User login
Enhanced recovery protocol speeds discharge, decreases readmissions for ventral hernia repair
A postsurgical recovery program featuring early feeding and multimodal pain management hastened the return of bowel function and shortened hospital stay by 2 days for patients undergoing complex ventral hernia repair.
Despite leaving the hospital sooner, however, patients were 75% less likely to be readmitted within 90 days, Dr. Arnab Majumder and his colleagues wrote in the June issue of the Journal of the American College of Surgeons (2016 Jun;222:1106-15). Most of those who did return had wound complications, a stark contrast to readmissions among patients who didn’t experience the enhanced recovery program. Among that group, 75% of the readmissions were caused by bowel obstruction/ileus, deep venous thrombosis or pulmonary embolism, pneumonia, and urinary tract infections – all of them “problems [that] could be related to prolonged hospitalizations,” said Dr. Majumder of the University Hospitals Case Medical Center, Cleveland.
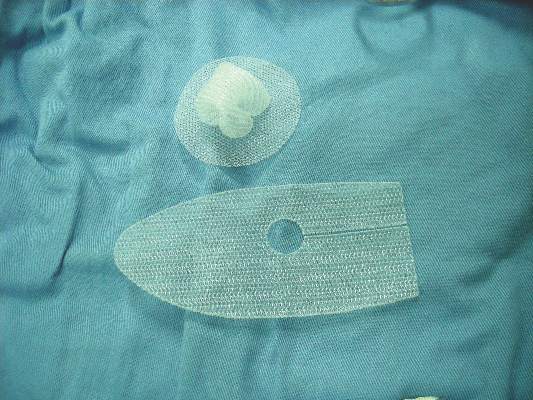
The investigators created an Enhanced Recovery After Surgery (ERAS) pathway specifically for patients undergoing complex ventral hernia repairs using transversus abdominis release and sublay synthetic mesh placement. The patients “present formidable challenges to the surgeon, not only in the operating room but also during perioperative management,” the authors noted.
The ERAS the team preemptively addressed patient issues in the preoperative, intra- and perioperative, and postoperative periods. They compared the outcomes of 100 patients treated with the protocol to those in a control group of 100 who underwent the same surgery before the protocol was implemented. The main outcomes measures were time to diet advancement, time to return of bowel function, time to oral narcotics, length of stay, and 90-day readmissions.
The ERAS begins with preoperative optimization. This consists of weight loss, smoking cessation, and managing diabetes and obstructive sleep apnea. No surgery occurs until the HbA1c is less than 8 and patients have been tobacco free for at least 1 month.
All patients receive an arginine and omega-3 supplement thrice daily for 5 days before surgery. The night before surgery, they have a nasal swab screen for methicillin-resistant Staphylococcus aureus (MRSA), and decolonization with mupirocin ointment and a chlorhexidine bath.
Preoperatively, they receive 5,000 units of unfractionated heparin, along with sequential compression devices for deep vein thrombosis protection. Use of both continue postoperatively, with heparin given every 8 hours until the patient is ambulatory.
Those without a history of narcotic use receive a preoperative dose of alvimopan. Everyone also receives oral gabapentin and preoperative antibiotics.
Intraoperatively, intravenous fluids are given judiciously to minimize bowel edema and decrease the risk of respiratory side effects. The surgeon also employs a transversus abdominis plane (TAP) block with liposomal bupivacaine.
There is a multimodal pain management program, which includes intravenous hydromorphone by patient-controlled anesthesia pump and oral gabapentin three times daily. Patients switch to oral analgesics on postoperative day 2. These consist of acetaminophen and NSAIDs on an alternating schedule. Intravenous diazepam can be added as an antispasmodic. Alvimopan is continued twice daily until first bowel movement or hospital discharge.
Clear liquids are limited to 250 mL/8 hours on postoperative day 1, along with a clear protein drink. By day 2, patients are advanced to unrestricted volumes of clear liquids, and on day 3, to a regular solid diet. At that point, the clear protein drink is switched for a regular protein drink (Boost Plus).
Patients who vomit or require a nasogastric tube for decompression, and those with severe persistent nausea are made NPO, but can resume diet when these symptoms improve. Those with mild-moderate nausea receive intravenous ondansetron and are allowed to self-limit oral intake.
Patients were a mean of 57 years old with a mean body mass index of about 33 kg/m2. The hernia was recurrent for about 60% of each group, with a mean area of about 300 cm2, and a mean width of 14 cm. The mean mesh size was about 1,000 cm2. The mean operative time was significantly shorter in the control group: 197 vs. 245 minutes.
Diet was advanced significantly more quickly in the ERAS group than the control group: 1 vs. 2 days on a liquid diet and 3 vs. 4.8 days to regular diet. Emesis after diet advancement was similar (4% for ERAS and 5% for control).
Compared with the control group, the ERAS group experienced significantly shorter average times to flatus (3.1 vs. 3.9 days), bowel movement (3.6 vs. 5.2 days), and reaching GI-3 status (3.4 vs. 4.8 days). Those in the ERAS group switched to oral narcotics sooner (2.2 vs. 3.6 days) also.
The average length of stay was significantly lower in ERAS group as well (4 vs. 6 days). About 18% of those in the ERAS group had a stay of less than 3 days, compared with 2% of the control group.
Readmissions within 90 days occurred in 16% of the control group and 4% of the ERAS group – a significant difference. There were four surgical site complications in the control group and three in the ERAS group. Bowel obstruction occurred in three control patients and one ERAS patient. All other complications requiring readmission occurred in the control group: two pulmonary embolisms, two deep vein thromboses, one pneumonia, one urinary tract infection and three other unspecified causes.
The authors noted that the shift to multimodal pain management and shorter-term use of IV opiates is a large contributor to the protocol’s good bowel outcomes. “Introduction of preoperative and postoperative gabapentin, intraoperative surgeon-delivered TAP block with long-acting liposomal bupivacaine, postoperative use of acetaminophen, and nonsteroidal agents have all appeared to contribute to better pain control and likely decrease in opioid consumption,” they said.
The use of diazepam as a pain medication is unusual, they said, but effective.
“We believe a large component of postoperative pain in hernia patients is due to muscle spasms after myofascial release, irritation from mesh placement, and transabdominal suture fixation. Therefore, in the context of our frequent use of myofascial releases for large incisional hernias, we believe the antispasmodic effects of diazepam potentially alleviate some of the postoperative discomfort caused by major abdominal wall reconstruction.”
None of the investigators reported financial conflicts.
A postsurgical recovery program featuring early feeding and multimodal pain management hastened the return of bowel function and shortened hospital stay by 2 days for patients undergoing complex ventral hernia repair.
Despite leaving the hospital sooner, however, patients were 75% less likely to be readmitted within 90 days, Dr. Arnab Majumder and his colleagues wrote in the June issue of the Journal of the American College of Surgeons (2016 Jun;222:1106-15). Most of those who did return had wound complications, a stark contrast to readmissions among patients who didn’t experience the enhanced recovery program. Among that group, 75% of the readmissions were caused by bowel obstruction/ileus, deep venous thrombosis or pulmonary embolism, pneumonia, and urinary tract infections – all of them “problems [that] could be related to prolonged hospitalizations,” said Dr. Majumder of the University Hospitals Case Medical Center, Cleveland.
The investigators created an Enhanced Recovery After Surgery (ERAS) pathway specifically for patients undergoing complex ventral hernia repairs using transversus abdominis release and sublay synthetic mesh placement. The patients “present formidable challenges to the surgeon, not only in the operating room but also during perioperative management,” the authors noted.
The ERAS the team preemptively addressed patient issues in the preoperative, intra- and perioperative, and postoperative periods. They compared the outcomes of 100 patients treated with the protocol to those in a control group of 100 who underwent the same surgery before the protocol was implemented. The main outcomes measures were time to diet advancement, time to return of bowel function, time to oral narcotics, length of stay, and 90-day readmissions.
The ERAS begins with preoperative optimization. This consists of weight loss, smoking cessation, and managing diabetes and obstructive sleep apnea. No surgery occurs until the HbA1c is less than 8 and patients have been tobacco free for at least 1 month.
All patients receive an arginine and omega-3 supplement thrice daily for 5 days before surgery. The night before surgery, they have a nasal swab screen for methicillin-resistant Staphylococcus aureus (MRSA), and decolonization with mupirocin ointment and a chlorhexidine bath.
Preoperatively, they receive 5,000 units of unfractionated heparin, along with sequential compression devices for deep vein thrombosis protection. Use of both continue postoperatively, with heparin given every 8 hours until the patient is ambulatory.
Those without a history of narcotic use receive a preoperative dose of alvimopan. Everyone also receives oral gabapentin and preoperative antibiotics.
Intraoperatively, intravenous fluids are given judiciously to minimize bowel edema and decrease the risk of respiratory side effects. The surgeon also employs a transversus abdominis plane (TAP) block with liposomal bupivacaine.
There is a multimodal pain management program, which includes intravenous hydromorphone by patient-controlled anesthesia pump and oral gabapentin three times daily. Patients switch to oral analgesics on postoperative day 2. These consist of acetaminophen and NSAIDs on an alternating schedule. Intravenous diazepam can be added as an antispasmodic. Alvimopan is continued twice daily until first bowel movement or hospital discharge.
Clear liquids are limited to 250 mL/8 hours on postoperative day 1, along with a clear protein drink. By day 2, patients are advanced to unrestricted volumes of clear liquids, and on day 3, to a regular solid diet. At that point, the clear protein drink is switched for a regular protein drink (Boost Plus).
Patients who vomit or require a nasogastric tube for decompression, and those with severe persistent nausea are made NPO, but can resume diet when these symptoms improve. Those with mild-moderate nausea receive intravenous ondansetron and are allowed to self-limit oral intake.
Patients were a mean of 57 years old with a mean body mass index of about 33 kg/m2. The hernia was recurrent for about 60% of each group, with a mean area of about 300 cm2, and a mean width of 14 cm. The mean mesh size was about 1,000 cm2. The mean operative time was significantly shorter in the control group: 197 vs. 245 minutes.
Diet was advanced significantly more quickly in the ERAS group than the control group: 1 vs. 2 days on a liquid diet and 3 vs. 4.8 days to regular diet. Emesis after diet advancement was similar (4% for ERAS and 5% for control).
Compared with the control group, the ERAS group experienced significantly shorter average times to flatus (3.1 vs. 3.9 days), bowel movement (3.6 vs. 5.2 days), and reaching GI-3 status (3.4 vs. 4.8 days). Those in the ERAS group switched to oral narcotics sooner (2.2 vs. 3.6 days) also.
The average length of stay was significantly lower in ERAS group as well (4 vs. 6 days). About 18% of those in the ERAS group had a stay of less than 3 days, compared with 2% of the control group.
Readmissions within 90 days occurred in 16% of the control group and 4% of the ERAS group – a significant difference. There were four surgical site complications in the control group and three in the ERAS group. Bowel obstruction occurred in three control patients and one ERAS patient. All other complications requiring readmission occurred in the control group: two pulmonary embolisms, two deep vein thromboses, one pneumonia, one urinary tract infection and three other unspecified causes.
The authors noted that the shift to multimodal pain management and shorter-term use of IV opiates is a large contributor to the protocol’s good bowel outcomes. “Introduction of preoperative and postoperative gabapentin, intraoperative surgeon-delivered TAP block with long-acting liposomal bupivacaine, postoperative use of acetaminophen, and nonsteroidal agents have all appeared to contribute to better pain control and likely decrease in opioid consumption,” they said.
