User login
Obesity blunts TNFi response in axial spondyloarthritis
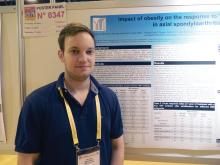
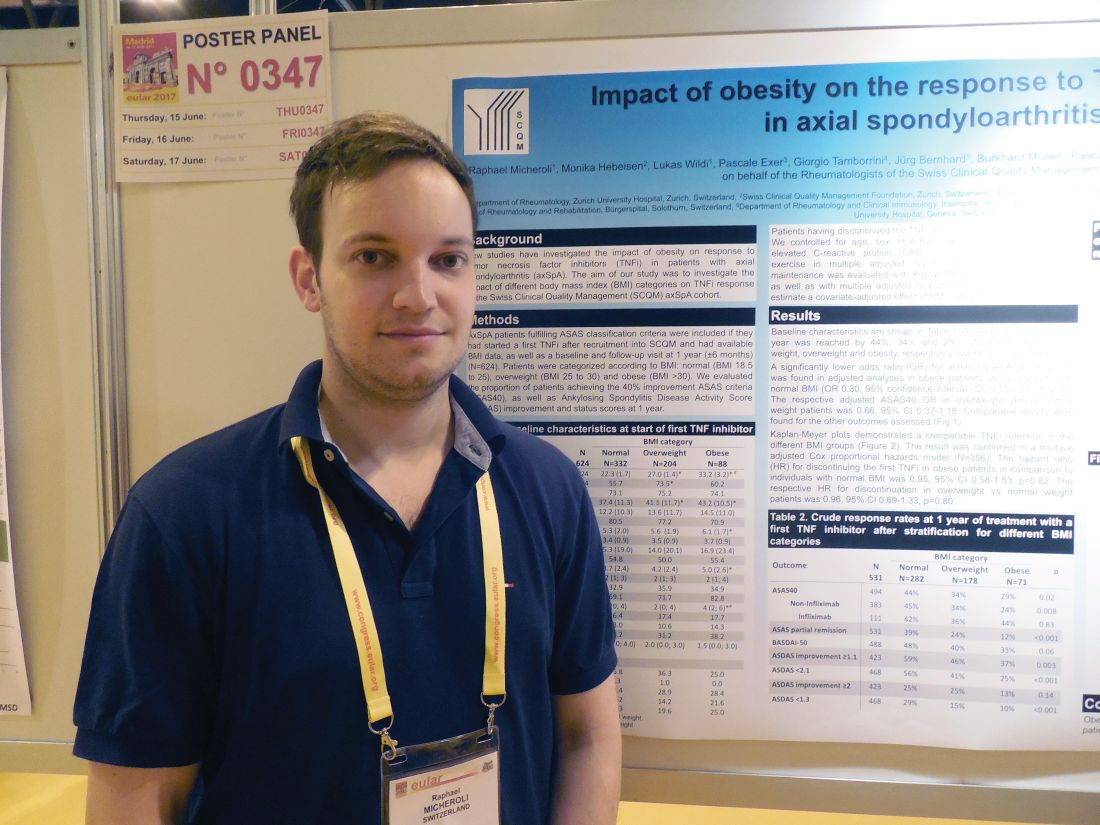
MADRID – Obese patients with axial spondyloarthritis were substantially less responsive to treatment with a tumor necrosis factor inhibitor than were healthy-weight patients in a multicenter Swiss study with 531 patients.
In a multivariate analysis that controlled for several demographic and clinical factors, including baseline disease severity, obese patients with axial spondyloarthritis (SpA) were 70% less likely to achieve a 40% or better improvement in their Assessment in SpondyloArthritis International Society improvement criteria (ASAS 40) when compared with patients with a healthy body mass index (BMI), Raphael Micheroli, MD, reported in a poster at the European Congress of Rheumatology.
The finding supplies a third reason why patients with newly diagnosed axial SpA should try to lose weight if they are obese (or overweight) – to potentially improve their responsiveness to a TNFi. The other two reasons are to reduce cardiovascular disease risk in patients who are already at risk for these complications because of their disease, and to also help improve their ability to perform physical activities, he explained in an interview.
Dr. Micheroli proposed three possible reasons why obese patients with axial SpA might be less responsive to a TNFi than healthy-weight patients: They receive an inadequate TNFi dosage, their increased adipose tissue produces excess proinflammatory cytokines that exacerbate their axial SpA, or it is possible that obese patients are more likely to be misdiagnosed with axial SpA and because they don’t really have this disease their symptoms cannot improve with TNFi treatment. They may instead have, for example, degenerative back pain, a condition that can be challenging to distinguish from axial SpA, he said.
A role for obesity in blunting the beneficial effects of TNFi treatment has been well described for psoriatic arthritis, for example, in an Italian study with 138 patients (Ann Rheum Dis. 2014 June;73[6]:1157-62), and in a Danish study with more than 1,200 patients (Rheumatology [Oxford]. 2016 Dec;55[12]:2191-9).
Dr. Micheroli’s study included 624 patients with axial SpA enrolled in the Swiss Clinical Quality Management in Rheumatic Diseases axial spondyloarthritis cohort who met the ASAS classification criteria for axial SpA and started treatment with their first TNFi after they entered the cohort. Follow-up data after 1 year on treatment were available for 531 of these patients. The entry group included 332 patients (53%) with a healthy BMI, 204 (33%) with an overweight BMI (25-30 kg/m2), and 88 (14%) obese patients (BMI more than 30 kg/m2). The patients averaged about 40 years old and had been symptomatic for an average of about 13 years. About one-third of patients started on adalimumab (Humira) treatment, about one-quarter started etanercept (Enbrel), more than one-fifth began infliximab (Remicade), and some patients started treatment with either golimumab (Simponi) or certolizumab pegol (Cimzia).
After 1 year on TNFi treatment, ASAS 40 improvement occurred in 44% of 282 healthy-BMI patients, 34% of 178 overweight patients, and in 29% of 71 obese patients, Dr. Micheroli reported. In a baseline-adjusted multivariate model, this difference translated into an odds ratio of 0.30 for obese patients achieving an ASAS 40 response, compared with the healthy-BMI patients after 1 year, a statistically significant difference. Further analysis showed no statistically significant differences in TNFi discontinuation rates among the three BMI subgroups.
Dr. Micheroli had no disclosures.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
MADRID – Obese patients with axial spondyloarthritis were substantially less responsive to treatment with a tumor necrosis factor inhibitor than were healthy-weight patients in a multicenter Swiss study with 531 patients.
In a multivariate analysis that controlled for several demographic and clinical factors, including baseline disease severity, obese patients with axial spondyloarthritis (SpA) were 70% less likely to achieve a 40% or better improvement in their Assessment in SpondyloArthritis International Society improvement criteria (ASAS 40) when compared with patients with a healthy body mass index (BMI), Raphael Micheroli, MD, reported in a poster at the European Congress of Rheumatology.
The finding supplies a third reason why patients with newly diagnosed axial SpA should try to lose weight if they are obese (or overweight) – to potentially improve their responsiveness to a TNFi. The other two reasons are to reduce cardiovascular disease risk in patients who are already at risk for these complications because of their disease, and to also help improve their ability to perform physical activities, he explained in an interview.
Dr. Micheroli proposed three possible reasons why obese patients with axial SpA might be less responsive to a TNFi than healthy-weight patients: They receive an inadequate TNFi dosage, their increased adipose tissue produces excess proinflammatory cytokines that exacerbate their axial SpA, or it is possible that obese patients are more likely to be misdiagnosed with axial SpA and because they don’t really have this disease their symptoms cannot improve with TNFi treatment. They may instead have, for example, degenerative back pain, a condition that can be challenging to distinguish from axial SpA, he said.
A role for obesity in blunting the beneficial effects of TNFi treatment has been well described for psoriatic arthritis, for example, in an Italian study with 138 patients (Ann Rheum Dis. 2014 June;73[6]:1157-62), and in a Danish study with more than 1,200 patients (Rheumatology [Oxford]. 2016 Dec;55[12]:2191-9).
Dr. Micheroli’s study included 624 patients with axial SpA enrolled in the Swiss Clinical Quality Management in Rheumatic Diseases axial spondyloarthritis cohort who met the ASAS classification criteria for axial SpA and started treatment with their first TNFi after they entered the cohort. Follow-up data after 1 year on treatment were available for 531 of these patients. The entry group included 332 patients (53%) with a healthy BMI, 204 (33%) with an overweight BMI (25-30 kg/m2), and 88 (14%) obese patients (BMI more than 30 kg/m2). The patients averaged about 40 years old and had been symptomatic for an average of about 13 years. About one-third of patients started on adalimumab (Humira) treatment, about one-quarter started etanercept (Enbrel), more than one-fifth began infliximab (Remicade), and some patients started treatment with either golimumab (Simponi) or certolizumab pegol (Cimzia).
After 1 year on TNFi treatment, ASAS 40 improvement occurred in 44% of 282 healthy-BMI patients, 34% of 178 overweight patients, and in 29% of 71 obese patients, Dr. Micheroli reported. In a baseline-adjusted multivariate model, this difference translated into an odds ratio of 0.30 for obese patients achieving an ASAS 40 response, compared with the healthy-BMI patients after 1 year, a statistically significant difference. Further analysis showed no statistically significant differences in TNFi discontinuation rates among the three BMI subgroups.
Dr. Micheroli had no disclosures.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
MADRID – Obese patients with axial spondyloarthritis were substantially less responsive to treatment with a tumor necrosis factor inhibitor than were healthy-weight patients in a multicenter Swiss study with 531 patients.
In a multivariate analysis that controlled for several demographic and clinical factors, including baseline disease severity, obese patients with axial spondyloarthritis (SpA) were 70% less likely to achieve a 40% or better improvement in their Assessment in SpondyloArthritis International Society improvement criteria (ASAS 40) when compared with patients with a healthy body mass index (BMI), Raphael Micheroli, MD, reported in a poster at the European Congress of Rheumatology.
The finding supplies a third reason why patients with newly diagnosed axial SpA should try to lose weight if they are obese (or overweight) – to potentially improve their responsiveness to a TNFi. The other two reasons are to reduce cardiovascular disease risk in patients who are already at risk for these complications because of their disease, and to also help improve their ability to perform physical activities, he explained in an interview.
Dr. Micheroli proposed three possible reasons why obese patients with axial SpA might be less responsive to a TNFi than healthy-weight patients: They receive an inadequate TNFi dosage, their increased adipose tissue produces excess proinflammatory cytokines that exacerbate their axial SpA, or it is possible that obese patients are more likely to be misdiagnosed with axial SpA and because they don’t really have this disease their symptoms cannot improve with TNFi treatment. They may instead have, for example, degenerative back pain, a condition that can be challenging to distinguish from axial SpA, he said.
A role for obesity in blunting the beneficial effects of TNFi treatment has been well described for psoriatic arthritis, for example, in an Italian study with 138 patients (Ann Rheum Dis. 2014 June;73[6]:1157-62), and in a Danish study with more than 1,200 patients (Rheumatology [Oxford]. 2016 Dec;55[12]:2191-9).
Dr. Micheroli’s study included 624 patients with axial SpA enrolled in the Swiss Clinical Quality Management in Rheumatic Diseases axial spondyloarthritis cohort who met the ASAS classification criteria for axial SpA and started treatment with their first TNFi after they entered the cohort. Follow-up data after 1 year on treatment were available for 531 of these patients. The entry group included 332 patients (53%) with a healthy BMI, 204 (33%) with an overweight BMI (25-30 kg/m2), and 88 (14%) obese patients (BMI more than 30 kg/m2). The patients averaged about 40 years old and had been symptomatic for an average of about 13 years. About one-third of patients started on adalimumab (Humira) treatment, about one-quarter started etanercept (Enbrel), more than one-fifth began infliximab (Remicade), and some patients started treatment with either golimumab (Simponi) or certolizumab pegol (Cimzia).
After 1 year on TNFi treatment, ASAS 40 improvement occurred in 44% of 282 healthy-BMI patients, 34% of 178 overweight patients, and in 29% of 71 obese patients, Dr. Micheroli reported. In a baseline-adjusted multivariate model, this difference translated into an odds ratio of 0.30 for obese patients achieving an ASAS 40 response, compared with the healthy-BMI patients after 1 year, a statistically significant difference. Further analysis showed no statistically significant differences in TNFi discontinuation rates among the three BMI subgroups.
Dr. Micheroli had no disclosures.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
AT THE EULAR 2017 CONGRESS
Key clinical point:
Major finding: Obese patients had a 70% lower response rate to a tumor necrosis factor inhibitor, compared with healthy-weight patients.
Data source: A cohort of 531 axial spondyloarthritis patients enrolled in the Swiss Clinical Quality Management in Rheumatic Diseases program.
Disclosures: Dr. Micheroli had no disclosures.
Panel revises spondyloarthritis treat-to-target recommendations
MADRID – The newly revised recommendations from an unaffiliated, international expert panel on a treat-to-target approach for axial spondyloarthritis and psoriatic arthritis has one conspicuous feature that the prior recommendations lacked: evidence.
The first treat-to-target recommendations for spondyloarthritis (SpA) and psoriatic arthritis (PsA) from 2013 were based entirely on expert opinion (Ann Rheum Dis. 2014 Jan;73[1]:6-16), but in the new update 4 of the 11 recommendations now have an evidence base as well as a fifth recommendation for the part that pertains to PsA, Désirée van der Heijde, MD, said at the European Congress of Rheumatology.
