User login
Shakespeare and suicide
The medical knowledge that William Shakespeare possessed has awed scholars for centuries. Theories about the provenance of his knowledge abound (such as his son-in-law being a physician), and the inclusion of medical terms and ailments throughout his plays suggests a broad knowledge of disease and sickness. Scholars have noted how he sprinkles references to dermatologic, neurologic, orthopedic, and metabolic ailments throughout his plays, mentioning carbuncles, fistulas, corpulence, rhinophyma, scurvy, ague, enuresis, kyphosis, epilepsy, and parkinsonism.1 What seems to strike post-Enlightenment audiences—and what sets Shakespeare apart from many of his contemporaries—is his portrayal of “complex” characters, those with what we envision as rich interior worlds and with whom a modern audience can resonate. There is a reason psychiatrists such as Sigmund Freud have rushed back to Shakespeare and (sometimes anachronistically) found in his characters various psychiatric diagnoses such as depression, anxiety, paranoia, jealous delusions, and obsessive-compulsive disorder. Suicide and suicidal ideation are prevalent themes in some of Shakespeare’s most well-known characters.
A surprisingly common theme
The gravest outcome of a psychiatric illness is death by suicide, which occurs in 13 of Shakespeare’s characters.2 There are additional characters who exhibit suicidal ideation without a completed act. Shakespearean characters whose lives end in suicide are variably portrayed, dying by various means and circumstances. Hamlet (who dies at the hand of his foe, Laertes), famously soliloquizes the theme of suicide and the afterlife. He ponders “tak[ing] arms against a sea of troubles.” Ophelia dies ambiguously. Immediately after, her mother and brother recount her death in a brook—having had “too much of water” when her garments “heavy with their drink, | pull’d the poor wretch from her melodious lay | To muddy death.” The 2 clowns/gravediggers then debate whether Ophelia deserves a Christian burial and if her death should be considered a suicide: did the water drown her, or did she drown herself?3
Lady Macbeth’s suicide is offstage, punctuated by a “night-shriek.” Romeo drinks poison and dies “with a kiss.” Juliet quickly follows, making her body the sword’s sheath which “there rust, and let [her] die.” Othello stabs himself after requesting that his peers will “speak of me as I am.” One of King Lear’s daughters poisons her sister “and after [slays] herself.” Timon dies by his cave, “entomb’d upon the very hem o’ the sea.” In Antony and Cleopatra, after being told that Cleopatra has killed herself with Antony’s name on her lips, Antony begs to be stabbed and then stabs himself; he is not defeated by Caesar, but rather conquered by himself: “none but Antony | Should conquer Antony.” Cleopatra and her lady-in-waiting, Charmian, kill themselves with an asp. In Julius Caesar, Brutus runs upon his sword. Cassius begs for his own death, asking that “this good sword, | That ran through Caesar’s bowels, search this bosom.” Portia, it is reported, “swallowed fire.”
Shakespeare uses specific stylized language to portray characters in psychological anguish and suicidal states. Scholars have discussed how he uses certain stylistic language to highlight the anguish that happens during solitary, solipsistic moments of contemplation.4 Moments of anguish and suicidal ideation are marked by verbal repetition. An example of this repetition comes in Hamlet’s speech after he returns to the kingdom where his uncle has usurped his father, when he laments that he cannot end his own life. He says:
O, that this too too sullied flesh would melt,
Thaw, and resolve itself into a dew!
Or that the Everlasting had not fix’d
His canon ’gainst self-slaughter! O God, God,
How weary, stale, flat, and unprofitable
Seem to me all the uses of this world.
In these 6 lines, there are 2 instances of verbal repetition: “too too” and “God, God.” In this moment of solitude and despair, Hamlet’s speech fractures; his fractured speech reflects his fractured psyche. While Hamlet speaks of staleness and stagnation in the world, his words represent a sterile excess. No meaning is elicited by their repetition; there is no forward momentum to his speech. The words reflect the extent to which Hamlet is stuck and divided in this moment. Something similar happens in Macbeth’s “Tomorrow and tomorrow and tomorrow” speech. The words march on, and with each repetition they become increasingly hollow and brittle.
Why does this discussion of suicide in Shakespeare hold value for a contemporary psychiatrist? First, there is no single prototypical suicidal character in Shakespeare. His characters who are suicidal vary in their demographics and incentives for ending their lives. In this way, he provides a rich framework, one with which many people can engage. Second, this discussion fits into an existing paradigm for using art therapy (specifically Shakespeare) as a treatment modality for trauma.5 Programs such as DE-CRUIT have used the recitation of Shakespearean verse as a means of processing trauma in veterans.5 While Shakespeare does not mention a remedy for suicide in his plays, perhaps the text can serve as medicine. Third, the repetitive speech that Shakespeare uses in times of anguish could be a fairly accurate reflection of speech patterns in patients who are suicidal. Research that completed a spoken language analysis of patients who were suicidal has found “mechanical and repetitive phrasing” as a quality of these patients’ speech.6,7
For hundreds of years, critics have searched beyond the text for Shakespeare’s voice and opinion; what did he himself think of melancholy, despair, or suicide? We cannot know. We, as readers, are invited to explore a nuanced and multifaceted view of suicide, one that neither chides nor valorizes the act, and provides ambiguity rather than condemnation.
1. Paciaroni M, Bogousslavsky J. William Shakespeare’s neurology. Prog Brain Res. 2013;206:3-18.
2. Kirkland LR. To end itself by death: suicide in Shakespeare’s tragedies. South Med J. 1999;92(7):660-666.
3. Sale C. The “Amending Hand”: Hales v. Petit, Eyston v. Studd, and Equitable Action in Hamlet. In: Jordan C, Cunningham K, eds. The Law in Shakespeare. Early Modern Literature in History. Palgrave Macmillan; 2007:189-207. https://doi.org/10.1057/9780230626348_11
4. Langley E. Narcissism and Suicide in Shakespeare and His Contemporaries. Oxford University Press; 2009.
5. Ali A, Wolfert S, Lam I, et al. Intersecting modes of aesthetic distance and mimetic induction in therapeutic process: examining a drama-based treatment for military-related traumatic stress. Drama Therapy Review. 2018;4(2):153-165.
6. Belouali A, Gupta S, Sourirajan V, et al. Acoustic and language analysis of speech for suicidal ideation among US veterans. BioData Min. 2021;14(1):11. doi:10.1186/s13040-021-00245-y
7. Cummins N, Scherer S, Krajewski J, et al. A review of depression and suicide risk assessment using speech analysis. Speech Commun. 2015;71:10-49.
The medical knowledge that William Shakespeare possessed has awed scholars for centuries. Theories about the provenance of his knowledge abound (such as his son-in-law being a physician), and the inclusion of medical terms and ailments throughout his plays suggests a broad knowledge of disease and sickness. Scholars have noted how he sprinkles references to dermatologic, neurologic, orthopedic, and metabolic ailments throughout his plays, mentioning carbuncles, fistulas, corpulence, rhinophyma, scurvy, ague, enuresis, kyphosis, epilepsy, and parkinsonism.1 What seems to strike post-Enlightenment audiences—and what sets Shakespeare apart from many of his contemporaries—is his portrayal of “complex” characters, those with what we envision as rich interior worlds and with whom a modern audience can resonate. There is a reason psychiatrists such as Sigmund Freud have rushed back to Shakespeare and (sometimes anachronistically) found in his characters various psychiatric diagnoses such as depression, anxiety, paranoia, jealous delusions, and obsessive-compulsive disorder. Suicide and suicidal ideation are prevalent themes in some of Shakespeare’s most well-known characters.
A surprisingly common theme
The gravest outcome of a psychiatric illness is death by suicide, which occurs in 13 of Shakespeare’s characters.2 There are additional characters who exhibit suicidal ideation without a completed act. Shakespearean characters whose lives end in suicide are variably portrayed, dying by various means and circumstances. Hamlet (who dies at the hand of his foe, Laertes), famously soliloquizes the theme of suicide and the afterlife. He ponders “tak[ing] arms against a sea of troubles.” Ophelia dies ambiguously. Immediately after, her mother and brother recount her death in a brook—having had “too much of water” when her garments “heavy with their drink, | pull’d the poor wretch from her melodious lay | To muddy death.” The 2 clowns/gravediggers then debate whether Ophelia deserves a Christian burial and if her death should be considered a suicide: did the water drown her, or did she drown herself?3
Lady Macbeth’s suicide is offstage, punctuated by a “night-shriek.” Romeo drinks poison and dies “with a kiss.” Juliet quickly follows, making her body the sword’s sheath which “there rust, and let [her] die.” Othello stabs himself after requesting that his peers will “speak of me as I am.” One of King Lear’s daughters poisons her sister “and after [slays] herself.” Timon dies by his cave, “entomb’d upon the very hem o’ the sea.” In Antony and Cleopatra, after being told that Cleopatra has killed herself with Antony’s name on her lips, Antony begs to be stabbed and then stabs himself; he is not defeated by Caesar, but rather conquered by himself: “none but Antony | Should conquer Antony.” Cleopatra and her lady-in-waiting, Charmian, kill themselves with an asp. In Julius Caesar, Brutus runs upon his sword. Cassius begs for his own death, asking that “this good sword, | That ran through Caesar’s bowels, search this bosom.” Portia, it is reported, “swallowed fire.”
Shakespeare uses specific stylized language to portray characters in psychological anguish and suicidal states. Scholars have discussed how he uses certain stylistic language to highlight the anguish that happens during solitary, solipsistic moments of contemplation.4 Moments of anguish and suicidal ideation are marked by verbal repetition. An example of this repetition comes in Hamlet’s speech after he returns to the kingdom where his uncle has usurped his father, when he laments that he cannot end his own life. He says:
O, that this too too sullied flesh would melt,
Thaw, and resolve itself into a dew!
Or that the Everlasting had not fix’d
His canon ’gainst self-slaughter! O God, God,
How weary, stale, flat, and unprofitable
Seem to me all the uses of this world.
In these 6 lines, there are 2 instances of verbal repetition: “too too” and “God, God.” In this moment of solitude and despair, Hamlet’s speech fractures; his fractured speech reflects his fractured psyche. While Hamlet speaks of staleness and stagnation in the world, his words represent a sterile excess. No meaning is elicited by their repetition; there is no forward momentum to his speech. The words reflect the extent to which Hamlet is stuck and divided in this moment. Something similar happens in Macbeth’s “Tomorrow and tomorrow and tomorrow” speech. The words march on, and with each repetition they become increasingly hollow and brittle.
Why does this discussion of suicide in Shakespeare hold value for a contemporary psychiatrist? First, there is no single prototypical suicidal character in Shakespeare. His characters who are suicidal vary in their demographics and incentives for ending their lives. In this way, he provides a rich framework, one with which many people can engage. Second, this discussion fits into an existing paradigm for using art therapy (specifically Shakespeare) as a treatment modality for trauma.5 Programs such as DE-CRUIT have used the recitation of Shakespearean verse as a means of processing trauma in veterans.5 While Shakespeare does not mention a remedy for suicide in his plays, perhaps the text can serve as medicine. Third, the repetitive speech that Shakespeare uses in times of anguish could be a fairly accurate reflection of speech patterns in patients who are suicidal. Research that completed a spoken language analysis of patients who were suicidal has found “mechanical and repetitive phrasing” as a quality of these patients’ speech.6,7
For hundreds of years, critics have searched beyond the text for Shakespeare’s voice and opinion; what did he himself think of melancholy, despair, or suicide? We cannot know. We, as readers, are invited to explore a nuanced and multifaceted view of suicide, one that neither chides nor valorizes the act, and provides ambiguity rather than condemnation.
The medical knowledge that William Shakespeare possessed has awed scholars for centuries. Theories about the provenance of his knowledge abound (such as his son-in-law being a physician), and the inclusion of medical terms and ailments throughout his plays suggests a broad knowledge of disease and sickness. Scholars have noted how he sprinkles references to dermatologic, neurologic, orthopedic, and metabolic ailments throughout his plays, mentioning carbuncles, fistulas, corpulence, rhinophyma, scurvy, ague, enuresis, kyphosis, epilepsy, and parkinsonism.1 What seems to strike post-Enlightenment audiences—and what sets Shakespeare apart from many of his contemporaries—is his portrayal of “complex” characters, those with what we envision as rich interior worlds and with whom a modern audience can resonate. There is a reason psychiatrists such as Sigmund Freud have rushed back to Shakespeare and (sometimes anachronistically) found in his characters various psychiatric diagnoses such as depression, anxiety, paranoia, jealous delusions, and obsessive-compulsive disorder. Suicide and suicidal ideation are prevalent themes in some of Shakespeare’s most well-known characters.
A surprisingly common theme
The gravest outcome of a psychiatric illness is death by suicide, which occurs in 13 of Shakespeare’s characters.2 There are additional characters who exhibit suicidal ideation without a completed act. Shakespearean characters whose lives end in suicide are variably portrayed, dying by various means and circumstances. Hamlet (who dies at the hand of his foe, Laertes), famously soliloquizes the theme of suicide and the afterlife. He ponders “tak[ing] arms against a sea of troubles.” Ophelia dies ambiguously. Immediately after, her mother and brother recount her death in a brook—having had “too much of water” when her garments “heavy with their drink, | pull’d the poor wretch from her melodious lay | To muddy death.” The 2 clowns/gravediggers then debate whether Ophelia deserves a Christian burial and if her death should be considered a suicide: did the water drown her, or did she drown herself?3
Lady Macbeth’s suicide is offstage, punctuated by a “night-shriek.” Romeo drinks poison and dies “with a kiss.” Juliet quickly follows, making her body the sword’s sheath which “there rust, and let [her] die.” Othello stabs himself after requesting that his peers will “speak of me as I am.” One of King Lear’s daughters poisons her sister “and after [slays] herself.” Timon dies by his cave, “entomb’d upon the very hem o’ the sea.” In Antony and Cleopatra, after being told that Cleopatra has killed herself with Antony’s name on her lips, Antony begs to be stabbed and then stabs himself; he is not defeated by Caesar, but rather conquered by himself: “none but Antony | Should conquer Antony.” Cleopatra and her lady-in-waiting, Charmian, kill themselves with an asp. In Julius Caesar, Brutus runs upon his sword. Cassius begs for his own death, asking that “this good sword, | That ran through Caesar’s bowels, search this bosom.” Portia, it is reported, “swallowed fire.”
Shakespeare uses specific stylized language to portray characters in psychological anguish and suicidal states. Scholars have discussed how he uses certain stylistic language to highlight the anguish that happens during solitary, solipsistic moments of contemplation.4 Moments of anguish and suicidal ideation are marked by verbal repetition. An example of this repetition comes in Hamlet’s speech after he returns to the kingdom where his uncle has usurped his father, when he laments that he cannot end his own life. He says:
O, that this too too sullied flesh would melt,
Thaw, and resolve itself into a dew!
Or that the Everlasting had not fix’d
His canon ’gainst self-slaughter! O God, God,
How weary, stale, flat, and unprofitable
Seem to me all the uses of this world.
In these 6 lines, there are 2 instances of verbal repetition: “too too” and “God, God.” In this moment of solitude and despair, Hamlet’s speech fractures; his fractured speech reflects his fractured psyche. While Hamlet speaks of staleness and stagnation in the world, his words represent a sterile excess. No meaning is elicited by their repetition; there is no forward momentum to his speech. The words reflect the extent to which Hamlet is stuck and divided in this moment. Something similar happens in Macbeth’s “Tomorrow and tomorrow and tomorrow” speech. The words march on, and with each repetition they become increasingly hollow and brittle.
Why does this discussion of suicide in Shakespeare hold value for a contemporary psychiatrist? First, there is no single prototypical suicidal character in Shakespeare. His characters who are suicidal vary in their demographics and incentives for ending their lives. In this way, he provides a rich framework, one with which many people can engage. Second, this discussion fits into an existing paradigm for using art therapy (specifically Shakespeare) as a treatment modality for trauma.5 Programs such as DE-CRUIT have used the recitation of Shakespearean verse as a means of processing trauma in veterans.5 While Shakespeare does not mention a remedy for suicide in his plays, perhaps the text can serve as medicine. Third, the repetitive speech that Shakespeare uses in times of anguish could be a fairly accurate reflection of speech patterns in patients who are suicidal. Research that completed a spoken language analysis of patients who were suicidal has found “mechanical and repetitive phrasing” as a quality of these patients’ speech.6,7
For hundreds of years, critics have searched beyond the text for Shakespeare’s voice and opinion; what did he himself think of melancholy, despair, or suicide? We cannot know. We, as readers, are invited to explore a nuanced and multifaceted view of suicide, one that neither chides nor valorizes the act, and provides ambiguity rather than condemnation.
1. Paciaroni M, Bogousslavsky J. William Shakespeare’s neurology. Prog Brain Res. 2013;206:3-18.
2. Kirkland LR. To end itself by death: suicide in Shakespeare’s tragedies. South Med J. 1999;92(7):660-666.
3. Sale C. The “Amending Hand”: Hales v. Petit, Eyston v. Studd, and Equitable Action in Hamlet. In: Jordan C, Cunningham K, eds. The Law in Shakespeare. Early Modern Literature in History. Palgrave Macmillan; 2007:189-207. https://doi.org/10.1057/9780230626348_11
4. Langley E. Narcissism and Suicide in Shakespeare and His Contemporaries. Oxford University Press; 2009.
5. Ali A, Wolfert S, Lam I, et al. Intersecting modes of aesthetic distance and mimetic induction in therapeutic process: examining a drama-based treatment for military-related traumatic stress. Drama Therapy Review. 2018;4(2):153-165.
6. Belouali A, Gupta S, Sourirajan V, et al. Acoustic and language analysis of speech for suicidal ideation among US veterans. BioData Min. 2021;14(1):11. doi:10.1186/s13040-021-00245-y
7. Cummins N, Scherer S, Krajewski J, et al. A review of depression and suicide risk assessment using speech analysis. Speech Commun. 2015;71:10-49.
1. Paciaroni M, Bogousslavsky J. William Shakespeare’s neurology. Prog Brain Res. 2013;206:3-18.
2. Kirkland LR. To end itself by death: suicide in Shakespeare’s tragedies. South Med J. 1999;92(7):660-666.
3. Sale C. The “Amending Hand”: Hales v. Petit, Eyston v. Studd, and Equitable Action in Hamlet. In: Jordan C, Cunningham K, eds. The Law in Shakespeare. Early Modern Literature in History. Palgrave Macmillan; 2007:189-207. https://doi.org/10.1057/9780230626348_11
4. Langley E. Narcissism and Suicide in Shakespeare and His Contemporaries. Oxford University Press; 2009.
5. Ali A, Wolfert S, Lam I, et al. Intersecting modes of aesthetic distance and mimetic induction in therapeutic process: examining a drama-based treatment for military-related traumatic stress. Drama Therapy Review. 2018;4(2):153-165.
6. Belouali A, Gupta S, Sourirajan V, et al. Acoustic and language analysis of speech for suicidal ideation among US veterans. BioData Min. 2021;14(1):11. doi:10.1186/s13040-021-00245-y
7. Cummins N, Scherer S, Krajewski J, et al. A review of depression and suicide risk assessment using speech analysis. Speech Commun. 2015;71:10-49.
Valedictory
All that’s bright must fade,
The brightest still the fleetest;
All that’s sweet was made
But to be lost when sweetest.
Thomas Moore
I sometimes hold it half a sin
To put in words the grief I feel;
For words, like Nature, half reveal
And half conceal the Soul within.
Alfred, Lord Tennyson, In Memoriam
Dear Readers,
I have sad news to share with you. This is the last issue of
During my travels around the country over the past 2 decades, countless psychiatrists have told me that
As the saying goes: All good things eventually come to an end. I am so grateful to have had the opportunity to collaborate with a wonderful, highly competent editorial staff, as well as with outstanding colleagues who served on the editorial board all those years. A special shout-out to Jeff Bauer, the publishing staff editor, with whom I worked so closely. I very much appreciated all the authors and peer reviewers who contributed timely clinical articles month after month and made
This has been a unique journey for all of us who strived to transform
All that’s bright must fade,
The brightest still the fleetest;
All that’s sweet was made
But to be lost when sweetest.
Thomas Moore
I sometimes hold it half a sin
To put in words the grief I feel;
For words, like Nature, half reveal
And half conceal the Soul within.
Alfred, Lord Tennyson, In Memoriam
Dear Readers,
I have sad news to share with you. This is the last issue of
During my travels around the country over the past 2 decades, countless psychiatrists have told me that
As the saying goes: All good things eventually come to an end. I am so grateful to have had the opportunity to collaborate with a wonderful, highly competent editorial staff, as well as with outstanding colleagues who served on the editorial board all those years. A special shout-out to Jeff Bauer, the publishing staff editor, with whom I worked so closely. I very much appreciated all the authors and peer reviewers who contributed timely clinical articles month after month and made
This has been a unique journey for all of us who strived to transform
All that’s bright must fade,
The brightest still the fleetest;
All that’s sweet was made
But to be lost when sweetest.
Thomas Moore
I sometimes hold it half a sin
To put in words the grief I feel;
For words, like Nature, half reveal
And half conceal the Soul within.
Alfred, Lord Tennyson, In Memoriam
Dear Readers,
I have sad news to share with you. This is the last issue of
During my travels around the country over the past 2 decades, countless psychiatrists have told me that
As the saying goes: All good things eventually come to an end. I am so grateful to have had the opportunity to collaborate with a wonderful, highly competent editorial staff, as well as with outstanding colleagues who served on the editorial board all those years. A special shout-out to Jeff Bauer, the publishing staff editor, with whom I worked so closely. I very much appreciated all the authors and peer reviewers who contributed timely clinical articles month after month and made
This has been a unique journey for all of us who strived to transform
Brain structural and cognitive changes during pregnancy
Pregnancy is unquestionably a major milestone in a woman’s life. During gestation, her body shape noticeably changes, but the invisible structural and cognitive changes in her brain are more striking. Some of those neurobiological changes are short-term, while others are long-lasting, well beyond delivery, and even into old age.
Physiological changes during pregnancy are extraordinary. The dramatic increases in estrogen, progesterone, and glucocorticoids help maintain pregnancy, ensure safe delivery of the baby, and trigger maternal behavior. However, other important changes also occur in the mother’s cardiac output, blood volume, renal function, respiratory output, and immune adaptations to accommodate the growth of the fetus. Gene expression also occurs to accomplish those changes, and there are lifelong repercussions from those drastic physiological changes.
During pregnancy, the brain is exposed to escalating levels of hormones released from the placenta, which the woman had never experienced. Those hormones regulate neuroplasticity, neuroinflammation, behavior, and cognition.
Structural brain changes1-6
Brain volume declines during pregnancy, reaching a nadir at the time of parturition. However, recovery occurs within 5 months after delivery. During the postpartum period, gray matter volume increases in the first 3 to 4 weeks, especially in areas involved in maternal behavior, including the amygdala, prefrontal cortex, and hypothalamus. Hippocampal gray matter decreases at 2 months postpartum compared to preconception levels, and reductions can still be observed up to 2 years following delivery. Gray matter reductions occur in multiple brain regions involved in social cognition, including the superior temporal gyrus, medial and inferior frontal cortex, fusiform areas, and hippocampus. Those changes correlate with positive maternal attachment. It is noteworthy that neural activity is highest in areas with reduced gray volume, so a decline in brain volume is associated with enhanced maternal attachment. Interestingly, those changes occur in fathers, too.
Childbearing improves stroke outcomes in middle age, but body weight will increase. The risk of Alzheimer’s disease increases with a higher number of gestations, but longevity is higher if the pregnancy occurs at an older age. Reproduction is also associated with shorter telomeres, which can elevate the risk of cancer, inflammation, diabetes, and dementia.
Cognitive changes7-10
The term “pregnancy brain” refers to cognitive changes during pregnancy and postpartum; these include decreased memory and concentration, absent-mindedness, heightened reactivity to threatening stimuli, and a decrease in motivation and executive functions. After delivery a mother has increased empathy (sometimes referred to as Theory of Mind) and greater activation in brain structures involved in empathy, including the paracingulate cortex, the posterior cingulate, and the insula. Also, the mirror neuron system becomes more activated in response to a woman’s own children compared to unfamiliar children. This incudes the ventral premotor cortex, the inferior frontal gyrus, and the posterior parietal cortex.
Certain forms of memory are impaired during pregnancy and early postpartum, including verbal free recall and working memory, as well as executive functions. Those are believed to correlate with glucocorticoids and estrogen levels.
Continue to: The following cognitive functions...
The following cognitive functions increase between the first and second trimester: verbal memory, attention, executive functions processing speed, verbal, and visuospatial abilities. Interestingly, mothers of a male fetus outperformed mothers of a female fetus on working memory and spatial ability.
Other changes11-16
- Cells from the fetus can traffic to the mother’s body and create microchimeric cells, which have short-term benefits (healing some of the other’s organs as stem cells do) but long-term downsides include future brain disorders such as Parkinson’s disease or Alzheimer’s disease, as well as autoimmune diseases and various types of cancer. The reverse also occurs with cells transferring from the mother to the fetus, persisting into infancy and childhood.
- Postpartum psychosis is associated with reductions in the volumes of the anterior cingulate, left parahippocampal gyrus, and superior temporal gyrus.
- A woman’s white matter increases during pregnancy compared to preconception. This is attributed to the high levels of prolactin, which proliferates oligodendrocytes, the glial cells that continuously manufacture myelin.
- The pituitary gland increases by 200% to 300% during pregnancy and returns to pre-pregnancy levels approximately 8 months following delivery. Prolactin also mediates the production of brain cells in the hippocampus (ie, neurogenesis).
- Sexual activity, even without pregnancy, increases neurogenesis. Plasma levels of prolactin increase significantly following an orgasm in both men and women, which indicates that sexual activity has beneficial brain effects.
- With pregnancy, the immune system shifts from proinflammatory to anti-inflammatory signaling. This protects the fetus from being attacked and rejected as foreign tissue. However, at the end of pregnancy, there is a “burst” of proinflammatory signaling, which serves as a major trigger to induce uterine contractions and initiate labor (to expel the foreign tissue).
- Brain levels of the anti-inflammatory cytokine interleukin-6 increase in the postpartum period, which represents a significant modification in the neuroimmune environment, and the maternal brain assumes an inflammatory-resistant state, which has cognitive and neuroplasticity implications. However, this neuroimmune dysregulation is implicated in postpartum depression and anxiety.
- Older females who were never pregnant or only had 1 pregnancy had better overall cognitive functioning than females who became pregnant at an young age.
- In animal studies, reproduction alleviates the negative effects of aging on several hippocampal functions, especially neurogenesis. Dendritic spine density in the CA1 region of the hippocampus is higher in pregnancy and early postpartum period compared to nulliparous females (based on animal studies).
Pregnancy is indispensable for the perpetuation of the species. Its hormonal, physiologic, neurobiological, and cognitive correlates are extensive. The cognitive changes in the postpartum period are designed by evolution to prepare a woman to care for her newborn and to ensure its survival. But the biological sequelae of pregnancy extend to the rest of a woman’s life and may predispose her to immune and brain disorders as she ages.
1. Barba-Müller E, Craddock S, Carmona S, et al. Brain plasticity in pregnancy and the postpartum period: links to maternal caregiving and mental health. Arch Womens Ment Health. 2019;22(2):289-299.
2. Pawluski JL, Hoekzema E, Leuner B, et al. Less can be more: fine tuning the maternal brain. Neurosci Biobehav Rev. 2022;133:104475. doi:10.1016/j.neubiorev.2021.11.045
3. Hoekzema E, Barba-Müller E, Pozzobon C, et al. Pregnancy leads to long-lasting changes in human brain structure. Nat Neurosci. 2017;20(2):287-296.
4. Cárdenas EF, Kujawa A, Humphreys KL. Neurobiological changes during the peripartum period: implications for health and behavior. Soc Cogn Affect Neurosci. 2020;15(10):1097-1110.
5. Eid RS, Chaiton JA, Lieblich SE, et al. Early and late effects of maternal experience on hippocampal neurogenesis, microglia, and the circulating cytokine milieu. Neurobiol Aging. 2019;78:1-17.
6. Galea LA, Leuner B, Slattery DA. Hippocampal plasticity during the peripartum period: influence of sex steroids, stress and ageing. J Neuroendocrinol. 2014;26(10):641-648.
7. Henry JF, Sherwin BB. Hormones and cognitive functioning during late pregnancy and postpartum: a longitudinal study. Behav Neurosci. 2012;126(1):73-85.
8. Barda G, Mizrachi Y, Borokchovich I, et al. The effect of pregnancy on maternal cognition. Sci Rep. 2011;11(1)12187. doi:10.1038/s41598-021-91504-9
9. Davies SJ, Lum JA, Skouteris H, et al. Cognitive impairment during pregnancy: a meta-analysis. Med J Aust. 2018;208(1):35-40.
10. Pownall M, Hutter RRC, Rockliffe L, et al. Memory and mood changes in pregnancy: a qualitative content analysis of women’s first-hand accounts. J Reprod Infant Psychol. 2023;41(5):516-527.
11. Hoekzema E, Barba-Müller E, Pozzobon C, et al. Pregnancy leads to long-lasting changes in human brain structure. Nat Neurosci. 2017;20(2):287-296.
12. Duarte-Guterman P, Leuner B, Galea LAM. The long and short term effects of motherhood on the brain. Front Neuroendocrinol. 2019;53:100740. doi:10.1016/j.yfrne.2019.02.004
13. Haim A, Julian D, Albin-Brooks C, et al. A survey of neuroimmune changes in pregnant and postpartum female rats. Brain Behav Immun. 2017;59:67-78.
