User login
Anxiety, inactivity linked to cognitive impairment in Parkinson’s
Parkinson’s disease patients who develop anxiety early in their disease are at risk for reduced physical activity, which promotes further anxiety and cognitive decline, data from nearly 500 individuals show.
Anxiety occurs in 20%-60% of Parkinson’s disease (PD) patients but often goes undiagnosed, wrote Jacob D. Jones, PhD, of California State University, San Bernardino, and colleagues.
“Anxiety can attenuate motivation to engage in physical activity leading to more anxiety and other negative cognitive outcomes,” although physical activity has been shown to improve cognitive function in PD patients, they said. However, physical activity as a mediator between anxiety and cognitive function in PD has not been well studied, they noted.
In a study published in Mental Health and Physical Activity Participants were followed for up to 5 years and completed neuropsychological tests, tests of motor severity, and self-reports on anxiety and physical activity. Anxiety was assessed using the State-Trait Anxiety Inventory-Trait (STAI-T) subscale. Physical activity was assessed using the Physical Activity Scale for the Elderly (PASE). Motor severity was assessed using the Unified Parkinson’s Disease Rating Scale-Part III (UPDRS). The average age of the participants was 61 years, 65% were men, and 96% were White.
Using a direct-effect model, the researchers found that individuals whose anxiety increased during the study period also showed signs of cognitive decline. A significant between-person effect showed that individuals who were generally more anxious also scored lower on cognitive tests over the 5-year study period.
In a mediation model computed with structural equation modeling, physical activity mediated the link between anxiety and cognition, most notably household activity.
“There was a significant within-person association between anxiety and household activities, meaning that individuals who became more anxious over the 5-year study also became less active in the home,” reported Dr. Jones and colleagues.
However, no significant indirect effect was noted regarding the between-person findings of the impact of physical activity on anxiety and cognitive decline. Although more severe anxiety was associated with less activity, cognitive performance was not associated with either type of physical activity.
The presence of a within-person effect “suggests that reductions in physical activity, specifically within the first 5 years of disease onset, may be detrimental to mental health,” the researchers emphasized. Given that the study population was newly diagnosed with PD “it is likely the within-person terms are more sensitive to changes in anxiety, physical activity, and cognition that are more directly the result of the PD process, as opposed to lifestyle/preexisting traits,” they said.
The study findings were limited by several factors, including the use of self-reports to measure physical activity, and the lack of granular information about the details of physical activity, the researchers noted. Another limitation was the inclusion of only newly diagnosed PD patients, which might limit generalizability.
“Future research is warranted to understand if other modes, intensities, or complexities of physical activity impact individuals with PD in a different manner in relation to cognition,” they said.
Dr. Jones and colleagues had no disclosures. The PPMI is supported by the Michael J. Fox Foundation for Parkinson’s Research and funding partners, including numerous pharmaceutical companies.
Parkinson’s disease patients who develop anxiety early in their disease are at risk for reduced physical activity, which promotes further anxiety and cognitive decline, data from nearly 500 individuals show.
Anxiety occurs in 20%-60% of Parkinson’s disease (PD) patients but often goes undiagnosed, wrote Jacob D. Jones, PhD, of California State University, San Bernardino, and colleagues.
“Anxiety can attenuate motivation to engage in physical activity leading to more anxiety and other negative cognitive outcomes,” although physical activity has been shown to improve cognitive function in PD patients, they said. However, physical activity as a mediator between anxiety and cognitive function in PD has not been well studied, they noted.
In a study published in Mental Health and Physical Activity Participants were followed for up to 5 years and completed neuropsychological tests, tests of motor severity, and self-reports on anxiety and physical activity. Anxiety was assessed using the State-Trait Anxiety Inventory-Trait (STAI-T) subscale. Physical activity was assessed using the Physical Activity Scale for the Elderly (PASE). Motor severity was assessed using the Unified Parkinson’s Disease Rating Scale-Part III (UPDRS). The average age of the participants was 61 years, 65% were men, and 96% were White.
Using a direct-effect model, the researchers found that individuals whose anxiety increased during the study period also showed signs of cognitive decline. A significant between-person effect showed that individuals who were generally more anxious also scored lower on cognitive tests over the 5-year study period.
In a mediation model computed with structural equation modeling, physical activity mediated the link between anxiety and cognition, most notably household activity.
“There was a significant within-person association between anxiety and household activities, meaning that individuals who became more anxious over the 5-year study also became less active in the home,” reported Dr. Jones and colleagues.
However, no significant indirect effect was noted regarding the between-person findings of the impact of physical activity on anxiety and cognitive decline. Although more severe anxiety was associated with less activity, cognitive performance was not associated with either type of physical activity.
The presence of a within-person effect “suggests that reductions in physical activity, specifically within the first 5 years of disease onset, may be detrimental to mental health,” the researchers emphasized. Given that the study population was newly diagnosed with PD “it is likely the within-person terms are more sensitive to changes in anxiety, physical activity, and cognition that are more directly the result of the PD process, as opposed to lifestyle/preexisting traits,” they said.
The study findings were limited by several factors, including the use of self-reports to measure physical activity, and the lack of granular information about the details of physical activity, the researchers noted. Another limitation was the inclusion of only newly diagnosed PD patients, which might limit generalizability.
“Future research is warranted to understand if other modes, intensities, or complexities of physical activity impact individuals with PD in a different manner in relation to cognition,” they said.
Dr. Jones and colleagues had no disclosures. The PPMI is supported by the Michael J. Fox Foundation for Parkinson’s Research and funding partners, including numerous pharmaceutical companies.
Parkinson’s disease patients who develop anxiety early in their disease are at risk for reduced physical activity, which promotes further anxiety and cognitive decline, data from nearly 500 individuals show.
Anxiety occurs in 20%-60% of Parkinson’s disease (PD) patients but often goes undiagnosed, wrote Jacob D. Jones, PhD, of California State University, San Bernardino, and colleagues.
“Anxiety can attenuate motivation to engage in physical activity leading to more anxiety and other negative cognitive outcomes,” although physical activity has been shown to improve cognitive function in PD patients, they said. However, physical activity as a mediator between anxiety and cognitive function in PD has not been well studied, they noted.
In a study published in Mental Health and Physical Activity Participants were followed for up to 5 years and completed neuropsychological tests, tests of motor severity, and self-reports on anxiety and physical activity. Anxiety was assessed using the State-Trait Anxiety Inventory-Trait (STAI-T) subscale. Physical activity was assessed using the Physical Activity Scale for the Elderly (PASE). Motor severity was assessed using the Unified Parkinson’s Disease Rating Scale-Part III (UPDRS). The average age of the participants was 61 years, 65% were men, and 96% were White.
Using a direct-effect model, the researchers found that individuals whose anxiety increased during the study period also showed signs of cognitive decline. A significant between-person effect showed that individuals who were generally more anxious also scored lower on cognitive tests over the 5-year study period.
In a mediation model computed with structural equation modeling, physical activity mediated the link between anxiety and cognition, most notably household activity.
“There was a significant within-person association between anxiety and household activities, meaning that individuals who became more anxious over the 5-year study also became less active in the home,” reported Dr. Jones and colleagues.
However, no significant indirect effect was noted regarding the between-person findings of the impact of physical activity on anxiety and cognitive decline. Although more severe anxiety was associated with less activity, cognitive performance was not associated with either type of physical activity.
The presence of a within-person effect “suggests that reductions in physical activity, specifically within the first 5 years of disease onset, may be detrimental to mental health,” the researchers emphasized. Given that the study population was newly diagnosed with PD “it is likely the within-person terms are more sensitive to changes in anxiety, physical activity, and cognition that are more directly the result of the PD process, as opposed to lifestyle/preexisting traits,” they said.
The study findings were limited by several factors, including the use of self-reports to measure physical activity, and the lack of granular information about the details of physical activity, the researchers noted. Another limitation was the inclusion of only newly diagnosed PD patients, which might limit generalizability.
“Future research is warranted to understand if other modes, intensities, or complexities of physical activity impact individuals with PD in a different manner in relation to cognition,” they said.
Dr. Jones and colleagues had no disclosures. The PPMI is supported by the Michael J. Fox Foundation for Parkinson’s Research and funding partners, including numerous pharmaceutical companies.
FROM MENTAL HEALTH AND PHYSICAL ACTIVITY
Early data for experimental THC drug ‘promising’ for Tourette’s
Oral delta-9-tetrahydracannabinol (delta-9-THC) and palmitoylethanolamide (PEA), in a proprietary combination known as THX-110, is promising for reducing tic symptoms in adults with Tourette syndrome (TS), new research suggests.
In a small phase 2 trial, investigators administered THX-110 to 16 adults with treatment-resistant TS for 12 weeks. Results showed a reduction of more than 20% in tic symptoms after the first week of treatment compared with baseline.
“We conducted an uncontrolled study in adults with severe TS and found that their tics improved over time while they took THX-110,” lead author Michael Bloch, MD, associate professor and co-director of the Tic and OCD Program at the Child Study Center, Yale University, New Haven, Conn., told this news organization.
Dr. Bloch added that the next step in this line of research will be to conduct a placebo-controlled trial of the compound in order to assess whether tic improvement observed over time in this study “was due to the effects of the medication and not related to the natural waxing-and-waning course of tic symptoms or treatment expectancy.”
The findings were published online August 2 in the Journal of Neuropsychiatry and Clinical Neurosciences.
‘Entourage effect’
“Several lines of evidence from clinical observation and even randomized controlled trials” suggest that cannabis (cannabis sativa) and delta-9-THC may be effective in treatment of tic disorders, Dr. Bloch said.
“Cannabinoid receptors are present in the motor regions important for tics, and thus, there is a potential mechanism of action to lead to improvement of tics,” he added.
However, “the major limitations of both cannabis and dronabinol [a synthetic form of delta-9-THC] use are the adverse psychoactive effects they induce in higher doses,” he said.
Dr. Bloch noted that PEA is a lipid messenger “known to mimic several endocannabinoid-driven activities.”
For this reason, combining delta-9-THC with PEA is hypothesized to reduce the dose of delta-9-THC needed to improve tics and also potentially lessen its side effects.
This initial open-label trial examined safety and tolerability of THX-110, as well as its effect on tic symptoms in adults with TS. The researchers hoped to “use the entourage effect to deliver the therapeutic benefits of delta-9-THC in reducing tics with decrease psychoactive effects by combining with PEA.”
The “entourage effect” refers to “endocannabinoid regulation by which multiple endogenous cannabinoid chemical species display a cooperative effect in eliciting a cellular response,” they write.
The investigators conducted a 12-week uncontrolled trial of THX-110, used at its maximum daily dose of delta-9-THC (10 mg) and a constant 800-mg dose of PEA in 16 adults with TS (mean age, 35 years; mean TS illness duration, 26.6 years).
Participants had a mean baseline Yale Global Tic Severity Scale (YGTSS) score of 38.1 and a mean worst-ever total tic score of 45.4.
All participants were experiencing persistent tics, despite having tried an array of previous evidence-based treatments for TS, including antipsychotics, alpha-2 agonists, VMAT2 inhibitors, benzodiazepines, and topiramate (Topamax).
Significant improvement
Results showed significant improvement in tic symptoms with TXH-110 treatment over time (general linear model time factor: F = 3.06, df = 7.91, P = .006).
At first assessment point, mean YGTSS improvement was 3.5 (95% confidence interval, 0.1-6.9; P = .047). The improvement not only remained significant but continued to increase throughout the 12-week trial period.
At 12 weeks, the maximal improvement in tic symptoms was observed, with a mean YGTSS improvement at endpoint of 7.6 (95% CI, 2.5-12.8; P = .007).
Four patients experienced a greater than 35% improvement in tic symptoms during the trial, whereas 6 experienced a 25% or greater improvement. The mean improvement in tic symptoms over the course of the trial was 20.6%.
There was also a significant improvement between baseline and endpoint on other measures of tic symptoms – but not on premonitory urges.
The patients experienced “modest” but not significant improvement in comorbid symptoms, including attentional, anxiety, depressive, and obsessive-compulsive symptoms.
Adverse events
All participants experienced some mild side effects for “a couple hours” after taking the medication, particularly during the course of dose escalation and maintenance. However, these were not serious enough to warrant stopping the medication.
These effects typically included fatigue/drowsiness, feeling “high,” dry mouth, dizziness/lightheadedness, and difficulty concentrating.
Side effects of moderate or greater severity necessitating changes in medication dosing were “less common,” the investigators report. No participants experienced significant laboratory abnormalities.
One patient discontinued the trial early because he felt that the study medication was not helpful, and a second discontinued because of drowsiness and fatigue related to the study medication.
Twelve participants elected to continue treatment with THX-110 during an open extension phase and 7 of these completed the additional 24 weeks.
“THX-110 treatment led to an average improvement in tic symptoms of roughly 20%, or a 7-point decrease in the YGTSS total tic score. This improvement translates to a large effect size (d = 0.92) of improvement over time,” the investigators write.
More data needed
Commenting on the findings, Yolanda Holler-Managan, MD, assistant professor of pediatrics (neurology), Northwestern University, Chicago, cautioned that this was not a randomized, double-blind, parallel-group placebo-controlled study.
Instead, it was a clinical study to prove safety, tolerability, and dosing of the combination medication in adult patients with TS and “does not provide as much weight, since we do not have many studies on the efficacy of cannabinoids,” said Dr. Holler-Managan, who was not involved with the research.
She noted that the American Academy of Neurology’s 2019 practice guideline recommendations for treatment of tics in individuals with TS and tic disorders reported “limited evidence” that delta-9-THC is “possibly more likely than placebo to reduce tic severity in adults with TS, therefore we need more data.”
The current investigators agree. “Although these initial data are promising, future randomized double-blind placebo-controlled trials are necessary to demonstrate efficacy of TXH-110 treatment,” they write.
They add that the psychoactive properties of cannabis-derived compounds make it challenging to design a properly blinded trial.
“Incorporation of physiologic biomarkers and objective measures of symptoms (e.g., videotaped tic counts by blinded raters) may be particularly important when examining these medications with psychoactive properties that may be prone to reporting bias,” the authors write.
The study was supported by an investigator-initiated grant to Dr. Bloch from Therapix Biosciences. The state of Connecticut also provided resource support via the Abraham Ribicoff Research Facilities at the Connecticut Mental Health Center. Dr. Bloch serves on the scientific advisory boards of Therapix Biosciences, and he receives research support from Biohaven Pharmaceuticals, Janssen Pharmaceuticals, NARSAD, Neurocrine Biosciences, NIH, and the Patterson Foundation. The other investigators and Dr. Holler-Managan have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Oral delta-9-tetrahydracannabinol (delta-9-THC) and palmitoylethanolamide (PEA), in a proprietary combination known as THX-110, is promising for reducing tic symptoms in adults with Tourette syndrome (TS), new research suggests.
In a small phase 2 trial, investigators administered THX-110 to 16 adults with treatment-resistant TS for 12 weeks. Results showed a reduction of more than 20% in tic symptoms after the first week of treatment compared with baseline.
“We conducted an uncontrolled study in adults with severe TS and found that their tics improved over time while they took THX-110,” lead author Michael Bloch, MD, associate professor and co-director of the Tic and OCD Program at the Child Study Center, Yale University, New Haven, Conn., told this news organization.
Dr. Bloch added that the next step in this line of research will be to conduct a placebo-controlled trial of the compound in order to assess whether tic improvement observed over time in this study “was due to the effects of the medication and not related to the natural waxing-and-waning course of tic symptoms or treatment expectancy.”
The findings were published online August 2 in the Journal of Neuropsychiatry and Clinical Neurosciences.
‘Entourage effect’
“Several lines of evidence from clinical observation and even randomized controlled trials” suggest that cannabis (cannabis sativa) and delta-9-THC may be effective in treatment of tic disorders, Dr. Bloch said.
“Cannabinoid receptors are present in the motor regions important for tics, and thus, there is a potential mechanism of action to lead to improvement of tics,” he added.
However, “the major limitations of both cannabis and dronabinol [a synthetic form of delta-9-THC] use are the adverse psychoactive effects they induce in higher doses,” he said.
Dr. Bloch noted that PEA is a lipid messenger “known to mimic several endocannabinoid-driven activities.”
For this reason, combining delta-9-THC with PEA is hypothesized to reduce the dose of delta-9-THC needed to improve tics and also potentially lessen its side effects.
This initial open-label trial examined safety and tolerability of THX-110, as well as its effect on tic symptoms in adults with TS. The researchers hoped to “use the entourage effect to deliver the therapeutic benefits of delta-9-THC in reducing tics with decrease psychoactive effects by combining with PEA.”
The “entourage effect” refers to “endocannabinoid regulation by which multiple endogenous cannabinoid chemical species display a cooperative effect in eliciting a cellular response,” they write.
The investigators conducted a 12-week uncontrolled trial of THX-110, used at its maximum daily dose of delta-9-THC (10 mg) and a constant 800-mg dose of PEA in 16 adults with TS (mean age, 35 years; mean TS illness duration, 26.6 years).
Participants had a mean baseline Yale Global Tic Severity Scale (YGTSS) score of 38.1 and a mean worst-ever total tic score of 45.4.
All participants were experiencing persistent tics, despite having tried an array of previous evidence-based treatments for TS, including antipsychotics, alpha-2 agonists, VMAT2 inhibitors, benzodiazepines, and topiramate (Topamax).
Significant improvement
Results showed significant improvement in tic symptoms with TXH-110 treatment over time (general linear model time factor: F = 3.06, df = 7.91, P = .006).
At first assessment point, mean YGTSS improvement was 3.5 (95% confidence interval, 0.1-6.9; P = .047). The improvement not only remained significant but continued to increase throughout the 12-week trial period.
At 12 weeks, the maximal improvement in tic symptoms was observed, with a mean YGTSS improvement at endpoint of 7.6 (95% CI, 2.5-12.8; P = .007).
Four patients experienced a greater than 35% improvement in tic symptoms during the trial, whereas 6 experienced a 25% or greater improvement. The mean improvement in tic symptoms over the course of the trial was 20.6%.
There was also a significant improvement between baseline and endpoint on other measures of tic symptoms – but not on premonitory urges.
The patients experienced “modest” but not significant improvement in comorbid symptoms, including attentional, anxiety, depressive, and obsessive-compulsive symptoms.
Adverse events
All participants experienced some mild side effects for “a couple hours” after taking the medication, particularly during the course of dose escalation and maintenance. However, these were not serious enough to warrant stopping the medication.
These effects typically included fatigue/drowsiness, feeling “high,” dry mouth, dizziness/lightheadedness, and difficulty concentrating.
Side effects of moderate or greater severity necessitating changes in medication dosing were “less common,” the investigators report. No participants experienced significant laboratory abnormalities.
One patient discontinued the trial early because he felt that the study medication was not helpful, and a second discontinued because of drowsiness and fatigue related to the study medication.
Twelve participants elected to continue treatment with THX-110 during an open extension phase and 7 of these completed the additional 24 weeks.
“THX-110 treatment led to an average improvement in tic symptoms of roughly 20%, or a 7-point decrease in the YGTSS total tic score. This improvement translates to a large effect size (d = 0.92) of improvement over time,” the investigators write.
More data needed
Commenting on the findings, Yolanda Holler-Managan, MD, assistant professor of pediatrics (neurology), Northwestern University, Chicago, cautioned that this was not a randomized, double-blind, parallel-group placebo-controlled study.
Instead, it was a clinical study to prove safety, tolerability, and dosing of the combination medication in adult patients with TS and “does not provide as much weight, since we do not have many studies on the efficacy of cannabinoids,” said Dr. Holler-Managan, who was not involved with the research.
She noted that the American Academy of Neurology’s 2019 practice guideline recommendations for treatment of tics in individuals with TS and tic disorders reported “limited evidence” that delta-9-THC is “possibly more likely than placebo to reduce tic severity in adults with TS, therefore we need more data.”
The current investigators agree. “Although these initial data are promising, future randomized double-blind placebo-controlled trials are necessary to demonstrate efficacy of TXH-110 treatment,” they write.
They add that the psychoactive properties of cannabis-derived compounds make it challenging to design a properly blinded trial.
“Incorporation of physiologic biomarkers and objective measures of symptoms (e.g., videotaped tic counts by blinded raters) may be particularly important when examining these medications with psychoactive properties that may be prone to reporting bias,” the authors write.
The study was supported by an investigator-initiated grant to Dr. Bloch from Therapix Biosciences. The state of Connecticut also provided resource support via the Abraham Ribicoff Research Facilities at the Connecticut Mental Health Center. Dr. Bloch serves on the scientific advisory boards of Therapix Biosciences, and he receives research support from Biohaven Pharmaceuticals, Janssen Pharmaceuticals, NARSAD, Neurocrine Biosciences, NIH, and the Patterson Foundation. The other investigators and Dr. Holler-Managan have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Oral delta-9-tetrahydracannabinol (delta-9-THC) and palmitoylethanolamide (PEA), in a proprietary combination known as THX-110, is promising for reducing tic symptoms in adults with Tourette syndrome (TS), new research suggests.
In a small phase 2 trial, investigators administered THX-110 to 16 adults with treatment-resistant TS for 12 weeks. Results showed a reduction of more than 20% in tic symptoms after the first week of treatment compared with baseline.
“We conducted an uncontrolled study in adults with severe TS and found that their tics improved over time while they took THX-110,” lead author Michael Bloch, MD, associate professor and co-director of the Tic and OCD Program at the Child Study Center, Yale University, New Haven, Conn., told this news organization.
Dr. Bloch added that the next step in this line of research will be to conduct a placebo-controlled trial of the compound in order to assess whether tic improvement observed over time in this study “was due to the effects of the medication and not related to the natural waxing-and-waning course of tic symptoms or treatment expectancy.”
The findings were published online August 2 in the Journal of Neuropsychiatry and Clinical Neurosciences.
‘Entourage effect’
“Several lines of evidence from clinical observation and even randomized controlled trials” suggest that cannabis (cannabis sativa) and delta-9-THC may be effective in treatment of tic disorders, Dr. Bloch said.
“Cannabinoid receptors are present in the motor regions important for tics, and thus, there is a potential mechanism of action to lead to improvement of tics,” he added.
However, “the major limitations of both cannabis and dronabinol [a synthetic form of delta-9-THC] use are the adverse psychoactive effects they induce in higher doses,” he said.
Dr. Bloch noted that PEA is a lipid messenger “known to mimic several endocannabinoid-driven activities.”
For this reason, combining delta-9-THC with PEA is hypothesized to reduce the dose of delta-9-THC needed to improve tics and also potentially lessen its side effects.
This initial open-label trial examined safety and tolerability of THX-110, as well as its effect on tic symptoms in adults with TS. The researchers hoped to “use the entourage effect to deliver the therapeutic benefits of delta-9-THC in reducing tics with decrease psychoactive effects by combining with PEA.”
The “entourage effect” refers to “endocannabinoid regulation by which multiple endogenous cannabinoid chemical species display a cooperative effect in eliciting a cellular response,” they write.
The investigators conducted a 12-week uncontrolled trial of THX-110, used at its maximum daily dose of delta-9-THC (10 mg) and a constant 800-mg dose of PEA in 16 adults with TS (mean age, 35 years; mean TS illness duration, 26.6 years).
Participants had a mean baseline Yale Global Tic Severity Scale (YGTSS) score of 38.1 and a mean worst-ever total tic score of 45.4.
All participants were experiencing persistent tics, despite having tried an array of previous evidence-based treatments for TS, including antipsychotics, alpha-2 agonists, VMAT2 inhibitors, benzodiazepines, and topiramate (Topamax).
Significant improvement
Results showed significant improvement in tic symptoms with TXH-110 treatment over time (general linear model time factor: F = 3.06, df = 7.91, P = .006).
At first assessment point, mean YGTSS improvement was 3.5 (95% confidence interval, 0.1-6.9; P = .047). The improvement not only remained significant but continued to increase throughout the 12-week trial period.
At 12 weeks, the maximal improvement in tic symptoms was observed, with a mean YGTSS improvement at endpoint of 7.6 (95% CI, 2.5-12.8; P = .007).
Four patients experienced a greater than 35% improvement in tic symptoms during the trial, whereas 6 experienced a 25% or greater improvement. The mean improvement in tic symptoms over the course of the trial was 20.6%.
There was also a significant improvement between baseline and endpoint on other measures of tic symptoms – but not on premonitory urges.
The patients experienced “modest” but not significant improvement in comorbid symptoms, including attentional, anxiety, depressive, and obsessive-compulsive symptoms.
Adverse events
All participants experienced some mild side effects for “a couple hours” after taking the medication, particularly during the course of dose escalation and maintenance. However, these were not serious enough to warrant stopping the medication.
These effects typically included fatigue/drowsiness, feeling “high,” dry mouth, dizziness/lightheadedness, and difficulty concentrating.
Side effects of moderate or greater severity necessitating changes in medication dosing were “less common,” the investigators report. No participants experienced significant laboratory abnormalities.
One patient discontinued the trial early because he felt that the study medication was not helpful, and a second discontinued because of drowsiness and fatigue related to the study medication.
Twelve participants elected to continue treatment with THX-110 during an open extension phase and 7 of these completed the additional 24 weeks.
“THX-110 treatment led to an average improvement in tic symptoms of roughly 20%, or a 7-point decrease in the YGTSS total tic score. This improvement translates to a large effect size (d = 0.92) of improvement over time,” the investigators write.
More data needed
Commenting on the findings, Yolanda Holler-Managan, MD, assistant professor of pediatrics (neurology), Northwestern University, Chicago, cautioned that this was not a randomized, double-blind, parallel-group placebo-controlled study.
Instead, it was a clinical study to prove safety, tolerability, and dosing of the combination medication in adult patients with TS and “does not provide as much weight, since we do not have many studies on the efficacy of cannabinoids,” said Dr. Holler-Managan, who was not involved with the research.
She noted that the American Academy of Neurology’s 2019 practice guideline recommendations for treatment of tics in individuals with TS and tic disorders reported “limited evidence” that delta-9-THC is “possibly more likely than placebo to reduce tic severity in adults with TS, therefore we need more data.”
The current investigators agree. “Although these initial data are promising, future randomized double-blind placebo-controlled trials are necessary to demonstrate efficacy of TXH-110 treatment,” they write.