Among the evidence-based recommendations, the most striking was a new formulation for how to measure disease activity. The new recommendations call the ASDAS (Ankylosing Spondylitis Disease Activity Score) the “preferred” disease activity measure for patients with axial SpA and cite both the DAPSA (Disease Activity Index for Psoriatic Arthritis) as well as minimal disease activity as “considered to define the target” when treating PsA.
“This recommendation just made it,” squeaking onto the list with a 52% vote of approval from the task force members, said Dr. van der Heijde. “It had the longest discussion,” with a significant minority of panelists taking a different view.
ASDAS shook out as the preferred measure for axial SpA because of evidence linking a patient’s ASDAS with syndesmophyte formation. “The idea is that by targeting ASDAS you should have better outcomes,” she explained.
“Applying a treat-to-target approach in axial SpA is feasible but requires systematic collection of outcome parameters in daily practice,” such as ASDAS, said Dr. Dougados, professor of rheumatology at Cochin Hospital in Paris. Another piece currently lacking in the case for treat-to-target is demonstration of the clinical benefit from this approach in a trial, he added.
According to Dr. van der Heijde, the other four recommendations that now have evidence backup are:
- Define clinical remission or minimal disease as the absence of clinical and laboratory evidence of significant disease activity.
- An alternative treatment target for PsA may be low or minimal disease activity.
- Measure disease activity by clinical signs and symptoms and by acute phase reactants.
- Once a treatment target is reached it should be maintained.
The task force also outlined “an extensive research agenda” where evidence is needed, specifying close to 50 individual research topics. Among them Dr. van der Heijde particularly called out the role of the Health Assessment Questionnaire (HAQ), validation of PsA target outcomes, and better parsing of the differences using remission or low disease activity as the treatment target.
Dr. van der Heijde, Dr. Dougados, and Dr. Braun are all consultants for several drug companies.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
The evidence we now have is the difference between the new recommendations and the prior version. We have evidence from trials in patients with psoriatic arthritis using minimal disease activity as a target. And we have indirect evidence from observational studies in patients with SpA that suggest the higher the ASDAS, the more progression occurs. In addition, results reported at the EULAR 2017 Congress showed that reductions in the ASDAS appeared to correlate with the effect of a tumor necrosis factor inhibitor on reduced radiographic progression in patients with ankylosing spondylitis. But this is just an association; data from a randomized, prospective trial should be available next year.
The recommendations say to manage patients with axial SpA or psoriatic arthritis by treating them to a target. To do that a clinician needs a standardized assessment of a patient’s disease and to perform follow-up measurements to see if the target is met. The data Dr. Dougados cited from Paris document that assessments such as an ASDAS are rarely made. Getting an ASDAS means knowing either a patient’s C-reactive protein level or erythrocyte sedimentation rate. That requires blood work before a clinic visit, something patients often don’t want.
Will these recommendations change practice and make the ASDAS more widely used? That depends to some extent on whether any benefits or penalties linked to ASDAS use go into place.
Next year, we expect to see results from trials that are testing whether the treat-to-target approach produces better outcomes. Evidence like that will be important to further spur adoption.
Lianne S. Gensler, MD , is director of the ankylosing spondylitis clinic at the University of California, San Francisco. She has been a consultant to Novartis and Janssen and has received research support from AbbVie and UCB. Dr. Gensler was a member of the task force that issued the revised recommendations. She made these comments in an interview.
The evidence we now have is the difference between the new recommendations and the prior version. We have evidence from trials in patients with psoriatic arthritis using minimal disease activity as a target. And we have indirect evidence from observational studies in patients with SpA that suggest the higher the ASDAS, the more progression occurs. In addition, results reported at the EULAR 2017 Congress showed that reductions in the ASDAS appeared to correlate with the effect of a tumor necrosis factor inhibitor on reduced radiographic progression in patients with ankylosing spondylitis. But this is just an association; data from a randomized, prospective trial should be available next year.
The recommendations say to manage patients with axial SpA or psoriatic arthritis by treating them to a target. To do that a clinician needs a standardized assessment of a patient’s disease and to perform follow-up measurements to see if the target is met. The data Dr. Dougados cited from Paris document that assessments such as an ASDAS are rarely made. Getting an ASDAS means knowing either a patient’s C-reactive protein level or erythrocyte sedimentation rate. That requires blood work before a clinic visit, something patients often don’t want.
Will these recommendations change practice and make the ASDAS more widely used? That depends to some extent on whether any benefits or penalties linked to ASDAS use go into place.
Next year, we expect to see results from trials that are testing whether the treat-to-target approach produces better outcomes. Evidence like that will be important to further spur adoption.
Lianne S. Gensler, MD , is director of the ankylosing spondylitis clinic at the University of California, San Francisco. She has been a consultant to Novartis and Janssen and has received research support from AbbVie and UCB. Dr. Gensler was a member of the task force that issued the revised recommendations. She made these comments in an interview.
The evidence we now have is the difference between the new recommendations and the prior version. We have evidence from trials in patients with psoriatic arthritis using minimal disease activity as a target. And we have indirect evidence from observational studies in patients with SpA that suggest the higher the ASDAS, the more progression occurs. In addition, results reported at the EULAR 2017 Congress showed that reductions in the ASDAS appeared to correlate with the effect of a tumor necrosis factor inhibitor on reduced radiographic progression in patients with ankylosing spondylitis. But this is just an association; data from a randomized, prospective trial should be available next year.
The recommendations say to manage patients with axial SpA or psoriatic arthritis by treating them to a target. To do that a clinician needs a standardized assessment of a patient’s disease and to perform follow-up measurements to see if the target is met. The data Dr. Dougados cited from Paris document that assessments such as an ASDAS are rarely made. Getting an ASDAS means knowing either a patient’s C-reactive protein level or erythrocyte sedimentation rate. That requires blood work before a clinic visit, something patients often don’t want.
Will these recommendations change practice and make the ASDAS more widely used? That depends to some extent on whether any benefits or penalties linked to ASDAS use go into place.
Next year, we expect to see results from trials that are testing whether the treat-to-target approach produces better outcomes. Evidence like that will be important to further spur adoption.
Lianne S. Gensler, MD , is director of the ankylosing spondylitis clinic at the University of California, San Francisco. She has been a consultant to Novartis and Janssen and has received research support from AbbVie and UCB. Dr. Gensler was a member of the task force that issued the revised recommendations. She made these comments in an interview.
MADRID – The newly revised recommendations from an unaffiliated, international expert panel on a treat-to-target approach for axial spondyloarthritis and psoriatic arthritis has one conspicuous feature that the prior recommendations lacked: evidence.
The first treat-to-target recommendations for spondyloarthritis (SpA) and psoriatic arthritis (PsA) from 2013 were based entirely on expert opinion (Ann Rheum Dis. 2014 Jan;73[1]:6-16), but in the new update 4 of the 11 recommendations now have an evidence base as well as a fifth recommendation for the part that pertains to PsA, Désirée van der Heijde, MD, said at the European Congress of Rheumatology.
Among the evidence-based recommendations, the most striking was a new formulation for how to measure disease activity. The new recommendations call the ASDAS (Ankylosing Spondylitis Disease Activity Score) the “preferred” disease activity measure for patients with axial SpA and cite both the DAPSA (Disease Activity Index for Psoriatic Arthritis) as well as minimal disease activity as “considered to define the target” when treating PsA.
“This recommendation just made it,” squeaking onto the list with a 52% vote of approval from the task force members, said Dr. van der Heijde. “It had the longest discussion,” with a significant minority of panelists taking a different view.
ASDAS shook out as the preferred measure for axial SpA because of evidence linking a patient’s ASDAS with syndesmophyte formation. “The idea is that by targeting ASDAS you should have better outcomes,” she explained.
“Applying a treat-to-target approach in axial SpA is feasible but requires systematic collection of outcome parameters in daily practice,” such as ASDAS, said Dr. Dougados, professor of rheumatology at Cochin Hospital in Paris. Another piece currently lacking in the case for treat-to-target is demonstration of the clinical benefit from this approach in a trial, he added.
According to Dr. van der Heijde, the other four recommendations that now have evidence backup are:
- Define clinical remission or minimal disease as the absence of clinical and laboratory evidence of significant disease activity.
- An alternative treatment target for PsA may be low or minimal disease activity.
- Measure disease activity by clinical signs and symptoms and by acute phase reactants.
- Once a treatment target is reached it should be maintained.
The task force also outlined “an extensive research agenda” where evidence is needed, specifying close to 50 individual research topics. Among them Dr. van der Heijde particularly called out the role of the Health Assessment Questionnaire (HAQ), validation of PsA target outcomes, and better parsing of the differences using remission or low disease activity as the treatment target.
Dr. van der Heijde, Dr. Dougados, and Dr. Braun are all consultants for several drug companies.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
MADRID – The newly revised recommendations from an unaffiliated, international expert panel on a treat-to-target approach for axial spondyloarthritis and psoriatic arthritis has one conspicuous feature that the prior recommendations lacked: evidence.
The first treat-to-target recommendations for spondyloarthritis (SpA) and psoriatic arthritis (PsA) from 2013 were based entirely on expert opinion (Ann Rheum Dis. 2014 Jan;73[1]:6-16), but in the new update 4 of the 11 recommendations now have an evidence base as well as a fifth recommendation for the part that pertains to PsA, Désirée van der Heijde, MD, said at the European Congress of Rheumatology.
Among the evidence-based recommendations, the most striking was a new formulation for how to measure disease activity. The new recommendations call the ASDAS (Ankylosing Spondylitis Disease Activity Score) the “preferred” disease activity measure for patients with axial SpA and cite both the DAPSA (Disease Activity Index for Psoriatic Arthritis) as well as minimal disease activity as “considered to define the target” when treating PsA.
“This recommendation just made it,” squeaking onto the list with a 52% vote of approval from the task force members, said Dr. van der Heijde. “It had the longest discussion,” with a significant minority of panelists taking a different view.
ASDAS shook out as the preferred measure for axial SpA because of evidence linking a patient’s ASDAS with syndesmophyte formation. “The idea is that by targeting ASDAS you should have better outcomes,” she explained.
“Applying a treat-to-target approach in axial SpA is feasible but requires systematic collection of outcome parameters in daily practice,” such as ASDAS, said Dr. Dougados, professor of rheumatology at Cochin Hospital in Paris. Another piece currently lacking in the case for treat-to-target is demonstration of the clinical benefit from this approach in a trial, he added.
According to Dr. van der Heijde, the other four recommendations that now have evidence backup are:
- Define clinical remission or minimal disease as the absence of clinical and laboratory evidence of significant disease activity.
- An alternative treatment target for PsA may be low or minimal disease activity.
- Measure disease activity by clinical signs and symptoms and by acute phase reactants.
- Once a treatment target is reached it should be maintained.
The task force also outlined “an extensive research agenda” where evidence is needed, specifying close to 50 individual research topics. Among them Dr. van der Heijde particularly called out the role of the Health Assessment Questionnaire (HAQ), validation of PsA target outcomes, and better parsing of the differences using remission or low disease activity as the treatment target.
Dr. van der Heijde, Dr. Dougados, and Dr. Braun are all consultants for several drug companies.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
EXPERT ANALYSIS FROM THE EULAR 2017 CONGRESS
VIDEO: Rheumatology biosimilars gain U.S. momentum
MADRID – With biosimilar infliximab on the U.S. market since November 2016 and producing an immediate, albeit modest, price drop for this tumor necrosis factor inhibitor (TNFi) and a second biosimilar infliximab now approved by the Food and Drug Administration and awaiting market entry, biosimilars are in a new phase of integration into U.S. practice.
“Physicians are willing to prescribe Inflectra,” the first biosimilar infliximab and the first TNFi to be sold in the United States last November, Jonathan Kay, MD, said in a video interview during the European Congress of Rheumatology. “Rheumatologists who were initially skeptical are now on the bandwagon and willing to prescribe biosimilars,” said Dr. Kay, a rheumatologist who has often consulted on biosimilar issues and has recently spoken to rheumatologists at various state society meetings to explain the U.S. biosimilar regulatory concepts and spread the message of the societal value of these agents.
“This is not a quick and casual drug evaluation” that produces “knockoff drugs,” but a “careful and extensive” FDA review that results in drugs that are equivalent in efficacy, safety, and immunogenicity to the reference drug and only compete on price, he explained.
When Pfizer began marketing Inflectra last Fall, it set the drug’s list price 15% lower than the list price at the time for Remicade, the reference-product infliximab. However, complex pricing and rebate strategies actually led to Remicade selling for a lower price than Inflectra, at least for some U.S. hospitals, including the University of Massachusetts in Worcester, where Dr. Kay is a professor of medicine.
“The effect of biosimilars is to reduce the cost to patients of an effective treatment. Whether that cost is for the reference drug or for the biosimilar drug doesn’t matter [from society’s perspective] as long as patients are able to receive an effective therapy at a [more] affordable cost, making the effective therapy available to more patients,” he said.
While Inflectra’s price impact my have been modest so far, the biosimilar effect on infliximab’s cost may soon intensify now that a second biosimilar of this TNFi, Renflexis – made by Samsung Bioepis and with U.S. marketing by Merck, received FDA approval on April 21, 2017. Until recently, U.S. pharmaceutical regulations had been understood to require a 180-day hiatus between FDA marketing approval for a biosimilar and the start of U.S. sales. But, on June 12, 2017, the U.S. Supreme Court, in a 9-0 decision, ruled that this 180-day wait was not required, making it possible for U.S. marketing of Renflexis to begin soon. (In mid-June, a statement on the Merck U.S. website for Renflexis says that the product is not currently available.)
