User login
VIDEO: Goserelin helps dodge ovarian failure in HR-negative breast cancer
CHICAGO – Adding the gonadotropin-releasing hormone agonist goserelin (Zoladex) to adjuvant or neoadjuvant chemotherapy boosted fertility prospects in premenopausal women with early-stage hormone-receptor–negative breast cancer.
Not only did goserelin reduce by 70% the risk of ovarian failure, a common consequence of chemotherapy, but the monthly injections also offered an intriguing boost in disease-free and overall survival.
Lead author of the intergroup POEMS (Prevention of Early Menopause Study) Dr. Halle Moore of the Cleveland Clinic spoke with us about the late-breaking trial at the annual meeting of the American Society of Clinical Oncology.
Click here to hear more about these practice-changing results.
The study was supported by the National Institutes of Health. Dr. Moore reported no disclosures; three coauthors have financial ties with AstraZeneca, the maker of goserelin.
Correction 5/31/14: An earlier version of this article carried a headline that misstated the cancer type.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
CHICAGO – Adding the gonadotropin-releasing hormone agonist goserelin (Zoladex) to adjuvant or neoadjuvant chemotherapy boosted fertility prospects in premenopausal women with early-stage hormone-receptor–negative breast cancer.
Not only did goserelin reduce by 70% the risk of ovarian failure, a common consequence of chemotherapy, but the monthly injections also offered an intriguing boost in disease-free and overall survival.
Lead author of the intergroup POEMS (Prevention of Early Menopause Study) Dr. Halle Moore of the Cleveland Clinic spoke with us about the late-breaking trial at the annual meeting of the American Society of Clinical Oncology.
Click here to hear more about these practice-changing results.
The study was supported by the National Institutes of Health. Dr. Moore reported no disclosures; three coauthors have financial ties with AstraZeneca, the maker of goserelin.
Correction 5/31/14: An earlier version of this article carried a headline that misstated the cancer type.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
CHICAGO – Adding the gonadotropin-releasing hormone agonist goserelin (Zoladex) to adjuvant or neoadjuvant chemotherapy boosted fertility prospects in premenopausal women with early-stage hormone-receptor–negative breast cancer.
Not only did goserelin reduce by 70% the risk of ovarian failure, a common consequence of chemotherapy, but the monthly injections also offered an intriguing boost in disease-free and overall survival.
Lead author of the intergroup POEMS (Prevention of Early Menopause Study) Dr. Halle Moore of the Cleveland Clinic spoke with us about the late-breaking trial at the annual meeting of the American Society of Clinical Oncology.
Click here to hear more about these practice-changing results.
The study was supported by the National Institutes of Health. Dr. Moore reported no disclosures; three coauthors have financial ties with AstraZeneca, the maker of goserelin.
Correction 5/31/14: An earlier version of this article carried a headline that misstated the cancer type.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT ASCO 2014
VIDEO: In SYMPLICITY, operator inexperience produced incomplete ablations
PARIS – A central problem with the SYMPLICITY HTN-3 trial of renal denervation was that the operators were inexperienced with the denervation procedure – and thus a majority of the renal denervations they carried out were not properly performed and left intact too many of the nerves that surround the renal arteries, commented Dr. Richard R. Heuser during the annual congress of the European Association of Percutaneous Cardiovascular Intervention.
"If you don’t get to the nerves and denervate them, you’re not going to have an effect," said Dr. Heuser, professor of medicine at the University of Arizona and chief of cardiology at St. Luke’s Medical Center in Phoenix.
Another limitation of the SYMPLICITY HTN-3 trial (N. Engl. J. Med. 2014;370:1393-1401) was that 25% of its enrolled patients were African Americans, and the trial’s results suggest that this patient subgroup does not respond to renal denervation with a significant fall in blood pressure.
In a video interview at the meeting, Dr. Heuser discussed the trial's potential limitations and renal denervation’s post-SYMPLICITY future.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
PARIS – A central problem with the SYMPLICITY HTN-3 trial of renal denervation was that the operators were inexperienced with the denervation procedure – and thus a majority of the renal denervations they carried out were not properly performed and left intact too many of the nerves that surround the renal arteries, commented Dr. Richard R. Heuser during the annual congress of the European Association of Percutaneous Cardiovascular Intervention.