They add that the psychoactive properties of cannabis-derived compounds make it challenging to design a properly blinded trial.
“Incorporation of physiologic biomarkers and objective measures of symptoms (e.g., videotaped tic counts by blinded raters) may be particularly important when examining these medications with psychoactive properties that may be prone to reporting bias,” the authors write.
The study was supported by an investigator-initiated grant to Dr. Bloch from Therapix Biosciences. The state of Connecticut also provided resource support via the Abraham Ribicoff Research Facilities at the Connecticut Mental Health Center. Dr. Bloch serves on the scientific advisory boards of Therapix Biosciences, and he receives research support from Biohaven Pharmaceuticals, Janssen Pharmaceuticals, NARSAD, Neurocrine Biosciences, NIH, and the Patterson Foundation. The other investigators and Dr. Holler-Managan have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Low depression scores may miss seniors with suicidal intent
Older adults may have a high degree of suicidal intent yet still have low scores on scales measuring psychiatric symptoms, such as depression, new research suggests.
In a cross-sectional cohort study of more than 800 adults who presented with self-harm to psychiatric EDs in Sweden, participants aged 65 years and older scored higher than younger and middle-aged adults on measures of suicidal intent.
However, only half of the older group fulfilled criteria for major depression, compared with three-quarters of both the middle-aged and young adult–aged groups.
“Suicidal older persons show a somewhat different clinical picture with relatively low levels of psychopathology but with high suicide intent compared to younger persons,” lead author Stefan Wiktorsson, PhD, University of Gothenburg (Sweden), said in an interview.
“It is therefore of importance for clinicians to carefully evaluate suicidal thinking in this age group. he said.
The findings were published online Aug. 9, 2021, in the American Journal of Geriatric Psychiatry.
Research by age groups ‘lacking’
“While there are large age differences in the prevalence of suicidal behavior, research studies that compare symptomatology and diagnostics in different age groups are lacking,” Dr. Wiktorsson said.
He and his colleagues “wanted to compare psychopathology in young, middle-aged, and older adults in order to increase knowledge about potential differences in symptomatology related to suicidal behavior over the life span.”
The researchers recruited patients aged 18 years and older who had sought or had been referred to emergency psychiatric services for self-harm at three psychiatric hospitals in Sweden between April 2012 and March 2016.
Among all patients, 821 fit inclusion criteria and agreed to participate. The researchers excluded participants who had engaged in nonsuicidal self-injury (NNSI), as determined on the basis of the Columbia Suicide Severity Rating Scale (C-SSRS). The remaining 683 participants, who had attempted suicide, were included in the analysis.
The participants were then divided into the following three groups: older (n = 96; age, 65-97 years; mean age, 77.2 years; 57% women), middle-aged (n = 164; age, 45-64 years; mean age, 53.4 years; 57% women), and younger (n = 423; age, 18-44 years; mean age, 28.3 years; 64% women)
Mental health staff interviewed participants within 7 days of the index episode. They collected information about sociodemographics, health, and contact with health care professionals. They used the C-SSRS to identify characteristics of the suicide attempts, and they used the Suicide Intent Scale (SIS) to evaluate circumstances surrounding the suicide attempt, such as active preparation.
Investigators also used the Mini International Neuropsychiatric Interview (MINI), the Suicide Assessment Scale (SUAS), and the Karolinska Affective and Borderline Symptoms Scale.
Greater disability, pain
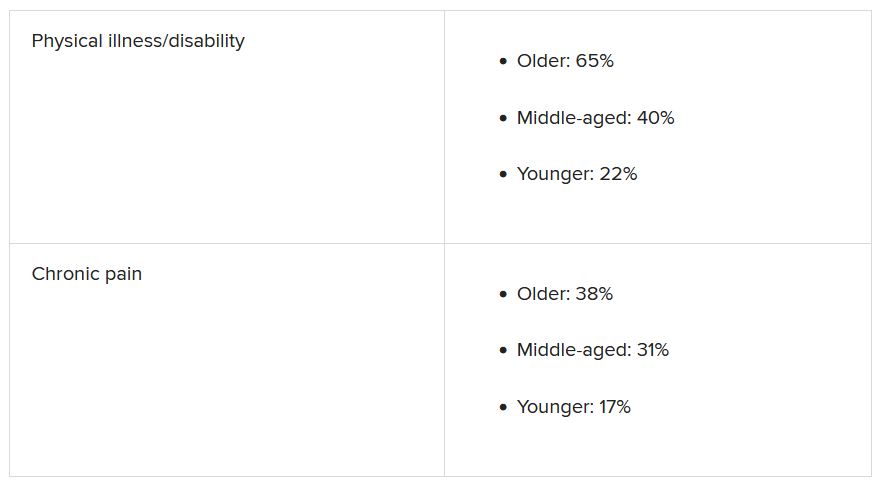
Of the older patients, 75% lived alone; 88% of the middle-aged and 48% of the younger participants lived alone. A higher proportion of older participants had severe physical illness/disability and severe chronic pain compared with younger participants (all comparisons, P < .001).
Older adults had less contact with psychiatric services, but they had more contact than the other age groups with primary care for mental health problems. Older adults were prescribed antidepressants at the time of the suicide attempt at a lower rate, compared with the middle-aged and younger groups (50% vs. 73% and 66%).
Slightly less than half (44%) of the older adults had a previous history of a suicide attempt – a proportion considerably lower than was reported by patients in the middle-aged and young adult groups (63% and 75%, respectively). Few older adults had a history of a previous NNSI (6% vs. 23% and 63%).
Three-quarters of older adults employed poisoning as the single method of suicide attempt at their index episode, compared with 67% and 59% of the middle-aged and younger groups.
Notably, only half of older adults (52%) met criteria for major depression, determined on the basis of the MINI, compared with three quarters of participants in the other groups (73% and 76%, respectively). Fewer members of the older group met criteria for other psychiatric conditions.
Clouded judgment
The mean total SUAS score was “considerably lower” in the older-adult group than in the other groups. This was also the case for the SUAS subscales for affect, bodily states, control, coping, and emotional reactivity.
Importantly, however, older adults scored higher than younger adults on the SIS total score and the subjective subscale, indicating a higher level of suicidal intent.
The mean SIS total score was 17.8 in the older group, 17.4 in the middle-aged group, and 15.9 in the younger group. The SIS subjective suicide intent score was 10.9 versus 10.6 and 9.4.
“While subjective suicidal intent was higher, compared to the young group, older adults were less likely to fulfill criteria for major depression and several other mental disorders and lower scores were observed on all symptom rating scales, compared to both middle-aged and younger adults,” the investigators wrote.
“Low levels of psychopathology may cloud the clinician’s assessment of the serious nature of suicide attempts in older patients,” they added.
‘Silent generation’
Commenting on the findings, Marnin Heisel, PhD, CPsych, associate professor, departments of psychiatry and of epidemiology and biostatistics, University of Western Ontario, London, said an important takeaway from the study is that, if health care professionals look only for depression or only consider suicide risk in individuals who present with depression, “they might miss older adults who are contemplating suicide or engaging in suicidal behavior.”
Dr. Heisel, who was not involved with the study, observed that older adults are sometimes called the “silent generation” because they often tend to downplay or underreport depressive symptoms, partially because of having been socialized to “keep things to themselves and not to air emotional laundry.”
He recommended that, when assessing potentially suicidal older adults, clinicians select tools specifically designed for use in this age group, particularly the Geriatric Suicide Ideation Scale and the Geriatric Depression Scale. Dr. Heisel also recommended the Center for Epidemiological Studies Depression Scale–Revised Version.
“Beyond a specific scale, the question is to walk into a clinical encounter with a much broader viewpoint, understand who the client is, where they come from, their attitudes, life experience, and what in their experience is going on, their reason for coming to see someone and what they’re struggling with,” he said.
“What we’re seeing with this study is that standard clinical tools don’t necessarily identify some of these richer issues that might contribute to emotional pain, so sometimes the best way to go is a broader clinical interview with a humanistic perspective,” Dr. Heisel concluded.
The study was funded by the Swedish Research Council, the Swedish Research Council for Health, Working Life and Welfare, and the Swedish state, Stockholm County Council and Västerbotten County Council. The investigators and Dr. Heisel have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Older adults may have a high degree of suicidal intent yet still have low scores on scales measuring psychiatric symptoms, such as depression, new research suggests.
In a cross-sectional cohort study of more than 800 adults who presented with self-harm to psychiatric EDs in Sweden, participants aged 65 years and older scored higher than younger and middle-aged adults on measures of suicidal intent.
However, only half of the older group fulfilled criteria for major depression, compared with three-quarters of both the middle-aged and young adult–aged groups.
“Suicidal older persons show a somewhat different clinical picture with relatively low levels of psychopathology but with high suicide intent compared to younger persons,” lead author Stefan Wiktorsson, PhD, University of Gothenburg (Sweden), said in an interview.
“It is therefore of importance for clinicians to carefully evaluate suicidal thinking in this age group. he said.
The findings were published online Aug. 9, 2021, in the American Journal of Geriatric Psychiatry.
Research by age groups ‘lacking’
“While there are large age differences in the prevalence of suicidal behavior, research studies that compare symptomatology and diagnostics in different age groups are lacking,” Dr. Wiktorsson said.
He and his colleagues “wanted to compare psychopathology in young, middle-aged, and older adults in order to increase knowledge about potential differences in symptomatology related to suicidal behavior over the life span.”
The researchers recruited patients aged 18 years and older who had sought or had been referred to emergency psychiatric services for self-harm at three psychiatric hospitals in Sweden between April 2012 and March 2016.
Among all patients, 821 fit inclusion criteria and agreed to participate. The researchers excluded participants who had engaged in nonsuicidal self-injury (NNSI), as determined on the basis of the Columbia Suicide Severity Rating Scale (C-SSRS). The remaining 683 participants, who had attempted suicide, were included in the analysis.
The participants were then divided into the following three groups: older (n = 96; age, 65-97 years; mean age, 77.2 years; 57% women), middle-aged (n = 164; age, 45-64 years; mean age, 53.4 years; 57% women), and younger (n = 423; age, 18-44 years; mean age, 28.3 years; 64% women)
Mental health staff interviewed participants within 7 days of the index episode. They collected information about sociodemographics, health, and contact with health care professionals. They used the C-SSRS to identify characteristics of the suicide attempts, and they used the Suicide Intent Scale (SIS) to evaluate circumstances surrounding the suicide attempt, such as active preparation.
Investigators also used the Mini International Neuropsychiatric Interview (MINI), the Suicide Assessment Scale (SUAS), and the Karolinska Affective and Borderline Symptoms Scale.
Greater disability, pain
Of the older patients, 75% lived alone; 88% of the middle-aged and 48% of the younger participants lived alone. A higher proportion of older participants had severe physical illness/disability and severe chronic pain compared with younger participants (all comparisons, P < .001).
Older adults had less contact with psychiatric services, but they had more contact than the other age groups with primary care for mental health problems. Older adults were prescribed antidepressants at the time of the suicide attempt at a lower rate, compared with the middle-aged and younger groups (50% vs. 73% and 66%).
Slightly less than half (44%) of the older adults had a previous history of a suicide attempt – a proportion considerably lower than was reported by patients in the middle-aged and young adult groups (63% and 75%, respectively). Few older adults had a history of a previous NNSI (6% vs. 23% and 63%).
Three-quarters of older adults employed poisoning as the single method of suicide attempt at their index episode, compared with 67% and 59% of the middle-aged and younger groups.
Notably, only half of older adults (52%) met criteria for major depression, determined on the basis of the MINI, compared with three quarters of participants in the other groups (73% and 76%, respectively). Fewer members of the older group met criteria for other psychiatric conditions.
Clouded judgment
The mean total SUAS score was “considerably lower” in the older-adult group than in the other groups. This was also the case for the SUAS subscales for affect, bodily states, control, coping, and emotional reactivity.
Importantly, however, older adults scored higher than younger adults on the SIS total score and the subjective subscale, indicating a higher level of suicidal intent.
The mean SIS total score was 17.8 in the older group, 17.4 in the middle-aged group, and 15.9 in the younger group. The SIS subjective suicide intent score was 10.9 versus 10.6 and 9.4.
“While subjective suicidal intent was higher, compared to the young group, older adults were less likely to fulfill criteria for major depression and several other mental disorders and lower scores were observed on all symptom rating scales, compared to both middle-aged and younger adults,” the investigators wrote.
“Low levels of psychopathology may cloud the clinician’s assessment of the serious nature of suicide attempts in older patients,” they added.
‘Silent generation’
Commenting on the findings, Marnin Heisel, PhD, CPsych, associate professor, departments of psychiatry and of epidemiology and biostatistics, University of Western Ontario, London, said an important takeaway from the study is that, if health care professionals look only for depression or only consider suicide risk in individuals who present with depression, “they might miss older adults who are contemplating suicide or engaging in suicidal behavior.”
Dr. Heisel, who was not involved with the study, observed that older adults are sometimes called the “silent generation” because they often tend to downplay or underreport depressive symptoms, partially because of having been socialized to “keep things to themselves and not to air emotional laundry.”
He recommended that, when assessing potentially suicidal older adults, clinicians select tools specifically designed for use in this age group, particularly the Geriatric Suicide Ideation Scale and the Geriatric Depression Scale. Dr. Heisel also recommended the Center for Epidemiological Studies Depression Scale–Revised Version.
“Beyond a specific scale, the question is to walk into a clinical encounter with a much broader viewpoint, understand who the client is, where they come from, their attitudes, life experience, and what in their experience is going on, their reason for coming to see someone and what they’re struggling with,” he said.
“What we’re seeing with this study is that standard clinical tools don’t necessarily identify some of these richer issues that might contribute to emotional pain, so sometimes the best way to go is a broader clinical interview with a humanistic perspective,” Dr. Heisel concluded.
The study was funded by the Swedish Research Council, the Swedish Research Council for Health, Working Life and Welfare, and the Swedish state, Stockholm County Council and Västerbotten County Council. The investigators and Dr. Heisel have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Older adults may have a high degree of suicidal intent yet still have low scores on scales measuring psychiatric symptoms, such as depression, new research suggests.
In a cross-sectional cohort study of more than 800 adults who presented with self-harm to psychiatric EDs in Sweden, participants aged 65 years and older scored higher than younger and middle-aged adults on measures of suicidal intent.
However, only half of the older group fulfilled criteria for major depression, compared with three-quarters of both the middle-aged and young adult–aged groups.
“Suicidal older persons show a somewhat different clinical picture with relatively low levels of psychopathology but with high suicide intent compared to younger persons,” lead author Stefan Wiktorsson, PhD, University of Gothenburg (Sweden), said in an interview.
“It is therefore of importance for clinicians to carefully evaluate suicidal thinking in this age group. he said.
The findings were published online Aug. 9, 2021, in the American Journal of Geriatric Psychiatry.
Research by age groups ‘lacking’
“While there are large age differences in the prevalence of suicidal behavior, research studies that compare symptomatology and diagnostics in different age groups are lacking,” Dr. Wiktorsson said.
He and his colleagues “wanted to compare psychopathology in young, middle-aged, and older adults in order to increase knowledge about potential differences in symptomatology related to suicidal behavior over the life span.”
The researchers recruited patients aged 18 years and older who had sought or had been referred to emergency psychiatric services for self-harm at three psychiatric hospitals in Sweden between April 2012 and March 2016.
Among all patients, 821 fit inclusion criteria and agreed to participate. The researchers excluded participants who had engaged in nonsuicidal self-injury (NNSI), as determined on the basis of the Columbia Suicide Severity Rating Scale (C-SSRS). The remaining 683 participants, who had attempted suicide, were included in the analysis.
The participants were then divided into the following three groups: older (n = 96; age, 65-97 years; mean age, 77.2 years; 57% women), middle-aged (n = 164; age, 45-64 years; mean age, 53.4 years; 57% women), and younger (n = 423; age, 18-44 years; mean age, 28.3 years; 64% women)
Mental health staff interviewed participants within 7 days of the index episode. They collected information about sociodemographics, health, and contact with health care professionals. They used the C-SSRS to identify characteristics of the suicide attempts, and they used the Suicide Intent Scale (SIS) to evaluate circumstances surrounding the suicide attempt, such as active preparation.
Investigators also used the Mini International Neuropsychiatric Interview (MINI), the Suicide Assessment Scale (SUAS), and the Karolinska Affective and Borderline Symptoms Scale.
Greater disability, pain
Of the older patients, 75% lived alone; 88% of the middle-aged and 48% of the younger participants lived alone. A higher proportion of older participants had severe physical illness/disability and severe chronic pain compared with younger participants (all comparisons, P < .001).
Older adults had less contact with psychiatric services, but they had more contact than the other age groups with primary care for mental health problems. Older adults were prescribed antidepressants at the time of the suicide attempt at a lower rate, compared with the middle-aged and younger groups (50% vs. 73% and 66%).
Slightly less than half (44%) of the older adults had a previous history of a suicide attempt – a proportion considerably lower than was reported by patients in the middle-aged and young adult groups (63% and 75%, respectively). Few older adults had a history of a previous NNSI (6% vs. 23% and 63%).
Three-quarters of older adults employed poisoning as the single method of suicide attempt at their index episode, compared with 67% and 59% of the middle-aged and younger groups.
Notably, only half of older adults (52%) met criteria for major depression, determined on the basis of the MINI, compared with three quarters of participants in the other groups (73% and 76%, respectively). Fewer members of the older group met criteria for other psychiatric conditions.
Clouded judgment
The mean total SUAS score was “considerably lower” in the older-adult group than in the other groups. This was also the case for the SUAS subscales for affect, bodily states, control, coping, and emotional reactivity.
Importantly, however, older adults scored higher than younger adults on the SIS total score and the subjective subscale, indicating a higher level of suicidal intent.
The mean SIS total score was 17.8 in the older group, 17.4 in the middle-aged group, and 15.9 in the younger group. The SIS subjective suicide intent score was 10.9 versus 10.6 and 9.4.
“While subjective suicidal intent was higher, compared to the young group, older adults were less likely to fulfill criteria for major depression and several other mental disorders and lower scores were observed on all symptom rating scales, compared to both middle-aged and younger adults,” the investigators wrote.
“Low levels of psychopathology may cloud the clinician’s assessment of the serious nature of suicide attempts in older patients,” they added.
‘Silent generation’
Commenting on the findings, Marnin Heisel, PhD, CPsych, associate professor, departments of psychiatry and of epidemiology and biostatistics, University of Western Ontario, London, said an important takeaway from the study is that, if health care professionals look only for depression or only consider suicide risk in individuals who present with depression, “they might miss older adults who are contemplating suicide or engaging in suicidal behavior.”
Dr. Heisel, who was not involved with the study, observed that older adults are sometimes called the “silent generation” because they often tend to downplay or underreport depressive symptoms, partially because of having been socialized to “keep things to themselves and not to air emotional laundry.”
He recommended that, when assessing potentially suicidal older adults, clinicians select tools specifically designed for use in this age group, particularly the Geriatric Suicide Ideation Scale and the Geriatric Depression Scale. Dr. Heisel also recommended the Center for Epidemiological Studies Depression Scale–Revised Version.
“Beyond a specific scale, the question is to walk into a clinical encounter with a much broader viewpoint, understand who the client is, where they come from, their attitudes, life experience, and what in their experience is going on, their reason for coming to see someone and what they’re struggling with,” he said.
“What we’re seeing with this study is that standard clinical tools don’t necessarily identify some of these richer issues that might contribute to emotional pain, so sometimes the best way to go is a broader clinical interview with a humanistic perspective,” Dr. Heisel concluded.
The study was funded by the Swedish Research Council, the Swedish Research Council for Health, Working Life and Welfare, and the Swedish state, Stockholm County Council and Västerbotten County Council. The investigators and Dr. Heisel have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Managing sleep in the elderly
Sleep problems are prevalent in older adults, and overmedication is a common cause. Insomnia is a concern, and it might not look the same in older adults as it does in younger populations, especially when neurodegenerative disorders may be present. “There’s often not only the inability to get to sleep and stay asleep in older adults but also changes in their biological rhythms, which is why treatments really need to be focused on both,” Ruth M. Benca, MD, PhD, said in an interview.
Dr. Benca spoke on the topic of insomnia in the elderly at a virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists. She is chair of psychiatry at Wake Forest Baptist Health, Winston-Salem, N.C.
Sleep issues strongly affect quality of life and health outcomes in the elderly, and there isn’t a lot of clear guidance for physicians to manage these issues. who spoke at the meeting presented by MedscapeLive. MedscapeLive and this news organization are owned by the same parent company.
Behavioral approaches are important, because quality of sleep is often affected by daytime activities, such as exercise and light exposure, according to Dr. Benca, who said that those factors can and should be addressed by behavioral interventions. Medications should be used as an adjunct to those treatments. “When we do need to use medications, we need to use ones that have been tested and found to be more helpful than harmful in older adults,” Dr. Benca said.
Many Food and Drug Administration–approved drugs should be used with caution or avoided in the elderly. The Beers criteria provide a useful list of potentially problematic drugs, and removing those drugs from consideration leaves just a few options, including the melatonin receptor agonist ramelteon, low doses of the tricyclic antidepressant doxepin, and dual orexin receptor antagonists, which are being tested in older adults, including some with dementia, Dr. Benca said.
Other drugs like benzodiazepines and related “Z” drugs can cause problems like amnesia, confusion, and psychomotor issues. “They’re advised against because there are some concerns about those side effects,” Dr. Benca said.
Sleep disturbance itself can be the result of polypharmacy. Even something as simple as a diuretic can interrupt slumber because of nocturnal bathroom visits. Antihypertensives and drugs that affect the central nervous system, including antidepressants, can affect sleep. “I’ve had patients get horrible dreams and nightmares from antihypertensive drugs. So there’s a very long laundry list of drugs that can affect sleep in a negative way,” said Dr. Benca.
Physicians have a tendency to prescribe more drugs to a patient without eliminating any, which can result in complex situations. “We see this sort of chasing the tail: You give a drug, it may have a positive effect on the primary thing you want to treat, but it has a side effect. When you give another drug to treat that side effect, it in turn has its own side effect. We keep piling on drugs,” Dr. Benca said.
“So if [a patient is] on medications for an indication, and particularly for sleep or other things, and the patient isn’t getting better, what we might want to do is slowly to withdraw things. Even for older adults who are on sleeping medications and maybe are doing better, sometimes we can decrease the dose [of the other drugs], or get them off those drugs or put them on something that might be less likely to have side effects,” Dr. Benca said.
To do that, she suggests taking a history to determine when the sleep problem began, and whether it coincided with adding or changing a medication. Another approach is to look at the list of current medications, and look for drugs that are prescribed for a problem and where the problem still persists. “You might want to take that away first, before you start adding something else,” said Dr. Benca.
Another challenge is that physicians are often unwilling to investigate sleep disorders, which are more common in older adults. Physicians can be reluctant to prescribe sleep medications, and may also be unfamiliar with behavioral interventions. “For a lot of providers, getting into sleep issues is like opening a Pandora’s Box. I think mostly physicians are taught: Don’t do this, and don’t do that. They’re not as well versed in the things that they can and should do,” said Dr. Benca.
If attempts to treat insomnia don’t succeed, or if the physician suspects a movement disorder or primary sleep disorder like sleep apnea, then the patients should be referred to a sleep specialist, according to Dr. Benca.
During the question-and-answer period following her talk, a questioner brought up the increasingly common use of cannabis to improve sleep. That can be tricky because it can be difficult to stop cannabis use, because of the rebound insomnia that may persist. She noted that there are ongoing studies on the potential impact of cannabidiol oil.
Dr. Benca was also asked about patients who take sedatives chronically and seem to be doing well. She emphasized the need for finding the lowest effective dose of a short-acting medication. “Patients should be monitored frequently, at least every 6 months. Just monitor your patient carefully.”
Dr. Benca is a consultant for Eisai, Genomind, Idorsia, Jazz, Merck, Sage, and Sunovion.
Sleep problems are prevalent in older adults, and overmedication is a common cause. Insomnia is a concern, and it might not look the same in older adults as it does in younger populations, especially when neurodegenerative disorders may be present. “There’s often not only the inability to get to sleep and stay asleep in older adults but also changes in their biological rhythms, which is why treatments really need to be focused on both,” Ruth M. Benca, MD, PhD, said in an interview.
Dr. Benca spoke on the topic of insomnia in the elderly at a virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists. She is chair of psychiatry at Wake Forest Baptist Health, Winston-Salem, N.C.
Sleep issues strongly affect quality of life and health outcomes in the elderly, and there isn’t a lot of clear guidance for physicians to manage these issues. who spoke at the meeting presented by MedscapeLive. MedscapeLive and this news organization are owned by the same parent company.
Behavioral approaches are important, because quality of sleep is often affected by daytime activities, such as exercise and light exposure, according to Dr. Benca, who said that those factors can and should be addressed by behavioral interventions. Medications should be used as an adjunct to those treatments. “When we do need to use medications, we need to use ones that have been tested and found to be more helpful than harmful in older adults,” Dr. Benca said.
Many Food and Drug Administration–approved drugs should be used with caution or avoided in the elderly. The Beers criteria provide a useful list of potentially problematic drugs, and removing those drugs from consideration leaves just a few options, including the melatonin receptor agonist ramelteon, low doses of the tricyclic antidepressant doxepin, and dual orexin receptor antagonists, which are being tested in older adults, including some with dementia, Dr. Benca said.
Other drugs like benzodiazepines and related “Z” drugs can cause problems like amnesia, confusion, and psychomotor issues. “They’re advised against because there are some concerns about those side effects,” Dr. Benca said.
Sleep disturbance itself can be the result of polypharmacy. Even something as simple as a diuretic can interrupt slumber because of nocturnal bathroom visits. Antihypertensives and drugs that affect the central nervous system, including antidepressants, can affect sleep. “I’ve had patients get horrible dreams and nightmares from antihypertensive drugs. So there’s a very long laundry list of drugs that can affect sleep in a negative way,” said Dr. Benca.
Physicians have a tendency to prescribe more drugs to a patient without eliminating any, which can result in complex situations. “We see this sort of chasing the tail: You give a drug, it may have a positive effect on the primary thing you want to treat, but it has a side effect. When you give another drug to treat that side effect, it in turn has its own side effect. We keep piling on drugs,” Dr. Benca said.