The use of diazepam as a pain medication is unusual, they said, but effective.
“We believe a large component of postoperative pain in hernia patients is due to muscle spasms after myofascial release, irritation from mesh placement, and transabdominal suture fixation. Therefore, in the context of our frequent use of myofascial releases for large incisional hernias, we believe the antispasmodic effects of diazepam potentially alleviate some of the postoperative discomfort caused by major abdominal wall reconstruction.”
None of the investigators reported financial conflicts.
A postsurgical recovery program featuring early feeding and multimodal pain management hastened the return of bowel function and shortened hospital stay by 2 days for patients undergoing complex ventral hernia repair.
Despite leaving the hospital sooner, however, patients were 75% less likely to be readmitted within 90 days, Dr. Arnab Majumder and his colleagues wrote in the June issue of the Journal of the American College of Surgeons (2016 Jun;222:1106-15). Most of those who did return had wound complications, a stark contrast to readmissions among patients who didn’t experience the enhanced recovery program. Among that group, 75% of the readmissions were caused by bowel obstruction/ileus, deep venous thrombosis or pulmonary embolism, pneumonia, and urinary tract infections – all of them “problems [that] could be related to prolonged hospitalizations,” said Dr. Majumder of the University Hospitals Case Medical Center, Cleveland.
The investigators created an Enhanced Recovery After Surgery (ERAS) pathway specifically for patients undergoing complex ventral hernia repairs using transversus abdominis release and sublay synthetic mesh placement. The patients “present formidable challenges to the surgeon, not only in the operating room but also during perioperative management,” the authors noted.
The ERAS the team preemptively addressed patient issues in the preoperative, intra- and perioperative, and postoperative periods. They compared the outcomes of 100 patients treated with the protocol to those in a control group of 100 who underwent the same surgery before the protocol was implemented. The main outcomes measures were time to diet advancement, time to return of bowel function, time to oral narcotics, length of stay, and 90-day readmissions.
The ERAS begins with preoperative optimization. This consists of weight loss, smoking cessation, and managing diabetes and obstructive sleep apnea. No surgery occurs until the HbA1c is less than 8 and patients have been tobacco free for at least 1 month.
All patients receive an arginine and omega-3 supplement thrice daily for 5 days before surgery. The night before surgery, they have a nasal swab screen for methicillin-resistant Staphylococcus aureus (MRSA), and decolonization with mupirocin ointment and a chlorhexidine bath.
Preoperatively, they receive 5,000 units of unfractionated heparin, along with sequential compression devices for deep vein thrombosis protection. Use of both continue postoperatively, with heparin given every 8 hours until the patient is ambulatory.
Those without a history of narcotic use receive a preoperative dose of alvimopan. Everyone also receives oral gabapentin and preoperative antibiotics.
Intraoperatively, intravenous fluids are given judiciously to minimize bowel edema and decrease the risk of respiratory side effects. The surgeon also employs a transversus abdominis plane (TAP) block with liposomal bupivacaine.
There is a multimodal pain management program, which includes intravenous hydromorphone by patient-controlled anesthesia pump and oral gabapentin three times daily. Patients switch to oral analgesics on postoperative day 2. These consist of acetaminophen and NSAIDs on an alternating schedule. Intravenous diazepam can be added as an antispasmodic. Alvimopan is continued twice daily until first bowel movement or hospital discharge.
Clear liquids are limited to 250 mL/8 hours on postoperative day 1, along with a clear protein drink. By day 2, patients are advanced to unrestricted volumes of clear liquids, and on day 3, to a regular solid diet. At that point, the clear protein drink is switched for a regular protein drink (Boost Plus).
Patients who vomit or require a nasogastric tube for decompression, and those with severe persistent nausea are made NPO, but can resume diet when these symptoms improve. Those with mild-moderate nausea receive intravenous ondansetron and are allowed to self-limit oral intake.
Patients were a mean of 57 years old with a mean body mass index of about 33 kg/m2. The hernia was recurrent for about 60% of each group, with a mean area of about 300 cm2, and a mean width of 14 cm. The mean mesh size was about 1,000 cm2. The mean operative time was significantly shorter in the control group: 197 vs. 245 minutes.
Diet was advanced significantly more quickly in the ERAS group than the control group: 1 vs. 2 days on a liquid diet and 3 vs. 4.8 days to regular diet. Emesis after diet advancement was similar (4% for ERAS and 5% for control).
Compared with the control group, the ERAS group experienced significantly shorter average times to flatus (3.1 vs. 3.9 days), bowel movement (3.6 vs. 5.2 days), and reaching GI-3 status (3.4 vs. 4.8 days). Those in the ERAS group switched to oral narcotics sooner (2.2 vs. 3.6 days) also.
The average length of stay was significantly lower in ERAS group as well (4 vs. 6 days). About 18% of those in the ERAS group had a stay of less than 3 days, compared with 2% of the control group.
Readmissions within 90 days occurred in 16% of the control group and 4% of the ERAS group – a significant difference. There were four surgical site complications in the control group and three in the ERAS group. Bowel obstruction occurred in three control patients and one ERAS patient. All other complications requiring readmission occurred in the control group: two pulmonary embolisms, two deep vein thromboses, one pneumonia, one urinary tract infection and three other unspecified causes.
The authors noted that the shift to multimodal pain management and shorter-term use of IV opiates is a large contributor to the protocol’s good bowel outcomes. “Introduction of preoperative and postoperative gabapentin, intraoperative surgeon-delivered TAP block with long-acting liposomal bupivacaine, postoperative use of acetaminophen, and nonsteroidal agents have all appeared to contribute to better pain control and likely decrease in opioid consumption,” they said.
The use of diazepam as a pain medication is unusual, they said, but effective.
“We believe a large component of postoperative pain in hernia patients is due to muscle spasms after myofascial release, irritation from mesh placement, and transabdominal suture fixation. Therefore, in the context of our frequent use of myofascial releases for large incisional hernias, we believe the antispasmodic effects of diazepam potentially alleviate some of the postoperative discomfort caused by major abdominal wall reconstruction.”
None of the investigators reported financial conflicts.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF SURGEONS
Key clinical point: Early enteral feeding and multimodal pain management both contributed to early return of bowel function.
Major finding: Length of stay was 2 days shorter, and readmissions decreased by 75%, compared with a control group.
Data source: The prospective study comprised 200 patients.
Disclosures: Neither Dr. Majumder nor his colleagues had any financial disclosures.
Consider patient-centered outcomes in ventral hernia repair decision
CHICAGO – Elective ventral hernia repair improves hernia-related quality of life for low- to moderate-risk patients, according to findings from a prospective patient-centered study.
The findings suggest that the risks and benefits of a conservative operative strategy should be reassessed, and that patient-centered outcomes should be considered, Dr. Julie Holihan reported at the annual meeting of the American Surgical Association.
Of 152 patients with a ventral hernia from a single hernia clinic, 97 were managed non-operatively, and 55 were managed operatively. In a propensity-matched cohort of 90 patients with similar demographics, baseline comorbidities, and quality of life scores, only operatively managed patients had improved quality of life scores at 6 months (improvement from 34.7 to 56.9 vs. from 35.6 to 36.6), according to Dr. Holihan of the University of Texas, Houston.
Further, satisfaction scores increased significantly more in the operative than in the non-operative group at follow-up (from a median score of 2 at baseline in both groups to scores of 9 and 3, respectively), and pain scores decreased significantly more in the operative group than in the non-operative group (from a baseline score of 5 down to 3 in the operative group, with no change [score of 6] in the non-operative group).
Two surgical site infections and one hernia recurrence occurred in the operative group.
Notably, the predicted risk of surgery in the cohort was much greater than the observed risk.
“We may be overestimating surgical risk in these patients,” she said.
Based on a multivariable analysis in the overall cohort, non-operative management was strongly associated with lower quality of life score (coefficient, -26.5), Dr. Holihan said.
Nonoperative management of ventral hernias is often recommended for patients, particularly in those with increased risk of surgical complications due to factors such as obesity, poorly controlled diabetes, smoking, or significant comorbidities like coronary artery disease, but this approach to management has not been well studied with respect to patient-centered outcomes such as quality of life and function, she explained.
Traditional outcomes that have been studied, including infection and hernia recurrence, may not be the outcomes that are most important to patients, she added.
For the current study, patients with ventral hernias were prospectively enrolled between June 2014 and June 2015. Non-operative management was recommended for smokers, those with a body mass index greater than 33 kg/m2, and those with poorly controlled diabetes. Measured outcomes included surgical site infection, hernia recurrence, and quality of life using a validated quality of life measure.
This is the first prospective study comparing management strategies in ventral hernia patients with comorbidities, Dr. Holihan said.
She concluded that “the elective repair of ventral hernia, compared with non-operative management, improves patient-centered outcomes in similar-risk patients.”
“Furthermore, the low occurrence of complications suggests that we may be overestimating surgical risk and that we may be too conservative in our patient selection for elective ventral hernia repair. It may be time to reevaluate patient selection criteria in order to better incorporate patient-centered outcomes,” she said.
In response to a question about managing patients with higher risk and/or higher BMI, Dr. Holihan’s coauthor, Dr. Mike K. Liang, also of the University of Texas, Houston, noted that the findings of the study provide estimates for potential future randomized trials. He also noted that the moderate-risk patients at the center often undergo “prehabilitation,” or a preoperative exercise and diet program designed to help optimize outcomes. Currently, patients with BMI of 30-40 kg/m2 are randomized to preoperative rehabilitation vs. current care.
“BMI is a very important decision making factor. We were not able to pick a standardized point [with respect to BMI] for when to operate vs. non-operate. Because of that, we used BMI as a factor in developing our propensity score,” he said, explaining that this is why the propensity-matched groups had similar BMI, while the non-operative group in the overall cohort had substantially higher BMI.
A randomized trial on prehabilitation may be able to provide some insight into the effects of rapid changes in weight and how they affect outcomes in order to make the best choices regarding surgery.
“We do hypothesize that significant weight loss prior to surgery may improve outcomes, and may make the abdominal wall more compliant and enable us to tackle more challenging hernias. We also hypothesize that patients who have a sudden increase in weight after having their ventral hernia repaired may end up having worse outcomes. Hopefully in the next year we will be able to shed more light on these very important questions.”
The authors reported having no disclosures.
The complete manuscript of this presentation is anticipated to be published in the Annals of Surgery pending editorial review.
CHICAGO – Elective ventral hernia repair improves hernia-related quality of life for low- to moderate-risk patients, according to findings from a prospective patient-centered study.
The findings suggest that the risks and benefits of a conservative operative strategy should be reassessed, and that patient-centered outcomes should be considered, Dr. Julie Holihan reported at the annual meeting of the American Surgical Association.
Of 152 patients with a ventral hernia from a single hernia clinic, 97 were managed non-operatively, and 55 were managed operatively. In a propensity-matched cohort of 90 patients with similar demographics, baseline comorbidities, and quality of life scores, only operatively managed patients had improved quality of life scores at 6 months (improvement from 34.7 to 56.9 vs. from 35.6 to 36.6), according to Dr. Holihan of the University of Texas, Houston.
