User login
COVID-19 leaves wake of medical debt among U.S. adults
Despite the passage of four major relief bills in 2020 and 2021 and federal efforts to offset pandemic- and job-related coverage loss, many people continued to face financial challenges, especially those with a low income and those who are Black or Latino.
The survey, which included responses from 5,450 adults, revealed that 10% of adults aged 19-64 were uninsured during the first half of 2021, a rate lower than what was recorded in 2020 and 2019 in both federal and private surveys. However, uninsured rates were highest among those with low income, those younger than 50 years old, and Black and Latino adults.
For most adults who lost employee health insurance, the coverage gap was relatively brief, with 54% saying their coverage gap lasted 3-4 months. Only 16% of adults said coverage gaps lasted a year or longer.
“The good news is that this survey is suggesting that the coverage losses during the pandemic may have been offset by federal efforts to help people get and maintain health insurance coverage,” lead author Sara Collins, PhD, Commonwealth Fund vice president for health care coverage, access, and tracking, said in an interview.
“The bad news is that a third of Americans continue to struggle with medical bills and medical debt, even among those who have health insurance coverage,” Dr. Collins added.
Indeed, the survey found that about one-third of insured adults reported a medical bill problem or that they were paying off medical debt, as did approximately half of those who were uninsured. Medical debt caused 35% of respondents to use up most or all of their savings to pay it off.
Meanwhile, 27% of adults said medical bills left them unable to pay for necessities such as food, heat, or rent. What surprised Dr. Collins was that 43% of adults said they received a lower credit rating as a result of their medical debt, and 35% said they had taken on more credit card debt to pay off these bills.
“The fact that it’s bleeding over into people’s financial security in terms of their credit scores, I think is something that really needs to be looked at by policymakers,” Dr. Collins said.
When analyzed by race/ethnicity, the researchers found that 55% of Black adults and 44% of Latino/Hispanic adults reported medical bills and debt problems, compared with 32% of White adults. In addition, 47% of those living below the poverty line also reported problems with medical bills.
According to the survey, 45% of respondents were directly affected by the pandemic in at least one of three ways – testing positive or getting sick from COVID-19, losing income, or losing employer coverage – with Black and Latinx adults and those with lower incomes at greater risk.
George Abraham, MD, president of the American College of Physicians, said the Commonwealth Fund’s findings were not surprising because it has always been known that underrepresented populations struggle for access to care because of socioeconomic factors. He said these populations were more vulnerable in terms of more severe infections and disease burden during the pandemic.
“[This study] validates what primary care physicians have been saying all along in regard to our patients’ access to care and their ability to cover health care costs,” said Dr. Abraham, who was not involved with the study. “This will hopefully be an eye-opener and wake-up call that reiterates that we still do not have equitable access to care and vulnerable populations are disproportionately affected.”
He believes that, although people are insured, many of them may contend with medical debt when they fall ill because they can’t afford the premiums.
“Even though they may have been registered for health coverage, they may not have active coverage at the time of illness simply because they weren’t able to make their last premium payments because they’ve been down, because they lost their job, or whatever else,” Dr. Abraham explained. “On paper, they appear to have health care coverage. But in reality, clearly, that coverage does not match their needs or it’s not affordable.”
For Dr. Abraham, the study emphasizes the need to continue support for health care reform, including pricing it so that insurance is available for those with fewer socioeconomic resources.
Yalda Jabbarpour, MD, medical director of the Robert Graham Center for Policy Studies, Washington, said high-deductible health plans need to be “reined in” because they can lead to greater debt, particularly among vulnerable populations.
“Hopefully this will encourage policymakers to look more closely at the problem of medical debt as a contributing factor to financial instability,” Dr. Jabbarpour said. “Federal relief is important, so is expanding access to comprehensive, affordable health care coverage.”
Dr. Collins said there should also be a way to raise awareness of the health care marketplace and coverage options so that people have an easier time getting insured.
A version of this article first appeared on Medscape.com.
Despite the passage of four major relief bills in 2020 and 2021 and federal efforts to offset pandemic- and job-related coverage loss, many people continued to face financial challenges, especially those with a low income and those who are Black or Latino.
The survey, which included responses from 5,450 adults, revealed that 10% of adults aged 19-64 were uninsured during the first half of 2021, a rate lower than what was recorded in 2020 and 2019 in both federal and private surveys. However, uninsured rates were highest among those with low income, those younger than 50 years old, and Black and Latino adults.
For most adults who lost employee health insurance, the coverage gap was relatively brief, with 54% saying their coverage gap lasted 3-4 months. Only 16% of adults said coverage gaps lasted a year or longer.
“The good news is that this survey is suggesting that the coverage losses during the pandemic may have been offset by federal efforts to help people get and maintain health insurance coverage,” lead author Sara Collins, PhD, Commonwealth Fund vice president for health care coverage, access, and tracking, said in an interview.
“The bad news is that a third of Americans continue to struggle with medical bills and medical debt, even among those who have health insurance coverage,” Dr. Collins added.
Indeed, the survey found that about one-third of insured adults reported a medical bill problem or that they were paying off medical debt, as did approximately half of those who were uninsured. Medical debt caused 35% of respondents to use up most or all of their savings to pay it off.
Meanwhile, 27% of adults said medical bills left them unable to pay for necessities such as food, heat, or rent. What surprised Dr. Collins was that 43% of adults said they received a lower credit rating as a result of their medical debt, and 35% said they had taken on more credit card debt to pay off these bills.
“The fact that it’s bleeding over into people’s financial security in terms of their credit scores, I think is something that really needs to be looked at by policymakers,” Dr. Collins said.
When analyzed by race/ethnicity, the researchers found that 55% of Black adults and 44% of Latino/Hispanic adults reported medical bills and debt problems, compared with 32% of White adults. In addition, 47% of those living below the poverty line also reported problems with medical bills.
According to the survey, 45% of respondents were directly affected by the pandemic in at least one of three ways – testing positive or getting sick from COVID-19, losing income, or losing employer coverage – with Black and Latinx adults and those with lower incomes at greater risk.
George Abraham, MD, president of the American College of Physicians, said the Commonwealth Fund’s findings were not surprising because it has always been known that underrepresented populations struggle for access to care because of socioeconomic factors. He said these populations were more vulnerable in terms of more severe infections and disease burden during the pandemic.
“[This study] validates what primary care physicians have been saying all along in regard to our patients’ access to care and their ability to cover health care costs,” said Dr. Abraham, who was not involved with the study. “This will hopefully be an eye-opener and wake-up call that reiterates that we still do not have equitable access to care and vulnerable populations are disproportionately affected.”
He believes that, although people are insured, many of them may contend with medical debt when they fall ill because they can’t afford the premiums.
“Even though they may have been registered for health coverage, they may not have active coverage at the time of illness simply because they weren’t able to make their last premium payments because they’ve been down, because they lost their job, or whatever else,” Dr. Abraham explained. “On paper, they appear to have health care coverage. But in reality, clearly, that coverage does not match their needs or it’s not affordable.”
For Dr. Abraham, the study emphasizes the need to continue support for health care reform, including pricing it so that insurance is available for those with fewer socioeconomic resources.
Yalda Jabbarpour, MD, medical director of the Robert Graham Center for Policy Studies, Washington, said high-deductible health plans need to be “reined in” because they can lead to greater debt, particularly among vulnerable populations.
“Hopefully this will encourage policymakers to look more closely at the problem of medical debt as a contributing factor to financial instability,” Dr. Jabbarpour said. “Federal relief is important, so is expanding access to comprehensive, affordable health care coverage.”
Dr. Collins said there should also be a way to raise awareness of the health care marketplace and coverage options so that people have an easier time getting insured.
A version of this article first appeared on Medscape.com.
Despite the passage of four major relief bills in 2020 and 2021 and federal efforts to offset pandemic- and job-related coverage loss, many people continued to face financial challenges, especially those with a low income and those who are Black or Latino.
The survey, which included responses from 5,450 adults, revealed that 10% of adults aged 19-64 were uninsured during the first half of 2021, a rate lower than what was recorded in 2020 and 2019 in both federal and private surveys. However, uninsured rates were highest among those with low income, those younger than 50 years old, and Black and Latino adults.
For most adults who lost employee health insurance, the coverage gap was relatively brief, with 54% saying their coverage gap lasted 3-4 months. Only 16% of adults said coverage gaps lasted a year or longer.
“The good news is that this survey is suggesting that the coverage losses during the pandemic may have been offset by federal efforts to help people get and maintain health insurance coverage,” lead author Sara Collins, PhD, Commonwealth Fund vice president for health care coverage, access, and tracking, said in an interview.
“The bad news is that a third of Americans continue to struggle with medical bills and medical debt, even among those who have health insurance coverage,” Dr. Collins added.
Indeed, the survey found that about one-third of insured adults reported a medical bill problem or that they were paying off medical debt, as did approximately half of those who were uninsured. Medical debt caused 35% of respondents to use up most or all of their savings to pay it off.
Meanwhile, 27% of adults said medical bills left them unable to pay for necessities such as food, heat, or rent. What surprised Dr. Collins was that 43% of adults said they received a lower credit rating as a result of their medical debt, and 35% said they had taken on more credit card debt to pay off these bills.
“The fact that it’s bleeding over into people’s financial security in terms of their credit scores, I think is something that really needs to be looked at by policymakers,” Dr. Collins said.
When analyzed by race/ethnicity, the researchers found that 55% of Black adults and 44% of Latino/Hispanic adults reported medical bills and debt problems, compared with 32% of White adults. In addition, 47% of those living below the poverty line also reported problems with medical bills.
According to the survey, 45% of respondents were directly affected by the pandemic in at least one of three ways – testing positive or getting sick from COVID-19, losing income, or losing employer coverage – with Black and Latinx adults and those with lower incomes at greater risk.
George Abraham, MD, president of the American College of Physicians, said the Commonwealth Fund’s findings were not surprising because it has always been known that underrepresented populations struggle for access to care because of socioeconomic factors. He said these populations were more vulnerable in terms of more severe infections and disease burden during the pandemic.
“[This study] validates what primary care physicians have been saying all along in regard to our patients’ access to care and their ability to cover health care costs,” said Dr. Abraham, who was not involved with the study. “This will hopefully be an eye-opener and wake-up call that reiterates that we still do not have equitable access to care and vulnerable populations are disproportionately affected.”
He believes that, although people are insured, many of them may contend with medical debt when they fall ill because they can’t afford the premiums.
“Even though they may have been registered for health coverage, they may not have active coverage at the time of illness simply because they weren’t able to make their last premium payments because they’ve been down, because they lost their job, or whatever else,” Dr. Abraham explained. “On paper, they appear to have health care coverage. But in reality, clearly, that coverage does not match their needs or it’s not affordable.”
For Dr. Abraham, the study emphasizes the need to continue support for health care reform, including pricing it so that insurance is available for those with fewer socioeconomic resources.
Yalda Jabbarpour, MD, medical director of the Robert Graham Center for Policy Studies, Washington, said high-deductible health plans need to be “reined in” because they can lead to greater debt, particularly among vulnerable populations.
“Hopefully this will encourage policymakers to look more closely at the problem of medical debt as a contributing factor to financial instability,” Dr. Jabbarpour said. “Federal relief is important, so is expanding access to comprehensive, affordable health care coverage.”
Dr. Collins said there should also be a way to raise awareness of the health care marketplace and coverage options so that people have an easier time getting insured.
A version of this article first appeared on Medscape.com.
As common respiratory viruses resurface, children are at serious risk
Younger children may be vulnerable to the reemergence of common respiratory viruses such as influenza and respiratory syncytial virus (RSV) as COVID-19 restrictions wane, experts say. The impact could be detrimental.
The COVID-19 pandemic and the implementation of preventative measures such as social distancing, travel restrictions, mask use, and shelter in place, reduced the transmission of respiratory viruses, according to the Centers for Disease Control and Prevention. However, because older infants and toddlers have not been exposed to these bugs during the pandemic, they are vulnerable to suffering severe viral infections.
“[We’ve] been in the honeymoon for 18 months,” said Christopher J. Harrison, MD, professor of pediatrics and pediatric infectious diseases at Children’s Mercy Hospitals and Clinics in Kansas City, Mo. “We are going to be coming out of the honeymoon and the children who didn’t get sick are going to start packing 2 years’ worth of infections into the next 9 months so there’s going to be twice as many as would be normal.”
The CDC issued a health advisory in June for parts of the southern United States, such as Texas, the Carolinas, and Oklahoma, encouraging broader testing for RSV – a virus that usually causes mild, cold-like symptoms and is the most common cause of bronchiolitis and pneumonia in children – among those who test negative for COVID-19. Virtually all children get an RSV infection by the time they are 2 years old, according to the CDC.
In previous years, RSV usually spread during the fall and spring seasons and usually peaked late December to mid-February. However, there’s been an offseason spike in the common illness this year, with nearly 2,000 confirmed cases each week of July.
Richard J. Webby, PhD, of the infectious diseases department at St. Jude Children’s Research Hospital, Memphis, Tenn., said that although RSV transmits more easily during the winter, the virus is able to thrive during this summer because many children have limited immunity and are more vulnerable to catching the virus than before. Population immunity normally limits a virus to circulating under its most favorable conditions, which is usually the winter. However, because there are a few more “susceptible hosts,” it gives the virus the ability to spread during a time when it typically wouldn’t be able to.
“Now we have a wider range of susceptible kids because they haven’t had that exposure over the past 18 months,” said Dr. Webby, who is on the World Health Organization’s Influenza Vaccine Composition Advisory Team. “It gives the virus more chances to transmit during conditions that are less favorable.”
Dr. Harrison said that, if children continue to take preventative measures such as wearing masks and sanitizing, they can delay catching the RSV – which can be severe in infants and young children – until they’re older and symptoms won’t be as severe.
“The swelling that these viruses cause in the trachea and the bronchial tubes is much bigger in proportion to the overall size of the tubes, so it takes less swelling to clog up the trachea or bronchial tube for the 9-month-old than it does of a 9-year-old,” Dr. Harrison said. “So if a 9-year-old was to get RSV, they’re not going to have nearly the same amount symptoms as the 9-month-old.
Dr. Harrison said delaying RSV in children was never an option before because it’s a virus that’s almost impossible to avoid.
“Hopefully, the mask means that if you get exposed, instead of getting a million virus particles from your classmate or your playmate, you may only get a couple thousand,” Dr. Harrison explained. “And maybe that’s enough that you can fight it off or it may be small enough that you get a mild infection instead of a severe infection.”
A summer surge of RSV has also occurred in Australia. A study published in Clinical Infectious Diseases found that Western Australia saw a 98% reduction in RSV cases. This suggests that COVID-19 restrictions also delayed the RSV season.
Dr. Webby said the lax in penetrative measures against COVID-19 may also affect this upcoming flu season. Usually, around 10%-30% of the population gets infected with the flu each year, but that hasn’t happened the past couple of seasons, he said.
“There might be slightly less overall immunity to these viruses,” Dr. Webby said. “When these viruses do come back, there’s a little bit more room for them to take off.”
Although a severe influenza season rebound this winter is a possibility, Australia continues to experience a historically low flu season. Dr. Harrison, who said the northern hemisphere looks at what’s happening in Australia and the rest of the “southern half of the world because their influenza season is during our summer,” hopes this is an indication that the northern hemisphere will also experience a mild season.
However, there’s no indication of how this upcoming flu season will hit the United States and there isn’t any guidance on what could happen because these historically low levels of respiratory viruses have never happened before, Dr. Webby explained.
He said that, if COVID-19’s delta variant continues to circulate during the fall and winter seasons, it will keep other viruses at low levels. This is because there is rarely a peak of activity of different viruses at the same time.
“When you get infected with the virus, your body’s immune response has this nonspecific reaction that protects you from anything else for a short period of time,” Dr. Webby explained. “When you get a lot of one virus circulating, it’s really hard for these other viruses to get into that population and sort of set off an epidemic of their own.”
To prepare for an unsure influenza season, Dr. Harrison suggests making the influenza vaccine available in August as opposed to October.
Dr. Harrison and Dr. Webby reported no conflicts of interest.
Younger children may be vulnerable to the reemergence of common respiratory viruses such as influenza and respiratory syncytial virus (RSV) as COVID-19 restrictions wane, experts say. The impact could be detrimental.
The COVID-19 pandemic and the implementation of preventative measures such as social distancing, travel restrictions, mask use, and shelter in place, reduced the transmission of respiratory viruses, according to the Centers for Disease Control and Prevention. However, because older infants and toddlers have not been exposed to these bugs during the pandemic, they are vulnerable to suffering severe viral infections.
“[We’ve] been in the honeymoon for 18 months,” said Christopher J. Harrison, MD, professor of pediatrics and pediatric infectious diseases at Children’s Mercy Hospitals and Clinics in Kansas City, Mo. “We are going to be coming out of the honeymoon and the children who didn’t get sick are going to start packing 2 years’ worth of infections into the next 9 months so there’s going to be twice as many as would be normal.”
The CDC issued a health advisory in June for parts of the southern United States, such as Texas, the Carolinas, and Oklahoma, encouraging broader testing for RSV – a virus that usually causes mild, cold-like symptoms and is the most common cause of bronchiolitis and pneumonia in children – among those who test negative for COVID-19. Virtually all children get an RSV infection by the time they are 2 years old, according to the CDC.