“So if [a patient is] on medications for an indication, and particularly for sleep or other things, and the patient isn’t getting better, what we might want to do is slowly to withdraw things. Even for older adults who are on sleeping medications and maybe are doing better, sometimes we can decrease the dose [of the other drugs], or get them off those drugs or put them on something that might be less likely to have side effects,” Dr. Benca said.
To do that, she suggests taking a history to determine when the sleep problem began, and whether it coincided with adding or changing a medication. Another approach is to look at the list of current medications, and look for drugs that are prescribed for a problem and where the problem still persists. “You might want to take that away first, before you start adding something else,” said Dr. Benca.
Another challenge is that physicians are often unwilling to investigate sleep disorders, which are more common in older adults. Physicians can be reluctant to prescribe sleep medications, and may also be unfamiliar with behavioral interventions. “For a lot of providers, getting into sleep issues is like opening a Pandora’s Box. I think mostly physicians are taught: Don’t do this, and don’t do that. They’re not as well versed in the things that they can and should do,” said Dr. Benca.
If attempts to treat insomnia don’t succeed, or if the physician suspects a movement disorder or primary sleep disorder like sleep apnea, then the patients should be referred to a sleep specialist, according to Dr. Benca.
During the question-and-answer period following her talk, a questioner brought up the increasingly common use of cannabis to improve sleep. That can be tricky because it can be difficult to stop cannabis use, because of the rebound insomnia that may persist. She noted that there are ongoing studies on the potential impact of cannabidiol oil.
Dr. Benca was also asked about patients who take sedatives chronically and seem to be doing well. She emphasized the need for finding the lowest effective dose of a short-acting medication. “Patients should be monitored frequently, at least every 6 months. Just monitor your patient carefully.”
Dr. Benca is a consultant for Eisai, Genomind, Idorsia, Jazz, Merck, Sage, and Sunovion.
Sleep problems are prevalent in older adults, and overmedication is a common cause. Insomnia is a concern, and it might not look the same in older adults as it does in younger populations, especially when neurodegenerative disorders may be present. “There’s often not only the inability to get to sleep and stay asleep in older adults but also changes in their biological rhythms, which is why treatments really need to be focused on both,” Ruth M. Benca, MD, PhD, said in an interview.
Dr. Benca spoke on the topic of insomnia in the elderly at a virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists. She is chair of psychiatry at Wake Forest Baptist Health, Winston-Salem, N.C.
Sleep issues strongly affect quality of life and health outcomes in the elderly, and there isn’t a lot of clear guidance for physicians to manage these issues. who spoke at the meeting presented by MedscapeLive. MedscapeLive and this news organization are owned by the same parent company.
Behavioral approaches are important, because quality of sleep is often affected by daytime activities, such as exercise and light exposure, according to Dr. Benca, who said that those factors can and should be addressed by behavioral interventions. Medications should be used as an adjunct to those treatments. “When we do need to use medications, we need to use ones that have been tested and found to be more helpful than harmful in older adults,” Dr. Benca said.
Many Food and Drug Administration–approved drugs should be used with caution or avoided in the elderly. The Beers criteria provide a useful list of potentially problematic drugs, and removing those drugs from consideration leaves just a few options, including the melatonin receptor agonist ramelteon, low doses of the tricyclic antidepressant doxepin, and dual orexin receptor antagonists, which are being tested in older adults, including some with dementia, Dr. Benca said.
Other drugs like benzodiazepines and related “Z” drugs can cause problems like amnesia, confusion, and psychomotor issues. “They’re advised against because there are some concerns about those side effects,” Dr. Benca said.
Sleep disturbance itself can be the result of polypharmacy. Even something as simple as a diuretic can interrupt slumber because of nocturnal bathroom visits. Antihypertensives and drugs that affect the central nervous system, including antidepressants, can affect sleep. “I’ve had patients get horrible dreams and nightmares from antihypertensive drugs. So there’s a very long laundry list of drugs that can affect sleep in a negative way,” said Dr. Benca.
Physicians have a tendency to prescribe more drugs to a patient without eliminating any, which can result in complex situations. “We see this sort of chasing the tail: You give a drug, it may have a positive effect on the primary thing you want to treat, but it has a side effect. When you give another drug to treat that side effect, it in turn has its own side effect. We keep piling on drugs,” Dr. Benca said.
“So if [a patient is] on medications for an indication, and particularly for sleep or other things, and the patient isn’t getting better, what we might want to do is slowly to withdraw things. Even for older adults who are on sleeping medications and maybe are doing better, sometimes we can decrease the dose [of the other drugs], or get them off those drugs or put them on something that might be less likely to have side effects,” Dr. Benca said.
To do that, she suggests taking a history to determine when the sleep problem began, and whether it coincided with adding or changing a medication. Another approach is to look at the list of current medications, and look for drugs that are prescribed for a problem and where the problem still persists. “You might want to take that away first, before you start adding something else,” said Dr. Benca.
Another challenge is that physicians are often unwilling to investigate sleep disorders, which are more common in older adults. Physicians can be reluctant to prescribe sleep medications, and may also be unfamiliar with behavioral interventions. “For a lot of providers, getting into sleep issues is like opening a Pandora’s Box. I think mostly physicians are taught: Don’t do this, and don’t do that. They’re not as well versed in the things that they can and should do,” said Dr. Benca.
If attempts to treat insomnia don’t succeed, or if the physician suspects a movement disorder or primary sleep disorder like sleep apnea, then the patients should be referred to a sleep specialist, according to Dr. Benca.
During the question-and-answer period following her talk, a questioner brought up the increasingly common use of cannabis to improve sleep. That can be tricky because it can be difficult to stop cannabis use, because of the rebound insomnia that may persist. She noted that there are ongoing studies on the potential impact of cannabidiol oil.
Dr. Benca was also asked about patients who take sedatives chronically and seem to be doing well. She emphasized the need for finding the lowest effective dose of a short-acting medication. “Patients should be monitored frequently, at least every 6 months. Just monitor your patient carefully.”
Dr. Benca is a consultant for Eisai, Genomind, Idorsia, Jazz, Merck, Sage, and Sunovion.
FROM FOCUS ON NEUROPSYCHIATRY 2021
FDA OKs stimulation device for anxiety in depression
The U.S. Food and Drug Administration has expanded the indication for the noninvasive BrainsWay Deep Transcranial Magnetic Stimulation (Deep TMS) System to include treatment of comorbid anxiety symptoms in adult patients with depression, the company has announced.
As reported by this news organization, the neurostimulation system has previously received FDA approval for treatment-resistant major depression, obsessive-compulsive disorder, and smoking addiction.
In the August 18 announcement, BrainsWay reported that it has also received 510(k) clearance from the FDA to market its TMS system for the reduction of anxious depression symptoms.
“This clearance is confirmation of what many have believed anecdotally for years – that Deep TMS is a unique form of therapy that can address comorbid anxiety symptoms using the same depression treatment protocol,” Aron Tendler, MD, chief medical officer at BrainsWay, said in a press release.
‘Consistent, robust’ effect
, which included both randomized controlled trials and open-label studies.
“The data demonstrated a treatment effect that was consistent, robust, and clinically meaningful for decreasing anxiety symptoms in adult patients suffering from major depressive disorder [MDD],” the company said in its release.
Data from three of the randomized trials showed an effect size of 0.3 when compared with a sham device and an effect size of 0.9 when compared with medication. The overall, weighted, pooled effect size was 0.55.
The company noted that in more than 70 published studies with about 16,000 total participants, effect sizes have ranged from 0.2-0.37 for drug-based anxiety treatments.
“The expanded FDA labeling now allows BrainsWay to market its Deep TMS System for the treatment of depressive episodes and for decreasing anxiety symptoms for those who may exhibit comorbid anxiety symptoms in adult patients suffering from [MDD] and who failed to achieve satisfactory improvement from previous antidepressant medication treatment in the current episode,” the company said.
A version of this article first appeared on Medscape.com.
The U.S. Food and Drug Administration has expanded the indication for the noninvasive BrainsWay Deep Transcranial Magnetic Stimulation (Deep TMS) System to include treatment of comorbid anxiety symptoms in adult patients with depression, the company has announced.
As reported by this news organization, the neurostimulation system has previously received FDA approval for treatment-resistant major depression, obsessive-compulsive disorder, and smoking addiction.
In the August 18 announcement, BrainsWay reported that it has also received 510(k) clearance from the FDA to market its TMS system for the reduction of anxious depression symptoms.
“This clearance is confirmation of what many have believed anecdotally for years – that Deep TMS is a unique form of therapy that can address comorbid anxiety symptoms using the same depression treatment protocol,” Aron Tendler, MD, chief medical officer at BrainsWay, said in a press release.
‘Consistent, robust’ effect
, which included both randomized controlled trials and open-label studies.
“The data demonstrated a treatment effect that was consistent, robust, and clinically meaningful for decreasing anxiety symptoms in adult patients suffering from major depressive disorder [MDD],” the company said in its release.
Data from three of the randomized trials showed an effect size of 0.3 when compared with a sham device and an effect size of 0.9 when compared with medication. The overall, weighted, pooled effect size was 0.55.
The company noted that in more than 70 published studies with about 16,000 total participants, effect sizes have ranged from 0.2-0.37 for drug-based anxiety treatments.
“The expanded FDA labeling now allows BrainsWay to market its Deep TMS System for the treatment of depressive episodes and for decreasing anxiety symptoms for those who may exhibit comorbid anxiety symptoms in adult patients suffering from [MDD] and who failed to achieve satisfactory improvement from previous antidepressant medication treatment in the current episode,” the company said.
A version of this article first appeared on Medscape.com.
The U.S. Food and Drug Administration has expanded the indication for the noninvasive BrainsWay Deep Transcranial Magnetic Stimulation (Deep TMS) System to include treatment of comorbid anxiety symptoms in adult patients with depression, the company has announced.
As reported by this news organization, the neurostimulation system has previously received FDA approval for treatment-resistant major depression, obsessive-compulsive disorder, and smoking addiction.
In the August 18 announcement, BrainsWay reported that it has also received 510(k) clearance from the FDA to market its TMS system for the reduction of anxious depression symptoms.
“This clearance is confirmation of what many have believed anecdotally for years – that Deep TMS is a unique form of therapy that can address comorbid anxiety symptoms using the same depression treatment protocol,” Aron Tendler, MD, chief medical officer at BrainsWay, said in a press release.
‘Consistent, robust’ effect
, which included both randomized controlled trials and open-label studies.
“The data demonstrated a treatment effect that was consistent, robust, and clinically meaningful for decreasing anxiety symptoms in adult patients suffering from major depressive disorder [MDD],” the company said in its release.
Data from three of the randomized trials showed an effect size of 0.3 when compared with a sham device and an effect size of 0.9 when compared with medication. The overall, weighted, pooled effect size was 0.55.
The company noted that in more than 70 published studies with about 16,000 total participants, effect sizes have ranged from 0.2-0.37 for drug-based anxiety treatments.
“The expanded FDA labeling now allows BrainsWay to market its Deep TMS System for the treatment of depressive episodes and for decreasing anxiety symptoms for those who may exhibit comorbid anxiety symptoms in adult patients suffering from [MDD] and who failed to achieve satisfactory improvement from previous antidepressant medication treatment in the current episode,” the company said.
A version of this article first appeared on Medscape.com.
Mental health after ICU: It’s complicated
It is well known that survivors of critical care are at heightened risk of mental health disorders even months afterward they are discharged, but it’s less clear what factors might contribute to those outcomes. A new attempt to identify risk factors for post-ICU depression, anxiety, or posttraumatic stress disorder, as well as worse quality of life, paints a complex picture.
Age, mental preexisting mental health concerns, acute emotional stress at the time of critical care, and post-care physical impairment all may play a role, according to the multicenter, prospective cohort study conducted in Brazil, which was published in CHEST .
Previous systematic reviews have shown raised frequencies mental health disorders following ICU discharge, including anxiety (32%-40%), depression (29%-34%), and PTSD (16%-23%). Few studies have looked at the potential impact of preexisting conditions or post-ICU disability on these outcomes, yet that information is critical to key to designing effective prevention and rehabilitation interventions.
The results suggest that preexisting mental health and factors associated with the critical illness, which have gained attention as potential factors, aren’t sufficient to explain these outcomes. “Our data suggest that the network of potential risk factors for mental illness among patients who have been discharged from the ICU is much more complex and may involve risk factors from multiple domains. ... Long-term mental health disorders after critical illness may be the result of the interaction among stressors before ICU stay, during ICU stay, and after ICU stay, calling attention to the need for interdisciplinary and multifaceted strategies aimed at preventing and screening for mental health disorders after ICU discharge,” Cassiano Teixeira, MD, PhD, of the Postgraduation of Pulmonology–Federal University of Rio Grande do Sul, Brazil, and colleagues wrote.
The researchers also noted that some risk factors could be screened and may be modifiable, including anxiety and depression symptoms at ICU discharge, as well as reduced physical function status.
Complications or risk factors?
The findings are significant, though they may represent complications of emotional distress following ICU stays, rather than risk factors that predict it, according to an accompanying editorial. The author, O. Joseph Bienvenu III, MD, PhD, who is a professor of psychiatry and behavioral sciences at Johns Hopkins Medicine, Baltimore. He called for prospective studies to determine the predictive value of these factors. “If we are to improve long-term mental health after critical illnesses, this predictive information will be vital to selective prevention efforts.”
Potential interventions could include psychological treatment in the ICU, ICU follow-up clinics, support groups, and cognitive-behavioral therapy, among others. Whichever approach is used, it should be targeted, according to Dr. Bienvenu, since patients who have greater emotional distress seem to gain the most benefit from such interventions.
The researchers examined outcomes among 579 adults who had spent at least 72 hours in the ICU. The median age was 61 years, and 47% were women.
Six months after release from the ICU, telephone assessments by trained researchers revealed that 48% had impairment in physical function, compared with the time preceding ICU admission. 36.2% of participants had a mental health disorder: 24.2% reported anxiety, 20.9% had depression, and 15.4% had PTSD.
Increasing numbers of psychiatric syndromes, from 0 to 3, was associated with worse scores on the mental dimension on the health-related quality of life (HRQoL) score, but there was no relationship with scores on the physical dimension.
Risks to mental health
Clinical characteristics associated with risk of anxiety at 6 months post discharge included being 65 years or older (prevalence ratio, 0.63; P = .009), a history of depression (PR, 1.52; P = .009), anxiety at discharge (PR, 1.65; P = .003), depression at discharge (HR, 1.44; P = .02), physical dependence (PR, 1.48; P = .01), and reduced physical functional status at 6 months post discharge (PR, 1.38; P = .04).
Characteristics associated with depression at 6 months post discharge included a history of depression (PR, 1.78; P = .001), symptoms of depression at discharge (PR, 3.04; P < .001), and reduced physical functional status at 6 months (PR, 1.53; P = .01).
Characteristics associated with PTSD at 6 months post discharge were depression symptoms at discharge (PR, 1.70; P = .01), physical dependence (PR, 1.79; P = .01), and reduced physical status at 6 months (PR, 1.62; P = .02).
Characteristics associated with any mental health disorder included higher education (PR, 0.74; P = .04), a history of depression (PR, 1.32; P = .02), anxiety symptoms at discharge (PR, 1.55; P = .001), depression symptoms at discharge (PR, 1.50; P = .001), and physical dependence at 6 months following discharge (PR, 1.66; P < .001).
“The lower HRQoL found in ICU survivors with mental health disorders in comparison with those without is a reason for concern. This finding, in association with the higher prevalence of psychiatric syndromes among ICU survivors, reinforces the importance of assessing anxiety, depression, and PTSD symptoms among ICU survivors, because these syndromes typically are long lasting and underdiagnosed, and their occurrence may affect quality of life, survival, and costs in the context of care after ICU discharge,” according to the researchers.
The authors of the study and Dr. Bienvenu have no relevant financial disclosures.
It is well known that survivors of critical care are at heightened risk of mental health disorders even months afterward they are discharged, but it’s less clear what factors might contribute to those outcomes. A new attempt to identify risk factors for post-ICU depression, anxiety, or posttraumatic stress disorder, as well as worse quality of life, paints a complex picture.
Age, mental preexisting mental health concerns, acute emotional stress at the time of critical care, and post-care physical impairment all may play a role, according to the multicenter, prospective cohort study conducted in Brazil, which was published in CHEST .
Previous systematic reviews have shown raised frequencies mental health disorders following ICU discharge, including anxiety (32%-40%), depression (29%-34%), and PTSD (16%-23%). Few studies have looked at the potential impact of preexisting conditions or post-ICU disability on these outcomes, yet that information is critical to key to designing effective prevention and rehabilitation interventions.
The results suggest that preexisting mental health and factors associated with the critical illness, which have gained attention as potential factors, aren’t sufficient to explain these outcomes. “Our data suggest that the network of potential risk factors for mental illness among patients who have been discharged from the ICU is much more complex and may involve risk factors from multiple domains. ... Long-term mental health disorders after critical illness may be the result of the interaction among stressors before ICU stay, during ICU stay, and after ICU stay, calling attention to the need for interdisciplinary and multifaceted strategies aimed at preventing and screening for mental health disorders after ICU discharge,” Cassiano Teixeira, MD, PhD, of the Postgraduation of Pulmonology–Federal University of Rio Grande do Sul, Brazil, and colleagues wrote.
The researchers also noted that some risk factors could be screened and may be modifiable, including anxiety and depression symptoms at ICU discharge, as well as reduced physical function status.
Complications or risk factors?
The findings are significant, though they may represent complications of emotional distress following ICU stays, rather than risk factors that predict it, according to an accompanying editorial. The author, O. Joseph Bienvenu III, MD, PhD, who is a professor of psychiatry and behavioral sciences at Johns Hopkins Medicine, Baltimore. He called for prospective studies to determine the predictive value of these factors. “If we are to improve long-term mental health after critical illnesses, this predictive information will be vital to selective prevention efforts.”
Potential interventions could include psychological treatment in the ICU, ICU follow-up clinics, support groups, and cognitive-behavioral therapy, among others. Whichever approach is used, it should be targeted, according to Dr. Bienvenu, since patients who have greater emotional distress seem to gain the most benefit from such interventions.
The researchers examined outcomes among 579 adults who had spent at least 72 hours in the ICU. The median age was 61 years, and 47% were women.
Six months after release from the ICU, telephone assessments by trained researchers revealed that 48% had impairment in physical function, compared with the time preceding ICU admission. 36.2% of participants had a mental health disorder: 24.2% reported anxiety, 20.9% had depression, and 15.4% had PTSD.
Increasing numbers of psychiatric syndromes, from 0 to 3, was associated with worse scores on the mental dimension on the health-related quality of life (HRQoL) score, but there was no relationship with scores on the physical dimension.
Risks to mental health
Clinical characteristics associated with risk of anxiety at 6 months post discharge included being 65 years or older (prevalence ratio, 0.63; P = .009), a history of depression (PR, 1.52; P = .009), anxiety at discharge (PR, 1.65; P = .003), depression at discharge (HR, 1.44; P = .02), physical dependence (PR, 1.48; P = .01), and reduced physical functional status at 6 months post discharge (PR, 1.38; P = .04).
Characteristics associated with depression at 6 months post discharge included a history of depression (PR, 1.78; P = .001), symptoms of depression at discharge (PR, 3.04; P < .001), and reduced physical functional status at 6 months (PR, 1.53; P = .01).
Characteristics associated with PTSD at 6 months post discharge were depression symptoms at discharge (PR, 1.70; P = .01), physical dependence (PR, 1.79; P = .01), and reduced physical status at 6 months (PR, 1.62; P = .02).
Characteristics associated with any mental health disorder included higher education (PR, 0.74; P = .04), a history of depression (PR, 1.32; P = .02), anxiety symptoms at discharge (PR, 1.55; P = .001), depression symptoms at discharge (PR, 1.50; P = .001), and physical dependence at 6 months following discharge (PR, 1.66; P < .001).
“The lower HRQoL found in ICU survivors with mental health disorders in comparison with those without is a reason for concern. This finding, in association with the higher prevalence of psychiatric syndromes among ICU survivors, reinforces the importance of assessing anxiety, depression, and PTSD symptoms among ICU survivors, because these syndromes typically are long lasting and underdiagnosed, and their occurrence may affect quality of life, survival, and costs in the context of care after ICU discharge,” according to the researchers.
The authors of the study and Dr. Bienvenu have no relevant financial disclosures.
It is well known that survivors of critical care are at heightened risk of mental health disorders even months afterward they are discharged, but it’s less clear what factors might contribute to those outcomes. A new attempt to identify risk factors for post-ICU depression, anxiety, or posttraumatic stress disorder, as well as worse quality of life, paints a complex picture.
Age, mental preexisting mental health concerns, acute emotional stress at the time of critical care, and post-care physical impairment all may play a role, according to the multicenter, prospective cohort study conducted in Brazil, which was published in CHEST .
Previous systematic reviews have shown raised frequencies mental health disorders following ICU discharge, including anxiety (32%-40%), depression (29%-34%), and PTSD (16%-23%). Few studies have looked at the potential impact of preexisting conditions or post-ICU disability on these outcomes, yet that information is critical to key to designing effective prevention and rehabilitation interventions.
The results suggest that preexisting mental health and factors associated with the critical illness, which have gained attention as potential factors, aren’t sufficient to explain these outcomes. “Our data suggest that the network of potential risk factors for mental illness among patients who have been discharged from the ICU is much more complex and may involve risk factors from multiple domains. ... Long-term mental health disorders after critical illness may be the result of the interaction among stressors before ICU stay, during ICU stay, and after ICU stay, calling attention to the need for interdisciplinary and multifaceted strategies aimed at preventing and screening for mental health disorders after ICU discharge,” Cassiano Teixeira, MD, PhD, of the Postgraduation of Pulmonology–Federal University of Rio Grande do Sul, Brazil, and colleagues wrote.
The researchers also noted that some risk factors could be screened and may be modifiable, including anxiety and depression symptoms at ICU discharge, as well as reduced physical function status.
Complications or risk factors?
The findings are significant, though they may represent complications of emotional distress following ICU stays, rather than risk factors that predict it, according to an accompanying editorial. The author, O. Joseph Bienvenu III, MD, PhD, who is a professor of psychiatry and behavioral sciences at Johns Hopkins Medicine, Baltimore. He called for prospective studies to determine the predictive value of these factors. “If we are to improve long-term mental health after critical illnesses, this predictive information will be vital to selective prevention efforts.”
Potential interventions could include psychological treatment in the ICU, ICU follow-up clinics, support groups, and cognitive-behavioral therapy, among others. Whichever approach is used, it should be targeted, according to Dr. Bienvenu, since patients who have greater emotional distress seem to gain the most benefit from such interventions.
The researchers examined outcomes among 579 adults who had spent at least 72 hours in the ICU. The median age was 61 years, and 47% were women.
Six months after release from the ICU, telephone assessments by trained researchers revealed that 48% had impairment in physical function, compared with the time preceding ICU admission. 36.2% of participants had a mental health disorder: 24.2% reported anxiety, 20.9% had depression, and 15.4% had PTSD.
Increasing numbers of psychiatric syndromes, from 0 to 3, was associated with worse scores on the mental dimension on the health-related quality of life (HRQoL) score, but there was no relationship with scores on the physical dimension.
Risks to mental health
Clinical characteristics associated with risk of anxiety at 6 months post discharge included being 65 years or older (prevalence ratio, 0.63; P = .009), a history of depression (PR, 1.52; P = .009), anxiety at discharge (PR, 1.65; P = .003), depression at discharge (HR, 1.44; P = .02), physical dependence (PR, 1.48; P = .01), and reduced physical functional status at 6 months post discharge (PR, 1.38; P = .04).
Characteristics associated with depression at 6 months post discharge included a history of depression (PR, 1.78; P = .001), symptoms of depression at discharge (PR, 3.04; P < .001), and reduced physical functional status at 6 months (PR, 1.53; P = .01).
Characteristics associated with PTSD at 6 months post discharge were depression symptoms at discharge (PR, 1.70; P = .01), physical dependence (PR, 1.79; P = .01), and reduced physical status at 6 months (PR, 1.62; P = .02).
Characteristics associated with any mental health disorder included higher education (PR, 0.74; P = .04), a history of depression (PR, 1.32; P = .02), anxiety symptoms at discharge (PR, 1.55; P = .001), depression symptoms at discharge (PR, 1.50; P = .001), and physical dependence at 6 months following discharge (PR, 1.66; P < .001).
“The lower HRQoL found in ICU survivors with mental health disorders in comparison with those without is a reason for concern. This finding, in association with the higher prevalence of psychiatric syndromes among ICU survivors, reinforces the importance of assessing anxiety, depression, and PTSD symptoms among ICU survivors, because these syndromes typically are long lasting and underdiagnosed, and their occurrence may affect quality of life, survival, and costs in the context of care after ICU discharge,” according to the researchers.
The authors of the study and Dr. Bienvenu have no relevant financial disclosures.
FROM CHEST
Comprehensive and Equitable Care for Vulnerable Veterans With Integrated Palliative, Psychology, and Oncology Care
Veterans living with cancer need comprehensive assessment that includes supportive psychosocial care. The National Comprehensive Cancer Network (NCCN) and American College of Surgeons Commission on Cancer require accredited cancer centers to evaluate psychosocial distress and provide appropriate triage and treatment for all patients.1-3 Implementing psychosocial distress screening can be difficult because of procedural barriers and time constraints, clinic and supportive care resources, and lack of knowledge about how to access supportive services.
Distress screening protocols must be designed to address the specific needs of each population. To improve screening for cancer-related distress, deliver effective supportive services, and gain agreement on distress screening standards of care, the Coleman Foundation supported development of the Coleman Supportive Oncology Collaborative (CSOC), a project of 135 interdisciplinary health care professionals from 25 Chicago-area cancer care institutions.4
The Jesse Brown US Department of Veterans Affairs (VA) Medical Center (JBVAMC) was chosen to assess cancer-related concerns among veterans using the CSOC screening tool and to improve access to supportive oncology. JBVAMC provides care to approximately 49,000 veterans in Chicago, Illinois, and northwestern Indiana. The JBVAMC patient population includes a large number of veterans with dual diagnoses (co-occurring substance use and mental health disorders) and veterans experiencing homelessness.
