User login
Postoperative Clostridium Difficile Infection Associated with Number of Antibiotics, Surgical Procedure Complexity
Clinical question: What are the factors that increase risk of Clostridium difficile infection (CDI) in postoperative patients?
Background: CDI has become an important infectious etiology for morbidity, lengthy and costly hospital admissions, and mortality. This study focused on the risks for postoperative patients to be infected with C. diff. Awareness of the risk factors for CDI allows for processes to be implemented that can decrease the rate of infection.
Study design: Retrospective, observational study.
Setting: Multiple Veterans Health Administration surgery programs.
Synopsis: The study investigated 468,386 surgical procedures in 134 surgical programs in 12 subspecialties over a four-year period. Overall, the postoperative CDI rate was 0.4% per year. Rates were higher in emergency or complex procedures, older patients, patients with longer preoperative hospital stays, and those who received three or more classes of antibiotics. CDI in postoperative patients was associated with five times higher risk of mortality, a 12 times higher risk of morbidity, and longer hospital stays (17.9 versus 3.6 days) compared with those without CDI. Further studies with a larger population size will confirm the findings of this study.
The study was conducted on middle-aged to elderly male veterans, and it can only be assumed that these results will translate to other populations. Nevertheless, CDI can lead to significant morbidity and mortality, and the study reinforces the importance of infection control and prevention to reduce CDI incidence and disease severity.
Bottom line: Postoperative CDI is significantly associated with the number of postoperative antibiotics, surgical procedure complexity, preoperative length of stay, and patient comorbidities.
Citation: Li X, Wilson M, Nylander W, Smith T, Lynn M, Gunnar W. Analysis of morbidity and mortality outcomes in postoperative Clostridium difficile infection in the Veterans Health Administration. JAMA Surg. 2015;25:1-9.
Clinical question: What are the factors that increase risk of Clostridium difficile infection (CDI) in postoperative patients?
Background: CDI has become an important infectious etiology for morbidity, lengthy and costly hospital admissions, and mortality. This study focused on the risks for postoperative patients to be infected with C. diff. Awareness of the risk factors for CDI allows for processes to be implemented that can decrease the rate of infection.
Study design: Retrospective, observational study.
Setting: Multiple Veterans Health Administration surgery programs.
Synopsis: The study investigated 468,386 surgical procedures in 134 surgical programs in 12 subspecialties over a four-year period. Overall, the postoperative CDI rate was 0.4% per year. Rates were higher in emergency or complex procedures, older patients, patients with longer preoperative hospital stays, and those who received three or more classes of antibiotics. CDI in postoperative patients was associated with five times higher risk of mortality, a 12 times higher risk of morbidity, and longer hospital stays (17.9 versus 3.6 days) compared with those without CDI. Further studies with a larger population size will confirm the findings of this study.
The study was conducted on middle-aged to elderly male veterans, and it can only be assumed that these results will translate to other populations. Nevertheless, CDI can lead to significant morbidity and mortality, and the study reinforces the importance of infection control and prevention to reduce CDI incidence and disease severity.
Bottom line: Postoperative CDI is significantly associated with the number of postoperative antibiotics, surgical procedure complexity, preoperative length of stay, and patient comorbidities.
Citation: Li X, Wilson M, Nylander W, Smith T, Lynn M, Gunnar W. Analysis of morbidity and mortality outcomes in postoperative Clostridium difficile infection in the Veterans Health Administration. JAMA Surg. 2015;25:1-9.
Clinical question: What are the factors that increase risk of Clostridium difficile infection (CDI) in postoperative patients?
Background: CDI has become an important infectious etiology for morbidity, lengthy and costly hospital admissions, and mortality. This study focused on the risks for postoperative patients to be infected with C. diff. Awareness of the risk factors for CDI allows for processes to be implemented that can decrease the rate of infection.
Study design: Retrospective, observational study.
Setting: Multiple Veterans Health Administration surgery programs.
Synopsis: The study investigated 468,386 surgical procedures in 134 surgical programs in 12 subspecialties over a four-year period. Overall, the postoperative CDI rate was 0.4% per year. Rates were higher in emergency or complex procedures, older patients, patients with longer preoperative hospital stays, and those who received three or more classes of antibiotics. CDI in postoperative patients was associated with five times higher risk of mortality, a 12 times higher risk of morbidity, and longer hospital stays (17.9 versus 3.6 days) compared with those without CDI. Further studies with a larger population size will confirm the findings of this study.
The study was conducted on middle-aged to elderly male veterans, and it can only be assumed that these results will translate to other populations. Nevertheless, CDI can lead to significant morbidity and mortality, and the study reinforces the importance of infection control and prevention to reduce CDI incidence and disease severity.
Bottom line: Postoperative CDI is significantly associated with the number of postoperative antibiotics, surgical procedure complexity, preoperative length of stay, and patient comorbidities.
Citation: Li X, Wilson M, Nylander W, Smith T, Lynn M, Gunnar W. Analysis of morbidity and mortality outcomes in postoperative Clostridium difficile infection in the Veterans Health Administration. JAMA Surg. 2015;25:1-9.
UK Report Shows Prevalence of Antibiotic Resistance in Pediatric Urinary Tract Infection
NEW YORK (Reuters Health) - The prevalence of antibiotic resistance in pediatric urinary tract infection (UTI) has reached such high levels in many countries that existing empiric therapies may no longer be effective, researchers from UK report."
Prevalence of resistance to commonly prescribed antibiotics in primary care in children with urinary tract infections caused by E. coli is high, and there was remarkable variability in E. coli resistance among countries in the study, particularly in countries outside the OECD (Organization for Economic Cooperation and Development), where one possible explanation is the availability of antibiotics over the counter," Ashley Bryce from the University of Bristol in the U.K. and Dr. Céire E. Costelloe from Imperial College London told Reuters Health in a joint email.
"This could render some antibiotics ineffective as first-line treatments for urinary tract infection," they said.
E. coli is responsible for more than 80% of all UTIs and is also the most common cause of bacteremia and foodborne infections and one cause of meningitis in neonates.
Bryce, Dr. Costelloe, and colleagues investigated the prevalence of resistance in community-acquired E. coli UTI to the most commonly prescribed antibiotics given to children in primary care in their systematic review of 58 published reports.
For all antibiotics tested, the prevalence of antibiotic resistance was higher in non-OECD countries than in OECD countries, the team reports in an article online March 15 in The BMJ.
The prevalence of resistance was highest for ampicillin, ranging from 41% in Switzerland to 100% in Ghana and Nigeria.
Resistance to co-trimoxazole and trimethoprim was 30% in OECD countries and 67% in Saudi Arabia, the only non-OECD country for which rates were available.
Pooled prevalences of resistance to ciprofloxacin and ceftazidime were around 2% in OECD countries but over 26% in non-OECD countries.
For all time periods analyzed, the odds of resistance were greater in children exposed to antibiotics than in those who were unexposed.
"The Infectious Diseases Society of America (IDSA) in collaboration with the European Society for Microbiology and Infectious Diseases (ESCMID) recommend that an antibiotic should be selected for first line empirical treatment of urinary tract infection only if the local prevalence of resistance is less than 20%," the researchers note.
"According to these guidelines, our review suggests ampicillin, co-trimoxazole, and trimethoprim are no longer suitable first line treatment options for urinary tract infection in many OECD countries and that as a result many guidelines, such as those published by the National Institute for Health and Care Excellence (NICE), might need updating," they write. "In non-OECD countries, resistance to all first line antibiotics specified for urinary tract infections was in excess of 20%, suggesting that choices of first line treatment might need to be re-evaluated in less well developed countries."
"We are not able to advise clinicians on which antibiotic is best to prescribe as this often depends on the individual case," Bryce and Dr. Costelloe said. "Clinicians should, however, adhere to local or national guidelines wherever possible, which is why it is of great importance that such guidelines are kept up to date and reflect current resistance rates."
"Clinicians may also wish to consider the antibiotic history of the child when they present to primary care with symptoms of an infection, especially in light of the suggestion of our results that previous treatment with an antibiotic is associated with resistance to that same antibiotic, and that this association may be present up to 6 months post treatment," they added.
Dr. Grant Russell from Monash University in Melbourne, Australia, wrote an editorial accompanying the report. He told Reuters Health by email, "I found the extent of the resistance (and the fact that it covered all of the regularly used empiric antibiotics) both concerning and surprising. The fact that choices are diminishing is disturbing, and the fact that the situation is dire in the developing world is deeply troubling."
"We need to do what we can do to prevent bacterial infections, and when treating them to consider that effective antibiotics are a finite resource," he said. "We all have a responsibility in attempting to conserve that resource."
"No new classes of antibiotics have been developed in the last 30 years - this and the dire situation in both the developed and the developing world suggests that the 'global problem' of antibiotic resistance is going to become more and more of an issue in years and decades to come," Dr. Russell concluded.
NEW YORK (Reuters Health) - The prevalence of antibiotic resistance in pediatric urinary tract infection (UTI) has reached such high levels in many countries that existing empiric therapies may no longer be effective, researchers from UK report."
Prevalence of resistance to commonly prescribed antibiotics in primary care in children with urinary tract infections caused by E. coli is high, and there was remarkable variability in E. coli resistance among countries in the study, particularly in countries outside the OECD (Organization for Economic Cooperation and Development), where one possible explanation is the availability of antibiotics over the counter," Ashley Bryce from the University of Bristol in the U.K. and Dr. Céire E. Costelloe from Imperial College London told Reuters Health in a joint email.
"This could render some antibiotics ineffective as first-line treatments for urinary tract infection," they said.
E. coli is responsible for more than 80% of all UTIs and is also the most common cause of bacteremia and foodborne infections and one cause of meningitis in neonates.
Bryce, Dr. Costelloe, and colleagues investigated the prevalence of resistance in community-acquired E. coli UTI to the most commonly prescribed antibiotics given to children in primary care in their systematic review of 58 published reports.
For all antibiotics tested, the prevalence of antibiotic resistance was higher in non-OECD countries than in OECD countries, the team reports in an article online March 15 in The BMJ.
The prevalence of resistance was highest for ampicillin, ranging from 41% in Switzerland to 100% in Ghana and Nigeria.
Resistance to co-trimoxazole and trimethoprim was 30% in OECD countries and 67% in Saudi Arabia, the only non-OECD country for which rates were available.
Pooled prevalences of resistance to ciprofloxacin and ceftazidime were around 2% in OECD countries but over 26% in non-OECD countries.
For all time periods analyzed, the odds of resistance were greater in children exposed to antibiotics than in those who were unexposed.
"The Infectious Diseases Society of America (IDSA) in collaboration with the European Society for Microbiology and Infectious Diseases (ESCMID) recommend that an antibiotic should be selected for first line empirical treatment of urinary tract infection only if the local prevalence of resistance is less than 20%," the researchers note.
