User login
Upfront Appendectomy Improves Survival Among Frail Older Adults
TOPLINE:
Older adults with acute uncomplicated appendicitis who were operated on within 1 day of admission were less likely to die in the hospital compared with those who were treated with nonsurgical management or who had a delayed surgery.
METHODOLOGY:
- Researchers conducted a retrospective cohort study of 24,320 older adults (median age, 72 years; 50.9% women; 75.6% White) with uncomplicated appendicitis over a 2-year period starting in 2016; of these, 7290 patients were frail.
- Patients received nonsurgical treatment, immediate appendectomy within 1 day of admission, or delayed surgery after more than 1 day of admission.
- The clinical outcomes included infectious complications using a composite, cardiopulmonary complications, in-hospital mortality, length of hospital stay, and total hospital costs.
- Frailty of patients was assessed using a claims-based index producing a score ranging from 0 to 1 on the basis of 93 variables.
TAKEAWAY:
- Patients with frailty had higher rates of infections (1.3% vs 0.4%), cardiopulmonary complications (24.1% vs 6.3%), overall complications (57.1% vs 28.8%), in-hospital deaths (3.9% vs 0.3%), longer hospital stays (6 vs 4 days), and higher hospital costs ($67,000 vs $42,000) than those without frailty (P < .001).
- Patients with frailty who had immediate surgery had lower risk for death than those who received nonsurgical treatment (odds ratio [OR], 2.89; P = .004) and delayed surgery (OR, 3.80; P = .001).
- In patients without frailty, immediate surgery was linked to a higher risk for hospital complications than nonsurgical treatment (OR, 0.77; P = .009), but it was linked to a lower risk than delayed appendectomy (OR, 2.05; P < .001).
- Black patients were less likely to receive immediate appendectomy compared with White patients (P < .001).
IN PRACTICE:
“Our results suggest that treatment of older adults with acute uncomplicated appendicitis may benefit from risk stratification based on patient frailty status,” the authors wrote. “Routine frailty assessments should be incorporated in the care of older adult patients to guide discussions for shared decision-making,” they added.
SOURCE:
The study was led by Matthew Ashbrook, MD, MPH, of the Department of Surgery, University of Southern California, Los Angeles, and published online in JAMA Network Open.
LIMITATIONS:
Modification of the frailty index and reliance on discharge diagnosis could have resulted in misclassification bias. The timing of presentation of symptoms was not assessed. Also, lack of long-term data prevented tracking of readmissions and related complications.
DISCLOSURES:
The authors declared no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
TOPLINE:
Older adults with acute uncomplicated appendicitis who were operated on within 1 day of admission were less likely to die in the hospital compared with those who were treated with nonsurgical management or who had a delayed surgery.
METHODOLOGY:
- Researchers conducted a retrospective cohort study of 24,320 older adults (median age, 72 years; 50.9% women; 75.6% White) with uncomplicated appendicitis over a 2-year period starting in 2016; of these, 7290 patients were frail.
- Patients received nonsurgical treatment, immediate appendectomy within 1 day of admission, or delayed surgery after more than 1 day of admission.
- The clinical outcomes included infectious complications using a composite, cardiopulmonary complications, in-hospital mortality, length of hospital stay, and total hospital costs.
- Frailty of patients was assessed using a claims-based index producing a score ranging from 0 to 1 on the basis of 93 variables.
TAKEAWAY:
- Patients with frailty had higher rates of infections (1.3% vs 0.4%), cardiopulmonary complications (24.1% vs 6.3%), overall complications (57.1% vs 28.8%), in-hospital deaths (3.9% vs 0.3%), longer hospital stays (6 vs 4 days), and higher hospital costs ($67,000 vs $42,000) than those without frailty (P < .001).
- Patients with frailty who had immediate surgery had lower risk for death than those who received nonsurgical treatment (odds ratio [OR], 2.89; P = .004) and delayed surgery (OR, 3.80; P = .001).
- In patients without frailty, immediate surgery was linked to a higher risk for hospital complications than nonsurgical treatment (OR, 0.77; P = .009), but it was linked to a lower risk than delayed appendectomy (OR, 2.05; P < .001).
- Black patients were less likely to receive immediate appendectomy compared with White patients (P < .001).
IN PRACTICE:
“Our results suggest that treatment of older adults with acute uncomplicated appendicitis may benefit from risk stratification based on patient frailty status,” the authors wrote. “Routine frailty assessments should be incorporated in the care of older adult patients to guide discussions for shared decision-making,” they added.
SOURCE:
The study was led by Matthew Ashbrook, MD, MPH, of the Department of Surgery, University of Southern California, Los Angeles, and published online in JAMA Network Open.
LIMITATIONS:
Modification of the frailty index and reliance on discharge diagnosis could have resulted in misclassification bias. The timing of presentation of symptoms was not assessed. Also, lack of long-term data prevented tracking of readmissions and related complications.
DISCLOSURES:
The authors declared no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
TOPLINE:
Older adults with acute uncomplicated appendicitis who were operated on within 1 day of admission were less likely to die in the hospital compared with those who were treated with nonsurgical management or who had a delayed surgery.
METHODOLOGY:
- Researchers conducted a retrospective cohort study of 24,320 older adults (median age, 72 years; 50.9% women; 75.6% White) with uncomplicated appendicitis over a 2-year period starting in 2016; of these, 7290 patients were frail.
- Patients received nonsurgical treatment, immediate appendectomy within 1 day of admission, or delayed surgery after more than 1 day of admission.
- The clinical outcomes included infectious complications using a composite, cardiopulmonary complications, in-hospital mortality, length of hospital stay, and total hospital costs.
- Frailty of patients was assessed using a claims-based index producing a score ranging from 0 to 1 on the basis of 93 variables.
TAKEAWAY:
- Patients with frailty had higher rates of infections (1.3% vs 0.4%), cardiopulmonary complications (24.1% vs 6.3%), overall complications (57.1% vs 28.8%), in-hospital deaths (3.9% vs 0.3%), longer hospital stays (6 vs 4 days), and higher hospital costs ($67,000 vs $42,000) than those without frailty (P < .001).
- Patients with frailty who had immediate surgery had lower risk for death than those who received nonsurgical treatment (odds ratio [OR], 2.89; P = .004) and delayed surgery (OR, 3.80; P = .001).
- In patients without frailty, immediate surgery was linked to a higher risk for hospital complications than nonsurgical treatment (OR, 0.77; P = .009), but it was linked to a lower risk than delayed appendectomy (OR, 2.05; P < .001).
- Black patients were less likely to receive immediate appendectomy compared with White patients (P < .001).
IN PRACTICE:
“Our results suggest that treatment of older adults with acute uncomplicated appendicitis may benefit from risk stratification based on patient frailty status,” the authors wrote. “Routine frailty assessments should be incorporated in the care of older adult patients to guide discussions for shared decision-making,” they added.
SOURCE:
The study was led by Matthew Ashbrook, MD, MPH, of the Department of Surgery, University of Southern California, Los Angeles, and published online in JAMA Network Open.
LIMITATIONS:
Modification of the frailty index and reliance on discharge diagnosis could have resulted in misclassification bias. The timing of presentation of symptoms was not assessed. Also, lack of long-term data prevented tracking of readmissions and related complications.
DISCLOSURES:
The authors declared no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Whether GLP-1 RAs Significantly Delay Gastric Emptying Called into Question
TOPLINE:
Patients taking a glucagon-like peptide 1 receptor agonist (GLP-1 RA) experience only a modest delay in gastric emptying of solid foods and no significant delay for liquids, compared with those receiving placebo, indicating that patients may not need to discontinue these medications before surgery.
METHODOLOGY:
- GLP-1 RAs, while effective in managing diabetes and obesity, are linked to delayed gastric emptying, which may pose risks during procedures requiring anesthesia or sedation due to potential aspiration of gastric contents.
- Researchers conducted a meta-analysis to quantify the duration of delay in gastric emptying caused by GLP-1 RAs in patients with diabetes and/or excessive body weight, which could guide periprocedural management decisions in the future.
- The primary outcome was halftime, the time required for 50% of solid gastric contents to empty, measured using scintigraphy. This analysis included data from five studies involving 247 patients who received either a GLP-1 RA or placebo.
- The secondary outcome was gastric emptying of liquids measured using the acetaminophen absorption test. Ten studies including 411 patients who received either a GLP-1 RA or placebo were included in this analysis.
TAKEAWAY:
- The mean gastric emptying halftime for solid foods was 138.4 minutes with a GLP-1 RA and 95.0 minutes with placebo, resulting in a pooled mean difference of 36.0 minutes (P < .01).
- Furthermore, the amount of gastric emptying noted at 4 or 5 hours on the acetaminophen absorption test was comparable between these groups.
- The gastric emptying time for both solids and liquids did not differ between GLP-1 RA formulations or between short-acting or long-acting GLP-1 RAs.
IN PRACTICE:
“Based on current evidence, a conservative approach with a liquid diet on the day before procedures while continuing GLP-1 RA therapy would represent the most sensible approach until more conclusive data on a solid diet are available,” the authors wrote.
SOURCE:
The study, led by Brent Hiramoto, MD, MPH, of the Center for Gastrointestinal Motility at Brigham and Women’s Hospital and Harvard Medical School, Boston, was published online in The American Journal of Gastroenterology.
LIMITATIONS:
The small number of studies utilizing some diagnostic modalities, such as breath testing, precluded a formal meta-analysis of these subgroups. The results could not be stratified by indication for GLP-1 RA (diabetes or obesity) because of insufficient studies in each category.
DISCLOSURES:
The lead author was supported by the National Institute of Diabetes and Digestive and Kidney Diseases. One author declared serving on the advisory boards of three pharmaceutical companies.
A version of this article first appeared on Medscape.com.
TOPLINE:
Patients taking a glucagon-like peptide 1 receptor agonist (GLP-1 RA) experience only a modest delay in gastric emptying of solid foods and no significant delay for liquids, compared with those receiving placebo, indicating that patients may not need to discontinue these medications before surgery.
METHODOLOGY:
- GLP-1 RAs, while effective in managing diabetes and obesity, are linked to delayed gastric emptying, which may pose risks during procedures requiring anesthesia or sedation due to potential aspiration of gastric contents.
- Researchers conducted a meta-analysis to quantify the duration of delay in gastric emptying caused by GLP-1 RAs in patients with diabetes and/or excessive body weight, which could guide periprocedural management decisions in the future.
- The primary outcome was halftime, the time required for 50% of solid gastric contents to empty, measured using scintigraphy. This analysis included data from five studies involving 247 patients who received either a GLP-1 RA or placebo.
- The secondary outcome was gastric emptying of liquids measured using the acetaminophen absorption test. Ten studies including 411 patients who received either a GLP-1 RA or placebo were included in this analysis.
TAKEAWAY:
- The mean gastric emptying halftime for solid foods was 138.4 minutes with a GLP-1 RA and 95.0 minutes with placebo, resulting in a pooled mean difference of 36.0 minutes (P < .01).
- Furthermore, the amount of gastric emptying noted at 4 or 5 hours on the acetaminophen absorption test was comparable between these groups.
- The gastric emptying time for both solids and liquids did not differ between GLP-1 RA formulations or between short-acting or long-acting GLP-1 RAs.
IN PRACTICE:
“Based on current evidence, a conservative approach with a liquid diet on the day before procedures while continuing GLP-1 RA therapy would represent the most sensible approach until more conclusive data on a solid diet are available,” the authors wrote.
SOURCE:
The study, led by Brent Hiramoto, MD, MPH, of the Center for Gastrointestinal Motility at Brigham and Women’s Hospital and Harvard Medical School, Boston, was published online in The American Journal of Gastroenterology.
LIMITATIONS:
The small number of studies utilizing some diagnostic modalities, such as breath testing, precluded a formal meta-analysis of these subgroups. The results could not be stratified by indication for GLP-1 RA (diabetes or obesity) because of insufficient studies in each category.
DISCLOSURES:
The lead author was supported by the National Institute of Diabetes and Digestive and Kidney Diseases. One author declared serving on the advisory boards of three pharmaceutical companies.
A version of this article first appeared on Medscape.com.
TOPLINE:
Patients taking a glucagon-like peptide 1 receptor agonist (GLP-1 RA) experience only a modest delay in gastric emptying of solid foods and no significant delay for liquids, compared with those receiving placebo, indicating that patients may not need to discontinue these medications before surgery.
METHODOLOGY:
- GLP-1 RAs, while effective in managing diabetes and obesity, are linked to delayed gastric emptying, which may pose risks during procedures requiring anesthesia or sedation due to potential aspiration of gastric contents.
- Researchers conducted a meta-analysis to quantify the duration of delay in gastric emptying caused by GLP-1 RAs in patients with diabetes and/or excessive body weight, which could guide periprocedural management decisions in the future.
- The primary outcome was halftime, the time required for 50% of solid gastric contents to empty, measured using scintigraphy. This analysis included data from five studies involving 247 patients who received either a GLP-1 RA or placebo.
- The secondary outcome was gastric emptying of liquids measured using the acetaminophen absorption test. Ten studies including 411 patients who received either a GLP-1 RA or placebo were included in this analysis.
TAKEAWAY:
- The mean gastric emptying halftime for solid foods was 138.4 minutes with a GLP-1 RA and 95.0 minutes with placebo, resulting in a pooled mean difference of 36.0 minutes (P < .01).
- Furthermore, the amount of gastric emptying noted at 4 or 5 hours on the acetaminophen absorption test was comparable between these groups.
- The gastric emptying time for both solids and liquids did not differ between GLP-1 RA formulations or between short-acting or long-acting GLP-1 RAs.
IN PRACTICE:
“Based on current evidence, a conservative approach with a liquid diet on the day before procedures while continuing GLP-1 RA therapy would represent the most sensible approach until more conclusive data on a solid diet are available,” the authors wrote.
SOURCE:
The study, led by Brent Hiramoto, MD, MPH, of the Center for Gastrointestinal Motility at Brigham and Women’s Hospital and Harvard Medical School, Boston, was published online in The American Journal of Gastroenterology.
LIMITATIONS:
The small number of studies utilizing some diagnostic modalities, such as breath testing, precluded a formal meta-analysis of these subgroups. The results could not be stratified by indication for GLP-1 RA (diabetes or obesity) because of insufficient studies in each category.
DISCLOSURES:
The lead author was supported by the National Institute of Diabetes and Digestive and Kidney Diseases. One author declared serving on the advisory boards of three pharmaceutical companies.
A version of this article first appeared on Medscape.com.
The Appendix: Is It ’Useless,’ or a Safe House and Immune Training Ground?
When doctors and patients consider the appendix, it’s often with urgency. In cases of appendicitis, the clock could be ticking down to a life-threatening burst. Thus, despite recent research suggesting antibiotics could be an alternative therapy, appendectomy remains standard for uncomplicated appendicitis.
But what if removing the appendix could raise the risk for gastrointestinal (GI) diseases like irritable bowel syndrome and colorectal cancer? That’s what some emerging science suggests. And though the research is early and mixed, it’s enough to give some health professionals pause.
“If there’s no reason to remove the appendix, then it’s better to have one,” said Heather Smith, PhD, a comparative anatomist at Midwestern University, Glendale, Arizona. Preemptive removal is not supported by the evidence, she said.
To be fair, we’ve come a long way since 1928, when American physician Miles Breuer, MD, suggested that people with infected appendixes should be left to perish, so as to remove their inferior DNA from the gene pool (he called such people “uncivilized” and “candidates for extinction”). Charles Darwin, while less radical, believed the appendix was at best useless — a mere vestige of our ancestors switching diets from leaves to fruits.
What we know now is that the appendix isn’t just a troublesome piece of worthless flesh. Instead, it may act as a safe house for friendly gut bacteria and a training camp for the immune system. It also appears to play a role in several medical conditions, from ulcerative colitis and colorectal cancer to Parkinson’s disease and lupus. The roughly 300,000 Americans who undergo appendectomy each year should be made aware of this, some experts say. But the frustrating truth is, scientists are still trying to figure out in which cases having an appendix is protective and in which we may be better off without it.
A ‘Worm’ as Intestinal Protection
The appendix is a blind pouch (meaning its ending is closed off) that extends from the large intestine. Not all mammals have one; it’s been found in several species of primates and rodents, as well as in rabbits, wombats, and Florida manatees, among others (dogs and cats don’t have it). While a human appendix “looks like a little worm,” Dr. Smith said, these anatomical structures come in various sizes and shapes. Some are thick, as in a beaver, while others are long and spiraling, like a rabbit’s.
Comparative anatomy studies reveal that the appendix has evolved independently at least 29 times throughout mammalian evolution. This suggests that “it has some kind of an adaptive function,” Dr. Smith said. When French scientists analyzed data from 258 species of mammals, they discovered that those that possess an appendix live longer than those without one. A possible explanation, the researchers wrote, may lie with the appendix’s role in preventing diarrhea.
Their 2023 study supported this hypothesis. Based on veterinary records of 45 different species of primates housed in a French zoo, the scientists established that primates with appendixes are far less likely to suffer severe diarrhea than those that don’t possess this organ. The appendix, it appears, might be our tiny weapon against bowel troubles.