14. Benson JC, Malyuk DF, Madhavan A, et al. Pituitary volume changes in pregnancy and the post-partum period. Neuroradiol J. 2023. doi:10.1177/19714009231196470
15. Schepanski S, Chini M, Sternemann V, et al. Pregnancy-induced maternal microchimerism shapes neurodevelopment and behavior in mice. Nat Commun. 2022;13(1):4571. doi:10.1038/s41467-022-32230-2
16. Larsen CM, Grattan DR. Prolactin, neurogenesis, and maternal behaviors. Brain Behav Immun. 2012;26(2):201-209.
Pregnancy is unquestionably a major milestone in a woman’s life. During gestation, her body shape noticeably changes, but the invisible structural and cognitive changes in her brain are more striking. Some of those neurobiological changes are short-term, while others are long-lasting, well beyond delivery, and even into old age.
Physiological changes during pregnancy are extraordinary. The dramatic increases in estrogen, progesterone, and glucocorticoids help maintain pregnancy, ensure safe delivery of the baby, and trigger maternal behavior. However, other important changes also occur in the mother’s cardiac output, blood volume, renal function, respiratory output, and immune adaptations to accommodate the growth of the fetus. Gene expression also occurs to accomplish those changes, and there are lifelong repercussions from those drastic physiological changes.
During pregnancy, the brain is exposed to escalating levels of hormones released from the placenta, which the woman had never experienced. Those hormones regulate neuroplasticity, neuroinflammation, behavior, and cognition.
Structural brain changes1-6
Brain volume declines during pregnancy, reaching a nadir at the time of parturition. However, recovery occurs within 5 months after delivery. During the postpartum period, gray matter volume increases in the first 3 to 4 weeks, especially in areas involved in maternal behavior, including the amygdala, prefrontal cortex, and hypothalamus. Hippocampal gray matter decreases at 2 months postpartum compared to preconception levels, and reductions can still be observed up to 2 years following delivery. Gray matter reductions occur in multiple brain regions involved in social cognition, including the superior temporal gyrus, medial and inferior frontal cortex, fusiform areas, and hippocampus. Those changes correlate with positive maternal attachment. It is noteworthy that neural activity is highest in areas with reduced gray volume, so a decline in brain volume is associated with enhanced maternal attachment. Interestingly, those changes occur in fathers, too.
Childbearing improves stroke outcomes in middle age, but body weight will increase. The risk of Alzheimer’s disease increases with a higher number of gestations, but longevity is higher if the pregnancy occurs at an older age. Reproduction is also associated with shorter telomeres, which can elevate the risk of cancer, inflammation, diabetes, and dementia.
Cognitive changes7-10
The term “pregnancy brain” refers to cognitive changes during pregnancy and postpartum; these include decreased memory and concentration, absent-mindedness, heightened reactivity to threatening stimuli, and a decrease in motivation and executive functions. After delivery a mother has increased empathy (sometimes referred to as Theory of Mind) and greater activation in brain structures involved in empathy, including the paracingulate cortex, the posterior cingulate, and the insula. Also, the mirror neuron system becomes more activated in response to a woman’s own children compared to unfamiliar children. This incudes the ventral premotor cortex, the inferior frontal gyrus, and the posterior parietal cortex.
Certain forms of memory are impaired during pregnancy and early postpartum, including verbal free recall and working memory, as well as executive functions. Those are believed to correlate with glucocorticoids and estrogen levels.
Continue to: The following cognitive functions...
The following cognitive functions increase between the first and second trimester: verbal memory, attention, executive functions processing speed, verbal, and visuospatial abilities. Interestingly, mothers of a male fetus outperformed mothers of a female fetus on working memory and spatial ability.
Other changes11-16
- Cells from the fetus can traffic to the mother’s body and create microchimeric cells, which have short-term benefits (healing some of the other’s organs as stem cells do) but long-term downsides include future brain disorders such as Parkinson’s disease or Alzheimer’s disease, as well as autoimmune diseases and various types of cancer. The reverse also occurs with cells transferring from the mother to the fetus, persisting into infancy and childhood.
- Postpartum psychosis is associated with reductions in the volumes of the anterior cingulate, left parahippocampal gyrus, and superior temporal gyrus.
- A woman’s white matter increases during pregnancy compared to preconception. This is attributed to the high levels of prolactin, which proliferates oligodendrocytes, the glial cells that continuously manufacture myelin.
- The pituitary gland increases by 200% to 300% during pregnancy and returns to pre-pregnancy levels approximately 8 months following delivery. Prolactin also mediates the production of brain cells in the hippocampus (ie, neurogenesis).
- Sexual activity, even without pregnancy, increases neurogenesis. Plasma levels of prolactin increase significantly following an orgasm in both men and women, which indicates that sexual activity has beneficial brain effects.
- With pregnancy, the immune system shifts from proinflammatory to anti-inflammatory signaling. This protects the fetus from being attacked and rejected as foreign tissue. However, at the end of pregnancy, there is a “burst” of proinflammatory signaling, which serves as a major trigger to induce uterine contractions and initiate labor (to expel the foreign tissue).
- Brain levels of the anti-inflammatory cytokine interleukin-6 increase in the postpartum period, which represents a significant modification in the neuroimmune environment, and the maternal brain assumes an inflammatory-resistant state, which has cognitive and neuroplasticity implications. However, this neuroimmune dysregulation is implicated in postpartum depression and anxiety.
- Older females who were never pregnant or only had 1 pregnancy had better overall cognitive functioning than females who became pregnant at an young age.
- In animal studies, reproduction alleviates the negative effects of aging on several hippocampal functions, especially neurogenesis. Dendritic spine density in the CA1 region of the hippocampus is higher in pregnancy and early postpartum period compared to nulliparous females (based on animal studies).
Pregnancy is indispensable for the perpetuation of the species. Its hormonal, physiologic, neurobiological, and cognitive correlates are extensive. The cognitive changes in the postpartum period are designed by evolution to prepare a woman to care for her newborn and to ensure its survival. But the biological sequelae of pregnancy extend to the rest of a woman’s life and may predispose her to immune and brain disorders as she ages.
Pregnancy is unquestionably a major milestone in a woman’s life. During gestation, her body shape noticeably changes, but the invisible structural and cognitive changes in her brain are more striking. Some of those neurobiological changes are short-term, while others are long-lasting, well beyond delivery, and even into old age.
Physiological changes during pregnancy are extraordinary. The dramatic increases in estrogen, progesterone, and glucocorticoids help maintain pregnancy, ensure safe delivery of the baby, and trigger maternal behavior. However, other important changes also occur in the mother’s cardiac output, blood volume, renal function, respiratory output, and immune adaptations to accommodate the growth of the fetus. Gene expression also occurs to accomplish those changes, and there are lifelong repercussions from those drastic physiological changes.
During pregnancy, the brain is exposed to escalating levels of hormones released from the placenta, which the woman had never experienced. Those hormones regulate neuroplasticity, neuroinflammation, behavior, and cognition.
Structural brain changes1-6
Brain volume declines during pregnancy, reaching a nadir at the time of parturition. However, recovery occurs within 5 months after delivery. During the postpartum period, gray matter volume increases in the first 3 to 4 weeks, especially in areas involved in maternal behavior, including the amygdala, prefrontal cortex, and hypothalamus. Hippocampal gray matter decreases at 2 months postpartum compared to preconception levels, and reductions can still be observed up to 2 years following delivery. Gray matter reductions occur in multiple brain regions involved in social cognition, including the superior temporal gyrus, medial and inferior frontal cortex, fusiform areas, and hippocampus. Those changes correlate with positive maternal attachment. It is noteworthy that neural activity is highest in areas with reduced gray volume, so a decline in brain volume is associated with enhanced maternal attachment. Interestingly, those changes occur in fathers, too.
Childbearing improves stroke outcomes in middle age, but body weight will increase. The risk of Alzheimer’s disease increases with a higher number of gestations, but longevity is higher if the pregnancy occurs at an older age. Reproduction is also associated with shorter telomeres, which can elevate the risk of cancer, inflammation, diabetes, and dementia.
Cognitive changes7-10
The term “pregnancy brain” refers to cognitive changes during pregnancy and postpartum; these include decreased memory and concentration, absent-mindedness, heightened reactivity to threatening stimuli, and a decrease in motivation and executive functions. After delivery a mother has increased empathy (sometimes referred to as Theory of Mind) and greater activation in brain structures involved in empathy, including the paracingulate cortex, the posterior cingulate, and the insula. Also, the mirror neuron system becomes more activated in response to a woman’s own children compared to unfamiliar children. This incudes the ventral premotor cortex, the inferior frontal gyrus, and the posterior parietal cortex.
Certain forms of memory are impaired during pregnancy and early postpartum, including verbal free recall and working memory, as well as executive functions. Those are believed to correlate with glucocorticoids and estrogen levels.
Continue to: The following cognitive functions...
The following cognitive functions increase between the first and second trimester: verbal memory, attention, executive functions processing speed, verbal, and visuospatial abilities. Interestingly, mothers of a male fetus outperformed mothers of a female fetus on working memory and spatial ability.
Other changes11-16
- Cells from the fetus can traffic to the mother’s body and create microchimeric cells, which have short-term benefits (healing some of the other’s organs as stem cells do) but long-term downsides include future brain disorders such as Parkinson’s disease or Alzheimer’s disease, as well as autoimmune diseases and various types of cancer. The reverse also occurs with cells transferring from the mother to the fetus, persisting into infancy and childhood.
- Postpartum psychosis is associated with reductions in the volumes of the anterior cingulate, left parahippocampal gyrus, and superior temporal gyrus.
- A woman’s white matter increases during pregnancy compared to preconception. This is attributed to the high levels of prolactin, which proliferates oligodendrocytes, the glial cells that continuously manufacture myelin.
- The pituitary gland increases by 200% to 300% during pregnancy and returns to pre-pregnancy levels approximately 8 months following delivery. Prolactin also mediates the production of brain cells in the hippocampus (ie, neurogenesis).
- Sexual activity, even without pregnancy, increases neurogenesis. Plasma levels of prolactin increase significantly following an orgasm in both men and women, which indicates that sexual activity has beneficial brain effects.
- With pregnancy, the immune system shifts from proinflammatory to anti-inflammatory signaling. This protects the fetus from being attacked and rejected as foreign tissue. However, at the end of pregnancy, there is a “burst” of proinflammatory signaling, which serves as a major trigger to induce uterine contractions and initiate labor (to expel the foreign tissue).
- Brain levels of the anti-inflammatory cytokine interleukin-6 increase in the postpartum period, which represents a significant modification in the neuroimmune environment, and the maternal brain assumes an inflammatory-resistant state, which has cognitive and neuroplasticity implications. However, this neuroimmune dysregulation is implicated in postpartum depression and anxiety.
- Older females who were never pregnant or only had 1 pregnancy had better overall cognitive functioning than females who became pregnant at an young age.
- In animal studies, reproduction alleviates the negative effects of aging on several hippocampal functions, especially neurogenesis. Dendritic spine density in the CA1 region of the hippocampus is higher in pregnancy and early postpartum period compared to nulliparous females (based on animal studies).
Pregnancy is indispensable for the perpetuation of the species. Its hormonal, physiologic, neurobiological, and cognitive correlates are extensive. The cognitive changes in the postpartum period are designed by evolution to prepare a woman to care for her newborn and to ensure its survival. But the biological sequelae of pregnancy extend to the rest of a woman’s life and may predispose her to immune and brain disorders as she ages.
1. Barba-Müller E, Craddock S, Carmona S, et al. Brain plasticity in pregnancy and the postpartum period: links to maternal caregiving and mental health. Arch Womens Ment Health. 2019;22(2):289-299.
2. Pawluski JL, Hoekzema E, Leuner B, et al. Less can be more: fine tuning the maternal brain. Neurosci Biobehav Rev. 2022;133:104475. doi:10.1016/j.neubiorev.2021.11.045
3. Hoekzema E, Barba-Müller E, Pozzobon C, et al. Pregnancy leads to long-lasting changes in human brain structure. Nat Neurosci. 2017;20(2):287-296.
4. Cárdenas EF, Kujawa A, Humphreys KL. Neurobiological changes during the peripartum period: implications for health and behavior. Soc Cogn Affect Neurosci. 2020;15(10):1097-1110.
5. Eid RS, Chaiton JA, Lieblich SE, et al. Early and late effects of maternal experience on hippocampal neurogenesis, microglia, and the circulating cytokine milieu. Neurobiol Aging. 2019;78:1-17.
6. Galea LA, Leuner B, Slattery DA. Hippocampal plasticity during the peripartum period: influence of sex steroids, stress and ageing. J Neuroendocrinol. 2014;26(10):641-648.
7. Henry JF, Sherwin BB. Hormones and cognitive functioning during late pregnancy and postpartum: a longitudinal study. Behav Neurosci. 2012;126(1):73-85.
8. Barda G, Mizrachi Y, Borokchovich I, et al. The effect of pregnancy on maternal cognition. Sci Rep. 2011;11(1)12187. doi:10.1038/s41598-021-91504-9
9. Davies SJ, Lum JA, Skouteris H, et al. Cognitive impairment during pregnancy: a meta-analysis. Med J Aust. 2018;208(1):35-40.
10. Pownall M, Hutter RRC, Rockliffe L, et al. Memory and mood changes in pregnancy: a qualitative content analysis of women’s first-hand accounts. J Reprod Infant Psychol. 2023;41(5):516-527.
11. Hoekzema E, Barba-Müller E, Pozzobon C, et al. Pregnancy leads to long-lasting changes in human brain structure. Nat Neurosci. 2017;20(2):287-296.
12. Duarte-Guterman P, Leuner B, Galea LAM. The long and short term effects of motherhood on the brain. Front Neuroendocrinol. 2019;53:100740. doi:10.1016/j.yfrne.2019.02.004
13. Haim A, Julian D, Albin-Brooks C, et al. A survey of neuroimmune changes in pregnant and postpartum female rats. Brain Behav Immun. 2017;59:67-78.
14. Benson JC, Malyuk DF, Madhavan A, et al. Pituitary volume changes in pregnancy and the post-partum period. Neuroradiol J. 2023. doi:10.1177/19714009231196470
15. Schepanski S, Chini M, Sternemann V, et al. Pregnancy-induced maternal microchimerism shapes neurodevelopment and behavior in mice. Nat Commun. 2022;13(1):4571. doi:10.1038/s41467-022-32230-2
16. Larsen CM, Grattan DR. Prolactin, neurogenesis, and maternal behaviors. Brain Behav Immun. 2012;26(2):201-209.
1. Barba-Müller E, Craddock S, Carmona S, et al. Brain plasticity in pregnancy and the postpartum period: links to maternal caregiving and mental health. Arch Womens Ment Health. 2019;22(2):289-299.
2. Pawluski JL, Hoekzema E, Leuner B, et al. Less can be more: fine tuning the maternal brain. Neurosci Biobehav Rev. 2022;133:104475. doi:10.1016/j.neubiorev.2021.11.045
3. Hoekzema E, Barba-Müller E, Pozzobon C, et al. Pregnancy leads to long-lasting changes in human brain structure. Nat Neurosci. 2017;20(2):287-296.
4. Cárdenas EF, Kujawa A, Humphreys KL. Neurobiological changes during the peripartum period: implications for health and behavior. Soc Cogn Affect Neurosci. 2020;15(10):1097-1110.
5. Eid RS, Chaiton JA, Lieblich SE, et al. Early and late effects of maternal experience on hippocampal neurogenesis, microglia, and the circulating cytokine milieu. Neurobiol Aging. 2019;78:1-17.
6. Galea LA, Leuner B, Slattery DA. Hippocampal plasticity during the peripartum period: influence of sex steroids, stress and ageing. J Neuroendocrinol. 2014;26(10):641-648.
7. Henry JF, Sherwin BB. Hormones and cognitive functioning during late pregnancy and postpartum: a longitudinal study. Behav Neurosci. 2012;126(1):73-85.
8. Barda G, Mizrachi Y, Borokchovich I, et al. The effect of pregnancy on maternal cognition. Sci Rep. 2011;11(1)12187. doi:10.1038/s41598-021-91504-9
9. Davies SJ, Lum JA, Skouteris H, et al. Cognitive impairment during pregnancy: a meta-analysis. Med J Aust. 2018;208(1):35-40.
10. Pownall M, Hutter RRC, Rockliffe L, et al. Memory and mood changes in pregnancy: a qualitative content analysis of women’s first-hand accounts. J Reprod Infant Psychol. 2023;41(5):516-527.
11. Hoekzema E, Barba-Müller E, Pozzobon C, et al. Pregnancy leads to long-lasting changes in human brain structure. Nat Neurosci. 2017;20(2):287-296.
12. Duarte-Guterman P, Leuner B, Galea LAM. The long and short term effects of motherhood on the brain. Front Neuroendocrinol. 2019;53:100740. doi:10.1016/j.yfrne.2019.02.004
13. Haim A, Julian D, Albin-Brooks C, et al. A survey of neuroimmune changes in pregnant and postpartum female rats. Brain Behav Immun. 2017;59:67-78.
14. Benson JC, Malyuk DF, Madhavan A, et al. Pituitary volume changes in pregnancy and the post-partum period. Neuroradiol J. 2023. doi:10.1177/19714009231196470
15. Schepanski S, Chini M, Sternemann V, et al. Pregnancy-induced maternal microchimerism shapes neurodevelopment and behavior in mice. Nat Commun. 2022;13(1):4571. doi:10.1038/s41467-022-32230-2
16. Larsen CM, Grattan DR. Prolactin, neurogenesis, and maternal behaviors. Brain Behav Immun. 2012;26(2):201-209.
The pandemic has permanently changed us, and its biopsychosocial sequelae linger…
Good riddance COVID-19 pandemic? Alas, that’s wishful thinking.
Many assume the pandemic is in our rearview mirror, but its biological, psychological, and social impacts continue to unfold. Its repercussions are etched into our brain, mind, emotions, behaviors, cognition, and outlook on life. Welcome to Pandemic 2.0.
Think of people who survive a heart attack. They experience multiple changes. Their initial ephemeral thrill of beating death is rapidly tempered with anxiety and worry about a future myocardial infarction and health issues in general. They become more risk-averse and more prone to dysphoria, irritability, and impatience. These individuals adopt a healthy lifestyle (diet and exercise), which they had neglected before. They develop more disciplined personality traits, feel a greater appreciation for being alive, and develop a closer affinity to family and friends. Simple things they had overlooked become more meaningful. They reevaluate their life goals, including career vs personal fulfilment. Some may overindulge in pleasurable activities in case their heart fails again. Some of those changes may be abrupt or transient, while others may become permanent features of their lives. And some may seek psychotherapy, which they may never have considered before.
The pandemic is the equivalent of a “societal cardiac arrest.” Its immediate impact was devastating. Bustling cities suddenly became ghost towns. Schools were closed, and children were locked at home with their parents, who were laid off. Businesses shut down; the economy tanked. Anxiety about being infected and dying skyrocketed, triggering a universal acute stress reaction that worsened the mental health of the population, but especially of the millions with preexisting psychiatric disorders. Routine medical and dental care stopped. Television and social media disseminated alarming updates about massive intensive care unit admissions and morgues overflowing with corpses of COVID-19 victims. Posttraumatic stress disorder (PTSD) was brewing across the nation as everyone faced this life-threatening pandemic.
The warp-speed development of vaccines for COVID-19 was equivalent to a defibrillator for the societal asystole, but the turmoil continued among the frazzled population. Some refused the vaccine due to conspiracy theories about their dangerous adverse effects. Employees in the private sector, state and federal government, and even the military who refused the mandatory vaccination lost their jobs. Controversy about shuttering schools and depriving children of face-to-face learning and socializing prompted some states to keep schools open, in contrast to most other states. Anger escalated about wearing masks, social distancing, and avoiding gatherings such as at restaurants or houses of worship. Cynicism and mistrust sprouted about the competence and reliability of health “experts” due to some conflicting signals, precluding wide adherence to medical advice.
The lingering effects of the COVID-19 pandemic
Those were the immediate repercussions of the pandemic. But what are its lingering effects? The sequelae extend across 1) the health care system; 2) the mental and emotional wellness of the population; 3) education; 4) work culture; 5) the economy; 6) societal operations; 7) technological and digital transformations; 8) mistrust in various societal institutions; 9) lack of confidence in medical information; and 10) preparedness for another pandemic due to a new strain.
As all psychiatrists know, the demand for mental health services continues to surge well after the pandemic has subsided, straining access to outpatient and inpatient care. Multiple lines of evidence confirm a deterioration in the long-term psychological well-being of children and adolescents because of lockdowns, social isolation, and anxiety about their own health and the health of their loved ones, leading to a serious rise in depression and suicidal behavior.1-3
Contunue to: Adults who survived pandemic...
Adults who survived the pandemic experienced grief during 2 very stressful years, with no peace of mind or “normal living.” Many began to contemplate the meaning of life and reevaluate the future, waxing more philosophical and embarking on “personal archeology.” The fragility of life suddenly became a ubiquitous epiphany that changed people’s habits. Working from home, which was necessary during the pandemic, became a preferred option for many, and home became an emotional refuge, not just a physical, brick-and-mortar refuge. Millions decided to quit working altogether (the “great resignation”).
Sexual activity declined precipitously during the pandemic for singles (French kissing became “the kiss of death”) but intercourse increased among couples, eventuating in a significant rise in births after the pandemic (a baby boomlet). Sexual interest among college students declined after the pandemic, which may be either due to fear of getting infected or a sublimation of libido to invest the energy in other, less risky activities.
At the societal level, the pandemic’s sequelae included a major shift to virtual communications, not just in health care (telepsychiatry and telemedicine) but also in business. Technology saved the day during the nadir of the pandemic by enabling psychiatrists and psychotherapists to treat their patients remotely. This was not technologically feasible during the past century’s influenza pandemics (1918, 1957, and 1968).
The intellectual and social development of an entire generation of children was stunted due to the COVID-19 pandemic. Consequences will continue to emerge in the years to come and may have ripple effects on this generation’s functioning. This may have particularly affected children of lower socioeconomic status, whose families cannot afford private schools and who are in dire need of good education to put them on the path of upward mobility.
As for adults who did not get infected by COVID-19, they suffered in 2 ways. First, they experienced a certain degree of brain atrophy, which is known to occur in chronic stress. This is attributed to persistent hypercortisolemia, which is toxic to the hippocampus. PTSD is well known to be associated with hippocampal atrophy.4 Additionally, a significant proportion of adults who contracted the COVID-19 virus and “recovered” were subsequently diagnosed with “long COVID,” with multiple neuropsychiatric symptoms, including psychosis, mania, depression, and panic attacks, as well as memory impairment and loss of the senses of smell and taste. For these individuals, the pandemic has not subsided; they will carry its neuropsychiatric scars for a long time.
Continue to: Economically, the pandemic...
Economically, the pandemic caused a horrific economic setback in its acute phase, which prompted the government to spend trillions to support the unemployed as well as blighted businesses. The economic sequalae of deficit spending of unprecedented proportions due to the pandemic triggered painful inflation that is ongoing. Interestingly, the numerical terms “billion” and “trillion” lost their loftiness as very huge numbers. Few people realize that counting to a billion (at one number per second) would take 31.7 years, while counting to a trillion would take 31,700 years! The inflationary impact of spending $6 trillion (which would take almost 200,000 years to count) becomes mathematically jarring. And despite the heroic measures to support the economy, some business perished, although others were created, changing the human architecture of the economy.
The pandemic drastically suppressed the “hunting and gathering” instinct of humans and demolished the fabled concept of work ethic. The “great resignation,” coupled with a desire to work from home on a mass scale, led to a glut of vacant office space in many large cities, lowering the value of commercial real estate. Following the pandemic, there was an uptick in moving away from urban areas, reflecting a creative destruction and reversal of a decades-long trend to gravitate to cities to work or live.
There was also political fallout from the pandemic. Staying at home is conducive to overdosing on television and social media, leading to an intensification and ossification of political hyperpartisanship and the further displacement of religious beliefs by passionately entrenched political beliefs. This continues to have seismic effects on political stability and harmony in our country. The pandemic may have instigated new models of national voting, which triggered further political friction.
Other examples of the pandemic’s aftereffects include a shortage of lifeguards and truck drivers, replacing the traditional handshake with a first bump, and increased spending on pleasurable activities (reminiscent of the Roaring 20s following the 1918 influenza pandemic), which may reflect an instinct to “live it up” before another deadly pandemic occurs.
Ironically, as I was finishing writing this article in early September 2023, the government announced that COVID-19 cases were again rising and a new vaccine was available for the new viral “strain.”
Here we go again: as the French saying goes: plus ça change, plus c’est la même chose…
1. Chavira DA, Ponting C, Ramos G. The impact of COVID-19 on child and adolescent mental health and treatment considerations. Behav Res Ther. 2022;157:104169. doi:10.1016/j.brat.2022.104169
2. Panchal U, Salazar de Pablo G, Franco M, et al. The impact of COVID-19 lockdown on child and adolescent mental health: systematic review. Eur Child Adolesc Psychiatry. 2023;32:1151-1177.
3. Mazrekaj D, De Witte K. The impact of school closures on learning and mental health of children: lessons from the COVID-19 pandemic. Perspectives on Psychological Science. 2023. https://doi.org/10.1177/17456916231181108
4. Logue MW, van Rooij SJH, Dennis EL, et al. A smaller hippocampal volume in posttraumatic stress disorder: a multisite ENIGMA-PGC study: subcortical volumetry results from posttraumatic stress disorder consortia. Biol Psychiatry. 2018;83(3):244-253.
Good riddance COVID-19 pandemic? Alas, that’s wishful thinking.
Many assume the pandemic is in our rearview mirror, but its biological, psychological, and social impacts continue to unfold. Its repercussions are etched into our brain, mind, emotions, behaviors, cognition, and outlook on life. Welcome to Pandemic 2.0.
Think of people who survive a heart attack. They experience multiple changes. Their initial ephemeral thrill of beating death is rapidly tempered with anxiety and worry about a future myocardial infarction and health issues in general. They become more risk-averse and more prone to dysphoria, irritability, and impatience. These individuals adopt a healthy lifestyle (diet and exercise), which they had neglected before. They develop more disciplined personality traits, feel a greater appreciation for being alive, and develop a closer affinity to family and friends. Simple things they had overlooked become more meaningful. They reevaluate their life goals, including career vs personal fulfilment. Some may overindulge in pleasurable activities in case their heart fails again. Some of those changes may be abrupt or transient, while others may become permanent features of their lives. And some may seek psychotherapy, which they may never have considered before.
The pandemic is the equivalent of a “societal cardiac arrest.” Its immediate impact was devastating. Bustling cities suddenly became ghost towns. Schools were closed, and children were locked at home with their parents, who were laid off. Businesses shut down; the economy tanked. Anxiety about being infected and dying skyrocketed, triggering a universal acute stress reaction that worsened the mental health of the population, but especially of the millions with preexisting psychiatric disorders. Routine medical and dental care stopped. Television and social media disseminated alarming updates about massive intensive care unit admissions and morgues overflowing with corpses of COVID-19 victims. Posttraumatic stress disorder (PTSD) was brewing across the nation as everyone faced this life-threatening pandemic.
The warp-speed development of vaccines for COVID-19 was equivalent to a defibrillator for the societal asystole, but the turmoil continued among the frazzled population. Some refused the vaccine due to conspiracy theories about their dangerous adverse effects. Employees in the private sector, state and federal government, and even the military who refused the mandatory vaccination lost their jobs. Controversy about shuttering schools and depriving children of face-to-face learning and socializing prompted some states to keep schools open, in contrast to most other states. Anger escalated about wearing masks, social distancing, and avoiding gatherings such as at restaurants or houses of worship. Cynicism and mistrust sprouted about the competence and reliability of health “experts” due to some conflicting signals, precluding wide adherence to medical advice.
The lingering effects of the COVID-19 pandemic
Those were the immediate repercussions of the pandemic. But what are its lingering effects? The sequelae extend across 1) the health care system; 2) the mental and emotional wellness of the population; 3) education; 4) work culture; 5) the economy; 6) societal operations; 7) technological and digital transformations; 8) mistrust in various societal institutions; 9) lack of confidence in medical information; and 10) preparedness for another pandemic due to a new strain.
As all psychiatrists know, the demand for mental health services continues to surge well after the pandemic has subsided, straining access to outpatient and inpatient care. Multiple lines of evidence confirm a deterioration in the long-term psychological well-being of children and adolescents because of lockdowns, social isolation, and anxiety about their own health and the health of their loved ones, leading to a serious rise in depression and suicidal behavior.1-3
Contunue to: Adults who survived pandemic...
Adults who survived the pandemic experienced grief during 2 very stressful years, with no peace of mind or “normal living.” Many began to contemplate the meaning of life and reevaluate the future, waxing more philosophical and embarking on “personal archeology.” The fragility of life suddenly became a ubiquitous epiphany that changed people’s habits. Working from home, which was necessary during the pandemic, became a preferred option for many, and home became an emotional refuge, not just a physical, brick-and-mortar refuge. Millions decided to quit working altogether (the “great resignation”).
Sexual activity declined precipitously during the pandemic for singles (French kissing became “the kiss of death”) but intercourse increased among couples, eventuating in a significant rise in births after the pandemic (a baby boomlet). Sexual interest among college students declined after the pandemic, which may be either due to fear of getting infected or a sublimation of libido to invest the energy in other, less risky activities.