"According to these guidelines, our review suggests ampicillin, co-trimoxazole, and trimethoprim are no longer suitable first line treatment options for urinary tract infection in many OECD countries and that as a result many guidelines, such as those published by the National Institute for Health and Care Excellence (NICE), might need updating," they write. "In non-OECD countries, resistance to all first line antibiotics specified for urinary tract infections was in excess of 20%, suggesting that choices of first line treatment might need to be re-evaluated in less well developed countries."
"We are not able to advise clinicians on which antibiotic is best to prescribe as this often depends on the individual case," Bryce and Dr. Costelloe said. "Clinicians should, however, adhere to local or national guidelines wherever possible, which is why it is of great importance that such guidelines are kept up to date and reflect current resistance rates."
"Clinicians may also wish to consider the antibiotic history of the child when they present to primary care with symptoms of an infection, especially in light of the suggestion of our results that previous treatment with an antibiotic is associated with resistance to that same antibiotic, and that this association may be present up to 6 months post treatment," they added.
Dr. Grant Russell from Monash University in Melbourne, Australia, wrote an editorial accompanying the report. He told Reuters Health by email, "I found the extent of the resistance (and the fact that it covered all of the regularly used empiric antibiotics) both concerning and surprising. The fact that choices are diminishing is disturbing, and the fact that the situation is dire in the developing world is deeply troubling."
"We need to do what we can do to prevent bacterial infections, and when treating them to consider that effective antibiotics are a finite resource," he said. "We all have a responsibility in attempting to conserve that resource."
"No new classes of antibiotics have been developed in the last 30 years - this and the dire situation in both the developed and the developing world suggests that the 'global problem' of antibiotic resistance is going to become more and more of an issue in years and decades to come," Dr. Russell concluded.
NEW YORK (Reuters Health) - The prevalence of antibiotic resistance in pediatric urinary tract infection (UTI) has reached such high levels in many countries that existing empiric therapies may no longer be effective, researchers from UK report."
Prevalence of resistance to commonly prescribed antibiotics in primary care in children with urinary tract infections caused by E. coli is high, and there was remarkable variability in E. coli resistance among countries in the study, particularly in countries outside the OECD (Organization for Economic Cooperation and Development), where one possible explanation is the availability of antibiotics over the counter," Ashley Bryce from the University of Bristol in the U.K. and Dr. Céire E. Costelloe from Imperial College London told Reuters Health in a joint email.
"This could render some antibiotics ineffective as first-line treatments for urinary tract infection," they said.
E. coli is responsible for more than 80% of all UTIs and is also the most common cause of bacteremia and foodborne infections and one cause of meningitis in neonates.
Bryce, Dr. Costelloe, and colleagues investigated the prevalence of resistance in community-acquired E. coli UTI to the most commonly prescribed antibiotics given to children in primary care in their systematic review of 58 published reports.
For all antibiotics tested, the prevalence of antibiotic resistance was higher in non-OECD countries than in OECD countries, the team reports in an article online March 15 in The BMJ.
The prevalence of resistance was highest for ampicillin, ranging from 41% in Switzerland to 100% in Ghana and Nigeria.
Resistance to co-trimoxazole and trimethoprim was 30% in OECD countries and 67% in Saudi Arabia, the only non-OECD country for which rates were available.
Pooled prevalences of resistance to ciprofloxacin and ceftazidime were around 2% in OECD countries but over 26% in non-OECD countries.
For all time periods analyzed, the odds of resistance were greater in children exposed to antibiotics than in those who were unexposed.
"The Infectious Diseases Society of America (IDSA) in collaboration with the European Society for Microbiology and Infectious Diseases (ESCMID) recommend that an antibiotic should be selected for first line empirical treatment of urinary tract infection only if the local prevalence of resistance is less than 20%," the researchers note.
"According to these guidelines, our review suggests ampicillin, co-trimoxazole, and trimethoprim are no longer suitable first line treatment options for urinary tract infection in many OECD countries and that as a result many guidelines, such as those published by the National Institute for Health and Care Excellence (NICE), might need updating," they write. "In non-OECD countries, resistance to all first line antibiotics specified for urinary tract infections was in excess of 20%, suggesting that choices of first line treatment might need to be re-evaluated in less well developed countries."
"We are not able to advise clinicians on which antibiotic is best to prescribe as this often depends on the individual case," Bryce and Dr. Costelloe said. "Clinicians should, however, adhere to local or national guidelines wherever possible, which is why it is of great importance that such guidelines are kept up to date and reflect current resistance rates."
"Clinicians may also wish to consider the antibiotic history of the child when they present to primary care with symptoms of an infection, especially in light of the suggestion of our results that previous treatment with an antibiotic is associated with resistance to that same antibiotic, and that this association may be present up to 6 months post treatment," they added.
Dr. Grant Russell from Monash University in Melbourne, Australia, wrote an editorial accompanying the report. He told Reuters Health by email, "I found the extent of the resistance (and the fact that it covered all of the regularly used empiric antibiotics) both concerning and surprising. The fact that choices are diminishing is disturbing, and the fact that the situation is dire in the developing world is deeply troubling."
"We need to do what we can do to prevent bacterial infections, and when treating them to consider that effective antibiotics are a finite resource," he said. "We all have a responsibility in attempting to conserve that resource."
"No new classes of antibiotics have been developed in the last 30 years - this and the dire situation in both the developed and the developing world suggests that the 'global problem' of antibiotic resistance is going to become more and more of an issue in years and decades to come," Dr. Russell concluded.
Increase in Broad-Spectrum Antibiotics Disproportionate to Rate of Resistant Organisms
Clinical question: Have healthcare-associated pneumonia (HCAP) guidelines improved treatment accuracy?
Background: Guidelines released in 2005 call for the use of broad-spectrum antibiotics for patients presenting with pneumonia who have had recent healthcare exposure. However, there is scant evidence to support the risk factors they identify, and the guidelines are likely to increase use of broad-spectrum antibiotics.
Study design: Observational, retrospective.
Setting: VA medical centers, 2006–2010.
Synopsis: In this study, VA medical center physicians evaluated 95,511 hospitalizations for pneumonia at 128 hospitals between 2006 and 2010, the years following the 2005 guidelines. Annual analyses were performed to assess antibiotics selection as well as evidence of resistant bacteria from blood and respiratory cultures. Researchers found that while the use of broad-spectrum antibiotics increased drastically during the study period (vancomycin from 16% to 31% and piperacillin-tazobactam from 16% to 27%, P<0.001 for both), the incidence of resistant organisms either decreased or remained stable.
Additionally, physicians were no better at matching broad-spectrum antibiotics to patients infected with resistant organisms at the end of the study period than they were at the start. They conclude that more research is urgently needed to identify patients at risk for resistant organisms in order to more appropriately prescribe broad-spectrum antibiotics.
This study did not evaluate patients’ clinical outcomes, so it is unclear whether they may have benefitted clinically from the implementation of the guidelines. For now, the optimal approach to empiric therapy for HCAP remains undefined.
Bottom line: Despite a marked increase in the use of broad-spectrum antibiotics for HCAP in the years following a change in treatment guidelines, doctors showed no improvement at matching these antibiotics to patients infected with resistant organisms.
Citation: Jones BE, Jones MM, Huttner B, et al. Trends in antibiotic use and nosocomial pathogens in hospitalized veterans with pneumonia at 128 medical centers, 2006-2010. Clin Infect Dis. 2015;61(9):1403-1410.
Clinical question: Have healthcare-associated pneumonia (HCAP) guidelines improved treatment accuracy?
Background: Guidelines released in 2005 call for the use of broad-spectrum antibiotics for patients presenting with pneumonia who have had recent healthcare exposure. However, there is scant evidence to support the risk factors they identify, and the guidelines are likely to increase use of broad-spectrum antibiotics.
Study design: Observational, retrospective.
Setting: VA medical centers, 2006–2010.
Synopsis: In this study, VA medical center physicians evaluated 95,511 hospitalizations for pneumonia at 128 hospitals between 2006 and 2010, the years following the 2005 guidelines. Annual analyses were performed to assess antibiotics selection as well as evidence of resistant bacteria from blood and respiratory cultures. Researchers found that while the use of broad-spectrum antibiotics increased drastically during the study period (vancomycin from 16% to 31% and piperacillin-tazobactam from 16% to 27%, P<0.001 for both), the incidence of resistant organisms either decreased or remained stable.
Additionally, physicians were no better at matching broad-spectrum antibiotics to patients infected with resistant organisms at the end of the study period than they were at the start. They conclude that more research is urgently needed to identify patients at risk for resistant organisms in order to more appropriately prescribe broad-spectrum antibiotics.
This study did not evaluate patients’ clinical outcomes, so it is unclear whether they may have benefitted clinically from the implementation of the guidelines. For now, the optimal approach to empiric therapy for HCAP remains undefined.
Bottom line: Despite a marked increase in the use of broad-spectrum antibiotics for HCAP in the years following a change in treatment guidelines, doctors showed no improvement at matching these antibiotics to patients infected with resistant organisms.
Citation: Jones BE, Jones MM, Huttner B, et al. Trends in antibiotic use and nosocomial pathogens in hospitalized veterans with pneumonia at 128 medical centers, 2006-2010. Clin Infect Dis. 2015;61(9):1403-1410.
Clinical question: Have healthcare-associated pneumonia (HCAP) guidelines improved treatment accuracy?
Background: Guidelines released in 2005 call for the use of broad-spectrum antibiotics for patients presenting with pneumonia who have had recent healthcare exposure. However, there is scant evidence to support the risk factors they identify, and the guidelines are likely to increase use of broad-spectrum antibiotics.
Study design: Observational, retrospective.
Setting: VA medical centers, 2006–2010.
Synopsis: In this study, VA medical center physicians evaluated 95,511 hospitalizations for pneumonia at 128 hospitals between 2006 and 2010, the years following the 2005 guidelines. Annual analyses were performed to assess antibiotics selection as well as evidence of resistant bacteria from blood and respiratory cultures. Researchers found that while the use of broad-spectrum antibiotics increased drastically during the study period (vancomycin from 16% to 31% and piperacillin-tazobactam from 16% to 27%, P<0.001 for both), the incidence of resistant organisms either decreased or remained stable.
Additionally, physicians were no better at matching broad-spectrum antibiotics to patients infected with resistant organisms at the end of the study period than they were at the start. They conclude that more research is urgently needed to identify patients at risk for resistant organisms in order to more appropriately prescribe broad-spectrum antibiotics.
This study did not evaluate patients’ clinical outcomes, so it is unclear whether they may have benefitted clinically from the implementation of the guidelines. For now, the optimal approach to empiric therapy for HCAP remains undefined.
Bottom line: Despite a marked increase in the use of broad-spectrum antibiotics for HCAP in the years following a change in treatment guidelines, doctors showed no improvement at matching these antibiotics to patients infected with resistant organisms.
Citation: Jones BE, Jones MM, Huttner B, et al. Trends in antibiotic use and nosocomial pathogens in hospitalized veterans with pneumonia at 128 medical centers, 2006-2010. Clin Infect Dis. 2015;61(9):1403-1410.
