User login
Light and heavy mesh deliver similar outcomes and QOL for lap inguinal repair
WASHINGTON – The weight of mesh used in laparoscopic inguinal hernia repairs was not a significant factor in postoperative outcomes and quality of life, in a large, long-term study.
“There are approximately 700,000 inguinal hernia repairs annually,” said Steve Groene, MD, of the Carolinas Medical Center, Charlotte, N.C. “The goal of our study was to utilize a large sample size of long-term follow-up and compare surgical and quality of life outcomes between light-weight and heavy-weight mesh in laparoscopic inguinal hernia repairs.”
The rates of postoperative complications such as surgical infection, urinary retention, and recurrence in the two groups were similar. Although the LW mesh group had a significantly higher rate of hematoma and seroma, that difference vanished with a multivariate analysis that accounted for confounding factors such as smoking, elective vs. emergent surgery, and surgical technique, Dr. Groene said at the annual clinical congress of the American College of Surgeons.
Quality of life (QOL) was measured with the Carolina Comfort Scale before surgery and at the 2-week, 1-month, 6-month, 12-month, 24-month, and 36-month follow-ups. The investigators looked at pain, movement limitation, and mesh sensation for outcomes and symptoms. There were no other statistically significant differences in QOL between the groups at any of the follow-up time points.
When asked during the discussion about the experience of the investigators in getting patients to continue through a 36-month follow-up, Dr. Groene said that “at 1 month, we were about 60%, [and] at 1 year about 40%; having about 40%-42% of people following up at 1 month is very good.”
Dr. Groene concluded that surgeons should continue to use the type of mesh they feel most comfortable with for laparoscopic inguinal hernia repair and expect to have similar outcomes.
He reported having no relevant financial disclosures.
WASHINGTON – The weight of mesh used in laparoscopic inguinal hernia repairs was not a significant factor in postoperative outcomes and quality of life, in a large, long-term study.
“There are approximately 700,000 inguinal hernia repairs annually,” said Steve Groene, MD, of the Carolinas Medical Center, Charlotte, N.C. “The goal of our study was to utilize a large sample size of long-term follow-up and compare surgical and quality of life outcomes between light-weight and heavy-weight mesh in laparoscopic inguinal hernia repairs.”
The rates of postoperative complications such as surgical infection, urinary retention, and recurrence in the two groups were similar. Although the LW mesh group had a significantly higher rate of hematoma and seroma, that difference vanished with a multivariate analysis that accounted for confounding factors such as smoking, elective vs. emergent surgery, and surgical technique, Dr. Groene said at the annual clinical congress of the American College of Surgeons.
Quality of life (QOL) was measured with the Carolina Comfort Scale before surgery and at the 2-week, 1-month, 6-month, 12-month, 24-month, and 36-month follow-ups. The investigators looked at pain, movement limitation, and mesh sensation for outcomes and symptoms. There were no other statistically significant differences in QOL between the groups at any of the follow-up time points.
When asked during the discussion about the experience of the investigators in getting patients to continue through a 36-month follow-up, Dr. Groene said that “at 1 month, we were about 60%, [and] at 1 year about 40%; having about 40%-42% of people following up at 1 month is very good.”
Dr. Groene concluded that surgeons should continue to use the type of mesh they feel most comfortable with for laparoscopic inguinal hernia repair and expect to have similar outcomes.
He reported having no relevant financial disclosures.
WASHINGTON – The weight of mesh used in laparoscopic inguinal hernia repairs was not a significant factor in postoperative outcomes and quality of life, in a large, long-term study.
“There are approximately 700,000 inguinal hernia repairs annually,” said Steve Groene, MD, of the Carolinas Medical Center, Charlotte, N.C. “The goal of our study was to utilize a large sample size of long-term follow-up and compare surgical and quality of life outcomes between light-weight and heavy-weight mesh in laparoscopic inguinal hernia repairs.”
The rates of postoperative complications such as surgical infection, urinary retention, and recurrence in the two groups were similar. Although the LW mesh group had a significantly higher rate of hematoma and seroma, that difference vanished with a multivariate analysis that accounted for confounding factors such as smoking, elective vs. emergent surgery, and surgical technique, Dr. Groene said at the annual clinical congress of the American College of Surgeons.
Quality of life (QOL) was measured with the Carolina Comfort Scale before surgery and at the 2-week, 1-month, 6-month, 12-month, 24-month, and 36-month follow-ups. The investigators looked at pain, movement limitation, and mesh sensation for outcomes and symptoms. There were no other statistically significant differences in QOL between the groups at any of the follow-up time points.
When asked during the discussion about the experience of the investigators in getting patients to continue through a 36-month follow-up, Dr. Groene said that “at 1 month, we were about 60%, [and] at 1 year about 40%; having about 40%-42% of people following up at 1 month is very good.”
Dr. Groene concluded that surgeons should continue to use the type of mesh they feel most comfortable with for laparoscopic inguinal hernia repair and expect to have similar outcomes.
He reported having no relevant financial disclosures.
FROM ACS CLINICAL CONGRESS
Key clinical point:
Major finding: For laparoscopic inguinal hernia repair, mesh weight was not a significant factor in postoperative complications or quality of life, as measured by the Carolinas Comfort Scale.
Data source: A prospective study of 1,270 laparoscopic inguinal hernia repair patients from a hernia-specific database.
Disclosures: Dr. Groene reported having no relevant financial disclosures.
Risk models for hernia recurrence don’t hold up to external validation
Five common variable selection strategies failed to produce a statistical model that accurately predicted ventral hernia recurrence in an investigation published in the Journal of Surgical Research.
The finding matters because those five techniques – expert opinion and various multivariate regression and bootstrapping strategies – have been widely used in previous studies to create risk scores for ventral hernia recurrence. The new study calls the value of existing scoring systems into question (J Surg Res. 2016 Nov;206[1]:159-67. doi: 10.1016/j.jss.2016.07.042).
The lack of external validation in many studies leads to medical findings that often can’t be confirmed by subsequent studies. It’s a problem that has contributed to skepticism about research results in both the medical community and the general public, they said.
“This study demonstrates the importance of true external validation on an external data set. Simply splitting a data set and validating [internally] does not appear to be an adequate assessment of predictive accuracy. … We recommend that future researchers consider using and presenting the results of multiple variable selection strategies [and] focus on presenting predictive accuracy on external data sets to validate their model,” the team concluded.
The original goal of the project was to identify the best predictors of ventral hernia recurrence since suggestions from past studies have varied. The team first used a prospective database of 790 ventral hernia repair patients to identify predictors of recurrence. Of that group, 526 patients – 173 (32.9%) of whom had a recurrence after a median follow-up of 20 months – were used to identify risk variables using expert opinion, selective stepwise regression, liberal stepwise regression, and bootstrapping with both restrictive and liberal internal resampling.
The team used the remaining 264 patients to confirm the findings. As in previous studies, internal validation worked: all five models had a Harrell’s C-statistic of about 0.76, which is considered reasonable, Dr. Holihan and her associates reported.
However, when the investigators applied their models to a second database of 1,225 patients followed for a median of 9 months – with 155 recurrences (12.7%) – they were not much better at predicting recurrence than a coin toss, with C-statistic values of about 0.56.
Some variables made the cut with all five selection techniques, including hernia type, wound class, and albumin levels, which are related to how well the wound heals. Other variables were significant in some selection strategies but not others, including smoking status, open versus laparoscopic approach, and mesh use.
At least for now, clinical intuition remains important for assessing rerupture risk, they said.
The National Institutes of Health funded the work. Author disclosures were not reported.
Five common variable selection strategies failed to produce a statistical model that accurately predicted ventral hernia recurrence in an investigation published in the Journal of Surgical Research.
The finding matters because those five techniques – expert opinion and various multivariate regression and bootstrapping strategies – have been widely used in previous studies to create risk scores for ventral hernia recurrence. The new study calls the value of existing scoring systems into question (J Surg Res. 2016 Nov;206[1]:159-67. doi: 10.1016/j.jss.2016.07.042).
The lack of external validation in many studies leads to medical findings that often can’t be confirmed by subsequent studies. It’s a problem that has contributed to skepticism about research results in both the medical community and the general public, they said.
“This study demonstrates the importance of true external validation on an external data set. Simply splitting a data set and validating [internally] does not appear to be an adequate assessment of predictive accuracy. … We recommend that future researchers consider using and presenting the results of multiple variable selection strategies [and] focus on presenting predictive accuracy on external data sets to validate their model,” the team concluded.
The original goal of the project was to identify the best predictors of ventral hernia recurrence since suggestions from past studies have varied. The team first used a prospective database of 790 ventral hernia repair patients to identify predictors of recurrence. Of that group, 526 patients – 173 (32.9%) of whom had a recurrence after a median follow-up of 20 months – were used to identify risk variables using expert opinion, selective stepwise regression, liberal stepwise regression, and bootstrapping with both restrictive and liberal internal resampling.
The team used the remaining 264 patients to confirm the findings. As in previous studies, internal validation worked: all five models had a Harrell’s C-statistic of about 0.76, which is considered reasonable, Dr. Holihan and her associates reported.
However, when the investigators applied their models to a second database of 1,225 patients followed for a median of 9 months – with 155 recurrences (12.7%) – they were not much better at predicting recurrence than a coin toss, with C-statistic values of about 0.56.
Some variables made the cut with all five selection techniques, including hernia type, wound class, and albumin levels, which are related to how well the wound heals. Other variables were significant in some selection strategies but not others, including smoking status, open versus laparoscopic approach, and mesh use.
At least for now, clinical intuition remains important for assessing rerupture risk, they said.
The National Institutes of Health funded the work. Author disclosures were not reported.
Five common variable selection strategies failed to produce a statistical model that accurately predicted ventral hernia recurrence in an investigation published in the Journal of Surgical Research.
The finding matters because those five techniques – expert opinion and various multivariate regression and bootstrapping strategies – have been widely used in previous studies to create risk scores for ventral hernia recurrence. The new study calls the value of existing scoring systems into question (J Surg Res. 2016 Nov;206[1]:159-67. doi: 10.1016/j.jss.2016.07.042).
The lack of external validation in many studies leads to medical findings that often can’t be confirmed by subsequent studies. It’s a problem that has contributed to skepticism about research results in both the medical community and the general public, they said.
“This study demonstrates the importance of true external validation on an external data set. Simply splitting a data set and validating [internally] does not appear to be an adequate assessment of predictive accuracy. … We recommend that future researchers consider using and presenting the results of multiple variable selection strategies [and] focus on presenting predictive accuracy on external data sets to validate their model,” the team concluded.
The original goal of the project was to identify the best predictors of ventral hernia recurrence since suggestions from past studies have varied. The team first used a prospective database of 790 ventral hernia repair patients to identify predictors of recurrence. Of that group, 526 patients – 173 (32.9%) of whom had a recurrence after a median follow-up of 20 months – were used to identify risk variables using expert opinion, selective stepwise regression, liberal stepwise regression, and bootstrapping with both restrictive and liberal internal resampling.
