User login
Stronger evidence links Zika to Guillain-Barré syndrome
Serological evidence from French Polynesia links an outbreak of Zika virus to a spike in cases of Guillain-Barré syndrome seen there in 2013-2014.
The research, published online Feb. 29 in The Lancet, is the first to use a case-control design to demonstrate that Zika, a mosquito-borne flavivirus, is associated with Guillain-Barré syndrome (Lancet. 2016 Feb 29. doi: 10.1016/S0140-6736(16)00562-6).
Guillain-Barré syndrome (GBS) is an immune-mediated flaccid paralysis that can follow viral or bacterial infections. Most patients with GBS recover with intensive care in hospitals, although the syndrome can be permanently debilitating or, in rare cases, fatal.
As a large outbreak of Zika continues in Central and South America, hospitals should be prepared for excess GBS cases, the authors of the study say, and assure adequate intensive-care capacity to treat them. Based on the 66% attack rate of Zika during the French Polynesia outbreak, investigators estimated the incidence of GBS at 0.24 per 1,000 Zika infections, but noted that it could be different in the current outbreak.
Dr. Van-Mai Cao-Lormeau of the Unit of Emerging Infectious Diseases at Institut Louis Malardé in Papeete, French Polynesia, alongside colleagues in France and French Polynesia, used a case-control design to compare serological samples from 42 patients (74% male) diagnosed at a Tahiti hospital with GBS with samples from age-and sex-matched patients who presented at the same hospital, also during the time of the outbreak, with a nonfebrile illness (n = 98) or with acute Zika disease without neurological symptoms (n = 70).
The investigators found that all but one patient with GBS had Zika virus antibodies, and all of them had neutralizing antibodies to Zika virus. By comparison, only 56% (n = 54) of the control group admitted with nonfebrile illness had neutralizing antibodies (P less than .0001).
Also, 93% of the GBS patients had Zika virus immunoglobulin M (IgM) and 88% reported symptoms consistent with Zika infection a mean of 6 days before onset of neurological symptoms. Acute Zika infection is usually characterized by rash, fever, and conjunctivitis.
Past dengue virus infection, which had been considered a possible risk factor for Zika-mediated GBS, did not differ significantly between patients in the control groups and those with GBS.
The investigators were also able to subtype the clinical characteristics of the GBS cases as consistent with acute motor axonal neuropathy, or AMAN, phenotype. However, the antibodies typically seen associated with AMAN were not seen in these patients, leading investigators to suspect that a different biological pathway was responsible.
More than a third of the GBS patients in the study required intensive care, most of these also with respiratory support, though none died.
The government of France, the European Union, and the Wellcome Trust funded the study. The researchers declared that they had no competing interests.
Zika virus can be added to our list of viruses that can cause Guillain-Barré syndrome, and investigation of these cases should include tests for Zika when there is a possibility of infection by that virus. Whether Zika will be proven to pose a greater threat in causing Guillain-Barré syndrome than its various flavivirus cousins remains to be determined. A little caution should be taken because the data are still scarce and we do not know whether the current Zika virus is identical to that in previous outbreaks, whether it will behave exactly the same in a different population with a different genetic and immunity background, or whether a cofactor or co-infection is responsible. Reassuringly, the investigators did not find any evidence that previous dengue infection enhanced the severity of the disease, which could substantially have increased the threat in areas of regular activity.
Dr. David W. Smith is a clinical professor of pathology and laboratory medicine at the University of Western Australia in Perth. John Mackenzie, Ph.D., is a professor of tropical and infectious diseases at Curtin University in Bentley, Australia. They had no competing interests to disclose.
Zika virus can be added to our list of viruses that can cause Guillain-Barré syndrome, and investigation of these cases should include tests for Zika when there is a possibility of infection by that virus. Whether Zika will be proven to pose a greater threat in causing Guillain-Barré syndrome than its various flavivirus cousins remains to be determined. A little caution should be taken because the data are still scarce and we do not know whether the current Zika virus is identical to that in previous outbreaks, whether it will behave exactly the same in a different population with a different genetic and immunity background, or whether a cofactor or co-infection is responsible. Reassuringly, the investigators did not find any evidence that previous dengue infection enhanced the severity of the disease, which could substantially have increased the threat in areas of regular activity.
Dr. David W. Smith is a clinical professor of pathology and laboratory medicine at the University of Western Australia in Perth. John Mackenzie, Ph.D., is a professor of tropical and infectious diseases at Curtin University in Bentley, Australia. They had no competing interests to disclose.
Zika virus can be added to our list of viruses that can cause Guillain-Barré syndrome, and investigation of these cases should include tests for Zika when there is a possibility of infection by that virus. Whether Zika will be proven to pose a greater threat in causing Guillain-Barré syndrome than its various flavivirus cousins remains to be determined. A little caution should be taken because the data are still scarce and we do not know whether the current Zika virus is identical to that in previous outbreaks, whether it will behave exactly the same in a different population with a different genetic and immunity background, or whether a cofactor or co-infection is responsible. Reassuringly, the investigators did not find any evidence that previous dengue infection enhanced the severity of the disease, which could substantially have increased the threat in areas of regular activity.
Dr. David W. Smith is a clinical professor of pathology and laboratory medicine at the University of Western Australia in Perth. John Mackenzie, Ph.D., is a professor of tropical and infectious diseases at Curtin University in Bentley, Australia. They had no competing interests to disclose.
Serological evidence from French Polynesia links an outbreak of Zika virus to a spike in cases of Guillain-Barré syndrome seen there in 2013-2014.
The research, published online Feb. 29 in The Lancet, is the first to use a case-control design to demonstrate that Zika, a mosquito-borne flavivirus, is associated with Guillain-Barré syndrome (Lancet. 2016 Feb 29. doi: 10.1016/S0140-6736(16)00562-6).
Guillain-Barré syndrome (GBS) is an immune-mediated flaccid paralysis that can follow viral or bacterial infections. Most patients with GBS recover with intensive care in hospitals, although the syndrome can be permanently debilitating or, in rare cases, fatal.
As a large outbreak of Zika continues in Central and South America, hospitals should be prepared for excess GBS cases, the authors of the study say, and assure adequate intensive-care capacity to treat them. Based on the 66% attack rate of Zika during the French Polynesia outbreak, investigators estimated the incidence of GBS at 0.24 per 1,000 Zika infections, but noted that it could be different in the current outbreak.
Dr. Van-Mai Cao-Lormeau of the Unit of Emerging Infectious Diseases at Institut Louis Malardé in Papeete, French Polynesia, alongside colleagues in France and French Polynesia, used a case-control design to compare serological samples from 42 patients (74% male) diagnosed at a Tahiti hospital with GBS with samples from age-and sex-matched patients who presented at the same hospital, also during the time of the outbreak, with a nonfebrile illness (n = 98) or with acute Zika disease without neurological symptoms (n = 70).
The investigators found that all but one patient with GBS had Zika virus antibodies, and all of them had neutralizing antibodies to Zika virus. By comparison, only 56% (n = 54) of the control group admitted with nonfebrile illness had neutralizing antibodies (P less than .0001).
Also, 93% of the GBS patients had Zika virus immunoglobulin M (IgM) and 88% reported symptoms consistent with Zika infection a mean of 6 days before onset of neurological symptoms. Acute Zika infection is usually characterized by rash, fever, and conjunctivitis.
Past dengue virus infection, which had been considered a possible risk factor for Zika-mediated GBS, did not differ significantly between patients in the control groups and those with GBS.
The investigators were also able to subtype the clinical characteristics of the GBS cases as consistent with acute motor axonal neuropathy, or AMAN, phenotype. However, the antibodies typically seen associated with AMAN were not seen in these patients, leading investigators to suspect that a different biological pathway was responsible.
More than a third of the GBS patients in the study required intensive care, most of these also with respiratory support, though none died.
The government of France, the European Union, and the Wellcome Trust funded the study. The researchers declared that they had no competing interests.
Serological evidence from French Polynesia links an outbreak of Zika virus to a spike in cases of Guillain-Barré syndrome seen there in 2013-2014.
The research, published online Feb. 29 in The Lancet, is the first to use a case-control design to demonstrate that Zika, a mosquito-borne flavivirus, is associated with Guillain-Barré syndrome (Lancet. 2016 Feb 29. doi: 10.1016/S0140-6736(16)00562-6).
Guillain-Barré syndrome (GBS) is an immune-mediated flaccid paralysis that can follow viral or bacterial infections. Most patients with GBS recover with intensive care in hospitals, although the syndrome can be permanently debilitating or, in rare cases, fatal.
As a large outbreak of Zika continues in Central and South America, hospitals should be prepared for excess GBS cases, the authors of the study say, and assure adequate intensive-care capacity to treat them. Based on the 66% attack rate of Zika during the French Polynesia outbreak, investigators estimated the incidence of GBS at 0.24 per 1,000 Zika infections, but noted that it could be different in the current outbreak.
Dr. Van-Mai Cao-Lormeau of the Unit of Emerging Infectious Diseases at Institut Louis Malardé in Papeete, French Polynesia, alongside colleagues in France and French Polynesia, used a case-control design to compare serological samples from 42 patients (74% male) diagnosed at a Tahiti hospital with GBS with samples from age-and sex-matched patients who presented at the same hospital, also during the time of the outbreak, with a nonfebrile illness (n = 98) or with acute Zika disease without neurological symptoms (n = 70).
The investigators found that all but one patient with GBS had Zika virus antibodies, and all of them had neutralizing antibodies to Zika virus. By comparison, only 56% (n = 54) of the control group admitted with nonfebrile illness had neutralizing antibodies (P less than .0001).
Also, 93% of the GBS patients had Zika virus immunoglobulin M (IgM) and 88% reported symptoms consistent with Zika infection a mean of 6 days before onset of neurological symptoms. Acute Zika infection is usually characterized by rash, fever, and conjunctivitis.
Past dengue virus infection, which had been considered a possible risk factor for Zika-mediated GBS, did not differ significantly between patients in the control groups and those with GBS.
The investigators were also able to subtype the clinical characteristics of the GBS cases as consistent with acute motor axonal neuropathy, or AMAN, phenotype. However, the antibodies typically seen associated with AMAN were not seen in these patients, leading investigators to suspect that a different biological pathway was responsible.
More than a third of the GBS patients in the study required intensive care, most of these also with respiratory support, though none died.
The government of France, the European Union, and the Wellcome Trust funded the study. The researchers declared that they had no competing interests.
FROM THE LANCET
Key clinical point: Acute infection with Zika virus in French Polynesia was associated with Guillain-Barré syndrome.
Major finding: Among GBS patients admitted to hospitals during an 2013-2014 outbreak of Zika virus, nearly all had antibodies or neutralizing antibodies to Zika, vs. 56% of age and sex-matched controls (P less than .0001).
