User login
HHS issues guidance on ransomware attacks
The U.S. Department of Health & Human Services’ Office of Civil Rights has issued new guidance to help physicians and their practices combat a ransomware attack.
Ransomware – a type of malicious software designed to block access to a computer system until a sum of money is paid – is becoming a bigger problem for U.S. businesses in general. Daily ransomware attacks against all types of computer systems increased 300% in early 2016 to 4,000, from 1,000 daily attacks in 2015, according to the Department of Justice.
The HHS fact sheet offers information on how HIPAA compliance can help protect and recover infected systems; how to detect if systems are infected; and what to do if a system becomes infected, including what is reportable.
There are “measures known to be effective to prevent the introduction of ransomware and to recover from a ransomware attack,” according to HHS.
The U.S. Department of Health & Human Services’ Office of Civil Rights has issued new guidance to help physicians and their practices combat a ransomware attack.
Ransomware – a type of malicious software designed to block access to a computer system until a sum of money is paid – is becoming a bigger problem for U.S. businesses in general. Daily ransomware attacks against all types of computer systems increased 300% in early 2016 to 4,000, from 1,000 daily attacks in 2015, according to the Department of Justice.
The HHS fact sheet offers information on how HIPAA compliance can help protect and recover infected systems; how to detect if systems are infected; and what to do if a system becomes infected, including what is reportable.
There are “measures known to be effective to prevent the introduction of ransomware and to recover from a ransomware attack,” according to HHS.
The U.S. Department of Health & Human Services’ Office of Civil Rights has issued new guidance to help physicians and their practices combat a ransomware attack.
Ransomware – a type of malicious software designed to block access to a computer system until a sum of money is paid – is becoming a bigger problem for U.S. businesses in general. Daily ransomware attacks against all types of computer systems increased 300% in early 2016 to 4,000, from 1,000 daily attacks in 2015, according to the Department of Justice.
The HHS fact sheet offers information on how HIPAA compliance can help protect and recover infected systems; how to detect if systems are infected; and what to do if a system becomes infected, including what is reportable.
There are “measures known to be effective to prevent the introduction of ransomware and to recover from a ransomware attack,” according to HHS.
Retiring Baby Boomers leave fewer workers to pay for Medicare
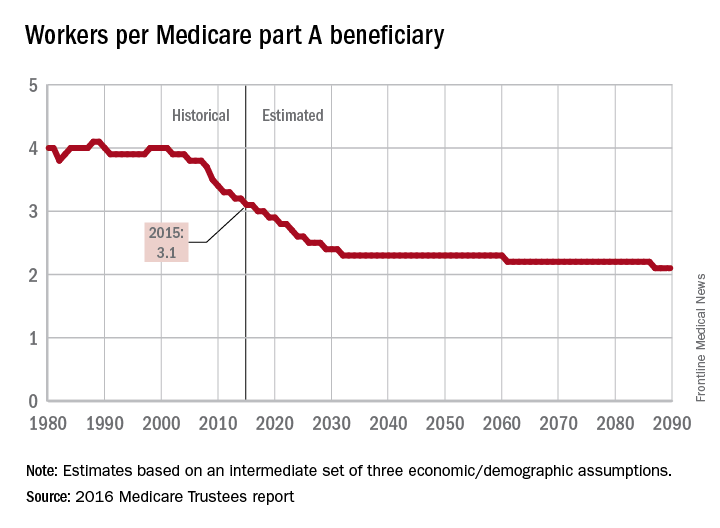
The influx of aging Baby Boomers into the ranks of the retired will reduce the ratio of workers available to pay for each Medicare part A beneficiary by 40% from 2000 to 2030, according to the 2016 report of the Medicare Trustees.
In 2015, there were 3.1 workers for each part A beneficiary, putting the United States in the middle of a projected drop from 4.0 workers per beneficiary in 2000 down to 2.4 in 2030. The Boomer-induced drop will largely be over by then, but the decline will continue until there are about 2.1 workers for each part A beneficiary by 2090, the report said.
“This reduction implies an increase in the [Medicare part A] cost rate of about 50% by 2090, relative to its current level, solely due to this demographic factor,” the trustees noted.
The projections are done using three sets – low-cost, intermediate, and high-cost – of economic and demographic assumptions. The figures presented here are from the intermediate assumption.
The influx of aging Baby Boomers into the ranks of the retired will reduce the ratio of workers available to pay for each Medicare part A beneficiary by 40% from 2000 to 2030, according to the 2016 report of the Medicare Trustees.
In 2015, there were 3.1 workers for each part A beneficiary, putting the United States in the middle of a projected drop from 4.0 workers per beneficiary in 2000 down to 2.4 in 2030. The Boomer-induced drop will largely be over by then, but the decline will continue until there are about 2.1 workers for each part A beneficiary by 2090, the report said.
“This reduction implies an increase in the [Medicare part A] cost rate of about 50% by 2090, relative to its current level, solely due to this demographic factor,” the trustees noted.
The projections are done using three sets – low-cost, intermediate, and high-cost – of economic and demographic assumptions. The figures presented here are from the intermediate assumption.
The influx of aging Baby Boomers into the ranks of the retired will reduce the ratio of workers available to pay for each Medicare part A beneficiary by 40% from 2000 to 2030, according to the 2016 report of the Medicare Trustees.
In 2015, there were 3.1 workers for each part A beneficiary, putting the United States in the middle of a projected drop from 4.0 workers per beneficiary in 2000 down to 2.4 in 2030. The Boomer-induced drop will largely be over by then, but the decline will continue until there are about 2.1 workers for each part A beneficiary by 2090, the report said.
“This reduction implies an increase in the [Medicare part A] cost rate of about 50% by 2090, relative to its current level, solely due to this demographic factor,” the trustees noted.
The projections are done using three sets – low-cost, intermediate, and high-cost – of economic and demographic assumptions. The figures presented here are from the intermediate assumption.
In Out-of-Hospital Care, IIb or Not IIb…
The 2015 American Heart Association CPR/ACLS update categorizes amiodarone and lidocaine as IIb drugs that “may be considered” for ventricular fibrillation or pulseless ventricular tachycardia unresponsive to CPR, defibrillation, or vasopressors. Out-of-hospital use of these drugs has previously been shown to increase survival rate to hospital admission, but not necessarily to hospital discharge.
The effects of amiodarone and lidocaine on the rate of survival to hospital discharge are addressed in a recent randomized, double-blind, out-of-hospital trial comparing amiodarone, lidocaine, and placebo in the treatment of shock-refractory ventricular fibrillation or pulseless ventricular tachycardia (N Engl J Med. 2016;374[18]:1711-1722). This study was conducted by the Resuscitation Outcomes Consortium (ROC) in 3,026 patients at 10 US and Canadian sites. The ROC authors concluded that “overall, neither amiodarone nor lidocaine resulted in a significantly higher rate of survival or favorable neurologic outcome than the rate with placebo.” But the article raises concerns about its methodology, appropriateness of its primary and secondary outcomes to out-of-hospital (or prehospital) care, and the manner in which its findings were reported.
Because of the condition (unconscious) and circumstances (out of hospital) of the patients at the time medication or placebo must be administered, this NIH-supported trial was conducted under exception from informed consent in emergency research, with FDA and Health Canada oversight, and with approval by trial-site Institutional Review Boards. Notwithstanding the list of regulatory bodies that approved the exception, is the trial appropriate for drugs previously demonstrated to be efficacious in improving survival rates to hospital admission—long considered the goal of prehospital care—when subsequent care from admission to hospital discharge is not standardized or controlled across multiple sites in two countries?
Another concern is the way the results were reported. Will the authors’ conclusion that overall, neither amiodarone nor lidocaine resulted in a significantly higher rate of survival suggest to hurried readers that there is no benefit to any patient to hospital discharge from either antiarrhythmic agent? In the results section, the authors report “active drugs were associated with a survival rate that was significantly higher than the rate with placebo among patients with bystander-witnessed arrest but not among those with unwitnessed arrest.” Also noted in the accompanying editorial entitled “Out-of-Hospital Cardiac Arrest—Are Drugs Ever the Answer?” (N Engl J Med. 2016;374[18]:1781-1782), both drugs were associated with nonsignificant increases in survival rate, fewer subsequent shocks, and less administration of rhythm-control medications or need for CPR during hospitalization, compared with patients’ courses after placebo.
