User login
Treating maternal subclinical hypothyroidism doesn’t improve childhood IQ
ATLANTA – Prenatal treatment of maternal subclinical hypothyroidism or hypothyroxinemia conferred no cognitive, behavioral, or neurodevelopmental benefit to children up to age 5.
The findings of two parallel randomized trials suggest that prenatal screening for these conditions is not necessary, Dr. Brian Casey said at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine. The data also support the American College of Obstetricians and Gynecologists’ 2007 recommendation against routine screening, said Dr. Casey, chief of maternal-fetal medicine and obstetrics at the University of Texas Southwestern Medical Center, Dallas.
The issue of whether to treat pregnant women for subclinical hypothyroidism has been debated for years. Studies in the early 2000s suggested that prenatal levothyroxine did improve child neurocognitive outcomes, but more recent studies, including a 2012 randomized trial, do not.
These data have led both the American College of Obstetricians and Gynecologists and the Endocrine Society to recommend against screening for subclinical hypothyroidism in pregnant women.
Dr. Casey and his colleagues conducted two large parallel randomized studies, one in women with subclinical hypothyroidism and another in women with hypothyroxinemia. Subclinical hypothyroidism was defined as a thyroid stimulating hormone (TSH) level of at least 4 mU/L with normal free T4. Hypothyroxinemia was defined as a normal TSH but a free T4 of less than 0.86 ng/dL.
The primary outcome in each group was child IQ at 5 years. Secondary outcomes were scores on neurodevelopmental and behavioral measures, including the presence of attention deficit hyperactivity disorder, conducted at ages 3, 4, and 5 years.
All women in the trials had a singleton pregnancy of less than 20 weeks’ gestation, with no known history of thyroid disease.
The subclinical hypothyroidism group comprised 677 women. They were a mean of 27 years old, with a mean gestational age of 16.5 weeks. Baseline TSH was 4.5 mU/L; baseline free T4 was 1 ng/dL. All had normal urinary iodide. They were randomized to placebo or to daily 100 mcg levothyroxine. The treatment goal was a TSH of 0.1-2.5 mU/L. Most (93%) achieved this by 21 weeks’ gestation.
There was no significant difference in the primary outcome of child IQ at 5 years between the treated and untreated groups (97 vs. 94). On the Bayley Scales of Infant and Toddler Development, scores of cognition, motor skills, and language were similar in each group at both 12 and 24 months. The Differential Ability Scales scores at 3 and 4 years were also similar. The Child Behavior Checklist scores at ages 4 years and 5 years were similar. There was no indication of an increase in ADHD.
The hypothyroxinemia trial comprised 467 women. They were randomized to placebo or to 50 mcg levothyroxine. These women were a mean of 28 years old with a mean gestational age of 18 weeks. Their baseline TSH was 1.5 mU/L, and baseline free T4 was 0.8 ng/dL. All had normal urinary iodide. The treatment goal was a free T4 of between 0.86 and 1.90 ng/dL. Most (83%) achieved this by 23 weeks’ gestation.
There was no difference on the primary outcome of child IQ at 5 years (94 vs. 91). On the Bayley Scales of Infant and Toddler Development, scores of cognition, motor skills, and language were similar in each group at both 12 and 24 months. The Differential Ability Scales scores at 3 years and 4 years were also similar. The Child Behavior Checklist scores at ages 4years and 5 years were similar. There was no indication of an increase in ADHD.
Dr. Casey added that there was no interaction between gestational age at baseline and treatment outcomes, suggesting that there may be little foundation to the argument that treating earlier in pregnancy is key.
He had no financial disclosures.
ATLANTA – Prenatal treatment of maternal subclinical hypothyroidism or hypothyroxinemia conferred no cognitive, behavioral, or neurodevelopmental benefit to children up to age 5.
The findings of two parallel randomized trials suggest that prenatal screening for these conditions is not necessary, Dr. Brian Casey said at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine. The data also support the American College of Obstetricians and Gynecologists’ 2007 recommendation against routine screening, said Dr. Casey, chief of maternal-fetal medicine and obstetrics at the University of Texas Southwestern Medical Center, Dallas.
The issue of whether to treat pregnant women for subclinical hypothyroidism has been debated for years. Studies in the early 2000s suggested that prenatal levothyroxine did improve child neurocognitive outcomes, but more recent studies, including a 2012 randomized trial, do not.
These data have led both the American College of Obstetricians and Gynecologists and the Endocrine Society to recommend against screening for subclinical hypothyroidism in pregnant women.
Dr. Casey and his colleagues conducted two large parallel randomized studies, one in women with subclinical hypothyroidism and another in women with hypothyroxinemia. Subclinical hypothyroidism was defined as a thyroid stimulating hormone (TSH) level of at least 4 mU/L with normal free T4. Hypothyroxinemia was defined as a normal TSH but a free T4 of less than 0.86 ng/dL.
The primary outcome in each group was child IQ at 5 years. Secondary outcomes were scores on neurodevelopmental and behavioral measures, including the presence of attention deficit hyperactivity disorder, conducted at ages 3, 4, and 5 years.
All women in the trials had a singleton pregnancy of less than 20 weeks’ gestation, with no known history of thyroid disease.
The subclinical hypothyroidism group comprised 677 women. They were a mean of 27 years old, with a mean gestational age of 16.5 weeks. Baseline TSH was 4.5 mU/L; baseline free T4 was 1 ng/dL. All had normal urinary iodide. They were randomized to placebo or to daily 100 mcg levothyroxine. The treatment goal was a TSH of 0.1-2.5 mU/L. Most (93%) achieved this by 21 weeks’ gestation.
There was no significant difference in the primary outcome of child IQ at 5 years between the treated and untreated groups (97 vs. 94). On the Bayley Scales of Infant and Toddler Development, scores of cognition, motor skills, and language were similar in each group at both 12 and 24 months. The Differential Ability Scales scores at 3 and 4 years were also similar. The Child Behavior Checklist scores at ages 4 years and 5 years were similar. There was no indication of an increase in ADHD.
The hypothyroxinemia trial comprised 467 women. They were randomized to placebo or to 50 mcg levothyroxine. These women were a mean of 28 years old with a mean gestational age of 18 weeks. Their baseline TSH was 1.5 mU/L, and baseline free T4 was 0.8 ng/dL. All had normal urinary iodide. The treatment goal was a free T4 of between 0.86 and 1.90 ng/dL. Most (83%) achieved this by 23 weeks’ gestation.
There was no difference on the primary outcome of child IQ at 5 years (94 vs. 91). On the Bayley Scales of Infant and Toddler Development, scores of cognition, motor skills, and language were similar in each group at both 12 and 24 months. The Differential Ability Scales scores at 3 years and 4 years were also similar. The Child Behavior Checklist scores at ages 4years and 5 years were similar. There was no indication of an increase in ADHD.
Dr. Casey added that there was no interaction between gestational age at baseline and treatment outcomes, suggesting that there may be little foundation to the argument that treating earlier in pregnancy is key.
He had no financial disclosures.
ATLANTA – Prenatal treatment of maternal subclinical hypothyroidism or hypothyroxinemia conferred no cognitive, behavioral, or neurodevelopmental benefit to children up to age 5.
The findings of two parallel randomized trials suggest that prenatal screening for these conditions is not necessary, Dr. Brian Casey said at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine. The data also support the American College of Obstetricians and Gynecologists’ 2007 recommendation against routine screening, said Dr. Casey, chief of maternal-fetal medicine and obstetrics at the University of Texas Southwestern Medical Center, Dallas.
The issue of whether to treat pregnant women for subclinical hypothyroidism has been debated for years. Studies in the early 2000s suggested that prenatal levothyroxine did improve child neurocognitive outcomes, but more recent studies, including a 2012 randomized trial, do not.
These data have led both the American College of Obstetricians and Gynecologists and the Endocrine Society to recommend against screening for subclinical hypothyroidism in pregnant women.
Dr. Casey and his colleagues conducted two large parallel randomized studies, one in women with subclinical hypothyroidism and another in women with hypothyroxinemia. Subclinical hypothyroidism was defined as a thyroid stimulating hormone (TSH) level of at least 4 mU/L with normal free T4. Hypothyroxinemia was defined as a normal TSH but a free T4 of less than 0.86 ng/dL.
The primary outcome in each group was child IQ at 5 years. Secondary outcomes were scores on neurodevelopmental and behavioral measures, including the presence of attention deficit hyperactivity disorder, conducted at ages 3, 4, and 5 years.
All women in the trials had a singleton pregnancy of less than 20 weeks’ gestation, with no known history of thyroid disease.
The subclinical hypothyroidism group comprised 677 women. They were a mean of 27 years old, with a mean gestational age of 16.5 weeks. Baseline TSH was 4.5 mU/L; baseline free T4 was 1 ng/dL. All had normal urinary iodide. They were randomized to placebo or to daily 100 mcg levothyroxine. The treatment goal was a TSH of 0.1-2.5 mU/L. Most (93%) achieved this by 21 weeks’ gestation.
There was no significant difference in the primary outcome of child IQ at 5 years between the treated and untreated groups (97 vs. 94). On the Bayley Scales of Infant and Toddler Development, scores of cognition, motor skills, and language were similar in each group at both 12 and 24 months. The Differential Ability Scales scores at 3 and 4 years were also similar. The Child Behavior Checklist scores at ages 4 years and 5 years were similar. There was no indication of an increase in ADHD.
The hypothyroxinemia trial comprised 467 women. They were randomized to placebo or to 50 mcg levothyroxine. These women were a mean of 28 years old with a mean gestational age of 18 weeks. Their baseline TSH was 1.5 mU/L, and baseline free T4 was 0.8 ng/dL. All had normal urinary iodide. The treatment goal was a free T4 of between 0.86 and 1.90 ng/dL. Most (83%) achieved this by 23 weeks’ gestation.
There was no difference on the primary outcome of child IQ at 5 years (94 vs. 91). On the Bayley Scales of Infant and Toddler Development, scores of cognition, motor skills, and language were similar in each group at both 12 and 24 months. The Differential Ability Scales scores at 3 years and 4 years were also similar. The Child Behavior Checklist scores at ages 4years and 5 years were similar. There was no indication of an increase in ADHD.
Dr. Casey added that there was no interaction between gestational age at baseline and treatment outcomes, suggesting that there may be little foundation to the argument that treating earlier in pregnancy is key.
He had no financial disclosures.
AT THE PREGNANCY MEETING
Key clinical point: Levothyroxine for women with subclinical hypothyroidism didn’t boost childhood cognition.
Major finding: Child IQ at 5 years old was 97 in the treated group and 94 in the placebo group – not a significant difference.
Data source: The parallel randomized controlled trials comprised a total of 1,144 women.
Disclosures: Dr. Casey had no financial disclosures.
Gender identity disorders in males associated with MS
An association between gender identity disorders (GIDs) and subsequent multiple sclerosis (MS) in males was found in an analysis of linked English Hospital Episode Statistics and mortality data from January 1999 to March 2012.
The findings “suggest that low testosterone levels and/or feminising gonadal hormones might influence MS risk in some men and highlight a need for further work to explore any potential role for gonadal hormones in management and/or prevention strategies,” wrote Dr. Julia Pakpoor of the Unit of Health-Care Epidemiology, Nuffield Department of Population Health, at University of Oxford (England).
She and her colleagues used the patient data to construct male and female cohorts (1,157 patients and 2,390 patients, respectively) of patients with GIDs. A patient was included in one of the two GID cohorts if he or she had an episode of care or hospital admission in which a GID or sexual transformation procedure was coded in any diagnostic position.
For males with GIDs transitioning to females, the most studied treatment regimen involves using feminizing hormones and anti-androgens, which reduce testosterone secretion or neutralize testosterone activity, the researchers noted.
