User login
First Senate vote to repeal and replace ACA fails
Senate Republicans’ first attempt to repeal and replace the Affordable Care Act failed July 25 as nine Republican senators crossed the aisle to vote against a measure that had no chance of passing.
The process started with a dramatic appearance by Sen. John McCain (R-Ariz.), recovering from surgery to diagnose glioblastoma, who returned to Washington to cast a key vote that would allow debate to move forward. The Senate split 50-50 on that vote, with Sen. Susan Collins (R-Maine) and Sen. Lisa Murkowski (R-Alaska) crossing the aisle to vote with all the chamber’s Democrats against the motion to proceed. Vice President Mike Pence cast the tie-breaking vote in favor of beginning debate.
However, the first amendment voted on would have replaced that language with the most recent version of the Senate GOP repeal-and-replace plan, the Better Care Reconciliation Act, with two additional provisions. One was from Sen. Ted Cruz (R-Tex.) and would allow insurers to offer more limited health insurance plans along side plans that cover the ACA’s essential benefits package. A second provision from Sen. Rob Portman (R-Ohio) would have added an additional $100 billion to the state stability fund to help low-income individuals whose Medicaid coverage was repealed.
The amendment was dead on arrival, as it would have needed 60 votes to pass. Throughout the repeal-and-replace effort, the 48 Senate Democrats have been firm in voting against any action. While much of the repeal-and-replace effort to date has relied on the budget reconciliation process, which requires a simple majority for passage, this legislation did not qualify and needed a supermajority of 60 votes for passage.
The nine GOP senators voting against the amendment included Collins, Murkowski, Bob Corker (Tenn.), Tom Cotton (Ark.), Lindsey Graham (S.C.), Dena Heller (Nev.), Mike Lee (Utah), Jerry Moran (Kan.), and Rand Paul (Ky.).
Earlier in the day, just after voting in favor of action on this legislation, Sen. McCain pleaded with his colleagues to return to regular order and write a bill that has bipartisan support. He criticized congressional Democrats for forcing the ACA through without bipartisan support 7 years ago and congressional Republicans for doing the exact same thing now with their repeal-and-replace efforts.
“Why don’t we try the old way of legislating in the Senate, the way our rules and customs encourage us to act,” Sen. McCain asked. “Let the Health, Education, Labor, and Pensions Committee under Chairman Alexander and Ranking Member Murray hold hearings, try to report a bill out of committee with contributions from both sides. Then bring it to the floor for amendment and debate and see if we can pass something that will be imperfect, full of compromises, and not very pleasing to implacable partisans on either side but that might provide workable solutions to problems Americans are struggling with today.”
Senate Republicans’ first attempt to repeal and replace the Affordable Care Act failed July 25 as nine Republican senators crossed the aisle to vote against a measure that had no chance of passing.
The process started with a dramatic appearance by Sen. John McCain (R-Ariz.), recovering from surgery to diagnose glioblastoma, who returned to Washington to cast a key vote that would allow debate to move forward. The Senate split 50-50 on that vote, with Sen. Susan Collins (R-Maine) and Sen. Lisa Murkowski (R-Alaska) crossing the aisle to vote with all the chamber’s Democrats against the motion to proceed. Vice President Mike Pence cast the tie-breaking vote in favor of beginning debate.
However, the first amendment voted on would have replaced that language with the most recent version of the Senate GOP repeal-and-replace plan, the Better Care Reconciliation Act, with two additional provisions. One was from Sen. Ted Cruz (R-Tex.) and would allow insurers to offer more limited health insurance plans along side plans that cover the ACA’s essential benefits package. A second provision from Sen. Rob Portman (R-Ohio) would have added an additional $100 billion to the state stability fund to help low-income individuals whose Medicaid coverage was repealed.
The amendment was dead on arrival, as it would have needed 60 votes to pass. Throughout the repeal-and-replace effort, the 48 Senate Democrats have been firm in voting against any action. While much of the repeal-and-replace effort to date has relied on the budget reconciliation process, which requires a simple majority for passage, this legislation did not qualify and needed a supermajority of 60 votes for passage.
The nine GOP senators voting against the amendment included Collins, Murkowski, Bob Corker (Tenn.), Tom Cotton (Ark.), Lindsey Graham (S.C.), Dena Heller (Nev.), Mike Lee (Utah), Jerry Moran (Kan.), and Rand Paul (Ky.).
Earlier in the day, just after voting in favor of action on this legislation, Sen. McCain pleaded with his colleagues to return to regular order and write a bill that has bipartisan support. He criticized congressional Democrats for forcing the ACA through without bipartisan support 7 years ago and congressional Republicans for doing the exact same thing now with their repeal-and-replace efforts.
“Why don’t we try the old way of legislating in the Senate, the way our rules and customs encourage us to act,” Sen. McCain asked. “Let the Health, Education, Labor, and Pensions Committee under Chairman Alexander and Ranking Member Murray hold hearings, try to report a bill out of committee with contributions from both sides. Then bring it to the floor for amendment and debate and see if we can pass something that will be imperfect, full of compromises, and not very pleasing to implacable partisans on either side but that might provide workable solutions to problems Americans are struggling with today.”
Senate Republicans’ first attempt to repeal and replace the Affordable Care Act failed July 25 as nine Republican senators crossed the aisle to vote against a measure that had no chance of passing.
The process started with a dramatic appearance by Sen. John McCain (R-Ariz.), recovering from surgery to diagnose glioblastoma, who returned to Washington to cast a key vote that would allow debate to move forward. The Senate split 50-50 on that vote, with Sen. Susan Collins (R-Maine) and Sen. Lisa Murkowski (R-Alaska) crossing the aisle to vote with all the chamber’s Democrats against the motion to proceed. Vice President Mike Pence cast the tie-breaking vote in favor of beginning debate.
However, the first amendment voted on would have replaced that language with the most recent version of the Senate GOP repeal-and-replace plan, the Better Care Reconciliation Act, with two additional provisions. One was from Sen. Ted Cruz (R-Tex.) and would allow insurers to offer more limited health insurance plans along side plans that cover the ACA’s essential benefits package. A second provision from Sen. Rob Portman (R-Ohio) would have added an additional $100 billion to the state stability fund to help low-income individuals whose Medicaid coverage was repealed.
The amendment was dead on arrival, as it would have needed 60 votes to pass. Throughout the repeal-and-replace effort, the 48 Senate Democrats have been firm in voting against any action. While much of the repeal-and-replace effort to date has relied on the budget reconciliation process, which requires a simple majority for passage, this legislation did not qualify and needed a supermajority of 60 votes for passage.
The nine GOP senators voting against the amendment included Collins, Murkowski, Bob Corker (Tenn.), Tom Cotton (Ark.), Lindsey Graham (S.C.), Dena Heller (Nev.), Mike Lee (Utah), Jerry Moran (Kan.), and Rand Paul (Ky.).
Earlier in the day, just after voting in favor of action on this legislation, Sen. McCain pleaded with his colleagues to return to regular order and write a bill that has bipartisan support. He criticized congressional Democrats for forcing the ACA through without bipartisan support 7 years ago and congressional Republicans for doing the exact same thing now with their repeal-and-replace efforts.
“Why don’t we try the old way of legislating in the Senate, the way our rules and customs encourage us to act,” Sen. McCain asked. “Let the Health, Education, Labor, and Pensions Committee under Chairman Alexander and Ranking Member Murray hold hearings, try to report a bill out of committee with contributions from both sides. Then bring it to the floor for amendment and debate and see if we can pass something that will be imperfect, full of compromises, and not very pleasing to implacable partisans on either side but that might provide workable solutions to problems Americans are struggling with today.”
Physician compensation growing but at a slightly slower pace
Physicians working in large multispecialty groups saw their compensation increase in 2016, albeit at a slower pace than in 2015, according to survey results reported by AMGA.
The 2017 Medical Group Compensation and Productivity Survey shows that the overall weighted average increase in physician compensation for the calendar year 2016 was 2.9%, slightly lower than the 3.1% increase seen in 2015. Doctors in more than three-quarters (77%) of specialties saw increases in 2016.
Opthalmologic surgery saw the largest compensation increase at 7.7%, followed by cardiothoracic surgery (7.0%), hematology and medical oncology (6.7%), allergy/immunology (5.9%) and pulmonary disease (5.6%). Emergency medicine saw a decrease in compensation of 2.0% in 2016 after experiencing a 9.6% increase in 2015.
Value-based payment is beginning to factor into the growth in payment by specialty. Overall, about 8% of compensation is being linked to value-based pay, and that number is expected to rise, with some medical practice groups linking 15% or more of compensation to value-based metrics.
