User login
Breaking the Cycle: Why Self-Compassion Is Essential for Today’s Physicians
Summary and Key Highlights
Summary: Dr Tyra Fainstad explores the ingrained culture in medicine that encourages self-criticism, with many physicians feeling that they must be hard on themselves to succeed. Dr Fainstad challenges this belief, advocating for self-compassion as a healthier alternative. The evolving medical field now includes physicians who prioritize well-being without sacrificing quality of care, underscoring the importance of self-kindness for sustainable practice.
Key Takeaways:
- Many physicians believe that self-criticism is necessary for success, a mindset rooted in medical culture.
- Practicing self-compassion can improve long-term resilience and prevent burnout.
- The changing landscape of healthcare supports a more balanced approach to physician well-being.
Our Editors Also Recommend:
Medscape Physician Burnout & Depression Report 2024: ‘We Have Much Work to Do’
Medscape Hospitalist Burnout & Depression Report 2024: Seeking Progress, Balance
Medscape Physician Lifestyle & Happiness Report 2024: The Ongoing Struggle for Balance
A Transformative Rx for Burnout, Grief, and Illness: Dance
Next Medscape Masters Event:
Stay at the forefront of obesity care. Register for exclusive insights and the latest treatment innovations.
Lotte Dyrbye, has disclosed the following relevant financial relationships: Co-inventor of the Well-being Index and its derivatives, which Mayo Clinic has licensed. Dyrbye receives royalties.
A version of this article first appeared on Medscape.com.
Summary and Key Highlights
Summary: Dr Tyra Fainstad explores the ingrained culture in medicine that encourages self-criticism, with many physicians feeling that they must be hard on themselves to succeed. Dr Fainstad challenges this belief, advocating for self-compassion as a healthier alternative. The evolving medical field now includes physicians who prioritize well-being without sacrificing quality of care, underscoring the importance of self-kindness for sustainable practice.
Key Takeaways:
- Many physicians believe that self-criticism is necessary for success, a mindset rooted in medical culture.
- Practicing self-compassion can improve long-term resilience and prevent burnout.
- The changing landscape of healthcare supports a more balanced approach to physician well-being.
Our Editors Also Recommend:
Medscape Physician Burnout & Depression Report 2024: ‘We Have Much Work to Do’
Medscape Hospitalist Burnout & Depression Report 2024: Seeking Progress, Balance
Medscape Physician Lifestyle & Happiness Report 2024: The Ongoing Struggle for Balance
A Transformative Rx for Burnout, Grief, and Illness: Dance
Next Medscape Masters Event:
Stay at the forefront of obesity care. Register for exclusive insights and the latest treatment innovations.
Lotte Dyrbye, has disclosed the following relevant financial relationships: Co-inventor of the Well-being Index and its derivatives, which Mayo Clinic has licensed. Dyrbye receives royalties.
A version of this article first appeared on Medscape.com.
Summary and Key Highlights
Summary: Dr Tyra Fainstad explores the ingrained culture in medicine that encourages self-criticism, with many physicians feeling that they must be hard on themselves to succeed. Dr Fainstad challenges this belief, advocating for self-compassion as a healthier alternative. The evolving medical field now includes physicians who prioritize well-being without sacrificing quality of care, underscoring the importance of self-kindness for sustainable practice.
Key Takeaways:
- Many physicians believe that self-criticism is necessary for success, a mindset rooted in medical culture.
- Practicing self-compassion can improve long-term resilience and prevent burnout.
- The changing landscape of healthcare supports a more balanced approach to physician well-being.
Our Editors Also Recommend:
Medscape Physician Burnout & Depression Report 2024: ‘We Have Much Work to Do’
Medscape Hospitalist Burnout & Depression Report 2024: Seeking Progress, Balance
Medscape Physician Lifestyle & Happiness Report 2024: The Ongoing Struggle for Balance
A Transformative Rx for Burnout, Grief, and Illness: Dance
Next Medscape Masters Event:
Stay at the forefront of obesity care. Register for exclusive insights and the latest treatment innovations.
Lotte Dyrbye, has disclosed the following relevant financial relationships: Co-inventor of the Well-being Index and its derivatives, which Mayo Clinic has licensed. Dyrbye receives royalties.
A version of this article first appeared on Medscape.com.
Finding Fulfillment Beyond Metrics: A Physician’s Path to Lasting Well-Being
Summary and Key Highlights
Summary: Dr Tyra Fainstad shares her personal experience with burnout and the journey to recovery through coaching and self-compassion. She describes the pressures of seeking validation through external achievements, which ultimately led to a crisis in self-worth after medical training. Through coaching, she learned to cultivate a sense of internal fulfillment, reconnecting with her passion for medicine and achieving a healthier balance.
Key Takeaways:
- Relying solely on external validation can deepen burnout and affect well-being.
- Coaching empowers physicians to develop self-compassion and sustainable coping strategies.
- Shifting from external to internal validation strengthens long-term fulfillment and job satisfaction.
Our Editors Also Recommend:
Medscape Physician Burnout & Depression Report 2024: ‘We Have Much Work to Do’
Medscape Hospitalist Burnout & Depression Report 2024: Seeking Progress, Balance
Medscape Physician Lifestyle & Happiness Report 2024: The Ongoing Struggle for Balance
A Transformative Rx for Burnout, Grief, and Illness: Dance
Next Medscape Masters Event:
Stay at the forefront of obesity care. Register for exclusive insights and the latest treatment innovations.
A version of this article first appeared on Medscape.com.
Summary and Key Highlights
Summary: Dr Tyra Fainstad shares her personal experience with burnout and the journey to recovery through coaching and self-compassion. She describes the pressures of seeking validation through external achievements, which ultimately led to a crisis in self-worth after medical training. Through coaching, she learned to cultivate a sense of internal fulfillment, reconnecting with her passion for medicine and achieving a healthier balance.
Key Takeaways:
- Relying solely on external validation can deepen burnout and affect well-being.
- Coaching empowers physicians to develop self-compassion and sustainable coping strategies.
- Shifting from external to internal validation strengthens long-term fulfillment and job satisfaction.
Our Editors Also Recommend:
Medscape Physician Burnout & Depression Report 2024: ‘We Have Much Work to Do’
Medscape Hospitalist Burnout & Depression Report 2024: Seeking Progress, Balance
Medscape Physician Lifestyle & Happiness Report 2024: The Ongoing Struggle for Balance
A Transformative Rx for Burnout, Grief, and Illness: Dance
Next Medscape Masters Event:
Stay at the forefront of obesity care. Register for exclusive insights and the latest treatment innovations.
A version of this article first appeared on Medscape.com.
Summary and Key Highlights
Summary: Dr Tyra Fainstad shares her personal experience with burnout and the journey to recovery through coaching and self-compassion. She describes the pressures of seeking validation through external achievements, which ultimately led to a crisis in self-worth after medical training. Through coaching, she learned to cultivate a sense of internal fulfillment, reconnecting with her passion for medicine and achieving a healthier balance.
Key Takeaways:
- Relying solely on external validation can deepen burnout and affect well-being.
- Coaching empowers physicians to develop self-compassion and sustainable coping strategies.
- Shifting from external to internal validation strengthens long-term fulfillment and job satisfaction.
Our Editors Also Recommend:
Medscape Physician Burnout & Depression Report 2024: ‘We Have Much Work to Do’
Medscape Hospitalist Burnout & Depression Report 2024: Seeking Progress, Balance
Medscape Physician Lifestyle & Happiness Report 2024: The Ongoing Struggle for Balance
A Transformative Rx for Burnout, Grief, and Illness: Dance
Next Medscape Masters Event:
Stay at the forefront of obesity care. Register for exclusive insights and the latest treatment innovations.
A version of this article first appeared on Medscape.com.
A Portrait of the Patient
Most of my writing starts on paper. I’ve stacks of Docket Gold legal pads, yellow and college ruled, filled with Sharpie S-Gel black ink. There are many scratch-outs and arrows, but no doodles. I’m genetically not a doodler. The draft of this essay however was interrupted by a graphic. It is a round figure with stick arms and legs. Somewhat centered are two intense scribbles, which represent eyes. A few loopy curls rest on top. It looks like a Mr. Potato Head, with owl eyes.
“Ah, art!” I say when I flip up the page and discover this spontaneous self-portrait of my 4-year-old. Using the media she had on hand, she let free her stored creative energy, an energy we all seem to have. “Tell me about what you’ve drawn here,” I say. She’s eager to share. Art is a natural way to connect.
My patients have shown me many similar self-portraits. Last week, the artist was a 71-year-old woman. She came with her friend, a 73-year-old woman, who is also my patient. They accompany each other on all their visits. She chose a small realtor pad with a color photo of a blonde with her arms folded and back against a graphic of a house. My patient managed to fit her sketch on the small, lined space, noting with tiny scribbles the lesions she wanted me to check. Although unnecessary, she added eyes, nose, and mouth.
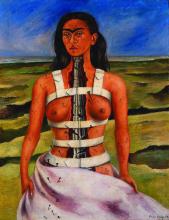
Another drawing was from a middle-aged white man. He has a look that suggests he rises early. His was on white printer paper, which he withdrew from a folder. He drew both a front and back view indicating with precision where I might find the spots he had mapped on his portrait. A retired teacher brought hers with a notably proportional anatomy and uniform tick marks on her face, arms, and legs. It reminded me of a self-portrait by the artist Frida Kahlo’s “The Broken Column.”
Kahlo was born with polio and suffered a severe bus accident as a young woman. She is one of many artists who shared their suffering through their art. “The Broken Column” depicts her with nails running from her face down her right short, weak leg. They look like the ticks my patient had added to her own self-portrait.
I remember in my neurology rotation asking patients to draw a clock. Stroke patients leave a whole half missing. Patients with dementia often crunch all the numbers into a little corner of the circle or forget to add the hands. Some of my dermatology patient self-portraits looked like that. I sometimes wonder if they also need a neurologist.
These pieces of patient art are utilitarian, drawn to narrate the story of what brought them to see me. Yet patients often add superfluous detail, demonstrating that utility and aesthetics are inseparable. I hold their drawings in the best light and notice the features and attributes. It helps me see their concerns from their point of view and primes me to notice other details during the physical exam. Viewing patients’ drawings can help build something called narrative competence the “ability to acknowledge, absorb, interpret, and act on the stories and plights of others.” Like Kahlo, patients are trying to share something with us, universal and recognizable. Art is how we connect to each other.
A few months ago, I walked in a room to see a consult. A white man in his 30s, he had prematurely graying hair and 80s-hip frames for glasses. He explained he was there for a skin screening and stood without warning, taking a step toward me. Like Michelangelo on wet plaster, he had grabbed a purple surgical marker to draw a self-portrait on the exam paper, the table set to just the right height and pitch to be an easel. It was the ginger-bread-man-type portrait with thick arms and legs and frosting-like dots marking the spots of concern. He marked L and R on the sheet, which were opposite what they would be if he was sitting facing me. But this was a self-portrait and he was drawing as it was with him facing the canvas, of course. “Ah, art!” I thought, and said, “Delightful! Tell me about what you’ve drawn here.” And so he did. A faint shadow of his portrait remains on that exam table to this day for every patient to see.
Benabio is chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on X. Write to him at dermnews@mdedge.com.
Most of my writing starts on paper. I’ve stacks of Docket Gold legal pads, yellow and college ruled, filled with Sharpie S-Gel black ink. There are many scratch-outs and arrows, but no doodles. I’m genetically not a doodler. The draft of this essay however was interrupted by a graphic. It is a round figure with stick arms and legs. Somewhat centered are two intense scribbles, which represent eyes. A few loopy curls rest on top. It looks like a Mr. Potato Head, with owl eyes.
“Ah, art!” I say when I flip up the page and discover this spontaneous self-portrait of my 4-year-old. Using the media she had on hand, she let free her stored creative energy, an energy we all seem to have. “Tell me about what you’ve drawn here,” I say. She’s eager to share. Art is a natural way to connect.
My patients have shown me many similar self-portraits. Last week, the artist was a 71-year-old woman. She came with her friend, a 73-year-old woman, who is also my patient. They accompany each other on all their visits. She chose a small realtor pad with a color photo of a blonde with her arms folded and back against a graphic of a house. My patient managed to fit her sketch on the small, lined space, noting with tiny scribbles the lesions she wanted me to check. Although unnecessary, she added eyes, nose, and mouth.
Another drawing was from a middle-aged white man. He has a look that suggests he rises early. His was on white printer paper, which he withdrew from a folder. He drew both a front and back view indicating with precision where I might find the spots he had mapped on his portrait. A retired teacher brought hers with a notably proportional anatomy and uniform tick marks on her face, arms, and legs. It reminded me of a self-portrait by the artist Frida Kahlo’s “The Broken Column.”
Kahlo was born with polio and suffered a severe bus accident as a young woman. She is one of many artists who shared their suffering through their art. “The Broken Column” depicts her with nails running from her face down her right short, weak leg. They look like the ticks my patient had added to her own self-portrait.
I remember in my neurology rotation asking patients to draw a clock. Stroke patients leave a whole half missing. Patients with dementia often crunch all the numbers into a little corner of the circle or forget to add the hands. Some of my dermatology patient self-portraits looked like that. I sometimes wonder if they also need a neurologist.
These pieces of patient art are utilitarian, drawn to narrate the story of what brought them to see me. Yet patients often add superfluous detail, demonstrating that utility and aesthetics are inseparable. I hold their drawings in the best light and notice the features and attributes. It helps me see their concerns from their point of view and primes me to notice other details during the physical exam. Viewing patients’ drawings can help build something called narrative competence the “ability to acknowledge, absorb, interpret, and act on the stories and plights of others.” Like Kahlo, patients are trying to share something with us, universal and recognizable. Art is how we connect to each other.
A few months ago, I walked in a room to see a consult. A white man in his 30s, he had prematurely graying hair and 80s-hip frames for glasses. He explained he was there for a skin screening and stood without warning, taking a step toward me. Like Michelangelo on wet plaster, he had grabbed a purple surgical marker to draw a self-portrait on the exam paper, the table set to just the right height and pitch to be an easel. It was the ginger-bread-man-type portrait with thick arms and legs and frosting-like dots marking the spots of concern. He marked L and R on the sheet, which were opposite what they would be if he was sitting facing me. But this was a self-portrait and he was drawing as it was with him facing the canvas, of course. “Ah, art!” I thought, and said, “Delightful! Tell me about what you’ve drawn here.” And so he did. A faint shadow of his portrait remains on that exam table to this day for every patient to see.
Benabio is chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on X. Write to him at dermnews@mdedge.com.
Most of my writing starts on paper. I’ve stacks of Docket Gold legal pads, yellow and college ruled, filled with Sharpie S-Gel black ink. There are many scratch-outs and arrows, but no doodles. I’m genetically not a doodler. The draft of this essay however was interrupted by a graphic. It is a round figure with stick arms and legs. Somewhat centered are two intense scribbles, which represent eyes. A few loopy curls rest on top. It looks like a Mr. Potato Head, with owl eyes.