They also used the database to construct male and female cohorts (4.6 million patients and 3.4 million patients, respectively) to serve as two control groups. For patients to be included in the control groups, they needed to have been first admitted to a hospital for a minor condition and to never have been admitted to a hospital for MS. Patients who had been admitted to a hospital for MS either before or at the same time they were admitted for GIDs were excluded from the GID cohorts. A patient stopped being followed upon diagnosis with MS.
“Our study design cannot give insights into mechanisms that might explain the association [between males with GIDs and MS]. However, there is evidence suggesting an association between gonadal hormones and MS, including animal models suggesting anti-inflammatory and/or neuroprotective actions of testosterone, studies indicating a high prevalence of hypogonadism in male MS patients, and improved cognitive function and slowed brain atrophy in a small pilot trial of testosterone,” the researchers noted.
The adjusted rate ratio of MS following GID in males was 6.63 (P = .0002), compared with 1.44 in females (P = .58). The adjusted rate ratios were based on 4 observed cases and 0.6 expected cases of MS in males and 5 observed cases and 3.5 expected cases of MS in females.
The authors reported no conflicts of interest.
Read the study in Multiple Sclerosis Journal (doi: 10.1177/1352458515627205).
An association between gender identity disorders (GIDs) and subsequent multiple sclerosis (MS) in males was found in an analysis of linked English Hospital Episode Statistics and mortality data from January 1999 to March 2012.
The findings “suggest that low testosterone levels and/or feminising gonadal hormones might influence MS risk in some men and highlight a need for further work to explore any potential role for gonadal hormones in management and/or prevention strategies,” wrote Dr. Julia Pakpoor of the Unit of Health-Care Epidemiology, Nuffield Department of Population Health, at University of Oxford (England).
She and her colleagues used the patient data to construct male and female cohorts (1,157 patients and 2,390 patients, respectively) of patients with GIDs. A patient was included in one of the two GID cohorts if he or she had an episode of care or hospital admission in which a GID or sexual transformation procedure was coded in any diagnostic position.
For males with GIDs transitioning to females, the most studied treatment regimen involves using feminizing hormones and anti-androgens, which reduce testosterone secretion or neutralize testosterone activity, the researchers noted.
They also used the database to construct male and female cohorts (4.6 million patients and 3.4 million patients, respectively) to serve as two control groups. For patients to be included in the control groups, they needed to have been first admitted to a hospital for a minor condition and to never have been admitted to a hospital for MS. Patients who had been admitted to a hospital for MS either before or at the same time they were admitted for GIDs were excluded from the GID cohorts. A patient stopped being followed upon diagnosis with MS.
“Our study design cannot give insights into mechanisms that might explain the association [between males with GIDs and MS]. However, there is evidence suggesting an association between gonadal hormones and MS, including animal models suggesting anti-inflammatory and/or neuroprotective actions of testosterone, studies indicating a high prevalence of hypogonadism in male MS patients, and improved cognitive function and slowed brain atrophy in a small pilot trial of testosterone,” the researchers noted.
The adjusted rate ratio of MS following GID in males was 6.63 (P = .0002), compared with 1.44 in females (P = .58). The adjusted rate ratios were based on 4 observed cases and 0.6 expected cases of MS in males and 5 observed cases and 3.5 expected cases of MS in females.
The authors reported no conflicts of interest.
Read the study in Multiple Sclerosis Journal (doi: 10.1177/1352458515627205).
An association between gender identity disorders (GIDs) and subsequent multiple sclerosis (MS) in males was found in an analysis of linked English Hospital Episode Statistics and mortality data from January 1999 to March 2012.
The findings “suggest that low testosterone levels and/or feminising gonadal hormones might influence MS risk in some men and highlight a need for further work to explore any potential role for gonadal hormones in management and/or prevention strategies,” wrote Dr. Julia Pakpoor of the Unit of Health-Care Epidemiology, Nuffield Department of Population Health, at University of Oxford (England).
She and her colleagues used the patient data to construct male and female cohorts (1,157 patients and 2,390 patients, respectively) of patients with GIDs. A patient was included in one of the two GID cohorts if he or she had an episode of care or hospital admission in which a GID or sexual transformation procedure was coded in any diagnostic position.
For males with GIDs transitioning to females, the most studied treatment regimen involves using feminizing hormones and anti-androgens, which reduce testosterone secretion or neutralize testosterone activity, the researchers noted.
They also used the database to construct male and female cohorts (4.6 million patients and 3.4 million patients, respectively) to serve as two control groups. For patients to be included in the control groups, they needed to have been first admitted to a hospital for a minor condition and to never have been admitted to a hospital for MS. Patients who had been admitted to a hospital for MS either before or at the same time they were admitted for GIDs were excluded from the GID cohorts. A patient stopped being followed upon diagnosis with MS.
“Our study design cannot give insights into mechanisms that might explain the association [between males with GIDs and MS]. However, there is evidence suggesting an association between gonadal hormones and MS, including animal models suggesting anti-inflammatory and/or neuroprotective actions of testosterone, studies indicating a high prevalence of hypogonadism in male MS patients, and improved cognitive function and slowed brain atrophy in a small pilot trial of testosterone,” the researchers noted.
The adjusted rate ratio of MS following GID in males was 6.63 (P = .0002), compared with 1.44 in females (P = .58). The adjusted rate ratios were based on 4 observed cases and 0.6 expected cases of MS in males and 5 observed cases and 3.5 expected cases of MS in females.
The authors reported no conflicts of interest.
Read the study in Multiple Sclerosis Journal (doi: 10.1177/1352458515627205).
FROM MULTIPLE SCLEROSIS JOURNAL
Endocrine Society issues first-ever guidelines for primary adrenal insufficiency
New guidelines on the diagnosis and management of primary adrenal insufficiency stress the importance of early recognition and the need to prevent life-threatening adrenal crises in these patients.
These are the first clinical practice guidelines on primary adrenal insufficiency (PAI), also known as Addison’s disease, issued by Endocrine Society (J Clin Endocrinol Metab. 2016 Jan 13:jc20151710 [Epub ahead of print]).
“Because it’s a rare disease and symptoms can mimic common conditions, adrenal insufficiency is often, at least initially, overlooked,” guideline co-author Dr. Deborah Merke, a senior investigator with the National Institutes of Health Clinical Center in Bethesda, Md., said. “So the main goal of these clinical practice guidelines is to improve patient care.”
The guidelines suggest clinicians should have a low diagnostic threshold in acutely ill patients with unexplained symptoms or signs suggestive of PAI such as volume depletion, hypotension, hyponatremia, hyperkalemia, fever, abdominal pain, hyperpigmentation, or, especially in children, hypoglycemia.
This low diagnostic threshold for PAI should also be extended to pregnant women with unexplained persistent nausea, fatigue, and hypotension.
For adult patients with a suspected adrenal crisis, an immediate parenteral injection of hydrocortisone 100 mg should be given, followed by appropriate fluid resuscitation and 200 mg of hydrocortisone for 24 hours, according to the guidelines, which were co-sponsored by the European Society of Endocrinology and American Association for Clinical Chemistry.
Despite a known association between adrenal crisis and mortality, there is a knowledge gap regarding how to prevent, recognize, and reduce the risk of these life-threatening events, Dr. Merke said.
To that end, the task force has taken a page from the diabetes community in recommending all PAI patients carry steroid emergency identification cards and be equipped with a glucocorticoid injection kit for emergency use and be educated on how to use it.
The guidelines also advocate education about stress dosing to counter the increased demand for corticosteroids during periods of stress, which can encompass something as common as the flu.
“Just like diabetics carry around emergency medicines, it’s important for patients with adrenal insufficiency to carry around an emergency kit and to realize that should they start to get sick, they need to increase their doses,” she said. “There often seems to be a lack of awareness among physicians as well that these patients have a potentially life-threatening condition, should they get a common illness.”
One of the key unanswered clinical questions the task force sought to address was whether the widely used high-dose (250 mcg) corticotropin stimulation test, also known as the adrenocorticotropin (ACTH) or short Synacthen test, should be replaced by the low-dose test (1 mcg) to diagnosis PAI.
Despite a review of published data and a systematic review commissioned by the task force, “We didn’t come up with much scientific evidence to say we should be changing the historic standard,” Dr. Merke said.
The systematic review identified only five studies of high-dose corticotropin testing specifically in PAI and none of low-dose testing. The low-dose test has shown higher sensitivity in the detection of adrenal insufficiency in critically ill patients and secondary adrenal insufficiency, but the limited available data suggest it does not provide better diagnostic accuracy for PAI than the high-dose test.
As a result, the guidelines recommend the standard, short corticotropin test (250 mcg for adults and children aged at least 2 years) as the “gold standard” diagnostic test to establish a PAI diagnosis.
The low-dose (1 mcg) test is recommended only when corticotropin is in short supply, which is not typically a problem in the United States, she said.
If corticotropin testing isn’t feasible, a combination of a morning plasma ACTH and cortisol levels (less than 5 mcg/dL) can be used as an initial screening, though confirmatory testing with corticotropin stimulation is strongly recommended.
Glucocorticoid therapy is recommended in all patients with confirmed PAI based on the highest quality of evidence, with a clear preference given for the short-acting steroids, Dr. Merke observed.
Hydrocortisone 15 mg-25 mg or cortisone acetate 20 mg-35 mg given in two to three divided doses per day is suggested for adults, with the highest dose to be given in the morning. Once- or twice-daily prednisolone 3 mg-5 mg is suggested as an alternative.
Hydrocortisone is also suggested over cortisone acetate, prednisolone, or prednisone for pregnant women and recommended for children (about 8 mg/m2 per day), but the evidence supporting these items was of low quality.
The guidelines suggest against using dexamethasone, the longest-acting glucocorticoid, because of the potential long-term side effects of overt-treatment and the frequent appearance of cushingoid side effects. They also recommend against dexamethasone in pregnant women because it is not inactivated in the placenta.
The guidelines are also quite clear in their suggestion against hormonal monitoring of glucocorticoid replacement and instead favor adjusting treatment based only on clinical response.
“This is a very important suggestion that we made because often clinicians use ACTH to adjust doses and this commonly results in overreplacement and there are side effects to overreplacement,” including weight gain, insomnia, and peripheral edema, Dr. Merke said.
A second systematic review commissioned by the task force involving 15 observational studies of glucocorticoid replacement regimens uncovered very sparse data on mortality, bone density, and incidence of adrenal crisis.
It has been suggested that newer extended-release and dual-release glucocorticoid formulations may result in higher health-reality quality of life than once-, twice-, or thrice-daily regimens, but once again, the evidence was insufficient to support a specific recommendation.
Dr. Merke acknowledged that many of the guidelines recommendations were ungraded or best practices, reflecting the lack of randomized clinical trials in PAI.
“I think that’s why it was so important for us to do this,” she said. “We had a group of experts that were very familiar with this disease providing guidance, but I think it’s also one reason why physicians out there in practice get confused about exactly what to do because of the lack of hard evidence. ... It does certainly cry for the need for more studies in these rare diseases.”
The guidelines were funded by the Endocrine Society, and the authors reported receiving no external funding or remuneration.
New guidelines on the diagnosis and management of primary adrenal insufficiency stress the importance of early recognition and the need to prevent life-threatening adrenal crises in these patients.
These are the first clinical practice guidelines on primary adrenal insufficiency (PAI), also known as Addison’s disease, issued by Endocrine Society (J Clin Endocrinol Metab. 2016 Jan 13:jc20151710 [Epub ahead of print]).
“Because it’s a rare disease and symptoms can mimic common conditions, adrenal insufficiency is often, at least initially, overlooked,” guideline co-author Dr. Deborah Merke, a senior investigator with the National Institutes of Health Clinical Center in Bethesda, Md., said. “So the main goal of these clinical practice guidelines is to improve patient care.”