Availability of a second biosimilar infliximab “is likely to drive the price down rapidly,” predicted Dr. Kay, citing what happened when multiple biosimilars for a reference drug came onto the European market.
Two other biosimilar TNFi have also received FDA marketing approvals but remain on hold as patent issues and litigation barriers play out. Erelzi – biosimilar etanercept – received FDA approval in August 2016, and Amjevita, biosimilar adalimumab, received FDA approval last September.
The efficacy and safety of Inflectra specifically, and by extension all biosimilars, received a recent boost with publication of findings from a randomized study with 482 patients that provided a real-world test of the core principle of biosimilar equivalence. After Inflectra came onto the Norwegian market, during July 2014 to August 2015, Norwegian researchers ran the NOR-SWTICH trial, which randomized patients who were on stable treatment with Remicade for a variety of indications (including 41% with a rheumatologic disease) to either stay on Remicade or to abruptly switch to treatment with Inflectra. During 1-year follow-up, the incidence of adverse effects and of episodes of disease worsening were virtually identical in the two treatment arms (Lancet. 2017 June 10;389[10086]:2304-16).
Dr. Kay has been a consultant to several companies that develop or market biosimilars, including Samsung Bioepis, Amgen, Pfizer, and Sandoz (Novartis), and to AbbVie, Boehringer Ingelheim, Bristol-Myers Squibb, Genentech, Janssen, Roche, and UCB.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
MADRID – With biosimilar infliximab on the U.S. market since November 2016 and producing an immediate, albeit modest, price drop for this tumor necrosis factor inhibitor (TNFi) and a second biosimilar infliximab now approved by the Food and Drug Administration and awaiting market entry, biosimilars are in a new phase of integration into U.S. practice.
“Physicians are willing to prescribe Inflectra,” the first biosimilar infliximab and the first TNFi to be sold in the United States last November, Jonathan Kay, MD, said in a video interview during the European Congress of Rheumatology. “Rheumatologists who were initially skeptical are now on the bandwagon and willing to prescribe biosimilars,” said Dr. Kay, a rheumatologist who has often consulted on biosimilar issues and has recently spoken to rheumatologists at various state society meetings to explain the U.S. biosimilar regulatory concepts and spread the message of the societal value of these agents.
“This is not a quick and casual drug evaluation” that produces “knockoff drugs,” but a “careful and extensive” FDA review that results in drugs that are equivalent in efficacy, safety, and immunogenicity to the reference drug and only compete on price, he explained.
When Pfizer began marketing Inflectra last Fall, it set the drug’s list price 15% lower than the list price at the time for Remicade, the reference-product infliximab. However, complex pricing and rebate strategies actually led to Remicade selling for a lower price than Inflectra, at least for some U.S. hospitals, including the University of Massachusetts in Worcester, where Dr. Kay is a professor of medicine.
“The effect of biosimilars is to reduce the cost to patients of an effective treatment. Whether that cost is for the reference drug or for the biosimilar drug doesn’t matter [from society’s perspective] as long as patients are able to receive an effective therapy at a [more] affordable cost, making the effective therapy available to more patients,” he said.
While Inflectra’s price impact my have been modest so far, the biosimilar effect on infliximab’s cost may soon intensify now that a second biosimilar of this TNFi, Renflexis – made by Samsung Bioepis and with U.S. marketing by Merck, received FDA approval on April 21, 2017. Until recently, U.S. pharmaceutical regulations had been understood to require a 180-day hiatus between FDA marketing approval for a biosimilar and the start of U.S. sales. But, on June 12, 2017, the U.S. Supreme Court, in a 9-0 decision, ruled that this 180-day wait was not required, making it possible for U.S. marketing of Renflexis to begin soon. (In mid-June, a statement on the Merck U.S. website for Renflexis says that the product is not currently available.)
Availability of a second biosimilar infliximab “is likely to drive the price down rapidly,” predicted Dr. Kay, citing what happened when multiple biosimilars for a reference drug came onto the European market.
Two other biosimilar TNFi have also received FDA marketing approvals but remain on hold as patent issues and litigation barriers play out. Erelzi – biosimilar etanercept – received FDA approval in August 2016, and Amjevita, biosimilar adalimumab, received FDA approval last September.
The efficacy and safety of Inflectra specifically, and by extension all biosimilars, received a recent boost with publication of findings from a randomized study with 482 patients that provided a real-world test of the core principle of biosimilar equivalence. After Inflectra came onto the Norwegian market, during July 2014 to August 2015, Norwegian researchers ran the NOR-SWTICH trial, which randomized patients who were on stable treatment with Remicade for a variety of indications (including 41% with a rheumatologic disease) to either stay on Remicade or to abruptly switch to treatment with Inflectra. During 1-year follow-up, the incidence of adverse effects and of episodes of disease worsening were virtually identical in the two treatment arms (Lancet. 2017 June 10;389[10086]:2304-16).
Dr. Kay has been a consultant to several companies that develop or market biosimilars, including Samsung Bioepis, Amgen, Pfizer, and Sandoz (Novartis), and to AbbVie, Boehringer Ingelheim, Bristol-Myers Squibb, Genentech, Janssen, Roche, and UCB.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
MADRID – With biosimilar infliximab on the U.S. market since November 2016 and producing an immediate, albeit modest, price drop for this tumor necrosis factor inhibitor (TNFi) and a second biosimilar infliximab now approved by the Food and Drug Administration and awaiting market entry, biosimilars are in a new phase of integration into U.S. practice.
“Physicians are willing to prescribe Inflectra,” the first biosimilar infliximab and the first TNFi to be sold in the United States last November, Jonathan Kay, MD, said in a video interview during the European Congress of Rheumatology. “Rheumatologists who were initially skeptical are now on the bandwagon and willing to prescribe biosimilars,” said Dr. Kay, a rheumatologist who has often consulted on biosimilar issues and has recently spoken to rheumatologists at various state society meetings to explain the U.S. biosimilar regulatory concepts and spread the message of the societal value of these agents.
“This is not a quick and casual drug evaluation” that produces “knockoff drugs,” but a “careful and extensive” FDA review that results in drugs that are equivalent in efficacy, safety, and immunogenicity to the reference drug and only compete on price, he explained.
When Pfizer began marketing Inflectra last Fall, it set the drug’s list price 15% lower than the list price at the time for Remicade, the reference-product infliximab. However, complex pricing and rebate strategies actually led to Remicade selling for a lower price than Inflectra, at least for some U.S. hospitals, including the University of Massachusetts in Worcester, where Dr. Kay is a professor of medicine.
“The effect of biosimilars is to reduce the cost to patients of an effective treatment. Whether that cost is for the reference drug or for the biosimilar drug doesn’t matter [from society’s perspective] as long as patients are able to receive an effective therapy at a [more] affordable cost, making the effective therapy available to more patients,” he said.
While Inflectra’s price impact my have been modest so far, the biosimilar effect on infliximab’s cost may soon intensify now that a second biosimilar of this TNFi, Renflexis – made by Samsung Bioepis and with U.S. marketing by Merck, received FDA approval on April 21, 2017. Until recently, U.S. pharmaceutical regulations had been understood to require a 180-day hiatus between FDA marketing approval for a biosimilar and the start of U.S. sales. But, on June 12, 2017, the U.S. Supreme Court, in a 9-0 decision, ruled that this 180-day wait was not required, making it possible for U.S. marketing of Renflexis to begin soon. (In mid-June, a statement on the Merck U.S. website for Renflexis says that the product is not currently available.)
Availability of a second biosimilar infliximab “is likely to drive the price down rapidly,” predicted Dr. Kay, citing what happened when multiple biosimilars for a reference drug came onto the European market.
Two other biosimilar TNFi have also received FDA marketing approvals but remain on hold as patent issues and litigation barriers play out. Erelzi – biosimilar etanercept – received FDA approval in August 2016, and Amjevita, biosimilar adalimumab, received FDA approval last September.
The efficacy and safety of Inflectra specifically, and by extension all biosimilars, received a recent boost with publication of findings from a randomized study with 482 patients that provided a real-world test of the core principle of biosimilar equivalence. After Inflectra came onto the Norwegian market, during July 2014 to August 2015, Norwegian researchers ran the NOR-SWTICH trial, which randomized patients who were on stable treatment with Remicade for a variety of indications (including 41% with a rheumatologic disease) to either stay on Remicade or to abruptly switch to treatment with Inflectra. During 1-year follow-up, the incidence of adverse effects and of episodes of disease worsening were virtually identical in the two treatment arms (Lancet. 2017 June 10;389[10086]:2304-16).
Dr. Kay has been a consultant to several companies that develop or market biosimilars, including Samsung Bioepis, Amgen, Pfizer, and Sandoz (Novartis), and to AbbVie, Boehringer Ingelheim, Bristol-Myers Squibb, Genentech, Janssen, Roche, and UCB.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
EXPERT ANALYSIS FROM THE EULAR 2017 CONGRESS
Sacroiliac structural changes show on MRI in nonradiographic axial SpA despite no inflammation
Structural lesions of the sacroiliac joints (SIJ) may be present on MRI in patients with nonradiographic axial spondyloarthritis (nr-axSpA), even when radiographs are normal or inconclusive for such lesions and there is no evidence of inflammation on MRI, according to findings from a cohort of patients in a randomized trial.
In the study, the patients who exhibited such lesions, especially erosions, were more likely to have more severe disease and greater spinal inflammation than were patients who did not have the structural lesions on MRI.
The presence of MRI structural lesions appeared to reflect more severe disease with greater spinal inflammation, the investigators said, based on higher mean SPARCC spinal scores in 23 discovertebral units. The mean number of discovertebral units involved was significantly greater overall among patients with structural lesions (6.5), compared with those without (3.3). Both Bath Ankylosing Spondylitis Activity Index and Bath Ankylosing Spondylitis Functional Index scores were also significantly higher for patients with BME but no MRI structural lesions (a mean of 6.4 cm and 4.6 cm, respectively), when compared with patients who had both (a mean of 5.7 cm and 3.7 cm, respectively).
Age, sex, and HLA-B27 status also appeared to play a role in the frequency with which MRI structural lesions coexisted with BME. The group of patients with both BME and structural lesions in the sacroiliac joint were significantly more often male (83% vs. 48%), younger (mean age of 30 vs. 34 years), and HLA-B27 positive (87% vs. 63%) than in those with only BME.
“These data support the concept that nr-axSpA is an early stage of axSpA and that structural lesions in the SIJ are associated with a more severe phenotype characterized by more active spinal inflammation,” the investigators wrote.
The presence of structural lesions might also identify patients who would benefit the most from early treatment with biologics, they suggested. “It has been suggested that there is a window of opportunity for disease modification with anti-inflammatory agents by treating acute inflammatory lesions before bone formation pathways are triggered in more complex inflammatory lesions. Consequently, the presence of structural lesions in the SIJ may help select patients for intervention with anti-TNF agents early in the disease course.”
The study was funded by Pfizer. Three of the authors are employees of Pfizer. Two authors have received consulting fees and/or research funding/grants from a variety of companies that make drugs for the treatment of ankylosing spondylitis, including Pfizer.
Structural lesions of the sacroiliac joints (SIJ) may be present on MRI in patients with nonradiographic axial spondyloarthritis (nr-axSpA), even when radiographs are normal or inconclusive for such lesions and there is no evidence of inflammation on MRI, according to findings from a cohort of patients in a randomized trial.
In the study, the patients who exhibited such lesions, especially erosions, were more likely to have more severe disease and greater spinal inflammation than were patients who did not have the structural lesions on MRI.
The presence of MRI structural lesions appeared to reflect more severe disease with greater spinal inflammation, the investigators said, based on higher mean SPARCC spinal scores in 23 discovertebral units. The mean number of discovertebral units involved was significantly greater overall among patients with structural lesions (6.5), compared with those without (3.3). Both Bath Ankylosing Spondylitis Activity Index and Bath Ankylosing Spondylitis Functional Index scores were also significantly higher for patients with BME but no MRI structural lesions (a mean of 6.4 cm and 4.6 cm, respectively), when compared with patients who had both (a mean of 5.7 cm and 3.7 cm, respectively).
Age, sex, and HLA-B27 status also appeared to play a role in the frequency with which MRI structural lesions coexisted with BME. The group of patients with both BME and structural lesions in the sacroiliac joint were significantly more often male (83% vs. 48%), younger (mean age of 30 vs. 34 years), and HLA-B27 positive (87% vs. 63%) than in those with only BME.
“These data support the concept that nr-axSpA is an early stage of axSpA and that structural lesions in the SIJ are associated with a more severe phenotype characterized by more active spinal inflammation,” the investigators wrote.
The presence of structural lesions might also identify patients who would benefit the most from early treatment with biologics, they suggested. “It has been suggested that there is a window of opportunity for disease modification with anti-inflammatory agents by treating acute inflammatory lesions before bone formation pathways are triggered in more complex inflammatory lesions. Consequently, the presence of structural lesions in the SIJ may help select patients for intervention with anti-TNF agents early in the disease course.”
The study was funded by Pfizer. Three of the authors are employees of Pfizer. Two authors have received consulting fees and/or research funding/grants from a variety of companies that make drugs for the treatment of ankylosing spondylitis, including Pfizer.
Structural lesions of the sacroiliac joints (SIJ) may be present on MRI in patients with nonradiographic axial spondyloarthritis (nr-axSpA), even when radiographs are normal or inconclusive for such lesions and there is no evidence of inflammation on MRI, according to findings from a cohort of patients in a randomized trial.
