User login
Katie Lennon is editor of MDedge's Family Practice News and Internal Medicine News. She has also served as editor of CHEST Physician; a staff writer for Financial Times publications; and a reporter for the Princeton Packet, Ocean County Observer, and South Bend Tribune. She is a graduate of the University of Notre Dame, South Bend, Ind. Follow her on Twitter @KatieWLennon.
ACP governmental affairs leaders discuss ACA, Title X
PHILADELPHIA – in a video interview conducted during the annual meeting of the American College of Physicians.

Robert B. Doherty, the ACP’s senior vice president, governmental affairs and public policy, and Shari M. Erickson, the organization’s vice president of governmental affairs and medical practice, addressed the future of the Affordable Care Act (ACA), cuts to the funding of Title X clinics, and the National Rifle Association’s urging of Congress to vote against the Violence Against Women Reauthorization Act.
“We’re very, very concerned by a decision by a Texas judge that, if upheld on appeal, would gut the entire ACA and the decision by the administration not to defend any part of the ACA,” said Mr. Doherty.
Ms. Erikson later discussed a final rule released by the administration that she said “significantly impacts access to care for women,” particularly for those in low-income and underserved areas who may be seen by clinics that receive Title X funding.
She also addressed the rule’s effects on federally qualified health centers and other health clinics near Title X–funded clinics that are forced to close.
On a positive note, Mr. Doherty noted that the ACP is supporting legislation that has been introduced in the House to stabilize the current insurance markets.
Mr. Doherty and Ms. Erikson concluded by discussing an ACP initiative focused on reducing administrative burden for ACP members.
PHILADELPHIA – in a video interview conducted during the annual meeting of the American College of Physicians.

Robert B. Doherty, the ACP’s senior vice president, governmental affairs and public policy, and Shari M. Erickson, the organization’s vice president of governmental affairs and medical practice, addressed the future of the Affordable Care Act (ACA), cuts to the funding of Title X clinics, and the National Rifle Association’s urging of Congress to vote against the Violence Against Women Reauthorization Act.
“We’re very, very concerned by a decision by a Texas judge that, if upheld on appeal, would gut the entire ACA and the decision by the administration not to defend any part of the ACA,” said Mr. Doherty.
Ms. Erikson later discussed a final rule released by the administration that she said “significantly impacts access to care for women,” particularly for those in low-income and underserved areas who may be seen by clinics that receive Title X funding.
She also addressed the rule’s effects on federally qualified health centers and other health clinics near Title X–funded clinics that are forced to close.
On a positive note, Mr. Doherty noted that the ACP is supporting legislation that has been introduced in the House to stabilize the current insurance markets.
Mr. Doherty and Ms. Erikson concluded by discussing an ACP initiative focused on reducing administrative burden for ACP members.
PHILADELPHIA – in a video interview conducted during the annual meeting of the American College of Physicians.

Robert B. Doherty, the ACP’s senior vice president, governmental affairs and public policy, and Shari M. Erickson, the organization’s vice president of governmental affairs and medical practice, addressed the future of the Affordable Care Act (ACA), cuts to the funding of Title X clinics, and the National Rifle Association’s urging of Congress to vote against the Violence Against Women Reauthorization Act.
“We’re very, very concerned by a decision by a Texas judge that, if upheld on appeal, would gut the entire ACA and the decision by the administration not to defend any part of the ACA,” said Mr. Doherty.
Ms. Erikson later discussed a final rule released by the administration that she said “significantly impacts access to care for women,” particularly for those in low-income and underserved areas who may be seen by clinics that receive Title X funding.
She also addressed the rule’s effects on federally qualified health centers and other health clinics near Title X–funded clinics that are forced to close.
On a positive note, Mr. Doherty noted that the ACP is supporting legislation that has been introduced in the House to stabilize the current insurance markets.
Mr. Doherty and Ms. Erikson concluded by discussing an ACP initiative focused on reducing administrative burden for ACP members.
REPORTING FROM INTERNAL MEDICINE 2019
Volunteerism: How and why to do it, according to Dr. Eileen Barrett
PHILADELPHIA –
“I think what we get out of it is the feeling of our commitment to our sense of purpose and mission, and you just feel great when you’re giving, and then you meet these really remarkable people who do really, really remarkable things. ... It’s tremendously inspiring,” Dr. Barrett said in a video interview at the annual meeting of the American College of Physicians. She is a hospitalist at the University of New Mexico, Albuquerque, and serves on the ACP Board of Regents.
In addition, Dr. Barrett has done disaster relief work in West Africa, provided patient care to refugees in a hospital on the Thailand side of the Thailand-Myanmar border, and even helped bring organization to a public radio station in rural New Mexico.
She also described some opportunities available to internists who are trying to get their feet wet in volunteering that are available through the organizations, Health Volunteers Overseas and the Maven Project.
PHILADELPHIA –
“I think what we get out of it is the feeling of our commitment to our sense of purpose and mission, and you just feel great when you’re giving, and then you meet these really remarkable people who do really, really remarkable things. ... It’s tremendously inspiring,” Dr. Barrett said in a video interview at the annual meeting of the American College of Physicians. She is a hospitalist at the University of New Mexico, Albuquerque, and serves on the ACP Board of Regents.
In addition, Dr. Barrett has done disaster relief work in West Africa, provided patient care to refugees in a hospital on the Thailand side of the Thailand-Myanmar border, and even helped bring organization to a public radio station in rural New Mexico.