Delivering integrated screening and oncologic care that is culture and age appropriate is particularly important for veterans given their unique risk factors. The veteran population is considered vulnerable in terms of health status, psychological functioning, and social context. Veterans who use the VA health system as a principal source of care have poorer health, greater comorbid medical conditions, and an increased risk of mortality and suicide compared with the general population.5,6 Poorer health status in veterans also may relate to old age, low income, poor education, psychological health, and minority race.7-9
Past studies point to unique risk factors for cancer and poor cancer adjustment among veterans, which may complicate cancer treatment and end-of-life/survivorship care. Veteran-specific risk factors include military-related exposures, particularly Agent Orange and morbidity/mortality secondary to comorbid medical and psychiatric conditions (eg, chronic obstructive pulmonary disease, diabetes mellitus, and posttraumatic stress disorder [PTSD]).10-12 Moreover, the geriatric veteran population continues to grow,with increasing rates of cancer that require unique considerations for effective cancer care.13,14 Despite this, there are minimal data to inform best practices and supportive care approaches for veterans with cancer. Lack of guidelines specific to veterans and other populations with increased psychosocial challenges may impede successful cancer care, making distress screening procedures particularly important. This is especially the case for the JBVAMC, which serves primarily African American urban-dwelling veterans who experience high rates of cancer disparities, including increased rates of mortality and increased levels of psychosocial distress.15,16
The goals of this program were to (1) examine levels of psychological, physical, financial, and treatment-related distress in a large sample of urban-dwelling veterans; (2) create a streamlined, sustainable process to screen a large number of veterans receiving cancer care in the outpatient setting and connect them with available supportive services; and (3) educate oncology physicians, nurses, and other staff about cancer-related distress and concerns using in-service trainings and interpersonal interactions to improve patient care. Our program was based on a Primary Care Mental Health Integration (PCMHI) model that embeds health psychologists in general medical clinics to better reach veterans dealing with mental health issues. We tailored for palliative care involvement.
Studies of this model have shown that mental health integration improves access to mental health services and mental health treatment outcomes and has higher patient and provider satisfaction.17 We were also influenced by the construct of the patient aligned care team (PACT) social worker who, in this veteran-centered approach, often functions as a care coordinator. Social work responsibilities include assessment of patients’ stressors including adjusting to the medical conditions, identifying untreated or undertreated mental health or substance abuse issues, economic instability, legal problems, and inadequate housing and transportation, which can often be exacerbated during cancer treatment.18
We screened for distress-related needs that included mental health concerns, physical needs including uncontrolled symptoms or adverse effects of cancer treatment, physical function complaints (eg, pain and fatigue), nutrition concerns, treatment or care related concerns, family and caregiver needs, along with financial challenges (housing and food) and insurance-related support. The goal of this article is to describe the development and implementation of this VA-specific distress screening program and reflect on the lessons learned for the application of streamlined distress screening and triage in similar settings throughout the VA health system and other similar settings.
Methods
This institutional review board at JBVAMC reviewed and exempted this quality improvement program using the SQUIRE framework.19 It was led by a group of palliative care clinicians, psychologists, and administrators who have worked with the oncology service for many years, primarily in the care of hospitalized patients. Common palliative care services include providing care for patients with serious illness diagnosis through the illness trajectory.
Setting
At the start of this program, we assessed the current clinic workflow to determine how to best screen and assist veterans experiencing distress. We met with team members individually to identify the best method of clinic integration, including attending medical oncologists, medical oncology fellows, psychology interns, oncology nursing staff, the oncology nurse coordinator, and clinic clerks.
The JBVAMC provides cancer care through 4 half-day medical hematology-oncology clinics that serve about 50 patients per half-day clinic. The clinics are staffed by hematology-oncology fellows supervised by hematology-oncology attending physicians, who are affiliated with 2 academic medical centers. These clinics are staffed by 3 registered nurses (RNs) and a licensed practical nurse (LPN) and are adjacent to a chemotherapy infusion clinic with unique nursing staff. The JBVAMC also provides a variety of supportive care services, including extensive mental health and substance use treatment, physical and occupational therapy, acupuncture, nutrition, social work, and housing services. Following our assessment, it was evident that there were a low number of referrals from oncology clinics to supportive care services, mostly due to lack of knowledge of resources and unclear referral procedures.
Based on clinical volume, we determined that our screening program could best be implemented through a stepped approach beginning in one clinic and expanding thereafter. We began by having a palliative care physician and health psychology intern embedded in 1 weekly half-day clinic and a health psychology intern embedded in a second weekly half-day clinic. Our program included 2 health psychology interns (for each academic year of the program) who were supervised by a JBVA health psychologist.
About 15 months after successful integration within the first 2 half-day clinics, we expanded the screening program to staff an additional half-day medical oncology clinic with a palliative care APRN. This allowed us to expand the screening tool distribution and collection to 3 of 4 of the weekly half-day oncology clinics as well as to meet individually with veterans experiencing high levels of distress. Veterans were flagged as having high distress levels by either the results of their completed screening tool or by referral from a medical oncology physician. We initially established screening in clinics that were sufficiently staffed to ensure that screens were appropriately distributed and reviewed. Patients seen in nonparticipating clinics were referred to outpatient social work, mental health and/or outpatient palliative care according to oncology fellows’ clinical assessments of the patient. All oncology fellows received education about distress screening and methods for referring to supportive care. Our clinic screening program extended from February 2017 through January 2020.
Screening
Program staff screened patients with new cancer diagnoses, then identified patients for follow-up screens. This tracking allowed staff to identify patients with oncology appointments that day and cross-reference patients needing a follow-up screen.
Following feedback from the clinic nurses, we determined that nurses would provide the distress tool to patients in paper form after they completed their assessment of vitals and waited to be seen by their medical oncologist. The patient would then deliver their completed form to the nurse who would combine it with the patient’s clinic notes for the oncologist to review.
Veterans referred for supportive care services were contacted by the relevant clinical administrator by phone to schedule an intake; for social work referrals, patients were either seen in a walk-in office located in a colocated building or contacted by a social worker by phone.
Our screening tool was the Coleman Foundation Supportive Oncology Collaborative Screening Tool, compiled from validated instruments. Patients completed this screening tool, which includes the PHQ-4, NCCN problem list concerns, adapted Mini Nutrition Assessment and PROMIS Pain and Fatigue measure (eAppendix B available at doi:10.12788/fp.0158).20-22
We also worked with the VA Computerized Patient Record System (CPRS) to create an electronic template for the screening tool. Completed screening tools were manually entered by the physician, psychologists, or APRN into the CPRS chart.
We analyzed the different supportive care services available at the JBVAMC and noticed that many supportive services were available, yet these services were often separated. Therefore, we created a consult flowsheet to assist oncologists in placing referrals. These supportive care services include mental health services, a cancer support group, home health care, social services, nutrition, physical medicine and rehabilitation, and other specialty services.
Patient Education
The psychology and nursing staff created a patient information bulletin board where patients could access information about supportive services available at JBVAMC. This board required frequent replenishment of handouts because patients consulted the board regularly. Handouts and folders about common clinical issues also were placed in the clinic treatment rooms. We partnered with 2 local cancer support centers, Gilda’s Club and the Cancer Support Center, to make referrals for family members and/or caregivers who would benefit from additional support.
We provided in-service trainings for oncology fellows, including trainings on PTSD and substance abuse and their relationship to cancer care at the VA. These topics were chosen based on the feedback program staff received about perceived knowledge gaps from the oncology fellows. This program allowed for multiple informal conversations between that program staff and oncology fellows about overall patient care. We held trainings with the cancer coordinator and clinical nursing staff on strategies to identify and follow-up on cancer-related distress, and with oncology fellows to review the importance of distress screening and to instruct fellows on instructions for the consult flowsheet.
Funding
This program was funded by the Chicago-based Coleman Foundation as part of the CSOC. Funding was used to support a portion of time for administrative and clinical work of program staff, as well as data collection and analysis.
Results
We established 3 half-day integrated clinics where patients were screened and referred for services based on supportive oncology needs. In addition to our primary activities to screen and refer veterans, we held multiple educational sessions for colleagues, developed a workflow template, and integrated patient education materials into the clinics.
Screening
Veterans completed 1010 distress screens in 3 of 4 half-day oncology clinics over the 2.5-year project period. Veterans were screened at initial diagnosis and every 3 months, or during changes in their clinical care or disease status. As a result, 579 patients completed screening, with some patients doing several follow-up screens during their care. Integration of palliative care providers and health psychologists was instrumental in facilitating screening in these busy general medical oncology clinics. Most veterans were receptive to completing surveys with few refusing to fill out the survey.23 Medical oncology fellows often used the completed screener to inform their review of systems (by reviewing the Coleman screener Physical and Other Concerns section) and connect with the supportive care staff present in clinic for patient’s identifying severe needs (ie, mental health distress or complex psychosocial needs). Veterans’ rates of distress needs and successfuloutcomes of integration with mental health and social work services have been reported elsewhere.23
The mean (SD) age for veterans in this cohort was 72 (9.5) years. Participants were primarily African American veterans (70%), with mostly advanced disease (Table 1). Participants endorsed elevated distress needs compared with other patient populations screened in Chicago through the CSOC for depressed mood, pain, housing, transportation, and physical, nutrition, and treatment concerns.23 Elevated presence of needs was especially prominent for food, housing and insurance/medical needs; physical concerns; nutrition, and treatment- or care-related concerns. Veterans in this cohort reported extensive financial and housing concerns: 10.4% reported food and housing concerns, 18.6% reported transportation concerns, and 9.0% reported issues paying for medical care or medications (Table 2).20 Anecdotally, many experienced job loss or strain with their cancer diagnosis or were living at the poverty level before their diagnosis.
Social work referrals were often triggered due to transportation barriers to appointments/medication access, and food and/or housing insecurity. Social workers assisted with referrals for housing, transportation, financial reimbursement, on-site or community-based food banks, home health support, familial support, and hospice services. Social work consults increased 166% from 2016 (the year before the program start date) to the end of 2019.
Based on this increased volume of referrals for social work in our oncology clinics, an oncology-specific social worker was hired at the completion of our program to be based in all 4 half-day oncology clinics in response to results of our quality improvement intervention. The social worker currently sees all patients with a new cancer diagnosis and supports oncology fellows to identify veterans needing a palliative care referral or referrals to other supportive services.
Throughout program implementation, traditional areas of palliative care focus were particularly important as veterans reported significant concerns with understanding their illness (67.4%), wanting to understand their prognosis (71.3%), and having questions about their treatment options (55.1%).20 The palliative care providers spent time educating patients about their disease, coordinating goals of care conversations, promoting patients’ engagement in decision making, and making a large number of referrals to hospice and home health to support veterans at home.
Discussion
This project created a successful program to screen veterans for psychosocial distress and triage them to appropriate services. During the project, patients in VA-outpatient oncology clinics reported significant cancer-related distress due to baseline psychosocial needs, changes in emotional and physical functioning, logistical and financial challenges of receiving cancer care, and lack of instrumental support.23
Staff education supported successful buy-in, development and implementation of supportive oncology programs. We used a combination of in-service trainings, online trainings, and handouts to provide evidence for distress screening.24 Highlighting the evidence-base that demonstrates how cancer-related distress screening improves cancer and quality of life outcomes helped to address physician reluctance to accept the additional requirements needed to address veterans’ psychosocial needs and care concerns. To increase buy-in and collaboration among team members and foster heightened understanding between providers and patients, we recommend creating accessible education for all staff levels.
One specific area of education we focused on was primary palliative care, which includes the core competencies of communication and symptom management recommended for generalists and specialists of all disciplines.25 Program staff supported oncology fellows in developing their primary palliative care skills by being available to discuss basic symptom management and communication issues. VA cancer care programs could benefit from ongoing palliative care education of oncology staff to facilitate primary palliative care as well as earlier integration of secondary palliative care when needed.26 Secondary palliative care or care provided directly by the palliative care team assists with complex symptom management or communication issues. For these needs, oncology fellows were encouraged to refer to either the palliative care staff available in one of the half-day clinics or to the outpatient palliative care clinic. As a unique strength, the VA allows veterans to receive concurrent cancer-directed therapy and hospice care, which enables earlier referrals to hospice care and higher quality end-of-life care and emphasizes the need for primary palliative care in oncology.27,28
Integrating supportive oncology team members, such as licensed clinical social worker and psychology interns, was successful. This was modeled on the VA PACT, which focuses on prevention, health promotion, coordination and chronic disease management.29 Social determinants of health have a major impact on health outcomes especially in veteran-specific and African American populations, making screening for distress critical.30-32 The VA Office of Health Equity actively addresses health inequities by supporting initiation of screening programs for social determinants of health, including education, employment, exposure to abuse and violence, food insecurity, housing instability, legal needs, social isolation, transportation needs, and utility needs. This is especially needed for African-American individuals who are not only more likely to experience cancer, but also more likely to be negatively impacted by the consequences of cancer diagnosis/treatment, such as complications related to one’s job security, access to care, adverse effects, and other highly distressing needs.33,34
Our program found that veterans with cancer often had concerns associated with food and housing insecurity, transportation and paying for medication or medical care, and screening allowed health care providers to detect and address these social determinants of health through referrals to VA and community-specific programs. Social workers integrated
Our ability to roll out distress screening was scaffolded by technological integration into existing VA systems (eg, screening results in CPRS and electronic referrals). Screening procedures could have been even more efficient with improved technology (Table 3). For example, technological limitations made it challenging to easily identify patients due for screening, requiring a cumbersome process of tracking, collecting and entering patients’ paper forms. Health care providers seeking to develop a distress screening program should consider investing in technology that allows for identification of patients requiring screening at a predetermined interval, completion of screening via tablet or personal device, integration of screening responses into the electronic health record, and automatic generation of notifications to the treating physician and appropriate support services.
We also established partnerships with community cancer support groups to offer both referral pathways and in-house programming. Veterans’ cancer care programs could benefit from identifying and securing community partnerships to capitalize on readily available low-cost or no-cost options for supportive oncology in the community. Further, as was the case in our program, cancer support centers may be willing to collaborate with VA hospitals to provide services on site (eg, support groups, art therapy). This would extend the reach of these supportive services while allowing VA employees to address the extensive psychosocial needs of individual veterans.
Conclusions
Veterans with cancer benefited from enhanced screening and psychosocial service availability, similar to a PCMHI model. Robust screening programs helped advocate for veterans dealing with the effects of poverty through identification of need and referral to existing VA programs and services quickly and efficiently. Providing comprehensive care within ambulatory cancer clinics can address cancer-related distress and any potential barriers to care in real time. VA hospitals typically offer an array of supportive services to address veterans’ psychosocial needs, yet these services tend to be siloed. Integrated referrals can help to resolve such access barriers. Since many veterans with burdensome cancers are not able to see their VA primary care physician regularly, offering comprehensive care within medical oncology ensures complete and integrated care that includes psychosocial screening.
We believe that this program is an example of a mechanism for oncologists and palliative care clinicians to integrate their care in a way that identifies needs and triages services for vulnerable veterans. As colleagues have written, “it is fundamental to our commitment to veterans that we ensure comparable, high quality care regardless of a veteran’s gender, race, or where they live.”34 Health care providers may underestimate the extensive change a cancer diagnosis can have on a patient’s quality of life. Cancer diagnosis and treatment have a large impact on all individuals, but this impact may be greater for individuals in poverty due to inability to work from home, inflexible work hours, and limited support structures. By creating screening programs with psychosocial integration in oncology clinics such as we have described, we hope to improve access to more equitable care for vulnerable veterans.
1. National Comprehensive Cancer Network. NCCN guidelines distress management. Version 2.2021. Updated January 5, 2021. Accessed July 8, 2021. http://www.nccn.org/professionals/physician_gls/pdf/distress.pdf
2. American College of Surgeons, Commission on Cancer. Cancer program standards 2012: ensuring patient-centered care. Version 1.2.1. Published 2021. Accessed July 8, 2021. https://www.facs.org/~/media/files/quality%20programs/cancer/coc/programstandards2012.ashx
3. Jacobsen PB, Ransom S. Implementation of NCCN distress management guidelines by member institutions. J Natl Compr Canc Netw. 2007;5(1):99-103. doi:10.6004/jnccn.2007.0010
4. The Coleman Supportive Oncology Collaborative. Training tools. Accessed July 14, 2021. https://www.supportiveoncologycollaborative.org/training-tools
5. Agha Z, Lofgren RP, VanRuiswyk JV, Layde PM. Are patients at Veterans Affairs medical centers sicker? A comparative analysis of health status and medical resource use. Arch Intern Med. 2000;160(21):3252-3257. doi:10.1001/archinte.160.21.3252
6. Bullman T, Schneiderman A, Gradus JL. Relative importance of posttraumatic stress disorder and depression in predicting risk of suicide among a cohort of Vietnam veterans. Suicide Life Threat Behav. 2019;49(3):838-845. doi:10.1111/sltb.12482
7. Kazis LE, Miller DR, Clark J, et al. Health-related quality of life in patients served by the Department of Veterans Affairs: results from the Veterans Health Study. Arch Intern Med. 1998;158(6):626-632. doi:10.1001/archinte.158.6.626
8. O’Toole BI, Marshall RP, Grayson DA, et al. The Australian Vietnam Veterans Health Study: III. Psychological health of Australian Vietnam veterans and its relationship to combat. Int J Epidemiol. 1996;25(2):331-340. doi:10.1093/ije/25.2.331
9. Vincent C, Chamberlain K, Long N. Mental and physical health status in a community sample of New Zealand Vietnam War veterans. Aust J Public Health. 1994;18(1):58-62. doi:10.1111/j.1753-6405.1994.tb00196.x
10. US Department of Veterans Affairs. Veterans’ diseases associated with Agent Orange. Updated June 16, 2021. Accessed July 8, 2021. http://www.publichealth.va.gov/exposures/agentorange/diseases.asp#veterans
11. Hwa KJ, Dua MM, Wren SM, Visser BC. Missing the obvious: psychosocial obstacles in Veterans with hepatocellular carcinoma. HBP (Oxford). 2015;17(12):1124-1129. doi:10.1111/hpb.12508
12. Saha S, Freeman M, Toure J, Tippens KM, Weeks C, Ibrahim S. Racial and ethnic disparities in the VA health care system: a systematic review. J Gen Intern Med. 2008;23(5):654-671. doi:10.1007/s11606-008-0521-4
13. Amaral EFL, Pollard MS, Mendelsohn J, Cefalu M. Current and future demographics of the veteran population, 2014-2024. Popul Rev. 2018;57(1):28-60. doi:10.1353/prv.2018.0002
14. Mohile SG, Dale W, Somerfield MR, et al. Practical assessment and management of vulnerabilities in older patients receiving chemotherapy: ASCO guideline for geriatric oncology. J Clin Oncol. 2018;36(22):2326-2347. doi:10.1200/JCO.2018.78.8687
15. Siegel R, Ward E, Brawley O, Jemal A. Cancer statistics, 2011: the impact of eliminating socioeconomic and racial disparities on premature cancer deaths. CA Cancer J Clin. 2011;61(4):212-236. doi:10.3322/caac.20121
16. Cimino T, Said K, Safier L, Harris H, Kinderman A. Psychosocial distress among oncology patients in the safety net. Psychooncology. 2020;29(11):1927-1935. doi:10.1002/pon.5525
17. Molander R, Hodgkins K, Johnson C, White A, Frazier E, Krahn D. Interprofessional education in patient aligned care team primary care-mental health integration. Fed Pract. 2017;34(6):40-48.
18. Parikh DA, Ragavan M, Dutta R, et al. Financial toxicity of cancer care: an analysis of financial burden in three distinct health care systems [published online ahead of print, 2021 Apr 7]. JCO Oncol Pract. 2021;OP2000890. doi:10.1200/OP.20.00890
19. Ogrinc G, Davies L, Goodman D, Batalden P, Davidoff F, Stevens D. SQUIRE 2.0 (Standards for QUality Improvement Reporting Excellence): revised publication guidelines from a detailed consensus process. BMJ Qual Saf. 2016;25(12):986-992. doi:10.1136/bmjqs-2015-004411
20. Weldon CB, Gerhart JI, Penedo FJ, et al. Correlates of distress for cancer patients: results from multi-institution use of holistic patient-reported screening tool. J Clin Oncol. 2019;37(15)(suppl):11587-11587. doi:10.1200/JCO.2019.37.15_suppl.11587
21. Kroenke K, Spitzer RL, Williams JB, Löwe B. The Patient Health Questionnaire Somatic, Anxiety, and Depressive Symptom Scales: a systematic review. Gen Hosp Psychiatry. 2010;32(4):345-359. doi:10.1016/j.genhosppsych.2010.03.006
22. Kaiser MJ, Bauer JM, Ramsch C, et al. Validation of the Mini Nutritional Assessment short-form (MNA-SF): a practical tool for identification of nutritional status. J Nutr Health Aging. 2009;13(9):782-788. doi:10.1007/s12603-009-0214-7
23. Azizoddin DR, Lakin JR, Hauser J, et al. Meeting the guidelines: implementing a distress screening intervention for veterans with cancer. Psychooncology. 2020;29(12):2067-2074. doi:10.1002/pon.5565
24. Carlson LE, Waller A, Mitchell AJ. Screening for distress and unmet needs in patients with cancer: review and recommendations. J Clin Oncol. 2012;30(11):1160-1177. doi:10.1200/JCO.2011.39.5509
25. Quill TE, Abernethy AP. Generalist plus specialist palliative care—creating a more sustainable model. N Engl J Med. 2013;368(13):1173-1175. doi:10.1056/NEJMp1215620
26. Weissman DE, Meier DE. Identifying patients in need of a palliative care assessment in the hospital setting: a consensus report from the Center to Advance Palliative Care. J Palliat Med. 2011;14(1):17-23. doi:10.1089/jpm.2010.0347
27. Kumar P, Wright AA, Hatfield LA, Temel JS, Keating NL. Family perspectives on hospice care experiences of patients with cancer. J Clin Oncol. 2017;35(4):432-439. doi:10.1200/JCO.2016.68.9257
28. Mor V, Joyce NR, Coté DL, et al. The rise of concurrent care for veterans with advanced cancer at the end of life. Cancer. 2016;122(5):782-790. doi:10.1002/cncr.29827
29. US Department of Veterans Affairs. Patient care services: Patient aligned care team (PACT). Updated November 5, 2020. Accessed July 8, 2021. https://www.patientcare.va.gov/primarycare/PACT.asp
30. US Department of Veterans Affairs, Veterans Health Administration. VHA health equity action plan. Published September 27, 2019. Accessed July 8, 2021. https://www.va.gov/HEALTHEQUITY/docs/Health_Equity_Action_Plan_Final_022020.pdf
31. Alcaraz KI, Wiedt TL, Daniels EC, Yabroff KR, Guerra CE, Wender RC. Understanding and addressing social determinants to advance cancer health equity in the United States: a blueprint for practice, research, and policy. CA Cancer J Clin. 2020;70(1):31-46. doi:10.3322/caac.21586
32. Atkins D, Kilbourne A, Lipson L. Health equity research in the Veterans Health Administration: we’ve come far but aren’t there yet. Am J Public Health. 2014;104(suppl 4):S525-526. doi:10.2105/AJPH.2014.302216
33. American Cancer Society. Cancer Facts & Figures for African Americans 2019-2021. Atlanta: American Cancer Society; 2019.
34. Hastert TA, Kirchhoff AC, Banegas MP, et al. Work changes and individual, cancer-related, and work-related predictors of decreased work participation among African American cancer survivors. Cancer Med. 2020;9(23):9168-9177. doi:10.1002/cam4.3512
35. Bekelman DB, Nowels CT, Allen LA, Shakar S, Kutner JS, Matlock DD. Outpatient palliative care for chronic heart failure: a case series. J Palliat Med. 2011;14(7):815-821. doi:10.1089/jpm.2010.050
Veterans living with cancer need comprehensive assessment that includes supportive psychosocial care. The National Comprehensive Cancer Network (NCCN) and American College of Surgeons Commission on Cancer require accredited cancer centers to evaluate psychosocial distress and provide appropriate triage and treatment for all patients.1-3 Implementing psychosocial distress screening can be difficult because of procedural barriers and time constraints, clinic and supportive care resources, and lack of knowledge about how to access supportive services.
Distress screening protocols must be designed to address the specific needs of each population. To improve screening for cancer-related distress, deliver effective supportive services, and gain agreement on distress screening standards of care, the Coleman Foundation supported development of the Coleman Supportive Oncology Collaborative (CSOC), a project of 135 interdisciplinary health care professionals from 25 Chicago-area cancer care institutions.4
The Jesse Brown US Department of Veterans Affairs (VA) Medical Center (JBVAMC) was chosen to assess cancer-related concerns among veterans using the CSOC screening tool and to improve access to supportive oncology. JBVAMC provides care to approximately 49,000 veterans in Chicago, Illinois, and northwestern Indiana. The JBVAMC patient population includes a large number of veterans with dual diagnoses (co-occurring substance use and mental health disorders) and veterans experiencing homelessness.
Delivering integrated screening and oncologic care that is culture and age appropriate is particularly important for veterans given their unique risk factors. The veteran population is considered vulnerable in terms of health status, psychological functioning, and social context. Veterans who use the VA health system as a principal source of care have poorer health, greater comorbid medical conditions, and an increased risk of mortality and suicide compared with the general population.5,6 Poorer health status in veterans also may relate to old age, low income, poor education, psychological health, and minority race.7-9
Past studies point to unique risk factors for cancer and poor cancer adjustment among veterans, which may complicate cancer treatment and end-of-life/survivorship care. Veteran-specific risk factors include military-related exposures, particularly Agent Orange and morbidity/mortality secondary to comorbid medical and psychiatric conditions (eg, chronic obstructive pulmonary disease, diabetes mellitus, and posttraumatic stress disorder [PTSD]).10-12 Moreover, the geriatric veteran population continues to grow,with increasing rates of cancer that require unique considerations for effective cancer care.13,14 Despite this, there are minimal data to inform best practices and supportive care approaches for veterans with cancer. Lack of guidelines specific to veterans and other populations with increased psychosocial challenges may impede successful cancer care, making distress screening procedures particularly important. This is especially the case for the JBVAMC, which serves primarily African American urban-dwelling veterans who experience high rates of cancer disparities, including increased rates of mortality and increased levels of psychosocial distress.15,16
The goals of this program were to (1) examine levels of psychological, physical, financial, and treatment-related distress in a large sample of urban-dwelling veterans; (2) create a streamlined, sustainable process to screen a large number of veterans receiving cancer care in the outpatient setting and connect them with available supportive services; and (3) educate oncology physicians, nurses, and other staff about cancer-related distress and concerns using in-service trainings and interpersonal interactions to improve patient care. Our program was based on a Primary Care Mental Health Integration (PCMHI) model that embeds health psychologists in general medical clinics to better reach veterans dealing with mental health issues. We tailored for palliative care involvement.