At the societal level, the pandemic’s sequelae included a major shift to virtual communications, not just in health care (telepsychiatry and telemedicine) but also in business. Technology saved the day during the nadir of the pandemic by enabling psychiatrists and psychotherapists to treat their patients remotely. This was not technologically feasible during the past century’s influenza pandemics (1918, 1957, and 1968).
The intellectual and social development of an entire generation of children was stunted due to the COVID-19 pandemic. Consequences will continue to emerge in the years to come and may have ripple effects on this generation’s functioning. This may have particularly affected children of lower socioeconomic status, whose families cannot afford private schools and who are in dire need of good education to put them on the path of upward mobility.
As for adults who did not get infected by COVID-19, they suffered in 2 ways. First, they experienced a certain degree of brain atrophy, which is known to occur in chronic stress. This is attributed to persistent hypercortisolemia, which is toxic to the hippocampus. PTSD is well known to be associated with hippocampal atrophy.4 Additionally, a significant proportion of adults who contracted the COVID-19 virus and “recovered” were subsequently diagnosed with “long COVID,” with multiple neuropsychiatric symptoms, including psychosis, mania, depression, and panic attacks, as well as memory impairment and loss of the senses of smell and taste. For these individuals, the pandemic has not subsided; they will carry its neuropsychiatric scars for a long time.
Continue to: Economically, the pandemic...
Economically, the pandemic caused a horrific economic setback in its acute phase, which prompted the government to spend trillions to support the unemployed as well as blighted businesses. The economic sequalae of deficit spending of unprecedented proportions due to the pandemic triggered painful inflation that is ongoing. Interestingly, the numerical terms “billion” and “trillion” lost their loftiness as very huge numbers. Few people realize that counting to a billion (at one number per second) would take 31.7 years, while counting to a trillion would take 31,700 years! The inflationary impact of spending $6 trillion (which would take almost 200,000 years to count) becomes mathematically jarring. And despite the heroic measures to support the economy, some business perished, although others were created, changing the human architecture of the economy.
The pandemic drastically suppressed the “hunting and gathering” instinct of humans and demolished the fabled concept of work ethic. The “great resignation,” coupled with a desire to work from home on a mass scale, led to a glut of vacant office space in many large cities, lowering the value of commercial real estate. Following the pandemic, there was an uptick in moving away from urban areas, reflecting a creative destruction and reversal of a decades-long trend to gravitate to cities to work or live.
There was also political fallout from the pandemic. Staying at home is conducive to overdosing on television and social media, leading to an intensification and ossification of political hyperpartisanship and the further displacement of religious beliefs by passionately entrenched political beliefs. This continues to have seismic effects on political stability and harmony in our country. The pandemic may have instigated new models of national voting, which triggered further political friction.
Other examples of the pandemic’s aftereffects include a shortage of lifeguards and truck drivers, replacing the traditional handshake with a first bump, and increased spending on pleasurable activities (reminiscent of the Roaring 20s following the 1918 influenza pandemic), which may reflect an instinct to “live it up” before another deadly pandemic occurs.
Ironically, as I was finishing writing this article in early September 2023, the government announced that COVID-19 cases were again rising and a new vaccine was available for the new viral “strain.”
Here we go again: as the French saying goes: plus ça change, plus c’est la même chose…
Good riddance COVID-19 pandemic? Alas, that’s wishful thinking.
Many assume the pandemic is in our rearview mirror, but its biological, psychological, and social impacts continue to unfold. Its repercussions are etched into our brain, mind, emotions, behaviors, cognition, and outlook on life. Welcome to Pandemic 2.0.
Think of people who survive a heart attack. They experience multiple changes. Their initial ephemeral thrill of beating death is rapidly tempered with anxiety and worry about a future myocardial infarction and health issues in general. They become more risk-averse and more prone to dysphoria, irritability, and impatience. These individuals adopt a healthy lifestyle (diet and exercise), which they had neglected before. They develop more disciplined personality traits, feel a greater appreciation for being alive, and develop a closer affinity to family and friends. Simple things they had overlooked become more meaningful. They reevaluate their life goals, including career vs personal fulfilment. Some may overindulge in pleasurable activities in case their heart fails again. Some of those changes may be abrupt or transient, while others may become permanent features of their lives. And some may seek psychotherapy, which they may never have considered before.
The pandemic is the equivalent of a “societal cardiac arrest.” Its immediate impact was devastating. Bustling cities suddenly became ghost towns. Schools were closed, and children were locked at home with their parents, who were laid off. Businesses shut down; the economy tanked. Anxiety about being infected and dying skyrocketed, triggering a universal acute stress reaction that worsened the mental health of the population, but especially of the millions with preexisting psychiatric disorders. Routine medical and dental care stopped. Television and social media disseminated alarming updates about massive intensive care unit admissions and morgues overflowing with corpses of COVID-19 victims. Posttraumatic stress disorder (PTSD) was brewing across the nation as everyone faced this life-threatening pandemic.
The warp-speed development of vaccines for COVID-19 was equivalent to a defibrillator for the societal asystole, but the turmoil continued among the frazzled population. Some refused the vaccine due to conspiracy theories about their dangerous adverse effects. Employees in the private sector, state and federal government, and even the military who refused the mandatory vaccination lost their jobs. Controversy about shuttering schools and depriving children of face-to-face learning and socializing prompted some states to keep schools open, in contrast to most other states. Anger escalated about wearing masks, social distancing, and avoiding gatherings such as at restaurants or houses of worship. Cynicism and mistrust sprouted about the competence and reliability of health “experts” due to some conflicting signals, precluding wide adherence to medical advice.
The lingering effects of the COVID-19 pandemic
Those were the immediate repercussions of the pandemic. But what are its lingering effects? The sequelae extend across 1) the health care system; 2) the mental and emotional wellness of the population; 3) education; 4) work culture; 5) the economy; 6) societal operations; 7) technological and digital transformations; 8) mistrust in various societal institutions; 9) lack of confidence in medical information; and 10) preparedness for another pandemic due to a new strain.
As all psychiatrists know, the demand for mental health services continues to surge well after the pandemic has subsided, straining access to outpatient and inpatient care. Multiple lines of evidence confirm a deterioration in the long-term psychological well-being of children and adolescents because of lockdowns, social isolation, and anxiety about their own health and the health of their loved ones, leading to a serious rise in depression and suicidal behavior.1-3
Contunue to: Adults who survived pandemic...
Adults who survived the pandemic experienced grief during 2 very stressful years, with no peace of mind or “normal living.” Many began to contemplate the meaning of life and reevaluate the future, waxing more philosophical and embarking on “personal archeology.” The fragility of life suddenly became a ubiquitous epiphany that changed people’s habits. Working from home, which was necessary during the pandemic, became a preferred option for many, and home became an emotional refuge, not just a physical, brick-and-mortar refuge. Millions decided to quit working altogether (the “great resignation”).
Sexual activity declined precipitously during the pandemic for singles (French kissing became “the kiss of death”) but intercourse increased among couples, eventuating in a significant rise in births after the pandemic (a baby boomlet). Sexual interest among college students declined after the pandemic, which may be either due to fear of getting infected or a sublimation of libido to invest the energy in other, less risky activities.
At the societal level, the pandemic’s sequelae included a major shift to virtual communications, not just in health care (telepsychiatry and telemedicine) but also in business. Technology saved the day during the nadir of the pandemic by enabling psychiatrists and psychotherapists to treat their patients remotely. This was not technologically feasible during the past century’s influenza pandemics (1918, 1957, and 1968).
The intellectual and social development of an entire generation of children was stunted due to the COVID-19 pandemic. Consequences will continue to emerge in the years to come and may have ripple effects on this generation’s functioning. This may have particularly affected children of lower socioeconomic status, whose families cannot afford private schools and who are in dire need of good education to put them on the path of upward mobility.
As for adults who did not get infected by COVID-19, they suffered in 2 ways. First, they experienced a certain degree of brain atrophy, which is known to occur in chronic stress. This is attributed to persistent hypercortisolemia, which is toxic to the hippocampus. PTSD is well known to be associated with hippocampal atrophy.4 Additionally, a significant proportion of adults who contracted the COVID-19 virus and “recovered” were subsequently diagnosed with “long COVID,” with multiple neuropsychiatric symptoms, including psychosis, mania, depression, and panic attacks, as well as memory impairment and loss of the senses of smell and taste. For these individuals, the pandemic has not subsided; they will carry its neuropsychiatric scars for a long time.
Continue to: Economically, the pandemic...
Economically, the pandemic caused a horrific economic setback in its acute phase, which prompted the government to spend trillions to support the unemployed as well as blighted businesses. The economic sequalae of deficit spending of unprecedented proportions due to the pandemic triggered painful inflation that is ongoing. Interestingly, the numerical terms “billion” and “trillion” lost their loftiness as very huge numbers. Few people realize that counting to a billion (at one number per second) would take 31.7 years, while counting to a trillion would take 31,700 years! The inflationary impact of spending $6 trillion (which would take almost 200,000 years to count) becomes mathematically jarring. And despite the heroic measures to support the economy, some business perished, although others were created, changing the human architecture of the economy.
The pandemic drastically suppressed the “hunting and gathering” instinct of humans and demolished the fabled concept of work ethic. The “great resignation,” coupled with a desire to work from home on a mass scale, led to a glut of vacant office space in many large cities, lowering the value of commercial real estate. Following the pandemic, there was an uptick in moving away from urban areas, reflecting a creative destruction and reversal of a decades-long trend to gravitate to cities to work or live.
There was also political fallout from the pandemic. Staying at home is conducive to overdosing on television and social media, leading to an intensification and ossification of political hyperpartisanship and the further displacement of religious beliefs by passionately entrenched political beliefs. This continues to have seismic effects on political stability and harmony in our country. The pandemic may have instigated new models of national voting, which triggered further political friction.
Other examples of the pandemic’s aftereffects include a shortage of lifeguards and truck drivers, replacing the traditional handshake with a first bump, and increased spending on pleasurable activities (reminiscent of the Roaring 20s following the 1918 influenza pandemic), which may reflect an instinct to “live it up” before another deadly pandemic occurs.
Ironically, as I was finishing writing this article in early September 2023, the government announced that COVID-19 cases were again rising and a new vaccine was available for the new viral “strain.”
Here we go again: as the French saying goes: plus ça change, plus c’est la même chose…
1. Chavira DA, Ponting C, Ramos G. The impact of COVID-19 on child and adolescent mental health and treatment considerations. Behav Res Ther. 2022;157:104169. doi:10.1016/j.brat.2022.104169
2. Panchal U, Salazar de Pablo G, Franco M, et al. The impact of COVID-19 lockdown on child and adolescent mental health: systematic review. Eur Child Adolesc Psychiatry. 2023;32:1151-1177.
3. Mazrekaj D, De Witte K. The impact of school closures on learning and mental health of children: lessons from the COVID-19 pandemic. Perspectives on Psychological Science. 2023. https://doi.org/10.1177/17456916231181108
4. Logue MW, van Rooij SJH, Dennis EL, et al. A smaller hippocampal volume in posttraumatic stress disorder: a multisite ENIGMA-PGC study: subcortical volumetry results from posttraumatic stress disorder consortia. Biol Psychiatry. 2018;83(3):244-253.
1. Chavira DA, Ponting C, Ramos G. The impact of COVID-19 on child and adolescent mental health and treatment considerations. Behav Res Ther. 2022;157:104169. doi:10.1016/j.brat.2022.104169
2. Panchal U, Salazar de Pablo G, Franco M, et al. The impact of COVID-19 lockdown on child and adolescent mental health: systematic review. Eur Child Adolesc Psychiatry. 2023;32:1151-1177.
3. Mazrekaj D, De Witte K. The impact of school closures on learning and mental health of children: lessons from the COVID-19 pandemic. Perspectives on Psychological Science. 2023. https://doi.org/10.1177/17456916231181108
4. Logue MW, van Rooij SJH, Dennis EL, et al. A smaller hippocampal volume in posttraumatic stress disorder: a multisite ENIGMA-PGC study: subcortical volumetry results from posttraumatic stress disorder consortia. Biol Psychiatry. 2018;83(3):244-253.
A toxic and fractured political system can breed angst and PTSD
As psychiatrists know, many of our severely traumatized adult patients were victims of abuse during childhood. We routinely ask every new patient about physical, emotional, or sexual abuse when they were growing up because of the well-established, serious neurobiological and mental repercussions.1,2
Perhaps one of the worst experiences for a child is to witness bitterly adversarial parents (their vital role models) who argue viciously, despise each other, and hurl insults (and even punches) at each other. Such a chronically and emotionally traumatic upbringing can haunt kids well into adulthood, disrupting their hypothalamic-pituitary-adrenal axis and triggering anxiety, depression, and even psychosis due to epigenetic changes that ultimately lead to abnormal brain development.3
It often feels that the governance of our country, or the national “political family,” is seriously fractured like a hopelessly dysfunctional family. Could that be negatively impacting the mental health of the citizenry? Having 2 antagonistic political parties expressing visceral hatred and undisguised contempt for each other 24/7 (thanks to the enabling era of cable TV, the internet, and social media) has transformed each party’s fanatic followers from fellow citizens to ideological combatants. In this poisonous societal zeitgeist of bidirectional acrimony and mutual detestation, the opposing parties and their “intellectual militias” label each other as “extremists” or “radicals.” They become completely blind to any redeeming social value in the ideas or principles of their political opponents. They spend enormous time and energy on undermining each other instead of attending to the myriad vital issues involved in the governance of a massive and complex country.
Winston Churchill said, “Democracy is the worst form of government, except for all the others that have been tried.”4 The current toxic cloud of intense “hyperpartisanship” is emblematic of the dark Machiavellian side of democracy. But those who lament the current distorted version of democracy should contemplate living in a dictatorship or totalitarian regime, where a despot would execute any dissenter or invade and destroy an adjacent country at a whim.
Churchill made that statement in 1947. The internet, social media, and smartphones were science fiction back then. Those technological advances have added fuel to the political process and significantly stoked the flames of hyperpartisanship. It’s now democracy on steroids, where freedom of expression goes to extremes, highlighting the warts and pitfalls of the democratic system. Political rivals can now communicate their ferocious disagreements to millions of their disciples instantaneously, triggering immediate rebuttals and counterattacks by their adversaries. This “virtual guerilla warfare” is mentally and emotionally exhausting to all involved, especially to the subset of neutral bystanders who are unaffiliated with either political party, which, due to the “religification” of politics, have become like secular religions.5 Chronic, unremitting, inescapable stress is a sure pathway for anxiety, depression, posttraumatic stress disorder, and even brain atrophy.
Optimists may point out that the United States has weathered and emerged stronger from many serious traumas, including the Civil War (with its lethal divisiveness), World War I, the deadly 1918 influenza pandemic, the Great Depression, Pearl Harbor, World War II, the Cold War, the Vietnam War, the Watergate political scandal, the 9/11 terrorist attacks, the banking collapse and recession, and most recently the COVID-19 pandemic, which brought society to a standstill and induced so much anxiety and uncertainty.
On the other hand, pessimists would insist those sequential crises left indelible scars that cumulatively altered the mindset of political rivals, predisposing them to extreme views of each other. Alienation inevitably leads to fanaticism. It’s perplexing but fascinating how the fierce bidirectional missives of weaponized ideas can be as virulent and destructive as a traditional physical war. Perhaps in this era, the pen is mightier than the sword after all.
Continue to: From a psychiatric perspective...
From a psychiatric perspective, the intransigent groupthink of political partisanship eerily resembles folie en masse, a psychiatric syndrome for which there is no established treatment. It has become a serious threat to our modern democracy. So I decided to ask the “know-it-all” artificial intelligence ChatGPT, whom I previously had “invited” to write a “guest editorial” about myths surrounding psychiatry,6 to answer 3 burning questions:
1. Is there toxic hyperpartisanship in the USA today? (Box 1)
Box 1
Yes, there is toxic hyperpartisanship in the United States today. Political polarization has been on the rise for several decades, and in recent years, it has become increasingly toxic and divisive. This toxic hyperpartisanship has contributed to a breakdown in civil discourse and a lack of cooperation and compromise in government.
The toxic hyperpartisanship is evident in many aspects of American society, including politics, media, and social media. Political leaders often engage in divisive rhetoric and focus on winning at all costs, rather than working towards solutions that benefit the country as a whole. Media outlets often present news in a partisan manner, further fueling political polarization. Social media platforms have also played a role in exacerbating toxic hyperpartisanship by allowing the spread of misinformation and creating echo chambers where people are only exposed to like-minded viewpoints.
The consequences of toxic hyperpartisanship are significant, as it can hinder progress on important issues and erode trust in institutions and government. It also makes it difficult for people to engage in productive dialogue and find common ground, leading to a lack of cooperation and compromise.
It is important for individuals to be aware of the impact of toxic hyperpartisanship and work towards finding ways to bridge the political divide and engage in constructive dialogue.
2. How can severe hyperpartisanship be corrected? (Supplemental Box 1)
Supplemental Box 1
Severe hyperpartisanship, characterized by intense and entrenched divisions between political parties, can be a challenging issue to address, but there are several steps that can be taken to work towards correcting it. Here are some potential approaches:
1. Promote civil discourse: Encourage respectful and constructive conversations between individuals with differing political views. This can be achieved through education programs, media campaigns, and initiatives to foster open dialogue.
2. Electoral reforms: Consider implementing electoral reforms that can reduce the influence of extreme partisanship. For example, ranked-choice voting or nonpartisan primaries may encourage candidates to appeal to a broader base of voters rather than just their party’s base.
3. Campaign finance reform: Limit the influence of money in politics, as it can exacerbate hyperpartisanship by allowing wealthy donors to have undue influence over candidates and parties.
4. Independent redistricting: Ensure that electoral district boundaries are drawn in a fair and nonpartisan manner. Gerrymandering, the manipulation of district lines to favor one party, can contribute to hyperpartisanship by creating “safe” districts where extreme candidates are more likely to be elected.
5. Promote media literacy: Encourage media literacy education to help citizens critically evaluate information sources and avoid echo chambers. A well-informed electorate is less susceptible to extreme partisanship.
6. Encourage bipartisan collaboration: Highlight and support instances of successful bipartisan collaboration. Elected officials who work across the aisle can serve as positive examples and encourage others to follow suit.
7. Address economic inequality: Tackling economic disparities can alleviate some of the underlying factors that contribute to polarization. When people feel economically secure, they may be more willing to seek common ground.
8. Civics education: Improve civics education in schools to foster a deeper understanding of democratic values, the political process, and the importance of civic engagement.
9. Leadership example: Encourage political leaders to model cooperation and compromise rather than relying on divisive rhetoric. Voters often take cues from their leaders’ behavior.
10. Promote third parties: Support and encourage the emergence of viable thirdparty candidates. A more diverse political landscape can provide alternatives to extreme partisanship.
11. Focus on common ground: Identify and prioritize issues where there is potential for bipartisan consensus and progress. Building success on these issues can create momentum for further cooperation.
12. Encourage grassroots activism: Support grassroots movements that seek to bridge divides and foster understanding between individuals and communities with different political perspectives.
It’s essential to recognize that addressing severe hyperpartisanship is a complex and long-term process that requires collective effort from citizens, political leaders, educators, and institutions. It won’t be achieved overnight, but through sustained and committed actions, progress can be made toward a more collaborative and less divisive political climate.
3. What can cause the collapse of a democracy? (Supplemental Box 2).
Supplemental Box 2
The collapse of a democracy can be a complex and multifaceted process, influenced by various factors and circumstances. Some of the common causes that can lead to the erosion or breakdown of a democratic system include:
1. Authoritarianism and power concentration: When leaders or institutions become increasingly authoritarian, centralizing power and weakening checks and balances, it can undermine democratic principles.
2. Corruption and lack of accountability: Rampant corruption among political leaders and institutions can erode public trust in the democratic system, leading to disillusionment and disengagement.
3. Economic instability: Prolonged economic crises or severe inequality can lead to social unrest, increasing the appeal of populist or extremist movements that may challenge democratic norms.
4. Weakening of rule of law: If the rule of law is weakened, and there is a lack of respect for judicial independence and constitutional principles, democratic institutions can become vulnerable to manipulation.
5. Erosion of civil liberties: Suppression of freedom of speech, media, assembly, and association can limit citizens’ ability to express their opinions and participate in the democratic process.
6. Polarization and divisive politics: Extreme political polarization and a breakdown of civil discourse can hinder cooperation and compromise essential for a functioning democracy.
7. External interference: Foreign intervention, propaganda, or cyberattacks can influence electoral processes and undermine democratic institutions.
8. Rise of populism and nationalism: Populist movements that challenge democratic norms, demonize minorities, or advocate for a strongman leadership can pose a threat to democracy.
9. Demographic and social shifts: Demographic changes and social tensions can exacerbate political divisions and weaken the fabric of democratic societies.
10. Lack of civic education and participation: A lack of civic education and low voter turnout can lead to reduced civic engagement and undermine the democratic process.
It is crucial to understand that no democracy is immune to these challenges, and the strength of a democratic system depends on the vigilance and engagement of its citizens, the integrity of its institutions, and the commitment to upholding democratic values. Safeguarding and strengthening democracy requires ongoing efforts to address these issues and protect the principles that underpin democratic governance.
Judge for yourself, but I believe the ChatGPT responses were spot-on.
1. Lippard ETC, Nemeroff CB. The devastating clinical consequences of child abuse and neglect: increased disease vulnerability and poor treatment response in mood disorders. Am J Psychiatry. 2023;180(8):548-564.
2. Nemeroff CB. Paradise lost: the neurobiological and clinical consequences of child abuse and neglect. Neuron. 2016;89(5):892-909.
3. Zhang ZZ, Moeckel C, Mustafa M, et al. The association of epigenetic age acceleration and depressive and anxiety symptom severity among children recently exposed to substantiated maltreatment. J Psychiatr Res. 2023;165:7-13.
4. International Churchill Society. The worst form of government. Accessed August 8, 2023. https://winstonchurchill.org/resources/quotes/the-worst-form-of-government/
5. Nasrallah HA. From ideology to articles of faith: the ‘religification’ of political beliefs. Current Psychiatry. 2021;20(7):4-5,19.
6. Nasrallah HA. A ‘guest editorial’ … generated by ChatGPT? Current Psychiatry. 2023;22(4):22:6-7.
As psychiatrists know, many of our severely traumatized adult patients were victims of abuse during childhood. We routinely ask every new patient about physical, emotional, or sexual abuse when they were growing up because of the well-established, serious neurobiological and mental repercussions.1,2
Perhaps one of the worst experiences for a child is to witness bitterly adversarial parents (their vital role models) who argue viciously, despise each other, and hurl insults (and even punches) at each other. Such a chronically and emotionally traumatic upbringing can haunt kids well into adulthood, disrupting their hypothalamic-pituitary-adrenal axis and triggering anxiety, depression, and even psychosis due to epigenetic changes that ultimately lead to abnormal brain development.3
It often feels that the governance of our country, or the national “political family,” is seriously fractured like a hopelessly dysfunctional family. Could that be negatively impacting the mental health of the citizenry? Having 2 antagonistic political parties expressing visceral hatred and undisguised contempt for each other 24/7 (thanks to the enabling era of cable TV, the internet, and social media) has transformed each party’s fanatic followers from fellow citizens to ideological combatants. In this poisonous societal zeitgeist of bidirectional acrimony and mutual detestation, the opposing parties and their “intellectual militias” label each other as “extremists” or “radicals.” They become completely blind to any redeeming social value in the ideas or principles of their political opponents. They spend enormous time and energy on undermining each other instead of attending to the myriad vital issues involved in the governance of a massive and complex country.
Winston Churchill said, “Democracy is the worst form of government, except for all the others that have been tried.”4 The current toxic cloud of intense “hyperpartisanship” is emblematic of the dark Machiavellian side of democracy. But those who lament the current distorted version of democracy should contemplate living in a dictatorship or totalitarian regime, where a despot would execute any dissenter or invade and destroy an adjacent country at a whim.
Churchill made that statement in 1947. The internet, social media, and smartphones were science fiction back then. Those technological advances have added fuel to the political process and significantly stoked the flames of hyperpartisanship. It’s now democracy on steroids, where freedom of expression goes to extremes, highlighting the warts and pitfalls of the democratic system. Political rivals can now communicate their ferocious disagreements to millions of their disciples instantaneously, triggering immediate rebuttals and counterattacks by their adversaries. This “virtual guerilla warfare” is mentally and emotionally exhausting to all involved, especially to the subset of neutral bystanders who are unaffiliated with either political party, which, due to the “religification” of politics, have become like secular religions.5 Chronic, unremitting, inescapable stress is a sure pathway for anxiety, depression, posttraumatic stress disorder, and even brain atrophy.
Optimists may point out that the United States has weathered and emerged stronger from many serious traumas, including the Civil War (with its lethal divisiveness), World War I, the deadly 1918 influenza pandemic, the Great Depression, Pearl Harbor, World War II, the Cold War, the Vietnam War, the Watergate political scandal, the 9/11 terrorist attacks, the banking collapse and recession, and most recently the COVID-19 pandemic, which brought society to a standstill and induced so much anxiety and uncertainty.
On the other hand, pessimists would insist those sequential crises left indelible scars that cumulatively altered the mindset of political rivals, predisposing them to extreme views of each other. Alienation inevitably leads to fanaticism. It’s perplexing but fascinating how the fierce bidirectional missives of weaponized ideas can be as virulent and destructive as a traditional physical war. Perhaps in this era, the pen is mightier than the sword after all.
Continue to: From a psychiatric perspective...
From a psychiatric perspective, the intransigent groupthink of political partisanship eerily resembles folie en masse, a psychiatric syndrome for which there is no established treatment. It has become a serious threat to our modern democracy. So I decided to ask the “know-it-all” artificial intelligence ChatGPT, whom I previously had “invited” to write a “guest editorial” about myths surrounding psychiatry,6 to answer 3 burning questions:
1. Is there toxic hyperpartisanship in the USA today? (Box 1)
Box 1
Yes, there is toxic hyperpartisanship in the United States today. Political polarization has been on the rise for several decades, and in recent years, it has become increasingly toxic and divisive. This toxic hyperpartisanship has contributed to a breakdown in civil discourse and a lack of cooperation and compromise in government.
The toxic hyperpartisanship is evident in many aspects of American society, including politics, media, and social media. Political leaders often engage in divisive rhetoric and focus on winning at all costs, rather than working towards solutions that benefit the country as a whole. Media outlets often present news in a partisan manner, further fueling political polarization. Social media platforms have also played a role in exacerbating toxic hyperpartisanship by allowing the spread of misinformation and creating echo chambers where people are only exposed to like-minded viewpoints.
The consequences of toxic hyperpartisanship are significant, as it can hinder progress on important issues and erode trust in institutions and government. It also makes it difficult for people to engage in productive dialogue and find common ground, leading to a lack of cooperation and compromise.
It is important for individuals to be aware of the impact of toxic hyperpartisanship and work towards finding ways to bridge the political divide and engage in constructive dialogue.
2. How can severe hyperpartisanship be corrected? (Supplemental Box 1)
Supplemental Box 1
Severe hyperpartisanship, characterized by intense and entrenched divisions between political parties, can be a challenging issue to address, but there are several steps that can be taken to work towards correcting it. Here are some potential approaches:
1. Promote civil discourse: Encourage respectful and constructive conversations between individuals with differing political views. This can be achieved through education programs, media campaigns, and initiatives to foster open dialogue.
2. Electoral reforms: Consider implementing electoral reforms that can reduce the influence of extreme partisanship. For example, ranked-choice voting or nonpartisan primaries may encourage candidates to appeal to a broader base of voters rather than just their party’s base.
3. Campaign finance reform: Limit the influence of money in politics, as it can exacerbate hyperpartisanship by allowing wealthy donors to have undue influence over candidates and parties.
4. Independent redistricting: Ensure that electoral district boundaries are drawn in a fair and nonpartisan manner. Gerrymandering, the manipulation of district lines to favor one party, can contribute to hyperpartisanship by creating “safe” districts where extreme candidates are more likely to be elected.
5. Promote media literacy: Encourage media literacy education to help citizens critically evaluate information sources and avoid echo chambers. A well-informed electorate is less susceptible to extreme partisanship.
6. Encourage bipartisan collaboration: Highlight and support instances of successful bipartisan collaboration. Elected officials who work across the aisle can serve as positive examples and encourage others to follow suit.
7. Address economic inequality: Tackling economic disparities can alleviate some of the underlying factors that contribute to polarization. When people feel economically secure, they may be more willing to seek common ground.
8. Civics education: Improve civics education in schools to foster a deeper understanding of democratic values, the political process, and the importance of civic engagement.
9. Leadership example: Encourage political leaders to model cooperation and compromise rather than relying on divisive rhetoric. Voters often take cues from their leaders’ behavior.
10. Promote third parties: Support and encourage the emergence of viable thirdparty candidates. A more diverse political landscape can provide alternatives to extreme partisanship.
11. Focus on common ground: Identify and prioritize issues where there is potential for bipartisan consensus and progress. Building success on these issues can create momentum for further cooperation.
12. Encourage grassroots activism: Support grassroots movements that seek to bridge divides and foster understanding between individuals and communities with different political perspectives.
