User login
Disability in medicine: My experience
What does a doctor look like? Throughout history, this concept has shifted due to societal norms and increased access to medical education. Today, the idea of a physician has expanded to incorporate a myriad of people; however, stigma still exists in medicine regarding mental illness and disability. I would like to share my personal journey through high school, college, medical school, and now residency, and how my identity and struggles have shaped me into the physician I am today. There are few conversations around disability—especially disability and mental health—in medicine, and through my own advocacy, I have met many students with disability who feel that medical school is unattainable. Additionally, I have met many medical students, residents, and pre-health advisors who are happy for the experience to learn more about a marginalized group in medicine. My hope in sharing my story is to offer a space for conversation about intersectionality within medical communities and how physicians and physicians in training can facilitate that change, regardless of their position or specialty. Additionally, I hope to shed light on the unique mental health needs of patients with disabilities and how mental health clinicians can address those needs.
Perceived weaknesses turned into strengths
“Why do you walk like that?” “What is that brace on your leg?” The early years of my childhood were marked by these questions and others like them. I was the kid with the limp, the kid with a brace on his leg, and the kid who disappeared multiple times a week for doctor’s appointments or physical therapy. I learned to deflect these questions or give nebulous answers about an accident or injury. The reality is that I was born with cerebral palsy (CP). My CP manifested as hemiparesis on the left side of my body. I was in aggressive physical therapy throughout childhood, received Botox injections for muscle spasticity, and underwent corrective surgery on my left leg to straighten my foot. In childhood, the diagnosis meant nothing more than 2 words that sounded like they belonged to superheroes in comic books. Even with supportive parents and family, I kept my disability a secret, much like the powers and abilities of my favorite superheroes.
However, like all great origin stories, what I once thought were weaknesses turned out to be strengths that pushed me through college, medical school, and now psychiatry residency. Living with a disability has shaped how I see the world and relate to my patients. My experience has helped me connect to my patients in ways others might not. These properties are important in any physician but vital in psychiatry, where many patients feel neglected or stigmatized; this is another reason there should be more doctors with disabilities in medicine. Unfortunately, systemic barriers are still in place that disincentivize those with a disability from pursuing careers in medicine. Stories like mine are important to inspire a reexamination of what a physician should be and how medicine, patients, and communities benefit from this change.
My experience through medical school
My path to psychiatry and residency was shaped by my early experience with the medical field and treatment. From the early days of my diagnosis at age 4, I was told that my brain was “wired differently” and that, because of this disruption in circuitry, I would have difficulty with physical activity. I grew to appreciate the intricacies of the brain and pathology to understand my body. With greater understanding came the existential realization that I would live with a disability for the rest of my life. Rather than dream of a future where I would be “normal,” I focused on adapting my life to my normal. An unfortunate reality of this normal was that no doctor would be able to relate to me, and my health care would focus on limitations rather than possibilities.
I focused on school as a distraction and slowly warmed to the idea of pursuing medicine as a career. The seed was planted years prior by the numerous doctors’ visits and procedures, and was cultivated by a desire to understand pathologies and offer treatment to patients from the perspective of a patient. When I applied to medical school, I did not know how to address my CP. Living as a person with CP was a core reason for my decision to pursue medicine, but I was afraid that a disclosure of disability would preclude any admission to medical school. Research into programs offered little guidance because most institutions only listed vague “physical expectations” of each student. There were times I doubted if I would be accepted anywhere. Many programs I reached out to about my situation seemed unenthusiastic about the prospect of a student with CP, and when I brought up my CP in interviews, the reaction was often of surprise and an admission that they had forgotten about “that part” of my application. Fortunately, I was accepted to medical school, but still struggled with the fear that one day I would be found out and not allowed to continue. No one in my class or school was like me, and a meeting with an Americans with Disabilities Act coordinator who asked me to reexamine the physical competencies of the school before advancing to clinical clerkships only further reinforced this fear. I decided to fly under the radar and not say anything about my disability to my attendings. I slowly worked my way through clerkships by making do with adapted ways to perform procedures and exams with additional practice and maneuvering at home. I found myself drawn to psychiatry because of the similarities I saw in the patients and myself. I empathized with how the patients struggled with chronic conditions that left them feeling separated from society and how they felt that their diagnosis was something they needed to hide. When medical school ended and I decided to pursue psychiatry, I wanted to share my story to inspire others with a disability to consider medicine as a career given their unique experiences. My experience thus far has been uplifting as my journey has echoed so many others.
A need for greater representation
Disability representation in medicine is needed more than ever. According to the CDC, >60 million adults in the United States (1 in 4) live with a disability.1 Although the physical health disparities are often discussed, there is less conversation surrounding mental health for individuals with disabilities. A 2018 study by Cree et al2 found that approximately 17.4 million adults with disabilities experienced frequent mental distress, defined as reporting ≥14 mentally unhealthy days in the past 30 days. Furthermore, compared to individuals without a disability, those with a disability are statistically more likely to have suicidal ideation, suicidal planning, and suicide attempts.3 One way to address this disparity is to recruit medical students with disabilities to become physicians with disabilities. Evidence suggests that physicians who are members of groups that are underrepresented in medicine are more likely to deliver care to underrepresented patients.4 However, medical schools and institutions have been slow to address the disparity. A 2019 survey found an estimated 4.6% of medical students responded “yes” when asked if they had a disability, with most students reporting a psychological or attention/hyperactive disorder.5 Existing barriers include restrictive language surrounding technical standards influenced by long-standing vestiges of what a physician should be.6
An opportunity to connect with patients
I now do not see myself as having a secret identity to hide. Although my CP does not give me any superpowers, it has given me the opportunity to connect with my patients and serve as an example of why medical school recruitment and admissions should expand. Psychiatrists have been on the forefront of change in medicine and can shift the perception of a physician. In doing so, we not only enrich our field but also the lives of our patients who may need it most.
1. Okoro CA, Hollis ND, Cyrus AC, et al. Prevalence of disabilities and health care access by disability status and type among adults—United States, 2016. MMWR Morb Mortal Wkly Rep. 2018;67(32):882-887.
2. Cree RA, Okoro CA, Zack MM, et al. Frequent mental distress among adults, by disability status, disability type, and selected characteristics—United States 2018. MMWR Morb Mortal Wkly Rep. 2020;69(36):1238-1243.
3. Marlow NM, Xie Z, Tanner R, et al. Association between disability and suicide-related outcomes among US adults. Am J Prev Med. 2021;61(6):852-862.
4. Thurmond VB, Kirch DG. Impact of minority physicians on health care. South Med J. 1998;91(11):1009-1013.
5. Meeks LM, Case B, Herzer K, et al. Change in prevalence of disabilities and accommodation practices among US medical schools, 2016 vs 2019. JAMA. 2019;322(20):2022-2024.
6. Stauffer C, Case B, Moreland CJ, et al. Technical standards from newly established medical schools: a review of disability inclusive practices. J Med Educ Curric Dev. 2022;9:23821205211072763.
What does a doctor look like? Throughout history, this concept has shifted due to societal norms and increased access to medical education. Today, the idea of a physician has expanded to incorporate a myriad of people; however, stigma still exists in medicine regarding mental illness and disability. I would like to share my personal journey through high school, college, medical school, and now residency, and how my identity and struggles have shaped me into the physician I am today. There are few conversations around disability—especially disability and mental health—in medicine, and through my own advocacy, I have met many students with disability who feel that medical school is unattainable. Additionally, I have met many medical students, residents, and pre-health advisors who are happy for the experience to learn more about a marginalized group in medicine. My hope in sharing my story is to offer a space for conversation about intersectionality within medical communities and how physicians and physicians in training can facilitate that change, regardless of their position or specialty. Additionally, I hope to shed light on the unique mental health needs of patients with disabilities and how mental health clinicians can address those needs.
Perceived weaknesses turned into strengths
“Why do you walk like that?” “What is that brace on your leg?” The early years of my childhood were marked by these questions and others like them. I was the kid with the limp, the kid with a brace on his leg, and the kid who disappeared multiple times a week for doctor’s appointments or physical therapy. I learned to deflect these questions or give nebulous answers about an accident or injury. The reality is that I was born with cerebral palsy (CP). My CP manifested as hemiparesis on the left side of my body. I was in aggressive physical therapy throughout childhood, received Botox injections for muscle spasticity, and underwent corrective surgery on my left leg to straighten my foot. In childhood, the diagnosis meant nothing more than 2 words that sounded like they belonged to superheroes in comic books. Even with supportive parents and family, I kept my disability a secret, much like the powers and abilities of my favorite superheroes.
However, like all great origin stories, what I once thought were weaknesses turned out to be strengths that pushed me through college, medical school, and now psychiatry residency. Living with a disability has shaped how I see the world and relate to my patients. My experience has helped me connect to my patients in ways others might not. These properties are important in any physician but vital in psychiatry, where many patients feel neglected or stigmatized; this is another reason there should be more doctors with disabilities in medicine. Unfortunately, systemic barriers are still in place that disincentivize those with a disability from pursuing careers in medicine. Stories like mine are important to inspire a reexamination of what a physician should be and how medicine, patients, and communities benefit from this change.
My experience through medical school
My path to psychiatry and residency was shaped by my early experience with the medical field and treatment. From the early days of my diagnosis at age 4, I was told that my brain was “wired differently” and that, because of this disruption in circuitry, I would have difficulty with physical activity. I grew to appreciate the intricacies of the brain and pathology to understand my body. With greater understanding came the existential realization that I would live with a disability for the rest of my life. Rather than dream of a future where I would be “normal,” I focused on adapting my life to my normal. An unfortunate reality of this normal was that no doctor would be able to relate to me, and my health care would focus on limitations rather than possibilities.
I focused on school as a distraction and slowly warmed to the idea of pursuing medicine as a career. The seed was planted years prior by the numerous doctors’ visits and procedures, and was cultivated by a desire to understand pathologies and offer treatment to patients from the perspective of a patient. When I applied to medical school, I did not know how to address my CP. Living as a person with CP was a core reason for my decision to pursue medicine, but I was afraid that a disclosure of disability would preclude any admission to medical school. Research into programs offered little guidance because most institutions only listed vague “physical expectations” of each student. There were times I doubted if I would be accepted anywhere. Many programs I reached out to about my situation seemed unenthusiastic about the prospect of a student with CP, and when I brought up my CP in interviews, the reaction was often of surprise and an admission that they had forgotten about “that part” of my application. Fortunately, I was accepted to medical school, but still struggled with the fear that one day I would be found out and not allowed to continue. No one in my class or school was like me, and a meeting with an Americans with Disabilities Act coordinator who asked me to reexamine the physical competencies of the school before advancing to clinical clerkships only further reinforced this fear. I decided to fly under the radar and not say anything about my disability to my attendings. I slowly worked my way through clerkships by making do with adapted ways to perform procedures and exams with additional practice and maneuvering at home. I found myself drawn to psychiatry because of the similarities I saw in the patients and myself. I empathized with how the patients struggled with chronic conditions that left them feeling separated from society and how they felt that their diagnosis was something they needed to hide. When medical school ended and I decided to pursue psychiatry, I wanted to share my story to inspire others with a disability to consider medicine as a career given their unique experiences. My experience thus far has been uplifting as my journey has echoed so many others.
A need for greater representation
Disability representation in medicine is needed more than ever. According to the CDC, >60 million adults in the United States (1 in 4) live with a disability.1 Although the physical health disparities are often discussed, there is less conversation surrounding mental health for individuals with disabilities. A 2018 study by Cree et al2 found that approximately 17.4 million adults with disabilities experienced frequent mental distress, defined as reporting ≥14 mentally unhealthy days in the past 30 days. Furthermore, compared to individuals without a disability, those with a disability are statistically more likely to have suicidal ideation, suicidal planning, and suicide attempts.3 One way to address this disparity is to recruit medical students with disabilities to become physicians with disabilities. Evidence suggests that physicians who are members of groups that are underrepresented in medicine are more likely to deliver care to underrepresented patients.4 However, medical schools and institutions have been slow to address the disparity. A 2019 survey found an estimated 4.6% of medical students responded “yes” when asked if they had a disability, with most students reporting a psychological or attention/hyperactive disorder.5 Existing barriers include restrictive language surrounding technical standards influenced by long-standing vestiges of what a physician should be.6
An opportunity to connect with patients
I now do not see myself as having a secret identity to hide. Although my CP does not give me any superpowers, it has given me the opportunity to connect with my patients and serve as an example of why medical school recruitment and admissions should expand. Psychiatrists have been on the forefront of change in medicine and can shift the perception of a physician. In doing so, we not only enrich our field but also the lives of our patients who may need it most.
What does a doctor look like? Throughout history, this concept has shifted due to societal norms and increased access to medical education. Today, the idea of a physician has expanded to incorporate a myriad of people; however, stigma still exists in medicine regarding mental illness and disability. I would like to share my personal journey through high school, college, medical school, and now residency, and how my identity and struggles have shaped me into the physician I am today. There are few conversations around disability—especially disability and mental health—in medicine, and through my own advocacy, I have met many students with disability who feel that medical school is unattainable. Additionally, I have met many medical students, residents, and pre-health advisors who are happy for the experience to learn more about a marginalized group in medicine. My hope in sharing my story is to offer a space for conversation about intersectionality within medical communities and how physicians and physicians in training can facilitate that change, regardless of their position or specialty. Additionally, I hope to shed light on the unique mental health needs of patients with disabilities and how mental health clinicians can address those needs.
Perceived weaknesses turned into strengths
“Why do you walk like that?” “What is that brace on your leg?” The early years of my childhood were marked by these questions and others like them. I was the kid with the limp, the kid with a brace on his leg, and the kid who disappeared multiple times a week for doctor’s appointments or physical therapy. I learned to deflect these questions or give nebulous answers about an accident or injury. The reality is that I was born with cerebral palsy (CP). My CP manifested as hemiparesis on the left side of my body. I was in aggressive physical therapy throughout childhood, received Botox injections for muscle spasticity, and underwent corrective surgery on my left leg to straighten my foot. In childhood, the diagnosis meant nothing more than 2 words that sounded like they belonged to superheroes in comic books. Even with supportive parents and family, I kept my disability a secret, much like the powers and abilities of my favorite superheroes.
However, like all great origin stories, what I once thought were weaknesses turned out to be strengths that pushed me through college, medical school, and now psychiatry residency. Living with a disability has shaped how I see the world and relate to my patients. My experience has helped me connect to my patients in ways others might not. These properties are important in any physician but vital in psychiatry, where many patients feel neglected or stigmatized; this is another reason there should be more doctors with disabilities in medicine. Unfortunately, systemic barriers are still in place that disincentivize those with a disability from pursuing careers in medicine. Stories like mine are important to inspire a reexamination of what a physician should be and how medicine, patients, and communities benefit from this change.
My experience through medical school
My path to psychiatry and residency was shaped by my early experience with the medical field and treatment. From the early days of my diagnosis at age 4, I was told that my brain was “wired differently” and that, because of this disruption in circuitry, I would have difficulty with physical activity. I grew to appreciate the intricacies of the brain and pathology to understand my body. With greater understanding came the existential realization that I would live with a disability for the rest of my life. Rather than dream of a future where I would be “normal,” I focused on adapting my life to my normal. An unfortunate reality of this normal was that no doctor would be able to relate to me, and my health care would focus on limitations rather than possibilities.
I focused on school as a distraction and slowly warmed to the idea of pursuing medicine as a career. The seed was planted years prior by the numerous doctors’ visits and procedures, and was cultivated by a desire to understand pathologies and offer treatment to patients from the perspective of a patient. When I applied to medical school, I did not know how to address my CP. Living as a person with CP was a core reason for my decision to pursue medicine, but I was afraid that a disclosure of disability would preclude any admission to medical school. Research into programs offered little guidance because most institutions only listed vague “physical expectations” of each student. There were times I doubted if I would be accepted anywhere. Many programs I reached out to about my situation seemed unenthusiastic about the prospect of a student with CP, and when I brought up my CP in interviews, the reaction was often of surprise and an admission that they had forgotten about “that part” of my application. Fortunately, I was accepted to medical school, but still struggled with the fear that one day I would be found out and not allowed to continue. No one in my class or school was like me, and a meeting with an Americans with Disabilities Act coordinator who asked me to reexamine the physical competencies of the school before advancing to clinical clerkships only further reinforced this fear. I decided to fly under the radar and not say anything about my disability to my attendings. I slowly worked my way through clerkships by making do with adapted ways to perform procedures and exams with additional practice and maneuvering at home. I found myself drawn to psychiatry because of the similarities I saw in the patients and myself. I empathized with how the patients struggled with chronic conditions that left them feeling separated from society and how they felt that their diagnosis was something they needed to hide. When medical school ended and I decided to pursue psychiatry, I wanted to share my story to inspire others with a disability to consider medicine as a career given their unique experiences. My experience thus far has been uplifting as my journey has echoed so many others.
A need for greater representation
Disability representation in medicine is needed more than ever. According to the CDC, >60 million adults in the United States (1 in 4) live with a disability.1 Although the physical health disparities are often discussed, there is less conversation surrounding mental health for individuals with disabilities. A 2018 study by Cree et al2 found that approximately 17.4 million adults with disabilities experienced frequent mental distress, defined as reporting ≥14 mentally unhealthy days in the past 30 days. Furthermore, compared to individuals without a disability, those with a disability are statistically more likely to have suicidal ideation, suicidal planning, and suicide attempts.3 One way to address this disparity is to recruit medical students with disabilities to become physicians with disabilities. Evidence suggests that physicians who are members of groups that are underrepresented in medicine are more likely to deliver care to underrepresented patients.4 However, medical schools and institutions have been slow to address the disparity. A 2019 survey found an estimated 4.6% of medical students responded “yes” when asked if they had a disability, with most students reporting a psychological or attention/hyperactive disorder.5 Existing barriers include restrictive language surrounding technical standards influenced by long-standing vestiges of what a physician should be.6
An opportunity to connect with patients
I now do not see myself as having a secret identity to hide. Although my CP does not give me any superpowers, it has given me the opportunity to connect with my patients and serve as an example of why medical school recruitment and admissions should expand. Psychiatrists have been on the forefront of change in medicine and can shift the perception of a physician. In doing so, we not only enrich our field but also the lives of our patients who may need it most.
1. Okoro CA, Hollis ND, Cyrus AC, et al. Prevalence of disabilities and health care access by disability status and type among adults—United States, 2016. MMWR Morb Mortal Wkly Rep. 2018;67(32):882-887.
2. Cree RA, Okoro CA, Zack MM, et al. Frequent mental distress among adults, by disability status, disability type, and selected characteristics—United States 2018. MMWR Morb Mortal Wkly Rep. 2020;69(36):1238-1243.
3. Marlow NM, Xie Z, Tanner R, et al. Association between disability and suicide-related outcomes among US adults. Am J Prev Med. 2021;61(6):852-862.
4. Thurmond VB, Kirch DG. Impact of minority physicians on health care. South Med J. 1998;91(11):1009-1013.
5. Meeks LM, Case B, Herzer K, et al. Change in prevalence of disabilities and accommodation practices among US medical schools, 2016 vs 2019. JAMA. 2019;322(20):2022-2024.
6. Stauffer C, Case B, Moreland CJ, et al. Technical standards from newly established medical schools: a review of disability inclusive practices. J Med Educ Curric Dev. 2022;9:23821205211072763.
1. Okoro CA, Hollis ND, Cyrus AC, et al. Prevalence of disabilities and health care access by disability status and type among adults—United States, 2016. MMWR Morb Mortal Wkly Rep. 2018;67(32):882-887.
2. Cree RA, Okoro CA, Zack MM, et al. Frequent mental distress among adults, by disability status, disability type, and selected characteristics—United States 2018. MMWR Morb Mortal Wkly Rep. 2020;69(36):1238-1243.
3. Marlow NM, Xie Z, Tanner R, et al. Association between disability and suicide-related outcomes among US adults. Am J Prev Med. 2021;61(6):852-862.
4. Thurmond VB, Kirch DG. Impact of minority physicians on health care. South Med J. 1998;91(11):1009-1013.
5. Meeks LM, Case B, Herzer K, et al. Change in prevalence of disabilities and accommodation practices among US medical schools, 2016 vs 2019. JAMA. 2019;322(20):2022-2024.
6. Stauffer C, Case B, Moreland CJ, et al. Technical standards from newly established medical schools: a review of disability inclusive practices. J Med Educ Curric Dev. 2022;9:23821205211072763.
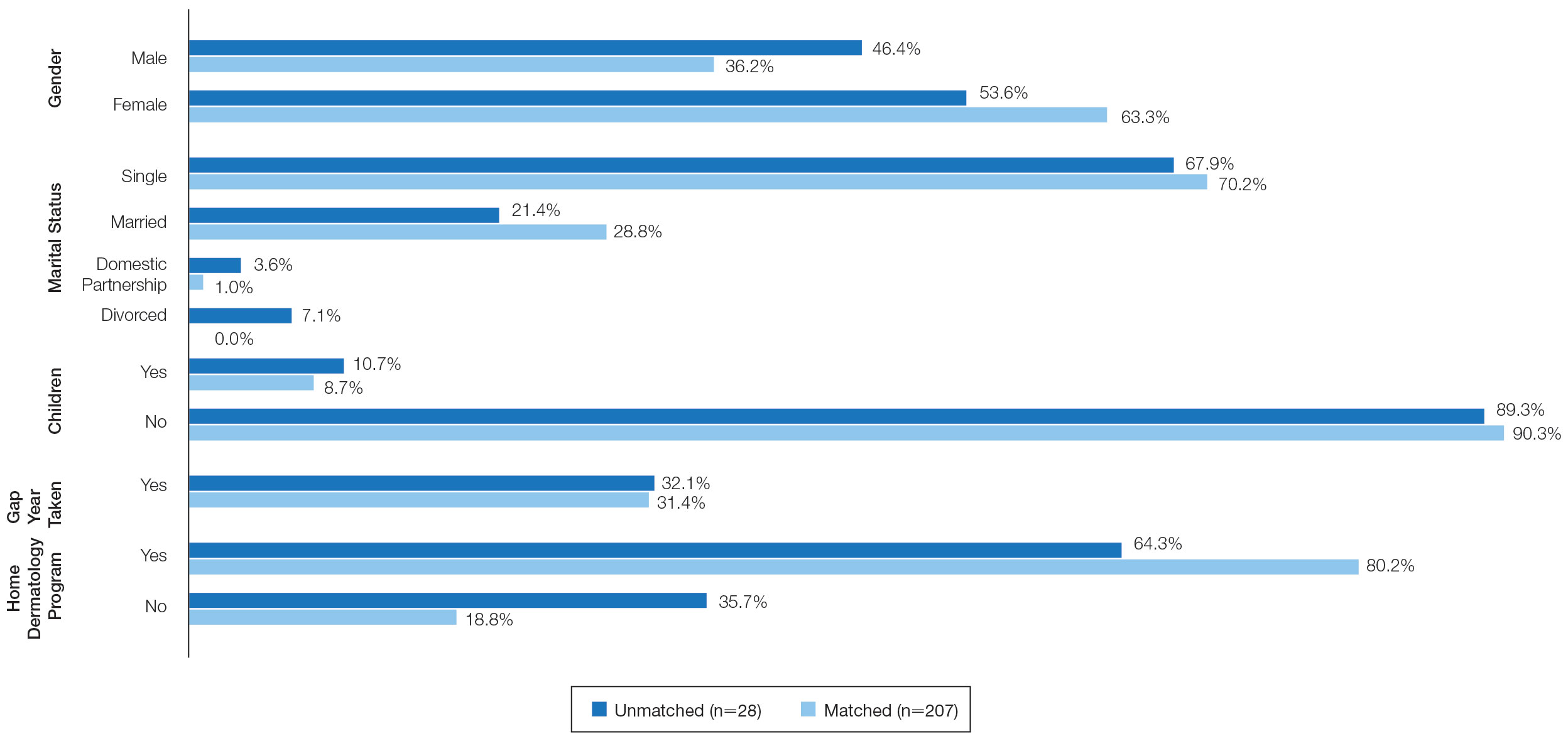
Characteristics of Matched vs Nonmatched Dermatology Applicants
Dermatology residency continues to be one of the most competitive specialties, with a match rate of 84.7% for US allopathic seniors in the 2019-2020 academic year.1 In the 2019-2020 cycle, dermatology applicants were tied with plastic surgery for the highest median US Medical Licensing Examination (USMLE) Step 1 score compared with other specialties, which suggests that the top medical students are applying, yet only approximately 5 of 6 students are matching.
Factors that have been cited with successful dermatology matching include USMLE Step 1 and Step 2 Clinical Knowledge (CK) scores,2 research accomplishments,3 letters of recommendation,4 medical school performance, personal statement, grades in required clerkships, and volunteer/extracurricular experiences, among others.5
The National Resident Matching Program (NRMP) publishes data each year regarding different academic factors—USMLE scores; number of abstracts, presentations, and papers; work, volunteer, and research experiences—and compares the mean between matched and nonmatched applicants.1 However, the USMLE does not report any demographic information of the applicants and the implication it has for matching. Additionally, the number of couples participating in the couples match continues to increase each year. In the 2019-2020 cycle, 1224 couples participated in the couples match.1 However, NRMP reports only limited data regarding the couples match, and it is not specialty specific.
We aimed to determine the characteristics of matched vs nonmatched dermatology applicants. Secondarily, we aimed to determine any differences among demographics regarding matching rates, academic performance, and research publications. We also aimed to characterize the strategy and outcomes of applicants that couples matched.
Materials and Methods
The Mayo Clinic institutional review board deemed this study exempt. All applicants who applied to Mayo Clinic dermatology residency in Scottsdale, Arizona, during the 2018-2019 cycle were emailed an initial survey (N=475) before Match Day that obtained demographic information, geographic information, gap-year information, USMLE Step 1 score, publications, medical school grades, number of away rotations, and number of interviews. A follow-up survey gathering match data and couples matching data was sent to the applicants who completed the first survey on Match Day. The survey was repeated for the 2019-2020 cycle. In the second survey, Step 2 CK data were obtained. The survey was sent to 629 applicants who applied to Mayo Clinic dermatology residencies in Arizona, Minnesota, and Florida to include a broader group of applicants. For publications, applicants were asked to count only published or accepted manuscripts, not abstracts, posters, conference presentations, or submitted manuscripts. Applicants who did not respond to the second survey (match data) were not included in that part of the analysis. One survey was excluded because of implausible answers (eg, scores outside of range for USMLE Step scores).
Statistical Analysis—For statistical analyses, the applicants from both applications cycles were combined. Descriptive statistics were reported in the form of mean, median, or counts (percentages), as applicable. Means were compared using 2-sided t tests. Group comparisons were examined using χ2 tests for categorical variables. Statistical analyses were performed using the BlueSky Statistics version 6.30. P<.05 was considered significant.
Results
In 2019, a total of 149 applicants completed the initial survey (31.4% response rate), and 112 completed the follow-up survey (75.2% response rate). In 2020, a total of 142 applicants completed the initial survey (22.6% response rate), and 124 completed the follow-up survey (87.3% response rate). Combining the 2 years, after removing 1 survey with implausible answers, there were 290 respondents from the initial survey and 235 from the follow-up survey. The median (SD) age for the total applicants over both years was 27 (3.0) years, and 180 applicants were female (61.9%).
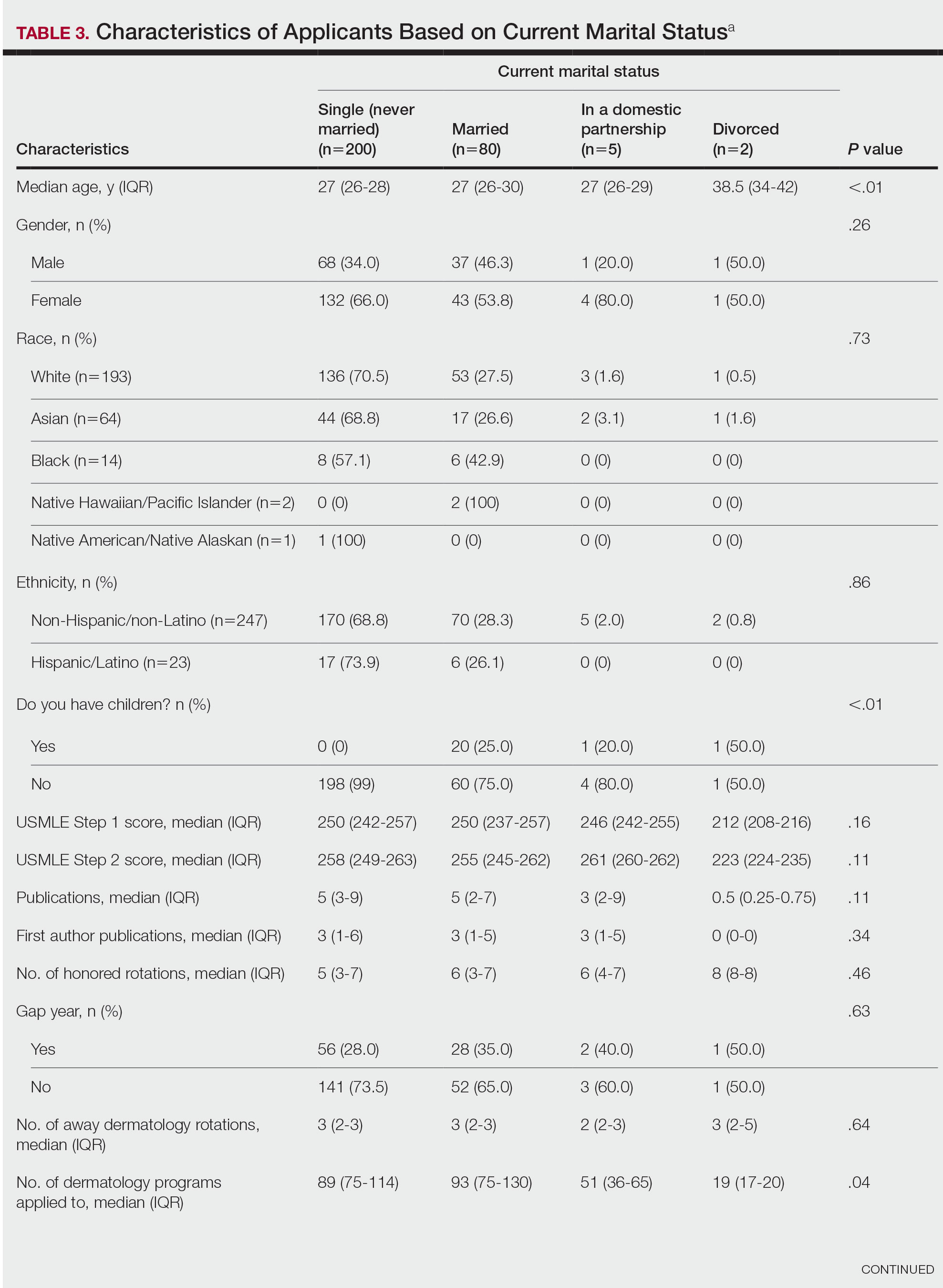
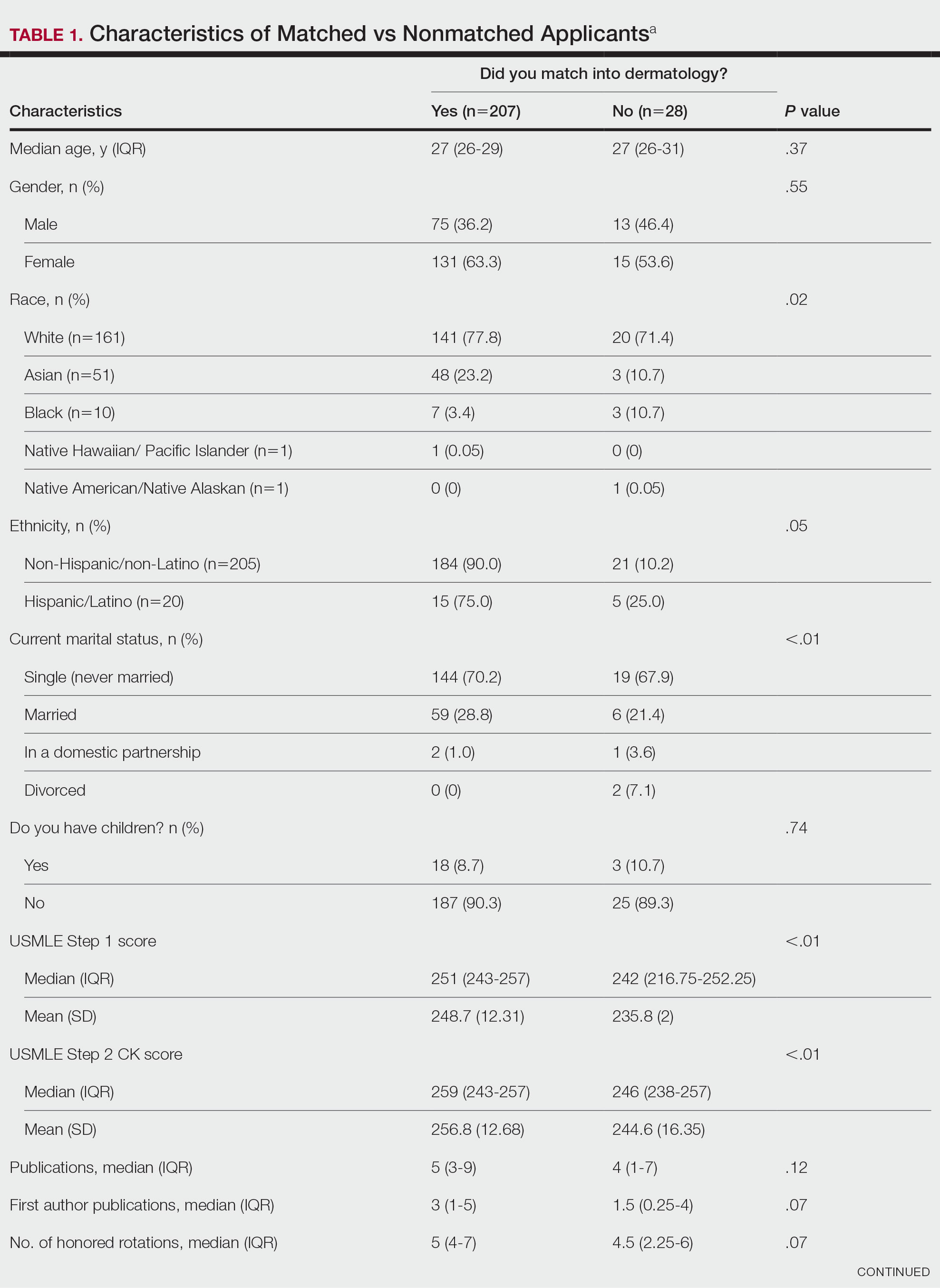
USMLE Scores—The median USMLE Step 1 score was 250, and scores ranged from 196 to 271. The median USMLE Step 2 CK score was 257, and scores ranged from 213 to 281. Higher USMLE Step 1 and Step 2 CK scores and more interviews were associated with higher match rates (Table 1). In addition, students with a dermatology program at their medical school were more likely to match than those without a home dermatology program.
