User login
Healing chronic venous ulcers? Compression, compression, compression
ESTES PARK, COLO. – Meg A. Lemon, MD, said at a conference on internal medicine sponsored by the University of Colorado at Denver, Aurora.
“The top nine ways of treating venous leg ulcers are compression,” explained Dr. Lemon, a Denver-area dermatologist in private practice. “You generally don’t have an active patient who’s moving around [and] allowing the calf to squeeze venous blood back into the circulation, so you have to compress externally. I spend a lot of time with patients saying, ‘If we don’t wear the compression stockings and we don’t elevate the legs, the wound will never heal.’ ”
Compression stockings are no longer frumpy – they have gotten hip. Endurance athletes have embraced them as a recovery aid, and they now come in a multitude of colorful styles. It’s best to start patients off at 15-20 mm Hg of compression so they don’t get discouraged by the initial challenges of getting the stockings on and off, Dr. Lemon explained, then work up to at least 30 mm Hg. Application devices that function much like a shoehorn can assist patients in getting the stockings on if they report difficulties.
As soon as patients get out of bed in the morning, their venous pressure skyrockets, and inflammatory compounds start accumulating in their legs: “I tell patients they need to put the stockings on before getting out of bed to pee in the morning,” the dermatologist said.
A meta-analysis has shown that adequate compression, coupled with wound debridement when indicated, resulted in the healing of 57% of longstanding chronic venous lower-extremity ulcers within 10 weeks and of 75% within 16 weeks, she reported.
Elevating the legs has therapeutic benefit as well, but it has to be done right. The legs must be above the heart for hours at a time, such as while sleeping or while laying on a couch to read or watch television. Putting three bed pillows under the entire calf – rather than under the feet – does the job. Simply sticking the pillows under the feet can result in painful knee hyperextension, which can lead to poor compliance.
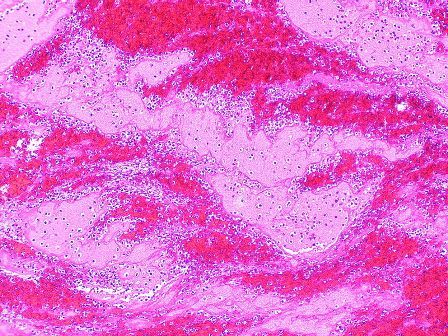
“We’re all basically large columns of fluid,” Dr. Lemon said. “We stand around or sit all the time, and the fluid pools in our legs because the valves in the veins stop closing properly as we age. The increased pressure in the vein causes the vein to leak inflammatory compounds into the surrounding tissue, producing edema and chronic inflammation. The chronicity of the disease leads to really profound changes in the skin that are extraordinarily helpful diagnostically.”
Diagnostic tips
These cutaneous changes include a dark brown discoloration – reminiscent of rust – because of deposition of hemosiderin in tissues. The skin becomes fibrous, hard, and ulcerated. The end stage of chronic venous insufficiency is lipodermatosclerosis, in which the skin becomes almost immobile and the lower leg takes on a champagne bottle shape because of hardening of the skin close to the ankle.
Venography, long preferred in definitively diagnosing venous lower-extremity ulcers, is giving way to venous duplex ultrasound, which is not quite as accurate but spares patients the pain associated with the older procedure.
Roughly 70% of chronic lower-extremity ulcers are of venous origin, Dr. Lemon noted.
She encounters quite a few patients who are hospitalized for what is mistakenly diagnosed as bilateral cellulitis, when their true problem is chronic venous insufficiency. The patient’s response to two questions makes it easy to differentiate the two disorders. One is, “Do your legs hurt more or itch more?”
“If the legs itch more, the patient doesn’t have cellulitis,” Dr. Lemon explained. “Cellulitis doesn’t itch. Also, ask the patient, ‘When did your legs last look normal?’ They usually say it was years ago. That’s not bilateral cellulitis – an acute problem requiring hospitalization. It’s a chronic problem requiring extensive chronic wound care.”
If the lower leg wound site looks like cellulitis, with redness, swelling, and warmth to touch, but it itches rather than hurts, she noted, it’s probably stasis dermatitis, which is very common in patients with venous lower-extremity ulcers. The treatment is a potent topical steroid.
“Don’t be afraid of potent steroids,” Dr. Lemon said. “There is so much inflammation in those tissues, they need a potent steroid on the leg. I usually prescribe fluocinonide 0.05% because it’s reliably beneficial.”
An exudative venous wound should receive a moist dressing.
“Forget what your granny told you, and stop telling patients their wounds need to breathe,” she cautioned. “Wounds generally need to be suffocated and covered with an ointment like Vaseline. A dry wound heals about six times slower than a moist one; that’s been extensively studied in the dermatology, surgery, and burn literature.”
If, after 5-6 months of Dr. Lemon’s efforts, a patient’s wound still isn’t healing, the dermatologist will obtain a venous surgical consultation. In some reported series, surgical treatment of insufficiency – venous stripping – has resulted in improved healing time and fewer recurrent ulcers.
Dr. Lemon reported having no financial conflicts regarding her presentation.
ESTES PARK, COLO. – Meg A. Lemon, MD, said at a conference on internal medicine sponsored by the University of Colorado at Denver, Aurora.
“The top nine ways of treating venous leg ulcers are compression,” explained Dr. Lemon, a Denver-area dermatologist in private practice. “You generally don’t have an active patient who’s moving around [and] allowing the calf to squeeze venous blood back into the circulation, so you have to compress externally. I spend a lot of time with patients saying, ‘If we don’t wear the compression stockings and we don’t elevate the legs, the wound will never heal.’ ”
Compression stockings are no longer frumpy – they have gotten hip. Endurance athletes have embraced them as a recovery aid, and they now come in a multitude of colorful styles. It’s best to start patients off at 15-20 mm Hg of compression so they don’t get discouraged by the initial challenges of getting the stockings on and off, Dr. Lemon explained, then work up to at least 30 mm Hg. Application devices that function much like a shoehorn can assist patients in getting the stockings on if they report difficulties.
As soon as patients get out of bed in the morning, their venous pressure skyrockets, and inflammatory compounds start accumulating in their legs: “I tell patients they need to put the stockings on before getting out of bed to pee in the morning,” the dermatologist said.
A meta-analysis has shown that adequate compression, coupled with wound debridement when indicated, resulted in the healing of 57% of longstanding chronic venous lower-extremity ulcers within 10 weeks and of 75% within 16 weeks, she reported.
Elevating the legs has therapeutic benefit as well, but it has to be done right. The legs must be above the heart for hours at a time, such as while sleeping or while laying on a couch to read or watch television. Putting three bed pillows under the entire calf – rather than under the feet – does the job. Simply sticking the pillows under the feet can result in painful knee hyperextension, which can lead to poor compliance.
“We’re all basically large columns of fluid,” Dr. Lemon said. “We stand around or sit all the time, and the fluid pools in our legs because the valves in the veins stop closing properly as we age. The increased pressure in the vein causes the vein to leak inflammatory compounds into the surrounding tissue, producing edema and chronic inflammation. The chronicity of the disease leads to really profound changes in the skin that are extraordinarily helpful diagnostically.”
Diagnostic tips
These cutaneous changes include a dark brown discoloration – reminiscent of rust – because of deposition of hemosiderin in tissues. The skin becomes fibrous, hard, and ulcerated. The end stage of chronic venous insufficiency is lipodermatosclerosis, in which the skin becomes almost immobile and the lower leg takes on a champagne bottle shape because of hardening of the skin close to the ankle.
Venography, long preferred in definitively diagnosing venous lower-extremity ulcers, is giving way to venous duplex ultrasound, which is not quite as accurate but spares patients the pain associated with the older procedure.
Roughly 70% of chronic lower-extremity ulcers are of venous origin, Dr. Lemon noted.
She encounters quite a few patients who are hospitalized for what is mistakenly diagnosed as bilateral cellulitis, when their true problem is chronic venous insufficiency. The patient’s response to two questions makes it easy to differentiate the two disorders. One is, “Do your legs hurt more or itch more?”
“If the legs itch more, the patient doesn’t have cellulitis,” Dr. Lemon explained. “Cellulitis doesn’t itch. Also, ask the patient, ‘When did your legs last look normal?’ They usually say it was years ago. That’s not bilateral cellulitis – an acute problem requiring hospitalization. It’s a chronic problem requiring extensive chronic wound care.”
If the lower leg wound site looks like cellulitis, with redness, swelling, and warmth to touch, but it itches rather than hurts, she noted, it’s probably stasis dermatitis, which is very common in patients with venous lower-extremity ulcers. The treatment is a potent topical steroid.
