Hirsh I. Introduction: History of Glucose Monitoring, in “Role of Continuous Glucose Monitoring in Diabetes Treatment.” American Diabetes Association. 2018.
2. Peters A. The Evidence Base for Continuous Glucose Monitoring, in “Role of Continuous Glucose Monitoring in Diabetes Treatment.” American Diabetes Association 2018.
3. “Medicare Loosening Restrictions for Continuous Glucose Monitor (CGM) Coverage,” Healthline. 2021 Jul 13.
Earlier this year, technology news sites reported that the Apple Watch Series 7 and the Samsung Galaxy Watch 4 were going to have integrated optical sensors for checking interstitial fluid glucose levels with no blood sampling needed. By the summer, new articles indicated that the glucose sensing watches would not be released this year for either Apple or Samsung.
For now, the newest technology available for monitoring glucose is continuous glucose monitoring (CGM), which involves a tiny sensor being inserted under the skin. The sensor tests glucose every few minutes, and a transmitter wirelessly sends the information to a monitor, which may be part of an insulin pump or a separate device. Some CGMs send information directly to a smartphone or tablet, according to the National Institutes of Health.
In 1999 the Food and Drug Administration approved the first CGM, which was only approved for downloading 3 days of data at a doctor’s office. Interestingly, the first real-time CGM device for patients to use on their own was a watch, the Glucowatch Biographer. Because of irritation and other issues, that watch never caught on. In 2006 and 2008, Dexcom and then Abbott released the first real-time CGMs that allowed patients to frequently check their own blood sugars.1,2
How CGM has advanced diabetes management
The advent of CGM has advanced the field of diabetes management in many ways.
It has allowed patients to get real time feedback on how their behavior affects their blood sugar. The use of CGM along with the ensuing behavioral changes actually leads to a decrease in hemoglobin A1c, along with a lower risk of hypoglycemia. CGM has also resulted in patients having a better understanding of several aspects of glucose control, including glucose variability and nocturnal hypoglycemia.
Affordable, readily accessible CGM monitors that allow patients to intermittently use CGM have become available over the last 3 years.
In the United States alone, 34.2 million people have diabetes – nearly 1 in every 10 people. Many do not do self-monitoring of blood glucose and most do not use CGM. The current alternative to CGM – self monitoring of blood glucose – is cumbersome, and, since it requires regular finger sticks, is painful. Also, there is significant cost to each test strip that is used to self-monitor, and most insurance limits the number of times a day a patient can check their blood sugar. CGM used to be reserved only for patients who use multiple doses of insulin daily, and only began being approved for use for patients on basal insulin alone in June 2021.3
Most primary care doctors are just beginning to learn how to interpret CGM data.
Smart watch glucose monitoring predictions
When smart watch glucose monitoring arrives, it will suddenly change the playing field for patients with diabetes and their doctors alike.
We expect it to bring down the price of CGM and make it readily available to any patient who owns a smart watch with that function.
For doctors, the new technology will result in them suddenly being asked to advise their patients on how to use the data generated by watch-based CGM.
Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington (Pa.) Hospital–Jefferson Health. They have no conflicts related to the content of this piece. Dr. Persampiere is a second-year resident in the family medicine residency program at Abington Jefferson Health. You can contact them at fpnews@mdedge.com.
References
1. Hirsh I. Introduction: History of Glucose Monitoring, in “Role of Continuous Glucose Monitoring in Diabetes Treatment.” American Diabetes Association. 2018.
2. Peters A. The Evidence Base for Continuous Glucose Monitoring, in “Role of Continuous Glucose Monitoring in Diabetes Treatment.” American Diabetes Association 2018.
3. “Medicare Loosening Restrictions for Continuous Glucose Monitor (CGM) Coverage,” Healthline. 2021 Jul 13.
What is the real risk of smart phones in medicine?
Over the 10 years we’ve been writing this column, we have often found inspiration for topics while traveling – especially while flying. This is not just because of the idle time spent in the air, but instead because of the many ways that air travel and health care experiences are similar. Both industries focus heavily on safety, are tightly regulated, and employ highly trained individuals.
Consumers may recognize the similarities as well – health care and air travel are both well-known for long waits, uncertainty, and implicit risk. Both sectors are also notorious drivers of innovation, constantly leveraging new technologies in pursuit of better outcomes and experiences. Occasionally, however, advancements in technology can present unforeseen challenges and even compromise safety, with the potential to produce unexpected consequences.
A familiar reminder of this potential was provided to us at the commencement of a recent flight, when we were instructed to turn off our personal electronic devices or flip them into “airplane mode.” This same admonishment is often given to patients and visitors in health care settings – everywhere from clinic waiting rooms to intensive care units – though the reason for this is typically left vague. This got us thinking. More importantly, what other emerging technologies have the potential to create issues we may not have anticipated?
Mayo Clinic findings on radio communication used by mobile phones
Once our flight landed, we did some research to answer our initial question about personal communication technology and its ability to interfere with sensitive electronic devices. Specifically, we wanted to know whether radio communication used by mobile phones could affect the operation of medical equipment, potentially leading to dire consequences for patients. Spoiler alert: There is very little evidence that this can occur. In fact, a well-documented study performed by the Mayo Clinic in 2007 found interference in 0 out of 300 tests performed. To quote the authors, “the incidence of clinically important interference was 0%.”
We could find no other studies since 2007 that strongly contradict Mayo’s findings, except for several anecdotal reports and articles that postulate the theoretical possibility.
This is confirmed by the American Heart Association, who maintains a list of devices that may interfere with ICDs and pacemakers on their website. According to the AHA, “wireless transmissions from the antennae of phones available in the United States are a very small risk to ICDs and even less of a risk for pacemakers.” And in case you’re wondering, the story is quite similar for airplanes as well.
The latest publication from NASA’s Aviation Safety Reporting System (ASRS) documents incidents related to personal electronic devices during air travel. Most involve smoke production – or even small fires – caused by malfunctioning phone batteries during charging. Only a few entries reference wireless interference, and these were all minor and unconfirmed events. As with health care environments, airplanes don’t appear to face significant risks from radio interference. But that doesn’t mean personal electronics are completely harmless to patients.
Smartphones’ risks to patient with cardiac devices
On May 13 of 2021, the FDA issued a warning to cardiac patients about their smart phones and smart watches. Many current personal electronic devices and accessories are equipped with strong magnets, such as those contained in the “MagSafe” connector on the iPhone 12, that can deactivate pacemakers and implanted cardiac defibrillators. These medical devices are designed to be manipulated by magnets for diagnostic and therapeutic purposes, but strong magnetic fields can disable them unintentionally, leading to catastrophic results.
Apple and other manufacturers have acknowledged this risk and recommend that smartphones and other devices be kept at least 6 inches from cardiac devices. Given the ubiquity of offending products, it is also imperative that we warn our patients about this risk to their physical wellbeing.
Dr. Notte is a family physician and chief medical officer of Abington (Pa.) Hospital–Jefferson Health. Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington Hospital–Jefferson Health. They have no conflicts related to the content of this piece.
Over the 10 years we’ve been writing this column, we have often found inspiration for topics while traveling – especially while flying. This is not just because of the idle time spent in the air, but instead because of the many ways that air travel and health care experiences are similar. Both industries focus heavily on safety, are tightly regulated, and employ highly trained individuals.
Consumers may recognize the similarities as well – health care and air travel are both well-known for long waits, uncertainty, and implicit risk. Both sectors are also notorious drivers of innovation, constantly leveraging new technologies in pursuit of better outcomes and experiences. Occasionally, however, advancements in technology can present unforeseen challenges and even compromise safety, with the potential to produce unexpected consequences.
A familiar reminder of this potential was provided to us at the commencement of a recent flight, when we were instructed to turn off our personal electronic devices or flip them into “airplane mode.” This same admonishment is often given to patients and visitors in health care settings – everywhere from clinic waiting rooms to intensive care units – though the reason for this is typically left vague. This got us thinking. More importantly, what other emerging technologies have the potential to create issues we may not have anticipated?
Mayo Clinic findings on radio communication used by mobile phones
Once our flight landed, we did some research to answer our initial question about personal communication technology and its ability to interfere with sensitive electronic devices. Specifically, we wanted to know whether radio communication used by mobile phones could affect the operation of medical equipment, potentially leading to dire consequences for patients. Spoiler alert: There is very little evidence that this can occur. In fact, a well-documented study performed by the Mayo Clinic in 2007 found interference in 0 out of 300 tests performed. To quote the authors, “the incidence of clinically important interference was 0%.”
We could find no other studies since 2007 that strongly contradict Mayo’s findings, except for several anecdotal reports and articles that postulate the theoretical possibility.
This is confirmed by the American Heart Association, who maintains a list of devices that may interfere with ICDs and pacemakers on their website. According to the AHA, “wireless transmissions from the antennae of phones available in the United States are a very small risk to ICDs and even less of a risk for pacemakers.” And in case you’re wondering, the story is quite similar for airplanes as well.
The latest publication from NASA’s Aviation Safety Reporting System (ASRS) documents incidents related to personal electronic devices during air travel. Most involve smoke production – or even small fires – caused by malfunctioning phone batteries during charging. Only a few entries reference wireless interference, and these were all minor and unconfirmed events. As with health care environments, airplanes don’t appear to face significant risks from radio interference. But that doesn’t mean personal electronics are completely harmless to patients.
Smartphones’ risks to patient with cardiac devices
On May 13 of 2021, the FDA issued a warning to cardiac patients about their smart phones and smart watches. Many current personal electronic devices and accessories are equipped with strong magnets, such as those contained in the “MagSafe” connector on the iPhone 12, that can deactivate pacemakers and implanted cardiac defibrillators. These medical devices are designed to be manipulated by magnets for diagnostic and therapeutic purposes, but strong magnetic fields can disable them unintentionally, leading to catastrophic results.
Apple and other manufacturers have acknowledged this risk and recommend that smartphones and other devices be kept at least 6 inches from cardiac devices. Given the ubiquity of offending products, it is also imperative that we warn our patients about this risk to their physical wellbeing.
Dr. Notte is a family physician and chief medical officer of Abington (Pa.) Hospital–Jefferson Health. Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington Hospital–Jefferson Health. They have no conflicts related to the content of this piece.
Over the 10 years we’ve been writing this column, we have often found inspiration for topics while traveling – especially while flying. This is not just because of the idle time spent in the air, but instead because of the many ways that air travel and health care experiences are similar. Both industries focus heavily on safety, are tightly regulated, and employ highly trained individuals.
Consumers may recognize the similarities as well – health care and air travel are both well-known for long waits, uncertainty, and implicit risk. Both sectors are also notorious drivers of innovation, constantly leveraging new technologies in pursuit of better outcomes and experiences. Occasionally, however, advancements in technology can present unforeseen challenges and even compromise safety, with the potential to produce unexpected consequences.
A familiar reminder of this potential was provided to us at the commencement of a recent flight, when we were instructed to turn off our personal electronic devices or flip them into “airplane mode.” This same admonishment is often given to patients and visitors in health care settings – everywhere from clinic waiting rooms to intensive care units – though the reason for this is typically left vague. This got us thinking. More importantly, what other emerging technologies have the potential to create issues we may not have anticipated?