The ROC trial is not the first or only out-of-hospital trial to use survival to hospital discharge as its primary outcome measure. A 1990-1991 study using death or discharge home to determine survival from out-of-hospital cardiac arrests in New York City found that of the 2,329 patients who met entry criteria for that study, overall survival was only 1.4%—which the authors attributed partly to lengthy elapsed time intervals at every step in the chain of survival, lack of adequate bystander CPR, and possibly sociodemographic features common to victims of cardiac arrest in large cities (JAMA. 1994;271[9]:678-683). The poor results led to increases in first responders and AED availability but not the abandonment of properly performed CPR and ACLS. In the ROC trial, length of time from cardiac arrest to administration of medications clearly was shown to be a significant outcome determinant and was emphasized in the accompanying editorial. Here too shouldn’t we concentrate on optimizing the setting and timing of CPR and ACLS measures?
The 2015 American Heart Association CPR/ACLS update categorizes amiodarone and lidocaine as IIb drugs that “may be considered” for ventricular fibrillation or pulseless ventricular tachycardia unresponsive to CPR, defibrillation, or vasopressors. Out-of-hospital use of these drugs has previously been shown to increase survival rate to hospital admission, but not necessarily to hospital discharge.
The effects of amiodarone and lidocaine on the rate of survival to hospital discharge are addressed in a recent randomized, double-blind, out-of-hospital trial comparing amiodarone, lidocaine, and placebo in the treatment of shock-refractory ventricular fibrillation or pulseless ventricular tachycardia (N Engl J Med. 2016;374[18]:1711-1722). This study was conducted by the Resuscitation Outcomes Consortium (ROC) in 3,026 patients at 10 US and Canadian sites. The ROC authors concluded that “overall, neither amiodarone nor lidocaine resulted in a significantly higher rate of survival or favorable neurologic outcome than the rate with placebo.” But the article raises concerns about its methodology, appropriateness of its primary and secondary outcomes to out-of-hospital (or prehospital) care, and the manner in which its findings were reported.
Because of the condition (unconscious) and circumstances (out of hospital) of the patients at the time medication or placebo must be administered, this NIH-supported trial was conducted under exception from informed consent in emergency research, with FDA and Health Canada oversight, and with approval by trial-site Institutional Review Boards. Notwithstanding the list of regulatory bodies that approved the exception, is the trial appropriate for drugs previously demonstrated to be efficacious in improving survival rates to hospital admission—long considered the goal of prehospital care—when subsequent care from admission to hospital discharge is not standardized or controlled across multiple sites in two countries?
Another concern is the way the results were reported. Will the authors’ conclusion that overall, neither amiodarone nor lidocaine resulted in a significantly higher rate of survival suggest to hurried readers that there is no benefit to any patient to hospital discharge from either antiarrhythmic agent? In the results section, the authors report “active drugs were associated with a survival rate that was significantly higher than the rate with placebo among patients with bystander-witnessed arrest but not among those with unwitnessed arrest.” Also noted in the accompanying editorial entitled “Out-of-Hospital Cardiac Arrest—Are Drugs Ever the Answer?” (N Engl J Med. 2016;374[18]:1781-1782), both drugs were associated with nonsignificant increases in survival rate, fewer subsequent shocks, and less administration of rhythm-control medications or need for CPR during hospitalization, compared with patients’ courses after placebo.
The ROC trial is not the first or only out-of-hospital trial to use survival to hospital discharge as its primary outcome measure. A 1990-1991 study using death or discharge home to determine survival from out-of-hospital cardiac arrests in New York City found that of the 2,329 patients who met entry criteria for that study, overall survival was only 1.4%—which the authors attributed partly to lengthy elapsed time intervals at every step in the chain of survival, lack of adequate bystander CPR, and possibly sociodemographic features common to victims of cardiac arrest in large cities (JAMA. 1994;271[9]:678-683). The poor results led to increases in first responders and AED availability but not the abandonment of properly performed CPR and ACLS. In the ROC trial, length of time from cardiac arrest to administration of medications clearly was shown to be a significant outcome determinant and was emphasized in the accompanying editorial. Here too shouldn’t we concentrate on optimizing the setting and timing of CPR and ACLS measures?
The 2015 American Heart Association CPR/ACLS update categorizes amiodarone and lidocaine as IIb drugs that “may be considered” for ventricular fibrillation or pulseless ventricular tachycardia unresponsive to CPR, defibrillation, or vasopressors. Out-of-hospital use of these drugs has previously been shown to increase survival rate to hospital admission, but not necessarily to hospital discharge.
The effects of amiodarone and lidocaine on the rate of survival to hospital discharge are addressed in a recent randomized, double-blind, out-of-hospital trial comparing amiodarone, lidocaine, and placebo in the treatment of shock-refractory ventricular fibrillation or pulseless ventricular tachycardia (N Engl J Med. 2016;374[18]:1711-1722). This study was conducted by the Resuscitation Outcomes Consortium (ROC) in 3,026 patients at 10 US and Canadian sites. The ROC authors concluded that “overall, neither amiodarone nor lidocaine resulted in a significantly higher rate of survival or favorable neurologic outcome than the rate with placebo.” But the article raises concerns about its methodology, appropriateness of its primary and secondary outcomes to out-of-hospital (or prehospital) care, and the manner in which its findings were reported.
Because of the condition (unconscious) and circumstances (out of hospital) of the patients at the time medication or placebo must be administered, this NIH-supported trial was conducted under exception from informed consent in emergency research, with FDA and Health Canada oversight, and with approval by trial-site Institutional Review Boards. Notwithstanding the list of regulatory bodies that approved the exception, is the trial appropriate for drugs previously demonstrated to be efficacious in improving survival rates to hospital admission—long considered the goal of prehospital care—when subsequent care from admission to hospital discharge is not standardized or controlled across multiple sites in two countries?
Another concern is the way the results were reported. Will the authors’ conclusion that overall, neither amiodarone nor lidocaine resulted in a significantly higher rate of survival suggest to hurried readers that there is no benefit to any patient to hospital discharge from either antiarrhythmic agent? In the results section, the authors report “active drugs were associated with a survival rate that was significantly higher than the rate with placebo among patients with bystander-witnessed arrest but not among those with unwitnessed arrest.” Also noted in the accompanying editorial entitled “Out-of-Hospital Cardiac Arrest—Are Drugs Ever the Answer?” (N Engl J Med. 2016;374[18]:1781-1782), both drugs were associated with nonsignificant increases in survival rate, fewer subsequent shocks, and less administration of rhythm-control medications or need for CPR during hospitalization, compared with patients’ courses after placebo.
The ROC trial is not the first or only out-of-hospital trial to use survival to hospital discharge as its primary outcome measure. A 1990-1991 study using death or discharge home to determine survival from out-of-hospital cardiac arrests in New York City found that of the 2,329 patients who met entry criteria for that study, overall survival was only 1.4%—which the authors attributed partly to lengthy elapsed time intervals at every step in the chain of survival, lack of adequate bystander CPR, and possibly sociodemographic features common to victims of cardiac arrest in large cities (JAMA. 1994;271[9]:678-683). The poor results led to increases in first responders and AED availability but not the abandonment of properly performed CPR and ACLS. In the ROC trial, length of time from cardiac arrest to administration of medications clearly was shown to be a significant outcome determinant and was emphasized in the accompanying editorial. Here too shouldn’t we concentrate on optimizing the setting and timing of CPR and ACLS measures?
Multisite NIH-sponsored research can now use single IRB
In an effort to streamline multisite clinical research, the National Institutes of Health announced a new policy related to the use of institutional review boards (IRBs).
The new policy sets “the expectation that multisite studies conducting the same protocol use a single IRB to carry out the ethical review of the proposed research,” NIH Director Francis S. Collins, MD, said in a June 21 statement. The policy goes into effect May 25, 2017, and applies only to domestic research.
Currently, for most multisite studies, the IRB at each site conducts an independent review of protocol and consent documents, which Dr. Collins said “adds time, but generally does not meaningfully enhance protections for the participants. This new NIH policy seeks to end duplicative reviews that slow down the start of the research.”
Michael Pichichero, MD, director of the research institute, Rochester (N.Y.) General Hospital, called the change “a good policy. Allowing a single IRB to review and not go through multiple reviews will help get clinical trials going faster,” he said in an interview. “The policies and principles of IRB review are the same for all U.S. Food and Drug Administration–approved IRBs, so the concern that inappropriate approval might be given is highly unlikely.”