It’s essential to recognize that addressing severe hyperpartisanship is a complex and long-term process that requires collective effort from citizens, political leaders, educators, and institutions. It won’t be achieved overnight, but through sustained and committed actions, progress can be made toward a more collaborative and less divisive political climate.
3. What can cause the collapse of a democracy? (Supplemental Box 2).
Supplemental Box 2
The collapse of a democracy can be a complex and multifaceted process, influenced by various factors and circumstances. Some of the common causes that can lead to the erosion or breakdown of a democratic system include:
1. Authoritarianism and power concentration: When leaders or institutions become increasingly authoritarian, centralizing power and weakening checks and balances, it can undermine democratic principles.
2. Corruption and lack of accountability: Rampant corruption among political leaders and institutions can erode public trust in the democratic system, leading to disillusionment and disengagement.
3. Economic instability: Prolonged economic crises or severe inequality can lead to social unrest, increasing the appeal of populist or extremist movements that may challenge democratic norms.
4. Weakening of rule of law: If the rule of law is weakened, and there is a lack of respect for judicial independence and constitutional principles, democratic institutions can become vulnerable to manipulation.
5. Erosion of civil liberties: Suppression of freedom of speech, media, assembly, and association can limit citizens’ ability to express their opinions and participate in the democratic process.
6. Polarization and divisive politics: Extreme political polarization and a breakdown of civil discourse can hinder cooperation and compromise essential for a functioning democracy.
7. External interference: Foreign intervention, propaganda, or cyberattacks can influence electoral processes and undermine democratic institutions.
8. Rise of populism and nationalism: Populist movements that challenge democratic norms, demonize minorities, or advocate for a strongman leadership can pose a threat to democracy.
9. Demographic and social shifts: Demographic changes and social tensions can exacerbate political divisions and weaken the fabric of democratic societies.
10. Lack of civic education and participation: A lack of civic education and low voter turnout can lead to reduced civic engagement and undermine the democratic process.
It is crucial to understand that no democracy is immune to these challenges, and the strength of a democratic system depends on the vigilance and engagement of its citizens, the integrity of its institutions, and the commitment to upholding democratic values. Safeguarding and strengthening democracy requires ongoing efforts to address these issues and protect the principles that underpin democratic governance.
Judge for yourself, but I believe the ChatGPT responses were spot-on.
As psychiatrists know, many of our severely traumatized adult patients were victims of abuse during childhood. We routinely ask every new patient about physical, emotional, or sexual abuse when they were growing up because of the well-established, serious neurobiological and mental repercussions.1,2
Perhaps one of the worst experiences for a child is to witness bitterly adversarial parents (their vital role models) who argue viciously, despise each other, and hurl insults (and even punches) at each other. Such a chronically and emotionally traumatic upbringing can haunt kids well into adulthood, disrupting their hypothalamic-pituitary-adrenal axis and triggering anxiety, depression, and even psychosis due to epigenetic changes that ultimately lead to abnormal brain development.3
It often feels that the governance of our country, or the national “political family,” is seriously fractured like a hopelessly dysfunctional family. Could that be negatively impacting the mental health of the citizenry? Having 2 antagonistic political parties expressing visceral hatred and undisguised contempt for each other 24/7 (thanks to the enabling era of cable TV, the internet, and social media) has transformed each party’s fanatic followers from fellow citizens to ideological combatants. In this poisonous societal zeitgeist of bidirectional acrimony and mutual detestation, the opposing parties and their “intellectual militias” label each other as “extremists” or “radicals.” They become completely blind to any redeeming social value in the ideas or principles of their political opponents. They spend enormous time and energy on undermining each other instead of attending to the myriad vital issues involved in the governance of a massive and complex country.
Winston Churchill said, “Democracy is the worst form of government, except for all the others that have been tried.”4 The current toxic cloud of intense “hyperpartisanship” is emblematic of the dark Machiavellian side of democracy. But those who lament the current distorted version of democracy should contemplate living in a dictatorship or totalitarian regime, where a despot would execute any dissenter or invade and destroy an adjacent country at a whim.
Churchill made that statement in 1947. The internet, social media, and smartphones were science fiction back then. Those technological advances have added fuel to the political process and significantly stoked the flames of hyperpartisanship. It’s now democracy on steroids, where freedom of expression goes to extremes, highlighting the warts and pitfalls of the democratic system. Political rivals can now communicate their ferocious disagreements to millions of their disciples instantaneously, triggering immediate rebuttals and counterattacks by their adversaries. This “virtual guerilla warfare” is mentally and emotionally exhausting to all involved, especially to the subset of neutral bystanders who are unaffiliated with either political party, which, due to the “religification” of politics, have become like secular religions.5 Chronic, unremitting, inescapable stress is a sure pathway for anxiety, depression, posttraumatic stress disorder, and even brain atrophy.
Optimists may point out that the United States has weathered and emerged stronger from many serious traumas, including the Civil War (with its lethal divisiveness), World War I, the deadly 1918 influenza pandemic, the Great Depression, Pearl Harbor, World War II, the Cold War, the Vietnam War, the Watergate political scandal, the 9/11 terrorist attacks, the banking collapse and recession, and most recently the COVID-19 pandemic, which brought society to a standstill and induced so much anxiety and uncertainty.
On the other hand, pessimists would insist those sequential crises left indelible scars that cumulatively altered the mindset of political rivals, predisposing them to extreme views of each other. Alienation inevitably leads to fanaticism. It’s perplexing but fascinating how the fierce bidirectional missives of weaponized ideas can be as virulent and destructive as a traditional physical war. Perhaps in this era, the pen is mightier than the sword after all.
Continue to: From a psychiatric perspective...
From a psychiatric perspective, the intransigent groupthink of political partisanship eerily resembles folie en masse, a psychiatric syndrome for which there is no established treatment. It has become a serious threat to our modern democracy. So I decided to ask the “know-it-all” artificial intelligence ChatGPT, whom I previously had “invited” to write a “guest editorial” about myths surrounding psychiatry,6 to answer 3 burning questions:
1. Is there toxic hyperpartisanship in the USA today? (Box 1)
Box 1
Yes, there is toxic hyperpartisanship in the United States today. Political polarization has been on the rise for several decades, and in recent years, it has become increasingly toxic and divisive. This toxic hyperpartisanship has contributed to a breakdown in civil discourse and a lack of cooperation and compromise in government.
The toxic hyperpartisanship is evident in many aspects of American society, including politics, media, and social media. Political leaders often engage in divisive rhetoric and focus on winning at all costs, rather than working towards solutions that benefit the country as a whole. Media outlets often present news in a partisan manner, further fueling political polarization. Social media platforms have also played a role in exacerbating toxic hyperpartisanship by allowing the spread of misinformation and creating echo chambers where people are only exposed to like-minded viewpoints.
The consequences of toxic hyperpartisanship are significant, as it can hinder progress on important issues and erode trust in institutions and government. It also makes it difficult for people to engage in productive dialogue and find common ground, leading to a lack of cooperation and compromise.
It is important for individuals to be aware of the impact of toxic hyperpartisanship and work towards finding ways to bridge the political divide and engage in constructive dialogue.
2. How can severe hyperpartisanship be corrected? (Supplemental Box 1)
Supplemental Box 1
Severe hyperpartisanship, characterized by intense and entrenched divisions between political parties, can be a challenging issue to address, but there are several steps that can be taken to work towards correcting it. Here are some potential approaches:
1. Promote civil discourse: Encourage respectful and constructive conversations between individuals with differing political views. This can be achieved through education programs, media campaigns, and initiatives to foster open dialogue.
2. Electoral reforms: Consider implementing electoral reforms that can reduce the influence of extreme partisanship. For example, ranked-choice voting or nonpartisan primaries may encourage candidates to appeal to a broader base of voters rather than just their party’s base.
3. Campaign finance reform: Limit the influence of money in politics, as it can exacerbate hyperpartisanship by allowing wealthy donors to have undue influence over candidates and parties.
4. Independent redistricting: Ensure that electoral district boundaries are drawn in a fair and nonpartisan manner. Gerrymandering, the manipulation of district lines to favor one party, can contribute to hyperpartisanship by creating “safe” districts where extreme candidates are more likely to be elected.
5. Promote media literacy: Encourage media literacy education to help citizens critically evaluate information sources and avoid echo chambers. A well-informed electorate is less susceptible to extreme partisanship.
6. Encourage bipartisan collaboration: Highlight and support instances of successful bipartisan collaboration. Elected officials who work across the aisle can serve as positive examples and encourage others to follow suit.
7. Address economic inequality: Tackling economic disparities can alleviate some of the underlying factors that contribute to polarization. When people feel economically secure, they may be more willing to seek common ground.
8. Civics education: Improve civics education in schools to foster a deeper understanding of democratic values, the political process, and the importance of civic engagement.
9. Leadership example: Encourage political leaders to model cooperation and compromise rather than relying on divisive rhetoric. Voters often take cues from their leaders’ behavior.
10. Promote third parties: Support and encourage the emergence of viable thirdparty candidates. A more diverse political landscape can provide alternatives to extreme partisanship.
11. Focus on common ground: Identify and prioritize issues where there is potential for bipartisan consensus and progress. Building success on these issues can create momentum for further cooperation.
12. Encourage grassroots activism: Support grassroots movements that seek to bridge divides and foster understanding between individuals and communities with different political perspectives.
It’s essential to recognize that addressing severe hyperpartisanship is a complex and long-term process that requires collective effort from citizens, political leaders, educators, and institutions. It won’t be achieved overnight, but through sustained and committed actions, progress can be made toward a more collaborative and less divisive political climate.
3. What can cause the collapse of a democracy? (Supplemental Box 2).
Supplemental Box 2
The collapse of a democracy can be a complex and multifaceted process, influenced by various factors and circumstances. Some of the common causes that can lead to the erosion or breakdown of a democratic system include:
1. Authoritarianism and power concentration: When leaders or institutions become increasingly authoritarian, centralizing power and weakening checks and balances, it can undermine democratic principles.
2. Corruption and lack of accountability: Rampant corruption among political leaders and institutions can erode public trust in the democratic system, leading to disillusionment and disengagement.
3. Economic instability: Prolonged economic crises or severe inequality can lead to social unrest, increasing the appeal of populist or extremist movements that may challenge democratic norms.
4. Weakening of rule of law: If the rule of law is weakened, and there is a lack of respect for judicial independence and constitutional principles, democratic institutions can become vulnerable to manipulation.
5. Erosion of civil liberties: Suppression of freedom of speech, media, assembly, and association can limit citizens’ ability to express their opinions and participate in the democratic process.
6. Polarization and divisive politics: Extreme political polarization and a breakdown of civil discourse can hinder cooperation and compromise essential for a functioning democracy.
7. External interference: Foreign intervention, propaganda, or cyberattacks can influence electoral processes and undermine democratic institutions.
8. Rise of populism and nationalism: Populist movements that challenge democratic norms, demonize minorities, or advocate for a strongman leadership can pose a threat to democracy.
9. Demographic and social shifts: Demographic changes and social tensions can exacerbate political divisions and weaken the fabric of democratic societies.
10. Lack of civic education and participation: A lack of civic education and low voter turnout can lead to reduced civic engagement and undermine the democratic process.
It is crucial to understand that no democracy is immune to these challenges, and the strength of a democratic system depends on the vigilance and engagement of its citizens, the integrity of its institutions, and the commitment to upholding democratic values. Safeguarding and strengthening democracy requires ongoing efforts to address these issues and protect the principles that underpin democratic governance.
Judge for yourself, but I believe the ChatGPT responses were spot-on.
1. Lippard ETC, Nemeroff CB. The devastating clinical consequences of child abuse and neglect: increased disease vulnerability and poor treatment response in mood disorders. Am J Psychiatry. 2023;180(8):548-564.
2. Nemeroff CB. Paradise lost: the neurobiological and clinical consequences of child abuse and neglect. Neuron. 2016;89(5):892-909.
3. Zhang ZZ, Moeckel C, Mustafa M, et al. The association of epigenetic age acceleration and depressive and anxiety symptom severity among children recently exposed to substantiated maltreatment. J Psychiatr Res. 2023;165:7-13.
4. International Churchill Society. The worst form of government. Accessed August 8, 2023. https://winstonchurchill.org/resources/quotes/the-worst-form-of-government/
5. Nasrallah HA. From ideology to articles of faith: the ‘religification’ of political beliefs. Current Psychiatry. 2021;20(7):4-5,19.
6. Nasrallah HA. A ‘guest editorial’ … generated by ChatGPT? Current Psychiatry. 2023;22(4):22:6-7.
1. Lippard ETC, Nemeroff CB. The devastating clinical consequences of child abuse and neglect: increased disease vulnerability and poor treatment response in mood disorders. Am J Psychiatry. 2023;180(8):548-564.
2. Nemeroff CB. Paradise lost: the neurobiological and clinical consequences of child abuse and neglect. Neuron. 2016;89(5):892-909.
3. Zhang ZZ, Moeckel C, Mustafa M, et al. The association of epigenetic age acceleration and depressive and anxiety symptom severity among children recently exposed to substantiated maltreatment. J Psychiatr Res. 2023;165:7-13.
4. International Churchill Society. The worst form of government. Accessed August 8, 2023. https://winstonchurchill.org/resources/quotes/the-worst-form-of-government/
5. Nasrallah HA. From ideology to articles of faith: the ‘religification’ of political beliefs. Current Psychiatry. 2021;20(7):4-5,19.
6. Nasrallah HA. A ‘guest editorial’ … generated by ChatGPT? Current Psychiatry. 2023;22(4):22:6-7.
Brain damage from recurrent relapses of bipolar mania: A call for early LAI use
Bipolar disorder (BD) is a psychotic mood disorder. Like schizophrenia, it has been shown to be associated with significant degeneration and structural brain abnormalities with multiple relapses.1,2
Just as I have always advocated preventing recurrences in schizophrenia by using long-acting injectable (LAI) antipsychotic formulations immediately after the first episode to prevent psychotic relapses and progressive brain damage,3 I strongly recommend using LAIs right after hospital discharge from the first manic episode. It is the most rational management approach for bipolar mania given the grave consequences of multiple episodes, which are so common in this psychotic mood disorder due to poor medication adherence.
In contrast to the depressive episodes of BD I, where patients have insight into their depression and seek psychiatric treatment, during a manic episode patients often have no insight (anosognosia) that they suffer from a serious brain disorder, and refuse treatment.4 In addition, young patients with BD I frequently discontinue their oral mood stabilizer or second-generation antipsychotic (which are approved for mania) because they miss the blissful euphoria and the buoyant physical and mental energy of their manic episodes. They are completely oblivious to (and uninformed about) the grave neurobiological damage of further manic episodes, which can condemn them to clinical, functional, and cognitive deterioration. These patients are also likely to become treatment-resistant, which has been labeled as “the malignant transformation of bipolar disorder.”5
The evidence for progressive brain tissue loss, clinical deterioration, functional decline, and treatment resistance is abundant.6 I was the lead investigator of the first study to report ventricular dilatation (which is a proxy for cortical atrophy) in bipolar mania,7 a discovery that was subsequently replicated by 2 dozen researchers. This was followed by numerous neuroimaging studies reporting a loss of volume across multiple brain regions, including the frontal lobe, temporal lobe, cerebellum, thalamus, hippocampus, and basal ganglia. BD is heterogeneous8 with 4 stages (Table 19), and patients experience progressively worse brain structure and function with each stage.
Many patients with bipolar mania end up with poor clinical and functional outcomes, even when they respond well to initial treatment with lithium, anticonvulsant mood stabilizers, or second-generation antipsychotics. With their intentional nonadherence to oral medications leading to multiple recurrent relapses, these patients are at serious risk for neuroprogression and brain atrophic changes driven by multiple factors: inflammatory cytokines, increased cortical steroids, decreased neurotrophins, deceased neurogenesis, increased oxidative stress, and mitochondrial energy dysfunction. The consequences include progressive shortening of the interval between episodes with every relapse and loss of responsiveness to pharmacotherapy as the illness progresses.6,10 Predictors of a downhill progression include genetic vulnerability, perinatal complication during fetal life, childhood trauma (physical, sexual, emotional, or neglect), substance use, stress, psychiatric/medial comorbidities, and especially the number of episodes.9,11
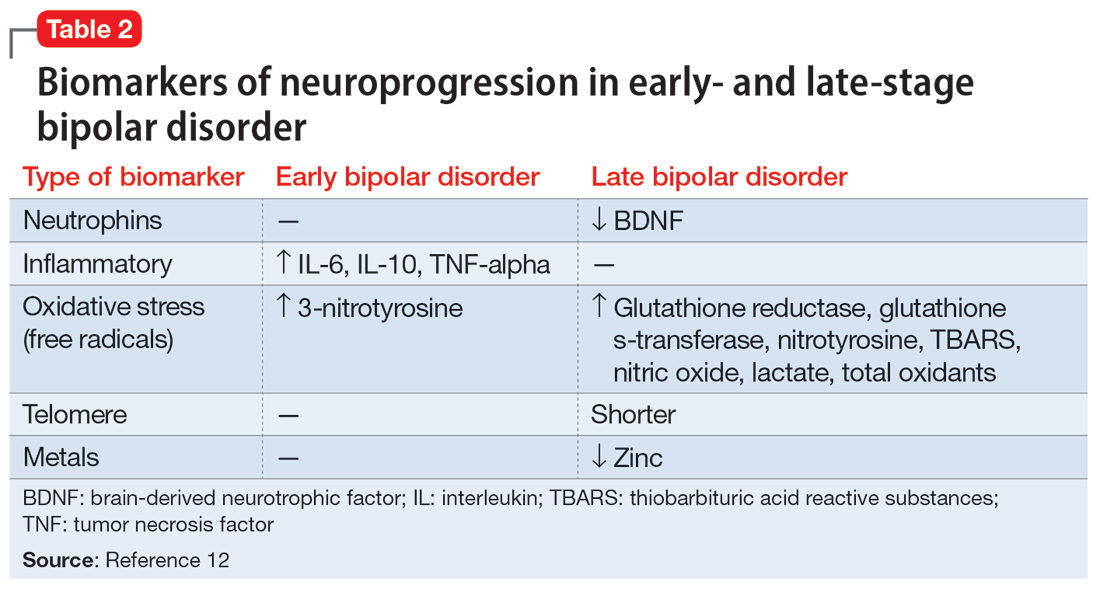
Biomarkers have been reported in both the early and late stages of BD (Table 212) as well as in postmortem studies (Table 38,13). They reflect the progressive neurodegenerative nature of recurrent BD I episodes as the disorder moves to the advanced stages. I summarize these stages in Table 19 and Table 212 for the benefit of psychiatric clinicians who do not have access to the neuroscience journals where such findings are usually published.
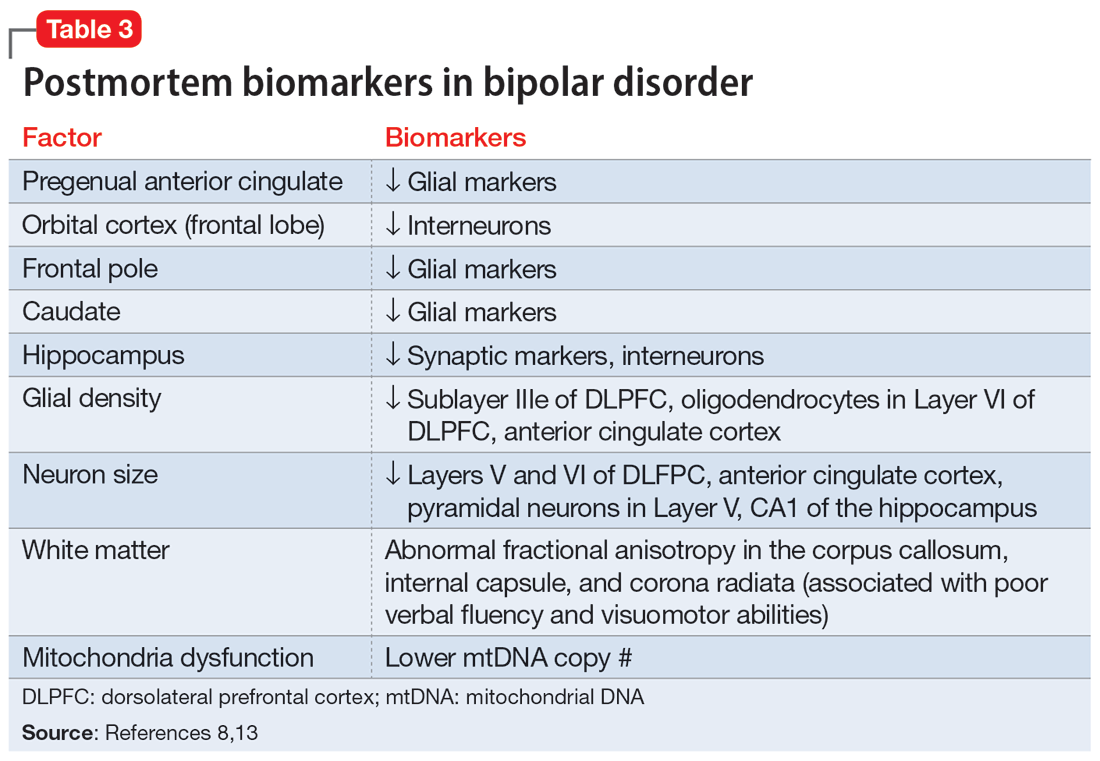
BD I is also believed to be associated with accelerated aging14,15 and an increased risk for dementia16 or cognitive deterioration.17 There is also an emerging hypothesis that neuroprogression and treatment resistance in BD is frequently associated with insulin resistance,18 peripheral inflammation,19 and blood-brain barrier permeability dysfunction.20
The bottom line is that like patients with schizophrenia, where relapses lead to devastating consequences,21 those with BD are at a similar high risk for neuroprogression, which includes atrophy in several brain regions, treatment resistance, and functional disability. This underscores the urgency for implementing LAI therapy early in the illness, when the first manic episode (Stage 2) emerges after the prodrome (Stage 1). This is the best strategy to preserve brain health in persons with BD22 and to allow them to remain functional with their many intellectual gifts, such as eloquence, poetry, artistic talents, humor, and social skills. It is unfortunate that the combination of patients’ and clinicians’ reluctance to use an LAI early in the illness dooms many patients with BD to a potentially avoidable malignant outcome.
1. Strakowski SM, DelBello MP, Adler CM. The functional neuroanatomy of bipolar disorder: a review of neuroimaging findings. Mol Psychiatry. 2005;10(1):105-106.
2. Kapezinski NS, Mwangi B, Cassidy RM, et al. Neuroprogression and illness trajectories in bipolar disorder. Expert Rev Neurother. 2017;17(3):277-285.
3. Nasrallah HA. Errors of omission and commission in psychiatric practice. Current Psychiatry. 2017;16(11):4,6,8.
4. Nasrallah HA. Is anosognosia a delusion, a negative symptom, or a cognitive deficit? Current Psychiatry. 2022;21(1):6-8,14.
5. Post RM. Preventing the malignant transformation of bipolar disorder. JAMA. 2018;319(12):1197-1198.
6. Berk M, Kapczinski F, Andreazza AC, et al. Pathways underlying neuroprogression in bipolar disorder: focus on inflammation, oxidative stress and neurotrophic factors. Neurosci Biobehav Rev. 2011;35(3):804-817.
7. Nasrallah HA, McCalley-Whitters M, Jacoby CG. Cerebral ventricular enlargement in young manic males. A controlled CT study. J Affective Dis. 1982;4(1):15-19.
8. Maletic V, Raison C. Integrated neurobiology of bipolar disorder. Front Psychiatry. 2014;5:98.
9. Berk M. Neuroprogression: pathways to progressive brain changes in bipolar disorder. Int J Neuropsychopharmacol. 2009;12(4):441-445.
10. Berk M, Conus P, Kapczinski F, et al. From neuroprogression to neuroprotection: implications for clinical care. Med J Aust. 2010;193(S4):S36-S40.
11. Passos IC, Mwangi B, Vieta E, et al. Areas of controversy in neuroprogression in bipolar disorder. Acta Psychiatr Scand. 2016;134(2):91-103.
12. Fries GR, Pfaffenseller B, Stertz L, et al. Staging and neuroprogression in bipolar disorder. Curr Psychiatry Rep. 2012;14(6):667-675.
13. Manji HK, Drevets WC, Charney DS. The cellular neurobiology of depression. Nat Med. 2001;7(5):541-547.
14. Fries GR, Zamzow MJ, Andrews T, et al. Accelerated aging in bipolar disorder: a comprehensive review of molecular findings and their clinical implications. Neurosci Biobehav Rev. 2020;112:107-116.
15. Fries GR, Bauer IE, Scaini G, et al. Accelerated hippocampal biological aging in bipolar disorder. Bipolar Dis. 2020;22(5):498-507.
16. Diniz BS, Teixeira AL, Cao F, et al. History of bipolar disorder and the risk of dementia: a systematic review and meta-analysis. Am J Geriatr Psychiatry. 2017;25(4):357-362.
17. Bauer IE, Ouyang A, Mwangi B, et al. Reduced white matter integrity and verbal fluency impairment in young adults with bipolar disorder: a diffusion tensor imaging study. J Psychiatr Res. 2015;62:115-122.
18. Calkin CV. Insulin resistance takes center stage: a new paradigm in the progression of bipolar disorder. Ann Med. 2019;51(5-6):281-293.
19. Grewal S, McKinlay S, Kapczinski F, et al. Biomarkers of neuroprogression and late staging in bipolar disorder: a systematic review. Aust N Z J Psychiatry. 2023;57(3):328-343.
20. Calkin C, McClelland C, Cairns K, et al. Insulin resistance and blood-brain barrier dysfunction underlie neuroprogression in bipolar disorder. Front Psychiatry. 2021;12:636174.
21. Nasrallah HA. 10 devastating consequences of psychotic relapses. Current Psychiatry. 2021;20(5):9-12.
22. Berk M, Hallam K, Malhi GS, et al. Evidence and implications for early intervention in bipolar disorder. J Ment Health. 2010;19(2):113-126.
Bipolar disorder (BD) is a psychotic mood disorder. Like schizophrenia, it has been shown to be associated with significant degeneration and structural brain abnormalities with multiple relapses.1,2
Just as I have always advocated preventing recurrences in schizophrenia by using long-acting injectable (LAI) antipsychotic formulations immediately after the first episode to prevent psychotic relapses and progressive brain damage,3 I strongly recommend using LAIs right after hospital discharge from the first manic episode. It is the most rational management approach for bipolar mania given the grave consequences of multiple episodes, which are so common in this psychotic mood disorder due to poor medication adherence.
In contrast to the depressive episodes of BD I, where patients have insight into their depression and seek psychiatric treatment, during a manic episode patients often have no insight (anosognosia) that they suffer from a serious brain disorder, and refuse treatment.4 In addition, young patients with BD I frequently discontinue their oral mood stabilizer or second-generation antipsychotic (which are approved for mania) because they miss the blissful euphoria and the buoyant physical and mental energy of their manic episodes. They are completely oblivious to (and uninformed about) the grave neurobiological damage of further manic episodes, which can condemn them to clinical, functional, and cognitive deterioration. These patients are also likely to become treatment-resistant, which has been labeled as “the malignant transformation of bipolar disorder.”5
The evidence for progressive brain tissue loss, clinical deterioration, functional decline, and treatment resistance is abundant.6 I was the lead investigator of the first study to report ventricular dilatation (which is a proxy for cortical atrophy) in bipolar mania,7 a discovery that was subsequently replicated by 2 dozen researchers. This was followed by numerous neuroimaging studies reporting a loss of volume across multiple brain regions, including the frontal lobe, temporal lobe, cerebellum, thalamus, hippocampus, and basal ganglia. BD is heterogeneous8 with 4 stages (Table 19), and patients experience progressively worse brain structure and function with each stage.
Many patients with bipolar mania end up with poor clinical and functional outcomes, even when they respond well to initial treatment with lithium, anticonvulsant mood stabilizers, or second-generation antipsychotics. With their intentional nonadherence to oral medications leading to multiple recurrent relapses, these patients are at serious risk for neuroprogression and brain atrophic changes driven by multiple factors: inflammatory cytokines, increased cortical steroids, decreased neurotrophins, deceased neurogenesis, increased oxidative stress, and mitochondrial energy dysfunction. The consequences include progressive shortening of the interval between episodes with every relapse and loss of responsiveness to pharmacotherapy as the illness progresses.6,10 Predictors of a downhill progression include genetic vulnerability, perinatal complication during fetal life, childhood trauma (physical, sexual, emotional, or neglect), substance use, stress, psychiatric/medial comorbidities, and especially the number of episodes.9,11
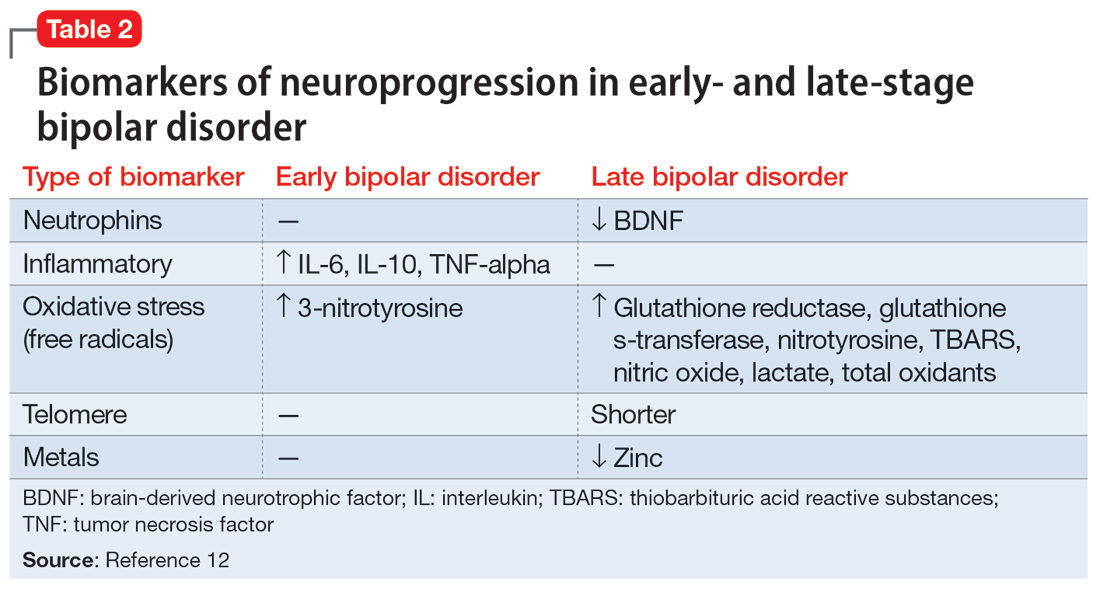
Biomarkers have been reported in both the early and late stages of BD (Table 212) as well as in postmortem studies (Table 38,13). They reflect the progressive neurodegenerative nature of recurrent BD I episodes as the disorder moves to the advanced stages. I summarize these stages in Table 19 and Table 212 for the benefit of psychiatric clinicians who do not have access to the neuroscience journals where such findings are usually published.