Data source: A case-cohort study comparing blood results from 42 GBS cases and two cohorts of controls, one with acute Zika infection without GBS (n = 70) and another admitted during the outbreak for other illnesses (n = 98).
Disclosures: The French government, the European Union, and the Wellcome Trust sponsored the study. Investigators disclosed no conflicts of interest.
ACA accelerated hospital readmission reduction efforts
Hospital readmissions have declined in recent years for three conditions targeted under the Affordable Care Act, with smaller declines for other conditions, according to new research.
The study, published online Feb. 24 in the New England Journal of Medicine, found that 30-day readmission rates declined quickly after the passage of the ACA in 2010 and then slowed at the end of 2012. The researchers also analyzed trends in the use of observation units during the same period and concluded that the drop in readmissions was not being masked by a similar uptick in patients being seen under observation status (N Engl J Med. 2016 Feb 24. doi: 10.1056/NEJMsa1513024).
Under the ACA’s Hospital Readmissions Reduction Program, hospitals are financially penalized if they have higher-than-expected readmission rates for acute myocardial infarction, heart failure, and pneumonia.
The researchers, led by Rachael B. Zuckerman, M.P.H., of the Department of Health & Human Services, examined Medicare data from 3,387 hospitals from October 2007 through May 2015. Overall readmissions for acute myocardial infarction, heart failure, and pneumonia – the three conditions targeted in the readmissions reduction program – dropped from 21.5% to 17.8% during this time period. Readmissions for nontargeted conditions also dropped from 15.3% to 13.1%.
The researchers reported that readmissions for the targeted conditions were already declining before the ACA implementation (slope of monthly rate, –0.017), accelerating between April 2010 and October 2010 (–0.103), then leveling off through 2015 (–0.05). A similar pattern was seen with readmissions for conditions not targeted under the health law, though the declines were less pronounced.
Observation rates for the targeted conditions increased from 2.6% to 4.7% during the study period, while rates for nontargeted conditions rose from 2.5% to 4.2%. The researchers did not observe any significant associations increases in observation-unit stays – which were steady throughout the study period – and the implementation of the ACA.
“It seems likely that the upward trend in observation-service use may be attributable to factors that are largely unrelated to the Hospital Readmissions Reduction Program, such as confusion over whether an inpatient stay would be deemed inappropriate by Medicare recovery audit contractors,” the researchers wrote.
Though the observational design of the study could not confirm a causal link between the ACA penalties and the drop in readmissions, the findings suggest that the declines are not solely a response to the ACA.
The health law likely “catalyzed behavioral change by many hospitals” that was already underway, possibly because of broader concern about readmissions and to earlier Medicare initiatives designed to reduce them. Also, the investigators noted, hospitals may have been helped by other government efforts on the readmission front, including the dissemination of best practices by the Centers for Medicare & Medicaid Services.
The study was funded by HHS and the researchers were agency employees. They reported having no other financial disclosures.
Hospital readmissions have declined in recent years for three conditions targeted under the Affordable Care Act, with smaller declines for other conditions, according to new research.
The study, published online Feb. 24 in the New England Journal of Medicine, found that 30-day readmission rates declined quickly after the passage of the ACA in 2010 and then slowed at the end of 2012. The researchers also analyzed trends in the use of observation units during the same period and concluded that the drop in readmissions was not being masked by a similar uptick in patients being seen under observation status (N Engl J Med. 2016 Feb 24. doi: 10.1056/NEJMsa1513024).
Under the ACA’s Hospital Readmissions Reduction Program, hospitals are financially penalized if they have higher-than-expected readmission rates for acute myocardial infarction, heart failure, and pneumonia.
The researchers, led by Rachael B. Zuckerman, M.P.H., of the Department of Health & Human Services, examined Medicare data from 3,387 hospitals from October 2007 through May 2015. Overall readmissions for acute myocardial infarction, heart failure, and pneumonia – the three conditions targeted in the readmissions reduction program – dropped from 21.5% to 17.8% during this time period. Readmissions for nontargeted conditions also dropped from 15.3% to 13.1%.
The researchers reported that readmissions for the targeted conditions were already declining before the ACA implementation (slope of monthly rate, –0.017), accelerating between April 2010 and October 2010 (–0.103), then leveling off through 2015 (–0.05). A similar pattern was seen with readmissions for conditions not targeted under the health law, though the declines were less pronounced.
Observation rates for the targeted conditions increased from 2.6% to 4.7% during the study period, while rates for nontargeted conditions rose from 2.5% to 4.2%. The researchers did not observe any significant associations increases in observation-unit stays – which were steady throughout the study period – and the implementation of the ACA.
“It seems likely that the upward trend in observation-service use may be attributable to factors that are largely unrelated to the Hospital Readmissions Reduction Program, such as confusion over whether an inpatient stay would be deemed inappropriate by Medicare recovery audit contractors,” the researchers wrote.
Though the observational design of the study could not confirm a causal link between the ACA penalties and the drop in readmissions, the findings suggest that the declines are not solely a response to the ACA.
The health law likely “catalyzed behavioral change by many hospitals” that was already underway, possibly because of broader concern about readmissions and to earlier Medicare initiatives designed to reduce them. Also, the investigators noted, hospitals may have been helped by other government efforts on the readmission front, including the dissemination of best practices by the Centers for Medicare & Medicaid Services.
The study was funded by HHS and the researchers were agency employees. They reported having no other financial disclosures.
Hospital readmissions have declined in recent years for three conditions targeted under the Affordable Care Act, with smaller declines for other conditions, according to new research.
The study, published online Feb. 24 in the New England Journal of Medicine, found that 30-day readmission rates declined quickly after the passage of the ACA in 2010 and then slowed at the end of 2012. The researchers also analyzed trends in the use of observation units during the same period and concluded that the drop in readmissions was not being masked by a similar uptick in patients being seen under observation status (N Engl J Med. 2016 Feb 24. doi: 10.1056/NEJMsa1513024).
Under the ACA’s Hospital Readmissions Reduction Program, hospitals are financially penalized if they have higher-than-expected readmission rates for acute myocardial infarction, heart failure, and pneumonia.
The researchers, led by Rachael B. Zuckerman, M.P.H., of the Department of Health & Human Services, examined Medicare data from 3,387 hospitals from October 2007 through May 2015. Overall readmissions for acute myocardial infarction, heart failure, and pneumonia – the three conditions targeted in the readmissions reduction program – dropped from 21.5% to 17.8% during this time period. Readmissions for nontargeted conditions also dropped from 15.3% to 13.1%.
The researchers reported that readmissions for the targeted conditions were already declining before the ACA implementation (slope of monthly rate, –0.017), accelerating between April 2010 and October 2010 (–0.103), then leveling off through 2015 (–0.05). A similar pattern was seen with readmissions for conditions not targeted under the health law, though the declines were less pronounced.
Observation rates for the targeted conditions increased from 2.6% to 4.7% during the study period, while rates for nontargeted conditions rose from 2.5% to 4.2%. The researchers did not observe any significant associations increases in observation-unit stays – which were steady throughout the study period – and the implementation of the ACA.
“It seems likely that the upward trend in observation-service use may be attributable to factors that are largely unrelated to the Hospital Readmissions Reduction Program, such as confusion over whether an inpatient stay would be deemed inappropriate by Medicare recovery audit contractors,” the researchers wrote.
Though the observational design of the study could not confirm a causal link between the ACA penalties and the drop in readmissions, the findings suggest that the declines are not solely a response to the ACA.
The health law likely “catalyzed behavioral change by many hospitals” that was already underway, possibly because of broader concern about readmissions and to earlier Medicare initiatives designed to reduce them. Also, the investigators noted, hospitals may have been helped by other government efforts on the readmission front, including the dissemination of best practices by the Centers for Medicare & Medicaid Services.
The study was funded by HHS and the researchers were agency employees. They reported having no other financial disclosures.
FROM NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Hospital readmission rates declined following ACA enactment in 2010, but increased use of observation units did not account for the change.
Major finding: During 2007-2015, 30-day hospital readmissions for three targeted conditions dropped from 21.5% to 17.8%.
Data source: An interrupted time-series analysis of readmission and observation unit stay data of elderly Medicare beneficiaries from nearly 3,400 hospitals from 2007-2015.
Disclosures: The Health and Human Services department funded the study and the researchers were agency employees. They reported having no other financial disclosures.
FDA gives breakthrough status to midostaurin for AML
An experimental treatment targeting a form of acute myeloid leukemia has been designated a breakthrough therapy by the Food and Drug Administration, according to the drug’s manufacturer.
Midostaurin (Novartis) is an oral drug used alongside standard chemotherapy for adults with newly-diagnosed AML who are positive for the FMS-like tyrosine 3 (FLT-3) mutation and can undergo chemotherapy. AML has the lowest survival rate of all leukemias, and about one-third of AML patients have the FLT-3 mutation.
The FDA’s breakthrough therapy designation, in place since 2012, is an intensive form of fast-tracking in which the agency offers the manufacturer more guidance on an efficient drug development program and a higher level of organizational support, though future approval is not guaranteed. To qualify, a therapy must come with preliminary clinical evidence demonstrating substantial improvement on at least one clinically significant endpoint over available therapy, according to the agency.
Results from a phase III clinical trial, presented in December 2015 at the 57th annual meeting of the American Society of Hematology, showed that among 717 patients randomized to receive midostaurin alongside standard induction and consolidation chemotherapy or the same chemotherapy protocol alone, the midostaurin group saw significant improvement in overall survival (hazard ratio, 0.77, P = .0074).
Mean OS for patients in the midostaurin arm was 74.7 months (95% CI: 31.7, not attained), compared with 25.6 months for the placebo arm (18.6, 42.9). Median follow-up in the study was 57 months for surviving patients.
In a news release Feb. 19, Novartis said that midostaurin would be submitted for FDA approval for FLT-3-positive AML and that the company had launched compassionate use and expanded access programs allowing newly diagnosed patients aged 18 and older to receive midostaurin alongside standard induction and consolidation therapy. No targeted AML treatments are currently approved by FDA.
FLT3 is a receptor tyrosine kinase that plays a role in the proliferation in the number of certain blood cells. Midostaurin is a multi-targeted kinase inhibitor that is also being investigated for the treatment of aggressive systemic mast cell leukemia, according to Novartis.
An experimental treatment targeting a form of acute myeloid leukemia has been designated a breakthrough therapy by the Food and Drug Administration, according to the drug’s manufacturer.
Midostaurin (Novartis) is an oral drug used alongside standard chemotherapy for adults with newly-diagnosed AML who are positive for the FMS-like tyrosine 3 (FLT-3) mutation and can undergo chemotherapy. AML has the lowest survival rate of all leukemias, and about one-third of AML patients have the FLT-3 mutation.