“In almost all of the groups that I have worked with in the last few years on [compensation] design, that has been one of the drivers of decision to do the compensation redesign is to allocate to the value-based metrics,” Wayne Hartley, vice president of AMGA Consulting, said in an interview. 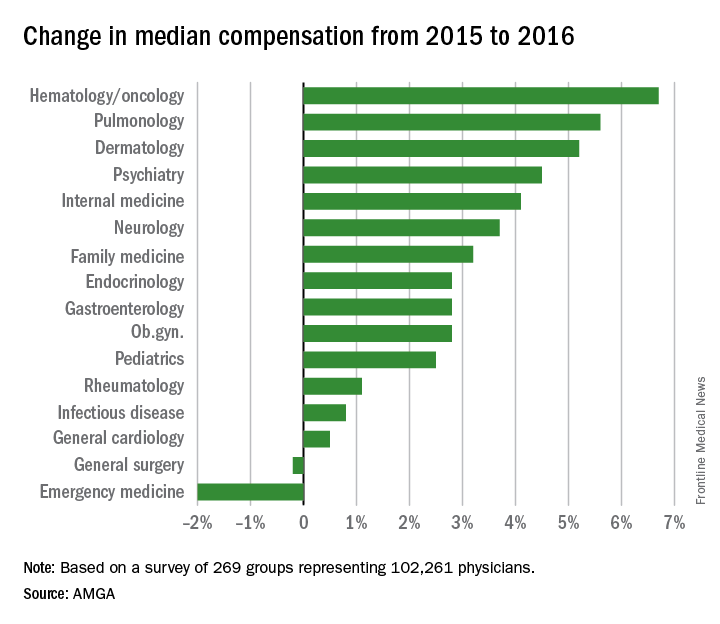
AMGA said that the data covers responses from 269 medical groups covering more than 102,000 providers and is representative of large multispecialty groups and integrated health systems that average 380 providers per group.
Physicians working in large multispecialty groups saw their compensation increase in 2016, albeit at a slower pace than in 2015, according to survey results reported by AMGA.
The 2017 Medical Group Compensation and Productivity Survey shows that the overall weighted average increase in physician compensation for the calendar year 2016 was 2.9%, slightly lower than the 3.1% increase seen in 2015. Doctors in more than three-quarters (77%) of specialties saw increases in 2016.
Opthalmologic surgery saw the largest compensation increase at 7.7%, followed by cardiothoracic surgery (7.0%), hematology and medical oncology (6.7%), allergy/immunology (5.9%) and pulmonary disease (5.6%). Emergency medicine saw a decrease in compensation of 2.0% in 2016 after experiencing a 9.6% increase in 2015.
Value-based payment is beginning to factor into the growth in payment by specialty. Overall, about 8% of compensation is being linked to value-based pay, and that number is expected to rise, with some medical practice groups linking 15% or more of compensation to value-based metrics.
“In almost all of the groups that I have worked with in the last few years on [compensation] design, that has been one of the drivers of decision to do the compensation redesign is to allocate to the value-based metrics,” Wayne Hartley, vice president of AMGA Consulting, said in an interview. 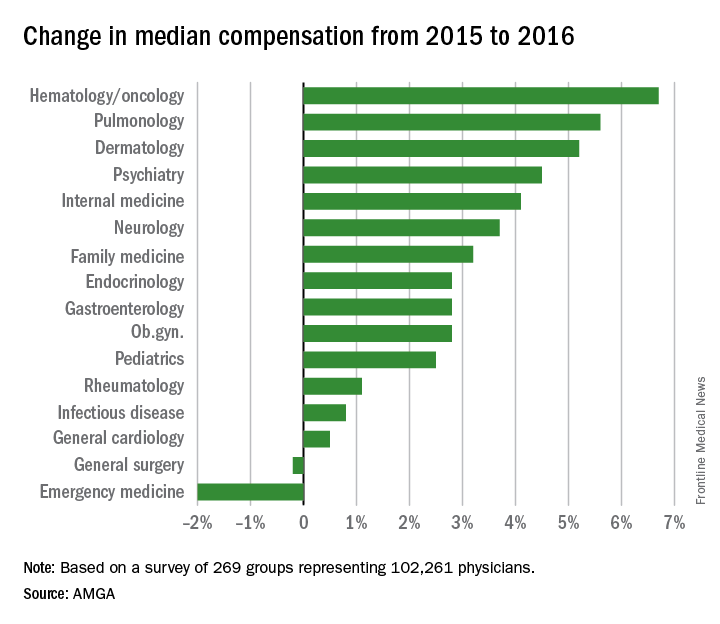
AMGA said that the data covers responses from 269 medical groups covering more than 102,000 providers and is representative of large multispecialty groups and integrated health systems that average 380 providers per group.
Physicians working in large multispecialty groups saw their compensation increase in 2016, albeit at a slower pace than in 2015, according to survey results reported by AMGA.
The 2017 Medical Group Compensation and Productivity Survey shows that the overall weighted average increase in physician compensation for the calendar year 2016 was 2.9%, slightly lower than the 3.1% increase seen in 2015. Doctors in more than three-quarters (77%) of specialties saw increases in 2016.
Opthalmologic surgery saw the largest compensation increase at 7.7%, followed by cardiothoracic surgery (7.0%), hematology and medical oncology (6.7%), allergy/immunology (5.9%) and pulmonary disease (5.6%). Emergency medicine saw a decrease in compensation of 2.0% in 2016 after experiencing a 9.6% increase in 2015.
Value-based payment is beginning to factor into the growth in payment by specialty. Overall, about 8% of compensation is being linked to value-based pay, and that number is expected to rise, with some medical practice groups linking 15% or more of compensation to value-based metrics.
“In almost all of the groups that I have worked with in the last few years on [compensation] design, that has been one of the drivers of decision to do the compensation redesign is to allocate to the value-based metrics,” Wayne Hartley, vice president of AMGA Consulting, said in an interview. 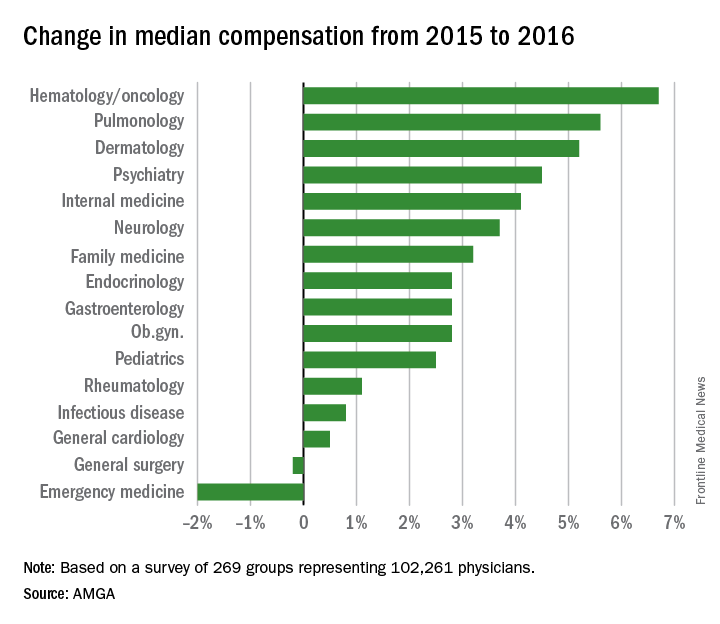
AMGA said that the data covers responses from 269 medical groups covering more than 102,000 providers and is representative of large multispecialty groups and integrated health systems that average 380 providers per group.
GOP health reform dead for now
Senate Republicans are scrambling to come up with another plan now that at least four member of their caucus have said that they would vote against moving forward with debate on the Better Care Reconciliation Act.
Support for the bill, which included dramatic Medicaid cuts and stripped many coverage provisions of the Affordable Care Act, was lacking after revisions were announced on July 13. At that time, conservative Sen. Ran Paul (R-Ky.) and moderate Susan Collins (R-Maine) voiced their opposition for different ideological reasons. They were joined by Sen. Mike Lee (R-Utah) and Sen. Jerry Moran (R-Kan.), who also declined to support the bill. Senate GOP leadership, with a slim 52-48 majority, could only afford to lose two votes (Vice President Mike Pence would have been the tie-breaking vote).
No new timeline has been revealed for the next steps.
“The health reform debate is by no means over,” David Barbe, MD, president of the American Medical Association, said in a statement. “Congress must begin a collaborative process that produces a bipartisan solution. ... Near-term action is needed to stabilize the individual/nongroup health insurance marketplace. In the long term, stakeholders and policymakers need to address the unsustainable trends in health care costs while achieving meaningful, affordable coverage for all Americans.”