She also described some opportunities available to internists who are trying to get their feet wet in volunteering that are available through the organizations, Health Volunteers Overseas and the Maven Project.
PHILADELPHIA –
“I think what we get out of it is the feeling of our commitment to our sense of purpose and mission, and you just feel great when you’re giving, and then you meet these really remarkable people who do really, really remarkable things. ... It’s tremendously inspiring,” Dr. Barrett said in a video interview at the annual meeting of the American College of Physicians. She is a hospitalist at the University of New Mexico, Albuquerque, and serves on the ACP Board of Regents.
In addition, Dr. Barrett has done disaster relief work in West Africa, provided patient care to refugees in a hospital on the Thailand side of the Thailand-Myanmar border, and even helped bring organization to a public radio station in rural New Mexico.
She also described some opportunities available to internists who are trying to get their feet wet in volunteering that are available through the organizations, Health Volunteers Overseas and the Maven Project.
REPORTING FROM INTERNAL MEDICINE 2019
ACP leaders explain why they value telehealth
PHILADELPHIA – according to the recently announced results of a questionnaire by the American College of Physicians.
The survey participants included 233 members of the ACP, who provided their responses between October 2018 and January 2019. ACP President Ana Maria Lopez, MD, as well as Tabassum Salam, MD, vice president for medical education, announced the survey’s results at a press briefing at the annual meeting of the American College of Physicians.
Dr. Lopez and Dr. Salam highlighted some of the findings and expressed their enthusiasm about the recent increases in the use of telemedicine in a video interview. They also explained how telehealth benefits patients and the barriers to more widespread use of telemedicine.
Dr. Lopez and Dr. Salam did not disclose any relevant conflicts of interest.
PHILADELPHIA – according to the recently announced results of a questionnaire by the American College of Physicians.
The survey participants included 233 members of the ACP, who provided their responses between October 2018 and January 2019. ACP President Ana Maria Lopez, MD, as well as Tabassum Salam, MD, vice president for medical education, announced the survey’s results at a press briefing at the annual meeting of the American College of Physicians.
Dr. Lopez and Dr. Salam highlighted some of the findings and expressed their enthusiasm about the recent increases in the use of telemedicine in a video interview. They also explained how telehealth benefits patients and the barriers to more widespread use of telemedicine.
Dr. Lopez and Dr. Salam did not disclose any relevant conflicts of interest.
PHILADELPHIA – according to the recently announced results of a questionnaire by the American College of Physicians.
The survey participants included 233 members of the ACP, who provided their responses between October 2018 and January 2019. ACP President Ana Maria Lopez, MD, as well as Tabassum Salam, MD, vice president for medical education, announced the survey’s results at a press briefing at the annual meeting of the American College of Physicians.
Dr. Lopez and Dr. Salam highlighted some of the findings and expressed their enthusiasm about the recent increases in the use of telemedicine in a video interview. They also explained how telehealth benefits patients and the barriers to more widespread use of telemedicine.
Dr. Lopez and Dr. Salam did not disclose any relevant conflicts of interest.
REPORTING FROM INTERNAL MEDICINE 2019
ACP launches program to better implement QI projects
PHILADELPHIA – .

The program includes 12 months of virtual coaching for a cost, and free online module training, according to Daisy Smith, MD, FACP, who spoke at a press conference at the annual meeting of the American College of Physicians.
Dr. Smith, the ACP’s vice president of clinical programs, discussed additional aspects of ACP Advance with Selam Wubu, director of the ACP’s Center for Quality, in a video interview.
“We launched ACP Advance to engage physicians and their teams [and] empower them to engage and implement quality improvement that results in meaningful improvement for them and their patients,” Ms. Wubu said.
Dr. Smith and Ms. Wubu have no relevant disclosures.
PHILADELPHIA – .

The program includes 12 months of virtual coaching for a cost, and free online module training, according to Daisy Smith, MD, FACP, who spoke at a press conference at the annual meeting of the American College of Physicians.
Dr. Smith, the ACP’s vice president of clinical programs, discussed additional aspects of ACP Advance with Selam Wubu, director of the ACP’s Center for Quality, in a video interview.
“We launched ACP Advance to engage physicians and their teams [and] empower them to engage and implement quality improvement that results in meaningful improvement for them and their patients,” Ms. Wubu said.
Dr. Smith and Ms. Wubu have no relevant disclosures.
PHILADELPHIA – .

The program includes 12 months of virtual coaching for a cost, and free online module training, according to Daisy Smith, MD, FACP, who spoke at a press conference at the annual meeting of the American College of Physicians.
Dr. Smith, the ACP’s vice president of clinical programs, discussed additional aspects of ACP Advance with Selam Wubu, director of the ACP’s Center for Quality, in a video interview.
“We launched ACP Advance to engage physicians and their teams [and] empower them to engage and implement quality improvement that results in meaningful improvement for them and their patients,” Ms. Wubu said.
Dr. Smith and Ms. Wubu have no relevant disclosures.
REPORTING FROM INTERNAL MEDICINE 2019
Palliative care may reduce suicide among lung cancer patients
according to new research that will be presented at an international conference of the American Thoracic Society.
“Suicide is a significant national public health problem, especially among lung cancer patients and among veterans,” said lead author, Donald R. Sullivan, MD, of the division of pulmonary and critical care medicine at Oregon Health & Science University and a member of the OHSU Knight Cancer Institute, in a statement.
The investigators found that veterans who experienced at least one “palliative care encounter” after learning they had lung cancer were 82% less likely to die by suicide (odds ratio, 0.18; 95% confidence interval, 0.07-0.46; P less than .001), when compared with veterans who were diagnosed with lung cancer but did not receive palliative care.