The team used the remaining 264 patients to confirm the findings. As in previous studies, internal validation worked: all five models had a Harrell’s C-statistic of about 0.76, which is considered reasonable, Dr. Holihan and her associates reported.
However, when the investigators applied their models to a second database of 1,225 patients followed for a median of 9 months – with 155 recurrences (12.7%) – they were not much better at predicting recurrence than a coin toss, with C-statistic values of about 0.56.
Some variables made the cut with all five selection techniques, including hernia type, wound class, and albumin levels, which are related to how well the wound heals. Other variables were significant in some selection strategies but not others, including smoking status, open versus laparoscopic approach, and mesh use.
At least for now, clinical intuition remains important for assessing rerupture risk, they said.
The National Institutes of Health funded the work. Author disclosures were not reported.
FROM THE JOURNAL OF SURGICAL RESEARCH
Key clinical point:
Major finding: Risk models developed from the five strategies weren’t much better at predicting recurrence than a coin toss, with C-statistic values of about 0.56.
Data source: Analysis of two datasets containing a total of 2,015 ventral hernia repair patients.
Disclosures: The National Institutes of Health funded the work. Author disclosures were not reported.
Ultrasound effective in diagnosing occult hernia in women
ORLANDO – Ultrasound appears to be an effective tool in diagnosing occult hernia in women with unexplained chronic pelvic pain, according to a retrospective cohort study of 96 women.
“As gynecologists, we are likely to see those patients with chronic pelvic pain in our clinic before other specialists due to the location of their pain,” said Joelle Aoun, MD, an ob.gyn. in the division of minimally invasive gynecologic surgery at Henry Ford Health System in Detroit. “So it’s very important to recognize women with a high clinical suspicion for occult hernia and evaluate them in order to prevent a delayed diagnosis and prolonged suffering.”
Hernias can be more difficult to diagnose in women than in men, Dr. Aoun said at the meeting sponsored by AAGL, and the literature offers conflicting findings since most hernia studies are conducted in men or with mixed gender cohorts.
Dr. Aoun and her coinvestigators conducted a retrospective cohort study from January 2005 to July 2016, identifying 96 women with chronic pelvic pain and focal inguinal tenderness. Protruding fat or visceral tissue on physical exam or observed visually led clinicians to suspect a hernia. A single sonographer performed the musculoskeletal ultrasound.
Investigators diagnosed an occult hernia in more than half of the patients (51 women) based on the physical exam and ultrasound findings. Diagnoses included inguinal, femoral, Spigelian, and umbilical hernias.
All women with an ultrasound-diagnosed hernia were referred to general surgery. A majority – 69% of women – underwent surgical exploration. The remaining 31% of women who declined tended to have lower pain scores, Dr. Aoun said. Surgeons confirmed the hernia diagnosis in 97% of the women, or 34 out of the 35 women who had consented to surgery.
The group with a hernia was older and more likely to have arthritis, but otherwise did not differ significantly from the nonhernia cohort.
“We believe musculoskeletal ultrasound is valuable as an initial imaging modality due to its high predictive value, low cost, and noninvasiveness,” Dr. Aoun said.
Chronic pelvic pain is not uncommon, affecting approximately 15% of women during their reproductive years often with significant impacts on quality of life, workplace productivity, and health care utilization, Dr. Aoun said. This presentation also accounts for about 10% outpatient gynecology consultations and approximately 40% of laparoscopies in the United States, she added.
Dr. Aoun and her colleagues are planning a subsequent study of all the women who opted not to undergo surgery to determine their follow-up pain profiles based on chart review and phone interviews.
Dr. Aoun reported having no relevant financial disclosures.
ORLANDO – Ultrasound appears to be an effective tool in diagnosing occult hernia in women with unexplained chronic pelvic pain, according to a retrospective cohort study of 96 women.
“As gynecologists, we are likely to see those patients with chronic pelvic pain in our clinic before other specialists due to the location of their pain,” said Joelle Aoun, MD, an ob.gyn. in the division of minimally invasive gynecologic surgery at Henry Ford Health System in Detroit. “So it’s very important to recognize women with a high clinical suspicion for occult hernia and evaluate them in order to prevent a delayed diagnosis and prolonged suffering.”
Hernias can be more difficult to diagnose in women than in men, Dr. Aoun said at the meeting sponsored by AAGL, and the literature offers conflicting findings since most hernia studies are conducted in men or with mixed gender cohorts.
Dr. Aoun and her coinvestigators conducted a retrospective cohort study from January 2005 to July 2016, identifying 96 women with chronic pelvic pain and focal inguinal tenderness. Protruding fat or visceral tissue on physical exam or observed visually led clinicians to suspect a hernia. A single sonographer performed the musculoskeletal ultrasound.
Investigators diagnosed an occult hernia in more than half of the patients (51 women) based on the physical exam and ultrasound findings. Diagnoses included inguinal, femoral, Spigelian, and umbilical hernias.
All women with an ultrasound-diagnosed hernia were referred to general surgery. A majority – 69% of women – underwent surgical exploration. The remaining 31% of women who declined tended to have lower pain scores, Dr. Aoun said. Surgeons confirmed the hernia diagnosis in 97% of the women, or 34 out of the 35 women who had consented to surgery.
The group with a hernia was older and more likely to have arthritis, but otherwise did not differ significantly from the nonhernia cohort.
“We believe musculoskeletal ultrasound is valuable as an initial imaging modality due to its high predictive value, low cost, and noninvasiveness,” Dr. Aoun said.
Chronic pelvic pain is not uncommon, affecting approximately 15% of women during their reproductive years often with significant impacts on quality of life, workplace productivity, and health care utilization, Dr. Aoun said. This presentation also accounts for about 10% outpatient gynecology consultations and approximately 40% of laparoscopies in the United States, she added.
Dr. Aoun and her colleagues are planning a subsequent study of all the women who opted not to undergo surgery to determine their follow-up pain profiles based on chart review and phone interviews.
Dr. Aoun reported having no relevant financial disclosures.
ORLANDO – Ultrasound appears to be an effective tool in diagnosing occult hernia in women with unexplained chronic pelvic pain, according to a retrospective cohort study of 96 women.
“As gynecologists, we are likely to see those patients with chronic pelvic pain in our clinic before other specialists due to the location of their pain,” said Joelle Aoun, MD, an ob.gyn. in the division of minimally invasive gynecologic surgery at Henry Ford Health System in Detroit. “So it’s very important to recognize women with a high clinical suspicion for occult hernia and evaluate them in order to prevent a delayed diagnosis and prolonged suffering.”
Hernias can be more difficult to diagnose in women than in men, Dr. Aoun said at the meeting sponsored by AAGL, and the literature offers conflicting findings since most hernia studies are conducted in men or with mixed gender cohorts.
Dr. Aoun and her coinvestigators conducted a retrospective cohort study from January 2005 to July 2016, identifying 96 women with chronic pelvic pain and focal inguinal tenderness. Protruding fat or visceral tissue on physical exam or observed visually led clinicians to suspect a hernia. A single sonographer performed the musculoskeletal ultrasound.
Investigators diagnosed an occult hernia in more than half of the patients (51 women) based on the physical exam and ultrasound findings. Diagnoses included inguinal, femoral, Spigelian, and umbilical hernias.
All women with an ultrasound-diagnosed hernia were referred to general surgery. A majority – 69% of women – underwent surgical exploration. The remaining 31% of women who declined tended to have lower pain scores, Dr. Aoun said. Surgeons confirmed the hernia diagnosis in 97% of the women, or 34 out of the 35 women who had consented to surgery.
The group with a hernia was older and more likely to have arthritis, but otherwise did not differ significantly from the nonhernia cohort.
“We believe musculoskeletal ultrasound is valuable as an initial imaging modality due to its high predictive value, low cost, and noninvasiveness,” Dr. Aoun said.
Chronic pelvic pain is not uncommon, affecting approximately 15% of women during their reproductive years often with significant impacts on quality of life, workplace productivity, and health care utilization, Dr. Aoun said. This presentation also accounts for about 10% outpatient gynecology consultations and approximately 40% of laparoscopies in the United States, she added.
Dr. Aoun and her colleagues are planning a subsequent study of all the women who opted not to undergo surgery to determine their follow-up pain profiles based on chart review and phone interviews.
Dr. Aoun reported having no relevant financial disclosures.
AT THE AAGL GLOBAL CONGRESS
Key clinical point:
Major finding: About 53% of women with chronic pelvic pain were diagnosed with an occult hernia following physical exam and ultrasound. Surgeons confirmed the hernia diagnosis in 34 out of 35 patients who consented to surgery.
Data source: A retrospective cohort study of 96 women with chronic pelvic pain and focal inguinal tenderness.
Disclosures: Dr. Aoun reported having no relevant financial disclosures.
Simulation model favors hernia surgery over watchful waiting
WASHINGTON – Surgical repair of ventral hernias at time of diagnosis is a more cost-effective approach than watchful waiting, according to the results of a state-transition microsimulation model presented by Lindsey Wolf, MD, at the annual clinical congress of the American College of Surgeons.
The benefit of surgical intervention, compared with observation or watchful waiting for reducible ventral hernias is not well described, reported Dr. Wolf, a general surgery resident at Brigham and Women’s Hospital, Boston.
In the model, cost was represented in U.S. dollars and benefit was indicated by quality-adjusted life years (QALY). Both measures accumulated for individual patients over time and then were averaged and reported for an entire cohort of simulated patients, Dr. Wolf explained. Incremental cost effectiveness, a measure represented as a ratio of cost per QALY gained for each strategy, “provides context by allowing us to compare each strategy to the next best strategy,” explained Dr. Wolf.
Willingness to pay, a threshold set by the government that represents the maximum amount a payer is willing to spend for additional quality, was set at a threshold of $50,000 dollars per QALY, which is a “commonly accepted willingness-to pay-threshold,” she said.
The model’s primary outcomes were lifetime costs, QALYs from time of diagnosis, and incremental cost-effectiveness ratios.
“We built a state-transition microsimulation model which represents the different health states a patient can occupy at any point in time,” Dr. Wolf reported. “Using a yearly cycle, a cohort of patients were simulated through the model one at a time.”
All patients entered the model in an asymptomatic state. For each year there was a probability for a patient to transition from the current state to another state in the model.
Patients who underwent surgical repair at diagnosis were transitioned to the no-hernia state in the first year after undergoing surgery. Those in the watchful-waiting group stayed in the asymptotic state and each year there was a probability of becoming symptomatic. Of those who became symptomatic, there was a small probability that they would present with an incarcerated hernia and would require emergent surgery rather than elective surgery. Patients were subjected to perioperative mortality rates, as well as background yearly risk of death.
Cohort characteristics, hospital and other costs, perioperative mortality, and quality of life were derived from best available published studies and the Nationwide Inpatient Sample, the largest all-payer inpatient care database in the United States.