AGA believes that, at a minimum, any replacement package must ensure patient access to and coverage of specialty care, ensure patient access to and coverage of evidence-based preventive screenings without cost-sharing, ensure that insurers cannot discriminate because of a pre-existing condition, ensure that insurers cannot discriminate based on gender, allow parents to keep their children on their plans until age 26, and there should be no annual or lifetime caps.
Senate Republicans are scrambling to come up with another plan now that at least four member of their caucus have said that they would vote against moving forward with debate on the Better Care Reconciliation Act.
Support for the bill, which included dramatic Medicaid cuts and stripped many coverage provisions of the Affordable Care Act, was lacking after revisions were announced on July 13. At that time, conservative Sen. Ran Paul (R-Ky.) and moderate Susan Collins (R-Maine) voiced their opposition for different ideological reasons. They were joined by Sen. Mike Lee (R-Utah) and Sen. Jerry Moran (R-Kan.), who also declined to support the bill. Senate GOP leadership, with a slim 52-48 majority, could only afford to lose two votes (Vice President Mike Pence would have been the tie-breaking vote).
No new timeline has been revealed for the next steps.
“The health reform debate is by no means over,” David Barbe, MD, president of the American Medical Association, said in a statement. “Congress must begin a collaborative process that produces a bipartisan solution. ... Near-term action is needed to stabilize the individual/nongroup health insurance marketplace. In the long term, stakeholders and policymakers need to address the unsustainable trends in health care costs while achieving meaningful, affordable coverage for all Americans.”
AGA believes that, at a minimum, any replacement package must ensure patient access to and coverage of specialty care, ensure patient access to and coverage of evidence-based preventive screenings without cost-sharing, ensure that insurers cannot discriminate because of a pre-existing condition, ensure that insurers cannot discriminate based on gender, allow parents to keep their children on their plans until age 26, and there should be no annual or lifetime caps.
Senate Republicans are scrambling to come up with another plan now that at least four member of their caucus have said that they would vote against moving forward with debate on the Better Care Reconciliation Act.
Support for the bill, which included dramatic Medicaid cuts and stripped many coverage provisions of the Affordable Care Act, was lacking after revisions were announced on July 13. At that time, conservative Sen. Ran Paul (R-Ky.) and moderate Susan Collins (R-Maine) voiced their opposition for different ideological reasons. They were joined by Sen. Mike Lee (R-Utah) and Sen. Jerry Moran (R-Kan.), who also declined to support the bill. Senate GOP leadership, with a slim 52-48 majority, could only afford to lose two votes (Vice President Mike Pence would have been the tie-breaking vote).
No new timeline has been revealed for the next steps.
“The health reform debate is by no means over,” David Barbe, MD, president of the American Medical Association, said in a statement. “Congress must begin a collaborative process that produces a bipartisan solution. ... Near-term action is needed to stabilize the individual/nongroup health insurance marketplace. In the long term, stakeholders and policymakers need to address the unsustainable trends in health care costs while achieving meaningful, affordable coverage for all Americans.”
AGA believes that, at a minimum, any replacement package must ensure patient access to and coverage of specialty care, ensure patient access to and coverage of evidence-based preventive screenings without cost-sharing, ensure that insurers cannot discriminate because of a pre-existing condition, ensure that insurers cannot discriminate based on gender, allow parents to keep their children on their plans until age 26, and there should be no annual or lifetime caps.
GOP health reform dead for now
Senate Republicans are scrambling to come up with another plan now that at least four member of their caucus have said that they would vote against moving forward with debate on the Better Care Reconciliation Act.
Support for the bill, which included dramatic Medicaid cuts and stripped many coverage provisions of the Affordable Care Act, was lacking after revisions were announced on July 13. At that time, conservative Sen. Ran Paul (R-Ky.) and moderate Susan Collins (R-Maine) voiced their opposition for different ideological reasons. They were joined by Sen. Mike Lee (R-Utah) and Sen. Jerry Moran (R-Kan.), who also declined to support the bill. Senate GOP leadership, with a slim 52-48 majority, could only afford to lose two votes (Vice President Mike Pence would have been the tie-breaking vote).
No new timeline has been revealed for the next steps.
“The health reform debate is by no means over,” David Barbe, MD, president of the American Medical Association, said in a statement. “Congress must begin a collaborative process that produces a bipartisan solution. ... Near-term action is needed to stabilize the individual/nongroup health insurance marketplace. In the long term, stakeholders and policymakers need to address the unsustainable trends in health care costs while achieving meaningful, affordable coverage for all Americans.”
Senate Republicans are scrambling to come up with another plan now that at least four member of their caucus have said that they would vote against moving forward with debate on the Better Care Reconciliation Act.
Support for the bill, which included dramatic Medicaid cuts and stripped many coverage provisions of the Affordable Care Act, was lacking after revisions were announced on July 13. At that time, conservative Sen. Ran Paul (R-Ky.) and moderate Susan Collins (R-Maine) voiced their opposition for different ideological reasons. They were joined by Sen. Mike Lee (R-Utah) and Sen. Jerry Moran (R-Kan.), who also declined to support the bill. Senate GOP leadership, with a slim 52-48 majority, could only afford to lose two votes (Vice President Mike Pence would have been the tie-breaking vote).
No new timeline has been revealed for the next steps.
“The health reform debate is by no means over,” David Barbe, MD, president of the American Medical Association, said in a statement. “Congress must begin a collaborative process that produces a bipartisan solution. ... Near-term action is needed to stabilize the individual/nongroup health insurance marketplace. In the long term, stakeholders and policymakers need to address the unsustainable trends in health care costs while achieving meaningful, affordable coverage for all Americans.”
Senate Republicans are scrambling to come up with another plan now that at least four member of their caucus have said that they would vote against moving forward with debate on the Better Care Reconciliation Act.
Support for the bill, which included dramatic Medicaid cuts and stripped many coverage provisions of the Affordable Care Act, was lacking after revisions were announced on July 13. At that time, conservative Sen. Ran Paul (R-Ky.) and moderate Susan Collins (R-Maine) voiced their opposition for different ideological reasons. They were joined by Sen. Mike Lee (R-Utah) and Sen. Jerry Moran (R-Kan.), who also declined to support the bill. Senate GOP leadership, with a slim 52-48 majority, could only afford to lose two votes (Vice President Mike Pence would have been the tie-breaking vote).
No new timeline has been revealed for the next steps.
“The health reform debate is by no means over,” David Barbe, MD, president of the American Medical Association, said in a statement. “Congress must begin a collaborative process that produces a bipartisan solution. ... Near-term action is needed to stabilize the individual/nongroup health insurance marketplace. In the long term, stakeholders and policymakers need to address the unsustainable trends in health care costs while achieving meaningful, affordable coverage for all Americans.”
Proposal would exempt more than half of physicians from MACRA/QPP
, thanks to a Centers for Medicare & Medicaid Services proposal exempting some physicians.
The proposed 2018 update to the Quality Payment Program (QPP), the payment system created as part of the Medicare Access and CHIP Reauthorization Act (MACRA), would increase the low-volume threshold for participation, exempting practices that receive $90,000 or less in Medicare Part B payments or have 200 or fewer Medicare patients would be exempt from participation in either the Merit-based Incentive Payment System (MIPS) or Advanced Alternative Payment Model (APM) tracks of the QPP.
According to the proposed rule, released June 20, the CMS “estimates that approximately 572,000 eligible clinicians would be required to participate in MIPS in the 2018 MIPS performance period. ... After restricting the population of eligible clinician types who are not newly enrolled, the proposed increase in the low-volume threshold is expected to exclude 585,560 clinicians who do not exceed the low-volume threshold.”
Overall, 96.6% of MIPS-eligible physicians will engage in quality reporting in 2020, with 96.1% receiving either a bonus to their Medicare Part B payments or no adjustment, according to CMS estimates. For all eligible clinicians, 76.8% will receive a bonus payment, with all payment bonuses totaling $673.3 million, while those losing money will see their Medicare payments reduced by $173.3 million. The overall aggregate impact will be a 0.9% increase in Part B payments to clinicians.
However, different practice sizes will have different experiences. For example, practices with 1-15 eligible clinicians (114,424 total eligible clinicians in this group) will see in the aggregate a 0.7% increase, while practices with 16-24 eligible clinicians (22,296) will see a 0.4% increase in the aggregate. Practices of 100 or more clinicians (318,841) stand to see the biggest bump in their Medicare payments, with a 1.4% bonus based on the provisions in the proposal.
