User login
Child of The New Gastroenterologist
Developing training pathways in advanced endoscopic resection and third-space endoscopy in the U.S.
As a gastroenterology and hepatology fellow, choosing a career path was a daunting prospect. Despite the additional specialization, there seemed to be endless career options to consider. Did I want to join an academic, private, or hybrid practice? Should I subspecialize within the field? Was it important to incorporate research or teaching into my practice? What about opportunities to take on administrative or leadership roles?
Fellowship training at a large academic research institution provided me the opportunity to work with expert faculty in inflammatory bowel disease, esophageal disease, motility and functional gastrointestinal disease, pancreaticobiliary disease, and hepatology. I enjoyed seeing patients in each of these subspecialty clinics. But, by the end of my second year of GI fellowship, I still wasn’t sure what I wanted to do professionally.
A career in academic general gastroenterology seemed to be a good fit for my personality and goals. Rather than focusing on research, I chose to position myself as a clinician educator. I knew that having a subspecialty area of expertise would help improve my clinical practice and make me a more attractive candidate to academic centers. To help narrow my choice, I looked at the clinical enterprise at our institution and assessed where the unmet clinical needs were most acute. Simultaneously, I identified potential mentors to support and guide me through the transition from fellow to independent practitioner. I decided to focus on acquiring the skills to care for patients with anorectal diseases and lower-GI motility disorders, as this area met both of my criteria – excellent mentorship and an unmet clinical need. Under the guidance of Dr. Yolanda Scarlett, I spent my 3rd year in clinic learning to interpret anorectal manometry tests, defecograms, and sitz marker studies and treating patients with refractory constipation, fecal incontinence, and anal fissures.
With a plan to develop an expertise in anorectal diseases and low-GI motility disorders, I also wanted to focus on improving my endoscopic skills to graduate as well rounded a clinician as possible. To achieve this goal, I sought out a separate endoscopy mentor, Dr. Ian Grimm, the director of endoscopy at the University of North Carolina at Chapel Hill. Dr. Grimm, a classically trained advanced endoscopist performing endoscopic ultrasound (EUS) and endoscopic retrograde cholangiopancreatography (ERCP), had a burgeoning interest in endoscopic mucosal resection (EMR) and had just returned from a few months in Japan learning to perform endoscopic submucosal dissection (ESD) and peroral endoscopic myotomy (POEM).
When I began working with Dr. Grimm, I had not even heard the term third-space endoscopy and knew nothing about ESD or POEM. I spent as much time as possible watching and assisting Dr. Grimm with complex endoscopic mucosal resection (EMR) during the first few months of my 3rd year. Soon after my exposure to advanced endoscopic resection, it was clear that I wanted to learn and incorporate this into my clinical practice. I watched Dr. Grimm perform the first POEM at UNC in the fall of 2016 and by that time I was hooked on learning third-space endoscopy. I observed and assisted with as many EMR, ESD, and POEM cases as I could that year. In addition to the hands-on and cognitive training with Dr. Grimm, I attended national meetings and workshops focused on learning third-space endoscopy. In the spring of my 3rd year I was honored to be the first fellow to complete the Olympus master class in ESD – a 2-day hands-on training course sponsored by Olympus. By the end of that year, I was performing complex EMR with minimal assistance and had completed multiple ESDs and POEMs with cognitive supervision only.
After fellowship, I joined the UNC faculty as a general gastroenterologist with expertise in anorectal disease and lower-GI motility disorders. While I was comfortable performing complex EMR, I still needed additional training and supervision before I felt ready to independently perform ESD or POEM. With the gracious support and encouragement of our division chief, I continued third-space endoscopy training with Dr. Grimm during dedicated protected time 2 days each month. Over the ensuing 4 years, I transitioned to fully independent practice performing all types of advanced EMR and third-space endoscopy including complex EMR, ESD, endoscopic full-thickness resection (EFTR), submucosal tunnel endoscopic resection (STER), esophageal POEM, gastric POEM, and Zenker’s POEM.
As one of the first gastroenterologists in the United States to perform third-space endoscopy without any formal training in advanced pancreaticobiliary endoscopy, I believe learning advanced endoscopic resection and third-space endoscopy is best achieved through a training pathway separate from the conventional advanced endoscopy fellowship focused on teaching EUS and ERCP. Although there are transferable skills learned from EUS and ERCP to the techniques used in third-space endoscopy, there is nothing inherent to performing EUS or ERCP that enables one to learn how to perform an ESD or a POEM.
There is a robust training pathway to teach advanced pancreaticobiliary endoscopy, but no formal training pathway exists to teach third-space endoscopy in the United States. Historically, a small number of interested and motivated advanced pancreaticobiliary endoscopists sought out opportunities to learn third-space endoscopy after completion of their advanced endoscopy fellowship, in some cases many years after graduation. For these early adopters in the United States, the only training opportunities required travel to Japan or another Eastern country with arrangements made to observe and participate in third-space endoscopy cases with experts there. With increased recognition of the benefits of ESD and POEM over the past 5-10 years in the United States, there has been greater adoption of third-space endoscopy and with it, more training opportunities. Still, there are very few institutions with formalized training programs in advanced endoscopic resection and third-space endoscopy in the United States to date.
Proof that this model works
In Eastern countries such as Japan, training endoscopists to perform ESD and POEM has been successfully achieved through an apprenticeship model whereby an expert in third-space endoscopy closely supervises a trainee who gains greater autonomy with increasing experience and skill over time. My personal experience is proof that this model works. But, adopting such a model more widely in the United States may prove difficult. We lack a sufficient number of experienced third-space endoscopy operators and, given the challenges to appropriate reimbursement for third-space endoscopy in the United States, there is understandable resistance to accepting the prolonged training period necessary for technical mastery of this skill.
In part, a long training period is needed because of a relative paucity of appropriate target lesions for ESD and the rarity of achalasia in the United States. While there is consensus among experts regarding the benefits of ESD for resection of early gastric cancer (EGC), relatively few EGCs are found in the United States and indications for ESD outside resection of EGC are less well defined with less clear benefits over more widely performed piecemeal EMR. Despite these challenges, it is critical that we continue to develop dedicated training pathways to teach advanced endoscopic resection and third-space endoscopy in the United States. My practice has evolved considerably since completion of fellowship nearly 6 years ago, and I now focus almost exclusively on advanced endoscopic resection and third-space endoscopy. Recently, Dr. Grimm and I began an advanced endoscopic resection elective for the general GI fellows at UNC and we are excited to welcome our first advanced endoscopic resection and third-space endoscopy fellow to UNC this July.
While there are many possible avenues to expertise in advanced endoscopic resection, few will likely follow the same path that I have taken. Trainees who are interested in pursuing this subspecialty should seek out supportive mentors in a setting where there is already a robust case volume of esophageal motility disorders and endoscopic resections. Success requires the persistent motivation to seek out diverse opportunities for self-study, exposure to experts, data on developments in the field, and hands-on exposure to as many ex-vivo and in-vivo cases as possible.
Dr. Kroch is assistant professor of medicine in the division of gastroenterology and hepatology at the University of North Carolina at Chapel Hill. He disclosed having no conflicts of interest.
As a gastroenterology and hepatology fellow, choosing a career path was a daunting prospect. Despite the additional specialization, there seemed to be endless career options to consider. Did I want to join an academic, private, or hybrid practice? Should I subspecialize within the field? Was it important to incorporate research or teaching into my practice? What about opportunities to take on administrative or leadership roles?
Fellowship training at a large academic research institution provided me the opportunity to work with expert faculty in inflammatory bowel disease, esophageal disease, motility and functional gastrointestinal disease, pancreaticobiliary disease, and hepatology. I enjoyed seeing patients in each of these subspecialty clinics. But, by the end of my second year of GI fellowship, I still wasn’t sure what I wanted to do professionally.
A career in academic general gastroenterology seemed to be a good fit for my personality and goals. Rather than focusing on research, I chose to position myself as a clinician educator. I knew that having a subspecialty area of expertise would help improve my clinical practice and make me a more attractive candidate to academic centers. To help narrow my choice, I looked at the clinical enterprise at our institution and assessed where the unmet clinical needs were most acute. Simultaneously, I identified potential mentors to support and guide me through the transition from fellow to independent practitioner. I decided to focus on acquiring the skills to care for patients with anorectal diseases and lower-GI motility disorders, as this area met both of my criteria – excellent mentorship and an unmet clinical need. Under the guidance of Dr. Yolanda Scarlett, I spent my 3rd year in clinic learning to interpret anorectal manometry tests, defecograms, and sitz marker studies and treating patients with refractory constipation, fecal incontinence, and anal fissures.
With a plan to develop an expertise in anorectal diseases and low-GI motility disorders, I also wanted to focus on improving my endoscopic skills to graduate as well rounded a clinician as possible. To achieve this goal, I sought out a separate endoscopy mentor, Dr. Ian Grimm, the director of endoscopy at the University of North Carolina at Chapel Hill. Dr. Grimm, a classically trained advanced endoscopist performing endoscopic ultrasound (EUS) and endoscopic retrograde cholangiopancreatography (ERCP), had a burgeoning interest in endoscopic mucosal resection (EMR) and had just returned from a few months in Japan learning to perform endoscopic submucosal dissection (ESD) and peroral endoscopic myotomy (POEM).
When I began working with Dr. Grimm, I had not even heard the term third-space endoscopy and knew nothing about ESD or POEM. I spent as much time as possible watching and assisting Dr. Grimm with complex endoscopic mucosal resection (EMR) during the first few months of my 3rd year. Soon after my exposure to advanced endoscopic resection, it was clear that I wanted to learn and incorporate this into my clinical practice. I watched Dr. Grimm perform the first POEM at UNC in the fall of 2016 and by that time I was hooked on learning third-space endoscopy. I observed and assisted with as many EMR, ESD, and POEM cases as I could that year. In addition to the hands-on and cognitive training with Dr. Grimm, I attended national meetings and workshops focused on learning third-space endoscopy. In the spring of my 3rd year I was honored to be the first fellow to complete the Olympus master class in ESD – a 2-day hands-on training course sponsored by Olympus. By the end of that year, I was performing complex EMR with minimal assistance and had completed multiple ESDs and POEMs with cognitive supervision only.
After fellowship, I joined the UNC faculty as a general gastroenterologist with expertise in anorectal disease and lower-GI motility disorders. While I was comfortable performing complex EMR, I still needed additional training and supervision before I felt ready to independently perform ESD or POEM. With the gracious support and encouragement of our division chief, I continued third-space endoscopy training with Dr. Grimm during dedicated protected time 2 days each month. Over the ensuing 4 years, I transitioned to fully independent practice performing all types of advanced EMR and third-space endoscopy including complex EMR, ESD, endoscopic full-thickness resection (EFTR), submucosal tunnel endoscopic resection (STER), esophageal POEM, gastric POEM, and Zenker’s POEM.
As one of the first gastroenterologists in the United States to perform third-space endoscopy without any formal training in advanced pancreaticobiliary endoscopy, I believe learning advanced endoscopic resection and third-space endoscopy is best achieved through a training pathway separate from the conventional advanced endoscopy fellowship focused on teaching EUS and ERCP. Although there are transferable skills learned from EUS and ERCP to the techniques used in third-space endoscopy, there is nothing inherent to performing EUS or ERCP that enables one to learn how to perform an ESD or a POEM.
There is a robust training pathway to teach advanced pancreaticobiliary endoscopy, but no formal training pathway exists to teach third-space endoscopy in the United States. Historically, a small number of interested and motivated advanced pancreaticobiliary endoscopists sought out opportunities to learn third-space endoscopy after completion of their advanced endoscopy fellowship, in some cases many years after graduation. For these early adopters in the United States, the only training opportunities required travel to Japan or another Eastern country with arrangements made to observe and participate in third-space endoscopy cases with experts there. With increased recognition of the benefits of ESD and POEM over the past 5-10 years in the United States, there has been greater adoption of third-space endoscopy and with it, more training opportunities. Still, there are very few institutions with formalized training programs in advanced endoscopic resection and third-space endoscopy in the United States to date.
Proof that this model works
In Eastern countries such as Japan, training endoscopists to perform ESD and POEM has been successfully achieved through an apprenticeship model whereby an expert in third-space endoscopy closely supervises a trainee who gains greater autonomy with increasing experience and skill over time. My personal experience is proof that this model works. But, adopting such a model more widely in the United States may prove difficult. We lack a sufficient number of experienced third-space endoscopy operators and, given the challenges to appropriate reimbursement for third-space endoscopy in the United States, there is understandable resistance to accepting the prolonged training period necessary for technical mastery of this skill.
In part, a long training period is needed because of a relative paucity of appropriate target lesions for ESD and the rarity of achalasia in the United States. While there is consensus among experts regarding the benefits of ESD for resection of early gastric cancer (EGC), relatively few EGCs are found in the United States and indications for ESD outside resection of EGC are less well defined with less clear benefits over more widely performed piecemeal EMR. Despite these challenges, it is critical that we continue to develop dedicated training pathways to teach advanced endoscopic resection and third-space endoscopy in the United States. My practice has evolved considerably since completion of fellowship nearly 6 years ago, and I now focus almost exclusively on advanced endoscopic resection and third-space endoscopy. Recently, Dr. Grimm and I began an advanced endoscopic resection elective for the general GI fellows at UNC and we are excited to welcome our first advanced endoscopic resection and third-space endoscopy fellow to UNC this July.
While there are many possible avenues to expertise in advanced endoscopic resection, few will likely follow the same path that I have taken. Trainees who are interested in pursuing this subspecialty should seek out supportive mentors in a setting where there is already a robust case volume of esophageal motility disorders and endoscopic resections. Success requires the persistent motivation to seek out diverse opportunities for self-study, exposure to experts, data on developments in the field, and hands-on exposure to as many ex-vivo and in-vivo cases as possible.
Dr. Kroch is assistant professor of medicine in the division of gastroenterology and hepatology at the University of North Carolina at Chapel Hill. He disclosed having no conflicts of interest.
As a gastroenterology and hepatology fellow, choosing a career path was a daunting prospect. Despite the additional specialization, there seemed to be endless career options to consider. Did I want to join an academic, private, or hybrid practice? Should I subspecialize within the field? Was it important to incorporate research or teaching into my practice? What about opportunities to take on administrative or leadership roles?
Fellowship training at a large academic research institution provided me the opportunity to work with expert faculty in inflammatory bowel disease, esophageal disease, motility and functional gastrointestinal disease, pancreaticobiliary disease, and hepatology. I enjoyed seeing patients in each of these subspecialty clinics. But, by the end of my second year of GI fellowship, I still wasn’t sure what I wanted to do professionally.
A career in academic general gastroenterology seemed to be a good fit for my personality and goals. Rather than focusing on research, I chose to position myself as a clinician educator. I knew that having a subspecialty area of expertise would help improve my clinical practice and make me a more attractive candidate to academic centers. To help narrow my choice, I looked at the clinical enterprise at our institution and assessed where the unmet clinical needs were most acute. Simultaneously, I identified potential mentors to support and guide me through the transition from fellow to independent practitioner. I decided to focus on acquiring the skills to care for patients with anorectal diseases and lower-GI motility disorders, as this area met both of my criteria – excellent mentorship and an unmet clinical need. Under the guidance of Dr. Yolanda Scarlett, I spent my 3rd year in clinic learning to interpret anorectal manometry tests, defecograms, and sitz marker studies and treating patients with refractory constipation, fecal incontinence, and anal fissures.
With a plan to develop an expertise in anorectal diseases and low-GI motility disorders, I also wanted to focus on improving my endoscopic skills to graduate as well rounded a clinician as possible. To achieve this goal, I sought out a separate endoscopy mentor, Dr. Ian Grimm, the director of endoscopy at the University of North Carolina at Chapel Hill. Dr. Grimm, a classically trained advanced endoscopist performing endoscopic ultrasound (EUS) and endoscopic retrograde cholangiopancreatography (ERCP), had a burgeoning interest in endoscopic mucosal resection (EMR) and had just returned from a few months in Japan learning to perform endoscopic submucosal dissection (ESD) and peroral endoscopic myotomy (POEM).
When I began working with Dr. Grimm, I had not even heard the term third-space endoscopy and knew nothing about ESD or POEM. I spent as much time as possible watching and assisting Dr. Grimm with complex endoscopic mucosal resection (EMR) during the first few months of my 3rd year. Soon after my exposure to advanced endoscopic resection, it was clear that I wanted to learn and incorporate this into my clinical practice. I watched Dr. Grimm perform the first POEM at UNC in the fall of 2016 and by that time I was hooked on learning third-space endoscopy. I observed and assisted with as many EMR, ESD, and POEM cases as I could that year. In addition to the hands-on and cognitive training with Dr. Grimm, I attended national meetings and workshops focused on learning third-space endoscopy. In the spring of my 3rd year I was honored to be the first fellow to complete the Olympus master class in ESD – a 2-day hands-on training course sponsored by Olympus. By the end of that year, I was performing complex EMR with minimal assistance and had completed multiple ESDs and POEMs with cognitive supervision only.
After fellowship, I joined the UNC faculty as a general gastroenterologist with expertise in anorectal disease and lower-GI motility disorders. While I was comfortable performing complex EMR, I still needed additional training and supervision before I felt ready to independently perform ESD or POEM. With the gracious support and encouragement of our division chief, I continued third-space endoscopy training with Dr. Grimm during dedicated protected time 2 days each month. Over the ensuing 4 years, I transitioned to fully independent practice performing all types of advanced EMR and third-space endoscopy including complex EMR, ESD, endoscopic full-thickness resection (EFTR), submucosal tunnel endoscopic resection (STER), esophageal POEM, gastric POEM, and Zenker’s POEM.