"If you don’t get to the nerves and denervate them, you’re not going to have an effect," said Dr. Heuser, professor of medicine at the University of Arizona and chief of cardiology at St. Luke’s Medical Center in Phoenix.
Another limitation of the SYMPLICITY HTN-3 trial (N. Engl. J. Med. 2014;370:1393-1401) was that 25% of its enrolled patients were African Americans, and the trial’s results suggest that this patient subgroup does not respond to renal denervation with a significant fall in blood pressure.
In a video interview at the meeting, Dr. Heuser discussed the trial's potential limitations and renal denervation’s post-SYMPLICITY future.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
PARIS – A central problem with the SYMPLICITY HTN-3 trial of renal denervation was that the operators were inexperienced with the denervation procedure – and thus a majority of the renal denervations they carried out were not properly performed and left intact too many of the nerves that surround the renal arteries, commented Dr. Richard R. Heuser during the annual congress of the European Association of Percutaneous Cardiovascular Intervention.
"If you don’t get to the nerves and denervate them, you’re not going to have an effect," said Dr. Heuser, professor of medicine at the University of Arizona and chief of cardiology at St. Luke’s Medical Center in Phoenix.
Another limitation of the SYMPLICITY HTN-3 trial (N. Engl. J. Med. 2014;370:1393-1401) was that 25% of its enrolled patients were African Americans, and the trial’s results suggest that this patient subgroup does not respond to renal denervation with a significant fall in blood pressure.
In a video interview at the meeting, Dr. Heuser discussed the trial's potential limitations and renal denervation’s post-SYMPLICITY future.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
AT EUROPCR 2014
VIDEO: New MS database could change practice
DALLAS – The North American Registry for Care and Research in MS, a national database of multiple sclerosis patients, and the first of its kind, is expected to change multiple sclerosis care in the next decade.
The NARCRMS, which acts as both a database and a registry, will collect patient information from MS centers across the United States over time. It is modeled after the Alzheimer’s Disease Neuroimaging Initiative (ADNI), and it’s a collaboration between the industry and MS centers to create an open source database, "available in real time to patients, physicians, and industry," Dr. Kottil W. Rammohan, professor of clinical neurology and director of the MS center of excellence at the University of Miami, said at a meeting of the Consortium of Multiple Sclerosis Centers and the Americas Committee for Treatment and Research in Multiple Sclerosis.
The NARCRMS, not to be confused with NARCOMS (North American Research Committee on Multiple Sclerosis), hasn’t launched yet – it will be established later this year – but the leaders have great hopes for it, and say that it will help find answers to questions that exist because of a lack of data.
For instance, there are very few head-to-head trials comparing drugs with each other. The database could provide insight and the answer, said Dr. Rammohan.
More information and details will be available once the database is launched, but Dr. Rammohan provided an overview of the NARCRMS, and explained why a database hasn’t been established until now.
Dr. Rammohan said he had no relevant financial disclosures.
On Twitter @naseemmiller
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
DALLAS – The North American Registry for Care and Research in MS, a national database of multiple sclerosis patients, and the first of its kind, is expected to change multiple sclerosis care in the next decade.
The NARCRMS, which acts as both a database and a registry, will collect patient information from MS centers across the United States over time. It is modeled after the Alzheimer’s Disease Neuroimaging Initiative (ADNI), and it’s a collaboration between the industry and MS centers to create an open source database, "available in real time to patients, physicians, and industry," Dr. Kottil W. Rammohan, professor of clinical neurology and director of the MS center of excellence at the University of Miami, said at a meeting of the Consortium of Multiple Sclerosis Centers and the Americas Committee for Treatment and Research in Multiple Sclerosis.
The NARCRMS, not to be confused with NARCOMS (North American Research Committee on Multiple Sclerosis), hasn’t launched yet – it will be established later this year – but the leaders have great hopes for it, and say that it will help find answers to questions that exist because of a lack of data.