Mayo Clinic findings on radio communication used by mobile phones
Once our flight landed, we did some research to answer our initial question about personal communication technology and its ability to interfere with sensitive electronic devices. Specifically, we wanted to know whether radio communication used by mobile phones could affect the operation of medical equipment, potentially leading to dire consequences for patients. Spoiler alert: There is very little evidence that this can occur. In fact, a well-documented study performed by the Mayo Clinic in 2007 found interference in 0 out of 300 tests performed. To quote the authors, “the incidence of clinically important interference was 0%.”
We could find no other studies since 2007 that strongly contradict Mayo’s findings, except for several anecdotal reports and articles that postulate the theoretical possibility.
This is confirmed by the American Heart Association, who maintains a list of devices that may interfere with ICDs and pacemakers on their website. According to the AHA, “wireless transmissions from the antennae of phones available in the United States are a very small risk to ICDs and even less of a risk for pacemakers.” And in case you’re wondering, the story is quite similar for airplanes as well.
The latest publication from NASA’s Aviation Safety Reporting System (ASRS) documents incidents related to personal electronic devices during air travel. Most involve smoke production – or even small fires – caused by malfunctioning phone batteries during charging. Only a few entries reference wireless interference, and these were all minor and unconfirmed events. As with health care environments, airplanes don’t appear to face significant risks from radio interference. But that doesn’t mean personal electronics are completely harmless to patients.
Smartphones’ risks to patient with cardiac devices
On May 13 of 2021, the FDA issued a warning to cardiac patients about their smart phones and smart watches. Many current personal electronic devices and accessories are equipped with strong magnets, such as those contained in the “MagSafe” connector on the iPhone 12, that can deactivate pacemakers and implanted cardiac defibrillators. These medical devices are designed to be manipulated by magnets for diagnostic and therapeutic purposes, but strong magnetic fields can disable them unintentionally, leading to catastrophic results.
Apple and other manufacturers have acknowledged this risk and recommend that smartphones and other devices be kept at least 6 inches from cardiac devices. Given the ubiquity of offending products, it is also imperative that we warn our patients about this risk to their physical wellbeing.
Dr. Notte is a family physician and chief medical officer of Abington (Pa.) Hospital–Jefferson Health. Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington Hospital–Jefferson Health. They have no conflicts related to the content of this piece.
The Cures Act: Is the “cure” worse than the disease?
There is a sudden spill of icy anxiety down your spine as you pick up your phone in your shaking hands. It’s 6 p.m.; your doctor’s office is closed. You open the message, and your worst fears are confirmed ... the cancer is back.
Or is it? You’re not sure. The biopsy sure sounds bad. But you’re an English teacher, not a doctor, and you spend the rest of the night Googling words like “tubulovillous” and “high-grade dysplasia.” You sit awake, terrified in front of the computer screen desperately trying to make sense of the possibly life-changing results. You wish you knew someone who could help you understand; you consider calling your doctor’s emergency line, or your cousin who is an ophthalmologist – anybody who can help you make sense of the results.
Or imagine another scenario: you’re a trans teen who has asked your doctor to refer to you by your preferred pronouns. You’re still presenting as your birth sex, in part because your family would disown you if they knew, and you’re not financially or emotionally ready for that step. You feel proud of yourself for advocating for your needs to your long-time physician, and excited about the resources they’ve included in your after visit summary and the referrals they’d made to gender-confirming specialists.
When you get home, you are confronted with a terrible reality that your doctor’s notes, orders, and recommendations are immediately viewable to anybody with your MyChart login – your parents knew the second your doctor signed the note. They received the notification, logged on as your guardians, and you have effectively been “outed” by the physician who took and oath to care for you and who you trusted implicitly.
How the Cures Act is affecting patients
While these examples may sound extreme, they are becoming more and more commonplace thanks to a recently enacted 21st Century Cures Act. The act was originally written to improve communication between physicians and patients. Part of the act stipulates that nearly all medical information – from notes to biopsies to lab results – must be available within 24 hours, published to a patient portal and a notification be sent to the patient by phone.
Oftentimes, this occurs before the ordering physician has even seen the results, much less interpreted them and made a plan for the patient. What happens now, not long after its enactment date, when it has become clear that the Cures Act is causing extreme harm to our patients?
Take, for example, the real example of a physician whose patient found out about her own intrauterine fetal demise by way of an EMR text message alert of “new imaging results!” sent directly to her phone. Or a physician colleague who witnessed firsthand the intrusive unhelpfulness of the Cures Act when she was informed via patient portal releasing her imaging information that she had a large, possibly malignant breast mass. “No phone call,” she said. “No human being for questions or comfort. Just a notification on my phone.”
The stories about the impact of the Cures Act across the medical community are an endless stream of anxiety, hurt, and broken trust. The relationship between a physician and a patient should be sacred, bolstered by communication and mutual respect.
In many ways, the new act feels like a third party to the patient-physician relationship – a digital imposter, oftentimes blurting out personal and life-altering medical information without any of the finesse, context, and perspective of an experienced physician.
Breaking ‘bad news’ to a patient
In training, some residents are taught how to “break bad news” to a patient. Some good practices for doing this are to have information available for the patient, provide emotional support, have a plan for their next steps already formulated, and call the appropriate specialist ahead of time if you can.
Above all, it’s most important to let the patient be the one to direct their own care. Give them time to ask questions and answer them honestly and clearly. Ask them how much they want to know and help them to understand the complex change in their usual state of health.
Now, unless physicians are keeping a very close eye on their inbox, results are slipping out to patients in a void. The bad news conversations aren’t happening at all, or if they are, they’re happening at 8 p.m. on a phone call after an exhausted physician ends their shift but has to slog through their results bin, calling all the patients who shouldn’t have to find out their results in solitude.
Reaching out to these patients immediately is an honorable, kind thing to, but for a physician, knowing they need to beat the patient to opening an email creates anxiety. Plus, making these calls at whatever hour the results are released to a patient is another burden added to doctors’ already-full plates.
Interpreting results
None of us want to harm our patients. All of us want to be there for them. But this act stands in the way of delivering quality, humanizing medical care.
It is true that patients have a right to access their own medical information. It is also true that waiting anxiously on results can cause undue harm to a patient. But the across-the-board, breakneck speed of information release mandated in this act causes irreparable harm not only to patients, but to the patient-physician relationship.
No patient should find out their cancer recurred while checking their emails at their desk. No patient should first learn of a life-altering diagnosis by way of scrolling through their smartphone in bed. The role of a physician is more than just a healer – we should also be educators, interpreters, partners and, first and foremost, advocates for our patients’ needs.
Our patients are depending on us to stand up and speak out about necessary changes to this act. Result releases should be delayed until they are viewed by a physician. Our patients deserve the dignity and opportunity of a conversation with their medical provider about their test results, and physicians deserve the chance to interpret results and frame the conversation in a way which is conducive to patient understanding and healing.
Dr. Persampiere is a first-year resident in the family medicine residency program at Abington (Pa.) Hospital–Jefferson Health. Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington Hospital–Jefferson Health. They have no conflicts related to the content of this piece. You can contact them at fpnews@mdedge.com.
There is a sudden spill of icy anxiety down your spine as you pick up your phone in your shaking hands. It’s 6 p.m.; your doctor’s office is closed. You open the message, and your worst fears are confirmed ... the cancer is back.
Or is it? You’re not sure. The biopsy sure sounds bad. But you’re an English teacher, not a doctor, and you spend the rest of the night Googling words like “tubulovillous” and “high-grade dysplasia.” You sit awake, terrified in front of the computer screen desperately trying to make sense of the possibly life-changing results. You wish you knew someone who could help you understand; you consider calling your doctor’s emergency line, or your cousin who is an ophthalmologist – anybody who can help you make sense of the results.
Or imagine another scenario: you’re a trans teen who has asked your doctor to refer to you by your preferred pronouns. You’re still presenting as your birth sex, in part because your family would disown you if they knew, and you’re not financially or emotionally ready for that step. You feel proud of yourself for advocating for your needs to your long-time physician, and excited about the resources they’ve included in your after visit summary and the referrals they’d made to gender-confirming specialists.
When you get home, you are confronted with a terrible reality that your doctor’s notes, orders, and recommendations are immediately viewable to anybody with your MyChart login – your parents knew the second your doctor signed the note. They received the notification, logged on as your guardians, and you have effectively been “outed” by the physician who took and oath to care for you and who you trusted implicitly.
How the Cures Act is affecting patients
While these examples may sound extreme, they are becoming more and more commonplace thanks to a recently enacted 21st Century Cures Act. The act was originally written to improve communication between physicians and patients. Part of the act stipulates that nearly all medical information – from notes to biopsies to lab results – must be available within 24 hours, published to a patient portal and a notification be sent to the patient by phone.
Oftentimes, this occurs before the ordering physician has even seen the results, much less interpreted them and made a plan for the patient. What happens now, not long after its enactment date, when it has become clear that the Cures Act is causing extreme harm to our patients?
Take, for example, the real example of a physician whose patient found out about her own intrauterine fetal demise by way of an EMR text message alert of “new imaging results!” sent directly to her phone. Or a physician colleague who witnessed firsthand the intrusive unhelpfulness of the Cures Act when she was informed via patient portal releasing her imaging information that she had a large, possibly malignant breast mass. “No phone call,” she said. “No human being for questions or comfort. Just a notification on my phone.”
The stories about the impact of the Cures Act across the medical community are an endless stream of anxiety, hurt, and broken trust. The relationship between a physician and a patient should be sacred, bolstered by communication and mutual respect.
In many ways, the new act feels like a third party to the patient-physician relationship – a digital imposter, oftentimes blurting out personal and life-altering medical information without any of the finesse, context, and perspective of an experienced physician.
Breaking ‘bad news’ to a patient
In training, some residents are taught how to “break bad news” to a patient. Some good practices for doing this are to have information available for the patient, provide emotional support, have a plan for their next steps already formulated, and call the appropriate specialist ahead of time if you can.
Above all, it’s most important to let the patient be the one to direct their own care. Give them time to ask questions and answer them honestly and clearly. Ask them how much they want to know and help them to understand the complex change in their usual state of health.
Now, unless physicians are keeping a very close eye on their inbox, results are slipping out to patients in a void. The bad news conversations aren’t happening at all, or if they are, they’re happening at 8 p.m. on a phone call after an exhausted physician ends their shift but has to slog through their results bin, calling all the patients who shouldn’t have to find out their results in solitude.
Reaching out to these patients immediately is an honorable, kind thing to, but for a physician, knowing they need to beat the patient to opening an email creates anxiety. Plus, making these calls at whatever hour the results are released to a patient is another burden added to doctors’ already-full plates.
Interpreting results
None of us want to harm our patients. All of us want to be there for them. But this act stands in the way of delivering quality, humanizing medical care.
It is true that patients have a right to access their own medical information. It is also true that waiting anxiously on results can cause undue harm to a patient. But the across-the-board, breakneck speed of information release mandated in this act causes irreparable harm not only to patients, but to the patient-physician relationship.