As one of the first gastroenterologists in the United States to perform third-space endoscopy without any formal training in advanced pancreaticobiliary endoscopy, I believe learning advanced endoscopic resection and third-space endoscopy is best achieved through a training pathway separate from the conventional advanced endoscopy fellowship focused on teaching EUS and ERCP. Although there are transferable skills learned from EUS and ERCP to the techniques used in third-space endoscopy, there is nothing inherent to performing EUS or ERCP that enables one to learn how to perform an ESD or a POEM.
There is a robust training pathway to teach advanced pancreaticobiliary endoscopy, but no formal training pathway exists to teach third-space endoscopy in the United States. Historically, a small number of interested and motivated advanced pancreaticobiliary endoscopists sought out opportunities to learn third-space endoscopy after completion of their advanced endoscopy fellowship, in some cases many years after graduation. For these early adopters in the United States, the only training opportunities required travel to Japan or another Eastern country with arrangements made to observe and participate in third-space endoscopy cases with experts there. With increased recognition of the benefits of ESD and POEM over the past 5-10 years in the United States, there has been greater adoption of third-space endoscopy and with it, more training opportunities. Still, there are very few institutions with formalized training programs in advanced endoscopic resection and third-space endoscopy in the United States to date.
Proof that this model works
In Eastern countries such as Japan, training endoscopists to perform ESD and POEM has been successfully achieved through an apprenticeship model whereby an expert in third-space endoscopy closely supervises a trainee who gains greater autonomy with increasing experience and skill over time. My personal experience is proof that this model works. But, adopting such a model more widely in the United States may prove difficult. We lack a sufficient number of experienced third-space endoscopy operators and, given the challenges to appropriate reimbursement for third-space endoscopy in the United States, there is understandable resistance to accepting the prolonged training period necessary for technical mastery of this skill.
In part, a long training period is needed because of a relative paucity of appropriate target lesions for ESD and the rarity of achalasia in the United States. While there is consensus among experts regarding the benefits of ESD for resection of early gastric cancer (EGC), relatively few EGCs are found in the United States and indications for ESD outside resection of EGC are less well defined with less clear benefits over more widely performed piecemeal EMR. Despite these challenges, it is critical that we continue to develop dedicated training pathways to teach advanced endoscopic resection and third-space endoscopy in the United States. My practice has evolved considerably since completion of fellowship nearly 6 years ago, and I now focus almost exclusively on advanced endoscopic resection and third-space endoscopy. Recently, Dr. Grimm and I began an advanced endoscopic resection elective for the general GI fellows at UNC and we are excited to welcome our first advanced endoscopic resection and third-space endoscopy fellow to UNC this July.
While there are many possible avenues to expertise in advanced endoscopic resection, few will likely follow the same path that I have taken. Trainees who are interested in pursuing this subspecialty should seek out supportive mentors in a setting where there is already a robust case volume of esophageal motility disorders and endoscopic resections. Success requires the persistent motivation to seek out diverse opportunities for self-study, exposure to experts, data on developments in the field, and hands-on exposure to as many ex-vivo and in-vivo cases as possible.
Dr. Kroch is assistant professor of medicine in the division of gastroenterology and hepatology at the University of North Carolina at Chapel Hill. He disclosed having no conflicts of interest.
From private practice to academic medicine: My journey and lessons learned
Loyalty.
This is a quality that I value in relationships. Loyalty was a significant factor contributing to my postfellowship commitment to private practice. In 2001, I graduated from physician assistant school and accepted a job with a private practice GI group in Omaha. I was fortunate to work with supportive gastroenterologists who encouraged me to pursue further training after I expressed an interest in medical school. My goal was to become a gastroenterologist but like every medical student, I would keep an open mind. My decision did not waver, and the support from my first mentors continued. As I graduated from fellowship in 2014, I gravitated toward the same private practice largely based on loyalty and my experience as a PA.

COURTESY AMERICAN GASTROENTEROLOGICAL ASSOCIATION
My experience in private practice was positive. My focus at that time and currently is clinical medicine with a focus on inflammatory bowel disease (IBD) patients. My colleagues were supportive, and I worked with a great team of nurses and APPs. I cared for many patients in both the inpatient and outpatient setting and had an opportunity to complete a high volume and variety of procedures. Overall, the various aspects of my job were rewarding. However, something was missing, and I made personal and professional adjustments. My schedule pulled me from valued family time with my kids (mostly) in the early mornings, therefore, I altered my work schedule. My clinical interest in IBD was diluted by the emphasis to see mostly general GI patients, as is the case for many in private practice. I missed the academic environment, especially working with medical students, residents, and fellows, so I occasionally had residents shadow me. Unfortunately, adjustments did not “fix” that missing component – to me, this was a job that did not feel like a career. I was not professionally fulfilled and on several occasions during the 6 years in private practice, I connected with mentors from my medical training to explore career options while trying to define what was missing.
During the latter part of years 5 and 6, it became apparent to me that loyalty pulled me toward working with a great group of supportive gastroenterologists, but it became increasingly more apparent that this job was not in line with my career goals. I had identified that I wanted to actively participate in medical education while practicing as a gastroenterologist in an academic setting. Additionally, time with my family was a critical part to the work-life integration.
My approach to the next step in my journey was different than my initial job. My goal was to define what was important, as in what were my absolute requirements for career satisfaction and where was I willing to be flexible. Each of us has different absolute and relative requirements based on our values, and I neglected to clearly identify these components with my first job. Admittedly, I have (at times) struggled to acknowledge my values, because I might somehow appear less committed to a career. Owning these values has provided clarity in my path from private practice to academic medicine. During the 3 years I have been in my current position, I have stepped into a leadership role in the University of Nebraska Medicine GI fellowship program while providing clinical medicine at the Fred Paustian IBD Center at Nebraska Medicine. In addition, I continue to have an active endoscopy schedule and derive great satisfaction teaching the fellows how to be effective endoscopists. Personally, the difference in compensation between academic medicine and private practice was not an important factor, although this is a factor for some people (and that’s okay).
When I graduated from fellowship, my path seemed clear, and I did not anticipate the road ahead. However, with each hurdle, I was gifted with lessons that would prove to be valuable as I moved ahead. Thank you for giving me the space to share my story.
Lessons that have helped in my journey from private practice to academics
- Mentorship: Find mentors, not just one mentor. Over the years, I have had several mentors, but what I recognize is that, early in my career, I did not have a mentor. Although a mentor cannot make decisions for you, he/she can provide guidance from a place of experience (both career and life experience).
- Define a mission statement: My mentor pushed me to first define my values and then my mission statement. This serves as the foundation that I reference when making decisions that will impact my family and my career. For example, if I am invited to participate on a committee, I look at how this will impact my family and whether it aligns with my mission. This helps to clarify what I am willing to say yes to and what to pass along to another colleague. Remember that last part ... if you are saying no to something, suggest another colleague for the opportunity.
- Advocate for yourself: Only you know what is best for you. Sometimes the path to discovering what that is can be tortuous and require guidance. Throughout my journey, I worked with colleagues who were supportive of my journey back to medical school and supportive of my job in private practice, but only I could define what a career meant to me.
- Assume positive intent: In medicine, we frequently work in a high-stakes, stressful environment. Assume positive intent in your interactions with others, especially colleagues. This will serve you well.
- Life happens: Each of us will experience an unexpected event in our personal life or career path or both. This will be okay. The path forward may look different and require a pivot. This unexpected event might be that you find your job leaves you wanting something more or something different. Your journey will be right for you.
Dr. Hutchins is an assistant professor in the division of gastroenterology and hepatology at the University of Nebraska Medical Center, Omaha. She reported no conflicts of interest.
Loyalty.
This is a quality that I value in relationships. Loyalty was a significant factor contributing to my postfellowship commitment to private practice. In 2001, I graduated from physician assistant school and accepted a job with a private practice GI group in Omaha. I was fortunate to work with supportive gastroenterologists who encouraged me to pursue further training after I expressed an interest in medical school. My goal was to become a gastroenterologist but like every medical student, I would keep an open mind. My decision did not waver, and the support from my first mentors continued. As I graduated from fellowship in 2014, I gravitated toward the same private practice largely based on loyalty and my experience as a PA.

COURTESY AMERICAN GASTROENTEROLOGICAL ASSOCIATION
My experience in private practice was positive. My focus at that time and currently is clinical medicine with a focus on inflammatory bowel disease (IBD) patients. My colleagues were supportive, and I worked with a great team of nurses and APPs. I cared for many patients in both the inpatient and outpatient setting and had an opportunity to complete a high volume and variety of procedures. Overall, the various aspects of my job were rewarding. However, something was missing, and I made personal and professional adjustments. My schedule pulled me from valued family time with my kids (mostly) in the early mornings, therefore, I altered my work schedule. My clinical interest in IBD was diluted by the emphasis to see mostly general GI patients, as is the case for many in private practice. I missed the academic environment, especially working with medical students, residents, and fellows, so I occasionally had residents shadow me. Unfortunately, adjustments did not “fix” that missing component – to me, this was a job that did not feel like a career. I was not professionally fulfilled and on several occasions during the 6 years in private practice, I connected with mentors from my medical training to explore career options while trying to define what was missing.
During the latter part of years 5 and 6, it became apparent to me that loyalty pulled me toward working with a great group of supportive gastroenterologists, but it became increasingly more apparent that this job was not in line with my career goals. I had identified that I wanted to actively participate in medical education while practicing as a gastroenterologist in an academic setting. Additionally, time with my family was a critical part to the work-life integration.
My approach to the next step in my journey was different than my initial job. My goal was to define what was important, as in what were my absolute requirements for career satisfaction and where was I willing to be flexible. Each of us has different absolute and relative requirements based on our values, and I neglected to clearly identify these components with my first job. Admittedly, I have (at times) struggled to acknowledge my values, because I might somehow appear less committed to a career. Owning these values has provided clarity in my path from private practice to academic medicine. During the 3 years I have been in my current position, I have stepped into a leadership role in the University of Nebraska Medicine GI fellowship program while providing clinical medicine at the Fred Paustian IBD Center at Nebraska Medicine. In addition, I continue to have an active endoscopy schedule and derive great satisfaction teaching the fellows how to be effective endoscopists. Personally, the difference in compensation between academic medicine and private practice was not an important factor, although this is a factor for some people (and that’s okay).
When I graduated from fellowship, my path seemed clear, and I did not anticipate the road ahead. However, with each hurdle, I was gifted with lessons that would prove to be valuable as I moved ahead. Thank you for giving me the space to share my story.
Lessons that have helped in my journey from private practice to academics
- Mentorship: Find mentors, not just one mentor. Over the years, I have had several mentors, but what I recognize is that, early in my career, I did not have a mentor. Although a mentor cannot make decisions for you, he/she can provide guidance from a place of experience (both career and life experience).
- Define a mission statement: My mentor pushed me to first define my values and then my mission statement. This serves as the foundation that I reference when making decisions that will impact my family and my career. For example, if I am invited to participate on a committee, I look at how this will impact my family and whether it aligns with my mission. This helps to clarify what I am willing to say yes to and what to pass along to another colleague. Remember that last part ... if you are saying no to something, suggest another colleague for the opportunity.
- Advocate for yourself: Only you know what is best for you. Sometimes the path to discovering what that is can be tortuous and require guidance. Throughout my journey, I worked with colleagues who were supportive of my journey back to medical school and supportive of my job in private practice, but only I could define what a career meant to me.
- Assume positive intent: In medicine, we frequently work in a high-stakes, stressful environment. Assume positive intent in your interactions with others, especially colleagues. This will serve you well.
- Life happens: Each of us will experience an unexpected event in our personal life or career path or both. This will be okay. The path forward may look different and require a pivot. This unexpected event might be that you find your job leaves you wanting something more or something different. Your journey will be right for you.
Dr. Hutchins is an assistant professor in the division of gastroenterology and hepatology at the University of Nebraska Medical Center, Omaha. She reported no conflicts of interest.
Loyalty.
This is a quality that I value in relationships. Loyalty was a significant factor contributing to my postfellowship commitment to private practice. In 2001, I graduated from physician assistant school and accepted a job with a private practice GI group in Omaha. I was fortunate to work with supportive gastroenterologists who encouraged me to pursue further training after I expressed an interest in medical school. My goal was to become a gastroenterologist but like every medical student, I would keep an open mind. My decision did not waver, and the support from my first mentors continued. As I graduated from fellowship in 2014, I gravitated toward the same private practice largely based on loyalty and my experience as a PA.

COURTESY AMERICAN GASTROENTEROLOGICAL ASSOCIATION
My experience in private practice was positive. My focus at that time and currently is clinical medicine with a focus on inflammatory bowel disease (IBD) patients. My colleagues were supportive, and I worked with a great team of nurses and APPs. I cared for many patients in both the inpatient and outpatient setting and had an opportunity to complete a high volume and variety of procedures. Overall, the various aspects of my job were rewarding. However, something was missing, and I made personal and professional adjustments. My schedule pulled me from valued family time with my kids (mostly) in the early mornings, therefore, I altered my work schedule. My clinical interest in IBD was diluted by the emphasis to see mostly general GI patients, as is the case for many in private practice. I missed the academic environment, especially working with medical students, residents, and fellows, so I occasionally had residents shadow me. Unfortunately, adjustments did not “fix” that missing component – to me, this was a job that did not feel like a career. I was not professionally fulfilled and on several occasions during the 6 years in private practice, I connected with mentors from my medical training to explore career options while trying to define what was missing.
During the latter part of years 5 and 6, it became apparent to me that loyalty pulled me toward working with a great group of supportive gastroenterologists, but it became increasingly more apparent that this job was not in line with my career goals. I had identified that I wanted to actively participate in medical education while practicing as a gastroenterologist in an academic setting. Additionally, time with my family was a critical part to the work-life integration.
My approach to the next step in my journey was different than my initial job. My goal was to define what was important, as in what were my absolute requirements for career satisfaction and where was I willing to be flexible. Each of us has different absolute and relative requirements based on our values, and I neglected to clearly identify these components with my first job. Admittedly, I have (at times) struggled to acknowledge my values, because I might somehow appear less committed to a career. Owning these values has provided clarity in my path from private practice to academic medicine. During the 3 years I have been in my current position, I have stepped into a leadership role in the University of Nebraska Medicine GI fellowship program while providing clinical medicine at the Fred Paustian IBD Center at Nebraska Medicine. In addition, I continue to have an active endoscopy schedule and derive great satisfaction teaching the fellows how to be effective endoscopists. Personally, the difference in compensation between academic medicine and private practice was not an important factor, although this is a factor for some people (and that’s okay).
When I graduated from fellowship, my path seemed clear, and I did not anticipate the road ahead. However, with each hurdle, I was gifted with lessons that would prove to be valuable as I moved ahead. Thank you for giving me the space to share my story.
Lessons that have helped in my journey from private practice to academics
- Mentorship: Find mentors, not just one mentor. Over the years, I have had several mentors, but what I recognize is that, early in my career, I did not have a mentor. Although a mentor cannot make decisions for you, he/she can provide guidance from a place of experience (both career and life experience).
- Define a mission statement: My mentor pushed me to first define my values and then my mission statement. This serves as the foundation that I reference when making decisions that will impact my family and my career. For example, if I am invited to participate on a committee, I look at how this will impact my family and whether it aligns with my mission. This helps to clarify what I am willing to say yes to and what to pass along to another colleague. Remember that last part ... if you are saying no to something, suggest another colleague for the opportunity.
- Advocate for yourself: Only you know what is best for you. Sometimes the path to discovering what that is can be tortuous and require guidance. Throughout my journey, I worked with colleagues who were supportive of my journey back to medical school and supportive of my job in private practice, but only I could define what a career meant to me.
- Assume positive intent: In medicine, we frequently work in a high-stakes, stressful environment. Assume positive intent in your interactions with others, especially colleagues. This will serve you well.
- Life happens: Each of us will experience an unexpected event in our personal life or career path or both. This will be okay. The path forward may look different and require a pivot. This unexpected event might be that you find your job leaves you wanting something more or something different. Your journey will be right for you.
Dr. Hutchins is an assistant professor in the division of gastroenterology and hepatology at the University of Nebraska Medical Center, Omaha. She reported no conflicts of interest.
My path: Challenges and decisions along the way
It took me a little while to get started on this assignment. What would be most useful to young gastroenterologists embarking on their careers? When I asked around, I heard that many of you wanted me to describe challenges and decision points. The following list is vaguely chronological, surely noncomprehensive, and meant to serve as a starting point.
1. To stay in basic science or return to patient care
My start in science was rocky. I had come to the United States for a post-doc after medical school in Germany. I had never pipetted before. It was the early days of array technologies, and the lab was very technical and basic. We made our own arrays and our own analytics, and none of my experiments worked. So, I spent 1 year feeling like I made no progress – but in hindsight I appreciate the tremendous growth in these formative years honing inquiry and persistence, as well as building resilience. I added a third year as some results were finally emerging; however, the bedside started to feel very far away. I could not ignore the tug back to the patient care, and after contemplating a PhD program, I decided to apply for residency in a physician-scientist pathway. Given the streamlined training that allowed for science and clinical education in an organized fashion, I also decided to stay in the U.S. This of course had vast personal consequences, which I did not fully appreciate at the time.
Residency was another time of immense growth, I was the only “foreign medical graduate” and had a lot to catch up on, but I enjoyed my amazing peers and the hands-on learning.
Pearl: Follow your passion. Not what makes most sense or what someone wants for you or what you could achieve given your past work. Do what will get you up in the morning and add a bounce to your step.