In previous years, RSV usually spread during the fall and spring seasons and usually peaked late December to mid-February. However, there’s been an offseason spike in the common illness this year, with nearly 2,000 confirmed cases each week of July.
Richard J. Webby, PhD, of the infectious diseases department at St. Jude Children’s Research Hospital, Memphis, Tenn., said that although RSV transmits more easily during the winter, the virus is able to thrive during this summer because many children have limited immunity and are more vulnerable to catching the virus than before. Population immunity normally limits a virus to circulating under its most favorable conditions, which is usually the winter. However, because there are a few more “susceptible hosts,” it gives the virus the ability to spread during a time when it typically wouldn’t be able to.
“Now we have a wider range of susceptible kids because they haven’t had that exposure over the past 18 months,” said Dr. Webby, who is on the World Health Organization’s Influenza Vaccine Composition Advisory Team. “It gives the virus more chances to transmit during conditions that are less favorable.”
Dr. Harrison said that, if children continue to take preventative measures such as wearing masks and sanitizing, they can delay catching the RSV – which can be severe in infants and young children – until they’re older and symptoms won’t be as severe.
“The swelling that these viruses cause in the trachea and the bronchial tubes is much bigger in proportion to the overall size of the tubes, so it takes less swelling to clog up the trachea or bronchial tube for the 9-month-old than it does of a 9-year-old,” Dr. Harrison said. “So if a 9-year-old was to get RSV, they’re not going to have nearly the same amount symptoms as the 9-month-old.
Dr. Harrison said delaying RSV in children was never an option before because it’s a virus that’s almost impossible to avoid.
“Hopefully, the mask means that if you get exposed, instead of getting a million virus particles from your classmate or your playmate, you may only get a couple thousand,” Dr. Harrison explained. “And maybe that’s enough that you can fight it off or it may be small enough that you get a mild infection instead of a severe infection.”
A summer surge of RSV has also occurred in Australia. A study published in Clinical Infectious Diseases found that Western Australia saw a 98% reduction in RSV cases. This suggests that COVID-19 restrictions also delayed the RSV season.
Dr. Webby said the lax in penetrative measures against COVID-19 may also affect this upcoming flu season. Usually, around 10%-30% of the population gets infected with the flu each year, but that hasn’t happened the past couple of seasons, he said.
“There might be slightly less overall immunity to these viruses,” Dr. Webby said. “When these viruses do come back, there’s a little bit more room for them to take off.”
Although a severe influenza season rebound this winter is a possibility, Australia continues to experience a historically low flu season. Dr. Harrison, who said the northern hemisphere looks at what’s happening in Australia and the rest of the “southern half of the world because their influenza season is during our summer,” hopes this is an indication that the northern hemisphere will also experience a mild season.
However, there’s no indication of how this upcoming flu season will hit the United States and there isn’t any guidance on what could happen because these historically low levels of respiratory viruses have never happened before, Dr. Webby explained.
He said that, if COVID-19’s delta variant continues to circulate during the fall and winter seasons, it will keep other viruses at low levels. This is because there is rarely a peak of activity of different viruses at the same time.
“When you get infected with the virus, your body’s immune response has this nonspecific reaction that protects you from anything else for a short period of time,” Dr. Webby explained. “When you get a lot of one virus circulating, it’s really hard for these other viruses to get into that population and sort of set off an epidemic of their own.”
To prepare for an unsure influenza season, Dr. Harrison suggests making the influenza vaccine available in August as opposed to October.
Dr. Harrison and Dr. Webby reported no conflicts of interest.
Younger children may be vulnerable to the reemergence of common respiratory viruses such as influenza and respiratory syncytial virus (RSV) as COVID-19 restrictions wane, experts say. The impact could be detrimental.
The COVID-19 pandemic and the implementation of preventative measures such as social distancing, travel restrictions, mask use, and shelter in place, reduced the transmission of respiratory viruses, according to the Centers for Disease Control and Prevention. However, because older infants and toddlers have not been exposed to these bugs during the pandemic, they are vulnerable to suffering severe viral infections.
“[We’ve] been in the honeymoon for 18 months,” said Christopher J. Harrison, MD, professor of pediatrics and pediatric infectious diseases at Children’s Mercy Hospitals and Clinics in Kansas City, Mo. “We are going to be coming out of the honeymoon and the children who didn’t get sick are going to start packing 2 years’ worth of infections into the next 9 months so there’s going to be twice as many as would be normal.”
The CDC issued a health advisory in June for parts of the southern United States, such as Texas, the Carolinas, and Oklahoma, encouraging broader testing for RSV – a virus that usually causes mild, cold-like symptoms and is the most common cause of bronchiolitis and pneumonia in children – among those who test negative for COVID-19. Virtually all children get an RSV infection by the time they are 2 years old, according to the CDC.
In previous years, RSV usually spread during the fall and spring seasons and usually peaked late December to mid-February. However, there’s been an offseason spike in the common illness this year, with nearly 2,000 confirmed cases each week of July.
Richard J. Webby, PhD, of the infectious diseases department at St. Jude Children’s Research Hospital, Memphis, Tenn., said that although RSV transmits more easily during the winter, the virus is able to thrive during this summer because many children have limited immunity and are more vulnerable to catching the virus than before. Population immunity normally limits a virus to circulating under its most favorable conditions, which is usually the winter. However, because there are a few more “susceptible hosts,” it gives the virus the ability to spread during a time when it typically wouldn’t be able to.
“Now we have a wider range of susceptible kids because they haven’t had that exposure over the past 18 months,” said Dr. Webby, who is on the World Health Organization’s Influenza Vaccine Composition Advisory Team. “It gives the virus more chances to transmit during conditions that are less favorable.”
Dr. Harrison said that, if children continue to take preventative measures such as wearing masks and sanitizing, they can delay catching the RSV – which can be severe in infants and young children – until they’re older and symptoms won’t be as severe.
“The swelling that these viruses cause in the trachea and the bronchial tubes is much bigger in proportion to the overall size of the tubes, so it takes less swelling to clog up the trachea or bronchial tube for the 9-month-old than it does of a 9-year-old,” Dr. Harrison said. “So if a 9-year-old was to get RSV, they’re not going to have nearly the same amount symptoms as the 9-month-old.
Dr. Harrison said delaying RSV in children was never an option before because it’s a virus that’s almost impossible to avoid.
“Hopefully, the mask means that if you get exposed, instead of getting a million virus particles from your classmate or your playmate, you may only get a couple thousand,” Dr. Harrison explained. “And maybe that’s enough that you can fight it off or it may be small enough that you get a mild infection instead of a severe infection.”
A summer surge of RSV has also occurred in Australia. A study published in Clinical Infectious Diseases found that Western Australia saw a 98% reduction in RSV cases. This suggests that COVID-19 restrictions also delayed the RSV season.
Dr. Webby said the lax in penetrative measures against COVID-19 may also affect this upcoming flu season. Usually, around 10%-30% of the population gets infected with the flu each year, but that hasn’t happened the past couple of seasons, he said.
“There might be slightly less overall immunity to these viruses,” Dr. Webby said. “When these viruses do come back, there’s a little bit more room for them to take off.”
Although a severe influenza season rebound this winter is a possibility, Australia continues to experience a historically low flu season. Dr. Harrison, who said the northern hemisphere looks at what’s happening in Australia and the rest of the “southern half of the world because their influenza season is during our summer,” hopes this is an indication that the northern hemisphere will also experience a mild season.
However, there’s no indication of how this upcoming flu season will hit the United States and there isn’t any guidance on what could happen because these historically low levels of respiratory viruses have never happened before, Dr. Webby explained.
He said that, if COVID-19’s delta variant continues to circulate during the fall and winter seasons, it will keep other viruses at low levels. This is because there is rarely a peak of activity of different viruses at the same time.
“When you get infected with the virus, your body’s immune response has this nonspecific reaction that protects you from anything else for a short period of time,” Dr. Webby explained. “When you get a lot of one virus circulating, it’s really hard for these other viruses to get into that population and sort of set off an epidemic of their own.”
To prepare for an unsure influenza season, Dr. Harrison suggests making the influenza vaccine available in August as opposed to October.
Dr. Harrison and Dr. Webby reported no conflicts of interest.
FM diversity has increased, but more physicians of color needed
The specialty has been on the path to a racially diverse workforce over the past few decades. Since family medicine is a discipline where doctors look not just at individual patients, but also at the health of the community, some family physicians see working in their specialty as a way to integrate public health with medicine to curb health inequities.
Maria Harsha Wusu, MD, MSEd, is an example of such a family physician.
Dr. Wusu, who is Black and of Japanese descent, chose to practice family medicine to address health in communities of color “which we know in the United States experience health inequities due to structural racism,” she said in an interview.
“It’s a discipline where you look at the health of the entire family and the community and you really look at the environmental, the political, the historical factors that are influencing the health of the community,” explained Dr. Wusu, who is currently the director of health equity at Morehouse School of Medicine, Atlanta. Family physicians are not just asking: “Does a patient have hypertension?” but also whether a patient has access to healthy food, green space and other things.
While the field of family medicine is more diverse in the 21st century than it was at its beginning, Dr. Wusu, who completed her residency in 2016, still faced challenges to achieving her goal of helping communities of color. These specifically stemmed from a lack of diversity among the people in the places where she studied to become a doctor and family physician.
There were moments when Dr. Wusu felt isolated while in medical school and residency, because so few students and faculty members she saw looked like her.
Plus, studies have shown that a racially and ethnically diverse physician workforce is necessary to address health inequities. Research published in 2018 in the Journal of Health Care for the Poor and Underserved, for example, found that underrepresented physicians are more likely to practice in underserved areas than their White peers.
“I went to medical school at a historically White institution, and so there were very few people who identified as what we would say are underrepresented minorities in medicine,” Dr. Wusu explained. “There are issues with both implicit and explicit racism, which I think could be echoed by colleagues across the country that are additional challenges that I think medical students, particularly students of color, experience during what is an already kind of challenging time of medical school and the rigorous training of residency.”
Ada Stewart, MD, FAAFP, president of the American Academy of Family Physicians, echoed Dr. Wusu’s medical school experience. Dr. Stewart, who finished her residency in 2003, said that, out of the 120 students in her graduating medical class, only 10 were Black.
Marginalized groups are still underrepresented in residences. According to data compiled by the Association of American Medical Colleges, only 9.3% of Black people, 10% of Latino, and 0.3% of Native Hawaiian or other Pacific Islanders are residents in family medicine residency programs in 2019-2020. Meanwhile, White residents make up 50.8% of the residency program.
“We really need to do all that we can to increase diversity within our medical schools and residencies,” Dr. Stewart said.
In regards to gender, there has been an increasing number of women in the family medicine specialty. A 2021 study found that the proportion of female physicians in family medicine has grown from 33.9% 2010 to 41.9% in 2020.
“There’s still room for growth and we have to change the system and those structures that created these problems,” noted Dr. Stewart.
The social responsibility of family medicine
The family medicine specialty was born during an era of protest of social change, alongside the Civil Rights Movement, the peace movement, and counterculture protests. In April 1966, 3 years before American Boards approved family practice as a new specialty; the National Commission on Community Health stated that every person should have a personal physician who is the “central point for the integration and continuity of all medical services to his patient.” They also said such physicians should be aware of the “many and varied social, emotional and environmental factors that influence the health of his patient and family.”
While the diversity of family medicine specialty has significantly increased since its beginnings, it continues to lag behind the general U.S. population. A 2018 study published in the Journal of the American Board of Family Medicine, which aggregated data from 1987 to 2017, found that the proportion of Black and Latino board certified family physicians increased from 1.3% to 7.8% and 2.3% to 9.1%, respectively, in 30 years.
A 2014 study included 2 decades worth of data from the U.S. Census and the Association of American Medical Colleges to examine trends in racial and ethnic composition among family medicine residents. The U.S. population increased from 9% to 17% for Latinos, 11.7% to 12.2% for Blacks/African Americans, and 0.87% to 0.89% for Native Americans from 1990 to 2012. Meanwhile, minority representation in family residencies increased 4.9% to 9.4% for Hispanics/Latinos, from 4.2% to 7.9% for Blacks/African Americans, and from 0.7% to 0.9% for Native Americans.
Furthermore, 13.4% of the U.S. population is Black and 18.5% of the population is Latino, while only 7.8% of family medicine residents in 2019 were Black and 9.1% of family medicine residents were Latino, according to a recent study published in Family Medicine.
Recruiting a diverse physician workforce
The AAFP has launched a few initiatives to increase diversity within the specialty. In 2017, the AAFP established the Center for Diversity and Health Equity, a center to address social determinants of health. The EveryONE Project, an initiative that’s part of the AAFP’s center, offers members education and resources to promote workforce diversity. Some of those resources include “The Ladder Program,” an initiative founded by an AAFP member which involves monthly meetings and events for students as young as 9 years old to introduce them to medicine at a young age.
“You can’t see what you don’t see,” noted Dr. Stewart, who is the first Black, female president of the AAFP, and the fourth woman in the role. “I really have seen how important it is to be a mentor and to be out there so that individuals who look like me can see that they too can become a family physician and be that member of their community.”
In addition to The Ladder Program, some other resources aimed at increasing diversity among family physicians include Tour for Diversity in Medicine and the Doctors Back to School Program.
The Tour for Diversity in Medicine involves a team of physicians, other clinicians and students hosting events nationwide for minority students to help them see a path to medicine and other health professions. Meanwhile, the AAFP’s Doctors Back to School Program involves family physicians visiting children at schools, clubs, community organizations, and other places to raise childhood awareness of family medicine and help them see their own potential in health care careers.
Dr. Stewart said these programs have been successful in increasing underrepresented groups.
“We are trying to see how best to measure their success,” the AAFP president said. “Looking at the high numbers of individuals who chose the specialty of family medicine last year is what I would deem a success.”
Dr. Wusu also believes outreach to children in elementary schools is important when it comes to increasing diversity in the family medicine specialty.
One organization that’s proving such outreach is the Student National Medical Association, a branch of the National Medical Association, which is a professional organization of Black physicians. This group’s initiative, the Health Professions Recruitment Exposure Programs, exposes teens to science-related activities while introducing them to careers in health professions. Another SMNA program, called Youth Science Enrichment Program, targets elementary and junior high school students.
Dr. Wusu led a 2019 project that focused on creating a more diverse family medicine residency program by developing and implementing a strategic plan for diversity recruitment, which involved increasing outreach to marginalized groups and revising interviews to minimize bias. In a paper published on the results of the initiative, Dr. Wusu and coauthors noted that, between 2014 and 2017, the total number of underrepresented minority applicants to the Boston Medical Center Family Medicine Residency Program increased by 80%. Before the intervention, the percentage of applicants who were part of an underrepresented group ranged from 0% to 20%. During the intervention, that range jumped to 25% to 50%, according to the paper.
While Dr. Wusu considers these programs to be beneficial for the specialty, she doesn’t believe they should be done in isolation. There should also be efforts to tackle lack of opportunities and structural racism.
“With any inequity, you have to address it on multiple levels,” Dr. Wusu explained. “It’s great that there has been recognition for a need for diversity in family medicine, but my hope is that the call for equity would reach beyond that.”
Fostering an inclusive environment
While family medicine has come a long way with regards to increasing the amount of underrepresented groups in its specialty, Stephen Richmond, MD, MPH, believes there also needs to be a focus on the infrastructure of support to help retain these physicians.
“The problem of diversity within family medicine and largely in other specialties cannot be summed up simply as a matter of poor representation. We must do be better to understand the lived experience of physicians of color, in particular Black physicians, once they arrive in the medical professional environment. Doing so will help institutions to provide that infrastructure of support – including antiracism policies and practices – that will enhance wellness and representation,” said Dr. Richmond, clinical assistant professor of medicine in the division of primary care and population health at Stanford (Calif.) University.
Dr. Wusu also suggested establishing an explicitly antiracist environment. This can be done in multiple ways, including by holding programs that acknowledge the impact of structural racism on both the patients, medical students and faculty, and by educating staff about the history of racism, she said.
Dr. Stewart and Dr. Wusu think the specialty has improved in its representation of minorities, but that it has a “long way to go.”
“I think family medicine is really one of the more inclusive specialties. I mean, it has higher numbers of Black and Brown residents and physicians than other specialties,” Dr. Wusu said. “We still have a very long way to go to be at numbers that match the general population. But I think, in that way, family medicine is a place where a lot of Black and Brown physicians can find a home.”
The specialty has been on the path to a racially diverse workforce over the past few decades. Since family medicine is a discipline where doctors look not just at individual patients, but also at the health of the community, some family physicians see working in their specialty as a way to integrate public health with medicine to curb health inequities.
Maria Harsha Wusu, MD, MSEd, is an example of such a family physician.
Dr. Wusu, who is Black and of Japanese descent, chose to practice family medicine to address health in communities of color “which we know in the United States experience health inequities due to structural racism,” she said in an interview.
“It’s a discipline where you look at the health of the entire family and the community and you really look at the environmental, the political, the historical factors that are influencing the health of the community,” explained Dr. Wusu, who is currently the director of health equity at Morehouse School of Medicine, Atlanta. Family physicians are not just asking: “Does a patient have hypertension?” but also whether a patient has access to healthy food, green space and other things.