No patient should find out their cancer recurred while checking their emails at their desk. No patient should first learn of a life-altering diagnosis by way of scrolling through their smartphone in bed. The role of a physician is more than just a healer – we should also be educators, interpreters, partners and, first and foremost, advocates for our patients’ needs.
Our patients are depending on us to stand up and speak out about necessary changes to this act. Result releases should be delayed until they are viewed by a physician. Our patients deserve the dignity and opportunity of a conversation with their medical provider about their test results, and physicians deserve the chance to interpret results and frame the conversation in a way which is conducive to patient understanding and healing.
Dr. Persampiere is a first-year resident in the family medicine residency program at Abington (Pa.) Hospital–Jefferson Health. Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington Hospital–Jefferson Health. They have no conflicts related to the content of this piece. You can contact them at fpnews@mdedge.com.
There is a sudden spill of icy anxiety down your spine as you pick up your phone in your shaking hands. It’s 6 p.m.; your doctor’s office is closed. You open the message, and your worst fears are confirmed ... the cancer is back.
Or is it? You’re not sure. The biopsy sure sounds bad. But you’re an English teacher, not a doctor, and you spend the rest of the night Googling words like “tubulovillous” and “high-grade dysplasia.” You sit awake, terrified in front of the computer screen desperately trying to make sense of the possibly life-changing results. You wish you knew someone who could help you understand; you consider calling your doctor’s emergency line, or your cousin who is an ophthalmologist – anybody who can help you make sense of the results.
Or imagine another scenario: you’re a trans teen who has asked your doctor to refer to you by your preferred pronouns. You’re still presenting as your birth sex, in part because your family would disown you if they knew, and you’re not financially or emotionally ready for that step. You feel proud of yourself for advocating for your needs to your long-time physician, and excited about the resources they’ve included in your after visit summary and the referrals they’d made to gender-confirming specialists.
When you get home, you are confronted with a terrible reality that your doctor’s notes, orders, and recommendations are immediately viewable to anybody with your MyChart login – your parents knew the second your doctor signed the note. They received the notification, logged on as your guardians, and you have effectively been “outed” by the physician who took and oath to care for you and who you trusted implicitly.
How the Cures Act is affecting patients
While these examples may sound extreme, they are becoming more and more commonplace thanks to a recently enacted 21st Century Cures Act. The act was originally written to improve communication between physicians and patients. Part of the act stipulates that nearly all medical information – from notes to biopsies to lab results – must be available within 24 hours, published to a patient portal and a notification be sent to the patient by phone.
Oftentimes, this occurs before the ordering physician has even seen the results, much less interpreted them and made a plan for the patient. What happens now, not long after its enactment date, when it has become clear that the Cures Act is causing extreme harm to our patients?
Take, for example, the real example of a physician whose patient found out about her own intrauterine fetal demise by way of an EMR text message alert of “new imaging results!” sent directly to her phone. Or a physician colleague who witnessed firsthand the intrusive unhelpfulness of the Cures Act when she was informed via patient portal releasing her imaging information that she had a large, possibly malignant breast mass. “No phone call,” she said. “No human being for questions or comfort. Just a notification on my phone.”
The stories about the impact of the Cures Act across the medical community are an endless stream of anxiety, hurt, and broken trust. The relationship between a physician and a patient should be sacred, bolstered by communication and mutual respect.
In many ways, the new act feels like a third party to the patient-physician relationship – a digital imposter, oftentimes blurting out personal and life-altering medical information without any of the finesse, context, and perspective of an experienced physician.
Breaking ‘bad news’ to a patient
In training, some residents are taught how to “break bad news” to a patient. Some good practices for doing this are to have information available for the patient, provide emotional support, have a plan for their next steps already formulated, and call the appropriate specialist ahead of time if you can.
Above all, it’s most important to let the patient be the one to direct their own care. Give them time to ask questions and answer them honestly and clearly. Ask them how much they want to know and help them to understand the complex change in their usual state of health.
Now, unless physicians are keeping a very close eye on their inbox, results are slipping out to patients in a void. The bad news conversations aren’t happening at all, or if they are, they’re happening at 8 p.m. on a phone call after an exhausted physician ends their shift but has to slog through their results bin, calling all the patients who shouldn’t have to find out their results in solitude.
Reaching out to these patients immediately is an honorable, kind thing to, but for a physician, knowing they need to beat the patient to opening an email creates anxiety. Plus, making these calls at whatever hour the results are released to a patient is another burden added to doctors’ already-full plates.
Interpreting results
None of us want to harm our patients. All of us want to be there for them. But this act stands in the way of delivering quality, humanizing medical care.
It is true that patients have a right to access their own medical information. It is also true that waiting anxiously on results can cause undue harm to a patient. But the across-the-board, breakneck speed of information release mandated in this act causes irreparable harm not only to patients, but to the patient-physician relationship.
No patient should find out their cancer recurred while checking their emails at their desk. No patient should first learn of a life-altering diagnosis by way of scrolling through their smartphone in bed. The role of a physician is more than just a healer – we should also be educators, interpreters, partners and, first and foremost, advocates for our patients’ needs.
Our patients are depending on us to stand up and speak out about necessary changes to this act. Result releases should be delayed until they are viewed by a physician. Our patients deserve the dignity and opportunity of a conversation with their medical provider about their test results, and physicians deserve the chance to interpret results and frame the conversation in a way which is conducive to patient understanding and healing.
Dr. Persampiere is a first-year resident in the family medicine residency program at Abington (Pa.) Hospital–Jefferson Health. Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington Hospital–Jefferson Health. They have no conflicts related to the content of this piece. You can contact them at fpnews@mdedge.com.
Change is hard: Lessons from an EHR conversion
During this “go-live,” 5 hospitals and approximately 300 ambulatory service and physician practice locations made the transition, consolidating over 100 disparate electronic systems and dozens of interfaces into one world-class medical record.
If you’ve ever been part of such an event, you know it is anything but simple. On the contrary, it requires an enormous financial investment along with years of planning, hours of meetings, and months of training. No matter how much preparation goes into it, there are sure to be bumps along the way. It is a traumatic and stressful time for all involved, but the end result is well worth the effort. Still, there are lessons to be learned and wisdom to be gleaned, and this month we’d like to share a few that we found most important. We believe that many of these are useful lessons even to those who will never live through a go-live.
Safety always comes first
Patient safety is a term so often used that it has a tendency to be taken for granted. Health systems build processes and procedures to ensure safety – some even win awards and recognition for their efforts. But the best (and safest) health care institutions build patient safety into their cultures. More than just being taught to use checklists or buzzwords, the staff at these institutions are encouraged to put the welfare of patients first, making all other activities secondary to this pursuit. We had the opportunity to witness the benefits of such a culture during this go-live and were incredibly impressed with the results.
To be successful in an EHR transition of any magnitude, an organization needs to hold patient safety as a core value and provide its employees with the tools to execute on that value. This enables staff to prepare adequately and to identify risks and opportunities before the conversion takes place. Once go-live occurs, staff also must feel empowered to speak up when they identify problem areas that might jeopardize patients’ care. They also must be given a clear escalation path to ensure their voices can be heard. Most importantly, everyone must understand that the electronic health record itself is just one piece of a major operational change.
As workflows are modified to adapt to the new technology, unsafe processes should be called out and fixed quickly. While the EHR may offer the latest in decision support and system integration, no advancement in technology can make up for bad outcomes, nor justify processes that lead to patient harm.
Training is no substitute for good support
It takes a long time to train thousands of employees, especially when that training must occur during the era of social distancing in the midst of a pandemic. Still, even in the best of times, education should be married to hands-on experience in order to have a real impact. Unfortunately, this is extremely challenging.
Trainees forget much of what they’ve learned in the weeks or months between education and go-live, so they must be given immediately accessible support to bridge the gap. This is known as “at-the-elbow” (ATE) support, and as the name implies, it consists of individuals who are familiar with the new system and are always available to end users, answering their questions and helping them navigate. Since health care never sleeps, this support needs to be offered 24/7, and it should also be flexible and plentiful.
There are many areas that will require more support than anticipated to accommodate the number of clinical and other staff who will use the system, so support staff must be nimble and available for redeployment. In addition, ensuring high-quality support is essential. As many ATE experts are hired contractors, their knowledge base and communications skills can vary widely. Accountability is key, and end users should feel empowered to identify gaps in coverage and deficits in knowledge base in the ATE.
As employees become more familiar with the new system, the need for ATE will wane, but there will still be questions that arise for many weeks to months, and new EHR users will also be added all the time. A good after–go-live support system should remain available so clinical and clerical employees can get just-in-time assistance whenever they need it.
Users should be given clear expectations
Clinicians going through an EHR conversion may be frustrated to discover that the data transferred from their old system into the new one is not quite what they expected. While structured elements such as allergies and immunizations may transfer, unstructured patient histories may not come over at all.
There may be gaps in data, or the opposite may even be true: an overabundance of useless information may transfer over, leaving doctors with dozens of meaningless data points to sift through and eliminate to clean up the chart. This can be extremely time-consuming and discouraging and may jeopardize the success of the go-live.
Providers deserve clear expectations prior to conversion. They should be told what will and will not transfer and be informed that there will be extra work required for documentation at the outset. They may also want the option to preemptively reduce patient volumes to accommodate the additional effort involved in preparing charts. No matter what, this will be a heavy lift, and physicians should understand the implications long before go-live to prepare accordingly.
Old habits die hard
One of the most common complaints we’ve heard following EHR conversions is that “things just worked better in the old system.” We always respond with a question: “Were things better, or just different?” The truth may lie somewhere in the middle, but there is no question that muscle memory develops over many years, and change is difficult no matter how much better the new system is. Still, appropriate expectations, access to just-in-time support, and a continual focus on safety will ensure that the long-term benefits of a patient-centered and integrated electronic record will far outweigh the initial challenges of go-live.
Dr. Notte is a family physician and chief medical officer of Abington (Pa.) Hospital–Jefferson Health. Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington Hospital–Jefferson Health. They have no conflicts related to the content of this piece.
During this “go-live,” 5 hospitals and approximately 300 ambulatory service and physician practice locations made the transition, consolidating over 100 disparate electronic systems and dozens of interfaces into one world-class medical record.
If you’ve ever been part of such an event, you know it is anything but simple. On the contrary, it requires an enormous financial investment along with years of planning, hours of meetings, and months of training. No matter how much preparation goes into it, there are sure to be bumps along the way. It is a traumatic and stressful time for all involved, but the end result is well worth the effort. Still, there are lessons to be learned and wisdom to be gleaned, and this month we’d like to share a few that we found most important. We believe that many of these are useful lessons even to those who will never live through a go-live.
Safety always comes first
Patient safety is a term so often used that it has a tendency to be taken for granted. Health systems build processes and procedures to ensure safety – some even win awards and recognition for their efforts. But the best (and safest) health care institutions build patient safety into their cultures. More than just being taught to use checklists or buzzwords, the staff at these institutions are encouraged to put the welfare of patients first, making all other activities secondary to this pursuit. We had the opportunity to witness the benefits of such a culture during this go-live and were incredibly impressed with the results.
