User login
Katie Lennon is editor of MDedge's Family Practice News and Internal Medicine News. She has also served as editor of CHEST Physician; a staff writer for Financial Times publications; and a reporter for the Princeton Packet, Ocean County Observer, and South Bend Tribune. She is a graduate of the University of Notre Dame, South Bend, Ind. Follow her on Twitter @KatieWLennon.
AAFP Congress adopts resolutions on physician privileges, medical education, employee benefits
PHILADELPHIA –
Practice enhancement
Hospital privileges were a hot topic for the reference committee on practice enhancement.
Adopted Resolution No. 304 calls on AAFP to oppose health insurance companies “privileging physicians based solely on their hospital privileges and hospital credentials.” The new rule also resolves that AAFP engage major national health insurance companies to develop methods to credential physicians that do not depend on hospital privileges.
The Congress also adopted Substitute Resolution No. 305, which calls on the AAFP to collaborate with the Joint Commission and other appropriate entities to create policy stating that hospitals remove undue barriers and restriction of privileges to hospitals and intensive care units for qualified family physicians who practice hospital medicine.
Delegates requested amendments to a resolution that called on AAFP to oppose nonphysician health care professionals making credentialing or privileging decisions regarding family physicians and that the AAFP oppose the use of nonphysician health care professionals in providing consultations requested of other physicians. The Congress could not agree on a final wording of the resolution.
Douglas J. Gruenbacher, MD, a Kansas delegate who works in a small hospital, said, “We actually credential in our hospital radiologists, orthopedists ... urologists. Do I know what they know? So we have to have many of our nonphysician providers, our nurse practitioners, help us. ... Should they be independent? No, of course not, but they do play an important part of our team.”
Douglas W. Curran, MD, a delegate from Texas, said, “I think we continue to give away stuff without taking care of ourselves. I have seen it for 4 years and, as result, we have seen this expansion of second-class care for people. ... Those are huge decisions, especially thinking about who’s going to do what in our hospitals. That includes small hospitals; I practice in a small hospital. I get all of that.”
After much debate, the Congress voted in favor of referring two proposed amendments to the board.
The Congress also adopted an amended version of Substitute Resolution No. 303, which calls on AAFP to support insurance coverage of acupuncture for pain control when ordered by a licensed physician or licensed collaborating advanced clinician on their practice team.
Education
Multipronged Substitute Resolution No. 606 – adopted by the Congress – aims to address racial inequities in medical education. Specifically, it calls on AAFP to do the following:
- Instruct the Liaison Committee for Medical Education to add race to its existing Cultural Competence and Health Care Disparities section 7.6 of Functions and Structure of a Medical School: Standards for Accreditation of Medical Education Programs Leading to the MD Degree.
- Ask the Accreditation Council for Graduate Medical Education to adopt an antiracism policy that includes corresponding curricular requirements,
- Develop and implement a policy on training in racism and implicit bias for officeholders and commission members.
- Take an active stance against racism when racist events occur within the medical community.
The Congress also adopted Resolution No. 611, which calls for the AAFP to encourage the expansion of clinical behavioral health fellowships for family medicine physicians.
The resolution received mixed testimony during the reference committee meeting, with those in favor of the resolution having cited the need for more education in behavioral health due to shortages in many communities. Opponents argued that completing the fellowship would not have added value in hospital privileging and insurance payment, because it would not lead physicians to earn a certificate of added qualification.
Delegates also passed Resolution 608, over the objections of the reference committee.
As adopted, the resolution calls for AAFP to express its concern that the American Board of Family Medicine (ABFM) Family Medicine Certification Longitudinal Assessment is the only alternative to 1-day-only certification exam, and for the AAFP to urge the ABFM to offer a longitudinal self-assessment process similar to the American Board of Obstetricians and Gynecologists self-assessment process to satisfy the cognitive component of ABFM’s continued certification requirement.
The Reference Committee on Education also referred several hotly debated resolutions back to the AAFP board of directors. No. 604 called on AAFP to support forgiving 1 year of federal medical student loans for every 2 years of full-time work in a primary care position, as well as tax credits for those working in rural or underserved areas.
Advocacy
The delegates also approved most of the recommendations of the reference committee on advocacy with little discussion.
Substitute Resolution No. 515, which was ultimately adopted with an amendment by the Congress, states that AAFP support policies that provide employees with reasonable benefits, including job security, wage replacement, and continued availability of health plan coverage in the event that leave by an employee becomes necessary for documented medical conditions, with protections for small businesses. Among the policies this resolution includes are the following:
- Medical leave for the employee, including pregnancy.
- Parental leave for the employee-parent, including leave for birth, adoption or foster care leading to adoption.
- Leave if medically appropriate to care for a member of the employee’s immediate family.
The Congress adopted several other resolutions recommended by the advocacy committee:
- Resolution No. 501, calling on AAFP to advocate for state-level adoption of the Interstate Medical Licensure Compact.
- Substitute Resolution No. 505, asking AAFP to request a National Coverage Determination for Cardiac Rehabilitation Programs to allow such programs to operate without physician supervision when an AED is immediately available, and the patient is attended by nursing staff currently trained in basic life support.
- Substitute Resolutions No. 506 and 507 to support and encourage the ability of parents to breastfeed in the workplace through its advocacy efforts, as well as promote the enforcements of current law.
- Resolution No. 508, to petition CMS, national health insurance companies, and pharmacy benefits managers to include all generic medications in a class within a health plan’s formulary and implement a system that informs the prescriber of all formulary alternatives to a medication when denying the same medication immediately upon denial, while also providing a mechanism to rapidly appeal the denial.
- Substitute Resolution No. 512, to petition the CMS to reevaluate its current policy on the time requirements for discharge summaries from hospitals and post-acute care facilities and specifically require such facilities to provide primary care physicians with discharge summaries within 7 days.
- Substitute Resolution No. 517, to unequivocally support the right of physicians to organize and bargain collectively.
- Substitute Resolution No. 519, to support legislation that decriminalizes people who are solicited for sex or sexual activities in exchange for money or goods, without supporting the legalization of the selling of sex, and advocate against legislation that decriminalizes sex-buying and third-parties who promote and/or profit from sex buying.
Some of the resolutions that incited many passionate responses during the reference committee on advocacy were not discussed during the Congress of Delegates meeting.
One of these asked the AAFP to oppose legislation of physician-patient decision making in child and adolescent gender-affirming care. Some in support of this resolution referred to this type of care as evidence-based medicine and said that legislators should be kept out of the exam room. Those opposed disagreed with classifying this type of care that way, noting that the long-term effects of some of the treatments are unknown.
During the reference committee, one opponent of the resolution, Lisa Gilbert, MD, claimed that gender-affirming care refers to blocking puberty, followed by cross-sex hormones,which would permanently sterilize the children. Dr. Gilbert, who identified herself as a member from Kansas speaking independently, added that if children have gone through puberty naturally, this would be a different discussion.
Kevin Wang, MD, an alternate delegate from Washington, who supported the resolution, noted that the rate of suicide in the transgender population is nine times that of the general population.
“I do want to emphasize that doing nothing does cause significant harm,” Dr. Wang said, The committee referred resolution No. 509 to the board for further clarification and study.
The merits of two other resolutions (No. 510 and No. 511), which called for the AAFP to no longer reject the use of “physician-assisted suicide” and “assisted suicide” and avoid the use of vague and euphemistic terms when referring to lethal medications prescribed with the intention of ending a patient’s life in statements and documents, also were heavily debated during the advocacy reference committee meeting. The committee recommended such resolutions be referred to the board for discussion.
The delegates approved the advocacy committee’s recommendations for Resolutions 509, 510, and 511.
PHILADELPHIA –
Practice enhancement
Hospital privileges were a hot topic for the reference committee on practice enhancement.
Adopted Resolution No. 304 calls on AAFP to oppose health insurance companies “privileging physicians based solely on their hospital privileges and hospital credentials.” The new rule also resolves that AAFP engage major national health insurance companies to develop methods to credential physicians that do not depend on hospital privileges.
The Congress also adopted Substitute Resolution No. 305, which calls on the AAFP to collaborate with the Joint Commission and other appropriate entities to create policy stating that hospitals remove undue barriers and restriction of privileges to hospitals and intensive care units for qualified family physicians who practice hospital medicine.
Delegates requested amendments to a resolution that called on AAFP to oppose nonphysician health care professionals making credentialing or privileging decisions regarding family physicians and that the AAFP oppose the use of nonphysician health care professionals in providing consultations requested of other physicians. The Congress could not agree on a final wording of the resolution.
Douglas J. Gruenbacher, MD, a Kansas delegate who works in a small hospital, said, “We actually credential in our hospital radiologists, orthopedists ... urologists. Do I know what they know? So we have to have many of our nonphysician providers, our nurse practitioners, help us. ... Should they be independent? No, of course not, but they do play an important part of our team.”
Douglas W. Curran, MD, a delegate from Texas, said, “I think we continue to give away stuff without taking care of ourselves. I have seen it for 4 years and, as result, we have seen this expansion of second-class care for people. ... Those are huge decisions, especially thinking about who’s going to do what in our hospitals. That includes small hospitals; I practice in a small hospital. I get all of that.”
After much debate, the Congress voted in favor of referring two proposed amendments to the board.
The Congress also adopted an amended version of Substitute Resolution No. 303, which calls on AAFP to support insurance coverage of acupuncture for pain control when ordered by a licensed physician or licensed collaborating advanced clinician on their practice team.
Education
Multipronged Substitute Resolution No. 606 – adopted by the Congress – aims to address racial inequities in medical education. Specifically, it calls on AAFP to do the following:
- Instruct the Liaison Committee for Medical Education to add race to its existing Cultural Competence and Health Care Disparities section 7.6 of Functions and Structure of a Medical School: Standards for Accreditation of Medical Education Programs Leading to the MD Degree.
- Ask the Accreditation Council for Graduate Medical Education to adopt an antiracism policy that includes corresponding curricular requirements,
- Develop and implement a policy on training in racism and implicit bias for officeholders and commission members.
- Take an active stance against racism when racist events occur within the medical community.
The Congress also adopted Resolution No. 611, which calls for the AAFP to encourage the expansion of clinical behavioral health fellowships for family medicine physicians.
The resolution received mixed testimony during the reference committee meeting, with those in favor of the resolution having cited the need for more education in behavioral health due to shortages in many communities. Opponents argued that completing the fellowship would not have added value in hospital privileging and insurance payment, because it would not lead physicians to earn a certificate of added qualification.
Delegates also passed Resolution 608, over the objections of the reference committee.
As adopted, the resolution calls for AAFP to express its concern that the American Board of Family Medicine (ABFM) Family Medicine Certification Longitudinal Assessment is the only alternative to 1-day-only certification exam, and for the AAFP to urge the ABFM to offer a longitudinal self-assessment process similar to the American Board of Obstetricians and Gynecologists self-assessment process to satisfy the cognitive component of ABFM’s continued certification requirement.
The Reference Committee on Education also referred several hotly debated resolutions back to the AAFP board of directors. No. 604 called on AAFP to support forgiving 1 year of federal medical student loans for every 2 years of full-time work in a primary care position, as well as tax credits for those working in rural or underserved areas.
Advocacy
The delegates also approved most of the recommendations of the reference committee on advocacy with little discussion.
Substitute Resolution No. 515, which was ultimately adopted with an amendment by the Congress, states that AAFP support policies that provide employees with reasonable benefits, including job security, wage replacement, and continued availability of health plan coverage in the event that leave by an employee becomes necessary for documented medical conditions, with protections for small businesses. Among the policies this resolution includes are the following:
- Medical leave for the employee, including pregnancy.
- Parental leave for the employee-parent, including leave for birth, adoption or foster care leading to adoption.
- Leave if medically appropriate to care for a member of the employee’s immediate family.
The Congress adopted several other resolutions recommended by the advocacy committee:
- Resolution No. 501, calling on AAFP to advocate for state-level adoption of the Interstate Medical Licensure Compact.
- Substitute Resolution No. 505, asking AAFP to request a National Coverage Determination for Cardiac Rehabilitation Programs to allow such programs to operate without physician supervision when an AED is immediately available, and the patient is attended by nursing staff currently trained in basic life support.
- Substitute Resolutions No. 506 and 507 to support and encourage the ability of parents to breastfeed in the workplace through its advocacy efforts, as well as promote the enforcements of current law.
- Resolution No. 508, to petition CMS, national health insurance companies, and pharmacy benefits managers to include all generic medications in a class within a health plan’s formulary and implement a system that informs the prescriber of all formulary alternatives to a medication when denying the same medication immediately upon denial, while also providing a mechanism to rapidly appeal the denial.
- Substitute Resolution No. 512, to petition the CMS to reevaluate its current policy on the time requirements for discharge summaries from hospitals and post-acute care facilities and specifically require such facilities to provide primary care physicians with discharge summaries within 7 days.
- Substitute Resolution No. 517, to unequivocally support the right of physicians to organize and bargain collectively.
- Substitute Resolution No. 519, to support legislation that decriminalizes people who are solicited for sex or sexual activities in exchange for money or goods, without supporting the legalization of the selling of sex, and advocate against legislation that decriminalizes sex-buying and third-parties who promote and/or profit from sex buying.
Some of the resolutions that incited many passionate responses during the reference committee on advocacy were not discussed during the Congress of Delegates meeting.
One of these asked the AAFP to oppose legislation of physician-patient decision making in child and adolescent gender-affirming care. Some in support of this resolution referred to this type of care as evidence-based medicine and said that legislators should be kept out of the exam room. Those opposed disagreed with classifying this type of care that way, noting that the long-term effects of some of the treatments are unknown.
During the reference committee, one opponent of the resolution, Lisa Gilbert, MD, claimed that gender-affirming care refers to blocking puberty, followed by cross-sex hormones,which would permanently sterilize the children. Dr. Gilbert, who identified herself as a member from Kansas speaking independently, added that if children have gone through puberty naturally, this would be a different discussion.
Kevin Wang, MD, an alternate delegate from Washington, who supported the resolution, noted that the rate of suicide in the transgender population is nine times that of the general population.
“I do want to emphasize that doing nothing does cause significant harm,” Dr. Wang said, The committee referred resolution No. 509 to the board for further clarification and study.
The merits of two other resolutions (No. 510 and No. 511), which called for the AAFP to no longer reject the use of “physician-assisted suicide” and “assisted suicide” and avoid the use of vague and euphemistic terms when referring to lethal medications prescribed with the intention of ending a patient’s life in statements and documents, also were heavily debated during the advocacy reference committee meeting. The committee recommended such resolutions be referred to the board for discussion.