While the field of family medicine is more diverse in the 21st century than it was at its beginning, Dr. Wusu, who completed her residency in 2016, still faced challenges to achieving her goal of helping communities of color. These specifically stemmed from a lack of diversity among the people in the places where she studied to become a doctor and family physician.
There were moments when Dr. Wusu felt isolated while in medical school and residency, because so few students and faculty members she saw looked like her.
Plus, studies have shown that a racially and ethnically diverse physician workforce is necessary to address health inequities. Research published in 2018 in the Journal of Health Care for the Poor and Underserved, for example, found that underrepresented physicians are more likely to practice in underserved areas than their White peers.
“I went to medical school at a historically White institution, and so there were very few people who identified as what we would say are underrepresented minorities in medicine,” Dr. Wusu explained. “There are issues with both implicit and explicit racism, which I think could be echoed by colleagues across the country that are additional challenges that I think medical students, particularly students of color, experience during what is an already kind of challenging time of medical school and the rigorous training of residency.”
Ada Stewart, MD, FAAFP, president of the American Academy of Family Physicians, echoed Dr. Wusu’s medical school experience. Dr. Stewart, who finished her residency in 2003, said that, out of the 120 students in her graduating medical class, only 10 were Black.
Marginalized groups are still underrepresented in residences. According to data compiled by the Association of American Medical Colleges, only 9.3% of Black people, 10% of Latino, and 0.3% of Native Hawaiian or other Pacific Islanders are residents in family medicine residency programs in 2019-2020. Meanwhile, White residents make up 50.8% of the residency program.
“We really need to do all that we can to increase diversity within our medical schools and residencies,” Dr. Stewart said.
In regards to gender, there has been an increasing number of women in the family medicine specialty. A 2021 study found that the proportion of female physicians in family medicine has grown from 33.9% 2010 to 41.9% in 2020.
“There’s still room for growth and we have to change the system and those structures that created these problems,” noted Dr. Stewart.
The social responsibility of family medicine
The family medicine specialty was born during an era of protest of social change, alongside the Civil Rights Movement, the peace movement, and counterculture protests. In April 1966, 3 years before American Boards approved family practice as a new specialty; the National Commission on Community Health stated that every person should have a personal physician who is the “central point for the integration and continuity of all medical services to his patient.” They also said such physicians should be aware of the “many and varied social, emotional and environmental factors that influence the health of his patient and family.”
While the diversity of family medicine specialty has significantly increased since its beginnings, it continues to lag behind the general U.S. population. A 2018 study published in the Journal of the American Board of Family Medicine, which aggregated data from 1987 to 2017, found that the proportion of Black and Latino board certified family physicians increased from 1.3% to 7.8% and 2.3% to 9.1%, respectively, in 30 years.
A 2014 study included 2 decades worth of data from the U.S. Census and the Association of American Medical Colleges to examine trends in racial and ethnic composition among family medicine residents. The U.S. population increased from 9% to 17% for Latinos, 11.7% to 12.2% for Blacks/African Americans, and 0.87% to 0.89% for Native Americans from 1990 to 2012. Meanwhile, minority representation in family residencies increased 4.9% to 9.4% for Hispanics/Latinos, from 4.2% to 7.9% for Blacks/African Americans, and from 0.7% to 0.9% for Native Americans.
Furthermore, 13.4% of the U.S. population is Black and 18.5% of the population is Latino, while only 7.8% of family medicine residents in 2019 were Black and 9.1% of family medicine residents were Latino, according to a recent study published in Family Medicine.
Recruiting a diverse physician workforce
The AAFP has launched a few initiatives to increase diversity within the specialty. In 2017, the AAFP established the Center for Diversity and Health Equity, a center to address social determinants of health. The EveryONE Project, an initiative that’s part of the AAFP’s center, offers members education and resources to promote workforce diversity. Some of those resources include “The Ladder Program,” an initiative founded by an AAFP member which involves monthly meetings and events for students as young as 9 years old to introduce them to medicine at a young age.
“You can’t see what you don’t see,” noted Dr. Stewart, who is the first Black, female president of the AAFP, and the fourth woman in the role. “I really have seen how important it is to be a mentor and to be out there so that individuals who look like me can see that they too can become a family physician and be that member of their community.”
In addition to The Ladder Program, some other resources aimed at increasing diversity among family physicians include Tour for Diversity in Medicine and the Doctors Back to School Program.
The Tour for Diversity in Medicine involves a team of physicians, other clinicians and students hosting events nationwide for minority students to help them see a path to medicine and other health professions. Meanwhile, the AAFP’s Doctors Back to School Program involves family physicians visiting children at schools, clubs, community organizations, and other places to raise childhood awareness of family medicine and help them see their own potential in health care careers.
Dr. Stewart said these programs have been successful in increasing underrepresented groups.
“We are trying to see how best to measure their success,” the AAFP president said. “Looking at the high numbers of individuals who chose the specialty of family medicine last year is what I would deem a success.”
Dr. Wusu also believes outreach to children in elementary schools is important when it comes to increasing diversity in the family medicine specialty.
One organization that’s proving such outreach is the Student National Medical Association, a branch of the National Medical Association, which is a professional organization of Black physicians. This group’s initiative, the Health Professions Recruitment Exposure Programs, exposes teens to science-related activities while introducing them to careers in health professions. Another SMNA program, called Youth Science Enrichment Program, targets elementary and junior high school students.
Dr. Wusu led a 2019 project that focused on creating a more diverse family medicine residency program by developing and implementing a strategic plan for diversity recruitment, which involved increasing outreach to marginalized groups and revising interviews to minimize bias. In a paper published on the results of the initiative, Dr. Wusu and coauthors noted that, between 2014 and 2017, the total number of underrepresented minority applicants to the Boston Medical Center Family Medicine Residency Program increased by 80%. Before the intervention, the percentage of applicants who were part of an underrepresented group ranged from 0% to 20%. During the intervention, that range jumped to 25% to 50%, according to the paper.
While Dr. Wusu considers these programs to be beneficial for the specialty, she doesn’t believe they should be done in isolation. There should also be efforts to tackle lack of opportunities and structural racism.
“With any inequity, you have to address it on multiple levels,” Dr. Wusu explained. “It’s great that there has been recognition for a need for diversity in family medicine, but my hope is that the call for equity would reach beyond that.”
Fostering an inclusive environment
While family medicine has come a long way with regards to increasing the amount of underrepresented groups in its specialty, Stephen Richmond, MD, MPH, believes there also needs to be a focus on the infrastructure of support to help retain these physicians.
“The problem of diversity within family medicine and largely in other specialties cannot be summed up simply as a matter of poor representation. We must do be better to understand the lived experience of physicians of color, in particular Black physicians, once they arrive in the medical professional environment. Doing so will help institutions to provide that infrastructure of support – including antiracism policies and practices – that will enhance wellness and representation,” said Dr. Richmond, clinical assistant professor of medicine in the division of primary care and population health at Stanford (Calif.) University.
Dr. Wusu also suggested establishing an explicitly antiracist environment. This can be done in multiple ways, including by holding programs that acknowledge the impact of structural racism on both the patients, medical students and faculty, and by educating staff about the history of racism, she said.
Dr. Stewart and Dr. Wusu think the specialty has improved in its representation of minorities, but that it has a “long way to go.”
“I think family medicine is really one of the more inclusive specialties. I mean, it has higher numbers of Black and Brown residents and physicians than other specialties,” Dr. Wusu said. “We still have a very long way to go to be at numbers that match the general population. But I think, in that way, family medicine is a place where a lot of Black and Brown physicians can find a home.”
The specialty has been on the path to a racially diverse workforce over the past few decades. Since family medicine is a discipline where doctors look not just at individual patients, but also at the health of the community, some family physicians see working in their specialty as a way to integrate public health with medicine to curb health inequities.
Maria Harsha Wusu, MD, MSEd, is an example of such a family physician.
Dr. Wusu, who is Black and of Japanese descent, chose to practice family medicine to address health in communities of color “which we know in the United States experience health inequities due to structural racism,” she said in an interview.
“It’s a discipline where you look at the health of the entire family and the community and you really look at the environmental, the political, the historical factors that are influencing the health of the community,” explained Dr. Wusu, who is currently the director of health equity at Morehouse School of Medicine, Atlanta. Family physicians are not just asking: “Does a patient have hypertension?” but also whether a patient has access to healthy food, green space and other things.
While the field of family medicine is more diverse in the 21st century than it was at its beginning, Dr. Wusu, who completed her residency in 2016, still faced challenges to achieving her goal of helping communities of color. These specifically stemmed from a lack of diversity among the people in the places where she studied to become a doctor and family physician.
There were moments when Dr. Wusu felt isolated while in medical school and residency, because so few students and faculty members she saw looked like her.
Plus, studies have shown that a racially and ethnically diverse physician workforce is necessary to address health inequities. Research published in 2018 in the Journal of Health Care for the Poor and Underserved, for example, found that underrepresented physicians are more likely to practice in underserved areas than their White peers.
“I went to medical school at a historically White institution, and so there were very few people who identified as what we would say are underrepresented minorities in medicine,” Dr. Wusu explained. “There are issues with both implicit and explicit racism, which I think could be echoed by colleagues across the country that are additional challenges that I think medical students, particularly students of color, experience during what is an already kind of challenging time of medical school and the rigorous training of residency.”
Ada Stewart, MD, FAAFP, president of the American Academy of Family Physicians, echoed Dr. Wusu’s medical school experience. Dr. Stewart, who finished her residency in 2003, said that, out of the 120 students in her graduating medical class, only 10 were Black.
Marginalized groups are still underrepresented in residences. According to data compiled by the Association of American Medical Colleges, only 9.3% of Black people, 10% of Latino, and 0.3% of Native Hawaiian or other Pacific Islanders are residents in family medicine residency programs in 2019-2020. Meanwhile, White residents make up 50.8% of the residency program.
“We really need to do all that we can to increase diversity within our medical schools and residencies,” Dr. Stewart said.
In regards to gender, there has been an increasing number of women in the family medicine specialty. A 2021 study found that the proportion of female physicians in family medicine has grown from 33.9% 2010 to 41.9% in 2020.
“There’s still room for growth and we have to change the system and those structures that created these problems,” noted Dr. Stewart.
The social responsibility of family medicine
The family medicine specialty was born during an era of protest of social change, alongside the Civil Rights Movement, the peace movement, and counterculture protests. In April 1966, 3 years before American Boards approved family practice as a new specialty; the National Commission on Community Health stated that every person should have a personal physician who is the “central point for the integration and continuity of all medical services to his patient.” They also said such physicians should be aware of the “many and varied social, emotional and environmental factors that influence the health of his patient and family.”
While the diversity of family medicine specialty has significantly increased since its beginnings, it continues to lag behind the general U.S. population. A 2018 study published in the Journal of the American Board of Family Medicine, which aggregated data from 1987 to 2017, found that the proportion of Black and Latino board certified family physicians increased from 1.3% to 7.8% and 2.3% to 9.1%, respectively, in 30 years.
A 2014 study included 2 decades worth of data from the U.S. Census and the Association of American Medical Colleges to examine trends in racial and ethnic composition among family medicine residents. The U.S. population increased from 9% to 17% for Latinos, 11.7% to 12.2% for Blacks/African Americans, and 0.87% to 0.89% for Native Americans from 1990 to 2012. Meanwhile, minority representation in family residencies increased 4.9% to 9.4% for Hispanics/Latinos, from 4.2% to 7.9% for Blacks/African Americans, and from 0.7% to 0.9% for Native Americans.
Furthermore, 13.4% of the U.S. population is Black and 18.5% of the population is Latino, while only 7.8% of family medicine residents in 2019 were Black and 9.1% of family medicine residents were Latino, according to a recent study published in Family Medicine.
Recruiting a diverse physician workforce
The AAFP has launched a few initiatives to increase diversity within the specialty. In 2017, the AAFP established the Center for Diversity and Health Equity, a center to address social determinants of health. The EveryONE Project, an initiative that’s part of the AAFP’s center, offers members education and resources to promote workforce diversity. Some of those resources include “The Ladder Program,” an initiative founded by an AAFP member which involves monthly meetings and events for students as young as 9 years old to introduce them to medicine at a young age.
“You can’t see what you don’t see,” noted Dr. Stewart, who is the first Black, female president of the AAFP, and the fourth woman in the role. “I really have seen how important it is to be a mentor and to be out there so that individuals who look like me can see that they too can become a family physician and be that member of their community.”
In addition to The Ladder Program, some other resources aimed at increasing diversity among family physicians include Tour for Diversity in Medicine and the Doctors Back to School Program.
The Tour for Diversity in Medicine involves a team of physicians, other clinicians and students hosting events nationwide for minority students to help them see a path to medicine and other health professions. Meanwhile, the AAFP’s Doctors Back to School Program involves family physicians visiting children at schools, clubs, community organizations, and other places to raise childhood awareness of family medicine and help them see their own potential in health care careers.
Dr. Stewart said these programs have been successful in increasing underrepresented groups.
“We are trying to see how best to measure their success,” the AAFP president said. “Looking at the high numbers of individuals who chose the specialty of family medicine last year is what I would deem a success.”
Dr. Wusu also believes outreach to children in elementary schools is important when it comes to increasing diversity in the family medicine specialty.
One organization that’s proving such outreach is the Student National Medical Association, a branch of the National Medical Association, which is a professional organization of Black physicians. This group’s initiative, the Health Professions Recruitment Exposure Programs, exposes teens to science-related activities while introducing them to careers in health professions. Another SMNA program, called Youth Science Enrichment Program, targets elementary and junior high school students.
Dr. Wusu led a 2019 project that focused on creating a more diverse family medicine residency program by developing and implementing a strategic plan for diversity recruitment, which involved increasing outreach to marginalized groups and revising interviews to minimize bias. In a paper published on the results of the initiative, Dr. Wusu and coauthors noted that, between 2014 and 2017, the total number of underrepresented minority applicants to the Boston Medical Center Family Medicine Residency Program increased by 80%. Before the intervention, the percentage of applicants who were part of an underrepresented group ranged from 0% to 20%. During the intervention, that range jumped to 25% to 50%, according to the paper.
While Dr. Wusu considers these programs to be beneficial for the specialty, she doesn’t believe they should be done in isolation. There should also be efforts to tackle lack of opportunities and structural racism.
“With any inequity, you have to address it on multiple levels,” Dr. Wusu explained. “It’s great that there has been recognition for a need for diversity in family medicine, but my hope is that the call for equity would reach beyond that.”
Fostering an inclusive environment
While family medicine has come a long way with regards to increasing the amount of underrepresented groups in its specialty, Stephen Richmond, MD, MPH, believes there also needs to be a focus on the infrastructure of support to help retain these physicians.
“The problem of diversity within family medicine and largely in other specialties cannot be summed up simply as a matter of poor representation. We must do be better to understand the lived experience of physicians of color, in particular Black physicians, once they arrive in the medical professional environment. Doing so will help institutions to provide that infrastructure of support – including antiracism policies and practices – that will enhance wellness and representation,” said Dr. Richmond, clinical assistant professor of medicine in the division of primary care and population health at Stanford (Calif.) University.
Dr. Wusu also suggested establishing an explicitly antiracist environment. This can be done in multiple ways, including by holding programs that acknowledge the impact of structural racism on both the patients, medical students and faculty, and by educating staff about the history of racism, she said.
Dr. Stewart and Dr. Wusu think the specialty has improved in its representation of minorities, but that it has a “long way to go.”
“I think family medicine is really one of the more inclusive specialties. I mean, it has higher numbers of Black and Brown residents and physicians than other specialties,” Dr. Wusu said. “We still have a very long way to go to be at numbers that match the general population. But I think, in that way, family medicine is a place where a lot of Black and Brown physicians can find a home.”
Hematologic cancer increases risk of delivery complications
The risk of in-hospital complications and poor birth outcomes were greater in pregnant women with current or historical cancer diagnoses, new research suggests.
The study, published in Mayo Clinic Proceedings, found that women with current and historical cancer diagnoses had an increased risk of death, kidney injury, and stroke during delivery hospitalizations, compared with those with no cancer. When it came to delivery outcomes, this group also had a higher risk for preterm birth and postpartum hemorrhage. Those with a current cancer diagnoses had a 1.7-fold increase in odds for a preterm birth, compared with women without cancer.
“Our study found that metastases increased the odds of mortality, cesarean delivery, preterm birth, and stillbirth,” the researchers noted. “Coupled with previous research reporting that pregnant women are more likely to be diagnosed with advanced disease, this implies that pregnant women with newly diagnosed cancer have poor prognoses.”
However, although women with prior cancer had increased odds of mortality, the researchers said it was not statistically significant.
“The study really did not show an increase of mortality [for women with prior cancer diagnosis],” said Justin Chura, MD, a specialist in gynecologic oncology who was not involved in the study. “And the reason might be because there is not or the reason might be because it’s such a rare event. You would need 100 million births to assess that. So I would actually use caution in that interpretation.”
Researchers analyzed more than 43 million delivery hospitalizations of women with or without current or historical cancer diagnoses between January 2004 and December 2014. They found that the most common cancer diagnoses were hematologic, thyroid, cervical, skin, and breast.
