User login
The Hospitalist only
COVID-19: Telehealth at the forefront of the pandemic
On Jan. 20, 2020, the first confirmed case of the 2019 novel coronavirus in the United States was admitted to Providence Regional Medical Center in Everett, Wash. Less than 3 months later, the COVID-19 pandemic has put enormous stress on the U.S. health care system, which is confronting acute resource shortage because of the surge of acute and critically ill patients, health care provider safety and burnout, and an ongoing need for managing vulnerable populations while minimizing the infection spread.
With the onset of these unprecedented challenges, telehealth has emerged as a powerful new resource for health care providers, hospitals, and health care systems across the country. This article offers a summary of government regulations that enabled telehealth expansion, and provides an overview of how two health care organizations, Providence St. Joseph Health and Sound Physicians, are employing telehealth services to combat the COVID-19 health care crisis.
The government response: Telehealth expansion
In response to the pandemic, the Centers for Medicare and Medicaid Services (CMS) have significantly increased access to telehealth services for Medicare and Medicaid beneficiaries. CMS swiftly put measures in place such as:
- Expanding telehealth beyond rural areas.
- Adding 80 services that can be provided in all settings, including patient homes
- Allowing providers to bill for telehealth visits at the same rate as in-person visits.
The U.S. Department of Health and Human Services also aided this effort by:
- Waiving requirements that physicians or other health care professionals must have licenses in the state in which they provide services, if they have an equivalent license from another state.
- Waving penalties for HIPAA violations against health care providers that serve patients in good faith through everyday communications technologies, such as FaceTime or Skype
Without prior regulatory and reimbursement restrictions, telehealth rapidly became a powerful tool in helping to solve some of the problems brought about by the COVID-19 pandemic.
Providence Telehealth for COVID-19
Providence St. Joseph Health is a not-for-profit health care system operating 51 hospitals and 1,085 clinics across Alaska, California, Montana, New Mexico, Oregon, Texas, and Washington. Providence has developed an enterprise telemedicine network with more than 100 virtual programs. Several of these services – including Telestroke, Telepsychiatry, TeleICU, and Telehospitalist – have been scaled across several states as a clinical cloud. More than 400 telemedicine endpoints are deployed, such as robotic carts and fixed InTouch TVs. In fact, the first U.S. COVID-19 patient was treated at Providence Regional Medical Center in Everett, Wash., using the telemedical robot Vici from InTouch Health.
According to Todd Czartoski, MD, chief medical technology officer at Providence, “while telehealth has been around for many years, COVID-19 opened a lot of people’s eyes to the value of virtual care delivery.”
Providence’s telehealth response to COVID-19 has encompassed five main areas: COVID-19 home care, COVID-19 acute care, ambulatory virtual visits, behavioral health concierge (BHC) expansion, and additional support for outside partnerships.
COVID-19 Home Care
Providence rapidly deployed home monitoring for nearly 2,000 positive or presumptive COVID-19 patients. Those symptomatic, clinically stable patients are given a thermometer and a pulse oximeter, and are monitored from home by a central team of nurses and physicians using the Xealth and Twistle programs.
Providence is evaluating expansion of home monitoring to other diagnoses, including higher acuity conditions.
COVID-19 Acute Care
TeleTriage expedites the triage of suspected COVID-19 patients and reduces the use of personal protective equipment (PPE) by 50% per patient per day. To date, TeleTriage has resulted in the conservation of more than 90,000 PPE units.
TeleHospitalist services expanded from traditional night coverage to caring for patients in COVID-19 units around the clock. Currently, there are 25 telehospitalists who practice both in-person and virtual medicine.
TeleICU offers remote management of more than 180 ICU beds across 17 hospitals from two central command centers in Washington state and Alaska. The services include night-time intensivist and ICU nurse coverage, including medication and ventilator management, and family conferences. COVID-19 increased the demand for TeleICU, with anticipated expansion to more than 300 beds.
Core TeleSpecialty services include TeleStroke and TelePsychiatry across 135 remote sites.
Ambulatory Virtual Visits
Providence launched the COVID-19 hub microsite to help educate patients by providing accurate and timely information. A chatbot named Grace helps screen patients who are worried about COVID-19. Grace also suggests next steps, such as a video visit with a patient’s primary care provider or a visit using Express Care/Virtual team, a direct-to-consumer service available to patients within and outside of the health care system.
In less than 2 weeks, Providence enabled virtual visits for more than 7,000 outpatient providers, with more than 14,000 alternative visits now occurring daily. This has allowed primary and specialty providers to continue to manage their patient panels remotely. The number of Express Care/Virtual visits increased from 60 to more than 1,000 per day.
BHC Expansion
In the effort to improve care for its caregivers, Providence launched a behavioral health concierge (BHC) service that offers employees and their dependents virtual access to licensed mental health professionals. Over the last half of 2019, BHC provided more than 1,000 phone and virtual visits, depending on the individual preference of patients. Notably, 21% percent of users were physicians; 65% of users were seen the same day and 100% of users were seen within 48 hours.
COVID-19 increased demand for services that initially started in Seattle and rapidly expanded to Montana, Oregon, and California.
Outside Partnerships
Providence has established partnerships with outside facilities by providing services to 135 sites across eight states. COVID-19 accelerated the employment of new services, including TeleICU.
Telemedicine at Sound Physicians
Sound Physicians is a national physician-founded and -led organization that provides emergency medicine, critical care, hospital medicine, population health, and physician advisory services. Five years ago, Sound launched a telemedicine service line. I spoke with Brian Carpenter, MD, national medical director for TeleHospitalist Services at Sound, to learn about his experience implementing Telehospitalist programs across 22 hospitals and 22 skilled nursing facilities.
Prior to COVID-19, Sound offered a spectrum of telemedicine services including night-time telephonic cross coverage, as well as video-assisted admissions, transfers, and rapid responses. In 2019, Sound Telehospitalists received 88,000 connect requests, including 6,400 video-assisted new admissions and 82 rapid responses. Typically, one physician covers four to eight hospitals with back-up available for surges. The team uses a predictive model for staffing and developed an acuity-based algorithm to ensure that patients in distress are evaluated immediately, new stable admissions on average are seen within 12 minutes, and order clarifications are provided within 30 minutes.
The COVID-19 pandemic created an urgent demand for providers to support an overwhelmed health care system. Without the traditional barriers to implementation – such as lack of acceptance by medical staff, nurses and patients, strict state licensing and technology requirements, lack of reimbursement, and delays in hospital credentialing – Sound was able to develop a rapid implementation model for telemedicine services. Currently, four new hospitals are in the active implementation phase, with 40 more hospitals in the pipeline.
Implementing a telemedicine program at your hospital
In order to successfully launch a telemedicine program, Dr. Carpenter outlined the following critical implementation steps:
- In collaboration with local leadership, define the problem you are trying to solve, which helps inform the scope of the telemedicine practice and technology requirements (for example, night-time cross-coverage vs. full telemedicine service).
- Complete a discovery process (for example, existing workflow for patient admission and transfer) with the end-goal of developing a workflow and rules of engagement.
- Obtain hospital credentialing/privileges and EMR access.
- Train end-users, including physicians and nurse telepresenters.
Dr. Carpenter offered this advice to those considering a telemedicine program: “Telemedicine is not just about technology; a true telemedicine program encompasses change management, workflow development, end-user training, compliance, and mechanisms for continuous process improvement. We want to make things better for the physicians, nurses, and patients.”
Telehealth is offering support to health care providers on the front lines, patients in need of care, and health care systems managing the unprecedented surges in volume.
Dr. Farah is a hospitalist, physician adviser, and Lean Six Sigma Black Belt. She is a performance improvement consultant based in Corvallis, Ore., and a member of The Hospitalist’s editorial advisory board.
On Jan. 20, 2020, the first confirmed case of the 2019 novel coronavirus in the United States was admitted to Providence Regional Medical Center in Everett, Wash. Less than 3 months later, the COVID-19 pandemic has put enormous stress on the U.S. health care system, which is confronting acute resource shortage because of the surge of acute and critically ill patients, health care provider safety and burnout, and an ongoing need for managing vulnerable populations while minimizing the infection spread.
With the onset of these unprecedented challenges, telehealth has emerged as a powerful new resource for health care providers, hospitals, and health care systems across the country. This article offers a summary of government regulations that enabled telehealth expansion, and provides an overview of how two health care organizations, Providence St. Joseph Health and Sound Physicians, are employing telehealth services to combat the COVID-19 health care crisis.
The government response: Telehealth expansion
In response to the pandemic, the Centers for Medicare and Medicaid Services (CMS) have significantly increased access to telehealth services for Medicare and Medicaid beneficiaries. CMS swiftly put measures in place such as:
- Expanding telehealth beyond rural areas.
- Adding 80 services that can be provided in all settings, including patient homes
- Allowing providers to bill for telehealth visits at the same rate as in-person visits.
The U.S. Department of Health and Human Services also aided this effort by:
- Waiving requirements that physicians or other health care professionals must have licenses in the state in which they provide services, if they have an equivalent license from another state.
- Waving penalties for HIPAA violations against health care providers that serve patients in good faith through everyday communications technologies, such as FaceTime or Skype
Without prior regulatory and reimbursement restrictions, telehealth rapidly became a powerful tool in helping to solve some of the problems brought about by the COVID-19 pandemic.
Providence Telehealth for COVID-19
Providence St. Joseph Health is a not-for-profit health care system operating 51 hospitals and 1,085 clinics across Alaska, California, Montana, New Mexico, Oregon, Texas, and Washington. Providence has developed an enterprise telemedicine network with more than 100 virtual programs. Several of these services – including Telestroke, Telepsychiatry, TeleICU, and Telehospitalist – have been scaled across several states as a clinical cloud. More than 400 telemedicine endpoints are deployed, such as robotic carts and fixed InTouch TVs. In fact, the first U.S. COVID-19 patient was treated at Providence Regional Medical Center in Everett, Wash., using the telemedical robot Vici from InTouch Health.
According to Todd Czartoski, MD, chief medical technology officer at Providence, “while telehealth has been around for many years, COVID-19 opened a lot of people’s eyes to the value of virtual care delivery.”
Providence’s telehealth response to COVID-19 has encompassed five main areas: COVID-19 home care, COVID-19 acute care, ambulatory virtual visits, behavioral health concierge (BHC) expansion, and additional support for outside partnerships.
COVID-19 Home Care
Providence rapidly deployed home monitoring for nearly 2,000 positive or presumptive COVID-19 patients. Those symptomatic, clinically stable patients are given a thermometer and a pulse oximeter, and are monitored from home by a central team of nurses and physicians using the Xealth and Twistle programs.
Providence is evaluating expansion of home monitoring to other diagnoses, including higher acuity conditions.
COVID-19 Acute Care
TeleTriage expedites the triage of suspected COVID-19 patients and reduces the use of personal protective equipment (PPE) by 50% per patient per day. To date, TeleTriage has resulted in the conservation of more than 90,000 PPE units.
TeleHospitalist services expanded from traditional night coverage to caring for patients in COVID-19 units around the clock. Currently, there are 25 telehospitalists who practice both in-person and virtual medicine.
TeleICU offers remote management of more than 180 ICU beds across 17 hospitals from two central command centers in Washington state and Alaska. The services include night-time intensivist and ICU nurse coverage, including medication and ventilator management, and family conferences. COVID-19 increased the demand for TeleICU, with anticipated expansion to more than 300 beds.
Core TeleSpecialty services include TeleStroke and TelePsychiatry across 135 remote sites.
Ambulatory Virtual Visits
Providence launched the COVID-19 hub microsite to help educate patients by providing accurate and timely information. A chatbot named Grace helps screen patients who are worried about COVID-19. Grace also suggests next steps, such as a video visit with a patient’s primary care provider or a visit using Express Care/Virtual team, a direct-to-consumer service available to patients within and outside of the health care system.
In less than 2 weeks, Providence enabled virtual visits for more than 7,000 outpatient providers, with more than 14,000 alternative visits now occurring daily. This has allowed primary and specialty providers to continue to manage their patient panels remotely. The number of Express Care/Virtual visits increased from 60 to more than 1,000 per day.
BHC Expansion
In the effort to improve care for its caregivers, Providence launched a behavioral health concierge (BHC) service that offers employees and their dependents virtual access to licensed mental health professionals. Over the last half of 2019, BHC provided more than 1,000 phone and virtual visits, depending on the individual preference of patients. Notably, 21% percent of users were physicians; 65% of users were seen the same day and 100% of users were seen within 48 hours.
COVID-19 increased demand for services that initially started in Seattle and rapidly expanded to Montana, Oregon, and California.
Outside Partnerships
Providence has established partnerships with outside facilities by providing services to 135 sites across eight states. COVID-19 accelerated the employment of new services, including TeleICU.
Telemedicine at Sound Physicians
Sound Physicians is a national physician-founded and -led organization that provides emergency medicine, critical care, hospital medicine, population health, and physician advisory services. Five years ago, Sound launched a telemedicine service line. I spoke with Brian Carpenter, MD, national medical director for TeleHospitalist Services at Sound, to learn about his experience implementing Telehospitalist programs across 22 hospitals and 22 skilled nursing facilities.
Prior to COVID-19, Sound offered a spectrum of telemedicine services including night-time telephonic cross coverage, as well as video-assisted admissions, transfers, and rapid responses. In 2019, Sound Telehospitalists received 88,000 connect requests, including 6,400 video-assisted new admissions and 82 rapid responses. Typically, one physician covers four to eight hospitals with back-up available for surges. The team uses a predictive model for staffing and developed an acuity-based algorithm to ensure that patients in distress are evaluated immediately, new stable admissions on average are seen within 12 minutes, and order clarifications are provided within 30 minutes.
The COVID-19 pandemic created an urgent demand for providers to support an overwhelmed health care system. Without the traditional barriers to implementation – such as lack of acceptance by medical staff, nurses and patients, strict state licensing and technology requirements, lack of reimbursement, and delays in hospital credentialing – Sound was able to develop a rapid implementation model for telemedicine services. Currently, four new hospitals are in the active implementation phase, with 40 more hospitals in the pipeline.
Implementing a telemedicine program at your hospital
In order to successfully launch a telemedicine program, Dr. Carpenter outlined the following critical implementation steps:
- In collaboration with local leadership, define the problem you are trying to solve, which helps inform the scope of the telemedicine practice and technology requirements (for example, night-time cross-coverage vs. full telemedicine service).
- Complete a discovery process (for example, existing workflow for patient admission and transfer) with the end-goal of developing a workflow and rules of engagement.
- Obtain hospital credentialing/privileges and EMR access.
- Train end-users, including physicians and nurse telepresenters.
Dr. Carpenter offered this advice to those considering a telemedicine program: “Telemedicine is not just about technology; a true telemedicine program encompasses change management, workflow development, end-user training, compliance, and mechanisms for continuous process improvement. We want to make things better for the physicians, nurses, and patients.”