The FDA’s breakthrough therapy designation, in place since 2012, is an intensive form of fast-tracking in which the agency offers the manufacturer more guidance on an efficient drug development program and a higher level of organizational support, though future approval is not guaranteed. To qualify, a therapy must come with preliminary clinical evidence demonstrating substantial improvement on at least one clinically significant endpoint over available therapy, according to the agency.
Results from a phase III clinical trial, presented in December 2015 at the 57th annual meeting of the American Society of Hematology, showed that among 717 patients randomized to receive midostaurin alongside standard induction and consolidation chemotherapy or the same chemotherapy protocol alone, the midostaurin group saw significant improvement in overall survival (hazard ratio, 0.77, P = .0074).
Mean OS for patients in the midostaurin arm was 74.7 months (95% CI: 31.7, not attained), compared with 25.6 months for the placebo arm (18.6, 42.9). Median follow-up in the study was 57 months for surviving patients.
In a news release Feb. 19, Novartis said that midostaurin would be submitted for FDA approval for FLT-3-positive AML and that the company had launched compassionate use and expanded access programs allowing newly diagnosed patients aged 18 and older to receive midostaurin alongside standard induction and consolidation therapy. No targeted AML treatments are currently approved by FDA.
FLT3 is a receptor tyrosine kinase that plays a role in the proliferation in the number of certain blood cells. Midostaurin is a multi-targeted kinase inhibitor that is also being investigated for the treatment of aggressive systemic mast cell leukemia, according to Novartis.
An experimental treatment targeting a form of acute myeloid leukemia has been designated a breakthrough therapy by the Food and Drug Administration, according to the drug’s manufacturer.
Midostaurin (Novartis) is an oral drug used alongside standard chemotherapy for adults with newly-diagnosed AML who are positive for the FMS-like tyrosine 3 (FLT-3) mutation and can undergo chemotherapy. AML has the lowest survival rate of all leukemias, and about one-third of AML patients have the FLT-3 mutation.
The FDA’s breakthrough therapy designation, in place since 2012, is an intensive form of fast-tracking in which the agency offers the manufacturer more guidance on an efficient drug development program and a higher level of organizational support, though future approval is not guaranteed. To qualify, a therapy must come with preliminary clinical evidence demonstrating substantial improvement on at least one clinically significant endpoint over available therapy, according to the agency.
Results from a phase III clinical trial, presented in December 2015 at the 57th annual meeting of the American Society of Hematology, showed that among 717 patients randomized to receive midostaurin alongside standard induction and consolidation chemotherapy or the same chemotherapy protocol alone, the midostaurin group saw significant improvement in overall survival (hazard ratio, 0.77, P = .0074).
Mean OS for patients in the midostaurin arm was 74.7 months (95% CI: 31.7, not attained), compared with 25.6 months for the placebo arm (18.6, 42.9). Median follow-up in the study was 57 months for surviving patients.
In a news release Feb. 19, Novartis said that midostaurin would be submitted for FDA approval for FLT-3-positive AML and that the company had launched compassionate use and expanded access programs allowing newly diagnosed patients aged 18 and older to receive midostaurin alongside standard induction and consolidation therapy. No targeted AML treatments are currently approved by FDA.
FLT3 is a receptor tyrosine kinase that plays a role in the proliferation in the number of certain blood cells. Midostaurin is a multi-targeted kinase inhibitor that is also being investigated for the treatment of aggressive systemic mast cell leukemia, according to Novartis.
Zika virus found in amniotic fluid
A case study conducted in Brazil revealed the presence of Zika virus in the amniotic fluid of two pregnant women, suggesting that the virus can cross the placental barrier and potentially infect the developing fetus.
Both women in the study had their amniotic fluid samples taken at 28 weeks, and later gave birth to babies with microcephaly.
The finding, published online Feb 17 in The Lancet Infectious Diseases (Lancet Infect Dis. 2016 Feb 17. doi: 10.1016/S1473-3099[16]00095-5), does not prove that Zika virus infection causes microcephaly but does suggest the biological plausibility of such a link.
In the same study, the researchers, led by Dr. Ana de Filippis of Oswaldo Cruz Institute in Rio de Janeiro, applied reverse transcription polymerase chain reaction and viral metagenomic sequencing to the viral samples, allowing them to establish that the virus was very closely related to the Zika virus that caused an outbreak in French Polynesia in 2013, and was not a recombinant strain.
The women in the study, age 27 and 35, were from the Brazilian state of Paraíba. Neither woman reported smoking, using recreational drugs or alcohol, or taking medications known to affect fetal development.
Zika virus was not found in the blood or urine of either woman when the amniotic samples were taken, though both had reported earlier symptoms consistent with Zika infection. Other infections, including HIV, dengue, chikungunya, rubella, and herpes viruses, were ruled out.
The results provide important insight into the origin of the Zika virus circulating in Brazil, the researchers wrote in their analysis. Moreover, “our group is the first, to our knowledge, to isolate the whole genome of Zika virus directly from the amniotic fluid of a pregnant woman before delivery, supporting the hypothesis that Zika virus infection could occur through transplacental transmission,” wrote Dr. de Filippis and her colleagues.
Still, little is known about the effects of Zika on the developing central nervous system, the researchers wrote. A connection between Zika virus infections and poor CNS outcomes “remains presumptive, and is based on a temporal association. New studies should be done to investigate whether the Zika virus can infect either neurological precursor cells or final differentiated cells.”
The researchers cautioned that congenital microcephaly has been associated with genetic disorders, chemical exposures, brain injury and uterine infections. Other possible contributors to the current high rate of microcephaly in Brazil, which last year was 20 times higher than in previous years, need to be investigated, they wrote.
Agencies within Brazil’s national government and the city of Rio de Janeiro funded the study, and investigators disclosed no conflicts of interest.
The temporal association between Zika virus outbreaks and microcephaly in Brazil strongly suggests that Zika virus infection during pregnancy might cause severe neurological damage in neonates. The challenge now is to provide empirical evidence for the link between Zika virus and microcephaly, and the demonstration that Zika virus can cross the placental barrier and infect the neonate strongly favors this association.
Even if all these data strongly suggest that Zika virus can cause microcephaly, the number of microcephaly cases related to Zika virus is still unknown. The next step will be to do case-control studies to estimate the potential risk of microcephaly after Zika virus infection during pregnancy, other fetal or neonatal complications, and long-term outcomes for infected symptomatic and asymptomatic neonates.
These comments were adapted from commentary by Dr. Didier Musso, Institut Louis Malardé, Tahiti, French Polynesia, and Dr. David Baud, University of Lausanne and University Hospital, Lausanne, Switzerland (Lancet Infect Dis. 2016 Feb 17. doi: 10.1016/S1473-3099[16]0096-7). Dr. Musso and Dr. Baud reported no conflicts of interest.
The temporal association between Zika virus outbreaks and microcephaly in Brazil strongly suggests that Zika virus infection during pregnancy might cause severe neurological damage in neonates. The challenge now is to provide empirical evidence for the link between Zika virus and microcephaly, and the demonstration that Zika virus can cross the placental barrier and infect the neonate strongly favors this association.
Even if all these data strongly suggest that Zika virus can cause microcephaly, the number of microcephaly cases related to Zika virus is still unknown. The next step will be to do case-control studies to estimate the potential risk of microcephaly after Zika virus infection during pregnancy, other fetal or neonatal complications, and long-term outcomes for infected symptomatic and asymptomatic neonates.
These comments were adapted from commentary by Dr. Didier Musso, Institut Louis Malardé, Tahiti, French Polynesia, and Dr. David Baud, University of Lausanne and University Hospital, Lausanne, Switzerland (Lancet Infect Dis. 2016 Feb 17. doi: 10.1016/S1473-3099[16]0096-7). Dr. Musso and Dr. Baud reported no conflicts of interest.
The temporal association between Zika virus outbreaks and microcephaly in Brazil strongly suggests that Zika virus infection during pregnancy might cause severe neurological damage in neonates. The challenge now is to provide empirical evidence for the link between Zika virus and microcephaly, and the demonstration that Zika virus can cross the placental barrier and infect the neonate strongly favors this association.
Even if all these data strongly suggest that Zika virus can cause microcephaly, the number of microcephaly cases related to Zika virus is still unknown. The next step will be to do case-control studies to estimate the potential risk of microcephaly after Zika virus infection during pregnancy, other fetal or neonatal complications, and long-term outcomes for infected symptomatic and asymptomatic neonates.
These comments were adapted from commentary by Dr. Didier Musso, Institut Louis Malardé, Tahiti, French Polynesia, and Dr. David Baud, University of Lausanne and University Hospital, Lausanne, Switzerland (Lancet Infect Dis. 2016 Feb 17. doi: 10.1016/S1473-3099[16]0096-7). Dr. Musso and Dr. Baud reported no conflicts of interest.
A case study conducted in Brazil revealed the presence of Zika virus in the amniotic fluid of two pregnant women, suggesting that the virus can cross the placental barrier and potentially infect the developing fetus.
Both women in the study had their amniotic fluid samples taken at 28 weeks, and later gave birth to babies with microcephaly.
The finding, published online Feb 17 in The Lancet Infectious Diseases (Lancet Infect Dis. 2016 Feb 17. doi: 10.1016/S1473-3099[16]00095-5), does not prove that Zika virus infection causes microcephaly but does suggest the biological plausibility of such a link.
In the same study, the researchers, led by Dr. Ana de Filippis of Oswaldo Cruz Institute in Rio de Janeiro, applied reverse transcription polymerase chain reaction and viral metagenomic sequencing to the viral samples, allowing them to establish that the virus was very closely related to the Zika virus that caused an outbreak in French Polynesia in 2013, and was not a recombinant strain.
The women in the study, age 27 and 35, were from the Brazilian state of Paraíba. Neither woman reported smoking, using recreational drugs or alcohol, or taking medications known to affect fetal development.
Zika virus was not found in the blood or urine of either woman when the amniotic samples were taken, though both had reported earlier symptoms consistent with Zika infection. Other infections, including HIV, dengue, chikungunya, rubella, and herpes viruses, were ruled out.
The results provide important insight into the origin of the Zika virus circulating in Brazil, the researchers wrote in their analysis. Moreover, “our group is the first, to our knowledge, to isolate the whole genome of Zika virus directly from the amniotic fluid of a pregnant woman before delivery, supporting the hypothesis that Zika virus infection could occur through transplacental transmission,” wrote Dr. de Filippis and her colleagues.
Still, little is known about the effects of Zika on the developing central nervous system, the researchers wrote. A connection between Zika virus infections and poor CNS outcomes “remains presumptive, and is based on a temporal association. New studies should be done to investigate whether the Zika virus can infect either neurological precursor cells or final differentiated cells.”
The researchers cautioned that congenital microcephaly has been associated with genetic disorders, chemical exposures, brain injury and uterine infections. Other possible contributors to the current high rate of microcephaly in Brazil, which last year was 20 times higher than in previous years, need to be investigated, they wrote.