Overall, laparoscopic surgery at diagnosis was the optimal hernia repair strategy, reported Dr. Wolf.
Although laparoscopic surgery was the most expensive, it was also the most effective and, compared with watchful waiting – the least expensive and least effective strategy – the incremental cost-effectiveness ratio was about $14,800 per QALY.
Open repair at diagnosis fell between the watchful-waiting and laparoscopic-repair strategies in terms of cost and effectiveness.
To understand the conditions in which the optimal strategy changed, the researchers performed sensitivity analysis using the net monetary benefit metric, which represented both costs and benefits in a single unit at a given willingness to pay threshold.
“For a cohort of high-risk patients, once the perioperative risk of death exceeds 3.4%, watchful waiting becomes the preferred strategy,” Dr. Wolf said. Watchful waiting also was the preferred strategy when the yearly risk of recurrence exceeded 24%.
A sensitivity analysis comparing quality of life for elective open and laparoscopic repair revealed that, when quality-of-life measures were similar between the two surgical repair groups, the open repair became the preferred strategy.
Finally, researchers performed probabilistic sensitivity analysis by simulating the cohort of 100,000 patients 100 times and each time deriving results that were similar – an indication of robust results.
“In conclusion, we found that, for a typical cohort of patients with ventral hernia, laparoscopic repair at diagnosis is very cost effective. As long-term outcomes for open and laparoscopic repair were very similar in the model, the decision between laparoscopic and open surgery depends on surgeon experience and preference for one method over another,” said Dr. Wolf.
This study was funded by the Resident Research Scholarship awarded by the American College of Surgeons. Dr. Wolf reported having no disclosures.
jcraig@frontlinemedcom.com
On Twitter @jessnicolecraig
WASHINGTON – Surgical repair of ventral hernias at time of diagnosis is a more cost-effective approach than watchful waiting, according to the results of a state-transition microsimulation model presented by Lindsey Wolf, MD, at the annual clinical congress of the American College of Surgeons.
The benefit of surgical intervention, compared with observation or watchful waiting for reducible ventral hernias is not well described, reported Dr. Wolf, a general surgery resident at Brigham and Women’s Hospital, Boston.
In the model, cost was represented in U.S. dollars and benefit was indicated by quality-adjusted life years (QALY). Both measures accumulated for individual patients over time and then were averaged and reported for an entire cohort of simulated patients, Dr. Wolf explained. Incremental cost effectiveness, a measure represented as a ratio of cost per QALY gained for each strategy, “provides context by allowing us to compare each strategy to the next best strategy,” explained Dr. Wolf.
Willingness to pay, a threshold set by the government that represents the maximum amount a payer is willing to spend for additional quality, was set at a threshold of $50,000 dollars per QALY, which is a “commonly accepted willingness-to pay-threshold,” she said.
The model’s primary outcomes were lifetime costs, QALYs from time of diagnosis, and incremental cost-effectiveness ratios.
“We built a state-transition microsimulation model which represents the different health states a patient can occupy at any point in time,” Dr. Wolf reported. “Using a yearly cycle, a cohort of patients were simulated through the model one at a time.”
All patients entered the model in an asymptomatic state. For each year there was a probability for a patient to transition from the current state to another state in the model.
Patients who underwent surgical repair at diagnosis were transitioned to the no-hernia state in the first year after undergoing surgery. Those in the watchful-waiting group stayed in the asymptotic state and each year there was a probability of becoming symptomatic. Of those who became symptomatic, there was a small probability that they would present with an incarcerated hernia and would require emergent surgery rather than elective surgery. Patients were subjected to perioperative mortality rates, as well as background yearly risk of death.
Cohort characteristics, hospital and other costs, perioperative mortality, and quality of life were derived from best available published studies and the Nationwide Inpatient Sample, the largest all-payer inpatient care database in the United States.
Overall, laparoscopic surgery at diagnosis was the optimal hernia repair strategy, reported Dr. Wolf.
Although laparoscopic surgery was the most expensive, it was also the most effective and, compared with watchful waiting – the least expensive and least effective strategy – the incremental cost-effectiveness ratio was about $14,800 per QALY.
Open repair at diagnosis fell between the watchful-waiting and laparoscopic-repair strategies in terms of cost and effectiveness.
To understand the conditions in which the optimal strategy changed, the researchers performed sensitivity analysis using the net monetary benefit metric, which represented both costs and benefits in a single unit at a given willingness to pay threshold.
“For a cohort of high-risk patients, once the perioperative risk of death exceeds 3.4%, watchful waiting becomes the preferred strategy,” Dr. Wolf said. Watchful waiting also was the preferred strategy when the yearly risk of recurrence exceeded 24%.
A sensitivity analysis comparing quality of life for elective open and laparoscopic repair revealed that, when quality-of-life measures were similar between the two surgical repair groups, the open repair became the preferred strategy.
Finally, researchers performed probabilistic sensitivity analysis by simulating the cohort of 100,000 patients 100 times and each time deriving results that were similar – an indication of robust results.
“In conclusion, we found that, for a typical cohort of patients with ventral hernia, laparoscopic repair at diagnosis is very cost effective. As long-term outcomes for open and laparoscopic repair were very similar in the model, the decision between laparoscopic and open surgery depends on surgeon experience and preference for one method over another,” said Dr. Wolf.
This study was funded by the Resident Research Scholarship awarded by the American College of Surgeons. Dr. Wolf reported having no disclosures.
jcraig@frontlinemedcom.com
On Twitter @jessnicolecraig
WASHINGTON – Surgical repair of ventral hernias at time of diagnosis is a more cost-effective approach than watchful waiting, according to the results of a state-transition microsimulation model presented by Lindsey Wolf, MD, at the annual clinical congress of the American College of Surgeons.
The benefit of surgical intervention, compared with observation or watchful waiting for reducible ventral hernias is not well described, reported Dr. Wolf, a general surgery resident at Brigham and Women’s Hospital, Boston.
In the model, cost was represented in U.S. dollars and benefit was indicated by quality-adjusted life years (QALY). Both measures accumulated for individual patients over time and then were averaged and reported for an entire cohort of simulated patients, Dr. Wolf explained. Incremental cost effectiveness, a measure represented as a ratio of cost per QALY gained for each strategy, “provides context by allowing us to compare each strategy to the next best strategy,” explained Dr. Wolf.
Willingness to pay, a threshold set by the government that represents the maximum amount a payer is willing to spend for additional quality, was set at a threshold of $50,000 dollars per QALY, which is a “commonly accepted willingness-to pay-threshold,” she said.
The model’s primary outcomes were lifetime costs, QALYs from time of diagnosis, and incremental cost-effectiveness ratios.
“We built a state-transition microsimulation model which represents the different health states a patient can occupy at any point in time,” Dr. Wolf reported. “Using a yearly cycle, a cohort of patients were simulated through the model one at a time.”
All patients entered the model in an asymptomatic state. For each year there was a probability for a patient to transition from the current state to another state in the model.
Patients who underwent surgical repair at diagnosis were transitioned to the no-hernia state in the first year after undergoing surgery. Those in the watchful-waiting group stayed in the asymptotic state and each year there was a probability of becoming symptomatic. Of those who became symptomatic, there was a small probability that they would present with an incarcerated hernia and would require emergent surgery rather than elective surgery. Patients were subjected to perioperative mortality rates, as well as background yearly risk of death.
Cohort characteristics, hospital and other costs, perioperative mortality, and quality of life were derived from best available published studies and the Nationwide Inpatient Sample, the largest all-payer inpatient care database in the United States.
Overall, laparoscopic surgery at diagnosis was the optimal hernia repair strategy, reported Dr. Wolf.
Although laparoscopic surgery was the most expensive, it was also the most effective and, compared with watchful waiting – the least expensive and least effective strategy – the incremental cost-effectiveness ratio was about $14,800 per QALY.
Open repair at diagnosis fell between the watchful-waiting and laparoscopic-repair strategies in terms of cost and effectiveness.
To understand the conditions in which the optimal strategy changed, the researchers performed sensitivity analysis using the net monetary benefit metric, which represented both costs and benefits in a single unit at a given willingness to pay threshold.
“For a cohort of high-risk patients, once the perioperative risk of death exceeds 3.4%, watchful waiting becomes the preferred strategy,” Dr. Wolf said. Watchful waiting also was the preferred strategy when the yearly risk of recurrence exceeded 24%.
A sensitivity analysis comparing quality of life for elective open and laparoscopic repair revealed that, when quality-of-life measures were similar between the two surgical repair groups, the open repair became the preferred strategy.
Finally, researchers performed probabilistic sensitivity analysis by simulating the cohort of 100,000 patients 100 times and each time deriving results that were similar – an indication of robust results.
“In conclusion, we found that, for a typical cohort of patients with ventral hernia, laparoscopic repair at diagnosis is very cost effective. As long-term outcomes for open and laparoscopic repair were very similar in the model, the decision between laparoscopic and open surgery depends on surgeon experience and preference for one method over another,” said Dr. Wolf.
This study was funded by the Resident Research Scholarship awarded by the American College of Surgeons. Dr. Wolf reported having no disclosures.
jcraig@frontlinemedcom.com
On Twitter @jessnicolecraig
AT THE ACS CLINICAL CONGRESS
Key clinical point:
Major finding: The incremental cost-effectiveness ratio for laparoscopic surgery, compared with watchful waiting, was about $14,800 per QALY.
Data source: A state-transition microsimulation model of 100,000 people.
Disclosures: This study was funded by the Resident Research Scholarship awarded by the American College of Surgeons. Dr. Wolf reported having no disclosures.
The mesh tradeoff: Lower recurrence risk vs. complicaitons
Among patients undergoing elective incisional repair of abdominal wall hernias, the use of mesh reinforcement decreases the short-term recurrence rate by 5% but increases major complications by approximately the same amount over the subsequent 5 years, Dunja Kokotovic, MB, reported at the annual clinical congress of the American College of Surgeons.
“Given the continuously increasing incidence of mesh-related complications with time, it is expected that, with even longer follow-up up than the 5 years observed in this study, mesh-related complications continue to accrue,” said Dr. Kokotovic of the Center for Surgical Science, Zealand University Hospital, Koge, Denmark. The findings of this observational registry-based cohort study were presented at the congress and simultaneously published online in JAMA (2016 Oct 17. doi: 10.1001/jama.2016.15217).
These results highlight the need to assess the long-term safety of interventions before making definitive conclusions about their benefits and widely adopting them. In the United States, manufacturers are required to demonstrate the long-term safety of drugs but not of some devices, including hernia meshes. There were approximately 190,000 such hernia repairs performed in the United States alone during the most recent year for which data are available, and mesh is estimated to have been used in at least half, Dr. Kokotovic noted.