Telehealth is offering support to health care providers on the front lines, patients in need of care, and health care systems managing the unprecedented surges in volume.
Dr. Farah is a hospitalist, physician adviser, and Lean Six Sigma Black Belt. She is a performance improvement consultant based in Corvallis, Ore., and a member of The Hospitalist’s editorial advisory board.
On Jan. 20, 2020, the first confirmed case of the 2019 novel coronavirus in the United States was admitted to Providence Regional Medical Center in Everett, Wash. Less than 3 months later, the COVID-19 pandemic has put enormous stress on the U.S. health care system, which is confronting acute resource shortage because of the surge of acute and critically ill patients, health care provider safety and burnout, and an ongoing need for managing vulnerable populations while minimizing the infection spread.
With the onset of these unprecedented challenges, telehealth has emerged as a powerful new resource for health care providers, hospitals, and health care systems across the country. This article offers a summary of government regulations that enabled telehealth expansion, and provides an overview of how two health care organizations, Providence St. Joseph Health and Sound Physicians, are employing telehealth services to combat the COVID-19 health care crisis.
The government response: Telehealth expansion
In response to the pandemic, the Centers for Medicare and Medicaid Services (CMS) have significantly increased access to telehealth services for Medicare and Medicaid beneficiaries. CMS swiftly put measures in place such as:
- Expanding telehealth beyond rural areas.
- Adding 80 services that can be provided in all settings, including patient homes
- Allowing providers to bill for telehealth visits at the same rate as in-person visits.
The U.S. Department of Health and Human Services also aided this effort by:
- Waiving requirements that physicians or other health care professionals must have licenses in the state in which they provide services, if they have an equivalent license from another state.
- Waving penalties for HIPAA violations against health care providers that serve patients in good faith through everyday communications technologies, such as FaceTime or Skype
Without prior regulatory and reimbursement restrictions, telehealth rapidly became a powerful tool in helping to solve some of the problems brought about by the COVID-19 pandemic.
Providence Telehealth for COVID-19
Providence St. Joseph Health is a not-for-profit health care system operating 51 hospitals and 1,085 clinics across Alaska, California, Montana, New Mexico, Oregon, Texas, and Washington. Providence has developed an enterprise telemedicine network with more than 100 virtual programs. Several of these services – including Telestroke, Telepsychiatry, TeleICU, and Telehospitalist – have been scaled across several states as a clinical cloud. More than 400 telemedicine endpoints are deployed, such as robotic carts and fixed InTouch TVs. In fact, the first U.S. COVID-19 patient was treated at Providence Regional Medical Center in Everett, Wash., using the telemedical robot Vici from InTouch Health.
According to Todd Czartoski, MD, chief medical technology officer at Providence, “while telehealth has been around for many years, COVID-19 opened a lot of people’s eyes to the value of virtual care delivery.”
Providence’s telehealth response to COVID-19 has encompassed five main areas: COVID-19 home care, COVID-19 acute care, ambulatory virtual visits, behavioral health concierge (BHC) expansion, and additional support for outside partnerships.
COVID-19 Home Care
Providence rapidly deployed home monitoring for nearly 2,000 positive or presumptive COVID-19 patients. Those symptomatic, clinically stable patients are given a thermometer and a pulse oximeter, and are monitored from home by a central team of nurses and physicians using the Xealth and Twistle programs.
Providence is evaluating expansion of home monitoring to other diagnoses, including higher acuity conditions.
COVID-19 Acute Care
TeleTriage expedites the triage of suspected COVID-19 patients and reduces the use of personal protective equipment (PPE) by 50% per patient per day. To date, TeleTriage has resulted in the conservation of more than 90,000 PPE units.
TeleHospitalist services expanded from traditional night coverage to caring for patients in COVID-19 units around the clock. Currently, there are 25 telehospitalists who practice both in-person and virtual medicine.
TeleICU offers remote management of more than 180 ICU beds across 17 hospitals from two central command centers in Washington state and Alaska. The services include night-time intensivist and ICU nurse coverage, including medication and ventilator management, and family conferences. COVID-19 increased the demand for TeleICU, with anticipated expansion to more than 300 beds.
Core TeleSpecialty services include TeleStroke and TelePsychiatry across 135 remote sites.
Ambulatory Virtual Visits
Providence launched the COVID-19 hub microsite to help educate patients by providing accurate and timely information. A chatbot named Grace helps screen patients who are worried about COVID-19. Grace also suggests next steps, such as a video visit with a patient’s primary care provider or a visit using Express Care/Virtual team, a direct-to-consumer service available to patients within and outside of the health care system.
In less than 2 weeks, Providence enabled virtual visits for more than 7,000 outpatient providers, with more than 14,000 alternative visits now occurring daily. This has allowed primary and specialty providers to continue to manage their patient panels remotely. The number of Express Care/Virtual visits increased from 60 to more than 1,000 per day.
BHC Expansion
In the effort to improve care for its caregivers, Providence launched a behavioral health concierge (BHC) service that offers employees and their dependents virtual access to licensed mental health professionals. Over the last half of 2019, BHC provided more than 1,000 phone and virtual visits, depending on the individual preference of patients. Notably, 21% percent of users were physicians; 65% of users were seen the same day and 100% of users were seen within 48 hours.
COVID-19 increased demand for services that initially started in Seattle and rapidly expanded to Montana, Oregon, and California.
Outside Partnerships
Providence has established partnerships with outside facilities by providing services to 135 sites across eight states. COVID-19 accelerated the employment of new services, including TeleICU.
Telemedicine at Sound Physicians
Sound Physicians is a national physician-founded and -led organization that provides emergency medicine, critical care, hospital medicine, population health, and physician advisory services. Five years ago, Sound launched a telemedicine service line. I spoke with Brian Carpenter, MD, national medical director for TeleHospitalist Services at Sound, to learn about his experience implementing Telehospitalist programs across 22 hospitals and 22 skilled nursing facilities.
Prior to COVID-19, Sound offered a spectrum of telemedicine services including night-time telephonic cross coverage, as well as video-assisted admissions, transfers, and rapid responses. In 2019, Sound Telehospitalists received 88,000 connect requests, including 6,400 video-assisted new admissions and 82 rapid responses. Typically, one physician covers four to eight hospitals with back-up available for surges. The team uses a predictive model for staffing and developed an acuity-based algorithm to ensure that patients in distress are evaluated immediately, new stable admissions on average are seen within 12 minutes, and order clarifications are provided within 30 minutes.
The COVID-19 pandemic created an urgent demand for providers to support an overwhelmed health care system. Without the traditional barriers to implementation – such as lack of acceptance by medical staff, nurses and patients, strict state licensing and technology requirements, lack of reimbursement, and delays in hospital credentialing – Sound was able to develop a rapid implementation model for telemedicine services. Currently, four new hospitals are in the active implementation phase, with 40 more hospitals in the pipeline.
Implementing a telemedicine program at your hospital
In order to successfully launch a telemedicine program, Dr. Carpenter outlined the following critical implementation steps:
- In collaboration with local leadership, define the problem you are trying to solve, which helps inform the scope of the telemedicine practice and technology requirements (for example, night-time cross-coverage vs. full telemedicine service).
- Complete a discovery process (for example, existing workflow for patient admission and transfer) with the end-goal of developing a workflow and rules of engagement.
- Obtain hospital credentialing/privileges and EMR access.
- Train end-users, including physicians and nurse telepresenters.
Dr. Carpenter offered this advice to those considering a telemedicine program: “Telemedicine is not just about technology; a true telemedicine program encompasses change management, workflow development, end-user training, compliance, and mechanisms for continuous process improvement. We want to make things better for the physicians, nurses, and patients.”
Telehealth is offering support to health care providers on the front lines, patients in need of care, and health care systems managing the unprecedented surges in volume.
Dr. Farah is a hospitalist, physician adviser, and Lean Six Sigma Black Belt. She is a performance improvement consultant based in Corvallis, Ore., and a member of The Hospitalist’s editorial advisory board.
How to expand the APP role in a crisis
An opportunity to better appreciate the value of PAs, NPs
Advanced practice providers – physician assistants and nurse practitioners – at the 733-bed Emory University Hospital in Atlanta are playing an expanded role in the admission of patients into the hospital, particularly those suspected of having COVID-19.
Before the pandemic crisis, evaluation visits by the APP would have been reviewed on the same day by the supervising physician through an in-person encounter with the patient. The new protocol is not outside of scope-of-practice regulations for APPs in Georgia or of the hospital’s bylaws. But it offers a way to help limit the overall exposure of hospital staff to patients suspected of COVID-19 infection, and the total amount of time providers spend in such patients’ room. Just one provider now needs to meet the patient during the admissions process, while the attending physician can fulfill a requirement for seeing the patient within 24 hours during rounds the following day. Emergency encounters would still be done as needed.
These protocols point toward future conversations about the limits to APPs’ scope of practice, and whether more expansive approaches could be widely adopted once the current crisis is over, say advocates for the APPs’ role.
“Our APPs are primarily doing the admissions to the hospital of COVID patients and of non-COVID patients, as we’ve always done. But with COVID-infected or -suspected patients, we’re trying to minimize exposure for our providers,” explained Susan Ortiz, a certified PA, lead APP at Emory University Hospital. “In this way, we can also see more patients more efficiently.” Ms. Ortiz said she finds in talking to other APP leads in the Emory system that “each facility has its own culture and way of doing things. But for the most part, they’re all trying to do something to limit providers’ time in patients’ rooms.”
In response to the rapidly moving crisis, tactics to limit personnel in COVID patients’ rooms to the “absolutely essential” include gathering much of the needed history and other information requested from the patient by telephone, Ms. Ortiz said. This can be done either over the patient’s own cell phone or a phone placed in the room by hospital staff. Family members may be called to supplement this information, with the patient’s consent.
Once vital sign monitoring equipment is hooked up, it is possible to monitor the patient’s vital signs remotely without making frequent trips into the room. That way, in-person vital sign monitoring doesn’t need to happen routinely – at least not as often. One observation by clinicians on Ms. Ortiz’s team: listening for lung sounds with a stethoscope has not been shown to alter treatment for these patients. Once a chest X-ray shows structural changes in a patient’s lung, all lung exams are going to sound bad.
The admitting provider still needs to meet the patient in person for part of the admission visit and physical exam, but the amount of time spent in close personal contact with the patient can be much shorter, Ms. Ortiz said. For patients who are admitted, if there is a question about difficulty swallowing, they will see a speech pathologist, and if evidence of malnutrition, a nutritionist. “But we have to be extremely thoughtful about when people go into the room. So we are not ordering these ancillary services as routinely as we do during non-COVID times,” she said.
Appropriate levels of fear
Emory’s hospitalists are communicating daily about a rapidly changing situation. “We get a note by email every day, and we have a Dropbox account for downloading more information,” Ms. Ortiz said. A joint on-call system is used to provide backup coverage of APPs at the seven Emory hospitals. When replacement shifts need filling in a hurry, practitioners are able to obtain emergency credentials at any of the other hospitals. “It’s a voluntary process to sign up to be on-call,” Ms. Ortiz said. So far, that has been sufficient.
All staff have their own level of “appropriate fear” of this infection, Ms. Ortiz noted. “We have an extremely supportive group here to back up those of us who, for good reason, don’t want to be admitting the COVID patients.” Ms. Ortiz opted out of doing COVID admissions because her husband’s health places him at particular risk. “But with the cross-coverage we have, sometimes I’ll provide assistance when needed if a patient is suspected of being infected.” APPs are critical to Emory’s hospital medicine group – not ancillaries. “Everyone here feels that way. So we want to give them a lot of support. We’re all pitching in, doing it together,” she said.
“We said when we started with this, a couple of weeks before the surge started, that you could volunteer to see COVID patients,” said Emory hospitalist Jessica Nave, MD. “As we came to realize that the demand would be greater, we said you would need to opt out of seeing these patients, rather than opt in, and have a reason for doing so.” An example is pregnant staff, of which there seems to be a lot at Emory right now, Dr. Nave said, or those who are immunocompromised for other reasons. Those who don’t opt out are seeing the majority of the COVID patients, depending on actual need.
Dr. Nave is married to another hospitalist at Emory. “We can’t isolate from each other or our children. He and I have a regimented protocol for how we handle the risk, which includes taking off our shoes and clothes in the garage, showering and wiping down every place we might have touched. But those steps are not guarantees.” Other staff at Emory are isolating from their families for weeks at a time. Emory has a conference hotel offering discounted rates to staff. Nine physicians at Emory have been tested for the infection based on presenting symptoms, but at press time none had tested positive.
Streamlining code blue
Another area in which Emory has revised its policies in response to COVID-19 is for in-hospital cardiac arrest code response. Codes are inherently unpredictable, and crowd control has always been an issue for them, Dr. Nave said. “Historically, you could have 15 or more people show up when a code was called. Now, more than ever, we need to limit the number of people involved, for the same reason, avoiding unnecessary patient contact.”
The hospital’s Resuscitation Committee took the lead on developing a new policy, approved by the its Critical Care Committee and COVID Task Force, to limit the number of professionals in the room when running a code to an essential six: two doing chest compression, two managing airways, a code leader, and a critical care nurse. Outside the patient’s door, wearing the same personal protective equipment (PPE), are a pharmacist, recorder, and runner. “If you’re not one of those nine, you don’t need to be involved and should leave the area,” Dr. Nave said.
Staff have been instructed that they need to don appropriate PPE, including gown, mask, and eye wear, before entering the room for a code – even if that delays the start of intervention. “We’ve also made a code kit for each unit with quickly accessible gowns and masks. It should be used only for code blues.”
Increasing flexibility for the team
PAs and NPs in other locations are also exploring opportunities for gearing up to play larger roles in hospital care in the current crisis situation. The American Association of Physician Assistants has urged all U.S. governors to issue executive orders to waive state-specific licensing requirements for physician supervision or collaboration during the crisis, in order to increase flexibility of health care teams to deploy APPs.
AAPA believes the supervisory requirement is the biggest current barrier to mobilizing PAs and NPs. That includes those who have been furloughed from outpatient or other settings but are limited in their ability to contribute to the COVID crisis by the need to sign a supervision agreement with a physician at a new hospital.
The crisis is creating an opportunity to better appreciate the value PAs and NPs bring to health care, said Tracy Cardin, ACNP-BC, SFHM, vice president for advanced practice providers at Sound Physicians, a national hospitalist company based in Tacoma, Wash. The company recently sent a memo to the leadership of hospital sites at which it has contracts, requesting suspension of the hospitals’ requirements for a daily physician supervisory visit for APPs – which can be a hurdle when trying to leverage all hands on deck in the crisis.