Further, satisfaction scores increased significantly more in the operative than in the non-operative group at follow-up (from a median score of 2 at baseline in both groups to scores of 9 and 3, respectively), and pain scores decreased significantly more in the operative group than in the non-operative group (from a baseline score of 5 down to 3 in the operative group, with no change [score of 6] in the non-operative group).
Two surgical site infections and one hernia recurrence occurred in the operative group.
Notably, the predicted risk of surgery in the cohort was much greater than the observed risk.
“We may be overestimating surgical risk in these patients,” she said.
Based on a multivariable analysis in the overall cohort, non-operative management was strongly associated with lower quality of life score (coefficient, -26.5), Dr. Holihan said.
Nonoperative management of ventral hernias is often recommended for patients, particularly in those with increased risk of surgical complications due to factors such as obesity, poorly controlled diabetes, smoking, or significant comorbidities like coronary artery disease, but this approach to management has not been well studied with respect to patient-centered outcomes such as quality of life and function, she explained.
Traditional outcomes that have been studied, including infection and hernia recurrence, may not be the outcomes that are most important to patients, she added.
For the current study, patients with ventral hernias were prospectively enrolled between June 2014 and June 2015. Non-operative management was recommended for smokers, those with a body mass index greater than 33 kg/m2, and those with poorly controlled diabetes. Measured outcomes included surgical site infection, hernia recurrence, and quality of life using a validated quality of life measure.
This is the first prospective study comparing management strategies in ventral hernia patients with comorbidities, Dr. Holihan said.
She concluded that “the elective repair of ventral hernia, compared with non-operative management, improves patient-centered outcomes in similar-risk patients.”
“Furthermore, the low occurrence of complications suggests that we may be overestimating surgical risk and that we may be too conservative in our patient selection for elective ventral hernia repair. It may be time to reevaluate patient selection criteria in order to better incorporate patient-centered outcomes,” she said.
In response to a question about managing patients with higher risk and/or higher BMI, Dr. Holihan’s coauthor, Dr. Mike K. Liang, also of the University of Texas, Houston, noted that the findings of the study provide estimates for potential future randomized trials. He also noted that the moderate-risk patients at the center often undergo “prehabilitation,” or a preoperative exercise and diet program designed to help optimize outcomes. Currently, patients with BMI of 30-40 kg/m2 are randomized to preoperative rehabilitation vs. current care.
“BMI is a very important decision making factor. We were not able to pick a standardized point [with respect to BMI] for when to operate vs. non-operate. Because of that, we used BMI as a factor in developing our propensity score,” he said, explaining that this is why the propensity-matched groups had similar BMI, while the non-operative group in the overall cohort had substantially higher BMI.
A randomized trial on prehabilitation may be able to provide some insight into the effects of rapid changes in weight and how they affect outcomes in order to make the best choices regarding surgery.
“We do hypothesize that significant weight loss prior to surgery may improve outcomes, and may make the abdominal wall more compliant and enable us to tackle more challenging hernias. We also hypothesize that patients who have a sudden increase in weight after having their ventral hernia repaired may end up having worse outcomes. Hopefully in the next year we will be able to shed more light on these very important questions.”
The authors reported having no disclosures.
The complete manuscript of this presentation is anticipated to be published in the Annals of Surgery pending editorial review.
CHICAGO – Elective ventral hernia repair improves hernia-related quality of life for low- to moderate-risk patients, according to findings from a prospective patient-centered study.
The findings suggest that the risks and benefits of a conservative operative strategy should be reassessed, and that patient-centered outcomes should be considered, Dr. Julie Holihan reported at the annual meeting of the American Surgical Association.
Of 152 patients with a ventral hernia from a single hernia clinic, 97 were managed non-operatively, and 55 were managed operatively. In a propensity-matched cohort of 90 patients with similar demographics, baseline comorbidities, and quality of life scores, only operatively managed patients had improved quality of life scores at 6 months (improvement from 34.7 to 56.9 vs. from 35.6 to 36.6), according to Dr. Holihan of the University of Texas, Houston.
Further, satisfaction scores increased significantly more in the operative than in the non-operative group at follow-up (from a median score of 2 at baseline in both groups to scores of 9 and 3, respectively), and pain scores decreased significantly more in the operative group than in the non-operative group (from a baseline score of 5 down to 3 in the operative group, with no change [score of 6] in the non-operative group).
Two surgical site infections and one hernia recurrence occurred in the operative group.
Notably, the predicted risk of surgery in the cohort was much greater than the observed risk.
“We may be overestimating surgical risk in these patients,” she said.
Based on a multivariable analysis in the overall cohort, non-operative management was strongly associated with lower quality of life score (coefficient, -26.5), Dr. Holihan said.
Nonoperative management of ventral hernias is often recommended for patients, particularly in those with increased risk of surgical complications due to factors such as obesity, poorly controlled diabetes, smoking, or significant comorbidities like coronary artery disease, but this approach to management has not been well studied with respect to patient-centered outcomes such as quality of life and function, she explained.
Traditional outcomes that have been studied, including infection and hernia recurrence, may not be the outcomes that are most important to patients, she added.
For the current study, patients with ventral hernias were prospectively enrolled between June 2014 and June 2015. Non-operative management was recommended for smokers, those with a body mass index greater than 33 kg/m2, and those with poorly controlled diabetes. Measured outcomes included surgical site infection, hernia recurrence, and quality of life using a validated quality of life measure.
This is the first prospective study comparing management strategies in ventral hernia patients with comorbidities, Dr. Holihan said.
She concluded that “the elective repair of ventral hernia, compared with non-operative management, improves patient-centered outcomes in similar-risk patients.”
“Furthermore, the low occurrence of complications suggests that we may be overestimating surgical risk and that we may be too conservative in our patient selection for elective ventral hernia repair. It may be time to reevaluate patient selection criteria in order to better incorporate patient-centered outcomes,” she said.
In response to a question about managing patients with higher risk and/or higher BMI, Dr. Holihan’s coauthor, Dr. Mike K. Liang, also of the University of Texas, Houston, noted that the findings of the study provide estimates for potential future randomized trials. He also noted that the moderate-risk patients at the center often undergo “prehabilitation,” or a preoperative exercise and diet program designed to help optimize outcomes. Currently, patients with BMI of 30-40 kg/m2 are randomized to preoperative rehabilitation vs. current care.
“BMI is a very important decision making factor. We were not able to pick a standardized point [with respect to BMI] for when to operate vs. non-operate. Because of that, we used BMI as a factor in developing our propensity score,” he said, explaining that this is why the propensity-matched groups had similar BMI, while the non-operative group in the overall cohort had substantially higher BMI.
A randomized trial on prehabilitation may be able to provide some insight into the effects of rapid changes in weight and how they affect outcomes in order to make the best choices regarding surgery.
“We do hypothesize that significant weight loss prior to surgery may improve outcomes, and may make the abdominal wall more compliant and enable us to tackle more challenging hernias. We also hypothesize that patients who have a sudden increase in weight after having their ventral hernia repaired may end up having worse outcomes. Hopefully in the next year we will be able to shed more light on these very important questions.”
The authors reported having no disclosures.
The complete manuscript of this presentation is anticipated to be published in the Annals of Surgery pending editorial review.
AT THE ASA ANNUAL MEETING
Key clinical point: Elective ventral hernia repair improves hernia-related quality of life for low- to moderate-risk patients, according to findings from a prospective patient-centered study.
Major finding: In a propensity-matched cohort, only operatively managed patients had improved quality of life scores at 6 months (improvement from 34.7 to 56.9 vs. from 35.6 to 36.6 for nonoperative patients).
Data source: A prospective patient-centered study of 152 patients.
Disclosures: The authors reported having no disclosures.
Pump-delivered anesthetic reduces pain post-hernia repair
MONTREAL – An elastomeric pump delivering local anesthetic to the site of a ventral hernia repair can significantly reduce postoperative pain, according to a small, single-center study.
The prospective, randomized, double-blind placebo-controlled trial of the use of an elastomeric bupivacaine-containing pump for pain management after laparoscopic ventral hernia repair (LVHR) found that patients receiving bupivacaine reported significantly less postoperative pain than did those receiving saline through the pump.
“The idea is that the use of this technology, in combination with standard postoperative pain medication, would do two things: It would maintain the same level of postoperative pain control, as well as reducing the amount of narcotic and non-narcotic pain medication used,” said Francis DeAsis, a medical student at Midwestern University, Chicago.
“For our project, we focused on the specific anatomic location of the catheter,” Mr. DeAsis said in a presentation at the annual meeting of the Central Surgical Association. A previous study, he said, had shown no efficacy for pump-delivered bupivacaine when it was delivered directly into the hernia sac.
In the present study, the cannula for the pump was placed inferior to the costochondral margin, with catheters tunnelled bilaterally between the transversalis fascia and the parietal peritoneum. “The idea behind this was to knock out as many pain receptors as possible,” said Mr. DeAsis.
Primary outcome measures were the self-reported level of postoperative pain and the amount of postoperative medication use. Adult patients at a single site who were undergoing nonemergent ventral hernia repair and who had no history of opioid abuse or adverse reactions to opioids or local anesthetics were enrolled.
Patients were then prospectively randomized to the placebo arm, where they received 400 mL of saline via pump, or to the intervention arm, where they received 400 mL of 0.5% bupivacaine following LVHR. The pump delivered the study drug for a period of 4 days after placement in both groups.
Patients completed a pain diary and medication log for the 7 days after discharge. They rated their current pain level, reported how frequently they had pain, and reported satisfaction with pain control.
In-hospital use of opioid pain medication did not differ significantly between groups, but patients receiving bupivacaine through their pumps used significantly less ketorolac as inpatients (mean 30 mg, compared with 53 mg in the saline group, P = .01).
“Ketorolac is our first-line; we try to avoid narcotics for many different reasons ... Ketorolac PRN was ordered for everybody,” said Dr. Michael Ujiki, a general surgeon at NorthShore University HealthSystem, Evanston, Ill., and senior investigator for the study.
The median pain score on a 1-10 Likert scale at discharge was 2.0 (interquartile range, 0.0-3.0) for the bupivacaine group and 4.0 (interquartile range, 2.0-5.0) for the saline group (P = .06).
Once patients were discharged from the hospital, patients receiving bupivacaine had significantly less postoperative pain through postoperative day 4 and significantly less frequent pain through postoperative day 4. Finally, they reported being significantly more satisfied with their pain management scores on postoperative days 1-3.
The study was limited by the small cohort size. “The primary reason behind this was that during recruitment, we had a lot of patients voice concern about potentially receiving placebo,” thereby forgoing the chance for additional pain relief, said Mr. DeAsis. “A well-powered study should be conducted in the future.”
The investigators reported no relevant financial disclosures, but all study pumps were provided by the manufacturer, On-Q.
On Twitter @karioakes
MONTREAL – An elastomeric pump delivering local anesthetic to the site of a ventral hernia repair can significantly reduce postoperative pain, according to a small, single-center study.
The prospective, randomized, double-blind placebo-controlled trial of the use of an elastomeric bupivacaine-containing pump for pain management after laparoscopic ventral hernia repair (LVHR) found that patients receiving bupivacaine reported significantly less postoperative pain than did those receiving saline through the pump.
