User login
Families as Care Partners: Implementing the Better Together Initiative Across a Large Health System
From the Institute for Patient- and Family-Centered Care, Bethesda, MD (Ms. Dokken and Ms. Johnson), and Northwell Health, New Hyde Park, NY (Dr. Barden, Ms. Tuomey, and Ms. Giammarinaro).
Abstract
Objective: To describe the growth of Better Together: Partnering with Families, a campaign launched in 2014 to eliminate restrictive hospital visiting policies and to put in place policies that recognize families as partners in care, and to discuss the processes involved in implementing the initiative in a large, integrated health system.
Methods: Descriptive report.
Results: In June 2014, the Institute for Patient- and Family-Centered Care (IPFCC) launched the Better Together campaign to emphasize the importance of family presence and participation to the quality, experience, safety, and outcomes of care. Since then, this initiative has expanded in both the United States and Canada. With support from 2 funders in the United States, special attention was focused on acute care hospitals across New York State. Nearly 50 hospitals participated in 2 separate but related projects. Fifteen of the hospitals are part of Northwell Health, New York State’s largest health system. Over a 10-month period, these hospitals made significant progress in changing policy, practice, and communication to support family presence.
Conclusion: The Better Together initiative was implemented across a health system with strong support from leadership and the involvement of patient and family advisors. An intervention offering structured training, coaching, and resources, like IPFCC’s Better Together initiative, can facilitate the change process.
Keywords: family presence; visiting policies; patient-centered care; family-centered care; patient experience.
The presence of families at the bedside of patients is often restricted by hospital visiting hours. Hospitals that maintain these restrictive policies cite concerns about negative impacts on security, infection control, privacy, and staff workload. But there are no data to support these concerns, and the experience of hospitals that have successfully changed policy and practice to welcome families demonstrates the potential positive impacts of less restrictive policies on patient care and outcomes.1 For example, hospitalization can lead to reduced cognitive function in elderly patients. Family members would recognize the changes and could provide valuable information to hospital staff, potentially improving outcomes.2
In June 2014, the Institute for Patient- and Family-Centered Care (IPFCC) launched the campaign Better Together: Partnering with Families.3 The campaign is is grounded in patient- and family- centered care, an approach to care that supports partnerships among health care providers, patients, and families, and, among other core principles, advocates that patients define their “families” and how they will participate in care and decision-making.
Emphasizing the importance of family presence and participation to quality and safety, the Better Together campaign seeks to eliminate restrictive visiting policies and calls upon hospitals to include families as members of the care team and to welcome them 24 hours a day, 7 days a week, according to patient preference. As part of the campaign, IPFCC developed an extensive toolkit of resources that is available to hospitals and other organizations at no cost. The resources include sample policies; profiles of hospitals that have implemented family presence policies; educational materials for staff, patients, and families; and a template for hospital websites. This article, a follow-up to an article published in the January 2015 issue of JCOM,1 discusses the growth of the Better Together initiative as well as the processes involved in implementing the initiative across a large health system.
Growth of the Initiative
Since its launch in 2014, the Better Together initiative has continued to expand in the United States and Canada. In Canada, under the leadership of the Canadian Foundation for Healthcare Improvement (CFHI), more than 50 organizations have made a commitment to the Better Together program and family presence.4 Utilizing and adapting IPFCC’s Toolkit, CFHI developed a change package of free resources for Canadian organizations.5 Some of the materials, including the Pocket Guide for Families (Manuel des Familles), were translated into French.6
With support from 2 funders in the United States, the United Hospital Fund and the New York State Health (NYSHealth) Foundation, through a subcontract with the New York Public Interest Research Group (NYPIRG), IPFCC has been able to focus on hospitals in New York City, including public hospitals, and, more broadly, acute care hospitals across New York State. Nearly 50 hospitals participated in these 2 separate but related projects.
Education and Support for New York City Hospitals
Supported by the United Hospital Fund, an 18-month project that focused specifically on New York City hospitals was completed in June 2017. The project began with a 1-day intensive training event with representatives of 21 hospitals. Eighteen of those hospitals were eligible to participate in follow-up consultation provided by IPFCC, and 14 participated in some kind of follow-up. NYC Health + Hospitals (H+H), the system of public hospitals in NYC, participated most fully in these activities.
The outcomes of the Better Together initiative in New York City are summarized in the report Sick, Scared, & Separated From Loved Ones,2 which is based on a pre/post review of hospital visitation/family presence policies and website communications. According to the report, hospitals that participated in the IPFCC training and consultation program performed better, as a group, with respect to improved policy and website scores on post review than those that did not. Of the 10 hospitals whose scores improved during the review period, 8 had participated in the IPFCC training and 1 hospital was part of a hospital network that did so. (Six of these hospitals are part of the H+H public hospital system.) Those 9 hospitals saw an average increase in scores of 4.9 points (out of a possible 11).
A Learning Community for Hospitals in New York State
With support from the NYSHealth Foundation, IPFCC again collaborated with NYPIRG and New Yorkers for Patient & Family Empowerment on a 2-year initiative, completed in November 2019, that involved 26 hospitals: 15 from Northwell Health, New York State’s largest health system, and 11 hospitals from health systems throughout the state (Greater Hudson Valley Health System, now Garnet Health; Mohawk Valley Health System; Rochester Regional Health; and University of Vermont Health Network). An update of the report Sick, Scared, & Separated From Loved Onescompared pre/post reviews of policies and website communications regarding hospital visitation/family presence.7 Its findings confirm that hospitals that participated in the Better Together Learning Community improved both their policy and website scores to a greater degree than hospitals that did not participate and that a planned intervention can help facilitate change.
During the survey period, 28 out of 40 hospitals’ website navigability scores improved. Of those, hospitals that did not participate in the Better Together Learning Community saw an average increase in scores of 1.2 points, out of a possible 11, while the participating hospitals saw an average increase of 2.7 points, with the top 5 largest increases in scores belonging to hospitals that participated in the Better Together Learning Community.7
The Northwell Health Experience
Northwell Health is a large integrated health care organization comprising more than 69,000 employees, 23 hospitals, and more than 750 medical practices, located geographically across New York State. Embracing patient- and family-centered care, Northwell is dedicated to improving the quality, experience, and safety of care for patients and their families. Welcoming and including patients, families, and care partners as members of the health care team has always been a core element of Northwell’s organizational goal of providing world-class patient care and experience.
Four years ago, the organization reorganized and formalized a system-wide Patient & Family Partnership Council (PFPC).8 Representatives on the PFPC include a Northwell patient experience leader and patient/family co-chair from local councils that have been established in nearly all 23 hospitals as well as service lines. Modeling partnership, the PFPC is grounded in listening to the “voice” of patients and families and promoting collaboration, with the goal of driving change across varied aspects and experiences of health care delivery.
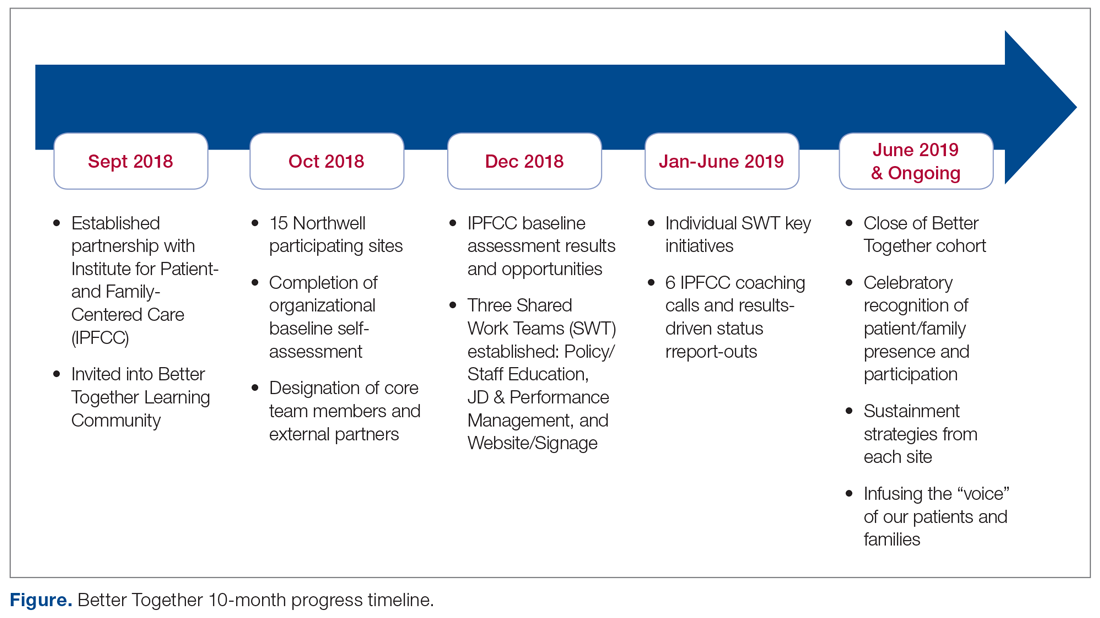
Through the Office of Patient and Customer Experience (OPCE), a partnership with IPFCC and the Better Together Learning Community for Hospitals in New York State was initiated as a fundamental next step in Northwell’s journey to enhance system-wide family presence and participation. Results from Better Together’s Organizational Self-Assessment Tool and process identified opportunities to influence 3 distinct areas: policy/staff education, position descriptions/performance management, and website/signage. Over a 10-month period (September 2018 through June 2019), 15 Northwell hospitals implemened significant patient- and family-centered improvements through multifaceted shared work teams (SWT) that partnered around the common goal of supporting the patient and family experience (Figure). Northwell’s SWT structure allowed teams to meet individually on specific tasks, led by a dedicated staff member of the OPCE to ensure progress, support, and accountability. Six monthly coaching calls or report-out meetings were attended by participating teams, where feedback and recommendations shared by IPFCC were discussed in order to maintain momentum and results.
Policy/Staff Education
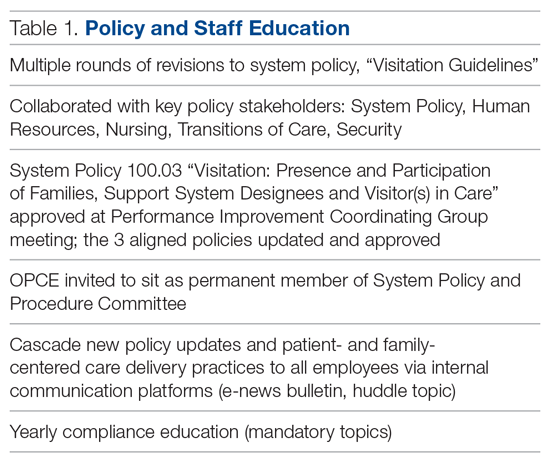
The policy/staff education SWT focused on appraising and updating existing policies to ensure alignment with key patient- and family-centered concepts and Better Together principles (Table 1). By establishing representation on the System Policy and Procedure Committee, OPCE enabled patients and families to have a voice at the decision-making table. OPCE leaders presented the ideology and scope of the transformation to this committee. After reviewing all system-wide policies, 4 were identified as key opportunities for revision. One overarching policy titled “Visitation Guidelines” was reviewed and updated to reflect Northwell’s mission of patient- and family-centered care, retiring the reference to “families” as “visitors” in definitions, incorporating language of inclusion and partnership, and citing other related policies. The policy was vetted through a multilayer process of review and stakeholder feedback and was ultimately approved at a system
Three additional related policies were also updated to reflect core principles of inclusion and partnership. These included system policies focused on discharge planning; identification of health care proxy, agent, support person and caregiver; and standards of behavior not conducive in a health care setting. As a result of this work, OPCE was invited to remain an active member of the System Policy and Procedure Committee, adding meaningful new perspectives to the clinical and administrative policy management process. Once policies were updated and approved, the SWT focused on educating leaders and teams. Using a diversified strategy, education was provided through various modes, including weekly system-wide internal communication channels, patient experience huddle messages, yearly mandatory topics training, and the incorporation of essential concepts in existing educational courses (classroom and e-learning modalities).
Position Descriptions/Performance Management
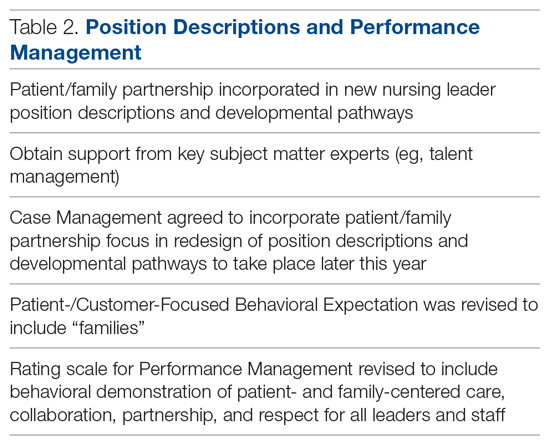
The position descriptions/performance management SWT focused its efforts on incorporating patient- and family-centered concepts and language into position descriptions and the performance appraisal process (Table 2). Due to the complex nature of this work, the process required collaboration from key subject matter experts in human resources, talent management, corporate compensation, and labor management. In 2019, Northwell began an initiative focused on streamlining and standardizing job titles, roles, and developmental pathways across the system. The overarching goal was to create system-wide consistency and standardization. The SWT was successful in advising the leaders overseeing this job architecture initiative on the importance of including language of patient- and family-centered care, like partnership and collaboration, and of highlighting the critical role of family members as part of the care team in subsequent documents.
Northwell has 6 behavioral expectations, standards to which all team members are held accountable: Patient/Customer Focus, Teamwork, Execution, Organizational Awareness, Enable Change, and Develop Self. As a result of the SWT’s work, Patient/Customer Focus was revised to include “families” as essential care partners, demonstrating Northwell’s ongoing commitment to honoring the role of families as members of the care team. It also ensures that all employees are aligned around this priority, as these expectations are utilized to support areas such as recognition and performance. Collaborating with talent management and organizational development, the SWT reviewed yearly performance management and new-hire evaluations. In doing so, they identified an opportunity to refresh the anchored qualitative rating scales to include behavioral demonstrations of patient- and family-centered care, collaboration, respect, and partnership with family members.
Website/Signage
Websites make an important first impression on patients and families looking for information to best prepare for a hospital experience. Therefore, the website/signage SWT worked to redesign hospital websites, enhance digital signage, and perform a baseline assessment of physical signage across facilities. Initial feedback on Northwell’s websites identified opportunities to include more patient- and family-centered, care-partner-infused language; improve navigation; and streamline click levels for easier access. Content for the websites was carefully crafted in collaboration with Northwell’s internal web team, utilizing IPFCC’s best practice standards as a framework and guide.