Agencies within Brazil’s national government and the city of Rio de Janeiro funded the study, and investigators disclosed no conflicts of interest.
A case study conducted in Brazil revealed the presence of Zika virus in the amniotic fluid of two pregnant women, suggesting that the virus can cross the placental barrier and potentially infect the developing fetus.
Both women in the study had their amniotic fluid samples taken at 28 weeks, and later gave birth to babies with microcephaly.
The finding, published online Feb 17 in The Lancet Infectious Diseases (Lancet Infect Dis. 2016 Feb 17. doi: 10.1016/S1473-3099[16]00095-5), does not prove that Zika virus infection causes microcephaly but does suggest the biological plausibility of such a link.
In the same study, the researchers, led by Dr. Ana de Filippis of Oswaldo Cruz Institute in Rio de Janeiro, applied reverse transcription polymerase chain reaction and viral metagenomic sequencing to the viral samples, allowing them to establish that the virus was very closely related to the Zika virus that caused an outbreak in French Polynesia in 2013, and was not a recombinant strain.
The women in the study, age 27 and 35, were from the Brazilian state of Paraíba. Neither woman reported smoking, using recreational drugs or alcohol, or taking medications known to affect fetal development.
Zika virus was not found in the blood or urine of either woman when the amniotic samples were taken, though both had reported earlier symptoms consistent with Zika infection. Other infections, including HIV, dengue, chikungunya, rubella, and herpes viruses, were ruled out.
The results provide important insight into the origin of the Zika virus circulating in Brazil, the researchers wrote in their analysis. Moreover, “our group is the first, to our knowledge, to isolate the whole genome of Zika virus directly from the amniotic fluid of a pregnant woman before delivery, supporting the hypothesis that Zika virus infection could occur through transplacental transmission,” wrote Dr. de Filippis and her colleagues.
Still, little is known about the effects of Zika on the developing central nervous system, the researchers wrote. A connection between Zika virus infections and poor CNS outcomes “remains presumptive, and is based on a temporal association. New studies should be done to investigate whether the Zika virus can infect either neurological precursor cells or final differentiated cells.”
The researchers cautioned that congenital microcephaly has been associated with genetic disorders, chemical exposures, brain injury and uterine infections. Other possible contributors to the current high rate of microcephaly in Brazil, which last year was 20 times higher than in previous years, need to be investigated, they wrote.
Agencies within Brazil’s national government and the city of Rio de Janeiro funded the study, and investigators disclosed no conflicts of interest.
FROM THE LANCET INFECTIOUS DISEASES
Key clinical point: Zika virus can cross the placental barrier in pregnant women and potentially infect a fetus.
Major finding: Genetic sequencing showed virus detected in amniotic fluid corresponded 97%-100% with the strain that caused a 2013 outbreak in French Polynesia.
Data source: A case study of two women in the same region of Brazil, using amniotic samples from 28 weeks’ gestation in which Zika virus was detected and sequenced.
Disclosures: Two government agencies in Brazil sponsored the study, and investigators disclosed no conflicts of interest.
Recent Active Asthma Raises AAA Rupture Risk
Patients aged 50 and older with recent active asthma are at elevated risk of abdominal aortic aneurysm and aneurysm rupture, according to new research.
A common inflammatory pathway between asthma and AAA, first observed nearly a decade ago in mice, is thought to be responsible.
The new findings, published online Feb. 11 in Arteriosclerosis, Thrombosis, and Vascular Biology (Arterioscler Thromb Vasc Biol. 2016. doi: 10.1161/ATVBAHA.115.306497) support the association in humans.
In a news release accompanying the findings, lead study author Guo-Ping Shi, D.Sc., of Brigham and Women’s Hospital and Harvard Medical School, Boston, said that the findings had clear clinical implications for older patients with a recent asthma diagnosis. Such patients, particularly older men, “should be checked for signs” of abdominal aortic aneurysm, Dr. Shi said.
For their research, Dr. Shi, along with colleagues at Zhengzhou (China) University, used data from a large Danish population-based cohort of nearly 16,000 patients (81% men) with AAA between 1996 and 2012, of which about 4,500 patients had rupture. They also looked at data from a comparison cohort of patients with and without AAA from a slightly larger population-based vascular screening trial of men in Denmark.
The investigators showed that hospital diagnosis of asthma within the previous year (n = 514) was associated with significantly higher risk of hospital admission with AAA rupture (n = 146) both before and after adjustment for AAA comorbidities (adjusted odds ratio 1.51-2.06). Higher risk of rupture also was seen for patients filling prescriptions for bronchodilators within the previous 3 months (aOR = 1.10-1.31), and for patients prescribed anti-asthma drugs (aOR OR = 1.09-1.48), which were seen as indicative of an outpatient asthma diagnosis.
“A hospital diagnosis of asthma or a recently filled prescription of an anti-asthmatic drug is associated with an increased risk of admission with rAAA compared with admission with intact AAA, both before and after adjusting for AAA comorbidities and relevant medications,” the researchers wrote in their analysis.
Moreover, “an asthma diagnosis or the use of bronchodilators or other anti-asthmatic drug prescriptions closer to the date of admission with AAA correlated directly with a higher risk of aortic rupture. The results remained robust after adjusting for a wide range of relevant possible confounders,” the researchers wrote.
In the cohort of patients from the vascular screening study, which included age-matched controls without AAA, asthma (measured by recent anti-asthmatic medication use) was seen associated with a significantly elevated risk of AAA before (OR = 1.45) and after adjustment for smoking (OR = 1.45) or other risk factors (OR = 1.46). This does not refer to rupture but just AAA.
Dr. Shi and colleagues noted that the AAA cohort lacked sufficient information on cigarette smoking, a known risk factor for AAA and AAA rupture, to preclude the possibility of confounding; however, the second all-male cohort did have extensive data on smoking, “and the risk of AAA among patients with asthma remained 45% higher than that of patients with nonasthma” even after adjustment.
The researchers hypothesized that an inflammatory response characterized by elevated immunoglobulin E may be the link between AAA pathogenesis and asthma, and that other allergic inflammatory diseases, including atopic dermatitis, allergic rhinitis, and some ocular allergic diseases, could potentially carry risks for AAA formation and rupture. Dr. Shi and colleagues previously investigated the IgE and aneurysm link in animal studies.
“The results have implications for the development of much needed advances in the prevention, screening criteria, and treatment of AAA, common conditions for which we currently lack sufficiently effective approaches,” the investigators wrote.
The Chinese, Danish, and U.S. governments sponsored the study. The investigators disclosed no conflicts of interest.
Patients aged 50 and older with recent active asthma are at elevated risk of abdominal aortic aneurysm and aneurysm rupture, according to new research.
A common inflammatory pathway between asthma and AAA, first observed nearly a decade ago in mice, is thought to be responsible.
The new findings, published online Feb. 11 in Arteriosclerosis, Thrombosis, and Vascular Biology (Arterioscler Thromb Vasc Biol. 2016. doi: 10.1161/ATVBAHA.115.306497) support the association in humans.
In a news release accompanying the findings, lead study author Guo-Ping Shi, D.Sc., of Brigham and Women’s Hospital and Harvard Medical School, Boston, said that the findings had clear clinical implications for older patients with a recent asthma diagnosis. Such patients, particularly older men, “should be checked for signs” of abdominal aortic aneurysm, Dr. Shi said.
For their research, Dr. Shi, along with colleagues at Zhengzhou (China) University, used data from a large Danish population-based cohort of nearly 16,000 patients (81% men) with AAA between 1996 and 2012, of which about 4,500 patients had rupture. They also looked at data from a comparison cohort of patients with and without AAA from a slightly larger population-based vascular screening trial of men in Denmark.
The investigators showed that hospital diagnosis of asthma within the previous year (n = 514) was associated with significantly higher risk of hospital admission with AAA rupture (n = 146) both before and after adjustment for AAA comorbidities (adjusted odds ratio 1.51-2.06). Higher risk of rupture also was seen for patients filling prescriptions for bronchodilators within the previous 3 months (aOR = 1.10-1.31), and for patients prescribed anti-asthma drugs (aOR OR = 1.09-1.48), which were seen as indicative of an outpatient asthma diagnosis.
“A hospital diagnosis of asthma or a recently filled prescription of an anti-asthmatic drug is associated with an increased risk of admission with rAAA compared with admission with intact AAA, both before and after adjusting for AAA comorbidities and relevant medications,” the researchers wrote in their analysis.
Moreover, “an asthma diagnosis or the use of bronchodilators or other anti-asthmatic drug prescriptions closer to the date of admission with AAA correlated directly with a higher risk of aortic rupture. The results remained robust after adjusting for a wide range of relevant possible confounders,” the researchers wrote.
In the cohort of patients from the vascular screening study, which included age-matched controls without AAA, asthma (measured by recent anti-asthmatic medication use) was seen associated with a significantly elevated risk of AAA before (OR = 1.45) and after adjustment for smoking (OR = 1.45) or other risk factors (OR = 1.46). This does not refer to rupture but just AAA.
Dr. Shi and colleagues noted that the AAA cohort lacked sufficient information on cigarette smoking, a known risk factor for AAA and AAA rupture, to preclude the possibility of confounding; however, the second all-male cohort did have extensive data on smoking, “and the risk of AAA among patients with asthma remained 45% higher than that of patients with nonasthma” even after adjustment.
The researchers hypothesized that an inflammatory response characterized by elevated immunoglobulin E may be the link between AAA pathogenesis and asthma, and that other allergic inflammatory diseases, including atopic dermatitis, allergic rhinitis, and some ocular allergic diseases, could potentially carry risks for AAA formation and rupture. Dr. Shi and colleagues previously investigated the IgE and aneurysm link in animal studies.
“The results have implications for the development of much needed advances in the prevention, screening criteria, and treatment of AAA, common conditions for which we currently lack sufficiently effective approaches,” the investigators wrote.
The Chinese, Danish, and U.S. governments sponsored the study. The investigators disclosed no conflicts of interest.
Patients aged 50 and older with recent active asthma are at elevated risk of abdominal aortic aneurysm and aneurysm rupture, according to new research.
A common inflammatory pathway between asthma and AAA, first observed nearly a decade ago in mice, is thought to be responsible.
The new findings, published online Feb. 11 in Arteriosclerosis, Thrombosis, and Vascular Biology (Arterioscler Thromb Vasc Biol. 2016. doi: 10.1161/ATVBAHA.115.306497) support the association in humans.
In a news release accompanying the findings, lead study author Guo-Ping Shi, D.Sc., of Brigham and Women’s Hospital and Harvard Medical School, Boston, said that the findings had clear clinical implications for older patients with a recent asthma diagnosis. Such patients, particularly older men, “should be checked for signs” of abdominal aortic aneurysm, Dr. Shi said.