“The idea is that the use of this technology, in combination with standard postoperative pain medication, would do two things: It would maintain the same level of postoperative pain control, as well as reducing the amount of narcotic and non-narcotic pain medication used,” said Francis DeAsis, a medical student at Midwestern University, Chicago.
“For our project, we focused on the specific anatomic location of the catheter,” Mr. DeAsis said in a presentation at the annual meeting of the Central Surgical Association. A previous study, he said, had shown no efficacy for pump-delivered bupivacaine when it was delivered directly into the hernia sac.
In the present study, the cannula for the pump was placed inferior to the costochondral margin, with catheters tunnelled bilaterally between the transversalis fascia and the parietal peritoneum. “The idea behind this was to knock out as many pain receptors as possible,” said Mr. DeAsis.
Primary outcome measures were the self-reported level of postoperative pain and the amount of postoperative medication use. Adult patients at a single site who were undergoing nonemergent ventral hernia repair and who had no history of opioid abuse or adverse reactions to opioids or local anesthetics were enrolled.
Patients were then prospectively randomized to the placebo arm, where they received 400 mL of saline via pump, or to the intervention arm, where they received 400 mL of 0.5% bupivacaine following LVHR. The pump delivered the study drug for a period of 4 days after placement in both groups.
Patients completed a pain diary and medication log for the 7 days after discharge. They rated their current pain level, reported how frequently they had pain, and reported satisfaction with pain control.
In-hospital use of opioid pain medication did not differ significantly between groups, but patients receiving bupivacaine through their pumps used significantly less ketorolac as inpatients (mean 30 mg, compared with 53 mg in the saline group, P = .01).
“Ketorolac is our first-line; we try to avoid narcotics for many different reasons ... Ketorolac PRN was ordered for everybody,” said Dr. Michael Ujiki, a general surgeon at NorthShore University HealthSystem, Evanston, Ill., and senior investigator for the study.
The median pain score on a 1-10 Likert scale at discharge was 2.0 (interquartile range, 0.0-3.0) for the bupivacaine group and 4.0 (interquartile range, 2.0-5.0) for the saline group (P = .06).
Once patients were discharged from the hospital, patients receiving bupivacaine had significantly less postoperative pain through postoperative day 4 and significantly less frequent pain through postoperative day 4. Finally, they reported being significantly more satisfied with their pain management scores on postoperative days 1-3.
The study was limited by the small cohort size. “The primary reason behind this was that during recruitment, we had a lot of patients voice concern about potentially receiving placebo,” thereby forgoing the chance for additional pain relief, said Mr. DeAsis. “A well-powered study should be conducted in the future.”
The investigators reported no relevant financial disclosures, but all study pumps were provided by the manufacturer, On-Q.
On Twitter @karioakes
MONTREAL – An elastomeric pump delivering local anesthetic to the site of a ventral hernia repair can significantly reduce postoperative pain, according to a small, single-center study.
The prospective, randomized, double-blind placebo-controlled trial of the use of an elastomeric bupivacaine-containing pump for pain management after laparoscopic ventral hernia repair (LVHR) found that patients receiving bupivacaine reported significantly less postoperative pain than did those receiving saline through the pump.
“The idea is that the use of this technology, in combination with standard postoperative pain medication, would do two things: It would maintain the same level of postoperative pain control, as well as reducing the amount of narcotic and non-narcotic pain medication used,” said Francis DeAsis, a medical student at Midwestern University, Chicago.
“For our project, we focused on the specific anatomic location of the catheter,” Mr. DeAsis said in a presentation at the annual meeting of the Central Surgical Association. A previous study, he said, had shown no efficacy for pump-delivered bupivacaine when it was delivered directly into the hernia sac.
In the present study, the cannula for the pump was placed inferior to the costochondral margin, with catheters tunnelled bilaterally between the transversalis fascia and the parietal peritoneum. “The idea behind this was to knock out as many pain receptors as possible,” said Mr. DeAsis.
Primary outcome measures were the self-reported level of postoperative pain and the amount of postoperative medication use. Adult patients at a single site who were undergoing nonemergent ventral hernia repair and who had no history of opioid abuse or adverse reactions to opioids or local anesthetics were enrolled.
Patients were then prospectively randomized to the placebo arm, where they received 400 mL of saline via pump, or to the intervention arm, where they received 400 mL of 0.5% bupivacaine following LVHR. The pump delivered the study drug for a period of 4 days after placement in both groups.
Patients completed a pain diary and medication log for the 7 days after discharge. They rated their current pain level, reported how frequently they had pain, and reported satisfaction with pain control.
In-hospital use of opioid pain medication did not differ significantly between groups, but patients receiving bupivacaine through their pumps used significantly less ketorolac as inpatients (mean 30 mg, compared with 53 mg in the saline group, P = .01).
“Ketorolac is our first-line; we try to avoid narcotics for many different reasons ... Ketorolac PRN was ordered for everybody,” said Dr. Michael Ujiki, a general surgeon at NorthShore University HealthSystem, Evanston, Ill., and senior investigator for the study.
The median pain score on a 1-10 Likert scale at discharge was 2.0 (interquartile range, 0.0-3.0) for the bupivacaine group and 4.0 (interquartile range, 2.0-5.0) for the saline group (P = .06).
Once patients were discharged from the hospital, patients receiving bupivacaine had significantly less postoperative pain through postoperative day 4 and significantly less frequent pain through postoperative day 4. Finally, they reported being significantly more satisfied with their pain management scores on postoperative days 1-3.
The study was limited by the small cohort size. “The primary reason behind this was that during recruitment, we had a lot of patients voice concern about potentially receiving placebo,” thereby forgoing the chance for additional pain relief, said Mr. DeAsis. “A well-powered study should be conducted in the future.”
The investigators reported no relevant financial disclosures, but all study pumps were provided by the manufacturer, On-Q.
On Twitter @karioakes
AT THE ANNUAL MEETING OF THE CENTRAL SURGICAL ASSOCIATION
Key clinical point: Pain scores were reduced when patients had pump-delivered local anesthetic after hernia repair.
Major finding: Pain level and frequency of pain were reduced, and satisfaction with pain control was increased, when patients received local anesthetic via pump after laparoscopic ventral hernia repair.
Data source: Single-center double-blind, placebo-controlled study of elastomeric pump-delivered bupivacaine vs. placebo in 29 patients undergoing laparoscopic ventral hernia repair.
Disclosures: The pump was supplied by the manufacturer (On-Q); the investigators reported no other relevant disclosures.
Pump-delivered anesthetic reduces pain post-hernia repair
MONTREAL – An elastomeric pump delivering local anesthetic to the site of a ventral hernia repair can significantly reduce postoperative pain, according to a small, single-center study.
The prospective, randomized, double-blind placebo-controlled trial of the use of an elastomeric bupivacaine-containing pump for pain management after laparoscopic ventral hernia repair (LVHR) found that patients receiving bupivacaine reported significantly less postoperative pain than did those receiving saline through the pump.
“The idea is that the use of this technology, in combination with standard postoperative pain medication, would do two things: It would maintain the same level of postoperative pain control, as well as reducing the amount of narcotic and non-narcotic pain medication used,” said Francis DeAsis, a medical student at Midwestern University, Chicago.
“For our project, we focused on the specific anatomic location of the catheter,” Mr. DeAsis said in a presentation at the annual meeting of the Central Surgical Association. A previous study, he said, had shown no efficacy for pump-delivered bupivacaine when it was delivered directly into the hernia sac.
In the present study, the cannula for the pump was placed inferior to the costochondral margin, with catheters tunnelled bilaterally between the transversalis fascia and the parietal peritoneum. “The idea behind this was to knock out as many pain receptors as possible,” said Mr. DeAsis.
Primary outcome measures were the self-reported level of postoperative pain and the amount of postoperative medication use. Adult patients at a single site who were undergoing nonemergent ventral hernia repair and who had no history of opioid abuse or adverse reactions to opioids or local anesthetics were enrolled.
Patients were then prospectively randomized to the placebo arm, where they received 400 mL of saline via pump, or to the intervention arm, where they received 400 mL of 0.5% bupivacaine following LVHR. The pump delivered the study drug for a period of 4 days after placement in both groups.
Patients completed a pain diary and medication log for the 7 days after discharge. They rated their current pain level, reported how frequently they had pain, and reported satisfaction with pain control.
In-hospital use of opioid pain medication did not differ significantly between groups, but patients receiving bupivacaine through their pumps used significantly less ketorolac as inpatients (mean 30 mg, compared with 53 mg in the saline group, P = .01).
“Ketorolac is our first-line; we try to avoid narcotics for many different reasons ... Ketorolac PRN was ordered for everybody,” said Dr. Michael Ujiki, a general surgeon at NorthShore University HealthSystem, Evanston, Ill., and senior investigator for the study.
The median pain score on a 1-10 Likert scale at discharge was 2.0 (interquartile range, 0.0-3.0) for the bupivacaine group and 4.0 (interquartile range, 2.0-5.0) for the saline group (P = .06).
Once patients were discharged from the hospital, patients receiving bupivacaine had significantly less postoperative pain through postoperative day 4 and significantly less frequent pain through postoperative day 4. Finally, they reported being significantly more satisfied with their pain management scores on postoperative days 1-3.
The study was limited by the small cohort size. “The primary reason behind this was that during recruitment, we had a lot of patients voice concern about potentially receiving placebo,” thereby forgoing the chance for additional pain relief, said Mr. DeAsis. “A well-powered study should be conducted in the future.”
The investigators reported no relevant financial disclosures, but all study pumps were provided by the manufacturer, On-Q.
On Twitter @karioakes
MONTREAL – An elastomeric pump delivering local anesthetic to the site of a ventral hernia repair can significantly reduce postoperative pain, according to a small, single-center study.
The prospective, randomized, double-blind placebo-controlled trial of the use of an elastomeric bupivacaine-containing pump for pain management after laparoscopic ventral hernia repair (LVHR) found that patients receiving bupivacaine reported significantly less postoperative pain than did those receiving saline through the pump.
“The idea is that the use of this technology, in combination with standard postoperative pain medication, would do two things: It would maintain the same level of postoperative pain control, as well as reducing the amount of narcotic and non-narcotic pain medication used,” said Francis DeAsis, a medical student at Midwestern University, Chicago.
“For our project, we focused on the specific anatomic location of the catheter,” Mr. DeAsis said in a presentation at the annual meeting of the Central Surgical Association. A previous study, he said, had shown no efficacy for pump-delivered bupivacaine when it was delivered directly into the hernia sac.
In the present study, the cannula for the pump was placed inferior to the costochondral margin, with catheters tunnelled bilaterally between the transversalis fascia and the parietal peritoneum. “The idea behind this was to knock out as many pain receptors as possible,” said Mr. DeAsis.
Primary outcome measures were the self-reported level of postoperative pain and the amount of postoperative medication use. Adult patients at a single site who were undergoing nonemergent ventral hernia repair and who had no history of opioid abuse or adverse reactions to opioids or local anesthetics were enrolled.
Patients were then prospectively randomized to the placebo arm, where they received 400 mL of saline via pump, or to the intervention arm, where they received 400 mL of 0.5% bupivacaine following LVHR. The pump delivered the study drug for a period of 4 days after placement in both groups.
Patients completed a pain diary and medication log for the 7 days after discharge. They rated their current pain level, reported how frequently they had pain, and reported satisfaction with pain control.