Of the five most common cancers, the prevalence of all maternal complications and negative delivery outcomes was the highest among women with hematologic cancers. They were more likely to experience peripartum cardiomyopathy, acute kidney injury, and arrhythmia, compared with other cancers. Postpartum hemorrhage, maternal mortality, and placental abruption was also more likely to occur in those with this type of cancer.
“I was surprised that it was the hematologic cancers that were worse when they did it by cancer type,” said Dr. Chura, who is the chief of surgery and the director of gynecologic oncology and robotic surgery at the Cancer Treatment Centers of America’s Eastern Regional Medical Center in Philadelphia. “I think this is a useful bit of information for counseling our patients and also to identify the cohort with the highest risk.”
The findings also suggested that those with skin cancer had the highest odds for stroke, while women with cervical and breast cancers were more likely to experience acute kidney injury and preterm birth.
Dr. Chura said cancer treatments can have an impact on a woman’s health when she’s giving birth. For example, if a woman is diagnosed with cervical cancer, doctors may perform a cone biopsy on her where they remove a large portion of the cervix and still leave them with the ability to conceive and become pregnant. However, those patients are left with a higher risk of a preterm delivery.
For women with a hematologic cancer like non-Hodgkin’s lymphoma, chest radiation may cause some subsequent damage to their heart muscles “and now the stress of pregnancy puts more demand on the heart that can lead to cardiac complications for that patient,” Dr. Chura said.
“There are potential long-term effects from radiation and chemotherapy,” Dr. Chura said.
Previous studies have shown that chemotherapy may affect pregnancy and delivery. A 2019 study published in the Journal of Cancer also found that 59 pregnant women with cancer had increased mortality compared with those without the long-term illness. Meanwhile, another 2018 study published in Cancer found that women who conceived less than a year after starting chemotherapy had higher risks of preterm birth in comparison with those who conceived more than a year after starting chemotherapy. The study also found that cancer survivors who conceived more than a year after finishing chemotherapy with or without radiation had no higher risk of a preterm birth than those without cancer.
Dr. Chura said the new study could force doctors to think about the long-term effects of their cancer therapies and make them more apt to think about how to make cancer therapy less toxic with less long-term health consequences, while still curing patients.
“Most oncologists, when dealing with younger patients, are very focused on curing the cancer at hand, but not necessarily thinking 5 or 10 years down the road,” Dr. Chura said. “[This study] could help inform or at least make us aware of the long-term consequences of our cancer therapies.”
Dr. Chura had no relevant financial disclosures.
The risk of in-hospital complications and poor birth outcomes were greater in pregnant women with current or historical cancer diagnoses, new research suggests.
The study, published in Mayo Clinic Proceedings, found that women with current and historical cancer diagnoses had an increased risk of death, kidney injury, and stroke during delivery hospitalizations, compared with those with no cancer. When it came to delivery outcomes, this group also had a higher risk for preterm birth and postpartum hemorrhage. Those with a current cancer diagnoses had a 1.7-fold increase in odds for a preterm birth, compared with women without cancer.
“Our study found that metastases increased the odds of mortality, cesarean delivery, preterm birth, and stillbirth,” the researchers noted. “Coupled with previous research reporting that pregnant women are more likely to be diagnosed with advanced disease, this implies that pregnant women with newly diagnosed cancer have poor prognoses.”
However, although women with prior cancer had increased odds of mortality, the researchers said it was not statistically significant.
“The study really did not show an increase of mortality [for women with prior cancer diagnosis],” said Justin Chura, MD, a specialist in gynecologic oncology who was not involved in the study. “And the reason might be because there is not or the reason might be because it’s such a rare event. You would need 100 million births to assess that. So I would actually use caution in that interpretation.”
Researchers analyzed more than 43 million delivery hospitalizations of women with or without current or historical cancer diagnoses between January 2004 and December 2014. They found that the most common cancer diagnoses were hematologic, thyroid, cervical, skin, and breast.
Of the five most common cancers, the prevalence of all maternal complications and negative delivery outcomes was the highest among women with hematologic cancers. They were more likely to experience peripartum cardiomyopathy, acute kidney injury, and arrhythmia, compared with other cancers. Postpartum hemorrhage, maternal mortality, and placental abruption was also more likely to occur in those with this type of cancer.
“I was surprised that it was the hematologic cancers that were worse when they did it by cancer type,” said Dr. Chura, who is the chief of surgery and the director of gynecologic oncology and robotic surgery at the Cancer Treatment Centers of America’s Eastern Regional Medical Center in Philadelphia. “I think this is a useful bit of information for counseling our patients and also to identify the cohort with the highest risk.”
The findings also suggested that those with skin cancer had the highest odds for stroke, while women with cervical and breast cancers were more likely to experience acute kidney injury and preterm birth.
Dr. Chura said cancer treatments can have an impact on a woman’s health when she’s giving birth. For example, if a woman is diagnosed with cervical cancer, doctors may perform a cone biopsy on her where they remove a large portion of the cervix and still leave them with the ability to conceive and become pregnant. However, those patients are left with a higher risk of a preterm delivery.
For women with a hematologic cancer like non-Hodgkin’s lymphoma, chest radiation may cause some subsequent damage to their heart muscles “and now the stress of pregnancy puts more demand on the heart that can lead to cardiac complications for that patient,” Dr. Chura said.
“There are potential long-term effects from radiation and chemotherapy,” Dr. Chura said.
Previous studies have shown that chemotherapy may affect pregnancy and delivery. A 2019 study published in the Journal of Cancer also found that 59 pregnant women with cancer had increased mortality compared with those without the long-term illness. Meanwhile, another 2018 study published in Cancer found that women who conceived less than a year after starting chemotherapy had higher risks of preterm birth in comparison with those who conceived more than a year after starting chemotherapy. The study also found that cancer survivors who conceived more than a year after finishing chemotherapy with or without radiation had no higher risk of a preterm birth than those without cancer.
Dr. Chura said the new study could force doctors to think about the long-term effects of their cancer therapies and make them more apt to think about how to make cancer therapy less toxic with less long-term health consequences, while still curing patients.
“Most oncologists, when dealing with younger patients, are very focused on curing the cancer at hand, but not necessarily thinking 5 or 10 years down the road,” Dr. Chura said. “[This study] could help inform or at least make us aware of the long-term consequences of our cancer therapies.”
Dr. Chura had no relevant financial disclosures.
The risk of in-hospital complications and poor birth outcomes were greater in pregnant women with current or historical cancer diagnoses, new research suggests.
The study, published in Mayo Clinic Proceedings, found that women with current and historical cancer diagnoses had an increased risk of death, kidney injury, and stroke during delivery hospitalizations, compared with those with no cancer. When it came to delivery outcomes, this group also had a higher risk for preterm birth and postpartum hemorrhage. Those with a current cancer diagnoses had a 1.7-fold increase in odds for a preterm birth, compared with women without cancer.
“Our study found that metastases increased the odds of mortality, cesarean delivery, preterm birth, and stillbirth,” the researchers noted. “Coupled with previous research reporting that pregnant women are more likely to be diagnosed with advanced disease, this implies that pregnant women with newly diagnosed cancer have poor prognoses.”
However, although women with prior cancer had increased odds of mortality, the researchers said it was not statistically significant.
“The study really did not show an increase of mortality [for women with prior cancer diagnosis],” said Justin Chura, MD, a specialist in gynecologic oncology who was not involved in the study. “And the reason might be because there is not or the reason might be because it’s such a rare event. You would need 100 million births to assess that. So I would actually use caution in that interpretation.”
Researchers analyzed more than 43 million delivery hospitalizations of women with or without current or historical cancer diagnoses between January 2004 and December 2014. They found that the most common cancer diagnoses were hematologic, thyroid, cervical, skin, and breast.
Of the five most common cancers, the prevalence of all maternal complications and negative delivery outcomes was the highest among women with hematologic cancers. They were more likely to experience peripartum cardiomyopathy, acute kidney injury, and arrhythmia, compared with other cancers. Postpartum hemorrhage, maternal mortality, and placental abruption was also more likely to occur in those with this type of cancer.
“I was surprised that it was the hematologic cancers that were worse when they did it by cancer type,” said Dr. Chura, who is the chief of surgery and the director of gynecologic oncology and robotic surgery at the Cancer Treatment Centers of America’s Eastern Regional Medical Center in Philadelphia. “I think this is a useful bit of information for counseling our patients and also to identify the cohort with the highest risk.”
The findings also suggested that those with skin cancer had the highest odds for stroke, while women with cervical and breast cancers were more likely to experience acute kidney injury and preterm birth.
Dr. Chura said cancer treatments can have an impact on a woman’s health when she’s giving birth. For example, if a woman is diagnosed with cervical cancer, doctors may perform a cone biopsy on her where they remove a large portion of the cervix and still leave them with the ability to conceive and become pregnant. However, those patients are left with a higher risk of a preterm delivery.
For women with a hematologic cancer like non-Hodgkin’s lymphoma, chest radiation may cause some subsequent damage to their heart muscles “and now the stress of pregnancy puts more demand on the heart that can lead to cardiac complications for that patient,” Dr. Chura said.
“There are potential long-term effects from radiation and chemotherapy,” Dr. Chura said.
Previous studies have shown that chemotherapy may affect pregnancy and delivery. A 2019 study published in the Journal of Cancer also found that 59 pregnant women with cancer had increased mortality compared with those without the long-term illness. Meanwhile, another 2018 study published in Cancer found that women who conceived less than a year after starting chemotherapy had higher risks of preterm birth in comparison with those who conceived more than a year after starting chemotherapy. The study also found that cancer survivors who conceived more than a year after finishing chemotherapy with or without radiation had no higher risk of a preterm birth than those without cancer.
Dr. Chura said the new study could force doctors to think about the long-term effects of their cancer therapies and make them more apt to think about how to make cancer therapy less toxic with less long-term health consequences, while still curing patients.
“Most oncologists, when dealing with younger patients, are very focused on curing the cancer at hand, but not necessarily thinking 5 or 10 years down the road,” Dr. Chura said. “[This study] could help inform or at least make us aware of the long-term consequences of our cancer therapies.”
Dr. Chura had no relevant financial disclosures.
FROM MAYO CLINIC PROCEEDINGS
The case for suicide-risk screening in primary care
Suicide-risk screening may identify cases that typically fall through the cracks during depression screening, new research suggests.
The study, published in Pediatrics, found that the Ask Suicide-Screening Questions (ASQ) identified 2.2% of additional cases compared with those screened for any type of depression or other mental illnesses, and 8.3% of additional cases compared with those who screened positive for major depressive disorder.
About 3.2% of U.S. children between the ages of 3 and 17 have been diagnosed with depression, according to the Centers for Disease Control and Prevention. The American Academy of Pediatrics and the U.S. Preventive Services Task Force recommends that all teens be routinely screened for depression. However, there’s no specific recommendation that adolescents should also be screened for suicide in addition to depression screening.
The study highlights the high baseline rates of depression and suicide risk and the need for pediatric practices to plan for them and develop strategies about how they’re going to provide follow-up care, including treatment for suicidal teens.
“We began this project because we were concerned that we might be missing teens with increased risk of suicide by screening only for depression,” study author Alex Kemper, MD, said in an interview. “Our goal with this project was really to compare standard depression screening tools that we’ve used for a long time with a suicide-specific instrument just to see if we would identify additional cases with a suicide-risk instrument.”
Dr. Kemper and colleagues collected data from 803 mostly Medicaid-enrolled adolescents across 12 primary care practices. The subjects were between the ages of 12 and 20 years, with no recent history of depression or self-harm, who were screened with the Patient Health Questionnaire–9 Modified for Adolescents (PHQ-9A) and ASQ. For the study, two PHQ-9A screening strategies were evaluated: screening for any type of depression or other mental illness (positive on any item) or screening for major depressive disorder.
In addition, the researchers found that 56.4% of patients had a positive PHQ-9A screen for any type of depression and 24.7% had a positive PHQ-9A screen for major depressive disorder. Meanwhile, 21.1% of the population received a positive screen result. Of those who responded on the PHQ-9A that they did not have suicidal thoughts in the past month, 13.2% had a positive ASQ result.
Dr. Kemper, division chief of primary care pediatrics at Nationwide Children’s Hospital and professor of pediatrics at the Ohio State University, both in Columbus, said the suicide-risk screening questions were more direct and clear than were the two suicide questions included in the PHQ-9A screening.
For example, the PHQ-9A includes the following suicide-risk questions: “Has there been a time in the past month when you have had serious thoughts about ending your life?” and “Have you EVER, in your WHOLE LIFE, tried to kill yourself or made a suicide attempt?” The teen can respond with “not at all,” “several days,” “more than half the days” or “nearly every day.”
Meanwhile, the ASQ questionnaire focuses on a more narrow time period and includes questions such as “In the past few weeks, have you wished you were dead?” and “Have you ever tried to kill yourself?” Teens respond by answering “yes” or “no.”
“So I think the difference is by asking questions that are really direct and very clear about suicide risk, you end up identifying more cases than this kind of general question about thoughts of killing yourself,” Dr. Kemper explained. “It makes sense when you think about where adolescents are in terms of their development, that the more specific you [are], the more likely you are to find what you’re looking for.”
Kelly Curran, MD, who was not involved in the study, said that because some of the ASQ questions “overlap” with the suicide-risk questions on the PHQ-9A, she didn’t expect the ASQ to identify more positive cases.
However, Dr. Curran said it is possible for suicidal teens to fall through the cracks during a depression screening because some of them may not self-identify as depressed.
“I don’t think we often think about the importance of linguistics or how something is asked,” said Dr. Curran, associate professor in the department of pediatrics at the University of Oklahoma, Oklahoma City.
“So asking [teens] these kind of direct questions about suicide may pick up on these cases of people who don’t necessarily have the insight into their sadness or their general kind of thought process.”
Dr. Kemper said he hopes the study would encourage pediatricians to adopt depression screening if they’re not already doing it and to think about whether they should implement suicide-risk screening in their practice. The study also highlights the importance of following up after a positive screening.
“There are a lot of teens who have depression or increased suicide risk that you wouldn’t identify if you didn’t screen, and a key aspect of any kind of screening is that you need to be prepared to provide follow-up care after a positive screening,” he explained.
Study limitations include the fact that the subjects were recruited from a single health care system that serves mostly urban and low-income communities, and that the study was not designed to determine test accuracy.
Dr. Kemper and Dr. Curran indicated that they have no financial disclosures.
Suicide-risk screening may identify cases that typically fall through the cracks during depression screening, new research suggests.
The study, published in Pediatrics, found that the Ask Suicide-Screening Questions (ASQ) identified 2.2% of additional cases compared with those screened for any type of depression or other mental illnesses, and 8.3% of additional cases compared with those who screened positive for major depressive disorder.
About 3.2% of U.S. children between the ages of 3 and 17 have been diagnosed with depression, according to the Centers for Disease Control and Prevention. The American Academy of Pediatrics and the U.S. Preventive Services Task Force recommends that all teens be routinely screened for depression. However, there’s no specific recommendation that adolescents should also be screened for suicide in addition to depression screening.
The study highlights the high baseline rates of depression and suicide risk and the need for pediatric practices to plan for them and develop strategies about how they’re going to provide follow-up care, including treatment for suicidal teens.
“We began this project because we were concerned that we might be missing teens with increased risk of suicide by screening only for depression,” study author Alex Kemper, MD, said in an interview. “Our goal with this project was really to compare standard depression screening tools that we’ve used for a long time with a suicide-specific instrument just to see if we would identify additional cases with a suicide-risk instrument.”
Dr. Kemper and colleagues collected data from 803 mostly Medicaid-enrolled adolescents across 12 primary care practices. The subjects were between the ages of 12 and 20 years, with no recent history of depression or self-harm, who were screened with the Patient Health Questionnaire–9 Modified for Adolescents (PHQ-9A) and ASQ. For the study, two PHQ-9A screening strategies were evaluated: screening for any type of depression or other mental illness (positive on any item) or screening for major depressive disorder.
In addition, the researchers found that 56.4% of patients had a positive PHQ-9A screen for any type of depression and 24.7% had a positive PHQ-9A screen for major depressive disorder. Meanwhile, 21.1% of the population received a positive screen result. Of those who responded on the PHQ-9A that they did not have suicidal thoughts in the past month, 13.2% had a positive ASQ result.
Dr. Kemper, division chief of primary care pediatrics at Nationwide Children’s Hospital and professor of pediatrics at the Ohio State University, both in Columbus, said the suicide-risk screening questions were more direct and clear than were the two suicide questions included in the PHQ-9A screening.
For example, the PHQ-9A includes the following suicide-risk questions: “Has there been a time in the past month when you have had serious thoughts about ending your life?” and “Have you EVER, in your WHOLE LIFE, tried to kill yourself or made a suicide attempt?” The teen can respond with “not at all,” “several days,” “more than half the days” or “nearly every day.”
Meanwhile, the ASQ questionnaire focuses on a more narrow time period and includes questions such as “In the past few weeks, have you wished you were dead?” and “Have you ever tried to kill yourself?” Teens respond by answering “yes” or “no.”
“So I think the difference is by asking questions that are really direct and very clear about suicide risk, you end up identifying more cases than this kind of general question about thoughts of killing yourself,” Dr. Kemper explained. “It makes sense when you think about where adolescents are in terms of their development, that the more specific you [are], the more likely you are to find what you’re looking for.”
