User login
Survival shorter in extended-criteria lung recipients
The availability of lungs for transplant has been severely limited by usable donors, but organs from so-called extended criteria donors – those aged 65 years or older, had a 20 pack-years or more smoking history or history of diabetes mellitus, or were black – were found to be associated with shorter survival than lungs from standard donor lungs, and recipients with more severe lung disease had the lowest survival rates from extended-criteria organs, an analysis of the national donor database found.
“Matching donor quality to recipient severity is critical to achieve optimal outcomes in lung transplantation,” Matthew J. Mulligan, MD, and his colleagues from the University of Maryland, Baltimore, said in the September issue of the Journal of Thoracic and Cardiovascular Surgery (2016;152:891-8). Dr. Mulligan previously presented the study results in April 2015 at the annual meeting of the American Association for Thoracic Surgery in Seattle.
The researchers analyzed 10,995 patients who received donor lungs between May 2005 and December 2012, 3,792 of whom received extended-criteria donor (ECD) organs. The study population was taken from the Organ Procurement and Transplantation Network/United Network for Organ Sharing database. Dr. Mulligan and his coauthors said this is the largest study examining ECD in lung transplants to date.
The goal of the study was to identify donor factors associated with reduced 1-year survival after transplantation, Dr. Mulligan and his colleagues said. “In the current literature, there is a paucity of data to guide the decision of matching donor quality to recipient severity,” the study authors said.
Recipients of extended-criteria lungs had a 41% increased risk of death, compared with recipients standard donor lungs, but individuals with more severe lung disease were at even greater risk with extended-criterial lungs, Dr. Mulligan and his colleagues said. Those who had a lung allocation score (LAS) less than 70 had a 1-year survival of 87% with standard donor lungs vs. 82% with extended-criteria lungs, while those who had a LAS of 70 or greater had survival rates of 80% and 72%, respectively.
Other donor factors that were inconsequential in recipient survival, Dr. Mulligan and his coauthors reported, included an abnormal chest x-ray, purulent secretions on bronchoscopy, blood type, mechanism of death (stroke, blunt trauma, gunshot, asphyxiation, and so on), or diagnosis of coronary artery disease and hypertension.
The researchers also did a Cox regression analysis, and found that recipients of extended-criteria lungs with a LAS greater than 70 had an 81% greater risk of death, compared with 37% for those with a LAS of 70 or greater who received standard-donor lungs, and 42% with a LAS of 70 or less and an extended-criteria donor lung.
These findings support the idea of not using ECD lungs in high-risk individuals with LAS greater than 70. “More important, ECD lungs were associated with the worst survival when transplanted into high-risk recipients,” Dr. Mulligan and his colleagues said.
The authors did acknowledge the inherent limitations of a retrospective analysis, but the large patient population is a redeeming factor of the study, Dr. Mulligan and his colleagues said. “Notwithstanding these limitations, the current study provides a rigorous analysis of a large number of lung transplants in the modern era, and the results reported will be useful to the lung transplant community,” the study authors said.
Dr. Mulligan and his coauthors had no relationships to disclose.
This study provides “greater clarity to the definition and significance of using lungs from an extended-criteria donor,” Benjamin Wei, MD, of the University of Alabama at Birmingham said in his invited commentary (J Thorac Cardiovasc Surg. 2016;152:899-900). “Now, we have more data about what constitutes an ECD for lung transplantation.”
The study also brought clarity on components of donor factors that do not affect survival – namely radiologic, bronchoscope, or laboratory criteria – Dr. Wei said. At the same time, the study raises questions about how transplant surgeons should use the findings. “Do we shy away from using donors with these high risk factors in low-risk recipients, high-risk recipients, neither, or both?” Dr. Wei asks. The study did not compare ECD lungs vs. no transplant, and becoming more selective in donors could cause more patients to die on the waiting list, he said.
A host of other questions also remain unanswered, Dr. Wei said, such as how a single standard-donor lung transplant compares with bilateral ECD transplants, or a single ECD lung vs. bilateral ECD lungs, and if use of ECD lungs by the criteria Dr. Mulligan and his coauthors outlined influences allograft patient survival.
“Of note, this study also did not include recipients receiving donor after cardiac death lungs or extracorporeal membrane oxygenation, both increasingly common situations,” he said. Nonetheless, the findings provide more information that transplant surgeons can base their decision-making on.
Dr. Wei had no financial relationships to disclose.
This study provides “greater clarity to the definition and significance of using lungs from an extended-criteria donor,” Benjamin Wei, MD, of the University of Alabama at Birmingham said in his invited commentary (J Thorac Cardiovasc Surg. 2016;152:899-900). “Now, we have more data about what constitutes an ECD for lung transplantation.”
The study also brought clarity on components of donor factors that do not affect survival – namely radiologic, bronchoscope, or laboratory criteria – Dr. Wei said. At the same time, the study raises questions about how transplant surgeons should use the findings. “Do we shy away from using donors with these high risk factors in low-risk recipients, high-risk recipients, neither, or both?” Dr. Wei asks. The study did not compare ECD lungs vs. no transplant, and becoming more selective in donors could cause more patients to die on the waiting list, he said.
A host of other questions also remain unanswered, Dr. Wei said, such as how a single standard-donor lung transplant compares with bilateral ECD transplants, or a single ECD lung vs. bilateral ECD lungs, and if use of ECD lungs by the criteria Dr. Mulligan and his coauthors outlined influences allograft patient survival.
“Of note, this study also did not include recipients receiving donor after cardiac death lungs or extracorporeal membrane oxygenation, both increasingly common situations,” he said. Nonetheless, the findings provide more information that transplant surgeons can base their decision-making on.
Dr. Wei had no financial relationships to disclose.
This study provides “greater clarity to the definition and significance of using lungs from an extended-criteria donor,” Benjamin Wei, MD, of the University of Alabama at Birmingham said in his invited commentary (J Thorac Cardiovasc Surg. 2016;152:899-900). “Now, we have more data about what constitutes an ECD for lung transplantation.”
The study also brought clarity on components of donor factors that do not affect survival – namely radiologic, bronchoscope, or laboratory criteria – Dr. Wei said. At the same time, the study raises questions about how transplant surgeons should use the findings. “Do we shy away from using donors with these high risk factors in low-risk recipients, high-risk recipients, neither, or both?” Dr. Wei asks. The study did not compare ECD lungs vs. no transplant, and becoming more selective in donors could cause more patients to die on the waiting list, he said.
A host of other questions also remain unanswered, Dr. Wei said, such as how a single standard-donor lung transplant compares with bilateral ECD transplants, or a single ECD lung vs. bilateral ECD lungs, and if use of ECD lungs by the criteria Dr. Mulligan and his coauthors outlined influences allograft patient survival.
“Of note, this study also did not include recipients receiving donor after cardiac death lungs or extracorporeal membrane oxygenation, both increasingly common situations,” he said. Nonetheless, the findings provide more information that transplant surgeons can base their decision-making on.
Dr. Wei had no financial relationships to disclose.
The availability of lungs for transplant has been severely limited by usable donors, but organs from so-called extended criteria donors – those aged 65 years or older, had a 20 pack-years or more smoking history or history of diabetes mellitus, or were black – were found to be associated with shorter survival than lungs from standard donor lungs, and recipients with more severe lung disease had the lowest survival rates from extended-criteria organs, an analysis of the national donor database found.
“Matching donor quality to recipient severity is critical to achieve optimal outcomes in lung transplantation,” Matthew J. Mulligan, MD, and his colleagues from the University of Maryland, Baltimore, said in the September issue of the Journal of Thoracic and Cardiovascular Surgery (2016;152:891-8). Dr. Mulligan previously presented the study results in April 2015 at the annual meeting of the American Association for Thoracic Surgery in Seattle.
The researchers analyzed 10,995 patients who received donor lungs between May 2005 and December 2012, 3,792 of whom received extended-criteria donor (ECD) organs. The study population was taken from the Organ Procurement and Transplantation Network/United Network for Organ Sharing database. Dr. Mulligan and his coauthors said this is the largest study examining ECD in lung transplants to date.
The goal of the study was to identify donor factors associated with reduced 1-year survival after transplantation, Dr. Mulligan and his colleagues said. “In the current literature, there is a paucity of data to guide the decision of matching donor quality to recipient severity,” the study authors said.
Recipients of extended-criteria lungs had a 41% increased risk of death, compared with recipients standard donor lungs, but individuals with more severe lung disease were at even greater risk with extended-criterial lungs, Dr. Mulligan and his colleagues said. Those who had a lung allocation score (LAS) less than 70 had a 1-year survival of 87% with standard donor lungs vs. 82% with extended-criteria lungs, while those who had a LAS of 70 or greater had survival rates of 80% and 72%, respectively.
Other donor factors that were inconsequential in recipient survival, Dr. Mulligan and his coauthors reported, included an abnormal chest x-ray, purulent secretions on bronchoscopy, blood type, mechanism of death (stroke, blunt trauma, gunshot, asphyxiation, and so on), or diagnosis of coronary artery disease and hypertension.
The researchers also did a Cox regression analysis, and found that recipients of extended-criteria lungs with a LAS greater than 70 had an 81% greater risk of death, compared with 37% for those with a LAS of 70 or greater who received standard-donor lungs, and 42% with a LAS of 70 or less and an extended-criteria donor lung.
These findings support the idea of not using ECD lungs in high-risk individuals with LAS greater than 70. “More important, ECD lungs were associated with the worst survival when transplanted into high-risk recipients,” Dr. Mulligan and his colleagues said.
The authors did acknowledge the inherent limitations of a retrospective analysis, but the large patient population is a redeeming factor of the study, Dr. Mulligan and his colleagues said. “Notwithstanding these limitations, the current study provides a rigorous analysis of a large number of lung transplants in the modern era, and the results reported will be useful to the lung transplant community,” the study authors said.
Dr. Mulligan and his coauthors had no relationships to disclose.
The availability of lungs for transplant has been severely limited by usable donors, but organs from so-called extended criteria donors – those aged 65 years or older, had a 20 pack-years or more smoking history or history of diabetes mellitus, or were black – were found to be associated with shorter survival than lungs from standard donor lungs, and recipients with more severe lung disease had the lowest survival rates from extended-criteria organs, an analysis of the national donor database found.
“Matching donor quality to recipient severity is critical to achieve optimal outcomes in lung transplantation,” Matthew J. Mulligan, MD, and his colleagues from the University of Maryland, Baltimore, said in the September issue of the Journal of Thoracic and Cardiovascular Surgery (2016;152:891-8). Dr. Mulligan previously presented the study results in April 2015 at the annual meeting of the American Association for Thoracic Surgery in Seattle.
The researchers analyzed 10,995 patients who received donor lungs between May 2005 and December 2012, 3,792 of whom received extended-criteria donor (ECD) organs. The study population was taken from the Organ Procurement and Transplantation Network/United Network for Organ Sharing database. Dr. Mulligan and his coauthors said this is the largest study examining ECD in lung transplants to date.
The goal of the study was to identify donor factors associated with reduced 1-year survival after transplantation, Dr. Mulligan and his colleagues said. “In the current literature, there is a paucity of data to guide the decision of matching donor quality to recipient severity,” the study authors said.
Recipients of extended-criteria lungs had a 41% increased risk of death, compared with recipients standard donor lungs, but individuals with more severe lung disease were at even greater risk with extended-criterial lungs, Dr. Mulligan and his colleagues said. Those who had a lung allocation score (LAS) less than 70 had a 1-year survival of 87% with standard donor lungs vs. 82% with extended-criteria lungs, while those who had a LAS of 70 or greater had survival rates of 80% and 72%, respectively.
Other donor factors that were inconsequential in recipient survival, Dr. Mulligan and his coauthors reported, included an abnormal chest x-ray, purulent secretions on bronchoscopy, blood type, mechanism of death (stroke, blunt trauma, gunshot, asphyxiation, and so on), or diagnosis of coronary artery disease and hypertension.
The researchers also did a Cox regression analysis, and found that recipients of extended-criteria lungs with a LAS greater than 70 had an 81% greater risk of death, compared with 37% for those with a LAS of 70 or greater who received standard-donor lungs, and 42% with a LAS of 70 or less and an extended-criteria donor lung.