ECCMID 2016: Antimicrobial resistance, the microbiome and systems vaccinology
The global infectious disease and clinical microbiology community meets every year at the European Congress of Clinical Microbiology and Infectious Diseases (ECCMID), the world’s largest congress on infectious diseases and medical microbiology, to present and discuss recent research results and to offer solutions to the most pressing infection problems.
The 2016 ECCMID annual conference, organized by the European Society of Clinical Microbiology and Infectious Diseases (ESCMID), will take place April 9-12 in Amsterdam. Discussions at this event not only help translate research findings into diagnostic tools, guidelines, best practices, and international policies; they also raise awareness of emerging health care challenges.
At ECCMID 2016, researchers will present more than 3,000 abstracts with the latest findings and recommendations to help improve diagnosis, prevention, and the clinical care given to patients. The Congress offers more than 150 oral presentations, including keynote lectures, symposia, oral sessions, educational workshops, and meet-the-experts sessions, as well as more than 2,000 poster presentations.
The main topics this year are strategies to detect and tackle antimicrobial resistance in various settings, approaches for prevention involving vaccines and infection control, as well as descriptions of novel diagnostic technologies. Always among the most popular sessions are lectures by winners of the ESCMID Award for Excellence and the Young Investigator Awards, as well as oral presentations on groundbreaking research, and late-breaking abstracts.
Also included will be mini oral “e-poster” presentations. Printed posters will be presented, but they will also be available at e-poster viewing stations, where visitors can scroll through abstracts of paper presentations.
Keynote speeches this year will feature innovative approaches to vaccines; microbiome and tuberculosis therapies; lectures on how nonhuman antibiotics affect public health; and an economic perspective on antimicrobial resistance.
Special topics
This year, the ECCMID Program Committee has decided to offer two special tracks for the late-breaking abstract sessions, focused on topics requiring a coordinated response from infection specialists across all disciplines.
The first topic is refugee and migrant health. The thousands of people who are currently migrating challenge public health systems in transition and the host countries. Clinicians and public health specialists need to develop strategies for the screening, prevention, and treatment of infectious diseases that were largely eradicated in Europe but are now gradually being reintroduced.
The second focus of the late-breaking abstracts is on emerging colistin resistance. Reports about the emergence of plasmid-borne resistance to this last-resort antibiotic have come from China, Canada, the United Kingdom, and most countries in continental Europe. Colistin resistance can spread easily between different types of bacteria, says Dr. Murat Akova, current ESCMID president and professor of medicine at Hacettepe University in Ankara, Turkey, and the world needs to wake up and take note.
In terms of viral infections, experts at the Congress will evaluate HIV and hepatitis C treatments in several interesting sessions. Researchers will also present results on emerging infections, including those caused by the Zika virus. Dr. Jean Paul Stahl, vice chairman of the ESCMID Study Group for Infectious Diseases of the Brain and professor of infectious diseases at University Hospital in Grenoble, France, says the current Zika virus epidemic is an important example of the great need we have for new evidence-based approaches on how to best manage emerging infections.
The outbreaks of Zika and Ebola in the last few years have seen the international community mobilize on infectious disease issues in a more collaborative manner than ever before, which should help reduce the severity of future outbreaks. But viral infections extend far beyond the recent outbreaks of unusual pathologies, and there are a number of important developments taking place among some of the more common viruses.
For more information on ECCMID 2016, visit http://www.eccmid.org/.
Dr. Winfried V. Kern is professor of medicine at the Albert Ludwigs University of Freiburg and head of the division of infectious diseases, department of medicine, and Centre for Infectious Diseases and Travel Medicine, University Hospital, Freiburg, Germany. His professional interests include bacterial multidrug resistance mechanisms and epidemiology, hospital antibiotic stewardship programs, health care–associated infections including infections in the immunocompromised host.
The global infectious disease and clinical microbiology community meets every year at the European Congress of Clinical Microbiology and Infectious Diseases (ECCMID), the world’s largest congress on infectious diseases and medical microbiology, to present and discuss recent research results and to offer solutions to the most pressing infection problems.
The 2016 ECCMID annual conference, organized by the European Society of Clinical Microbiology and Infectious Diseases (ESCMID), will take place April 9-12 in Amsterdam. Discussions at this event not only help translate research findings into diagnostic tools, guidelines, best practices, and international policies; they also raise awareness of emerging health care challenges.
At ECCMID 2016, researchers will present more than 3,000 abstracts with the latest findings and recommendations to help improve diagnosis, prevention, and the clinical care given to patients. The Congress offers more than 150 oral presentations, including keynote lectures, symposia, oral sessions, educational workshops, and meet-the-experts sessions, as well as more than 2,000 poster presentations.
The main topics this year are strategies to detect and tackle antimicrobial resistance in various settings, approaches for prevention involving vaccines and infection control, as well as descriptions of novel diagnostic technologies. Always among the most popular sessions are lectures by winners of the ESCMID Award for Excellence and the Young Investigator Awards, as well as oral presentations on groundbreaking research, and late-breaking abstracts.
Also included will be mini oral “e-poster” presentations. Printed posters will be presented, but they will also be available at e-poster viewing stations, where visitors can scroll through abstracts of paper presentations.
Keynote speeches this year will feature innovative approaches to vaccines; microbiome and tuberculosis therapies; lectures on how nonhuman antibiotics affect public health; and an economic perspective on antimicrobial resistance.
Special topics
This year, the ECCMID Program Committee has decided to offer two special tracks for the late-breaking abstract sessions, focused on topics requiring a coordinated response from infection specialists across all disciplines.
The first topic is refugee and migrant health. The thousands of people who are currently migrating challenge public health systems in transition and the host countries. Clinicians and public health specialists need to develop strategies for the screening, prevention, and treatment of infectious diseases that were largely eradicated in Europe but are now gradually being reintroduced.
The second focus of the late-breaking abstracts is on emerging colistin resistance. Reports about the emergence of plasmid-borne resistance to this last-resort antibiotic have come from China, Canada, the United Kingdom, and most countries in continental Europe. Colistin resistance can spread easily between different types of bacteria, says Dr. Murat Akova, current ESCMID president and professor of medicine at Hacettepe University in Ankara, Turkey, and the world needs to wake up and take note.
In terms of viral infections, experts at the Congress will evaluate HIV and hepatitis C treatments in several interesting sessions. Researchers will also present results on emerging infections, including those caused by the Zika virus. Dr. Jean Paul Stahl, vice chairman of the ESCMID Study Group for Infectious Diseases of the Brain and professor of infectious diseases at University Hospital in Grenoble, France, says the current Zika virus epidemic is an important example of the great need we have for new evidence-based approaches on how to best manage emerging infections.
The outbreaks of Zika and Ebola in the last few years have seen the international community mobilize on infectious disease issues in a more collaborative manner than ever before, which should help reduce the severity of future outbreaks. But viral infections extend far beyond the recent outbreaks of unusual pathologies, and there are a number of important developments taking place among some of the more common viruses.
For more information on ECCMID 2016, visit http://www.eccmid.org/.
Dr. Winfried V. Kern is professor of medicine at the Albert Ludwigs University of Freiburg and head of the division of infectious diseases, department of medicine, and Centre for Infectious Diseases and Travel Medicine, University Hospital, Freiburg, Germany. His professional interests include bacterial multidrug resistance mechanisms and epidemiology, hospital antibiotic stewardship programs, health care–associated infections including infections in the immunocompromised host.
The global infectious disease and clinical microbiology community meets every year at the European Congress of Clinical Microbiology and Infectious Diseases (ECCMID), the world’s largest congress on infectious diseases and medical microbiology, to present and discuss recent research results and to offer solutions to the most pressing infection problems.
The 2016 ECCMID annual conference, organized by the European Society of Clinical Microbiology and Infectious Diseases (ESCMID), will take place April 9-12 in Amsterdam. Discussions at this event not only help translate research findings into diagnostic tools, guidelines, best practices, and international policies; they also raise awareness of emerging health care challenges.
At ECCMID 2016, researchers will present more than 3,000 abstracts with the latest findings and recommendations to help improve diagnosis, prevention, and the clinical care given to patients. The Congress offers more than 150 oral presentations, including keynote lectures, symposia, oral sessions, educational workshops, and meet-the-experts sessions, as well as more than 2,000 poster presentations.
The main topics this year are strategies to detect and tackle antimicrobial resistance in various settings, approaches for prevention involving vaccines and infection control, as well as descriptions of novel diagnostic technologies. Always among the most popular sessions are lectures by winners of the ESCMID Award for Excellence and the Young Investigator Awards, as well as oral presentations on groundbreaking research, and late-breaking abstracts.
Also included will be mini oral “e-poster” presentations. Printed posters will be presented, but they will also be available at e-poster viewing stations, where visitors can scroll through abstracts of paper presentations.
Keynote speeches this year will feature innovative approaches to vaccines; microbiome and tuberculosis therapies; lectures on how nonhuman antibiotics affect public health; and an economic perspective on antimicrobial resistance.
Special topics
This year, the ECCMID Program Committee has decided to offer two special tracks for the late-breaking abstract sessions, focused on topics requiring a coordinated response from infection specialists across all disciplines.
The first topic is refugee and migrant health. The thousands of people who are currently migrating challenge public health systems in transition and the host countries. Clinicians and public health specialists need to develop strategies for the screening, prevention, and treatment of infectious diseases that were largely eradicated in Europe but are now gradually being reintroduced.
The second focus of the late-breaking abstracts is on emerging colistin resistance. Reports about the emergence of plasmid-borne resistance to this last-resort antibiotic have come from China, Canada, the United Kingdom, and most countries in continental Europe. Colistin resistance can spread easily between different types of bacteria, says Dr. Murat Akova, current ESCMID president and professor of medicine at Hacettepe University in Ankara, Turkey, and the world needs to wake up and take note.
In terms of viral infections, experts at the Congress will evaluate HIV and hepatitis C treatments in several interesting sessions. Researchers will also present results on emerging infections, including those caused by the Zika virus. Dr. Jean Paul Stahl, vice chairman of the ESCMID Study Group for Infectious Diseases of the Brain and professor of infectious diseases at University Hospital in Grenoble, France, says the current Zika virus epidemic is an important example of the great need we have for new evidence-based approaches on how to best manage emerging infections.
The outbreaks of Zika and Ebola in the last few years have seen the international community mobilize on infectious disease issues in a more collaborative manner than ever before, which should help reduce the severity of future outbreaks. But viral infections extend far beyond the recent outbreaks of unusual pathologies, and there are a number of important developments taking place among some of the more common viruses.
For more information on ECCMID 2016, visit http://www.eccmid.org/.
Dr. Winfried V. Kern is professor of medicine at the Albert Ludwigs University of Freiburg and head of the division of infectious diseases, department of medicine, and Centre for Infectious Diseases and Travel Medicine, University Hospital, Freiburg, Germany. His professional interests include bacterial multidrug resistance mechanisms and epidemiology, hospital antibiotic stewardship programs, health care–associated infections including infections in the immunocompromised host.
SHM’s Twitter Contest Encourages Appropriate Antibiotic Prescribing
- Identify opportunities to engage with all hospital-based clinicians to improve antibiotic stewardship in your hospital.