The guidelines suggest clinicians should have a low diagnostic threshold in acutely ill patients with unexplained symptoms or signs suggestive of PAI such as volume depletion, hypotension, hyponatremia, hyperkalemia, fever, abdominal pain, hyperpigmentation, or, especially in children, hypoglycemia.
This low diagnostic threshold for PAI should also be extended to pregnant women with unexplained persistent nausea, fatigue, and hypotension.
For adult patients with a suspected adrenal crisis, an immediate parenteral injection of hydrocortisone 100 mg should be given, followed by appropriate fluid resuscitation and 200 mg of hydrocortisone for 24 hours, according to the guidelines, which were co-sponsored by the European Society of Endocrinology and American Association for Clinical Chemistry.
Despite a known association between adrenal crisis and mortality, there is a knowledge gap regarding how to prevent, recognize, and reduce the risk of these life-threatening events, Dr. Merke said.
To that end, the task force has taken a page from the diabetes community in recommending all PAI patients carry steroid emergency identification cards and be equipped with a glucocorticoid injection kit for emergency use and be educated on how to use it.
The guidelines also advocate education about stress dosing to counter the increased demand for corticosteroids during periods of stress, which can encompass something as common as the flu.
“Just like diabetics carry around emergency medicines, it’s important for patients with adrenal insufficiency to carry around an emergency kit and to realize that should they start to get sick, they need to increase their doses,” she said. “There often seems to be a lack of awareness among physicians as well that these patients have a potentially life-threatening condition, should they get a common illness.”
One of the key unanswered clinical questions the task force sought to address was whether the widely used high-dose (250 mcg) corticotropin stimulation test, also known as the adrenocorticotropin (ACTH) or short Synacthen test, should be replaced by the low-dose test (1 mcg) to diagnosis PAI.
Despite a review of published data and a systematic review commissioned by the task force, “We didn’t come up with much scientific evidence to say we should be changing the historic standard,” Dr. Merke said.
The systematic review identified only five studies of high-dose corticotropin testing specifically in PAI and none of low-dose testing. The low-dose test has shown higher sensitivity in the detection of adrenal insufficiency in critically ill patients and secondary adrenal insufficiency, but the limited available data suggest it does not provide better diagnostic accuracy for PAI than the high-dose test.
As a result, the guidelines recommend the standard, short corticotropin test (250 mcg for adults and children aged at least 2 years) as the “gold standard” diagnostic test to establish a PAI diagnosis.
The low-dose (1 mcg) test is recommended only when corticotropin is in short supply, which is not typically a problem in the United States, she said.
If corticotropin testing isn’t feasible, a combination of a morning plasma ACTH and cortisol levels (less than 5 mcg/dL) can be used as an initial screening, though confirmatory testing with corticotropin stimulation is strongly recommended.
Glucocorticoid therapy is recommended in all patients with confirmed PAI based on the highest quality of evidence, with a clear preference given for the short-acting steroids, Dr. Merke observed.
Hydrocortisone 15 mg-25 mg or cortisone acetate 20 mg-35 mg given in two to three divided doses per day is suggested for adults, with the highest dose to be given in the morning. Once- or twice-daily prednisolone 3 mg-5 mg is suggested as an alternative.
Hydrocortisone is also suggested over cortisone acetate, prednisolone, or prednisone for pregnant women and recommended for children (about 8 mg/m2 per day), but the evidence supporting these items was of low quality.
The guidelines suggest against using dexamethasone, the longest-acting glucocorticoid, because of the potential long-term side effects of overt-treatment and the frequent appearance of cushingoid side effects. They also recommend against dexamethasone in pregnant women because it is not inactivated in the placenta.
The guidelines are also quite clear in their suggestion against hormonal monitoring of glucocorticoid replacement and instead favor adjusting treatment based only on clinical response.
“This is a very important suggestion that we made because often clinicians use ACTH to adjust doses and this commonly results in overreplacement and there are side effects to overreplacement,” including weight gain, insomnia, and peripheral edema, Dr. Merke said.
A second systematic review commissioned by the task force involving 15 observational studies of glucocorticoid replacement regimens uncovered very sparse data on mortality, bone density, and incidence of adrenal crisis.
It has been suggested that newer extended-release and dual-release glucocorticoid formulations may result in higher health-reality quality of life than once-, twice-, or thrice-daily regimens, but once again, the evidence was insufficient to support a specific recommendation.
Dr. Merke acknowledged that many of the guidelines recommendations were ungraded or best practices, reflecting the lack of randomized clinical trials in PAI.
“I think that’s why it was so important for us to do this,” she said. “We had a group of experts that were very familiar with this disease providing guidance, but I think it’s also one reason why physicians out there in practice get confused about exactly what to do because of the lack of hard evidence. ... It does certainly cry for the need for more studies in these rare diseases.”
The guidelines were funded by the Endocrine Society, and the authors reported receiving no external funding or remuneration.
New guidelines on the diagnosis and management of primary adrenal insufficiency stress the importance of early recognition and the need to prevent life-threatening adrenal crises in these patients.
These are the first clinical practice guidelines on primary adrenal insufficiency (PAI), also known as Addison’s disease, issued by Endocrine Society (J Clin Endocrinol Metab. 2016 Jan 13:jc20151710 [Epub ahead of print]).
“Because it’s a rare disease and symptoms can mimic common conditions, adrenal insufficiency is often, at least initially, overlooked,” guideline co-author Dr. Deborah Merke, a senior investigator with the National Institutes of Health Clinical Center in Bethesda, Md., said. “So the main goal of these clinical practice guidelines is to improve patient care.”
The guidelines suggest clinicians should have a low diagnostic threshold in acutely ill patients with unexplained symptoms or signs suggestive of PAI such as volume depletion, hypotension, hyponatremia, hyperkalemia, fever, abdominal pain, hyperpigmentation, or, especially in children, hypoglycemia.
This low diagnostic threshold for PAI should also be extended to pregnant women with unexplained persistent nausea, fatigue, and hypotension.
For adult patients with a suspected adrenal crisis, an immediate parenteral injection of hydrocortisone 100 mg should be given, followed by appropriate fluid resuscitation and 200 mg of hydrocortisone for 24 hours, according to the guidelines, which were co-sponsored by the European Society of Endocrinology and American Association for Clinical Chemistry.
Despite a known association between adrenal crisis and mortality, there is a knowledge gap regarding how to prevent, recognize, and reduce the risk of these life-threatening events, Dr. Merke said.
To that end, the task force has taken a page from the diabetes community in recommending all PAI patients carry steroid emergency identification cards and be equipped with a glucocorticoid injection kit for emergency use and be educated on how to use it.
The guidelines also advocate education about stress dosing to counter the increased demand for corticosteroids during periods of stress, which can encompass something as common as the flu.
“Just like diabetics carry around emergency medicines, it’s important for patients with adrenal insufficiency to carry around an emergency kit and to realize that should they start to get sick, they need to increase their doses,” she said. “There often seems to be a lack of awareness among physicians as well that these patients have a potentially life-threatening condition, should they get a common illness.”
One of the key unanswered clinical questions the task force sought to address was whether the widely used high-dose (250 mcg) corticotropin stimulation test, also known as the adrenocorticotropin (ACTH) or short Synacthen test, should be replaced by the low-dose test (1 mcg) to diagnosis PAI.
Despite a review of published data and a systematic review commissioned by the task force, “We didn’t come up with much scientific evidence to say we should be changing the historic standard,” Dr. Merke said.
The systematic review identified only five studies of high-dose corticotropin testing specifically in PAI and none of low-dose testing. The low-dose test has shown higher sensitivity in the detection of adrenal insufficiency in critically ill patients and secondary adrenal insufficiency, but the limited available data suggest it does not provide better diagnostic accuracy for PAI than the high-dose test.
As a result, the guidelines recommend the standard, short corticotropin test (250 mcg for adults and children aged at least 2 years) as the “gold standard” diagnostic test to establish a PAI diagnosis.
The low-dose (1 mcg) test is recommended only when corticotropin is in short supply, which is not typically a problem in the United States, she said.
If corticotropin testing isn’t feasible, a combination of a morning plasma ACTH and cortisol levels (less than 5 mcg/dL) can be used as an initial screening, though confirmatory testing with corticotropin stimulation is strongly recommended.
Glucocorticoid therapy is recommended in all patients with confirmed PAI based on the highest quality of evidence, with a clear preference given for the short-acting steroids, Dr. Merke observed.
Hydrocortisone 15 mg-25 mg or cortisone acetate 20 mg-35 mg given in two to three divided doses per day is suggested for adults, with the highest dose to be given in the morning. Once- or twice-daily prednisolone 3 mg-5 mg is suggested as an alternative.
Hydrocortisone is also suggested over cortisone acetate, prednisolone, or prednisone for pregnant women and recommended for children (about 8 mg/m2 per day), but the evidence supporting these items was of low quality.
The guidelines suggest against using dexamethasone, the longest-acting glucocorticoid, because of the potential long-term side effects of overt-treatment and the frequent appearance of cushingoid side effects. They also recommend against dexamethasone in pregnant women because it is not inactivated in the placenta.
The guidelines are also quite clear in their suggestion against hormonal monitoring of glucocorticoid replacement and instead favor adjusting treatment based only on clinical response.
“This is a very important suggestion that we made because often clinicians use ACTH to adjust doses and this commonly results in overreplacement and there are side effects to overreplacement,” including weight gain, insomnia, and peripheral edema, Dr. Merke said.
A second systematic review commissioned by the task force involving 15 observational studies of glucocorticoid replacement regimens uncovered very sparse data on mortality, bone density, and incidence of adrenal crisis.
It has been suggested that newer extended-release and dual-release glucocorticoid formulations may result in higher health-reality quality of life than once-, twice-, or thrice-daily regimens, but once again, the evidence was insufficient to support a specific recommendation.
Dr. Merke acknowledged that many of the guidelines recommendations were ungraded or best practices, reflecting the lack of randomized clinical trials in PAI.
“I think that’s why it was so important for us to do this,” she said. “We had a group of experts that were very familiar with this disease providing guidance, but I think it’s also one reason why physicians out there in practice get confused about exactly what to do because of the lack of hard evidence. ... It does certainly cry for the need for more studies in these rare diseases.”
The guidelines were funded by the Endocrine Society, and the authors reported receiving no external funding or remuneration.
FROM THE JOURNAL OF CLINICAL ENDOCRINOLOGY & METABOLISM
Novel agent for adult GH can be administered once weekly
Use of a novel reversible albumin-binding human growth hormone (GH) derivative administered subcutaneously once weekly for 4 weeks was safe and effective in adults with growth hormone deficiency, according to a phase I, randomized, open-label trial.
Results from a recent clinical trial of the agent, known as NNC0195-0092 and being developed by Norvo Nordisk, indicated the feasibility of a once-weekly dosing regimen in healthy men (J Clin Endocrinol Metab. 2014;99:E1819-29). The purpose of the current study was to report the first data obtained from a multiple-dose trial of NNC0195-0092 conducted in men and women at three hospitals in Denmark and one in Sweden.
“GH is currently administered as daily subcutaneous injections; however, a long-acting GH formulation that decreases injection frequency may improve treatment adherence and reduce the inconvenience associated with daily injections,” researchers led by Dr. Michael Højby Rasmussen wrote in the article published online Jan. 4 in the Journal of Clinical Endocrinology and Metabolism (2016. doi: 10.1210/jc.2015-1991). They went on to note that the plasma half-life of therapeutic peptides such as GH can be extended through binding to serum albumin, which “has a high affinity and binding capacity for fatty acids, and acylation of fatty acids to therapeutic proteins has been used to facilitate binding of these molecules to circulating albumin. In NNC0195-0092, fatty acids with noncovalent albumin-binding properties have been attached by acylation.”