NPs and PAs are stepping up and volunteering for COVID patients, Ms. Cardin said. Some have even taken leaves from their jobs to go to New York to help out at the epicenter of the U.S. crisis. “They want to make a difference. We’ve been deploying nonhospital medicine APPs from surgery, primary care, and elsewhere, embedding them on the hospital medicine team.”
Before the crisis, APPs at Sound Physicians weren’t always able to practice at the top of their licenses, depending on the hospital setting, added Alicia Scheffer, CNP, the company’s Great Lakes regional director for APPs. “Then COVID-19 showed up and really expedited conversations about how to maximize caseloads using APPs and about the fear of failing patients due to lack of capacity.”
In several locales, Sound Physicians is using quarantined providers to do telephone triage, or staffing ICUs with APPs backed up by telemedicine. “In APP-led ICUs, where the nurses are leading, they are intubating patients, placing central lines, things we weren’t allowed to do before,” Ms. Scheffer said.
A spirit of improvisation
There is a lot of tension at Emory University Hospital these days, reflecting the fears and uncertainties about the crisis, Dr. Nave said. “But there’s also a strangely powerful camaraderie like I’ve never seen before. When you walk onto the COVID units, you feel immediately bonded to the nurses, the techs, the phlebotomists. And you feel like you could talk about anything.”
Changes such as those made at Emory, have been talked about for a while, for example when hospitalists are having a busy night, she said. “But because this is a big cultural change, some physicians resisted it. We trust our APPs. But if the doctor’s name is on a patient chart, they want to see the patient – just for their own comfort level.”
Ms. Ortiz thinks the experience with the COVID crisis could help to advance the conversation about the appropriate role for APPs and their scope of practice in hospital medicine, once the current crisis has passed. “People were used to always doing things a certain way. This experience, hopefully, will get us to the point where attending physicians have more comfort with the APP’s ability to act autonomously,” she said.
“We’ve also talked about piloting telemedicine examinations using Zoom,” Dr. Nave added. “It’s making us think a lot of remote cross-coverage could be done that way. We’ve talked about using the hospital’s iPads with patients. This crisis really makes you think you want to innovate, in a spirit of improvisation,” she said. “Now is the time to try some of these things.”
Editors note: During the COVID-19 pandemic, many hospitals are seeing unprecedented volumes of patients requiring hospital medicine groups to stretch their current resources and recruit providers from outside their groups to bolster their inpatient services. The Society of Hospital Medicine has put together the following stepwise guide for onboarding traditional outpatient and subspecialty-based providers to work on general medicine wards: COVID-19 nonhospitalist onboarding resources.
An opportunity to better appreciate the value of PAs, NPs
An opportunity to better appreciate the value of PAs, NPs
Advanced practice providers – physician assistants and nurse practitioners – at the 733-bed Emory University Hospital in Atlanta are playing an expanded role in the admission of patients into the hospital, particularly those suspected of having COVID-19.
Before the pandemic crisis, evaluation visits by the APP would have been reviewed on the same day by the supervising physician through an in-person encounter with the patient. The new protocol is not outside of scope-of-practice regulations for APPs in Georgia or of the hospital’s bylaws. But it offers a way to help limit the overall exposure of hospital staff to patients suspected of COVID-19 infection, and the total amount of time providers spend in such patients’ room. Just one provider now needs to meet the patient during the admissions process, while the attending physician can fulfill a requirement for seeing the patient within 24 hours during rounds the following day. Emergency encounters would still be done as needed.
These protocols point toward future conversations about the limits to APPs’ scope of practice, and whether more expansive approaches could be widely adopted once the current crisis is over, say advocates for the APPs’ role.
“Our APPs are primarily doing the admissions to the hospital of COVID patients and of non-COVID patients, as we’ve always done. But with COVID-infected or -suspected patients, we’re trying to minimize exposure for our providers,” explained Susan Ortiz, a certified PA, lead APP at Emory University Hospital. “In this way, we can also see more patients more efficiently.” Ms. Ortiz said she finds in talking to other APP leads in the Emory system that “each facility has its own culture and way of doing things. But for the most part, they’re all trying to do something to limit providers’ time in patients’ rooms.”
In response to the rapidly moving crisis, tactics to limit personnel in COVID patients’ rooms to the “absolutely essential” include gathering much of the needed history and other information requested from the patient by telephone, Ms. Ortiz said. This can be done either over the patient’s own cell phone or a phone placed in the room by hospital staff. Family members may be called to supplement this information, with the patient’s consent.
Once vital sign monitoring equipment is hooked up, it is possible to monitor the patient’s vital signs remotely without making frequent trips into the room. That way, in-person vital sign monitoring doesn’t need to happen routinely – at least not as often. One observation by clinicians on Ms. Ortiz’s team: listening for lung sounds with a stethoscope has not been shown to alter treatment for these patients. Once a chest X-ray shows structural changes in a patient’s lung, all lung exams are going to sound bad.
The admitting provider still needs to meet the patient in person for part of the admission visit and physical exam, but the amount of time spent in close personal contact with the patient can be much shorter, Ms. Ortiz said. For patients who are admitted, if there is a question about difficulty swallowing, they will see a speech pathologist, and if evidence of malnutrition, a nutritionist. “But we have to be extremely thoughtful about when people go into the room. So we are not ordering these ancillary services as routinely as we do during non-COVID times,” she said.
Appropriate levels of fear
Emory’s hospitalists are communicating daily about a rapidly changing situation. “We get a note by email every day, and we have a Dropbox account for downloading more information,” Ms. Ortiz said. A joint on-call system is used to provide backup coverage of APPs at the seven Emory hospitals. When replacement shifts need filling in a hurry, practitioners are able to obtain emergency credentials at any of the other hospitals. “It’s a voluntary process to sign up to be on-call,” Ms. Ortiz said. So far, that has been sufficient.
All staff have their own level of “appropriate fear” of this infection, Ms. Ortiz noted. “We have an extremely supportive group here to back up those of us who, for good reason, don’t want to be admitting the COVID patients.” Ms. Ortiz opted out of doing COVID admissions because her husband’s health places him at particular risk. “But with the cross-coverage we have, sometimes I’ll provide assistance when needed if a patient is suspected of being infected.” APPs are critical to Emory’s hospital medicine group – not ancillaries. “Everyone here feels that way. So we want to give them a lot of support. We’re all pitching in, doing it together,” she said.
“We said when we started with this, a couple of weeks before the surge started, that you could volunteer to see COVID patients,” said Emory hospitalist Jessica Nave, MD. “As we came to realize that the demand would be greater, we said you would need to opt out of seeing these patients, rather than opt in, and have a reason for doing so.” An example is pregnant staff, of which there seems to be a lot at Emory right now, Dr. Nave said, or those who are immunocompromised for other reasons. Those who don’t opt out are seeing the majority of the COVID patients, depending on actual need.
Dr. Nave is married to another hospitalist at Emory. “We can’t isolate from each other or our children. He and I have a regimented protocol for how we handle the risk, which includes taking off our shoes and clothes in the garage, showering and wiping down every place we might have touched. But those steps are not guarantees.” Other staff at Emory are isolating from their families for weeks at a time. Emory has a conference hotel offering discounted rates to staff. Nine physicians at Emory have been tested for the infection based on presenting symptoms, but at press time none had tested positive.
Streamlining code blue
Another area in which Emory has revised its policies in response to COVID-19 is for in-hospital cardiac arrest code response. Codes are inherently unpredictable, and crowd control has always been an issue for them, Dr. Nave said. “Historically, you could have 15 or more people show up when a code was called. Now, more than ever, we need to limit the number of people involved, for the same reason, avoiding unnecessary patient contact.”
The hospital’s Resuscitation Committee took the lead on developing a new policy, approved by the its Critical Care Committee and COVID Task Force, to limit the number of professionals in the room when running a code to an essential six: two doing chest compression, two managing airways, a code leader, and a critical care nurse. Outside the patient’s door, wearing the same personal protective equipment (PPE), are a pharmacist, recorder, and runner. “If you’re not one of those nine, you don’t need to be involved and should leave the area,” Dr. Nave said.
Staff have been instructed that they need to don appropriate PPE, including gown, mask, and eye wear, before entering the room for a code – even if that delays the start of intervention. “We’ve also made a code kit for each unit with quickly accessible gowns and masks. It should be used only for code blues.”
Increasing flexibility for the team
PAs and NPs in other locations are also exploring opportunities for gearing up to play larger roles in hospital care in the current crisis situation. The American Association of Physician Assistants has urged all U.S. governors to issue executive orders to waive state-specific licensing requirements for physician supervision or collaboration during the crisis, in order to increase flexibility of health care teams to deploy APPs.
AAPA believes the supervisory requirement is the biggest current barrier to mobilizing PAs and NPs. That includes those who have been furloughed from outpatient or other settings but are limited in their ability to contribute to the COVID crisis by the need to sign a supervision agreement with a physician at a new hospital.
The crisis is creating an opportunity to better appreciate the value PAs and NPs bring to health care, said Tracy Cardin, ACNP-BC, SFHM, vice president for advanced practice providers at Sound Physicians, a national hospitalist company based in Tacoma, Wash. The company recently sent a memo to the leadership of hospital sites at which it has contracts, requesting suspension of the hospitals’ requirements for a daily physician supervisory visit for APPs – which can be a hurdle when trying to leverage all hands on deck in the crisis.
NPs and PAs are stepping up and volunteering for COVID patients, Ms. Cardin said. Some have even taken leaves from their jobs to go to New York to help out at the epicenter of the U.S. crisis. “They want to make a difference. We’ve been deploying nonhospital medicine APPs from surgery, primary care, and elsewhere, embedding them on the hospital medicine team.”
Before the crisis, APPs at Sound Physicians weren’t always able to practice at the top of their licenses, depending on the hospital setting, added Alicia Scheffer, CNP, the company’s Great Lakes regional director for APPs. “Then COVID-19 showed up and really expedited conversations about how to maximize caseloads using APPs and about the fear of failing patients due to lack of capacity.”
In several locales, Sound Physicians is using quarantined providers to do telephone triage, or staffing ICUs with APPs backed up by telemedicine. “In APP-led ICUs, where the nurses are leading, they are intubating patients, placing central lines, things we weren’t allowed to do before,” Ms. Scheffer said.
A spirit of improvisation
There is a lot of tension at Emory University Hospital these days, reflecting the fears and uncertainties about the crisis, Dr. Nave said. “But there’s also a strangely powerful camaraderie like I’ve never seen before. When you walk onto the COVID units, you feel immediately bonded to the nurses, the techs, the phlebotomists. And you feel like you could talk about anything.”
Changes such as those made at Emory, have been talked about for a while, for example when hospitalists are having a busy night, she said. “But because this is a big cultural change, some physicians resisted it. We trust our APPs. But if the doctor’s name is on a patient chart, they want to see the patient – just for their own comfort level.”
Ms. Ortiz thinks the experience with the COVID crisis could help to advance the conversation about the appropriate role for APPs and their scope of practice in hospital medicine, once the current crisis has passed. “People were used to always doing things a certain way. This experience, hopefully, will get us to the point where attending physicians have more comfort with the APP’s ability to act autonomously,” she said.
“We’ve also talked about piloting telemedicine examinations using Zoom,” Dr. Nave added. “It’s making us think a lot of remote cross-coverage could be done that way. We’ve talked about using the hospital’s iPads with patients. This crisis really makes you think you want to innovate, in a spirit of improvisation,” she said. “Now is the time to try some of these things.”
Editors note: During the COVID-19 pandemic, many hospitals are seeing unprecedented volumes of patients requiring hospital medicine groups to stretch their current resources and recruit providers from outside their groups to bolster their inpatient services. The Society of Hospital Medicine has put together the following stepwise guide for onboarding traditional outpatient and subspecialty-based providers to work on general medicine wards: COVID-19 nonhospitalist onboarding resources.
Advanced practice providers – physician assistants and nurse practitioners – at the 733-bed Emory University Hospital in Atlanta are playing an expanded role in the admission of patients into the hospital, particularly those suspected of having COVID-19.
Before the pandemic crisis, evaluation visits by the APP would have been reviewed on the same day by the supervising physician through an in-person encounter with the patient. The new protocol is not outside of scope-of-practice regulations for APPs in Georgia or of the hospital’s bylaws. But it offers a way to help limit the overall exposure of hospital staff to patients suspected of COVID-19 infection, and the total amount of time providers spend in such patients’ room. Just one provider now needs to meet the patient during the admissions process, while the attending physician can fulfill a requirement for seeing the patient within 24 hours during rounds the following day. Emergency encounters would still be done as needed.
These protocols point toward future conversations about the limits to APPs’ scope of practice, and whether more expansive approaches could be widely adopted once the current crisis is over, say advocates for the APPs’ role.
“Our APPs are primarily doing the admissions to the hospital of COVID patients and of non-COVID patients, as we’ve always done. But with COVID-infected or -suspected patients, we’re trying to minimize exposure for our providers,” explained Susan Ortiz, a certified PA, lead APP at Emory University Hospital. “In this way, we can also see more patients more efficiently.” Ms. Ortiz said she finds in talking to other APP leads in the Emory system that “each facility has its own culture and way of doing things. But for the most part, they’re all trying to do something to limit providers’ time in patients’ rooms.”
In response to the rapidly moving crisis, tactics to limit personnel in COVID patients’ rooms to the “absolutely essential” include gathering much of the needed history and other information requested from the patient by telephone, Ms. Ortiz said. This can be done either over the patient’s own cell phone or a phone placed in the room by hospital staff. Family members may be called to supplement this information, with the patient’s consent.
Once vital sign monitoring equipment is hooked up, it is possible to monitor the patient’s vital signs remotely without making frequent trips into the room. That way, in-person vital sign monitoring doesn’t need to happen routinely – at least not as often. One observation by clinicians on Ms. Ortiz’s team: listening for lung sounds with a stethoscope has not been shown to alter treatment for these patients. Once a chest X-ray shows structural changes in a patient’s lung, all lung exams are going to sound bad.
The admitting provider still needs to meet the patient in person for part of the admission visit and physical exam, but the amount of time spent in close personal contact with the patient can be much shorter, Ms. Ortiz said. For patients who are admitted, if there is a question about difficulty swallowing, they will see a speech pathologist, and if evidence of malnutrition, a nutritionist. “But we have to be extremely thoughtful about when people go into the room. So we are not ordering these ancillary services as routinely as we do during non-COVID times,” she said.
Appropriate levels of fear
Emory’s hospitalists are communicating daily about a rapidly changing situation. “We get a note by email every day, and we have a Dropbox account for downloading more information,” Ms. Ortiz said. A joint on-call system is used to provide backup coverage of APPs at the seven Emory hospitals. When replacement shifts need filling in a hurry, practitioners are able to obtain emergency credentials at any of the other hospitals. “It’s a voluntary process to sign up to be on-call,” Ms. Ortiz said. So far, that has been sufficient.