The delegates approved the advocacy committee’s recommendations for Resolutions 509, 510, and 511.
PHILADELPHIA –
Practice enhancement
Hospital privileges were a hot topic for the reference committee on practice enhancement.
Adopted Resolution No. 304 calls on AAFP to oppose health insurance companies “privileging physicians based solely on their hospital privileges and hospital credentials.” The new rule also resolves that AAFP engage major national health insurance companies to develop methods to credential physicians that do not depend on hospital privileges.
The Congress also adopted Substitute Resolution No. 305, which calls on the AAFP to collaborate with the Joint Commission and other appropriate entities to create policy stating that hospitals remove undue barriers and restriction of privileges to hospitals and intensive care units for qualified family physicians who practice hospital medicine.
Delegates requested amendments to a resolution that called on AAFP to oppose nonphysician health care professionals making credentialing or privileging decisions regarding family physicians and that the AAFP oppose the use of nonphysician health care professionals in providing consultations requested of other physicians. The Congress could not agree on a final wording of the resolution.
Douglas J. Gruenbacher, MD, a Kansas delegate who works in a small hospital, said, “We actually credential in our hospital radiologists, orthopedists ... urologists. Do I know what they know? So we have to have many of our nonphysician providers, our nurse practitioners, help us. ... Should they be independent? No, of course not, but they do play an important part of our team.”
Douglas W. Curran, MD, a delegate from Texas, said, “I think we continue to give away stuff without taking care of ourselves. I have seen it for 4 years and, as result, we have seen this expansion of second-class care for people. ... Those are huge decisions, especially thinking about who’s going to do what in our hospitals. That includes small hospitals; I practice in a small hospital. I get all of that.”
After much debate, the Congress voted in favor of referring two proposed amendments to the board.
The Congress also adopted an amended version of Substitute Resolution No. 303, which calls on AAFP to support insurance coverage of acupuncture for pain control when ordered by a licensed physician or licensed collaborating advanced clinician on their practice team.
Education
Multipronged Substitute Resolution No. 606 – adopted by the Congress – aims to address racial inequities in medical education. Specifically, it calls on AAFP to do the following:
- Instruct the Liaison Committee for Medical Education to add race to its existing Cultural Competence and Health Care Disparities section 7.6 of Functions and Structure of a Medical School: Standards for Accreditation of Medical Education Programs Leading to the MD Degree.
- Ask the Accreditation Council for Graduate Medical Education to adopt an antiracism policy that includes corresponding curricular requirements,
- Develop and implement a policy on training in racism and implicit bias for officeholders and commission members.
- Take an active stance against racism when racist events occur within the medical community.
The Congress also adopted Resolution No. 611, which calls for the AAFP to encourage the expansion of clinical behavioral health fellowships for family medicine physicians.
The resolution received mixed testimony during the reference committee meeting, with those in favor of the resolution having cited the need for more education in behavioral health due to shortages in many communities. Opponents argued that completing the fellowship would not have added value in hospital privileging and insurance payment, because it would not lead physicians to earn a certificate of added qualification.
Delegates also passed Resolution 608, over the objections of the reference committee.
As adopted, the resolution calls for AAFP to express its concern that the American Board of Family Medicine (ABFM) Family Medicine Certification Longitudinal Assessment is the only alternative to 1-day-only certification exam, and for the AAFP to urge the ABFM to offer a longitudinal self-assessment process similar to the American Board of Obstetricians and Gynecologists self-assessment process to satisfy the cognitive component of ABFM’s continued certification requirement.
The Reference Committee on Education also referred several hotly debated resolutions back to the AAFP board of directors. No. 604 called on AAFP to support forgiving 1 year of federal medical student loans for every 2 years of full-time work in a primary care position, as well as tax credits for those working in rural or underserved areas.
Advocacy
The delegates also approved most of the recommendations of the reference committee on advocacy with little discussion.
Substitute Resolution No. 515, which was ultimately adopted with an amendment by the Congress, states that AAFP support policies that provide employees with reasonable benefits, including job security, wage replacement, and continued availability of health plan coverage in the event that leave by an employee becomes necessary for documented medical conditions, with protections for small businesses. Among the policies this resolution includes are the following:
- Medical leave for the employee, including pregnancy.
- Parental leave for the employee-parent, including leave for birth, adoption or foster care leading to adoption.
- Leave if medically appropriate to care for a member of the employee’s immediate family.
The Congress adopted several other resolutions recommended by the advocacy committee:
- Resolution No. 501, calling on AAFP to advocate for state-level adoption of the Interstate Medical Licensure Compact.
- Substitute Resolution No. 505, asking AAFP to request a National Coverage Determination for Cardiac Rehabilitation Programs to allow such programs to operate without physician supervision when an AED is immediately available, and the patient is attended by nursing staff currently trained in basic life support.
- Substitute Resolutions No. 506 and 507 to support and encourage the ability of parents to breastfeed in the workplace through its advocacy efforts, as well as promote the enforcements of current law.
- Resolution No. 508, to petition CMS, national health insurance companies, and pharmacy benefits managers to include all generic medications in a class within a health plan’s formulary and implement a system that informs the prescriber of all formulary alternatives to a medication when denying the same medication immediately upon denial, while also providing a mechanism to rapidly appeal the denial.
- Substitute Resolution No. 512, to petition the CMS to reevaluate its current policy on the time requirements for discharge summaries from hospitals and post-acute care facilities and specifically require such facilities to provide primary care physicians with discharge summaries within 7 days.
- Substitute Resolution No. 517, to unequivocally support the right of physicians to organize and bargain collectively.
- Substitute Resolution No. 519, to support legislation that decriminalizes people who are solicited for sex or sexual activities in exchange for money or goods, without supporting the legalization of the selling of sex, and advocate against legislation that decriminalizes sex-buying and third-parties who promote and/or profit from sex buying.
Some of the resolutions that incited many passionate responses during the reference committee on advocacy were not discussed during the Congress of Delegates meeting.
One of these asked the AAFP to oppose legislation of physician-patient decision making in child and adolescent gender-affirming care. Some in support of this resolution referred to this type of care as evidence-based medicine and said that legislators should be kept out of the exam room. Those opposed disagreed with classifying this type of care that way, noting that the long-term effects of some of the treatments are unknown.
During the reference committee, one opponent of the resolution, Lisa Gilbert, MD, claimed that gender-affirming care refers to blocking puberty, followed by cross-sex hormones,which would permanently sterilize the children. Dr. Gilbert, who identified herself as a member from Kansas speaking independently, added that if children have gone through puberty naturally, this would be a different discussion.
Kevin Wang, MD, an alternate delegate from Washington, who supported the resolution, noted that the rate of suicide in the transgender population is nine times that of the general population.
“I do want to emphasize that doing nothing does cause significant harm,” Dr. Wang said, The committee referred resolution No. 509 to the board for further clarification and study.
The merits of two other resolutions (No. 510 and No. 511), which called for the AAFP to no longer reject the use of “physician-assisted suicide” and “assisted suicide” and avoid the use of vague and euphemistic terms when referring to lethal medications prescribed with the intention of ending a patient’s life in statements and documents, also were heavily debated during the advocacy reference committee meeting. The committee recommended such resolutions be referred to the board for discussion.
The delegates approved the advocacy committee’s recommendations for Resolutions 509, 510, and 511.
REPORTING FROM AAFP Congress
CDC activates Emergency Operations Center to investigate vaping-associated lung injury
This move allows the CDC “to provide increased operational support” to CDC staff to meet the evolving challenges of the outbreak of vaping-related injuries and deaths, says a statement from the CDC.
“CDC has made it a priority to find out what is causing this outbreak,” noted CDC Director Robert Redfield, MD, in the statement.
The agency “continues to work closely with the U.S. Food and Drug Administration to collect information about recent e-cigarette product use, or vaping, among patients and to test the substances or chemicals within e-cigarette products used by case patients,” according to the statement.
The CDC provided email addresses and site addresses for gathering information and communicating about e-cigarettes.
Information about the collection of e-cigarettes for possible testing by FDA can be obtained through contacting FDAVapingSampleInquiries@fda.hhs.gov.
To communicate with CDC about this public health response, clinicians and health officials can contact LungDiseaseOutbreak@cdc.gov.
More information on the current outbreak related to e-cigarettes is available at https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease.html.
General information on electronic cigarette products, can be found at www.cdc.gov/e-cigarettes.
Individuals concerned about health risks of vaping should consider refraining from e-cigarette use while the cases of lung injury are being investigated, the CDC said.
This move allows the CDC “to provide increased operational support” to CDC staff to meet the evolving challenges of the outbreak of vaping-related injuries and deaths, says a statement from the CDC.
“CDC has made it a priority to find out what is causing this outbreak,” noted CDC Director Robert Redfield, MD, in the statement.
The agency “continues to work closely with the U.S. Food and Drug Administration to collect information about recent e-cigarette product use, or vaping, among patients and to test the substances or chemicals within e-cigarette products used by case patients,” according to the statement.
The CDC provided email addresses and site addresses for gathering information and communicating about e-cigarettes.
Information about the collection of e-cigarettes for possible testing by FDA can be obtained through contacting FDAVapingSampleInquiries@fda.hhs.gov.
To communicate with CDC about this public health response, clinicians and health officials can contact LungDiseaseOutbreak@cdc.gov.
More information on the current outbreak related to e-cigarettes is available at https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease.html.
General information on electronic cigarette products, can be found at www.cdc.gov/e-cigarettes.
Individuals concerned about health risks of vaping should consider refraining from e-cigarette use while the cases of lung injury are being investigated, the CDC said.
This move allows the CDC “to provide increased operational support” to CDC staff to meet the evolving challenges of the outbreak of vaping-related injuries and deaths, says a statement from the CDC.
“CDC has made it a priority to find out what is causing this outbreak,” noted CDC Director Robert Redfield, MD, in the statement.
The agency “continues to work closely with the U.S. Food and Drug Administration to collect information about recent e-cigarette product use, or vaping, among patients and to test the substances or chemicals within e-cigarette products used by case patients,” according to the statement.
The CDC provided email addresses and site addresses for gathering information and communicating about e-cigarettes.
Information about the collection of e-cigarettes for possible testing by FDA can be obtained through contacting FDAVapingSampleInquiries@fda.hhs.gov.
To communicate with CDC about this public health response, clinicians and health officials can contact LungDiseaseOutbreak@cdc.gov.
More information on the current outbreak related to e-cigarettes is available at https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease.html.
General information on electronic cigarette products, can be found at www.cdc.gov/e-cigarettes.
Individuals concerned about health risks of vaping should consider refraining from e-cigarette use while the cases of lung injury are being investigated, the CDC said.
Medical societies urge action to reduce gun violence
“With nearly 40,000 firearm-related deaths in 2017, the United States has reached a 20-year high, according to the Centers for Disease Control and Prevention,” the authors noted in the call to action (Ann Intern Med. 2019 Aug 7. doi: 10.7326/M19-2441).
The recommendations “stem largely from the individual positions previously approved by our organizations and ongoing collaborative discussion among leaders,” wrote the authors, who included leaders of the American Academy of Family Physicians, American Academy of Pediatrics, American College of Physicians, American College of Surgeons, American Medical Association, and American Psychiatric Association, as well as the American Public Health Association.
“Our organizations support a multifaceted public health approach to prevention of firearm injury and death similar to approaches that have successfully reduced the ill effects of tobacco use, motor vehicle accidents, and unintentional poisoning,” wrote Robert McLean, MD, president of the American College of Physicians, and colleagues. “While we recognize the significant political and philosophical differences about firearm ownership and regulation in the United States, we are committed to reaching out to bridge these differences to improve the health and safety of our patients, their families, and communities, while respecting the U.S. Constitution.”
The organizations specifically call for the following:
- Comprehensive criminal background checks for all firearm purchases and transfers between individuals, with limited exceptions.
- Research into the causes and consequences of firearm-related injury and death and the development and implementation of strategies to reduce these events.
- Extension of federal laws prohibiting access to firearms for domestic abusers to dating partners.
- The passage of child access prevention laws that hold accountable firearm owners who negligently store firearms under circumstances where minors could or do gain access to them.
- Improving access to mental health care for all individuals, while not broadly including all individuals with a mental health or substance use disorder in a category of individuals prohibited from purchasing firearms.
- Enactment of extreme risk protection order (ERPO) laws, which allow a judge to temporarily remove firearms from those who might be at imminent risk for using them to harm themselves or others. ERPO laws should be enacted in a manner consistent with due process.
- Physicians can and must be able to counsel at-risk patients about mitigating firearms-associated risks in the home.
- High-capacity magazines and firearms with features designed to increase their rapid and extended killing capacity should be the subject of special scrutiny and regulation.
For more than 2 decades, the American College of Physicians “has advocated for the urgent need for impactful legislation that would reduce firearms-related injuries and deaths,” ACP officials said in a statement.
“We need to protect our patients, their families, and our communities across the country from needless injuries and deaths; it’s time for the [United States] to put firearms violence prevention at the forefront of the health care conversation,” Dr. McLean said in a statement.“We are committed to working with all stakeholders, and continuing to speak out, to address this public health threat.”
Leaders at the American Academy of Family Physicians concurred.
“We need to come together as a nation on this issue,” AAFP President John Cullen, MD, said in a statement. “Treating firearm injuries as a public health issue is an important first step. We did this for motor vehicle accidents and have seen a significant decrease in injuries. We didn’t try to remove cars, we made them safer ... Both sides of the debate should come together now and work on solutions—including safe storage laws, expanded background checks, research and improved access to mental health services—we can all agree on.”
Additional firearms-related health policy content that has been published in Annals of Internal Medicine is available at: http://annals.org/aim/pages/firearm-related-content.
“With nearly 40,000 firearm-related deaths in 2017, the United States has reached a 20-year high, according to the Centers for Disease Control and Prevention,” the authors noted in the call to action (Ann Intern Med. 2019 Aug 7. doi: 10.7326/M19-2441).
The recommendations “stem largely from the individual positions previously approved by our organizations and ongoing collaborative discussion among leaders,” wrote the authors, who included leaders of the American Academy of Family Physicians, American Academy of Pediatrics, American College of Physicians, American College of Surgeons, American Medical Association, and American Psychiatric Association, as well as the American Public Health Association.
“Our organizations support a multifaceted public health approach to prevention of firearm injury and death similar to approaches that have successfully reduced the ill effects of tobacco use, motor vehicle accidents, and unintentional poisoning,” wrote Robert McLean, MD, president of the American College of Physicians, and colleagues. “While we recognize the significant political and philosophical differences about firearm ownership and regulation in the United States, we are committed to reaching out to bridge these differences to improve the health and safety of our patients, their families, and communities, while respecting the U.S. Constitution.”