These findings support the idea of not using ECD lungs in high-risk individuals with LAS greater than 70. “More important, ECD lungs were associated with the worst survival when transplanted into high-risk recipients,” Dr. Mulligan and his colleagues said.
The authors did acknowledge the inherent limitations of a retrospective analysis, but the large patient population is a redeeming factor of the study, Dr. Mulligan and his colleagues said. “Notwithstanding these limitations, the current study provides a rigorous analysis of a large number of lung transplants in the modern era, and the results reported will be useful to the lung transplant community,” the study authors said.
Dr. Mulligan and his coauthors had no relationships to disclose.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: Lung transplant recipients who received extended-criteria donor (ECD) lungs have lower rates of 1-year survival than recipients of standard donor lungs.
Major finding: Recipients of ECD lungs had a 41% higher risk of death than recipients of standard lungs, and those who had more severe lung disease had lower rates of 1-year survival after receiving ECD lungs, compared with standard donor lungs.
Data source: Retrospective analysis of 10,995 lung recipients, from the Organ Procurement and Transplantation Network/United Network for Organ Sharing database, 3,792 of whom who received extended-criteria donor organs over 7.5 years.
Disclosures: Dr. Mulligan and his coauthors had no financial relationships to disclose.
Antibiotic susceptibility differs in transplant recipients
Antibiotic susceptibility in bacteria cultured from transplant recipients at a single hospital differed markedly from that in hospital-wide antibiograms, according to a report published in Diagnostic Microbiology and Infectious Disease.
Understanding the differences in antibiotic susceptibility among these highly immunocompromised patients can help guide treatment when they develop infection, and reduce the delay before they begin receiving appropriate antibiotics, said Rossana Rosa, MD, of Jackson Memorial Hospital, Miami, and her associates.
The investigators examined the antibiotic susceptibility of 1,889 isolates from blood and urine specimens taken from patients who had received solid-organ transplants at a single tertiary-care teaching hospital and then developed bacterial infections during a 2-year period. These patients included both children and adults who had received kidney, pancreas, liver, heart, lung, or intestinal transplants and were treated in numerous, “geographically distributed” units throughout the hospital. Their culture results were compared with those from 10,439 other patients with bacterial infections, which comprised the hospital-wide antibiograms developed every 6 months during the study period.
The Escherichia coli, Klebsiella pneumoniae, and Pseudomonas aeruginosa isolates from the transplant recipients showed markedly less susceptibility to first-line antibiotics than would have been predicted by the hospital-antibiograms. In particular, in the transplant recipients E. coli infections were resistant to trimethoprim-sulfamethoxazole, levofloxacin, and ceftriaxone; K. pneumoniae infections were resistant to every antibiotic except amikacin; and P. aeruginosa infections were resistant to levofloxacin, cefepime, and amikacin (Diag Microbiol Infect Dis. 2016 Aug 25. doi: 10.1016/j.diagmicrobio.2016.08.018).
“We advocate for the development of antibiograms specific to solid-organ transplant recipients. This may allow intrahospital comparisons and intertransplant-center monitoring of trends in antimicrobial resistance over time,” Dr. Rosa and her associates said.
Antibiotic susceptibility in bacteria cultured from transplant recipients at a single hospital differed markedly from that in hospital-wide antibiograms, according to a report published in Diagnostic Microbiology and Infectious Disease.
Understanding the differences in antibiotic susceptibility among these highly immunocompromised patients can help guide treatment when they develop infection, and reduce the delay before they begin receiving appropriate antibiotics, said Rossana Rosa, MD, of Jackson Memorial Hospital, Miami, and her associates.
The investigators examined the antibiotic susceptibility of 1,889 isolates from blood and urine specimens taken from patients who had received solid-organ transplants at a single tertiary-care teaching hospital and then developed bacterial infections during a 2-year period. These patients included both children and adults who had received kidney, pancreas, liver, heart, lung, or intestinal transplants and were treated in numerous, “geographically distributed” units throughout the hospital. Their culture results were compared with those from 10,439 other patients with bacterial infections, which comprised the hospital-wide antibiograms developed every 6 months during the study period.
The Escherichia coli, Klebsiella pneumoniae, and Pseudomonas aeruginosa isolates from the transplant recipients showed markedly less susceptibility to first-line antibiotics than would have been predicted by the hospital-antibiograms. In particular, in the transplant recipients E. coli infections were resistant to trimethoprim-sulfamethoxazole, levofloxacin, and ceftriaxone; K. pneumoniae infections were resistant to every antibiotic except amikacin; and P. aeruginosa infections were resistant to levofloxacin, cefepime, and amikacin (Diag Microbiol Infect Dis. 2016 Aug 25. doi: 10.1016/j.diagmicrobio.2016.08.018).
“We advocate for the development of antibiograms specific to solid-organ transplant recipients. This may allow intrahospital comparisons and intertransplant-center monitoring of trends in antimicrobial resistance over time,” Dr. Rosa and her associates said.
Antibiotic susceptibility in bacteria cultured from transplant recipients at a single hospital differed markedly from that in hospital-wide antibiograms, according to a report published in Diagnostic Microbiology and Infectious Disease.
Understanding the differences in antibiotic susceptibility among these highly immunocompromised patients can help guide treatment when they develop infection, and reduce the delay before they begin receiving appropriate antibiotics, said Rossana Rosa, MD, of Jackson Memorial Hospital, Miami, and her associates.
The investigators examined the antibiotic susceptibility of 1,889 isolates from blood and urine specimens taken from patients who had received solid-organ transplants at a single tertiary-care teaching hospital and then developed bacterial infections during a 2-year period. These patients included both children and adults who had received kidney, pancreas, liver, heart, lung, or intestinal transplants and were treated in numerous, “geographically distributed” units throughout the hospital. Their culture results were compared with those from 10,439 other patients with bacterial infections, which comprised the hospital-wide antibiograms developed every 6 months during the study period.
The Escherichia coli, Klebsiella pneumoniae, and Pseudomonas aeruginosa isolates from the transplant recipients showed markedly less susceptibility to first-line antibiotics than would have been predicted by the hospital-antibiograms. In particular, in the transplant recipients E. coli infections were resistant to trimethoprim-sulfamethoxazole, levofloxacin, and ceftriaxone; K. pneumoniae infections were resistant to every antibiotic except amikacin; and P. aeruginosa infections were resistant to levofloxacin, cefepime, and amikacin (Diag Microbiol Infect Dis. 2016 Aug 25. doi: 10.1016/j.diagmicrobio.2016.08.018).
“We advocate for the development of antibiograms specific to solid-organ transplant recipients. This may allow intrahospital comparisons and intertransplant-center monitoring of trends in antimicrobial resistance over time,” Dr. Rosa and her associates said.
FROM DIAGNOSTIC MICROBIOLOGY AND INFECTIOUS DISEASE
Key clinical point: Antibiotic susceptibility in bacteria cultured from transplant recipients differs markedly from that in hospital-wide antibiograms.
Major finding: In the transplant recipients, E. coli infections were resistant to trimethoprim-sulfamethoxazole, levofloxacin, and ceftriaxone; K. pneumoniae infections were resistant to every antibiotic except amikacin; and P. aeruginosa infections were resistant to levofloxacin, cefepime, and amikacin.
Data source: A single-center study comparing the antibiotic susceptibility of 1,889 bacterial isolates from transplant recipients with 10,439 isolates from other patients.
Disclosures: This study was not supported by funding from any public, commercial, or not-for-profit entities. Dr. Rosa and her associates reported having no relevant financial disclosures.
VIDEO: EVLP may extend lung preservation, quality for transplants
BALTIMORE – The use of ex vivo lung perfusion (EVLP) may allow for the safe transplantation of lungs preserved for more than 12 hours, according to a study presented at the annual meeting of the American Association for Thoracic Surgery.
A research team at the University of Toronto evaluated the outcomes of transplant patients who received a lung with a preservation time of over 12 hours between January 2006 and April 2015 and compared them to the general lung transplant population. Median hospital and ICU length of stay were similar between the two groups, and Kaplan-Meier survival curves between the two groups did not show any difference. Preservation time, donor PO2, and use of EVLP were not significant variables affecting survival.
Dr. Bartley P. Griffith, chief of cardiac surgery at the University of Maryland, Baltimore, and a discussant on the paper at the meeting, said that the findings of the study open up the possibility of a more “planned” approach to transplantation.
“Anything that not only extends preservation time, but perhaps even improves quality of preservation, would be a godsend,” Dr. Griffith said in a video interview. He cautioned that the “devil is in the details,” and that the data had to be examined closely. Nevertheless, Dr. Griffith said transplant surgeons should be grateful for the important work done by the University of Toronto team.
Dr. Griffith reported no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @richpizzi
BALTIMORE – The use of ex vivo lung perfusion (EVLP) may allow for the safe transplantation of lungs preserved for more than 12 hours, according to a study presented at the annual meeting of the American Association for Thoracic Surgery.
A research team at the University of Toronto evaluated the outcomes of transplant patients who received a lung with a preservation time of over 12 hours between January 2006 and April 2015 and compared them to the general lung transplant population. Median hospital and ICU length of stay were similar between the two groups, and Kaplan-Meier survival curves between the two groups did not show any difference. Preservation time, donor PO2, and use of EVLP were not significant variables affecting survival.
Dr. Bartley P. Griffith, chief of cardiac surgery at the University of Maryland, Baltimore, and a discussant on the paper at the meeting, said that the findings of the study open up the possibility of a more “planned” approach to transplantation.
“Anything that not only extends preservation time, but perhaps even improves quality of preservation, would be a godsend,” Dr. Griffith said in a video interview. He cautioned that the “devil is in the details,” and that the data had to be examined closely. Nevertheless, Dr. Griffith said transplant surgeons should be grateful for the important work done by the University of Toronto team.
Dr. Griffith reported no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @richpizzi
BALTIMORE – The use of ex vivo lung perfusion (EVLP) may allow for the safe transplantation of lungs preserved for more than 12 hours, according to a study presented at the annual meeting of the American Association for Thoracic Surgery.
A research team at the University of Toronto evaluated the outcomes of transplant patients who received a lung with a preservation time of over 12 hours between January 2006 and April 2015 and compared them to the general lung transplant population. Median hospital and ICU length of stay were similar between the two groups, and Kaplan-Meier survival curves between the two groups did not show any difference. Preservation time, donor PO2, and use of EVLP were not significant variables affecting survival.
Dr. Bartley P. Griffith, chief of cardiac surgery at the University of Maryland, Baltimore, and a discussant on the paper at the meeting, said that the findings of the study open up the possibility of a more “planned” approach to transplantation.
“Anything that not only extends preservation time, but perhaps even improves quality of preservation, would be a godsend,” Dr. Griffith said in a video interview. He cautioned that the “devil is in the details,” and that the data had to be examined closely. Nevertheless, Dr. Griffith said transplant surgeons should be grateful for the important work done by the University of Toronto team.
Dr. Griffith reported no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @richpizzi
AT THE AATS ANNUAL MEETING
Tacrolimus worsens IBD post liver transplant for primary sclerosing cholangitis
SAN DIEGO – A retrospective study provides insight as to why some patients have a milder versus a more severe course of inflammatory bowel disease (IBD) after liver transplant for primary sclerosing cholangitis (PSC).
Recurrent PSC, prolonged use of steroids, and cancer development after liver transplant were associated with a milder course of IBD, but tacrolimus use was associated with increased IBD flare post transplant.
“The course of IBD is highly variable after liver transplant for PSC. PSC is associated with IBD in 60% to 90% of patients, and IBD worsens in about 30% of PSC-IBD patients after transplant. We wanted to explore the risk factors for worsening IBD in this setting,” Dr. Mohamad Mouchli of the Mayo Clinic in Rochester, Minn., explained at the annual Digestive Disease Week.
For purposes of this study, progression of IBD was defined as the need for escalation of medical therapy, compared with before liver transplant, or need for colectomy for medically refractory IBD.
The study population included patients with PSC-IBD who underwent liver transplant for noncholangiocarcinoma indications at the Mayo Clinic from 1998 to 2012. Patients were followed through February 2015.