All staff have their own level of “appropriate fear” of this infection, Ms. Ortiz noted. “We have an extremely supportive group here to back up those of us who, for good reason, don’t want to be admitting the COVID patients.” Ms. Ortiz opted out of doing COVID admissions because her husband’s health places him at particular risk. “But with the cross-coverage we have, sometimes I’ll provide assistance when needed if a patient is suspected of being infected.” APPs are critical to Emory’s hospital medicine group – not ancillaries. “Everyone here feels that way. So we want to give them a lot of support. We’re all pitching in, doing it together,” she said.
“We said when we started with this, a couple of weeks before the surge started, that you could volunteer to see COVID patients,” said Emory hospitalist Jessica Nave, MD. “As we came to realize that the demand would be greater, we said you would need to opt out of seeing these patients, rather than opt in, and have a reason for doing so.” An example is pregnant staff, of which there seems to be a lot at Emory right now, Dr. Nave said, or those who are immunocompromised for other reasons. Those who don’t opt out are seeing the majority of the COVID patients, depending on actual need.
Dr. Nave is married to another hospitalist at Emory. “We can’t isolate from each other or our children. He and I have a regimented protocol for how we handle the risk, which includes taking off our shoes and clothes in the garage, showering and wiping down every place we might have touched. But those steps are not guarantees.” Other staff at Emory are isolating from their families for weeks at a time. Emory has a conference hotel offering discounted rates to staff. Nine physicians at Emory have been tested for the infection based on presenting symptoms, but at press time none had tested positive.
Streamlining code blue
Another area in which Emory has revised its policies in response to COVID-19 is for in-hospital cardiac arrest code response. Codes are inherently unpredictable, and crowd control has always been an issue for them, Dr. Nave said. “Historically, you could have 15 or more people show up when a code was called. Now, more than ever, we need to limit the number of people involved, for the same reason, avoiding unnecessary patient contact.”
The hospital’s Resuscitation Committee took the lead on developing a new policy, approved by the its Critical Care Committee and COVID Task Force, to limit the number of professionals in the room when running a code to an essential six: two doing chest compression, two managing airways, a code leader, and a critical care nurse. Outside the patient’s door, wearing the same personal protective equipment (PPE), are a pharmacist, recorder, and runner. “If you’re not one of those nine, you don’t need to be involved and should leave the area,” Dr. Nave said.
Staff have been instructed that they need to don appropriate PPE, including gown, mask, and eye wear, before entering the room for a code – even if that delays the start of intervention. “We’ve also made a code kit for each unit with quickly accessible gowns and masks. It should be used only for code blues.”
Increasing flexibility for the team
PAs and NPs in other locations are also exploring opportunities for gearing up to play larger roles in hospital care in the current crisis situation. The American Association of Physician Assistants has urged all U.S. governors to issue executive orders to waive state-specific licensing requirements for physician supervision or collaboration during the crisis, in order to increase flexibility of health care teams to deploy APPs.
AAPA believes the supervisory requirement is the biggest current barrier to mobilizing PAs and NPs. That includes those who have been furloughed from outpatient or other settings but are limited in their ability to contribute to the COVID crisis by the need to sign a supervision agreement with a physician at a new hospital.
The crisis is creating an opportunity to better appreciate the value PAs and NPs bring to health care, said Tracy Cardin, ACNP-BC, SFHM, vice president for advanced practice providers at Sound Physicians, a national hospitalist company based in Tacoma, Wash. The company recently sent a memo to the leadership of hospital sites at which it has contracts, requesting suspension of the hospitals’ requirements for a daily physician supervisory visit for APPs – which can be a hurdle when trying to leverage all hands on deck in the crisis.
NPs and PAs are stepping up and volunteering for COVID patients, Ms. Cardin said. Some have even taken leaves from their jobs to go to New York to help out at the epicenter of the U.S. crisis. “They want to make a difference. We’ve been deploying nonhospital medicine APPs from surgery, primary care, and elsewhere, embedding them on the hospital medicine team.”
Before the crisis, APPs at Sound Physicians weren’t always able to practice at the top of their licenses, depending on the hospital setting, added Alicia Scheffer, CNP, the company’s Great Lakes regional director for APPs. “Then COVID-19 showed up and really expedited conversations about how to maximize caseloads using APPs and about the fear of failing patients due to lack of capacity.”
In several locales, Sound Physicians is using quarantined providers to do telephone triage, or staffing ICUs with APPs backed up by telemedicine. “In APP-led ICUs, where the nurses are leading, they are intubating patients, placing central lines, things we weren’t allowed to do before,” Ms. Scheffer said.
A spirit of improvisation
There is a lot of tension at Emory University Hospital these days, reflecting the fears and uncertainties about the crisis, Dr. Nave said. “But there’s also a strangely powerful camaraderie like I’ve never seen before. When you walk onto the COVID units, you feel immediately bonded to the nurses, the techs, the phlebotomists. And you feel like you could talk about anything.”
Changes such as those made at Emory, have been talked about for a while, for example when hospitalists are having a busy night, she said. “But because this is a big cultural change, some physicians resisted it. We trust our APPs. But if the doctor’s name is on a patient chart, they want to see the patient – just for their own comfort level.”
Ms. Ortiz thinks the experience with the COVID crisis could help to advance the conversation about the appropriate role for APPs and their scope of practice in hospital medicine, once the current crisis has passed. “People were used to always doing things a certain way. This experience, hopefully, will get us to the point where attending physicians have more comfort with the APP’s ability to act autonomously,” she said.
“We’ve also talked about piloting telemedicine examinations using Zoom,” Dr. Nave added. “It’s making us think a lot of remote cross-coverage could be done that way. We’ve talked about using the hospital’s iPads with patients. This crisis really makes you think you want to innovate, in a spirit of improvisation,” she said. “Now is the time to try some of these things.”
Editors note: During the COVID-19 pandemic, many hospitals are seeing unprecedented volumes of patients requiring hospital medicine groups to stretch their current resources and recruit providers from outside their groups to bolster their inpatient services. The Society of Hospital Medicine has put together the following stepwise guide for onboarding traditional outpatient and subspecialty-based providers to work on general medicine wards: COVID-19 nonhospitalist onboarding resources.
MRSA decolonization reduces postdischarge infections
Background: MRSA carriers are at higher risk of infection and rehospitalization after hospital discharge. Education regarding hygiene, environmental cleaning, and decolonization of MRSA carriers have been used as possible preventive strategies. Decolonization has been effective in reducing surgical-site infections, recurrent skin infections, and infections in ICU. However, there is sparsity of data on the efficacy of routine decolonization of MRSA carriers after hospital discharge.
Study design: Multicenter, randomized, unblinded controlled trial.
Setting: A total of 17 hospitals and seven nursing homes in Southern California.
Synopsis: The study included 2,121 inpatients hospitalized within the previous 30 days and found to be MRSA carriers. Patients were randomized to education only (1,063) or decolonization plus education (1,058), with both groups followed for 12 months after discharge. Decolonization consisted of 4% rinse-off chlorhexidine for daily bathing or showering, 0.12% chlorhexidine mouthwash twice daily, and 2% nasal mupirocin twice daily. The primary outcome was MRSA infection as defined by the CDC. Secondary outcomes included MRSA infection based on clinical judgment, infection from any cause, and infection-related hospitalization. Per protocol analysis showed that MRSA infection occurred in 9.2% in the education group and 6.3% in the decolonization plus education group, with 30% reduction in the risk of infection (HR, 0.70; 95% CI, 0.51-0.99; number needed to treat to prevent one infection, 30). The decolonization group also had a lower hazard of clinically judged infection from any cause (HR, 0.83; 95% CI, 0.70-0.99) and infection-related hospitalization (HR, 0.76; 95% CI, 0.62-0.93).
Limitations of the study include unblinded intervention, missing of milder infections that might not have required hospitalization, and frequent insufficient documentation in charts for events to be deemed infection according to the CDC criteria.
Bottom line: Decolonization of MRSA carriers post discharge may lower MRSA-related infections and infections more than hygiene education alone.
Citation: Huang SS et al. Decolonization to reduce postdischarge infection risk among MRSA carriers. N Eng J Med. 2019;380:638-50.
Dr. Vedamurthy is a hospitalist at Massachusetts General Hospital.
Background: MRSA carriers are at higher risk of infection and rehospitalization after hospital discharge. Education regarding hygiene, environmental cleaning, and decolonization of MRSA carriers have been used as possible preventive strategies. Decolonization has been effective in reducing surgical-site infections, recurrent skin infections, and infections in ICU. However, there is sparsity of data on the efficacy of routine decolonization of MRSA carriers after hospital discharge.
Study design: Multicenter, randomized, unblinded controlled trial.
Setting: A total of 17 hospitals and seven nursing homes in Southern California.
Synopsis: The study included 2,121 inpatients hospitalized within the previous 30 days and found to be MRSA carriers. Patients were randomized to education only (1,063) or decolonization plus education (1,058), with both groups followed for 12 months after discharge. Decolonization consisted of 4% rinse-off chlorhexidine for daily bathing or showering, 0.12% chlorhexidine mouthwash twice daily, and 2% nasal mupirocin twice daily. The primary outcome was MRSA infection as defined by the CDC. Secondary outcomes included MRSA infection based on clinical judgment, infection from any cause, and infection-related hospitalization. Per protocol analysis showed that MRSA infection occurred in 9.2% in the education group and 6.3% in the decolonization plus education group, with 30% reduction in the risk of infection (HR, 0.70; 95% CI, 0.51-0.99; number needed to treat to prevent one infection, 30). The decolonization group also had a lower hazard of clinically judged infection from any cause (HR, 0.83; 95% CI, 0.70-0.99) and infection-related hospitalization (HR, 0.76; 95% CI, 0.62-0.93).
Limitations of the study include unblinded intervention, missing of milder infections that might not have required hospitalization, and frequent insufficient documentation in charts for events to be deemed infection according to the CDC criteria.
Bottom line: Decolonization of MRSA carriers post discharge may lower MRSA-related infections and infections more than hygiene education alone.
Citation: Huang SS et al. Decolonization to reduce postdischarge infection risk among MRSA carriers. N Eng J Med. 2019;380:638-50.
Dr. Vedamurthy is a hospitalist at Massachusetts General Hospital.
Background: MRSA carriers are at higher risk of infection and rehospitalization after hospital discharge. Education regarding hygiene, environmental cleaning, and decolonization of MRSA carriers have been used as possible preventive strategies. Decolonization has been effective in reducing surgical-site infections, recurrent skin infections, and infections in ICU. However, there is sparsity of data on the efficacy of routine decolonization of MRSA carriers after hospital discharge.
Study design: Multicenter, randomized, unblinded controlled trial.
Setting: A total of 17 hospitals and seven nursing homes in Southern California.
Synopsis: The study included 2,121 inpatients hospitalized within the previous 30 days and found to be MRSA carriers. Patients were randomized to education only (1,063) or decolonization plus education (1,058), with both groups followed for 12 months after discharge. Decolonization consisted of 4% rinse-off chlorhexidine for daily bathing or showering, 0.12% chlorhexidine mouthwash twice daily, and 2% nasal mupirocin twice daily. The primary outcome was MRSA infection as defined by the CDC. Secondary outcomes included MRSA infection based on clinical judgment, infection from any cause, and infection-related hospitalization. Per protocol analysis showed that MRSA infection occurred in 9.2% in the education group and 6.3% in the decolonization plus education group, with 30% reduction in the risk of infection (HR, 0.70; 95% CI, 0.51-0.99; number needed to treat to prevent one infection, 30). The decolonization group also had a lower hazard of clinically judged infection from any cause (HR, 0.83; 95% CI, 0.70-0.99) and infection-related hospitalization (HR, 0.76; 95% CI, 0.62-0.93).
Limitations of the study include unblinded intervention, missing of milder infections that might not have required hospitalization, and frequent insufficient documentation in charts for events to be deemed infection according to the CDC criteria.
Bottom line: Decolonization of MRSA carriers post discharge may lower MRSA-related infections and infections more than hygiene education alone.
Citation: Huang SS et al. Decolonization to reduce postdischarge infection risk among MRSA carriers. N Eng J Med. 2019;380:638-50.
Dr. Vedamurthy is a hospitalist at Massachusetts General Hospital.
Andexanet alfa reverses factor Xa inhibitors
Background: Factor Xa inhibitors have become increasingly popular in the treatment and prevention of thrombotic events, but the lack of specific reversal agents in the event of life-threatening or uncontrolled bleeding may limit their use. Andexanet alfa is a new Food and Drug Administration–approved reversal agent which rapidly reduces anti–factor Xa activity, thereby reversing the anticoagulation effects of factor Xa inhibitors.
Study design: A prospective, open-label, single-group cohort study.
Setting: An industry-sponsored, multicenter study.
Synopsis: The study evaluated 352 adult patients who had acute major bleeding (such as intracranial hemorrhage [64%] or GI bleeding [26%] within 18 hours after administration of a factor Xa inhibitor, including apixaban, rivaroxaban, or edoxaban). Efficacy was assessed in 254 patients who met criteria for severe bleeding and elevated baseline anti–factor Xa activity. Patients were administered a bolus dose of andexanet alfa followed by a 2-hour infusion. The median anti–factor Xa activity reduced by 92% each among patients receiving apixaban or rivaroxaban. The majority (82%) of evaluable patients achieved excellent or good hemostasis at 12 hours after andexanet alfa administration, which compares favorably with the hemostatic efficacy of 72% observed with prothrombin complex concentrate used to reverse anticoagulation in patients treated with vitamin K antagonists. Of patients in the study, 10% experienced a thrombotic event during the 30-day follow-up period, and 14% died.
Limitations of the study include lack of a control group and absence of a significant relationship between a reduction in anti–factor Xa activity and hemostasis. The sponsor is planning to conduct a randomized trial with FDA guidance in the near future.
Bottom line: Andexanet alfa is an FDA-approved agent and appears effective in achieving hemostasis in patients with a factor Xa inhibitor–associated major acute bleeding.
Citation: Connolly SJ et al. Full study report of andexanet alfa for bleeding associated with factor Xa inhibitors. N Eng J Med. 2019 Feb 7. doi: 10.1056/NEJMoa1814051.
Dr. Vedamurthy is a hospitalist at Massachusetts General Hospital.
Background: Factor Xa inhibitors have become increasingly popular in the treatment and prevention of thrombotic events, but the lack of specific reversal agents in the event of life-threatening or uncontrolled bleeding may limit their use. Andexanet alfa is a new Food and Drug Administration–approved reversal agent which rapidly reduces anti–factor Xa activity, thereby reversing the anticoagulation effects of factor Xa inhibitors.
Study design: A prospective, open-label, single-group cohort study.
Setting: An industry-sponsored, multicenter study.