The organizations specifically call for the following:
- Comprehensive criminal background checks for all firearm purchases and transfers between individuals, with limited exceptions.
- Research into the causes and consequences of firearm-related injury and death and the development and implementation of strategies to reduce these events.
- Extension of federal laws prohibiting access to firearms for domestic abusers to dating partners.
- The passage of child access prevention laws that hold accountable firearm owners who negligently store firearms under circumstances where minors could or do gain access to them.
- Improving access to mental health care for all individuals, while not broadly including all individuals with a mental health or substance use disorder in a category of individuals prohibited from purchasing firearms.
- Enactment of extreme risk protection order (ERPO) laws, which allow a judge to temporarily remove firearms from those who might be at imminent risk for using them to harm themselves or others. ERPO laws should be enacted in a manner consistent with due process.
- Physicians can and must be able to counsel at-risk patients about mitigating firearms-associated risks in the home.
- High-capacity magazines and firearms with features designed to increase their rapid and extended killing capacity should be the subject of special scrutiny and regulation.
For more than 2 decades, the American College of Physicians “has advocated for the urgent need for impactful legislation that would reduce firearms-related injuries and deaths,” ACP officials said in a statement.
“We need to protect our patients, their families, and our communities across the country from needless injuries and deaths; it’s time for the [United States] to put firearms violence prevention at the forefront of the health care conversation,” Dr. McLean said in a statement.“We are committed to working with all stakeholders, and continuing to speak out, to address this public health threat.”
Leaders at the American Academy of Family Physicians concurred.
“We need to come together as a nation on this issue,” AAFP President John Cullen, MD, said in a statement. “Treating firearm injuries as a public health issue is an important first step. We did this for motor vehicle accidents and have seen a significant decrease in injuries. We didn’t try to remove cars, we made them safer ... Both sides of the debate should come together now and work on solutions—including safe storage laws, expanded background checks, research and improved access to mental health services—we can all agree on.”
Additional firearms-related health policy content that has been published in Annals of Internal Medicine is available at: http://annals.org/aim/pages/firearm-related-content.
“With nearly 40,000 firearm-related deaths in 2017, the United States has reached a 20-year high, according to the Centers for Disease Control and Prevention,” the authors noted in the call to action (Ann Intern Med. 2019 Aug 7. doi: 10.7326/M19-2441).
The recommendations “stem largely from the individual positions previously approved by our organizations and ongoing collaborative discussion among leaders,” wrote the authors, who included leaders of the American Academy of Family Physicians, American Academy of Pediatrics, American College of Physicians, American College of Surgeons, American Medical Association, and American Psychiatric Association, as well as the American Public Health Association.
“Our organizations support a multifaceted public health approach to prevention of firearm injury and death similar to approaches that have successfully reduced the ill effects of tobacco use, motor vehicle accidents, and unintentional poisoning,” wrote Robert McLean, MD, president of the American College of Physicians, and colleagues. “While we recognize the significant political and philosophical differences about firearm ownership and regulation in the United States, we are committed to reaching out to bridge these differences to improve the health and safety of our patients, their families, and communities, while respecting the U.S. Constitution.”
The organizations specifically call for the following:
- Comprehensive criminal background checks for all firearm purchases and transfers between individuals, with limited exceptions.
- Research into the causes and consequences of firearm-related injury and death and the development and implementation of strategies to reduce these events.
- Extension of federal laws prohibiting access to firearms for domestic abusers to dating partners.
- The passage of child access prevention laws that hold accountable firearm owners who negligently store firearms under circumstances where minors could or do gain access to them.
- Improving access to mental health care for all individuals, while not broadly including all individuals with a mental health or substance use disorder in a category of individuals prohibited from purchasing firearms.
- Enactment of extreme risk protection order (ERPO) laws, which allow a judge to temporarily remove firearms from those who might be at imminent risk for using them to harm themselves or others. ERPO laws should be enacted in a manner consistent with due process.
- Physicians can and must be able to counsel at-risk patients about mitigating firearms-associated risks in the home.
- High-capacity magazines and firearms with features designed to increase their rapid and extended killing capacity should be the subject of special scrutiny and regulation.
For more than 2 decades, the American College of Physicians “has advocated for the urgent need for impactful legislation that would reduce firearms-related injuries and deaths,” ACP officials said in a statement.
“We need to protect our patients, their families, and our communities across the country from needless injuries and deaths; it’s time for the [United States] to put firearms violence prevention at the forefront of the health care conversation,” Dr. McLean said in a statement.“We are committed to working with all stakeholders, and continuing to speak out, to address this public health threat.”
Leaders at the American Academy of Family Physicians concurred.
“We need to come together as a nation on this issue,” AAFP President John Cullen, MD, said in a statement. “Treating firearm injuries as a public health issue is an important first step. We did this for motor vehicle accidents and have seen a significant decrease in injuries. We didn’t try to remove cars, we made them safer ... Both sides of the debate should come together now and work on solutions—including safe storage laws, expanded background checks, research and improved access to mental health services—we can all agree on.”
Additional firearms-related health policy content that has been published in Annals of Internal Medicine is available at: http://annals.org/aim/pages/firearm-related-content.
FROM ANNALS OF INTERNAL MEDICINE
Commentary: Medical educators must do more to prevent physician suicides
while describing two exemplars at providing physicians with mental health support, in a recently published commentary.
“I want to call attention to the gap between what educators think and say is available, in terms of mental health support, and what trainees experience,” Dr. Poorman said in a statement on her piece in the Journal of Patient Safety and Risk Management. She shared the results of an anonymous depression survey of interns, which showed that 41.8% of participants screened positive for depression. Dr. Poorman also provided statistics on physician suicide, including that at least 66 residents killed themselves between 2000 and 2014, according to ACGME, and that another source estimated that 300-400 physician suicide deaths occur annually.
“When it comes to mental illness and suicide, we are all at risk, but we too often lacked compassion in the way we approach our colleagues. We have lacked the courage to fight the stigma that is killing us. We have not asked whether our unwillingness to reform medical training has eroded the empathy of generations of doctors. We have not done enough to fight medical boards that ask doctors about mental health diagnoses in the same way they ask if we have domestic violence charges,” wrote Dr. Poorman, who practices at a University of Washington neighborhood clinic in Kent.
“A focus on the occupational risks we face would shift us away from ‘wellness’ and ‘resilience,’ and place the onus on schools, training programs, and hospitals to do better for providers and patients,” continued Dr. Poorman, who serves on the editorial advisory board of Internal Medicine News.
She commended Oregon Health and Science University, Portland, and Stanford (Calif.) University’s divisions of general surgery for providing “rigorously confidential mental health support” through a wellness and suicide prevention program for residents and faculty, and a wellness program for residents “that emphasizes relationships, structural support, and psychological safety,” respectively. Dr. Poorman also applauded both for speaking openly about physician suicides.
SOURCE: Poorman E. J Patient Saf Risk Manag. 2019 Aug 5. doi: 10.1177/2516043519866993.
This article was updated 8/5/19.
while describing two exemplars at providing physicians with mental health support, in a recently published commentary.
“I want to call attention to the gap between what educators think and say is available, in terms of mental health support, and what trainees experience,” Dr. Poorman said in a statement on her piece in the Journal of Patient Safety and Risk Management. She shared the results of an anonymous depression survey of interns, which showed that 41.8% of participants screened positive for depression. Dr. Poorman also provided statistics on physician suicide, including that at least 66 residents killed themselves between 2000 and 2014, according to ACGME, and that another source estimated that 300-400 physician suicide deaths occur annually.
“When it comes to mental illness and suicide, we are all at risk, but we too often lacked compassion in the way we approach our colleagues. We have lacked the courage to fight the stigma that is killing us. We have not asked whether our unwillingness to reform medical training has eroded the empathy of generations of doctors. We have not done enough to fight medical boards that ask doctors about mental health diagnoses in the same way they ask if we have domestic violence charges,” wrote Dr. Poorman, who practices at a University of Washington neighborhood clinic in Kent.
“A focus on the occupational risks we face would shift us away from ‘wellness’ and ‘resilience,’ and place the onus on schools, training programs, and hospitals to do better for providers and patients,” continued Dr. Poorman, who serves on the editorial advisory board of Internal Medicine News.
She commended Oregon Health and Science University, Portland, and Stanford (Calif.) University’s divisions of general surgery for providing “rigorously confidential mental health support” through a wellness and suicide prevention program for residents and faculty, and a wellness program for residents “that emphasizes relationships, structural support, and psychological safety,” respectively. Dr. Poorman also applauded both for speaking openly about physician suicides.
SOURCE: Poorman E. J Patient Saf Risk Manag. 2019 Aug 5. doi: 10.1177/2516043519866993.
This article was updated 8/5/19.
while describing two exemplars at providing physicians with mental health support, in a recently published commentary.
“I want to call attention to the gap between what educators think and say is available, in terms of mental health support, and what trainees experience,” Dr. Poorman said in a statement on her piece in the Journal of Patient Safety and Risk Management. She shared the results of an anonymous depression survey of interns, which showed that 41.8% of participants screened positive for depression. Dr. Poorman also provided statistics on physician suicide, including that at least 66 residents killed themselves between 2000 and 2014, according to ACGME, and that another source estimated that 300-400 physician suicide deaths occur annually.
“When it comes to mental illness and suicide, we are all at risk, but we too often lacked compassion in the way we approach our colleagues. We have lacked the courage to fight the stigma that is killing us. We have not asked whether our unwillingness to reform medical training has eroded the empathy of generations of doctors. We have not done enough to fight medical boards that ask doctors about mental health diagnoses in the same way they ask if we have domestic violence charges,” wrote Dr. Poorman, who practices at a University of Washington neighborhood clinic in Kent.
“A focus on the occupational risks we face would shift us away from ‘wellness’ and ‘resilience,’ and place the onus on schools, training programs, and hospitals to do better for providers and patients,” continued Dr. Poorman, who serves on the editorial advisory board of Internal Medicine News.
She commended Oregon Health and Science University, Portland, and Stanford (Calif.) University’s divisions of general surgery for providing “rigorously confidential mental health support” through a wellness and suicide prevention program for residents and faculty, and a wellness program for residents “that emphasizes relationships, structural support, and psychological safety,” respectively. Dr. Poorman also applauded both for speaking openly about physician suicides.
SOURCE: Poorman E. J Patient Saf Risk Manag. 2019 Aug 5. doi: 10.1177/2516043519866993.
This article was updated 8/5/19.
FROM THE JOURNAL OF PATIENT SAFETY AND RISK MANAGEMENT
The costs and benefits of SGLT2 inhibitors & GLP-1 RAs
The options for treating type 2 diabetes without insulin have grown beyond metformin to include a long list of sodium-glucose cotransporter 2 (SGLT2) inhibitors and glucagonlike peptide–1 (GLP-1) receptor agonists that can be taken with or without metformin. These new drugs have cardiovascular and kidney benefits and help with weight loss, but they also carry risks and, according to some experts, their costs can be prohibitively expensive.
Given the medical community’s long-term experience with treating patients with metformin, and metformin’s lower cost, most of the physicians interviewed for this article advise using SGLT2 inhibitors and GLP-1 receptor agonists as second-line treatments. Others said that they would prefer to use the newer drugs as first-line therapies in select high-risk patients, but prior authorization hurdles created by insurance companies make that approach too burdensome.
“The economics of U.S. health care is stacked against many of our patients with diabetes in the current era,” Robert H. Hopkins Jr., MD, said in an interview.
Even when their insurance approves the drugs, patients still may not be able to afford the copay, explained Dr. Hopkins, professor of internal medicine and pediatrics and director of the division of general internal medicine at the University of Arkansas for Medical Sciences, Little Rock. “Sometimes patients can purchase drugs at a lower cost than the copay to purchase with the ‘drug coverage’ in their insurance plan – unfortunately, this is not the case with the newer diabetes medications we are discussing here.”
“SGLT2 inhibitors and GLP-1 agonists can cost several hundred dollars a month, and insurers often balk at paying for them. They’ll say, ‘Have you tried metformin?’ ” explained endocrinologist Victor Lawrence Roberts, MD, in a interview. “We have to work with insurance companies the best we can in a stepwise fashion.”
According to Dr. Roberts, 80% of his patients with diabetes struggle with the cost of medicine in general. “They’re either underinsured or not insured or their formulary is limited.
Douglas S. Paauw, MD, agreed in an interview that the newer drugs can be problematic on the insurance front.
“For some patients they aren’t affordable, especially for the uninsured if you can’t get them on an assistance program,” said Dr. Paauw, who is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and serves as third-year medical student clerkship director at the university.
Dr. Hopkins, who is on the Internal Medicine News board, noted that “unfortunately, the treatment of type 2 diabetes in patients who cannot achieve control with metformin, diet, weight control, and exercise is a story of the ‘haves’ and the ‘have nots.’ The ‘haves’ are those who have pharmacy benefits which make access to newer agents like SGLT2 inhibitors and GLP-1 agonists a possibility.”
“I have had very few of the ‘have nots’ who have been able to even consider these newer agents, which carry price tags of $600-$1,300 a month even with the availability of discounting coupons in the marketplace,” he added. “Most of these patients end up requiring a sulfonylurea or TZD [thiazolidinedione] as a second agent to achieve glycemic control. This makes it very difficult to achieve sufficient weight and metabolic control to avoid an eventual switch to insulin.”
Fatima Z. Syed, MD, an endocrine-trained general internist at DukeHealth in Durham, N.C., said she prescribes SGLT2 inhibitors and GLP-1 receptor agonists in combination with metformin. “I prescribe them frequently, but they are not first-line treatments,” she explained.
“Nothing replaces diet and exercise” as therapy for patients with type 2 diabetes, she added.
Neil S. Skolnik, MD, said that insurance companies were not preventing patients from using these drugs in his experience. He also provided an optimistic take on the accessibility of these drugs in the near future.
“Most insurance companies are now covering select SGLT2 inhibitors and GLP-1 receptor agonists for appropriate patients and those companies that currently do not will soon have to,” said Dr. Skolnik, who is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington (Pa.) Jefferson Health.
“The outcomes [associated with use of the new drugs] are robust, the benefits are large, and are well worth the cost,” he added.
The side effects
While others praised these drugs for their beneficial effects, they also noted that the side effects of these drugs are serious and must be discussed with patients.