For instance, there are very few head-to-head trials comparing drugs with each other. The database could provide insight and the answer, said Dr. Rammohan.
More information and details will be available once the database is launched, but Dr. Rammohan provided an overview of the NARCRMS, and explained why a database hasn’t been established until now.
Dr. Rammohan said he had no relevant financial disclosures.
On Twitter @naseemmiller
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
DALLAS – The North American Registry for Care and Research in MS, a national database of multiple sclerosis patients, and the first of its kind, is expected to change multiple sclerosis care in the next decade.
The NARCRMS, which acts as both a database and a registry, will collect patient information from MS centers across the United States over time. It is modeled after the Alzheimer’s Disease Neuroimaging Initiative (ADNI), and it’s a collaboration between the industry and MS centers to create an open source database, "available in real time to patients, physicians, and industry," Dr. Kottil W. Rammohan, professor of clinical neurology and director of the MS center of excellence at the University of Miami, said at a meeting of the Consortium of Multiple Sclerosis Centers and the Americas Committee for Treatment and Research in Multiple Sclerosis.
The NARCRMS, not to be confused with NARCOMS (North American Research Committee on Multiple Sclerosis), hasn’t launched yet – it will be established later this year – but the leaders have great hopes for it, and say that it will help find answers to questions that exist because of a lack of data.
For instance, there are very few head-to-head trials comparing drugs with each other. The database could provide insight and the answer, said Dr. Rammohan.
More information and details will be available once the database is launched, but Dr. Rammohan provided an overview of the NARCRMS, and explained why a database hasn’t been established until now.
Dr. Rammohan said he had no relevant financial disclosures.
On Twitter @naseemmiller
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE CMSC/ACTRIMS ANNUAL MEETING
Clozapine trials
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
VIDEO: Abnormal endocrinology labs? Look beyond ‘usual suspects’
PHILADELPHIA – Psychiatric medications can affect prolactin levels, while antibodies can affect thyroid-stimulating hormone levels. Hirsutism may be the result of polycystic ovary syndrome – but it may also be caused by congenital adrenal hyperplasia.
And if that’s not confounding enough, physicians should add to the medical factors that can influence lab reports what Dr. Ellen L. Connor says is the importance of "knowing the typical ranges of the assays you are using, and what the ranges considered normal are at the [laboratory] you’re working with."
In a video interview at the annual meeting of the North American Society for Pediatric and Adolescent Gynecology, Dr. Connor of the department of pediatric endocrinology at the University of Wisconsin, Madison, reviews what can change prolactin levels, how to get the most clinical utility out of thyroid tests, what is the gold standard for testosterone testing in women, how best to test and interpret vitamin D levels, and what adrenal malfunctions are possible in young women. She also stresses the value of working with knowledgeable lab personnel.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @whitneymcknight
PHILADELPHIA – Psychiatric medications can affect prolactin levels, while antibodies can affect thyroid-stimulating hormone levels. Hirsutism may be the result of polycystic ovary syndrome – but it may also be caused by congenital adrenal hyperplasia.
And if that’s not confounding enough, physicians should add to the medical factors that can influence lab reports what Dr. Ellen L. Connor says is the importance of "knowing the typical ranges of the assays you are using, and what the ranges considered normal are at the [laboratory] you’re working with."
In a video interview at the annual meeting of the North American Society for Pediatric and Adolescent Gynecology, Dr. Connor of the department of pediatric endocrinology at the University of Wisconsin, Madison, reviews what can change prolactin levels, how to get the most clinical utility out of thyroid tests, what is the gold standard for testosterone testing in women, how best to test and interpret vitamin D levels, and what adrenal malfunctions are possible in young women. She also stresses the value of working with knowledgeable lab personnel.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @whitneymcknight
PHILADELPHIA – Psychiatric medications can affect prolactin levels, while antibodies can affect thyroid-stimulating hormone levels. Hirsutism may be the result of polycystic ovary syndrome – but it may also be caused by congenital adrenal hyperplasia.