The suicide rate for the advanced-stage lung cancer patients was 200/100,000 patient-years, which was more than five times higher than the suicide rate – adjusted for age, sex, and year – for all veterans using VA health care (37.5/100,000), according to the study abstract.
Of the 20,900 lung cancer patients analyzed, 30 committed suicide. Only six (20%) of the patients who died by suicide had received palliative care. Overall, most patients (18,192 or 87%) in the registry died of lung cancer. Other cancers, heart disease, and chronic obstructive pulmonary disease were some of the other common causes of death for the lung cancer patients, according to the abstract.
While several medical societies recommend palliative care for all patients with advanced-stage lung cancer, there is a gap between those recommendations and practice, noted Dr. Sullivan. “There are many barriers to palliative care, and unfortunately, some are related to clinician referrals. Not all doctors are aware of the benefits of palliative care,” he said in the statement.
Dr. Sullivan added that palliative care should be offered to all patients shortly after receiving a diagnosis of advanced-stage lung cancer.
More details on this study will be presented at the conference on Monday, May 21, at 2:30 p.m. in Room 14 A-B (Mezzanine Level) of the San Diego Convention Center.
according to new research that will be presented at an international conference of the American Thoracic Society.
“Suicide is a significant national public health problem, especially among lung cancer patients and among veterans,” said lead author, Donald R. Sullivan, MD, of the division of pulmonary and critical care medicine at Oregon Health & Science University and a member of the OHSU Knight Cancer Institute, in a statement.
The investigators found that veterans who experienced at least one “palliative care encounter” after learning they had lung cancer were 82% less likely to die by suicide (odds ratio, 0.18; 95% confidence interval, 0.07-0.46; P less than .001), when compared with veterans who were diagnosed with lung cancer but did not receive palliative care.
The suicide rate for the advanced-stage lung cancer patients was 200/100,000 patient-years, which was more than five times higher than the suicide rate – adjusted for age, sex, and year – for all veterans using VA health care (37.5/100,000), according to the study abstract.
Of the 20,900 lung cancer patients analyzed, 30 committed suicide. Only six (20%) of the patients who died by suicide had received palliative care. Overall, most patients (18,192 or 87%) in the registry died of lung cancer. Other cancers, heart disease, and chronic obstructive pulmonary disease were some of the other common causes of death for the lung cancer patients, according to the abstract.
While several medical societies recommend palliative care for all patients with advanced-stage lung cancer, there is a gap between those recommendations and practice, noted Dr. Sullivan. “There are many barriers to palliative care, and unfortunately, some are related to clinician referrals. Not all doctors are aware of the benefits of palliative care,” he said in the statement.
Dr. Sullivan added that palliative care should be offered to all patients shortly after receiving a diagnosis of advanced-stage lung cancer.
More details on this study will be presented at the conference on Monday, May 21, at 2:30 p.m. in Room 14 A-B (Mezzanine Level) of the San Diego Convention Center.
according to new research that will be presented at an international conference of the American Thoracic Society.
“Suicide is a significant national public health problem, especially among lung cancer patients and among veterans,” said lead author, Donald R. Sullivan, MD, of the division of pulmonary and critical care medicine at Oregon Health & Science University and a member of the OHSU Knight Cancer Institute, in a statement.
The investigators found that veterans who experienced at least one “palliative care encounter” after learning they had lung cancer were 82% less likely to die by suicide (odds ratio, 0.18; 95% confidence interval, 0.07-0.46; P less than .001), when compared with veterans who were diagnosed with lung cancer but did not receive palliative care.
The suicide rate for the advanced-stage lung cancer patients was 200/100,000 patient-years, which was more than five times higher than the suicide rate – adjusted for age, sex, and year – for all veterans using VA health care (37.5/100,000), according to the study abstract.
Of the 20,900 lung cancer patients analyzed, 30 committed suicide. Only six (20%) of the patients who died by suicide had received palliative care. Overall, most patients (18,192 or 87%) in the registry died of lung cancer. Other cancers, heart disease, and chronic obstructive pulmonary disease were some of the other common causes of death for the lung cancer patients, according to the abstract.
While several medical societies recommend palliative care for all patients with advanced-stage lung cancer, there is a gap between those recommendations and practice, noted Dr. Sullivan. “There are many barriers to palliative care, and unfortunately, some are related to clinician referrals. Not all doctors are aware of the benefits of palliative care,” he said in the statement.
Dr. Sullivan added that palliative care should be offered to all patients shortly after receiving a diagnosis of advanced-stage lung cancer.
More details on this study will be presented at the conference on Monday, May 21, at 2:30 p.m. in Room 14 A-B (Mezzanine Level) of the San Diego Convention Center.
FROM ATS 2018
Americans are getting more sleep
an analysis of data from the American Time Use Survey (ATUS) has suggested.
Many people living in the United States habitually sleep less than the recommended 7-9 hours each day. “Experimental studies have demonstrated that both acute total and chronic partial sleep restriction in healthy adults are associated with physiological changes that can be considered precursors of manifest diseases (e.g. decreased insulin sensitivity),” noted Mathias Basner, MD, PhD, and David F. Dinges, PhD, both of the division of sleep and chronobiology at the University of Pennsylvania, Philadelphia, in their paper, which was published in the journal Sleep.
This new study is the first to have demonstrated that large parts of the U.S. population significantly increased their sleep between 2003 and 2016.