2. To go for big impact or climate
At UCSD at the time, there was a culture of impactful mega-labs, up 30 post-docs, often with many working on the same project with the ones finishing first garnering the publication. This created a “go big or go home” (literally) atmosphere. As part of the PSTP program, I was supported by the GI T32 and, being “free labor,” had a pretty wide array of labs to choose from. To the program director’s surprise, I settled on a fairly junior investigator, who was a fellow gastroenterologist and took a personal interest in my career. When making that decision, I prioritized climate over outcome. I remember thinking to myself that how I spent my time was just as important as the potential outcome of the time spent. Through my years in Dr. John Carethers’ lab, I gained insight into his administrative and leadership roles which added another dimension to our mentorship relationship. These years were fun and productive, and our mentorship grew into a friendship.
Pearl: Look for the right people to work with. Particularly who you work for. Everything else is secondary as the right people will set the tone and most influence your day-to-day experience, which is the foundation of your success.
3. To cultivate a life outside of academia
When I turned 30, I remember driving down Interstate 5 in San Diego and taking stock. Yes, I loved clinical work, I felt valued, and was in a stimulating supportive environment. Yet, I was so immersed that everything else seemed to take a back seat. I made the conscious decision on that drive to prioritize life outside of academia. It is not like I did not have one, I just decided to set an intention so it would not get away from me. I continue to make a conscious effort to be present for my husband, my kids, my family – to take time and spend it together without work bleeding into it. And since this is a goal in and of itself, there is no conflict! Through less travel and no more late nights or weekends, your nonacademic life will flourish.
Pearl: Deliberately prioritize your family and hobbies in the long run. Make key decisions with that in mind.
4. To grow your own program or lead others
When we moved to Chicago for my husband’s residency (he went to medical school as his third career at age 35), I was very excited to build my own comprehensive GI cancer genetics program at Northwestern. It was a little scary but also fun to now run my own lab and try to connect the clinical community around hereditary GI cancers. The program was moving along nicely when I received a generic letter asking for applications to become division chief at the neighboring University of Illinois. The letter concluded with an enticing “Chicago is a vibrant city,” so clearly it was meant for a broad audience. I was not sure what to do and again took stock. Did I want to continue to increase the impact of my own work – clearly there was a lot more ground to cover. Or, did I want to be part of making further-reaching decisions? I had been approached by fellows who wanted to be recruited, and I had ideas for programs and thoughts around processes. While my input was valued, I was not the ultimate decision maker. I decided that I either focus on one or the other and so applied for the position and then took the leap.
Pearl: There are many forks and they will present when you do not expect them. Assess and consider. Also know yourself – not everything that is attainable is desirable.
5. To have greater influence or stay with what you know
Becoming a division chief was transformative. Learning to integrate the needs of various and sometimes conflicting stakeholders, running an operation but also thinking strategically and mission-based – I was drinking from a firehose. How to measure success as a leader? I was fortunate to enter the division at a turbulent time where much rebuilding was needed and it was easy to implement and see change.
Pearl: Again know yourself – not everything that is attainable is desirable. But also – take risks. What is the worst that can happen? Growth may not be attained by waiting.
6. To be spread too thin or close doors
As you develop your focus and expertise while implementing No. 3, you will run out of hours in the day. This means you will need to become more and more efficient, as in delegating (and letting go) where you can and doing fewer nonessential tasks. However, you want to think hard about closing doors completely. I have been careful to hone and keep my endoscopy skills as well as my scientific output. To leave the doors ajar, I have tried to find ways to be very deliberate with my involvement and also understand that at some point it may make sense to close a door.
Pearl: Do not try to do everything well, you will risk doing everything poorly. Work on “good enough” for tasks that can be very involved. Think hard before permanently leaving something behind as you may lose flexibility down the road.
7. To enjoy fruits of labor or continue to grow
A question I get asked often is regarding the ideal time to move. In my mind, there is no perfect time. It depends on your satisfaction with your current position (see No. 2), your personal situation (see No. 3), and what you want at that juncture (see No. 5). At some point, one may want to stay awhile and enjoy. Or continue to change and grow – both have their merits and there is no right or wrong.
Pearl: When contemplating next steps, go back to your passion and priorities. Has anything shifted? Are your goals being met? Are you enjoying yourself? Advice can be helpful but also confusing. Remember, no one knows you like you do.
8. To show tangible results or build out relationships
Over time, as you become more and more efficient, you simultaneously need to spend more time fostering relationships. This feels strange at first as it is the opposite of a fast-paced to-do list and the “results” appear elusive. Build in time for relating – with peers, superiors, fellows, members of your lab.
Pearl: Form relationships early and often. Take care of them (No. 3) and include relationship building into your workstream – I promise it will make your path more successful and satisfying.
I hope this list shows that there are many forks and no one right way. Advice is helpful and subjective. No path is the same, and it truly is yours to shape. Be thoughtful and enjoy – your journey will be amazing and full of surprises.
Dr. Jung is professor and chair, and the Robert G. Petersdorf Endowed Chair in Medicine, in the department of medicine at the University of Washington, Seattle. She is on Twitter @barbarahjung. She has no conflicts of interest.
It took me a little while to get started on this assignment. What would be most useful to young gastroenterologists embarking on their careers? When I asked around, I heard that many of you wanted me to describe challenges and decision points. The following list is vaguely chronological, surely noncomprehensive, and meant to serve as a starting point.
1. To stay in basic science or return to patient care
My start in science was rocky. I had come to the United States for a post-doc after medical school in Germany. I had never pipetted before. It was the early days of array technologies, and the lab was very technical and basic. We made our own arrays and our own analytics, and none of my experiments worked. So, I spent 1 year feeling like I made no progress – but in hindsight I appreciate the tremendous growth in these formative years honing inquiry and persistence, as well as building resilience. I added a third year as some results were finally emerging; however, the bedside started to feel very far away. I could not ignore the tug back to the patient care, and after contemplating a PhD program, I decided to apply for residency in a physician-scientist pathway. Given the streamlined training that allowed for science and clinical education in an organized fashion, I also decided to stay in the U.S. This of course had vast personal consequences, which I did not fully appreciate at the time.
Residency was another time of immense growth, I was the only “foreign medical graduate” and had a lot to catch up on, but I enjoyed my amazing peers and the hands-on learning.
Pearl: Follow your passion. Not what makes most sense or what someone wants for you or what you could achieve given your past work. Do what will get you up in the morning and add a bounce to your step.
2. To go for big impact or climate
At UCSD at the time, there was a culture of impactful mega-labs, up 30 post-docs, often with many working on the same project with the ones finishing first garnering the publication. This created a “go big or go home” (literally) atmosphere. As part of the PSTP program, I was supported by the GI T32 and, being “free labor,” had a pretty wide array of labs to choose from. To the program director’s surprise, I settled on a fairly junior investigator, who was a fellow gastroenterologist and took a personal interest in my career. When making that decision, I prioritized climate over outcome. I remember thinking to myself that how I spent my time was just as important as the potential outcome of the time spent. Through my years in Dr. John Carethers’ lab, I gained insight into his administrative and leadership roles which added another dimension to our mentorship relationship. These years were fun and productive, and our mentorship grew into a friendship.
Pearl: Look for the right people to work with. Particularly who you work for. Everything else is secondary as the right people will set the tone and most influence your day-to-day experience, which is the foundation of your success.
3. To cultivate a life outside of academia
When I turned 30, I remember driving down Interstate 5 in San Diego and taking stock. Yes, I loved clinical work, I felt valued, and was in a stimulating supportive environment. Yet, I was so immersed that everything else seemed to take a back seat. I made the conscious decision on that drive to prioritize life outside of academia. It is not like I did not have one, I just decided to set an intention so it would not get away from me. I continue to make a conscious effort to be present for my husband, my kids, my family – to take time and spend it together without work bleeding into it. And since this is a goal in and of itself, there is no conflict! Through less travel and no more late nights or weekends, your nonacademic life will flourish.
Pearl: Deliberately prioritize your family and hobbies in the long run. Make key decisions with that in mind.
4. To grow your own program or lead others
When we moved to Chicago for my husband’s residency (he went to medical school as his third career at age 35), I was very excited to build my own comprehensive GI cancer genetics program at Northwestern. It was a little scary but also fun to now run my own lab and try to connect the clinical community around hereditary GI cancers. The program was moving along nicely when I received a generic letter asking for applications to become division chief at the neighboring University of Illinois. The letter concluded with an enticing “Chicago is a vibrant city,” so clearly it was meant for a broad audience. I was not sure what to do and again took stock. Did I want to continue to increase the impact of my own work – clearly there was a lot more ground to cover. Or, did I want to be part of making further-reaching decisions? I had been approached by fellows who wanted to be recruited, and I had ideas for programs and thoughts around processes. While my input was valued, I was not the ultimate decision maker. I decided that I either focus on one or the other and so applied for the position and then took the leap.
Pearl: There are many forks and they will present when you do not expect them. Assess and consider. Also know yourself – not everything that is attainable is desirable.
5. To have greater influence or stay with what you know
Becoming a division chief was transformative. Learning to integrate the needs of various and sometimes conflicting stakeholders, running an operation but also thinking strategically and mission-based – I was drinking from a firehose. How to measure success as a leader? I was fortunate to enter the division at a turbulent time where much rebuilding was needed and it was easy to implement and see change.
Pearl: Again know yourself – not everything that is attainable is desirable. But also – take risks. What is the worst that can happen? Growth may not be attained by waiting.
6. To be spread too thin or close doors
As you develop your focus and expertise while implementing No. 3, you will run out of hours in the day. This means you will need to become more and more efficient, as in delegating (and letting go) where you can and doing fewer nonessential tasks. However, you want to think hard about closing doors completely. I have been careful to hone and keep my endoscopy skills as well as my scientific output. To leave the doors ajar, I have tried to find ways to be very deliberate with my involvement and also understand that at some point it may make sense to close a door.
Pearl: Do not try to do everything well, you will risk doing everything poorly. Work on “good enough” for tasks that can be very involved. Think hard before permanently leaving something behind as you may lose flexibility down the road.
7. To enjoy fruits of labor or continue to grow
A question I get asked often is regarding the ideal time to move. In my mind, there is no perfect time. It depends on your satisfaction with your current position (see No. 2), your personal situation (see No. 3), and what you want at that juncture (see No. 5). At some point, one may want to stay awhile and enjoy. Or continue to change and grow – both have their merits and there is no right or wrong.
Pearl: When contemplating next steps, go back to your passion and priorities. Has anything shifted? Are your goals being met? Are you enjoying yourself? Advice can be helpful but also confusing. Remember, no one knows you like you do.
8. To show tangible results or build out relationships
Over time, as you become more and more efficient, you simultaneously need to spend more time fostering relationships. This feels strange at first as it is the opposite of a fast-paced to-do list and the “results” appear elusive. Build in time for relating – with peers, superiors, fellows, members of your lab.
Pearl: Form relationships early and often. Take care of them (No. 3) and include relationship building into your workstream – I promise it will make your path more successful and satisfying.
I hope this list shows that there are many forks and no one right way. Advice is helpful and subjective. No path is the same, and it truly is yours to shape. Be thoughtful and enjoy – your journey will be amazing and full of surprises.
Dr. Jung is professor and chair, and the Robert G. Petersdorf Endowed Chair in Medicine, in the department of medicine at the University of Washington, Seattle. She is on Twitter @barbarahjung. She has no conflicts of interest.
It took me a little while to get started on this assignment. What would be most useful to young gastroenterologists embarking on their careers? When I asked around, I heard that many of you wanted me to describe challenges and decision points. The following list is vaguely chronological, surely noncomprehensive, and meant to serve as a starting point.
1. To stay in basic science or return to patient care
My start in science was rocky. I had come to the United States for a post-doc after medical school in Germany. I had never pipetted before. It was the early days of array technologies, and the lab was very technical and basic. We made our own arrays and our own analytics, and none of my experiments worked. So, I spent 1 year feeling like I made no progress – but in hindsight I appreciate the tremendous growth in these formative years honing inquiry and persistence, as well as building resilience. I added a third year as some results were finally emerging; however, the bedside started to feel very far away. I could not ignore the tug back to the patient care, and after contemplating a PhD program, I decided to apply for residency in a physician-scientist pathway. Given the streamlined training that allowed for science and clinical education in an organized fashion, I also decided to stay in the U.S. This of course had vast personal consequences, which I did not fully appreciate at the time.
Residency was another time of immense growth, I was the only “foreign medical graduate” and had a lot to catch up on, but I enjoyed my amazing peers and the hands-on learning.
Pearl: Follow your passion. Not what makes most sense or what someone wants for you or what you could achieve given your past work. Do what will get you up in the morning and add a bounce to your step.
2. To go for big impact or climate
At UCSD at the time, there was a culture of impactful mega-labs, up 30 post-docs, often with many working on the same project with the ones finishing first garnering the publication. This created a “go big or go home” (literally) atmosphere. As part of the PSTP program, I was supported by the GI T32 and, being “free labor,” had a pretty wide array of labs to choose from. To the program director’s surprise, I settled on a fairly junior investigator, who was a fellow gastroenterologist and took a personal interest in my career. When making that decision, I prioritized climate over outcome. I remember thinking to myself that how I spent my time was just as important as the potential outcome of the time spent. Through my years in Dr. John Carethers’ lab, I gained insight into his administrative and leadership roles which added another dimension to our mentorship relationship. These years were fun and productive, and our mentorship grew into a friendship.
Pearl: Look for the right people to work with. Particularly who you work for. Everything else is secondary as the right people will set the tone and most influence your day-to-day experience, which is the foundation of your success.
3. To cultivate a life outside of academia
When I turned 30, I remember driving down Interstate 5 in San Diego and taking stock. Yes, I loved clinical work, I felt valued, and was in a stimulating supportive environment. Yet, I was so immersed that everything else seemed to take a back seat. I made the conscious decision on that drive to prioritize life outside of academia. It is not like I did not have one, I just decided to set an intention so it would not get away from me. I continue to make a conscious effort to be present for my husband, my kids, my family – to take time and spend it together without work bleeding into it. And since this is a goal in and of itself, there is no conflict! Through less travel and no more late nights or weekends, your nonacademic life will flourish.
Pearl: Deliberately prioritize your family and hobbies in the long run. Make key decisions with that in mind.
4. To grow your own program or lead others
When we moved to Chicago for my husband’s residency (he went to medical school as his third career at age 35), I was very excited to build my own comprehensive GI cancer genetics program at Northwestern. It was a little scary but also fun to now run my own lab and try to connect the clinical community around hereditary GI cancers. The program was moving along nicely when I received a generic letter asking for applications to become division chief at the neighboring University of Illinois. The letter concluded with an enticing “Chicago is a vibrant city,” so clearly it was meant for a broad audience. I was not sure what to do and again took stock. Did I want to continue to increase the impact of my own work – clearly there was a lot more ground to cover. Or, did I want to be part of making further-reaching decisions? I had been approached by fellows who wanted to be recruited, and I had ideas for programs and thoughts around processes. While my input was valued, I was not the ultimate decision maker. I decided that I either focus on one or the other and so applied for the position and then took the leap.
Pearl: There are many forks and they will present when you do not expect them. Assess and consider. Also know yourself – not everything that is attainable is desirable.
5. To have greater influence or stay with what you know
Becoming a division chief was transformative. Learning to integrate the needs of various and sometimes conflicting stakeholders, running an operation but also thinking strategically and mission-based – I was drinking from a firehose. How to measure success as a leader? I was fortunate to enter the division at a turbulent time where much rebuilding was needed and it was easy to implement and see change.
Pearl: Again know yourself – not everything that is attainable is desirable. But also – take risks. What is the worst that can happen? Growth may not be attained by waiting.
6. To be spread too thin or close doors
As you develop your focus and expertise while implementing No. 3, you will run out of hours in the day. This means you will need to become more and more efficient, as in delegating (and letting go) where you can and doing fewer nonessential tasks. However, you want to think hard about closing doors completely. I have been careful to hone and keep my endoscopy skills as well as my scientific output. To leave the doors ajar, I have tried to find ways to be very deliberate with my involvement and also understand that at some point it may make sense to close a door.
Pearl: Do not try to do everything well, you will risk doing everything poorly. Work on “good enough” for tasks that can be very involved. Think hard before permanently leaving something behind as you may lose flexibility down the road.
7. To enjoy fruits of labor or continue to grow
A question I get asked often is regarding the ideal time to move. In my mind, there is no perfect time. It depends on your satisfaction with your current position (see No. 2), your personal situation (see No. 3), and what you want at that juncture (see No. 5). At some point, one may want to stay awhile and enjoy. Or continue to change and grow – both have their merits and there is no right or wrong.
Pearl: When contemplating next steps, go back to your passion and priorities. Has anything shifted? Are your goals being met? Are you enjoying yourself? Advice can be helpful but also confusing. Remember, no one knows you like you do.
8. To show tangible results or build out relationships
Over time, as you become more and more efficient, you simultaneously need to spend more time fostering relationships. This feels strange at first as it is the opposite of a fast-paced to-do list and the “results” appear elusive. Build in time for relating – with peers, superiors, fellows, members of your lab.
Pearl: Form relationships early and often. Take care of them (No. 3) and include relationship building into your workstream – I promise it will make your path more successful and satisfying.
I hope this list shows that there are many forks and no one right way. Advice is helpful and subjective. No path is the same, and it truly is yours to shape. Be thoughtful and enjoy – your journey will be amazing and full of surprises.
Dr. Jung is professor and chair, and the Robert G. Petersdorf Endowed Chair in Medicine, in the department of medicine at the University of Washington, Seattle. She is on Twitter @barbarahjung. She has no conflicts of interest.
The road less traveled in gastroenterology and hepatology: Becoming a medical educator
How did you realize medical education was the pathway for you?