And if that’s not confounding enough, physicians should add to the medical factors that can influence lab reports what Dr. Ellen L. Connor says is the importance of "knowing the typical ranges of the assays you are using, and what the ranges considered normal are at the [laboratory] you’re working with."
In a video interview at the annual meeting of the North American Society for Pediatric and Adolescent Gynecology, Dr. Connor of the department of pediatric endocrinology at the University of Wisconsin, Madison, reviews what can change prolactin levels, how to get the most clinical utility out of thyroid tests, what is the gold standard for testosterone testing in women, how best to test and interpret vitamin D levels, and what adrenal malfunctions are possible in young women. She also stresses the value of working with knowledgeable lab personnel.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @whitneymcknight
EXPERT ANALYSIS FROM NASPAG 2014
VIDEO: Endocrinology initiatives can improve transgender care
LAS VEGAS – Dr. Joshua D. Safer is a man on a mission. He wants to incorporate transgender medicine into medical school curricula across North America to help increase the number of specialists who can treat individuals with gender identity disorders.
"The number of endocrinologists who do this is very small," said Dr. Safer of the departments of medicine and molecular medicine and director of the endocrinology fellowship training program at Boston University. This is partly because many physicians aren’t comfortable with the topic, said Dr. Safer. Endocrinologists should recognize that "gender identity is usually fixed," and once they accept this fact, hormone treatment for transgender individuals "follows a conventional endocrinology paradigm," he said at the annual meeting of the American Association of Clinical Endocrinologists.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
By his count, there may be a dozen endocrinologists in the United States who specialize in transgender medicine. Yet, some statistics suggest that 0.3% of the population has gender identity disorder, Dr. Safer noted, "and that’s not a small number – you’re talking about hundreds of thousands of people." Also, the age of Internet and social media has helped transgender individuals recognize that they’re not alone in their battle, and "many are showing up at a younger age," he added.
Several protocols are available for physicians, including one published by the Endocrine Society and another by the World Professional Association for Transgender Health (WPATH), which is one of the oldest organizations to focus on understanding and treatment of gender identity disorders. Both groups are working to create treatment paradigms that are reproducible by physicians in multiple specialties, Dr. Safer said. The American Congress of Obstetricians and Gynecologists also has a complete list of available resources.
Dr. Safer said that endocrinologists can also contact experts like him for advice. (For instance, Dr. Safer works closely with a mental health counselor who helps patients navigate their way through the changes.)
In the meantime, he continues to give talks around the nation to raise awareness and is planning on conducting studies and surveying physicians on their knowledge of the field. Transgender medicine is already incorporated into Boston University’s medical school curriculum, he said.
Dr. Safer has no relevant financial relationships with commercial interests.
On Twitter @naseemmiller
LAS VEGAS – Dr. Joshua D. Safer is a man on a mission. He wants to incorporate transgender medicine into medical school curricula across North America to help increase the number of specialists who can treat individuals with gender identity disorders.
"The number of endocrinologists who do this is very small," said Dr. Safer of the departments of medicine and molecular medicine and director of the endocrinology fellowship training program at Boston University. This is partly because many physicians aren’t comfortable with the topic, said Dr. Safer. Endocrinologists should recognize that "gender identity is usually fixed," and once they accept this fact, hormone treatment for transgender individuals "follows a conventional endocrinology paradigm," he said at the annual meeting of the American Association of Clinical Endocrinologists.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
By his count, there may be a dozen endocrinologists in the United States who specialize in transgender medicine. Yet, some statistics suggest that 0.3% of the population has gender identity disorder, Dr. Safer noted, "and that’s not a small number – you’re talking about hundreds of thousands of people." Also, the age of Internet and social media has helped transgender individuals recognize that they’re not alone in their battle, and "many are showing up at a younger age," he added.
Several protocols are available for physicians, including one published by the Endocrine Society and another by the World Professional Association for Transgender Health (WPATH), which is one of the oldest organizations to focus on understanding and treatment of gender identity disorders. Both groups are working to create treatment paradigms that are reproducible by physicians in multiple specialties, Dr. Safer said. The American Congress of Obstetricians and Gynecologists also has a complete list of available resources.
