User login
USPSTF updates recommendations for syphilis screening
Because syphilis infection rates have increased over the last decade, health care providers should screen patients for the disease more frequently to detect and treat it earlier and more effectively, particular in high-risk subgroups.
The United States Preventive Services Task Force made this recommendation in a JAMA article published online, the first update to the syphilis screening recommendation since 2004 (JAMA. 2016;315[21]:2321-2327. doi: 10.1001/jama.2016.5824).
“Individuals with previous syphilis infection, an infected sexual partner, current HIV infection, or more than 4 sex partners in the preceding year are at increased risk of acquiring syphilis,” the report states. “Higher prevalence rates are associated with sociodemographic groups including men who have sex with men (MSM), young adult men, sex workers, adults in correctional facilities, and individuals who are black or live in metropolitan areas in the southern and western United States. Men who have sex with men accounted for 61% of all primary and secondary syphilis cases reported in 2014.”
A systematic review of trials and studies investigating syphilis screening effectiveness, testing accuracy, and screening risks in nonpregnant adults and adolescents – all of which were included in the Cochrane Central Register of Controlled Trials and Cochrane Database of Systematic Reviews through October 2015, along with the Ovid MEDLINE database from January 2004 through October 2015 – was undertaken to update the 2004 recommendations.
Studies with clinical application were emphasized more heavily, along with those that focused on target populations of asymptomatic, sexually active, adolescent and older men and women. In total, 2,000 English-language titles and abstracts were reviewed, from which 448 full-text studies underwent further review for inclusion. From these, only nine were ultimately selected for inclusion, four of which were observational studies, three of which were observational studies of test accuracy, and two of which were observational studies of testing sequences.
The first four studies – Bissessor et al. 2010, Cohen et al. 2005, Zou et al. 2013, and Bissessor et al. 2011 – were included to answer the investigation’s key question 1 (KQ1) – “What is the effectiveness of screening for syphilis in reducing complications of the disease and transmission or acquisition of other sexually transmitted infections in asymptomatic, nonpregnant, sexually active adults and adolescents? What is the effectiveness of specific screening intervals and screening among population subgroups?”
The remaining five studies – Wong et al. 2011, Tsang et al. 2007, Juárez-Figueroa et al. 2007, Mishra et al. 2011, and Binnicker et al. 2012 – were aimed at KQ3, asking “What is the accuracy of currently used screening tests and strategies (e.g., sequence of tests) for detecting syphilis infection?”
Regarding KQ1, all four studies found that MSM and HIV-infected men who were screened routinely every 3 months had a significantly higher rate of syphilis detection compared with those who were screened annually. The studies, all of which came from Europe and Australia, detected syphilis early in those who were screened every 3 months in 8.1% of HIV-infected MSM versus 3.1% of those who screened annually (P = .001), detected early-latent syphilis in 1.7% of routine screeners versus 0.4% of annual screeners (P = .008), and detected early syphilis in higher-risk MSM in 53% of regular screeners versus just 16% of annual screeners (P = .001). The cohort comprised 6,789 asymptomatic MSM.
In addition, newly acquired syphilis in HIV-positive MSM was found in 7.3 cases per 1,000 patient-years (95% CI, 5.2-9.9) for those who were regularly screened, versus 2.8 cases per 1,000 patient-years (95% CI, 1.8-4.0) for those who were screened annually.
Of the five studies investigating KQ3, three (Wong, Tsang, Juárez-Figueroa) were observational studies of treponemal and nontreponemal tests to detect syphilis. Results indicated that both tests had a sensitivity of 85.3%-98%, and specificity of 91%-100%. However, the remaining two studies (Mishra, Binnicker) used reverse screening algorithms to confirm positive test results from treponemal and nontreponemal, finding higher rates of false positives in the rapid plasma reagin than in the traditional enzyme analyses: 0.6% vs. 0.0% in one study (P = .03) and 0.26% vs. 0.13% in the other.
“Additional research on syphilis screening is needed to directly compare the effectiveness of different screening strategies for identifying individuals at increased risk of infection, co-testing for concurrent STIs, and different screening intervals among various patient populations,” wrote the USPSTF investigators, adding that research also is needed on evaluating the instruments used in risk assessment, as well as diagnostic accuracy.
Furthermore, while the data from these studies have shed light on syphilis testing and screening, several other important components of disease treatment and prevention – namely, “the effectiveness of screening in reducing syphilis complications and transmission, effectiveness of risk assessment methods, and harms related to screening” – were not adequately addressed.
This study was funded by the Agency for Healthcare Research and Quality, “under a contract to support the USPSTF.” The authors did not report any relevant financial disclosures.
As the 1990s ended, syphilis was on the decline. At least in part due to safer sexual behaviors prompted by the AIDS epidemic, the rate of incident syphilis declined to fewer than 4 cases per 100,000 by the year 2000, a historic nadir. Now, in 2016, hopes for eradication have long since faded, as have many of the gains realized by the effort. Rates of syphilis have trended steadily upward since 2000, and the CDC’s syphilis elimination efforts officially ended as of December 2013.
The good news is that fixing what has gone wrong does not require huge capital investment, breakthrough technological advances, or massive restructuring of our health care system. Improvements are at hand and require mostly focus and commitment on the part of the health care community. First, awareness of the problem needs to be increased, particularly in clinical settings where patients at higher risk for syphilis are being followed up. These high-risk populations include MSM, HIV-infected persons, and younger sexually active persons, particularly persons of color and those from socioeconomically disadvantaged populations. The syphilis demographic overlaps considerably with the HIV demographic. For example, in 2014, half of all MSM diagnosed with syphilis were also coinfected with HIV. Younger men (aged 20-29 years) have a prevalence rate nearly 3 times that of the national average for men, and persons of color are particularly at risk, with black individuals disproportionately affected in the United States. Rates of primary and secondary syphilis were 18.9 cases per 100000 in blacks compared with 3.5 per 100000 in whites. Rates in other ethnic groups (aside from Asians, whose rates were lowest of all) were intermediate between blacks and whites.
Although imperfect, serologic syphilis screening is highly sensitive and specific in high-prevalence populations, is inexpensive and technically simple, and has minimal potential for harm. These factors argue for much more widespread and comprehensive screening of groups at high risk for syphilis. Because treatment of early syphilis is also highly effective, identifying untreated infected persons by means of the recommended screening strategy has great potential for both eliminating the consequences of later-stage infection and substantially reducing transmission from those with early infection.
Dr. Meredith E. Clement is with the division of infectious diseases at Duke University, Durham, N.C. Dr. Charles B. Hicks is with the department of medicine at the University of California, San Diego. Dr Hicks reported ties with Bristol-Myers Squibb, Gilead Sciences, Merck, Janssen Virology, ViiV Healthcare, AstraZeneca, and UpToDate. He served as associate editor and author for NEJM Journal Watch. Dr. Clement has received royalties from UpToDate. These comments were excerpted from the editorial accompanying the study (JAMA. 2016;315[21]:2281-3).
As the 1990s ended, syphilis was on the decline. At least in part due to safer sexual behaviors prompted by the AIDS epidemic, the rate of incident syphilis declined to fewer than 4 cases per 100,000 by the year 2000, a historic nadir. Now, in 2016, hopes for eradication have long since faded, as have many of the gains realized by the effort. Rates of syphilis have trended steadily upward since 2000, and the CDC’s syphilis elimination efforts officially ended as of December 2013.
The good news is that fixing what has gone wrong does not require huge capital investment, breakthrough technological advances, or massive restructuring of our health care system. Improvements are at hand and require mostly focus and commitment on the part of the health care community. First, awareness of the problem needs to be increased, particularly in clinical settings where patients at higher risk for syphilis are being followed up. These high-risk populations include MSM, HIV-infected persons, and younger sexually active persons, particularly persons of color and those from socioeconomically disadvantaged populations. The syphilis demographic overlaps considerably with the HIV demographic. For example, in 2014, half of all MSM diagnosed with syphilis were also coinfected with HIV. Younger men (aged 20-29 years) have a prevalence rate nearly 3 times that of the national average for men, and persons of color are particularly at risk, with black individuals disproportionately affected in the United States. Rates of primary and secondary syphilis were 18.9 cases per 100000 in blacks compared with 3.5 per 100000 in whites. Rates in other ethnic groups (aside from Asians, whose rates were lowest of all) were intermediate between blacks and whites.
Although imperfect, serologic syphilis screening is highly sensitive and specific in high-prevalence populations, is inexpensive and technically simple, and has minimal potential for harm. These factors argue for much more widespread and comprehensive screening of groups at high risk for syphilis. Because treatment of early syphilis is also highly effective, identifying untreated infected persons by means of the recommended screening strategy has great potential for both eliminating the consequences of later-stage infection and substantially reducing transmission from those with early infection.
Dr. Meredith E. Clement is with the division of infectious diseases at Duke University, Durham, N.C. Dr. Charles B. Hicks is with the department of medicine at the University of California, San Diego. Dr Hicks reported ties with Bristol-Myers Squibb, Gilead Sciences, Merck, Janssen Virology, ViiV Healthcare, AstraZeneca, and UpToDate. He served as associate editor and author for NEJM Journal Watch. Dr. Clement has received royalties from UpToDate. These comments were excerpted from the editorial accompanying the study (JAMA. 2016;315[21]:2281-3).
As the 1990s ended, syphilis was on the decline. At least in part due to safer sexual behaviors prompted by the AIDS epidemic, the rate of incident syphilis declined to fewer than 4 cases per 100,000 by the year 2000, a historic nadir. Now, in 2016, hopes for eradication have long since faded, as have many of the gains realized by the effort. Rates of syphilis have trended steadily upward since 2000, and the CDC’s syphilis elimination efforts officially ended as of December 2013.
The good news is that fixing what has gone wrong does not require huge capital investment, breakthrough technological advances, or massive restructuring of our health care system. Improvements are at hand and require mostly focus and commitment on the part of the health care community. First, awareness of the problem needs to be increased, particularly in clinical settings where patients at higher risk for syphilis are being followed up. These high-risk populations include MSM, HIV-infected persons, and younger sexually active persons, particularly persons of color and those from socioeconomically disadvantaged populations. The syphilis demographic overlaps considerably with the HIV demographic. For example, in 2014, half of all MSM diagnosed with syphilis were also coinfected with HIV. Younger men (aged 20-29 years) have a prevalence rate nearly 3 times that of the national average for men, and persons of color are particularly at risk, with black individuals disproportionately affected in the United States. Rates of primary and secondary syphilis were 18.9 cases per 100000 in blacks compared with 3.5 per 100000 in whites. Rates in other ethnic groups (aside from Asians, whose rates were lowest of all) were intermediate between blacks and whites.