The investigators analyzed ATUS responses from 181,335 Americans aged 15 years and older; respondents included in the analysis were not active in the military or residing in institutions such as nursing homes or prisons. In 15- to 20-minute computer-assisted telephone interviews, the survey participants reported the activities they performed over a 24-hour period on a minute-by-minute basis. In-depth analyses only included groups “that showed a significant increase in sleep duration across survey years either on weekdays or weekends (or both): employed respondents, full-time students, and retirees.”
Using this data from ATUS, Dr. Basner and Dr. Dinges found that on workdays the prevalence of people who were sleeping 7 hours or less a day decreased by 0.44% per year (P less than .0001), while the percentage people who were sleeping more than 9 hours a day increased by 0.48% per year (P less than .0001).
Overall, respondents’ sleep increased by an average of 1.40 minutes during a weekday and 0.83 minutes during a weekend day every year.
These findings will be welcome news for organizations, such as the American Academy of Sleep Medicine, the Sleep Research Society, and the Centers for Disease Control and Prevention, that have been campaigning for years to increase sleep time among Americans.
The researchers also observed that the percentage of respondents in short sleep duration categories decreased significantly, and the percentage of respondents in long sleep duration categories increased significantly across survey years. One of the “most pronounced changes” occurred in the size of the group of patients receiving 6-7 hours of sleep. This group decreased by 0.23% per year. The biggest change was seen in the category of patients receiving 9-10 hours of sleep, which increased by 0.24% per year.
“[The] change in sleep duration across survey years on weekdays can mostly be explained by respondents going to bed earlier at night and, to a lesser degree, by getting up later in the morning,” the researchers said. “On weekends/holidays, ‘time to bed’ shifted significantly to earlier bed times by 1.1 min/year across survey years, which was comparable to the shift observed on weekdays.”
Study participants aged 18-24 slept the most, with hours slept having “decreased with increasing age.” On weekdays, adults aged 45-54 years slept the least, and on weekends, adults aged 55-64 years got the least shuteye. Hispanic, Asian, and black respondents slept more than white and “other race/ethnicity” survey participants. The researchers also found that women overall got more sleep than men.
Dr. Basner and Dr. Dinges expressed optimism about Americans’ ongoing battle against chronic sleep deficiency. “These findings presented here suggest that we are on the right track ... even if there is still a long way to go,” they said.
The authors reported no conflicts of interest.
David Schulman, MD, FCCP, comments: For more than fifteen years, we have had evidence that sleep deprivation is not only associated with increased accident risk, but also other common causes of mortality, including cardiovascular disease and cancer. Despite this knowledge, decades of trending in sleep patterns of the United States population have continued to show declines in total sleep time, which have been attributed to multiple factors, including longer work hours and the pervasive use of electronics, which can serve both as a distraction from sleep and a contributor to circadian dysrhythmia.
While our work in improving public awareness of sleep deprivation is far from done, perhaps this study is the first sign that a new day is dawning on improved sleep health for the country.
David Schulman, MD, FCCP, comments: For more than fifteen years, we have had evidence that sleep deprivation is not only associated with increased accident risk, but also other common causes of mortality, including cardiovascular disease and cancer. Despite this knowledge, decades of trending in sleep patterns of the United States population have continued to show declines in total sleep time, which have been attributed to multiple factors, including longer work hours and the pervasive use of electronics, which can serve both as a distraction from sleep and a contributor to circadian dysrhythmia.
While our work in improving public awareness of sleep deprivation is far from done, perhaps this study is the first sign that a new day is dawning on improved sleep health for the country.
David Schulman, MD, FCCP, comments: For more than fifteen years, we have had evidence that sleep deprivation is not only associated with increased accident risk, but also other common causes of mortality, including cardiovascular disease and cancer. Despite this knowledge, decades of trending in sleep patterns of the United States population have continued to show declines in total sleep time, which have been attributed to multiple factors, including longer work hours and the pervasive use of electronics, which can serve both as a distraction from sleep and a contributor to circadian dysrhythmia.
While our work in improving public awareness of sleep deprivation is far from done, perhaps this study is the first sign that a new day is dawning on improved sleep health for the country.
an analysis of data from the American Time Use Survey (ATUS) has suggested.
Many people living in the United States habitually sleep less than the recommended 7-9 hours each day. “Experimental studies have demonstrated that both acute total and chronic partial sleep restriction in healthy adults are associated with physiological changes that can be considered precursors of manifest diseases (e.g. decreased insulin sensitivity),” noted Mathias Basner, MD, PhD, and David F. Dinges, PhD, both of the division of sleep and chronobiology at the University of Pennsylvania, Philadelphia, in their paper, which was published in the journal Sleep.
This new study is the first to have demonstrated that large parts of the U.S. population significantly increased their sleep between 2003 and 2016.
The investigators analyzed ATUS responses from 181,335 Americans aged 15 years and older; respondents included in the analysis were not active in the military or residing in institutions such as nursing homes or prisons. In 15- to 20-minute computer-assisted telephone interviews, the survey participants reported the activities they performed over a 24-hour period on a minute-by-minute basis. In-depth analyses only included groups “that showed a significant increase in sleep duration across survey years either on weekdays or weekends (or both): employed respondents, full-time students, and retirees.”
Using this data from ATUS, Dr. Basner and Dr. Dinges found that on workdays the prevalence of people who were sleeping 7 hours or less a day decreased by 0.44% per year (P less than .0001), while the percentage people who were sleeping more than 9 hours a day increased by 0.48% per year (P less than .0001).