To be successful in an EHR transition of any magnitude, an organization needs to hold patient safety as a core value and provide its employees with the tools to execute on that value. This enables staff to prepare adequately and to identify risks and opportunities before the conversion takes place. Once go-live occurs, staff also must feel empowered to speak up when they identify problem areas that might jeopardize patients’ care. They also must be given a clear escalation path to ensure their voices can be heard. Most importantly, everyone must understand that the electronic health record itself is just one piece of a major operational change.
As workflows are modified to adapt to the new technology, unsafe processes should be called out and fixed quickly. While the EHR may offer the latest in decision support and system integration, no advancement in technology can make up for bad outcomes, nor justify processes that lead to patient harm.
Training is no substitute for good support
It takes a long time to train thousands of employees, especially when that training must occur during the era of social distancing in the midst of a pandemic. Still, even in the best of times, education should be married to hands-on experience in order to have a real impact. Unfortunately, this is extremely challenging.
Trainees forget much of what they’ve learned in the weeks or months between education and go-live, so they must be given immediately accessible support to bridge the gap. This is known as “at-the-elbow” (ATE) support, and as the name implies, it consists of individuals who are familiar with the new system and are always available to end users, answering their questions and helping them navigate. Since health care never sleeps, this support needs to be offered 24/7, and it should also be flexible and plentiful.
There are many areas that will require more support than anticipated to accommodate the number of clinical and other staff who will use the system, so support staff must be nimble and available for redeployment. In addition, ensuring high-quality support is essential. As many ATE experts are hired contractors, their knowledge base and communications skills can vary widely. Accountability is key, and end users should feel empowered to identify gaps in coverage and deficits in knowledge base in the ATE.
As employees become more familiar with the new system, the need for ATE will wane, but there will still be questions that arise for many weeks to months, and new EHR users will also be added all the time. A good after–go-live support system should remain available so clinical and clerical employees can get just-in-time assistance whenever they need it.
Users should be given clear expectations
Clinicians going through an EHR conversion may be frustrated to discover that the data transferred from their old system into the new one is not quite what they expected. While structured elements such as allergies and immunizations may transfer, unstructured patient histories may not come over at all.
There may be gaps in data, or the opposite may even be true: an overabundance of useless information may transfer over, leaving doctors with dozens of meaningless data points to sift through and eliminate to clean up the chart. This can be extremely time-consuming and discouraging and may jeopardize the success of the go-live.
Providers deserve clear expectations prior to conversion. They should be told what will and will not transfer and be informed that there will be extra work required for documentation at the outset. They may also want the option to preemptively reduce patient volumes to accommodate the additional effort involved in preparing charts. No matter what, this will be a heavy lift, and physicians should understand the implications long before go-live to prepare accordingly.
Old habits die hard
One of the most common complaints we’ve heard following EHR conversions is that “things just worked better in the old system.” We always respond with a question: “Were things better, or just different?” The truth may lie somewhere in the middle, but there is no question that muscle memory develops over many years, and change is difficult no matter how much better the new system is. Still, appropriate expectations, access to just-in-time support, and a continual focus on safety will ensure that the long-term benefits of a patient-centered and integrated electronic record will far outweigh the initial challenges of go-live.
Dr. Notte is a family physician and chief medical officer of Abington (Pa.) Hospital–Jefferson Health. Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington Hospital–Jefferson Health. They have no conflicts related to the content of this piece.
During this “go-live,” 5 hospitals and approximately 300 ambulatory service and physician practice locations made the transition, consolidating over 100 disparate electronic systems and dozens of interfaces into one world-class medical record.
If you’ve ever been part of such an event, you know it is anything but simple. On the contrary, it requires an enormous financial investment along with years of planning, hours of meetings, and months of training. No matter how much preparation goes into it, there are sure to be bumps along the way. It is a traumatic and stressful time for all involved, but the end result is well worth the effort. Still, there are lessons to be learned and wisdom to be gleaned, and this month we’d like to share a few that we found most important. We believe that many of these are useful lessons even to those who will never live through a go-live.
Safety always comes first
Patient safety is a term so often used that it has a tendency to be taken for granted. Health systems build processes and procedures to ensure safety – some even win awards and recognition for their efforts. But the best (and safest) health care institutions build patient safety into their cultures. More than just being taught to use checklists or buzzwords, the staff at these institutions are encouraged to put the welfare of patients first, making all other activities secondary to this pursuit. We had the opportunity to witness the benefits of such a culture during this go-live and were incredibly impressed with the results.
To be successful in an EHR transition of any magnitude, an organization needs to hold patient safety as a core value and provide its employees with the tools to execute on that value. This enables staff to prepare adequately and to identify risks and opportunities before the conversion takes place. Once go-live occurs, staff also must feel empowered to speak up when they identify problem areas that might jeopardize patients’ care. They also must be given a clear escalation path to ensure their voices can be heard. Most importantly, everyone must understand that the electronic health record itself is just one piece of a major operational change.
As workflows are modified to adapt to the new technology, unsafe processes should be called out and fixed quickly. While the EHR may offer the latest in decision support and system integration, no advancement in technology can make up for bad outcomes, nor justify processes that lead to patient harm.
Training is no substitute for good support
It takes a long time to train thousands of employees, especially when that training must occur during the era of social distancing in the midst of a pandemic. Still, even in the best of times, education should be married to hands-on experience in order to have a real impact. Unfortunately, this is extremely challenging.
Trainees forget much of what they’ve learned in the weeks or months between education and go-live, so they must be given immediately accessible support to bridge the gap. This is known as “at-the-elbow” (ATE) support, and as the name implies, it consists of individuals who are familiar with the new system and are always available to end users, answering their questions and helping them navigate. Since health care never sleeps, this support needs to be offered 24/7, and it should also be flexible and plentiful.
There are many areas that will require more support than anticipated to accommodate the number of clinical and other staff who will use the system, so support staff must be nimble and available for redeployment. In addition, ensuring high-quality support is essential. As many ATE experts are hired contractors, their knowledge base and communications skills can vary widely. Accountability is key, and end users should feel empowered to identify gaps in coverage and deficits in knowledge base in the ATE.
As employees become more familiar with the new system, the need for ATE will wane, but there will still be questions that arise for many weeks to months, and new EHR users will also be added all the time. A good after–go-live support system should remain available so clinical and clerical employees can get just-in-time assistance whenever they need it.
Users should be given clear expectations
Clinicians going through an EHR conversion may be frustrated to discover that the data transferred from their old system into the new one is not quite what they expected. While structured elements such as allergies and immunizations may transfer, unstructured patient histories may not come over at all.
There may be gaps in data, or the opposite may even be true: an overabundance of useless information may transfer over, leaving doctors with dozens of meaningless data points to sift through and eliminate to clean up the chart. This can be extremely time-consuming and discouraging and may jeopardize the success of the go-live.
Providers deserve clear expectations prior to conversion. They should be told what will and will not transfer and be informed that there will be extra work required for documentation at the outset. They may also want the option to preemptively reduce patient volumes to accommodate the additional effort involved in preparing charts. No matter what, this will be a heavy lift, and physicians should understand the implications long before go-live to prepare accordingly.
Old habits die hard
One of the most common complaints we’ve heard following EHR conversions is that “things just worked better in the old system.” We always respond with a question: “Were things better, or just different?” The truth may lie somewhere in the middle, but there is no question that muscle memory develops over many years, and change is difficult no matter how much better the new system is. Still, appropriate expectations, access to just-in-time support, and a continual focus on safety will ensure that the long-term benefits of a patient-centered and integrated electronic record will far outweigh the initial challenges of go-live.
Dr. Notte is a family physician and chief medical officer of Abington (Pa.) Hospital–Jefferson Health. Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington Hospital–Jefferson Health. They have no conflicts related to the content of this piece.
Home devices screen for atrial fibrillation
In an ad for one of these products, KardiaMobile, a cardiologist says this device “detects atrial fibrillation, one of the major causes of stroke.” You might also have heard that the Apple Watch has an opt-in feature that constantly screens for atrial fibrillation without any effort being made by the patient, or can check on-demand for AFib if a wearer experiences palpitations or an abnormal heart beat. Both of these devices generate a standard limb–lead ECG (essentially lead I) by connecting the device to both arms and producing a 30-second rhythm strip.
KardiaMobile recently introduced a newer device. When you place this device on a bare knee and touch one electrode with fingers from the right hand and another electrode with fingers from the left hand, the device produces a six-lead ECG. These small devices send an image of the ECG to a patient’s smartphone over Bluetooth, and the results can be easily read, printed out, or sent to the doctor for further analysis. Additionally, both of KardiaMobile’s devices utilize artificial intelligence to analyze a rhythm strip in real time and let the patient know if the ECG is normal, shows AFib, or is unable to be analyzed.
The electrocardiographic technology was formerly only available in a medical setting. It required an expensive machine and could only be interpreted by someone with expertise developed through years of training. Now it is readily available to patients in their homes. But how accurate is the technology and how are we going to use it?
How effective is KardiaMobile at detecting AFib?
Studies have looked at both KardiaMobile and the Apple Watch. One study of KardiaMobile in patients with Afib who were admitted for antiarrhythmic drug initiation showed that about a quarter of readings could not be classified because of artifact and other reasons. After exclusion of unclassified recordings, the KardiaMobile interpretation had 97% sensitivity and 94% specificity for AFib detection when compared with physician-interpreted ECGs.1 In a large review of the device’s accuracy, there was about 85% sensitivity and specificity of the automated readings.2
How does the Apple Watch find AFib?
Like the KardiaMobile device, the Apple Watch can be used whenever patients notice symptoms or whenever they and their physicians decide the device would be useful. In addition, though, the Apple Watch has a function where the wearer can opt in to have the watch screen for AFib in the background whenever the watch is worn.
The watch monitors heart rate using photoplethysmography, where light-sensitive photodiodes detect blood pulses to assess heart rate variability. When an irregular heart rate is detected, the AW alerts the user of possible AFib. Once alerted, the wearer can then utilize a second function to obtain a single-lead ECG. Heart rate, rhythm, and a 30-second ECG tracing are saved in the Bluetooth-linked iPhone’s health app and can be exported for review by a physician.
In a study of over 400,000 participants, among participants notified of an irregular pulse through screening there was a positive predictive value of 84%.3 Single-lead EKGs initiated by watch wearers had a specificity for AFib of 99.6% among tracings with good wave forms, indicating very few false positives. Only 1 individual of the 263 individuals who had normal sinus rhythm on 12-lead ECG was classified as having AFib, though in 7% sinus rhythm could not be confirmed because of poor tracings.4,5
What should we do with the results?
It’s impressive that these devices deliver accurate information with very good specificity. Our hope is that detecting AFib with one of these devices will lead to an intervention being made that will decrease a patient’s risk of stroke. But it is not clear if routine screening in asymptomatic adults will accomplish this.