“Ah, art!” I say when I flip up the page and discover this spontaneous self-portrait of my 4-year-old. Using the media she had on hand, she let free her stored creative energy, an energy we all seem to have. “Tell me about what you’ve drawn here,” I say. She’s eager to share. Art is a natural way to connect.
My patients have shown me many similar self-portraits. Last week, the artist was a 71-year-old woman. She came with her friend, a 73-year-old woman, who is also my patient. They accompany each other on all their visits. She chose a small realtor pad with a color photo of a blonde with her arms folded and back against a graphic of a house. My patient managed to fit her sketch on the small, lined space, noting with tiny scribbles the lesions she wanted me to check. Although unnecessary, she added eyes, nose, and mouth.
Another drawing was from a middle-aged white man. He has a look that suggests he rises early. His was on white printer paper, which he withdrew from a folder. He drew both a front and back view indicating with precision where I might find the spots he had mapped on his portrait. A retired teacher brought hers with a notably proportional anatomy and uniform tick marks on her face, arms, and legs. It reminded me of a self-portrait by the artist Frida Kahlo’s “The Broken Column.”
Kahlo was born with polio and suffered a severe bus accident as a young woman. She is one of many artists who shared their suffering through their art. “The Broken Column” depicts her with nails running from her face down her right short, weak leg. They look like the ticks my patient had added to her own self-portrait.
I remember in my neurology rotation asking patients to draw a clock. Stroke patients leave a whole half missing. Patients with dementia often crunch all the numbers into a little corner of the circle or forget to add the hands. Some of my dermatology patient self-portraits looked like that. I sometimes wonder if they also need a neurologist.
These pieces of patient art are utilitarian, drawn to narrate the story of what brought them to see me. Yet patients often add superfluous detail, demonstrating that utility and aesthetics are inseparable. I hold their drawings in the best light and notice the features and attributes. It helps me see their concerns from their point of view and primes me to notice other details during the physical exam. Viewing patients’ drawings can help build something called narrative competence the “ability to acknowledge, absorb, interpret, and act on the stories and plights of others.” Like Kahlo, patients are trying to share something with us, universal and recognizable. Art is how we connect to each other.
A few months ago, I walked in a room to see a consult. A white man in his 30s, he had prematurely graying hair and 80s-hip frames for glasses. He explained he was there for a skin screening and stood without warning, taking a step toward me. Like Michelangelo on wet plaster, he had grabbed a purple surgical marker to draw a self-portrait on the exam paper, the table set to just the right height and pitch to be an easel. It was the ginger-bread-man-type portrait with thick arms and legs and frosting-like dots marking the spots of concern. He marked L and R on the sheet, which were opposite what they would be if he was sitting facing me. But this was a self-portrait and he was drawing as it was with him facing the canvas, of course. “Ah, art!” I thought, and said, “Delightful! Tell me about what you’ve drawn here.” And so he did. A faint shadow of his portrait remains on that exam table to this day for every patient to see.
Benabio is chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on X. Write to him at dermnews@mdedge.com.
Telehealth Vs In-Person Diabetes Care: Is One Better?
Adults with diabetes who participated in telehealth visits reported similar levels of care, trust in the healthcare system, and patient-centered communication compared to those who had in-person visits, a cross-sectional study suggested.
The authors urged continued integration of telehealth into diabetes care beyond December 31, 2024, when the pandemic public health emergency ends, potentially limiting such services.
The study “provides population-level evidence that telehealth can deliver care quality comparable to in-person visits in diabetes management,” lead author Young-Rock Hong, PhD, MPH, an assistant professor in the University of Florida, Gainesville, told this news organization.
“Perhaps the most meaningful finding was the high utilization of telephone-only visits among older adults,” he said. “This has important policy implications, particularly as some insurers and healthcare systems have pushed to restrict telehealth coverage to video-only visits.”
“Maintaining telephone visit coverage is crucial for equitable access, especially for older adults who may be less comfortable with video technology; those with limited internet access; or patients facing other barriers to video visits,” he explained.
The study was published online in BMJ Open.
Video-only, Voice-only, Both
The researchers did a secondary analysis of data from the 2022 Health Information National Trends Survey, a nationally representative survey that includes information on health communication and knowledge and perceptions about all health conditions among US adults aged ≥ 18 years.
Participants had a self-reported diagnosis of type 1 or type 2 diabetes. The mean age was 59.4 years; 50% were women; and 53% were non-Hispanic White individuals.
Primary and secondary outcomes were use of telehealth in the last 12-months; telehealth modality; overall perception of quality of care; perceived trust in the healthcare system; and patient-centered communication score.
In the analysis of 1116 participants representing 33.6 million individuals, 48.1% reported telehealth use in the past 12 months.
Telehealth users were more likely to be younger and women with higher household incomes and health insurance coverage; live in metropolitan areas; and have multiple chronic conditions, poorer perceived health status, and more frequent physician visits than nonusers.
After adjustment, adults aged ≥ 65 years had a significantly lower likelihood of telehealth use than those ages 18-49 years (odds ratio [OR], 0.43).
Higher income and more frequent healthcare visits were predictors of telehealth usage, with no significant differences across race, education, or location.
Those with a household income between $35,000 and $74,999 had more than double the likelihood of telehealth use (OR, 2.14) than those with incomes below $35,000.
Among telehealth users, 39.3% reported having video-only; 35%, phone (voice)-only; and 25.7%, both modalities. Among those aged ≥ 65 years, 55.5% used phone calls only and 25.5% used video only. In contrast, those aged 18-49 years had higher rates of video-only use (36.1%) and combined video/phone use (31.2%).
Healthcare provider recommendation (68.1%) was the most common reason for telehealth use, followed by convenience (57.7%), avoiding potential COVID-19 exposure (48.1%), and obtaining advice about the need for in-person care (23.6%).
Nonusers said they preferred in-person visits and also cited privacy concerns and technology challenges.
Patient-reported quality-of-care outcomes were comparable between telehealth users and nonusers, with no significant differences by telehealth modality or area of residence (urban or rural).
Around 70% of individuals with diabetes in both groups rated their quality of care as “excellent” and “very good;” fewer than 10% rated their care as “fair” and “poor.”
Similarly, trust in the healthcare system was comparable between users and nonusers: 41.3% of telehealth users 41% of nonusers reported trusting the healthcare system “very much.” Patient-centered communication scores were also similar between users and nonusers.
Telehealth appears to be a good option from the providers’ perspective as well, according to the authors. A previous study by the team found more than 80% of US physicians intended to continue telehealth beyond the pandemic.
“The recent unanimous bipartisan passage of the Telehealth Modernization Act by the House Energy & Commerce Committee signals strong political support for extending telehealth flexibilities through 2026,” Hong said. “The bill addresses key access issues by permanently removing geographic restrictions, expanding eligible providers, and maintaining audio-only coverage — provisions that align with our study’s findings about the importance of telephone visits, particularly for older adults and underserved populations.”
There is concern that extending telehealth services might increase Medicare spending by over $2 billion, he added. “While this may be a valid concern, there is a need for more robust evidence regarding the overall value of telehealth services — ie, the ‘benefits’ they provide relative to their costs and outcomes.”
Reassuring, but More Research Needed
COVID prompted “dramatic shifts” in care delivery from in-person to telehealth, Kevin Peterson, MD, MPH, American Diabetes Association vice president of primary care told this news organization. “The authors’ findings provide reassurance that these changes provided for additional convenience in care delivery without being associated with compromises in patient-reported care quality.”
However, he said, “the study does not necessarily capture representative samples of rural and underserved populations, making the impact of telehealth on health equity difficult to determine.” In addition, although patient-perceived care quality did not change with telehealth delivery, the study “does not address impacts on safety, clinical outcomes, equity, costs, or other important measures.”
Furthermore, he noted, “this is an association study that occurred during the dramatic changes brought about by COVID. It may not represent provider or patient preferences that characterize the role of telehealth under more normal circumstances.”
For now, clinicians should be aware that “initial evidence suggests that telehealth can be integrated into care without significantly compromising the patient’s perception of the quality of care,” he concluded.
No funding was declared. Hong and Peterson reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
Adults with diabetes who participated in telehealth visits reported similar levels of care, trust in the healthcare system, and patient-centered communication compared to those who had in-person visits, a cross-sectional study suggested.
The authors urged continued integration of telehealth into diabetes care beyond December 31, 2024, when the pandemic public health emergency ends, potentially limiting such services.
The study “provides population-level evidence that telehealth can deliver care quality comparable to in-person visits in diabetes management,” lead author Young-Rock Hong, PhD, MPH, an assistant professor in the University of Florida, Gainesville, told this news organization.
“Perhaps the most meaningful finding was the high utilization of telephone-only visits among older adults,” he said. “This has important policy implications, particularly as some insurers and healthcare systems have pushed to restrict telehealth coverage to video-only visits.”
“Maintaining telephone visit coverage is crucial for equitable access, especially for older adults who may be less comfortable with video technology; those with limited internet access; or patients facing other barriers to video visits,” he explained.
The study was published online in BMJ Open.
Video-only, Voice-only, Both
The researchers did a secondary analysis of data from the 2022 Health Information National Trends Survey, a nationally representative survey that includes information on health communication and knowledge and perceptions about all health conditions among US adults aged ≥ 18 years.
Participants had a self-reported diagnosis of type 1 or type 2 diabetes. The mean age was 59.4 years; 50% were women; and 53% were non-Hispanic White individuals.
Primary and secondary outcomes were use of telehealth in the last 12-months; telehealth modality; overall perception of quality of care; perceived trust in the healthcare system; and patient-centered communication score.
In the analysis of 1116 participants representing 33.6 million individuals, 48.1% reported telehealth use in the past 12 months.
Telehealth users were more likely to be younger and women with higher household incomes and health insurance coverage; live in metropolitan areas; and have multiple chronic conditions, poorer perceived health status, and more frequent physician visits than nonusers.
After adjustment, adults aged ≥ 65 years had a significantly lower likelihood of telehealth use than those ages 18-49 years (odds ratio [OR], 0.43).
Higher income and more frequent healthcare visits were predictors of telehealth usage, with no significant differences across race, education, or location.
Those with a household income between $35,000 and $74,999 had more than double the likelihood of telehealth use (OR, 2.14) than those with incomes below $35,000.
Among telehealth users, 39.3% reported having video-only; 35%, phone (voice)-only; and 25.7%, both modalities. Among those aged ≥ 65 years, 55.5% used phone calls only and 25.5% used video only. In contrast, those aged 18-49 years had higher rates of video-only use (36.1%) and combined video/phone use (31.2%).
Healthcare provider recommendation (68.1%) was the most common reason for telehealth use, followed by convenience (57.7%), avoiding potential COVID-19 exposure (48.1%), and obtaining advice about the need for in-person care (23.6%).
Nonusers said they preferred in-person visits and also cited privacy concerns and technology challenges.
Patient-reported quality-of-care outcomes were comparable between telehealth users and nonusers, with no significant differences by telehealth modality or area of residence (urban or rural).
Around 70% of individuals with diabetes in both groups rated their quality of care as “excellent” and “very good;” fewer than 10% rated their care as “fair” and “poor.”
Similarly, trust in the healthcare system was comparable between users and nonusers: 41.3% of telehealth users 41% of nonusers reported trusting the healthcare system “very much.” Patient-centered communication scores were also similar between users and nonusers.
Telehealth appears to be a good option from the providers’ perspective as well, according to the authors. A previous study by the team found more than 80% of US physicians intended to continue telehealth beyond the pandemic.
“The recent unanimous bipartisan passage of the Telehealth Modernization Act by the House Energy & Commerce Committee signals strong political support for extending telehealth flexibilities through 2026,” Hong said. “The bill addresses key access issues by permanently removing geographic restrictions, expanding eligible providers, and maintaining audio-only coverage — provisions that align with our study’s findings about the importance of telephone visits, particularly for older adults and underserved populations.”
There is concern that extending telehealth services might increase Medicare spending by over $2 billion, he added. “While this may be a valid concern, there is a need for more robust evidence regarding the overall value of telehealth services — ie, the ‘benefits’ they provide relative to their costs and outcomes.”
Reassuring, but More Research Needed
COVID prompted “dramatic shifts” in care delivery from in-person to telehealth, Kevin Peterson, MD, MPH, American Diabetes Association vice president of primary care told this news organization. “The authors’ findings provide reassurance that these changes provided for additional convenience in care delivery without being associated with compromises in patient-reported care quality.”
However, he said, “the study does not necessarily capture representative samples of rural and underserved populations, making the impact of telehealth on health equity difficult to determine.” In addition, although patient-perceived care quality did not change with telehealth delivery, the study “does not address impacts on safety, clinical outcomes, equity, costs, or other important measures.”
Furthermore, he noted, “this is an association study that occurred during the dramatic changes brought about by COVID. It may not represent provider or patient preferences that characterize the role of telehealth under more normal circumstances.”
For now, clinicians should be aware that “initial evidence suggests that telehealth can be integrated into care without significantly compromising the patient’s perception of the quality of care,” he concluded.
No funding was declared. Hong and Peterson reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
Adults with diabetes who participated in telehealth visits reported similar levels of care, trust in the healthcare system, and patient-centered communication compared to those who had in-person visits, a cross-sectional study suggested.
The authors urged continued integration of telehealth into diabetes care beyond December 31, 2024, when the pandemic public health emergency ends, potentially limiting such services.
The study “provides population-level evidence that telehealth can deliver care quality comparable to in-person visits in diabetes management,” lead author Young-Rock Hong, PhD, MPH, an assistant professor in the University of Florida, Gainesville, told this news organization.
“Perhaps the most meaningful finding was the high utilization of telephone-only visits among older adults,” he said. “This has important policy implications, particularly as some insurers and healthcare systems have pushed to restrict telehealth coverage to video-only visits.”
“Maintaining telephone visit coverage is crucial for equitable access, especially for older adults who may be less comfortable with video technology; those with limited internet access; or patients facing other barriers to video visits,” he explained.
The study was published online in BMJ Open.
Video-only, Voice-only, Both
The researchers did a secondary analysis of data from the 2022 Health Information National Trends Survey, a nationally representative survey that includes information on health communication and knowledge and perceptions about all health conditions among US adults aged ≥ 18 years.
Participants had a self-reported diagnosis of type 1 or type 2 diabetes. The mean age was 59.4 years; 50% were women; and 53% were non-Hispanic White individuals.
Primary and secondary outcomes were use of telehealth in the last 12-months; telehealth modality; overall perception of quality of care; perceived trust in the healthcare system; and patient-centered communication score.
In the analysis of 1116 participants representing 33.6 million individuals, 48.1% reported telehealth use in the past 12 months.