- Pay attention to appropriate antibiotic choice and resistance patterns and identify mechanisms to educate providers on overprescribing in your hospital.
- Consider the following:
Adhere to antibiotic treatment guidelines.
Track the day.
Set a stop date.
Reevaluate therapy.
Streamline therapy.
Avoid automatic time courses.
Not only did participants receive recognition for their efforts hanging up the posters and engaging their teams, the posters’ presence in various hospitals and offices around the country created thousands of impressions among hospital-based staff and others directly responsible for proper antibiotic prescribing.
Although the contest is over, you can still help facilitate culture change related to appropriate antibiotic prescribing. Follow SHM on Twitter @SHMLive, and continue to visit FightTheResistance.org for the latest updates on the campaign and new tools to promote antibiotic stewardship. TH
Brett Radler is SHM’s communications coordinator.
- Identify opportunities to engage with all hospital-based clinicians to improve antibiotic stewardship in your hospital.
- Pay attention to appropriate antibiotic choice and resistance patterns and identify mechanisms to educate providers on overprescribing in your hospital.
- Consider the following:
Adhere to antibiotic treatment guidelines.
Track the day.
Set a stop date.
Reevaluate therapy.
Streamline therapy.
Avoid automatic time courses.
Not only did participants receive recognition for their efforts hanging up the posters and engaging their teams, the posters’ presence in various hospitals and offices around the country created thousands of impressions among hospital-based staff and others directly responsible for proper antibiotic prescribing.
Although the contest is over, you can still help facilitate culture change related to appropriate antibiotic prescribing. Follow SHM on Twitter @SHMLive, and continue to visit FightTheResistance.org for the latest updates on the campaign and new tools to promote antibiotic stewardship. TH
Brett Radler is SHM’s communications coordinator.
- Identify opportunities to engage with all hospital-based clinicians to improve antibiotic stewardship in your hospital.
- Pay attention to appropriate antibiotic choice and resistance patterns and identify mechanisms to educate providers on overprescribing in your hospital.
- Consider the following:
Adhere to antibiotic treatment guidelines.
Track the day.
Set a stop date.
Reevaluate therapy.
Streamline therapy.
Avoid automatic time courses.
Not only did participants receive recognition for their efforts hanging up the posters and engaging their teams, the posters’ presence in various hospitals and offices around the country created thousands of impressions among hospital-based staff and others directly responsible for proper antibiotic prescribing.
Although the contest is over, you can still help facilitate culture change related to appropriate antibiotic prescribing. Follow SHM on Twitter @SHMLive, and continue to visit FightTheResistance.org for the latest updates on the campaign and new tools to promote antibiotic stewardship. TH
Brett Radler is SHM’s communications coordinator.
Antibiotic-resistant infections remain a persistent threat
One in every seven infections in acute care hospitals related to catheters and surgeries was caused by antibiotic-resistant bacteria. In long-term acute care hospitals, that number increased to one in four.
Those are key findings from a study published March 3 in the Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report that is the first to combine national data on antibiotic-resistant (AR) bacteria threats with progress on health care–associated infections (HAIs).
“Antibiotic resistance threatens to return us to a time when a simple infection could kill,” CDC Director Thomas Frieden said during a March 3 telebriefing. “The more people who get infected with resistant bacteria, the more people who suffer complications, the more who, tragically, may die from preventable infections. On any given day about one in 25 hospitalized patients has at least one health care–associated infection that they didn’t come in with. No one should get sick when they’re trying to get well.”
For the study, researchers led by Dr. Clifford McDonald of the CDC’s Division of Healthcare Quality Promotion, collected data on specific infections that were reported to the National Healthcare Safety Network in 2014 by approximately 4,000 short-term acute care hospitals, 501 long-term acute care hospitals, and 1,135 inpatient rehabilitation facilities in all 50 states (MMWR. 2016 Mar 3. doi: 10.15585/mmwr.mm6509e1er). Next, they determined the proportions of AR pathogens and HAIs caused by any of six resistant bacteria highlighted by the CDC in 2013 as urgent or serious threats: CRE (carbapenem-resistant Enterobacteriaceae), MRSA (methicillin-resistant Staphylococcus aureus), ESBL-producing Enterobacteriaceae (extended-spectrum beta-lactamases), VRE (vancomycin-resistant enterococci), multidrug-resistant pseudomonas, and multidrug-resistant Acinetobacter.
The researchers found that, compared with historical data from 5-8 years earlier, central line–associated bloodstream infections decreased by 50% and surgical site infections (SSIs) by 17% in 2014.
“There is encouraging news here,” Dr. Frieden said. “Doctors, nurses, hospitals, health care systems and other partners have made progress preventing some health care–associated infections.” However, the study found that one in six remaining central line-associated bloodstream infections were caused by urgent or serious antibiotic-resistant bacteria, while one in seven remaining surgical site infections were caused by urgent or serious antibiotic-resistant bacteria.
While catheter-associated urinary tract infections appear unchanged from baseline, there have been recent decreases, according to the study. In addition, C. difficile infections in hospitals decreased 8% between 2011 and 2014.
Dr. McDonald and his associates determined that in 2014, one in seven infections in acute care hospitals related to catheters and surgeries was caused by one of the six antibiotic-resistance threat bacteria, “which is deeply concerning,” Dr. Frieden said. That number increased to one in four infections in long-term acute care hospitals, a proportion that he characterized as “chilling.”
The CDC recommends three strategies that doctors, nurses, and other health care providers should take with every patient, to prevent HAIs and stop the spread of antibiotic resistance:
• Prevent the spread of bacteria between patients. Dr. Peter Pronovost, who participated in the telebriefing, said that he and his associates at Johns Hopkins University in Baltimore “do this by practicing good hand hygiene techniques by wearing sterile equipment when inserting lines.”
• Prevent surgery-related infections and/or placement of a catheter. “Check catheters frequently and remove them when you no longer need them,” advised Dr. Pronovost, director of the Armstrong Institute for Patient Safety and Quality at Johns Hopkins. “Ask if you actually need them before you even place them.”
• Improve antibiotic use through stewardship. This means using “the right antibiotics for the right duration,” Dr. Pronovost said. “Antibiotics could be lifesaving and are necessary for critically ill patients, especially those with septic shock. But these antibiotics need to be adjusted based on lab results and new information about the organisms that are causing these infections. Forty-eight hours after antibiotics are initiated, take a ‘time out.’ Perform a brief but focused assessment to determine if antibiotic therapy is still needed, or if it should be refined. A common mistake we make is to continue vancomycin when there is no presence of MRSA. We often tell our staff at Johns Hopkins, ‘if it doesn’t grow, let it go.’ ”
Dr. Frieden concluded his remarks by noting that physicians and other clinicians on the front lines “need support of their facility leadership,” to prevent HAIs. “Health care facilities, CEOs, and administrators are a major part of the solution. It’s important that they make a priority of infection prevention, sepsis prevention, and antibiotic stewardship. Know your facility’s data and target prevention efforts to ensure improvements in patient safety.”
One in every seven infections in acute care hospitals related to catheters and surgeries was caused by antibiotic-resistant bacteria. In long-term acute care hospitals, that number increased to one in four.
Those are key findings from a study published March 3 in the Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report that is the first to combine national data on antibiotic-resistant (AR) bacteria threats with progress on health care–associated infections (HAIs).
“Antibiotic resistance threatens to return us to a time when a simple infection could kill,” CDC Director Thomas Frieden said during a March 3 telebriefing. “The more people who get infected with resistant bacteria, the more people who suffer complications, the more who, tragically, may die from preventable infections. On any given day about one in 25 hospitalized patients has at least one health care–associated infection that they didn’t come in with. No one should get sick when they’re trying to get well.”
For the study, researchers led by Dr. Clifford McDonald of the CDC’s Division of Healthcare Quality Promotion, collected data on specific infections that were reported to the National Healthcare Safety Network in 2014 by approximately 4,000 short-term acute care hospitals, 501 long-term acute care hospitals, and 1,135 inpatient rehabilitation facilities in all 50 states (MMWR. 2016 Mar 3. doi: 10.15585/mmwr.mm6509e1er). Next, they determined the proportions of AR pathogens and HAIs caused by any of six resistant bacteria highlighted by the CDC in 2013 as urgent or serious threats: CRE (carbapenem-resistant Enterobacteriaceae), MRSA (methicillin-resistant Staphylococcus aureus), ESBL-producing Enterobacteriaceae (extended-spectrum beta-lactamases), VRE (vancomycin-resistant enterococci), multidrug-resistant pseudomonas, and multidrug-resistant Acinetobacter.
The researchers found that, compared with historical data from 5-8 years earlier, central line–associated bloodstream infections decreased by 50% and surgical site infections (SSIs) by 17% in 2014.
“There is encouraging news here,” Dr. Frieden said. “Doctors, nurses, hospitals, health care systems and other partners have made progress preventing some health care–associated infections.” However, the study found that one in six remaining central line-associated bloodstream infections were caused by urgent or serious antibiotic-resistant bacteria, while one in seven remaining surgical site infections were caused by urgent or serious antibiotic-resistant bacteria.
While catheter-associated urinary tract infections appear unchanged from baseline, there have been recent decreases, according to the study. In addition, C. difficile infections in hospitals decreased 8% between 2011 and 2014.
Dr. McDonald and his associates determined that in 2014, one in seven infections in acute care hospitals related to catheters and surgeries was caused by one of the six antibiotic-resistance threat bacteria, “which is deeply concerning,” Dr. Frieden said. That number increased to one in four infections in long-term acute care hospitals, a proportion that he characterized as “chilling.”
The CDC recommends three strategies that doctors, nurses, and other health care providers should take with every patient, to prevent HAIs and stop the spread of antibiotic resistance:
• Prevent the spread of bacteria between patients. Dr. Peter Pronovost, who participated in the telebriefing, said that he and his associates at Johns Hopkins University in Baltimore “do this by practicing good hand hygiene techniques by wearing sterile equipment when inserting lines.”
• Prevent surgery-related infections and/or placement of a catheter. “Check catheters frequently and remove them when you no longer need them,” advised Dr. Pronovost, director of the Armstrong Institute for Patient Safety and Quality at Johns Hopkins. “Ask if you actually need them before you even place them.”
• Improve antibiotic use through stewardship. This means using “the right antibiotics for the right duration,” Dr. Pronovost said. “Antibiotics could be lifesaving and are necessary for critically ill patients, especially those with septic shock. But these antibiotics need to be adjusted based on lab results and new information about the organisms that are causing these infections. Forty-eight hours after antibiotics are initiated, take a ‘time out.’ Perform a brief but focused assessment to determine if antibiotic therapy is still needed, or if it should be refined. A common mistake we make is to continue vancomycin when there is no presence of MRSA. We often tell our staff at Johns Hopkins, ‘if it doesn’t grow, let it go.’ ”
Dr. Frieden concluded his remarks by noting that physicians and other clinicians on the front lines “need support of their facility leadership,” to prevent HAIs. “Health care facilities, CEOs, and administrators are a major part of the solution. It’s important that they make a priority of infection prevention, sepsis prevention, and antibiotic stewardship. Know your facility’s data and target prevention efforts to ensure improvements in patient safety.”