While more data is needed, we must acknowledge that our patients will soon be bringing us results from home. Regardless of what we think of this technology, we need to decide what to do when patients call us with results from these devices.
Dr. Notte is a family physician and chief medical officer of Abington (Pa.) Hospital–Jefferson Health. Follow him on Twitter (@doctornotte). Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington Hospital–Jefferson Health. They have no conflicts related to the content of this piece.
References
1. William A et al. Heart Rhythm. 2018 Oct;15(10):1561-5.
2. KardiaMobile for the ambulatory detection of atrial fibrillation. NICE Medtech innovation briefing. 29 October 2020 Oct 29. www.nice.org.uk/guidance/mib232.
3. Perez MV et al. N Engl J Med. 2019; 381:1909-17.
4. Using Apple Watch for Arrhythmia Detection, December 2018. Apple. https://www.apple.com/healthcare/site/docs/Apple_Watch_Arrhythmia_Detection.pdf. Accessed 2019 Apr 5.
5. De Novo Classification Request for ECG App. https://www.accessdata.fda.gov/cdrh_docs/reviews/DEN180044.pdf. Accessed 2019 Apr 29.
In an ad for one of these products, KardiaMobile, a cardiologist says this device “detects atrial fibrillation, one of the major causes of stroke.” You might also have heard that the Apple Watch has an opt-in feature that constantly screens for atrial fibrillation without any effort being made by the patient, or can check on-demand for AFib if a wearer experiences palpitations or an abnormal heart beat. Both of these devices generate a standard limb–lead ECG (essentially lead I) by connecting the device to both arms and producing a 30-second rhythm strip.
KardiaMobile recently introduced a newer device. When you place this device on a bare knee and touch one electrode with fingers from the right hand and another electrode with fingers from the left hand, the device produces a six-lead ECG. These small devices send an image of the ECG to a patient’s smartphone over Bluetooth, and the results can be easily read, printed out, or sent to the doctor for further analysis. Additionally, both of KardiaMobile’s devices utilize artificial intelligence to analyze a rhythm strip in real time and let the patient know if the ECG is normal, shows AFib, or is unable to be analyzed.
The electrocardiographic technology was formerly only available in a medical setting. It required an expensive machine and could only be interpreted by someone with expertise developed through years of training. Now it is readily available to patients in their homes. But how accurate is the technology and how are we going to use it?
How effective is KardiaMobile at detecting AFib?
Studies have looked at both KardiaMobile and the Apple Watch. One study of KardiaMobile in patients with Afib who were admitted for antiarrhythmic drug initiation showed that about a quarter of readings could not be classified because of artifact and other reasons. After exclusion of unclassified recordings, the KardiaMobile interpretation had 97% sensitivity and 94% specificity for AFib detection when compared with physician-interpreted ECGs.1 In a large review of the device’s accuracy, there was about 85% sensitivity and specificity of the automated readings.2
How does the Apple Watch find AFib?
Like the KardiaMobile device, the Apple Watch can be used whenever patients notice symptoms or whenever they and their physicians decide the device would be useful. In addition, though, the Apple Watch has a function where the wearer can opt in to have the watch screen for AFib in the background whenever the watch is worn.
The watch monitors heart rate using photoplethysmography, where light-sensitive photodiodes detect blood pulses to assess heart rate variability. When an irregular heart rate is detected, the AW alerts the user of possible AFib. Once alerted, the wearer can then utilize a second function to obtain a single-lead ECG. Heart rate, rhythm, and a 30-second ECG tracing are saved in the Bluetooth-linked iPhone’s health app and can be exported for review by a physician.
In a study of over 400,000 participants, among participants notified of an irregular pulse through screening there was a positive predictive value of 84%.3 Single-lead EKGs initiated by watch wearers had a specificity for AFib of 99.6% among tracings with good wave forms, indicating very few false positives. Only 1 individual of the 263 individuals who had normal sinus rhythm on 12-lead ECG was classified as having AFib, though in 7% sinus rhythm could not be confirmed because of poor tracings.4,5
What should we do with the results?
It’s impressive that these devices deliver accurate information with very good specificity. Our hope is that detecting AFib with one of these devices will lead to an intervention being made that will decrease a patient’s risk of stroke. But it is not clear if routine screening in asymptomatic adults will accomplish this.
While more data is needed, we must acknowledge that our patients will soon be bringing us results from home. Regardless of what we think of this technology, we need to decide what to do when patients call us with results from these devices.
Dr. Notte is a family physician and chief medical officer of Abington (Pa.) Hospital–Jefferson Health. Follow him on Twitter (@doctornotte). Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington Hospital–Jefferson Health. They have no conflicts related to the content of this piece.
References
1. William A et al. Heart Rhythm. 2018 Oct;15(10):1561-5.
2. KardiaMobile for the ambulatory detection of atrial fibrillation. NICE Medtech innovation briefing. 29 October 2020 Oct 29. www.nice.org.uk/guidance/mib232.
3. Perez MV et al. N Engl J Med. 2019; 381:1909-17.
4. Using Apple Watch for Arrhythmia Detection, December 2018. Apple. https://www.apple.com/healthcare/site/docs/Apple_Watch_Arrhythmia_Detection.pdf. Accessed 2019 Apr 5.
5. De Novo Classification Request for ECG App. https://www.accessdata.fda.gov/cdrh_docs/reviews/DEN180044.pdf. Accessed 2019 Apr 29.
In an ad for one of these products, KardiaMobile, a cardiologist says this device “detects atrial fibrillation, one of the major causes of stroke.” You might also have heard that the Apple Watch has an opt-in feature that constantly screens for atrial fibrillation without any effort being made by the patient, or can check on-demand for AFib if a wearer experiences palpitations or an abnormal heart beat. Both of these devices generate a standard limb–lead ECG (essentially lead I) by connecting the device to both arms and producing a 30-second rhythm strip.
KardiaMobile recently introduced a newer device. When you place this device on a bare knee and touch one electrode with fingers from the right hand and another electrode with fingers from the left hand, the device produces a six-lead ECG. These small devices send an image of the ECG to a patient’s smartphone over Bluetooth, and the results can be easily read, printed out, or sent to the doctor for further analysis. Additionally, both of KardiaMobile’s devices utilize artificial intelligence to analyze a rhythm strip in real time and let the patient know if the ECG is normal, shows AFib, or is unable to be analyzed.
The electrocardiographic technology was formerly only available in a medical setting. It required an expensive machine and could only be interpreted by someone with expertise developed through years of training. Now it is readily available to patients in their homes. But how accurate is the technology and how are we going to use it?
How effective is KardiaMobile at detecting AFib?
Studies have looked at both KardiaMobile and the Apple Watch. One study of KardiaMobile in patients with Afib who were admitted for antiarrhythmic drug initiation showed that about a quarter of readings could not be classified because of artifact and other reasons. After exclusion of unclassified recordings, the KardiaMobile interpretation had 97% sensitivity and 94% specificity for AFib detection when compared with physician-interpreted ECGs.1 In a large review of the device’s accuracy, there was about 85% sensitivity and specificity of the automated readings.2
How does the Apple Watch find AFib?
Like the KardiaMobile device, the Apple Watch can be used whenever patients notice symptoms or whenever they and their physicians decide the device would be useful. In addition, though, the Apple Watch has a function where the wearer can opt in to have the watch screen for AFib in the background whenever the watch is worn.
The watch monitors heart rate using photoplethysmography, where light-sensitive photodiodes detect blood pulses to assess heart rate variability. When an irregular heart rate is detected, the AW alerts the user of possible AFib. Once alerted, the wearer can then utilize a second function to obtain a single-lead ECG. Heart rate, rhythm, and a 30-second ECG tracing are saved in the Bluetooth-linked iPhone’s health app and can be exported for review by a physician.
In a study of over 400,000 participants, among participants notified of an irregular pulse through screening there was a positive predictive value of 84%.3 Single-lead EKGs initiated by watch wearers had a specificity for AFib of 99.6% among tracings with good wave forms, indicating very few false positives. Only 1 individual of the 263 individuals who had normal sinus rhythm on 12-lead ECG was classified as having AFib, though in 7% sinus rhythm could not be confirmed because of poor tracings.4,5
What should we do with the results?
It’s impressive that these devices deliver accurate information with very good specificity. Our hope is that detecting AFib with one of these devices will lead to an intervention being made that will decrease a patient’s risk of stroke. But it is not clear if routine screening in asymptomatic adults will accomplish this.
While more data is needed, we must acknowledge that our patients will soon be bringing us results from home. Regardless of what we think of this technology, we need to decide what to do when patients call us with results from these devices.
Dr. Notte is a family physician and chief medical officer of Abington (Pa.) Hospital–Jefferson Health. Follow him on Twitter (@doctornotte). Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington Hospital–Jefferson Health. They have no conflicts related to the content of this piece.
References
1. William A et al. Heart Rhythm. 2018 Oct;15(10):1561-5.
2. KardiaMobile for the ambulatory detection of atrial fibrillation. NICE Medtech innovation briefing. 29 October 2020 Oct 29. www.nice.org.uk/guidance/mib232.
3. Perez MV et al. N Engl J Med. 2019; 381:1909-17.
4. Using Apple Watch for Arrhythmia Detection, December 2018. Apple. https://www.apple.com/healthcare/site/docs/Apple_Watch_Arrhythmia_Detection.pdf. Accessed 2019 Apr 5.
5. De Novo Classification Request for ECG App. https://www.accessdata.fda.gov/cdrh_docs/reviews/DEN180044.pdf. Accessed 2019 Apr 29.
Medication adherence challenges and helpers
For most chronic diseases, up to 20%-30% of the pills that are prescribed are not taken. In the case of inhalers for asthma and COPD, patients miss over half of the prescribed doses.
There are many things that contribute to the problem of poor adherence, but people often just simply forget. Thankfully, there are tools designed to help remind patients of what they need to take and when. A survey of apps developed to help patients remember to take their medicines found more than 700 available in Apple and Android app stores.1 Most apps focus on medication alerts, reminders, and medication logs.2 A recent review showed that apps have some – yet limited – effectiveness in increasing adherence, with patient self-reported improvements of 7%-40%.3
Another perhaps more promising area of improving adherence involves high-tech advances in the way medications can be taken. Inhalers are a primary target as they are complicated devices. A patient has to breathe in at the correct time after the inhaler is actuated, and the inhaler works optimally only if the rate of inhalation is sufficient to carry the medication into the lungs.
A number of companies have developed attachments for inhalers (and even inhalers themselves) that can record when the medication is taken through a Bluetooth connection to a patient’s smartphone. These can also assess inspiratory flow. Reminders to take the medication are built into the app, and those reminders disappear if the medication is taken. Patients can receive feedback about the quality of their timing and inspiratory rate to maximize medication delivery to the lungs.4
We learned long ago that it is difficult to take medications three to four times a day, so extended-release tablets were developed to reduce the frequency to once or twice a day. A great deal of work is now being done behind the scenes to develop medications that decrease the need for patients to remember to take their medications. The best examples of this are the long-acting reversible contraception (LARC) devices, specifically IUDs and Nexplanon. Compared with traditional oral contraceptives that need to be taken daily, LARCs reduce the rate of pregnancy by five- to tenfold.