For immunologist William Parker, PhD, a visiting scholar at the University of North Carolina at Chapel Hill, these data are “about as good as we could hope for” in support of the idea that the appendix might protect mammals from GI problems. An experiment on humans would be unethical, Dr. Parker said. But observational studies offer clues.
One study showed that compared with people with an intact appendix, young adults with a history of appendectomy have more than double the risk of developing a serious infection with non-typhoidal Salmonella of the kind that would require hospitalization.
A ‘Safe House’ for Bacteria
Such studies add weight to a theory that Dr. Parker and his colleagues developed back in 2007: That the appendix acts as a “safe house” for beneficial gut bacteria.
Think of the colon as a wide pipe, Dr. Parker said, that may become contaminated with a pathogen such as Salmonella. Diarrhea follows, and the pipe gets repeatedly flushed, wiping everything clean, including your friendly gut microbiome. Luckily, “you’ve got this little offshoot of that pipe,” where the flow can’t really get in “because it’s so constricted,” Dr. Parker said. The friendly gut microbes can survive inside the appendix and repopulate the colon once diarrhea is over. Dr. Parker and his colleagues found that the human appendix contains a thick layer of beneficial bacteria. “They were right where we predicted they would be,” he said.
This safe house hypothesis could explain why the gut microbiome may be different in people who no longer have an appendix. In one small study, people who’d had an appendectomy had a less diverse microbiome, with a lower abundance of beneficial strains such as Butyricicoccus and Barnesiella, than did those with intact appendixes.
The appendix likely has a second function, too, Dr. Smith said: It may serve as a training camp for the immune system. “When there is an invading pathogen in the gut, it helps the GI system to mount the immune response,” she said. The human appendix is rich in special cells known as M cells. These act as scouts, detecting and capturing invasive bacteria and viruses and presenting them to the body’s defense team, such as the T lymphocytes.
If the appendix shelters beneficial bacteria and boosts immune response, that may explain its links to various diseases. According to an epidemiological study from Taiwan,patients who underwent an appendectomy have a 46% higher risk of developing irritable bowel syndrome (IBS) — a disease associated with a low abundance of Butyricicoccus bacteria. This is why, the study authors wrote, doctors should pay careful attention to people who’ve had their appendixes removed, monitoring them for potential symptoms of IBS.
The same database helped uncover other connections between appendectomy and disease. For one, there was type 2 diabetes: Within 3 years of the surgery, patients under 30 had double the risk of developing this disorder. Then there was lupus: While those who underwent appendectomy generally had higher risk for this autoimmune disease, women were particularly affected.
The Contentious Connections
The most heated scientific discussion surrounds the links between the appendix and conditions such as Parkinson’s disease, ulcerative colitis, and colorectal cancer. A small 2019 study showed, for example, that appendectomy may improve symptoms of certain forms of ulcerative colitis that don’t respond to standard medical treatments. A third of patients improved after their appendix was removed, and 17% fully recovered.
Why? According to Dr. Parker, appendectomy may work for ulcerative colitis because it’s “a way of suppressing the immune system, especially in the lower intestinal areas.” A 2023 meta-analysis found that people who’d had their appendix removed before being diagnosed with ulcerative colitis were less likely to need their colon removed later on.
Such a procedure may have a serious side effect, however: Colorectal cancer. French scientists discovered that removing the appendix may reduce the numbers of certain immune cells called CD3+ and CD8+ T cells, causing a weakened immune surveillance. As a result, tumor cells might escape detection.
Yet the links between appendix removal and cancer are far from clear. A recent meta-analysis found that while people with appendectomies generally had a higher risk for colorectal cancer, for Europeans, these effects were insignificant. In fact, removal of the appendix actually protected European women from this particular form of cancer. For Parker, such mixed results may stem from the fact that treatments and populations vary widely. The issue “may depend on complex social and medical factors,” Dr. Parker said.
Things also appear complicated with Parkinson’s disease — another condition linked to the appendix. A large epidemiological study showed that appendectomy is associated with a lower risk for Parkinson’s disease and a delayed age of Parkinson’s onset. It also found that a normal appendix contains α-synuclein, a protein that may accumulate in the brain and contribute to the development of Parkinson’s. “Although α-synuclein is toxic when in the brain, it appears to be quite normal when present in the appendix,” said Luis Vitetta, PhD, MD, a clinical epidemiologist at the University of Sydney, Camperdown, Australia. Yet, not all studies find that removing the appendix lowers the risk for Parkinson’s. In fact, some show the opposite results.
How Should Doctors View the Appendix?
Even with these mysteries and contradictions, Dr. Vitetta said, a healthy appendix in a healthy body appears to be protective. This is why, he said, when someone is diagnosed with appendicitis, careful assessment is essential before surgery is performed.
“Perhaps an antibiotic can actually help fix it,” he said. A 2020 study published in The New England Journal of Medicine showed that antibiotics may indeed be a good alternative to surgery for the treatment of appendicitis. “We don’t want necessarily to remove an appendix that could be beneficial,” Dr. Smith said.
The many links between the appendix and various diseases mean that doctors should be more vigilant when treating patients who’ve had this organ removed, Dr. Parker said. “When a patient loses an appendix, depending on their environment, there may be effects on infection and cancer. So they might need more regular checkups,” he said. This could include monitoring for IBS and colorectal cancer.
What’s more, Dr. Parker believes that research on the appendix puts even more emphasis on the need to protect the gut microbiome — such as taking probiotics with antibiotics. And while we are still a long way from understanding how exactly this worm-like structure affects various diseases, one thing appears quite certain: The appendix is not useless. “If Darwin had the information that we have, he would not have drawn these conclusions,” Dr. Parker said.
A version of this article first appeared on Medscape.com.
When doctors and patients consider the appendix, it’s often with urgency. In cases of appendicitis, the clock could be ticking down to a life-threatening burst. Thus, despite recent research suggesting antibiotics could be an alternative therapy, appendectomy remains standard for uncomplicated appendicitis.
But what if removing the appendix could raise the risk for gastrointestinal (GI) diseases like irritable bowel syndrome and colorectal cancer? That’s what some emerging science suggests. And though the research is early and mixed, it’s enough to give some health professionals pause.
“If there’s no reason to remove the appendix, then it’s better to have one,” said Heather Smith, PhD, a comparative anatomist at Midwestern University, Glendale, Arizona. Preemptive removal is not supported by the evidence, she said.
To be fair, we’ve come a long way since 1928, when American physician Miles Breuer, MD, suggested that people with infected appendixes should be left to perish, so as to remove their inferior DNA from the gene pool (he called such people “uncivilized” and “candidates for extinction”). Charles Darwin, while less radical, believed the appendix was at best useless — a mere vestige of our ancestors switching diets from leaves to fruits.
What we know now is that the appendix isn’t just a troublesome piece of worthless flesh. Instead, it may act as a safe house for friendly gut bacteria and a training camp for the immune system. It also appears to play a role in several medical conditions, from ulcerative colitis and colorectal cancer to Parkinson’s disease and lupus. The roughly 300,000 Americans who undergo appendectomy each year should be made aware of this, some experts say. But the frustrating truth is, scientists are still trying to figure out in which cases having an appendix is protective and in which we may be better off without it.
A ‘Worm’ as Intestinal Protection
The appendix is a blind pouch (meaning its ending is closed off) that extends from the large intestine. Not all mammals have one; it’s been found in several species of primates and rodents, as well as in rabbits, wombats, and Florida manatees, among others (dogs and cats don’t have it). While a human appendix “looks like a little worm,” Dr. Smith said, these anatomical structures come in various sizes and shapes. Some are thick, as in a beaver, while others are long and spiraling, like a rabbit’s.
Comparative anatomy studies reveal that the appendix has evolved independently at least 29 times throughout mammalian evolution. This suggests that “it has some kind of an adaptive function,” Dr. Smith said. When French scientists analyzed data from 258 species of mammals, they discovered that those that possess an appendix live longer than those without one. A possible explanation, the researchers wrote, may lie with the appendix’s role in preventing diarrhea.
Their 2023 study supported this hypothesis. Based on veterinary records of 45 different species of primates housed in a French zoo, the scientists established that primates with appendixes are far less likely to suffer severe diarrhea than those that don’t possess this organ. The appendix, it appears, might be our tiny weapon against bowel troubles.
For immunologist William Parker, PhD, a visiting scholar at the University of North Carolina at Chapel Hill, these data are “about as good as we could hope for” in support of the idea that the appendix might protect mammals from GI problems. An experiment on humans would be unethical, Dr. Parker said. But observational studies offer clues.
One study showed that compared with people with an intact appendix, young adults with a history of appendectomy have more than double the risk of developing a serious infection with non-typhoidal Salmonella of the kind that would require hospitalization.
A ‘Safe House’ for Bacteria
Such studies add weight to a theory that Dr. Parker and his colleagues developed back in 2007: That the appendix acts as a “safe house” for beneficial gut bacteria.
Think of the colon as a wide pipe, Dr. Parker said, that may become contaminated with a pathogen such as Salmonella. Diarrhea follows, and the pipe gets repeatedly flushed, wiping everything clean, including your friendly gut microbiome. Luckily, “you’ve got this little offshoot of that pipe,” where the flow can’t really get in “because it’s so constricted,” Dr. Parker said. The friendly gut microbes can survive inside the appendix and repopulate the colon once diarrhea is over. Dr. Parker and his colleagues found that the human appendix contains a thick layer of beneficial bacteria. “They were right where we predicted they would be,” he said.
This safe house hypothesis could explain why the gut microbiome may be different in people who no longer have an appendix. In one small study, people who’d had an appendectomy had a less diverse microbiome, with a lower abundance of beneficial strains such as Butyricicoccus and Barnesiella, than did those with intact appendixes.
The appendix likely has a second function, too, Dr. Smith said: It may serve as a training camp for the immune system. “When there is an invading pathogen in the gut, it helps the GI system to mount the immune response,” she said. The human appendix is rich in special cells known as M cells. These act as scouts, detecting and capturing invasive bacteria and viruses and presenting them to the body’s defense team, such as the T lymphocytes.
If the appendix shelters beneficial bacteria and boosts immune response, that may explain its links to various diseases. According to an epidemiological study from Taiwan,patients who underwent an appendectomy have a 46% higher risk of developing irritable bowel syndrome (IBS) — a disease associated with a low abundance of Butyricicoccus bacteria. This is why, the study authors wrote, doctors should pay careful attention to people who’ve had their appendixes removed, monitoring them for potential symptoms of IBS.
The same database helped uncover other connections between appendectomy and disease. For one, there was type 2 diabetes: Within 3 years of the surgery, patients under 30 had double the risk of developing this disorder. Then there was lupus: While those who underwent appendectomy generally had higher risk for this autoimmune disease, women were particularly affected.
The Contentious Connections
The most heated scientific discussion surrounds the links between the appendix and conditions such as Parkinson’s disease, ulcerative colitis, and colorectal cancer. A small 2019 study showed, for example, that appendectomy may improve symptoms of certain forms of ulcerative colitis that don’t respond to standard medical treatments. A third of patients improved after their appendix was removed, and 17% fully recovered.
Why? According to Dr. Parker, appendectomy may work for ulcerative colitis because it’s “a way of suppressing the immune system, especially in the lower intestinal areas.” A 2023 meta-analysis found that people who’d had their appendix removed before being diagnosed with ulcerative colitis were less likely to need their colon removed later on.
Such a procedure may have a serious side effect, however: Colorectal cancer. French scientists discovered that removing the appendix may reduce the numbers of certain immune cells called CD3+ and CD8+ T cells, causing a weakened immune surveillance. As a result, tumor cells might escape detection.
Yet the links between appendix removal and cancer are far from clear. A recent meta-analysis found that while people with appendectomies generally had a higher risk for colorectal cancer, for Europeans, these effects were insignificant. In fact, removal of the appendix actually protected European women from this particular form of cancer. For Parker, such mixed results may stem from the fact that treatments and populations vary widely. The issue “may depend on complex social and medical factors,” Dr. Parker said.
Things also appear complicated with Parkinson’s disease — another condition linked to the appendix. A large epidemiological study showed that appendectomy is associated with a lower risk for Parkinson’s disease and a delayed age of Parkinson’s onset. It also found that a normal appendix contains α-synuclein, a protein that may accumulate in the brain and contribute to the development of Parkinson’s. “Although α-synuclein is toxic when in the brain, it appears to be quite normal when present in the appendix,” said Luis Vitetta, PhD, MD, a clinical epidemiologist at the University of Sydney, Camperdown, Australia. Yet, not all studies find that removing the appendix lowers the risk for Parkinson’s. In fact, some show the opposite results.
How Should Doctors View the Appendix?
Even with these mysteries and contradictions, Dr. Vitetta said, a healthy appendix in a healthy body appears to be protective. This is why, he said, when someone is diagnosed with appendicitis, careful assessment is essential before surgery is performed.
“Perhaps an antibiotic can actually help fix it,” he said. A 2020 study published in The New England Journal of Medicine showed that antibiotics may indeed be a good alternative to surgery for the treatment of appendicitis. “We don’t want necessarily to remove an appendix that could be beneficial,” Dr. Smith said.
The many links between the appendix and various diseases mean that doctors should be more vigilant when treating patients who’ve had this organ removed, Dr. Parker said. “When a patient loses an appendix, depending on their environment, there may be effects on infection and cancer. So they might need more regular checkups,” he said. This could include monitoring for IBS and colorectal cancer.
What’s more, Dr. Parker believes that research on the appendix puts even more emphasis on the need to protect the gut microbiome — such as taking probiotics with antibiotics. And while we are still a long way from understanding how exactly this worm-like structure affects various diseases, one thing appears quite certain: The appendix is not useless. “If Darwin had the information that we have, he would not have drawn these conclusions,” Dr. Parker said.
A version of this article first appeared on Medscape.com.
When doctors and patients consider the appendix, it’s often with urgency. In cases of appendicitis, the clock could be ticking down to a life-threatening burst. Thus, despite recent research suggesting antibiotics could be an alternative therapy, appendectomy remains standard for uncomplicated appendicitis.
But what if removing the appendix could raise the risk for gastrointestinal (GI) diseases like irritable bowel syndrome and colorectal cancer? That’s what some emerging science suggests. And though the research is early and mixed, it’s enough to give some health professionals pause.
“If there’s no reason to remove the appendix, then it’s better to have one,” said Heather Smith, PhD, a comparative anatomist at Midwestern University, Glendale, Arizona. Preemptive removal is not supported by the evidence, she said.
To be fair, we’ve come a long way since 1928, when American physician Miles Breuer, MD, suggested that people with infected appendixes should be left to perish, so as to remove their inferior DNA from the gene pool (he called such people “uncivilized” and “candidates for extinction”). Charles Darwin, while less radical, believed the appendix was at best useless — a mere vestige of our ancestors switching diets from leaves to fruits.
What we know now is that the appendix isn’t just a troublesome piece of worthless flesh. Instead, it may act as a safe house for friendly gut bacteria and a training camp for the immune system. It also appears to play a role in several medical conditions, from ulcerative colitis and colorectal cancer to Parkinson’s disease and lupus. The roughly 300,000 Americans who undergo appendectomy each year should be made aware of this, some experts say. But the frustrating truth is, scientists are still trying to figure out in which cases having an appendix is protective and in which we may be better off without it.
A ‘Worm’ as Intestinal Protection
The appendix is a blind pouch (meaning its ending is closed off) that extends from the large intestine. Not all mammals have one; it’s been found in several species of primates and rodents, as well as in rabbits, wombats, and Florida manatees, among others (dogs and cats don’t have it). While a human appendix “looks like a little worm,” Dr. Smith said, these anatomical structures come in various sizes and shapes. Some are thick, as in a beaver, while others are long and spiraling, like a rabbit’s.
Comparative anatomy studies reveal that the appendix has evolved independently at least 29 times throughout mammalian evolution. This suggests that “it has some kind of an adaptive function,” Dr. Smith said. When French scientists analyzed data from 258 species of mammals, they discovered that those that possess an appendix live longer than those without one. A possible explanation, the researchers wrote, may lie with the appendix’s role in preventing diarrhea.
Their 2023 study supported this hypothesis. Based on veterinary records of 45 different species of primates housed in a French zoo, the scientists established that primates with appendixes are far less likely to suffer severe diarrhea than those that don’t possess this organ. The appendix, it appears, might be our tiny weapon against bowel troubles.
For immunologist William Parker, PhD, a visiting scholar at the University of North Carolina at Chapel Hill, these data are “about as good as we could hope for” in support of the idea that the appendix might protect mammals from GI problems. An experiment on humans would be unethical, Dr. Parker said. But observational studies offer clues.
One study showed that compared with people with an intact appendix, young adults with a history of appendectomy have more than double the risk of developing a serious infection with non-typhoidal Salmonella of the kind that would require hospitalization.
A ‘Safe House’ for Bacteria
Such studies add weight to a theory that Dr. Parker and his colleagues developed back in 2007: That the appendix acts as a “safe house” for beneficial gut bacteria.
Think of the colon as a wide pipe, Dr. Parker said, that may become contaminated with a pathogen such as Salmonella. Diarrhea follows, and the pipe gets repeatedly flushed, wiping everything clean, including your friendly gut microbiome. Luckily, “you’ve got this little offshoot of that pipe,” where the flow can’t really get in “because it’s so constricted,” Dr. Parker said. The friendly gut microbes can survive inside the appendix and repopulate the colon once diarrhea is over. Dr. Parker and his colleagues found that the human appendix contains a thick layer of beneficial bacteria. “They were right where we predicted they would be,” he said.