Next, a multidisciplinary website shared-governance team was established by the OPCE to ensure that key stakeholders were represented and had the opportunity to review and make recommendations for appropriate language and messaging about family presence and participation. This 13-person team was comprised of patient/family partners, patient-experience culture leaders, quality, compliance, human resources, policy, a chief nursing officer, a medical director, and representation from the Institute for Nursing. After careful review and consideration from Northwell’s family partners and teams, all participating hospital websites were enhanced as of June 2019 to include prominent 1-click access from homepages to information for “patients, families and visitors,” as well as “your care partners” information on the important role of families and care partners.
Along with refreshing websites, another step in Northwell’s work to strengthen messaging about family presence and participation was to partner and collaborate with the system’s digital web team as well as local facility councils to understand the capacity to adjust digital signage across facilities. Opportunities were found to make simple yet effective enhancements to the language and imagery of digital signage upon entry, creating a warmer and more welcoming first impression for patients and families. With patient and family partner feedback, the team designed digital signage with inclusive messaging and images that would circulate appropriately based on the facility. Signage specifically welcomes families and refers to them as members of patients’ care teams.
Northwell’s website/signage SWT also directed a 2-phase physical signage assessment to determine ongoing opportunities to alter signs in areas that particularly impact patients and families, such as emergency departments, main lobbies, cafeterias, surgical waiting areas, and intensive care units. Each hospital’s local PFPC did a “walk-about”9 to make enhancements to physical signage, such as removing paper and overcrowded signs, adjusting negative language, ensuring alignment with brand guidelines, and including language that welcomed families. As a result of the team’s efforts around signage, collaboration began with the health system’s signage committee to help standardize signage terminology to reflect family inclusiveness, and to implement the recommendation for a standardized signage shared-governance team to ensure accountability and a patient- and family-centered structure.
Sustainment
Since implementing Better Together, Northwell has been able to infuse a more patient- and family-centered emphasis into its overall patient experience message of “Every role, every person, every moment matters.” As a strategic tool aimed at encouraging leaders, clinicians, and staff to pause and reflect about the “heart” of their work, patient and family stories are now included at the beginning of meetings, forums, and team huddles. Elements of the initiative have been integrated in current Patient and Family Partnership sustainment plans at participating hospitals. Some highlights include continued integration of patient/family partners on committees and councils that impact areas such as way finding, signage, recruitment, new-hire orientation, and community outreach; focus on enhancing partner retention and development programs; and inclusion of patient- and family-centered care and Better Together principles in ongoing leadership meetings.
Factors Contributing to Success
Health care is a complex, regulated, and often bureaucratic world that can be very difficult for patients and families to navigate. The system’s partnership with the Better Together Learning Community for Hospitals in New York State enhanced its efforts to improve family presence and participation and created powerful synergy. The success of this partnership was based on a number of important factors:
A solid foundation of support, structure, and accountability. The OPCE initiated the IPFCC Better Together partnership and established a synergistic collaboration inclusive of leadership, frontline teams, multiple departments, and patient and family partners. As a major strategic component of Northwell’s mission to deliver high-quality, patient- and family-centered care, OPCE was instrumental in connecting key areas and stakeholders and mobilizing the recommendations coming from patients and families.
A visible commitment of leadership at all levels. Partnering with leadership across Northwell’s system required a delineated vision, clear purpose and ownership, and comprehensive implementation and sustainment strategies. The existing format of Northwell’s PFPC provided the structure and framework needed for engaged patient and family input; the OPCE motivated and organized key areas of involvement and led communication efforts across the organization. The IPFCC coaching calls provided the underlying guidance and accountability needed to sustain momentum. As leadership and frontline teams became aware of the vision, they understood the larger connection to the system’s purpose, which ultimately created a clear path for positive change.
Meaningful involvement and input of patient and family partners. Throughout this project, Northwell’s patient/family partners were involved through the PFPC and local councils. For example, patient/family partners attended every IPFCC coaching call; members had a central voice in every decision made within each SWT; and local PFPCs actively participated in physical signage “walk-abouts” across facilities, making key recommendations for improvement. This multifaceted, supportive collaboration created a rejuvenated and purposeful focus for all council members involved. Some of their reactions include, “…I am so happy to be able to help other families in crisis, so that they don’t have to be alone, like I was,” and “I feel how important the patient and family’s voice is … it’s truly a partnership between patients, families, and staff.”
Regular access to IPFCC as a best practice coach and expert resource. Throughout the 10-month process, IPFCC’s Better Together Learning Community for Hospitals in New York State provided ongoing learning interventions for members of the SWT; multiple and varied resources from the Better Together toolkit for adaptation; and opportunities to share and reinforce new, learned expertise with colleagues within the Northwell Health system and beyond through IPFCC’s free online learning community, PFCC.Connect.
Conclusion
Family presence and participation are important to the quality, experience, safety, and outcomes of care. IPFCC’s campaign, Better Together: Partnering with Families, encourages hospitals to change restrictive visiting policies and, instead, to welcome families and caregivers 24 hours a day.
Two projects within Better Together involving almost 50 acute care hospitals in New York State confirm that change in policy, practice, and communication is particularly effective when implemented with strong support from leadership. An intervention like the Better Together Learning Community, offering structured training, coaching, and resources, can facilitate the change process.
Corresponding author: IPFCC, Deborah L. Dokken, 6917 Arlington Rd., Ste. 309, Bethesda, MD 20814; ddokken@ipfcc.org.
Funding disclosures: None.
1. Dokken DL, Kaufman J, Johnson BJ et al. Changing hospital visiting policies: from families as “visitors” to families as partners. J Clin Outcomes Manag. 2015; 22:29-36.
2. New York Public Interest Research Group and New Yorkers for Patient & Family Empowerment. Sick, scared and separated from loved ones. third edition: A pathway to improvement in New York City. New York: NYPIRG: 2018. www.nypirg.org/pubs/201801/NYPIRG_SICK_SCARED_FINAL.pdf. Accessed December 12, 2019.
3. Institute for Patient- and Family-Centered Care. Better Together: Partnering with Families. www.ipfcc.org/bestpractices/better-together.html. Accessed December 12, 2019.
4. Canadian Foundation for Healthcare Improvement. Better Together. www.cfhi-fcass.ca/WhatWeDo/better-together. Accessed December 12, 2019.
5. Canadian Foundation for Healthcare Improvement. Better Together: A change package to support the adoption of family presence and participation in acute care hospitals and accelerate healthcare improvement. www.cfhi-fcass.ca/sf-docs/default-source/patient-engagement/better-together-change-package.pdf?sfvrsn=9656d044_4. Accessed December 12, 2019.
6. Canadian Foundation for Healthcare Improvement. L’Objectif santé: main dans la main avec les familles. www.cfhi-fcass.ca/sf-docs/default-source/patient-engagement/families-pocket-screen_fr.pdf. Accessed December 12, 2019.
7. New York Public Interest Research Group and New Yorkers for Patient & Family Empowerment. Sick, scared and separated from loved ones. fourth edition: A pathway to improvement in New York. New York: NYPIRG: 2019. www.nypirg.org/pubs/201911/Sick_Scared_Separated_2019_web_FINAL.pdf. Accessed December 12, 2019.
8. Northwell Health. Patient and Family Partnership Councils. www.northwell.edu/about/commitment-to-excellence/patient-and-customer-experience/care-delivery-hospitality. Accessed December 12, 2019.
9 . Institute for Patient- and Family-Centered Care. How to conduct a “walk-about” from the patient and family perspective. www.ipfcc.org/resources/How_To_Conduct_A_Walk-About.pdf. Accessed December 12, 2019.
From the Institute for Patient- and Family-Centered Care, Bethesda, MD (Ms. Dokken and Ms. Johnson), and Northwell Health, New Hyde Park, NY (Dr. Barden, Ms. Tuomey, and Ms. Giammarinaro).
Abstract
Objective: To describe the growth of Better Together: Partnering with Families, a campaign launched in 2014 to eliminate restrictive hospital visiting policies and to put in place policies that recognize families as partners in care, and to discuss the processes involved in implementing the initiative in a large, integrated health system.
Methods: Descriptive report.
Results: In June 2014, the Institute for Patient- and Family-Centered Care (IPFCC) launched the Better Together campaign to emphasize the importance of family presence and participation to the quality, experience, safety, and outcomes of care. Since then, this initiative has expanded in both the United States and Canada. With support from 2 funders in the United States, special attention was focused on acute care hospitals across New York State. Nearly 50 hospitals participated in 2 separate but related projects. Fifteen of the hospitals are part of Northwell Health, New York State’s largest health system. Over a 10-month period, these hospitals made significant progress in changing policy, practice, and communication to support family presence.
Conclusion: The Better Together initiative was implemented across a health system with strong support from leadership and the involvement of patient and family advisors. An intervention offering structured training, coaching, and resources, like IPFCC’s Better Together initiative, can facilitate the change process.
Keywords: family presence; visiting policies; patient-centered care; family-centered care; patient experience.
The presence of families at the bedside of patients is often restricted by hospital visiting hours. Hospitals that maintain these restrictive policies cite concerns about negative impacts on security, infection control, privacy, and staff workload. But there are no data to support these concerns, and the experience of hospitals that have successfully changed policy and practice to welcome families demonstrates the potential positive impacts of less restrictive policies on patient care and outcomes.1 For example, hospitalization can lead to reduced cognitive function in elderly patients. Family members would recognize the changes and could provide valuable information to hospital staff, potentially improving outcomes.2
In June 2014, the Institute for Patient- and Family-Centered Care (IPFCC) launched the campaign Better Together: Partnering with Families.3 The campaign is is grounded in patient- and family- centered care, an approach to care that supports partnerships among health care providers, patients, and families, and, among other core principles, advocates that patients define their “families” and how they will participate in care and decision-making.
Emphasizing the importance of family presence and participation to quality and safety, the Better Together campaign seeks to eliminate restrictive visiting policies and calls upon hospitals to include families as members of the care team and to welcome them 24 hours a day, 7 days a week, according to patient preference. As part of the campaign, IPFCC developed an extensive toolkit of resources that is available to hospitals and other organizations at no cost. The resources include sample policies; profiles of hospitals that have implemented family presence policies; educational materials for staff, patients, and families; and a template for hospital websites. This article, a follow-up to an article published in the January 2015 issue of JCOM,1 discusses the growth of the Better Together initiative as well as the processes involved in implementing the initiative across a large health system.
Growth of the Initiative
Since its launch in 2014, the Better Together initiative has continued to expand in the United States and Canada. In Canada, under the leadership of the Canadian Foundation for Healthcare Improvement (CFHI), more than 50 organizations have made a commitment to the Better Together program and family presence.4 Utilizing and adapting IPFCC’s Toolkit, CFHI developed a change package of free resources for Canadian organizations.5 Some of the materials, including the Pocket Guide for Families (Manuel des Familles), were translated into French.6
With support from 2 funders in the United States, the United Hospital Fund and the New York State Health (NYSHealth) Foundation, through a subcontract with the New York Public Interest Research Group (NYPIRG), IPFCC has been able to focus on hospitals in New York City, including public hospitals, and, more broadly, acute care hospitals across New York State. Nearly 50 hospitals participated in these 2 separate but related projects.
Education and Support for New York City Hospitals
Supported by the United Hospital Fund, an 18-month project that focused specifically on New York City hospitals was completed in June 2017. The project began with a 1-day intensive training event with representatives of 21 hospitals. Eighteen of those hospitals were eligible to participate in follow-up consultation provided by IPFCC, and 14 participated in some kind of follow-up. NYC Health + Hospitals (H+H), the system of public hospitals in NYC, participated most fully in these activities.
The outcomes of the Better Together initiative in New York City are summarized in the report Sick, Scared, & Separated From Loved Ones,2 which is based on a pre/post review of hospital visitation/family presence policies and website communications. According to the report, hospitals that participated in the IPFCC training and consultation program performed better, as a group, with respect to improved policy and website scores on post review than those that did not. Of the 10 hospitals whose scores improved during the review period, 8 had participated in the IPFCC training and 1 hospital was part of a hospital network that did so. (Six of these hospitals are part of the H+H public hospital system.) Those 9 hospitals saw an average increase in scores of 4.9 points (out of a possible 11).
A Learning Community for Hospitals in New York State
With support from the NYSHealth Foundation, IPFCC again collaborated with NYPIRG and New Yorkers for Patient & Family Empowerment on a 2-year initiative, completed in November 2019, that involved 26 hospitals: 15 from Northwell Health, New York State’s largest health system, and 11 hospitals from health systems throughout the state (Greater Hudson Valley Health System, now Garnet Health; Mohawk Valley Health System; Rochester Regional Health; and University of Vermont Health Network). An update of the report Sick, Scared, & Separated From Loved Onescompared pre/post reviews of policies and website communications regarding hospital visitation/family presence.7 Its findings confirm that hospitals that participated in the Better Together Learning Community improved both their policy and website scores to a greater degree than hospitals that did not participate and that a planned intervention can help facilitate change.
During the survey period, 28 out of 40 hospitals’ website navigability scores improved. Of those, hospitals that did not participate in the Better Together Learning Community saw an average increase in scores of 1.2 points, out of a possible 11, while the participating hospitals saw an average increase of 2.7 points, with the top 5 largest increases in scores belonging to hospitals that participated in the Better Together Learning Community.7
The Northwell Health Experience
Northwell Health is a large integrated health care organization comprising more than 69,000 employees, 23 hospitals, and more than 750 medical practices, located geographically across New York State. Embracing patient- and family-centered care, Northwell is dedicated to improving the quality, experience, and safety of care for patients and their families. Welcoming and including patients, families, and care partners as members of the health care team has always been a core element of Northwell’s organizational goal of providing world-class patient care and experience.
Four years ago, the organization reorganized and formalized a system-wide Patient & Family Partnership Council (PFPC).8 Representatives on the PFPC include a Northwell patient experience leader and patient/family co-chair from local councils that have been established in nearly all 23 hospitals as well as service lines. Modeling partnership, the PFPC is grounded in listening to the “voice” of patients and families and promoting collaboration, with the goal of driving change across varied aspects and experiences of health care delivery.
Through the Office of Patient and Customer Experience (OPCE), a partnership with IPFCC and the Better Together Learning Community for Hospitals in New York State was initiated as a fundamental next step in Northwell’s journey to enhance system-wide family presence and participation. Results from Better Together’s Organizational Self-Assessment Tool and process identified opportunities to influence 3 distinct areas: policy/staff education, position descriptions/performance management, and website/signage. Over a 10-month period (September 2018 through June 2019), 15 Northwell hospitals implemened significant patient- and family-centered improvements through multifaceted shared work teams (SWT) that partnered around the common goal of supporting the patient and family experience (Figure). Northwell’s SWT structure allowed teams to meet individually on specific tasks, led by a dedicated staff member of the OPCE to ensure progress, support, and accountability. Six monthly coaching calls or report-out meetings were attended by participating teams, where feedback and recommendations shared by IPFCC were discussed in order to maintain momentum and results.