Ten percent of practices with 1-15 MIPS-eligible clinicians and 10.9% of practices with 16-24 MIPS-eligible clinicians are estimated to receive a decrease in their Medicare payments based on the proposal, while 0.8% of clinicians in practices of 100 or more are expected to see the penalty.
The increased low-volume threshold would help out a lot of physicians who might otherwise struggle to meet the requirements, but some view it as a penalty against those who have made the investment and are ready to fully transition into the new value-based payment program, particularly the larger health care systems.
According to the MACRA legislation language, the MIPS program will be a budget-neutral program – so, the more practices that are exempt from having to participate, the less money will be available for potential bonuses for those who perform well.
“It compresses the potential reward for those who are ready and ready to do well,” Chet Speed, vice president of public policy at AMGA, said in an interview, adding that the projected 1.4% aggregate bonus payments for large practices and health systems “does not really reflect or reward all the work they have done to get to this point.” AMGA is an association representing large practices and health systems.
Comments on the proposed update to the QPP are due to the CMS by Aug. 21, 2017.
, thanks to a Centers for Medicare & Medicaid Services proposal exempting some physicians.
The proposed 2018 update to the Quality Payment Program (QPP), the payment system created as part of the Medicare Access and CHIP Reauthorization Act (MACRA), would increase the low-volume threshold for participation, exempting practices that receive $90,000 or less in Medicare Part B payments or have 200 or fewer Medicare patients would be exempt from participation in either the Merit-based Incentive Payment System (MIPS) or Advanced Alternative Payment Model (APM) tracks of the QPP.
According to the proposed rule, released June 20, the CMS “estimates that approximately 572,000 eligible clinicians would be required to participate in MIPS in the 2018 MIPS performance period. ... After restricting the population of eligible clinician types who are not newly enrolled, the proposed increase in the low-volume threshold is expected to exclude 585,560 clinicians who do not exceed the low-volume threshold.”
Overall, 96.6% of MIPS-eligible physicians will engage in quality reporting in 2020, with 96.1% receiving either a bonus to their Medicare Part B payments or no adjustment, according to CMS estimates. For all eligible clinicians, 76.8% will receive a bonus payment, with all payment bonuses totaling $673.3 million, while those losing money will see their Medicare payments reduced by $173.3 million. The overall aggregate impact will be a 0.9% increase in Part B payments to clinicians.
However, different practice sizes will have different experiences. For example, practices with 1-15 eligible clinicians (114,424 total eligible clinicians in this group) will see in the aggregate a 0.7% increase, while practices with 16-24 eligible clinicians (22,296) will see a 0.4% increase in the aggregate. Practices of 100 or more clinicians (318,841) stand to see the biggest bump in their Medicare payments, with a 1.4% bonus based on the provisions in the proposal.
Ten percent of practices with 1-15 MIPS-eligible clinicians and 10.9% of practices with 16-24 MIPS-eligible clinicians are estimated to receive a decrease in their Medicare payments based on the proposal, while 0.8% of clinicians in practices of 100 or more are expected to see the penalty.
The increased low-volume threshold would help out a lot of physicians who might otherwise struggle to meet the requirements, but some view it as a penalty against those who have made the investment and are ready to fully transition into the new value-based payment program, particularly the larger health care systems.
According to the MACRA legislation language, the MIPS program will be a budget-neutral program – so, the more practices that are exempt from having to participate, the less money will be available for potential bonuses for those who perform well.
“It compresses the potential reward for those who are ready and ready to do well,” Chet Speed, vice president of public policy at AMGA, said in an interview, adding that the projected 1.4% aggregate bonus payments for large practices and health systems “does not really reflect or reward all the work they have done to get to this point.” AMGA is an association representing large practices and health systems.
Comments on the proposed update to the QPP are due to the CMS by Aug. 21, 2017.
, thanks to a Centers for Medicare & Medicaid Services proposal exempting some physicians.
The proposed 2018 update to the Quality Payment Program (QPP), the payment system created as part of the Medicare Access and CHIP Reauthorization Act (MACRA), would increase the low-volume threshold for participation, exempting practices that receive $90,000 or less in Medicare Part B payments or have 200 or fewer Medicare patients would be exempt from participation in either the Merit-based Incentive Payment System (MIPS) or Advanced Alternative Payment Model (APM) tracks of the QPP.
According to the proposed rule, released June 20, the CMS “estimates that approximately 572,000 eligible clinicians would be required to participate in MIPS in the 2018 MIPS performance period. ... After restricting the population of eligible clinician types who are not newly enrolled, the proposed increase in the low-volume threshold is expected to exclude 585,560 clinicians who do not exceed the low-volume threshold.”
Overall, 96.6% of MIPS-eligible physicians will engage in quality reporting in 2020, with 96.1% receiving either a bonus to their Medicare Part B payments or no adjustment, according to CMS estimates. For all eligible clinicians, 76.8% will receive a bonus payment, with all payment bonuses totaling $673.3 million, while those losing money will see their Medicare payments reduced by $173.3 million. The overall aggregate impact will be a 0.9% increase in Part B payments to clinicians.
However, different practice sizes will have different experiences. For example, practices with 1-15 eligible clinicians (114,424 total eligible clinicians in this group) will see in the aggregate a 0.7% increase, while practices with 16-24 eligible clinicians (22,296) will see a 0.4% increase in the aggregate. Practices of 100 or more clinicians (318,841) stand to see the biggest bump in their Medicare payments, with a 1.4% bonus based on the provisions in the proposal.
Ten percent of practices with 1-15 MIPS-eligible clinicians and 10.9% of practices with 16-24 MIPS-eligible clinicians are estimated to receive a decrease in their Medicare payments based on the proposal, while 0.8% of clinicians in practices of 100 or more are expected to see the penalty.
The increased low-volume threshold would help out a lot of physicians who might otherwise struggle to meet the requirements, but some view it as a penalty against those who have made the investment and are ready to fully transition into the new value-based payment program, particularly the larger health care systems.
According to the MACRA legislation language, the MIPS program will be a budget-neutral program – so, the more practices that are exempt from having to participate, the less money will be available for potential bonuses for those who perform well.
“It compresses the potential reward for those who are ready and ready to do well,” Chet Speed, vice president of public policy at AMGA, said in an interview, adding that the projected 1.4% aggregate bonus payments for large practices and health systems “does not really reflect or reward all the work they have done to get to this point.” AMGA is an association representing large practices and health systems.
Comments on the proposed update to the QPP are due to the CMS by Aug. 21, 2017.
Senate GOP tweaks health care reform proposal, but it still lacks support
in the upper chamber of Congress.
The update, released July 13, includes a number of provisions to sweeten the pot for conservatives, but it does little to address the concerns of the moderates in the party, particularly of those who are worried about cuts to the Medicaid program.
The GOP leadership also is putting an additional $45 billion into the fight against opioid addiction. Plus, the revised bill includes a provision to allow tax credits to be used to purchase plans that offer only catastrophic coverage.
What the new revision doesn’t do is alter the cuts in the Medicaid program, leaving unchanged the plan to phase out the expansion of Medicaid in 2021 and complete it by 2024; allowing state governors to choose between block grants and per capita allotments to help pay for their Medicaid populations; and allowing states to institute a work requirement for nonpregnant, nondisabled, and nonelderly individuals eligible to receive Medicaid coverage.
Despite the changes, the bill still faces an uphill climb.
Sen. Rand Paul (R-Ky.), Sen. Susan Collins (R-Maine), and Sen. Rob Portman (R-Ohio) have publicly stated that they are opposed to the bill. With only a 52-seat majority and no Democrats expected to vote in favor of the bill, Senate Majority Leader Mitch McConnell (R-Ky.) needs at least 50 votes under budget reconciliation rules to pass the bill. (Vice President Mike Pence would be the tie-breaking vote if the GOP can get to 50 votes.) There are other moderate Republican senators who have opposed previous iterations of the bill, and it remains to be seen if the current tweaks will swing their votes.
The increased funding for the opioid crisis could draw some of the opposing GOP moderates. But, as Julius Hobson, a health care lobbyist with the Washington-based firm Polsinelli, noted, there is “not enough money to deal with” the opioid crisis.
The bill also has provisions allowing insurers to offer catastrophic coverage policies with minimal coverage alongside more comprehensive policies, an effort to bring in healthy younger individuals who may not want more comprehensive coverage. But those provisions have sparked pushback from state insurance directors, America’s Health Insurance Plans, and the Blue Cross Blue Shield Association.
“I can’t see how this bill got better in terms of health care access,” added Mr. Hobson, a former lobbyist with the American Medical Association.
AMA President David Barbe, MD, said that the tweaks do not do enough.
“The revised bill does not address the key concerns of physicians and patients regarding proposed Medicaid cuts and inadequate subsidies that will result in millions of Americans losing health insurance coverage,” Dr. Barbe said in a statement.