Overall, respondents’ sleep increased by an average of 1.40 minutes during a weekday and 0.83 minutes during a weekend day every year.
These findings will be welcome news for organizations, such as the American Academy of Sleep Medicine, the Sleep Research Society, and the Centers for Disease Control and Prevention, that have been campaigning for years to increase sleep time among Americans.
The researchers also observed that the percentage of respondents in short sleep duration categories decreased significantly, and the percentage of respondents in long sleep duration categories increased significantly across survey years. One of the “most pronounced changes” occurred in the size of the group of patients receiving 6-7 hours of sleep. This group decreased by 0.23% per year. The biggest change was seen in the category of patients receiving 9-10 hours of sleep, which increased by 0.24% per year.
“[The] change in sleep duration across survey years on weekdays can mostly be explained by respondents going to bed earlier at night and, to a lesser degree, by getting up later in the morning,” the researchers said. “On weekends/holidays, ‘time to bed’ shifted significantly to earlier bed times by 1.1 min/year across survey years, which was comparable to the shift observed on weekdays.”
Study participants aged 18-24 slept the most, with hours slept having “decreased with increasing age.” On weekdays, adults aged 45-54 years slept the least, and on weekends, adults aged 55-64 years got the least shuteye. Hispanic, Asian, and black respondents slept more than white and “other race/ethnicity” survey participants. The researchers also found that women overall got more sleep than men.
Dr. Basner and Dr. Dinges expressed optimism about Americans’ ongoing battle against chronic sleep deficiency. “These findings presented here suggest that we are on the right track ... even if there is still a long way to go,” they said.
The authors reported no conflicts of interest.
an analysis of data from the American Time Use Survey (ATUS) has suggested.
Many people living in the United States habitually sleep less than the recommended 7-9 hours each day. “Experimental studies have demonstrated that both acute total and chronic partial sleep restriction in healthy adults are associated with physiological changes that can be considered precursors of manifest diseases (e.g. decreased insulin sensitivity),” noted Mathias Basner, MD, PhD, and David F. Dinges, PhD, both of the division of sleep and chronobiology at the University of Pennsylvania, Philadelphia, in their paper, which was published in the journal Sleep.
This new study is the first to have demonstrated that large parts of the U.S. population significantly increased their sleep between 2003 and 2016.
The investigators analyzed ATUS responses from 181,335 Americans aged 15 years and older; respondents included in the analysis were not active in the military or residing in institutions such as nursing homes or prisons. In 15- to 20-minute computer-assisted telephone interviews, the survey participants reported the activities they performed over a 24-hour period on a minute-by-minute basis. In-depth analyses only included groups “that showed a significant increase in sleep duration across survey years either on weekdays or weekends (or both): employed respondents, full-time students, and retirees.”
Using this data from ATUS, Dr. Basner and Dr. Dinges found that on workdays the prevalence of people who were sleeping 7 hours or less a day decreased by 0.44% per year (P less than .0001), while the percentage people who were sleeping more than 9 hours a day increased by 0.48% per year (P less than .0001).
Overall, respondents’ sleep increased by an average of 1.40 minutes during a weekday and 0.83 minutes during a weekend day every year.
These findings will be welcome news for organizations, such as the American Academy of Sleep Medicine, the Sleep Research Society, and the Centers for Disease Control and Prevention, that have been campaigning for years to increase sleep time among Americans.
The researchers also observed that the percentage of respondents in short sleep duration categories decreased significantly, and the percentage of respondents in long sleep duration categories increased significantly across survey years. One of the “most pronounced changes” occurred in the size of the group of patients receiving 6-7 hours of sleep. This group decreased by 0.23% per year. The biggest change was seen in the category of patients receiving 9-10 hours of sleep, which increased by 0.24% per year.
“[The] change in sleep duration across survey years on weekdays can mostly be explained by respondents going to bed earlier at night and, to a lesser degree, by getting up later in the morning,” the researchers said. “On weekends/holidays, ‘time to bed’ shifted significantly to earlier bed times by 1.1 min/year across survey years, which was comparable to the shift observed on weekdays.”
Study participants aged 18-24 slept the most, with hours slept having “decreased with increasing age.” On weekdays, adults aged 45-54 years slept the least, and on weekends, adults aged 55-64 years got the least shuteye. Hispanic, Asian, and black respondents slept more than white and “other race/ethnicity” survey participants. The researchers also found that women overall got more sleep than men.
Dr. Basner and Dr. Dinges expressed optimism about Americans’ ongoing battle against chronic sleep deficiency. “These findings presented here suggest that we are on the right track ... even if there is still a long way to go,” they said.
The authors reported no conflicts of interest.
FROM SLEEP
Key clinical point: The amount of time people in the United States spend sleeping has increased.
Major finding: On workdays, the prevalence of people who were sleeping 7 hours or less a day decreased by 0.44% per year, and the percentage of people who were sleeping more than 9 hours a day increased by 0.48% per year.
Study details: An analysis of survey responses from 181,335 Americans over 2003-2016.
Disclosures: The authors reported no conflicts of interest.
Source: Basner M et al. Sleep. 2018 Apr 1;41(4):1-16.
FDA: More COPD patients can use triple therapy
The Food and Drug Administration has approved a new indication for the chronic obstructive pulmonary disease (COPD) therapy fluticasone furoate/umeclidinium/vilanterol (Trelegy Ellipta), which allows physicians to prescribe the drug to a broader class of COPD patients, according to a statement from two pharmaceutical companies.