One in every seven infections in acute care hospitals related to catheters and surgeries was caused by antibiotic-resistant bacteria. In long-term acute care hospitals, that number increased to one in four.
Those are key findings from a study published March 3 in the Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report that is the first to combine national data on antibiotic-resistant (AR) bacteria threats with progress on health care–associated infections (HAIs).
“Antibiotic resistance threatens to return us to a time when a simple infection could kill,” CDC Director Thomas Frieden said during a March 3 telebriefing. “The more people who get infected with resistant bacteria, the more people who suffer complications, the more who, tragically, may die from preventable infections. On any given day about one in 25 hospitalized patients has at least one health care–associated infection that they didn’t come in with. No one should get sick when they’re trying to get well.”
For the study, researchers led by Dr. Clifford McDonald of the CDC’s Division of Healthcare Quality Promotion, collected data on specific infections that were reported to the National Healthcare Safety Network in 2014 by approximately 4,000 short-term acute care hospitals, 501 long-term acute care hospitals, and 1,135 inpatient rehabilitation facilities in all 50 states (MMWR. 2016 Mar 3. doi: 10.15585/mmwr.mm6509e1er). Next, they determined the proportions of AR pathogens and HAIs caused by any of six resistant bacteria highlighted by the CDC in 2013 as urgent or serious threats: CRE (carbapenem-resistant Enterobacteriaceae), MRSA (methicillin-resistant Staphylococcus aureus), ESBL-producing Enterobacteriaceae (extended-spectrum beta-lactamases), VRE (vancomycin-resistant enterococci), multidrug-resistant pseudomonas, and multidrug-resistant Acinetobacter.
The researchers found that, compared with historical data from 5-8 years earlier, central line–associated bloodstream infections decreased by 50% and surgical site infections (SSIs) by 17% in 2014.
“There is encouraging news here,” Dr. Frieden said. “Doctors, nurses, hospitals, health care systems and other partners have made progress preventing some health care–associated infections.” However, the study found that one in six remaining central line-associated bloodstream infections were caused by urgent or serious antibiotic-resistant bacteria, while one in seven remaining surgical site infections were caused by urgent or serious antibiotic-resistant bacteria.
While catheter-associated urinary tract infections appear unchanged from baseline, there have been recent decreases, according to the study. In addition, C. difficile infections in hospitals decreased 8% between 2011 and 2014.
Dr. McDonald and his associates determined that in 2014, one in seven infections in acute care hospitals related to catheters and surgeries was caused by one of the six antibiotic-resistance threat bacteria, “which is deeply concerning,” Dr. Frieden said. That number increased to one in four infections in long-term acute care hospitals, a proportion that he characterized as “chilling.”
The CDC recommends three strategies that doctors, nurses, and other health care providers should take with every patient, to prevent HAIs and stop the spread of antibiotic resistance:
• Prevent the spread of bacteria between patients. Dr. Peter Pronovost, who participated in the telebriefing, said that he and his associates at Johns Hopkins University in Baltimore “do this by practicing good hand hygiene techniques by wearing sterile equipment when inserting lines.”
• Prevent surgery-related infections and/or placement of a catheter. “Check catheters frequently and remove them when you no longer need them,” advised Dr. Pronovost, director of the Armstrong Institute for Patient Safety and Quality at Johns Hopkins. “Ask if you actually need them before you even place them.”
• Improve antibiotic use through stewardship. This means using “the right antibiotics for the right duration,” Dr. Pronovost said. “Antibiotics could be lifesaving and are necessary for critically ill patients, especially those with septic shock. But these antibiotics need to be adjusted based on lab results and new information about the organisms that are causing these infections. Forty-eight hours after antibiotics are initiated, take a ‘time out.’ Perform a brief but focused assessment to determine if antibiotic therapy is still needed, or if it should be refined. A common mistake we make is to continue vancomycin when there is no presence of MRSA. We often tell our staff at Johns Hopkins, ‘if it doesn’t grow, let it go.’ ”
Dr. Frieden concluded his remarks by noting that physicians and other clinicians on the front lines “need support of their facility leadership,” to prevent HAIs. “Health care facilities, CEOs, and administrators are a major part of the solution. It’s important that they make a priority of infection prevention, sepsis prevention, and antibiotic stewardship. Know your facility’s data and target prevention efforts to ensure improvements in patient safety.”
FROM MMWR
MRSA incidence decreased in children as clindamycin resistance increased
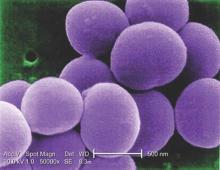
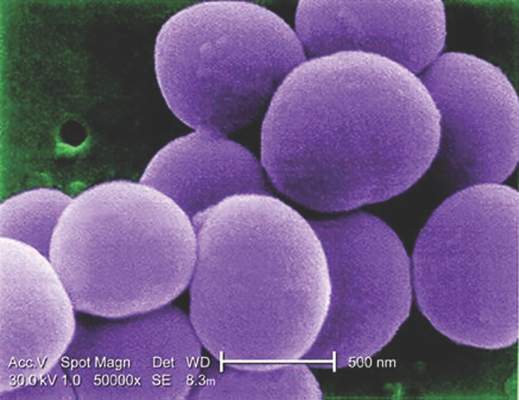
The incidence of methicillin-resistant Staphylococcus aureus (MRSA) infections has decreased in children in recent years, but resistance to clindamycin has increased over the same period, a study showed.
“The epidemic of skin and soft tissue infections and invasive MRSA led to modifications of antimicrobial prescribing practices for suspected S. aureus infections,” reported Dr. Deena E. Sutter of the San Antonio Military Medical Center in Fort Sam Houston, Tex., and her associates. “Over the study period, erythromycin susceptibility among methicillin-susceptible S. aureus (MSSA) remained stable, suggesting that declining clindamycin susceptibility is a result of an increase in inducible resistance.”
The steady decline in clindamycin susceptibility “may lead to some concern about the continued reliance on clindamycin for the empirical treatment of presumptive S. aureus infections, although it is probably premature to abandon this effective antibiotic choice,” they wrote (Pediatrics. 2016 Mar. 1. doi: 10.1542/peds.2015-3099). “It is crucial that clinicians remain knowledgeable about local susceptibility rates as it would be prudent to consider [alternative] antimicrobial agents for empirical use when the local clindamycin susceptibility rate drops below 85%.”
The researchers retrospectively analyzed lab results from 39,209 patients under age 18 who were treated for S. aureus infections at one of the 266 U.S. facilities of the Military Health System from 2005 to 2014. The data included 41,745 S. aureus isolates, classified as MRSA if found resistant to cefoxitin, methicillin, or oxacillin and as methicillin susceptible (MSSA) if susceptible to those antimicrobials. The isolates had also been tested for susceptibility to ciprofloxacin, clindamycin, erythromycin, gentamicin, oxacillin, penicillin, rifampin, tetracycline, and trimethoprim/sulfamethoxazole (TMP/SMX).
During that decade, overall S. aureus susceptibility to clindamycin, ciprofloxacin, and TMP/SMX decreased – although susceptibility to TMP/SMX in 2014 stayed high at 98% – while overall susceptibility to erythromycin, gentamicin, and oxacillin increased. Specifically, 59% of S. aureus isolates were susceptible to oxacillin in 2005, which dropped briefly to 54% in 2007 before climbing to the 2014 rate of 68%.
Meanwhile, overall susceptibility to clindamycin dropped from 91% in 2005 to 86% in 2014, and MSSA susceptibility to clindamycin dropped from 91% in 2005 to 84% in 2014. “Erythromycin susceptibility remained stable among MSSA isolates throughout the study period at 63.5%, whereas MRSA susceptibility to erythromycin increased from 12.1% to 20.5%,” Dr. Sutter and her associates reported. “Ciprofloxacin susceptibility significantly decreased overall, although an initial decrease of 10.6% over the first 7 years of the study was subsequently followed by an increase of 6% between 2011 and 2014.”
Most of the isolates came from patients with skin and soft tissue infections, which were less likely to be susceptible to oxacillin than were other infections. Infections in children aged 1-5 years also were less likely to be susceptible to oxacillin, compared with infections in children of other age groups.
If the local clindamycin susceptibility rate falls below 85%, “beta-lactams, TMP/SMX, or tetracyclines may be used for less severe infections with intravenous vancomycin employed in severe cases,” the investigators said. “If overall MRSA rates continue to decline and clindamycin resistance among MSSA continues to increase, we may see a return to antistaphylococcal beta-lactam antimicrobial agents such as oxacillin or first-generation cephalosporins as preferred empirical therapy for presumed S. aureus infections.”
The research did not use external funding, and the authors reported no relevant financial disclosures.
Staphylococcus aureus is one of the most common organisms isolated from children with health care–associated infections, regardless of whether these infections had their onset in the community or were acquired in the hospital. Thus, the initial empiric treatment of a skin or soft tissue infection or invasive infection in a child almost always includes an antibiotic effective against S. aureus.
However, over the years, clindamycin susceptibility among S. aureus isolates has declined, likely related to the increased use of this agent for empiric as well as definitive treatment of community-acquired (CA) MRSA infections, encouraging the transmission of the genes associated with clindamycin resistance.
What are the implications of the findings from the report by Sutter et al. with respect to the selection of empiric antibiotics for children with suspected S. aureus infections? Currently, considering the still substantial MRSA resistance rates that exceed the 10%-15% level suggested by many experts as the threshold above which agents effective against CA-MRSA isolates should be administered for empiric treatment, changes in the selection of empiric antibiotics are not warranted. If rates of MRSA among S. aureus isolates from otherwise normal children are documented to drop below the 10%-15% threshold in different communities, a modification of current recommendations should be considered. It would also be important to understand why methicillin resistance is declining among S. aureus isolates from CA infections; this information may provide clues for preventing CA-MRSA infections with the use of vaccines or other means. The epidemiology of S. aureus infections in children has been changing over the past 2 decades, which is why it is critical to keep a very close eye on this common pathogen.
These comments were excerpted from an accompanying commentary by Dr. Sheldon L. Kaplan of the infectious disease service at Texas Children’s Hospital in Houston (Pediatrics. 2016 Mar 1. doi: 10.1542/peds.2016-0101). Dr. Kaplan has received research funds from Pfizer, Forest Laboratories, and Cubist.
Staphylococcus aureus is one of the most common organisms isolated from children with health care–associated infections, regardless of whether these infections had their onset in the community or were acquired in the hospital. Thus, the initial empiric treatment of a skin or soft tissue infection or invasive infection in a child almost always includes an antibiotic effective against S. aureus.
However, over the years, clindamycin susceptibility among S. aureus isolates has declined, likely related to the increased use of this agent for empiric as well as definitive treatment of community-acquired (CA) MRSA infections, encouraging the transmission of the genes associated with clindamycin resistance.