GLP-1 receptor agonists are linked to gastrointestinal symptoms, especially nausea, while SGLT2 inhibitors have been linked to kidney failure, ketoacidosis, and more. The Food and Drug Administration warned in 2018 that the SGLT2 inhibitors can cause a rare serious infection known as Fournier’s gangrene – necrotizing fasciitis of the perineum.
“We have to tell our patients to let us know right away if they get pain or swelling in the genital area,” Dr. Paauw, who is on the Internal Medicine News board, noted. “The chance that an infection could explode quickly is higher in those who take these drugs.”
Amputation risks also are associated with taking the SGLT2 inhibitor canagliflozin (Invokana). The FDA requires the manufacturer of this drug to include a black-box warning about the risk of “lower-limb amputations, most frequently of the toe and midfoot,” but also the leg. In approval trials, the risk doubled versus placebo.
These amputation risks “put a damper on some of the enthusiasm on behalf of physicians and patients ... for taking this drug,” noted Dr. Roberts, who is a professor of internal medicine at the University of Central Florida, Orlando.
While a manufacturer-funded study released last year found no link to amputations, the results weren’t powerful enough to rule out a moderately increased risk.
“[If] you are at high risk for having an amputation, we really have to take this risk very seriously,” said John B. Buse, MD, chief of the division of endocrinology at the University of North Carolina at Chapel Hill, in a presentation about the study at the 2018 annual scientific sessions of the American Diabetes Association.
The benefits
Despite these risks of adverse events, most interviewed agreed that the many benefits observed in those taking SGLT2 inhibitors or GLP-1 receptor agonists make them worth prescribing, at least to those who are able to afford them.
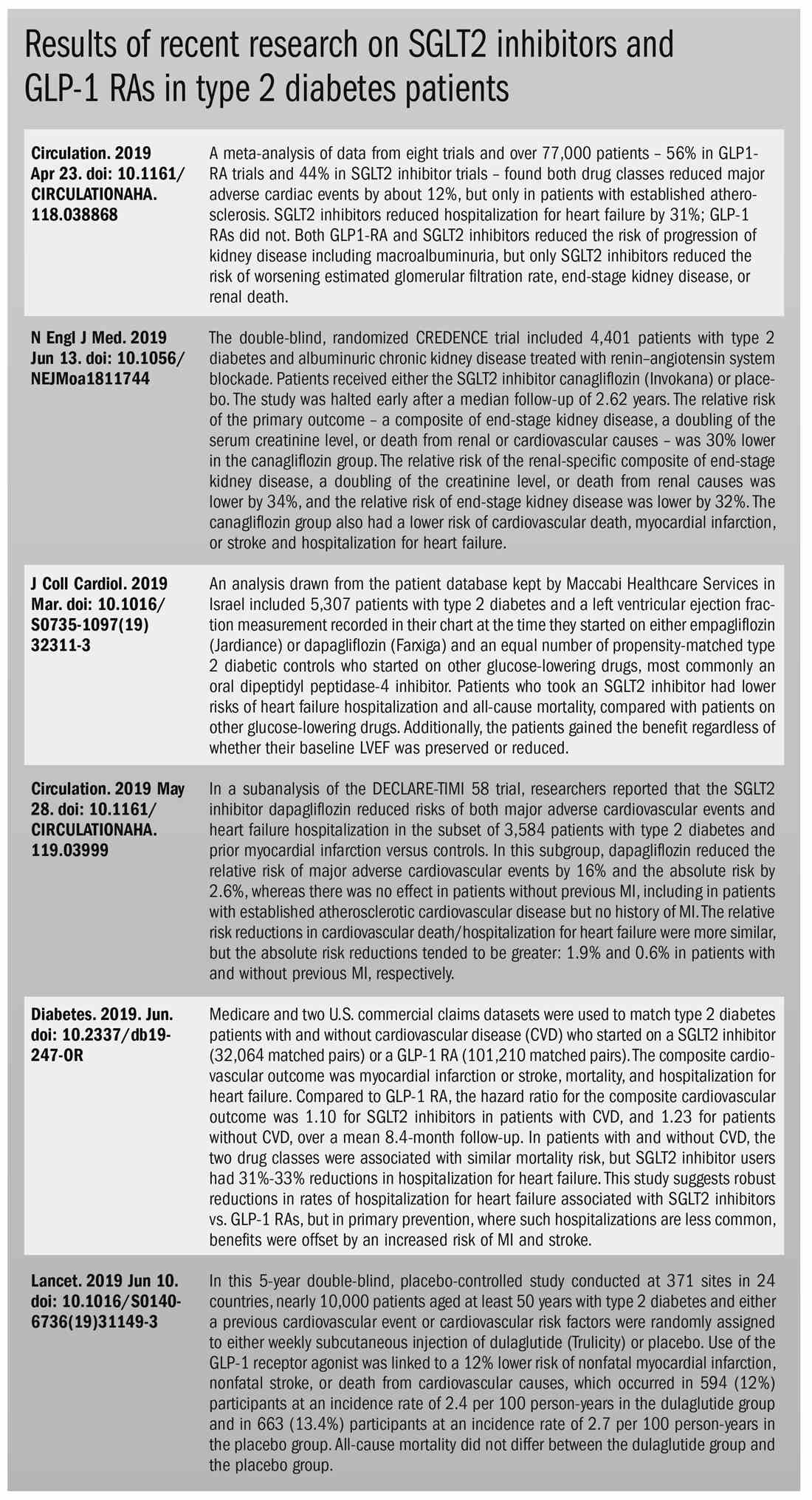
Both SGLT2 inhibitors and GLP-1 receptor agonists appear to have significant cardiovascular benefits. A 2019 meta-analysis and systematic review found that both drugs reduced major adverse cardiac events by about 12% (Circulation. 2019 Apr 23;139[17]:2022-31).
“They don’t cause hypoglycemia, they lower blood pressure, they don’t cause weight gain, and they might promote weight loss,” noted Dr. Paauw.
SGLT2 inhibitors also have shown signs of kidney benefits. The CREDENCE trial linked canagliflozin to a lowering of kidney disorders versus placebo (N Engl J Med. 2019 Jun 13;380[24]:2295-306). “The relative risk of the renal-specific composite of end-stage kidney disease, a doubling of the creatinine level, or death from renal causes was lower by 34% (hazard ratio, 0.66; 95% confidence interval, 0.53-0.81; P less than .001), and the relative risk of end-stage kidney disease was lower by 32% (HR, 0.68; 95% CI, 0.54-0.86; P = .002),” the trial investigators wrote.
“They showed very nicely that the drug improved the kidney function of those patients and reduced the kidney deterioration,” said Yehuda Handelsman, MD, an endocrinologist in Tarzana, Calif., who chaired the 2011 and 2015 American Association of Clinical Endocrinologists’ Comprehensive Diabetes Guidelines. The study was especially impressive, he added, because it included patients with low kidney function.
SGLT2 inhibitors’ “diuretic mechanism explains why there is a substantial reduction in heart failure hospitalizations in patients who take these drugs,” said cardiologist Marc E. Goldschmidt, MD, director of the Heart Success Program at Atlantic Health System’s Morristown (N.J.) Medical Center, in an interview. “Both the EMPA-REG Outcome and the CREDENCE trials demonstrated substantial benefit of this class of medications by showing a lower risk of cardiovascular death as well as death from any cause and a lower risk of hospitalization for heart failure."
Overall, the SGLT2 trial data have been very consistent with a benefit for cardiovascular risk reduction, particularly in regard to heart failure hospitalizations and even in potentially preventing heart failure in diabetics,” he added.
Dr. Skolnik, a columnist for Family Practice News, cited SGLT2 inhibitors and GLP-1 receptor agonists’ ability to slow renal disease progression, promote weight loss, and prevent poor cardiac outcomes.“These drugs should be used, in addition to metformin, in all patients with diabetes and vascular disease. These proven outcomes are far better than we ever were able to achieve previously and the strength of the evidence at this point is very strong,” said Dr. Skolnik. “In addition to the benefits of decreasing the development of cardiovascular disease, serious heart failure, and slowing progression of renal disease, these two classes of medication have additional benefits. Both classes help patients lose weight, which is very different from what was found with either sulfonylureas or insulin, which cause patients to gain weight. Also both the SGLT2 inhibitors and the GLP-1 RAs [receptor agonists] have a low incidence of hypoglycemia. For all these reasons, these have become important medications for us to use in primary care.”
Other recent trials offer “very powerful data” about SGLT2 inhibitors, Dr. Roberts said. That’s good news, since “our approach needs to be toward cardiovascular protection and preservation as well as managing blood sugar.”An Israeli trial, whose results were released in May 2019 at the annual meeting of the American College of Cardiology, found that, compared with other glucose-lowering drugs, taking an SGLT2 inhibitor was associated with lower risks of heart failure hospitalization and all-cause mortality (HR, 0.54; 95% CI, 0.44-0.65; P less than .001). This trial also offered a new detail: The patients gained the benefit regardless of whether their baseline left ventricular ejection fraction was preserved or reduced (J Coll Cardiol. 2019 Mar;73[9]:suppl 1). The SGLT2 inhibitors used in this trial included dapagliflozin (Farxiga) and empagliflozin (Jardiance).
In another study released this year, a subanalysis of the DECLARE-TIMI 58 trial, researchers reported that the SGLT2 inhibitor dapagliflozin reduced risks of both major adverse cardiovascular events and heart failure hospitalization in the subset of patients with type 2 diabetes and prior myocardial infarction versus controls (Circulation. 2019 May 28;139[22]:2516-27). The absolute risk reduction for major adverse cardiovascular events was 1.9% (HR, 0.81; 95% CI, 0.65-1.00; P = .046), while it was 0.6% for heart failure hospitalization (HR, 0.85; 95% CI, 0.72-1.00; P = .055).
These and other studies “speak volumes about the efficacy of managing blood sugar and addressing our biggest nemesis, which is cardiovascular disease,” Dr. Roberts said. “It’s irrefutable. The data [are] very good.”
Dr. Paauw said an SGLT2 inhibitor or GLP-1 receptor agonist is best reserved for use in select patients with cardiovascular risks and type 2 diabetes that need management beyond metformin.
For example, they might fit a 70-year-old with persistent hypertension who’s already taking a couple of blood pressure medications. “If they have another cardiovascular risk factor, the cardiovascular protection piece will be a bigger deal,” he said. Also, “it will probably help lower their blood pressure so they can avoid taking another blood pressure medicine.”
Trials of both GLP-1 receptor agonists and SGLT2 inhibitors have shown benefits “in improving [major adverse cardiac events], with the SGLT2 class showing substantial benefit in improving both heart failure and renal outcomes as well,” noted Dr. Skolnik. “It is in this context that one must address the question of whether the price of the medications are worthwhile. With such substantial benefit, there is no question in my mind that – for patients who have underlying cardiovascular illness, which includes patients with existent coronary disease, history of stroke, transient ischemic attack, or peripheral vascular disease – it is far and away worth it to prescribe these classes of medications.”
Indeed, the American Diabetes Association and the European Association for the Study of Diabetes’ most recent guidelines now call for a GLP-1 receptor agonist – instead of insulin – to be the first injectable used to treat type 2 diabetes (Diabetes Care 2018 Dec; 41[12]:2669-701).
“For the relatively small number of my patients who have been able to access and use these medications for months or longer, more have tolerated the GLP-1 agonists than SGLT2 inhibitors primarily due to urinary issues,” noted Dr. Hopkins.
Dipeptidyl peptidase–4 inhibitors are another option in patients with type 2 diabetes, but research suggests they may not be a top option for patients with cardiovascular risk. A 2018 review noted that cardiovascular outcome trials for alogliptin (Nesina), saxagliptin (Onglyza), and sitagliptin (Januvia) showed noninferiority but failed to demonstrate any superiority, compared with placebo in patients with type 2 diabetes mellitus and high cardiovascular risk (Circ Res. 2018 May 11;122[10]:1439-59).
The combination therapies
Many of the newer drugs are available as combinations with other types of diabetes drugs. In some cases, physicians create their own form of combination therapy by separately prescribing two or more diabetes drugs. Earlier this year, a study suggested the benefits of this kind of add-on therapy: Diabetes outcomes improved in patients who took the GLP-1 receptor agonist semaglutide and an SGLT2 inhibitor (Lancet Diabetes Endocrinol. 2019 Mar 1. doi: 10.1016/S2213-8587[19]30066-X).
Dr. Roberts suggested caution, however, when prescribing combination therapies. “My recommendation is always to begin with the individual medications to see if the patient tolerates the drugs and then decide which component needs to be titrated. It’s hard to titrate a combination drug, and it doesn’t leave a lot of flexibility. You never know which drug is doing what.
Dr. Handelsman said some patients may need to take three medications such as metformin, an SGLT2 inhibitor, and a GLP-1 receptor agonist.
“I don’t recommend using the combinations if you’re not familiar with the drugs ... These are relatively new pharmaceuticals, and most of us are on a learning curve as to how they fit into the armamentarium. If a drug is tolerated with a good response, you can certainly consider going to the combination tablets,” he added.
There is at least one drug that combines these three classes: The newly FDA-approved Qternmet XR, which combines dapagliflozin (an SGLT2 inhibitor), saxagliptin (a GLP-1 receptor agonist), and metformin. As of mid-June 2019, it was not yet available in the United States. Its sister drug Qtern, which combines dapagliflozin and saxagliptin, costs more than $500 a month with a free coupon, according to goodrx.com. In contrast, metformin is extremely inexpensive, costing just a few dollars a month for a common starting dose.
What about adding insulin?
“Both [SGLT2 inhibitors and GLP-1 receptor agonists] work very well with insulin,” Dr. Handelsman said. “There is a nice additive effect on the reduction of [hemoglobin] A1c. The only caution is that, although neither SGLT2 inhibitors nor GLP-1 receptor agonists cause hypoglycemia, in combination with insulin they do increase the risk of hypoglycemia. You may have to adjust the dose of insulin.”
Dr. Hopkins warned that cost becomes an even bigger issue when you add insulin into the mix.
“When insulin comes into the discussion, we are again stuck with astronomical costs which many struggle to afford,” he explained.
Indeed, the price tag on these drugs seems to be the biggest problem physicians have with them.
“The challenges in managing patients with diabetes aren’t the risks associated with the drugs. It’s dealing with their insurers,” noted Dr. Roberts.