Although imperfect, serologic syphilis screening is highly sensitive and specific in high-prevalence populations, is inexpensive and technically simple, and has minimal potential for harm. These factors argue for much more widespread and comprehensive screening of groups at high risk for syphilis. Because treatment of early syphilis is also highly effective, identifying untreated infected persons by means of the recommended screening strategy has great potential for both eliminating the consequences of later-stage infection and substantially reducing transmission from those with early infection.
Dr. Meredith E. Clement is with the division of infectious diseases at Duke University, Durham, N.C. Dr. Charles B. Hicks is with the department of medicine at the University of California, San Diego. Dr Hicks reported ties with Bristol-Myers Squibb, Gilead Sciences, Merck, Janssen Virology, ViiV Healthcare, AstraZeneca, and UpToDate. He served as associate editor and author for NEJM Journal Watch. Dr. Clement has received royalties from UpToDate. These comments were excerpted from the editorial accompanying the study (JAMA. 2016;315[21]:2281-3).
Because syphilis infection rates have increased over the last decade, health care providers should screen patients for the disease more frequently to detect and treat it earlier and more effectively, particular in high-risk subgroups.
The United States Preventive Services Task Force made this recommendation in a JAMA article published online, the first update to the syphilis screening recommendation since 2004 (JAMA. 2016;315[21]:2321-2327. doi: 10.1001/jama.2016.5824).
“Individuals with previous syphilis infection, an infected sexual partner, current HIV infection, or more than 4 sex partners in the preceding year are at increased risk of acquiring syphilis,” the report states. “Higher prevalence rates are associated with sociodemographic groups including men who have sex with men (MSM), young adult men, sex workers, adults in correctional facilities, and individuals who are black or live in metropolitan areas in the southern and western United States. Men who have sex with men accounted for 61% of all primary and secondary syphilis cases reported in 2014.”
A systematic review of trials and studies investigating syphilis screening effectiveness, testing accuracy, and screening risks in nonpregnant adults and adolescents – all of which were included in the Cochrane Central Register of Controlled Trials and Cochrane Database of Systematic Reviews through October 2015, along with the Ovid MEDLINE database from January 2004 through October 2015 – was undertaken to update the 2004 recommendations.
Studies with clinical application were emphasized more heavily, along with those that focused on target populations of asymptomatic, sexually active, adolescent and older men and women. In total, 2,000 English-language titles and abstracts were reviewed, from which 448 full-text studies underwent further review for inclusion. From these, only nine were ultimately selected for inclusion, four of which were observational studies, three of which were observational studies of test accuracy, and two of which were observational studies of testing sequences.
The first four studies – Bissessor et al. 2010, Cohen et al. 2005, Zou et al. 2013, and Bissessor et al. 2011 – were included to answer the investigation’s key question 1 (KQ1) – “What is the effectiveness of screening for syphilis in reducing complications of the disease and transmission or acquisition of other sexually transmitted infections in asymptomatic, nonpregnant, sexually active adults and adolescents? What is the effectiveness of specific screening intervals and screening among population subgroups?”
The remaining five studies – Wong et al. 2011, Tsang et al. 2007, Juárez-Figueroa et al. 2007, Mishra et al. 2011, and Binnicker et al. 2012 – were aimed at KQ3, asking “What is the accuracy of currently used screening tests and strategies (e.g., sequence of tests) for detecting syphilis infection?”
Regarding KQ1, all four studies found that MSM and HIV-infected men who were screened routinely every 3 months had a significantly higher rate of syphilis detection compared with those who were screened annually. The studies, all of which came from Europe and Australia, detected syphilis early in those who were screened every 3 months in 8.1% of HIV-infected MSM versus 3.1% of those who screened annually (P = .001), detected early-latent syphilis in 1.7% of routine screeners versus 0.4% of annual screeners (P = .008), and detected early syphilis in higher-risk MSM in 53% of regular screeners versus just 16% of annual screeners (P = .001). The cohort comprised 6,789 asymptomatic MSM.
In addition, newly acquired syphilis in HIV-positive MSM was found in 7.3 cases per 1,000 patient-years (95% CI, 5.2-9.9) for those who were regularly screened, versus 2.8 cases per 1,000 patient-years (95% CI, 1.8-4.0) for those who were screened annually.
Of the five studies investigating KQ3, three (Wong, Tsang, Juárez-Figueroa) were observational studies of treponemal and nontreponemal tests to detect syphilis. Results indicated that both tests had a sensitivity of 85.3%-98%, and specificity of 91%-100%. However, the remaining two studies (Mishra, Binnicker) used reverse screening algorithms to confirm positive test results from treponemal and nontreponemal, finding higher rates of false positives in the rapid plasma reagin than in the traditional enzyme analyses: 0.6% vs. 0.0% in one study (P = .03) and 0.26% vs. 0.13% in the other.
“Additional research on syphilis screening is needed to directly compare the effectiveness of different screening strategies for identifying individuals at increased risk of infection, co-testing for concurrent STIs, and different screening intervals among various patient populations,” wrote the USPSTF investigators, adding that research also is needed on evaluating the instruments used in risk assessment, as well as diagnostic accuracy.
Furthermore, while the data from these studies have shed light on syphilis testing and screening, several other important components of disease treatment and prevention – namely, “the effectiveness of screening in reducing syphilis complications and transmission, effectiveness of risk assessment methods, and harms related to screening” – were not adequately addressed.
This study was funded by the Agency for Healthcare Research and Quality, “under a contract to support the USPSTF.” The authors did not report any relevant financial disclosures.
Because syphilis infection rates have increased over the last decade, health care providers should screen patients for the disease more frequently to detect and treat it earlier and more effectively, particular in high-risk subgroups.
The United States Preventive Services Task Force made this recommendation in a JAMA article published online, the first update to the syphilis screening recommendation since 2004 (JAMA. 2016;315[21]:2321-2327. doi: 10.1001/jama.2016.5824).
“Individuals with previous syphilis infection, an infected sexual partner, current HIV infection, or more than 4 sex partners in the preceding year are at increased risk of acquiring syphilis,” the report states. “Higher prevalence rates are associated with sociodemographic groups including men who have sex with men (MSM), young adult men, sex workers, adults in correctional facilities, and individuals who are black or live in metropolitan areas in the southern and western United States. Men who have sex with men accounted for 61% of all primary and secondary syphilis cases reported in 2014.”
A systematic review of trials and studies investigating syphilis screening effectiveness, testing accuracy, and screening risks in nonpregnant adults and adolescents – all of which were included in the Cochrane Central Register of Controlled Trials and Cochrane Database of Systematic Reviews through October 2015, along with the Ovid MEDLINE database from January 2004 through October 2015 – was undertaken to update the 2004 recommendations.
Studies with clinical application were emphasized more heavily, along with those that focused on target populations of asymptomatic, sexually active, adolescent and older men and women. In total, 2,000 English-language titles and abstracts were reviewed, from which 448 full-text studies underwent further review for inclusion. From these, only nine were ultimately selected for inclusion, four of which were observational studies, three of which were observational studies of test accuracy, and two of which were observational studies of testing sequences.
The first four studies – Bissessor et al. 2010, Cohen et al. 2005, Zou et al. 2013, and Bissessor et al. 2011 – were included to answer the investigation’s key question 1 (KQ1) – “What is the effectiveness of screening for syphilis in reducing complications of the disease and transmission or acquisition of other sexually transmitted infections in asymptomatic, nonpregnant, sexually active adults and adolescents? What is the effectiveness of specific screening intervals and screening among population subgroups?”
The remaining five studies – Wong et al. 2011, Tsang et al. 2007, Juárez-Figueroa et al. 2007, Mishra et al. 2011, and Binnicker et al. 2012 – were aimed at KQ3, asking “What is the accuracy of currently used screening tests and strategies (e.g., sequence of tests) for detecting syphilis infection?”
Regarding KQ1, all four studies found that MSM and HIV-infected men who were screened routinely every 3 months had a significantly higher rate of syphilis detection compared with those who were screened annually. The studies, all of which came from Europe and Australia, detected syphilis early in those who were screened every 3 months in 8.1% of HIV-infected MSM versus 3.1% of those who screened annually (P = .001), detected early-latent syphilis in 1.7% of routine screeners versus 0.4% of annual screeners (P = .008), and detected early syphilis in higher-risk MSM in 53% of regular screeners versus just 16% of annual screeners (P = .001). The cohort comprised 6,789 asymptomatic MSM.
In addition, newly acquired syphilis in HIV-positive MSM was found in 7.3 cases per 1,000 patient-years (95% CI, 5.2-9.9) for those who were regularly screened, versus 2.8 cases per 1,000 patient-years (95% CI, 1.8-4.0) for those who were screened annually.
Of the five studies investigating KQ3, three (Wong, Tsang, Juárez-Figueroa) were observational studies of treponemal and nontreponemal tests to detect syphilis. Results indicated that both tests had a sensitivity of 85.3%-98%, and specificity of 91%-100%. However, the remaining two studies (Mishra, Binnicker) used reverse screening algorithms to confirm positive test results from treponemal and nontreponemal, finding higher rates of false positives in the rapid plasma reagin than in the traditional enzyme analyses: 0.6% vs. 0.0% in one study (P = .03) and 0.26% vs. 0.13% in the other.
“Additional research on syphilis screening is needed to directly compare the effectiveness of different screening strategies for identifying individuals at increased risk of infection, co-testing for concurrent STIs, and different screening intervals among various patient populations,” wrote the USPSTF investigators, adding that research also is needed on evaluating the instruments used in risk assessment, as well as diagnostic accuracy.
Furthermore, while the data from these studies have shed light on syphilis testing and screening, several other important components of disease treatment and prevention – namely, “the effectiveness of screening in reducing syphilis complications and transmission, effectiveness of risk assessment methods, and harms related to screening” – were not adequately addressed.
This study was funded by the Agency for Healthcare Research and Quality, “under a contract to support the USPSTF.” The authors did not report any relevant financial disclosures.
FROM JAMA
Key clinical point: Screening for syphilis every 3 months in high-risk individuals is associated with greater detection of the disease.
Major finding: Of 6,789 asymptomatic men who have sex with men, 53% of those tested every 3 months received a diagnosis of early syphilis, versus 16% of those tested annually.
Data source: Review of nine full-text articles in the Cochrane Central Register of Controlled Trials, the Cochrane Database of Systematic Reviews, and the Ovid MEDLINE database from January 2004 through October 2015.
Disclosures: The Agency for Healthcare Research and Quality funded the study. The authors did not report any relevant financial disclosures.
CDC Updates Guidelines for Zika Virus Testing, Interpretation of Results
Patients with suspected Zika virus infection who have negative real-time reverse transcription–polymerase chain reaction (rRT-PCR) test results are not automatically in the clear, officials at the Centers for Disease Control and Prevention warned in new guidelines on the interpretation of Zika virus antibody test results.
