User login
MADRID – Obese patients with axial spondyloarthritis were substantially less responsive to treatment with a tumor necrosis factor inhibitor than were healthy-weight patients in a multicenter Swiss study with 531 patients.
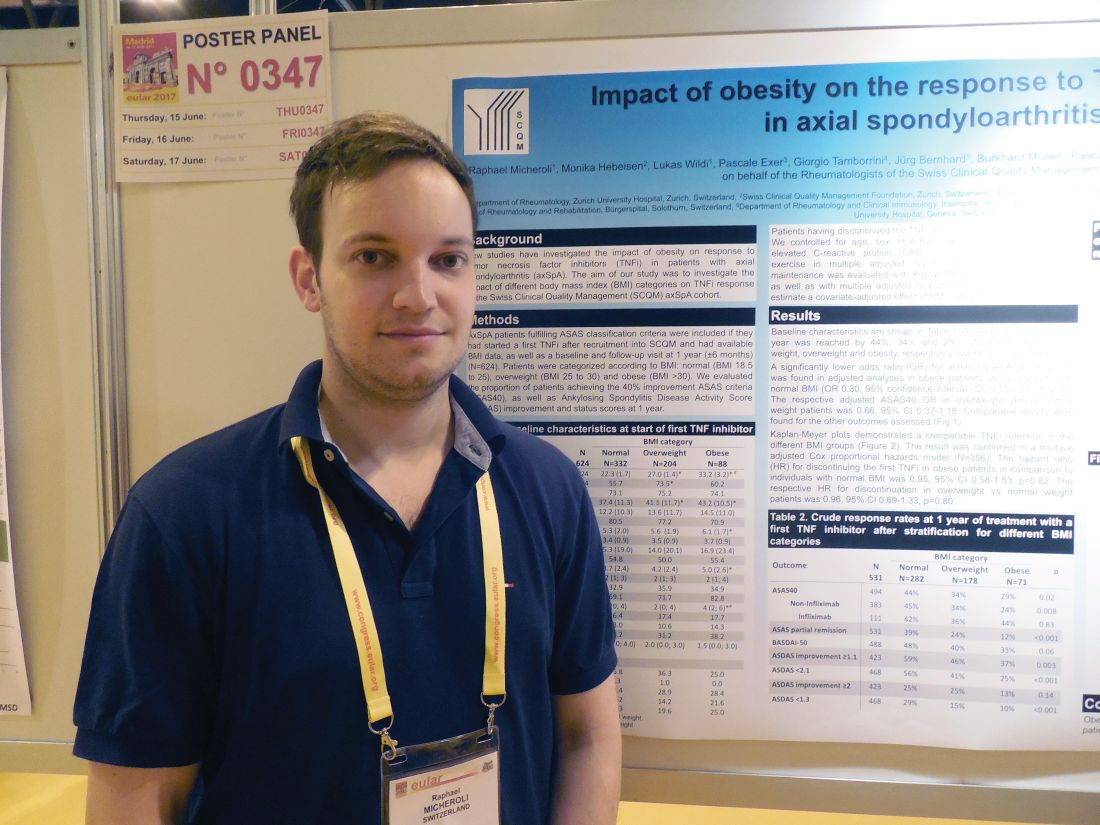
In a multivariate analysis that controlled for several demographic and clinical factors, including baseline disease severity, obese patients with axial spondyloarthritis (SpA) were 70% less likely to achieve a 40% or better improvement in their Assessment in SpondyloArthritis International Society improvement criteria (ASAS 40) when compared with patients with a healthy body mass index (BMI), Raphael Micheroli, MD, reported in a poster at the European Congress of Rheumatology.
The finding supplies a third reason why patients with newly diagnosed axial SpA should try to lose weight if they are obese (or overweight) – to potentially improve their responsiveness to a TNFi. The other two reasons are to reduce cardiovascular disease risk in patients who are already at risk for these complications because of their disease, and to also help improve their ability to perform physical activities, he explained in an interview.
Dr. Micheroli proposed three possible reasons why obese patients with axial SpA might be less responsive to a TNFi than healthy-weight patients: They receive an inadequate TNFi dosage, their increased adipose tissue produces excess proinflammatory cytokines that exacerbate their axial SpA, or it is possible that obese patients are more likely to be misdiagnosed with axial SpA and because they don’t really have this disease their symptoms cannot improve with TNFi treatment. They may instead have, for example, degenerative back pain, a condition that can be challenging to distinguish from axial SpA, he said.