Dr. Rasmussen of Novo Nordisk, Denmark, and his associates reported results from 25 men and nine women with a mean age of 53 years who were assigned into four cohorts of eight subjects and randomized to receive once-weekly NNC0195-0092 for 4 weeks in doses that ranged from 0.02 to 0.12 mg/kg, or daily injections of Norditropin NordiFlex for 4 weeks with a dose replicating the pretrial dose of somatropin. They found that the number of adverse events was similar at the 0.02, 0.04, and 0.08 mg/kg doses of NNC0195-0092, compared with the daily injections of Norditropin NordiFlex, while the number of adverse events was greatest at the 0.12 mg/kg dose of NNC0195-0092.
“No clinically significant safety and tolerability signals causally related to NNC0195-0092 were identified, nor were any immunogenicity concerns revealed,” the investigators concluded. “The IGF-I profiles were consistent with a once-weekly treatment profile of NNC0195-0092 at a starting dose of 0.02-0.04 mg/kg/wk.”
The trial was supported by Novo Nordisk. Dr. Rasmussen disclosed that he is an employee of the company.
Use of a novel reversible albumin-binding human growth hormone (GH) derivative administered subcutaneously once weekly for 4 weeks was safe and effective in adults with growth hormone deficiency, according to a phase I, randomized, open-label trial.
Results from a recent clinical trial of the agent, known as NNC0195-0092 and being developed by Norvo Nordisk, indicated the feasibility of a once-weekly dosing regimen in healthy men (J Clin Endocrinol Metab. 2014;99:E1819-29). The purpose of the current study was to report the first data obtained from a multiple-dose trial of NNC0195-0092 conducted in men and women at three hospitals in Denmark and one in Sweden.
“GH is currently administered as daily subcutaneous injections; however, a long-acting GH formulation that decreases injection frequency may improve treatment adherence and reduce the inconvenience associated with daily injections,” researchers led by Dr. Michael Højby Rasmussen wrote in the article published online Jan. 4 in the Journal of Clinical Endocrinology and Metabolism (2016. doi: 10.1210/jc.2015-1991). They went on to note that the plasma half-life of therapeutic peptides such as GH can be extended through binding to serum albumin, which “has a high affinity and binding capacity for fatty acids, and acylation of fatty acids to therapeutic proteins has been used to facilitate binding of these molecules to circulating albumin. In NNC0195-0092, fatty acids with noncovalent albumin-binding properties have been attached by acylation.”
Dr. Rasmussen of Novo Nordisk, Denmark, and his associates reported results from 25 men and nine women with a mean age of 53 years who were assigned into four cohorts of eight subjects and randomized to receive once-weekly NNC0195-0092 for 4 weeks in doses that ranged from 0.02 to 0.12 mg/kg, or daily injections of Norditropin NordiFlex for 4 weeks with a dose replicating the pretrial dose of somatropin. They found that the number of adverse events was similar at the 0.02, 0.04, and 0.08 mg/kg doses of NNC0195-0092, compared with the daily injections of Norditropin NordiFlex, while the number of adverse events was greatest at the 0.12 mg/kg dose of NNC0195-0092.
“No clinically significant safety and tolerability signals causally related to NNC0195-0092 were identified, nor were any immunogenicity concerns revealed,” the investigators concluded. “The IGF-I profiles were consistent with a once-weekly treatment profile of NNC0195-0092 at a starting dose of 0.02-0.04 mg/kg/wk.”
The trial was supported by Novo Nordisk. Dr. Rasmussen disclosed that he is an employee of the company.
Use of a novel reversible albumin-binding human growth hormone (GH) derivative administered subcutaneously once weekly for 4 weeks was safe and effective in adults with growth hormone deficiency, according to a phase I, randomized, open-label trial.
Results from a recent clinical trial of the agent, known as NNC0195-0092 and being developed by Norvo Nordisk, indicated the feasibility of a once-weekly dosing regimen in healthy men (J Clin Endocrinol Metab. 2014;99:E1819-29). The purpose of the current study was to report the first data obtained from a multiple-dose trial of NNC0195-0092 conducted in men and women at three hospitals in Denmark and one in Sweden.
“GH is currently administered as daily subcutaneous injections; however, a long-acting GH formulation that decreases injection frequency may improve treatment adherence and reduce the inconvenience associated with daily injections,” researchers led by Dr. Michael Højby Rasmussen wrote in the article published online Jan. 4 in the Journal of Clinical Endocrinology and Metabolism (2016. doi: 10.1210/jc.2015-1991). They went on to note that the plasma half-life of therapeutic peptides such as GH can be extended through binding to serum albumin, which “has a high affinity and binding capacity for fatty acids, and acylation of fatty acids to therapeutic proteins has been used to facilitate binding of these molecules to circulating albumin. In NNC0195-0092, fatty acids with noncovalent albumin-binding properties have been attached by acylation.”
Dr. Rasmussen of Novo Nordisk, Denmark, and his associates reported results from 25 men and nine women with a mean age of 53 years who were assigned into four cohorts of eight subjects and randomized to receive once-weekly NNC0195-0092 for 4 weeks in doses that ranged from 0.02 to 0.12 mg/kg, or daily injections of Norditropin NordiFlex for 4 weeks with a dose replicating the pretrial dose of somatropin. They found that the number of adverse events was similar at the 0.02, 0.04, and 0.08 mg/kg doses of NNC0195-0092, compared with the daily injections of Norditropin NordiFlex, while the number of adverse events was greatest at the 0.12 mg/kg dose of NNC0195-0092.
“No clinically significant safety and tolerability signals causally related to NNC0195-0092 were identified, nor were any immunogenicity concerns revealed,” the investigators concluded. “The IGF-I profiles were consistent with a once-weekly treatment profile of NNC0195-0092 at a starting dose of 0.02-0.04 mg/kg/wk.”
The trial was supported by Novo Nordisk. Dr. Rasmussen disclosed that he is an employee of the company.
FROM THE JOURNAL OF CLINICAL ENDOCRINOLOGY AND METABOLISM
Key clinical point: Four once-weekly doses of NNC0195-0092 administered to patients with adult growth hormone deficiency were well tolerated.
Major finding: The number of adverse events was similar at the 0.02, 0.04, and 0.08 mg/kg doses of NNC0195-0092, compared with the daily injections of Norditropin NordiFlex, while the number of adverse events was greatest at the 0.12 mg/kg dose of NNC0195-0092.
Data source: A phase I, open-label, randomized study that set out to evaluate the safety and tolerability of multiple once-weekly doses of NNC0195-0092, compared with daily GH in 34 patients with adult growth hormone deficiency.
Disclosures: The trial was supported by Novo Nordisk. Dr. Rasmussen disclosed that he is an employee of the company.
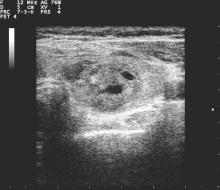
Wide variation in clinical management of thyroid nodules seen in first-ever survey
LAKE BUENA VISTA, FLA. – When making diagnostic and treatment decisions about thyroid nodules, many endocrinologists are not following current clinical practice guidelines, according to a recent survey. Further, according to a recent international survey of endocrinologists, there is wide regional variation in the use of molecular testing and calcitonin levels.
Dr. Nicole Vietor of the department of endocrinology at Walter Reed National Military Medical Center, Bethesda, Md., and her collaborators contacted members of the American Thyroid Association (ATA), the Endocrine Society (TES), and the American Association of Clinical Endocrinologists (AACE). Members of these societies were contacted directly by investigators and asked to complete a web-based survey regarding their practices for diagnosing and managing thyroid nodules.
The survey consisted of 36 questions, with an index case with variations presented to respondents, who then answered questions about diagnostic and management decisionmaking practices. The hypothetical index patient was a 52 year old woman with an incidental finding of a 1.5 cm right thyroid nodule. The patient was healthy and without risk factors; the patient’s nodule was not palpable on physical exam and she had no cervical lymphadenopathy.
Almost all respondents (99.4%) would order a thyroid-stimulating hormone for initial lab testing. Other commonly ordered exams included free T4 levels and thyroid peroxidase antibody requested by 41.5% and 24.3% of respondents, respectively. Fewer than 15% of respondents would have ordered any further lab exams.
All but 1.5% of respondents would order an anatomic or functional test for this index patient, with 57.2% ordering a thyroid ultrasound to be performed in radiology and 52.1% ordering an ultrasound in clinic (multiple responses were permitted). Cervical lymph nodes were included in the initial ultrasound assessment by 68.5% of respondents. Overall, more than half (56.6%) of thyroid ultrasounds were performed by endocrinologists, and about a third (31.9%) done by radiologists.
Practice variation from guidelines became apparent when respondents were asked how various nodule characteristics affected the decision to perform a fine needle aspiration (FNA). For a 1.5-cm solid hypoechoic nodule, 93.8% of respondents would perform FNA, while two thirds (67.0%) would perform an FNA for a 0.7-cm hypoechoic nodule with microcalcifications.
When performing FNAs, 83.3% of respondents use ultrasound to guide the biopsy, with most operators performing two (19.2%), three (28.5%), or four (23.0%) passes per nodule.
Of the 897 respondents, 80.5% were TES members, 56.5% were AACE members, and 44.5% were ATA members; most respondents belonged to more than one society. Almost two thirds of respondents (63.0%) were from North America, while 12.2% were from Europe, 10.8% were from Latin America, 6.5% were from Asia, 5.6% were from the Middle East or Africa, and just 1.9% were from Oceania. More men (60.2%) than women responded.
The AACE issued clinical practice guidelines for the management of thyroid nodules in 2010, as did the ATA in 2009 and 2015.
“In summary, management of a thyroid nodule is highly variable and differs from societal guidelines in multiple areas,” wrote Dr. Vietor and her colleagues in the presentation abstract.
On Twitter @karioakes
LAKE BUENA VISTA, FLA. – When making diagnostic and treatment decisions about thyroid nodules, many endocrinologists are not following current clinical practice guidelines, according to a recent survey. Further, according to a recent international survey of endocrinologists, there is wide regional variation in the use of molecular testing and calcitonin levels.
Dr. Nicole Vietor of the department of endocrinology at Walter Reed National Military Medical Center, Bethesda, Md., and her collaborators contacted members of the American Thyroid Association (ATA), the Endocrine Society (TES), and the American Association of Clinical Endocrinologists (AACE). Members of these societies were contacted directly by investigators and asked to complete a web-based survey regarding their practices for diagnosing and managing thyroid nodules.
The survey consisted of 36 questions, with an index case with variations presented to respondents, who then answered questions about diagnostic and management decisionmaking practices. The hypothetical index patient was a 52 year old woman with an incidental finding of a 1.5 cm right thyroid nodule. The patient was healthy and without risk factors; the patient’s nodule was not palpable on physical exam and she had no cervical lymphadenopathy.
Almost all respondents (99.4%) would order a thyroid-stimulating hormone for initial lab testing. Other commonly ordered exams included free T4 levels and thyroid peroxidase antibody requested by 41.5% and 24.3% of respondents, respectively. Fewer than 15% of respondents would have ordered any further lab exams.
All but 1.5% of respondents would order an anatomic or functional test for this index patient, with 57.2% ordering a thyroid ultrasound to be performed in radiology and 52.1% ordering an ultrasound in clinic (multiple responses were permitted). Cervical lymph nodes were included in the initial ultrasound assessment by 68.5% of respondents. Overall, more than half (56.6%) of thyroid ultrasounds were performed by endocrinologists, and about a third (31.9%) done by radiologists.
Practice variation from guidelines became apparent when respondents were asked how various nodule characteristics affected the decision to perform a fine needle aspiration (FNA). For a 1.5-cm solid hypoechoic nodule, 93.8% of respondents would perform FNA, while two thirds (67.0%) would perform an FNA for a 0.7-cm hypoechoic nodule with microcalcifications.
When performing FNAs, 83.3% of respondents use ultrasound to guide the biopsy, with most operators performing two (19.2%), three (28.5%), or four (23.0%) passes per nodule.