Studies of this model have shown that mental health integration improves access to mental health services and mental health treatment outcomes and has higher patient and provider satisfaction.17 We were also influenced by the construct of the patient aligned care team (PACT) social worker who, in this veteran-centered approach, often functions as a care coordinator. Social work responsibilities include assessment of patients’ stressors including adjusting to the medical conditions, identifying untreated or undertreated mental health or substance abuse issues, economic instability, legal problems, and inadequate housing and transportation, which can often be exacerbated during cancer treatment.18
We screened for distress-related needs that included mental health concerns, physical needs including uncontrolled symptoms or adverse effects of cancer treatment, physical function complaints (eg, pain and fatigue), nutrition concerns, treatment or care related concerns, family and caregiver needs, along with financial challenges (housing and food) and insurance-related support. The goal of this article is to describe the development and implementation of this VA-specific distress screening program and reflect on the lessons learned for the application of streamlined distress screening and triage in similar settings throughout the VA health system and other similar settings.
Methods
This institutional review board at JBVAMC reviewed and exempted this quality improvement program using the SQUIRE framework.19 It was led by a group of palliative care clinicians, psychologists, and administrators who have worked with the oncology service for many years, primarily in the care of hospitalized patients. Common palliative care services include providing care for patients with serious illness diagnosis through the illness trajectory.
Setting
At the start of this program, we assessed the current clinic workflow to determine how to best screen and assist veterans experiencing distress. We met with team members individually to identify the best method of clinic integration, including attending medical oncologists, medical oncology fellows, psychology interns, oncology nursing staff, the oncology nurse coordinator, and clinic clerks.
The JBVAMC provides cancer care through 4 half-day medical hematology-oncology clinics that serve about 50 patients per half-day clinic. The clinics are staffed by hematology-oncology fellows supervised by hematology-oncology attending physicians, who are affiliated with 2 academic medical centers. These clinics are staffed by 3 registered nurses (RNs) and a licensed practical nurse (LPN) and are adjacent to a chemotherapy infusion clinic with unique nursing staff. The JBVAMC also provides a variety of supportive care services, including extensive mental health and substance use treatment, physical and occupational therapy, acupuncture, nutrition, social work, and housing services. Following our assessment, it was evident that there were a low number of referrals from oncology clinics to supportive care services, mostly due to lack of knowledge of resources and unclear referral procedures.
Based on clinical volume, we determined that our screening program could best be implemented through a stepped approach beginning in one clinic and expanding thereafter. We began by having a palliative care physician and health psychology intern embedded in 1 weekly half-day clinic and a health psychology intern embedded in a second weekly half-day clinic. Our program included 2 health psychology interns (for each academic year of the program) who were supervised by a JBVA health psychologist.
About 15 months after successful integration within the first 2 half-day clinics, we expanded the screening program to staff an additional half-day medical oncology clinic with a palliative care APRN. This allowed us to expand the screening tool distribution and collection to 3 of 4 of the weekly half-day oncology clinics as well as to meet individually with veterans experiencing high levels of distress. Veterans were flagged as having high distress levels by either the results of their completed screening tool or by referral from a medical oncology physician. We initially established screening in clinics that were sufficiently staffed to ensure that screens were appropriately distributed and reviewed. Patients seen in nonparticipating clinics were referred to outpatient social work, mental health and/or outpatient palliative care according to oncology fellows’ clinical assessments of the patient. All oncology fellows received education about distress screening and methods for referring to supportive care. Our clinic screening program extended from February 2017 through January 2020.
Screening
Program staff screened patients with new cancer diagnoses, then identified patients for follow-up screens. This tracking allowed staff to identify patients with oncology appointments that day and cross-reference patients needing a follow-up screen.
Following feedback from the clinic nurses, we determined that nurses would provide the distress tool to patients in paper form after they completed their assessment of vitals and waited to be seen by their medical oncologist. The patient would then deliver their completed form to the nurse who would combine it with the patient’s clinic notes for the oncologist to review.
Veterans referred for supportive care services were contacted by the relevant clinical administrator by phone to schedule an intake; for social work referrals, patients were either seen in a walk-in office located in a colocated building or contacted by a social worker by phone.
Our screening tool was the Coleman Foundation Supportive Oncology Collaborative Screening Tool, compiled from validated instruments. Patients completed this screening tool, which includes the PHQ-4, NCCN problem list concerns, adapted Mini Nutrition Assessment and PROMIS Pain and Fatigue measure (eAppendix B available at doi:10.12788/fp.0158).20-22
We also worked with the VA Computerized Patient Record System (CPRS) to create an electronic template for the screening tool. Completed screening tools were manually entered by the physician, psychologists, or APRN into the CPRS chart.
We analyzed the different supportive care services available at the JBVAMC and noticed that many supportive services were available, yet these services were often separated. Therefore, we created a consult flowsheet to assist oncologists in placing referrals. These supportive care services include mental health services, a cancer support group, home health care, social services, nutrition, physical medicine and rehabilitation, and other specialty services.
Patient Education
The psychology and nursing staff created a patient information bulletin board where patients could access information about supportive services available at JBVAMC. This board required frequent replenishment of handouts because patients consulted the board regularly. Handouts and folders about common clinical issues also were placed in the clinic treatment rooms. We partnered with 2 local cancer support centers, Gilda’s Club and the Cancer Support Center, to make referrals for family members and/or caregivers who would benefit from additional support.
We provided in-service trainings for oncology fellows, including trainings on PTSD and substance abuse and their relationship to cancer care at the VA. These topics were chosen based on the feedback program staff received about perceived knowledge gaps from the oncology fellows. This program allowed for multiple informal conversations between that program staff and oncology fellows about overall patient care. We held trainings with the cancer coordinator and clinical nursing staff on strategies to identify and follow-up on cancer-related distress, and with oncology fellows to review the importance of distress screening and to instruct fellows on instructions for the consult flowsheet.
Funding
This program was funded by the Chicago-based Coleman Foundation as part of the CSOC. Funding was used to support a portion of time for administrative and clinical work of program staff, as well as data collection and analysis.
Results
We established 3 half-day integrated clinics where patients were screened and referred for services based on supportive oncology needs. In addition to our primary activities to screen and refer veterans, we held multiple educational sessions for colleagues, developed a workflow template, and integrated patient education materials into the clinics.
Screening
Veterans completed 1010 distress screens in 3 of 4 half-day oncology clinics over the 2.5-year project period. Veterans were screened at initial diagnosis and every 3 months, or during changes in their clinical care or disease status. As a result, 579 patients completed screening, with some patients doing several follow-up screens during their care. Integration of palliative care providers and health psychologists was instrumental in facilitating screening in these busy general medical oncology clinics. Most veterans were receptive to completing surveys with few refusing to fill out the survey.23 Medical oncology fellows often used the completed screener to inform their review of systems (by reviewing the Coleman screener Physical and Other Concerns section) and connect with the supportive care staff present in clinic for patient’s identifying severe needs (ie, mental health distress or complex psychosocial needs). Veterans’ rates of distress needs and successfuloutcomes of integration with mental health and social work services have been reported elsewhere.23
The mean (SD) age for veterans in this cohort was 72 (9.5) years. Participants were primarily African American veterans (70%), with mostly advanced disease (Table 1). Participants endorsed elevated distress needs compared with other patient populations screened in Chicago through the CSOC for depressed mood, pain, housing, transportation, and physical, nutrition, and treatment concerns.23 Elevated presence of needs was especially prominent for food, housing and insurance/medical needs; physical concerns; nutrition, and treatment- or care-related concerns. Veterans in this cohort reported extensive financial and housing concerns: 10.4% reported food and housing concerns, 18.6% reported transportation concerns, and 9.0% reported issues paying for medical care or medications (Table 2).20 Anecdotally, many experienced job loss or strain with their cancer diagnosis or were living at the poverty level before their diagnosis.
Social work referrals were often triggered due to transportation barriers to appointments/medication access, and food and/or housing insecurity. Social workers assisted with referrals for housing, transportation, financial reimbursement, on-site or community-based food banks, home health support, familial support, and hospice services. Social work consults increased 166% from 2016 (the year before the program start date) to the end of 2019.
Based on this increased volume of referrals for social work in our oncology clinics, an oncology-specific social worker was hired at the completion of our program to be based in all 4 half-day oncology clinics in response to results of our quality improvement intervention. The social worker currently sees all patients with a new cancer diagnosis and supports oncology fellows to identify veterans needing a palliative care referral or referrals to other supportive services.
Throughout program implementation, traditional areas of palliative care focus were particularly important as veterans reported significant concerns with understanding their illness (67.4%), wanting to understand their prognosis (71.3%), and having questions about their treatment options (55.1%).20 The palliative care providers spent time educating patients about their disease, coordinating goals of care conversations, promoting patients’ engagement in decision making, and making a large number of referrals to hospice and home health to support veterans at home.
Discussion
This project created a successful program to screen veterans for psychosocial distress and triage them to appropriate services. During the project, patients in VA-outpatient oncology clinics reported significant cancer-related distress due to baseline psychosocial needs, changes in emotional and physical functioning, logistical and financial challenges of receiving cancer care, and lack of instrumental support.23
Staff education supported successful buy-in, development and implementation of supportive oncology programs. We used a combination of in-service trainings, online trainings, and handouts to provide evidence for distress screening.24 Highlighting the evidence-base that demonstrates how cancer-related distress screening improves cancer and quality of life outcomes helped to address physician reluctance to accept the additional requirements needed to address veterans’ psychosocial needs and care concerns. To increase buy-in and collaboration among team members and foster heightened understanding between providers and patients, we recommend creating accessible education for all staff levels.
One specific area of education we focused on was primary palliative care, which includes the core competencies of communication and symptom management recommended for generalists and specialists of all disciplines.25 Program staff supported oncology fellows in developing their primary palliative care skills by being available to discuss basic symptom management and communication issues. VA cancer care programs could benefit from ongoing palliative care education of oncology staff to facilitate primary palliative care as well as earlier integration of secondary palliative care when needed.26 Secondary palliative care or care provided directly by the palliative care team assists with complex symptom management or communication issues. For these needs, oncology fellows were encouraged to refer to either the palliative care staff available in one of the half-day clinics or to the outpatient palliative care clinic. As a unique strength, the VA allows veterans to receive concurrent cancer-directed therapy and hospice care, which enables earlier referrals to hospice care and higher quality end-of-life care and emphasizes the need for primary palliative care in oncology.27,28
Integrating supportive oncology team members, such as licensed clinical social worker and psychology interns, was successful. This was modeled on the VA PACT, which focuses on prevention, health promotion, coordination and chronic disease management.29 Social determinants of health have a major impact on health outcomes especially in veteran-specific and African American populations, making screening for distress critical.30-32 The VA Office of Health Equity actively addresses health inequities by supporting initiation of screening programs for social determinants of health, including education, employment, exposure to abuse and violence, food insecurity, housing instability, legal needs, social isolation, transportation needs, and utility needs. This is especially needed for African-American individuals who are not only more likely to experience cancer, but also more likely to be negatively impacted by the consequences of cancer diagnosis/treatment, such as complications related to one’s job security, access to care, adverse effects, and other highly distressing needs.33,34
Our program found that veterans with cancer often had concerns associated with food and housing insecurity, transportation and paying for medication or medical care, and screening allowed health care providers to detect and address these social determinants of health through referrals to VA and community-specific programs. Social workers integrated
Our ability to roll out distress screening was scaffolded by technological integration into existing VA systems (eg, screening results in CPRS and electronic referrals). Screening procedures could have been even more efficient with improved technology (Table 3). For example, technological limitations made it challenging to easily identify patients due for screening, requiring a cumbersome process of tracking, collecting and entering patients’ paper forms. Health care providers seeking to develop a distress screening program should consider investing in technology that allows for identification of patients requiring screening at a predetermined interval, completion of screening via tablet or personal device, integration of screening responses into the electronic health record, and automatic generation of notifications to the treating physician and appropriate support services.
We also established partnerships with community cancer support groups to offer both referral pathways and in-house programming. Veterans’ cancer care programs could benefit from identifying and securing community partnerships to capitalize on readily available low-cost or no-cost options for supportive oncology in the community. Further, as was the case in our program, cancer support centers may be willing to collaborate with VA hospitals to provide services on site (eg, support groups, art therapy). This would extend the reach of these supportive services while allowing VA employees to address the extensive psychosocial needs of individual veterans.
Conclusions
Veterans with cancer benefited from enhanced screening and psychosocial service availability, similar to a PCMHI model. Robust screening programs helped advocate for veterans dealing with the effects of poverty through identification of need and referral to existing VA programs and services quickly and efficiently. Providing comprehensive care within ambulatory cancer clinics can address cancer-related distress and any potential barriers to care in real time. VA hospitals typically offer an array of supportive services to address veterans’ psychosocial needs, yet these services tend to be siloed. Integrated referrals can help to resolve such access barriers. Since many veterans with burdensome cancers are not able to see their VA primary care physician regularly, offering comprehensive care within medical oncology ensures complete and integrated care that includes psychosocial screening.
We believe that this program is an example of a mechanism for oncologists and palliative care clinicians to integrate their care in a way that identifies needs and triages services for vulnerable veterans. As colleagues have written, “it is fundamental to our commitment to veterans that we ensure comparable, high quality care regardless of a veteran’s gender, race, or where they live.”34 Health care providers may underestimate the extensive change a cancer diagnosis can have on a patient’s quality of life. Cancer diagnosis and treatment have a large impact on all individuals, but this impact may be greater for individuals in poverty due to inability to work from home, inflexible work hours, and limited support structures. By creating screening programs with psychosocial integration in oncology clinics such as we have described, we hope to improve access to more equitable care for vulnerable veterans.
Veterans living with cancer need comprehensive assessment that includes supportive psychosocial care. The National Comprehensive Cancer Network (NCCN) and American College of Surgeons Commission on Cancer require accredited cancer centers to evaluate psychosocial distress and provide appropriate triage and treatment for all patients.1-3 Implementing psychosocial distress screening can be difficult because of procedural barriers and time constraints, clinic and supportive care resources, and lack of knowledge about how to access supportive services.
Distress screening protocols must be designed to address the specific needs of each population. To improve screening for cancer-related distress, deliver effective supportive services, and gain agreement on distress screening standards of care, the Coleman Foundation supported development of the Coleman Supportive Oncology Collaborative (CSOC), a project of 135 interdisciplinary health care professionals from 25 Chicago-area cancer care institutions.4
The Jesse Brown US Department of Veterans Affairs (VA) Medical Center (JBVAMC) was chosen to assess cancer-related concerns among veterans using the CSOC screening tool and to improve access to supportive oncology. JBVAMC provides care to approximately 49,000 veterans in Chicago, Illinois, and northwestern Indiana. The JBVAMC patient population includes a large number of veterans with dual diagnoses (co-occurring substance use and mental health disorders) and veterans experiencing homelessness.
Delivering integrated screening and oncologic care that is culture and age appropriate is particularly important for veterans given their unique risk factors. The veteran population is considered vulnerable in terms of health status, psychological functioning, and social context. Veterans who use the VA health system as a principal source of care have poorer health, greater comorbid medical conditions, and an increased risk of mortality and suicide compared with the general population.5,6 Poorer health status in veterans also may relate to old age, low income, poor education, psychological health, and minority race.7-9
Past studies point to unique risk factors for cancer and poor cancer adjustment among veterans, which may complicate cancer treatment and end-of-life/survivorship care. Veteran-specific risk factors include military-related exposures, particularly Agent Orange and morbidity/mortality secondary to comorbid medical and psychiatric conditions (eg, chronic obstructive pulmonary disease, diabetes mellitus, and posttraumatic stress disorder [PTSD]).10-12 Moreover, the geriatric veteran population continues to grow,with increasing rates of cancer that require unique considerations for effective cancer care.13,14 Despite this, there are minimal data to inform best practices and supportive care approaches for veterans with cancer. Lack of guidelines specific to veterans and other populations with increased psychosocial challenges may impede successful cancer care, making distress screening procedures particularly important. This is especially the case for the JBVAMC, which serves primarily African American urban-dwelling veterans who experience high rates of cancer disparities, including increased rates of mortality and increased levels of psychosocial distress.15,16
The goals of this program were to (1) examine levels of psychological, physical, financial, and treatment-related distress in a large sample of urban-dwelling veterans; (2) create a streamlined, sustainable process to screen a large number of veterans receiving cancer care in the outpatient setting and connect them with available supportive services; and (3) educate oncology physicians, nurses, and other staff about cancer-related distress and concerns using in-service trainings and interpersonal interactions to improve patient care. Our program was based on a Primary Care Mental Health Integration (PCMHI) model that embeds health psychologists in general medical clinics to better reach veterans dealing with mental health issues. We tailored for palliative care involvement.
Studies of this model have shown that mental health integration improves access to mental health services and mental health treatment outcomes and has higher patient and provider satisfaction.17 We were also influenced by the construct of the patient aligned care team (PACT) social worker who, in this veteran-centered approach, often functions as a care coordinator. Social work responsibilities include assessment of patients’ stressors including adjusting to the medical conditions, identifying untreated or undertreated mental health or substance abuse issues, economic instability, legal problems, and inadequate housing and transportation, which can often be exacerbated during cancer treatment.18
We screened for distress-related needs that included mental health concerns, physical needs including uncontrolled symptoms or adverse effects of cancer treatment, physical function complaints (eg, pain and fatigue), nutrition concerns, treatment or care related concerns, family and caregiver needs, along with financial challenges (housing and food) and insurance-related support. The goal of this article is to describe the development and implementation of this VA-specific distress screening program and reflect on the lessons learned for the application of streamlined distress screening and triage in similar settings throughout the VA health system and other similar settings.
Methods
This institutional review board at JBVAMC reviewed and exempted this quality improvement program using the SQUIRE framework.19 It was led by a group of palliative care clinicians, psychologists, and administrators who have worked with the oncology service for many years, primarily in the care of hospitalized patients. Common palliative care services include providing care for patients with serious illness diagnosis through the illness trajectory.
Setting
At the start of this program, we assessed the current clinic workflow to determine how to best screen and assist veterans experiencing distress. We met with team members individually to identify the best method of clinic integration, including attending medical oncologists, medical oncology fellows, psychology interns, oncology nursing staff, the oncology nurse coordinator, and clinic clerks.
The JBVAMC provides cancer care through 4 half-day medical hematology-oncology clinics that serve about 50 patients per half-day clinic. The clinics are staffed by hematology-oncology fellows supervised by hematology-oncology attending physicians, who are affiliated with 2 academic medical centers. These clinics are staffed by 3 registered nurses (RNs) and a licensed practical nurse (LPN) and are adjacent to a chemotherapy infusion clinic with unique nursing staff. The JBVAMC also provides a variety of supportive care services, including extensive mental health and substance use treatment, physical and occupational therapy, acupuncture, nutrition, social work, and housing services. Following our assessment, it was evident that there were a low number of referrals from oncology clinics to supportive care services, mostly due to lack of knowledge of resources and unclear referral procedures.
Based on clinical volume, we determined that our screening program could best be implemented through a stepped approach beginning in one clinic and expanding thereafter. We began by having a palliative care physician and health psychology intern embedded in 1 weekly half-day clinic and a health psychology intern embedded in a second weekly half-day clinic. Our program included 2 health psychology interns (for each academic year of the program) who were supervised by a JBVA health psychologist.
About 15 months after successful integration within the first 2 half-day clinics, we expanded the screening program to staff an additional half-day medical oncology clinic with a palliative care APRN. This allowed us to expand the screening tool distribution and collection to 3 of 4 of the weekly half-day oncology clinics as well as to meet individually with veterans experiencing high levels of distress. Veterans were flagged as having high distress levels by either the results of their completed screening tool or by referral from a medical oncology physician. We initially established screening in clinics that were sufficiently staffed to ensure that screens were appropriately distributed and reviewed. Patients seen in nonparticipating clinics were referred to outpatient social work, mental health and/or outpatient palliative care according to oncology fellows’ clinical assessments of the patient. All oncology fellows received education about distress screening and methods for referring to supportive care. Our clinic screening program extended from February 2017 through January 2020.
Screening
Program staff screened patients with new cancer diagnoses, then identified patients for follow-up screens. This tracking allowed staff to identify patients with oncology appointments that day and cross-reference patients needing a follow-up screen.
Following feedback from the clinic nurses, we determined that nurses would provide the distress tool to patients in paper form after they completed their assessment of vitals and waited to be seen by their medical oncologist. The patient would then deliver their completed form to the nurse who would combine it with the patient’s clinic notes for the oncologist to review.
Veterans referred for supportive care services were contacted by the relevant clinical administrator by phone to schedule an intake; for social work referrals, patients were either seen in a walk-in office located in a colocated building or contacted by a social worker by phone.
Our screening tool was the Coleman Foundation Supportive Oncology Collaborative Screening Tool, compiled from validated instruments. Patients completed this screening tool, which includes the PHQ-4, NCCN problem list concerns, adapted Mini Nutrition Assessment and PROMIS Pain and Fatigue measure (eAppendix B available at doi:10.12788/fp.0158).20-22
We also worked with the VA Computerized Patient Record System (CPRS) to create an electronic template for the screening tool. Completed screening tools were manually entered by the physician, psychologists, or APRN into the CPRS chart.
We analyzed the different supportive care services available at the JBVAMC and noticed that many supportive services were available, yet these services were often separated. Therefore, we created a consult flowsheet to assist oncologists in placing referrals. These supportive care services include mental health services, a cancer support group, home health care, social services, nutrition, physical medicine and rehabilitation, and other specialty services.
Patient Education
The psychology and nursing staff created a patient information bulletin board where patients could access information about supportive services available at JBVAMC. This board required frequent replenishment of handouts because patients consulted the board regularly. Handouts and folders about common clinical issues also were placed in the clinic treatment rooms. We partnered with 2 local cancer support centers, Gilda’s Club and the Cancer Support Center, to make referrals for family members and/or caregivers who would benefit from additional support.
We provided in-service trainings for oncology fellows, including trainings on PTSD and substance abuse and their relationship to cancer care at the VA. These topics were chosen based on the feedback program staff received about perceived knowledge gaps from the oncology fellows. This program allowed for multiple informal conversations between that program staff and oncology fellows about overall patient care. We held trainings with the cancer coordinator and clinical nursing staff on strategies to identify and follow-up on cancer-related distress, and with oncology fellows to review the importance of distress screening and to instruct fellows on instructions for the consult flowsheet.
Funding
This program was funded by the Chicago-based Coleman Foundation as part of the CSOC. Funding was used to support a portion of time for administrative and clinical work of program staff, as well as data collection and analysis.
Results
We established 3 half-day integrated clinics where patients were screened and referred for services based on supportive oncology needs. In addition to our primary activities to screen and refer veterans, we held multiple educational sessions for colleagues, developed a workflow template, and integrated patient education materials into the clinics.
Screening
Veterans completed 1010 distress screens in 3 of 4 half-day oncology clinics over the 2.5-year project period. Veterans were screened at initial diagnosis and every 3 months, or during changes in their clinical care or disease status. As a result, 579 patients completed screening, with some patients doing several follow-up screens during their care. Integration of palliative care providers and health psychologists was instrumental in facilitating screening in these busy general medical oncology clinics. Most veterans were receptive to completing surveys with few refusing to fill out the survey.23 Medical oncology fellows often used the completed screener to inform their review of systems (by reviewing the Coleman screener Physical and Other Concerns section) and connect with the supportive care staff present in clinic for patient’s identifying severe needs (ie, mental health distress or complex psychosocial needs). Veterans’ rates of distress needs and successfuloutcomes of integration with mental health and social work services have been reported elsewhere.23
The mean (SD) age for veterans in this cohort was 72 (9.5) years. Participants were primarily African American veterans (70%), with mostly advanced disease (Table 1). Participants endorsed elevated distress needs compared with other patient populations screened in Chicago through the CSOC for depressed mood, pain, housing, transportation, and physical, nutrition, and treatment concerns.23 Elevated presence of needs was especially prominent for food, housing and insurance/medical needs; physical concerns; nutrition, and treatment- or care-related concerns. Veterans in this cohort reported extensive financial and housing concerns: 10.4% reported food and housing concerns, 18.6% reported transportation concerns, and 9.0% reported issues paying for medical care or medications (Table 2).20 Anecdotally, many experienced job loss or strain with their cancer diagnosis or were living at the poverty level before their diagnosis.
Social work referrals were often triggered due to transportation barriers to appointments/medication access, and food and/or housing insecurity. Social workers assisted with referrals for housing, transportation, financial reimbursement, on-site or community-based food banks, home health support, familial support, and hospice services. Social work consults increased 166% from 2016 (the year before the program start date) to the end of 2019.
Based on this increased volume of referrals for social work in our oncology clinics, an oncology-specific social worker was hired at the completion of our program to be based in all 4 half-day oncology clinics in response to results of our quality improvement intervention. The social worker currently sees all patients with a new cancer diagnosis and supports oncology fellows to identify veterans needing a palliative care referral or referrals to other supportive services.
Throughout program implementation, traditional areas of palliative care focus were particularly important as veterans reported significant concerns with understanding their illness (67.4%), wanting to understand their prognosis (71.3%), and having questions about their treatment options (55.1%).20 The palliative care providers spent time educating patients about their disease, coordinating goals of care conversations, promoting patients’ engagement in decision making, and making a large number of referrals to hospice and home health to support veterans at home.