In-hospital use of opioid pain medication did not differ significantly between groups, but patients receiving bupivacaine through their pumps used significantly less ketorolac as inpatients (mean 30 mg, compared with 53 mg in the saline group, P = .01).
“Ketorolac is our first-line; we try to avoid narcotics for many different reasons ... Ketorolac PRN was ordered for everybody,” said Dr. Michael Ujiki, a general surgeon at NorthShore University HealthSystem, Evanston, Ill., and senior investigator for the study.
The median pain score on a 1-10 Likert scale at discharge was 2.0 (interquartile range, 0.0-3.0) for the bupivacaine group and 4.0 (interquartile range, 2.0-5.0) for the saline group (P = .06).
Once patients were discharged from the hospital, patients receiving bupivacaine had significantly less postoperative pain through postoperative day 4 and significantly less frequent pain through postoperative day 4. Finally, they reported being significantly more satisfied with their pain management scores on postoperative days 1-3.
The study was limited by the small cohort size. “The primary reason behind this was that during recruitment, we had a lot of patients voice concern about potentially receiving placebo,” thereby forgoing the chance for additional pain relief, said Mr. DeAsis. “A well-powered study should be conducted in the future.”
The investigators reported no relevant financial disclosures, but all study pumps were provided by the manufacturer, On-Q.
On Twitter @karioakes
MONTREAL – An elastomeric pump delivering local anesthetic to the site of a ventral hernia repair can significantly reduce postoperative pain, according to a small, single-center study.
The prospective, randomized, double-blind placebo-controlled trial of the use of an elastomeric bupivacaine-containing pump for pain management after laparoscopic ventral hernia repair (LVHR) found that patients receiving bupivacaine reported significantly less postoperative pain than did those receiving saline through the pump.
“The idea is that the use of this technology, in combination with standard postoperative pain medication, would do two things: It would maintain the same level of postoperative pain control, as well as reducing the amount of narcotic and non-narcotic pain medication used,” said Francis DeAsis, a medical student at Midwestern University, Chicago.
“For our project, we focused on the specific anatomic location of the catheter,” Mr. DeAsis said in a presentation at the annual meeting of the Central Surgical Association. A previous study, he said, had shown no efficacy for pump-delivered bupivacaine when it was delivered directly into the hernia sac.
In the present study, the cannula for the pump was placed inferior to the costochondral margin, with catheters tunnelled bilaterally between the transversalis fascia and the parietal peritoneum. “The idea behind this was to knock out as many pain receptors as possible,” said Mr. DeAsis.
Primary outcome measures were the self-reported level of postoperative pain and the amount of postoperative medication use. Adult patients at a single site who were undergoing nonemergent ventral hernia repair and who had no history of opioid abuse or adverse reactions to opioids or local anesthetics were enrolled.
Patients were then prospectively randomized to the placebo arm, where they received 400 mL of saline via pump, or to the intervention arm, where they received 400 mL of 0.5% bupivacaine following LVHR. The pump delivered the study drug for a period of 4 days after placement in both groups.
Patients completed a pain diary and medication log for the 7 days after discharge. They rated their current pain level, reported how frequently they had pain, and reported satisfaction with pain control.
In-hospital use of opioid pain medication did not differ significantly between groups, but patients receiving bupivacaine through their pumps used significantly less ketorolac as inpatients (mean 30 mg, compared with 53 mg in the saline group, P = .01).
“Ketorolac is our first-line; we try to avoid narcotics for many different reasons ... Ketorolac PRN was ordered for everybody,” said Dr. Michael Ujiki, a general surgeon at NorthShore University HealthSystem, Evanston, Ill., and senior investigator for the study.
The median pain score on a 1-10 Likert scale at discharge was 2.0 (interquartile range, 0.0-3.0) for the bupivacaine group and 4.0 (interquartile range, 2.0-5.0) for the saline group (P = .06).
Once patients were discharged from the hospital, patients receiving bupivacaine had significantly less postoperative pain through postoperative day 4 and significantly less frequent pain through postoperative day 4. Finally, they reported being significantly more satisfied with their pain management scores on postoperative days 1-3.
The study was limited by the small cohort size. “The primary reason behind this was that during recruitment, we had a lot of patients voice concern about potentially receiving placebo,” thereby forgoing the chance for additional pain relief, said Mr. DeAsis. “A well-powered study should be conducted in the future.”
The investigators reported no relevant financial disclosures, but all study pumps were provided by the manufacturer, On-Q.
On Twitter @karioakes
AT THE ANNUAL MEETING OF THE CENTRAL SURGICAL ASSOCIATION
Key clinical point: Pain scores were reduced when patients had pump-delivered local anesthetic after hernia repair.
Major finding: Pain level and frequency of pain were reduced, and satisfaction with pain control was increased, when patients received local anesthetic via pump after laparoscopic ventral hernia repair.
Data source: Single-center double-blind, placebo-controlled study of elastomeric pump-delivered bupivacaine vs. placebo in 29 patients undergoing laparoscopic ventral hernia repair.
Disclosures: The pump was supplied by the manufacturer (On-Q); the investigators reported no other relevant disclosures.
Damage to nearby structure common cause of hernia malpractice claim
JACKSONVILLE, FLA. – General surgeons are among the most sued physicians, and hernia repair is one of the most common operations they perform, so a study was conducted to drill down into the legal data on hernia repair to determine what about the operation is most likely to get surgeons in trouble.
They found that a failure to diagnose a complication caused by damage to a nearby structure during the operation was the most common cause for a malpractice suit for hernia repair, Dr. Nadeem Haddad of the Mayo Clinic in Rochester, Minn., reported at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
“Hernia repair with more than 1 million cases annually is one of the most common surgical procedures,” Dr. Haddad said. “The most common type of operation for malpractice was inguinal hernia repair. The majority of cases were elective cases where the informed consent was not breached.”
The researchers sampled data on 250 malpractice cases arising from hernia surgery filed with the Westlaw Next legal database between 1985 and 2015, Dr. Haddad said. He added that the sample is not inclusive of all malpractice cases related to hernia repair in that time. “Our objective was to analyze reasons for litigation related to hernia repairs,” he said.
Among the hernia cases from the database, physicians (defendants) won 59%, patients (plaintiffs) won around 27%, and the remainder went to settlement before a verdict. Award payments ranged from $10,000 for a case where a Penrose drain was left in the patient to $16 million in the case of death of an infant due to perioperative hyperkalemia.
Eighty-four percent of the cases in the study involved inguinal or ventral hernia repair, Dr. Haddad said, but the Westlaw Next database did not differentiate between the two types of procedures. Nor did it separate out pediatric or adult repairs. Westlaw Next provides the alleged reason for litigation and gives details about lawsuits. The researchers classified the alleged reasons for the lawsuits based on the time period in which they happened: preoperatively, intraoperatively, and postoperatively.
“The single most common reason for malpractice in hernia repair was failure to diagnose a complication following damage to a surrounding structure,” Dr. Haddad said.
The state of New York had the highest number of medical malpractice cases (46), followed closely by California (42). In 15% of cases (38) the patients claimed a breach of informed consent by the surgeon
“While understanding the reasons why surgeons go to trial, the risk of future lawsuits may lessen if measures are enacted to prevent such outcomes,” Dr. Haddad said. “Following protocols in diagnosis and management, attention to good surgical technique, and keeping a checklist of possible complications are some of the ways to improve patients safety and decrease chances of litigation.”
Dr. Haddad and coauthors had no financial relationships to disclose.
JACKSONVILLE, FLA. – General surgeons are among the most sued physicians, and hernia repair is one of the most common operations they perform, so a study was conducted to drill down into the legal data on hernia repair to determine what about the operation is most likely to get surgeons in trouble.
They found that a failure to diagnose a complication caused by damage to a nearby structure during the operation was the most common cause for a malpractice suit for hernia repair, Dr. Nadeem Haddad of the Mayo Clinic in Rochester, Minn., reported at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
“Hernia repair with more than 1 million cases annually is one of the most common surgical procedures,” Dr. Haddad said. “The most common type of operation for malpractice was inguinal hernia repair. The majority of cases were elective cases where the informed consent was not breached.”
The researchers sampled data on 250 malpractice cases arising from hernia surgery filed with the Westlaw Next legal database between 1985 and 2015, Dr. Haddad said. He added that the sample is not inclusive of all malpractice cases related to hernia repair in that time. “Our objective was to analyze reasons for litigation related to hernia repairs,” he said.
Among the hernia cases from the database, physicians (defendants) won 59%, patients (plaintiffs) won around 27%, and the remainder went to settlement before a verdict. Award payments ranged from $10,000 for a case where a Penrose drain was left in the patient to $16 million in the case of death of an infant due to perioperative hyperkalemia.
Eighty-four percent of the cases in the study involved inguinal or ventral hernia repair, Dr. Haddad said, but the Westlaw Next database did not differentiate between the two types of procedures. Nor did it separate out pediatric or adult repairs. Westlaw Next provides the alleged reason for litigation and gives details about lawsuits. The researchers classified the alleged reasons for the lawsuits based on the time period in which they happened: preoperatively, intraoperatively, and postoperatively.
“The single most common reason for malpractice in hernia repair was failure to diagnose a complication following damage to a surrounding structure,” Dr. Haddad said.
The state of New York had the highest number of medical malpractice cases (46), followed closely by California (42). In 15% of cases (38) the patients claimed a breach of informed consent by the surgeon
“While understanding the reasons why surgeons go to trial, the risk of future lawsuits may lessen if measures are enacted to prevent such outcomes,” Dr. Haddad said. “Following protocols in diagnosis and management, attention to good surgical technique, and keeping a checklist of possible complications are some of the ways to improve patients safety and decrease chances of litigation.”
Dr. Haddad and coauthors had no financial relationships to disclose.
JACKSONVILLE, FLA. – General surgeons are among the most sued physicians, and hernia repair is one of the most common operations they perform, so a study was conducted to drill down into the legal data on hernia repair to determine what about the operation is most likely to get surgeons in trouble.
They found that a failure to diagnose a complication caused by damage to a nearby structure during the operation was the most common cause for a malpractice suit for hernia repair, Dr. Nadeem Haddad of the Mayo Clinic in Rochester, Minn., reported at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
“Hernia repair with more than 1 million cases annually is one of the most common surgical procedures,” Dr. Haddad said. “The most common type of operation for malpractice was inguinal hernia repair. The majority of cases were elective cases where the informed consent was not breached.”
The researchers sampled data on 250 malpractice cases arising from hernia surgery filed with the Westlaw Next legal database between 1985 and 2015, Dr. Haddad said. He added that the sample is not inclusive of all malpractice cases related to hernia repair in that time. “Our objective was to analyze reasons for litigation related to hernia repairs,” he said.
Among the hernia cases from the database, physicians (defendants) won 59%, patients (plaintiffs) won around 27%, and the remainder went to settlement before a verdict. Award payments ranged from $10,000 for a case where a Penrose drain was left in the patient to $16 million in the case of death of an infant due to perioperative hyperkalemia.
Eighty-four percent of the cases in the study involved inguinal or ventral hernia repair, Dr. Haddad said, but the Westlaw Next database did not differentiate between the two types of procedures. Nor did it separate out pediatric or adult repairs. Westlaw Next provides the alleged reason for litigation and gives details about lawsuits. The researchers classified the alleged reasons for the lawsuits based on the time period in which they happened: preoperatively, intraoperatively, and postoperatively.