Synopsis: The study evaluated 352 adult patients who had acute major bleeding (such as intracranial hemorrhage [64%] or GI bleeding [26%] within 18 hours after administration of a factor Xa inhibitor, including apixaban, rivaroxaban, or edoxaban). Efficacy was assessed in 254 patients who met criteria for severe bleeding and elevated baseline anti–factor Xa activity. Patients were administered a bolus dose of andexanet alfa followed by a 2-hour infusion. The median anti–factor Xa activity reduced by 92% each among patients receiving apixaban or rivaroxaban. The majority (82%) of evaluable patients achieved excellent or good hemostasis at 12 hours after andexanet alfa administration, which compares favorably with the hemostatic efficacy of 72% observed with prothrombin complex concentrate used to reverse anticoagulation in patients treated with vitamin K antagonists. Of patients in the study, 10% experienced a thrombotic event during the 30-day follow-up period, and 14% died.
Limitations of the study include lack of a control group and absence of a significant relationship between a reduction in anti–factor Xa activity and hemostasis. The sponsor is planning to conduct a randomized trial with FDA guidance in the near future.
Bottom line: Andexanet alfa is an FDA-approved agent and appears effective in achieving hemostasis in patients with a factor Xa inhibitor–associated major acute bleeding.
Citation: Connolly SJ et al. Full study report of andexanet alfa for bleeding associated with factor Xa inhibitors. N Eng J Med. 2019 Feb 7. doi: 10.1056/NEJMoa1814051.
Dr. Vedamurthy is a hospitalist at Massachusetts General Hospital.
Background: Factor Xa inhibitors have become increasingly popular in the treatment and prevention of thrombotic events, but the lack of specific reversal agents in the event of life-threatening or uncontrolled bleeding may limit their use. Andexanet alfa is a new Food and Drug Administration–approved reversal agent which rapidly reduces anti–factor Xa activity, thereby reversing the anticoagulation effects of factor Xa inhibitors.
Study design: A prospective, open-label, single-group cohort study.
Setting: An industry-sponsored, multicenter study.
Synopsis: The study evaluated 352 adult patients who had acute major bleeding (such as intracranial hemorrhage [64%] or GI bleeding [26%] within 18 hours after administration of a factor Xa inhibitor, including apixaban, rivaroxaban, or edoxaban). Efficacy was assessed in 254 patients who met criteria for severe bleeding and elevated baseline anti–factor Xa activity. Patients were administered a bolus dose of andexanet alfa followed by a 2-hour infusion. The median anti–factor Xa activity reduced by 92% each among patients receiving apixaban or rivaroxaban. The majority (82%) of evaluable patients achieved excellent or good hemostasis at 12 hours after andexanet alfa administration, which compares favorably with the hemostatic efficacy of 72% observed with prothrombin complex concentrate used to reverse anticoagulation in patients treated with vitamin K antagonists. Of patients in the study, 10% experienced a thrombotic event during the 30-day follow-up period, and 14% died.
Limitations of the study include lack of a control group and absence of a significant relationship between a reduction in anti–factor Xa activity and hemostasis. The sponsor is planning to conduct a randomized trial with FDA guidance in the near future.
Bottom line: Andexanet alfa is an FDA-approved agent and appears effective in achieving hemostasis in patients with a factor Xa inhibitor–associated major acute bleeding.
Citation: Connolly SJ et al. Full study report of andexanet alfa for bleeding associated with factor Xa inhibitors. N Eng J Med. 2019 Feb 7. doi: 10.1056/NEJMoa1814051.
Dr. Vedamurthy is a hospitalist at Massachusetts General Hospital.
COVID-19: Eight steps for getting ready to see patients again
After COVID-19 hit the Denver area, internist Jean Kutner, MD, and her clinical colleagues drastically reduced the number of patients they saw and kept a minimum number of people in the office. A small team sees patients who still require in-person visits on one side of the clinic; on the other side, another team conducts clinic-based telehealth visits. A rotating schedule allows for social distancing.
The rest of the practice’s physicians are home, conducting more virtual visits.
Dr. Kutner said she is looking forward to reopening her practice completely at some point. She said she realizes that the practice probably won’t be exactly the same as before.
“We have to embrace the fact that the way we practice medicine has fundamentally changed,” said Dr. Kutner, professor of medicine at the University of Colorado at Denver, Aurora, and incoming president of the Society of General Internal Medicine. She anticipates keeping many of these changes in place for the foreseeable future.
Nearly half of 2,600 primary care physicians who responded to a recent national survey said they were struggling to remain open during the crisis. Most have had to limit wellness/chronic-disease management visits, and nearly half reported that physicians or staff were out sick. Layoffs, furloughs, and reduced hours are commonplace; some practices were forced to shut down entirely.
Social distancing helps reduce the rates of hospitalizations and deaths.
For example, remote monitoring capabilities have reduced the need for in-person checks of vital signs, such as respiratory rate oxygenation, blood glucose levels, and heart rate. “We can’t go back,” she said.
Dr. Kutner sees the pandemic as an opportunity to innovate, to think about how primary practices can best utilize their resources, face-to-face time with patients, and when and how to best leverage virtual visits in a way that improves patient health. The goal, of course, is to meet the needs of the patients while keeping everyone safe.
Like many physicians in private practice, Dr. Kutner is concerned about revenue. She hopes the Centers for Medicare & Medicaid Services makes its temporary waivers permanent.
What you need to consider when planning to reopen your office
Physicians say their post-COVID-19 practices will look very different from their prepandemic practices. Many plan to maintain guidelines, such as those from the AAFP, long after the pandemic has peaked.
If you are starting to think about reopening, here are some major considerations.
1. Develop procedures and practices that will keep your patients and staff safe.
“When we return, the first thing we need to do is limit the number of patients in the waiting room,” said Clinton Coleman, MD, who practices internal medicine and nephrology in Teaneck, N.J. “No one is comfortable in a waiting room any longer,” said Dr. Coleman, chief of internal medicine at Holy Name Medical Center in Teaneck.
Careful planning is required to resume in-person care of patients requiring non-COVID-19 care, as well as all aspects of care, according to the CMS. Adequate staff, testing, supplies, and support services, such as pathology services, are just a few considerations. The CMS recommends that physicians “evaluate the necessity of the care based on clinical needs. Providers should prioritize surgical/procedural care and high-complexity chronic disease management; however, select preventive services may also be highly necessary.”
The American Medical Association recently unveiled a checklist for reopening. One key recommendation was for practices to select a date for reopening the office, ideally preceded by a “soft” or incremental reopening to ensure that new procedures are working. The AMA also recommends opening incrementally, continuing telehealth while also inviting patients back into the office.
2. Figure out how to safely see patients, particularly in your waiting areas and common spaces.
Logistic factors, such as managing patient flow, will change. Waiting rooms will be emptier; in some locations, patients may be asked to wait in their cars until an exam room is available.
The AMA also suggests limiting nonpatient visitors by posting the practice’s policy at the entrance and on the practice’s website. If service calls for repairs are needed, have those visitors come outside of normal operating hours.
Commonly shared objects such magazines or toys in pediatric offices will likely disappear. Wipes, hand sanitizers, and the wearing of masks will become even more commonplace. Those who suspect they’re ill or who have respiratory symptoms may be relegated to specific “sick visit” appointment times or taken to designated exam rooms, which will be thoroughly sanitized between patients.
3. Prepare for routine screening of staff and other facility workers.
According to recent CMS guidelines, you and your staff will need to undergo routine screening, as will others who work in the facility (housekeeping, delivery personnel, and anyone else who enters the area). This may mean regularly stocking screening tests and setting guidelines for what to do if one of your staff tests positive.
You may need to hire temporary workers if your staff tests positive. The CDC recommends at the very least understanding the minimum staffing requirements to ensure good patient care and a safe work environment. Consider adjusting staff schedules and rotating clinical personnel to positions that support patient care activities. You may also want to look into cross-training your office staff so that they can fill in or help out with each other’s responsibilities if one or more persons are ill.
Dr. Kutner is on board with these changes. “We don’t want to get rid of social distancing right away, because it will give us a new spike in cases – how do we figure out patient flow while honoring that?”
4. Develop a strategy for triaging and caring for a potential backlog of patients.
“Many of my partners are scared right now because they have no income except for emergencies,” said Andrew Gonzalez, MD, JD, MPH, a vascular surgeon and assistant professor of surgery at Indiana University, Indianapolis. Almost all nonemergency surgery has been put on hold.
“If we don’t operate, the practice makes no money,” he said. He thinks revenue will continue to be a problem as long as patients fear in-person consultations or undergoing surgery for nonacute problems such as hernias.
As restrictions ease, most physicians will face an enormous backlog of patients and will need to find new ways of triaging the most serious cases, he says. Telehealth will help, but Dr. Gonzalez predicts many of his colleagues will be working longer hours and on weekends to catch up. “Physicians are going to have to really think about ways of optimizing their time and workflow to be very efficient, because the backlog is going to prodigious.”
5. Anticipate changes in patient expectations.
This may entail your reconsidering tests and procedures you previously performed and considering developing new sources for some services, phasing some others out, and revising your current approach. It will most likely also mean that you make telemedicine and televisits a greater part of your practice.
Carolyn Kaloostian, MD, a family medicine and geriatric practitioner in Los Angeles, points to increased reliance on community agencies for conducting common office-based procedures, such as performing blood tests and taking ECGs and x-rays. “A lot of patients are using telemedicine or telephone visits and get the lab work or x-rays somewhere that’s less congested,” she said. To become sustainable, many of these changes will hinge on economics – whether and how they are reimbursed.
The pandemic will leave lasting effects in our health care delivery, according to Dr. Kaloostian. She is sure many of her colleagues’ and patients’ current experiences will be infused into future care. “I can’t say we’ll ever be back to normal, necessarily.”
Even if the CMS rolls back its telehealth waivers, some physicians, like Dr. Coleman, plan to continue using the technology extensively. He’s confident about the level of care he’s currently providing patients in his practice. It allows him to better manage many low-income patients who can’t access his office regularly. Not only does splitting his time between the clinic and telehealth allow him to be more available for more patients, he says it also empowers patients to take better care of themselves.
6. Consider a new way to conduct “check-in visits.”
One thing that will likely go by the wayside are “check-in” visits, or so-called “social visits,” those interval appointments that can just as easily be completed virtually. “Patients are going to ask why they need to drive 3 hours so you can tell them their incision looks fine from an operation you did 5 years ago,” Dr. Gonzalez said.
He’s concerned that some people will remain so fearful of the health care system that a formerly busy practice may see the pendulum swing in the opposite direction. If an aneurysm patient skips a visit, that person may also decide not to undergo a CT scan – and something preventable will be missed. “Not everybody has the option to stay away until they feel comfortable. They’re basically playing hot potato. And at some point, the music’s going to stop,” Dr. Gonzalez said.
The pandemic has prompted some very honest conversations with his patients about what truly needs to get done and what may be optional. “Everyone has now become a hyper-rational user of health care,” he said.
7. If you haven’t yet, consider becoming more involved with technology.
In addition to greater use of telehealth, Dr. Kaloostian, assistant professor of clinical family medicine at the University of Southern California, Los Angeles, foresees continued reliance upon technology such as smartphone apps that connect with a user’s smartwatch. This allows for more proactive, remote monitoring.
“For example, any time a patient is having recurrent nighttime trips to the bathroom, I’ll get pinged and know that,” she explained. It means she can reach out and ask about any changes before a fall occurs or a condition worsens. “It provides reassurance to the provider and to the patient that you’re doing all you can to keep an eye on them from afar.”
8. Update or reformulate your business plans.
Some physicians in smaller practices may have to temporarily or permanently rethink their situation. Those who have struggled or who have closed down and are considering reopening need to update their business plans. It may be safer economically to become part of a bigger group that is affiliated with an academic center or join a larger health care system that has more funds or resources.
In addition, Dr. Kaloostian suggests that primary care physicians become more flexible in the short term, perhaps working part time in an urgent care clinic or larger organization to gain additional sources of revenue until their own practice finances pick back up.
For offices that reopen, the AMA recommends contacting medical malpractice insurance carriers to check on possible liability concerns. Congress has provided certain protections for clinicians during this time, but malpractice carriers may have more information and may offer more coverage.
Dr. Coleman said a hybrid model of fewer in-person and more telehealth visits “will allow me to practice in a different way.” If the CMS reimposes prior restrictions, reimbursement may be affected initially, but that will likely change once insurers see the increased cost-effectiveness of this approach. Patients with minor complaints, those who need to have medications refilled, and patients with chronic diseases that need managing won’t have to deal with crowded waiting rooms, and it will help mitigate problems with infection control.
If there’s any upside to the pandemic, it’s an increase in attention given to advanced care planning, said Dr. Kutner. It’s something she hopes continues after everyone stops being in crisis mode. “We’re realizing how important it is to have these conversations and document people’s goals and values and code status,” she said.
Are offices likely to open soon?
An assumption that may or may not be valid is that a practice will remain viable and can return to former capacity. Prior to passage of the CARES Act on March 27, a survey from Kareo, a company in Irvine, California, that makes a technology platform for independent physician practices, found that 9% of respondents reported practice closures. Many more reported concern about potential closures as patient office visits plummet because of stay-at-home orders and other concerns.
By mid-April, a survey from the Primary Care Collaborative and the Larry A. Green Center found that 42% of practices had experienced layoffs and had furloughed staff. Most (85%) have seen dramatic decreases in patient volume.
“Reopening the economy or loosening physical distancing restrictions will be difficult when 20% of primary care practices predict closure within 4 weeks,” the survey concluded.
For the practices and the doctors who make it through this, we’re going to probably be better, stronger, and more efficient, Dr. Gonzalez predicts. This shock has uncovered a lot of weaknesses in the American health care system that doctors have known about and have been complaining about for a long time. It will take an open mind and lots of continued flexibility on the part of physicians, hospitals, health care systems, and the government for these changes to stick.
A version of this article originally appeared on Medscape.com.
After COVID-19 hit the Denver area, internist Jean Kutner, MD, and her clinical colleagues drastically reduced the number of patients they saw and kept a minimum number of people in the office. A small team sees patients who still require in-person visits on one side of the clinic; on the other side, another team conducts clinic-based telehealth visits. A rotating schedule allows for social distancing.
The rest of the practice’s physicians are home, conducting more virtual visits.
Dr. Kutner said she is looking forward to reopening her practice completely at some point. She said she realizes that the practice probably won’t be exactly the same as before.
“We have to embrace the fact that the way we practice medicine has fundamentally changed,” said Dr. Kutner, professor of medicine at the University of Colorado at Denver, Aurora, and incoming president of the Society of General Internal Medicine. She anticipates keeping many of these changes in place for the foreseeable future.