Dr. Hopkins, Dr. Paauw, Dr. Roberts, and Dr. Syed reported no disclosures. Dr. Buse is an investigator for Johnson and Johnson. Dr. Goldschmidt is paid to speak by Novartis. Dr. Handelsman reported research grants, consulting work, and speaker honoraria from Amgen, Gilead, Lilly, Merck, Novo Nordisk, and others. Dr Skolnik reported nonfinancial support from AstraZeneca, Boehringer Ingelheim, Sanofi, and GlaxoSmithKline and personal fees from AstraZeneca, Boehringer Ingelheim, and Eli Lilly. He also serves on the advisory boards of AstraZeneca, Boehringer Ingelheim, Teva Pharmaceutical, Eli Lilly, Sanofi, Janssen Pharmaceuticals, Intarcia, Mylan, and GlaxoSmithKline.
Dr. Paauw and Dr. Skolnik are columnists for Family Practice News and Internal Medicine News.
M. Alexander Otto contributed to this report.
The options for treating type 2 diabetes without insulin have grown beyond metformin to include a long list of sodium-glucose cotransporter 2 (SGLT2) inhibitors and glucagonlike peptide–1 (GLP-1) receptor agonists that can be taken with or without metformin. These new drugs have cardiovascular and kidney benefits and help with weight loss, but they also carry risks and, according to some experts, their costs can be prohibitively expensive.
Given the medical community’s long-term experience with treating patients with metformin, and metformin’s lower cost, most of the physicians interviewed for this article advise using SGLT2 inhibitors and GLP-1 receptor agonists as second-line treatments. Others said that they would prefer to use the newer drugs as first-line therapies in select high-risk patients, but prior authorization hurdles created by insurance companies make that approach too burdensome.
“The economics of U.S. health care is stacked against many of our patients with diabetes in the current era,” Robert H. Hopkins Jr., MD, said in an interview.
Even when their insurance approves the drugs, patients still may not be able to afford the copay, explained Dr. Hopkins, professor of internal medicine and pediatrics and director of the division of general internal medicine at the University of Arkansas for Medical Sciences, Little Rock. “Sometimes patients can purchase drugs at a lower cost than the copay to purchase with the ‘drug coverage’ in their insurance plan – unfortunately, this is not the case with the newer diabetes medications we are discussing here.”
“SGLT2 inhibitors and GLP-1 agonists can cost several hundred dollars a month, and insurers often balk at paying for them. They’ll say, ‘Have you tried metformin?’ ” explained endocrinologist Victor Lawrence Roberts, MD, in a interview. “We have to work with insurance companies the best we can in a stepwise fashion.”
According to Dr. Roberts, 80% of his patients with diabetes struggle with the cost of medicine in general. “They’re either underinsured or not insured or their formulary is limited.
Douglas S. Paauw, MD, agreed in an interview that the newer drugs can be problematic on the insurance front.
“For some patients they aren’t affordable, especially for the uninsured if you can’t get them on an assistance program,” said Dr. Paauw, who is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and serves as third-year medical student clerkship director at the university.
Dr. Hopkins, who is on the Internal Medicine News board, noted that “unfortunately, the treatment of type 2 diabetes in patients who cannot achieve control with metformin, diet, weight control, and exercise is a story of the ‘haves’ and the ‘have nots.’ The ‘haves’ are those who have pharmacy benefits which make access to newer agents like SGLT2 inhibitors and GLP-1 agonists a possibility.”
“I have had very few of the ‘have nots’ who have been able to even consider these newer agents, which carry price tags of $600-$1,300 a month even with the availability of discounting coupons in the marketplace,” he added. “Most of these patients end up requiring a sulfonylurea or TZD [thiazolidinedione] as a second agent to achieve glycemic control. This makes it very difficult to achieve sufficient weight and metabolic control to avoid an eventual switch to insulin.”
Fatima Z. Syed, MD, an endocrine-trained general internist at DukeHealth in Durham, N.C., said she prescribes SGLT2 inhibitors and GLP-1 receptor agonists in combination with metformin. “I prescribe them frequently, but they are not first-line treatments,” she explained.
“Nothing replaces diet and exercise” as therapy for patients with type 2 diabetes, she added.
Neil S. Skolnik, MD, said that insurance companies were not preventing patients from using these drugs in his experience. He also provided an optimistic take on the accessibility of these drugs in the near future.
“Most insurance companies are now covering select SGLT2 inhibitors and GLP-1 receptor agonists for appropriate patients and those companies that currently do not will soon have to,” said Dr. Skolnik, who is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington (Pa.) Jefferson Health.
“The outcomes [associated with use of the new drugs] are robust, the benefits are large, and are well worth the cost,” he added.
The side effects
While others praised these drugs for their beneficial effects, they also noted that the side effects of these drugs are serious and must be discussed with patients.
GLP-1 receptor agonists are linked to gastrointestinal symptoms, especially nausea, while SGLT2 inhibitors have been linked to kidney failure, ketoacidosis, and more. The Food and Drug Administration warned in 2018 that the SGLT2 inhibitors can cause a rare serious infection known as Fournier’s gangrene – necrotizing fasciitis of the perineum.
“We have to tell our patients to let us know right away if they get pain or swelling in the genital area,” Dr. Paauw, who is on the Internal Medicine News board, noted. “The chance that an infection could explode quickly is higher in those who take these drugs.”
Amputation risks also are associated with taking the SGLT2 inhibitor canagliflozin (Invokana). The FDA requires the manufacturer of this drug to include a black-box warning about the risk of “lower-limb amputations, most frequently of the toe and midfoot,” but also the leg. In approval trials, the risk doubled versus placebo.
These amputation risks “put a damper on some of the enthusiasm on behalf of physicians and patients ... for taking this drug,” noted Dr. Roberts, who is a professor of internal medicine at the University of Central Florida, Orlando.
While a manufacturer-funded study released last year found no link to amputations, the results weren’t powerful enough to rule out a moderately increased risk.
“[If] you are at high risk for having an amputation, we really have to take this risk very seriously,” said John B. Buse, MD, chief of the division of endocrinology at the University of North Carolina at Chapel Hill, in a presentation about the study at the 2018 annual scientific sessions of the American Diabetes Association.
The benefits
Despite these risks of adverse events, most interviewed agreed that the many benefits observed in those taking SGLT2 inhibitors or GLP-1 receptor agonists make them worth prescribing, at least to those who are able to afford them.
Both SGLT2 inhibitors and GLP-1 receptor agonists appear to have significant cardiovascular benefits. A 2019 meta-analysis and systematic review found that both drugs reduced major adverse cardiac events by about 12% (Circulation. 2019 Apr 23;139[17]:2022-31).
“They don’t cause hypoglycemia, they lower blood pressure, they don’t cause weight gain, and they might promote weight loss,” noted Dr. Paauw.
SGLT2 inhibitors also have shown signs of kidney benefits. The CREDENCE trial linked canagliflozin to a lowering of kidney disorders versus placebo (N Engl J Med. 2019 Jun 13;380[24]:2295-306). “The relative risk of the renal-specific composite of end-stage kidney disease, a doubling of the creatinine level, or death from renal causes was lower by 34% (hazard ratio, 0.66; 95% confidence interval, 0.53-0.81; P less than .001), and the relative risk of end-stage kidney disease was lower by 32% (HR, 0.68; 95% CI, 0.54-0.86; P = .002),” the trial investigators wrote.
“They showed very nicely that the drug improved the kidney function of those patients and reduced the kidney deterioration,” said Yehuda Handelsman, MD, an endocrinologist in Tarzana, Calif., who chaired the 2011 and 2015 American Association of Clinical Endocrinologists’ Comprehensive Diabetes Guidelines. The study was especially impressive, he added, because it included patients with low kidney function.
SGLT2 inhibitors’ “diuretic mechanism explains why there is a substantial reduction in heart failure hospitalizations in patients who take these drugs,” said cardiologist Marc E. Goldschmidt, MD, director of the Heart Success Program at Atlantic Health System’s Morristown (N.J.) Medical Center, in an interview. “Both the EMPA-REG Outcome and the CREDENCE trials demonstrated substantial benefit of this class of medications by showing a lower risk of cardiovascular death as well as death from any cause and a lower risk of hospitalization for heart failure."
Overall, the SGLT2 trial data have been very consistent with a benefit for cardiovascular risk reduction, particularly in regard to heart failure hospitalizations and even in potentially preventing heart failure in diabetics,” he added.
Dr. Skolnik, a columnist for Family Practice News, cited SGLT2 inhibitors and GLP-1 receptor agonists’ ability to slow renal disease progression, promote weight loss, and prevent poor cardiac outcomes.“These drugs should be used, in addition to metformin, in all patients with diabetes and vascular disease. These proven outcomes are far better than we ever were able to achieve previously and the strength of the evidence at this point is very strong,” said Dr. Skolnik. “In addition to the benefits of decreasing the development of cardiovascular disease, serious heart failure, and slowing progression of renal disease, these two classes of medication have additional benefits. Both classes help patients lose weight, which is very different from what was found with either sulfonylureas or insulin, which cause patients to gain weight. Also both the SGLT2 inhibitors and the GLP-1 RAs [receptor agonists] have a low incidence of hypoglycemia. For all these reasons, these have become important medications for us to use in primary care.”
Other recent trials offer “very powerful data” about SGLT2 inhibitors, Dr. Roberts said. That’s good news, since “our approach needs to be toward cardiovascular protection and preservation as well as managing blood sugar.”An Israeli trial, whose results were released in May 2019 at the annual meeting of the American College of Cardiology, found that, compared with other glucose-lowering drugs, taking an SGLT2 inhibitor was associated with lower risks of heart failure hospitalization and all-cause mortality (HR, 0.54; 95% CI, 0.44-0.65; P less than .001). This trial also offered a new detail: The patients gained the benefit regardless of whether their baseline left ventricular ejection fraction was preserved or reduced (J Coll Cardiol. 2019 Mar;73[9]:suppl 1). The SGLT2 inhibitors used in this trial included dapagliflozin (Farxiga) and empagliflozin (Jardiance).
In another study released this year, a subanalysis of the DECLARE-TIMI 58 trial, researchers reported that the SGLT2 inhibitor dapagliflozin reduced risks of both major adverse cardiovascular events and heart failure hospitalization in the subset of patients with type 2 diabetes and prior myocardial infarction versus controls (Circulation. 2019 May 28;139[22]:2516-27). The absolute risk reduction for major adverse cardiovascular events was 1.9% (HR, 0.81; 95% CI, 0.65-1.00; P = .046), while it was 0.6% for heart failure hospitalization (HR, 0.85; 95% CI, 0.72-1.00; P = .055).
These and other studies “speak volumes about the efficacy of managing blood sugar and addressing our biggest nemesis, which is cardiovascular disease,” Dr. Roberts said. “It’s irrefutable. The data [are] very good.”
Dr. Paauw said an SGLT2 inhibitor or GLP-1 receptor agonist is best reserved for use in select patients with cardiovascular risks and type 2 diabetes that need management beyond metformin.
For example, they might fit a 70-year-old with persistent hypertension who’s already taking a couple of blood pressure medications. “If they have another cardiovascular risk factor, the cardiovascular protection piece will be a bigger deal,” he said. Also, “it will probably help lower their blood pressure so they can avoid taking another blood pressure medicine.”
Trials of both GLP-1 receptor agonists and SGLT2 inhibitors have shown benefits “in improving [major adverse cardiac events], with the SGLT2 class showing substantial benefit in improving both heart failure and renal outcomes as well,” noted Dr. Skolnik. “It is in this context that one must address the question of whether the price of the medications are worthwhile. With such substantial benefit, there is no question in my mind that – for patients who have underlying cardiovascular illness, which includes patients with existent coronary disease, history of stroke, transient ischemic attack, or peripheral vascular disease – it is far and away worth it to prescribe these classes of medications.”
Indeed, the American Diabetes Association and the European Association for the Study of Diabetes’ most recent guidelines now call for a GLP-1 receptor agonist – instead of insulin – to be the first injectable used to treat type 2 diabetes (Diabetes Care 2018 Dec; 41[12]:2669-701).
“For the relatively small number of my patients who have been able to access and use these medications for months or longer, more have tolerated the GLP-1 agonists than SGLT2 inhibitors primarily due to urinary issues,” noted Dr. Hopkins.
Dipeptidyl peptidase–4 inhibitors are another option in patients with type 2 diabetes, but research suggests they may not be a top option for patients with cardiovascular risk. A 2018 review noted that cardiovascular outcome trials for alogliptin (Nesina), saxagliptin (Onglyza), and sitagliptin (Januvia) showed noninferiority but failed to demonstrate any superiority, compared with placebo in patients with type 2 diabetes mellitus and high cardiovascular risk (Circ Res. 2018 May 11;122[10]:1439-59).
The combination therapies
Many of the newer drugs are available as combinations with other types of diabetes drugs. In some cases, physicians create their own form of combination therapy by separately prescribing two or more diabetes drugs. Earlier this year, a study suggested the benefits of this kind of add-on therapy: Diabetes outcomes improved in patients who took the GLP-1 receptor agonist semaglutide and an SGLT2 inhibitor (Lancet Diabetes Endocrinol. 2019 Mar 1. doi: 10.1016/S2213-8587[19]30066-X).
Dr. Roberts suggested caution, however, when prescribing combination therapies. “My recommendation is always to begin with the individual medications to see if the patient tolerates the drugs and then decide which component needs to be titrated. It’s hard to titrate a combination drug, and it doesn’t leave a lot of flexibility. You never know which drug is doing what.
Dr. Handelsman said some patients may need to take three medications such as metformin, an SGLT2 inhibitor, and a GLP-1 receptor agonist.
“I don’t recommend using the combinations if you’re not familiar with the drugs ... These are relatively new pharmaceuticals, and most of us are on a learning curve as to how they fit into the armamentarium. If a drug is tolerated with a good response, you can certainly consider going to the combination tablets,” he added.
There is at least one drug that combines these three classes: The newly FDA-approved Qternmet XR, which combines dapagliflozin (an SGLT2 inhibitor), saxagliptin (a GLP-1 receptor agonist), and metformin. As of mid-June 2019, it was not yet available in the United States. Its sister drug Qtern, which combines dapagliflozin and saxagliptin, costs more than $500 a month with a free coupon, according to goodrx.com. In contrast, metformin is extremely inexpensive, costing just a few dollars a month for a common starting dose.
What about adding insulin?
“Both [SGLT2 inhibitors and GLP-1 receptor agonists] work very well with insulin,” Dr. Handelsman said. “There is a nice additive effect on the reduction of [hemoglobin] A1c. The only caution is that, although neither SGLT2 inhibitors nor GLP-1 receptor agonists cause hypoglycemia, in combination with insulin they do increase the risk of hypoglycemia. You may have to adjust the dose of insulin.”
Dr. Hopkins warned that cost becomes an even bigger issue when you add insulin into the mix.