“The additional funding to address the opioid epidemic is a positive step; however, those suffering from substance use disorder have other health care needs that are not likely to be addressed if they lose coverage through a rollback of the Medicaid expansion,” he added. “While stabilizing the individual market is an initial step, more bipartisan collaboration is needed in the months ahead to improve the delivery and financing of health care.”
in the upper chamber of Congress.
The update, released July 13, includes a number of provisions to sweeten the pot for conservatives, but it does little to address the concerns of the moderates in the party, particularly of those who are worried about cuts to the Medicaid program.
The GOP leadership also is putting an additional $45 billion into the fight against opioid addiction. Plus, the revised bill includes a provision to allow tax credits to be used to purchase plans that offer only catastrophic coverage.
What the new revision doesn’t do is alter the cuts in the Medicaid program, leaving unchanged the plan to phase out the expansion of Medicaid in 2021 and complete it by 2024; allowing state governors to choose between block grants and per capita allotments to help pay for their Medicaid populations; and allowing states to institute a work requirement for nonpregnant, nondisabled, and nonelderly individuals eligible to receive Medicaid coverage.
Despite the changes, the bill still faces an uphill climb.
Sen. Rand Paul (R-Ky.), Sen. Susan Collins (R-Maine), and Sen. Rob Portman (R-Ohio) have publicly stated that they are opposed to the bill. With only a 52-seat majority and no Democrats expected to vote in favor of the bill, Senate Majority Leader Mitch McConnell (R-Ky.) needs at least 50 votes under budget reconciliation rules to pass the bill. (Vice President Mike Pence would be the tie-breaking vote if the GOP can get to 50 votes.) There are other moderate Republican senators who have opposed previous iterations of the bill, and it remains to be seen if the current tweaks will swing their votes.
The increased funding for the opioid crisis could draw some of the opposing GOP moderates. But, as Julius Hobson, a health care lobbyist with the Washington-based firm Polsinelli, noted, there is “not enough money to deal with” the opioid crisis.
The bill also has provisions allowing insurers to offer catastrophic coverage policies with minimal coverage alongside more comprehensive policies, an effort to bring in healthy younger individuals who may not want more comprehensive coverage. But those provisions have sparked pushback from state insurance directors, America’s Health Insurance Plans, and the Blue Cross Blue Shield Association.
“I can’t see how this bill got better in terms of health care access,” added Mr. Hobson, a former lobbyist with the American Medical Association.
AMA President David Barbe, MD, said that the tweaks do not do enough.
“The revised bill does not address the key concerns of physicians and patients regarding proposed Medicaid cuts and inadequate subsidies that will result in millions of Americans losing health insurance coverage,” Dr. Barbe said in a statement.
“The additional funding to address the opioid epidemic is a positive step; however, those suffering from substance use disorder have other health care needs that are not likely to be addressed if they lose coverage through a rollback of the Medicaid expansion,” he added. “While stabilizing the individual market is an initial step, more bipartisan collaboration is needed in the months ahead to improve the delivery and financing of health care.”
in the upper chamber of Congress.
The update, released July 13, includes a number of provisions to sweeten the pot for conservatives, but it does little to address the concerns of the moderates in the party, particularly of those who are worried about cuts to the Medicaid program.
The GOP leadership also is putting an additional $45 billion into the fight against opioid addiction. Plus, the revised bill includes a provision to allow tax credits to be used to purchase plans that offer only catastrophic coverage.
What the new revision doesn’t do is alter the cuts in the Medicaid program, leaving unchanged the plan to phase out the expansion of Medicaid in 2021 and complete it by 2024; allowing state governors to choose between block grants and per capita allotments to help pay for their Medicaid populations; and allowing states to institute a work requirement for nonpregnant, nondisabled, and nonelderly individuals eligible to receive Medicaid coverage.
Despite the changes, the bill still faces an uphill climb.
Sen. Rand Paul (R-Ky.), Sen. Susan Collins (R-Maine), and Sen. Rob Portman (R-Ohio) have publicly stated that they are opposed to the bill. With only a 52-seat majority and no Democrats expected to vote in favor of the bill, Senate Majority Leader Mitch McConnell (R-Ky.) needs at least 50 votes under budget reconciliation rules to pass the bill. (Vice President Mike Pence would be the tie-breaking vote if the GOP can get to 50 votes.) There are other moderate Republican senators who have opposed previous iterations of the bill, and it remains to be seen if the current tweaks will swing their votes.
The increased funding for the opioid crisis could draw some of the opposing GOP moderates. But, as Julius Hobson, a health care lobbyist with the Washington-based firm Polsinelli, noted, there is “not enough money to deal with” the opioid crisis.
The bill also has provisions allowing insurers to offer catastrophic coverage policies with minimal coverage alongside more comprehensive policies, an effort to bring in healthy younger individuals who may not want more comprehensive coverage. But those provisions have sparked pushback from state insurance directors, America’s Health Insurance Plans, and the Blue Cross Blue Shield Association.
“I can’t see how this bill got better in terms of health care access,” added Mr. Hobson, a former lobbyist with the American Medical Association.
AMA President David Barbe, MD, said that the tweaks do not do enough.
“The revised bill does not address the key concerns of physicians and patients regarding proposed Medicaid cuts and inadequate subsidies that will result in millions of Americans losing health insurance coverage,” Dr. Barbe said in a statement.
“The additional funding to address the opioid epidemic is a positive step; however, those suffering from substance use disorder have other health care needs that are not likely to be addressed if they lose coverage through a rollback of the Medicaid expansion,” he added. “While stabilizing the individual market is an initial step, more bipartisan collaboration is needed in the months ahead to improve the delivery and financing of health care.”
New federal health IT leadership, same goals
WASHINGTON – Although the leadership at the Office of the National Coordinator for Health Information Technology is new, the focus of the federal office – reducing physician burden and improving interoperability of electronic heath records – remains the same.
“One priority is on the whole question of burden of [EHR] usability,” said Don Rucker, MD, the new national coordinator, at a July 11 press briefing. “The other is interoperability. We’ve obviously spent a lot of money collectively in the country on these systems, and there’s a widespread dissatisfaction with the level of interoperability.”
“We are looking at documentation and the whole quality framework around value-based purchasing,” he said. “For a lot of practices now, this has become a challenge that we just have to think about what’s the win. At some point, the expense of complying with the quality measures is a much greater expense than the innate value of the quality measures. ”
EHRs “have become symbolic of physician administrative burden, but by no means are they the whole cause,” John Flemming, MD, ONC deputy assistant secretary for health technology reform, said at the briefing. “The physician, particularly in an independent practice, must manage the practice. So he or she is the CEO. They are also on the assembly line, seeing patients. Now with EHRs, they have to be the data input person as well. It’s time consuming.”
Dr. Fleming is a family physician from Louisiana and a former Republican member of congress.
Dr. Rucker acknowledged that reducing the burden of EHRs has been discussed for quite a long time now. He recalled beginning working with them in his private practice back in 1988 and figured, based on the quick rate of technological innovation demonstrated in Silicon Valley, the issues would be solved by 1992 or 1993 at the latest.
“Right now, [EHRs] are really about documentation, about billing, but that is a funny kind of beast,” he said. “Every other industry uses their enterprise computer software to do automation, to become more efficient. We are the only business that I am aware of to have used computers to become less efficient. ... I think part of what we are trying to do ... is let some of these newer technologies that will actually reduce costs, reduce variance, have those technologies have an entrée into some of these data collections that are out there.”
WASHINGTON – Although the leadership at the Office of the National Coordinator for Health Information Technology is new, the focus of the federal office – reducing physician burden and improving interoperability of electronic heath records – remains the same.
“One priority is on the whole question of burden of [EHR] usability,” said Don Rucker, MD, the new national coordinator, at a July 11 press briefing. “The other is interoperability. We’ve obviously spent a lot of money collectively in the country on these systems, and there’s a widespread dissatisfaction with the level of interoperability.”
“We are looking at documentation and the whole quality framework around value-based purchasing,” he said. “For a lot of practices now, this has become a challenge that we just have to think about what’s the win. At some point, the expense of complying with the quality measures is a much greater expense than the innate value of the quality measures. ”
EHRs “have become symbolic of physician administrative burden, but by no means are they the whole cause,” John Flemming, MD, ONC deputy assistant secretary for health technology reform, said at the briefing. “The physician, particularly in an independent practice, must manage the practice. So he or she is the CEO. They are also on the assembly line, seeing patients. Now with EHRs, they have to be the data input person as well. It’s time consuming.”