Near the end of medical school, I recall my friends and I casting predictions about what each person would be doing in twenty years. The projections offered up about my ultimate landing place were unanimous: a clinical researcher leading a gastroenterology division. I was excited when they said this to me. It made sense, as I had already done over 3 years of clinical research on inflammatory bowel disease at the time. But as I began leading various clinical research projects during my internal medicine residency, I realized that they were not generating a strong sense of fulfillment or passion for me. I greatly enjoyed the process of research and writing, but there still was something missing; I could no longer see the role of a funded clinical researcher sustaining me for the length of my medical and academic career.
Thus, at the end of my 2nd year of residency, I began to self-reflect more on the various aspects of my medical journey to elucidate my path forward. This process was jump-started by a humbling recognition from that year’s graduating class of medical students for my contributions to their education over the past 3 years. I had served as a teaching assistant for their pathophysiology course and then subsequently worked alongside many of them on their medicine rotations. I realized that helping foster their growth as physicians in a longitudinal way was unquestionably the most rewarding experience that I had had to date. With further reflection, I recognized that, amid the chaos of a busy call day, I most looked forward to the moments when I could teach the interns and students about the nuances of the patients being admitted. It never felt like an obligation but rather always left me feeling revitalized. So, by the beginning of my 3rd year of residency, I knew that I wanted to pursue a career within medical education.
Once you decided to become a medical educator, what were your next steps?
As I began to vocalize this change in career trajectory, I did not always encounter enthusiastic support. Because the medical educator pathway is more typical amongst the general medicine community, some faculty members advised me to avoid solely focusing on medical education as a specialist because academic success would be difficult to attain. But I had just recognized this could be my vocation within medicine, so I could not turn back now. Thus, I began to seek the mentorship of educators at my institution, and many of them wisely advised me to consider pursuing additional training in medical education to accrue the skill sets needed to lay the groundwork for a lifelong career. So, I participated in a 1-year medical education fellowship in conjunction with my chief residency year. This training was profoundly formative; I learned about the various theories on adult learning, as well as how to create curricula, how to teach effectively in a clinical environment, and how to deliver meaningful feedback to learners. But perhaps most importantly, I learned how to generate tangible evidence of productivity within medical education to allow for advancement in academia. This included rigorously studying the impact of educational interventions. It became clear to me by the end of this year that the pathways of medical education and researcher were not incongruent but could actually be quite complementary. In light of this, I designed and implemented a mandatory inpatient hepatology curriculum for internal medicine residents, for which I studied its immediate and long-term effects throughout my gastroenterology and hepatology fellowships as well as during my time as an attending. Currently, I am also investigating medical students’ exposure to liver disease through a multicenter assessment. Projects such as these would not have been feasible without dedicated mentorship, but as alluded to above, in contrast to the traditional clinical research paradigm, my mentors have often been from outside the fields of gastroenterology and hepatology.
What advice would you offer a junior faculty member interested in a career in medical education within gastroenterology and hepatology?
1. Just before I completed fellowship, I asked Holly Humphrey, MD, the former dean of the Pritzker School of Medicine at the University of Chicago, this same question. Her answer was simple and is worth sharing: “In the beginning, just focus on becoming the best clinician possible. The rest will fall into place with time.” So, I did exactly this. I continually tried to push the limits of my knowledge, always questioning standard clinical practices to understand the evidence behind (or not behind) them. This knowledge then naturally became the content of my teaching for trainees in the clinical environment so that eventually patient care and teaching were seamlessly integrated into the same day-to-day workflow. The more I taught trainees, the more my commitment to education was recognized by my institution.
2. Meet with leadership of your medical school, internal medicine residency program, and gastroenterology and hepatology fellowships early in the course of your career to assert your desire to contribute to their respective educational missions.
3. Create a teaching philosophy that clearly communicates “your fundamental beliefs about teaching and learning, why you hold those values and beliefs, and how you translate these claims into practice.”1 This document will act as a guiding force in your career by highlighting the themes and principles that you have already incorporated and will continue to incorporate into your teaching practices and educational activities. For example, it can provide clarity when you are in doubt of how to address a difficult learning environment or whether to accept a certain position.
4. Because of No. 1 and No. 2, you will start to be offered opportunities to formally become involved in curricula within undergraduate (UME) and graduate medical education (GME). It will likely begin with requests to lecture or precept small group sessions. Use these smaller opportunities not only to refine your teaching skills but to explore whether your career aspirations better align with UME or GME. With hard work and perseverance, the opportunities can progress to invitations to become a course director, join a curriculum committee, or become an associate program director for a residency or fellowship program (which at this point is why you want to know if you prefer working in UME, GME, or both).
5. Seek feedback often from your learners. It is the only way you will continue to improve your teaching skills and the learning environment you create. Furthermore, formal evaluations can be used in the promotion process.
6. Collaborate with and seek mentorship from fellow medical educators both at your own institution and at others. As previously mentioned, these relationships do not need to be (and are often not) with other gastroenterologists or hepatologists.
7. Seek out national opportunities related to medical education. Most of the gastroenterology and hepatology societies have one or more committees focused on medical training. The AGA Academy of Educators is a fantastic community of education-focused individuals within our specialty that provides opportunities for networking, funding, and career development. Furthermore, other general societies (for example, the Association of American Medical Colleges, American College of Physicians) may be interested in including subspecialty members in their educational committees and activities.
Dr. Mikolajczyk is an assistant professor of medicine and an associate program director for the Internal Medicine Residency Program at the University of Illinois Chicago. He is the lead faculty adviser for the Liver Fellow Network. He has no conflicts of interest to disclose.
How did you realize medical education was the pathway for you?
Near the end of medical school, I recall my friends and I casting predictions about what each person would be doing in twenty years. The projections offered up about my ultimate landing place were unanimous: a clinical researcher leading a gastroenterology division. I was excited when they said this to me. It made sense, as I had already done over 3 years of clinical research on inflammatory bowel disease at the time. But as I began leading various clinical research projects during my internal medicine residency, I realized that they were not generating a strong sense of fulfillment or passion for me. I greatly enjoyed the process of research and writing, but there still was something missing; I could no longer see the role of a funded clinical researcher sustaining me for the length of my medical and academic career.
Thus, at the end of my 2nd year of residency, I began to self-reflect more on the various aspects of my medical journey to elucidate my path forward. This process was jump-started by a humbling recognition from that year’s graduating class of medical students for my contributions to their education over the past 3 years. I had served as a teaching assistant for their pathophysiology course and then subsequently worked alongside many of them on their medicine rotations. I realized that helping foster their growth as physicians in a longitudinal way was unquestionably the most rewarding experience that I had had to date. With further reflection, I recognized that, amid the chaos of a busy call day, I most looked forward to the moments when I could teach the interns and students about the nuances of the patients being admitted. It never felt like an obligation but rather always left me feeling revitalized. So, by the beginning of my 3rd year of residency, I knew that I wanted to pursue a career within medical education.
Once you decided to become a medical educator, what were your next steps?
As I began to vocalize this change in career trajectory, I did not always encounter enthusiastic support. Because the medical educator pathway is more typical amongst the general medicine community, some faculty members advised me to avoid solely focusing on medical education as a specialist because academic success would be difficult to attain. But I had just recognized this could be my vocation within medicine, so I could not turn back now. Thus, I began to seek the mentorship of educators at my institution, and many of them wisely advised me to consider pursuing additional training in medical education to accrue the skill sets needed to lay the groundwork for a lifelong career. So, I participated in a 1-year medical education fellowship in conjunction with my chief residency year. This training was profoundly formative; I learned about the various theories on adult learning, as well as how to create curricula, how to teach effectively in a clinical environment, and how to deliver meaningful feedback to learners. But perhaps most importantly, I learned how to generate tangible evidence of productivity within medical education to allow for advancement in academia. This included rigorously studying the impact of educational interventions. It became clear to me by the end of this year that the pathways of medical education and researcher were not incongruent but could actually be quite complementary. In light of this, I designed and implemented a mandatory inpatient hepatology curriculum for internal medicine residents, for which I studied its immediate and long-term effects throughout my gastroenterology and hepatology fellowships as well as during my time as an attending. Currently, I am also investigating medical students’ exposure to liver disease through a multicenter assessment. Projects such as these would not have been feasible without dedicated mentorship, but as alluded to above, in contrast to the traditional clinical research paradigm, my mentors have often been from outside the fields of gastroenterology and hepatology.
What advice would you offer a junior faculty member interested in a career in medical education within gastroenterology and hepatology?
1. Just before I completed fellowship, I asked Holly Humphrey, MD, the former dean of the Pritzker School of Medicine at the University of Chicago, this same question. Her answer was simple and is worth sharing: “In the beginning, just focus on becoming the best clinician possible. The rest will fall into place with time.” So, I did exactly this. I continually tried to push the limits of my knowledge, always questioning standard clinical practices to understand the evidence behind (or not behind) them. This knowledge then naturally became the content of my teaching for trainees in the clinical environment so that eventually patient care and teaching were seamlessly integrated into the same day-to-day workflow. The more I taught trainees, the more my commitment to education was recognized by my institution.
2. Meet with leadership of your medical school, internal medicine residency program, and gastroenterology and hepatology fellowships early in the course of your career to assert your desire to contribute to their respective educational missions.
3. Create a teaching philosophy that clearly communicates “your fundamental beliefs about teaching and learning, why you hold those values and beliefs, and how you translate these claims into practice.”1 This document will act as a guiding force in your career by highlighting the themes and principles that you have already incorporated and will continue to incorporate into your teaching practices and educational activities. For example, it can provide clarity when you are in doubt of how to address a difficult learning environment or whether to accept a certain position.
4. Because of No. 1 and No. 2, you will start to be offered opportunities to formally become involved in curricula within undergraduate (UME) and graduate medical education (GME). It will likely begin with requests to lecture or precept small group sessions. Use these smaller opportunities not only to refine your teaching skills but to explore whether your career aspirations better align with UME or GME. With hard work and perseverance, the opportunities can progress to invitations to become a course director, join a curriculum committee, or become an associate program director for a residency or fellowship program (which at this point is why you want to know if you prefer working in UME, GME, or both).
5. Seek feedback often from your learners. It is the only way you will continue to improve your teaching skills and the learning environment you create. Furthermore, formal evaluations can be used in the promotion process.
6. Collaborate with and seek mentorship from fellow medical educators both at your own institution and at others. As previously mentioned, these relationships do not need to be (and are often not) with other gastroenterologists or hepatologists.
7. Seek out national opportunities related to medical education. Most of the gastroenterology and hepatology societies have one or more committees focused on medical training. The AGA Academy of Educators is a fantastic community of education-focused individuals within our specialty that provides opportunities for networking, funding, and career development. Furthermore, other general societies (for example, the Association of American Medical Colleges, American College of Physicians) may be interested in including subspecialty members in their educational committees and activities.
Dr. Mikolajczyk is an assistant professor of medicine and an associate program director for the Internal Medicine Residency Program at the University of Illinois Chicago. He is the lead faculty adviser for the Liver Fellow Network. He has no conflicts of interest to disclose.
How did you realize medical education was the pathway for you?
Near the end of medical school, I recall my friends and I casting predictions about what each person would be doing in twenty years. The projections offered up about my ultimate landing place were unanimous: a clinical researcher leading a gastroenterology division. I was excited when they said this to me. It made sense, as I had already done over 3 years of clinical research on inflammatory bowel disease at the time. But as I began leading various clinical research projects during my internal medicine residency, I realized that they were not generating a strong sense of fulfillment or passion for me. I greatly enjoyed the process of research and writing, but there still was something missing; I could no longer see the role of a funded clinical researcher sustaining me for the length of my medical and academic career.
Thus, at the end of my 2nd year of residency, I began to self-reflect more on the various aspects of my medical journey to elucidate my path forward. This process was jump-started by a humbling recognition from that year’s graduating class of medical students for my contributions to their education over the past 3 years. I had served as a teaching assistant for their pathophysiology course and then subsequently worked alongside many of them on their medicine rotations. I realized that helping foster their growth as physicians in a longitudinal way was unquestionably the most rewarding experience that I had had to date. With further reflection, I recognized that, amid the chaos of a busy call day, I most looked forward to the moments when I could teach the interns and students about the nuances of the patients being admitted. It never felt like an obligation but rather always left me feeling revitalized. So, by the beginning of my 3rd year of residency, I knew that I wanted to pursue a career within medical education.
Once you decided to become a medical educator, what were your next steps?
As I began to vocalize this change in career trajectory, I did not always encounter enthusiastic support. Because the medical educator pathway is more typical amongst the general medicine community, some faculty members advised me to avoid solely focusing on medical education as a specialist because academic success would be difficult to attain. But I had just recognized this could be my vocation within medicine, so I could not turn back now. Thus, I began to seek the mentorship of educators at my institution, and many of them wisely advised me to consider pursuing additional training in medical education to accrue the skill sets needed to lay the groundwork for a lifelong career. So, I participated in a 1-year medical education fellowship in conjunction with my chief residency year. This training was profoundly formative; I learned about the various theories on adult learning, as well as how to create curricula, how to teach effectively in a clinical environment, and how to deliver meaningful feedback to learners. But perhaps most importantly, I learned how to generate tangible evidence of productivity within medical education to allow for advancement in academia. This included rigorously studying the impact of educational interventions. It became clear to me by the end of this year that the pathways of medical education and researcher were not incongruent but could actually be quite complementary. In light of this, I designed and implemented a mandatory inpatient hepatology curriculum for internal medicine residents, for which I studied its immediate and long-term effects throughout my gastroenterology and hepatology fellowships as well as during my time as an attending. Currently, I am also investigating medical students’ exposure to liver disease through a multicenter assessment. Projects such as these would not have been feasible without dedicated mentorship, but as alluded to above, in contrast to the traditional clinical research paradigm, my mentors have often been from outside the fields of gastroenterology and hepatology.
What advice would you offer a junior faculty member interested in a career in medical education within gastroenterology and hepatology?
1. Just before I completed fellowship, I asked Holly Humphrey, MD, the former dean of the Pritzker School of Medicine at the University of Chicago, this same question. Her answer was simple and is worth sharing: “In the beginning, just focus on becoming the best clinician possible. The rest will fall into place with time.” So, I did exactly this. I continually tried to push the limits of my knowledge, always questioning standard clinical practices to understand the evidence behind (or not behind) them. This knowledge then naturally became the content of my teaching for trainees in the clinical environment so that eventually patient care and teaching were seamlessly integrated into the same day-to-day workflow. The more I taught trainees, the more my commitment to education was recognized by my institution.
2. Meet with leadership of your medical school, internal medicine residency program, and gastroenterology and hepatology fellowships early in the course of your career to assert your desire to contribute to their respective educational missions.
3. Create a teaching philosophy that clearly communicates “your fundamental beliefs about teaching and learning, why you hold those values and beliefs, and how you translate these claims into practice.”1 This document will act as a guiding force in your career by highlighting the themes and principles that you have already incorporated and will continue to incorporate into your teaching practices and educational activities. For example, it can provide clarity when you are in doubt of how to address a difficult learning environment or whether to accept a certain position.
4. Because of No. 1 and No. 2, you will start to be offered opportunities to formally become involved in curricula within undergraduate (UME) and graduate medical education (GME). It will likely begin with requests to lecture or precept small group sessions. Use these smaller opportunities not only to refine your teaching skills but to explore whether your career aspirations better align with UME or GME. With hard work and perseverance, the opportunities can progress to invitations to become a course director, join a curriculum committee, or become an associate program director for a residency or fellowship program (which at this point is why you want to know if you prefer working in UME, GME, or both).
5. Seek feedback often from your learners. It is the only way you will continue to improve your teaching skills and the learning environment you create. Furthermore, formal evaluations can be used in the promotion process.
6. Collaborate with and seek mentorship from fellow medical educators both at your own institution and at others. As previously mentioned, these relationships do not need to be (and are often not) with other gastroenterologists or hepatologists.
7. Seek out national opportunities related to medical education. Most of the gastroenterology and hepatology societies have one or more committees focused on medical training. The AGA Academy of Educators is a fantastic community of education-focused individuals within our specialty that provides opportunities for networking, funding, and career development. Furthermore, other general societies (for example, the Association of American Medical Colleges, American College of Physicians) may be interested in including subspecialty members in their educational committees and activities.
Dr. Mikolajczyk is an assistant professor of medicine and an associate program director for the Internal Medicine Residency Program at the University of Illinois Chicago. He is the lead faculty adviser for the Liver Fellow Network. He has no conflicts of interest to disclose.
Developing a career in medical pancreatology: An emerging postfellowship career path
Although described by the Greek physician Herophilos around 300 B.C., it was not until the 19th century that enzymes began to be isolated from pancreatic secretions and their digestive action described, and not until early in the 20th century that Banting, Macleod, and Best received the Nobel prize for purifying insulin from the pancreata of dogs. For centuries in between, the pancreas was considered to be just a ‘beautiful piece of flesh’ (kallikreas), the main role of which was to protect the blood vessels in the abdomen and to serve as a cushion to the stomach.1 Certainly, the pancreas has come a long way since then but, like most other organs in the body, is oft ignored until it develops issues.