This safe house hypothesis could explain why the gut microbiome may be different in people who no longer have an appendix. In one small study, people who’d had an appendectomy had a less diverse microbiome, with a lower abundance of beneficial strains such as Butyricicoccus and Barnesiella, than did those with intact appendixes.
The appendix likely has a second function, too, Dr. Smith said: It may serve as a training camp for the immune system. “When there is an invading pathogen in the gut, it helps the GI system to mount the immune response,” she said. The human appendix is rich in special cells known as M cells. These act as scouts, detecting and capturing invasive bacteria and viruses and presenting them to the body’s defense team, such as the T lymphocytes.
If the appendix shelters beneficial bacteria and boosts immune response, that may explain its links to various diseases. According to an epidemiological study from Taiwan,patients who underwent an appendectomy have a 46% higher risk of developing irritable bowel syndrome (IBS) — a disease associated with a low abundance of Butyricicoccus bacteria. This is why, the study authors wrote, doctors should pay careful attention to people who’ve had their appendixes removed, monitoring them for potential symptoms of IBS.
The same database helped uncover other connections between appendectomy and disease. For one, there was type 2 diabetes: Within 3 years of the surgery, patients under 30 had double the risk of developing this disorder. Then there was lupus: While those who underwent appendectomy generally had higher risk for this autoimmune disease, women were particularly affected.
The Contentious Connections
The most heated scientific discussion surrounds the links between the appendix and conditions such as Parkinson’s disease, ulcerative colitis, and colorectal cancer. A small 2019 study showed, for example, that appendectomy may improve symptoms of certain forms of ulcerative colitis that don’t respond to standard medical treatments. A third of patients improved after their appendix was removed, and 17% fully recovered.
Why? According to Dr. Parker, appendectomy may work for ulcerative colitis because it’s “a way of suppressing the immune system, especially in the lower intestinal areas.” A 2023 meta-analysis found that people who’d had their appendix removed before being diagnosed with ulcerative colitis were less likely to need their colon removed later on.
Such a procedure may have a serious side effect, however: Colorectal cancer. French scientists discovered that removing the appendix may reduce the numbers of certain immune cells called CD3+ and CD8+ T cells, causing a weakened immune surveillance. As a result, tumor cells might escape detection.
Yet the links between appendix removal and cancer are far from clear. A recent meta-analysis found that while people with appendectomies generally had a higher risk for colorectal cancer, for Europeans, these effects were insignificant. In fact, removal of the appendix actually protected European women from this particular form of cancer. For Parker, such mixed results may stem from the fact that treatments and populations vary widely. The issue “may depend on complex social and medical factors,” Dr. Parker said.
Things also appear complicated with Parkinson’s disease — another condition linked to the appendix. A large epidemiological study showed that appendectomy is associated with a lower risk for Parkinson’s disease and a delayed age of Parkinson’s onset. It also found that a normal appendix contains α-synuclein, a protein that may accumulate in the brain and contribute to the development of Parkinson’s. “Although α-synuclein is toxic when in the brain, it appears to be quite normal when present in the appendix,” said Luis Vitetta, PhD, MD, a clinical epidemiologist at the University of Sydney, Camperdown, Australia. Yet, not all studies find that removing the appendix lowers the risk for Parkinson’s. In fact, some show the opposite results.
How Should Doctors View the Appendix?
Even with these mysteries and contradictions, Dr. Vitetta said, a healthy appendix in a healthy body appears to be protective. This is why, he said, when someone is diagnosed with appendicitis, careful assessment is essential before surgery is performed.
“Perhaps an antibiotic can actually help fix it,” he said. A 2020 study published in The New England Journal of Medicine showed that antibiotics may indeed be a good alternative to surgery for the treatment of appendicitis. “We don’t want necessarily to remove an appendix that could be beneficial,” Dr. Smith said.
The many links between the appendix and various diseases mean that doctors should be more vigilant when treating patients who’ve had this organ removed, Dr. Parker said. “When a patient loses an appendix, depending on their environment, there may be effects on infection and cancer. So they might need more regular checkups,” he said. This could include monitoring for IBS and colorectal cancer.
What’s more, Dr. Parker believes that research on the appendix puts even more emphasis on the need to protect the gut microbiome — such as taking probiotics with antibiotics. And while we are still a long way from understanding how exactly this worm-like structure affects various diseases, one thing appears quite certain: The appendix is not useless. “If Darwin had the information that we have, he would not have drawn these conclusions,” Dr. Parker said.
A version of this article first appeared on Medscape.com.
Do People With Diabetes Need to Fast Longer Before Surgery?
People with diabetes don’t have higher gastric volumes than those without diabetes after following standard preoperative fasting instructions, suggested a study from a team of anesthesiologist researchers.
Moreover, the issue is now further complicated by the widespread use of glucagon-like peptide-1 (GLP-1) receptor agonists for the treatment of both type 2 diabetes and weight loss. These drugs, which were introduced after the study’s enrollment period, work in part by delaying gastric emptying.
The new data come from a prospective study of 84 people with diabetes (85% with type 2) and 96 without diabetes, all with a body mass index (BMI) < 40, who were undergoing elective surgery. A gastric ultrasound was used to assess their gastric contents after they had followed the standard preoperative fasting guidelines of stopping solids 8 hours prior to the procedure and clearing liquids 2 hours prior.
There was no significant difference between the two groups in gastric volume (0.81 mL/kg with diabetes vs 0.87 mL/kg without) or in the proportion with “full stomach,” as designated by the American Society of Anesthesiologists (ASA) guidelines (any solid content or > 1.5 mL/kg of clear fluid), which was seen in 13 with diabetes (15.5%) and 11 (11.5%) without.
Published in Anesthesiology, the findings offer reassurance that different fasting instructions generally aren’t needed for people with diabetes in order to minimize the risk for perioperative pulmonary aspiration, lead author Anahi Perlas, MD, professor of anesthesiology and pain medicine at the University of Toronto, told this news organization.
“We never change practice completely based on a single study, but I think in general, based on our findings, that most diabetic patients aren’t any different from nondiabetics when it comes to their gastric content after fasting, and our standard fasting instructions seem to be just as effective in ensuring an empty stomach.”
But, she added, “If someone has symptoms of gastroparesis or when in doubt, we can always do a gastric ultrasound exam at the bedside and see whether the stomach is full or empty ... it’s very quick, and it’s not difficult to do.”
Expert Identifies Noteworthy Study Limitations
In an accompanying editorial, Mark A. Warner, MD, professor of anesthesiology at the Mayo Clinic in Rochester, Minnesota, said the findings “will be very helpful to anesthesiologists,” although he noted that the exclusion of people with a BMI > 40 is a limitation.
However, Michael Horowitz, MBBS, PhD, FRACP, director of the Endocrine and Metabolic Unit at the Royal Adelaide Hospital and professor of medicine at Adelaide Medical School in Adelaide, Australia, disputed the study’s conclusions. He noted that the sample was small, and the participants had an average A1c of 7.2%. Fewer than half had microvascular or neuropathic complications. Thus, they were healthier than the general population with diabetes.
“They’ve picked the wrong group of diabetics,” said Dr. Horowitz, who specializes in gastrointestinal complications of diabetes. “This is not a group where you would expect a very high prevalence of delayed emptying.”
Gastric emptying of solids and liquids varies widely even among healthy people and more so in those with type 2 diabetes. About a third of those with above-target A1c levels have gastroparesis, while those more in the target range tend to have accelerated emptying, he explained.
And regarding the use of gastric ultrasound for those who are symptomatic, Dr. Horowitz said, “The relationship of symptoms such as nausea, vomiting, fullness, whatever it may be, with the rate of gastric emptying is weak at best. The association is not simply cause and effect.”
Are the Fasting Guidelines Flawed, Regardless of Diabetes Status?
Dr. Horowitz also faulted the ASA’s 2017 guidance revision for allowing clear liquids to be consumed up to 2 hours in advance of anesthesia because it doesn’t distinguish between liquids with and without calories.
“Whether you have diabetes or not, if you are allowed to have a sugar drink up to 2 hours before your operation, the majority of people empty at about 4 kcal/min, so they will still have some of that drink in their stomach,” he said. “If you want an empty stomach, the ASA guidelines are wrong.”
That explains why the study found relatively high rates of “full stomach” in both groups, 15.5% of those with diabetes and 11.5% of those without, he said.
The GLP-1 Agonist Factor
Although the study didn’t address GLP-1 receptor agonist use, Dr. Warner did in his accompanying editorial, noting that the drugs’ rapid expansion “will likely change how we use perioperative fasting guidelines. With these medications delaying gastric emptying times, we now have another risk factor for pulmonary aspiration to consider when applying fasting guidelines. The inconsistent impact of GLP-1 agonists on gastric emptying, ranging from little to significant, makes it difficult for anesthesiologists to gauge whether or not patients taking GLP-1 agonists are likely to have preoperative gastric liquid or solid contents that could cause subsequent damage if regurgitated.”
Gastric ultrasound can be helpful in this situation, Dr. Warner wrote. In addition, he endorsed the 2023 ASA guidance, which calls for withholding daily-dosed GLP-1 agonists on the day of the surgery and the weekly formulations for a week. And if gastrointestinal symptoms are present, delay elective procedures.
But Dr. Horowitz said those recommendations are likely insufficient as well, pointing to data suggesting that daily liraglutide can delay gastric emptying for up to 16 weeks in about a third of patients. Such studies haven’t been conducted by the manufacturers, particularly on the once-weekly formulations, and the ensuing risk for aspiration isn’t known.
“The slowing occurs in much lower doses than are used for glucose lowering,” Dr. Horowitz said. “It is very likely that plasma levels will need to be extremely low to avoid gastric slowing. The current guidelines fail to appreciate this. So, to withhold the short-acting drugs for 1 day is probably wrong. And to stop long-acting drugs for 1 week is almost certainly wrong too.”
But as for what should be done, he said, “I don’t actually know what you do about it. And no one does because there are no data available to answer the question.”
The study received funding from the Physicians’ Services Incorporated Foundation and the Canadian Society of Anesthesiologists. Dr. Perlas received support for nonclinical time through a merit award from the Department of Anesthesiology and Pain Medicine, University of Toronto, and the Department of Anesthesia and Pain Management, Toronto Western Hospital, University Health Network. She is an executive editor of the journal Regional Anesthesia and Pain Medicine and does consulting work for FujiFilm SonoSite. Dr. Horowitz had no relevant disclosures.
A version of this article appeared on Medscape.com.
People with diabetes don’t have higher gastric volumes than those without diabetes after following standard preoperative fasting instructions, suggested a study from a team of anesthesiologist researchers.
Moreover, the issue is now further complicated by the widespread use of glucagon-like peptide-1 (GLP-1) receptor agonists for the treatment of both type 2 diabetes and weight loss. These drugs, which were introduced after the study’s enrollment period, work in part by delaying gastric emptying.
The new data come from a prospective study of 84 people with diabetes (85% with type 2) and 96 without diabetes, all with a body mass index (BMI) < 40, who were undergoing elective surgery. A gastric ultrasound was used to assess their gastric contents after they had followed the standard preoperative fasting guidelines of stopping solids 8 hours prior to the procedure and clearing liquids 2 hours prior.
There was no significant difference between the two groups in gastric volume (0.81 mL/kg with diabetes vs 0.87 mL/kg without) or in the proportion with “full stomach,” as designated by the American Society of Anesthesiologists (ASA) guidelines (any solid content or > 1.5 mL/kg of clear fluid), which was seen in 13 with diabetes (15.5%) and 11 (11.5%) without.
Published in Anesthesiology, the findings offer reassurance that different fasting instructions generally aren’t needed for people with diabetes in order to minimize the risk for perioperative pulmonary aspiration, lead author Anahi Perlas, MD, professor of anesthesiology and pain medicine at the University of Toronto, told this news organization.
“We never change practice completely based on a single study, but I think in general, based on our findings, that most diabetic patients aren’t any different from nondiabetics when it comes to their gastric content after fasting, and our standard fasting instructions seem to be just as effective in ensuring an empty stomach.”
But, she added, “If someone has symptoms of gastroparesis or when in doubt, we can always do a gastric ultrasound exam at the bedside and see whether the stomach is full or empty ... it’s very quick, and it’s not difficult to do.”
Expert Identifies Noteworthy Study Limitations
In an accompanying editorial, Mark A. Warner, MD, professor of anesthesiology at the Mayo Clinic in Rochester, Minnesota, said the findings “will be very helpful to anesthesiologists,” although he noted that the exclusion of people with a BMI > 40 is a limitation.
However, Michael Horowitz, MBBS, PhD, FRACP, director of the Endocrine and Metabolic Unit at the Royal Adelaide Hospital and professor of medicine at Adelaide Medical School in Adelaide, Australia, disputed the study’s conclusions. He noted that the sample was small, and the participants had an average A1c of 7.2%. Fewer than half had microvascular or neuropathic complications. Thus, they were healthier than the general population with diabetes.
“They’ve picked the wrong group of diabetics,” said Dr. Horowitz, who specializes in gastrointestinal complications of diabetes. “This is not a group where you would expect a very high prevalence of delayed emptying.”
Gastric emptying of solids and liquids varies widely even among healthy people and more so in those with type 2 diabetes. About a third of those with above-target A1c levels have gastroparesis, while those more in the target range tend to have accelerated emptying, he explained.
And regarding the use of gastric ultrasound for those who are symptomatic, Dr. Horowitz said, “The relationship of symptoms such as nausea, vomiting, fullness, whatever it may be, with the rate of gastric emptying is weak at best. The association is not simply cause and effect.”
Are the Fasting Guidelines Flawed, Regardless of Diabetes Status?
Dr. Horowitz also faulted the ASA’s 2017 guidance revision for allowing clear liquids to be consumed up to 2 hours in advance of anesthesia because it doesn’t distinguish between liquids with and without calories.
“Whether you have diabetes or not, if you are allowed to have a sugar drink up to 2 hours before your operation, the majority of people empty at about 4 kcal/min, so they will still have some of that drink in their stomach,” he said. “If you want an empty stomach, the ASA guidelines are wrong.”
That explains why the study found relatively high rates of “full stomach” in both groups, 15.5% of those with diabetes and 11.5% of those without, he said.
The GLP-1 Agonist Factor
Although the study didn’t address GLP-1 receptor agonist use, Dr. Warner did in his accompanying editorial, noting that the drugs’ rapid expansion “will likely change how we use perioperative fasting guidelines. With these medications delaying gastric emptying times, we now have another risk factor for pulmonary aspiration to consider when applying fasting guidelines. The inconsistent impact of GLP-1 agonists on gastric emptying, ranging from little to significant, makes it difficult for anesthesiologists to gauge whether or not patients taking GLP-1 agonists are likely to have preoperative gastric liquid or solid contents that could cause subsequent damage if regurgitated.”
Gastric ultrasound can be helpful in this situation, Dr. Warner wrote. In addition, he endorsed the 2023 ASA guidance, which calls for withholding daily-dosed GLP-1 agonists on the day of the surgery and the weekly formulations for a week. And if gastrointestinal symptoms are present, delay elective procedures.
But Dr. Horowitz said those recommendations are likely insufficient as well, pointing to data suggesting that daily liraglutide can delay gastric emptying for up to 16 weeks in about a third of patients. Such studies haven’t been conducted by the manufacturers, particularly on the once-weekly formulations, and the ensuing risk for aspiration isn’t known.
“The slowing occurs in much lower doses than are used for glucose lowering,” Dr. Horowitz said. “It is very likely that plasma levels will need to be extremely low to avoid gastric slowing. The current guidelines fail to appreciate this. So, to withhold the short-acting drugs for 1 day is probably wrong. And to stop long-acting drugs for 1 week is almost certainly wrong too.”
But as for what should be done, he said, “I don’t actually know what you do about it. And no one does because there are no data available to answer the question.”
The study received funding from the Physicians’ Services Incorporated Foundation and the Canadian Society of Anesthesiologists. Dr. Perlas received support for nonclinical time through a merit award from the Department of Anesthesiology and Pain Medicine, University of Toronto, and the Department of Anesthesia and Pain Management, Toronto Western Hospital, University Health Network. She is an executive editor of the journal Regional Anesthesia and Pain Medicine and does consulting work for FujiFilm SonoSite. Dr. Horowitz had no relevant disclosures.
A version of this article appeared on Medscape.com.
People with diabetes don’t have higher gastric volumes than those without diabetes after following standard preoperative fasting instructions, suggested a study from a team of anesthesiologist researchers.
Moreover, the issue is now further complicated by the widespread use of glucagon-like peptide-1 (GLP-1) receptor agonists for the treatment of both type 2 diabetes and weight loss. These drugs, which were introduced after the study’s enrollment period, work in part by delaying gastric emptying.
The new data come from a prospective study of 84 people with diabetes (85% with type 2) and 96 without diabetes, all with a body mass index (BMI) < 40, who were undergoing elective surgery. A gastric ultrasound was used to assess their gastric contents after they had followed the standard preoperative fasting guidelines of stopping solids 8 hours prior to the procedure and clearing liquids 2 hours prior.