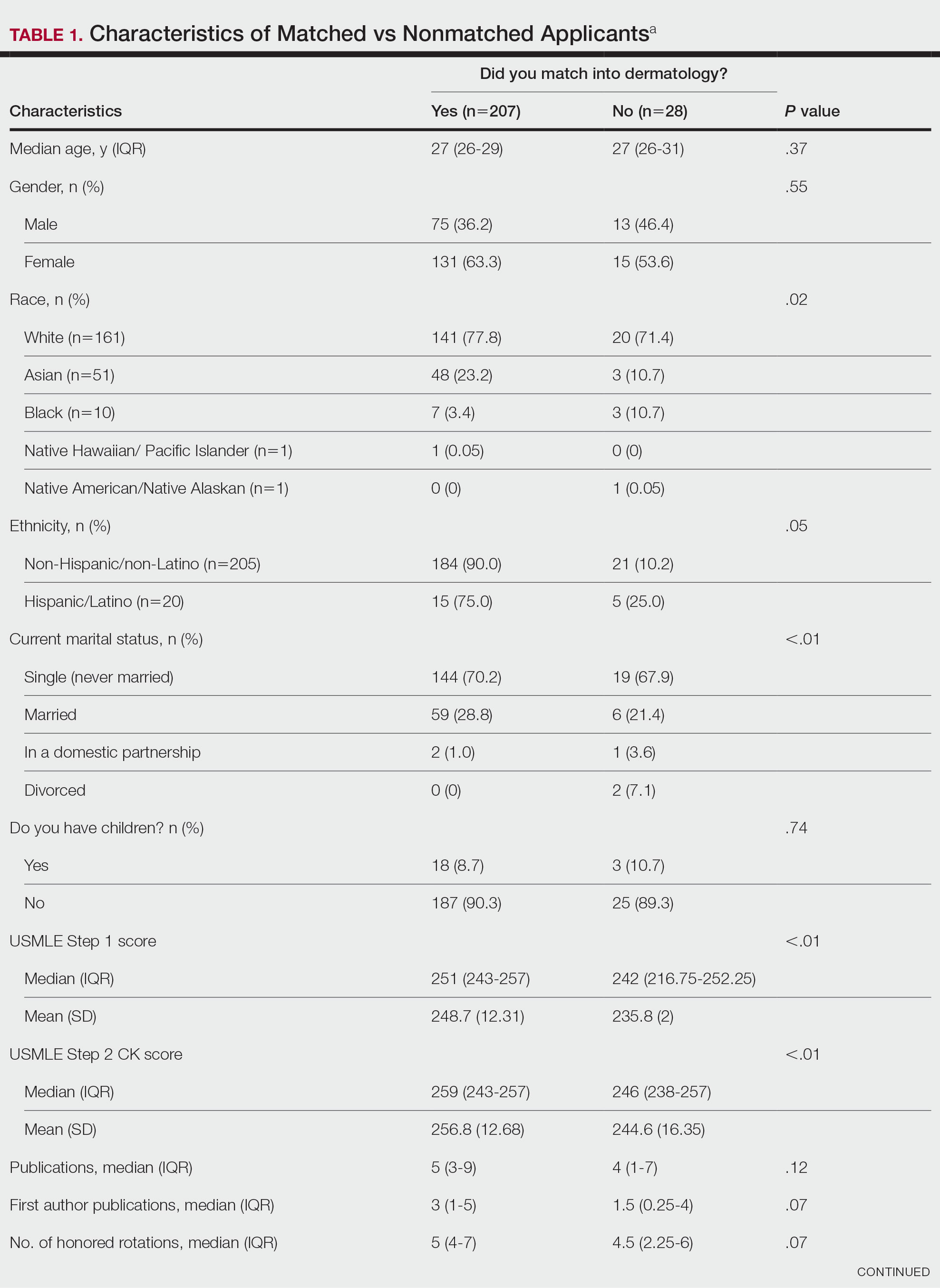

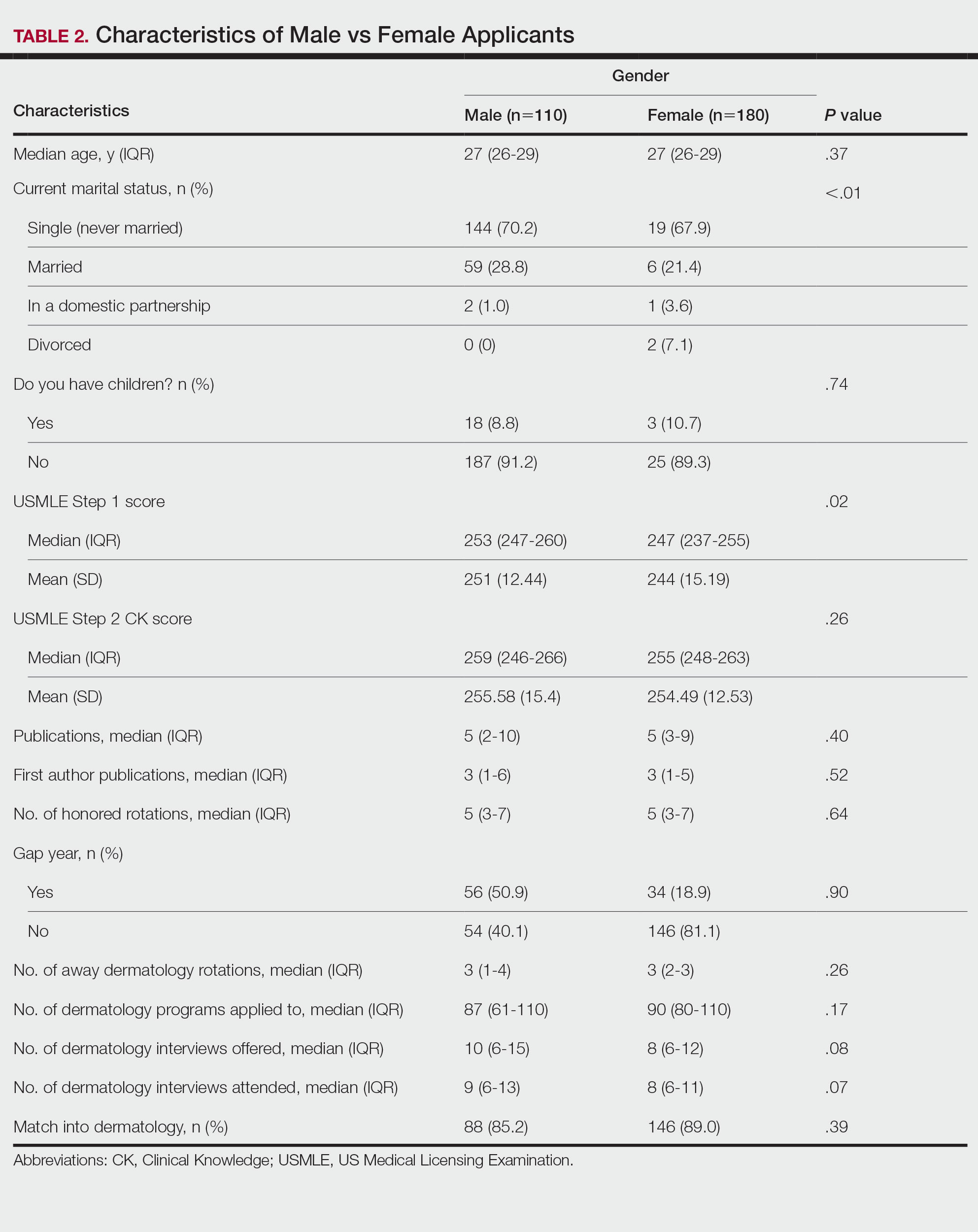
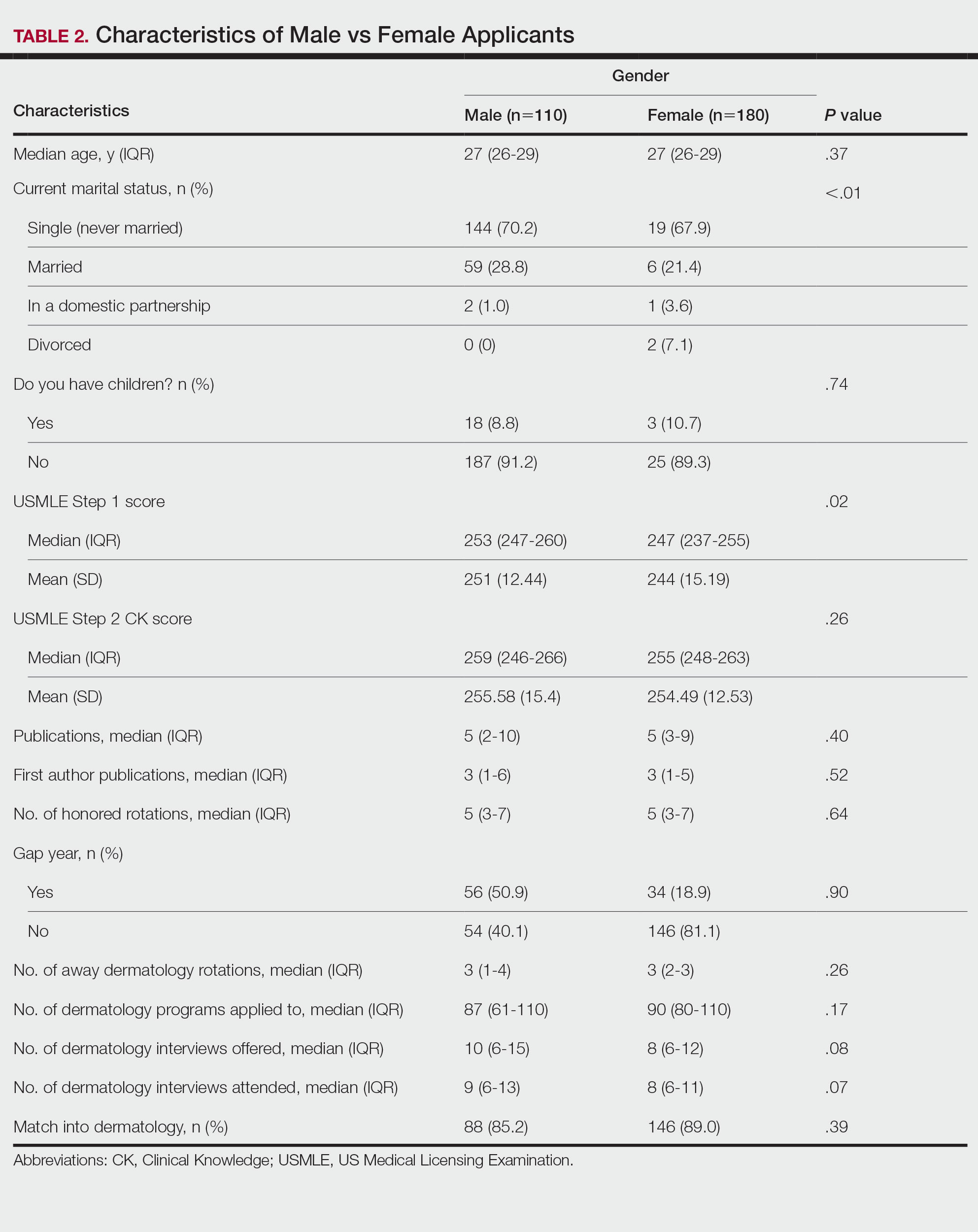
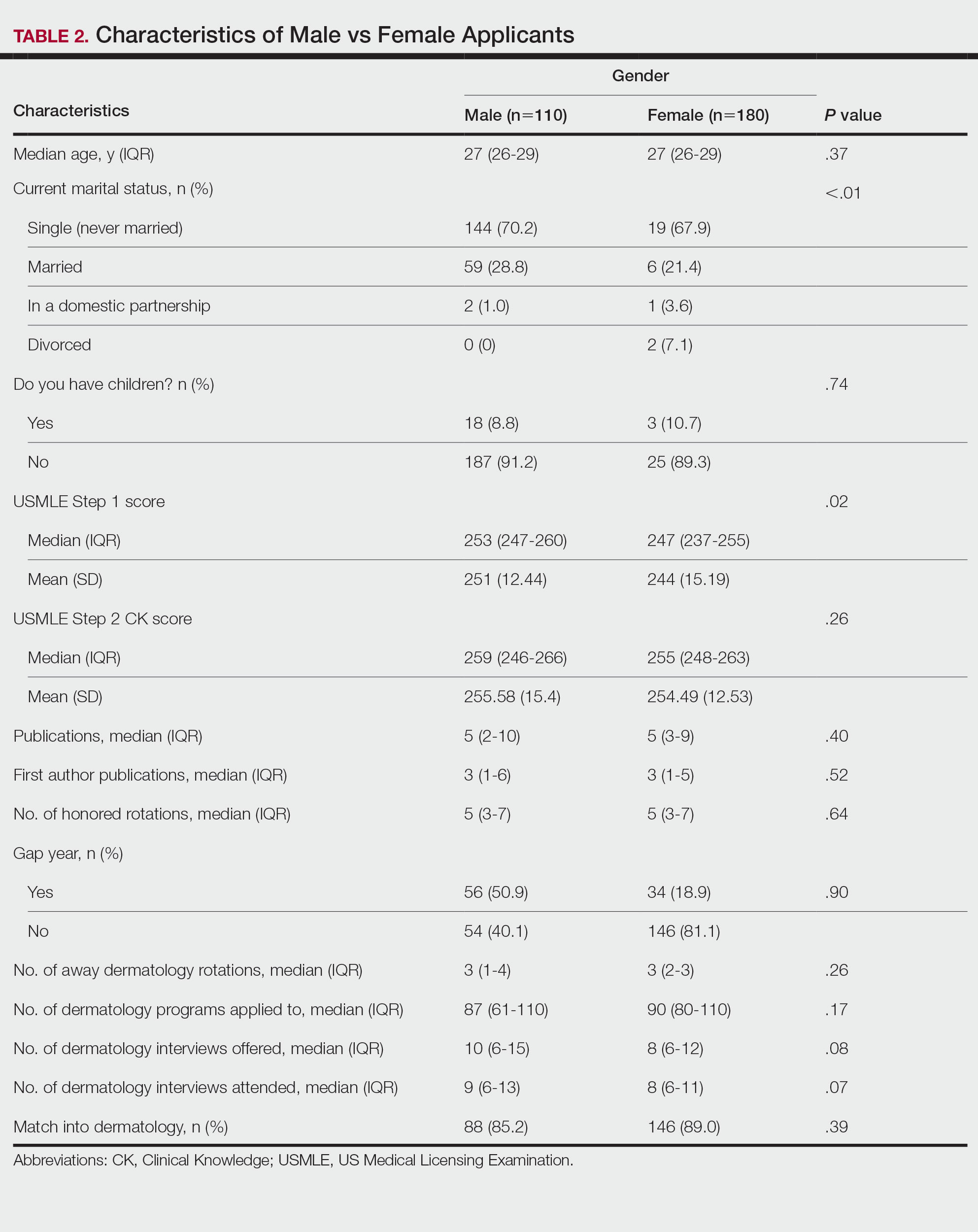
Gender Differences—There were 180 females and 110 males who completed the surveys. Males and females had similar match rates (85.2% vs 89.0%; P=.39)(Table 2).
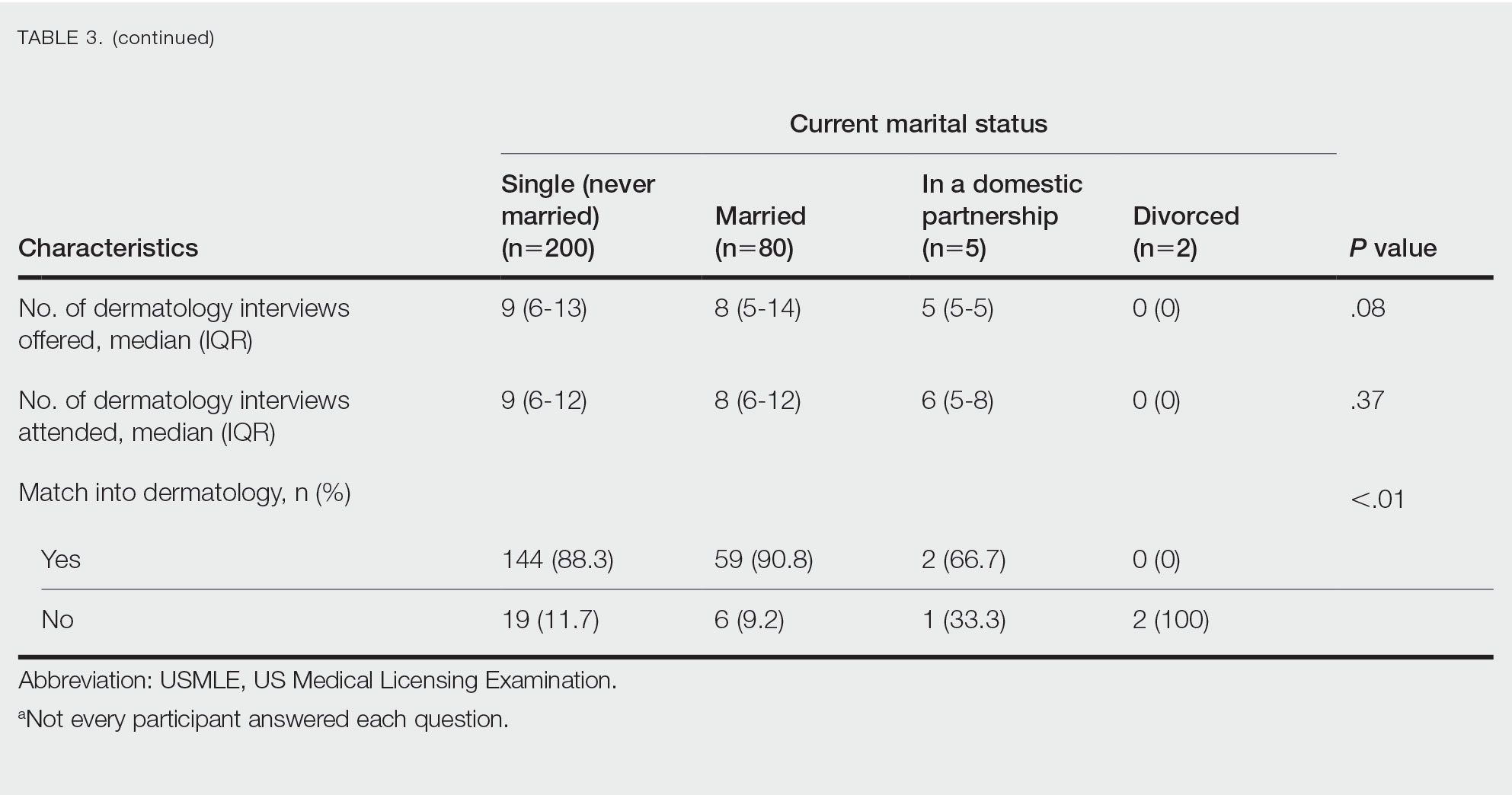
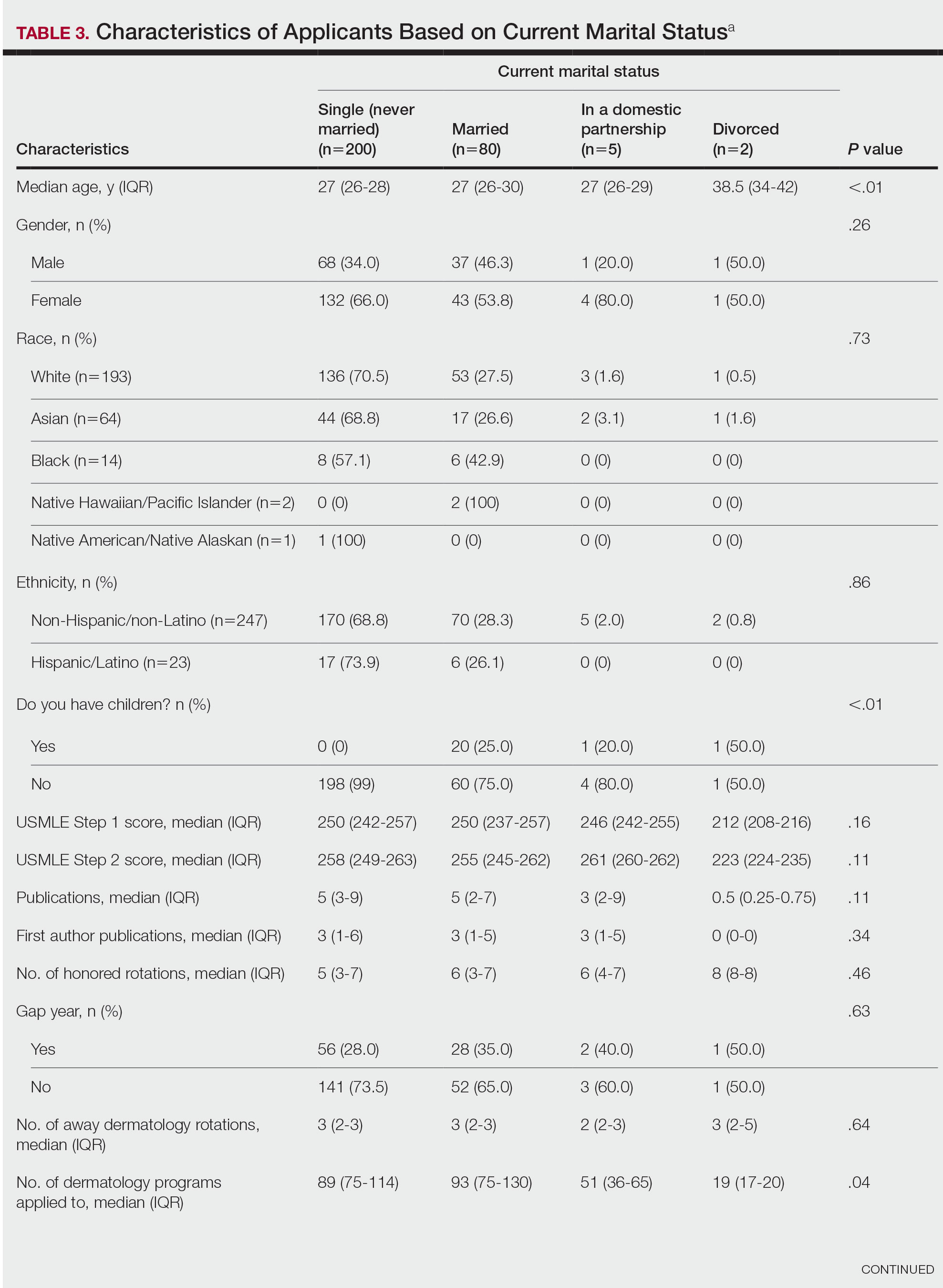
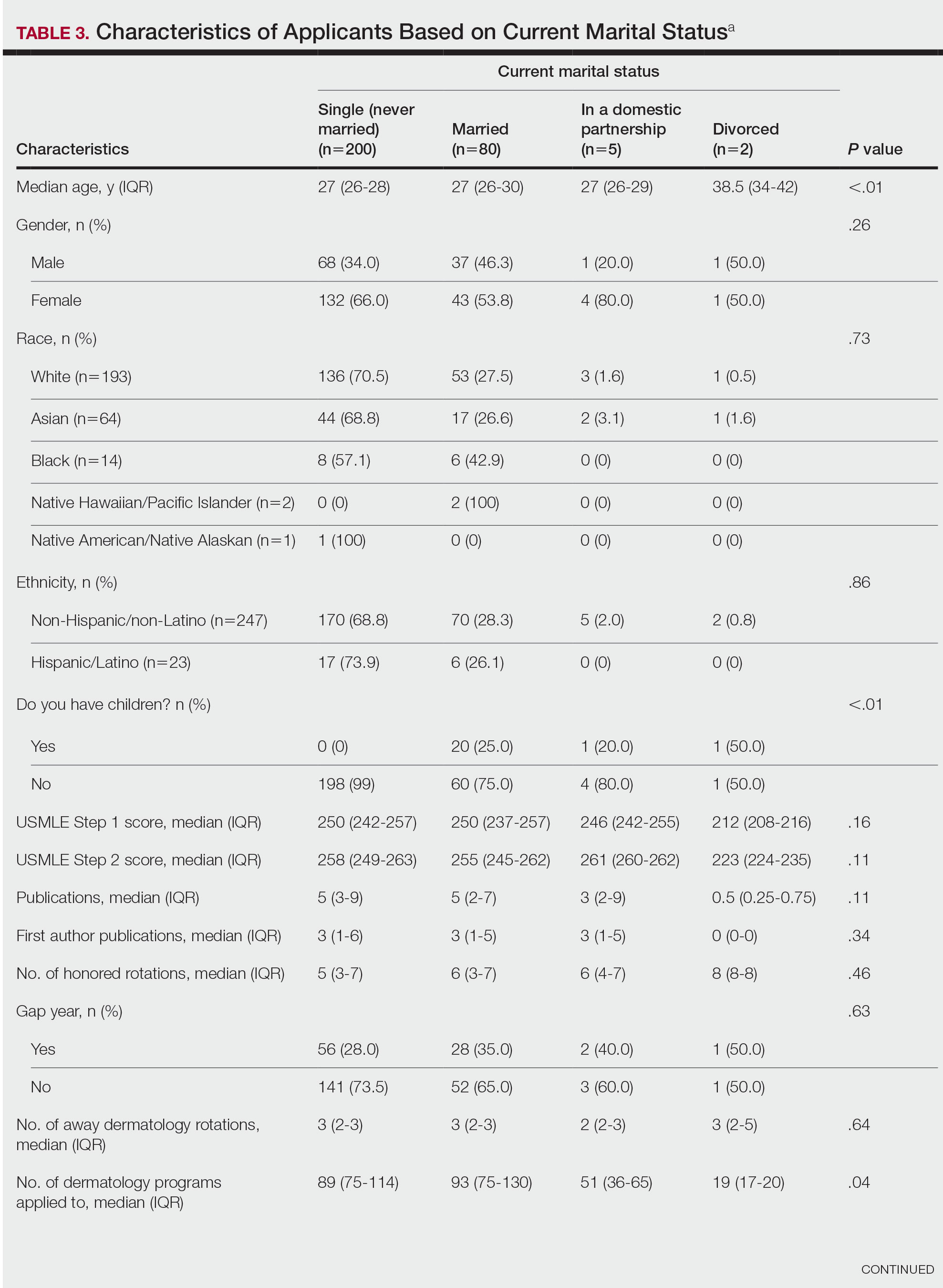
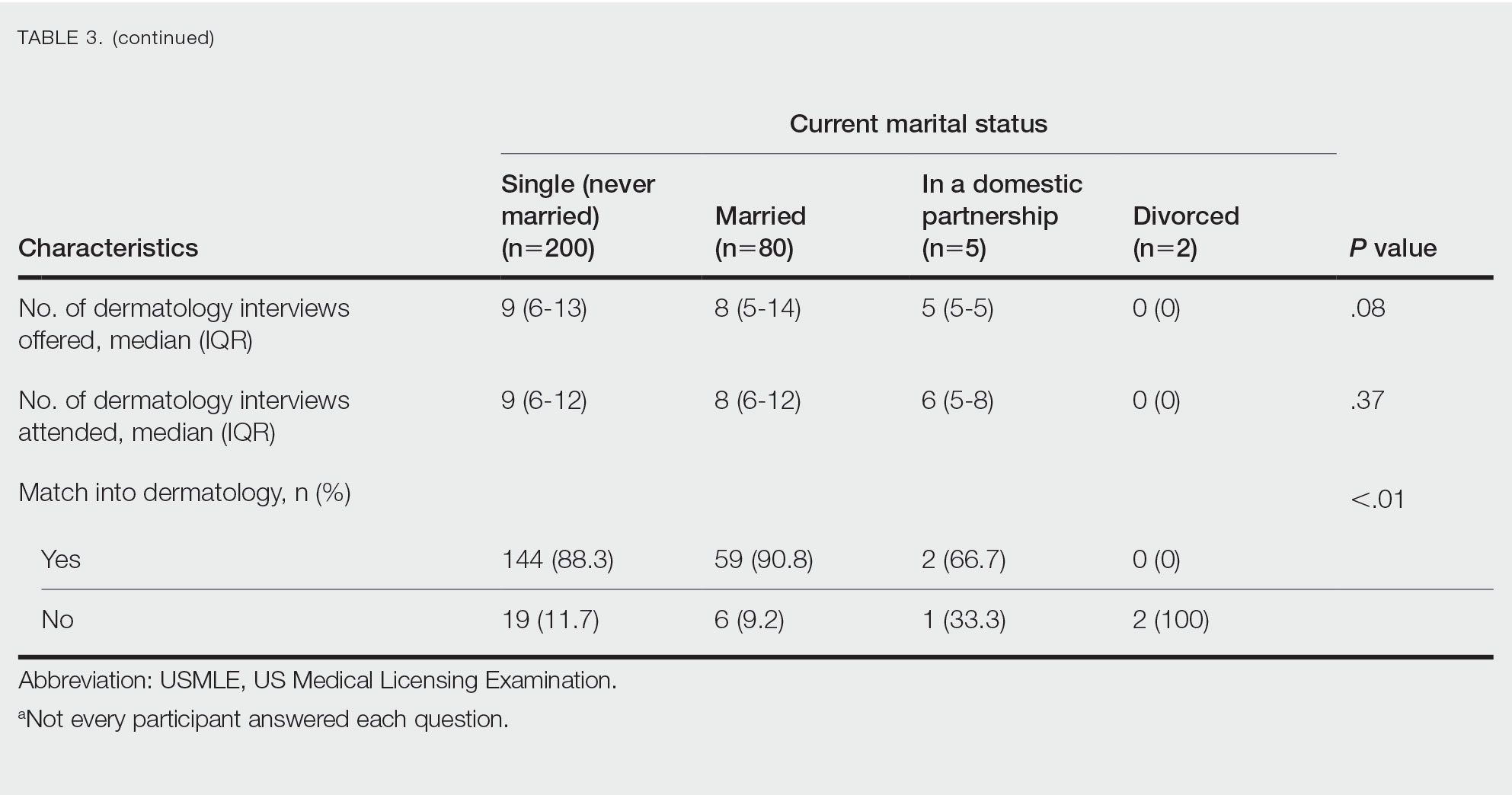
Family Life—In comparing marital status, applicants who were divorced had a higher median age (38.5 years) compared with applicants who were single, married, or in a domestic partnership (all 27 years; P<.01). Differences are outlined in Table 3.
