User login
Don’t discontinue osteoporosis meds for COVID-19 vaccines, expert guidance says
COVID-19 vaccines are safe and effective for patients taking osteoporosis medications, according to joint guidance from six endocrine and osteoporosis societies and foundations.
They noted, though, that some timing modifications with certain medications should be considered to help distinguish between adverse events from the medication versus the vaccine.
The American Society for Bone and Mineral Research “is an international organization, so we brought together our sister societies that have a vested interested in bone health. Vaccination is happening worldwide, and we wanted to present a united front and united recommendations about how to handle osteoporosis medications appropriately during vaccination,” said Suzanne Jan De Beur, MD, who is president of ASBMR and an associate professor of medicine at Johns Hopkins University, Baltimore.
There has been quite a lot of concern from the community about vaccine and medications, from both physicians and patients wondering whether treatments and vaccines should occur in a certain order, and whether there should be a time gap between the two, said Dr. Jan De Beur. “There was a dearth of information about the best practices for osteoporosis treatment management during vaccination, and we didn’t want people missing their opportunity for a vaccine, and we also didn’t want them unnecessarily delaying their osteoporosis treatment.”
There is no evidence that osteoporosis therapies affect the risk or severity of COVID-19 disease, nor do they appear to change the disease course. Osteoporosis itself does not appear associated with increased risk of infection or severe outcomes, so patients with osteoporosis do not need to be prioritized for vaccination based on that condition alone.
There is no evidence that osteoporosis therapies affect the safety or efficacy of vaccination, but given that vaccine availability is currently inconsistent, patients may need to make temporary changes to their osteoporosis regimens to ensure they can receive vaccine when it is available, such as ensuring a delay between medication and vaccination injections.
A key reason for a delay between injectable or infusion medications and a vaccine is to distinguish between adverse events that could occur, so that an adverse reaction to vaccine isn’t mistaken for an adverse reaction to a drug. Nevertheless, the real world is messy. Dr. Jan De Beur noted a recent patient who arrived at her clinic for an injectable treatment who had just received a COVID-19 vaccination that morning. “We decided to put the injection in the other arm, rather than reschedule the person and put them through the risk of coming back. We could distinguish between injection-site reactions, at least,” she said.
No changes should be made to general bone health therapies, such as calcium and vitamin D supplementation, weight-bearing exercises, and maintenance of a balanced diet.
The guidance includes some recommendations for specific osteoporosis medications.
- Oral bisphosphonates: Alendronate, risedronate, and ibandronate should be continued.
- Intravenous bisphosphonates: a 7-day interval (4-day minimum) is recommended between intravenous bisphosphonate (zoledronic acid and ibandronate) infusion and COVID-19 vaccination in order to distinguish potential autoimmune or inflammatory reactions that could be attributable to either intravenous bisphosphonate or the vaccine.
- Denosumab: There should be a 4- to 7-day delay between denosumab infusion and COVID-19 vaccination to account for injection-site reactions. Another option is to have denosumab injected into the contralateral arm or another site like the abdomen or upper thigh, if spacing the injections is not possible. In any case, denosumab injections should be performed within 7 months of the previous dose.
- Teriparatide and abaloparatide should be continued.
- Romosozumab: There should be a 4- to 7-day delay between a romosozumab injection and COVID-19 vaccine, or romosozumab can be injected in the abdomen (with the exception of a 2-inch area around the naval) or thigh if spacing is not possible.
- Raloxifene should be continued in patients receiving COVID-19 vaccination.
Guidance signatories include ASBMR, the American Association of Clinical Endocrinology, the Endocrine Society, the European Calcified Tissue Society, the National Osteoporosis Foundation, and the International Osteoporosis Foundation.
Dr. Jan De Beur has no relevant financial disclosures.
COVID-19 vaccines are safe and effective for patients taking osteoporosis medications, according to joint guidance from six endocrine and osteoporosis societies and foundations.
They noted, though, that some timing modifications with certain medications should be considered to help distinguish between adverse events from the medication versus the vaccine.
The American Society for Bone and Mineral Research “is an international organization, so we brought together our sister societies that have a vested interested in bone health. Vaccination is happening worldwide, and we wanted to present a united front and united recommendations about how to handle osteoporosis medications appropriately during vaccination,” said Suzanne Jan De Beur, MD, who is president of ASBMR and an associate professor of medicine at Johns Hopkins University, Baltimore.
There has been quite a lot of concern from the community about vaccine and medications, from both physicians and patients wondering whether treatments and vaccines should occur in a certain order, and whether there should be a time gap between the two, said Dr. Jan De Beur. “There was a dearth of information about the best practices for osteoporosis treatment management during vaccination, and we didn’t want people missing their opportunity for a vaccine, and we also didn’t want them unnecessarily delaying their osteoporosis treatment.”
There is no evidence that osteoporosis therapies affect the risk or severity of COVID-19 disease, nor do they appear to change the disease course. Osteoporosis itself does not appear associated with increased risk of infection or severe outcomes, so patients with osteoporosis do not need to be prioritized for vaccination based on that condition alone.
There is no evidence that osteoporosis therapies affect the safety or efficacy of vaccination, but given that vaccine availability is currently inconsistent, patients may need to make temporary changes to their osteoporosis regimens to ensure they can receive vaccine when it is available, such as ensuring a delay between medication and vaccination injections.
A key reason for a delay between injectable or infusion medications and a vaccine is to distinguish between adverse events that could occur, so that an adverse reaction to vaccine isn’t mistaken for an adverse reaction to a drug. Nevertheless, the real world is messy. Dr. Jan De Beur noted a recent patient who arrived at her clinic for an injectable treatment who had just received a COVID-19 vaccination that morning. “We decided to put the injection in the other arm, rather than reschedule the person and put them through the risk of coming back. We could distinguish between injection-site reactions, at least,” she said.
No changes should be made to general bone health therapies, such as calcium and vitamin D supplementation, weight-bearing exercises, and maintenance of a balanced diet.
The guidance includes some recommendations for specific osteoporosis medications.
- Oral bisphosphonates: Alendronate, risedronate, and ibandronate should be continued.
- Intravenous bisphosphonates: a 7-day interval (4-day minimum) is recommended between intravenous bisphosphonate (zoledronic acid and ibandronate) infusion and COVID-19 vaccination in order to distinguish potential autoimmune or inflammatory reactions that could be attributable to either intravenous bisphosphonate or the vaccine.
- Denosumab: There should be a 4- to 7-day delay between denosumab infusion and COVID-19 vaccination to account for injection-site reactions. Another option is to have denosumab injected into the contralateral arm or another site like the abdomen or upper thigh, if spacing the injections is not possible. In any case, denosumab injections should be performed within 7 months of the previous dose.
- Teriparatide and abaloparatide should be continued.
- Romosozumab: There should be a 4- to 7-day delay between a romosozumab injection and COVID-19 vaccine, or romosozumab can be injected in the abdomen (with the exception of a 2-inch area around the naval) or thigh if spacing is not possible.
- Raloxifene should be continued in patients receiving COVID-19 vaccination.
Guidance signatories include ASBMR, the American Association of Clinical Endocrinology, the Endocrine Society, the European Calcified Tissue Society, the National Osteoporosis Foundation, and the International Osteoporosis Foundation.
Dr. Jan De Beur has no relevant financial disclosures.
COVID-19 vaccines are safe and effective for patients taking osteoporosis medications, according to joint guidance from six endocrine and osteoporosis societies and foundations.
They noted, though, that some timing modifications with certain medications should be considered to help distinguish between adverse events from the medication versus the vaccine.
The American Society for Bone and Mineral Research “is an international organization, so we brought together our sister societies that have a vested interested in bone health. Vaccination is happening worldwide, and we wanted to present a united front and united recommendations about how to handle osteoporosis medications appropriately during vaccination,” said Suzanne Jan De Beur, MD, who is president of ASBMR and an associate professor of medicine at Johns Hopkins University, Baltimore.
There has been quite a lot of concern from the community about vaccine and medications, from both physicians and patients wondering whether treatments and vaccines should occur in a certain order, and whether there should be a time gap between the two, said Dr. Jan De Beur. “There was a dearth of information about the best practices for osteoporosis treatment management during vaccination, and we didn’t want people missing their opportunity for a vaccine, and we also didn’t want them unnecessarily delaying their osteoporosis treatment.”
There is no evidence that osteoporosis therapies affect the risk or severity of COVID-19 disease, nor do they appear to change the disease course. Osteoporosis itself does not appear associated with increased risk of infection or severe outcomes, so patients with osteoporosis do not need to be prioritized for vaccination based on that condition alone.
There is no evidence that osteoporosis therapies affect the safety or efficacy of vaccination, but given that vaccine availability is currently inconsistent, patients may need to make temporary changes to their osteoporosis regimens to ensure they can receive vaccine when it is available, such as ensuring a delay between medication and vaccination injections.
A key reason for a delay between injectable or infusion medications and a vaccine is to distinguish between adverse events that could occur, so that an adverse reaction to vaccine isn’t mistaken for an adverse reaction to a drug. Nevertheless, the real world is messy. Dr. Jan De Beur noted a recent patient who arrived at her clinic for an injectable treatment who had just received a COVID-19 vaccination that morning. “We decided to put the injection in the other arm, rather than reschedule the person and put them through the risk of coming back. We could distinguish between injection-site reactions, at least,” she said.
No changes should be made to general bone health therapies, such as calcium and vitamin D supplementation, weight-bearing exercises, and maintenance of a balanced diet.
The guidance includes some recommendations for specific osteoporosis medications.
- Oral bisphosphonates: Alendronate, risedronate, and ibandronate should be continued.
- Intravenous bisphosphonates: a 7-day interval (4-day minimum) is recommended between intravenous bisphosphonate (zoledronic acid and ibandronate) infusion and COVID-19 vaccination in order to distinguish potential autoimmune or inflammatory reactions that could be attributable to either intravenous bisphosphonate or the vaccine.
- Denosumab: There should be a 4- to 7-day delay between denosumab infusion and COVID-19 vaccination to account for injection-site reactions. Another option is to have denosumab injected into the contralateral arm or another site like the abdomen or upper thigh, if spacing the injections is not possible. In any case, denosumab injections should be performed within 7 months of the previous dose.
- Teriparatide and abaloparatide should be continued.
- Romosozumab: There should be a 4- to 7-day delay between a romosozumab injection and COVID-19 vaccine, or romosozumab can be injected in the abdomen (with the exception of a 2-inch area around the naval) or thigh if spacing is not possible.
- Raloxifene should be continued in patients receiving COVID-19 vaccination.
Guidance signatories include ASBMR, the American Association of Clinical Endocrinology, the Endocrine Society, the European Calcified Tissue Society, the National Osteoporosis Foundation, and the International Osteoporosis Foundation.
Dr. Jan De Beur has no relevant financial disclosures.
Bone loss common in kidney stone patients, yet rarely detected
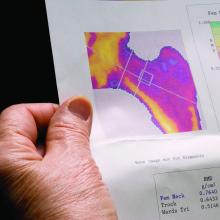
Almost one in four men and women diagnosed with kidney stones have osteoporosis or a history of fracture at the time of their diagnosis, yet fewer than 10% undergo bone mineral density (BMD) screening, a retrospective analysis of a Veterans Health Administration database shows.
Because the majority of those analyzed in the VA dataset were men, this means that middle-aged and older men with kidney stones have about the same risk for osteoporosis as postmenopausal women do, but BMD screening for such men is not currently recommended, the study notes.
“These findings suggest that the risk of osteoporosis or fractures in patients with kidney stone disease is not restricted to postmenopausal women but is also observed in men, a group that is less well recognized to be at risk,” Calyani Ganesan, MD, of Stanford (Calif.) University and colleagues say in their article, published online March 3 in the Journal of Bone and Mineral Research.
“We hope this work raises awareness regarding the possibility of reduced bone strength in patients with kidney stones, [and] in our future work, we hope to identify which patients with kidney stones are at higher risk for osteoporosis or fracture to help guide bone density screening efforts by clinicians in this population,” Dr. Ganesan added in a statement.
VA dataset: Just 9.1% had DXA after kidney stone diagnosed
A total of 531,431 patients with a history of kidney stone disease were identified in the VA dataset. Of these, 23.6% either had been diagnosed with osteoporosis or had a history of fracture around the time of their kidney stone diagnosis. The most common diagnosis was a non-hip fracture, seen in 19% of patients, Dr. Ganesan and colleagues note, followed by osteoporosis in 6.1%, and hip fracture in 2.1%.
The mean age of the patients who concurrently had received a diagnosis of kidney stone disease and osteoporosis or had a fracture history was 64.2 years. In this cohort, more than 91% were men. The majority of the patients were White.
Among some 462,681 patients who had no prior history of either osteoporosis or fracture before their diagnosis of kidney stones, only 9.1% had undergone dual-energy x-ray absorptiometry (DXA) screening for BMD in the 5 years after their kidney stone diagnosis.
“Of those who completed DXA ... 20% were subsequently diagnosed with osteoporosis,” the authors note – 19% with non-hip fracture, and 2.4% with hip fracture.
Importantly, 85% of patients with kidney stone disease who were screened with DXA and were later diagnosed with osteoporosis were men.
“Given that almost 20% of patients in our cohort had a non-hip fracture, we contend that osteoporosis is underdiagnosed and undertreated in older men with kidney stone disease,” the authors stress.
Perform DXA screen in older men, even in absence of hypercalciuria
The authors also explain that the most common metabolic abnormality associated with kidney stones is high urine calcium excretion, or hypercalciuria.
“In a subset of patients with kidney stones, dysregulated calcium homeostasis may be present in which calcium is resorbed from bone and excreted into the urine, which can lead to osteoporosis and the formation of calcium stones,” they explain.
However, when they carried out a 24-hour assessment of urine calcium excretion on a small subset of patients with kidney stones, “we found no correlation between osteoporosis and the level of 24-hour urine calcium excretion,” they point out.
Even when the authors excluded patients who were taking a thiazide diuretic – a class of drugs that decreases urine calcium excretion – there was no correlation between osteoporosis and the level of 24-hour urine calcium excretion.
The investigators suggest it is possible that, in the majority of patients with kidney stones, the cause of hypercalciuria is more closely related to overabsorption of calcium from the gut, not to overresorption of calcium from the bone.
“Nonetheless, our findings indicate that patients with kidney stone disease could benefit from DXA screening even in the absence of hypercalciuria,” they state.
“And our findings provide support for wider use of bone mineral density screening in patients with kidney stone disease, including middle-aged and older men, for whom efforts to mitigate risks of osteoporosis and fractures are not commonly emphasized,” they reaffirm.
The study was funded by the VA Merit Review and the National Institute of Diabetes and Digestive and Kidney Diseases. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Almost one in four men and women diagnosed with kidney stones have osteoporosis or a history of fracture at the time of their diagnosis, yet fewer than 10% undergo bone mineral density (BMD) screening, a retrospective analysis of a Veterans Health Administration database shows.
Because the majority of those analyzed in the VA dataset were men, this means that middle-aged and older men with kidney stones have about the same risk for osteoporosis as postmenopausal women do, but BMD screening for such men is not currently recommended, the study notes.
“These findings suggest that the risk of osteoporosis or fractures in patients with kidney stone disease is not restricted to postmenopausal women but is also observed in men, a group that is less well recognized to be at risk,” Calyani Ganesan, MD, of Stanford (Calif.) University and colleagues say in their article, published online March 3 in the Journal of Bone and Mineral Research.
“We hope this work raises awareness regarding the possibility of reduced bone strength in patients with kidney stones, [and] in our future work, we hope to identify which patients with kidney stones are at higher risk for osteoporosis or fracture to help guide bone density screening efforts by clinicians in this population,” Dr. Ganesan added in a statement.
VA dataset: Just 9.1% had DXA after kidney stone diagnosed
A total of 531,431 patients with a history of kidney stone disease were identified in the VA dataset. Of these, 23.6% either had been diagnosed with osteoporosis or had a history of fracture around the time of their kidney stone diagnosis. The most common diagnosis was a non-hip fracture, seen in 19% of patients, Dr. Ganesan and colleagues note, followed by osteoporosis in 6.1%, and hip fracture in 2.1%.
The mean age of the patients who concurrently had received a diagnosis of kidney stone disease and osteoporosis or had a fracture history was 64.2 years. In this cohort, more than 91% were men. The majority of the patients were White.
Among some 462,681 patients who had no prior history of either osteoporosis or fracture before their diagnosis of kidney stones, only 9.1% had undergone dual-energy x-ray absorptiometry (DXA) screening for BMD in the 5 years after their kidney stone diagnosis.
“Of those who completed DXA ... 20% were subsequently diagnosed with osteoporosis,” the authors note – 19% with non-hip fracture, and 2.4% with hip fracture.
Importantly, 85% of patients with kidney stone disease who were screened with DXA and were later diagnosed with osteoporosis were men.