Of the 897 respondents, 80.5% were TES members, 56.5% were AACE members, and 44.5% were ATA members; most respondents belonged to more than one society. Almost two thirds of respondents (63.0%) were from North America, while 12.2% were from Europe, 10.8% were from Latin America, 6.5% were from Asia, 5.6% were from the Middle East or Africa, and just 1.9% were from Oceania. More men (60.2%) than women responded.
The AACE issued clinical practice guidelines for the management of thyroid nodules in 2010, as did the ATA in 2009 and 2015.
“In summary, management of a thyroid nodule is highly variable and differs from societal guidelines in multiple areas,” wrote Dr. Vietor and her colleagues in the presentation abstract.
On Twitter @karioakes
LAKE BUENA VISTA, FLA. – When making diagnostic and treatment decisions about thyroid nodules, many endocrinologists are not following current clinical practice guidelines, according to a recent survey. Further, according to a recent international survey of endocrinologists, there is wide regional variation in the use of molecular testing and calcitonin levels.
Dr. Nicole Vietor of the department of endocrinology at Walter Reed National Military Medical Center, Bethesda, Md., and her collaborators contacted members of the American Thyroid Association (ATA), the Endocrine Society (TES), and the American Association of Clinical Endocrinologists (AACE). Members of these societies were contacted directly by investigators and asked to complete a web-based survey regarding their practices for diagnosing and managing thyroid nodules.
The survey consisted of 36 questions, with an index case with variations presented to respondents, who then answered questions about diagnostic and management decisionmaking practices. The hypothetical index patient was a 52 year old woman with an incidental finding of a 1.5 cm right thyroid nodule. The patient was healthy and without risk factors; the patient’s nodule was not palpable on physical exam and she had no cervical lymphadenopathy.
Almost all respondents (99.4%) would order a thyroid-stimulating hormone for initial lab testing. Other commonly ordered exams included free T4 levels and thyroid peroxidase antibody requested by 41.5% and 24.3% of respondents, respectively. Fewer than 15% of respondents would have ordered any further lab exams.
All but 1.5% of respondents would order an anatomic or functional test for this index patient, with 57.2% ordering a thyroid ultrasound to be performed in radiology and 52.1% ordering an ultrasound in clinic (multiple responses were permitted). Cervical lymph nodes were included in the initial ultrasound assessment by 68.5% of respondents. Overall, more than half (56.6%) of thyroid ultrasounds were performed by endocrinologists, and about a third (31.9%) done by radiologists.
Practice variation from guidelines became apparent when respondents were asked how various nodule characteristics affected the decision to perform a fine needle aspiration (FNA). For a 1.5-cm solid hypoechoic nodule, 93.8% of respondents would perform FNA, while two thirds (67.0%) would perform an FNA for a 0.7-cm hypoechoic nodule with microcalcifications.
When performing FNAs, 83.3% of respondents use ultrasound to guide the biopsy, with most operators performing two (19.2%), three (28.5%), or four (23.0%) passes per nodule.
Of the 897 respondents, 80.5% were TES members, 56.5% were AACE members, and 44.5% were ATA members; most respondents belonged to more than one society. Almost two thirds of respondents (63.0%) were from North America, while 12.2% were from Europe, 10.8% were from Latin America, 6.5% were from Asia, 5.6% were from the Middle East or Africa, and just 1.9% were from Oceania. More men (60.2%) than women responded.
The AACE issued clinical practice guidelines for the management of thyroid nodules in 2010, as did the ATA in 2009 and 2015.
“In summary, management of a thyroid nodule is highly variable and differs from societal guidelines in multiple areas,” wrote Dr. Vietor and her colleagues in the presentation abstract.
On Twitter @karioakes
AT THE 15TH INTERNATIONAL THYROID CONGRESS
Key clinical point: A first-ever international survey of endocrinologists showed wide variation in clinical management of thyroid nodules.
Major finding: Respondents reported performing more fine needle aspiration (FNA) biopsies of thyroid nodules than recommended by practice guidelines.
Data source: Web-based survey of 897 members of three different professional organizations.
Disclosures: No disclosures were identified.
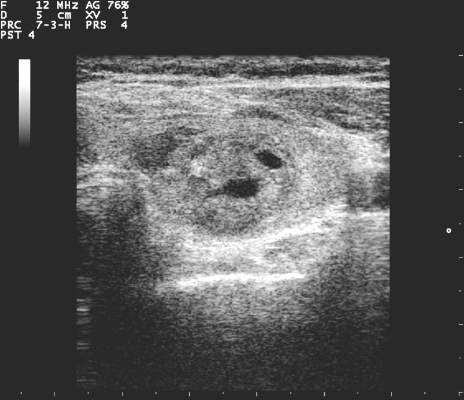
Core needle biopsy proves sensitive for first-line thyroid nodule diagnosis
LAKE BUENA VISTA, FLA. – The nondiagnostic result rate was significantly lower with core needle biopsy than with fine needle aspiration as a first-line biopsy method for newly detected thyroid nodules in a comparative study.
In 631 pairs of initially detected thyroid nodules that were matched based on propensity score analysis, the nondiagnostic result rate was 1.4% when core needle biopsy (CNB) was used, compared with 8.1% with ultrasound-guided fine-needle aspiration. The indeterminate result rate was 5.1% vs. 8.1% with the two approaches, respectively, and the differences between the groups were statistically significant, Dr. Hyun Kyung Lim of Soonchunhyang University Seoul Hospital, Korea, reported at the International Thyroid Congress.
The nondiagnostic rate with CNB was also significantly lower than with fine-needle aspiration for nodules with calcifications, posterior location, or diameter less than 1 cm, Dr. Lim said at the meeting at the meeting held by the American Thyroid Association, Asia-Oceania Thyroid Association, European Thyroid Association, and Latin American Thyroid Society.
No difference was seen between the groups with respect to diagnostic performance based on degree of clinician experience.
The complication rate was higher with CNB than with fine -needle aspiration (3.6% vs. 1.6%), but complications were minor, Dr. Lim said.
Core needle biopsy has been suggested as a complementary tool for the diagnosis of thyroid nodules when the results of fine-needle aspiration are inconclusive, and the approach has been shown to be both safe and accurate for biopsy. However, its role as a first-line approach for thyroid nodule biopsy has been controversial and few studies have evaluated it as a first-line tool, she noted.
The current findings suggest that CNB is a safe and highly sensitive first-line biopsy method for such nodules, she concluded.
Dr. Lim reported having no disclosures.
LAKE BUENA VISTA, FLA. – The nondiagnostic result rate was significantly lower with core needle biopsy than with fine needle aspiration as a first-line biopsy method for newly detected thyroid nodules in a comparative study.
In 631 pairs of initially detected thyroid nodules that were matched based on propensity score analysis, the nondiagnostic result rate was 1.4% when core needle biopsy (CNB) was used, compared with 8.1% with ultrasound-guided fine-needle aspiration. The indeterminate result rate was 5.1% vs. 8.1% with the two approaches, respectively, and the differences between the groups were statistically significant, Dr. Hyun Kyung Lim of Soonchunhyang University Seoul Hospital, Korea, reported at the International Thyroid Congress.
The nondiagnostic rate with CNB was also significantly lower than with fine-needle aspiration for nodules with calcifications, posterior location, or diameter less than 1 cm, Dr. Lim said at the meeting at the meeting held by the American Thyroid Association, Asia-Oceania Thyroid Association, European Thyroid Association, and Latin American Thyroid Society.
No difference was seen between the groups with respect to diagnostic performance based on degree of clinician experience.
The complication rate was higher with CNB than with fine -needle aspiration (3.6% vs. 1.6%), but complications were minor, Dr. Lim said.
Core needle biopsy has been suggested as a complementary tool for the diagnosis of thyroid nodules when the results of fine-needle aspiration are inconclusive, and the approach has been shown to be both safe and accurate for biopsy. However, its role as a first-line approach for thyroid nodule biopsy has been controversial and few studies have evaluated it as a first-line tool, she noted.
The current findings suggest that CNB is a safe and highly sensitive first-line biopsy method for such nodules, she concluded.
Dr. Lim reported having no disclosures.
LAKE BUENA VISTA, FLA. – The nondiagnostic result rate was significantly lower with core needle biopsy than with fine needle aspiration as a first-line biopsy method for newly detected thyroid nodules in a comparative study.
In 631 pairs of initially detected thyroid nodules that were matched based on propensity score analysis, the nondiagnostic result rate was 1.4% when core needle biopsy (CNB) was used, compared with 8.1% with ultrasound-guided fine-needle aspiration. The indeterminate result rate was 5.1% vs. 8.1% with the two approaches, respectively, and the differences between the groups were statistically significant, Dr. Hyun Kyung Lim of Soonchunhyang University Seoul Hospital, Korea, reported at the International Thyroid Congress.
The nondiagnostic rate with CNB was also significantly lower than with fine-needle aspiration for nodules with calcifications, posterior location, or diameter less than 1 cm, Dr. Lim said at the meeting at the meeting held by the American Thyroid Association, Asia-Oceania Thyroid Association, European Thyroid Association, and Latin American Thyroid Society.
No difference was seen between the groups with respect to diagnostic performance based on degree of clinician experience.
The complication rate was higher with CNB than with fine -needle aspiration (3.6% vs. 1.6%), but complications were minor, Dr. Lim said.
Core needle biopsy has been suggested as a complementary tool for the diagnosis of thyroid nodules when the results of fine-needle aspiration are inconclusive, and the approach has been shown to be both safe and accurate for biopsy. However, its role as a first-line approach for thyroid nodule biopsy has been controversial and few studies have evaluated it as a first-line tool, she noted.
The current findings suggest that CNB is a safe and highly sensitive first-line biopsy method for such nodules, she concluded.
Dr. Lim reported having no disclosures.
AT THE INTERNATIONAL THYROID CONGRESS
Key clinical point: The nondiagnostic result rate was significantly lower with core needle biopsy than with fine-needle aspiration as a first-line biopsy method for newly detected thyroid nodules in a comparative study.
Major finding: The nondiagnostic result rate was 1.4% with core needle biopsy vs. 8.1% with fine-needle aspiration.
Data source: A comparative study in 631 propensity score–matched pairs of thyroid nodules.
Disclosures: Dr. Lim reported having no disclosures.
ADT linked to increased risk of Alzheimer’s disease
The use of androgen deprivation therapy (ADT) for treatment of prostate cancer was associated with increased risk of Alzheimer’s disease, and patients with greater duration of ADT use had higher risks, according to medical records data analysis.
ADT use was significantly associated with Alzheimer’s disease risk, with a hazard ratio (HR) of 1.88 by propensity score–matched Cox regression analysis (95% confidence interval, 1.10-3.20; P = .021), and HR of 1.66 by traditional multivariable-adjusted Cox regression analysis (95% CI, 1.05-2.64; P = .031).
Patients who used ADT for 12 months or more had the greatest risk observed (HR, 2.12; 95% CI, 1.11-4.03; P = .011), and the risk increased by category of ADT duration (P for trend = .016).
Investigators used a novel text-processing pipeline to analyze clinical data, extracting disease and terminology codes, medication lists, and positive-present mentions of drug and disease concepts from clinical notes.
“Use of the electronic medical record in this way allows rapid investigation of a rich data source to study a broad range of postmarketing outcome, including those unlikely to be seen in smaller clinical trials,” wrote Dr. Kevin T. Nead of the University of Pennsylvania, Philadelphia, and his colleagues (J Clin Oncol. 2015 Dec 7. doi: 10.1200/JCO.2015.63.6266).
The study evaluated 16,888 patients with prostate cancer; in total, 2,397 received ADT and 125 were diagnosed with Alzheimer’s disease during a median follow-up of 2.7 years. The median time to Alzheimer’s disease diagnosis was 4 years.
The analysis replicated previously known associations between Alzheimer’s disease and age (HR, 1.06; P less than .001) and cardiovascular disease (HR, 1.60; P = .031), supporting the validity of the method, according to the researchers.