The CDC cautions that while a positive rRT-PCR test confirms a Zika virus infection, a negative test cannot exclude infection, because of Zika’s viremic similarity to other mosquito-borne flaviviruses such as dengue, West Nile, Japanese encephalitis, and yellow fever. In cases of a negative rRT-PCR results, patients should undergo immunoglobulin M (IgM) antibody testing; IgM testing should be done on any patient with a negative rRT-PCR test, regardless of the day on which the sample was originally collected. For confirmation of a positive, equivocal, or inconclusive result on the IgM test, patients will require a plaque reduction neutralization test (PRNT) as well.
“Recent evidence suggests that a 4-fold higher titer by PRNT might not discriminate between anti-Zika virus antibodies and crossreacting antibodies in all persons who have been previously infected with or vaccinated against a related flavivirus. Thus, a more conservative approach to interpreting PRNT results is now recommended to reduce the possibility of missing the diagnosis of either Zika or dengue virus infection,” CDC officials wrote. The report is in the May 31 issue of Morbidity and Mortality Weekly Report (doi: http://dx.doi.org/10.15585/mmwr.mm6521e1).
Any PRNT titer greater than 10 should be interpreted as proof of infection with the specific tested flavivirus, if the titer is less than 10 for other tested flaviviruses. If multiple flaviviruses are tested and all result in a titer of 10 or greater, than the result is proof of a recent infection with a flavivirus, not Zika specifically. And if the PRNT titer is less than 10 for a specific flavivirus, then that should be interpreted as there being no evidence of infection with that virus.
The CDC urges health care providers who have patients suspected of Zika virus infection to consult with their local and state health agencies to properly interpret any test results. Any pregnant women who have a confirmed Zika virus infection should be reported to the U.S. Zika Pregnancy Registry or the Puerto Rico Zika Active Pregnancy Surveillance System, with continued monitoring for any possible adverse effects to the pregnancy.
“If serologic testing indicates recent flavivirus infection that could be caused by either Zika or dengue virus, patients should be clinically managed for both infections because they might have been infected with either virus,” the CDC cautioned.
Patients with suspected Zika virus infection who have negative real-time reverse transcription–polymerase chain reaction (rRT-PCR) test results are not automatically in the clear, officials at the Centers for Disease Control and Prevention warned in new guidelines on the interpretation of Zika virus antibody test results.
The CDC cautions that while a positive rRT-PCR test confirms a Zika virus infection, a negative test cannot exclude infection, because of Zika’s viremic similarity to other mosquito-borne flaviviruses such as dengue, West Nile, Japanese encephalitis, and yellow fever. In cases of a negative rRT-PCR results, patients should undergo immunoglobulin M (IgM) antibody testing; IgM testing should be done on any patient with a negative rRT-PCR test, regardless of the day on which the sample was originally collected. For confirmation of a positive, equivocal, or inconclusive result on the IgM test, patients will require a plaque reduction neutralization test (PRNT) as well.
“Recent evidence suggests that a 4-fold higher titer by PRNT might not discriminate between anti-Zika virus antibodies and crossreacting antibodies in all persons who have been previously infected with or vaccinated against a related flavivirus. Thus, a more conservative approach to interpreting PRNT results is now recommended to reduce the possibility of missing the diagnosis of either Zika or dengue virus infection,” CDC officials wrote. The report is in the May 31 issue of Morbidity and Mortality Weekly Report (doi: http://dx.doi.org/10.15585/mmwr.mm6521e1).
Any PRNT titer greater than 10 should be interpreted as proof of infection with the specific tested flavivirus, if the titer is less than 10 for other tested flaviviruses. If multiple flaviviruses are tested and all result in a titer of 10 or greater, than the result is proof of a recent infection with a flavivirus, not Zika specifically. And if the PRNT titer is less than 10 for a specific flavivirus, then that should be interpreted as there being no evidence of infection with that virus.
The CDC urges health care providers who have patients suspected of Zika virus infection to consult with their local and state health agencies to properly interpret any test results. Any pregnant women who have a confirmed Zika virus infection should be reported to the U.S. Zika Pregnancy Registry or the Puerto Rico Zika Active Pregnancy Surveillance System, with continued monitoring for any possible adverse effects to the pregnancy.
“If serologic testing indicates recent flavivirus infection that could be caused by either Zika or dengue virus, patients should be clinically managed for both infections because they might have been infected with either virus,” the CDC cautioned.
Patients with suspected Zika virus infection who have negative real-time reverse transcription–polymerase chain reaction (rRT-PCR) test results are not automatically in the clear, officials at the Centers for Disease Control and Prevention warned in new guidelines on the interpretation of Zika virus antibody test results.
The CDC cautions that while a positive rRT-PCR test confirms a Zika virus infection, a negative test cannot exclude infection, because of Zika’s viremic similarity to other mosquito-borne flaviviruses such as dengue, West Nile, Japanese encephalitis, and yellow fever. In cases of a negative rRT-PCR results, patients should undergo immunoglobulin M (IgM) antibody testing; IgM testing should be done on any patient with a negative rRT-PCR test, regardless of the day on which the sample was originally collected. For confirmation of a positive, equivocal, or inconclusive result on the IgM test, patients will require a plaque reduction neutralization test (PRNT) as well.
“Recent evidence suggests that a 4-fold higher titer by PRNT might not discriminate between anti-Zika virus antibodies and crossreacting antibodies in all persons who have been previously infected with or vaccinated against a related flavivirus. Thus, a more conservative approach to interpreting PRNT results is now recommended to reduce the possibility of missing the diagnosis of either Zika or dengue virus infection,” CDC officials wrote. The report is in the May 31 issue of Morbidity and Mortality Weekly Report (doi: http://dx.doi.org/10.15585/mmwr.mm6521e1).
Any PRNT titer greater than 10 should be interpreted as proof of infection with the specific tested flavivirus, if the titer is less than 10 for other tested flaviviruses. If multiple flaviviruses are tested and all result in a titer of 10 or greater, than the result is proof of a recent infection with a flavivirus, not Zika specifically. And if the PRNT titer is less than 10 for a specific flavivirus, then that should be interpreted as there being no evidence of infection with that virus.
The CDC urges health care providers who have patients suspected of Zika virus infection to consult with their local and state health agencies to properly interpret any test results. Any pregnant women who have a confirmed Zika virus infection should be reported to the U.S. Zika Pregnancy Registry or the Puerto Rico Zika Active Pregnancy Surveillance System, with continued monitoring for any possible adverse effects to the pregnancy.
“If serologic testing indicates recent flavivirus infection that could be caused by either Zika or dengue virus, patients should be clinically managed for both infections because they might have been infected with either virus,” the CDC cautioned.
FROM MMWR
CDC updates guidelines for Zika virus testing, interpretation of results
Patients with suspected Zika virus infection who have negative real-time reverse transcription–polymerase chain reaction (rRT-PCR) test results are not automatically in the clear, officials at the Centers for Disease Control and Prevention warned in new guidelines on the interpretation of Zika virus antibody test results.
The CDC cautions that while a positive rRT-PCR test confirms a Zika virus infection, a negative test cannot exclude infection, because of Zika’s viremic similarity to other mosquito-borne flaviviruses such as dengue, West Nile, Japanese encephalitis, and yellow fever. In cases of a negative rRT-PCR results, patients should undergo immunoglobulin M (IgM) antibody testing; IgM testing should be done on any patient with a negative rRT-PCR test, regardless of the day on which the sample was originally collected. For confirmation of a positive, equivocal, or inconclusive result on the IgM test, patients will require a plaque reduction neutralization test (PRNT) as well.
“Recent evidence suggests that a 4-fold higher titer by PRNT might not discriminate between anti-Zika virus antibodies and crossreacting antibodies in all persons who have been previously infected with or vaccinated against a related flavivirus. Thus, a more conservative approach to interpreting PRNT results is now recommended to reduce the possibility of missing the diagnosis of either Zika or dengue virus infection,” CDC officials wrote. The report is in the May 31 issue of Morbidity and Mortality Weekly Report (doi: http://dx.doi.org/10.15585/mmwr.mm6521e1).
Any PRNT titer greater than 10 should be interpreted as proof of infection with the specific tested flavivirus, if the titer is less than 10 for other tested flaviviruses. If multiple flaviviruses are tested and all result in a titer of 10 or greater, than the result is proof of a recent infection with a flavivirus, not Zika specifically. And if the PRNT titer is less than 10 for a specific flavivirus, then that should be interpreted as there being no evidence of infection with that virus.
The CDC urges health care providers who have patients suspected of Zika virus infection to consult with their local and state health agencies to properly interpret any test results. Any pregnant women who have a confirmed Zika virus infection should be reported to the U.S. Zika Pregnancy Registry or the Puerto Rico Zika Active Pregnancy Surveillance System, with continued monitoring for any possible adverse effects to the pregnancy.
“If serologic testing indicates recent flavivirus infection that could be caused by either Zika or dengue virus, patients should be clinically managed for both infections because they might have been infected with either virus,” the CDC cautioned.
Patients with suspected Zika virus infection who have negative real-time reverse transcription–polymerase chain reaction (rRT-PCR) test results are not automatically in the clear, officials at the Centers for Disease Control and Prevention warned in new guidelines on the interpretation of Zika virus antibody test results.
The CDC cautions that while a positive rRT-PCR test confirms a Zika virus infection, a negative test cannot exclude infection, because of Zika’s viremic similarity to other mosquito-borne flaviviruses such as dengue, West Nile, Japanese encephalitis, and yellow fever. In cases of a negative rRT-PCR results, patients should undergo immunoglobulin M (IgM) antibody testing; IgM testing should be done on any patient with a negative rRT-PCR test, regardless of the day on which the sample was originally collected. For confirmation of a positive, equivocal, or inconclusive result on the IgM test, patients will require a plaque reduction neutralization test (PRNT) as well.
“Recent evidence suggests that a 4-fold higher titer by PRNT might not discriminate between anti-Zika virus antibodies and crossreacting antibodies in all persons who have been previously infected with or vaccinated against a related flavivirus. Thus, a more conservative approach to interpreting PRNT results is now recommended to reduce the possibility of missing the diagnosis of either Zika or dengue virus infection,” CDC officials wrote. The report is in the May 31 issue of Morbidity and Mortality Weekly Report (doi: http://dx.doi.org/10.15585/mmwr.mm6521e1).
Any PRNT titer greater than 10 should be interpreted as proof of infection with the specific tested flavivirus, if the titer is less than 10 for other tested flaviviruses. If multiple flaviviruses are tested and all result in a titer of 10 or greater, than the result is proof of a recent infection with a flavivirus, not Zika specifically. And if the PRNT titer is less than 10 for a specific flavivirus, then that should be interpreted as there being no evidence of infection with that virus.