“Given that almost 20% of patients in our cohort had a non-hip fracture, we contend that osteoporosis is underdiagnosed and undertreated in older men with kidney stone disease,” the authors stress.
Perform DXA screen in older men, even in absence of hypercalciuria
The authors also explain that the most common metabolic abnormality associated with kidney stones is high urine calcium excretion, or hypercalciuria.
“In a subset of patients with kidney stones, dysregulated calcium homeostasis may be present in which calcium is resorbed from bone and excreted into the urine, which can lead to osteoporosis and the formation of calcium stones,” they explain.
However, when they carried out a 24-hour assessment of urine calcium excretion on a small subset of patients with kidney stones, “we found no correlation between osteoporosis and the level of 24-hour urine calcium excretion,” they point out.
Even when the authors excluded patients who were taking a thiazide diuretic – a class of drugs that decreases urine calcium excretion – there was no correlation between osteoporosis and the level of 24-hour urine calcium excretion.
The investigators suggest it is possible that, in the majority of patients with kidney stones, the cause of hypercalciuria is more closely related to overabsorption of calcium from the gut, not to overresorption of calcium from the bone.
“Nonetheless, our findings indicate that patients with kidney stone disease could benefit from DXA screening even in the absence of hypercalciuria,” they state.
“And our findings provide support for wider use of bone mineral density screening in patients with kidney stone disease, including middle-aged and older men, for whom efforts to mitigate risks of osteoporosis and fractures are not commonly emphasized,” they reaffirm.
The study was funded by the VA Merit Review and the National Institute of Diabetes and Digestive and Kidney Diseases. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Almost one in four men and women diagnosed with kidney stones have osteoporosis or a history of fracture at the time of their diagnosis, yet fewer than 10% undergo bone mineral density (BMD) screening, a retrospective analysis of a Veterans Health Administration database shows.
Because the majority of those analyzed in the VA dataset were men, this means that middle-aged and older men with kidney stones have about the same risk for osteoporosis as postmenopausal women do, but BMD screening for such men is not currently recommended, the study notes.
“These findings suggest that the risk of osteoporosis or fractures in patients with kidney stone disease is not restricted to postmenopausal women but is also observed in men, a group that is less well recognized to be at risk,” Calyani Ganesan, MD, of Stanford (Calif.) University and colleagues say in their article, published online March 3 in the Journal of Bone and Mineral Research.
“We hope this work raises awareness regarding the possibility of reduced bone strength in patients with kidney stones, [and] in our future work, we hope to identify which patients with kidney stones are at higher risk for osteoporosis or fracture to help guide bone density screening efforts by clinicians in this population,” Dr. Ganesan added in a statement.
VA dataset: Just 9.1% had DXA after kidney stone diagnosed
A total of 531,431 patients with a history of kidney stone disease were identified in the VA dataset. Of these, 23.6% either had been diagnosed with osteoporosis or had a history of fracture around the time of their kidney stone diagnosis. The most common diagnosis was a non-hip fracture, seen in 19% of patients, Dr. Ganesan and colleagues note, followed by osteoporosis in 6.1%, and hip fracture in 2.1%.
The mean age of the patients who concurrently had received a diagnosis of kidney stone disease and osteoporosis or had a fracture history was 64.2 years. In this cohort, more than 91% were men. The majority of the patients were White.
Among some 462,681 patients who had no prior history of either osteoporosis or fracture before their diagnosis of kidney stones, only 9.1% had undergone dual-energy x-ray absorptiometry (DXA) screening for BMD in the 5 years after their kidney stone diagnosis.
“Of those who completed DXA ... 20% were subsequently diagnosed with osteoporosis,” the authors note – 19% with non-hip fracture, and 2.4% with hip fracture.
Importantly, 85% of patients with kidney stone disease who were screened with DXA and were later diagnosed with osteoporosis were men.
“Given that almost 20% of patients in our cohort had a non-hip fracture, we contend that osteoporosis is underdiagnosed and undertreated in older men with kidney stone disease,” the authors stress.
Perform DXA screen in older men, even in absence of hypercalciuria
The authors also explain that the most common metabolic abnormality associated with kidney stones is high urine calcium excretion, or hypercalciuria.
“In a subset of patients with kidney stones, dysregulated calcium homeostasis may be present in which calcium is resorbed from bone and excreted into the urine, which can lead to osteoporosis and the formation of calcium stones,” they explain.
However, when they carried out a 24-hour assessment of urine calcium excretion on a small subset of patients with kidney stones, “we found no correlation between osteoporosis and the level of 24-hour urine calcium excretion,” they point out.
Even when the authors excluded patients who were taking a thiazide diuretic – a class of drugs that decreases urine calcium excretion – there was no correlation between osteoporosis and the level of 24-hour urine calcium excretion.
The investigators suggest it is possible that, in the majority of patients with kidney stones, the cause of hypercalciuria is more closely related to overabsorption of calcium from the gut, not to overresorption of calcium from the bone.
“Nonetheless, our findings indicate that patients with kidney stone disease could benefit from DXA screening even in the absence of hypercalciuria,” they state.
“And our findings provide support for wider use of bone mineral density screening in patients with kidney stone disease, including middle-aged and older men, for whom efforts to mitigate risks of osteoporosis and fractures are not commonly emphasized,” they reaffirm.
The study was funded by the VA Merit Review and the National Institute of Diabetes and Digestive and Kidney Diseases. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Vitamin D deficiency linked to early cognitive impairment in MS
according to new research that adds to the known adverse relationship between low vitamin D and MS.
“We confirmed that low vitamin D may affect not only early disability but also cognition in newly MS diagnosed patients,” said lead author Eleonora Virgilio, MD, of the MS Center, neurology unit, at the University of Eastern Piedmont, Novara, Italy.
“The possible effects of vitamin D on both cognition (in particular, information processing speed) and early disability in newly diagnosed MS patients needs to be further investigated because this association might represent a marker of future disability, supporting the need for prompt supplementation,” she said.
The findings were presented at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
Low vitamin D and MS
Previous studies have linked insufficient serum vitamin D with everything from the development of MS to activity and disease progression, but less has been reported on a specific link to the impairment of cognitive function, an important complication of MS.
“Cognitive impairment, and, in particular, slowed information processing speed, is very frequent in the MS population from the early stages of disease, and frequently underestimated,” Dr. Virgilio noted. “It has yet to be completely elucidated what the exact underlying mechanisms are.”
To evaluate the relationship, Dr. Virgilio and colleagues enrolled 60 patients in Italy with MS who were newly diagnosed and had serum vitamin D levels collected upon diagnosis. The participants were also tested at diagnosis with the Symbol Digit Modalities Test (SDMT) for information processing speed, which is a hallmark of the cognitive impairment that can occur in MS and is typically the first cognitive domain to show effects of the disease.
Among the patients, 40 were female and the mean age at diagnosis was 39.5 years; 90% had relapsing remitting MS at baseline and 10% had progressive MS. Their median Expanded Disability Status Scale score at diagnosis was 1.5.
At baseline, as many as 85% of the participants (51) had low serum vitamin D levels, defined as below 30 ng/mL, which Dr. Virgilio noted is consistent with other rates reported among people with MS in the Lombardy region of Italy, where the study was conducted.
The patients had a mean vitamin D level of 21.17 ng/mL (± 10.02), with 51.7% considered to have a deficiency (less than 20 ng/mL) and 33.3% with an insufficiency (20-30 ng/mL).
Of the patients, 16 (27%) had cognitive impairment, defined as a z score of 1.5 or less. Their mean raw SDMT score was 46.50 (± 14.73) and mean z score was –0.62 (± 1.29).
Importantly, those with cognitive impairment were significantly more likely to have severe hypovitaminosis D, compared with those with sufficient vitamin D levels, none of whom showed cognitive impairment (P = .02).
Furthermore, vitamin D levels positively correlated with SDMT raw values (P = .001) and z score (P = .008).
Over a mean follow-up of 2 years, a significant correlation was observed between serum vitamin D levels at diagnosis and early disability on the MS severity score (MSSS; P = .02) and a weak correlation with age-related MSSS (ARMSS; P = .08) at the last clinical follow-up.
Dr. Virgilio noted that factors including disease treatment effects or other factors could have played a role in the weaker results. “It is possible that the linear correlation we found was not as strong as expected [because of] an effect of treatment with disease-modifying therapies or vitamin D supplementation, or because of the short follow-up available at the moment for our population – only for a mean period of 2 years after MS diagnosis.”
The mechanisms for vitamin D deficiency in the MS population are likely multifactorial, with genetic as well as environmental links, she noted.
“The immunomodulatory effects of vitamin D are well known,” Dr. Virgilio said.
“Vitamin D was already linked to cognitive function in other neurodegenerative diseases, [including] Alzheimer’s disease, but more importantly, also in other autoimmune diseases, such as systemic lupus erythematosus,” she explained.
Vitamin D also linked to long-term cognitive function
The study adds to recent research showing longer-term effects of vitamin D deficiency and cognitive impairment in MS: In the longitudinal BENEFIT trial published in 2020, researchers following 278 patients with MS over the course of 11 years found that a 50 ng/L higher mean vitamin D level in the first 2 years of the study was associated with a 65% lower odds of a poor performance on Paced Auditory Serial Addition Test scores at the 11-year follow-up.
That study also looked at neurofilament light chain concentrations, which are associated with MS disease activity, and found they were 20% lower among those with higher vitamin D at baseline. Smokers also had lower cognitive scores.
“Lower vitamin D and smoking after clinical onset predicted worse long-term cognitive function and neuronal integrity in patients with MS,” the authors concluded.
The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to new research that adds to the known adverse relationship between low vitamin D and MS.
“We confirmed that low vitamin D may affect not only early disability but also cognition in newly MS diagnosed patients,” said lead author Eleonora Virgilio, MD, of the MS Center, neurology unit, at the University of Eastern Piedmont, Novara, Italy.
“The possible effects of vitamin D on both cognition (in particular, information processing speed) and early disability in newly diagnosed MS patients needs to be further investigated because this association might represent a marker of future disability, supporting the need for prompt supplementation,” she said.
The findings were presented at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
Low vitamin D and MS
Previous studies have linked insufficient serum vitamin D with everything from the development of MS to activity and disease progression, but less has been reported on a specific link to the impairment of cognitive function, an important complication of MS.
“Cognitive impairment, and, in particular, slowed information processing speed, is very frequent in the MS population from the early stages of disease, and frequently underestimated,” Dr. Virgilio noted. “It has yet to be completely elucidated what the exact underlying mechanisms are.”
To evaluate the relationship, Dr. Virgilio and colleagues enrolled 60 patients in Italy with MS who were newly diagnosed and had serum vitamin D levels collected upon diagnosis. The participants were also tested at diagnosis with the Symbol Digit Modalities Test (SDMT) for information processing speed, which is a hallmark of the cognitive impairment that can occur in MS and is typically the first cognitive domain to show effects of the disease.
Among the patients, 40 were female and the mean age at diagnosis was 39.5 years; 90% had relapsing remitting MS at baseline and 10% had progressive MS. Their median Expanded Disability Status Scale score at diagnosis was 1.5.
At baseline, as many as 85% of the participants (51) had low serum vitamin D levels, defined as below 30 ng/mL, which Dr. Virgilio noted is consistent with other rates reported among people with MS in the Lombardy region of Italy, where the study was conducted.
The patients had a mean vitamin D level of 21.17 ng/mL (± 10.02), with 51.7% considered to have a deficiency (less than 20 ng/mL) and 33.3% with an insufficiency (20-30 ng/mL).
Of the patients, 16 (27%) had cognitive impairment, defined as a z score of 1.5 or less. Their mean raw SDMT score was 46.50 (± 14.73) and mean z score was –0.62 (± 1.29).
Importantly, those with cognitive impairment were significantly more likely to have severe hypovitaminosis D, compared with those with sufficient vitamin D levels, none of whom showed cognitive impairment (P = .02).
Furthermore, vitamin D levels positively correlated with SDMT raw values (P = .001) and z score (P = .008).
Over a mean follow-up of 2 years, a significant correlation was observed between serum vitamin D levels at diagnosis and early disability on the MS severity score (MSSS; P = .02) and a weak correlation with age-related MSSS (ARMSS; P = .08) at the last clinical follow-up.
Dr. Virgilio noted that factors including disease treatment effects or other factors could have played a role in the weaker results. “It is possible that the linear correlation we found was not as strong as expected [because of] an effect of treatment with disease-modifying therapies or vitamin D supplementation, or because of the short follow-up available at the moment for our population – only for a mean period of 2 years after MS diagnosis.”
The mechanisms for vitamin D deficiency in the MS population are likely multifactorial, with genetic as well as environmental links, she noted.
“The immunomodulatory effects of vitamin D are well known,” Dr. Virgilio said.
“Vitamin D was already linked to cognitive function in other neurodegenerative diseases, [including] Alzheimer’s disease, but more importantly, also in other autoimmune diseases, such as systemic lupus erythematosus,” she explained.
Vitamin D also linked to long-term cognitive function
The study adds to recent research showing longer-term effects of vitamin D deficiency and cognitive impairment in MS: In the longitudinal BENEFIT trial published in 2020, researchers following 278 patients with MS over the course of 11 years found that a 50 ng/L higher mean vitamin D level in the first 2 years of the study was associated with a 65% lower odds of a poor performance on Paced Auditory Serial Addition Test scores at the 11-year follow-up.
That study also looked at neurofilament light chain concentrations, which are associated with MS disease activity, and found they were 20% lower among those with higher vitamin D at baseline. Smokers also had lower cognitive scores.
“Lower vitamin D and smoking after clinical onset predicted worse long-term cognitive function and neuronal integrity in patients with MS,” the authors concluded.
The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to new research that adds to the known adverse relationship between low vitamin D and MS.
“We confirmed that low vitamin D may affect not only early disability but also cognition in newly MS diagnosed patients,” said lead author Eleonora Virgilio, MD, of the MS Center, neurology unit, at the University of Eastern Piedmont, Novara, Italy.
“The possible effects of vitamin D on both cognition (in particular, information processing speed) and early disability in newly diagnosed MS patients needs to be further investigated because this association might represent a marker of future disability, supporting the need for prompt supplementation,” she said.
The findings were presented at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
Low vitamin D and MS
Previous studies have linked insufficient serum vitamin D with everything from the development of MS to activity and disease progression, but less has been reported on a specific link to the impairment of cognitive function, an important complication of MS.
“Cognitive impairment, and, in particular, slowed information processing speed, is very frequent in the MS population from the early stages of disease, and frequently underestimated,” Dr. Virgilio noted. “It has yet to be completely elucidated what the exact underlying mechanisms are.”
To evaluate the relationship, Dr. Virgilio and colleagues enrolled 60 patients in Italy with MS who were newly diagnosed and had serum vitamin D levels collected upon diagnosis. The participants were also tested at diagnosis with the Symbol Digit Modalities Test (SDMT) for information processing speed, which is a hallmark of the cognitive impairment that can occur in MS and is typically the first cognitive domain to show effects of the disease.
Among the patients, 40 were female and the mean age at diagnosis was 39.5 years; 90% had relapsing remitting MS at baseline and 10% had progressive MS. Their median Expanded Disability Status Scale score at diagnosis was 1.5.
At baseline, as many as 85% of the participants (51) had low serum vitamin D levels, defined as below 30 ng/mL, which Dr. Virgilio noted is consistent with other rates reported among people with MS in the Lombardy region of Italy, where the study was conducted.
The patients had a mean vitamin D level of 21.17 ng/mL (± 10.02), with 51.7% considered to have a deficiency (less than 20 ng/mL) and 33.3% with an insufficiency (20-30 ng/mL).
Of the patients, 16 (27%) had cognitive impairment, defined as a z score of 1.5 or less. Their mean raw SDMT score was 46.50 (± 14.73) and mean z score was –0.62 (± 1.29).
Importantly, those with cognitive impairment were significantly more likely to have severe hypovitaminosis D, compared with those with sufficient vitamin D levels, none of whom showed cognitive impairment (P = .02).
Furthermore, vitamin D levels positively correlated with SDMT raw values (P = .001) and z score (P = .008).
Over a mean follow-up of 2 years, a significant correlation was observed between serum vitamin D levels at diagnosis and early disability on the MS severity score (MSSS; P = .02) and a weak correlation with age-related MSSS (ARMSS; P = .08) at the last clinical follow-up.
Dr. Virgilio noted that factors including disease treatment effects or other factors could have played a role in the weaker results. “It is possible that the linear correlation we found was not as strong as expected [because of] an effect of treatment with disease-modifying therapies or vitamin D supplementation, or because of the short follow-up available at the moment for our population – only for a mean period of 2 years after MS diagnosis.”
The mechanisms for vitamin D deficiency in the MS population are likely multifactorial, with genetic as well as environmental links, she noted.