She and her associates analyzed the 5-year outcomes for virtually all incisional hernia repairs performed in Denmark from 2007 through 2010 using data in a mandatory national registry. Their analysis included 3,242 patients (mean age, 58 years): 1,119 (34.5%) who had open mesh repair, 1,757 (54.2%) who had laparoscopic mesh repair, and 366 (11.3%) who had nonmesh repair.
The cumulative risk of reoperation for hernia recurrence was significantly lower for patients who had open mesh repair (12.3%) or laparoscopic mesh repair (10.6%) than for those who had nonmesh repair (17.1%). However, this benefit was offset by the rate of major mesh-related complications requiring surgical intervention – including surgical site infection, formation of a chronic sinus tract, late-onset intra-abdominal abscess, enterocutaneous fistula, bowel obstruction, and bowel perforation – which progressively increased over time. The cumulative incidence of such complications was 5.6% for open mesh repair and 3.7% for laparoscopic mesh repair.
This study was limited in that it was observational rather than being based on randomized data, so selection bias and imbalances among the study groups couldn’t be fully controlled for. However, two strengths of this study were that it reflects the real-world experience of an entire country and all the surgeons performing hernia repairs there, and it had 100% follow-up, the researchers said.
This study was partly funded by the Edgar Schnohr and Wife Gilberte Schnohr’s Foundation supporting independent surgical and anesthesiological research. Dr. Kokotovic reported having no relevant financial disclosures; one investigator reported receiving personal fees from Bard and Etichon for educational presentations.
These study findings suggest that the risk-benefit ratio of mesh reinforcement is not as clear as previously thought and call into question the current widespread use of mesh, even for repair of small hernias, when mesh is the norm for all incisional hernia repairs of any size.
Although the study by Kokotovic and colleagues is one of the most comprehensive long-term studies in hernia surgery, many questions remain about the optimal approach for repairing ventral hernia. To provide more rigorous data to better understand optimal approaches to this common clinical problem, surgeons will need to design large multicenter pragmatic trials with long-term follow-up.
Kamal M. F. Itani, MD, is at the VA Boston Health Care System, Boston University, West Roxbury, Mass., and Harvard Medical School in Boston. He reported having served as a research consultant to Davol 4 years ago regarding an antibiotic-coated mesh product. These remarks are excerpted from an editorial accompanying Dr. Kokotovic’s report (JAMA 2016 Oct 17. doi: 10.1001/jama.2016.15722).
These study findings suggest that the risk-benefit ratio of mesh reinforcement is not as clear as previously thought and call into question the current widespread use of mesh, even for repair of small hernias, when mesh is the norm for all incisional hernia repairs of any size.
Although the study by Kokotovic and colleagues is one of the most comprehensive long-term studies in hernia surgery, many questions remain about the optimal approach for repairing ventral hernia. To provide more rigorous data to better understand optimal approaches to this common clinical problem, surgeons will need to design large multicenter pragmatic trials with long-term follow-up.
Kamal M. F. Itani, MD, is at the VA Boston Health Care System, Boston University, West Roxbury, Mass., and Harvard Medical School in Boston. He reported having served as a research consultant to Davol 4 years ago regarding an antibiotic-coated mesh product. These remarks are excerpted from an editorial accompanying Dr. Kokotovic’s report (JAMA 2016 Oct 17. doi: 10.1001/jama.2016.15722).
These study findings suggest that the risk-benefit ratio of mesh reinforcement is not as clear as previously thought and call into question the current widespread use of mesh, even for repair of small hernias, when mesh is the norm for all incisional hernia repairs of any size.
Although the study by Kokotovic and colleagues is one of the most comprehensive long-term studies in hernia surgery, many questions remain about the optimal approach for repairing ventral hernia. To provide more rigorous data to better understand optimal approaches to this common clinical problem, surgeons will need to design large multicenter pragmatic trials with long-term follow-up.
Kamal M. F. Itani, MD, is at the VA Boston Health Care System, Boston University, West Roxbury, Mass., and Harvard Medical School in Boston. He reported having served as a research consultant to Davol 4 years ago regarding an antibiotic-coated mesh product. These remarks are excerpted from an editorial accompanying Dr. Kokotovic’s report (JAMA 2016 Oct 17. doi: 10.1001/jama.2016.15722).
Among patients undergoing elective incisional repair of abdominal wall hernias, the use of mesh reinforcement decreases the short-term recurrence rate by 5% but increases major complications by approximately the same amount over the subsequent 5 years, Dunja Kokotovic, MB, reported at the annual clinical congress of the American College of Surgeons.
“Given the continuously increasing incidence of mesh-related complications with time, it is expected that, with even longer follow-up up than the 5 years observed in this study, mesh-related complications continue to accrue,” said Dr. Kokotovic of the Center for Surgical Science, Zealand University Hospital, Koge, Denmark. The findings of this observational registry-based cohort study were presented at the congress and simultaneously published online in JAMA (2016 Oct 17. doi: 10.1001/jama.2016.15217).
These results highlight the need to assess the long-term safety of interventions before making definitive conclusions about their benefits and widely adopting them. In the United States, manufacturers are required to demonstrate the long-term safety of drugs but not of some devices, including hernia meshes. There were approximately 190,000 such hernia repairs performed in the United States alone during the most recent year for which data are available, and mesh is estimated to have been used in at least half, Dr. Kokotovic noted.
She and her associates analyzed the 5-year outcomes for virtually all incisional hernia repairs performed in Denmark from 2007 through 2010 using data in a mandatory national registry. Their analysis included 3,242 patients (mean age, 58 years): 1,119 (34.5%) who had open mesh repair, 1,757 (54.2%) who had laparoscopic mesh repair, and 366 (11.3%) who had nonmesh repair.
The cumulative risk of reoperation for hernia recurrence was significantly lower for patients who had open mesh repair (12.3%) or laparoscopic mesh repair (10.6%) than for those who had nonmesh repair (17.1%). However, this benefit was offset by the rate of major mesh-related complications requiring surgical intervention – including surgical site infection, formation of a chronic sinus tract, late-onset intra-abdominal abscess, enterocutaneous fistula, bowel obstruction, and bowel perforation – which progressively increased over time. The cumulative incidence of such complications was 5.6% for open mesh repair and 3.7% for laparoscopic mesh repair.
This study was limited in that it was observational rather than being based on randomized data, so selection bias and imbalances among the study groups couldn’t be fully controlled for. However, two strengths of this study were that it reflects the real-world experience of an entire country and all the surgeons performing hernia repairs there, and it had 100% follow-up, the researchers said.
This study was partly funded by the Edgar Schnohr and Wife Gilberte Schnohr’s Foundation supporting independent surgical and anesthesiological research. Dr. Kokotovic reported having no relevant financial disclosures; one investigator reported receiving personal fees from Bard and Etichon for educational presentations.
Among patients undergoing elective incisional repair of abdominal wall hernias, the use of mesh reinforcement decreases the short-term recurrence rate by 5% but increases major complications by approximately the same amount over the subsequent 5 years, Dunja Kokotovic, MB, reported at the annual clinical congress of the American College of Surgeons.
“Given the continuously increasing incidence of mesh-related complications with time, it is expected that, with even longer follow-up up than the 5 years observed in this study, mesh-related complications continue to accrue,” said Dr. Kokotovic of the Center for Surgical Science, Zealand University Hospital, Koge, Denmark. The findings of this observational registry-based cohort study were presented at the congress and simultaneously published online in JAMA (2016 Oct 17. doi: 10.1001/jama.2016.15217).
These results highlight the need to assess the long-term safety of interventions before making definitive conclusions about their benefits and widely adopting them. In the United States, manufacturers are required to demonstrate the long-term safety of drugs but not of some devices, including hernia meshes. There were approximately 190,000 such hernia repairs performed in the United States alone during the most recent year for which data are available, and mesh is estimated to have been used in at least half, Dr. Kokotovic noted.
She and her associates analyzed the 5-year outcomes for virtually all incisional hernia repairs performed in Denmark from 2007 through 2010 using data in a mandatory national registry. Their analysis included 3,242 patients (mean age, 58 years): 1,119 (34.5%) who had open mesh repair, 1,757 (54.2%) who had laparoscopic mesh repair, and 366 (11.3%) who had nonmesh repair.
The cumulative risk of reoperation for hernia recurrence was significantly lower for patients who had open mesh repair (12.3%) or laparoscopic mesh repair (10.6%) than for those who had nonmesh repair (17.1%). However, this benefit was offset by the rate of major mesh-related complications requiring surgical intervention – including surgical site infection, formation of a chronic sinus tract, late-onset intra-abdominal abscess, enterocutaneous fistula, bowel obstruction, and bowel perforation – which progressively increased over time. The cumulative incidence of such complications was 5.6% for open mesh repair and 3.7% for laparoscopic mesh repair.
This study was limited in that it was observational rather than being based on randomized data, so selection bias and imbalances among the study groups couldn’t be fully controlled for. However, two strengths of this study were that it reflects the real-world experience of an entire country and all the surgeons performing hernia repairs there, and it had 100% follow-up, the researchers said.
This study was partly funded by the Edgar Schnohr and Wife Gilberte Schnohr’s Foundation supporting independent surgical and anesthesiological research. Dr. Kokotovic reported having no relevant financial disclosures; one investigator reported receiving personal fees from Bard and Etichon for educational presentations.
FROM THE ACS CLINICAL CONGRESS
Key clinical point: Among patients undergoing elective incisional repair of abdominal wall hernias, the use of mesh reinforcement decreases the short-term recurrence rate by 5% but increases major complications by 5.6% over the subsequent 5 years.
Major finding: The cumulative rate of major mesh-related complications requiring surgical intervention was 5.6% for open mesh repair and 3.7% for laparoscopic mesh repair, compared with 0% for nonmesh repair.
Data source: A nationwide observational registry-based cohort study involving virtually all incisional hernia repairs (3,242) performed in Denmark from 2007 through 2010.
Disclosures: This study was partly funded by the Edgar Schnohr and Wife Gilberte Schnohr’s Foundation supporting independent surgical and anesthesiological research. Dr. Kokotovic reported having no relevant financial disclosures; one investigator reported receiving personal fees from Bard and Etichon for educational presentations.
Patients want surgery for ventral hernia despite risks and comorbidity obstacles
An in-depth qualitative survey of patients’ expectations and satisfaction regarding ventral hernia management showed that while most were satisfied with surgical outcomes, many were uninformed about postoperative adverse outcomes and many were dissatisfied with nonoperative management.
Zeinab M. Alawadi, MD, and a team of researchers at the University of Texas Health Sciences Center, Houston, initially interviewed 30 patients seeking care for ventral hernia at a safety-net hospital prior to their surgical consultation about factors guiding their decision-making framework. A second interview was conducted 6 months later, asking about their level of satisfaction with their care and outcomes. The study appeared online Oct. 11 in the Journal of the American College of Surgeons.