In an effort to streamline multisite clinical research, the National Institutes of Health announced a new policy related to the use of institutional review boards (IRBs).
The new policy sets “the expectation that multisite studies conducting the same protocol use a single IRB to carry out the ethical review of the proposed research,” NIH Director Francis S. Collins, MD, said in a June 21 statement. The policy goes into effect May 25, 2017, and applies only to domestic research.
Currently, for most multisite studies, the IRB at each site conducts an independent review of protocol and consent documents, which Dr. Collins said “adds time, but generally does not meaningfully enhance protections for the participants. This new NIH policy seeks to end duplicative reviews that slow down the start of the research.”
Michael Pichichero, MD, director of the research institute, Rochester (N.Y.) General Hospital, called the change “a good policy. Allowing a single IRB to review and not go through multiple reviews will help get clinical trials going faster,” he said in an interview. “The policies and principles of IRB review are the same for all U.S. Food and Drug Administration–approved IRBs, so the concern that inappropriate approval might be given is highly unlikely.”
In an effort to streamline multisite clinical research, the National Institutes of Health announced a new policy related to the use of institutional review boards (IRBs).
The new policy sets “the expectation that multisite studies conducting the same protocol use a single IRB to carry out the ethical review of the proposed research,” NIH Director Francis S. Collins, MD, said in a June 21 statement. The policy goes into effect May 25, 2017, and applies only to domestic research.
Currently, for most multisite studies, the IRB at each site conducts an independent review of protocol and consent documents, which Dr. Collins said “adds time, but generally does not meaningfully enhance protections for the participants. This new NIH policy seeks to end duplicative reviews that slow down the start of the research.”
Michael Pichichero, MD, director of the research institute, Rochester (N.Y.) General Hospital, called the change “a good policy. Allowing a single IRB to review and not go through multiple reviews will help get clinical trials going faster,” he said in an interview. “The policies and principles of IRB review are the same for all U.S. Food and Drug Administration–approved IRBs, so the concern that inappropriate approval might be given is highly unlikely.”
Reducing Drug Expenditure with Computerized Alerts
Hospitalists face ever-increasing pressure to reduce drug expenditures without compromising the quality of care provided to patients, and as a consequence, are creating new ways to approach the issue. A recent study published in the American Journal of Medical Quality assessed the effectiveness of computerized provider order entry alerts as one method. The alerts displayed the cost of a high-cost medication alongside a lower-cost alternative.
“We regularly scrutinize our drug budgets and look for medications that display changing costs/utilization,” says Gregory K. Gipson, PharmD, cardiothoracic surgery and cardiology pharmacist at the University of Washington and lead author of “Optimizing Prescribing Practices of High-Cost Medications with Computerized Alerts in the Inpatient Setting.”
“We were able to identify a few medications that were both high in cost and utilization but had lower-cost alternatives that could be substituted in certain situations,” Dr. Gipson says. “These higher-cost medications also had formulary restrictions for use; however, it was felt that very few people knew about these restrictions or had any idea how much any of these medications cost. In an attempt to reduce unnecessary use of these high-cost medications, we created alerts that informed providers of the cost of both high- and low-cost medications and restrictions for use, and we gave them the ability to convert the order to the lower-cost alternative.”
The study looked specifically at three high-cost medications and their utilization during the year prior to the intervention and compared it to usage in the year after implementation, and it found reduced utilization of high-cost medications.
“Ipratropium hydrofluoroalkane and fluticasone hydrofluoroalkane metered dose inhaler utilization were reduced by 29% and 62%, respectively (P
Overall, they saw this as a success. “This type of interruptive electronic order entry alert containing cost information and therapeutic alternatives is an effective educational tool that reduces medication costs,” Dr. Gipson says. “… This suggests that new computerized alerts can be implemented in thoughtful ways to minimize the interference with hospital workflow and alert fatigue yet still achieve their desired outcome.”
Reference
- Gipson G, Kelly JL, McKinney CM, White AA. Optimizing prescribing practices of high-cost medications with computerized alerts in the inpatient setting. Am J Med Qual. doi:10.1177/1062860616649660.
Quick Byte
Telehealth Expansion
In 2014, reimbursements for telehealth accounted for less than $14 million out of the more than $600 billion spent through the Medicare program, according to “Integrating Health Care and Housing to Promote Healthy Aging,” a recent Health Affairs blog. But, the authors suggest, the Centers for Medicare & Medicaid Services and state Medicaid programs should encourage greater reimbursement of telehealth and other technologies that have the potential to improve health outcomes and reduce costs, especially for seniors who could remain at home. “The shift away from fee-for-service payment toward value-based delivery and payment models represents a key opportunity for broader integration of telehealth,” according to the post.
Reference
1. Schwartz A, Parekh A. Integrating health care and housing to promote healthy aging. Health Aff. Available at: http://healthaffairs.org/blog/2016/05/23/integrating-health-care-and-housing-to-promote-healthy-aging/. Accessed May 31, 2016.
Hospitalists face ever-increasing pressure to reduce drug expenditures without compromising the quality of care provided to patients, and as a consequence, are creating new ways to approach the issue. A recent study published in the American Journal of Medical Quality assessed the effectiveness of computerized provider order entry alerts as one method. The alerts displayed the cost of a high-cost medication alongside a lower-cost alternative.
“We regularly scrutinize our drug budgets and look for medications that display changing costs/utilization,” says Gregory K. Gipson, PharmD, cardiothoracic surgery and cardiology pharmacist at the University of Washington and lead author of “Optimizing Prescribing Practices of High-Cost Medications with Computerized Alerts in the Inpatient Setting.”
“We were able to identify a few medications that were both high in cost and utilization but had lower-cost alternatives that could be substituted in certain situations,” Dr. Gipson says. “These higher-cost medications also had formulary restrictions for use; however, it was felt that very few people knew about these restrictions or had any idea how much any of these medications cost. In an attempt to reduce unnecessary use of these high-cost medications, we created alerts that informed providers of the cost of both high- and low-cost medications and restrictions for use, and we gave them the ability to convert the order to the lower-cost alternative.”
The study looked specifically at three high-cost medications and their utilization during the year prior to the intervention and compared it to usage in the year after implementation, and it found reduced utilization of high-cost medications.
“Ipratropium hydrofluoroalkane and fluticasone hydrofluoroalkane metered dose inhaler utilization were reduced by 29% and 62%, respectively (P
Overall, they saw this as a success. “This type of interruptive electronic order entry alert containing cost information and therapeutic alternatives is an effective educational tool that reduces medication costs,” Dr. Gipson says. “… This suggests that new computerized alerts can be implemented in thoughtful ways to minimize the interference with hospital workflow and alert fatigue yet still achieve their desired outcome.”
Reference
- Gipson G, Kelly JL, McKinney CM, White AA. Optimizing prescribing practices of high-cost medications with computerized alerts in the inpatient setting. Am J Med Qual. doi:10.1177/1062860616649660.
Quick Byte
Telehealth Expansion
In 2014, reimbursements for telehealth accounted for less than $14 million out of the more than $600 billion spent through the Medicare program, according to “Integrating Health Care and Housing to Promote Healthy Aging,” a recent Health Affairs blog. But, the authors suggest, the Centers for Medicare & Medicaid Services and state Medicaid programs should encourage greater reimbursement of telehealth and other technologies that have the potential to improve health outcomes and reduce costs, especially for seniors who could remain at home. “The shift away from fee-for-service payment toward value-based delivery and payment models represents a key opportunity for broader integration of telehealth,” according to the post.
Reference
1. Schwartz A, Parekh A. Integrating health care and housing to promote healthy aging. Health Aff. Available at: http://healthaffairs.org/blog/2016/05/23/integrating-health-care-and-housing-to-promote-healthy-aging/. Accessed May 31, 2016.
Hospitalists face ever-increasing pressure to reduce drug expenditures without compromising the quality of care provided to patients, and as a consequence, are creating new ways to approach the issue. A recent study published in the American Journal of Medical Quality assessed the effectiveness of computerized provider order entry alerts as one method. The alerts displayed the cost of a high-cost medication alongside a lower-cost alternative.