For their research, Dr. Shi, along with colleagues at Zhengzhou (China) University, used data from a large Danish population-based cohort of nearly 16,000 patients (81% men) with AAA between 1996 and 2012, of which about 4,500 patients had rupture. They also looked at data from a comparison cohort of patients with and without AAA from a slightly larger population-based vascular screening trial of men in Denmark.
The investigators showed that hospital diagnosis of asthma within the previous year (n = 514) was associated with significantly higher risk of hospital admission with AAA rupture (n = 146) both before and after adjustment for AAA comorbidities (adjusted odds ratio 1.51-2.06). Higher risk of rupture also was seen for patients filling prescriptions for bronchodilators within the previous 3 months (aOR = 1.10-1.31), and for patients prescribed anti-asthma drugs (aOR OR = 1.09-1.48), which were seen as indicative of an outpatient asthma diagnosis.
“A hospital diagnosis of asthma or a recently filled prescription of an anti-asthmatic drug is associated with an increased risk of admission with rAAA compared with admission with intact AAA, both before and after adjusting for AAA comorbidities and relevant medications,” the researchers wrote in their analysis.
Moreover, “an asthma diagnosis or the use of bronchodilators or other anti-asthmatic drug prescriptions closer to the date of admission with AAA correlated directly with a higher risk of aortic rupture. The results remained robust after adjusting for a wide range of relevant possible confounders,” the researchers wrote.
In the cohort of patients from the vascular screening study, which included age-matched controls without AAA, asthma (measured by recent anti-asthmatic medication use) was seen associated with a significantly elevated risk of AAA before (OR = 1.45) and after adjustment for smoking (OR = 1.45) or other risk factors (OR = 1.46). This does not refer to rupture but just AAA.
Dr. Shi and colleagues noted that the AAA cohort lacked sufficient information on cigarette smoking, a known risk factor for AAA and AAA rupture, to preclude the possibility of confounding; however, the second all-male cohort did have extensive data on smoking, “and the risk of AAA among patients with asthma remained 45% higher than that of patients with nonasthma” even after adjustment.
The researchers hypothesized that an inflammatory response characterized by elevated immunoglobulin E may be the link between AAA pathogenesis and asthma, and that other allergic inflammatory diseases, including atopic dermatitis, allergic rhinitis, and some ocular allergic diseases, could potentially carry risks for AAA formation and rupture. Dr. Shi and colleagues previously investigated the IgE and aneurysm link in animal studies.
“The results have implications for the development of much needed advances in the prevention, screening criteria, and treatment of AAA, common conditions for which we currently lack sufficiently effective approaches,” the investigators wrote.
The Chinese, Danish, and U.S. governments sponsored the study. The investigators disclosed no conflicts of interest.
FROM ARTERIOSCLEROSIS, THROMBOSIS, AND VASCULAR BIOLOGY
Recent active asthma raises AAA rupture risk
Patients aged 50 and older with recent active asthma are at elevated risk of abdominal aortic aneurysm and aneurysm rupture, according to new research.
A common inflammatory pathway between asthma and AAA, first observed nearly a decade ago in mice, is thought to be responsible.
The new findings, published online Feb. 11 in Arteriosclerosis, Thrombosis, and Vascular Biology (Arterioscler Thromb Vasc Biol. 2016. doi: 10.1161/ATVBAHA.115.306497) support the association in humans.
In a news release accompanying the findings, lead study author Guo-Ping Shi, ScD, of Brigham and Women’s Hospital and Harvard Medical School, Boston, said that the findings had clear clinical implications for older patients with a recent asthma diagnosis. Such patients, particularly older men, “should be checked for signs” of abdominal aortic aneurysm, Dr. Shi said.*
For their research, Dr. Shi, along with colleagues at Zhengzhou (China) University, used data from a large Danish population-based cohort of nearly 16,000 patients (81% men) with AAA between 1996 and 2012, of which about 4,500 patients had rupture. They also looked at data from a comparison cohort of patients with and without AAA from a slightly larger population-based vascular screening trial of men in Denmark.
The investigators showed that hospital diagnosis of asthma within the previous year (n = 514) was associated with significantly higher risk of hospital admission with AAA rupture (n = 146) both before and after adjustment for AAA comorbidities (adjusted odds ratio 1.51-2.06). Higher risk of rupture also was seen for patients filling prescriptions for bronchodilators within the previous 3 months (aOR = 1.10-1.31), and for patients prescribed anti-asthma drugs (aOR OR = 1.09-1.48), which were seen as indicative of an outpatient asthma diagnosis.
“A hospital diagnosis of asthma or a recently filled prescription of an anti-asthmatic drug is associated with an increased risk of admission with rAAA compared with admission with intact AAA, both before and after adjusting for AAA comorbidities and relevant medications,” the researchers wrote in their analysis.
Moreover, “an asthma diagnosis or the use of bronchodilators or other anti-asthmatic drug prescriptions closer to the date of admission with AAA correlated directly with a higher risk of aortic rupture. The results remained robust after adjusting for a wide range of relevant possible confounders,” the researchers wrote.
In the cohort of patients from the vascular screening study, which included age-matched controls without AAA, asthma (measured by recent anti-asthmatic medication use) was seen associated with a significantly elevated risk of AAA before (OR = 1.45) and after adjustment for smoking (OR = 1.45) or other risk factors (OR = 1.46). This does not refer to rupture but just AAA.
Dr. Shi and colleagues noted that the AAA cohort lacked sufficient information on cigarette smoking, a known risk factor for AAA and AAA rupture, to preclude the possibility of confounding; however, the second all-male cohort did have extensive data on smoking, “and the risk of AAA among patients with asthma remained 45% higher than that of patients with nonasthma” even after adjustment.
The researchers hypothesized that an inflammatory response characterized by elevated immunoglobulin E may be the link between AAA pathogenesis and asthma, and that other allergic inflammatory diseases, including atopic dermatitis, allergic rhinitis, and some ocular allergic diseases, could potentially carry risks for AAA formation and rupture. Dr. Shi and colleagues previously investigated the IgE and aneurysm link in animal studies.
“The results have implications for the development of much needed advances in the prevention, screening criteria, and treatment of AAA, common conditions for which we currently lack sufficiently effective approaches,” the investigators wrote.
The Chinese, Danish, and U.S. governments sponsored the study. The investigators disclosed no conflicts of interest.
*CORRECTION 8/12/2020: Dr. Shi's credential was misstated in the original version on this article and has been corrected to ScD.
Patients aged 50 and older with recent active asthma are at elevated risk of abdominal aortic aneurysm and aneurysm rupture, according to new research.
A common inflammatory pathway between asthma and AAA, first observed nearly a decade ago in mice, is thought to be responsible.
The new findings, published online Feb. 11 in Arteriosclerosis, Thrombosis, and Vascular Biology (Arterioscler Thromb Vasc Biol. 2016. doi: 10.1161/ATVBAHA.115.306497) support the association in humans.
In a news release accompanying the findings, lead study author Guo-Ping Shi, ScD, of Brigham and Women’s Hospital and Harvard Medical School, Boston, said that the findings had clear clinical implications for older patients with a recent asthma diagnosis. Such patients, particularly older men, “should be checked for signs” of abdominal aortic aneurysm, Dr. Shi said.*
For their research, Dr. Shi, along with colleagues at Zhengzhou (China) University, used data from a large Danish population-based cohort of nearly 16,000 patients (81% men) with AAA between 1996 and 2012, of which about 4,500 patients had rupture. They also looked at data from a comparison cohort of patients with and without AAA from a slightly larger population-based vascular screening trial of men in Denmark.
The investigators showed that hospital diagnosis of asthma within the previous year (n = 514) was associated with significantly higher risk of hospital admission with AAA rupture (n = 146) both before and after adjustment for AAA comorbidities (adjusted odds ratio 1.51-2.06). Higher risk of rupture also was seen for patients filling prescriptions for bronchodilators within the previous 3 months (aOR = 1.10-1.31), and for patients prescribed anti-asthma drugs (aOR OR = 1.09-1.48), which were seen as indicative of an outpatient asthma diagnosis.
“A hospital diagnosis of asthma or a recently filled prescription of an anti-asthmatic drug is associated with an increased risk of admission with rAAA compared with admission with intact AAA, both before and after adjusting for AAA comorbidities and relevant medications,” the researchers wrote in their analysis.
Moreover, “an asthma diagnosis or the use of bronchodilators or other anti-asthmatic drug prescriptions closer to the date of admission with AAA correlated directly with a higher risk of aortic rupture. The results remained robust after adjusting for a wide range of relevant possible confounders,” the researchers wrote.
In the cohort of patients from the vascular screening study, which included age-matched controls without AAA, asthma (measured by recent anti-asthmatic medication use) was seen associated with a significantly elevated risk of AAA before (OR = 1.45) and after adjustment for smoking (OR = 1.45) or other risk factors (OR = 1.46). This does not refer to rupture but just AAA.
Dr. Shi and colleagues noted that the AAA cohort lacked sufficient information on cigarette smoking, a known risk factor for AAA and AAA rupture, to preclude the possibility of confounding; however, the second all-male cohort did have extensive data on smoking, “and the risk of AAA among patients with asthma remained 45% higher than that of patients with nonasthma” even after adjustment.
The researchers hypothesized that an inflammatory response characterized by elevated immunoglobulin E may be the link between AAA pathogenesis and asthma, and that other allergic inflammatory diseases, including atopic dermatitis, allergic rhinitis, and some ocular allergic diseases, could potentially carry risks for AAA formation and rupture. Dr. Shi and colleagues previously investigated the IgE and aneurysm link in animal studies.
“The results have implications for the development of much needed advances in the prevention, screening criteria, and treatment of AAA, common conditions for which we currently lack sufficiently effective approaches,” the investigators wrote.
The Chinese, Danish, and U.S. governments sponsored the study. The investigators disclosed no conflicts of interest.
*CORRECTION 8/12/2020: Dr. Shi's credential was misstated in the original version on this article and has been corrected to ScD.
Patients aged 50 and older with recent active asthma are at elevated risk of abdominal aortic aneurysm and aneurysm rupture, according to new research.
A common inflammatory pathway between asthma and AAA, first observed nearly a decade ago in mice, is thought to be responsible.
The new findings, published online Feb. 11 in Arteriosclerosis, Thrombosis, and Vascular Biology (Arterioscler Thromb Vasc Biol. 2016. doi: 10.1161/ATVBAHA.115.306497) support the association in humans.