Telehealth users were more likely to be younger and women with higher household incomes and health insurance coverage; live in metropolitan areas; and have multiple chronic conditions, poorer perceived health status, and more frequent physician visits than nonusers.
After adjustment, adults aged ≥ 65 years had a significantly lower likelihood of telehealth use than those ages 18-49 years (odds ratio [OR], 0.43).
Higher income and more frequent healthcare visits were predictors of telehealth usage, with no significant differences across race, education, or location.
Those with a household income between $35,000 and $74,999 had more than double the likelihood of telehealth use (OR, 2.14) than those with incomes below $35,000.
Among telehealth users, 39.3% reported having video-only; 35%, phone (voice)-only; and 25.7%, both modalities. Among those aged ≥ 65 years, 55.5% used phone calls only and 25.5% used video only. In contrast, those aged 18-49 years had higher rates of video-only use (36.1%) and combined video/phone use (31.2%).
Healthcare provider recommendation (68.1%) was the most common reason for telehealth use, followed by convenience (57.7%), avoiding potential COVID-19 exposure (48.1%), and obtaining advice about the need for in-person care (23.6%).
Nonusers said they preferred in-person visits and also cited privacy concerns and technology challenges.
Patient-reported quality-of-care outcomes were comparable between telehealth users and nonusers, with no significant differences by telehealth modality or area of residence (urban or rural).
Around 70% of individuals with diabetes in both groups rated their quality of care as “excellent” and “very good;” fewer than 10% rated their care as “fair” and “poor.”
Similarly, trust in the healthcare system was comparable between users and nonusers: 41.3% of telehealth users 41% of nonusers reported trusting the healthcare system “very much.” Patient-centered communication scores were also similar between users and nonusers.
Telehealth appears to be a good option from the providers’ perspective as well, according to the authors. A previous study by the team found more than 80% of US physicians intended to continue telehealth beyond the pandemic.
“The recent unanimous bipartisan passage of the Telehealth Modernization Act by the House Energy & Commerce Committee signals strong political support for extending telehealth flexibilities through 2026,” Hong said. “The bill addresses key access issues by permanently removing geographic restrictions, expanding eligible providers, and maintaining audio-only coverage — provisions that align with our study’s findings about the importance of telephone visits, particularly for older adults and underserved populations.”
There is concern that extending telehealth services might increase Medicare spending by over $2 billion, he added. “While this may be a valid concern, there is a need for more robust evidence regarding the overall value of telehealth services — ie, the ‘benefits’ they provide relative to their costs and outcomes.”
Reassuring, but More Research Needed
COVID prompted “dramatic shifts” in care delivery from in-person to telehealth, Kevin Peterson, MD, MPH, American Diabetes Association vice president of primary care told this news organization. “The authors’ findings provide reassurance that these changes provided for additional convenience in care delivery without being associated with compromises in patient-reported care quality.”
However, he said, “the study does not necessarily capture representative samples of rural and underserved populations, making the impact of telehealth on health equity difficult to determine.” In addition, although patient-perceived care quality did not change with telehealth delivery, the study “does not address impacts on safety, clinical outcomes, equity, costs, or other important measures.”
Furthermore, he noted, “this is an association study that occurred during the dramatic changes brought about by COVID. It may not represent provider or patient preferences that characterize the role of telehealth under more normal circumstances.”
For now, clinicians should be aware that “initial evidence suggests that telehealth can be integrated into care without significantly compromising the patient’s perception of the quality of care,” he concluded.
No funding was declared. Hong and Peterson reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
FROM BMJ OPEN
The Emotional Cost of Nursing School: Depression
Nursing is a competitive field. In 2022, nursing schools rejected more than 78,000 qualified applications, and the students whose applications were accepted faced demanding schedules and rigorous academics and clinical rotations. Is this a recipe for depression?
In 2024, 38% of nursing students experienced depression — a 9.3% increase over 2019, according to research from higher education research group Degreechoices. Catherine A. Stubin, PhD, RN, assistant professor of nursing at Rutgers University–Camden in New Jersey, calls it “a mental health crisis in nursing.”
“Nursing is a very rigorous, difficult, psychologically and physically demanding profession,” she said. “If students don’t have the tools and resources to adequately deal with these stressors in nursing school, it’s going to carry over to their professional practice.”
A growing recognition of the toll that nursing programs may have on students’ mental health has led schools to launch initiatives to better support the next generation of nurses.
Diagnosing the Problem
Higher than average rates of depression among nursing students are not new. Nursing students often work long shifts with limited breaks. The academic rigors and clinical demands of caring for patients with acute and chronic conditions while instructors evaluate and watch for mistakes can cause high levels of stress, Stubin told this news organization. “Eventually, something has to give, and it’s usually their mental health.”
Clinical practicums often start when nursing students are still freshmen, and asking 18-year-old students to provide patient care in often-chaotic clinical environments is “overwhelming,” according to Stubin. The COVID-19 pandemic further exacerbated the issue.
During lockdown, more than half the nursing students reported moderate to severe symptoms of anxiety and depression, which was attributed to the transition to online learning, fear of infection, burnout, and the psychological distress of lockdown.
“The pandemic exacerbated existing mental health problems in undergraduate nursing students,” said Stubin. “In the wake of it ... a lot of [registered nurses] have mental health issues and are leaving the profession.”
Helping Nurses Heal
A significant shift in the willingness to talk about mental health and seek treatment could help. In 2011, just one third of students participated in the treatment for a mental health disorder. The latest data show that 61% of students experiencing symptoms of depression or anxiety take medication or seek therapy or counseling.
Incoming health sciences students at Ohio State University (OSU), Columbus, are screened for depression, anxiety, and suicidal ideation and directed to campus health services as needed. Bernadette Mazurek Melnyk, PhD, APRN-CNP, OSU’s chief wellness officer and former dean in the College of Nursing, believes it’s an essential step in supporting students, adding, “If you don’t screen, you don’t know the students are suffering, and we’re able to get help to the students who need it quickly.”
Prioritizing Solutions
Counseling services available through campus health centers are just one part of a multipronged approach that nursing schools have taken to improve the health and well-being of students. Nursing programs have also introduced initiatives to lower stress, prevent burnout, and relieve emotional trauma.
“In nursing education, we have to lay the groundwork for the self-care, wellness, and resilience practices that can, hopefully, be carried over into their professional practices,” Stubin said.
At Rutgers University–Camden, the wellness center provides counseling services, and the Student Nursing Association offers a pet therapy program. Stubin also incorporates self-care, resilience-building strategies, and wellness programming into the curriculum.
During the pandemic, the University of Colorado College of Nursing, Aurora, created a class called Stress Impact and Care for COVID-19 to provide content, exercises, and support groups for nursing students. The class was so popular that it was adapted and integrated into the curriculum.
The University of Vermont, Burlington, introduced the Benson-Henry Institute Stress Management and Resiliency Training program in 2021. The 8-week program was designed to teach nursing students coping strategies to reduce stress.
Offering stress management programs to first-year nursing students has been linked to improved problem-solving skills and fewer emotional and social behavioral symptoms. However, for programs to be effective, Melnyk believes that they need to be integrated into the curriculum, not offered as electives.
“We know mindfulness works, we know cognitive behavior skills-building works, and these types of evidence-based programs with such efficacy behind them should not be optional,” she said. “Students are overwhelmed just with their coursework, so if these programs exist for extra credit, students won’t take them.”
Creating a Culture of Wellness
Teaching nursing students how to manage stress and providing the resources to combat depression and anxiety is just the first step in building a healthy, resilient nursing workforce.
Prioritizing wellness in nursing isn’t just essential for addressing the nationwide nursing shortage. Burnout in the medical field costs the United States healthcare system $4.6 billion per year, and preventable medical errors are the third leading cause of death in the United States.
“There is a nice movement across the United States to reduce these mental health issues because they’re so costly,” Melnyk said.
There are also national efforts to address the issue. The National Academy of Medicine introduced the Action Collaborative on Clinician Well-Being and Resilience, which has grown to include more than 200 organizations committed to reversing burnout and improving mental health in the clinical workforce. The American Nurses Foundation created The Nurse Well-Being: Building Peer and Leadership Support Program to provide resources and peer support to help nurses manage stress.
Health systems and hospitals also need to prioritize clinical well-being to reduce stress and burnout — and these efforts must be ongoing.
“These resources have to be extended into the working world ... and not just once a year for Nurses Week in May, but on a regular continued basis,” said Stubin. “Healthcare corporations and hospitals have to continue these resources and this help; it has to be a priority.”
Until the culture changes, Stubin fears that nursing students will continue facing barriers to completing their programs and maintaining nursing careers. Currently, 43% of college students considered leaving their program for mental health reasons, and 21.7% of nurses reported suicidal ideation.
“There’s a nursing shortage, and the acuity of patient care is increasing, so the stressors in the clinical area aren’t going to decrease,” Stubin said. “We as nursing faculty must teach our students how to manage these stressors to build a resilient, mentally and physically healthy workforce.”
A version of this article first appeared on Medscape.com.
Nursing is a competitive field. In 2022, nursing schools rejected more than 78,000 qualified applications, and the students whose applications were accepted faced demanding schedules and rigorous academics and clinical rotations. Is this a recipe for depression?
In 2024, 38% of nursing students experienced depression — a 9.3% increase over 2019, according to research from higher education research group Degreechoices. Catherine A. Stubin, PhD, RN, assistant professor of nursing at Rutgers University–Camden in New Jersey, calls it “a mental health crisis in nursing.”
“Nursing is a very rigorous, difficult, psychologically and physically demanding profession,” she said. “If students don’t have the tools and resources to adequately deal with these stressors in nursing school, it’s going to carry over to their professional practice.”
A growing recognition of the toll that nursing programs may have on students’ mental health has led schools to launch initiatives to better support the next generation of nurses.
Diagnosing the Problem
Higher than average rates of depression among nursing students are not new. Nursing students often work long shifts with limited breaks. The academic rigors and clinical demands of caring for patients with acute and chronic conditions while instructors evaluate and watch for mistakes can cause high levels of stress, Stubin told this news organization. “Eventually, something has to give, and it’s usually their mental health.”
Clinical practicums often start when nursing students are still freshmen, and asking 18-year-old students to provide patient care in often-chaotic clinical environments is “overwhelming,” according to Stubin. The COVID-19 pandemic further exacerbated the issue.
During lockdown, more than half the nursing students reported moderate to severe symptoms of anxiety and depression, which was attributed to the transition to online learning, fear of infection, burnout, and the psychological distress of lockdown.
“The pandemic exacerbated existing mental health problems in undergraduate nursing students,” said Stubin. “In the wake of it ... a lot of [registered nurses] have mental health issues and are leaving the profession.”
Helping Nurses Heal
A significant shift in the willingness to talk about mental health and seek treatment could help. In 2011, just one third of students participated in the treatment for a mental health disorder. The latest data show that 61% of students experiencing symptoms of depression or anxiety take medication or seek therapy or counseling.
Incoming health sciences students at Ohio State University (OSU), Columbus, are screened for depression, anxiety, and suicidal ideation and directed to campus health services as needed. Bernadette Mazurek Melnyk, PhD, APRN-CNP, OSU’s chief wellness officer and former dean in the College of Nursing, believes it’s an essential step in supporting students, adding, “If you don’t screen, you don’t know the students are suffering, and we’re able to get help to the students who need it quickly.”
Prioritizing Solutions
Counseling services available through campus health centers are just one part of a multipronged approach that nursing schools have taken to improve the health and well-being of students. Nursing programs have also introduced initiatives to lower stress, prevent burnout, and relieve emotional trauma.
“In nursing education, we have to lay the groundwork for the self-care, wellness, and resilience practices that can, hopefully, be carried over into their professional practices,” Stubin said.
At Rutgers University–Camden, the wellness center provides counseling services, and the Student Nursing Association offers a pet therapy program. Stubin also incorporates self-care, resilience-building strategies, and wellness programming into the curriculum.
During the pandemic, the University of Colorado College of Nursing, Aurora, created a class called Stress Impact and Care for COVID-19 to provide content, exercises, and support groups for nursing students. The class was so popular that it was adapted and integrated into the curriculum.
The University of Vermont, Burlington, introduced the Benson-Henry Institute Stress Management and Resiliency Training program in 2021. The 8-week program was designed to teach nursing students coping strategies to reduce stress.
Offering stress management programs to first-year nursing students has been linked to improved problem-solving skills and fewer emotional and social behavioral symptoms. However, for programs to be effective, Melnyk believes that they need to be integrated into the curriculum, not offered as electives.
“We know mindfulness works, we know cognitive behavior skills-building works, and these types of evidence-based programs with such efficacy behind them should not be optional,” she said. “Students are overwhelmed just with their coursework, so if these programs exist for extra credit, students won’t take them.”
Creating a Culture of Wellness
Teaching nursing students how to manage stress and providing the resources to combat depression and anxiety is just the first step in building a healthy, resilient nursing workforce.
Prioritizing wellness in nursing isn’t just essential for addressing the nationwide nursing shortage. Burnout in the medical field costs the United States healthcare system $4.6 billion per year, and preventable medical errors are the third leading cause of death in the United States.
“There is a nice movement across the United States to reduce these mental health issues because they’re so costly,” Melnyk said.
There are also national efforts to address the issue. The National Academy of Medicine introduced the Action Collaborative on Clinician Well-Being and Resilience, which has grown to include more than 200 organizations committed to reversing burnout and improving mental health in the clinical workforce. The American Nurses Foundation created The Nurse Well-Being: Building Peer and Leadership Support Program to provide resources and peer support to help nurses manage stress.
Health systems and hospitals also need to prioritize clinical well-being to reduce stress and burnout — and these efforts must be ongoing.
“These resources have to be extended into the working world ... and not just once a year for Nurses Week in May, but on a regular continued basis,” said Stubin. “Healthcare corporations and hospitals have to continue these resources and this help; it has to be a priority.”
Until the culture changes, Stubin fears that nursing students will continue facing barriers to completing their programs and maintaining nursing careers. Currently, 43% of college students considered leaving their program for mental health reasons, and 21.7% of nurses reported suicidal ideation.
“There’s a nursing shortage, and the acuity of patient care is increasing, so the stressors in the clinical area aren’t going to decrease,” Stubin said. “We as nursing faculty must teach our students how to manage these stressors to build a resilient, mentally and physically healthy workforce.”
A version of this article first appeared on Medscape.com.
Nursing is a competitive field. In 2022, nursing schools rejected more than 78,000 qualified applications, and the students whose applications were accepted faced demanding schedules and rigorous academics and clinical rotations. Is this a recipe for depression?
In 2024, 38% of nursing students experienced depression — a 9.3% increase over 2019, according to research from higher education research group Degreechoices. Catherine A. Stubin, PhD, RN, assistant professor of nursing at Rutgers University–Camden in New Jersey, calls it “a mental health crisis in nursing.”