“The immunomodulatory effects of vitamin D are well known,” Dr. Virgilio said.
“Vitamin D was already linked to cognitive function in other neurodegenerative diseases, [including] Alzheimer’s disease, but more importantly, also in other autoimmune diseases, such as systemic lupus erythematosus,” she explained.
Vitamin D also linked to long-term cognitive function
The study adds to recent research showing longer-term effects of vitamin D deficiency and cognitive impairment in MS: In the longitudinal BENEFIT trial published in 2020, researchers following 278 patients with MS over the course of 11 years found that a 50 ng/L higher mean vitamin D level in the first 2 years of the study was associated with a 65% lower odds of a poor performance on Paced Auditory Serial Addition Test scores at the 11-year follow-up.
That study also looked at neurofilament light chain concentrations, which are associated with MS disease activity, and found they were 20% lower among those with higher vitamin D at baseline. Smokers also had lower cognitive scores.
“Lower vitamin D and smoking after clinical onset predicted worse long-term cognitive function and neuronal integrity in patients with MS,” the authors concluded.
The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ACTRIMS FORUM 2021
Metformin for pediatric obesity? Researchers review the evidence
Metformin has a modest favorable effect on body mass index z score and insulin resistance in children and adolescents with obesity, compared with placebo, according to a systematic review of trial data.
“The available evidence is of varying quality,” however, and the drug increases the likelihood of gastrointestinal adverse effects, reported Reem Masarwa, PharmD, PhD, and colleagues in Pediatrics. “Nonetheless, metformin may be considered for use as a pharmacologic therapy in this pediatric population because of its modest efficacy, availability, cost, and safety profile.”
The Food and Drug Administration has approved metformin for the treatment of type 2 diabetes in children and adolescents. Doctors have used the drug off label for weight loss in children with obesity, but this use “remains controversial,” the review authors said.
To assess the efficacy and safety of metformin plus lifestyle interventions compared with placebo plus lifestyle interventions in children and adolescents with obesity, Dr. Masarwa, with the Center for Clinical Epidemiology, Lady Davis Institute, Jewish General Hospital, and the department of epidemiology, biostatistics, and occupational health, McGill University, Montreal, and colleagues systematically reviewed data from randomized controlled trials (RCTs). Their review was published online in Pediatrics.
The investigators focused on studies that examined outcomes such as body mass index, BMI z score, insulin resistance, and gastrointestinal adverse effects. They excluded studies of children with type 2 diabetes.
The researchers included 24 RCTs in their review. The studies included 1,623 children and adolescents who received metformin (861 participants) or placebo (762 participants). Indications included uncomplicated obesity in 10 studies, obesity with insulin resistance in 9 studies, prediabetes in 3 studies, and nonalcoholic fatty liver disease in 2 studies. One of the trials did not incorporate a lifestyle cointervention.
Participants ranged in age from 4 years to 19 years, and trial durations ranged from 2 months to 2 years. The total daily dose of metformin ranged from 500 mg to 2,000 mg.
In 14 RCTs that reported BMI, metformin generally decreased BMI (range of mean changes: –2.70 to 1.30), compared with placebo (range of mean changes: –1.12 to 1.90), although three trials suggested that metformin increased BMI. The average difference in the treatment effect between the metformin and placebo groups ranged from –2.72 to 0.70. “Importantly, the authors of many RCTs reported variable treatment effects, preventing definitive conclusions from being drawn from individual trials,” Dr. Masarwa and coauthors wrote.
In seven RCTs that reported BMI z score, metformin consistently decreased BMI z score (range of mean changes: –0.37 to –0.03), compared with placebo (range of mean changes: –0.22 to 0.15). The mean difference in the treatment effect between treatment groups ranged from –0.15 to –0.07. The largest decrease occurred in patients with nonalcoholic fatty liver disease.
The rate of gastrointestinal adverse events nearly doubled with metformin treatment, relative to placebo (rate range: 2%-74% for metformin vs. 0%-42% for placebo).
Metformin adherence rates ranged from 60% to 90%, and lifestyle cointerventions varied substantially across the trials, the researchers noted. The clinical significance and long-term effects of metformin treatment in this population “remain uncertain,” they said.
Off-label use may not be ideal
“Ideally, children with obesity should be entered into a clinical trial rather than placed on an off-label medication,” Vandana Raman, MD, and Carol M. Foster, MD, said in a related commentary. Still, treatment with metformin may be reasonable in certain cases, said Dr. Raman and Dr. Foster of the division of endocrinology in the department of pediatrics at the University of Utah in Salt Lake City. “Metformin is a low-cost option and may provide modest clinical benefit for weight loss with minimal side effects. If lifestyle modification has been pursued but has achieved minimal weight loss, it may be reasonable to try an agent such as metformin as adjunctive therapy,” they said.
Lifestyle modification therapy – including nutritional changes, physical activity, and behavior modification – has been the “mainstay of management” for patients with obesity, and this approach underpins successful weight loss, they said. But durable weight loss with lifestyle modification may be challenging, and pharmacologic treatments “are attractive options before proceeding to bariatric surgery,” they said.
For younger patients, FDA-approved medications for obesity include orlistat and liraglutide for patients aged 12 years and older, and phentermine for patients aged 16 years and older.
“Orlistat has been associated with modest BMI reduction but may cause intolerable gastrointestinal side effects and possible fat-soluble vitamin deficiency,” they said. “Phentermine is approved for short-term therapy only and may increase heart rate and blood pressure and cause irritability and insomnia.”
Liraglutide, which was approved for the treatment of pediatric obesity in December 2020, reduced BMI in a trial that included adolescents with obesity. About 43% of the participants who received liraglutide, compared with 18% who received placebo, had a 5% reduction in BMI. In addition, 26% and 8%, respectively, had a 10% reduction in BMI. The use of liraglutide “is limited by the need for daily subcutaneous injections and high frequency of gastrointestinal side effects and high cost,” however, the commentary authors noted.
In addition, the FDA has approved setmelanotide for children older than 6 years with obesity caused by three rare genetic conditions.
Some small studies have suggested that topiramate may lead to meaningful weight loss in children, but the medication has been associated with cognitive dysfunction, they said.
Considering surgery
“This is an important review of the efficacy of metformin as a tool for weight loss in children with obesity,” said Suzanne C. Boulter, MD, adjunct professor emeritus of pediatrics and community and family medicine at the Geisel School of Medicine at Dartmouth in Hanover, N.H. “Results showed modest decreases in BMI z scores compared to placebo but there were a significant percentage of GI side effects and dropouts from the trials.”
“Tools other than lifestyle changes are needed to address” pediatric obesity, Dr. Boulter said. “Another tool is gastric bypass which is now a recommended intervention in selected clinical sites for adolescents 14 years of age and older with BMIs greater than 35.”
Dr. Boulter highlighted a recent study in Pediatrics that examined data from more than 200 adolescents who underwent bariatric surgery. The researchers found that outcomes were similar for older and younger patients.
“It would be interesting to pediatricians in practice to see a comparison study between metformin and bariatric surgery long-term results,” Dr. Boulter added.
Dr. Masarwa and coauthors received support from the Quebec Foundation for Health Research and the Canadian Institutes of Health Research Drug Safety and Effectiveness Cross-Disciplinary Training Program. One coauthor also is supported by an award from McGill University.
The authors of the systematic review and the accompanying commentary had no relevant financial disclosures. Dr. Boulter is a member of the editorial advisory board for Pediatric News and had no relevant financial disclosures.
Metformin has a modest favorable effect on body mass index z score and insulin resistance in children and adolescents with obesity, compared with placebo, according to a systematic review of trial data.
“The available evidence is of varying quality,” however, and the drug increases the likelihood of gastrointestinal adverse effects, reported Reem Masarwa, PharmD, PhD, and colleagues in Pediatrics. “Nonetheless, metformin may be considered for use as a pharmacologic therapy in this pediatric population because of its modest efficacy, availability, cost, and safety profile.”
The Food and Drug Administration has approved metformin for the treatment of type 2 diabetes in children and adolescents. Doctors have used the drug off label for weight loss in children with obesity, but this use “remains controversial,” the review authors said.
To assess the efficacy and safety of metformin plus lifestyle interventions compared with placebo plus lifestyle interventions in children and adolescents with obesity, Dr. Masarwa, with the Center for Clinical Epidemiology, Lady Davis Institute, Jewish General Hospital, and the department of epidemiology, biostatistics, and occupational health, McGill University, Montreal, and colleagues systematically reviewed data from randomized controlled trials (RCTs). Their review was published online in Pediatrics.
The investigators focused on studies that examined outcomes such as body mass index, BMI z score, insulin resistance, and gastrointestinal adverse effects. They excluded studies of children with type 2 diabetes.
The researchers included 24 RCTs in their review. The studies included 1,623 children and adolescents who received metformin (861 participants) or placebo (762 participants). Indications included uncomplicated obesity in 10 studies, obesity with insulin resistance in 9 studies, prediabetes in 3 studies, and nonalcoholic fatty liver disease in 2 studies. One of the trials did not incorporate a lifestyle cointervention.
Participants ranged in age from 4 years to 19 years, and trial durations ranged from 2 months to 2 years. The total daily dose of metformin ranged from 500 mg to 2,000 mg.
In 14 RCTs that reported BMI, metformin generally decreased BMI (range of mean changes: –2.70 to 1.30), compared with placebo (range of mean changes: –1.12 to 1.90), although three trials suggested that metformin increased BMI. The average difference in the treatment effect between the metformin and placebo groups ranged from –2.72 to 0.70. “Importantly, the authors of many RCTs reported variable treatment effects, preventing definitive conclusions from being drawn from individual trials,” Dr. Masarwa and coauthors wrote.
In seven RCTs that reported BMI z score, metformin consistently decreased BMI z score (range of mean changes: –0.37 to –0.03), compared with placebo (range of mean changes: –0.22 to 0.15). The mean difference in the treatment effect between treatment groups ranged from –0.15 to –0.07. The largest decrease occurred in patients with nonalcoholic fatty liver disease.
The rate of gastrointestinal adverse events nearly doubled with metformin treatment, relative to placebo (rate range: 2%-74% for metformin vs. 0%-42% for placebo).
Metformin adherence rates ranged from 60% to 90%, and lifestyle cointerventions varied substantially across the trials, the researchers noted. The clinical significance and long-term effects of metformin treatment in this population “remain uncertain,” they said.
Off-label use may not be ideal
“Ideally, children with obesity should be entered into a clinical trial rather than placed on an off-label medication,” Vandana Raman, MD, and Carol M. Foster, MD, said in a related commentary. Still, treatment with metformin may be reasonable in certain cases, said Dr. Raman and Dr. Foster of the division of endocrinology in the department of pediatrics at the University of Utah in Salt Lake City. “Metformin is a low-cost option and may provide modest clinical benefit for weight loss with minimal side effects. If lifestyle modification has been pursued but has achieved minimal weight loss, it may be reasonable to try an agent such as metformin as adjunctive therapy,” they said.
Lifestyle modification therapy – including nutritional changes, physical activity, and behavior modification – has been the “mainstay of management” for patients with obesity, and this approach underpins successful weight loss, they said. But durable weight loss with lifestyle modification may be challenging, and pharmacologic treatments “are attractive options before proceeding to bariatric surgery,” they said.
For younger patients, FDA-approved medications for obesity include orlistat and liraglutide for patients aged 12 years and older, and phentermine for patients aged 16 years and older.
“Orlistat has been associated with modest BMI reduction but may cause intolerable gastrointestinal side effects and possible fat-soluble vitamin deficiency,” they said. “Phentermine is approved for short-term therapy only and may increase heart rate and blood pressure and cause irritability and insomnia.”
Liraglutide, which was approved for the treatment of pediatric obesity in December 2020, reduced BMI in a trial that included adolescents with obesity. About 43% of the participants who received liraglutide, compared with 18% who received placebo, had a 5% reduction in BMI. In addition, 26% and 8%, respectively, had a 10% reduction in BMI. The use of liraglutide “is limited by the need for daily subcutaneous injections and high frequency of gastrointestinal side effects and high cost,” however, the commentary authors noted.
In addition, the FDA has approved setmelanotide for children older than 6 years with obesity caused by three rare genetic conditions.
Some small studies have suggested that topiramate may lead to meaningful weight loss in children, but the medication has been associated with cognitive dysfunction, they said.
Considering surgery
“This is an important review of the efficacy of metformin as a tool for weight loss in children with obesity,” said Suzanne C. Boulter, MD, adjunct professor emeritus of pediatrics and community and family medicine at the Geisel School of Medicine at Dartmouth in Hanover, N.H. “Results showed modest decreases in BMI z scores compared to placebo but there were a significant percentage of GI side effects and dropouts from the trials.”
“Tools other than lifestyle changes are needed to address” pediatric obesity, Dr. Boulter said. “Another tool is gastric bypass which is now a recommended intervention in selected clinical sites for adolescents 14 years of age and older with BMIs greater than 35.”
Dr. Boulter highlighted a recent study in Pediatrics that examined data from more than 200 adolescents who underwent bariatric surgery. The researchers found that outcomes were similar for older and younger patients.
“It would be interesting to pediatricians in practice to see a comparison study between metformin and bariatric surgery long-term results,” Dr. Boulter added.
Dr. Masarwa and coauthors received support from the Quebec Foundation for Health Research and the Canadian Institutes of Health Research Drug Safety and Effectiveness Cross-Disciplinary Training Program. One coauthor also is supported by an award from McGill University.
The authors of the systematic review and the accompanying commentary had no relevant financial disclosures. Dr. Boulter is a member of the editorial advisory board for Pediatric News and had no relevant financial disclosures.
Metformin has a modest favorable effect on body mass index z score and insulin resistance in children and adolescents with obesity, compared with placebo, according to a systematic review of trial data.
“The available evidence is of varying quality,” however, and the drug increases the likelihood of gastrointestinal adverse effects, reported Reem Masarwa, PharmD, PhD, and colleagues in Pediatrics. “Nonetheless, metformin may be considered for use as a pharmacologic therapy in this pediatric population because of its modest efficacy, availability, cost, and safety profile.”
The Food and Drug Administration has approved metformin for the treatment of type 2 diabetes in children and adolescents. Doctors have used the drug off label for weight loss in children with obesity, but this use “remains controversial,” the review authors said.
To assess the efficacy and safety of metformin plus lifestyle interventions compared with placebo plus lifestyle interventions in children and adolescents with obesity, Dr. Masarwa, with the Center for Clinical Epidemiology, Lady Davis Institute, Jewish General Hospital, and the department of epidemiology, biostatistics, and occupational health, McGill University, Montreal, and colleagues systematically reviewed data from randomized controlled trials (RCTs). Their review was published online in Pediatrics.
The investigators focused on studies that examined outcomes such as body mass index, BMI z score, insulin resistance, and gastrointestinal adverse effects. They excluded studies of children with type 2 diabetes.
The researchers included 24 RCTs in their review. The studies included 1,623 children and adolescents who received metformin (861 participants) or placebo (762 participants). Indications included uncomplicated obesity in 10 studies, obesity with insulin resistance in 9 studies, prediabetes in 3 studies, and nonalcoholic fatty liver disease in 2 studies. One of the trials did not incorporate a lifestyle cointervention.
Participants ranged in age from 4 years to 19 years, and trial durations ranged from 2 months to 2 years. The total daily dose of metformin ranged from 500 mg to 2,000 mg.
In 14 RCTs that reported BMI, metformin generally decreased BMI (range of mean changes: –2.70 to 1.30), compared with placebo (range of mean changes: –1.12 to 1.90), although three trials suggested that metformin increased BMI. The average difference in the treatment effect between the metformin and placebo groups ranged from –2.72 to 0.70. “Importantly, the authors of many RCTs reported variable treatment effects, preventing definitive conclusions from being drawn from individual trials,” Dr. Masarwa and coauthors wrote.
In seven RCTs that reported BMI z score, metformin consistently decreased BMI z score (range of mean changes: –0.37 to –0.03), compared with placebo (range of mean changes: –0.22 to 0.15). The mean difference in the treatment effect between treatment groups ranged from –0.15 to –0.07. The largest decrease occurred in patients with nonalcoholic fatty liver disease.
The rate of gastrointestinal adverse events nearly doubled with metformin treatment, relative to placebo (rate range: 2%-74% for metformin vs. 0%-42% for placebo).
Metformin adherence rates ranged from 60% to 90%, and lifestyle cointerventions varied substantially across the trials, the researchers noted. The clinical significance and long-term effects of metformin treatment in this population “remain uncertain,” they said.