Kelly Curran, MD, who was not involved in the study, said that because some of the ASQ questions “overlap” with the suicide-risk questions on the PHQ-9A, she didn’t expect the ASQ to identify more positive cases.
However, Dr. Curran said it is possible for suicidal teens to fall through the cracks during a depression screening because some of them may not self-identify as depressed.
“I don’t think we often think about the importance of linguistics or how something is asked,” said Dr. Curran, associate professor in the department of pediatrics at the University of Oklahoma, Oklahoma City.
“So asking [teens] these kind of direct questions about suicide may pick up on these cases of people who don’t necessarily have the insight into their sadness or their general kind of thought process.”
Dr. Kemper said he hopes the study would encourage pediatricians to adopt depression screening if they’re not already doing it and to think about whether they should implement suicide-risk screening in their practice. The study also highlights the importance of following up after a positive screening.
“There are a lot of teens who have depression or increased suicide risk that you wouldn’t identify if you didn’t screen, and a key aspect of any kind of screening is that you need to be prepared to provide follow-up care after a positive screening,” he explained.
Study limitations include the fact that the subjects were recruited from a single health care system that serves mostly urban and low-income communities, and that the study was not designed to determine test accuracy.
Dr. Kemper and Dr. Curran indicated that they have no financial disclosures.
Suicide-risk screening may identify cases that typically fall through the cracks during depression screening, new research suggests.
The study, published in Pediatrics, found that the Ask Suicide-Screening Questions (ASQ) identified 2.2% of additional cases compared with those screened for any type of depression or other mental illnesses, and 8.3% of additional cases compared with those who screened positive for major depressive disorder.
About 3.2% of U.S. children between the ages of 3 and 17 have been diagnosed with depression, according to the Centers for Disease Control and Prevention. The American Academy of Pediatrics and the U.S. Preventive Services Task Force recommends that all teens be routinely screened for depression. However, there’s no specific recommendation that adolescents should also be screened for suicide in addition to depression screening.
The study highlights the high baseline rates of depression and suicide risk and the need for pediatric practices to plan for them and develop strategies about how they’re going to provide follow-up care, including treatment for suicidal teens.
“We began this project because we were concerned that we might be missing teens with increased risk of suicide by screening only for depression,” study author Alex Kemper, MD, said in an interview. “Our goal with this project was really to compare standard depression screening tools that we’ve used for a long time with a suicide-specific instrument just to see if we would identify additional cases with a suicide-risk instrument.”
Dr. Kemper and colleagues collected data from 803 mostly Medicaid-enrolled adolescents across 12 primary care practices. The subjects were between the ages of 12 and 20 years, with no recent history of depression or self-harm, who were screened with the Patient Health Questionnaire–9 Modified for Adolescents (PHQ-9A) and ASQ. For the study, two PHQ-9A screening strategies were evaluated: screening for any type of depression or other mental illness (positive on any item) or screening for major depressive disorder.
In addition, the researchers found that 56.4% of patients had a positive PHQ-9A screen for any type of depression and 24.7% had a positive PHQ-9A screen for major depressive disorder. Meanwhile, 21.1% of the population received a positive screen result. Of those who responded on the PHQ-9A that they did not have suicidal thoughts in the past month, 13.2% had a positive ASQ result.
Dr. Kemper, division chief of primary care pediatrics at Nationwide Children’s Hospital and professor of pediatrics at the Ohio State University, both in Columbus, said the suicide-risk screening questions were more direct and clear than were the two suicide questions included in the PHQ-9A screening.
For example, the PHQ-9A includes the following suicide-risk questions: “Has there been a time in the past month when you have had serious thoughts about ending your life?” and “Have you EVER, in your WHOLE LIFE, tried to kill yourself or made a suicide attempt?” The teen can respond with “not at all,” “several days,” “more than half the days” or “nearly every day.”
Meanwhile, the ASQ questionnaire focuses on a more narrow time period and includes questions such as “In the past few weeks, have you wished you were dead?” and “Have you ever tried to kill yourself?” Teens respond by answering “yes” or “no.”
“So I think the difference is by asking questions that are really direct and very clear about suicide risk, you end up identifying more cases than this kind of general question about thoughts of killing yourself,” Dr. Kemper explained. “It makes sense when you think about where adolescents are in terms of their development, that the more specific you [are], the more likely you are to find what you’re looking for.”
Kelly Curran, MD, who was not involved in the study, said that because some of the ASQ questions “overlap” with the suicide-risk questions on the PHQ-9A, she didn’t expect the ASQ to identify more positive cases.
However, Dr. Curran said it is possible for suicidal teens to fall through the cracks during a depression screening because some of them may not self-identify as depressed.
“I don’t think we often think about the importance of linguistics or how something is asked,” said Dr. Curran, associate professor in the department of pediatrics at the University of Oklahoma, Oklahoma City.
“So asking [teens] these kind of direct questions about suicide may pick up on these cases of people who don’t necessarily have the insight into their sadness or their general kind of thought process.”
Dr. Kemper said he hopes the study would encourage pediatricians to adopt depression screening if they’re not already doing it and to think about whether they should implement suicide-risk screening in their practice. The study also highlights the importance of following up after a positive screening.
“There are a lot of teens who have depression or increased suicide risk that you wouldn’t identify if you didn’t screen, and a key aspect of any kind of screening is that you need to be prepared to provide follow-up care after a positive screening,” he explained.
Study limitations include the fact that the subjects were recruited from a single health care system that serves mostly urban and low-income communities, and that the study was not designed to determine test accuracy.
Dr. Kemper and Dr. Curran indicated that they have no financial disclosures.
Drug effective in treating symptoms of postpartum depression
Those suffering from postpartum depression may have a more convenient treatment option, compared with the only drug approved by the Food and Drug Administration to specifically treat this mood disorder.
Observations from phase 3 of a clinical trial published in JAMA Psychiatry shows that zuranolone, an oral drug, improved the core symptoms of postpartum depression after just 3 days.
Postpartum depression affects approximately one in eight women, according to the Centers for Disease Control and Prevention. Brexanolone (Zulresso), which was approved by the FDA in 2019 to treat this condition, is administered intravenously over a 60-hour period with medical supervision.
“Many women don’t have child care and are unable to go to a hospital setting for 72 hours to receive treatment,” study author Kristina Deligiannidis, MD, associate professor at the Feinstein Institutes for Medical Research, Manhasset, N.Y., said in an interview. “The field really does need a variety of new and novel treatments that are fast acting. It is of utmost importance that we treat [postpartum depression] as quickly as possible because it has significant effects on maternal function, mood, and the ability to care for infants.”
Dr. Deligiannidis and colleagues randomly placed 153 volunteers between the ages of 18 and 45 years, who were 6 months or less post partum, into a group that would receive either a placebo or 30 mg of zuranolone daily for 2 weeks. The participants were followed for 45 days to test the effect of the drug.
Researchers measured depression using the Hamilton Rating Scale for Depression (HAMD-17) – where a score of 10-13 means a patient has mild symptoms, 14-17 means mild to moderate symptoms, and anything over 17 equals moderate to severe symptoms. At the baseline of the study, the average HAMD-17 score of those in the zuranolone and placebo groups were 28.4 and 28.8, respectively.
Researchers found that after day 3, 41% of those in the zuranolone group had a 50% or greater reduction in HAMD-17 score from baseline. By day 15, the day after their last dose, 72% of those who had taken zuranolone had a reduction in HAMD-17 compared with 56% of those who had taken the placebo. By day 45, that increased to 75% in the zuranolone group and 57% in the placebo group.
Dr. Deligiannidis, who initially wasn’t sure how long it would take for patients to see the beneficial effects of zuranolone, was surprised by how fast-acting the oral drug appeared to be in the clinical trial. Unlike brexanolone, which is infused into the veins and has rapid access to the brain and nervous system, zuranolone is an oral medicine that has to go through the stomach and the gastrointestinal tract, and then it has to go into the blood system and then has to cross the blood-brain barrier, she explained.
By day 15, 45% of women who took zuranolone received a HAMD-17 score of 7 or under, meaning they have remitted depression. By day 45, 53% of women who had taken the drug were in remission.
Although the zuranolone was well tolerated, about 5% of the group experienced adverse events. Of those who experienced side effects, 15% experienced drowsiness, 9% suffered from headaches, and 8% experienced dizziness and developed an upper respiratory infection. Participants also suffered diarrhea and sedation.
Lissette Tanner, MD, MPH, FACOG, who was not involved with the study, thought the current study’s findings were promising and would be a great alternative to brexanolone.
“You have the additional benefit that it’s an oral agent as opposed to injection, which I know a lot of patients often have concerns about,” said Dr. Tanner, assistant professor of gynecology and obstetrics at Emory University, Atlanta. “[It’s] an exciting prospect for clinical care to be able to prescribe an oral agent patients can feel comfortable taking at home.”
When it comes to the study’s method, Dr. Tanner noted that the researchers used the HAMD-17 scale as opposed to the Edinburgh Postnatal Depression Scale (EPDS), something that is used “a lot more in clinical situations and providers are a lot more familiar with.” Using the EPDS score would be more applicable “in terms of introducing these medications into true clinical care.”
In terms of follow-up, Dr. Tanner said there may be a need for ongoing research that follows the study participants for more than 45 days.
“For depressive symptoms in particular, oftentimes those symptoms ebb and flow. So seeing if there is a long-term response to these medications or just kind of an immediate onset then wane will be important in the future,” she added.
Dr. Tanner is also interested in pharmacokinetic studies involving zuranolone to see how much of the medication may potentially pass into breast milk.
Dr. Deligiannidis and Dr. Tanner had no financial disclosures.
Those suffering from postpartum depression may have a more convenient treatment option, compared with the only drug approved by the Food and Drug Administration to specifically treat this mood disorder.
Observations from phase 3 of a clinical trial published in JAMA Psychiatry shows that zuranolone, an oral drug, improved the core symptoms of postpartum depression after just 3 days.
Postpartum depression affects approximately one in eight women, according to the Centers for Disease Control and Prevention. Brexanolone (Zulresso), which was approved by the FDA in 2019 to treat this condition, is administered intravenously over a 60-hour period with medical supervision.
“Many women don’t have child care and are unable to go to a hospital setting for 72 hours to receive treatment,” study author Kristina Deligiannidis, MD, associate professor at the Feinstein Institutes for Medical Research, Manhasset, N.Y., said in an interview. “The field really does need a variety of new and novel treatments that are fast acting. It is of utmost importance that we treat [postpartum depression] as quickly as possible because it has significant effects on maternal function, mood, and the ability to care for infants.”
Dr. Deligiannidis and colleagues randomly placed 153 volunteers between the ages of 18 and 45 years, who were 6 months or less post partum, into a group that would receive either a placebo or 30 mg of zuranolone daily for 2 weeks. The participants were followed for 45 days to test the effect of the drug.
Researchers measured depression using the Hamilton Rating Scale for Depression (HAMD-17) – where a score of 10-13 means a patient has mild symptoms, 14-17 means mild to moderate symptoms, and anything over 17 equals moderate to severe symptoms. At the baseline of the study, the average HAMD-17 score of those in the zuranolone and placebo groups were 28.4 and 28.8, respectively.
Researchers found that after day 3, 41% of those in the zuranolone group had a 50% or greater reduction in HAMD-17 score from baseline. By day 15, the day after their last dose, 72% of those who had taken zuranolone had a reduction in HAMD-17 compared with 56% of those who had taken the placebo. By day 45, that increased to 75% in the zuranolone group and 57% in the placebo group.
Dr. Deligiannidis, who initially wasn’t sure how long it would take for patients to see the beneficial effects of zuranolone, was surprised by how fast-acting the oral drug appeared to be in the clinical trial. Unlike brexanolone, which is infused into the veins and has rapid access to the brain and nervous system, zuranolone is an oral medicine that has to go through the stomach and the gastrointestinal tract, and then it has to go into the blood system and then has to cross the blood-brain barrier, she explained.
By day 15, 45% of women who took zuranolone received a HAMD-17 score of 7 or under, meaning they have remitted depression. By day 45, 53% of women who had taken the drug were in remission.
Although the zuranolone was well tolerated, about 5% of the group experienced adverse events. Of those who experienced side effects, 15% experienced drowsiness, 9% suffered from headaches, and 8% experienced dizziness and developed an upper respiratory infection. Participants also suffered diarrhea and sedation.
Lissette Tanner, MD, MPH, FACOG, who was not involved with the study, thought the current study’s findings were promising and would be a great alternative to brexanolone.
“You have the additional benefit that it’s an oral agent as opposed to injection, which I know a lot of patients often have concerns about,” said Dr. Tanner, assistant professor of gynecology and obstetrics at Emory University, Atlanta. “[It’s] an exciting prospect for clinical care to be able to prescribe an oral agent patients can feel comfortable taking at home.”
When it comes to the study’s method, Dr. Tanner noted that the researchers used the HAMD-17 scale as opposed to the Edinburgh Postnatal Depression Scale (EPDS), something that is used “a lot more in clinical situations and providers are a lot more familiar with.” Using the EPDS score would be more applicable “in terms of introducing these medications into true clinical care.”
In terms of follow-up, Dr. Tanner said there may be a need for ongoing research that follows the study participants for more than 45 days.
“For depressive symptoms in particular, oftentimes those symptoms ebb and flow. So seeing if there is a long-term response to these medications or just kind of an immediate onset then wane will be important in the future,” she added.
Dr. Tanner is also interested in pharmacokinetic studies involving zuranolone to see how much of the medication may potentially pass into breast milk.
Dr. Deligiannidis and Dr. Tanner had no financial disclosures.
Those suffering from postpartum depression may have a more convenient treatment option, compared with the only drug approved by the Food and Drug Administration to specifically treat this mood disorder.
Observations from phase 3 of a clinical trial published in JAMA Psychiatry shows that zuranolone, an oral drug, improved the core symptoms of postpartum depression after just 3 days.
Postpartum depression affects approximately one in eight women, according to the Centers for Disease Control and Prevention. Brexanolone (Zulresso), which was approved by the FDA in 2019 to treat this condition, is administered intravenously over a 60-hour period with medical supervision.
“Many women don’t have child care and are unable to go to a hospital setting for 72 hours to receive treatment,” study author Kristina Deligiannidis, MD, associate professor at the Feinstein Institutes for Medical Research, Manhasset, N.Y., said in an interview. “The field really does need a variety of new and novel treatments that are fast acting. It is of utmost importance that we treat [postpartum depression] as quickly as possible because it has significant effects on maternal function, mood, and the ability to care for infants.”
Dr. Deligiannidis and colleagues randomly placed 153 volunteers between the ages of 18 and 45 years, who were 6 months or less post partum, into a group that would receive either a placebo or 30 mg of zuranolone daily for 2 weeks. The participants were followed for 45 days to test the effect of the drug.
Researchers measured depression using the Hamilton Rating Scale for Depression (HAMD-17) – where a score of 10-13 means a patient has mild symptoms, 14-17 means mild to moderate symptoms, and anything over 17 equals moderate to severe symptoms. At the baseline of the study, the average HAMD-17 score of those in the zuranolone and placebo groups were 28.4 and 28.8, respectively.
Researchers found that after day 3, 41% of those in the zuranolone group had a 50% or greater reduction in HAMD-17 score from baseline. By day 15, the day after their last dose, 72% of those who had taken zuranolone had a reduction in HAMD-17 compared with 56% of those who had taken the placebo. By day 45, that increased to 75% in the zuranolone group and 57% in the placebo group.
Dr. Deligiannidis, who initially wasn’t sure how long it would take for patients to see the beneficial effects of zuranolone, was surprised by how fast-acting the oral drug appeared to be in the clinical trial. Unlike brexanolone, which is infused into the veins and has rapid access to the brain and nervous system, zuranolone is an oral medicine that has to go through the stomach and the gastrointestinal tract, and then it has to go into the blood system and then has to cross the blood-brain barrier, she explained.
By day 15, 45% of women who took zuranolone received a HAMD-17 score of 7 or under, meaning they have remitted depression. By day 45, 53% of women who had taken the drug were in remission.
Although the zuranolone was well tolerated, about 5% of the group experienced adverse events. Of those who experienced side effects, 15% experienced drowsiness, 9% suffered from headaches, and 8% experienced dizziness and developed an upper respiratory infection. Participants also suffered diarrhea and sedation.
Lissette Tanner, MD, MPH, FACOG, who was not involved with the study, thought the current study’s findings were promising and would be a great alternative to brexanolone.
“You have the additional benefit that it’s an oral agent as opposed to injection, which I know a lot of patients often have concerns about,” said Dr. Tanner, assistant professor of gynecology and obstetrics at Emory University, Atlanta. “[It’s] an exciting prospect for clinical care to be able to prescribe an oral agent patients can feel comfortable taking at home.”
When it comes to the study’s method, Dr. Tanner noted that the researchers used the HAMD-17 scale as opposed to the Edinburgh Postnatal Depression Scale (EPDS), something that is used “a lot more in clinical situations and providers are a lot more familiar with.” Using the EPDS score would be more applicable “in terms of introducing these medications into true clinical care.”