There was no significant difference between the two groups in gastric volume (0.81 mL/kg with diabetes vs 0.87 mL/kg without) or in the proportion with “full stomach,” as designated by the American Society of Anesthesiologists (ASA) guidelines (any solid content or > 1.5 mL/kg of clear fluid), which was seen in 13 with diabetes (15.5%) and 11 (11.5%) without.
Published in Anesthesiology, the findings offer reassurance that different fasting instructions generally aren’t needed for people with diabetes in order to minimize the risk for perioperative pulmonary aspiration, lead author Anahi Perlas, MD, professor of anesthesiology and pain medicine at the University of Toronto, told this news organization.
“We never change practice completely based on a single study, but I think in general, based on our findings, that most diabetic patients aren’t any different from nondiabetics when it comes to their gastric content after fasting, and our standard fasting instructions seem to be just as effective in ensuring an empty stomach.”
But, she added, “If someone has symptoms of gastroparesis or when in doubt, we can always do a gastric ultrasound exam at the bedside and see whether the stomach is full or empty ... it’s very quick, and it’s not difficult to do.”
Expert Identifies Noteworthy Study Limitations
In an accompanying editorial, Mark A. Warner, MD, professor of anesthesiology at the Mayo Clinic in Rochester, Minnesota, said the findings “will be very helpful to anesthesiologists,” although he noted that the exclusion of people with a BMI > 40 is a limitation.
However, Michael Horowitz, MBBS, PhD, FRACP, director of the Endocrine and Metabolic Unit at the Royal Adelaide Hospital and professor of medicine at Adelaide Medical School in Adelaide, Australia, disputed the study’s conclusions. He noted that the sample was small, and the participants had an average A1c of 7.2%. Fewer than half had microvascular or neuropathic complications. Thus, they were healthier than the general population with diabetes.
“They’ve picked the wrong group of diabetics,” said Dr. Horowitz, who specializes in gastrointestinal complications of diabetes. “This is not a group where you would expect a very high prevalence of delayed emptying.”
Gastric emptying of solids and liquids varies widely even among healthy people and more so in those with type 2 diabetes. About a third of those with above-target A1c levels have gastroparesis, while those more in the target range tend to have accelerated emptying, he explained.
And regarding the use of gastric ultrasound for those who are symptomatic, Dr. Horowitz said, “The relationship of symptoms such as nausea, vomiting, fullness, whatever it may be, with the rate of gastric emptying is weak at best. The association is not simply cause and effect.”
Are the Fasting Guidelines Flawed, Regardless of Diabetes Status?
Dr. Horowitz also faulted the ASA’s 2017 guidance revision for allowing clear liquids to be consumed up to 2 hours in advance of anesthesia because it doesn’t distinguish between liquids with and without calories.
“Whether you have diabetes or not, if you are allowed to have a sugar drink up to 2 hours before your operation, the majority of people empty at about 4 kcal/min, so they will still have some of that drink in their stomach,” he said. “If you want an empty stomach, the ASA guidelines are wrong.”
That explains why the study found relatively high rates of “full stomach” in both groups, 15.5% of those with diabetes and 11.5% of those without, he said.
The GLP-1 Agonist Factor
Although the study didn’t address GLP-1 receptor agonist use, Dr. Warner did in his accompanying editorial, noting that the drugs’ rapid expansion “will likely change how we use perioperative fasting guidelines. With these medications delaying gastric emptying times, we now have another risk factor for pulmonary aspiration to consider when applying fasting guidelines. The inconsistent impact of GLP-1 agonists on gastric emptying, ranging from little to significant, makes it difficult for anesthesiologists to gauge whether or not patients taking GLP-1 agonists are likely to have preoperative gastric liquid or solid contents that could cause subsequent damage if regurgitated.”
Gastric ultrasound can be helpful in this situation, Dr. Warner wrote. In addition, he endorsed the 2023 ASA guidance, which calls for withholding daily-dosed GLP-1 agonists on the day of the surgery and the weekly formulations for a week. And if gastrointestinal symptoms are present, delay elective procedures.
But Dr. Horowitz said those recommendations are likely insufficient as well, pointing to data suggesting that daily liraglutide can delay gastric emptying for up to 16 weeks in about a third of patients. Such studies haven’t been conducted by the manufacturers, particularly on the once-weekly formulations, and the ensuing risk for aspiration isn’t known.
“The slowing occurs in much lower doses than are used for glucose lowering,” Dr. Horowitz said. “It is very likely that plasma levels will need to be extremely low to avoid gastric slowing. The current guidelines fail to appreciate this. So, to withhold the short-acting drugs for 1 day is probably wrong. And to stop long-acting drugs for 1 week is almost certainly wrong too.”
But as for what should be done, he said, “I don’t actually know what you do about it. And no one does because there are no data available to answer the question.”
The study received funding from the Physicians’ Services Incorporated Foundation and the Canadian Society of Anesthesiologists. Dr. Perlas received support for nonclinical time through a merit award from the Department of Anesthesiology and Pain Medicine, University of Toronto, and the Department of Anesthesia and Pain Management, Toronto Western Hospital, University Health Network. She is an executive editor of the journal Regional Anesthesia and Pain Medicine and does consulting work for FujiFilm SonoSite. Dr. Horowitz had no relevant disclosures.
A version of this article appeared on Medscape.com.
Cancer Surgery Tied to Increased Venous Thromboembolism Risk
TOPLINE:
Cancer surgery poses an elevated risk for venous thromboembolism, which can vary depending on the type of cancer and the timing of surgery, a study suggested.
METHODOLOGY:
- Both major surgery and cancer increase the risk for venous thromboembolism, which can lead to severe illness and death. Research showed that approximately 2% of patients who have cancer surgery experience clinically significant venous thromboembolism, which accounts for about half of the deaths that occur immediately after surgery.
- The American Society of Clinical Oncology and European Association of Urology guidelines recommend an extended 28-day prophylaxis for patients undergoing cancer surgery. These guidelines also provide specific estimates of the excess risk for thromboembolic events for each disease.
- This retrospective study included data on 432,218 patients (median age, 67 years) from Swedish nationwide registers who underwent major surgery for eight types of cancer (bladder, breast, colorectal, gynecologic, lung, prostate, gastroesophageal, and kidney or upper tract urothelial cancer) from 1998 to 2016.
- The researchers matched the patients with 4,009,343 cancer-free individuals from the general population in a 1:10 ratio.
- The primary outcome was the incidence of venous thromboembolic events, including subsegmental pulmonary embolism and deep venous thromboembolism in the calf, within 1 year after the surgery.
TAKEAWAY:
- The researchers found an increased absolute risk for pulmonary embolism at 1 year following cancer surgery, with the highest increase in patients with bladder cancer (a 2.69 percentage point difference), followed by lung (a 2.61 percentage point difference), gastroesophageal (2.13), colorectal (1.57), kidney or upper urinary tract (1.38), gynecologic (1.32), breast (0.59), and prostate cancer (0.57).
- The increased 1-year absolute risk for deep vein thrombosis (in percentage points) was highest for the bladder (a 4.67 percentage point difference), followed by gastroesophageal (2.19), colorectal (2.15), upper urinary tract (2.14), gynecologic (2.02), lung (1.40), breast (1.36), and prostate cancer (0.75).
- The temporal trends showed that the risk for pulmonary embolism and deep vein thrombosis peaked immediately after surgery and plateaued within 120 days for most cancers. At 30 days after surgery, the risk for pulmonary embolism following cancer surgery was 10- to 30-fold times higher than with no surgery for all cancers aside from breast cancer (hazard ratio, 5.18). The researchers observed a similar elevated risk for deep vein thrombosis 30 days following surgery.
- The risk for pulmonary embolism and deep vein thrombosis remained significant at 1 year for all cancer types, except prostate.
IN PRACTICE:
“The marked variation in the occurrence patterns of postoperative venous thromboembolic events indicates a need for a more tailored approach to prophylaxis,” the authors noted, advocating for individualized venous thromboembolism risk evaluation and prophylaxis regimens.
SOURCE:
This study, led by Johan Björklund, MD, PhD, from Karolinska Institute, Stockholm, Sweden, was published online in JAMA Network Open.
LIMITATIONS:
The information regarding treatments other than surgery that might be linked to an elevated risk for venous thromboembolism was not available. Additionally, changes in clinical practices and diagnostics over time could affect both the occurrence and detection of outcomes. Adoption of minimally invasive surgical techniques, increased use of thromboprophylaxis over time, improved diagnostic capabilities, and a trend toward operating on older patients with more comorbidities over time may have influenced outcomes.
DISCLOSURES:
The work was funded by the Karolinska Institute and the Swedish Cancer Society. Two study authors reported receiving personal or consulting fees. Other authors reported no conflicts of interest.
A version of this article appeared on Medscape.com.
TOPLINE:
Cancer surgery poses an elevated risk for venous thromboembolism, which can vary depending on the type of cancer and the timing of surgery, a study suggested.
METHODOLOGY:
- Both major surgery and cancer increase the risk for venous thromboembolism, which can lead to severe illness and death. Research showed that approximately 2% of patients who have cancer surgery experience clinically significant venous thromboembolism, which accounts for about half of the deaths that occur immediately after surgery.
- The American Society of Clinical Oncology and European Association of Urology guidelines recommend an extended 28-day prophylaxis for patients undergoing cancer surgery. These guidelines also provide specific estimates of the excess risk for thromboembolic events for each disease.
- This retrospective study included data on 432,218 patients (median age, 67 years) from Swedish nationwide registers who underwent major surgery for eight types of cancer (bladder, breast, colorectal, gynecologic, lung, prostate, gastroesophageal, and kidney or upper tract urothelial cancer) from 1998 to 2016.
- The researchers matched the patients with 4,009,343 cancer-free individuals from the general population in a 1:10 ratio.
- The primary outcome was the incidence of venous thromboembolic events, including subsegmental pulmonary embolism and deep venous thromboembolism in the calf, within 1 year after the surgery.
TAKEAWAY:
- The researchers found an increased absolute risk for pulmonary embolism at 1 year following cancer surgery, with the highest increase in patients with bladder cancer (a 2.69 percentage point difference), followed by lung (a 2.61 percentage point difference), gastroesophageal (2.13), colorectal (1.57), kidney or upper urinary tract (1.38), gynecologic (1.32), breast (0.59), and prostate cancer (0.57).
- The increased 1-year absolute risk for deep vein thrombosis (in percentage points) was highest for the bladder (a 4.67 percentage point difference), followed by gastroesophageal (2.19), colorectal (2.15), upper urinary tract (2.14), gynecologic (2.02), lung (1.40), breast (1.36), and prostate cancer (0.75).
- The temporal trends showed that the risk for pulmonary embolism and deep vein thrombosis peaked immediately after surgery and plateaued within 120 days for most cancers. At 30 days after surgery, the risk for pulmonary embolism following cancer surgery was 10- to 30-fold times higher than with no surgery for all cancers aside from breast cancer (hazard ratio, 5.18). The researchers observed a similar elevated risk for deep vein thrombosis 30 days following surgery.
- The risk for pulmonary embolism and deep vein thrombosis remained significant at 1 year for all cancer types, except prostate.
IN PRACTICE:
“The marked variation in the occurrence patterns of postoperative venous thromboembolic events indicates a need for a more tailored approach to prophylaxis,” the authors noted, advocating for individualized venous thromboembolism risk evaluation and prophylaxis regimens.
SOURCE:
This study, led by Johan Björklund, MD, PhD, from Karolinska Institute, Stockholm, Sweden, was published online in JAMA Network Open.
LIMITATIONS:
The information regarding treatments other than surgery that might be linked to an elevated risk for venous thromboembolism was not available. Additionally, changes in clinical practices and diagnostics over time could affect both the occurrence and detection of outcomes. Adoption of minimally invasive surgical techniques, increased use of thromboprophylaxis over time, improved diagnostic capabilities, and a trend toward operating on older patients with more comorbidities over time may have influenced outcomes.
DISCLOSURES:
The work was funded by the Karolinska Institute and the Swedish Cancer Society. Two study authors reported receiving personal or consulting fees. Other authors reported no conflicts of interest.
A version of this article appeared on Medscape.com.
TOPLINE:
Cancer surgery poses an elevated risk for venous thromboembolism, which can vary depending on the type of cancer and the timing of surgery, a study suggested.
METHODOLOGY:
- Both major surgery and cancer increase the risk for venous thromboembolism, which can lead to severe illness and death. Research showed that approximately 2% of patients who have cancer surgery experience clinically significant venous thromboembolism, which accounts for about half of the deaths that occur immediately after surgery.
- The American Society of Clinical Oncology and European Association of Urology guidelines recommend an extended 28-day prophylaxis for patients undergoing cancer surgery. These guidelines also provide specific estimates of the excess risk for thromboembolic events for each disease.
- This retrospective study included data on 432,218 patients (median age, 67 years) from Swedish nationwide registers who underwent major surgery for eight types of cancer (bladder, breast, colorectal, gynecologic, lung, prostate, gastroesophageal, and kidney or upper tract urothelial cancer) from 1998 to 2016.
- The researchers matched the patients with 4,009,343 cancer-free individuals from the general population in a 1:10 ratio.
- The primary outcome was the incidence of venous thromboembolic events, including subsegmental pulmonary embolism and deep venous thromboembolism in the calf, within 1 year after the surgery.
TAKEAWAY:
- The researchers found an increased absolute risk for pulmonary embolism at 1 year following cancer surgery, with the highest increase in patients with bladder cancer (a 2.69 percentage point difference), followed by lung (a 2.61 percentage point difference), gastroesophageal (2.13), colorectal (1.57), kidney or upper urinary tract (1.38), gynecologic (1.32), breast (0.59), and prostate cancer (0.57).
- The increased 1-year absolute risk for deep vein thrombosis (in percentage points) was highest for the bladder (a 4.67 percentage point difference), followed by gastroesophageal (2.19), colorectal (2.15), upper urinary tract (2.14), gynecologic (2.02), lung (1.40), breast (1.36), and prostate cancer (0.75).
- The temporal trends showed that the risk for pulmonary embolism and deep vein thrombosis peaked immediately after surgery and plateaued within 120 days for most cancers. At 30 days after surgery, the risk for pulmonary embolism following cancer surgery was 10- to 30-fold times higher than with no surgery for all cancers aside from breast cancer (hazard ratio, 5.18). The researchers observed a similar elevated risk for deep vein thrombosis 30 days following surgery.
- The risk for pulmonary embolism and deep vein thrombosis remained significant at 1 year for all cancer types, except prostate.
IN PRACTICE:
“The marked variation in the occurrence patterns of postoperative venous thromboembolic events indicates a need for a more tailored approach to prophylaxis,” the authors noted, advocating for individualized venous thromboembolism risk evaluation and prophylaxis regimens.
SOURCE:
This study, led by Johan Björklund, MD, PhD, from Karolinska Institute, Stockholm, Sweden, was published online in JAMA Network Open.
LIMITATIONS:
The information regarding treatments other than surgery that might be linked to an elevated risk for venous thromboembolism was not available. Additionally, changes in clinical practices and diagnostics over time could affect both the occurrence and detection of outcomes. Adoption of minimally invasive surgical techniques, increased use of thromboprophylaxis over time, improved diagnostic capabilities, and a trend toward operating on older patients with more comorbidities over time may have influenced outcomes.
DISCLOSURES:
The work was funded by the Karolinska Institute and the Swedish Cancer Society. Two study authors reported receiving personal or consulting fees. Other authors reported no conflicts of interest.
A version of this article appeared on Medscape.com.
Magnetic System May Improve Kidney Stone Removal
Kidney stones afflict approximately one in nine individuals, causing intense pain and serious infections. With over 1.3 million emergency room visits and healthcare expenditures exceeding $5 billion annually in the United States, they pose a significant health burden. Small, hard-to-extract fragments are often left behind, risking natural elimination. While technologies like focused ultrasound, fragment adhesion with biopolymers, and negative pressure aspiration have been explored, they face limitations, especially with standard ureteroscope channel sizes.
Magnetizing Renal Calculus Fragments
A published study introduced the Magnetic System for Total Nephrolith Extraction, a system designed to enhance the efficiency of renal calculus fragment removal. In this system, the stones are coated with a magnetic hydrogel and retrieved using a magnetic guidewire compatible with standard ureteroscopes.
In vitro, laser-obtained renal calculus fragments were separated by size and coated with either ferumoxytol alone or combined with chitosan (Hydrogel CF). Treated fragments were then subjected to a magnetic wire for fragment removal assessment. Additional tests included scanning electron microscopy and cell culture with human urothelial cells to evaluate the cytotoxicity of the magnetic hydrogel components. The hydrogel and its components underwent safety and efficacy evaluations in in vitro studies, human tissue samples, and murine models to assess their impact on urothelium and antibacterial properties.
Safe Fragment Removal
The Hydrogel CF, composed of ferumoxytol and chitosan, demonstrated 100% effectiveness in eliminating all tested fragments, even those measuring up to 4 mm, across various stone compositions. Particle tracing simulations indicated that small-sized stones (1 and 3 mm) could be captured several millimeters away. Scanning electron microscopy confirmed the binding of ferumoxytol and Hydrogel CF to the surface of calcium oxalate stones.