“Nursing is a very rigorous, difficult, psychologically and physically demanding profession,” she said. “If students don’t have the tools and resources to adequately deal with these stressors in nursing school, it’s going to carry over to their professional practice.”
A growing recognition of the toll that nursing programs may have on students’ mental health has led schools to launch initiatives to better support the next generation of nurses.
Diagnosing the Problem
Higher than average rates of depression among nursing students are not new. Nursing students often work long shifts with limited breaks. The academic rigors and clinical demands of caring for patients with acute and chronic conditions while instructors evaluate and watch for mistakes can cause high levels of stress, Stubin told this news organization. “Eventually, something has to give, and it’s usually their mental health.”
Clinical practicums often start when nursing students are still freshmen, and asking 18-year-old students to provide patient care in often-chaotic clinical environments is “overwhelming,” according to Stubin. The COVID-19 pandemic further exacerbated the issue.
During lockdown, more than half the nursing students reported moderate to severe symptoms of anxiety and depression, which was attributed to the transition to online learning, fear of infection, burnout, and the psychological distress of lockdown.
“The pandemic exacerbated existing mental health problems in undergraduate nursing students,” said Stubin. “In the wake of it ... a lot of [registered nurses] have mental health issues and are leaving the profession.”
Helping Nurses Heal
A significant shift in the willingness to talk about mental health and seek treatment could help. In 2011, just one third of students participated in the treatment for a mental health disorder. The latest data show that 61% of students experiencing symptoms of depression or anxiety take medication or seek therapy or counseling.
Incoming health sciences students at Ohio State University (OSU), Columbus, are screened for depression, anxiety, and suicidal ideation and directed to campus health services as needed. Bernadette Mazurek Melnyk, PhD, APRN-CNP, OSU’s chief wellness officer and former dean in the College of Nursing, believes it’s an essential step in supporting students, adding, “If you don’t screen, you don’t know the students are suffering, and we’re able to get help to the students who need it quickly.”
Prioritizing Solutions
Counseling services available through campus health centers are just one part of a multipronged approach that nursing schools have taken to improve the health and well-being of students. Nursing programs have also introduced initiatives to lower stress, prevent burnout, and relieve emotional trauma.
“In nursing education, we have to lay the groundwork for the self-care, wellness, and resilience practices that can, hopefully, be carried over into their professional practices,” Stubin said.
At Rutgers University–Camden, the wellness center provides counseling services, and the Student Nursing Association offers a pet therapy program. Stubin also incorporates self-care, resilience-building strategies, and wellness programming into the curriculum.
During the pandemic, the University of Colorado College of Nursing, Aurora, created a class called Stress Impact and Care for COVID-19 to provide content, exercises, and support groups for nursing students. The class was so popular that it was adapted and integrated into the curriculum.
The University of Vermont, Burlington, introduced the Benson-Henry Institute Stress Management and Resiliency Training program in 2021. The 8-week program was designed to teach nursing students coping strategies to reduce stress.
Offering stress management programs to first-year nursing students has been linked to improved problem-solving skills and fewer emotional and social behavioral symptoms. However, for programs to be effective, Melnyk believes that they need to be integrated into the curriculum, not offered as electives.
“We know mindfulness works, we know cognitive behavior skills-building works, and these types of evidence-based programs with such efficacy behind them should not be optional,” she said. “Students are overwhelmed just with their coursework, so if these programs exist for extra credit, students won’t take them.”
Creating a Culture of Wellness
Teaching nursing students how to manage stress and providing the resources to combat depression and anxiety is just the first step in building a healthy, resilient nursing workforce.
Prioritizing wellness in nursing isn’t just essential for addressing the nationwide nursing shortage. Burnout in the medical field costs the United States healthcare system $4.6 billion per year, and preventable medical errors are the third leading cause of death in the United States.
“There is a nice movement across the United States to reduce these mental health issues because they’re so costly,” Melnyk said.
There are also national efforts to address the issue. The National Academy of Medicine introduced the Action Collaborative on Clinician Well-Being and Resilience, which has grown to include more than 200 organizations committed to reversing burnout and improving mental health in the clinical workforce. The American Nurses Foundation created The Nurse Well-Being: Building Peer and Leadership Support Program to provide resources and peer support to help nurses manage stress.
Health systems and hospitals also need to prioritize clinical well-being to reduce stress and burnout — and these efforts must be ongoing.
“These resources have to be extended into the working world ... and not just once a year for Nurses Week in May, but on a regular continued basis,” said Stubin. “Healthcare corporations and hospitals have to continue these resources and this help; it has to be a priority.”
Until the culture changes, Stubin fears that nursing students will continue facing barriers to completing their programs and maintaining nursing careers. Currently, 43% of college students considered leaving their program for mental health reasons, and 21.7% of nurses reported suicidal ideation.
“There’s a nursing shortage, and the acuity of patient care is increasing, so the stressors in the clinical area aren’t going to decrease,” Stubin said. “We as nursing faculty must teach our students how to manage these stressors to build a resilient, mentally and physically healthy workforce.”
A version of this article first appeared on Medscape.com.
Lessons Learned: What Docs Wish Med Students Knew
Despite 4 years of med school and 3-7 years in residency, when you enter the workforce as a doctor, you still have much to learn. There is only so much your professors and attending physicians can pack in. Going forward, you’ll continue to learn on the job and via continuing education.
Some of that lifelong learning will involve soft skills — how to compassionately work with your patients and their families, for instance. Other lessons will get down to the business of medicine — the paperwork, the work/life balance, and the moral dilemmas you never saw coming. And still others will involve learning how to take care of yourself in the middle of seemingly endless hours on the job.
“We all have things we wish we had known upon starting our careers,” said Daniel Opris, MD, a primary care physician at Ohio-based Executive Medical Centers.
We tapped several veteran physicians and an educator to learn what they wish med students knew as they enter the workforce. We’ve compiled them here to give you a head start on the lessons ahead.
You Won’t Know Everything, and That’s Okay
When you go through your medical training, it can feel overwhelming to absorb all the knowledge your professors and attendings impart. The bottom line, said Shoshana Ungerleider, MD, an internal medicine specialist, is that you shouldn’t worry about it.
David Lenihan, PhD, CEO at Ponce Health Sciences University, agrees. “What we’ve lost in recent years, is the ability to apply your skill set and say, ‘let me take a day and get back to you,’” he said. “Doctors love it when you do that because it shows you can pitch in and work as part of a team.”
Medicine is a collaborative field, said Ungerleider, and learning from others, whether peers, nurses, or specialists, is “not a weakness.” She recommends embracing uncertainty and getting comfortable with the unknown.
You’ll Take Your Work Home With You
Doctors enter the field because they care about their patients and want to help. Successful outcomes are never guaranteed, however, no matter how much you try. The result? Some days you’ll bring home those upsetting and haunting cases, said Lenihan.
“We often believe that we should leave our work at the office, but sometimes you need to bring it home and think it through,” he said. “It can’t overwhelm you, but you should digest what happened.”
When you do, said Lenihan, you’ll come out the other end more empathetic and that helps the healthcare system in the long run. “The more you reflect on your day, the better you’ll get at reading the room and treating your patients.”
Drew Remignanti, MD, a retired emergency medicine physician from New Hampshire, agrees, but puts a different spin on bringing work home.
“We revisit the patient care decisions we made, second-guess ourselves, and worry about our patients’ welfare and outcomes,” he said. “I think it can only lead to better outcomes down the road, however, if you learn from that bad decision, preventing you from committing a similar mistake.”
Burnout Is Real — Make Self-Care a Priority
As a retired physician who spent 40 years practicing medicine, Remignanti experienced the evolution of healthcare as it has become what he calls a “consumer-provider” model. “Productivity didn’t use to be part of the equation, but now it’s the focus,” he said.
The result is burnout, a very real threat to incoming physicians. Remignanti holds that if you are aware of the risk, you can resist it. Part of avoiding burnout is self-care, according to Ungerleider. “The sooner you prioritize your mental, emotional, and physical well-being, the better,” she said. “Balancing work and life may feel impossible at times but taking care of yourself is essential to being a better physician in the long run.”
That means carving out time for exercise, hobbies, and connections outside of the medical field. It also means making sleep and nutrition a priority, even when that feels hard to accomplish. “If you don’t take care of yourself, you can’t take care of others,” added Opris. “It’s so common to lose yourself in your career, but you need to hold onto your physical, emotional, and spiritual self.”
Avoid Relying Too Heavily on Tech
Technology is invading every aspect of our lives — often for the greater good — but in medicine, it’s important to always return to your core knowledge above all else. Case in point, said Opris, the UpToDate app. While it can be a useful tool, it’s important not to become too reliant on it. “UpToDate is expert opinion-based guidance, and it’s a fantastic resource,” he said. “But you need to use your references and knowledge in every case.”
It’s key to remember that every patient is different, and their case may not line up perfectly with the guidance presented in UpToDate or other technology source. Piggybacking on that, Ungerleider added that it’s important to remember medicine is about people, not just conditions.
“It’s easy to focus on mastering the science, but the real art of medicine comes from seeing the whole person in front of you,” she said. “Your patients are more than their diagnoses — they come with complex emotions, life stories, and needs.” Being compassionate, listening carefully, and building trust should match up to your clinical skills.
Partner With Your Patients, Even When It’s Difficult
Perhaps the most difficult lesson of all is remembering that your patients may not always agree with your recommendations and choose to ignore them. After all your years spent learning, there may be times when it feels your education is going to waste.
“Remember that the landscape today is so varied, and that bleeds into medicine,” said Opris. “We go into cases with our own biases, and it’s important to take a step back to reset, every time.”
Opris reminds himself of Sir William Osler’s famous essay, “Aequanimitas,” in which he tells graduating medical students to practice with “coolness and presence of mind under all circumstances.”
Remignanti offers this advice: “Physicians need to be able to partner with their patients and jointly decide which courses of action are most effective,” he said. “Cling to the idea that you are forming a partnership with your patients — what can we together determine is the best course?”
At the same time, the path the patient chooses may not be what’s best for them — potentially even leading to a poor outcome.
“You may not always understand their choices,” said Opris. “But they do have a choice. Think of yourself almost like a consultant.”
A version of this article first appeared on Medscape.com.
Despite 4 years of med school and 3-7 years in residency, when you enter the workforce as a doctor, you still have much to learn. There is only so much your professors and attending physicians can pack in. Going forward, you’ll continue to learn on the job and via continuing education.
Some of that lifelong learning will involve soft skills — how to compassionately work with your patients and their families, for instance. Other lessons will get down to the business of medicine — the paperwork, the work/life balance, and the moral dilemmas you never saw coming. And still others will involve learning how to take care of yourself in the middle of seemingly endless hours on the job.
“We all have things we wish we had known upon starting our careers,” said Daniel Opris, MD, a primary care physician at Ohio-based Executive Medical Centers.
We tapped several veteran physicians and an educator to learn what they wish med students knew as they enter the workforce. We’ve compiled them here to give you a head start on the lessons ahead.
You Won’t Know Everything, and That’s Okay
When you go through your medical training, it can feel overwhelming to absorb all the knowledge your professors and attendings impart. The bottom line, said Shoshana Ungerleider, MD, an internal medicine specialist, is that you shouldn’t worry about it.
David Lenihan, PhD, CEO at Ponce Health Sciences University, agrees. “What we’ve lost in recent years, is the ability to apply your skill set and say, ‘let me take a day and get back to you,’” he said. “Doctors love it when you do that because it shows you can pitch in and work as part of a team.”
Medicine is a collaborative field, said Ungerleider, and learning from others, whether peers, nurses, or specialists, is “not a weakness.” She recommends embracing uncertainty and getting comfortable with the unknown.
You’ll Take Your Work Home With You
Doctors enter the field because they care about their patients and want to help. Successful outcomes are never guaranteed, however, no matter how much you try. The result? Some days you’ll bring home those upsetting and haunting cases, said Lenihan.
“We often believe that we should leave our work at the office, but sometimes you need to bring it home and think it through,” he said. “It can’t overwhelm you, but you should digest what happened.”
When you do, said Lenihan, you’ll come out the other end more empathetic and that helps the healthcare system in the long run. “The more you reflect on your day, the better you’ll get at reading the room and treating your patients.”
Drew Remignanti, MD, a retired emergency medicine physician from New Hampshire, agrees, but puts a different spin on bringing work home.
“We revisit the patient care decisions we made, second-guess ourselves, and worry about our patients’ welfare and outcomes,” he said. “I think it can only lead to better outcomes down the road, however, if you learn from that bad decision, preventing you from committing a similar mistake.”
Burnout Is Real — Make Self-Care a Priority
As a retired physician who spent 40 years practicing medicine, Remignanti experienced the evolution of healthcare as it has become what he calls a “consumer-provider” model. “Productivity didn’t use to be part of the equation, but now it’s the focus,” he said.
The result is burnout, a very real threat to incoming physicians. Remignanti holds that if you are aware of the risk, you can resist it. Part of avoiding burnout is self-care, according to Ungerleider. “The sooner you prioritize your mental, emotional, and physical well-being, the better,” she said. “Balancing work and life may feel impossible at times but taking care of yourself is essential to being a better physician in the long run.”
That means carving out time for exercise, hobbies, and connections outside of the medical field. It also means making sleep and nutrition a priority, even when that feels hard to accomplish. “If you don’t take care of yourself, you can’t take care of others,” added Opris. “It’s so common to lose yourself in your career, but you need to hold onto your physical, emotional, and spiritual self.”
Avoid Relying Too Heavily on Tech
Technology is invading every aspect of our lives — often for the greater good — but in medicine, it’s important to always return to your core knowledge above all else. Case in point, said Opris, the UpToDate app. While it can be a useful tool, it’s important not to become too reliant on it. “UpToDate is expert opinion-based guidance, and it’s a fantastic resource,” he said. “But you need to use your references and knowledge in every case.”
It’s key to remember that every patient is different, and their case may not line up perfectly with the guidance presented in UpToDate or other technology source. Piggybacking on that, Ungerleider added that it’s important to remember medicine is about people, not just conditions.
“It’s easy to focus on mastering the science, but the real art of medicine comes from seeing the whole person in front of you,” she said. “Your patients are more than their diagnoses — they come with complex emotions, life stories, and needs.” Being compassionate, listening carefully, and building trust should match up to your clinical skills.
Partner With Your Patients, Even When It’s Difficult
Perhaps the most difficult lesson of all is remembering that your patients may not always agree with your recommendations and choose to ignore them. After all your years spent learning, there may be times when it feels your education is going to waste.
“Remember that the landscape today is so varied, and that bleeds into medicine,” said Opris. “We go into cases with our own biases, and it’s important to take a step back to reset, every time.”
Opris reminds himself of Sir William Osler’s famous essay, “Aequanimitas,” in which he tells graduating medical students to practice with “coolness and presence of mind under all circumstances.”