The investigators screened 373 patients: After exclusions for cancer, no IBD at transplant, and pretransplant colectomy, 151 patients with an intact colon were left and formed the basis of further analysis.
Median age at transplant was 46 years and two-thirds of the patients were male. Transplant-related variables included the following: 23% experienced allograft failure, 36% had recurrent PSC, 25.2% had CMV infection, 19.2% were retransplanted, 22.5% developed cancer after liver transplant, and 52.3% had acute cellular rejection.
Before transplant, 69 patients had quiescent IBD with no therapy and 62 were maintained on 5-aminosalicylates. Post transplant, despite transplant-related immunosuppression, 56 patients (37.1%) required escalation of therapy, 87 patients (57.6%) had a stable course, and 8 patients (5.3%) improved.
Risk of IBD progression at 1, 5, and 10 years was 4%, 18.5%, and 25.5%, respectively. Thirty-five patients underwent colectomy after transplant: the 1-, 5-, and 10-year risks of colectomy were 2%, 9.3%, and 17.2%, respectively. Fourteen percent of patients required anti–tumor necrosis factor therapy after transplant.
On multivariate analysis, tacrolimus exposure emerged as a risk factor for progression of IBD. Tacrolimus immunosuppression was twice as likely as cyclosporine-based immunosuppression to lead to IBD progression. By contrast, recurrent PSC, use of steroids for longer than 6 months, and cancer development after liver transplant were protective of IBD progression.
No association was found between progression of IBD and transplant-related infection or mismatch, immunosuppression with mycophenolate or azathioprine, or IBD-related factors such as pretransplant IBD status or empirical initiation of 5-aminosalicylates within 4 months of liver transplant. During the question-and-answer session following his presentation, Dr. Mouchli was asked whether these results justify prophylactic colectomy. He said that could be considered in patients with active IBD before transplant, but on a case-by-case basis.
SAN DIEGO – A retrospective study provides insight as to why some patients have a milder versus a more severe course of inflammatory bowel disease (IBD) after liver transplant for primary sclerosing cholangitis (PSC).
Recurrent PSC, prolonged use of steroids, and cancer development after liver transplant were associated with a milder course of IBD, but tacrolimus use was associated with increased IBD flare post transplant.
“The course of IBD is highly variable after liver transplant for PSC. PSC is associated with IBD in 60% to 90% of patients, and IBD worsens in about 30% of PSC-IBD patients after transplant. We wanted to explore the risk factors for worsening IBD in this setting,” Dr. Mohamad Mouchli of the Mayo Clinic in Rochester, Minn., explained at the annual Digestive Disease Week.
For purposes of this study, progression of IBD was defined as the need for escalation of medical therapy, compared with before liver transplant, or need for colectomy for medically refractory IBD.
The study population included patients with PSC-IBD who underwent liver transplant for noncholangiocarcinoma indications at the Mayo Clinic from 1998 to 2012. Patients were followed through February 2015.
The investigators screened 373 patients: After exclusions for cancer, no IBD at transplant, and pretransplant colectomy, 151 patients with an intact colon were left and formed the basis of further analysis.
Median age at transplant was 46 years and two-thirds of the patients were male. Transplant-related variables included the following: 23% experienced allograft failure, 36% had recurrent PSC, 25.2% had CMV infection, 19.2% were retransplanted, 22.5% developed cancer after liver transplant, and 52.3% had acute cellular rejection.
Before transplant, 69 patients had quiescent IBD with no therapy and 62 were maintained on 5-aminosalicylates. Post transplant, despite transplant-related immunosuppression, 56 patients (37.1%) required escalation of therapy, 87 patients (57.6%) had a stable course, and 8 patients (5.3%) improved.
Risk of IBD progression at 1, 5, and 10 years was 4%, 18.5%, and 25.5%, respectively. Thirty-five patients underwent colectomy after transplant: the 1-, 5-, and 10-year risks of colectomy were 2%, 9.3%, and 17.2%, respectively. Fourteen percent of patients required anti–tumor necrosis factor therapy after transplant.
On multivariate analysis, tacrolimus exposure emerged as a risk factor for progression of IBD. Tacrolimus immunosuppression was twice as likely as cyclosporine-based immunosuppression to lead to IBD progression. By contrast, recurrent PSC, use of steroids for longer than 6 months, and cancer development after liver transplant were protective of IBD progression.
No association was found between progression of IBD and transplant-related infection or mismatch, immunosuppression with mycophenolate or azathioprine, or IBD-related factors such as pretransplant IBD status or empirical initiation of 5-aminosalicylates within 4 months of liver transplant. During the question-and-answer session following his presentation, Dr. Mouchli was asked whether these results justify prophylactic colectomy. He said that could be considered in patients with active IBD before transplant, but on a case-by-case basis.
SAN DIEGO – A retrospective study provides insight as to why some patients have a milder versus a more severe course of inflammatory bowel disease (IBD) after liver transplant for primary sclerosing cholangitis (PSC).
Recurrent PSC, prolonged use of steroids, and cancer development after liver transplant were associated with a milder course of IBD, but tacrolimus use was associated with increased IBD flare post transplant.
“The course of IBD is highly variable after liver transplant for PSC. PSC is associated with IBD in 60% to 90% of patients, and IBD worsens in about 30% of PSC-IBD patients after transplant. We wanted to explore the risk factors for worsening IBD in this setting,” Dr. Mohamad Mouchli of the Mayo Clinic in Rochester, Minn., explained at the annual Digestive Disease Week.
For purposes of this study, progression of IBD was defined as the need for escalation of medical therapy, compared with before liver transplant, or need for colectomy for medically refractory IBD.
The study population included patients with PSC-IBD who underwent liver transplant for noncholangiocarcinoma indications at the Mayo Clinic from 1998 to 2012. Patients were followed through February 2015.
The investigators screened 373 patients: After exclusions for cancer, no IBD at transplant, and pretransplant colectomy, 151 patients with an intact colon were left and formed the basis of further analysis.
Median age at transplant was 46 years and two-thirds of the patients were male. Transplant-related variables included the following: 23% experienced allograft failure, 36% had recurrent PSC, 25.2% had CMV infection, 19.2% were retransplanted, 22.5% developed cancer after liver transplant, and 52.3% had acute cellular rejection.
Before transplant, 69 patients had quiescent IBD with no therapy and 62 were maintained on 5-aminosalicylates. Post transplant, despite transplant-related immunosuppression, 56 patients (37.1%) required escalation of therapy, 87 patients (57.6%) had a stable course, and 8 patients (5.3%) improved.
Risk of IBD progression at 1, 5, and 10 years was 4%, 18.5%, and 25.5%, respectively. Thirty-five patients underwent colectomy after transplant: the 1-, 5-, and 10-year risks of colectomy were 2%, 9.3%, and 17.2%, respectively. Fourteen percent of patients required anti–tumor necrosis factor therapy after transplant.
On multivariate analysis, tacrolimus exposure emerged as a risk factor for progression of IBD. Tacrolimus immunosuppression was twice as likely as cyclosporine-based immunosuppression to lead to IBD progression. By contrast, recurrent PSC, use of steroids for longer than 6 months, and cancer development after liver transplant were protective of IBD progression.
No association was found between progression of IBD and transplant-related infection or mismatch, immunosuppression with mycophenolate or azathioprine, or IBD-related factors such as pretransplant IBD status or empirical initiation of 5-aminosalicylates within 4 months of liver transplant. During the question-and-answer session following his presentation, Dr. Mouchli was asked whether these results justify prophylactic colectomy. He said that could be considered in patients with active IBD before transplant, but on a case-by-case basis.
AT DDW® 2016
Key clinical point: Tacrolimus exposure was an independent risk factor for IBD progression after liver transplant in patients with PSC-IBD.
Major finding: Tacrolimus immunosuppression was twice as likely as cyclosporine-based immunosuppression to lead to worsening IBC post liver transplant.
Data source: Retrospective study of the natural history of IBD following liver transplant in 151 patients with PSC-IBD.
Disclosures: Dr. Mouchli had no financial disclosures to report.
Parathyroidectomy before kidney transplant may reduce complications
BALTIMORE – Performing a parathyroidectomy in kidney transplant patients before their transplant can reduce the risk of graft failure and provide other benefits, the findings of a retrospective study of 913 patients suggest.
Uremic hyperparathyroidism (UHPT) is common in patients with end-stage kidney disease, and elevated parathyroid hormone (PTH) levels have been linked with delayed graft function after kidney transplants, but current guidelines for PTH levels may not go far enough to reduce the risk of graft failure and other post–kidney transplant complications in people with elevated PTH before transplant, according to Dr. Glenda G. Callender of Yale University, New Haven, Conn., and her colleagues.
“Uremic hyperparathyroidism was associated with an increased risk of complications in the first year post kidney transplant,” Dr. Callender said at the annual meeting of the American Association of Endocrine Surgeons. “Pre–kidney transplant parathyroidectomy was associated with a decreased risk of post–kidney transplant graft failure. This implies that pre–kidney transplant reduction of PTH levels should be considered in patients with UPHT.”
The Yale researchers reviewed outcomes of 913 patients at their institution who had a kidney transplant from 2005 to 2014. They analyzed biochemical values before kidney transplant and at three intervals post transplant: at 1 month, 6 months, and 1 year. Among the outcomes they evaluated were calcium and PTH levels, estimated glomerular filtration rate, complications, delayed graft function, and graft failure. The overall graft survival rate was 97.8% 1 year after kidney transplantation.
Overall, 49.4% of patients (451) had a diagnosis with UHPT before kidney transplant; 6.2% of all patients (57) had parathyroidectomy before kidney transplant and another 2% (18) had parathyroidectomy at some point after their kidney transplant operations. Median baseline PTH levels were higher in the UHPT patients: 206 pg/mL vs. 159 pg/mL for the non-UHPT group, Dr. Callender reported.
The researchers captured complete data on 37 of the 57 patients who had pretransplant parathyroidectomy. Twenty-four (65% of the group) had subtotal parathyroidectomy in which 3.5 glands were removed, and 12 (32%) had fewer than 3.5 glands removed. One patient had total parathyroidectomy, she said.
Among the patients with UHPT, the median pre–kidney transplant PTH was similar between the pretransplant parathyroidectomy and the no-parathyroidectomy groups: 218 pg/mL and 180 pg/mL, respectively, Dr. Callender said.
Pre–kidney transplant diagnosis of UHPT had an odds ratio of 1.44 for complications in the first year after transplant surgery, but not necessarily a greater risk for graft function or graft failure, she said. However, those relative risks changed with the degree of PTH above normal. Patients with UHPT who had pretransplant parathyroidectomy had a lower risk of graft failure, with an odds ratio of 0.547.
Current Kidney Disease Improving Global Outcomes (KDIGO) guidelines recommend maintaining PTH levels in patients with UHPT before they have kidney transplant surgery at no more than nine times normal. To test the optimal PTH levels before kidney transplant, the researchers analyzed thresholds ranging from two to nine times the normal limit.
“A pre–kidney transplant [PTH] level greater than or equal to six times normal was associated with post-transplant graft failure but not with delayed graft function or complications in the first year post kidney transplant,” Dr. Callender said. “Although the thresholds at two and four times normal were statistically significant, there was a continued risk significant for graft failure above six times normal.”
This finding “suggests that perhaps the current KDIGO guideline of maintaining patient PTH at up to nine times normal is too liberal,” Dr. Callender said.
She acknowledged several limitations of the study: its retrospective nature, small sample size, and “many missing data points” because a wide variety of dialysis centers with varying documentation standards collected information.
“However,” Dr. Callender said, “we believe these findings support the design and implementation of a multi-institutional, prospective, randomized control trial to evaluate whether a change in management of patients with uremic hyperparathyroidism is warranted.”
Dr. Callender and her coauthors had no financial relationships to disclose.
BALTIMORE – Performing a parathyroidectomy in kidney transplant patients before their transplant can reduce the risk of graft failure and provide other benefits, the findings of a retrospective study of 913 patients suggest.
Uremic hyperparathyroidism (UHPT) is common in patients with end-stage kidney disease, and elevated parathyroid hormone (PTH) levels have been linked with delayed graft function after kidney transplants, but current guidelines for PTH levels may not go far enough to reduce the risk of graft failure and other post–kidney transplant complications in people with elevated PTH before transplant, according to Dr. Glenda G. Callender of Yale University, New Haven, Conn., and her colleagues.