Nearly half of 2,600 primary care physicians who responded to a recent national survey said they were struggling to remain open during the crisis. Most have had to limit wellness/chronic-disease management visits, and nearly half reported that physicians or staff were out sick. Layoffs, furloughs, and reduced hours are commonplace; some practices were forced to shut down entirely.
Social distancing helps reduce the rates of hospitalizations and deaths.
For example, remote monitoring capabilities have reduced the need for in-person checks of vital signs, such as respiratory rate oxygenation, blood glucose levels, and heart rate. “We can’t go back,” she said.
Dr. Kutner sees the pandemic as an opportunity to innovate, to think about how primary practices can best utilize their resources, face-to-face time with patients, and when and how to best leverage virtual visits in a way that improves patient health. The goal, of course, is to meet the needs of the patients while keeping everyone safe.
Like many physicians in private practice, Dr. Kutner is concerned about revenue. She hopes the Centers for Medicare & Medicaid Services makes its temporary waivers permanent.
What you need to consider when planning to reopen your office
Physicians say their post-COVID-19 practices will look very different from their prepandemic practices. Many plan to maintain guidelines, such as those from the AAFP, long after the pandemic has peaked.
If you are starting to think about reopening, here are some major considerations.
1. Develop procedures and practices that will keep your patients and staff safe.
“When we return, the first thing we need to do is limit the number of patients in the waiting room,” said Clinton Coleman, MD, who practices internal medicine and nephrology in Teaneck, N.J. “No one is comfortable in a waiting room any longer,” said Dr. Coleman, chief of internal medicine at Holy Name Medical Center in Teaneck.
Careful planning is required to resume in-person care of patients requiring non-COVID-19 care, as well as all aspects of care, according to the CMS. Adequate staff, testing, supplies, and support services, such as pathology services, are just a few considerations. The CMS recommends that physicians “evaluate the necessity of the care based on clinical needs. Providers should prioritize surgical/procedural care and high-complexity chronic disease management; however, select preventive services may also be highly necessary.”
The American Medical Association recently unveiled a checklist for reopening. One key recommendation was for practices to select a date for reopening the office, ideally preceded by a “soft” or incremental reopening to ensure that new procedures are working. The AMA also recommends opening incrementally, continuing telehealth while also inviting patients back into the office.
2. Figure out how to safely see patients, particularly in your waiting areas and common spaces.
Logistic factors, such as managing patient flow, will change. Waiting rooms will be emptier; in some locations, patients may be asked to wait in their cars until an exam room is available.
The AMA also suggests limiting nonpatient visitors by posting the practice’s policy at the entrance and on the practice’s website. If service calls for repairs are needed, have those visitors come outside of normal operating hours.
Commonly shared objects such magazines or toys in pediatric offices will likely disappear. Wipes, hand sanitizers, and the wearing of masks will become even more commonplace. Those who suspect they’re ill or who have respiratory symptoms may be relegated to specific “sick visit” appointment times or taken to designated exam rooms, which will be thoroughly sanitized between patients.
3. Prepare for routine screening of staff and other facility workers.
According to recent CMS guidelines, you and your staff will need to undergo routine screening, as will others who work in the facility (housekeeping, delivery personnel, and anyone else who enters the area). This may mean regularly stocking screening tests and setting guidelines for what to do if one of your staff tests positive.
You may need to hire temporary workers if your staff tests positive. The CDC recommends at the very least understanding the minimum staffing requirements to ensure good patient care and a safe work environment. Consider adjusting staff schedules and rotating clinical personnel to positions that support patient care activities. You may also want to look into cross-training your office staff so that they can fill in or help out with each other’s responsibilities if one or more persons are ill.
Dr. Kutner is on board with these changes. “We don’t want to get rid of social distancing right away, because it will give us a new spike in cases – how do we figure out patient flow while honoring that?”
4. Develop a strategy for triaging and caring for a potential backlog of patients.
“Many of my partners are scared right now because they have no income except for emergencies,” said Andrew Gonzalez, MD, JD, MPH, a vascular surgeon and assistant professor of surgery at Indiana University, Indianapolis. Almost all nonemergency surgery has been put on hold.
“If we don’t operate, the practice makes no money,” he said. He thinks revenue will continue to be a problem as long as patients fear in-person consultations or undergoing surgery for nonacute problems such as hernias.
As restrictions ease, most physicians will face an enormous backlog of patients and will need to find new ways of triaging the most serious cases, he says. Telehealth will help, but Dr. Gonzalez predicts many of his colleagues will be working longer hours and on weekends to catch up. “Physicians are going to have to really think about ways of optimizing their time and workflow to be very efficient, because the backlog is going to prodigious.”
5. Anticipate changes in patient expectations.
This may entail your reconsidering tests and procedures you previously performed and considering developing new sources for some services, phasing some others out, and revising your current approach. It will most likely also mean that you make telemedicine and televisits a greater part of your practice.
Carolyn Kaloostian, MD, a family medicine and geriatric practitioner in Los Angeles, points to increased reliance on community agencies for conducting common office-based procedures, such as performing blood tests and taking ECGs and x-rays. “A lot of patients are using telemedicine or telephone visits and get the lab work or x-rays somewhere that’s less congested,” she said. To become sustainable, many of these changes will hinge on economics – whether and how they are reimbursed.
The pandemic will leave lasting effects in our health care delivery, according to Dr. Kaloostian. She is sure many of her colleagues’ and patients’ current experiences will be infused into future care. “I can’t say we’ll ever be back to normal, necessarily.”
Even if the CMS rolls back its telehealth waivers, some physicians, like Dr. Coleman, plan to continue using the technology extensively. He’s confident about the level of care he’s currently providing patients in his practice. It allows him to better manage many low-income patients who can’t access his office regularly. Not only does splitting his time between the clinic and telehealth allow him to be more available for more patients, he says it also empowers patients to take better care of themselves.
6. Consider a new way to conduct “check-in visits.”
One thing that will likely go by the wayside are “check-in” visits, or so-called “social visits,” those interval appointments that can just as easily be completed virtually. “Patients are going to ask why they need to drive 3 hours so you can tell them their incision looks fine from an operation you did 5 years ago,” Dr. Gonzalez said.
He’s concerned that some people will remain so fearful of the health care system that a formerly busy practice may see the pendulum swing in the opposite direction. If an aneurysm patient skips a visit, that person may also decide not to undergo a CT scan – and something preventable will be missed. “Not everybody has the option to stay away until they feel comfortable. They’re basically playing hot potato. And at some point, the music’s going to stop,” Dr. Gonzalez said.
The pandemic has prompted some very honest conversations with his patients about what truly needs to get done and what may be optional. “Everyone has now become a hyper-rational user of health care,” he said.
7. If you haven’t yet, consider becoming more involved with technology.
In addition to greater use of telehealth, Dr. Kaloostian, assistant professor of clinical family medicine at the University of Southern California, Los Angeles, foresees continued reliance upon technology such as smartphone apps that connect with a user’s smartwatch. This allows for more proactive, remote monitoring.
“For example, any time a patient is having recurrent nighttime trips to the bathroom, I’ll get pinged and know that,” she explained. It means she can reach out and ask about any changes before a fall occurs or a condition worsens. “It provides reassurance to the provider and to the patient that you’re doing all you can to keep an eye on them from afar.”
8. Update or reformulate your business plans.
Some physicians in smaller practices may have to temporarily or permanently rethink their situation. Those who have struggled or who have closed down and are considering reopening need to update their business plans. It may be safer economically to become part of a bigger group that is affiliated with an academic center or join a larger health care system that has more funds or resources.
In addition, Dr. Kaloostian suggests that primary care physicians become more flexible in the short term, perhaps working part time in an urgent care clinic or larger organization to gain additional sources of revenue until their own practice finances pick back up.
For offices that reopen, the AMA recommends contacting medical malpractice insurance carriers to check on possible liability concerns. Congress has provided certain protections for clinicians during this time, but malpractice carriers may have more information and may offer more coverage.
Dr. Coleman said a hybrid model of fewer in-person and more telehealth visits “will allow me to practice in a different way.” If the CMS reimposes prior restrictions, reimbursement may be affected initially, but that will likely change once insurers see the increased cost-effectiveness of this approach. Patients with minor complaints, those who need to have medications refilled, and patients with chronic diseases that need managing won’t have to deal with crowded waiting rooms, and it will help mitigate problems with infection control.
If there’s any upside to the pandemic, it’s an increase in attention given to advanced care planning, said Dr. Kutner. It’s something she hopes continues after everyone stops being in crisis mode. “We’re realizing how important it is to have these conversations and document people’s goals and values and code status,” she said.
Are offices likely to open soon?
An assumption that may or may not be valid is that a practice will remain viable and can return to former capacity. Prior to passage of the CARES Act on March 27, a survey from Kareo, a company in Irvine, California, that makes a technology platform for independent physician practices, found that 9% of respondents reported practice closures. Many more reported concern about potential closures as patient office visits plummet because of stay-at-home orders and other concerns.
By mid-April, a survey from the Primary Care Collaborative and the Larry A. Green Center found that 42% of practices had experienced layoffs and had furloughed staff. Most (85%) have seen dramatic decreases in patient volume.
“Reopening the economy or loosening physical distancing restrictions will be difficult when 20% of primary care practices predict closure within 4 weeks,” the survey concluded.
For the practices and the doctors who make it through this, we’re going to probably be better, stronger, and more efficient, Dr. Gonzalez predicts. This shock has uncovered a lot of weaknesses in the American health care system that doctors have known about and have been complaining about for a long time. It will take an open mind and lots of continued flexibility on the part of physicians, hospitals, health care systems, and the government for these changes to stick.
A version of this article originally appeared on Medscape.com.
After COVID-19 hit the Denver area, internist Jean Kutner, MD, and her clinical colleagues drastically reduced the number of patients they saw and kept a minimum number of people in the office. A small team sees patients who still require in-person visits on one side of the clinic; on the other side, another team conducts clinic-based telehealth visits. A rotating schedule allows for social distancing.
The rest of the practice’s physicians are home, conducting more virtual visits.
Dr. Kutner said she is looking forward to reopening her practice completely at some point. She said she realizes that the practice probably won’t be exactly the same as before.
“We have to embrace the fact that the way we practice medicine has fundamentally changed,” said Dr. Kutner, professor of medicine at the University of Colorado at Denver, Aurora, and incoming president of the Society of General Internal Medicine. She anticipates keeping many of these changes in place for the foreseeable future.
Nearly half of 2,600 primary care physicians who responded to a recent national survey said they were struggling to remain open during the crisis. Most have had to limit wellness/chronic-disease management visits, and nearly half reported that physicians or staff were out sick. Layoffs, furloughs, and reduced hours are commonplace; some practices were forced to shut down entirely.
Social distancing helps reduce the rates of hospitalizations and deaths.
For example, remote monitoring capabilities have reduced the need for in-person checks of vital signs, such as respiratory rate oxygenation, blood glucose levels, and heart rate. “We can’t go back,” she said.
Dr. Kutner sees the pandemic as an opportunity to innovate, to think about how primary practices can best utilize their resources, face-to-face time with patients, and when and how to best leverage virtual visits in a way that improves patient health. The goal, of course, is to meet the needs of the patients while keeping everyone safe.
Like many physicians in private practice, Dr. Kutner is concerned about revenue. She hopes the Centers for Medicare & Medicaid Services makes its temporary waivers permanent.
What you need to consider when planning to reopen your office
Physicians say their post-COVID-19 practices will look very different from their prepandemic practices. Many plan to maintain guidelines, such as those from the AAFP, long after the pandemic has peaked.
If you are starting to think about reopening, here are some major considerations.
1. Develop procedures and practices that will keep your patients and staff safe.
“When we return, the first thing we need to do is limit the number of patients in the waiting room,” said Clinton Coleman, MD, who practices internal medicine and nephrology in Teaneck, N.J. “No one is comfortable in a waiting room any longer,” said Dr. Coleman, chief of internal medicine at Holy Name Medical Center in Teaneck.
Careful planning is required to resume in-person care of patients requiring non-COVID-19 care, as well as all aspects of care, according to the CMS. Adequate staff, testing, supplies, and support services, such as pathology services, are just a few considerations. The CMS recommends that physicians “evaluate the necessity of the care based on clinical needs. Providers should prioritize surgical/procedural care and high-complexity chronic disease management; however, select preventive services may also be highly necessary.”
The American Medical Association recently unveiled a checklist for reopening. One key recommendation was for practices to select a date for reopening the office, ideally preceded by a “soft” or incremental reopening to ensure that new procedures are working. The AMA also recommends opening incrementally, continuing telehealth while also inviting patients back into the office.
2. Figure out how to safely see patients, particularly in your waiting areas and common spaces.
Logistic factors, such as managing patient flow, will change. Waiting rooms will be emptier; in some locations, patients may be asked to wait in their cars until an exam room is available.
The AMA also suggests limiting nonpatient visitors by posting the practice’s policy at the entrance and on the practice’s website. If service calls for repairs are needed, have those visitors come outside of normal operating hours.
Commonly shared objects such magazines or toys in pediatric offices will likely disappear. Wipes, hand sanitizers, and the wearing of masks will become even more commonplace. Those who suspect they’re ill or who have respiratory symptoms may be relegated to specific “sick visit” appointment times or taken to designated exam rooms, which will be thoroughly sanitized between patients.
3. Prepare for routine screening of staff and other facility workers.
According to recent CMS guidelines, you and your staff will need to undergo routine screening, as will others who work in the facility (housekeeping, delivery personnel, and anyone else who enters the area). This may mean regularly stocking screening tests and setting guidelines for what to do if one of your staff tests positive.
You may need to hire temporary workers if your staff tests positive. The CDC recommends at the very least understanding the minimum staffing requirements to ensure good patient care and a safe work environment. Consider adjusting staff schedules and rotating clinical personnel to positions that support patient care activities. You may also want to look into cross-training your office staff so that they can fill in or help out with each other’s responsibilities if one or more persons are ill.
Dr. Kutner is on board with these changes. “We don’t want to get rid of social distancing right away, because it will give us a new spike in cases – how do we figure out patient flow while honoring that?”
4. Develop a strategy for triaging and caring for a potential backlog of patients.
“Many of my partners are scared right now because they have no income except for emergencies,” said Andrew Gonzalez, MD, JD, MPH, a vascular surgeon and assistant professor of surgery at Indiana University, Indianapolis. Almost all nonemergency surgery has been put on hold.
“If we don’t operate, the practice makes no money,” he said. He thinks revenue will continue to be a problem as long as patients fear in-person consultations or undergoing surgery for nonacute problems such as hernias.
As restrictions ease, most physicians will face an enormous backlog of patients and will need to find new ways of triaging the most serious cases, he says. Telehealth will help, but Dr. Gonzalez predicts many of his colleagues will be working longer hours and on weekends to catch up. “Physicians are going to have to really think about ways of optimizing their time and workflow to be very efficient, because the backlog is going to prodigious.”