The components of Hydrogel CF did not induce significant cytotoxicity on human urothelial cells, even after a 4-hour exposure. Moreover, live mouse studies showed that Hydrogel CF caused less bladder urothelium exfoliation compared with chitosan, and the urothelium returned to normal within 12 hours. In addition, these components exhibited antibacterial properties, inhibiting the growth of uropathogenic bacteria such as Escherichia coli and Proteus mirabilis, comparable to that of ciprofloxacin.
The ability to eliminate lithiasic fragments, the absence of significant urothelial toxicity, and antibacterial activity suggest that the use of magnetic hydrogel could be integrated into laser treatments for renal stones through ureteroscopy without immediate complications. The antibacterial properties could offer potential postoperative benefits while reducing procedural time. Further animal studies are underway to assess the safety of Hydrogel CF before proceeding to human clinical trials.
This article was translated from JIM, which is part of the Medscape Professional Network. A version of this article appeared on Medscape.com.
Kidney stones afflict approximately one in nine individuals, causing intense pain and serious infections. With over 1.3 million emergency room visits and healthcare expenditures exceeding $5 billion annually in the United States, they pose a significant health burden. Small, hard-to-extract fragments are often left behind, risking natural elimination. While technologies like focused ultrasound, fragment adhesion with biopolymers, and negative pressure aspiration have been explored, they face limitations, especially with standard ureteroscope channel sizes.
Magnetizing Renal Calculus Fragments
A published study introduced the Magnetic System for Total Nephrolith Extraction, a system designed to enhance the efficiency of renal calculus fragment removal. In this system, the stones are coated with a magnetic hydrogel and retrieved using a magnetic guidewire compatible with standard ureteroscopes.
In vitro, laser-obtained renal calculus fragments were separated by size and coated with either ferumoxytol alone or combined with chitosan (Hydrogel CF). Treated fragments were then subjected to a magnetic wire for fragment removal assessment. Additional tests included scanning electron microscopy and cell culture with human urothelial cells to evaluate the cytotoxicity of the magnetic hydrogel components. The hydrogel and its components underwent safety and efficacy evaluations in in vitro studies, human tissue samples, and murine models to assess their impact on urothelium and antibacterial properties.
Safe Fragment Removal
The Hydrogel CF, composed of ferumoxytol and chitosan, demonstrated 100% effectiveness in eliminating all tested fragments, even those measuring up to 4 mm, across various stone compositions. Particle tracing simulations indicated that small-sized stones (1 and 3 mm) could be captured several millimeters away. Scanning electron microscopy confirmed the binding of ferumoxytol and Hydrogel CF to the surface of calcium oxalate stones.
The components of Hydrogel CF did not induce significant cytotoxicity on human urothelial cells, even after a 4-hour exposure. Moreover, live mouse studies showed that Hydrogel CF caused less bladder urothelium exfoliation compared with chitosan, and the urothelium returned to normal within 12 hours. In addition, these components exhibited antibacterial properties, inhibiting the growth of uropathogenic bacteria such as Escherichia coli and Proteus mirabilis, comparable to that of ciprofloxacin.
The ability to eliminate lithiasic fragments, the absence of significant urothelial toxicity, and antibacterial activity suggest that the use of magnetic hydrogel could be integrated into laser treatments for renal stones through ureteroscopy without immediate complications. The antibacterial properties could offer potential postoperative benefits while reducing procedural time. Further animal studies are underway to assess the safety of Hydrogel CF before proceeding to human clinical trials.
This article was translated from JIM, which is part of the Medscape Professional Network. A version of this article appeared on Medscape.com.
Kidney stones afflict approximately one in nine individuals, causing intense pain and serious infections. With over 1.3 million emergency room visits and healthcare expenditures exceeding $5 billion annually in the United States, they pose a significant health burden. Small, hard-to-extract fragments are often left behind, risking natural elimination. While technologies like focused ultrasound, fragment adhesion with biopolymers, and negative pressure aspiration have been explored, they face limitations, especially with standard ureteroscope channel sizes.
Magnetizing Renal Calculus Fragments
A published study introduced the Magnetic System for Total Nephrolith Extraction, a system designed to enhance the efficiency of renal calculus fragment removal. In this system, the stones are coated with a magnetic hydrogel and retrieved using a magnetic guidewire compatible with standard ureteroscopes.
In vitro, laser-obtained renal calculus fragments were separated by size and coated with either ferumoxytol alone or combined with chitosan (Hydrogel CF). Treated fragments were then subjected to a magnetic wire for fragment removal assessment. Additional tests included scanning electron microscopy and cell culture with human urothelial cells to evaluate the cytotoxicity of the magnetic hydrogel components. The hydrogel and its components underwent safety and efficacy evaluations in in vitro studies, human tissue samples, and murine models to assess their impact on urothelium and antibacterial properties.
Safe Fragment Removal
The Hydrogel CF, composed of ferumoxytol and chitosan, demonstrated 100% effectiveness in eliminating all tested fragments, even those measuring up to 4 mm, across various stone compositions. Particle tracing simulations indicated that small-sized stones (1 and 3 mm) could be captured several millimeters away. Scanning electron microscopy confirmed the binding of ferumoxytol and Hydrogel CF to the surface of calcium oxalate stones.
The components of Hydrogel CF did not induce significant cytotoxicity on human urothelial cells, even after a 4-hour exposure. Moreover, live mouse studies showed that Hydrogel CF caused less bladder urothelium exfoliation compared with chitosan, and the urothelium returned to normal within 12 hours. In addition, these components exhibited antibacterial properties, inhibiting the growth of uropathogenic bacteria such as Escherichia coli and Proteus mirabilis, comparable to that of ciprofloxacin.
The ability to eliminate lithiasic fragments, the absence of significant urothelial toxicity, and antibacterial activity suggest that the use of magnetic hydrogel could be integrated into laser treatments for renal stones through ureteroscopy without immediate complications. The antibacterial properties could offer potential postoperative benefits while reducing procedural time. Further animal studies are underway to assess the safety of Hydrogel CF before proceeding to human clinical trials.
This article was translated from JIM, which is part of the Medscape Professional Network. A version of this article appeared on Medscape.com.
Antireflux surgery may not reduce cancer risk in Barrett’s esophagus
, according to a Nordic retrospective study.
Risk of EAC was higher among patients who underwent surgery, and risk appeared to increase over time, suggesting that postoperative patients should continue to participate in surveillance programs, reported lead author Jesper Lagergren, MD, PhD, of the Karolinska Institutet, Stockholm, and colleagues.
“Antireflux surgery with fundoplication increases the ability of the gastroesophageal anatomic and physiological barrier to prevent reflux, and can thus prevent any carcinogenic gastric content from reaching the esophagus, including both acid and bile,” the investigators wrote in Gastroenterology, noting that surgery reduces esophageal acid exposure to a greater degree than medication. “Antireflux surgery may thus prevent esophageal adenocarcinoma better than antireflux medication.”
Three meta-analyses to date, however, have failed to provide consistent support for this hypothesis.
“Most of the studies included in these meta-analyses came from single centers, were of small sample size, examined only one treatment arm, and had a short or incomplete follow-up, and ... were hampered by heterogeneity among the included studies,” they noted.
For the present study, Dr. Lagergren and colleagues analyzed national registry data from 33,939 patients with Barrett’s esophagus in Denmark, Finland, Norway, and Sweden. Out of this group, 542 patients (1.6%) had undergone antireflux surgery, while the remainder were managed with antireflux medication.
In both groups, approximately two-thirds of the patients were men. The median age at enrollment was about a decade higher in the medication group (66 vs. 54 years), and this group also tended to have more comorbidities.
After a follow-up period as long as 32 years, the absolute rates of EAC were 1.3% and 2.6% in the medication and surgery groups, respectively. Multivariate analysis, with adjustments for sex, age, year, comorbidities, and age, revealed that postsurgical patients had a 90% increased risk of EAC (hazard ratio [HR], 1.9; 95% CI, 1.1-3.5), versus patients treated with antireflux medication alone.
The relatively higher risk of EAC appeared to increase over time, based on a nonsignificant hazard ratio of 1.8 during the 1- to 4-year follow-up period (HR, 1.8; 95% CI, 0.6-5.0), versus a significant, fourfold risk elevation during the 10- to 32-year follow-up period (HR, 4.4; 95% CI, 1.4-13.5).
“In this cohort of patients with Barrett’s esophagus, the risk of esophageal adenocarcinoma did not decrease after antireflux surgery compared with antireflux medication,” the investigators wrote. “Instead, the risk was increased throughout the follow-up among patients having undergone antireflux surgery.”
Dr. Lagergren and colleagues suggested that the reason for relatively higher cancer risk in the group that underwent surgery likely stems from early and prolonged acid exposure.
“[P]erforming antireflux surgery after years of GERD may be too late to enable a cancer-preventative effect, and most of the patients first diagnosed with Barrett’s esophagus reported a history of many years of GERD symptoms,” they wrote, suggesting that carcinogenic processes had already been set in motion by the time surgery was performed.
“[P]atients with Barrett’s esophagus who undergo antireflux surgery remain at an increased risk of esophageal adenocarcinoma and should continue taking part in surveillance programs,” the investigators concluded.
The study was funded by the Swedish Cancer Society, Swedish Research Council, and Stockholm County Council. The investigators disclosed no conflicts of interest.
Esophageal adenocarcinoma (EAC) has been increasing in frequency for decades. EAC’s only known precursor is Barrett’s esophagus (BE), a complication of GERD with chronic esophageal inflammation (reflux esophagitis). Chronic inflammation can predispose to cancer and refluxed acid itself can cause potentially carcinogenic double-strand DNA breaks in Barrett’s metaplasia. PPIs, which block secretion of the gastric acid that causes reflux esophagitis and DNA damage, are recommended to BE patients for cancer prevention. Logical as that practice may seem, meta-analyses have reached contradictory conclusions regarding the cancer-preventive benefits of PPIs. PPIs do not stop the reflux of other potential carcinogens such as bile salts, and thus it has been argued that fundoplication, which blocks the reflux of all gastric material, should be superior to PPIs for cancer prevention. Plausible as that argument sounds, meta-analyses of the generally small and heterogeneous studies on this issue have not found consistently that antireflux surgery is superior to medical therapy for cancer prevention in BE.
Now, a large, population-based cohort study by Åkerström et al. of Nordic BE patients followed for up to 32 years has found that the overall risk of EAC was higher for patients treated with fundoplication than for those treated with medication (adjusted HR 1.9, 95%CI 1.1-3.5). Furthermore, the EAC risk increased over time in the surgical patients. Well done as this study was, it has important limitations. The overall BE population was large (n=33,939), but only 1.6% (542 patients) had antireflux surgery, and only 14 of those developed EAC during follow-up. Those small numbers limit statistical power. Moreover, important residual confounding cannot be excluded. The surgical patients might have had more severe GERD than medical patients, and it is difficult to make a plausible argument for why fundoplication should increase EAC risk. Nevertheless, this study provides a good lesson on why a plausible argument needs supportive evidence before acting on it in clinical practice. While there may be some excellent reasons for recommending antireflux surgery over medication for patients with severe GERD, better esophageal cancer prevention does not appear to be one of them.
Stuart Jon Spechler, MD, is chief of the division of gastroenterology and codirector of the Center for Esophageal Diseases at Baylor University Medical Center, and codirector of the Center for Esophageal Research at Baylor Scott & White Research Institute, Dallas, Texas. Dr. Spechler is a consultant for Phathom Pharmaceuticals and ISOThrive, LLC.
Esophageal adenocarcinoma (EAC) has been increasing in frequency for decades. EAC’s only known precursor is Barrett’s esophagus (BE), a complication of GERD with chronic esophageal inflammation (reflux esophagitis). Chronic inflammation can predispose to cancer and refluxed acid itself can cause potentially carcinogenic double-strand DNA breaks in Barrett’s metaplasia. PPIs, which block secretion of the gastric acid that causes reflux esophagitis and DNA damage, are recommended to BE patients for cancer prevention. Logical as that practice may seem, meta-analyses have reached contradictory conclusions regarding the cancer-preventive benefits of PPIs. PPIs do not stop the reflux of other potential carcinogens such as bile salts, and thus it has been argued that fundoplication, which blocks the reflux of all gastric material, should be superior to PPIs for cancer prevention. Plausible as that argument sounds, meta-analyses of the generally small and heterogeneous studies on this issue have not found consistently that antireflux surgery is superior to medical therapy for cancer prevention in BE.
Now, a large, population-based cohort study by Åkerström et al. of Nordic BE patients followed for up to 32 years has found that the overall risk of EAC was higher for patients treated with fundoplication than for those treated with medication (adjusted HR 1.9, 95%CI 1.1-3.5). Furthermore, the EAC risk increased over time in the surgical patients. Well done as this study was, it has important limitations. The overall BE population was large (n=33,939), but only 1.6% (542 patients) had antireflux surgery, and only 14 of those developed EAC during follow-up. Those small numbers limit statistical power. Moreover, important residual confounding cannot be excluded. The surgical patients might have had more severe GERD than medical patients, and it is difficult to make a plausible argument for why fundoplication should increase EAC risk. Nevertheless, this study provides a good lesson on why a plausible argument needs supportive evidence before acting on it in clinical practice. While there may be some excellent reasons for recommending antireflux surgery over medication for patients with severe GERD, better esophageal cancer prevention does not appear to be one of them.
Stuart Jon Spechler, MD, is chief of the division of gastroenterology and codirector of the Center for Esophageal Diseases at Baylor University Medical Center, and codirector of the Center for Esophageal Research at Baylor Scott & White Research Institute, Dallas, Texas. Dr. Spechler is a consultant for Phathom Pharmaceuticals and ISOThrive, LLC.
Esophageal adenocarcinoma (EAC) has been increasing in frequency for decades. EAC’s only known precursor is Barrett’s esophagus (BE), a complication of GERD with chronic esophageal inflammation (reflux esophagitis). Chronic inflammation can predispose to cancer and refluxed acid itself can cause potentially carcinogenic double-strand DNA breaks in Barrett’s metaplasia. PPIs, which block secretion of the gastric acid that causes reflux esophagitis and DNA damage, are recommended to BE patients for cancer prevention. Logical as that practice may seem, meta-analyses have reached contradictory conclusions regarding the cancer-preventive benefits of PPIs. PPIs do not stop the reflux of other potential carcinogens such as bile salts, and thus it has been argued that fundoplication, which blocks the reflux of all gastric material, should be superior to PPIs for cancer prevention. Plausible as that argument sounds, meta-analyses of the generally small and heterogeneous studies on this issue have not found consistently that antireflux surgery is superior to medical therapy for cancer prevention in BE.
Now, a large, population-based cohort study by Åkerström et al. of Nordic BE patients followed for up to 32 years has found that the overall risk of EAC was higher for patients treated with fundoplication than for those treated with medication (adjusted HR 1.9, 95%CI 1.1-3.5). Furthermore, the EAC risk increased over time in the surgical patients. Well done as this study was, it has important limitations. The overall BE population was large (n=33,939), but only 1.6% (542 patients) had antireflux surgery, and only 14 of those developed EAC during follow-up. Those small numbers limit statistical power. Moreover, important residual confounding cannot be excluded. The surgical patients might have had more severe GERD than medical patients, and it is difficult to make a plausible argument for why fundoplication should increase EAC risk. Nevertheless, this study provides a good lesson on why a plausible argument needs supportive evidence before acting on it in clinical practice. While there may be some excellent reasons for recommending antireflux surgery over medication for patients with severe GERD, better esophageal cancer prevention does not appear to be one of them.
Stuart Jon Spechler, MD, is chief of the division of gastroenterology and codirector of the Center for Esophageal Diseases at Baylor University Medical Center, and codirector of the Center for Esophageal Research at Baylor Scott & White Research Institute, Dallas, Texas. Dr. Spechler is a consultant for Phathom Pharmaceuticals and ISOThrive, LLC.
, according to a Nordic retrospective study.
Risk of EAC was higher among patients who underwent surgery, and risk appeared to increase over time, suggesting that postoperative patients should continue to participate in surveillance programs, reported lead author Jesper Lagergren, MD, PhD, of the Karolinska Institutet, Stockholm, and colleagues.
“Antireflux surgery with fundoplication increases the ability of the gastroesophageal anatomic and physiological barrier to prevent reflux, and can thus prevent any carcinogenic gastric content from reaching the esophagus, including both acid and bile,” the investigators wrote in Gastroenterology, noting that surgery reduces esophageal acid exposure to a greater degree than medication. “Antireflux surgery may thus prevent esophageal adenocarcinoma better than antireflux medication.”
Three meta-analyses to date, however, have failed to provide consistent support for this hypothesis.
“Most of the studies included in these meta-analyses came from single centers, were of small sample size, examined only one treatment arm, and had a short or incomplete follow-up, and ... were hampered by heterogeneity among the included studies,” they noted.
For the present study, Dr. Lagergren and colleagues analyzed national registry data from 33,939 patients with Barrett’s esophagus in Denmark, Finland, Norway, and Sweden. Out of this group, 542 patients (1.6%) had undergone antireflux surgery, while the remainder were managed with antireflux medication.
In both groups, approximately two-thirds of the patients were men. The median age at enrollment was about a decade higher in the medication group (66 vs. 54 years), and this group also tended to have more comorbidities.