The CDC urges health care providers who have patients suspected of Zika virus infection to consult with their local and state health agencies to properly interpret any test results. Any pregnant women who have a confirmed Zika virus infection should be reported to the U.S. Zika Pregnancy Registry or the Puerto Rico Zika Active Pregnancy Surveillance System, with continued monitoring for any possible adverse effects to the pregnancy.
“If serologic testing indicates recent flavivirus infection that could be caused by either Zika or dengue virus, patients should be clinically managed for both infections because they might have been infected with either virus,” the CDC cautioned.
Patients with suspected Zika virus infection who have negative real-time reverse transcription–polymerase chain reaction (rRT-PCR) test results are not automatically in the clear, officials at the Centers for Disease Control and Prevention warned in new guidelines on the interpretation of Zika virus antibody test results.
The CDC cautions that while a positive rRT-PCR test confirms a Zika virus infection, a negative test cannot exclude infection, because of Zika’s viremic similarity to other mosquito-borne flaviviruses such as dengue, West Nile, Japanese encephalitis, and yellow fever. In cases of a negative rRT-PCR results, patients should undergo immunoglobulin M (IgM) antibody testing; IgM testing should be done on any patient with a negative rRT-PCR test, regardless of the day on which the sample was originally collected. For confirmation of a positive, equivocal, or inconclusive result on the IgM test, patients will require a plaque reduction neutralization test (PRNT) as well.
“Recent evidence suggests that a 4-fold higher titer by PRNT might not discriminate between anti-Zika virus antibodies and crossreacting antibodies in all persons who have been previously infected with or vaccinated against a related flavivirus. Thus, a more conservative approach to interpreting PRNT results is now recommended to reduce the possibility of missing the diagnosis of either Zika or dengue virus infection,” CDC officials wrote. The report is in the May 31 issue of Morbidity and Mortality Weekly Report (doi: http://dx.doi.org/10.15585/mmwr.mm6521e1).
Any PRNT titer greater than 10 should be interpreted as proof of infection with the specific tested flavivirus, if the titer is less than 10 for other tested flaviviruses. If multiple flaviviruses are tested and all result in a titer of 10 or greater, than the result is proof of a recent infection with a flavivirus, not Zika specifically. And if the PRNT titer is less than 10 for a specific flavivirus, then that should be interpreted as there being no evidence of infection with that virus.
The CDC urges health care providers who have patients suspected of Zika virus infection to consult with their local and state health agencies to properly interpret any test results. Any pregnant women who have a confirmed Zika virus infection should be reported to the U.S. Zika Pregnancy Registry or the Puerto Rico Zika Active Pregnancy Surveillance System, with continued monitoring for any possible adverse effects to the pregnancy.
“If serologic testing indicates recent flavivirus infection that could be caused by either Zika or dengue virus, patients should be clinically managed for both infections because they might have been infected with either virus,” the CDC cautioned.
FROM MMWR
Methylphenidate Tied to Greater Risk for Arrhythmia in Children, Adolescents
Children and adolescents with attention-deficit/hyperactivity disorder who are prescribed methylphenidate to manage their conditions stand at a higher risk for arrhythmia and other, more serious, cardiac conditions.
In a study published in the BMJ, Ju-Young Shin, Ph.D., and colleagues examined records of 1,224 patients aged 17 years and younger from a nationwide South Korean health insurance database submitted between January 2007 and December 2011. All of the patients had experienced a cardiovascular event and at least one recorded prescription for methylphenidate to treat attention-deficit/hyperactivity disorder (ADHD) (BMJ 2016;353:i2550 doi:10.1136/bmj.i2550).
Of the 1,224 subjects, 864 (70.5%) had experienced arrhythmias, and the mean duration of exposure to methylphenidate was 0.5 years. During periods of methylphenidate treatment, subjects had an increased risk of arrhythmia, as Dr. Shin and coinvestigators calculated an adjusted incidence rate ratio of 1.61 (95% confidence interval, 1.48-1.74). This incidence rate ratio jumped up to 2.01 (95% CI, 1.74-2.31) during the first 3 days of methylphenidate treatment.
The risk was even higher for subjects with congenital heart disease; this subgroup had an adjusted incidence rate ratio of 3.49 (95% CI, 2.33-5.22), compared with 1.34 (95% CI, 1.23-1.46) in patients without it. Both the median age of first exposure to methylphenidate and occurrence of the first cardiac event were in patients aged 11-13 years, reported Dr. Shin of the Centre for Clinical Epidemiology at Jewish General Hospital and McGill University, both in Montreal, and colleagues in Australia and Korea.
“These results are consistent with the biological plausibility that the mechanism of action relates to the effect of methylphenidate on the heart rate,” the authors concluded. “Delayed effects would be expected with myocardial infarction, while more immediate effects would be expected with arrhythmias, as we observed.”
Dr. Shin and colleagues cited several limitations. For example, coding mistakes and incomplete records could not be ruled out in their study. In addition, they said, the “outcome measures were limited to patients with diagnoses of cardiovascular adverse events, and we could have missed outcomes not diagnosed.”
Nevertheless, they said, in light of the increased use of methylphenidate to treat ADHD across the globe, the benefits of using the drug “should be carefully weighed against potential cardiovascular risks of these drugs in children and adolescents.”
Two of the authors disclosed receiving support via fellowships from Australia’s National Health and Medical Research Council.
Children and adolescents with attention-deficit/hyperactivity disorder who are prescribed methylphenidate to manage their conditions stand at a higher risk for arrhythmia and other, more serious, cardiac conditions.
In a study published in the BMJ, Ju-Young Shin, Ph.D., and colleagues examined records of 1,224 patients aged 17 years and younger from a nationwide South Korean health insurance database submitted between January 2007 and December 2011. All of the patients had experienced a cardiovascular event and at least one recorded prescription for methylphenidate to treat attention-deficit/hyperactivity disorder (ADHD) (BMJ 2016;353:i2550 doi:10.1136/bmj.i2550).
Of the 1,224 subjects, 864 (70.5%) had experienced arrhythmias, and the mean duration of exposure to methylphenidate was 0.5 years. During periods of methylphenidate treatment, subjects had an increased risk of arrhythmia, as Dr. Shin and coinvestigators calculated an adjusted incidence rate ratio of 1.61 (95% confidence interval, 1.48-1.74). This incidence rate ratio jumped up to 2.01 (95% CI, 1.74-2.31) during the first 3 days of methylphenidate treatment.
The risk was even higher for subjects with congenital heart disease; this subgroup had an adjusted incidence rate ratio of 3.49 (95% CI, 2.33-5.22), compared with 1.34 (95% CI, 1.23-1.46) in patients without it. Both the median age of first exposure to methylphenidate and occurrence of the first cardiac event were in patients aged 11-13 years, reported Dr. Shin of the Centre for Clinical Epidemiology at Jewish General Hospital and McGill University, both in Montreal, and colleagues in Australia and Korea.
“These results are consistent with the biological plausibility that the mechanism of action relates to the effect of methylphenidate on the heart rate,” the authors concluded. “Delayed effects would be expected with myocardial infarction, while more immediate effects would be expected with arrhythmias, as we observed.”
Dr. Shin and colleagues cited several limitations. For example, coding mistakes and incomplete records could not be ruled out in their study. In addition, they said, the “outcome measures were limited to patients with diagnoses of cardiovascular adverse events, and we could have missed outcomes not diagnosed.”
Nevertheless, they said, in light of the increased use of methylphenidate to treat ADHD across the globe, the benefits of using the drug “should be carefully weighed against potential cardiovascular risks of these drugs in children and adolescents.”
Two of the authors disclosed receiving support via fellowships from Australia’s National Health and Medical Research Council.
Children and adolescents with attention-deficit/hyperactivity disorder who are prescribed methylphenidate to manage their conditions stand at a higher risk for arrhythmia and other, more serious, cardiac conditions.
In a study published in the BMJ, Ju-Young Shin, Ph.D., and colleagues examined records of 1,224 patients aged 17 years and younger from a nationwide South Korean health insurance database submitted between January 2007 and December 2011. All of the patients had experienced a cardiovascular event and at least one recorded prescription for methylphenidate to treat attention-deficit/hyperactivity disorder (ADHD) (BMJ 2016;353:i2550 doi:10.1136/bmj.i2550).
Of the 1,224 subjects, 864 (70.5%) had experienced arrhythmias, and the mean duration of exposure to methylphenidate was 0.5 years. During periods of methylphenidate treatment, subjects had an increased risk of arrhythmia, as Dr. Shin and coinvestigators calculated an adjusted incidence rate ratio of 1.61 (95% confidence interval, 1.48-1.74). This incidence rate ratio jumped up to 2.01 (95% CI, 1.74-2.31) during the first 3 days of methylphenidate treatment.
The risk was even higher for subjects with congenital heart disease; this subgroup had an adjusted incidence rate ratio of 3.49 (95% CI, 2.33-5.22), compared with 1.34 (95% CI, 1.23-1.46) in patients without it. Both the median age of first exposure to methylphenidate and occurrence of the first cardiac event were in patients aged 11-13 years, reported Dr. Shin of the Centre for Clinical Epidemiology at Jewish General Hospital and McGill University, both in Montreal, and colleagues in Australia and Korea.
“These results are consistent with the biological plausibility that the mechanism of action relates to the effect of methylphenidate on the heart rate,” the authors concluded. “Delayed effects would be expected with myocardial infarction, while more immediate effects would be expected with arrhythmias, as we observed.”
Dr. Shin and colleagues cited several limitations. For example, coding mistakes and incomplete records could not be ruled out in their study. In addition, they said, the “outcome measures were limited to patients with diagnoses of cardiovascular adverse events, and we could have missed outcomes not diagnosed.”
Nevertheless, they said, in light of the increased use of methylphenidate to treat ADHD across the globe, the benefits of using the drug “should be carefully weighed against potential cardiovascular risks of these drugs in children and adolescents.”
Two of the authors disclosed receiving support via fellowships from Australia’s National Health and Medical Research Council.
FROM THE BMJ
Methylphenidate tied to greater risk of arrhythmia in children, adolescents
Children and adolescents with attention-deficit/hyperactivity disorder who are prescribed methylphenidate to manage their conditions stand at a higher risk for arrhythmia and other, more serious, cardiac conditions.
In a study published in the BMJ, Ju-Young Shin, Ph.D., and colleagues examined records of 1,224 patients aged 17 years and younger from a nationwide South Korean health insurance database submitted between January 2007 and December 2011. All of the patients had experienced a cardiovascular event and at least one recorded prescription for methylphenidate to treat attention-deficit/hyperactivity disorder (ADHD) (BMJ 2016;353:i2550 doi:10.1136/bmj.i2550).