“Don’t be afraid of potent steroids,” Dr. Lemon said. “There is so much inflammation in those tissues, they need a potent steroid on the leg. I usually prescribe fluocinonide 0.05% because it’s reliably beneficial.”
An exudative venous wound should receive a moist dressing.
“Forget what your granny told you, and stop telling patients their wounds need to breathe,” she cautioned. “Wounds generally need to be suffocated and covered with an ointment like Vaseline. A dry wound heals about six times slower than a moist one; that’s been extensively studied in the dermatology, surgery, and burn literature.”
If, after 5-6 months of Dr. Lemon’s efforts, a patient’s wound still isn’t healing, the dermatologist will obtain a venous surgical consultation. In some reported series, surgical treatment of insufficiency – venous stripping – has resulted in improved healing time and fewer recurrent ulcers.
Dr. Lemon reported having no financial conflicts regarding her presentation.
ESTES PARK, COLO. – Meg A. Lemon, MD, said at a conference on internal medicine sponsored by the University of Colorado at Denver, Aurora.
“The top nine ways of treating venous leg ulcers are compression,” explained Dr. Lemon, a Denver-area dermatologist in private practice. “You generally don’t have an active patient who’s moving around [and] allowing the calf to squeeze venous blood back into the circulation, so you have to compress externally. I spend a lot of time with patients saying, ‘If we don’t wear the compression stockings and we don’t elevate the legs, the wound will never heal.’ ”
Compression stockings are no longer frumpy – they have gotten hip. Endurance athletes have embraced them as a recovery aid, and they now come in a multitude of colorful styles. It’s best to start patients off at 15-20 mm Hg of compression so they don’t get discouraged by the initial challenges of getting the stockings on and off, Dr. Lemon explained, then work up to at least 30 mm Hg. Application devices that function much like a shoehorn can assist patients in getting the stockings on if they report difficulties.
As soon as patients get out of bed in the morning, their venous pressure skyrockets, and inflammatory compounds start accumulating in their legs: “I tell patients they need to put the stockings on before getting out of bed to pee in the morning,” the dermatologist said.
A meta-analysis has shown that adequate compression, coupled with wound debridement when indicated, resulted in the healing of 57% of longstanding chronic venous lower-extremity ulcers within 10 weeks and of 75% within 16 weeks, she reported.
Elevating the legs has therapeutic benefit as well, but it has to be done right. The legs must be above the heart for hours at a time, such as while sleeping or while laying on a couch to read or watch television. Putting three bed pillows under the entire calf – rather than under the feet – does the job. Simply sticking the pillows under the feet can result in painful knee hyperextension, which can lead to poor compliance.
“We’re all basically large columns of fluid,” Dr. Lemon said. “We stand around or sit all the time, and the fluid pools in our legs because the valves in the veins stop closing properly as we age. The increased pressure in the vein causes the vein to leak inflammatory compounds into the surrounding tissue, producing edema and chronic inflammation. The chronicity of the disease leads to really profound changes in the skin that are extraordinarily helpful diagnostically.”
Diagnostic tips
These cutaneous changes include a dark brown discoloration – reminiscent of rust – because of deposition of hemosiderin in tissues. The skin becomes fibrous, hard, and ulcerated. The end stage of chronic venous insufficiency is lipodermatosclerosis, in which the skin becomes almost immobile and the lower leg takes on a champagne bottle shape because of hardening of the skin close to the ankle.
Venography, long preferred in definitively diagnosing venous lower-extremity ulcers, is giving way to venous duplex ultrasound, which is not quite as accurate but spares patients the pain associated with the older procedure.
Roughly 70% of chronic lower-extremity ulcers are of venous origin, Dr. Lemon noted.
She encounters quite a few patients who are hospitalized for what is mistakenly diagnosed as bilateral cellulitis, when their true problem is chronic venous insufficiency. The patient’s response to two questions makes it easy to differentiate the two disorders. One is, “Do your legs hurt more or itch more?”
“If the legs itch more, the patient doesn’t have cellulitis,” Dr. Lemon explained. “Cellulitis doesn’t itch. Also, ask the patient, ‘When did your legs last look normal?’ They usually say it was years ago. That’s not bilateral cellulitis – an acute problem requiring hospitalization. It’s a chronic problem requiring extensive chronic wound care.”
If the lower leg wound site looks like cellulitis, with redness, swelling, and warmth to touch, but it itches rather than hurts, she noted, it’s probably stasis dermatitis, which is very common in patients with venous lower-extremity ulcers. The treatment is a potent topical steroid.
“Don’t be afraid of potent steroids,” Dr. Lemon said. “There is so much inflammation in those tissues, they need a potent steroid on the leg. I usually prescribe fluocinonide 0.05% because it’s reliably beneficial.”
An exudative venous wound should receive a moist dressing.
“Forget what your granny told you, and stop telling patients their wounds need to breathe,” she cautioned. “Wounds generally need to be suffocated and covered with an ointment like Vaseline. A dry wound heals about six times slower than a moist one; that’s been extensively studied in the dermatology, surgery, and burn literature.”
If, after 5-6 months of Dr. Lemon’s efforts, a patient’s wound still isn’t healing, the dermatologist will obtain a venous surgical consultation. In some reported series, surgical treatment of insufficiency – venous stripping – has resulted in improved healing time and fewer recurrent ulcers.
Dr. Lemon reported having no financial conflicts regarding her presentation.
EXPERT ANALYSIS FROM THE ANNUAL INTERNAL MEDICINE PROGRAM
Exercise program speeds healing of venous leg ulcers
A supervised exercise program for patients with venous leg ulcers has shown improved healing times over compression therapy alone, according to a paper published online on Oct. 27 in the British Journal of Dermatology.
In a parallel group feasibility trial, researchers randomized 39 patients with venous ulcers either to a 12-week program of supervised exercise three times a week plus compression therapy (18 patients), or compression therapy alone (21 patients). The exercise program combined aerobic, resistance, and flexibility exercises.
This group showed a median ulcer healing time of 13 weeks (3.9-52 weeks), compared with 34.7 weeks (4.3-52 weeks) for the compression therapy–only group, although the median ulcer size was similar between the two groups at 12 months. At last follow-up of 12 months, 83% of the ulcers in the exercise group had healed, compared with 60% in the control group (Br J Dermatol. 2017 Oct 27. doi: 10.1111/bjd.16089).
The intervention group had a slightly higher quality of life at baseline, as measured by the EQ-5D utility score, and this difference was maintained throughout the study.
Nearly three-quarters (72%) of the exercise group participants went to all the scheduled exercise sessions, with an overall attendance rate of 79%, which the authors noted was high considering many were old, frail, and had no previous exercise experience.
“This was achieved without employing any specific adherence-enhancing components or provision of behavioral change support, which could have potentially improved attendance rates and the effect of the intervention even further,” wrote Markos Klonizakis, DPhil, from the Centre for Sport and Exercise Science at Sheffield (England) Hallam University, and his coinvestigators.
There were no serious adverse events, and only two exercise-related adverse events in the intervention group – both excessive discharge from the ulcer – which resulted in postponement of the exercise sessions for those two individuals.
The exercise regimen was associated with modest reductions in weight, while those in the control group showed an overall increase in weight.
Researchers also assessed the relative costs of the two interventions by getting participants to keep a diary of their use of National Health Service resources, health care visits, prescriptions, and other out-of-pocket expenses.
They calculated that the total mean National Health Service cost per participant for the exercise intervention was £813.27, and £2,298.57 for the control group who received compression therapy only.
The investigators noted that their initial plan had been met with some skepticism from clinicians and patients, some of whom felt that exercise would have a detrimental rather than positive effect on venous ulcer healing.
“Our results suggest that there may be significant potential benefit in healing rates and that, if this were confirmed in a full trial, the introduction of supervised exercise for venous leg ulcers may well also be cost-saving for the National Health Service.”
The study was funded by the National Institute for Health Research. No conflicts of interest were declared.
A supervised exercise program for patients with venous leg ulcers has shown improved healing times over compression therapy alone, according to a paper published online on Oct. 27 in the British Journal of Dermatology.
In a parallel group feasibility trial, researchers randomized 39 patients with venous ulcers either to a 12-week program of supervised exercise three times a week plus compression therapy (18 patients), or compression therapy alone (21 patients). The exercise program combined aerobic, resistance, and flexibility exercises.