“Uremic hyperparathyroidism was associated with an increased risk of complications in the first year post kidney transplant,” Dr. Callender said at the annual meeting of the American Association of Endocrine Surgeons. “Pre–kidney transplant parathyroidectomy was associated with a decreased risk of post–kidney transplant graft failure. This implies that pre–kidney transplant reduction of PTH levels should be considered in patients with UPHT.”
The Yale researchers reviewed outcomes of 913 patients at their institution who had a kidney transplant from 2005 to 2014. They analyzed biochemical values before kidney transplant and at three intervals post transplant: at 1 month, 6 months, and 1 year. Among the outcomes they evaluated were calcium and PTH levels, estimated glomerular filtration rate, complications, delayed graft function, and graft failure. The overall graft survival rate was 97.8% 1 year after kidney transplantation.
Overall, 49.4% of patients (451) had a diagnosis with UHPT before kidney transplant; 6.2% of all patients (57) had parathyroidectomy before kidney transplant and another 2% (18) had parathyroidectomy at some point after their kidney transplant operations. Median baseline PTH levels were higher in the UHPT patients: 206 pg/mL vs. 159 pg/mL for the non-UHPT group, Dr. Callender reported.
The researchers captured complete data on 37 of the 57 patients who had pretransplant parathyroidectomy. Twenty-four (65% of the group) had subtotal parathyroidectomy in which 3.5 glands were removed, and 12 (32%) had fewer than 3.5 glands removed. One patient had total parathyroidectomy, she said.
Among the patients with UHPT, the median pre–kidney transplant PTH was similar between the pretransplant parathyroidectomy and the no-parathyroidectomy groups: 218 pg/mL and 180 pg/mL, respectively, Dr. Callender said.
Pre–kidney transplant diagnosis of UHPT had an odds ratio of 1.44 for complications in the first year after transplant surgery, but not necessarily a greater risk for graft function or graft failure, she said. However, those relative risks changed with the degree of PTH above normal. Patients with UHPT who had pretransplant parathyroidectomy had a lower risk of graft failure, with an odds ratio of 0.547.
Current Kidney Disease Improving Global Outcomes (KDIGO) guidelines recommend maintaining PTH levels in patients with UHPT before they have kidney transplant surgery at no more than nine times normal. To test the optimal PTH levels before kidney transplant, the researchers analyzed thresholds ranging from two to nine times the normal limit.
“A pre–kidney transplant [PTH] level greater than or equal to six times normal was associated with post-transplant graft failure but not with delayed graft function or complications in the first year post kidney transplant,” Dr. Callender said. “Although the thresholds at two and four times normal were statistically significant, there was a continued risk significant for graft failure above six times normal.”
This finding “suggests that perhaps the current KDIGO guideline of maintaining patient PTH at up to nine times normal is too liberal,” Dr. Callender said.
She acknowledged several limitations of the study: its retrospective nature, small sample size, and “many missing data points” because a wide variety of dialysis centers with varying documentation standards collected information.
“However,” Dr. Callender said, “we believe these findings support the design and implementation of a multi-institutional, prospective, randomized control trial to evaluate whether a change in management of patients with uremic hyperparathyroidism is warranted.”
Dr. Callender and her coauthors had no financial relationships to disclose.
BALTIMORE – Performing a parathyroidectomy in kidney transplant patients before their transplant can reduce the risk of graft failure and provide other benefits, the findings of a retrospective study of 913 patients suggest.
Uremic hyperparathyroidism (UHPT) is common in patients with end-stage kidney disease, and elevated parathyroid hormone (PTH) levels have been linked with delayed graft function after kidney transplants, but current guidelines for PTH levels may not go far enough to reduce the risk of graft failure and other post–kidney transplant complications in people with elevated PTH before transplant, according to Dr. Glenda G. Callender of Yale University, New Haven, Conn., and her colleagues.
“Uremic hyperparathyroidism was associated with an increased risk of complications in the first year post kidney transplant,” Dr. Callender said at the annual meeting of the American Association of Endocrine Surgeons. “Pre–kidney transplant parathyroidectomy was associated with a decreased risk of post–kidney transplant graft failure. This implies that pre–kidney transplant reduction of PTH levels should be considered in patients with UPHT.”
The Yale researchers reviewed outcomes of 913 patients at their institution who had a kidney transplant from 2005 to 2014. They analyzed biochemical values before kidney transplant and at three intervals post transplant: at 1 month, 6 months, and 1 year. Among the outcomes they evaluated were calcium and PTH levels, estimated glomerular filtration rate, complications, delayed graft function, and graft failure. The overall graft survival rate was 97.8% 1 year after kidney transplantation.
Overall, 49.4% of patients (451) had a diagnosis with UHPT before kidney transplant; 6.2% of all patients (57) had parathyroidectomy before kidney transplant and another 2% (18) had parathyroidectomy at some point after their kidney transplant operations. Median baseline PTH levels were higher in the UHPT patients: 206 pg/mL vs. 159 pg/mL for the non-UHPT group, Dr. Callender reported.
The researchers captured complete data on 37 of the 57 patients who had pretransplant parathyroidectomy. Twenty-four (65% of the group) had subtotal parathyroidectomy in which 3.5 glands were removed, and 12 (32%) had fewer than 3.5 glands removed. One patient had total parathyroidectomy, she said.
Among the patients with UHPT, the median pre–kidney transplant PTH was similar between the pretransplant parathyroidectomy and the no-parathyroidectomy groups: 218 pg/mL and 180 pg/mL, respectively, Dr. Callender said.
Pre–kidney transplant diagnosis of UHPT had an odds ratio of 1.44 for complications in the first year after transplant surgery, but not necessarily a greater risk for graft function or graft failure, she said. However, those relative risks changed with the degree of PTH above normal. Patients with UHPT who had pretransplant parathyroidectomy had a lower risk of graft failure, with an odds ratio of 0.547.
Current Kidney Disease Improving Global Outcomes (KDIGO) guidelines recommend maintaining PTH levels in patients with UHPT before they have kidney transplant surgery at no more than nine times normal. To test the optimal PTH levels before kidney transplant, the researchers analyzed thresholds ranging from two to nine times the normal limit.
“A pre–kidney transplant [PTH] level greater than or equal to six times normal was associated with post-transplant graft failure but not with delayed graft function or complications in the first year post kidney transplant,” Dr. Callender said. “Although the thresholds at two and four times normal were statistically significant, there was a continued risk significant for graft failure above six times normal.”
This finding “suggests that perhaps the current KDIGO guideline of maintaining patient PTH at up to nine times normal is too liberal,” Dr. Callender said.
She acknowledged several limitations of the study: its retrospective nature, small sample size, and “many missing data points” because a wide variety of dialysis centers with varying documentation standards collected information.
“However,” Dr. Callender said, “we believe these findings support the design and implementation of a multi-institutional, prospective, randomized control trial to evaluate whether a change in management of patients with uremic hyperparathyroidism is warranted.”
Dr. Callender and her coauthors had no financial relationships to disclose.
AT AAES 2016
Key clinical point: Parathyroidectomy reduces graft failure in individuals with uremic hyperparathyroidism (UHPT) who undergo kidney transplant.
Major finding: Pre–kidney transplant diagnosis of UHPT had an odds ratio of 1.44 of complications a year after transplant; patients who had parathyroidectomy before transplant had a reduced 0.547 odds ratio risk of graft failure.
Data source: Review of 913 patients who had kidney transplant from 2005 to 2014 at a single institution.
Disclosures: Dr. Callender and her coauthors reported having no financial disclosures.
Infections kill many waiting for liver transplant, force others off list
AMSTERDAM – Infection is a major cause of death among patients waiting for a liver transplant, killing more than half of those who contracted one.
Infection also was the biggest reason that patients with end-stage liver disease withdrew from the transplant waiting list, a 9-year-long study has shown. Patients who developed an infection were six times more likely to withdraw than were those who did not, Dr. Loes Alferink wrote in a poster presented at the European Society of Clinical Microbiology and Infectious Diseases annual congress.
“We need to focus on better prophylactic antibiotic strategies to save lives in patients with end-stage liver disease who are on the waiting list,” said Dr. Alferink of Erasmus Medical Center, Rotterdam, the Netherlands.
She and her colleagues examined the effect of infections on 312 patients who were waiting for a transplant at Erasmus Medical Center from the period of 2006-2013. During that time, a total of 317 infections developed in 144 patients. The infections were fatal in 58% of these patients.
These included spontaneous primary cholangitis (75); spontaneous bacterial peritonitis (61); urogenital (38), respiratory (30), and skin (25) infections; as well as primary bacteremia (22). Also, there were 18 cases of gastroenteritis and 12 cases of Candida esophagitis. The remainder were unspecified infections.
The death rate was highest in primary bacteremia, which killed about 40% of those who developed it. The rate was about 25% in respiratory infections, 20% in spontaneous primary bacteremia, 15% in esophagitis, 10% in gastroenteritis and urinary tract infections, and 10% in patients with multiple site infections.
The pathogens were gram negative (70) and gram positive (37) bacteria; Enterococcus faecium (15) and faecalis (3); yeasts (13); viruses (7); and mold (2). The remainder of the infections yielded a negative culture.
In 24 patients, multiple pathogens were identified. These patients had the highest rate of mortality, with almost half of them dying from their infection; one of the two patients with a mold infection also died. The death rate was 20% in patients with yeast infections, 18% in those with E. faecium, 15% in gram-positive infections, and 10% in gram-negative infections.
A multivariate analysis found several factors that increased the risk of dying from an infection. For every 10 years of increasing age, the risk of infection-related mortality doubled (odds ratio, 2); worse MELD (Model for End-Stage Liver Disease) scores increased the risk by 12%.
Patients with hepatic encephalopathy were 76% more likely to die from an infection, and those with refractory ascites faced a 2.5-fold increased risk. Mechanical ventilation was associated with more than a fivefold increased risk (OR, 5.72).
Patients who developed an infection were almost six times more likely to be withdrawn from the transplant waiting list (hazard ratio, 5.87). The regression analysis for withdrawal identified several factors that significantly increased the risk, including age, MELD score, and serum albumin. The biggest risk factor for withdrawal related to infection was refractory ascites, which more than doubled the risk (HR, 2.2).
Dr. Alferink had no financial disclosures.
On Twitter @Alz_Gal
AMSTERDAM – Infection is a major cause of death among patients waiting for a liver transplant, killing more than half of those who contracted one.
Infection also was the biggest reason that patients with end-stage liver disease withdrew from the transplant waiting list, a 9-year-long study has shown. Patients who developed an infection were six times more likely to withdraw than were those who did not, Dr. Loes Alferink wrote in a poster presented at the European Society of Clinical Microbiology and Infectious Diseases annual congress.
“We need to focus on better prophylactic antibiotic strategies to save lives in patients with end-stage liver disease who are on the waiting list,” said Dr. Alferink of Erasmus Medical Center, Rotterdam, the Netherlands.
She and her colleagues examined the effect of infections on 312 patients who were waiting for a transplant at Erasmus Medical Center from the period of 2006-2013. During that time, a total of 317 infections developed in 144 patients. The infections were fatal in 58% of these patients.
These included spontaneous primary cholangitis (75); spontaneous bacterial peritonitis (61); urogenital (38), respiratory (30), and skin (25) infections; as well as primary bacteremia (22). Also, there were 18 cases of gastroenteritis and 12 cases of Candida esophagitis. The remainder were unspecified infections.
The death rate was highest in primary bacteremia, which killed about 40% of those who developed it. The rate was about 25% in respiratory infections, 20% in spontaneous primary bacteremia, 15% in esophagitis, 10% in gastroenteritis and urinary tract infections, and 10% in patients with multiple site infections.
The pathogens were gram negative (70) and gram positive (37) bacteria; Enterococcus faecium (15) and faecalis (3); yeasts (13); viruses (7); and mold (2). The remainder of the infections yielded a negative culture.