Like many other disorders in gastroenterology, pancreatic disorders were historically approached as mechanical or “plumbing” issues. As modern technology and innovation percolated through the world of endoscopy, a wide array of state-of-the-art tools were devised. Availability of newer “toys” and development of newer techniques also means that an ever-increasing curriculum has been squeezed into a generally single year of therapeutic endoscopy training, such that trainees can no longer limit themselves to learning only endoscopic ultrasound (EUS) and endoscopic retrograde cholangiopancreatography (ERCP) or intervening on pancreatic disease alone. Modern, subspecialized approaches to disease and economic considerations often dictate that the therapeutic endoscopist of today must perform a wide range of procedures besides ERCP and EUS, such as advanced resection using endoscopic mucosal resection (EMR), endoscopic submucosal dissection (ESD), per-oral endoscopic myotomy (POEM), endoscopic bariatric procedures, and newer techniques and acronyms that continue to evolve on a regular basis. This leaves the therapeutic endoscopist with little time for outpatient management of many patients that don’t need interventional procedures but are often very complex and need ongoing, long-term follow-up. In addition, any clinic slots available for interventional endoscopists may be utilized by patients coming in to discuss complex procedures or for postprocedure follow-up. Endoscopic management is not the definitive treatment for most pancreatic disorders. In fact, as our knowledge of pancreatic disease has continued to evolve, endoscopic intervention is now required in a minority of cases.
Role of the medical pancreatologist
Patient Care
As part of a comprehensive, multidisciplinary team that also includes an interventional gastroenterologist, pancreatic surgeon, transplant surgeon (in centers offering islet autotransplantation with total pancreatectomy), radiology, endocrinology, and GI pathologist, the medical pancreatologist helps lead the care of patients with pancreatic disorders, such as pancreatic cysts, acute and chronic pancreatitis (especially in cases where there is no role for active endoscopic intervention), autoimmune pancreatitis, indeterminate pancreatic masses, as well as screens high-risk patients for pancreatic cancer in conjunction with a genetic counselor. The medical pancreatologist often also serves as a bridge between various members of a large multidisciplinary team that, formally in the form of conferences or informally, discusses the management of complex patients, with each member available to help the other based on the patient’s most immediate clinical need at that time. A schematic showing how the medical pancreatologist collaborates with the therapeutic endoscopist is provided in Figure 1.
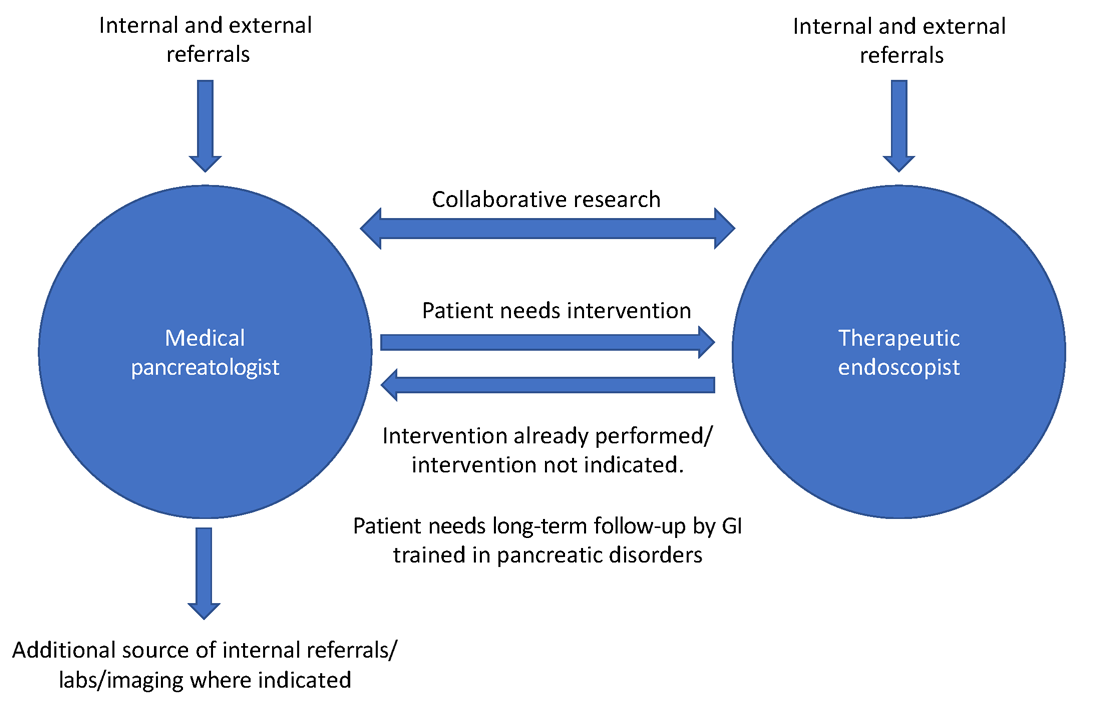
Uzma Siddiqui, MD, director for the Center for Endoscopic Research and Technology (CERT) at the University of Chicago said, “The management of pancreatic diseases is often challenging. Surgeons and endoscopists can offer some treatments that focus on one aspect or symptom, but the medical pancreatologist brings focus to the patient as a whole and helps organize care. It is only with everyone’s combined efforts and the added perspective of the medical pancreatologist that we can provide the best care for our shared patients.”
David Xin, MD, MPH, a medical pancreatologist at Brigham and Women’s Hospital, Boston, added, “I am often asked what it means to be a medical pancreatologist. What do I do if not EUS and ERCP? I provide longitudinal care, coordinate multidisciplinary management, assess nutritional status, optimize quality of life, and manage pain. But perhaps most importantly, I make myself available for patients who seek understanding and sympathy regarding their complex disease. I became a medical pancreatologist because my mentors during training helped me recognize how rewarding this career would be.”
Insights from other medical pancreatologists and therapeutic endoscopists are provided in Figure 2.
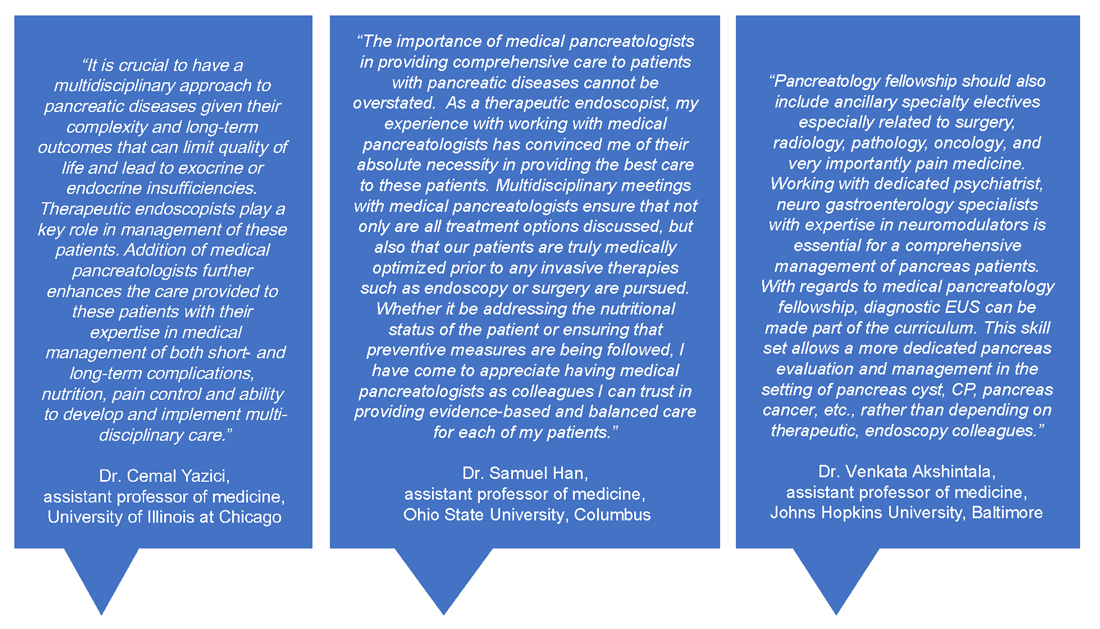
Education
Having a dedicated medical pancreatology clinic has the potential to add a unique element to the training of gastroenterology fellows. In my own experience, besides fellows interested in medical pancreatology, even those interested in therapeutic endoscopy find it useful to rotate through the pancreas clinic and follow patients after or leading to their procedures, becoming comfortable with noninterventional pain management of patients with pancreatic disorders and risk stratification of pancreatic cystic lesions, and learning about the management of rare disorders such as autoimmune pancreatitis. Most importantly, this allows trainees to identify cases where endoscopic intervention may not offer definitive treatment for complex conditions such as pancreatic pain. Trainee-centered organizations such as the Collaborative Alliance for Pancreatic Education and Research (CAPER) enable trainees and young investigators to network with other physicians who are passionate about the pancreas and establish early research collaborations for current and future research endeavors that will help advance this field.
Research
Having a trained medical pancreatologist adds the possibility of adding a unique angle to ongoing research within a gastroenterology division, especially in collaboration with others. For example, during my fellowship training I was able to focus on histological changes in pancreatic islets of patients with pancreatic cancer that develop diabetes, compared with those that do not, in collaboration with a pathologist who focused on studying islet pathology and under the guidance of my mentor, Dr. Suresh Chari, a medical pancreatologist.2 I was also part of other studies within the GI division with other medical pancreatologists, such as Dr. Santhi Vege and Dr. Shounak Majumder, who have continued to serve as career and research mentors.3 Collaborative, multicenter studies on pancreatic disease are also conducted by CAPER, the organization mentioned above. A list of potential collaborations for the fellow interested
in medical pancreatology is provided in Figure 3.
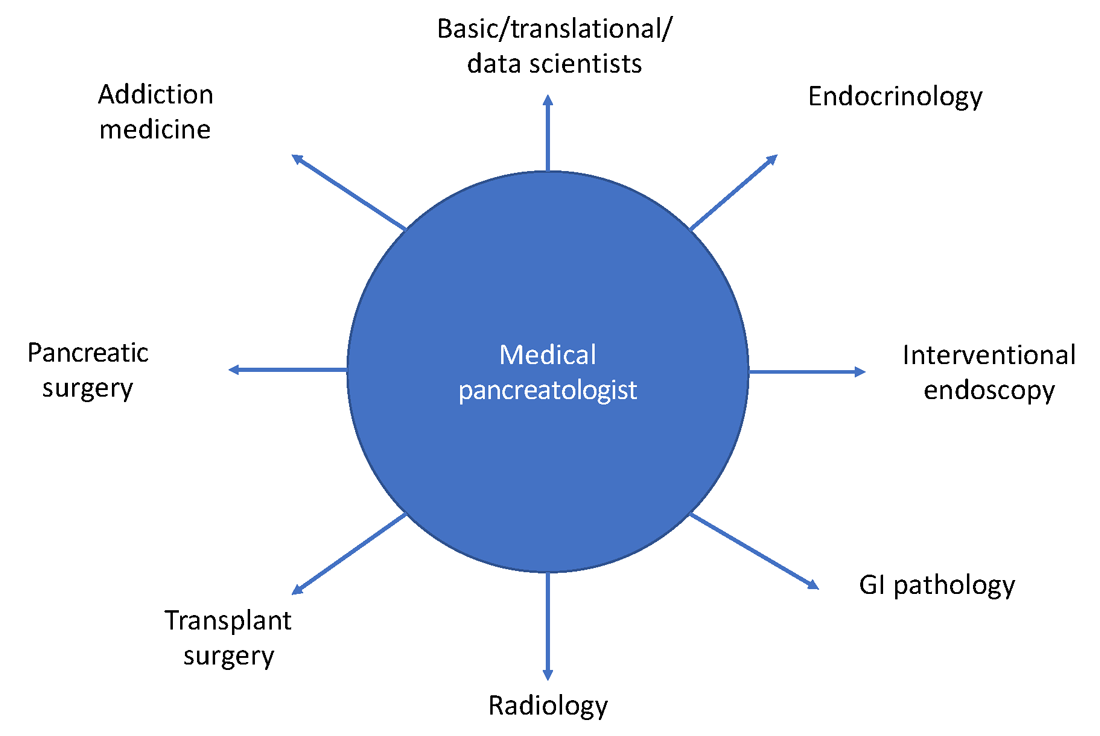
Marketing considerations for the gastroenterology division
Having a medical pancreatologist in the team is not only attractive for referring physicians within an institution but is often a great asset from a marketing standpoint, especially for tertiary care academic centers and large community practices with a broad referral base. Given that there are a limited number of medical pancreatologists in the country, having one as part of the faculty can certainly provide a competitive edge to that center within the area, especially with an ever-increasing preference of patients for hyperspecialized care.
How to develop a career in medical pancreatology
Gastroenterology fellows often start their fellowships “undifferentiated” and try to get exposed to a wide variety of GI pathology, either through general GI clinics or as part of subspecialized clinics, as they attempt to decide how they want their careers to look down the line. Similar to other subspecialities, if a trainee has already decided to pursue medical pancreatology (as happened in my case), they should strongly consider ranking programs with available opportunities for research/clinic in medical pancreatology and ideally undergo an additional year of training. Fellows who decide during the course of their fellowship that they want to pursue a career in medical pancreatology should consider applying for a 4th year in the subject to not only obtain further training in the field but to also conduct research in the area and become more “marketable” as a person that could start a medical pancreatology program at their future academic or community position. Trainees interested in medical pancreatology should try to focus their time on long-term, clinical management of patients with pancreatic disorders, engaging a multidisciplinary team composed of interventional endoscopists, pancreatic surgeons, transplant surgeons (if total pancreatectomy and islet autotransplantation is available), radiology, addiction medicine (if available), endocrinology, and pathology. The list of places that offer a 4th year in medical pancreatology is increasing every year, and as of the writing of this article there are six programs that have this opportunity, which include:
- Mayo Clinic, Rochester, Minn.
- Beth Israel Deaconess Medical Center, Boston
- Brigham and Women’s Hospital, Boston
- Johns Hopkins Hospital, Baltimore
- University of Pittsburgh Medical Center, Pittsburgh, Penn.
The CAPER website is also a great resource for education as well as for identifying potential medical pancreatology programs.
In summary, medical pancreatology is an evolving and rapidly growing career path for gastroenterology fellows interested in providing care to patients with pancreatic disease in close collaboration with multiple other subspecialties, especially therapeutic endoscopy and pancreatic surgery. The field is also ripe for fellows interested in clinical, translational, and basic science research related to pancreatic disorders.
Dr. Nagpal is assistant professor of medicine, director, pancreas clinic, University of Chicago. He had no conflicts to disclose.
References
1. Feldman M et al. “Sleisenger and Fordtran’s Gastrointestinal and Liver Disease,” 11th ed. (Philadelphia: Elsevier, 2021).
2. Nagpal SJS et al. Pancreatology. 2020 Jul;20(5):929-35.
3. Nagpal SJS et al. Pancreatology. 2019 Mar;19(2):290-5.
Although described by the Greek physician Herophilos around 300 B.C., it was not until the 19th century that enzymes began to be isolated from pancreatic secretions and their digestive action described, and not until early in the 20th century that Banting, Macleod, and Best received the Nobel prize for purifying insulin from the pancreata of dogs. For centuries in between, the pancreas was considered to be just a ‘beautiful piece of flesh’ (kallikreas), the main role of which was to protect the blood vessels in the abdomen and to serve as a cushion to the stomach.1 Certainly, the pancreas has come a long way since then but, like most other organs in the body, is oft ignored until it develops issues.
Like many other disorders in gastroenterology, pancreatic disorders were historically approached as mechanical or “plumbing” issues. As modern technology and innovation percolated through the world of endoscopy, a wide array of state-of-the-art tools were devised. Availability of newer “toys” and development of newer techniques also means that an ever-increasing curriculum has been squeezed into a generally single year of therapeutic endoscopy training, such that trainees can no longer limit themselves to learning only endoscopic ultrasound (EUS) and endoscopic retrograde cholangiopancreatography (ERCP) or intervening on pancreatic disease alone. Modern, subspecialized approaches to disease and economic considerations often dictate that the therapeutic endoscopist of today must perform a wide range of procedures besides ERCP and EUS, such as advanced resection using endoscopic mucosal resection (EMR), endoscopic submucosal dissection (ESD), per-oral endoscopic myotomy (POEM), endoscopic bariatric procedures, and newer techniques and acronyms that continue to evolve on a regular basis. This leaves the therapeutic endoscopist with little time for outpatient management of many patients that don’t need interventional procedures but are often very complex and need ongoing, long-term follow-up. In addition, any clinic slots available for interventional endoscopists may be utilized by patients coming in to discuss complex procedures or for postprocedure follow-up. Endoscopic management is not the definitive treatment for most pancreatic disorders. In fact, as our knowledge of pancreatic disease has continued to evolve, endoscopic intervention is now required in a minority of cases.
Role of the medical pancreatologist
Patient Care
As part of a comprehensive, multidisciplinary team that also includes an interventional gastroenterologist, pancreatic surgeon, transplant surgeon (in centers offering islet autotransplantation with total pancreatectomy), radiology, endocrinology, and GI pathologist, the medical pancreatologist helps lead the care of patients with pancreatic disorders, such as pancreatic cysts, acute and chronic pancreatitis (especially in cases where there is no role for active endoscopic intervention), autoimmune pancreatitis, indeterminate pancreatic masses, as well as screens high-risk patients for pancreatic cancer in conjunction with a genetic counselor. The medical pancreatologist often also serves as a bridge between various members of a large multidisciplinary team that, formally in the form of conferences or informally, discusses the management of complex patients, with each member available to help the other based on the patient’s most immediate clinical need at that time. A schematic showing how the medical pancreatologist collaborates with the therapeutic endoscopist is provided in Figure 1.