In the study, the patients who exhibited such lesions, especially erosions, were more likely to have more severe disease and greater spinal inflammation than were patients who did not have the structural lesions on MRI.
The presence of MRI structural lesions appeared to reflect more severe disease with greater spinal inflammation, the investigators said, based on higher mean SPARCC spinal scores in 23 discovertebral units. The mean number of discovertebral units involved was significantly greater overall among patients with structural lesions (6.5), compared with those without (3.3). Both Bath Ankylosing Spondylitis Activity Index and Bath Ankylosing Spondylitis Functional Index scores were also significantly higher for patients with BME but no MRI structural lesions (a mean of 6.4 cm and 4.6 cm, respectively), when compared with patients who had both (a mean of 5.7 cm and 3.7 cm, respectively).
Age, sex, and HLA-B27 status also appeared to play a role in the frequency with which MRI structural lesions coexisted with BME. The group of patients with both BME and structural lesions in the sacroiliac joint were significantly more often male (83% vs. 48%), younger (mean age of 30 vs. 34 years), and HLA-B27 positive (87% vs. 63%) than in those with only BME.
“These data support the concept that nr-axSpA is an early stage of axSpA and that structural lesions in the SIJ are associated with a more severe phenotype characterized by more active spinal inflammation,” the investigators wrote.
The presence of structural lesions might also identify patients who would benefit the most from early treatment with biologics, they suggested. “It has been suggested that there is a window of opportunity for disease modification with anti-inflammatory agents by treating acute inflammatory lesions before bone formation pathways are triggered in more complex inflammatory lesions. Consequently, the presence of structural lesions in the SIJ may help select patients for intervention with anti-TNF agents early in the disease course.”
The study was funded by Pfizer. Three of the authors are employees of Pfizer. Two authors have received consulting fees and/or research funding/grants from a variety of companies that make drugs for the treatment of ankylosing spondylitis, including Pfizer.
FROM ARTHRITIS RESEARCH & THERAPY
Key clinical point:
Major finding: Sacroiliac joint erosions on MRI occurred in 11% of patients who did not have bone marrow edema, which was significantly less than its occurrence in 45% of those with BME.
Data source: A study of 183 patients with nr-axSpA who had participated in a treatment trial.
Disclosures: The study was funded by Pfizer. Three of the authors are employees of Pfizer. Two authors have received consulting fees and/or research funding/grants from a variety of companies that make drugs for the treatment of ankylosing spondylitis, including Pfizer.
EULAR program features novel treatments and targets in immune pathways and key overviews of the field
Novel treatments involving the interleukin-17, IL-23, and Janus kinase (JAK) pathways and the growing importance of early diagnosis and treatment will be some of the key themes covered in the scientific program at this year’s EULAR congress in Madrid, June 14-17.
The annual EULAR congress’ traditional spirit of giving congress attendees a thorough scientific update of the evidence published in peer-reviewed journals across the broad spectrum of rheumatic diseases is reflected in the wide range of state-of-the-art lectures, clinical and basic science symposia, practical workshops, and special interest sessions running throughout the packed 4-day congress, said João Eurico Cabral da Fonseca, MD, PhD, chair of the Scientific Programme Committee.
“Our program is driven by novelty and not by a particular area we need to cover,” said Dr. Fonseca of the rheumatology and metabolic bone disease department at the Santa Maria Hospital in Lisbon.
“There has been a lot of research in the past year on the IL-17 and IL-23 pathway, on the use of IL-6 inhibitors in vasculitis, and exploring the several diseases in rheumatology where the inhibition of the JAK pathway and other intracellular pathways will be relevant,” he said.
Some of these advances and innovation in rheumatology will be highlighted in the many “What is New” (WIN) and “How to Treat” (HOT) sessions scattered throughout the scientific program. WIN sessions are a review of the evidence that has been published during the year on a specific area of rheumatology, whereas the purpose of the HOT sessions is to update attendees on the new research in that space while also allowing experts to impart some of their hands-on experience in the area.
“For the HOT and WIN sessions, we invite people to present who are not only scientifically active but are clinically active in order to give some input, particularly for the HOT sessions. They are also usually well skilled in speaking to and engaging with large audiences.”
In WIN and HOT sessions to be held on the afternoon of Saturday, June 17, Josef Smolen, MD, of the Medical University of Vienna will update attendees on the latest developments in the treatment of rheumatoid arthritis.
Dr. Smolen’s talk will be followed by a presentation from pediatric rheumatologist Nico Wulffraat, MD, PhD, of the Wilhelmina Children’s Hospital, Utrecht, the Netherlands on the latest developments in juvenile idiopathic arthritis.
Another WIN session that has been popular with attendees in previous years is EULAR’s collaborative session with The Lancet. The purpose of the collaborative session with The Lancet is twofold: to give attendees an excellent state-of-the-art session on the latest developments in rheumatoid arthritis and also to showcase to the wider global medical community the latest developments in the field of rheumatology, Dr. Fonseca said.
“The long-term goal is to distribute the information we’re gathering in rheumatology journals and at the congress to a broader audience,” he said, noting the relevance of bringing the innovations in rheumatology to audiences outside the field.
The Lancet session this year is on Saturday morning and will focus on the pathogenesis and treatment of rheumatoid arthritis. High-profile speakers at this session include Iain McInnes, PhD, professor of experimental medicine and rheumatology at the University of Glasgow, who will be presenting a WIN session entitled “Dissecting the pathogenesis of rheumatoid arthritis – what have therapeutics taught us?” and EULAR President Gerd Burmester, MD, director of the department of rheumatology and clinical immunology and professor of medicine at Charité University Hospital and Free University and Humboldt University of Berlin, who will present the WIN session “Don’t delay – new treatment concepts in rheumatoid arthritis.”
The importance of diagnosing and treating patients early is a message that is close to EULAR’s heart, Dr. Fonseca said.
The organization, which celebrates its 70th birthday this year, will launch its first awareness campaign‚ “Don’t delay, connect today!” at the congress. The message of the campaign is that “early diagnosis and access to treatment are the key to preventing further damage and burden on individuals and society.”
He said that while the sessions cover all the major rheumatology disciplines, there are some particularly interesting sessions on psoriatic arthritis and spondyloarthritis.
“There’s a lot more interest in these areas than compared to 5 years ago,” he said in an interview. On the morning of Thursday, June 15, there will be an abstract session titled “PsA: A fascinating disease,” followed by a session the next morning called “PsA: The options grow!”
Attendees can also join a poster tour on Thursday morning to discover exactly what progress has been made in the management of spondyloarthritis.
There are new developments in systemic diseases such as lupus and scleroderma that will be highlighted at this year’s congress. However, osteoarthritis is still waiting for its time in the sun, Dr. Landewé said.
“I would say keep an eye on OA over the next few years. ... There are not many sessions this year, but I am very certain there are many new developments on the horizon, perhaps not at this congress, but in the next couple of years,” he said.
Perhaps the pièce de résistance of the scientific program is the conference highlights session on the last day of the congress. Attendees will need to arrive early to get a seat as this session represents a huge effort by two experts who are selected by the Scientific Programme Committee to summarize the most important research published since EULAR 2016 from a clinical, translational, and basic science perspective.
This year, Loreto Carmona, MD, PhD, an epidemiologist and rheumatologist from the Musculoskeletal Health Institute in Madrid, will take the podium to present the clinical highlights. She will be followed by Thomas Dörner, MD, of the Charité University Hospital, Berlin, who will present the translational and basic science highlights.
“This session is a very useful one for delegates as it simplifies the major bits of the congress,” Dr. Fonseca said.
Novel treatments involving the interleukin-17, IL-23, and Janus kinase (JAK) pathways and the growing importance of early diagnosis and treatment will be some of the key themes covered in the scientific program at this year’s EULAR congress in Madrid, June 14-17.
The annual EULAR congress’ traditional spirit of giving congress attendees a thorough scientific update of the evidence published in peer-reviewed journals across the broad spectrum of rheumatic diseases is reflected in the wide range of state-of-the-art lectures, clinical and basic science symposia, practical workshops, and special interest sessions running throughout the packed 4-day congress, said João Eurico Cabral da Fonseca, MD, PhD, chair of the Scientific Programme Committee.
“Our program is driven by novelty and not by a particular area we need to cover,” said Dr. Fonseca of the rheumatology and metabolic bone disease department at the Santa Maria Hospital in Lisbon.
“There has been a lot of research in the past year on the IL-17 and IL-23 pathway, on the use of IL-6 inhibitors in vasculitis, and exploring the several diseases in rheumatology where the inhibition of the JAK pathway and other intracellular pathways will be relevant,” he said.
Some of these advances and innovation in rheumatology will be highlighted in the many “What is New” (WIN) and “How to Treat” (HOT) sessions scattered throughout the scientific program. WIN sessions are a review of the evidence that has been published during the year on a specific area of rheumatology, whereas the purpose of the HOT sessions is to update attendees on the new research in that space while also allowing experts to impart some of their hands-on experience in the area.
“For the HOT and WIN sessions, we invite people to present who are not only scientifically active but are clinically active in order to give some input, particularly for the HOT sessions. They are also usually well skilled in speaking to and engaging with large audiences.”
In WIN and HOT sessions to be held on the afternoon of Saturday, June 17, Josef Smolen, MD, of the Medical University of Vienna will update attendees on the latest developments in the treatment of rheumatoid arthritis.
Dr. Smolen’s talk will be followed by a presentation from pediatric rheumatologist Nico Wulffraat, MD, PhD, of the Wilhelmina Children’s Hospital, Utrecht, the Netherlands on the latest developments in juvenile idiopathic arthritis.
Another WIN session that has been popular with attendees in previous years is EULAR’s collaborative session with The Lancet. The purpose of the collaborative session with The Lancet is twofold: to give attendees an excellent state-of-the-art session on the latest developments in rheumatoid arthritis and also to showcase to the wider global medical community the latest developments in the field of rheumatology, Dr. Fonseca said.
“The long-term goal is to distribute the information we’re gathering in rheumatology journals and at the congress to a broader audience,” he said, noting the relevance of bringing the innovations in rheumatology to audiences outside the field.
The Lancet session this year is on Saturday morning and will focus on the pathogenesis and treatment of rheumatoid arthritis. High-profile speakers at this session include Iain McInnes, PhD, professor of experimental medicine and rheumatology at the University of Glasgow, who will be presenting a WIN session entitled “Dissecting the pathogenesis of rheumatoid arthritis – what have therapeutics taught us?” and EULAR President Gerd Burmester, MD, director of the department of rheumatology and clinical immunology and professor of medicine at Charité University Hospital and Free University and Humboldt University of Berlin, who will present the WIN session “Don’t delay – new treatment concepts in rheumatoid arthritis.”
The importance of diagnosing and treating patients early is a message that is close to EULAR’s heart, Dr. Fonseca said.
The organization, which celebrates its 70th birthday this year, will launch its first awareness campaign‚ “Don’t delay, connect today!” at the congress. The message of the campaign is that “early diagnosis and access to treatment are the key to preventing further damage and burden on individuals and society.”
He said that while the sessions cover all the major rheumatology disciplines, there are some particularly interesting sessions on psoriatic arthritis and spondyloarthritis.
“There’s a lot more interest in these areas than compared to 5 years ago,” he said in an interview. On the morning of Thursday, June 15, there will be an abstract session titled “PsA: A fascinating disease,” followed by a session the next morning called “PsA: The options grow!”
Attendees can also join a poster tour on Thursday morning to discover exactly what progress has been made in the management of spondyloarthritis.
There are new developments in systemic diseases such as lupus and scleroderma that will be highlighted at this year’s congress. However, osteoarthritis is still waiting for its time in the sun, Dr. Landewé said.
“I would say keep an eye on OA over the next few years. ... There are not many sessions this year, but I am very certain there are many new developments on the horizon, perhaps not at this congress, but in the next couple of years,” he said.
Perhaps the pièce de résistance of the scientific program is the conference highlights session on the last day of the congress. Attendees will need to arrive early to get a seat as this session represents a huge effort by two experts who are selected by the Scientific Programme Committee to summarize the most important research published since EULAR 2016 from a clinical, translational, and basic science perspective.
This year, Loreto Carmona, MD, PhD, an epidemiologist and rheumatologist from the Musculoskeletal Health Institute in Madrid, will take the podium to present the clinical highlights. She will be followed by Thomas Dörner, MD, of the Charité University Hospital, Berlin, who will present the translational and basic science highlights.
“This session is a very useful one for delegates as it simplifies the major bits of the congress,” Dr. Fonseca said.
Novel treatments involving the interleukin-17, IL-23, and Janus kinase (JAK) pathways and the growing importance of early diagnosis and treatment will be some of the key themes covered in the scientific program at this year’s EULAR congress in Madrid, June 14-17.
The annual EULAR congress’ traditional spirit of giving congress attendees a thorough scientific update of the evidence published in peer-reviewed journals across the broad spectrum of rheumatic diseases is reflected in the wide range of state-of-the-art lectures, clinical and basic science symposia, practical workshops, and special interest sessions running throughout the packed 4-day congress, said João Eurico Cabral da Fonseca, MD, PhD, chair of the Scientific Programme Committee.
“Our program is driven by novelty and not by a particular area we need to cover,” said Dr. Fonseca of the rheumatology and metabolic bone disease department at the Santa Maria Hospital in Lisbon.
“There has been a lot of research in the past year on the IL-17 and IL-23 pathway, on the use of IL-6 inhibitors in vasculitis, and exploring the several diseases in rheumatology where the inhibition of the JAK pathway and other intracellular pathways will be relevant,” he said.
