User login
BOSTON – For many surgeons, hours in the OR can translate into serious or chronic neck, back, and hand pain.
Studies of occupational injury related to performing surgery took off in the 1990s when laparoscopic surgery became widespread and put new physical demands on surgeons (Surg Endosc 1999:13:466-468; Arch Surg 1999;134:1011-1016). Findings from a study presented at the Society for Surgical Oncology suggest that the problem remains widespread.
Dr. Rachael K. Voss, a research resident at the University of Texas MD Anderson Cancer Center, Houston, and her colleagues conducted a survey among oncologic surgeons at the Center to explore the extent, sources and risk factors of workplace injuries.
“[Workplace injury] is a serious issue for surgeons, but it is something we don’t talk about and there is very little training and information as we are going through training. But these occupational hazards are something we need to acknowledge. We need to do more work in the future with ergonomics experts and occupational hygiene experts that can help us improve our posture and positions in the OR so we can prevent these injuries,” Dr. Voss said.
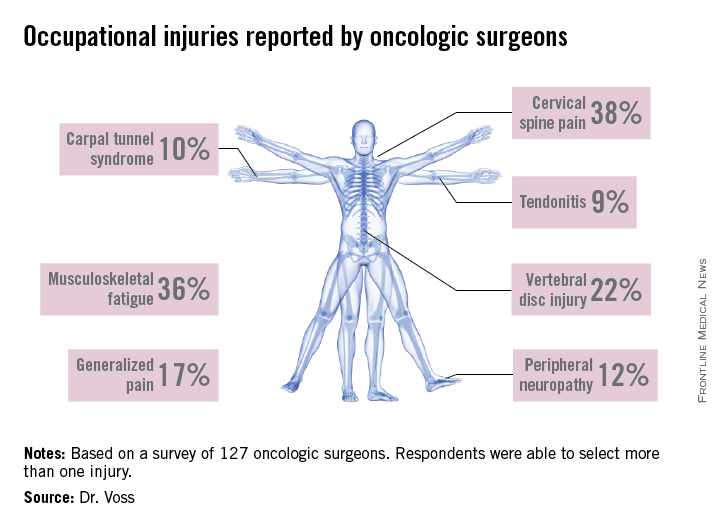
A high response rate of 58% yielded a total of 127 completed surveys. Most of the respondents were aged 35-64 and three-quarters spent 10 hours or more per week working in the OR. Among those responding, 92.3% experienced at least one occupation-related symptom over the past 6 weeks, and 27.6% reported sustaining an injury or chronic condition which they attributed to operating. The majority of injuries reported were cervical spine injury, musculoskeletal fatigue and vertebral disc injury. Other conditions mentioned were brachial plexus damage, carpal tunnel syndrome, peripheral neuropathy, and tendonitis.
A multivariate analysis identified some independent risk factors for injury: male gender, average case duration of 4 hours or longer, neck pain, and frequent use of a step for height adjustment. Age and years in practice were not associated with injury risk.
The good news is that, in this sample, 72% of the respondents reported seeking treatment for their injury. Physical therapy and medication were the most commonly utilized treatments, with about 20% resorting to surgery.
Plenty of evidence
The MD Anderson findings confirmed what other studies in this area have reported. William T. Davis and his colleagues surveyed Fellows of the Tennessee chapter of the American College of Surgeons on the issue of occupational musculoskeletal injury (J Surg Res 2014;184:207-212). Of the 793 surveys sent, 33% were completed. General surgeons accounted for 64% of respondents and 80% were male. Forty percent of respondents had sustained at least one injury related to operating. Most reported spine, hand, and neck injuries, but hip, knee, and shoulder pain was also mentioned. The majority of respondents reported the cause of their injury as chronic and 51% sought medical treatment. As with the MD Anderson study, no association was found between age or years in practice and workplace injury.