In terms of follow-up, Dr. Tanner said there may be a need for ongoing research that follows the study participants for more than 45 days.
“For depressive symptoms in particular, oftentimes those symptoms ebb and flow. So seeing if there is a long-term response to these medications or just kind of an immediate onset then wane will be important in the future,” she added.
Dr. Tanner is also interested in pharmacokinetic studies involving zuranolone to see how much of the medication may potentially pass into breast milk.
Dr. Deligiannidis and Dr. Tanner had no financial disclosures.
FROM JAMA PSYCHIATRY
Opioid prescriptions decrease in young kids, long dosages increase
The opioid prescription rates have significantly decreased for children, teens, and younger adults between 2006 and 2018, according to new research.
“What’s important about this new study is that it documented that these improvements were also occurring for children and young adults specifically,” said Kao-Ping Chua, MD, PhD, primary care physician and assistant professor of pediatrics at the University of Michigan, Ann Arbor, who was not involved in the study. “The reason that’s important is that changes in medical practice for adults aren’t always reflected in pediatrics.”
The study, published in JAMA Pediatrics, found that dispensed opioid prescriptions for this population have decreased by 15% annually since 2013. However, the study also examined specific prescribing variables, such as duration of opioid prescription and high-dosage prescriptions. Researchers found reduced rates of high-dosage and long-duration prescriptions for adolescents and younger adults. However, these types of prescription practices increased in children aged 0-5 years.
“I think [the findings are] promising, suggesting that opiate prescribing practices may be improving,” study author Madeline Renny, MD, pediatric emergency medicine doctor at New York University Langone Health, said in an interview. “But we did find that there were increases in the young children for the practice variables, which we didn’t expect. I think that was kind of one of the findings that we were a bit surprised about and want to explore further.”
Previous studies have linked prescription opioid use in children and teens to an increased risk of future opioid misuse. A 2015 study published in Pediatrics found that using prescribed opioids before the 12th grade is associated with a 33% increase in the risk of future opioid misuse by the age of 23. The study also found that for those with a low predicted risk of future opioid misuse, an opioid prescription increases the risk for misuse after high school threefold.
Furthermore, a 2018 study published in JAMA Network Open found that, between 1999 and 2016, the annual estimated mortality rate for all children and adolescents from prescription and illicit opioid use rose 268.2%.
In the new study, Dr. Renny and colleagues examined data from 2006 to 2018 from IQVIA Longitudinal Prescription Data, which captured 74%-92% of U.S. retail outpatient opioid prescriptions dispensed to people up to the age of 24. Researchers also examined prescribing practice variables, which included opioid dispensing rates, average amount of opioid dispensed per prescription, duration of opioid prescription, high-dosage opioid prescription for individuals, and the rate in which extended-release or long-acting opioids are prescribed.
Researchers found that between 2006 and 2018, the total U.S. annual opioid prescriptions dispensed to patients younger than 25 years was highest in 2007 at 15,689,779 prescriptions, and since 2012 has steadily decreased to 6,705,478 in 2018.
“Our study did show that there were declines, but opioids remain readily dispensed,” Dr. Renny said. “And I think it’s good that rates have gone down, but I think opioids are still commonly dispensed to children and adolescents and young adults and all of our age groups.”
Dr. Chua said that the study was important, but when it came to younger children, it didn’t account for the fact that “the underlying population of patients who were getting opioids changed because it’s not the same group of children.”
“Maybe at the beginning there were more surgical patients who are getting shorter duration, lower dosage opioids,” he added. “Now some of those surgical exceptions kind of went away and who’s left in the population of people who get opioids is a sicker population.”
“Who are the 0 to 5-year-olds who are getting opioids now?” Dr. Chua asked. “Well, some of them are going to be cancer or surgical patients. If you think about it, over time their surgeons may be more judicious and they stop prescribing opioids for some things like circumcision or something like that. So that means that who’s left in the population of children who get opiate prescriptions are the cancer patients. Cancer patients’ opioid dosages are going to be higher because they have chronic pain.”
Dr. Chua said it is important to remember that the number of children who are affected by those high-risk prescriptions are lower because the overall number of opioid prescriptions has gone down. He added that the key piece of missing information is the absolute number of prescriptions that were high risk.
Researchers of the current study suggested that, because of the differences between pediatric and adult pain and indications for opioid prescribing, there should be national guidelines on general opioid prescribing for children and adolescents.
Experts did not disclose relevant financial relationships.
The opioid prescription rates have significantly decreased for children, teens, and younger adults between 2006 and 2018, according to new research.
“What’s important about this new study is that it documented that these improvements were also occurring for children and young adults specifically,” said Kao-Ping Chua, MD, PhD, primary care physician and assistant professor of pediatrics at the University of Michigan, Ann Arbor, who was not involved in the study. “The reason that’s important is that changes in medical practice for adults aren’t always reflected in pediatrics.”
The study, published in JAMA Pediatrics, found that dispensed opioid prescriptions for this population have decreased by 15% annually since 2013. However, the study also examined specific prescribing variables, such as duration of opioid prescription and high-dosage prescriptions. Researchers found reduced rates of high-dosage and long-duration prescriptions for adolescents and younger adults. However, these types of prescription practices increased in children aged 0-5 years.
“I think [the findings are] promising, suggesting that opiate prescribing practices may be improving,” study author Madeline Renny, MD, pediatric emergency medicine doctor at New York University Langone Health, said in an interview. “But we did find that there were increases in the young children for the practice variables, which we didn’t expect. I think that was kind of one of the findings that we were a bit surprised about and want to explore further.”
Previous studies have linked prescription opioid use in children and teens to an increased risk of future opioid misuse. A 2015 study published in Pediatrics found that using prescribed opioids before the 12th grade is associated with a 33% increase in the risk of future opioid misuse by the age of 23. The study also found that for those with a low predicted risk of future opioid misuse, an opioid prescription increases the risk for misuse after high school threefold.
Furthermore, a 2018 study published in JAMA Network Open found that, between 1999 and 2016, the annual estimated mortality rate for all children and adolescents from prescription and illicit opioid use rose 268.2%.
In the new study, Dr. Renny and colleagues examined data from 2006 to 2018 from IQVIA Longitudinal Prescription Data, which captured 74%-92% of U.S. retail outpatient opioid prescriptions dispensed to people up to the age of 24. Researchers also examined prescribing practice variables, which included opioid dispensing rates, average amount of opioid dispensed per prescription, duration of opioid prescription, high-dosage opioid prescription for individuals, and the rate in which extended-release or long-acting opioids are prescribed.
Researchers found that between 2006 and 2018, the total U.S. annual opioid prescriptions dispensed to patients younger than 25 years was highest in 2007 at 15,689,779 prescriptions, and since 2012 has steadily decreased to 6,705,478 in 2018.
“Our study did show that there were declines, but opioids remain readily dispensed,” Dr. Renny said. “And I think it’s good that rates have gone down, but I think opioids are still commonly dispensed to children and adolescents and young adults and all of our age groups.”
Dr. Chua said that the study was important, but when it came to younger children, it didn’t account for the fact that “the underlying population of patients who were getting opioids changed because it’s not the same group of children.”
“Maybe at the beginning there were more surgical patients who are getting shorter duration, lower dosage opioids,” he added. “Now some of those surgical exceptions kind of went away and who’s left in the population of people who get opioids is a sicker population.”
“Who are the 0 to 5-year-olds who are getting opioids now?” Dr. Chua asked. “Well, some of them are going to be cancer or surgical patients. If you think about it, over time their surgeons may be more judicious and they stop prescribing opioids for some things like circumcision or something like that. So that means that who’s left in the population of children who get opiate prescriptions are the cancer patients. Cancer patients’ opioid dosages are going to be higher because they have chronic pain.”
Dr. Chua said it is important to remember that the number of children who are affected by those high-risk prescriptions are lower because the overall number of opioid prescriptions has gone down. He added that the key piece of missing information is the absolute number of prescriptions that were high risk.
Researchers of the current study suggested that, because of the differences between pediatric and adult pain and indications for opioid prescribing, there should be national guidelines on general opioid prescribing for children and adolescents.
Experts did not disclose relevant financial relationships.
The opioid prescription rates have significantly decreased for children, teens, and younger adults between 2006 and 2018, according to new research.
“What’s important about this new study is that it documented that these improvements were also occurring for children and young adults specifically,” said Kao-Ping Chua, MD, PhD, primary care physician and assistant professor of pediatrics at the University of Michigan, Ann Arbor, who was not involved in the study. “The reason that’s important is that changes in medical practice for adults aren’t always reflected in pediatrics.”
The study, published in JAMA Pediatrics, found that dispensed opioid prescriptions for this population have decreased by 15% annually since 2013. However, the study also examined specific prescribing variables, such as duration of opioid prescription and high-dosage prescriptions. Researchers found reduced rates of high-dosage and long-duration prescriptions for adolescents and younger adults. However, these types of prescription practices increased in children aged 0-5 years.
“I think [the findings are] promising, suggesting that opiate prescribing practices may be improving,” study author Madeline Renny, MD, pediatric emergency medicine doctor at New York University Langone Health, said in an interview. “But we did find that there were increases in the young children for the practice variables, which we didn’t expect. I think that was kind of one of the findings that we were a bit surprised about and want to explore further.”
Previous studies have linked prescription opioid use in children and teens to an increased risk of future opioid misuse. A 2015 study published in Pediatrics found that using prescribed opioids before the 12th grade is associated with a 33% increase in the risk of future opioid misuse by the age of 23. The study also found that for those with a low predicted risk of future opioid misuse, an opioid prescription increases the risk for misuse after high school threefold.
Furthermore, a 2018 study published in JAMA Network Open found that, between 1999 and 2016, the annual estimated mortality rate for all children and adolescents from prescription and illicit opioid use rose 268.2%.
In the new study, Dr. Renny and colleagues examined data from 2006 to 2018 from IQVIA Longitudinal Prescription Data, which captured 74%-92% of U.S. retail outpatient opioid prescriptions dispensed to people up to the age of 24. Researchers also examined prescribing practice variables, which included opioid dispensing rates, average amount of opioid dispensed per prescription, duration of opioid prescription, high-dosage opioid prescription for individuals, and the rate in which extended-release or long-acting opioids are prescribed.
Researchers found that between 2006 and 2018, the total U.S. annual opioid prescriptions dispensed to patients younger than 25 years was highest in 2007 at 15,689,779 prescriptions, and since 2012 has steadily decreased to 6,705,478 in 2018.
“Our study did show that there were declines, but opioids remain readily dispensed,” Dr. Renny said. “And I think it’s good that rates have gone down, but I think opioids are still commonly dispensed to children and adolescents and young adults and all of our age groups.”
Dr. Chua said that the study was important, but when it came to younger children, it didn’t account for the fact that “the underlying population of patients who were getting opioids changed because it’s not the same group of children.”
“Maybe at the beginning there were more surgical patients who are getting shorter duration, lower dosage opioids,” he added. “Now some of those surgical exceptions kind of went away and who’s left in the population of people who get opioids is a sicker population.”
“Who are the 0 to 5-year-olds who are getting opioids now?” Dr. Chua asked. “Well, some of them are going to be cancer or surgical patients. If you think about it, over time their surgeons may be more judicious and they stop prescribing opioids for some things like circumcision or something like that. So that means that who’s left in the population of children who get opiate prescriptions are the cancer patients. Cancer patients’ opioid dosages are going to be higher because they have chronic pain.”
Dr. Chua said it is important to remember that the number of children who are affected by those high-risk prescriptions are lower because the overall number of opioid prescriptions has gone down. He added that the key piece of missing information is the absolute number of prescriptions that were high risk.
Researchers of the current study suggested that, because of the differences between pediatric and adult pain and indications for opioid prescribing, there should be national guidelines on general opioid prescribing for children and adolescents.
Experts did not disclose relevant financial relationships.
FROM JAMA PEDIATRICS
Diversity of pediatric residents, fellows continues to lag
The proportion of underrepresented groups in pediatric fellowships decreased between 2007 and 2019, while those in pediatric residencies remained stagnant, new research revealed.
Researchers acknowledged that some of the factors contributing to the low proportion of minorities in the pediatric workforce may include educational disparities starting in primary or secondary school, such as underfunded schools and lack of educational resources.
“Something I really appreciated about the paper is that this goes beyond a student stepping into medical school, finding a mentor in pediatrics, and then eventually matriculating into a pediatric residency,” said Christle Nwora, MD, an internal medicine–pediatrics resident physician at Johns Hopkins Urban Health Residency Program in Baltimore, who was not involved in the study. “I like the idea of knowing that people aren’t going into the field and being very critical as to why.”
Prior studies, including a 2019 study published in JAMA Network Open, has found that minority students remain underrepresented in medical schools. However, this most recent study, published in Pediatrics, is one of the first to report trends in the race or ethnicity of pediatric residents and fellows.
“It’s been pretty well documented throughout the medical literature that the representation of underrepresented [groups] in medicine is low among all specialties,” study author Kimberly Montez, MD, MPH, FAAP, said in an interview. “This is one of the first studies that [show this trend] in pediatrics, [but] we were kind of expecting [these findings] knowing the rest of the literature out there.”
Dr. Montez and colleagues examined self-reported race and ethnicity data from 2007 to 2019 for pediatric residents and fellows from the GME Census reports. The annual number of pediatric trainees increased from 7,964 to 8,950 between 2007 and 2019. For pediatric subspecialty fellows, that number increased from 2,684 to 3,966.
The number of underrepresented pediatric trainees also increased over time, from 1,277 to 1,478 residents and 382 to 532 subspecialty fellows. However, researchers found that the trend in proportion of underrepresented in medicine (URiM) trainees was unchanged in pediatric residencies – 16% in 2007 to 16.5% in 2019 – and, overall, decreased for URiM subspecialty fellows from 14.2% in 2007 to 13.5% in 2019.
“I was shocked at the fact that there has been no significant increase either over the last 12 years,” said Joan Park, MD, a pediatric resident at Johns Hopkins Hospital, Baltimore, who was not involved in the study. “In the news, we’re seeing way more discussions in regards to racism and representation and the fact that that hasn’t really fueled or caught fire yet in medicine at all to really move that arrow is definitely really shocking.”
The recent study also pointed out that the percentage of underrepresented groups in pediatric residencies and fellowships is considerably lower in comparison with those groups’ representations in the U.S. population. For example, Black or African American people make up 13.4% of the U.S. population but just 5.6% of pediatric trainees. Meanwhile, American Indian or Alaskan Native people make up 1.3% of the U.S. population but make up 0.2% of pediatric trainees.
Dr. Montez hypothesized that the lack of underrepresented groups as pediatric trainees – or in the medical field, in general – may have to do with systemic barriers that span the entire educational continuum and affects them even before they reach medical school, including attendance at underfunded primary and secondary schools.
“Just think about all the barriers that exist for underrepresented minorities in medicine,” said Dr. Montez, assistant professor of pediatrics at Wake Forest University, Winston-Salem, N.C. “We know that underrepresented minorities are accepted and matriculate at lower rates than [those of] their nonminority counterparts. All of this occurs even just before getting into the field of pediatrics. So multiple barriers exist.”
Those barriers may also include racism, bias, and discrimination, which may play out unconsciously when members of an underrepresented group are applying for residencies or med school, such as “recognizing a name that may be from a different ethnic or racial background and then unconsciously biasing yourself against that applicant, for example,” Dr. Montez explained.
Dr. Montez said that although there has been progress, there is still a long way to go. She hopes the study will help academic institutions and professional organizations recognize the importance of diversity in pediatrics. She noted that pediatric trainees are more likely to experience microaggressions, which could potentially cause them to leave a program.
“I hope this will galvanize pediatric programs to really think a lot about the environment that they create for underrepresented minority trainees and also about their recruitment process in terms of making sure it’s standardized, using a holistic review,” Dr. Montez explained.
In 2016, the Association of American Medical Colleges published a diversity and inclusion strategic planning guide to improve training programs. Furthermore, in 2019, the Accreditation Council for Graduate Medical Education instituted a new common program requirement on diversity that requires programs to focus on systematic recruitment and retention of a diverse and inclusive workforce of residents and fellows.
“The same way pediatricians are aware of how the environment will shape the way a child grows up, we have to be mindful of the way an environment that surrounds the medical student will shape where they eventually end up as well,” said Dr. Nwora.
The experts disclosed no conflicts of interest.
The proportion of underrepresented groups in pediatric fellowships decreased between 2007 and 2019, while those in pediatric residencies remained stagnant, new research revealed.
Researchers acknowledged that some of the factors contributing to the low proportion of minorities in the pediatric workforce may include educational disparities starting in primary or secondary school, such as underfunded schools and lack of educational resources.
“Something I really appreciated about the paper is that this goes beyond a student stepping into medical school, finding a mentor in pediatrics, and then eventually matriculating into a pediatric residency,” said Christle Nwora, MD, an internal medicine–pediatrics resident physician at Johns Hopkins Urban Health Residency Program in Baltimore, who was not involved in the study. “I like the idea of knowing that people aren’t going into the field and being very critical as to why.”
Prior studies, including a 2019 study published in JAMA Network Open, has found that minority students remain underrepresented in medical schools. However, this most recent study, published in Pediatrics, is one of the first to report trends in the race or ethnicity of pediatric residents and fellows.