Of the 1,224 subjects, 864 (70.5%) had experienced arrhythmias, and the mean duration of exposure to methylphenidate was 0.5 years. During periods of methylphenidate treatment, subjects had an increased risk of arrhythmia, as Dr. Shin and coinvestigators calculated an adjusted incidence rate ratio of 1.61 (95% confidence interval, 1.48-1.74). This incidence rate ratio jumped up to 2.01 (95% CI, 1.74-2.31) during the first 3 days of methylphenidate treatment.
The risk was even higher for subjects with congenital heart disease; this subgroup had an adjusted incidence rate ratio of 3.49 (95% CI, 2.33-5.22), compared with 1.34 (95% CI, 1.23-1.46) in patients without it. Both the median age of first exposure to methylphenidate and occurrence of the first cardiac event were in patients aged 11-13 years, reported Dr. Shin of the Centre for Clinical Epidemiology at Jewish General Hospital and McGill University, both in Montreal, and colleagues in Australia and Korea.
“These results are consistent with the biological plausibility that the mechanism of action relates to the effect of methylphenidate on the heart rate,” the authors concluded. “Delayed effects would be expected with myocardial infarction, while more immediate effects would be expected with arrhythmias, as we observed.”
Dr. Shin and colleagues cited several limitations. For example, coding mistakes and incomplete records could not be ruled out in their study. In addition, they said, the “outcome measures were limited to patients with diagnoses of cardiovascular adverse events, and we could have missed outcomes not diagnosed.”
Nevertheless, they said, in light of the increased use of methylphenidate to treat ADHD across the globe, the benefits of using the drug “should be carefully weighed against potential cardiovascular risks of these drugs in children and adolescents.”
Two of the authors disclosed receiving support via fellowships from Australia’s National Health and Medical Research Council.
Children and adolescents with attention-deficit/hyperactivity disorder who are prescribed methylphenidate to manage their conditions stand at a higher risk for arrhythmia and other, more serious, cardiac conditions.
In a study published in the BMJ, Ju-Young Shin, Ph.D., and colleagues examined records of 1,224 patients aged 17 years and younger from a nationwide South Korean health insurance database submitted between January 2007 and December 2011. All of the patients had experienced a cardiovascular event and at least one recorded prescription for methylphenidate to treat attention-deficit/hyperactivity disorder (ADHD) (BMJ 2016;353:i2550 doi:10.1136/bmj.i2550).
Of the 1,224 subjects, 864 (70.5%) had experienced arrhythmias, and the mean duration of exposure to methylphenidate was 0.5 years. During periods of methylphenidate treatment, subjects had an increased risk of arrhythmia, as Dr. Shin and coinvestigators calculated an adjusted incidence rate ratio of 1.61 (95% confidence interval, 1.48-1.74). This incidence rate ratio jumped up to 2.01 (95% CI, 1.74-2.31) during the first 3 days of methylphenidate treatment.
The risk was even higher for subjects with congenital heart disease; this subgroup had an adjusted incidence rate ratio of 3.49 (95% CI, 2.33-5.22), compared with 1.34 (95% CI, 1.23-1.46) in patients without it. Both the median age of first exposure to methylphenidate and occurrence of the first cardiac event were in patients aged 11-13 years, reported Dr. Shin of the Centre for Clinical Epidemiology at Jewish General Hospital and McGill University, both in Montreal, and colleagues in Australia and Korea.
“These results are consistent with the biological plausibility that the mechanism of action relates to the effect of methylphenidate on the heart rate,” the authors concluded. “Delayed effects would be expected with myocardial infarction, while more immediate effects would be expected with arrhythmias, as we observed.”
Dr. Shin and colleagues cited several limitations. For example, coding mistakes and incomplete records could not be ruled out in their study. In addition, they said, the “outcome measures were limited to patients with diagnoses of cardiovascular adverse events, and we could have missed outcomes not diagnosed.”
Nevertheless, they said, in light of the increased use of methylphenidate to treat ADHD across the globe, the benefits of using the drug “should be carefully weighed against potential cardiovascular risks of these drugs in children and adolescents.”
Two of the authors disclosed receiving support via fellowships from Australia’s National Health and Medical Research Council.
Children and adolescents with attention-deficit/hyperactivity disorder who are prescribed methylphenidate to manage their conditions stand at a higher risk for arrhythmia and other, more serious, cardiac conditions.
In a study published in the BMJ, Ju-Young Shin, Ph.D., and colleagues examined records of 1,224 patients aged 17 years and younger from a nationwide South Korean health insurance database submitted between January 2007 and December 2011. All of the patients had experienced a cardiovascular event and at least one recorded prescription for methylphenidate to treat attention-deficit/hyperactivity disorder (ADHD) (BMJ 2016;353:i2550 doi:10.1136/bmj.i2550).
Of the 1,224 subjects, 864 (70.5%) had experienced arrhythmias, and the mean duration of exposure to methylphenidate was 0.5 years. During periods of methylphenidate treatment, subjects had an increased risk of arrhythmia, as Dr. Shin and coinvestigators calculated an adjusted incidence rate ratio of 1.61 (95% confidence interval, 1.48-1.74). This incidence rate ratio jumped up to 2.01 (95% CI, 1.74-2.31) during the first 3 days of methylphenidate treatment.
The risk was even higher for subjects with congenital heart disease; this subgroup had an adjusted incidence rate ratio of 3.49 (95% CI, 2.33-5.22), compared with 1.34 (95% CI, 1.23-1.46) in patients without it. Both the median age of first exposure to methylphenidate and occurrence of the first cardiac event were in patients aged 11-13 years, reported Dr. Shin of the Centre for Clinical Epidemiology at Jewish General Hospital and McGill University, both in Montreal, and colleagues in Australia and Korea.
“These results are consistent with the biological plausibility that the mechanism of action relates to the effect of methylphenidate on the heart rate,” the authors concluded. “Delayed effects would be expected with myocardial infarction, while more immediate effects would be expected with arrhythmias, as we observed.”
Dr. Shin and colleagues cited several limitations. For example, coding mistakes and incomplete records could not be ruled out in their study. In addition, they said, the “outcome measures were limited to patients with diagnoses of cardiovascular adverse events, and we could have missed outcomes not diagnosed.”
Nevertheless, they said, in light of the increased use of methylphenidate to treat ADHD across the globe, the benefits of using the drug “should be carefully weighed against potential cardiovascular risks of these drugs in children and adolescents.”
Two of the authors disclosed receiving support via fellowships from Australia’s National Health and Medical Research Council.
FROM THE BMJ
Key clinical point: Use of methylphenidate to treat children with attention-deficit/hyperactivity disorder (ADHD) can lead to higher risk for arrhythmia, especially in the first 3 days of use.
Major finding: The risk of arrhythmia increased during periods of treatment with methylphenidate when compared with other treatment periods (incidence rate ratio, 1.61), and reached 2.01 during the first 1-3 days of methylphenidate treatment.
Data source: A retrospective case series analysis of 1,224 patients at or younger than 17 years of age, who had at least one recorded cardiovascular event and one prescription for methylphenidate.
Disclosures: Two coauthors disclosed receiving support via fellowships from Australia’s National Health and Medical Research Council.
VIDEO: Post legalization, what effect is recreational marijuana use having on children?
BALTIMORE – Experts from Colorado and Washington – two states which have legalized recreational use of the drug – came together at the annual meeting of the Pediatric Academic Societies to discuss the challenges of treating and preventing short-term and long-term illness brought on by marijuana use.
“In Colorado, a lot of [mothers] use [marijuana] for depression, anxiety, as well as for nausea, and they’re not disclosing that” to their primary care doctors, explained Dr. Maya Bunik of the University of Colorado in Aurora. “Then they’re sort of surprised at birth when we tell them that we don’t know what [marijuana] does in terms of affecting [their] baby.”
In a series of interviews, presenters at the roundtable discussed the importance of talking to parents – particularly pregnant mothers – about the dangers of marijuana use around kids, keeping marijuana and related products away from children, what’s being done on the legislative side to keep marijuana away from children and adolescents, and the long-term ramifications of marijuana use by children and their parents.
Joining Dr. Bunik for this discussion are Dr. George Sam Wang, Ayelet Talmi, Ph.D., Dr. Karen M. Wilson, Dr. Kathryn M. Wells, and Dr. Erica M. Wymore of the University of Colorado at Aurora, and Dr. Leslie R. Walker of the University of Washington in Seattle.
Dr. Wang disclosed receiving a grant from the Colorado Department of Public Health and Environments, and royalties from author contributions. The other presenters had no relevant financial disclosures.
BALTIMORE – Experts from Colorado and Washington – two states which have legalized recreational use of the drug – came together at the annual meeting of the Pediatric Academic Societies to discuss the challenges of treating and preventing short-term and long-term illness brought on by marijuana use.
“In Colorado, a lot of [mothers] use [marijuana] for depression, anxiety, as well as for nausea, and they’re not disclosing that” to their primary care doctors, explained Dr. Maya Bunik of the University of Colorado in Aurora. “Then they’re sort of surprised at birth when we tell them that we don’t know what [marijuana] does in terms of affecting [their] baby.”
In a series of interviews, presenters at the roundtable discussed the importance of talking to parents – particularly pregnant mothers – about the dangers of marijuana use around kids, keeping marijuana and related products away from children, what’s being done on the legislative side to keep marijuana away from children and adolescents, and the long-term ramifications of marijuana use by children and their parents.
Joining Dr. Bunik for this discussion are Dr. George Sam Wang, Ayelet Talmi, Ph.D., Dr. Karen M. Wilson, Dr. Kathryn M. Wells, and Dr. Erica M. Wymore of the University of Colorado at Aurora, and Dr. Leslie R. Walker of the University of Washington in Seattle.
Dr. Wang disclosed receiving a grant from the Colorado Department of Public Health and Environments, and royalties from author contributions. The other presenters had no relevant financial disclosures.
BALTIMORE – Experts from Colorado and Washington – two states which have legalized recreational use of the drug – came together at the annual meeting of the Pediatric Academic Societies to discuss the challenges of treating and preventing short-term and long-term illness brought on by marijuana use.
“In Colorado, a lot of [mothers] use [marijuana] for depression, anxiety, as well as for nausea, and they’re not disclosing that” to their primary care doctors, explained Dr. Maya Bunik of the University of Colorado in Aurora. “Then they’re sort of surprised at birth when we tell them that we don’t know what [marijuana] does in terms of affecting [their] baby.”
In a series of interviews, presenters at the roundtable discussed the importance of talking to parents – particularly pregnant mothers – about the dangers of marijuana use around kids, keeping marijuana and related products away from children, what’s being done on the legislative side to keep marijuana away from children and adolescents, and the long-term ramifications of marijuana use by children and their parents.