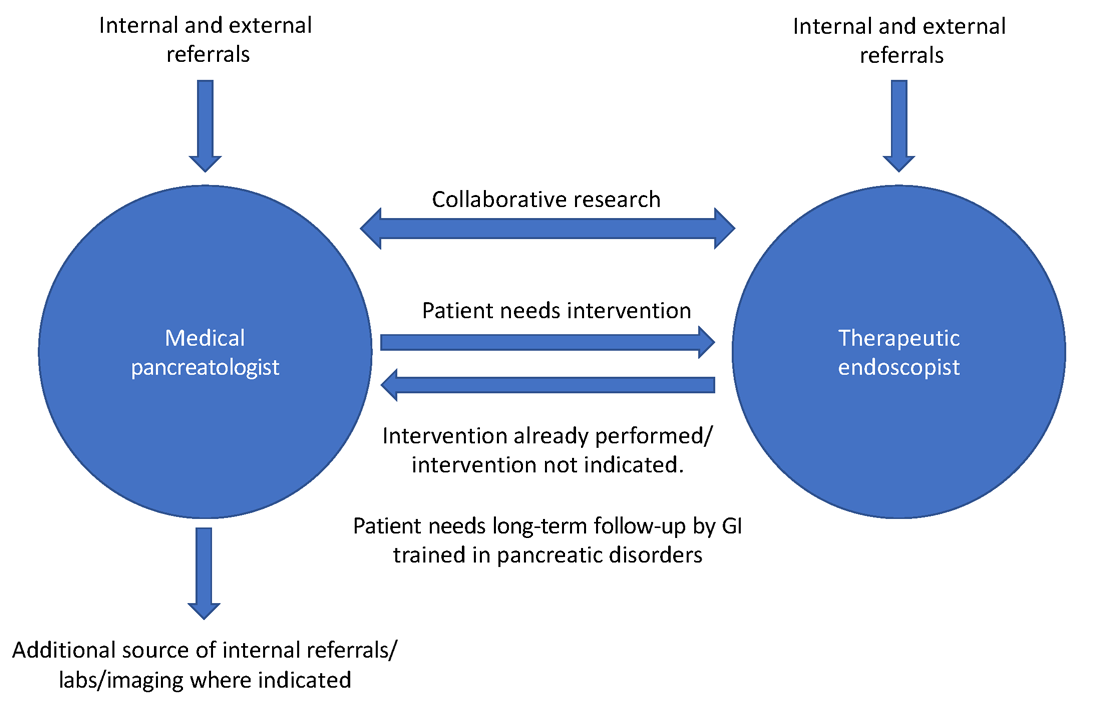
Uzma Siddiqui, MD, director for the Center for Endoscopic Research and Technology (CERT) at the University of Chicago said, “The management of pancreatic diseases is often challenging. Surgeons and endoscopists can offer some treatments that focus on one aspect or symptom, but the medical pancreatologist brings focus to the patient as a whole and helps organize care. It is only with everyone’s combined efforts and the added perspective of the medical pancreatologist that we can provide the best care for our shared patients.”
David Xin, MD, MPH, a medical pancreatologist at Brigham and Women’s Hospital, Boston, added, “I am often asked what it means to be a medical pancreatologist. What do I do if not EUS and ERCP? I provide longitudinal care, coordinate multidisciplinary management, assess nutritional status, optimize quality of life, and manage pain. But perhaps most importantly, I make myself available for patients who seek understanding and sympathy regarding their complex disease. I became a medical pancreatologist because my mentors during training helped me recognize how rewarding this career would be.”
Insights from other medical pancreatologists and therapeutic endoscopists are provided in Figure 2.
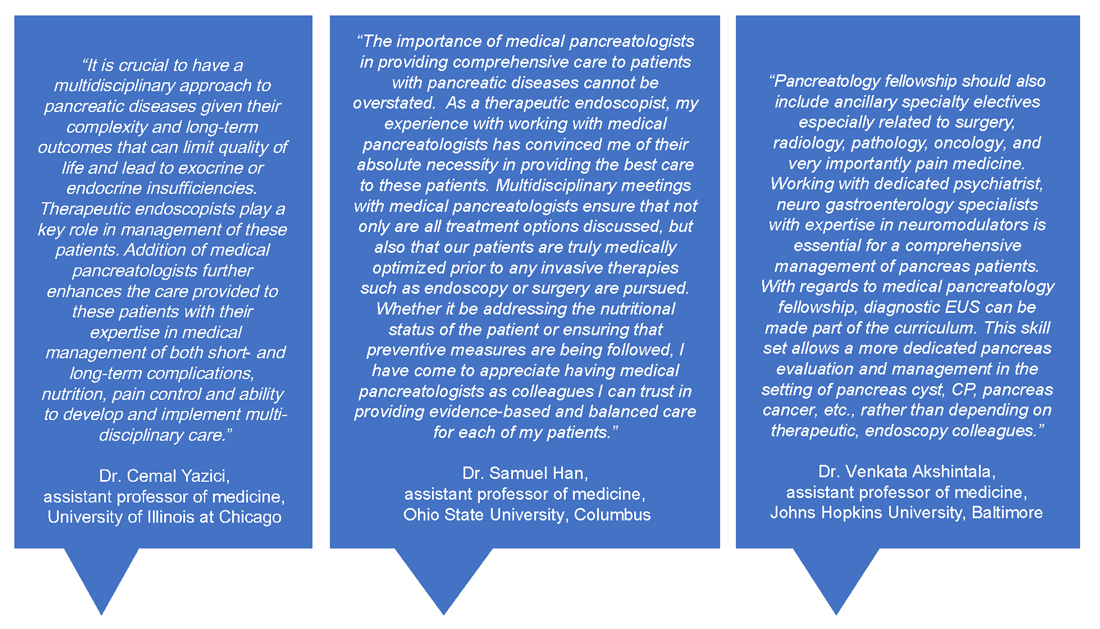
Education
Having a dedicated medical pancreatology clinic has the potential to add a unique element to the training of gastroenterology fellows. In my own experience, besides fellows interested in medical pancreatology, even those interested in therapeutic endoscopy find it useful to rotate through the pancreas clinic and follow patients after or leading to their procedures, becoming comfortable with noninterventional pain management of patients with pancreatic disorders and risk stratification of pancreatic cystic lesions, and learning about the management of rare disorders such as autoimmune pancreatitis. Most importantly, this allows trainees to identify cases where endoscopic intervention may not offer definitive treatment for complex conditions such as pancreatic pain. Trainee-centered organizations such as the Collaborative Alliance for Pancreatic Education and Research (CAPER) enable trainees and young investigators to network with other physicians who are passionate about the pancreas and establish early research collaborations for current and future research endeavors that will help advance this field.
Research
Having a trained medical pancreatologist adds the possibility of adding a unique angle to ongoing research within a gastroenterology division, especially in collaboration with others. For example, during my fellowship training I was able to focus on histological changes in pancreatic islets of patients with pancreatic cancer that develop diabetes, compared with those that do not, in collaboration with a pathologist who focused on studying islet pathology and under the guidance of my mentor, Dr. Suresh Chari, a medical pancreatologist.2 I was also part of other studies within the GI division with other medical pancreatologists, such as Dr. Santhi Vege and Dr. Shounak Majumder, who have continued to serve as career and research mentors.3 Collaborative, multicenter studies on pancreatic disease are also conducted by CAPER, the organization mentioned above. A list of potential collaborations for the fellow interested
in medical pancreatology is provided in Figure 3.
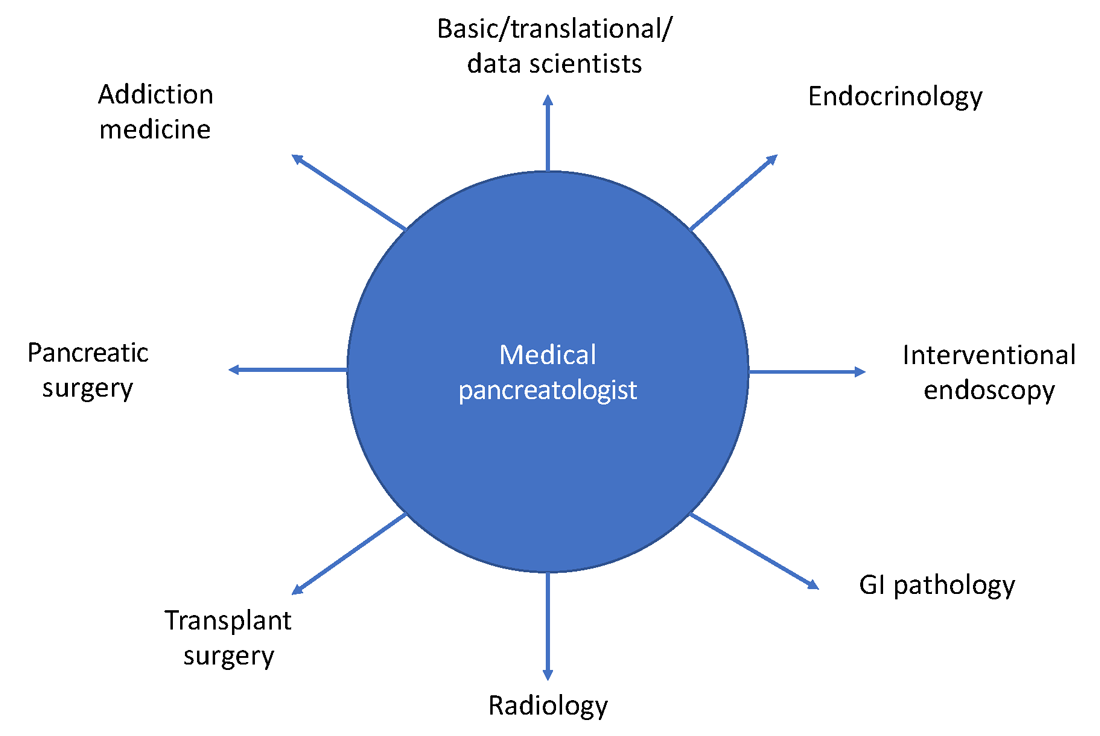
Marketing considerations for the gastroenterology division
Having a medical pancreatologist in the team is not only attractive for referring physicians within an institution but is often a great asset from a marketing standpoint, especially for tertiary care academic centers and large community practices with a broad referral base. Given that there are a limited number of medical pancreatologists in the country, having one as part of the faculty can certainly provide a competitive edge to that center within the area, especially with an ever-increasing preference of patients for hyperspecialized care.
How to develop a career in medical pancreatology
Gastroenterology fellows often start their fellowships “undifferentiated” and try to get exposed to a wide variety of GI pathology, either through general GI clinics or as part of subspecialized clinics, as they attempt to decide how they want their careers to look down the line. Similar to other subspecialities, if a trainee has already decided to pursue medical pancreatology (as happened in my case), they should strongly consider ranking programs with available opportunities for research/clinic in medical pancreatology and ideally undergo an additional year of training. Fellows who decide during the course of their fellowship that they want to pursue a career in medical pancreatology should consider applying for a 4th year in the subject to not only obtain further training in the field but to also conduct research in the area and become more “marketable” as a person that could start a medical pancreatology program at their future academic or community position. Trainees interested in medical pancreatology should try to focus their time on long-term, clinical management of patients with pancreatic disorders, engaging a multidisciplinary team composed of interventional endoscopists, pancreatic surgeons, transplant surgeons (if total pancreatectomy and islet autotransplantation is available), radiology, addiction medicine (if available), endocrinology, and pathology. The list of places that offer a 4th year in medical pancreatology is increasing every year, and as of the writing of this article there are six programs that have this opportunity, which include:
- Mayo Clinic, Rochester, Minn.
- Beth Israel Deaconess Medical Center, Boston
- Brigham and Women’s Hospital, Boston
- Johns Hopkins Hospital, Baltimore
- University of Pittsburgh Medical Center, Pittsburgh, Penn.
The CAPER website is also a great resource for education as well as for identifying potential medical pancreatology programs.
In summary, medical pancreatology is an evolving and rapidly growing career path for gastroenterology fellows interested in providing care to patients with pancreatic disease in close collaboration with multiple other subspecialties, especially therapeutic endoscopy and pancreatic surgery. The field is also ripe for fellows interested in clinical, translational, and basic science research related to pancreatic disorders.
Dr. Nagpal is assistant professor of medicine, director, pancreas clinic, University of Chicago. He had no conflicts to disclose.
References
1. Feldman M et al. “Sleisenger and Fordtran’s Gastrointestinal and Liver Disease,” 11th ed. (Philadelphia: Elsevier, 2021).
2. Nagpal SJS et al. Pancreatology. 2020 Jul;20(5):929-35.
3. Nagpal SJS et al. Pancreatology. 2019 Mar;19(2):290-5.
Although described by the Greek physician Herophilos around 300 B.C., it was not until the 19th century that enzymes began to be isolated from pancreatic secretions and their digestive action described, and not until early in the 20th century that Banting, Macleod, and Best received the Nobel prize for purifying insulin from the pancreata of dogs. For centuries in between, the pancreas was considered to be just a ‘beautiful piece of flesh’ (kallikreas), the main role of which was to protect the blood vessels in the abdomen and to serve as a cushion to the stomach.1 Certainly, the pancreas has come a long way since then but, like most other organs in the body, is oft ignored until it develops issues.
Like many other disorders in gastroenterology, pancreatic disorders were historically approached as mechanical or “plumbing” issues. As modern technology and innovation percolated through the world of endoscopy, a wide array of state-of-the-art tools were devised. Availability of newer “toys” and development of newer techniques also means that an ever-increasing curriculum has been squeezed into a generally single year of therapeutic endoscopy training, such that trainees can no longer limit themselves to learning only endoscopic ultrasound (EUS) and endoscopic retrograde cholangiopancreatography (ERCP) or intervening on pancreatic disease alone. Modern, subspecialized approaches to disease and economic considerations often dictate that the therapeutic endoscopist of today must perform a wide range of procedures besides ERCP and EUS, such as advanced resection using endoscopic mucosal resection (EMR), endoscopic submucosal dissection (ESD), per-oral endoscopic myotomy (POEM), endoscopic bariatric procedures, and newer techniques and acronyms that continue to evolve on a regular basis. This leaves the therapeutic endoscopist with little time for outpatient management of many patients that don’t need interventional procedures but are often very complex and need ongoing, long-term follow-up. In addition, any clinic slots available for interventional endoscopists may be utilized by patients coming in to discuss complex procedures or for postprocedure follow-up. Endoscopic management is not the definitive treatment for most pancreatic disorders. In fact, as our knowledge of pancreatic disease has continued to evolve, endoscopic intervention is now required in a minority of cases.
Role of the medical pancreatologist
Patient Care
As part of a comprehensive, multidisciplinary team that also includes an interventional gastroenterologist, pancreatic surgeon, transplant surgeon (in centers offering islet autotransplantation with total pancreatectomy), radiology, endocrinology, and GI pathologist, the medical pancreatologist helps lead the care of patients with pancreatic disorders, such as pancreatic cysts, acute and chronic pancreatitis (especially in cases where there is no role for active endoscopic intervention), autoimmune pancreatitis, indeterminate pancreatic masses, as well as screens high-risk patients for pancreatic cancer in conjunction with a genetic counselor. The medical pancreatologist often also serves as a bridge between various members of a large multidisciplinary team that, formally in the form of conferences or informally, discusses the management of complex patients, with each member available to help the other based on the patient’s most immediate clinical need at that time. A schematic showing how the medical pancreatologist collaborates with the therapeutic endoscopist is provided in Figure 1.
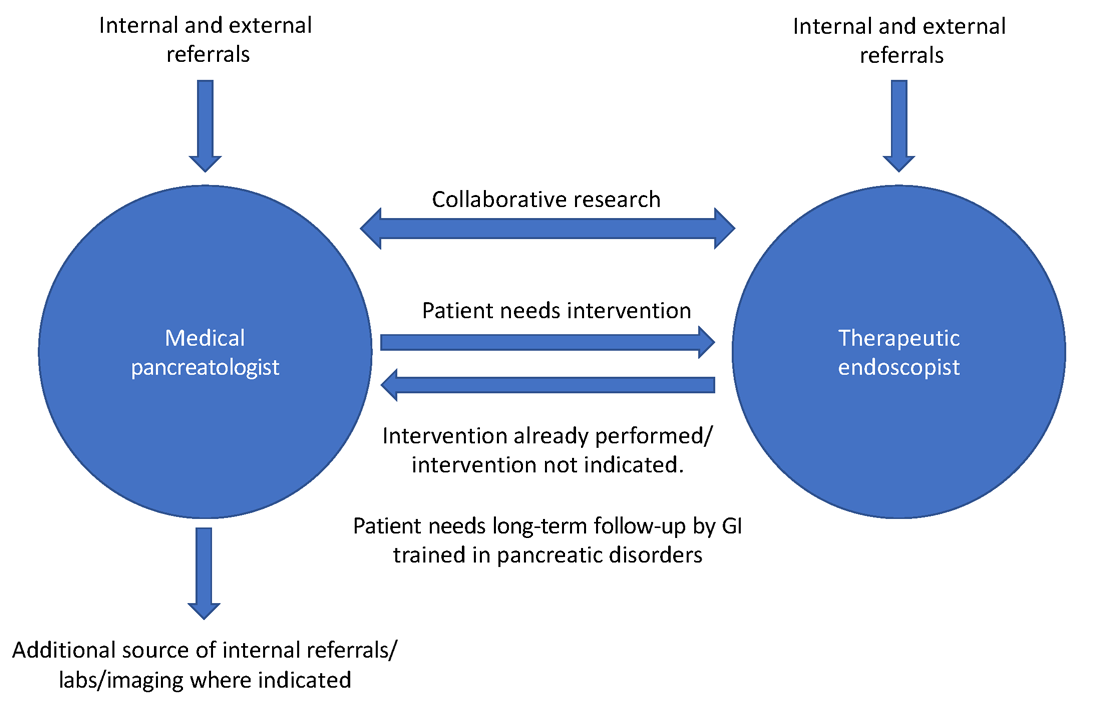
Uzma Siddiqui, MD, director for the Center for Endoscopic Research and Technology (CERT) at the University of Chicago said, “The management of pancreatic diseases is often challenging. Surgeons and endoscopists can offer some treatments that focus on one aspect or symptom, but the medical pancreatologist brings focus to the patient as a whole and helps organize care. It is only with everyone’s combined efforts and the added perspective of the medical pancreatologist that we can provide the best care for our shared patients.”