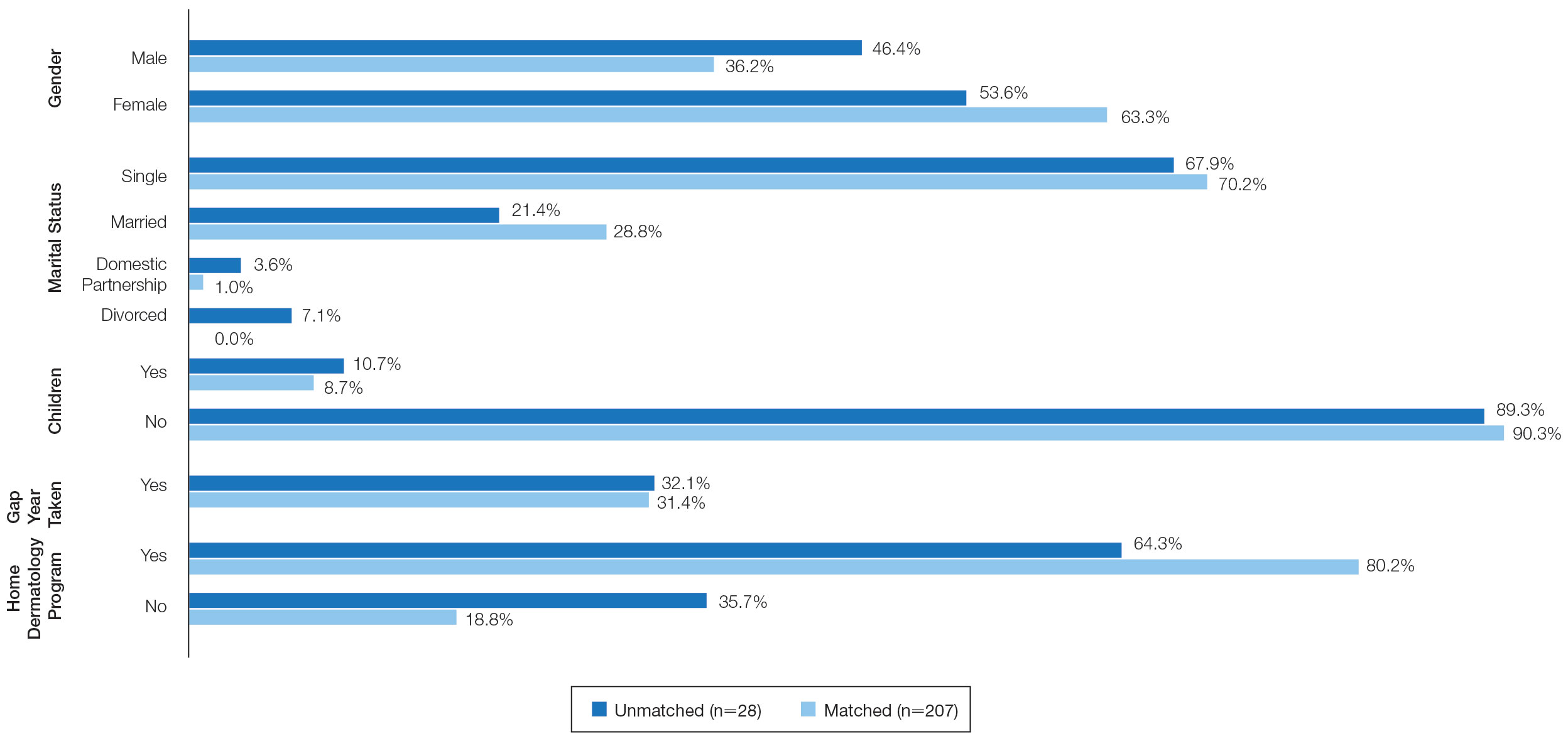
On average, applicants with children (n=27 [15 male, 12 female]; P=.13) were 3 years older than those without (30.5 vs 27; P<.01) and were more likely to be married (88.9% vs 21.5%; P<.01). Applicants with children had a mean USMLE Step 1 score of 241 compared to 251 for those without children (P=.02) and a mean USMLE Step 2 CK score of 246 compared to 258 for those without children (P<.01). Applicants with children had similar debt, number of publications, number of honored rotations, and match rates compared to applicants without children (Figure).
Couples Match—Seventeen individuals in our survey participated in the couples match (7.8%), and all 17 (100%) matched into dermatology. The mean age was 26.7 years, 12 applicants were female, 2 applicants were married, and 1 applicant had children. The mean number of interviews offered was 13.6, and the mean number of interviews attended was 11.3. This was higher than participants who were not couples matching (13.6 vs 9.8 [P=.02] and 11.3 vs 8.9 [P=.04], respectively). Applicants and their partners applied to programs and received interviews in a mean of 10 cities. Sixteen applicants reported that they contacted programs where their partner had interview offers. All participants’ rank lists included programs located in different cities than their partners’ ranked programs, and all but 1 participant ranked programs located in a different state than their partners’ ranked programs. Fifteen participants had options in their rank list for the applicant not to match, even if the partner would match. Similarly, 12 had the option for the applicant to match, even if the partner would not match. Fourteen (82.4%) matched at the same institution as their significant other. Three (17.6%) applicants matched to a program in a different state than the partner’s matched program. Two (11.8%) participants felt their relationship with their partner suffered because of the match, and 1 (5.9%) applicant was undetermined. One applicant described their relationship suffering from “unnecessary tension and anxiety” and noted “difficult conversations” about potentially matching into dermatology in a different location from their partner that could have been “devastating and not something [he or she] should have to choose.”
Comment
Factors for Matching in Dermatology—In our survey, we found the statistically significant factors of matching into dermatology included high USMLE Step 1 and Step 2 CK scores (P<.01), having a home dermatology program (P=.04), and attending a higher number of dermatology interviews (P<.01). These data are similar to NRMP results1; however, the higher likelihood of matching if the medical school has a home dermatology program has not been reported. This finding could be due to multiple factors such as students have less access to academic dermatologists for research projects, letters of recommendations, mentorship, and clinical rotations.
Gender and having children were factors that had no correlation with the match rate. There was a statistical difference of matching based on marital status (P<.01), but this is likely due to the low number of applicants in the divorced category. There were differences among demographics with USMLE Step 1 and Step 2 CK scores, which is a known factor in matching.1,2 Applicants with children had lower USMLE Step 1 and Step 2 CK scores compared to applicants without children. Females also had lower median USMLE Step 1 scores compared to males. This finding may serve as a reminder to programs when comparing USMLE Step examination scores that demographic factors may play a role. The race and ethnicity of applicants likely play a role. It has been reported that underrepresented minorities had lower match rates than White and Asian applicants in dermatology.6 There have been several published articles discussing the lack of diversity in dermatology, with a call to action.7-9
Factors for Couples Matching—The number of applicants participating in the couples match continues to increase yearly. The NMRP does publish data regarding “successful” couples matching but does not specify how many couples match together. There also is little published regarding advice for participation in the couples match. Although we had a limited number of couples that participated in the match, it is interesting to note they had similar strategies, including contacting programs at institutions that had offered interviews to their partners. This strategy may be effective, as dermatology programs offer interviews relatively late compared with other specialties.5 Additionally, this strategy may increase the number of interviews offered and received, as evidenced by the higher number of interviews offered compared with those who were not couples matching. Additionally, this survey highlights the sacrifice often needed by couples in the couples match as revealed by the inclusion of rank-list options in which the couples reside long distance or in which 1 partner does not match. This information may be helpful to applicants who are planning a strategy for the couples match in dermatology. Although this study does not encompass all dermatology applicants in the 2019-2020 cycle, we do believe it may be representative. The USMLE Step 1 scores in this study were similar to the published NRMP data.1,10 According to NRMP data from the 2019-2020 cycle, the mean USMLE Step 1 score was 248 for matched applicants and 239 for unmatched.1 The NRMP reported the mean USMLE Step 2 CK score for matched was 256 and 248 for unmatched, which also is similar to our data. The NRMP reported the mean number of programs ranked was 9.9 for matched and 4.5 for unmatched applicants.1 Again, our data were similar for number of dermatology interviews attended.
Limitations—There are limitations to this study. The main limitation is that the survey is from a single institution and had a limited number of respondents. Given the nature of the study, the accuracy of the data is dependent on the applicants’ honesty in self-reporting academic performance and other variables. There also may be a selection bias given the low response rate. The subanalyses—children and couples matching—were underpowered with the limited number of participants. Further studies that include multiple residency programs and multiple years could be helpful to provide more power and less risk of bias. We did not gather information such as the Medical Student Performance Evaluation letter, letters of recommendation, or personal statements, which do play an important role in the assessment of an applicant. However, because the applicants completed these surveys, and given these are largely blinded to applicants, we did not feel the applicants could accurately respond to those aspects of the application.
Conclusion
Our survey finds that factors associated with matching included a higher USMLE Step 1 score, having a home dermatology program, and a higher number of interviews offered and attended. Some demographics had varying USMLE Step 1 scores but similar match rates.
- National Resident Matching Program. Results and Data: 2020 Main Residency Match. National Resident Matching Program; May 2020. Accessed January 9, 2023. https://www.nrmp.org/wp-content/uploads/2021/12/MM_Results_and-Data_2020-1.pdf
- Gauer JL, Jackson JB. The association of USMLE Step 1 and Step 2 CK scores with residency match specialty and location. Med Educ Online. 2017;22:1358579.
- Wang JV, Keller M. Pressure to publish for residency applicants in dermatology. Dermatol Online J. 2016;22:13030/qt56x1t7ww.
- Wang RF, Zhang M, Kaffenberger JA. Does the dermatology standardized letter of recommendation alter applicants’ chances of matching into residency. J Am Acad Dermatol. 2017;77:e139-e140.
- National Resident Matching Program, Data Release and Research Committee: results of the 2018 NRMP Program Director Survey. Accessed December 19, 2022. https://www.nrmp.org/wp-content/uploads/2021/07/NRMP-2018-Program-Director-Survey-for-WWW.pdf
- Costello CM, Harvey JA, Besch-Stokes JG, et al. The role of race and ethnicity in the dermatology applicant match process. J Natl Med Assoc. 2022;113:666-670.
- Chen A, Shinkai K. Rethinking how we select dermatology applicants-turning the tide. JAMA Dermatol. 2017;153:259-260.
- Pandya AG, Alexis AF, Berger TG, et al. Increasing racial and ethnic diversity in dermatology: a call to action. J Am Acad Dermatol. 2016;74:584-587.
- Van Voorhees AS, Enos CW. Diversity in dermatology residency programs. J Investig Dermatol Symp Proc. 2017;18:S46-S49.
- National Resident Matching Program. Charting outcomes in the match: U.S. allopathic seniors. Characteristics of U.S. allopathic seniors who matched to their preferred specialty in the 2018 main residency match. 2nd ed. Accessed December 19, 2022. https://www.nrmp.org/wp-content/uploads/2021/07/Charting-Outcomes-in-the-Match-2018_Seniors-1.pdf
Dermatology residency continues to be one of the most competitive specialties, with a match rate of 84.7% for US allopathic seniors in the 2019-2020 academic year.1 In the 2019-2020 cycle, dermatology applicants were tied with plastic surgery for the highest median US Medical Licensing Examination (USMLE) Step 1 score compared with other specialties, which suggests that the top medical students are applying, yet only approximately 5 of 6 students are matching.
Factors that have been cited with successful dermatology matching include USMLE Step 1 and Step 2 Clinical Knowledge (CK) scores,2 research accomplishments,3 letters of recommendation,4 medical school performance, personal statement, grades in required clerkships, and volunteer/extracurricular experiences, among others.5
The National Resident Matching Program (NRMP) publishes data each year regarding different academic factors—USMLE scores; number of abstracts, presentations, and papers; work, volunteer, and research experiences—and compares the mean between matched and nonmatched applicants.1 However, the USMLE does not report any demographic information of the applicants and the implication it has for matching. Additionally, the number of couples participating in the couples match continues to increase each year. In the 2019-2020 cycle, 1224 couples participated in the couples match.1 However, NRMP reports only limited data regarding the couples match, and it is not specialty specific.
We aimed to determine the characteristics of matched vs nonmatched dermatology applicants. Secondarily, we aimed to determine any differences among demographics regarding matching rates, academic performance, and research publications. We also aimed to characterize the strategy and outcomes of applicants that couples matched.
Materials and Methods
The Mayo Clinic institutional review board deemed this study exempt. All applicants who applied to Mayo Clinic dermatology residency in Scottsdale, Arizona, during the 2018-2019 cycle were emailed an initial survey (N=475) before Match Day that obtained demographic information, geographic information, gap-year information, USMLE Step 1 score, publications, medical school grades, number of away rotations, and number of interviews. A follow-up survey gathering match data and couples matching data was sent to the applicants who completed the first survey on Match Day. The survey was repeated for the 2019-2020 cycle. In the second survey, Step 2 CK data were obtained. The survey was sent to 629 applicants who applied to Mayo Clinic dermatology residencies in Arizona, Minnesota, and Florida to include a broader group of applicants. For publications, applicants were asked to count only published or accepted manuscripts, not abstracts, posters, conference presentations, or submitted manuscripts. Applicants who did not respond to the second survey (match data) were not included in that part of the analysis. One survey was excluded because of implausible answers (eg, scores outside of range for USMLE Step scores).
Statistical Analysis—For statistical analyses, the applicants from both applications cycles were combined. Descriptive statistics were reported in the form of mean, median, or counts (percentages), as applicable. Means were compared using 2-sided t tests. Group comparisons were examined using χ2 tests for categorical variables. Statistical analyses were performed using the BlueSky Statistics version 6.30. P<.05 was considered significant.
Results
In 2019, a total of 149 applicants completed the initial survey (31.4% response rate), and 112 completed the follow-up survey (75.2% response rate). In 2020, a total of 142 applicants completed the initial survey (22.6% response rate), and 124 completed the follow-up survey (87.3% response rate). Combining the 2 years, after removing 1 survey with implausible answers, there were 290 respondents from the initial survey and 235 from the follow-up survey. The median (SD) age for the total applicants over both years was 27 (3.0) years, and 180 applicants were female (61.9%).
USMLE Scores—The median USMLE Step 1 score was 250, and scores ranged from 196 to 271. The median USMLE Step 2 CK score was 257, and scores ranged from 213 to 281. Higher USMLE Step 1 and Step 2 CK scores and more interviews were associated with higher match rates (Table 1). In addition, students with a dermatology program at their medical school were more likely to match than those without a home dermatology program.
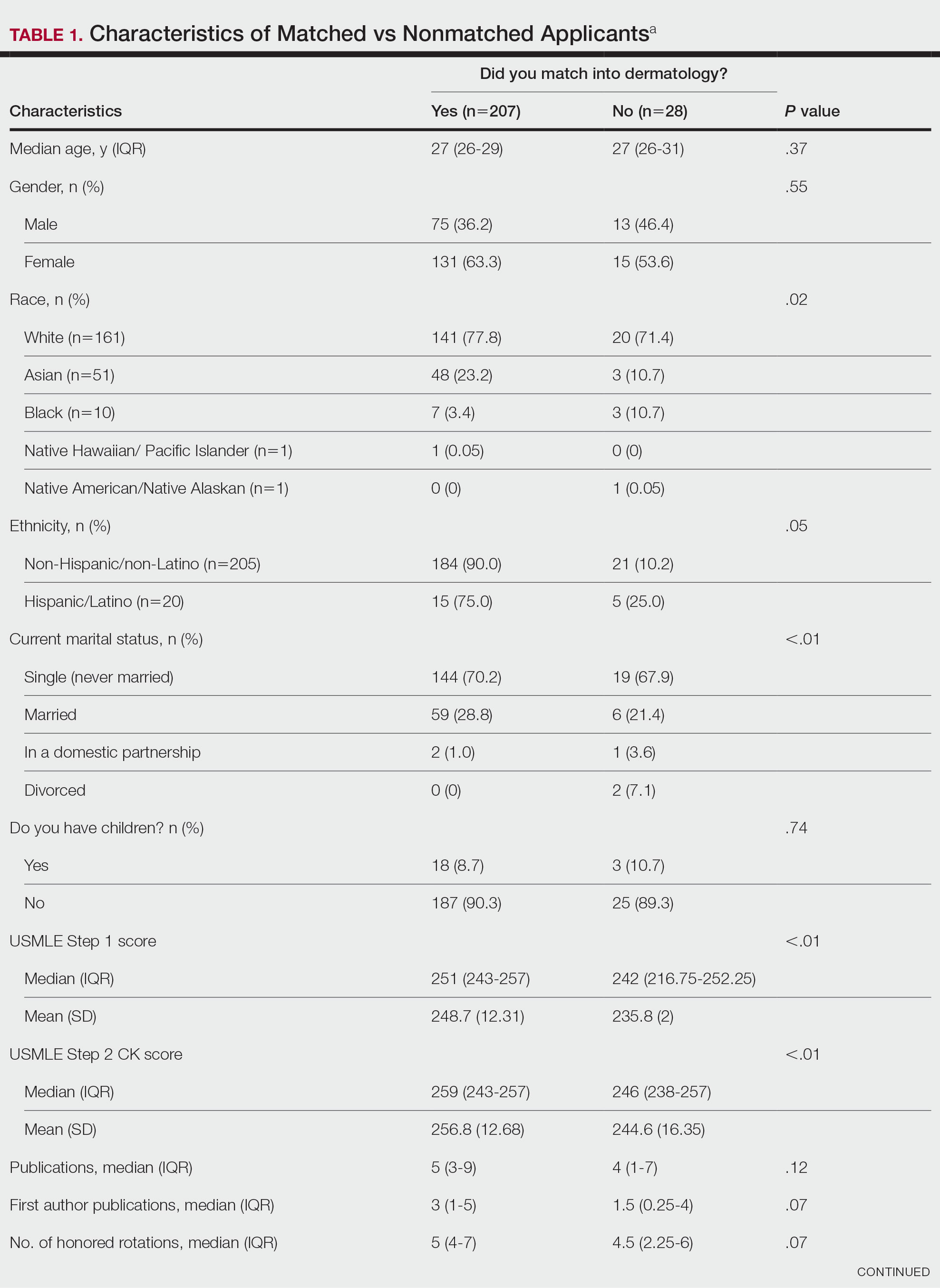

Gender Differences—There were 180 females and 110 males who completed the surveys. Males and females had similar match rates (85.2% vs 89.0%; P=.39)(Table 2).
Family Life—In comparing marital status, applicants who were divorced had a higher median age (38.5 years) compared with applicants who were single, married, or in a domestic partnership (all 27 years; P<.01). Differences are outlined in Table 3.
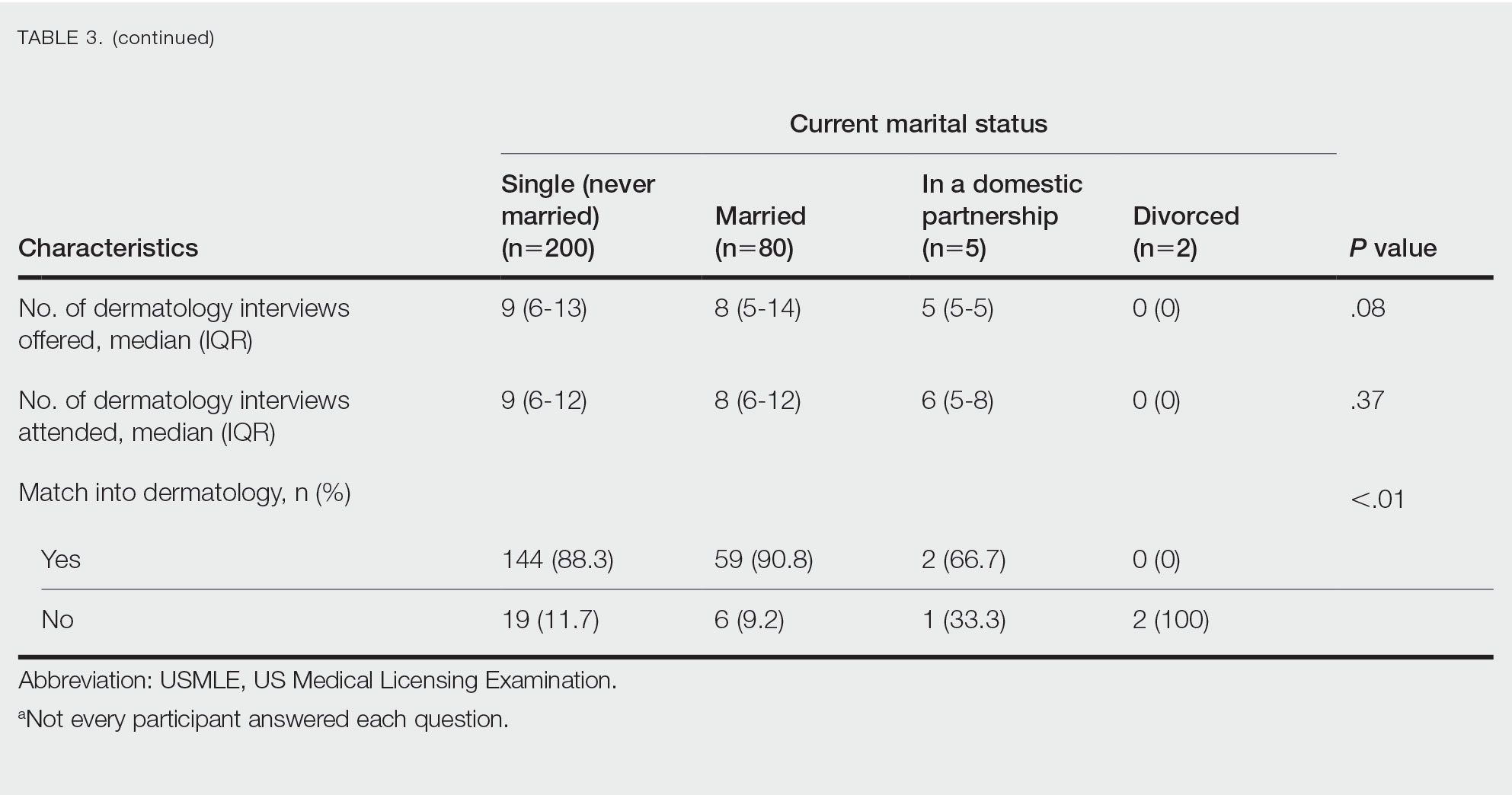
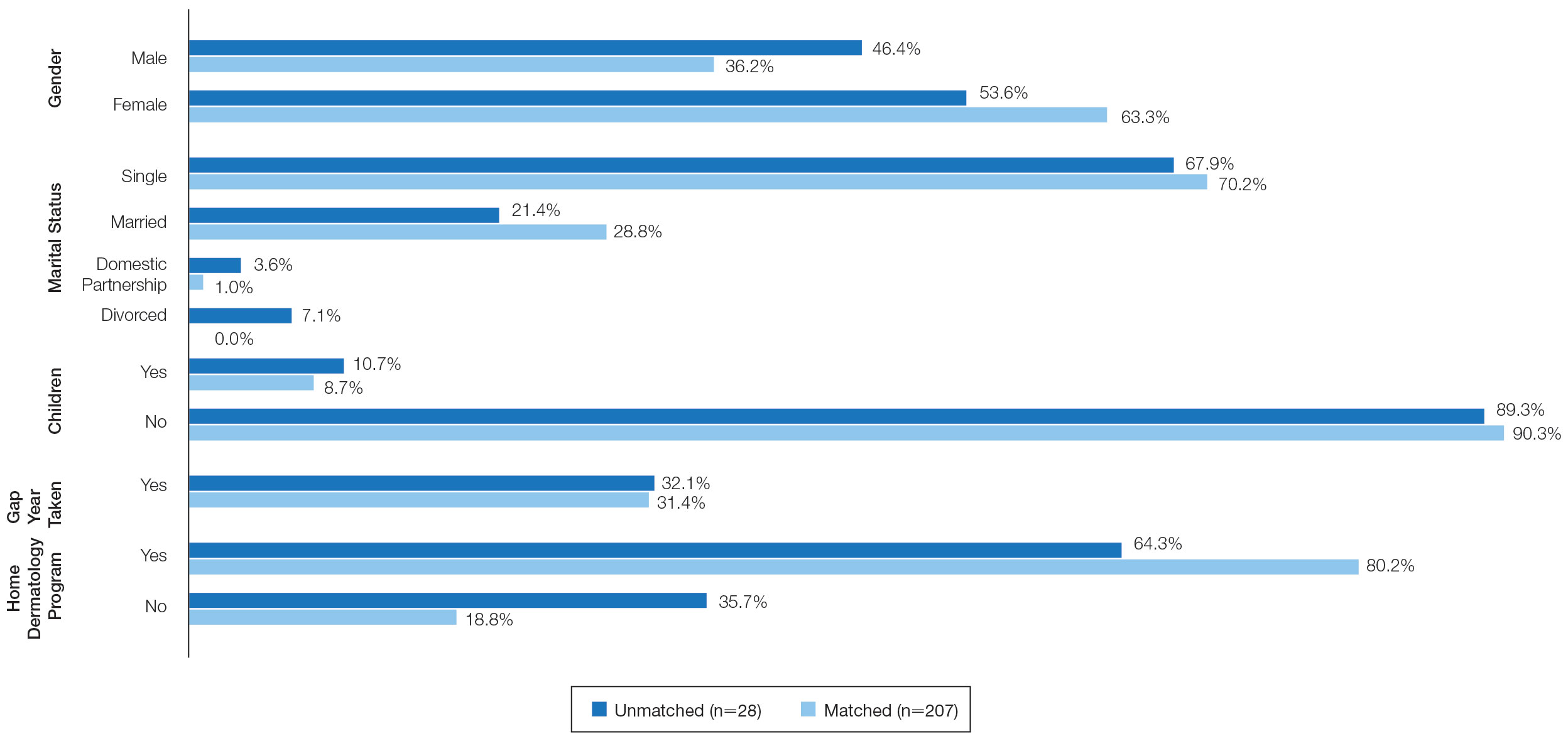
On average, applicants with children (n=27 [15 male, 12 female]; P=.13) were 3 years older than those without (30.5 vs 27; P<.01) and were more likely to be married (88.9% vs 21.5%; P<.01). Applicants with children had a mean USMLE Step 1 score of 241 compared to 251 for those without children (P=.02) and a mean USMLE Step 2 CK score of 246 compared to 258 for those without children (P<.01). Applicants with children had similar debt, number of publications, number of honored rotations, and match rates compared to applicants without children (Figure).
Couples Match—Seventeen individuals in our survey participated in the couples match (7.8%), and all 17 (100%) matched into dermatology. The mean age was 26.7 years, 12 applicants were female, 2 applicants were married, and 1 applicant had children. The mean number of interviews offered was 13.6, and the mean number of interviews attended was 11.3. This was higher than participants who were not couples matching (13.6 vs 9.8 [P=.02] and 11.3 vs 8.9 [P=.04], respectively). Applicants and their partners applied to programs and received interviews in a mean of 10 cities. Sixteen applicants reported that they contacted programs where their partner had interview offers. All participants’ rank lists included programs located in different cities than their partners’ ranked programs, and all but 1 participant ranked programs located in a different state than their partners’ ranked programs. Fifteen participants had options in their rank list for the applicant not to match, even if the partner would match. Similarly, 12 had the option for the applicant to match, even if the partner would not match. Fourteen (82.4%) matched at the same institution as their significant other. Three (17.6%) applicants matched to a program in a different state than the partner’s matched program. Two (11.8%) participants felt their relationship with their partner suffered because of the match, and 1 (5.9%) applicant was undetermined. One applicant described their relationship suffering from “unnecessary tension and anxiety” and noted “difficult conversations” about potentially matching into dermatology in a different location from their partner that could have been “devastating and not something [he or she] should have to choose.”
Comment
Factors for Matching in Dermatology—In our survey, we found the statistically significant factors of matching into dermatology included high USMLE Step 1 and Step 2 CK scores (P<.01), having a home dermatology program (P=.04), and attending a higher number of dermatology interviews (P<.01). These data are similar to NRMP results1; however, the higher likelihood of matching if the medical school has a home dermatology program has not been reported. This finding could be due to multiple factors such as students have less access to academic dermatologists for research projects, letters of recommendations, mentorship, and clinical rotations.
Gender and having children were factors that had no correlation with the match rate. There was a statistical difference of matching based on marital status (P<.01), but this is likely due to the low number of applicants in the divorced category. There were differences among demographics with USMLE Step 1 and Step 2 CK scores, which is a known factor in matching.1,2 Applicants with children had lower USMLE Step 1 and Step 2 CK scores compared to applicants without children. Females also had lower median USMLE Step 1 scores compared to males. This finding may serve as a reminder to programs when comparing USMLE Step examination scores that demographic factors may play a role. The race and ethnicity of applicants likely play a role. It has been reported that underrepresented minorities had lower match rates than White and Asian applicants in dermatology.6 There have been several published articles discussing the lack of diversity in dermatology, with a call to action.7-9
Factors for Couples Matching—The number of applicants participating in the couples match continues to increase yearly. The NMRP does publish data regarding “successful” couples matching but does not specify how many couples match together. There also is little published regarding advice for participation in the couples match. Although we had a limited number of couples that participated in the match, it is interesting to note they had similar strategies, including contacting programs at institutions that had offered interviews to their partners. This strategy may be effective, as dermatology programs offer interviews relatively late compared with other specialties.5 Additionally, this strategy may increase the number of interviews offered and received, as evidenced by the higher number of interviews offered compared with those who were not couples matching. Additionally, this survey highlights the sacrifice often needed by couples in the couples match as revealed by the inclusion of rank-list options in which the couples reside long distance or in which 1 partner does not match. This information may be helpful to applicants who are planning a strategy for the couples match in dermatology. Although this study does not encompass all dermatology applicants in the 2019-2020 cycle, we do believe it may be representative. The USMLE Step 1 scores in this study were similar to the published NRMP data.1,10 According to NRMP data from the 2019-2020 cycle, the mean USMLE Step 1 score was 248 for matched applicants and 239 for unmatched.1 The NRMP reported the mean USMLE Step 2 CK score for matched was 256 and 248 for unmatched, which also is similar to our data. The NRMP reported the mean number of programs ranked was 9.9 for matched and 4.5 for unmatched applicants.1 Again, our data were similar for number of dermatology interviews attended.