What are the implications of the findings from the report by Sutter et al. with respect to the selection of empiric antibiotics for children with suspected S. aureus infections? Currently, considering the still substantial MRSA resistance rates that exceed the 10%-15% level suggested by many experts as the threshold above which agents effective against CA-MRSA isolates should be administered for empiric treatment, changes in the selection of empiric antibiotics are not warranted. If rates of MRSA among S. aureus isolates from otherwise normal children are documented to drop below the 10%-15% threshold in different communities, a modification of current recommendations should be considered. It would also be important to understand why methicillin resistance is declining among S. aureus isolates from CA infections; this information may provide clues for preventing CA-MRSA infections with the use of vaccines or other means. The epidemiology of S. aureus infections in children has been changing over the past 2 decades, which is why it is critical to keep a very close eye on this common pathogen.
These comments were excerpted from an accompanying commentary by Dr. Sheldon L. Kaplan of the infectious disease service at Texas Children’s Hospital in Houston (Pediatrics. 2016 Mar 1. doi: 10.1542/peds.2016-0101). Dr. Kaplan has received research funds from Pfizer, Forest Laboratories, and Cubist.
Staphylococcus aureus is one of the most common organisms isolated from children with health care–associated infections, regardless of whether these infections had their onset in the community or were acquired in the hospital. Thus, the initial empiric treatment of a skin or soft tissue infection or invasive infection in a child almost always includes an antibiotic effective against S. aureus.
However, over the years, clindamycin susceptibility among S. aureus isolates has declined, likely related to the increased use of this agent for empiric as well as definitive treatment of community-acquired (CA) MRSA infections, encouraging the transmission of the genes associated with clindamycin resistance.
What are the implications of the findings from the report by Sutter et al. with respect to the selection of empiric antibiotics for children with suspected S. aureus infections? Currently, considering the still substantial MRSA resistance rates that exceed the 10%-15% level suggested by many experts as the threshold above which agents effective against CA-MRSA isolates should be administered for empiric treatment, changes in the selection of empiric antibiotics are not warranted. If rates of MRSA among S. aureus isolates from otherwise normal children are documented to drop below the 10%-15% threshold in different communities, a modification of current recommendations should be considered. It would also be important to understand why methicillin resistance is declining among S. aureus isolates from CA infections; this information may provide clues for preventing CA-MRSA infections with the use of vaccines or other means. The epidemiology of S. aureus infections in children has been changing over the past 2 decades, which is why it is critical to keep a very close eye on this common pathogen.
These comments were excerpted from an accompanying commentary by Dr. Sheldon L. Kaplan of the infectious disease service at Texas Children’s Hospital in Houston (Pediatrics. 2016 Mar 1. doi: 10.1542/peds.2016-0101). Dr. Kaplan has received research funds from Pfizer, Forest Laboratories, and Cubist.
The incidence of methicillin-resistant Staphylococcus aureus (MRSA) infections has decreased in children in recent years, but resistance to clindamycin has increased over the same period, a study showed.
“The epidemic of skin and soft tissue infections and invasive MRSA led to modifications of antimicrobial prescribing practices for suspected S. aureus infections,” reported Dr. Deena E. Sutter of the San Antonio Military Medical Center in Fort Sam Houston, Tex., and her associates. “Over the study period, erythromycin susceptibility among methicillin-susceptible S. aureus (MSSA) remained stable, suggesting that declining clindamycin susceptibility is a result of an increase in inducible resistance.”
The steady decline in clindamycin susceptibility “may lead to some concern about the continued reliance on clindamycin for the empirical treatment of presumptive S. aureus infections, although it is probably premature to abandon this effective antibiotic choice,” they wrote (Pediatrics. 2016 Mar. 1. doi: 10.1542/peds.2015-3099). “It is crucial that clinicians remain knowledgeable about local susceptibility rates as it would be prudent to consider [alternative] antimicrobial agents for empirical use when the local clindamycin susceptibility rate drops below 85%.”
The researchers retrospectively analyzed lab results from 39,209 patients under age 18 who were treated for S. aureus infections at one of the 266 U.S. facilities of the Military Health System from 2005 to 2014. The data included 41,745 S. aureus isolates, classified as MRSA if found resistant to cefoxitin, methicillin, or oxacillin and as methicillin susceptible (MSSA) if susceptible to those antimicrobials. The isolates had also been tested for susceptibility to ciprofloxacin, clindamycin, erythromycin, gentamicin, oxacillin, penicillin, rifampin, tetracycline, and trimethoprim/sulfamethoxazole (TMP/SMX).
During that decade, overall S. aureus susceptibility to clindamycin, ciprofloxacin, and TMP/SMX decreased – although susceptibility to TMP/SMX in 2014 stayed high at 98% – while overall susceptibility to erythromycin, gentamicin, and oxacillin increased. Specifically, 59% of S. aureus isolates were susceptible to oxacillin in 2005, which dropped briefly to 54% in 2007 before climbing to the 2014 rate of 68%.
Meanwhile, overall susceptibility to clindamycin dropped from 91% in 2005 to 86% in 2014, and MSSA susceptibility to clindamycin dropped from 91% in 2005 to 84% in 2014. “Erythromycin susceptibility remained stable among MSSA isolates throughout the study period at 63.5%, whereas MRSA susceptibility to erythromycin increased from 12.1% to 20.5%,” Dr. Sutter and her associates reported. “Ciprofloxacin susceptibility significantly decreased overall, although an initial decrease of 10.6% over the first 7 years of the study was subsequently followed by an increase of 6% between 2011 and 2014.”
Most of the isolates came from patients with skin and soft tissue infections, which were less likely to be susceptible to oxacillin than were other infections. Infections in children aged 1-5 years also were less likely to be susceptible to oxacillin, compared with infections in children of other age groups.
If the local clindamycin susceptibility rate falls below 85%, “beta-lactams, TMP/SMX, or tetracyclines may be used for less severe infections with intravenous vancomycin employed in severe cases,” the investigators said. “If overall MRSA rates continue to decline and clindamycin resistance among MSSA continues to increase, we may see a return to antistaphylococcal beta-lactam antimicrobial agents such as oxacillin or first-generation cephalosporins as preferred empirical therapy for presumed S. aureus infections.”
The research did not use external funding, and the authors reported no relevant financial disclosures.
The incidence of methicillin-resistant Staphylococcus aureus (MRSA) infections has decreased in children in recent years, but resistance to clindamycin has increased over the same period, a study showed.
“The epidemic of skin and soft tissue infections and invasive MRSA led to modifications of antimicrobial prescribing practices for suspected S. aureus infections,” reported Dr. Deena E. Sutter of the San Antonio Military Medical Center in Fort Sam Houston, Tex., and her associates. “Over the study period, erythromycin susceptibility among methicillin-susceptible S. aureus (MSSA) remained stable, suggesting that declining clindamycin susceptibility is a result of an increase in inducible resistance.”
The steady decline in clindamycin susceptibility “may lead to some concern about the continued reliance on clindamycin for the empirical treatment of presumptive S. aureus infections, although it is probably premature to abandon this effective antibiotic choice,” they wrote (Pediatrics. 2016 Mar. 1. doi: 10.1542/peds.2015-3099). “It is crucial that clinicians remain knowledgeable about local susceptibility rates as it would be prudent to consider [alternative] antimicrobial agents for empirical use when the local clindamycin susceptibility rate drops below 85%.”
The researchers retrospectively analyzed lab results from 39,209 patients under age 18 who were treated for S. aureus infections at one of the 266 U.S. facilities of the Military Health System from 2005 to 2014. The data included 41,745 S. aureus isolates, classified as MRSA if found resistant to cefoxitin, methicillin, or oxacillin and as methicillin susceptible (MSSA) if susceptible to those antimicrobials. The isolates had also been tested for susceptibility to ciprofloxacin, clindamycin, erythromycin, gentamicin, oxacillin, penicillin, rifampin, tetracycline, and trimethoprim/sulfamethoxazole (TMP/SMX).
During that decade, overall S. aureus susceptibility to clindamycin, ciprofloxacin, and TMP/SMX decreased – although susceptibility to TMP/SMX in 2014 stayed high at 98% – while overall susceptibility to erythromycin, gentamicin, and oxacillin increased. Specifically, 59% of S. aureus isolates were susceptible to oxacillin in 2005, which dropped briefly to 54% in 2007 before climbing to the 2014 rate of 68%.
Meanwhile, overall susceptibility to clindamycin dropped from 91% in 2005 to 86% in 2014, and MSSA susceptibility to clindamycin dropped from 91% in 2005 to 84% in 2014. “Erythromycin susceptibility remained stable among MSSA isolates throughout the study period at 63.5%, whereas MRSA susceptibility to erythromycin increased from 12.1% to 20.5%,” Dr. Sutter and her associates reported. “Ciprofloxacin susceptibility significantly decreased overall, although an initial decrease of 10.6% over the first 7 years of the study was subsequently followed by an increase of 6% between 2011 and 2014.”
Most of the isolates came from patients with skin and soft tissue infections, which were less likely to be susceptible to oxacillin than were other infections. Infections in children aged 1-5 years also were less likely to be susceptible to oxacillin, compared with infections in children of other age groups.
If the local clindamycin susceptibility rate falls below 85%, “beta-lactams, TMP/SMX, or tetracyclines may be used for less severe infections with intravenous vancomycin employed in severe cases,” the investigators said. “If overall MRSA rates continue to decline and clindamycin resistance among MSSA continues to increase, we may see a return to antistaphylococcal beta-lactam antimicrobial agents such as oxacillin or first-generation cephalosporins as preferred empirical therapy for presumed S. aureus infections.”
The research did not use external funding, and the authors reported no relevant financial disclosures.
FROM PEDIATRICS
Key clinical point: The incidence of methicillin-resistant Staphylococcus aureus infections has decreased in children in recent years while resistance to clindamycin has increased.
Major finding: MRSA susceptibility to oxacillin increased to 68.4% in 2014, and susceptibility dropped to 86% for clindamycin.
Data source: A retrospective analysis of 41,745 S. aureus isolates from 39,209 patients under age 18 years in the U.S. Military Health System between 2005 and 2014.
Disclosures: The research did not use external funding, and the authors reported no relevant financial disclosures.
Fecal microbiota transplants achieved C. difficile resolution
An open-label study of fecal microbiota transfer in patients with recurrent Clostridium difficile infection has achieved clinical resolution in 96.7% of patients, according to a paper published online Feb. 8 in the Journal of Infectious Diseases.
Researchers treated 30 patients with two different dosing regimens of fractionated and encapsulated stool specimens from healthy donors, given after antibiotic therapy for a current episode of C. difficile infection.
At 8 weeks after dosing, 26 patients (86.7%) had had no C. difficile–positive diarrhea, and of the 4 who did have symptoms, 3 had early self-limiting diarrhea but tested negative for C. difficile carriage at 8 weeks, meaning that overall, 29 of the 30 patients achieved clinical resolution.
Patients also showed significant increases in microbial diversity from day 4 after treatment, and by week 8, the engrafted spore-forming bacteria made up around one-third of the total gut microbial carriage, with no serious adverse events related to the treatment (J Infect Diseases. 2016 Feb. 8. doi: 10.1093/infdis/jiv766).