Discussion
This project created a successful program to screen veterans for psychosocial distress and triage them to appropriate services. During the project, patients in VA-outpatient oncology clinics reported significant cancer-related distress due to baseline psychosocial needs, changes in emotional and physical functioning, logistical and financial challenges of receiving cancer care, and lack of instrumental support.23
Staff education supported successful buy-in, development and implementation of supportive oncology programs. We used a combination of in-service trainings, online trainings, and handouts to provide evidence for distress screening.24 Highlighting the evidence-base that demonstrates how cancer-related distress screening improves cancer and quality of life outcomes helped to address physician reluctance to accept the additional requirements needed to address veterans’ psychosocial needs and care concerns. To increase buy-in and collaboration among team members and foster heightened understanding between providers and patients, we recommend creating accessible education for all staff levels.
One specific area of education we focused on was primary palliative care, which includes the core competencies of communication and symptom management recommended for generalists and specialists of all disciplines.25 Program staff supported oncology fellows in developing their primary palliative care skills by being available to discuss basic symptom management and communication issues. VA cancer care programs could benefit from ongoing palliative care education of oncology staff to facilitate primary palliative care as well as earlier integration of secondary palliative care when needed.26 Secondary palliative care or care provided directly by the palliative care team assists with complex symptom management or communication issues. For these needs, oncology fellows were encouraged to refer to either the palliative care staff available in one of the half-day clinics or to the outpatient palliative care clinic. As a unique strength, the VA allows veterans to receive concurrent cancer-directed therapy and hospice care, which enables earlier referrals to hospice care and higher quality end-of-life care and emphasizes the need for primary palliative care in oncology.27,28
Integrating supportive oncology team members, such as licensed clinical social worker and psychology interns, was successful. This was modeled on the VA PACT, which focuses on prevention, health promotion, coordination and chronic disease management.29 Social determinants of health have a major impact on health outcomes especially in veteran-specific and African American populations, making screening for distress critical.30-32 The VA Office of Health Equity actively addresses health inequities by supporting initiation of screening programs for social determinants of health, including education, employment, exposure to abuse and violence, food insecurity, housing instability, legal needs, social isolation, transportation needs, and utility needs. This is especially needed for African-American individuals who are not only more likely to experience cancer, but also more likely to be negatively impacted by the consequences of cancer diagnosis/treatment, such as complications related to one’s job security, access to care, adverse effects, and other highly distressing needs.33,34
Our program found that veterans with cancer often had concerns associated with food and housing insecurity, transportation and paying for medication or medical care, and screening allowed health care providers to detect and address these social determinants of health through referrals to VA and community-specific programs. Social workers integrated
Our ability to roll out distress screening was scaffolded by technological integration into existing VA systems (eg, screening results in CPRS and electronic referrals). Screening procedures could have been even more efficient with improved technology (Table 3). For example, technological limitations made it challenging to easily identify patients due for screening, requiring a cumbersome process of tracking, collecting and entering patients’ paper forms. Health care providers seeking to develop a distress screening program should consider investing in technology that allows for identification of patients requiring screening at a predetermined interval, completion of screening via tablet or personal device, integration of screening responses into the electronic health record, and automatic generation of notifications to the treating physician and appropriate support services.
We also established partnerships with community cancer support groups to offer both referral pathways and in-house programming. Veterans’ cancer care programs could benefit from identifying and securing community partnerships to capitalize on readily available low-cost or no-cost options for supportive oncology in the community. Further, as was the case in our program, cancer support centers may be willing to collaborate with VA hospitals to provide services on site (eg, support groups, art therapy). This would extend the reach of these supportive services while allowing VA employees to address the extensive psychosocial needs of individual veterans.
Conclusions
Veterans with cancer benefited from enhanced screening and psychosocial service availability, similar to a PCMHI model. Robust screening programs helped advocate for veterans dealing with the effects of poverty through identification of need and referral to existing VA programs and services quickly and efficiently. Providing comprehensive care within ambulatory cancer clinics can address cancer-related distress and any potential barriers to care in real time. VA hospitals typically offer an array of supportive services to address veterans’ psychosocial needs, yet these services tend to be siloed. Integrated referrals can help to resolve such access barriers. Since many veterans with burdensome cancers are not able to see their VA primary care physician regularly, offering comprehensive care within medical oncology ensures complete and integrated care that includes psychosocial screening.
We believe that this program is an example of a mechanism for oncologists and palliative care clinicians to integrate their care in a way that identifies needs and triages services for vulnerable veterans. As colleagues have written, “it is fundamental to our commitment to veterans that we ensure comparable, high quality care regardless of a veteran’s gender, race, or where they live.”34 Health care providers may underestimate the extensive change a cancer diagnosis can have on a patient’s quality of life. Cancer diagnosis and treatment have a large impact on all individuals, but this impact may be greater for individuals in poverty due to inability to work from home, inflexible work hours, and limited support structures. By creating screening programs with psychosocial integration in oncology clinics such as we have described, we hope to improve access to more equitable care for vulnerable veterans.
1. National Comprehensive Cancer Network. NCCN guidelines distress management. Version 2.2021. Updated January 5, 2021. Accessed July 8, 2021. http://www.nccn.org/professionals/physician_gls/pdf/distress.pdf
2. American College of Surgeons, Commission on Cancer. Cancer program standards 2012: ensuring patient-centered care. Version 1.2.1. Published 2021. Accessed July 8, 2021. https://www.facs.org/~/media/files/quality%20programs/cancer/coc/programstandards2012.ashx
3. Jacobsen PB, Ransom S. Implementation of NCCN distress management guidelines by member institutions. J Natl Compr Canc Netw. 2007;5(1):99-103. doi:10.6004/jnccn.2007.0010
4. The Coleman Supportive Oncology Collaborative. Training tools. Accessed July 14, 2021. https://www.supportiveoncologycollaborative.org/training-tools
5. Agha Z, Lofgren RP, VanRuiswyk JV, Layde PM. Are patients at Veterans Affairs medical centers sicker? A comparative analysis of health status and medical resource use. Arch Intern Med. 2000;160(21):3252-3257. doi:10.1001/archinte.160.21.3252
6. Bullman T, Schneiderman A, Gradus JL. Relative importance of posttraumatic stress disorder and depression in predicting risk of suicide among a cohort of Vietnam veterans. Suicide Life Threat Behav. 2019;49(3):838-845. doi:10.1111/sltb.12482
7. Kazis LE, Miller DR, Clark J, et al. Health-related quality of life in patients served by the Department of Veterans Affairs: results from the Veterans Health Study. Arch Intern Med. 1998;158(6):626-632. doi:10.1001/archinte.158.6.626
8. O’Toole BI, Marshall RP, Grayson DA, et al. The Australian Vietnam Veterans Health Study: III. Psychological health of Australian Vietnam veterans and its relationship to combat. Int J Epidemiol. 1996;25(2):331-340. doi:10.1093/ije/25.2.331
9. Vincent C, Chamberlain K, Long N. Mental and physical health status in a community sample of New Zealand Vietnam War veterans. Aust J Public Health. 1994;18(1):58-62. doi:10.1111/j.1753-6405.1994.tb00196.x
10. US Department of Veterans Affairs. Veterans’ diseases associated with Agent Orange. Updated June 16, 2021. Accessed July 8, 2021. http://www.publichealth.va.gov/exposures/agentorange/diseases.asp#veterans
11. Hwa KJ, Dua MM, Wren SM, Visser BC. Missing the obvious: psychosocial obstacles in Veterans with hepatocellular carcinoma. HBP (Oxford). 2015;17(12):1124-1129. doi:10.1111/hpb.12508
12. Saha S, Freeman M, Toure J, Tippens KM, Weeks C, Ibrahim S. Racial and ethnic disparities in the VA health care system: a systematic review. J Gen Intern Med. 2008;23(5):654-671. doi:10.1007/s11606-008-0521-4
13. Amaral EFL, Pollard MS, Mendelsohn J, Cefalu M. Current and future demographics of the veteran population, 2014-2024. Popul Rev. 2018;57(1):28-60. doi:10.1353/prv.2018.0002
14. Mohile SG, Dale W, Somerfield MR, et al. Practical assessment and management of vulnerabilities in older patients receiving chemotherapy: ASCO guideline for geriatric oncology. J Clin Oncol. 2018;36(22):2326-2347. doi:10.1200/JCO.2018.78.8687
15. Siegel R, Ward E, Brawley O, Jemal A. Cancer statistics, 2011: the impact of eliminating socioeconomic and racial disparities on premature cancer deaths. CA Cancer J Clin. 2011;61(4):212-236. doi:10.3322/caac.20121
16. Cimino T, Said K, Safier L, Harris H, Kinderman A. Psychosocial distress among oncology patients in the safety net. Psychooncology. 2020;29(11):1927-1935. doi:10.1002/pon.5525
17. Molander R, Hodgkins K, Johnson C, White A, Frazier E, Krahn D. Interprofessional education in patient aligned care team primary care-mental health integration. Fed Pract. 2017;34(6):40-48.
18. Parikh DA, Ragavan M, Dutta R, et al. Financial toxicity of cancer care: an analysis of financial burden in three distinct health care systems [published online ahead of print, 2021 Apr 7]. JCO Oncol Pract. 2021;OP2000890. doi:10.1200/OP.20.00890
19. Ogrinc G, Davies L, Goodman D, Batalden P, Davidoff F, Stevens D. SQUIRE 2.0 (Standards for QUality Improvement Reporting Excellence): revised publication guidelines from a detailed consensus process. BMJ Qual Saf. 2016;25(12):986-992. doi:10.1136/bmjqs-2015-004411
20. Weldon CB, Gerhart JI, Penedo FJ, et al. Correlates of distress for cancer patients: results from multi-institution use of holistic patient-reported screening tool. J Clin Oncol. 2019;37(15)(suppl):11587-11587. doi:10.1200/JCO.2019.37.15_suppl.11587
21. Kroenke K, Spitzer RL, Williams JB, Löwe B. The Patient Health Questionnaire Somatic, Anxiety, and Depressive Symptom Scales: a systematic review. Gen Hosp Psychiatry. 2010;32(4):345-359. doi:10.1016/j.genhosppsych.2010.03.006
22. Kaiser MJ, Bauer JM, Ramsch C, et al. Validation of the Mini Nutritional Assessment short-form (MNA-SF): a practical tool for identification of nutritional status. J Nutr Health Aging. 2009;13(9):782-788. doi:10.1007/s12603-009-0214-7
23. Azizoddin DR, Lakin JR, Hauser J, et al. Meeting the guidelines: implementing a distress screening intervention for veterans with cancer. Psychooncology. 2020;29(12):2067-2074. doi:10.1002/pon.5565
24. Carlson LE, Waller A, Mitchell AJ. Screening for distress and unmet needs in patients with cancer: review and recommendations. J Clin Oncol. 2012;30(11):1160-1177. doi:10.1200/JCO.2011.39.5509
25. Quill TE, Abernethy AP. Generalist plus specialist palliative care—creating a more sustainable model. N Engl J Med. 2013;368(13):1173-1175. doi:10.1056/NEJMp1215620
26. Weissman DE, Meier DE. Identifying patients in need of a palliative care assessment in the hospital setting: a consensus report from the Center to Advance Palliative Care. J Palliat Med. 2011;14(1):17-23. doi:10.1089/jpm.2010.0347
27. Kumar P, Wright AA, Hatfield LA, Temel JS, Keating NL. Family perspectives on hospice care experiences of patients with cancer. J Clin Oncol. 2017;35(4):432-439. doi:10.1200/JCO.2016.68.9257
28. Mor V, Joyce NR, Coté DL, et al. The rise of concurrent care for veterans with advanced cancer at the end of life. Cancer. 2016;122(5):782-790. doi:10.1002/cncr.29827
29. US Department of Veterans Affairs. Patient care services: Patient aligned care team (PACT). Updated November 5, 2020. Accessed July 8, 2021. https://www.patientcare.va.gov/primarycare/PACT.asp
30. US Department of Veterans Affairs, Veterans Health Administration. VHA health equity action plan. Published September 27, 2019. Accessed July 8, 2021. https://www.va.gov/HEALTHEQUITY/docs/Health_Equity_Action_Plan_Final_022020.pdf
31. Alcaraz KI, Wiedt TL, Daniels EC, Yabroff KR, Guerra CE, Wender RC. Understanding and addressing social determinants to advance cancer health equity in the United States: a blueprint for practice, research, and policy. CA Cancer J Clin. 2020;70(1):31-46. doi:10.3322/caac.21586
32. Atkins D, Kilbourne A, Lipson L. Health equity research in the Veterans Health Administration: we’ve come far but aren’t there yet. Am J Public Health. 2014;104(suppl 4):S525-526. doi:10.2105/AJPH.2014.302216
33. American Cancer Society. Cancer Facts & Figures for African Americans 2019-2021. Atlanta: American Cancer Society; 2019.
34. Hastert TA, Kirchhoff AC, Banegas MP, et al. Work changes and individual, cancer-related, and work-related predictors of decreased work participation among African American cancer survivors. Cancer Med. 2020;9(23):9168-9177. doi:10.1002/cam4.3512
35. Bekelman DB, Nowels CT, Allen LA, Shakar S, Kutner JS, Matlock DD. Outpatient palliative care for chronic heart failure: a case series. J Palliat Med. 2011;14(7):815-821. doi:10.1089/jpm.2010.050
1. National Comprehensive Cancer Network. NCCN guidelines distress management. Version 2.2021. Updated January 5, 2021. Accessed July 8, 2021. http://www.nccn.org/professionals/physician_gls/pdf/distress.pdf
2. American College of Surgeons, Commission on Cancer. Cancer program standards 2012: ensuring patient-centered care. Version 1.2.1. Published 2021. Accessed July 8, 2021. https://www.facs.org/~/media/files/quality%20programs/cancer/coc/programstandards2012.ashx
3. Jacobsen PB, Ransom S. Implementation of NCCN distress management guidelines by member institutions. J Natl Compr Canc Netw. 2007;5(1):99-103. doi:10.6004/jnccn.2007.0010
4. The Coleman Supportive Oncology Collaborative. Training tools. Accessed July 14, 2021. https://www.supportiveoncologycollaborative.org/training-tools
5. Agha Z, Lofgren RP, VanRuiswyk JV, Layde PM. Are patients at Veterans Affairs medical centers sicker? A comparative analysis of health status and medical resource use. Arch Intern Med. 2000;160(21):3252-3257. doi:10.1001/archinte.160.21.3252
6. Bullman T, Schneiderman A, Gradus JL. Relative importance of posttraumatic stress disorder and depression in predicting risk of suicide among a cohort of Vietnam veterans. Suicide Life Threat Behav. 2019;49(3):838-845. doi:10.1111/sltb.12482
7. Kazis LE, Miller DR, Clark J, et al. Health-related quality of life in patients served by the Department of Veterans Affairs: results from the Veterans Health Study. Arch Intern Med. 1998;158(6):626-632. doi:10.1001/archinte.158.6.626
8. O’Toole BI, Marshall RP, Grayson DA, et al. The Australian Vietnam Veterans Health Study: III. Psychological health of Australian Vietnam veterans and its relationship to combat. Int J Epidemiol. 1996;25(2):331-340. doi:10.1093/ije/25.2.331
9. Vincent C, Chamberlain K, Long N. Mental and physical health status in a community sample of New Zealand Vietnam War veterans. Aust J Public Health. 1994;18(1):58-62. doi:10.1111/j.1753-6405.1994.tb00196.x
10. US Department of Veterans Affairs. Veterans’ diseases associated with Agent Orange. Updated June 16, 2021. Accessed July 8, 2021. http://www.publichealth.va.gov/exposures/agentorange/diseases.asp#veterans
11. Hwa KJ, Dua MM, Wren SM, Visser BC. Missing the obvious: psychosocial obstacles in Veterans with hepatocellular carcinoma. HBP (Oxford). 2015;17(12):1124-1129. doi:10.1111/hpb.12508
12. Saha S, Freeman M, Toure J, Tippens KM, Weeks C, Ibrahim S. Racial and ethnic disparities in the VA health care system: a systematic review. J Gen Intern Med. 2008;23(5):654-671. doi:10.1007/s11606-008-0521-4
13. Amaral EFL, Pollard MS, Mendelsohn J, Cefalu M. Current and future demographics of the veteran population, 2014-2024. Popul Rev. 2018;57(1):28-60. doi:10.1353/prv.2018.0002
14. Mohile SG, Dale W, Somerfield MR, et al. Practical assessment and management of vulnerabilities in older patients receiving chemotherapy: ASCO guideline for geriatric oncology. J Clin Oncol. 2018;36(22):2326-2347. doi:10.1200/JCO.2018.78.8687
15. Siegel R, Ward E, Brawley O, Jemal A. Cancer statistics, 2011: the impact of eliminating socioeconomic and racial disparities on premature cancer deaths. CA Cancer J Clin. 2011;61(4):212-236. doi:10.3322/caac.20121
16. Cimino T, Said K, Safier L, Harris H, Kinderman A. Psychosocial distress among oncology patients in the safety net. Psychooncology. 2020;29(11):1927-1935. doi:10.1002/pon.5525
17. Molander R, Hodgkins K, Johnson C, White A, Frazier E, Krahn D. Interprofessional education in patient aligned care team primary care-mental health integration. Fed Pract. 2017;34(6):40-48.
18. Parikh DA, Ragavan M, Dutta R, et al. Financial toxicity of cancer care: an analysis of financial burden in three distinct health care systems [published online ahead of print, 2021 Apr 7]. JCO Oncol Pract. 2021;OP2000890. doi:10.1200/OP.20.00890
19. Ogrinc G, Davies L, Goodman D, Batalden P, Davidoff F, Stevens D. SQUIRE 2.0 (Standards for QUality Improvement Reporting Excellence): revised publication guidelines from a detailed consensus process. BMJ Qual Saf. 2016;25(12):986-992. doi:10.1136/bmjqs-2015-004411
20. Weldon CB, Gerhart JI, Penedo FJ, et al. Correlates of distress for cancer patients: results from multi-institution use of holistic patient-reported screening tool. J Clin Oncol. 2019;37(15)(suppl):11587-11587. doi:10.1200/JCO.2019.37.15_suppl.11587
21. Kroenke K, Spitzer RL, Williams JB, Löwe B. The Patient Health Questionnaire Somatic, Anxiety, and Depressive Symptom Scales: a systematic review. Gen Hosp Psychiatry. 2010;32(4):345-359. doi:10.1016/j.genhosppsych.2010.03.006
22. Kaiser MJ, Bauer JM, Ramsch C, et al. Validation of the Mini Nutritional Assessment short-form (MNA-SF): a practical tool for identification of nutritional status. J Nutr Health Aging. 2009;13(9):782-788. doi:10.1007/s12603-009-0214-7
23. Azizoddin DR, Lakin JR, Hauser J, et al. Meeting the guidelines: implementing a distress screening intervention for veterans with cancer. Psychooncology. 2020;29(12):2067-2074. doi:10.1002/pon.5565
24. Carlson LE, Waller A, Mitchell AJ. Screening for distress and unmet needs in patients with cancer: review and recommendations. J Clin Oncol. 2012;30(11):1160-1177. doi:10.1200/JCO.2011.39.5509
25. Quill TE, Abernethy AP. Generalist plus specialist palliative care—creating a more sustainable model. N Engl J Med. 2013;368(13):1173-1175. doi:10.1056/NEJMp1215620
26. Weissman DE, Meier DE. Identifying patients in need of a palliative care assessment in the hospital setting: a consensus report from the Center to Advance Palliative Care. J Palliat Med. 2011;14(1):17-23. doi:10.1089/jpm.2010.0347
27. Kumar P, Wright AA, Hatfield LA, Temel JS, Keating NL. Family perspectives on hospice care experiences of patients with cancer. J Clin Oncol. 2017;35(4):432-439. doi:10.1200/JCO.2016.68.9257
28. Mor V, Joyce NR, Coté DL, et al. The rise of concurrent care for veterans with advanced cancer at the end of life. Cancer. 2016;122(5):782-790. doi:10.1002/cncr.29827
29. US Department of Veterans Affairs. Patient care services: Patient aligned care team (PACT). Updated November 5, 2020. Accessed July 8, 2021. https://www.patientcare.va.gov/primarycare/PACT.asp
30. US Department of Veterans Affairs, Veterans Health Administration. VHA health equity action plan. Published September 27, 2019. Accessed July 8, 2021. https://www.va.gov/HEALTHEQUITY/docs/Health_Equity_Action_Plan_Final_022020.pdf
31. Alcaraz KI, Wiedt TL, Daniels EC, Yabroff KR, Guerra CE, Wender RC. Understanding and addressing social determinants to advance cancer health equity in the United States: a blueprint for practice, research, and policy. CA Cancer J Clin. 2020;70(1):31-46. doi:10.3322/caac.21586
32. Atkins D, Kilbourne A, Lipson L. Health equity research in the Veterans Health Administration: we’ve come far but aren’t there yet. Am J Public Health. 2014;104(suppl 4):S525-526. doi:10.2105/AJPH.2014.302216
33. American Cancer Society. Cancer Facts & Figures for African Americans 2019-2021. Atlanta: American Cancer Society; 2019.
34. Hastert TA, Kirchhoff AC, Banegas MP, et al. Work changes and individual, cancer-related, and work-related predictors of decreased work participation among African American cancer survivors. Cancer Med. 2020;9(23):9168-9177. doi:10.1002/cam4.3512
35. Bekelman DB, Nowels CT, Allen LA, Shakar S, Kutner JS, Matlock DD. Outpatient palliative care for chronic heart failure: a case series. J Palliat Med. 2011;14(7):815-821. doi:10.1089/jpm.2010.050
‘Reassuring’ findings for second-generation antipsychotics during pregnancy
Second-generation antipsychotics (SGAs) taken by pregnant women are linked to a low rate of adverse effects in their children, new research suggests.
Data from a large registry study of almost 2,000 women showed that 2.5% of the live births in a group that had been exposed to antipsychotics had confirmed major malformations compared with 2% of the live births in a non-exposed group. This translated into an estimated odds ratio of 1.5 for major malformations.
“The 2.5% absolute risk for major malformations is consistent with the estimates of the Centers for Disease Control and Prevention’s national baseline rate of major malformations in the general population,” lead author Adele Viguera, MD, MPH, director of research for women’s mental health, Cleveland Clinic Neurological Institute, told this news organization.
“Our results are reassuring and suggest that second-generation antipsychotics, as a class, do not substantially increase the risk of major malformations,” Dr. Viguera said.
The findings were published online August 3 in the Journal of Clinical Psychiatry.
Safety data scarce
Despite the increasing use of SGAs to treat a “spectrum of psychiatric disorders,” relatively little data are available on the reproductive safety of these agents, Dr. Viguera said.
The National Pregnancy Registry for Atypical Antipsychotics (NPRAA) was established in 2008 to determine risk for major malformation among infants exposed to these medications during the first trimester, relative to a comparison group of unexposed infants of mothers with histories of psychiatric morbidity.
The NPRAA follows pregnant women (aged 18 to 45 years) with psychiatric illness who are exposed or unexposed to SGAs during pregnancy. Participants are recruited through nationwide provider referral, self-referral, and advertisement through the Massachusetts General Hospital Center for Women’s Mental Health website.
Specific data collected are shown in the following table.
Since publication of the first results in 2015, the sample size for the trial has increased – and the absolute and relative risk for major malformations observed in the study population are “more precise,” the investigators note. The current study presented updated previous findings.
Demographic differences
Of the 1,906 women who enrolled as of April 2020, 1,311 (mean age, 32.6 years; 81.3% White) completed the study and were eligible for inclusion in the analysis.
Although the groups had a virtually identical mean age, fewer women in the exposure group were married compared with those in the non-exposure group (77% vs. 90%, respectively) and fewer had a college education (71.2% vs. 87.8%). There was also a higher percentage of first-trimester cigarette smokers in the exposure group (18.4% vs. 5.1%).
On the other hand, more women in the non-exposure group used alcohol than in the exposure group (28.6% vs. 21.4%, respectively).
The most frequent psychiatric disorder in the exposure group was bipolar disorder (63.9%), followed by major depression (12.9%), anxiety (5.8%), and schizophrenia (4.5%). Only 11.4% of women in the non-exposure group were diagnosed with bipolar disorder, whereas 34.1% were diagnosed with major depression, 31.3% with anxiety, and none with schizophrenia.
Notably, a large percentage of women in both groups had a history of postpartum depression and/or psychosis (41.4% and 35.5%, respectively).
The most frequently used SGAs in the exposure group were quetiapine (Seroquel), aripiprazole (Abilify), and lurasidone (Latuda).
Participants in the exposure group had a higher age at initial onset of primary psychiatric diagnosis and a lower proportion of lifetime illness compared with those in the non-exposure group.
Major clinical implication?
Among 640 live births in the exposure group, which included 17 twin pregnancies and 1 triplet pregnancy, 2.5% reported major malformations. Among 704 live births in the control group, which included 14 twin pregnancies, 1.99% reported major malformations.
The estimated OR for major malformations comparing exposed and unexposed infants was 1.48 (95% confidence interval, 0.625-3.517).
The authors note that their findings were consistent with one of the largest studies to date, which included a nationwide sample of more than 1 million women. Its results showed that, among infants exposed to SGAs versus those who were not exposed, the estimated risk ratio after adjusting for psychiatric conditions was 1.05 (95% CI, 0.96-1.16).
Additionally, “a hallmark of a teratogen is that it tends to cause a specific type or pattern of malformations, and we found no preponderance of one single type of major malformation or specific pattern of malformations among the exposed and unexposed groups,” Dr. Viguera said
“A major clinical implication of these findings is that for women with major mood and/or psychotic disorders, treatment with an atypical antipsychotic during pregnancy may be the most prudent clinical decision, much as continued treatment is recommended for pregnant women with other serious and chronic medical conditions, such as epilepsy,” she added.
The concept of ‘satisficing’
Commenting on the study, Vivien Burt, MD, PhD, founder and director/consultant of the Women’s Life Center at the Resnick University of California, Los Angeles (UCLA) Neuropsychiatric Hospital, called the findings “reassuring.”
The results “support the conclusion that in pregnant women with serious psychiatric illnesses, the use of SGAs is often a better option than avoiding these medications and exposing both the women and their offspring to the adverse consequences of maternal mental illness,” she said.