Some of these advances and innovation in rheumatology will be highlighted in the many “What is New” (WIN) and “How to Treat” (HOT) sessions scattered throughout the scientific program. WIN sessions are a review of the evidence that has been published during the year on a specific area of rheumatology, whereas the purpose of the HOT sessions is to update attendees on the new research in that space while also allowing experts to impart some of their hands-on experience in the area.
“For the HOT and WIN sessions, we invite people to present who are not only scientifically active but are clinically active in order to give some input, particularly for the HOT sessions. They are also usually well skilled in speaking to and engaging with large audiences.”
In WIN and HOT sessions to be held on the afternoon of Saturday, June 17, Josef Smolen, MD, of the Medical University of Vienna will update attendees on the latest developments in the treatment of rheumatoid arthritis.
Dr. Smolen’s talk will be followed by a presentation from pediatric rheumatologist Nico Wulffraat, MD, PhD, of the Wilhelmina Children’s Hospital, Utrecht, the Netherlands on the latest developments in juvenile idiopathic arthritis.
Another WIN session that has been popular with attendees in previous years is EULAR’s collaborative session with The Lancet. The purpose of the collaborative session with The Lancet is twofold: to give attendees an excellent state-of-the-art session on the latest developments in rheumatoid arthritis and also to showcase to the wider global medical community the latest developments in the field of rheumatology, Dr. Fonseca said.
“The long-term goal is to distribute the information we’re gathering in rheumatology journals and at the congress to a broader audience,” he said, noting the relevance of bringing the innovations in rheumatology to audiences outside the field.
The Lancet session this year is on Saturday morning and will focus on the pathogenesis and treatment of rheumatoid arthritis. High-profile speakers at this session include Iain McInnes, PhD, professor of experimental medicine and rheumatology at the University of Glasgow, who will be presenting a WIN session entitled “Dissecting the pathogenesis of rheumatoid arthritis – what have therapeutics taught us?” and EULAR President Gerd Burmester, MD, director of the department of rheumatology and clinical immunology and professor of medicine at Charité University Hospital and Free University and Humboldt University of Berlin, who will present the WIN session “Don’t delay – new treatment concepts in rheumatoid arthritis.”
The importance of diagnosing and treating patients early is a message that is close to EULAR’s heart, Dr. Fonseca said.
The organization, which celebrates its 70th birthday this year, will launch its first awareness campaign‚ “Don’t delay, connect today!” at the congress. The message of the campaign is that “early diagnosis and access to treatment are the key to preventing further damage and burden on individuals and society.”
He said that while the sessions cover all the major rheumatology disciplines, there are some particularly interesting sessions on psoriatic arthritis and spondyloarthritis.
“There’s a lot more interest in these areas than compared to 5 years ago,” he said in an interview. On the morning of Thursday, June 15, there will be an abstract session titled “PsA: A fascinating disease,” followed by a session the next morning called “PsA: The options grow!”
Attendees can also join a poster tour on Thursday morning to discover exactly what progress has been made in the management of spondyloarthritis.
There are new developments in systemic diseases such as lupus and scleroderma that will be highlighted at this year’s congress. However, osteoarthritis is still waiting for its time in the sun, Dr. Landewé said.
“I would say keep an eye on OA over the next few years. ... There are not many sessions this year, but I am very certain there are many new developments on the horizon, perhaps not at this congress, but in the next couple of years,” he said.
Perhaps the pièce de résistance of the scientific program is the conference highlights session on the last day of the congress. Attendees will need to arrive early to get a seat as this session represents a huge effort by two experts who are selected by the Scientific Programme Committee to summarize the most important research published since EULAR 2016 from a clinical, translational, and basic science perspective.
This year, Loreto Carmona, MD, PhD, an epidemiologist and rheumatologist from the Musculoskeletal Health Institute in Madrid, will take the podium to present the clinical highlights. She will be followed by Thomas Dörner, MD, of the Charité University Hospital, Berlin, who will present the translational and basic science highlights.
“This session is a very useful one for delegates as it simplifies the major bits of the congress,” Dr. Fonseca said.
EMEUNET tailors EULAR experience for young rheumatologists
Young rheumatologists and researchers will find plenty of relevant content at this year’s EULAR Congress in Madrid, June 14-17, thanks to a dedicated presentation track. Other tailored opportunities include networking events, mentorship for first-time attendees to help them make the most of their EULAR experience, and a unique opportunity for small group discussion and networking with key opinion leaders in rheumatology in the so-called mentor-mentee meetings.
The Young Rheumatologists track provides three sessions with a special focus on researchers and clinicians who are early in their careers, Sofia Ramiro, MD, PhD, explained in an interview. Dr. Ramiro chairs the steering committee of the Emerging Eular Network (EMEUNET), a network of young clinicians and researchers in the field of rheumatology in Europe.
Another session will zero in on osteoarthritis, vasculitis, spondyloarthritis, and rheumatoid arthritis, with a shorter lecture format and more time left for a question-and-answer session and discussion. With a group of younger rheumatologists in attendance, “the sessions are somewhat more informal,” promoting a comfortable and interactive environment for discussion and learning, Dr. Ramiro said.
The third session in the Young Rheumatologists track will consist of case discussions focused on how to counsel and take care of women who have rheumatoid arthritis and would like to become pregnant. Two patient cases will be presented and discussed by leaders in the field. “Again, the idea is to make these presentations as real-world as possible,” Dr. Ramiro said.
The EMEUNET booth will be in the EULAR Village, and, for the first time, the booth will be incorporated in the EULAR booth, as a “pillar” under the bigger EULAR umbrella. Dr. Ramiro said to be sure to stay tuned for a surprise associated with EULAR’s 70th anniversary. On the evening of Thursday, June 15, EMEUNET will host a networking event.
On the morning of Friday, June 16, mentor-mentee meetings organized by EMEUNET link five to six young attendees with mentors, according to area of interest. Sign up is available online, allowing small group discussion with leaders in academic rheumatology. This year, meetings will be led by Iain McInnes, PhD (Glasgow, Scotland), Josef Smolen, MD (Vienna), and William Dixon, MBBS, PhD (Manchester, England). Mentorship topics can include the incorporation of research into a clinical career, general career advice, and insight into international collaboration, Dr. Ramiro said.
“These are usually very well-attended meetings and very popular,” she said. “People who have participated in them always give us very good feedback and are very enthusiastic about how easily accessible these very famous key opinion leaders are and what good advice they give to them.”
Finally, the Ambassador program helps first-time attendees get the most out of EULAR. “I think that we all know that the first time we attend such a huge conference the experience can be daunting,” Dr. Ramiro said. Now in its third year, the ambassador program pairs an EMEUNET member with up to six first-timers. The ambassador helps the newcomers decide which sessions to attend and remains available through mobile phone, social media, and the meeting app throughout the meeting.
All of EMEUNET’s activities during EULAR support the organization’s aim of “widening collaboration and fostering collaboration among young researchers and clinicians,” Dr. Ramiro said. “The ultimate aim is to improve and promote education in the area of our diseases and to foster research collaborations,” she said of the 1,500-member strong organization.
Young rheumatologists and researchers will find plenty of relevant content at this year’s EULAR Congress in Madrid, June 14-17, thanks to a dedicated presentation track. Other tailored opportunities include networking events, mentorship for first-time attendees to help them make the most of their EULAR experience, and a unique opportunity for small group discussion and networking with key opinion leaders in rheumatology in the so-called mentor-mentee meetings.
The Young Rheumatologists track provides three sessions with a special focus on researchers and clinicians who are early in their careers, Sofia Ramiro, MD, PhD, explained in an interview. Dr. Ramiro chairs the steering committee of the Emerging Eular Network (EMEUNET), a network of young clinicians and researchers in the field of rheumatology in Europe.
Another session will zero in on osteoarthritis, vasculitis, spondyloarthritis, and rheumatoid arthritis, with a shorter lecture format and more time left for a question-and-answer session and discussion. With a group of younger rheumatologists in attendance, “the sessions are somewhat more informal,” promoting a comfortable and interactive environment for discussion and learning, Dr. Ramiro said.
The third session in the Young Rheumatologists track will consist of case discussions focused on how to counsel and take care of women who have rheumatoid arthritis and would like to become pregnant. Two patient cases will be presented and discussed by leaders in the field. “Again, the idea is to make these presentations as real-world as possible,” Dr. Ramiro said.
The EMEUNET booth will be in the EULAR Village, and, for the first time, the booth will be incorporated in the EULAR booth, as a “pillar” under the bigger EULAR umbrella. Dr. Ramiro said to be sure to stay tuned for a surprise associated with EULAR’s 70th anniversary. On the evening of Thursday, June 15, EMEUNET will host a networking event.
On the morning of Friday, June 16, mentor-mentee meetings organized by EMEUNET link five to six young attendees with mentors, according to area of interest. Sign up is available online, allowing small group discussion with leaders in academic rheumatology. This year, meetings will be led by Iain McInnes, PhD (Glasgow, Scotland), Josef Smolen, MD (Vienna), and William Dixon, MBBS, PhD (Manchester, England). Mentorship topics can include the incorporation of research into a clinical career, general career advice, and insight into international collaboration, Dr. Ramiro said.
“These are usually very well-attended meetings and very popular,” she said. “People who have participated in them always give us very good feedback and are very enthusiastic about how easily accessible these very famous key opinion leaders are and what good advice they give to them.”
Finally, the Ambassador program helps first-time attendees get the most out of EULAR. “I think that we all know that the first time we attend such a huge conference the experience can be daunting,” Dr. Ramiro said. Now in its third year, the ambassador program pairs an EMEUNET member with up to six first-timers. The ambassador helps the newcomers decide which sessions to attend and remains available through mobile phone, social media, and the meeting app throughout the meeting.
All of EMEUNET’s activities during EULAR support the organization’s aim of “widening collaboration and fostering collaboration among young researchers and clinicians,” Dr. Ramiro said. “The ultimate aim is to improve and promote education in the area of our diseases and to foster research collaborations,” she said of the 1,500-member strong organization.
Young rheumatologists and researchers will find plenty of relevant content at this year’s EULAR Congress in Madrid, June 14-17, thanks to a dedicated presentation track. Other tailored opportunities include networking events, mentorship for first-time attendees to help them make the most of their EULAR experience, and a unique opportunity for small group discussion and networking with key opinion leaders in rheumatology in the so-called mentor-mentee meetings.
The Young Rheumatologists track provides three sessions with a special focus on researchers and clinicians who are early in their careers, Sofia Ramiro, MD, PhD, explained in an interview. Dr. Ramiro chairs the steering committee of the Emerging Eular Network (EMEUNET), a network of young clinicians and researchers in the field of rheumatology in Europe.
Another session will zero in on osteoarthritis, vasculitis, spondyloarthritis, and rheumatoid arthritis, with a shorter lecture format and more time left for a question-and-answer session and discussion. With a group of younger rheumatologists in attendance, “the sessions are somewhat more informal,” promoting a comfortable and interactive environment for discussion and learning, Dr. Ramiro said.
The third session in the Young Rheumatologists track will consist of case discussions focused on how to counsel and take care of women who have rheumatoid arthritis and would like to become pregnant. Two patient cases will be presented and discussed by leaders in the field. “Again, the idea is to make these presentations as real-world as possible,” Dr. Ramiro said.
The EMEUNET booth will be in the EULAR Village, and, for the first time, the booth will be incorporated in the EULAR booth, as a “pillar” under the bigger EULAR umbrella. Dr. Ramiro said to be sure to stay tuned for a surprise associated with EULAR’s 70th anniversary. On the evening of Thursday, June 15, EMEUNET will host a networking event.
On the morning of Friday, June 16, mentor-mentee meetings organized by EMEUNET link five to six young attendees with mentors, according to area of interest. Sign up is available online, allowing small group discussion with leaders in academic rheumatology. This year, meetings will be led by Iain McInnes, PhD (Glasgow, Scotland), Josef Smolen, MD (Vienna), and William Dixon, MBBS, PhD (Manchester, England). Mentorship topics can include the incorporation of research into a clinical career, general career advice, and insight into international collaboration, Dr. Ramiro said.
“These are usually very well-attended meetings and very popular,” she said. “People who have participated in them always give us very good feedback and are very enthusiastic about how easily accessible these very famous key opinion leaders are and what good advice they give to them.”
Finally, the Ambassador program helps first-time attendees get the most out of EULAR. “I think that we all know that the first time we attend such a huge conference the experience can be daunting,” Dr. Ramiro said. Now in its third year, the ambassador program pairs an EMEUNET member with up to six first-timers. The ambassador helps the newcomers decide which sessions to attend and remains available through mobile phone, social media, and the meeting app throughout the meeting.
All of EMEUNET’s activities during EULAR support the organization’s aim of “widening collaboration and fostering collaboration among young researchers and clinicians,” Dr. Ramiro said. “The ultimate aim is to improve and promote education in the area of our diseases and to foster research collaborations,” she said of the 1,500-member strong organization.
Long-term TNFi tapering possible for some with ankylosing spondylitis
BIRMINGHAM, ENGLAND – A proportion of patients with ankylosing spondylitis (AS) were able to remain on a reduced-dose regimen of a tumor necrosis factor inhibitor (TNFi) for almost 4 years, according to data from a small study presented at the British Society for Rheumatology annual conference.