This group showed a median ulcer healing time of 13 weeks (3.9-52 weeks), compared with 34.7 weeks (4.3-52 weeks) for the compression therapy–only group, although the median ulcer size was similar between the two groups at 12 months. At last follow-up of 12 months, 83% of the ulcers in the exercise group had healed, compared with 60% in the control group (Br J Dermatol. 2017 Oct 27. doi: 10.1111/bjd.16089).
The intervention group had a slightly higher quality of life at baseline, as measured by the EQ-5D utility score, and this difference was maintained throughout the study.
Nearly three-quarters (72%) of the exercise group participants went to all the scheduled exercise sessions, with an overall attendance rate of 79%, which the authors noted was high considering many were old, frail, and had no previous exercise experience.
“This was achieved without employing any specific adherence-enhancing components or provision of behavioral change support, which could have potentially improved attendance rates and the effect of the intervention even further,” wrote Markos Klonizakis, DPhil, from the Centre for Sport and Exercise Science at Sheffield (England) Hallam University, and his coinvestigators.
There were no serious adverse events, and only two exercise-related adverse events in the intervention group – both excessive discharge from the ulcer – which resulted in postponement of the exercise sessions for those two individuals.
The exercise regimen was associated with modest reductions in weight, while those in the control group showed an overall increase in weight.
Researchers also assessed the relative costs of the two interventions by getting participants to keep a diary of their use of National Health Service resources, health care visits, prescriptions, and other out-of-pocket expenses.
They calculated that the total mean National Health Service cost per participant for the exercise intervention was £813.27, and £2,298.57 for the control group who received compression therapy only.
The investigators noted that their initial plan had been met with some skepticism from clinicians and patients, some of whom felt that exercise would have a detrimental rather than positive effect on venous ulcer healing.
“Our results suggest that there may be significant potential benefit in healing rates and that, if this were confirmed in a full trial, the introduction of supervised exercise for venous leg ulcers may well also be cost-saving for the National Health Service.”
The study was funded by the National Institute for Health Research. No conflicts of interest were declared.
A supervised exercise program for patients with venous leg ulcers has shown improved healing times over compression therapy alone, according to a paper published online on Oct. 27 in the British Journal of Dermatology.
In a parallel group feasibility trial, researchers randomized 39 patients with venous ulcers either to a 12-week program of supervised exercise three times a week plus compression therapy (18 patients), or compression therapy alone (21 patients). The exercise program combined aerobic, resistance, and flexibility exercises.
This group showed a median ulcer healing time of 13 weeks (3.9-52 weeks), compared with 34.7 weeks (4.3-52 weeks) for the compression therapy–only group, although the median ulcer size was similar between the two groups at 12 months. At last follow-up of 12 months, 83% of the ulcers in the exercise group had healed, compared with 60% in the control group (Br J Dermatol. 2017 Oct 27. doi: 10.1111/bjd.16089).
The intervention group had a slightly higher quality of life at baseline, as measured by the EQ-5D utility score, and this difference was maintained throughout the study.
Nearly three-quarters (72%) of the exercise group participants went to all the scheduled exercise sessions, with an overall attendance rate of 79%, which the authors noted was high considering many were old, frail, and had no previous exercise experience.
“This was achieved without employing any specific adherence-enhancing components or provision of behavioral change support, which could have potentially improved attendance rates and the effect of the intervention even further,” wrote Markos Klonizakis, DPhil, from the Centre for Sport and Exercise Science at Sheffield (England) Hallam University, and his coinvestigators.
There were no serious adverse events, and only two exercise-related adverse events in the intervention group – both excessive discharge from the ulcer – which resulted in postponement of the exercise sessions for those two individuals.
The exercise regimen was associated with modest reductions in weight, while those in the control group showed an overall increase in weight.
Researchers also assessed the relative costs of the two interventions by getting participants to keep a diary of their use of National Health Service resources, health care visits, prescriptions, and other out-of-pocket expenses.
They calculated that the total mean National Health Service cost per participant for the exercise intervention was £813.27, and £2,298.57 for the control group who received compression therapy only.
The investigators noted that their initial plan had been met with some skepticism from clinicians and patients, some of whom felt that exercise would have a detrimental rather than positive effect on venous ulcer healing.
“Our results suggest that there may be significant potential benefit in healing rates and that, if this were confirmed in a full trial, the introduction of supervised exercise for venous leg ulcers may well also be cost-saving for the National Health Service.”
The study was funded by the National Institute for Health Research. No conflicts of interest were declared.
FROM THE BRITISH JOURNAL OF DERMATOLOGY
Key clinical point: A supervised exercise program for patients with venous leg ulcers has shown significantly improved healing times over compression therapy alone.
Major finding: Patients who underwent a program of supervised exercise in addition to compression therapy showed a median ulcer healing time of 13 weeks, compared with 35 weeks for patients who received compression therapy alone.
Data source: A randomized, parallel group feasibility trial in 39 patients with venous ulcers.
Disclosures: The study was funded by the National Institute for Health Research. No conflicts of interest were declared.
Topical timolol improved chronic leg ulcer healing
The use of topical timolol maleate as a treatment for chronic diabetic and chronic venous ulcers showed increased wound healing compared with controls, according to the results of a prospective observational study of 60 patients.
In the treatment group, 30 patients with chronic leg ulcer (15 diabetic ulcers; 15 venous) received topical application of 0.5% timolol maleate (a beta-blocker) plus conventional antibiotic and wound dressing therapy. In the control group, 30 patients (identical split between diabetic and venous ulcers) were treated with conventional therapy alone, according to a report published in the November issue of the Journal of Vascular Surgery: Venous and Lymphatic Disorders.
The researchers found no significant difference in healing rates due to sex, between smokers and nonsmokers, or alcohol consumers vs. nonconsumers and they saw no major adverse effects due to timolol application (J Vasc Surg: Venous and Lym Dis 2017;5:844-50).
They reported that the limitations of their study included the lack of randomization and a formal power assessment.
“Topical application of timolol maleate is an effective therapeutic option for the treatment of chronic diabetic ulcer and chronic venous ulcer patients to improve ulcer healing by promoting keratinocyte migration,” the researchers concluded.
They reported having no relevant conflicts.
The use of topical timolol maleate as a treatment for chronic diabetic and chronic venous ulcers showed increased wound healing compared with controls, according to the results of a prospective observational study of 60 patients.
In the treatment group, 30 patients with chronic leg ulcer (15 diabetic ulcers; 15 venous) received topical application of 0.5% timolol maleate (a beta-blocker) plus conventional antibiotic and wound dressing therapy. In the control group, 30 patients (identical split between diabetic and venous ulcers) were treated with conventional therapy alone, according to a report published in the November issue of the Journal of Vascular Surgery: Venous and Lymphatic Disorders.
The researchers found no significant difference in healing rates due to sex, between smokers and nonsmokers, or alcohol consumers vs. nonconsumers and they saw no major adverse effects due to timolol application (J Vasc Surg: Venous and Lym Dis 2017;5:844-50).
They reported that the limitations of their study included the lack of randomization and a formal power assessment.
“Topical application of timolol maleate is an effective therapeutic option for the treatment of chronic diabetic ulcer and chronic venous ulcer patients to improve ulcer healing by promoting keratinocyte migration,” the researchers concluded.
They reported having no relevant conflicts.
The use of topical timolol maleate as a treatment for chronic diabetic and chronic venous ulcers showed increased wound healing compared with controls, according to the results of a prospective observational study of 60 patients.
In the treatment group, 30 patients with chronic leg ulcer (15 diabetic ulcers; 15 venous) received topical application of 0.5% timolol maleate (a beta-blocker) plus conventional antibiotic and wound dressing therapy. In the control group, 30 patients (identical split between diabetic and venous ulcers) were treated with conventional therapy alone, according to a report published in the November issue of the Journal of Vascular Surgery: Venous and Lymphatic Disorders.
The researchers found no significant difference in healing rates due to sex, between smokers and nonsmokers, or alcohol consumers vs. nonconsumers and they saw no major adverse effects due to timolol application (J Vasc Surg: Venous and Lym Dis 2017;5:844-50).
They reported that the limitations of their study included the lack of randomization and a formal power assessment.
“Topical application of timolol maleate is an effective therapeutic option for the treatment of chronic diabetic ulcer and chronic venous ulcer patients to improve ulcer healing by promoting keratinocyte migration,” the researchers concluded.
They reported having no relevant conflicts.