Joining Dr. Bunik for this discussion are Dr. George Sam Wang, Ayelet Talmi, Ph.D., Dr. Karen M. Wilson, Dr. Kathryn M. Wells, and Dr. Erica M. Wymore of the University of Colorado at Aurora, and Dr. Leslie R. Walker of the University of Washington in Seattle.
Dr. Wang disclosed receiving a grant from the Colorado Department of Public Health and Environments, and royalties from author contributions. The other presenters had no relevant financial disclosures.
AT THE PAS ANNUAL MEETING
VIDEO: Children exposed to marijuana at risk for long-term neurocognitive issues
BALTIMORE – The legalization of recreational marijuana in certain states has brought with it a host of new challenges to health care professionals, particularly ob.gyns. and pediatricians, who may be faced with parents who use the drug but are unaware – or unwilling to recognize – the dangers of marijuana exposure to their children.
“A longitudinal, very good study that [showed] regular use [of marijuana] by adolescents [is] associated with about a 6-8 point reduction in adult IQ, and persistent neurocognitive deficits [that] may not even be fully reversible,” said Dr. Paula D. Riggs of the University of Colorado in Aurora.
In an interview at the annual meeting of the Pediatric Academic Societies, Dr. Riggs discussed this and other key studies that point to the dangers of marijuana exposure to children, both before and after birth, and how important it is that all health care professionals ask parents the right questions to ensure that children aren’t being put in danger of long-term cognitive repercussions of marijuana use.
Dr. Riggs did not report any relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BALTIMORE – The legalization of recreational marijuana in certain states has brought with it a host of new challenges to health care professionals, particularly ob.gyns. and pediatricians, who may be faced with parents who use the drug but are unaware – or unwilling to recognize – the dangers of marijuana exposure to their children.
“A longitudinal, very good study that [showed] regular use [of marijuana] by adolescents [is] associated with about a 6-8 point reduction in adult IQ, and persistent neurocognitive deficits [that] may not even be fully reversible,” said Dr. Paula D. Riggs of the University of Colorado in Aurora.
In an interview at the annual meeting of the Pediatric Academic Societies, Dr. Riggs discussed this and other key studies that point to the dangers of marijuana exposure to children, both before and after birth, and how important it is that all health care professionals ask parents the right questions to ensure that children aren’t being put in danger of long-term cognitive repercussions of marijuana use.
Dr. Riggs did not report any relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BALTIMORE – The legalization of recreational marijuana in certain states has brought with it a host of new challenges to health care professionals, particularly ob.gyns. and pediatricians, who may be faced with parents who use the drug but are unaware – or unwilling to recognize – the dangers of marijuana exposure to their children.
“A longitudinal, very good study that [showed] regular use [of marijuana] by adolescents [is] associated with about a 6-8 point reduction in adult IQ, and persistent neurocognitive deficits [that] may not even be fully reversible,” said Dr. Paula D. Riggs of the University of Colorado in Aurora.
In an interview at the annual meeting of the Pediatric Academic Societies, Dr. Riggs discussed this and other key studies that point to the dangers of marijuana exposure to children, both before and after birth, and how important it is that all health care professionals ask parents the right questions to ensure that children aren’t being put in danger of long-term cognitive repercussions of marijuana use.
Dr. Riggs did not report any relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE PAS ANNUAL MEETING
Operating with pain: Surgeon workplace injury underrecognized
BOSTON – For many surgeons, hours in the OR can translate into serious or chronic neck, back, and hand pain.
Studies of occupational injury related to performing surgery took off in the 1990s when laparoscopic surgery became widespread and put new physical demands on surgeons (Surg Endosc 1999:13:466-468; Arch Surg 1999;134:1011-1016). Findings from a study presented at the Society for Surgical Oncology suggest that the problem remains widespread.
Dr. Rachael K. Voss, a research resident at the University of Texas MD Anderson Cancer Center, Houston, and her colleagues conducted a survey among oncologic surgeons at the Center to explore the extent, sources and risk factors of workplace injuries.
“[Workplace injury] is a serious issue for surgeons, but it is something we don’t talk about and there is very little training and information as we are going through training. But these occupational hazards are something we need to acknowledge. We need to do more work in the future with ergonomics experts and occupational hygiene experts that can help us improve our posture and positions in the OR so we can prevent these injuries,” Dr. Voss said.
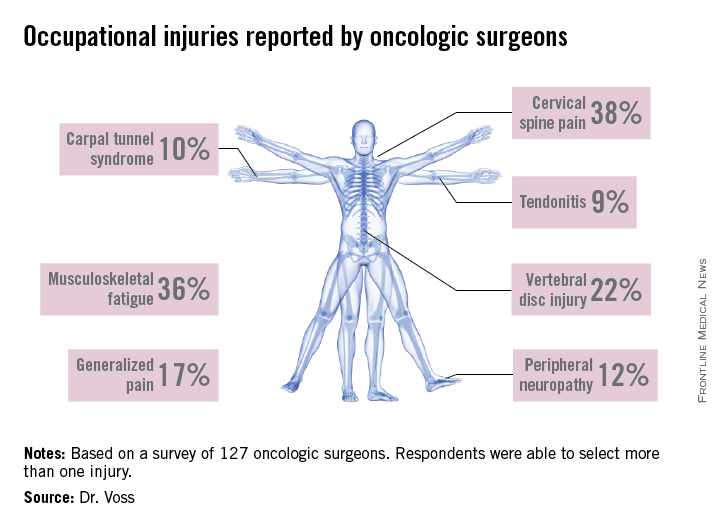
A high response rate of 58% yielded a total of 127 completed surveys. Most of the respondents were aged 35-64 and three-quarters spent 10 hours or more per week working in the OR. Among those responding, 92.3% experienced at least one occupation-related symptom over the past 6 weeks, and 27.6% reported sustaining an injury or chronic condition which they attributed to operating. The majority of injuries reported were cervical spine injury, musculoskeletal fatigue and vertebral disc injury. Other conditions mentioned were brachial plexus damage, carpal tunnel syndrome, peripheral neuropathy, and tendonitis.
A multivariate analysis identified some independent risk factors for injury: male gender, average case duration of 4 hours or longer, neck pain, and frequent use of a step for height adjustment. Age and years in practice were not associated with injury risk.
The good news is that, in this sample, 72% of the respondents reported seeking treatment for their injury. Physical therapy and medication were the most commonly utilized treatments, with about 20% resorting to surgery.
Plenty of evidence
The MD Anderson findings confirmed what other studies in this area have reported. William T. Davis and his colleagues surveyed Fellows of the Tennessee chapter of the American College of Surgeons on the issue of occupational musculoskeletal injury (J Surg Res 2014;184:207-212). Of the 793 surveys sent, 33% were completed. General surgeons accounted for 64% of respondents and 80% were male. Forty percent of respondents had sustained at least one injury related to operating. Most reported spine, hand, and neck injuries, but hip, knee, and shoulder pain was also mentioned. The majority of respondents reported the cause of their injury as chronic and 51% sought medical treatment. As with the MD Anderson study, no association was found between age or years in practice and workplace injury.
Mr. Davis and his colleagues conducted a similar study of orthopaedic surgeons and found similar rates of occupational injury (44%) among their 140 survey respondents (J Bone Joint Surg Am. 2013;95:e107). This study found that responding orthopaedic surgeons had more hand and lower back injuries, and correlation was found between years in practice and prevalence of injury.
A limitation of all of these studies is that the injury data are self-reported, and there is a potential selection bias. It is likely that the true extent of workplace injury among surgeons, and the costs and impact on surgeons’ life quality and productivity, are still largely unknown.
“There have been a few studies on this, but I think we’re just scratching the surface,” explained Dr. Adrian Park, chair of surgery at the Anne Arundel Medical Center in Annapolis, Md. Dr. Park was the lead author of a 2010 study that identified chronic pain among surgeons as a serious and underreported issue within medicine (J Am Coll Surg 2010;210;306-313).
The study, which evaluated 317 surgeons using a 23-question survey, found that 86.9% of surgeons experience “physical symptoms or discomfort,” with the most significant indicator of such symptoms being a high case load. Subsequent studies from Europe and eastern Asia also found rates of 80% or higher among surgeons in those regions.
Injuries downplayed
With so pervasive a problem, however, the relative paucity of data and conversation among medical professionals is something Dr. Park finds alarming. “As a surgeon leader, I can tell you surgeons complain about a lot of stuff, but one of the things they tend not to complain about is themselves and their own health and well-being,” said Dr. Park.
Dr. Mario Cerame is well aware of what a seemingly innocuous, relatively small chronic pain can do to a surgeon. A general surgeon practicing in North Carolina, Dr. Cerame began to experience symptoms of repetitive motion injury about 2 years ago, symptoms which he says “crept up on me.”
It began as numbness at the tips of his fingers, affecting the way he held laparoscopic tools during surgery and other, more menial, daily tasks. Initially suspecting it was carpal tunnel syndrome, Dr. Cerame brushed it off, until the numbness spread to three whole fingers and, eventually, his entire hand. His physician explained what was happening, instructing him that if he didn’t undergo orthopaedic surgery immediately, he ran the risk of paralysis.
“I got the diagnosis on Thursday, and had the operation on Tuesday,” said Dr. Cerame, explaining that the diagnosis was spinal stenosis. Two areas of his spinal column were pinching inward, causing the slow but steady paralysis he was experiencing. With physical therapy, Dr. Cerame could have returning function within 2 years of the operation.
“I’ve published an awful lot of papers, but the thing that struck me about [the 2010] paper is the response I got,” said Dr. Park. “Surgeons, literally from around the country, would call me saying ‘I used to be able to do this operation, I no longer can do that,’ or ‘this used to be what my case list looked like, I can no longer do this, you can use me as an example.’ People came forward.”
Risks of ignoring, self-medicating
Then there is the dark side of coping with chronic pain: risk of substance abuse. A study published in the Journal of Addiction Medicine (2013;7;349-353) on misuse of prescription medication among physicians found that surgeons were among the specialists at highest risk for substance abuse. According to this study, the beginning of addiction for many doctors is a prescription or self-medication for chronic pain. For surgeons, chronic pain from occupational injuries could lead to dependence on pain medication.
“When livelihoods are at stake, I think folks will take opportunities to stay in the game,” admitted Dr. Park.
The bottom line, according to both Dr. Park and Dr. Cerame, is for surgeons not to keep quiet about these issues if they ever do experience them. Asking for help and getting things checked right away is better, not only for a surgeon, but for family and patients, too. While Dr. Cerame has gone back to work, he is unable to handle the caseload he once had and isn’t sure if he’ll ever be able to.