Off-label use may not be ideal
“Ideally, children with obesity should be entered into a clinical trial rather than placed on an off-label medication,” Vandana Raman, MD, and Carol M. Foster, MD, said in a related commentary. Still, treatment with metformin may be reasonable in certain cases, said Dr. Raman and Dr. Foster of the division of endocrinology in the department of pediatrics at the University of Utah in Salt Lake City. “Metformin is a low-cost option and may provide modest clinical benefit for weight loss with minimal side effects. If lifestyle modification has been pursued but has achieved minimal weight loss, it may be reasonable to try an agent such as metformin as adjunctive therapy,” they said.
Lifestyle modification therapy – including nutritional changes, physical activity, and behavior modification – has been the “mainstay of management” for patients with obesity, and this approach underpins successful weight loss, they said. But durable weight loss with lifestyle modification may be challenging, and pharmacologic treatments “are attractive options before proceeding to bariatric surgery,” they said.
For younger patients, FDA-approved medications for obesity include orlistat and liraglutide for patients aged 12 years and older, and phentermine for patients aged 16 years and older.
“Orlistat has been associated with modest BMI reduction but may cause intolerable gastrointestinal side effects and possible fat-soluble vitamin deficiency,” they said. “Phentermine is approved for short-term therapy only and may increase heart rate and blood pressure and cause irritability and insomnia.”
Liraglutide, which was approved for the treatment of pediatric obesity in December 2020, reduced BMI in a trial that included adolescents with obesity. About 43% of the participants who received liraglutide, compared with 18% who received placebo, had a 5% reduction in BMI. In addition, 26% and 8%, respectively, had a 10% reduction in BMI. The use of liraglutide “is limited by the need for daily subcutaneous injections and high frequency of gastrointestinal side effects and high cost,” however, the commentary authors noted.
In addition, the FDA has approved setmelanotide for children older than 6 years with obesity caused by three rare genetic conditions.
Some small studies have suggested that topiramate may lead to meaningful weight loss in children, but the medication has been associated with cognitive dysfunction, they said.
Considering surgery
“This is an important review of the efficacy of metformin as a tool for weight loss in children with obesity,” said Suzanne C. Boulter, MD, adjunct professor emeritus of pediatrics and community and family medicine at the Geisel School of Medicine at Dartmouth in Hanover, N.H. “Results showed modest decreases in BMI z scores compared to placebo but there were a significant percentage of GI side effects and dropouts from the trials.”
“Tools other than lifestyle changes are needed to address” pediatric obesity, Dr. Boulter said. “Another tool is gastric bypass which is now a recommended intervention in selected clinical sites for adolescents 14 years of age and older with BMIs greater than 35.”
Dr. Boulter highlighted a recent study in Pediatrics that examined data from more than 200 adolescents who underwent bariatric surgery. The researchers found that outcomes were similar for older and younger patients.
“It would be interesting to pediatricians in practice to see a comparison study between metformin and bariatric surgery long-term results,” Dr. Boulter added.
Dr. Masarwa and coauthors received support from the Quebec Foundation for Health Research and the Canadian Institutes of Health Research Drug Safety and Effectiveness Cross-Disciplinary Training Program. One coauthor also is supported by an award from McGill University.
The authors of the systematic review and the accompanying commentary had no relevant financial disclosures. Dr. Boulter is a member of the editorial advisory board for Pediatric News and had no relevant financial disclosures.
FROM PEDIATRICS
COVID-19 vaccination recommended for rheumatology patients
People with rheumatic diseases should get vaccinated against SARS-CoV-2 as soon as possible, the American College of Rheumatology (ACR) recommends.
“It may be that people with rheumatic diseases are at increased risk of developing COVID or serious COVID-related complications,” Jonathan Hausmann, MD, assistant professor of medicine at Harvard Medical School, Boston, said in an ACR podcast. “So the need to prevent COVID-19 is incredibly important in this group of patients.”
The guidelines recommend a delay in vaccination only in rare circumstances, such as for patients with very severe illness or who have recently been administered rituximab, Jeffrey R. Curtis, MD, MPH, lead author of the guidelines, said in the podcast.
“Our members have been inundated with questions and concerns from their patients on whether they should receive the vaccine,” ACR President David Karp, MD, PhD, said in a press release.
So the ACR convened a panel of nine rheumatologists, two infectious disease specialists, and two public health experts. Over the course of 8 weeks, the task force reviewed the literature and agreed on recommendations. The organization posted a summary of the guidelines on its website after its board of directors approved it Feb. 8. The paper is pending journal peer review.
Some risks are real
The task force confined its research to the COVID-19 vaccines being offered by Pfizer and Moderna because they are currently the only ones approved by the Food and Drug Administration. It found no reason to distinguish between the two vaccines in its recommendations.
Because little research has directly addressed the question concerning COVID-19 vaccination for patients with rheumatic diseases, the task force extrapolated from data on other vaccinations in people with rheumatic disease and on the COVID-19 vaccinations in other populations.
It analyzed reports that other types of vaccination, such as for influenza, triggered flares of rheumatic conditions. “It is really individual case reports or small cohorts where there may be a somewhat higher incidence of flare, but it’s usually not very large in its magnitude nor duration,” said Dr. Curtis of the University of Alabama at Birmingham.
The task force also considered the possibility that vaccinations could lead to a new autoimmune disorder, such as Guillain-Barré syndrome or Bell palsy. The risk is real, the task force decided, but not significant enough to influence their recommendations.
Likewise, in immunocompromised people, vaccinations with live virus, such as those for shingles, might trigger the infection the vaccination is meant to prevent. But this can’t happen with the Pfizer and Moderna COVID-19 vaccines because they contain messenger RNA instead of live viruses, Dr. Curtis said.
Although it might be optimal to administer the vaccines when rheumatic diseases are quiescent, the urgency of getting vaccinated overrides that consideration, Dr. Curtis said. “By and large, there was a general consensus to not want to delay vaccination until somebody was stable and doing great, because you don’t know how long that’s going to be,” he said.
How well does it work?
One unanswered question is whether the COVID-19 vaccines work as well for patients with rheumatic diseases. The task force was reassured by data showing efficacy across a range of subgroups, including some with immunosenescence, Dr. Curtis said. “But until we have data in rheumatology patients, we’re just not going to know,” he said.
The guidelines specify that some drug regimens be modified when patients are vaccinated.
For patients taking rituximab, vaccination should be delayed, but only for those who are able to maintain safe social distancing to reduce the risk for COVID-19 exposure, Dr. Curtis said. “If somebody has just gotten rituximab recently, it might be more ideal to complete the vaccine series about 2-4 weeks before the next rituximab dose,” he said. “So if you are giving that therapy, say, at 6-month intervals, if you could vaccinate them at around month 5 from the most recent rituximab cycle, that might be more ideal.”
The guidance calls for withholding JAK inhibitors for a week after each vaccine dose is administered.
It calls for holding SQ abatacept 1 week prior and 1 week after the first COVID-19 vaccine dose, with no interruption after the second dose.
For abatacept IV, clinicians should “time vaccine administration so that the first vaccination will occur 4 weeks after abatacept infusion (i.e., the entire dosing interval), and postpone the subsequent abatacept infusion by 1 week (i.e., a 5-week gap in total).” It recommends no medication adjustment for the second vaccine dose.
For cyclophosphamide, the guidance recommends timing administration to occur about a week after each vaccine dose, when feasible.
None of this advice should supersede clinical judgment, Dr. Curtis said.
A version of this article first appeared on Medscape.com.
People with rheumatic diseases should get vaccinated against SARS-CoV-2 as soon as possible, the American College of Rheumatology (ACR) recommends.
“It may be that people with rheumatic diseases are at increased risk of developing COVID or serious COVID-related complications,” Jonathan Hausmann, MD, assistant professor of medicine at Harvard Medical School, Boston, said in an ACR podcast. “So the need to prevent COVID-19 is incredibly important in this group of patients.”
The guidelines recommend a delay in vaccination only in rare circumstances, such as for patients with very severe illness or who have recently been administered rituximab, Jeffrey R. Curtis, MD, MPH, lead author of the guidelines, said in the podcast.
“Our members have been inundated with questions and concerns from their patients on whether they should receive the vaccine,” ACR President David Karp, MD, PhD, said in a press release.
So the ACR convened a panel of nine rheumatologists, two infectious disease specialists, and two public health experts. Over the course of 8 weeks, the task force reviewed the literature and agreed on recommendations. The organization posted a summary of the guidelines on its website after its board of directors approved it Feb. 8. The paper is pending journal peer review.
Some risks are real
The task force confined its research to the COVID-19 vaccines being offered by Pfizer and Moderna because they are currently the only ones approved by the Food and Drug Administration. It found no reason to distinguish between the two vaccines in its recommendations.
Because little research has directly addressed the question concerning COVID-19 vaccination for patients with rheumatic diseases, the task force extrapolated from data on other vaccinations in people with rheumatic disease and on the COVID-19 vaccinations in other populations.
It analyzed reports that other types of vaccination, such as for influenza, triggered flares of rheumatic conditions. “It is really individual case reports or small cohorts where there may be a somewhat higher incidence of flare, but it’s usually not very large in its magnitude nor duration,” said Dr. Curtis of the University of Alabama at Birmingham.
The task force also considered the possibility that vaccinations could lead to a new autoimmune disorder, such as Guillain-Barré syndrome or Bell palsy. The risk is real, the task force decided, but not significant enough to influence their recommendations.
Likewise, in immunocompromised people, vaccinations with live virus, such as those for shingles, might trigger the infection the vaccination is meant to prevent. But this can’t happen with the Pfizer and Moderna COVID-19 vaccines because they contain messenger RNA instead of live viruses, Dr. Curtis said.
Although it might be optimal to administer the vaccines when rheumatic diseases are quiescent, the urgency of getting vaccinated overrides that consideration, Dr. Curtis said. “By and large, there was a general consensus to not want to delay vaccination until somebody was stable and doing great, because you don’t know how long that’s going to be,” he said.
How well does it work?
One unanswered question is whether the COVID-19 vaccines work as well for patients with rheumatic diseases. The task force was reassured by data showing efficacy across a range of subgroups, including some with immunosenescence, Dr. Curtis said. “But until we have data in rheumatology patients, we’re just not going to know,” he said.
The guidelines specify that some drug regimens be modified when patients are vaccinated.
For patients taking rituximab, vaccination should be delayed, but only for those who are able to maintain safe social distancing to reduce the risk for COVID-19 exposure, Dr. Curtis said. “If somebody has just gotten rituximab recently, it might be more ideal to complete the vaccine series about 2-4 weeks before the next rituximab dose,” he said. “So if you are giving that therapy, say, at 6-month intervals, if you could vaccinate them at around month 5 from the most recent rituximab cycle, that might be more ideal.”
The guidance calls for withholding JAK inhibitors for a week after each vaccine dose is administered.
It calls for holding SQ abatacept 1 week prior and 1 week after the first COVID-19 vaccine dose, with no interruption after the second dose.
For abatacept IV, clinicians should “time vaccine administration so that the first vaccination will occur 4 weeks after abatacept infusion (i.e., the entire dosing interval), and postpone the subsequent abatacept infusion by 1 week (i.e., a 5-week gap in total).” It recommends no medication adjustment for the second vaccine dose.
For cyclophosphamide, the guidance recommends timing administration to occur about a week after each vaccine dose, when feasible.
None of this advice should supersede clinical judgment, Dr. Curtis said.
A version of this article first appeared on Medscape.com.
People with rheumatic diseases should get vaccinated against SARS-CoV-2 as soon as possible, the American College of Rheumatology (ACR) recommends.
“It may be that people with rheumatic diseases are at increased risk of developing COVID or serious COVID-related complications,” Jonathan Hausmann, MD, assistant professor of medicine at Harvard Medical School, Boston, said in an ACR podcast. “So the need to prevent COVID-19 is incredibly important in this group of patients.”
The guidelines recommend a delay in vaccination only in rare circumstances, such as for patients with very severe illness or who have recently been administered rituximab, Jeffrey R. Curtis, MD, MPH, lead author of the guidelines, said in the podcast.
“Our members have been inundated with questions and concerns from their patients on whether they should receive the vaccine,” ACR President David Karp, MD, PhD, said in a press release.
So the ACR convened a panel of nine rheumatologists, two infectious disease specialists, and two public health experts. Over the course of 8 weeks, the task force reviewed the literature and agreed on recommendations. The organization posted a summary of the guidelines on its website after its board of directors approved it Feb. 8. The paper is pending journal peer review.
Some risks are real
The task force confined its research to the COVID-19 vaccines being offered by Pfizer and Moderna because they are currently the only ones approved by the Food and Drug Administration. It found no reason to distinguish between the two vaccines in its recommendations.
Because little research has directly addressed the question concerning COVID-19 vaccination for patients with rheumatic diseases, the task force extrapolated from data on other vaccinations in people with rheumatic disease and on the COVID-19 vaccinations in other populations.
It analyzed reports that other types of vaccination, such as for influenza, triggered flares of rheumatic conditions. “It is really individual case reports or small cohorts where there may be a somewhat higher incidence of flare, but it’s usually not very large in its magnitude nor duration,” said Dr. Curtis of the University of Alabama at Birmingham.
The task force also considered the possibility that vaccinations could lead to a new autoimmune disorder, such as Guillain-Barré syndrome or Bell palsy. The risk is real, the task force decided, but not significant enough to influence their recommendations.
Likewise, in immunocompromised people, vaccinations with live virus, such as those for shingles, might trigger the infection the vaccination is meant to prevent. But this can’t happen with the Pfizer and Moderna COVID-19 vaccines because they contain messenger RNA instead of live viruses, Dr. Curtis said.
Although it might be optimal to administer the vaccines when rheumatic diseases are quiescent, the urgency of getting vaccinated overrides that consideration, Dr. Curtis said. “By and large, there was a general consensus to not want to delay vaccination until somebody was stable and doing great, because you don’t know how long that’s going to be,” he said.
How well does it work?
One unanswered question is whether the COVID-19 vaccines work as well for patients with rheumatic diseases. The task force was reassured by data showing efficacy across a range of subgroups, including some with immunosenescence, Dr. Curtis said. “But until we have data in rheumatology patients, we’re just not going to know,” he said.
The guidelines specify that some drug regimens be modified when patients are vaccinated.
For patients taking rituximab, vaccination should be delayed, but only for those who are able to maintain safe social distancing to reduce the risk for COVID-19 exposure, Dr. Curtis said. “If somebody has just gotten rituximab recently, it might be more ideal to complete the vaccine series about 2-4 weeks before the next rituximab dose,” he said. “So if you are giving that therapy, say, at 6-month intervals, if you could vaccinate them at around month 5 from the most recent rituximab cycle, that might be more ideal.”
The guidance calls for withholding JAK inhibitors for a week after each vaccine dose is administered.
It calls for holding SQ abatacept 1 week prior and 1 week after the first COVID-19 vaccine dose, with no interruption after the second dose.
For abatacept IV, clinicians should “time vaccine administration so that the first vaccination will occur 4 weeks after abatacept infusion (i.e., the entire dosing interval), and postpone the subsequent abatacept infusion by 1 week (i.e., a 5-week gap in total).” It recommends no medication adjustment for the second vaccine dose.
For cyclophosphamide, the guidance recommends timing administration to occur about a week after each vaccine dose, when feasible.
None of this advice should supersede clinical judgment, Dr. Curtis said.
A version of this article first appeared on Medscape.com.
Romosozumab may not increase cardiovascular risk after all
The potent anabolic, antiosteoporosis agent romosozumab has been saddled with an Food and Drug Administration–mandated black-box warning for increased cardiovascular risk that may not be warranted, Glenn Haugeberg, MD, PhD, asserted at the 2021 Rheumatology Winter Clinical Symposium.
The black-box warning states that romosozumab (Evenity), a monoclonal antibody approved in 2019 for fracture prevention in patients with osteoporosis, may increase the risk of MI, stroke, and cardiovascular death. The warning arose from FDA concerns raised by the results of the phase 3 ARCH trial in which 4,093 postmenopausal women at high fracture risk were randomized to monthly subcutaneous injections of romosozumab or weekly dosing of the oral bisphosphonate alendronate (Fosamax) for 1 year, followed by 12 months of open-label alendronate for all. Alarm bells went off at the FDA because during year 1, the incidence of adjudicated major adverse cardiovascular events was 2.5% in the romosozumab arm, compared with 1.9% with alendronate.
Could a cardioprotective effect of bisphosphonates explain cardiovascular concerns?
However, evidence from multiple animal and human studies suggests that bisphosphonates actually have a cardioprotective effect. For example, a Taiwanese population-based cohort study of 1,548 patients on bisphosphonate therapy for osteoporotic fractures and 4,644 individuals with hip or vertebral fractures who were not on a bisphosphonate showed a 65% reduction in the risk of acute MI during 2 years of follow-up in those who received a bisphosphonate.