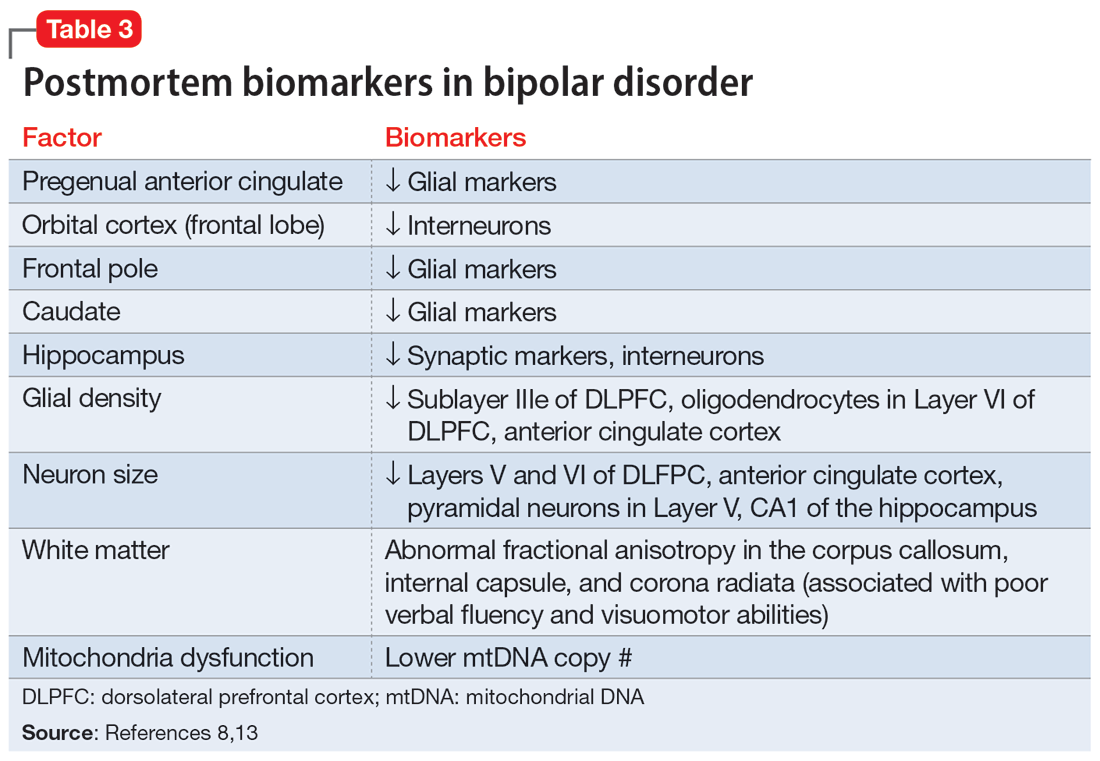
BD I is also believed to be associated with accelerated aging14,15 and an increased risk for dementia16 or cognitive deterioration.17 There is also an emerging hypothesis that neuroprogression and treatment resistance in BD is frequently associated with insulin resistance,18 peripheral inflammation,19 and blood-brain barrier permeability dysfunction.20
The bottom line is that like patients with schizophrenia, where relapses lead to devastating consequences,21 those with BD are at a similar high risk for neuroprogression, which includes atrophy in several brain regions, treatment resistance, and functional disability. This underscores the urgency for implementing LAI therapy early in the illness, when the first manic episode (Stage 2) emerges after the prodrome (Stage 1). This is the best strategy to preserve brain health in persons with BD22 and to allow them to remain functional with their many intellectual gifts, such as eloquence, poetry, artistic talents, humor, and social skills. It is unfortunate that the combination of patients’ and clinicians’ reluctance to use an LAI early in the illness dooms many patients with BD to a potentially avoidable malignant outcome.
Bipolar disorder (BD) is a psychotic mood disorder. Like schizophrenia, it has been shown to be associated with significant degeneration and structural brain abnormalities with multiple relapses.1,2
Just as I have always advocated preventing recurrences in schizophrenia by using long-acting injectable (LAI) antipsychotic formulations immediately after the first episode to prevent psychotic relapses and progressive brain damage,3 I strongly recommend using LAIs right after hospital discharge from the first manic episode. It is the most rational management approach for bipolar mania given the grave consequences of multiple episodes, which are so common in this psychotic mood disorder due to poor medication adherence.
In contrast to the depressive episodes of BD I, where patients have insight into their depression and seek psychiatric treatment, during a manic episode patients often have no insight (anosognosia) that they suffer from a serious brain disorder, and refuse treatment.4 In addition, young patients with BD I frequently discontinue their oral mood stabilizer or second-generation antipsychotic (which are approved for mania) because they miss the blissful euphoria and the buoyant physical and mental energy of their manic episodes. They are completely oblivious to (and uninformed about) the grave neurobiological damage of further manic episodes, which can condemn them to clinical, functional, and cognitive deterioration. These patients are also likely to become treatment-resistant, which has been labeled as “the malignant transformation of bipolar disorder.”5
The evidence for progressive brain tissue loss, clinical deterioration, functional decline, and treatment resistance is abundant.6 I was the lead investigator of the first study to report ventricular dilatation (which is a proxy for cortical atrophy) in bipolar mania,7 a discovery that was subsequently replicated by 2 dozen researchers. This was followed by numerous neuroimaging studies reporting a loss of volume across multiple brain regions, including the frontal lobe, temporal lobe, cerebellum, thalamus, hippocampus, and basal ganglia. BD is heterogeneous8 with 4 stages (Table 19), and patients experience progressively worse brain structure and function with each stage.
Many patients with bipolar mania end up with poor clinical and functional outcomes, even when they respond well to initial treatment with lithium, anticonvulsant mood stabilizers, or second-generation antipsychotics. With their intentional nonadherence to oral medications leading to multiple recurrent relapses, these patients are at serious risk for neuroprogression and brain atrophic changes driven by multiple factors: inflammatory cytokines, increased cortical steroids, decreased neurotrophins, deceased neurogenesis, increased oxidative stress, and mitochondrial energy dysfunction. The consequences include progressive shortening of the interval between episodes with every relapse and loss of responsiveness to pharmacotherapy as the illness progresses.6,10 Predictors of a downhill progression include genetic vulnerability, perinatal complication during fetal life, childhood trauma (physical, sexual, emotional, or neglect), substance use, stress, psychiatric/medial comorbidities, and especially the number of episodes.9,11
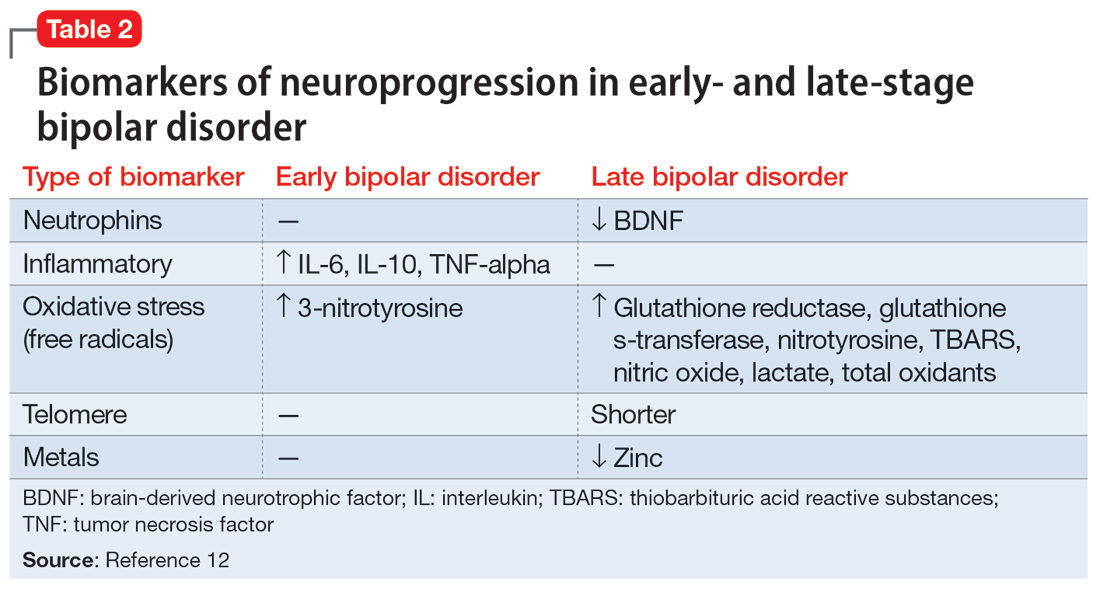
Biomarkers have been reported in both the early and late stages of BD (Table 212) as well as in postmortem studies (Table 38,13). They reflect the progressive neurodegenerative nature of recurrent BD I episodes as the disorder moves to the advanced stages. I summarize these stages in Table 19 and Table 212 for the benefit of psychiatric clinicians who do not have access to the neuroscience journals where such findings are usually published.
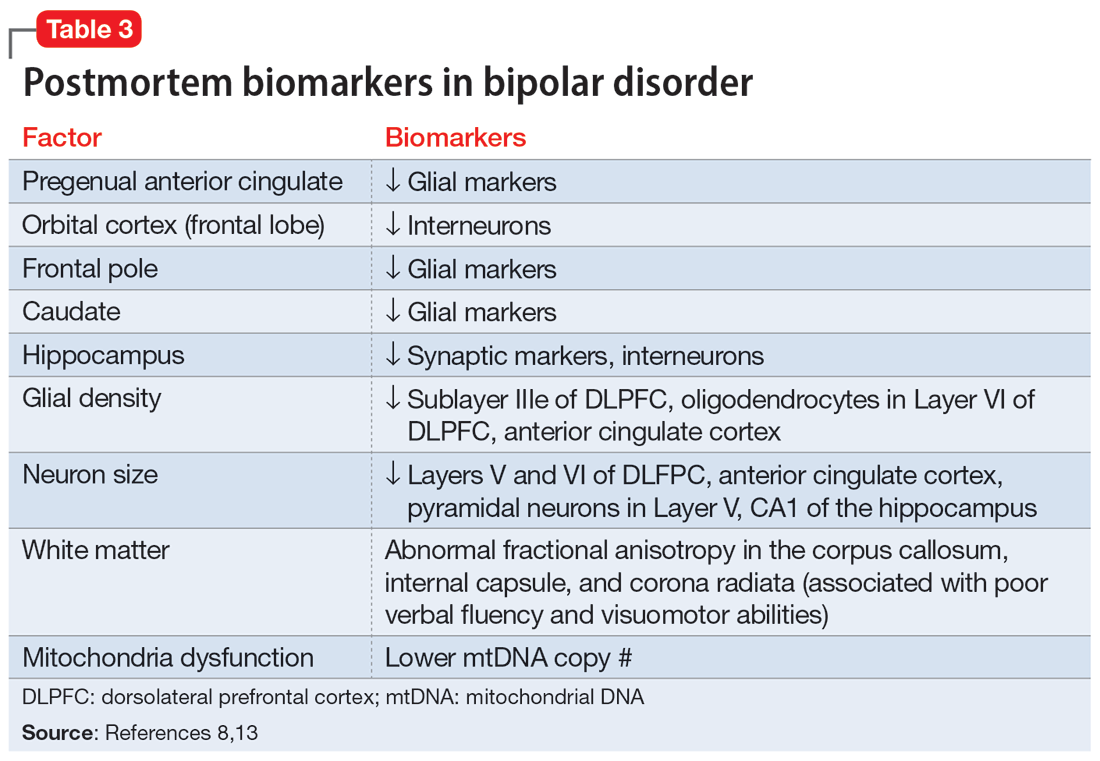
BD I is also believed to be associated with accelerated aging14,15 and an increased risk for dementia16 or cognitive deterioration.17 There is also an emerging hypothesis that neuroprogression and treatment resistance in BD is frequently associated with insulin resistance,18 peripheral inflammation,19 and blood-brain barrier permeability dysfunction.20
The bottom line is that like patients with schizophrenia, where relapses lead to devastating consequences,21 those with BD are at a similar high risk for neuroprogression, which includes atrophy in several brain regions, treatment resistance, and functional disability. This underscores the urgency for implementing LAI therapy early in the illness, when the first manic episode (Stage 2) emerges after the prodrome (Stage 1). This is the best strategy to preserve brain health in persons with BD22 and to allow them to remain functional with their many intellectual gifts, such as eloquence, poetry, artistic talents, humor, and social skills. It is unfortunate that the combination of patients’ and clinicians’ reluctance to use an LAI early in the illness dooms many patients with BD to a potentially avoidable malignant outcome.
1. Strakowski SM, DelBello MP, Adler CM. The functional neuroanatomy of bipolar disorder: a review of neuroimaging findings. Mol Psychiatry. 2005;10(1):105-106.
2. Kapezinski NS, Mwangi B, Cassidy RM, et al. Neuroprogression and illness trajectories in bipolar disorder. Expert Rev Neurother. 2017;17(3):277-285.
3. Nasrallah HA. Errors of omission and commission in psychiatric practice. Current Psychiatry. 2017;16(11):4,6,8.
4. Nasrallah HA. Is anosognosia a delusion, a negative symptom, or a cognitive deficit? Current Psychiatry. 2022;21(1):6-8,14.
5. Post RM. Preventing the malignant transformation of bipolar disorder. JAMA. 2018;319(12):1197-1198.
6. Berk M, Kapczinski F, Andreazza AC, et al. Pathways underlying neuroprogression in bipolar disorder: focus on inflammation, oxidative stress and neurotrophic factors. Neurosci Biobehav Rev. 2011;35(3):804-817.
7. Nasrallah HA, McCalley-Whitters M, Jacoby CG. Cerebral ventricular enlargement in young manic males. A controlled CT study. J Affective Dis. 1982;4(1):15-19.
8. Maletic V, Raison C. Integrated neurobiology of bipolar disorder. Front Psychiatry. 2014;5:98.
9. Berk M. Neuroprogression: pathways to progressive brain changes in bipolar disorder. Int J Neuropsychopharmacol. 2009;12(4):441-445.
10. Berk M, Conus P, Kapczinski F, et al. From neuroprogression to neuroprotection: implications for clinical care. Med J Aust. 2010;193(S4):S36-S40.
11. Passos IC, Mwangi B, Vieta E, et al. Areas of controversy in neuroprogression in bipolar disorder. Acta Psychiatr Scand. 2016;134(2):91-103.
12. Fries GR, Pfaffenseller B, Stertz L, et al. Staging and neuroprogression in bipolar disorder. Curr Psychiatry Rep. 2012;14(6):667-675.
13. Manji HK, Drevets WC, Charney DS. The cellular neurobiology of depression. Nat Med. 2001;7(5):541-547.
14. Fries GR, Zamzow MJ, Andrews T, et al. Accelerated aging in bipolar disorder: a comprehensive review of molecular findings and their clinical implications. Neurosci Biobehav Rev. 2020;112:107-116.
15. Fries GR, Bauer IE, Scaini G, et al. Accelerated hippocampal biological aging in bipolar disorder. Bipolar Dis. 2020;22(5):498-507.
16. Diniz BS, Teixeira AL, Cao F, et al. History of bipolar disorder and the risk of dementia: a systematic review and meta-analysis. Am J Geriatr Psychiatry. 2017;25(4):357-362.
17. Bauer IE, Ouyang A, Mwangi B, et al. Reduced white matter integrity and verbal fluency impairment in young adults with bipolar disorder: a diffusion tensor imaging study. J Psychiatr Res. 2015;62:115-122.
18. Calkin CV. Insulin resistance takes center stage: a new paradigm in the progression of bipolar disorder. Ann Med. 2019;51(5-6):281-293.
19. Grewal S, McKinlay S, Kapczinski F, et al. Biomarkers of neuroprogression and late staging in bipolar disorder: a systematic review. Aust N Z J Psychiatry. 2023;57(3):328-343.
20. Calkin C, McClelland C, Cairns K, et al. Insulin resistance and blood-brain barrier dysfunction underlie neuroprogression in bipolar disorder. Front Psychiatry. 2021;12:636174.
21. Nasrallah HA. 10 devastating consequences of psychotic relapses. Current Psychiatry. 2021;20(5):9-12.
22. Berk M, Hallam K, Malhi GS, et al. Evidence and implications for early intervention in bipolar disorder. J Ment Health. 2010;19(2):113-126.
1. Strakowski SM, DelBello MP, Adler CM. The functional neuroanatomy of bipolar disorder: a review of neuroimaging findings. Mol Psychiatry. 2005;10(1):105-106.
2. Kapezinski NS, Mwangi B, Cassidy RM, et al. Neuroprogression and illness trajectories in bipolar disorder. Expert Rev Neurother. 2017;17(3):277-285.
3. Nasrallah HA. Errors of omission and commission in psychiatric practice. Current Psychiatry. 2017;16(11):4,6,8.
4. Nasrallah HA. Is anosognosia a delusion, a negative symptom, or a cognitive deficit? Current Psychiatry. 2022;21(1):6-8,14.
5. Post RM. Preventing the malignant transformation of bipolar disorder. JAMA. 2018;319(12):1197-1198.
6. Berk M, Kapczinski F, Andreazza AC, et al. Pathways underlying neuroprogression in bipolar disorder: focus on inflammation, oxidative stress and neurotrophic factors. Neurosci Biobehav Rev. 2011;35(3):804-817.
7. Nasrallah HA, McCalley-Whitters M, Jacoby CG. Cerebral ventricular enlargement in young manic males. A controlled CT study. J Affective Dis. 1982;4(1):15-19.
8. Maletic V, Raison C. Integrated neurobiology of bipolar disorder. Front Psychiatry. 2014;5:98.
9. Berk M. Neuroprogression: pathways to progressive brain changes in bipolar disorder. Int J Neuropsychopharmacol. 2009;12(4):441-445.
10. Berk M, Conus P, Kapczinski F, et al. From neuroprogression to neuroprotection: implications for clinical care. Med J Aust. 2010;193(S4):S36-S40.
11. Passos IC, Mwangi B, Vieta E, et al. Areas of controversy in neuroprogression in bipolar disorder. Acta Psychiatr Scand. 2016;134(2):91-103.
12. Fries GR, Pfaffenseller B, Stertz L, et al. Staging and neuroprogression in bipolar disorder. Curr Psychiatry Rep. 2012;14(6):667-675.
13. Manji HK, Drevets WC, Charney DS. The cellular neurobiology of depression. Nat Med. 2001;7(5):541-547.
14. Fries GR, Zamzow MJ, Andrews T, et al. Accelerated aging in bipolar disorder: a comprehensive review of molecular findings and their clinical implications. Neurosci Biobehav Rev. 2020;112:107-116.
15. Fries GR, Bauer IE, Scaini G, et al. Accelerated hippocampal biological aging in bipolar disorder. Bipolar Dis. 2020;22(5):498-507.
16. Diniz BS, Teixeira AL, Cao F, et al. History of bipolar disorder and the risk of dementia: a systematic review and meta-analysis. Am J Geriatr Psychiatry. 2017;25(4):357-362.
17. Bauer IE, Ouyang A, Mwangi B, et al. Reduced white matter integrity and verbal fluency impairment in young adults with bipolar disorder: a diffusion tensor imaging study. J Psychiatr Res. 2015;62:115-122.
18. Calkin CV. Insulin resistance takes center stage: a new paradigm in the progression of bipolar disorder. Ann Med. 2019;51(5-6):281-293.
19. Grewal S, McKinlay S, Kapczinski F, et al. Biomarkers of neuroprogression and late staging in bipolar disorder: a systematic review. Aust N Z J Psychiatry. 2023;57(3):328-343.
20. Calkin C, McClelland C, Cairns K, et al. Insulin resistance and blood-brain barrier dysfunction underlie neuroprogression in bipolar disorder. Front Psychiatry. 2021;12:636174.
21. Nasrallah HA. 10 devastating consequences of psychotic relapses. Current Psychiatry. 2021;20(5):9-12.
22. Berk M, Hallam K, Malhi GS, et al. Evidence and implications for early intervention in bipolar disorder. J Ment Health. 2010;19(2):113-126.
Is the contemporary mental health crisis among youth due to DMN disruption?
The advent of unprecedented technologies drastically altering the behavior of children and adolescents, compounded by prolonged isolation from a once-in-a-century pandemic, may have negatively impacted the normal connectivity of the human brain among youth, leading to the current alarming increase of depression, anxiety, and suicidality among this population.
The human brain is comprised of multiple large-scale networks that are functionally connected and control feelings, thoughts, and behaviors. As clinical neuroscientists, psychiatrists must consider the profound impact of a massive societal shift in human behavior on the functional connectivity of brain networks in health and disease. The advent of smartphones, social media, and video game addiction may have disrupted the developing brain networks in children and adolescents, leading to the current escalating epidemic of mental disorders in youth.
The major networks in the human brain include the default mode network (DMN), the salience network, the limbic system, the dorsal attention network, the central executive network, and the visual system.1 Each network connects several brain regions. Researchers can use functional MRI to detect the connectivity of those networks. When blood flow increases concurrently across 2 or 3 networks, this indicates those networks are functionally connected.
There was an old “dogma” that brain regions use energy only when activated and being used. Hans Berger, who developed the EEG in 1929, noticed electrical activity at rest and proposed that the brain is constantly busy, but his neurology peers did not take him seriously.2 In the 1950s, Louis Sokoloff noticed that brain metabolism was the same whether a person is at rest or doing math. In the 1970s, David Ingvar discovered that the highest blood flow in the frontal lobe occurred when a person was at rest.3 Finally, in 2007, Raichle et al4 used positron emission tomography scans to confirm that the frontal lobe is most active when a person is not doing anything. He labeled this phenomenon the DMN, comprising the medial fronto-parietal cortex, the posterior cingulate gyrus, the precuneus, and the angular gyrus. Interestingly, the number of publications about the DMN has skyrocketed since 2007.
The many roles of the DMN
Ongoing research has revealed that the DMN is most active at rest, and its anatomical hubs mediate several key functions5:
- Posterior cingulate gyrus (the central core of the DMN): remembering the past and thinking about the future
- Medial prefrontal cortex: autobiographical memories, future goals and events, reflecting on one’s emotional self, and considering decisions about family members
- Dorsal medial subsystem: thinking about others, determining and inferring the purpose of other people’s actions
- Temporo-parietal junction: reflecting on the beliefs and emotions of others (known as “theory of mind”6)
- Lateral parietal junction: retrieval of social and conceptual knowledge
- Hippocampus: forming new memories, remembering the past, imagining the future
- Posterior-inferior parietal lobe: junction of auditory, visual, and somatic sensory information and attention
- Precuneus: Visual, sensory-motor, and attention.
Many terms have been used to describe the function of the DMN, including “daydreaming,” “auto-pilot,” “mind-wondering,” “reminiscing,” “contemplating,” “self-reflection,” “the neurological basis of the self,” and “seat of literary creativity.”
Psychiatric consequences of DMN deactivation
When another brain network, the attention network (which is also referred to as the task-positive network), is activated consciously and volitionally to perform a task that demands focus (such as text messaging, playing video games, or continuously interacting with social media sites), DMN activity declines.
Continue to: The DMN does not exist...
The DMN does not exist in infants, but starts to develop in childhood.7 It is enhanced by exercise, daydreaming, and sleep, activities that are common in childhood but have declined drastically with the widespread use of smartphones, video games, and social media, which for many youth occupy the bulk of their waking hours. Those tasks, which require continuous attention, deactivate the DMN. In fact, research has shown that addictive behavior decreases the connectivity of the DMN and suppresses its activity.8 Most children and adolescents can be regarded as essentially addicted to social media, text messaging, and video games. Unsurprisingly, serious psychiatric consequences follow.9
DMN dysfunction has been reported in several psychiatric conditions, including depression, posttraumatic stress disorder, autism, schizophrenia, anxiety, obsessive-compulsive disorder, and substance use.10-12 Impaired social interactions and communications, negative ruminations, suicidal ideas, and impaired encoding of long-term memories are some of the adverse effects of DMN dysfunction. The good news is that the DMN’s connectivity and functioning can be modulated and restored by meditation, mentalizing, exercise, psychotherapy, antidepressants, and psychedelics.13,14
The lockdown and stress of the COVID-19 pandemic added insult to injury and exacerbated mental illness in children by isolating them from each other and intensifying their technological addiction to fill the void of isolation. This crisis in youth mental health continues unabated, and calls for action to prevent grim outcomes. DMN dysfunction in youth can be reversed with treatment, but access to mental health care has become more challenging due to workforce shortages and insurance restrictions. Psychiatrists and parents must work diligently to treat psychiatrically affected youth, which has become a DaMN serious problem…
1. Yao Z, Hu B, Xie Y, et al. A review of structural and functional brain networks: small world and atlas. Brain Inform. 2015;2(1):45-52. doi:10.1007/s40708-015-0009-z
2. Raichle ME. The brain’s dark energy. Sci Am. 2010;302(3):44-49. doi:10.1038/scientific american0310-44
3. Buckner RL, Andrews-Hanna JR, Schacter DL. The brain’s default network: anatomy, function, and relevance to disease. Ann N Y Acad Sci. 2008;1124:1-38. doi:10.1196/annals.1440.011
4. Raichle ME, Snyder AZ. A default mode of brain function: a brief history of an evolving idea. Neuroimage. 2007;37(4):1083-1090; discussion 1097-1099. doi:10.1016/j.neuroimage.2007.02.041
5. Andrews-Hanna JR. The brain’s default network and its adaptive role in internal mentation. Neuroscientist. 2012;18(3):251-270. doi:10.1177/1073858411403316
6. Tsoukalas I. Theory of mind: towards an evolutionary theory. Evolutionary Psychological Science. 2018;4(1):38-66. https://doi.org/10.1007/s40806-017-0112-x
7. Broyd SJ, Demanuele C, Debener S, et al. Default-mode brain dysfunction in mental disorders: a systematic review. Neurosci Biobehav Rev. 2009;33(3):279-296. doi:10.1016/j.neubiorev.2008.09.002
8. Zhang R, Volkow ND. Brain default-mode network dysfunction in addiction. Neuroimage. 2019;200:313-331. doi:10.1016/j.neuroimage.2019.06.036
9. Bommersbach TJ, McKean AJ, Olfson M, et al. National trends in mental health-related emergency department visits among youth, 2011-2020. JAMA. 2023;329(17):1469-1477. doi:10.1001/jama.2023.4809
10. Whitfield-Gabrieli S, Ford JM. Default mode network activity and connectivity in psychopathology. Annu Rev Clin Psychol. 2012;8:49-76. doi:10.1146/annurev-clinpsy-032511-143049
11. Akiki TJ, Averill CL, Wrocklage KM, et al. Default mode network abnormalities in posttraumatic stress disorder: a novel network-restricted topology approach. Neuroimage. 2018;176:489-498. doi:10.1016/j.neuroimage.2018.05.005
12. Nagata JM, Chu J, Zamora G, et al. Screen time and obsessive-compulsive disorder among children 9-10 years old: a prospective cohort study. J Adolesc Health. 2023;72(3):390-396. doi:10.1016/j.jadohealth.2022.10.023
13. Fox KC, Nijeboer S, Dixon ML, et al. Is meditation associated with altered brain structure? A systematic review and meta-analysis of morphometric neuroimaging in meditation practitioners. Neurosci Biobehav Rev. 2014;43:48-73. doi:10.1016/j.neubiorev.2014.03.016
14. Gattuso JJ, Perkins D, Ruffell S, et al. Default mode network modulation by psychedelics: a systematic review. Int J Neuropsychopharmacol. 2023;26(3):155-188. doi:10.1093/ijnp/pyac074
The advent of unprecedented technologies drastically altering the behavior of children and adolescents, compounded by prolonged isolation from a once-in-a-century pandemic, may have negatively impacted the normal connectivity of the human brain among youth, leading to the current alarming increase of depression, anxiety, and suicidality among this population.