“Following the initial approval of Trelegy Ellipta in September, we have analysed the data from the IMPACT study and identified additional benefits that this important medicine offers patients with [COPD],” said Hal Barron, MD, chief scientific officer and president of research and development at GlaxoSmithKline, in the statement. “We are pleased that the robust data from the IMPACT study has enabled the expanded indication announced today and the FDA action has been taken so swiftly.”
The results of the IMPACT trial, which was the first study to compare a single-inhaler triple therapy with two dual therapies, were published on April 18 (N Engl J Med 2018. doi: 10.1056/NEJMoa1713901).
This study randomized patients to 52 weeks of either triple inhaled therapy involving a once-daily combination of 100 mcg fluticasone furoate, 62.5 mcg of umeclidinium, and 25 mcg of vilanterol; or dual inhaled therapy involving either 100 mcg fluticasone furoate plus 25 mcg of vilanterol, or 62.5 mcg of umeclidinium plus 25 mcg of vilanterol.
After 1 year, the rate of moderate to severe COPD exacerbations in the triple-therapy group was 0.91 per year, compared with 1.07 in the fluticasone furoate–vilanterol group and 1.21 in the vilanterol-umeclidinium group. This translated to a 15% reduction with triple therapy compared with fluticasone furoate–vilanterol and a 25% reduction, compared with vilanterol-umeclidinium (P less than .001 for both).
The Food and Drug Administration has approved a new indication for the chronic obstructive pulmonary disease (COPD) therapy fluticasone furoate/umeclidinium/vilanterol (Trelegy Ellipta), which allows physicians to prescribe the drug to a broader class of COPD patients, according to a statement from two pharmaceutical companies.
“Following the initial approval of Trelegy Ellipta in September, we have analysed the data from the IMPACT study and identified additional benefits that this important medicine offers patients with [COPD],” said Hal Barron, MD, chief scientific officer and president of research and development at GlaxoSmithKline, in the statement. “We are pleased that the robust data from the IMPACT study has enabled the expanded indication announced today and the FDA action has been taken so swiftly.”
The results of the IMPACT trial, which was the first study to compare a single-inhaler triple therapy with two dual therapies, were published on April 18 (N Engl J Med 2018. doi: 10.1056/NEJMoa1713901).
This study randomized patients to 52 weeks of either triple inhaled therapy involving a once-daily combination of 100 mcg fluticasone furoate, 62.5 mcg of umeclidinium, and 25 mcg of vilanterol; or dual inhaled therapy involving either 100 mcg fluticasone furoate plus 25 mcg of vilanterol, or 62.5 mcg of umeclidinium plus 25 mcg of vilanterol.
After 1 year, the rate of moderate to severe COPD exacerbations in the triple-therapy group was 0.91 per year, compared with 1.07 in the fluticasone furoate–vilanterol group and 1.21 in the vilanterol-umeclidinium group. This translated to a 15% reduction with triple therapy compared with fluticasone furoate–vilanterol and a 25% reduction, compared with vilanterol-umeclidinium (P less than .001 for both).
The Food and Drug Administration has approved a new indication for the chronic obstructive pulmonary disease (COPD) therapy fluticasone furoate/umeclidinium/vilanterol (Trelegy Ellipta), which allows physicians to prescribe the drug to a broader class of COPD patients, according to a statement from two pharmaceutical companies.
“Following the initial approval of Trelegy Ellipta in September, we have analysed the data from the IMPACT study and identified additional benefits that this important medicine offers patients with [COPD],” said Hal Barron, MD, chief scientific officer and president of research and development at GlaxoSmithKline, in the statement. “We are pleased that the robust data from the IMPACT study has enabled the expanded indication announced today and the FDA action has been taken so swiftly.”
The results of the IMPACT trial, which was the first study to compare a single-inhaler triple therapy with two dual therapies, were published on April 18 (N Engl J Med 2018. doi: 10.1056/NEJMoa1713901).
This study randomized patients to 52 weeks of either triple inhaled therapy involving a once-daily combination of 100 mcg fluticasone furoate, 62.5 mcg of umeclidinium, and 25 mcg of vilanterol; or dual inhaled therapy involving either 100 mcg fluticasone furoate plus 25 mcg of vilanterol, or 62.5 mcg of umeclidinium plus 25 mcg of vilanterol.
After 1 year, the rate of moderate to severe COPD exacerbations in the triple-therapy group was 0.91 per year, compared with 1.07 in the fluticasone furoate–vilanterol group and 1.21 in the vilanterol-umeclidinium group. This translated to a 15% reduction with triple therapy compared with fluticasone furoate–vilanterol and a 25% reduction, compared with vilanterol-umeclidinium (P less than .001 for both).
Smoking Sped Progression of Multiple Sclerosis
Patients with multiple sclerosis who continued to smoke after diagnosis had faster disease progression in a population-based, case-control study.
Each additional year of smoking after diagnosis accelerated the time to conversion to secondary progressive multiple sclerosis (SPMS) by 4.7%, and those who smoked continuously each year after diagnosis converted to SPMS an estimated 8 years earlier than did those who quit smoking at diagnosis, according to Ryan Ramanujam, Ph.D., and his colleagues.
They analyzed data from a survey of 2,538 MS patients living in Sweden, including 728 who smoked at diagnosis, 1,012 who never had smoked, and 618 who had smoked prior to having been diagnosed. The group of smokers included 118 who stopped smoking during the year after diagnosis, 332 who continued smoking, and 278 who smoked intermittently, meaning they continued smoking for at least 1 year after being diagnosed with MS and were not smoking for at least 1 year after diagnosis.