FROM THE JOURNAL OF VASCULAR SURGERY: VENOUS AND LYMPHATIC DISORDERS
Infections increase risk of idiopathic VTE
Infection and infection sites have been found to be associated with a significant increased risk of venous thromboembolism, according to results of a population-based, matched, case-control analysis of medical records covering the 13-year period 1988-2000.
Dr. Kevin P. Cohoon and his colleagues at the Mayo Clinic, Rochester, Minn., developed models using conditional logistic regression analysis to stratify the risk associated with specific infections and infection sites.
Five hundred thirteen (39.4%) cases and 189 (12.7%) controls had an infection within the previous 92 days (odds ratio, 4.5; P less than .0001). Known VTE risk factors and potentially confounding variables were used in the adjusted univariate and multivariate models, as reported in the American Journal of Medicine (2017. doi: 10.1016/j.amjmed.2017.09.015).
Dr. Cohoon and his colleagues reported that univariate analysis showed “most infection sites were strongly associated with venous thromboembolism” and the adjusted multivariate model resulted in 2.4-fold (P less than .0001) higher odds for VTE incidence, compared with uninfected controls.
Adjusted multivariate analysis ranked the odds of VTE according to specific infections. Dr. Cohoon and his colleagues reported that this modeling showed that the “highest magnitude of risk, compared with no infection, was imparted by intra-abdominal infection (OR, 18) followed by oral infection (OR, 12), systematic blood stream infection (OR, 11), lower respiratory infection such as pneumonia (OR, 3.6), and symptomatic urinary tract infection (OR, 2.2).”
The researchers concluded that their findings may allow for further refinement of inpatient VTE risk-prediction models such as the Padua prediction score and “future studies are required to assess the utility of venous thromboembolism prophylaxis among outpatients with high venous thromboembolism risk infections.”
The authors reported that they had no conflicts of interest.
Infection and infection sites have been found to be associated with a significant increased risk of venous thromboembolism, according to results of a population-based, matched, case-control analysis of medical records covering the 13-year period 1988-2000.
Dr. Kevin P. Cohoon and his colleagues at the Mayo Clinic, Rochester, Minn., developed models using conditional logistic regression analysis to stratify the risk associated with specific infections and infection sites.
Five hundred thirteen (39.4%) cases and 189 (12.7%) controls had an infection within the previous 92 days (odds ratio, 4.5; P less than .0001). Known VTE risk factors and potentially confounding variables were used in the adjusted univariate and multivariate models, as reported in the American Journal of Medicine (2017. doi: 10.1016/j.amjmed.2017.09.015).
Dr. Cohoon and his colleagues reported that univariate analysis showed “most infection sites were strongly associated with venous thromboembolism” and the adjusted multivariate model resulted in 2.4-fold (P less than .0001) higher odds for VTE incidence, compared with uninfected controls.
Adjusted multivariate analysis ranked the odds of VTE according to specific infections. Dr. Cohoon and his colleagues reported that this modeling showed that the “highest magnitude of risk, compared with no infection, was imparted by intra-abdominal infection (OR, 18) followed by oral infection (OR, 12), systematic blood stream infection (OR, 11), lower respiratory infection such as pneumonia (OR, 3.6), and symptomatic urinary tract infection (OR, 2.2).”
The researchers concluded that their findings may allow for further refinement of inpatient VTE risk-prediction models such as the Padua prediction score and “future studies are required to assess the utility of venous thromboembolism prophylaxis among outpatients with high venous thromboembolism risk infections.”
The authors reported that they had no conflicts of interest.
Infection and infection sites have been found to be associated with a significant increased risk of venous thromboembolism, according to results of a population-based, matched, case-control analysis of medical records covering the 13-year period 1988-2000.
Dr. Kevin P. Cohoon and his colleagues at the Mayo Clinic, Rochester, Minn., developed models using conditional logistic regression analysis to stratify the risk associated with specific infections and infection sites.
Five hundred thirteen (39.4%) cases and 189 (12.7%) controls had an infection within the previous 92 days (odds ratio, 4.5; P less than .0001). Known VTE risk factors and potentially confounding variables were used in the adjusted univariate and multivariate models, as reported in the American Journal of Medicine (2017. doi: 10.1016/j.amjmed.2017.09.015).
Dr. Cohoon and his colleagues reported that univariate analysis showed “most infection sites were strongly associated with venous thromboembolism” and the adjusted multivariate model resulted in 2.4-fold (P less than .0001) higher odds for VTE incidence, compared with uninfected controls.
Adjusted multivariate analysis ranked the odds of VTE according to specific infections. Dr. Cohoon and his colleagues reported that this modeling showed that the “highest magnitude of risk, compared with no infection, was imparted by intra-abdominal infection (OR, 18) followed by oral infection (OR, 12), systematic blood stream infection (OR, 11), lower respiratory infection such as pneumonia (OR, 3.6), and symptomatic urinary tract infection (OR, 2.2).”
The researchers concluded that their findings may allow for further refinement of inpatient VTE risk-prediction models such as the Padua prediction score and “future studies are required to assess the utility of venous thromboembolism prophylaxis among outpatients with high venous thromboembolism risk infections.”
The authors reported that they had no conflicts of interest.
FROM THE AMERICAN JOURNAL OF MEDICINE
Key clinical point:
Major finding: A significantly greater number of patients with infections developed VTE as compared with uninfected controls (OR, 4.5; P less than .0001).
Data source: Study was a retrospective database analysis of 1,303 VTE patients and 1,494 paired controls.
Disclosures: The authors reported that they had no conflicts of interest.
Atrial fibrillation boosts VTE risk
BARCELONA – Atrial fibrillation is at least as strong a risk factor for venous thromboembolism as for ischemic stroke, Bjorn Hornestam, MD, asserted at the annual congress of the European Society of Cardiology.
This novel finding from a Swedish national registry study suggests it’s time for thoughtful consideration of a revision of risk scores in patients with atrial fibrillation (AF), according to Dr. Hornestam, director of cardiology at Sahlgrenska University Hospital in Gothenburg, Sweden.
“VTE risk is not included as an outcome in the CHA2DS2-VASc score, so we underestimate the total thromboembolic risk in AF patients,” he said.
Dr. Hornestam presented a Swedish registry study of 1.36 million patients, including 470,738 patients with new-onset AF and no previous diagnosis of VTE or ischemic stroke and twice as many controls without AF who were matched to the AF patients by age, gender, and county.
The VTE risk was highest during the first 30 days after diagnosis of AF. Women with new-onset AF had an 8.3-fold increased risk of VTE compared with controls during this early period, by a margin of 55.8 versus 6.4 cases per 1,000 person-years. Men with newly diagnosed AF had a 7.2-fold increased risk of VTE in the first 30 days, reflecting a rate of 40.1 per 1,000 person-years compared to 5.6 per 1,000 in controls.
The VTE risk dropped off precipitously in men after the first month. The rate was cut in half by 2 months after AF diagnosis and was no different from that of controls by 9 months.
In women, too, the early elevated VTE risk was halved by 2 months out, but thereafter the rate of decline in VTE risk slowed. Even 10 years after AF diagnosis, women had a 21% greater VTE risk than did matched controls.
Of note, the risk of VTE during the first 12 months after diagnosis of AF was nearly twice as great in both men and women under age 65 than in those older than 75.
These data raise the question of whether standard therapy in AF patients needs to be modified, especially during what now appears to be the critical time frame of the first 3-6 months after diagnosis of the arrhythmia, Dr. Hornestam said.
He reported having no financial conflicts of interest regarding this study.
BARCELONA – Atrial fibrillation is at least as strong a risk factor for venous thromboembolism as for ischemic stroke, Bjorn Hornestam, MD, asserted at the annual congress of the European Society of Cardiology.
This novel finding from a Swedish national registry study suggests it’s time for thoughtful consideration of a revision of risk scores in patients with atrial fibrillation (AF), according to Dr. Hornestam, director of cardiology at Sahlgrenska University Hospital in Gothenburg, Sweden.
“VTE risk is not included as an outcome in the CHA2DS2-VASc score, so we underestimate the total thromboembolic risk in AF patients,” he said.
Dr. Hornestam presented a Swedish registry study of 1.36 million patients, including 470,738 patients with new-onset AF and no previous diagnosis of VTE or ischemic stroke and twice as many controls without AF who were matched to the AF patients by age, gender, and county.
The VTE risk was highest during the first 30 days after diagnosis of AF. Women with new-onset AF had an 8.3-fold increased risk of VTE compared with controls during this early period, by a margin of 55.8 versus 6.4 cases per 1,000 person-years. Men with newly diagnosed AF had a 7.2-fold increased risk of VTE in the first 30 days, reflecting a rate of 40.1 per 1,000 person-years compared to 5.6 per 1,000 in controls.