“It’s been pretty well documented throughout the medical literature that the representation of underrepresented [groups] in medicine is low among all specialties,” study author Kimberly Montez, MD, MPH, FAAP, said in an interview. “This is one of the first studies that [show this trend] in pediatrics, [but] we were kind of expecting [these findings] knowing the rest of the literature out there.”
Dr. Montez and colleagues examined self-reported race and ethnicity data from 2007 to 2019 for pediatric residents and fellows from the GME Census reports. The annual number of pediatric trainees increased from 7,964 to 8,950 between 2007 and 2019. For pediatric subspecialty fellows, that number increased from 2,684 to 3,966.
The number of underrepresented pediatric trainees also increased over time, from 1,277 to 1,478 residents and 382 to 532 subspecialty fellows. However, researchers found that the trend in proportion of underrepresented in medicine (URiM) trainees was unchanged in pediatric residencies – 16% in 2007 to 16.5% in 2019 – and, overall, decreased for URiM subspecialty fellows from 14.2% in 2007 to 13.5% in 2019.
“I was shocked at the fact that there has been no significant increase either over the last 12 years,” said Joan Park, MD, a pediatric resident at Johns Hopkins Hospital, Baltimore, who was not involved in the study. “In the news, we’re seeing way more discussions in regards to racism and representation and the fact that that hasn’t really fueled or caught fire yet in medicine at all to really move that arrow is definitely really shocking.”
The recent study also pointed out that the percentage of underrepresented groups in pediatric residencies and fellowships is considerably lower in comparison with those groups’ representations in the U.S. population. For example, Black or African American people make up 13.4% of the U.S. population but just 5.6% of pediatric trainees. Meanwhile, American Indian or Alaskan Native people make up 1.3% of the U.S. population but make up 0.2% of pediatric trainees.
Dr. Montez hypothesized that the lack of underrepresented groups as pediatric trainees – or in the medical field, in general – may have to do with systemic barriers that span the entire educational continuum and affects them even before they reach medical school, including attendance at underfunded primary and secondary schools.
“Just think about all the barriers that exist for underrepresented minorities in medicine,” said Dr. Montez, assistant professor of pediatrics at Wake Forest University, Winston-Salem, N.C. “We know that underrepresented minorities are accepted and matriculate at lower rates than [those of] their nonminority counterparts. All of this occurs even just before getting into the field of pediatrics. So multiple barriers exist.”
Those barriers may also include racism, bias, and discrimination, which may play out unconsciously when members of an underrepresented group are applying for residencies or med school, such as “recognizing a name that may be from a different ethnic or racial background and then unconsciously biasing yourself against that applicant, for example,” Dr. Montez explained.
Dr. Montez said that although there has been progress, there is still a long way to go. She hopes the study will help academic institutions and professional organizations recognize the importance of diversity in pediatrics. She noted that pediatric trainees are more likely to experience microaggressions, which could potentially cause them to leave a program.
“I hope this will galvanize pediatric programs to really think a lot about the environment that they create for underrepresented minority trainees and also about their recruitment process in terms of making sure it’s standardized, using a holistic review,” Dr. Montez explained.
In 2016, the Association of American Medical Colleges published a diversity and inclusion strategic planning guide to improve training programs. Furthermore, in 2019, the Accreditation Council for Graduate Medical Education instituted a new common program requirement on diversity that requires programs to focus on systematic recruitment and retention of a diverse and inclusive workforce of residents and fellows.
“The same way pediatricians are aware of how the environment will shape the way a child grows up, we have to be mindful of the way an environment that surrounds the medical student will shape where they eventually end up as well,” said Dr. Nwora.
The experts disclosed no conflicts of interest.
The proportion of underrepresented groups in pediatric fellowships decreased between 2007 and 2019, while those in pediatric residencies remained stagnant, new research revealed.
Researchers acknowledged that some of the factors contributing to the low proportion of minorities in the pediatric workforce may include educational disparities starting in primary or secondary school, such as underfunded schools and lack of educational resources.
“Something I really appreciated about the paper is that this goes beyond a student stepping into medical school, finding a mentor in pediatrics, and then eventually matriculating into a pediatric residency,” said Christle Nwora, MD, an internal medicine–pediatrics resident physician at Johns Hopkins Urban Health Residency Program in Baltimore, who was not involved in the study. “I like the idea of knowing that people aren’t going into the field and being very critical as to why.”
Prior studies, including a 2019 study published in JAMA Network Open, has found that minority students remain underrepresented in medical schools. However, this most recent study, published in Pediatrics, is one of the first to report trends in the race or ethnicity of pediatric residents and fellows.
“It’s been pretty well documented throughout the medical literature that the representation of underrepresented [groups] in medicine is low among all specialties,” study author Kimberly Montez, MD, MPH, FAAP, said in an interview. “This is one of the first studies that [show this trend] in pediatrics, [but] we were kind of expecting [these findings] knowing the rest of the literature out there.”
Dr. Montez and colleagues examined self-reported race and ethnicity data from 2007 to 2019 for pediatric residents and fellows from the GME Census reports. The annual number of pediatric trainees increased from 7,964 to 8,950 between 2007 and 2019. For pediatric subspecialty fellows, that number increased from 2,684 to 3,966.
The number of underrepresented pediatric trainees also increased over time, from 1,277 to 1,478 residents and 382 to 532 subspecialty fellows. However, researchers found that the trend in proportion of underrepresented in medicine (URiM) trainees was unchanged in pediatric residencies – 16% in 2007 to 16.5% in 2019 – and, overall, decreased for URiM subspecialty fellows from 14.2% in 2007 to 13.5% in 2019.
“I was shocked at the fact that there has been no significant increase either over the last 12 years,” said Joan Park, MD, a pediatric resident at Johns Hopkins Hospital, Baltimore, who was not involved in the study. “In the news, we’re seeing way more discussions in regards to racism and representation and the fact that that hasn’t really fueled or caught fire yet in medicine at all to really move that arrow is definitely really shocking.”
The recent study also pointed out that the percentage of underrepresented groups in pediatric residencies and fellowships is considerably lower in comparison with those groups’ representations in the U.S. population. For example, Black or African American people make up 13.4% of the U.S. population but just 5.6% of pediatric trainees. Meanwhile, American Indian or Alaskan Native people make up 1.3% of the U.S. population but make up 0.2% of pediatric trainees.
Dr. Montez hypothesized that the lack of underrepresented groups as pediatric trainees – or in the medical field, in general – may have to do with systemic barriers that span the entire educational continuum and affects them even before they reach medical school, including attendance at underfunded primary and secondary schools.
“Just think about all the barriers that exist for underrepresented minorities in medicine,” said Dr. Montez, assistant professor of pediatrics at Wake Forest University, Winston-Salem, N.C. “We know that underrepresented minorities are accepted and matriculate at lower rates than [those of] their nonminority counterparts. All of this occurs even just before getting into the field of pediatrics. So multiple barriers exist.”
Those barriers may also include racism, bias, and discrimination, which may play out unconsciously when members of an underrepresented group are applying for residencies or med school, such as “recognizing a name that may be from a different ethnic or racial background and then unconsciously biasing yourself against that applicant, for example,” Dr. Montez explained.
Dr. Montez said that although there has been progress, there is still a long way to go. She hopes the study will help academic institutions and professional organizations recognize the importance of diversity in pediatrics. She noted that pediatric trainees are more likely to experience microaggressions, which could potentially cause them to leave a program.
“I hope this will galvanize pediatric programs to really think a lot about the environment that they create for underrepresented minority trainees and also about their recruitment process in terms of making sure it’s standardized, using a holistic review,” Dr. Montez explained.
In 2016, the Association of American Medical Colleges published a diversity and inclusion strategic planning guide to improve training programs. Furthermore, in 2019, the Accreditation Council for Graduate Medical Education instituted a new common program requirement on diversity that requires programs to focus on systematic recruitment and retention of a diverse and inclusive workforce of residents and fellows.
“The same way pediatricians are aware of how the environment will shape the way a child grows up, we have to be mindful of the way an environment that surrounds the medical student will shape where they eventually end up as well,” said Dr. Nwora.
The experts disclosed no conflicts of interest.
Toxic chemicals found in many cosmetics
People may be absorbing and ingesting potentially toxic chemicals from their cosmetic products, a new study suggests.
– per- and polyfluoroalkyl substances. Many of these chemicals were not included on the product labels, making it difficult for consumers to consciously avoid them.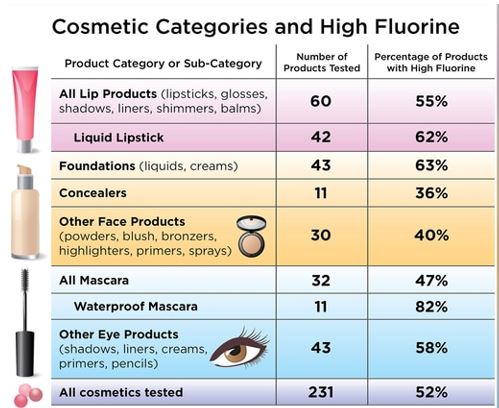
“This study is very helpful for elucidating the PFAS content of different types of cosmetics in the U.S. and Canadian markets,” said Elsie Sunderland, PhD, an environmental scientist who was not involved with the study.
“Previously, all the data had been collected in Europe, and this study shows we are dealing with similar problems in the North American marketplace,” said Dr. Sunderland, a professor of environmental chemistry at the Harvard School of Public Health, Boston.
PFAS are a class of chemicals used in a variety of consumer products, such as nonstick cookware, stain-resistant carpeting, and water-repellent clothing, according to the Centers for Disease Control and Prevention. They are added to cosmetics to make the products more durable and spreadable, researchers said in the study.
“[PFAS] are added to change the properties of surfaces, to make them nonstick or resistant to stay in water or oils,” said study coauthor Tom Bruton, PhD, senior scientist at the Green Science Policy Institute in Berkeley, Calif. “The concerning thing about cosmetics is that these are products that you’re applying to your skin and face every day, so there’s the skin absorption route that’s of concern, but also incidental ingestion of cosmetics is also a concern as well.”
The CDC says some of the potential health effects of PFAS exposure includes increased cholesterol levels, increased risk of kidney and testicular cancer, changes in liver enzymes, decreased vaccine response in children, and a higher risk of high blood pressure or preeclampsia in pregnant women.
“PFAS are a large class of chemicals. In humans, exposure to some of these chemicals has been associated with impaired immune function, certain cancers, increased risks of diabetes, obesity and endocrine disruption,” Dr. Sunderland said. “They appear to be harmful to every major organ system in the human body.”
For the current study, published online in Environmental Science & Technology Letters, Dr. Bruton and colleagues purchased 231 cosmetic products in the United States and Canada from retailers such as Ulta Beauty, Sephora, Target, and Bed Bath & Beyond. They then screened them for fluorine.Three-quarters of waterproof mascara samples contained high fluorine concentrations, as did nearly two-thirds of foundations and liquid lipsticks, and more than half of the eye and lip products tested.
The authors found that different categories of makeup tended to have higher or lower fluorine concentrations. “High fluorine levels were found in products commonly advertised as ‘wear-resistant’ to water and oils or ‘long-lasting,’ including foundations, liquid lipsticks, and waterproof mascaras,” Dr. Bruton and colleagues wrote.
When they further analyzed a subset of 29 products to determine what types of chemicals were present, they found that each cosmetic product contained at least 4 PFAS, with one product containing 13.The PFAS substances found included some that break down into other chemicals that are known to be highly toxic and environmentally harmful.
“It’s concerning that some of the products we tested appear to be intentionally using PFAS, but not listing those ingredients on the label,” Dr. Bruton said. “I do think that it is helpful for consumers to read labels, but beyond that, there’s not a lot of ways that consumers themselves can solve this problem. ... We think that the industry needs to be more proactive about moving away from this group of chemicals.”
Dr. Sunderland said a resource people can use when trying to avoid PFAS is the Environmental Working Group, a nonprofit organization that maintains an extensive database of cosmetics and personal care products.
“At this point, there is very little regulatory activity related to PFAS in cosmetics,” Dr. Sunderland said. “The best thing to happen now would be for consumers to indicate that they prefer products without PFAS and to demand better transparency in product ingredient lists.”
A similar study done in 2018 by the Danish Environmental Protection Agency found high levels of PFAS in nearly one-third of the cosmetics products it tested.
People can also be exposed to PFAS by eating or drinking contaminated food or water and through food packaging. Dr. Sunderland said some wild foods like seafood are known to accumulate these compounds in the environment.
“There are examples of contaminated biosolids leading to accumulation of PFAS in vegetables and milk,” Dr. Sunderland explained. “Food packaging is another concern because it can also result in PFAS accumulation in the foods we eat.”
Although it’s difficult to avoid PFAS altogether, the CDC suggests lowering exposure rates by avoiding contaminated water and food. If you’re not sure if your water is contaminated, you should ask your local or state health and environmental quality departments for fish or water advisories in your area.
A version of this article first appeared on WebMD.com.
People may be absorbing and ingesting potentially toxic chemicals from their cosmetic products, a new study suggests.
– per- and polyfluoroalkyl substances. Many of these chemicals were not included on the product labels, making it difficult for consumers to consciously avoid them.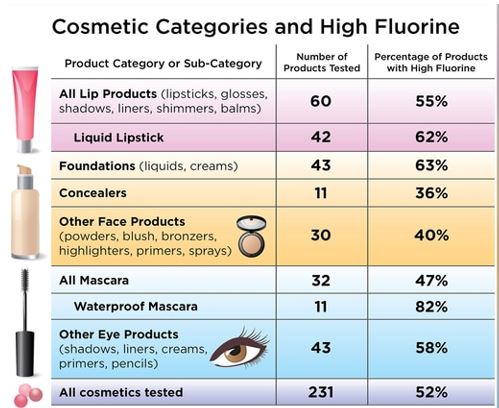
“This study is very helpful for elucidating the PFAS content of different types of cosmetics in the U.S. and Canadian markets,” said Elsie Sunderland, PhD, an environmental scientist who was not involved with the study.
“Previously, all the data had been collected in Europe, and this study shows we are dealing with similar problems in the North American marketplace,” said Dr. Sunderland, a professor of environmental chemistry at the Harvard School of Public Health, Boston.
PFAS are a class of chemicals used in a variety of consumer products, such as nonstick cookware, stain-resistant carpeting, and water-repellent clothing, according to the Centers for Disease Control and Prevention. They are added to cosmetics to make the products more durable and spreadable, researchers said in the study.
“[PFAS] are added to change the properties of surfaces, to make them nonstick or resistant to stay in water or oils,” said study coauthor Tom Bruton, PhD, senior scientist at the Green Science Policy Institute in Berkeley, Calif. “The concerning thing about cosmetics is that these are products that you’re applying to your skin and face every day, so there’s the skin absorption route that’s of concern, but also incidental ingestion of cosmetics is also a concern as well.”
The CDC says some of the potential health effects of PFAS exposure includes increased cholesterol levels, increased risk of kidney and testicular cancer, changes in liver enzymes, decreased vaccine response in children, and a higher risk of high blood pressure or preeclampsia in pregnant women.
“PFAS are a large class of chemicals. In humans, exposure to some of these chemicals has been associated with impaired immune function, certain cancers, increased risks of diabetes, obesity and endocrine disruption,” Dr. Sunderland said. “They appear to be harmful to every major organ system in the human body.”
For the current study, published online in Environmental Science & Technology Letters, Dr. Bruton and colleagues purchased 231 cosmetic products in the United States and Canada from retailers such as Ulta Beauty, Sephora, Target, and Bed Bath & Beyond. They then screened them for fluorine.Three-quarters of waterproof mascara samples contained high fluorine concentrations, as did nearly two-thirds of foundations and liquid lipsticks, and more than half of the eye and lip products tested.
The authors found that different categories of makeup tended to have higher or lower fluorine concentrations. “High fluorine levels were found in products commonly advertised as ‘wear-resistant’ to water and oils or ‘long-lasting,’ including foundations, liquid lipsticks, and waterproof mascaras,” Dr. Bruton and colleagues wrote.
When they further analyzed a subset of 29 products to determine what types of chemicals were present, they found that each cosmetic product contained at least 4 PFAS, with one product containing 13.The PFAS substances found included some that break down into other chemicals that are known to be highly toxic and environmentally harmful.
“It’s concerning that some of the products we tested appear to be intentionally using PFAS, but not listing those ingredients on the label,” Dr. Bruton said. “I do think that it is helpful for consumers to read labels, but beyond that, there’s not a lot of ways that consumers themselves can solve this problem. ... We think that the industry needs to be more proactive about moving away from this group of chemicals.”
Dr. Sunderland said a resource people can use when trying to avoid PFAS is the Environmental Working Group, a nonprofit organization that maintains an extensive database of cosmetics and personal care products.
“At this point, there is very little regulatory activity related to PFAS in cosmetics,” Dr. Sunderland said. “The best thing to happen now would be for consumers to indicate that they prefer products without PFAS and to demand better transparency in product ingredient lists.”
A similar study done in 2018 by the Danish Environmental Protection Agency found high levels of PFAS in nearly one-third of the cosmetics products it tested.
People can also be exposed to PFAS by eating or drinking contaminated food or water and through food packaging. Dr. Sunderland said some wild foods like seafood are known to accumulate these compounds in the environment.