An accompanying editorial co-authored by Dr. Burt and colleague Sonya Rasminsky, MD, introduced the concept of “satisficing” – a term coined by Herbert Simon, a behavioral economist and Nobel Laureate. “Satisficing” is a “decision-making strategy that aims for a satisfactory (‘good enough’) outcome rather than a perfect one.”
The concept applies to decision-making beyond the field of economics “and is critical to how physicians help patients make decisions when they are faced with multiple treatment options,” said Dr. Burt, a professor emeritus of psychiatry at UCLA.
“The goal of ‘satisficing’ is to plan for the most satisfactory outcome, knowing that there are always unknowns, so in an uncertain world, clinicians should carefully help their patients make decisions that will allow them to achieve an outcome they can best live with,” she noted.
The investigators note that their findings may not be generalizable to the larger population of women taking SGAs, given that their participants were “overwhelmingly White, married, and well-educated women.”
They add that enrollment into the NPRAA registry is ongoing and larger sample sizes will “further narrow the confidence interval around the risk estimates and allow for adjustment of likely sources of confounding.”
The NPRAA is supported by Alkermes, Johnson & Johnson/Janssen Pharmaceuticals, Otsuka America Pharmaceutical, Sunovion Pharmaceuticals, SAGE Therapeutics, Teva Pharmaceuticals, and Aurobindo Pharma. Past sponsors of the NPRAA are listed in the original paper. Dr. Viguera receives research support from the NPRAA, Alkermes Biopharmaceuticals, Aurobindo Pharma, Janssen Pharmaceuticals, Otsuka Pharmaceutical, Sunovion Pharmaceuticals, Teva Pharmaceuticals, and SAGE Therapeutics and receives adviser/consulting fees from Up-to-Date. Dr. Burt has been a consultant/speaker for Sage Therapeutics. Dr. Rasminsky has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Second-generation antipsychotics (SGAs) taken by pregnant women are linked to a low rate of adverse effects in their children, new research suggests.
Data from a large registry study of almost 2,000 women showed that 2.5% of the live births in a group that had been exposed to antipsychotics had confirmed major malformations compared with 2% of the live births in a non-exposed group. This translated into an estimated odds ratio of 1.5 for major malformations.
“The 2.5% absolute risk for major malformations is consistent with the estimates of the Centers for Disease Control and Prevention’s national baseline rate of major malformations in the general population,” lead author Adele Viguera, MD, MPH, director of research for women’s mental health, Cleveland Clinic Neurological Institute, told this news organization.
“Our results are reassuring and suggest that second-generation antipsychotics, as a class, do not substantially increase the risk of major malformations,” Dr. Viguera said.
The findings were published online August 3 in the Journal of Clinical Psychiatry.
Safety data scarce
Despite the increasing use of SGAs to treat a “spectrum of psychiatric disorders,” relatively little data are available on the reproductive safety of these agents, Dr. Viguera said.
The National Pregnancy Registry for Atypical Antipsychotics (NPRAA) was established in 2008 to determine risk for major malformation among infants exposed to these medications during the first trimester, relative to a comparison group of unexposed infants of mothers with histories of psychiatric morbidity.
The NPRAA follows pregnant women (aged 18 to 45 years) with psychiatric illness who are exposed or unexposed to SGAs during pregnancy. Participants are recruited through nationwide provider referral, self-referral, and advertisement through the Massachusetts General Hospital Center for Women’s Mental Health website.
Specific data collected are shown in the following table.
Since publication of the first results in 2015, the sample size for the trial has increased – and the absolute and relative risk for major malformations observed in the study population are “more precise,” the investigators note. The current study presented updated previous findings.
Demographic differences
Of the 1,906 women who enrolled as of April 2020, 1,311 (mean age, 32.6 years; 81.3% White) completed the study and were eligible for inclusion in the analysis.
Although the groups had a virtually identical mean age, fewer women in the exposure group were married compared with those in the non-exposure group (77% vs. 90%, respectively) and fewer had a college education (71.2% vs. 87.8%). There was also a higher percentage of first-trimester cigarette smokers in the exposure group (18.4% vs. 5.1%).
On the other hand, more women in the non-exposure group used alcohol than in the exposure group (28.6% vs. 21.4%, respectively).
The most frequent psychiatric disorder in the exposure group was bipolar disorder (63.9%), followed by major depression (12.9%), anxiety (5.8%), and schizophrenia (4.5%). Only 11.4% of women in the non-exposure group were diagnosed with bipolar disorder, whereas 34.1% were diagnosed with major depression, 31.3% with anxiety, and none with schizophrenia.
Notably, a large percentage of women in both groups had a history of postpartum depression and/or psychosis (41.4% and 35.5%, respectively).
The most frequently used SGAs in the exposure group were quetiapine (Seroquel), aripiprazole (Abilify), and lurasidone (Latuda).
Participants in the exposure group had a higher age at initial onset of primary psychiatric diagnosis and a lower proportion of lifetime illness compared with those in the non-exposure group.
Major clinical implication?
Among 640 live births in the exposure group, which included 17 twin pregnancies and 1 triplet pregnancy, 2.5% reported major malformations. Among 704 live births in the control group, which included 14 twin pregnancies, 1.99% reported major malformations.
The estimated OR for major malformations comparing exposed and unexposed infants was 1.48 (95% confidence interval, 0.625-3.517).
The authors note that their findings were consistent with one of the largest studies to date, which included a nationwide sample of more than 1 million women. Its results showed that, among infants exposed to SGAs versus those who were not exposed, the estimated risk ratio after adjusting for psychiatric conditions was 1.05 (95% CI, 0.96-1.16).
Additionally, “a hallmark of a teratogen is that it tends to cause a specific type or pattern of malformations, and we found no preponderance of one single type of major malformation or specific pattern of malformations among the exposed and unexposed groups,” Dr. Viguera said
“A major clinical implication of these findings is that for women with major mood and/or psychotic disorders, treatment with an atypical antipsychotic during pregnancy may be the most prudent clinical decision, much as continued treatment is recommended for pregnant women with other serious and chronic medical conditions, such as epilepsy,” she added.
The concept of ‘satisficing’
Commenting on the study, Vivien Burt, MD, PhD, founder and director/consultant of the Women’s Life Center at the Resnick University of California, Los Angeles (UCLA) Neuropsychiatric Hospital, called the findings “reassuring.”
The results “support the conclusion that in pregnant women with serious psychiatric illnesses, the use of SGAs is often a better option than avoiding these medications and exposing both the women and their offspring to the adverse consequences of maternal mental illness,” she said.
An accompanying editorial co-authored by Dr. Burt and colleague Sonya Rasminsky, MD, introduced the concept of “satisficing” – a term coined by Herbert Simon, a behavioral economist and Nobel Laureate. “Satisficing” is a “decision-making strategy that aims for a satisfactory (‘good enough’) outcome rather than a perfect one.”
The concept applies to decision-making beyond the field of economics “and is critical to how physicians help patients make decisions when they are faced with multiple treatment options,” said Dr. Burt, a professor emeritus of psychiatry at UCLA.
“The goal of ‘satisficing’ is to plan for the most satisfactory outcome, knowing that there are always unknowns, so in an uncertain world, clinicians should carefully help their patients make decisions that will allow them to achieve an outcome they can best live with,” she noted.
The investigators note that their findings may not be generalizable to the larger population of women taking SGAs, given that their participants were “overwhelmingly White, married, and well-educated women.”
They add that enrollment into the NPRAA registry is ongoing and larger sample sizes will “further narrow the confidence interval around the risk estimates and allow for adjustment of likely sources of confounding.”
The NPRAA is supported by Alkermes, Johnson & Johnson/Janssen Pharmaceuticals, Otsuka America Pharmaceutical, Sunovion Pharmaceuticals, SAGE Therapeutics, Teva Pharmaceuticals, and Aurobindo Pharma. Past sponsors of the NPRAA are listed in the original paper. Dr. Viguera receives research support from the NPRAA, Alkermes Biopharmaceuticals, Aurobindo Pharma, Janssen Pharmaceuticals, Otsuka Pharmaceutical, Sunovion Pharmaceuticals, Teva Pharmaceuticals, and SAGE Therapeutics and receives adviser/consulting fees from Up-to-Date. Dr. Burt has been a consultant/speaker for Sage Therapeutics. Dr. Rasminsky has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Second-generation antipsychotics (SGAs) taken by pregnant women are linked to a low rate of adverse effects in their children, new research suggests.
Data from a large registry study of almost 2,000 women showed that 2.5% of the live births in a group that had been exposed to antipsychotics had confirmed major malformations compared with 2% of the live births in a non-exposed group. This translated into an estimated odds ratio of 1.5 for major malformations.
“The 2.5% absolute risk for major malformations is consistent with the estimates of the Centers for Disease Control and Prevention’s national baseline rate of major malformations in the general population,” lead author Adele Viguera, MD, MPH, director of research for women’s mental health, Cleveland Clinic Neurological Institute, told this news organization.
“Our results are reassuring and suggest that second-generation antipsychotics, as a class, do not substantially increase the risk of major malformations,” Dr. Viguera said.
The findings were published online August 3 in the Journal of Clinical Psychiatry.
Safety data scarce
Despite the increasing use of SGAs to treat a “spectrum of psychiatric disorders,” relatively little data are available on the reproductive safety of these agents, Dr. Viguera said.
The National Pregnancy Registry for Atypical Antipsychotics (NPRAA) was established in 2008 to determine risk for major malformation among infants exposed to these medications during the first trimester, relative to a comparison group of unexposed infants of mothers with histories of psychiatric morbidity.
The NPRAA follows pregnant women (aged 18 to 45 years) with psychiatric illness who are exposed or unexposed to SGAs during pregnancy. Participants are recruited through nationwide provider referral, self-referral, and advertisement through the Massachusetts General Hospital Center for Women’s Mental Health website.
Specific data collected are shown in the following table.
Since publication of the first results in 2015, the sample size for the trial has increased – and the absolute and relative risk for major malformations observed in the study population are “more precise,” the investigators note. The current study presented updated previous findings.
Demographic differences
Of the 1,906 women who enrolled as of April 2020, 1,311 (mean age, 32.6 years; 81.3% White) completed the study and were eligible for inclusion in the analysis.
Although the groups had a virtually identical mean age, fewer women in the exposure group were married compared with those in the non-exposure group (77% vs. 90%, respectively) and fewer had a college education (71.2% vs. 87.8%). There was also a higher percentage of first-trimester cigarette smokers in the exposure group (18.4% vs. 5.1%).
On the other hand, more women in the non-exposure group used alcohol than in the exposure group (28.6% vs. 21.4%, respectively).
The most frequent psychiatric disorder in the exposure group was bipolar disorder (63.9%), followed by major depression (12.9%), anxiety (5.8%), and schizophrenia (4.5%). Only 11.4% of women in the non-exposure group were diagnosed with bipolar disorder, whereas 34.1% were diagnosed with major depression, 31.3% with anxiety, and none with schizophrenia.
Notably, a large percentage of women in both groups had a history of postpartum depression and/or psychosis (41.4% and 35.5%, respectively).
The most frequently used SGAs in the exposure group were quetiapine (Seroquel), aripiprazole (Abilify), and lurasidone (Latuda).
Participants in the exposure group had a higher age at initial onset of primary psychiatric diagnosis and a lower proportion of lifetime illness compared with those in the non-exposure group.
Major clinical implication?
Among 640 live births in the exposure group, which included 17 twin pregnancies and 1 triplet pregnancy, 2.5% reported major malformations. Among 704 live births in the control group, which included 14 twin pregnancies, 1.99% reported major malformations.
The estimated OR for major malformations comparing exposed and unexposed infants was 1.48 (95% confidence interval, 0.625-3.517).
The authors note that their findings were consistent with one of the largest studies to date, which included a nationwide sample of more than 1 million women. Its results showed that, among infants exposed to SGAs versus those who were not exposed, the estimated risk ratio after adjusting for psychiatric conditions was 1.05 (95% CI, 0.96-1.16).
Additionally, “a hallmark of a teratogen is that it tends to cause a specific type or pattern of malformations, and we found no preponderance of one single type of major malformation or specific pattern of malformations among the exposed and unexposed groups,” Dr. Viguera said
“A major clinical implication of these findings is that for women with major mood and/or psychotic disorders, treatment with an atypical antipsychotic during pregnancy may be the most prudent clinical decision, much as continued treatment is recommended for pregnant women with other serious and chronic medical conditions, such as epilepsy,” she added.
The concept of ‘satisficing’
Commenting on the study, Vivien Burt, MD, PhD, founder and director/consultant of the Women’s Life Center at the Resnick University of California, Los Angeles (UCLA) Neuropsychiatric Hospital, called the findings “reassuring.”
The results “support the conclusion that in pregnant women with serious psychiatric illnesses, the use of SGAs is often a better option than avoiding these medications and exposing both the women and their offspring to the adverse consequences of maternal mental illness,” she said.
An accompanying editorial co-authored by Dr. Burt and colleague Sonya Rasminsky, MD, introduced the concept of “satisficing” – a term coined by Herbert Simon, a behavioral economist and Nobel Laureate. “Satisficing” is a “decision-making strategy that aims for a satisfactory (‘good enough’) outcome rather than a perfect one.”
The concept applies to decision-making beyond the field of economics “and is critical to how physicians help patients make decisions when they are faced with multiple treatment options,” said Dr. Burt, a professor emeritus of psychiatry at UCLA.
“The goal of ‘satisficing’ is to plan for the most satisfactory outcome, knowing that there are always unknowns, so in an uncertain world, clinicians should carefully help their patients make decisions that will allow them to achieve an outcome they can best live with,” she noted.
The investigators note that their findings may not be generalizable to the larger population of women taking SGAs, given that their participants were “overwhelmingly White, married, and well-educated women.”
They add that enrollment into the NPRAA registry is ongoing and larger sample sizes will “further narrow the confidence interval around the risk estimates and allow for adjustment of likely sources of confounding.”
The NPRAA is supported by Alkermes, Johnson & Johnson/Janssen Pharmaceuticals, Otsuka America Pharmaceutical, Sunovion Pharmaceuticals, SAGE Therapeutics, Teva Pharmaceuticals, and Aurobindo Pharma. Past sponsors of the NPRAA are listed in the original paper. Dr. Viguera receives research support from the NPRAA, Alkermes Biopharmaceuticals, Aurobindo Pharma, Janssen Pharmaceuticals, Otsuka Pharmaceutical, Sunovion Pharmaceuticals, Teva Pharmaceuticals, and SAGE Therapeutics and receives adviser/consulting fees from Up-to-Date. Dr. Burt has been a consultant/speaker for Sage Therapeutics. Dr. Rasminsky has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Shedding the super-doctor myth requires an honest look at systemic racism
An overwhelmingly loud and high-pitched screech rattles against your hip. You startle and groan into the pillow as your thoughts settle into conscious awareness. It is 3 a.m. You are a 2nd-year resident trudging through the night shift, alerted to the presence of a new patient awaiting an emergency assessment. You are the only in-house physician. Walking steadfastly toward the emergency unit, you enter and greet the patient. Immediately, you observe a look of surprise followed immediately by a scowl.
You extend a hand, but your greeting is abruptly cut short with: “I want to see a doctor!” You pace your breaths to quell annoyance and resume your introduction, asserting that you are a doctor and indeed the only doctor on duty. After moments of deep sighs and questions regarding your credentials, you persuade the patient to start the interview.
It is now 8 a.m. The frustration of the night starts to ease as you prepare to leave. While gathering your things, a visitor is overheard inquiring the whereabouts of a hospital unit. Volunteering as a guide, you walk the person toward the opposite end of the hospital. Bleary eyed, muscle laxed, and bone weary, you point out the entrance, then turn to leave. The steady rhythm of your steps suddenly halts as you hear from behind: “Thank you! You speak English really well!” Blankly, you stare. Your voice remains mute while your brain screams: “What is that supposed to mean?” But you do not utter a sound, because intuitively, you know the answer.
While reading this scenario, what did you feel? Pride in knowing that the physician was able to successfully navigate a busy night? Relief in the physician’s ability to maintain a professional demeanor despite belittling microaggressions? Are you angry? Would you replay those moments like reruns of a bad TV show? Can you imagine entering your home and collapsing onto the bed as your tears of fury pool over your rumpled sheets?
The emotional release of that morning is seared into my memory. Over the years, I questioned my reactions. Was I too passive? Should I have schooled them on their ignorance? Had I done so, would I have incurred reprimands? Would standing up for myself cause years of hard work to fall away? Moreover, had I defended myself, would I forever have been viewed as “The Angry Black Woman?”
This story is more than a vignette. For me, it is another reminder that, despite how far we have come, we have much further to go. As a Black woman in a professional sphere, I stand upon the shoulders of those who sacrificed for a dream, a greater purpose. My foremothers and forefathers fought bravely and tirelessly so that we could attain levels of success that were only once but a dream. Despite this progress, a grimace, carelessly spoken words, or a mindless gesture remind me that, no matter how much I toil and what levels of success I achieve, when I meet someone for the first time or encounter someone from my past, I find myself wondering whether I am remembered for me or because I am “The Black One.”
Honest look at medicine is imperative
It is important to consider multiple facets of the super-doctor myth. We are dedicated, fearless, authoritative, ambitious individuals. We do not yield to sickness, family obligations, or fatigue. Medicine is a calling, and the patient deserves the utmost respect and professional behavior. Impervious to ethnicity, race, nationality, or creed, we are unbiased and always in service of the greater good. Often, however, I wonder how the expectations of patient-focused, patient-centered care can prevail without an honest look at the vicissitudes facing medicine.
We find ourselves amid a tumultuous year overshadowed by a devastating pandemic that skews heavily toward Black and Brown communities, in addition to political turmoil and racial reckoning that sprang forth from fear, anger, and determination ignited by the murders of Breonna Taylor and George Floyd – communities united in outrage lamenting the cries of Black Lives Matter.
I remember the tears briskly falling upon my blouse as I watched Mr. Floyd’s life violently ripped from this Earth. Shortly thereafter, I remember the phone calls, emails, and texts from close friends, acquaintances, and colleagues offering support, listening ears, pledging to learn and endeavoring to understand the struggle for recognition and the fight for human rights. Even so, the deafening support was clouded by the preternatural silence of some medical organizations. Within the Black physician community, outrage was palpable. We reflected upon years of sacrifice and perseverance despite the challenge of bigotry, ignorance, and racism – not only from patients and their families – but also colleagues and administrators. Yet, in our time of horror and need, in those moments of vulnerability ... silence. Eventually, lengthy proclamations of support were expressed through various media. However, it felt too safe, too corporate, and too generic and inauthentic. As a result, an exodus of Black physicians from leadership positions and academic medicine took hold as the blatant continuation of rhetoric – coupled with ineffective outreach and support – finally took its toll.
Frequently, I question how the obstacles of medical school, residency, and beyond are expected to be traversed while living in a world that consistently affords additional challenges to those who look, act, or speak in a manner that varies from the perceived standard. In a culture where the myth of the super doctor reigns, how do we reconcile attainment of a false and detrimental narrative while the overarching pressure acutely felt by Black physicians magnifies in the setting of stereotypes, sociopolitical turbulence, bigotry, and racism? How can one sacrifice for an entity that is unwilling to acknowledge the psychological implications of that sacrifice?
For instance, while in medical school, I transitioned my hair to its natural state but was counseled against doing so because of the risk of losing residency opportunities as a direct result of my “unprofessional” appearance. Throughout residency, multiple incidents come to mind, including frequent demands to see my hospital badge despite the same not being of asked of my White cohorts; denial of entry into physician entrance within the residency building because, despite my professional attire, I was presumed to be a member of the custodial staff; and patients being confused and asking for a doctor despite my long white coat and clear introductions.
Furthermore, the fluency of my speech and the absence of regional dialect or vernacular are quite often lauded by patients. Inquiries to touch my hair as well as hypotheses regarding my nationality or degree of “blackness” with respect to the shape of my nose, eyes, and lips are openly questioned. Unfortunately, those uncomfortable incidents have not been limited to patient encounters.
In one instance, while presenting a patient in the presence of my attending and a 3rd-year medical student, I was sternly admonished for disclosing the race of the patient. I sat still and resolute as this doctor spoke on increased risk of bias in diagnosis and treatment when race is identified. Outwardly, I projected patience but inside, I seethed. In that moment, I realized that I would never have the luxury of ignorance or denial. Although I desire to be valued for my prowess in medicine, the mythical status was not created with my skin color in mind. For is avoidance not but a reflection of denial?
In these chaotic and uncertain times, how can we continue to promote a pathological ideal when the roads traveled are so fundamentally skewed? If a White physician faces a belligerent and argumentative patient, there is opportunity for debriefing both individually and among a larger cohort via classes, conferences, and supervisions. Conversely, when a Black physician is derided with racist sentiment, will they have the same opportunity for reflection and support? Despite identical expectations of professionalism and growth, how can one be successful in a system that either directly or indirectly encourages the opposite?
As we try to shed the super-doctor myth, we must recognize that this unattainable and detrimental persona hinders progress. This myth undermines our ability to understand our fragility, the limitations of our capabilities, and the strength of our vulnerability. We must take an honest look at the manner in which our individual biases and the deeply ingrained (and potentially unconscious) systemic biases are counterintuitive to the success and support of physicians of color.
Dr. Thomas is a board-certified adult psychiatrist with an interest in chronic illness, women’s behavioral health, and minority mental health. She currently practices in North Kingstown and East Providence, R.I. She has no conflicts of interest.
An overwhelmingly loud and high-pitched screech rattles against your hip. You startle and groan into the pillow as your thoughts settle into conscious awareness. It is 3 a.m. You are a 2nd-year resident trudging through the night shift, alerted to the presence of a new patient awaiting an emergency assessment. You are the only in-house physician. Walking steadfastly toward the emergency unit, you enter and greet the patient. Immediately, you observe a look of surprise followed immediately by a scowl.
You extend a hand, but your greeting is abruptly cut short with: “I want to see a doctor!” You pace your breaths to quell annoyance and resume your introduction, asserting that you are a doctor and indeed the only doctor on duty. After moments of deep sighs and questions regarding your credentials, you persuade the patient to start the interview.
It is now 8 a.m. The frustration of the night starts to ease as you prepare to leave. While gathering your things, a visitor is overheard inquiring the whereabouts of a hospital unit. Volunteering as a guide, you walk the person toward the opposite end of the hospital. Bleary eyed, muscle laxed, and bone weary, you point out the entrance, then turn to leave. The steady rhythm of your steps suddenly halts as you hear from behind: “Thank you! You speak English really well!” Blankly, you stare. Your voice remains mute while your brain screams: “What is that supposed to mean?” But you do not utter a sound, because intuitively, you know the answer.
While reading this scenario, what did you feel? Pride in knowing that the physician was able to successfully navigate a busy night? Relief in the physician’s ability to maintain a professional demeanor despite belittling microaggressions? Are you angry? Would you replay those moments like reruns of a bad TV show? Can you imagine entering your home and collapsing onto the bed as your tears of fury pool over your rumpled sheets?
The emotional release of that morning is seared into my memory. Over the years, I questioned my reactions. Was I too passive? Should I have schooled them on their ignorance? Had I done so, would I have incurred reprimands? Would standing up for myself cause years of hard work to fall away? Moreover, had I defended myself, would I forever have been viewed as “The Angry Black Woman?”
This story is more than a vignette. For me, it is another reminder that, despite how far we have come, we have much further to go. As a Black woman in a professional sphere, I stand upon the shoulders of those who sacrificed for a dream, a greater purpose. My foremothers and forefathers fought bravely and tirelessly so that we could attain levels of success that were only once but a dream. Despite this progress, a grimace, carelessly spoken words, or a mindless gesture remind me that, no matter how much I toil and what levels of success I achieve, when I meet someone for the first time or encounter someone from my past, I find myself wondering whether I am remembered for me or because I am “The Black One.”
Honest look at medicine is imperative
It is important to consider multiple facets of the super-doctor myth. We are dedicated, fearless, authoritative, ambitious individuals. We do not yield to sickness, family obligations, or fatigue. Medicine is a calling, and the patient deserves the utmost respect and professional behavior. Impervious to ethnicity, race, nationality, or creed, we are unbiased and always in service of the greater good. Often, however, I wonder how the expectations of patient-focused, patient-centered care can prevail without an honest look at the vicissitudes facing medicine.
We find ourselves amid a tumultuous year overshadowed by a devastating pandemic that skews heavily toward Black and Brown communities, in addition to political turmoil and racial reckoning that sprang forth from fear, anger, and determination ignited by the murders of Breonna Taylor and George Floyd – communities united in outrage lamenting the cries of Black Lives Matter.
I remember the tears briskly falling upon my blouse as I watched Mr. Floyd’s life violently ripped from this Earth. Shortly thereafter, I remember the phone calls, emails, and texts from close friends, acquaintances, and colleagues offering support, listening ears, pledging to learn and endeavoring to understand the struggle for recognition and the fight for human rights. Even so, the deafening support was clouded by the preternatural silence of some medical organizations. Within the Black physician community, outrage was palpable. We reflected upon years of sacrifice and perseverance despite the challenge of bigotry, ignorance, and racism – not only from patients and their families – but also colleagues and administrators. Yet, in our time of horror and need, in those moments of vulnerability ... silence. Eventually, lengthy proclamations of support were expressed through various media. However, it felt too safe, too corporate, and too generic and inauthentic. As a result, an exodus of Black physicians from leadership positions and academic medicine took hold as the blatant continuation of rhetoric – coupled with ineffective outreach and support – finally took its toll.
Frequently, I question how the obstacles of medical school, residency, and beyond are expected to be traversed while living in a world that consistently affords additional challenges to those who look, act, or speak in a manner that varies from the perceived standard. In a culture where the myth of the super doctor reigns, how do we reconcile attainment of a false and detrimental narrative while the overarching pressure acutely felt by Black physicians magnifies in the setting of stereotypes, sociopolitical turbulence, bigotry, and racism? How can one sacrifice for an entity that is unwilling to acknowledge the psychological implications of that sacrifice?