The VTE risk dropped off precipitously in men after the first month. The rate was cut in half by 2 months after AF diagnosis and was no different from that of controls by 9 months.
In women, too, the early elevated VTE risk was halved by 2 months out, but thereafter the rate of decline in VTE risk slowed. Even 10 years after AF diagnosis, women had a 21% greater VTE risk than did matched controls.
Of note, the risk of VTE during the first 12 months after diagnosis of AF was nearly twice as great in both men and women under age 65 than in those older than 75.
These data raise the question of whether standard therapy in AF patients needs to be modified, especially during what now appears to be the critical time frame of the first 3-6 months after diagnosis of the arrhythmia, Dr. Hornestam said.
He reported having no financial conflicts of interest regarding this study.
BARCELONA – Atrial fibrillation is at least as strong a risk factor for venous thromboembolism as for ischemic stroke, Bjorn Hornestam, MD, asserted at the annual congress of the European Society of Cardiology.
This novel finding from a Swedish national registry study suggests it’s time for thoughtful consideration of a revision of risk scores in patients with atrial fibrillation (AF), according to Dr. Hornestam, director of cardiology at Sahlgrenska University Hospital in Gothenburg, Sweden.
“VTE risk is not included as an outcome in the CHA2DS2-VASc score, so we underestimate the total thromboembolic risk in AF patients,” he said.
Dr. Hornestam presented a Swedish registry study of 1.36 million patients, including 470,738 patients with new-onset AF and no previous diagnosis of VTE or ischemic stroke and twice as many controls without AF who were matched to the AF patients by age, gender, and county.
The VTE risk was highest during the first 30 days after diagnosis of AF. Women with new-onset AF had an 8.3-fold increased risk of VTE compared with controls during this early period, by a margin of 55.8 versus 6.4 cases per 1,000 person-years. Men with newly diagnosed AF had a 7.2-fold increased risk of VTE in the first 30 days, reflecting a rate of 40.1 per 1,000 person-years compared to 5.6 per 1,000 in controls.
The VTE risk dropped off precipitously in men after the first month. The rate was cut in half by 2 months after AF diagnosis and was no different from that of controls by 9 months.
In women, too, the early elevated VTE risk was halved by 2 months out, but thereafter the rate of decline in VTE risk slowed. Even 10 years after AF diagnosis, women had a 21% greater VTE risk than did matched controls.
Of note, the risk of VTE during the first 12 months after diagnosis of AF was nearly twice as great in both men and women under age 65 than in those older than 75.
These data raise the question of whether standard therapy in AF patients needs to be modified, especially during what now appears to be the critical time frame of the first 3-6 months after diagnosis of the arrhythmia, Dr. Hornestam said.
He reported having no financial conflicts of interest regarding this study.
AT THE ESC CONGRESS 2017
Key clinical point:
Major finding: The risk of a first venous thromboembolism is increased 7.2- to 8.3-fold during the first 30 days following diagnosis of AF and remains moderately elevated in women even 10 years later.
Data source: An observational Swedish national registry study of more than 1.3 million patients, including 470,738 with newly diagnosed atrial fibrillation and their matched controls.
Disclosures: The presenter reported having no financial conflicts of interest regarding this study, which was conducted free of commercial support.
Caprini score is not a good predictor of PE in patients with DVT
The Caprini score, commonly used to risk stratify patients for the development of venous thromboembolism and to determine the optimal dose of prophylaxis, failed to predict the development of pulmonary embolism and hemodynamically significant PE in patients presenting with deep vein thrombosis (DVT), according to the results of a large, retrospective single-center study.
Recent surgery was not associated with the development of hemodynamically significant PE, but the presence of proximal DVT was, according to a report published online in the Journal of Vascular Surgery: Venous and Lymphatic Disorders (2017. doi: 10.1016/j.jvsv.2017.08.015).
Their results showed that patients who had undergone recent surgery were less likely to develop hemodynamically significant PE (13.3% vs. 27.2%; P = .01). In contrast, patients with proximal DVT were at higher risk for development of hemodynamically significant PE (80.7% vs. 64.2%; P = .007). They found no association between Caprini score and PE severity (P = .17) or the Caprini score and proximal DVT (P = .89).
“This study shows that the Caprini score does not correlate with the occurrence of PE or the severity of PE. On the other hand, a proximal location of DVT seems to have a high association with hemodynamically significant PE. Such patients may benefit from more aggressive anticoagulant therapy and work-up for PE,” the researchers concluded.
The authors reported that they had no conflicts of interest.
The Caprini score, commonly used to risk stratify patients for the development of venous thromboembolism and to determine the optimal dose of prophylaxis, failed to predict the development of pulmonary embolism and hemodynamically significant PE in patients presenting with deep vein thrombosis (DVT), according to the results of a large, retrospective single-center study.
Recent surgery was not associated with the development of hemodynamically significant PE, but the presence of proximal DVT was, according to a report published online in the Journal of Vascular Surgery: Venous and Lymphatic Disorders (2017. doi: 10.1016/j.jvsv.2017.08.015).
Their results showed that patients who had undergone recent surgery were less likely to develop hemodynamically significant PE (13.3% vs. 27.2%; P = .01). In contrast, patients with proximal DVT were at higher risk for development of hemodynamically significant PE (80.7% vs. 64.2%; P = .007). They found no association between Caprini score and PE severity (P = .17) or the Caprini score and proximal DVT (P = .89).
“This study shows that the Caprini score does not correlate with the occurrence of PE or the severity of PE. On the other hand, a proximal location of DVT seems to have a high association with hemodynamically significant PE. Such patients may benefit from more aggressive anticoagulant therapy and work-up for PE,” the researchers concluded.
The authors reported that they had no conflicts of interest.
The Caprini score, commonly used to risk stratify patients for the development of venous thromboembolism and to determine the optimal dose of prophylaxis, failed to predict the development of pulmonary embolism and hemodynamically significant PE in patients presenting with deep vein thrombosis (DVT), according to the results of a large, retrospective single-center study.
Recent surgery was not associated with the development of hemodynamically significant PE, but the presence of proximal DVT was, according to a report published online in the Journal of Vascular Surgery: Venous and Lymphatic Disorders (2017. doi: 10.1016/j.jvsv.2017.08.015).
Their results showed that patients who had undergone recent surgery were less likely to develop hemodynamically significant PE (13.3% vs. 27.2%; P = .01). In contrast, patients with proximal DVT were at higher risk for development of hemodynamically significant PE (80.7% vs. 64.2%; P = .007). They found no association between Caprini score and PE severity (P = .17) or the Caprini score and proximal DVT (P = .89).
“This study shows that the Caprini score does not correlate with the occurrence of PE or the severity of PE. On the other hand, a proximal location of DVT seems to have a high association with hemodynamically significant PE. Such patients may benefit from more aggressive anticoagulant therapy and work-up for PE,” the researchers concluded.
The authors reported that they had no conflicts of interest.
FROM THE JOURNAL OF VASCULAR SURGERY: VENOUS AND LYMPHATIC DISORDERS
Key clinical point:
Major finding: Among 838 patients presenting with DVT, nearly 26% had concomitant PE, more than half of which was hemodynamically significant.
Data source: A single-center, retrospective review of 838 patients diagnosed with DVT.
Disclosures: The authors reported that they had no conflicts of interest.
News from SVS: Post-thrombotic venous obstructions and stenting
Endovascular treatment of iliocaval and infrainguinal post-thrombotic venous obstruction results do not appear to be adversely affected by extension of the iliac vein stents into the femoral venous system, according to a report in the November edition of the Journal of Vascular Surgery: Venous and Lymphatic Diseases (J Vasc Surg: Venous and Lym Dis 2017;5:789-99).
Deep venous thrombosis remains a significant problem with well over 500,000 people affected in the United States. Over a quarter of these patients will experience post-thrombotic syndrome (PTS), despite appropriate anti-coagulation. Patients with iliocaval thrombosis face a three-fold risk of PTS. Treatment of the complications of PTS, including leg swelling, venous claudication, skin changes and ulceration, results in healthcare costs estimated at $7 to $10 billion per year.
Popularized by Drs. Seshadri Raju and Peter Neglen, venous stenting for symptomatic patients has increased significantly in this setting. Several large series since then have demonstrated safety, efficacy and good durability of this technique in iliocaval obstruction. Questions, however, remain as to the outcomes with regards to etiology (i.e., thrombotic versus non-thrombotic occlusion) and extent of stenting (i.e., extension below the inguinal ligament). Concern for the latter is raised as the mobility of the common femoral vein may result in stent fracture and thrombosis.