“We regularly scrutinize our drug budgets and look for medications that display changing costs/utilization,” says Gregory K. Gipson, PharmD, cardiothoracic surgery and cardiology pharmacist at the University of Washington and lead author of “Optimizing Prescribing Practices of High-Cost Medications with Computerized Alerts in the Inpatient Setting.”
“We were able to identify a few medications that were both high in cost and utilization but had lower-cost alternatives that could be substituted in certain situations,” Dr. Gipson says. “These higher-cost medications also had formulary restrictions for use; however, it was felt that very few people knew about these restrictions or had any idea how much any of these medications cost. In an attempt to reduce unnecessary use of these high-cost medications, we created alerts that informed providers of the cost of both high- and low-cost medications and restrictions for use, and we gave them the ability to convert the order to the lower-cost alternative.”
The study looked specifically at three high-cost medications and their utilization during the year prior to the intervention and compared it to usage in the year after implementation, and it found reduced utilization of high-cost medications.
“Ipratropium hydrofluoroalkane and fluticasone hydrofluoroalkane metered dose inhaler utilization were reduced by 29% and 62%, respectively (P
Overall, they saw this as a success. “This type of interruptive electronic order entry alert containing cost information and therapeutic alternatives is an effective educational tool that reduces medication costs,” Dr. Gipson says. “… This suggests that new computerized alerts can be implemented in thoughtful ways to minimize the interference with hospital workflow and alert fatigue yet still achieve their desired outcome.”
Reference
- Gipson G, Kelly JL, McKinney CM, White AA. Optimizing prescribing practices of high-cost medications with computerized alerts in the inpatient setting. Am J Med Qual. doi:10.1177/1062860616649660.
Quick Byte
Telehealth Expansion
In 2014, reimbursements for telehealth accounted for less than $14 million out of the more than $600 billion spent through the Medicare program, according to “Integrating Health Care and Housing to Promote Healthy Aging,” a recent Health Affairs blog. But, the authors suggest, the Centers for Medicare & Medicaid Services and state Medicaid programs should encourage greater reimbursement of telehealth and other technologies that have the potential to improve health outcomes and reduce costs, especially for seniors who could remain at home. “The shift away from fee-for-service payment toward value-based delivery and payment models represents a key opportunity for broader integration of telehealth,” according to the post.
Reference
1. Schwartz A, Parekh A. Integrating health care and housing to promote healthy aging. Health Aff. Available at: http://healthaffairs.org/blog/2016/05/23/integrating-health-care-and-housing-to-promote-healthy-aging/. Accessed May 31, 2016.
As Summer—and Interns—Roll In, Try a Little Empathy on Your Patients, Colleagues
It’s July, the month that marks the annual rite of passage for both newly minted physicians starting their internships and somewhat-less-fresh trainees completing their residencies and moving on to the next stage of their professional journey. I would imagine that many of you, like me, spend at least a fleeting moment this time of year thinking back to your first days as interns and, hopefully, extend at least a little empathy to those anxious souls who are being called upon to serve as “doctors” for the very first time.
When I reflect a little further, I am also reminded of the immense power and influence of role models over the course of our training. Although internal medicine was certainly interesting to me, even during medical school, I will candidly also say that the residents and attendings who I served with on teams during medical school at the University of Pennsylvania had at least as much if not more to do with my choice to match in internal medicine. I remember many of their names to this day. While I am not in touch with them, I will always be grateful for the way they demonstrated enthusiasm for medicine; compassion for their patients; partnership with nurses, therapists, and the many other members of our teams; and a genuine love for teaching and conveying a sense of mission in what they did.
I had many great teachers in other areas (particularly, I have to admit, surgery, where some of us students were so enamored of the clinical clerkship director that we memorialized him in a sendup of Forrest Gump in our annual comedy show). However, the consistency of this enthusiasm in the medicine teams was incomparable. In short, these were physicians who I wanted to be like, to emulate. They were role models.
Likewise, during residency, it was those attendings who were among the earliest of academic hospitalists who demonstrated those same skills. I will always remember an encounter with one of my chief residents at the Veterans Affairs early in my internship, when I was struggling with a particular issue. Perhaps it was a foreshadowing of my ultimate career choice, but I was disappointed with my ambulatory clinic experience. As a chief resident, he could have dismissed my frustration or told me to suck it up. He didn’t. He empathized, acknowledging my exasperation and assuring me that I wasn’t alone in how I felt. He also helped me frame the experience to find positive learning aspects—after all, it wasn’t a problem he could just fix and make go away.
Most important, he listened and didn’t judge.
Long before we started thinking of empathy as a teachable communication skill, I experienced it firsthand, and it turned my entire experience around. To this day, I try to emulate that empathy when frustrated physicians or employees come to me with issues.
As hospitalists and physicians, the spotlight is on us almost every minute of every day. We are watched (yes, we are judged) all the time by nurses, pharmacists, case managers, and our patients to see if we live the values of teamwork, collaboration, and emotional intelligence that we claim to embody as system thinkers and system reformers.
But no one watches us more closely than those who we are charged with training. From the very earliest medical student to the most seasoned resident and fellow, how we act is how they will act. When we demonstrate that the bar is highest for us in terms of professionalism, collegiality, and empathy, we imprint upon our trainees those same behaviors and the values that they reflect.
We also show trainees a way of practicing medicine that has the ability to be profoundly satisfying to not only ourselves but also to those who collaborate with us and the patients who benefit from that teamwork. And, hopefully, by doing so we are guiding students, interns, and residents to become hospitalists like us.
So, this July, I call upon all of us in the hospitalist teaching community to reach out and welcome the new trainees in your institution and to remember what it was like to be where they are now. Appreciate the profound impact that you have on them by not only the medicine you teach but the way you practice and communicate and your body language and attitude.
As we think about the continuous need to focus on building up the pipeline of future hospital-based practitioners, there is no better way to develop that bench strength than by using our presence as role models to positively influence our new trainees.
Happy July, everyone! TH
It’s July, the month that marks the annual rite of passage for both newly minted physicians starting their internships and somewhat-less-fresh trainees completing their residencies and moving on to the next stage of their professional journey. I would imagine that many of you, like me, spend at least a fleeting moment this time of year thinking back to your first days as interns and, hopefully, extend at least a little empathy to those anxious souls who are being called upon to serve as “doctors” for the very first time.
When I reflect a little further, I am also reminded of the immense power and influence of role models over the course of our training. Although internal medicine was certainly interesting to me, even during medical school, I will candidly also say that the residents and attendings who I served with on teams during medical school at the University of Pennsylvania had at least as much if not more to do with my choice to match in internal medicine. I remember many of their names to this day. While I am not in touch with them, I will always be grateful for the way they demonstrated enthusiasm for medicine; compassion for their patients; partnership with nurses, therapists, and the many other members of our teams; and a genuine love for teaching and conveying a sense of mission in what they did.
I had many great teachers in other areas (particularly, I have to admit, surgery, where some of us students were so enamored of the clinical clerkship director that we memorialized him in a sendup of Forrest Gump in our annual comedy show). However, the consistency of this enthusiasm in the medicine teams was incomparable. In short, these were physicians who I wanted to be like, to emulate. They were role models.
Likewise, during residency, it was those attendings who were among the earliest of academic hospitalists who demonstrated those same skills. I will always remember an encounter with one of my chief residents at the Veterans Affairs early in my internship, when I was struggling with a particular issue. Perhaps it was a foreshadowing of my ultimate career choice, but I was disappointed with my ambulatory clinic experience. As a chief resident, he could have dismissed my frustration or told me to suck it up. He didn’t. He empathized, acknowledging my exasperation and assuring me that I wasn’t alone in how I felt. He also helped me frame the experience to find positive learning aspects—after all, it wasn’t a problem he could just fix and make go away.
Most important, he listened and didn’t judge.
Long before we started thinking of empathy as a teachable communication skill, I experienced it firsthand, and it turned my entire experience around. To this day, I try to emulate that empathy when frustrated physicians or employees come to me with issues.
As hospitalists and physicians, the spotlight is on us almost every minute of every day. We are watched (yes, we are judged) all the time by nurses, pharmacists, case managers, and our patients to see if we live the values of teamwork, collaboration, and emotional intelligence that we claim to embody as system thinkers and system reformers.
But no one watches us more closely than those who we are charged with training. From the very earliest medical student to the most seasoned resident and fellow, how we act is how they will act. When we demonstrate that the bar is highest for us in terms of professionalism, collegiality, and empathy, we imprint upon our trainees those same behaviors and the values that they reflect.