5. Anticipate changes in patient expectations.
This may entail your reconsidering tests and procedures you previously performed and considering developing new sources for some services, phasing some others out, and revising your current approach. It will most likely also mean that you make telemedicine and televisits a greater part of your practice.
Carolyn Kaloostian, MD, a family medicine and geriatric practitioner in Los Angeles, points to increased reliance on community agencies for conducting common office-based procedures, such as performing blood tests and taking ECGs and x-rays. “A lot of patients are using telemedicine or telephone visits and get the lab work or x-rays somewhere that’s less congested,” she said. To become sustainable, many of these changes will hinge on economics – whether and how they are reimbursed.
The pandemic will leave lasting effects in our health care delivery, according to Dr. Kaloostian. She is sure many of her colleagues’ and patients’ current experiences will be infused into future care. “I can’t say we’ll ever be back to normal, necessarily.”
Even if the CMS rolls back its telehealth waivers, some physicians, like Dr. Coleman, plan to continue using the technology extensively. He’s confident about the level of care he’s currently providing patients in his practice. It allows him to better manage many low-income patients who can’t access his office regularly. Not only does splitting his time between the clinic and telehealth allow him to be more available for more patients, he says it also empowers patients to take better care of themselves.
6. Consider a new way to conduct “check-in visits.”
One thing that will likely go by the wayside are “check-in” visits, or so-called “social visits,” those interval appointments that can just as easily be completed virtually. “Patients are going to ask why they need to drive 3 hours so you can tell them their incision looks fine from an operation you did 5 years ago,” Dr. Gonzalez said.
He’s concerned that some people will remain so fearful of the health care system that a formerly busy practice may see the pendulum swing in the opposite direction. If an aneurysm patient skips a visit, that person may also decide not to undergo a CT scan – and something preventable will be missed. “Not everybody has the option to stay away until they feel comfortable. They’re basically playing hot potato. And at some point, the music’s going to stop,” Dr. Gonzalez said.
The pandemic has prompted some very honest conversations with his patients about what truly needs to get done and what may be optional. “Everyone has now become a hyper-rational user of health care,” he said.
7. If you haven’t yet, consider becoming more involved with technology.
In addition to greater use of telehealth, Dr. Kaloostian, assistant professor of clinical family medicine at the University of Southern California, Los Angeles, foresees continued reliance upon technology such as smartphone apps that connect with a user’s smartwatch. This allows for more proactive, remote monitoring.
“For example, any time a patient is having recurrent nighttime trips to the bathroom, I’ll get pinged and know that,” she explained. It means she can reach out and ask about any changes before a fall occurs or a condition worsens. “It provides reassurance to the provider and to the patient that you’re doing all you can to keep an eye on them from afar.”
8. Update or reformulate your business plans.
Some physicians in smaller practices may have to temporarily or permanently rethink their situation. Those who have struggled or who have closed down and are considering reopening need to update their business plans. It may be safer economically to become part of a bigger group that is affiliated with an academic center or join a larger health care system that has more funds or resources.
In addition, Dr. Kaloostian suggests that primary care physicians become more flexible in the short term, perhaps working part time in an urgent care clinic or larger organization to gain additional sources of revenue until their own practice finances pick back up.
For offices that reopen, the AMA recommends contacting medical malpractice insurance carriers to check on possible liability concerns. Congress has provided certain protections for clinicians during this time, but malpractice carriers may have more information and may offer more coverage.
Dr. Coleman said a hybrid model of fewer in-person and more telehealth visits “will allow me to practice in a different way.” If the CMS reimposes prior restrictions, reimbursement may be affected initially, but that will likely change once insurers see the increased cost-effectiveness of this approach. Patients with minor complaints, those who need to have medications refilled, and patients with chronic diseases that need managing won’t have to deal with crowded waiting rooms, and it will help mitigate problems with infection control.
If there’s any upside to the pandemic, it’s an increase in attention given to advanced care planning, said Dr. Kutner. It’s something she hopes continues after everyone stops being in crisis mode. “We’re realizing how important it is to have these conversations and document people’s goals and values and code status,” she said.
Are offices likely to open soon?
An assumption that may or may not be valid is that a practice will remain viable and can return to former capacity. Prior to passage of the CARES Act on March 27, a survey from Kareo, a company in Irvine, California, that makes a technology platform for independent physician practices, found that 9% of respondents reported practice closures. Many more reported concern about potential closures as patient office visits plummet because of stay-at-home orders and other concerns.
By mid-April, a survey from the Primary Care Collaborative and the Larry A. Green Center found that 42% of practices had experienced layoffs and had furloughed staff. Most (85%) have seen dramatic decreases in patient volume.
“Reopening the economy or loosening physical distancing restrictions will be difficult when 20% of primary care practices predict closure within 4 weeks,” the survey concluded.
For the practices and the doctors who make it through this, we’re going to probably be better, stronger, and more efficient, Dr. Gonzalez predicts. This shock has uncovered a lot of weaknesses in the American health care system that doctors have known about and have been complaining about for a long time. It will take an open mind and lots of continued flexibility on the part of physicians, hospitals, health care systems, and the government for these changes to stick.
A version of this article originally appeared on Medscape.com.
IV-to-oral antibiotics can benefit patients with MRSA bloodstream infection
Background: Methicillin-resistant Staphylococcus aureus bloodstream infections carry a high risk of morbidity and relapse with most published guidelines recommending prolonged courses of IV antibiotics to ensure complete clearance of the infection. However, long-term IV antibiotic therapy may also be costly and is not without its own complications. An equally effective IV-to-oral antibiotic therapy would be welcome.
Study design: Retrospective cohort study.
Setting: A single academic center in the United States.
Synopsis: The investigators reviewed data from 492 adults with at least one positive blood culture for MRSA who had not yet completed their antibiotic course at the time of discharge during the index hospitalization but were sufficiently stable to complete outpatient antibiotic treatment. Of this cohort, 70 patients were switched to oral antibiotic therapy on discharge, while the rest received OPAT. The primary outcome was clinical failure, a 90-day composite measure of MRSA bloodstream infection recurrence, deep MRSA infection, or all-cause mortality. The most commonly used oral antibiotics were linezolid, trimethoprim/sulfamethoxazole, and clindamycin, all with high bioavailability. Endovascular infection was present in 21.5% of the study population. After propensity score adjustment for covariates, patients who received oral antibiotics had a nonsignificant reduction in the rate of clinical failure (hazard ratio, 0.379; 95% CI, 0.131-1.101).
Limitations of the study included its observational design with potential for significant residual confounding despite the propensity score–adjusted analysis, its single-center setting, the low frequency of endovascular infections, and the uncertainty in how the loss of patients to follow-up might have affected the results.
Bottom line: Selected patients with MRSA BSI may be successfully treated with sequential IV-to-oral antibiotic therapy.
Citation: Jorgensen SCJ et al. Sequential intravenous-to-oral outpatient antibiotic therapy for MRSA bacteraemia: One step closer. J Antimicrob Chemother. 2019 Feb;74(2):489-98.
Dr. Torres is a hospitalist at Massachusetts General Hospital.
Background: Methicillin-resistant Staphylococcus aureus bloodstream infections carry a high risk of morbidity and relapse with most published guidelines recommending prolonged courses of IV antibiotics to ensure complete clearance of the infection. However, long-term IV antibiotic therapy may also be costly and is not without its own complications. An equally effective IV-to-oral antibiotic therapy would be welcome.
Study design: Retrospective cohort study.
Setting: A single academic center in the United States.
Synopsis: The investigators reviewed data from 492 adults with at least one positive blood culture for MRSA who had not yet completed their antibiotic course at the time of discharge during the index hospitalization but were sufficiently stable to complete outpatient antibiotic treatment. Of this cohort, 70 patients were switched to oral antibiotic therapy on discharge, while the rest received OPAT. The primary outcome was clinical failure, a 90-day composite measure of MRSA bloodstream infection recurrence, deep MRSA infection, or all-cause mortality. The most commonly used oral antibiotics were linezolid, trimethoprim/sulfamethoxazole, and clindamycin, all with high bioavailability. Endovascular infection was present in 21.5% of the study population. After propensity score adjustment for covariates, patients who received oral antibiotics had a nonsignificant reduction in the rate of clinical failure (hazard ratio, 0.379; 95% CI, 0.131-1.101).
Limitations of the study included its observational design with potential for significant residual confounding despite the propensity score–adjusted analysis, its single-center setting, the low frequency of endovascular infections, and the uncertainty in how the loss of patients to follow-up might have affected the results.
Bottom line: Selected patients with MRSA BSI may be successfully treated with sequential IV-to-oral antibiotic therapy.
Citation: Jorgensen SCJ et al. Sequential intravenous-to-oral outpatient antibiotic therapy for MRSA bacteraemia: One step closer. J Antimicrob Chemother. 2019 Feb;74(2):489-98.
Dr. Torres is a hospitalist at Massachusetts General Hospital.
Background: Methicillin-resistant Staphylococcus aureus bloodstream infections carry a high risk of morbidity and relapse with most published guidelines recommending prolonged courses of IV antibiotics to ensure complete clearance of the infection. However, long-term IV antibiotic therapy may also be costly and is not without its own complications. An equally effective IV-to-oral antibiotic therapy would be welcome.
Study design: Retrospective cohort study.
Setting: A single academic center in the United States.
Synopsis: The investigators reviewed data from 492 adults with at least one positive blood culture for MRSA who had not yet completed their antibiotic course at the time of discharge during the index hospitalization but were sufficiently stable to complete outpatient antibiotic treatment. Of this cohort, 70 patients were switched to oral antibiotic therapy on discharge, while the rest received OPAT. The primary outcome was clinical failure, a 90-day composite measure of MRSA bloodstream infection recurrence, deep MRSA infection, or all-cause mortality. The most commonly used oral antibiotics were linezolid, trimethoprim/sulfamethoxazole, and clindamycin, all with high bioavailability. Endovascular infection was present in 21.5% of the study population. After propensity score adjustment for covariates, patients who received oral antibiotics had a nonsignificant reduction in the rate of clinical failure (hazard ratio, 0.379; 95% CI, 0.131-1.101).
Limitations of the study included its observational design with potential for significant residual confounding despite the propensity score–adjusted analysis, its single-center setting, the low frequency of endovascular infections, and the uncertainty in how the loss of patients to follow-up might have affected the results.
Bottom line: Selected patients with MRSA BSI may be successfully treated with sequential IV-to-oral antibiotic therapy.
Citation: Jorgensen SCJ et al. Sequential intravenous-to-oral outpatient antibiotic therapy for MRSA bacteraemia: One step closer. J Antimicrob Chemother. 2019 Feb;74(2):489-98.
Dr. Torres is a hospitalist at Massachusetts General Hospital.
Don’t delay antibiotic treatment in elderly patients with UTI
Background: If left untreated, UTIs may lead to severe complications. Although campaigns aimed at decreasing unnecessary prescriptions have reduced the number of antibiotic prescriptions for UTI, a concurrent rise in the rates of gram-negative bloodstream infections (BSIs) has also been observed.
Study design: Retrospective, population-based cohort study with data compiled from primary care records from 2007 to 2015 linked to hospital episode statistics and death records.
Setting: General practices in England.
Synopsis: The investigators analyzed 312,896 UTI episodes among 157,264 unique patients (65 years of age or older) during the study period. Exclusion criteria included asymptomatic bacteriuria and complicated UTI. Of 271,070 patients who received antibiotics on the day of presentation with symptoms, 0.2% developed BSI within 60 days versus 2.2% of patients in whom antibiotics were delayed and 2.9% among patients not prescribed antibiotics. After adjustment for comorbidities, sex, and socioeconomic status, patients in whom antibiotics were deferred had a 7.12-fold greater odds of BSI, compared with the immediate-antibiotic group. BSIs were more common among men and older patients. All-cause mortality, a secondary outcome, was 1.16-fold higher with deferred antibiotics and 2.18 times higher with no antibiotics.
While the cohort studied was very large, a causal relationship cannot be firmly established in this observational study. Also, researchers were unable to include laboratory data, such as urinalysis and culture, in their analysis.
Bottom line: Delayed prescription of antibiotics for elderly patients presenting with UTI in primary care settings was associated with higher rates of BSI and death.
Citation: Gharbi M et al. Antibiotic management of urinary tract infection in elderly patients in primary care and its association with bloodstream infections and all-cause mortality: Population-based cohort study. BMJ. 2019 Feb;364:1525.
Dr. Torres is a hospitalist at Massachusetts General Hospital.
Background: If left untreated, UTIs may lead to severe complications. Although campaigns aimed at decreasing unnecessary prescriptions have reduced the number of antibiotic prescriptions for UTI, a concurrent rise in the rates of gram-negative bloodstream infections (BSIs) has also been observed.
Study design: Retrospective, population-based cohort study with data compiled from primary care records from 2007 to 2015 linked to hospital episode statistics and death records.
Setting: General practices in England.
Synopsis: The investigators analyzed 312,896 UTI episodes among 157,264 unique patients (65 years of age or older) during the study period. Exclusion criteria included asymptomatic bacteriuria and complicated UTI. Of 271,070 patients who received antibiotics on the day of presentation with symptoms, 0.2% developed BSI within 60 days versus 2.2% of patients in whom antibiotics were delayed and 2.9% among patients not prescribed antibiotics. After adjustment for comorbidities, sex, and socioeconomic status, patients in whom antibiotics were deferred had a 7.12-fold greater odds of BSI, compared with the immediate-antibiotic group. BSIs were more common among men and older patients. All-cause mortality, a secondary outcome, was 1.16-fold higher with deferred antibiotics and 2.18 times higher with no antibiotics.
While the cohort studied was very large, a causal relationship cannot be firmly established in this observational study. Also, researchers were unable to include laboratory data, such as urinalysis and culture, in their analysis.
Bottom line: Delayed prescription of antibiotics for elderly patients presenting with UTI in primary care settings was associated with higher rates of BSI and death.
Citation: Gharbi M et al. Antibiotic management of urinary tract infection in elderly patients in primary care and its association with bloodstream infections and all-cause mortality: Population-based cohort study. BMJ. 2019 Feb;364:1525.
Dr. Torres is a hospitalist at Massachusetts General Hospital.
Background: If left untreated, UTIs may lead to severe complications. Although campaigns aimed at decreasing unnecessary prescriptions have reduced the number of antibiotic prescriptions for UTI, a concurrent rise in the rates of gram-negative bloodstream infections (BSIs) has also been observed.
Study design: Retrospective, population-based cohort study with data compiled from primary care records from 2007 to 2015 linked to hospital episode statistics and death records.
Setting: General practices in England.