The use of androgen deprivation therapy (ADT) for treatment of prostate cancer was associated with increased risk of Alzheimer’s disease, and patients with greater duration of ADT use had higher risks, according to medical records data analysis.
ADT use was significantly associated with Alzheimer’s disease risk, with a hazard ratio (HR) of 1.88 by propensity score–matched Cox regression analysis (95% confidence interval, 1.10-3.20; P = .021), and HR of 1.66 by traditional multivariable-adjusted Cox regression analysis (95% CI, 1.05-2.64; P = .031).
Patients who used ADT for 12 months or more had the greatest risk observed (HR, 2.12; 95% CI, 1.11-4.03; P = .011), and the risk increased by category of ADT duration (P for trend = .016).
Investigators used a novel text-processing pipeline to analyze clinical data, extracting disease and terminology codes, medication lists, and positive-present mentions of drug and disease concepts from clinical notes.
“Use of the electronic medical record in this way allows rapid investigation of a rich data source to study a broad range of postmarketing outcome, including those unlikely to be seen in smaller clinical trials,” wrote Dr. Kevin T. Nead of the University of Pennsylvania, Philadelphia, and his colleagues (J Clin Oncol. 2015 Dec 7. doi: 10.1200/JCO.2015.63.6266).
The study evaluated 16,888 patients with prostate cancer; in total, 2,397 received ADT and 125 were diagnosed with Alzheimer’s disease during a median follow-up of 2.7 years. The median time to Alzheimer’s disease diagnosis was 4 years.
The analysis replicated previously known associations between Alzheimer’s disease and age (HR, 1.06; P less than .001) and cardiovascular disease (HR, 1.60; P = .031), supporting the validity of the method, according to the researchers.
The use of androgen deprivation therapy (ADT) for treatment of prostate cancer was associated with increased risk of Alzheimer’s disease, and patients with greater duration of ADT use had higher risks, according to medical records data analysis.
ADT use was significantly associated with Alzheimer’s disease risk, with a hazard ratio (HR) of 1.88 by propensity score–matched Cox regression analysis (95% confidence interval, 1.10-3.20; P = .021), and HR of 1.66 by traditional multivariable-adjusted Cox regression analysis (95% CI, 1.05-2.64; P = .031).
Patients who used ADT for 12 months or more had the greatest risk observed (HR, 2.12; 95% CI, 1.11-4.03; P = .011), and the risk increased by category of ADT duration (P for trend = .016).
Investigators used a novel text-processing pipeline to analyze clinical data, extracting disease and terminology codes, medication lists, and positive-present mentions of drug and disease concepts from clinical notes.
“Use of the electronic medical record in this way allows rapid investigation of a rich data source to study a broad range of postmarketing outcome, including those unlikely to be seen in smaller clinical trials,” wrote Dr. Kevin T. Nead of the University of Pennsylvania, Philadelphia, and his colleagues (J Clin Oncol. 2015 Dec 7. doi: 10.1200/JCO.2015.63.6266).
The study evaluated 16,888 patients with prostate cancer; in total, 2,397 received ADT and 125 were diagnosed with Alzheimer’s disease during a median follow-up of 2.7 years. The median time to Alzheimer’s disease diagnosis was 4 years.
The analysis replicated previously known associations between Alzheimer’s disease and age (HR, 1.06; P less than .001) and cardiovascular disease (HR, 1.60; P = .031), supporting the validity of the method, according to the researchers.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Patients who underwent ADT for prostate cancer had significantly increased risk of future Alzheimer’s disease diagnosis.
Major finding: ADT use was significantly associated with Alzheimer’s disease risk, with an HR of 1.88 by propensity score–matched Cox regression analysis (95% CI, 1.10-3.20; P = .021).
Data source: The electronic medical record analysis evaluated 16,888 patients with prostate cancer. Of 2,397 patients who received ADT, 125 were diagnosed with Alzheimer’s disease during a median follow-up of 2.7 years.
Disclosures: Research was supported by grants from the National Institutes of Health, National Library of Medicine, and National Institute of General Medical Sciences, which owns the patent by Stanford on data mining techniques. Dr. Nead reported having no disclosures.
Iron deficiency may explain persistent hypothyroidism symptoms
LAKE BUENA VISTA, FLA. – Between 30% and 50% of hypothyroid patients with persistent symptoms despite adequate levothyroxine therapy may have covert iron deficiency, findings from a small study suggest.
The findings cast “a dark shadow of doubt on the validity of the studies on the effect of T3 therapy in these patients,” Dr. Esa Soppi reported in a poster at the International Thyroid Congress.
Study subjects were women with a history of overt hypothyroidism who had persistent symptoms after appropriate and ongoing treatment with L-T4. L-T4 dosing was adjusted as necessary to achieve a thyroid-stimulating hormone concentration of 1-2 mU/L, and diabetes, B12-vitamin deficiency, celiac disease, hypercalcemia, and vitamin D deficiency were ruled out as causes for the persistent symptoms.
Further, none of the patients had anemia, and red cell indices were within the reference range.
Five of the women had serum ferritin of less than 15 mcg/L, and two of those had serum iron, transferrin, or soluble transferrin receptor concentration or transferrin saturation out of range, suggesting iron deficiency. The remaining 20 women had a serum ferritin concentration between 15 mcg/L and 60 mcg/L, Dr. Soppi of Eira Hospital, Helsinki, noted at the meeting held by the American Thyroid Association, Asia-Oceania Thyroid Association , European Thyroid Association, and Latin American Thyroid Society.
Four of the five women with serum ferritin less than 15 mcg/L, and 14 of the 20 with less than 15-60 mcg/L became symptom free when treated with oral iron substitution therapy for 6-12 months, Dr. Soppi said.
“All patients were advised to take their thyroxine dose at the fasting state in the morning and start breakfast 30 minutes later. The interval between the iron and thyroxine was at least 4 hours. The response was observed at a serum ferritin concentration approaching 70-100 mcg/L,” Dr. Soppi wrote, noting that in one patient – a 28-year-old woman with type 1 diabetes and hypothyroidism – all symptoms of fatigue, failure to thrive, and lethargy experienced before the start of the iron therapy disappeared after about 4 months of oral iron therapy at a dose of 100 mg twice daily.
However, another patient – an 18-year-old woman with hypothyroidism after total thyroidectomy performed because of a suspected thyroid malignancy – was found to have no malignancy; disabling tiredness, and failure to thrive emerged after the thyroidectomy and persisted despite iron therapy given at 100 mg twice daily.
“Iron deficiency is as common as hypothyroidism and its symptoms resemble those of hypothyroidism. However, the diagnosis of iron deficiency without anemia is extremely challenging since all indicators of iron status may be ‘normal.’ A clinical suspicion is key to diagnosis of covert iron deficiency,” Dr. Soppi wrote, noting that the serum ferritin concentration may be helpful, and restoration of ferritin above 100 mcg/L seems to ameliorate symptoms in about two-thirds of patients, and that it is not currently known why some iron-deficient patients fail to respond to restoration of their functional iron stores.
LAKE BUENA VISTA, FLA. – Between 30% and 50% of hypothyroid patients with persistent symptoms despite adequate levothyroxine therapy may have covert iron deficiency, findings from a small study suggest.
The findings cast “a dark shadow of doubt on the validity of the studies on the effect of T3 therapy in these patients,” Dr. Esa Soppi reported in a poster at the International Thyroid Congress.
Study subjects were women with a history of overt hypothyroidism who had persistent symptoms after appropriate and ongoing treatment with L-T4. L-T4 dosing was adjusted as necessary to achieve a thyroid-stimulating hormone concentration of 1-2 mU/L, and diabetes, B12-vitamin deficiency, celiac disease, hypercalcemia, and vitamin D deficiency were ruled out as causes for the persistent symptoms.
Further, none of the patients had anemia, and red cell indices were within the reference range.
Five of the women had serum ferritin of less than 15 mcg/L, and two of those had serum iron, transferrin, or soluble transferrin receptor concentration or transferrin saturation out of range, suggesting iron deficiency. The remaining 20 women had a serum ferritin concentration between 15 mcg/L and 60 mcg/L, Dr. Soppi of Eira Hospital, Helsinki, noted at the meeting held by the American Thyroid Association, Asia-Oceania Thyroid Association , European Thyroid Association, and Latin American Thyroid Society.
Four of the five women with serum ferritin less than 15 mcg/L, and 14 of the 20 with less than 15-60 mcg/L became symptom free when treated with oral iron substitution therapy for 6-12 months, Dr. Soppi said.
“All patients were advised to take their thyroxine dose at the fasting state in the morning and start breakfast 30 minutes later. The interval between the iron and thyroxine was at least 4 hours. The response was observed at a serum ferritin concentration approaching 70-100 mcg/L,” Dr. Soppi wrote, noting that in one patient – a 28-year-old woman with type 1 diabetes and hypothyroidism – all symptoms of fatigue, failure to thrive, and lethargy experienced before the start of the iron therapy disappeared after about 4 months of oral iron therapy at a dose of 100 mg twice daily.
However, another patient – an 18-year-old woman with hypothyroidism after total thyroidectomy performed because of a suspected thyroid malignancy – was found to have no malignancy; disabling tiredness, and failure to thrive emerged after the thyroidectomy and persisted despite iron therapy given at 100 mg twice daily.
“Iron deficiency is as common as hypothyroidism and its symptoms resemble those of hypothyroidism. However, the diagnosis of iron deficiency without anemia is extremely challenging since all indicators of iron status may be ‘normal.’ A clinical suspicion is key to diagnosis of covert iron deficiency,” Dr. Soppi wrote, noting that the serum ferritin concentration may be helpful, and restoration of ferritin above 100 mcg/L seems to ameliorate symptoms in about two-thirds of patients, and that it is not currently known why some iron-deficient patients fail to respond to restoration of their functional iron stores.
LAKE BUENA VISTA, FLA. – Between 30% and 50% of hypothyroid patients with persistent symptoms despite adequate levothyroxine therapy may have covert iron deficiency, findings from a small study suggest.
The findings cast “a dark shadow of doubt on the validity of the studies on the effect of T3 therapy in these patients,” Dr. Esa Soppi reported in a poster at the International Thyroid Congress.
Study subjects were women with a history of overt hypothyroidism who had persistent symptoms after appropriate and ongoing treatment with L-T4. L-T4 dosing was adjusted as necessary to achieve a thyroid-stimulating hormone concentration of 1-2 mU/L, and diabetes, B12-vitamin deficiency, celiac disease, hypercalcemia, and vitamin D deficiency were ruled out as causes for the persistent symptoms.
Further, none of the patients had anemia, and red cell indices were within the reference range.
Five of the women had serum ferritin of less than 15 mcg/L, and two of those had serum iron, transferrin, or soluble transferrin receptor concentration or transferrin saturation out of range, suggesting iron deficiency. The remaining 20 women had a serum ferritin concentration between 15 mcg/L and 60 mcg/L, Dr. Soppi of Eira Hospital, Helsinki, noted at the meeting held by the American Thyroid Association, Asia-Oceania Thyroid Association , European Thyroid Association, and Latin American Thyroid Society.
Four of the five women with serum ferritin less than 15 mcg/L, and 14 of the 20 with less than 15-60 mcg/L became symptom free when treated with oral iron substitution therapy for 6-12 months, Dr. Soppi said.
“All patients were advised to take their thyroxine dose at the fasting state in the morning and start breakfast 30 minutes later. The interval between the iron and thyroxine was at least 4 hours. The response was observed at a serum ferritin concentration approaching 70-100 mcg/L,” Dr. Soppi wrote, noting that in one patient – a 28-year-old woman with type 1 diabetes and hypothyroidism – all symptoms of fatigue, failure to thrive, and lethargy experienced before the start of the iron therapy disappeared after about 4 months of oral iron therapy at a dose of 100 mg twice daily.