The human brain is comprised of multiple large-scale networks that are functionally connected and control feelings, thoughts, and behaviors. As clinical neuroscientists, psychiatrists must consider the profound impact of a massive societal shift in human behavior on the functional connectivity of brain networks in health and disease. The advent of smartphones, social media, and video game addiction may have disrupted the developing brain networks in children and adolescents, leading to the current escalating epidemic of mental disorders in youth.
The major networks in the human brain include the default mode network (DMN), the salience network, the limbic system, the dorsal attention network, the central executive network, and the visual system.1 Each network connects several brain regions. Researchers can use functional MRI to detect the connectivity of those networks. When blood flow increases concurrently across 2 or 3 networks, this indicates those networks are functionally connected.
There was an old “dogma” that brain regions use energy only when activated and being used. Hans Berger, who developed the EEG in 1929, noticed electrical activity at rest and proposed that the brain is constantly busy, but his neurology peers did not take him seriously.2 In the 1950s, Louis Sokoloff noticed that brain metabolism was the same whether a person is at rest or doing math. In the 1970s, David Ingvar discovered that the highest blood flow in the frontal lobe occurred when a person was at rest.3 Finally, in 2007, Raichle et al4 used positron emission tomography scans to confirm that the frontal lobe is most active when a person is not doing anything. He labeled this phenomenon the DMN, comprising the medial fronto-parietal cortex, the posterior cingulate gyrus, the precuneus, and the angular gyrus. Interestingly, the number of publications about the DMN has skyrocketed since 2007.
The many roles of the DMN
Ongoing research has revealed that the DMN is most active at rest, and its anatomical hubs mediate several key functions5:
- Posterior cingulate gyrus (the central core of the DMN): remembering the past and thinking about the future
- Medial prefrontal cortex: autobiographical memories, future goals and events, reflecting on one’s emotional self, and considering decisions about family members
- Dorsal medial subsystem: thinking about others, determining and inferring the purpose of other people’s actions
- Temporo-parietal junction: reflecting on the beliefs and emotions of others (known as “theory of mind”6)
- Lateral parietal junction: retrieval of social and conceptual knowledge
- Hippocampus: forming new memories, remembering the past, imagining the future
- Posterior-inferior parietal lobe: junction of auditory, visual, and somatic sensory information and attention
- Precuneus: Visual, sensory-motor, and attention.
Many terms have been used to describe the function of the DMN, including “daydreaming,” “auto-pilot,” “mind-wondering,” “reminiscing,” “contemplating,” “self-reflection,” “the neurological basis of the self,” and “seat of literary creativity.”
Psychiatric consequences of DMN deactivation
When another brain network, the attention network (which is also referred to as the task-positive network), is activated consciously and volitionally to perform a task that demands focus (such as text messaging, playing video games, or continuously interacting with social media sites), DMN activity declines.
Continue to: The DMN does not exist...
The DMN does not exist in infants, but starts to develop in childhood.7 It is enhanced by exercise, daydreaming, and sleep, activities that are common in childhood but have declined drastically with the widespread use of smartphones, video games, and social media, which for many youth occupy the bulk of their waking hours. Those tasks, which require continuous attention, deactivate the DMN. In fact, research has shown that addictive behavior decreases the connectivity of the DMN and suppresses its activity.8 Most children and adolescents can be regarded as essentially addicted to social media, text messaging, and video games. Unsurprisingly, serious psychiatric consequences follow.9
DMN dysfunction has been reported in several psychiatric conditions, including depression, posttraumatic stress disorder, autism, schizophrenia, anxiety, obsessive-compulsive disorder, and substance use.10-12 Impaired social interactions and communications, negative ruminations, suicidal ideas, and impaired encoding of long-term memories are some of the adverse effects of DMN dysfunction. The good news is that the DMN’s connectivity and functioning can be modulated and restored by meditation, mentalizing, exercise, psychotherapy, antidepressants, and psychedelics.13,14
The lockdown and stress of the COVID-19 pandemic added insult to injury and exacerbated mental illness in children by isolating them from each other and intensifying their technological addiction to fill the void of isolation. This crisis in youth mental health continues unabated, and calls for action to prevent grim outcomes. DMN dysfunction in youth can be reversed with treatment, but access to mental health care has become more challenging due to workforce shortages and insurance restrictions. Psychiatrists and parents must work diligently to treat psychiatrically affected youth, which has become a DaMN serious problem…
The advent of unprecedented technologies drastically altering the behavior of children and adolescents, compounded by prolonged isolation from a once-in-a-century pandemic, may have negatively impacted the normal connectivity of the human brain among youth, leading to the current alarming increase of depression, anxiety, and suicidality among this population.
The human brain is comprised of multiple large-scale networks that are functionally connected and control feelings, thoughts, and behaviors. As clinical neuroscientists, psychiatrists must consider the profound impact of a massive societal shift in human behavior on the functional connectivity of brain networks in health and disease. The advent of smartphones, social media, and video game addiction may have disrupted the developing brain networks in children and adolescents, leading to the current escalating epidemic of mental disorders in youth.
The major networks in the human brain include the default mode network (DMN), the salience network, the limbic system, the dorsal attention network, the central executive network, and the visual system.1 Each network connects several brain regions. Researchers can use functional MRI to detect the connectivity of those networks. When blood flow increases concurrently across 2 or 3 networks, this indicates those networks are functionally connected.
There was an old “dogma” that brain regions use energy only when activated and being used. Hans Berger, who developed the EEG in 1929, noticed electrical activity at rest and proposed that the brain is constantly busy, but his neurology peers did not take him seriously.2 In the 1950s, Louis Sokoloff noticed that brain metabolism was the same whether a person is at rest or doing math. In the 1970s, David Ingvar discovered that the highest blood flow in the frontal lobe occurred when a person was at rest.3 Finally, in 2007, Raichle et al4 used positron emission tomography scans to confirm that the frontal lobe is most active when a person is not doing anything. He labeled this phenomenon the DMN, comprising the medial fronto-parietal cortex, the posterior cingulate gyrus, the precuneus, and the angular gyrus. Interestingly, the number of publications about the DMN has skyrocketed since 2007.
The many roles of the DMN
Ongoing research has revealed that the DMN is most active at rest, and its anatomical hubs mediate several key functions5:
- Posterior cingulate gyrus (the central core of the DMN): remembering the past and thinking about the future
- Medial prefrontal cortex: autobiographical memories, future goals and events, reflecting on one’s emotional self, and considering decisions about family members
- Dorsal medial subsystem: thinking about others, determining and inferring the purpose of other people’s actions
- Temporo-parietal junction: reflecting on the beliefs and emotions of others (known as “theory of mind”6)
- Lateral parietal junction: retrieval of social and conceptual knowledge
- Hippocampus: forming new memories, remembering the past, imagining the future
- Posterior-inferior parietal lobe: junction of auditory, visual, and somatic sensory information and attention
- Precuneus: Visual, sensory-motor, and attention.
Many terms have been used to describe the function of the DMN, including “daydreaming,” “auto-pilot,” “mind-wondering,” “reminiscing,” “contemplating,” “self-reflection,” “the neurological basis of the self,” and “seat of literary creativity.”
Psychiatric consequences of DMN deactivation
When another brain network, the attention network (which is also referred to as the task-positive network), is activated consciously and volitionally to perform a task that demands focus (such as text messaging, playing video games, or continuously interacting with social media sites), DMN activity declines.
Continue to: The DMN does not exist...
The DMN does not exist in infants, but starts to develop in childhood.7 It is enhanced by exercise, daydreaming, and sleep, activities that are common in childhood but have declined drastically with the widespread use of smartphones, video games, and social media, which for many youth occupy the bulk of their waking hours. Those tasks, which require continuous attention, deactivate the DMN. In fact, research has shown that addictive behavior decreases the connectivity of the DMN and suppresses its activity.8 Most children and adolescents can be regarded as essentially addicted to social media, text messaging, and video games. Unsurprisingly, serious psychiatric consequences follow.9
DMN dysfunction has been reported in several psychiatric conditions, including depression, posttraumatic stress disorder, autism, schizophrenia, anxiety, obsessive-compulsive disorder, and substance use.10-12 Impaired social interactions and communications, negative ruminations, suicidal ideas, and impaired encoding of long-term memories are some of the adverse effects of DMN dysfunction. The good news is that the DMN’s connectivity and functioning can be modulated and restored by meditation, mentalizing, exercise, psychotherapy, antidepressants, and psychedelics.13,14
The lockdown and stress of the COVID-19 pandemic added insult to injury and exacerbated mental illness in children by isolating them from each other and intensifying their technological addiction to fill the void of isolation. This crisis in youth mental health continues unabated, and calls for action to prevent grim outcomes. DMN dysfunction in youth can be reversed with treatment, but access to mental health care has become more challenging due to workforce shortages and insurance restrictions. Psychiatrists and parents must work diligently to treat psychiatrically affected youth, which has become a DaMN serious problem…
1. Yao Z, Hu B, Xie Y, et al. A review of structural and functional brain networks: small world and atlas. Brain Inform. 2015;2(1):45-52. doi:10.1007/s40708-015-0009-z
2. Raichle ME. The brain’s dark energy. Sci Am. 2010;302(3):44-49. doi:10.1038/scientific american0310-44
3. Buckner RL, Andrews-Hanna JR, Schacter DL. The brain’s default network: anatomy, function, and relevance to disease. Ann N Y Acad Sci. 2008;1124:1-38. doi:10.1196/annals.1440.011
4. Raichle ME, Snyder AZ. A default mode of brain function: a brief history of an evolving idea. Neuroimage. 2007;37(4):1083-1090; discussion 1097-1099. doi:10.1016/j.neuroimage.2007.02.041
5. Andrews-Hanna JR. The brain’s default network and its adaptive role in internal mentation. Neuroscientist. 2012;18(3):251-270. doi:10.1177/1073858411403316
6. Tsoukalas I. Theory of mind: towards an evolutionary theory. Evolutionary Psychological Science. 2018;4(1):38-66. https://doi.org/10.1007/s40806-017-0112-x
7. Broyd SJ, Demanuele C, Debener S, et al. Default-mode brain dysfunction in mental disorders: a systematic review. Neurosci Biobehav Rev. 2009;33(3):279-296. doi:10.1016/j.neubiorev.2008.09.002
8. Zhang R, Volkow ND. Brain default-mode network dysfunction in addiction. Neuroimage. 2019;200:313-331. doi:10.1016/j.neuroimage.2019.06.036
9. Bommersbach TJ, McKean AJ, Olfson M, et al. National trends in mental health-related emergency department visits among youth, 2011-2020. JAMA. 2023;329(17):1469-1477. doi:10.1001/jama.2023.4809
10. Whitfield-Gabrieli S, Ford JM. Default mode network activity and connectivity in psychopathology. Annu Rev Clin Psychol. 2012;8:49-76. doi:10.1146/annurev-clinpsy-032511-143049
11. Akiki TJ, Averill CL, Wrocklage KM, et al. Default mode network abnormalities in posttraumatic stress disorder: a novel network-restricted topology approach. Neuroimage. 2018;176:489-498. doi:10.1016/j.neuroimage.2018.05.005
12. Nagata JM, Chu J, Zamora G, et al. Screen time and obsessive-compulsive disorder among children 9-10 years old: a prospective cohort study. J Adolesc Health. 2023;72(3):390-396. doi:10.1016/j.jadohealth.2022.10.023
13. Fox KC, Nijeboer S, Dixon ML, et al. Is meditation associated with altered brain structure? A systematic review and meta-analysis of morphometric neuroimaging in meditation practitioners. Neurosci Biobehav Rev. 2014;43:48-73. doi:10.1016/j.neubiorev.2014.03.016
14. Gattuso JJ, Perkins D, Ruffell S, et al. Default mode network modulation by psychedelics: a systematic review. Int J Neuropsychopharmacol. 2023;26(3):155-188. doi:10.1093/ijnp/pyac074
1. Yao Z, Hu B, Xie Y, et al. A review of structural and functional brain networks: small world and atlas. Brain Inform. 2015;2(1):45-52. doi:10.1007/s40708-015-0009-z
2. Raichle ME. The brain’s dark energy. Sci Am. 2010;302(3):44-49. doi:10.1038/scientific american0310-44
3. Buckner RL, Andrews-Hanna JR, Schacter DL. The brain’s default network: anatomy, function, and relevance to disease. Ann N Y Acad Sci. 2008;1124:1-38. doi:10.1196/annals.1440.011
4. Raichle ME, Snyder AZ. A default mode of brain function: a brief history of an evolving idea. Neuroimage. 2007;37(4):1083-1090; discussion 1097-1099. doi:10.1016/j.neuroimage.2007.02.041
5. Andrews-Hanna JR. The brain’s default network and its adaptive role in internal mentation. Neuroscientist. 2012;18(3):251-270. doi:10.1177/1073858411403316
6. Tsoukalas I. Theory of mind: towards an evolutionary theory. Evolutionary Psychological Science. 2018;4(1):38-66. https://doi.org/10.1007/s40806-017-0112-x
7. Broyd SJ, Demanuele C, Debener S, et al. Default-mode brain dysfunction in mental disorders: a systematic review. Neurosci Biobehav Rev. 2009;33(3):279-296. doi:10.1016/j.neubiorev.2008.09.002
8. Zhang R, Volkow ND. Brain default-mode network dysfunction in addiction. Neuroimage. 2019;200:313-331. doi:10.1016/j.neuroimage.2019.06.036
9. Bommersbach TJ, McKean AJ, Olfson M, et al. National trends in mental health-related emergency department visits among youth, 2011-2020. JAMA. 2023;329(17):1469-1477. doi:10.1001/jama.2023.4809
10. Whitfield-Gabrieli S, Ford JM. Default mode network activity and connectivity in psychopathology. Annu Rev Clin Psychol. 2012;8:49-76. doi:10.1146/annurev-clinpsy-032511-143049
11. Akiki TJ, Averill CL, Wrocklage KM, et al. Default mode network abnormalities in posttraumatic stress disorder: a novel network-restricted topology approach. Neuroimage. 2018;176:489-498. doi:10.1016/j.neuroimage.2018.05.005
12. Nagata JM, Chu J, Zamora G, et al. Screen time and obsessive-compulsive disorder among children 9-10 years old: a prospective cohort study. J Adolesc Health. 2023;72(3):390-396. doi:10.1016/j.jadohealth.2022.10.023
13. Fox KC, Nijeboer S, Dixon ML, et al. Is meditation associated with altered brain structure? A systematic review and meta-analysis of morphometric neuroimaging in meditation practitioners. Neurosci Biobehav Rev. 2014;43:48-73. doi:10.1016/j.neubiorev.2014.03.016
14. Gattuso JJ, Perkins D, Ruffell S, et al. Default mode network modulation by psychedelics: a systematic review. Int J Neuropsychopharmacol. 2023;26(3):155-188. doi:10.1093/ijnp/pyac074
The joys and rewards of an asymmetric life
The benefits of living a balanced life is a very popular concept. But I beg to differ. Balance in one’s life is overrated. Allocating equal time to the various components of one’s life may sound admirable, but it is a recipe for an ordinary life, with no major achievements or a memorable legacy. Scoring a “moonshot” achievement while living a balanced life is highly unlikely.
The benefits of deliberately leading an “asymmetric life” is an epiphany I acquired as a young boy addicted to watching stellar Olympic athletes win gold medals. I dreamed about being the best in the world in a sport, or in something else. As I read about the lives of my Olympic idols, my mind was opened to the fact that each of them led an unbalanced life in the pursuit of their cherished goal to be the best in the world: a gold medalist. I found out that for several years before the Olympic games, these athletes spent a disproportionate amount of their waking time (≥10 hours a day) practicing their sport, strengthening their muscles, building up their stamina, and honing their physical skills and mental toughness. Those sacrifices were necessary—in fact, indispensable—to set themselves apart from us mere mortals. Their social life was quite restricted, and even their educational pursuits had to be reduced or deferred.
I realized at a young age that to be the world’s best athlete, one must lead a purpose-driven life and channel a tremendous amount of time and energy to achieve the cherished goal of an Olympic gold medal. I understood the sacrifices necessary to excel in sports, and concluded the same was also true outside of sports, such as for Nobel Laureates, world-class pianists, prodigious authors, ballet dancers, opera divas, or self-employed entrepreneurs.
As I grew up, I repeatedly heard people praise “the balanced life,” but in my heart, I knew that was a fallacy. I had already decided in high school that I wanted to become a psychiatric physician. I was a premed major in college and very aware that our medical school enrolled only 44 students into the Med 1 class. There were >350 other premed undergraduates. Thus, without hesitation, and with gusto, I deliberately led an unbalanced life, studying countless hours each day to achieve an A grade in all required and elective courses to earn a spot on the Dean’s list. I already had confidence in my academic skills because of my excellent performance in high school, but I was not going to take any chances because I recalled a quote commonly attributed to Thomas Edison: “Genius is 1% inspiration and 99% perspiration.” This is obviously antithetical to living a balanced life.
I matriculated in medical school, and my unbalanced lifestyle continued unabated. Most readers of this journal are fellow physicians who know well the heavy demands of medical school on our lives, in both the preclinical and clinical years. Trying to lead a balanced life during the 4 years of medical school can have disastrous consequences. We all led an “asymmetric existence” with 75% (or more) of our waking hours invested in our careers and 25% (or less) directed to our social lives (and fortunately, our families and friends generally understood). That is what it takes to earn the coveted MD, the equivalent of an Olympic medal for intellectual athletes.
Then came 4 more years of psychiatric residency training, and the long hours of work continued, along with many nights and weekends on call. As a resident, I treasured the modest but precious amount of time I had outside work. I was lucky to have a very supportive and competent wife (a psychologist), who spared me from having to wake up at night to feed our first baby or do various household chores, so I could read the many articles and books on my desk and catch up on my sleep after my frequent night and weekend call shifts.
My unbalanced life continued when I pursued a postresidency fellowship at the National Institutes of Health, where I conducted numerous clinical research trials, brain imaging studies, and postmortem research on a large collection of brains from deceased patients with schizophrenia or bipolar disorder. I worked 12 to 15 hours a day to write up the data I had collected, submit it to scientific journals, and revise it as needed. I knew from the strategic plan I had set for my life that the neuroscience fellowship would launch my academic career, and indeed it did.
Continue to: Reaping the benefits
Reaping the benefits
Fast forward 30 years and you will still find me leading an unbalanced but joyful and fulfilling life. People often ask me how I was able to achieve so much (authoring several hundred scientific publications; publishing 13 books; receiving dozens of grants; editing 3 scientific journals; founding an international schizophrenia society; assuming many leadership positions, including becoming a department chair at 2 universities and being elected to the presidency of several associations; lecturing around the world and making hundreds of scientific presentations at national and international conferences; seeing thousands of patients; teaching, supervising, and mentoring countless medical students, psychiatric residents, and young faculty members; and creating a nonprofit foundation [CURESZ.org] with a former patient who recovered completely after 5 years of home classes and treatment-refractory command hallucinations who then graduated from college with honors in molecular biology after I prescribed clozapine to “cure” her from what was deemed a hopeless and irreversible mental disability1). In all, thanks to my unbalanced life, I have achieved 12 moonshots and each is a major achievement of which I am proud.
My answer to those who ask me how I did all that is simple: I have strategically led an unbalanced life, enjoying every minute of it, and reaping the fruits of my labor. I do not waste an inordinate amount of time watching TV or participating in social media like many others might. And more importantly, despite this unbalanced life, I have been married to my college sweetheart for several decades and have a son and a daughter who are very high achievers and make me proud. I do budget time to regularly take my children and grandchildren on family vacations to exotic locations. I have dinner with my family every night. I am very happy with this so-called unbalanced life. I have received numerous awards and recognitions for my accomplishments, including the Distinguished Scholar Award (the highest academic recognition at The Ohio State University), the coveted Stanley Dean Award for research into schizophrenia from the American College of Psychiatrists, 4 Golden Apple Teaching Awards, and the Daniel Drake Medal, the highest honor that the University of Cincinnati College of Medicine bestows on a faculty member. (Dr. Drake founded the University of Cincinnati College of Medicine 200 years ago, a major moonshot, and among his many accomplishments, he also established the first psychiatric hospital in Ohio, another consequential moonshot. I am sure he led a very productive, unbalanced life, and that is why he is still remembered and revered 200 years later.)
It is said that at the height of his prominence 90 years ago, Sigmund Freud was asked, “What is life all about?” He responded with 2 words: “Liebe und arbeit” (love and work). Importantly, he did not specify which proportions those 2 major functions should occupy in one’s life. It was left up to each individual to make that choice. In the constitution of our country, that freedom of choice is the secret sauce of “the pursuit of happiness.”
1. The CURESZ Foundation. Who we are. Accessed April 11, 2023. https://curesz.org/about/who-we-are/
The benefits of living a balanced life is a very popular concept. But I beg to differ. Balance in one’s life is overrated. Allocating equal time to the various components of one’s life may sound admirable, but it is a recipe for an ordinary life, with no major achievements or a memorable legacy. Scoring a “moonshot” achievement while living a balanced life is highly unlikely.
The benefits of deliberately leading an “asymmetric life” is an epiphany I acquired as a young boy addicted to watching stellar Olympic athletes win gold medals. I dreamed about being the best in the world in a sport, or in something else. As I read about the lives of my Olympic idols, my mind was opened to the fact that each of them led an unbalanced life in the pursuit of their cherished goal to be the best in the world: a gold medalist. I found out that for several years before the Olympic games, these athletes spent a disproportionate amount of their waking time (≥10 hours a day) practicing their sport, strengthening their muscles, building up their stamina, and honing their physical skills and mental toughness. Those sacrifices were necessary—in fact, indispensable—to set themselves apart from us mere mortals. Their social life was quite restricted, and even their educational pursuits had to be reduced or deferred.
I realized at a young age that to be the world’s best athlete, one must lead a purpose-driven life and channel a tremendous amount of time and energy to achieve the cherished goal of an Olympic gold medal. I understood the sacrifices necessary to excel in sports, and concluded the same was also true outside of sports, such as for Nobel Laureates, world-class pianists, prodigious authors, ballet dancers, opera divas, or self-employed entrepreneurs.
As I grew up, I repeatedly heard people praise “the balanced life,” but in my heart, I knew that was a fallacy. I had already decided in high school that I wanted to become a psychiatric physician. I was a premed major in college and very aware that our medical school enrolled only 44 students into the Med 1 class. There were >350 other premed undergraduates. Thus, without hesitation, and with gusto, I deliberately led an unbalanced life, studying countless hours each day to achieve an A grade in all required and elective courses to earn a spot on the Dean’s list. I already had confidence in my academic skills because of my excellent performance in high school, but I was not going to take any chances because I recalled a quote commonly attributed to Thomas Edison: “Genius is 1% inspiration and 99% perspiration.” This is obviously antithetical to living a balanced life.
I matriculated in medical school, and my unbalanced lifestyle continued unabated. Most readers of this journal are fellow physicians who know well the heavy demands of medical school on our lives, in both the preclinical and clinical years. Trying to lead a balanced life during the 4 years of medical school can have disastrous consequences. We all led an “asymmetric existence” with 75% (or more) of our waking hours invested in our careers and 25% (or less) directed to our social lives (and fortunately, our families and friends generally understood). That is what it takes to earn the coveted MD, the equivalent of an Olympic medal for intellectual athletes.
Then came 4 more years of psychiatric residency training, and the long hours of work continued, along with many nights and weekends on call. As a resident, I treasured the modest but precious amount of time I had outside work. I was lucky to have a very supportive and competent wife (a psychologist), who spared me from having to wake up at night to feed our first baby or do various household chores, so I could read the many articles and books on my desk and catch up on my sleep after my frequent night and weekend call shifts.
My unbalanced life continued when I pursued a postresidency fellowship at the National Institutes of Health, where I conducted numerous clinical research trials, brain imaging studies, and postmortem research on a large collection of brains from deceased patients with schizophrenia or bipolar disorder. I worked 12 to 15 hours a day to write up the data I had collected, submit it to scientific journals, and revise it as needed. I knew from the strategic plan I had set for my life that the neuroscience fellowship would launch my academic career, and indeed it did.
Continue to: Reaping the benefits
Reaping the benefits
Fast forward 30 years and you will still find me leading an unbalanced but joyful and fulfilling life. People often ask me how I was able to achieve so much (authoring several hundred scientific publications; publishing 13 books; receiving dozens of grants; editing 3 scientific journals; founding an international schizophrenia society; assuming many leadership positions, including becoming a department chair at 2 universities and being elected to the presidency of several associations; lecturing around the world and making hundreds of scientific presentations at national and international conferences; seeing thousands of patients; teaching, supervising, and mentoring countless medical students, psychiatric residents, and young faculty members; and creating a nonprofit foundation [CURESZ.org] with a former patient who recovered completely after 5 years of home classes and treatment-refractory command hallucinations who then graduated from college with honors in molecular biology after I prescribed clozapine to “cure” her from what was deemed a hopeless and irreversible mental disability1). In all, thanks to my unbalanced life, I have achieved 12 moonshots and each is a major achievement of which I am proud.
My answer to those who ask me how I did all that is simple: I have strategically led an unbalanced life, enjoying every minute of it, and reaping the fruits of my labor. I do not waste an inordinate amount of time watching TV or participating in social media like many others might. And more importantly, despite this unbalanced life, I have been married to my college sweetheart for several decades and have a son and a daughter who are very high achievers and make me proud. I do budget time to regularly take my children and grandchildren on family vacations to exotic locations. I have dinner with my family every night. I am very happy with this so-called unbalanced life. I have received numerous awards and recognitions for my accomplishments, including the Distinguished Scholar Award (the highest academic recognition at The Ohio State University), the coveted Stanley Dean Award for research into schizophrenia from the American College of Psychiatrists, 4 Golden Apple Teaching Awards, and the Daniel Drake Medal, the highest honor that the University of Cincinnati College of Medicine bestows on a faculty member. (Dr. Drake founded the University of Cincinnati College of Medicine 200 years ago, a major moonshot, and among his many accomplishments, he also established the first psychiatric hospital in Ohio, another consequential moonshot. I am sure he led a very productive, unbalanced life, and that is why he is still remembered and revered 200 years later.)
It is said that at the height of his prominence 90 years ago, Sigmund Freud was asked, “What is life all about?” He responded with 2 words: “Liebe und arbeit” (love and work). Importantly, he did not specify which proportions those 2 major functions should occupy in one’s life. It was left up to each individual to make that choice. In the constitution of our country, that freedom of choice is the secret sauce of “the pursuit of happiness.”
The benefits of living a balanced life is a very popular concept. But I beg to differ. Balance in one’s life is overrated. Allocating equal time to the various components of one’s life may sound admirable, but it is a recipe for an ordinary life, with no major achievements or a memorable legacy. Scoring a “moonshot” achievement while living a balanced life is highly unlikely.
The benefits of deliberately leading an “asymmetric life” is an epiphany I acquired as a young boy addicted to watching stellar Olympic athletes win gold medals. I dreamed about being the best in the world in a sport, or in something else. As I read about the lives of my Olympic idols, my mind was opened to the fact that each of them led an unbalanced life in the pursuit of their cherished goal to be the best in the world: a gold medalist. I found out that for several years before the Olympic games, these athletes spent a disproportionate amount of their waking time (≥10 hours a day) practicing their sport, strengthening their muscles, building up their stamina, and honing their physical skills and mental toughness. Those sacrifices were necessary—in fact, indispensable—to set themselves apart from us mere mortals. Their social life was quite restricted, and even their educational pursuits had to be reduced or deferred.
I realized at a young age that to be the world’s best athlete, one must lead a purpose-driven life and channel a tremendous amount of time and energy to achieve the cherished goal of an Olympic gold medal. I understood the sacrifices necessary to excel in sports, and concluded the same was also true outside of sports, such as for Nobel Laureates, world-class pianists, prodigious authors, ballet dancers, opera divas, or self-employed entrepreneurs.
As I grew up, I repeatedly heard people praise “the balanced life,” but in my heart, I knew that was a fallacy. I had already decided in high school that I wanted to become a psychiatric physician. I was a premed major in college and very aware that our medical school enrolled only 44 students into the Med 1 class. There were >350 other premed undergraduates. Thus, without hesitation, and with gusto, I deliberately led an unbalanced life, studying countless hours each day to achieve an A grade in all required and elective courses to earn a spot on the Dean’s list. I already had confidence in my academic skills because of my excellent performance in high school, but I was not going to take any chances because I recalled a quote commonly attributed to Thomas Edison: “Genius is 1% inspiration and 99% perspiration.” This is obviously antithetical to living a balanced life.
I matriculated in medical school, and my unbalanced lifestyle continued unabated. Most readers of this journal are fellow physicians who know well the heavy demands of medical school on our lives, in both the preclinical and clinical years. Trying to lead a balanced life during the 4 years of medical school can have disastrous consequences. We all led an “asymmetric existence” with 75% (or more) of our waking hours invested in our careers and 25% (or less) directed to our social lives (and fortunately, our families and friends generally understood). That is what it takes to earn the coveted MD, the equivalent of an Olympic medal for intellectual athletes.
Then came 4 more years of psychiatric residency training, and the long hours of work continued, along with many nights and weekends on call. As a resident, I treasured the modest but precious amount of time I had outside work. I was lucky to have a very supportive and competent wife (a psychologist), who spared me from having to wake up at night to feed our first baby or do various household chores, so I could read the many articles and books on my desk and catch up on my sleep after my frequent night and weekend call shifts.