In a news release accompanying the findings, lead study author Guo-Ping Shi, ScD, of Brigham and Women’s Hospital and Harvard Medical School, Boston, said that the findings had clear clinical implications for older patients with a recent asthma diagnosis. Such patients, particularly older men, “should be checked for signs” of abdominal aortic aneurysm, Dr. Shi said.*
For their research, Dr. Shi, along with colleagues at Zhengzhou (China) University, used data from a large Danish population-based cohort of nearly 16,000 patients (81% men) with AAA between 1996 and 2012, of which about 4,500 patients had rupture. They also looked at data from a comparison cohort of patients with and without AAA from a slightly larger population-based vascular screening trial of men in Denmark.
The investigators showed that hospital diagnosis of asthma within the previous year (n = 514) was associated with significantly higher risk of hospital admission with AAA rupture (n = 146) both before and after adjustment for AAA comorbidities (adjusted odds ratio 1.51-2.06). Higher risk of rupture also was seen for patients filling prescriptions for bronchodilators within the previous 3 months (aOR = 1.10-1.31), and for patients prescribed anti-asthma drugs (aOR OR = 1.09-1.48), which were seen as indicative of an outpatient asthma diagnosis.
“A hospital diagnosis of asthma or a recently filled prescription of an anti-asthmatic drug is associated with an increased risk of admission with rAAA compared with admission with intact AAA, both before and after adjusting for AAA comorbidities and relevant medications,” the researchers wrote in their analysis.
Moreover, “an asthma diagnosis or the use of bronchodilators or other anti-asthmatic drug prescriptions closer to the date of admission with AAA correlated directly with a higher risk of aortic rupture. The results remained robust after adjusting for a wide range of relevant possible confounders,” the researchers wrote.
In the cohort of patients from the vascular screening study, which included age-matched controls without AAA, asthma (measured by recent anti-asthmatic medication use) was seen associated with a significantly elevated risk of AAA before (OR = 1.45) and after adjustment for smoking (OR = 1.45) or other risk factors (OR = 1.46). This does not refer to rupture but just AAA.
Dr. Shi and colleagues noted that the AAA cohort lacked sufficient information on cigarette smoking, a known risk factor for AAA and AAA rupture, to preclude the possibility of confounding; however, the second all-male cohort did have extensive data on smoking, “and the risk of AAA among patients with asthma remained 45% higher than that of patients with nonasthma” even after adjustment.
The researchers hypothesized that an inflammatory response characterized by elevated immunoglobulin E may be the link between AAA pathogenesis and asthma, and that other allergic inflammatory diseases, including atopic dermatitis, allergic rhinitis, and some ocular allergic diseases, could potentially carry risks for AAA formation and rupture. Dr. Shi and colleagues previously investigated the IgE and aneurysm link in animal studies.
“The results have implications for the development of much needed advances in the prevention, screening criteria, and treatment of AAA, common conditions for which we currently lack sufficiently effective approaches,” the investigators wrote.
The Chinese, Danish, and U.S. governments sponsored the study. The investigators disclosed no conflicts of interest.
*CORRECTION 8/12/2020: Dr. Shi's credential was misstated in the original version on this article and has been corrected to ScD.
FROM ARTERIOSCLEROSIS, THROMBOSIS, AND VASCULAR BIOLOGY
Key clinical point: Older patients with a recent asthma diagnosis, particularly men, should be checked for abdominal aortic aneurysms.
Major finding: People over 50 with recent active asthma and abdominal aortic aneurysm saw a more than 50% greater risk of rupture compared with patients without asthma.
Data source: Two large cohorts from Denmark of AAA patients 50 and older (n = 15,942) and men 65 and older with and without AAA (n = 18,749), with information on asthma diagnosis and rupture.
Disclosures: The Chinese, Danish, and U.S. governments sponsored the study. The investigators disclosed no conflicts of interest.
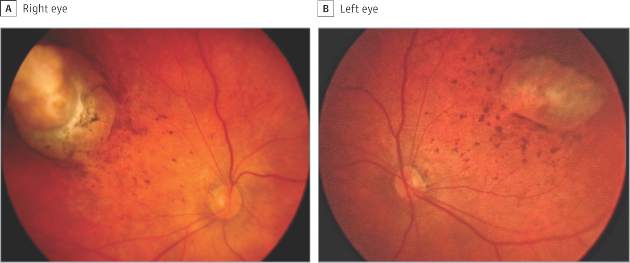
Ocular symptoms accompany microcephaly in Brazilian newborns
In a sample of infants born with microcephaly and a presumed diagnosis of congenital Zika virus, about one-third were found to have vision-threatening eye abnormalities, according to researchers working in a Zika hot spot in Brazil.
The group, led by Dr. Bruno de Paula Freitas of the Hospital Geral Roberto Santos, in Salvador, Brazil, evaluated 29 infants with microcephaly born at a single hospital in December following suspected maternal infection with the mosquito-borne Zika virus. In a paper published online Feb 9., Dr. de Paula Freitas and his colleagues reported eye abnormalities in 10 of these children (34.5%) (JAMA Ophthalmol. doi:10.1001/jamaophthalmol.2016.0267.).
Brazil first reported an outbreak of Zika virus infections in April 2015, followed months later by a spike in the number of infants born with microcephaly, a birth defect defined by a cephalic circumference of 32 cm or less in newborns. The most common ocular abnormalities seen in the cohort of affected infants were pigment mottling of the retina and chorioretinal atrophy (11 of 17 abnormal eyes); optic nerve abnormalities (8 eyes); and iris coloboma (affecting 2 eyes in one infant).
While a previous study of a Zika virus outbreak in Micronesia found conjunctivitis among infected individuals, none of the mothers of the current cohort of infants disclosed having had conjunctivitis. Altogether 23 of the mothers (79%) reported having had any symptoms of Zika virus infection during pregnancy.
Dr. de Paula Freitas and his colleagues acknowledged that their results were limited by a small sample size and single-site study design. However, the investigators noted, the findings suggest the possibility “that even oligosymptomatic or asymptomatic pregnant patients presumably infected [with Zika virus] may have microcephalic newborns with ophthalmoscopic lesions” and those newborns should be routinely evaluated for ocular symptoms.
An important question that requires further investigation, they noted, is whether newborns without microcephaly, but whose mothers may have been infected with the Zika virus, should be screened to identify possible ocular lesions.
Funding for the study came from Hospital Geral Roberto Santos, Federal University of São Paulo, Vision Institute, and Conselho Nacional de Desenvolvimento Científico e Tecnológico in Brasília, Brazil. The authors reported having no financial disclosures.
Ophthalmologic manifestations of congenital Zika virus infection are not yet well described. The report by de Paula Freitas et al. implicates this infection as the cause of chorioretinal scarring and possibly other ocular abnormalities in infants with microcephaly recently born in Brazil.
Microcephaly can be genetic, metabolic, drug related, or caused by perinatal insults such as hypoxia, malnutrition, or infection. The present 20-fold reported increase of microcephaly in parts of Brazil is temporally associated with the outbreak of Zika virus. However, this association is still presumptive because definitive serologic testing for Zika virus was not available in Brazil at the time of the outbreak, and confusion may occur with other causes of microcephaly. Similarly, the currently described eye lesions are presumptively associated with the virus.
Based on current information, in our opinion, clinicians in areas where Zika virus is present should perform ophthalmologic examinations on all microcephalic babies. Because it is still unclear whether the eye lesions occur in the absence of microcephaly, it is premature to suggest ophthalmic screening of all babies born in epidemic areas.
Dr. Lee M. Jampol and Dr. Debra A Goldstein are from the department of ophthalmology, Northwestern University, Chicago. These comments are excerpted from an accompanying editorial (JAMA Ophthalmol. doi:10.1001/jamaopthalmol.2016.0284.). The authors reported having no financial disclosures.
Ophthalmologic manifestations of congenital Zika virus infection are not yet well described. The report by de Paula Freitas et al. implicates this infection as the cause of chorioretinal scarring and possibly other ocular abnormalities in infants with microcephaly recently born in Brazil.
Microcephaly can be genetic, metabolic, drug related, or caused by perinatal insults such as hypoxia, malnutrition, or infection. The present 20-fold reported increase of microcephaly in parts of Brazil is temporally associated with the outbreak of Zika virus. However, this association is still presumptive because definitive serologic testing for Zika virus was not available in Brazil at the time of the outbreak, and confusion may occur with other causes of microcephaly. Similarly, the currently described eye lesions are presumptively associated with the virus.
Based on current information, in our opinion, clinicians in areas where Zika virus is present should perform ophthalmologic examinations on all microcephalic babies. Because it is still unclear whether the eye lesions occur in the absence of microcephaly, it is premature to suggest ophthalmic screening of all babies born in epidemic areas.
Dr. Lee M. Jampol and Dr. Debra A Goldstein are from the department of ophthalmology, Northwestern University, Chicago. These comments are excerpted from an accompanying editorial (JAMA Ophthalmol. doi:10.1001/jamaopthalmol.2016.0284.). The authors reported having no financial disclosures.
Ophthalmologic manifestations of congenital Zika virus infection are not yet well described. The report by de Paula Freitas et al. implicates this infection as the cause of chorioretinal scarring and possibly other ocular abnormalities in infants with microcephaly recently born in Brazil.
Microcephaly can be genetic, metabolic, drug related, or caused by perinatal insults such as hypoxia, malnutrition, or infection. The present 20-fold reported increase of microcephaly in parts of Brazil is temporally associated with the outbreak of Zika virus. However, this association is still presumptive because definitive serologic testing for Zika virus was not available in Brazil at the time of the outbreak, and confusion may occur with other causes of microcephaly. Similarly, the currently described eye lesions are presumptively associated with the virus.
Based on current information, in our opinion, clinicians in areas where Zika virus is present should perform ophthalmologic examinations on all microcephalic babies. Because it is still unclear whether the eye lesions occur in the absence of microcephaly, it is premature to suggest ophthalmic screening of all babies born in epidemic areas.
Dr. Lee M. Jampol and Dr. Debra A Goldstein are from the department of ophthalmology, Northwestern University, Chicago. These comments are excerpted from an accompanying editorial (JAMA Ophthalmol. doi:10.1001/jamaopthalmol.2016.0284.). The authors reported having no financial disclosures.
In a sample of infants born with microcephaly and a presumed diagnosis of congenital Zika virus, about one-third were found to have vision-threatening eye abnormalities, according to researchers working in a Zika hot spot in Brazil.
The group, led by Dr. Bruno de Paula Freitas of the Hospital Geral Roberto Santos, in Salvador, Brazil, evaluated 29 infants with microcephaly born at a single hospital in December following suspected maternal infection with the mosquito-borne Zika virus. In a paper published online Feb 9., Dr. de Paula Freitas and his colleagues reported eye abnormalities in 10 of these children (34.5%) (JAMA Ophthalmol. doi:10.1001/jamaophthalmol.2016.0267.).