We also now have medications for osteoporosis that can be taken monthly, or even annually. When bisphosphonates were first developed for osteoporosis prevention, they needed to be taken daily. Then a weekly bisphosphonate was developed. Now there is a once-monthly oral bisphosphonate, Ibandronate, and even a once yearly IV bisphosphonate.
Exciting developments have also occurred in the management of diabetes. We may be tempted to take for granted how once-daily long-acting insulin, which releases insulin slowly over the course of a day, has revolutionized the diabetic treatment since its Food and Drug Administration approval in 2000. Yet progress did not end there. The first GLP-1 receptor agonist for diabetes was approved in 2005 and was a twice-a-day medicine. Shortly afterward, a daily GLP-1 was approved, and now there are three once-weekly GLP-1 receptor agonists.
Several pharmaceutical manufacturers are now working on a once-weekly insulin,5 as well as an implantable GLP-1 receptor agonist that will need to be replaced every 6-12 months.6 Imagine your patient coming in once a year to replace his or her potent glucose lowering medication – one that offers a low incidence of hypoglycemia, maintains glucose control all year long, and requires no adherence to a complicated medication regimen.
Similar technology is being used to develop a once-yearly anti-HIV prophylactic medication delivery system.7 This could help prevent the spread of HIV in areas of the world where it may be difficult for people to take daily medications.7
The many technological advances we have described may help us reduce our likelihood of missing a dose of a medication. We are hopeful that progress in this area will continue, and that one day medication adherence will require even less effort from patients than it does today.
Dr. Notte is a family physician and chief medical officer of Abington (Pa.) Hospital–Jefferson Health. Follow him on Twitter (@doctornotte). Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington Hospital–Jefferson Health. They have no conflicts related to the content of this piece.
References
1. Tabi K et al. Mobile apps for medication management: Review and analysis. JMIR Mhealth Uhealth. 2019 Sep 7(9):13608.
2. Park JYE et al. Mobile phone apps targeting medication adherence: Quality assessment and content analysis of user reviews. JMIR Mhealth Uhealth. 2019 Jan 31;7(1):e11919.
3. Pérez-Jover V et al. Mobile apps for increasing treatment adherence: Systematic review. J Med Internet Res. 2019;21(6):e12505. doi: 10.2196/12505.
4. 4 Smart inhalers that could be lifesaving for people living with asthma & COPD. MyTherapy, July 11, 2019.
5. Rosenstock J et al. Once-weekly insulin for type 2 diabetes without previous insulin treatment. N Engl J Med. 2020 Sep 22. doi: 10.1056/NEJMoa2022474.
6. GLP-1 agonists: From 2 daily injections to 1 per week and beyond. DiaTribe, Jan. 10, 2018.
7. Long-acting HIV prevention tools. Hiv.gov, July 20, 2019.
For most chronic diseases, up to 20%-30% of the pills that are prescribed are not taken. In the case of inhalers for asthma and COPD, patients miss over half of the prescribed doses.
There are many things that contribute to the problem of poor adherence, but people often just simply forget. Thankfully, there are tools designed to help remind patients of what they need to take and when. A survey of apps developed to help patients remember to take their medicines found more than 700 available in Apple and Android app stores.1 Most apps focus on medication alerts, reminders, and medication logs.2 A recent review showed that apps have some – yet limited – effectiveness in increasing adherence, with patient self-reported improvements of 7%-40%.3
Another perhaps more promising area of improving adherence involves high-tech advances in the way medications can be taken. Inhalers are a primary target as they are complicated devices. A patient has to breathe in at the correct time after the inhaler is actuated, and the inhaler works optimally only if the rate of inhalation is sufficient to carry the medication into the lungs.
A number of companies have developed attachments for inhalers (and even inhalers themselves) that can record when the medication is taken through a Bluetooth connection to a patient’s smartphone. These can also assess inspiratory flow. Reminders to take the medication are built into the app, and those reminders disappear if the medication is taken. Patients can receive feedback about the quality of their timing and inspiratory rate to maximize medication delivery to the lungs.4
We learned long ago that it is difficult to take medications three to four times a day, so extended-release tablets were developed to reduce the frequency to once or twice a day. A great deal of work is now being done behind the scenes to develop medications that decrease the need for patients to remember to take their medications. The best examples of this are the long-acting reversible contraception (LARC) devices, specifically IUDs and Nexplanon. Compared with traditional oral contraceptives that need to be taken daily, LARCs reduce the rate of pregnancy by five- to tenfold.
We also now have medications for osteoporosis that can be taken monthly, or even annually. When bisphosphonates were first developed for osteoporosis prevention, they needed to be taken daily. Then a weekly bisphosphonate was developed. Now there is a once-monthly oral bisphosphonate, Ibandronate, and even a once yearly IV bisphosphonate.
Exciting developments have also occurred in the management of diabetes. We may be tempted to take for granted how once-daily long-acting insulin, which releases insulin slowly over the course of a day, has revolutionized the diabetic treatment since its Food and Drug Administration approval in 2000. Yet progress did not end there. The first GLP-1 receptor agonist for diabetes was approved in 2005 and was a twice-a-day medicine. Shortly afterward, a daily GLP-1 was approved, and now there are three once-weekly GLP-1 receptor agonists.
Several pharmaceutical manufacturers are now working on a once-weekly insulin,5 as well as an implantable GLP-1 receptor agonist that will need to be replaced every 6-12 months.6 Imagine your patient coming in once a year to replace his or her potent glucose lowering medication – one that offers a low incidence of hypoglycemia, maintains glucose control all year long, and requires no adherence to a complicated medication regimen.
Similar technology is being used to develop a once-yearly anti-HIV prophylactic medication delivery system.7 This could help prevent the spread of HIV in areas of the world where it may be difficult for people to take daily medications.7
The many technological advances we have described may help us reduce our likelihood of missing a dose of a medication. We are hopeful that progress in this area will continue, and that one day medication adherence will require even less effort from patients than it does today.
Dr. Notte is a family physician and chief medical officer of Abington (Pa.) Hospital–Jefferson Health. Follow him on Twitter (@doctornotte). Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington Hospital–Jefferson Health. They have no conflicts related to the content of this piece.
References
1. Tabi K et al. Mobile apps for medication management: Review and analysis. JMIR Mhealth Uhealth. 2019 Sep 7(9):13608.
2. Park JYE et al. Mobile phone apps targeting medication adherence: Quality assessment and content analysis of user reviews. JMIR Mhealth Uhealth. 2019 Jan 31;7(1):e11919.
3. Pérez-Jover V et al. Mobile apps for increasing treatment adherence: Systematic review. J Med Internet Res. 2019;21(6):e12505. doi: 10.2196/12505.
4. 4 Smart inhalers that could be lifesaving for people living with asthma & COPD. MyTherapy, July 11, 2019.
5. Rosenstock J et al. Once-weekly insulin for type 2 diabetes without previous insulin treatment. N Engl J Med. 2020 Sep 22. doi: 10.1056/NEJMoa2022474.
6. GLP-1 agonists: From 2 daily injections to 1 per week and beyond. DiaTribe, Jan. 10, 2018.
7. Long-acting HIV prevention tools. Hiv.gov, July 20, 2019.
For most chronic diseases, up to 20%-30% of the pills that are prescribed are not taken. In the case of inhalers for asthma and COPD, patients miss over half of the prescribed doses.
There are many things that contribute to the problem of poor adherence, but people often just simply forget. Thankfully, there are tools designed to help remind patients of what they need to take and when. A survey of apps developed to help patients remember to take their medicines found more than 700 available in Apple and Android app stores.1 Most apps focus on medication alerts, reminders, and medication logs.2 A recent review showed that apps have some – yet limited – effectiveness in increasing adherence, with patient self-reported improvements of 7%-40%.3
Another perhaps more promising area of improving adherence involves high-tech advances in the way medications can be taken. Inhalers are a primary target as they are complicated devices. A patient has to breathe in at the correct time after the inhaler is actuated, and the inhaler works optimally only if the rate of inhalation is sufficient to carry the medication into the lungs.
A number of companies have developed attachments for inhalers (and even inhalers themselves) that can record when the medication is taken through a Bluetooth connection to a patient’s smartphone. These can also assess inspiratory flow. Reminders to take the medication are built into the app, and those reminders disappear if the medication is taken. Patients can receive feedback about the quality of their timing and inspiratory rate to maximize medication delivery to the lungs.4
We learned long ago that it is difficult to take medications three to four times a day, so extended-release tablets were developed to reduce the frequency to once or twice a day. A great deal of work is now being done behind the scenes to develop medications that decrease the need for patients to remember to take their medications. The best examples of this are the long-acting reversible contraception (LARC) devices, specifically IUDs and Nexplanon. Compared with traditional oral contraceptives that need to be taken daily, LARCs reduce the rate of pregnancy by five- to tenfold.
We also now have medications for osteoporosis that can be taken monthly, or even annually. When bisphosphonates were first developed for osteoporosis prevention, they needed to be taken daily. Then a weekly bisphosphonate was developed. Now there is a once-monthly oral bisphosphonate, Ibandronate, and even a once yearly IV bisphosphonate.
Exciting developments have also occurred in the management of diabetes. We may be tempted to take for granted how once-daily long-acting insulin, which releases insulin slowly over the course of a day, has revolutionized the diabetic treatment since its Food and Drug Administration approval in 2000. Yet progress did not end there. The first GLP-1 receptor agonist for diabetes was approved in 2005 and was a twice-a-day medicine. Shortly afterward, a daily GLP-1 was approved, and now there are three once-weekly GLP-1 receptor agonists.
Several pharmaceutical manufacturers are now working on a once-weekly insulin,5 as well as an implantable GLP-1 receptor agonist that will need to be replaced every 6-12 months.6 Imagine your patient coming in once a year to replace his or her potent glucose lowering medication – one that offers a low incidence of hypoglycemia, maintains glucose control all year long, and requires no adherence to a complicated medication regimen.
Similar technology is being used to develop a once-yearly anti-HIV prophylactic medication delivery system.7 This could help prevent the spread of HIV in areas of the world where it may be difficult for people to take daily medications.7
The many technological advances we have described may help us reduce our likelihood of missing a dose of a medication. We are hopeful that progress in this area will continue, and that one day medication adherence will require even less effort from patients than it does today.
Dr. Notte is a family physician and chief medical officer of Abington (Pa.) Hospital–Jefferson Health. Follow him on Twitter (@doctornotte). Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington Hospital–Jefferson Health. They have no conflicts related to the content of this piece.
References
1. Tabi K et al. Mobile apps for medication management: Review and analysis. JMIR Mhealth Uhealth. 2019 Sep 7(9):13608.
2. Park JYE et al. Mobile phone apps targeting medication adherence: Quality assessment and content analysis of user reviews. JMIR Mhealth Uhealth. 2019 Jan 31;7(1):e11919.
3. Pérez-Jover V et al. Mobile apps for increasing treatment adherence: Systematic review. J Med Internet Res. 2019;21(6):e12505. doi: 10.2196/12505.