“When insulin comes into the discussion, we are again stuck with astronomical costs which many struggle to afford,” he explained.
Indeed, the price tag on these drugs seems to be the biggest problem physicians have with them.
“The challenges in managing patients with diabetes aren’t the risks associated with the drugs. It’s dealing with their insurers,” noted Dr. Roberts.
Dr. Hopkins, Dr. Paauw, Dr. Roberts, and Dr. Syed reported no disclosures. Dr. Buse is an investigator for Johnson and Johnson. Dr. Goldschmidt is paid to speak by Novartis. Dr. Handelsman reported research grants, consulting work, and speaker honoraria from Amgen, Gilead, Lilly, Merck, Novo Nordisk, and others. Dr Skolnik reported nonfinancial support from AstraZeneca, Boehringer Ingelheim, Sanofi, and GlaxoSmithKline and personal fees from AstraZeneca, Boehringer Ingelheim, and Eli Lilly. He also serves on the advisory boards of AstraZeneca, Boehringer Ingelheim, Teva Pharmaceutical, Eli Lilly, Sanofi, Janssen Pharmaceuticals, Intarcia, Mylan, and GlaxoSmithKline.
Dr. Paauw and Dr. Skolnik are columnists for Family Practice News and Internal Medicine News.
M. Alexander Otto contributed to this report.
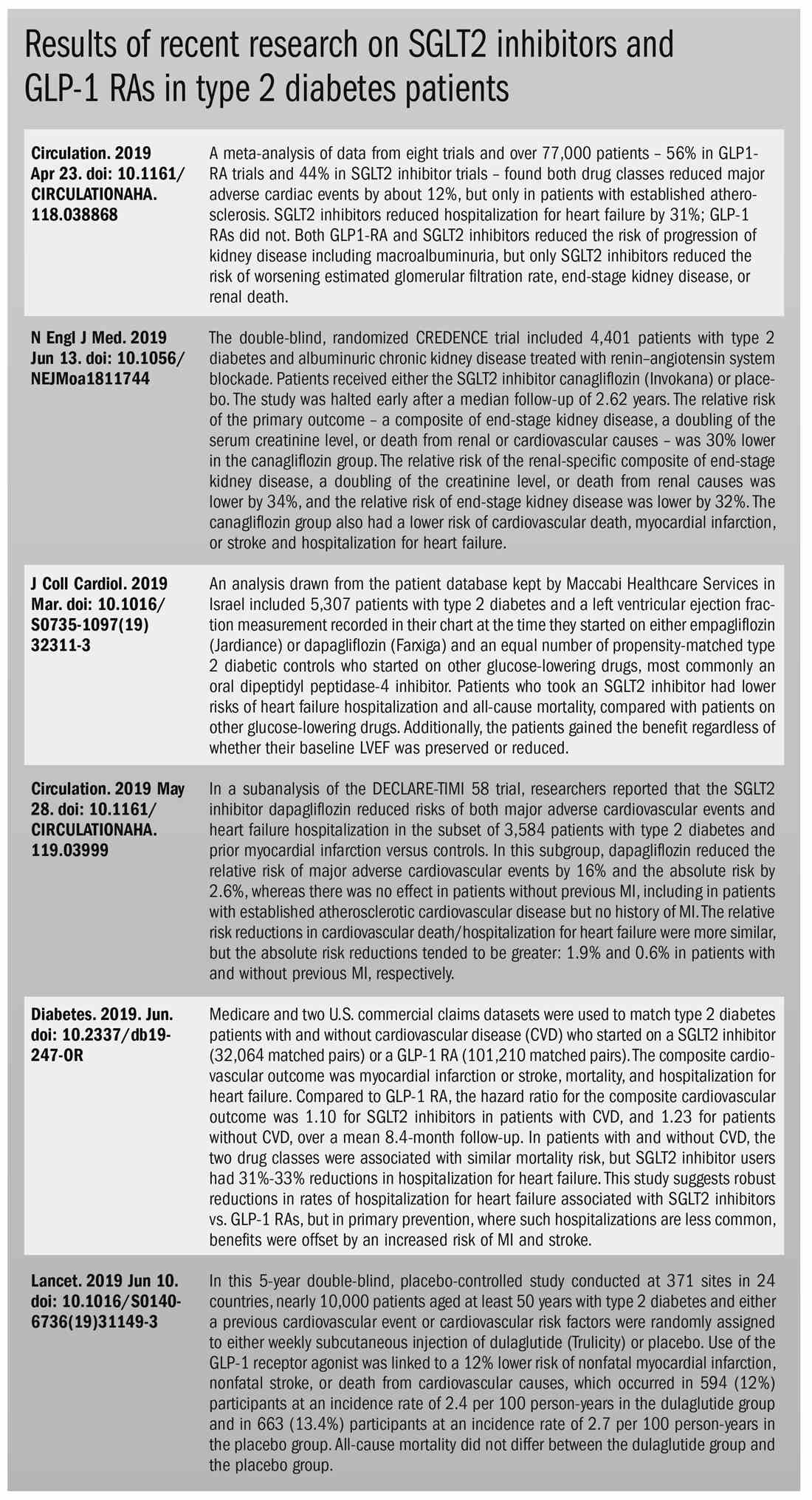
The options for treating type 2 diabetes without insulin have grown beyond metformin to include a long list of sodium-glucose cotransporter 2 (SGLT2) inhibitors and glucagonlike peptide–1 (GLP-1) receptor agonists that can be taken with or without metformin. These new drugs have cardiovascular and kidney benefits and help with weight loss, but they also carry risks and, according to some experts, their costs can be prohibitively expensive.
Given the medical community’s long-term experience with treating patients with metformin, and metformin’s lower cost, most of the physicians interviewed for this article advise using SGLT2 inhibitors and GLP-1 receptor agonists as second-line treatments. Others said that they would prefer to use the newer drugs as first-line therapies in select high-risk patients, but prior authorization hurdles created by insurance companies make that approach too burdensome.
“The economics of U.S. health care is stacked against many of our patients with diabetes in the current era,” Robert H. Hopkins Jr., MD, said in an interview.
Even when their insurance approves the drugs, patients still may not be able to afford the copay, explained Dr. Hopkins, professor of internal medicine and pediatrics and director of the division of general internal medicine at the University of Arkansas for Medical Sciences, Little Rock. “Sometimes patients can purchase drugs at a lower cost than the copay to purchase with the ‘drug coverage’ in their insurance plan – unfortunately, this is not the case with the newer diabetes medications we are discussing here.”
“SGLT2 inhibitors and GLP-1 agonists can cost several hundred dollars a month, and insurers often balk at paying for them. They’ll say, ‘Have you tried metformin?’ ” explained endocrinologist Victor Lawrence Roberts, MD, in a interview. “We have to work with insurance companies the best we can in a stepwise fashion.”
According to Dr. Roberts, 80% of his patients with diabetes struggle with the cost of medicine in general. “They’re either underinsured or not insured or their formulary is limited.
Douglas S. Paauw, MD, agreed in an interview that the newer drugs can be problematic on the insurance front.
“For some patients they aren’t affordable, especially for the uninsured if you can’t get them on an assistance program,” said Dr. Paauw, who is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and serves as third-year medical student clerkship director at the university.
Dr. Hopkins, who is on the Internal Medicine News board, noted that “unfortunately, the treatment of type 2 diabetes in patients who cannot achieve control with metformin, diet, weight control, and exercise is a story of the ‘haves’ and the ‘have nots.’ The ‘haves’ are those who have pharmacy benefits which make access to newer agents like SGLT2 inhibitors and GLP-1 agonists a possibility.”
“I have had very few of the ‘have nots’ who have been able to even consider these newer agents, which carry price tags of $600-$1,300 a month even with the availability of discounting coupons in the marketplace,” he added. “Most of these patients end up requiring a sulfonylurea or TZD [thiazolidinedione] as a second agent to achieve glycemic control. This makes it very difficult to achieve sufficient weight and metabolic control to avoid an eventual switch to insulin.”
Fatima Z. Syed, MD, an endocrine-trained general internist at DukeHealth in Durham, N.C., said she prescribes SGLT2 inhibitors and GLP-1 receptor agonists in combination with metformin. “I prescribe them frequently, but they are not first-line treatments,” she explained.
“Nothing replaces diet and exercise” as therapy for patients with type 2 diabetes, she added.
Neil S. Skolnik, MD, said that insurance companies were not preventing patients from using these drugs in his experience. He also provided an optimistic take on the accessibility of these drugs in the near future.
“Most insurance companies are now covering select SGLT2 inhibitors and GLP-1 receptor agonists for appropriate patients and those companies that currently do not will soon have to,” said Dr. Skolnik, who is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington (Pa.) Jefferson Health.
“The outcomes [associated with use of the new drugs] are robust, the benefits are large, and are well worth the cost,” he added.
The side effects
While others praised these drugs for their beneficial effects, they also noted that the side effects of these drugs are serious and must be discussed with patients.
GLP-1 receptor agonists are linked to gastrointestinal symptoms, especially nausea, while SGLT2 inhibitors have been linked to kidney failure, ketoacidosis, and more. The Food and Drug Administration warned in 2018 that the SGLT2 inhibitors can cause a rare serious infection known as Fournier’s gangrene – necrotizing fasciitis of the perineum.
“We have to tell our patients to let us know right away if they get pain or swelling in the genital area,” Dr. Paauw, who is on the Internal Medicine News board, noted. “The chance that an infection could explode quickly is higher in those who take these drugs.”
Amputation risks also are associated with taking the SGLT2 inhibitor canagliflozin (Invokana). The FDA requires the manufacturer of this drug to include a black-box warning about the risk of “lower-limb amputations, most frequently of the toe and midfoot,” but also the leg. In approval trials, the risk doubled versus placebo.
These amputation risks “put a damper on some of the enthusiasm on behalf of physicians and patients ... for taking this drug,” noted Dr. Roberts, who is a professor of internal medicine at the University of Central Florida, Orlando.
While a manufacturer-funded study released last year found no link to amputations, the results weren’t powerful enough to rule out a moderately increased risk.
“[If] you are at high risk for having an amputation, we really have to take this risk very seriously,” said John B. Buse, MD, chief of the division of endocrinology at the University of North Carolina at Chapel Hill, in a presentation about the study at the 2018 annual scientific sessions of the American Diabetes Association.
The benefits
Despite these risks of adverse events, most interviewed agreed that the many benefits observed in those taking SGLT2 inhibitors or GLP-1 receptor agonists make them worth prescribing, at least to those who are able to afford them.
Both SGLT2 inhibitors and GLP-1 receptor agonists appear to have significant cardiovascular benefits. A 2019 meta-analysis and systematic review found that both drugs reduced major adverse cardiac events by about 12% (Circulation. 2019 Apr 23;139[17]:2022-31).
“They don’t cause hypoglycemia, they lower blood pressure, they don’t cause weight gain, and they might promote weight loss,” noted Dr. Paauw.
SGLT2 inhibitors also have shown signs of kidney benefits. The CREDENCE trial linked canagliflozin to a lowering of kidney disorders versus placebo (N Engl J Med. 2019 Jun 13;380[24]:2295-306). “The relative risk of the renal-specific composite of end-stage kidney disease, a doubling of the creatinine level, or death from renal causes was lower by 34% (hazard ratio, 0.66; 95% confidence interval, 0.53-0.81; P less than .001), and the relative risk of end-stage kidney disease was lower by 32% (HR, 0.68; 95% CI, 0.54-0.86; P = .002),” the trial investigators wrote.
“They showed very nicely that the drug improved the kidney function of those patients and reduced the kidney deterioration,” said Yehuda Handelsman, MD, an endocrinologist in Tarzana, Calif., who chaired the 2011 and 2015 American Association of Clinical Endocrinologists’ Comprehensive Diabetes Guidelines. The study was especially impressive, he added, because it included patients with low kidney function.
SGLT2 inhibitors’ “diuretic mechanism explains why there is a substantial reduction in heart failure hospitalizations in patients who take these drugs,” said cardiologist Marc E. Goldschmidt, MD, director of the Heart Success Program at Atlantic Health System’s Morristown (N.J.) Medical Center, in an interview. “Both the EMPA-REG Outcome and the CREDENCE trials demonstrated substantial benefit of this class of medications by showing a lower risk of cardiovascular death as well as death from any cause and a lower risk of hospitalization for heart failure."
Overall, the SGLT2 trial data have been very consistent with a benefit for cardiovascular risk reduction, particularly in regard to heart failure hospitalizations and even in potentially preventing heart failure in diabetics,” he added.
Dr. Skolnik, a columnist for Family Practice News, cited SGLT2 inhibitors and GLP-1 receptor agonists’ ability to slow renal disease progression, promote weight loss, and prevent poor cardiac outcomes.“These drugs should be used, in addition to metformin, in all patients with diabetes and vascular disease. These proven outcomes are far better than we ever were able to achieve previously and the strength of the evidence at this point is very strong,” said Dr. Skolnik. “In addition to the benefits of decreasing the development of cardiovascular disease, serious heart failure, and slowing progression of renal disease, these two classes of medication have additional benefits. Both classes help patients lose weight, which is very different from what was found with either sulfonylureas or insulin, which cause patients to gain weight. Also both the SGLT2 inhibitors and the GLP-1 RAs [receptor agonists] have a low incidence of hypoglycemia. For all these reasons, these have become important medications for us to use in primary care.”
Other recent trials offer “very powerful data” about SGLT2 inhibitors, Dr. Roberts said. That’s good news, since “our approach needs to be toward cardiovascular protection and preservation as well as managing blood sugar.”An Israeli trial, whose results were released in May 2019 at the annual meeting of the American College of Cardiology, found that, compared with other glucose-lowering drugs, taking an SGLT2 inhibitor was associated with lower risks of heart failure hospitalization and all-cause mortality (HR, 0.54; 95% CI, 0.44-0.65; P less than .001). This trial also offered a new detail: The patients gained the benefit regardless of whether their baseline left ventricular ejection fraction was preserved or reduced (J Coll Cardiol. 2019 Mar;73[9]:suppl 1). The SGLT2 inhibitors used in this trial included dapagliflozin (Farxiga) and empagliflozin (Jardiance).
In another study released this year, a subanalysis of the DECLARE-TIMI 58 trial, researchers reported that the SGLT2 inhibitor dapagliflozin reduced risks of both major adverse cardiovascular events and heart failure hospitalization in the subset of patients with type 2 diabetes and prior myocardial infarction versus controls (Circulation. 2019 May 28;139[22]:2516-27). The absolute risk reduction for major adverse cardiovascular events was 1.9% (HR, 0.81; 95% CI, 0.65-1.00; P = .046), while it was 0.6% for heart failure hospitalization (HR, 0.85; 95% CI, 0.72-1.00; P = .055).