After a follow-up period as long as 32 years, the absolute rates of EAC were 1.3% and 2.6% in the medication and surgery groups, respectively. Multivariate analysis, with adjustments for sex, age, year, comorbidities, and age, revealed that postsurgical patients had a 90% increased risk of EAC (hazard ratio [HR], 1.9; 95% CI, 1.1-3.5), versus patients treated with antireflux medication alone.
The relatively higher risk of EAC appeared to increase over time, based on a nonsignificant hazard ratio of 1.8 during the 1- to 4-year follow-up period (HR, 1.8; 95% CI, 0.6-5.0), versus a significant, fourfold risk elevation during the 10- to 32-year follow-up period (HR, 4.4; 95% CI, 1.4-13.5).
“In this cohort of patients with Barrett’s esophagus, the risk of esophageal adenocarcinoma did not decrease after antireflux surgery compared with antireflux medication,” the investigators wrote. “Instead, the risk was increased throughout the follow-up among patients having undergone antireflux surgery.”
Dr. Lagergren and colleagues suggested that the reason for relatively higher cancer risk in the group that underwent surgery likely stems from early and prolonged acid exposure.
“[P]erforming antireflux surgery after years of GERD may be too late to enable a cancer-preventative effect, and most of the patients first diagnosed with Barrett’s esophagus reported a history of many years of GERD symptoms,” they wrote, suggesting that carcinogenic processes had already been set in motion by the time surgery was performed.
“[P]atients with Barrett’s esophagus who undergo antireflux surgery remain at an increased risk of esophageal adenocarcinoma and should continue taking part in surveillance programs,” the investigators concluded.
The study was funded by the Swedish Cancer Society, Swedish Research Council, and Stockholm County Council. The investigators disclosed no conflicts of interest.
, according to a Nordic retrospective study.
Risk of EAC was higher among patients who underwent surgery, and risk appeared to increase over time, suggesting that postoperative patients should continue to participate in surveillance programs, reported lead author Jesper Lagergren, MD, PhD, of the Karolinska Institutet, Stockholm, and colleagues.
“Antireflux surgery with fundoplication increases the ability of the gastroesophageal anatomic and physiological barrier to prevent reflux, and can thus prevent any carcinogenic gastric content from reaching the esophagus, including both acid and bile,” the investigators wrote in Gastroenterology, noting that surgery reduces esophageal acid exposure to a greater degree than medication. “Antireflux surgery may thus prevent esophageal adenocarcinoma better than antireflux medication.”
Three meta-analyses to date, however, have failed to provide consistent support for this hypothesis.
“Most of the studies included in these meta-analyses came from single centers, were of small sample size, examined only one treatment arm, and had a short or incomplete follow-up, and ... were hampered by heterogeneity among the included studies,” they noted.
For the present study, Dr. Lagergren and colleagues analyzed national registry data from 33,939 patients with Barrett’s esophagus in Denmark, Finland, Norway, and Sweden. Out of this group, 542 patients (1.6%) had undergone antireflux surgery, while the remainder were managed with antireflux medication.
In both groups, approximately two-thirds of the patients were men. The median age at enrollment was about a decade higher in the medication group (66 vs. 54 years), and this group also tended to have more comorbidities.
After a follow-up period as long as 32 years, the absolute rates of EAC were 1.3% and 2.6% in the medication and surgery groups, respectively. Multivariate analysis, with adjustments for sex, age, year, comorbidities, and age, revealed that postsurgical patients had a 90% increased risk of EAC (hazard ratio [HR], 1.9; 95% CI, 1.1-3.5), versus patients treated with antireflux medication alone.
The relatively higher risk of EAC appeared to increase over time, based on a nonsignificant hazard ratio of 1.8 during the 1- to 4-year follow-up period (HR, 1.8; 95% CI, 0.6-5.0), versus a significant, fourfold risk elevation during the 10- to 32-year follow-up period (HR, 4.4; 95% CI, 1.4-13.5).
“In this cohort of patients with Barrett’s esophagus, the risk of esophageal adenocarcinoma did not decrease after antireflux surgery compared with antireflux medication,” the investigators wrote. “Instead, the risk was increased throughout the follow-up among patients having undergone antireflux surgery.”
Dr. Lagergren and colleagues suggested that the reason for relatively higher cancer risk in the group that underwent surgery likely stems from early and prolonged acid exposure.
“[P]erforming antireflux surgery after years of GERD may be too late to enable a cancer-preventative effect, and most of the patients first diagnosed with Barrett’s esophagus reported a history of many years of GERD symptoms,” they wrote, suggesting that carcinogenic processes had already been set in motion by the time surgery was performed.
“[P]atients with Barrett’s esophagus who undergo antireflux surgery remain at an increased risk of esophageal adenocarcinoma and should continue taking part in surveillance programs,” the investigators concluded.
The study was funded by the Swedish Cancer Society, Swedish Research Council, and Stockholm County Council. The investigators disclosed no conflicts of interest.
FROM GASTROENTEROLOGY
Thyroid ablation safety addressed by expert consensus
“There are no documents to date in the United States focusing primarily on the safe adoption and implementation of ablation techniques, including learning curve considerations and necessary pre-procedural skillsets,” reports the ATA task force in the consensus statement, which was published in Thyroid.
“Although these emerging technologies hold great promise, they are not without risk and require development of a unique skill set and environment for optimal, safe performance and consistent outcomes,” task force co-author Catherine F. Sinclair, MD, an associate professor at the Icahn School of Medicine at Mount Sinai, New York, said in an interview.
Chemical ablation has long been utilized as a nonsurgical option for benign thyroid nodule ablation. However, the current array of treatment options has expanded with thermal ablation. Techniques such as radiofrequency ablation (RFA), laser ablation, microwave ablation, and high-intensity focused ultrasound have gained favor as minimally invasive alternatives to surgery.
Much has been published on indications and outcomes with the use of the techniques. The multidisciplinary global task force was convened to address key issues regarding safety and utilization. The report is directed toward specialists, including surgeons, endocrinologists, and interventional radiologists.
The recommendations cover three broad categories: safety considerations spanning preprocedural to postprocedural periods; necessary skill sets for optimal, safe performance with the approaches; and the expectations for success in the context of risks and benefits.
Ablation methods can depend on nodule type
Among key issues addressed are which ablation methods are most appropriate for which types of nodules. Recommendations include chemical ablation, typically involving the injection of dehydrated ethanol in a target nodule. In solid nodules, diffusion with chemical ablation can be unpredictable, which makes it more appropriate for cystic nodules.
Thermal ablation is considered best suited for patients with compressive and/or cosmetic complaints that clearly involve a single or dominant nodule, as well as for autonomously functioning thyroid nodules that cause subclinical or overt hyperthyroidism.
While ethanol ablation is recommended as a first-line treatment for benign cystic thyroid nodules, its efficacy decreases when there is an increase of more than 20% of the solid component. In such cases, RFA or a combination of ethanol ablation and RFA may be considered, the task force recommends.
Patient counseling – managing expectations
Another key consideration in treatment with thyroid nodule ablation is managing patients’ expectations.
Patients should be advised of benefits, such as the avoidance of surgery and general anesthesia and less recovery time. Risks can include thermal or chemical injury to the recurrent laryngeal nerve and other vital structures. The task force underscores discussion of alternative options with patients.
Alternative management options to ablation, including observation, radioactive iodine for functioning nodules, and surgery should also be discussed, and “their relative advantages and disadvantages should be presented without bias such that the patient can make an informed, individual treatment decision,” the task force recommends.
Patients should be informed that, in contrast to surgical management, the benefits of ablation are not immediate; rather, they accrue over the course of months. Reduction in nodule size within the first month is often limited.
Pain, soreness, and some swelling of the nodule and surrounding tissues are common in the first week. These symptoms usually peak in the first 3-5 days after the procedure. Importantly, patients rarely require opioid medications, and their use should be avoided, the task force recommends.
Patients should also be informed about the possibilities of nodule regrowth following ablation and the possible need for more than one ablation procedure.
“Although regrowth definitions in the literature vary, risk of regrowth after thermal ablation is 5%-40% and increases the larger the baseline nodule volume,” the task force notes.
Of note, most studies on ablation to date have shown that thermal ablation complication rates are low. Twelve months post procedure, volume reductions are typically greater than 50%.
Follow-up
For long-term monitoring following ablation, follow-up neck ultrasound is typically recommended at 1-3 months and at 6 and 12 months post ablation to assess volume reduction, nodule appearance, nodule vascularity, and areas at risk for regrowth, the authors note.
Prolonged serial biochemical evaluation of thyroid function is only recommended in cases of hyperfunctioning thyroid nodules.
Key considerations for additional ablative sessions for nodules greater than 20-30 mL in volume should include a failure to achieve adequate reduction in volume, nodule regrowth in previously untreated peripheral areas, and/or persistent or new compressive symptoms.
Learning curve
Dr. Sinclair underscored that successful thyroid nodule ablation requires skill – and experience.
“Probably the greatest concern shared by the writing group on this statement was the potential for clinicians to start ablation practices without having an appropriate prior skill set,” she said.
“Ablation is an advanced, ultrasound-guided procedure, and clinicians need to be experienced in performing neck ultrasounds and biopsies,” she added. “To consider performing ablations without this skill set is both unrealistic and dangerous.”
RFA, currently the most commonly used thermal ablation method for benign thyroid nodule ablation in the U.S., “has a good safety profile but can have a steep learning curve initially,” she said.
Among the most important recommendations is that for their first 20-60 ablation procedures, clinicians should consider limiting treatment to small- to medium-sized benign nodules rather than large-volume disease, Dr. Sinclair added.
“In addition, prior to starting thyroid ablation practices, clinicians should be proficient in ultrasound imaging and fine-needle biopsies and can gain valuable experience by practicing on phantoms and having expert proctoring for the first few cases,” she said.
For initial ablative cases, the task force recommends that clinicians select moderate-size (< 20-30 mL), nonvascular nodules with favorable characteristics and location. The final volume reduction should be based not only on baseline nodule characteristics, such as volume and vascularity, but also on the practitioner’s skill.
Clinicians furthermore should be board certified or eligible in an appropriate medical specialty, have extensive background knowledge, and “should have clinical experience in the clinical diagnosis and treatment of thyroid nodules; neck imaging anatomy; thyroid ultrasound imaging and fine needle aspiration biopsy procedures; and ultrasound risk stratification for benign and malignant thyroid tumors,” the group recommends.
Importantly, the statement is designed to reflect a consensus opinion of the panel of experts but is not meant to serve as a formal guideline or a standard of care for the clinical practice of thermal ablation, Dr. Sinclair added.
“It is not the intent of the statement to replace individual decision-making, the wishes of the patient or family, or clinical judgment.”
The authors’ disclosures are detailed in the published report.
A version of this article first appeared on Medscape.com.
“There are no documents to date in the United States focusing primarily on the safe adoption and implementation of ablation techniques, including learning curve considerations and necessary pre-procedural skillsets,” reports the ATA task force in the consensus statement, which was published in Thyroid.
“Although these emerging technologies hold great promise, they are not without risk and require development of a unique skill set and environment for optimal, safe performance and consistent outcomes,” task force co-author Catherine F. Sinclair, MD, an associate professor at the Icahn School of Medicine at Mount Sinai, New York, said in an interview.
Chemical ablation has long been utilized as a nonsurgical option for benign thyroid nodule ablation. However, the current array of treatment options has expanded with thermal ablation. Techniques such as radiofrequency ablation (RFA), laser ablation, microwave ablation, and high-intensity focused ultrasound have gained favor as minimally invasive alternatives to surgery.
Much has been published on indications and outcomes with the use of the techniques. The multidisciplinary global task force was convened to address key issues regarding safety and utilization. The report is directed toward specialists, including surgeons, endocrinologists, and interventional radiologists.
The recommendations cover three broad categories: safety considerations spanning preprocedural to postprocedural periods; necessary skill sets for optimal, safe performance with the approaches; and the expectations for success in the context of risks and benefits.
Ablation methods can depend on nodule type
Among key issues addressed are which ablation methods are most appropriate for which types of nodules. Recommendations include chemical ablation, typically involving the injection of dehydrated ethanol in a target nodule. In solid nodules, diffusion with chemical ablation can be unpredictable, which makes it more appropriate for cystic nodules.
Thermal ablation is considered best suited for patients with compressive and/or cosmetic complaints that clearly involve a single or dominant nodule, as well as for autonomously functioning thyroid nodules that cause subclinical or overt hyperthyroidism.
While ethanol ablation is recommended as a first-line treatment for benign cystic thyroid nodules, its efficacy decreases when there is an increase of more than 20% of the solid component. In such cases, RFA or a combination of ethanol ablation and RFA may be considered, the task force recommends.
Patient counseling – managing expectations
Another key consideration in treatment with thyroid nodule ablation is managing patients’ expectations.
Patients should be advised of benefits, such as the avoidance of surgery and general anesthesia and less recovery time. Risks can include thermal or chemical injury to the recurrent laryngeal nerve and other vital structures. The task force underscores discussion of alternative options with patients.
Alternative management options to ablation, including observation, radioactive iodine for functioning nodules, and surgery should also be discussed, and “their relative advantages and disadvantages should be presented without bias such that the patient can make an informed, individual treatment decision,” the task force recommends.
Patients should be informed that, in contrast to surgical management, the benefits of ablation are not immediate; rather, they accrue over the course of months. Reduction in nodule size within the first month is often limited.
Pain, soreness, and some swelling of the nodule and surrounding tissues are common in the first week. These symptoms usually peak in the first 3-5 days after the procedure. Importantly, patients rarely require opioid medications, and their use should be avoided, the task force recommends.
Patients should also be informed about the possibilities of nodule regrowth following ablation and the possible need for more than one ablation procedure.
“Although regrowth definitions in the literature vary, risk of regrowth after thermal ablation is 5%-40% and increases the larger the baseline nodule volume,” the task force notes.
Of note, most studies on ablation to date have shown that thermal ablation complication rates are low. Twelve months post procedure, volume reductions are typically greater than 50%.
Follow-up
For long-term monitoring following ablation, follow-up neck ultrasound is typically recommended at 1-3 months and at 6 and 12 months post ablation to assess volume reduction, nodule appearance, nodule vascularity, and areas at risk for regrowth, the authors note.
Prolonged serial biochemical evaluation of thyroid function is only recommended in cases of hyperfunctioning thyroid nodules.
Key considerations for additional ablative sessions for nodules greater than 20-30 mL in volume should include a failure to achieve adequate reduction in volume, nodule regrowth in previously untreated peripheral areas, and/or persistent or new compressive symptoms.
Learning curve
Dr. Sinclair underscored that successful thyroid nodule ablation requires skill – and experience.
“Probably the greatest concern shared by the writing group on this statement was the potential for clinicians to start ablation practices without having an appropriate prior skill set,” she said.
“Ablation is an advanced, ultrasound-guided procedure, and clinicians need to be experienced in performing neck ultrasounds and biopsies,” she added. “To consider performing ablations without this skill set is both unrealistic and dangerous.”
RFA, currently the most commonly used thermal ablation method for benign thyroid nodule ablation in the U.S., “has a good safety profile but can have a steep learning curve initially,” she said.
Among the most important recommendations is that for their first 20-60 ablation procedures, clinicians should consider limiting treatment to small- to medium-sized benign nodules rather than large-volume disease, Dr. Sinclair added.
“In addition, prior to starting thyroid ablation practices, clinicians should be proficient in ultrasound imaging and fine-needle biopsies and can gain valuable experience by practicing on phantoms and having expert proctoring for the first few cases,” she said.
For initial ablative cases, the task force recommends that clinicians select moderate-size (< 20-30 mL), nonvascular nodules with favorable characteristics and location. The final volume reduction should be based not only on baseline nodule characteristics, such as volume and vascularity, but also on the practitioner’s skill.
Clinicians furthermore should be board certified or eligible in an appropriate medical specialty, have extensive background knowledge, and “should have clinical experience in the clinical diagnosis and treatment of thyroid nodules; neck imaging anatomy; thyroid ultrasound imaging and fine needle aspiration biopsy procedures; and ultrasound risk stratification for benign and malignant thyroid tumors,” the group recommends.
Importantly, the statement is designed to reflect a consensus opinion of the panel of experts but is not meant to serve as a formal guideline or a standard of care for the clinical practice of thermal ablation, Dr. Sinclair added.
“It is not the intent of the statement to replace individual decision-making, the wishes of the patient or family, or clinical judgment.”
The authors’ disclosures are detailed in the published report.
A version of this article first appeared on Medscape.com.
“There are no documents to date in the United States focusing primarily on the safe adoption and implementation of ablation techniques, including learning curve considerations and necessary pre-procedural skillsets,” reports the ATA task force in the consensus statement, which was published in Thyroid.
“Although these emerging technologies hold great promise, they are not without risk and require development of a unique skill set and environment for optimal, safe performance and consistent outcomes,” task force co-author Catherine F. Sinclair, MD, an associate professor at the Icahn School of Medicine at Mount Sinai, New York, said in an interview.
Chemical ablation has long been utilized as a nonsurgical option for benign thyroid nodule ablation. However, the current array of treatment options has expanded with thermal ablation. Techniques such as radiofrequency ablation (RFA), laser ablation, microwave ablation, and high-intensity focused ultrasound have gained favor as minimally invasive alternatives to surgery.