The initial interview revealed that most patients had limited knowledge about risks and potential adverse outcomes of surgery, but nearly three-quarters of them wanted to undergo surgery for their ventral hernias. Only 7 of the 30 patients were treated surgically and of those, 2 reported an unexpected level of postoperative pain and dissatisfaction with the surgery outcome. The remaining five patients who had surgery were extremely satisfied with their decision.
Most of those interviewed had nonoperative management of their hernias, due to factors such as obesity, diabetes, and smoking. These patients expressed dissatisfaction with the obstacles of meeting surgical criteria, in particular the difficulties of losing weight and coping with diabetes. “From patients’ perspectives, the additional challenges of managing their diabetes and difficulties with exercising due to painful hernias represent overwhelming barriers to treating their obesity. Patients’ accounts do not reflect a simple failure to adhere to medical recommendations but substantial obstacles to losing weight,” the researchers noted. But these patients also expressed willingness to try to meet surgical criteria and to take responsibility for recurrence prevention by self-management.
This study provides insight into patient perceptions and expectation of ventral hernia surgery. “Several findings in this study suggest a need for better education and counseling of patients regarding the natural history of hernias and the risks and benefits of different management strategies. Self-contradicting patient responses regarding knowledge of surgical risks and benefits may represent poor communication by the physicians or poor understanding by the patients. As a result, patients appeared to have unrealistic expectations of surgery. In addition, contrary to the literature, patients appeared to disregard the physicians’ risk assessment and persisted in their preferences for surgical management, even after counseling.”
This work was supported by the Center for Clinical and Translational Sciences, which is funded by National Institutes of Health Clinical and Translational Award UL1 TR000371 and KL2 TR000370 from the National Center for Advancing Translational Sciences. The authors had no disclosures.
Read the complete study at goo.gl/pq4fjz.
An in-depth qualitative survey of patients’ expectations and satisfaction regarding ventral hernia management showed that while most were satisfied with surgical outcomes, many were uninformed about postoperative adverse outcomes and many were dissatisfied with nonoperative management.
Zeinab M. Alawadi, MD, and a team of researchers at the University of Texas Health Sciences Center, Houston, initially interviewed 30 patients seeking care for ventral hernia at a safety-net hospital prior to their surgical consultation about factors guiding their decision-making framework. A second interview was conducted 6 months later, asking about their level of satisfaction with their care and outcomes. The study appeared online Oct. 11 in the Journal of the American College of Surgeons.
The initial interview revealed that most patients had limited knowledge about risks and potential adverse outcomes of surgery, but nearly three-quarters of them wanted to undergo surgery for their ventral hernias. Only 7 of the 30 patients were treated surgically and of those, 2 reported an unexpected level of postoperative pain and dissatisfaction with the surgery outcome. The remaining five patients who had surgery were extremely satisfied with their decision.
Most of those interviewed had nonoperative management of their hernias, due to factors such as obesity, diabetes, and smoking. These patients expressed dissatisfaction with the obstacles of meeting surgical criteria, in particular the difficulties of losing weight and coping with diabetes. “From patients’ perspectives, the additional challenges of managing their diabetes and difficulties with exercising due to painful hernias represent overwhelming barriers to treating their obesity. Patients’ accounts do not reflect a simple failure to adhere to medical recommendations but substantial obstacles to losing weight,” the researchers noted. But these patients also expressed willingness to try to meet surgical criteria and to take responsibility for recurrence prevention by self-management.
This study provides insight into patient perceptions and expectation of ventral hernia surgery. “Several findings in this study suggest a need for better education and counseling of patients regarding the natural history of hernias and the risks and benefits of different management strategies. Self-contradicting patient responses regarding knowledge of surgical risks and benefits may represent poor communication by the physicians or poor understanding by the patients. As a result, patients appeared to have unrealistic expectations of surgery. In addition, contrary to the literature, patients appeared to disregard the physicians’ risk assessment and persisted in their preferences for surgical management, even after counseling.”
This work was supported by the Center for Clinical and Translational Sciences, which is funded by National Institutes of Health Clinical and Translational Award UL1 TR000371 and KL2 TR000370 from the National Center for Advancing Translational Sciences. The authors had no disclosures.
Read the complete study at goo.gl/pq4fjz.
An in-depth qualitative survey of patients’ expectations and satisfaction regarding ventral hernia management showed that while most were satisfied with surgical outcomes, many were uninformed about postoperative adverse outcomes and many were dissatisfied with nonoperative management.
Zeinab M. Alawadi, MD, and a team of researchers at the University of Texas Health Sciences Center, Houston, initially interviewed 30 patients seeking care for ventral hernia at a safety-net hospital prior to their surgical consultation about factors guiding their decision-making framework. A second interview was conducted 6 months later, asking about their level of satisfaction with their care and outcomes. The study appeared online Oct. 11 in the Journal of the American College of Surgeons.
The initial interview revealed that most patients had limited knowledge about risks and potential adverse outcomes of surgery, but nearly three-quarters of them wanted to undergo surgery for their ventral hernias. Only 7 of the 30 patients were treated surgically and of those, 2 reported an unexpected level of postoperative pain and dissatisfaction with the surgery outcome. The remaining five patients who had surgery were extremely satisfied with their decision.
Most of those interviewed had nonoperative management of their hernias, due to factors such as obesity, diabetes, and smoking. These patients expressed dissatisfaction with the obstacles of meeting surgical criteria, in particular the difficulties of losing weight and coping with diabetes. “From patients’ perspectives, the additional challenges of managing their diabetes and difficulties with exercising due to painful hernias represent overwhelming barriers to treating their obesity. Patients’ accounts do not reflect a simple failure to adhere to medical recommendations but substantial obstacles to losing weight,” the researchers noted. But these patients also expressed willingness to try to meet surgical criteria and to take responsibility for recurrence prevention by self-management.
This study provides insight into patient perceptions and expectation of ventral hernia surgery. “Several findings in this study suggest a need for better education and counseling of patients regarding the natural history of hernias and the risks and benefits of different management strategies. Self-contradicting patient responses regarding knowledge of surgical risks and benefits may represent poor communication by the physicians or poor understanding by the patients. As a result, patients appeared to have unrealistic expectations of surgery. In addition, contrary to the literature, patients appeared to disregard the physicians’ risk assessment and persisted in their preferences for surgical management, even after counseling.”
This work was supported by the Center for Clinical and Translational Sciences, which is funded by National Institutes of Health Clinical and Translational Award UL1 TR000371 and KL2 TR000370 from the National Center for Advancing Translational Sciences. The authors had no disclosures.
Read the complete study at goo.gl/pq4fjz.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF SURGEONS
Risk model predicts chronic postop pain for VHR patients
Postoperative pain that lingers for months is a common outcome of ventral hernia repair surgery. A predictive model has been developed by investigators at the Carolina Medical Center in Charlotte, N.C., to determine which hernia patients are at risk for chronic postoperative pain.
Tiffany C. Cox, MD, and the research team used the International Hernia Mesh Registry to obtain a sample of 887 ventral hernia repair patients that had surgery between 2007 and 2014. Data on postoperative pain was based on the Carolinas Comfort Scale questionnaire administered at 1, 6 and 12 months after surgery. Logistic regression analyses were used to determine independent predictors of postoperative chronic pain and a risk model was developed (Am J Surg. 2016 Sep; 212[3]:501-10).
The investigators concluded that the statistically significant predictors of risk for developing chronic postoperative pain at 1 year were preoperative pain and pain at 1 month of 2 or greater on the Carolina Comfort Scale (odds ratio, 2.97 and 2.64, respectively), female sex (OR, 1.74), and repair of recurrent hernias (OR, 1.59).
The predictive model for chronic postoperative pain may be helpful to surgeons in counseling patients and in devising postoperative interventions.
The investigators had no disclosures.
Read the full study at goo.gl/MRjM66.
Postoperative pain that lingers for months is a common outcome of ventral hernia repair surgery. A predictive model has been developed by investigators at the Carolina Medical Center in Charlotte, N.C., to determine which hernia patients are at risk for chronic postoperative pain.
Tiffany C. Cox, MD, and the research team used the International Hernia Mesh Registry to obtain a sample of 887 ventral hernia repair patients that had surgery between 2007 and 2014. Data on postoperative pain was based on the Carolinas Comfort Scale questionnaire administered at 1, 6 and 12 months after surgery. Logistic regression analyses were used to determine independent predictors of postoperative chronic pain and a risk model was developed (Am J Surg. 2016 Sep; 212[3]:501-10).
The investigators concluded that the statistically significant predictors of risk for developing chronic postoperative pain at 1 year were preoperative pain and pain at 1 month of 2 or greater on the Carolina Comfort Scale (odds ratio, 2.97 and 2.64, respectively), female sex (OR, 1.74), and repair of recurrent hernias (OR, 1.59).
The predictive model for chronic postoperative pain may be helpful to surgeons in counseling patients and in devising postoperative interventions.
The investigators had no disclosures.
Read the full study at goo.gl/MRjM66.
Postoperative pain that lingers for months is a common outcome of ventral hernia repair surgery. A predictive model has been developed by investigators at the Carolina Medical Center in Charlotte, N.C., to determine which hernia patients are at risk for chronic postoperative pain.
Tiffany C. Cox, MD, and the research team used the International Hernia Mesh Registry to obtain a sample of 887 ventral hernia repair patients that had surgery between 2007 and 2014. Data on postoperative pain was based on the Carolinas Comfort Scale questionnaire administered at 1, 6 and 12 months after surgery. Logistic regression analyses were used to determine independent predictors of postoperative chronic pain and a risk model was developed (Am J Surg. 2016 Sep; 212[3]:501-10).
The investigators concluded that the statistically significant predictors of risk for developing chronic postoperative pain at 1 year were preoperative pain and pain at 1 month of 2 or greater on the Carolina Comfort Scale (odds ratio, 2.97 and 2.64, respectively), female sex (OR, 1.74), and repair of recurrent hernias (OR, 1.59).
The predictive model for chronic postoperative pain may be helpful to surgeons in counseling patients and in devising postoperative interventions.
The investigators had no disclosures.
Read the full study at goo.gl/MRjM66.
FROM THE AMERICAN JOURNAL OF SURGERY
Underlay mesh for hernia repair yields better postop pain outcomes
Chronic pain that typically follows primary inguinal hernia repair can be significantly reduced by adopting procedures that use underlay mesh rather than overlay mesh, according to a new study published in the Journal of Surgical Research.
“Although chronic pain and discomfort is still one of the greatest problems after inguinal hernia repair due to the fact that it interferes with patients’ quality of life, there are very little data available from previous studies concerning presentation, diagnosis, and modes of treatment of this issue. In particular, the data in the literature concerning the cause of chronic pain are very limited,” wrote the authors, led by Hideyuki Takata, MD, of Nippon Medical School, Tokyo.