Remignanti offers this advice: “Physicians need to be able to partner with their patients and jointly decide which courses of action are most effective,” he said. “Cling to the idea that you are forming a partnership with your patients — what can we together determine is the best course?”
At the same time, the path the patient chooses may not be what’s best for them — potentially even leading to a poor outcome.
“You may not always understand their choices,” said Opris. “But they do have a choice. Think of yourself almost like a consultant.”
A version of this article first appeared on Medscape.com.
Despite 4 years of med school and 3-7 years in residency, when you enter the workforce as a doctor, you still have much to learn. There is only so much your professors and attending physicians can pack in. Going forward, you’ll continue to learn on the job and via continuing education.
Some of that lifelong learning will involve soft skills — how to compassionately work with your patients and their families, for instance. Other lessons will get down to the business of medicine — the paperwork, the work/life balance, and the moral dilemmas you never saw coming. And still others will involve learning how to take care of yourself in the middle of seemingly endless hours on the job.
“We all have things we wish we had known upon starting our careers,” said Daniel Opris, MD, a primary care physician at Ohio-based Executive Medical Centers.
We tapped several veteran physicians and an educator to learn what they wish med students knew as they enter the workforce. We’ve compiled them here to give you a head start on the lessons ahead.
You Won’t Know Everything, and That’s Okay
When you go through your medical training, it can feel overwhelming to absorb all the knowledge your professors and attendings impart. The bottom line, said Shoshana Ungerleider, MD, an internal medicine specialist, is that you shouldn’t worry about it.
David Lenihan, PhD, CEO at Ponce Health Sciences University, agrees. “What we’ve lost in recent years, is the ability to apply your skill set and say, ‘let me take a day and get back to you,’” he said. “Doctors love it when you do that because it shows you can pitch in and work as part of a team.”
Medicine is a collaborative field, said Ungerleider, and learning from others, whether peers, nurses, or specialists, is “not a weakness.” She recommends embracing uncertainty and getting comfortable with the unknown.
You’ll Take Your Work Home With You
Doctors enter the field because they care about their patients and want to help. Successful outcomes are never guaranteed, however, no matter how much you try. The result? Some days you’ll bring home those upsetting and haunting cases, said Lenihan.
“We often believe that we should leave our work at the office, but sometimes you need to bring it home and think it through,” he said. “It can’t overwhelm you, but you should digest what happened.”
When you do, said Lenihan, you’ll come out the other end more empathetic and that helps the healthcare system in the long run. “The more you reflect on your day, the better you’ll get at reading the room and treating your patients.”
Drew Remignanti, MD, a retired emergency medicine physician from New Hampshire, agrees, but puts a different spin on bringing work home.
“We revisit the patient care decisions we made, second-guess ourselves, and worry about our patients’ welfare and outcomes,” he said. “I think it can only lead to better outcomes down the road, however, if you learn from that bad decision, preventing you from committing a similar mistake.”
Burnout Is Real — Make Self-Care a Priority
As a retired physician who spent 40 years practicing medicine, Remignanti experienced the evolution of healthcare as it has become what he calls a “consumer-provider” model. “Productivity didn’t use to be part of the equation, but now it’s the focus,” he said.
The result is burnout, a very real threat to incoming physicians. Remignanti holds that if you are aware of the risk, you can resist it. Part of avoiding burnout is self-care, according to Ungerleider. “The sooner you prioritize your mental, emotional, and physical well-being, the better,” she said. “Balancing work and life may feel impossible at times but taking care of yourself is essential to being a better physician in the long run.”
That means carving out time for exercise, hobbies, and connections outside of the medical field. It also means making sleep and nutrition a priority, even when that feels hard to accomplish. “If you don’t take care of yourself, you can’t take care of others,” added Opris. “It’s so common to lose yourself in your career, but you need to hold onto your physical, emotional, and spiritual self.”
Avoid Relying Too Heavily on Tech
Technology is invading every aspect of our lives — often for the greater good — but in medicine, it’s important to always return to your core knowledge above all else. Case in point, said Opris, the UpToDate app. While it can be a useful tool, it’s important not to become too reliant on it. “UpToDate is expert opinion-based guidance, and it’s a fantastic resource,” he said. “But you need to use your references and knowledge in every case.”
It’s key to remember that every patient is different, and their case may not line up perfectly with the guidance presented in UpToDate or other technology source. Piggybacking on that, Ungerleider added that it’s important to remember medicine is about people, not just conditions.
“It’s easy to focus on mastering the science, but the real art of medicine comes from seeing the whole person in front of you,” she said. “Your patients are more than their diagnoses — they come with complex emotions, life stories, and needs.” Being compassionate, listening carefully, and building trust should match up to your clinical skills.
Partner With Your Patients, Even When It’s Difficult
Perhaps the most difficult lesson of all is remembering that your patients may not always agree with your recommendations and choose to ignore them. After all your years spent learning, there may be times when it feels your education is going to waste.
“Remember that the landscape today is so varied, and that bleeds into medicine,” said Opris. “We go into cases with our own biases, and it’s important to take a step back to reset, every time.”
Opris reminds himself of Sir William Osler’s famous essay, “Aequanimitas,” in which he tells graduating medical students to practice with “coolness and presence of mind under all circumstances.”
Remignanti offers this advice: “Physicians need to be able to partner with their patients and jointly decide which courses of action are most effective,” he said. “Cling to the idea that you are forming a partnership with your patients — what can we together determine is the best course?”
At the same time, the path the patient chooses may not be what’s best for them — potentially even leading to a poor outcome.
“You may not always understand their choices,” said Opris. “But they do have a choice. Think of yourself almost like a consultant.”
A version of this article first appeared on Medscape.com.
How Do Novel CRC Blood Tests Fare Against Established Tests?
TOPLINE:
METHODOLOGY:
- Researchers estimated the clinical and economic impacts of emerging blood- and stool-based CRC screening tests with established alternatives in average-risk adults aged 45 years and older.
- The established screening tools were colonoscopy, a fecal immunochemical test (FIT), and a multitarget stool DNA test (MT-sDNA, Exact Sciences Cologuard).
- The four emerging screening methods were two cf-bDNA tests (Guardant Shield and Freenome); an enhanced, a next-generation multitarget stool test (ngMT-sDNA), and a novel FIT-RNA test (Geneoscopy ColoSense).
TAKEAWAY:
- Assuming 100% participation in all screening steps, colonoscopy and FIT yielded reductions of more than 70% in CRC incidence and 75% in mortality vs no screening.
- The MT-sDNA test reduced CRC incidence by 68% and mortality by 73%, with similar rates for the ngMT-sDNA and FIT-RNA tests vs no screening. The cf-bDNA tests yielded CRC incidence and mortality reductions of only 42% and 56%.
- Colonoscopy and FIT were more effective and less costly than the cf-bDNA and MT-sDNA tests, and the MT-sDNA test was more effective and less costly than the cf-bDNA test.
- Population benefits from blood tests were seen only in those who declined colonoscopy and stool tests. Substituting a blood test for those already using colonoscopy or stool tests led to worse population-level outcomes.
IN PRACTICE:
“First-generation novel cf-bDNA tests have the potential to decrease meaningfully the incidence and mortality of CRC compared with no screening but substantially less profoundly than screening colonoscopy or stool tests. Net population benefit or harm can follow incorporation of first-generation cf-bDNA CRC screening tests into practice, depending on the balance between bringing unscreened persons into screening (addition) vs shifting persons away from the more effective strategies of colonoscopy or stool testing (substitution),” the authors concluded.
SOURCE:
The study, with first author Uri Ladabaum, MD, MS, Stanford University School of Medicine, California, was published online in Annals of Internal Medicine.
LIMITATIONS:
Limitations included test-specific participation patterns being unknown over time.
DISCLOSURES:
Disclosure forms for the authors are available with the article online. Funding was provided by the Gorrindo Family Fund.
A version of this article appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Researchers estimated the clinical and economic impacts of emerging blood- and stool-based CRC screening tests with established alternatives in average-risk adults aged 45 years and older.
- The established screening tools were colonoscopy, a fecal immunochemical test (FIT), and a multitarget stool DNA test (MT-sDNA, Exact Sciences Cologuard).
- The four emerging screening methods were two cf-bDNA tests (Guardant Shield and Freenome); an enhanced, a next-generation multitarget stool test (ngMT-sDNA), and a novel FIT-RNA test (Geneoscopy ColoSense).
TAKEAWAY:
- Assuming 100% participation in all screening steps, colonoscopy and FIT yielded reductions of more than 70% in CRC incidence and 75% in mortality vs no screening.
- The MT-sDNA test reduced CRC incidence by 68% and mortality by 73%, with similar rates for the ngMT-sDNA and FIT-RNA tests vs no screening. The cf-bDNA tests yielded CRC incidence and mortality reductions of only 42% and 56%.
- Colonoscopy and FIT were more effective and less costly than the cf-bDNA and MT-sDNA tests, and the MT-sDNA test was more effective and less costly than the cf-bDNA test.
- Population benefits from blood tests were seen only in those who declined colonoscopy and stool tests. Substituting a blood test for those already using colonoscopy or stool tests led to worse population-level outcomes.
IN PRACTICE:
“First-generation novel cf-bDNA tests have the potential to decrease meaningfully the incidence and mortality of CRC compared with no screening but substantially less profoundly than screening colonoscopy or stool tests. Net population benefit or harm can follow incorporation of first-generation cf-bDNA CRC screening tests into practice, depending on the balance between bringing unscreened persons into screening (addition) vs shifting persons away from the more effective strategies of colonoscopy or stool testing (substitution),” the authors concluded.
SOURCE:
The study, with first author Uri Ladabaum, MD, MS, Stanford University School of Medicine, California, was published online in Annals of Internal Medicine.
LIMITATIONS:
Limitations included test-specific participation patterns being unknown over time.
DISCLOSURES:
Disclosure forms for the authors are available with the article online. Funding was provided by the Gorrindo Family Fund.
A version of this article appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Researchers estimated the clinical and economic impacts of emerging blood- and stool-based CRC screening tests with established alternatives in average-risk adults aged 45 years and older.
- The established screening tools were colonoscopy, a fecal immunochemical test (FIT), and a multitarget stool DNA test (MT-sDNA, Exact Sciences Cologuard).
- The four emerging screening methods were two cf-bDNA tests (Guardant Shield and Freenome); an enhanced, a next-generation multitarget stool test (ngMT-sDNA), and a novel FIT-RNA test (Geneoscopy ColoSense).
TAKEAWAY:
- Assuming 100% participation in all screening steps, colonoscopy and FIT yielded reductions of more than 70% in CRC incidence and 75% in mortality vs no screening.
- The MT-sDNA test reduced CRC incidence by 68% and mortality by 73%, with similar rates for the ngMT-sDNA and FIT-RNA tests vs no screening. The cf-bDNA tests yielded CRC incidence and mortality reductions of only 42% and 56%.
- Colonoscopy and FIT were more effective and less costly than the cf-bDNA and MT-sDNA tests, and the MT-sDNA test was more effective and less costly than the cf-bDNA test.
- Population benefits from blood tests were seen only in those who declined colonoscopy and stool tests. Substituting a blood test for those already using colonoscopy or stool tests led to worse population-level outcomes.
IN PRACTICE:
“First-generation novel cf-bDNA tests have the potential to decrease meaningfully the incidence and mortality of CRC compared with no screening but substantially less profoundly than screening colonoscopy or stool tests. Net population benefit or harm can follow incorporation of first-generation cf-bDNA CRC screening tests into practice, depending on the balance between bringing unscreened persons into screening (addition) vs shifting persons away from the more effective strategies of colonoscopy or stool testing (substitution),” the authors concluded.
SOURCE:
The study, with first author Uri Ladabaum, MD, MS, Stanford University School of Medicine, California, was published online in Annals of Internal Medicine.
LIMITATIONS:
Limitations included test-specific participation patterns being unknown over time.
DISCLOSURES:
Disclosure forms for the authors are available with the article online. Funding was provided by the Gorrindo Family Fund.
A version of this article appeared on Medscape.com.
Tips on Handling a Negative Patient Review
LAS VEGAS —
“It said something like, ‘Do not see Joe the fake doctor. Joe should have his medical license pulled. He didn’t listen to me. He threw drugs at me and he only talked to me for 5 minutes,’ ” Cari, who practices at the University of Colorado Anschutz Medical Campus, Aurora, said at the Society of Dermatology Physician Associates (SDPA) 22nd Annual Fall Dermatology Conference. “Being early in my practice, that hurt; it was a jab to the heart. I had about 20-30 five-star reviews, but I laser-focused on the bad one.”
When a review questions competence, it can feel personal, he continued, even though it often reflects the reviewer’s emotions or experience. Cari, a former Marine, said that clinicians can mitigate emotional responses to negative reviews by building emotional resilience. He draws inspiration from Stoicism (the school of philosophy that originated during the Hellenistic period), which emphasizes developing inner resilience, managing emotions, “and cultivating virtues such as wisdom, courage, and self-discipline,” he said.
Cari often cites a quote from Marcus Aurelius, the former Roman Emperor and Stoic philosopher: “You have power over your mind — not outside events. Realize this, and you will find strength.” Another quote that changed his perspective comes from the Stoic Epictetus: “We cannot control the external events around us, but we can control our reactions to them.”
On a practical level, Cari shared several ways that clinicians can cultivate emotional resilience when faced with a negative review.
Practice mindfulness. Reading reviews in a nonjudgmental way “allows us to pause, reflect, and respond thoughtfully rather than react emotionally,” he explained. He also recommended setting clear boundaries between work and personal life to prevent burnout and maintain a healthy work–life balance. Realizing he needed time to decompress after a previous job that involved a 1-hour drive, he began listening to audiobooks on his way home. “I set that time aside for myself to listen, relax, and let all my troubles from work melt away,” Cari said.
Develop a support network. This includes both professionals, such as therapists, and personal connections, such as colleagues, mentors, and friends.
Practice self-care. Whether it’s yoga, running, jogging, spending time with loved ones, or playing with your dog, find activities that help you recharge. “Most importantly, get some rest and take a vacation,” Cari advised. “Your body is like a machine. If you do not rest it and take care of it, it will slowly breakdown and burnout.”
Practice equanimity. Cari defined this as mental calmness, composure, and evenness of temper, especially in a difficult situation. “Maintaining a calm and balanced state of mind, regardless of external circumstances, is a core Stoic and military practice,” he said.
According to data he attributed to reviewtrackers, an estimated 60% of reviews are influenced by the reviewer’s personal stress or mood, “so don’t take [bad reviews] personally,” he said. Instead, view criticism as an opportunity for self-improvement and to gain insight into others’ perspectives. Cari recommended practicing indifference to both praise and blame. “Do not seek validation or be disheartened by negative reviews,” he said. “Remain focused on your own standards of excellence.”