“That may explain the ARCH finding. It may – I say may – be that this concern in the ARCH study can be explained by the positive effect of the bisphosphonates on cardiovascular events,” according to Dr. Haugeberg, head of the division of rheumatology at the Southern Norway Hospital Trust, Kristiansand, and professor of medicine at the Norwegian University of Science and Technology, Trondheim.
He noted that, in the FRAME trial, another pivotal phase 3 trial of romosozumab, there was no signal of increased cardiovascular risk, compared with placebo. In FRAME, which included 7,180 osteoporotic postmenopausal women, rates of major adverse cardiovascular events and other adverse events were balanced between the two study arms at 12 months. Indeed, the incidence of adjudicated serious cardiovascular events was 0.5% with romosozumab and 0.4% with placebo injections. After 12 months, all participants were transitioned to denosumab (Prolia) for another 12 months. At 24 months, there remained no significant between-group difference in cardiovascular events, cancer, osteoarthritis, hyperostosis, or other major adverse events.
Potency of romosozumab
Romosozumab’s efficacy for fracture prevention in these two pivotal trials was striking. The risk of new vertebral fractures was reduced by 73% with romosozumab, compared with placebo at 12 months in FRAME, and by 75% at 24 months in the romosozumab-to-denosumab group.
“FRAME was a 12-month study for the primary endpoint. The bisphosphonate studies typically had a 3-year design in order to show benefit, but here you see only 12-month follow-up. This illustrates the potency of this drug. We saw rapid increase in bone density and a huge decrease in new vertebral fractures versus placebo in the first 12 months, then during follow-up with denosumab the reduction in fractures was maintained,” the rheumatologist commented.
In the ARCH trial, where romosozumab went head to head with a very effective oral bisphosphonate, the risk of new vertebral fractures was 48% lower at 24 months in the romosozumab-to-alendronate group than in women on alendronate for the full 24 months, while the risk of hip fractures was reduced by 38%.
Romosozumab is a humanized monoclonal antibody with a novel mechanism of anabolic action: This agent binds to sclerostin, which is produced in osteocytes. When sclerostin binds to receptors on osteoblasts it reduces their activity, thereby inhibiting bone formation. Romosozumab takes away this inhibition of osteoblasts, boosting their activity. The result is increased bone formation accompanied by decreased bone resorption. This allows for a logical treatment approach: first using an anabolic agent – in this instance, subcutaneously injected romosozumab at 210 mg once monthly for 12 months – then switching to an antiresorptive agent in order to maintain the gain in bone mineral density and decrease fracture risk. This is the same treatment strategy recommended when using the anabolic agents teriparatide (Forteo) and abaloparatide (Tymlos); however, those parathyroid hormone and parathyroid hormone–related protein analogs are seldom used in Norway because their cost is substantially greater than for romosozumab, he explained.
Updated Endocrine Society guidelines
Dr. Haugeberg called romosozumab “a new and wonderful drug.” The Endocrine Society also considers romosozumab an important new drug, as evidenced by the release of an 8-page update of the group’s clinical practice guideline on the pharmacologic management of osteoporosis in postmenopausal women; the update was devoted specifically to the use of romosozumab. The update, published in response to the biologic’s recent approval by U.S., Canadian, and European regulatory agencies, came just 10 months after release of the Endocrine Society’s comprehensive 28-page clinical practice guideline.
Dr. Haugeberg is a fan of the Endocrine Society guideline, which recommends romosozumab as a first-line therapy in postmenopausal women at very high risk of osteoporotic fracture, defined as those with a history of multiple vertebral fractures or severe osteoporosis with a T score of –2.5 or less at the hip or spine plus fractures. The updated guideline also recommends consideration of the antisclerostin biologic in high-risk patients who have failed on antiresorptive treatments.
The practice guideline states that the issue of a possible cardioprotective effect of alendronate in the ARCH trial “remains uncertain at this time.”
“Women at high risk of cardiovascular disease and stroke should not be considered for romosozumab pending further studies on cardiovascular risk associated with this treatment,” according to the Endocrine Society.
Dr. Haugeberg reported receiving research grants from Pfizer and Biogen and serving as a consultant to and/or on speakers’ bureaus for Amgen, which markets romosozumab, and more than a dozen other pharmaceutical companies.
The potent anabolic, antiosteoporosis agent romosozumab has been saddled with an Food and Drug Administration–mandated black-box warning for increased cardiovascular risk that may not be warranted, Glenn Haugeberg, MD, PhD, asserted at the 2021 Rheumatology Winter Clinical Symposium.
The black-box warning states that romosozumab (Evenity), a monoclonal antibody approved in 2019 for fracture prevention in patients with osteoporosis, may increase the risk of MI, stroke, and cardiovascular death. The warning arose from FDA concerns raised by the results of the phase 3 ARCH trial in which 4,093 postmenopausal women at high fracture risk were randomized to monthly subcutaneous injections of romosozumab or weekly dosing of the oral bisphosphonate alendronate (Fosamax) for 1 year, followed by 12 months of open-label alendronate for all. Alarm bells went off at the FDA because during year 1, the incidence of adjudicated major adverse cardiovascular events was 2.5% in the romosozumab arm, compared with 1.9% with alendronate.
Could a cardioprotective effect of bisphosphonates explain cardiovascular concerns?
However, evidence from multiple animal and human studies suggests that bisphosphonates actually have a cardioprotective effect. For example, a Taiwanese population-based cohort study of 1,548 patients on bisphosphonate therapy for osteoporotic fractures and 4,644 individuals with hip or vertebral fractures who were not on a bisphosphonate showed a 65% reduction in the risk of acute MI during 2 years of follow-up in those who received a bisphosphonate.
“That may explain the ARCH finding. It may – I say may – be that this concern in the ARCH study can be explained by the positive effect of the bisphosphonates on cardiovascular events,” according to Dr. Haugeberg, head of the division of rheumatology at the Southern Norway Hospital Trust, Kristiansand, and professor of medicine at the Norwegian University of Science and Technology, Trondheim.
He noted that, in the FRAME trial, another pivotal phase 3 trial of romosozumab, there was no signal of increased cardiovascular risk, compared with placebo. In FRAME, which included 7,180 osteoporotic postmenopausal women, rates of major adverse cardiovascular events and other adverse events were balanced between the two study arms at 12 months. Indeed, the incidence of adjudicated serious cardiovascular events was 0.5% with romosozumab and 0.4% with placebo injections. After 12 months, all participants were transitioned to denosumab (Prolia) for another 12 months. At 24 months, there remained no significant between-group difference in cardiovascular events, cancer, osteoarthritis, hyperostosis, or other major adverse events.
Potency of romosozumab
Romosozumab’s efficacy for fracture prevention in these two pivotal trials was striking. The risk of new vertebral fractures was reduced by 73% with romosozumab, compared with placebo at 12 months in FRAME, and by 75% at 24 months in the romosozumab-to-denosumab group.
“FRAME was a 12-month study for the primary endpoint. The bisphosphonate studies typically had a 3-year design in order to show benefit, but here you see only 12-month follow-up. This illustrates the potency of this drug. We saw rapid increase in bone density and a huge decrease in new vertebral fractures versus placebo in the first 12 months, then during follow-up with denosumab the reduction in fractures was maintained,” the rheumatologist commented.
In the ARCH trial, where romosozumab went head to head with a very effective oral bisphosphonate, the risk of new vertebral fractures was 48% lower at 24 months in the romosozumab-to-alendronate group than in women on alendronate for the full 24 months, while the risk of hip fractures was reduced by 38%.
Romosozumab is a humanized monoclonal antibody with a novel mechanism of anabolic action: This agent binds to sclerostin, which is produced in osteocytes. When sclerostin binds to receptors on osteoblasts it reduces their activity, thereby inhibiting bone formation. Romosozumab takes away this inhibition of osteoblasts, boosting their activity. The result is increased bone formation accompanied by decreased bone resorption. This allows for a logical treatment approach: first using an anabolic agent – in this instance, subcutaneously injected romosozumab at 210 mg once monthly for 12 months – then switching to an antiresorptive agent in order to maintain the gain in bone mineral density and decrease fracture risk. This is the same treatment strategy recommended when using the anabolic agents teriparatide (Forteo) and abaloparatide (Tymlos); however, those parathyroid hormone and parathyroid hormone–related protein analogs are seldom used in Norway because their cost is substantially greater than for romosozumab, he explained.
Updated Endocrine Society guidelines
Dr. Haugeberg called romosozumab “a new and wonderful drug.” The Endocrine Society also considers romosozumab an important new drug, as evidenced by the release of an 8-page update of the group’s clinical practice guideline on the pharmacologic management of osteoporosis in postmenopausal women; the update was devoted specifically to the use of romosozumab. The update, published in response to the biologic’s recent approval by U.S., Canadian, and European regulatory agencies, came just 10 months after release of the Endocrine Society’s comprehensive 28-page clinical practice guideline.
Dr. Haugeberg is a fan of the Endocrine Society guideline, which recommends romosozumab as a first-line therapy in postmenopausal women at very high risk of osteoporotic fracture, defined as those with a history of multiple vertebral fractures or severe osteoporosis with a T score of –2.5 or less at the hip or spine plus fractures. The updated guideline also recommends consideration of the antisclerostin biologic in high-risk patients who have failed on antiresorptive treatments.
The practice guideline states that the issue of a possible cardioprotective effect of alendronate in the ARCH trial “remains uncertain at this time.”
“Women at high risk of cardiovascular disease and stroke should not be considered for romosozumab pending further studies on cardiovascular risk associated with this treatment,” according to the Endocrine Society.
Dr. Haugeberg reported receiving research grants from Pfizer and Biogen and serving as a consultant to and/or on speakers’ bureaus for Amgen, which markets romosozumab, and more than a dozen other pharmaceutical companies.
The potent anabolic, antiosteoporosis agent romosozumab has been saddled with an Food and Drug Administration–mandated black-box warning for increased cardiovascular risk that may not be warranted, Glenn Haugeberg, MD, PhD, asserted at the 2021 Rheumatology Winter Clinical Symposium.
The black-box warning states that romosozumab (Evenity), a monoclonal antibody approved in 2019 for fracture prevention in patients with osteoporosis, may increase the risk of MI, stroke, and cardiovascular death. The warning arose from FDA concerns raised by the results of the phase 3 ARCH trial in which 4,093 postmenopausal women at high fracture risk were randomized to monthly subcutaneous injections of romosozumab or weekly dosing of the oral bisphosphonate alendronate (Fosamax) for 1 year, followed by 12 months of open-label alendronate for all. Alarm bells went off at the FDA because during year 1, the incidence of adjudicated major adverse cardiovascular events was 2.5% in the romosozumab arm, compared with 1.9% with alendronate.
Could a cardioprotective effect of bisphosphonates explain cardiovascular concerns?
However, evidence from multiple animal and human studies suggests that bisphosphonates actually have a cardioprotective effect. For example, a Taiwanese population-based cohort study of 1,548 patients on bisphosphonate therapy for osteoporotic fractures and 4,644 individuals with hip or vertebral fractures who were not on a bisphosphonate showed a 65% reduction in the risk of acute MI during 2 years of follow-up in those who received a bisphosphonate.
“That may explain the ARCH finding. It may – I say may – be that this concern in the ARCH study can be explained by the positive effect of the bisphosphonates on cardiovascular events,” according to Dr. Haugeberg, head of the division of rheumatology at the Southern Norway Hospital Trust, Kristiansand, and professor of medicine at the Norwegian University of Science and Technology, Trondheim.
He noted that, in the FRAME trial, another pivotal phase 3 trial of romosozumab, there was no signal of increased cardiovascular risk, compared with placebo. In FRAME, which included 7,180 osteoporotic postmenopausal women, rates of major adverse cardiovascular events and other adverse events were balanced between the two study arms at 12 months. Indeed, the incidence of adjudicated serious cardiovascular events was 0.5% with romosozumab and 0.4% with placebo injections. After 12 months, all participants were transitioned to denosumab (Prolia) for another 12 months. At 24 months, there remained no significant between-group difference in cardiovascular events, cancer, osteoarthritis, hyperostosis, or other major adverse events.
Potency of romosozumab
Romosozumab’s efficacy for fracture prevention in these two pivotal trials was striking. The risk of new vertebral fractures was reduced by 73% with romosozumab, compared with placebo at 12 months in FRAME, and by 75% at 24 months in the romosozumab-to-denosumab group.
“FRAME was a 12-month study for the primary endpoint. The bisphosphonate studies typically had a 3-year design in order to show benefit, but here you see only 12-month follow-up. This illustrates the potency of this drug. We saw rapid increase in bone density and a huge decrease in new vertebral fractures versus placebo in the first 12 months, then during follow-up with denosumab the reduction in fractures was maintained,” the rheumatologist commented.
In the ARCH trial, where romosozumab went head to head with a very effective oral bisphosphonate, the risk of new vertebral fractures was 48% lower at 24 months in the romosozumab-to-alendronate group than in women on alendronate for the full 24 months, while the risk of hip fractures was reduced by 38%.
Romosozumab is a humanized monoclonal antibody with a novel mechanism of anabolic action: This agent binds to sclerostin, which is produced in osteocytes. When sclerostin binds to receptors on osteoblasts it reduces their activity, thereby inhibiting bone formation. Romosozumab takes away this inhibition of osteoblasts, boosting their activity. The result is increased bone formation accompanied by decreased bone resorption. This allows for a logical treatment approach: first using an anabolic agent – in this instance, subcutaneously injected romosozumab at 210 mg once monthly for 12 months – then switching to an antiresorptive agent in order to maintain the gain in bone mineral density and decrease fracture risk. This is the same treatment strategy recommended when using the anabolic agents teriparatide (Forteo) and abaloparatide (Tymlos); however, those parathyroid hormone and parathyroid hormone–related protein analogs are seldom used in Norway because their cost is substantially greater than for romosozumab, he explained.
Updated Endocrine Society guidelines
Dr. Haugeberg called romosozumab “a new and wonderful drug.” The Endocrine Society also considers romosozumab an important new drug, as evidenced by the release of an 8-page update of the group’s clinical practice guideline on the pharmacologic management of osteoporosis in postmenopausal women; the update was devoted specifically to the use of romosozumab. The update, published in response to the biologic’s recent approval by U.S., Canadian, and European regulatory agencies, came just 10 months after release of the Endocrine Society’s comprehensive 28-page clinical practice guideline.
Dr. Haugeberg is a fan of the Endocrine Society guideline, which recommends romosozumab as a first-line therapy in postmenopausal women at very high risk of osteoporotic fracture, defined as those with a history of multiple vertebral fractures or severe osteoporosis with a T score of –2.5 or less at the hip or spine plus fractures. The updated guideline also recommends consideration of the antisclerostin biologic in high-risk patients who have failed on antiresorptive treatments.
The practice guideline states that the issue of a possible cardioprotective effect of alendronate in the ARCH trial “remains uncertain at this time.”
“Women at high risk of cardiovascular disease and stroke should not be considered for romosozumab pending further studies on cardiovascular risk associated with this treatment,” according to the Endocrine Society.
Dr. Haugeberg reported receiving research grants from Pfizer and Biogen and serving as a consultant to and/or on speakers’ bureaus for Amgen, which markets romosozumab, and more than a dozen other pharmaceutical companies.
FROM RWCS 2021
Cumulative exposure to high-potency topical steroid doses drives osteoporosis fractures
In support of previously published case reports, in a dose-response relationship.
In a stepwise manner, the hazard ratios for major osteoporotic fracture (MOF) were found to start climbing incrementally for those with a cumulative topical steroid dose equivalent of more than 500 g of mometasone furoate when compared with exposure of 200-499 g, according to the team of investigators from the University of Copenhagen.
“Use of these drugs is very common, and we found an estimated population-attributable risk of as much as 4.3%,” the investigators reported in the study, published in JAMA Dermatology.
The retrospective cohort study drew data from the Danish National Patient Registry, which covers 99% of the country’s population. It was linked to the Danish National Prescription Registry, which captures data on pharmacy-dispensed medications. Data collected from the beginning of 2003 to the end of 2017 were evaluated.
Exposures to potent or very potent topical corticosteroids were converted into a single standard with potency equivalent to 1 mg/g of mometasone furoate. Four strata of exposure were compared to a reference exposure of 200-499 g. These were 500-999 g, 1,000-1,999 g, 2,000-9,999 g, and 10,000 g or greater.
For the first strata, the small increased risk for MOF did not reach significance (HR, 1.01; 95% confidence interval, 0.99-1.03), but each of the others did. These climbed from a 5% greater risk (HR 1.05 95% CI 1.02-1.08) for a cumulative exposure of 1,000 to 1,999 g, to a 10% greater risk (HR, 1.10; 95% CI, 1.07-1.13) for a cumulative exposure of 2,000-9,999 g, and finally to a 27% greater risk (HR, 1.27; 95% CI, 1.19-1.35) for a cumulative exposure of 10,000 g or higher.