“There are examples of contaminated biosolids leading to accumulation of PFAS in vegetables and milk,” Dr. Sunderland explained. “Food packaging is another concern because it can also result in PFAS accumulation in the foods we eat.”
Although it’s difficult to avoid PFAS altogether, the CDC suggests lowering exposure rates by avoiding contaminated water and food. If you’re not sure if your water is contaminated, you should ask your local or state health and environmental quality departments for fish or water advisories in your area.
A version of this article first appeared on WebMD.com.
People may be absorbing and ingesting potentially toxic chemicals from their cosmetic products, a new study suggests.
– per- and polyfluoroalkyl substances. Many of these chemicals were not included on the product labels, making it difficult for consumers to consciously avoid them.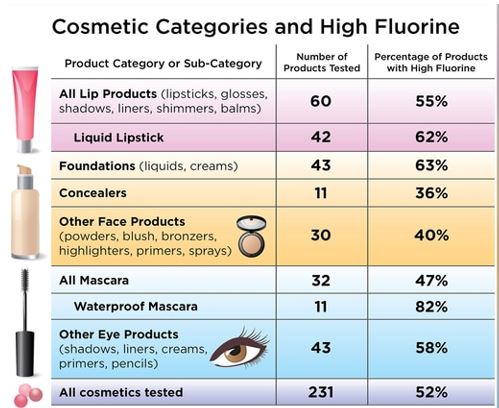
“This study is very helpful for elucidating the PFAS content of different types of cosmetics in the U.S. and Canadian markets,” said Elsie Sunderland, PhD, an environmental scientist who was not involved with the study.
“Previously, all the data had been collected in Europe, and this study shows we are dealing with similar problems in the North American marketplace,” said Dr. Sunderland, a professor of environmental chemistry at the Harvard School of Public Health, Boston.
PFAS are a class of chemicals used in a variety of consumer products, such as nonstick cookware, stain-resistant carpeting, and water-repellent clothing, according to the Centers for Disease Control and Prevention. They are added to cosmetics to make the products more durable and spreadable, researchers said in the study.
“[PFAS] are added to change the properties of surfaces, to make them nonstick or resistant to stay in water or oils,” said study coauthor Tom Bruton, PhD, senior scientist at the Green Science Policy Institute in Berkeley, Calif. “The concerning thing about cosmetics is that these are products that you’re applying to your skin and face every day, so there’s the skin absorption route that’s of concern, but also incidental ingestion of cosmetics is also a concern as well.”
The CDC says some of the potential health effects of PFAS exposure includes increased cholesterol levels, increased risk of kidney and testicular cancer, changes in liver enzymes, decreased vaccine response in children, and a higher risk of high blood pressure or preeclampsia in pregnant women.
“PFAS are a large class of chemicals. In humans, exposure to some of these chemicals has been associated with impaired immune function, certain cancers, increased risks of diabetes, obesity and endocrine disruption,” Dr. Sunderland said. “They appear to be harmful to every major organ system in the human body.”
For the current study, published online in Environmental Science & Technology Letters, Dr. Bruton and colleagues purchased 231 cosmetic products in the United States and Canada from retailers such as Ulta Beauty, Sephora, Target, and Bed Bath & Beyond. They then screened them for fluorine.Three-quarters of waterproof mascara samples contained high fluorine concentrations, as did nearly two-thirds of foundations and liquid lipsticks, and more than half of the eye and lip products tested.
The authors found that different categories of makeup tended to have higher or lower fluorine concentrations. “High fluorine levels were found in products commonly advertised as ‘wear-resistant’ to water and oils or ‘long-lasting,’ including foundations, liquid lipsticks, and waterproof mascaras,” Dr. Bruton and colleagues wrote.
When they further analyzed a subset of 29 products to determine what types of chemicals were present, they found that each cosmetic product contained at least 4 PFAS, with one product containing 13.The PFAS substances found included some that break down into other chemicals that are known to be highly toxic and environmentally harmful.
“It’s concerning that some of the products we tested appear to be intentionally using PFAS, but not listing those ingredients on the label,” Dr. Bruton said. “I do think that it is helpful for consumers to read labels, but beyond that, there’s not a lot of ways that consumers themselves can solve this problem. ... We think that the industry needs to be more proactive about moving away from this group of chemicals.”
Dr. Sunderland said a resource people can use when trying to avoid PFAS is the Environmental Working Group, a nonprofit organization that maintains an extensive database of cosmetics and personal care products.
“At this point, there is very little regulatory activity related to PFAS in cosmetics,” Dr. Sunderland said. “The best thing to happen now would be for consumers to indicate that they prefer products without PFAS and to demand better transparency in product ingredient lists.”
A similar study done in 2018 by the Danish Environmental Protection Agency found high levels of PFAS in nearly one-third of the cosmetics products it tested.
People can also be exposed to PFAS by eating or drinking contaminated food or water and through food packaging. Dr. Sunderland said some wild foods like seafood are known to accumulate these compounds in the environment.
“There are examples of contaminated biosolids leading to accumulation of PFAS in vegetables and milk,” Dr. Sunderland explained. “Food packaging is another concern because it can also result in PFAS accumulation in the foods we eat.”
Although it’s difficult to avoid PFAS altogether, the CDC suggests lowering exposure rates by avoiding contaminated water and food. If you’re not sure if your water is contaminated, you should ask your local or state health and environmental quality departments for fish or water advisories in your area.
A version of this article first appeared on WebMD.com.
LDCT lung cancer screening may ID aortic stenosis risk
says new research published in Annals of Internal Medicine.
Aortic stenosis is one of the most common valve disease problems and is characterized by the narrowing of the aortic valve opening, according to the American Heart Association. The condition impedes the delivery of blood from the heart to the body.
Researchers found that LDCT, which according to the Centers for Disease Control and Prevention is the only recommended screening test for lung cancer, also can be used to identify aortic valve calcification – a condition in which calcium deposits form on the aortic valve, narrowing it.
Since cardiovascular events and lung cancer are known to have the same modifiable risk factors, people screened for lung cancer could also be diagnosed with cardiovascular diseases, the authors noted in their paper.
Furthermore, a 2019 study published in the Journal of Thoracic Imaging found that LDCT can be useful for identifying not just lung cancer, but the early stages of chronic obstructive pulmonary disease and coronary artery disease.
“LDCT has been described as useful for identifying the early stages of chronic obstructive pulmonary disease and coronary artery disease, but it can also [screen for] calcified aortic valve [which corresponds] with the risk of severe aortic stenosis,” study author Marcin Fijalkowski, MD, PhD, of the Medical University of Gdansk, said in an interview. “This additional evaluation is not time-consuming and is easy to perform.”
Methods and results
For the study, Dr. Fijalkowski and his colleagues examined data from 6,631 people between the ages of 50 and 80 years of age with a smoking history of 30 or more pack-years. The group was enrolled in the MOLTEST BIS lung cancer screening program between 2016 and 2018, which assessed the usefulness of LDCT performed during lung cancer screening in determining the degree of aortic valve calcification as an additional finding. The researchers arbitrarily determined a calcium score of 900 as a cutoff point indicating a positive test result. Positive patients were sent for an echocardiogram for confirmation of diagnosis.
Aortic valve calcification was identified in 869 patients, 13.1% of the group. Sixty-eight participants, which is about 8% of this group, were identified as having a calcium score of 900 at least and were referred for echocardiography to confirm these results. Of this group, 0.5% were diagnosed with at least moderate aortic stenosis after receiving an echocardiogram. About 55% of the participants with this condition were unaware of their valvular heart disease, including 23% with a severe form of the disease.
Study identified patients who had not been aware of disease
Dr. Fijalkowski said while he was not surprised by the findings, he was surprised that the study may have saved some of the participants’ lives.
“We were expecting the same degree of calcification of aortic valve and correlation with aortic stenosis severity, but what surprised us was that half of diagnosed patients were not aware of disease,” he said. “This additional finding was lifesaving.”
In the paper, the authors noted that cardiology societies do not yet recognize LDCT as a diagnostic tool for aortic stenosis. Based on their findings, they propose that aortic valve calcification become a routine assessment procedure in the LDCT protocol for lung cancer screening.
Findings are ‘important’ but not practice changing
Salim S. Virani, MD, FACC, who was not involved in the study, said this new research is important.
The analyses were done well and push the needle further in a direction that suggests “when we are doing imaging for one reason, we should use the totality of information that we have available,” he noted.
“I mean, if you are looking at a lung nodule, if you see an aortic valve that’s very calcified, then it should prompt you to at least ask the patient about some symptoms related to that,” Dr. Virani explained.
However, he said more research is needed on a larger population before LDCT can be considered a diagnostic tool for aortic stenosis.
“I think we have to understand that this study was done in a very specific group of patients,” said Dr. Virani, professor in the sections of cardiology and cardiovascular research at Baylor College of Medicine, Houston. “If you were to do it in a population that was much younger, with much lower risk of even lung cancer, then the yield of a CT to pick up aortic stenosis would be lower.”
Before any practice changes are made regarding LDCT and the diagnosis of aortic stenosis, there needs to be more research on how many people in the general population are getting non–cardiology-related chest imaging and then come up with a population-based metric as to what calcium score cutoff could be used, he said.
Dr. Fijalkowski said he believes the results of his study will encourage physicians to focus not only on pulmonary nodules but also to look for additional things such as aortic valve calcification.
The experts did not disclose any relevant financial relationships.
says new research published in Annals of Internal Medicine.
Aortic stenosis is one of the most common valve disease problems and is characterized by the narrowing of the aortic valve opening, according to the American Heart Association. The condition impedes the delivery of blood from the heart to the body.
Researchers found that LDCT, which according to the Centers for Disease Control and Prevention is the only recommended screening test for lung cancer, also can be used to identify aortic valve calcification – a condition in which calcium deposits form on the aortic valve, narrowing it.
Since cardiovascular events and lung cancer are known to have the same modifiable risk factors, people screened for lung cancer could also be diagnosed with cardiovascular diseases, the authors noted in their paper.
Furthermore, a 2019 study published in the Journal of Thoracic Imaging found that LDCT can be useful for identifying not just lung cancer, but the early stages of chronic obstructive pulmonary disease and coronary artery disease.
“LDCT has been described as useful for identifying the early stages of chronic obstructive pulmonary disease and coronary artery disease, but it can also [screen for] calcified aortic valve [which corresponds] with the risk of severe aortic stenosis,” study author Marcin Fijalkowski, MD, PhD, of the Medical University of Gdansk, said in an interview. “This additional evaluation is not time-consuming and is easy to perform.”
Methods and results
For the study, Dr. Fijalkowski and his colleagues examined data from 6,631 people between the ages of 50 and 80 years of age with a smoking history of 30 or more pack-years. The group was enrolled in the MOLTEST BIS lung cancer screening program between 2016 and 2018, which assessed the usefulness of LDCT performed during lung cancer screening in determining the degree of aortic valve calcification as an additional finding. The researchers arbitrarily determined a calcium score of 900 as a cutoff point indicating a positive test result. Positive patients were sent for an echocardiogram for confirmation of diagnosis.
Aortic valve calcification was identified in 869 patients, 13.1% of the group. Sixty-eight participants, which is about 8% of this group, were identified as having a calcium score of 900 at least and were referred for echocardiography to confirm these results. Of this group, 0.5% were diagnosed with at least moderate aortic stenosis after receiving an echocardiogram. About 55% of the participants with this condition were unaware of their valvular heart disease, including 23% with a severe form of the disease.
Study identified patients who had not been aware of disease
Dr. Fijalkowski said while he was not surprised by the findings, he was surprised that the study may have saved some of the participants’ lives.
“We were expecting the same degree of calcification of aortic valve and correlation with aortic stenosis severity, but what surprised us was that half of diagnosed patients were not aware of disease,” he said. “This additional finding was lifesaving.”
In the paper, the authors noted that cardiology societies do not yet recognize LDCT as a diagnostic tool for aortic stenosis. Based on their findings, they propose that aortic valve calcification become a routine assessment procedure in the LDCT protocol for lung cancer screening.
Findings are ‘important’ but not practice changing
Salim S. Virani, MD, FACC, who was not involved in the study, said this new research is important.
The analyses were done well and push the needle further in a direction that suggests “when we are doing imaging for one reason, we should use the totality of information that we have available,” he noted.
“I mean, if you are looking at a lung nodule, if you see an aortic valve that’s very calcified, then it should prompt you to at least ask the patient about some symptoms related to that,” Dr. Virani explained.
However, he said more research is needed on a larger population before LDCT can be considered a diagnostic tool for aortic stenosis.
“I think we have to understand that this study was done in a very specific group of patients,” said Dr. Virani, professor in the sections of cardiology and cardiovascular research at Baylor College of Medicine, Houston. “If you were to do it in a population that was much younger, with much lower risk of even lung cancer, then the yield of a CT to pick up aortic stenosis would be lower.”
Before any practice changes are made regarding LDCT and the diagnosis of aortic stenosis, there needs to be more research on how many people in the general population are getting non–cardiology-related chest imaging and then come up with a population-based metric as to what calcium score cutoff could be used, he said.
Dr. Fijalkowski said he believes the results of his study will encourage physicians to focus not only on pulmonary nodules but also to look for additional things such as aortic valve calcification.
The experts did not disclose any relevant financial relationships.
says new research published in Annals of Internal Medicine.
Aortic stenosis is one of the most common valve disease problems and is characterized by the narrowing of the aortic valve opening, according to the American Heart Association. The condition impedes the delivery of blood from the heart to the body.
Researchers found that LDCT, which according to the Centers for Disease Control and Prevention is the only recommended screening test for lung cancer, also can be used to identify aortic valve calcification – a condition in which calcium deposits form on the aortic valve, narrowing it.
Since cardiovascular events and lung cancer are known to have the same modifiable risk factors, people screened for lung cancer could also be diagnosed with cardiovascular diseases, the authors noted in their paper.
Furthermore, a 2019 study published in the Journal of Thoracic Imaging found that LDCT can be useful for identifying not just lung cancer, but the early stages of chronic obstructive pulmonary disease and coronary artery disease.
“LDCT has been described as useful for identifying the early stages of chronic obstructive pulmonary disease and coronary artery disease, but it can also [screen for] calcified aortic valve [which corresponds] with the risk of severe aortic stenosis,” study author Marcin Fijalkowski, MD, PhD, of the Medical University of Gdansk, said in an interview. “This additional evaluation is not time-consuming and is easy to perform.”
Methods and results
For the study, Dr. Fijalkowski and his colleagues examined data from 6,631 people between the ages of 50 and 80 years of age with a smoking history of 30 or more pack-years. The group was enrolled in the MOLTEST BIS lung cancer screening program between 2016 and 2018, which assessed the usefulness of LDCT performed during lung cancer screening in determining the degree of aortic valve calcification as an additional finding. The researchers arbitrarily determined a calcium score of 900 as a cutoff point indicating a positive test result. Positive patients were sent for an echocardiogram for confirmation of diagnosis.
Aortic valve calcification was identified in 869 patients, 13.1% of the group. Sixty-eight participants, which is about 8% of this group, were identified as having a calcium score of 900 at least and were referred for echocardiography to confirm these results. Of this group, 0.5% were diagnosed with at least moderate aortic stenosis after receiving an echocardiogram. About 55% of the participants with this condition were unaware of their valvular heart disease, including 23% with a severe form of the disease.
Study identified patients who had not been aware of disease
Dr. Fijalkowski said while he was not surprised by the findings, he was surprised that the study may have saved some of the participants’ lives.
“We were expecting the same degree of calcification of aortic valve and correlation with aortic stenosis severity, but what surprised us was that half of diagnosed patients were not aware of disease,” he said. “This additional finding was lifesaving.”
In the paper, the authors noted that cardiology societies do not yet recognize LDCT as a diagnostic tool for aortic stenosis. Based on their findings, they propose that aortic valve calcification become a routine assessment procedure in the LDCT protocol for lung cancer screening.
Findings are ‘important’ but not practice changing
Salim S. Virani, MD, FACC, who was not involved in the study, said this new research is important.
The analyses were done well and push the needle further in a direction that suggests “when we are doing imaging for one reason, we should use the totality of information that we have available,” he noted.
“I mean, if you are looking at a lung nodule, if you see an aortic valve that’s very calcified, then it should prompt you to at least ask the patient about some symptoms related to that,” Dr. Virani explained.
However, he said more research is needed on a larger population before LDCT can be considered a diagnostic tool for aortic stenosis.
“I think we have to understand that this study was done in a very specific group of patients,” said Dr. Virani, professor in the sections of cardiology and cardiovascular research at Baylor College of Medicine, Houston. “If you were to do it in a population that was much younger, with much lower risk of even lung cancer, then the yield of a CT to pick up aortic stenosis would be lower.”
Before any practice changes are made regarding LDCT and the diagnosis of aortic stenosis, there needs to be more research on how many people in the general population are getting non–cardiology-related chest imaging and then come up with a population-based metric as to what calcium score cutoff could be used, he said.
Dr. Fijalkowski said he believes the results of his study will encourage physicians to focus not only on pulmonary nodules but also to look for additional things such as aortic valve calcification.
The experts did not disclose any relevant financial relationships.
FROM ANNALS OF INTERNAL MEDICINE