“Surgeons and physicians in general have a tendency to get so consumed with other people’s health that they don’t focus on their own health issues,” said Dr. Cerame. “It took me almost 8 months from the time I had symptoms to actually get it checked out [because] I thought it would go away, [so] if you find something that you feel isn’t normal, take care of it.”
Dr. Voss, Dr. Park, and Dr. Cerame had no relevant financial disclosures.
Neil Osterweil contributed to this article.
BOSTON – For many surgeons, hours in the OR can translate into serious or chronic neck, back, and hand pain.
Studies of occupational injury related to performing surgery took off in the 1990s when laparoscopic surgery became widespread and put new physical demands on surgeons (Surg Endosc 1999:13:466-468; Arch Surg 1999;134:1011-1016). Findings from a study presented at the Society for Surgical Oncology suggest that the problem remains widespread.
Dr. Rachael K. Voss, a research resident at the University of Texas MD Anderson Cancer Center, Houston, and her colleagues conducted a survey among oncologic surgeons at the Center to explore the extent, sources and risk factors of workplace injuries.
“[Workplace injury] is a serious issue for surgeons, but it is something we don’t talk about and there is very little training and information as we are going through training. But these occupational hazards are something we need to acknowledge. We need to do more work in the future with ergonomics experts and occupational hygiene experts that can help us improve our posture and positions in the OR so we can prevent these injuries,” Dr. Voss said.
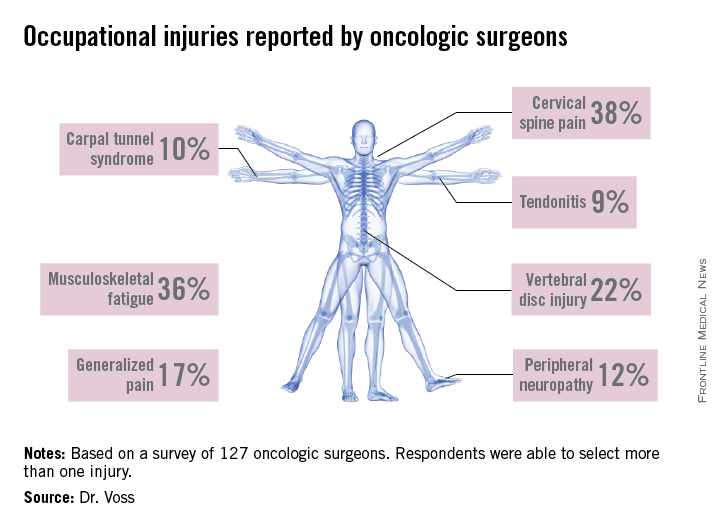
A high response rate of 58% yielded a total of 127 completed surveys. Most of the respondents were aged 35-64 and three-quarters spent 10 hours or more per week working in the OR. Among those responding, 92.3% experienced at least one occupation-related symptom over the past 6 weeks, and 27.6% reported sustaining an injury or chronic condition which they attributed to operating. The majority of injuries reported were cervical spine injury, musculoskeletal fatigue and vertebral disc injury. Other conditions mentioned were brachial plexus damage, carpal tunnel syndrome, peripheral neuropathy, and tendonitis.
A multivariate analysis identified some independent risk factors for injury: male gender, average case duration of 4 hours or longer, neck pain, and frequent use of a step for height adjustment. Age and years in practice were not associated with injury risk.
The good news is that, in this sample, 72% of the respondents reported seeking treatment for their injury. Physical therapy and medication were the most commonly utilized treatments, with about 20% resorting to surgery.
Plenty of evidence
The MD Anderson findings confirmed what other studies in this area have reported. William T. Davis and his colleagues surveyed Fellows of the Tennessee chapter of the American College of Surgeons on the issue of occupational musculoskeletal injury (J Surg Res 2014;184:207-212). Of the 793 surveys sent, 33% were completed. General surgeons accounted for 64% of respondents and 80% were male. Forty percent of respondents had sustained at least one injury related to operating. Most reported spine, hand, and neck injuries, but hip, knee, and shoulder pain was also mentioned. The majority of respondents reported the cause of their injury as chronic and 51% sought medical treatment. As with the MD Anderson study, no association was found between age or years in practice and workplace injury.
Mr. Davis and his colleagues conducted a similar study of orthopaedic surgeons and found similar rates of occupational injury (44%) among their 140 survey respondents (J Bone Joint Surg Am. 2013;95:e107). This study found that responding orthopaedic surgeons had more hand and lower back injuries, and correlation was found between years in practice and prevalence of injury.
A limitation of all of these studies is that the injury data are self-reported, and there is a potential selection bias. It is likely that the true extent of workplace injury among surgeons, and the costs and impact on surgeons’ life quality and productivity, are still largely unknown.
“There have been a few studies on this, but I think we’re just scratching the surface,” explained Dr. Adrian Park, chair of surgery at the Anne Arundel Medical Center in Annapolis, Md. Dr. Park was the lead author of a 2010 study that identified chronic pain among surgeons as a serious and underreported issue within medicine (J Am Coll Surg 2010;210;306-313).
The study, which evaluated 317 surgeons using a 23-question survey, found that 86.9% of surgeons experience “physical symptoms or discomfort,” with the most significant indicator of such symptoms being a high case load. Subsequent studies from Europe and eastern Asia also found rates of 80% or higher among surgeons in those regions.
Injuries downplayed
With so pervasive a problem, however, the relative paucity of data and conversation among medical professionals is something Dr. Park finds alarming. “As a surgeon leader, I can tell you surgeons complain about a lot of stuff, but one of the things they tend not to complain about is themselves and their own health and well-being,” said Dr. Park.
Dr. Mario Cerame is well aware of what a seemingly innocuous, relatively small chronic pain can do to a surgeon. A general surgeon practicing in North Carolina, Dr. Cerame began to experience symptoms of repetitive motion injury about 2 years ago, symptoms which he says “crept up on me.”
It began as numbness at the tips of his fingers, affecting the way he held laparoscopic tools during surgery and other, more menial, daily tasks. Initially suspecting it was carpal tunnel syndrome, Dr. Cerame brushed it off, until the numbness spread to three whole fingers and, eventually, his entire hand. His physician explained what was happening, instructing him that if he didn’t undergo orthopaedic surgery immediately, he ran the risk of paralysis.
“I got the diagnosis on Thursday, and had the operation on Tuesday,” said Dr. Cerame, explaining that the diagnosis was spinal stenosis. Two areas of his spinal column were pinching inward, causing the slow but steady paralysis he was experiencing. With physical therapy, Dr. Cerame could have returning function within 2 years of the operation.
“I’ve published an awful lot of papers, but the thing that struck me about [the 2010] paper is the response I got,” said Dr. Park. “Surgeons, literally from around the country, would call me saying ‘I used to be able to do this operation, I no longer can do that,’ or ‘this used to be what my case list looked like, I can no longer do this, you can use me as an example.’ People came forward.”
Risks of ignoring, self-medicating
Then there is the dark side of coping with chronic pain: risk of substance abuse. A study published in the Journal of Addiction Medicine (2013;7;349-353) on misuse of prescription medication among physicians found that surgeons were among the specialists at highest risk for substance abuse. According to this study, the beginning of addiction for many doctors is a prescription or self-medication for chronic pain. For surgeons, chronic pain from occupational injuries could lead to dependence on pain medication.
“When livelihoods are at stake, I think folks will take opportunities to stay in the game,” admitted Dr. Park.
The bottom line, according to both Dr. Park and Dr. Cerame, is for surgeons not to keep quiet about these issues if they ever do experience them. Asking for help and getting things checked right away is better, not only for a surgeon, but for family and patients, too. While Dr. Cerame has gone back to work, he is unable to handle the caseload he once had and isn’t sure if he’ll ever be able to.
“Surgeons and physicians in general have a tendency to get so consumed with other people’s health that they don’t focus on their own health issues,” said Dr. Cerame. “It took me almost 8 months from the time I had symptoms to actually get it checked out [because] I thought it would go away, [so] if you find something that you feel isn’t normal, take care of it.”
Dr. Voss, Dr. Park, and Dr. Cerame had no relevant financial disclosures.
Neil Osterweil contributed to this article.
BOSTON – For many surgeons, hours in the OR can translate into serious or chronic neck, back, and hand pain.
Studies of occupational injury related to performing surgery took off in the 1990s when laparoscopic surgery became widespread and put new physical demands on surgeons (Surg Endosc 1999:13:466-468; Arch Surg 1999;134:1011-1016). Findings from a study presented at the Society for Surgical Oncology suggest that the problem remains widespread.
Dr. Rachael K. Voss, a research resident at the University of Texas MD Anderson Cancer Center, Houston, and her colleagues conducted a survey among oncologic surgeons at the Center to explore the extent, sources and risk factors of workplace injuries.
“[Workplace injury] is a serious issue for surgeons, but it is something we don’t talk about and there is very little training and information as we are going through training. But these occupational hazards are something we need to acknowledge. We need to do more work in the future with ergonomics experts and occupational hygiene experts that can help us improve our posture and positions in the OR so we can prevent these injuries,” Dr. Voss said.
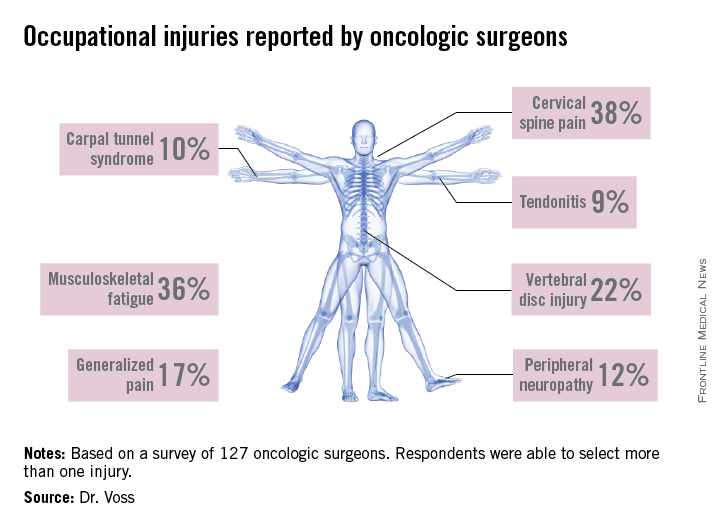
A high response rate of 58% yielded a total of 127 completed surveys. Most of the respondents were aged 35-64 and three-quarters spent 10 hours or more per week working in the OR. Among those responding, 92.3% experienced at least one occupation-related symptom over the past 6 weeks, and 27.6% reported sustaining an injury or chronic condition which they attributed to operating. The majority of injuries reported were cervical spine injury, musculoskeletal fatigue and vertebral disc injury. Other conditions mentioned were brachial plexus damage, carpal tunnel syndrome, peripheral neuropathy, and tendonitis.