We also show trainees a way of practicing medicine that has the ability to be profoundly satisfying to not only ourselves but also to those who collaborate with us and the patients who benefit from that teamwork. And, hopefully, by doing so we are guiding students, interns, and residents to become hospitalists like us.
So, this July, I call upon all of us in the hospitalist teaching community to reach out and welcome the new trainees in your institution and to remember what it was like to be where they are now. Appreciate the profound impact that you have on them by not only the medicine you teach but the way you practice and communicate and your body language and attitude.
As we think about the continuous need to focus on building up the pipeline of future hospital-based practitioners, there is no better way to develop that bench strength than by using our presence as role models to positively influence our new trainees.
Happy July, everyone! TH
It’s July, the month that marks the annual rite of passage for both newly minted physicians starting their internships and somewhat-less-fresh trainees completing their residencies and moving on to the next stage of their professional journey. I would imagine that many of you, like me, spend at least a fleeting moment this time of year thinking back to your first days as interns and, hopefully, extend at least a little empathy to those anxious souls who are being called upon to serve as “doctors” for the very first time.
When I reflect a little further, I am also reminded of the immense power and influence of role models over the course of our training. Although internal medicine was certainly interesting to me, even during medical school, I will candidly also say that the residents and attendings who I served with on teams during medical school at the University of Pennsylvania had at least as much if not more to do with my choice to match in internal medicine. I remember many of their names to this day. While I am not in touch with them, I will always be grateful for the way they demonstrated enthusiasm for medicine; compassion for their patients; partnership with nurses, therapists, and the many other members of our teams; and a genuine love for teaching and conveying a sense of mission in what they did.
I had many great teachers in other areas (particularly, I have to admit, surgery, where some of us students were so enamored of the clinical clerkship director that we memorialized him in a sendup of Forrest Gump in our annual comedy show). However, the consistency of this enthusiasm in the medicine teams was incomparable. In short, these were physicians who I wanted to be like, to emulate. They were role models.
Likewise, during residency, it was those attendings who were among the earliest of academic hospitalists who demonstrated those same skills. I will always remember an encounter with one of my chief residents at the Veterans Affairs early in my internship, when I was struggling with a particular issue. Perhaps it was a foreshadowing of my ultimate career choice, but I was disappointed with my ambulatory clinic experience. As a chief resident, he could have dismissed my frustration or told me to suck it up. He didn’t. He empathized, acknowledging my exasperation and assuring me that I wasn’t alone in how I felt. He also helped me frame the experience to find positive learning aspects—after all, it wasn’t a problem he could just fix and make go away.
Most important, he listened and didn’t judge.
Long before we started thinking of empathy as a teachable communication skill, I experienced it firsthand, and it turned my entire experience around. To this day, I try to emulate that empathy when frustrated physicians or employees come to me with issues.
As hospitalists and physicians, the spotlight is on us almost every minute of every day. We are watched (yes, we are judged) all the time by nurses, pharmacists, case managers, and our patients to see if we live the values of teamwork, collaboration, and emotional intelligence that we claim to embody as system thinkers and system reformers.
But no one watches us more closely than those who we are charged with training. From the very earliest medical student to the most seasoned resident and fellow, how we act is how they will act. When we demonstrate that the bar is highest for us in terms of professionalism, collegiality, and empathy, we imprint upon our trainees those same behaviors and the values that they reflect.
We also show trainees a way of practicing medicine that has the ability to be profoundly satisfying to not only ourselves but also to those who collaborate with us and the patients who benefit from that teamwork. And, hopefully, by doing so we are guiding students, interns, and residents to become hospitalists like us.
So, this July, I call upon all of us in the hospitalist teaching community to reach out and welcome the new trainees in your institution and to remember what it was like to be where they are now. Appreciate the profound impact that you have on them by not only the medicine you teach but the way you practice and communicate and your body language and attitude.
As we think about the continuous need to focus on building up the pipeline of future hospital-based practitioners, there is no better way to develop that bench strength than by using our presence as role models to positively influence our new trainees.
Happy July, everyone! TH
Supreme Court deadlocks on immigration policy case
Supreme Court justices have deadlocked on whether protections for undocumented immigrants can be expanded under an executive order by the President.
In a June 23 decision, justices were equally divided on the constitutionality of two of President Obama’s immigration policies: the Deferred Action for Parents of Americans and Lawful Permanent Residents (DAPA) and an expanded version of the Deferred Action for Childhood Arrivals (DACA). The former protects undocumented immigrants who are parents of U.S. citizens from deportation, if they meet certain criteria. The second extends work authorization under the original DACA program from 2 years to 3 years and broadens age requirements.
The 4-to-4 split decision in Texas v. United States mean the policies remain blocked by the lower court, and the expanded programs will not go forward anytime soon. The decision does not affect original DACA, which protects from deportation undocumented immigrants brought to the United States as children and offers access to work authorization.
President Obama expressed disappointment at the lack of agreement, saying the tie vote underscores the need for nine justices on the court.
“As disappointing as it was to be challenged for taking the kind of action that other administrations have taken, the country was looking to the Supreme Court to resolve the important legal questions raised in this case,” President Obama said during a June 23 press conference. “Today, the Supreme Court was unable to reach a decision ... it means the expanded set of common sense deferred action policies that I announced 2 years ago cannot go forward at this stage until there is a ninth justice on the court to break the tie.”
Texas Attorney General Ken Paxton was satisfied with the decision, calling it a victory for the state plaintiffs.
“Today’s decision keeps in place what we have maintained from the very start: one person, even a president, cannot unilaterally change the law,” Mr. Paxton said in a statement. “This is a major setback to President Obama’s attempts to expand executive power, and a victory for those who believe in the separation of powers and the rule of law.”
Texas was 1 of 26 states that sued over DAPA and expanded DACA. The states argued the president does not have the authority to issue the new immigration policies, and that the programs violate the Constitution as well as the Administrative Procedure Act for notice-and-comment rule making. Justices heard oral arguments April 18.
Immigration advocates were worried that if expanded DACA were struck down, a similar fate would follow for the original DACA policy. As it stands, undocumented immigrants who benefit from deportation protection and work authorization under original DACA, including undocumented medical students, will not be affected by the Supreme Court decision.
Marielena Hincapié, executive director for the National Immigration Law Center, vowed to continue fighting for the policies to take effect.
“Immigrants and allies fought for and won these significant policy victories, which would have brought much-needed emotional and economic stability to millions of our community members, and we will not sit back,” she said in a statement. “We urge the Department of Justice to seek a rehearing for when a ninth justice is confirmed for the Supreme Court.”
Federation for American Immigration Reform President Dan Stein said the split decision upholds the rule of law and helps preserve the balance of power in the United States.
“By ruling in favor of the federal court’s injunction, half of the nation’s Supreme Court Justices have shown that they have deep concerns about this president’s attempt at a power grab by his efforts to amend federal laws from the Oval Office,” Mr. Stein said in a statement.
Texas v. United States will be sent back to U.S. District Court Judge Andrew Hanen in Texas who will hear the case on its merits. The case could wind its way back to the U.S. Supreme Court for a rehearing after a ninth justice is confirmed.
On Twitter @legal_med
Supreme Court justices have deadlocked on whether protections for undocumented immigrants can be expanded under an executive order by the President.
In a June 23 decision, justices were equally divided on the constitutionality of two of President Obama’s immigration policies: the Deferred Action for Parents of Americans and Lawful Permanent Residents (DAPA) and an expanded version of the Deferred Action for Childhood Arrivals (DACA). The former protects undocumented immigrants who are parents of U.S. citizens from deportation, if they meet certain criteria. The second extends work authorization under the original DACA program from 2 years to 3 years and broadens age requirements.
The 4-to-4 split decision in Texas v. United States mean the policies remain blocked by the lower court, and the expanded programs will not go forward anytime soon. The decision does not affect original DACA, which protects from deportation undocumented immigrants brought to the United States as children and offers access to work authorization.
President Obama expressed disappointment at the lack of agreement, saying the tie vote underscores the need for nine justices on the court.
“As disappointing as it was to be challenged for taking the kind of action that other administrations have taken, the country was looking to the Supreme Court to resolve the important legal questions raised in this case,” President Obama said during a June 23 press conference. “Today, the Supreme Court was unable to reach a decision ... it means the expanded set of common sense deferred action policies that I announced 2 years ago cannot go forward at this stage until there is a ninth justice on the court to break the tie.”