Limitations—There are limitations to this study. The main limitation is that the survey is from a single institution and had a limited number of respondents. Given the nature of the study, the accuracy of the data is dependent on the applicants’ honesty in self-reporting academic performance and other variables. There also may be a selection bias given the low response rate. The subanalyses—children and couples matching—were underpowered with the limited number of participants. Further studies that include multiple residency programs and multiple years could be helpful to provide more power and less risk of bias. We did not gather information such as the Medical Student Performance Evaluation letter, letters of recommendation, or personal statements, which do play an important role in the assessment of an applicant. However, because the applicants completed these surveys, and given these are largely blinded to applicants, we did not feel the applicants could accurately respond to those aspects of the application.
Conclusion
Our survey finds that factors associated with matching included a higher USMLE Step 1 score, having a home dermatology program, and a higher number of interviews offered and attended. Some demographics had varying USMLE Step 1 scores but similar match rates.
Dermatology residency continues to be one of the most competitive specialties, with a match rate of 84.7% for US allopathic seniors in the 2019-2020 academic year.1 In the 2019-2020 cycle, dermatology applicants were tied with plastic surgery for the highest median US Medical Licensing Examination (USMLE) Step 1 score compared with other specialties, which suggests that the top medical students are applying, yet only approximately 5 of 6 students are matching.
Factors that have been cited with successful dermatology matching include USMLE Step 1 and Step 2 Clinical Knowledge (CK) scores,2 research accomplishments,3 letters of recommendation,4 medical school performance, personal statement, grades in required clerkships, and volunteer/extracurricular experiences, among others.5
The National Resident Matching Program (NRMP) publishes data each year regarding different academic factors—USMLE scores; number of abstracts, presentations, and papers; work, volunteer, and research experiences—and compares the mean between matched and nonmatched applicants.1 However, the USMLE does not report any demographic information of the applicants and the implication it has for matching. Additionally, the number of couples participating in the couples match continues to increase each year. In the 2019-2020 cycle, 1224 couples participated in the couples match.1 However, NRMP reports only limited data regarding the couples match, and it is not specialty specific.
We aimed to determine the characteristics of matched vs nonmatched dermatology applicants. Secondarily, we aimed to determine any differences among demographics regarding matching rates, academic performance, and research publications. We also aimed to characterize the strategy and outcomes of applicants that couples matched.
Materials and Methods
The Mayo Clinic institutional review board deemed this study exempt. All applicants who applied to Mayo Clinic dermatology residency in Scottsdale, Arizona, during the 2018-2019 cycle were emailed an initial survey (N=475) before Match Day that obtained demographic information, geographic information, gap-year information, USMLE Step 1 score, publications, medical school grades, number of away rotations, and number of interviews. A follow-up survey gathering match data and couples matching data was sent to the applicants who completed the first survey on Match Day. The survey was repeated for the 2019-2020 cycle. In the second survey, Step 2 CK data were obtained. The survey was sent to 629 applicants who applied to Mayo Clinic dermatology residencies in Arizona, Minnesota, and Florida to include a broader group of applicants. For publications, applicants were asked to count only published or accepted manuscripts, not abstracts, posters, conference presentations, or submitted manuscripts. Applicants who did not respond to the second survey (match data) were not included in that part of the analysis. One survey was excluded because of implausible answers (eg, scores outside of range for USMLE Step scores).
Statistical Analysis—For statistical analyses, the applicants from both applications cycles were combined. Descriptive statistics were reported in the form of mean, median, or counts (percentages), as applicable. Means were compared using 2-sided t tests. Group comparisons were examined using χ2 tests for categorical variables. Statistical analyses were performed using the BlueSky Statistics version 6.30. P<.05 was considered significant.
Results
In 2019, a total of 149 applicants completed the initial survey (31.4% response rate), and 112 completed the follow-up survey (75.2% response rate). In 2020, a total of 142 applicants completed the initial survey (22.6% response rate), and 124 completed the follow-up survey (87.3% response rate). Combining the 2 years, after removing 1 survey with implausible answers, there were 290 respondents from the initial survey and 235 from the follow-up survey. The median (SD) age for the total applicants over both years was 27 (3.0) years, and 180 applicants were female (61.9%).
USMLE Scores—The median USMLE Step 1 score was 250, and scores ranged from 196 to 271. The median USMLE Step 2 CK score was 257, and scores ranged from 213 to 281. Higher USMLE Step 1 and Step 2 CK scores and more interviews were associated with higher match rates (Table 1). In addition, students with a dermatology program at their medical school were more likely to match than those without a home dermatology program.

Gender Differences—There were 180 females and 110 males who completed the surveys. Males and females had similar match rates (85.2% vs 89.0%; P=.39)(Table 2).
Family Life—In comparing marital status, applicants who were divorced had a higher median age (38.5 years) compared with applicants who were single, married, or in a domestic partnership (all 27 years; P<.01). Differences are outlined in Table 3.
On average, applicants with children (n=27 [15 male, 12 female]; P=.13) were 3 years older than those without (30.5 vs 27; P<.01) and were more likely to be married (88.9% vs 21.5%; P<.01). Applicants with children had a mean USMLE Step 1 score of 241 compared to 251 for those without children (P=.02) and a mean USMLE Step 2 CK score of 246 compared to 258 for those without children (P<.01). Applicants with children had similar debt, number of publications, number of honored rotations, and match rates compared to applicants without children (Figure).
Couples Match—Seventeen individuals in our survey participated in the couples match (7.8%), and all 17 (100%) matched into dermatology. The mean age was 26.7 years, 12 applicants were female, 2 applicants were married, and 1 applicant had children. The mean number of interviews offered was 13.6, and the mean number of interviews attended was 11.3. This was higher than participants who were not couples matching (13.6 vs 9.8 [P=.02] and 11.3 vs 8.9 [P=.04], respectively). Applicants and their partners applied to programs and received interviews in a mean of 10 cities. Sixteen applicants reported that they contacted programs where their partner had interview offers. All participants’ rank lists included programs located in different cities than their partners’ ranked programs, and all but 1 participant ranked programs located in a different state than their partners’ ranked programs. Fifteen participants had options in their rank list for the applicant not to match, even if the partner would match. Similarly, 12 had the option for the applicant to match, even if the partner would not match. Fourteen (82.4%) matched at the same institution as their significant other. Three (17.6%) applicants matched to a program in a different state than the partner’s matched program. Two (11.8%) participants felt their relationship with their partner suffered because of the match, and 1 (5.9%) applicant was undetermined. One applicant described their relationship suffering from “unnecessary tension and anxiety” and noted “difficult conversations” about potentially matching into dermatology in a different location from their partner that could have been “devastating and not something [he or she] should have to choose.”
Comment
Factors for Matching in Dermatology—In our survey, we found the statistically significant factors of matching into dermatology included high USMLE Step 1 and Step 2 CK scores (P<.01), having a home dermatology program (P=.04), and attending a higher number of dermatology interviews (P<.01). These data are similar to NRMP results1; however, the higher likelihood of matching if the medical school has a home dermatology program has not been reported. This finding could be due to multiple factors such as students have less access to academic dermatologists for research projects, letters of recommendations, mentorship, and clinical rotations.
Gender and having children were factors that had no correlation with the match rate. There was a statistical difference of matching based on marital status (P<.01), but this is likely due to the low number of applicants in the divorced category. There were differences among demographics with USMLE Step 1 and Step 2 CK scores, which is a known factor in matching.1,2 Applicants with children had lower USMLE Step 1 and Step 2 CK scores compared to applicants without children. Females also had lower median USMLE Step 1 scores compared to males. This finding may serve as a reminder to programs when comparing USMLE Step examination scores that demographic factors may play a role. The race and ethnicity of applicants likely play a role. It has been reported that underrepresented minorities had lower match rates than White and Asian applicants in dermatology.6 There have been several published articles discussing the lack of diversity in dermatology, with a call to action.7-9
Factors for Couples Matching—The number of applicants participating in the couples match continues to increase yearly. The NMRP does publish data regarding “successful” couples matching but does not specify how many couples match together. There also is little published regarding advice for participation in the couples match. Although we had a limited number of couples that participated in the match, it is interesting to note they had similar strategies, including contacting programs at institutions that had offered interviews to their partners. This strategy may be effective, as dermatology programs offer interviews relatively late compared with other specialties.5 Additionally, this strategy may increase the number of interviews offered and received, as evidenced by the higher number of interviews offered compared with those who were not couples matching. Additionally, this survey highlights the sacrifice often needed by couples in the couples match as revealed by the inclusion of rank-list options in which the couples reside long distance or in which 1 partner does not match. This information may be helpful to applicants who are planning a strategy for the couples match in dermatology. Although this study does not encompass all dermatology applicants in the 2019-2020 cycle, we do believe it may be representative. The USMLE Step 1 scores in this study were similar to the published NRMP data.1,10 According to NRMP data from the 2019-2020 cycle, the mean USMLE Step 1 score was 248 for matched applicants and 239 for unmatched.1 The NRMP reported the mean USMLE Step 2 CK score for matched was 256 and 248 for unmatched, which also is similar to our data. The NRMP reported the mean number of programs ranked was 9.9 for matched and 4.5 for unmatched applicants.1 Again, our data were similar for number of dermatology interviews attended.
Limitations—There are limitations to this study. The main limitation is that the survey is from a single institution and had a limited number of respondents. Given the nature of the study, the accuracy of the data is dependent on the applicants’ honesty in self-reporting academic performance and other variables. There also may be a selection bias given the low response rate. The subanalyses—children and couples matching—were underpowered with the limited number of participants. Further studies that include multiple residency programs and multiple years could be helpful to provide more power and less risk of bias. We did not gather information such as the Medical Student Performance Evaluation letter, letters of recommendation, or personal statements, which do play an important role in the assessment of an applicant. However, because the applicants completed these surveys, and given these are largely blinded to applicants, we did not feel the applicants could accurately respond to those aspects of the application.
Conclusion
Our survey finds that factors associated with matching included a higher USMLE Step 1 score, having a home dermatology program, and a higher number of interviews offered and attended. Some demographics had varying USMLE Step 1 scores but similar match rates.
- National Resident Matching Program. Results and Data: 2020 Main Residency Match. National Resident Matching Program; May 2020. Accessed January 9, 2023. https://www.nrmp.org/wp-content/uploads/2021/12/MM_Results_and-Data_2020-1.pdf
- Gauer JL, Jackson JB. The association of USMLE Step 1 and Step 2 CK scores with residency match specialty and location. Med Educ Online. 2017;22:1358579.
- Wang JV, Keller M. Pressure to publish for residency applicants in dermatology. Dermatol Online J. 2016;22:13030/qt56x1t7ww.
- Wang RF, Zhang M, Kaffenberger JA. Does the dermatology standardized letter of recommendation alter applicants’ chances of matching into residency. J Am Acad Dermatol. 2017;77:e139-e140.
- National Resident Matching Program, Data Release and Research Committee: results of the 2018 NRMP Program Director Survey. Accessed December 19, 2022. https://www.nrmp.org/wp-content/uploads/2021/07/NRMP-2018-Program-Director-Survey-for-WWW.pdf
- Costello CM, Harvey JA, Besch-Stokes JG, et al. The role of race and ethnicity in the dermatology applicant match process. J Natl Med Assoc. 2022;113:666-670.
- Chen A, Shinkai K. Rethinking how we select dermatology applicants-turning the tide. JAMA Dermatol. 2017;153:259-260.
- Pandya AG, Alexis AF, Berger TG, et al. Increasing racial and ethnic diversity in dermatology: a call to action. J Am Acad Dermatol. 2016;74:584-587.
- Van Voorhees AS, Enos CW. Diversity in dermatology residency programs. J Investig Dermatol Symp Proc. 2017;18:S46-S49.
- National Resident Matching Program. Charting outcomes in the match: U.S. allopathic seniors. Characteristics of U.S. allopathic seniors who matched to their preferred specialty in the 2018 main residency match. 2nd ed. Accessed December 19, 2022. https://www.nrmp.org/wp-content/uploads/2021/07/Charting-Outcomes-in-the-Match-2018_Seniors-1.pdf
- National Resident Matching Program. Results and Data: 2020 Main Residency Match. National Resident Matching Program; May 2020. Accessed January 9, 2023. https://www.nrmp.org/wp-content/uploads/2021/12/MM_Results_and-Data_2020-1.pdf
- Gauer JL, Jackson JB. The association of USMLE Step 1 and Step 2 CK scores with residency match specialty and location. Med Educ Online. 2017;22:1358579.
- Wang JV, Keller M. Pressure to publish for residency applicants in dermatology. Dermatol Online J. 2016;22:13030/qt56x1t7ww.
- Wang RF, Zhang M, Kaffenberger JA. Does the dermatology standardized letter of recommendation alter applicants’ chances of matching into residency. J Am Acad Dermatol. 2017;77:e139-e140.
- National Resident Matching Program, Data Release and Research Committee: results of the 2018 NRMP Program Director Survey. Accessed December 19, 2022. https://www.nrmp.org/wp-content/uploads/2021/07/NRMP-2018-Program-Director-Survey-for-WWW.pdf
- Costello CM, Harvey JA, Besch-Stokes JG, et al. The role of race and ethnicity in the dermatology applicant match process. J Natl Med Assoc. 2022;113:666-670.
- Chen A, Shinkai K. Rethinking how we select dermatology applicants-turning the tide. JAMA Dermatol. 2017;153:259-260.
- Pandya AG, Alexis AF, Berger TG, et al. Increasing racial and ethnic diversity in dermatology: a call to action. J Am Acad Dermatol. 2016;74:584-587.
- Van Voorhees AS, Enos CW. Diversity in dermatology residency programs. J Investig Dermatol Symp Proc. 2017;18:S46-S49.
- National Resident Matching Program. Charting outcomes in the match: U.S. allopathic seniors. Characteristics of U.S. allopathic seniors who matched to their preferred specialty in the 2018 main residency match. 2nd ed. Accessed December 19, 2022. https://www.nrmp.org/wp-content/uploads/2021/07/Charting-Outcomes-in-the-Match-2018_Seniors-1.pdf
PRACTICE POINTS
- Dermatology residency continues to be one of the most competitive specialties, with a match rate of 84.7% in 2019.
- A high US Medical Licensing Examination (USMLE) Step 1 score and having a home dermatology program and a greater number of interviews may lead to higher likeliness of matching in dermatology.
- Most applicants (82.4%) applied to programs their partner had interviews at, suggesting this may be a helpful strategy.
Insights From the 2020-2021 Dermatology Residency Match
To the Editor:
Data from the program director survey of the National Resident Matching Program offer key insights into the 2021 dermatology application process.1,2 Examination of data from the 2020 (N=12) and 2021 (N=17) program director survey regarding interviewing applicants revealed that specialty-specific letters of recommendation (LORs), personal prior knowledge of an applicant, and personal statement increased in importance by 17%, 7.4%, and 17%, respectively, whereas away rotations within the department decreased in importance by 44.9% (Table).1,2 Interestingly, for ranking applicants, programs decreased their emphasis on specialty-specific LORs by 25.8% and away rotations within the department by 22.7% and increased emphasis on personal statements by 14.7% and personal prior knowledge of an applicant by 0.8% from 2020 to 2021 (Table).1,2 These findings align with the prior recommendation to limit away rotations; data are contradictory—when comparing factors for interviewing as compared to ranking applicants—for specialty-specific LORs.

We further compared data from the otolaryngology cycle, which implemented preference signaling by which an applicant can signal their interest in a particular residency program in the 2021 Match, to data from dermatology with no preference signaling. A 90% probability of matching is estimated to require approximately 8 or 9 interviews for dermatology or 12 interviews for otolaryngology for MD senior students in 2020.4 In prior dermatology application cycles, the most highly qualified candidates constituted 7% to 21% of all applicants but were estimated to receive half of all interviews, causing a maldistribution of interviews.5,6
For the 2021 otolaryngology match, the Society of University Otolaryngologists implemented a novel preference signaling system that allowed candidates to show interest in programs by sending 5 preferences, or tokens.7 Recent data reports from the otolaryngology cycle demonstrated at least a 2-fold increase in the rate of receiving an interview invitation for signaled programs compared to the closest nonsignaled program if applicants were provided an additional token.7 Regarding overall applicant competitiveness (ie, dividing participants into quartiles based on their competitiveness), the highest increase in the overall rate of interview invitations (3.5 [total invitations/total applications]) was demonstrated for fourth-quartile (ie, “lowest quartile”) applicants compared with the increase in the overall rate of interview invitations seen in other quartiles (first quartile, an increase of 2.3; second quartile, an increase of 2.6; and third quartile, an increase of 2.4).7 We look forward to seeing the impact of preference signaling on the results of the 2022 dermatology cycle.
Despite changes in the interviewing process to accommodate COVID-19 pandemic safety recommendations, the overall dermatology postgraduate year (PGY) 2 fill rate remained unchanged from 2018 (98.6%) to 2021 (98.7%). Zero PGY-1 positions and 5 PGY-2 positions were unfilled in the 2021 Main Residency Match compared to 1 unfilled PGY-1 position and 4 unfilled PGY-2 positions in 2018.8 The coordinated interview invitation release, holistic review of applications, increased number of rankings, and virtual interviews might have helped offset potential obstacles imparted by inability to complete away rotations, inability to obtain LORs, and conducting interviews virtually.5
A limitation of our analysis is the low response rate of program directors to National Resident Matching Program surveys.
These strategies—holistic application review and coordinated interview release—may be considered in future cycles given their convenience and negligible impact on the dermatology match rate. For example, virtual interviews relieve the financial and time burdens of in-person interviews—approximately $10,000 for each US senior applicant—thus potentially allowing for a more equitable matching process.3 Inversely, in-person interviews allow participants to effectively network and form more meaningful connections while obtaining a better understanding of facilities and surrounding locales. As such, the medical community should continue to come to a consensus on the optimal format to host interviews.
- Results of the 2021 NRMP Program Director Survey. National Resident Matching Program. August 2021. Accessed December 6, 2021. https://www.nrmp.org/wp-content/uploads/2021/11/2021-PD-Survey-Report-for-WWW.pdf
- Results of the 2020 NRMP Program Director Survey. National Resident Matching Program. August 2020. Accessed December 6, 2021. https://www.nrmp.org/wp-content/uploads/2022/01/2020-PD-Survey.pdf
- Rojek NW, Shinkai K, Fett N. Dermatology faculty and residents’ perspectives on the dermatology residency application process: a nationwide survey. J Am Acad Dermatol. 2018;79:157-159. doi:10.1016/j.jaad.2018.01.00
- Charting Outcomes in the Match: Senior Students of U.S. MD Medical Schools. National Resident Matching Program. July 2020. Accessed December 6, 2021. https://www.nrmp.org/wp-content/uploads/2021/08/Charting-Outcomes-in-the-Match-2020_MD-Senior_final.pdf
- Thatiparthi A, Martin A, Liu J, et al. Preliminary outcomes of 2020-2021 dermatology residency application cycle and adverse effects of COVID-19. J Am Acad Dermatol. 2021;84:e263-e264. doi:10.1016/j.jaad.2021.03.034
- Hammoud MM, Standiford T, Carmody JB. Potential implications of COVID-19 for the 2020-2021 residency application cycle. JAMA. 2020;324:29-30. doi:10.1001/jama.2020.8911
- Interview offer rate with/without ENTSignaling. Society of University Otolaryngologists. Updated July 19, 2022. Accessed December 12, 2022. https://opdo-hns.org/mpage/signaling-updates
- Results and Data: 2021 Main Residency Match. National Resident Matching Program. May 2021. Accessed December 6, 2021. https://www.nrmp.org/wp-content/uploads/2021/08/MRM-Results_and-Data_2021.pdf
To the Editor:
Data from the program director survey of the National Resident Matching Program offer key insights into the 2021 dermatology application process.1,2 Examination of data from the 2020 (N=12) and 2021 (N=17) program director survey regarding interviewing applicants revealed that specialty-specific letters of recommendation (LORs), personal prior knowledge of an applicant, and personal statement increased in importance by 17%, 7.4%, and 17%, respectively, whereas away rotations within the department decreased in importance by 44.9% (Table).1,2 Interestingly, for ranking applicants, programs decreased their emphasis on specialty-specific LORs by 25.8% and away rotations within the department by 22.7% and increased emphasis on personal statements by 14.7% and personal prior knowledge of an applicant by 0.8% from 2020 to 2021 (Table).1,2 These findings align with the prior recommendation to limit away rotations; data are contradictory—when comparing factors for interviewing as compared to ranking applicants—for specialty-specific LORs.

We further compared data from the otolaryngology cycle, which implemented preference signaling by which an applicant can signal their interest in a particular residency program in the 2021 Match, to data from dermatology with no preference signaling. A 90% probability of matching is estimated to require approximately 8 or 9 interviews for dermatology or 12 interviews for otolaryngology for MD senior students in 2020.4 In prior dermatology application cycles, the most highly qualified candidates constituted 7% to 21% of all applicants but were estimated to receive half of all interviews, causing a maldistribution of interviews.5,6
For the 2021 otolaryngology match, the Society of University Otolaryngologists implemented a novel preference signaling system that allowed candidates to show interest in programs by sending 5 preferences, or tokens.7 Recent data reports from the otolaryngology cycle demonstrated at least a 2-fold increase in the rate of receiving an interview invitation for signaled programs compared to the closest nonsignaled program if applicants were provided an additional token.7 Regarding overall applicant competitiveness (ie, dividing participants into quartiles based on their competitiveness), the highest increase in the overall rate of interview invitations (3.5 [total invitations/total applications]) was demonstrated for fourth-quartile (ie, “lowest quartile”) applicants compared with the increase in the overall rate of interview invitations seen in other quartiles (first quartile, an increase of 2.3; second quartile, an increase of 2.6; and third quartile, an increase of 2.4).7 We look forward to seeing the impact of preference signaling on the results of the 2022 dermatology cycle.
Despite changes in the interviewing process to accommodate COVID-19 pandemic safety recommendations, the overall dermatology postgraduate year (PGY) 2 fill rate remained unchanged from 2018 (98.6%) to 2021 (98.7%). Zero PGY-1 positions and 5 PGY-2 positions were unfilled in the 2021 Main Residency Match compared to 1 unfilled PGY-1 position and 4 unfilled PGY-2 positions in 2018.8 The coordinated interview invitation release, holistic review of applications, increased number of rankings, and virtual interviews might have helped offset potential obstacles imparted by inability to complete away rotations, inability to obtain LORs, and conducting interviews virtually.5
A limitation of our analysis is the low response rate of program directors to National Resident Matching Program surveys.
These strategies—holistic application review and coordinated interview release—may be considered in future cycles given their convenience and negligible impact on the dermatology match rate. For example, virtual interviews relieve the financial and time burdens of in-person interviews—approximately $10,000 for each US senior applicant—thus potentially allowing for a more equitable matching process.3 Inversely, in-person interviews allow participants to effectively network and form more meaningful connections while obtaining a better understanding of facilities and surrounding locales. As such, the medical community should continue to come to a consensus on the optimal format to host interviews.
To the Editor:
Data from the program director survey of the National Resident Matching Program offer key insights into the 2021 dermatology application process.1,2 Examination of data from the 2020 (N=12) and 2021 (N=17) program director survey regarding interviewing applicants revealed that specialty-specific letters of recommendation (LORs), personal prior knowledge of an applicant, and personal statement increased in importance by 17%, 7.4%, and 17%, respectively, whereas away rotations within the department decreased in importance by 44.9% (Table).1,2 Interestingly, for ranking applicants, programs decreased their emphasis on specialty-specific LORs by 25.8% and away rotations within the department by 22.7% and increased emphasis on personal statements by 14.7% and personal prior knowledge of an applicant by 0.8% from 2020 to 2021 (Table).1,2 These findings align with the prior recommendation to limit away rotations; data are contradictory—when comparing factors for interviewing as compared to ranking applicants—for specialty-specific LORs.

We further compared data from the otolaryngology cycle, which implemented preference signaling by which an applicant can signal their interest in a particular residency program in the 2021 Match, to data from dermatology with no preference signaling. A 90% probability of matching is estimated to require approximately 8 or 9 interviews for dermatology or 12 interviews for otolaryngology for MD senior students in 2020.4 In prior dermatology application cycles, the most highly qualified candidates constituted 7% to 21% of all applicants but were estimated to receive half of all interviews, causing a maldistribution of interviews.5,6
For the 2021 otolaryngology match, the Society of University Otolaryngologists implemented a novel preference signaling system that allowed candidates to show interest in programs by sending 5 preferences, or tokens.7 Recent data reports from the otolaryngology cycle demonstrated at least a 2-fold increase in the rate of receiving an interview invitation for signaled programs compared to the closest nonsignaled program if applicants were provided an additional token.7 Regarding overall applicant competitiveness (ie, dividing participants into quartiles based on their competitiveness), the highest increase in the overall rate of interview invitations (3.5 [total invitations/total applications]) was demonstrated for fourth-quartile (ie, “lowest quartile”) applicants compared with the increase in the overall rate of interview invitations seen in other quartiles (first quartile, an increase of 2.3; second quartile, an increase of 2.6; and third quartile, an increase of 2.4).7 We look forward to seeing the impact of preference signaling on the results of the 2022 dermatology cycle.
Despite changes in the interviewing process to accommodate COVID-19 pandemic safety recommendations, the overall dermatology postgraduate year (PGY) 2 fill rate remained unchanged from 2018 (98.6%) to 2021 (98.7%). Zero PGY-1 positions and 5 PGY-2 positions were unfilled in the 2021 Main Residency Match compared to 1 unfilled PGY-1 position and 4 unfilled PGY-2 positions in 2018.8 The coordinated interview invitation release, holistic review of applications, increased number of rankings, and virtual interviews might have helped offset potential obstacles imparted by inability to complete away rotations, inability to obtain LORs, and conducting interviews virtually.5
A limitation of our analysis is the low response rate of program directors to National Resident Matching Program surveys.
These strategies—holistic application review and coordinated interview release—may be considered in future cycles given their convenience and negligible impact on the dermatology match rate. For example, virtual interviews relieve the financial and time burdens of in-person interviews—approximately $10,000 for each US senior applicant—thus potentially allowing for a more equitable matching process.3 Inversely, in-person interviews allow participants to effectively network and form more meaningful connections while obtaining a better understanding of facilities and surrounding locales. As such, the medical community should continue to come to a consensus on the optimal format to host interviews.
- Results of the 2021 NRMP Program Director Survey. National Resident Matching Program. August 2021. Accessed December 6, 2021. https://www.nrmp.org/wp-content/uploads/2021/11/2021-PD-Survey-Report-for-WWW.pdf
- Results of the 2020 NRMP Program Director Survey. National Resident Matching Program. August 2020. Accessed December 6, 2021. https://www.nrmp.org/wp-content/uploads/2022/01/2020-PD-Survey.pdf
- Rojek NW, Shinkai K, Fett N. Dermatology faculty and residents’ perspectives on the dermatology residency application process: a nationwide survey. J Am Acad Dermatol. 2018;79:157-159. doi:10.1016/j.jaad.2018.01.00
- Charting Outcomes in the Match: Senior Students of U.S. MD Medical Schools. National Resident Matching Program. July 2020. Accessed December 6, 2021. https://www.nrmp.org/wp-content/uploads/2021/08/Charting-Outcomes-in-the-Match-2020_MD-Senior_final.pdf
- Thatiparthi A, Martin A, Liu J, et al. Preliminary outcomes of 2020-2021 dermatology residency application cycle and adverse effects of COVID-19. J Am Acad Dermatol. 2021;84:e263-e264. doi:10.1016/j.jaad.2021.03.034
- Hammoud MM, Standiford T, Carmody JB. Potential implications of COVID-19 for the 2020-2021 residency application cycle. JAMA. 2020;324:29-30. doi:10.1001/jama.2020.8911
- Interview offer rate with/without ENTSignaling. Society of University Otolaryngologists. Updated July 19, 2022. Accessed December 12, 2022. https://opdo-hns.org/mpage/signaling-updates
- Results and Data: 2021 Main Residency Match. National Resident Matching Program. May 2021. Accessed December 6, 2021. https://www.nrmp.org/wp-content/uploads/2021/08/MRM-Results_and-Data_2021.pdf
- Results of the 2021 NRMP Program Director Survey. National Resident Matching Program. August 2021. Accessed December 6, 2021. https://www.nrmp.org/wp-content/uploads/2021/11/2021-PD-Survey-Report-for-WWW.pdf
- Results of the 2020 NRMP Program Director Survey. National Resident Matching Program. August 2020. Accessed December 6, 2021. https://www.nrmp.org/wp-content/uploads/2022/01/2020-PD-Survey.pdf
- Rojek NW, Shinkai K, Fett N. Dermatology faculty and residents’ perspectives on the dermatology residency application process: a nationwide survey. J Am Acad Dermatol. 2018;79:157-159. doi:10.1016/j.jaad.2018.01.00
- Charting Outcomes in the Match: Senior Students of U.S. MD Medical Schools. National Resident Matching Program. July 2020. Accessed December 6, 2021. https://www.nrmp.org/wp-content/uploads/2021/08/Charting-Outcomes-in-the-Match-2020_MD-Senior_final.pdf
- Thatiparthi A, Martin A, Liu J, et al. Preliminary outcomes of 2020-2021 dermatology residency application cycle and adverse effects of COVID-19. J Am Acad Dermatol. 2021;84:e263-e264. doi:10.1016/j.jaad.2021.03.034
- Hammoud MM, Standiford T, Carmody JB. Potential implications of COVID-19 for the 2020-2021 residency application cycle. JAMA. 2020;324:29-30. doi:10.1001/jama.2020.8911
- Interview offer rate with/without ENTSignaling. Society of University Otolaryngologists. Updated July 19, 2022. Accessed December 12, 2022. https://opdo-hns.org/mpage/signaling-updates
- Results and Data: 2021 Main Residency Match. National Resident Matching Program. May 2021. Accessed December 6, 2021. https://www.nrmp.org/wp-content/uploads/2021/08/MRM-Results_and-Data_2021.pdf
PRACTICE POINTS
- Although there have been numerous changes to the dermatology interview process due to the COVID-19 pandemic, the overall fill rate for postgraduate year 2 positions remained unchanged from 2018 (prepandemic) to 2021 (postpandemic).
- Strategies to accommodate new safety recommendations for interviews may reduce the financial burden (approximately $10,000 for each senior applicant) and time constraints on applicants. These strategies should be considered for implementation in future cycles.
Feedback and Education in Dermatology Residency
A dermatology resident has more education and experience than a medical student or intern but less than a fellow or attending physician. Because of this position, residents have a unique opportunity to provide feedback and education to those with less knowledge and experience as a teacher and also to provide feedback to their more senior colleagues about their teaching effectiveness while simultaneously learning from them. The reciprocal exchange of information—from patients and colleagues in clinic, co-residents or attendings in lectures, or in other environments such as pathology at the microscope or skills during simulation training sessions—is the cornerstone of medical education. Being able to give effective feedback while also learning to accept it is one of the most vital skills a resident can learn to thrive in medical education.
The importance of feedback cannot be understated. The art of medicine involves the scientific knowledge needed to treat disease, as well as the social ability to educate, comfort, and heal those afflicted. Mastering this art takes a lifetime. The direct imparting of knowledge from those more experienced to those learning occurs via feedback. In addition, the desire to better oneself leads to more satisfaction with work and improved performance.1 The ability to give and receive feedback is vital for the field of dermatology and medicine in general.