A role for obesity in blunting the beneficial effects of TNFi treatment has been well described for psoriatic arthritis, for example, in an Italian study with 138 patients (Ann Rheum Dis. 2014 June;73[6]:1157-62), and in a Danish study with more than 1,200 patients (Rheumatology [Oxford]. 2016 Dec;55[12]:2191-9).
Dr. Micheroli’s study included 624 patients with axial SpA enrolled in the Swiss Clinical Quality Management in Rheumatic Diseases axial spondyloarthritis cohort who met the ASAS classification criteria for axial SpA and started treatment with their first TNFi after they entered the cohort. Follow-up data after 1 year on treatment were available for 531 of these patients. The entry group included 332 patients (53%) with a healthy BMI, 204 (33%) with an overweight BMI (25-30 kg/m2), and 88 (14%) obese patients (BMI more than 30 kg/m2). The patients averaged about 40 years old and had been symptomatic for an average of about 13 years. About one-third of patients started on adalimumab (Humira) treatment, about one-quarter started etanercept (Enbrel), more than one-fifth began infliximab (Remicade), and some patients started treatment with either golimumab (Simponi) or certolizumab pegol (Cimzia).
After 1 year on TNFi treatment, ASAS 40 improvement occurred in 44% of 282 healthy-BMI patients, 34% of 178 overweight patients, and in 29% of 71 obese patients, Dr. Micheroli reported. In a baseline-adjusted multivariate model, this difference translated into an odds ratio of 0.30 for obese patients achieving an ASAS 40 response, compared with the healthy-BMI patients after 1 year, a statistically significant difference. Further analysis showed no statistically significant differences in TNFi discontinuation rates among the three BMI subgroups.
Dr. Micheroli had no disclosures.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
MADRID – Obese patients with axial spondyloarthritis were substantially less responsive to treatment with a tumor necrosis factor inhibitor than were healthy-weight patients in a multicenter Swiss study with 531 patients.
In a multivariate analysis that controlled for several demographic and clinical factors, including baseline disease severity, obese patients with axial spondyloarthritis (SpA) were 70% less likely to achieve a 40% or better improvement in their Assessment in SpondyloArthritis International Society improvement criteria (ASAS 40) when compared with patients with a healthy body mass index (BMI), Raphael Micheroli, MD, reported in a poster at the European Congress of Rheumatology.
The finding supplies a third reason why patients with newly diagnosed axial SpA should try to lose weight if they are obese (or overweight) – to potentially improve their responsiveness to a TNFi. The other two reasons are to reduce cardiovascular disease risk in patients who are already at risk for these complications because of their disease, and to also help improve their ability to perform physical activities, he explained in an interview.
Dr. Micheroli proposed three possible reasons why obese patients with axial SpA might be less responsive to a TNFi than healthy-weight patients: They receive an inadequate TNFi dosage, their increased adipose tissue produces excess proinflammatory cytokines that exacerbate their axial SpA, or it is possible that obese patients are more likely to be misdiagnosed with axial SpA and because they don’t really have this disease their symptoms cannot improve with TNFi treatment. They may instead have, for example, degenerative back pain, a condition that can be challenging to distinguish from axial SpA, he said.
A role for obesity in blunting the beneficial effects of TNFi treatment has been well described for psoriatic arthritis, for example, in an Italian study with 138 patients (Ann Rheum Dis. 2014 June;73[6]:1157-62), and in a Danish study with more than 1,200 patients (Rheumatology [Oxford]. 2016 Dec;55[12]:2191-9).
Dr. Micheroli’s study included 624 patients with axial SpA enrolled in the Swiss Clinical Quality Management in Rheumatic Diseases axial spondyloarthritis cohort who met the ASAS classification criteria for axial SpA and started treatment with their first TNFi after they entered the cohort. Follow-up data after 1 year on treatment were available for 531 of these patients. The entry group included 332 patients (53%) with a healthy BMI, 204 (33%) with an overweight BMI (25-30 kg/m2), and 88 (14%) obese patients (BMI more than 30 kg/m2). The patients averaged about 40 years old and had been symptomatic for an average of about 13 years. About one-third of patients started on adalimumab (Humira) treatment, about one-quarter started etanercept (Enbrel), more than one-fifth began infliximab (Remicade), and some patients started treatment with either golimumab (Simponi) or certolizumab pegol (Cimzia).