Dr. Takata and his coinvestigators looked at patients who underwent a mesh repair operation for primary inguinal hernia at a single institution – Nippon Medical School – between May 2011 and May 2014. All patients were aged 40 years or older, and the overwhelming majority were male. A total of 334 patients were identified, with 378 lesions among them; all patients’ operations were performed via the Lichtenstein (onlay mesh only), Ultrapro Plug (onlay and plug mesh), modified Kugel Patch (onlay and underlay mesh), or laparoscopic transabdominal preperitoneal (underlay mesh only, TAPP) surgical routes.
Forty-four patients had bilateral lesions, 152 had lesions on the right, and 138 on the left; 76 patients received Lichtenstein operations, 85 received Ultrapro Plug, 156 received modified Kugel Patch, and 61 received TAPP. (J Surg Res 2016 Aug 11. doi: 10.1016/j.jss.2016.08.027).
Patients received questionnaires at 2-3 weeks, 3 months, and 6 months after the operation to determine their pain and discomfort levels. Responses for all 378 lesions (100%) were received at the first follow-up, with questionnaires received for 229 lesions (60.5%) at the 3-month follow-up and 249 lesions (65.9%) at the 6-month follow-up. Of those who responded at the 6-month follow-up, 46 received Lichtenstein, 59 received Ultrapro Plug, 101 received modified Kugel Patch, and 61 received TAPP.
No patients reported moderate or severe pain while at rest. Mild pain was reported by 11 (4.4%) of all respondents; 0 of those who received Lichtenstein, 4 (6.8%) of those who received Ultrapro Plug, 7 (6.9%) of those who received modified Kugel Patch, and 0 of those who received TAPP (P less than .01).
Pain with movement was reported in 35 (14.1%) of respondents: 6 (13.0%) of those who received Lichtenstein, 7 (11.9%) of those who received Ultrapro Plug, 20 (19.8%) of those who received modified Kugel Patch, and 2 (4.7%) of those who received TAPP (P less than .05). One respondent reported experiencing moderate pain with movement, and that individual received Ultrapro Plug (1.7%). No patients reported experiencing severe pain with movement.
“We conclude that the sensory nerves in the inguinal region should be kept away from the mesh to prevent the development of chronic pain and discomfort,” the investigators concluded. “Further study is required to determine the mechanism involved in the generation of chronic pain and discomfort to improve the patient’s quality of life after primary inguinal hernia repair.”
No funding source was disclosed for this study. Dr. Takata and his coauthors did not report any relevant financial disclosures.
Chronic pain that typically follows primary inguinal hernia repair can be significantly reduced by adopting procedures that use underlay mesh rather than overlay mesh, according to a new study published in the Journal of Surgical Research.
“Although chronic pain and discomfort is still one of the greatest problems after inguinal hernia repair due to the fact that it interferes with patients’ quality of life, there are very little data available from previous studies concerning presentation, diagnosis, and modes of treatment of this issue. In particular, the data in the literature concerning the cause of chronic pain are very limited,” wrote the authors, led by Hideyuki Takata, MD, of Nippon Medical School, Tokyo.
Dr. Takata and his coinvestigators looked at patients who underwent a mesh repair operation for primary inguinal hernia at a single institution – Nippon Medical School – between May 2011 and May 2014. All patients were aged 40 years or older, and the overwhelming majority were male. A total of 334 patients were identified, with 378 lesions among them; all patients’ operations were performed via the Lichtenstein (onlay mesh only), Ultrapro Plug (onlay and plug mesh), modified Kugel Patch (onlay and underlay mesh), or laparoscopic transabdominal preperitoneal (underlay mesh only, TAPP) surgical routes.
Forty-four patients had bilateral lesions, 152 had lesions on the right, and 138 on the left; 76 patients received Lichtenstein operations, 85 received Ultrapro Plug, 156 received modified Kugel Patch, and 61 received TAPP. (J Surg Res 2016 Aug 11. doi: 10.1016/j.jss.2016.08.027).
Patients received questionnaires at 2-3 weeks, 3 months, and 6 months after the operation to determine their pain and discomfort levels. Responses for all 378 lesions (100%) were received at the first follow-up, with questionnaires received for 229 lesions (60.5%) at the 3-month follow-up and 249 lesions (65.9%) at the 6-month follow-up. Of those who responded at the 6-month follow-up, 46 received Lichtenstein, 59 received Ultrapro Plug, 101 received modified Kugel Patch, and 61 received TAPP.
No patients reported moderate or severe pain while at rest. Mild pain was reported by 11 (4.4%) of all respondents; 0 of those who received Lichtenstein, 4 (6.8%) of those who received Ultrapro Plug, 7 (6.9%) of those who received modified Kugel Patch, and 0 of those who received TAPP (P less than .01).
Pain with movement was reported in 35 (14.1%) of respondents: 6 (13.0%) of those who received Lichtenstein, 7 (11.9%) of those who received Ultrapro Plug, 20 (19.8%) of those who received modified Kugel Patch, and 2 (4.7%) of those who received TAPP (P less than .05). One respondent reported experiencing moderate pain with movement, and that individual received Ultrapro Plug (1.7%). No patients reported experiencing severe pain with movement.
“We conclude that the sensory nerves in the inguinal region should be kept away from the mesh to prevent the development of chronic pain and discomfort,” the investigators concluded. “Further study is required to determine the mechanism involved in the generation of chronic pain and discomfort to improve the patient’s quality of life after primary inguinal hernia repair.”
No funding source was disclosed for this study. Dr. Takata and his coauthors did not report any relevant financial disclosures.
Chronic pain that typically follows primary inguinal hernia repair can be significantly reduced by adopting procedures that use underlay mesh rather than overlay mesh, according to a new study published in the Journal of Surgical Research.
“Although chronic pain and discomfort is still one of the greatest problems after inguinal hernia repair due to the fact that it interferes with patients’ quality of life, there are very little data available from previous studies concerning presentation, diagnosis, and modes of treatment of this issue. In particular, the data in the literature concerning the cause of chronic pain are very limited,” wrote the authors, led by Hideyuki Takata, MD, of Nippon Medical School, Tokyo.
Dr. Takata and his coinvestigators looked at patients who underwent a mesh repair operation for primary inguinal hernia at a single institution – Nippon Medical School – between May 2011 and May 2014. All patients were aged 40 years or older, and the overwhelming majority were male. A total of 334 patients were identified, with 378 lesions among them; all patients’ operations were performed via the Lichtenstein (onlay mesh only), Ultrapro Plug (onlay and plug mesh), modified Kugel Patch (onlay and underlay mesh), or laparoscopic transabdominal preperitoneal (underlay mesh only, TAPP) surgical routes.
Forty-four patients had bilateral lesions, 152 had lesions on the right, and 138 on the left; 76 patients received Lichtenstein operations, 85 received Ultrapro Plug, 156 received modified Kugel Patch, and 61 received TAPP. (J Surg Res 2016 Aug 11. doi: 10.1016/j.jss.2016.08.027).
Patients received questionnaires at 2-3 weeks, 3 months, and 6 months after the operation to determine their pain and discomfort levels. Responses for all 378 lesions (100%) were received at the first follow-up, with questionnaires received for 229 lesions (60.5%) at the 3-month follow-up and 249 lesions (65.9%) at the 6-month follow-up. Of those who responded at the 6-month follow-up, 46 received Lichtenstein, 59 received Ultrapro Plug, 101 received modified Kugel Patch, and 61 received TAPP.
No patients reported moderate or severe pain while at rest. Mild pain was reported by 11 (4.4%) of all respondents; 0 of those who received Lichtenstein, 4 (6.8%) of those who received Ultrapro Plug, 7 (6.9%) of those who received modified Kugel Patch, and 0 of those who received TAPP (P less than .01).
Pain with movement was reported in 35 (14.1%) of respondents: 6 (13.0%) of those who received Lichtenstein, 7 (11.9%) of those who received Ultrapro Plug, 20 (19.8%) of those who received modified Kugel Patch, and 2 (4.7%) of those who received TAPP (P less than .05). One respondent reported experiencing moderate pain with movement, and that individual received Ultrapro Plug (1.7%). No patients reported experiencing severe pain with movement.
“We conclude that the sensory nerves in the inguinal region should be kept away from the mesh to prevent the development of chronic pain and discomfort,” the investigators concluded. “Further study is required to determine the mechanism involved in the generation of chronic pain and discomfort to improve the patient’s quality of life after primary inguinal hernia repair.”
No funding source was disclosed for this study. Dr. Takata and his coauthors did not report any relevant financial disclosures.
Key clinical point:
Major finding: Mild pain at rest and with movement were both significantly lower in patients who received TAPP than in those who received one of three other surgical procedures.
Data source: Retrospective analysis of 334 primary inguinal hernia patients with 378 lesions undergoing TAPP or Lichtenstein procedures.
Disclosures: The authors did not report any relevant financial disclosures.
Biologic mesh for ventral hernia repair compared for recurrence, cost
The porcine acellular dermal mesh product Strattice was associated with significantly lower odds of hernia recurrence, compared with several other biologic mesh products, in a study of 223 patients who underwent open ventral hernia repair.
Prospective operative outcomes data from a tertiary referral hernia center showed that at a mean follow-up of 18.2 months, the rate of hernia recurrence was 35% in 40 patients who were treated with Alloderm (LifeCell Corporation), 34.5% in 23 patients treated with AlloMax (Bard/Davol), 37.1% in 70 patients treated with FlexHD (Ethicon), and 59.1% in 22 patients treated with Xenmatrix (Bard/Davol), compared with 14.7% in 68 patients treated with Strattice (LifeCell Corporation). Alloderm, AlloMax, and FlexHD are all human acellular dermal mesh products, and Strattice and Xenmatrix are both porcine acellular dermal mesh products, Ciara R. Huntington, MD, and her colleagues at the Carolinas Medical Center in Charlotte, N.C., reported.
 |
| Photo courtesy Acelity. STRATTICETM Reconstructive Tissue Matrix |
After multivariate analysis to adjust for factors such as comorbidities, hernia size, and intraoperative techniques, the odds ratios for recurrence with each product as compared with Strattice were 2.4 with Alloderm, 2.9 with FlexHD, 3.4 with AlloMax, and 7.8 with Xenmatrix. The odds for recurrence were significantly greater with all except Alloderm, the investigators said (Surgery. 2016. doi: 10.1016/j.surg.2016.07.008).
The significant differences between the two porcine acellular dermal meshes (Xenmatrix and Strattice) may reflect variation in tissue processing and design in biomesh engineering, they noted.
Study subjects were adults with a mean age of 57.7 years and mean body mass index of 34.8 kg/m2. Overall, 9.8% had an American Society of Anesthesiology classification of 4, 54.6% had a classification of 3, and 35.6% had a classification of 1 or 2. Average operative time was 241 minutes with estimated blood loss of 202 mL.
Average hernia defect size was 257 cm2, with average mesh size of 384 cm2.