Cari has reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
LAS VEGAS —
“It said something like, ‘Do not see Joe the fake doctor. Joe should have his medical license pulled. He didn’t listen to me. He threw drugs at me and he only talked to me for 5 minutes,’ ” Cari, who practices at the University of Colorado Anschutz Medical Campus, Aurora, said at the Society of Dermatology Physician Associates (SDPA) 22nd Annual Fall Dermatology Conference. “Being early in my practice, that hurt; it was a jab to the heart. I had about 20-30 five-star reviews, but I laser-focused on the bad one.”
When a review questions competence, it can feel personal, he continued, even though it often reflects the reviewer’s emotions or experience. Cari, a former Marine, said that clinicians can mitigate emotional responses to negative reviews by building emotional resilience. He draws inspiration from Stoicism (the school of philosophy that originated during the Hellenistic period), which emphasizes developing inner resilience, managing emotions, “and cultivating virtues such as wisdom, courage, and self-discipline,” he said.
Cari often cites a quote from Marcus Aurelius, the former Roman Emperor and Stoic philosopher: “You have power over your mind — not outside events. Realize this, and you will find strength.” Another quote that changed his perspective comes from the Stoic Epictetus: “We cannot control the external events around us, but we can control our reactions to them.”
On a practical level, Cari shared several ways that clinicians can cultivate emotional resilience when faced with a negative review.
Practice mindfulness. Reading reviews in a nonjudgmental way “allows us to pause, reflect, and respond thoughtfully rather than react emotionally,” he explained. He also recommended setting clear boundaries between work and personal life to prevent burnout and maintain a healthy work–life balance. Realizing he needed time to decompress after a previous job that involved a 1-hour drive, he began listening to audiobooks on his way home. “I set that time aside for myself to listen, relax, and let all my troubles from work melt away,” Cari said.
Develop a support network. This includes both professionals, such as therapists, and personal connections, such as colleagues, mentors, and friends.
Practice self-care. Whether it’s yoga, running, jogging, spending time with loved ones, or playing with your dog, find activities that help you recharge. “Most importantly, get some rest and take a vacation,” Cari advised. “Your body is like a machine. If you do not rest it and take care of it, it will slowly breakdown and burnout.”
Practice equanimity. Cari defined this as mental calmness, composure, and evenness of temper, especially in a difficult situation. “Maintaining a calm and balanced state of mind, regardless of external circumstances, is a core Stoic and military practice,” he said.
According to data he attributed to reviewtrackers, an estimated 60% of reviews are influenced by the reviewer’s personal stress or mood, “so don’t take [bad reviews] personally,” he said. Instead, view criticism as an opportunity for self-improvement and to gain insight into others’ perspectives. Cari recommended practicing indifference to both praise and blame. “Do not seek validation or be disheartened by negative reviews,” he said. “Remain focused on your own standards of excellence.”
Cari has reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
LAS VEGAS —
“It said something like, ‘Do not see Joe the fake doctor. Joe should have his medical license pulled. He didn’t listen to me. He threw drugs at me and he only talked to me for 5 minutes,’ ” Cari, who practices at the University of Colorado Anschutz Medical Campus, Aurora, said at the Society of Dermatology Physician Associates (SDPA) 22nd Annual Fall Dermatology Conference. “Being early in my practice, that hurt; it was a jab to the heart. I had about 20-30 five-star reviews, but I laser-focused on the bad one.”
When a review questions competence, it can feel personal, he continued, even though it often reflects the reviewer’s emotions or experience. Cari, a former Marine, said that clinicians can mitigate emotional responses to negative reviews by building emotional resilience. He draws inspiration from Stoicism (the school of philosophy that originated during the Hellenistic period), which emphasizes developing inner resilience, managing emotions, “and cultivating virtues such as wisdom, courage, and self-discipline,” he said.
Cari often cites a quote from Marcus Aurelius, the former Roman Emperor and Stoic philosopher: “You have power over your mind — not outside events. Realize this, and you will find strength.” Another quote that changed his perspective comes from the Stoic Epictetus: “We cannot control the external events around us, but we can control our reactions to them.”
On a practical level, Cari shared several ways that clinicians can cultivate emotional resilience when faced with a negative review.
Practice mindfulness. Reading reviews in a nonjudgmental way “allows us to pause, reflect, and respond thoughtfully rather than react emotionally,” he explained. He also recommended setting clear boundaries between work and personal life to prevent burnout and maintain a healthy work–life balance. Realizing he needed time to decompress after a previous job that involved a 1-hour drive, he began listening to audiobooks on his way home. “I set that time aside for myself to listen, relax, and let all my troubles from work melt away,” Cari said.
Develop a support network. This includes both professionals, such as therapists, and personal connections, such as colleagues, mentors, and friends.
Practice self-care. Whether it’s yoga, running, jogging, spending time with loved ones, or playing with your dog, find activities that help you recharge. “Most importantly, get some rest and take a vacation,” Cari advised. “Your body is like a machine. If you do not rest it and take care of it, it will slowly breakdown and burnout.”
Practice equanimity. Cari defined this as mental calmness, composure, and evenness of temper, especially in a difficult situation. “Maintaining a calm and balanced state of mind, regardless of external circumstances, is a core Stoic and military practice,” he said.
According to data he attributed to reviewtrackers, an estimated 60% of reviews are influenced by the reviewer’s personal stress or mood, “so don’t take [bad reviews] personally,” he said. Instead, view criticism as an opportunity for self-improvement and to gain insight into others’ perspectives. Cari recommended practicing indifference to both praise and blame. “Do not seek validation or be disheartened by negative reviews,” he said. “Remain focused on your own standards of excellence.”
Cari has reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
FROM SDPA 24
From Primary Care to Specialization: How PAs Make a Specialty Switch
Physician assistants (PAs) are educated as generalists — with the ability to switch medical specialties during their careers. Andrzej Kozikowski, PhD, senior director of research at the National Commission on Certification of Physician Assistants (NCCPA), said that having that kind of career flexibility is often a motivating factor for students who pursue the PA path.
“If you look at the research literature on physicians, you can see that choosing a specialty can be quite stressful,” he told this news organization. “It’s a lifelong decision. You have to commit to a residency, maybe fellowship training, and if you don’t like it and want to switch your specialty, you have to go back and do it again. It’s a decision that weighs heavily on your [physicians] shoulders.”
The PA profession, however, offers lateral movement. Rachel Porter, PhD, interim director of preclinical education at PA program, Duke University, Durham, North Carolina, said that the didactic portion of a PA’s medical education is very broad to support that kind of flexibility. And most PA students, depending on their program, have the opportunity to go through several clinical rotations to see which specialty might be the best fit.
“That initial medical education is meant to provide a good foundation across all systems, across all age groups, subpopulations, and settings — hospital, ambulatory, or outpatient,” she explained. “Once they are exposed to clinical experiences later, we find that students discover their niche and where they want to be once they start their career.”
Making a Lateral Move
According to the 2022 Statistical Profile of Board-Certified PAs by Specialty, based on a survey conducted by the NCCPA, approximately half of board-certified PAs have switched to a different specialty at least once during their career. Nearly 31% have done so at least twice.
Eric Van Hecke, DMSc, MPAS, PA-C, CAQ-EM, assistant professor and PA program director at Concordia University, St. Paul in St. Paul, Minnesota, works in emergency medicine, thanks to his clinical rotations during PA school, which helped him determine that a surgical specialty was not for him.
“I did some surgical rotations, and I found I hated being in the operating room,” he said. “I didn’t like the way PAs were utilized there. But then, toward the end of my PA program, I had the opportunity to do an emergency department rotation and found it was a much better fit.”
Other PAs, however, may not be as lucky to find the right practice straight out of school. Some may be limited by job availability in a specific geographic area, while others may feel more comfortable starting in a hospital setting. Lyndsey Milcarek, PA-C, MPH, a PA in Buffalo, New York, said she started in a primary care role after school but moved to geriatric home health after a year. Then, 3 years later, she switched specialties again to join an emergency department. She said her decisions to move were largely driven by organizational issues.
“In one case, I saw the organization was headed for a buyout and I wanted to get ahead of it,” she said. “In another, the workload was a lot, and you couldn’t go home at the end of your shift if there were still patients to see. It was a recipe for burnout.”
Amanda Michaud, DMSc, PA-C, in Jacksonville, Florida, said she initially enjoyed the “fast-paced environment” of emergency medicine after graduating from PA school. But when her family was looking at a move out of state, she started to consider a specialty change and ultimately ended up joining an allergy practice.
“I wanted to have a more nine-to-five kind of job. I wanted my weekends. I had missed a lot of holidays with my family,” she said. “But I also was interested in becoming more of an expert in a particular field. In the ER, you become an expert in saving lives and stabilizing patients. But I wanted an opportunity to truly learn the medicine and science behind one area.”
Understand Your Why — and Do the Work
The reasons a PA might choose to make a specialty switch aren’t unlike the reasons a corporate attorney might want to practice family law or a nurse practitioner might want to switch from the ICU to the pediatric ward. People might consider it a change of scenery. Some may be looking to relocate, support a better work-life balance, reduce their stress, expand their skills and knowledge, find a more palatable work environment, or make more money. But those who have made lateral moves said it isn’t as easy as it may look.
“It will take time, not just to learn the new specialty but to understand how your new practice does things,” said Michaud. “You need to expect a huge learning curve ahead when you make a change.”
Milcarek added that PAs who are considering a switch should think long and hard about the kind of environment they want to work in and, as they look at other departments or practices, spend time talking to and shadowing PAs to understand what working there will look like. Just because a particular specialty has a reputation for being low stress (or high paying) doesn’t mean that’s what you’ll find once you come on board. So much depends on your employer — and the people you work with.
“There are a lot of opportunities for PA jobs, but employers aren’t always transparent about workflows and management,” Milcarek said. “You want to have good intel upfront before you make a decision.”
Kozikowski agreed. “It takes a while to adapt to a new environment and to understand how things are done,” he explained. “Research suggests that having a good network, mentors, and good onboarding programs are really important. It’s not just finding continuing medical education, you also need to have the right support system in place.”
Despite the challenges involved with a specialty switch, Milcarek said her moves have made her a stronger overall clinician.
“I have a unique perspective because I’ve worked in so many different areas,” she said. “I’ve learned a lot in each and can apply those things in my new roles. I feel fortunate that I’ve been able to make these switches and continue to learn and grow and become a better PA.”
A version of this article first appeared on Medscape.com.
Physician assistants (PAs) are educated as generalists — with the ability to switch medical specialties during their careers. Andrzej Kozikowski, PhD, senior director of research at the National Commission on Certification of Physician Assistants (NCCPA), said that having that kind of career flexibility is often a motivating factor for students who pursue the PA path.
“If you look at the research literature on physicians, you can see that choosing a specialty can be quite stressful,” he told this news organization. “It’s a lifelong decision. You have to commit to a residency, maybe fellowship training, and if you don’t like it and want to switch your specialty, you have to go back and do it again. It’s a decision that weighs heavily on your [physicians] shoulders.”
The PA profession, however, offers lateral movement. Rachel Porter, PhD, interim director of preclinical education at PA program, Duke University, Durham, North Carolina, said that the didactic portion of a PA’s medical education is very broad to support that kind of flexibility. And most PA students, depending on their program, have the opportunity to go through several clinical rotations to see which specialty might be the best fit.
“That initial medical education is meant to provide a good foundation across all systems, across all age groups, subpopulations, and settings — hospital, ambulatory, or outpatient,” she explained. “Once they are exposed to clinical experiences later, we find that students discover their niche and where they want to be once they start their career.”
Making a Lateral Move
According to the 2022 Statistical Profile of Board-Certified PAs by Specialty, based on a survey conducted by the NCCPA, approximately half of board-certified PAs have switched to a different specialty at least once during their career. Nearly 31% have done so at least twice.
Eric Van Hecke, DMSc, MPAS, PA-C, CAQ-EM, assistant professor and PA program director at Concordia University, St. Paul in St. Paul, Minnesota, works in emergency medicine, thanks to his clinical rotations during PA school, which helped him determine that a surgical specialty was not for him.
“I did some surgical rotations, and I found I hated being in the operating room,” he said. “I didn’t like the way PAs were utilized there. But then, toward the end of my PA program, I had the opportunity to do an emergency department rotation and found it was a much better fit.”
Other PAs, however, may not be as lucky to find the right practice straight out of school. Some may be limited by job availability in a specific geographic area, while others may feel more comfortable starting in a hospital setting. Lyndsey Milcarek, PA-C, MPH, a PA in Buffalo, New York, said she started in a primary care role after school but moved to geriatric home health after a year. Then, 3 years later, she switched specialties again to join an emergency department. She said her decisions to move were largely driven by organizational issues.
“In one case, I saw the organization was headed for a buyout and I wanted to get ahead of it,” she said. “In another, the workload was a lot, and you couldn’t go home at the end of your shift if there were still patients to see. It was a recipe for burnout.”
Amanda Michaud, DMSc, PA-C, in Jacksonville, Florida, said she initially enjoyed the “fast-paced environment” of emergency medicine after graduating from PA school. But when her family was looking at a move out of state, she started to consider a specialty change and ultimately ended up joining an allergy practice.
“I wanted to have a more nine-to-five kind of job. I wanted my weekends. I had missed a lot of holidays with my family,” she said. “But I also was interested in becoming more of an expert in a particular field. In the ER, you become an expert in saving lives and stabilizing patients. But I wanted an opportunity to truly learn the medicine and science behind one area.”
Understand Your Why — and Do the Work
The reasons a PA might choose to make a specialty switch aren’t unlike the reasons a corporate attorney might want to practice family law or a nurse practitioner might want to switch from the ICU to the pediatric ward. People might consider it a change of scenery. Some may be looking to relocate, support a better work-life balance, reduce their stress, expand their skills and knowledge, find a more palatable work environment, or make more money. But those who have made lateral moves said it isn’t as easy as it may look.
“It will take time, not just to learn the new specialty but to understand how your new practice does things,” said Michaud. “You need to expect a huge learning curve ahead when you make a change.”
Milcarek added that PAs who are considering a switch should think long and hard about the kind of environment they want to work in and, as they look at other departments or practices, spend time talking to and shadowing PAs to understand what working there will look like. Just because a particular specialty has a reputation for being low stress (or high paying) doesn’t mean that’s what you’ll find once you come on board. So much depends on your employer — and the people you work with.
“There are a lot of opportunities for PA jobs, but employers aren’t always transparent about workflows and management,” Milcarek said. “You want to have good intel upfront before you make a decision.”
Kozikowski agreed. “It takes a while to adapt to a new environment and to understand how things are done,” he explained. “Research suggests that having a good network, mentors, and good onboarding programs are really important. It’s not just finding continuing medical education, you also need to have the right support system in place.”
Despite the challenges involved with a specialty switch, Milcarek said her moves have made her a stronger overall clinician.
“I have a unique perspective because I’ve worked in so many different areas,” she said. “I’ve learned a lot in each and can apply those things in my new roles. I feel fortunate that I’ve been able to make these switches and continue to learn and grow and become a better PA.”