Texas Attorney General Ken Paxton was satisfied with the decision, calling it a victory for the state plaintiffs.
“Today’s decision keeps in place what we have maintained from the very start: one person, even a president, cannot unilaterally change the law,” Mr. Paxton said in a statement. “This is a major setback to President Obama’s attempts to expand executive power, and a victory for those who believe in the separation of powers and the rule of law.”
Texas was 1 of 26 states that sued over DAPA and expanded DACA. The states argued the president does not have the authority to issue the new immigration policies, and that the programs violate the Constitution as well as the Administrative Procedure Act for notice-and-comment rule making. Justices heard oral arguments April 18.
Immigration advocates were worried that if expanded DACA were struck down, a similar fate would follow for the original DACA policy. As it stands, undocumented immigrants who benefit from deportation protection and work authorization under original DACA, including undocumented medical students, will not be affected by the Supreme Court decision.
Marielena Hincapié, executive director for the National Immigration Law Center, vowed to continue fighting for the policies to take effect.
“Immigrants and allies fought for and won these significant policy victories, which would have brought much-needed emotional and economic stability to millions of our community members, and we will not sit back,” she said in a statement. “We urge the Department of Justice to seek a rehearing for when a ninth justice is confirmed for the Supreme Court.”
Federation for American Immigration Reform President Dan Stein said the split decision upholds the rule of law and helps preserve the balance of power in the United States.
“By ruling in favor of the federal court’s injunction, half of the nation’s Supreme Court Justices have shown that they have deep concerns about this president’s attempt at a power grab by his efforts to amend federal laws from the Oval Office,” Mr. Stein said in a statement.
Texas v. United States will be sent back to U.S. District Court Judge Andrew Hanen in Texas who will hear the case on its merits. The case could wind its way back to the U.S. Supreme Court for a rehearing after a ninth justice is confirmed.
On Twitter @legal_med
Supreme Court justices have deadlocked on whether protections for undocumented immigrants can be expanded under an executive order by the President.
In a June 23 decision, justices were equally divided on the constitutionality of two of President Obama’s immigration policies: the Deferred Action for Parents of Americans and Lawful Permanent Residents (DAPA) and an expanded version of the Deferred Action for Childhood Arrivals (DACA). The former protects undocumented immigrants who are parents of U.S. citizens from deportation, if they meet certain criteria. The second extends work authorization under the original DACA program from 2 years to 3 years and broadens age requirements.
The 4-to-4 split decision in Texas v. United States mean the policies remain blocked by the lower court, and the expanded programs will not go forward anytime soon. The decision does not affect original DACA, which protects from deportation undocumented immigrants brought to the United States as children and offers access to work authorization.
President Obama expressed disappointment at the lack of agreement, saying the tie vote underscores the need for nine justices on the court.
“As disappointing as it was to be challenged for taking the kind of action that other administrations have taken, the country was looking to the Supreme Court to resolve the important legal questions raised in this case,” President Obama said during a June 23 press conference. “Today, the Supreme Court was unable to reach a decision ... it means the expanded set of common sense deferred action policies that I announced 2 years ago cannot go forward at this stage until there is a ninth justice on the court to break the tie.”
Texas Attorney General Ken Paxton was satisfied with the decision, calling it a victory for the state plaintiffs.
“Today’s decision keeps in place what we have maintained from the very start: one person, even a president, cannot unilaterally change the law,” Mr. Paxton said in a statement. “This is a major setback to President Obama’s attempts to expand executive power, and a victory for those who believe in the separation of powers and the rule of law.”
Texas was 1 of 26 states that sued over DAPA and expanded DACA. The states argued the president does not have the authority to issue the new immigration policies, and that the programs violate the Constitution as well as the Administrative Procedure Act for notice-and-comment rule making. Justices heard oral arguments April 18.
Immigration advocates were worried that if expanded DACA were struck down, a similar fate would follow for the original DACA policy. As it stands, undocumented immigrants who benefit from deportation protection and work authorization under original DACA, including undocumented medical students, will not be affected by the Supreme Court decision.
Marielena Hincapié, executive director for the National Immigration Law Center, vowed to continue fighting for the policies to take effect.
“Immigrants and allies fought for and won these significant policy victories, which would have brought much-needed emotional and economic stability to millions of our community members, and we will not sit back,” she said in a statement. “We urge the Department of Justice to seek a rehearing for when a ninth justice is confirmed for the Supreme Court.”
Federation for American Immigration Reform President Dan Stein said the split decision upholds the rule of law and helps preserve the balance of power in the United States.
“By ruling in favor of the federal court’s injunction, half of the nation’s Supreme Court Justices have shown that they have deep concerns about this president’s attempt at a power grab by his efforts to amend federal laws from the Oval Office,” Mr. Stein said in a statement.
Texas v. United States will be sent back to U.S. District Court Judge Andrew Hanen in Texas who will hear the case on its merits. The case could wind its way back to the U.S. Supreme Court for a rehearing after a ninth justice is confirmed.
On Twitter @legal_med
Who to Blame for Surgical Readmissions?
When too many surgery patients are readmitted, the hospital can be fined by the federal government - but a new study suggests many of those readmissions are not the hospital's fault.
Many readmissions were due to issues like drug abuse or homelessness, the researchers found. Less than one in five patients returned to the hospital due to something doctors could have managed better.
"Very few were due to reasons we could control with better medical care at the index admission," said lead author Dr. Lisa McIntyre, of Harbourview Medical Center in Seattle.
McIntyre and her colleagues noted June 15 in JAMA Surgery that the U.S. government began fining hospitals in 2015 for surgery readmission rates that are higher than expected. Fines were already being imposed since 2012 for readmissions following treatments for various medical conditions.
The researchers studied the medical records of patients who were discharged from their hospital's general surgery department in 2014 or 2015 and readmitted within 30 days.
Out of the 2,100 discharges during that time, there were 173 unplanned readmissions. About 17% of those readmissions were due to injection drug use and about 15% were due to issues like homelessness or difficulty getting to follow-up appointments.
Only about 18% of readmissions - about 2% of all discharges - were due to potentially avoidable problems following surgery.
While the results are only from a single hospital, that hospital is also a safety-net facility for the local area - and McIntyre pointed out that all hospitals have some amount of disadvantaged patients.
"To be able to affect this rate, there are going to need to be new interventions that require money and a more global care package of each individual patient that doesn't stop at discharge," said McIntyre, who is also affiliated with the University of Washington.
Being female, having diabetes, having sepsis upon admission, being in the ICU and being discharged to respite care were all tied to an increased risk of readmission, the researchers found.
The results raise the question of whether readmission rates are valuable measures of surgical quality, write Drs. Alexander Schwed and Christian de Virgilio of the University of California, Los Angeles in an editorial.
Some would argue that readmitting patients is a sound medical decision that is tied to lower risks of death, they write.
"Should such an inexact marker of quality be used to financially penalize hospitals?" they ask. "Health services researchers (need to find) a better marker for surgical quality that is reliably calculable and clinically useful."
SOURCE: http://bit.ly/28Km3aH and http://bit.ly/28Km3Ye JAMA Surgery 2016.
When too many surgery patients are readmitted, the hospital can be fined by the federal government - but a new study suggests many of those readmissions are not the hospital's fault.
Many readmissions were due to issues like drug abuse or homelessness, the researchers found. Less than one in five patients returned to the hospital due to something doctors could have managed better.
"Very few were due to reasons we could control with better medical care at the index admission," said lead author Dr. Lisa McIntyre, of Harbourview Medical Center in Seattle.
McIntyre and her colleagues noted June 15 in JAMA Surgery that the U.S. government began fining hospitals in 2015 for surgery readmission rates that are higher than expected. Fines were already being imposed since 2012 for readmissions following treatments for various medical conditions.
The researchers studied the medical records of patients who were discharged from their hospital's general surgery department in 2014 or 2015 and readmitted within 30 days.
Out of the 2,100 discharges during that time, there were 173 unplanned readmissions. About 17% of those readmissions were due to injection drug use and about 15% were due to issues like homelessness or difficulty getting to follow-up appointments.
Only about 18% of readmissions - about 2% of all discharges - were due to potentially avoidable problems following surgery.