“Component separation was performed in 47.5% of cases, and abdomen was left open prior to definitive closure in 10.7%. Biologic mesh was used to bridge fascial defects in 19.6% of cases. The mesh was placed in the preperitoneal space in 38.2% of cases,” the investigators wrote, noting that a concomitant procedure was performed in 82% of cases.
Sepsis developed in 6.7% of patients, 36.3% had a wound infection, and 24.3% required a negative pressure dressing for healing. The inpatient mortality rate was 1.4%.
However, mesh infections requiring explantation occurred in less than 1% of cases.
On adjusted analysis, Xenmatrix was the most expensive mesh and AlloMax was the least expensive (mean of $59,122 and $22,304, respectively). Strattice costs averaged $40,490.
Ventral hernia repair (VHR) is a common operation, with about 350,000 performed each year. Rates of postoperative wound infection and hernia recurrence vary widely, but may be improved with appropriate mesh selection. However, prospective data to guide selection are lacking, the investigators said.
“The great number of meshes available for use complicates the debate surrounding the best timing and use of biologic mesh in VHR, and the search for the better mesh for use in the abdominal wall reconstruction continues. Biologic mesh usually is reserved for the patients at the highest risk for developing a postoperative wound complication, and although there is a current dearth of high-level evidence supporting its use, this report confirms that complications are low despite obvious surgical complexity presented herein,” they wrote.
The findings of this study – the largest report of outcomes with biologic mesh in ventral hernia repair to date, according to the authors – support the safety of using biologic mesh in high-risk patients, they said.
They noted, however, that the study may still be underpowered to make final clinical decisions.
“Although our study provides useful information to the practicing surgeon, there is much work to be done regarding the selection of biologic mesh,” they wrote, adding that while “a well-performing biologic mesh should be in the toolkit of every general surgeon who may face complex abdominal walls requiring reconstruction in patients that are at high risk for a postoperative wound complication,” additional research is necessary to further clarify the role of biologic mesh in these operations.
Dr. Huntington reported having no disclosures. Other authors reported having been awarded honoraria, speaking fees, surgical research funding, and education grants from W.L. Gore and Associates, Ethicon, Novadaq, Bard/Davol, and LifeCell Corporation.
The porcine acellular dermal mesh product Strattice was associated with significantly lower odds of hernia recurrence, compared with several other biologic mesh products, in a study of 223 patients who underwent open ventral hernia repair.
Prospective operative outcomes data from a tertiary referral hernia center showed that at a mean follow-up of 18.2 months, the rate of hernia recurrence was 35% in 40 patients who were treated with Alloderm (LifeCell Corporation), 34.5% in 23 patients treated with AlloMax (Bard/Davol), 37.1% in 70 patients treated with FlexHD (Ethicon), and 59.1% in 22 patients treated with Xenmatrix (Bard/Davol), compared with 14.7% in 68 patients treated with Strattice (LifeCell Corporation). Alloderm, AlloMax, and FlexHD are all human acellular dermal mesh products, and Strattice and Xenmatrix are both porcine acellular dermal mesh products, Ciara R. Huntington, MD, and her colleagues at the Carolinas Medical Center in Charlotte, N.C., reported.
 |
| Photo courtesy Acelity. STRATTICETM Reconstructive Tissue Matrix |
After multivariate analysis to adjust for factors such as comorbidities, hernia size, and intraoperative techniques, the odds ratios for recurrence with each product as compared with Strattice were 2.4 with Alloderm, 2.9 with FlexHD, 3.4 with AlloMax, and 7.8 with Xenmatrix. The odds for recurrence were significantly greater with all except Alloderm, the investigators said (Surgery. 2016. doi: 10.1016/j.surg.2016.07.008).
The significant differences between the two porcine acellular dermal meshes (Xenmatrix and Strattice) may reflect variation in tissue processing and design in biomesh engineering, they noted.
Study subjects were adults with a mean age of 57.7 years and mean body mass index of 34.8 kg/m2. Overall, 9.8% had an American Society of Anesthesiology classification of 4, 54.6% had a classification of 3, and 35.6% had a classification of 1 or 2. Average operative time was 241 minutes with estimated blood loss of 202 mL.
Average hernia defect size was 257 cm2, with average mesh size of 384 cm2.
“Component separation was performed in 47.5% of cases, and abdomen was left open prior to definitive closure in 10.7%. Biologic mesh was used to bridge fascial defects in 19.6% of cases. The mesh was placed in the preperitoneal space in 38.2% of cases,” the investigators wrote, noting that a concomitant procedure was performed in 82% of cases.
Sepsis developed in 6.7% of patients, 36.3% had a wound infection, and 24.3% required a negative pressure dressing for healing. The inpatient mortality rate was 1.4%.
However, mesh infections requiring explantation occurred in less than 1% of cases.
On adjusted analysis, Xenmatrix was the most expensive mesh and AlloMax was the least expensive (mean of $59,122 and $22,304, respectively). Strattice costs averaged $40,490.
Ventral hernia repair (VHR) is a common operation, with about 350,000 performed each year. Rates of postoperative wound infection and hernia recurrence vary widely, but may be improved with appropriate mesh selection. However, prospective data to guide selection are lacking, the investigators said.
“The great number of meshes available for use complicates the debate surrounding the best timing and use of biologic mesh in VHR, and the search for the better mesh for use in the abdominal wall reconstruction continues. Biologic mesh usually is reserved for the patients at the highest risk for developing a postoperative wound complication, and although there is a current dearth of high-level evidence supporting its use, this report confirms that complications are low despite obvious surgical complexity presented herein,” they wrote.
The findings of this study – the largest report of outcomes with biologic mesh in ventral hernia repair to date, according to the authors – support the safety of using biologic mesh in high-risk patients, they said.
They noted, however, that the study may still be underpowered to make final clinical decisions.
“Although our study provides useful information to the practicing surgeon, there is much work to be done regarding the selection of biologic mesh,” they wrote, adding that while “a well-performing biologic mesh should be in the toolkit of every general surgeon who may face complex abdominal walls requiring reconstruction in patients that are at high risk for a postoperative wound complication,” additional research is necessary to further clarify the role of biologic mesh in these operations.
Dr. Huntington reported having no disclosures. Other authors reported having been awarded honoraria, speaking fees, surgical research funding, and education grants from W.L. Gore and Associates, Ethicon, Novadaq, Bard/Davol, and LifeCell Corporation.
The porcine acellular dermal mesh product Strattice was associated with significantly lower odds of hernia recurrence, compared with several other biologic mesh products, in a study of 223 patients who underwent open ventral hernia repair.
Prospective operative outcomes data from a tertiary referral hernia center showed that at a mean follow-up of 18.2 months, the rate of hernia recurrence was 35% in 40 patients who were treated with Alloderm (LifeCell Corporation), 34.5% in 23 patients treated with AlloMax (Bard/Davol), 37.1% in 70 patients treated with FlexHD (Ethicon), and 59.1% in 22 patients treated with Xenmatrix (Bard/Davol), compared with 14.7% in 68 patients treated with Strattice (LifeCell Corporation). Alloderm, AlloMax, and FlexHD are all human acellular dermal mesh products, and Strattice and Xenmatrix are both porcine acellular dermal mesh products, Ciara R. Huntington, MD, and her colleagues at the Carolinas Medical Center in Charlotte, N.C., reported.
 |
| Photo courtesy Acelity. STRATTICETM Reconstructive Tissue Matrix |
After multivariate analysis to adjust for factors such as comorbidities, hernia size, and intraoperative techniques, the odds ratios for recurrence with each product as compared with Strattice were 2.4 with Alloderm, 2.9 with FlexHD, 3.4 with AlloMax, and 7.8 with Xenmatrix. The odds for recurrence were significantly greater with all except Alloderm, the investigators said (Surgery. 2016. doi: 10.1016/j.surg.2016.07.008).
The significant differences between the two porcine acellular dermal meshes (Xenmatrix and Strattice) may reflect variation in tissue processing and design in biomesh engineering, they noted.
Study subjects were adults with a mean age of 57.7 years and mean body mass index of 34.8 kg/m2. Overall, 9.8% had an American Society of Anesthesiology classification of 4, 54.6% had a classification of 3, and 35.6% had a classification of 1 or 2. Average operative time was 241 minutes with estimated blood loss of 202 mL.
Average hernia defect size was 257 cm2, with average mesh size of 384 cm2.
“Component separation was performed in 47.5% of cases, and abdomen was left open prior to definitive closure in 10.7%. Biologic mesh was used to bridge fascial defects in 19.6% of cases. The mesh was placed in the preperitoneal space in 38.2% of cases,” the investigators wrote, noting that a concomitant procedure was performed in 82% of cases.
Sepsis developed in 6.7% of patients, 36.3% had a wound infection, and 24.3% required a negative pressure dressing for healing. The inpatient mortality rate was 1.4%.
However, mesh infections requiring explantation occurred in less than 1% of cases.
On adjusted analysis, Xenmatrix was the most expensive mesh and AlloMax was the least expensive (mean of $59,122 and $22,304, respectively). Strattice costs averaged $40,490.
Ventral hernia repair (VHR) is a common operation, with about 350,000 performed each year. Rates of postoperative wound infection and hernia recurrence vary widely, but may be improved with appropriate mesh selection. However, prospective data to guide selection are lacking, the investigators said.
“The great number of meshes available for use complicates the debate surrounding the best timing and use of biologic mesh in VHR, and the search for the better mesh for use in the abdominal wall reconstruction continues. Biologic mesh usually is reserved for the patients at the highest risk for developing a postoperative wound complication, and although there is a current dearth of high-level evidence supporting its use, this report confirms that complications are low despite obvious surgical complexity presented herein,” they wrote.
The findings of this study – the largest report of outcomes with biologic mesh in ventral hernia repair to date, according to the authors – support the safety of using biologic mesh in high-risk patients, they said.
They noted, however, that the study may still be underpowered to make final clinical decisions.
“Although our study provides useful information to the practicing surgeon, there is much work to be done regarding the selection of biologic mesh,” they wrote, adding that while “a well-performing biologic mesh should be in the toolkit of every general surgeon who may face complex abdominal walls requiring reconstruction in patients that are at high risk for a postoperative wound complication,” additional research is necessary to further clarify the role of biologic mesh in these operations.
Dr. Huntington reported having no disclosures. Other authors reported having been awarded honoraria, speaking fees, surgical research funding, and education grants from W.L. Gore and Associates, Ethicon, Novadaq, Bard/Davol, and LifeCell Corporation.
FROM SURGERY
Key clinical point: The porcine acellular dermal mesh product Strattice was associated with significantly lower odds of hernia recurrence, compared with several other biologic mesh products, in a study of 223 patients who underwent open ventral hernia repair.
Major finding: The adjusted odds ratios for recurrence, compared with Strattice, were 2.4 with Alloderm, 2.9 with FlexHD, 3.4 with AlloMax, and 7.8 with Xenmatrix.
Data source: 223 cases from a prospective operative outcomes database.