Brazil first reported an outbreak of Zika virus infections in April 2015, followed months later by a spike in the number of infants born with microcephaly, a birth defect defined by a cephalic circumference of 32 cm or less in newborns. The most common ocular abnormalities seen in the cohort of affected infants were pigment mottling of the retina and chorioretinal atrophy (11 of 17 abnormal eyes); optic nerve abnormalities (8 eyes); and iris coloboma (affecting 2 eyes in one infant).
While a previous study of a Zika virus outbreak in Micronesia found conjunctivitis among infected individuals, none of the mothers of the current cohort of infants disclosed having had conjunctivitis. Altogether 23 of the mothers (79%) reported having had any symptoms of Zika virus infection during pregnancy.
Dr. de Paula Freitas and his colleagues acknowledged that their results were limited by a small sample size and single-site study design. However, the investigators noted, the findings suggest the possibility “that even oligosymptomatic or asymptomatic pregnant patients presumably infected [with Zika virus] may have microcephalic newborns with ophthalmoscopic lesions” and those newborns should be routinely evaluated for ocular symptoms.
An important question that requires further investigation, they noted, is whether newborns without microcephaly, but whose mothers may have been infected with the Zika virus, should be screened to identify possible ocular lesions.
Funding for the study came from Hospital Geral Roberto Santos, Federal University of São Paulo, Vision Institute, and Conselho Nacional de Desenvolvimento Científico e Tecnológico in Brasília, Brazil. The authors reported having no financial disclosures.
In a sample of infants born with microcephaly and a presumed diagnosis of congenital Zika virus, about one-third were found to have vision-threatening eye abnormalities, according to researchers working in a Zika hot spot in Brazil.
The group, led by Dr. Bruno de Paula Freitas of the Hospital Geral Roberto Santos, in Salvador, Brazil, evaluated 29 infants with microcephaly born at a single hospital in December following suspected maternal infection with the mosquito-borne Zika virus. In a paper published online Feb 9., Dr. de Paula Freitas and his colleagues reported eye abnormalities in 10 of these children (34.5%) (JAMA Ophthalmol. doi:10.1001/jamaophthalmol.2016.0267.).
Brazil first reported an outbreak of Zika virus infections in April 2015, followed months later by a spike in the number of infants born with microcephaly, a birth defect defined by a cephalic circumference of 32 cm or less in newborns. The most common ocular abnormalities seen in the cohort of affected infants were pigment mottling of the retina and chorioretinal atrophy (11 of 17 abnormal eyes); optic nerve abnormalities (8 eyes); and iris coloboma (affecting 2 eyes in one infant).
While a previous study of a Zika virus outbreak in Micronesia found conjunctivitis among infected individuals, none of the mothers of the current cohort of infants disclosed having had conjunctivitis. Altogether 23 of the mothers (79%) reported having had any symptoms of Zika virus infection during pregnancy.
Dr. de Paula Freitas and his colleagues acknowledged that their results were limited by a small sample size and single-site study design. However, the investigators noted, the findings suggest the possibility “that even oligosymptomatic or asymptomatic pregnant patients presumably infected [with Zika virus] may have microcephalic newborns with ophthalmoscopic lesions” and those newborns should be routinely evaluated for ocular symptoms.
An important question that requires further investigation, they noted, is whether newborns without microcephaly, but whose mothers may have been infected with the Zika virus, should be screened to identify possible ocular lesions.
Funding for the study came from Hospital Geral Roberto Santos, Federal University of São Paulo, Vision Institute, and Conselho Nacional de Desenvolvimento Científico e Tecnológico in Brasília, Brazil. The authors reported having no financial disclosures.
FROM JAMA OPTHALMOLOGY
Key clinical point: Serious ocular abnormalities may accompany microcephaly in babies born to mothers infected with the Zika virus.
Major finding: More than one-third (34.5%) of a cohort of 29 infants born with microcephaly and with a presumed diagnosis of congenital Zika virus had ocular abnormalities in one or both eyes.
Data source: A single-site cohort study evaluating 29 infants born with microcephaly in a single hospital in Salvador, Brazil.
Disclosures: Funding for the study came from Hospital Geral Roberto Santos, Federal University of São Paulo, Vision Institute, and Conselho Nacional de Desenvolvimento Científico e Tecnológico in Brasília, Brazil. The authors reported having no financial disclosures.
TEP hernia repair superior to Lichtenstein in pain outcomes
Patients undergoing endoscopic total extraperitoneal repair (TEP) of hernias had less persistent pain and greater mobility than those whose hernias were repaired using the Lichtenstein technique.
For their research, conducted in Sweden, researchers led by Dr. Linn Westin of the Karolinska Institutet in Stockholm and colleagues randomized 384 adult men with primary unilateral inguinal hernia to surgery with Lichtenstein using local anesthesia (n = 191) or TEP with general anesthesia (n = 193). Patients underwent operations in two hospitals between 2006 and 2011, with four surgeons participating, and the same heavyweight mesh was used in both groups.
All patients were followed for 1 year for postoperative pain, recurrence of hernias, difficulty in performing daily activities, complications, and use of analgesics. Pain was measured using the Inguinal Pain Questionnaire (IPQ).
In a paper published in the February issue of Annals of Surgery (2016;263:240-3), Dr. Westin and colleagues reported that the group randomized to TEP saw significantly less persistent mild pain at 1 year, compared with the Lichtenstein group. In the TEP group 39 patients reported such pain, compared with 62 in the Lichtenstein group (20.7% vs. 33.2,% P = .007).
Five TEP patients reported pain in the groin that limited their ability to perform physical exercise, while 14 in the Lichtenstein group reported similar pain, a difference that reached statistical significance (2.7% vs. 7.5%, P = .034). Severe pain, defined as pain affecting most activities, was comparable in both groups, with four patients in the TEP group and six in the Lichtenstein group reporting severe pain (2.1% and 3.2%, P = .543).
No significant between-group differences were seen in recurrences, use of pain medications, or specific measures of mobility, such as being able to sit or stand for more than 30 minutes at a stretch.
“Our results show a clinically significant advantage in favor of TEP regarding long-term postoperative pain, and justify the use of TEP for routine inguinal hernia surgery,” Dr. Westin and colleagues noted in their analysis. Their findings, they said, should prompt more extensive training of surgeons in the TEP technique.
The investigators noted as a limitation of their study that it was not powered to detect differences in severe pain, which could be considered more clinically relevant than mild persistent pain.
Patients’ pain outcomes may have been related to surgeons’ handling of the nerves in the inguinal tract, they wrote.
Also, they noted, the same heavyweight mesh was used in all operations in the study, for consistency, despite the fact that, after the initiation of the trial, lightweight mesh was shown in studies to be associated with less pain. Dr. Westin and colleagues wrote that their findings would be applicable to surgeries using lightweight mesh, which might further limit pain.
Their results, they wrote, suggested that TEP should be considered a valid first choice not only for the study population, which included only men with primary unilateral hernias, but for those with bilateral or recurrent hernias and also for women.
The study was funded by the Uppsala-Orebro Regional Research Council, Stockholm County Council, Swedish Society of Medicine, and Olle Engqvist Research Foundation. None of the investigators declared conflicts of interest.
Patients undergoing endoscopic total extraperitoneal repair (TEP) of hernias had less persistent pain and greater mobility than those whose hernias were repaired using the Lichtenstein technique.
For their research, conducted in Sweden, researchers led by Dr. Linn Westin of the Karolinska Institutet in Stockholm and colleagues randomized 384 adult men with primary unilateral inguinal hernia to surgery with Lichtenstein using local anesthesia (n = 191) or TEP with general anesthesia (n = 193). Patients underwent operations in two hospitals between 2006 and 2011, with four surgeons participating, and the same heavyweight mesh was used in both groups.
All patients were followed for 1 year for postoperative pain, recurrence of hernias, difficulty in performing daily activities, complications, and use of analgesics. Pain was measured using the Inguinal Pain Questionnaire (IPQ).
In a paper published in the February issue of Annals of Surgery (2016;263:240-3), Dr. Westin and colleagues reported that the group randomized to TEP saw significantly less persistent mild pain at 1 year, compared with the Lichtenstein group. In the TEP group 39 patients reported such pain, compared with 62 in the Lichtenstein group (20.7% vs. 33.2,% P = .007).
Five TEP patients reported pain in the groin that limited their ability to perform physical exercise, while 14 in the Lichtenstein group reported similar pain, a difference that reached statistical significance (2.7% vs. 7.5%, P = .034). Severe pain, defined as pain affecting most activities, was comparable in both groups, with four patients in the TEP group and six in the Lichtenstein group reporting severe pain (2.1% and 3.2%, P = .543).
No significant between-group differences were seen in recurrences, use of pain medications, or specific measures of mobility, such as being able to sit or stand for more than 30 minutes at a stretch.
“Our results show a clinically significant advantage in favor of TEP regarding long-term postoperative pain, and justify the use of TEP for routine inguinal hernia surgery,” Dr. Westin and colleagues noted in their analysis. Their findings, they said, should prompt more extensive training of surgeons in the TEP technique.
The investigators noted as a limitation of their study that it was not powered to detect differences in severe pain, which could be considered more clinically relevant than mild persistent pain.
Patients’ pain outcomes may have been related to surgeons’ handling of the nerves in the inguinal tract, they wrote.
Also, they noted, the same heavyweight mesh was used in all operations in the study, for consistency, despite the fact that, after the initiation of the trial, lightweight mesh was shown in studies to be associated with less pain. Dr. Westin and colleagues wrote that their findings would be applicable to surgeries using lightweight mesh, which might further limit pain.
Their results, they wrote, suggested that TEP should be considered a valid first choice not only for the study population, which included only men with primary unilateral hernias, but for those with bilateral or recurrent hernias and also for women.
The study was funded by the Uppsala-Orebro Regional Research Council, Stockholm County Council, Swedish Society of Medicine, and Olle Engqvist Research Foundation. None of the investigators declared conflicts of interest.
Patients undergoing endoscopic total extraperitoneal repair (TEP) of hernias had less persistent pain and greater mobility than those whose hernias were repaired using the Lichtenstein technique.
For their research, conducted in Sweden, researchers led by Dr. Linn Westin of the Karolinska Institutet in Stockholm and colleagues randomized 384 adult men with primary unilateral inguinal hernia to surgery with Lichtenstein using local anesthesia (n = 191) or TEP with general anesthesia (n = 193). Patients underwent operations in two hospitals between 2006 and 2011, with four surgeons participating, and the same heavyweight mesh was used in both groups.
All patients were followed for 1 year for postoperative pain, recurrence of hernias, difficulty in performing daily activities, complications, and use of analgesics. Pain was measured using the Inguinal Pain Questionnaire (IPQ).
In a paper published in the February issue of Annals of Surgery (2016;263:240-3), Dr. Westin and colleagues reported that the group randomized to TEP saw significantly less persistent mild pain at 1 year, compared with the Lichtenstein group. In the TEP group 39 patients reported such pain, compared with 62 in the Lichtenstein group (20.7% vs. 33.2,% P = .007).