In 24 patients, multiple pathogens were identified. These patients had the highest rate of mortality, with almost half of them dying from their infection; one of the two patients with a mold infection also died. The death rate was 20% in patients with yeast infections, 18% in those with E. faecium, 15% in gram-positive infections, and 10% in gram-negative infections.
A multivariate analysis found several factors that increased the risk of dying from an infection. For every 10 years of increasing age, the risk of infection-related mortality doubled (odds ratio, 2); worse MELD (Model for End-Stage Liver Disease) scores increased the risk by 12%.
Patients with hepatic encephalopathy were 76% more likely to die from an infection, and those with refractory ascites faced a 2.5-fold increased risk. Mechanical ventilation was associated with more than a fivefold increased risk (OR, 5.72).
Patients who developed an infection were almost six times more likely to be withdrawn from the transplant waiting list (hazard ratio, 5.87). The regression analysis for withdrawal identified several factors that significantly increased the risk, including age, MELD score, and serum albumin. The biggest risk factor for withdrawal related to infection was refractory ascites, which more than doubled the risk (HR, 2.2).
Dr. Alferink had no financial disclosures.
On Twitter @Alz_Gal
AMSTERDAM – Infection is a major cause of death among patients waiting for a liver transplant, killing more than half of those who contracted one.
Infection also was the biggest reason that patients with end-stage liver disease withdrew from the transplant waiting list, a 9-year-long study has shown. Patients who developed an infection were six times more likely to withdraw than were those who did not, Dr. Loes Alferink wrote in a poster presented at the European Society of Clinical Microbiology and Infectious Diseases annual congress.
“We need to focus on better prophylactic antibiotic strategies to save lives in patients with end-stage liver disease who are on the waiting list,” said Dr. Alferink of Erasmus Medical Center, Rotterdam, the Netherlands.
She and her colleagues examined the effect of infections on 312 patients who were waiting for a transplant at Erasmus Medical Center from the period of 2006-2013. During that time, a total of 317 infections developed in 144 patients. The infections were fatal in 58% of these patients.
These included spontaneous primary cholangitis (75); spontaneous bacterial peritonitis (61); urogenital (38), respiratory (30), and skin (25) infections; as well as primary bacteremia (22). Also, there were 18 cases of gastroenteritis and 12 cases of Candida esophagitis. The remainder were unspecified infections.
The death rate was highest in primary bacteremia, which killed about 40% of those who developed it. The rate was about 25% in respiratory infections, 20% in spontaneous primary bacteremia, 15% in esophagitis, 10% in gastroenteritis and urinary tract infections, and 10% in patients with multiple site infections.
The pathogens were gram negative (70) and gram positive (37) bacteria; Enterococcus faecium (15) and faecalis (3); yeasts (13); viruses (7); and mold (2). The remainder of the infections yielded a negative culture.
In 24 patients, multiple pathogens were identified. These patients had the highest rate of mortality, with almost half of them dying from their infection; one of the two patients with a mold infection also died. The death rate was 20% in patients with yeast infections, 18% in those with E. faecium, 15% in gram-positive infections, and 10% in gram-negative infections.
A multivariate analysis found several factors that increased the risk of dying from an infection. For every 10 years of increasing age, the risk of infection-related mortality doubled (odds ratio, 2); worse MELD (Model for End-Stage Liver Disease) scores increased the risk by 12%.
Patients with hepatic encephalopathy were 76% more likely to die from an infection, and those with refractory ascites faced a 2.5-fold increased risk. Mechanical ventilation was associated with more than a fivefold increased risk (OR, 5.72).
Patients who developed an infection were almost six times more likely to be withdrawn from the transplant waiting list (hazard ratio, 5.87). The regression analysis for withdrawal identified several factors that significantly increased the risk, including age, MELD score, and serum albumin. The biggest risk factor for withdrawal related to infection was refractory ascites, which more than doubled the risk (HR, 2.2).
Dr. Alferink had no financial disclosures.
On Twitter @Alz_Gal
AT ECCMID 2016
Key clinical point: Infections are a major cause of transplant wait-list withdrawal and death in patients with end-stage liver disease.
Major finding: Infections increased the risk of withdrawal by sixfold, and killed 58% of those who developed one.
Data source: A retrospective study of 144 patients who developed a total of 317 infections.
Disclosures: Dr. Alferink had no financial disclosures.
Fatty liver risk rises in years after transplant
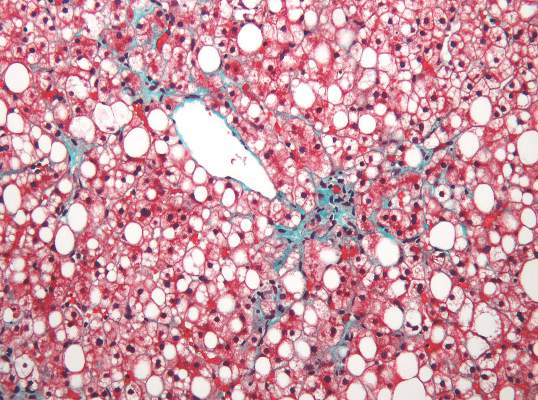
Steatosis may be present in at least half of liver transplant recipients, and the prevalence increases significantly over time, according to data from a retrospective study of 548 adult patients.
Although steatosis is common after transplantation, the prevalence, risk factors, and impact on patient survival has not been well studied, wrote Dr. Irena Hejlova of the Institute for Clinical and Experimental Medicine in Prague, Czech Republic, and her colleagues.
“Our study was the first to document that the prevalence of steatosis in LT [liver transplant] recipients may be far higher than previously reported,” they said.
The researchers reviewed liver biopsies and patient survival data and found steatosis in 309 (56%) of the patients, including 93 (17%) with significant steatosis (defined as greater than 33%). Pretransplant factors associated with significant steatosis included cirrhosis caused by alcohol consumption as well as a high body mass index. Post-transplant risk factors associated with increased risk of significant steatosis included increased body mass index, increased serum triglycerides, alcohol consumption, and type 2 diabetes. However, “Although patients transplanted for alcoholic cirrhosis are at an increased risk, the vast majority of post-transplant steatosis is nonalcohol-related,” the researchers noted.
The overall prevalence of steatosis increased from 30% at 1 year after transplant to 48% at 10 years after transplant. Post-transplant steatosis was not associated with worse patient survival in the short term, but the long-term survival of patients with significant steatosis tended to be worse.
Read the full study here (Liver Transpl. 2016 Apr 5. doi: 10.1002/lt.24393).
Steatosis may be present in at least half of liver transplant recipients, and the prevalence increases significantly over time, according to data from a retrospective study of 548 adult patients.
Although steatosis is common after transplantation, the prevalence, risk factors, and impact on patient survival has not been well studied, wrote Dr. Irena Hejlova of the Institute for Clinical and Experimental Medicine in Prague, Czech Republic, and her colleagues.
“Our study was the first to document that the prevalence of steatosis in LT [liver transplant] recipients may be far higher than previously reported,” they said.
The researchers reviewed liver biopsies and patient survival data and found steatosis in 309 (56%) of the patients, including 93 (17%) with significant steatosis (defined as greater than 33%). Pretransplant factors associated with significant steatosis included cirrhosis caused by alcohol consumption as well as a high body mass index. Post-transplant risk factors associated with increased risk of significant steatosis included increased body mass index, increased serum triglycerides, alcohol consumption, and type 2 diabetes. However, “Although patients transplanted for alcoholic cirrhosis are at an increased risk, the vast majority of post-transplant steatosis is nonalcohol-related,” the researchers noted.
The overall prevalence of steatosis increased from 30% at 1 year after transplant to 48% at 10 years after transplant. Post-transplant steatosis was not associated with worse patient survival in the short term, but the long-term survival of patients with significant steatosis tended to be worse.
Read the full study here (Liver Transpl. 2016 Apr 5. doi: 10.1002/lt.24393).
Steatosis may be present in at least half of liver transplant recipients, and the prevalence increases significantly over time, according to data from a retrospective study of 548 adult patients.
Although steatosis is common after transplantation, the prevalence, risk factors, and impact on patient survival has not been well studied, wrote Dr. Irena Hejlova of the Institute for Clinical and Experimental Medicine in Prague, Czech Republic, and her colleagues.
“Our study was the first to document that the prevalence of steatosis in LT [liver transplant] recipients may be far higher than previously reported,” they said.
The researchers reviewed liver biopsies and patient survival data and found steatosis in 309 (56%) of the patients, including 93 (17%) with significant steatosis (defined as greater than 33%). Pretransplant factors associated with significant steatosis included cirrhosis caused by alcohol consumption as well as a high body mass index. Post-transplant risk factors associated with increased risk of significant steatosis included increased body mass index, increased serum triglycerides, alcohol consumption, and type 2 diabetes. However, “Although patients transplanted for alcoholic cirrhosis are at an increased risk, the vast majority of post-transplant steatosis is nonalcohol-related,” the researchers noted.
The overall prevalence of steatosis increased from 30% at 1 year after transplant to 48% at 10 years after transplant. Post-transplant steatosis was not associated with worse patient survival in the short term, but the long-term survival of patients with significant steatosis tended to be worse.
Read the full study here (Liver Transpl. 2016 Apr 5. doi: 10.1002/lt.24393).
FROM LIVER TRANSPLANTATION
Aortic aneurysms pose unique challenges in transplant recipients
CHICAGO – Surgeons can expect to see more abdominal organ transplant recipients presenting with aortic aneurysms, as transplant survival rates increase along with the age of organ donors and recipients.
“The consensus is that abdominal aortic aneurysms (AAAs) have a more aggressive course post-transplant and within that context, probably need to be managed more aggressively,” Dr. Michael J. Englesbe of the University of Michigan, Ann Arbor said at the annual Northwestern Vascular Symposium.
Some 270,000 Americans are living with a functioning liver or kidney graft, and their average age has risen from 47 years to 57 years over the last decade.
Though the data isn’t great, it’s hypothesized that the immunosuppression prerequisite for successful organ transplantation promotes the progression of atherosclerosis and aneurysm growth in transplant patients, he said.
New-onset diabetes, hyperlipidemia, and hypertension are all common post-transplant due to immunosuppression therapy. Aortic aneurysms are also reported to rupture at smaller sizes in transplant recipients.
Intriguingly, the opposite effect has been observed in experimental animal models, where immunosuppression with calcineurin inhibitors and mammalian target of rapamycin (mTOR) inhibitors has been shown to stabilize atherosclerotic lesions and inhibit aneurysm expansion.
The reason for this disparity is unclear, but immunosuppressants likely augment other cardiovascular comorbidities such as hypertension and atherosclerosis and this may trump their anti-inflammatory effects and lead to worse aneurysm disease and faster expansion in humans, Dr. Englesbe speculated in an interview.
As for when aneurysms should be fixed, kidney transplant candidates should undergo AAA repair prior to transplantation since the risk of renal complications after aneurysm repair puts the allograft at risk, Dr. Englesbe advised. Either an open or endovascular approach can be used.
In liver transplant candidates, elective AAA repair should be avoided if possible and is contraindicated if any signs of hepatic decompensation are present such as muscle wasting, ascites, platelet count less than 50 x 109/L, or encephalopathy. For well-compensated cirrhotic patients, endovascular repair is best.
One of the most important considerations for any solid-organ transplant patient undergoing aneurysm repair is perioperative management of immunosuppression, Dr. Englesbe stressed.
Transplant patients are maintained on oral calcineurin inhibitors such as cyclosporine and tacrolimus (Prograf) throughout the perioperative period to prevent organ rejection, but these drugs have nephrotoxic effects. About 10% of recipients, typically the sicker patients, will be switched to mTOR inhibitors such as everolimus (Afinitor) and sirolumus (Rapamune) as a kidney-sparing alternative.
“Part of the mechanism of these [mTOR] drugs is that they really affect fibroblast functioning, so patients that are on these medications, their wound will fall apart and they will invariably get a hernia,” Dr. Englesbe said. “You have to stop them upwards of about 6 weeks before surgical intervention, and I think this is also true for many endografts.”
He highlighted a case in which an mTOR inhibitor was started three months after liver transplant due to renal dysfunction in a patient who was fully healed, but within three weeks, “her wound fell apart, completely fell apart.” She developed several seromas underneath her incision, one of which became infected and took months to close.