A multivariate analysis identified some independent risk factors for injury: male gender, average case duration of 4 hours or longer, neck pain, and frequent use of a step for height adjustment. Age and years in practice were not associated with injury risk.
The good news is that, in this sample, 72% of the respondents reported seeking treatment for their injury. Physical therapy and medication were the most commonly utilized treatments, with about 20% resorting to surgery.
Plenty of evidence
The MD Anderson findings confirmed what other studies in this area have reported. William T. Davis and his colleagues surveyed Fellows of the Tennessee chapter of the American College of Surgeons on the issue of occupational musculoskeletal injury (J Surg Res 2014;184:207-212). Of the 793 surveys sent, 33% were completed. General surgeons accounted for 64% of respondents and 80% were male. Forty percent of respondents had sustained at least one injury related to operating. Most reported spine, hand, and neck injuries, but hip, knee, and shoulder pain was also mentioned. The majority of respondents reported the cause of their injury as chronic and 51% sought medical treatment. As with the MD Anderson study, no association was found between age or years in practice and workplace injury.
Mr. Davis and his colleagues conducted a similar study of orthopaedic surgeons and found similar rates of occupational injury (44%) among their 140 survey respondents (J Bone Joint Surg Am. 2013;95:e107). This study found that responding orthopaedic surgeons had more hand and lower back injuries, and correlation was found between years in practice and prevalence of injury.
A limitation of all of these studies is that the injury data are self-reported, and there is a potential selection bias. It is likely that the true extent of workplace injury among surgeons, and the costs and impact on surgeons’ life quality and productivity, are still largely unknown.
“There have been a few studies on this, but I think we’re just scratching the surface,” explained Dr. Adrian Park, chair of surgery at the Anne Arundel Medical Center in Annapolis, Md. Dr. Park was the lead author of a 2010 study that identified chronic pain among surgeons as a serious and underreported issue within medicine (J Am Coll Surg 2010;210;306-313).
The study, which evaluated 317 surgeons using a 23-question survey, found that 86.9% of surgeons experience “physical symptoms or discomfort,” with the most significant indicator of such symptoms being a high case load. Subsequent studies from Europe and eastern Asia also found rates of 80% or higher among surgeons in those regions.
Injuries downplayed
With so pervasive a problem, however, the relative paucity of data and conversation among medical professionals is something Dr. Park finds alarming. “As a surgeon leader, I can tell you surgeons complain about a lot of stuff, but one of the things they tend not to complain about is themselves and their own health and well-being,” said Dr. Park.
Dr. Mario Cerame is well aware of what a seemingly innocuous, relatively small chronic pain can do to a surgeon. A general surgeon practicing in North Carolina, Dr. Cerame began to experience symptoms of repetitive motion injury about 2 years ago, symptoms which he says “crept up on me.”
It began as numbness at the tips of his fingers, affecting the way he held laparoscopic tools during surgery and other, more menial, daily tasks. Initially suspecting it was carpal tunnel syndrome, Dr. Cerame brushed it off, until the numbness spread to three whole fingers and, eventually, his entire hand. His physician explained what was happening, instructing him that if he didn’t undergo orthopaedic surgery immediately, he ran the risk of paralysis.
“I got the diagnosis on Thursday, and had the operation on Tuesday,” said Dr. Cerame, explaining that the diagnosis was spinal stenosis. Two areas of his spinal column were pinching inward, causing the slow but steady paralysis he was experiencing. With physical therapy, Dr. Cerame could have returning function within 2 years of the operation.
“I’ve published an awful lot of papers, but the thing that struck me about [the 2010] paper is the response I got,” said Dr. Park. “Surgeons, literally from around the country, would call me saying ‘I used to be able to do this operation, I no longer can do that,’ or ‘this used to be what my case list looked like, I can no longer do this, you can use me as an example.’ People came forward.”
Risks of ignoring, self-medicating
Then there is the dark side of coping with chronic pain: risk of substance abuse. A study published in the Journal of Addiction Medicine (2013;7;349-353) on misuse of prescription medication among physicians found that surgeons were among the specialists at highest risk for substance abuse. According to this study, the beginning of addiction for many doctors is a prescription or self-medication for chronic pain. For surgeons, chronic pain from occupational injuries could lead to dependence on pain medication.
“When livelihoods are at stake, I think folks will take opportunities to stay in the game,” admitted Dr. Park.
The bottom line, according to both Dr. Park and Dr. Cerame, is for surgeons not to keep quiet about these issues if they ever do experience them. Asking for help and getting things checked right away is better, not only for a surgeon, but for family and patients, too. While Dr. Cerame has gone back to work, he is unable to handle the caseload he once had and isn’t sure if he’ll ever be able to.
“Surgeons and physicians in general have a tendency to get so consumed with other people’s health that they don’t focus on their own health issues,” said Dr. Cerame. “It took me almost 8 months from the time I had symptoms to actually get it checked out [because] I thought it would go away, [so] if you find something that you feel isn’t normal, take care of it.”
Dr. Voss, Dr. Park, and Dr. Cerame had no relevant financial disclosures.
Neil Osterweil contributed to this article.
VIDEO: Caring for transgender youth will require care across specialties
BALTIMORE – Training in transgender care needs to be amplified across all specialties, including pediatrics, as the number of transgender individuals, both young and old, continues to climb.
“We all have a gender, we all have a gender identity, we all have a way in which we express that to the world around us, and to ignore that part of a human being [and] a patient would be a real detriment [to] our society,” explained Dr. Kristen Eckstrand a resident in the child psychiatry program at the University of Pittsburgh.
In an interview at the annual meeting of the Pediatric Academic Societies, Dr. Eckstrand discussed strategies for talking to transgender patients to provide the best care for them, and the importance of working across professions and specialties when the situation calls for it.
Dr. Eckstrand did not report any relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Go to LGBT Youth Consult on our site for articles on the nature of sexuality and gender identity and how they affect health, advice on how to talk with your patients about these topics, and how to make your office a safe place for LGBT youth.
BALTIMORE – Training in transgender care needs to be amplified across all specialties, including pediatrics, as the number of transgender individuals, both young and old, continues to climb.
“We all have a gender, we all have a gender identity, we all have a way in which we express that to the world around us, and to ignore that part of a human being [and] a patient would be a real detriment [to] our society,” explained Dr. Kristen Eckstrand a resident in the child psychiatry program at the University of Pittsburgh.
In an interview at the annual meeting of the Pediatric Academic Societies, Dr. Eckstrand discussed strategies for talking to transgender patients to provide the best care for them, and the importance of working across professions and specialties when the situation calls for it.
Dr. Eckstrand did not report any relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Go to LGBT Youth Consult on our site for articles on the nature of sexuality and gender identity and how they affect health, advice on how to talk with your patients about these topics, and how to make your office a safe place for LGBT youth.
BALTIMORE – Training in transgender care needs to be amplified across all specialties, including pediatrics, as the number of transgender individuals, both young and old, continues to climb.
“We all have a gender, we all have a gender identity, we all have a way in which we express that to the world around us, and to ignore that part of a human being [and] a patient would be a real detriment [to] our society,” explained Dr. Kristen Eckstrand a resident in the child psychiatry program at the University of Pittsburgh.
In an interview at the annual meeting of the Pediatric Academic Societies, Dr. Eckstrand discussed strategies for talking to transgender patients to provide the best care for them, and the importance of working across professions and specialties when the situation calls for it.
Dr. Eckstrand did not report any relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Go to LGBT Youth Consult on our site for articles on the nature of sexuality and gender identity and how they affect health, advice on how to talk with your patients about these topics, and how to make your office a safe place for LGBT youth.
AT THE PAS ANNUAL MEETING
VIDEO: Transgender care becoming an increasingly important component of pediatric care
BALTIMORE – With a growing number of youth coming out as transgender, it’s becoming increasingly important for both the current and upcoming generation of pediatricians to know how to provide the best possible health care to this population.
“It’s now very common for pediatricians to be approached by parents or teens, and asked for help or support with a transition,” explained Dr. Daniel E. Shumer of the University of Michigan in Ann Arbor. He added, “I think it’s incumbent upon pediatricians to figure out how to provide that education to trainees so that the next generation of pediatricians is able to provide excellent care for transgender kids and their families.”
In an interview at the annual meeting of the Pediatric Academic Societies, Dr. Shumer elaborated on the importance of training new pediatricians on how to handle LGBT patients, exactly what such training should entail, and why it’s equally important for current pediatricians to educate themselves on this very issue.
Dr. Shumer did not report any relevant financial disclosures.
Go to LGBT Youth Consult on our site for articles on the nature of sexuality and gender identity and how they affect health, advice on how to talk with your patients about these topics, and how to make your office a safe place for LGBT youth.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BALTIMORE – With a growing number of youth coming out as transgender, it’s becoming increasingly important for both the current and upcoming generation of pediatricians to know how to provide the best possible health care to this population.
“It’s now very common for pediatricians to be approached by parents or teens, and asked for help or support with a transition,” explained Dr. Daniel E. Shumer of the University of Michigan in Ann Arbor. He added, “I think it’s incumbent upon pediatricians to figure out how to provide that education to trainees so that the next generation of pediatricians is able to provide excellent care for transgender kids and their families.”
In an interview at the annual meeting of the Pediatric Academic Societies, Dr. Shumer elaborated on the importance of training new pediatricians on how to handle LGBT patients, exactly what such training should entail, and why it’s equally important for current pediatricians to educate themselves on this very issue.
Dr. Shumer did not report any relevant financial disclosures.
Go to LGBT Youth Consult on our site for articles on the nature of sexuality and gender identity and how they affect health, advice on how to talk with your patients about these topics, and how to make your office a safe place for LGBT youth.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BALTIMORE – With a growing number of youth coming out as transgender, it’s becoming increasingly important for both the current and upcoming generation of pediatricians to know how to provide the best possible health care to this population.
“It’s now very common for pediatricians to be approached by parents or teens, and asked for help or support with a transition,” explained Dr. Daniel E. Shumer of the University of Michigan in Ann Arbor. He added, “I think it’s incumbent upon pediatricians to figure out how to provide that education to trainees so that the next generation of pediatricians is able to provide excellent care for transgender kids and their families.”
In an interview at the annual meeting of the Pediatric Academic Societies, Dr. Shumer elaborated on the importance of training new pediatricians on how to handle LGBT patients, exactly what such training should entail, and why it’s equally important for current pediatricians to educate themselves on this very issue.
Dr. Shumer did not report any relevant financial disclosures.
Go to LGBT Youth Consult on our site for articles on the nature of sexuality and gender identity and how they affect health, advice on how to talk with your patients about these topics, and how to make your office a safe place for LGBT youth.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
EXPERT ANALYSIS FROM THE PAS ANNUAL MEETING
