In an extension of the ANSWERS (Ankylosing Spondylitis with Etanercept Regimens) trial, 4 of 12 patients receiving a once-weekly 25-mg dose of etanercept (Enbrel) had a sustained response as did 14 of 21 patients who remained on the usual once-weekly dose of 50 mg.
“Although a minority of patients maintained response to the lower dose of etanercept over the longer term, the costs savings are substantial,” said Lauren Steel and coauthors from the Norfolk and Norwich Hospitals NHS Foundation Trust in a poster presentation. Almost 18,000 pounds sterling ($23,000) could be saved per each patient who is able to stay on the lower dose for 50 months.
Further, patients who did not maintain a response on the lower dose were usually able to regain their responses when the higher dose therapy was reinstituted. On average, disease control was reestablished in three out of four patients within 14 months of reverting to standard therapy.
ANSWERS was an open-label, multicenter, randomized, pilot study that sought to determine if tapering the dose of etanercept from the recommended 50 mg to 25 mg was feasible in 47 patients with AS (J Rheumatol. 2015;42:1177–85). The premise was that dose tapering in patients who achieved a response would perhaps reduce the risk for side effects in the long term, as well as provide considerable cost savings.
About half of the patients studied achieved a response to full-dose etanercept and were able to reduce their dose. At 6 months, a clinical response was maintained by 52% of the patients taking 25 mg and 92% of the patients taking 50 mg (P = .003).
The current prospective extension of the study looked at the longer-term outcomes of the patients who successfully maintained a response to the lower dose of etanercept.
Maintenance of response was defined as no change in the primary outcome of a reduction of 50% or more or a fall of at least 2 units in the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI), and at least a 2-unit reduction in spinal pain measured using a 10-point scale.
In all, 12 patients, 9 of them male, with a mean age of 52 years entered the extension study. The comparator group consisted of 21 patients who had continued taking the 50-mg dose, 20 of them male, with a mean age of 60 years.
Of the 12 patients in the 25-mg group, 1 discontinued treatment because of side effects and did not restart any further biologic treatment; 7 patients experienced a disease flare after a median of 16 months and were retreated with the 50-mg dose. Five of the seven patients who reverted to the higher dose of etanercept regained a good response; the other two patients were switched to adalimumab (Humira) because of a loss of efficacy.
Pfizer funded the original study. One author disclosed he had received research funding and acted as an adviser to Pfizer and other pharmaceutical companies.
BIRMINGHAM, ENGLAND – A proportion of patients with ankylosing spondylitis (AS) were able to remain on a reduced-dose regimen of a tumor necrosis factor inhibitor (TNFi) for almost 4 years, according to data from a small study presented at the British Society for Rheumatology annual conference.
In an extension of the ANSWERS (Ankylosing Spondylitis with Etanercept Regimens) trial, 4 of 12 patients receiving a once-weekly 25-mg dose of etanercept (Enbrel) had a sustained response as did 14 of 21 patients who remained on the usual once-weekly dose of 50 mg.
“Although a minority of patients maintained response to the lower dose of etanercept over the longer term, the costs savings are substantial,” said Lauren Steel and coauthors from the Norfolk and Norwich Hospitals NHS Foundation Trust in a poster presentation. Almost 18,000 pounds sterling ($23,000) could be saved per each patient who is able to stay on the lower dose for 50 months.
Further, patients who did not maintain a response on the lower dose were usually able to regain their responses when the higher dose therapy was reinstituted. On average, disease control was reestablished in three out of four patients within 14 months of reverting to standard therapy.
ANSWERS was an open-label, multicenter, randomized, pilot study that sought to determine if tapering the dose of etanercept from the recommended 50 mg to 25 mg was feasible in 47 patients with AS (J Rheumatol. 2015;42:1177–85). The premise was that dose tapering in patients who achieved a response would perhaps reduce the risk for side effects in the long term, as well as provide considerable cost savings.
About half of the patients studied achieved a response to full-dose etanercept and were able to reduce their dose. At 6 months, a clinical response was maintained by 52% of the patients taking 25 mg and 92% of the patients taking 50 mg (P = .003).
The current prospective extension of the study looked at the longer-term outcomes of the patients who successfully maintained a response to the lower dose of etanercept.
Maintenance of response was defined as no change in the primary outcome of a reduction of 50% or more or a fall of at least 2 units in the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI), and at least a 2-unit reduction in spinal pain measured using a 10-point scale.
In all, 12 patients, 9 of them male, with a mean age of 52 years entered the extension study. The comparator group consisted of 21 patients who had continued taking the 50-mg dose, 20 of them male, with a mean age of 60 years.
Of the 12 patients in the 25-mg group, 1 discontinued treatment because of side effects and did not restart any further biologic treatment; 7 patients experienced a disease flare after a median of 16 months and were retreated with the 50-mg dose. Five of the seven patients who reverted to the higher dose of etanercept regained a good response; the other two patients were switched to adalimumab (Humira) because of a loss of efficacy.
Pfizer funded the original study. One author disclosed he had received research funding and acted as an adviser to Pfizer and other pharmaceutical companies.
BIRMINGHAM, ENGLAND – A proportion of patients with ankylosing spondylitis (AS) were able to remain on a reduced-dose regimen of a tumor necrosis factor inhibitor (TNFi) for almost 4 years, according to data from a small study presented at the British Society for Rheumatology annual conference.
In an extension of the ANSWERS (Ankylosing Spondylitis with Etanercept Regimens) trial, 4 of 12 patients receiving a once-weekly 25-mg dose of etanercept (Enbrel) had a sustained response as did 14 of 21 patients who remained on the usual once-weekly dose of 50 mg.
“Although a minority of patients maintained response to the lower dose of etanercept over the longer term, the costs savings are substantial,” said Lauren Steel and coauthors from the Norfolk and Norwich Hospitals NHS Foundation Trust in a poster presentation. Almost 18,000 pounds sterling ($23,000) could be saved per each patient who is able to stay on the lower dose for 50 months.
Further, patients who did not maintain a response on the lower dose were usually able to regain their responses when the higher dose therapy was reinstituted. On average, disease control was reestablished in three out of four patients within 14 months of reverting to standard therapy.
ANSWERS was an open-label, multicenter, randomized, pilot study that sought to determine if tapering the dose of etanercept from the recommended 50 mg to 25 mg was feasible in 47 patients with AS (J Rheumatol. 2015;42:1177–85). The premise was that dose tapering in patients who achieved a response would perhaps reduce the risk for side effects in the long term, as well as provide considerable cost savings.
About half of the patients studied achieved a response to full-dose etanercept and were able to reduce their dose. At 6 months, a clinical response was maintained by 52% of the patients taking 25 mg and 92% of the patients taking 50 mg (P = .003).
The current prospective extension of the study looked at the longer-term outcomes of the patients who successfully maintained a response to the lower dose of etanercept.
Maintenance of response was defined as no change in the primary outcome of a reduction of 50% or more or a fall of at least 2 units in the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI), and at least a 2-unit reduction in spinal pain measured using a 10-point scale.
In all, 12 patients, 9 of them male, with a mean age of 52 years entered the extension study. The comparator group consisted of 21 patients who had continued taking the 50-mg dose, 20 of them male, with a mean age of 60 years.
Of the 12 patients in the 25-mg group, 1 discontinued treatment because of side effects and did not restart any further biologic treatment; 7 patients experienced a disease flare after a median of 16 months and were retreated with the 50-mg dose. Five of the seven patients who reverted to the higher dose of etanercept regained a good response; the other two patients were switched to adalimumab (Humira) because of a loss of efficacy.
Pfizer funded the original study. One author disclosed he had received research funding and acted as an adviser to Pfizer and other pharmaceutical companies.
AT RHEUMATOLOGY 2017
Key clinical point:
Major finding: Four of 12 patients treated with etanercept 25 mg once weekly maintained a response at 50 months.
Data source: An extension study of 33 patients in the open-label, multicenter, randomized Ankylosing Spondylitis with Etanercept Regimens (ANSWERS) trial.
Disclosures: Pfizer funded the original study. One author disclosed he had received research funding and acted as an adviser to Pfizer and other pharmaceutical companies.
Ankylosing spondylitis disease severity worsened by smoking
BIRMINGHAM, ENGLAND – Patients with axial spondyloarthritis who currently smoke have been found to have worse disease activity than those who do not in an early analysis of data from the British Society for Rheumatology Biologics Register for Ankylosing Spondylitis (BSRBR-AS).
Smoking was associated with worse disease not only when comparing ever smokers with never smokers, but also when current smokers were compared to ex-smokers, and there was some evidence that the amount of smoking was important with heavier smokers having worse disease activity than light smokers.
Dr. Zhao, of Aintree University Hospital in Liverpool, England, added that, as in previous studies, these data show that “smoking is associated with worse disease activity at baseline and this needs to be accounted for in the next stage of longitudinal analysis.”
An association between smoking and worse disease activity in patients with axSpA has been reported previously, Dr. Zhao acknowledged, but this is not as clear cut as in rheumatoid arthritis where smoking is known to have a pathogenic effect. The small number of earlier studies looking at the possible effect of smoking in AS have been limited by their size and varying methodology, he added, and the studies’ researchers were not able to see if there was any potential dose effect of smoking.
The BSRBR-AS, which started recruiting patients with an Assessment of SpondyloArthritis international Society (ASAS) classification of axSpA in 2012, offers a unique opportunity to explore the association between smoking and axSpA further, he said. More than 2,500 patients are included in the register at present, none of whom should have not been treated with biologic agents at the time of recruitment.
The aim of the present analysis that looked at data on 932 patients was to quantify the effect of smoking status and quantity on several disease outcomes as measured by the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI), the Bath Ankylosing Spondylitis Functional Index (BASFI), and the Bath Ankylosing Spondylitis Metrology Index (BASMI). Spinal pain was also assessed, by way of a visual analog scale (VAS), and quality of life was determined via the disease-specific Ankylosing Spondylitis Quality of Life Instruments (ASQoL).
Most of the patients recruited were male (71%), and the mean age was 50 years. HLA-B27 data were available for 64% of the cohort, and 84% were positive.
Self-reported smoking status was recorded, with 19% saying they were current smokers, 37% saying they were ex-smokers, and 44% saying they had never smoked. If patients reported being ever smokers, the frequency with which they smoked (daily, weekly, monthly, once or twice, or never) was recorded, and if patients smoked daily, then the number of cigarettes smoked per day was obtained. Heavy smoking was defined as smoking 10 or more cigarettes per day and light smoking as fewer than 10 cigarettes per day. By this definition, around 37% of daily smokers were classed as heavy smokers.
In a comparison of ever smokers with never smokers, the mean BASDAI, BASFI, BASMI, spinal VAS, and ASQoL were significantly higher if patients had smoked at some point. All comparisons were adjusted for age, gender, body mass index, and HLA-B27 status.
The mean BASDAI score, for example, was more than 1 unit higher in a comparison of ever smokers with never smokers, with an adjusted regression coefficient of 1.04 and a 95% confidence interval (CI) of 0.72-1.36.
The adjusted regression coefficients for the other measures assessed were 1.34 (95% CI, 0.98-1.69) for BASFI, 0.61 (95% CI 0.36-0.87) for BASMI, 1.11 (95% CI, 0.74-1.49) for spinal VAS, and 2.71 (95% CI, 2.01–3.41) for ASQoL.
Similar findings were seen in the analysis comparing current with ex-smokers across all measures studied, and there was a trend for disease activity to be worse in heavier than in lighter smokers. The latter may not have reached significance because of the smaller number of patients (n = 172) involved in that part of the analysis. Nevertheless, these preliminary findings suggest that even being a light smoker can affect disease outcomes and so cutting down (i.e., to fewer than 10 cigarettes per day) may not be sufficient to reduce the effect that smoking has on disease activity.
“We should be actively encouraging our patients [with axSpA] to stop smoking,” Dr. Zhao concluded.
The BSRBR-AS is managed by a team of investigators based at the University of Aberdeen in collaboration with 83 centers throughout the United Kingdom. It is funded by the BSR, which in turn receives funding from the manufacturers of the biologic therapies included in this study (currently AbbVie, Pfizer, and UCB). Dr. Zhao and coauthors had no conflicts of interest to disclose.
BIRMINGHAM, ENGLAND – Patients with axial spondyloarthritis who currently smoke have been found to have worse disease activity than those who do not in an early analysis of data from the British Society for Rheumatology Biologics Register for Ankylosing Spondylitis (BSRBR-AS).
Smoking was associated with worse disease not only when comparing ever smokers with never smokers, but also when current smokers were compared to ex-smokers, and there was some evidence that the amount of smoking was important with heavier smokers having worse disease activity than light smokers.
Dr. Zhao, of Aintree University Hospital in Liverpool, England, added that, as in previous studies, these data show that “smoking is associated with worse disease activity at baseline and this needs to be accounted for in the next stage of longitudinal analysis.”
An association between smoking and worse disease activity in patients with axSpA has been reported previously, Dr. Zhao acknowledged, but this is not as clear cut as in rheumatoid arthritis where smoking is known to have a pathogenic effect. The small number of earlier studies looking at the possible effect of smoking in AS have been limited by their size and varying methodology, he added, and the studies’ researchers were not able to see if there was any potential dose effect of smoking.
The BSRBR-AS, which started recruiting patients with an Assessment of SpondyloArthritis international Society (ASAS) classification of axSpA in 2012, offers a unique opportunity to explore the association between smoking and axSpA further, he said. More than 2,500 patients are included in the register at present, none of whom should have not been treated with biologic agents at the time of recruitment.