My unbalanced life continued when I pursued a postresidency fellowship at the National Institutes of Health, where I conducted numerous clinical research trials, brain imaging studies, and postmortem research on a large collection of brains from deceased patients with schizophrenia or bipolar disorder. I worked 12 to 15 hours a day to write up the data I had collected, submit it to scientific journals, and revise it as needed. I knew from the strategic plan I had set for my life that the neuroscience fellowship would launch my academic career, and indeed it did.
Continue to: Reaping the benefits
Reaping the benefits
Fast forward 30 years and you will still find me leading an unbalanced but joyful and fulfilling life. People often ask me how I was able to achieve so much (authoring several hundred scientific publications; publishing 13 books; receiving dozens of grants; editing 3 scientific journals; founding an international schizophrenia society; assuming many leadership positions, including becoming a department chair at 2 universities and being elected to the presidency of several associations; lecturing around the world and making hundreds of scientific presentations at national and international conferences; seeing thousands of patients; teaching, supervising, and mentoring countless medical students, psychiatric residents, and young faculty members; and creating a nonprofit foundation [CURESZ.org] with a former patient who recovered completely after 5 years of home classes and treatment-refractory command hallucinations who then graduated from college with honors in molecular biology after I prescribed clozapine to “cure” her from what was deemed a hopeless and irreversible mental disability1). In all, thanks to my unbalanced life, I have achieved 12 moonshots and each is a major achievement of which I am proud.
My answer to those who ask me how I did all that is simple: I have strategically led an unbalanced life, enjoying every minute of it, and reaping the fruits of my labor. I do not waste an inordinate amount of time watching TV or participating in social media like many others might. And more importantly, despite this unbalanced life, I have been married to my college sweetheart for several decades and have a son and a daughter who are very high achievers and make me proud. I do budget time to regularly take my children and grandchildren on family vacations to exotic locations. I have dinner with my family every night. I am very happy with this so-called unbalanced life. I have received numerous awards and recognitions for my accomplishments, including the Distinguished Scholar Award (the highest academic recognition at The Ohio State University), the coveted Stanley Dean Award for research into schizophrenia from the American College of Psychiatrists, 4 Golden Apple Teaching Awards, and the Daniel Drake Medal, the highest honor that the University of Cincinnati College of Medicine bestows on a faculty member. (Dr. Drake founded the University of Cincinnati College of Medicine 200 years ago, a major moonshot, and among his many accomplishments, he also established the first psychiatric hospital in Ohio, another consequential moonshot. I am sure he led a very productive, unbalanced life, and that is why he is still remembered and revered 200 years later.)
It is said that at the height of his prominence 90 years ago, Sigmund Freud was asked, “What is life all about?” He responded with 2 words: “Liebe und arbeit” (love and work). Importantly, he did not specify which proportions those 2 major functions should occupy in one’s life. It was left up to each individual to make that choice. In the constitution of our country, that freedom of choice is the secret sauce of “the pursuit of happiness.”
1. The CURESZ Foundation. Who we are. Accessed April 11, 2023. https://curesz.org/about/who-we-are/
1. The CURESZ Foundation. Who we are. Accessed April 11, 2023. https://curesz.org/about/who-we-are/
For artificial intelligence, the future is finally here
We are currently on the verge of yet another societal “revolution” that will exert an unprecedented impact on our lives. It may surpass prior seismic cultural breakthroughs like the internet, smartphones, and social media. Artificial intelligence (AI) has been fermenting for several decades, gathering steam to become equivalent (and eventually superior) to human intelligence. The escalation of AI sophistication will be jarring and perhaps change human life in completely unpredictable ways.
Composing thoughts into words and coherent sentences has always been a uniquely human attribute among all living organisms. Now, that sublime feature of the human mind is being simulated, thanks to advances in AI software, ironically created by the human mind itself! On November 30, 2022, Open AI introduced ChatGPT (generative pre-trained transformer), which can generate an article on any topic a user requests. Within a few weeks, it was used by more than 100 million people. ChatGPT is taking the world by storm because it is a harbinger (some pessimists may label it an omen) of how human existence will be radically impacted in the future. Such AI breakthroughs to surpass human intelligence are, ironically, the product of the advanced human brain, which I previously described as concurrently a triumph and a blunder by evolution.1
How we got here, and what’s next
ChatGPT is a large language model based on neural networks.2 It generates realistic text responses to a wide range of questions by mimicking the pattern of language in gargantuan online databases. One Hong Kong–based, AI-powered drug discovery company (Insilico Medicine) declared it published articles generated by AI tools, even before ChatGPT became available. This indicates how AI can be misused in scientific publications and may be hard to detect as a new form of plagiarism.3
The roots of AI date back to the 1950s, when Alan Turing, now considered the father of AI, published a seminal article about creating a machine to “imitate the brain” and to “mimic the behavior of the human.”4 The term “artificial intelligence” was coined in 1989 by McCarthy,5 who defined it as “the science of engineering for making intelligent machines.” Since then, several subsets of AI have been developed:
- Machine learning: The study of computer algorithms to generate hypotheses
- Deep learning: A type of machine learning algorithm that uses multiple layers to progressively extract higher-level features from raw input. (Both machine learning and deep learning are used in the burgeoning fields of computational psychiatry6 and neuroscience research7)
- Expert knowledge system: A computer-based system that mimics human decision-making ability
- Neural networks: An interconnected group of artificial neurons that uses a math or computer model for information processing
- Predictive analytics: An algorithm to predict future outcomes based on historical data.
These subsets of AI have been used to identify psychiatric disorders using neuroimaging data8 and to classify brain disorders.9 There are many potential uses of AI in psychiatry.10,11 My first experience with AI was 13 years ago, when we conducted a project to distinguish fake suicide notes from genuine ones.12 AI was more successful in correctly identifying fake notes (78% correctly detected) than senior psychiatric residents (49%) or even faculty (53%).
AI will dramatically change how humans interact with the world and may lead to enhanced creativity and new explorations and forays into novel, previously unknown horizons. It is expected to significantly boost the global economy by many trillions of dollars over the next decade. Major high-tech companies are vigorously competing to develop their own AI tools like ChatGPT (Microsoft invested $10 billion in Open AI). Google, which owns DeepMind (an AI lab that invented the T in GPT) developed its own chatbot called Bard. Amazon has invested heavily in Stability AI by giving its founder and CEO Emad Mostaque 4,000 Nvidia AI chips to assemble the world’s largest supercomputer (1 year ago, Stability had only 32 AI chips!). Apple recently integrated Stable Diffusion into its latest operating system. Chinese tech giants Alibaba and Baidu also announced their own chatbots to be released soon.
Other competitors include Cohere, Hugging Face, Midjourney, GitHub Copilot, Game Changer, Jasper, and Anthropic, which released Claude as its chatbot at a lower cost than ChatGPT. Open AI also developed Dall-E2 in April 2022, which can generate very realistic images from text, one of which recently won an award at an art competition.
Continue to: One of the major...
One of the major concerns about these AI developments is that chatbots can make errors or disseminate misinformation and even enunciate racist or misogynist statements. The greatest worry is that the ultimate implicit goal of AI is what is called artificial general intelligence (AGI), which can think and learn better than humans. Some fear AGI may wipe out humans as a species, a grave outcome indeed. That’s why AI developers intend to align AGI with “basic human values” in the event it surpasses human intelligence. Some are even calling for a transition from AI to AW (artificial wisdom), with built-in empathy, kindness, self-reflection, acceptance of diverse perspectives, and promotion of prosocial ideas.13
Creating content: artificial intelligence vs human authors
ChatGPT has opened a Pandora’s box of concern about potential plagiarism by students or scientific authors. This has prompted several journals,14 including
- Anosognosia in schizophrenia (Box 1); based on “Is anosognosia a delusion, a negative symptom, or a cognitive deficit?”
Current Psychiatry , January 2022, p. 6-8,14. doi: 10.12788/cp.0210 - Benefits of metformin in psychiatry (Box 2); based on “Beyond diabetes: The beneficial uses of metformin in psychiatry,”
Current Psychiatry , March 2022, p. 7-9. doi: 10.12788/cp.0225 - Epidemic of intellectual constipation (Box 3); based on “From debate to stalemate and hate: An epidemic of intellectual constipation,”
Current Psychiatry , January 2023, p. 3-4. doi: 10.12788/cp.0321 - SWOT analysis of psychiatry (Box 4); based on “Contemporary psychiatry: A SWOT analysis,”
Current Psychiatry , January 2023, p. 16-19,27. doi: 10.12788/cp.0320.
These ChatGPT articles are verbatim as generated, without any copyediting, fact-checking, or addition of reference citations. One can easily notice that while factually acceptable, the ChatGPT articles tend to be rather synthetic, simple, bland, and lacking creative language or going beyond the facts to express personal viewpoints. However, I have no doubt that future versions of ChatGPT or other chatbots will evolve into far more sophisticated products and may match what a human can compose in terms of quality and complexity.
AI has arrived with a bang. Going forward, I predict it will continue to surprise us, with elements of “future shock.” The credit (or blame) belongs to the boundless creativity of human intelligence that is seeking to invent an intelligence higher than its own. Caveat emptor!
Box 1
Anosognosia is a condition in which a person is unaware or unable to recognize their own illness or disability. In schizophrenia, anosognosia can be present in up to 50% of cases and is characterized by a lack of insight into the presence and severity of symptoms.
People with anosognosia in schizophrenia may not believe that they have a mental illness, may deny the reality of their symptoms, or may attribute them to external causes. This can make it difficult for them to comply with treatment, as they may not see the need for medication or other interventions.
Anosognosia is thought to be caused by structural and functional changes in the brain, particularly in areas associated with self-awareness and insight. It is often more severe in people with more severe forms of schizophrenia and may be associated with poorer treatment outcomes.
Effective treatment for anosognosia in schizophrenia typically involves a combination of medication and therapy, as well as strategies for improving insight and awareness of symptoms. Family members and caregivers can also play an important role in helping people with schizophrenia to recognize the presence and impact of their illness, and encouraging them to engage in treatment.
a Based on “Is anosognosia a delusion, a negative symptom, or a cognitive deficit?” Current Psychiatry, January 2022, p. 6-8,14. doi: 10.12788/cp.0210
Box 2
Metformin is a medication commonly used in the treatment of type 2 diabetes. However, there is growing interest in its potential use in psychiatry, particularly in the treatment of certain mental health conditions. Some potential benefits of metformin in psychiatry include:
1. Treatment of mood disorders: Studies have suggested that metformin may be helpful in the treatment of mood disorders, such as depression and bipolar disorder. One proposed mechanism is that metformin may help to regulate glucose metabolism and insulin sensitivity, which in turn may help to stabilize mood.
2. Treatment of schizophrenia: Some studies have suggested that metformin may be helpful in reducing symptoms of schizophrenia, particularly negative symptoms such as social withdrawal and apathy. One proposed mechanism is that metformin may improve brain energy metabolism, which may in turn improve cognitive function and reduce symptoms.
3. Weight management: Metformin has been shown to be effective in weight management, which can be particularly important for people with certain mental health conditions, such as bipolar disorder, where weight gain can be a side effect of medication.
4. Neuroprotection: Metformin has been shown to have neuroprotective effects, which may be beneficial for people with certain mental health conditions, such as Alzheimer’s disease and Parkinson’s disease.
It is important to note that while there is some evidence for the potential benefits of metformin in psychiatry, further research is needed to fully understand its effectiveness and safety in this context. People with mental health conditions should not start taking metformin without first consulting with their healthcare provider.
a Based on “Beyond diabetes: The beneficial uses of metformin in psychiatry,” Current Psychiatry, March 2022, p. 7-9. doi: 10.12788/cp.0225
Box 3
The term “epidemic of intellectual constipation” refers to a phenomenon in which individuals, groups, or even entire societies are seen as lacking the ability to think critically, creatively, or expansively. It can be characterized by a lack of curiosity, a narrow range of interests, and a reluctance to engage with new or challenging ideas.
The cause of this phenomenon can be attributed to a variety of factors, including cultural, social, and educational influences. For example, some argue that a narrow and standardized educational system, as well as a lack of exposure to diverse perspectives, can limit creativity and critical thinking skills. Additionally, the prevalence of social media and other forms of digital media may encourage a focus on immediate gratification and quick information, rather than more in-depth and meaningful engagement with information.
The consequences of this epidemic can be far-reaching and can impact personal, social, and political aspects of life. For instance, a lack of critical thinking skills can lead to the spread of misinformation, while a narrow range of interests can limit personal growth and the ability to connect with others.
To combat the epidemic of intellectual constipation, it’s important to foster critical thinking skills, encourage exposure to diverse perspectives, and encourage a lifelong love of learning. This can be achieved through education, community engagement, and personal effort.
In conclusion, the “epidemic of intellectual constipation” refers to a phenomenon in which individuals, groups, or entire societies lack the ability to think critically, creatively, and expansively. To combat this epidemic, it’s important to foster critical thinking skills, encourage exposure to diverse perspectives, and encourage a lifelong love of learning.
a Based on “From debate to stalemate and hate: An epidemic of intellectual constipation,” Current Psychiatry, January 2023, p. 3-4. doi: 10.12788/cp.0321
Box 4
SWOT analysis is a tool used to assess the strengths, weaknesses, opportunities, and threats of a particular entity or industry. In this case, we will conduct a SWOT analysis of psychiatry as a field of medicine.
Strengths
• Psychiatry plays a crucial role in addressing mental health issues and improving the quality of life of individuals who struggle with them.
• Psychiatry has made significant advances in understanding the biological and psychological underpinnings of mental illness, which has led to the development of more effective treatments.
• There is growing public awareness and acceptance of the importance of mental health, which has led to increased demand for psychiatric services.
• The field of psychiatry attracts many talented and compassionate professionals who are dedicated to helping those in need.
Weaknesses
• There is still a significant stigma associated with mental illness, which can deter individuals from seeking treatment.
• The effectiveness of some psychiatric treatments can be limited, particularly in cases of severe mental illness.
• The shortage of mental health professionals in many areas means that access to psychiatric services may be limited, particularly for individuals with lower incomes.
• The cost of psychiatric treatment can be prohibitively expensive, particularly for individuals without insurance coverage.
Opportunities
• New advances in neuroscience and technology, such as brain imaging and genetic testing, hold promise for improving the accuracy of psychiatric diagnoses and developing more targeted treatments.
• Telepsychiatry and other online mental health services offer new ways to increase access to care and reach individuals in underserved areas.
• Greater collaboration with primary care physicians and other healthcare professionals could improve the integration of mental health services into routine healthcare.
• The ongoing destigmatization of mental illness could lead to greater public acceptance and support for mental health services.
Threats
• The ongoing COVID-19 pandemic has increased the prevalence of mental health issues and placed additional strain on mental health services.
• The shortage of mental health professionals, particularly in certain areas of the country, could worsen in the coming years.
• Changes in healthcare policy, such as cuts to mental health funding or changes to insurance coverage, could limit access to care.
• Misinformation and stigma surrounding mental illness could continue to deter individuals from seeking treatment.
a Based on “Contemporary psychiatry: A SWOT analysis,” Current Psychiatry, January 2023, p. 16-19,27. doi: 10.12788/cp.0320
1. Nasrallah HA. Is evolution’s greatest triumph its worst blunder? Current Psychiatry. 2022;21(11):5-11. doi: 10.12788/cp.0301
2. Macpherson T, Churchland A, Sejnowski T, et al. Natural and artificial intelligence: a brief introduction to the interplay between AI and neuroscience research. Neural Netw. 2021;144:603-613.
3. Dehbouche N. Plagiarism in the age of massive Generative Pre-trained Transformers (GPT-3): “The best time to act was yesterday. The next best time is now.” Ethics Sci Environ Polit. 2021;21:17-23.
4. Turing AM. Computing machinery and intelligence. Mind. 1950;59(236):433-460.
5. McCarthy J. Artificial intelligence, logic, and formulising common sense. In: Richard H. Thomason, ed. Philosophical Logic and Artificial Intelligence. Kluwer Academic Publishing; 1989:161-190.
6. Koppe G, Meyer-Lindenberg A, Durstewitz D. Deep learning for small and big data in psychiatry. Neuropsychopharmacology. 2021;46(1):176-190.
7. Dabney W, Kurth-Nelson Z, Uchida N, et al. A distributional code for value in dopamine-based reinforcement learning. Nature. 2020;577(7792):671-675.
8. Zhou Z, Wu TC, Wang B, et al. Machine learning methods in psychiatry: a brief introduction. Gen Psychiatr. 2020;33(1):e100171.
9. Sun J, Cao R, Zhou M, et al. A hybrid deep neural network for classification of schizophrenia using EEG Data. Sci Rep. 2021;11(1):4706.
10. Kalenderian H, Nasrallah HA. Artificial intelligence in psychiatry. Current Psychiatry. 2019;18(8):33-38.
11. Ray A, Bhardwaj A, Malik YK, et al. Artificial intelligence and psychiatry: an overview. Asian J Psychiatr. 2022;70:103021.
12. Pestian E, Nasrallah HA, Matykiewicz P, et al. Suicide note classification using natural language processing: a content analysis. Biomed Inform Insights. 2010(3):19-28.
13. Chen Y, Wei Z, Gou H, et al. How far is brain-inspired artificial intelligence away from brain? Frontiers Neurosci. 2022;16:1096737.
14. Tools such as ChatGPT threaten transparent science; here are our ground rules for their use. Nature. 2023;613(7945):612. doi:10.1038/d41586-023-00191-1
We are currently on the verge of yet another societal “revolution” that will exert an unprecedented impact on our lives. It may surpass prior seismic cultural breakthroughs like the internet, smartphones, and social media. Artificial intelligence (AI) has been fermenting for several decades, gathering steam to become equivalent (and eventually superior) to human intelligence. The escalation of AI sophistication will be jarring and perhaps change human life in completely unpredictable ways.
Composing thoughts into words and coherent sentences has always been a uniquely human attribute among all living organisms. Now, that sublime feature of the human mind is being simulated, thanks to advances in AI software, ironically created by the human mind itself! On November 30, 2022, Open AI introduced ChatGPT (generative pre-trained transformer), which can generate an article on any topic a user requests. Within a few weeks, it was used by more than 100 million people. ChatGPT is taking the world by storm because it is a harbinger (some pessimists may label it an omen) of how human existence will be radically impacted in the future. Such AI breakthroughs to surpass human intelligence are, ironically, the product of the advanced human brain, which I previously described as concurrently a triumph and a blunder by evolution.1
How we got here, and what’s next
ChatGPT is a large language model based on neural networks.2 It generates realistic text responses to a wide range of questions by mimicking the pattern of language in gargantuan online databases. One Hong Kong–based, AI-powered drug discovery company (Insilico Medicine) declared it published articles generated by AI tools, even before ChatGPT became available. This indicates how AI can be misused in scientific publications and may be hard to detect as a new form of plagiarism.3
The roots of AI date back to the 1950s, when Alan Turing, now considered the father of AI, published a seminal article about creating a machine to “imitate the brain” and to “mimic the behavior of the human.”4 The term “artificial intelligence” was coined in 1989 by McCarthy,5 who defined it as “the science of engineering for making intelligent machines.” Since then, several subsets of AI have been developed:
- Machine learning: The study of computer algorithms to generate hypotheses
- Deep learning: A type of machine learning algorithm that uses multiple layers to progressively extract higher-level features from raw input. (Both machine learning and deep learning are used in the burgeoning fields of computational psychiatry6 and neuroscience research7)
- Expert knowledge system: A computer-based system that mimics human decision-making ability
- Neural networks: An interconnected group of artificial neurons that uses a math or computer model for information processing
- Predictive analytics: An algorithm to predict future outcomes based on historical data.
These subsets of AI have been used to identify psychiatric disorders using neuroimaging data8 and to classify brain disorders.9 There are many potential uses of AI in psychiatry.10,11 My first experience with AI was 13 years ago, when we conducted a project to distinguish fake suicide notes from genuine ones.12 AI was more successful in correctly identifying fake notes (78% correctly detected) than senior psychiatric residents (49%) or even faculty (53%).
AI will dramatically change how humans interact with the world and may lead to enhanced creativity and new explorations and forays into novel, previously unknown horizons. It is expected to significantly boost the global economy by many trillions of dollars over the next decade. Major high-tech companies are vigorously competing to develop their own AI tools like ChatGPT (Microsoft invested $10 billion in Open AI). Google, which owns DeepMind (an AI lab that invented the T in GPT) developed its own chatbot called Bard. Amazon has invested heavily in Stability AI by giving its founder and CEO Emad Mostaque 4,000 Nvidia AI chips to assemble the world’s largest supercomputer (1 year ago, Stability had only 32 AI chips!). Apple recently integrated Stable Diffusion into its latest operating system. Chinese tech giants Alibaba and Baidu also announced their own chatbots to be released soon.
Other competitors include Cohere, Hugging Face, Midjourney, GitHub Copilot, Game Changer, Jasper, and Anthropic, which released Claude as its chatbot at a lower cost than ChatGPT. Open AI also developed Dall-E2 in April 2022, which can generate very realistic images from text, one of which recently won an award at an art competition.
Continue to: One of the major...
One of the major concerns about these AI developments is that chatbots can make errors or disseminate misinformation and even enunciate racist or misogynist statements. The greatest worry is that the ultimate implicit goal of AI is what is called artificial general intelligence (AGI), which can think and learn better than humans. Some fear AGI may wipe out humans as a species, a grave outcome indeed. That’s why AI developers intend to align AGI with “basic human values” in the event it surpasses human intelligence. Some are even calling for a transition from AI to AW (artificial wisdom), with built-in empathy, kindness, self-reflection, acceptance of diverse perspectives, and promotion of prosocial ideas.13
Creating content: artificial intelligence vs human authors
ChatGPT has opened a Pandora’s box of concern about potential plagiarism by students or scientific authors. This has prompted several journals,14 including
- Anosognosia in schizophrenia (Box 1); based on “Is anosognosia a delusion, a negative symptom, or a cognitive deficit?”
Current Psychiatry , January 2022, p. 6-8,14. doi: 10.12788/cp.0210 - Benefits of metformin in psychiatry (Box 2); based on “Beyond diabetes: The beneficial uses of metformin in psychiatry,”
Current Psychiatry , March 2022, p. 7-9. doi: 10.12788/cp.0225 - Epidemic of intellectual constipation (Box 3); based on “From debate to stalemate and hate: An epidemic of intellectual constipation,”
Current Psychiatry , January 2023, p. 3-4. doi: 10.12788/cp.0321 - SWOT analysis of psychiatry (Box 4); based on “Contemporary psychiatry: A SWOT analysis,”
Current Psychiatry , January 2023, p. 16-19,27. doi: 10.12788/cp.0320.
These ChatGPT articles are verbatim as generated, without any copyediting, fact-checking, or addition of reference citations. One can easily notice that while factually acceptable, the ChatGPT articles tend to be rather synthetic, simple, bland, and lacking creative language or going beyond the facts to express personal viewpoints. However, I have no doubt that future versions of ChatGPT or other chatbots will evolve into far more sophisticated products and may match what a human can compose in terms of quality and complexity.
AI has arrived with a bang. Going forward, I predict it will continue to surprise us, with elements of “future shock.” The credit (or blame) belongs to the boundless creativity of human intelligence that is seeking to invent an intelligence higher than its own. Caveat emptor!
Box 1
Anosognosia is a condition in which a person is unaware or unable to recognize their own illness or disability. In schizophrenia, anosognosia can be present in up to 50% of cases and is characterized by a lack of insight into the presence and severity of symptoms.
People with anosognosia in schizophrenia may not believe that they have a mental illness, may deny the reality of their symptoms, or may attribute them to external causes. This can make it difficult for them to comply with treatment, as they may not see the need for medication or other interventions.
Anosognosia is thought to be caused by structural and functional changes in the brain, particularly in areas associated with self-awareness and insight. It is often more severe in people with more severe forms of schizophrenia and may be associated with poorer treatment outcomes.
Effective treatment for anosognosia in schizophrenia typically involves a combination of medication and therapy, as well as strategies for improving insight and awareness of symptoms. Family members and caregivers can also play an important role in helping people with schizophrenia to recognize the presence and impact of their illness, and encouraging them to engage in treatment.
a Based on “Is anosognosia a delusion, a negative symptom, or a cognitive deficit?” Current Psychiatry, January 2022, p. 6-8,14. doi: 10.12788/cp.0210
Box 2
Metformin is a medication commonly used in the treatment of type 2 diabetes. However, there is growing interest in its potential use in psychiatry, particularly in the treatment of certain mental health conditions. Some potential benefits of metformin in psychiatry include:
1. Treatment of mood disorders: Studies have suggested that metformin may be helpful in the treatment of mood disorders, such as depression and bipolar disorder. One proposed mechanism is that metformin may help to regulate glucose metabolism and insulin sensitivity, which in turn may help to stabilize mood.
2. Treatment of schizophrenia: Some studies have suggested that metformin may be helpful in reducing symptoms of schizophrenia, particularly negative symptoms such as social withdrawal and apathy. One proposed mechanism is that metformin may improve brain energy metabolism, which may in turn improve cognitive function and reduce symptoms.
3. Weight management: Metformin has been shown to be effective in weight management, which can be particularly important for people with certain mental health conditions, such as bipolar disorder, where weight gain can be a side effect of medication.
4. Neuroprotection: Metformin has been shown to have neuroprotective effects, which may be beneficial for people with certain mental health conditions, such as Alzheimer’s disease and Parkinson’s disease.
It is important to note that while there is some evidence for the potential benefits of metformin in psychiatry, further research is needed to fully understand its effectiveness and safety in this context. People with mental health conditions should not start taking metformin without first consulting with their healthcare provider.
a Based on “Beyond diabetes: The beneficial uses of metformin in psychiatry,” Current Psychiatry, March 2022, p. 7-9. doi: 10.12788/cp.0225
Box 3
The term “epidemic of intellectual constipation” refers to a phenomenon in which individuals, groups, or even entire societies are seen as lacking the ability to think critically, creatively, or expansively. It can be characterized by a lack of curiosity, a narrow range of interests, and a reluctance to engage with new or challenging ideas.
The cause of this phenomenon can be attributed to a variety of factors, including cultural, social, and educational influences. For example, some argue that a narrow and standardized educational system, as well as a lack of exposure to diverse perspectives, can limit creativity and critical thinking skills. Additionally, the prevalence of social media and other forms of digital media may encourage a focus on immediate gratification and quick information, rather than more in-depth and meaningful engagement with information.
The consequences of this epidemic can be far-reaching and can impact personal, social, and political aspects of life. For instance, a lack of critical thinking skills can lead to the spread of misinformation, while a narrow range of interests can limit personal growth and the ability to connect with others.
To combat the epidemic of intellectual constipation, it’s important to foster critical thinking skills, encourage exposure to diverse perspectives, and encourage a lifelong love of learning. This can be achieved through education, community engagement, and personal effort.
In conclusion, the “epidemic of intellectual constipation” refers to a phenomenon in which individuals, groups, or entire societies lack the ability to think critically, creatively, and expansively. To combat this epidemic, it’s important to foster critical thinking skills, encourage exposure to diverse perspectives, and encourage a lifelong love of learning.
a Based on “From debate to stalemate and hate: An epidemic of intellectual constipation,” Current Psychiatry, January 2023, p. 3-4. doi: 10.12788/cp.0321
Box 4
SWOT analysis is a tool used to assess the strengths, weaknesses, opportunities, and threats of a particular entity or industry. In this case, we will conduct a SWOT analysis of psychiatry as a field of medicine.
Strengths
• Psychiatry plays a crucial role in addressing mental health issues and improving the quality of life of individuals who struggle with them.
• Psychiatry has made significant advances in understanding the biological and psychological underpinnings of mental illness, which has led to the development of more effective treatments.
• There is growing public awareness and acceptance of the importance of mental health, which has led to increased demand for psychiatric services.
• The field of psychiatry attracts many talented and compassionate professionals who are dedicated to helping those in need.
Weaknesses
• There is still a significant stigma associated with mental illness, which can deter individuals from seeking treatment.
• The effectiveness of some psychiatric treatments can be limited, particularly in cases of severe mental illness.
• The shortage of mental health professionals in many areas means that access to psychiatric services may be limited, particularly for individuals with lower incomes.
• The cost of psychiatric treatment can be prohibitively expensive, particularly for individuals without insurance coverage.
Opportunities
• New advances in neuroscience and technology, such as brain imaging and genetic testing, hold promise for improving the accuracy of psychiatric diagnoses and developing more targeted treatments.
• Telepsychiatry and other online mental health services offer new ways to increase access to care and reach individuals in underserved areas.
• Greater collaboration with primary care physicians and other healthcare professionals could improve the integration of mental health services into routine healthcare.
• The ongoing destigmatization of mental illness could lead to greater public acceptance and support for mental health services.
Threats
• The ongoing COVID-19 pandemic has increased the prevalence of mental health issues and placed additional strain on mental health services.
• The shortage of mental health professionals, particularly in certain areas of the country, could worsen in the coming years.
• Changes in healthcare policy, such as cuts to mental health funding or changes to insurance coverage, could limit access to care.
• Misinformation and stigma surrounding mental illness could continue to deter individuals from seeking treatment.
a Based on “Contemporary psychiatry: A SWOT analysis,” Current Psychiatry, January 2023, p. 16-19,27. doi: 10.12788/cp.0320
We are currently on the verge of yet another societal “revolution” that will exert an unprecedented impact on our lives. It may surpass prior seismic cultural breakthroughs like the internet, smartphones, and social media. Artificial intelligence (AI) has been fermenting for several decades, gathering steam to become equivalent (and eventually superior) to human intelligence. The escalation of AI sophistication will be jarring and perhaps change human life in completely unpredictable ways.