“This study demonstrates that smoking after MS diagnosis has a negative impact on the progression of the disease, whereas reduced smoking may improve patient quality of life, with more years before the development of SP disease,” the investigators wrote.
“We suggest that these results should be regarded as sufficient to recommend smoking cessation to patients,” they added.
Read the full study in JAMA Neurology (doi: 10.1001/jamaneurol.2015.1788).
Patients with multiple sclerosis who continued to smoke after diagnosis had faster disease progression in a population-based, case-control study.
Each additional year of smoking after diagnosis accelerated the time to conversion to secondary progressive multiple sclerosis (SPMS) by 4.7%, and those who smoked continuously each year after diagnosis converted to SPMS an estimated 8 years earlier than did those who quit smoking at diagnosis, according to Ryan Ramanujam, Ph.D., and his colleagues.
They analyzed data from a survey of 2,538 MS patients living in Sweden, including 728 who smoked at diagnosis, 1,012 who never had smoked, and 618 who had smoked prior to having been diagnosed. The group of smokers included 118 who stopped smoking during the year after diagnosis, 332 who continued smoking, and 278 who smoked intermittently, meaning they continued smoking for at least 1 year after being diagnosed with MS and were not smoking for at least 1 year after diagnosis.
“This study demonstrates that smoking after MS diagnosis has a negative impact on the progression of the disease, whereas reduced smoking may improve patient quality of life, with more years before the development of SP disease,” the investigators wrote.
“We suggest that these results should be regarded as sufficient to recommend smoking cessation to patients,” they added.
Read the full study in JAMA Neurology (doi: 10.1001/jamaneurol.2015.1788).
Patients with multiple sclerosis who continued to smoke after diagnosis had faster disease progression in a population-based, case-control study.
Each additional year of smoking after diagnosis accelerated the time to conversion to secondary progressive multiple sclerosis (SPMS) by 4.7%, and those who smoked continuously each year after diagnosis converted to SPMS an estimated 8 years earlier than did those who quit smoking at diagnosis, according to Ryan Ramanujam, Ph.D., and his colleagues.
They analyzed data from a survey of 2,538 MS patients living in Sweden, including 728 who smoked at diagnosis, 1,012 who never had smoked, and 618 who had smoked prior to having been diagnosed. The group of smokers included 118 who stopped smoking during the year after diagnosis, 332 who continued smoking, and 278 who smoked intermittently, meaning they continued smoking for at least 1 year after being diagnosed with MS and were not smoking for at least 1 year after diagnosis.
“This study demonstrates that smoking after MS diagnosis has a negative impact on the progression of the disease, whereas reduced smoking may improve patient quality of life, with more years before the development of SP disease,” the investigators wrote.
“We suggest that these results should be regarded as sufficient to recommend smoking cessation to patients,” they added.
Read the full study in JAMA Neurology (doi: 10.1001/jamaneurol.2015.1788).
Smoking sped progression of multiple sclerosis
Patients with multiple sclerosis who continued to smoke after diagnosis had faster disease progression in a population-based, case-control study.
Each additional year of smoking after diagnosis accelerated the time to conversion to secondary progressive multiple sclerosis (SPMS) by 4.7%, and those who smoked continuously each year after diagnosis converted to SPMS an estimated 8 years earlier than did those who quit smoking at diagnosis, according to Ryan Ramanujam, Ph.D., and his colleagues.
They analyzed data from a survey of 2,538 MS patients living in Sweden, including 728 who smoked at diagnosis, 1,012 who never had smoked, and 618 who had smoked prior to having been diagnosed. The group of smokers included 118 who stopped smoking during the year after diagnosis, 332 who continued smoking, and 278 who smoked intermittently, meaning they continued smoking for at least 1 year after being diagnosed with MS and were not smoking for at least 1 year after diagnosis.
“This study demonstrates that smoking after MS diagnosis has a negative impact on the progression of the disease, whereas reduced smoking may improve patient quality of life, with more years before the development of SP disease,” the investigators wrote.
“We suggest that these results should be regarded as sufficient to recommend smoking cessation to patients,” they added.
Read the full study in JAMA Neurology (doi: 10.1001/jamaneurol.2015.1788).
Patients with multiple sclerosis who continued to smoke after diagnosis had faster disease progression in a population-based, case-control study.
Each additional year of smoking after diagnosis accelerated the time to conversion to secondary progressive multiple sclerosis (SPMS) by 4.7%, and those who smoked continuously each year after diagnosis converted to SPMS an estimated 8 years earlier than did those who quit smoking at diagnosis, according to Ryan Ramanujam, Ph.D., and his colleagues.
They analyzed data from a survey of 2,538 MS patients living in Sweden, including 728 who smoked at diagnosis, 1,012 who never had smoked, and 618 who had smoked prior to having been diagnosed. The group of smokers included 118 who stopped smoking during the year after diagnosis, 332 who continued smoking, and 278 who smoked intermittently, meaning they continued smoking for at least 1 year after being diagnosed with MS and were not smoking for at least 1 year after diagnosis.
“This study demonstrates that smoking after MS diagnosis has a negative impact on the progression of the disease, whereas reduced smoking may improve patient quality of life, with more years before the development of SP disease,” the investigators wrote.
“We suggest that these results should be regarded as sufficient to recommend smoking cessation to patients,” they added.
Read the full study in JAMA Neurology (doi: 10.1001/jamaneurol.2015.1788).
Patients with multiple sclerosis who continued to smoke after diagnosis had faster disease progression in a population-based, case-control study.