“Although our study is limited by the lack of a placebo arm, the single clinical recurrence of C. difficile diarrhea in this study contrasts starkly with the recurrence rates documented in the placebo arms of three randomized, controlled trials involving patients with similar demographic characteristics and histories of recurrent episodes of [C. difficile infection],” wrote Dr. Sahil Khanna of the Mayo Clinic, Rochester, Minn., and coauthors.
The study was sponsored by Seres Therapeutics. One author reported a consultancy with Seres Therapeutics, and eight authors were employees of and held equity positions in Seres Therapeutics.
The development of SER-109 represents another major step toward fully engineered microbiota transfer, but we are still only halfway there.
Long-term safety databases are likely to play an important role in documenting currently unknown safety aspects of fecal microbiota transfer, and input from basic and clinical research is crucial to the identification of new indications.
Dr. Maria J.G.T. Vehreschild and Dr. Oliver A. Cornely are from the department of internal medicine at the University Hospital Cologne (Germany). These comments are adapted from an accompanying editorial (J Infect Diseases. 2016 Feb 8. doi: 10.1093/infdis/jiv768). The authors declared speakers bureau positions, lecture honoraria, research funding, and consultancies from a range of pharmaceutical companies. Dr. Cornely disclosed a consultancy with Seres.
The development of SER-109 represents another major step toward fully engineered microbiota transfer, but we are still only halfway there.
Long-term safety databases are likely to play an important role in documenting currently unknown safety aspects of fecal microbiota transfer, and input from basic and clinical research is crucial to the identification of new indications.
Dr. Maria J.G.T. Vehreschild and Dr. Oliver A. Cornely are from the department of internal medicine at the University Hospital Cologne (Germany). These comments are adapted from an accompanying editorial (J Infect Diseases. 2016 Feb 8. doi: 10.1093/infdis/jiv768). The authors declared speakers bureau positions, lecture honoraria, research funding, and consultancies from a range of pharmaceutical companies. Dr. Cornely disclosed a consultancy with Seres.
The development of SER-109 represents another major step toward fully engineered microbiota transfer, but we are still only halfway there.
Long-term safety databases are likely to play an important role in documenting currently unknown safety aspects of fecal microbiota transfer, and input from basic and clinical research is crucial to the identification of new indications.
Dr. Maria J.G.T. Vehreschild and Dr. Oliver A. Cornely are from the department of internal medicine at the University Hospital Cologne (Germany). These comments are adapted from an accompanying editorial (J Infect Diseases. 2016 Feb 8. doi: 10.1093/infdis/jiv768). The authors declared speakers bureau positions, lecture honoraria, research funding, and consultancies from a range of pharmaceutical companies. Dr. Cornely disclosed a consultancy with Seres.
An open-label study of fecal microbiota transfer in patients with recurrent Clostridium difficile infection has achieved clinical resolution in 96.7% of patients, according to a paper published online Feb. 8 in the Journal of Infectious Diseases.
Researchers treated 30 patients with two different dosing regimens of fractionated and encapsulated stool specimens from healthy donors, given after antibiotic therapy for a current episode of C. difficile infection.
At 8 weeks after dosing, 26 patients (86.7%) had had no C. difficile–positive diarrhea, and of the 4 who did have symptoms, 3 had early self-limiting diarrhea but tested negative for C. difficile carriage at 8 weeks, meaning that overall, 29 of the 30 patients achieved clinical resolution.
Patients also showed significant increases in microbial diversity from day 4 after treatment, and by week 8, the engrafted spore-forming bacteria made up around one-third of the total gut microbial carriage, with no serious adverse events related to the treatment (J Infect Diseases. 2016 Feb. 8. doi: 10.1093/infdis/jiv766).
“Although our study is limited by the lack of a placebo arm, the single clinical recurrence of C. difficile diarrhea in this study contrasts starkly with the recurrence rates documented in the placebo arms of three randomized, controlled trials involving patients with similar demographic characteristics and histories of recurrent episodes of [C. difficile infection],” wrote Dr. Sahil Khanna of the Mayo Clinic, Rochester, Minn., and coauthors.
The study was sponsored by Seres Therapeutics. One author reported a consultancy with Seres Therapeutics, and eight authors were employees of and held equity positions in Seres Therapeutics.
An open-label study of fecal microbiota transfer in patients with recurrent Clostridium difficile infection has achieved clinical resolution in 96.7% of patients, according to a paper published online Feb. 8 in the Journal of Infectious Diseases.
Researchers treated 30 patients with two different dosing regimens of fractionated and encapsulated stool specimens from healthy donors, given after antibiotic therapy for a current episode of C. difficile infection.
At 8 weeks after dosing, 26 patients (86.7%) had had no C. difficile–positive diarrhea, and of the 4 who did have symptoms, 3 had early self-limiting diarrhea but tested negative for C. difficile carriage at 8 weeks, meaning that overall, 29 of the 30 patients achieved clinical resolution.
Patients also showed significant increases in microbial diversity from day 4 after treatment, and by week 8, the engrafted spore-forming bacteria made up around one-third of the total gut microbial carriage, with no serious adverse events related to the treatment (J Infect Diseases. 2016 Feb. 8. doi: 10.1093/infdis/jiv766).
“Although our study is limited by the lack of a placebo arm, the single clinical recurrence of C. difficile diarrhea in this study contrasts starkly with the recurrence rates documented in the placebo arms of three randomized, controlled trials involving patients with similar demographic characteristics and histories of recurrent episodes of [C. difficile infection],” wrote Dr. Sahil Khanna of the Mayo Clinic, Rochester, Minn., and coauthors.
The study was sponsored by Seres Therapeutics. One author reported a consultancy with Seres Therapeutics, and eight authors were employees of and held equity positions in Seres Therapeutics.
FROM THE JOURNAL OF INFECTIOUS DISEASES
Key clinical point: Fecal microbiota transplants were highly efficacious in the treatment of recurrent Clostridium difficile infection in a study of 30 patients.
Major finding: Fecal microbiota transplants achieved clinical resolution of C. difficile infection in 96.7% of patients by 8 weeks.
Data source: An open-label study in 30 patients with recurrent C. difficile infection.
Disclosures: The study was sponsored by Seres Therapeutics. One author reported a consultancy with Seres Therapeutics, and eight authors were employees of and held equity positions in Seres Therapeutics.
Infection control is everyone’s responsibility
Big things come in small packages, very small – so small they may even be invisible to the naked eye. Take for instance a huge infection causing multiorgan system failure, disseminated intravascular coagulation, even septic shock refractory to high-dose pressors. This catastrophe may be the end result of exposure to tiny pathogenic microbes that can take down an otherwise healthy 300-pound man, tout suite!
Microorganisms are everywhere. We can’t live without them, but we can’t live with certain ones either. Unless you live in a bubble you are going to be exposed to countless bacteria each and every day. They are in the air we breathe, the water we drink, the beds we sleep in. While it is a given that we all will be continuously exposed to bacteria, having a well-considered strategy to curtail the spread of disease can dramatically decrease the risk that we, our families, and our patients are needlessly exposed to potentially life-threatening organisms.
We all know we are to wash our hands on the way in, and out, of patients’ rooms. This practice is our front line of defense against the spread of numerous potentially lethal diseases. Yet, many clinicians, as well as ancillary hospital personnel, repeatedly fail to abide by this rule, thinking that ‘this one time won’t hurt anything.’ Whether it’s the nurse who rushes into a patient’s room to stop a beeping IV pole or the doctor who eyes a family member in the room and makes a beeline to discuss the discharge plan, all of us have been guilty of entering or leaving a patient’s room without following appropriate infection control standards.
Or, how many times have you followed the protocol meticulously, at least initially, and removed your gown and gloves and washed your hands on your way out the door when the patient remembers another question, or asks you to hand him something that leads to more contact with him or his surroundings? You already washed your hands once, so must you really do it again? After all, what is the likelihood that you pick up (or pass along) any germs anyway? Sometimes, more than we realize. Something as simple as handing a patient his nurses’ call button can expose us to enough C. difficile spores to cause infection in us or others we come into contact with unwittingly. So wash those hands, and wash them again if you touch anything in a patient’s room, even if it is not the patient himself.
Direct observation (AKA “Secret Santas”) can provide invaluable information about adherence to hand hygiene among health care workers and providing feedback is key. This can be unit based, group based, and even provider based. Once collected, this information should be used to drive changes in behavior, which could be punitive or positive; each hospital should decide how to best use its data.
Visitor contact is another important issue and not everyone agrees on how to enforce, or whether to even try to enforce, infection control procedures. The Society for Healthcare Epidemiology of America (SHEA) has several helpful pocket guidelines to address this and other infection control issues. For instance, the society recommends that hospitals consider adopting guidelines to minimize horizontal transmission by visitors, though these guidelines should be feasible to enforce. Factors such as the specific organism and its potential to cause harm are important to consider when developing these guidelines. For instance, the spouse of a patient admitted with influenza has likely already been exposed, and postexposure prophylaxis may be more feasible to her than wearing an uncomfortable mask during an 8-hour hospital visit.
A pharmacy stewardship program is another invaluable infection control tool. With this model, a group of pharmacists, under the direction of an infectious disease specialist, reviews culture results daily and makes recommendations to the physician regarding narrowing antibiotic coverage. I greatly appreciate receiving calls to notify me that the final culture results are in long before I would have actually seen them myself. This allows me to adjust antibiotics in a timely fashion, thus reducing the emergence of drug-resistant organisms or precipitating an unnecessary case of C. difficile.
In addition, written guidelines should be established for indwelling catheters, both urinary and venous. The indication for continued use should be reassessed daily; a computer alert that requires a response is very helpful, as is a call from the friendly floor nurse asking, “Does this patient really still need his catheter?”
Infection control is everyone’s responsibility and we all need to work together toward this common goal.
Dr. Hester is a hospitalist at Baltimore-Washington Medical Center in Glen Burnie, Md. She is the creator of the Patient Whiz, a patient-engagement app for iOS. Reach her at healthsavvy@aol.com.
Big things come in small packages, very small – so small they may even be invisible to the naked eye. Take for instance a huge infection causing multiorgan system failure, disseminated intravascular coagulation, even septic shock refractory to high-dose pressors. This catastrophe may be the end result of exposure to tiny pathogenic microbes that can take down an otherwise healthy 300-pound man, tout suite!
Microorganisms are everywhere. We can’t live without them, but we can’t live with certain ones either. Unless you live in a bubble you are going to be exposed to countless bacteria each and every day. They are in the air we breathe, the water we drink, the beds we sleep in. While it is a given that we all will be continuously exposed to bacteria, having a well-considered strategy to curtail the spread of disease can dramatically decrease the risk that we, our families, and our patients are needlessly exposed to potentially life-threatening organisms.