Types and Implementation of Feedback
Feedback comes in many forms and can be classified via different characteristics such as formal vs informal, written vs spoken, real time vs delayed, and single observer vs pooled data. Each style of feedback has positive and negative aspects, and a feedback provider will need to weigh the pros and cons when deciding the most appropriate one. Although there is no one correct way to provide feedback, the literature shows that some forms of feedback may be more effective and better received than others. This can depend on the context of what is being evaluated.
Many dermatology residencies employ formal scheduled feedback as part of their curricula, ensuring that residents will receive feedback at preset time intervals and providing residency directors with information to assess improvement and areas where more growth is needed. The Accreditation Council for Graduate Medical Education provides a reference for programs on how to give this formal standardized feedback in The Milestones Guidebook.2 This feedback is a minimum required amount, with a survey of residents showing preference for frequent informal feedback sessions in addition to standardized formal feedback.3 Another study showed that residents want feedback that is confidential, in person, shortly after experiences, and specific to their actions.4 Medical students also voiced a need for frequent, transparent, and actionable feedback during protected, predetermined, and communicated times.5 Clearly, learners appreciate spoken intentional feedback as opposed to the traditional formal model of feedback.
Finally, a study was performed analyzing how prior generations of physician educators view millennial trainees.6 Because most current dermatology residents were born between 1981 and 1996, this study seemed to pinpoint thoughts toward teaching current residents. The study found that although negative judgments such as millennial entitlement (P<.001), impoliteness (P<.001), oversensitivity (P<.001), and inferior work ethic (P<.001) reached significance, millennial ideals of social justice (P<.001) and savviness with technology (P<.001) also were notable. Overall, millennials were thought to be good colleagues (P<.001), were equally competent to more experienced clinicians (P<.001), and would lead medicine to a good future (P=.039).6
Identifying and Maximizing the Impact of Feedback
In addition to how and when to provide feedback, there are discrepancies between attending and resident perception of what is considered feedback. This disconnect can be seen in a study of 122 respondents (67 residents and 55 attendings) that showed 31% of attendings reported giving feedback daily, as opposed to only 9% of residents who reported receiving daily feedback.4 When feedback is to be performed, it may be important to specifically announce the process so that it can be properly acknowledged.7
Beach8 provided a systematic breakdown of clinical teaching to those who may be unfamiliar with the process. This method is divided into preclinic, in-clinic, and postclinic strategies to maximize learning. The author recommended establishing the objectives of the rotation from the teacher’s perspective and inquiring about the objectives of the learner. Both perspectives should inform the lessons to be learned; for example, if a medical student expresses specific interest in psoriasis (a well-established part of a medical student curriculum), all efforts should be placed on arranging for that student to see those specific patients. Beach8 also recommended providing resources and creating a positive supportive learning environment to better utilize precious clinic time and create investment in all learning parties. The author recommended matching trainees during clinic to competence-specific challenges in clinical practice where appropriate technical skill is needed. Appropriate autonomy also is promoted, as it requires higher levels of learning and knowledge consolidation. Group discussions can be facilitated by asking questions of increasing levels of difficulty as experience increases. Finally, postclinic feedback should be timely and constructive.8
One technique discussed by Beach8 is the “1-minute preceptor plus” approach. In this approach, the teacher wants to establish 5 “micro-skills” by first getting a commitment, then checking for supportive evidence of this initial plan, teaching a general principle, reinforcing what was properly performed, and correcting errors. The “plus” comes from trying to take that lesson and apply it to a broader concept. Although this concept is meant to be used in a time-limited setting, it can be expanded to larger conversations. A common example could be made when residents teach rotating medical students through direct observation and supervision during clinic. In this hypothetical situation, the resident and medical student see a patient with erythematous silver-scaled plaques on the elbows and knees. During the patient encounter, the student then inquires about any personal history of cardiovascular disease, diabetes mellitus, and hypertension. After leaving the examination room, the medical student asserts the diagnosis is plaque psoriasis because of the physical examination findings and distribution of lesions. A discussion about the relationship between psoriasis and metabolic syndrome commences, emphasizing the pathophysiology of type 1 helper T-cell–mediated and type 17 helper T-cell–mediated inflammation with vascular damage and growth from inflammatory cytokines.9 The student subsequently is praised on inquiring about relevant comorbidities, and a relevant journal article is retrieved for the student’s future studies. Teaching points regarding the Koebner phenomenon, such as that it is not an instantaneous process and comes with a differential diagnosis, are then provided.
Situation-Behavior-Impact is another teaching method developed by the Center for Creative Leadership. In this technique, one will identify what specifically happened, how the learner responded, and what occurred because of the response.10 This technique is exemplified in the following mock conversation between an attending and their resident following a challenging patient situation: “When you walked into the room and asked the patient coming in for a follow-up appointment ‘What brings you in today?,’ they immediately tensed up and responded that you should already know and check your electronic medical record. This tension could be ameliorated by reviewing the patient’s medical record and addressing what they initially presented for, followed by inquiring if there are other skin problems they want to discuss afterwards.” By identifying the cause-and-effect relationship, helpful and unhelpful responses can be identified and ways to mitigate or continue behaviors can be brainstormed.
The Learning Process
Brodell et all11 outlined techniques to augment the education process that are specific to dermatology. They recommended learning general applicable concepts instead of contextless memorization, mnemonic devices to assist memory for associations and lists, and repetition and practice of learned material. For teaching, they divided techniques into Aristotelian or Socratic; Aristotelian teaching is the formal lecture style, whereas Socratic is conversation based. Both have a place in teaching—as fundamental knowledge grows via Aristotelian teaching, critical thinking can be enhanced via the Socratic method. The authors then outlined tips to create the most conducive learning environment for students.11
Feedback is a reciprocal process with information being given and received by both the teacher and the learner. This is paramount because perfecting the art of teaching is a career-long process and can only be achieved via correction of oversights and mistakes. A questionnaire-based study found that when critiquing the teacher, a combination of self-assessment with assessment from learners was effective in stimulating the greatest level of change in the teacher.12 This finding likely is because the educator was able to see the juxtaposition of how they think they performed with how students interpreted the same situation. Another survey-based study showed that of 68 attending physicians, 28 attendings saw utility in specialized feedback training; an additional 11 attendings agreed with online modules to improve their feedback skills. A recommendation that trainees receive training on the acceptance feedback also was proposed.13 Specialized training to give and receive feedback could be initiated for both attending and resident physicians to fully create an environment emphasizing improvement and teamwork.
Final Thoughts
The art of giving and receiving feedback is a deliberate process that develops with experience and training. Because residents are early in their medical career, being familiar with techniques such as those outlined in this article can enhance teaching and the reception of feedback. Residents are in a unique position, as residency itself is a time of dramatic learning and teaching. Providing feedback gives us a way to advance medicine and better ourselves by solidifying good habits and knowledge.
Acknowledgment—I thank Warren R. Heymann, MD (Camden, New Jersey), for assisting in the creation of this topic and reviewing this article.
- Crommelinck M, Anseel F. Understanding and encouraging feedback-seeking behavior: a literature review. Med Educ. 2013;47:232-241.
- Edgar L, McLean S, Hogan SO, et al. The Milestones Guidebook. Accreditation Council for Graduate Medical Education; 2020. Accessed December 12, 2022. https://www.acgme.org/globalassets/milestonesguidebook.pdf
- Wang JV, O’Connor M, McGuinn K, et al. Feedback practices in dermatology residency programs: building a culture for millennials. Clin Dermatol. 2019;37:282-283.
- Hajar T, Wanat KA, Fett N. Survey of resident physician and attending physician feedback perceptions: there is still work to be done. Dermatol Online J. 2020;25:13030/qt2sg354p6.
- Yoon J, Said JT, Thompson LL, et al. Medical student perceptions of assessment systems, subjectivity, and variability on introductory dermatology clerkships. Int J Womens Dermatol. 2021;7:232-330.
- Marka A, LeBoeuf MR, Vidal NY. Perspectives of dermatology faculty toward millennial trainees and colleagues: a national survey. Mayo Clin Proc Innov Qual Outcomes. 2021;5:65-71.
- Bernard AW, Kman NE, Khandelwal S. Feedback in the emergency medicine clerkship. West J Emerg Med. 2011;12:537-542.
- Beach RA. Strategies to maximise teaching in your next ambulatory clinic. Clin Teach. 2017;14:85-89.
- Takeshita J, Grewal S, Langan SM, et al. Psoriasis and comorbid diseases part I. epidemiology. J Am Acad Dermatol. 2017;76:377-390.
- Olbricht SM. What makes feedback productive? Cutis. 2016;98:222-223.
- Brodell RT, Wile MZ, Chren M, et al. Learning and teaching in dermatology: a practitioner’s guide. Arch Dermatol. 1996;132:946-952.
- Stalmeijer RE, Dolmans DHJM, Wolfhagen IHAP, et al. Combined student ratings and self-assessment provide useful feedback for clinical teachers. Adv in Health Sci Educ. 2010;15:315-328.
- Chelliah P, Srivastava D, Nijhawan RI. What makes giving feedback challenging? a survey of the Association of Professors of Dermatology (APD)[published online July 19, 2022]. Arch Dermatol Res. doi:10.1007/s00403-022-02370-y
A dermatology resident has more education and experience than a medical student or intern but less than a fellow or attending physician. Because of this position, residents have a unique opportunity to provide feedback and education to those with less knowledge and experience as a teacher and also to provide feedback to their more senior colleagues about their teaching effectiveness while simultaneously learning from them. The reciprocal exchange of information—from patients and colleagues in clinic, co-residents or attendings in lectures, or in other environments such as pathology at the microscope or skills during simulation training sessions—is the cornerstone of medical education. Being able to give effective feedback while also learning to accept it is one of the most vital skills a resident can learn to thrive in medical education.
The importance of feedback cannot be understated. The art of medicine involves the scientific knowledge needed to treat disease, as well as the social ability to educate, comfort, and heal those afflicted. Mastering this art takes a lifetime. The direct imparting of knowledge from those more experienced to those learning occurs via feedback. In addition, the desire to better oneself leads to more satisfaction with work and improved performance.1 The ability to give and receive feedback is vital for the field of dermatology and medicine in general.
Types and Implementation of Feedback
Feedback comes in many forms and can be classified via different characteristics such as formal vs informal, written vs spoken, real time vs delayed, and single observer vs pooled data. Each style of feedback has positive and negative aspects, and a feedback provider will need to weigh the pros and cons when deciding the most appropriate one. Although there is no one correct way to provide feedback, the literature shows that some forms of feedback may be more effective and better received than others. This can depend on the context of what is being evaluated.
Many dermatology residencies employ formal scheduled feedback as part of their curricula, ensuring that residents will receive feedback at preset time intervals and providing residency directors with information to assess improvement and areas where more growth is needed. The Accreditation Council for Graduate Medical Education provides a reference for programs on how to give this formal standardized feedback in The Milestones Guidebook.2 This feedback is a minimum required amount, with a survey of residents showing preference for frequent informal feedback sessions in addition to standardized formal feedback.3 Another study showed that residents want feedback that is confidential, in person, shortly after experiences, and specific to their actions.4 Medical students also voiced a need for frequent, transparent, and actionable feedback during protected, predetermined, and communicated times.5 Clearly, learners appreciate spoken intentional feedback as opposed to the traditional formal model of feedback.
Finally, a study was performed analyzing how prior generations of physician educators view millennial trainees.6 Because most current dermatology residents were born between 1981 and 1996, this study seemed to pinpoint thoughts toward teaching current residents. The study found that although negative judgments such as millennial entitlement (P<.001), impoliteness (P<.001), oversensitivity (P<.001), and inferior work ethic (P<.001) reached significance, millennial ideals of social justice (P<.001) and savviness with technology (P<.001) also were notable. Overall, millennials were thought to be good colleagues (P<.001), were equally competent to more experienced clinicians (P<.001), and would lead medicine to a good future (P=.039).6
Identifying and Maximizing the Impact of Feedback
In addition to how and when to provide feedback, there are discrepancies between attending and resident perception of what is considered feedback. This disconnect can be seen in a study of 122 respondents (67 residents and 55 attendings) that showed 31% of attendings reported giving feedback daily, as opposed to only 9% of residents who reported receiving daily feedback.4 When feedback is to be performed, it may be important to specifically announce the process so that it can be properly acknowledged.7
Beach8 provided a systematic breakdown of clinical teaching to those who may be unfamiliar with the process. This method is divided into preclinic, in-clinic, and postclinic strategies to maximize learning. The author recommended establishing the objectives of the rotation from the teacher’s perspective and inquiring about the objectives of the learner. Both perspectives should inform the lessons to be learned; for example, if a medical student expresses specific interest in psoriasis (a well-established part of a medical student curriculum), all efforts should be placed on arranging for that student to see those specific patients. Beach8 also recommended providing resources and creating a positive supportive learning environment to better utilize precious clinic time and create investment in all learning parties. The author recommended matching trainees during clinic to competence-specific challenges in clinical practice where appropriate technical skill is needed. Appropriate autonomy also is promoted, as it requires higher levels of learning and knowledge consolidation. Group discussions can be facilitated by asking questions of increasing levels of difficulty as experience increases. Finally, postclinic feedback should be timely and constructive.8
One technique discussed by Beach8 is the “1-minute preceptor plus” approach. In this approach, the teacher wants to establish 5 “micro-skills” by first getting a commitment, then checking for supportive evidence of this initial plan, teaching a general principle, reinforcing what was properly performed, and correcting errors. The “plus” comes from trying to take that lesson and apply it to a broader concept. Although this concept is meant to be used in a time-limited setting, it can be expanded to larger conversations. A common example could be made when residents teach rotating medical students through direct observation and supervision during clinic. In this hypothetical situation, the resident and medical student see a patient with erythematous silver-scaled plaques on the elbows and knees. During the patient encounter, the student then inquires about any personal history of cardiovascular disease, diabetes mellitus, and hypertension. After leaving the examination room, the medical student asserts the diagnosis is plaque psoriasis because of the physical examination findings and distribution of lesions. A discussion about the relationship between psoriasis and metabolic syndrome commences, emphasizing the pathophysiology of type 1 helper T-cell–mediated and type 17 helper T-cell–mediated inflammation with vascular damage and growth from inflammatory cytokines.9 The student subsequently is praised on inquiring about relevant comorbidities, and a relevant journal article is retrieved for the student’s future studies. Teaching points regarding the Koebner phenomenon, such as that it is not an instantaneous process and comes with a differential diagnosis, are then provided.
Situation-Behavior-Impact is another teaching method developed by the Center for Creative Leadership. In this technique, one will identify what specifically happened, how the learner responded, and what occurred because of the response.10 This technique is exemplified in the following mock conversation between an attending and their resident following a challenging patient situation: “When you walked into the room and asked the patient coming in for a follow-up appointment ‘What brings you in today?,’ they immediately tensed up and responded that you should already know and check your electronic medical record. This tension could be ameliorated by reviewing the patient’s medical record and addressing what they initially presented for, followed by inquiring if there are other skin problems they want to discuss afterwards.” By identifying the cause-and-effect relationship, helpful and unhelpful responses can be identified and ways to mitigate or continue behaviors can be brainstormed.
The Learning Process
Brodell et all11 outlined techniques to augment the education process that are specific to dermatology. They recommended learning general applicable concepts instead of contextless memorization, mnemonic devices to assist memory for associations and lists, and repetition and practice of learned material. For teaching, they divided techniques into Aristotelian or Socratic; Aristotelian teaching is the formal lecture style, whereas Socratic is conversation based. Both have a place in teaching—as fundamental knowledge grows via Aristotelian teaching, critical thinking can be enhanced via the Socratic method. The authors then outlined tips to create the most conducive learning environment for students.11
Feedback is a reciprocal process with information being given and received by both the teacher and the learner. This is paramount because perfecting the art of teaching is a career-long process and can only be achieved via correction of oversights and mistakes. A questionnaire-based study found that when critiquing the teacher, a combination of self-assessment with assessment from learners was effective in stimulating the greatest level of change in the teacher.12 This finding likely is because the educator was able to see the juxtaposition of how they think they performed with how students interpreted the same situation. Another survey-based study showed that of 68 attending physicians, 28 attendings saw utility in specialized feedback training; an additional 11 attendings agreed with online modules to improve their feedback skills. A recommendation that trainees receive training on the acceptance feedback also was proposed.13 Specialized training to give and receive feedback could be initiated for both attending and resident physicians to fully create an environment emphasizing improvement and teamwork.
Final Thoughts
The art of giving and receiving feedback is a deliberate process that develops with experience and training. Because residents are early in their medical career, being familiar with techniques such as those outlined in this article can enhance teaching and the reception of feedback. Residents are in a unique position, as residency itself is a time of dramatic learning and teaching. Providing feedback gives us a way to advance medicine and better ourselves by solidifying good habits and knowledge.
Acknowledgment—I thank Warren R. Heymann, MD (Camden, New Jersey), for assisting in the creation of this topic and reviewing this article.
A dermatology resident has more education and experience than a medical student or intern but less than a fellow or attending physician. Because of this position, residents have a unique opportunity to provide feedback and education to those with less knowledge and experience as a teacher and also to provide feedback to their more senior colleagues about their teaching effectiveness while simultaneously learning from them. The reciprocal exchange of information—from patients and colleagues in clinic, co-residents or attendings in lectures, or in other environments such as pathology at the microscope or skills during simulation training sessions—is the cornerstone of medical education. Being able to give effective feedback while also learning to accept it is one of the most vital skills a resident can learn to thrive in medical education.
The importance of feedback cannot be understated. The art of medicine involves the scientific knowledge needed to treat disease, as well as the social ability to educate, comfort, and heal those afflicted. Mastering this art takes a lifetime. The direct imparting of knowledge from those more experienced to those learning occurs via feedback. In addition, the desire to better oneself leads to more satisfaction with work and improved performance.1 The ability to give and receive feedback is vital for the field of dermatology and medicine in general.
Types and Implementation of Feedback
Feedback comes in many forms and can be classified via different characteristics such as formal vs informal, written vs spoken, real time vs delayed, and single observer vs pooled data. Each style of feedback has positive and negative aspects, and a feedback provider will need to weigh the pros and cons when deciding the most appropriate one. Although there is no one correct way to provide feedback, the literature shows that some forms of feedback may be more effective and better received than others. This can depend on the context of what is being evaluated.
Many dermatology residencies employ formal scheduled feedback as part of their curricula, ensuring that residents will receive feedback at preset time intervals and providing residency directors with information to assess improvement and areas where more growth is needed. The Accreditation Council for Graduate Medical Education provides a reference for programs on how to give this formal standardized feedback in The Milestones Guidebook.2 This feedback is a minimum required amount, with a survey of residents showing preference for frequent informal feedback sessions in addition to standardized formal feedback.3 Another study showed that residents want feedback that is confidential, in person, shortly after experiences, and specific to their actions.4 Medical students also voiced a need for frequent, transparent, and actionable feedback during protected, predetermined, and communicated times.5 Clearly, learners appreciate spoken intentional feedback as opposed to the traditional formal model of feedback.
Finally, a study was performed analyzing how prior generations of physician educators view millennial trainees.6 Because most current dermatology residents were born between 1981 and 1996, this study seemed to pinpoint thoughts toward teaching current residents. The study found that although negative judgments such as millennial entitlement (P<.001), impoliteness (P<.001), oversensitivity (P<.001), and inferior work ethic (P<.001) reached significance, millennial ideals of social justice (P<.001) and savviness with technology (P<.001) also were notable. Overall, millennials were thought to be good colleagues (P<.001), were equally competent to more experienced clinicians (P<.001), and would lead medicine to a good future (P=.039).6
Identifying and Maximizing the Impact of Feedback
In addition to how and when to provide feedback, there are discrepancies between attending and resident perception of what is considered feedback. This disconnect can be seen in a study of 122 respondents (67 residents and 55 attendings) that showed 31% of attendings reported giving feedback daily, as opposed to only 9% of residents who reported receiving daily feedback.4 When feedback is to be performed, it may be important to specifically announce the process so that it can be properly acknowledged.7
Beach8 provided a systematic breakdown of clinical teaching to those who may be unfamiliar with the process. This method is divided into preclinic, in-clinic, and postclinic strategies to maximize learning. The author recommended establishing the objectives of the rotation from the teacher’s perspective and inquiring about the objectives of the learner. Both perspectives should inform the lessons to be learned; for example, if a medical student expresses specific interest in psoriasis (a well-established part of a medical student curriculum), all efforts should be placed on arranging for that student to see those specific patients. Beach8 also recommended providing resources and creating a positive supportive learning environment to better utilize precious clinic time and create investment in all learning parties. The author recommended matching trainees during clinic to competence-specific challenges in clinical practice where appropriate technical skill is needed. Appropriate autonomy also is promoted, as it requires higher levels of learning and knowledge consolidation. Group discussions can be facilitated by asking questions of increasing levels of difficulty as experience increases. Finally, postclinic feedback should be timely and constructive.8
One technique discussed by Beach8 is the “1-minute preceptor plus” approach. In this approach, the teacher wants to establish 5 “micro-skills” by first getting a commitment, then checking for supportive evidence of this initial plan, teaching a general principle, reinforcing what was properly performed, and correcting errors. The “plus” comes from trying to take that lesson and apply it to a broader concept. Although this concept is meant to be used in a time-limited setting, it can be expanded to larger conversations. A common example could be made when residents teach rotating medical students through direct observation and supervision during clinic. In this hypothetical situation, the resident and medical student see a patient with erythematous silver-scaled plaques on the elbows and knees. During the patient encounter, the student then inquires about any personal history of cardiovascular disease, diabetes mellitus, and hypertension. After leaving the examination room, the medical student asserts the diagnosis is plaque psoriasis because of the physical examination findings and distribution of lesions. A discussion about the relationship between psoriasis and metabolic syndrome commences, emphasizing the pathophysiology of type 1 helper T-cell–mediated and type 17 helper T-cell–mediated inflammation with vascular damage and growth from inflammatory cytokines.9 The student subsequently is praised on inquiring about relevant comorbidities, and a relevant journal article is retrieved for the student’s future studies. Teaching points regarding the Koebner phenomenon, such as that it is not an instantaneous process and comes with a differential diagnosis, are then provided.
Situation-Behavior-Impact is another teaching method developed by the Center for Creative Leadership. In this technique, one will identify what specifically happened, how the learner responded, and what occurred because of the response.10 This technique is exemplified in the following mock conversation between an attending and their resident following a challenging patient situation: “When you walked into the room and asked the patient coming in for a follow-up appointment ‘What brings you in today?,’ they immediately tensed up and responded that you should already know and check your electronic medical record. This tension could be ameliorated by reviewing the patient’s medical record and addressing what they initially presented for, followed by inquiring if there are other skin problems they want to discuss afterwards.” By identifying the cause-and-effect relationship, helpful and unhelpful responses can be identified and ways to mitigate or continue behaviors can be brainstormed.
The Learning Process
Brodell et all11 outlined techniques to augment the education process that are specific to dermatology. They recommended learning general applicable concepts instead of contextless memorization, mnemonic devices to assist memory for associations and lists, and repetition and practice of learned material. For teaching, they divided techniques into Aristotelian or Socratic; Aristotelian teaching is the formal lecture style, whereas Socratic is conversation based. Both have a place in teaching—as fundamental knowledge grows via Aristotelian teaching, critical thinking can be enhanced via the Socratic method. The authors then outlined tips to create the most conducive learning environment for students.11
Feedback is a reciprocal process with information being given and received by both the teacher and the learner. This is paramount because perfecting the art of teaching is a career-long process and can only be achieved via correction of oversights and mistakes. A questionnaire-based study found that when critiquing the teacher, a combination of self-assessment with assessment from learners was effective in stimulating the greatest level of change in the teacher.12 This finding likely is because the educator was able to see the juxtaposition of how they think they performed with how students interpreted the same situation. Another survey-based study showed that of 68 attending physicians, 28 attendings saw utility in specialized feedback training; an additional 11 attendings agreed with online modules to improve their feedback skills. A recommendation that trainees receive training on the acceptance feedback also was proposed.13 Specialized training to give and receive feedback could be initiated for both attending and resident physicians to fully create an environment emphasizing improvement and teamwork.
Final Thoughts
The art of giving and receiving feedback is a deliberate process that develops with experience and training. Because residents are early in their medical career, being familiar with techniques such as those outlined in this article can enhance teaching and the reception of feedback. Residents are in a unique position, as residency itself is a time of dramatic learning and teaching. Providing feedback gives us a way to advance medicine and better ourselves by solidifying good habits and knowledge.
Acknowledgment—I thank Warren R. Heymann, MD (Camden, New Jersey), for assisting in the creation of this topic and reviewing this article.
- Crommelinck M, Anseel F. Understanding and encouraging feedback-seeking behavior: a literature review. Med Educ. 2013;47:232-241.
- Edgar L, McLean S, Hogan SO, et al. The Milestones Guidebook. Accreditation Council for Graduate Medical Education; 2020. Accessed December 12, 2022. https://www.acgme.org/globalassets/milestonesguidebook.pdf
- Wang JV, O’Connor M, McGuinn K, et al. Feedback practices in dermatology residency programs: building a culture for millennials. Clin Dermatol. 2019;37:282-283.
- Hajar T, Wanat KA, Fett N. Survey of resident physician and attending physician feedback perceptions: there is still work to be done. Dermatol Online J. 2020;25:13030/qt2sg354p6.
- Yoon J, Said JT, Thompson LL, et al. Medical student perceptions of assessment systems, subjectivity, and variability on introductory dermatology clerkships. Int J Womens Dermatol. 2021;7:232-330.
- Marka A, LeBoeuf MR, Vidal NY. Perspectives of dermatology faculty toward millennial trainees and colleagues: a national survey. Mayo Clin Proc Innov Qual Outcomes. 2021;5:65-71.
- Bernard AW, Kman NE, Khandelwal S. Feedback in the emergency medicine clerkship. West J Emerg Med. 2011;12:537-542.
- Beach RA. Strategies to maximise teaching in your next ambulatory clinic. Clin Teach. 2017;14:85-89.
- Takeshita J, Grewal S, Langan SM, et al. Psoriasis and comorbid diseases part I. epidemiology. J Am Acad Dermatol. 2017;76:377-390.
- Olbricht SM. What makes feedback productive? Cutis. 2016;98:222-223.
- Brodell RT, Wile MZ, Chren M, et al. Learning and teaching in dermatology: a practitioner’s guide. Arch Dermatol. 1996;132:946-952.
- Stalmeijer RE, Dolmans DHJM, Wolfhagen IHAP, et al. Combined student ratings and self-assessment provide useful feedback for clinical teachers. Adv in Health Sci Educ. 2010;15:315-328.
- Chelliah P, Srivastava D, Nijhawan RI. What makes giving feedback challenging? a survey of the Association of Professors of Dermatology (APD)[published online July 19, 2022]. Arch Dermatol Res. doi:10.1007/s00403-022-02370-y
- Crommelinck M, Anseel F. Understanding and encouraging feedback-seeking behavior: a literature review. Med Educ. 2013;47:232-241.
- Edgar L, McLean S, Hogan SO, et al. The Milestones Guidebook. Accreditation Council for Graduate Medical Education; 2020. Accessed December 12, 2022. https://www.acgme.org/globalassets/milestonesguidebook.pdf
- Wang JV, O’Connor M, McGuinn K, et al. Feedback practices in dermatology residency programs: building a culture for millennials. Clin Dermatol. 2019;37:282-283.
- Hajar T, Wanat KA, Fett N. Survey of resident physician and attending physician feedback perceptions: there is still work to be done. Dermatol Online J. 2020;25:13030/qt2sg354p6.
- Yoon J, Said JT, Thompson LL, et al. Medical student perceptions of assessment systems, subjectivity, and variability on introductory dermatology clerkships. Int J Womens Dermatol. 2021;7:232-330.
- Marka A, LeBoeuf MR, Vidal NY. Perspectives of dermatology faculty toward millennial trainees and colleagues: a national survey. Mayo Clin Proc Innov Qual Outcomes. 2021;5:65-71.
- Bernard AW, Kman NE, Khandelwal S. Feedback in the emergency medicine clerkship. West J Emerg Med. 2011;12:537-542.
- Beach RA. Strategies to maximise teaching in your next ambulatory clinic. Clin Teach. 2017;14:85-89.
- Takeshita J, Grewal S, Langan SM, et al. Psoriasis and comorbid diseases part I. epidemiology. J Am Acad Dermatol. 2017;76:377-390.
- Olbricht SM. What makes feedback productive? Cutis. 2016;98:222-223.
- Brodell RT, Wile MZ, Chren M, et al. Learning and teaching in dermatology: a practitioner’s guide. Arch Dermatol. 1996;132:946-952.
- Stalmeijer RE, Dolmans DHJM, Wolfhagen IHAP, et al. Combined student ratings and self-assessment provide useful feedback for clinical teachers. Adv in Health Sci Educ. 2010;15:315-328.
- Chelliah P, Srivastava D, Nijhawan RI. What makes giving feedback challenging? a survey of the Association of Professors of Dermatology (APD)[published online July 19, 2022]. Arch Dermatol Res. doi:10.1007/s00403-022-02370-y
RESIDENT PEARLS
- Feedback between dermatology trainees and their educators should be provided in a private and constructive way soon after the observation was performed.
- One method to improve education and feedback in a residency program is a specialty course to improve giving and receiving feedback by both residents and attending physicians.
Rheumatology Match Day follows same pattern as previous years
Rheumatology joined six other Medicine specialties that filled more than 95% of fellowship positions in 2022.
The National Resident Matching Program in its 2022 Medicine and Pediatric Specialties Match reported that rheumatology filled 123 of 127 certified programs (96.9%) along with 265 certified positions (97.8%).
Matched applicants for adult rheumatology programs included 40 U.S. foreign applicants (15.1%), 123 MD graduates (46.4%), 66 foreign (24.9%), and 36 DO graduates (13.6%).
A total of 352 applicants showed a preference for this specialty, and 75% matched to the specialty. Another 23% did not match to any program.
2022 was the first year that NRMP combined medical specialties, pediatric specialties, and adolescent medicine fellowship matches into the “Medicine and Pediatric Specialties Match.”
“We engaged the leadership of both pediatrics and internal medicine organizations to work with the NRMP to brainstorm solutions and were successful in combining pediatrics and internal medicine into one fellowship match,” said Jill Fussell, MD, immediate past chair of the Council of Pediatric Subspecialties in a statement. “It was an incredibly rewarding experience to work across pediatrics and internal medicine on behalf of resident well-being to make this collaborative change happen.”
Similar to 2021, pediatric rheumatology didn’t do as well as adult programs, filling just 18 of 32 certified programs (56.3%) and 27 out of 43 certified positions (62.8%). More than 66% of the applicants represented MD graduates. Eight were foreign, and one was a DO graduate.
The 2022 match was the largest on record, comprising 39 subspecialties in internal medicine, pediatrics, addiction, and multidisciplinary specialties. A total of 3,361 programs filled 7,648 (87.7%) of 8,724 positions in 2022. Three specialties – cardiovascular disease, interventional pulmonology, and oncology – filled all their positions offered in the match.
In addition to rheumatology, six other specialties filled 95% or more of their positions. This included clinical cardiac electrophysiology, critical care medicine, endocrinology, gastroenterology, hematology/oncology, and pulmonary/critical care medicine. Allergy and immunology, which accepts applicants from either internal medicine or pediatrics, also filled more than 95% of positions offered.
Matched applicants will start fellowship training in July 2023.
Rheumatology joined six other Medicine specialties that filled more than 95% of fellowship positions in 2022.
The National Resident Matching Program in its 2022 Medicine and Pediatric Specialties Match reported that rheumatology filled 123 of 127 certified programs (96.9%) along with 265 certified positions (97.8%).