4. 4 Smart inhalers that could be lifesaving for people living with asthma & COPD. MyTherapy, July 11, 2019.
5. Rosenstock J et al. Once-weekly insulin for type 2 diabetes without previous insulin treatment. N Engl J Med. 2020 Sep 22. doi: 10.1056/NEJMoa2022474.
6. GLP-1 agonists: From 2 daily injections to 1 per week and beyond. DiaTribe, Jan. 10, 2018.
7. Long-acting HIV prevention tools. Hiv.gov, July 20, 2019.
What to do when a patient is not ready to stop smoking
Recommendations from the American Thoracic Society
Below is a case involving a patient who is not yet ready to quit smoking. We later provide treatment recommendations for this patient based on a new guideline from the American Thoracic Society.
Case
A 58-year-old female comes into the office for a physical exam. She has been smoking two packs a day since she was 23 years of age. You have tried at previous visits to get her to quit, but she hasn’t been interested. The patient says she has a lot of stress, and that it is still not the right time for her to stop smoking. You tell her she needs to quit and, though the patient understands that quitting would be beneficial for her health, she just isn’t ready to try to kick the habit. How do you proceed?
The Guideline in context
Even though this patient stated that she is not ready to stop smoking, she is still a candidate for pharmacological treatment for her tobacco dependence and can be offered varenicline, according to the ATS guideline.1
In a previously published column, we have discussed the ATS’ recommended approaches for treating patients who are ready to stop smoking cigarettes. The reality is that many patients, if not most, are not ready to quit when we speak to them during any given office visit. The ATS guideline addresses this critical issue by recommending treatment with varenicline in patients who are not ready to stop smoking. It also states that this is a better strategy than waiting to start treatment until patients say they are ready for it.
This recommendation – to prescribe varenicline to smokers even when they are not ready to quit smoking – is based on solid clinical trial evidence. Research has shown that behavior change is dynamic and that the decision to stop smoking is not always a planned one.1 Patients often make quit attempts between office visits, and are often successful in those attempts. Because the decision to try to stop smoking is influenced by the satisfaction and physical addiction that comes from smoking, a medication such as varenicline that is a partial agonist/antagonist at the alpha4-beta2 nicotinic receptor might increase the likelihood that a patient would decide to try to stop smoking. This is because taking this type of a drug would lead the patient to no longer experience the reinforcing effects of nicotine.2 This hypothesis was examined in five randomized trials.1
In these studies, regular smokers who were not ready to make a quit attempt were randomized to varenicline versus placebo. Twice as many individuals who took varenicline stopped smoking 6 months after starting treatment.1
Suggested treatment
This patient should be offered varenicline. This individual meets the criteria for this treatment according to the ATS guideline in that the patient is a regular smoker who doesn’t think she is ready to stop smoking but understands she needs to stop and is open to taking medication to assist her with quitting.
Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington (Pa.) Hospital–Jefferson Health. Dr. Sprogell is a third-year resident in the family medicine residency program at Abington Jefferson Health. They have no conflicts related to the content of this piece. For questions or comments, feel free to contact Dr. Skolnik on Twitter @NeilSkolnik.
References
1. Leone F T et al. Initiating pharmacologic treatment in tobacco-dependent adults: An official American Thoracic Society Clinical Practice Guideline. Am J Respir Crit Care Med. 2020 Jul 15;202(2):e5–e31.
2. Ebbert JO et al. Varenicline for smoking cessation: Efficacy, safety, and treatment recommendations. Patient Prefer Adherence. 2010;4:355-62.
Recommendations from the American Thoracic Society
Recommendations from the American Thoracic Society
Below is a case involving a patient who is not yet ready to quit smoking. We later provide treatment recommendations for this patient based on a new guideline from the American Thoracic Society.
Case
A 58-year-old female comes into the office for a physical exam. She has been smoking two packs a day since she was 23 years of age. You have tried at previous visits to get her to quit, but she hasn’t been interested. The patient says she has a lot of stress, and that it is still not the right time for her to stop smoking. You tell her she needs to quit and, though the patient understands that quitting would be beneficial for her health, she just isn’t ready to try to kick the habit. How do you proceed?
The Guideline in context
Even though this patient stated that she is not ready to stop smoking, she is still a candidate for pharmacological treatment for her tobacco dependence and can be offered varenicline, according to the ATS guideline.1
In a previously published column, we have discussed the ATS’ recommended approaches for treating patients who are ready to stop smoking cigarettes. The reality is that many patients, if not most, are not ready to quit when we speak to them during any given office visit. The ATS guideline addresses this critical issue by recommending treatment with varenicline in patients who are not ready to stop smoking. It also states that this is a better strategy than waiting to start treatment until patients say they are ready for it.
This recommendation – to prescribe varenicline to smokers even when they are not ready to quit smoking – is based on solid clinical trial evidence. Research has shown that behavior change is dynamic and that the decision to stop smoking is not always a planned one.1 Patients often make quit attempts between office visits, and are often successful in those attempts. Because the decision to try to stop smoking is influenced by the satisfaction and physical addiction that comes from smoking, a medication such as varenicline that is a partial agonist/antagonist at the alpha4-beta2 nicotinic receptor might increase the likelihood that a patient would decide to try to stop smoking. This is because taking this type of a drug would lead the patient to no longer experience the reinforcing effects of nicotine.2 This hypothesis was examined in five randomized trials.1
In these studies, regular smokers who were not ready to make a quit attempt were randomized to varenicline versus placebo. Twice as many individuals who took varenicline stopped smoking 6 months after starting treatment.1
Suggested treatment
This patient should be offered varenicline. This individual meets the criteria for this treatment according to the ATS guideline in that the patient is a regular smoker who doesn’t think she is ready to stop smoking but understands she needs to stop and is open to taking medication to assist her with quitting.
Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington (Pa.) Hospital–Jefferson Health. Dr. Sprogell is a third-year resident in the family medicine residency program at Abington Jefferson Health. They have no conflicts related to the content of this piece. For questions or comments, feel free to contact Dr. Skolnik on Twitter @NeilSkolnik.
References
1. Leone F T et al. Initiating pharmacologic treatment in tobacco-dependent adults: An official American Thoracic Society Clinical Practice Guideline. Am J Respir Crit Care Med. 2020 Jul 15;202(2):e5–e31.
2. Ebbert JO et al. Varenicline for smoking cessation: Efficacy, safety, and treatment recommendations. Patient Prefer Adherence. 2010;4:355-62.
Below is a case involving a patient who is not yet ready to quit smoking. We later provide treatment recommendations for this patient based on a new guideline from the American Thoracic Society.
Case
A 58-year-old female comes into the office for a physical exam. She has been smoking two packs a day since she was 23 years of age. You have tried at previous visits to get her to quit, but she hasn’t been interested. The patient says she has a lot of stress, and that it is still not the right time for her to stop smoking. You tell her she needs to quit and, though the patient understands that quitting would be beneficial for her health, she just isn’t ready to try to kick the habit. How do you proceed?
The Guideline in context
Even though this patient stated that she is not ready to stop smoking, she is still a candidate for pharmacological treatment for her tobacco dependence and can be offered varenicline, according to the ATS guideline.1
In a previously published column, we have discussed the ATS’ recommended approaches for treating patients who are ready to stop smoking cigarettes. The reality is that many patients, if not most, are not ready to quit when we speak to them during any given office visit. The ATS guideline addresses this critical issue by recommending treatment with varenicline in patients who are not ready to stop smoking. It also states that this is a better strategy than waiting to start treatment until patients say they are ready for it.
This recommendation – to prescribe varenicline to smokers even when they are not ready to quit smoking – is based on solid clinical trial evidence. Research has shown that behavior change is dynamic and that the decision to stop smoking is not always a planned one.1 Patients often make quit attempts between office visits, and are often successful in those attempts. Because the decision to try to stop smoking is influenced by the satisfaction and physical addiction that comes from smoking, a medication such as varenicline that is a partial agonist/antagonist at the alpha4-beta2 nicotinic receptor might increase the likelihood that a patient would decide to try to stop smoking. This is because taking this type of a drug would lead the patient to no longer experience the reinforcing effects of nicotine.2 This hypothesis was examined in five randomized trials.1
In these studies, regular smokers who were not ready to make a quit attempt were randomized to varenicline versus placebo. Twice as many individuals who took varenicline stopped smoking 6 months after starting treatment.1
Suggested treatment
This patient should be offered varenicline. This individual meets the criteria for this treatment according to the ATS guideline in that the patient is a regular smoker who doesn’t think she is ready to stop smoking but understands she needs to stop and is open to taking medication to assist her with quitting.
Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington (Pa.) Hospital–Jefferson Health. Dr. Sprogell is a third-year resident in the family medicine residency program at Abington Jefferson Health. They have no conflicts related to the content of this piece. For questions or comments, feel free to contact Dr. Skolnik on Twitter @NeilSkolnik.
References
1. Leone F T et al. Initiating pharmacologic treatment in tobacco-dependent adults: An official American Thoracic Society Clinical Practice Guideline. Am J Respir Crit Care Med. 2020 Jul 15;202(2):e5–e31.
2. Ebbert JO et al. Varenicline for smoking cessation: Efficacy, safety, and treatment recommendations. Patient Prefer Adherence. 2010;4:355-62.
Smart health devices – promises and pitfalls
What needs to be done before the data deluge hits the office
Hurricane Sally recently crossed the Gulf of Mexico and landed with torrential rainfalls along the Alabama coast. A little rainfall is important for crops; too much leads to devastation. As physicians, we need data in order to help manage patients’ illnesses and to help to keep them healthy. Our fear though is that too much data provided too quickly may have the opposite effect.
Personal monitoring devices
When I bought my first Fitbit 7 years ago, I was enamored with the technology. The Fitbit was little more than a step tracker, yet I proudly wore its black rubber strap on my wrist. It was my first foray into wearable technology, and it felt quite empowering to have an objective way to track my fitness beyond just using my bathroom scale. Now less than a decade later, that Fitbit looks archaic in comparison with the wrist-top technology currently available.
As I write this, the world’s largest technology company is in the process of releasing its sixth-generation Apple Watch. In addition to acting as a smartphone, this new device, which is barely larger than a postage stamp, offers GPS-based movement tracking, the ability to detect falls, continuous heart rate monitoring, a built-in EKG capable of diagnosing atrial fibrillation, and an oxygen saturation sensor. These features weren’t added thoughtlessly. Apple is marketing this as a health-focused device, with their primary advertising campaign claiming that “the future of health is on your wrist,” and they aren’t the only company making this play.
Along with Apple, Samsung, Withings, Fitbit, and other companies continue to bring products to market that monitor our activity and provide new insights into our health. Typically linked to smartphone-based apps, these devices record all of their measurements for later review, while software helps interpret the findings to make them actionable. From heart rate tracking to sleep analysis, these options now provide access to volumes of data that promise to improve our wellness and change our lives. Of course, those promises will only be fulfilled if our behavior is altered as a consequence of having more detailed information. Whether that will happen remains to be seen.