“The single most common reason for malpractice in hernia repair was failure to diagnose a complication following damage to a surrounding structure,” Dr. Haddad said.
The state of New York had the highest number of medical malpractice cases (46), followed closely by California (42). In 15% of cases (38) the patients claimed a breach of informed consent by the surgeon
“While understanding the reasons why surgeons go to trial, the risk of future lawsuits may lessen if measures are enacted to prevent such outcomes,” Dr. Haddad said. “Following protocols in diagnosis and management, attention to good surgical technique, and keeping a checklist of possible complications are some of the ways to improve patients safety and decrease chances of litigation.”
Dr. Haddad and coauthors had no financial relationships to disclose.
AT THE ANNUAL ACADEMIC SURGICAL CONGRESS
Key clinical point: Failure to diagnose a complication caused by damage to a nearby structure during hernia repair surgery is the most common cause for a malpractice claim for hernia repair.
Major finding: In malpractice cases involving hernia surgery that go to trial, 59% of the rulings are for the plaintiff physicians and about 14% go to settlement before a judge or jury decision.
Data source: Sample of 250 hernia surgical malpractice cases from 1985 to 2015 in the Westlaw Next legal database.
Disclosures: The study authors reported having no financial disclosures.
Emergency hernia surgery risk predicted by access, age, and race
JACKSONVILLE, FLA. – Age and access to medical care may be key drivers of emergency surgery for ventral hernia repair, a large retrospective study has found.
Patients who do not have health insurance, are advanced in age, are black or Hispanic, or have unrelated health problems are at significantly higher risk than other patients with hernias of having emergency surgery for ventral hernia repair, facing a higher risk of death, a higher cost, and a longer hospital stay, Dr. Lindsey Wolf said at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress. “This study demonstrates persistent disparities in access to elective surgery care that must be understood and mitigated,” she said. “The strongest predictor was being uninsured. The self-pay group had an odds ratio of 3.5 for undergoing emergency surgery, compared with those who were primarily insured.”
The goal of the study was to identify patient and hospital factors associated with emergency ventral hernia surgery in the U.S. population, said Dr. Wolf of Brigham and Women’s Hospital in Boston. “Prior studies that have been done on predictors of emergency repair are from universally insured populations,” she said. One was a national cohort study in Denmark, and another involved the Veterans Affairs population, she said. “Both of these identified several demographic and clinical risk factors for emergency hernia repair,” she said.
The current Brigham and Women’s study involved a retrospective cross-sectional data analysis of approximately 453,000 elective and emergency ventral hernia repairs performed from 2003 to 2011 in the Nationwide Inpatient Sample. Any cases that involved a trauma diagnosis were excluded. Forty percent of the cases in the sample were emergency admissions.
When considering the effect of age, the investigators found that the aged 65-75 group had the lowest risk of emergency hernia surgery of all age groups with an odds ratio of 0.77, compared with those under 45 years. Those aged 85 and older, however, had the highest risk of all age groups with an odds ratio of 2.23. “The proportion of the cohort undergoing emergency surgery really increases drastically with age after 75 years,” Dr. Wolf said.
Other factors that had an impact on emergency hernia repair were Medicaid coverage (OR, 1.29, compared with private insurance), black race (OR, 1.64, compared with white race), Hispanic ethnicity (OR, 1.44, compared with non-Hispanic white race/ethnicity), and comorbidities, ranging from 1.13 for one comorbidity to 1.68 for three or more, compared with none.
The study also elucidated a few consequences of emergency ventral hernia repair: 2.58 times higher odds of death, a 15% greater cost per hospital stay, and 26% longer hospital stays.
“Looking forward there are both patient and provider areas to target,” Dr. Wolf said. “For patients, interventions must be designed to populations that may have poor access to elective surgical services.” She acknowledged that race was a strong predictor, “but race is a social construct that may be a proxy to many barriers to access and care.”
The study findings may also help inform surgeons on when to operate on ventral hernias. “In the absence of any clinical guidelines for when a hernia should be repaired, our results with regard to age and multiple comorbidities may assist surgeons in risk stratifying patients when considering [whether] to perform an elective repair,” she said.
Dr. Wolf and her coauthors had no relevant financial conflicts to disclose.
JACKSONVILLE, FLA. – Age and access to medical care may be key drivers of emergency surgery for ventral hernia repair, a large retrospective study has found.
Patients who do not have health insurance, are advanced in age, are black or Hispanic, or have unrelated health problems are at significantly higher risk than other patients with hernias of having emergency surgery for ventral hernia repair, facing a higher risk of death, a higher cost, and a longer hospital stay, Dr. Lindsey Wolf said at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress. “This study demonstrates persistent disparities in access to elective surgery care that must be understood and mitigated,” she said. “The strongest predictor was being uninsured. The self-pay group had an odds ratio of 3.5 for undergoing emergency surgery, compared with those who were primarily insured.”
The goal of the study was to identify patient and hospital factors associated with emergency ventral hernia surgery in the U.S. population, said Dr. Wolf of Brigham and Women’s Hospital in Boston. “Prior studies that have been done on predictors of emergency repair are from universally insured populations,” she said. One was a national cohort study in Denmark, and another involved the Veterans Affairs population, she said. “Both of these identified several demographic and clinical risk factors for emergency hernia repair,” she said.
The current Brigham and Women’s study involved a retrospective cross-sectional data analysis of approximately 453,000 elective and emergency ventral hernia repairs performed from 2003 to 2011 in the Nationwide Inpatient Sample. Any cases that involved a trauma diagnosis were excluded. Forty percent of the cases in the sample were emergency admissions.
When considering the effect of age, the investigators found that the aged 65-75 group had the lowest risk of emergency hernia surgery of all age groups with an odds ratio of 0.77, compared with those under 45 years. Those aged 85 and older, however, had the highest risk of all age groups with an odds ratio of 2.23. “The proportion of the cohort undergoing emergency surgery really increases drastically with age after 75 years,” Dr. Wolf said.
Other factors that had an impact on emergency hernia repair were Medicaid coverage (OR, 1.29, compared with private insurance), black race (OR, 1.64, compared with white race), Hispanic ethnicity (OR, 1.44, compared with non-Hispanic white race/ethnicity), and comorbidities, ranging from 1.13 for one comorbidity to 1.68 for three or more, compared with none.
The study also elucidated a few consequences of emergency ventral hernia repair: 2.58 times higher odds of death, a 15% greater cost per hospital stay, and 26% longer hospital stays.
“Looking forward there are both patient and provider areas to target,” Dr. Wolf said. “For patients, interventions must be designed to populations that may have poor access to elective surgical services.” She acknowledged that race was a strong predictor, “but race is a social construct that may be a proxy to many barriers to access and care.”
The study findings may also help inform surgeons on when to operate on ventral hernias. “In the absence of any clinical guidelines for when a hernia should be repaired, our results with regard to age and multiple comorbidities may assist surgeons in risk stratifying patients when considering [whether] to perform an elective repair,” she said.
Dr. Wolf and her coauthors had no relevant financial conflicts to disclose.
JACKSONVILLE, FLA. – Age and access to medical care may be key drivers of emergency surgery for ventral hernia repair, a large retrospective study has found.
Patients who do not have health insurance, are advanced in age, are black or Hispanic, or have unrelated health problems are at significantly higher risk than other patients with hernias of having emergency surgery for ventral hernia repair, facing a higher risk of death, a higher cost, and a longer hospital stay, Dr. Lindsey Wolf said at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress. “This study demonstrates persistent disparities in access to elective surgery care that must be understood and mitigated,” she said. “The strongest predictor was being uninsured. The self-pay group had an odds ratio of 3.5 for undergoing emergency surgery, compared with those who were primarily insured.”
The goal of the study was to identify patient and hospital factors associated with emergency ventral hernia surgery in the U.S. population, said Dr. Wolf of Brigham and Women’s Hospital in Boston. “Prior studies that have been done on predictors of emergency repair are from universally insured populations,” she said. One was a national cohort study in Denmark, and another involved the Veterans Affairs population, she said. “Both of these identified several demographic and clinical risk factors for emergency hernia repair,” she said.
The current Brigham and Women’s study involved a retrospective cross-sectional data analysis of approximately 453,000 elective and emergency ventral hernia repairs performed from 2003 to 2011 in the Nationwide Inpatient Sample. Any cases that involved a trauma diagnosis were excluded. Forty percent of the cases in the sample were emergency admissions.
When considering the effect of age, the investigators found that the aged 65-75 group had the lowest risk of emergency hernia surgery of all age groups with an odds ratio of 0.77, compared with those under 45 years. Those aged 85 and older, however, had the highest risk of all age groups with an odds ratio of 2.23. “The proportion of the cohort undergoing emergency surgery really increases drastically with age after 75 years,” Dr. Wolf said.
Other factors that had an impact on emergency hernia repair were Medicaid coverage (OR, 1.29, compared with private insurance), black race (OR, 1.64, compared with white race), Hispanic ethnicity (OR, 1.44, compared with non-Hispanic white race/ethnicity), and comorbidities, ranging from 1.13 for one comorbidity to 1.68 for three or more, compared with none.
The study also elucidated a few consequences of emergency ventral hernia repair: 2.58 times higher odds of death, a 15% greater cost per hospital stay, and 26% longer hospital stays.
“Looking forward there are both patient and provider areas to target,” Dr. Wolf said. “For patients, interventions must be designed to populations that may have poor access to elective surgical services.” She acknowledged that race was a strong predictor, “but race is a social construct that may be a proxy to many barriers to access and care.”
The study findings may also help inform surgeons on when to operate on ventral hernias. “In the absence of any clinical guidelines for when a hernia should be repaired, our results with regard to age and multiple comorbidities may assist surgeons in risk stratifying patients when considering [whether] to perform an elective repair,” she said.
Dr. Wolf and her coauthors had no relevant financial conflicts to disclose.
AT THE ACADEMIC SURGICAL CONGRESS
Key clinical point: Disparities among patients more likely to get emergency rather than elective ventral hernia repair include race, insurance status, and advanced age.
Major finding: Among demographic groups with a significantly higher likelihood of undergoing emergency ventral hernia repair were blacks (odds ratio, 1.64), Hispanics (OR, 1.44), and people over age 85 (OR, 2.23).
Data source: Nationwide Inpatient Sample of 453,000 adults who had inpatient ventral hernia repair from 2003 to 2011.
Disclosures: The study authors reported having no relevant financial disclosures.
TEP hernia repair superior to Lichtenstein in pain outcomes
Patients undergoing endoscopic total extraperitoneal repair (TEP) of hernias had less persistent pain and greater mobility than those whose hernias were repaired using the Lichtenstein technique.
For their research, conducted in Sweden, researchers led by Dr. Linn Westin of the Karolinska Institutet in Stockholm and colleagues randomized 384 adult men with primary unilateral inguinal hernia to surgery with Lichtenstein using local anesthesia (n = 191) or TEP with general anesthesia (n = 193). Patients underwent operations in two hospitals between 2006 and 2011, with four surgeons participating, and the same heavyweight mesh was used in both groups.
All patients were followed for 1 year for postoperative pain, recurrence of hernias, difficulty in performing daily activities, complications, and use of analgesics. Pain was measured using the Inguinal Pain Questionnaire (IPQ).