Synopsis: The investigators analyzed 312,896 UTI episodes among 157,264 unique patients (65 years of age or older) during the study period. Exclusion criteria included asymptomatic bacteriuria and complicated UTI. Of 271,070 patients who received antibiotics on the day of presentation with symptoms, 0.2% developed BSI within 60 days versus 2.2% of patients in whom antibiotics were delayed and 2.9% among patients not prescribed antibiotics. After adjustment for comorbidities, sex, and socioeconomic status, patients in whom antibiotics were deferred had a 7.12-fold greater odds of BSI, compared with the immediate-antibiotic group. BSIs were more common among men and older patients. All-cause mortality, a secondary outcome, was 1.16-fold higher with deferred antibiotics and 2.18 times higher with no antibiotics.
While the cohort studied was very large, a causal relationship cannot be firmly established in this observational study. Also, researchers were unable to include laboratory data, such as urinalysis and culture, in their analysis.
Bottom line: Delayed prescription of antibiotics for elderly patients presenting with UTI in primary care settings was associated with higher rates of BSI and death.
Citation: Gharbi M et al. Antibiotic management of urinary tract infection in elderly patients in primary care and its association with bloodstream infections and all-cause mortality: Population-based cohort study. BMJ. 2019 Feb;364:1525.
Dr. Torres is a hospitalist at Massachusetts General Hospital.
Pandemic effect: All other health care visits can wait
according to survey conducted at the end of April.
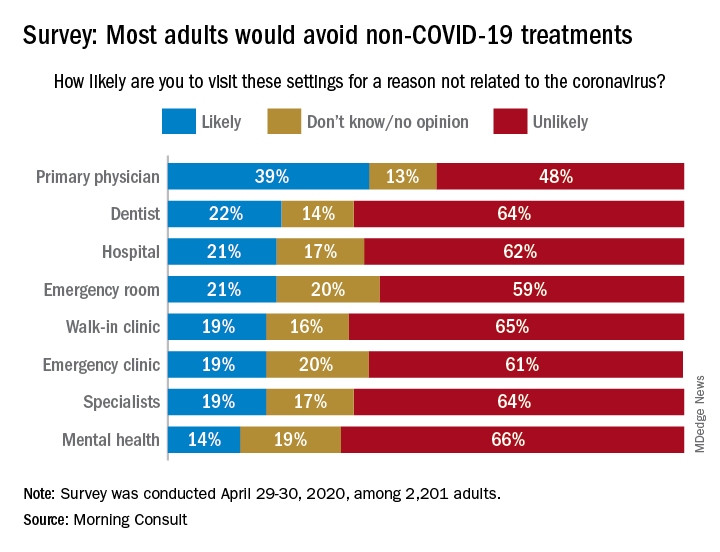
When asked how likely they were to visit a variety of health care settings for treatment not related to the coronavirus, 62% of respondents said it was unlikely that they would go to a hospital, 64% wouldn’t go to a specialist, and 65% would avoid walk-in clinics, digital media company Morning Consult reported May 4.
The only setting with less than a majority on the unlikely-to-visit side was primary physicians, who managed to combine a 39% likely vote with a 13% undecided/no-opinion tally, Morning Consult said after surveying 2,201 adults on April 29-30 (margin of error, ±2 percentage points).
As to when they might feel comfortable making such an in-person visit with their primary physician, 24% of respondents said they would willing to go in the next month, 14% said 2 months, 18% said 3 months, 13% said 6 months, and 10% said more than 6 months, the Morning Consult data show.
“Hospitals, despite being overburdened in recent weeks in coronavirus hot spots such as New York City, have reported dips in revenue as a result of potential patients opting against receiving elective surgeries out of fear of contracting COVID-19,” Morning Consult wrote, and these poll results suggest that “health care companies could continue to feel the pinch as long as the coronavirus lingers.”
according to survey conducted at the end of April.
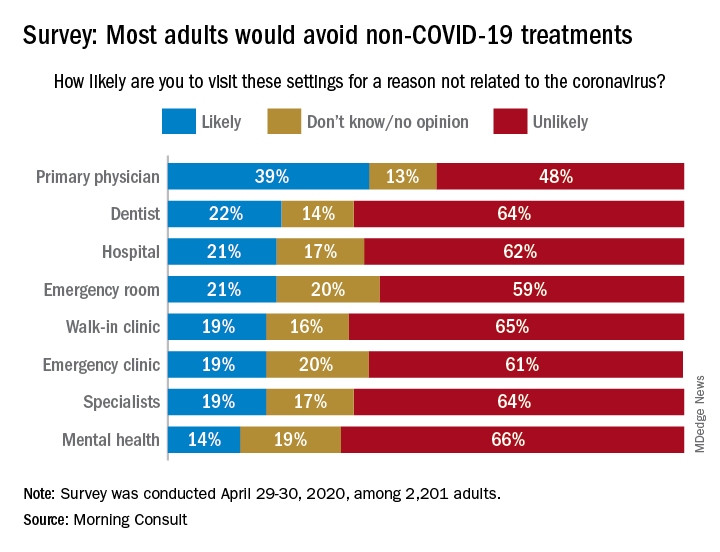
When asked how likely they were to visit a variety of health care settings for treatment not related to the coronavirus, 62% of respondents said it was unlikely that they would go to a hospital, 64% wouldn’t go to a specialist, and 65% would avoid walk-in clinics, digital media company Morning Consult reported May 4.
The only setting with less than a majority on the unlikely-to-visit side was primary physicians, who managed to combine a 39% likely vote with a 13% undecided/no-opinion tally, Morning Consult said after surveying 2,201 adults on April 29-30 (margin of error, ±2 percentage points).
As to when they might feel comfortable making such an in-person visit with their primary physician, 24% of respondents said they would willing to go in the next month, 14% said 2 months, 18% said 3 months, 13% said 6 months, and 10% said more than 6 months, the Morning Consult data show.
“Hospitals, despite being overburdened in recent weeks in coronavirus hot spots such as New York City, have reported dips in revenue as a result of potential patients opting against receiving elective surgeries out of fear of contracting COVID-19,” Morning Consult wrote, and these poll results suggest that “health care companies could continue to feel the pinch as long as the coronavirus lingers.”
according to survey conducted at the end of April.
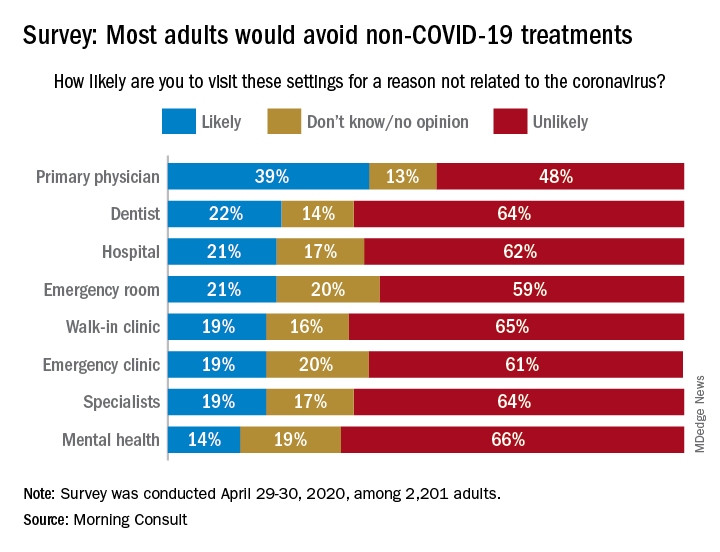
When asked how likely they were to visit a variety of health care settings for treatment not related to the coronavirus, 62% of respondents said it was unlikely that they would go to a hospital, 64% wouldn’t go to a specialist, and 65% would avoid walk-in clinics, digital media company Morning Consult reported May 4.
The only setting with less than a majority on the unlikely-to-visit side was primary physicians, who managed to combine a 39% likely vote with a 13% undecided/no-opinion tally, Morning Consult said after surveying 2,201 adults on April 29-30 (margin of error, ±2 percentage points).
As to when they might feel comfortable making such an in-person visit with their primary physician, 24% of respondents said they would willing to go in the next month, 14% said 2 months, 18% said 3 months, 13% said 6 months, and 10% said more than 6 months, the Morning Consult data show.
“Hospitals, despite being overburdened in recent weeks in coronavirus hot spots such as New York City, have reported dips in revenue as a result of potential patients opting against receiving elective surgeries out of fear of contracting COVID-19,” Morning Consult wrote, and these poll results suggest that “health care companies could continue to feel the pinch as long as the coronavirus lingers.”
Sepsis patients with hypothermia face greater mortality risk
Background: Fevers (like other vital sign abnormalities) often trigger interventions from providers. However, hypothermia (temperature under 36° C) may also be associated with higher mortality.
Study design: Retrospective subanalysis of a previous study (Focused Outcome Research on Emergency Care for Acute respiratory distress syndrome, Sepsis and Trauma [FORECAST]).
Setting: Adult patients with severe sepsis based on Sepsis-2 in 59 ICUs in Japan.
Synopsis: The study involved 1,143 patients admitted to ICUs with severe sepsis (62.6% with septic shock). The median age was 73 years with a median APACHE II and SOFA scores of 22 and 9, respectively. Core temperatures were measured on admission to ICU with patients categorized into three arms: temperature under 36° C (hypothermic), temperature 36°-38° C, and febrile patients with temperature greater than 38° C. Of studied patients, 11.1% were hypothermic on presentation. These patients were older, sicker (higher APACHE/SOFA scores), had lower body mass indexes, and had higher prevalence of septic shock than did the febrile patients. Hypothermic patients fared worse in every clinical outcome measured – in-hospital mortality, 28-day mortality, ventilator-free days, ICU-free days, length of hospital stay, and likelihood of discharge home. The odds ratio of in-hospital mortality for hypothermic patients, compared with reference febrile patients, was 1.76 (95% CI, 1.14-2.73). Patients with hypothermia were also significantly less likely to receive the entire 3-hour resuscitation bundle, including broad-spectrum antibiotics (56.3%) versus 60.8% of patients with temperature 36-38° C and 71.1% for febrile group (P = .003).
Bottom line: Hypothermia in patients with severe sepsis is associated with a significantly higher disease severity, mortality risk, and lower implementation of sepsis bundles. More emphasis on earlier identification and treatment of this specific patient population appears needed.
Citation: Kushimoto S et al. Impact of body temperature abnormalities on the implementation of sepsis bundles and outcomes in patients with severe sepsis: A retrospective sub-analysis of the focused outcome of research of emergency care for acute respiratory distress syndrome, sepsis and trauma study. Crit Care Med. 2019 May;47(5):691-9.
Dr. Sekaran is a hospitalist at Massachusetts General Hospital.
Background: Fevers (like other vital sign abnormalities) often trigger interventions from providers. However, hypothermia (temperature under 36° C) may also be associated with higher mortality.
Study design: Retrospective subanalysis of a previous study (Focused Outcome Research on Emergency Care for Acute respiratory distress syndrome, Sepsis and Trauma [FORECAST]).
Setting: Adult patients with severe sepsis based on Sepsis-2 in 59 ICUs in Japan.
Synopsis: The study involved 1,143 patients admitted to ICUs with severe sepsis (62.6% with septic shock). The median age was 73 years with a median APACHE II and SOFA scores of 22 and 9, respectively. Core temperatures were measured on admission to ICU with patients categorized into three arms: temperature under 36° C (hypothermic), temperature 36°-38° C, and febrile patients with temperature greater than 38° C. Of studied patients, 11.1% were hypothermic on presentation. These patients were older, sicker (higher APACHE/SOFA scores), had lower body mass indexes, and had higher prevalence of septic shock than did the febrile patients. Hypothermic patients fared worse in every clinical outcome measured – in-hospital mortality, 28-day mortality, ventilator-free days, ICU-free days, length of hospital stay, and likelihood of discharge home. The odds ratio of in-hospital mortality for hypothermic patients, compared with reference febrile patients, was 1.76 (95% CI, 1.14-2.73). Patients with hypothermia were also significantly less likely to receive the entire 3-hour resuscitation bundle, including broad-spectrum antibiotics (56.3%) versus 60.8% of patients with temperature 36-38° C and 71.1% for febrile group (P = .003).
Bottom line: Hypothermia in patients with severe sepsis is associated with a significantly higher disease severity, mortality risk, and lower implementation of sepsis bundles. More emphasis on earlier identification and treatment of this specific patient population appears needed.
Citation: Kushimoto S et al. Impact of body temperature abnormalities on the implementation of sepsis bundles and outcomes in patients with severe sepsis: A retrospective sub-analysis of the focused outcome of research of emergency care for acute respiratory distress syndrome, sepsis and trauma study. Crit Care Med. 2019 May;47(5):691-9.
Dr. Sekaran is a hospitalist at Massachusetts General Hospital.
Background: Fevers (like other vital sign abnormalities) often trigger interventions from providers. However, hypothermia (temperature under 36° C) may also be associated with higher mortality.
Study design: Retrospective subanalysis of a previous study (Focused Outcome Research on Emergency Care for Acute respiratory distress syndrome, Sepsis and Trauma [FORECAST]).
Setting: Adult patients with severe sepsis based on Sepsis-2 in 59 ICUs in Japan.
Synopsis: The study involved 1,143 patients admitted to ICUs with severe sepsis (62.6% with septic shock). The median age was 73 years with a median APACHE II and SOFA scores of 22 and 9, respectively. Core temperatures were measured on admission to ICU with patients categorized into three arms: temperature under 36° C (hypothermic), temperature 36°-38° C, and febrile patients with temperature greater than 38° C. Of studied patients, 11.1% were hypothermic on presentation. These patients were older, sicker (higher APACHE/SOFA scores), had lower body mass indexes, and had higher prevalence of septic shock than did the febrile patients. Hypothermic patients fared worse in every clinical outcome measured – in-hospital mortality, 28-day mortality, ventilator-free days, ICU-free days, length of hospital stay, and likelihood of discharge home. The odds ratio of in-hospital mortality for hypothermic patients, compared with reference febrile patients, was 1.76 (95% CI, 1.14-2.73). Patients with hypothermia were also significantly less likely to receive the entire 3-hour resuscitation bundle, including broad-spectrum antibiotics (56.3%) versus 60.8% of patients with temperature 36-38° C and 71.1% for febrile group (P = .003).
Bottom line: Hypothermia in patients with severe sepsis is associated with a significantly higher disease severity, mortality risk, and lower implementation of sepsis bundles. More emphasis on earlier identification and treatment of this specific patient population appears needed.
Citation: Kushimoto S et al. Impact of body temperature abnormalities on the implementation of sepsis bundles and outcomes in patients with severe sepsis: A retrospective sub-analysis of the focused outcome of research of emergency care for acute respiratory distress syndrome, sepsis and trauma study. Crit Care Med. 2019 May;47(5):691-9.
Dr. Sekaran is a hospitalist at Massachusetts General Hospital.