David Xin, MD, MPH, a medical pancreatologist at Brigham and Women’s Hospital, Boston, added, “I am often asked what it means to be a medical pancreatologist. What do I do if not EUS and ERCP? I provide longitudinal care, coordinate multidisciplinary management, assess nutritional status, optimize quality of life, and manage pain. But perhaps most importantly, I make myself available for patients who seek understanding and sympathy regarding their complex disease. I became a medical pancreatologist because my mentors during training helped me recognize how rewarding this career would be.”
Insights from other medical pancreatologists and therapeutic endoscopists are provided in Figure 2.
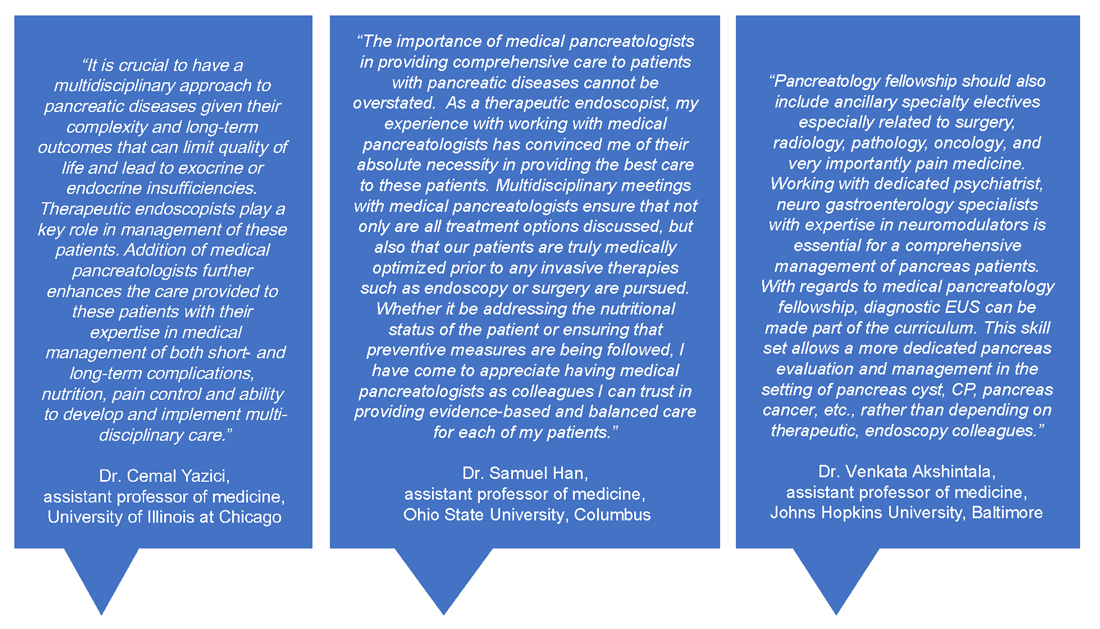
Education
Having a dedicated medical pancreatology clinic has the potential to add a unique element to the training of gastroenterology fellows. In my own experience, besides fellows interested in medical pancreatology, even those interested in therapeutic endoscopy find it useful to rotate through the pancreas clinic and follow patients after or leading to their procedures, becoming comfortable with noninterventional pain management of patients with pancreatic disorders and risk stratification of pancreatic cystic lesions, and learning about the management of rare disorders such as autoimmune pancreatitis. Most importantly, this allows trainees to identify cases where endoscopic intervention may not offer definitive treatment for complex conditions such as pancreatic pain. Trainee-centered organizations such as the Collaborative Alliance for Pancreatic Education and Research (CAPER) enable trainees and young investigators to network with other physicians who are passionate about the pancreas and establish early research collaborations for current and future research endeavors that will help advance this field.
Research
Having a trained medical pancreatologist adds the possibility of adding a unique angle to ongoing research within a gastroenterology division, especially in collaboration with others. For example, during my fellowship training I was able to focus on histological changes in pancreatic islets of patients with pancreatic cancer that develop diabetes, compared with those that do not, in collaboration with a pathologist who focused on studying islet pathology and under the guidance of my mentor, Dr. Suresh Chari, a medical pancreatologist.2 I was also part of other studies within the GI division with other medical pancreatologists, such as Dr. Santhi Vege and Dr. Shounak Majumder, who have continued to serve as career and research mentors.3 Collaborative, multicenter studies on pancreatic disease are also conducted by CAPER, the organization mentioned above. A list of potential collaborations for the fellow interested
in medical pancreatology is provided in Figure 3.
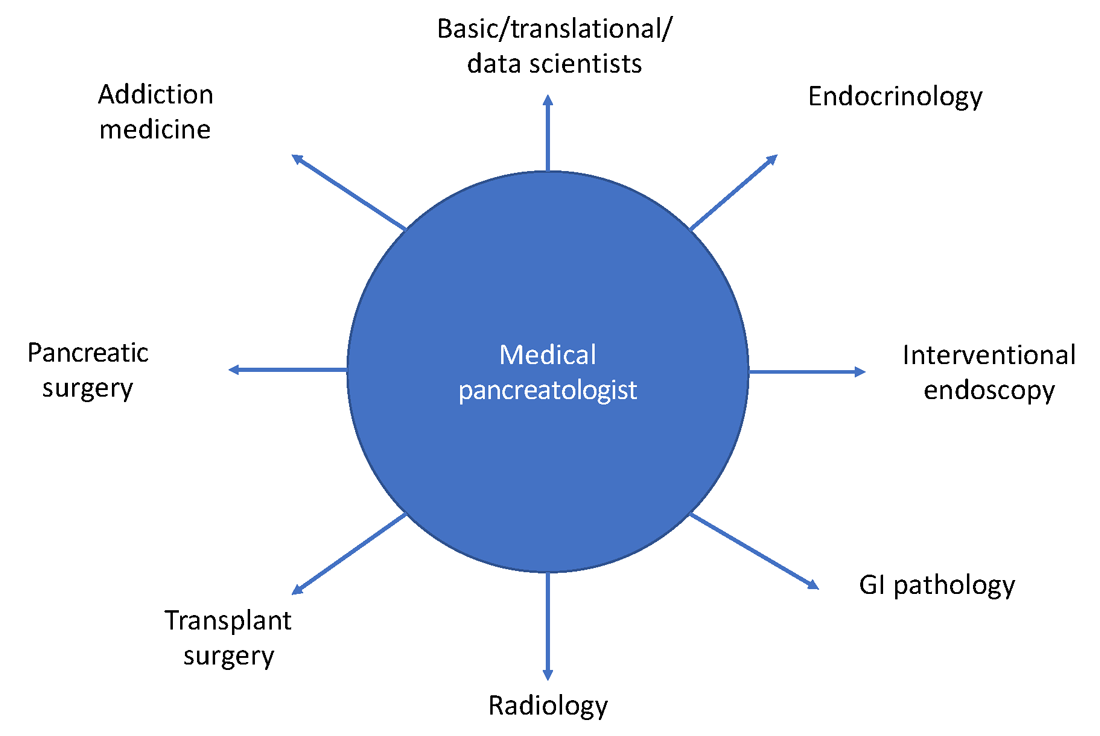
Marketing considerations for the gastroenterology division
Having a medical pancreatologist in the team is not only attractive for referring physicians within an institution but is often a great asset from a marketing standpoint, especially for tertiary care academic centers and large community practices with a broad referral base. Given that there are a limited number of medical pancreatologists in the country, having one as part of the faculty can certainly provide a competitive edge to that center within the area, especially with an ever-increasing preference of patients for hyperspecialized care.
How to develop a career in medical pancreatology
Gastroenterology fellows often start their fellowships “undifferentiated” and try to get exposed to a wide variety of GI pathology, either through general GI clinics or as part of subspecialized clinics, as they attempt to decide how they want their careers to look down the line. Similar to other subspecialities, if a trainee has already decided to pursue medical pancreatology (as happened in my case), they should strongly consider ranking programs with available opportunities for research/clinic in medical pancreatology and ideally undergo an additional year of training. Fellows who decide during the course of their fellowship that they want to pursue a career in medical pancreatology should consider applying for a 4th year in the subject to not only obtain further training in the field but to also conduct research in the area and become more “marketable” as a person that could start a medical pancreatology program at their future academic or community position. Trainees interested in medical pancreatology should try to focus their time on long-term, clinical management of patients with pancreatic disorders, engaging a multidisciplinary team composed of interventional endoscopists, pancreatic surgeons, transplant surgeons (if total pancreatectomy and islet autotransplantation is available), radiology, addiction medicine (if available), endocrinology, and pathology. The list of places that offer a 4th year in medical pancreatology is increasing every year, and as of the writing of this article there are six programs that have this opportunity, which include:
- Mayo Clinic, Rochester, Minn.
- Beth Israel Deaconess Medical Center, Boston
- Brigham and Women’s Hospital, Boston
- Johns Hopkins Hospital, Baltimore
- University of Pittsburgh Medical Center, Pittsburgh, Penn.
The CAPER website is also a great resource for education as well as for identifying potential medical pancreatology programs.
In summary, medical pancreatology is an evolving and rapidly growing career path for gastroenterology fellows interested in providing care to patients with pancreatic disease in close collaboration with multiple other subspecialties, especially therapeutic endoscopy and pancreatic surgery. The field is also ripe for fellows interested in clinical, translational, and basic science research related to pancreatic disorders.
Dr. Nagpal is assistant professor of medicine, director, pancreas clinic, University of Chicago. He had no conflicts to disclose.
References
1. Feldman M et al. “Sleisenger and Fordtran’s Gastrointestinal and Liver Disease,” 11th ed. (Philadelphia: Elsevier, 2021).
2. Nagpal SJS et al. Pancreatology. 2020 Jul;20(5):929-35.
3. Nagpal SJS et al. Pancreatology. 2019 Mar;19(2):290-5.
Choosing a career as chief medical officer at a health technology startup
How did your career pathway lead you to working at a health tech startup?
I’ve always had an interest in technology – in fact, it was part of the reason I chose gastroenterology. When I finished GI fellowship, I decided to stay in academics because of an opportunity to lead clinical innovation efforts at my institution’s patient safety institute. This role provided protected time to foster external and internal partnerships around technology. It also gave me an opportunity to pursue clinical research and administrative experiences. While I enjoyed all three paths, it became clear that health technology was my passion. While the opportunity to join a startup was largely serendipitous – I met the founder of the company after presenting at a digital medicine conference – it also happened as a result of the steps outlined in a subsequent question. Not long after learning about the company, I made the transition to part-time faculty/clinical status and full-time chief medical officer (CMO).
What do you do as CMO?
There is no one answer to this question. It will depend on a number of variables, especially the type of business (for example, diagnostic, drug, digital, direct care management, and so on), stage of company (for example, concept, seed, series A/B/C, public), and the existing background of company founders (for example, technical, clinical, operations, and so on). Generally speaking, the earlier the stage of the company, the more hats you’ll wear (though this also means more risk; more on that later). An early-stage company was appealing to me because it gave me an opportunity to apply many of the same critical-thinking and problem-solving skills in clinical medicine to a host of other challenges. For example, as a practicing gastroenterologist, I know the pain points in the delivery of GI care and the challenges that my patients encounter. I then ask how can I develop our technology and product platform to address these issues. Also understanding how value and quality are measured in GI practice makes it easier to convey the effect of the solutions that are built and prioritize their development. In my current role I contribute to the following areas:
- Clinical strategy and vision. This means understanding the clinical need the company is trying to address at a fundamental level and designing how the technology or solution can address that need in a meaningful way. This includes working directly with technology and product teams to create a roadmap for how the technology/solution will continue to drive impact.
- Clinical care leadership. If the company employs or works with health professionals in any capacity, this usually involves developing clinical protocols and providing clinical direction.
- Clinical outcomes. This means being responsible for understanding and/or developing the metrics that will be used to demonstrate impact of the technology/solution. This includes designing clinical studies and being responsible for their execution.
- Stakeholder engagement. This means interfacing internally with nearly every aspect of the company and interacting externally with customers (usually medical peers and executives), investors, other companies, and key opinion leaders in the field.
- Regulatory. For companies pursuing Food and Drug Administration clearance or approval for their product, this entails developing a strategy and executing it.
- Research & development. This involves creating and executing a roadmap for integrating new technologies/ideas that generally complement the initial problem you are trying to solve.
What do you enjoy most about working at a startup?
The variety of experience, the flexibility, the fast pace, the ability to work creatively, and the potential to make a large-scale impact are all aspects of the job that I enjoy. The ability to continue clinical practice is important to me and is a major plus.
What do you find most challenging about working at a startup?
One of the biggest differences between a startup and a traditional clinical role is the degree of uncertainty that permeates the entire experience. It took some time for me to adjust to the relative volatility/risk associated with this type of work. Unlike an academic, administrative, or private practice job, things can change very quickly (as in a 24-hour period or less!). This can encompass a number of changes, such as funding, leadership, strategic direction, business model, and staffing, to name a few. What I’ve learned is that this doesn’t always mean changing for the worse, but it does mean things changing near constantly. Being mentally prepared to adapt quickly and frequently to big changes is part of the experience.
What are the ways that GIs can get involved in startups?
Gastroenterologists have more opportunities than most physicians due to the diversity of conditions we treat and the large corresponding number of unmet needs we encounter. There is also the inherent innovation potential associated with new applications in endoscopy, diagnostics, and drug therapies. As a result, there are a number of ways to get involved:
- This often takes the form of “spinning out” research from an academic institution but can also be done successfully from private practice, particularly in the context of new devices/services. Another related option is to license your technology to a company, which offloads the operational aspects of running a business.
- Provide consulting/advisory support. Many early-stage companies cannot afford to hire a full-time physician, but they are open to consulting arrangements (and of course volunteer work). Don’t hesitate to directly contact companies that are interesting to you. These opportunities are possible even while in clinical training.
- Work part time or full time. The majority of startups are supportive of physicians continuing to practice clinically. This makes engaging in a part-time position financially feasible for both parties. Given the relatively high remuneration for gastroenterologists working clinically, a full-time position at a startup may require a financial tradeoff (that is, lower short-term salary for a potential larger long-term gain – note the emphasis on “potential”).
- Invest in early-stage companies. Physicians can become angel investors for early-stage companies. Given the relatively time-intensive process of finding new opportunities and conducting due diligence, this often takes the form of pooling funds into angel networks that can distribute the execution of investments more efficiently.
How would a fellow or early-career GI who is interested in startups pursue this career pathway?
The first step I recommend is self-reflection – what about the startup experience is interesting to you? Not all aspects appeal to everyone, and not all options provide the same opportunities. Spending time deciding which specific aspects of the startup experience appeal to you will make it easier to find the right opportunity. A concurrent step is to build expertise. This can take many forms, including traditional basic science or clinical research, but also includes implementation, evaluation/analysis, design, education, regulation, policy, and so on. The next step is to proactively meet people who are doing what you are interested in doing. Reach out to mentors, alumni, faculty, and friends. Conferences and social media are also great places to network. Other potential paths can include developing expertise in an allied functional area that can be later leveraged into a startup role (for example, experience at pharma, payer, regulatory, and so on). Many of these organizations have programs specifically geared toward physicians making a transition. In addition, another potential option is to seek additional education through an MBA where internships, recruitment programs, and robust alumni networks can be helpful in finding placement.
What if I want to learn more about the health technology startup experience?
The AGA Center for GI Innovation and Technology (CGIT) has a number of programs throughout the year, including the annual Tech Summit where you can learn about new companies, ideas, and technologies from like-minded individuals. I also invite you to reach out to me directly via Twitter, LinkedIn, or email with specific questions. As gastroenterologists, we are fortunate to work in a field full of innovation and new ideas. As a result, there are many meaningful career paths available to those interested in gastroenterology and technology. Whether providing direct clinical care with the latest endoscopic techniques or developing the next digital therapy, the opportunities for gastroenterologists will only continue to grow.
Dr. Mathews is chief medical officer at Vivante Health and assistant professor of medicine at Johns Hopkins Medicine in Baltimore. He is an officer at Vivante Health with stock options, but he reports having nothing else to disclose.
How did your career pathway lead you to working at a health tech startup?
I’ve always had an interest in technology – in fact, it was part of the reason I chose gastroenterology. When I finished GI fellowship, I decided to stay in academics because of an opportunity to lead clinical innovation efforts at my institution’s patient safety institute. This role provided protected time to foster external and internal partnerships around technology. It also gave me an opportunity to pursue clinical research and administrative experiences. While I enjoyed all three paths, it became clear that health technology was my passion. While the opportunity to join a startup was largely serendipitous – I met the founder of the company after presenting at a digital medicine conference – it also happened as a result of the steps outlined in a subsequent question. Not long after learning about the company, I made the transition to part-time faculty/clinical status and full-time chief medical officer (CMO).
What do you do as CMO?