In a paper published in the February issue of Annals of Surgery (2016;263:240-3), Dr. Westin and colleagues reported that the group randomized to TEP saw significantly less persistent mild pain at 1 year, compared with the Lichtenstein group. In the TEP group 39 patients reported such pain, compared with 62 in the Lichtenstein group (20.7% vs. 33.2,% P = .007).
Five TEP patients reported pain in the groin that limited their ability to perform physical exercise, while 14 in the Lichtenstein group reported similar pain, a difference that reached statistical significance (2.7% vs. 7.5%, P = .034). Severe pain, defined as pain affecting most activities, was comparable in both groups, with four patients in the TEP group and six in the Lichtenstein group reporting severe pain (2.1% and 3.2%, P = .543).
No significant between-group differences were seen in recurrences, use of pain medications, or specific measures of mobility, such as being able to sit or stand for more than 30 minutes at a stretch.
“Our results show a clinically significant advantage in favor of TEP regarding long-term postoperative pain, and justify the use of TEP for routine inguinal hernia surgery,” Dr. Westin and colleagues noted in their analysis. Their findings, they said, should prompt more extensive training of surgeons in the TEP technique.
The investigators noted as a limitation of their study that it was not powered to detect differences in severe pain, which could be considered more clinically relevant than mild persistent pain.
Patients’ pain outcomes may have been related to surgeons’ handling of the nerves in the inguinal tract, they wrote.
Also, they noted, the same heavyweight mesh was used in all operations in the study, for consistency, despite the fact that, after the initiation of the trial, lightweight mesh was shown in studies to be associated with less pain. Dr. Westin and colleagues wrote that their findings would be applicable to surgeries using lightweight mesh, which might further limit pain.
Their results, they wrote, suggested that TEP should be considered a valid first choice not only for the study population, which included only men with primary unilateral hernias, but for those with bilateral or recurrent hernias and also for women.
The study was funded by the Uppsala-Orebro Regional Research Council, Stockholm County Council, Swedish Society of Medicine, and Olle Engqvist Research Foundation. None of the investigators declared conflicts of interest.
Patients undergoing endoscopic total extraperitoneal repair (TEP) of hernias had less persistent pain and greater mobility than those whose hernias were repaired using the Lichtenstein technique.
For their research, conducted in Sweden, researchers led by Dr. Linn Westin of the Karolinska Institutet in Stockholm and colleagues randomized 384 adult men with primary unilateral inguinal hernia to surgery with Lichtenstein using local anesthesia (n = 191) or TEP with general anesthesia (n = 193). Patients underwent operations in two hospitals between 2006 and 2011, with four surgeons participating, and the same heavyweight mesh was used in both groups.
All patients were followed for 1 year for postoperative pain, recurrence of hernias, difficulty in performing daily activities, complications, and use of analgesics. Pain was measured using the Inguinal Pain Questionnaire (IPQ).
In a paper published in the February issue of Annals of Surgery (2016;263:240-3), Dr. Westin and colleagues reported that the group randomized to TEP saw significantly less persistent mild pain at 1 year, compared with the Lichtenstein group. In the TEP group 39 patients reported such pain, compared with 62 in the Lichtenstein group (20.7% vs. 33.2,% P = .007).
Five TEP patients reported pain in the groin that limited their ability to perform physical exercise, while 14 in the Lichtenstein group reported similar pain, a difference that reached statistical significance (2.7% vs. 7.5%, P = .034). Severe pain, defined as pain affecting most activities, was comparable in both groups, with four patients in the TEP group and six in the Lichtenstein group reporting severe pain (2.1% and 3.2%, P = .543).
No significant between-group differences were seen in recurrences, use of pain medications, or specific measures of mobility, such as being able to sit or stand for more than 30 minutes at a stretch.
“Our results show a clinically significant advantage in favor of TEP regarding long-term postoperative pain, and justify the use of TEP for routine inguinal hernia surgery,” Dr. Westin and colleagues noted in their analysis. Their findings, they said, should prompt more extensive training of surgeons in the TEP technique.
The investigators noted as a limitation of their study that it was not powered to detect differences in severe pain, which could be considered more clinically relevant than mild persistent pain.
Patients’ pain outcomes may have been related to surgeons’ handling of the nerves in the inguinal tract, they wrote.
Also, they noted, the same heavyweight mesh was used in all operations in the study, for consistency, despite the fact that, after the initiation of the trial, lightweight mesh was shown in studies to be associated with less pain. Dr. Westin and colleagues wrote that their findings would be applicable to surgeries using lightweight mesh, which might further limit pain.
Their results, they wrote, suggested that TEP should be considered a valid first choice not only for the study population, which included only men with primary unilateral hernias, but for those with bilateral or recurrent hernias and also for women.
The study was funded by the Uppsala-Orebro Regional Research Council, Stockholm County Council, Swedish Society of Medicine, and Olle Engqvist Research Foundation. None of the investigators declared conflicts of interest.
Patients undergoing endoscopic total extraperitoneal repair (TEP) of hernias had less persistent pain and greater mobility than those whose hernias were repaired using the Lichtenstein technique.
For their research, conducted in Sweden, researchers led by Dr. Linn Westin of the Karolinska Institutet in Stockholm and colleagues randomized 384 adult men with primary unilateral inguinal hernia to surgery with Lichtenstein using local anesthesia (n = 191) or TEP with general anesthesia (n = 193). Patients underwent operations in two hospitals between 2006 and 2011, with four surgeons participating, and the same heavyweight mesh was used in both groups.
All patients were followed for 1 year for postoperative pain, recurrence of hernias, difficulty in performing daily activities, complications, and use of analgesics. Pain was measured using the Inguinal Pain Questionnaire (IPQ).
In a paper published in the February issue of Annals of Surgery (2016;263:240-3), Dr. Westin and colleagues reported that the group randomized to TEP saw significantly less persistent mild pain at 1 year, compared with the Lichtenstein group. In the TEP group 39 patients reported such pain, compared with 62 in the Lichtenstein group (20.7% vs. 33.2,% P = .007).
Five TEP patients reported pain in the groin that limited their ability to perform physical exercise, while 14 in the Lichtenstein group reported similar pain, a difference that reached statistical significance (2.7% vs. 7.5%, P = .034). Severe pain, defined as pain affecting most activities, was comparable in both groups, with four patients in the TEP group and six in the Lichtenstein group reporting severe pain (2.1% and 3.2%, P = .543).
No significant between-group differences were seen in recurrences, use of pain medications, or specific measures of mobility, such as being able to sit or stand for more than 30 minutes at a stretch.
“Our results show a clinically significant advantage in favor of TEP regarding long-term postoperative pain, and justify the use of TEP for routine inguinal hernia surgery,” Dr. Westin and colleagues noted in their analysis. Their findings, they said, should prompt more extensive training of surgeons in the TEP technique.
The investigators noted as a limitation of their study that it was not powered to detect differences in severe pain, which could be considered more clinically relevant than mild persistent pain.
Patients’ pain outcomes may have been related to surgeons’ handling of the nerves in the inguinal tract, they wrote.
Also, they noted, the same heavyweight mesh was used in all operations in the study, for consistency, despite the fact that, after the initiation of the trial, lightweight mesh was shown in studies to be associated with less pain. Dr. Westin and colleagues wrote that their findings would be applicable to surgeries using lightweight mesh, which might further limit pain.
Their results, they wrote, suggested that TEP should be considered a valid first choice not only for the study population, which included only men with primary unilateral hernias, but for those with bilateral or recurrent hernias and also for women.
The study was funded by the Uppsala-Orebro Regional Research Council, Stockholm County Council, Swedish Society of Medicine, and Olle Engqvist Research Foundation. None of the investigators declared conflicts of interest.
FROM ANNALS OF SURGERY
Key clinical point: Patients undergoing TEP for hernia repair were less likely to report persistent pain after 1 year than those undergoing Lichtenstein procedures.
Major finding: In the TEP group, 39 (20.7%) patients reported persistent pain, compared with 62 (33.2%) in the Lichtenstein group (P = .007).
Data source: A randomized multisite surgical trial in Sweden enrolling 384 men with unilateral primary inguinal hernias, with 375 followed up at 1 year.
Disclosures: The study was funded by Swedish government grants, the Swedish Society of Medicine, and the Olle Engqvist Research Foundation. Investigators disclosed no conflicts of interest.
Hernia repair: Studies don’t support use of higher-cost biological mesh
The jury is still out on the costs and efficacy of biological mesh implants for abdominal wall hernia repair, according to a systematic review of the literature.
Of 20 articles that met search criteria, only 3 were comparative studies and none was a randomized clinical trial. In fact, most were case series involving convenience samples of patients at single institutions, Dr. Sergio Huerta of the University of Texas Southwestern Medical Center, Dallas, and his colleagues reported online Jan. 27 in JAMA Surgery.
The authors used multiple electronic databases to identify articles published between 1948 and June 30, 2015, on the use of biological mesh materials for reinforcement of the abdominal wall for hernia repair. Included were 14 articles that described outcomes with human acellular dermal matrix, 2 that reported results for porcine collagen intestinal submucosa derivatives, 3 that reported on porcine acelluar collagen skin derivatives, and 1 that described results for bovine pericardium.
Several problems were noted with respect to the studies, including widely varying follow-up time, operative technique, types of mesh used, and patient selection criteria. Also, outcome measures were not reported consistently across studies.
In addition, 16 of the 20 studies that met search criteria did not report investigator conflicts of interest, the authors reported (JAMA Surg. 2016 Jan 27. doi: 10.10001/jamasurg.2015.5234).
Notably, all the meshes used in the studies were approved by the Food and Drug Administration and were considered to be comparable to a group of nonbiological predicate devices, which cost up to 25% less than the biological equivalents, they noted.
“We were unable to find any evidence that supported the use of expensive biological material relative to low-cost synthetic mesh. In fact, with one exception, the biological materials became commercially available by showing that these materials were equivalent to low-cost established synthetic mesh material in an FDA 510(k) approval process. This process does not require phase 0 through IV clinical trials as required for drugs or biological agents,” they wrote, noting that the one material that bypassed the 510(k) process (Alloderm) was not required to demonstrate equivalence because it was classified as human transplanted tissue.
Biological mesh materials were introduced in the 1990s to minimize the risk of complications commonly seen with the use of synthetic mesh for abdominal wall hernia repair – one of the most common procedures performed by general surgeons, the authors explained.
“Because the outcomes for biological mesh material are perceived to be better than those for polymer-based prosthetic mesh replacement materials, the use of biological grafts increased exponentially without clear clinical evidence of efficacy,” they wrote.
The current review suggests that the evidence remains insufficient to determine whether cost and clinical benefits exist.
“It is generally assumed that FDA-approved drug or biological agents have been rigorously evaluated and that there is demonstrable safety and efficacy. This is not the case for 510(k) medical devices. Before using a new medical device, physicians should know the approval basis for the device and recognize that if it is a 510(k) device neither safety nor efficacy is ensured,” they said, adding that physicians should assume such devices are no better than predicate devices to which they are equivalent, and that “there can be no justification for purchasing a more expensive device when a lower-cost predicate device, which is equivalent, is available.”
Though limited by certain factors such as lack of access to detailed FDA information such as the specific criteria used to determine equivalence, and a lack of published literature on the full market penetration of biological mesh materials vs. nonbiological counterparts, the authors maintained that until evidence demonstrates superiority of biological materials, the expense associated with their use cannot be justified.