“The transplant professionals – your nephrologists, your cardiologists – aren’t going to know this fact, but as a transplant surgeon it’s usually the first question we’re going to ask with respect to any post-transplant patient we’re going to operate on, so it’s something to keep in mind,” Dr. Englesbe said.
Another take-home message was the importance of maintaining kidney function in kidney recipients presenting with aortic aneurysm, as mortality in these patients is about 10-fold higher once the kidney fails, he said. A recent study reported that AAAs are significantly more common in kidney than liver transplant recipients (29.6% vs. 11.4%; P = .02), despite a similar prevalence for any aneurysm (4%) in both groups (J Vasc Surg. 2014 Mar;59;594-8).
When kidney recipients present, preoperative imaging of the aorta from the aneurysm to the kidney allograft is mandatory, he said. Endovascular repair is preferred, whenever possible.
The renal graft is typically sewn to the external iliac artery 3 cm to 10 cm from the bifurcation of the external and internal iliac arteries. Because of this, repair is challenging when aneurysmal disease involves the iliac artery, Dr. Englesbe observed. Aneurysmal dilation is less common in the external iliac, but stenting an iliac aneurysm can still compromise inflow to the transplanted kidney.
Several surgical techniques including axillofemoral bypass, aortofemoral shunt, or extracorporeal circuit have been reported to preserve renal function during open AAA repair in renal transplant recipients. These techniques are not without their own risk of complications and should be avoided in patients with low creatinine, but are appropriate in patients with marginal or impaired renal function, according to Dr. Englesbe, who reported having no relevant disclosures.
CHICAGO – Surgeons can expect to see more abdominal organ transplant recipients presenting with aortic aneurysms, as transplant survival rates increase along with the age of organ donors and recipients.
“The consensus is that abdominal aortic aneurysms (AAAs) have a more aggressive course post-transplant and within that context, probably need to be managed more aggressively,” Dr. Michael J. Englesbe of the University of Michigan, Ann Arbor said at the annual Northwestern Vascular Symposium.
Some 270,000 Americans are living with a functioning liver or kidney graft, and their average age has risen from 47 years to 57 years over the last decade.
Though the data isn’t great, it’s hypothesized that the immunosuppression prerequisite for successful organ transplantation promotes the progression of atherosclerosis and aneurysm growth in transplant patients, he said.
New-onset diabetes, hyperlipidemia, and hypertension are all common post-transplant due to immunosuppression therapy. Aortic aneurysms are also reported to rupture at smaller sizes in transplant recipients.
Intriguingly, the opposite effect has been observed in experimental animal models, where immunosuppression with calcineurin inhibitors and mammalian target of rapamycin (mTOR) inhibitors has been shown to stabilize atherosclerotic lesions and inhibit aneurysm expansion.
The reason for this disparity is unclear, but immunosuppressants likely augment other cardiovascular comorbidities such as hypertension and atherosclerosis and this may trump their anti-inflammatory effects and lead to worse aneurysm disease and faster expansion in humans, Dr. Englesbe speculated in an interview.
As for when aneurysms should be fixed, kidney transplant candidates should undergo AAA repair prior to transplantation since the risk of renal complications after aneurysm repair puts the allograft at risk, Dr. Englesbe advised. Either an open or endovascular approach can be used.
In liver transplant candidates, elective AAA repair should be avoided if possible and is contraindicated if any signs of hepatic decompensation are present such as muscle wasting, ascites, platelet count less than 50 x 109/L, or encephalopathy. For well-compensated cirrhotic patients, endovascular repair is best.
One of the most important considerations for any solid-organ transplant patient undergoing aneurysm repair is perioperative management of immunosuppression, Dr. Englesbe stressed.
Transplant patients are maintained on oral calcineurin inhibitors such as cyclosporine and tacrolimus (Prograf) throughout the perioperative period to prevent organ rejection, but these drugs have nephrotoxic effects. About 10% of recipients, typically the sicker patients, will be switched to mTOR inhibitors such as everolimus (Afinitor) and sirolumus (Rapamune) as a kidney-sparing alternative.
“Part of the mechanism of these [mTOR] drugs is that they really affect fibroblast functioning, so patients that are on these medications, their wound will fall apart and they will invariably get a hernia,” Dr. Englesbe said. “You have to stop them upwards of about 6 weeks before surgical intervention, and I think this is also true for many endografts.”
He highlighted a case in which an mTOR inhibitor was started three months after liver transplant due to renal dysfunction in a patient who was fully healed, but within three weeks, “her wound fell apart, completely fell apart.” She developed several seromas underneath her incision, one of which became infected and took months to close.
“The transplant professionals – your nephrologists, your cardiologists – aren’t going to know this fact, but as a transplant surgeon it’s usually the first question we’re going to ask with respect to any post-transplant patient we’re going to operate on, so it’s something to keep in mind,” Dr. Englesbe said.
Another take-home message was the importance of maintaining kidney function in kidney recipients presenting with aortic aneurysm, as mortality in these patients is about 10-fold higher once the kidney fails, he said. A recent study reported that AAAs are significantly more common in kidney than liver transplant recipients (29.6% vs. 11.4%; P = .02), despite a similar prevalence for any aneurysm (4%) in both groups (J Vasc Surg. 2014 Mar;59;594-8).
When kidney recipients present, preoperative imaging of the aorta from the aneurysm to the kidney allograft is mandatory, he said. Endovascular repair is preferred, whenever possible.
The renal graft is typically sewn to the external iliac artery 3 cm to 10 cm from the bifurcation of the external and internal iliac arteries. Because of this, repair is challenging when aneurysmal disease involves the iliac artery, Dr. Englesbe observed. Aneurysmal dilation is less common in the external iliac, but stenting an iliac aneurysm can still compromise inflow to the transplanted kidney.
Several surgical techniques including axillofemoral bypass, aortofemoral shunt, or extracorporeal circuit have been reported to preserve renal function during open AAA repair in renal transplant recipients. These techniques are not without their own risk of complications and should be avoided in patients with low creatinine, but are appropriate in patients with marginal or impaired renal function, according to Dr. Englesbe, who reported having no relevant disclosures.
CHICAGO – Surgeons can expect to see more abdominal organ transplant recipients presenting with aortic aneurysms, as transplant survival rates increase along with the age of organ donors and recipients.
“The consensus is that abdominal aortic aneurysms (AAAs) have a more aggressive course post-transplant and within that context, probably need to be managed more aggressively,” Dr. Michael J. Englesbe of the University of Michigan, Ann Arbor said at the annual Northwestern Vascular Symposium.
Some 270,000 Americans are living with a functioning liver or kidney graft, and their average age has risen from 47 years to 57 years over the last decade.
Though the data isn’t great, it’s hypothesized that the immunosuppression prerequisite for successful organ transplantation promotes the progression of atherosclerosis and aneurysm growth in transplant patients, he said.
New-onset diabetes, hyperlipidemia, and hypertension are all common post-transplant due to immunosuppression therapy. Aortic aneurysms are also reported to rupture at smaller sizes in transplant recipients.
Intriguingly, the opposite effect has been observed in experimental animal models, where immunosuppression with calcineurin inhibitors and mammalian target of rapamycin (mTOR) inhibitors has been shown to stabilize atherosclerotic lesions and inhibit aneurysm expansion.
The reason for this disparity is unclear, but immunosuppressants likely augment other cardiovascular comorbidities such as hypertension and atherosclerosis and this may trump their anti-inflammatory effects and lead to worse aneurysm disease and faster expansion in humans, Dr. Englesbe speculated in an interview.
As for when aneurysms should be fixed, kidney transplant candidates should undergo AAA repair prior to transplantation since the risk of renal complications after aneurysm repair puts the allograft at risk, Dr. Englesbe advised. Either an open or endovascular approach can be used.
In liver transplant candidates, elective AAA repair should be avoided if possible and is contraindicated if any signs of hepatic decompensation are present such as muscle wasting, ascites, platelet count less than 50 x 109/L, or encephalopathy. For well-compensated cirrhotic patients, endovascular repair is best.
One of the most important considerations for any solid-organ transplant patient undergoing aneurysm repair is perioperative management of immunosuppression, Dr. Englesbe stressed.
Transplant patients are maintained on oral calcineurin inhibitors such as cyclosporine and tacrolimus (Prograf) throughout the perioperative period to prevent organ rejection, but these drugs have nephrotoxic effects. About 10% of recipients, typically the sicker patients, will be switched to mTOR inhibitors such as everolimus (Afinitor) and sirolumus (Rapamune) as a kidney-sparing alternative.
“Part of the mechanism of these [mTOR] drugs is that they really affect fibroblast functioning, so patients that are on these medications, their wound will fall apart and they will invariably get a hernia,” Dr. Englesbe said. “You have to stop them upwards of about 6 weeks before surgical intervention, and I think this is also true for many endografts.”
He highlighted a case in which an mTOR inhibitor was started three months after liver transplant due to renal dysfunction in a patient who was fully healed, but within three weeks, “her wound fell apart, completely fell apart.” She developed several seromas underneath her incision, one of which became infected and took months to close.
“The transplant professionals – your nephrologists, your cardiologists – aren’t going to know this fact, but as a transplant surgeon it’s usually the first question we’re going to ask with respect to any post-transplant patient we’re going to operate on, so it’s something to keep in mind,” Dr. Englesbe said.
Another take-home message was the importance of maintaining kidney function in kidney recipients presenting with aortic aneurysm, as mortality in these patients is about 10-fold higher once the kidney fails, he said. A recent study reported that AAAs are significantly more common in kidney than liver transplant recipients (29.6% vs. 11.4%; P = .02), despite a similar prevalence for any aneurysm (4%) in both groups (J Vasc Surg. 2014 Mar;59;594-8).
When kidney recipients present, preoperative imaging of the aorta from the aneurysm to the kidney allograft is mandatory, he said. Endovascular repair is preferred, whenever possible.
The renal graft is typically sewn to the external iliac artery 3 cm to 10 cm from the bifurcation of the external and internal iliac arteries. Because of this, repair is challenging when aneurysmal disease involves the iliac artery, Dr. Englesbe observed. Aneurysmal dilation is less common in the external iliac, but stenting an iliac aneurysm can still compromise inflow to the transplanted kidney.
Several surgical techniques including axillofemoral bypass, aortofemoral shunt, or extracorporeal circuit have been reported to preserve renal function during open AAA repair in renal transplant recipients. These techniques are not without their own risk of complications and should be avoided in patients with low creatinine, but are appropriate in patients with marginal or impaired renal function, according to Dr. Englesbe, who reported having no relevant disclosures.
EXPERT ANALYSIS FROM THE NORTHWESTERN VASCULAR SYMPOSIUM
Organ transplant recipients face increased risk of BCC
Recipients of a solid organ transplant face up to a sixfold increase in the risk of developing a basal cell carcinoma – a risk that seems to increase as time passes.
A pretransplant history of squamous cell carcinoma (SCC) increased this risk to 55 times that seen in the general population, Dr. Britta Krynitz and her colleagues reported (Br J Dermatol. 2015. doi: 10.1111/bjd.14153).
But even when the pretransplant SCC group was removed from the final analysis, the risk of basal cell carcinoma after transplant was five times that of the general population, “indicating that a pretransplant SCC has limited effect on BCC risk overall and that organ transplantation per se is a strong driver of posttransplant BCC risk,” wrote Dr. Krynitz of Karolinska Institute, Stockholm, and her coauthors.
“Our results strongly suggest tumor promoter effects of the immunosuppressive drugs in the pathogenesis of post-transplantation BCC,” the team said. “We speculate that calcineurin inhibitors and also antiproliferative drugs, often used in combination with corticosteroids, play a role.”
The researchers investigated the incidence of both BCC and SCC in a cohort of 4,023 patients who underwent solid organ transplant from 2004 to 2011. Their median age at the time of transplant was 53 years; most (59%) received a kidney. Other organs transplanted were liver (22%), heart and/or lung (15%), and other organs (4%). The median follow-up time was 3.4 years; the longest follow-up was 5.5 years.
Only 17 of patients had a history of melanoma, and 19 patients a history of SCC – less than 1% for each skin cancer. Seven percent (301) of patients had experienced some form of nonskin cancer.
By the end of follow-up, 341 BCCs had developed among 175 patients – an incidence of 6.7%. About half developed more than one BCC.
The researchers compared these patients to a group of almost 200,000 nontransplant patients who had developed BCC. Among these, the median age at BCC appearance was significantly older (71 years); 39% had more than one lesion.
The overall relative risk of BCC was increased sixfold in transplant recipients and was similar between the genders. However, the risk varied according to the type of organ received. Kidney recipients were at the highest risk (relative risk, 7.2), and those who received other organs had a lower risk (heart/lung: RR, 5.8; liver: RR, 2.6).
The risk also appeared to increase over time, the authors noted. From 0 to 2 years, it was 5.8; from 3 to 5 years, it increased to 7.0.
Among men, 54% of lesions appeared in the head/neck area and 35% on the trunk – a similar distribution to that seen in the nontransplant control group. Among women, there were differences between transplant patients and controls: 44% of lesions appeared on patients’ head/neck, compared with 60% in the control group, and 34% appeared on the truck, compared with 24% in the control group.
Histology was similar, as were the proportions of aggressive type II and highly aggressive type III lesions.
A total of 199 SCCs developed among 87 patients during follow-up, a ratio to BCC of 1:1.7. “The low ratio was probably due to the short follow-up in our study,” the authors noted.
The Welander Foundation, the Westerberg Foundation, and the Strategic Research Program in Epidemiology at Karolinska Institute sponsored the study. None of the authors had any financial declarations.
Recipients of a solid organ transplant face up to a sixfold increase in the risk of developing a basal cell carcinoma – a risk that seems to increase as time passes.
A pretransplant history of squamous cell carcinoma (SCC) increased this risk to 55 times that seen in the general population, Dr. Britta Krynitz and her colleagues reported (Br J Dermatol. 2015. doi: 10.1111/bjd.14153).
But even when the pretransplant SCC group was removed from the final analysis, the risk of basal cell carcinoma after transplant was five times that of the general population, “indicating that a pretransplant SCC has limited effect on BCC risk overall and that organ transplantation per se is a strong driver of posttransplant BCC risk,” wrote Dr. Krynitz of Karolinska Institute, Stockholm, and her coauthors.
“Our results strongly suggest tumor promoter effects of the immunosuppressive drugs in the pathogenesis of post-transplantation BCC,” the team said. “We speculate that calcineurin inhibitors and also antiproliferative drugs, often used in combination with corticosteroids, play a role.”
The researchers investigated the incidence of both BCC and SCC in a cohort of 4,023 patients who underwent solid organ transplant from 2004 to 2011. Their median age at the time of transplant was 53 years; most (59%) received a kidney. Other organs transplanted were liver (22%), heart and/or lung (15%), and other organs (4%). The median follow-up time was 3.4 years; the longest follow-up was 5.5 years.
Only 17 of patients had a history of melanoma, and 19 patients a history of SCC – less than 1% for each skin cancer. Seven percent (301) of patients had experienced some form of nonskin cancer.
By the end of follow-up, 341 BCCs had developed among 175 patients – an incidence of 6.7%. About half developed more than one BCC.
The researchers compared these patients to a group of almost 200,000 nontransplant patients who had developed BCC. Among these, the median age at BCC appearance was significantly older (71 years); 39% had more than one lesion.
The overall relative risk of BCC was increased sixfold in transplant recipients and was similar between the genders. However, the risk varied according to the type of organ received. Kidney recipients were at the highest risk (relative risk, 7.2), and those who received other organs had a lower risk (heart/lung: RR, 5.8; liver: RR, 2.6).
The risk also appeared to increase over time, the authors noted. From 0 to 2 years, it was 5.8; from 3 to 5 years, it increased to 7.0.
Among men, 54% of lesions appeared in the head/neck area and 35% on the trunk – a similar distribution to that seen in the nontransplant control group. Among women, there were differences between transplant patients and controls: 44% of lesions appeared on patients’ head/neck, compared with 60% in the control group, and 34% appeared on the truck, compared with 24% in the control group.
Histology was similar, as were the proportions of aggressive type II and highly aggressive type III lesions.
A total of 199 SCCs developed among 87 patients during follow-up, a ratio to BCC of 1:1.7. “The low ratio was probably due to the short follow-up in our study,” the authors noted.
The Welander Foundation, the Westerberg Foundation, and the Strategic Research Program in Epidemiology at Karolinska Institute sponsored the study. None of the authors had any financial declarations.
Recipients of a solid organ transplant face up to a sixfold increase in the risk of developing a basal cell carcinoma – a risk that seems to increase as time passes.
A pretransplant history of squamous cell carcinoma (SCC) increased this risk to 55 times that seen in the general population, Dr. Britta Krynitz and her colleagues reported (Br J Dermatol. 2015. doi: 10.1111/bjd.14153).
But even when the pretransplant SCC group was removed from the final analysis, the risk of basal cell carcinoma after transplant was five times that of the general population, “indicating that a pretransplant SCC has limited effect on BCC risk overall and that organ transplantation per se is a strong driver of posttransplant BCC risk,” wrote Dr. Krynitz of Karolinska Institute, Stockholm, and her coauthors.
“Our results strongly suggest tumor promoter effects of the immunosuppressive drugs in the pathogenesis of post-transplantation BCC,” the team said. “We speculate that calcineurin inhibitors and also antiproliferative drugs, often used in combination with corticosteroids, play a role.”
The researchers investigated the incidence of both BCC and SCC in a cohort of 4,023 patients who underwent solid organ transplant from 2004 to 2011. Their median age at the time of transplant was 53 years; most (59%) received a kidney. Other organs transplanted were liver (22%), heart and/or lung (15%), and other organs (4%). The median follow-up time was 3.4 years; the longest follow-up was 5.5 years.
Only 17 of patients had a history of melanoma, and 19 patients a history of SCC – less than 1% for each skin cancer. Seven percent (301) of patients had experienced some form of nonskin cancer.
By the end of follow-up, 341 BCCs had developed among 175 patients – an incidence of 6.7%. About half developed more than one BCC.
The researchers compared these patients to a group of almost 200,000 nontransplant patients who had developed BCC. Among these, the median age at BCC appearance was significantly older (71 years); 39% had more than one lesion.
The overall relative risk of BCC was increased sixfold in transplant recipients and was similar between the genders. However, the risk varied according to the type of organ received. Kidney recipients were at the highest risk (relative risk, 7.2), and those who received other organs had a lower risk (heart/lung: RR, 5.8; liver: RR, 2.6).
The risk also appeared to increase over time, the authors noted. From 0 to 2 years, it was 5.8; from 3 to 5 years, it increased to 7.0.
Among men, 54% of lesions appeared in the head/neck area and 35% on the trunk – a similar distribution to that seen in the nontransplant control group. Among women, there were differences between transplant patients and controls: 44% of lesions appeared on patients’ head/neck, compared with 60% in the control group, and 34% appeared on the truck, compared with 24% in the control group.
Histology was similar, as were the proportions of aggressive type II and highly aggressive type III lesions.
A total of 199 SCCs developed among 87 patients during follow-up, a ratio to BCC of 1:1.7. “The low ratio was probably due to the short follow-up in our study,” the authors noted.
The Welander Foundation, the Westerberg Foundation, and the Strategic Research Program in Epidemiology at Karolinska Institute sponsored the study. None of the authors had any financial declarations.
FROM BRITISH JOURNAL OF DERMATOLOGY
Key clinical point: The risk of a basal cell carcinoma increases after solid organ transplant.
Major finding: Transplant patients have a sixfold increased risk of BCC.
Data source: A retrospective database study of 4,000 transplant patients and almost 200,000 controls.
Disclosures: The Welander Foundation, the Westerberg Foundation, and the Strategic Research Program in Epidemiology at Karolinska Institute sponsored the study. None of the authors had any financial declarations.
Finding more transplant hearts but not more donors
Heart transplant volumes in the United States have remained static since the start of the century because of improved trauma prevention and treatment, but that has challenged cardiologists to find enough donor hearts for the growing ranks of advanced heart failure patients. So a multidisciplinary team at the University of Washington in Seattle initiated a quality improvement program that doubled transplant volume without any change in transplant-related deaths by accepting hearts they would have otherwise discarded.
The study came about after the researchers determined that a large number of donor hearts from their own organ procurement program were being sent to other transplant centers. So they gathered a multidisciplinary team of transplant surgeons, cardiologists, and members of the organ procurement program to study ways to improve its center-specific organ utilization rate. The endeavor resulted in an increase in utilization rates from 28% to 49% in a year, a rate that has been sustained through a second year, according to study findings published in the January issue of the Journal of Thoracic and Cardiovascular Surgery (2016;151:238-43).
“The simple process of systematically reviewing donor turn down events as a group tended to reduce variability [and] increase confidence in expanded criteria donors and resulted in improved donor organ utilization and transplant volumes,” lead author Dr. Jason Smith and colleagues said.
The 30-day and 1-year death rates were similar before and after the quality improvement program started, but the death rates of those on the heart wait list declined from 17.2% to 12%, “which was not statistically significant,” Dr. Smith and coauthors said, “but does show that increasing use of organs that may be outside of the usual pattern has a trend toward improved wait list survival and needs to be considered when assessing donor hearts.”
Because of excellent results of heart transplants in patients with advanced heart failure, a number of investigators have proposed expanding the population of heart donors to include older people, those with higher risk of infectious disease, or with heart disease such as coronary artery disease and left ventricular hypertrophy, Dr. Smith and coauthors said. Their own review found a higher-than-expected rate of donor hearts sent to other centers from the University of Washington organ procurement program.
The multidisciplinary team analyzed the organs the University of Washington surgeons refused and sent to other institutions from July 2012 to June 2013.
For a year after that, the multidisciplinary group did real-time analysis of organ refusal along with quarterly reviews “in a non-confrontational, proactive” setting, as Dr. Smith and his colleagues described it. The group held open discussions on refused organs that were ultimately transplanted elsewhere. “The review process was facilitated to provide a constructive environment to encourage development of best practices and consistency,” the researchers noted. The quality improvement program led to an increase in the unit’s transplant volume despite fewer donor offers.
The researchers acknowledged that donor assessment has been the focus of much controversy. They pointed out that average donor age has increased over the last 20 years from 29 years to 33 years and has since retreated to 31 years, and some programs utilize donors up to their mid-60s. Also, previous studies have advocated for the use of donors who meet the criteria of the Centers for Disease Control and Prevention high risk behavior of infection as well as some drug abusers because of the low-risk of transmission and emerging evidence affirming the safety of hearts of drug users.
“The individual decision to utilize or discard a donor organ is one of the most challenging aspects of transplant medicine,” Dr. Smith and colleagues said. “It requires balancing donor risks against the exigencies of the recipient.”
Today, the multidisciplinary team evaluates each heart offered for donation and is exploring ways to accept even more donor hearts, even discarded hearts. “This represents a large, untapped pool of potential donor hearts that might add to the net number of transplants performed nationally and not merely redistribute organ usage,” Dr. Smith and colleagues said.
Dr. Smith is a consultant for Thoratec and is a primary site investigator for the EXPAND Trial sponsored by TransMedics. Dr. Todd Dardas is supported by the American College of Cardiology/Daiichi Sankyo Career Development Award. Dr. Jay Pal receives grant support from Tenax. Dr. Wayne Levy is a consultant for HeartWare, Novartis, GE Healthcare, Pharmin, and Biotronik. Dr. Claudius Mahr is a consultant for Thoratec, HeartWare and Abiomed. Dr. Nahush Mokadam is a consultant for Thoratec, HeartWare, Syncardia and St. Jude Medical, and has research grants from Thoratec, HeartWare and Syncardia. The other coauthors had no relationships to disclose.
How the University of Washington researchers brought about such a dramatic increase in donor heart utilization raises a number of questions, Dr. Nicholas Smedira of Cleveland Clinic said in his invited commentary (J Thorac Cardiovasc Surg 2016;151:243-4).
“They refer euphemistically to ‘behavioral adaptation’ and ‘frank discussions’ regarding ‘individual and group bias’ as explanations, but understanding exactly how this is accomplished is not easy,” Dr. Smedira said.