These and other studies “speak volumes about the efficacy of managing blood sugar and addressing our biggest nemesis, which is cardiovascular disease,” Dr. Roberts said. “It’s irrefutable. The data [are] very good.”
Dr. Paauw said an SGLT2 inhibitor or GLP-1 receptor agonist is best reserved for use in select patients with cardiovascular risks and type 2 diabetes that need management beyond metformin.
For example, they might fit a 70-year-old with persistent hypertension who’s already taking a couple of blood pressure medications. “If they have another cardiovascular risk factor, the cardiovascular protection piece will be a bigger deal,” he said. Also, “it will probably help lower their blood pressure so they can avoid taking another blood pressure medicine.”
Trials of both GLP-1 receptor agonists and SGLT2 inhibitors have shown benefits “in improving [major adverse cardiac events], with the SGLT2 class showing substantial benefit in improving both heart failure and renal outcomes as well,” noted Dr. Skolnik. “It is in this context that one must address the question of whether the price of the medications are worthwhile. With such substantial benefit, there is no question in my mind that – for patients who have underlying cardiovascular illness, which includes patients with existent coronary disease, history of stroke, transient ischemic attack, or peripheral vascular disease – it is far and away worth it to prescribe these classes of medications.”
Indeed, the American Diabetes Association and the European Association for the Study of Diabetes’ most recent guidelines now call for a GLP-1 receptor agonist – instead of insulin – to be the first injectable used to treat type 2 diabetes (Diabetes Care 2018 Dec; 41[12]:2669-701).
“For the relatively small number of my patients who have been able to access and use these medications for months or longer, more have tolerated the GLP-1 agonists than SGLT2 inhibitors primarily due to urinary issues,” noted Dr. Hopkins.
Dipeptidyl peptidase–4 inhibitors are another option in patients with type 2 diabetes, but research suggests they may not be a top option for patients with cardiovascular risk. A 2018 review noted that cardiovascular outcome trials for alogliptin (Nesina), saxagliptin (Onglyza), and sitagliptin (Januvia) showed noninferiority but failed to demonstrate any superiority, compared with placebo in patients with type 2 diabetes mellitus and high cardiovascular risk (Circ Res. 2018 May 11;122[10]:1439-59).
The combination therapies
Many of the newer drugs are available as combinations with other types of diabetes drugs. In some cases, physicians create their own form of combination therapy by separately prescribing two or more diabetes drugs. Earlier this year, a study suggested the benefits of this kind of add-on therapy: Diabetes outcomes improved in patients who took the GLP-1 receptor agonist semaglutide and an SGLT2 inhibitor (Lancet Diabetes Endocrinol. 2019 Mar 1. doi: 10.1016/S2213-8587[19]30066-X).
Dr. Roberts suggested caution, however, when prescribing combination therapies. “My recommendation is always to begin with the individual medications to see if the patient tolerates the drugs and then decide which component needs to be titrated. It’s hard to titrate a combination drug, and it doesn’t leave a lot of flexibility. You never know which drug is doing what.
Dr. Handelsman said some patients may need to take three medications such as metformin, an SGLT2 inhibitor, and a GLP-1 receptor agonist.
“I don’t recommend using the combinations if you’re not familiar with the drugs ... These are relatively new pharmaceuticals, and most of us are on a learning curve as to how they fit into the armamentarium. If a drug is tolerated with a good response, you can certainly consider going to the combination tablets,” he added.
There is at least one drug that combines these three classes: The newly FDA-approved Qternmet XR, which combines dapagliflozin (an SGLT2 inhibitor), saxagliptin (a GLP-1 receptor agonist), and metformin. As of mid-June 2019, it was not yet available in the United States. Its sister drug Qtern, which combines dapagliflozin and saxagliptin, costs more than $500 a month with a free coupon, according to goodrx.com. In contrast, metformin is extremely inexpensive, costing just a few dollars a month for a common starting dose.
What about adding insulin?
“Both [SGLT2 inhibitors and GLP-1 receptor agonists] work very well with insulin,” Dr. Handelsman said. “There is a nice additive effect on the reduction of [hemoglobin] A1c. The only caution is that, although neither SGLT2 inhibitors nor GLP-1 receptor agonists cause hypoglycemia, in combination with insulin they do increase the risk of hypoglycemia. You may have to adjust the dose of insulin.”
Dr. Hopkins warned that cost becomes an even bigger issue when you add insulin into the mix.
“When insulin comes into the discussion, we are again stuck with astronomical costs which many struggle to afford,” he explained.
Indeed, the price tag on these drugs seems to be the biggest problem physicians have with them.
“The challenges in managing patients with diabetes aren’t the risks associated with the drugs. It’s dealing with their insurers,” noted Dr. Roberts.
Dr. Hopkins, Dr. Paauw, Dr. Roberts, and Dr. Syed reported no disclosures. Dr. Buse is an investigator for Johnson and Johnson. Dr. Goldschmidt is paid to speak by Novartis. Dr. Handelsman reported research grants, consulting work, and speaker honoraria from Amgen, Gilead, Lilly, Merck, Novo Nordisk, and others. Dr Skolnik reported nonfinancial support from AstraZeneca, Boehringer Ingelheim, Sanofi, and GlaxoSmithKline and personal fees from AstraZeneca, Boehringer Ingelheim, and Eli Lilly. He also serves on the advisory boards of AstraZeneca, Boehringer Ingelheim, Teva Pharmaceutical, Eli Lilly, Sanofi, Janssen Pharmaceuticals, Intarcia, Mylan, and GlaxoSmithKline.
Dr. Paauw and Dr. Skolnik are columnists for Family Practice News and Internal Medicine News.
M. Alexander Otto contributed to this report.
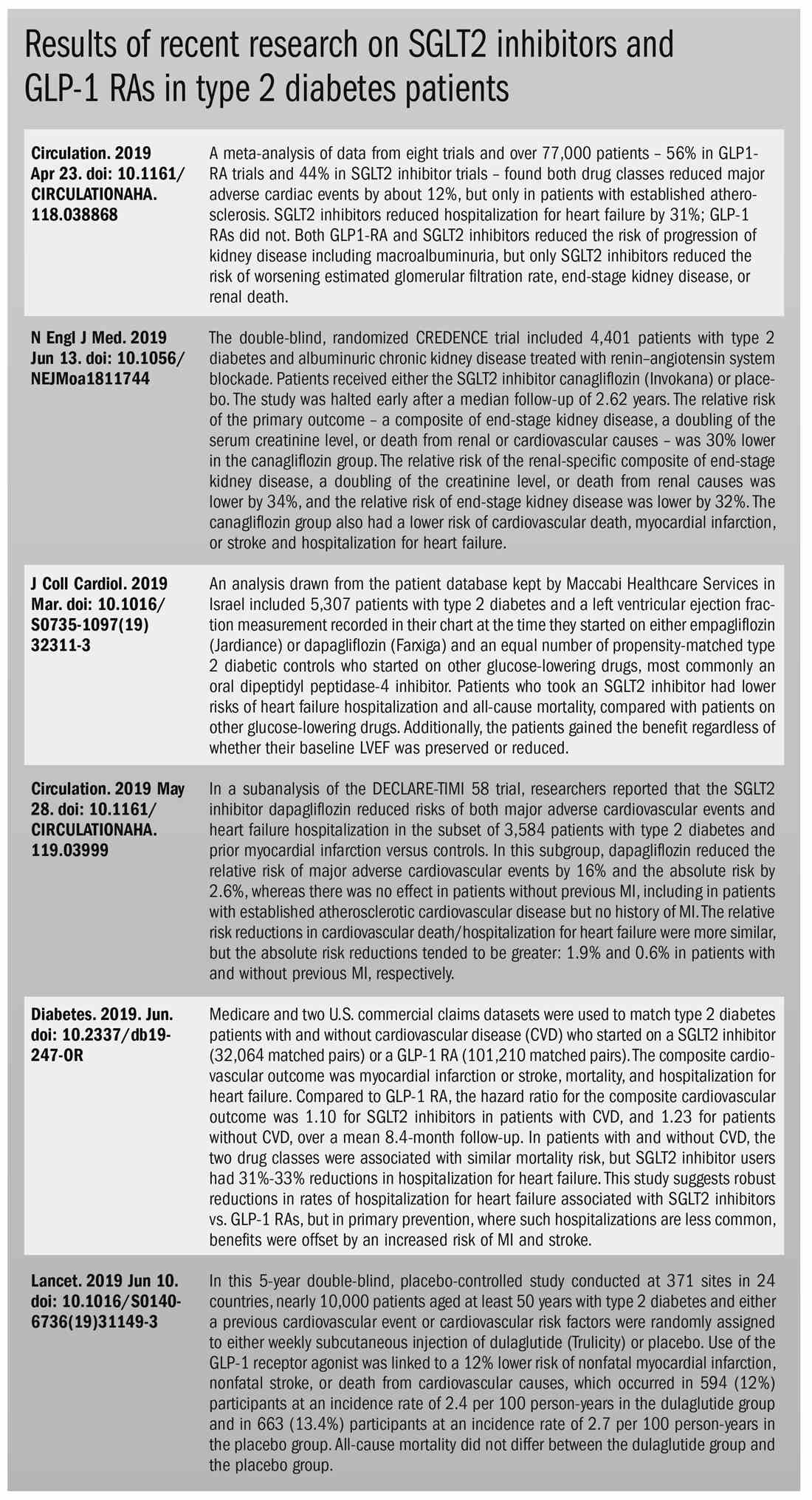
SGLT2 inhibitors, GLP-1 RAs are effective, but costly in T2D
FDA grants marketing clearance for chlamydia and gonorrhea extragenital tests
The new tests, the Aptima Combo 2 Assay and Xpert CT/NG, use samples from the throat and rectum to test for chlamydia and gonorrhea, according to a statement from the FDA.
“It is best for patients if both [chlamydia and gonorrhea] are caught and treated right away, as significant complications can occur if left untreated,” noted Tim Stenzel, MD, in the statement.
“Today’s clearances provide a mechanism for more easily diagnosing these infections,” said Dr. Stenzel, director of the Office of In Vitro Diagnostics and Radiological Health in the FDA’s Center for Devices and Radiological Health.
The two tests were reviewed through the premarket notification – or 510(k) – pathway, which seeks to demonstrate to the FDA that the device to be marketed is equivalent or better in safety and effectiveness to the legally marketed device.
In the FDA’s evaluation of the tests, it reviewed clinical data from a multisite study of more than 2,500 patients. This study evaluated the diagnostic accuracy of multiple commercially available nucleic acid amplification tests for detection of Neisseria gonorrhoeae and Chlamydia trachomatis from throat and rectal sites. The results of this study and other information reviewed by the FDA demonstrated that the two tests “are safe and effective for extragenital testing for chlamydia and gonorrhea,” according to the statement.
The data were collected through a cross-sectional study coordinated by the Antibacterial Resistance Leadership Group, which is funded and supported by the National Institute of Allergy and Infectious Diseases.
The FDA granted marketing clearance to Hologic and Cepheid for the Aptima Combo 2 Assay and the Xpert CT/NG, respectively.
The new tests, the Aptima Combo 2 Assay and Xpert CT/NG, use samples from the throat and rectum to test for chlamydia and gonorrhea, according to a statement from the FDA.
“It is best for patients if both [chlamydia and gonorrhea] are caught and treated right away, as significant complications can occur if left untreated,” noted Tim Stenzel, MD, in the statement.
“Today’s clearances provide a mechanism for more easily diagnosing these infections,” said Dr. Stenzel, director of the Office of In Vitro Diagnostics and Radiological Health in the FDA’s Center for Devices and Radiological Health.
The two tests were reviewed through the premarket notification – or 510(k) – pathway, which seeks to demonstrate to the FDA that the device to be marketed is equivalent or better in safety and effectiveness to the legally marketed device.
In the FDA’s evaluation of the tests, it reviewed clinical data from a multisite study of more than 2,500 patients. This study evaluated the diagnostic accuracy of multiple commercially available nucleic acid amplification tests for detection of Neisseria gonorrhoeae and Chlamydia trachomatis from throat and rectal sites. The results of this study and other information reviewed by the FDA demonstrated that the two tests “are safe and effective for extragenital testing for chlamydia and gonorrhea,” according to the statement.
The data were collected through a cross-sectional study coordinated by the Antibacterial Resistance Leadership Group, which is funded and supported by the National Institute of Allergy and Infectious Diseases.
The FDA granted marketing clearance to Hologic and Cepheid for the Aptima Combo 2 Assay and the Xpert CT/NG, respectively.
The new tests, the Aptima Combo 2 Assay and Xpert CT/NG, use samples from the throat and rectum to test for chlamydia and gonorrhea, according to a statement from the FDA.
“It is best for patients if both [chlamydia and gonorrhea] are caught and treated right away, as significant complications can occur if left untreated,” noted Tim Stenzel, MD, in the statement.
“Today’s clearances provide a mechanism for more easily diagnosing these infections,” said Dr. Stenzel, director of the Office of In Vitro Diagnostics and Radiological Health in the FDA’s Center for Devices and Radiological Health.
The two tests were reviewed through the premarket notification – or 510(k) – pathway, which seeks to demonstrate to the FDA that the device to be marketed is equivalent or better in safety and effectiveness to the legally marketed device.
In the FDA’s evaluation of the tests, it reviewed clinical data from a multisite study of more than 2,500 patients. This study evaluated the diagnostic accuracy of multiple commercially available nucleic acid amplification tests for detection of Neisseria gonorrhoeae and Chlamydia trachomatis from throat and rectal sites. The results of this study and other information reviewed by the FDA demonstrated that the two tests “are safe and effective for extragenital testing for chlamydia and gonorrhea,” according to the statement.
The data were collected through a cross-sectional study coordinated by the Antibacterial Resistance Leadership Group, which is funded and supported by the National Institute of Allergy and Infectious Diseases.
The FDA granted marketing clearance to Hologic and Cepheid for the Aptima Combo 2 Assay and the Xpert CT/NG, respectively.
Confronting physician depression and suicide

Please join us Monday, June 3, at 8:00 p.m. ET as we discuss depression in physicians and the resulting tragedies, as well as how to help physicians receive the treatment they need to prevent suicide.