We all know we are to wash our hands on the way in, and out, of patients’ rooms. This practice is our front line of defense against the spread of numerous potentially lethal diseases. Yet, many clinicians, as well as ancillary hospital personnel, repeatedly fail to abide by this rule, thinking that ‘this one time won’t hurt anything.’ Whether it’s the nurse who rushes into a patient’s room to stop a beeping IV pole or the doctor who eyes a family member in the room and makes a beeline to discuss the discharge plan, all of us have been guilty of entering or leaving a patient’s room without following appropriate infection control standards.
Or, how many times have you followed the protocol meticulously, at least initially, and removed your gown and gloves and washed your hands on your way out the door when the patient remembers another question, or asks you to hand him something that leads to more contact with him or his surroundings? You already washed your hands once, so must you really do it again? After all, what is the likelihood that you pick up (or pass along) any germs anyway? Sometimes, more than we realize. Something as simple as handing a patient his nurses’ call button can expose us to enough C. difficile spores to cause infection in us or others we come into contact with unwittingly. So wash those hands, and wash them again if you touch anything in a patient’s room, even if it is not the patient himself.
Direct observation (AKA “Secret Santas”) can provide invaluable information about adherence to hand hygiene among health care workers and providing feedback is key. This can be unit based, group based, and even provider based. Once collected, this information should be used to drive changes in behavior, which could be punitive or positive; each hospital should decide how to best use its data.
Visitor contact is another important issue and not everyone agrees on how to enforce, or whether to even try to enforce, infection control procedures. The Society for Healthcare Epidemiology of America (SHEA) has several helpful pocket guidelines to address this and other infection control issues. For instance, the society recommends that hospitals consider adopting guidelines to minimize horizontal transmission by visitors, though these guidelines should be feasible to enforce. Factors such as the specific organism and its potential to cause harm are important to consider when developing these guidelines. For instance, the spouse of a patient admitted with influenza has likely already been exposed, and postexposure prophylaxis may be more feasible to her than wearing an uncomfortable mask during an 8-hour hospital visit.
A pharmacy stewardship program is another invaluable infection control tool. With this model, a group of pharmacists, under the direction of an infectious disease specialist, reviews culture results daily and makes recommendations to the physician regarding narrowing antibiotic coverage. I greatly appreciate receiving calls to notify me that the final culture results are in long before I would have actually seen them myself. This allows me to adjust antibiotics in a timely fashion, thus reducing the emergence of drug-resistant organisms or precipitating an unnecessary case of C. difficile.
In addition, written guidelines should be established for indwelling catheters, both urinary and venous. The indication for continued use should be reassessed daily; a computer alert that requires a response is very helpful, as is a call from the friendly floor nurse asking, “Does this patient really still need his catheter?”
Infection control is everyone’s responsibility and we all need to work together toward this common goal.
Dr. Hester is a hospitalist at Baltimore-Washington Medical Center in Glen Burnie, Md. She is the creator of the Patient Whiz, a patient-engagement app for iOS. Reach her at healthsavvy@aol.com.
Big things come in small packages, very small – so small they may even be invisible to the naked eye. Take for instance a huge infection causing multiorgan system failure, disseminated intravascular coagulation, even septic shock refractory to high-dose pressors. This catastrophe may be the end result of exposure to tiny pathogenic microbes that can take down an otherwise healthy 300-pound man, tout suite!
Microorganisms are everywhere. We can’t live without them, but we can’t live with certain ones either. Unless you live in a bubble you are going to be exposed to countless bacteria each and every day. They are in the air we breathe, the water we drink, the beds we sleep in. While it is a given that we all will be continuously exposed to bacteria, having a well-considered strategy to curtail the spread of disease can dramatically decrease the risk that we, our families, and our patients are needlessly exposed to potentially life-threatening organisms.
We all know we are to wash our hands on the way in, and out, of patients’ rooms. This practice is our front line of defense against the spread of numerous potentially lethal diseases. Yet, many clinicians, as well as ancillary hospital personnel, repeatedly fail to abide by this rule, thinking that ‘this one time won’t hurt anything.’ Whether it’s the nurse who rushes into a patient’s room to stop a beeping IV pole or the doctor who eyes a family member in the room and makes a beeline to discuss the discharge plan, all of us have been guilty of entering or leaving a patient’s room without following appropriate infection control standards.
Or, how many times have you followed the protocol meticulously, at least initially, and removed your gown and gloves and washed your hands on your way out the door when the patient remembers another question, or asks you to hand him something that leads to more contact with him or his surroundings? You already washed your hands once, so must you really do it again? After all, what is the likelihood that you pick up (or pass along) any germs anyway? Sometimes, more than we realize. Something as simple as handing a patient his nurses’ call button can expose us to enough C. difficile spores to cause infection in us or others we come into contact with unwittingly. So wash those hands, and wash them again if you touch anything in a patient’s room, even if it is not the patient himself.
Direct observation (AKA “Secret Santas”) can provide invaluable information about adherence to hand hygiene among health care workers and providing feedback is key. This can be unit based, group based, and even provider based. Once collected, this information should be used to drive changes in behavior, which could be punitive or positive; each hospital should decide how to best use its data.
Visitor contact is another important issue and not everyone agrees on how to enforce, or whether to even try to enforce, infection control procedures. The Society for Healthcare Epidemiology of America (SHEA) has several helpful pocket guidelines to address this and other infection control issues. For instance, the society recommends that hospitals consider adopting guidelines to minimize horizontal transmission by visitors, though these guidelines should be feasible to enforce. Factors such as the specific organism and its potential to cause harm are important to consider when developing these guidelines. For instance, the spouse of a patient admitted with influenza has likely already been exposed, and postexposure prophylaxis may be more feasible to her than wearing an uncomfortable mask during an 8-hour hospital visit.
A pharmacy stewardship program is another invaluable infection control tool. With this model, a group of pharmacists, under the direction of an infectious disease specialist, reviews culture results daily and makes recommendations to the physician regarding narrowing antibiotic coverage. I greatly appreciate receiving calls to notify me that the final culture results are in long before I would have actually seen them myself. This allows me to adjust antibiotics in a timely fashion, thus reducing the emergence of drug-resistant organisms or precipitating an unnecessary case of C. difficile.
In addition, written guidelines should be established for indwelling catheters, both urinary and venous. The indication for continued use should be reassessed daily; a computer alert that requires a response is very helpful, as is a call from the friendly floor nurse asking, “Does this patient really still need his catheter?”
Infection control is everyone’s responsibility and we all need to work together toward this common goal.
Dr. Hester is a hospitalist at Baltimore-Washington Medical Center in Glen Burnie, Md. She is the creator of the Patient Whiz, a patient-engagement app for iOS. Reach her at healthsavvy@aol.com.
Manufacturer issues new reprocessing instructions for ED-3490TK video duodenoscope
PENTAX, the manufacturer of the ED-3490TK video duodenoscope, has issued updated validated manual reprocessing instructions to replace those provided in the original device labeling in response to a Food and Drug Administration Safety Communication released last February concerning the design of endoscopic retrograde cholangiopancreatography (ERCP) duodenoscopes and the risk of multidrug-resistant bacterial infections.
The FDA has reviewed these updated reprocessing instructions and recommends that staff be trained to implement them as soon as possible. Several changes have been made to the protocol for precleaning, manual cleaning, and high-level disinfection that the FDA found to be adequate.
Olympus, the manufacturer of the TJF-Q180V duodenoscope has also issued updated manual reprocessing instructions.
In February 2015, the FDA first announced that the agency had received reports of multidrug-resistant bacterial infections in patients who had undergone ERCP with duodenoscopes that had been cleaned and disinfected properly (according to manufacturer instructions) and determined that the “complex design of ERCP endoscopes (also called duodenoscopes) may impede effective reprocessing.”
Since then, the FDA has been working with duodenoscope manufacturers to revise their manual reprocessing instructions to devise standard procedures to eliminate the risk of spreading infection between patients and better survey any contamination of the duodenoscopes.
The American Gastroenterological Association's Center for GI Innovation and Technology has been working closely with the FDA and device manufacturers to develop a path forward with zero device-associated infections.
Adverse events associated with duodenoscopes should be reported to the FDA’s MedWatch program at 800-332-1088 or www.accessdata.fda.gov/scripts/medwatch.
PENTAX, the manufacturer of the ED-3490TK video duodenoscope, has issued updated validated manual reprocessing instructions to replace those provided in the original device labeling in response to a Food and Drug Administration Safety Communication released last February concerning the design of endoscopic retrograde cholangiopancreatography (ERCP) duodenoscopes and the risk of multidrug-resistant bacterial infections.
The FDA has reviewed these updated reprocessing instructions and recommends that staff be trained to implement them as soon as possible. Several changes have been made to the protocol for precleaning, manual cleaning, and high-level disinfection that the FDA found to be adequate.
Olympus, the manufacturer of the TJF-Q180V duodenoscope has also issued updated manual reprocessing instructions.
In February 2015, the FDA first announced that the agency had received reports of multidrug-resistant bacterial infections in patients who had undergone ERCP with duodenoscopes that had been cleaned and disinfected properly (according to manufacturer instructions) and determined that the “complex design of ERCP endoscopes (also called duodenoscopes) may impede effective reprocessing.”
Since then, the FDA has been working with duodenoscope manufacturers to revise their manual reprocessing instructions to devise standard procedures to eliminate the risk of spreading infection between patients and better survey any contamination of the duodenoscopes.
The American Gastroenterological Association's Center for GI Innovation and Technology has been working closely with the FDA and device manufacturers to develop a path forward with zero device-associated infections.
Adverse events associated with duodenoscopes should be reported to the FDA’s MedWatch program at 800-332-1088 or www.accessdata.fda.gov/scripts/medwatch.
PENTAX, the manufacturer of the ED-3490TK video duodenoscope, has issued updated validated manual reprocessing instructions to replace those provided in the original device labeling in response to a Food and Drug Administration Safety Communication released last February concerning the design of endoscopic retrograde cholangiopancreatography (ERCP) duodenoscopes and the risk of multidrug-resistant bacterial infections.
The FDA has reviewed these updated reprocessing instructions and recommends that staff be trained to implement them as soon as possible. Several changes have been made to the protocol for precleaning, manual cleaning, and high-level disinfection that the FDA found to be adequate.
Olympus, the manufacturer of the TJF-Q180V duodenoscope has also issued updated manual reprocessing instructions.
In February 2015, the FDA first announced that the agency had received reports of multidrug-resistant bacterial infections in patients who had undergone ERCP with duodenoscopes that had been cleaned and disinfected properly (according to manufacturer instructions) and determined that the “complex design of ERCP endoscopes (also called duodenoscopes) may impede effective reprocessing.”
Since then, the FDA has been working with duodenoscope manufacturers to revise their manual reprocessing instructions to devise standard procedures to eliminate the risk of spreading infection between patients and better survey any contamination of the duodenoscopes.
The American Gastroenterological Association's Center for GI Innovation and Technology has been working closely with the FDA and device manufacturers to develop a path forward with zero device-associated infections.
Adverse events associated with duodenoscopes should be reported to the FDA’s MedWatch program at 800-332-1088 or www.accessdata.fda.gov/scripts/medwatch.