A version of this article first appeared on Medscape.com.
Physician assistants (PAs) are educated as generalists — with the ability to switch medical specialties during their careers. Andrzej Kozikowski, PhD, senior director of research at the National Commission on Certification of Physician Assistants (NCCPA), said that having that kind of career flexibility is often a motivating factor for students who pursue the PA path.
“If you look at the research literature on physicians, you can see that choosing a specialty can be quite stressful,” he told this news organization. “It’s a lifelong decision. You have to commit to a residency, maybe fellowship training, and if you don’t like it and want to switch your specialty, you have to go back and do it again. It’s a decision that weighs heavily on your [physicians] shoulders.”
The PA profession, however, offers lateral movement. Rachel Porter, PhD, interim director of preclinical education at PA program, Duke University, Durham, North Carolina, said that the didactic portion of a PA’s medical education is very broad to support that kind of flexibility. And most PA students, depending on their program, have the opportunity to go through several clinical rotations to see which specialty might be the best fit.
“That initial medical education is meant to provide a good foundation across all systems, across all age groups, subpopulations, and settings — hospital, ambulatory, or outpatient,” she explained. “Once they are exposed to clinical experiences later, we find that students discover their niche and where they want to be once they start their career.”
Making a Lateral Move
According to the 2022 Statistical Profile of Board-Certified PAs by Specialty, based on a survey conducted by the NCCPA, approximately half of board-certified PAs have switched to a different specialty at least once during their career. Nearly 31% have done so at least twice.
Eric Van Hecke, DMSc, MPAS, PA-C, CAQ-EM, assistant professor and PA program director at Concordia University, St. Paul in St. Paul, Minnesota, works in emergency medicine, thanks to his clinical rotations during PA school, which helped him determine that a surgical specialty was not for him.
“I did some surgical rotations, and I found I hated being in the operating room,” he said. “I didn’t like the way PAs were utilized there. But then, toward the end of my PA program, I had the opportunity to do an emergency department rotation and found it was a much better fit.”
Other PAs, however, may not be as lucky to find the right practice straight out of school. Some may be limited by job availability in a specific geographic area, while others may feel more comfortable starting in a hospital setting. Lyndsey Milcarek, PA-C, MPH, a PA in Buffalo, New York, said she started in a primary care role after school but moved to geriatric home health after a year. Then, 3 years later, she switched specialties again to join an emergency department. She said her decisions to move were largely driven by organizational issues.
“In one case, I saw the organization was headed for a buyout and I wanted to get ahead of it,” she said. “In another, the workload was a lot, and you couldn’t go home at the end of your shift if there were still patients to see. It was a recipe for burnout.”
Amanda Michaud, DMSc, PA-C, in Jacksonville, Florida, said she initially enjoyed the “fast-paced environment” of emergency medicine after graduating from PA school. But when her family was looking at a move out of state, she started to consider a specialty change and ultimately ended up joining an allergy practice.
“I wanted to have a more nine-to-five kind of job. I wanted my weekends. I had missed a lot of holidays with my family,” she said. “But I also was interested in becoming more of an expert in a particular field. In the ER, you become an expert in saving lives and stabilizing patients. But I wanted an opportunity to truly learn the medicine and science behind one area.”
Understand Your Why — and Do the Work
The reasons a PA might choose to make a specialty switch aren’t unlike the reasons a corporate attorney might want to practice family law or a nurse practitioner might want to switch from the ICU to the pediatric ward. People might consider it a change of scenery. Some may be looking to relocate, support a better work-life balance, reduce their stress, expand their skills and knowledge, find a more palatable work environment, or make more money. But those who have made lateral moves said it isn’t as easy as it may look.
“It will take time, not just to learn the new specialty but to understand how your new practice does things,” said Michaud. “You need to expect a huge learning curve ahead when you make a change.”
Milcarek added that PAs who are considering a switch should think long and hard about the kind of environment they want to work in and, as they look at other departments or practices, spend time talking to and shadowing PAs to understand what working there will look like. Just because a particular specialty has a reputation for being low stress (or high paying) doesn’t mean that’s what you’ll find once you come on board. So much depends on your employer — and the people you work with.
“There are a lot of opportunities for PA jobs, but employers aren’t always transparent about workflows and management,” Milcarek said. “You want to have good intel upfront before you make a decision.”
Kozikowski agreed. “It takes a while to adapt to a new environment and to understand how things are done,” he explained. “Research suggests that having a good network, mentors, and good onboarding programs are really important. It’s not just finding continuing medical education, you also need to have the right support system in place.”
Despite the challenges involved with a specialty switch, Milcarek said her moves have made her a stronger overall clinician.
“I have a unique perspective because I’ve worked in so many different areas,” she said. “I’ve learned a lot in each and can apply those things in my new roles. I feel fortunate that I’ve been able to make these switches and continue to learn and grow and become a better PA.”
A version of this article first appeared on Medscape.com.
Weight Loss Treatments Beyond the Reach of Many in Need
SAN ANTONIO — Weight loss treatments aren’t reaching many of the people who need them most because of coverage barriers, new data suggested.
Findings from three studies presented at The Obesity Society’s Obesity Week 2024 meeting illustrate different aspects of the problem.
One, presented by Alissa S. Chen, MD, MPH, a postdoctoral fellow at Yale University, New Haven, Connecticut, found that people with obesity, particularly those with cardiovascular disease (CVD) and those who are Black and Hispanic, have high rates of cost-related prescription drug rationing. Those findings were simultaneously published as a research letter in JAMA Network Open.
“The implications are that structural barriers impede access to medications for Black and Hispanic adults with obesity, which might worsen if there’s not expanding coverage for GLP-1 RAs [glucagon-like peptide 1 receptor agonists], and it’s possible that broader insurance coverage could ameliorate some of these issues,” Chen said.
She noted that patients don’t always volunteer that information. “In my clinical practice, I always start by saying something like, ‘I have a lot of patients who can’t afford their medications. In the last week, was there a time [you didn’t take your medications due to cost]?’ ”
State Medicaid programs vary widely in the degree to which they cover weight loss treatments. But not a single one covers all modalities — nutrition counseling (NC), intensive behavioral therapy (IBT), obesity medications (OMs), and metabolic and bariatric surgery (MBS) — without restrictions or limitations, and only seven states cover them all with restrictions, according to a dual presentation by Christine Gallagher, MPAff, associate director for research and policy with the STOP Obesity Alliance at George Washington University, Washington, DC, and Tracy Zvenyach, PhD, MS, RN, director of policy strategy and alliances at the Obesity Action Coalition, also in Washington, DC.
Detailed Medicaid coverage data for each state are posted on the STOP Obesity Alliance website. (As of now, Medicare doesn’t cover medications specifically for obesity at all.)
A third presentation, by Treah Haggerty, MD, of the Department of Family Medicine and director of the Pediatric Medical Weight Management program at West Virginia University, Morgantown, was of a qualitative descriptive study exploring the impact on 22 individuals enrolled in a medical weight loss management program whose state employee insurance carrier made a policy decision to stop covering all anti-OMs in March 2024. All had been prescribed GLP-1 agonists for weight loss, and the decision forced most to stop using them.
Those findings were published in the September 2024 issue of Obesity Pillars.
“Patients perceive the discontinuation of anti-obesity medication coverage as stigmatizing and unjust, leading to feelings of hopelessness and fear. With more insurance companies denying coverage for these costly medications, more information is needed to identify best ways to address the loss of coverage with patients. Clinical management of these patients should incorporate evidence-based obesity treatments while navigating insurance constraints,” Haggerty said.
Create a Safe Space to Discuss the Barriers
Asked to comment, Session Moderator John D. Clark, MD, PhD, chief population health officer at Sharp Rees-Stealy Medical Group, San Diego, California, told Medscape Medical News, “Health systems and payers are determining what can and can’t be covered, and at the end of the day, it frequently comes down to finances…I think the big challenge is really identifying patients who may have the greatest need. ... If we have limited resources, how and where should we be directing those resources? I would say the current system hasn’t really answered that question or identified patients for whom we would say that the cost truly is less than either the financial or long-term health benefits.”
But Clark said, “When some of these newer anti-obesity medications are able to go generic and be less expensive, which will happen eventually, I think things will change ... and in the future, there will be more options on the market as well.”
In the meantime, he advised that clinicians “try to have conversations with patients about these barriers, acknowledge that these barriers exist, and create a safe space to discuss those barriers. ... Let’s see where we are right now, and let’s come up with a plan.”
People With Obesity More Susceptible to Drug Rationing
Chen reported on a sample of 51,720 adults who participated in the 2020-2022 National Health Interview Survey who did not have diabetes and who used at least one prescription medication of any type. Of those, 80% were White, 9.7% were Hispanic, and 9.7% were Black, and 33.9% overall had obesity.
Cost-related prescription rationing, defined as any self-reported skipping, taking less, or delaying filling a prescription to save money, was reported by 8.3% of those with obesity vs 5.9% without. After adjustment, rationing among those with obesity was significantly associated with younger age (aged 18-44 years), female sex, lower incomes, lack of health insurance coverage, and CVD.
The adjusted estimated probability of cost-related prescription drug rationing was 7.4% for those with CVD vs 4.4% for those without. By race/ethnicity, the proportions reporting rationing were 7.7%, 9.8%, and 10.7% for White, Black, and Hispanics, respectively.
“Given that few insurance providers cover GLP-1 RAs for obesity, cost-related prescription drug rationing could be exacerbated if patients were prescribed GLP-1 RAs at their current price of more than $1000 a month,” Chen noted, adding that the high prices could worsen health disparities among Black and Hispanic individuals with obesity.
Medicaid Coverage Lacking for All Obesity Treatments
For their project, Gallagher and Zvenyach delved into a database that aggregates Medicaid manuals, fee schedules, statutes, regulations, and preferred drug lists for each US state, both for Medicaid fee for service and top Medicaid managed care plans, in order to determine 2024 levels of coverage for NC, IBT, OMs, and MBS for adults with obesity.
No state provides coverage for all those treatments without either limitations — such as body mass index (BMI) cutoffs, age, or “comorbidity regardless of body mass index (BMI)” for OM and MBS — or outright restrictions, such as “proof of failed attempts.” And only seven states provide coverage for the four modalities “with limitations”: California, Arizona, New Mexico, South Carolina, Delaware, Rhode Island, and Massachusetts.
Twenty-two states don’t cover NC, although just one state doesn’t cover IBT. Overall, 37 states don’t cover OMs, and other states ranged considerably in various restrictions and limitations for OMs and MBS. Only four states fully covered the surgery without limitations or restrictions.
“The vast majority of states have significant barriers and conditions of coverage for obesity care,” Gallagher said.
Zvenyach added, “Most of the applied exclusions, limitations, or restrictions do not align with evidence-based practice standards or guidelines.”
When Coverage Stops, Hopelessness and Anger Emerge
Haggerty and colleagues’ research involved semi-structured interviews of the 22 participants — all of them women — who had lost their obesity medication coverage due to their insurers’ decision. Four themes emerged:
- 1. Feelings of hope replaced by hopelessness upon loss of medication coverage: One person said, “I’m afraid for my mental health. It’s tough to be in a situation where you’re never right. And it doesn’t matter what you do; it’s not going to work, and then to have just a glimmer of hope, a little spark of hey, look, this might help. And for someone else to take that away from you for no reason. I don’t know what am I supposed to do.”
- 2. Anger regarding the perceived injustice of anti-obesity medication coverage termination: For example, “They can pay for heart attacks, they could pay for me to have a stroke, they could pay for me to have diabetes, but they won’t let me have this one medicine that could take all of that away. Makes no sense.”
- 3. Perceptions of past and present stigma within the healthcare system and insurance company: “I’m not trying for vanity. I’m way too old to be a Victoria’s Secret model. I’m not trying to do it to be cute and skinny and hot. I just want to make it through a day of work and not be exhausted.”
- 4. Generational influences on obesity treatment: “I’m married, and my husband, since I’ve started this medicine, he’s been eating better. He’s been eating what I eat, and he’s been losing weight as well.”
- Some participants said they planned to cope in different ways, including trying to obtain compounded versions of the drugs from “spas” or online pharmacies, as well as skipping doses, reducing doses, or sharing medications — in other words, rationing.
Asked by this news organization what clinicians should keep in mind, Haggerty said, “that there are big barriers and that we need to take care of the patients within this system that has their arm tied behind their back.
Chen was funded by a grant from the National Institute on Aging outside the submitted work, and she was funded as a Yale National Clinician Scholar. A coauthor received grants from the Food and Drug Administration, Johnson & Johnson, the National Institutes of Health, the Agency for Healthcare Research and Quality, and Arnold Ventures. Another coauthor reported receiving personal fees from UpToDate and the Centers for Medicare & Medicaid Services. Gallagher has received research funding from Altimmune, Amgen, Boehringer Ingelheim, Currax, Eli Lilly and Company, Found, Novo Nordisk, Pfizer, Structure Therapeutics, and WeightWatchers. Haggerty reported article publishing charge was provided by West Virginia Alliance for Creative Health Solutions. Zvenyach and Clark had no disclosures.
A version of this article first appeared on Medscape.com.
SAN ANTONIO — Weight loss treatments aren’t reaching many of the people who need them most because of coverage barriers, new data suggested.
Findings from three studies presented at The Obesity Society’s Obesity Week 2024 meeting illustrate different aspects of the problem.
One, presented by Alissa S. Chen, MD, MPH, a postdoctoral fellow at Yale University, New Haven, Connecticut, found that people with obesity, particularly those with cardiovascular disease (CVD) and those who are Black and Hispanic, have high rates of cost-related prescription drug rationing. Those findings were simultaneously published as a research letter in JAMA Network Open.
“The implications are that structural barriers impede access to medications for Black and Hispanic adults with obesity, which might worsen if there’s not expanding coverage for GLP-1 RAs [glucagon-like peptide 1 receptor agonists], and it’s possible that broader insurance coverage could ameliorate some of these issues,” Chen said.
She noted that patients don’t always volunteer that information. “In my clinical practice, I always start by saying something like, ‘I have a lot of patients who can’t afford their medications. In the last week, was there a time [you didn’t take your medications due to cost]?’ ”
State Medicaid programs vary widely in the degree to which they cover weight loss treatments. But not a single one covers all modalities — nutrition counseling (NC), intensive behavioral therapy (IBT), obesity medications (OMs), and metabolic and bariatric surgery (MBS) — without restrictions or limitations, and only seven states cover them all with restrictions, according to a dual presentation by Christine Gallagher, MPAff, associate director for research and policy with the STOP Obesity Alliance at George Washington University, Washington, DC, and Tracy Zvenyach, PhD, MS, RN, director of policy strategy and alliances at the Obesity Action Coalition, also in Washington, DC.