However, another patient – an 18-year-old woman with hypothyroidism after total thyroidectomy performed because of a suspected thyroid malignancy – was found to have no malignancy; disabling tiredness, and failure to thrive emerged after the thyroidectomy and persisted despite iron therapy given at 100 mg twice daily.
“Iron deficiency is as common as hypothyroidism and its symptoms resemble those of hypothyroidism. However, the diagnosis of iron deficiency without anemia is extremely challenging since all indicators of iron status may be ‘normal.’ A clinical suspicion is key to diagnosis of covert iron deficiency,” Dr. Soppi wrote, noting that the serum ferritin concentration may be helpful, and restoration of ferritin above 100 mcg/L seems to ameliorate symptoms in about two-thirds of patients, and that it is not currently known why some iron-deficient patients fail to respond to restoration of their functional iron stores.
AT THE INTERNATIONAL THYROID CONGRESS
Key clinical point: Between 30% and 50% of hypothyroid patients with persistent symptoms despite adequate levothyroxine therapy may have covert iron deficiency, findings from a small study suggest.
Major finding: Four of five women with serum ferritin less than 15 mcg/L, and 14 of 20 with less than 15-60 mcg/L became symptom free when treated with oral iron substitution therapy for 6-12 months.
Data source: A prospective study of 25 women.
Disclosures: Dr. Soppi reported having no disclosures.
Survivors of childhood cancers at increased risk for autoimmune diseases
Analysis of cancer registry data from Denmark, Iceland, and Sweden over more than 60 years found that survivors of childhood cancer had a 1.4-fold higher risk of autoimmune disease compared with matched controls.
Results showed significantly increased rates of hospital visits for 11 of 33 autoimmune diseases investigated. The most prominent excesses were for insulin-dependent diabetes mellitus, Addison’s disease, and Hashimoto’s thyroiditis, accounting for more than half the total number of excess autoimmune cases (Ann Rheum Dis 2015 Nov 6. doi: 10.1136/annrheumdis-2015-207659). The investigators could not rule out the influence of surveillance bias, given that hospitalization rate ratios were highest in the first 5 years after cancer diagnosis, potentially a consequence of closer surveillance during that period. For most autoimmune diseases, however, the excess risk persisted through the second and third decades after cancer diagnosis.
The Nordic childhood cancer survivor cohort comprised 25,635 individuals diagnosed with cancer before the age of 20 years, from the 1940s-1950s (start of cancer registries in Denmark, Iceland, and Sweden) to 2008. Expected autoimmune disease rates were based on rates of hospital visits for the comparison cohort, which included 128,023 individuals matched for age, sex, and country of the corresponding survivor. The standardized hospitalization rate ratio is the observed number of autoimmune diseases among survivors divided by the expected rate. Childhood malignancies with the most pronounced risk increases were leukemia (standardized hospitalization rate ratio, 1.6), Hodgkin lymphoma (1.6), renal tumors (1.6), and central nervous system neoplasms (1.4).
“Cure is no longer a sufficient goal in childhood cancer care. As the vast majority of these patients survive, attention must be to paid to their long-term quality of life and health challenges,” wrote Dr. Anna Salifors Holmqvist of the department of clinical sciences, pediatric oncology and hematology, Skane University Hospital, Lund University, Sweden.
Increased risks were noted for a wide range of relatively rare autoimmune diseases after treatment for several types of childhood malignancies, and underlying mechanisms should be addressed in future studies, noted Dr. Holmqvist and her colleagues.
Analysis of cancer registry data from Denmark, Iceland, and Sweden over more than 60 years found that survivors of childhood cancer had a 1.4-fold higher risk of autoimmune disease compared with matched controls.
Results showed significantly increased rates of hospital visits for 11 of 33 autoimmune diseases investigated. The most prominent excesses were for insulin-dependent diabetes mellitus, Addison’s disease, and Hashimoto’s thyroiditis, accounting for more than half the total number of excess autoimmune cases (Ann Rheum Dis 2015 Nov 6. doi: 10.1136/annrheumdis-2015-207659). The investigators could not rule out the influence of surveillance bias, given that hospitalization rate ratios were highest in the first 5 years after cancer diagnosis, potentially a consequence of closer surveillance during that period. For most autoimmune diseases, however, the excess risk persisted through the second and third decades after cancer diagnosis.
The Nordic childhood cancer survivor cohort comprised 25,635 individuals diagnosed with cancer before the age of 20 years, from the 1940s-1950s (start of cancer registries in Denmark, Iceland, and Sweden) to 2008. Expected autoimmune disease rates were based on rates of hospital visits for the comparison cohort, which included 128,023 individuals matched for age, sex, and country of the corresponding survivor. The standardized hospitalization rate ratio is the observed number of autoimmune diseases among survivors divided by the expected rate. Childhood malignancies with the most pronounced risk increases were leukemia (standardized hospitalization rate ratio, 1.6), Hodgkin lymphoma (1.6), renal tumors (1.6), and central nervous system neoplasms (1.4).
“Cure is no longer a sufficient goal in childhood cancer care. As the vast majority of these patients survive, attention must be to paid to their long-term quality of life and health challenges,” wrote Dr. Anna Salifors Holmqvist of the department of clinical sciences, pediatric oncology and hematology, Skane University Hospital, Lund University, Sweden.
Increased risks were noted for a wide range of relatively rare autoimmune diseases after treatment for several types of childhood malignancies, and underlying mechanisms should be addressed in future studies, noted Dr. Holmqvist and her colleagues.
Analysis of cancer registry data from Denmark, Iceland, and Sweden over more than 60 years found that survivors of childhood cancer had a 1.4-fold higher risk of autoimmune disease compared with matched controls.
Results showed significantly increased rates of hospital visits for 11 of 33 autoimmune diseases investigated. The most prominent excesses were for insulin-dependent diabetes mellitus, Addison’s disease, and Hashimoto’s thyroiditis, accounting for more than half the total number of excess autoimmune cases (Ann Rheum Dis 2015 Nov 6. doi: 10.1136/annrheumdis-2015-207659). The investigators could not rule out the influence of surveillance bias, given that hospitalization rate ratios were highest in the first 5 years after cancer diagnosis, potentially a consequence of closer surveillance during that period. For most autoimmune diseases, however, the excess risk persisted through the second and third decades after cancer diagnosis.
The Nordic childhood cancer survivor cohort comprised 25,635 individuals diagnosed with cancer before the age of 20 years, from the 1940s-1950s (start of cancer registries in Denmark, Iceland, and Sweden) to 2008. Expected autoimmune disease rates were based on rates of hospital visits for the comparison cohort, which included 128,023 individuals matched for age, sex, and country of the corresponding survivor. The standardized hospitalization rate ratio is the observed number of autoimmune diseases among survivors divided by the expected rate. Childhood malignancies with the most pronounced risk increases were leukemia (standardized hospitalization rate ratio, 1.6), Hodgkin lymphoma (1.6), renal tumors (1.6), and central nervous system neoplasms (1.4).
“Cure is no longer a sufficient goal in childhood cancer care. As the vast majority of these patients survive, attention must be to paid to their long-term quality of life and health challenges,” wrote Dr. Anna Salifors Holmqvist of the department of clinical sciences, pediatric oncology and hematology, Skane University Hospital, Lund University, Sweden.
Increased risks were noted for a wide range of relatively rare autoimmune diseases after treatment for several types of childhood malignancies, and underlying mechanisms should be addressed in future studies, noted Dr. Holmqvist and her colleagues.
FROM ANNALS OF RHEUMATIC DISEASES
Key clinical point: Survivors of childhood cancers, especially leukemia, Hodgkin lymphoma, and renal tumors, had a significantly increased risk of autoimmune disease.
Major finding: Compared with matched controls, survivors had a 1.4-fold increased risk for hospital contact concerning an autoimmune disease.
Data source: The Nordic childhood cancer survivor cohort comprised 25,635 individuals diagnosed with cancer before age 20 years, from the 1940s-1950s (start of cancer registries in Denmark, Iceland, and Sweden) to 2008.
Disclosures: Dr. Holmqvist and coauthors reported having no disclosures.
Experimental LOXO-101 induces regression in several hard-to-treat cancers
BOSTON – An experimental agent that targets the byproducts of gene fusions has shown surprising clinical activity against notoriously treatment-refractory cancers in early results from a phase I trial.
“I think that’s what remarkable about this is that we have all these different histologies and many different fusions, but all seem to be having some kind of [response] to this molecule,” said lead investigator Dr. David S. Hong, deputy chair and associate professor in the department of investigational cancer therapeutics at the University of Texas MD Anderson Cancer Center, Houston.
The molecule, LOXO-101 is a selective inhibitor of abnormal TRKA, TRKAB, and TRKC kinases that arise from gene fusions. TRK fusions have been implicated in tumor development in preclinical studies, he reported at the AACR–NCI–EORTC International Conference on Molecular Targets and Cancer Therapeutics.
One patient, a 41-year-old woman with undifferentiated soft tissue sarcoma of the groin that had metastasized to her lungs had rapid and “substantial” tumor and lung-nodule regression that radiographically fell just shy of a complete response, Dr. Hong said.
The drug also induced robust partial responses in a 55-year-old man with a gastrointestinal stromal tumor (GIST) for whom five prior targeted agents had failed, and a 33-year-old man with mammary analogue secretory carcinoma of the salivary gland (MASC) that had progressed on chemotherapy with docetaxel, carboplatin, and 5-fluorauracil.
A fourth patient, a man (age unspecified) who had papillary thyroid cancer with palpable lymphadenopathy, had no palpable nodes at 1-month follow-up, and appears to be responding to the drug, Dr. Hong added.
“This is really a dramatic example, I think, of a targeted therapy that is not histology specific, and this is another area in oncology where it’s new, and we’re just feeling our way,” commented Dr. Lee C. Helman, a sarcoma specialist at the National Cancer Institute in Bethesda, Md., who moderated the briefing where Dr. Hong presented the data.
Tumor promoters
The TRK family of proteins consists of separate tyrosine kinases that, when functioning normally, are important for the development of peripheral central nervous system processes such as pain and thermoregulation, Dr. Hong explained.
“The NTRK 1, 2, and 3 genes which encode for the TRK proteins are subject to these gene rearrangements and fusions, and the resulting TRK gene fusions may become erroneously expressed, and the kinase domain constitutively activated,” he said.
Gene fusions resulting in constitutively active TRKA, B, and C kinases can occur in the range of about 2%-25% in a wide variety of tumors, including adenocarcinomas of the lung, gliomas, thyroid tumors, head and neck cancers, sarcomas, and other types. These fusions have also been detected in more than 75% of MASC tumors, secretory breast carcinomas, and infantile (congenital) fibrosarcoma.
LOXO-101 is an orally delivered small molecule that was rationally designed to target the TRK fusions while largely leaving other kinases alone. In preclinical studies, the compound showed potent tumor growth inhibition and regression in mice bearing NTRK fusions.
The phase I trial is a dose-finding study including a total of 24 patients with various treatment-refractory advanced or metastatic solid tumors. Patients were enrolled regardless of fusional status.
Well tolerated
At the selected dose of 100 mg twice daily, patients appeared to tolerate the drug very well, with few off-target adverse events, Dr. Hong said. The most common side effect was mild dizziness. Grade 3 or 4 adverse events occurring at all doses levels include fatigue (one patient), anemia (two), abdominal pain (one), increased alkaline phosphatase (one), increased aspartate aminotransferase, delirium, and syncope (two each).
A total of six of the 24 patients had TRK fusions in their tumors, and three of these patients were available for assessment as of Oct. 20, 2015.