Policy/Staff Education
The policy/staff education SWT focused on appraising and updating existing policies to ensure alignment with key patient- and family-centered concepts and Better Together principles (Table 1). By establishing representation on the System Policy and Procedure Committee, OPCE enabled patients and families to have a voice at the decision-making table. OPCE leaders presented the ideology and scope of the transformation to this committee. After reviewing all system-wide policies, 4 were identified as key opportunities for revision. One overarching policy titled “Visitation Guidelines” was reviewed and updated to reflect Northwell’s mission of patient- and family-centered care, retiring the reference to “families” as “visitors” in definitions, incorporating language of inclusion and partnership, and citing other related policies. The policy was vetted through a multilayer process of review and stakeholder feedback and was ultimately approved at a system
Three additional related policies were also updated to reflect core principles of inclusion and partnership. These included system policies focused on discharge planning; identification of health care proxy, agent, support person and caregiver; and standards of behavior not conducive in a health care setting. As a result of this work, OPCE was invited to remain an active member of the System Policy and Procedure Committee, adding meaningful new perspectives to the clinical and administrative policy management process. Once policies were updated and approved, the SWT focused on educating leaders and teams. Using a diversified strategy, education was provided through various modes, including weekly system-wide internal communication channels, patient experience huddle messages, yearly mandatory topics training, and the incorporation of essential concepts in existing educational courses (classroom and e-learning modalities).
Position Descriptions/Performance Management
The position descriptions/performance management SWT focused its efforts on incorporating patient- and family-centered concepts and language into position descriptions and the performance appraisal process (Table 2). Due to the complex nature of this work, the process required collaboration from key subject matter experts in human resources, talent management, corporate compensation, and labor management. In 2019, Northwell began an initiative focused on streamlining and standardizing job titles, roles, and developmental pathways across the system. The overarching goal was to create system-wide consistency and standardization. The SWT was successful in advising the leaders overseeing this job architecture initiative on the importance of including language of patient- and family-centered care, like partnership and collaboration, and of highlighting the critical role of family members as part of the care team in subsequent documents.
Northwell has 6 behavioral expectations, standards to which all team members are held accountable: Patient/Customer Focus, Teamwork, Execution, Organizational Awareness, Enable Change, and Develop Self. As a result of the SWT’s work, Patient/Customer Focus was revised to include “families” as essential care partners, demonstrating Northwell’s ongoing commitment to honoring the role of families as members of the care team. It also ensures that all employees are aligned around this priority, as these expectations are utilized to support areas such as recognition and performance. Collaborating with talent management and organizational development, the SWT reviewed yearly performance management and new-hire evaluations. In doing so, they identified an opportunity to refresh the anchored qualitative rating scales to include behavioral demonstrations of patient- and family-centered care, collaboration, respect, and partnership with family members.
Website/Signage
Websites make an important first impression on patients and families looking for information to best prepare for a hospital experience. Therefore, the website/signage SWT worked to redesign hospital websites, enhance digital signage, and perform a baseline assessment of physical signage across facilities. Initial feedback on Northwell’s websites identified opportunities to include more patient- and family-centered, care-partner-infused language; improve navigation; and streamline click levels for easier access. Content for the websites was carefully crafted in collaboration with Northwell’s internal web team, utilizing IPFCC’s best practice standards as a framework and guide.
Next, a multidisciplinary website shared-governance team was established by the OPCE to ensure that key stakeholders were represented and had the opportunity to review and make recommendations for appropriate language and messaging about family presence and participation. This 13-person team was comprised of patient/family partners, patient-experience culture leaders, quality, compliance, human resources, policy, a chief nursing officer, a medical director, and representation from the Institute for Nursing. After careful review and consideration from Northwell’s family partners and teams, all participating hospital websites were enhanced as of June 2019 to include prominent 1-click access from homepages to information for “patients, families and visitors,” as well as “your care partners” information on the important role of families and care partners.
Along with refreshing websites, another step in Northwell’s work to strengthen messaging about family presence and participation was to partner and collaborate with the system’s digital web team as well as local facility councils to understand the capacity to adjust digital signage across facilities. Opportunities were found to make simple yet effective enhancements to the language and imagery of digital signage upon entry, creating a warmer and more welcoming first impression for patients and families. With patient and family partner feedback, the team designed digital signage with inclusive messaging and images that would circulate appropriately based on the facility. Signage specifically welcomes families and refers to them as members of patients’ care teams.
Northwell’s website/signage SWT also directed a 2-phase physical signage assessment to determine ongoing opportunities to alter signs in areas that particularly impact patients and families, such as emergency departments, main lobbies, cafeterias, surgical waiting areas, and intensive care units. Each hospital’s local PFPC did a “walk-about”9 to make enhancements to physical signage, such as removing paper and overcrowded signs, adjusting negative language, ensuring alignment with brand guidelines, and including language that welcomed families. As a result of the team’s efforts around signage, collaboration began with the health system’s signage committee to help standardize signage terminology to reflect family inclusiveness, and to implement the recommendation for a standardized signage shared-governance team to ensure accountability and a patient- and family-centered structure.
Sustainment
Since implementing Better Together, Northwell has been able to infuse a more patient- and family-centered emphasis into its overall patient experience message of “Every role, every person, every moment matters.” As a strategic tool aimed at encouraging leaders, clinicians, and staff to pause and reflect about the “heart” of their work, patient and family stories are now included at the beginning of meetings, forums, and team huddles. Elements of the initiative have been integrated in current Patient and Family Partnership sustainment plans at participating hospitals. Some highlights include continued integration of patient/family partners on committees and councils that impact areas such as way finding, signage, recruitment, new-hire orientation, and community outreach; focus on enhancing partner retention and development programs; and inclusion of patient- and family-centered care and Better Together principles in ongoing leadership meetings.
Factors Contributing to Success
Health care is a complex, regulated, and often bureaucratic world that can be very difficult for patients and families to navigate. The system’s partnership with the Better Together Learning Community for Hospitals in New York State enhanced its efforts to improve family presence and participation and created powerful synergy. The success of this partnership was based on a number of important factors:
A solid foundation of support, structure, and accountability. The OPCE initiated the IPFCC Better Together partnership and established a synergistic collaboration inclusive of leadership, frontline teams, multiple departments, and patient and family partners. As a major strategic component of Northwell’s mission to deliver high-quality, patient- and family-centered care, OPCE was instrumental in connecting key areas and stakeholders and mobilizing the recommendations coming from patients and families.
A visible commitment of leadership at all levels. Partnering with leadership across Northwell’s system required a delineated vision, clear purpose and ownership, and comprehensive implementation and sustainment strategies. The existing format of Northwell’s PFPC provided the structure and framework needed for engaged patient and family input; the OPCE motivated and organized key areas of involvement and led communication efforts across the organization. The IPFCC coaching calls provided the underlying guidance and accountability needed to sustain momentum. As leadership and frontline teams became aware of the vision, they understood the larger connection to the system’s purpose, which ultimately created a clear path for positive change.
Meaningful involvement and input of patient and family partners. Throughout this project, Northwell’s patient/family partners were involved through the PFPC and local councils. For example, patient/family partners attended every IPFCC coaching call; members had a central voice in every decision made within each SWT; and local PFPCs actively participated in physical signage “walk-abouts” across facilities, making key recommendations for improvement. This multifaceted, supportive collaboration created a rejuvenated and purposeful focus for all council members involved. Some of their reactions include, “…I am so happy to be able to help other families in crisis, so that they don’t have to be alone, like I was,” and “I feel how important the patient and family’s voice is … it’s truly a partnership between patients, families, and staff.”
Regular access to IPFCC as a best practice coach and expert resource. Throughout the 10-month process, IPFCC’s Better Together Learning Community for Hospitals in New York State provided ongoing learning interventions for members of the SWT; multiple and varied resources from the Better Together toolkit for adaptation; and opportunities to share and reinforce new, learned expertise with colleagues within the Northwell Health system and beyond through IPFCC’s free online learning community, PFCC.Connect.
Conclusion
Family presence and participation are important to the quality, experience, safety, and outcomes of care. IPFCC’s campaign, Better Together: Partnering with Families, encourages hospitals to change restrictive visiting policies and, instead, to welcome families and caregivers 24 hours a day.
Two projects within Better Together involving almost 50 acute care hospitals in New York State confirm that change in policy, practice, and communication is particularly effective when implemented with strong support from leadership. An intervention like the Better Together Learning Community, offering structured training, coaching, and resources, can facilitate the change process.
Corresponding author: IPFCC, Deborah L. Dokken, 6917 Arlington Rd., Ste. 309, Bethesda, MD 20814; ddokken@ipfcc.org.
Funding disclosures: None.
From the Institute for Patient- and Family-Centered Care, Bethesda, MD (Ms. Dokken and Ms. Johnson), and Northwell Health, New Hyde Park, NY (Dr. Barden, Ms. Tuomey, and Ms. Giammarinaro).
Abstract
Objective: To describe the growth of Better Together: Partnering with Families, a campaign launched in 2014 to eliminate restrictive hospital visiting policies and to put in place policies that recognize families as partners in care, and to discuss the processes involved in implementing the initiative in a large, integrated health system.
Methods: Descriptive report.
Results: In June 2014, the Institute for Patient- and Family-Centered Care (IPFCC) launched the Better Together campaign to emphasize the importance of family presence and participation to the quality, experience, safety, and outcomes of care. Since then, this initiative has expanded in both the United States and Canada. With support from 2 funders in the United States, special attention was focused on acute care hospitals across New York State. Nearly 50 hospitals participated in 2 separate but related projects. Fifteen of the hospitals are part of Northwell Health, New York State’s largest health system. Over a 10-month period, these hospitals made significant progress in changing policy, practice, and communication to support family presence.
Conclusion: The Better Together initiative was implemented across a health system with strong support from leadership and the involvement of patient and family advisors. An intervention offering structured training, coaching, and resources, like IPFCC’s Better Together initiative, can facilitate the change process.
Keywords: family presence; visiting policies; patient-centered care; family-centered care; patient experience.
The presence of families at the bedside of patients is often restricted by hospital visiting hours. Hospitals that maintain these restrictive policies cite concerns about negative impacts on security, infection control, privacy, and staff workload. But there are no data to support these concerns, and the experience of hospitals that have successfully changed policy and practice to welcome families demonstrates the potential positive impacts of less restrictive policies on patient care and outcomes.1 For example, hospitalization can lead to reduced cognitive function in elderly patients. Family members would recognize the changes and could provide valuable information to hospital staff, potentially improving outcomes.2
In June 2014, the Institute for Patient- and Family-Centered Care (IPFCC) launched the campaign Better Together: Partnering with Families.3 The campaign is is grounded in patient- and family- centered care, an approach to care that supports partnerships among health care providers, patients, and families, and, among other core principles, advocates that patients define their “families” and how they will participate in care and decision-making.
Emphasizing the importance of family presence and participation to quality and safety, the Better Together campaign seeks to eliminate restrictive visiting policies and calls upon hospitals to include families as members of the care team and to welcome them 24 hours a day, 7 days a week, according to patient preference. As part of the campaign, IPFCC developed an extensive toolkit of resources that is available to hospitals and other organizations at no cost. The resources include sample policies; profiles of hospitals that have implemented family presence policies; educational materials for staff, patients, and families; and a template for hospital websites. This article, a follow-up to an article published in the January 2015 issue of JCOM,1 discusses the growth of the Better Together initiative as well as the processes involved in implementing the initiative across a large health system.
Growth of the Initiative
Since its launch in 2014, the Better Together initiative has continued to expand in the United States and Canada. In Canada, under the leadership of the Canadian Foundation for Healthcare Improvement (CFHI), more than 50 organizations have made a commitment to the Better Together program and family presence.4 Utilizing and adapting IPFCC’s Toolkit, CFHI developed a change package of free resources for Canadian organizations.5 Some of the materials, including the Pocket Guide for Families (Manuel des Familles), were translated into French.6
With support from 2 funders in the United States, the United Hospital Fund and the New York State Health (NYSHealth) Foundation, through a subcontract with the New York Public Interest Research Group (NYPIRG), IPFCC has been able to focus on hospitals in New York City, including public hospitals, and, more broadly, acute care hospitals across New York State. Nearly 50 hospitals participated in these 2 separate but related projects.
Education and Support for New York City Hospitals
Supported by the United Hospital Fund, an 18-month project that focused specifically on New York City hospitals was completed in June 2017. The project began with a 1-day intensive training event with representatives of 21 hospitals. Eighteen of those hospitals were eligible to participate in follow-up consultation provided by IPFCC, and 14 participated in some kind of follow-up. NYC Health + Hospitals (H+H), the system of public hospitals in NYC, participated most fully in these activities.
The outcomes of the Better Together initiative in New York City are summarized in the report Sick, Scared, & Separated From Loved Ones,2 which is based on a pre/post review of hospital visitation/family presence policies and website communications. According to the report, hospitals that participated in the IPFCC training and consultation program performed better, as a group, with respect to improved policy and website scores on post review than those that did not. Of the 10 hospitals whose scores improved during the review period, 8 had participated in the IPFCC training and 1 hospital was part of a hospital network that did so. (Six of these hospitals are part of the H+H public hospital system.) Those 9 hospitals saw an average increase in scores of 4.9 points (out of a possible 11).
A Learning Community for Hospitals in New York State
With support from the NYSHealth Foundation, IPFCC again collaborated with NYPIRG and New Yorkers for Patient & Family Empowerment on a 2-year initiative, completed in November 2019, that involved 26 hospitals: 15 from Northwell Health, New York State’s largest health system, and 11 hospitals from health systems throughout the state (Greater Hudson Valley Health System, now Garnet Health; Mohawk Valley Health System; Rochester Regional Health; and University of Vermont Health Network). An update of the report Sick, Scared, & Separated From Loved Onescompared pre/post reviews of policies and website communications regarding hospital visitation/family presence.7 Its findings confirm that hospitals that participated in the Better Together Learning Community improved both their policy and website scores to a greater degree than hospitals that did not participate and that a planned intervention can help facilitate change.
During the survey period, 28 out of 40 hospitals’ website navigability scores improved. Of those, hospitals that did not participate in the Better Together Learning Community saw an average increase in scores of 1.2 points, out of a possible 11, while the participating hospitals saw an average increase of 2.7 points, with the top 5 largest increases in scores belonging to hospitals that participated in the Better Together Learning Community.7
The Northwell Health Experience
Northwell Health is a large integrated health care organization comprising more than 69,000 employees, 23 hospitals, and more than 750 medical practices, located geographically across New York State. Embracing patient- and family-centered care, Northwell is dedicated to improving the quality, experience, and safety of care for patients and their families. Welcoming and including patients, families, and care partners as members of the health care team has always been a core element of Northwell’s organizational goal of providing world-class patient care and experience.
Four years ago, the organization reorganized and formalized a system-wide Patient & Family Partnership Council (PFPC).8 Representatives on the PFPC include a Northwell patient experience leader and patient/family co-chair from local councils that have been established in nearly all 23 hospitals as well as service lines. Modeling partnership, the PFPC is grounded in listening to the “voice” of patients and families and promoting collaboration, with the goal of driving change across varied aspects and experiences of health care delivery.