This study was supported by the Hudson-Penn Endowment fund at the University of Texas Southwestern Medical Center. The authors reported having no relevant financial disclosures.
Balancing the need for innovation against the practicalities of demonstrating clinical benefit for novel ideas is a fundamental problem in surgery – a problem highlighted by Heurta et al., Dr. Benjamin K. Poulose and his colleagues said in an editorial.
“This issue is particularly timely given an unsustainable trajectory of health care spending in the United States,” they wrote (JAMA Surg 2016 Jan 27. doi: 10.1001/jamasurg2015.5236).
Like the authors of the literature review, the editorial authors stressed the importance of understanding the limitations of the 510(k) process, and noted that surgeons should consider that the FDA sees them as “the group responsible for understanding and evaluating the data before using expensive medical devices.
“Understanding who is in charge of making sure that the devices that we use during surgery are safe and effective is critical. Likely, it will require a collaborative effort of the FDA, medical device companies, and physicians,” they wrote. Establishing a more formal system of postmarketing surveillance for higher-risk medical devices will benefit patients, they added. Current efforts suffer from reliance on self-reporting and lack of standardized data collection.
Postmarketing surveillance can be greatly improved by directly linking medical device approval with the support of high-quality registries, and the end result should provide transparent data for monitoring effectiveness and safety to drive value-based care and maintain innovation, they said.
Dr. Poulose is with Vanderbilt University Medical Center, Nashville, Tenn. Dr. Poulose reported receiving personal fees from Ariste Medical for consulting work, and research grants from Bard-Davol outside the submitted work.
Balancing the need for innovation against the practicalities of demonstrating clinical benefit for novel ideas is a fundamental problem in surgery – a problem highlighted by Heurta et al., Dr. Benjamin K. Poulose and his colleagues said in an editorial.
“This issue is particularly timely given an unsustainable trajectory of health care spending in the United States,” they wrote (JAMA Surg 2016 Jan 27. doi: 10.1001/jamasurg2015.5236).
Like the authors of the literature review, the editorial authors stressed the importance of understanding the limitations of the 510(k) process, and noted that surgeons should consider that the FDA sees them as “the group responsible for understanding and evaluating the data before using expensive medical devices.
“Understanding who is in charge of making sure that the devices that we use during surgery are safe and effective is critical. Likely, it will require a collaborative effort of the FDA, medical device companies, and physicians,” they wrote. Establishing a more formal system of postmarketing surveillance for higher-risk medical devices will benefit patients, they added. Current efforts suffer from reliance on self-reporting and lack of standardized data collection.
Postmarketing surveillance can be greatly improved by directly linking medical device approval with the support of high-quality registries, and the end result should provide transparent data for monitoring effectiveness and safety to drive value-based care and maintain innovation, they said.
Dr. Poulose is with Vanderbilt University Medical Center, Nashville, Tenn. Dr. Poulose reported receiving personal fees from Ariste Medical for consulting work, and research grants from Bard-Davol outside the submitted work.
Balancing the need for innovation against the practicalities of demonstrating clinical benefit for novel ideas is a fundamental problem in surgery – a problem highlighted by Heurta et al., Dr. Benjamin K. Poulose and his colleagues said in an editorial.
“This issue is particularly timely given an unsustainable trajectory of health care spending in the United States,” they wrote (JAMA Surg 2016 Jan 27. doi: 10.1001/jamasurg2015.5236).
Like the authors of the literature review, the editorial authors stressed the importance of understanding the limitations of the 510(k) process, and noted that surgeons should consider that the FDA sees them as “the group responsible for understanding and evaluating the data before using expensive medical devices.
“Understanding who is in charge of making sure that the devices that we use during surgery are safe and effective is critical. Likely, it will require a collaborative effort of the FDA, medical device companies, and physicians,” they wrote. Establishing a more formal system of postmarketing surveillance for higher-risk medical devices will benefit patients, they added. Current efforts suffer from reliance on self-reporting and lack of standardized data collection.
Postmarketing surveillance can be greatly improved by directly linking medical device approval with the support of high-quality registries, and the end result should provide transparent data for monitoring effectiveness and safety to drive value-based care and maintain innovation, they said.
Dr. Poulose is with Vanderbilt University Medical Center, Nashville, Tenn. Dr. Poulose reported receiving personal fees from Ariste Medical for consulting work, and research grants from Bard-Davol outside the submitted work.
The jury is still out on the costs and efficacy of biological mesh implants for abdominal wall hernia repair, according to a systematic review of the literature.
Of 20 articles that met search criteria, only 3 were comparative studies and none was a randomized clinical trial. In fact, most were case series involving convenience samples of patients at single institutions, Dr. Sergio Huerta of the University of Texas Southwestern Medical Center, Dallas, and his colleagues reported online Jan. 27 in JAMA Surgery.
The authors used multiple electronic databases to identify articles published between 1948 and June 30, 2015, on the use of biological mesh materials for reinforcement of the abdominal wall for hernia repair. Included were 14 articles that described outcomes with human acellular dermal matrix, 2 that reported results for porcine collagen intestinal submucosa derivatives, 3 that reported on porcine acelluar collagen skin derivatives, and 1 that described results for bovine pericardium.
Several problems were noted with respect to the studies, including widely varying follow-up time, operative technique, types of mesh used, and patient selection criteria. Also, outcome measures were not reported consistently across studies.
In addition, 16 of the 20 studies that met search criteria did not report investigator conflicts of interest, the authors reported (JAMA Surg. 2016 Jan 27. doi: 10.10001/jamasurg.2015.5234).
Notably, all the meshes used in the studies were approved by the Food and Drug Administration and were considered to be comparable to a group of nonbiological predicate devices, which cost up to 25% less than the biological equivalents, they noted.
“We were unable to find any evidence that supported the use of expensive biological material relative to low-cost synthetic mesh. In fact, with one exception, the biological materials became commercially available by showing that these materials were equivalent to low-cost established synthetic mesh material in an FDA 510(k) approval process. This process does not require phase 0 through IV clinical trials as required for drugs or biological agents,” they wrote, noting that the one material that bypassed the 510(k) process (Alloderm) was not required to demonstrate equivalence because it was classified as human transplanted tissue.
Biological mesh materials were introduced in the 1990s to minimize the risk of complications commonly seen with the use of synthetic mesh for abdominal wall hernia repair – one of the most common procedures performed by general surgeons, the authors explained.
“Because the outcomes for biological mesh material are perceived to be better than those for polymer-based prosthetic mesh replacement materials, the use of biological grafts increased exponentially without clear clinical evidence of efficacy,” they wrote.
The current review suggests that the evidence remains insufficient to determine whether cost and clinical benefits exist.
“It is generally assumed that FDA-approved drug or biological agents have been rigorously evaluated and that there is demonstrable safety and efficacy. This is not the case for 510(k) medical devices. Before using a new medical device, physicians should know the approval basis for the device and recognize that if it is a 510(k) device neither safety nor efficacy is ensured,” they said, adding that physicians should assume such devices are no better than predicate devices to which they are equivalent, and that “there can be no justification for purchasing a more expensive device when a lower-cost predicate device, which is equivalent, is available.”
Though limited by certain factors such as lack of access to detailed FDA information such as the specific criteria used to determine equivalence, and a lack of published literature on the full market penetration of biological mesh materials vs. nonbiological counterparts, the authors maintained that until evidence demonstrates superiority of biological materials, the expense associated with their use cannot be justified.
This study was supported by the Hudson-Penn Endowment fund at the University of Texas Southwestern Medical Center. The authors reported having no relevant financial disclosures.
The jury is still out on the costs and efficacy of biological mesh implants for abdominal wall hernia repair, according to a systematic review of the literature.
Of 20 articles that met search criteria, only 3 were comparative studies and none was a randomized clinical trial. In fact, most were case series involving convenience samples of patients at single institutions, Dr. Sergio Huerta of the University of Texas Southwestern Medical Center, Dallas, and his colleagues reported online Jan. 27 in JAMA Surgery.
The authors used multiple electronic databases to identify articles published between 1948 and June 30, 2015, on the use of biological mesh materials for reinforcement of the abdominal wall for hernia repair. Included were 14 articles that described outcomes with human acellular dermal matrix, 2 that reported results for porcine collagen intestinal submucosa derivatives, 3 that reported on porcine acelluar collagen skin derivatives, and 1 that described results for bovine pericardium.
Several problems were noted with respect to the studies, including widely varying follow-up time, operative technique, types of mesh used, and patient selection criteria. Also, outcome measures were not reported consistently across studies.
In addition, 16 of the 20 studies that met search criteria did not report investigator conflicts of interest, the authors reported (JAMA Surg. 2016 Jan 27. doi: 10.10001/jamasurg.2015.5234).
Notably, all the meshes used in the studies were approved by the Food and Drug Administration and were considered to be comparable to a group of nonbiological predicate devices, which cost up to 25% less than the biological equivalents, they noted.
“We were unable to find any evidence that supported the use of expensive biological material relative to low-cost synthetic mesh. In fact, with one exception, the biological materials became commercially available by showing that these materials were equivalent to low-cost established synthetic mesh material in an FDA 510(k) approval process. This process does not require phase 0 through IV clinical trials as required for drugs or biological agents,” they wrote, noting that the one material that bypassed the 510(k) process (Alloderm) was not required to demonstrate equivalence because it was classified as human transplanted tissue.
Biological mesh materials were introduced in the 1990s to minimize the risk of complications commonly seen with the use of synthetic mesh for abdominal wall hernia repair – one of the most common procedures performed by general surgeons, the authors explained.
“Because the outcomes for biological mesh material are perceived to be better than those for polymer-based prosthetic mesh replacement materials, the use of biological grafts increased exponentially without clear clinical evidence of efficacy,” they wrote.
The current review suggests that the evidence remains insufficient to determine whether cost and clinical benefits exist.
“It is generally assumed that FDA-approved drug or biological agents have been rigorously evaluated and that there is demonstrable safety and efficacy. This is not the case for 510(k) medical devices. Before using a new medical device, physicians should know the approval basis for the device and recognize that if it is a 510(k) device neither safety nor efficacy is ensured,” they said, adding that physicians should assume such devices are no better than predicate devices to which they are equivalent, and that “there can be no justification for purchasing a more expensive device when a lower-cost predicate device, which is equivalent, is available.”
Though limited by certain factors such as lack of access to detailed FDA information such as the specific criteria used to determine equivalence, and a lack of published literature on the full market penetration of biological mesh materials vs. nonbiological counterparts, the authors maintained that until evidence demonstrates superiority of biological materials, the expense associated with their use cannot be justified.
This study was supported by the Hudson-Penn Endowment fund at the University of Texas Southwestern Medical Center. The authors reported having no relevant financial disclosures.
FROM JAMA SURGERY
Key clinical point: The jury is still out on the costs and efficacy of biological mesh implants for abdominal wall hernia repair, and the expense associated with their use cannot be justified at this time, a systematic review of the literature suggested.
Major finding: Available evidence remains insufficient to determine whether cost and clinical benefits exist with the use of biological mesh for abdominal wall hernia repair.
Data source: A systematic review of the literature, yielding 20 eligible studies.
Disclosures: This study was supported by the Hudson-Penn Endowment fund at University of Texas Southwestern Medical Center. The authors reported having no relevant financial disclosures.