Each additional year of smoking after diagnosis accelerated the time to conversion to secondary progressive multiple sclerosis (SPMS) by 4.7%, and those who smoked continuously each year after diagnosis converted to SPMS an estimated 8 years earlier than did those who quit smoking at diagnosis, according to Ryan Ramanujam, Ph.D., and his colleagues.
They analyzed data from a survey of 2,538 MS patients living in Sweden, including 728 who smoked at diagnosis, 1,012 who never had smoked, and 618 who had smoked prior to having been diagnosed. The group of smokers included 118 who stopped smoking during the year after diagnosis, 332 who continued smoking, and 278 who smoked intermittently, meaning they continued smoking for at least 1 year after being diagnosed with MS and were not smoking for at least 1 year after diagnosis.
“This study demonstrates that smoking after MS diagnosis has a negative impact on the progression of the disease, whereas reduced smoking may improve patient quality of life, with more years before the development of SP disease,” the investigators wrote.
“We suggest that these results should be regarded as sufficient to recommend smoking cessation to patients,” they added.
Read the full study in JAMA Neurology (doi: 10.1001/jamaneurol.2015.1788).
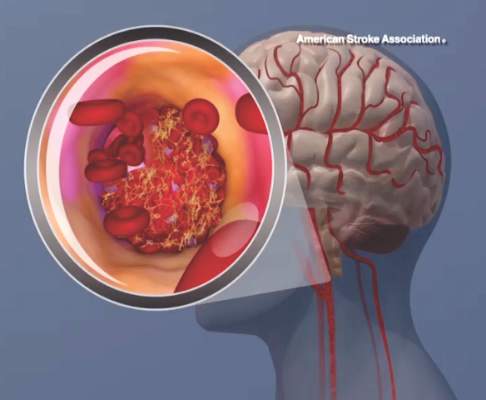
AHA begins Cryptogenic Stroke Initiative
Cryptogenic stroke patients and their caregivers recently surveyed by the American Heart Association/American Stroke Association said that they experience several negative consequences of having an undetermined cause of their stroke, and only one-fifth received information about cryptogenic stroke at the time of diagnosis.
This lack of information prompted the organization to start the Cryptogenic Stroke Initiative. The initiative will inform cryptogenic stroke patients and help “them to work with their healthcare team to prevent a second stroke,” Dr. Mary Ann Bauman, chair of the American Stroke Association Advisory Committee, said in an announcement.
This month, the American Heart Association/American Stroke Association, with support from Medtronic, published a free informational document. This Patient Guide to Cryptogenic Stroke is the first of several guides that the American Stroke Association plans to create for cryptogenic stroke patients. This edition of the guide includes “information on cryptogenic stroke diagnosis, what happens during a stroke, secondary prevention information, questions [for patients to ask their doctor, and] support resources,” the Association said.
In the organizations’ survey, which included 309 cryptogenic stroke patients and caregivers, more than 50% reported anxiety and frustration when the cause of stroke is undetermined. Of the 20% of patients and caregivers who received information about cryptogenic stroke at the time of diagnosis, the information was verbally communicated 75% of the time.
Cryptogenic stroke patients and their caregivers recently surveyed by the American Heart Association/American Stroke Association said that they experience several negative consequences of having an undetermined cause of their stroke, and only one-fifth received information about cryptogenic stroke at the time of diagnosis.
This lack of information prompted the organization to start the Cryptogenic Stroke Initiative. The initiative will inform cryptogenic stroke patients and help “them to work with their healthcare team to prevent a second stroke,” Dr. Mary Ann Bauman, chair of the American Stroke Association Advisory Committee, said in an announcement.
This month, the American Heart Association/American Stroke Association, with support from Medtronic, published a free informational document. This Patient Guide to Cryptogenic Stroke is the first of several guides that the American Stroke Association plans to create for cryptogenic stroke patients. This edition of the guide includes “information on cryptogenic stroke diagnosis, what happens during a stroke, secondary prevention information, questions [for patients to ask their doctor, and] support resources,” the Association said.
In the organizations’ survey, which included 309 cryptogenic stroke patients and caregivers, more than 50% reported anxiety and frustration when the cause of stroke is undetermined. Of the 20% of patients and caregivers who received information about cryptogenic stroke at the time of diagnosis, the information was verbally communicated 75% of the time.
Cryptogenic stroke patients and their caregivers recently surveyed by the American Heart Association/American Stroke Association said that they experience several negative consequences of having an undetermined cause of their stroke, and only one-fifth received information about cryptogenic stroke at the time of diagnosis.
This lack of information prompted the organization to start the Cryptogenic Stroke Initiative. The initiative will inform cryptogenic stroke patients and help “them to work with their healthcare team to prevent a second stroke,” Dr. Mary Ann Bauman, chair of the American Stroke Association Advisory Committee, said in an announcement.
This month, the American Heart Association/American Stroke Association, with support from Medtronic, published a free informational document. This Patient Guide to Cryptogenic Stroke is the first of several guides that the American Stroke Association plans to create for cryptogenic stroke patients. This edition of the guide includes “information on cryptogenic stroke diagnosis, what happens during a stroke, secondary prevention information, questions [for patients to ask their doctor, and] support resources,” the Association said.
In the organizations’ survey, which included 309 cryptogenic stroke patients and caregivers, more than 50% reported anxiety and frustration when the cause of stroke is undetermined. Of the 20% of patients and caregivers who received information about cryptogenic stroke at the time of diagnosis, the information was verbally communicated 75% of the time.