Mr. Davis and his colleagues conducted a similar study of orthopaedic surgeons and found similar rates of occupational injury (44%) among their 140 survey respondents (J Bone Joint Surg Am. 2013;95:e107). This study found that responding orthopaedic surgeons had more hand and lower back injuries, and correlation was found between years in practice and prevalence of injury.
A limitation of all of these studies is that the injury data are self-reported, and there is a potential selection bias. It is likely that the true extent of workplace injury among surgeons, and the costs and impact on surgeons’ life quality and productivity, are still largely unknown.
“There have been a few studies on this, but I think we’re just scratching the surface,” explained Dr. Adrian Park, chair of surgery at the Anne Arundel Medical Center in Annapolis, Md. Dr. Park was the lead author of a 2010 study that identified chronic pain among surgeons as a serious and underreported issue within medicine (J Am Coll Surg 2010;210;306-313).
The study, which evaluated 317 surgeons using a 23-question survey, found that 86.9% of surgeons experience “physical symptoms or discomfort,” with the most significant indicator of such symptoms being a high case load. Subsequent studies from Europe and eastern Asia also found rates of 80% or higher among surgeons in those regions.
Injuries downplayed
With so pervasive a problem, however, the relative paucity of data and conversation among medical professionals is something Dr. Park finds alarming. “As a surgeon leader, I can tell you surgeons complain about a lot of stuff, but one of the things they tend not to complain about is themselves and their own health and well-being,” said Dr. Park.
Dr. Mario Cerame is well aware of what a seemingly innocuous, relatively small chronic pain can do to a surgeon. A general surgeon practicing in North Carolina, Dr. Cerame began to experience symptoms of repetitive motion injury about 2 years ago, symptoms which he says “crept up on me.”
It began as numbness at the tips of his fingers, affecting the way he held laparoscopic tools during surgery and other, more menial, daily tasks. Initially suspecting it was carpal tunnel syndrome, Dr. Cerame brushed it off, until the numbness spread to three whole fingers and, eventually, his entire hand. His physician explained what was happening, instructing him that if he didn’t undergo orthopaedic surgery immediately, he ran the risk of paralysis.
“I got the diagnosis on Thursday, and had the operation on Tuesday,” said Dr. Cerame, explaining that the diagnosis was spinal stenosis. Two areas of his spinal column were pinching inward, causing the slow but steady paralysis he was experiencing. With physical therapy, Dr. Cerame could have returning function within 2 years of the operation.
“I’ve published an awful lot of papers, but the thing that struck me about [the 2010] paper is the response I got,” said Dr. Park. “Surgeons, literally from around the country, would call me saying ‘I used to be able to do this operation, I no longer can do that,’ or ‘this used to be what my case list looked like, I can no longer do this, you can use me as an example.’ People came forward.”
Risks of ignoring, self-medicating
Then there is the dark side of coping with chronic pain: risk of substance abuse. A study published in the Journal of Addiction Medicine (2013;7;349-353) on misuse of prescription medication among physicians found that surgeons were among the specialists at highest risk for substance abuse. According to this study, the beginning of addiction for many doctors is a prescription or self-medication for chronic pain. For surgeons, chronic pain from occupational injuries could lead to dependence on pain medication.
“When livelihoods are at stake, I think folks will take opportunities to stay in the game,” admitted Dr. Park.
The bottom line, according to both Dr. Park and Dr. Cerame, is for surgeons not to keep quiet about these issues if they ever do experience them. Asking for help and getting things checked right away is better, not only for a surgeon, but for family and patients, too. While Dr. Cerame has gone back to work, he is unable to handle the caseload he once had and isn’t sure if he’ll ever be able to.
“Surgeons and physicians in general have a tendency to get so consumed with other people’s health that they don’t focus on their own health issues,” said Dr. Cerame. “It took me almost 8 months from the time I had symptoms to actually get it checked out [because] I thought it would go away, [so] if you find something that you feel isn’t normal, take care of it.”
Dr. Voss, Dr. Park, and Dr. Cerame had no relevant financial disclosures.
Neil Osterweil contributed to this article.
BOSTON – For many surgeons, hours in the OR can translate into serious or chronic neck, back, and hand pain.
Studies of occupational injury related to performing surgery took off in the 1990s when laparoscopic surgery became widespread and put new physical demands on surgeons (Surg Endosc 1999:13:466-468; Arch Surg 1999;134:1011-1016). Findings from a study presented at the Society for Surgical Oncology suggest that the problem remains widespread.
Dr. Rachael K. Voss, a research resident at the University of Texas MD Anderson Cancer Center, Houston, and her colleagues conducted a survey among oncologic surgeons at the Center to explore the extent, sources and risk factors of workplace injuries.
“[Workplace injury] is a serious issue for surgeons, but it is something we don’t talk about and there is very little training and information as we are going through training. But these occupational hazards are something we need to acknowledge. We need to do more work in the future with ergonomics experts and occupational hygiene experts that can help us improve our posture and positions in the OR so we can prevent these injuries,” Dr. Voss said.
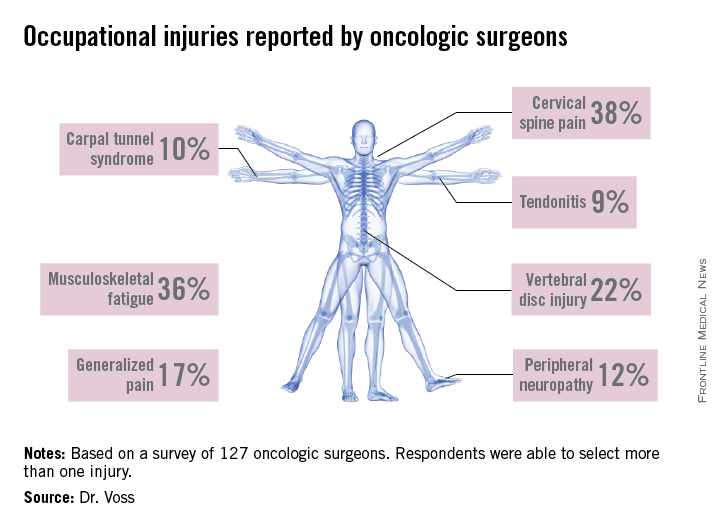
A high response rate of 58% yielded a total of 127 completed surveys. Most of the respondents were aged 35-64 and three-quarters spent 10 hours or more per week working in the OR. Among those responding, 92.3% experienced at least one occupation-related symptom over the past 6 weeks, and 27.6% reported sustaining an injury or chronic condition which they attributed to operating. The majority of injuries reported were cervical spine injury, musculoskeletal fatigue and vertebral disc injury. Other conditions mentioned were brachial plexus damage, carpal tunnel syndrome, peripheral neuropathy, and tendonitis.
A multivariate analysis identified some independent risk factors for injury: male gender, average case duration of 4 hours or longer, neck pain, and frequent use of a step for height adjustment. Age and years in practice were not associated with injury risk.
The good news is that, in this sample, 72% of the respondents reported seeking treatment for their injury. Physical therapy and medication were the most commonly utilized treatments, with about 20% resorting to surgery.
Plenty of evidence
The MD Anderson findings confirmed what other studies in this area have reported. William T. Davis and his colleagues surveyed Fellows of the Tennessee chapter of the American College of Surgeons on the issue of occupational musculoskeletal injury (J Surg Res 2014;184:207-212). Of the 793 surveys sent, 33% were completed. General surgeons accounted for 64% of respondents and 80% were male. Forty percent of respondents had sustained at least one injury related to operating. Most reported spine, hand, and neck injuries, but hip, knee, and shoulder pain was also mentioned. The majority of respondents reported the cause of their injury as chronic and 51% sought medical treatment. As with the MD Anderson study, no association was found between age or years in practice and workplace injury.
Mr. Davis and his colleagues conducted a similar study of orthopaedic surgeons and found similar rates of occupational injury (44%) among their 140 survey respondents (J Bone Joint Surg Am. 2013;95:e107). This study found that responding orthopaedic surgeons had more hand and lower back injuries, and correlation was found between years in practice and prevalence of injury.
A limitation of all of these studies is that the injury data are self-reported, and there is a potential selection bias. It is likely that the true extent of workplace injury among surgeons, and the costs and impact on surgeons’ life quality and productivity, are still largely unknown.
“There have been a few studies on this, but I think we’re just scratching the surface,” explained Dr. Adrian Park, chair of surgery at the Anne Arundel Medical Center in Annapolis, Md. Dr. Park was the lead author of a 2010 study that identified chronic pain among surgeons as a serious and underreported issue within medicine (J Am Coll Surg 2010;210;306-313).
The study, which evaluated 317 surgeons using a 23-question survey, found that 86.9% of surgeons experience “physical symptoms or discomfort,” with the most significant indicator of such symptoms being a high case load. Subsequent studies from Europe and eastern Asia also found rates of 80% or higher among surgeons in those regions.
Injuries downplayed
With so pervasive a problem, however, the relative paucity of data and conversation among medical professionals is something Dr. Park finds alarming. “As a surgeon leader, I can tell you surgeons complain about a lot of stuff, but one of the things they tend not to complain about is themselves and their own health and well-being,” said Dr. Park.
Dr. Mario Cerame is well aware of what a seemingly innocuous, relatively small chronic pain can do to a surgeon. A general surgeon practicing in North Carolina, Dr. Cerame began to experience symptoms of repetitive motion injury about 2 years ago, symptoms which he says “crept up on me.”
It began as numbness at the tips of his fingers, affecting the way he held laparoscopic tools during surgery and other, more menial, daily tasks. Initially suspecting it was carpal tunnel syndrome, Dr. Cerame brushed it off, until the numbness spread to three whole fingers and, eventually, his entire hand. His physician explained what was happening, instructing him that if he didn’t undergo orthopaedic surgery immediately, he ran the risk of paralysis.
“I got the diagnosis on Thursday, and had the operation on Tuesday,” said Dr. Cerame, explaining that the diagnosis was spinal stenosis. Two areas of his spinal column were pinching inward, causing the slow but steady paralysis he was experiencing. With physical therapy, Dr. Cerame could have returning function within 2 years of the operation.
“I’ve published an awful lot of papers, but the thing that struck me about [the 2010] paper is the response I got,” said Dr. Park. “Surgeons, literally from around the country, would call me saying ‘I used to be able to do this operation, I no longer can do that,’ or ‘this used to be what my case list looked like, I can no longer do this, you can use me as an example.’ People came forward.”
Risks of ignoring, self-medicating
Then there is the dark side of coping with chronic pain: risk of substance abuse. A study published in the Journal of Addiction Medicine (2013;7;349-353) on misuse of prescription medication among physicians found that surgeons were among the specialists at highest risk for substance abuse. According to this study, the beginning of addiction for many doctors is a prescription or self-medication for chronic pain. For surgeons, chronic pain from occupational injuries could lead to dependence on pain medication.
“When livelihoods are at stake, I think folks will take opportunities to stay in the game,” admitted Dr. Park.
The bottom line, according to both Dr. Park and Dr. Cerame, is for surgeons not to keep quiet about these issues if they ever do experience them. Asking for help and getting things checked right away is better, not only for a surgeon, but for family and patients, too. While Dr. Cerame has gone back to work, he is unable to handle the caseload he once had and isn’t sure if he’ll ever be able to.
“Surgeons and physicians in general have a tendency to get so consumed with other people’s health that they don’t focus on their own health issues,” said Dr. Cerame. “It took me almost 8 months from the time I had symptoms to actually get it checked out [because] I thought it would go away, [so] if you find something that you feel isn’t normal, take care of it.”
Dr. Voss, Dr. Park, and Dr. Cerame had no relevant financial disclosures.
Neil Osterweil contributed to this article.
BOSTON – For many surgeons, hours in the OR can translate into serious or chronic neck, back, and hand pain.
Studies of occupational injury related to performing surgery took off in the 1990s when laparoscopic surgery became widespread and put new physical demands on surgeons (Surg Endosc 1999:13:466-468; Arch Surg 1999;134:1011-1016). Findings from a study presented at the Society for Surgical Oncology suggest that the problem remains widespread.
Dr. Rachael K. Voss, a research resident at the University of Texas MD Anderson Cancer Center, Houston, and her colleagues conducted a survey among oncologic surgeons at the Center to explore the extent, sources and risk factors of workplace injuries.
“[Workplace injury] is a serious issue for surgeons, but it is something we don’t talk about and there is very little training and information as we are going through training. But these occupational hazards are something we need to acknowledge. We need to do more work in the future with ergonomics experts and occupational hygiene experts that can help us improve our posture and positions in the OR so we can prevent these injuries,” Dr. Voss said.
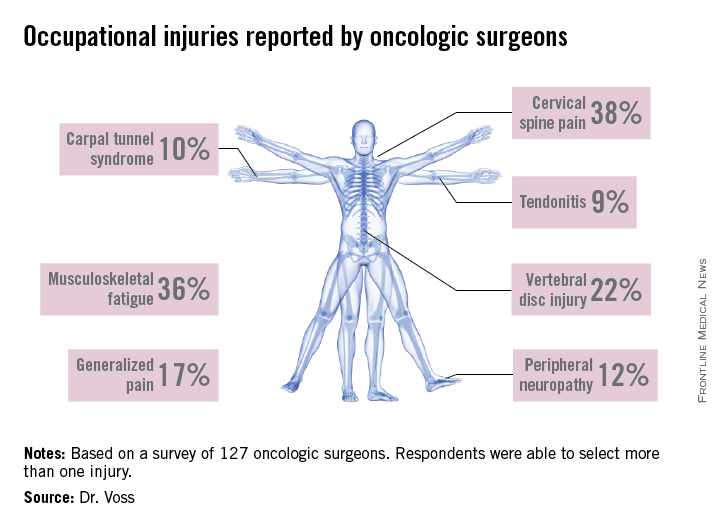
A high response rate of 58% yielded a total of 127 completed surveys. Most of the respondents were aged 35-64 and three-quarters spent 10 hours or more per week working in the OR. Among those responding, 92.3% experienced at least one occupation-related symptom over the past 6 weeks, and 27.6% reported sustaining an injury or chronic condition which they attributed to operating. The majority of injuries reported were cervical spine injury, musculoskeletal fatigue and vertebral disc injury. Other conditions mentioned were brachial plexus damage, carpal tunnel syndrome, peripheral neuropathy, and tendonitis.
A multivariate analysis identified some independent risk factors for injury: male gender, average case duration of 4 hours or longer, neck pain, and frequent use of a step for height adjustment. Age and years in practice were not associated with injury risk.
The good news is that, in this sample, 72% of the respondents reported seeking treatment for their injury. Physical therapy and medication were the most commonly utilized treatments, with about 20% resorting to surgery.
Plenty of evidence
The MD Anderson findings confirmed what other studies in this area have reported. William T. Davis and his colleagues surveyed Fellows of the Tennessee chapter of the American College of Surgeons on the issue of occupational musculoskeletal injury (J Surg Res 2014;184:207-212). Of the 793 surveys sent, 33% were completed. General surgeons accounted for 64% of respondents and 80% were male. Forty percent of respondents had sustained at least one injury related to operating. Most reported spine, hand, and neck injuries, but hip, knee, and shoulder pain was also mentioned. The majority of respondents reported the cause of their injury as chronic and 51% sought medical treatment. As with the MD Anderson study, no association was found between age or years in practice and workplace injury.
Mr. Davis and his colleagues conducted a similar study of orthopaedic surgeons and found similar rates of occupational injury (44%) among their 140 survey respondents (J Bone Joint Surg Am. 2013;95:e107). This study found that responding orthopaedic surgeons had more hand and lower back injuries, and correlation was found between years in practice and prevalence of injury.
A limitation of all of these studies is that the injury data are self-reported, and there is a potential selection bias. It is likely that the true extent of workplace injury among surgeons, and the costs and impact on surgeons’ life quality and productivity, are still largely unknown.
“There have been a few studies on this, but I think we’re just scratching the surface,” explained Dr. Adrian Park, chair of surgery at the Anne Arundel Medical Center in Annapolis, Md. Dr. Park was the lead author of a 2010 study that identified chronic pain among surgeons as a serious and underreported issue within medicine (J Am Coll Surg 2010;210;306-313).
The study, which evaluated 317 surgeons using a 23-question survey, found that 86.9% of surgeons experience “physical symptoms or discomfort,” with the most significant indicator of such symptoms being a high case load. Subsequent studies from Europe and eastern Asia also found rates of 80% or higher among surgeons in those regions.
Injuries downplayed
With so pervasive a problem, however, the relative paucity of data and conversation among medical professionals is something Dr. Park finds alarming. “As a surgeon leader, I can tell you surgeons complain about a lot of stuff, but one of the things they tend not to complain about is themselves and their own health and well-being,” said Dr. Park.
Dr. Mario Cerame is well aware of what a seemingly innocuous, relatively small chronic pain can do to a surgeon. A general surgeon practicing in North Carolina, Dr. Cerame began to experience symptoms of repetitive motion injury about 2 years ago, symptoms which he says “crept up on me.”
It began as numbness at the tips of his fingers, affecting the way he held laparoscopic tools during surgery and other, more menial, daily tasks. Initially suspecting it was carpal tunnel syndrome, Dr. Cerame brushed it off, until the numbness spread to three whole fingers and, eventually, his entire hand. His physician explained what was happening, instructing him that if he didn’t undergo orthopaedic surgery immediately, he ran the risk of paralysis.
“I got the diagnosis on Thursday, and had the operation on Tuesday,” said Dr. Cerame, explaining that the diagnosis was spinal stenosis. Two areas of his spinal column were pinching inward, causing the slow but steady paralysis he was experiencing. With physical therapy, Dr. Cerame could have returning function within 2 years of the operation.
“I’ve published an awful lot of papers, but the thing that struck me about [the 2010] paper is the response I got,” said Dr. Park. “Surgeons, literally from around the country, would call me saying ‘I used to be able to do this operation, I no longer can do that,’ or ‘this used to be what my case list looked like, I can no longer do this, you can use me as an example.’ People came forward.”
Risks of ignoring, self-medicating
Then there is the dark side of coping with chronic pain: risk of substance abuse. A study published in the Journal of Addiction Medicine (2013;7;349-353) on misuse of prescription medication among physicians found that surgeons were among the specialists at highest risk for substance abuse. According to this study, the beginning of addiction for many doctors is a prescription or self-medication for chronic pain. For surgeons, chronic pain from occupational injuries could lead to dependence on pain medication.
“When livelihoods are at stake, I think folks will take opportunities to stay in the game,” admitted Dr. Park.
The bottom line, according to both Dr. Park and Dr. Cerame, is for surgeons not to keep quiet about these issues if they ever do experience them. Asking for help and getting things checked right away is better, not only for a surgeon, but for family and patients, too. While Dr. Cerame has gone back to work, he is unable to handle the caseload he once had and isn’t sure if he’ll ever be able to.
“Surgeons and physicians in general have a tendency to get so consumed with other people’s health that they don’t focus on their own health issues,” said Dr. Cerame. “It took me almost 8 months from the time I had symptoms to actually get it checked out [because] I thought it would go away, [so] if you find something that you feel isn’t normal, take care of it.”
Dr. Voss, Dr. Park, and Dr. Cerame had no relevant financial disclosures.
Neil Osterweil contributed to this article.