Dr. Safer said that endocrinologists can also contact experts like him for advice. (For instance, Dr. Safer works closely with a mental health counselor who helps patients navigate their way through the changes.)
In the meantime, he continues to give talks around the nation to raise awareness and is planning on conducting studies and surveying physicians on their knowledge of the field. Transgender medicine is already incorporated into Boston University’s medical school curriculum, he said.
Dr. Safer has no relevant financial relationships with commercial interests.
On Twitter @naseemmiller
LAS VEGAS – Dr. Joshua D. Safer is a man on a mission. He wants to incorporate transgender medicine into medical school curricula across North America to help increase the number of specialists who can treat individuals with gender identity disorders.
"The number of endocrinologists who do this is very small," said Dr. Safer of the departments of medicine and molecular medicine and director of the endocrinology fellowship training program at Boston University. This is partly because many physicians aren’t comfortable with the topic, said Dr. Safer. Endocrinologists should recognize that "gender identity is usually fixed," and once they accept this fact, hormone treatment for transgender individuals "follows a conventional endocrinology paradigm," he said at the annual meeting of the American Association of Clinical Endocrinologists.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
By his count, there may be a dozen endocrinologists in the United States who specialize in transgender medicine. Yet, some statistics suggest that 0.3% of the population has gender identity disorder, Dr. Safer noted, "and that’s not a small number – you’re talking about hundreds of thousands of people." Also, the age of Internet and social media has helped transgender individuals recognize that they’re not alone in their battle, and "many are showing up at a younger age," he added.
Several protocols are available for physicians, including one published by the Endocrine Society and another by the World Professional Association for Transgender Health (WPATH), which is one of the oldest organizations to focus on understanding and treatment of gender identity disorders. Both groups are working to create treatment paradigms that are reproducible by physicians in multiple specialties, Dr. Safer said. The American Congress of Obstetricians and Gynecologists also has a complete list of available resources.
Dr. Safer said that endocrinologists can also contact experts like him for advice. (For instance, Dr. Safer works closely with a mental health counselor who helps patients navigate their way through the changes.)
In the meantime, he continues to give talks around the nation to raise awareness and is planning on conducting studies and surveying physicians on their knowledge of the field. Transgender medicine is already incorporated into Boston University’s medical school curriculum, he said.
Dr. Safer has no relevant financial relationships with commercial interests.
On Twitter @naseemmiller
AT AACE 14
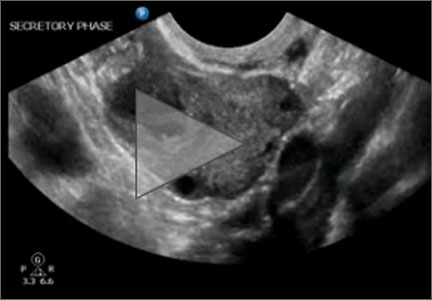
Transvaginal ultrasonography of ovarian cyst
VIDEO: Hypogonadism, hypercortisolemia may mean anorexia in men
LAS VEGAS – Anorexia nervosa in men may present in unusual ways, confounding the diagnosis and leading to inappropriate treatment, according to a case series reported at the annual meeting of the American Association of Clinical Endocrinologists.
In a video interview, Dr. Aren H. Skolnick, an endocrinology fellow at Hofstra University, Hempstead, N.Y., Jewish Medical Center, explains the signs of anorexia in men, how the condition presents itself, and what clinicians should do.
On Twitter @naseemmiller
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LAS VEGAS – Anorexia nervosa in men may present in unusual ways, confounding the diagnosis and leading to inappropriate treatment, according to a case series reported at the annual meeting of the American Association of Clinical Endocrinologists.
In a video interview, Dr. Aren H. Skolnick, an endocrinology fellow at Hofstra University, Hempstead, N.Y., Jewish Medical Center, explains the signs of anorexia in men, how the condition presents itself, and what clinicians should do.