Matched applicants for adult rheumatology programs included 40 U.S. foreign applicants (15.1%), 123 MD graduates (46.4%), 66 foreign (24.9%), and 36 DO graduates (13.6%).
A total of 352 applicants showed a preference for this specialty, and 75% matched to the specialty. Another 23% did not match to any program.
2022 was the first year that NRMP combined medical specialties, pediatric specialties, and adolescent medicine fellowship matches into the “Medicine and Pediatric Specialties Match.”
“We engaged the leadership of both pediatrics and internal medicine organizations to work with the NRMP to brainstorm solutions and were successful in combining pediatrics and internal medicine into one fellowship match,” said Jill Fussell, MD, immediate past chair of the Council of Pediatric Subspecialties in a statement. “It was an incredibly rewarding experience to work across pediatrics and internal medicine on behalf of resident well-being to make this collaborative change happen.”
Similar to 2021, pediatric rheumatology didn’t do as well as adult programs, filling just 18 of 32 certified programs (56.3%) and 27 out of 43 certified positions (62.8%). More than 66% of the applicants represented MD graduates. Eight were foreign, and one was a DO graduate.
The 2022 match was the largest on record, comprising 39 subspecialties in internal medicine, pediatrics, addiction, and multidisciplinary specialties. A total of 3,361 programs filled 7,648 (87.7%) of 8,724 positions in 2022. Three specialties – cardiovascular disease, interventional pulmonology, and oncology – filled all their positions offered in the match.
In addition to rheumatology, six other specialties filled 95% or more of their positions. This included clinical cardiac electrophysiology, critical care medicine, endocrinology, gastroenterology, hematology/oncology, and pulmonary/critical care medicine. Allergy and immunology, which accepts applicants from either internal medicine or pediatrics, also filled more than 95% of positions offered.
Matched applicants will start fellowship training in July 2023.
Rheumatology joined six other Medicine specialties that filled more than 95% of fellowship positions in 2022.
The National Resident Matching Program in its 2022 Medicine and Pediatric Specialties Match reported that rheumatology filled 123 of 127 certified programs (96.9%) along with 265 certified positions (97.8%).
Matched applicants for adult rheumatology programs included 40 U.S. foreign applicants (15.1%), 123 MD graduates (46.4%), 66 foreign (24.9%), and 36 DO graduates (13.6%).
A total of 352 applicants showed a preference for this specialty, and 75% matched to the specialty. Another 23% did not match to any program.
2022 was the first year that NRMP combined medical specialties, pediatric specialties, and adolescent medicine fellowship matches into the “Medicine and Pediatric Specialties Match.”
“We engaged the leadership of both pediatrics and internal medicine organizations to work with the NRMP to brainstorm solutions and were successful in combining pediatrics and internal medicine into one fellowship match,” said Jill Fussell, MD, immediate past chair of the Council of Pediatric Subspecialties in a statement. “It was an incredibly rewarding experience to work across pediatrics and internal medicine on behalf of resident well-being to make this collaborative change happen.”
Similar to 2021, pediatric rheumatology didn’t do as well as adult programs, filling just 18 of 32 certified programs (56.3%) and 27 out of 43 certified positions (62.8%). More than 66% of the applicants represented MD graduates. Eight were foreign, and one was a DO graduate.
The 2022 match was the largest on record, comprising 39 subspecialties in internal medicine, pediatrics, addiction, and multidisciplinary specialties. A total of 3,361 programs filled 7,648 (87.7%) of 8,724 positions in 2022. Three specialties – cardiovascular disease, interventional pulmonology, and oncology – filled all their positions offered in the match.
In addition to rheumatology, six other specialties filled 95% or more of their positions. This included clinical cardiac electrophysiology, critical care medicine, endocrinology, gastroenterology, hematology/oncology, and pulmonary/critical care medicine. Allergy and immunology, which accepts applicants from either internal medicine or pediatrics, also filled more than 95% of positions offered.
Matched applicants will start fellowship training in July 2023.
How to Foster Camaraderie in Dermatology Residency
Change is inevitable in residency as well as in life. Every year on July 1, the atmosphere and social structure of residencies change with the new postgraduate year 2 class. Each class brings a unique perspective and energy. Residents come together from different backgrounds and life situations. Some residents are single, some are engaged or married, and some are starting or expanding their families. Some residents will have prior careers, others will have graduate degrees or expertise in various fields. They will have different ethnic backgrounds, religious and/or spiritual beliefs, familial upbringings, personalities, and methods of communicating. These differences all are important to consider when developing a mindset of inclusion and camaraderie. As residents start their journey together, it is important to remember that residency is a team endeavor. The principles of teamwork apply directly to residents and are founded on creating a climate of trust and building strong relationships with one another.1 Trust is the foundation of good relationships in the workplace; it allows people to communicate freely and foster the belief that everyone is working for each other’s best interests. Being open and sharing knowledge about networking opportunities, scholarships, and research projects is one way to foster collaboration and trust in residency.
Diversity, equity, and inclusion in dermatology is a work in progress. In the 2020-2021 dermatology application cycle, only 4.8% of applicants identified as Hispanic or Latino, and 7.8% identified as Black or African American.2 The American Academy of Dermatology took an active role in promoting diversity by creating a task force in 2018 to increase the exposure and recruitment into dermatology of medical students who are underrepresented in medicine.2 As standards for diversity are met in dermatology, we will have the wonderful opportunity to welcome even more diversity into our lives.
Listening, showing curiosity about your co-residents’ lives outside of work, and asking questions can help build respect, friendships, and camaraderie. Ask your co-residents what makes them happy and what their goals are in residency. Finding common goals and cultivating the mindset that you all work together to achieve your goals is key to the success of a residency class. Now that we discussed accepting and welcoming differences, how do you foster camaraderie in a social setting?
Establish a Social Committee
As a class, consider 1 or 2 residents who are always excited to try new activities such as attend restaurant openings, exercise classes, concerts, or movie nights. Consider nominating these co-residents along with one attending to be social chairs of your residency. The social chairs should meet and establish at least 1 social event per season, with 4 total for the academic year. There are only 2 rules with social events: (1) they must be held outside of clinic, and (2) everyone should try their best to attend.
Social chairs should try to prioritize a location-specific event that allows the residents who are not from the area to experience something local, which can be anything from apple picking at an orchard in the fall to beach volleyball in the summer. Planning these parties gives everyone an event to look forward to and a chance to spend time together and grow closer. The memories and inside jokes that arise from these outings are invaluable and increase joy inside and outside of clinic.
Utilize Social Media
Another project can be developing a social media account for your program with the approval of your faculty. @unmcdermatology, @uwderm, and @gwdermres can help foster social relationships by establishing a lighthearted space to celebrate the residency’s achievements, new publications, volunteer events, or social gatherings.
Encourage Local and National Conference Attendance
All residents should be encouraged to submit abstracts to local and national conferences and attend with their co-residents. Conferences are peak opportunities to foster camaraderie within residency classes, as they involve a sense of togetherness in the specialty along with the excitement of traveling to a new city and meeting other like-minded individuals. Conferences allow collaboration within the specialty on a national level and foster relationships between residency programs.
In addition, national groups such as the Women’s Dermatologic Society, the Skin of Color Society, and the American Academy of Dermatology Diversity, Equity, and Inclusion task force meet at the national conferences and discuss their next initiatives and projects. Joining a society of your interest can lead to many new networks and relationships you may not have had before. Even if you are not interested in specializing after general dermatology, consider attending a surgery, dermatopathology, or pediatric or cosmetic dermatology conference to learn more about the field from the experts.
Repair Conflicts and Build a Climate of Collaboration
Conflicts and disagreements unfortunately are inevitable during residency. Whether they involve planning vacation times or coordinating call schedules, everyone will not agree on every decision. Learning how to handle and approach conflict with co-residents is of utmost importance to maintaining the hard work you have put in to create trust, camaraderie, and a good social atmosphere. If you are having an issue with a circumstance involving a co-resident, holding a grudge will only sour your experience and the experience of others. Talking to your co-resident directly about your concerns before escalating the issue to a chief resident or faculty member is a great start. Consider asking them about their thought process and show concern for their point of view. Listen to them openly before going into your preferences. It is important to remember that working as a team requires sacrifices, and sometimes you will not be satisfied with the outcome of a conflict.
It also is important to remember that feelings change, and an issue you feel you must address immediately can wait to be addressed at a better time when you have calmed down. You may even find that you decide not to address it at all. At the end of the day, if a conflict cannot be worked out between those involved, consider confiding in a chief resident or a faculty mentor for advice on the next steps to take to resolve the problem. Ultimately, having a good foundation of respect and strong bonds with your residents will help tremendously when conflicts arise.
Final Thoughts
Fostering camaraderie in residency will improve the overall experience and lives of the residents, as well as the experience of the faculty, staff, and patients by the trickle-down effect. Creating a cheerful and fun atmosphere filled with inside jokes and excitement regarding upcoming social events or conferences will certainly result in a time you will cherish for the rest of your life.
- Kouzes JM, Posner BZ. Foster collaboration. In: Kouzes JM, Posner BZ, eds. The Leadership Challenge. 6th ed. John Wiley & Sons, Inc; 2017:195-217.
- Cooper J, Shao K, Feng H. Racial/ethnic health disparities in dermatology in the United States, part 1: overview of contributing factors and management strategies [published online February 7, 2022]. J Am Acad Dermatol. 2022;87:723-730. doi:10.1016/j.jaad.2021.12.061
Change is inevitable in residency as well as in life. Every year on July 1, the atmosphere and social structure of residencies change with the new postgraduate year 2 class. Each class brings a unique perspective and energy. Residents come together from different backgrounds and life situations. Some residents are single, some are engaged or married, and some are starting or expanding their families. Some residents will have prior careers, others will have graduate degrees or expertise in various fields. They will have different ethnic backgrounds, religious and/or spiritual beliefs, familial upbringings, personalities, and methods of communicating. These differences all are important to consider when developing a mindset of inclusion and camaraderie. As residents start their journey together, it is important to remember that residency is a team endeavor. The principles of teamwork apply directly to residents and are founded on creating a climate of trust and building strong relationships with one another.1 Trust is the foundation of good relationships in the workplace; it allows people to communicate freely and foster the belief that everyone is working for each other’s best interests. Being open and sharing knowledge about networking opportunities, scholarships, and research projects is one way to foster collaboration and trust in residency.
Diversity, equity, and inclusion in dermatology is a work in progress. In the 2020-2021 dermatology application cycle, only 4.8% of applicants identified as Hispanic or Latino, and 7.8% identified as Black or African American.2 The American Academy of Dermatology took an active role in promoting diversity by creating a task force in 2018 to increase the exposure and recruitment into dermatology of medical students who are underrepresented in medicine.2 As standards for diversity are met in dermatology, we will have the wonderful opportunity to welcome even more diversity into our lives.
Listening, showing curiosity about your co-residents’ lives outside of work, and asking questions can help build respect, friendships, and camaraderie. Ask your co-residents what makes them happy and what their goals are in residency. Finding common goals and cultivating the mindset that you all work together to achieve your goals is key to the success of a residency class. Now that we discussed accepting and welcoming differences, how do you foster camaraderie in a social setting?
Establish a Social Committee
As a class, consider 1 or 2 residents who are always excited to try new activities such as attend restaurant openings, exercise classes, concerts, or movie nights. Consider nominating these co-residents along with one attending to be social chairs of your residency. The social chairs should meet and establish at least 1 social event per season, with 4 total for the academic year. There are only 2 rules with social events: (1) they must be held outside of clinic, and (2) everyone should try their best to attend.
Social chairs should try to prioritize a location-specific event that allows the residents who are not from the area to experience something local, which can be anything from apple picking at an orchard in the fall to beach volleyball in the summer. Planning these parties gives everyone an event to look forward to and a chance to spend time together and grow closer. The memories and inside jokes that arise from these outings are invaluable and increase joy inside and outside of clinic.
Utilize Social Media
Another project can be developing a social media account for your program with the approval of your faculty. @unmcdermatology, @uwderm, and @gwdermres can help foster social relationships by establishing a lighthearted space to celebrate the residency’s achievements, new publications, volunteer events, or social gatherings.
Encourage Local and National Conference Attendance
All residents should be encouraged to submit abstracts to local and national conferences and attend with their co-residents. Conferences are peak opportunities to foster camaraderie within residency classes, as they involve a sense of togetherness in the specialty along with the excitement of traveling to a new city and meeting other like-minded individuals. Conferences allow collaboration within the specialty on a national level and foster relationships between residency programs.
In addition, national groups such as the Women’s Dermatologic Society, the Skin of Color Society, and the American Academy of Dermatology Diversity, Equity, and Inclusion task force meet at the national conferences and discuss their next initiatives and projects. Joining a society of your interest can lead to many new networks and relationships you may not have had before. Even if you are not interested in specializing after general dermatology, consider attending a surgery, dermatopathology, or pediatric or cosmetic dermatology conference to learn more about the field from the experts.
Repair Conflicts and Build a Climate of Collaboration
Conflicts and disagreements unfortunately are inevitable during residency. Whether they involve planning vacation times or coordinating call schedules, everyone will not agree on every decision. Learning how to handle and approach conflict with co-residents is of utmost importance to maintaining the hard work you have put in to create trust, camaraderie, and a good social atmosphere. If you are having an issue with a circumstance involving a co-resident, holding a grudge will only sour your experience and the experience of others. Talking to your co-resident directly about your concerns before escalating the issue to a chief resident or faculty member is a great start. Consider asking them about their thought process and show concern for their point of view. Listen to them openly before going into your preferences. It is important to remember that working as a team requires sacrifices, and sometimes you will not be satisfied with the outcome of a conflict.
It also is important to remember that feelings change, and an issue you feel you must address immediately can wait to be addressed at a better time when you have calmed down. You may even find that you decide not to address it at all. At the end of the day, if a conflict cannot be worked out between those involved, consider confiding in a chief resident or a faculty mentor for advice on the next steps to take to resolve the problem. Ultimately, having a good foundation of respect and strong bonds with your residents will help tremendously when conflicts arise.
Final Thoughts
Fostering camaraderie in residency will improve the overall experience and lives of the residents, as well as the experience of the faculty, staff, and patients by the trickle-down effect. Creating a cheerful and fun atmosphere filled with inside jokes and excitement regarding upcoming social events or conferences will certainly result in a time you will cherish for the rest of your life.
Change is inevitable in residency as well as in life. Every year on July 1, the atmosphere and social structure of residencies change with the new postgraduate year 2 class. Each class brings a unique perspective and energy. Residents come together from different backgrounds and life situations. Some residents are single, some are engaged or married, and some are starting or expanding their families. Some residents will have prior careers, others will have graduate degrees or expertise in various fields. They will have different ethnic backgrounds, religious and/or spiritual beliefs, familial upbringings, personalities, and methods of communicating. These differences all are important to consider when developing a mindset of inclusion and camaraderie. As residents start their journey together, it is important to remember that residency is a team endeavor. The principles of teamwork apply directly to residents and are founded on creating a climate of trust and building strong relationships with one another.1 Trust is the foundation of good relationships in the workplace; it allows people to communicate freely and foster the belief that everyone is working for each other’s best interests. Being open and sharing knowledge about networking opportunities, scholarships, and research projects is one way to foster collaboration and trust in residency.
Diversity, equity, and inclusion in dermatology is a work in progress. In the 2020-2021 dermatology application cycle, only 4.8% of applicants identified as Hispanic or Latino, and 7.8% identified as Black or African American.2 The American Academy of Dermatology took an active role in promoting diversity by creating a task force in 2018 to increase the exposure and recruitment into dermatology of medical students who are underrepresented in medicine.2 As standards for diversity are met in dermatology, we will have the wonderful opportunity to welcome even more diversity into our lives.
Listening, showing curiosity about your co-residents’ lives outside of work, and asking questions can help build respect, friendships, and camaraderie. Ask your co-residents what makes them happy and what their goals are in residency. Finding common goals and cultivating the mindset that you all work together to achieve your goals is key to the success of a residency class. Now that we discussed accepting and welcoming differences, how do you foster camaraderie in a social setting?
Establish a Social Committee
As a class, consider 1 or 2 residents who are always excited to try new activities such as attend restaurant openings, exercise classes, concerts, or movie nights. Consider nominating these co-residents along with one attending to be social chairs of your residency. The social chairs should meet and establish at least 1 social event per season, with 4 total for the academic year. There are only 2 rules with social events: (1) they must be held outside of clinic, and (2) everyone should try their best to attend.
Social chairs should try to prioritize a location-specific event that allows the residents who are not from the area to experience something local, which can be anything from apple picking at an orchard in the fall to beach volleyball in the summer. Planning these parties gives everyone an event to look forward to and a chance to spend time together and grow closer. The memories and inside jokes that arise from these outings are invaluable and increase joy inside and outside of clinic.
Utilize Social Media
Another project can be developing a social media account for your program with the approval of your faculty. @unmcdermatology, @uwderm, and @gwdermres can help foster social relationships by establishing a lighthearted space to celebrate the residency’s achievements, new publications, volunteer events, or social gatherings.
Encourage Local and National Conference Attendance
All residents should be encouraged to submit abstracts to local and national conferences and attend with their co-residents. Conferences are peak opportunities to foster camaraderie within residency classes, as they involve a sense of togetherness in the specialty along with the excitement of traveling to a new city and meeting other like-minded individuals. Conferences allow collaboration within the specialty on a national level and foster relationships between residency programs.
In addition, national groups such as the Women’s Dermatologic Society, the Skin of Color Society, and the American Academy of Dermatology Diversity, Equity, and Inclusion task force meet at the national conferences and discuss their next initiatives and projects. Joining a society of your interest can lead to many new networks and relationships you may not have had before. Even if you are not interested in specializing after general dermatology, consider attending a surgery, dermatopathology, or pediatric or cosmetic dermatology conference to learn more about the field from the experts.
Repair Conflicts and Build a Climate of Collaboration
Conflicts and disagreements unfortunately are inevitable during residency. Whether they involve planning vacation times or coordinating call schedules, everyone will not agree on every decision. Learning how to handle and approach conflict with co-residents is of utmost importance to maintaining the hard work you have put in to create trust, camaraderie, and a good social atmosphere. If you are having an issue with a circumstance involving a co-resident, holding a grudge will only sour your experience and the experience of others. Talking to your co-resident directly about your concerns before escalating the issue to a chief resident or faculty member is a great start. Consider asking them about their thought process and show concern for their point of view. Listen to them openly before going into your preferences. It is important to remember that working as a team requires sacrifices, and sometimes you will not be satisfied with the outcome of a conflict.
It also is important to remember that feelings change, and an issue you feel you must address immediately can wait to be addressed at a better time when you have calmed down. You may even find that you decide not to address it at all. At the end of the day, if a conflict cannot be worked out between those involved, consider confiding in a chief resident or a faculty mentor for advice on the next steps to take to resolve the problem. Ultimately, having a good foundation of respect and strong bonds with your residents will help tremendously when conflicts arise.
Final Thoughts
Fostering camaraderie in residency will improve the overall experience and lives of the residents, as well as the experience of the faculty, staff, and patients by the trickle-down effect. Creating a cheerful and fun atmosphere filled with inside jokes and excitement regarding upcoming social events or conferences will certainly result in a time you will cherish for the rest of your life.
- Kouzes JM, Posner BZ. Foster collaboration. In: Kouzes JM, Posner BZ, eds. The Leadership Challenge. 6th ed. John Wiley & Sons, Inc; 2017:195-217.
- Cooper J, Shao K, Feng H. Racial/ethnic health disparities in dermatology in the United States, part 1: overview of contributing factors and management strategies [published online February 7, 2022]. J Am Acad Dermatol. 2022;87:723-730. doi:10.1016/j.jaad.2021.12.061
- Kouzes JM, Posner BZ. Foster collaboration. In: Kouzes JM, Posner BZ, eds. The Leadership Challenge. 6th ed. John Wiley & Sons, Inc; 2017:195-217.
- Cooper J, Shao K, Feng H. Racial/ethnic health disparities in dermatology in the United States, part 1: overview of contributing factors and management strategies [published online February 7, 2022]. J Am Acad Dermatol. 2022;87:723-730. doi:10.1016/j.jaad.2021.12.061
Resident Pearls
- Camaraderie in residency is a special dynamic that can be enhanced and fostered in many different ways.
- The relationships among residents should be treated with importance, as some of the friends you make will last a career and/or a lifetime.
- Conflicts inevitably will arise and learning how to handle them effectively can improve the residency experience.
Should residents be taught how to prescribe monoamine oxidase inhibitors?
What else can I offer this patient?
This thought passed through my mind as the patient’s desperation grew palpable. He had experienced intractable major depressive disorder (MDD) for years and had exhausted multiple classes of antidepressants, trying various combinations without any relief.
The previous resident had arranged for intranasal ketamine treatment, but the patient was unable to receive it due to lack of transportation. As I combed through the list of the dozens of medications the patient previously had been prescribed, I noticed the absence of a certain class of agents: monoamine oxidase inhibitors (MAOIs).
My knowledge of MAOIs stemmed from medical school, where the dietary restrictions, potential for hypertensive crisis, and capricious drug-drug interactions were heavily emphasized while their value was minimized. I did not have any practical experience with these medications, and even the attending physician disclosed he had not prescribed an MAOI in more than 30 years. Nonetheless, both the attending physician and patient agreed that the patient would try one.
Following a washout period, the patient began tranylcypromine. After taking tranylcypromine 40 mg/d for 3 months, he reported he felt like a weight had been lifted off his chest. He felt less irritable and depressed, more energetic, and more hopeful for the future. He also felt that his symptoms were improving for the first time in many years.
An older but still potentially helpful class of medications
MDD is one of the leading causes of disability in the United States, affecting millions of people. Its economic burden is estimated to be more than $200 billion, with a large contingent consisting of direct medical cost and suicide-related costs.1 MDD is often recurrent—60% of patients experience another episode within 5 years.2 Most of these patients are classified as having treatment-resistant depression (TRD), which typically is defined as the failure to respond to 2 different medications given at adequate doses for a sufficient duration.3 The Sequenced Treatment Alternatives to Relieve Depression trial suggested that after each medication failure, depression becomes increasingly difficult to treat, with many patients developing TRD.4 For some patients with TRD, MAOIs may be a powerful and beneficial option.5,6 Studies have shown that MAOIs (at adequate doses) can be effective in approximately one-half of patients with TRD. Patients with anxious, endogenous, or atypical depression may also respond to MAOIs.7
MAOIs were among the earliest antidepressants on the market, starting in the late 1950s with isocarboxazid, phenelzine, tranylcypromine, and selegiline. The use of MAOIs as a treatment for depression was serendipitously discovered when iproniazid, a tuberculosis drug, was observed to have mood-elevating adverse effects that were explained by its monoamine oxidase (MAO) inhibitory properties.8 This sparked the hypothesis that a deficiency in serotonin, norepinephrine, and dopamine played a central role in depressive disorders. MAOs encompass a class of enzymes that metabolize catecholamines, which include the previously mentioned neurotransmitters and the trace amine tyramine. The MAO isoenzymes also inhabit many tissues, including the central and peripheral nervous system, liver, and intestines.
There are 2 subtypes of MAOs: MAO-A and MAO-B. MAO-A inhibits tyramine, serotonin, norepinephrine, and dopamine. MAO-B is mainly responsible for the degradation of dopamine, which makes MAO-B inhibitors (ie, rasagiline) useful in treating Parkinson disease.9
Continue to: For most psychiatrists...
For most psychiatrists, MAOIs have fallen out of favor due to their discomfort with their potential adverse effects and drug-drug interactions, the dietary restrictions patients must face, and the perception that newer medications have fewer adverse effects.10 Prescribing an MAOI requires the clinician to remain vigilant of any new medication the patient is taking that may potentiate intrasynaptic serotonin, which may include certain antibiotics or analgesics, causing serotonin syndrome. Close monitoring of the patient’s diet also is necessary so the patient avoids foods rich in tyramine that may trigger a hypertensive crisis. This is because excess tyramine can precipitate an increase in catecholamine release, causing a dangerous increase in blood pressure. However, many foods have safe levels of tyramine (<6 mg/serving), although the perception of tyramine levels in modern foods remains overestimated.5
Residents need to know how to use MAOIs
Psychiatrists should weigh the risks and benefits prior to prescribing any new medication, and MAOIs should be no exception. A patient’s enduring pain is often overshadowed by the potential for adverse effects, which occasionally is overemphasized. Other treatments for severe psychiatric illnesses (such as lithium and clozapine) are also declining due to these agents’ requirement for cumbersome monitoring and potential for adverse effects despite evidence of their superior efficacy and antisuicidal properties.11,12
Fortunately, there are many novel therapies available that can be effective for patients with TRD, including transcranial magnetic stimulation, ketamine, and vagal nerve stimulation. However, as psychiatrists, especially during training, our armamentarium should be equipped with all modalities of psychopharmacology. Training and teaching residents to prescribe MAOIs safely and effectively may add a glimmer of hope for an otherwise hopeless patient.
1. Greenberg PE, Fournier AA, Sisitsky T, et al. The economic burden of adults with major depressive disorder in the United States (2010 and 2018). Pharmacoeconomics. 2021;39(6):653-665.
2. Hardeveld F, Spijker J, De Graaf R, et al. Prevalence and predictors of recurrence of major depressive disorder in the adult population. Acta Psychiatr Scand. 2010;122(3):184-191.
3. Gaynes BN, Lux L, Gartlehner G, et al. Defining treatment-resistant depression. Depress Anxiety. 2020;37(2):134-145.
4. Trivedi MH, Rush AJ, Wisniewski SR, et al. Evaluation of outcomes with citalopram for depression using measurement-based care in STAR*D: implications for clinical practice. Am J Psychiatry. 2006;163(1):28-40.
5. Fiedorowicz JG, Swartz KL. The role of monoamine oxidase inhibitors in current psychiatric practice. J Psychiatr Pract. 2004;10(4):239-248.
6. Amsterdam JD, Shults J. MAOI efficacy and safety in advanced stage treatment-resistant depression--a retrospective study. J Affect Disord. 2005;89(1-3):183-188.
7. Amsterdam JD, Hornig-Rohan M. Treatment algorithms in treatment-resistant depression. Psychiatr Clin North Am. 1996;19(2):371-386.
8. Ramachandraih CT, Subramanyam N, Bar KJ, et al. Antidepressants: from MAOIs to SSRIs and more. Indian J Psychiatry. 2011;53(2):180-182.
9. Tipton KF. 90 years of monoamine oxidase: some progress and some confusion. J Neural Transm (Vienna). 2018;125(11):1519-1551.
10. Gillman PK, Feinberg SS, Fochtmann LJ. Revitalizing monoamine oxidase inhibitors: a call for action. CNS Spectr. 2020;25(4):452-454.
11. Kelly DL, Wehring HJ, Vyas G. Current status of clozapine in the United States. Shanghai Arch Psychiatry. 2012;24(2):110-113.
12. Tibrewal P, Ng T, Bastiampillai T, et al. Why is lithium use declining? Asian J Psychiatr. 2019;43:219-220.
What else can I offer this patient?
This thought passed through my mind as the patient’s desperation grew palpable. He had experienced intractable major depressive disorder (MDD) for years and had exhausted multiple classes of antidepressants, trying various combinations without any relief.
The previous resident had arranged for intranasal ketamine treatment, but the patient was unable to receive it due to lack of transportation. As I combed through the list of the dozens of medications the patient previously had been prescribed, I noticed the absence of a certain class of agents: monoamine oxidase inhibitors (MAOIs).
My knowledge of MAOIs stemmed from medical school, where the dietary restrictions, potential for hypertensive crisis, and capricious drug-drug interactions were heavily emphasized while their value was minimized. I did not have any practical experience with these medications, and even the attending physician disclosed he had not prescribed an MAOI in more than 30 years. Nonetheless, both the attending physician and patient agreed that the patient would try one.
Following a washout period, the patient began tranylcypromine. After taking tranylcypromine 40 mg/d for 3 months, he reported he felt like a weight had been lifted off his chest. He felt less irritable and depressed, more energetic, and more hopeful for the future. He also felt that his symptoms were improving for the first time in many years.
An older but still potentially helpful class of medications
MDD is one of the leading causes of disability in the United States, affecting millions of people. Its economic burden is estimated to be more than $200 billion, with a large contingent consisting of direct medical cost and suicide-related costs.1 MDD is often recurrent—60% of patients experience another episode within 5 years.2 Most of these patients are classified as having treatment-resistant depression (TRD), which typically is defined as the failure to respond to 2 different medications given at adequate doses for a sufficient duration.3 The Sequenced Treatment Alternatives to Relieve Depression trial suggested that after each medication failure, depression becomes increasingly difficult to treat, with many patients developing TRD.4 For some patients with TRD, MAOIs may be a powerful and beneficial option.5,6 Studies have shown that MAOIs (at adequate doses) can be effective in approximately one-half of patients with TRD. Patients with anxious, endogenous, or atypical depression may also respond to MAOIs.7
MAOIs were among the earliest antidepressants on the market, starting in the late 1950s with isocarboxazid, phenelzine, tranylcypromine, and selegiline. The use of MAOIs as a treatment for depression was serendipitously discovered when iproniazid, a tuberculosis drug, was observed to have mood-elevating adverse effects that were explained by its monoamine oxidase (MAO) inhibitory properties.8 This sparked the hypothesis that a deficiency in serotonin, norepinephrine, and dopamine played a central role in depressive disorders. MAOs encompass a class of enzymes that metabolize catecholamines, which include the previously mentioned neurotransmitters and the trace amine tyramine. The MAO isoenzymes also inhabit many tissues, including the central and peripheral nervous system, liver, and intestines.
There are 2 subtypes of MAOs: MAO-A and MAO-B. MAO-A inhibits tyramine, serotonin, norepinephrine, and dopamine. MAO-B is mainly responsible for the degradation of dopamine, which makes MAO-B inhibitors (ie, rasagiline) useful in treating Parkinson disease.9
Continue to: For most psychiatrists...
For most psychiatrists, MAOIs have fallen out of favor due to their discomfort with their potential adverse effects and drug-drug interactions, the dietary restrictions patients must face, and the perception that newer medications have fewer adverse effects.10 Prescribing an MAOI requires the clinician to remain vigilant of any new medication the patient is taking that may potentiate intrasynaptic serotonin, which may include certain antibiotics or analgesics, causing serotonin syndrome. Close monitoring of the patient’s diet also is necessary so the patient avoids foods rich in tyramine that may trigger a hypertensive crisis. This is because excess tyramine can precipitate an increase in catecholamine release, causing a dangerous increase in blood pressure. However, many foods have safe levels of tyramine (<6 mg/serving), although the perception of tyramine levels in modern foods remains overestimated.5
Residents need to know how to use MAOIs
Psychiatrists should weigh the risks and benefits prior to prescribing any new medication, and MAOIs should be no exception. A patient’s enduring pain is often overshadowed by the potential for adverse effects, which occasionally is overemphasized. Other treatments for severe psychiatric illnesses (such as lithium and clozapine) are also declining due to these agents’ requirement for cumbersome monitoring and potential for adverse effects despite evidence of their superior efficacy and antisuicidal properties.11,12
Fortunately, there are many novel therapies available that can be effective for patients with TRD, including transcranial magnetic stimulation, ketamine, and vagal nerve stimulation. However, as psychiatrists, especially during training, our armamentarium should be equipped with all modalities of psychopharmacology. Training and teaching residents to prescribe MAOIs safely and effectively may add a glimmer of hope for an otherwise hopeless patient.
What else can I offer this patient?
This thought passed through my mind as the patient’s desperation grew palpable. He had experienced intractable major depressive disorder (MDD) for years and had exhausted multiple classes of antidepressants, trying various combinations without any relief.
The previous resident had arranged for intranasal ketamine treatment, but the patient was unable to receive it due to lack of transportation. As I combed through the list of the dozens of medications the patient previously had been prescribed, I noticed the absence of a certain class of agents: monoamine oxidase inhibitors (MAOIs).