Health system–linked devices
Major advancements in medical monitoring technology are now enabling physicians to get much deeper insight into their patients’ health status. Internet-connected scales, blood pressure cuffs, and exercise equipment offer the ability to upload information into patient portals and integrate that information into EHRs. New devices provide access to information that previously was impossible to obtain. For example, wearable continuous blood glucose monitors, such as the FreeStyle Libre or DexCom’s G6, allow patients and physicians to follow blood sugar readings 24 hours a day. This provides unprecedented awareness of diabetes control and relieves the pain and inconvenience of finger sticks and blood draws. It also aids with compliance because patients don’t need to remember to check their sugar levels on a schedule.
Other compliance-boosting breakthroughs, such as Bluetooth-enabled asthma inhalers and cellular-connected continuous positive airway pressure machines, assist patients with managing chronic respiratory conditions. Many companies are developing technologies to manage acute conditions as well. One such company, an on-demand telemedicine provider called TytoCare, has developed a $299 suite of instruments that includes a digital stethoscope, thermometer, and camera-based otoscope. In concert with a virtual visit, their providers can remotely use these tools to examine and assess sick individuals. This virtual “laying on of hands” may have sounded like science fiction and likely would have been rejected by patients just a few years ago. Now it is becoming commonplace and will soon be an expectation of many seeking care.
But if we are to be successful, everyone must acknowledge that this revolution in health care brings many challenges along with it. One of those is the deluge of data that connected devices provide.
Information overload
There is such a thing as “too much of a good thing.” Described by journalist David Shenk as “data smog” in his 1997 book of the same name, the idea is clear: There is only so much information we can assimilate.
Even after years of using EHRs and with government-implemented incentives that promote “meaningful use,” physicians are still struggling with EHRs. Additionally, many have expressed frustration with the connectedness that EHRs provide and lament their inability to ever really “leave the office.” As more and more data become available to physicians, the challenge of how to assimilate and act on those data will continue to grow. The addition of patient-provided health statistics will only make information overload worse, with clinicians will feeling an ever-growing burden to know, understand, and act on this information.
Unless we develop systems to sort, filter, and prioritize the flow of information, there is potential for liability from not acting on the amount of virtual information doctors receive. This new risk for already fatigued and overburdened physicians combined with an increase in the amount of virtual information at doctors’ fingertips may lead to the value of patient data being lost.
Dr. Notte is a family physician and chief medical officer of Abington (Pa.) Hospital–Jefferson Health. Follow him on Twitter (@doctornotte). Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington Hospital–Jefferson Health. They have no conflicts related to the content of this piece.
What needs to be done before the data deluge hits the office
What needs to be done before the data deluge hits the office
Hurricane Sally recently crossed the Gulf of Mexico and landed with torrential rainfalls along the Alabama coast. A little rainfall is important for crops; too much leads to devastation. As physicians, we need data in order to help manage patients’ illnesses and to help to keep them healthy. Our fear though is that too much data provided too quickly may have the opposite effect.
Personal monitoring devices
When I bought my first Fitbit 7 years ago, I was enamored with the technology. The Fitbit was little more than a step tracker, yet I proudly wore its black rubber strap on my wrist. It was my first foray into wearable technology, and it felt quite empowering to have an objective way to track my fitness beyond just using my bathroom scale. Now less than a decade later, that Fitbit looks archaic in comparison with the wrist-top technology currently available.
As I write this, the world’s largest technology company is in the process of releasing its sixth-generation Apple Watch. In addition to acting as a smartphone, this new device, which is barely larger than a postage stamp, offers GPS-based movement tracking, the ability to detect falls, continuous heart rate monitoring, a built-in EKG capable of diagnosing atrial fibrillation, and an oxygen saturation sensor. These features weren’t added thoughtlessly. Apple is marketing this as a health-focused device, with their primary advertising campaign claiming that “the future of health is on your wrist,” and they aren’t the only company making this play.
Along with Apple, Samsung, Withings, Fitbit, and other companies continue to bring products to market that monitor our activity and provide new insights into our health. Typically linked to smartphone-based apps, these devices record all of their measurements for later review, while software helps interpret the findings to make them actionable. From heart rate tracking to sleep analysis, these options now provide access to volumes of data that promise to improve our wellness and change our lives. Of course, those promises will only be fulfilled if our behavior is altered as a consequence of having more detailed information. Whether that will happen remains to be seen.
Health system–linked devices
Major advancements in medical monitoring technology are now enabling physicians to get much deeper insight into their patients’ health status. Internet-connected scales, blood pressure cuffs, and exercise equipment offer the ability to upload information into patient portals and integrate that information into EHRs. New devices provide access to information that previously was impossible to obtain. For example, wearable continuous blood glucose monitors, such as the FreeStyle Libre or DexCom’s G6, allow patients and physicians to follow blood sugar readings 24 hours a day. This provides unprecedented awareness of diabetes control and relieves the pain and inconvenience of finger sticks and blood draws. It also aids with compliance because patients don’t need to remember to check their sugar levels on a schedule.
Other compliance-boosting breakthroughs, such as Bluetooth-enabled asthma inhalers and cellular-connected continuous positive airway pressure machines, assist patients with managing chronic respiratory conditions. Many companies are developing technologies to manage acute conditions as well. One such company, an on-demand telemedicine provider called TytoCare, has developed a $299 suite of instruments that includes a digital stethoscope, thermometer, and camera-based otoscope. In concert with a virtual visit, their providers can remotely use these tools to examine and assess sick individuals. This virtual “laying on of hands” may have sounded like science fiction and likely would have been rejected by patients just a few years ago. Now it is becoming commonplace and will soon be an expectation of many seeking care.
But if we are to be successful, everyone must acknowledge that this revolution in health care brings many challenges along with it. One of those is the deluge of data that connected devices provide.
Information overload
There is such a thing as “too much of a good thing.” Described by journalist David Shenk as “data smog” in his 1997 book of the same name, the idea is clear: There is only so much information we can assimilate.
Even after years of using EHRs and with government-implemented incentives that promote “meaningful use,” physicians are still struggling with EHRs. Additionally, many have expressed frustration with the connectedness that EHRs provide and lament their inability to ever really “leave the office.” As more and more data become available to physicians, the challenge of how to assimilate and act on those data will continue to grow. The addition of patient-provided health statistics will only make information overload worse, with clinicians will feeling an ever-growing burden to know, understand, and act on this information.
Unless we develop systems to sort, filter, and prioritize the flow of information, there is potential for liability from not acting on the amount of virtual information doctors receive. This new risk for already fatigued and overburdened physicians combined with an increase in the amount of virtual information at doctors’ fingertips may lead to the value of patient data being lost.
Dr. Notte is a family physician and chief medical officer of Abington (Pa.) Hospital–Jefferson Health. Follow him on Twitter (@doctornotte). Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington Hospital–Jefferson Health. They have no conflicts related to the content of this piece.
Hurricane Sally recently crossed the Gulf of Mexico and landed with torrential rainfalls along the Alabama coast. A little rainfall is important for crops; too much leads to devastation. As physicians, we need data in order to help manage patients’ illnesses and to help to keep them healthy. Our fear though is that too much data provided too quickly may have the opposite effect.
Personal monitoring devices
When I bought my first Fitbit 7 years ago, I was enamored with the technology. The Fitbit was little more than a step tracker, yet I proudly wore its black rubber strap on my wrist. It was my first foray into wearable technology, and it felt quite empowering to have an objective way to track my fitness beyond just using my bathroom scale. Now less than a decade later, that Fitbit looks archaic in comparison with the wrist-top technology currently available.
As I write this, the world’s largest technology company is in the process of releasing its sixth-generation Apple Watch. In addition to acting as a smartphone, this new device, which is barely larger than a postage stamp, offers GPS-based movement tracking, the ability to detect falls, continuous heart rate monitoring, a built-in EKG capable of diagnosing atrial fibrillation, and an oxygen saturation sensor. These features weren’t added thoughtlessly. Apple is marketing this as a health-focused device, with their primary advertising campaign claiming that “the future of health is on your wrist,” and they aren’t the only company making this play.
Along with Apple, Samsung, Withings, Fitbit, and other companies continue to bring products to market that monitor our activity and provide new insights into our health. Typically linked to smartphone-based apps, these devices record all of their measurements for later review, while software helps interpret the findings to make them actionable. From heart rate tracking to sleep analysis, these options now provide access to volumes of data that promise to improve our wellness and change our lives. Of course, those promises will only be fulfilled if our behavior is altered as a consequence of having more detailed information. Whether that will happen remains to be seen.
Health system–linked devices
Major advancements in medical monitoring technology are now enabling physicians to get much deeper insight into their patients’ health status. Internet-connected scales, blood pressure cuffs, and exercise equipment offer the ability to upload information into patient portals and integrate that information into EHRs. New devices provide access to information that previously was impossible to obtain. For example, wearable continuous blood glucose monitors, such as the FreeStyle Libre or DexCom’s G6, allow patients and physicians to follow blood sugar readings 24 hours a day. This provides unprecedented awareness of diabetes control and relieves the pain and inconvenience of finger sticks and blood draws. It also aids with compliance because patients don’t need to remember to check their sugar levels on a schedule.
Other compliance-boosting breakthroughs, such as Bluetooth-enabled asthma inhalers and cellular-connected continuous positive airway pressure machines, assist patients with managing chronic respiratory conditions. Many companies are developing technologies to manage acute conditions as well. One such company, an on-demand telemedicine provider called TytoCare, has developed a $299 suite of instruments that includes a digital stethoscope, thermometer, and camera-based otoscope. In concert with a virtual visit, their providers can remotely use these tools to examine and assess sick individuals. This virtual “laying on of hands” may have sounded like science fiction and likely would have been rejected by patients just a few years ago. Now it is becoming commonplace and will soon be an expectation of many seeking care.
But if we are to be successful, everyone must acknowledge that this revolution in health care brings many challenges along with it. One of those is the deluge of data that connected devices provide.
Information overload
There is such a thing as “too much of a good thing.” Described by journalist David Shenk as “data smog” in his 1997 book of the same name, the idea is clear: There is only so much information we can assimilate.
Even after years of using EHRs and with government-implemented incentives that promote “meaningful use,” physicians are still struggling with EHRs. Additionally, many have expressed frustration with the connectedness that EHRs provide and lament their inability to ever really “leave the office.” As more and more data become available to physicians, the challenge of how to assimilate and act on those data will continue to grow. The addition of patient-provided health statistics will only make information overload worse, with clinicians will feeling an ever-growing burden to know, understand, and act on this information.
Unless we develop systems to sort, filter, and prioritize the flow of information, there is potential for liability from not acting on the amount of virtual information doctors receive. This new risk for already fatigued and overburdened physicians combined with an increase in the amount of virtual information at doctors’ fingertips may lead to the value of patient data being lost.
Dr. Notte is a family physician and chief medical officer of Abington (Pa.) Hospital–Jefferson Health. Follow him on Twitter (@doctornotte). Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington Hospital–Jefferson Health. They have no conflicts related to the content of this piece.