Dr. Hong and colleagues previously reportedon the case of the 41-year old woman with sarcoma. She was found to have a fusion of LMNA (a gene that encodes for nuclear membrane proteins) with NTRK1. She was started on the 100-mg b.i.d. dose of LOX-101 and had rapid resolution of dyspnea and hypoxemia. She had a confirmed partial response, and a CT scan showed that her multiple pulmonary nodules had regressed, with just a single, small disease site remaining at most recent follow-up. This patient continues on treatment and has been followed for more than 8 months.
The man with GIST had experienced disease progression while on therapy with imatinib, sunitinib, sorafenib, nilotinib, and regorafenib. He was treated in the 150-mg b.i.d. dose cohort, had a confirmed partial response, and remains on study after 4-plus months.
The third patient, the 33-year-old man with MASC, was assigned to the 100-mg b.i.d. dose. He too had a partial response, with radiologic evidence of substantial tumor shrinkage, and a persistent, tumor-related cough that disappeared after about 10 days of treatment, and remains on study after more than 3 months of follow-up.
The investigators have begun accruing patients for a phase II “basket” trial in adult patients with advanced or metastatic solid tumors displaying TRK fusions, including non–small cell lung cancers, thyroid tumors, sarcomas, colorectal cancer, salivary gland cancers, primary central nervous system cancers, and all other solid tumors.
Dr. Hong said that the results indicate the importance of tumor profiling for the majority of patients, especially those whose disease is refractory to standard therapies.
The study was funded by Loxo Oncology. Dr. Hong disclosed receiving travel expenses from the company. Three coauthors are employees and shareholders of the company.
BOSTON – An experimental agent that targets the byproducts of gene fusions has shown surprising clinical activity against notoriously treatment-refractory cancers in early results from a phase I trial.
“I think that’s what remarkable about this is that we have all these different histologies and many different fusions, but all seem to be having some kind of [response] to this molecule,” said lead investigator Dr. David S. Hong, deputy chair and associate professor in the department of investigational cancer therapeutics at the University of Texas MD Anderson Cancer Center, Houston.
The molecule, LOXO-101 is a selective inhibitor of abnormal TRKA, TRKAB, and TRKC kinases that arise from gene fusions. TRK fusions have been implicated in tumor development in preclinical studies, he reported at the AACR–NCI–EORTC International Conference on Molecular Targets and Cancer Therapeutics.
One patient, a 41-year-old woman with undifferentiated soft tissue sarcoma of the groin that had metastasized to her lungs had rapid and “substantial” tumor and lung-nodule regression that radiographically fell just shy of a complete response, Dr. Hong said.
The drug also induced robust partial responses in a 55-year-old man with a gastrointestinal stromal tumor (GIST) for whom five prior targeted agents had failed, and a 33-year-old man with mammary analogue secretory carcinoma of the salivary gland (MASC) that had progressed on chemotherapy with docetaxel, carboplatin, and 5-fluorauracil.
A fourth patient, a man (age unspecified) who had papillary thyroid cancer with palpable lymphadenopathy, had no palpable nodes at 1-month follow-up, and appears to be responding to the drug, Dr. Hong added.
“This is really a dramatic example, I think, of a targeted therapy that is not histology specific, and this is another area in oncology where it’s new, and we’re just feeling our way,” commented Dr. Lee C. Helman, a sarcoma specialist at the National Cancer Institute in Bethesda, Md., who moderated the briefing where Dr. Hong presented the data.
Tumor promoters
The TRK family of proteins consists of separate tyrosine kinases that, when functioning normally, are important for the development of peripheral central nervous system processes such as pain and thermoregulation, Dr. Hong explained.
“The NTRK 1, 2, and 3 genes which encode for the TRK proteins are subject to these gene rearrangements and fusions, and the resulting TRK gene fusions may become erroneously expressed, and the kinase domain constitutively activated,” he said.
Gene fusions resulting in constitutively active TRKA, B, and C kinases can occur in the range of about 2%-25% in a wide variety of tumors, including adenocarcinomas of the lung, gliomas, thyroid tumors, head and neck cancers, sarcomas, and other types. These fusions have also been detected in more than 75% of MASC tumors, secretory breast carcinomas, and infantile (congenital) fibrosarcoma.
LOXO-101 is an orally delivered small molecule that was rationally designed to target the TRK fusions while largely leaving other kinases alone. In preclinical studies, the compound showed potent tumor growth inhibition and regression in mice bearing NTRK fusions.
The phase I trial is a dose-finding study including a total of 24 patients with various treatment-refractory advanced or metastatic solid tumors. Patients were enrolled regardless of fusional status.
Well tolerated
At the selected dose of 100 mg twice daily, patients appeared to tolerate the drug very well, with few off-target adverse events, Dr. Hong said. The most common side effect was mild dizziness. Grade 3 or 4 adverse events occurring at all doses levels include fatigue (one patient), anemia (two), abdominal pain (one), increased alkaline phosphatase (one), increased aspartate aminotransferase, delirium, and syncope (two each).
A total of six of the 24 patients had TRK fusions in their tumors, and three of these patients were available for assessment as of Oct. 20, 2015.
Dr. Hong and colleagues previously reportedon the case of the 41-year old woman with sarcoma. She was found to have a fusion of LMNA (a gene that encodes for nuclear membrane proteins) with NTRK1. She was started on the 100-mg b.i.d. dose of LOX-101 and had rapid resolution of dyspnea and hypoxemia. She had a confirmed partial response, and a CT scan showed that her multiple pulmonary nodules had regressed, with just a single, small disease site remaining at most recent follow-up. This patient continues on treatment and has been followed for more than 8 months.
The man with GIST had experienced disease progression while on therapy with imatinib, sunitinib, sorafenib, nilotinib, and regorafenib. He was treated in the 150-mg b.i.d. dose cohort, had a confirmed partial response, and remains on study after 4-plus months.
The third patient, the 33-year-old man with MASC, was assigned to the 100-mg b.i.d. dose. He too had a partial response, with radiologic evidence of substantial tumor shrinkage, and a persistent, tumor-related cough that disappeared after about 10 days of treatment, and remains on study after more than 3 months of follow-up.
The investigators have begun accruing patients for a phase II “basket” trial in adult patients with advanced or metastatic solid tumors displaying TRK fusions, including non–small cell lung cancers, thyroid tumors, sarcomas, colorectal cancer, salivary gland cancers, primary central nervous system cancers, and all other solid tumors.
Dr. Hong said that the results indicate the importance of tumor profiling for the majority of patients, especially those whose disease is refractory to standard therapies.
The study was funded by Loxo Oncology. Dr. Hong disclosed receiving travel expenses from the company. Three coauthors are employees and shareholders of the company.
BOSTON – An experimental agent that targets the byproducts of gene fusions has shown surprising clinical activity against notoriously treatment-refractory cancers in early results from a phase I trial.
“I think that’s what remarkable about this is that we have all these different histologies and many different fusions, but all seem to be having some kind of [response] to this molecule,” said lead investigator Dr. David S. Hong, deputy chair and associate professor in the department of investigational cancer therapeutics at the University of Texas MD Anderson Cancer Center, Houston.
The molecule, LOXO-101 is a selective inhibitor of abnormal TRKA, TRKAB, and TRKC kinases that arise from gene fusions. TRK fusions have been implicated in tumor development in preclinical studies, he reported at the AACR–NCI–EORTC International Conference on Molecular Targets and Cancer Therapeutics.
One patient, a 41-year-old woman with undifferentiated soft tissue sarcoma of the groin that had metastasized to her lungs had rapid and “substantial” tumor and lung-nodule regression that radiographically fell just shy of a complete response, Dr. Hong said.
The drug also induced robust partial responses in a 55-year-old man with a gastrointestinal stromal tumor (GIST) for whom five prior targeted agents had failed, and a 33-year-old man with mammary analogue secretory carcinoma of the salivary gland (MASC) that had progressed on chemotherapy with docetaxel, carboplatin, and 5-fluorauracil.
A fourth patient, a man (age unspecified) who had papillary thyroid cancer with palpable lymphadenopathy, had no palpable nodes at 1-month follow-up, and appears to be responding to the drug, Dr. Hong added.
“This is really a dramatic example, I think, of a targeted therapy that is not histology specific, and this is another area in oncology where it’s new, and we’re just feeling our way,” commented Dr. Lee C. Helman, a sarcoma specialist at the National Cancer Institute in Bethesda, Md., who moderated the briefing where Dr. Hong presented the data.
Tumor promoters
The TRK family of proteins consists of separate tyrosine kinases that, when functioning normally, are important for the development of peripheral central nervous system processes such as pain and thermoregulation, Dr. Hong explained.
“The NTRK 1, 2, and 3 genes which encode for the TRK proteins are subject to these gene rearrangements and fusions, and the resulting TRK gene fusions may become erroneously expressed, and the kinase domain constitutively activated,” he said.
Gene fusions resulting in constitutively active TRKA, B, and C kinases can occur in the range of about 2%-25% in a wide variety of tumors, including adenocarcinomas of the lung, gliomas, thyroid tumors, head and neck cancers, sarcomas, and other types. These fusions have also been detected in more than 75% of MASC tumors, secretory breast carcinomas, and infantile (congenital) fibrosarcoma.
LOXO-101 is an orally delivered small molecule that was rationally designed to target the TRK fusions while largely leaving other kinases alone. In preclinical studies, the compound showed potent tumor growth inhibition and regression in mice bearing NTRK fusions.
The phase I trial is a dose-finding study including a total of 24 patients with various treatment-refractory advanced or metastatic solid tumors. Patients were enrolled regardless of fusional status.
Well tolerated
At the selected dose of 100 mg twice daily, patients appeared to tolerate the drug very well, with few off-target adverse events, Dr. Hong said. The most common side effect was mild dizziness. Grade 3 or 4 adverse events occurring at all doses levels include fatigue (one patient), anemia (two), abdominal pain (one), increased alkaline phosphatase (one), increased aspartate aminotransferase, delirium, and syncope (two each).
A total of six of the 24 patients had TRK fusions in their tumors, and three of these patients were available for assessment as of Oct. 20, 2015.
Dr. Hong and colleagues previously reportedon the case of the 41-year old woman with sarcoma. She was found to have a fusion of LMNA (a gene that encodes for nuclear membrane proteins) with NTRK1. She was started on the 100-mg b.i.d. dose of LOX-101 and had rapid resolution of dyspnea and hypoxemia. She had a confirmed partial response, and a CT scan showed that her multiple pulmonary nodules had regressed, with just a single, small disease site remaining at most recent follow-up. This patient continues on treatment and has been followed for more than 8 months.
The man with GIST had experienced disease progression while on therapy with imatinib, sunitinib, sorafenib, nilotinib, and regorafenib. He was treated in the 150-mg b.i.d. dose cohort, had a confirmed partial response, and remains on study after 4-plus months.
The third patient, the 33-year-old man with MASC, was assigned to the 100-mg b.i.d. dose. He too had a partial response, with radiologic evidence of substantial tumor shrinkage, and a persistent, tumor-related cough that disappeared after about 10 days of treatment, and remains on study after more than 3 months of follow-up.
The investigators have begun accruing patients for a phase II “basket” trial in adult patients with advanced or metastatic solid tumors displaying TRK fusions, including non–small cell lung cancers, thyroid tumors, sarcomas, colorectal cancer, salivary gland cancers, primary central nervous system cancers, and all other solid tumors.
Dr. Hong said that the results indicate the importance of tumor profiling for the majority of patients, especially those whose disease is refractory to standard therapies.
The study was funded by Loxo Oncology. Dr. Hong disclosed receiving travel expenses from the company. Three coauthors are employees and shareholders of the company.
Key clinical point:Inhibition of TRK gene fusion products is a novel strategy for treating cancer.
Major finding: Three of three patients evaluable for response had near-complete responses.
Data source: Phase I dose-finding study in 24 patients, with and without TRK gene fusions.
Disclosures: The study was funded by Loxo Oncology. Dr. Hong disclosed receiving travel expenses from the company. Three coauthors are employees and shareholders of the company.