Researchers from UCLA, led by vascular surgeon Dr. Brian DeRubertis, retrospectively evaluated their single-center experience with percutaneous treatment of post-thrombotic iliocaval obstruction. In this series, 31 patients (42 limbs) presented with pain/swelling (100%) including venous claudication (81%) and active ulceration (10%). Percutaneous interventions, including iliocaval angioplasty/stent in 81% with extension into the femoral system (38%), resulted in 100% technical success. Of those with IVC filters, 46% were able to be removed.
At an average of 15 months follow-up (range 2-49 months), the following results were achieved:
- Improvement in pain/swelling 84%
- Resolved pain/swelling 42%
- Decreased CEAP classification 65%
- 1 year primary stent patency 66%
- 1 year secondary stent patency 75%
Those requiring infrainguinal extension of the stent realized no significant difference in primary stent patency at one year compared to those who did not (68% versus 65%). However, in those whose IVC filter could not be removed, resolution of symptoms was achieved in only 17%.
“Our aim was to better understand risk factors for poor clinical outcomes in patients undergoing percutaneous intervention for symptomatic chronic venous obstruction secondary to post-thrombotic lesions,” comments first author Dr. Johnathon Rollo. “Our results suggest that stenting below the inguinal ligament does not result in inferior outcomes, at least in the short-term, and may be necessary in a higher percentage of patients than previously reported. Additionally, the failure to remove an IVC filter in this setting appears to result in inferior outcome and an attempt to safely remove the filter should be made in this high-risk population.”
This data suggests a role for early filter removal after, or not even placing them at all, during ileocaval lytic therapy.
The authors emphasize stenting from normal vein above to normal vein below the occlusive disease, if technically possible. Based on these results, going below the inguinal ligament to achieve adequate inflow makes sense.
To download the complete article (link available free through 12/31/2017), click here.
Endovascular treatment of iliocaval and infrainguinal post-thrombotic venous obstruction results do not appear to be adversely affected by extension of the iliac vein stents into the femoral venous system, according to a report in the November edition of the Journal of Vascular Surgery: Venous and Lymphatic Diseases (J Vasc Surg: Venous and Lym Dis 2017;5:789-99).
Deep venous thrombosis remains a significant problem with well over 500,000 people affected in the United States. Over a quarter of these patients will experience post-thrombotic syndrome (PTS), despite appropriate anti-coagulation. Patients with iliocaval thrombosis face a three-fold risk of PTS. Treatment of the complications of PTS, including leg swelling, venous claudication, skin changes and ulceration, results in healthcare costs estimated at $7 to $10 billion per year.
Popularized by Drs. Seshadri Raju and Peter Neglen, venous stenting for symptomatic patients has increased significantly in this setting. Several large series since then have demonstrated safety, efficacy and good durability of this technique in iliocaval obstruction. Questions, however, remain as to the outcomes with regards to etiology (i.e., thrombotic versus non-thrombotic occlusion) and extent of stenting (i.e., extension below the inguinal ligament). Concern for the latter is raised as the mobility of the common femoral vein may result in stent fracture and thrombosis.
Researchers from UCLA, led by vascular surgeon Dr. Brian DeRubertis, retrospectively evaluated their single-center experience with percutaneous treatment of post-thrombotic iliocaval obstruction. In this series, 31 patients (42 limbs) presented with pain/swelling (100%) including venous claudication (81%) and active ulceration (10%). Percutaneous interventions, including iliocaval angioplasty/stent in 81% with extension into the femoral system (38%), resulted in 100% technical success. Of those with IVC filters, 46% were able to be removed.
At an average of 15 months follow-up (range 2-49 months), the following results were achieved:
- Improvement in pain/swelling 84%
- Resolved pain/swelling 42%
- Decreased CEAP classification 65%
- 1 year primary stent patency 66%
- 1 year secondary stent patency 75%
Those requiring infrainguinal extension of the stent realized no significant difference in primary stent patency at one year compared to those who did not (68% versus 65%). However, in those whose IVC filter could not be removed, resolution of symptoms was achieved in only 17%.
“Our aim was to better understand risk factors for poor clinical outcomes in patients undergoing percutaneous intervention for symptomatic chronic venous obstruction secondary to post-thrombotic lesions,” comments first author Dr. Johnathon Rollo. “Our results suggest that stenting below the inguinal ligament does not result in inferior outcomes, at least in the short-term, and may be necessary in a higher percentage of patients than previously reported. Additionally, the failure to remove an IVC filter in this setting appears to result in inferior outcome and an attempt to safely remove the filter should be made in this high-risk population.”
This data suggests a role for early filter removal after, or not even placing them at all, during ileocaval lytic therapy.
The authors emphasize stenting from normal vein above to normal vein below the occlusive disease, if technically possible. Based on these results, going below the inguinal ligament to achieve adequate inflow makes sense.
To download the complete article (link available free through 12/31/2017), click here.
Endovascular treatment of iliocaval and infrainguinal post-thrombotic venous obstruction results do not appear to be adversely affected by extension of the iliac vein stents into the femoral venous system, according to a report in the November edition of the Journal of Vascular Surgery: Venous and Lymphatic Diseases (J Vasc Surg: Venous and Lym Dis 2017;5:789-99).
Deep venous thrombosis remains a significant problem with well over 500,000 people affected in the United States. Over a quarter of these patients will experience post-thrombotic syndrome (PTS), despite appropriate anti-coagulation. Patients with iliocaval thrombosis face a three-fold risk of PTS. Treatment of the complications of PTS, including leg swelling, venous claudication, skin changes and ulceration, results in healthcare costs estimated at $7 to $10 billion per year.
Popularized by Drs. Seshadri Raju and Peter Neglen, venous stenting for symptomatic patients has increased significantly in this setting. Several large series since then have demonstrated safety, efficacy and good durability of this technique in iliocaval obstruction. Questions, however, remain as to the outcomes with regards to etiology (i.e., thrombotic versus non-thrombotic occlusion) and extent of stenting (i.e., extension below the inguinal ligament). Concern for the latter is raised as the mobility of the common femoral vein may result in stent fracture and thrombosis.
Researchers from UCLA, led by vascular surgeon Dr. Brian DeRubertis, retrospectively evaluated their single-center experience with percutaneous treatment of post-thrombotic iliocaval obstruction. In this series, 31 patients (42 limbs) presented with pain/swelling (100%) including venous claudication (81%) and active ulceration (10%). Percutaneous interventions, including iliocaval angioplasty/stent in 81% with extension into the femoral system (38%), resulted in 100% technical success. Of those with IVC filters, 46% were able to be removed.
At an average of 15 months follow-up (range 2-49 months), the following results were achieved:
- Improvement in pain/swelling 84%
- Resolved pain/swelling 42%
- Decreased CEAP classification 65%
- 1 year primary stent patency 66%
- 1 year secondary stent patency 75%
Those requiring infrainguinal extension of the stent realized no significant difference in primary stent patency at one year compared to those who did not (68% versus 65%). However, in those whose IVC filter could not be removed, resolution of symptoms was achieved in only 17%.
“Our aim was to better understand risk factors for poor clinical outcomes in patients undergoing percutaneous intervention for symptomatic chronic venous obstruction secondary to post-thrombotic lesions,” comments first author Dr. Johnathon Rollo. “Our results suggest that stenting below the inguinal ligament does not result in inferior outcomes, at least in the short-term, and may be necessary in a higher percentage of patients than previously reported. Additionally, the failure to remove an IVC filter in this setting appears to result in inferior outcome and an attempt to safely remove the filter should be made in this high-risk population.”
This data suggests a role for early filter removal after, or not even placing them at all, during ileocaval lytic therapy.
The authors emphasize stenting from normal vein above to normal vein below the occlusive disease, if technically possible. Based on these results, going below the inguinal ligament to achieve adequate inflow makes sense.
To download the complete article (link available free through 12/31/2017), click here.
Beware the risks associated with greater saphenous vein thrombosis
Isolated greater saphenous vein thrombosis is not as benign as generally thought, according to the results of a single institution retrospective study of 61 patients (67 limbs) with isolated GSVT.
Instead, patients had a significant risk of persistent symptoms, recurrence, deep vein thrombosis (DVT), and pulmonary embolism (PE), according to a report published in the Annals of Vascular Surgery by Elizabeth Kudlaty, MD, Ohio State University, Columbus, and her colleagues.