My knowledge of MAOIs stemmed from medical school, where the dietary restrictions, potential for hypertensive crisis, and capricious drug-drug interactions were heavily emphasized while their value was minimized. I did not have any practical experience with these medications, and even the attending physician disclosed he had not prescribed an MAOI in more than 30 years. Nonetheless, both the attending physician and patient agreed that the patient would try one.
Following a washout period, the patient began tranylcypromine. After taking tranylcypromine 40 mg/d for 3 months, he reported he felt like a weight had been lifted off his chest. He felt less irritable and depressed, more energetic, and more hopeful for the future. He also felt that his symptoms were improving for the first time in many years.
An older but still potentially helpful class of medications
MDD is one of the leading causes of disability in the United States, affecting millions of people. Its economic burden is estimated to be more than $200 billion, with a large contingent consisting of direct medical cost and suicide-related costs.1 MDD is often recurrent—60% of patients experience another episode within 5 years.2 Most of these patients are classified as having treatment-resistant depression (TRD), which typically is defined as the failure to respond to 2 different medications given at adequate doses for a sufficient duration.3 The Sequenced Treatment Alternatives to Relieve Depression trial suggested that after each medication failure, depression becomes increasingly difficult to treat, with many patients developing TRD.4 For some patients with TRD, MAOIs may be a powerful and beneficial option.5,6 Studies have shown that MAOIs (at adequate doses) can be effective in approximately one-half of patients with TRD. Patients with anxious, endogenous, or atypical depression may also respond to MAOIs.7
MAOIs were among the earliest antidepressants on the market, starting in the late 1950s with isocarboxazid, phenelzine, tranylcypromine, and selegiline. The use of MAOIs as a treatment for depression was serendipitously discovered when iproniazid, a tuberculosis drug, was observed to have mood-elevating adverse effects that were explained by its monoamine oxidase (MAO) inhibitory properties.8 This sparked the hypothesis that a deficiency in serotonin, norepinephrine, and dopamine played a central role in depressive disorders. MAOs encompass a class of enzymes that metabolize catecholamines, which include the previously mentioned neurotransmitters and the trace amine tyramine. The MAO isoenzymes also inhabit many tissues, including the central and peripheral nervous system, liver, and intestines.
There are 2 subtypes of MAOs: MAO-A and MAO-B. MAO-A inhibits tyramine, serotonin, norepinephrine, and dopamine. MAO-B is mainly responsible for the degradation of dopamine, which makes MAO-B inhibitors (ie, rasagiline) useful in treating Parkinson disease.9
Continue to: For most psychiatrists...
For most psychiatrists, MAOIs have fallen out of favor due to their discomfort with their potential adverse effects and drug-drug interactions, the dietary restrictions patients must face, and the perception that newer medications have fewer adverse effects.10 Prescribing an MAOI requires the clinician to remain vigilant of any new medication the patient is taking that may potentiate intrasynaptic serotonin, which may include certain antibiotics or analgesics, causing serotonin syndrome. Close monitoring of the patient’s diet also is necessary so the patient avoids foods rich in tyramine that may trigger a hypertensive crisis. This is because excess tyramine can precipitate an increase in catecholamine release, causing a dangerous increase in blood pressure. However, many foods have safe levels of tyramine (<6 mg/serving), although the perception of tyramine levels in modern foods remains overestimated.5
Residents need to know how to use MAOIs
Psychiatrists should weigh the risks and benefits prior to prescribing any new medication, and MAOIs should be no exception. A patient’s enduring pain is often overshadowed by the potential for adverse effects, which occasionally is overemphasized. Other treatments for severe psychiatric illnesses (such as lithium and clozapine) are also declining due to these agents’ requirement for cumbersome monitoring and potential for adverse effects despite evidence of their superior efficacy and antisuicidal properties.11,12
Fortunately, there are many novel therapies available that can be effective for patients with TRD, including transcranial magnetic stimulation, ketamine, and vagal nerve stimulation. However, as psychiatrists, especially during training, our armamentarium should be equipped with all modalities of psychopharmacology. Training and teaching residents to prescribe MAOIs safely and effectively may add a glimmer of hope for an otherwise hopeless patient.
1. Greenberg PE, Fournier AA, Sisitsky T, et al. The economic burden of adults with major depressive disorder in the United States (2010 and 2018). Pharmacoeconomics. 2021;39(6):653-665.
2. Hardeveld F, Spijker J, De Graaf R, et al. Prevalence and predictors of recurrence of major depressive disorder in the adult population. Acta Psychiatr Scand. 2010;122(3):184-191.
3. Gaynes BN, Lux L, Gartlehner G, et al. Defining treatment-resistant depression. Depress Anxiety. 2020;37(2):134-145.
4. Trivedi MH, Rush AJ, Wisniewski SR, et al. Evaluation of outcomes with citalopram for depression using measurement-based care in STAR*D: implications for clinical practice. Am J Psychiatry. 2006;163(1):28-40.
5. Fiedorowicz JG, Swartz KL. The role of monoamine oxidase inhibitors in current psychiatric practice. J Psychiatr Pract. 2004;10(4):239-248.
6. Amsterdam JD, Shults J. MAOI efficacy and safety in advanced stage treatment-resistant depression--a retrospective study. J Affect Disord. 2005;89(1-3):183-188.
7. Amsterdam JD, Hornig-Rohan M. Treatment algorithms in treatment-resistant depression. Psychiatr Clin North Am. 1996;19(2):371-386.
8. Ramachandraih CT, Subramanyam N, Bar KJ, et al. Antidepressants: from MAOIs to SSRIs and more. Indian J Psychiatry. 2011;53(2):180-182.
9. Tipton KF. 90 years of monoamine oxidase: some progress and some confusion. J Neural Transm (Vienna). 2018;125(11):1519-1551.
10. Gillman PK, Feinberg SS, Fochtmann LJ. Revitalizing monoamine oxidase inhibitors: a call for action. CNS Spectr. 2020;25(4):452-454.
11. Kelly DL, Wehring HJ, Vyas G. Current status of clozapine in the United States. Shanghai Arch Psychiatry. 2012;24(2):110-113.
12. Tibrewal P, Ng T, Bastiampillai T, et al. Why is lithium use declining? Asian J Psychiatr. 2019;43:219-220.
1. Greenberg PE, Fournier AA, Sisitsky T, et al. The economic burden of adults with major depressive disorder in the United States (2010 and 2018). Pharmacoeconomics. 2021;39(6):653-665.
2. Hardeveld F, Spijker J, De Graaf R, et al. Prevalence and predictors of recurrence of major depressive disorder in the adult population. Acta Psychiatr Scand. 2010;122(3):184-191.
3. Gaynes BN, Lux L, Gartlehner G, et al. Defining treatment-resistant depression. Depress Anxiety. 2020;37(2):134-145.
4. Trivedi MH, Rush AJ, Wisniewski SR, et al. Evaluation of outcomes with citalopram for depression using measurement-based care in STAR*D: implications for clinical practice. Am J Psychiatry. 2006;163(1):28-40.
5. Fiedorowicz JG, Swartz KL. The role of monoamine oxidase inhibitors in current psychiatric practice. J Psychiatr Pract. 2004;10(4):239-248.
6. Amsterdam JD, Shults J. MAOI efficacy and safety in advanced stage treatment-resistant depression--a retrospective study. J Affect Disord. 2005;89(1-3):183-188.
7. Amsterdam JD, Hornig-Rohan M. Treatment algorithms in treatment-resistant depression. Psychiatr Clin North Am. 1996;19(2):371-386.
8. Ramachandraih CT, Subramanyam N, Bar KJ, et al. Antidepressants: from MAOIs to SSRIs and more. Indian J Psychiatry. 2011;53(2):180-182.
9. Tipton KF. 90 years of monoamine oxidase: some progress and some confusion. J Neural Transm (Vienna). 2018;125(11):1519-1551.
10. Gillman PK, Feinberg SS, Fochtmann LJ. Revitalizing monoamine oxidase inhibitors: a call for action. CNS Spectr. 2020;25(4):452-454.
11. Kelly DL, Wehring HJ, Vyas G. Current status of clozapine in the United States. Shanghai Arch Psychiatry. 2012;24(2):110-113.
12. Tibrewal P, Ng T, Bastiampillai T, et al. Why is lithium use declining? Asian J Psychiatr. 2019;43:219-220.
Disaster Preparedness in Dermatology Residency Programs
In an age of changing climate and emerging global pandemics, the ability of residency programs to prepare for and adapt to potential disasters may be paramount in preserving the training of physicians. The current literature regarding residency program disaster preparedness, which focuses predominantly on hurricanes and COVID-19,1-8 is lacking in recommendations specific to dermatology residency programs. Likewise, the Accreditation Council for Graduate Medical Education (ACGME) guidelines9 do not address dermatology-specific concerns in disaster preparedness or response. Herein, we propose recommendations to mitigate the impact of various types of disasters on dermatology residency programs and their trainees with regard to resident safety and wellness, resident education, and patient care (Table).

Resident Safety and Wellness
Role of the Program Director—The role of the program director is critical, serving as a figure of structure and reassurance.4,7,10 Once concern of disaster arises, the program director should contact the Designated Institutional Official (DIO) to express concerns about possible disruptions to resident training. The DIO should then contact the ACGME within 10 days to report the disaster and submit a request for emergency (eg, pandemic) or extraordinary circumstances (eg, natural disaster) categorization.4,9 Program directors should promptly prepare plans for program reconfiguration and resident transfers in alignment with ACGME requirements to maintain evaluation and completion of core competencies of training during disasters.9 Program directors should prioritize the safety of trainees during the immediate threat with clear guidelines on sheltering, evacuations, or quarantines; a timeline of program recovery based on communication with residents, faculty, and administration should then be established.10,11
Communication—Establishing a strong line of communication between program directors and residents is paramount. Collection of emergency noninstitutional contact information, establishment of a centralized website for information dissemination, use of noninstitutional email and proxy servers outside of the location of impact, social media updates, on-site use of 2-way radios, and program-wide conference calls when possible should be strongly considered as part of the disaster response.2-4,12,13
Resident Accommodations and Mental Health—If training is disrupted, residents should be reassured of continued access to salary, housing, food, or other resources as necessary.3,4,11 There should be clear contingency plans if residents need to leave the program for extended periods of time due to injury, illness, or personal circumstances. Although relevant in all types of disasters, resident mental health and response to trauma also must be addressed. Access to counseling, morale-building opportunities (eg, resident social events), and screening for depression or posttraumatic stress disorder may help promote well-being among residents following traumatic events.14
Resident Education
Participation in Disaster Relief—Residents may seek to aid in the disaster response, which may prove challenging in the setting of programs with high patient volume.4 In coordination with the ACGME and graduate medical education governing bodies, program directors should consider how residents may fulfill dermatology training requirements in conjunction with disaster relief efforts, such as working in an inpatient setting or providing wound care.10
Continued Didactic Education—The use of online learning and conference calls for continuing the dermatology curriculum is an efficient means to maintaining resident education when meeting in person poses risks to residents.15 Projections of microscopy images, clinical photographs, or other instructional materials allow for continued instruction on resident examination, histopathology, and diagnostic skills.
Continued Clinical Training—If the home institution cannot support the operation of dermatology clinics, residents should be guaranteed continued training at other institutions. Agreements with other dermatology programs, community hospitals, or private dermatology practices should be established in advance, with consideration given to the number of residents a program can support, funding transfers, and credentialing requirements.2,4,5
Prolonged Disruptions—Nonessential departments of medical institutions may cease to function during war or mass casualty disasters, and it may be unsafe to send dermatology residents to other institutions or clinical areas. If the threat is prolonged, programs may need to consider allowing current residents a longer duration of training despite potential overlap with incoming dermatology residents.7
Patient Care
Disruptions to Clinic Operations—Regarding threats of violence, dangerous exposures, or natural disasters, there should be clear guidelines on sheltering in the clinical setting or stabilizing patients during a procedure.11 Equipment used by residents such as laptops, microscopes, and treatment devices (eg, lasers) should be stored in weather-safe locations that would not be notably impacted by moisture or structural damage to the clinic building. If electricity or internet access are compromised, paper medical records should be available to residents to continue clinical operations. Electronic health records used by residents should regularly be backed up on remote servers or cloud storage to allow continued access to patient health information if on-site servers are not functional.12 If disruptions are prolonged, residency program administration should coordinate with the institution to ensure there is adequate supply and storage of medications (eg, lidocaine, botulinum toxin) as well as a continued means of delivering biologic medications to patients and an ability to obtain laboratory or dermatopathology services.
In-Person Appointments vs Telemedicine—There are benefits to both residency training and patient care when physicians are able to perform in-person examinations, biopsies, and in-office treatments.16 Programs should ensure an adequate supply of personal protective equipment to continue in-office appointments, vaccinations, and medical care if a resident or other members of the team are exposed to an infectious disease.7 If in-person appointments are limited or impossible, telemedicine capabilities may still allow residents to meet program requirements.7,10,15 However, reduced patient volume due to decreased elective visits or procedures may complicate the fulfillment of clinical requirements, which may need to be adjusted in the wake of a disaster.7
Use of Immunosuppressive Therapies—Residency programs should address the risks of prescribing immunosuppressive therapies (eg, biologics) during an infectious threat with their residents and encourage trainees to counsel patients on the importance of preventative measures to reduce risks for severe infection.17
Final Thoughts
- Davis W. Hurricane Katrina: the challenge to graduate medical education. Ochsner J. 2006;6:39.
- Cefalu CA, Schwartz RS. Salvaging a geriatric medicine academic program in disaster mode—the LSU training program post-Katrina.J Natl Med Assoc. 2007;99:590-596.
- Ayyala R. Lessons from Katrina: a program director’s perspective. Ophthalmology. 2007;114:1425-1426.
- Wiese JG. Leadership in graduate medical education: eleven steps instrumental in recovering residency programs after a disaster. Am J Med Sci. 2008;336:168-173.
- Griffies WS. Post-Katrina stabilization of the LSU/Ochsner Psychiatry Residency Program: caveats for disaster preparedness. Acad Psychiatry. 2009;33:418-422.
- Kearns DG, Chat VS, Uppal S, et al. Applying to dermatology residency during the COVID-19 pandemic. J Am Acad Dermatol. 2020;83:1214-1215.
- Matthews JB, Blair PG, Ellison EC, et al. Checklist framework for surgical education disaster plans. J Am Coll Surg. 2021;233:557-563.
- Litchman GH, Marson JW, Rigel DS. The continuing impact of COVID-19 on dermatology practice: office workflow, economics, and future implications. J Am Acad Dermatol. 2021;84:576-579.
- Accreditation Council for Graduate Medical Education. Sponsoring institution emergency categorization. Accessed October 20, 2022. https://www.acgme.org/covid-19/sponsoring-institution-emergency-categorization/
- Li YM, Galimberti F, Abrouk M, et al. US dermatology resident responses about the COVID-19 pandemic: results from a nationwide survey. South Med J. 2020;113:462-465.
- Newman B, Gallion C. Hurricane Harvey: firsthand perspectives for disaster preparedness in graduate medical education. Acad Med. 2019;94:1267-1269.
- Pero CD, Pou AM, Arriaga MA, et al. Post-Katrina: study in crisis-related program adaptability. Otolaryngol Head Neck Surg. 2008;138:394-397.
- Hattaway R, Singh N, Rais-Bahrami S, et al. Adaptations of dermatology residency programs to changes in medical education amid the COVID-19 pandemic: virtual opportunities and social media. SKIN. 2021;5:94-100.
- Hillier K, Paskaradevan J, Wilkes JK, et al. Disaster plans: resident involvement and well-being during Hurricane Harvey. J Grad Med Educ. 2019;11:129-131.
- Samimi S, Choi J, Rosman IS, et al. Impact of COVID-19 on dermatology residency. Dermatol Clin. 2021;39:609-618.
- Bastola M, Locatis C, Fontelo P. Diagnostic reliability of in-person versus remote dermatology: a meta-analysis. Telemed J E Health. 2021;27:247-250.
- Bashyam AM, Feldman SR. Should patients stop their biologic treatment during the COVID-19 pandemic? J Dermatolog Treat. 2020;31:317-318.
In an age of changing climate and emerging global pandemics, the ability of residency programs to prepare for and adapt to potential disasters may be paramount in preserving the training of physicians. The current literature regarding residency program disaster preparedness, which focuses predominantly on hurricanes and COVID-19,1-8 is lacking in recommendations specific to dermatology residency programs. Likewise, the Accreditation Council for Graduate Medical Education (ACGME) guidelines9 do not address dermatology-specific concerns in disaster preparedness or response. Herein, we propose recommendations to mitigate the impact of various types of disasters on dermatology residency programs and their trainees with regard to resident safety and wellness, resident education, and patient care (Table).

Resident Safety and Wellness
Role of the Program Director—The role of the program director is critical, serving as a figure of structure and reassurance.4,7,10 Once concern of disaster arises, the program director should contact the Designated Institutional Official (DIO) to express concerns about possible disruptions to resident training. The DIO should then contact the ACGME within 10 days to report the disaster and submit a request for emergency (eg, pandemic) or extraordinary circumstances (eg, natural disaster) categorization.4,9 Program directors should promptly prepare plans for program reconfiguration and resident transfers in alignment with ACGME requirements to maintain evaluation and completion of core competencies of training during disasters.9 Program directors should prioritize the safety of trainees during the immediate threat with clear guidelines on sheltering, evacuations, or quarantines; a timeline of program recovery based on communication with residents, faculty, and administration should then be established.10,11
Communication—Establishing a strong line of communication between program directors and residents is paramount. Collection of emergency noninstitutional contact information, establishment of a centralized website for information dissemination, use of noninstitutional email and proxy servers outside of the location of impact, social media updates, on-site use of 2-way radios, and program-wide conference calls when possible should be strongly considered as part of the disaster response.2-4,12,13
Resident Accommodations and Mental Health—If training is disrupted, residents should be reassured of continued access to salary, housing, food, or other resources as necessary.3,4,11 There should be clear contingency plans if residents need to leave the program for extended periods of time due to injury, illness, or personal circumstances. Although relevant in all types of disasters, resident mental health and response to trauma also must be addressed. Access to counseling, morale-building opportunities (eg, resident social events), and screening for depression or posttraumatic stress disorder may help promote well-being among residents following traumatic events.14
Resident Education
Participation in Disaster Relief—Residents may seek to aid in the disaster response, which may prove challenging in the setting of programs with high patient volume.4 In coordination with the ACGME and graduate medical education governing bodies, program directors should consider how residents may fulfill dermatology training requirements in conjunction with disaster relief efforts, such as working in an inpatient setting or providing wound care.10
Continued Didactic Education—The use of online learning and conference calls for continuing the dermatology curriculum is an efficient means to maintaining resident education when meeting in person poses risks to residents.15 Projections of microscopy images, clinical photographs, or other instructional materials allow for continued instruction on resident examination, histopathology, and diagnostic skills.
Continued Clinical Training—If the home institution cannot support the operation of dermatology clinics, residents should be guaranteed continued training at other institutions. Agreements with other dermatology programs, community hospitals, or private dermatology practices should be established in advance, with consideration given to the number of residents a program can support, funding transfers, and credentialing requirements.2,4,5
Prolonged Disruptions—Nonessential departments of medical institutions may cease to function during war or mass casualty disasters, and it may be unsafe to send dermatology residents to other institutions or clinical areas. If the threat is prolonged, programs may need to consider allowing current residents a longer duration of training despite potential overlap with incoming dermatology residents.7
Patient Care
Disruptions to Clinic Operations—Regarding threats of violence, dangerous exposures, or natural disasters, there should be clear guidelines on sheltering in the clinical setting or stabilizing patients during a procedure.11 Equipment used by residents such as laptops, microscopes, and treatment devices (eg, lasers) should be stored in weather-safe locations that would not be notably impacted by moisture or structural damage to the clinic building. If electricity or internet access are compromised, paper medical records should be available to residents to continue clinical operations. Electronic health records used by residents should regularly be backed up on remote servers or cloud storage to allow continued access to patient health information if on-site servers are not functional.12 If disruptions are prolonged, residency program administration should coordinate with the institution to ensure there is adequate supply and storage of medications (eg, lidocaine, botulinum toxin) as well as a continued means of delivering biologic medications to patients and an ability to obtain laboratory or dermatopathology services.
In-Person Appointments vs Telemedicine—There are benefits to both residency training and patient care when physicians are able to perform in-person examinations, biopsies, and in-office treatments.16 Programs should ensure an adequate supply of personal protective equipment to continue in-office appointments, vaccinations, and medical care if a resident or other members of the team are exposed to an infectious disease.7 If in-person appointments are limited or impossible, telemedicine capabilities may still allow residents to meet program requirements.7,10,15 However, reduced patient volume due to decreased elective visits or procedures may complicate the fulfillment of clinical requirements, which may need to be adjusted in the wake of a disaster.7
Use of Immunosuppressive Therapies—Residency programs should address the risks of prescribing immunosuppressive therapies (eg, biologics) during an infectious threat with their residents and encourage trainees to counsel patients on the importance of preventative measures to reduce risks for severe infection.17
Final Thoughts
In an age of changing climate and emerging global pandemics, the ability of residency programs to prepare for and adapt to potential disasters may be paramount in preserving the training of physicians. The current literature regarding residency program disaster preparedness, which focuses predominantly on hurricanes and COVID-19,1-8 is lacking in recommendations specific to dermatology residency programs. Likewise, the Accreditation Council for Graduate Medical Education (ACGME) guidelines9 do not address dermatology-specific concerns in disaster preparedness or response. Herein, we propose recommendations to mitigate the impact of various types of disasters on dermatology residency programs and their trainees with regard to resident safety and wellness, resident education, and patient care (Table).

Resident Safety and Wellness
Role of the Program Director—The role of the program director is critical, serving as a figure of structure and reassurance.4,7,10 Once concern of disaster arises, the program director should contact the Designated Institutional Official (DIO) to express concerns about possible disruptions to resident training. The DIO should then contact the ACGME within 10 days to report the disaster and submit a request for emergency (eg, pandemic) or extraordinary circumstances (eg, natural disaster) categorization.4,9 Program directors should promptly prepare plans for program reconfiguration and resident transfers in alignment with ACGME requirements to maintain evaluation and completion of core competencies of training during disasters.9 Program directors should prioritize the safety of trainees during the immediate threat with clear guidelines on sheltering, evacuations, or quarantines; a timeline of program recovery based on communication with residents, faculty, and administration should then be established.10,11
Communication—Establishing a strong line of communication between program directors and residents is paramount. Collection of emergency noninstitutional contact information, establishment of a centralized website for information dissemination, use of noninstitutional email and proxy servers outside of the location of impact, social media updates, on-site use of 2-way radios, and program-wide conference calls when possible should be strongly considered as part of the disaster response.2-4,12,13
Resident Accommodations and Mental Health—If training is disrupted, residents should be reassured of continued access to salary, housing, food, or other resources as necessary.3,4,11 There should be clear contingency plans if residents need to leave the program for extended periods of time due to injury, illness, or personal circumstances. Although relevant in all types of disasters, resident mental health and response to trauma also must be addressed. Access to counseling, morale-building opportunities (eg, resident social events), and screening for depression or posttraumatic stress disorder may help promote well-being among residents following traumatic events.14
Resident Education
Participation in Disaster Relief—Residents may seek to aid in the disaster response, which may prove challenging in the setting of programs with high patient volume.4 In coordination with the ACGME and graduate medical education governing bodies, program directors should consider how residents may fulfill dermatology training requirements in conjunction with disaster relief efforts, such as working in an inpatient setting or providing wound care.10
Continued Didactic Education—The use of online learning and conference calls for continuing the dermatology curriculum is an efficient means to maintaining resident education when meeting in person poses risks to residents.15 Projections of microscopy images, clinical photographs, or other instructional materials allow for continued instruction on resident examination, histopathology, and diagnostic skills.
Continued Clinical Training—If the home institution cannot support the operation of dermatology clinics, residents should be guaranteed continued training at other institutions. Agreements with other dermatology programs, community hospitals, or private dermatology practices should be established in advance, with consideration given to the number of residents a program can support, funding transfers, and credentialing requirements.2,4,5
Prolonged Disruptions—Nonessential departments of medical institutions may cease to function during war or mass casualty disasters, and it may be unsafe to send dermatology residents to other institutions or clinical areas. If the threat is prolonged, programs may need to consider allowing current residents a longer duration of training despite potential overlap with incoming dermatology residents.7
Patient Care
Disruptions to Clinic Operations—Regarding threats of violence, dangerous exposures, or natural disasters, there should be clear guidelines on sheltering in the clinical setting or stabilizing patients during a procedure.11 Equipment used by residents such as laptops, microscopes, and treatment devices (eg, lasers) should be stored in weather-safe locations that would not be notably impacted by moisture or structural damage to the clinic building. If electricity or internet access are compromised, paper medical records should be available to residents to continue clinical operations. Electronic health records used by residents should regularly be backed up on remote servers or cloud storage to allow continued access to patient health information if on-site servers are not functional.12 If disruptions are prolonged, residency program administration should coordinate with the institution to ensure there is adequate supply and storage of medications (eg, lidocaine, botulinum toxin) as well as a continued means of delivering biologic medications to patients and an ability to obtain laboratory or dermatopathology services.
In-Person Appointments vs Telemedicine—There are benefits to both residency training and patient care when physicians are able to perform in-person examinations, biopsies, and in-office treatments.16 Programs should ensure an adequate supply of personal protective equipment to continue in-office appointments, vaccinations, and medical care if a resident or other members of the team are exposed to an infectious disease.7 If in-person appointments are limited or impossible, telemedicine capabilities may still allow residents to meet program requirements.7,10,15 However, reduced patient volume due to decreased elective visits or procedures may complicate the fulfillment of clinical requirements, which may need to be adjusted in the wake of a disaster.7
Use of Immunosuppressive Therapies—Residency programs should address the risks of prescribing immunosuppressive therapies (eg, biologics) during an infectious threat with their residents and encourage trainees to counsel patients on the importance of preventative measures to reduce risks for severe infection.17
Final Thoughts
- Davis W. Hurricane Katrina: the challenge to graduate medical education. Ochsner J. 2006;6:39.
- Cefalu CA, Schwartz RS. Salvaging a geriatric medicine academic program in disaster mode—the LSU training program post-Katrina.J Natl Med Assoc. 2007;99:590-596.
- Ayyala R. Lessons from Katrina: a program director’s perspective. Ophthalmology. 2007;114:1425-1426.
- Wiese JG. Leadership in graduate medical education: eleven steps instrumental in recovering residency programs after a disaster. Am J Med Sci. 2008;336:168-173.
- Griffies WS. Post-Katrina stabilization of the LSU/Ochsner Psychiatry Residency Program: caveats for disaster preparedness. Acad Psychiatry. 2009;33:418-422.
- Kearns DG, Chat VS, Uppal S, et al. Applying to dermatology residency during the COVID-19 pandemic. J Am Acad Dermatol. 2020;83:1214-1215.
- Matthews JB, Blair PG, Ellison EC, et al. Checklist framework for surgical education disaster plans. J Am Coll Surg. 2021;233:557-563.
- Litchman GH, Marson JW, Rigel DS. The continuing impact of COVID-19 on dermatology practice: office workflow, economics, and future implications. J Am Acad Dermatol. 2021;84:576-579.
- Accreditation Council for Graduate Medical Education. Sponsoring institution emergency categorization. Accessed October 20, 2022. https://www.acgme.org/covid-19/sponsoring-institution-emergency-categorization/
- Li YM, Galimberti F, Abrouk M, et al. US dermatology resident responses about the COVID-19 pandemic: results from a nationwide survey. South Med J. 2020;113:462-465.
- Newman B, Gallion C. Hurricane Harvey: firsthand perspectives for disaster preparedness in graduate medical education. Acad Med. 2019;94:1267-1269.
- Pero CD, Pou AM, Arriaga MA, et al. Post-Katrina: study in crisis-related program adaptability. Otolaryngol Head Neck Surg. 2008;138:394-397.
- Hattaway R, Singh N, Rais-Bahrami S, et al. Adaptations of dermatology residency programs to changes in medical education amid the COVID-19 pandemic: virtual opportunities and social media. SKIN. 2021;5:94-100.
- Hillier K, Paskaradevan J, Wilkes JK, et al. Disaster plans: resident involvement and well-being during Hurricane Harvey. J Grad Med Educ. 2019;11:129-131.
- Samimi S, Choi J, Rosman IS, et al. Impact of COVID-19 on dermatology residency. Dermatol Clin. 2021;39:609-618.
- Bastola M, Locatis C, Fontelo P. Diagnostic reliability of in-person versus remote dermatology: a meta-analysis. Telemed J E Health. 2021;27:247-250.
- Bashyam AM, Feldman SR. Should patients stop their biologic treatment during the COVID-19 pandemic? J Dermatolog Treat. 2020;31:317-318.
- Davis W. Hurricane Katrina: the challenge to graduate medical education. Ochsner J. 2006;6:39.
- Cefalu CA, Schwartz RS. Salvaging a geriatric medicine academic program in disaster mode—the LSU training program post-Katrina.J Natl Med Assoc. 2007;99:590-596.
- Ayyala R. Lessons from Katrina: a program director’s perspective. Ophthalmology. 2007;114:1425-1426.
- Wiese JG. Leadership in graduate medical education: eleven steps instrumental in recovering residency programs after a disaster. Am J Med Sci. 2008;336:168-173.
- Griffies WS. Post-Katrina stabilization of the LSU/Ochsner Psychiatry Residency Program: caveats for disaster preparedness. Acad Psychiatry. 2009;33:418-422.
- Kearns DG, Chat VS, Uppal S, et al. Applying to dermatology residency during the COVID-19 pandemic. J Am Acad Dermatol. 2020;83:1214-1215.
- Matthews JB, Blair PG, Ellison EC, et al. Checklist framework for surgical education disaster plans. J Am Coll Surg. 2021;233:557-563.
- Litchman GH, Marson JW, Rigel DS. The continuing impact of COVID-19 on dermatology practice: office workflow, economics, and future implications. J Am Acad Dermatol. 2021;84:576-579.
- Accreditation Council for Graduate Medical Education. Sponsoring institution emergency categorization. Accessed October 20, 2022. https://www.acgme.org/covid-19/sponsoring-institution-emergency-categorization/
- Li YM, Galimberti F, Abrouk M, et al. US dermatology resident responses about the COVID-19 pandemic: results from a nationwide survey. South Med J. 2020;113:462-465.
- Newman B, Gallion C. Hurricane Harvey: firsthand perspectives for disaster preparedness in graduate medical education. Acad Med. 2019;94:1267-1269.
- Pero CD, Pou AM, Arriaga MA, et al. Post-Katrina: study in crisis-related program adaptability. Otolaryngol Head Neck Surg. 2008;138:394-397.
- Hattaway R, Singh N, Rais-Bahrami S, et al. Adaptations of dermatology residency programs to changes in medical education amid the COVID-19 pandemic: virtual opportunities and social media. SKIN. 2021;5:94-100.
- Hillier K, Paskaradevan J, Wilkes JK, et al. Disaster plans: resident involvement and well-being during Hurricane Harvey. J Grad Med Educ. 2019;11:129-131.
- Samimi S, Choi J, Rosman IS, et al. Impact of COVID-19 on dermatology residency. Dermatol Clin. 2021;39:609-618.
- Bastola M, Locatis C, Fontelo P. Diagnostic reliability of in-person versus remote dermatology: a meta-analysis. Telemed J E Health. 2021;27:247-250.
- Bashyam AM, Feldman SR. Should patients stop their biologic treatment during the COVID-19 pandemic? J Dermatolog Treat. 2020;31:317-318.
Practice Points
- Dermatology residency programs should prioritize the development of disaster preparedness plans prior to the onset of disasters.