Dr. Fleming is a family physician from Louisiana and a former Republican member of congress.
Dr. Rucker acknowledged that reducing the burden of EHRs has been discussed for quite a long time now. He recalled beginning working with them in his private practice back in 1988 and figured, based on the quick rate of technological innovation demonstrated in Silicon Valley, the issues would be solved by 1992 or 1993 at the latest.
“Right now, [EHRs] are really about documentation, about billing, but that is a funny kind of beast,” he said. “Every other industry uses their enterprise computer software to do automation, to become more efficient. We are the only business that I am aware of to have used computers to become less efficient. ... I think part of what we are trying to do ... is let some of these newer technologies that will actually reduce costs, reduce variance, have those technologies have an entrée into some of these data collections that are out there.”
WASHINGTON – Although the leadership at the Office of the National Coordinator for Health Information Technology is new, the focus of the federal office – reducing physician burden and improving interoperability of electronic heath records – remains the same.
“One priority is on the whole question of burden of [EHR] usability,” said Don Rucker, MD, the new national coordinator, at a July 11 press briefing. “The other is interoperability. We’ve obviously spent a lot of money collectively in the country on these systems, and there’s a widespread dissatisfaction with the level of interoperability.”
“We are looking at documentation and the whole quality framework around value-based purchasing,” he said. “For a lot of practices now, this has become a challenge that we just have to think about what’s the win. At some point, the expense of complying with the quality measures is a much greater expense than the innate value of the quality measures. ”
EHRs “have become symbolic of physician administrative burden, but by no means are they the whole cause,” John Flemming, MD, ONC deputy assistant secretary for health technology reform, said at the briefing. “The physician, particularly in an independent practice, must manage the practice. So he or she is the CEO. They are also on the assembly line, seeing patients. Now with EHRs, they have to be the data input person as well. It’s time consuming.”
Dr. Fleming is a family physician from Louisiana and a former Republican member of congress.
Dr. Rucker acknowledged that reducing the burden of EHRs has been discussed for quite a long time now. He recalled beginning working with them in his private practice back in 1988 and figured, based on the quick rate of technological innovation demonstrated in Silicon Valley, the issues would be solved by 1992 or 1993 at the latest.
“Right now, [EHRs] are really about documentation, about billing, but that is a funny kind of beast,” he said. “Every other industry uses their enterprise computer software to do automation, to become more efficient. We are the only business that I am aware of to have used computers to become less efficient. ... I think part of what we are trying to do ... is let some of these newer technologies that will actually reduce costs, reduce variance, have those technologies have an entrée into some of these data collections that are out there.”
Consequence of change? Medicaid disenrollment delayed breast cancer diagnosis
A spike in later-stage breast cancers is a potential byproduct of the Republican-proposed Medicaid reductions, according to Wafa Tarazi, PhD, and her colleagues.
The team looked at breast cancer stage at diagnosis following the 2005 Medicaid disenrollment of nearly 170,000 nonelderly adults in Tennessee that occurred because of state financial issues.
“Overall, nonelderly women in Tennessee were diagnosed at later stages of disease and experienced more delays in treatment in the period after disenrollment,” wrote Dr. Tarazi of Virginia Commonwealth University, Richmond, and her colleagues. “Disenrollment was found to be associated with a 3.3 percentage point increase in late stage of disease at the time of diagnosis” (Cancer 2016 June 26. doi: 10.1002/cncr.30771).
The investigators offered a few explanations for why this could be the case.
While disenrollment was associated with later stage of breast cancer at diagnosis, it also was associated with a 1.9 percentage-point decrease in a 60-day–plus delay in surgical treatment and a 1.4 percentage-point decrease in a greater-than-90-day–plus delay in treatment for women living in low-income ZIP codes, compared with women living in high-income ZIP codes.
Contractions “in the availability of Medicaid coverage have important health consequences for low-income women, and may increase income-related disparities, morbidity, and mortality for those diagnosed with breast cancer,” the authors wrote. “These negative health consequences should be considered by policymakers who weigh the costs and benefits of implementing or discontinuing expanded Medicaid coverage under the Patient Protection and Affordable Care Act and future federal and state policies.”
The Susan G. Komen Breast Cancer Foundation funded the study. The authors reported no conflicts of interest.
A spike in later-stage breast cancers is a potential byproduct of the Republican-proposed Medicaid reductions, according to Wafa Tarazi, PhD, and her colleagues.
The team looked at breast cancer stage at diagnosis following the 2005 Medicaid disenrollment of nearly 170,000 nonelderly adults in Tennessee that occurred because of state financial issues.
“Overall, nonelderly women in Tennessee were diagnosed at later stages of disease and experienced more delays in treatment in the period after disenrollment,” wrote Dr. Tarazi of Virginia Commonwealth University, Richmond, and her colleagues. “Disenrollment was found to be associated with a 3.3 percentage point increase in late stage of disease at the time of diagnosis” (Cancer 2016 June 26. doi: 10.1002/cncr.30771).
The investigators offered a few explanations for why this could be the case.
While disenrollment was associated with later stage of breast cancer at diagnosis, it also was associated with a 1.9 percentage-point decrease in a 60-day–plus delay in surgical treatment and a 1.4 percentage-point decrease in a greater-than-90-day–plus delay in treatment for women living in low-income ZIP codes, compared with women living in high-income ZIP codes.
Contractions “in the availability of Medicaid coverage have important health consequences for low-income women, and may increase income-related disparities, morbidity, and mortality for those diagnosed with breast cancer,” the authors wrote. “These negative health consequences should be considered by policymakers who weigh the costs and benefits of implementing or discontinuing expanded Medicaid coverage under the Patient Protection and Affordable Care Act and future federal and state policies.”
The Susan G. Komen Breast Cancer Foundation funded the study. The authors reported no conflicts of interest.
A spike in later-stage breast cancers is a potential byproduct of the Republican-proposed Medicaid reductions, according to Wafa Tarazi, PhD, and her colleagues.
The team looked at breast cancer stage at diagnosis following the 2005 Medicaid disenrollment of nearly 170,000 nonelderly adults in Tennessee that occurred because of state financial issues.
“Overall, nonelderly women in Tennessee were diagnosed at later stages of disease and experienced more delays in treatment in the period after disenrollment,” wrote Dr. Tarazi of Virginia Commonwealth University, Richmond, and her colleagues. “Disenrollment was found to be associated with a 3.3 percentage point increase in late stage of disease at the time of diagnosis” (Cancer 2016 June 26. doi: 10.1002/cncr.30771).
The investigators offered a few explanations for why this could be the case.
While disenrollment was associated with later stage of breast cancer at diagnosis, it also was associated with a 1.9 percentage-point decrease in a 60-day–plus delay in surgical treatment and a 1.4 percentage-point decrease in a greater-than-90-day–plus delay in treatment for women living in low-income ZIP codes, compared with women living in high-income ZIP codes.
Contractions “in the availability of Medicaid coverage have important health consequences for low-income women, and may increase income-related disparities, morbidity, and mortality for those diagnosed with breast cancer,” the authors wrote. “These negative health consequences should be considered by policymakers who weigh the costs and benefits of implementing or discontinuing expanded Medicaid coverage under the Patient Protection and Affordable Care Act and future federal and state policies.”
The Susan G. Komen Breast Cancer Foundation funded the study. The authors reported no conflicts of interest.
FROM CANCER
Docs still don’t get MACRA
Seven months into the first year of the Quality Payment Program, the new value-based payment plan set up by the Medicare Access and CHIP Reauthorization Act (MACRA), and doctors’ knowledge of the program is still light.
“Physicians, especially those in small practices, need more help in preparing” for participation in QPP either through the Merit-Based Incentive Payment System (MIPS) or advanced Alternative Payment Models (APMs), according to a new report issued by the American Medical Association and consulting firm KPMG.
That said, about 70% of those surveyed responded that they have begun preparing to meet the requirements of the QPP in 2017. The survey did not make clear whether this meant meeting the minimum requirements to avoid any penalties or doing more to become eligible for potential bonus Medicare payments.
“Even those who feel prepared still don’t fully understand the financial ramifications of the program,” the report said. “In short, they may be prepared to ‘check the box’ of reporting requirements, but may lack the long-term strategic financial vision to succeed in 2018 and beyond,” noting that only 8% of the respondents said they are “very prepared” for long-term financial success. On the other side of the that spectrum, 26% said they are not at all prepared and 58% said they were slightly prepared.