Our special guests include physicians with expertise on the triggers of physician depression and solutions for fighting this epidemic, Sarah Candler, MD, (@sarahgcandler) and Elisabeth Poorman, MD, (@DrPoorman). We hope you will participate in our Twitter chat on June 3 at 8 p.m. ET. #MDedgeChats
Physicians have higher rates of depression and suicide, compared with the general population, according to the American Foundation for Suicide Prevention. Suicide rates for male physicians are 1.41 times higher than in the general population and, for female physicians, 2.27 times greater.
“But these numbers come from only those deaths that are reported publicly,” Dr. Poorman wrote in an article that was published by WBUR, Boston’s NPR News Station. In fact, as Dr. Poorman was writing this story, she learned of five separate deaths that were widely known to be suicides, but never publicly identified as such, she said.
One possible explanation for physicians’ higher likelihood of becoming depressed or dying by suicide, compared with other professionals, is their hesitance to receive mental health treatment, experts have suggested. Psychiatrist Michael F. Myers, MD, found anecdotal evidence of this tendency when he interviewed the loved ones, friends, and colleagues of physicians who took their own lives.
In this chat we will discuss this topic and other possible reasons for the high rate of depression and suicide among physicians.
Topics of conversation
Question 1: What are the causes of physician depression and suicide in training and practice?
Question 2: How can we end stigma against seeking mental health treatment among physicians?
Question 3: How can we prevent depression and suicide among medical students and physicians?
Question 4: Which institutions or programs are exemplars in providing resources to improve mental health?
Question 5: What organizational and political changes are likely to reduce physician suicides?

Resources
1. Getting Back to Medicine as a Community
2. What stops physicians from getting mental health care?
3. Risk considerations for suicidal physicians
4. Two more and counting: Suicide in medical trainees
5. How to talk with a struggling physician colleague
6. Healthcare industry takes on high physician suicide rates, mental health stigma
7. The Curbsiders episode #129 Depression and Suicide: Occupational Hazards of Practicing Medicine
8. Creating Joy in Medicine in St. Paul, MN: A Case Study
About Dr. Poorman
Dr. Poorman (@DrPoorman) is a primary care physician at the University of Washington in Seattle, a freelance journalist covering issues related to medicine, and a frequent speaker on the causes of and solutions to mental illness among providers.
Her writing has been featured in Self, The Guardian. Medpage Today’s KevinMD.com, and other publications. She produces the blog: https://www.drpoorman.org/what-we-do.
About Dr. Candler
Dr. Candler (@sarahgcandler) is a primary care physician in Houston. She is coeditor of the Annals Fresh Look blog, and a member of Internal Medicine News’ Editorial Advisory Board.
She is currently consulting for a tech firm and will later be joining Iora Health to start a Medicare Advantage clinic.

Please join us Monday, June 3, at 8:00 p.m. ET as we discuss depression in physicians and the resulting tragedies, as well as how to help physicians receive the treatment they need to prevent suicide.
Our special guests include physicians with expertise on the triggers of physician depression and solutions for fighting this epidemic, Sarah Candler, MD, (@sarahgcandler) and Elisabeth Poorman, MD, (@DrPoorman). We hope you will participate in our Twitter chat on June 3 at 8 p.m. ET. #MDedgeChats
Physicians have higher rates of depression and suicide, compared with the general population, according to the American Foundation for Suicide Prevention. Suicide rates for male physicians are 1.41 times higher than in the general population and, for female physicians, 2.27 times greater.
“But these numbers come from only those deaths that are reported publicly,” Dr. Poorman wrote in an article that was published by WBUR, Boston’s NPR News Station. In fact, as Dr. Poorman was writing this story, she learned of five separate deaths that were widely known to be suicides, but never publicly identified as such, she said.
One possible explanation for physicians’ higher likelihood of becoming depressed or dying by suicide, compared with other professionals, is their hesitance to receive mental health treatment, experts have suggested. Psychiatrist Michael F. Myers, MD, found anecdotal evidence of this tendency when he interviewed the loved ones, friends, and colleagues of physicians who took their own lives.
In this chat we will discuss this topic and other possible reasons for the high rate of depression and suicide among physicians.
Topics of conversation
Question 1: What are the causes of physician depression and suicide in training and practice?
Question 2: How can we end stigma against seeking mental health treatment among physicians?
Question 3: How can we prevent depression and suicide among medical students and physicians?
Question 4: Which institutions or programs are exemplars in providing resources to improve mental health?
Question 5: What organizational and political changes are likely to reduce physician suicides?

Resources
1. Getting Back to Medicine as a Community
2. What stops physicians from getting mental health care?
3. Risk considerations for suicidal physicians
4. Two more and counting: Suicide in medical trainees
5. How to talk with a struggling physician colleague
6. Healthcare industry takes on high physician suicide rates, mental health stigma
7. The Curbsiders episode #129 Depression and Suicide: Occupational Hazards of Practicing Medicine
8. Creating Joy in Medicine in St. Paul, MN: A Case Study
About Dr. Poorman
Dr. Poorman (@DrPoorman) is a primary care physician at the University of Washington in Seattle, a freelance journalist covering issues related to medicine, and a frequent speaker on the causes of and solutions to mental illness among providers.
Her writing has been featured in Self, The Guardian. Medpage Today’s KevinMD.com, and other publications. She produces the blog: https://www.drpoorman.org/what-we-do.
About Dr. Candler
Dr. Candler (@sarahgcandler) is a primary care physician in Houston. She is coeditor of the Annals Fresh Look blog, and a member of Internal Medicine News’ Editorial Advisory Board.
She is currently consulting for a tech firm and will later be joining Iora Health to start a Medicare Advantage clinic.

Please join us Monday, June 3, at 8:00 p.m. ET as we discuss depression in physicians and the resulting tragedies, as well as how to help physicians receive the treatment they need to prevent suicide.
Our special guests include physicians with expertise on the triggers of physician depression and solutions for fighting this epidemic, Sarah Candler, MD, (@sarahgcandler) and Elisabeth Poorman, MD, (@DrPoorman). We hope you will participate in our Twitter chat on June 3 at 8 p.m. ET. #MDedgeChats
Physicians have higher rates of depression and suicide, compared with the general population, according to the American Foundation for Suicide Prevention. Suicide rates for male physicians are 1.41 times higher than in the general population and, for female physicians, 2.27 times greater.
“But these numbers come from only those deaths that are reported publicly,” Dr. Poorman wrote in an article that was published by WBUR, Boston’s NPR News Station. In fact, as Dr. Poorman was writing this story, she learned of five separate deaths that were widely known to be suicides, but never publicly identified as such, she said.
One possible explanation for physicians’ higher likelihood of becoming depressed or dying by suicide, compared with other professionals, is their hesitance to receive mental health treatment, experts have suggested. Psychiatrist Michael F. Myers, MD, found anecdotal evidence of this tendency when he interviewed the loved ones, friends, and colleagues of physicians who took their own lives.
In this chat we will discuss this topic and other possible reasons for the high rate of depression and suicide among physicians.
Topics of conversation
Question 1: What are the causes of physician depression and suicide in training and practice?
Question 2: How can we end stigma against seeking mental health treatment among physicians?
Question 3: How can we prevent depression and suicide among medical students and physicians?
Question 4: Which institutions or programs are exemplars in providing resources to improve mental health?
Question 5: What organizational and political changes are likely to reduce physician suicides?

Resources
1. Getting Back to Medicine as a Community
2. What stops physicians from getting mental health care?
3. Risk considerations for suicidal physicians
4. Two more and counting: Suicide in medical trainees
5. How to talk with a struggling physician colleague
6. Healthcare industry takes on high physician suicide rates, mental health stigma
7. The Curbsiders episode #129 Depression and Suicide: Occupational Hazards of Practicing Medicine
8. Creating Joy in Medicine in St. Paul, MN: A Case Study
About Dr. Poorman
Dr. Poorman (@DrPoorman) is a primary care physician at the University of Washington in Seattle, a freelance journalist covering issues related to medicine, and a frequent speaker on the causes of and solutions to mental illness among providers.
Her writing has been featured in Self, The Guardian. Medpage Today’s KevinMD.com, and other publications. She produces the blog: https://www.drpoorman.org/what-we-do.
About Dr. Candler
Dr. Candler (@sarahgcandler) is a primary care physician in Houston. She is coeditor of the Annals Fresh Look blog, and a member of Internal Medicine News’ Editorial Advisory Board.
She is currently consulting for a tech firm and will later be joining Iora Health to start a Medicare Advantage clinic.
Dr. Douglas Paauw gives updates on antihypertensives, statins, SGLT2 inhibitors
PHILADELPHIA – in a video interview at the annual meeting of the American College of Physicians.
Dr. Paauw, professor of medicine at the University of Washington, Seattle, began by discussing some of the issues that occurred with antihypertensive drugs in the past year. These included the link between hydrochlorothiazide use and the increased risk of nonmelanoma skin cancers, the recalls of many drug lots of angiotensin II receptor blockers, and a study that found an increased risk of lung cancer in people who were taking ACE inhibitors.
He then described the findings of studies that examined the links between statins and muscle pain and other new research on these drugs.
He also warned physicians to be particularity cautious about prescribing sodium-glucose cotransporter 2 inhibitors to certain kinds of patients.
Dr. Paauw concluded by explaining why clarithromycin is his most hated drug.
Dr. Paauw is also the Rathmann Family Foundation Endowed Chair for Patient-Centered Clinical Education and the medicine clerkship director at the University of Washington.
klennon@mdedge.com
PHILADELPHIA – in a video interview at the annual meeting of the American College of Physicians.
Dr. Paauw, professor of medicine at the University of Washington, Seattle, began by discussing some of the issues that occurred with antihypertensive drugs in the past year. These included the link between hydrochlorothiazide use and the increased risk of nonmelanoma skin cancers, the recalls of many drug lots of angiotensin II receptor blockers, and a study that found an increased risk of lung cancer in people who were taking ACE inhibitors.
He then described the findings of studies that examined the links between statins and muscle pain and other new research on these drugs.
He also warned physicians to be particularity cautious about prescribing sodium-glucose cotransporter 2 inhibitors to certain kinds of patients.
Dr. Paauw concluded by explaining why clarithromycin is his most hated drug.
Dr. Paauw is also the Rathmann Family Foundation Endowed Chair for Patient-Centered Clinical Education and the medicine clerkship director at the University of Washington.
klennon@mdedge.com
PHILADELPHIA – in a video interview at the annual meeting of the American College of Physicians.
Dr. Paauw, professor of medicine at the University of Washington, Seattle, began by discussing some of the issues that occurred with antihypertensive drugs in the past year. These included the link between hydrochlorothiazide use and the increased risk of nonmelanoma skin cancers, the recalls of many drug lots of angiotensin II receptor blockers, and a study that found an increased risk of lung cancer in people who were taking ACE inhibitors.
He then described the findings of studies that examined the links between statins and muscle pain and other new research on these drugs.
He also warned physicians to be particularity cautious about prescribing sodium-glucose cotransporter 2 inhibitors to certain kinds of patients.
Dr. Paauw concluded by explaining why clarithromycin is his most hated drug.
Dr. Paauw is also the Rathmann Family Foundation Endowed Chair for Patient-Centered Clinical Education and the medicine clerkship director at the University of Washington.
klennon@mdedge.com
REPORTING FROM INTERNAL MEDICINE 2019
Physicians discuss bringing cultural humility to medicine
PHILADELPHIA – during a panel discussion moderated by Sarah Candler, MD, an internist in Houston.
Dr. Candler, former chair, Council of Resident and Fellow Members, Board of Regents, American College of Physicians, began the discussion by asking Dr. DeLisser, to describe his role in teaching medical students about the social determinants of health, at the annual Internal Medicine meeting of the ACP.
Dr. DeLisser, associate dean for professionalism and humanism at the University of Pennsylvania, Philadelphia, said he focuses on a number of issues, including social medicine, cultural competency, and cultural humility.
“We look at health care disparities and try to do a lot of innovation around service learning that will bring our students into the community, one to learn about these determinants but more importantly to be able to see how these issues can be addressed both on a provider level but also on a more structural systemic level,” he noted.
Dr. Poorman, an internist at the University of Washington, later discussed the importance of practicing cultural humility as it related to her experience providing care to migrant workers while she was a medical school student.
Dr. Candler, an internist in Houston, concluded the discussion by describing some of the ACP’s newest resources designed to address the social determinants of health for specific groups of patients.
The full panel discussion was recorded as a video.
PHILADELPHIA – during a panel discussion moderated by Sarah Candler, MD, an internist in Houston.
Dr. Candler, former chair, Council of Resident and Fellow Members, Board of Regents, American College of Physicians, began the discussion by asking Dr. DeLisser, to describe his role in teaching medical students about the social determinants of health, at the annual Internal Medicine meeting of the ACP.
Dr. DeLisser, associate dean for professionalism and humanism at the University of Pennsylvania, Philadelphia, said he focuses on a number of issues, including social medicine, cultural competency, and cultural humility.
“We look at health care disparities and try to do a lot of innovation around service learning that will bring our students into the community, one to learn about these determinants but more importantly to be able to see how these issues can be addressed both on a provider level but also on a more structural systemic level,” he noted.
Dr. Poorman, an internist at the University of Washington, later discussed the importance of practicing cultural humility as it related to her experience providing care to migrant workers while she was a medical school student.
Dr. Candler, an internist in Houston, concluded the discussion by describing some of the ACP’s newest resources designed to address the social determinants of health for specific groups of patients.
The full panel discussion was recorded as a video.
PHILADELPHIA – during a panel discussion moderated by Sarah Candler, MD, an internist in Houston.
Dr. Candler, former chair, Council of Resident and Fellow Members, Board of Regents, American College of Physicians, began the discussion by asking Dr. DeLisser, to describe his role in teaching medical students about the social determinants of health, at the annual Internal Medicine meeting of the ACP.
Dr. DeLisser, associate dean for professionalism and humanism at the University of Pennsylvania, Philadelphia, said he focuses on a number of issues, including social medicine, cultural competency, and cultural humility.
“We look at health care disparities and try to do a lot of innovation around service learning that will bring our students into the community, one to learn about these determinants but more importantly to be able to see how these issues can be addressed both on a provider level but also on a more structural systemic level,” he noted.
Dr. Poorman, an internist at the University of Washington, later discussed the importance of practicing cultural humility as it related to her experience providing care to migrant workers while she was a medical school student.
Dr. Candler, an internist in Houston, concluded the discussion by describing some of the ACP’s newest resources designed to address the social determinants of health for specific groups of patients.
The full panel discussion was recorded as a video.
REPORTING FROM INTERNAL MEDICINE 2019

