The study included more than 700,000 individuals exposed to topical mometasone at a potency equivalent of 200 g or more over the study period. The reference group (200-499 g) was the largest (317,907 individuals). The first strata (500-999 g) included 186,359 patients; the second (1,000-1,999 g), 111,203 patients; the third (2,000-9,999 g), 94,334 patients; and the fifth (10,000 g or more), 13,448 patients.
“A 3% increase in the relative risk of osteoporosis and MOF was observed per doubling of the TCS dose,” according to the investigators.
Patients exposed to doses of high-potency topical steroids that put them at risk of MOF is limited but substantial, according to the senior author, Alexander Egeberg, MD, PhD, of the department of dermatology and allergy at Herlev and Gentofte Hospital, Copenhagen.
“It is true that the risk is modest for the average user of topical steroids,” Dr. Egeberg said in an interview. However, despite the fact that topical steroids are intended for short-term use, “2% of all our users had been exposed to the equivalent of 10,000 g of mometasone, which mean 100 tubes of 100 g.”
If the other two strata at significantly increased risk of MOF (greater than 1,000 g) are included, an additional 28% of all users are facing the potential for clinically significant osteoporosis, according to the Danish data.
The adverse effect of steroids on bone metabolism has been established previously, and several studies have linked systemic corticosteroid exposure, including inhaled corticosteroids, with increased risk of osteoporotic fracture. For example, one study showed that patients with chronic obstructive pulmonary disease on daily inhaled doses of the equivalent of fluticasone at or above 1,000 mcg for more than 4 years had about a 10% increased risk of MOF relative to those not exposed.
The data associate topical steroids with increased risk of osteoporotic fracture, but Dr. Egeberg said osteoporosis is not the only reason to use topical steroids prudently.
“It is important to keep in mind that osteoporosis and fractures are at the extreme end of the side-effect profile and that other side effects, such as striae formation, skin thinning, and dysregulated diabetes, can occur with much lower quantities of topical steroids,” Dr. Egeberg said
For avoiding this risk, “there are no specific cutoffs” recommended for topical steroids in current guidelines, but dermatologists should be aware that many of the indications for topical steroids, such as psoriasis and atopic dermatitis, involve skin with an impaired barrier function, exposing patients to an increased likelihood of absorption, according to Dr. Egeberg.
“A general rule of thumb that we use is that, if a patient with persistent disease activity requires a new prescription of the equivalent of 100 g mometasone every 1-2 months, it might be worth considering if there is a suitable alternative,” Dr. Egeberg said.
In an accompanying editorial, Rebecca D. Jackson, MD, of the division of endocrinology, diabetes, and metabolism in the department of internal medicine at Ohio State University, Columbus, agreed that no guidelines specific to avoiding the risks of topical corticosteroids are currently available, but she advised clinicians to be considering these risks nonetheless. In general, she suggested that topical steroids, like oral steroids, should be used at “the lowest dose for the shortest duration necessary to manage the underlying medical condition.”
The correlation between topical corticosteroids and increased risk of osteoporotic fracture, although not established previously in a large study, is not surprising, according to Victoria Werth, MD, chief of dermatology at the Philadelphia Veterans Affairs Hospital and professor of dermatology at the University of Pennsylvania, also in Philadelphia.
“Systemic absorption of potent topical steroids has previously been demonstrated with a rapid decrease in serum cortisol levels,” Dr. Werth said in an interview. She indicated that concern about the risk of osteoporosis imposed by use of potent steroids over large body surface areas is appropriate.
To minimize this risk, “it is reasonable to use the lowest dose of steroid possible and to try to substitute other medications when possible,” she said.
Dr. Egeberg reported financial relationships with Abbvie, Almirall, Bristol-Myers Squibb, Dermavant Sciences, Galderma, Janssen Pharmaceuticals, Eli Lilly, Novartis, Pfizer, Samsung, Bioepis, and UCB. Five authors had disclosures related to some of those pharmaceutical companies and/or others. Dr. Jackson had no disclosures.
In support of previously published case reports, in a dose-response relationship.
In a stepwise manner, the hazard ratios for major osteoporotic fracture (MOF) were found to start climbing incrementally for those with a cumulative topical steroid dose equivalent of more than 500 g of mometasone furoate when compared with exposure of 200-499 g, according to the team of investigators from the University of Copenhagen.
“Use of these drugs is very common, and we found an estimated population-attributable risk of as much as 4.3%,” the investigators reported in the study, published in JAMA Dermatology.
The retrospective cohort study drew data from the Danish National Patient Registry, which covers 99% of the country’s population. It was linked to the Danish National Prescription Registry, which captures data on pharmacy-dispensed medications. Data collected from the beginning of 2003 to the end of 2017 were evaluated.
Exposures to potent or very potent topical corticosteroids were converted into a single standard with potency equivalent to 1 mg/g of mometasone furoate. Four strata of exposure were compared to a reference exposure of 200-499 g. These were 500-999 g, 1,000-1,999 g, 2,000-9,999 g, and 10,000 g or greater.
For the first strata, the small increased risk for MOF did not reach significance (HR, 1.01; 95% confidence interval, 0.99-1.03), but each of the others did. These climbed from a 5% greater risk (HR 1.05 95% CI 1.02-1.08) for a cumulative exposure of 1,000 to 1,999 g, to a 10% greater risk (HR, 1.10; 95% CI, 1.07-1.13) for a cumulative exposure of 2,000-9,999 g, and finally to a 27% greater risk (HR, 1.27; 95% CI, 1.19-1.35) for a cumulative exposure of 10,000 g or higher.
The study included more than 700,000 individuals exposed to topical mometasone at a potency equivalent of 200 g or more over the study period. The reference group (200-499 g) was the largest (317,907 individuals). The first strata (500-999 g) included 186,359 patients; the second (1,000-1,999 g), 111,203 patients; the third (2,000-9,999 g), 94,334 patients; and the fifth (10,000 g or more), 13,448 patients.
“A 3% increase in the relative risk of osteoporosis and MOF was observed per doubling of the TCS dose,” according to the investigators.
Patients exposed to doses of high-potency topical steroids that put them at risk of MOF is limited but substantial, according to the senior author, Alexander Egeberg, MD, PhD, of the department of dermatology and allergy at Herlev and Gentofte Hospital, Copenhagen.
“It is true that the risk is modest for the average user of topical steroids,” Dr. Egeberg said in an interview. However, despite the fact that topical steroids are intended for short-term use, “2% of all our users had been exposed to the equivalent of 10,000 g of mometasone, which mean 100 tubes of 100 g.”
If the other two strata at significantly increased risk of MOF (greater than 1,000 g) are included, an additional 28% of all users are facing the potential for clinically significant osteoporosis, according to the Danish data.
The adverse effect of steroids on bone metabolism has been established previously, and several studies have linked systemic corticosteroid exposure, including inhaled corticosteroids, with increased risk of osteoporotic fracture. For example, one study showed that patients with chronic obstructive pulmonary disease on daily inhaled doses of the equivalent of fluticasone at or above 1,000 mcg for more than 4 years had about a 10% increased risk of MOF relative to those not exposed.
The data associate topical steroids with increased risk of osteoporotic fracture, but Dr. Egeberg said osteoporosis is not the only reason to use topical steroids prudently.
“It is important to keep in mind that osteoporosis and fractures are at the extreme end of the side-effect profile and that other side effects, such as striae formation, skin thinning, and dysregulated diabetes, can occur with much lower quantities of topical steroids,” Dr. Egeberg said
For avoiding this risk, “there are no specific cutoffs” recommended for topical steroids in current guidelines, but dermatologists should be aware that many of the indications for topical steroids, such as psoriasis and atopic dermatitis, involve skin with an impaired barrier function, exposing patients to an increased likelihood of absorption, according to Dr. Egeberg.
“A general rule of thumb that we use is that, if a patient with persistent disease activity requires a new prescription of the equivalent of 100 g mometasone every 1-2 months, it might be worth considering if there is a suitable alternative,” Dr. Egeberg said.
In an accompanying editorial, Rebecca D. Jackson, MD, of the division of endocrinology, diabetes, and metabolism in the department of internal medicine at Ohio State University, Columbus, agreed that no guidelines specific to avoiding the risks of topical corticosteroids are currently available, but she advised clinicians to be considering these risks nonetheless. In general, she suggested that topical steroids, like oral steroids, should be used at “the lowest dose for the shortest duration necessary to manage the underlying medical condition.”
The correlation between topical corticosteroids and increased risk of osteoporotic fracture, although not established previously in a large study, is not surprising, according to Victoria Werth, MD, chief of dermatology at the Philadelphia Veterans Affairs Hospital and professor of dermatology at the University of Pennsylvania, also in Philadelphia.
“Systemic absorption of potent topical steroids has previously been demonstrated with a rapid decrease in serum cortisol levels,” Dr. Werth said in an interview. She indicated that concern about the risk of osteoporosis imposed by use of potent steroids over large body surface areas is appropriate.
To minimize this risk, “it is reasonable to use the lowest dose of steroid possible and to try to substitute other medications when possible,” she said.
Dr. Egeberg reported financial relationships with Abbvie, Almirall, Bristol-Myers Squibb, Dermavant Sciences, Galderma, Janssen Pharmaceuticals, Eli Lilly, Novartis, Pfizer, Samsung, Bioepis, and UCB. Five authors had disclosures related to some of those pharmaceutical companies and/or others. Dr. Jackson had no disclosures.
In support of previously published case reports, in a dose-response relationship.
In a stepwise manner, the hazard ratios for major osteoporotic fracture (MOF) were found to start climbing incrementally for those with a cumulative topical steroid dose equivalent of more than 500 g of mometasone furoate when compared with exposure of 200-499 g, according to the team of investigators from the University of Copenhagen.
“Use of these drugs is very common, and we found an estimated population-attributable risk of as much as 4.3%,” the investigators reported in the study, published in JAMA Dermatology.
The retrospective cohort study drew data from the Danish National Patient Registry, which covers 99% of the country’s population. It was linked to the Danish National Prescription Registry, which captures data on pharmacy-dispensed medications. Data collected from the beginning of 2003 to the end of 2017 were evaluated.
Exposures to potent or very potent topical corticosteroids were converted into a single standard with potency equivalent to 1 mg/g of mometasone furoate. Four strata of exposure were compared to a reference exposure of 200-499 g. These were 500-999 g, 1,000-1,999 g, 2,000-9,999 g, and 10,000 g or greater.
For the first strata, the small increased risk for MOF did not reach significance (HR, 1.01; 95% confidence interval, 0.99-1.03), but each of the others did. These climbed from a 5% greater risk (HR 1.05 95% CI 1.02-1.08) for a cumulative exposure of 1,000 to 1,999 g, to a 10% greater risk (HR, 1.10; 95% CI, 1.07-1.13) for a cumulative exposure of 2,000-9,999 g, and finally to a 27% greater risk (HR, 1.27; 95% CI, 1.19-1.35) for a cumulative exposure of 10,000 g or higher.
The study included more than 700,000 individuals exposed to topical mometasone at a potency equivalent of 200 g or more over the study period. The reference group (200-499 g) was the largest (317,907 individuals). The first strata (500-999 g) included 186,359 patients; the second (1,000-1,999 g), 111,203 patients; the third (2,000-9,999 g), 94,334 patients; and the fifth (10,000 g or more), 13,448 patients.
“A 3% increase in the relative risk of osteoporosis and MOF was observed per doubling of the TCS dose,” according to the investigators.
Patients exposed to doses of high-potency topical steroids that put them at risk of MOF is limited but substantial, according to the senior author, Alexander Egeberg, MD, PhD, of the department of dermatology and allergy at Herlev and Gentofte Hospital, Copenhagen.
“It is true that the risk is modest for the average user of topical steroids,” Dr. Egeberg said in an interview. However, despite the fact that topical steroids are intended for short-term use, “2% of all our users had been exposed to the equivalent of 10,000 g of mometasone, which mean 100 tubes of 100 g.”
If the other two strata at significantly increased risk of MOF (greater than 1,000 g) are included, an additional 28% of all users are facing the potential for clinically significant osteoporosis, according to the Danish data.
The adverse effect of steroids on bone metabolism has been established previously, and several studies have linked systemic corticosteroid exposure, including inhaled corticosteroids, with increased risk of osteoporotic fracture. For example, one study showed that patients with chronic obstructive pulmonary disease on daily inhaled doses of the equivalent of fluticasone at or above 1,000 mcg for more than 4 years had about a 10% increased risk of MOF relative to those not exposed.
The data associate topical steroids with increased risk of osteoporotic fracture, but Dr. Egeberg said osteoporosis is not the only reason to use topical steroids prudently.
“It is important to keep in mind that osteoporosis and fractures are at the extreme end of the side-effect profile and that other side effects, such as striae formation, skin thinning, and dysregulated diabetes, can occur with much lower quantities of topical steroids,” Dr. Egeberg said
For avoiding this risk, “there are no specific cutoffs” recommended for topical steroids in current guidelines, but dermatologists should be aware that many of the indications for topical steroids, such as psoriasis and atopic dermatitis, involve skin with an impaired barrier function, exposing patients to an increased likelihood of absorption, according to Dr. Egeberg.
“A general rule of thumb that we use is that, if a patient with persistent disease activity requires a new prescription of the equivalent of 100 g mometasone every 1-2 months, it might be worth considering if there is a suitable alternative,” Dr. Egeberg said.
In an accompanying editorial, Rebecca D. Jackson, MD, of the division of endocrinology, diabetes, and metabolism in the department of internal medicine at Ohio State University, Columbus, agreed that no guidelines specific to avoiding the risks of topical corticosteroids are currently available, but she advised clinicians to be considering these risks nonetheless. In general, she suggested that topical steroids, like oral steroids, should be used at “the lowest dose for the shortest duration necessary to manage the underlying medical condition.”
The correlation between topical corticosteroids and increased risk of osteoporotic fracture, although not established previously in a large study, is not surprising, according to Victoria Werth, MD, chief of dermatology at the Philadelphia Veterans Affairs Hospital and professor of dermatology at the University of Pennsylvania, also in Philadelphia.
“Systemic absorption of potent topical steroids has previously been demonstrated with a rapid decrease in serum cortisol levels,” Dr. Werth said in an interview. She indicated that concern about the risk of osteoporosis imposed by use of potent steroids over large body surface areas is appropriate.
To minimize this risk, “it is reasonable to use the lowest dose of steroid possible and to try to substitute other medications when possible,” she said.
Dr. Egeberg reported financial relationships with Abbvie, Almirall, Bristol-Myers Squibb, Dermavant Sciences, Galderma, Janssen Pharmaceuticals, Eli Lilly, Novartis, Pfizer, Samsung, Bioepis, and UCB. Five authors had disclosures related to some of those pharmaceutical companies and/or others. Dr. Jackson had no disclosures.
FROM JAMA DERMATOLOGY
Could an osteoporosis drug reduce need for hip revision surgery?
A single injection of denosumab (Prolia, Amgen), frequently used to treat osteoporosis, may reduce the need for revision surgery in patients with symptomatic osteolysis following total hip arthroplasty, a new proof-of-concept study suggests.
Aseptic loosening is the result of wear-induced osteolysis caused by the prosthetic hip and is a major contributor to the need for revision surgery in many parts of the world.
“The only established treatment for prosthesis-related osteolysis after joint replacement is revision surgery, which carries substantially greater morbidity and mortality than primary joint replacement,” Mohit M. Mahatma, MRes, of the University of Sheffield, England, and colleagues wrote in their article, published online Jan. 11 in The Lancet Rheumatology.
As well as an increased risk of infection and other complications, revision surgery is much more costly than a first-time operation, they added.
“The results of this proof-of-concept clinical trial indicate that denosumab is effective at reducing bone resorption activity within osteolytic lesion tissue and is well tolerated within the limitations of the single dose used here,” they concluded.
Commenting on the findings, Antonia Chen, MD, associate professor of orthopedic surgery, Harvard Medical School, Boston, emphasized that further studies are needed to assess the effectiveness of this strategy to reduce the need for hip revision surgery.
Nevertheless, “osteolysis is still unfortunately a problem we do have to deal with and we do not have any other way to prevent it,” she said in an interview. “So it’s a good start ... although further studies are definitely needed,” Dr. Chen added.
In an accompanying editorial, Hannu Aro, MD, Turku University Hospital in Finland, agreed: “Without a doubt, the trial is a breakthrough, but it represents only the first step in the development of pharmacological therapy aiming to slow, prevent, or even reverse the process of wear-induced periprosthetic osteolysis.”
Small single-center study
The phase 2, single-center, randomized, controlled trial involved 22 patients who had previously undergone hip replacement surgery at Sheffield Teaching Hospitals and were scheduled for revision surgery due to symptomatic osteolysis. They were randomized to a single subcutaneous injection of denosumab at a dose of 60 mg, or placebo, on their second hospital visit.