Composing thoughts into words and coherent sentences has always been a uniquely human attribute among all living organisms. Now, that sublime feature of the human mind is being simulated, thanks to advances in AI software, ironically created by the human mind itself! On November 30, 2022, Open AI introduced ChatGPT (generative pre-trained transformer), which can generate an article on any topic a user requests. Within a few weeks, it was used by more than 100 million people. ChatGPT is taking the world by storm because it is a harbinger (some pessimists may label it an omen) of how human existence will be radically impacted in the future. Such AI breakthroughs to surpass human intelligence are, ironically, the product of the advanced human brain, which I previously described as concurrently a triumph and a blunder by evolution.1
How we got here, and what’s next
ChatGPT is a large language model based on neural networks.2 It generates realistic text responses to a wide range of questions by mimicking the pattern of language in gargantuan online databases. One Hong Kong–based, AI-powered drug discovery company (Insilico Medicine) declared it published articles generated by AI tools, even before ChatGPT became available. This indicates how AI can be misused in scientific publications and may be hard to detect as a new form of plagiarism.3
The roots of AI date back to the 1950s, when Alan Turing, now considered the father of AI, published a seminal article about creating a machine to “imitate the brain” and to “mimic the behavior of the human.”4 The term “artificial intelligence” was coined in 1989 by McCarthy,5 who defined it as “the science of engineering for making intelligent machines.” Since then, several subsets of AI have been developed:
- Machine learning: The study of computer algorithms to generate hypotheses
- Deep learning: A type of machine learning algorithm that uses multiple layers to progressively extract higher-level features from raw input. (Both machine learning and deep learning are used in the burgeoning fields of computational psychiatry6 and neuroscience research7)
- Expert knowledge system: A computer-based system that mimics human decision-making ability
- Neural networks: An interconnected group of artificial neurons that uses a math or computer model for information processing
- Predictive analytics: An algorithm to predict future outcomes based on historical data.
These subsets of AI have been used to identify psychiatric disorders using neuroimaging data8 and to classify brain disorders.9 There are many potential uses of AI in psychiatry.10,11 My first experience with AI was 13 years ago, when we conducted a project to distinguish fake suicide notes from genuine ones.12 AI was more successful in correctly identifying fake notes (78% correctly detected) than senior psychiatric residents (49%) or even faculty (53%).
AI will dramatically change how humans interact with the world and may lead to enhanced creativity and new explorations and forays into novel, previously unknown horizons. It is expected to significantly boost the global economy by many trillions of dollars over the next decade. Major high-tech companies are vigorously competing to develop their own AI tools like ChatGPT (Microsoft invested $10 billion in Open AI). Google, which owns DeepMind (an AI lab that invented the T in GPT) developed its own chatbot called Bard. Amazon has invested heavily in Stability AI by giving its founder and CEO Emad Mostaque 4,000 Nvidia AI chips to assemble the world’s largest supercomputer (1 year ago, Stability had only 32 AI chips!). Apple recently integrated Stable Diffusion into its latest operating system. Chinese tech giants Alibaba and Baidu also announced their own chatbots to be released soon.
Other competitors include Cohere, Hugging Face, Midjourney, GitHub Copilot, Game Changer, Jasper, and Anthropic, which released Claude as its chatbot at a lower cost than ChatGPT. Open AI also developed Dall-E2 in April 2022, which can generate very realistic images from text, one of which recently won an award at an art competition.
Continue to: One of the major...
One of the major concerns about these AI developments is that chatbots can make errors or disseminate misinformation and even enunciate racist or misogynist statements. The greatest worry is that the ultimate implicit goal of AI is what is called artificial general intelligence (AGI), which can think and learn better than humans. Some fear AGI may wipe out humans as a species, a grave outcome indeed. That’s why AI developers intend to align AGI with “basic human values” in the event it surpasses human intelligence. Some are even calling for a transition from AI to AW (artificial wisdom), with built-in empathy, kindness, self-reflection, acceptance of diverse perspectives, and promotion of prosocial ideas.13
Creating content: artificial intelligence vs human authors
ChatGPT has opened a Pandora’s box of concern about potential plagiarism by students or scientific authors. This has prompted several journals,14 including
- Anosognosia in schizophrenia (Box 1); based on “Is anosognosia a delusion, a negative symptom, or a cognitive deficit?”
Current Psychiatry , January 2022, p. 6-8,14. doi: 10.12788/cp.0210 - Benefits of metformin in psychiatry (Box 2); based on “Beyond diabetes: The beneficial uses of metformin in psychiatry,”
Current Psychiatry , March 2022, p. 7-9. doi: 10.12788/cp.0225 - Epidemic of intellectual constipation (Box 3); based on “From debate to stalemate and hate: An epidemic of intellectual constipation,”
Current Psychiatry , January 2023, p. 3-4. doi: 10.12788/cp.0321 - SWOT analysis of psychiatry (Box 4); based on “Contemporary psychiatry: A SWOT analysis,”
Current Psychiatry , January 2023, p. 16-19,27. doi: 10.12788/cp.0320.
These ChatGPT articles are verbatim as generated, without any copyediting, fact-checking, or addition of reference citations. One can easily notice that while factually acceptable, the ChatGPT articles tend to be rather synthetic, simple, bland, and lacking creative language or going beyond the facts to express personal viewpoints. However, I have no doubt that future versions of ChatGPT or other chatbots will evolve into far more sophisticated products and may match what a human can compose in terms of quality and complexity.
AI has arrived with a bang. Going forward, I predict it will continue to surprise us, with elements of “future shock.” The credit (or blame) belongs to the boundless creativity of human intelligence that is seeking to invent an intelligence higher than its own. Caveat emptor!
Box 1
Anosognosia is a condition in which a person is unaware or unable to recognize their own illness or disability. In schizophrenia, anosognosia can be present in up to 50% of cases and is characterized by a lack of insight into the presence and severity of symptoms.
People with anosognosia in schizophrenia may not believe that they have a mental illness, may deny the reality of their symptoms, or may attribute them to external causes. This can make it difficult for them to comply with treatment, as they may not see the need for medication or other interventions.
Anosognosia is thought to be caused by structural and functional changes in the brain, particularly in areas associated with self-awareness and insight. It is often more severe in people with more severe forms of schizophrenia and may be associated with poorer treatment outcomes.
Effective treatment for anosognosia in schizophrenia typically involves a combination of medication and therapy, as well as strategies for improving insight and awareness of symptoms. Family members and caregivers can also play an important role in helping people with schizophrenia to recognize the presence and impact of their illness, and encouraging them to engage in treatment.
a Based on “Is anosognosia a delusion, a negative symptom, or a cognitive deficit?” Current Psychiatry, January 2022, p. 6-8,14. doi: 10.12788/cp.0210
Box 2
Metformin is a medication commonly used in the treatment of type 2 diabetes. However, there is growing interest in its potential use in psychiatry, particularly in the treatment of certain mental health conditions. Some potential benefits of metformin in psychiatry include:
1. Treatment of mood disorders: Studies have suggested that metformin may be helpful in the treatment of mood disorders, such as depression and bipolar disorder. One proposed mechanism is that metformin may help to regulate glucose metabolism and insulin sensitivity, which in turn may help to stabilize mood.
2. Treatment of schizophrenia: Some studies have suggested that metformin may be helpful in reducing symptoms of schizophrenia, particularly negative symptoms such as social withdrawal and apathy. One proposed mechanism is that metformin may improve brain energy metabolism, which may in turn improve cognitive function and reduce symptoms.
3. Weight management: Metformin has been shown to be effective in weight management, which can be particularly important for people with certain mental health conditions, such as bipolar disorder, where weight gain can be a side effect of medication.
4. Neuroprotection: Metformin has been shown to have neuroprotective effects, which may be beneficial for people with certain mental health conditions, such as Alzheimer’s disease and Parkinson’s disease.
It is important to note that while there is some evidence for the potential benefits of metformin in psychiatry, further research is needed to fully understand its effectiveness and safety in this context. People with mental health conditions should not start taking metformin without first consulting with their healthcare provider.
a Based on “Beyond diabetes: The beneficial uses of metformin in psychiatry,” Current Psychiatry, March 2022, p. 7-9. doi: 10.12788/cp.0225
Box 3
The term “epidemic of intellectual constipation” refers to a phenomenon in which individuals, groups, or even entire societies are seen as lacking the ability to think critically, creatively, or expansively. It can be characterized by a lack of curiosity, a narrow range of interests, and a reluctance to engage with new or challenging ideas.
The cause of this phenomenon can be attributed to a variety of factors, including cultural, social, and educational influences. For example, some argue that a narrow and standardized educational system, as well as a lack of exposure to diverse perspectives, can limit creativity and critical thinking skills. Additionally, the prevalence of social media and other forms of digital media may encourage a focus on immediate gratification and quick information, rather than more in-depth and meaningful engagement with information.
The consequences of this epidemic can be far-reaching and can impact personal, social, and political aspects of life. For instance, a lack of critical thinking skills can lead to the spread of misinformation, while a narrow range of interests can limit personal growth and the ability to connect with others.
To combat the epidemic of intellectual constipation, it’s important to foster critical thinking skills, encourage exposure to diverse perspectives, and encourage a lifelong love of learning. This can be achieved through education, community engagement, and personal effort.
In conclusion, the “epidemic of intellectual constipation” refers to a phenomenon in which individuals, groups, or entire societies lack the ability to think critically, creatively, and expansively. To combat this epidemic, it’s important to foster critical thinking skills, encourage exposure to diverse perspectives, and encourage a lifelong love of learning.
a Based on “From debate to stalemate and hate: An epidemic of intellectual constipation,” Current Psychiatry, January 2023, p. 3-4. doi: 10.12788/cp.0321
Box 4
SWOT analysis is a tool used to assess the strengths, weaknesses, opportunities, and threats of a particular entity or industry. In this case, we will conduct a SWOT analysis of psychiatry as a field of medicine.
Strengths
• Psychiatry plays a crucial role in addressing mental health issues and improving the quality of life of individuals who struggle with them.
• Psychiatry has made significant advances in understanding the biological and psychological underpinnings of mental illness, which has led to the development of more effective treatments.
• There is growing public awareness and acceptance of the importance of mental health, which has led to increased demand for psychiatric services.
• The field of psychiatry attracts many talented and compassionate professionals who are dedicated to helping those in need.
Weaknesses
• There is still a significant stigma associated with mental illness, which can deter individuals from seeking treatment.
• The effectiveness of some psychiatric treatments can be limited, particularly in cases of severe mental illness.
• The shortage of mental health professionals in many areas means that access to psychiatric services may be limited, particularly for individuals with lower incomes.
• The cost of psychiatric treatment can be prohibitively expensive, particularly for individuals without insurance coverage.
Opportunities
• New advances in neuroscience and technology, such as brain imaging and genetic testing, hold promise for improving the accuracy of psychiatric diagnoses and developing more targeted treatments.
• Telepsychiatry and other online mental health services offer new ways to increase access to care and reach individuals in underserved areas.
• Greater collaboration with primary care physicians and other healthcare professionals could improve the integration of mental health services into routine healthcare.
• The ongoing destigmatization of mental illness could lead to greater public acceptance and support for mental health services.
Threats
• The ongoing COVID-19 pandemic has increased the prevalence of mental health issues and placed additional strain on mental health services.
• The shortage of mental health professionals, particularly in certain areas of the country, could worsen in the coming years.
• Changes in healthcare policy, such as cuts to mental health funding or changes to insurance coverage, could limit access to care.
• Misinformation and stigma surrounding mental illness could continue to deter individuals from seeking treatment.
a Based on “Contemporary psychiatry: A SWOT analysis,” Current Psychiatry, January 2023, p. 16-19,27. doi: 10.12788/cp.0320
1. Nasrallah HA. Is evolution’s greatest triumph its worst blunder? Current Psychiatry. 2022;21(11):5-11. doi: 10.12788/cp.0301
2. Macpherson T, Churchland A, Sejnowski T, et al. Natural and artificial intelligence: a brief introduction to the interplay between AI and neuroscience research. Neural Netw. 2021;144:603-613.
3. Dehbouche N. Plagiarism in the age of massive Generative Pre-trained Transformers (GPT-3): “The best time to act was yesterday. The next best time is now.” Ethics Sci Environ Polit. 2021;21:17-23.
4. Turing AM. Computing machinery and intelligence. Mind. 1950;59(236):433-460.
5. McCarthy J. Artificial intelligence, logic, and formulising common sense. In: Richard H. Thomason, ed. Philosophical Logic and Artificial Intelligence. Kluwer Academic Publishing; 1989:161-190.
6. Koppe G, Meyer-Lindenberg A, Durstewitz D. Deep learning for small and big data in psychiatry. Neuropsychopharmacology. 2021;46(1):176-190.
7. Dabney W, Kurth-Nelson Z, Uchida N, et al. A distributional code for value in dopamine-based reinforcement learning. Nature. 2020;577(7792):671-675.
8. Zhou Z, Wu TC, Wang B, et al. Machine learning methods in psychiatry: a brief introduction. Gen Psychiatr. 2020;33(1):e100171.
9. Sun J, Cao R, Zhou M, et al. A hybrid deep neural network for classification of schizophrenia using EEG Data. Sci Rep. 2021;11(1):4706.
10. Kalenderian H, Nasrallah HA. Artificial intelligence in psychiatry. Current Psychiatry. 2019;18(8):33-38.
11. Ray A, Bhardwaj A, Malik YK, et al. Artificial intelligence and psychiatry: an overview. Asian J Psychiatr. 2022;70:103021.
12. Pestian E, Nasrallah HA, Matykiewicz P, et al. Suicide note classification using natural language processing: a content analysis. Biomed Inform Insights. 2010(3):19-28.
13. Chen Y, Wei Z, Gou H, et al. How far is brain-inspired artificial intelligence away from brain? Frontiers Neurosci. 2022;16:1096737.
14. Tools such as ChatGPT threaten transparent science; here are our ground rules for their use. Nature. 2023;613(7945):612. doi:10.1038/d41586-023-00191-1
1. Nasrallah HA. Is evolution’s greatest triumph its worst blunder? Current Psychiatry. 2022;21(11):5-11. doi: 10.12788/cp.0301
2. Macpherson T, Churchland A, Sejnowski T, et al. Natural and artificial intelligence: a brief introduction to the interplay between AI and neuroscience research. Neural Netw. 2021;144:603-613.
3. Dehbouche N. Plagiarism in the age of massive Generative Pre-trained Transformers (GPT-3): “The best time to act was yesterday. The next best time is now.” Ethics Sci Environ Polit. 2021;21:17-23.
4. Turing AM. Computing machinery and intelligence. Mind. 1950;59(236):433-460.
5. McCarthy J. Artificial intelligence, logic, and formulising common sense. In: Richard H. Thomason, ed. Philosophical Logic and Artificial Intelligence. Kluwer Academic Publishing; 1989:161-190.
6. Koppe G, Meyer-Lindenberg A, Durstewitz D. Deep learning for small and big data in psychiatry. Neuropsychopharmacology. 2021;46(1):176-190.
7. Dabney W, Kurth-Nelson Z, Uchida N, et al. A distributional code for value in dopamine-based reinforcement learning. Nature. 2020;577(7792):671-675.
8. Zhou Z, Wu TC, Wang B, et al. Machine learning methods in psychiatry: a brief introduction. Gen Psychiatr. 2020;33(1):e100171.
9. Sun J, Cao R, Zhou M, et al. A hybrid deep neural network for classification of schizophrenia using EEG Data. Sci Rep. 2021;11(1):4706.
10. Kalenderian H, Nasrallah HA. Artificial intelligence in psychiatry. Current Psychiatry. 2019;18(8):33-38.
11. Ray A, Bhardwaj A, Malik YK, et al. Artificial intelligence and psychiatry: an overview. Asian J Psychiatr. 2022;70:103021.
12. Pestian E, Nasrallah HA, Matykiewicz P, et al. Suicide note classification using natural language processing: a content analysis. Biomed Inform Insights. 2010(3):19-28.
13. Chen Y, Wei Z, Gou H, et al. How far is brain-inspired artificial intelligence away from brain? Frontiers Neurosci. 2022;16:1096737.
14. Tools such as ChatGPT threaten transparent science; here are our ground rules for their use. Nature. 2023;613(7945):612. doi:10.1038/d41586-023-00191-1
A ‘guest editorial’ … generated by ChatGPT?
The artificial intelligence (AI) program ChatGPT (generative pre-trained transformer) was introduced to the public by Open AI on November 30, 2022. It has been described as a game-changer for society, culture, literature, arts, and science, with a potential impact that rivals that of the internet and social media.
ChatGPT can produce human-like essays in response to queries. Some researchers used ChatGPT to generate abstracts based on the titles of articles published in 5 high-impact journals. These abstracts were so “real” that they escaped detection by expert peer reviewers in 32% of cases.1 In addition, several medical/science articles were published that included ChatGPT as a bylined author.2
Like other journals,3-7
- Nonhuman AI technologies do not qualify for named authorship.
- Authors should be transparent about the use of AI technologies to aid in writing content. Authors should disclose which tool was used and how it was applied in the article submitted to the journal.
- Human authors are responsible for the accuracy of work compiled by an AI tool, including the absence of plagiarism. Proper referencing of statements is necessary.
- Images created by AI tools are not permitted for publication.
Because the overwhelming majority of articles published in
Can AI generate an acceptable ‘guest editorial?’
In addition to creating formulaic writing, some of the concerns about using AI in scientific publishing is that the results might be outdated, incorrect, or lacking appropriate references, and that it can produce “plausible-sounding but incorrect or nonsensical” answers to questions.3 To test this, I asked ChatGPT to write an article on the same topic as 4 of my articles published in
Box
There are many myths and misconceptions surrounding psychiatry, the branch of medicine that deals with the diagnosis, treatment, and prevention of mental illness. Some of the most common myths include:
1. Psychiatry is not a real medical specialty: This is a false myth. Psychiatry is a recognized medical specialty, and psychiatrists are licensed medical doctors who have undergone extensive training in the diagnosis and treatment of mental illness.
2. Mental illness is not a real illness: Mental illness is a real and biologically based medical condition, just like physical illness. Research has shown that mental illness is caused by a combination of genetic, environmental, and lifestyle factors.
3. Antidepressants are not effective: Antidepressants have been shown to be effective in treating depression and other mental illnesses. While they are not a cure, they can provide significant symptom relief and improve quality of life for many people.
4. Psychiatric drugs are dangerous and have serious side effects: While all drugs have potential side effects, psychiatric medications have been proven to be safe and effective for many people. The risks and benefits of taking any medication should be carefully considered and discussed with a healthcare professional.
5. Therapy is not effective: Therapy, also known as psychotherapy, has been shown to be effective in treating a wide range of mental illnesses, including depression, anxiety, and post-traumatic stress disorder (PTSD).
6. People with mental illness are violent: People with mental illness are no more likely to be violent than the general population. In fact, people with mental illness are more likely to be victims of violence than perpetrators.
It is important to dispel these myths and misconceptions about psychiatry, as they can prevent people from seeking the help they need and can also contribute to stigma and discrimination towards those with mental illness.
In conclusion, there are many myths and misconceptions surrounding psychiatry. Dispelling these myths and increasing public understanding about mental illness and its treatment can help reduce stigma and encourage more people to seek the help they need.
What do you think? I encourage you to send me your take on this AI-generated “guest editorial,” and whether you deem its quality to be similar to that of an article authored by a human psychiatrist.
1. Else H. Abstracts written by ChatGPT fool scientists. Nature. 2023;613(7944):423. doi: 10.1038/d41586-023-00056-7
2. Stokel-Walker C. ChatGPT listed as author on research papers: many scientists disapprove. Nature. 2023;613(7945):620-621. doi:10.1038/d41586-023-00107-z
3. Flanagin A, Bibbins-Domingo K, Berkwits M, et al. Nonhuman “authors” and implications for the integrity of scientific publication and medical knowledge. JAMA. 2023;329(8):637-639. doi:10.1001/jama.2023.1344
4. Tools such as ChatGPT threaten transparent science; here are our ground rules for their use. Nature. 2023;613(7945):612. doi:10.1038/d41586-023-00191-1
5. Thorp HH. ChatGPT is fun, but not an author. Science. 2023;379(6630):313. doi:10.1126/science.adg7879
6. PNAS. The PNAS journals outline their policies for ChatGPT and generative AI. February 21, 2023. Accessed March 9, 2023. https://www.pnas.org/post/update/pnas-policy-for-chatgpt-generative-ai
7. Marušic’ A. JoGH policy on the use of artificial intelligence in scholarly manuscripts. J Glob Health. 2023;13:01002. doi:10.7189/jogh.13.01002
The artificial intelligence (AI) program ChatGPT (generative pre-trained transformer) was introduced to the public by Open AI on November 30, 2022. It has been described as a game-changer for society, culture, literature, arts, and science, with a potential impact that rivals that of the internet and social media.
ChatGPT can produce human-like essays in response to queries. Some researchers used ChatGPT to generate abstracts based on the titles of articles published in 5 high-impact journals. These abstracts were so “real” that they escaped detection by expert peer reviewers in 32% of cases.1 In addition, several medical/science articles were published that included ChatGPT as a bylined author.2
Like other journals,3-7
- Nonhuman AI technologies do not qualify for named authorship.
- Authors should be transparent about the use of AI technologies to aid in writing content. Authors should disclose which tool was used and how it was applied in the article submitted to the journal.
- Human authors are responsible for the accuracy of work compiled by an AI tool, including the absence of plagiarism. Proper referencing of statements is necessary.
- Images created by AI tools are not permitted for publication.
Because the overwhelming majority of articles published in
Can AI generate an acceptable ‘guest editorial?’
In addition to creating formulaic writing, some of the concerns about using AI in scientific publishing is that the results might be outdated, incorrect, or lacking appropriate references, and that it can produce “plausible-sounding but incorrect or nonsensical” answers to questions.3 To test this, I asked ChatGPT to write an article on the same topic as 4 of my articles published in
Box
There are many myths and misconceptions surrounding psychiatry, the branch of medicine that deals with the diagnosis, treatment, and prevention of mental illness. Some of the most common myths include:
1. Psychiatry is not a real medical specialty: This is a false myth. Psychiatry is a recognized medical specialty, and psychiatrists are licensed medical doctors who have undergone extensive training in the diagnosis and treatment of mental illness.
2. Mental illness is not a real illness: Mental illness is a real and biologically based medical condition, just like physical illness. Research has shown that mental illness is caused by a combination of genetic, environmental, and lifestyle factors.
3. Antidepressants are not effective: Antidepressants have been shown to be effective in treating depression and other mental illnesses. While they are not a cure, they can provide significant symptom relief and improve quality of life for many people.
4. Psychiatric drugs are dangerous and have serious side effects: While all drugs have potential side effects, psychiatric medications have been proven to be safe and effective for many people. The risks and benefits of taking any medication should be carefully considered and discussed with a healthcare professional.
5. Therapy is not effective: Therapy, also known as psychotherapy, has been shown to be effective in treating a wide range of mental illnesses, including depression, anxiety, and post-traumatic stress disorder (PTSD).
6. People with mental illness are violent: People with mental illness are no more likely to be violent than the general population. In fact, people with mental illness are more likely to be victims of violence than perpetrators.
It is important to dispel these myths and misconceptions about psychiatry, as they can prevent people from seeking the help they need and can also contribute to stigma and discrimination towards those with mental illness.
In conclusion, there are many myths and misconceptions surrounding psychiatry. Dispelling these myths and increasing public understanding about mental illness and its treatment can help reduce stigma and encourage more people to seek the help they need.
What do you think? I encourage you to send me your take on this AI-generated “guest editorial,” and whether you deem its quality to be similar to that of an article authored by a human psychiatrist.
The artificial intelligence (AI) program ChatGPT (generative pre-trained transformer) was introduced to the public by Open AI on November 30, 2022. It has been described as a game-changer for society, culture, literature, arts, and science, with a potential impact that rivals that of the internet and social media.
ChatGPT can produce human-like essays in response to queries. Some researchers used ChatGPT to generate abstracts based on the titles of articles published in 5 high-impact journals. These abstracts were so “real” that they escaped detection by expert peer reviewers in 32% of cases.1 In addition, several medical/science articles were published that included ChatGPT as a bylined author.2
Like other journals,3-7
- Nonhuman AI technologies do not qualify for named authorship.
- Authors should be transparent about the use of AI technologies to aid in writing content. Authors should disclose which tool was used and how it was applied in the article submitted to the journal.
- Human authors are responsible for the accuracy of work compiled by an AI tool, including the absence of plagiarism. Proper referencing of statements is necessary.
- Images created by AI tools are not permitted for publication.
Because the overwhelming majority of articles published in
Can AI generate an acceptable ‘guest editorial?’
In addition to creating formulaic writing, some of the concerns about using AI in scientific publishing is that the results might be outdated, incorrect, or lacking appropriate references, and that it can produce “plausible-sounding but incorrect or nonsensical” answers to questions.3 To test this, I asked ChatGPT to write an article on the same topic as 4 of my articles published in
Box
There are many myths and misconceptions surrounding psychiatry, the branch of medicine that deals with the diagnosis, treatment, and prevention of mental illness. Some of the most common myths include:
1. Psychiatry is not a real medical specialty: This is a false myth. Psychiatry is a recognized medical specialty, and psychiatrists are licensed medical doctors who have undergone extensive training in the diagnosis and treatment of mental illness.
2. Mental illness is not a real illness: Mental illness is a real and biologically based medical condition, just like physical illness. Research has shown that mental illness is caused by a combination of genetic, environmental, and lifestyle factors.
3. Antidepressants are not effective: Antidepressants have been shown to be effective in treating depression and other mental illnesses. While they are not a cure, they can provide significant symptom relief and improve quality of life for many people.
4. Psychiatric drugs are dangerous and have serious side effects: While all drugs have potential side effects, psychiatric medications have been proven to be safe and effective for many people. The risks and benefits of taking any medication should be carefully considered and discussed with a healthcare professional.
5. Therapy is not effective: Therapy, also known as psychotherapy, has been shown to be effective in treating a wide range of mental illnesses, including depression, anxiety, and post-traumatic stress disorder (PTSD).
6. People with mental illness are violent: People with mental illness are no more likely to be violent than the general population. In fact, people with mental illness are more likely to be victims of violence than perpetrators.
It is important to dispel these myths and misconceptions about psychiatry, as they can prevent people from seeking the help they need and can also contribute to stigma and discrimination towards those with mental illness.
In conclusion, there are many myths and misconceptions surrounding psychiatry. Dispelling these myths and increasing public understanding about mental illness and its treatment can help reduce stigma and encourage more people to seek the help they need.
What do you think? I encourage you to send me your take on this AI-generated “guest editorial,” and whether you deem its quality to be similar to that of an article authored by a human psychiatrist.
1. Else H. Abstracts written by ChatGPT fool scientists. Nature. 2023;613(7944):423. doi: 10.1038/d41586-023-00056-7
2. Stokel-Walker C. ChatGPT listed as author on research papers: many scientists disapprove. Nature. 2023;613(7945):620-621. doi:10.1038/d41586-023-00107-z
3. Flanagin A, Bibbins-Domingo K, Berkwits M, et al. Nonhuman “authors” and implications for the integrity of scientific publication and medical knowledge. JAMA. 2023;329(8):637-639. doi:10.1001/jama.2023.1344
4. Tools such as ChatGPT threaten transparent science; here are our ground rules for their use. Nature. 2023;613(7945):612. doi:10.1038/d41586-023-00191-1
5. Thorp HH. ChatGPT is fun, but not an author. Science. 2023;379(6630):313. doi:10.1126/science.adg7879
6. PNAS. The PNAS journals outline their policies for ChatGPT and generative AI. February 21, 2023. Accessed March 9, 2023. https://www.pnas.org/post/update/pnas-policy-for-chatgpt-generative-ai
7. Marušic’ A. JoGH policy on the use of artificial intelligence in scholarly manuscripts. J Glob Health. 2023;13:01002. doi:10.7189/jogh.13.01002
1. Else H. Abstracts written by ChatGPT fool scientists. Nature. 2023;613(7944):423. doi: 10.1038/d41586-023-00056-7
2. Stokel-Walker C. ChatGPT listed as author on research papers: many scientists disapprove. Nature. 2023;613(7945):620-621. doi:10.1038/d41586-023-00107-z
3. Flanagin A, Bibbins-Domingo K, Berkwits M, et al. Nonhuman “authors” and implications for the integrity of scientific publication and medical knowledge. JAMA. 2023;329(8):637-639. doi:10.1001/jama.2023.1344
4. Tools such as ChatGPT threaten transparent science; here are our ground rules for their use. Nature. 2023;613(7945):612. doi:10.1038/d41586-023-00191-1
5. Thorp HH. ChatGPT is fun, but not an author. Science. 2023;379(6630):313. doi:10.1126/science.adg7879
6. PNAS. The PNAS journals outline their policies for ChatGPT and generative AI. February 21, 2023. Accessed March 9, 2023. https://www.pnas.org/post/update/pnas-policy-for-chatgpt-generative-ai
7. Marušic’ A. JoGH policy on the use of artificial intelligence in scholarly manuscripts. J Glob Health. 2023;13:01002. doi:10.7189/jogh.13.01002