Location of the GSVT within 5 cm of the saphenous vein junction (SVJ; 32 patients) as compared with GSVT greater than 5 cm from the SVJ (29 patients) was significantly associated with malignancy (37.5% vs. 6.9%, respectively; P = .01), in-patient status (71.9% vs. 41.4%; P = .02), and diabetes (37.5% vs. 10.3%; P = .02). PE also was significantly greater in patients with GSVT within 5 cm of the SVJ (18.8% vs. 0.0%; P = .02). Patients with GSVT greater than 5 cm from the SVJ showed significantly more GSVT propagation/new saphenous vein thrombosis (0% vs. 31.3%, P = .048). There was a nonsignificant trend toward greater mortality for patients with GSVT within 5 cm of the SVJ (P = .052).
Dr. Kudlaty and her colleagues found that the different management options used, including anticoagulation, observation, and aspirin use, did not significantly affect outcomes (Ann Vasc Surg. 2017 Nov;45:154-9).
“Isolated GSVT can be viewed as a marker of more serious systemic diseases, notably diabetes and cancer, and leaves patients at high risk for thromboembolic events, recurrence, and persistent symptoms, despite a variety of managements,” the researchers concluded.
The authors reported that they had no conflicts of interest and that there were no outside funding sources.
Isolated greater saphenous vein thrombosis is not as benign as generally thought, according to the results of a single institution retrospective study of 61 patients (67 limbs) with isolated GSVT.
Instead, patients had a significant risk of persistent symptoms, recurrence, deep vein thrombosis (DVT), and pulmonary embolism (PE), according to a report published in the Annals of Vascular Surgery by Elizabeth Kudlaty, MD, Ohio State University, Columbus, and her colleagues.
Location of the GSVT within 5 cm of the saphenous vein junction (SVJ; 32 patients) as compared with GSVT greater than 5 cm from the SVJ (29 patients) was significantly associated with malignancy (37.5% vs. 6.9%, respectively; P = .01), in-patient status (71.9% vs. 41.4%; P = .02), and diabetes (37.5% vs. 10.3%; P = .02). PE also was significantly greater in patients with GSVT within 5 cm of the SVJ (18.8% vs. 0.0%; P = .02). Patients with GSVT greater than 5 cm from the SVJ showed significantly more GSVT propagation/new saphenous vein thrombosis (0% vs. 31.3%, P = .048). There was a nonsignificant trend toward greater mortality for patients with GSVT within 5 cm of the SVJ (P = .052).
Dr. Kudlaty and her colleagues found that the different management options used, including anticoagulation, observation, and aspirin use, did not significantly affect outcomes (Ann Vasc Surg. 2017 Nov;45:154-9).
“Isolated GSVT can be viewed as a marker of more serious systemic diseases, notably diabetes and cancer, and leaves patients at high risk for thromboembolic events, recurrence, and persistent symptoms, despite a variety of managements,” the researchers concluded.
The authors reported that they had no conflicts of interest and that there were no outside funding sources.
Isolated greater saphenous vein thrombosis is not as benign as generally thought, according to the results of a single institution retrospective study of 61 patients (67 limbs) with isolated GSVT.
Instead, patients had a significant risk of persistent symptoms, recurrence, deep vein thrombosis (DVT), and pulmonary embolism (PE), according to a report published in the Annals of Vascular Surgery by Elizabeth Kudlaty, MD, Ohio State University, Columbus, and her colleagues.
Location of the GSVT within 5 cm of the saphenous vein junction (SVJ; 32 patients) as compared with GSVT greater than 5 cm from the SVJ (29 patients) was significantly associated with malignancy (37.5% vs. 6.9%, respectively; P = .01), in-patient status (71.9% vs. 41.4%; P = .02), and diabetes (37.5% vs. 10.3%; P = .02). PE also was significantly greater in patients with GSVT within 5 cm of the SVJ (18.8% vs. 0.0%; P = .02). Patients with GSVT greater than 5 cm from the SVJ showed significantly more GSVT propagation/new saphenous vein thrombosis (0% vs. 31.3%, P = .048). There was a nonsignificant trend toward greater mortality for patients with GSVT within 5 cm of the SVJ (P = .052).
Dr. Kudlaty and her colleagues found that the different management options used, including anticoagulation, observation, and aspirin use, did not significantly affect outcomes (Ann Vasc Surg. 2017 Nov;45:154-9).
“Isolated GSVT can be viewed as a marker of more serious systemic diseases, notably diabetes and cancer, and leaves patients at high risk for thromboembolic events, recurrence, and persistent symptoms, despite a variety of managements,” the researchers concluded.
The authors reported that they had no conflicts of interest and that there were no outside funding sources.
FROM THE ANNALS OF VASCULAR SURGERY
Key clinical point:
Major finding: Patients with GSVT show a significant risk of persistent symptoms, recurrence, deep vein thrombosis, and pulmonary embolism.
Data source: A retrospective review of all 61 patients with isolated GSVT at a single institution between 2008 and 2014.
Disclosures: The authors reported that they had no conflicts of interest and that there were no outside funding sources.
Study: Varicose vein procedures should be offered to patients 65 years and older
Older and younger patients benefited from varicose vein procedures, a finding that calls into question the use of compression therapy as the primary treatment for patients aged 65 years and older, according to the results of a prospectively maintained database study of all patients in the Vascular Quality Initiative Varicose Vein Registry–participating centers.
Procedures for varicose veins in 1,068 patients aged 65 years or older showed similar improvement in Clinical, Etiology, Anatomy, and Pathophysiology class and Venous Clinical Severity Score, compared with a group of 2,691 younger patients, according to a report published in Journal of Vascular Surgery: Venous and Lymphatic Disorders. Among patients younger than 65 years, 57.4% had an improvement, compared with 52% of patients aged 65 years or older.
However, the younger patients had more improvement in patient-reported outcomes, according to Danielle C. Sutzko, MD, of the University of Michigan, Ann Arbor, and her colleagues (J Vasc Surg Venous Lymphat Disord. 2017 Sep;5[5]:647-57).
One of the main limitations of the study was the fact that only 62% of procedures within the Vascular Quality Initiative Varicose Vein Registry had follow-up.
“Patients older than 65 years appear to benefit from appropriate varicose vein procedures and should not be denied interventions on their varicose veins and venous insufficiency on the basis of their age only,” the researchers concluded.
Dr. Sutzko and her colleagues reported having no conflicts of interest.
Older and younger patients benefited from varicose vein procedures, a finding that calls into question the use of compression therapy as the primary treatment for patients aged 65 years and older, according to the results of a prospectively maintained database study of all patients in the Vascular Quality Initiative Varicose Vein Registry–participating centers.
Procedures for varicose veins in 1,068 patients aged 65 years or older showed similar improvement in Clinical, Etiology, Anatomy, and Pathophysiology class and Venous Clinical Severity Score, compared with a group of 2,691 younger patients, according to a report published in Journal of Vascular Surgery: Venous and Lymphatic Disorders. Among patients younger than 65 years, 57.4% had an improvement, compared with 52% of patients aged 65 years or older.
However, the younger patients had more improvement in patient-reported outcomes, according to Danielle C. Sutzko, MD, of the University of Michigan, Ann Arbor, and her colleagues (J Vasc Surg Venous Lymphat Disord. 2017 Sep;5[5]:647-57).
One of the main limitations of the study was the fact that only 62% of procedures within the Vascular Quality Initiative Varicose Vein Registry had follow-up.
“Patients older than 65 years appear to benefit from appropriate varicose vein procedures and should not be denied interventions on their varicose veins and venous insufficiency on the basis of their age only,” the researchers concluded.
Dr. Sutzko and her colleagues reported having no conflicts of interest.
Older and younger patients benefited from varicose vein procedures, a finding that calls into question the use of compression therapy as the primary treatment for patients aged 65 years and older, according to the results of a prospectively maintained database study of all patients in the Vascular Quality Initiative Varicose Vein Registry–participating centers.
Procedures for varicose veins in 1,068 patients aged 65 years or older showed similar improvement in Clinical, Etiology, Anatomy, and Pathophysiology class and Venous Clinical Severity Score, compared with a group of 2,691 younger patients, according to a report published in Journal of Vascular Surgery: Venous and Lymphatic Disorders. Among patients younger than 65 years, 57.4% had an improvement, compared with 52% of patients aged 65 years or older.
However, the younger patients had more improvement in patient-reported outcomes, according to Danielle C. Sutzko, MD, of the University of Michigan, Ann Arbor, and her colleagues (J Vasc Surg Venous Lymphat Disord. 2017 Sep;5[5]:647-57).