Survey respondents indicated a number of areas where they need help:
• Time required to accurately capture and report performance data (66%)
• Understanding reporting requirements (58%)
• Understanding the overall MIPS scoring process (57%)
• Cost required to accurately capture and report performance data (53%)
• Organizational infrastructure needed to report performance (49%)
The report also noted the significant differences when it comes to practice size, although the differences were “not unexpected.” For example, solo practices, compared to those groups of 50 or more physicians, were “significantly more likely (56%) to view reporting requirements as very burdensome, ... significantly more like to feel ‘not at all prepared’ for long-term financial success, ... less likely to be participating in an advanced APM, [and] less likely to have begun preparing.”
Specialists, more so than primary care physicians were “slightly more likely to be deeply knowledgeable about MACRA/QPP, [and] more likely to expect to participate in MIPS (61% versus 48%) and less likely to participate in an advanced APM (15% versus 22%),” the report adds.
“Ongoing educational assistance from CMS, as well as those in the private sector, should focus on the areas where physicians need the most help: understanding requirements and potential financial impact, selection of quality measures, and clinical practice transformation strategies,” the report states.
The survey comes on the heels of CMS releasing its proposed update to the regulations surrounding the QPP for 2018. Comments on the proposed regulatory update are due to CMS on Aug. 21, 2017.
Seven months into the first year of the Quality Payment Program, the new value-based payment plan set up by the Medicare Access and CHIP Reauthorization Act (MACRA), and doctors’ knowledge of the program is still light.
“Physicians, especially those in small practices, need more help in preparing” for participation in QPP either through the Merit-Based Incentive Payment System (MIPS) or advanced Alternative Payment Models (APMs), according to a new report issued by the American Medical Association and consulting firm KPMG.
That said, about 70% of those surveyed responded that they have begun preparing to meet the requirements of the QPP in 2017. The survey did not make clear whether this meant meeting the minimum requirements to avoid any penalties or doing more to become eligible for potential bonus Medicare payments.
“Even those who feel prepared still don’t fully understand the financial ramifications of the program,” the report said. “In short, they may be prepared to ‘check the box’ of reporting requirements, but may lack the long-term strategic financial vision to succeed in 2018 and beyond,” noting that only 8% of the respondents said they are “very prepared” for long-term financial success. On the other side of the that spectrum, 26% said they are not at all prepared and 58% said they were slightly prepared.
Survey respondents indicated a number of areas where they need help:
• Time required to accurately capture and report performance data (66%)
• Understanding reporting requirements (58%)
• Understanding the overall MIPS scoring process (57%)
• Cost required to accurately capture and report performance data (53%)
• Organizational infrastructure needed to report performance (49%)
The report also noted the significant differences when it comes to practice size, although the differences were “not unexpected.” For example, solo practices, compared to those groups of 50 or more physicians, were “significantly more likely (56%) to view reporting requirements as very burdensome, ... significantly more like to feel ‘not at all prepared’ for long-term financial success, ... less likely to be participating in an advanced APM, [and] less likely to have begun preparing.”
Specialists, more so than primary care physicians were “slightly more likely to be deeply knowledgeable about MACRA/QPP, [and] more likely to expect to participate in MIPS (61% versus 48%) and less likely to participate in an advanced APM (15% versus 22%),” the report adds.
“Ongoing educational assistance from CMS, as well as those in the private sector, should focus on the areas where physicians need the most help: understanding requirements and potential financial impact, selection of quality measures, and clinical practice transformation strategies,” the report states.
The survey comes on the heels of CMS releasing its proposed update to the regulations surrounding the QPP for 2018. Comments on the proposed regulatory update are due to CMS on Aug. 21, 2017.
Seven months into the first year of the Quality Payment Program, the new value-based payment plan set up by the Medicare Access and CHIP Reauthorization Act (MACRA), and doctors’ knowledge of the program is still light.
“Physicians, especially those in small practices, need more help in preparing” for participation in QPP either through the Merit-Based Incentive Payment System (MIPS) or advanced Alternative Payment Models (APMs), according to a new report issued by the American Medical Association and consulting firm KPMG.
That said, about 70% of those surveyed responded that they have begun preparing to meet the requirements of the QPP in 2017. The survey did not make clear whether this meant meeting the minimum requirements to avoid any penalties or doing more to become eligible for potential bonus Medicare payments.
“Even those who feel prepared still don’t fully understand the financial ramifications of the program,” the report said. “In short, they may be prepared to ‘check the box’ of reporting requirements, but may lack the long-term strategic financial vision to succeed in 2018 and beyond,” noting that only 8% of the respondents said they are “very prepared” for long-term financial success. On the other side of the that spectrum, 26% said they are not at all prepared and 58% said they were slightly prepared.
Survey respondents indicated a number of areas where they need help:
• Time required to accurately capture and report performance data (66%)
• Understanding reporting requirements (58%)
• Understanding the overall MIPS scoring process (57%)
• Cost required to accurately capture and report performance data (53%)
• Organizational infrastructure needed to report performance (49%)
The report also noted the significant differences when it comes to practice size, although the differences were “not unexpected.” For example, solo practices, compared to those groups of 50 or more physicians, were “significantly more likely (56%) to view reporting requirements as very burdensome, ... significantly more like to feel ‘not at all prepared’ for long-term financial success, ... less likely to be participating in an advanced APM, [and] less likely to have begun preparing.”
Specialists, more so than primary care physicians were “slightly more likely to be deeply knowledgeable about MACRA/QPP, [and] more likely to expect to participate in MIPS (61% versus 48%) and less likely to participate in an advanced APM (15% versus 22%),” the report adds.
“Ongoing educational assistance from CMS, as well as those in the private sector, should focus on the areas where physicians need the most help: understanding requirements and potential financial impact, selection of quality measures, and clinical practice transformation strategies,” the report states.
The survey comes on the heels of CMS releasing its proposed update to the regulations surrounding the QPP for 2018. Comments on the proposed regulatory update are due to CMS on Aug. 21, 2017.
CBO: Senate health care proposal marginally better than House-passed bill
The Senate health care proposal is only marginally better in terms of the number of uninsured Americans, compared with the House-passed bill it aims to replace, but it still would leave 22 million more Americans without insurance coverage, according to a June 26 analysis by the Congressional Budget Office.
The analysis raised voices of opposition from the medical community.
BCRA would lower the federal deficit by $321 billion between 2017-2026, driven by the dramatic cuts in spending on Medicaid (estimated to be $772 billion), as well as $408 billion saved from reduced tax credits and other subsidies to help people afford health insurance.
The CBO’s estimate also addresses how the bill could impact access to health care.
Initially, patients can expect another short-term spike in insurance premiums, with average premiums in 2018 increasing by 20%, compared with current law, “mainly because the penalty for not having insurance would be eliminated, inducing fewer comparatively healthy people to sign up.” In 2019, premiums are predicted to be about 10% higher than under current law; however, by 2020, premiums for benchmark plans would be 30% lower than with current law.
However, as premiums come down, deductibles would continue to rise for plans that would offer lower levels of coverage, according to the CBO report. Additionally, “starting in 2020, the premium for a silver plan would typically be a relatively high percentage of income for low income people. The deductible for a plan ... would be a significantly higher percentage of income – also making such a plan unattractive but for a different reason. As a result, despite being eligible for premium tax credits, few low-income people would purchase any plan.”
The report also notes that the Senate proposal would not necessarily reverse current concerns regarding consumer choice in the individual markets, stating that “a small fraction of the population resides in areas which – because of this legislation, for at least some of the years after 2019 – no insurers will participate in the nongroup market or insurance would be offered only with very high premiums.” Additionally, removing the employer mandate could result in employers forgoing offering health insurance to their employees.
The bill faces an uphill battle in the Senate as there seemingly are not enough votes to pass the bill at this time. The measure is using the budget reconciliation process, meaning it will need 50 of the 52 Senate Republicans to pass it (all 48 Democrats are expected to vote against it). At least six GOP senators have said they are not ready to start debate. Senate Majority Leader Mitch McConnell (R-Ky) will not present the bill to the chamber for consideration until after the July 4 recess in an effort to tweak the language to garner the 50 votes needed to pass.
Medical societies are pushing back against the bill as well.
The American Medical Association, in a letter to Senate leaders, notes that the first principal that medical professionals operate under is to do no harm. “The draft legislation violates that standard on many levels,” according to the AMA letter.
In a statement from the American Gastroenterological Association, it was pointed out that both the House and Senate bills allow states to opt out of the Affordable Care Act’s essential health benefits package, which includes coverage of colorectal cancer screenings. “A core mission of AGA is to ensure that patients have access to high-quality medical care,“ said Timothy Wang, MD, AGAF, AGA chair. “We have made great strides in the increase in screening and prevention of colorectal cancer, which reduces deaths and downstream health care costs. Erecting barriers to screening will only reverse this process.” The budget cuts and restrictions on patient access under the congressional proposals will create tremendous burdens for the health care system as patients will increasingly rely on practices and academic medical centers to provide uncompensated care, according to the AGA.