After 1 year on TNFi treatment, ASAS 40 improvement occurred in 44% of 282 healthy-BMI patients, 34% of 178 overweight patients, and in 29% of 71 obese patients, Dr. Micheroli reported. In a baseline-adjusted multivariate model, this difference translated into an odds ratio of 0.30 for obese patients achieving an ASAS 40 response, compared with the healthy-BMI patients after 1 year, a statistically significant difference. Further analysis showed no statistically significant differences in TNFi discontinuation rates among the three BMI subgroups.
Dr. Micheroli had no disclosures.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
MADRID – Obese patients with axial spondyloarthritis were substantially less responsive to treatment with a tumor necrosis factor inhibitor than were healthy-weight patients in a multicenter Swiss study with 531 patients.
In a multivariate analysis that controlled for several demographic and clinical factors, including baseline disease severity, obese patients with axial spondyloarthritis (SpA) were 70% less likely to achieve a 40% or better improvement in their Assessment in SpondyloArthritis International Society improvement criteria (ASAS 40) when compared with patients with a healthy body mass index (BMI), Raphael Micheroli, MD, reported in a poster at the European Congress of Rheumatology.
The finding supplies a third reason why patients with newly diagnosed axial SpA should try to lose weight if they are obese (or overweight) – to potentially improve their responsiveness to a TNFi. The other two reasons are to reduce cardiovascular disease risk in patients who are already at risk for these complications because of their disease, and to also help improve their ability to perform physical activities, he explained in an interview.
Dr. Micheroli proposed three possible reasons why obese patients with axial SpA might be less responsive to a TNFi than healthy-weight patients: They receive an inadequate TNFi dosage, their increased adipose tissue produces excess proinflammatory cytokines that exacerbate their axial SpA, or it is possible that obese patients are more likely to be misdiagnosed with axial SpA and because they don’t really have this disease their symptoms cannot improve with TNFi treatment. They may instead have, for example, degenerative back pain, a condition that can be challenging to distinguish from axial SpA, he said.
A role for obesity in blunting the beneficial effects of TNFi treatment has been well described for psoriatic arthritis, for example, in an Italian study with 138 patients (Ann Rheum Dis. 2014 June;73[6]:1157-62), and in a Danish study with more than 1,200 patients (Rheumatology [Oxford]. 2016 Dec;55[12]:2191-9).
Dr. Micheroli’s study included 624 patients with axial SpA enrolled in the Swiss Clinical Quality Management in Rheumatic Diseases axial spondyloarthritis cohort who met the ASAS classification criteria for axial SpA and started treatment with their first TNFi after they entered the cohort. Follow-up data after 1 year on treatment were available for 531 of these patients. The entry group included 332 patients (53%) with a healthy BMI, 204 (33%) with an overweight BMI (25-30 kg/m2), and 88 (14%) obese patients (BMI more than 30 kg/m2). The patients averaged about 40 years old and had been symptomatic for an average of about 13 years. About one-third of patients started on adalimumab (Humira) treatment, about one-quarter started etanercept (Enbrel), more than one-fifth began infliximab (Remicade), and some patients started treatment with either golimumab (Simponi) or certolizumab pegol (Cimzia).
After 1 year on TNFi treatment, ASAS 40 improvement occurred in 44% of 282 healthy-BMI patients, 34% of 178 overweight patients, and in 29% of 71 obese patients, Dr. Micheroli reported. In a baseline-adjusted multivariate model, this difference translated into an odds ratio of 0.30 for obese patients achieving an ASAS 40 response, compared with the healthy-BMI patients after 1 year, a statistically significant difference. Further analysis showed no statistically significant differences in TNFi discontinuation rates among the three BMI subgroups.
Dr. Micheroli had no disclosures.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
AT THE EULAR 2017 CONGRESS
Key clinical point:
Major finding: Obese patients had a 70% lower response rate to a tumor necrosis factor inhibitor, compared with healthy-weight patients.
Data source: A cohort of 531 axial spondyloarthritis patients enrolled in the Swiss Clinical Quality Management in Rheumatic Diseases program.
Disclosures: Dr. Micheroli had no disclosures.