One of the main limitations of the study was the fact that only 62% of procedures within the Vascular Quality Initiative Varicose Vein Registry had follow-up.
“Patients older than 65 years appear to benefit from appropriate varicose vein procedures and should not be denied interventions on their varicose veins and venous insufficiency on the basis of their age only,” the researchers concluded.
Dr. Sutzko and her colleagues reported having no conflicts of interest.
FROM JOURNAL OF VASCULAR SURGERY: VENOUS AND LYMPHATIC DISORDERS
Key clinical point:
Major finding: Among patients younger than 65, 57.4% had an improvement, compared to 52% of patients aged 65 years or older.
Data source: Prospectively captured data for all patients in the Vascular Quality Initiative Varicose Vein Registry–participating centers.
Disclosures: Dr. Sutzko and her colleagues reported having no conflicts of interest.
Wait at least 2 days to replace central venous catheters in patients with candidemia
SAN DIEGO – Wait at least 2 days before replacing central venous catheters (CVC) in patients with catheter-associated candidemia, according to the results of a single-center retrospective cohort study of 228 patients.
Waiting less than 2 days to replace a CVC increased the odds of 30-day mortality nearly sixfold among patients with catheter-related bloodstream infections due to candidemia, even after controlling for potential confounders, Takahiro Matsuo, MD, said at an annual scientific meeting on infectious diseases. No other factor significantly predicted mortality in univariate or multivariate analyses, he said. “This is the first study to demonstrate the optimal timing of central venous catheter replacement in catheter-related [bloodstream infection] due to Candida.”
Invasive candidiasis is associated with mortality rates of up to 50%, noted Dr. Matsuo, who is a fellow in infectious diseases at St. Luke’s International Hospital, Tokyo. Antifungal therapy improves outcomes, and most physicians agree that removing a CVC does, too. To better pinpoint optimal timing of catheter replacement, Dr. Matsuo and his associates examined risk factors for 30-day mortality among patients with candidemia who were treated at St. Luke’s between 2004 and 2015.
Among 228 patients with candidemia, 166 had CVCs, and 144 had their CVC removed. Among 71 patients who needed their CVC replaced, 15 died within 30 days. Central venous catheters were replaced less than 2 days after removal in 87% of patients who died and in 54% of survivors (P = .04). The association remained statistically significant after the researchers accounted for potential confounders (adjusted odds ratio, 5.9; 95% confidence interval, 1.2-29.7; P = .03).
Patients who died within 30 days of CVC replacement also were more likely to have hematologic malignancies (20% versus 4%), diabetes (13% vs. 11%), to be on hemodialysis (27% vs. 16%), and to have a history of recent corticosteroid exposure (20% versus 11%) compared with survivors, but none of these associations reached statistical significance. Furthermore, 30-day mortality was not associated with gender, age, Candida species, endophthalmitis, or type of antifungal therapy, said Dr. Matsuo, who spoke at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
An infectious disease consultation was associated with about a 70% reduction in the odds of mortality in the multivariate analysis, but the 95% confidence interval crossed 1.0, rendering the link statistically insignificant.
Given the small sample size and single-center design of this study, its findings ideally should be confirmed in a larger randomized controlled trial, Dr. Matsuo said. The investigators also did not track whether patients were fungemic at the time of CVC replacement, he noted.
The researchers reported having no conflicts of interest.
SAN DIEGO – Wait at least 2 days before replacing central venous catheters (CVC) in patients with catheter-associated candidemia, according to the results of a single-center retrospective cohort study of 228 patients.
Waiting less than 2 days to replace a CVC increased the odds of 30-day mortality nearly sixfold among patients with catheter-related bloodstream infections due to candidemia, even after controlling for potential confounders, Takahiro Matsuo, MD, said at an annual scientific meeting on infectious diseases. No other factor significantly predicted mortality in univariate or multivariate analyses, he said. “This is the first study to demonstrate the optimal timing of central venous catheter replacement in catheter-related [bloodstream infection] due to Candida.”
Invasive candidiasis is associated with mortality rates of up to 50%, noted Dr. Matsuo, who is a fellow in infectious diseases at St. Luke’s International Hospital, Tokyo. Antifungal therapy improves outcomes, and most physicians agree that removing a CVC does, too. To better pinpoint optimal timing of catheter replacement, Dr. Matsuo and his associates examined risk factors for 30-day mortality among patients with candidemia who were treated at St. Luke’s between 2004 and 2015.
Among 228 patients with candidemia, 166 had CVCs, and 144 had their CVC removed. Among 71 patients who needed their CVC replaced, 15 died within 30 days. Central venous catheters were replaced less than 2 days after removal in 87% of patients who died and in 54% of survivors (P = .04). The association remained statistically significant after the researchers accounted for potential confounders (adjusted odds ratio, 5.9; 95% confidence interval, 1.2-29.7; P = .03).
Patients who died within 30 days of CVC replacement also were more likely to have hematologic malignancies (20% versus 4%), diabetes (13% vs. 11%), to be on hemodialysis (27% vs. 16%), and to have a history of recent corticosteroid exposure (20% versus 11%) compared with survivors, but none of these associations reached statistical significance. Furthermore, 30-day mortality was not associated with gender, age, Candida species, endophthalmitis, or type of antifungal therapy, said Dr. Matsuo, who spoke at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
An infectious disease consultation was associated with about a 70% reduction in the odds of mortality in the multivariate analysis, but the 95% confidence interval crossed 1.0, rendering the link statistically insignificant.
Given the small sample size and single-center design of this study, its findings ideally should be confirmed in a larger randomized controlled trial, Dr. Matsuo said. The investigators also did not track whether patients were fungemic at the time of CVC replacement, he noted.
The researchers reported having no conflicts of interest.
SAN DIEGO – Wait at least 2 days before replacing central venous catheters (CVC) in patients with catheter-associated candidemia, according to the results of a single-center retrospective cohort study of 228 patients.
Waiting less than 2 days to replace a CVC increased the odds of 30-day mortality nearly sixfold among patients with catheter-related bloodstream infections due to candidemia, even after controlling for potential confounders, Takahiro Matsuo, MD, said at an annual scientific meeting on infectious diseases. No other factor significantly predicted mortality in univariate or multivariate analyses, he said. “This is the first study to demonstrate the optimal timing of central venous catheter replacement in catheter-related [bloodstream infection] due to Candida.”
Invasive candidiasis is associated with mortality rates of up to 50%, noted Dr. Matsuo, who is a fellow in infectious diseases at St. Luke’s International Hospital, Tokyo. Antifungal therapy improves outcomes, and most physicians agree that removing a CVC does, too. To better pinpoint optimal timing of catheter replacement, Dr. Matsuo and his associates examined risk factors for 30-day mortality among patients with candidemia who were treated at St. Luke’s between 2004 and 2015.
Among 228 patients with candidemia, 166 had CVCs, and 144 had their CVC removed. Among 71 patients who needed their CVC replaced, 15 died within 30 days. Central venous catheters were replaced less than 2 days after removal in 87% of patients who died and in 54% of survivors (P = .04). The association remained statistically significant after the researchers accounted for potential confounders (adjusted odds ratio, 5.9; 95% confidence interval, 1.2-29.7; P = .03).
Patients who died within 30 days of CVC replacement also were more likely to have hematologic malignancies (20% versus 4%), diabetes (13% vs. 11%), to be on hemodialysis (27% vs. 16%), and to have a history of recent corticosteroid exposure (20% versus 11%) compared with survivors, but none of these associations reached statistical significance. Furthermore, 30-day mortality was not associated with gender, age, Candida species, endophthalmitis, or type of antifungal therapy, said Dr. Matsuo, who spoke at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
An infectious disease consultation was associated with about a 70% reduction in the odds of mortality in the multivariate analysis, but the 95% confidence interval crossed 1.0, rendering the link statistically insignificant.
Given the small sample size and single-center design of this study, its findings ideally should be confirmed in a larger randomized controlled trial, Dr. Matsuo said. The investigators also did not track whether patients were fungemic at the time of CVC replacement, he noted.
The researchers reported having no conflicts of interest.
AT IDWEEK 2017
Key clinical point: Consider waiting at least 2 days to replace a central venous catheter that has been removed because of candidemia.
Major finding: (odds ratio, 5.9; 95% confidence interval, 1.2-27.3).
Data source: A single-center retrospective cohort study of 228 patients with candidemia.
Disclosures: The researchers reported having no conflicts of interest.