Disclosures: Dr. Huntington reported having no disclosures. Other authors reported having been awarded honoraria, speaking fees, surgical research funding, and education grants from W.L. Gore and Associates, Ethicon, Novadaq, Bard/Davol, and LifeCell Corporation.
Prevention of postop GI disorders may reduce ‘failed discharges’ for laparoscopic hernia surgery
Postoperative hospital readmissions after ventral hernia repair may be both predictable and preventable if type of operation and patient characteristics are taken into account, a large retrospective study has found.
Early readmissions, or ‘failed discharges,’ are potentially more preventable than are later readmissions, according to Adam C. Celio, MD, of East Carolina University, Greenville, N.C., and his colleagues. Medical literature “demonstrates that patients readmitted within a few days of discharge return for different reasons than patients who are readmitted later; very early readmissions are likely due to poor coordination of care or inadequate recognition of postdischarge needs, while later readmissions (still within the 30-day window) are more likely due to patient disease or procedural complications.”
Dr. Celio and his coinvestigators examined data from the American College of Surgeons’ National Surgical Quality Improvement Program, looking for patients who underwent either open (n = 9,009) or laparoscopic (n = 3,360) ventral hernia repair (VHR) in 2012. The primary endpoint was defined as readmission within 30 days of discharge following a VHR procedure; early readmission was defined as occurring within 5 days of discharge for laparoscopic VHR and within 9 days of discharge for open VHR, while late readmission was defined as any readmission that occurred after the aforementioned time frames (Surgery. 2016;160[2]:413-17).
The researchers analyzed each readmission to determine its cause among nine classifications: bleeding, cardiovascular events, dehydration, gastrointestinal causes (nausea, emesis, ileus, and bowel obstruction), pain, venous thromboembolic event, wound occurrences (superficial site infection, deep operative site infection, wound disruptions), other infection, and other causes.
Of the 12,369 individuals included in the study, 1,057 (8.5%) were readmitted within 30 days of undergoing VHR. Generally, the patients who had open procedures had higher ASA scores than did those who had laparoscopic surgery, reflecting a greater likelihood of preoperative physical impairment and chronic disease. The researchers then analyzed which patients were mostly likely to be readmitted and the correlation between type of operation, cause of readmission, and timing of readmission (early or late).
Open-VHR patients were more likely to be readmitted within 30 days than were those who underwent laparoscopic VHR: 9.2% vs. 6.9% readmission rates, respectively (OR 0.73, 95% CI 0.63-0.85). Among all the patients readmitted, wound complications were the most common cause (32.2%), followed by gastrointestinal disorders (14.3%), most which were attributed to emesis or nausea.
Wound complications were more highly associated with late readmission than with early ones, at 52% vs. 23%, respectively (OR 3.68, 95% CI 2.56-5.29). As might be expected, wound complications were more likely to occur in open-VHR patients than in laparoscopic-VHR patients: 49.6% vs. 24.4% (OR 3.05, 95% CI 2.06-4.52).
Of the entire cohort, 279 patients (2.3%) were classified as early readmissions, and gastrointestinal causes were more highly associated with early readmission than with late ones: 39% vs.13% (OR 4.45, 95% CI 3.06-6.47). Gastrointestinal issues occurred more often after laparoscopic VHR than after open VHR: 33% vs. 16% (OR 2.59, 95% CI 1.75-3.84). These early readmissions, occurring within days of discharge, are potentially preventable with a stepped up focus on control of nausea and emesis experienced by these patients, the researchers noted.
A funding source for this study was not disclosed. Dr. Celio and his coauthors did not report any relevant disclosures.
Postoperative hospital readmissions after ventral hernia repair may be both predictable and preventable if type of operation and patient characteristics are taken into account, a large retrospective study has found.
Early readmissions, or ‘failed discharges,’ are potentially more preventable than are later readmissions, according to Adam C. Celio, MD, of East Carolina University, Greenville, N.C., and his colleagues. Medical literature “demonstrates that patients readmitted within a few days of discharge return for different reasons than patients who are readmitted later; very early readmissions are likely due to poor coordination of care or inadequate recognition of postdischarge needs, while later readmissions (still within the 30-day window) are more likely due to patient disease or procedural complications.”
Dr. Celio and his coinvestigators examined data from the American College of Surgeons’ National Surgical Quality Improvement Program, looking for patients who underwent either open (n = 9,009) or laparoscopic (n = 3,360) ventral hernia repair (VHR) in 2012. The primary endpoint was defined as readmission within 30 days of discharge following a VHR procedure; early readmission was defined as occurring within 5 days of discharge for laparoscopic VHR and within 9 days of discharge for open VHR, while late readmission was defined as any readmission that occurred after the aforementioned time frames (Surgery. 2016;160[2]:413-17).
The researchers analyzed each readmission to determine its cause among nine classifications: bleeding, cardiovascular events, dehydration, gastrointestinal causes (nausea, emesis, ileus, and bowel obstruction), pain, venous thromboembolic event, wound occurrences (superficial site infection, deep operative site infection, wound disruptions), other infection, and other causes.
Of the 12,369 individuals included in the study, 1,057 (8.5%) were readmitted within 30 days of undergoing VHR. Generally, the patients who had open procedures had higher ASA scores than did those who had laparoscopic surgery, reflecting a greater likelihood of preoperative physical impairment and chronic disease. The researchers then analyzed which patients were mostly likely to be readmitted and the correlation between type of operation, cause of readmission, and timing of readmission (early or late).
Open-VHR patients were more likely to be readmitted within 30 days than were those who underwent laparoscopic VHR: 9.2% vs. 6.9% readmission rates, respectively (OR 0.73, 95% CI 0.63-0.85). Among all the patients readmitted, wound complications were the most common cause (32.2%), followed by gastrointestinal disorders (14.3%), most which were attributed to emesis or nausea.
Wound complications were more highly associated with late readmission than with early ones, at 52% vs. 23%, respectively (OR 3.68, 95% CI 2.56-5.29). As might be expected, wound complications were more likely to occur in open-VHR patients than in laparoscopic-VHR patients: 49.6% vs. 24.4% (OR 3.05, 95% CI 2.06-4.52).
Of the entire cohort, 279 patients (2.3%) were classified as early readmissions, and gastrointestinal causes were more highly associated with early readmission than with late ones: 39% vs.13% (OR 4.45, 95% CI 3.06-6.47). Gastrointestinal issues occurred more often after laparoscopic VHR than after open VHR: 33% vs. 16% (OR 2.59, 95% CI 1.75-3.84). These early readmissions, occurring within days of discharge, are potentially preventable with a stepped up focus on control of nausea and emesis experienced by these patients, the researchers noted.
A funding source for this study was not disclosed. Dr. Celio and his coauthors did not report any relevant disclosures.
Postoperative hospital readmissions after ventral hernia repair may be both predictable and preventable if type of operation and patient characteristics are taken into account, a large retrospective study has found.
Early readmissions, or ‘failed discharges,’ are potentially more preventable than are later readmissions, according to Adam C. Celio, MD, of East Carolina University, Greenville, N.C., and his colleagues. Medical literature “demonstrates that patients readmitted within a few days of discharge return for different reasons than patients who are readmitted later; very early readmissions are likely due to poor coordination of care or inadequate recognition of postdischarge needs, while later readmissions (still within the 30-day window) are more likely due to patient disease or procedural complications.”
Dr. Celio and his coinvestigators examined data from the American College of Surgeons’ National Surgical Quality Improvement Program, looking for patients who underwent either open (n = 9,009) or laparoscopic (n = 3,360) ventral hernia repair (VHR) in 2012. The primary endpoint was defined as readmission within 30 days of discharge following a VHR procedure; early readmission was defined as occurring within 5 days of discharge for laparoscopic VHR and within 9 days of discharge for open VHR, while late readmission was defined as any readmission that occurred after the aforementioned time frames (Surgery. 2016;160[2]:413-17).
The researchers analyzed each readmission to determine its cause among nine classifications: bleeding, cardiovascular events, dehydration, gastrointestinal causes (nausea, emesis, ileus, and bowel obstruction), pain, venous thromboembolic event, wound occurrences (superficial site infection, deep operative site infection, wound disruptions), other infection, and other causes.
Of the 12,369 individuals included in the study, 1,057 (8.5%) were readmitted within 30 days of undergoing VHR. Generally, the patients who had open procedures had higher ASA scores than did those who had laparoscopic surgery, reflecting a greater likelihood of preoperative physical impairment and chronic disease. The researchers then analyzed which patients were mostly likely to be readmitted and the correlation between type of operation, cause of readmission, and timing of readmission (early or late).
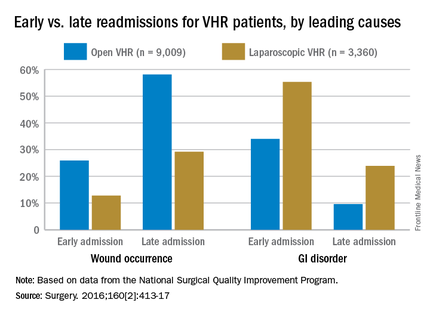
Open-VHR patients were more likely to be readmitted within 30 days than were those who underwent laparoscopic VHR: 9.2% vs. 6.9% readmission rates, respectively (OR 0.73, 95% CI 0.63-0.85). Among all the patients readmitted, wound complications were the most common cause (32.2%), followed by gastrointestinal disorders (14.3%), most which were attributed to emesis or nausea.
Wound complications were more highly associated with late readmission than with early ones, at 52% vs. 23%, respectively (OR 3.68, 95% CI 2.56-5.29). As might be expected, wound complications were more likely to occur in open-VHR patients than in laparoscopic-VHR patients: 49.6% vs. 24.4% (OR 3.05, 95% CI 2.06-4.52).
Of the entire cohort, 279 patients (2.3%) were classified as early readmissions, and gastrointestinal causes were more highly associated with early readmission than with late ones: 39% vs.13% (OR 4.45, 95% CI 3.06-6.47). Gastrointestinal issues occurred more often after laparoscopic VHR than after open VHR: 33% vs. 16% (OR 2.59, 95% CI 1.75-3.84). These early readmissions, occurring within days of discharge, are potentially preventable with a stepped up focus on control of nausea and emesis experienced by these patients, the researchers noted.
A funding source for this study was not disclosed. Dr. Celio and his coauthors did not report any relevant disclosures.
FROM SURGERY
Key clinical point: Postoperative complications and likelihood of readmission differ according to the type of ventral hernia repair procedure (open or laparoscopic).
Major finding: Thirty-day readmissions occurred among 6.9% of patients who had laparoscopic surgery, compared with 9.2% of open-procedure patients; gastrointestinal disorders were more common in early readmissions but wound occurrences were more common in late readmissions.
Data source: Retrospective cohort study of 12,369 ventral hernia repair patients (open and laparoscopic) in 2012.
Disclosures: Funding source not disclosed. Authors did not report any relevant financial disclosures.