While the results are only from a single hospital, that hospital is also a safety-net facility for the local area - and McIntyre pointed out that all hospitals have some amount of disadvantaged patients.
"To be able to affect this rate, there are going to need to be new interventions that require money and a more global care package of each individual patient that doesn't stop at discharge," said McIntyre, who is also affiliated with the University of Washington.
Being female, having diabetes, having sepsis upon admission, being in the ICU and being discharged to respite care were all tied to an increased risk of readmission, the researchers found.
The results raise the question of whether readmission rates are valuable measures of surgical quality, write Drs. Alexander Schwed and Christian de Virgilio of the University of California, Los Angeles in an editorial.
Some would argue that readmitting patients is a sound medical decision that is tied to lower risks of death, they write.
"Should such an inexact marker of quality be used to financially penalize hospitals?" they ask. "Health services researchers (need to find) a better marker for surgical quality that is reliably calculable and clinically useful."
SOURCE: http://bit.ly/28Km3aH and http://bit.ly/28Km3Ye JAMA Surgery 2016.
When too many surgery patients are readmitted, the hospital can be fined by the federal government - but a new study suggests many of those readmissions are not the hospital's fault.
Many readmissions were due to issues like drug abuse or homelessness, the researchers found. Less than one in five patients returned to the hospital due to something doctors could have managed better.
"Very few were due to reasons we could control with better medical care at the index admission," said lead author Dr. Lisa McIntyre, of Harbourview Medical Center in Seattle.
McIntyre and her colleagues noted June 15 in JAMA Surgery that the U.S. government began fining hospitals in 2015 for surgery readmission rates that are higher than expected. Fines were already being imposed since 2012 for readmissions following treatments for various medical conditions.
The researchers studied the medical records of patients who were discharged from their hospital's general surgery department in 2014 or 2015 and readmitted within 30 days.
Out of the 2,100 discharges during that time, there were 173 unplanned readmissions. About 17% of those readmissions were due to injection drug use and about 15% were due to issues like homelessness or difficulty getting to follow-up appointments.
Only about 18% of readmissions - about 2% of all discharges - were due to potentially avoidable problems following surgery.
While the results are only from a single hospital, that hospital is also a safety-net facility for the local area - and McIntyre pointed out that all hospitals have some amount of disadvantaged patients.
"To be able to affect this rate, there are going to need to be new interventions that require money and a more global care package of each individual patient that doesn't stop at discharge," said McIntyre, who is also affiliated with the University of Washington.
Being female, having diabetes, having sepsis upon admission, being in the ICU and being discharged to respite care were all tied to an increased risk of readmission, the researchers found.
The results raise the question of whether readmission rates are valuable measures of surgical quality, write Drs. Alexander Schwed and Christian de Virgilio of the University of California, Los Angeles in an editorial.
Some would argue that readmitting patients is a sound medical decision that is tied to lower risks of death, they write.
"Should such an inexact marker of quality be used to financially penalize hospitals?" they ask. "Health services researchers (need to find) a better marker for surgical quality that is reliably calculable and clinically useful."
SOURCE: http://bit.ly/28Km3aH and http://bit.ly/28Km3Ye JAMA Surgery 2016.
House Republicans unveil long-awaited plan to replace health law
Six years after promising a plan to “repeal and replace” the federal health law, House Republicans are finally ready to deliver.
The 37-page white paper, called “A Better Way,” includes virtually every idea on health care proposed by Republicans going back at least 2 decades. It would bring back “high-risk pools” for people with very high medical expenses, end open-ended funding for the Medicaid program, and encourage small businesses to band together to get better bargaining power in “Association Health Plans.”
What the plan does not include, however, is any idea of how much it would cost, or how it would be financed. Also unclear is how many of the 20 million Americans who have gained coverage since the law took effect would be able to remain insured.
“It’s a framework,” a senior House Republican leadership aide said on a conference call with reporters Tuesday, with the specifics to be determined next year by congressional committees, assuming the GOP maintains its majority. He likened the document to the white paper issued just after President Barack Obama’s election by then–Senate Finance Committee Chairman Max Baucus (D-Mont.). That document foreshadowed many of the key elements of the Affordable Care Act.
The plan starts with repeal of the health law and its requirements and taxes, but it would then put back many of its most popular elements: Allowing young adults to stay on their parents’ health plan to age 26; banning insurers from charging people with preexisting health problems higher premiums; and forbidding insurers from dropping coverage if a policyholder gets sick.
It would repeal the current scheme of exchanges where consumers buy insurance and government tax credits to help moderate-income Americans pay their premiums if they don’t have an employer to help. Instead, everyone buying policies in the individual market would receive tax credits. Older people charged more by insurers would receive larger credits, though the House Republicans don’t specify how much.
But the GOP plan also would likely make insurance more expensive for older people by proposing a broader range for premiums based on age. Current premiums can vary only threefold based on age, which is “driving out younger and healthier patients” who can’t afford them, the GOP aide said.
Under the plan, insurance companies could not charge higher rates to people with preexisting conditions so long as they maintain continuous coverage, whether from an employer or in a policy they purchase themselves. The new high-risk pools would be available for those who have a break in coverage, or who fail to purchase during a one-time open enrollment under the plan.
The plan would get rid of most of the coverage requirements under the Medicaid program for the poor, so states could make them more or less generous than they are currently. It would also limit funding. States could opt for either a per-person cap or a block grant to spend much as they wish.
On Medicare, the proposal would encourage the existing movement of patients from the program’s traditional fee-for-service program to managed care plans, and would transition from the existing financing structure based on benefits to a controversial structure called “premium support” that puts cost-controlling responsibilities more on private insurance companies. That change has been pushed by House Speaker Paul Ryan (R-Wisc.) for nearly a decade.
Backers of the existing health law were quick to criticize the GOP outline.
“The proposal introduced by Speaker Ryan is nothing more than vague and recycled ideas to take health insurance away from millions and increase costs for seniors and hardworking families,” said White House Assistant Press Secretary Katie Hill.
Families USA Executive Director Ron Pollack, who pushed hard for passage of the Affordable Care Act, said: “Make no mistake, Ryan’s approach is not a better way forward, but a bitter path backward that returns us to the bad old days when vast swaths of Americans were left to the tender mercies of the insurance industry and could not afford needed care.”
This story appears courtesy of Kaiser Health News, a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
Six years after promising a plan to “repeal and replace” the federal health law, House Republicans are finally ready to deliver.
The 37-page white paper, called “A Better Way,” includes virtually every idea on health care proposed by Republicans going back at least 2 decades. It would bring back “high-risk pools” for people with very high medical expenses, end open-ended funding for the Medicaid program, and encourage small businesses to band together to get better bargaining power in “Association Health Plans.”
What the plan does not include, however, is any idea of how much it would cost, or how it would be financed. Also unclear is how many of the 20 million Americans who have gained coverage since the law took effect would be able to remain insured.
“It’s a framework,” a senior House Republican leadership aide said on a conference call with reporters Tuesday, with the specifics to be determined next year by congressional committees, assuming the GOP maintains its majority. He likened the document to the white paper issued just after President Barack Obama’s election by then–Senate Finance Committee Chairman Max Baucus (D-Mont.). That document foreshadowed many of the key elements of the Affordable Care Act.
The plan starts with repeal of the health law and its requirements and taxes, but it would then put back many of its most popular elements: Allowing young adults to stay on their parents’ health plan to age 26; banning insurers from charging people with preexisting health problems higher premiums; and forbidding insurers from dropping coverage if a policyholder gets sick.
It would repeal the current scheme of exchanges where consumers buy insurance and government tax credits to help moderate-income Americans pay their premiums if they don’t have an employer to help. Instead, everyone buying policies in the individual market would receive tax credits. Older people charged more by insurers would receive larger credits, though the House Republicans don’t specify how much.
But the GOP plan also would likely make insurance more expensive for older people by proposing a broader range for premiums based on age. Current premiums can vary only threefold based on age, which is “driving out younger and healthier patients” who can’t afford them, the GOP aide said.
Under the plan, insurance companies could not charge higher rates to people with preexisting conditions so long as they maintain continuous coverage, whether from an employer or in a policy they purchase themselves. The new high-risk pools would be available for those who have a break in coverage, or who fail to purchase during a one-time open enrollment under the plan.
The plan would get rid of most of the coverage requirements under the Medicaid program for the poor, so states could make them more or less generous than they are currently. It would also limit funding. States could opt for either a per-person cap or a block grant to spend much as they wish.