Much has been published on indications and outcomes with the use of the techniques. The multidisciplinary global task force was convened to address key issues regarding safety and utilization. The report is directed toward specialists, including surgeons, endocrinologists, and interventional radiologists.
The recommendations cover three broad categories: safety considerations spanning preprocedural to postprocedural periods; necessary skill sets for optimal, safe performance with the approaches; and the expectations for success in the context of risks and benefits.
Ablation methods can depend on nodule type
Among key issues addressed are which ablation methods are most appropriate for which types of nodules. Recommendations include chemical ablation, typically involving the injection of dehydrated ethanol in a target nodule. In solid nodules, diffusion with chemical ablation can be unpredictable, which makes it more appropriate for cystic nodules.
Thermal ablation is considered best suited for patients with compressive and/or cosmetic complaints that clearly involve a single or dominant nodule, as well as for autonomously functioning thyroid nodules that cause subclinical or overt hyperthyroidism.
While ethanol ablation is recommended as a first-line treatment for benign cystic thyroid nodules, its efficacy decreases when there is an increase of more than 20% of the solid component. In such cases, RFA or a combination of ethanol ablation and RFA may be considered, the task force recommends.
Patient counseling – managing expectations
Another key consideration in treatment with thyroid nodule ablation is managing patients’ expectations.
Patients should be advised of benefits, such as the avoidance of surgery and general anesthesia and less recovery time. Risks can include thermal or chemical injury to the recurrent laryngeal nerve and other vital structures. The task force underscores discussion of alternative options with patients.
Alternative management options to ablation, including observation, radioactive iodine for functioning nodules, and surgery should also be discussed, and “their relative advantages and disadvantages should be presented without bias such that the patient can make an informed, individual treatment decision,” the task force recommends.
Patients should be informed that, in contrast to surgical management, the benefits of ablation are not immediate; rather, they accrue over the course of months. Reduction in nodule size within the first month is often limited.
Pain, soreness, and some swelling of the nodule and surrounding tissues are common in the first week. These symptoms usually peak in the first 3-5 days after the procedure. Importantly, patients rarely require opioid medications, and their use should be avoided, the task force recommends.
Patients should also be informed about the possibilities of nodule regrowth following ablation and the possible need for more than one ablation procedure.
“Although regrowth definitions in the literature vary, risk of regrowth after thermal ablation is 5%-40% and increases the larger the baseline nodule volume,” the task force notes.
Of note, most studies on ablation to date have shown that thermal ablation complication rates are low. Twelve months post procedure, volume reductions are typically greater than 50%.
Follow-up
For long-term monitoring following ablation, follow-up neck ultrasound is typically recommended at 1-3 months and at 6 and 12 months post ablation to assess volume reduction, nodule appearance, nodule vascularity, and areas at risk for regrowth, the authors note.
Prolonged serial biochemical evaluation of thyroid function is only recommended in cases of hyperfunctioning thyroid nodules.
Key considerations for additional ablative sessions for nodules greater than 20-30 mL in volume should include a failure to achieve adequate reduction in volume, nodule regrowth in previously untreated peripheral areas, and/or persistent or new compressive symptoms.
Learning curve
Dr. Sinclair underscored that successful thyroid nodule ablation requires skill – and experience.
“Probably the greatest concern shared by the writing group on this statement was the potential for clinicians to start ablation practices without having an appropriate prior skill set,” she said.
“Ablation is an advanced, ultrasound-guided procedure, and clinicians need to be experienced in performing neck ultrasounds and biopsies,” she added. “To consider performing ablations without this skill set is both unrealistic and dangerous.”
RFA, currently the most commonly used thermal ablation method for benign thyroid nodule ablation in the U.S., “has a good safety profile but can have a steep learning curve initially,” she said.
Among the most important recommendations is that for their first 20-60 ablation procedures, clinicians should consider limiting treatment to small- to medium-sized benign nodules rather than large-volume disease, Dr. Sinclair added.
“In addition, prior to starting thyroid ablation practices, clinicians should be proficient in ultrasound imaging and fine-needle biopsies and can gain valuable experience by practicing on phantoms and having expert proctoring for the first few cases,” she said.
For initial ablative cases, the task force recommends that clinicians select moderate-size (< 20-30 mL), nonvascular nodules with favorable characteristics and location. The final volume reduction should be based not only on baseline nodule characteristics, such as volume and vascularity, but also on the practitioner’s skill.
Clinicians furthermore should be board certified or eligible in an appropriate medical specialty, have extensive background knowledge, and “should have clinical experience in the clinical diagnosis and treatment of thyroid nodules; neck imaging anatomy; thyroid ultrasound imaging and fine needle aspiration biopsy procedures; and ultrasound risk stratification for benign and malignant thyroid tumors,” the group recommends.
Importantly, the statement is designed to reflect a consensus opinion of the panel of experts but is not meant to serve as a formal guideline or a standard of care for the clinical practice of thermal ablation, Dr. Sinclair added.
“It is not the intent of the statement to replace individual decision-making, the wishes of the patient or family, or clinical judgment.”
The authors’ disclosures are detailed in the published report.
A version of this article first appeared on Medscape.com.
FROM THYROID
Atypical antipsychotics no safer than haloperidol for postoperative delirium: Study
Dae Hyun Kim, MD, ScD, associate professor of medicine at Harvard Medical School, in Boston, who is the lead author of the study, said the findings were especially relevant, as the use of atypical antipsychotics, such as quetiapine, olanzapine, and risperidone, has increased while use of haloperidol has fallen.
A separate but related study led by Dr. Kim, which was recently published in the Journal of the American Geriatrics Society, showed that between 2008 and 2018, use of haloperidol and benzodiazepines in community hospitals and academic medical centers decreased while use of atypical antipsychotics, antidepressants, antiepileptics, and dexmedetomidine rose (P < .01).
“Clinicians should not think atypical antipsychotics are the safer option to haloperidol,” Dr. Kim said. “We should focus on reducing prescriptions.”
Postoperative delirium
Postoperative delirium is the among the most common complications of surgery in older adults, affecting between 15% and 50% of those patients who undergo major operations. Postoperative delirium is associated with longer hospital stays, poor functional recovery, institutionalization, dementia, and death.
According to research from Harvard Medical School, postoperative delirium is linked to a 40% faster rate of cognitive decline among patients who develop the condition, compared with those who do not experience the complication.
While older patients often feel tired or a bit off after surgery, marked changes in mental function, such as confusion, disorientation, agitation, aggression, hallucinations, or persistent sleepiness, could indicate postoperative delirium.
“Antipsychotic medications are most commonly used off label for managing those symptoms of delirium,” Dr. Kim said. “What we’ve done is look at the comparative safety of two other drugs.”
Results
In the retrospective cohort study, researchers analyzed data from 17,115 patients aged 65 years and older who were without psychiatric disorders and who received oral antipsychotics after major surgery requiring general anesthesia.
“These results don’t apply to people in emergent situations where there is severe behavior that threatens their safety and others,” Dr. Kim noted.
There was no statistically significant difference in the risk for in-hospital death among patients treated with haloperidol (3.7%), olanzapine (2.8%; relative risk, 0.74; 95% confidence interval, 0.42-1.27), quetiapine (2.6%; RR, 0.70; 95% CI, 0.47-1.04), or risperidone (3.3%; RR, 0.90; CI, 0.53-1.41).
The study also found statistically insignificant differences in the risk for nonfatal clinical events. Those risks ranged from 2% to 2.6% for a cardiac arrhythmia, from 4.2% to 4.6% for pneumonia, and from 0.6% to 1.2% for strokes or transient ischemic attacks.
Esther Oh, MD, PhD, an associate professor at Johns Hopkins University, Baltimore, said that caring for patients who experience acute changes in mental status or behaviors during hospitalization can be difficult.
“Although there is a lot of evidence in the literature that nonpharmacological methods to address these problems are effective, staff shortages of recent years have made it even more difficult for the care team to institute these methods,” Dr. Oh said in an interview.
Prevention
Dr. Oh and Dr. Kim agreed that nonpharmacologic strategies, such as ensuring good nutrition and hydration, daily walking, cognitive-stimulating activities, and good sleep hygiene, are effective and safe in preventing postoperative delirium.
“These are common sense interventions, but they require a lot of staffing and training,” Dr. Kim said. “It’s a resource-intensive intervention that requires really changing the way hospital staff interacts with older patients in the hospital.”
Second-generation antipsychotic medications often are thought to be safer than haloperidol in terms of side effects, Dr. Oh said, but the new findings challenge that assumption.
“Based on the findings from this study and on prior studies of antipsychotic use for older adults, use of all antipsychotics, both first and second generation, should be reviewed carefully to ensure they are being administered at the lowest effective dose for the shortest duration possible,” she said.
The study was supported by the National Institute on Aging of the National Institutes of Health. Dr. Kim and Dr. Oh disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Dae Hyun Kim, MD, ScD, associate professor of medicine at Harvard Medical School, in Boston, who is the lead author of the study, said the findings were especially relevant, as the use of atypical antipsychotics, such as quetiapine, olanzapine, and risperidone, has increased while use of haloperidol has fallen.
A separate but related study led by Dr. Kim, which was recently published in the Journal of the American Geriatrics Society, showed that between 2008 and 2018, use of haloperidol and benzodiazepines in community hospitals and academic medical centers decreased while use of atypical antipsychotics, antidepressants, antiepileptics, and dexmedetomidine rose (P < .01).
“Clinicians should not think atypical antipsychotics are the safer option to haloperidol,” Dr. Kim said. “We should focus on reducing prescriptions.”
Postoperative delirium
Postoperative delirium is the among the most common complications of surgery in older adults, affecting between 15% and 50% of those patients who undergo major operations. Postoperative delirium is associated with longer hospital stays, poor functional recovery, institutionalization, dementia, and death.
According to research from Harvard Medical School, postoperative delirium is linked to a 40% faster rate of cognitive decline among patients who develop the condition, compared with those who do not experience the complication.
While older patients often feel tired or a bit off after surgery, marked changes in mental function, such as confusion, disorientation, agitation, aggression, hallucinations, or persistent sleepiness, could indicate postoperative delirium.
“Antipsychotic medications are most commonly used off label for managing those symptoms of delirium,” Dr. Kim said. “What we’ve done is look at the comparative safety of two other drugs.”
Results
In the retrospective cohort study, researchers analyzed data from 17,115 patients aged 65 years and older who were without psychiatric disorders and who received oral antipsychotics after major surgery requiring general anesthesia.
“These results don’t apply to people in emergent situations where there is severe behavior that threatens their safety and others,” Dr. Kim noted.
There was no statistically significant difference in the risk for in-hospital death among patients treated with haloperidol (3.7%), olanzapine (2.8%; relative risk, 0.74; 95% confidence interval, 0.42-1.27), quetiapine (2.6%; RR, 0.70; 95% CI, 0.47-1.04), or risperidone (3.3%; RR, 0.90; CI, 0.53-1.41).
The study also found statistically insignificant differences in the risk for nonfatal clinical events. Those risks ranged from 2% to 2.6% for a cardiac arrhythmia, from 4.2% to 4.6% for pneumonia, and from 0.6% to 1.2% for strokes or transient ischemic attacks.
Esther Oh, MD, PhD, an associate professor at Johns Hopkins University, Baltimore, said that caring for patients who experience acute changes in mental status or behaviors during hospitalization can be difficult.
“Although there is a lot of evidence in the literature that nonpharmacological methods to address these problems are effective, staff shortages of recent years have made it even more difficult for the care team to institute these methods,” Dr. Oh said in an interview.
Prevention
Dr. Oh and Dr. Kim agreed that nonpharmacologic strategies, such as ensuring good nutrition and hydration, daily walking, cognitive-stimulating activities, and good sleep hygiene, are effective and safe in preventing postoperative delirium.
“These are common sense interventions, but they require a lot of staffing and training,” Dr. Kim said. “It’s a resource-intensive intervention that requires really changing the way hospital staff interacts with older patients in the hospital.”
Second-generation antipsychotic medications often are thought to be safer than haloperidol in terms of side effects, Dr. Oh said, but the new findings challenge that assumption.
“Based on the findings from this study and on prior studies of antipsychotic use for older adults, use of all antipsychotics, both first and second generation, should be reviewed carefully to ensure they are being administered at the lowest effective dose for the shortest duration possible,” she said.
The study was supported by the National Institute on Aging of the National Institutes of Health. Dr. Kim and Dr. Oh disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Dae Hyun Kim, MD, ScD, associate professor of medicine at Harvard Medical School, in Boston, who is the lead author of the study, said the findings were especially relevant, as the use of atypical antipsychotics, such as quetiapine, olanzapine, and risperidone, has increased while use of haloperidol has fallen.
A separate but related study led by Dr. Kim, which was recently published in the Journal of the American Geriatrics Society, showed that between 2008 and 2018, use of haloperidol and benzodiazepines in community hospitals and academic medical centers decreased while use of atypical antipsychotics, antidepressants, antiepileptics, and dexmedetomidine rose (P < .01).
“Clinicians should not think atypical antipsychotics are the safer option to haloperidol,” Dr. Kim said. “We should focus on reducing prescriptions.”
Postoperative delirium
Postoperative delirium is the among the most common complications of surgery in older adults, affecting between 15% and 50% of those patients who undergo major operations. Postoperative delirium is associated with longer hospital stays, poor functional recovery, institutionalization, dementia, and death.
According to research from Harvard Medical School, postoperative delirium is linked to a 40% faster rate of cognitive decline among patients who develop the condition, compared with those who do not experience the complication.
While older patients often feel tired or a bit off after surgery, marked changes in mental function, such as confusion, disorientation, agitation, aggression, hallucinations, or persistent sleepiness, could indicate postoperative delirium.
“Antipsychotic medications are most commonly used off label for managing those symptoms of delirium,” Dr. Kim said. “What we’ve done is look at the comparative safety of two other drugs.”
Results
In the retrospective cohort study, researchers analyzed data from 17,115 patients aged 65 years and older who were without psychiatric disorders and who received oral antipsychotics after major surgery requiring general anesthesia.
“These results don’t apply to people in emergent situations where there is severe behavior that threatens their safety and others,” Dr. Kim noted.
There was no statistically significant difference in the risk for in-hospital death among patients treated with haloperidol (3.7%), olanzapine (2.8%; relative risk, 0.74; 95% confidence interval, 0.42-1.27), quetiapine (2.6%; RR, 0.70; 95% CI, 0.47-1.04), or risperidone (3.3%; RR, 0.90; CI, 0.53-1.41).
The study also found statistically insignificant differences in the risk for nonfatal clinical events. Those risks ranged from 2% to 2.6% for a cardiac arrhythmia, from 4.2% to 4.6% for pneumonia, and from 0.6% to 1.2% for strokes or transient ischemic attacks.
Esther Oh, MD, PhD, an associate professor at Johns Hopkins University, Baltimore, said that caring for patients who experience acute changes in mental status or behaviors during hospitalization can be difficult.
“Although there is a lot of evidence in the literature that nonpharmacological methods to address these problems are effective, staff shortages of recent years have made it even more difficult for the care team to institute these methods,” Dr. Oh said in an interview.
Prevention
Dr. Oh and Dr. Kim agreed that nonpharmacologic strategies, such as ensuring good nutrition and hydration, daily walking, cognitive-stimulating activities, and good sleep hygiene, are effective and safe in preventing postoperative delirium.
“These are common sense interventions, but they require a lot of staffing and training,” Dr. Kim said. “It’s a resource-intensive intervention that requires really changing the way hospital staff interacts with older patients in the hospital.”
Second-generation antipsychotic medications often are thought to be safer than haloperidol in terms of side effects, Dr. Oh said, but the new findings challenge that assumption.
“Based on the findings from this study and on prior studies of antipsychotic use for older adults, use of all antipsychotics, both first and second generation, should be reviewed carefully to ensure they are being administered at the lowest effective dose for the shortest duration possible,” she said.
The study was supported by the National Institute on Aging of the National Institutes of Health. Dr. Kim and Dr. Oh disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ANNALS OF INTERNAL MEDICINE
Gender-affirming surgeries nearly tripled between 2016 and 2019: Study
a new study published in JAMA Network Open found.
Breast and chest surgeries were the most common procedures performed, and the number of surgical procedures carried out increased with age. The researchers said that, in addition to legal shifts, the established safety of the surgeries and resulting increase in quality of life may also help explain the increase.
“The point of this is to raise awareness and to really document the patterns of care in the United States,” said Jason Wright, MD, an associate professor at Columbia University, New York. “We hope that people understand that these procedures are being performed more commonly and they’re out there.”
A study published in 2022 in JAMA Pediatrics found that the number of chest reconstruction surgeries among U.S. adolescents rose fourfold between 2016 and 2019.
The new study included data from 2016 to 2020 in the Nationwide Ambulatory Surgery Sample and the National Inpatient Sample. More than 48,000 patients with diagnosis codes for gender identity disorder, transsexualism, or a personal history of sex reassignment were identified. Age ranges were grouped as 12-18 (7.7%), 19-30 (52.3%), and 31-40 (21.8%).