The aim of the present analysis that looked at data on 932 patients was to quantify the effect of smoking status and quantity on several disease outcomes as measured by the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI), the Bath Ankylosing Spondylitis Functional Index (BASFI), and the Bath Ankylosing Spondylitis Metrology Index (BASMI). Spinal pain was also assessed, by way of a visual analog scale (VAS), and quality of life was determined via the disease-specific Ankylosing Spondylitis Quality of Life Instruments (ASQoL).
Most of the patients recruited were male (71%), and the mean age was 50 years. HLA-B27 data were available for 64% of the cohort, and 84% were positive.
Self-reported smoking status was recorded, with 19% saying they were current smokers, 37% saying they were ex-smokers, and 44% saying they had never smoked. If patients reported being ever smokers, the frequency with which they smoked (daily, weekly, monthly, once or twice, or never) was recorded, and if patients smoked daily, then the number of cigarettes smoked per day was obtained. Heavy smoking was defined as smoking 10 or more cigarettes per day and light smoking as fewer than 10 cigarettes per day. By this definition, around 37% of daily smokers were classed as heavy smokers.
In a comparison of ever smokers with never smokers, the mean BASDAI, BASFI, BASMI, spinal VAS, and ASQoL were significantly higher if patients had smoked at some point. All comparisons were adjusted for age, gender, body mass index, and HLA-B27 status.
The mean BASDAI score, for example, was more than 1 unit higher in a comparison of ever smokers with never smokers, with an adjusted regression coefficient of 1.04 and a 95% confidence interval (CI) of 0.72-1.36.
The adjusted regression coefficients for the other measures assessed were 1.34 (95% CI, 0.98-1.69) for BASFI, 0.61 (95% CI 0.36-0.87) for BASMI, 1.11 (95% CI, 0.74-1.49) for spinal VAS, and 2.71 (95% CI, 2.01–3.41) for ASQoL.
Similar findings were seen in the analysis comparing current with ex-smokers across all measures studied, and there was a trend for disease activity to be worse in heavier than in lighter smokers. The latter may not have reached significance because of the smaller number of patients (n = 172) involved in that part of the analysis. Nevertheless, these preliminary findings suggest that even being a light smoker can affect disease outcomes and so cutting down (i.e., to fewer than 10 cigarettes per day) may not be sufficient to reduce the effect that smoking has on disease activity.
“We should be actively encouraging our patients [with axSpA] to stop smoking,” Dr. Zhao concluded.
The BSRBR-AS is managed by a team of investigators based at the University of Aberdeen in collaboration with 83 centers throughout the United Kingdom. It is funded by the BSR, which in turn receives funding from the manufacturers of the biologic therapies included in this study (currently AbbVie, Pfizer, and UCB). Dr. Zhao and coauthors had no conflicts of interest to disclose.
BIRMINGHAM, ENGLAND – Patients with axial spondyloarthritis who currently smoke have been found to have worse disease activity than those who do not in an early analysis of data from the British Society for Rheumatology Biologics Register for Ankylosing Spondylitis (BSRBR-AS).
Smoking was associated with worse disease not only when comparing ever smokers with never smokers, but also when current smokers were compared to ex-smokers, and there was some evidence that the amount of smoking was important with heavier smokers having worse disease activity than light smokers.
Dr. Zhao, of Aintree University Hospital in Liverpool, England, added that, as in previous studies, these data show that “smoking is associated with worse disease activity at baseline and this needs to be accounted for in the next stage of longitudinal analysis.”
An association between smoking and worse disease activity in patients with axSpA has been reported previously, Dr. Zhao acknowledged, but this is not as clear cut as in rheumatoid arthritis where smoking is known to have a pathogenic effect. The small number of earlier studies looking at the possible effect of smoking in AS have been limited by their size and varying methodology, he added, and the studies’ researchers were not able to see if there was any potential dose effect of smoking.
The BSRBR-AS, which started recruiting patients with an Assessment of SpondyloArthritis international Society (ASAS) classification of axSpA in 2012, offers a unique opportunity to explore the association between smoking and axSpA further, he said. More than 2,500 patients are included in the register at present, none of whom should have not been treated with biologic agents at the time of recruitment.
The aim of the present analysis that looked at data on 932 patients was to quantify the effect of smoking status and quantity on several disease outcomes as measured by the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI), the Bath Ankylosing Spondylitis Functional Index (BASFI), and the Bath Ankylosing Spondylitis Metrology Index (BASMI). Spinal pain was also assessed, by way of a visual analog scale (VAS), and quality of life was determined via the disease-specific Ankylosing Spondylitis Quality of Life Instruments (ASQoL).
Most of the patients recruited were male (71%), and the mean age was 50 years. HLA-B27 data were available for 64% of the cohort, and 84% were positive.
Self-reported smoking status was recorded, with 19% saying they were current smokers, 37% saying they were ex-smokers, and 44% saying they had never smoked. If patients reported being ever smokers, the frequency with which they smoked (daily, weekly, monthly, once or twice, or never) was recorded, and if patients smoked daily, then the number of cigarettes smoked per day was obtained. Heavy smoking was defined as smoking 10 or more cigarettes per day and light smoking as fewer than 10 cigarettes per day. By this definition, around 37% of daily smokers were classed as heavy smokers.
In a comparison of ever smokers with never smokers, the mean BASDAI, BASFI, BASMI, spinal VAS, and ASQoL were significantly higher if patients had smoked at some point. All comparisons were adjusted for age, gender, body mass index, and HLA-B27 status.
The mean BASDAI score, for example, was more than 1 unit higher in a comparison of ever smokers with never smokers, with an adjusted regression coefficient of 1.04 and a 95% confidence interval (CI) of 0.72-1.36.
The adjusted regression coefficients for the other measures assessed were 1.34 (95% CI, 0.98-1.69) for BASFI, 0.61 (95% CI 0.36-0.87) for BASMI, 1.11 (95% CI, 0.74-1.49) for spinal VAS, and 2.71 (95% CI, 2.01–3.41) for ASQoL.
Similar findings were seen in the analysis comparing current with ex-smokers across all measures studied, and there was a trend for disease activity to be worse in heavier than in lighter smokers. The latter may not have reached significance because of the smaller number of patients (n = 172) involved in that part of the analysis. Nevertheless, these preliminary findings suggest that even being a light smoker can affect disease outcomes and so cutting down (i.e., to fewer than 10 cigarettes per day) may not be sufficient to reduce the effect that smoking has on disease activity.
“We should be actively encouraging our patients [with axSpA] to stop smoking,” Dr. Zhao concluded.
The BSRBR-AS is managed by a team of investigators based at the University of Aberdeen in collaboration with 83 centers throughout the United Kingdom. It is funded by the BSR, which in turn receives funding from the manufacturers of the biologic therapies included in this study (currently AbbVie, Pfizer, and UCB). Dr. Zhao and coauthors had no conflicts of interest to disclose.
AT RHEUMATOLOGY 2017
Key clinical point:
Major finding: Mean BASDAI, BASFI, BASMI, spinal VAS, and ASQoL were all significantly higher in ever vs. never smokers.
Data source: The British Society for Rheumatology Biologics Register for Ankylosing Spondylitis (BSRBR-AS).
Disclosures: The BSRBR-AS is managed by a team of investigators based at the University of Aberdeen in collaboration with 83 centers throughout the United Kingdom. It is funded by the BSR, which in turn receives funding from the manufacturers of the biologic therapies included in this study (currently AbbVie, Pfizer, and UCB). Dr. Zhao and coauthors had no conflicts of interest to disclose.
Fibromyalgia may affect one in five with ankylosing spondylitis
BIRMINGHAM, ENGLAND – One in five people with ankylosing spondylitis could have comorbid fibromyalgia, according to data from the British Society for Rheumatology Biologics Register for Ankylosing Spondylitis (BSRBR-AS).
The analysis, which included more than 880 patients with axial spondyloarthritis (SpA), found that 20.7% met 2011 research criteria for the chronic pain condition.
The prevalence of fibromyalgia was similar when the modified New York (mNY) criteria were used to diagnose SpA, at 19.7%, but slightly higher at 25.2% when SpA patients met the Assessment of SpondyloArthritis international Society (ASAS) imaging criteria but not mNY criteria, and substantially lower at 9.5% when SpA patients met ASAS clinical criteria only.
Dr. Macfarlane, chief investigator of the BSRBR-AS and professor and chair of clinical epidemiology at the University of Aberdeen (Scotland), added that having comorbid fibromyalgia might “distort the responses of some of the key patient-reported measures and that may lead to some patients having inappropriate therapy.”
So the aim of the present analysis was to provide data on the frequency of SpA and fibromyalgia co-occurrence, characterize which patients might be more likely to have both conditions, and also provide information that would inform future studies looking at the optimal management of such patients.
“The patients most likely to meet fibromyalgia criteria were female, either HLA-B27 negative or untested, and there was a particularly strong association with higher levels of [social] deprivation,” Dr. Macfarlane reported.
Patients who had both SpA and fibromyalgia also were found to be more likely to have been treated with a biologic than those who had SpA alone (51% vs. 32%), and there also was an associated with the time missed (15.1% vs. 2.5%) or impaired (50.8% vs. 22.8%) at work.
In a comparison of the characteristics of patients with SpA who met the fibromyalgia research criteria with those who did not, Dr. Macfarlane observed that they had worse disease activity, function, metrology, and global scores as measured using Bath Ankylosing Spondylitis disease indices:
• Disease activity scores were a respective 6.7 and 3.6, giving a difference of 3.1 (95% confidence interval, 2.9-3.3).
• Function scores were a respective 6.6 and 3.7, with a difference of 2.9 (95% CI, 2.6-3.3).
• Metrology scores were a respective 4.2 and 3.6, with a difference of 0.6 (95% CI, 0.3-0.9).
• Global scores were a respective 6.9 and 3.7, with a different of 3.2 (95% CI, 2.9-3.6).
Dr. Macfarlane reported that there were “extremely large differences” on the patient-reported measures of quality of life, depression, and anxiety. Other common problems in the group meeting the fibromyalgia criteria were sleeping difficulties and high levels of fatigue, he said.
Patients with both SpA and fibromyalgia fared worse on quality of life scores measured using the disease-specific Ankylosing Spondylitis Quality of Life (ASQoL) questionnaire where they scored a mean of 7.1 points (95% CI, 6.4-7.7) higher than did those with SpA alone.
The mean differences in depression and anxiety, both measured using the Hospital Anxiety and Depression Scale (HADS), was 4.8 (95% CI, 4.3-5.2) and 4.7 (95% CI, 4.1-5.2).
The mean difference in the sleep disturbance scale was 5.3 (95% CI, 4.5-6.0), and the mean difference in Chalder Fatigue Scale scores was 4.0 (95% CI, 3.5-4.4).
In contrast, there was no difference in the proportion of patients who had levels of C-reactive protein above 1 mg/dL or in the number of proportion of patients who had extraspinal manifestations of SpA, with the exception of tender or swollen joint counts.
Dr. Macfarlane noted that the fibromyalgia research criteria had not been validated for use in patients with axial SpA but that a grant had been awarded by Arthritis Research UK to look at this and also to look into optimizing options for managing patients with both conditions.
The BSRBR-AS is currently the newest of the biologics registries and began recruiting patients with axial SpA as of December 2012 from 82 centers across the United Kingdom. The register enrolls patients who have not previously been treated with a tumor necrosis factor inhibitor drug and are then followed-up for a 5-year period. The 2011 fibromyalgia research criteria have been used as part of the baseline assessment since September 2015, and clinicians also are asked to report whether they think that patients have fibromyalgia.
The BSRBR-AS is funded by the British Society for Rheumatology, which receives funds from AbbVie, Pfizer, and UCB. Dr. Macfarlane did not report having any conflicts of interest.
BIRMINGHAM, ENGLAND – One in five people with ankylosing spondylitis could have comorbid fibromyalgia, according to data from the British Society for Rheumatology Biologics Register for Ankylosing Spondylitis (BSRBR-AS).
The analysis, which included more than 880 patients with axial spondyloarthritis (SpA), found that 20.7% met 2011 research criteria for the chronic pain condition.
The prevalence of fibromyalgia was similar when the modified New York (mNY) criteria were used to diagnose SpA, at 19.7%, but slightly higher at 25.2% when SpA patients met the Assessment of SpondyloArthritis international Society (ASAS) imaging criteria but not mNY criteria, and substantially lower at 9.5% when SpA patients met ASAS clinical criteria only.
Dr. Macfarlane, chief investigator of the BSRBR-AS and professor and chair of clinical epidemiology at the University of Aberdeen (Scotland), added that having comorbid fibromyalgia might “distort the responses of some of the key patient-reported measures and that may lead to some patients having inappropriate therapy.”
So the aim of the present analysis was to provide data on the frequency of SpA and fibromyalgia co-occurrence, characterize which patients might be more likely to have both conditions, and also provide information that would inform future studies looking at the optimal management of such patients.
“The patients most likely to meet fibromyalgia criteria were female, either HLA-B27 negative or untested, and there was a particularly strong association with higher levels of [social] deprivation,” Dr. Macfarlane reported.
Patients who had both SpA and fibromyalgia also were found to be more likely to have been treated with a biologic than those who had SpA alone (51% vs. 32%), and there also was an associated with the time missed (15.1% vs. 2.5%) or impaired (50.8% vs. 22.8%) at work.
In a comparison of the characteristics of patients with SpA who met the fibromyalgia research criteria with those who did not, Dr. Macfarlane observed that they had worse disease activity, function, metrology, and global scores as measured using Bath Ankylosing Spondylitis disease indices:
• Disease activity scores were a respective 6.7 and 3.6, giving a difference of 3.1 (95% confidence interval, 2.9-3.3).
• Function scores were a respective 6.6 and 3.7, with a difference of 2.9 (95% CI, 2.6-3.3).
• Metrology scores were a respective 4.2 and 3.6, with a difference of 0.6 (95% CI, 0.3-0.9).
• Global scores were a respective 6.9 and 3.7, with a different of 3.2 (95% CI, 2.9-3.6).
Dr. Macfarlane reported that there were “extremely large differences” on the patient-reported measures of quality of life, depression, and anxiety. Other common problems in the group meeting the fibromyalgia criteria were sleeping difficulties and high levels of fatigue, he said.
Patients with both SpA and fibromyalgia fared worse on quality of life scores measured using the disease-specific Ankylosing Spondylitis Quality of Life (ASQoL) questionnaire where they scored a mean of 7.1 points (95% CI, 6.4-7.7) higher than did those with SpA alone.
The mean differences in depression and anxiety, both measured using the Hospital Anxiety and Depression Scale (HADS), was 4.8 (95% CI, 4.3-5.2) and 4.7 (95% CI, 4.1-5.2).
The mean difference in the sleep disturbance scale was 5.3 (95% CI, 4.5-6.0), and the mean difference in Chalder Fatigue Scale scores was 4.0 (95% CI, 3.5-4.4).
In contrast, there was no difference in the proportion of patients who had levels of C-reactive protein above 1 mg/dL or in the number of proportion of patients who had extraspinal manifestations of SpA, with the exception of tender or swollen joint counts.
Dr. Macfarlane noted that the fibromyalgia research criteria had not been validated for use in patients with axial SpA but that a grant had been awarded by Arthritis Research UK to look at this and also to look into optimizing options for managing patients with both conditions.
The BSRBR-AS is currently the newest of the biologics registries and began recruiting patients with axial SpA as of December 2012 from 82 centers across the United Kingdom. The register enrolls patients who have not previously been treated with a tumor necrosis factor inhibitor drug and are then followed-up for a 5-year period. The 2011 fibromyalgia research criteria have been used as part of the baseline assessment since September 2015, and clinicians also are asked to report whether they think that patients have fibromyalgia.
The BSRBR-AS is funded by the British Society for Rheumatology, which receives funds from AbbVie, Pfizer, and UCB. Dr. Macfarlane did not report having any conflicts of interest.
BIRMINGHAM, ENGLAND – One in five people with ankylosing spondylitis could have comorbid fibromyalgia, according to data from the British Society for Rheumatology Biologics Register for Ankylosing Spondylitis (BSRBR-AS).
The analysis, which included more than 880 patients with axial spondyloarthritis (SpA), found that 20.7% met 2011 research criteria for the chronic pain condition.
The prevalence of fibromyalgia was similar when the modified New York (mNY) criteria were used to diagnose SpA, at 19.7%, but slightly higher at 25.2% when SpA patients met the Assessment of SpondyloArthritis international Society (ASAS) imaging criteria but not mNY criteria, and substantially lower at 9.5% when SpA patients met ASAS clinical criteria only.
Dr. Macfarlane, chief investigator of the BSRBR-AS and professor and chair of clinical epidemiology at the University of Aberdeen (Scotland), added that having comorbid fibromyalgia might “distort the responses of some of the key patient-reported measures and that may lead to some patients having inappropriate therapy.”
So the aim of the present analysis was to provide data on the frequency of SpA and fibromyalgia co-occurrence, characterize which patients might be more likely to have both conditions, and also provide information that would inform future studies looking at the optimal management of such patients.
“The patients most likely to meet fibromyalgia criteria were female, either HLA-B27 negative or untested, and there was a particularly strong association with higher levels of [social] deprivation,” Dr. Macfarlane reported.
Patients who had both SpA and fibromyalgia also were found to be more likely to have been treated with a biologic than those who had SpA alone (51% vs. 32%), and there also was an associated with the time missed (15.1% vs. 2.5%) or impaired (50.8% vs. 22.8%) at work.
In a comparison of the characteristics of patients with SpA who met the fibromyalgia research criteria with those who did not, Dr. Macfarlane observed that they had worse disease activity, function, metrology, and global scores as measured using Bath Ankylosing Spondylitis disease indices:
• Disease activity scores were a respective 6.7 and 3.6, giving a difference of 3.1 (95% confidence interval, 2.9-3.3).
• Function scores were a respective 6.6 and 3.7, with a difference of 2.9 (95% CI, 2.6-3.3).
• Metrology scores were a respective 4.2 and 3.6, with a difference of 0.6 (95% CI, 0.3-0.9).
• Global scores were a respective 6.9 and 3.7, with a different of 3.2 (95% CI, 2.9-3.6).
Dr. Macfarlane reported that there were “extremely large differences” on the patient-reported measures of quality of life, depression, and anxiety. Other common problems in the group meeting the fibromyalgia criteria were sleeping difficulties and high levels of fatigue, he said.
Patients with both SpA and fibromyalgia fared worse on quality of life scores measured using the disease-specific Ankylosing Spondylitis Quality of Life (ASQoL) questionnaire where they scored a mean of 7.1 points (95% CI, 6.4-7.7) higher than did those with SpA alone.
The mean differences in depression and anxiety, both measured using the Hospital Anxiety and Depression Scale (HADS), was 4.8 (95% CI, 4.3-5.2) and 4.7 (95% CI, 4.1-5.2).
The mean difference in the sleep disturbance scale was 5.3 (95% CI, 4.5-6.0), and the mean difference in Chalder Fatigue Scale scores was 4.0 (95% CI, 3.5-4.4).
In contrast, there was no difference in the proportion of patients who had levels of C-reactive protein above 1 mg/dL or in the number of proportion of patients who had extraspinal manifestations of SpA, with the exception of tender or swollen joint counts.
Dr. Macfarlane noted that the fibromyalgia research criteria had not been validated for use in patients with axial SpA but that a grant had been awarded by Arthritis Research UK to look at this and also to look into optimizing options for managing patients with both conditions.
The BSRBR-AS is currently the newest of the biologics registries and began recruiting patients with axial SpA as of December 2012 from 82 centers across the United Kingdom. The register enrolls patients who have not previously been treated with a tumor necrosis factor inhibitor drug and are then followed-up for a 5-year period. The 2011 fibromyalgia research criteria have been used as part of the baseline assessment since September 2015, and clinicians also are asked to report whether they think that patients have fibromyalgia.
The BSRBR-AS is funded by the British Society for Rheumatology, which receives funds from AbbVie, Pfizer, and UCB. Dr. Macfarlane did not report having any conflicts of interest.
AT RHEUMATOLOGY 2017
Key clinical point:
Major finding: Of more than 880 patients with axial SpA, 20.7% met 2011 research criteria for the chronic pain condition.
Data source: British Society for Rheumatology Biologics Register for Ankylosing Spondylitis (BSRBR-AS).
Disclosures: The BSRBR-AS is funded by the British Society for Rheumatology, which receives funds from AbbVie, Pfizer, and UCB. Dr. Macfarlane did not report having any conflicts of interest.
Dactylitis, enthesitis, anterior uveitis less frequent in IBD-SpA
In patients with inflammatory bowel disease and spondyloarthritis (IBD-SpA), dactylitis, enthesitis, and anterior uveitis (AU) are significantly less frequent than in patients with other types of SpA, according to Fabrizio Cantini, MD, and his associates.
In a 12-month, case-control study, 88 patients with IBD-SpA, 29 with ulcerative colitis (UC), and 59 with Crohn’s disease (CD) were examined along with the 176 patients with SpA in the control group. Results showed a significantly lower occurrence of dactylitis in case patients, with 4 episodes (4.5%) in IBD-SpA patients and 30 (17.4%) in controls (P = .008). The comparison of the frequency of dactylitis in patients with UC-SpA and in patients with CD-SpA found no significant differences between the two (3.4% and 5.08%, respectively; P = .843). Enthesitis was significantly lower in IBD-SpA, occurring in 16 out of 88 patients (18.1%), compared with in 78 out of 176 controls (44.3%; P less than .001). AU was also recorded in 3 (3.4%) of the patients with IBD-SpA and in 26 controls (14.7%; P = .010), and B27 positivity was recorded in 10 (11.3%) of patients with IBD-SpA and in 70 (39.8%) of patients with SpA (P less than .001).
There was a significantly lower occurrence of dactylitis reported in IBD-SpA patients without psoriasis (1 case in 74 patients; P = .001) compared with the control group, while dactylitis occurrence was not significantly different in 3 out of 14 patients (21.4%) with coexistent psoriasis (P = .960). Enthesitis was significantly higher in 14 IBD-SpA patients with associated psoriasis (50%), compared with the remaining 74 cases (12.1%; P = .003). It was noted that enthesitis occurrence was not different in patients with UC and in those with CD (P = .103).
“The results of our case-control study show that dactylitis, enthesitis, and AU are significantly less frequent in IBD-SpA, compared with other types of SpA,” researchers concluded. “Owing to the frequent association of psoriasis with IBD, and especially with CD, the coexistence of skin disease should be taken into account when evaluating the prevalence of dactylitis and enthesitis in patients with IBD-SpA.”
Find the full study in the Journal of Rheumatology (doi: 10.3899/jrheum.161518).
In patients with inflammatory bowel disease and spondyloarthritis (IBD-SpA), dactylitis, enthesitis, and anterior uveitis (AU) are significantly less frequent than in patients with other types of SpA, according to Fabrizio Cantini, MD, and his associates.
In a 12-month, case-control study, 88 patients with IBD-SpA, 29 with ulcerative colitis (UC), and 59 with Crohn’s disease (CD) were examined along with the 176 patients with SpA in the control group. Results showed a significantly lower occurrence of dactylitis in case patients, with 4 episodes (4.5%) in IBD-SpA patients and 30 (17.4%) in controls (P = .008). The comparison of the frequency of dactylitis in patients with UC-SpA and in patients with CD-SpA found no significant differences between the two (3.4% and 5.08%, respectively; P = .843). Enthesitis was significantly lower in IBD-SpA, occurring in 16 out of 88 patients (18.1%), compared with in 78 out of 176 controls (44.3%; P less than .001). AU was also recorded in 3 (3.4%) of the patients with IBD-SpA and in 26 controls (14.7%; P = .010), and B27 positivity was recorded in 10 (11.3%) of patients with IBD-SpA and in 70 (39.8%) of patients with SpA (P less than .001).
There was a significantly lower occurrence of dactylitis reported in IBD-SpA patients without psoriasis (1 case in 74 patients; P = .001) compared with the control group, while dactylitis occurrence was not significantly different in 3 out of 14 patients (21.4%) with coexistent psoriasis (P = .960). Enthesitis was significantly higher in 14 IBD-SpA patients with associated psoriasis (50%), compared with the remaining 74 cases (12.1%; P = .003). It was noted that enthesitis occurrence was not different in patients with UC and in those with CD (P = .103).
“The results of our case-control study show that dactylitis, enthesitis, and AU are significantly less frequent in IBD-SpA, compared with other types of SpA,” researchers concluded. “Owing to the frequent association of psoriasis with IBD, and especially with CD, the coexistence of skin disease should be taken into account when evaluating the prevalence of dactylitis and enthesitis in patients with IBD-SpA.”
Find the full study in the Journal of Rheumatology (doi: 10.3899/jrheum.161518).
In patients with inflammatory bowel disease and spondyloarthritis (IBD-SpA), dactylitis, enthesitis, and anterior uveitis (AU) are significantly less frequent than in patients with other types of SpA, according to Fabrizio Cantini, MD, and his associates.
In a 12-month, case-control study, 88 patients with IBD-SpA, 29 with ulcerative colitis (UC), and 59 with Crohn’s disease (CD) were examined along with the 176 patients with SpA in the control group. Results showed a significantly lower occurrence of dactylitis in case patients, with 4 episodes (4.5%) in IBD-SpA patients and 30 (17.4%) in controls (P = .008). The comparison of the frequency of dactylitis in patients with UC-SpA and in patients with CD-SpA found no significant differences between the two (3.4% and 5.08%, respectively; P = .843). Enthesitis was significantly lower in IBD-SpA, occurring in 16 out of 88 patients (18.1%), compared with in 78 out of 176 controls (44.3%; P less than .001). AU was also recorded in 3 (3.4%) of the patients with IBD-SpA and in 26 controls (14.7%; P = .010), and B27 positivity was recorded in 10 (11.3%) of patients with IBD-SpA and in 70 (39.8%) of patients with SpA (P less than .001).
There was a significantly lower occurrence of dactylitis reported in IBD-SpA patients without psoriasis (1 case in 74 patients; P = .001) compared with the control group, while dactylitis occurrence was not significantly different in 3 out of 14 patients (21.4%) with coexistent psoriasis (P = .960). Enthesitis was significantly higher in 14 IBD-SpA patients with associated psoriasis (50%), compared with the remaining 74 cases (12.1%; P = .003). It was noted that enthesitis occurrence was not different in patients with UC and in those with CD (P = .103).
“The results of our case-control study show that dactylitis, enthesitis, and AU are significantly less frequent in IBD-SpA, compared with other types of SpA,” researchers concluded. “Owing to the frequent association of psoriasis with IBD, and especially with CD, the coexistence of skin disease should be taken into account when evaluating the prevalence of dactylitis and enthesitis in patients with IBD-SpA.”
Find the full study in the Journal of Rheumatology (doi: 10.3899/jrheum.161518).