Noteworthy is that the researchers used more donors who meet Center for Disease Control and Prevention high risk criteria for infectious disease. However, cardiologists tend to weigh their decision for accepting donor hearts “by the last memorable or distressful experience,” Dr. Smedira said. Hence, many of these donor hearts go unused. At the same time, assessing risk without complete information is challenging, he said.
Besides their thought processes, other factors that influence cardiologists’ decisions on accepting donor hearts include fatigue, scheduling conflicts, reimbursement issues, and outcome metrics. He credited the University of Washington for its “courage” to examine their decision-making process, including exploring biases as well as working “collectively and blamelessly” to support their decisions. “I would encourage more transplant centers to follow a program similar to the University of Washington’s and maybe we will be hearing more yeses and fewer nos,” Dr. Smedira said.
He had no relationships to disclose.
How the University of Washington researchers brought about such a dramatic increase in donor heart utilization raises a number of questions, Dr. Nicholas Smedira of Cleveland Clinic said in his invited commentary (J Thorac Cardiovasc Surg 2016;151:243-4).
“They refer euphemistically to ‘behavioral adaptation’ and ‘frank discussions’ regarding ‘individual and group bias’ as explanations, but understanding exactly how this is accomplished is not easy,” Dr. Smedira said.
Noteworthy is that the researchers used more donors who meet Center for Disease Control and Prevention high risk criteria for infectious disease. However, cardiologists tend to weigh their decision for accepting donor hearts “by the last memorable or distressful experience,” Dr. Smedira said. Hence, many of these donor hearts go unused. At the same time, assessing risk without complete information is challenging, he said.
Besides their thought processes, other factors that influence cardiologists’ decisions on accepting donor hearts include fatigue, scheduling conflicts, reimbursement issues, and outcome metrics. He credited the University of Washington for its “courage” to examine their decision-making process, including exploring biases as well as working “collectively and blamelessly” to support their decisions. “I would encourage more transplant centers to follow a program similar to the University of Washington’s and maybe we will be hearing more yeses and fewer nos,” Dr. Smedira said.
He had no relationships to disclose.
How the University of Washington researchers brought about such a dramatic increase in donor heart utilization raises a number of questions, Dr. Nicholas Smedira of Cleveland Clinic said in his invited commentary (J Thorac Cardiovasc Surg 2016;151:243-4).
“They refer euphemistically to ‘behavioral adaptation’ and ‘frank discussions’ regarding ‘individual and group bias’ as explanations, but understanding exactly how this is accomplished is not easy,” Dr. Smedira said.
Noteworthy is that the researchers used more donors who meet Center for Disease Control and Prevention high risk criteria for infectious disease. However, cardiologists tend to weigh their decision for accepting donor hearts “by the last memorable or distressful experience,” Dr. Smedira said. Hence, many of these donor hearts go unused. At the same time, assessing risk without complete information is challenging, he said.
Besides their thought processes, other factors that influence cardiologists’ decisions on accepting donor hearts include fatigue, scheduling conflicts, reimbursement issues, and outcome metrics. He credited the University of Washington for its “courage” to examine their decision-making process, including exploring biases as well as working “collectively and blamelessly” to support their decisions. “I would encourage more transplant centers to follow a program similar to the University of Washington’s and maybe we will be hearing more yeses and fewer nos,” Dr. Smedira said.
He had no relationships to disclose.
Heart transplant volumes in the United States have remained static since the start of the century because of improved trauma prevention and treatment, but that has challenged cardiologists to find enough donor hearts for the growing ranks of advanced heart failure patients. So a multidisciplinary team at the University of Washington in Seattle initiated a quality improvement program that doubled transplant volume without any change in transplant-related deaths by accepting hearts they would have otherwise discarded.
The study came about after the researchers determined that a large number of donor hearts from their own organ procurement program were being sent to other transplant centers. So they gathered a multidisciplinary team of transplant surgeons, cardiologists, and members of the organ procurement program to study ways to improve its center-specific organ utilization rate. The endeavor resulted in an increase in utilization rates from 28% to 49% in a year, a rate that has been sustained through a second year, according to study findings published in the January issue of the Journal of Thoracic and Cardiovascular Surgery (2016;151:238-43).
“The simple process of systematically reviewing donor turn down events as a group tended to reduce variability [and] increase confidence in expanded criteria donors and resulted in improved donor organ utilization and transplant volumes,” lead author Dr. Jason Smith and colleagues said.
The 30-day and 1-year death rates were similar before and after the quality improvement program started, but the death rates of those on the heart wait list declined from 17.2% to 12%, “which was not statistically significant,” Dr. Smith and coauthors said, “but does show that increasing use of organs that may be outside of the usual pattern has a trend toward improved wait list survival and needs to be considered when assessing donor hearts.”
Because of excellent results of heart transplants in patients with advanced heart failure, a number of investigators have proposed expanding the population of heart donors to include older people, those with higher risk of infectious disease, or with heart disease such as coronary artery disease and left ventricular hypertrophy, Dr. Smith and coauthors said. Their own review found a higher-than-expected rate of donor hearts sent to other centers from the University of Washington organ procurement program.
The multidisciplinary team analyzed the organs the University of Washington surgeons refused and sent to other institutions from July 2012 to June 2013.
For a year after that, the multidisciplinary group did real-time analysis of organ refusal along with quarterly reviews “in a non-confrontational, proactive” setting, as Dr. Smith and his colleagues described it. The group held open discussions on refused organs that were ultimately transplanted elsewhere. “The review process was facilitated to provide a constructive environment to encourage development of best practices and consistency,” the researchers noted. The quality improvement program led to an increase in the unit’s transplant volume despite fewer donor offers.
The researchers acknowledged that donor assessment has been the focus of much controversy. They pointed out that average donor age has increased over the last 20 years from 29 years to 33 years and has since retreated to 31 years, and some programs utilize donors up to their mid-60s. Also, previous studies have advocated for the use of donors who meet the criteria of the Centers for Disease Control and Prevention high risk behavior of infection as well as some drug abusers because of the low-risk of transmission and emerging evidence affirming the safety of hearts of drug users.
“The individual decision to utilize or discard a donor organ is one of the most challenging aspects of transplant medicine,” Dr. Smith and colleagues said. “It requires balancing donor risks against the exigencies of the recipient.”
Today, the multidisciplinary team evaluates each heart offered for donation and is exploring ways to accept even more donor hearts, even discarded hearts. “This represents a large, untapped pool of potential donor hearts that might add to the net number of transplants performed nationally and not merely redistribute organ usage,” Dr. Smith and colleagues said.
Dr. Smith is a consultant for Thoratec and is a primary site investigator for the EXPAND Trial sponsored by TransMedics. Dr. Todd Dardas is supported by the American College of Cardiology/Daiichi Sankyo Career Development Award. Dr. Jay Pal receives grant support from Tenax. Dr. Wayne Levy is a consultant for HeartWare, Novartis, GE Healthcare, Pharmin, and Biotronik. Dr. Claudius Mahr is a consultant for Thoratec, HeartWare and Abiomed. Dr. Nahush Mokadam is a consultant for Thoratec, HeartWare, Syncardia and St. Jude Medical, and has research grants from Thoratec, HeartWare and Syncardia. The other coauthors had no relationships to disclose.
Heart transplant volumes in the United States have remained static since the start of the century because of improved trauma prevention and treatment, but that has challenged cardiologists to find enough donor hearts for the growing ranks of advanced heart failure patients. So a multidisciplinary team at the University of Washington in Seattle initiated a quality improvement program that doubled transplant volume without any change in transplant-related deaths by accepting hearts they would have otherwise discarded.
The study came about after the researchers determined that a large number of donor hearts from their own organ procurement program were being sent to other transplant centers. So they gathered a multidisciplinary team of transplant surgeons, cardiologists, and members of the organ procurement program to study ways to improve its center-specific organ utilization rate. The endeavor resulted in an increase in utilization rates from 28% to 49% in a year, a rate that has been sustained through a second year, according to study findings published in the January issue of the Journal of Thoracic and Cardiovascular Surgery (2016;151:238-43).
“The simple process of systematically reviewing donor turn down events as a group tended to reduce variability [and] increase confidence in expanded criteria donors and resulted in improved donor organ utilization and transplant volumes,” lead author Dr. Jason Smith and colleagues said.
The 30-day and 1-year death rates were similar before and after the quality improvement program started, but the death rates of those on the heart wait list declined from 17.2% to 12%, “which was not statistically significant,” Dr. Smith and coauthors said, “but does show that increasing use of organs that may be outside of the usual pattern has a trend toward improved wait list survival and needs to be considered when assessing donor hearts.”
Because of excellent results of heart transplants in patients with advanced heart failure, a number of investigators have proposed expanding the population of heart donors to include older people, those with higher risk of infectious disease, or with heart disease such as coronary artery disease and left ventricular hypertrophy, Dr. Smith and coauthors said. Their own review found a higher-than-expected rate of donor hearts sent to other centers from the University of Washington organ procurement program.
The multidisciplinary team analyzed the organs the University of Washington surgeons refused and sent to other institutions from July 2012 to June 2013.
For a year after that, the multidisciplinary group did real-time analysis of organ refusal along with quarterly reviews “in a non-confrontational, proactive” setting, as Dr. Smith and his colleagues described it. The group held open discussions on refused organs that were ultimately transplanted elsewhere. “The review process was facilitated to provide a constructive environment to encourage development of best practices and consistency,” the researchers noted. The quality improvement program led to an increase in the unit’s transplant volume despite fewer donor offers.
The researchers acknowledged that donor assessment has been the focus of much controversy. They pointed out that average donor age has increased over the last 20 years from 29 years to 33 years and has since retreated to 31 years, and some programs utilize donors up to their mid-60s. Also, previous studies have advocated for the use of donors who meet the criteria of the Centers for Disease Control and Prevention high risk behavior of infection as well as some drug abusers because of the low-risk of transmission and emerging evidence affirming the safety of hearts of drug users.
“The individual decision to utilize or discard a donor organ is one of the most challenging aspects of transplant medicine,” Dr. Smith and colleagues said. “It requires balancing donor risks against the exigencies of the recipient.”
Today, the multidisciplinary team evaluates each heart offered for donation and is exploring ways to accept even more donor hearts, even discarded hearts. “This represents a large, untapped pool of potential donor hearts that might add to the net number of transplants performed nationally and not merely redistribute organ usage,” Dr. Smith and colleagues said.
Dr. Smith is a consultant for Thoratec and is a primary site investigator for the EXPAND Trial sponsored by TransMedics. Dr. Todd Dardas is supported by the American College of Cardiology/Daiichi Sankyo Career Development Award. Dr. Jay Pal receives grant support from Tenax. Dr. Wayne Levy is a consultant for HeartWare, Novartis, GE Healthcare, Pharmin, and Biotronik. Dr. Claudius Mahr is a consultant for Thoratec, HeartWare and Abiomed. Dr. Nahush Mokadam is a consultant for Thoratec, HeartWare, Syncardia and St. Jude Medical, and has research grants from Thoratec, HeartWare and Syncardia. The other coauthors had no relationships to disclose.
Key clinical point: A group approach to systematically review rejected donor organs has led to expanded donor criteria and resulted in improved donor organ utilization and transplant volume.
Major finding: Transplant utilization rate increased from 28% to 49% with no significant change in 30-day survival after implementation of a donor review protocol.
Data source: Retrospective review of 293 total donor heart offers at a single center from July 2012 to June 2013 compared with review of 279 heart offers from July 2013 to June 2014.
Disclosures: Lead author Dr. Jason Smith is a consultant for Thoratec and is a primary site investigator for the EXPAND Trial sponsored by TransMedics. Dr. Todd Dardas is supported by the American College of Cardiology/Daiichi Sankyo Career Development Award. Dr. Jay Pal receives grant support from Tenax. Dr. Wayne Levy is a consultant for HeartWare, Novartis, GE Healthcare, Pharmin, and Biotronik. Dr. Claudius Mahr is a consultant for Thoratec, HeartWare and Abiomed. Dr. Nahush Mokadam is a consultant for Thoratec, HeartWare, Syncardia, and St. Jude Medical, and has research grants from Thoratec, HeartWare and Syncardia. The other coauthors had no relationships to disclose.