On Twitter @naseemmiller
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LAS VEGAS – Anorexia nervosa in men may present in unusual ways, confounding the diagnosis and leading to inappropriate treatment, according to a case series reported at the annual meeting of the American Association of Clinical Endocrinologists.
In a video interview, Dr. Aren H. Skolnick, an endocrinology fellow at Hofstra University, Hempstead, N.Y., Jewish Medical Center, explains the signs of anorexia in men, how the condition presents itself, and what clinicians should do.
On Twitter @naseemmiller
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
EXPERT ANALYSIS FROM AACE 14
VIDEO: Glycogen storage disease – easy to miss, easy to fix
VANCOUVER, B.C. – Recently, it’s become clear that milder forms of glycogen storage disease (GSD) – a genetic aberration in sugar metabolism – can cause problems with attention, mood, and growth that are easy to mistake for something else. GSD type 9 is a particularly potent imposter that occurs in boys and men only.
Once recognized, the solution is easy – cornstarch doses about every 4 hours. At the annual meeting of the Pediatric Academic Societies, a team lead by Dr. David A. Weinstein, a professor of pediatric endocrinology and the director of the glycogen storage disease program at the University of Florida, Gainesville, reported that a new, slow-release form of cornstarch called Glycosade lets patients skip their night dose so they can get a full 8 hours of sleep.
At the meeting, Dr. Weinstein told us how to recognize, diagnose, and treat glycogen storage disease, and a little bit about how effective intervention can change the lives of people who have it.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
VANCOUVER, B.C. – Recently, it’s become clear that milder forms of glycogen storage disease (GSD) – a genetic aberration in sugar metabolism – can cause problems with attention, mood, and growth that are easy to mistake for something else. GSD type 9 is a particularly potent imposter that occurs in boys and men only.
Once recognized, the solution is easy – cornstarch doses about every 4 hours. At the annual meeting of the Pediatric Academic Societies, a team lead by Dr. David A. Weinstein, a professor of pediatric endocrinology and the director of the glycogen storage disease program at the University of Florida, Gainesville, reported that a new, slow-release form of cornstarch called Glycosade lets patients skip their night dose so they can get a full 8 hours of sleep.
At the meeting, Dr. Weinstein told us how to recognize, diagnose, and treat glycogen storage disease, and a little bit about how effective intervention can change the lives of people who have it.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
VANCOUVER, B.C. – Recently, it’s become clear that milder forms of glycogen storage disease (GSD) – a genetic aberration in sugar metabolism – can cause problems with attention, mood, and growth that are easy to mistake for something else. GSD type 9 is a particularly potent imposter that occurs in boys and men only.
Once recognized, the solution is easy – cornstarch doses about every 4 hours. At the annual meeting of the Pediatric Academic Societies, a team lead by Dr. David A. Weinstein, a professor of pediatric endocrinology and the director of the glycogen storage disease program at the University of Florida, Gainesville, reported that a new, slow-release form of cornstarch called Glycosade lets patients skip their night dose so they can get a full 8 hours of sleep.
At the meeting, Dr. Weinstein told us how to recognize, diagnose, and treat glycogen storage disease, and a little bit about how effective intervention can change the lives of people who have it.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
EXPERT ANALYSIS FROM THE PAS ANNUAL MEETING
VIDEO: Coffee break at AACE – What I’ve learned
LAS VEGAS – With so many sessions to attend, we were curious what stood out to attendees at the annual meeting of the American Association of Clinical Endocrinologists.
In this video, attendees share the lessons they learned that they will be applying to their practices.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @naseemmiller
LAS VEGAS – With so many sessions to attend, we were curious what stood out to attendees at the annual meeting of the American Association of Clinical Endocrinologists.
In this video, attendees share the lessons they learned that they will be applying to their practices.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @naseemmiller
LAS VEGAS – With so many sessions to attend, we were curious what stood out to attendees at the annual meeting of the American Association of Clinical Endocrinologists.
In this video, attendees share the lessons they learned that they will be applying to their practices.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @naseemmiller
AT AACE 14