For instance, while in medical school, I transitioned my hair to its natural state but was counseled against doing so because of the risk of losing residency opportunities as a direct result of my “unprofessional” appearance. Throughout residency, multiple incidents come to mind, including frequent demands to see my hospital badge despite the same not being of asked of my White cohorts; denial of entry into physician entrance within the residency building because, despite my professional attire, I was presumed to be a member of the custodial staff; and patients being confused and asking for a doctor despite my long white coat and clear introductions.
Furthermore, the fluency of my speech and the absence of regional dialect or vernacular are quite often lauded by patients. Inquiries to touch my hair as well as hypotheses regarding my nationality or degree of “blackness” with respect to the shape of my nose, eyes, and lips are openly questioned. Unfortunately, those uncomfortable incidents have not been limited to patient encounters.
In one instance, while presenting a patient in the presence of my attending and a 3rd-year medical student, I was sternly admonished for disclosing the race of the patient. I sat still and resolute as this doctor spoke on increased risk of bias in diagnosis and treatment when race is identified. Outwardly, I projected patience but inside, I seethed. In that moment, I realized that I would never have the luxury of ignorance or denial. Although I desire to be valued for my prowess in medicine, the mythical status was not created with my skin color in mind. For is avoidance not but a reflection of denial?
In these chaotic and uncertain times, how can we continue to promote a pathological ideal when the roads traveled are so fundamentally skewed? If a White physician faces a belligerent and argumentative patient, there is opportunity for debriefing both individually and among a larger cohort via classes, conferences, and supervisions. Conversely, when a Black physician is derided with racist sentiment, will they have the same opportunity for reflection and support? Despite identical expectations of professionalism and growth, how can one be successful in a system that either directly or indirectly encourages the opposite?
As we try to shed the super-doctor myth, we must recognize that this unattainable and detrimental persona hinders progress. This myth undermines our ability to understand our fragility, the limitations of our capabilities, and the strength of our vulnerability. We must take an honest look at the manner in which our individual biases and the deeply ingrained (and potentially unconscious) systemic biases are counterintuitive to the success and support of physicians of color.
Dr. Thomas is a board-certified adult psychiatrist with an interest in chronic illness, women’s behavioral health, and minority mental health. She currently practices in North Kingstown and East Providence, R.I. She has no conflicts of interest.
An overwhelmingly loud and high-pitched screech rattles against your hip. You startle and groan into the pillow as your thoughts settle into conscious awareness. It is 3 a.m. You are a 2nd-year resident trudging through the night shift, alerted to the presence of a new patient awaiting an emergency assessment. You are the only in-house physician. Walking steadfastly toward the emergency unit, you enter and greet the patient. Immediately, you observe a look of surprise followed immediately by a scowl.
You extend a hand, but your greeting is abruptly cut short with: “I want to see a doctor!” You pace your breaths to quell annoyance and resume your introduction, asserting that you are a doctor and indeed the only doctor on duty. After moments of deep sighs and questions regarding your credentials, you persuade the patient to start the interview.
It is now 8 a.m. The frustration of the night starts to ease as you prepare to leave. While gathering your things, a visitor is overheard inquiring the whereabouts of a hospital unit. Volunteering as a guide, you walk the person toward the opposite end of the hospital. Bleary eyed, muscle laxed, and bone weary, you point out the entrance, then turn to leave. The steady rhythm of your steps suddenly halts as you hear from behind: “Thank you! You speak English really well!” Blankly, you stare. Your voice remains mute while your brain screams: “What is that supposed to mean?” But you do not utter a sound, because intuitively, you know the answer.
While reading this scenario, what did you feel? Pride in knowing that the physician was able to successfully navigate a busy night? Relief in the physician’s ability to maintain a professional demeanor despite belittling microaggressions? Are you angry? Would you replay those moments like reruns of a bad TV show? Can you imagine entering your home and collapsing onto the bed as your tears of fury pool over your rumpled sheets?
The emotional release of that morning is seared into my memory. Over the years, I questioned my reactions. Was I too passive? Should I have schooled them on their ignorance? Had I done so, would I have incurred reprimands? Would standing up for myself cause years of hard work to fall away? Moreover, had I defended myself, would I forever have been viewed as “The Angry Black Woman?”
This story is more than a vignette. For me, it is another reminder that, despite how far we have come, we have much further to go. As a Black woman in a professional sphere, I stand upon the shoulders of those who sacrificed for a dream, a greater purpose. My foremothers and forefathers fought bravely and tirelessly so that we could attain levels of success that were only once but a dream. Despite this progress, a grimace, carelessly spoken words, or a mindless gesture remind me that, no matter how much I toil and what levels of success I achieve, when I meet someone for the first time or encounter someone from my past, I find myself wondering whether I am remembered for me or because I am “The Black One.”
Honest look at medicine is imperative
It is important to consider multiple facets of the super-doctor myth. We are dedicated, fearless, authoritative, ambitious individuals. We do not yield to sickness, family obligations, or fatigue. Medicine is a calling, and the patient deserves the utmost respect and professional behavior. Impervious to ethnicity, race, nationality, or creed, we are unbiased and always in service of the greater good. Often, however, I wonder how the expectations of patient-focused, patient-centered care can prevail without an honest look at the vicissitudes facing medicine.
We find ourselves amid a tumultuous year overshadowed by a devastating pandemic that skews heavily toward Black and Brown communities, in addition to political turmoil and racial reckoning that sprang forth from fear, anger, and determination ignited by the murders of Breonna Taylor and George Floyd – communities united in outrage lamenting the cries of Black Lives Matter.
I remember the tears briskly falling upon my blouse as I watched Mr. Floyd’s life violently ripped from this Earth. Shortly thereafter, I remember the phone calls, emails, and texts from close friends, acquaintances, and colleagues offering support, listening ears, pledging to learn and endeavoring to understand the struggle for recognition and the fight for human rights. Even so, the deafening support was clouded by the preternatural silence of some medical organizations. Within the Black physician community, outrage was palpable. We reflected upon years of sacrifice and perseverance despite the challenge of bigotry, ignorance, and racism – not only from patients and their families – but also colleagues and administrators. Yet, in our time of horror and need, in those moments of vulnerability ... silence. Eventually, lengthy proclamations of support were expressed through various media. However, it felt too safe, too corporate, and too generic and inauthentic. As a result, an exodus of Black physicians from leadership positions and academic medicine took hold as the blatant continuation of rhetoric – coupled with ineffective outreach and support – finally took its toll.
Frequently, I question how the obstacles of medical school, residency, and beyond are expected to be traversed while living in a world that consistently affords additional challenges to those who look, act, or speak in a manner that varies from the perceived standard. In a culture where the myth of the super doctor reigns, how do we reconcile attainment of a false and detrimental narrative while the overarching pressure acutely felt by Black physicians magnifies in the setting of stereotypes, sociopolitical turbulence, bigotry, and racism? How can one sacrifice for an entity that is unwilling to acknowledge the psychological implications of that sacrifice?
For instance, while in medical school, I transitioned my hair to its natural state but was counseled against doing so because of the risk of losing residency opportunities as a direct result of my “unprofessional” appearance. Throughout residency, multiple incidents come to mind, including frequent demands to see my hospital badge despite the same not being of asked of my White cohorts; denial of entry into physician entrance within the residency building because, despite my professional attire, I was presumed to be a member of the custodial staff; and patients being confused and asking for a doctor despite my long white coat and clear introductions.
Furthermore, the fluency of my speech and the absence of regional dialect or vernacular are quite often lauded by patients. Inquiries to touch my hair as well as hypotheses regarding my nationality or degree of “blackness” with respect to the shape of my nose, eyes, and lips are openly questioned. Unfortunately, those uncomfortable incidents have not been limited to patient encounters.
In one instance, while presenting a patient in the presence of my attending and a 3rd-year medical student, I was sternly admonished for disclosing the race of the patient. I sat still and resolute as this doctor spoke on increased risk of bias in diagnosis and treatment when race is identified. Outwardly, I projected patience but inside, I seethed. In that moment, I realized that I would never have the luxury of ignorance or denial. Although I desire to be valued for my prowess in medicine, the mythical status was not created with my skin color in mind. For is avoidance not but a reflection of denial?
In these chaotic and uncertain times, how can we continue to promote a pathological ideal when the roads traveled are so fundamentally skewed? If a White physician faces a belligerent and argumentative patient, there is opportunity for debriefing both individually and among a larger cohort via classes, conferences, and supervisions. Conversely, when a Black physician is derided with racist sentiment, will they have the same opportunity for reflection and support? Despite identical expectations of professionalism and growth, how can one be successful in a system that either directly or indirectly encourages the opposite?
As we try to shed the super-doctor myth, we must recognize that this unattainable and detrimental persona hinders progress. This myth undermines our ability to understand our fragility, the limitations of our capabilities, and the strength of our vulnerability. We must take an honest look at the manner in which our individual biases and the deeply ingrained (and potentially unconscious) systemic biases are counterintuitive to the success and support of physicians of color.
Dr. Thomas is a board-certified adult psychiatrist with an interest in chronic illness, women’s behavioral health, and minority mental health. She currently practices in North Kingstown and East Providence, R.I. She has no conflicts of interest.
Is this a psychiatric emergency? How to screen, assess, and triage safety concerns from the primary care office
Case vignette: Laura is a 14-year-old biological girl who presents to your office for a routine well-child visit. She is doing well medically but notes that over the past 3 months she has been having increasing thoughts of suicide and has self-harmed via cutting on her wrists with a blade removed from a shaving razor. You contemplate what the most salient questions are in order to determine the best disposition for your patient.
The case vignette above may sound like one that you have heard before, and if not, you undoubtedly will encounter such a situation moving forward. The rate of suicidal ideation amongst youth ages 10-24 has increased by 57.4% between 2007 and 2018.1 Furthermore, suicide is the second leading cause of death in those aged 10 through young adulthood.2 According to the Centers for Disease Control and Prevention’s 2019 High School Youth Risk Behavior Survey, 18.8% of high school students seriously considered attempting suicide, 15.7% made a plan about how they would attempt suicide, and 8.9% actually attempted suicide, with 2.5% having a suicide attempt that resulted in an injury, poisoning, or overdose that had to be treated by a doctor or nurse during the 12 months before the survey.3 Children often present first to their primary care provider, and they may be the first individual who the child shares their suicidal or self-harm thoughts with. It may be useful to have a standardized approach, while using your own clinical judgment, to determine best next steps. Given the significant recent surge in children presenting to the emergency department for psychiatric needs and that environment having its own limitations (for example, long wait times, nontherapeutic space, etc.), a simple screen and brief assessment may lead to being able to maintain a patient safely outside of the hospital.
Screen all appropriate patients for suicide
There are, at minimum, three validated screening tools that can be used as to determine what the best next step should be. They include the Ask Suicide-Screening Questions (ASQ) developed by the National Institute of Mental Health, the Columbia-Suicide Severity Rating Scale (C-SSRS), and the PHQ-9 (modified for adolescents). We can highlight one of the screening tools here as noted below, but the choice of screener may be based on facility and/or clinician preference.
The Ask Suicide-Screening Questions
The ASQ, developed by the National Institute of Mental Health, include the following four binary questions plus a fifth acuity question, as follows:
1. In the past few weeks, have you wished you were dead?
2. In the past few weeks, have you felt that you or your family would be better off if you were dead?
3. In the past week, have you been having thoughts about killing yourself?
4. Have you ever tried to kill yourself?
a. If yes, how?
b. When?
The following acuity question is to be asked if any of the above are answered “yes”:
5. Are you having thoughts of killing yourself right now?
a. If yes, please describe.
Assess the level of risk
Once you have screened a patient, you need to assess the level of risk to help determine the level of care required. Returning to our original case vignette, does the patient warrant outpatient management, crisis evaluation, or an emergency psychiatric evaluation? You may have already decided that the patient needs an emergency mental health evaluation from a local crisis clinician evaluation and/or the emergency department. However, you may also find that the screen did not elicit imminent concern, but it does warrant a brief assessment to further elucidate the level of risk and proper disposition. One such instrument that may be helpful is the Brief Suicide Safety Assessment (BSSA) – also developed by the NIMH as a tool linked to the ASQ. There are clear and specific instructions in the BSSA with suggestions on how to ask questions. Important components to the BSSA include:
- A focus on a more thorough clinical history – including frequency of suicidal ideation, suicide plan, past behavior, associated symptoms, and social support/stressors
- Collateral information (e.g., further details from those who know the patient such as family/friends).
- Safety planning.
- Determining disposition.
The BSSA may suggest that a crisis/psychiatric evaluation is warranted or suggest that a safety plan with a mental health referral will likely be sufficient.
Triage and safety planning
A safety plan should be created if you determine that a patient can be safely maintained as an outpatient based on your screening, assessment, and triaging. Traditional safety plans come in many different forms and can be found online (Example of a Safety Plan Template). However, most safety plans include some version of the following:
- Increased supervision: 24/7 supervision with doors open/unlocked.
- Reduced access: medications (prescription and OTC) locked away; sharps and firearms secured.
- Adaptive coping strategies (e.g., relaxation techniques such as drawing or listening to music).
- Reliable persons for support (e.g., parent, therapist, school counselor).
- Outpatient mental health provider follow-up and/or referral.
- Provision of local crisis and national hotline contact information.
- Use of a safety plan phone app completed with patient.
Envision a safety plan as a living document that evolves, grows, and changes with your patient/family – one that can be easily reviewed/updated at each visit.
Returning to our case vignette
Laura returns to your office for a follow-up after a 10-day stay at a hospital-diversion program or inpatient psychiatric unit. The decision is made to use the primary care NIMH ASQ/BSSA algorithm, and you determine the patient to not be at imminent risk following the screen and assessment. Laura is triaged as appropriate for outpatient care, you collaborate to update the safety plan, regular follow-ups are scheduled, and a mental health referral has been placed. Thus, there are tools to assist with screening, assessing, and triaging pediatric patients with suicidal ideation that provide the patient with appropriate care and treatment and may help alleviate the need to have a patient present to the emergency department.
Dr. Abdul-Karim is a child psychiatrist at the University of Vermont University Children’s Hospital in Burlington.
Additional resources
The American Academy of Child and Adolescent Psychiatry has developed information that can be provided to families about suicide safety precautions that can be taken at home, which can be found here: Facts for Families. Suicide Safety: Precautions at Home.
Screening tools listed above can be found here:
ASQ Toolkit.
C-SSRS.
PHQ-9 Modified for Adolescents (PHQ-A).
References
1. Curtin SC. National Center for Health Statistics. “State Suicide Rates Among Adolescents and Young Adults Aged 10-24: United States, 2000-2018” National Vital Statistics Reports..
2. Centers for Disease Control and Prevention, National Center for Health Statistics. “Underlying Cause of Death 2018-2019” CDC WONDER Online Database. Accessed 2021 Jul 31, 6:57:39 p.m.
3. Centers for Disease Control and Prevention. 1991-2019 High School Youth Risk Behavior Survey Data.
Case vignette: Laura is a 14-year-old biological girl who presents to your office for a routine well-child visit. She is doing well medically but notes that over the past 3 months she has been having increasing thoughts of suicide and has self-harmed via cutting on her wrists with a blade removed from a shaving razor. You contemplate what the most salient questions are in order to determine the best disposition for your patient.
The case vignette above may sound like one that you have heard before, and if not, you undoubtedly will encounter such a situation moving forward. The rate of suicidal ideation amongst youth ages 10-24 has increased by 57.4% between 2007 and 2018.1 Furthermore, suicide is the second leading cause of death in those aged 10 through young adulthood.2 According to the Centers for Disease Control and Prevention’s 2019 High School Youth Risk Behavior Survey, 18.8% of high school students seriously considered attempting suicide, 15.7% made a plan about how they would attempt suicide, and 8.9% actually attempted suicide, with 2.5% having a suicide attempt that resulted in an injury, poisoning, or overdose that had to be treated by a doctor or nurse during the 12 months before the survey.3 Children often present first to their primary care provider, and they may be the first individual who the child shares their suicidal or self-harm thoughts with. It may be useful to have a standardized approach, while using your own clinical judgment, to determine best next steps. Given the significant recent surge in children presenting to the emergency department for psychiatric needs and that environment having its own limitations (for example, long wait times, nontherapeutic space, etc.), a simple screen and brief assessment may lead to being able to maintain a patient safely outside of the hospital.
Screen all appropriate patients for suicide
There are, at minimum, three validated screening tools that can be used as to determine what the best next step should be. They include the Ask Suicide-Screening Questions (ASQ) developed by the National Institute of Mental Health, the Columbia-Suicide Severity Rating Scale (C-SSRS), and the PHQ-9 (modified for adolescents). We can highlight one of the screening tools here as noted below, but the choice of screener may be based on facility and/or clinician preference.
The Ask Suicide-Screening Questions
The ASQ, developed by the National Institute of Mental Health, include the following four binary questions plus a fifth acuity question, as follows:
1. In the past few weeks, have you wished you were dead?
2. In the past few weeks, have you felt that you or your family would be better off if you were dead?
3. In the past week, have you been having thoughts about killing yourself?
4. Have you ever tried to kill yourself?
a. If yes, how?
b. When?
The following acuity question is to be asked if any of the above are answered “yes”:
5. Are you having thoughts of killing yourself right now?
a. If yes, please describe.
Assess the level of risk
Once you have screened a patient, you need to assess the level of risk to help determine the level of care required. Returning to our original case vignette, does the patient warrant outpatient management, crisis evaluation, or an emergency psychiatric evaluation? You may have already decided that the patient needs an emergency mental health evaluation from a local crisis clinician evaluation and/or the emergency department. However, you may also find that the screen did not elicit imminent concern, but it does warrant a brief assessment to further elucidate the level of risk and proper disposition. One such instrument that may be helpful is the Brief Suicide Safety Assessment (BSSA) – also developed by the NIMH as a tool linked to the ASQ. There are clear and specific instructions in the BSSA with suggestions on how to ask questions. Important components to the BSSA include:
- A focus on a more thorough clinical history – including frequency of suicidal ideation, suicide plan, past behavior, associated symptoms, and social support/stressors
- Collateral information (e.g., further details from those who know the patient such as family/friends).
- Safety planning.
- Determining disposition.
The BSSA may suggest that a crisis/psychiatric evaluation is warranted or suggest that a safety plan with a mental health referral will likely be sufficient.
Triage and safety planning
A safety plan should be created if you determine that a patient can be safely maintained as an outpatient based on your screening, assessment, and triaging. Traditional safety plans come in many different forms and can be found online (Example of a Safety Plan Template). However, most safety plans include some version of the following:
- Increased supervision: 24/7 supervision with doors open/unlocked.
- Reduced access: medications (prescription and OTC) locked away; sharps and firearms secured.
- Adaptive coping strategies (e.g., relaxation techniques such as drawing or listening to music).
- Reliable persons for support (e.g., parent, therapist, school counselor).
- Outpatient mental health provider follow-up and/or referral.
- Provision of local crisis and national hotline contact information.
- Use of a safety plan phone app completed with patient.
Envision a safety plan as a living document that evolves, grows, and changes with your patient/family – one that can be easily reviewed/updated at each visit.
Returning to our case vignette
Laura returns to your office for a follow-up after a 10-day stay at a hospital-diversion program or inpatient psychiatric unit. The decision is made to use the primary care NIMH ASQ/BSSA algorithm, and you determine the patient to not be at imminent risk following the screen and assessment. Laura is triaged as appropriate for outpatient care, you collaborate to update the safety plan, regular follow-ups are scheduled, and a mental health referral has been placed. Thus, there are tools to assist with screening, assessing, and triaging pediatric patients with suicidal ideation that provide the patient with appropriate care and treatment and may help alleviate the need to have a patient present to the emergency department.
Dr. Abdul-Karim is a child psychiatrist at the University of Vermont University Children’s Hospital in Burlington.
Additional resources
The American Academy of Child and Adolescent Psychiatry has developed information that can be provided to families about suicide safety precautions that can be taken at home, which can be found here: Facts for Families. Suicide Safety: Precautions at Home.
Screening tools listed above can be found here:
ASQ Toolkit.
C-SSRS.
PHQ-9 Modified for Adolescents (PHQ-A).
References
1. Curtin SC. National Center for Health Statistics. “State Suicide Rates Among Adolescents and Young Adults Aged 10-24: United States, 2000-2018” National Vital Statistics Reports..
2. Centers for Disease Control and Prevention, National Center for Health Statistics. “Underlying Cause of Death 2018-2019” CDC WONDER Online Database. Accessed 2021 Jul 31, 6:57:39 p.m.
3. Centers for Disease Control and Prevention. 1991-2019 High School Youth Risk Behavior Survey Data.
Case vignette: Laura is a 14-year-old biological girl who presents to your office for a routine well-child visit. She is doing well medically but notes that over the past 3 months she has been having increasing thoughts of suicide and has self-harmed via cutting on her wrists with a blade removed from a shaving razor. You contemplate what the most salient questions are in order to determine the best disposition for your patient.
The case vignette above may sound like one that you have heard before, and if not, you undoubtedly will encounter such a situation moving forward. The rate of suicidal ideation amongst youth ages 10-24 has increased by 57.4% between 2007 and 2018.1 Furthermore, suicide is the second leading cause of death in those aged 10 through young adulthood.2 According to the Centers for Disease Control and Prevention’s 2019 High School Youth Risk Behavior Survey, 18.8% of high school students seriously considered attempting suicide, 15.7% made a plan about how they would attempt suicide, and 8.9% actually attempted suicide, with 2.5% having a suicide attempt that resulted in an injury, poisoning, or overdose that had to be treated by a doctor or nurse during the 12 months before the survey.3 Children often present first to their primary care provider, and they may be the first individual who the child shares their suicidal or self-harm thoughts with. It may be useful to have a standardized approach, while using your own clinical judgment, to determine best next steps. Given the significant recent surge in children presenting to the emergency department for psychiatric needs and that environment having its own limitations (for example, long wait times, nontherapeutic space, etc.), a simple screen and brief assessment may lead to being able to maintain a patient safely outside of the hospital.
Screen all appropriate patients for suicide
There are, at minimum, three validated screening tools that can be used as to determine what the best next step should be. They include the Ask Suicide-Screening Questions (ASQ) developed by the National Institute of Mental Health, the Columbia-Suicide Severity Rating Scale (C-SSRS), and the PHQ-9 (modified for adolescents). We can highlight one of the screening tools here as noted below, but the choice of screener may be based on facility and/or clinician preference.
The Ask Suicide-Screening Questions
The ASQ, developed by the National Institute of Mental Health, include the following four binary questions plus a fifth acuity question, as follows:
1. In the past few weeks, have you wished you were dead?
2. In the past few weeks, have you felt that you or your family would be better off if you were dead?
3. In the past week, have you been having thoughts about killing yourself?
4. Have you ever tried to kill yourself?
a. If yes, how?
b. When?
The following acuity question is to be asked if any of the above are answered “yes”:
5. Are you having thoughts of killing yourself right now?
a. If yes, please describe.
Assess the level of risk
Once you have screened a patient, you need to assess the level of risk to help determine the level of care required. Returning to our original case vignette, does the patient warrant outpatient management, crisis evaluation, or an emergency psychiatric evaluation? You may have already decided that the patient needs an emergency mental health evaluation from a local crisis clinician evaluation and/or the emergency department. However, you may also find that the screen did not elicit imminent concern, but it does warrant a brief assessment to further elucidate the level of risk and proper disposition. One such instrument that may be helpful is the Brief Suicide Safety Assessment (BSSA) – also developed by the NIMH as a tool linked to the ASQ. There are clear and specific instructions in the BSSA with suggestions on how to ask questions. Important components to the BSSA include:
- A focus on a more thorough clinical history – including frequency of suicidal ideation, suicide plan, past behavior, associated symptoms, and social support/stressors
- Collateral information (e.g., further details from those who know the patient such as family/friends).
- Safety planning.
- Determining disposition.
The BSSA may suggest that a crisis/psychiatric evaluation is warranted or suggest that a safety plan with a mental health referral will likely be sufficient.
Triage and safety planning
A safety plan should be created if you determine that a patient can be safely maintained as an outpatient based on your screening, assessment, and triaging. Traditional safety plans come in many different forms and can be found online (Example of a Safety Plan Template). However, most safety plans include some version of the following:
- Increased supervision: 24/7 supervision with doors open/unlocked.
- Reduced access: medications (prescription and OTC) locked away; sharps and firearms secured.
- Adaptive coping strategies (e.g., relaxation techniques such as drawing or listening to music).
- Reliable persons for support (e.g., parent, therapist, school counselor).
- Outpatient mental health provider follow-up and/or referral.
- Provision of local crisis and national hotline contact information.
- Use of a safety plan phone app completed with patient.
Envision a safety plan as a living document that evolves, grows, and changes with your patient/family – one that can be easily reviewed/updated at each visit.
Returning to our case vignette
Laura returns to your office for a follow-up after a 10-day stay at a hospital-diversion program or inpatient psychiatric unit. The decision is made to use the primary care NIMH ASQ/BSSA algorithm, and you determine the patient to not be at imminent risk following the screen and assessment. Laura is triaged as appropriate for outpatient care, you collaborate to update the safety plan, regular follow-ups are scheduled, and a mental health referral has been placed. Thus, there are tools to assist with screening, assessing, and triaging pediatric patients with suicidal ideation that provide the patient with appropriate care and treatment and may help alleviate the need to have a patient present to the emergency department.
Dr. Abdul-Karim is a child psychiatrist at the University of Vermont University Children’s Hospital in Burlington.
Additional resources
The American Academy of Child and Adolescent Psychiatry has developed information that can be provided to families about suicide safety precautions that can be taken at home, which can be found here: Facts for Families. Suicide Safety: Precautions at Home.
Screening tools listed above can be found here:
ASQ Toolkit.
C-SSRS.
PHQ-9 Modified for Adolescents (PHQ-A).
References
1. Curtin SC. National Center for Health Statistics. “State Suicide Rates Among Adolescents and Young Adults Aged 10-24: United States, 2000-2018” National Vital Statistics Reports..
2. Centers for Disease Control and Prevention, National Center for Health Statistics. “Underlying Cause of Death 2018-2019” CDC WONDER Online Database. Accessed 2021 Jul 31, 6:57:39 p.m.
3. Centers for Disease Control and Prevention. 1991-2019 High School Youth Risk Behavior Survey Data.