The American Osteopathic Association reiterated its objections to BCRA in a statement, citing the CBO’s determination that 22 million would lose coverage.
“As patient advocates, we cannot accept that under [BCRA] patients in need will no longer have the coverage they require to access health care services,” the association said in a statement. “The BCRA does nothing to control health costs but instead focuses on reducing federal health care expenditures by cutting coverage of our nation’s most vulnerable individuals and eliminating policies that promote access to preventive care services that can actually drive down expenses while improving patient outcomes.”
The American College of Cardiology noted that CBO analysis “makes it clear that the [BCRA] would lead to loss of coverage for millions of Americans and limit access to care for our most vulnerable populations. ... The ACC opposes the BCRA as it does not align with our Principles for Health Reform, which stress the need for patient access to meaningful insurance coverage and high-quality care.”
The Senate health care proposal is only marginally better in terms of the number of uninsured Americans, compared with the House-passed bill it aims to replace, but it still would leave 22 million more Americans without insurance coverage, according to a June 26 analysis by the Congressional Budget Office.
The analysis raised voices of opposition from the medical community.
BCRA would lower the federal deficit by $321 billion between 2017-2026, driven by the dramatic cuts in spending on Medicaid (estimated to be $772 billion), as well as $408 billion saved from reduced tax credits and other subsidies to help people afford health insurance.
The CBO’s estimate also addresses how the bill could impact access to health care.
Initially, patients can expect another short-term spike in insurance premiums, with average premiums in 2018 increasing by 20%, compared with current law, “mainly because the penalty for not having insurance would be eliminated, inducing fewer comparatively healthy people to sign up.” In 2019, premiums are predicted to be about 10% higher than under current law; however, by 2020, premiums for benchmark plans would be 30% lower than with current law.
However, as premiums come down, deductibles would continue to rise for plans that would offer lower levels of coverage, according to the CBO report. Additionally, “starting in 2020, the premium for a silver plan would typically be a relatively high percentage of income for low income people. The deductible for a plan ... would be a significantly higher percentage of income – also making such a plan unattractive but for a different reason. As a result, despite being eligible for premium tax credits, few low-income people would purchase any plan.”
The report also notes that the Senate proposal would not necessarily reverse current concerns regarding consumer choice in the individual markets, stating that “a small fraction of the population resides in areas which – because of this legislation, for at least some of the years after 2019 – no insurers will participate in the nongroup market or insurance would be offered only with very high premiums.” Additionally, removing the employer mandate could result in employers forgoing offering health insurance to their employees.
The bill faces an uphill battle in the Senate as there seemingly are not enough votes to pass the bill at this time. The measure is using the budget reconciliation process, meaning it will need 50 of the 52 Senate Republicans to pass it (all 48 Democrats are expected to vote against it). At least six GOP senators have said they are not ready to start debate. Senate Majority Leader Mitch McConnell (R-Ky) will not present the bill to the chamber for consideration until after the July 4 recess in an effort to tweak the language to garner the 50 votes needed to pass.
Medical societies are pushing back against the bill as well.
The American Medical Association, in a letter to Senate leaders, notes that the first principal that medical professionals operate under is to do no harm. “The draft legislation violates that standard on many levels,” according to the AMA letter.
In a statement from the American Gastroenterological Association, it was pointed out that both the House and Senate bills allow states to opt out of the Affordable Care Act’s essential health benefits package, which includes coverage of colorectal cancer screenings. “A core mission of AGA is to ensure that patients have access to high-quality medical care,“ said Timothy Wang, MD, AGAF, AGA chair. “We have made great strides in the increase in screening and prevention of colorectal cancer, which reduces deaths and downstream health care costs. Erecting barriers to screening will only reverse this process.” The budget cuts and restrictions on patient access under the congressional proposals will create tremendous burdens for the health care system as patients will increasingly rely on practices and academic medical centers to provide uncompensated care, according to the AGA.
The American Osteopathic Association reiterated its objections to BCRA in a statement, citing the CBO’s determination that 22 million would lose coverage.
“As patient advocates, we cannot accept that under [BCRA] patients in need will no longer have the coverage they require to access health care services,” the association said in a statement. “The BCRA does nothing to control health costs but instead focuses on reducing federal health care expenditures by cutting coverage of our nation’s most vulnerable individuals and eliminating policies that promote access to preventive care services that can actually drive down expenses while improving patient outcomes.”
The American College of Cardiology noted that CBO analysis “makes it clear that the [BCRA] would lead to loss of coverage for millions of Americans and limit access to care for our most vulnerable populations. ... The ACC opposes the BCRA as it does not align with our Principles for Health Reform, which stress the need for patient access to meaningful insurance coverage and high-quality care.”
The Senate health care proposal is only marginally better in terms of the number of uninsured Americans, compared with the House-passed bill it aims to replace, but it still would leave 22 million more Americans without insurance coverage, according to a June 26 analysis by the Congressional Budget Office.
The analysis raised voices of opposition from the medical community.
BCRA would lower the federal deficit by $321 billion between 2017-2026, driven by the dramatic cuts in spending on Medicaid (estimated to be $772 billion), as well as $408 billion saved from reduced tax credits and other subsidies to help people afford health insurance.
The CBO’s estimate also addresses how the bill could impact access to health care.
Initially, patients can expect another short-term spike in insurance premiums, with average premiums in 2018 increasing by 20%, compared with current law, “mainly because the penalty for not having insurance would be eliminated, inducing fewer comparatively healthy people to sign up.” In 2019, premiums are predicted to be about 10% higher than under current law; however, by 2020, premiums for benchmark plans would be 30% lower than with current law.
However, as premiums come down, deductibles would continue to rise for plans that would offer lower levels of coverage, according to the CBO report. Additionally, “starting in 2020, the premium for a silver plan would typically be a relatively high percentage of income for low income people. The deductible for a plan ... would be a significantly higher percentage of income – also making such a plan unattractive but for a different reason. As a result, despite being eligible for premium tax credits, few low-income people would purchase any plan.”
The report also notes that the Senate proposal would not necessarily reverse current concerns regarding consumer choice in the individual markets, stating that “a small fraction of the population resides in areas which – because of this legislation, for at least some of the years after 2019 – no insurers will participate in the nongroup market or insurance would be offered only with very high premiums.” Additionally, removing the employer mandate could result in employers forgoing offering health insurance to their employees.
The bill faces an uphill battle in the Senate as there seemingly are not enough votes to pass the bill at this time. The measure is using the budget reconciliation process, meaning it will need 50 of the 52 Senate Republicans to pass it (all 48 Democrats are expected to vote against it). At least six GOP senators have said they are not ready to start debate. Senate Majority Leader Mitch McConnell (R-Ky) will not present the bill to the chamber for consideration until after the July 4 recess in an effort to tweak the language to garner the 50 votes needed to pass.
Medical societies are pushing back against the bill as well.
The American Medical Association, in a letter to Senate leaders, notes that the first principal that medical professionals operate under is to do no harm. “The draft legislation violates that standard on many levels,” according to the AMA letter.
In a statement from the American Gastroenterological Association, it was pointed out that both the House and Senate bills allow states to opt out of the Affordable Care Act’s essential health benefits package, which includes coverage of colorectal cancer screenings. “A core mission of AGA is to ensure that patients have access to high-quality medical care,“ said Timothy Wang, MD, AGAF, AGA chair. “We have made great strides in the increase in screening and prevention of colorectal cancer, which reduces deaths and downstream health care costs. Erecting barriers to screening will only reverse this process.” The budget cuts and restrictions on patient access under the congressional proposals will create tremendous burdens for the health care system as patients will increasingly rely on practices and academic medical centers to provide uncompensated care, according to the AGA.
The American Osteopathic Association reiterated its objections to BCRA in a statement, citing the CBO’s determination that 22 million would lose coverage.
“As patient advocates, we cannot accept that under [BCRA] patients in need will no longer have the coverage they require to access health care services,” the association said in a statement. “The BCRA does nothing to control health costs but instead focuses on reducing federal health care expenditures by cutting coverage of our nation’s most vulnerable individuals and eliminating policies that promote access to preventive care services that can actually drive down expenses while improving patient outcomes.”
The American College of Cardiology noted that CBO analysis “makes it clear that the [BCRA] would lead to loss of coverage for millions of Americans and limit access to care for our most vulnerable populations. ... The ACC opposes the BCRA as it does not align with our Principles for Health Reform, which stress the need for patient access to meaningful insurance coverage and high-quality care.”