The number of gender-affirming procedures rose from 4,552 in 2016 to a peak of 13,011 in 2019. (A slight decline to 12,818 procedures in 2020 was attributed to the COVID-19 pandemic.) The surgeries were grouped into three categories: breast and chest procedures, which occurred in 56.6% of patients; genital reconstructive surgeries (35.1%), and other facial cosmetic procedures (13.9%).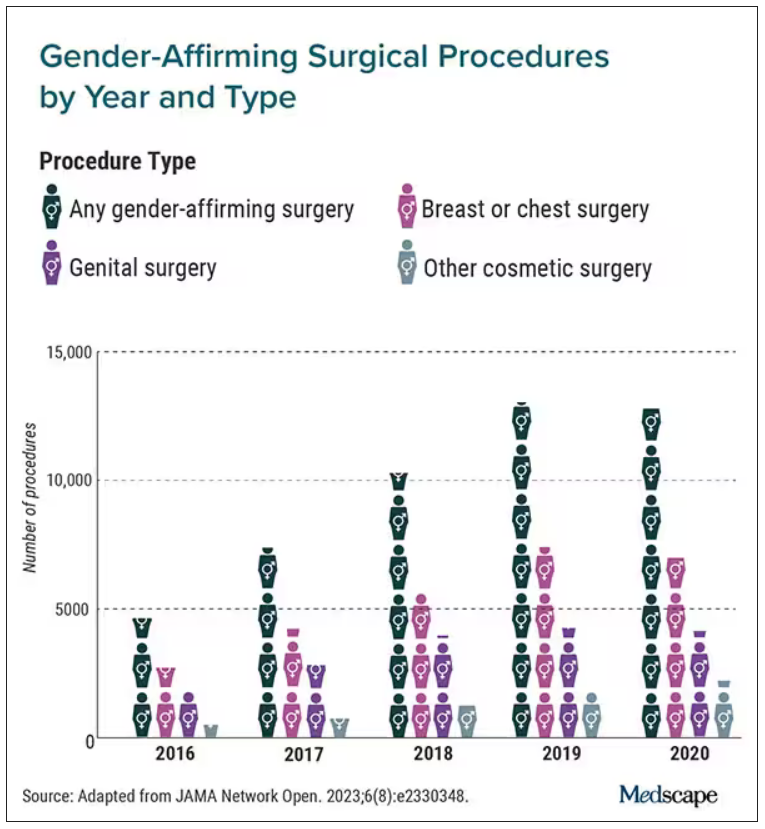
“We really wanted to try to make this as representative as we could,” Dr. Wright said. “I think this is really the best estimates that are available to date.”
Chest and breast procedures made up a higher percentage of surgeries in younger patients, while genital surgical procedures made up a higher percentage in older patients. For example, patients aged 19-30 made up 59.1% of breast or chest surgeries and 44.2% of genital surgeries. However, those aged 31-40 accounted for 26.2% of genital surgeries and 18.1% of breast or chest surgeries. For ages 41-50, the spread was more than double, accounting for 12.8% of genital surgeries and only 6.1% of breast or chest surgeries, according to the researchers.
Undocumented uptick
In addition to more inclusive health insurance, Dr. Wright said the increase in these procedures can also be attributed to studies showing their safety and the long-term association with high patient satisfaction.
Kevin Wang, MD, medical director of Providence–Swedish Health Services’ LGBTQIA+ program in Seattle, agreed that changes in health insurance coverage for gender-affirming surgery likely account in part for their increase. But he added that more clinicians are performing these procedures.
He said gender-affirming surgeries improve quality of life for the people who undergo them. The American Academy of Pediatrics has said it would be conducting a thorough review of the effects of transgender care on youth. A 2018 policy statement from the group said transgender youth should “have access to comprehensive, gender-affirming, and developmentally appropriate health care that is provided in a safe and inclusive clinical space.”
Dr. Wright cited several limitations to his group’s study that may result in the undercapture of transgender individuals and gender-affirming surgery; in particular, while the study captured inpatient and ambulatory surgical procedures in large, nationwide datasets, a small number of the procedures could have been performed in other settings.
Guiding a patient through gender-affirming care and surgical procedures can be an arduous process, including understanding their goals, using hormone therapy, and making referrals to specialists. Dr. Wang said he works to maximize his patients’ physical, mental, and emotional health, and helps them understand the risks.
He cited the double standard of a cisgender woman wanting breast augmentation without justification, but someone who identifies as transgender has many more boxes to check – for example, seeing a behavior health specialist to demonstrate they understand the risks and securing a letter of support from their primary care physician to undergo a similar procedure.
“It’s just interesting how the transgender community has to jump through so many more barriers and hoops for affirming, lifesaving procedures where you have other people who are doing it for aesthetic purposes and do not require any type of authorization,” Dr. Wang said.
Dr. Wright said he hopes the findings call attention to the need for more professionals working in the gender-affirming care field.
“I think for the medical community, it’s important to raise the idea that these procedures are becoming more common,” Dr. Wright said. “We are going to need specialists who have expertise in transgender care and surgeons who have the ability to perform these operations. Hopefully, this sheds light on the resources that are going to be required to care for these patients going forward.”
Dr. Wright reported receiving grants from Merck and personal fees from UpToDate outside the submitted work. No other disclosures were reported.
A version of this article first appeared on Medscape.com.
a new study published in JAMA Network Open found.
Breast and chest surgeries were the most common procedures performed, and the number of surgical procedures carried out increased with age. The researchers said that, in addition to legal shifts, the established safety of the surgeries and resulting increase in quality of life may also help explain the increase.
“The point of this is to raise awareness and to really document the patterns of care in the United States,” said Jason Wright, MD, an associate professor at Columbia University, New York. “We hope that people understand that these procedures are being performed more commonly and they’re out there.”
A study published in 2022 in JAMA Pediatrics found that the number of chest reconstruction surgeries among U.S. adolescents rose fourfold between 2016 and 2019.
The new study included data from 2016 to 2020 in the Nationwide Ambulatory Surgery Sample and the National Inpatient Sample. More than 48,000 patients with diagnosis codes for gender identity disorder, transsexualism, or a personal history of sex reassignment were identified. Age ranges were grouped as 12-18 (7.7%), 19-30 (52.3%), and 31-40 (21.8%).
The number of gender-affirming procedures rose from 4,552 in 2016 to a peak of 13,011 in 2019. (A slight decline to 12,818 procedures in 2020 was attributed to the COVID-19 pandemic.) The surgeries were grouped into three categories: breast and chest procedures, which occurred in 56.6% of patients; genital reconstructive surgeries (35.1%), and other facial cosmetic procedures (13.9%).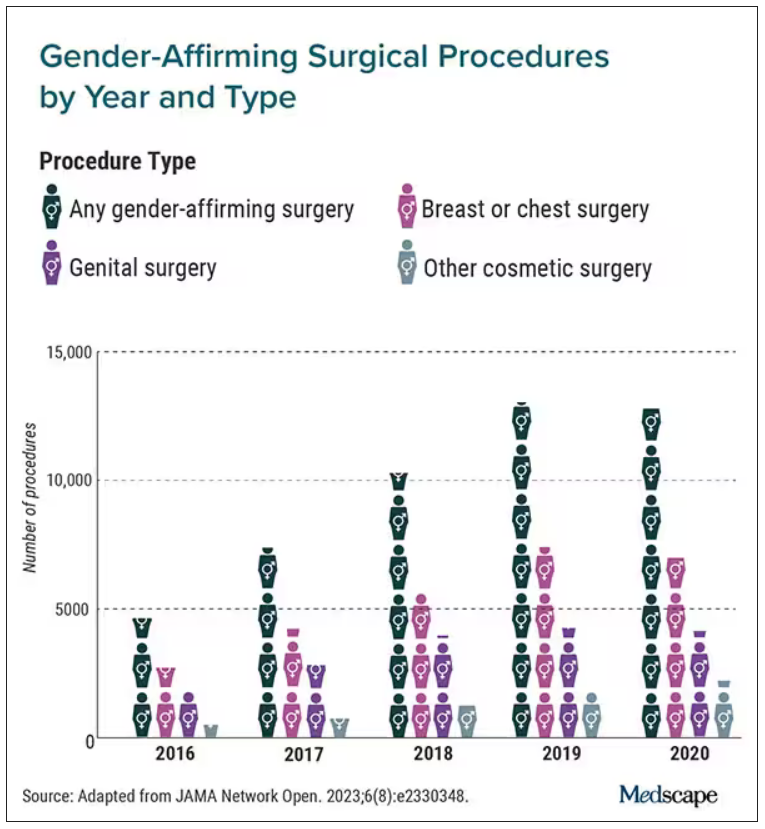
“We really wanted to try to make this as representative as we could,” Dr. Wright said. “I think this is really the best estimates that are available to date.”
Chest and breast procedures made up a higher percentage of surgeries in younger patients, while genital surgical procedures made up a higher percentage in older patients. For example, patients aged 19-30 made up 59.1% of breast or chest surgeries and 44.2% of genital surgeries. However, those aged 31-40 accounted for 26.2% of genital surgeries and 18.1% of breast or chest surgeries. For ages 41-50, the spread was more than double, accounting for 12.8% of genital surgeries and only 6.1% of breast or chest surgeries, according to the researchers.
Undocumented uptick
In addition to more inclusive health insurance, Dr. Wright said the increase in these procedures can also be attributed to studies showing their safety and the long-term association with high patient satisfaction.
Kevin Wang, MD, medical director of Providence–Swedish Health Services’ LGBTQIA+ program in Seattle, agreed that changes in health insurance coverage for gender-affirming surgery likely account in part for their increase. But he added that more clinicians are performing these procedures.
He said gender-affirming surgeries improve quality of life for the people who undergo them. The American Academy of Pediatrics has said it would be conducting a thorough review of the effects of transgender care on youth. A 2018 policy statement from the group said transgender youth should “have access to comprehensive, gender-affirming, and developmentally appropriate health care that is provided in a safe and inclusive clinical space.”
Dr. Wright cited several limitations to his group’s study that may result in the undercapture of transgender individuals and gender-affirming surgery; in particular, while the study captured inpatient and ambulatory surgical procedures in large, nationwide datasets, a small number of the procedures could have been performed in other settings.
Guiding a patient through gender-affirming care and surgical procedures can be an arduous process, including understanding their goals, using hormone therapy, and making referrals to specialists. Dr. Wang said he works to maximize his patients’ physical, mental, and emotional health, and helps them understand the risks.
He cited the double standard of a cisgender woman wanting breast augmentation without justification, but someone who identifies as transgender has many more boxes to check – for example, seeing a behavior health specialist to demonstrate they understand the risks and securing a letter of support from their primary care physician to undergo a similar procedure.
“It’s just interesting how the transgender community has to jump through so many more barriers and hoops for affirming, lifesaving procedures where you have other people who are doing it for aesthetic purposes and do not require any type of authorization,” Dr. Wang said.
Dr. Wright said he hopes the findings call attention to the need for more professionals working in the gender-affirming care field.
“I think for the medical community, it’s important to raise the idea that these procedures are becoming more common,” Dr. Wright said. “We are going to need specialists who have expertise in transgender care and surgeons who have the ability to perform these operations. Hopefully, this sheds light on the resources that are going to be required to care for these patients going forward.”
Dr. Wright reported receiving grants from Merck and personal fees from UpToDate outside the submitted work. No other disclosures were reported.
A version of this article first appeared on Medscape.com.
a new study published in JAMA Network Open found.
Breast and chest surgeries were the most common procedures performed, and the number of surgical procedures carried out increased with age. The researchers said that, in addition to legal shifts, the established safety of the surgeries and resulting increase in quality of life may also help explain the increase.
“The point of this is to raise awareness and to really document the patterns of care in the United States,” said Jason Wright, MD, an associate professor at Columbia University, New York. “We hope that people understand that these procedures are being performed more commonly and they’re out there.”
A study published in 2022 in JAMA Pediatrics found that the number of chest reconstruction surgeries among U.S. adolescents rose fourfold between 2016 and 2019.
The new study included data from 2016 to 2020 in the Nationwide Ambulatory Surgery Sample and the National Inpatient Sample. More than 48,000 patients with diagnosis codes for gender identity disorder, transsexualism, or a personal history of sex reassignment were identified. Age ranges were grouped as 12-18 (7.7%), 19-30 (52.3%), and 31-40 (21.8%).
The number of gender-affirming procedures rose from 4,552 in 2016 to a peak of 13,011 in 2019. (A slight decline to 12,818 procedures in 2020 was attributed to the COVID-19 pandemic.) The surgeries were grouped into three categories: breast and chest procedures, which occurred in 56.6% of patients; genital reconstructive surgeries (35.1%), and other facial cosmetic procedures (13.9%).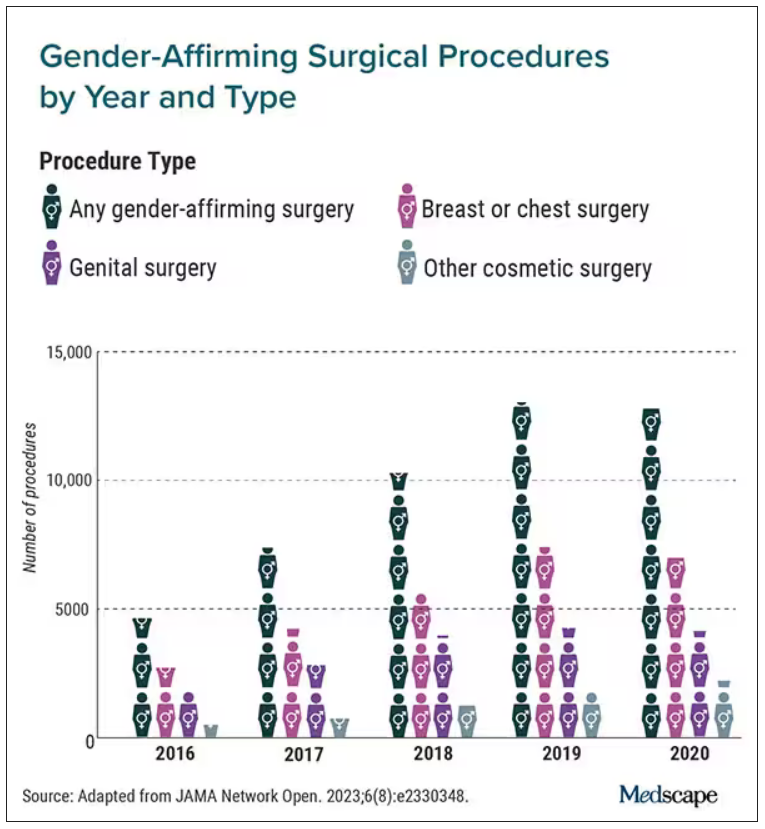
“We really wanted to try to make this as representative as we could,” Dr. Wright said. “I think this is really the best estimates that are available to date.”
Chest and breast procedures made up a higher percentage of surgeries in younger patients, while genital surgical procedures made up a higher percentage in older patients. For example, patients aged 19-30 made up 59.1% of breast or chest surgeries and 44.2% of genital surgeries. However, those aged 31-40 accounted for 26.2% of genital surgeries and 18.1% of breast or chest surgeries. For ages 41-50, the spread was more than double, accounting for 12.8% of genital surgeries and only 6.1% of breast or chest surgeries, according to the researchers.
Undocumented uptick
In addition to more inclusive health insurance, Dr. Wright said the increase in these procedures can also be attributed to studies showing their safety and the long-term association with high patient satisfaction.
Kevin Wang, MD, medical director of Providence–Swedish Health Services’ LGBTQIA+ program in Seattle, agreed that changes in health insurance coverage for gender-affirming surgery likely account in part for their increase. But he added that more clinicians are performing these procedures.
He said gender-affirming surgeries improve quality of life for the people who undergo them. The American Academy of Pediatrics has said it would be conducting a thorough review of the effects of transgender care on youth. A 2018 policy statement from the group said transgender youth should “have access to comprehensive, gender-affirming, and developmentally appropriate health care that is provided in a safe and inclusive clinical space.”
Dr. Wright cited several limitations to his group’s study that may result in the undercapture of transgender individuals and gender-affirming surgery; in particular, while the study captured inpatient and ambulatory surgical procedures in large, nationwide datasets, a small number of the procedures could have been performed in other settings.
Guiding a patient through gender-affirming care and surgical procedures can be an arduous process, including understanding their goals, using hormone therapy, and making referrals to specialists. Dr. Wang said he works to maximize his patients’ physical, mental, and emotional health, and helps them understand the risks.
He cited the double standard of a cisgender woman wanting breast augmentation without justification, but someone who identifies as transgender has many more boxes to check – for example, seeing a behavior health specialist to demonstrate they understand the risks and securing a letter of support from their primary care physician to undergo a similar procedure.
“It’s just interesting how the transgender community has to jump through so many more barriers and hoops for affirming, lifesaving procedures where you have other people who are doing it for aesthetic purposes and do not require any type of authorization,” Dr. Wang said.
Dr. Wright said he hopes the findings call attention to the need for more professionals working in the gender-affirming care field.
“I think for the medical community, it’s important to raise the idea that these procedures are becoming more common,” Dr. Wright said. “We are going to need specialists who have expertise in transgender care and surgeons who have the ability to perform these operations. Hopefully, this sheds light on the resources that are going to be required to care for these patients going forward.”
Dr. Wright reported receiving grants from Merck and personal fees from UpToDate outside the submitted work. No other disclosures were reported.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN


