User login
Number of malpractice payments down 28% since 2004
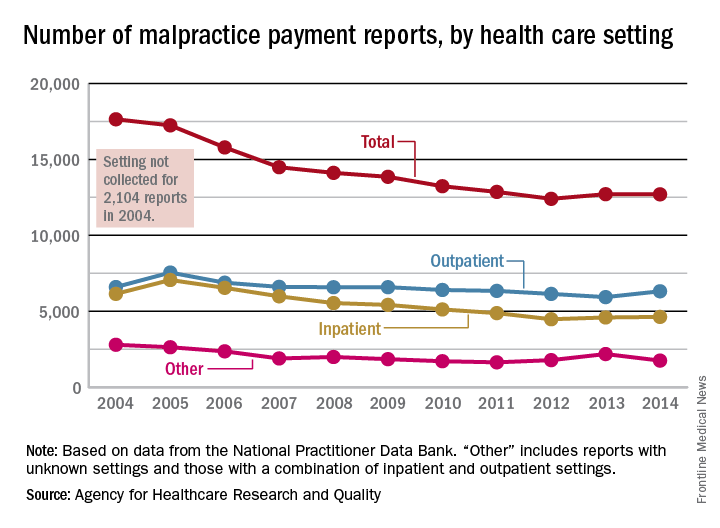
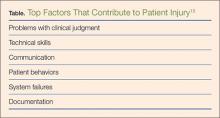
The annual number of medical malpractice payment reports fell 28% from 2004 to 2014, according to the Agency for Healthcare Research and Quality.
The total number of medical malpractice payment reports (MMPRs) for 2014 was 12,699, a decrease of 28% since 2004, when there were 17,641. The total had gone down every year until a slight increase in 2013, but the number held steady in 2014, the AHRQ reported in the Chartbook on Patient Safety.
Since 2004, MMPRs related to inpatient settings have been dropping slightly faster than outpatient-related MMPRs, with the exception, again, of 2013, when the number of inpatient MMPRs went up while the outpatient total dropped. Both types went up in 2014, but the category of “other” – reports related to unknown settings and those from a combination of the two – dropped in 2014 to keep the overall number from going up again, data from the National Practitioner Data Bank show.
Looking at the types of allegation leading to MMPRs, treatment was highest, accounting for 27.4% of the total from 2004 to 2014, with diagnosis right behind at 27.1%, followed by surgery at 23.5% and obstetrics at 6.7%. Medication-related cases represented 5.3% of all MMPRs over that period, the AHRQ noted.
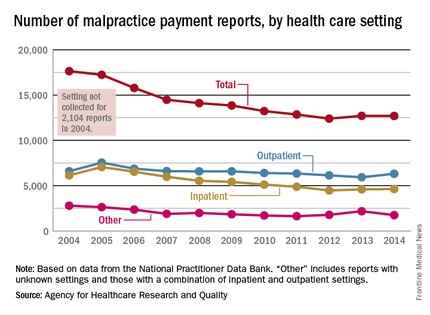
The annual number of medical malpractice payment reports fell 28% from 2004 to 2014, according to the Agency for Healthcare Research and Quality.
The total number of medical malpractice payment reports (MMPRs) for 2014 was 12,699, a decrease of 28% since 2004, when there were 17,641. The total had gone down every year until a slight increase in 2013, but the number held steady in 2014, the AHRQ reported in the Chartbook on Patient Safety.
Since 2004, MMPRs related to inpatient settings have been dropping slightly faster than outpatient-related MMPRs, with the exception, again, of 2013, when the number of inpatient MMPRs went up while the outpatient total dropped. Both types went up in 2014, but the category of “other” – reports related to unknown settings and those from a combination of the two – dropped in 2014 to keep the overall number from going up again, data from the National Practitioner Data Bank show.
Looking at the types of allegation leading to MMPRs, treatment was highest, accounting for 27.4% of the total from 2004 to 2014, with diagnosis right behind at 27.1%, followed by surgery at 23.5% and obstetrics at 6.7%. Medication-related cases represented 5.3% of all MMPRs over that period, the AHRQ noted.
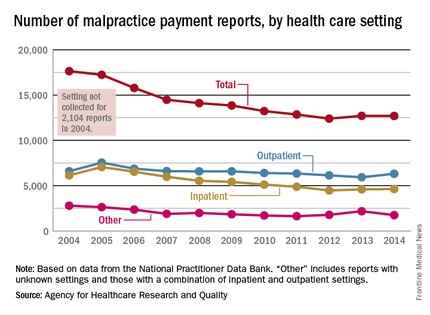
The annual number of medical malpractice payment reports fell 28% from 2004 to 2014, according to the Agency for Healthcare Research and Quality.
The total number of medical malpractice payment reports (MMPRs) for 2014 was 12,699, a decrease of 28% since 2004, when there were 17,641. The total had gone down every year until a slight increase in 2013, but the number held steady in 2014, the AHRQ reported in the Chartbook on Patient Safety.
Since 2004, MMPRs related to inpatient settings have been dropping slightly faster than outpatient-related MMPRs, with the exception, again, of 2013, when the number of inpatient MMPRs went up while the outpatient total dropped. Both types went up in 2014, but the category of “other” – reports related to unknown settings and those from a combination of the two – dropped in 2014 to keep the overall number from going up again, data from the National Practitioner Data Bank show.
Looking at the types of allegation leading to MMPRs, treatment was highest, accounting for 27.4% of the total from 2004 to 2014, with diagnosis right behind at 27.1%, followed by surgery at 23.5% and obstetrics at 6.7%. Medication-related cases represented 5.3% of all MMPRs over that period, the AHRQ noted.
Hospital computerized physician order entry systems often miss prescribing errors
Medical errors are estimated to be the third-highest cause of death in the country. Experts and patient safety advocates are trying to change that. But at least one of the tools that has been considered a fix isn’t yet working as well as it should, suggests a report released April 7.
That’s according to the Leapfrog Group, a nonprofit organization known for rating hospitals on patient safety. Leapfrog conducted a voluntary survey of almost 1,800 hospitals to determine how many use computerized-physician-order-entry systems to make sure patients are prescribed and receive the correct drugs, and that medications won’t cause harm.
The takeaway? While a vast majority of hospitals surveyed had some kind of computer-based medication system in place, the systems still fall short in catching possible problems.
“These systems are not always catching the potential errors inherent in prescribing,” said Erica Mobley, Leapfrog’s director of development and communications.
Almost 40 percent of potentially harmful drug orders weren’t flagged as dangerous by the systems, Leapfrog found. These included medication orders for the wrong condition or in the wrong dose based on things like a patient’s size, other illnesses or likely drug interactions.
Meanwhile, systems missed about 13 percent of errors that could have killed patients.
According to 2015 figures from the federal Agency for Healthcare Research and Quality, about 1 of every 20 patients in hospitals suffers harm because of medications. Of those, the agency estimates, half are avoidable.
Meanwhile, in a push to improve patient safety and health care quality, the federal government has been encouraging hospitals to adopt electronic health records – particularly with medication ordering systems – thanks to parts of the 2009 stimulus package and 2010 health reform. But there has been pushback from many doctors and advocates, who say design issues can make the software difficult to use or even counterproductive.
The Leapfrog survey – which is not peer-reviewed – asked participating hospitals to use “dummy patients” to test their system, Mobley said. Participants would put in information for fake patients and submit a set of medication orders to see which ones got flagged. Mistakes might include orders prescribing an adult dosage to a child, for instance.
The results are “alarming,” said Helen Haskell, a prominent patient safety advocate. “It shows that the technology is not as foolproof as we would like to think.”
But it’s difficult to know how many of those missed errors result in actual harm, Mobley acknowledged. Ordering the wrong medication can be inconvenient or problematic. But it isn’t always dangerous. And, for those that are, hospitals may have other safeguards in place to catch mistakes before they actually hurt patients. “It really does vary significantly by hospital,” she said.
The survey, Mobley suggested, underscores the need for hospitals and patients to be vigilant when it comes to overseeing their medications. For hospitals, that means instituting “checks and balances” – system-wide initiatives like requiring manual reviews of a patient’s drugs, on top of the computer checks.
And hospitals are increasingly taking such steps to make medication errors less common, said Jesse Pines, who directs the Office for Clinical Practice Innovation at George Washington University, Washington, and is a professor of emergency medicine. Technology is also improving, so medication ordering systems should get better, he added.
“Technology exists to help with detecting medical errors at the point of when you’re entering drug orders in the hospital or health care settings,” he said. “But they’re not perfect. They still need a lot of work.”
Patients, meanwhile, should make sure to have someone with them when they go into the hospital, who can check out what drugs they’re being prescribed, Mobley said.
“It’s absolutely critical that whenever the patient or somebody with them notices that this maze [of medications] looks slightly different from what’s been done in the past, they ask about that,” she said.
But even with that vigilance, Haskell said, “your knowledge is not infinite – so there’s a limit to what patients can do.”
Hospitals can try to customize their medication ordering systems to do things like identify frequently ordered drugs or better match the patients they’re likely to treat.
How well they do at adapting the software can also play a role in how good hospitals are at catching and preventing mistakes when it comes to ordering medications, said Raj Ratwani, who researches health care safety and is the scientific director for MedStar Health’s National Center for Human Factors in Healthcare in Washington. To that end, hospitals and safety experts should figure out what are the best practices when it comes to customizing tools like medication ordering software.
A number of Leapfrog’s surveys have come under scrutiny from some hospitals, who question their methodology and metrics. Here, Mobley said, the survey may inflate the number of hospitals with a computer-based medication ordering system. But when it comes to how effective the systems are, the findings are unsurprising, both Haskell and Ratwani said.
“What these findings indicate – and what many other researchers have shown – is that computerized physician order entry is effective at reducing adverse drug events,” Ratwani said. “What we also know…is these electronic health record systems are complex.”
Kaiser Health News is a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
On Twitter @Shefalil
Medical errors are estimated to be the third-highest cause of death in the country. Experts and patient safety advocates are trying to change that. But at least one of the tools that has been considered a fix isn’t yet working as well as it should, suggests a report released April 7.
That’s according to the Leapfrog Group, a nonprofit organization known for rating hospitals on patient safety. Leapfrog conducted a voluntary survey of almost 1,800 hospitals to determine how many use computerized-physician-order-entry systems to make sure patients are prescribed and receive the correct drugs, and that medications won’t cause harm.
The takeaway? While a vast majority of hospitals surveyed had some kind of computer-based medication system in place, the systems still fall short in catching possible problems.
“These systems are not always catching the potential errors inherent in prescribing,” said Erica Mobley, Leapfrog’s director of development and communications.
Almost 40 percent of potentially harmful drug orders weren’t flagged as dangerous by the systems, Leapfrog found. These included medication orders for the wrong condition or in the wrong dose based on things like a patient’s size, other illnesses or likely drug interactions.
Meanwhile, systems missed about 13 percent of errors that could have killed patients.
According to 2015 figures from the federal Agency for Healthcare Research and Quality, about 1 of every 20 patients in hospitals suffers harm because of medications. Of those, the agency estimates, half are avoidable.
Meanwhile, in a push to improve patient safety and health care quality, the federal government has been encouraging hospitals to adopt electronic health records – particularly with medication ordering systems – thanks to parts of the 2009 stimulus package and 2010 health reform. But there has been pushback from many doctors and advocates, who say design issues can make the software difficult to use or even counterproductive.
The Leapfrog survey – which is not peer-reviewed – asked participating hospitals to use “dummy patients” to test their system, Mobley said. Participants would put in information for fake patients and submit a set of medication orders to see which ones got flagged. Mistakes might include orders prescribing an adult dosage to a child, for instance.
The results are “alarming,” said Helen Haskell, a prominent patient safety advocate. “It shows that the technology is not as foolproof as we would like to think.”
But it’s difficult to know how many of those missed errors result in actual harm, Mobley acknowledged. Ordering the wrong medication can be inconvenient or problematic. But it isn’t always dangerous. And, for those that are, hospitals may have other safeguards in place to catch mistakes before they actually hurt patients. “It really does vary significantly by hospital,” she said.
The survey, Mobley suggested, underscores the need for hospitals and patients to be vigilant when it comes to overseeing their medications. For hospitals, that means instituting “checks and balances” – system-wide initiatives like requiring manual reviews of a patient’s drugs, on top of the computer checks.
And hospitals are increasingly taking such steps to make medication errors less common, said Jesse Pines, who directs the Office for Clinical Practice Innovation at George Washington University, Washington, and is a professor of emergency medicine. Technology is also improving, so medication ordering systems should get better, he added.
“Technology exists to help with detecting medical errors at the point of when you’re entering drug orders in the hospital or health care settings,” he said. “But they’re not perfect. They still need a lot of work.”
Patients, meanwhile, should make sure to have someone with them when they go into the hospital, who can check out what drugs they’re being prescribed, Mobley said.
“It’s absolutely critical that whenever the patient or somebody with them notices that this maze [of medications] looks slightly different from what’s been done in the past, they ask about that,” she said.
But even with that vigilance, Haskell said, “your knowledge is not infinite – so there’s a limit to what patients can do.”
Hospitals can try to customize their medication ordering systems to do things like identify frequently ordered drugs or better match the patients they’re likely to treat.
How well they do at adapting the software can also play a role in how good hospitals are at catching and preventing mistakes when it comes to ordering medications, said Raj Ratwani, who researches health care safety and is the scientific director for MedStar Health’s National Center for Human Factors in Healthcare in Washington. To that end, hospitals and safety experts should figure out what are the best practices when it comes to customizing tools like medication ordering software.
A number of Leapfrog’s surveys have come under scrutiny from some hospitals, who question their methodology and metrics. Here, Mobley said, the survey may inflate the number of hospitals with a computer-based medication ordering system. But when it comes to how effective the systems are, the findings are unsurprising, both Haskell and Ratwani said.
“What these findings indicate – and what many other researchers have shown – is that computerized physician order entry is effective at reducing adverse drug events,” Ratwani said. “What we also know…is these electronic health record systems are complex.”
Kaiser Health News is a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
On Twitter @Shefalil
Medical errors are estimated to be the third-highest cause of death in the country. Experts and patient safety advocates are trying to change that. But at least one of the tools that has been considered a fix isn’t yet working as well as it should, suggests a report released April 7.
That’s according to the Leapfrog Group, a nonprofit organization known for rating hospitals on patient safety. Leapfrog conducted a voluntary survey of almost 1,800 hospitals to determine how many use computerized-physician-order-entry systems to make sure patients are prescribed and receive the correct drugs, and that medications won’t cause harm.
The takeaway? While a vast majority of hospitals surveyed had some kind of computer-based medication system in place, the systems still fall short in catching possible problems.
“These systems are not always catching the potential errors inherent in prescribing,” said Erica Mobley, Leapfrog’s director of development and communications.
Almost 40 percent of potentially harmful drug orders weren’t flagged as dangerous by the systems, Leapfrog found. These included medication orders for the wrong condition or in the wrong dose based on things like a patient’s size, other illnesses or likely drug interactions.
Meanwhile, systems missed about 13 percent of errors that could have killed patients.
According to 2015 figures from the federal Agency for Healthcare Research and Quality, about 1 of every 20 patients in hospitals suffers harm because of medications. Of those, the agency estimates, half are avoidable.
Meanwhile, in a push to improve patient safety and health care quality, the federal government has been encouraging hospitals to adopt electronic health records – particularly with medication ordering systems – thanks to parts of the 2009 stimulus package and 2010 health reform. But there has been pushback from many doctors and advocates, who say design issues can make the software difficult to use or even counterproductive.
The Leapfrog survey – which is not peer-reviewed – asked participating hospitals to use “dummy patients” to test their system, Mobley said. Participants would put in information for fake patients and submit a set of medication orders to see which ones got flagged. Mistakes might include orders prescribing an adult dosage to a child, for instance.
The results are “alarming,” said Helen Haskell, a prominent patient safety advocate. “It shows that the technology is not as foolproof as we would like to think.”
But it’s difficult to know how many of those missed errors result in actual harm, Mobley acknowledged. Ordering the wrong medication can be inconvenient or problematic. But it isn’t always dangerous. And, for those that are, hospitals may have other safeguards in place to catch mistakes before they actually hurt patients. “It really does vary significantly by hospital,” she said.
The survey, Mobley suggested, underscores the need for hospitals and patients to be vigilant when it comes to overseeing their medications. For hospitals, that means instituting “checks and balances” – system-wide initiatives like requiring manual reviews of a patient’s drugs, on top of the computer checks.
And hospitals are increasingly taking such steps to make medication errors less common, said Jesse Pines, who directs the Office for Clinical Practice Innovation at George Washington University, Washington, and is a professor of emergency medicine. Technology is also improving, so medication ordering systems should get better, he added.
“Technology exists to help with detecting medical errors at the point of when you’re entering drug orders in the hospital or health care settings,” he said. “But they’re not perfect. They still need a lot of work.”
Patients, meanwhile, should make sure to have someone with them when they go into the hospital, who can check out what drugs they’re being prescribed, Mobley said.
“It’s absolutely critical that whenever the patient or somebody with them notices that this maze [of medications] looks slightly different from what’s been done in the past, they ask about that,” she said.
But even with that vigilance, Haskell said, “your knowledge is not infinite – so there’s a limit to what patients can do.”
Hospitals can try to customize their medication ordering systems to do things like identify frequently ordered drugs or better match the patients they’re likely to treat.
How well they do at adapting the software can also play a role in how good hospitals are at catching and preventing mistakes when it comes to ordering medications, said Raj Ratwani, who researches health care safety and is the scientific director for MedStar Health’s National Center for Human Factors in Healthcare in Washington. To that end, hospitals and safety experts should figure out what are the best practices when it comes to customizing tools like medication ordering software.
A number of Leapfrog’s surveys have come under scrutiny from some hospitals, who question their methodology and metrics. Here, Mobley said, the survey may inflate the number of hospitals with a computer-based medication ordering system. But when it comes to how effective the systems are, the findings are unsurprising, both Haskell and Ratwani said.
“What these findings indicate – and what many other researchers have shown – is that computerized physician order entry is effective at reducing adverse drug events,” Ratwani said. “What we also know…is these electronic health record systems are complex.”
Kaiser Health News is a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
On Twitter @Shefalil
SURVEY: Telemedicine high priority, but reimbursement remains challenging
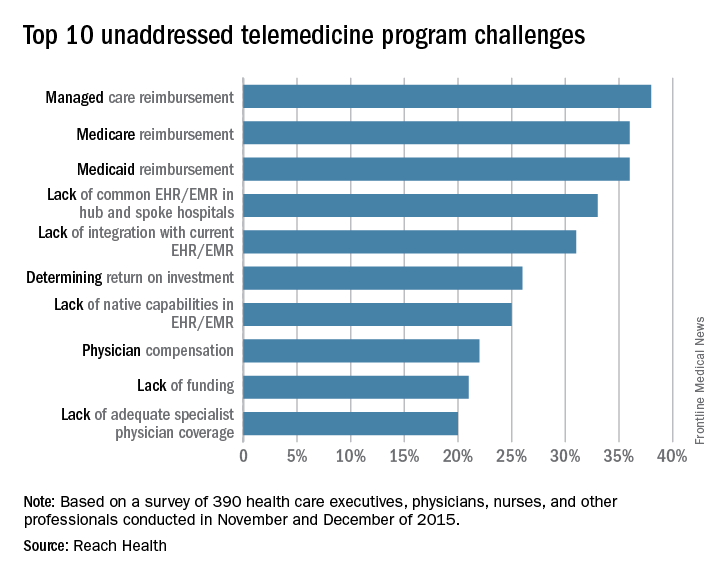
Nearly two-thirds of health care providers rank telemedicine as a top priority in 2016, a 10% increase from last year, according to a survey.
Telemedicine software company REACH Health surveyed 390 U.S. health care professionals between November 2015 and December 2015, including physicians, nurses, and health care executives. Participants answered questions related to their objectives, challenges, telemedicine program models, and management structures, among other inquiries.
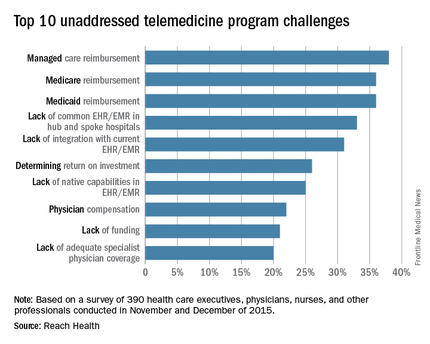
Of those polled, 96% of respondents said improving patient outcome was a top objective in developing telemedicine programs, according to the survey. Increasing patient convenience (87%) and improving patient engagement (86%) also rated highly. Other objectives included providing remote and rural patients with access to specialists (83%) and improving leverage of limited physician resources (81%). Percentages do not equal 100% because respondents could choose more than one objective.
The maturity of telemedicine programs varied widely depending on care setting. In general, settings requiring highly specialized treatment had more mature telemedicine programs than those requiring more generalized treatment. Stroke, neurology, and psychiatric/behavioral health settings had the most mature telemedicine programs, according to the survey.
Reimbursement ranked as the top barrier to telemedicine. Respondents rated private plan payment as the No. 1 challenge (38%), followed by Medicare reimbursement (36%) and Medicaid reimbursement (36%). Electronic health record incapabilities and liability risks also ranked as primary challenges.
“Telemedicine reimbursement poses the primary obstacle to success, but EMR-related challenges are persistent and widely noted in the survey,” Steve McGraw, president and CEO of REACH Health said in a statement. “There is clearly a high demand in the industry for EMR integration, specifically the two-way flow of individual data elements between telemedicine platforms and EMR systems.”
On Twitter @legal_med
Nearly two-thirds of health care providers rank telemedicine as a top priority in 2016, a 10% increase from last year, according to a survey.
Telemedicine software company REACH Health surveyed 390 U.S. health care professionals between November 2015 and December 2015, including physicians, nurses, and health care executives. Participants answered questions related to their objectives, challenges, telemedicine program models, and management structures, among other inquiries.
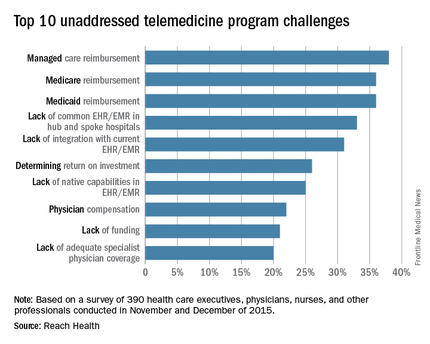
Of those polled, 96% of respondents said improving patient outcome was a top objective in developing telemedicine programs, according to the survey. Increasing patient convenience (87%) and improving patient engagement (86%) also rated highly. Other objectives included providing remote and rural patients with access to specialists (83%) and improving leverage of limited physician resources (81%). Percentages do not equal 100% because respondents could choose more than one objective.
The maturity of telemedicine programs varied widely depending on care setting. In general, settings requiring highly specialized treatment had more mature telemedicine programs than those requiring more generalized treatment. Stroke, neurology, and psychiatric/behavioral health settings had the most mature telemedicine programs, according to the survey.
Reimbursement ranked as the top barrier to telemedicine. Respondents rated private plan payment as the No. 1 challenge (38%), followed by Medicare reimbursement (36%) and Medicaid reimbursement (36%). Electronic health record incapabilities and liability risks also ranked as primary challenges.
“Telemedicine reimbursement poses the primary obstacle to success, but EMR-related challenges are persistent and widely noted in the survey,” Steve McGraw, president and CEO of REACH Health said in a statement. “There is clearly a high demand in the industry for EMR integration, specifically the two-way flow of individual data elements between telemedicine platforms and EMR systems.”
On Twitter @legal_med
Nearly two-thirds of health care providers rank telemedicine as a top priority in 2016, a 10% increase from last year, according to a survey.
Telemedicine software company REACH Health surveyed 390 U.S. health care professionals between November 2015 and December 2015, including physicians, nurses, and health care executives. Participants answered questions related to their objectives, challenges, telemedicine program models, and management structures, among other inquiries.
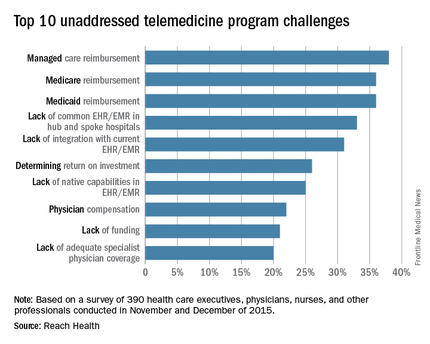
Of those polled, 96% of respondents said improving patient outcome was a top objective in developing telemedicine programs, according to the survey. Increasing patient convenience (87%) and improving patient engagement (86%) also rated highly. Other objectives included providing remote and rural patients with access to specialists (83%) and improving leverage of limited physician resources (81%). Percentages do not equal 100% because respondents could choose more than one objective.
The maturity of telemedicine programs varied widely depending on care setting. In general, settings requiring highly specialized treatment had more mature telemedicine programs than those requiring more generalized treatment. Stroke, neurology, and psychiatric/behavioral health settings had the most mature telemedicine programs, according to the survey.
Reimbursement ranked as the top barrier to telemedicine. Respondents rated private plan payment as the No. 1 challenge (38%), followed by Medicare reimbursement (36%) and Medicaid reimbursement (36%). Electronic health record incapabilities and liability risks also ranked as primary challenges.
“Telemedicine reimbursement poses the primary obstacle to success, but EMR-related challenges are persistent and widely noted in the survey,” Steve McGraw, president and CEO of REACH Health said in a statement. “There is clearly a high demand in the industry for EMR integration, specifically the two-way flow of individual data elements between telemedicine platforms and EMR systems.”
On Twitter @legal_med
Administrators Share Strategies for High-Performing Hospitalist Groups at HM16
In November, Barbara Weisenbach took a new job as practice manager for the hospitalist group at Northwest Hospital in Seattle. She’s an experienced administrator but as for hospital medicine, not so much. And she is the group’s first full-fledged practice manager—as in, she’s not a physician taking on admin responsibilities and seeing a partial census.
She’s doing a lot of reshaping and a lot of learning, she said, standing outside Room 10 of the San Diego Convention Center, where a daylong pre-course on practice management was being held at SHM’s annual meeting.
“There have been a lot of business things that have been overlooked and not addressed ever before,” she said.
The pre-course, “The Highly Effective Hospital Medicine Group: Using SHM’s Key Characteristics to Drive Performance,” was led by John Nelson, MD, MHM, and Leslie Flores, MHA, SFHM, and offered one useful lesson after another, Weisenbach said.
“One of the most practical portions of the session this morning was about dashboards, which is something I’m currently working on and could definitely use some insight,” Weisenbach said, adding that a list of metrics a dashboard should include and general guidelines on effective dashboards were things she’ll find useful in her own implementation.
The pre-course expanded on the key principles and traits for effective groups, including effective leadership, engaged hospitalists, adequate resources, alignment with the hospital, and care coordination across settings.
HM16 also included two and a half days of practice management sessions. Plus, management themes were woven through workshops and sprinkled into other sessions.
In one session on handling change, presenters used a surfing analogy: Like a surfer’s intensity just before riding a wave, a laser focus is called for when the moment arrives to execute change.
“Get ready for the ride,” said Steve Behnke, MD, president of Columbus, Ohio–based MedOne Hospital Physicians.
He discussed details of introducing the electronic health record system Epic at their group. There was 18 months of planning involving the practice’s whole operational team, then a doubling of the staffing ratios when the system went live, followed by catered lunches to gather feedback and identify problems.
Presenters emphasized the idea of agility in responding to obstacles and realizing that change affects everyone. Successful change, they said, involves seeing the process from all perspectives and leaders should expect resistance.
“Court them. Listen to them. I can’t tell you how many times I’ve done that,” said Dea Robinson, MA, MedOne’s vice president of operations. “Just listening and giving a platform.”
Back at the pre-course, Dr. Nelson, a hospital medicine consultant, talked about the importance of effective leadership.
“An effective group leader is a really key element of a successful group,” said The Hospitalist’s resident practice management columnist. “I’ve worked on-site with many hundreds of hospitalist groups around the country. There’s pretty good correlation between the effectiveness of the leader and the success of the group overall. But a good leader alone is not enough.”
He added that there are too “few leaders to go around.”
A good leader is an active one, he said, adding with funny-because-it’s-true humor that a lot of leaders say their main job is to make the schedule. Good leaders, he said, need to be focused on making the group high-functioning, should be available for administrative work even when not on a clinical shift, and must be able to delegate.
Another critical ingredient for a successful group, he said, is having engaged frontline hospitalists. Reviews need to be meaningful, and meetings should be held regularly with attendance essentially mandatory. Meetings, he said, might need a “tune-up,” with actual voting, written agendas, minutes taken, and group problem-solving above one-way information.
Win Whitcomb, MD, MHM, on care coordination, said the relationship with primary care physicians is crucial though difficult.
“I think we have to go out of our way to build relationships,” he said. “And we don’t have occasion to see them, so we need to figure out a way to get to know our community.”
He suggested:
- Having dedicated transcriptionists for hospitalists,
- Tracking the rate at which discharge summaries are generated within 24 hours,
- Making sure PCPs know how to reach hospitalists, and
- Scheduling events—perhaps an annual event—for meeting PCPs and skill-nursing facility healthcare professionals.
It was clear that, in a field whose dimensions seem to be changing all the time, practice management remained a top interest at HM16. Robert Clothier, RN, a practice manager for the hospitalist group at ThedaCare in Wisconsin, recently switched from managing a cardiology clinic. He said there were huge differences in hospital medicine.
“The profession is growing so fast, and really nobody knows where the end is,” he said. “I can’t even think of anything where you could say, ‘Well, no, they’ll never do that.’ It’s endless. That’s going to be hardest thing. People are going to be pulling on us, and leadership from the hospital is going to be saying, ‘You guys need to do this.’
“So how can I control what we pick, and how can I make sure that we have the resources to do it?” TH
In November, Barbara Weisenbach took a new job as practice manager for the hospitalist group at Northwest Hospital in Seattle. She’s an experienced administrator but as for hospital medicine, not so much. And she is the group’s first full-fledged practice manager—as in, she’s not a physician taking on admin responsibilities and seeing a partial census.
She’s doing a lot of reshaping and a lot of learning, she said, standing outside Room 10 of the San Diego Convention Center, where a daylong pre-course on practice management was being held at SHM’s annual meeting.
“There have been a lot of business things that have been overlooked and not addressed ever before,” she said.
The pre-course, “The Highly Effective Hospital Medicine Group: Using SHM’s Key Characteristics to Drive Performance,” was led by John Nelson, MD, MHM, and Leslie Flores, MHA, SFHM, and offered one useful lesson after another, Weisenbach said.
“One of the most practical portions of the session this morning was about dashboards, which is something I’m currently working on and could definitely use some insight,” Weisenbach said, adding that a list of metrics a dashboard should include and general guidelines on effective dashboards were things she’ll find useful in her own implementation.
The pre-course expanded on the key principles and traits for effective groups, including effective leadership, engaged hospitalists, adequate resources, alignment with the hospital, and care coordination across settings.
HM16 also included two and a half days of practice management sessions. Plus, management themes were woven through workshops and sprinkled into other sessions.
In one session on handling change, presenters used a surfing analogy: Like a surfer’s intensity just before riding a wave, a laser focus is called for when the moment arrives to execute change.
“Get ready for the ride,” said Steve Behnke, MD, president of Columbus, Ohio–based MedOne Hospital Physicians.
He discussed details of introducing the electronic health record system Epic at their group. There was 18 months of planning involving the practice’s whole operational team, then a doubling of the staffing ratios when the system went live, followed by catered lunches to gather feedback and identify problems.
Presenters emphasized the idea of agility in responding to obstacles and realizing that change affects everyone. Successful change, they said, involves seeing the process from all perspectives and leaders should expect resistance.
“Court them. Listen to them. I can’t tell you how many times I’ve done that,” said Dea Robinson, MA, MedOne’s vice president of operations. “Just listening and giving a platform.”
Back at the pre-course, Dr. Nelson, a hospital medicine consultant, talked about the importance of effective leadership.
“An effective group leader is a really key element of a successful group,” said The Hospitalist’s resident practice management columnist. “I’ve worked on-site with many hundreds of hospitalist groups around the country. There’s pretty good correlation between the effectiveness of the leader and the success of the group overall. But a good leader alone is not enough.”
He added that there are too “few leaders to go around.”
A good leader is an active one, he said, adding with funny-because-it’s-true humor that a lot of leaders say their main job is to make the schedule. Good leaders, he said, need to be focused on making the group high-functioning, should be available for administrative work even when not on a clinical shift, and must be able to delegate.
Another critical ingredient for a successful group, he said, is having engaged frontline hospitalists. Reviews need to be meaningful, and meetings should be held regularly with attendance essentially mandatory. Meetings, he said, might need a “tune-up,” with actual voting, written agendas, minutes taken, and group problem-solving above one-way information.
Win Whitcomb, MD, MHM, on care coordination, said the relationship with primary care physicians is crucial though difficult.
“I think we have to go out of our way to build relationships,” he said. “And we don’t have occasion to see them, so we need to figure out a way to get to know our community.”
He suggested:
- Having dedicated transcriptionists for hospitalists,
- Tracking the rate at which discharge summaries are generated within 24 hours,
- Making sure PCPs know how to reach hospitalists, and
- Scheduling events—perhaps an annual event—for meeting PCPs and skill-nursing facility healthcare professionals.
It was clear that, in a field whose dimensions seem to be changing all the time, practice management remained a top interest at HM16. Robert Clothier, RN, a practice manager for the hospitalist group at ThedaCare in Wisconsin, recently switched from managing a cardiology clinic. He said there were huge differences in hospital medicine.
“The profession is growing so fast, and really nobody knows where the end is,” he said. “I can’t even think of anything where you could say, ‘Well, no, they’ll never do that.’ It’s endless. That’s going to be hardest thing. People are going to be pulling on us, and leadership from the hospital is going to be saying, ‘You guys need to do this.’
“So how can I control what we pick, and how can I make sure that we have the resources to do it?” TH
In November, Barbara Weisenbach took a new job as practice manager for the hospitalist group at Northwest Hospital in Seattle. She’s an experienced administrator but as for hospital medicine, not so much. And she is the group’s first full-fledged practice manager—as in, she’s not a physician taking on admin responsibilities and seeing a partial census.
She’s doing a lot of reshaping and a lot of learning, she said, standing outside Room 10 of the San Diego Convention Center, where a daylong pre-course on practice management was being held at SHM’s annual meeting.
“There have been a lot of business things that have been overlooked and not addressed ever before,” she said.
The pre-course, “The Highly Effective Hospital Medicine Group: Using SHM’s Key Characteristics to Drive Performance,” was led by John Nelson, MD, MHM, and Leslie Flores, MHA, SFHM, and offered one useful lesson after another, Weisenbach said.
“One of the most practical portions of the session this morning was about dashboards, which is something I’m currently working on and could definitely use some insight,” Weisenbach said, adding that a list of metrics a dashboard should include and general guidelines on effective dashboards were things she’ll find useful in her own implementation.
The pre-course expanded on the key principles and traits for effective groups, including effective leadership, engaged hospitalists, adequate resources, alignment with the hospital, and care coordination across settings.
HM16 also included two and a half days of practice management sessions. Plus, management themes were woven through workshops and sprinkled into other sessions.
In one session on handling change, presenters used a surfing analogy: Like a surfer’s intensity just before riding a wave, a laser focus is called for when the moment arrives to execute change.
“Get ready for the ride,” said Steve Behnke, MD, president of Columbus, Ohio–based MedOne Hospital Physicians.
He discussed details of introducing the electronic health record system Epic at their group. There was 18 months of planning involving the practice’s whole operational team, then a doubling of the staffing ratios when the system went live, followed by catered lunches to gather feedback and identify problems.
Presenters emphasized the idea of agility in responding to obstacles and realizing that change affects everyone. Successful change, they said, involves seeing the process from all perspectives and leaders should expect resistance.
“Court them. Listen to them. I can’t tell you how many times I’ve done that,” said Dea Robinson, MA, MedOne’s vice president of operations. “Just listening and giving a platform.”
Back at the pre-course, Dr. Nelson, a hospital medicine consultant, talked about the importance of effective leadership.
“An effective group leader is a really key element of a successful group,” said The Hospitalist’s resident practice management columnist. “I’ve worked on-site with many hundreds of hospitalist groups around the country. There’s pretty good correlation between the effectiveness of the leader and the success of the group overall. But a good leader alone is not enough.”
He added that there are too “few leaders to go around.”
A good leader is an active one, he said, adding with funny-because-it’s-true humor that a lot of leaders say their main job is to make the schedule. Good leaders, he said, need to be focused on making the group high-functioning, should be available for administrative work even when not on a clinical shift, and must be able to delegate.
Another critical ingredient for a successful group, he said, is having engaged frontline hospitalists. Reviews need to be meaningful, and meetings should be held regularly with attendance essentially mandatory. Meetings, he said, might need a “tune-up,” with actual voting, written agendas, minutes taken, and group problem-solving above one-way information.
Win Whitcomb, MD, MHM, on care coordination, said the relationship with primary care physicians is crucial though difficult.
“I think we have to go out of our way to build relationships,” he said. “And we don’t have occasion to see them, so we need to figure out a way to get to know our community.”
He suggested:
- Having dedicated transcriptionists for hospitalists,
- Tracking the rate at which discharge summaries are generated within 24 hours,
- Making sure PCPs know how to reach hospitalists, and
- Scheduling events—perhaps an annual event—for meeting PCPs and skill-nursing facility healthcare professionals.
It was clear that, in a field whose dimensions seem to be changing all the time, practice management remained a top interest at HM16. Robert Clothier, RN, a practice manager for the hospitalist group at ThedaCare in Wisconsin, recently switched from managing a cardiology clinic. He said there were huge differences in hospital medicine.
“The profession is growing so fast, and really nobody knows where the end is,” he said. “I can’t even think of anything where you could say, ‘Well, no, they’ll never do that.’ It’s endless. That’s going to be hardest thing. People are going to be pulling on us, and leadership from the hospital is going to be saying, ‘You guys need to do this.’
“So how can I control what we pick, and how can I make sure that we have the resources to do it?” TH
Could value-based care raise False Claims Act liability?
As you begin to consider the switch to value-based care systems, be sure to safeguard against risks that could fuel false claims scrutiny by the government, legal experts advise.
A primary consideration is arrangements that include shared savings through coordinated care, said George B. Breen, a Washington-based health law attorney. For example, he said that the Stark Law could be implicated if a physician within a shared savings model receives a bonus payment for referring patients to specific providers. The Stark Law prohibits a physician from referring Medicare patients for designated health services to an entity with which the physician has a financial relationship.
“While there are a number of exceptions and safe harbors which would validate any such relationship, it’s something that needs to be thought through” from the start, Mr. Breen said in an interview. “You have to look at each factual circumstance separately because each is fact and circumstance dependent.”
The Anti-Kickback Statute also could come into play if value-based arrangements generate renumeration. The Anti-Kickback Statute prohibits offering, paying, soliciting, or receiving anything of value to induce or reward referrals or generate federal health care program business. Exceptions to the statute can be applied and should also be examined during arrangement development, Mr. Breen said.
Data collection and reporting also may present a problem, according to Seattle-based health law attorney Robert G. Homchick. Inaccurate data that become the basis for quality-based payments could lead to overpayment liability and indirect False Claims Act (FCA) exposure, he said.
In addition, “If the facts support that you were acting with intentional or deliberate ignorance or reckless disregard for how the data were gathered and reported that supported your value-based comp kicker, there could be direct False Claims Act liability,” Mr. Homchick said in an interview.
But Mr. Homchick stressed there are still many unknowns when it comes to how data-driven measurements will unfold.
“With MACRA, this is such a moving target as to exactly what type of data is going to form the basis for the metrics, and how the data need to be gathered and reported,” he said. “Many of those issues are still in play or still being developed at the agency level in terms of regulatory guidance.”
Current lawsuit could influence future cases
While it is too early to know every legal theory that could intersect with quality-based care, legal experts are closely watching a case that could offer insight into future claims.
In Duffy v. Lawrence Memorial Hospital, a former employee turned whistle-blower alleges that the Lawrence, Kan.–based hospital inflated its performance scores under the Hospital Value-Based Purchasing Program to increase federal incentive payments. Hospital leaders deny they falsified data and claim the allegations are based on the whistle-blower’s “improper understanding of acceptable reporting times for patient arrival,” according the hospital’s court response. The FCA lawsuit is before the U.S. District Court for the District of Kansas.
Notably, the government has declined to intervene in the lawsuit twice, Mr. Breen said. The case is continuing without government intervention, a trend that has become more common in recent years, he said. In 2015, whistle-blower cases in which U.S. Department of Justice declined to intervene led to $1.1 billion in recoveries for the government and $335 million in rewards for whistle-blowers, according to government data.
Mr. Homchick called the Lawrence Memorial lawsuit “troubling.”
“Providers are struggling with the complexity of the reporting requirements imposed by the layers of value-based payment programs implemented by both government and private payers,” he said. “The Lawrence Memorial case illustrates that the whistle-blower community will likely exploit the inevitable mistakes or missteps of providers attempting to comply with the increasingly byzantine quality-reporting requirements.”
The outcome of the Lawrence Memorial case could influence similar lawsuits involving value-based programs, Mr. Breen said.
“I think this theory that there is some false reporting, or false certification, is a theory that you will see being pursed in connection with some of these quality-based programs,” Mr. Breen said.
Early steps can curb legal risk
Asking questions and being proactive as new value-based models develop is key to mitigating legal dangers, experts said.
Ensure that new arrangements are analyzed for fraud and abuse risk exposure before finalizing, Mr. Breen advised.
“Have a comfort level about the arrangement” that’s being entered into, he added, and “have those arrangements vetted.”
Pay attention to data, added Michael E. Paulhus, an Atlanta-based health law attorney who specializes in FCA cases.
“The more data they collect, the more the government is paying attention to where you are in the range,” he said in an interview. “If you stick out on either end, that would be a risk profile that, as a physician, I would want to know. I would want to know where I sit in the data.”
When making reports regarding quality measures, include such reports in internal audits as part of regular compliance efforts, the experts suggested.
In addition, seek out resources early that can help prepare the practice for new quality-based regulations, Mr. Homchick said.
“There will be guidance coming out [regarding] eligibility for these value-based incentives,” he said. “That will require you and your staff to really pay attention and seek out resources and guidance to try to do this right. If you have the bandwidth to get out ahead of this, that would certainly be the best approach.”
On Twitter @legal_med
As you begin to consider the switch to value-based care systems, be sure to safeguard against risks that could fuel false claims scrutiny by the government, legal experts advise.
A primary consideration is arrangements that include shared savings through coordinated care, said George B. Breen, a Washington-based health law attorney. For example, he said that the Stark Law could be implicated if a physician within a shared savings model receives a bonus payment for referring patients to specific providers. The Stark Law prohibits a physician from referring Medicare patients for designated health services to an entity with which the physician has a financial relationship.
“While there are a number of exceptions and safe harbors which would validate any such relationship, it’s something that needs to be thought through” from the start, Mr. Breen said in an interview. “You have to look at each factual circumstance separately because each is fact and circumstance dependent.”
The Anti-Kickback Statute also could come into play if value-based arrangements generate renumeration. The Anti-Kickback Statute prohibits offering, paying, soliciting, or receiving anything of value to induce or reward referrals or generate federal health care program business. Exceptions to the statute can be applied and should also be examined during arrangement development, Mr. Breen said.
Data collection and reporting also may present a problem, according to Seattle-based health law attorney Robert G. Homchick. Inaccurate data that become the basis for quality-based payments could lead to overpayment liability and indirect False Claims Act (FCA) exposure, he said.
In addition, “If the facts support that you were acting with intentional or deliberate ignorance or reckless disregard for how the data were gathered and reported that supported your value-based comp kicker, there could be direct False Claims Act liability,” Mr. Homchick said in an interview.
But Mr. Homchick stressed there are still many unknowns when it comes to how data-driven measurements will unfold.
“With MACRA, this is such a moving target as to exactly what type of data is going to form the basis for the metrics, and how the data need to be gathered and reported,” he said. “Many of those issues are still in play or still being developed at the agency level in terms of regulatory guidance.”
Current lawsuit could influence future cases
While it is too early to know every legal theory that could intersect with quality-based care, legal experts are closely watching a case that could offer insight into future claims.
In Duffy v. Lawrence Memorial Hospital, a former employee turned whistle-blower alleges that the Lawrence, Kan.–based hospital inflated its performance scores under the Hospital Value-Based Purchasing Program to increase federal incentive payments. Hospital leaders deny they falsified data and claim the allegations are based on the whistle-blower’s “improper understanding of acceptable reporting times for patient arrival,” according the hospital’s court response. The FCA lawsuit is before the U.S. District Court for the District of Kansas.
Notably, the government has declined to intervene in the lawsuit twice, Mr. Breen said. The case is continuing without government intervention, a trend that has become more common in recent years, he said. In 2015, whistle-blower cases in which U.S. Department of Justice declined to intervene led to $1.1 billion in recoveries for the government and $335 million in rewards for whistle-blowers, according to government data.
Mr. Homchick called the Lawrence Memorial lawsuit “troubling.”
“Providers are struggling with the complexity of the reporting requirements imposed by the layers of value-based payment programs implemented by both government and private payers,” he said. “The Lawrence Memorial case illustrates that the whistle-blower community will likely exploit the inevitable mistakes or missteps of providers attempting to comply with the increasingly byzantine quality-reporting requirements.”
The outcome of the Lawrence Memorial case could influence similar lawsuits involving value-based programs, Mr. Breen said.
“I think this theory that there is some false reporting, or false certification, is a theory that you will see being pursed in connection with some of these quality-based programs,” Mr. Breen said.
Early steps can curb legal risk
Asking questions and being proactive as new value-based models develop is key to mitigating legal dangers, experts said.
Ensure that new arrangements are analyzed for fraud and abuse risk exposure before finalizing, Mr. Breen advised.
“Have a comfort level about the arrangement” that’s being entered into, he added, and “have those arrangements vetted.”
Pay attention to data, added Michael E. Paulhus, an Atlanta-based health law attorney who specializes in FCA cases.
“The more data they collect, the more the government is paying attention to where you are in the range,” he said in an interview. “If you stick out on either end, that would be a risk profile that, as a physician, I would want to know. I would want to know where I sit in the data.”
When making reports regarding quality measures, include such reports in internal audits as part of regular compliance efforts, the experts suggested.
In addition, seek out resources early that can help prepare the practice for new quality-based regulations, Mr. Homchick said.
“There will be guidance coming out [regarding] eligibility for these value-based incentives,” he said. “That will require you and your staff to really pay attention and seek out resources and guidance to try to do this right. If you have the bandwidth to get out ahead of this, that would certainly be the best approach.”
On Twitter @legal_med
As you begin to consider the switch to value-based care systems, be sure to safeguard against risks that could fuel false claims scrutiny by the government, legal experts advise.
A primary consideration is arrangements that include shared savings through coordinated care, said George B. Breen, a Washington-based health law attorney. For example, he said that the Stark Law could be implicated if a physician within a shared savings model receives a bonus payment for referring patients to specific providers. The Stark Law prohibits a physician from referring Medicare patients for designated health services to an entity with which the physician has a financial relationship.
“While there are a number of exceptions and safe harbors which would validate any such relationship, it’s something that needs to be thought through” from the start, Mr. Breen said in an interview. “You have to look at each factual circumstance separately because each is fact and circumstance dependent.”
The Anti-Kickback Statute also could come into play if value-based arrangements generate renumeration. The Anti-Kickback Statute prohibits offering, paying, soliciting, or receiving anything of value to induce or reward referrals or generate federal health care program business. Exceptions to the statute can be applied and should also be examined during arrangement development, Mr. Breen said.
Data collection and reporting also may present a problem, according to Seattle-based health law attorney Robert G. Homchick. Inaccurate data that become the basis for quality-based payments could lead to overpayment liability and indirect False Claims Act (FCA) exposure, he said.
In addition, “If the facts support that you were acting with intentional or deliberate ignorance or reckless disregard for how the data were gathered and reported that supported your value-based comp kicker, there could be direct False Claims Act liability,” Mr. Homchick said in an interview.
But Mr. Homchick stressed there are still many unknowns when it comes to how data-driven measurements will unfold.
“With MACRA, this is such a moving target as to exactly what type of data is going to form the basis for the metrics, and how the data need to be gathered and reported,” he said. “Many of those issues are still in play or still being developed at the agency level in terms of regulatory guidance.”
Current lawsuit could influence future cases
While it is too early to know every legal theory that could intersect with quality-based care, legal experts are closely watching a case that could offer insight into future claims.
In Duffy v. Lawrence Memorial Hospital, a former employee turned whistle-blower alleges that the Lawrence, Kan.–based hospital inflated its performance scores under the Hospital Value-Based Purchasing Program to increase federal incentive payments. Hospital leaders deny they falsified data and claim the allegations are based on the whistle-blower’s “improper understanding of acceptable reporting times for patient arrival,” according the hospital’s court response. The FCA lawsuit is before the U.S. District Court for the District of Kansas.
Notably, the government has declined to intervene in the lawsuit twice, Mr. Breen said. The case is continuing without government intervention, a trend that has become more common in recent years, he said. In 2015, whistle-blower cases in which U.S. Department of Justice declined to intervene led to $1.1 billion in recoveries for the government and $335 million in rewards for whistle-blowers, according to government data.
Mr. Homchick called the Lawrence Memorial lawsuit “troubling.”
“Providers are struggling with the complexity of the reporting requirements imposed by the layers of value-based payment programs implemented by both government and private payers,” he said. “The Lawrence Memorial case illustrates that the whistle-blower community will likely exploit the inevitable mistakes or missteps of providers attempting to comply with the increasingly byzantine quality-reporting requirements.”
The outcome of the Lawrence Memorial case could influence similar lawsuits involving value-based programs, Mr. Breen said.
“I think this theory that there is some false reporting, or false certification, is a theory that you will see being pursed in connection with some of these quality-based programs,” Mr. Breen said.
Early steps can curb legal risk
Asking questions and being proactive as new value-based models develop is key to mitigating legal dangers, experts said.
Ensure that new arrangements are analyzed for fraud and abuse risk exposure before finalizing, Mr. Breen advised.
“Have a comfort level about the arrangement” that’s being entered into, he added, and “have those arrangements vetted.”
Pay attention to data, added Michael E. Paulhus, an Atlanta-based health law attorney who specializes in FCA cases.
“The more data they collect, the more the government is paying attention to where you are in the range,” he said in an interview. “If you stick out on either end, that would be a risk profile that, as a physician, I would want to know. I would want to know where I sit in the data.”
When making reports regarding quality measures, include such reports in internal audits as part of regular compliance efforts, the experts suggested.
In addition, seek out resources early that can help prepare the practice for new quality-based regulations, Mr. Homchick said.
“There will be guidance coming out [regarding] eligibility for these value-based incentives,” he said. “That will require you and your staff to really pay attention and seek out resources and guidance to try to do this right. If you have the bandwidth to get out ahead of this, that would certainly be the best approach.”
On Twitter @legal_med
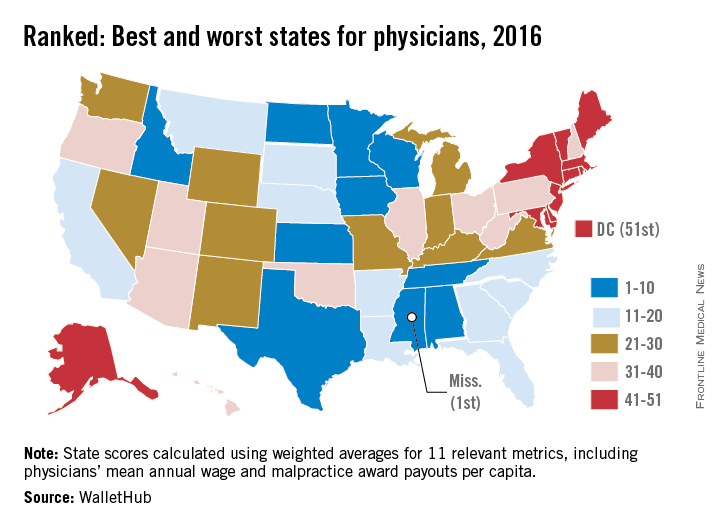
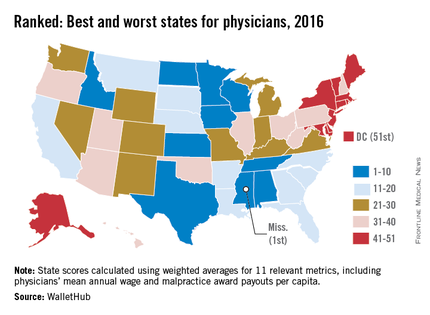
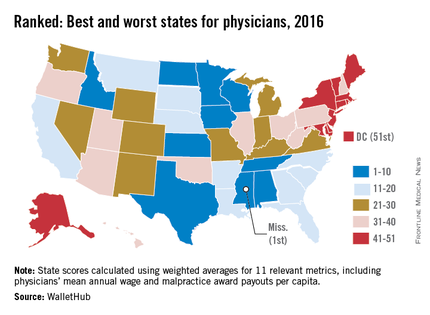
What are the best, worst states for physicians?
Should your future include a move to the South? A new report finds that Mississippi ranks as the best state to practice medicine, while the District of Columbia and New York are the least doctor-friendly areas in the United States.
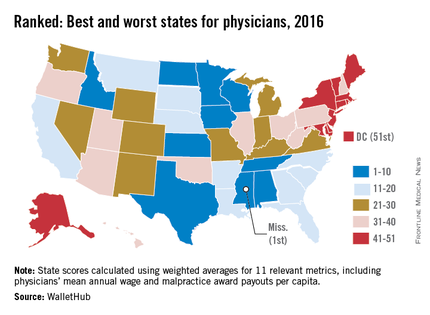
The survey, conducted by personal finance website WalletHub, compares all 50 states and D.C. across 11 metrics, including physician starting salary, medical malpractice climate, provider competition, and annual wages – adjusted for cost of living. Data was derived from the U.S. Census Bureau, the Bureau of Labor Statistics, the U.S. Department of Health and Human Services, and the Missouri Economic Research & Information Center, among other sources.
Researchers gave each metric a value between 0 and 100 and then calculated an overall score for each state using the weighted average across all metrics. Behind Mississippi, Iowa, Minnesota, and North Dakota ranked among the best states to practice medicine, according to the report. Rhode Island, Maryland, and Connecticut ranked among the worst, just slightly better than New York and D.C.
“There are an abundance of differences in terms of the working environments faced by doctors across the nation,” WalletHub analyst Jill Gonzalez said in an interview. “The results, while not too surprising, may certainly be eye opening for many new or soon-to-be doctors. Doctors should understand what they’re signing up for in terms of wages, malpractice rates, and job security when they move to another state to practice.”
View the entire WalletHub analysis here.
On Twitter @legal_med
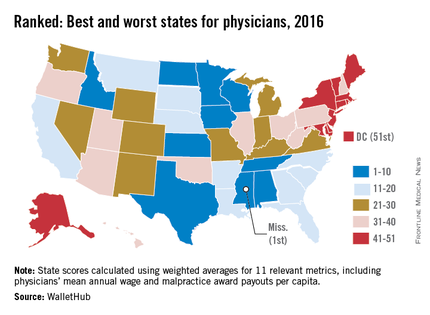
Should your future include a move to the South? A new report finds that Mississippi ranks as the best state to practice medicine, while the District of Columbia and New York are the least doctor-friendly areas in the United States.
The survey, conducted by personal finance website WalletHub, compares all 50 states and D.C. across 11 metrics, including physician starting salary, medical malpractice climate, provider competition, and annual wages – adjusted for cost of living. Data was derived from the U.S. Census Bureau, the Bureau of Labor Statistics, the U.S. Department of Health and Human Services, and the Missouri Economic Research & Information Center, among other sources.
Researchers gave each metric a value between 0 and 100 and then calculated an overall score for each state using the weighted average across all metrics. Behind Mississippi, Iowa, Minnesota, and North Dakota ranked among the best states to practice medicine, according to the report. Rhode Island, Maryland, and Connecticut ranked among the worst, just slightly better than New York and D.C.
“There are an abundance of differences in terms of the working environments faced by doctors across the nation,” WalletHub analyst Jill Gonzalez said in an interview. “The results, while not too surprising, may certainly be eye opening for many new or soon-to-be doctors. Doctors should understand what they’re signing up for in terms of wages, malpractice rates, and job security when they move to another state to practice.”
View the entire WalletHub analysis here.
On Twitter @legal_med
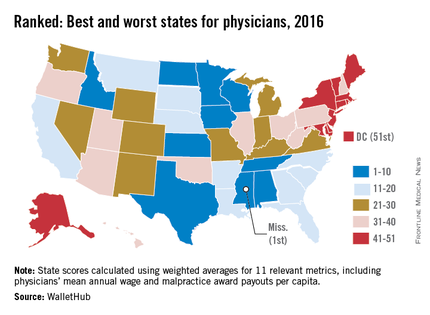
Should your future include a move to the South? A new report finds that Mississippi ranks as the best state to practice medicine, while the District of Columbia and New York are the least doctor-friendly areas in the United States.
The survey, conducted by personal finance website WalletHub, compares all 50 states and D.C. across 11 metrics, including physician starting salary, medical malpractice climate, provider competition, and annual wages – adjusted for cost of living. Data was derived from the U.S. Census Bureau, the Bureau of Labor Statistics, the U.S. Department of Health and Human Services, and the Missouri Economic Research & Information Center, among other sources.
Researchers gave each metric a value between 0 and 100 and then calculated an overall score for each state using the weighted average across all metrics. Behind Mississippi, Iowa, Minnesota, and North Dakota ranked among the best states to practice medicine, according to the report. Rhode Island, Maryland, and Connecticut ranked among the worst, just slightly better than New York and D.C.
“There are an abundance of differences in terms of the working environments faced by doctors across the nation,” WalletHub analyst Jill Gonzalez said in an interview. “The results, while not too surprising, may certainly be eye opening for many new or soon-to-be doctors. Doctors should understand what they’re signing up for in terms of wages, malpractice rates, and job security when they move to another state to practice.”
View the entire WalletHub analysis here.
On Twitter @legal_med
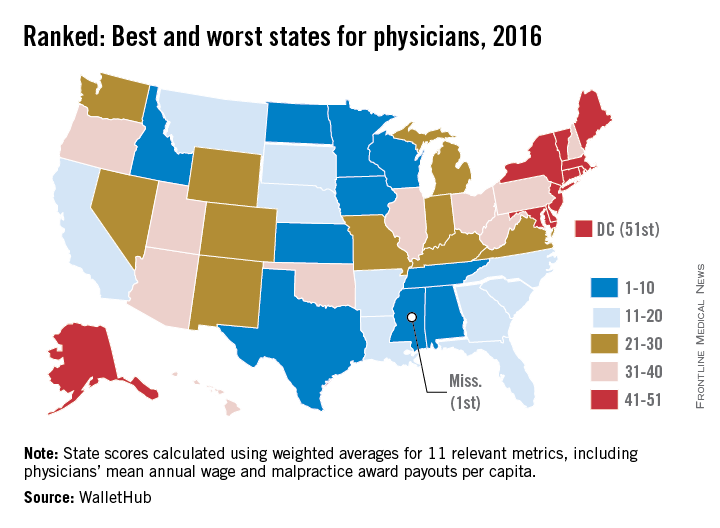
What are the best, worst states for physicians?
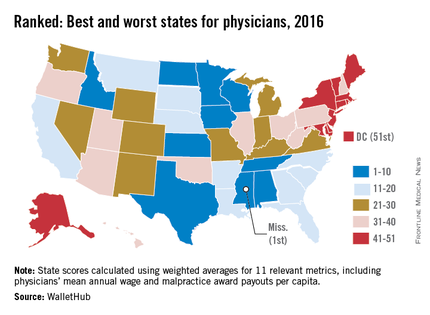
Should your future include a move to the South? A new report finds that Mississippi ranks as the best state to practice medicine, while the District of Columbia and New York are the least doctor-friendly areas in the United States.
The survey, conducted by personal finance website WalletHub, compares all 50 states and D.C. across 11 metrics, including physician starting salary, medical malpractice climate, provider competition, and annual wages – adjusted for cost of living. Data was derived from the U.S. Census Bureau, the Bureau of Labor Statistics, the U.S. Department of Health and Human Services, and the Missouri Economic Research & Information Center, among other sources.
Researchers gave each metric a value between 0 and 100 and then calculated an overall score for each state using the weighted average across all metrics. Behind Mississippi, Iowa, Minnesota, and North Dakota ranked among the best states to practice medicine, according to the report. Rhode Island, Maryland, and Connecticut ranked among the worst, just slightly better than New York and D.C.
“There are an abundance of differences in terms of the working environments faced by doctors across the nation,” WalletHub analyst Jill Gonzalez said in an interview. “The results, while not too surprising, may certainly be eye opening for many new or soon-to-be doctors. Doctors should understand what they’re signing up for in terms of wages, malpractice rates, and job security when they move to another state to practice.”
View the entire WalletHub analysis here.
On Twitter @legal_med
Should your future include a move to the South? A new report finds that Mississippi ranks as the best state to practice medicine, while the District of Columbia and New York are the least doctor-friendly areas in the United States.
The survey, conducted by personal finance website WalletHub, compares all 50 states and D.C. across 11 metrics, including physician starting salary, medical malpractice climate, provider competition, and annual wages – adjusted for cost of living. Data was derived from the U.S. Census Bureau, the Bureau of Labor Statistics, the U.S. Department of Health and Human Services, and the Missouri Economic Research & Information Center, among other sources.
Researchers gave each metric a value between 0 and 100 and then calculated an overall score for each state using the weighted average across all metrics. Behind Mississippi, Iowa, Minnesota, and North Dakota ranked among the best states to practice medicine, according to the report. Rhode Island, Maryland, and Connecticut ranked among the worst, just slightly better than New York and D.C.
“There are an abundance of differences in terms of the working environments faced by doctors across the nation,” WalletHub analyst Jill Gonzalez said in an interview. “The results, while not too surprising, may certainly be eye opening for many new or soon-to-be doctors. Doctors should understand what they’re signing up for in terms of wages, malpractice rates, and job security when they move to another state to practice.”
View the entire WalletHub analysis here.
On Twitter @legal_med
Should your future include a move to the South? A new report finds that Mississippi ranks as the best state to practice medicine, while the District of Columbia and New York are the least doctor-friendly areas in the United States.
The survey, conducted by personal finance website WalletHub, compares all 50 states and D.C. across 11 metrics, including physician starting salary, medical malpractice climate, provider competition, and annual wages – adjusted for cost of living. Data was derived from the U.S. Census Bureau, the Bureau of Labor Statistics, the U.S. Department of Health and Human Services, and the Missouri Economic Research & Information Center, among other sources.
Researchers gave each metric a value between 0 and 100 and then calculated an overall score for each state using the weighted average across all metrics. Behind Mississippi, Iowa, Minnesota, and North Dakota ranked among the best states to practice medicine, according to the report. Rhode Island, Maryland, and Connecticut ranked among the worst, just slightly better than New York and D.C.
“There are an abundance of differences in terms of the working environments faced by doctors across the nation,” WalletHub analyst Jill Gonzalez said in an interview. “The results, while not too surprising, may certainly be eye opening for many new or soon-to-be doctors. Doctors should understand what they’re signing up for in terms of wages, malpractice rates, and job security when they move to another state to practice.”
View the entire WalletHub analysis here.
On Twitter @legal_med
Allegations: Current Trends in Medical Malpractice, Part 2
Most medical malpractice cases are still resolved in a courtroom—typically after years of preparation and personal torment. Yet, overall rates of paid medical malpractice claims among all physicians have been steadily decreasing over the past two decades, with reports showing decreases of 30% to 50% in paid claims since 2000.1-3 At the same time, while median payments and insurance premiums continued to increase until the mid-2000s, they now appear to have plateaued.1
None of these changes occurred in isolation. More than 30 states now have caps on noneconomic or total damages.2 As noted in part 1, since 2000, some states have enacted comprehensive tort reform.4 However, whether these changes in malpractice patterns can be attributed directly to specific policy changes remains a hotly contested issue.
Malpractice Risk in Emergency Medicine
To what extent do the trends in medical malpractice apply to emergency medicine (EM)? While emergency physicians’ (EPs’) perception of malpractice risk ranks higher than any other medical specialty,5 in a review of a large sample of malpractice claims from 1991 through 2005, EPs ranked in the middle among specialties with respect to annual risk of a malpractice claim.6 Moreover, the annual risk of a claim for EPs is just under 8%, compared to 7.4% for all physicians. Yet, for neurosurgery and cardiothoracic surgery—the specialties with the highest overall risk of malpractice claims—the annual risk approaches 20%.6 Regarding payout statistics, less than one-fifth of the claims against EPs resulted in payment.6 In a review of a separate insurance database of closed claims, EPs were named as the primary defendant in only 19% of cases.7
Despite the discrepancies between perceived risk and absolute risk of malpractice claims among EPs, malpractice lawsuits continue to affect the practice of EM. This is evidenced in several surveys, in which the majority of EP participants admitted to practicing “defensive medicine” by ordering tests that were felt to be unnecessary and did so in response to perceived malpractice risk.8-10 Perceived risk also accounts for the significant variation in decision-making in the ED with respect to diagnostic testing and hospitalization of patients.11 One would expect that lowering malpractice risk would result in less so-called unnecessary testing, but whether or not this is truly the case remains to be seen.
Effects of Malpractice Reform
A study by Waxman et al12 on the effects of significant malpractice tort reform in ED care in Texas, Georgia, and South Carolina found no difference in rates of imaging studies, charges, or patient admissions. Furthermore, legislation reform did not increase plaintiff onus to prove proximate “gross negligence” rather than simply a breach from “reasonably skillful and careful” medicine.12 These findings suggest that perception of malpractice risk might simply be serving as a proxy for physicians’ underlying risk tolerance, and be less subject to influence by external forces.
Areas Associated With Malpractice Risk
A number of closed-claim databases attempted to identify the characteristics of patient encounters that can lead to malpractice claims, including patient conditions and sources of error. Diagnostic errors have consistently been found to be the leading cause of malpractice claims, accounting for 28% to 65% of claims, followed by inappropriate management of medical treatment and improper performance of a procedure.7,13-16 A January 2016 benchmarking system report by CRICO Strategies found that 30% of 23,658 medical malpractice claims filed between 2009 through 2013 cited failures in communication as a factor.17 The report also revealed that among these failed communications, those that occurred between health care providers are more likely to result in payout compared to miscommunications between providers and patients.17 This report further noted 70% to 80% of claims closed without payment.7,16 Closed claims were significantly more likely to involve serious injuries or death.7,18 Leading conditions that resulted in claims include myocardial infarction, nonspecific chest pain, symptoms involving the abdomen or pelvis, appendicitis, and orthopedic injuries.7,13,16
Diagnostic Errors
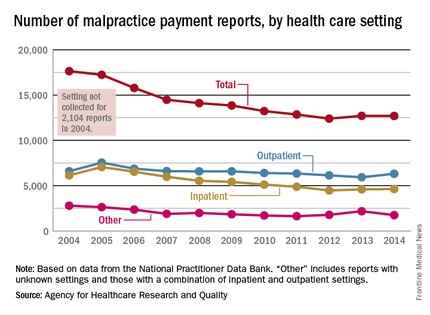
Errors in diagnosis have been attributed to multiple factors in the ED. The two most common factors were failure to order tests and failure to perform an adequate history and physical examination, both of which contribute to rationalization of the practice of defensive medicine under the current tort system.13 Other significant factors associated with errors in diagnosis include misinterpretation of test results or imaging studies and failure to obtain an appropriate consultation. Processes contributing to each of these potential errors include mistakes in judgment, lack of knowledge, miscommunication, and insufficient documentation (Table).15
Strategies for Reducing Malpractice Risk
In part 1, we listed several strategies EPs could adopt to help reduce malpractice risk. In this section, we will discuss in further detail how these strategies help mitigate malpractice claims.
Patient Communication
Open communication with patients is paramount in reducing the risk of a malpractice allegation. Patients are more likely to become angry or frustrated if they sense a physician is not listening to or addressing their concerns. These patients are in turn more likely to file a complaint if they are harmed or experience a bad outcome during their stay in the ED.
Situations in which patients are unable to provide pertinent information also place the EP at significant risk, as the provider must make decisions without full knowledge of the case. Communication with potential resources such as nursing home staff, the patient’s family, and emergency medical service providers to obtain additional information can help reduce risk.
Of course, when evaluating and treating patients, the EP should always take the time to listen to the patient’s concerns during the encounter to ensure his or her needs have been addressed. In the event of a patient allegation or complaint, the EP should make the effort to explore and de-escalate the situation before the patient is discharged.
Discharge Care and Instructions
According to CRICO, premature discharge as a factor in medical malpractice liability results from inadequate assessment and missed opportunities in 41% of diagnosis-related ED cases.16 The following situation illustrates a brief example of such a missed opportunity: A provider makes a diagnosis of urinary tract infection (UTI) in a patient presenting with fever and abdominal pain but whose urinalysis is suspect for contamination and in whom no pelvic examination was performed to rule out other etiologies. When the same patient later returns to the ED with worse abdominal pain, a sterile urine culture invalidates the diagnosis of UTI, and further evaluation leads to a final diagnosis of ruptured appendix.
Prior to discharging any patient, the EP should provide clear and concise at-home care instructions in a manner in which the patient can understand. Clear instructions on how the patient is to manage his or her care after discharge are vital, and failure to do so in terms the patient can understand can create problems if a harmful result occurs. This is especially important in patients with whom there is a communication barrier—eg, language barrier, hearing impairment, cognitive deficit, intoxication, or violent or irrational behavior. In these situations, the EP should always take advantage of available resources and tools such as language lines, interpreters, discharge planners, psychiatric staff, and supportive family members to help reconcile any communication barriers. These measures will in turn optimize patient outcome and reduce the risk of a later malpractice allegation.
Board Certification
All physicians should maintain their respective board certification and specialty training requirements. Efforts in this area help providers to stay up to date in current practice standards and new developments, thus reducing one’s risk of incurring a malpractice claim.
Patient Safety
All members of the care team should engender an environment that is focused on patient safety, including open communication between providers and with nursing staff and technical support teams. Although interruptions can be detrimental to patient care, simply having an understanding of this phenomenon among all staff members can alleviate some of the working stressors in the ED. Effort must be made to create an environment that allows for clarification between nursing staff and physicians without causing undue antagonism. Fostering supportive communication, having a questioning attitude, and seeking clarification can only enhance patient safety.
The importance of the supervisory role of attending physicians to trainees, physician extenders, and nursing staff must be emphasized, and appropriate guidance from the ED attending is germane in keeping patients safe in teaching environments. Additionally, in departments that suffer the burden of high numbers of admitted patient boarders in the ED, attention must be given to the transitional period between decision to admit and termination of ED care and the acquisition of care of the admitting physician. A clear plan of responsibility must be in place for these high-risk situations.
Policies and Procedures
Departmental policies and procedures should be designed to identify and address all late laboratory results data, radiological discrepancies, and culture results in a timely and uniform manner. Since unaddressed results and discrepancies can result in patient harm, patient-callback processes should be designed to reduce risk by addressing these hazards regularly, thoroughly, and in a timely fashion.
Cognitive Biases
An awareness of inherent biases in the medical decision-making process is also helpful to maintain mindfulness in the routine practice of EM and avoid medical errors. The EP should take care not to be influenced by recent events and diagnostic information that is easy to recall or common, and to ensure the differential addresses possibilities beyond the readily available diagnoses. Further, reliance on an existing opinion may be misleading if subsequent judgments are based on this “anchor,” whether it is true or false.
If the data points of the case do not line up as expected, or if there are unexplained outliers, the EP should expand the frame of reference to seek more appropriate possibilities, and avoid attempts to make the data fit a preferred or favored conclusion.
When one fails to recognize that data do not fit the diagnostic presumption, the true diagnosis can be undermined. Such confirmation bias in turn challenges diagnostic success. Hasty judgment without considering and seeking out relevant information can set up diagnostic failure and premature closure.
Remembering the Basics
Finally, providers should follow the basic principles for every patient. Vital signs are vital for a reason, and all abnormal data must be accounted for prior to patient hand off or discharge. Patient turnover is a high-risk occasion, and demands careful attention to case details between the off-going physician, the accepting physician, and the patient.
All patients presenting to the ED for care should leave the ED at their baseline functional level (ie, if they walk independently, they should still walk independently at discharge). If not, the reason should be sought out and clarified with appropriate recommendations for treatment and follow-up.
Patients and staff should always be treated with respect, which in turn will encourage effective communication. Providers should be honest with patients, document truthfully, respect privacy and confidentiality, practice within one’s competence, confirm information, and avoid assumptions. Compassion goes hand in hand with respectful and open communication. Physicians perceived as compassionate and trustworthy are less likely to be the target of a malpractice suit, even when harm has occurred.
Conclusion
Even though the number of paid medical malpractice claims has continued to decrease over the past 20 years, a discrepancy between perceived and absolute risk persists among EPs—one that perpetuates the practice of defensive medicine and continues to affect EM. Despite the current perceptions and climate, EPs can allay their risk of incurring a malpractice claim by employing the strategies outlined above.
1. Mello MM, Studdert DM, Kachalia A. The medical liability climate and prospects for reform. JAMA. 2014;312(20):2146-2155.
2. Paik M, Black B, Hyman DA. The receding tide of medical malpractice: part 1 - national trends. J Empirical Leg Stud. 2013;10(4):612-638.
3. Bishop TF, Ryan AM, Caslino LP. Paid malpractice claims for adverse events in inpatient and outpatient settings. JAMA. 2011;305(23):2427-2431.
4. Kachalia A, Mello MM. New directions in medical liability reform. N Engl J Med. 2011;364(16):
1564-1572.
5. Carrier ER, Reschovsky JD, Mello MM, Mayrell RC, Katz D. Physicians’ fears of malpractice lawsuits are not assured by tort reforms. Health Aff. 2010;29(9):1585-1592.
6. Jena AB, Seabury S, Lakdawalla D, Chandra A. Malpractice risk according to physician specialty. N Engl J Med. 2011;365(7):629-636.
7. Brown TW, McCarthy ML, Kelen GD, Levy F. An epidemiologic study of closed emergency department malpractice claims in a national database of physician malpractice insurers. Acad Emerg Med. 2010;17(5):553-560.
8. Studdert DM, Mello MM, Sage WM, et al. Defensive medicine among high-risk specialist physicians in a volatile malpractice environment. JAMA. 2005;293(21):2609-2617.
9. Bishop TF, Federman AD, Keyhani S. Physicians’ views on defensive medicine: a national survey. Arch Intern Med. 2010;170(12):1081-1083.
10. Massachusetts Medical Society. Investigation of defensive medicine in Massachusetts. November 2008. Available at http://www.massmed.org/defensivemedicine. Accessed March 16, 2016.
11. Katz DA, Williams GC, Brown RL, et al. Emergency physicians’ fear of malpractice in evaluating patient with possible acute cardiac ischemia. Ann Emerg Med. 2005;46(6):525-533.
12. Waxman DA, Greenberg MD, Ridgely MS, Kellermann AL, Heaton P. The effect of malpractice reform on emergency department care. N Engl J Med. 2014;371(16):1518-1525.
13. Kachalia A, Gandhi TK, Puopolo AL, et al. Missed and delayed diagnoses in the emergency department: a study of closed malpractice claims from 4 liability insurers. Ann Emerg Med. 2007;49(2):196-205.
14. Saber Tehrani AS, Lee H, Mathews SC, et al. 25-Year summary of US malpractice claims for diagnostic errors 1986-2010: an analysis from the National Practitioner Data Bank. BMJ Qual Saf. 2013;22(8):672-680.
15. Ross J, Ranum D, Troxel DB. Emergency medicine closed claims study. The Doctors Company. Available at http://www.thedoctors.com/ecm/groups/public/@tdc/@web/@kc/@patientsafety/documents/article/con_id_004776.pdf. Accessed March 16, 2016.
16. Ruoff G, ed. 2011 Annual benchmarking report: malpractice risks in emergency medicine. CRICO strategies. 2012. Available at https://www.rmf.harvard.edu/Strategies/Home/Products-and-Services/Comparative-Data/Annual-Benchmark-Reports. Accessed March 16, 2016.
17. Failures in communication contribute to medical malpractice. January 31, 2016. https://www.rmf.harvard.edu/About-CRICO/Media/Press-Releases/News/2016/February/Failures-in-Communication-Contribute-to-Medical-Malpractice.
18. Studdert DM, Mello MM, Gawande AA, et al. Claims, errors, and compensation payments in medical malpractice litigation. N Engl J Med. 2006;354(19):2024-2033. Accessed March 16, 2016.
Most medical malpractice cases are still resolved in a courtroom—typically after years of preparation and personal torment. Yet, overall rates of paid medical malpractice claims among all physicians have been steadily decreasing over the past two decades, with reports showing decreases of 30% to 50% in paid claims since 2000.1-3 At the same time, while median payments and insurance premiums continued to increase until the mid-2000s, they now appear to have plateaued.1
None of these changes occurred in isolation. More than 30 states now have caps on noneconomic or total damages.2 As noted in part 1, since 2000, some states have enacted comprehensive tort reform.4 However, whether these changes in malpractice patterns can be attributed directly to specific policy changes remains a hotly contested issue.
Malpractice Risk in Emergency Medicine
To what extent do the trends in medical malpractice apply to emergency medicine (EM)? While emergency physicians’ (EPs’) perception of malpractice risk ranks higher than any other medical specialty,5 in a review of a large sample of malpractice claims from 1991 through 2005, EPs ranked in the middle among specialties with respect to annual risk of a malpractice claim.6 Moreover, the annual risk of a claim for EPs is just under 8%, compared to 7.4% for all physicians. Yet, for neurosurgery and cardiothoracic surgery—the specialties with the highest overall risk of malpractice claims—the annual risk approaches 20%.6 Regarding payout statistics, less than one-fifth of the claims against EPs resulted in payment.6 In a review of a separate insurance database of closed claims, EPs were named as the primary defendant in only 19% of cases.7
Despite the discrepancies between perceived risk and absolute risk of malpractice claims among EPs, malpractice lawsuits continue to affect the practice of EM. This is evidenced in several surveys, in which the majority of EP participants admitted to practicing “defensive medicine” by ordering tests that were felt to be unnecessary and did so in response to perceived malpractice risk.8-10 Perceived risk also accounts for the significant variation in decision-making in the ED with respect to diagnostic testing and hospitalization of patients.11 One would expect that lowering malpractice risk would result in less so-called unnecessary testing, but whether or not this is truly the case remains to be seen.
Effects of Malpractice Reform
A study by Waxman et al12 on the effects of significant malpractice tort reform in ED care in Texas, Georgia, and South Carolina found no difference in rates of imaging studies, charges, or patient admissions. Furthermore, legislation reform did not increase plaintiff onus to prove proximate “gross negligence” rather than simply a breach from “reasonably skillful and careful” medicine.12 These findings suggest that perception of malpractice risk might simply be serving as a proxy for physicians’ underlying risk tolerance, and be less subject to influence by external forces.
Areas Associated With Malpractice Risk
A number of closed-claim databases attempted to identify the characteristics of patient encounters that can lead to malpractice claims, including patient conditions and sources of error. Diagnostic errors have consistently been found to be the leading cause of malpractice claims, accounting for 28% to 65% of claims, followed by inappropriate management of medical treatment and improper performance of a procedure.7,13-16 A January 2016 benchmarking system report by CRICO Strategies found that 30% of 23,658 medical malpractice claims filed between 2009 through 2013 cited failures in communication as a factor.17 The report also revealed that among these failed communications, those that occurred between health care providers are more likely to result in payout compared to miscommunications between providers and patients.17 This report further noted 70% to 80% of claims closed without payment.7,16 Closed claims were significantly more likely to involve serious injuries or death.7,18 Leading conditions that resulted in claims include myocardial infarction, nonspecific chest pain, symptoms involving the abdomen or pelvis, appendicitis, and orthopedic injuries.7,13,16
Diagnostic Errors
Errors in diagnosis have been attributed to multiple factors in the ED. The two most common factors were failure to order tests and failure to perform an adequate history and physical examination, both of which contribute to rationalization of the practice of defensive medicine under the current tort system.13 Other significant factors associated with errors in diagnosis include misinterpretation of test results or imaging studies and failure to obtain an appropriate consultation. Processes contributing to each of these potential errors include mistakes in judgment, lack of knowledge, miscommunication, and insufficient documentation (Table).15
Strategies for Reducing Malpractice Risk
In part 1, we listed several strategies EPs could adopt to help reduce malpractice risk. In this section, we will discuss in further detail how these strategies help mitigate malpractice claims.
Patient Communication
Open communication with patients is paramount in reducing the risk of a malpractice allegation. Patients are more likely to become angry or frustrated if they sense a physician is not listening to or addressing their concerns. These patients are in turn more likely to file a complaint if they are harmed or experience a bad outcome during their stay in the ED.
Situations in which patients are unable to provide pertinent information also place the EP at significant risk, as the provider must make decisions without full knowledge of the case. Communication with potential resources such as nursing home staff, the patient’s family, and emergency medical service providers to obtain additional information can help reduce risk.
Of course, when evaluating and treating patients, the EP should always take the time to listen to the patient’s concerns during the encounter to ensure his or her needs have been addressed. In the event of a patient allegation or complaint, the EP should make the effort to explore and de-escalate the situation before the patient is discharged.
Discharge Care and Instructions
According to CRICO, premature discharge as a factor in medical malpractice liability results from inadequate assessment and missed opportunities in 41% of diagnosis-related ED cases.16 The following situation illustrates a brief example of such a missed opportunity: A provider makes a diagnosis of urinary tract infection (UTI) in a patient presenting with fever and abdominal pain but whose urinalysis is suspect for contamination and in whom no pelvic examination was performed to rule out other etiologies. When the same patient later returns to the ED with worse abdominal pain, a sterile urine culture invalidates the diagnosis of UTI, and further evaluation leads to a final diagnosis of ruptured appendix.
Prior to discharging any patient, the EP should provide clear and concise at-home care instructions in a manner in which the patient can understand. Clear instructions on how the patient is to manage his or her care after discharge are vital, and failure to do so in terms the patient can understand can create problems if a harmful result occurs. This is especially important in patients with whom there is a communication barrier—eg, language barrier, hearing impairment, cognitive deficit, intoxication, or violent or irrational behavior. In these situations, the EP should always take advantage of available resources and tools such as language lines, interpreters, discharge planners, psychiatric staff, and supportive family members to help reconcile any communication barriers. These measures will in turn optimize patient outcome and reduce the risk of a later malpractice allegation.
Board Certification
All physicians should maintain their respective board certification and specialty training requirements. Efforts in this area help providers to stay up to date in current practice standards and new developments, thus reducing one’s risk of incurring a malpractice claim.
Patient Safety
All members of the care team should engender an environment that is focused on patient safety, including open communication between providers and with nursing staff and technical support teams. Although interruptions can be detrimental to patient care, simply having an understanding of this phenomenon among all staff members can alleviate some of the working stressors in the ED. Effort must be made to create an environment that allows for clarification between nursing staff and physicians without causing undue antagonism. Fostering supportive communication, having a questioning attitude, and seeking clarification can only enhance patient safety.
The importance of the supervisory role of attending physicians to trainees, physician extenders, and nursing staff must be emphasized, and appropriate guidance from the ED attending is germane in keeping patients safe in teaching environments. Additionally, in departments that suffer the burden of high numbers of admitted patient boarders in the ED, attention must be given to the transitional period between decision to admit and termination of ED care and the acquisition of care of the admitting physician. A clear plan of responsibility must be in place for these high-risk situations.
Policies and Procedures
Departmental policies and procedures should be designed to identify and address all late laboratory results data, radiological discrepancies, and culture results in a timely and uniform manner. Since unaddressed results and discrepancies can result in patient harm, patient-callback processes should be designed to reduce risk by addressing these hazards regularly, thoroughly, and in a timely fashion.
Cognitive Biases
An awareness of inherent biases in the medical decision-making process is also helpful to maintain mindfulness in the routine practice of EM and avoid medical errors. The EP should take care not to be influenced by recent events and diagnostic information that is easy to recall or common, and to ensure the differential addresses possibilities beyond the readily available diagnoses. Further, reliance on an existing opinion may be misleading if subsequent judgments are based on this “anchor,” whether it is true or false.
If the data points of the case do not line up as expected, or if there are unexplained outliers, the EP should expand the frame of reference to seek more appropriate possibilities, and avoid attempts to make the data fit a preferred or favored conclusion.
When one fails to recognize that data do not fit the diagnostic presumption, the true diagnosis can be undermined. Such confirmation bias in turn challenges diagnostic success. Hasty judgment without considering and seeking out relevant information can set up diagnostic failure and premature closure.
Remembering the Basics
Finally, providers should follow the basic principles for every patient. Vital signs are vital for a reason, and all abnormal data must be accounted for prior to patient hand off or discharge. Patient turnover is a high-risk occasion, and demands careful attention to case details between the off-going physician, the accepting physician, and the patient.
All patients presenting to the ED for care should leave the ED at their baseline functional level (ie, if they walk independently, they should still walk independently at discharge). If not, the reason should be sought out and clarified with appropriate recommendations for treatment and follow-up.
Patients and staff should always be treated with respect, which in turn will encourage effective communication. Providers should be honest with patients, document truthfully, respect privacy and confidentiality, practice within one’s competence, confirm information, and avoid assumptions. Compassion goes hand in hand with respectful and open communication. Physicians perceived as compassionate and trustworthy are less likely to be the target of a malpractice suit, even when harm has occurred.
Conclusion
Even though the number of paid medical malpractice claims has continued to decrease over the past 20 years, a discrepancy between perceived and absolute risk persists among EPs—one that perpetuates the practice of defensive medicine and continues to affect EM. Despite the current perceptions and climate, EPs can allay their risk of incurring a malpractice claim by employing the strategies outlined above.
Most medical malpractice cases are still resolved in a courtroom—typically after years of preparation and personal torment. Yet, overall rates of paid medical malpractice claims among all physicians have been steadily decreasing over the past two decades, with reports showing decreases of 30% to 50% in paid claims since 2000.1-3 At the same time, while median payments and insurance premiums continued to increase until the mid-2000s, they now appear to have plateaued.1
None of these changes occurred in isolation. More than 30 states now have caps on noneconomic or total damages.2 As noted in part 1, since 2000, some states have enacted comprehensive tort reform.4 However, whether these changes in malpractice patterns can be attributed directly to specific policy changes remains a hotly contested issue.
Malpractice Risk in Emergency Medicine
To what extent do the trends in medical malpractice apply to emergency medicine (EM)? While emergency physicians’ (EPs’) perception of malpractice risk ranks higher than any other medical specialty,5 in a review of a large sample of malpractice claims from 1991 through 2005, EPs ranked in the middle among specialties with respect to annual risk of a malpractice claim.6 Moreover, the annual risk of a claim for EPs is just under 8%, compared to 7.4% for all physicians. Yet, for neurosurgery and cardiothoracic surgery—the specialties with the highest overall risk of malpractice claims—the annual risk approaches 20%.6 Regarding payout statistics, less than one-fifth of the claims against EPs resulted in payment.6 In a review of a separate insurance database of closed claims, EPs were named as the primary defendant in only 19% of cases.7
Despite the discrepancies between perceived risk and absolute risk of malpractice claims among EPs, malpractice lawsuits continue to affect the practice of EM. This is evidenced in several surveys, in which the majority of EP participants admitted to practicing “defensive medicine” by ordering tests that were felt to be unnecessary and did so in response to perceived malpractice risk.8-10 Perceived risk also accounts for the significant variation in decision-making in the ED with respect to diagnostic testing and hospitalization of patients.11 One would expect that lowering malpractice risk would result in less so-called unnecessary testing, but whether or not this is truly the case remains to be seen.
Effects of Malpractice Reform
A study by Waxman et al12 on the effects of significant malpractice tort reform in ED care in Texas, Georgia, and South Carolina found no difference in rates of imaging studies, charges, or patient admissions. Furthermore, legislation reform did not increase plaintiff onus to prove proximate “gross negligence” rather than simply a breach from “reasonably skillful and careful” medicine.12 These findings suggest that perception of malpractice risk might simply be serving as a proxy for physicians’ underlying risk tolerance, and be less subject to influence by external forces.
Areas Associated With Malpractice Risk
A number of closed-claim databases attempted to identify the characteristics of patient encounters that can lead to malpractice claims, including patient conditions and sources of error. Diagnostic errors have consistently been found to be the leading cause of malpractice claims, accounting for 28% to 65% of claims, followed by inappropriate management of medical treatment and improper performance of a procedure.7,13-16 A January 2016 benchmarking system report by CRICO Strategies found that 30% of 23,658 medical malpractice claims filed between 2009 through 2013 cited failures in communication as a factor.17 The report also revealed that among these failed communications, those that occurred between health care providers are more likely to result in payout compared to miscommunications between providers and patients.17 This report further noted 70% to 80% of claims closed without payment.7,16 Closed claims were significantly more likely to involve serious injuries or death.7,18 Leading conditions that resulted in claims include myocardial infarction, nonspecific chest pain, symptoms involving the abdomen or pelvis, appendicitis, and orthopedic injuries.7,13,16
Diagnostic Errors
Errors in diagnosis have been attributed to multiple factors in the ED. The two most common factors were failure to order tests and failure to perform an adequate history and physical examination, both of which contribute to rationalization of the practice of defensive medicine under the current tort system.13 Other significant factors associated with errors in diagnosis include misinterpretation of test results or imaging studies and failure to obtain an appropriate consultation. Processes contributing to each of these potential errors include mistakes in judgment, lack of knowledge, miscommunication, and insufficient documentation (Table).15
Strategies for Reducing Malpractice Risk
In part 1, we listed several strategies EPs could adopt to help reduce malpractice risk. In this section, we will discuss in further detail how these strategies help mitigate malpractice claims.
Patient Communication
Open communication with patients is paramount in reducing the risk of a malpractice allegation. Patients are more likely to become angry or frustrated if they sense a physician is not listening to or addressing their concerns. These patients are in turn more likely to file a complaint if they are harmed or experience a bad outcome during their stay in the ED.
Situations in which patients are unable to provide pertinent information also place the EP at significant risk, as the provider must make decisions without full knowledge of the case. Communication with potential resources such as nursing home staff, the patient’s family, and emergency medical service providers to obtain additional information can help reduce risk.
Of course, when evaluating and treating patients, the EP should always take the time to listen to the patient’s concerns during the encounter to ensure his or her needs have been addressed. In the event of a patient allegation or complaint, the EP should make the effort to explore and de-escalate the situation before the patient is discharged.
Discharge Care and Instructions
According to CRICO, premature discharge as a factor in medical malpractice liability results from inadequate assessment and missed opportunities in 41% of diagnosis-related ED cases.16 The following situation illustrates a brief example of such a missed opportunity: A provider makes a diagnosis of urinary tract infection (UTI) in a patient presenting with fever and abdominal pain but whose urinalysis is suspect for contamination and in whom no pelvic examination was performed to rule out other etiologies. When the same patient later returns to the ED with worse abdominal pain, a sterile urine culture invalidates the diagnosis of UTI, and further evaluation leads to a final diagnosis of ruptured appendix.
Prior to discharging any patient, the EP should provide clear and concise at-home care instructions in a manner in which the patient can understand. Clear instructions on how the patient is to manage his or her care after discharge are vital, and failure to do so in terms the patient can understand can create problems if a harmful result occurs. This is especially important in patients with whom there is a communication barrier—eg, language barrier, hearing impairment, cognitive deficit, intoxication, or violent or irrational behavior. In these situations, the EP should always take advantage of available resources and tools such as language lines, interpreters, discharge planners, psychiatric staff, and supportive family members to help reconcile any communication barriers. These measures will in turn optimize patient outcome and reduce the risk of a later malpractice allegation.
Board Certification
All physicians should maintain their respective board certification and specialty training requirements. Efforts in this area help providers to stay up to date in current practice standards and new developments, thus reducing one’s risk of incurring a malpractice claim.
Patient Safety
All members of the care team should engender an environment that is focused on patient safety, including open communication between providers and with nursing staff and technical support teams. Although interruptions can be detrimental to patient care, simply having an understanding of this phenomenon among all staff members can alleviate some of the working stressors in the ED. Effort must be made to create an environment that allows for clarification between nursing staff and physicians without causing undue antagonism. Fostering supportive communication, having a questioning attitude, and seeking clarification can only enhance patient safety.
The importance of the supervisory role of attending physicians to trainees, physician extenders, and nursing staff must be emphasized, and appropriate guidance from the ED attending is germane in keeping patients safe in teaching environments. Additionally, in departments that suffer the burden of high numbers of admitted patient boarders in the ED, attention must be given to the transitional period between decision to admit and termination of ED care and the acquisition of care of the admitting physician. A clear plan of responsibility must be in place for these high-risk situations.
Policies and Procedures
Departmental policies and procedures should be designed to identify and address all late laboratory results data, radiological discrepancies, and culture results in a timely and uniform manner. Since unaddressed results and discrepancies can result in patient harm, patient-callback processes should be designed to reduce risk by addressing these hazards regularly, thoroughly, and in a timely fashion.
Cognitive Biases
An awareness of inherent biases in the medical decision-making process is also helpful to maintain mindfulness in the routine practice of EM and avoid medical errors. The EP should take care not to be influenced by recent events and diagnostic information that is easy to recall or common, and to ensure the differential addresses possibilities beyond the readily available diagnoses. Further, reliance on an existing opinion may be misleading if subsequent judgments are based on this “anchor,” whether it is true or false.
If the data points of the case do not line up as expected, or if there are unexplained outliers, the EP should expand the frame of reference to seek more appropriate possibilities, and avoid attempts to make the data fit a preferred or favored conclusion.
When one fails to recognize that data do not fit the diagnostic presumption, the true diagnosis can be undermined. Such confirmation bias in turn challenges diagnostic success. Hasty judgment without considering and seeking out relevant information can set up diagnostic failure and premature closure.
Remembering the Basics
Finally, providers should follow the basic principles for every patient. Vital signs are vital for a reason, and all abnormal data must be accounted for prior to patient hand off or discharge. Patient turnover is a high-risk occasion, and demands careful attention to case details between the off-going physician, the accepting physician, and the patient.
All patients presenting to the ED for care should leave the ED at their baseline functional level (ie, if they walk independently, they should still walk independently at discharge). If not, the reason should be sought out and clarified with appropriate recommendations for treatment and follow-up.
Patients and staff should always be treated with respect, which in turn will encourage effective communication. Providers should be honest with patients, document truthfully, respect privacy and confidentiality, practice within one’s competence, confirm information, and avoid assumptions. Compassion goes hand in hand with respectful and open communication. Physicians perceived as compassionate and trustworthy are less likely to be the target of a malpractice suit, even when harm has occurred.
Conclusion
Even though the number of paid medical malpractice claims has continued to decrease over the past 20 years, a discrepancy between perceived and absolute risk persists among EPs—one that perpetuates the practice of defensive medicine and continues to affect EM. Despite the current perceptions and climate, EPs can allay their risk of incurring a malpractice claim by employing the strategies outlined above.
1. Mello MM, Studdert DM, Kachalia A. The medical liability climate and prospects for reform. JAMA. 2014;312(20):2146-2155.
2. Paik M, Black B, Hyman DA. The receding tide of medical malpractice: part 1 - national trends. J Empirical Leg Stud. 2013;10(4):612-638.
3. Bishop TF, Ryan AM, Caslino LP. Paid malpractice claims for adverse events in inpatient and outpatient settings. JAMA. 2011;305(23):2427-2431.
4. Kachalia A, Mello MM. New directions in medical liability reform. N Engl J Med. 2011;364(16):
1564-1572.
5. Carrier ER, Reschovsky JD, Mello MM, Mayrell RC, Katz D. Physicians’ fears of malpractice lawsuits are not assured by tort reforms. Health Aff. 2010;29(9):1585-1592.
6. Jena AB, Seabury S, Lakdawalla D, Chandra A. Malpractice risk according to physician specialty. N Engl J Med. 2011;365(7):629-636.
7. Brown TW, McCarthy ML, Kelen GD, Levy F. An epidemiologic study of closed emergency department malpractice claims in a national database of physician malpractice insurers. Acad Emerg Med. 2010;17(5):553-560.
8. Studdert DM, Mello MM, Sage WM, et al. Defensive medicine among high-risk specialist physicians in a volatile malpractice environment. JAMA. 2005;293(21):2609-2617.
9. Bishop TF, Federman AD, Keyhani S. Physicians’ views on defensive medicine: a national survey. Arch Intern Med. 2010;170(12):1081-1083.
10. Massachusetts Medical Society. Investigation of defensive medicine in Massachusetts. November 2008. Available at http://www.massmed.org/defensivemedicine. Accessed March 16, 2016.
11. Katz DA, Williams GC, Brown RL, et al. Emergency physicians’ fear of malpractice in evaluating patient with possible acute cardiac ischemia. Ann Emerg Med. 2005;46(6):525-533.
12. Waxman DA, Greenberg MD, Ridgely MS, Kellermann AL, Heaton P. The effect of malpractice reform on emergency department care. N Engl J Med. 2014;371(16):1518-1525.
13. Kachalia A, Gandhi TK, Puopolo AL, et al. Missed and delayed diagnoses in the emergency department: a study of closed malpractice claims from 4 liability insurers. Ann Emerg Med. 2007;49(2):196-205.
14. Saber Tehrani AS, Lee H, Mathews SC, et al. 25-Year summary of US malpractice claims for diagnostic errors 1986-2010: an analysis from the National Practitioner Data Bank. BMJ Qual Saf. 2013;22(8):672-680.
15. Ross J, Ranum D, Troxel DB. Emergency medicine closed claims study. The Doctors Company. Available at http://www.thedoctors.com/ecm/groups/public/@tdc/@web/@kc/@patientsafety/documents/article/con_id_004776.pdf. Accessed March 16, 2016.
16. Ruoff G, ed. 2011 Annual benchmarking report: malpractice risks in emergency medicine. CRICO strategies. 2012. Available at https://www.rmf.harvard.edu/Strategies/Home/Products-and-Services/Comparative-Data/Annual-Benchmark-Reports. Accessed March 16, 2016.
17. Failures in communication contribute to medical malpractice. January 31, 2016. https://www.rmf.harvard.edu/About-CRICO/Media/Press-Releases/News/2016/February/Failures-in-Communication-Contribute-to-Medical-Malpractice.
18. Studdert DM, Mello MM, Gawande AA, et al. Claims, errors, and compensation payments in medical malpractice litigation. N Engl J Med. 2006;354(19):2024-2033. Accessed March 16, 2016.
1. Mello MM, Studdert DM, Kachalia A. The medical liability climate and prospects for reform. JAMA. 2014;312(20):2146-2155.
2. Paik M, Black B, Hyman DA. The receding tide of medical malpractice: part 1 - national trends. J Empirical Leg Stud. 2013;10(4):612-638.
3. Bishop TF, Ryan AM, Caslino LP. Paid malpractice claims for adverse events in inpatient and outpatient settings. JAMA. 2011;305(23):2427-2431.
4. Kachalia A, Mello MM. New directions in medical liability reform. N Engl J Med. 2011;364(16):
1564-1572.
5. Carrier ER, Reschovsky JD, Mello MM, Mayrell RC, Katz D. Physicians’ fears of malpractice lawsuits are not assured by tort reforms. Health Aff. 2010;29(9):1585-1592.
6. Jena AB, Seabury S, Lakdawalla D, Chandra A. Malpractice risk according to physician specialty. N Engl J Med. 2011;365(7):629-636.
7. Brown TW, McCarthy ML, Kelen GD, Levy F. An epidemiologic study of closed emergency department malpractice claims in a national database of physician malpractice insurers. Acad Emerg Med. 2010;17(5):553-560.
8. Studdert DM, Mello MM, Sage WM, et al. Defensive medicine among high-risk specialist physicians in a volatile malpractice environment. JAMA. 2005;293(21):2609-2617.
9. Bishop TF, Federman AD, Keyhani S. Physicians’ views on defensive medicine: a national survey. Arch Intern Med. 2010;170(12):1081-1083.
10. Massachusetts Medical Society. Investigation of defensive medicine in Massachusetts. November 2008. Available at http://www.massmed.org/defensivemedicine. Accessed March 16, 2016.
11. Katz DA, Williams GC, Brown RL, et al. Emergency physicians’ fear of malpractice in evaluating patient with possible acute cardiac ischemia. Ann Emerg Med. 2005;46(6):525-533.
12. Waxman DA, Greenberg MD, Ridgely MS, Kellermann AL, Heaton P. The effect of malpractice reform on emergency department care. N Engl J Med. 2014;371(16):1518-1525.
13. Kachalia A, Gandhi TK, Puopolo AL, et al. Missed and delayed diagnoses in the emergency department: a study of closed malpractice claims from 4 liability insurers. Ann Emerg Med. 2007;49(2):196-205.
14. Saber Tehrani AS, Lee H, Mathews SC, et al. 25-Year summary of US malpractice claims for diagnostic errors 1986-2010: an analysis from the National Practitioner Data Bank. BMJ Qual Saf. 2013;22(8):672-680.
15. Ross J, Ranum D, Troxel DB. Emergency medicine closed claims study. The Doctors Company. Available at http://www.thedoctors.com/ecm/groups/public/@tdc/@web/@kc/@patientsafety/documents/article/con_id_004776.pdf. Accessed March 16, 2016.
16. Ruoff G, ed. 2011 Annual benchmarking report: malpractice risks in emergency medicine. CRICO strategies. 2012. Available at https://www.rmf.harvard.edu/Strategies/Home/Products-and-Services/Comparative-Data/Annual-Benchmark-Reports. Accessed March 16, 2016.
17. Failures in communication contribute to medical malpractice. January 31, 2016. https://www.rmf.harvard.edu/About-CRICO/Media/Press-Releases/News/2016/February/Failures-in-Communication-Contribute-to-Medical-Malpractice.
18. Studdert DM, Mello MM, Gawande AA, et al. Claims, errors, and compensation payments in medical malpractice litigation. N Engl J Med. 2006;354(19):2024-2033. Accessed March 16, 2016.
Feds extend behavioral health parity to Medicaid, CHIP
A final federal rule brings behavioral health parity to Medicaid managed care and the Children’s Health Insurance Plan – a move that earned an initial thumbs-up from the American Psychiatric Association.
The Centers for Medicare & Medicaid Services issued a final rule March 30 that extends to Medicaid and CHIP certain aspects of the of the Paul Wellstone and Pete Domenici Mental Health Parity and Addiction Equity Act. That 2008 law requires private health insurance to cover mental health and substance abuse treatments as they do medical and surgical services.
“Many of our recommendations to the proposed rule were adopted, and our preliminary analysis does not indicate any major disappointments,” APA President Renée Binder said in an interview. “There were considerable health plan industry pressures to dilute the essential features of the parity rule, but their approach was not adopted by CMS. The end result is that Medicaid patients will enjoy the same protections under the parity law that commercially insured patients get.”
The final rule, published in the Federal Register, subjects Medicaid managed care organizations, states that offer Medicaid alternative benefit plans, and all CHIP programs to the same financial treatment and limitations consistent with regulations applied to private insurers in that state. It does not apply to fee-for-service Medicaid.
In addition, in contrast to the proposed rule, “this final rule also extends parity protections to apply to long-term care services for mental health and substance abuse disorders in the same manner as they are applied to other services,” the agency noted in a fact sheet issued March 29.
The new rule will be effective in getting treatment for Medicaid and CHIP patients, the APA’s Dr. Binder predicted.
“The prevalence of these conditions is significant and costly,” she said. “Setting requirements that level the playing field for managing access to mental health and substance use disorder services will remove discriminatory entry barriers to treatment for these beneficiaries.”
When plans do restrict access, the rule directs plans to make reasons for denial of reimbursement or payment for services available to enrollees.
The rule “seemingly closed any possible loopholes or workarounds to the parity requirements,” Dr. Binder noted. “Given the often-complex managed care arrangements states have to provide these benefits, this is a significant achievement.”
Indeed, CMS rejected a request for more liberal use of prior authorization. The rule highlights a specific request for plans to be able to require prior authorization to move patients from emergency departments to inpatient care.
“The factors used to determine whether and when the use of prior authorization is appropriate must be comparable and applied no more stringently for [mental health/substance use disorder] benefits than they are for medical/surgical conditions,” CMS stated.
A final federal rule brings behavioral health parity to Medicaid managed care and the Children’s Health Insurance Plan – a move that earned an initial thumbs-up from the American Psychiatric Association.
The Centers for Medicare & Medicaid Services issued a final rule March 30 that extends to Medicaid and CHIP certain aspects of the of the Paul Wellstone and Pete Domenici Mental Health Parity and Addiction Equity Act. That 2008 law requires private health insurance to cover mental health and substance abuse treatments as they do medical and surgical services.
“Many of our recommendations to the proposed rule were adopted, and our preliminary analysis does not indicate any major disappointments,” APA President Renée Binder said in an interview. “There were considerable health plan industry pressures to dilute the essential features of the parity rule, but their approach was not adopted by CMS. The end result is that Medicaid patients will enjoy the same protections under the parity law that commercially insured patients get.”
The final rule, published in the Federal Register, subjects Medicaid managed care organizations, states that offer Medicaid alternative benefit plans, and all CHIP programs to the same financial treatment and limitations consistent with regulations applied to private insurers in that state. It does not apply to fee-for-service Medicaid.
In addition, in contrast to the proposed rule, “this final rule also extends parity protections to apply to long-term care services for mental health and substance abuse disorders in the same manner as they are applied to other services,” the agency noted in a fact sheet issued March 29.
The new rule will be effective in getting treatment for Medicaid and CHIP patients, the APA’s Dr. Binder predicted.
“The prevalence of these conditions is significant and costly,” she said. “Setting requirements that level the playing field for managing access to mental health and substance use disorder services will remove discriminatory entry barriers to treatment for these beneficiaries.”
When plans do restrict access, the rule directs plans to make reasons for denial of reimbursement or payment for services available to enrollees.
The rule “seemingly closed any possible loopholes or workarounds to the parity requirements,” Dr. Binder noted. “Given the often-complex managed care arrangements states have to provide these benefits, this is a significant achievement.”
Indeed, CMS rejected a request for more liberal use of prior authorization. The rule highlights a specific request for plans to be able to require prior authorization to move patients from emergency departments to inpatient care.
“The factors used to determine whether and when the use of prior authorization is appropriate must be comparable and applied no more stringently for [mental health/substance use disorder] benefits than they are for medical/surgical conditions,” CMS stated.
A final federal rule brings behavioral health parity to Medicaid managed care and the Children’s Health Insurance Plan – a move that earned an initial thumbs-up from the American Psychiatric Association.
The Centers for Medicare & Medicaid Services issued a final rule March 30 that extends to Medicaid and CHIP certain aspects of the of the Paul Wellstone and Pete Domenici Mental Health Parity and Addiction Equity Act. That 2008 law requires private health insurance to cover mental health and substance abuse treatments as they do medical and surgical services.
“Many of our recommendations to the proposed rule were adopted, and our preliminary analysis does not indicate any major disappointments,” APA President Renée Binder said in an interview. “There were considerable health plan industry pressures to dilute the essential features of the parity rule, but their approach was not adopted by CMS. The end result is that Medicaid patients will enjoy the same protections under the parity law that commercially insured patients get.”
The final rule, published in the Federal Register, subjects Medicaid managed care organizations, states that offer Medicaid alternative benefit plans, and all CHIP programs to the same financial treatment and limitations consistent with regulations applied to private insurers in that state. It does not apply to fee-for-service Medicaid.
In addition, in contrast to the proposed rule, “this final rule also extends parity protections to apply to long-term care services for mental health and substance abuse disorders in the same manner as they are applied to other services,” the agency noted in a fact sheet issued March 29.
The new rule will be effective in getting treatment for Medicaid and CHIP patients, the APA’s Dr. Binder predicted.
“The prevalence of these conditions is significant and costly,” she said. “Setting requirements that level the playing field for managing access to mental health and substance use disorder services will remove discriminatory entry barriers to treatment for these beneficiaries.”
When plans do restrict access, the rule directs plans to make reasons for denial of reimbursement or payment for services available to enrollees.
The rule “seemingly closed any possible loopholes or workarounds to the parity requirements,” Dr. Binder noted. “Given the often-complex managed care arrangements states have to provide these benefits, this is a significant achievement.”
Indeed, CMS rejected a request for more liberal use of prior authorization. The rule highlights a specific request for plans to be able to require prior authorization to move patients from emergency departments to inpatient care.
“The factors used to determine whether and when the use of prior authorization is appropriate must be comparable and applied no more stringently for [mental health/substance use disorder] benefits than they are for medical/surgical conditions,” CMS stated.
Tips for Policy and Procedure Manuals, Along with Roles for NP/PAs
Editor’s note: Second in a three-part series.
This month continues my list of important issues that help position your hospitalist group for greatest success. SHM’s “Key Principles and Characteristics of an Effective Hospital Medicine Group” is the definitive list, and this is my much smaller list. Last month, I discussed a culture (or mindset) of practice ownership, a formal system of group decision-making, and the importance of hospitalists themselves playing an active role in recruitment.
Policy and Procedure Manual
New protocols and decisions are being implemented every day. It is impossible to keep track of them, especially the ones that come into play infrequently. For example, many adult hospitalist groups have reached decisions about whether to admit teenagers (e.g., admit only 16 and older or 18 and older, etc.) and whether a hospitalist or obstetrician serves as attending for pregnant women admitted for a medical problem like asthma or pneumonia. But ask everyone in your group to recite the policies, and I bet the answers will differ.
My experience is that only about 20% to 25% of hospitalist groups have written these things down in one place, but all should. It doesn’t need to be fancy and could just start as a Word document in which the lead hospitalist or other designated person writes down a handful of policies and then updates them on an ongoing basis. For example, if a group meeting results in adopting a new policy, it could be added to the document as soon as the meeting adjourns. In some cases, a policy is communicated by email; it would be fine to just copy the body of that email into the manual.
This “living” document could be maintained on a shared computer drive accessible from anywhere in or out of the hospital. That way, when the solo night doctor thinks, “Do we admit 17-year-olds or not?,” she has a place to find the answer right away. And the manual will be a real asset to orient new providers to your practice.
You could start the policy and procedure manual by listing categories, including human resource issues like sick-day policy, how to request days off or scheduling changes, clinical policies like which hip fractures are admitted by hospitalists versus orthopedics, billing and coding practices such as always turn in charges at end of each day, and so on.
I’ve seen useful manuals that are about 10 pages and others that run more than 50 pages.
An Effective Performance Dashboard
Every hospitalist group should have some sort of routine performance report (dashboard) provided in the same format at regular intervals, yet in my experience many, or even most, don’t. It is worth the sometimes considerable effort to develop a meaningful dashboard, and in 2006, SHM published a helpful guide. Even though it is getting old, most of the advice is still very relevant even if the metrics we care most about have changed.
I’m a big believer in providing unblinded performance data to all in the hospitalist group. For example, a report of individual work relative value unit (wRVU) productivity would show productivity for each doctor by name. I think it is healthy to be transparent and ensure all in the group know how others are performing. There is nothing like finding out you are a performance outlier to spark an interest in understanding why and what should be done about it.
Roles for NPs and PAs
Nurse practitioners (NPs) and physician assistants (PAs) can be valuable contributors to a successful hospitalist program, and according to the 2014 State of Hospital Medicine Report, 65% of hospitalist groups nationally had at least one such clinician—an increase over prior years.
While the idea of NP/PAs contributing to the practice is a sound one, my experience is that many groups execute the idea poorly and end up creating a role that can be both professionally unsatisfying and not serve as a platform to contribute effectively to the group. A common scenario is a hospitalist group has trouble with recruiting physicians, so it turns to NP/PAs because they are more readily available. But so often the group has thought little about the precise role NP/PAs will serve (nothing more than “they will help out the docs”). Too often the result is NP/PAs who will say many physician hospitalists simply repeat all the work on each patient, which certainly isn’t a rewarding or cost-effective role.
All should be convinced that the practice is better off in terms of increased overall productivity and/or other benefits by investing in NP/PAs than if those same dollars were instead invested in physician staffing. So one economic model to consider is to calculate the total cost (salary, benefits, malpractice, etc.) for an NP/PA and divide that by those costs for a physician. Let’s say that shows an NP/PA costs half as much as a physician (ranges 40% to 60% in my experience). That staffing cost could be considered in “physician FTE equivalents” so that, for example, a practice with four NP/PAs each costing 50% as much as a physician, or two physician equivalents, could be said to have a total of two physician-equivalent FTEs of staffing. Is the practice better off configured that way, or would it be better to have two physicians instead of the four NP/PAs? The answer will vary, but I think every practice should look at NP/PA staffing through this lens, as well as other considerations, to determine whether they’ve made the best choice.
Having NP/PAs and physicians share rounding duties can be tricky to do efficiently. In my experience, NP/PAs can be better positioned to contribute optimally and find greater professional satisfaction if responsible for a specific portion of the group’s work. For example, at a large hospital, NP/PAs might see all orthopedic consults or psych unit admissions reasonably independently, though with physician backup available. Or NP/PAs could serve as evening (“swing”) shift staffing and manage cross-cover and some admissions. In these roles, the division of labor between NP/PAs and physicians is clearer and allows NP/PAs to contribute most effectively. TH

Editor’s note: Second in a three-part series.
This month continues my list of important issues that help position your hospitalist group for greatest success. SHM’s “Key Principles and Characteristics of an Effective Hospital Medicine Group” is the definitive list, and this is my much smaller list. Last month, I discussed a culture (or mindset) of practice ownership, a formal system of group decision-making, and the importance of hospitalists themselves playing an active role in recruitment.
Policy and Procedure Manual
New protocols and decisions are being implemented every day. It is impossible to keep track of them, especially the ones that come into play infrequently. For example, many adult hospitalist groups have reached decisions about whether to admit teenagers (e.g., admit only 16 and older or 18 and older, etc.) and whether a hospitalist or obstetrician serves as attending for pregnant women admitted for a medical problem like asthma or pneumonia. But ask everyone in your group to recite the policies, and I bet the answers will differ.
My experience is that only about 20% to 25% of hospitalist groups have written these things down in one place, but all should. It doesn’t need to be fancy and could just start as a Word document in which the lead hospitalist or other designated person writes down a handful of policies and then updates them on an ongoing basis. For example, if a group meeting results in adopting a new policy, it could be added to the document as soon as the meeting adjourns. In some cases, a policy is communicated by email; it would be fine to just copy the body of that email into the manual.
This “living” document could be maintained on a shared computer drive accessible from anywhere in or out of the hospital. That way, when the solo night doctor thinks, “Do we admit 17-year-olds or not?,” she has a place to find the answer right away. And the manual will be a real asset to orient new providers to your practice.
You could start the policy and procedure manual by listing categories, including human resource issues like sick-day policy, how to request days off or scheduling changes, clinical policies like which hip fractures are admitted by hospitalists versus orthopedics, billing and coding practices such as always turn in charges at end of each day, and so on.
I’ve seen useful manuals that are about 10 pages and others that run more than 50 pages.
An Effective Performance Dashboard
Every hospitalist group should have some sort of routine performance report (dashboard) provided in the same format at regular intervals, yet in my experience many, or even most, don’t. It is worth the sometimes considerable effort to develop a meaningful dashboard, and in 2006, SHM published a helpful guide. Even though it is getting old, most of the advice is still very relevant even if the metrics we care most about have changed.
I’m a big believer in providing unblinded performance data to all in the hospitalist group. For example, a report of individual work relative value unit (wRVU) productivity would show productivity for each doctor by name. I think it is healthy to be transparent and ensure all in the group know how others are performing. There is nothing like finding out you are a performance outlier to spark an interest in understanding why and what should be done about it.
Roles for NPs and PAs
Nurse practitioners (NPs) and physician assistants (PAs) can be valuable contributors to a successful hospitalist program, and according to the 2014 State of Hospital Medicine Report, 65% of hospitalist groups nationally had at least one such clinician—an increase over prior years.
While the idea of NP/PAs contributing to the practice is a sound one, my experience is that many groups execute the idea poorly and end up creating a role that can be both professionally unsatisfying and not serve as a platform to contribute effectively to the group. A common scenario is a hospitalist group has trouble with recruiting physicians, so it turns to NP/PAs because they are more readily available. But so often the group has thought little about the precise role NP/PAs will serve (nothing more than “they will help out the docs”). Too often the result is NP/PAs who will say many physician hospitalists simply repeat all the work on each patient, which certainly isn’t a rewarding or cost-effective role.
All should be convinced that the practice is better off in terms of increased overall productivity and/or other benefits by investing in NP/PAs than if those same dollars were instead invested in physician staffing. So one economic model to consider is to calculate the total cost (salary, benefits, malpractice, etc.) for an NP/PA and divide that by those costs for a physician. Let’s say that shows an NP/PA costs half as much as a physician (ranges 40% to 60% in my experience). That staffing cost could be considered in “physician FTE equivalents” so that, for example, a practice with four NP/PAs each costing 50% as much as a physician, or two physician equivalents, could be said to have a total of two physician-equivalent FTEs of staffing. Is the practice better off configured that way, or would it be better to have two physicians instead of the four NP/PAs? The answer will vary, but I think every practice should look at NP/PA staffing through this lens, as well as other considerations, to determine whether they’ve made the best choice.
Having NP/PAs and physicians share rounding duties can be tricky to do efficiently. In my experience, NP/PAs can be better positioned to contribute optimally and find greater professional satisfaction if responsible for a specific portion of the group’s work. For example, at a large hospital, NP/PAs might see all orthopedic consults or psych unit admissions reasonably independently, though with physician backup available. Or NP/PAs could serve as evening (“swing”) shift staffing and manage cross-cover and some admissions. In these roles, the division of labor between NP/PAs and physicians is clearer and allows NP/PAs to contribute most effectively. TH

Editor’s note: Second in a three-part series.
This month continues my list of important issues that help position your hospitalist group for greatest success. SHM’s “Key Principles and Characteristics of an Effective Hospital Medicine Group” is the definitive list, and this is my much smaller list. Last month, I discussed a culture (or mindset) of practice ownership, a formal system of group decision-making, and the importance of hospitalists themselves playing an active role in recruitment.
Policy and Procedure Manual
New protocols and decisions are being implemented every day. It is impossible to keep track of them, especially the ones that come into play infrequently. For example, many adult hospitalist groups have reached decisions about whether to admit teenagers (e.g., admit only 16 and older or 18 and older, etc.) and whether a hospitalist or obstetrician serves as attending for pregnant women admitted for a medical problem like asthma or pneumonia. But ask everyone in your group to recite the policies, and I bet the answers will differ.
My experience is that only about 20% to 25% of hospitalist groups have written these things down in one place, but all should. It doesn’t need to be fancy and could just start as a Word document in which the lead hospitalist or other designated person writes down a handful of policies and then updates them on an ongoing basis. For example, if a group meeting results in adopting a new policy, it could be added to the document as soon as the meeting adjourns. In some cases, a policy is communicated by email; it would be fine to just copy the body of that email into the manual.
This “living” document could be maintained on a shared computer drive accessible from anywhere in or out of the hospital. That way, when the solo night doctor thinks, “Do we admit 17-year-olds or not?,” she has a place to find the answer right away. And the manual will be a real asset to orient new providers to your practice.
You could start the policy and procedure manual by listing categories, including human resource issues like sick-day policy, how to request days off or scheduling changes, clinical policies like which hip fractures are admitted by hospitalists versus orthopedics, billing and coding practices such as always turn in charges at end of each day, and so on.
I’ve seen useful manuals that are about 10 pages and others that run more than 50 pages.
An Effective Performance Dashboard
Every hospitalist group should have some sort of routine performance report (dashboard) provided in the same format at regular intervals, yet in my experience many, or even most, don’t. It is worth the sometimes considerable effort to develop a meaningful dashboard, and in 2006, SHM published a helpful guide. Even though it is getting old, most of the advice is still very relevant even if the metrics we care most about have changed.
I’m a big believer in providing unblinded performance data to all in the hospitalist group. For example, a report of individual work relative value unit (wRVU) productivity would show productivity for each doctor by name. I think it is healthy to be transparent and ensure all in the group know how others are performing. There is nothing like finding out you are a performance outlier to spark an interest in understanding why and what should be done about it.
Roles for NPs and PAs
Nurse practitioners (NPs) and physician assistants (PAs) can be valuable contributors to a successful hospitalist program, and according to the 2014 State of Hospital Medicine Report, 65% of hospitalist groups nationally had at least one such clinician—an increase over prior years.
While the idea of NP/PAs contributing to the practice is a sound one, my experience is that many groups execute the idea poorly and end up creating a role that can be both professionally unsatisfying and not serve as a platform to contribute effectively to the group. A common scenario is a hospitalist group has trouble with recruiting physicians, so it turns to NP/PAs because they are more readily available. But so often the group has thought little about the precise role NP/PAs will serve (nothing more than “they will help out the docs”). Too often the result is NP/PAs who will say many physician hospitalists simply repeat all the work on each patient, which certainly isn’t a rewarding or cost-effective role.
All should be convinced that the practice is better off in terms of increased overall productivity and/or other benefits by investing in NP/PAs than if those same dollars were instead invested in physician staffing. So one economic model to consider is to calculate the total cost (salary, benefits, malpractice, etc.) for an NP/PA and divide that by those costs for a physician. Let’s say that shows an NP/PA costs half as much as a physician (ranges 40% to 60% in my experience). That staffing cost could be considered in “physician FTE equivalents” so that, for example, a practice with four NP/PAs each costing 50% as much as a physician, or two physician equivalents, could be said to have a total of two physician-equivalent FTEs of staffing. Is the practice better off configured that way, or would it be better to have two physicians instead of the four NP/PAs? The answer will vary, but I think every practice should look at NP/PA staffing through this lens, as well as other considerations, to determine whether they’ve made the best choice.
Having NP/PAs and physicians share rounding duties can be tricky to do efficiently. In my experience, NP/PAs can be better positioned to contribute optimally and find greater professional satisfaction if responsible for a specific portion of the group’s work. For example, at a large hospital, NP/PAs might see all orthopedic consults or psych unit admissions reasonably independently, though with physician backup available. Or NP/PAs could serve as evening (“swing”) shift staffing and manage cross-cover and some admissions. In these roles, the division of labor between NP/PAs and physicians is clearer and allows NP/PAs to contribute most effectively. TH