On Medicare, the proposal would encourage the existing movement of patients from the program’s traditional fee-for-service program to managed care plans, and would transition from the existing financing structure based on benefits to a controversial structure called “premium support” that puts cost-controlling responsibilities more on private insurance companies. That change has been pushed by House Speaker Paul Ryan (R-Wisc.) for nearly a decade.
Backers of the existing health law were quick to criticize the GOP outline.
“The proposal introduced by Speaker Ryan is nothing more than vague and recycled ideas to take health insurance away from millions and increase costs for seniors and hardworking families,” said White House Assistant Press Secretary Katie Hill.
Families USA Executive Director Ron Pollack, who pushed hard for passage of the Affordable Care Act, said: “Make no mistake, Ryan’s approach is not a better way forward, but a bitter path backward that returns us to the bad old days when vast swaths of Americans were left to the tender mercies of the insurance industry and could not afford needed care.”
This story appears courtesy of Kaiser Health News, a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
Six years after promising a plan to “repeal and replace” the federal health law, House Republicans are finally ready to deliver.
The 37-page white paper, called “A Better Way,” includes virtually every idea on health care proposed by Republicans going back at least 2 decades. It would bring back “high-risk pools” for people with very high medical expenses, end open-ended funding for the Medicaid program, and encourage small businesses to band together to get better bargaining power in “Association Health Plans.”
What the plan does not include, however, is any idea of how much it would cost, or how it would be financed. Also unclear is how many of the 20 million Americans who have gained coverage since the law took effect would be able to remain insured.
“It’s a framework,” a senior House Republican leadership aide said on a conference call with reporters Tuesday, with the specifics to be determined next year by congressional committees, assuming the GOP maintains its majority. He likened the document to the white paper issued just after President Barack Obama’s election by then–Senate Finance Committee Chairman Max Baucus (D-Mont.). That document foreshadowed many of the key elements of the Affordable Care Act.
The plan starts with repeal of the health law and its requirements and taxes, but it would then put back many of its most popular elements: Allowing young adults to stay on their parents’ health plan to age 26; banning insurers from charging people with preexisting health problems higher premiums; and forbidding insurers from dropping coverage if a policyholder gets sick.
It would repeal the current scheme of exchanges where consumers buy insurance and government tax credits to help moderate-income Americans pay their premiums if they don’t have an employer to help. Instead, everyone buying policies in the individual market would receive tax credits. Older people charged more by insurers would receive larger credits, though the House Republicans don’t specify how much.
But the GOP plan also would likely make insurance more expensive for older people by proposing a broader range for premiums based on age. Current premiums can vary only threefold based on age, which is “driving out younger and healthier patients” who can’t afford them, the GOP aide said.
Under the plan, insurance companies could not charge higher rates to people with preexisting conditions so long as they maintain continuous coverage, whether from an employer or in a policy they purchase themselves. The new high-risk pools would be available for those who have a break in coverage, or who fail to purchase during a one-time open enrollment under the plan.
The plan would get rid of most of the coverage requirements under the Medicaid program for the poor, so states could make them more or less generous than they are currently. It would also limit funding. States could opt for either a per-person cap or a block grant to spend much as they wish.
On Medicare, the proposal would encourage the existing movement of patients from the program’s traditional fee-for-service program to managed care plans, and would transition from the existing financing structure based on benefits to a controversial structure called “premium support” that puts cost-controlling responsibilities more on private insurance companies. That change has been pushed by House Speaker Paul Ryan (R-Wisc.) for nearly a decade.
Backers of the existing health law were quick to criticize the GOP outline.
“The proposal introduced by Speaker Ryan is nothing more than vague and recycled ideas to take health insurance away from millions and increase costs for seniors and hardworking families,” said White House Assistant Press Secretary Katie Hill.
Families USA Executive Director Ron Pollack, who pushed hard for passage of the Affordable Care Act, said: “Make no mistake, Ryan’s approach is not a better way forward, but a bitter path backward that returns us to the bad old days when vast swaths of Americans were left to the tender mercies of the insurance industry and could not afford needed care.”
This story appears courtesy of Kaiser Health News, a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
Medicare Trust Fund projected to run dry in 2028
The Medicare Trust Fund is projected to become insolvent in 2028, 2 years earlier than projected this time last year.
The change is based on two key factors: an expected reduction in payroll taxes and a slowdown in declining rate of inpatient utilization, Andy Slavitt, acting administrator of the Centers for Medicare & Medicaid Services said at a June 22 press conference to review the annual Medicare Trustees report.
“The good news is inpatient utilization is still declining, it’s just declining at a slightly lower rate,” Mr. Slavitt said.
He also highlighted the continuing rising cost of prescription medications, which he called “a major driver” in Medicare spending growth.
“For the second year in a row, we saw spending growth for prescription drugs dramatically outpace cost growth for other Medicare services,” Mr. Slavitt said. “Through 2025, Medicare Part D expenditures per enrollee are estimated to increase nearly 50% higher than the estimated increase in GDP per capita and higher than the combined per enrollee growth rate of Medicare Part A and Medicare Part B combined.”
Overall, total Medicare expenditures “are slightly lower than estimated last year,” Mr. Slavitt said, adding that over the next decade, “Medicare per-enrollee spending is projected to continue to grow slower than historical rates, at 4.3%, lower than the growth in overall per capita national health expenditures.”
The growth rate is not projected to trigger the activation of the Independent Payment Advisory Board, according to the report.
In 2015, Medicare covered 55.3 million people, including 46.3 million aged 65 and older, and 9 million disabled individuals.
The Medicare Trust Fund is projected to become insolvent in 2028, 2 years earlier than projected this time last year.
The change is based on two key factors: an expected reduction in payroll taxes and a slowdown in declining rate of inpatient utilization, Andy Slavitt, acting administrator of the Centers for Medicare & Medicaid Services said at a June 22 press conference to review the annual Medicare Trustees report.
“The good news is inpatient utilization is still declining, it’s just declining at a slightly lower rate,” Mr. Slavitt said.
He also highlighted the continuing rising cost of prescription medications, which he called “a major driver” in Medicare spending growth.
“For the second year in a row, we saw spending growth for prescription drugs dramatically outpace cost growth for other Medicare services,” Mr. Slavitt said. “Through 2025, Medicare Part D expenditures per enrollee are estimated to increase nearly 50% higher than the estimated increase in GDP per capita and higher than the combined per enrollee growth rate of Medicare Part A and Medicare Part B combined.”
Overall, total Medicare expenditures “are slightly lower than estimated last year,” Mr. Slavitt said, adding that over the next decade, “Medicare per-enrollee spending is projected to continue to grow slower than historical rates, at 4.3%, lower than the growth in overall per capita national health expenditures.”
The growth rate is not projected to trigger the activation of the Independent Payment Advisory Board, according to the report.
In 2015, Medicare covered 55.3 million people, including 46.3 million aged 65 and older, and 9 million disabled individuals.
The Medicare Trust Fund is projected to become insolvent in 2028, 2 years earlier than projected this time last year.
The change is based on two key factors: an expected reduction in payroll taxes and a slowdown in declining rate of inpatient utilization, Andy Slavitt, acting administrator of the Centers for Medicare & Medicaid Services said at a June 22 press conference to review the annual Medicare Trustees report.
“The good news is inpatient utilization is still declining, it’s just declining at a slightly lower rate,” Mr. Slavitt said.
He also highlighted the continuing rising cost of prescription medications, which he called “a major driver” in Medicare spending growth.
“For the second year in a row, we saw spending growth for prescription drugs dramatically outpace cost growth for other Medicare services,” Mr. Slavitt said. “Through 2025, Medicare Part D expenditures per enrollee are estimated to increase nearly 50% higher than the estimated increase in GDP per capita and higher than the combined per enrollee growth rate of Medicare Part A and Medicare Part B combined.”
Overall, total Medicare expenditures “are slightly lower than estimated last year,” Mr. Slavitt said, adding that over the next decade, “Medicare per-enrollee spending is projected to continue to grow slower than historical rates, at 4.3%, lower than the growth in overall per capita national health expenditures.”
The growth rate is not projected to trigger the activation of the Independent Payment Advisory Board, according to the report.
In 2015, Medicare covered 55.3 million people, including 46.3 million aged 65 and older, and 9 million disabled individuals.