- Comprehensive disaster preparedness addresses many possible disruptions to dermatology resident training and clinic operations, including natural and manmade disasters and threats of widespread infectious disease.
- Safety being paramount, dermatology residency programs may be tasked with maintaining resident wellness, continuing resident education—potentially in unconventional ways—and adapting clinical operations to continue patient care.
The light at the end of the tunnel: Reflecting on a 7-year training journey
Throughout my training, a common refrain from more senior colleagues was that training “goes by quickly.” At the risk of sounding cliché, and even after a 7-year journey spanning psychiatry and preventive medicine residencies as well as a consultation-liaison psychiatry fellowship, I agree without reservations that it does indeed go quickly. In the waning days of my training, reflection and nostalgia have become commonplace, as one might expect after such a meaningful pursuit. In sharing my reflections, I hope others progressing through training will also reflect on elements that added meaning to their experience and how they might improve the journey for future trainees.
Residency is a team sport
One realization that quickly struck me was that residency is a team sport, and finding supportive communities is essential to survival. Other residents, colleagues, and mentors played integral roles in making my experience rewarding. Training might be considered a shared traumatic experience, but having peers to commiserate with at each step has been among its greatest rewards. Residency automatically provided a cohort of colleagues who shared and validated my experiences. Additionally, having mentors who have been through it themselves and find ways to improve the training experience made mine superlative. Mentors assisted me in tailoring my training and developing interests that I could integrate into my future practice. The interpersonal connections I made were critical in helping me survive and thrive during training.
See one, do one, teach one
Residency and fellowship programs might be considered “see one, do one, teach one”1 at large scale. Since their inception, these programs—designed to develop junior physicians—have been inherently educational in nature. The structure is elegant, allowing trainees to continue learning while incrementally gaining more autonomy and teaching responsibility.2 Naively, I did not understand that implicit within my education was an expectation to become an educator and hone my teaching skills. Initially, being a newly minted resident receiving brand-new 3rd-year medical students charged me with apprehension. Thoughts I internalized, such as “these students probably know more than me” or “how can I be responsible for patients and students simultaneously,” may have resulted from a paucity of instruction about teaching available during medical school.3,4 I quickly found, though, that teaching was among the most rewarding facets of training. Helping other learners grow became one of my passions and added to my experience.
Iron sharpens iron
Although my experience was enjoyable, I would be remiss without also considering accompanying trials and tribulations. Seemingly interminable night shifts, sleep deprivation, lack of autonomy, and system inefficiencies frustrated me. Eventually, these frustrations seemed less bothersome. These challenges likely had not vanished with time, but perhaps my capacity to tolerate distress improved—likely corresponding with increasing skill and confidence. These challenges allowed me to hone my clinical decision-making abilities while under duress. My struggles and frustrations were not unique but perhaps lessons themselves.
Residency is not meant to be easy. The crucible of residency taught me that I had resilience to draw upon during challenging times. “Iron sharpens iron,” as the adage goes, and I believe adversity ultimately helped me become a better psychiatrist.
Self-reflection is part of completing training
Reminders that my journey is at an end are everywhere. Seeing notes written by past residents or fellows reminds me that soon I too will merely be a name in the chart to future trainees. Perhaps this line of thought is unfair, reducing my training experience to notes I signed—whereas my training experience was defined by connections made with colleagues and mentors, opportunities to teach junior learners, and confidence gained by overcoming adversity.
While becoming an attending psychiatrist fills me with trepidation, fear need not be an inherent aspect of new beginnings. Reflection has been a powerful practice, allowing me to realize what made my experience so meaningful, and that training is meant to be process-oriented rather than outcome-oriented. My reflection has underscored the realization that challenges are inherent in training, although not without purpose. I believe these struggles were meant to allow me to build meaningful relationships with colleagues, discover joy in teaching, and build resiliency.
The purpose of residencies and fellowships should be to produce clinically excellent psychiatrists, but I feel the journey was as important as the destination. Psychiatrists likely understand this better than most, as we were trained to thoughtfully approach the process of termination with patients.5 While the conclusion of our training journeys may seem unceremonious or anticlimactic, the termination process should include self-reflection on meaningful facets of training. For me, this reflection has itself been invaluable, while also making me hopeful to contribute value to the training journeys of future psychiatrists.
1. Gorrindo T, Beresin EV. Is “See one, do one, teach one” dead? Implications for the professionalization of medical educators in the twenty-first century. Acad Psychiatry. 2015;39(6):613-614. doi:10.1007/s40596-015-0424-8
2. Wright Jr. JR, Schachar NS. Necessity is the mother of invention: William Stewart Halsted’s addiction and its influence on the development of residency training in North America. Can J Surg. 2020;63(1):E13-E19. doi:10.1503/cjs.003319
3. Dandavino M, Snell L, Wiseman J. Why medical students should learn how to teach. Med Teach. 2007;29(6):558-565. doi:10.1080/01421590701477449
4. Liu AC, Liu M, Dannaway J, et al. Are Australian medical students being taught to teach? Clin Teach. 2017;14(5):330-335. doi:10.1111/tct.12591
5. Vasquez MJ, Bingham RP, Barnett JE. Psychotherapy termination: clinical and ethical responsibilities. J Clin Psychol. 2008;64(5):653-665. doi:10.1002/jclp.20478
Throughout my training, a common refrain from more senior colleagues was that training “goes by quickly.” At the risk of sounding cliché, and even after a 7-year journey spanning psychiatry and preventive medicine residencies as well as a consultation-liaison psychiatry fellowship, I agree without reservations that it does indeed go quickly. In the waning days of my training, reflection and nostalgia have become commonplace, as one might expect after such a meaningful pursuit. In sharing my reflections, I hope others progressing through training will also reflect on elements that added meaning to their experience and how they might improve the journey for future trainees.
Residency is a team sport
One realization that quickly struck me was that residency is a team sport, and finding supportive communities is essential to survival. Other residents, colleagues, and mentors played integral roles in making my experience rewarding. Training might be considered a shared traumatic experience, but having peers to commiserate with at each step has been among its greatest rewards. Residency automatically provided a cohort of colleagues who shared and validated my experiences. Additionally, having mentors who have been through it themselves and find ways to improve the training experience made mine superlative. Mentors assisted me in tailoring my training and developing interests that I could integrate into my future practice. The interpersonal connections I made were critical in helping me survive and thrive during training.
See one, do one, teach one
Residency and fellowship programs might be considered “see one, do one, teach one”1 at large scale. Since their inception, these programs—designed to develop junior physicians—have been inherently educational in nature. The structure is elegant, allowing trainees to continue learning while incrementally gaining more autonomy and teaching responsibility.2 Naively, I did not understand that implicit within my education was an expectation to become an educator and hone my teaching skills. Initially, being a newly minted resident receiving brand-new 3rd-year medical students charged me with apprehension. Thoughts I internalized, such as “these students probably know more than me” or “how can I be responsible for patients and students simultaneously,” may have resulted from a paucity of instruction about teaching available during medical school.3,4 I quickly found, though, that teaching was among the most rewarding facets of training. Helping other learners grow became one of my passions and added to my experience.
Iron sharpens iron
Although my experience was enjoyable, I would be remiss without also considering accompanying trials and tribulations. Seemingly interminable night shifts, sleep deprivation, lack of autonomy, and system inefficiencies frustrated me. Eventually, these frustrations seemed less bothersome. These challenges likely had not vanished with time, but perhaps my capacity to tolerate distress improved—likely corresponding with increasing skill and confidence. These challenges allowed me to hone my clinical decision-making abilities while under duress. My struggles and frustrations were not unique but perhaps lessons themselves.
Residency is not meant to be easy. The crucible of residency taught me that I had resilience to draw upon during challenging times. “Iron sharpens iron,” as the adage goes, and I believe adversity ultimately helped me become a better psychiatrist.
Self-reflection is part of completing training
Reminders that my journey is at an end are everywhere. Seeing notes written by past residents or fellows reminds me that soon I too will merely be a name in the chart to future trainees. Perhaps this line of thought is unfair, reducing my training experience to notes I signed—whereas my training experience was defined by connections made with colleagues and mentors, opportunities to teach junior learners, and confidence gained by overcoming adversity.
While becoming an attending psychiatrist fills me with trepidation, fear need not be an inherent aspect of new beginnings. Reflection has been a powerful practice, allowing me to realize what made my experience so meaningful, and that training is meant to be process-oriented rather than outcome-oriented. My reflection has underscored the realization that challenges are inherent in training, although not without purpose. I believe these struggles were meant to allow me to build meaningful relationships with colleagues, discover joy in teaching, and build resiliency.
The purpose of residencies and fellowships should be to produce clinically excellent psychiatrists, but I feel the journey was as important as the destination. Psychiatrists likely understand this better than most, as we were trained to thoughtfully approach the process of termination with patients.5 While the conclusion of our training journeys may seem unceremonious or anticlimactic, the termination process should include self-reflection on meaningful facets of training. For me, this reflection has itself been invaluable, while also making me hopeful to contribute value to the training journeys of future psychiatrists.
Throughout my training, a common refrain from more senior colleagues was that training “goes by quickly.” At the risk of sounding cliché, and even after a 7-year journey spanning psychiatry and preventive medicine residencies as well as a consultation-liaison psychiatry fellowship, I agree without reservations that it does indeed go quickly. In the waning days of my training, reflection and nostalgia have become commonplace, as one might expect after such a meaningful pursuit. In sharing my reflections, I hope others progressing through training will also reflect on elements that added meaning to their experience and how they might improve the journey for future trainees.
Residency is a team sport
One realization that quickly struck me was that residency is a team sport, and finding supportive communities is essential to survival. Other residents, colleagues, and mentors played integral roles in making my experience rewarding. Training might be considered a shared traumatic experience, but having peers to commiserate with at each step has been among its greatest rewards. Residency automatically provided a cohort of colleagues who shared and validated my experiences. Additionally, having mentors who have been through it themselves and find ways to improve the training experience made mine superlative. Mentors assisted me in tailoring my training and developing interests that I could integrate into my future practice. The interpersonal connections I made were critical in helping me survive and thrive during training.
See one, do one, teach one
Residency and fellowship programs might be considered “see one, do one, teach one”1 at large scale. Since their inception, these programs—designed to develop junior physicians—have been inherently educational in nature. The structure is elegant, allowing trainees to continue learning while incrementally gaining more autonomy and teaching responsibility.2 Naively, I did not understand that implicit within my education was an expectation to become an educator and hone my teaching skills. Initially, being a newly minted resident receiving brand-new 3rd-year medical students charged me with apprehension. Thoughts I internalized, such as “these students probably know more than me” or “how can I be responsible for patients and students simultaneously,” may have resulted from a paucity of instruction about teaching available during medical school.3,4 I quickly found, though, that teaching was among the most rewarding facets of training. Helping other learners grow became one of my passions and added to my experience.
Iron sharpens iron
Although my experience was enjoyable, I would be remiss without also considering accompanying trials and tribulations. Seemingly interminable night shifts, sleep deprivation, lack of autonomy, and system inefficiencies frustrated me. Eventually, these frustrations seemed less bothersome. These challenges likely had not vanished with time, but perhaps my capacity to tolerate distress improved—likely corresponding with increasing skill and confidence. These challenges allowed me to hone my clinical decision-making abilities while under duress. My struggles and frustrations were not unique but perhaps lessons themselves.
Residency is not meant to be easy. The crucible of residency taught me that I had resilience to draw upon during challenging times. “Iron sharpens iron,” as the adage goes, and I believe adversity ultimately helped me become a better psychiatrist.
Self-reflection is part of completing training
Reminders that my journey is at an end are everywhere. Seeing notes written by past residents or fellows reminds me that soon I too will merely be a name in the chart to future trainees. Perhaps this line of thought is unfair, reducing my training experience to notes I signed—whereas my training experience was defined by connections made with colleagues and mentors, opportunities to teach junior learners, and confidence gained by overcoming adversity.
While becoming an attending psychiatrist fills me with trepidation, fear need not be an inherent aspect of new beginnings. Reflection has been a powerful practice, allowing me to realize what made my experience so meaningful, and that training is meant to be process-oriented rather than outcome-oriented. My reflection has underscored the realization that challenges are inherent in training, although not without purpose. I believe these struggles were meant to allow me to build meaningful relationships with colleagues, discover joy in teaching, and build resiliency.
The purpose of residencies and fellowships should be to produce clinically excellent psychiatrists, but I feel the journey was as important as the destination. Psychiatrists likely understand this better than most, as we were trained to thoughtfully approach the process of termination with patients.5 While the conclusion of our training journeys may seem unceremonious or anticlimactic, the termination process should include self-reflection on meaningful facets of training. For me, this reflection has itself been invaluable, while also making me hopeful to contribute value to the training journeys of future psychiatrists.
1. Gorrindo T, Beresin EV. Is “See one, do one, teach one” dead? Implications for the professionalization of medical educators in the twenty-first century. Acad Psychiatry. 2015;39(6):613-614. doi:10.1007/s40596-015-0424-8
2. Wright Jr. JR, Schachar NS. Necessity is the mother of invention: William Stewart Halsted’s addiction and its influence on the development of residency training in North America. Can J Surg. 2020;63(1):E13-E19. doi:10.1503/cjs.003319
3. Dandavino M, Snell L, Wiseman J. Why medical students should learn how to teach. Med Teach. 2007;29(6):558-565. doi:10.1080/01421590701477449
4. Liu AC, Liu M, Dannaway J, et al. Are Australian medical students being taught to teach? Clin Teach. 2017;14(5):330-335. doi:10.1111/tct.12591
5. Vasquez MJ, Bingham RP, Barnett JE. Psychotherapy termination: clinical and ethical responsibilities. J Clin Psychol. 2008;64(5):653-665. doi:10.1002/jclp.20478
1. Gorrindo T, Beresin EV. Is “See one, do one, teach one” dead? Implications for the professionalization of medical educators in the twenty-first century. Acad Psychiatry. 2015;39(6):613-614. doi:10.1007/s40596-015-0424-8
2. Wright Jr. JR, Schachar NS. Necessity is the mother of invention: William Stewart Halsted’s addiction and its influence on the development of residency training in North America. Can J Surg. 2020;63(1):E13-E19. doi:10.1503/cjs.003319
3. Dandavino M, Snell L, Wiseman J. Why medical students should learn how to teach. Med Teach. 2007;29(6):558-565. doi:10.1080/01421590701477449
4. Liu AC, Liu M, Dannaway J, et al. Are Australian medical students being taught to teach? Clin Teach. 2017;14(5):330-335. doi:10.1111/tct.12591
5. Vasquez MJ, Bingham RP, Barnett JE. Psychotherapy termination: clinical and ethical responsibilities. J Clin Psychol. 2008;64(5):653-665. doi:10.1002/jclp.20478
Younger doctors call for more attention to patients with disabilities
As an undergraduate student at Northeastern University in Boston, Meghan Chin spent her summers working for a day program in Rhode Island. Her charges were adults with various forms of intellectual and developmental disabilities (IDD).
“I was very much a caretaker,” Ms. Chin, now 29, said. “It was everything from helping them get dressed in the morning to getting them to medical appointments.”
During one such visit Ms. Chin got a lesson about how health care looks from the viewpoint of someone with an IDD.
The patient was a woman in her 60s and she was having gastrointestinal issues; symptoms she could have articulated, if asked. “She was perfectly capable of telling a clinician where it hurt, how long she had experienced the problem, and what she had done or not done to alleviate it,” Ms. Chin said.
And of comprehending a response. But she was not given the opportunity.
“She would explain what was going on to the clinician,” Ms. Chin recalled. “And the clinician would turn to me and answer. It was this weird three-way conversation – as if she wasn’t even there in the room with us.”
Ms. Chin was incensed at the rude and disrespectful way the patient had been treated. But her charge didn’t seem upset or surprised. Just resigned. “Sadly, she had become used to this,” Ms. Chin said.
For the young aide, however, the experience was searing. “It didn’t seem right to me,” Ms. Chin said. “That’s why, when I went to medical school, I knew I wanted to do better for this population.”
Serendipity led her to Georgetown University, Washington, where she met Kim Bullock, MD, one of the country’s leading advocates for improved health care delivery to those with IDDs.
Dr. Bullock, an associate professor of family medicine, seeks to create better training and educational opportunities for medical students who will likely encounter patients with these disabilities in their practices.
When Dr. Bullock heard Ms. Chin’s story about the patient being ignored, she was not surprised.
“This is not an unusual or unique situation,” said Dr. Bullock, who is also director of Georgetown’s community health division and a faculty member of the university’s Center for Excellence for Developmental Disabilities. “In fact, it’s quite common and is part of what spurred my own interest in educating pre-med and medical students about effective communication techniques, particularly when addressing neurodiverse patients.”
More than 13% of Americans, or roughly 44 million people, have some form of disability, according to the National Institute on Disability at the University of New Hampshire, a figure that does not include those who are institutionalized. The Centers for Disease Control and Prevention estimates that 17% of children aged 3-17 years have a developmental disability.
Even so, many physicians feel ill-prepared to care for disabled patients. A survey of physicians, published in the journal Health Affairs, found that some lacked the resources and training to properly care for patients with disabilities, or that they struggled to coordinate care for such individuals. Some said they did not know which types of accessible equipment, like adjustable tables and chair scales, were needed or how to use them. And some said they actively try to avoid treating patients with disabilities.
Don’t assume
The first step at correcting the problem, Dr. Bullock said, is to not assume that all IDD patients are incapable of communicating. By talking not to the patient but to their caregiver or spouse or child, as the clinician did with Ms. Chin years ago, “we are taking away their agency, their autonomy to speak for and about themselves.”
Change involves altering physicians’ attitudes and assumptions toward this population, through education. But how?
“The medical school curriculum is tight as it is,” Dr. Bullock acknowledged. “There’s a lot of things students have to learn. People wonder: where we will add this?”
Her suggestion: Incorporate IDD all along the way, through programs or experiences that will enable medical students to see such patients “not as something separate, but as people that have special needs just as other populations have.”
Case in point: Operation House Call, a program in Massachusetts designed to support young health care professionals, by building “confidence, interest, and sensitivity” toward individuals with IDD.
Eight medical and allied health schools, including those at Harvard Medical School and Yale School of Nursing, participate in the program, the centerpiece of which is time spent by teams of medical students in the homes of families with neurodiverse members. “It’s transformational,” said Susan Feeney, DNP, NP-C, director of adult gerontology and family nurse practitioner programs at the graduate school of nursing at the University of Massachusetts, Worcester. “They spend a few hours at the homes of these families, have this interaction with them, and journal about their experiences.”
Dr. Feeney described as “transformational” the experience of the students after getting to know these families. “They all come back profoundly changed,” she told this news organization. “As a medical or health care professional, you meet people in an artificial environment of the clinic and hospital. Here, they become human, like you. It takes the stigma away.”
One area of medicine in which this is an exception is pediatrics, where interaction with children with IDD and their families is common – and close. “They’re going to be much more attuned to this,” Dr. Feeney said. “The problem is primary care or internal medicine. Once these children get into their mid and later 20s, and they need a practitioner to talk to about adult concerns.”
And with adulthood come other medical needs, as the physical demands of age fall no less heavily on individuals with IDDs than those without. For example: “Neurodiverse people get pregnant,” Dr. Bullock said. They also can get heart disease as they age; or require the care of a rheumatologist, a neurologist, an orthopedic surgeon, or any other medical specialty.
Generation gap
Fortunately, the next generation of physicians may be more open to this more inclusionary approach toward a widely misunderstood population.
Like Ms. Chin, Sarah Bdeir had experience with this population prior to beginning her training in medicine. She had volunteered at a school for people with IDD.
“It was one of the best experiences I’ve ever had,” Ms. Bdeir, now 23 and a first-year medical student at Wayne State University, Detroit, said. She found that the neurodiverse individuals she worked with had as many abilities as disabilities. “They are capable of learning, but they do it differently,” she said. “You have to adjust to the way they learn. And you have to step out of your own box.”
Ms. Bdeir also heard about Dr. Bullock’s work and is assisting her in a research project on how to better improve nutritional education for people with IDDs. And although she said it may take time for curriculum boards at medical schools to integrate this kind of training into their programs, she believes they will, in part because the rising cohort of medical students today have an eagerness to engage with and learn more about IDD patients.
As does Ms. Chin.
“When I talk to my peers about this, they’re very receptive,” Ms. Chin said. “They want to learn how to better support the IDD population. And they will learn. I believe in my generation of future doctors.”
A version of this article first appeared on Medscape.com.
As an undergraduate student at Northeastern University in Boston, Meghan Chin spent her summers working for a day program in Rhode Island. Her charges were adults with various forms of intellectual and developmental disabilities (IDD).
“I was very much a caretaker,” Ms. Chin, now 29, said. “It was everything from helping them get dressed in the morning to getting them to medical appointments.”
During one such visit Ms. Chin got a lesson about how health care looks from the viewpoint of someone with an IDD.
The patient was a woman in her 60s and she was having gastrointestinal issues; symptoms she could have articulated, if asked. “She was perfectly capable of telling a clinician where it hurt, how long she had experienced the problem, and what she had done or not done to alleviate it,” Ms. Chin said.
And of comprehending a response. But she was not given the opportunity.
“She would explain what was going on to the clinician,” Ms. Chin recalled. “And the clinician would turn to me and answer. It was this weird three-way conversation – as if she wasn’t even there in the room with us.”
Ms. Chin was incensed at the rude and disrespectful way the patient had been treated. But her charge didn’t seem upset or surprised. Just resigned. “Sadly, she had become used to this,” Ms. Chin said.
For the young aide, however, the experience was searing. “It didn’t seem right to me,” Ms. Chin said. “That’s why, when I went to medical school, I knew I wanted to do better for this population.”
Serendipity led her to Georgetown University, Washington, where she met Kim Bullock, MD, one of the country’s leading advocates for improved health care delivery to those with IDDs.
Dr. Bullock, an associate professor of family medicine, seeks to create better training and educational opportunities for medical students who will likely encounter patients with these disabilities in their practices.
When Dr. Bullock heard Ms. Chin’s story about the patient being ignored, she was not surprised.
“This is not an unusual or unique situation,” said Dr. Bullock, who is also director of Georgetown’s community health division and a faculty member of the university’s Center for Excellence for Developmental Disabilities. “In fact, it’s quite common and is part of what spurred my own interest in educating pre-med and medical students about effective communication techniques, particularly when addressing neurodiverse patients.”
More than 13% of Americans, or roughly 44 million people, have some form of disability, according to the National Institute on Disability at the University of New Hampshire, a figure that does not include those who are institutionalized. The Centers for Disease Control and Prevention estimates that 17% of children aged 3-17 years have a developmental disability.
Even so, many physicians feel ill-prepared to care for disabled patients. A survey of physicians, published in the journal Health Affairs, found that some lacked the resources and training to properly care for patients with disabilities, or that they struggled to coordinate care for such individuals. Some said they did not know which types of accessible equipment, like adjustable tables and chair scales, were needed or how to use them. And some said they actively try to avoid treating patients with disabilities.
Don’t assume
The first step at correcting the problem, Dr. Bullock said, is to not assume that all IDD patients are incapable of communicating. By talking not to the patient but to their caregiver or spouse or child, as the clinician did with Ms. Chin years ago, “we are taking away their agency, their autonomy to speak for and about themselves.”
Change involves altering physicians’ attitudes and assumptions toward this population, through education. But how?
“The medical school curriculum is tight as it is,” Dr. Bullock acknowledged. “There’s a lot of things students have to learn. People wonder: where we will add this?”
Her suggestion: Incorporate IDD all along the way, through programs or experiences that will enable medical students to see such patients “not as something separate, but as people that have special needs just as other populations have.”
Case in point: Operation House Call, a program in Massachusetts designed to support young health care professionals, by building “confidence, interest, and sensitivity” toward individuals with IDD.
Eight medical and allied health schools, including those at Harvard Medical School and Yale School of Nursing, participate in the program, the centerpiece of which is time spent by teams of medical students in the homes of families with neurodiverse members. “It’s transformational,” said Susan Feeney, DNP, NP-C, director of adult gerontology and family nurse practitioner programs at the graduate school of nursing at the University of Massachusetts, Worcester. “They spend a few hours at the homes of these families, have this interaction with them, and journal about their experiences.”
Dr. Feeney described as “transformational” the experience of the students after getting to know these families. “They all come back profoundly changed,” she told this news organization. “As a medical or health care professional, you meet people in an artificial environment of the clinic and hospital. Here, they become human, like you. It takes the stigma away.”
One area of medicine in which this is an exception is pediatrics, where interaction with children with IDD and their families is common – and close. “They’re going to be much more attuned to this,” Dr. Feeney said. “The problem is primary care or internal medicine. Once these children get into their mid and later 20s, and they need a practitioner to talk to about adult concerns.”
And with adulthood come other medical needs, as the physical demands of age fall no less heavily on individuals with IDDs than those without. For example: “Neurodiverse people get pregnant,” Dr. Bullock said. They also can get heart disease as they age; or require the care of a rheumatologist, a neurologist, an orthopedic surgeon, or any other medical specialty.
Generation gap
Fortunately, the next generation of physicians may be more open to this more inclusionary approach toward a widely misunderstood population.
Like Ms. Chin, Sarah Bdeir had experience with this population prior to beginning her training in medicine. She had volunteered at a school for people with IDD.
“It was one of the best experiences I’ve ever had,” Ms. Bdeir, now 23 and a first-year medical student at Wayne State University, Detroit, said. She found that the neurodiverse individuals she worked with had as many abilities as disabilities. “They are capable of learning, but they do it differently,” she said. “You have to adjust to the way they learn. And you have to step out of your own box.”
Ms. Bdeir also heard about Dr. Bullock’s work and is assisting her in a research project on how to better improve nutritional education for people with IDDs. And although she said it may take time for curriculum boards at medical schools to integrate this kind of training into their programs, she believes they will, in part because the rising cohort of medical students today have an eagerness to engage with and learn more about IDD patients.
As does Ms. Chin.
“When I talk to my peers about this, they’re very receptive,” Ms. Chin said. “They want to learn how to better support the IDD population. And they will learn. I believe in my generation of future doctors.”
A version of this article first appeared on Medscape.com.
As an undergraduate student at Northeastern University in Boston, Meghan Chin spent her summers working for a day program in Rhode Island. Her charges were adults with various forms of intellectual and developmental disabilities (IDD).
“I was very much a caretaker,” Ms. Chin, now 29, said. “It was everything from helping them get dressed in the morning to getting them to medical appointments.”
During one such visit Ms. Chin got a lesson about how health care looks from the viewpoint of someone with an IDD.
The patient was a woman in her 60s and she was having gastrointestinal issues; symptoms she could have articulated, if asked. “She was perfectly capable of telling a clinician where it hurt, how long she had experienced the problem, and what she had done or not done to alleviate it,” Ms. Chin said.
And of comprehending a response. But she was not given the opportunity.
“She would explain what was going on to the clinician,” Ms. Chin recalled. “And the clinician would turn to me and answer. It was this weird three-way conversation – as if she wasn’t even there in the room with us.”
Ms. Chin was incensed at the rude and disrespectful way the patient had been treated. But her charge didn’t seem upset or surprised. Just resigned. “Sadly, she had become used to this,” Ms. Chin said.
For the young aide, however, the experience was searing. “It didn’t seem right to me,” Ms. Chin said. “That’s why, when I went to medical school, I knew I wanted to do better for this population.”
Serendipity led her to Georgetown University, Washington, where she met Kim Bullock, MD, one of the country’s leading advocates for improved health care delivery to those with IDDs.
Dr. Bullock, an associate professor of family medicine, seeks to create better training and educational opportunities for medical students who will likely encounter patients with these disabilities in their practices.
When Dr. Bullock heard Ms. Chin’s story about the patient being ignored, she was not surprised.
“This is not an unusual or unique situation,” said Dr. Bullock, who is also director of Georgetown’s community health division and a faculty member of the university’s Center for Excellence for Developmental Disabilities. “In fact, it’s quite common and is part of what spurred my own interest in educating pre-med and medical students about effective communication techniques, particularly when addressing neurodiverse patients.”
More than 13% of Americans, or roughly 44 million people, have some form of disability, according to the National Institute on Disability at the University of New Hampshire, a figure that does not include those who are institutionalized. The Centers for Disease Control and Prevention estimates that 17% of children aged 3-17 years have a developmental disability.
Even so, many physicians feel ill-prepared to care for disabled patients. A survey of physicians, published in the journal Health Affairs, found that some lacked the resources and training to properly care for patients with disabilities, or that they struggled to coordinate care for such individuals. Some said they did not know which types of accessible equipment, like adjustable tables and chair scales, were needed or how to use them. And some said they actively try to avoid treating patients with disabilities.
Don’t assume
The first step at correcting the problem, Dr. Bullock said, is to not assume that all IDD patients are incapable of communicating. By talking not to the patient but to their caregiver or spouse or child, as the clinician did with Ms. Chin years ago, “we are taking away their agency, their autonomy to speak for and about themselves.”
Change involves altering physicians’ attitudes and assumptions toward this population, through education. But how?
“The medical school curriculum is tight as it is,” Dr. Bullock acknowledged. “There’s a lot of things students have to learn. People wonder: where we will add this?”
Her suggestion: Incorporate IDD all along the way, through programs or experiences that will enable medical students to see such patients “not as something separate, but as people that have special needs just as other populations have.”
Case in point: Operation House Call, a program in Massachusetts designed to support young health care professionals, by building “confidence, interest, and sensitivity” toward individuals with IDD.
Eight medical and allied health schools, including those at Harvard Medical School and Yale School of Nursing, participate in the program, the centerpiece of which is time spent by teams of medical students in the homes of families with neurodiverse members. “It’s transformational,” said Susan Feeney, DNP, NP-C, director of adult gerontology and family nurse practitioner programs at the graduate school of nursing at the University of Massachusetts, Worcester. “They spend a few hours at the homes of these families, have this interaction with them, and journal about their experiences.”
Dr. Feeney described as “transformational” the experience of the students after getting to know these families. “They all come back profoundly changed,” she told this news organization. “As a medical or health care professional, you meet people in an artificial environment of the clinic and hospital. Here, they become human, like you. It takes the stigma away.”
One area of medicine in which this is an exception is pediatrics, where interaction with children with IDD and their families is common – and close. “They’re going to be much more attuned to this,” Dr. Feeney said. “The problem is primary care or internal medicine. Once these children get into their mid and later 20s, and they need a practitioner to talk to about adult concerns.”
And with adulthood come other medical needs, as the physical demands of age fall no less heavily on individuals with IDDs than those without. For example: “Neurodiverse people get pregnant,” Dr. Bullock said. They also can get heart disease as they age; or require the care of a rheumatologist, a neurologist, an orthopedic surgeon, or any other medical specialty.
Generation gap
Fortunately, the next generation of physicians may be more open to this more inclusionary approach toward a widely misunderstood population.
Like Ms. Chin, Sarah Bdeir had experience with this population prior to beginning her training in medicine. She had volunteered at a school for people with IDD.
“It was one of the best experiences I’ve ever had,” Ms. Bdeir, now 23 and a first-year medical student at Wayne State University, Detroit, said. She found that the neurodiverse individuals she worked with had as many abilities as disabilities. “They are capable of learning, but they do it differently,” she said. “You have to adjust to the way they learn. And you have to step out of your own box.”
Ms. Bdeir also heard about Dr. Bullock’s work and is assisting her in a research project on how to better improve nutritional education for people with IDDs. And although she said it may take time for curriculum boards at medical schools to integrate this kind of training into their programs, she believes they will, in part because the rising cohort of medical students today have an eagerness to engage with and learn more about IDD patients.
As does Ms. Chin.
“When I talk to my peers about this, they’re very receptive,” Ms. Chin said. “They want to learn how to better support the IDD population. And they will learn. I believe in my generation of future doctors.”
A version of this article first appeared on Medscape.com.