“The primary outcome was the between-group difference in the number of osteoclasts per mm of osteolytic membrane at the osteolytic membrane-bone interface at week 8,” the authors noted.
At this time point, there were 83% fewer osteoclasts at the interface in the denosumab group compared with placebo, at a median of 0.05 per mm in the treatment group compared with 0.30 per mm in the placebo group (P = .011).
Secondary histological outcomes were also significantly improved in favor of the denosumab group compared with placebo.
Potential to prevent half of all hip revision surgeries?
Patients who received denosumab also demonstrated an acute fall in serum and urinary markers of bone resorption following administration of the drug, reaching a nadir at week 4, which was maintained until revision surgery at week 8.
In contrast, “no change in these markers was observed in the placebo group [P < .0003 for all biomarkers],” the investigators noted. Rates of adverse events were comparable in both treatment groups.
As the authors explained, osteolysis occurs following joint replacement surgery when particles of plastic wear off from the prosthesis, triggering an immune reaction that attacks the bone around the implant, causing the joint to loosen.
“It is very clear from our bone biopsies and bone imaging that the [denosumab] injection stops the bone absorbing the microplastic particles from the replacement joint and therefore could prevent the bone from being eaten away and the need for revision surgery,” senior author Mark Wilkinson, MBChB, PhD, honorary consultant orthopedic surgeon, Sheffield Teaching Hospitals, said in a press release from his institution.
“This study is a significant breakthrough as we’ve demonstrated that there is a drug, already available and successful in the treatment of osteoporosis, that has the potential to prevent up to half of all revised replacement surgeries which are caused by osteolysis,” he added.
Dr. Wilkinson and coauthors said their results justify the need for future trials targeting earlier-stage disease to further test the use of denosumab to prevent or reduce the need for revision surgery.
In 2018, aseptic loosening accounted for over half of all revision procedures, as reported to the National Joint Registry in England and Wales.
Older polyethylene prostheses are the main culprit
Commenting further on the study, Dr. Chen noted that osteolysis still plagues orthopedic surgeons because the original polyethylene prostheses were not very good. A better prosthesis developed at Massachusetts General Hospital is made up of highly crossed-link polyethylene and still wears over time but to a much lesser extent than the older polyethylene prostheses.
Metal and ceramic prostheses also can induce osteolysis, but again to a much lesser extent than the older polyethylene implants.
“Any particle can technically cause osteolysis but plastic produces the most particles,” Dr. Chen explained. Although hip revision rates in the United States are low to begin with, aseptic loosening is still one of the main reasons that patients need to undergo revision surgery, she observed.
“A lot of patients are still living with the old plastic [implants] so there is still a need for something like this,” she stressed.
However, many questions about this potential new strategy remain to be answered, including when best to initiate treatment and how to manage patients at risk for osteolysis 20-30 years after they have received their original implant.
In his editorial, Dr. Aro said that serious adverse consequences often become evident 10-20 years after patients have undergone the original hip replacement procedures, when they are potentially less physically fit than they were at the time of the operation and thus less able to withstand the rigors of a difficult revision surgery.
“In this context, the concept of nonsurgical pharmacological treatment of periprosthetic osteolysis ... brings a new hope for the ever-increasing population of patients with total hip arthroplasty to avoid revision surgery,” Dr. Aro suggested.
However, Dr. Aro cautioned that reduction of bone turnover by antiresorptive agents such as denosumab has been associated with the development of atypical femoral fractures.
The study was funded by Amgen. Dr. Wilkinson has reported receiving a grant from Amgen. Dr. Chen has reported serving as a consultant for Striker and b-One Ortho. Dr. Aro has reported receiving a grant to his institution from Amgen Finland and the Academy of Finland. He has also served as a member of an advisory scientific board for Amgen Finland.
A version of this article first appeared on Medscape.com.
A single injection of denosumab (Prolia, Amgen), frequently used to treat osteoporosis, may reduce the need for revision surgery in patients with symptomatic osteolysis following total hip arthroplasty, a new proof-of-concept study suggests.
Aseptic loosening is the result of wear-induced osteolysis caused by the prosthetic hip and is a major contributor to the need for revision surgery in many parts of the world.
“The only established treatment for prosthesis-related osteolysis after joint replacement is revision surgery, which carries substantially greater morbidity and mortality than primary joint replacement,” Mohit M. Mahatma, MRes, of the University of Sheffield, England, and colleagues wrote in their article, published online Jan. 11 in The Lancet Rheumatology.
As well as an increased risk of infection and other complications, revision surgery is much more costly than a first-time operation, they added.
“The results of this proof-of-concept clinical trial indicate that denosumab is effective at reducing bone resorption activity within osteolytic lesion tissue and is well tolerated within the limitations of the single dose used here,” they concluded.
Commenting on the findings, Antonia Chen, MD, associate professor of orthopedic surgery, Harvard Medical School, Boston, emphasized that further studies are needed to assess the effectiveness of this strategy to reduce the need for hip revision surgery.
Nevertheless, “osteolysis is still unfortunately a problem we do have to deal with and we do not have any other way to prevent it,” she said in an interview. “So it’s a good start ... although further studies are definitely needed,” Dr. Chen added.
In an accompanying editorial, Hannu Aro, MD, Turku University Hospital in Finland, agreed: “Without a doubt, the trial is a breakthrough, but it represents only the first step in the development of pharmacological therapy aiming to slow, prevent, or even reverse the process of wear-induced periprosthetic osteolysis.”
Small single-center study
The phase 2, single-center, randomized, controlled trial involved 22 patients who had previously undergone hip replacement surgery at Sheffield Teaching Hospitals and were scheduled for revision surgery due to symptomatic osteolysis. They were randomized to a single subcutaneous injection of denosumab at a dose of 60 mg, or placebo, on their second hospital visit.
“The primary outcome was the between-group difference in the number of osteoclasts per mm of osteolytic membrane at the osteolytic membrane-bone interface at week 8,” the authors noted.
At this time point, there were 83% fewer osteoclasts at the interface in the denosumab group compared with placebo, at a median of 0.05 per mm in the treatment group compared with 0.30 per mm in the placebo group (P = .011).
Secondary histological outcomes were also significantly improved in favor of the denosumab group compared with placebo.
Potential to prevent half of all hip revision surgeries?
Patients who received denosumab also demonstrated an acute fall in serum and urinary markers of bone resorption following administration of the drug, reaching a nadir at week 4, which was maintained until revision surgery at week 8.
In contrast, “no change in these markers was observed in the placebo group [P < .0003 for all biomarkers],” the investigators noted. Rates of adverse events were comparable in both treatment groups.
As the authors explained, osteolysis occurs following joint replacement surgery when particles of plastic wear off from the prosthesis, triggering an immune reaction that attacks the bone around the implant, causing the joint to loosen.
“It is very clear from our bone biopsies and bone imaging that the [denosumab] injection stops the bone absorbing the microplastic particles from the replacement joint and therefore could prevent the bone from being eaten away and the need for revision surgery,” senior author Mark Wilkinson, MBChB, PhD, honorary consultant orthopedic surgeon, Sheffield Teaching Hospitals, said in a press release from his institution.
“This study is a significant breakthrough as we’ve demonstrated that there is a drug, already available and successful in the treatment of osteoporosis, that has the potential to prevent up to half of all revised replacement surgeries which are caused by osteolysis,” he added.
Dr. Wilkinson and coauthors said their results justify the need for future trials targeting earlier-stage disease to further test the use of denosumab to prevent or reduce the need for revision surgery.
In 2018, aseptic loosening accounted for over half of all revision procedures, as reported to the National Joint Registry in England and Wales.
Older polyethylene prostheses are the main culprit
Commenting further on the study, Dr. Chen noted that osteolysis still plagues orthopedic surgeons because the original polyethylene prostheses were not very good. A better prosthesis developed at Massachusetts General Hospital is made up of highly crossed-link polyethylene and still wears over time but to a much lesser extent than the older polyethylene prostheses.
Metal and ceramic prostheses also can induce osteolysis, but again to a much lesser extent than the older polyethylene implants.
“Any particle can technically cause osteolysis but plastic produces the most particles,” Dr. Chen explained. Although hip revision rates in the United States are low to begin with, aseptic loosening is still one of the main reasons that patients need to undergo revision surgery, she observed.
“A lot of patients are still living with the old plastic [implants] so there is still a need for something like this,” she stressed.
However, many questions about this potential new strategy remain to be answered, including when best to initiate treatment and how to manage patients at risk for osteolysis 20-30 years after they have received their original implant.
In his editorial, Dr. Aro said that serious adverse consequences often become evident 10-20 years after patients have undergone the original hip replacement procedures, when they are potentially less physically fit than they were at the time of the operation and thus less able to withstand the rigors of a difficult revision surgery.
“In this context, the concept of nonsurgical pharmacological treatment of periprosthetic osteolysis ... brings a new hope for the ever-increasing population of patients with total hip arthroplasty to avoid revision surgery,” Dr. Aro suggested.
However, Dr. Aro cautioned that reduction of bone turnover by antiresorptive agents such as denosumab has been associated with the development of atypical femoral fractures.
The study was funded by Amgen. Dr. Wilkinson has reported receiving a grant from Amgen. Dr. Chen has reported serving as a consultant for Striker and b-One Ortho. Dr. Aro has reported receiving a grant to his institution from Amgen Finland and the Academy of Finland. He has also served as a member of an advisory scientific board for Amgen Finland.
A version of this article first appeared on Medscape.com.
A single injection of denosumab (Prolia, Amgen), frequently used to treat osteoporosis, may reduce the need for revision surgery in patients with symptomatic osteolysis following total hip arthroplasty, a new proof-of-concept study suggests.
Aseptic loosening is the result of wear-induced osteolysis caused by the prosthetic hip and is a major contributor to the need for revision surgery in many parts of the world.
“The only established treatment for prosthesis-related osteolysis after joint replacement is revision surgery, which carries substantially greater morbidity and mortality than primary joint replacement,” Mohit M. Mahatma, MRes, of the University of Sheffield, England, and colleagues wrote in their article, published online Jan. 11 in The Lancet Rheumatology.
As well as an increased risk of infection and other complications, revision surgery is much more costly than a first-time operation, they added.
“The results of this proof-of-concept clinical trial indicate that denosumab is effective at reducing bone resorption activity within osteolytic lesion tissue and is well tolerated within the limitations of the single dose used here,” they concluded.
Commenting on the findings, Antonia Chen, MD, associate professor of orthopedic surgery, Harvard Medical School, Boston, emphasized that further studies are needed to assess the effectiveness of this strategy to reduce the need for hip revision surgery.
Nevertheless, “osteolysis is still unfortunately a problem we do have to deal with and we do not have any other way to prevent it,” she said in an interview. “So it’s a good start ... although further studies are definitely needed,” Dr. Chen added.
In an accompanying editorial, Hannu Aro, MD, Turku University Hospital in Finland, agreed: “Without a doubt, the trial is a breakthrough, but it represents only the first step in the development of pharmacological therapy aiming to slow, prevent, or even reverse the process of wear-induced periprosthetic osteolysis.”
Small single-center study
The phase 2, single-center, randomized, controlled trial involved 22 patients who had previously undergone hip replacement surgery at Sheffield Teaching Hospitals and were scheduled for revision surgery due to symptomatic osteolysis. They were randomized to a single subcutaneous injection of denosumab at a dose of 60 mg, or placebo, on their second hospital visit.
“The primary outcome was the between-group difference in the number of osteoclasts per mm of osteolytic membrane at the osteolytic membrane-bone interface at week 8,” the authors noted.
At this time point, there were 83% fewer osteoclasts at the interface in the denosumab group compared with placebo, at a median of 0.05 per mm in the treatment group compared with 0.30 per mm in the placebo group (P = .011).
Secondary histological outcomes were also significantly improved in favor of the denosumab group compared with placebo.
Potential to prevent half of all hip revision surgeries?
Patients who received denosumab also demonstrated an acute fall in serum and urinary markers of bone resorption following administration of the drug, reaching a nadir at week 4, which was maintained until revision surgery at week 8.
In contrast, “no change in these markers was observed in the placebo group [P < .0003 for all biomarkers],” the investigators noted. Rates of adverse events were comparable in both treatment groups.
As the authors explained, osteolysis occurs following joint replacement surgery when particles of plastic wear off from the prosthesis, triggering an immune reaction that attacks the bone around the implant, causing the joint to loosen.
“It is very clear from our bone biopsies and bone imaging that the [denosumab] injection stops the bone absorbing the microplastic particles from the replacement joint and therefore could prevent the bone from being eaten away and the need for revision surgery,” senior author Mark Wilkinson, MBChB, PhD, honorary consultant orthopedic surgeon, Sheffield Teaching Hospitals, said in a press release from his institution.
“This study is a significant breakthrough as we’ve demonstrated that there is a drug, already available and successful in the treatment of osteoporosis, that has the potential to prevent up to half of all revised replacement surgeries which are caused by osteolysis,” he added.
Dr. Wilkinson and coauthors said their results justify the need for future trials targeting earlier-stage disease to further test the use of denosumab to prevent or reduce the need for revision surgery.
In 2018, aseptic loosening accounted for over half of all revision procedures, as reported to the National Joint Registry in England and Wales.
Older polyethylene prostheses are the main culprit
Commenting further on the study, Dr. Chen noted that osteolysis still plagues orthopedic surgeons because the original polyethylene prostheses were not very good. A better prosthesis developed at Massachusetts General Hospital is made up of highly crossed-link polyethylene and still wears over time but to a much lesser extent than the older polyethylene prostheses.
Metal and ceramic prostheses also can induce osteolysis, but again to a much lesser extent than the older polyethylene implants.
“Any particle can technically cause osteolysis but plastic produces the most particles,” Dr. Chen explained. Although hip revision rates in the United States are low to begin with, aseptic loosening is still one of the main reasons that patients need to undergo revision surgery, she observed.
“A lot of patients are still living with the old plastic [implants] so there is still a need for something like this,” she stressed.
However, many questions about this potential new strategy remain to be answered, including when best to initiate treatment and how to manage patients at risk for osteolysis 20-30 years after they have received their original implant.
In his editorial, Dr. Aro said that serious adverse consequences often become evident 10-20 years after patients have undergone the original hip replacement procedures, when they are potentially less physically fit than they were at the time of the operation and thus less able to withstand the rigors of a difficult revision surgery.
“In this context, the concept of nonsurgical pharmacological treatment of periprosthetic osteolysis ... brings a new hope for the ever-increasing population of patients with total hip arthroplasty to avoid revision surgery,” Dr. Aro suggested.
However, Dr. Aro cautioned that reduction of bone turnover by antiresorptive agents such as denosumab has been associated with the development of atypical femoral fractures.
The study was funded by Amgen. Dr. Wilkinson has reported receiving a grant from Amgen. Dr. Chen has reported serving as a consultant for Striker and b-One Ortho. Dr. Aro has reported receiving a grant to his institution from Amgen Finland and the Academy of Finland. He has also served as a member of an advisory scientific board for Amgen Finland.
A version of this article first appeared on Medscape.com.
Osteoporosis prevalence in PsA similar to general population
The rates of osteopenia and osteoporosis among individuals with psoriatic arthritis are comparable to those seen in the general population, research suggests.
The cohort study, published in Arthritis Care & Research, also found that clinicians are likely to refer patients for bone mineral density (BMD) testing based on osteoporosis risk factors or psoriatic arthritis disease severity markers.
Timothy S.H. Kwok, MD, of the University of Toronto, and coauthors wrote that previous research suggested a possible link between psoriatic arthritis and osteoporosis or osteopenia. However, no cohort studies appear to have examined this association.
The study involved 201 individuals with psoriatic arthritis attending a single specialist clinic, who were enrolled in a longitudinal study of psoriatic arthritis (PsA) and who were also referred for BMD testing with dual-energy x-ray absorptiometry.
Of these participants, 13% had a BMD in the osteoporotic range, 45% were in the osteopenic range, and 42% were in the normal range for BMD. The prevalence of osteoporosis observed in the general population aged 50 or above, observed in an earlier large prospective study, ranged from 7% to 16%, and osteopenia ranged from 27% to 46%.
“Our study suggests that patients with PsA have similar BMDs compared to the general population,” the authors wrote.
Researchers did note the suggestion that patients with polyarthritis had lower BMDs over time. Because of the small number of events, this did not achieve statistical significance, but “this relationship warrants further research, given that multiple cohort studies have independently demonstrated polyarticular onset of disease predicting clinical deformities and erosive disease in PsA,” they wrote.
They also saw that patients with increased body mass index had a significant 21% lower odds of having a BMD in the osteoporotic range, while those using biologics had a significant 83% lower odds.
Among participants with BMD scores in the osteopenic or osteoporotic range, these scores were seen in the lumbar spine in 63% of measurements, the femoral neck in 88%, and the total hip in 39%. Mean T-scores for the lumbar spine were –0.30±0.32, and for the femoral neck were –1.10±1.04 and the total hip, –0.45±0.42.