Five TEP patients reported pain in the groin that limited their ability to perform physical exercise, while 14 in the Lichtenstein group reported similar pain, a difference that reached statistical significance (2.7% vs. 7.5%, P = .034). Severe pain, defined as pain affecting most activities, was comparable in both groups, with four patients in the TEP group and six in the Lichtenstein group reporting severe pain (2.1% and 3.2%, P = .543).
No significant between-group differences were seen in recurrences, use of pain medications, or specific measures of mobility, such as being able to sit or stand for more than 30 minutes at a stretch.
“Our results show a clinically significant advantage in favor of TEP regarding long-term postoperative pain, and justify the use of TEP for routine inguinal hernia surgery,” Dr. Westin and colleagues noted in their analysis. Their findings, they said, should prompt more extensive training of surgeons in the TEP technique.
The investigators noted as a limitation of their study that it was not powered to detect differences in severe pain, which could be considered more clinically relevant than mild persistent pain.
Patients’ pain outcomes may have been related to surgeons’ handling of the nerves in the inguinal tract, they wrote.
Also, they noted, the same heavyweight mesh was used in all operations in the study, for consistency, despite the fact that, after the initiation of the trial, lightweight mesh was shown in studies to be associated with less pain. Dr. Westin and colleagues wrote that their findings would be applicable to surgeries using lightweight mesh, which might further limit pain.
Their results, they wrote, suggested that TEP should be considered a valid first choice not only for the study population, which included only men with primary unilateral hernias, but for those with bilateral or recurrent hernias and also for women.
The study was funded by the Uppsala-Orebro Regional Research Council, Stockholm County Council, Swedish Society of Medicine, and Olle Engqvist Research Foundation. None of the investigators declared conflicts of interest.
FROM ANNALS OF SURGERY
Key clinical point: Patients undergoing TEP for hernia repair were less likely to report persistent pain after 1 year than those undergoing Lichtenstein procedures.
Major finding: In the TEP group, 39 (20.7%) patients reported persistent pain, compared with 62 (33.2%) in the Lichtenstein group (P = .007).
Data source: A randomized multisite surgical trial in Sweden enrolling 384 men with unilateral primary inguinal hernias, with 375 followed up at 1 year.
Disclosures: The study was funded by Swedish government grants, the Swedish Society of Medicine, and the Olle Engqvist Research Foundation. Investigators disclosed no conflicts of interest.
More Than 15% of Reproductive Age Women Use Antidepressants
About 15% of women of childbearing age filled prescriptions for antidepressants at least once a year during 2008-2013, according to a new report from the Centers for Disease Control and Prevention.
Women between the ages of 35 and 44 years made up the largest share of those filling an antidepressant prescription. The most commonly filled prescriptions were for sertraline, bupropion, and citalopram (Morb Mortal Wkly Rep. 2016 Jan 29;65:41-6).
The analysis is based on prescription information from a database of employer-sponsored insurance plans representing an average of 5.8 million women aged 15-44 years for each year of the study.
The findings raise public health concerns given the possible association between some antidepressants and birth defects and the large number of unintended pregnancies, wrote the investigators, led by April L. Dawson of the CDC’s National Center on Birth Defects and Developmental Disabilities.
A recent analysis of the National Birth Defects Prevention Study data found that paroxetine and fluoxetine, both SSRIs, were linked with a higher rate of some birth defects, including cardiac abnormalities, though the increase in absolute risk was small (BMJ 2015;351:h3190).
“Prescribing of antidepressants is common, and research on antidepressant safety during pregnancy needs to be accelerated to provide evidence-based information to health care providers and women about the potential risks for antidepressant exposure before and during pregnancy and between pregnancies,” Ms. Dawson and her colleagues wrote.
The study authors were employees of the CDC or the March of Dimes Foundation.
About 15% of women of childbearing age filled prescriptions for antidepressants at least once a year during 2008-2013, according to a new report from the Centers for Disease Control and Prevention.
Women between the ages of 35 and 44 years made up the largest share of those filling an antidepressant prescription. The most commonly filled prescriptions were for sertraline, bupropion, and citalopram (Morb Mortal Wkly Rep. 2016 Jan 29;65:41-6).
The analysis is based on prescription information from a database of employer-sponsored insurance plans representing an average of 5.8 million women aged 15-44 years for each year of the study.
The findings raise public health concerns given the possible association between some antidepressants and birth defects and the large number of unintended pregnancies, wrote the investigators, led by April L. Dawson of the CDC’s National Center on Birth Defects and Developmental Disabilities.
A recent analysis of the National Birth Defects Prevention Study data found that paroxetine and fluoxetine, both SSRIs, were linked with a higher rate of some birth defects, including cardiac abnormalities, though the increase in absolute risk was small (BMJ 2015;351:h3190).
“Prescribing of antidepressants is common, and research on antidepressant safety during pregnancy needs to be accelerated to provide evidence-based information to health care providers and women about the potential risks for antidepressant exposure before and during pregnancy and between pregnancies,” Ms. Dawson and her colleagues wrote.
The study authors were employees of the CDC or the March of Dimes Foundation.
About 15% of women of childbearing age filled prescriptions for antidepressants at least once a year during 2008-2013, according to a new report from the Centers for Disease Control and Prevention.
Women between the ages of 35 and 44 years made up the largest share of those filling an antidepressant prescription. The most commonly filled prescriptions were for sertraline, bupropion, and citalopram (Morb Mortal Wkly Rep. 2016 Jan 29;65:41-6).
The analysis is based on prescription information from a database of employer-sponsored insurance plans representing an average of 5.8 million women aged 15-44 years for each year of the study.
The findings raise public health concerns given the possible association between some antidepressants and birth defects and the large number of unintended pregnancies, wrote the investigators, led by April L. Dawson of the CDC’s National Center on Birth Defects and Developmental Disabilities.
A recent analysis of the National Birth Defects Prevention Study data found that paroxetine and fluoxetine, both SSRIs, were linked with a higher rate of some birth defects, including cardiac abnormalities, though the increase in absolute risk was small (BMJ 2015;351:h3190).
“Prescribing of antidepressants is common, and research on antidepressant safety during pregnancy needs to be accelerated to provide evidence-based information to health care providers and women about the potential risks for antidepressant exposure before and during pregnancy and between pregnancies,” Ms. Dawson and her colleagues wrote.
The study authors were employees of the CDC or the March of Dimes Foundation.
FROM MMWR
More than 15% of reproductive age women use antidepressants
About 15% of women of childbearing age filled prescriptions for antidepressants at least once a year during 2008-2013, according to a new report from the Centers for Disease Control and Prevention.
Women between the ages of 35 and 44 years made up the largest share of those filling an antidepressant prescription. The most commonly filled prescriptions were for sertraline, bupropion, and citalopram (Morb Mortal Wkly Rep. 2016 Jan 29;65:41-6).
The analysis is based on prescription information from a database of employer-sponsored insurance plans representing an average of 5.8 million women aged 15-44 years for each year of the study.
The findings raise public health concerns given the possible association between some antidepressants and birth defects and the large number of unintended pregnancies, wrote the investigators, led by April L. Dawson of the CDC’s National Center on Birth Defects and Developmental Disabilities.
A recent analysis of the National Birth Defects Prevention Study data found that paroxetine and fluoxetine, both SSRIs, were linked with a higher rate of some birth defects, including cardiac abnormalities, though the increase in absolute risk was small (BMJ 2015;351:h3190).
“Prescribing of antidepressants is common, and research on antidepressant safety during pregnancy needs to be accelerated to provide evidence-based information to health care providers and women about the potential risks for antidepressant exposure before and during pregnancy and between pregnancies,” Ms. Dawson and her colleagues wrote.
The study authors were employees of the CDC or the March of Dimes Foundation.
About 15% of women of childbearing age filled prescriptions for antidepressants at least once a year during 2008-2013, according to a new report from the Centers for Disease Control and Prevention.
Women between the ages of 35 and 44 years made up the largest share of those filling an antidepressant prescription. The most commonly filled prescriptions were for sertraline, bupropion, and citalopram (Morb Mortal Wkly Rep. 2016 Jan 29;65:41-6).
The analysis is based on prescription information from a database of employer-sponsored insurance plans representing an average of 5.8 million women aged 15-44 years for each year of the study.
The findings raise public health concerns given the possible association between some antidepressants and birth defects and the large number of unintended pregnancies, wrote the investigators, led by April L. Dawson of the CDC’s National Center on Birth Defects and Developmental Disabilities.
A recent analysis of the National Birth Defects Prevention Study data found that paroxetine and fluoxetine, both SSRIs, were linked with a higher rate of some birth defects, including cardiac abnormalities, though the increase in absolute risk was small (BMJ 2015;351:h3190).
“Prescribing of antidepressants is common, and research on antidepressant safety during pregnancy needs to be accelerated to provide evidence-based information to health care providers and women about the potential risks for antidepressant exposure before and during pregnancy and between pregnancies,” Ms. Dawson and her colleagues wrote.
The study authors were employees of the CDC or the March of Dimes Foundation.
About 15% of women of childbearing age filled prescriptions for antidepressants at least once a year during 2008-2013, according to a new report from the Centers for Disease Control and Prevention.
Women between the ages of 35 and 44 years made up the largest share of those filling an antidepressant prescription. The most commonly filled prescriptions were for sertraline, bupropion, and citalopram (Morb Mortal Wkly Rep. 2016 Jan 29;65:41-6).
The analysis is based on prescription information from a database of employer-sponsored insurance plans representing an average of 5.8 million women aged 15-44 years for each year of the study.
The findings raise public health concerns given the possible association between some antidepressants and birth defects and the large number of unintended pregnancies, wrote the investigators, led by April L. Dawson of the CDC’s National Center on Birth Defects and Developmental Disabilities.
A recent analysis of the National Birth Defects Prevention Study data found that paroxetine and fluoxetine, both SSRIs, were linked with a higher rate of some birth defects, including cardiac abnormalities, though the increase in absolute risk was small (BMJ 2015;351:h3190).
“Prescribing of antidepressants is common, and research on antidepressant safety during pregnancy needs to be accelerated to provide evidence-based information to health care providers and women about the potential risks for antidepressant exposure before and during pregnancy and between pregnancies,” Ms. Dawson and her colleagues wrote.
The study authors were employees of the CDC or the March of Dimes Foundation.
FROM MMWR
Key clinical point: About 15% of reproductive-age women use antidepressants each year.
Major finding: A total of 15.4% of women aged 15-44 years filled at least one prescription annually for an antidepressant during 2008-2013.
Data source: A retrospective analysis of data from a commercial database that included an average of 5.8 million women with private, employer-sponsored insurance.
Disclosures: Study authors were employees of the CDC or the March of Dimes Foundation.