Detailed Medicaid coverage data for each state are posted on the STOP Obesity Alliance website. (As of now, Medicare doesn’t cover medications specifically for obesity at all.)
A third presentation, by Treah Haggerty, MD, of the Department of Family Medicine and director of the Pediatric Medical Weight Management program at West Virginia University, Morgantown, was of a qualitative descriptive study exploring the impact on 22 individuals enrolled in a medical weight loss management program whose state employee insurance carrier made a policy decision to stop covering all anti-OMs in March 2024. All had been prescribed GLP-1 agonists for weight loss, and the decision forced most to stop using them.
Those findings were published in the September 2024 issue of Obesity Pillars.
“Patients perceive the discontinuation of anti-obesity medication coverage as stigmatizing and unjust, leading to feelings of hopelessness and fear. With more insurance companies denying coverage for these costly medications, more information is needed to identify best ways to address the loss of coverage with patients. Clinical management of these patients should incorporate evidence-based obesity treatments while navigating insurance constraints,” Haggerty said.
Create a Safe Space to Discuss the Barriers
Asked to comment, Session Moderator John D. Clark, MD, PhD, chief population health officer at Sharp Rees-Stealy Medical Group, San Diego, California, told Medscape Medical News, “Health systems and payers are determining what can and can’t be covered, and at the end of the day, it frequently comes down to finances…I think the big challenge is really identifying patients who may have the greatest need. ... If we have limited resources, how and where should we be directing those resources? I would say the current system hasn’t really answered that question or identified patients for whom we would say that the cost truly is less than either the financial or long-term health benefits.”
But Clark said, “When some of these newer anti-obesity medications are able to go generic and be less expensive, which will happen eventually, I think things will change ... and in the future, there will be more options on the market as well.”
In the meantime, he advised that clinicians “try to have conversations with patients about these barriers, acknowledge that these barriers exist, and create a safe space to discuss those barriers. ... Let’s see where we are right now, and let’s come up with a plan.”
People With Obesity More Susceptible to Drug Rationing
Chen reported on a sample of 51,720 adults who participated in the 2020-2022 National Health Interview Survey who did not have diabetes and who used at least one prescription medication of any type. Of those, 80% were White, 9.7% were Hispanic, and 9.7% were Black, and 33.9% overall had obesity.
Cost-related prescription rationing, defined as any self-reported skipping, taking less, or delaying filling a prescription to save money, was reported by 8.3% of those with obesity vs 5.9% without. After adjustment, rationing among those with obesity was significantly associated with younger age (aged 18-44 years), female sex, lower incomes, lack of health insurance coverage, and CVD.
The adjusted estimated probability of cost-related prescription drug rationing was 7.4% for those with CVD vs 4.4% for those without. By race/ethnicity, the proportions reporting rationing were 7.7%, 9.8%, and 10.7% for White, Black, and Hispanics, respectively.
“Given that few insurance providers cover GLP-1 RAs for obesity, cost-related prescription drug rationing could be exacerbated if patients were prescribed GLP-1 RAs at their current price of more than $1000 a month,” Chen noted, adding that the high prices could worsen health disparities among Black and Hispanic individuals with obesity.
Medicaid Coverage Lacking for All Obesity Treatments
For their project, Gallagher and Zvenyach delved into a database that aggregates Medicaid manuals, fee schedules, statutes, regulations, and preferred drug lists for each US state, both for Medicaid fee for service and top Medicaid managed care plans, in order to determine 2024 levels of coverage for NC, IBT, OMs, and MBS for adults with obesity.
No state provides coverage for all those treatments without either limitations — such as body mass index (BMI) cutoffs, age, or “comorbidity regardless of body mass index (BMI)” for OM and MBS — or outright restrictions, such as “proof of failed attempts.” And only seven states provide coverage for the four modalities “with limitations”: California, Arizona, New Mexico, South Carolina, Delaware, Rhode Island, and Massachusetts.
Twenty-two states don’t cover NC, although just one state doesn’t cover IBT. Overall, 37 states don’t cover OMs, and other states ranged considerably in various restrictions and limitations for OMs and MBS. Only four states fully covered the surgery without limitations or restrictions.
“The vast majority of states have significant barriers and conditions of coverage for obesity care,” Gallagher said.
Zvenyach added, “Most of the applied exclusions, limitations, or restrictions do not align with evidence-based practice standards or guidelines.”
When Coverage Stops, Hopelessness and Anger Emerge
Haggerty and colleagues’ research involved semi-structured interviews of the 22 participants — all of them women — who had lost their obesity medication coverage due to their insurers’ decision. Four themes emerged:
- 1. Feelings of hope replaced by hopelessness upon loss of medication coverage: One person said, “I’m afraid for my mental health. It’s tough to be in a situation where you’re never right. And it doesn’t matter what you do; it’s not going to work, and then to have just a glimmer of hope, a little spark of hey, look, this might help. And for someone else to take that away from you for no reason. I don’t know what am I supposed to do.”
- 2. Anger regarding the perceived injustice of anti-obesity medication coverage termination: For example, “They can pay for heart attacks, they could pay for me to have a stroke, they could pay for me to have diabetes, but they won’t let me have this one medicine that could take all of that away. Makes no sense.”
- 3. Perceptions of past and present stigma within the healthcare system and insurance company: “I’m not trying for vanity. I’m way too old to be a Victoria’s Secret model. I’m not trying to do it to be cute and skinny and hot. I just want to make it through a day of work and not be exhausted.”
- 4. Generational influences on obesity treatment: “I’m married, and my husband, since I’ve started this medicine, he’s been eating better. He’s been eating what I eat, and he’s been losing weight as well.”
- Some participants said they planned to cope in different ways, including trying to obtain compounded versions of the drugs from “spas” or online pharmacies, as well as skipping doses, reducing doses, or sharing medications — in other words, rationing.
Asked by this news organization what clinicians should keep in mind, Haggerty said, “that there are big barriers and that we need to take care of the patients within this system that has their arm tied behind their back.
Chen was funded by a grant from the National Institute on Aging outside the submitted work, and she was funded as a Yale National Clinician Scholar. A coauthor received grants from the Food and Drug Administration, Johnson & Johnson, the National Institutes of Health, the Agency for Healthcare Research and Quality, and Arnold Ventures. Another coauthor reported receiving personal fees from UpToDate and the Centers for Medicare & Medicaid Services. Gallagher has received research funding from Altimmune, Amgen, Boehringer Ingelheim, Currax, Eli Lilly and Company, Found, Novo Nordisk, Pfizer, Structure Therapeutics, and WeightWatchers. Haggerty reported article publishing charge was provided by West Virginia Alliance for Creative Health Solutions. Zvenyach and Clark had no disclosures.
A version of this article first appeared on Medscape.com.
SAN ANTONIO — Weight loss treatments aren’t reaching many of the people who need them most because of coverage barriers, new data suggested.
Findings from three studies presented at The Obesity Society’s Obesity Week 2024 meeting illustrate different aspects of the problem.
One, presented by Alissa S. Chen, MD, MPH, a postdoctoral fellow at Yale University, New Haven, Connecticut, found that people with obesity, particularly those with cardiovascular disease (CVD) and those who are Black and Hispanic, have high rates of cost-related prescription drug rationing. Those findings were simultaneously published as a research letter in JAMA Network Open.
“The implications are that structural barriers impede access to medications for Black and Hispanic adults with obesity, which might worsen if there’s not expanding coverage for GLP-1 RAs [glucagon-like peptide 1 receptor agonists], and it’s possible that broader insurance coverage could ameliorate some of these issues,” Chen said.
She noted that patients don’t always volunteer that information. “In my clinical practice, I always start by saying something like, ‘I have a lot of patients who can’t afford their medications. In the last week, was there a time [you didn’t take your medications due to cost]?’ ”
State Medicaid programs vary widely in the degree to which they cover weight loss treatments. But not a single one covers all modalities — nutrition counseling (NC), intensive behavioral therapy (IBT), obesity medications (OMs), and metabolic and bariatric surgery (MBS) — without restrictions or limitations, and only seven states cover them all with restrictions, according to a dual presentation by Christine Gallagher, MPAff, associate director for research and policy with the STOP Obesity Alliance at George Washington University, Washington, DC, and Tracy Zvenyach, PhD, MS, RN, director of policy strategy and alliances at the Obesity Action Coalition, also in Washington, DC.
Detailed Medicaid coverage data for each state are posted on the STOP Obesity Alliance website. (As of now, Medicare doesn’t cover medications specifically for obesity at all.)
A third presentation, by Treah Haggerty, MD, of the Department of Family Medicine and director of the Pediatric Medical Weight Management program at West Virginia University, Morgantown, was of a qualitative descriptive study exploring the impact on 22 individuals enrolled in a medical weight loss management program whose state employee insurance carrier made a policy decision to stop covering all anti-OMs in March 2024. All had been prescribed GLP-1 agonists for weight loss, and the decision forced most to stop using them.
Those findings were published in the September 2024 issue of Obesity Pillars.
“Patients perceive the discontinuation of anti-obesity medication coverage as stigmatizing and unjust, leading to feelings of hopelessness and fear. With more insurance companies denying coverage for these costly medications, more information is needed to identify best ways to address the loss of coverage with patients. Clinical management of these patients should incorporate evidence-based obesity treatments while navigating insurance constraints,” Haggerty said.
Create a Safe Space to Discuss the Barriers
Asked to comment, Session Moderator John D. Clark, MD, PhD, chief population health officer at Sharp Rees-Stealy Medical Group, San Diego, California, told Medscape Medical News, “Health systems and payers are determining what can and can’t be covered, and at the end of the day, it frequently comes down to finances…I think the big challenge is really identifying patients who may have the greatest need. ... If we have limited resources, how and where should we be directing those resources? I would say the current system hasn’t really answered that question or identified patients for whom we would say that the cost truly is less than either the financial or long-term health benefits.”
But Clark said, “When some of these newer anti-obesity medications are able to go generic and be less expensive, which will happen eventually, I think things will change ... and in the future, there will be more options on the market as well.”
In the meantime, he advised that clinicians “try to have conversations with patients about these barriers, acknowledge that these barriers exist, and create a safe space to discuss those barriers. ... Let’s see where we are right now, and let’s come up with a plan.”
People With Obesity More Susceptible to Drug Rationing
Chen reported on a sample of 51,720 adults who participated in the 2020-2022 National Health Interview Survey who did not have diabetes and who used at least one prescription medication of any type. Of those, 80% were White, 9.7% were Hispanic, and 9.7% were Black, and 33.9% overall had obesity.
Cost-related prescription rationing, defined as any self-reported skipping, taking less, or delaying filling a prescription to save money, was reported by 8.3% of those with obesity vs 5.9% without. After adjustment, rationing among those with obesity was significantly associated with younger age (aged 18-44 years), female sex, lower incomes, lack of health insurance coverage, and CVD.
The adjusted estimated probability of cost-related prescription drug rationing was 7.4% for those with CVD vs 4.4% for those without. By race/ethnicity, the proportions reporting rationing were 7.7%, 9.8%, and 10.7% for White, Black, and Hispanics, respectively.
“Given that few insurance providers cover GLP-1 RAs for obesity, cost-related prescription drug rationing could be exacerbated if patients were prescribed GLP-1 RAs at their current price of more than $1000 a month,” Chen noted, adding that the high prices could worsen health disparities among Black and Hispanic individuals with obesity.
Medicaid Coverage Lacking for All Obesity Treatments
For their project, Gallagher and Zvenyach delved into a database that aggregates Medicaid manuals, fee schedules, statutes, regulations, and preferred drug lists for each US state, both for Medicaid fee for service and top Medicaid managed care plans, in order to determine 2024 levels of coverage for NC, IBT, OMs, and MBS for adults with obesity.
No state provides coverage for all those treatments without either limitations — such as body mass index (BMI) cutoffs, age, or “comorbidity regardless of body mass index (BMI)” for OM and MBS — or outright restrictions, such as “proof of failed attempts.” And only seven states provide coverage for the four modalities “with limitations”: California, Arizona, New Mexico, South Carolina, Delaware, Rhode Island, and Massachusetts.
Twenty-two states don’t cover NC, although just one state doesn’t cover IBT. Overall, 37 states don’t cover OMs, and other states ranged considerably in various restrictions and limitations for OMs and MBS. Only four states fully covered the surgery without limitations or restrictions.
“The vast majority of states have significant barriers and conditions of coverage for obesity care,” Gallagher said.
Zvenyach added, “Most of the applied exclusions, limitations, or restrictions do not align with evidence-based practice standards or guidelines.”
When Coverage Stops, Hopelessness and Anger Emerge
Haggerty and colleagues’ research involved semi-structured interviews of the 22 participants — all of them women — who had lost their obesity medication coverage due to their insurers’ decision. Four themes emerged:
- 1. Feelings of hope replaced by hopelessness upon loss of medication coverage: One person said, “I’m afraid for my mental health. It’s tough to be in a situation where you’re never right. And it doesn’t matter what you do; it’s not going to work, and then to have just a glimmer of hope, a little spark of hey, look, this might help. And for someone else to take that away from you for no reason. I don’t know what am I supposed to do.”
- 2. Anger regarding the perceived injustice of anti-obesity medication coverage termination: For example, “They can pay for heart attacks, they could pay for me to have a stroke, they could pay for me to have diabetes, but they won’t let me have this one medicine that could take all of that away. Makes no sense.”
- 3. Perceptions of past and present stigma within the healthcare system and insurance company: “I’m not trying for vanity. I’m way too old to be a Victoria’s Secret model. I’m not trying to do it to be cute and skinny and hot. I just want to make it through a day of work and not be exhausted.”
- 4. Generational influences on obesity treatment: “I’m married, and my husband, since I’ve started this medicine, he’s been eating better. He’s been eating what I eat, and he’s been losing weight as well.”
- Some participants said they planned to cope in different ways, including trying to obtain compounded versions of the drugs from “spas” or online pharmacies, as well as skipping doses, reducing doses, or sharing medications — in other words, rationing.
Asked by this news organization what clinicians should keep in mind, Haggerty said, “that there are big barriers and that we need to take care of the patients within this system that has their arm tied behind their back.
Chen was funded by a grant from the National Institute on Aging outside the submitted work, and she was funded as a Yale National Clinician Scholar. A coauthor received grants from the Food and Drug Administration, Johnson & Johnson, the National Institutes of Health, the Agency for Healthcare Research and Quality, and Arnold Ventures. Another coauthor reported receiving personal fees from UpToDate and the Centers for Medicare & Medicaid Services. Gallagher has received research funding from Altimmune, Amgen, Boehringer Ingelheim, Currax, Eli Lilly and Company, Found, Novo Nordisk, Pfizer, Structure Therapeutics, and WeightWatchers. Haggerty reported article publishing charge was provided by West Virginia Alliance for Creative Health Solutions. Zvenyach and Clark had no disclosures.
A version of this article first appeared on Medscape.com.
FROM OBESITY WEEK 2024