Through the Office of Patient and Customer Experience (OPCE), a partnership with IPFCC and the Better Together Learning Community for Hospitals in New York State was initiated as a fundamental next step in Northwell’s journey to enhance system-wide family presence and participation. Results from Better Together’s Organizational Self-Assessment Tool and process identified opportunities to influence 3 distinct areas: policy/staff education, position descriptions/performance management, and website/signage. Over a 10-month period (September 2018 through June 2019), 15 Northwell hospitals implemened significant patient- and family-centered improvements through multifaceted shared work teams (SWT) that partnered around the common goal of supporting the patient and family experience (Figure). Northwell’s SWT structure allowed teams to meet individually on specific tasks, led by a dedicated staff member of the OPCE to ensure progress, support, and accountability. Six monthly coaching calls or report-out meetings were attended by participating teams, where feedback and recommendations shared by IPFCC were discussed in order to maintain momentum and results.
Policy/Staff Education
The policy/staff education SWT focused on appraising and updating existing policies to ensure alignment with key patient- and family-centered concepts and Better Together principles (Table 1). By establishing representation on the System Policy and Procedure Committee, OPCE enabled patients and families to have a voice at the decision-making table. OPCE leaders presented the ideology and scope of the transformation to this committee. After reviewing all system-wide policies, 4 were identified as key opportunities for revision. One overarching policy titled “Visitation Guidelines” was reviewed and updated to reflect Northwell’s mission of patient- and family-centered care, retiring the reference to “families” as “visitors” in definitions, incorporating language of inclusion and partnership, and citing other related policies. The policy was vetted through a multilayer process of review and stakeholder feedback and was ultimately approved at a system
Three additional related policies were also updated to reflect core principles of inclusion and partnership. These included system policies focused on discharge planning; identification of health care proxy, agent, support person and caregiver; and standards of behavior not conducive in a health care setting. As a result of this work, OPCE was invited to remain an active member of the System Policy and Procedure Committee, adding meaningful new perspectives to the clinical and administrative policy management process. Once policies were updated and approved, the SWT focused on educating leaders and teams. Using a diversified strategy, education was provided through various modes, including weekly system-wide internal communication channels, patient experience huddle messages, yearly mandatory topics training, and the incorporation of essential concepts in existing educational courses (classroom and e-learning modalities).
Position Descriptions/Performance Management
The position descriptions/performance management SWT focused its efforts on incorporating patient- and family-centered concepts and language into position descriptions and the performance appraisal process (Table 2). Due to the complex nature of this work, the process required collaboration from key subject matter experts in human resources, talent management, corporate compensation, and labor management. In 2019, Northwell began an initiative focused on streamlining and standardizing job titles, roles, and developmental pathways across the system. The overarching goal was to create system-wide consistency and standardization. The SWT was successful in advising the leaders overseeing this job architecture initiative on the importance of including language of patient- and family-centered care, like partnership and collaboration, and of highlighting the critical role of family members as part of the care team in subsequent documents.
Northwell has 6 behavioral expectations, standards to which all team members are held accountable: Patient/Customer Focus, Teamwork, Execution, Organizational Awareness, Enable Change, and Develop Self. As a result of the SWT’s work, Patient/Customer Focus was revised to include “families” as essential care partners, demonstrating Northwell’s ongoing commitment to honoring the role of families as members of the care team. It also ensures that all employees are aligned around this priority, as these expectations are utilized to support areas such as recognition and performance. Collaborating with talent management and organizational development, the SWT reviewed yearly performance management and new-hire evaluations. In doing so, they identified an opportunity to refresh the anchored qualitative rating scales to include behavioral demonstrations of patient- and family-centered care, collaboration, respect, and partnership with family members.
Website/Signage
Websites make an important first impression on patients and families looking for information to best prepare for a hospital experience. Therefore, the website/signage SWT worked to redesign hospital websites, enhance digital signage, and perform a baseline assessment of physical signage across facilities. Initial feedback on Northwell’s websites identified opportunities to include more patient- and family-centered, care-partner-infused language; improve navigation; and streamline click levels for easier access. Content for the websites was carefully crafted in collaboration with Northwell’s internal web team, utilizing IPFCC’s best practice standards as a framework and guide.
Next, a multidisciplinary website shared-governance team was established by the OPCE to ensure that key stakeholders were represented and had the opportunity to review and make recommendations for appropriate language and messaging about family presence and participation. This 13-person team was comprised of patient/family partners, patient-experience culture leaders, quality, compliance, human resources, policy, a chief nursing officer, a medical director, and representation from the Institute for Nursing. After careful review and consideration from Northwell’s family partners and teams, all participating hospital websites were enhanced as of June 2019 to include prominent 1-click access from homepages to information for “patients, families and visitors,” as well as “your care partners” information on the important role of families and care partners.
Along with refreshing websites, another step in Northwell’s work to strengthen messaging about family presence and participation was to partner and collaborate with the system’s digital web team as well as local facility councils to understand the capacity to adjust digital signage across facilities. Opportunities were found to make simple yet effective enhancements to the language and imagery of digital signage upon entry, creating a warmer and more welcoming first impression for patients and families. With patient and family partner feedback, the team designed digital signage with inclusive messaging and images that would circulate appropriately based on the facility. Signage specifically welcomes families and refers to them as members of patients’ care teams.
Northwell’s website/signage SWT also directed a 2-phase physical signage assessment to determine ongoing opportunities to alter signs in areas that particularly impact patients and families, such as emergency departments, main lobbies, cafeterias, surgical waiting areas, and intensive care units. Each hospital’s local PFPC did a “walk-about”9 to make enhancements to physical signage, such as removing paper and overcrowded signs, adjusting negative language, ensuring alignment with brand guidelines, and including language that welcomed families. As a result of the team’s efforts around signage, collaboration began with the health system’s signage committee to help standardize signage terminology to reflect family inclusiveness, and to implement the recommendation for a standardized signage shared-governance team to ensure accountability and a patient- and family-centered structure.
Sustainment
Since implementing Better Together, Northwell has been able to infuse a more patient- and family-centered emphasis into its overall patient experience message of “Every role, every person, every moment matters.” As a strategic tool aimed at encouraging leaders, clinicians, and staff to pause and reflect about the “heart” of their work, patient and family stories are now included at the beginning of meetings, forums, and team huddles. Elements of the initiative have been integrated in current Patient and Family Partnership sustainment plans at participating hospitals. Some highlights include continued integration of patient/family partners on committees and councils that impact areas such as way finding, signage, recruitment, new-hire orientation, and community outreach; focus on enhancing partner retention and development programs; and inclusion of patient- and family-centered care and Better Together principles in ongoing leadership meetings.
Factors Contributing to Success
Health care is a complex, regulated, and often bureaucratic world that can be very difficult for patients and families to navigate. The system’s partnership with the Better Together Learning Community for Hospitals in New York State enhanced its efforts to improve family presence and participation and created powerful synergy. The success of this partnership was based on a number of important factors:
A solid foundation of support, structure, and accountability. The OPCE initiated the IPFCC Better Together partnership and established a synergistic collaboration inclusive of leadership, frontline teams, multiple departments, and patient and family partners. As a major strategic component of Northwell’s mission to deliver high-quality, patient- and family-centered care, OPCE was instrumental in connecting key areas and stakeholders and mobilizing the recommendations coming from patients and families.
A visible commitment of leadership at all levels. Partnering with leadership across Northwell’s system required a delineated vision, clear purpose and ownership, and comprehensive implementation and sustainment strategies. The existing format of Northwell’s PFPC provided the structure and framework needed for engaged patient and family input; the OPCE motivated and organized key areas of involvement and led communication efforts across the organization. The IPFCC coaching calls provided the underlying guidance and accountability needed to sustain momentum. As leadership and frontline teams became aware of the vision, they understood the larger connection to the system’s purpose, which ultimately created a clear path for positive change.
Meaningful involvement and input of patient and family partners. Throughout this project, Northwell’s patient/family partners were involved through the PFPC and local councils. For example, patient/family partners attended every IPFCC coaching call; members had a central voice in every decision made within each SWT; and local PFPCs actively participated in physical signage “walk-abouts” across facilities, making key recommendations for improvement. This multifaceted, supportive collaboration created a rejuvenated and purposeful focus for all council members involved. Some of their reactions include, “…I am so happy to be able to help other families in crisis, so that they don’t have to be alone, like I was,” and “I feel how important the patient and family’s voice is … it’s truly a partnership between patients, families, and staff.”
Regular access to IPFCC as a best practice coach and expert resource. Throughout the 10-month process, IPFCC’s Better Together Learning Community for Hospitals in New York State provided ongoing learning interventions for members of the SWT; multiple and varied resources from the Better Together toolkit for adaptation; and opportunities to share and reinforce new, learned expertise with colleagues within the Northwell Health system and beyond through IPFCC’s free online learning community, PFCC.Connect.
Conclusion
Family presence and participation are important to the quality, experience, safety, and outcomes of care. IPFCC’s campaign, Better Together: Partnering with Families, encourages hospitals to change restrictive visiting policies and, instead, to welcome families and caregivers 24 hours a day.
Two projects within Better Together involving almost 50 acute care hospitals in New York State confirm that change in policy, practice, and communication is particularly effective when implemented with strong support from leadership. An intervention like the Better Together Learning Community, offering structured training, coaching, and resources, can facilitate the change process.
Corresponding author: IPFCC, Deborah L. Dokken, 6917 Arlington Rd., Ste. 309, Bethesda, MD 20814; ddokken@ipfcc.org.
Funding disclosures: None.
1. Dokken DL, Kaufman J, Johnson BJ et al. Changing hospital visiting policies: from families as “visitors” to families as partners. J Clin Outcomes Manag. 2015; 22:29-36.
2. New York Public Interest Research Group and New Yorkers for Patient & Family Empowerment. Sick, scared and separated from loved ones. third edition: A pathway to improvement in New York City. New York: NYPIRG: 2018. www.nypirg.org/pubs/201801/NYPIRG_SICK_SCARED_FINAL.pdf. Accessed December 12, 2019.
3. Institute for Patient- and Family-Centered Care. Better Together: Partnering with Families. www.ipfcc.org/bestpractices/better-together.html. Accessed December 12, 2019.
4. Canadian Foundation for Healthcare Improvement. Better Together. www.cfhi-fcass.ca/WhatWeDo/better-together. Accessed December 12, 2019.
5. Canadian Foundation for Healthcare Improvement. Better Together: A change package to support the adoption of family presence and participation in acute care hospitals and accelerate healthcare improvement. www.cfhi-fcass.ca/sf-docs/default-source/patient-engagement/better-together-change-package.pdf?sfvrsn=9656d044_4. Accessed December 12, 2019.
6. Canadian Foundation for Healthcare Improvement. L’Objectif santé: main dans la main avec les familles. www.cfhi-fcass.ca/sf-docs/default-source/patient-engagement/families-pocket-screen_fr.pdf. Accessed December 12, 2019.
7. New York Public Interest Research Group and New Yorkers for Patient & Family Empowerment. Sick, scared and separated from loved ones. fourth edition: A pathway to improvement in New York. New York: NYPIRG: 2019. www.nypirg.org/pubs/201911/Sick_Scared_Separated_2019_web_FINAL.pdf. Accessed December 12, 2019.
8. Northwell Health. Patient and Family Partnership Councils. www.northwell.edu/about/commitment-to-excellence/patient-and-customer-experience/care-delivery-hospitality. Accessed December 12, 2019.
9 . Institute for Patient- and Family-Centered Care. How to conduct a “walk-about” from the patient and family perspective. www.ipfcc.org/resources/How_To_Conduct_A_Walk-About.pdf. Accessed December 12, 2019.
1. Dokken DL, Kaufman J, Johnson BJ et al. Changing hospital visiting policies: from families as “visitors” to families as partners. J Clin Outcomes Manag. 2015; 22:29-36.
2. New York Public Interest Research Group and New Yorkers for Patient & Family Empowerment. Sick, scared and separated from loved ones. third edition: A pathway to improvement in New York City. New York: NYPIRG: 2018. www.nypirg.org/pubs/201801/NYPIRG_SICK_SCARED_FINAL.pdf. Accessed December 12, 2019.
3. Institute for Patient- and Family-Centered Care. Better Together: Partnering with Families. www.ipfcc.org/bestpractices/better-together.html. Accessed December 12, 2019.
4. Canadian Foundation for Healthcare Improvement. Better Together. www.cfhi-fcass.ca/WhatWeDo/better-together. Accessed December 12, 2019.
5. Canadian Foundation for Healthcare Improvement. Better Together: A change package to support the adoption of family presence and participation in acute care hospitals and accelerate healthcare improvement. www.cfhi-fcass.ca/sf-docs/default-source/patient-engagement/better-together-change-package.pdf?sfvrsn=9656d044_4. Accessed December 12, 2019.
6. Canadian Foundation for Healthcare Improvement. L’Objectif santé: main dans la main avec les familles. www.cfhi-fcass.ca/sf-docs/default-source/patient-engagement/families-pocket-screen_fr.pdf. Accessed December 12, 2019.
7. New York Public Interest Research Group and New Yorkers for Patient & Family Empowerment. Sick, scared and separated from loved ones. fourth edition: A pathway to improvement in New York. New York: NYPIRG: 2019. www.nypirg.org/pubs/201911/Sick_Scared_Separated_2019_web_FINAL.pdf. Accessed December 12, 2019.
8. Northwell Health. Patient and Family Partnership Councils. www.northwell.edu/about/commitment-to-excellence/patient-and-customer-experience/care-delivery-hospitality. Accessed December 12, 2019.
9 . Institute for Patient- and Family-Centered Care. How to conduct a “walk-about” from the patient and family perspective. www.ipfcc.org/resources/How_To_Conduct_A_Walk-About.pdf. Accessed December 12, 2019.
Changing Hospital Visiting Policies: From Families as “Visitors” to Families as Partners
From the Institute for Patient- and Family-Centered Care, Bethesda, MD (Ms. Dokken, Ms. Kaufman, and Ms. Johnson), Anne Arundel Medical Center, Annapolis, MD (Dr. Perkins), Contra Costa Regional Medical Center & Health Centers, Martinez, CA (Ms. Benepal, Ms. Roth, and Vidant Health, Greenville, NC (Ms. Dutton and Ms. Jones).
Abstract
- Objective: To describe a campaign to eliminate restrictive hospital visiting policies and to put in place policies that recognize families as partners in care.
- Methods: Descriptive report.
- Results: Many hospitals still have “visiting” hours that limit family presence, often counter to patient preferences. To change the concept of families as visitors and eliminate restrictive hospital visiting policies, the Institute for Patient- and Family-Centered Care (IPFCC) launched the campaign Better Together: Partnering with Families, calling on all hospitals to welcome families 24 hours a day and transform their policies and approaches to care so that patients’ families and loved ones are included in care and decision making, according to patient preferences. As part of the campaign, IPFCC recognized 12 hospitals that exemplify success in eliminating restrictive visiting policies and have changed the concept of families from “visitors” to partners. Leaders at these hospitals attest to the benefits of the changes through improved experience of care and other outcomes. Three exemplar hospitals are highlighted in this article and share their processes of change as well as key learnings and outcomes.
- Conclusion: Hospital policies and practices that encourage and support families as partners in care are essential to patients’ health, well-being, and safety.
Many families are restricted from the bedsides of loved ones because of hospital visiting policies [1–3]. Restrictive policies are often based on long-held beliefs that the presence and participation of families interferes with care, exhausts patients, is a burden to families, spreads infection, or violates HIPAA. However, there is no evidence to support those beliefs. In fact, isolating patients at their most vulnerable time from the people who know them best places them at risk for medical error, emotional harm, inconsistencies in care, and lack of preparedness for transitions in care [4,5]. Jackie Gruzenski’s story “Behind a Locked Door” (printed below) affectingly describes the impact of restrictive policies on a couple's last days.
Fortunately, a growing number of hospitals are lifting these restrictions. But opening the door is not enough. Hospitals need to change the concept of families as “visitors” to families as partners in care. Changing policies is a foundational step in creating a patient- and family-centered culture where families are recognized as essential to patients’ health and well-being and where they are respected as allies for quality and safety.
In response to this critical need for change, in June 2014 the Institute for Patient- and Family-Centered Care (IPFCC) launched the campaign Better Together: Partnering with Families. IPFCC, founded in 1992, is a nonprofit organization that provides essential leadership to advance the understanding and practice of patient- and family-centered care [6]. Emphasizing the importance of family presence and participation to quality and safety, the campaign seeks to eliminate restrictive “visiting” policies and calls upon hospitals to include families as members of the care team and to welcome them 24 hours a day, 7 days a week, according to patient preference [7]. The goal of the campaign is to change visiting policies in 1000 hospitals by 2017. Partnering with IPFCC in this initiative are the American Society for Healthcare Risk Management, American Association of Critical Care Nurses, National Partnership for Women & Families, New Yorkers for Patient and Family Empowerment, Health In Aging Foundation, and the Canadian Foundation for Healthcare Improvement.
Anne Arundel Medical Center
A regional not-for-profit hospital founded in 1902, Anne Arundel Medical Center in Annapolis, MD, provides acute inpatient and outpatient care to residents of 4 counties in Maryland. A 380-bed facility, Anne Arundel has a cancer institute, heart and vascular institute, joint center, spine center, and a women’s and children’s center. In April 2011, the hospital completed a $424 million expansion project, which included a pediatric emergency room, an expanded general emergency room, 50 new patient beds, and 8 new operating rooms.
In 2010, based on a desire to concretely implement the principles of patient- and family-centered care, leaders at Anne Arundel began working with patient and family advisors and initiated a process to change the hospital’s restrictive visiting policy. Now, there are no restrictions on family presence anywhere in the hospital, from ICUs to medical/surgical units to other clinical areas. Patients have the power to choose who they want to stay with them—24 hours a day, 7 days a week. According to Anne Arundel’s policy, each patient determines who is defined as “family.” A “Revisiting Visiting” task force, comprising support staff, providers, and patient and family advisors, worked for 9 months to develop the new family presence policy and support its implementation.
With Anne Arundel leadership encouragement and support, patient and family advisors participated in all phases of the development and implementation of the new family presence policy and in other ways to advance the practice of patient- and family-centered care. The advisors also participated in the process to change the way nurse change of shift report was conducted, and they made recommendations for changes in the directional signs throughout the hospital. New signs, featuring a pineapple (a symbol of hospitality) and the words “Welcome Families” replaced old ones displaying the former restrictive visiting policy.
Supporting patient and family involvement in transitions in care is an integral aspect of implementing family presence policies and practices. Through an “Always Events” grant from the Picker Institute (for information about the Always Events program, see www.ihi.org/Engage/Initiatives/PatientFamilyCenteredCare/Pages/AlwaysEvents.aspx), patient and family advisors, staff, and providers at Anne Arundel developed the SMART discharge protocol, which includes a simple 5-item checklist that is reviewed and discussed with the patient and family prior to discharge. SMART is an acronym for Signs, Medications, Appointments, Results, and Talk. In its work, the SMART team built on current evidence, created urgency and expectation for use with patients, families, and caregivers, disseminated findings, and promoted the protocol as a national standard. The tool is available at www.ihi.org/resources/Pages/Tools/SMARTDischargeProtocol.aspx.
According to Anne Arundel’s COO and CNO, Sherry Perkins, a critical part of the change process was to first understand staff’s fears and then learn what the evidence says. For example, with regard to the impact of additional family presence on infection control, they learned that family presence did not pose additional infection control concerns.
In 2009, there were no patient and family advisors volunteering at Anne Arundel. In 2014, there are approximately 80 advisors. Since 2009, the overall HCAHPS rating of the hospital has gone from 75.4% to 82% (the national average is 70%). While patient satisfaction scores have previously been in the top deciles at Anne Arundel, they have consistently risen since expanding family presence and implementing additional patient- and family-centered strategies.
Contra Costa Regional Medical Center and Health Centers
Contra Costa Health Services in Martinez, CA, includes Contra Costa Regional Medical Center and 10 health centers as part of a comprehensive county health system. Its 164-bed public hospital is dedicated to offering services that are welcoming, accessible, safe and respectful for everyone.
Like many hospitals in the country, for years Contra Costa Regional Medical Center restricted the hours when family members and loved ones could visit patients. However, the hospital’s medical staff often felt uncomfortable that they had to usher family and care partners away from patients when visiting hours were over. Anna Roth, Contra Costa’s CEO, recalls an incident that caused great anguish and contributed to the hospital’s decision to eliminate its restrictive visiting policy. A young boy whose grandfather was in the ICU was denied visitation. The grandfather, who had raised him, passed away, with the two having had no chance to say goodbye. Roth said that the incident hit home for her and the entire staff, and they knew they could do better. “Our old policies treated family members like visitors, until we realized that we are the visitors in people’s lives, not the other way around,” she noted.
In 2012, the hospital established an interdisciplinary team to transform its existing visiting policy into a “welcoming policy.” The team comprised the director of inpatient nursing, the chief of nursing, the chief of security, a public health program specialist, the facilities manager, and a patient partner. The new policy would support family presence 24/7 as well as change the concept of families as “visitors.”
Over the course of a year, the team designed the framework for a 3-day pilot and developed a check-in process to help loved ones gain access to patients after regular hospital hours. Working closely with nursing leadership, front-line staff, patient partners, and security, the team made necessary adjustments to the policy throughout the pilot period. The pilot was well-received and the policy was implemented soon after.
In the policy’s first year, more than 7000 family members and care partners were able to be with their loved ones between 8 pm and 6 am, the time period formerly restricted. The feedback from staff, patients and loved ones has been overwhelmingly positive. Front-line nurses are currently strengthening their skills and confidence in conducting change of shift report at bedside with patients and families. Other “welcoming” measures have also been implemented, including making signage more user-friendly, providing comfortable chairs to sleep in, and installing new vending machines with healthy snacks and drinks.
Vidant Health
Vidant Health serves 1.4 million people in a 29-county region of eastern North Carolina and comprises over 70 primary and specialty physician office practices, a 900-bed academic medical center, 7 community hospitals, an ambulatory surgery center, and home health and hospice services. Vidant Health’s efforts to advance a culture of patient- and family-centered care began in the late 1990s in the James and Connie Maynard Children’s Hospital and the regional rehabilitation center, but this culture did not spread consistently throughout Vidant Health, leading to differing experiences of care for patients and families.
The Vidant Health executive team and senior leaders heard about these inconsistencies firsthand in the spring of 2007 when an employee shared her family’s experiences during her brother’s ICU stay. Christie Odom described how the visitation policy restricted her family’s access to her brother to 15-minute increments, 6 times a day, which led to heightened fear and anxiety for her brother, family, and friends and impeded patient and family engagement in care and decision-making. Odom’s brother died alone with no family by his side. A physical therapist, Odom observed that in the regional rehabilitation center, families were partners in care, yet in the adult ICU, they were visitors.
After hearing Christie’s story, the system’s executive team, board of directors, and physician leaders made a commitment to eliminate these restrictive visitation guidelines. Leaders understood that this would require the organization’s culture to change from viewing patients and families as passive recipients of care to recognizing them as partners. Subsequently, the commitment to patient-family partnerships was imbedded in key documents including the corporation’s strategic and 5-year quality plans. An Office of Patient-Family Experience was established at Vidant Medical Center in 2008 and, a year later, a corporate office was established to guide system transformation. Emphasis was placed on building a solid team of patient-family advisors and staff champions. An initial focus was to replace the restrictive visitation policy with family presence guidelines. A key tenet of these guidelines is that patients define who their family members are and how they should be included in care and decision-making.
This policy and practice change provided the impetus for ongoing evolution of patient-family partnerships. Patient-family advisors are now integrated across the health care system. They serve on performance improvement teams, make safety rounds, serve as faculty in education programs, interview applicants for key positions, and develop and edit patient education materials. The outcomes achieved by this system transformation are evidenced in exceptional HCAHPS performance, significant reductions in serious safety events and hospital acquired infections and national recognition for commitment to patient-family partnerships.
Conclusion
Changing the concept of families as visitors to families as partners in care, according to patient preference, is foundational to advancing the practice of patient- and family-centered care and to building a safe, high-quality, cost-effective system of care. In 2009, Lucian Leape and colleagues envisioned a transformed health care culture in which “the family is respected as part of the care team—never visitors—in every area of the hospital, including the emergency department and the intensive care unit” [8]. A 2014 report by the National Patient Safety Foundation’s Lucian Leape Institute affirmed, “patients and families can play a critical role in preventing medical errors and reducing harm” [9].
Many hospitals still do not encourage family presence and participation and do not embrace the concept of families as true partners in care. But as demonstrated by the actions of the exemplar hospitals described here, it is possible to make this critical culture shift. The exemplar hospitals understand the importance of partnering with patients’ families instead of treating them as outsiders who are interfering in their loved one’s care. These hospitals are proving that giving patients the access they want to their loved ones actually helps themget better.
Through its campaign Better Together: Partnering with Families, IPFCC challenges hospitals across the United States and Canada to pledge to join this important initiative. Now is the time for all hospitals to embrace family presence and participation and to welcome families and other care partners 24 hours a day, 7 days a week.
Hospitals are invited to join this initiative. Steps to begin the change process may be found at www.ipfcc.org/advance/topics/better-together-pledge.html. Also available at IPFCC website is the Better Together toolkit, other materials and information that support the initiative, and a complete list of the exemplar hospitals and their processes and policies. The toolkit includes an organizational self-assessment, sample processes and policies, videos, and guides for families and staff to use in developing partnership. It is available at no charge at www.ipfcc.org/bettertogether/.
Corresponding author: Beverley H. Johnson, 6917 Arlington Rd., Ste. 309, Bethesda, MD 20814, bjohson@ipfcc.org.
Behind a Locked Door
This is our story as I remember it.
One day I came home from work, and my husband was confused. In all the years we’d been married, I’d never known him to be confused. He was sitting in the family room, and he looked frightened.
I said, “Bill, what’s going on?” He said, “Well, I was just going to get up and go look outside for Joey.” I said, “Bill, Joey’s not here.” He insisted, “Oh yes, we just came back from vacation. Joey just went outside, and I was going to check on him.”
I was alarmed and said, “Bill, I think you’re a little confused. I’m concerned because this morning you told me you had a headache. Maybe we should go to the hospital.” He resisted, but I simply told him, “Bill, if something was to happen to you, I might be held responsible because I didn’t do what was in your best interest. We can come home if everything is okay.”
And so we went to the emergency room, where we learned that my husband had a small bleed in his brain. We were told that we needed to go to another hospital that had a neurosurgeon on staff. My husband was transported by ambulance to a hospital about a mile away, and I followed him there in our car.
I want to stop here and tell you a bit about my husband and about myself. My name is Jackie Gruzenski, and I am a nurse involved in the field of psychiatric nursing. My husband’s name was Dr. William Gruzenski. He was a psychiatrist for forty years, and he was a chief medical officer for the last twelve years of his career.
Bill was a very good doctor and a very good husband. And toward the end of his life, he realized that all of his degrees, along with money and material possessions, didn’t matter. They were nothing. He just wanted to have me with him. We loved each other very deeply, and we wanted to share our last days and moments together, but I’m getting ahead of myself.
When we got to the second hospital, my husband was in the emergency room from about 7:00 p.m. until about 6:00 a.m. the next morning. At some point, he started to develop a hypertensive crisis, and the staff could not bring his blood pressure down. They started an IV medication, which required that he be monitored closely in the intensive care unit (ICU).
Of course, I went with him as he was transferred from emergency to ICU. When we got to the ICU door, I was told, “Now, just go into the waiting room. We’re going to settle your husband, and then we’ll come and get you.”
I was a nervous wreck while I waited. I knew my husband had been pretty sick while in emergency. What if he got more confused? What if he lost even this current level of functioning and wouldn’t
remember me? The longer I waited, the more my anxiety grew.
The waiting room was a small area, with chairs around the perimeter, except by the locked door. After an hour with no news, I saw a phone on the wall and called. I said to the voice on the other end, “My name is Mrs. Gruzenski. I was informed that my husband was going to be settled and that someone would come and get me.”
The next thing I knew a young, perky nurse came out, greeted me, and then directed me totally away from my husband, away from the door to the ICU, to a little room. She proceeded to give me the strict policies and procedures for the ICU, including that visitation was allowed only four times a day for thirty minutes each time.
Not believing what I was hearing, I said, “But my husband is going to be worried that I am not with him. We are the center of each other’s lives—we are only apart when we are at work!” Her response was, “Well, you can’t be with him. Those are the rules.”
I lived ten miles away. What was I supposed to do between these widely spaced thirty-minute visits? I felt I had to play by the rules. I was afraid that if I questioned too much or was abrupt with someone, they would treat my husband meanly. And because he was behind a locked door, I would never know.
I didn’t know what else to do and so, shortly before 8:00 a.m., I went home to get some rest. Ironically, just after I got home and started to settle after our long night in the ER, I got a flurry of calls from different residents who wanted information about my husband. They never said, “Come over and visit. He’s missing you.” They called because they needed the information I could give them, but they kept me locked out.
When I was able to have my first visit the next day, my husband asked where I had been. I explained that there were very limited visiting hours. This prompted my husband to speak to his nurse and say, “You know, she’s not a visitor. She’s my wife!” But he was informed that didn’t matter, that there were rules, and that I was a visitor and had to be treated as a visitor.
The rule trumped both of us and what we wanted. The rule meant he had to suffer alone. This was an accredited hospital, but in my view it was archaic. Staff hid behind the rules rather than using their heads and their hearts.
Over the next few days, I saw that my not being there with my husband was leading to more and more distress for him. As he became more ill, he would not allow the nurses to wash him, and he would not eat their food. He was doing everything he could do to get the staff’s attention to revisit the visiting restrictions. If I’d been allowed to stay, I’m sure I could have helped with feeding, with bathing, and with toileting. I’m certain I could have calmed him and helped lower his blood pressure.
I was treated as though I was an enemy, but all I wanted was to be with him, to share the last days of his life. I had always been his anchor. I was the person who navigated the everyday waters of his life. The hospital’s rules meant that he was adrift, and I was lost.
During his hospitalization, he was not afforded the respect he had given to all his patients and the nurses and doctors he had worked with each day. For example, the ICU staff never asked him how he would like to be addressed. They called him “Bill” when he should have been addressed as “Doctor Gruzenski.” He wouldn’t have thought of calling a resident by his first name, and there were only a few people in his life, his inner circle of family and friends, who called him “Bill.”
One day, I actually witnessed one doctor refer to my husband not even as “Bill” but as “Billy.”
I followed this doctor out of the ICU and challenged him saying “Would you think you were valued as a medical professional, and that your life had meant something if, in forty years’ time, someone called you ‘Billy’? ‘Billy’ is what you call some young boy you like, not someone who is sixty-eight years old and is a dignified gentleman and physician.”
My husband earned the title of “Doctor.” He attended four years of medical school, one year of internship, four years as a resident psychiatrist, and he was board certified in psychiatry. He had earned respect by exceeding all the societal standards for being addressed as “Doctor.” These achievements should not be washed away once you are hospitalized. In fact, I believe my husband might have felt a little safer if he had been addressed as “Doctor.”
My husband was in the ICU for eight of the last sixteen days of his life, and there were lots of missed opportunities for us. He wanted me there more than I was allowed. We missed time together we could have had. I feel it was a very cruel thing that was done to us.
We both knew the gravity of his condition, and my husband wanted quality of life, not quantity. I was a large part of the quality he wanted, but I was locked out for the greater part of his last days.
After my husband died, I felt I had to do something so that what happened to us wouldn’t happen to anyone else. I wrote letters to the chief executive officer of the hospital. I wrote to the chief of the medical staff. I wrote to the chief of nursing. And I wrote to the chaplain. The only person I ever heard from was the chaplain. No one apologized or said they would change the rules.
I believe more harm comes when family are not actively involved, and research is proving my belief is sound. And so I will continue to tell my story. I hope that if I tell it enough times, maybe people who write the rules in hospitals will realize that loved ones are advocates, not visitors.
I will never stop advocating for the elimination of visiting hours.
Reprinted from Crocker L, Johnson B. Privileged presence. Personal stories of connections in health care. 2nd ed. Boulder, CO: Bull Publishing; 2014.
1. American Association of Critical-Care Nurses. Practice alert: Family presence: Visitation in the adult ICU. Accessed at www.aacn.org/WD/practice/docs/practicealerts/family-visitation-adult-icu-practicealert.pdf.
2. New Yorkers for Patient & Family Empowerment and the New York Public Interest Research Group. Sick, scared and separated from loved ones: A report on NYS hospital visiting policies and how patient-centered approaches can promote wellness and safer healthcare. August 2012. Accessed at www.patientandfamily/default.html.
3. Liu V, Read JL, Scruth E, Cheng E. Visitation policies and practices in US ICUs. Crit Care 2013;17:R71.
4. Institute for Patient- and Family-Centered Care. Facts and figures about family presence and participation. Accessed at www.ipfcc.org/advance/topics/Better-Together-Facts-and-Figures.pdf.
5. Better together: partnering with families. Changing the concept of families as visitors bibliography. Accessed at www.ipfcc.org/advance/topics/Changing-the-Concept-of-Families-as-Visitors-Bibliography.pdf.
6. Institute for Patient- and Family-Centered Care. Accessed at www.ipfcc.org/about/index.html.
7. Institute for Patient- and Family-Centered Care. Better together: Partnering with families. Accessed at www.ipfcc.org/advance/topics/better-together.html.
8. Leape L, Berwick D, Clancy C, et al; Lucian Leape Institute at the National Patient Safety Foundation. Transforming healthcare: a safety imperative. Qual Saf Health Care 2009;18:424–8.
9. The National Patient Safety Foundation’s Lucien Leape Institute. Safety is personal: Partnering with patients and families for the safest care. Report of the Roundtable on Consumer Engagement in Patient Safety. Boston: National Patient Safety Foundation; 2014.
From the Institute for Patient- and Family-Centered Care, Bethesda, MD (Ms. Dokken, Ms. Kaufman, and Ms. Johnson), Anne Arundel Medical Center, Annapolis, MD (Dr. Perkins), Contra Costa Regional Medical Center & Health Centers, Martinez, CA (Ms. Benepal, Ms. Roth, and Vidant Health, Greenville, NC (Ms. Dutton and Ms. Jones).
Abstract
- Objective: To describe a campaign to eliminate restrictive hospital visiting policies and to put in place policies that recognize families as partners in care.
- Methods: Descriptive report.
- Results: Many hospitals still have “visiting” hours that limit family presence, often counter to patient preferences. To change the concept of families as visitors and eliminate restrictive hospital visiting policies, the Institute for Patient- and Family-Centered Care (IPFCC) launched the campaign Better Together: Partnering with Families, calling on all hospitals to welcome families 24 hours a day and transform their policies and approaches to care so that patients’ families and loved ones are included in care and decision making, according to patient preferences. As part of the campaign, IPFCC recognized 12 hospitals that exemplify success in eliminating restrictive visiting policies and have changed the concept of families from “visitors” to partners. Leaders at these hospitals attest to the benefits of the changes through improved experience of care and other outcomes. Three exemplar hospitals are highlighted in this article and share their processes of change as well as key learnings and outcomes.
- Conclusion: Hospital policies and practices that encourage and support families as partners in care are essential to patients’ health, well-being, and safety.
Many families are restricted from the bedsides of loved ones because of hospital visiting policies [1–3]. Restrictive policies are often based on long-held beliefs that the presence and participation of families interferes with care, exhausts patients, is a burden to families, spreads infection, or violates HIPAA. However, there is no evidence to support those beliefs. In fact, isolating patients at their most vulnerable time from the people who know them best places them at risk for medical error, emotional harm, inconsistencies in care, and lack of preparedness for transitions in care [4,5]. Jackie Gruzenski’s story “Behind a Locked Door” (printed below) affectingly describes the impact of restrictive policies on a couple's last days.
Fortunately, a growing number of hospitals are lifting these restrictions. But opening the door is not enough. Hospitals need to change the concept of families as “visitors” to families as partners in care. Changing policies is a foundational step in creating a patient- and family-centered culture where families are recognized as essential to patients’ health and well-being and where they are respected as allies for quality and safety.
In response to this critical need for change, in June 2014 the Institute for Patient- and Family-Centered Care (IPFCC) launched the campaign Better Together: Partnering with Families. IPFCC, founded in 1992, is a nonprofit organization that provides essential leadership to advance the understanding and practice of patient- and family-centered care [6]. Emphasizing the importance of family presence and participation to quality and safety, the campaign seeks to eliminate restrictive “visiting” policies and calls upon hospitals to include families as members of the care team and to welcome them 24 hours a day, 7 days a week, according to patient preference [7]. The goal of the campaign is to change visiting policies in 1000 hospitals by 2017. Partnering with IPFCC in this initiative are the American Society for Healthcare Risk Management, American Association of Critical Care Nurses, National Partnership for Women & Families, New Yorkers for Patient and Family Empowerment, Health In Aging Foundation, and the Canadian Foundation for Healthcare Improvement.
Anne Arundel Medical Center
A regional not-for-profit hospital founded in 1902, Anne Arundel Medical Center in Annapolis, MD, provides acute inpatient and outpatient care to residents of 4 counties in Maryland. A 380-bed facility, Anne Arundel has a cancer institute, heart and vascular institute, joint center, spine center, and a women’s and children’s center. In April 2011, the hospital completed a $424 million expansion project, which included a pediatric emergency room, an expanded general emergency room, 50 new patient beds, and 8 new operating rooms.
In 2010, based on a desire to concretely implement the principles of patient- and family-centered care, leaders at Anne Arundel began working with patient and family advisors and initiated a process to change the hospital’s restrictive visiting policy. Now, there are no restrictions on family presence anywhere in the hospital, from ICUs to medical/surgical units to other clinical areas. Patients have the power to choose who they want to stay with them—24 hours a day, 7 days a week. According to Anne Arundel’s policy, each patient determines who is defined as “family.” A “Revisiting Visiting” task force, comprising support staff, providers, and patient and family advisors, worked for 9 months to develop the new family presence policy and support its implementation.
With Anne Arundel leadership encouragement and support, patient and family advisors participated in all phases of the development and implementation of the new family presence policy and in other ways to advance the practice of patient- and family-centered care. The advisors also participated in the process to change the way nurse change of shift report was conducted, and they made recommendations for changes in the directional signs throughout the hospital. New signs, featuring a pineapple (a symbol of hospitality) and the words “Welcome Families” replaced old ones displaying the former restrictive visiting policy.
Supporting patient and family involvement in transitions in care is an integral aspect of implementing family presence policies and practices. Through an “Always Events” grant from the Picker Institute (for information about the Always Events program, see www.ihi.org/Engage/Initiatives/PatientFamilyCenteredCare/Pages/AlwaysEvents.aspx), patient and family advisors, staff, and providers at Anne Arundel developed the SMART discharge protocol, which includes a simple 5-item checklist that is reviewed and discussed with the patient and family prior to discharge. SMART is an acronym for Signs, Medications, Appointments, Results, and Talk. In its work, the SMART team built on current evidence, created urgency and expectation for use with patients, families, and caregivers, disseminated findings, and promoted the protocol as a national standard. The tool is available at www.ihi.org/resources/Pages/Tools/SMARTDischargeProtocol.aspx.
According to Anne Arundel’s COO and CNO, Sherry Perkins, a critical part of the change process was to first understand staff’s fears and then learn what the evidence says. For example, with regard to the impact of additional family presence on infection control, they learned that family presence did not pose additional infection control concerns.
In 2009, there were no patient and family advisors volunteering at Anne Arundel. In 2014, there are approximately 80 advisors. Since 2009, the overall HCAHPS rating of the hospital has gone from 75.4% to 82% (the national average is 70%). While patient satisfaction scores have previously been in the top deciles at Anne Arundel, they have consistently risen since expanding family presence and implementing additional patient- and family-centered strategies.
Contra Costa Regional Medical Center and Health Centers
Contra Costa Health Services in Martinez, CA, includes Contra Costa Regional Medical Center and 10 health centers as part of a comprehensive county health system. Its 164-bed public hospital is dedicated to offering services that are welcoming, accessible, safe and respectful for everyone.
Like many hospitals in the country, for years Contra Costa Regional Medical Center restricted the hours when family members and loved ones could visit patients. However, the hospital’s medical staff often felt uncomfortable that they had to usher family and care partners away from patients when visiting hours were over. Anna Roth, Contra Costa’s CEO, recalls an incident that caused great anguish and contributed to the hospital’s decision to eliminate its restrictive visiting policy. A young boy whose grandfather was in the ICU was denied visitation. The grandfather, who had raised him, passed away, with the two having had no chance to say goodbye. Roth said that the incident hit home for her and the entire staff, and they knew they could do better. “Our old policies treated family members like visitors, until we realized that we are the visitors in people’s lives, not the other way around,” she noted.
In 2012, the hospital established an interdisciplinary team to transform its existing visiting policy into a “welcoming policy.” The team comprised the director of inpatient nursing, the chief of nursing, the chief of security, a public health program specialist, the facilities manager, and a patient partner. The new policy would support family presence 24/7 as well as change the concept of families as “visitors.”
Over the course of a year, the team designed the framework for a 3-day pilot and developed a check-in process to help loved ones gain access to patients after regular hospital hours. Working closely with nursing leadership, front-line staff, patient partners, and security, the team made necessary adjustments to the policy throughout the pilot period. The pilot was well-received and the policy was implemented soon after.
In the policy’s first year, more than 7000 family members and care partners were able to be with their loved ones between 8 pm and 6 am, the time period formerly restricted. The feedback from staff, patients and loved ones has been overwhelmingly positive. Front-line nurses are currently strengthening their skills and confidence in conducting change of shift report at bedside with patients and families. Other “welcoming” measures have also been implemented, including making signage more user-friendly, providing comfortable chairs to sleep in, and installing new vending machines with healthy snacks and drinks.
Vidant Health
Vidant Health serves 1.4 million people in a 29-county region of eastern North Carolina and comprises over 70 primary and specialty physician office practices, a 900-bed academic medical center, 7 community hospitals, an ambulatory surgery center, and home health and hospice services. Vidant Health’s efforts to advance a culture of patient- and family-centered care began in the late 1990s in the James and Connie Maynard Children’s Hospital and the regional rehabilitation center, but this culture did not spread consistently throughout Vidant Health, leading to differing experiences of care for patients and families.
The Vidant Health executive team and senior leaders heard about these inconsistencies firsthand in the spring of 2007 when an employee shared her family’s experiences during her brother’s ICU stay. Christie Odom described how the visitation policy restricted her family’s access to her brother to 15-minute increments, 6 times a day, which led to heightened fear and anxiety for her brother, family, and friends and impeded patient and family engagement in care and decision-making. Odom’s brother died alone with no family by his side. A physical therapist, Odom observed that in the regional rehabilitation center, families were partners in care, yet in the adult ICU, they were visitors.
After hearing Christie’s story, the system’s executive team, board of directors, and physician leaders made a commitment to eliminate these restrictive visitation guidelines. Leaders understood that this would require the organization’s culture to change from viewing patients and families as passive recipients of care to recognizing them as partners. Subsequently, the commitment to patient-family partnerships was imbedded in key documents including the corporation’s strategic and 5-year quality plans. An Office of Patient-Family Experience was established at Vidant Medical Center in 2008 and, a year later, a corporate office was established to guide system transformation. Emphasis was placed on building a solid team of patient-family advisors and staff champions. An initial focus was to replace the restrictive visitation policy with family presence guidelines. A key tenet of these guidelines is that patients define who their family members are and how they should be included in care and decision-making.
This policy and practice change provided the impetus for ongoing evolution of patient-family partnerships. Patient-family advisors are now integrated across the health care system. They serve on performance improvement teams, make safety rounds, serve as faculty in education programs, interview applicants for key positions, and develop and edit patient education materials. The outcomes achieved by this system transformation are evidenced in exceptional HCAHPS performance, significant reductions in serious safety events and hospital acquired infections and national recognition for commitment to patient-family partnerships.
Conclusion
Changing the concept of families as visitors to families as partners in care, according to patient preference, is foundational to advancing the practice of patient- and family-centered care and to building a safe, high-quality, cost-effective system of care. In 2009, Lucian Leape and colleagues envisioned a transformed health care culture in which “the family is respected as part of the care team—never visitors—in every area of the hospital, including the emergency department and the intensive care unit” [8]. A 2014 report by the National Patient Safety Foundation’s Lucian Leape Institute affirmed, “patients and families can play a critical role in preventing medical errors and reducing harm” [9].
Many hospitals still do not encourage family presence and participation and do not embrace the concept of families as true partners in care. But as demonstrated by the actions of the exemplar hospitals described here, it is possible to make this critical culture shift. The exemplar hospitals understand the importance of partnering with patients’ families instead of treating them as outsiders who are interfering in their loved one’s care. These hospitals are proving that giving patients the access they want to their loved ones actually helps themget better.
Through its campaign Better Together: Partnering with Families, IPFCC challenges hospitals across the United States and Canada to pledge to join this important initiative. Now is the time for all hospitals to embrace family presence and participation and to welcome families and other care partners 24 hours a day, 7 days a week.
Hospitals are invited to join this initiative. Steps to begin the change process may be found at www.ipfcc.org/advance/topics/better-together-pledge.html. Also available at IPFCC website is the Better Together toolkit, other materials and information that support the initiative, and a complete list of the exemplar hospitals and their processes and policies. The toolkit includes an organizational self-assessment, sample processes and policies, videos, and guides for families and staff to use in developing partnership. It is available at no charge at www.ipfcc.org/bettertogether/.
Corresponding author: Beverley H. Johnson, 6917 Arlington Rd., Ste. 309, Bethesda, MD 20814, bjohson@ipfcc.org.
Behind a Locked Door
This is our story as I remember it.
One day I came home from work, and my husband was confused. In all the years we’d been married, I’d never known him to be confused. He was sitting in the family room, and he looked frightened.
I said, “Bill, what’s going on?” He said, “Well, I was just going to get up and go look outside for Joey.” I said, “Bill, Joey’s not here.” He insisted, “Oh yes, we just came back from vacation. Joey just went outside, and I was going to check on him.”
I was alarmed and said, “Bill, I think you’re a little confused. I’m concerned because this morning you told me you had a headache. Maybe we should go to the hospital.” He resisted, but I simply told him, “Bill, if something was to happen to you, I might be held responsible because I didn’t do what was in your best interest. We can come home if everything is okay.”
And so we went to the emergency room, where we learned that my husband had a small bleed in his brain. We were told that we needed to go to another hospital that had a neurosurgeon on staff. My husband was transported by ambulance to a hospital about a mile away, and I followed him there in our car.
I want to stop here and tell you a bit about my husband and about myself. My name is Jackie Gruzenski, and I am a nurse involved in the field of psychiatric nursing. My husband’s name was Dr. William Gruzenski. He was a psychiatrist for forty years, and he was a chief medical officer for the last twelve years of his career.
Bill was a very good doctor and a very good husband. And toward the end of his life, he realized that all of his degrees, along with money and material possessions, didn’t matter. They were nothing. He just wanted to have me with him. We loved each other very deeply, and we wanted to share our last days and moments together, but I’m getting ahead of myself.
When we got to the second hospital, my husband was in the emergency room from about 7:00 p.m. until about 6:00 a.m. the next morning. At some point, he started to develop a hypertensive crisis, and the staff could not bring his blood pressure down. They started an IV medication, which required that he be monitored closely in the intensive care unit (ICU).
Of course, I went with him as he was transferred from emergency to ICU. When we got to the ICU door, I was told, “Now, just go into the waiting room. We’re going to settle your husband, and then we’ll come and get you.”
I was a nervous wreck while I waited. I knew my husband had been pretty sick while in emergency. What if he got more confused? What if he lost even this current level of functioning and wouldn’t
remember me? The longer I waited, the more my anxiety grew.
The waiting room was a small area, with chairs around the perimeter, except by the locked door. After an hour with no news, I saw a phone on the wall and called. I said to the voice on the other end, “My name is Mrs. Gruzenski. I was informed that my husband was going to be settled and that someone would come and get me.”
The next thing I knew a young, perky nurse came out, greeted me, and then directed me totally away from my husband, away from the door to the ICU, to a little room. She proceeded to give me the strict policies and procedures for the ICU, including that visitation was allowed only four times a day for thirty minutes each time.
Not believing what I was hearing, I said, “But my husband is going to be worried that I am not with him. We are the center of each other’s lives—we are only apart when we are at work!” Her response was, “Well, you can’t be with him. Those are the rules.”
I lived ten miles away. What was I supposed to do between these widely spaced thirty-minute visits? I felt I had to play by the rules. I was afraid that if I questioned too much or was abrupt with someone, they would treat my husband meanly. And because he was behind a locked door, I would never know.
I didn’t know what else to do and so, shortly before 8:00 a.m., I went home to get some rest. Ironically, just after I got home and started to settle after our long night in the ER, I got a flurry of calls from different residents who wanted information about my husband. They never said, “Come over and visit. He’s missing you.” They called because they needed the information I could give them, but they kept me locked out.
When I was able to have my first visit the next day, my husband asked where I had been. I explained that there were very limited visiting hours. This prompted my husband to speak to his nurse and say, “You know, she’s not a visitor. She’s my wife!” But he was informed that didn’t matter, that there were rules, and that I was a visitor and had to be treated as a visitor.
The rule trumped both of us and what we wanted. The rule meant he had to suffer alone. This was an accredited hospital, but in my view it was archaic. Staff hid behind the rules rather than using their heads and their hearts.
Over the next few days, I saw that my not being there with my husband was leading to more and more distress for him. As he became more ill, he would not allow the nurses to wash him, and he would not eat their food. He was doing everything he could do to get the staff’s attention to revisit the visiting restrictions. If I’d been allowed to stay, I’m sure I could have helped with feeding, with bathing, and with toileting. I’m certain I could have calmed him and helped lower his blood pressure.
I was treated as though I was an enemy, but all I wanted was to be with him, to share the last days of his life. I had always been his anchor. I was the person who navigated the everyday waters of his life. The hospital’s rules meant that he was adrift, and I was lost.
During his hospitalization, he was not afforded the respect he had given to all his patients and the nurses and doctors he had worked with each day. For example, the ICU staff never asked him how he would like to be addressed. They called him “Bill” when he should have been addressed as “Doctor Gruzenski.” He wouldn’t have thought of calling a resident by his first name, and there were only a few people in his life, his inner circle of family and friends, who called him “Bill.”
One day, I actually witnessed one doctor refer to my husband not even as “Bill” but as “Billy.”
I followed this doctor out of the ICU and challenged him saying “Would you think you were valued as a medical professional, and that your life had meant something if, in forty years’ time, someone called you ‘Billy’? ‘Billy’ is what you call some young boy you like, not someone who is sixty-eight years old and is a dignified gentleman and physician.”
My husband earned the title of “Doctor.” He attended four years of medical school, one year of internship, four years as a resident psychiatrist, and he was board certified in psychiatry. He had earned respect by exceeding all the societal standards for being addressed as “Doctor.” These achievements should not be washed away once you are hospitalized. In fact, I believe my husband might have felt a little safer if he had been addressed as “Doctor.”
My husband was in the ICU for eight of the last sixteen days of his life, and there were lots of missed opportunities for us. He wanted me there more than I was allowed. We missed time together we could have had. I feel it was a very cruel thing that was done to us.
We both knew the gravity of his condition, and my husband wanted quality of life, not quantity. I was a large part of the quality he wanted, but I was locked out for the greater part of his last days.
After my husband died, I felt I had to do something so that what happened to us wouldn’t happen to anyone else. I wrote letters to the chief executive officer of the hospital. I wrote to the chief of the medical staff. I wrote to the chief of nursing. And I wrote to the chaplain. The only person I ever heard from was the chaplain. No one apologized or said they would change the rules.
I believe more harm comes when family are not actively involved, and research is proving my belief is sound. And so I will continue to tell my story. I hope that if I tell it enough times, maybe people who write the rules in hospitals will realize that loved ones are advocates, not visitors.
I will never stop advocating for the elimination of visiting hours.
Reprinted from Crocker L, Johnson B. Privileged presence. Personal stories of connections in health care. 2nd ed. Boulder, CO: Bull Publishing; 2014.
From the Institute for Patient- and Family-Centered Care, Bethesda, MD (Ms. Dokken, Ms. Kaufman, and Ms. Johnson), Anne Arundel Medical Center, Annapolis, MD (Dr. Perkins), Contra Costa Regional Medical Center & Health Centers, Martinez, CA (Ms. Benepal, Ms. Roth, and Vidant Health, Greenville, NC (Ms. Dutton and Ms. Jones).
Abstract
- Objective: To describe a campaign to eliminate restrictive hospital visiting policies and to put in place policies that recognize families as partners in care.
- Methods: Descriptive report.
- Results: Many hospitals still have “visiting” hours that limit family presence, often counter to patient preferences. To change the concept of families as visitors and eliminate restrictive hospital visiting policies, the Institute for Patient- and Family-Centered Care (IPFCC) launched the campaign Better Together: Partnering with Families, calling on all hospitals to welcome families 24 hours a day and transform their policies and approaches to care so that patients’ families and loved ones are included in care and decision making, according to patient preferences. As part of the campaign, IPFCC recognized 12 hospitals that exemplify success in eliminating restrictive visiting policies and have changed the concept of families from “visitors” to partners. Leaders at these hospitals attest to the benefits of the changes through improved experience of care and other outcomes. Three exemplar hospitals are highlighted in this article and share their processes of change as well as key learnings and outcomes.
- Conclusion: Hospital policies and practices that encourage and support families as partners in care are essential to patients’ health, well-being, and safety.
Many families are restricted from the bedsides of loved ones because of hospital visiting policies [1–3]. Restrictive policies are often based on long-held beliefs that the presence and participation of families interferes with care, exhausts patients, is a burden to families, spreads infection, or violates HIPAA. However, there is no evidence to support those beliefs. In fact, isolating patients at their most vulnerable time from the people who know them best places them at risk for medical error, emotional harm, inconsistencies in care, and lack of preparedness for transitions in care [4,5]. Jackie Gruzenski’s story “Behind a Locked Door” (printed below) affectingly describes the impact of restrictive policies on a couple's last days.
Fortunately, a growing number of hospitals are lifting these restrictions. But opening the door is not enough. Hospitals need to change the concept of families as “visitors” to families as partners in care. Changing policies is a foundational step in creating a patient- and family-centered culture where families are recognized as essential to patients’ health and well-being and where they are respected as allies for quality and safety.
In response to this critical need for change, in June 2014 the Institute for Patient- and Family-Centered Care (IPFCC) launched the campaign Better Together: Partnering with Families. IPFCC, founded in 1992, is a nonprofit organization that provides essential leadership to advance the understanding and practice of patient- and family-centered care [6]. Emphasizing the importance of family presence and participation to quality and safety, the campaign seeks to eliminate restrictive “visiting” policies and calls upon hospitals to include families as members of the care team and to welcome them 24 hours a day, 7 days a week, according to patient preference [7]. The goal of the campaign is to change visiting policies in 1000 hospitals by 2017. Partnering with IPFCC in this initiative are the American Society for Healthcare Risk Management, American Association of Critical Care Nurses, National Partnership for Women & Families, New Yorkers for Patient and Family Empowerment, Health In Aging Foundation, and the Canadian Foundation for Healthcare Improvement.
Anne Arundel Medical Center
A regional not-for-profit hospital founded in 1902, Anne Arundel Medical Center in Annapolis, MD, provides acute inpatient and outpatient care to residents of 4 counties in Maryland. A 380-bed facility, Anne Arundel has a cancer institute, heart and vascular institute, joint center, spine center, and a women’s and children’s center. In April 2011, the hospital completed a $424 million expansion project, which included a pediatric emergency room, an expanded general emergency room, 50 new patient beds, and 8 new operating rooms.
In 2010, based on a desire to concretely implement the principles of patient- and family-centered care, leaders at Anne Arundel began working with patient and family advisors and initiated a process to change the hospital’s restrictive visiting policy. Now, there are no restrictions on family presence anywhere in the hospital, from ICUs to medical/surgical units to other clinical areas. Patients have the power to choose who they want to stay with them—24 hours a day, 7 days a week. According to Anne Arundel’s policy, each patient determines who is defined as “family.” A “Revisiting Visiting” task force, comprising support staff, providers, and patient and family advisors, worked for 9 months to develop the new family presence policy and support its implementation.
With Anne Arundel leadership encouragement and support, patient and family advisors participated in all phases of the development and implementation of the new family presence policy and in other ways to advance the practice of patient- and family-centered care. The advisors also participated in the process to change the way nurse change of shift report was conducted, and they made recommendations for changes in the directional signs throughout the hospital. New signs, featuring a pineapple (a symbol of hospitality) and the words “Welcome Families” replaced old ones displaying the former restrictive visiting policy.
Supporting patient and family involvement in transitions in care is an integral aspect of implementing family presence policies and practices. Through an “Always Events” grant from the Picker Institute (for information about the Always Events program, see www.ihi.org/Engage/Initiatives/PatientFamilyCenteredCare/Pages/AlwaysEvents.aspx), patient and family advisors, staff, and providers at Anne Arundel developed the SMART discharge protocol, which includes a simple 5-item checklist that is reviewed and discussed with the patient and family prior to discharge. SMART is an acronym for Signs, Medications, Appointments, Results, and Talk. In its work, the SMART team built on current evidence, created urgency and expectation for use with patients, families, and caregivers, disseminated findings, and promoted the protocol as a national standard. The tool is available at www.ihi.org/resources/Pages/Tools/SMARTDischargeProtocol.aspx.
According to Anne Arundel’s COO and CNO, Sherry Perkins, a critical part of the change process was to first understand staff’s fears and then learn what the evidence says. For example, with regard to the impact of additional family presence on infection control, they learned that family presence did not pose additional infection control concerns.
In 2009, there were no patient and family advisors volunteering at Anne Arundel. In 2014, there are approximately 80 advisors. Since 2009, the overall HCAHPS rating of the hospital has gone from 75.4% to 82% (the national average is 70%). While patient satisfaction scores have previously been in the top deciles at Anne Arundel, they have consistently risen since expanding family presence and implementing additional patient- and family-centered strategies.
Contra Costa Regional Medical Center and Health Centers
Contra Costa Health Services in Martinez, CA, includes Contra Costa Regional Medical Center and 10 health centers as part of a comprehensive county health system. Its 164-bed public hospital is dedicated to offering services that are welcoming, accessible, safe and respectful for everyone.
Like many hospitals in the country, for years Contra Costa Regional Medical Center restricted the hours when family members and loved ones could visit patients. However, the hospital’s medical staff often felt uncomfortable that they had to usher family and care partners away from patients when visiting hours were over. Anna Roth, Contra Costa’s CEO, recalls an incident that caused great anguish and contributed to the hospital’s decision to eliminate its restrictive visiting policy. A young boy whose grandfather was in the ICU was denied visitation. The grandfather, who had raised him, passed away, with the two having had no chance to say goodbye. Roth said that the incident hit home for her and the entire staff, and they knew they could do better. “Our old policies treated family members like visitors, until we realized that we are the visitors in people’s lives, not the other way around,” she noted.
In 2012, the hospital established an interdisciplinary team to transform its existing visiting policy into a “welcoming policy.” The team comprised the director of inpatient nursing, the chief of nursing, the chief of security, a public health program specialist, the facilities manager, and a patient partner. The new policy would support family presence 24/7 as well as change the concept of families as “visitors.”
Over the course of a year, the team designed the framework for a 3-day pilot and developed a check-in process to help loved ones gain access to patients after regular hospital hours. Working closely with nursing leadership, front-line staff, patient partners, and security, the team made necessary adjustments to the policy throughout the pilot period. The pilot was well-received and the policy was implemented soon after.
In the policy’s first year, more than 7000 family members and care partners were able to be with their loved ones between 8 pm and 6 am, the time period formerly restricted. The feedback from staff, patients and loved ones has been overwhelmingly positive. Front-line nurses are currently strengthening their skills and confidence in conducting change of shift report at bedside with patients and families. Other “welcoming” measures have also been implemented, including making signage more user-friendly, providing comfortable chairs to sleep in, and installing new vending machines with healthy snacks and drinks.
Vidant Health
Vidant Health serves 1.4 million people in a 29-county region of eastern North Carolina and comprises over 70 primary and specialty physician office practices, a 900-bed academic medical center, 7 community hospitals, an ambulatory surgery center, and home health and hospice services. Vidant Health’s efforts to advance a culture of patient- and family-centered care began in the late 1990s in the James and Connie Maynard Children’s Hospital and the regional rehabilitation center, but this culture did not spread consistently throughout Vidant Health, leading to differing experiences of care for patients and families.
The Vidant Health executive team and senior leaders heard about these inconsistencies firsthand in the spring of 2007 when an employee shared her family’s experiences during her brother’s ICU stay. Christie Odom described how the visitation policy restricted her family’s access to her brother to 15-minute increments, 6 times a day, which led to heightened fear and anxiety for her brother, family, and friends and impeded patient and family engagement in care and decision-making. Odom’s brother died alone with no family by his side. A physical therapist, Odom observed that in the regional rehabilitation center, families were partners in care, yet in the adult ICU, they were visitors.
After hearing Christie’s story, the system’s executive team, board of directors, and physician leaders made a commitment to eliminate these restrictive visitation guidelines. Leaders understood that this would require the organization’s culture to change from viewing patients and families as passive recipients of care to recognizing them as partners. Subsequently, the commitment to patient-family partnerships was imbedded in key documents including the corporation’s strategic and 5-year quality plans. An Office of Patient-Family Experience was established at Vidant Medical Center in 2008 and, a year later, a corporate office was established to guide system transformation. Emphasis was placed on building a solid team of patient-family advisors and staff champions. An initial focus was to replace the restrictive visitation policy with family presence guidelines. A key tenet of these guidelines is that patients define who their family members are and how they should be included in care and decision-making.
This policy and practice change provided the impetus for ongoing evolution of patient-family partnerships. Patient-family advisors are now integrated across the health care system. They serve on performance improvement teams, make safety rounds, serve as faculty in education programs, interview applicants for key positions, and develop and edit patient education materials. The outcomes achieved by this system transformation are evidenced in exceptional HCAHPS performance, significant reductions in serious safety events and hospital acquired infections and national recognition for commitment to patient-family partnerships.
Conclusion
Changing the concept of families as visitors to families as partners in care, according to patient preference, is foundational to advancing the practice of patient- and family-centered care and to building a safe, high-quality, cost-effective system of care. In 2009, Lucian Leape and colleagues envisioned a transformed health care culture in which “the family is respected as part of the care team—never visitors—in every area of the hospital, including the emergency department and the intensive care unit” [8]. A 2014 report by the National Patient Safety Foundation’s Lucian Leape Institute affirmed, “patients and families can play a critical role in preventing medical errors and reducing harm” [9].
Many hospitals still do not encourage family presence and participation and do not embrace the concept of families as true partners in care. But as demonstrated by the actions of the exemplar hospitals described here, it is possible to make this critical culture shift. The exemplar hospitals understand the importance of partnering with patients’ families instead of treating them as outsiders who are interfering in their loved one’s care. These hospitals are proving that giving patients the access they want to their loved ones actually helps themget better.
Through its campaign Better Together: Partnering with Families, IPFCC challenges hospitals across the United States and Canada to pledge to join this important initiative. Now is the time for all hospitals to embrace family presence and participation and to welcome families and other care partners 24 hours a day, 7 days a week.
Hospitals are invited to join this initiative. Steps to begin the change process may be found at www.ipfcc.org/advance/topics/better-together-pledge.html. Also available at IPFCC website is the Better Together toolkit, other materials and information that support the initiative, and a complete list of the exemplar hospitals and their processes and policies. The toolkit includes an organizational self-assessment, sample processes and policies, videos, and guides for families and staff to use in developing partnership. It is available at no charge at www.ipfcc.org/bettertogether/.
Corresponding author: Beverley H. Johnson, 6917 Arlington Rd., Ste. 309, Bethesda, MD 20814, bjohson@ipfcc.org.
Behind a Locked Door
This is our story as I remember it.
One day I came home from work, and my husband was confused. In all the years we’d been married, I’d never known him to be confused. He was sitting in the family room, and he looked frightened.
I said, “Bill, what’s going on?” He said, “Well, I was just going to get up and go look outside for Joey.” I said, “Bill, Joey’s not here.” He insisted, “Oh yes, we just came back from vacation. Joey just went outside, and I was going to check on him.”
I was alarmed and said, “Bill, I think you’re a little confused. I’m concerned because this morning you told me you had a headache. Maybe we should go to the hospital.” He resisted, but I simply told him, “Bill, if something was to happen to you, I might be held responsible because I didn’t do what was in your best interest. We can come home if everything is okay.”
And so we went to the emergency room, where we learned that my husband had a small bleed in his brain. We were told that we needed to go to another hospital that had a neurosurgeon on staff. My husband was transported by ambulance to a hospital about a mile away, and I followed him there in our car.
I want to stop here and tell you a bit about my husband and about myself. My name is Jackie Gruzenski, and I am a nurse involved in the field of psychiatric nursing. My husband’s name was Dr. William Gruzenski. He was a psychiatrist for forty years, and he was a chief medical officer for the last twelve years of his career.
Bill was a very good doctor and a very good husband. And toward the end of his life, he realized that all of his degrees, along with money and material possessions, didn’t matter. They were nothing. He just wanted to have me with him. We loved each other very deeply, and we wanted to share our last days and moments together, but I’m getting ahead of myself.
When we got to the second hospital, my husband was in the emergency room from about 7:00 p.m. until about 6:00 a.m. the next morning. At some point, he started to develop a hypertensive crisis, and the staff could not bring his blood pressure down. They started an IV medication, which required that he be monitored closely in the intensive care unit (ICU).
Of course, I went with him as he was transferred from emergency to ICU. When we got to the ICU door, I was told, “Now, just go into the waiting room. We’re going to settle your husband, and then we’ll come and get you.”
I was a nervous wreck while I waited. I knew my husband had been pretty sick while in emergency. What if he got more confused? What if he lost even this current level of functioning and wouldn’t
remember me? The longer I waited, the more my anxiety grew.
The waiting room was a small area, with chairs around the perimeter, except by the locked door. After an hour with no news, I saw a phone on the wall and called. I said to the voice on the other end, “My name is Mrs. Gruzenski. I was informed that my husband was going to be settled and that someone would come and get me.”
The next thing I knew a young, perky nurse came out, greeted me, and then directed me totally away from my husband, away from the door to the ICU, to a little room. She proceeded to give me the strict policies and procedures for the ICU, including that visitation was allowed only four times a day for thirty minutes each time.
Not believing what I was hearing, I said, “But my husband is going to be worried that I am not with him. We are the center of each other’s lives—we are only apart when we are at work!” Her response was, “Well, you can’t be with him. Those are the rules.”
I lived ten miles away. What was I supposed to do between these widely spaced thirty-minute visits? I felt I had to play by the rules. I was afraid that if I questioned too much or was abrupt with someone, they would treat my husband meanly. And because he was behind a locked door, I would never know.
I didn’t know what else to do and so, shortly before 8:00 a.m., I went home to get some rest. Ironically, just after I got home and started to settle after our long night in the ER, I got a flurry of calls from different residents who wanted information about my husband. They never said, “Come over and visit. He’s missing you.” They called because they needed the information I could give them, but they kept me locked out.
When I was able to have my first visit the next day, my husband asked where I had been. I explained that there were very limited visiting hours. This prompted my husband to speak to his nurse and say, “You know, she’s not a visitor. She’s my wife!” But he was informed that didn’t matter, that there were rules, and that I was a visitor and had to be treated as a visitor.
The rule trumped both of us and what we wanted. The rule meant he had to suffer alone. This was an accredited hospital, but in my view it was archaic. Staff hid behind the rules rather than using their heads and their hearts.
Over the next few days, I saw that my not being there with my husband was leading to more and more distress for him. As he became more ill, he would not allow the nurses to wash him, and he would not eat their food. He was doing everything he could do to get the staff’s attention to revisit the visiting restrictions. If I’d been allowed to stay, I’m sure I could have helped with feeding, with bathing, and with toileting. I’m certain I could have calmed him and helped lower his blood pressure.
I was treated as though I was an enemy, but all I wanted was to be with him, to share the last days of his life. I had always been his anchor. I was the person who navigated the everyday waters of his life. The hospital’s rules meant that he was adrift, and I was lost.
During his hospitalization, he was not afforded the respect he had given to all his patients and the nurses and doctors he had worked with each day. For example, the ICU staff never asked him how he would like to be addressed. They called him “Bill” when he should have been addressed as “Doctor Gruzenski.” He wouldn’t have thought of calling a resident by his first name, and there were only a few people in his life, his inner circle of family and friends, who called him “Bill.”
One day, I actually witnessed one doctor refer to my husband not even as “Bill” but as “Billy.”
I followed this doctor out of the ICU and challenged him saying “Would you think you were valued as a medical professional, and that your life had meant something if, in forty years’ time, someone called you ‘Billy’? ‘Billy’ is what you call some young boy you like, not someone who is sixty-eight years old and is a dignified gentleman and physician.”
My husband earned the title of “Doctor.” He attended four years of medical school, one year of internship, four years as a resident psychiatrist, and he was board certified in psychiatry. He had earned respect by exceeding all the societal standards for being addressed as “Doctor.” These achievements should not be washed away once you are hospitalized. In fact, I believe my husband might have felt a little safer if he had been addressed as “Doctor.”
My husband was in the ICU for eight of the last sixteen days of his life, and there were lots of missed opportunities for us. He wanted me there more than I was allowed. We missed time together we could have had. I feel it was a very cruel thing that was done to us.
We both knew the gravity of his condition, and my husband wanted quality of life, not quantity. I was a large part of the quality he wanted, but I was locked out for the greater part of his last days.
After my husband died, I felt I had to do something so that what happened to us wouldn’t happen to anyone else. I wrote letters to the chief executive officer of the hospital. I wrote to the chief of the medical staff. I wrote to the chief of nursing. And I wrote to the chaplain. The only person I ever heard from was the chaplain. No one apologized or said they would change the rules.
I believe more harm comes when family are not actively involved, and research is proving my belief is sound. And so I will continue to tell my story. I hope that if I tell it enough times, maybe people who write the rules in hospitals will realize that loved ones are advocates, not visitors.
I will never stop advocating for the elimination of visiting hours.
Reprinted from Crocker L, Johnson B. Privileged presence. Personal stories of connections in health care. 2nd ed. Boulder, CO: Bull Publishing; 2014.
1. American Association of Critical-Care Nurses. Practice alert: Family presence: Visitation in the adult ICU. Accessed at www.aacn.org/WD/practice/docs/practicealerts/family-visitation-adult-icu-practicealert.pdf.
2. New Yorkers for Patient & Family Empowerment and the New York Public Interest Research Group. Sick, scared and separated from loved ones: A report on NYS hospital visiting policies and how patient-centered approaches can promote wellness and safer healthcare. August 2012. Accessed at www.patientandfamily/default.html.
3. Liu V, Read JL, Scruth E, Cheng E. Visitation policies and practices in US ICUs. Crit Care 2013;17:R71.
4. Institute for Patient- and Family-Centered Care. Facts and figures about family presence and participation. Accessed at www.ipfcc.org/advance/topics/Better-Together-Facts-and-Figures.pdf.
5. Better together: partnering with families. Changing the concept of families as visitors bibliography. Accessed at www.ipfcc.org/advance/topics/Changing-the-Concept-of-Families-as-Visitors-Bibliography.pdf.
6. Institute for Patient- and Family-Centered Care. Accessed at www.ipfcc.org/about/index.html.
7. Institute for Patient- and Family-Centered Care. Better together: Partnering with families. Accessed at www.ipfcc.org/advance/topics/better-together.html.
8. Leape L, Berwick D, Clancy C, et al; Lucian Leape Institute at the National Patient Safety Foundation. Transforming healthcare: a safety imperative. Qual Saf Health Care 2009;18:424–8.
9. The National Patient Safety Foundation’s Lucien Leape Institute. Safety is personal: Partnering with patients and families for the safest care. Report of the Roundtable on Consumer Engagement in Patient Safety. Boston: National Patient Safety Foundation; 2014.
1. American Association of Critical-Care Nurses. Practice alert: Family presence: Visitation in the adult ICU. Accessed at www.aacn.org/WD/practice/docs/practicealerts/family-visitation-adult-icu-practicealert.pdf.
2. New Yorkers for Patient & Family Empowerment and the New York Public Interest Research Group. Sick, scared and separated from loved ones: A report on NYS hospital visiting policies and how patient-centered approaches can promote wellness and safer healthcare. August 2012. Accessed at www.patientandfamily/default.html.
3. Liu V, Read JL, Scruth E, Cheng E. Visitation policies and practices in US ICUs. Crit Care 2013;17:R71.
4. Institute for Patient- and Family-Centered Care. Facts and figures about family presence and participation. Accessed at www.ipfcc.org/advance/topics/Better-Together-Facts-and-Figures.pdf.
5. Better together: partnering with families. Changing the concept of families as visitors bibliography. Accessed at www.ipfcc.org/advance/topics/Changing-the-Concept-of-Families-as-Visitors-Bibliography.pdf.
6. Institute for Patient- and Family-Centered Care. Accessed at www.ipfcc.org/about/index.html.
7. Institute for Patient- and Family-Centered Care. Better together: Partnering with families. Accessed at www.ipfcc.org/advance/topics/better-together.html.
8. Leape L, Berwick D, Clancy C, et al; Lucian Leape Institute at the National Patient Safety Foundation. Transforming healthcare: a safety imperative. Qual Saf Health Care 2009;18:424–8.
9. The National Patient Safety Foundation’s Lucien Leape Institute. Safety is personal: Partnering with patients and families for the safest care. Report of the Roundtable on Consumer Engagement in Patient Safety. Boston: National Patient Safety Foundation; 2014.