The study also examined what factors were associated with referral for BMD testing. They found that increasing age, menopause, elevated acute phase reactants, or use of biologics, methotrexate, and systemic glucocorticoids were associated with a higher likelihood of undergoing BMD testing.
Noting that the latest Canadian clinical practice guidelines on BMD testing advise that age, menopause, and use of systemic glucocorticoids use are risk factors that should prompt testing, the authors suggested clinicians were using a combination of traditional osteoporosis risk factors and markers of psoriatic disease severity to underpin their decision to refer.
However, they commented that none of the factors associated with a higher likelihood of having a BMD test were actually associated with lower BMD scores.
“This suggests that clinicians may be over-screening patients with PsA for osteopenia/osteoporosis, as they do not appear to be at baseline higher risk for lower BMD scores than the general population,” they wrote. “This is of importance, as there are currently no formal recommendations with regards to the optimal interval or time to commence BMD testing within the recent major PsA guidelines.”
The study was supported by a grant from the Krembil Foundation. No conflicts of interest were declared.
SOURCE: Kwok TSH et al. Arthritis Care Res. 2020 Dec 16. doi: 10.1002/acr.24538.
The rates of osteopenia and osteoporosis among individuals with psoriatic arthritis are comparable to those seen in the general population, research suggests.
The cohort study, published in Arthritis Care & Research, also found that clinicians are likely to refer patients for bone mineral density (BMD) testing based on osteoporosis risk factors or psoriatic arthritis disease severity markers.
Timothy S.H. Kwok, MD, of the University of Toronto, and coauthors wrote that previous research suggested a possible link between psoriatic arthritis and osteoporosis or osteopenia. However, no cohort studies appear to have examined this association.
The study involved 201 individuals with psoriatic arthritis attending a single specialist clinic, who were enrolled in a longitudinal study of psoriatic arthritis (PsA) and who were also referred for BMD testing with dual-energy x-ray absorptiometry.
Of these participants, 13% had a BMD in the osteoporotic range, 45% were in the osteopenic range, and 42% were in the normal range for BMD. The prevalence of osteoporosis observed in the general population aged 50 or above, observed in an earlier large prospective study, ranged from 7% to 16%, and osteopenia ranged from 27% to 46%.
“Our study suggests that patients with PsA have similar BMDs compared to the general population,” the authors wrote.
Researchers did note the suggestion that patients with polyarthritis had lower BMDs over time. Because of the small number of events, this did not achieve statistical significance, but “this relationship warrants further research, given that multiple cohort studies have independently demonstrated polyarticular onset of disease predicting clinical deformities and erosive disease in PsA,” they wrote.
They also saw that patients with increased body mass index had a significant 21% lower odds of having a BMD in the osteoporotic range, while those using biologics had a significant 83% lower odds.
Among participants with BMD scores in the osteopenic or osteoporotic range, these scores were seen in the lumbar spine in 63% of measurements, the femoral neck in 88%, and the total hip in 39%. Mean T-scores for the lumbar spine were –0.30±0.32, and for the femoral neck were –1.10±1.04 and the total hip, –0.45±0.42.
The study also examined what factors were associated with referral for BMD testing. They found that increasing age, menopause, elevated acute phase reactants, or use of biologics, methotrexate, and systemic glucocorticoids were associated with a higher likelihood of undergoing BMD testing.
Noting that the latest Canadian clinical practice guidelines on BMD testing advise that age, menopause, and use of systemic glucocorticoids use are risk factors that should prompt testing, the authors suggested clinicians were using a combination of traditional osteoporosis risk factors and markers of psoriatic disease severity to underpin their decision to refer.
However, they commented that none of the factors associated with a higher likelihood of having a BMD test were actually associated with lower BMD scores.
“This suggests that clinicians may be over-screening patients with PsA for osteopenia/osteoporosis, as they do not appear to be at baseline higher risk for lower BMD scores than the general population,” they wrote. “This is of importance, as there are currently no formal recommendations with regards to the optimal interval or time to commence BMD testing within the recent major PsA guidelines.”
The study was supported by a grant from the Krembil Foundation. No conflicts of interest were declared.
SOURCE: Kwok TSH et al. Arthritis Care Res. 2020 Dec 16. doi: 10.1002/acr.24538.
The rates of osteopenia and osteoporosis among individuals with psoriatic arthritis are comparable to those seen in the general population, research suggests.
The cohort study, published in Arthritis Care & Research, also found that clinicians are likely to refer patients for bone mineral density (BMD) testing based on osteoporosis risk factors or psoriatic arthritis disease severity markers.
Timothy S.H. Kwok, MD, of the University of Toronto, and coauthors wrote that previous research suggested a possible link between psoriatic arthritis and osteoporosis or osteopenia. However, no cohort studies appear to have examined this association.
The study involved 201 individuals with psoriatic arthritis attending a single specialist clinic, who were enrolled in a longitudinal study of psoriatic arthritis (PsA) and who were also referred for BMD testing with dual-energy x-ray absorptiometry.
Of these participants, 13% had a BMD in the osteoporotic range, 45% were in the osteopenic range, and 42% were in the normal range for BMD. The prevalence of osteoporosis observed in the general population aged 50 or above, observed in an earlier large prospective study, ranged from 7% to 16%, and osteopenia ranged from 27% to 46%.
“Our study suggests that patients with PsA have similar BMDs compared to the general population,” the authors wrote.
Researchers did note the suggestion that patients with polyarthritis had lower BMDs over time. Because of the small number of events, this did not achieve statistical significance, but “this relationship warrants further research, given that multiple cohort studies have independently demonstrated polyarticular onset of disease predicting clinical deformities and erosive disease in PsA,” they wrote.
They also saw that patients with increased body mass index had a significant 21% lower odds of having a BMD in the osteoporotic range, while those using biologics had a significant 83% lower odds.
Among participants with BMD scores in the osteopenic or osteoporotic range, these scores were seen in the lumbar spine in 63% of measurements, the femoral neck in 88%, and the total hip in 39%. Mean T-scores for the lumbar spine were –0.30±0.32, and for the femoral neck were –1.10±1.04 and the total hip, –0.45±0.42.
The study also examined what factors were associated with referral for BMD testing. They found that increasing age, menopause, elevated acute phase reactants, or use of biologics, methotrexate, and systemic glucocorticoids were associated with a higher likelihood of undergoing BMD testing.
Noting that the latest Canadian clinical practice guidelines on BMD testing advise that age, menopause, and use of systemic glucocorticoids use are risk factors that should prompt testing, the authors suggested clinicians were using a combination of traditional osteoporosis risk factors and markers of psoriatic disease severity to underpin their decision to refer.
However, they commented that none of the factors associated with a higher likelihood of having a BMD test were actually associated with lower BMD scores.
“This suggests that clinicians may be over-screening patients with PsA for osteopenia/osteoporosis, as they do not appear to be at baseline higher risk for lower BMD scores than the general population,” they wrote. “This is of importance, as there are currently no formal recommendations with regards to the optimal interval or time to commence BMD testing within the recent major PsA guidelines.”
The study was supported by a grant from the Krembil Foundation. No conflicts of interest were declared.
SOURCE: Kwok TSH et al. Arthritis Care Res. 2020 Dec 16. doi: 10.1002/acr.24538.
FROM ARTHRITIS CARE & RESEARCH
EULAR recommendations define strategies to improve adherence in RMDs
Clinicians who care for patients with rheumatic and musculoskeletal diseases (RMDs) can now refer to a new set of strategies and points to consider from a European League Against Rheumatism (EULAR) task force in building a patient-centered approach to improve adherence to treatments.
Nonadherence to treatments is concerning given that 30%-80% of patients who have RMDs are thought to not follow a recommended treatment plan according to their physicians’ instructions, according to first author Valentin Ritschl of the Medical University of Vienna and colleagues.
“The problem of poor adherence is addressed in some EULAR recommendations/points to consider on the management of specific health conditions or on the role of professionals,” Mr. Ritschl said in an interview. “However, all these recommendations focus on limited aspects of nonadherence and do not cover the multifaceted nature of this phenomenon.”
Mr. Ritschl and colleagues conducted an extensive systematic literature review, the results of which they presented to a task force consisting of a panel of international experts hailing from 12 different countries. The task force included rheumatologists and other health professionals in rheumatology, as well as patient representatives.
The collaboration resulted in investigators crafting a definition of adherence in addition to drafting four overarching principles and nine points to consider, which were published Dec. 18 in Annals of the Rheumatic Diseases.
They defined adherence as “the extent to which a person’s behavior corresponds with the agreed prescription, of pharmacological or nonpharmacological treatments, by a health care provider.”
The four overarching principles emphasize the following concepts: that adherence affects outcomes in people who have RMDs; the importance of shared decision-making, with the understanding that the adherence describes the patient’s behavior “following an agreed prescription”; that numerous factors can affect adherence; and the notion of adherence being a dynamic process that, consequently, requires continuous evaluation.
Among the nine points to consider, Mr. Ritschl and coauthors encouraged all health care providers involved in caring for RMD patients to assume responsibility for promoting adherence. Practitioners should also strive to create an ongoing, open dialogue to discuss adherence, especially in cases in which the patient’s RMD is not well controlled. The patient-centered recommendations include taking into account the patient’s goals and preferences because these greatly contribute to the patient’s ability to adhere to any medication regimen. Another arm of that exploration also requires the medical professional to evaluate any circumstances that could bear a negative effect on the patient’s adherence – whether it be medication access issues related to cost or availability, or functional challenges such as memory, motivation, or complexity of the medication regimen.
Mr. Ritschl believed the task force’s recommendations will add value and help improve overall outcomes in RMD population management.
“Until today, there are no recommendations or points to consider developed in order to support our patients to be adherent to the agreed treatment plan,” he said. “In our project/initiative, we therefore developed for the first time points to consider to detect, assess, and manage nonadherence in people with RMDs.”
Additionally, the recommendations offer some strategic insights to help improve clinical trials because the deleterious effects of nonadherence also affect study results.
Looking ahead, Mr. Ritschl said randomized, controlled trials are necessary to test strategies that might improve adherence. He strongly emphasized the importance of designing future research studies that are heavily patient centered and effective for shared decision-making.
The project was funded by EULAR. Mr. Ritschl reported having no disclosures, but many of his coauthors reported financial relationships with pharmaceutical companies.
SOURCE: Ritschl V et al. Ann Rheum Dis. 2020 Dec 18. doi: 10.1136/annrheumdis-2020-218986.
Clinicians who care for patients with rheumatic and musculoskeletal diseases (RMDs) can now refer to a new set of strategies and points to consider from a European League Against Rheumatism (EULAR) task force in building a patient-centered approach to improve adherence to treatments.
Nonadherence to treatments is concerning given that 30%-80% of patients who have RMDs are thought to not follow a recommended treatment plan according to their physicians’ instructions, according to first author Valentin Ritschl of the Medical University of Vienna and colleagues.
“The problem of poor adherence is addressed in some EULAR recommendations/points to consider on the management of specific health conditions or on the role of professionals,” Mr. Ritschl said in an interview. “However, all these recommendations focus on limited aspects of nonadherence and do not cover the multifaceted nature of this phenomenon.”
Mr. Ritschl and colleagues conducted an extensive systematic literature review, the results of which they presented to a task force consisting of a panel of international experts hailing from 12 different countries. The task force included rheumatologists and other health professionals in rheumatology, as well as patient representatives.
The collaboration resulted in investigators crafting a definition of adherence in addition to drafting four overarching principles and nine points to consider, which were published Dec. 18 in Annals of the Rheumatic Diseases.
They defined adherence as “the extent to which a person’s behavior corresponds with the agreed prescription, of pharmacological or nonpharmacological treatments, by a health care provider.”
The four overarching principles emphasize the following concepts: that adherence affects outcomes in people who have RMDs; the importance of shared decision-making, with the understanding that the adherence describes the patient’s behavior “following an agreed prescription”; that numerous factors can affect adherence; and the notion of adherence being a dynamic process that, consequently, requires continuous evaluation.
Among the nine points to consider, Mr. Ritschl and coauthors encouraged all health care providers involved in caring for RMD patients to assume responsibility for promoting adherence. Practitioners should also strive to create an ongoing, open dialogue to discuss adherence, especially in cases in which the patient’s RMD is not well controlled. The patient-centered recommendations include taking into account the patient’s goals and preferences because these greatly contribute to the patient’s ability to adhere to any medication regimen. Another arm of that exploration also requires the medical professional to evaluate any circumstances that could bear a negative effect on the patient’s adherence – whether it be medication access issues related to cost or availability, or functional challenges such as memory, motivation, or complexity of the medication regimen.
Mr. Ritschl believed the task force’s recommendations will add value and help improve overall outcomes in RMD population management.
“Until today, there are no recommendations or points to consider developed in order to support our patients to be adherent to the agreed treatment plan,” he said. “In our project/initiative, we therefore developed for the first time points to consider to detect, assess, and manage nonadherence in people with RMDs.”
Additionally, the recommendations offer some strategic insights to help improve clinical trials because the deleterious effects of nonadherence also affect study results.
Looking ahead, Mr. Ritschl said randomized, controlled trials are necessary to test strategies that might improve adherence. He strongly emphasized the importance of designing future research studies that are heavily patient centered and effective for shared decision-making.
The project was funded by EULAR. Mr. Ritschl reported having no disclosures, but many of his coauthors reported financial relationships with pharmaceutical companies.
SOURCE: Ritschl V et al. Ann Rheum Dis. 2020 Dec 18. doi: 10.1136/annrheumdis-2020-218986.
Clinicians who care for patients with rheumatic and musculoskeletal diseases (RMDs) can now refer to a new set of strategies and points to consider from a European League Against Rheumatism (EULAR) task force in building a patient-centered approach to improve adherence to treatments.
Nonadherence to treatments is concerning given that 30%-80% of patients who have RMDs are thought to not follow a recommended treatment plan according to their physicians’ instructions, according to first author Valentin Ritschl of the Medical University of Vienna and colleagues.
“The problem of poor adherence is addressed in some EULAR recommendations/points to consider on the management of specific health conditions or on the role of professionals,” Mr. Ritschl said in an interview. “However, all these recommendations focus on limited aspects of nonadherence and do not cover the multifaceted nature of this phenomenon.”
Mr. Ritschl and colleagues conducted an extensive systematic literature review, the results of which they presented to a task force consisting of a panel of international experts hailing from 12 different countries. The task force included rheumatologists and other health professionals in rheumatology, as well as patient representatives.
The collaboration resulted in investigators crafting a definition of adherence in addition to drafting four overarching principles and nine points to consider, which were published Dec. 18 in Annals of the Rheumatic Diseases.
They defined adherence as “the extent to which a person’s behavior corresponds with the agreed prescription, of pharmacological or nonpharmacological treatments, by a health care provider.”
The four overarching principles emphasize the following concepts: that adherence affects outcomes in people who have RMDs; the importance of shared decision-making, with the understanding that the adherence describes the patient’s behavior “following an agreed prescription”; that numerous factors can affect adherence; and the notion of adherence being a dynamic process that, consequently, requires continuous evaluation.
Among the nine points to consider, Mr. Ritschl and coauthors encouraged all health care providers involved in caring for RMD patients to assume responsibility for promoting adherence. Practitioners should also strive to create an ongoing, open dialogue to discuss adherence, especially in cases in which the patient’s RMD is not well controlled. The patient-centered recommendations include taking into account the patient’s goals and preferences because these greatly contribute to the patient’s ability to adhere to any medication regimen. Another arm of that exploration also requires the medical professional to evaluate any circumstances that could bear a negative effect on the patient’s adherence – whether it be medication access issues related to cost or availability, or functional challenges such as memory, motivation, or complexity of the medication regimen.
Mr. Ritschl believed the task force’s recommendations will add value and help improve overall outcomes in RMD population management.
“Until today, there are no recommendations or points to consider developed in order to support our patients to be adherent to the agreed treatment plan,” he said. “In our project/initiative, we therefore developed for the first time points to consider to detect, assess, and manage nonadherence in people with RMDs.”
Additionally, the recommendations offer some strategic insights to help improve clinical trials because the deleterious effects of nonadherence also affect study results.
Looking ahead, Mr. Ritschl said randomized, controlled trials are necessary to test strategies that might improve adherence. He strongly emphasized the importance of designing future research studies that are heavily patient centered and effective for shared decision-making.
The project was funded by EULAR. Mr. Ritschl reported having no disclosures, but many of his coauthors reported financial relationships with pharmaceutical companies.
SOURCE: Ritschl V et al. Ann Rheum Dis. 2020 Dec 18. doi: 10.1136/annrheumdis-2020-218986.
FROM ANNALS OF THE RHEUMATIC DISEASES