There is no one answer to this question. It will depend on a number of variables, especially the type of business (for example, diagnostic, drug, digital, direct care management, and so on), stage of company (for example, concept, seed, series A/B/C, public), and the existing background of company founders (for example, technical, clinical, operations, and so on). Generally speaking, the earlier the stage of the company, the more hats you’ll wear (though this also means more risk; more on that later). An early-stage company was appealing to me because it gave me an opportunity to apply many of the same critical-thinking and problem-solving skills in clinical medicine to a host of other challenges. For example, as a practicing gastroenterologist, I know the pain points in the delivery of GI care and the challenges that my patients encounter. I then ask how can I develop our technology and product platform to address these issues. Also understanding how value and quality are measured in GI practice makes it easier to convey the effect of the solutions that are built and prioritize their development. In my current role I contribute to the following areas:
- Clinical strategy and vision. This means understanding the clinical need the company is trying to address at a fundamental level and designing how the technology or solution can address that need in a meaningful way. This includes working directly with technology and product teams to create a roadmap for how the technology/solution will continue to drive impact.
- Clinical care leadership. If the company employs or works with health professionals in any capacity, this usually involves developing clinical protocols and providing clinical direction.
- Clinical outcomes. This means being responsible for understanding and/or developing the metrics that will be used to demonstrate impact of the technology/solution. This includes designing clinical studies and being responsible for their execution.
- Stakeholder engagement. This means interfacing internally with nearly every aspect of the company and interacting externally with customers (usually medical peers and executives), investors, other companies, and key opinion leaders in the field.
- Regulatory. For companies pursuing Food and Drug Administration clearance or approval for their product, this entails developing a strategy and executing it.
- Research & development. This involves creating and executing a roadmap for integrating new technologies/ideas that generally complement the initial problem you are trying to solve.
What do you enjoy most about working at a startup?
The variety of experience, the flexibility, the fast pace, the ability to work creatively, and the potential to make a large-scale impact are all aspects of the job that I enjoy. The ability to continue clinical practice is important to me and is a major plus.
What do you find most challenging about working at a startup?
One of the biggest differences between a startup and a traditional clinical role is the degree of uncertainty that permeates the entire experience. It took some time for me to adjust to the relative volatility/risk associated with this type of work. Unlike an academic, administrative, or private practice job, things can change very quickly (as in a 24-hour period or less!). This can encompass a number of changes, such as funding, leadership, strategic direction, business model, and staffing, to name a few. What I’ve learned is that this doesn’t always mean changing for the worse, but it does mean things changing near constantly. Being mentally prepared to adapt quickly and frequently to big changes is part of the experience.
What are the ways that GIs can get involved in startups?
Gastroenterologists have more opportunities than most physicians due to the diversity of conditions we treat and the large corresponding number of unmet needs we encounter. There is also the inherent innovation potential associated with new applications in endoscopy, diagnostics, and drug therapies. As a result, there are a number of ways to get involved:
- This often takes the form of “spinning out” research from an academic institution but can also be done successfully from private practice, particularly in the context of new devices/services. Another related option is to license your technology to a company, which offloads the operational aspects of running a business.
- Provide consulting/advisory support. Many early-stage companies cannot afford to hire a full-time physician, but they are open to consulting arrangements (and of course volunteer work). Don’t hesitate to directly contact companies that are interesting to you. These opportunities are possible even while in clinical training.
- Work part time or full time. The majority of startups are supportive of physicians continuing to practice clinically. This makes engaging in a part-time position financially feasible for both parties. Given the relatively high remuneration for gastroenterologists working clinically, a full-time position at a startup may require a financial tradeoff (that is, lower short-term salary for a potential larger long-term gain – note the emphasis on “potential”).
- Invest in early-stage companies. Physicians can become angel investors for early-stage companies. Given the relatively time-intensive process of finding new opportunities and conducting due diligence, this often takes the form of pooling funds into angel networks that can distribute the execution of investments more efficiently.
How would a fellow or early-career GI who is interested in startups pursue this career pathway?
The first step I recommend is self-reflection – what about the startup experience is interesting to you? Not all aspects appeal to everyone, and not all options provide the same opportunities. Spending time deciding which specific aspects of the startup experience appeal to you will make it easier to find the right opportunity. A concurrent step is to build expertise. This can take many forms, including traditional basic science or clinical research, but also includes implementation, evaluation/analysis, design, education, regulation, policy, and so on. The next step is to proactively meet people who are doing what you are interested in doing. Reach out to mentors, alumni, faculty, and friends. Conferences and social media are also great places to network. Other potential paths can include developing expertise in an allied functional area that can be later leveraged into a startup role (for example, experience at pharma, payer, regulatory, and so on). Many of these organizations have programs specifically geared toward physicians making a transition. In addition, another potential option is to seek additional education through an MBA where internships, recruitment programs, and robust alumni networks can be helpful in finding placement.
What if I want to learn more about the health technology startup experience?
The AGA Center for GI Innovation and Technology (CGIT) has a number of programs throughout the year, including the annual Tech Summit where you can learn about new companies, ideas, and technologies from like-minded individuals. I also invite you to reach out to me directly via Twitter, LinkedIn, or email with specific questions. As gastroenterologists, we are fortunate to work in a field full of innovation and new ideas. As a result, there are many meaningful career paths available to those interested in gastroenterology and technology. Whether providing direct clinical care with the latest endoscopic techniques or developing the next digital therapy, the opportunities for gastroenterologists will only continue to grow.
Dr. Mathews is chief medical officer at Vivante Health and assistant professor of medicine at Johns Hopkins Medicine in Baltimore. He is an officer at Vivante Health with stock options, but he reports having nothing else to disclose.
How did your career pathway lead you to working at a health tech startup?
I’ve always had an interest in technology – in fact, it was part of the reason I chose gastroenterology. When I finished GI fellowship, I decided to stay in academics because of an opportunity to lead clinical innovation efforts at my institution’s patient safety institute. This role provided protected time to foster external and internal partnerships around technology. It also gave me an opportunity to pursue clinical research and administrative experiences. While I enjoyed all three paths, it became clear that health technology was my passion. While the opportunity to join a startup was largely serendipitous – I met the founder of the company after presenting at a digital medicine conference – it also happened as a result of the steps outlined in a subsequent question. Not long after learning about the company, I made the transition to part-time faculty/clinical status and full-time chief medical officer (CMO).
What do you do as CMO?
There is no one answer to this question. It will depend on a number of variables, especially the type of business (for example, diagnostic, drug, digital, direct care management, and so on), stage of company (for example, concept, seed, series A/B/C, public), and the existing background of company founders (for example, technical, clinical, operations, and so on). Generally speaking, the earlier the stage of the company, the more hats you’ll wear (though this also means more risk; more on that later). An early-stage company was appealing to me because it gave me an opportunity to apply many of the same critical-thinking and problem-solving skills in clinical medicine to a host of other challenges. For example, as a practicing gastroenterologist, I know the pain points in the delivery of GI care and the challenges that my patients encounter. I then ask how can I develop our technology and product platform to address these issues. Also understanding how value and quality are measured in GI practice makes it easier to convey the effect of the solutions that are built and prioritize their development. In my current role I contribute to the following areas:
- Clinical strategy and vision. This means understanding the clinical need the company is trying to address at a fundamental level and designing how the technology or solution can address that need in a meaningful way. This includes working directly with technology and product teams to create a roadmap for how the technology/solution will continue to drive impact.
- Clinical care leadership. If the company employs or works with health professionals in any capacity, this usually involves developing clinical protocols and providing clinical direction.
- Clinical outcomes. This means being responsible for understanding and/or developing the metrics that will be used to demonstrate impact of the technology/solution. This includes designing clinical studies and being responsible for their execution.
- Stakeholder engagement. This means interfacing internally with nearly every aspect of the company and interacting externally with customers (usually medical peers and executives), investors, other companies, and key opinion leaders in the field.
- Regulatory. For companies pursuing Food and Drug Administration clearance or approval for their product, this entails developing a strategy and executing it.
- Research & development. This involves creating and executing a roadmap for integrating new technologies/ideas that generally complement the initial problem you are trying to solve.
What do you enjoy most about working at a startup?
The variety of experience, the flexibility, the fast pace, the ability to work creatively, and the potential to make a large-scale impact are all aspects of the job that I enjoy. The ability to continue clinical practice is important to me and is a major plus.
What do you find most challenging about working at a startup?
One of the biggest differences between a startup and a traditional clinical role is the degree of uncertainty that permeates the entire experience. It took some time for me to adjust to the relative volatility/risk associated with this type of work. Unlike an academic, administrative, or private practice job, things can change very quickly (as in a 24-hour period or less!). This can encompass a number of changes, such as funding, leadership, strategic direction, business model, and staffing, to name a few. What I’ve learned is that this doesn’t always mean changing for the worse, but it does mean things changing near constantly. Being mentally prepared to adapt quickly and frequently to big changes is part of the experience.
What are the ways that GIs can get involved in startups?
Gastroenterologists have more opportunities than most physicians due to the diversity of conditions we treat and the large corresponding number of unmet needs we encounter. There is also the inherent innovation potential associated with new applications in endoscopy, diagnostics, and drug therapies. As a result, there are a number of ways to get involved:
- This often takes the form of “spinning out” research from an academic institution but can also be done successfully from private practice, particularly in the context of new devices/services. Another related option is to license your technology to a company, which offloads the operational aspects of running a business.
- Provide consulting/advisory support. Many early-stage companies cannot afford to hire a full-time physician, but they are open to consulting arrangements (and of course volunteer work). Don’t hesitate to directly contact companies that are interesting to you. These opportunities are possible even while in clinical training.
- Work part time or full time. The majority of startups are supportive of physicians continuing to practice clinically. This makes engaging in a part-time position financially feasible for both parties. Given the relatively high remuneration for gastroenterologists working clinically, a full-time position at a startup may require a financial tradeoff (that is, lower short-term salary for a potential larger long-term gain – note the emphasis on “potential”).
- Invest in early-stage companies. Physicians can become angel investors for early-stage companies. Given the relatively time-intensive process of finding new opportunities and conducting due diligence, this often takes the form of pooling funds into angel networks that can distribute the execution of investments more efficiently.
How would a fellow or early-career GI who is interested in startups pursue this career pathway?
The first step I recommend is self-reflection – what about the startup experience is interesting to you? Not all aspects appeal to everyone, and not all options provide the same opportunities. Spending time deciding which specific aspects of the startup experience appeal to you will make it easier to find the right opportunity. A concurrent step is to build expertise. This can take many forms, including traditional basic science or clinical research, but also includes implementation, evaluation/analysis, design, education, regulation, policy, and so on. The next step is to proactively meet people who are doing what you are interested in doing. Reach out to mentors, alumni, faculty, and friends. Conferences and social media are also great places to network. Other potential paths can include developing expertise in an allied functional area that can be later leveraged into a startup role (for example, experience at pharma, payer, regulatory, and so on). Many of these organizations have programs specifically geared toward physicians making a transition. In addition, another potential option is to seek additional education through an MBA where internships, recruitment programs, and robust alumni networks can be helpful in finding placement.
What if I want to learn more about the health technology startup experience?
The AGA Center for GI Innovation and Technology (CGIT) has a number of programs throughout the year, including the annual Tech Summit where you can learn about new companies, ideas, and technologies from like-minded individuals. I also invite you to reach out to me directly via Twitter, LinkedIn, or email with specific questions. As gastroenterologists, we are fortunate to work in a field full of innovation and new ideas. As a result, there are many meaningful career paths available to those interested in gastroenterology and technology. Whether providing direct clinical care with the latest endoscopic techniques or developing the next digital therapy, the opportunities for gastroenterologists will only continue to grow.
Dr. Mathews is chief medical officer at Vivante Health and assistant professor of medicine at Johns Hopkins Medicine in Baltimore. He is an officer at Vivante Health with stock options, but he reports having nothing else to disclose.
The path to becoming an esophagologist
Esophagology was a term coined in 1948 to describe a medical specialty devoted to the study of the anatomy, physiology, and pathology of the esophagus. The term was born out of increased interest and evolution in esophagology and supported by development in esophagoscopy.1 While still rooted in these basic tenets, the landscape of esophagology is dramatically different in 2020. The last decade alone has seen unprecedented technological advances in esophagology, from the transformation of line tracings to high-resolution esophageal pressure topography to more recent innovations such as the functional lumen imaging probe. Successful therapeutic developments have increased opportunities for effective and less invasive treatment approaches for achalasia and gastroesophageal reflux disease (GERD). With changing concepts in esophageal diseases such as eosinophilic esophagitis, successful management now incorporates findings from recent discoveries that have revolutionized care pathways. (see Figure 1).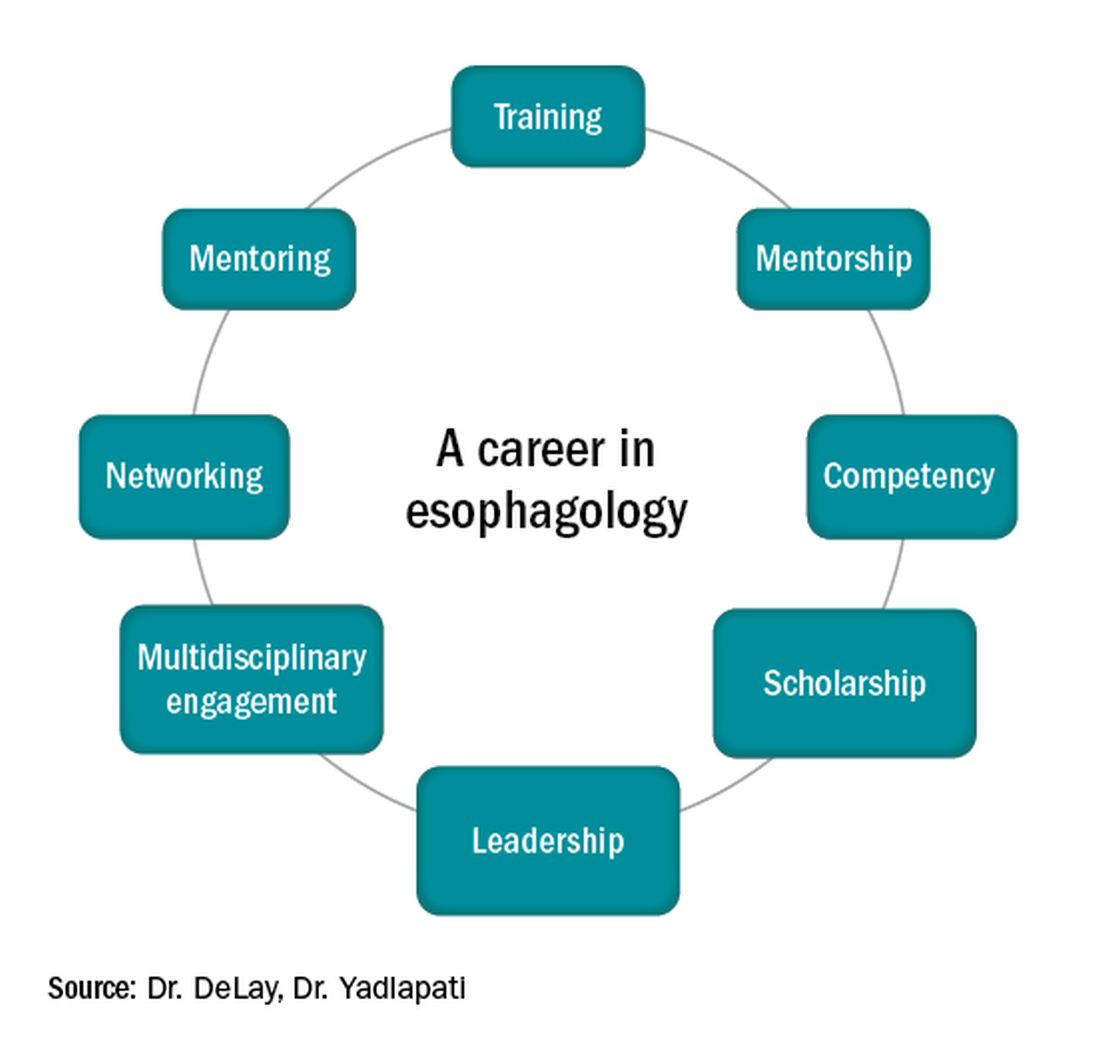
Figure 1
Optimizing esophagology training during fellowship
First, and most importantly, an esophagologist must have a foundation in the basic principles of esophageal anatomy, physiology, and pathology (see Figure 2). While newer digital learning resources exist, tried and true book-based resources – text books, chapters, and reviews – related to esophageal mechanics, the interplay between muscle function and neurogenics, and factors associated with nociception, remain the optimal learning strategy.
Once equipped with a foundation in esophageal physiology, one can readily engage with esophageal technologies, as there exists a vast array of testing to assess esophageal function. A comprehensive understanding of each, including device configuration, clinical protocol, and data storage, promotes a depth of knowledge every esophagologist should develop. Aspiring esophagologists should take time to observe and perform procedures in their motility labs, particularly esophageal high-resolution manometry and ambulatory reflux monitoring studies. If afforded the opportunity through a research study or a clinical indication, esophagologists should also undergo the tests themselves. Empathy regarding the discomfort and tolerability of motility tests, which are notoriously challenging for patients, can promote rapport and trust with patients, increase patient satisfaction, and enhance one’s own understanding of resource utilization and safety.
Perhaps most critical to becoming an esophagologist, is acquiring sufficient competency in interpretation of esophageal studies. Prior research highlights the limitations in achieving competency when trainees adhere to the minimum case volume of studies recommended by the GI core curriculum.2,3 With the bar set higher for the burgeoning esophagologist, one must not only practice with a higher case volume, but also engage in competency-based assessments and performance feedback.4 Trainees should start by reviewing tracings for their own patients. Preliminary interpretation of pending studies and review with a mentor before the final sign-off, participation in research that requires study, or even teaching co-trainees basic tenets of motility are other creative approaches to learning. Esophagologists will be expected to know how to navigate the software to access studies, manually review tracings, and generate reports. Trainees should refer to the multitude of societal guidelines and classification scheme recommendations available when developing competency in diagnostic impression.5
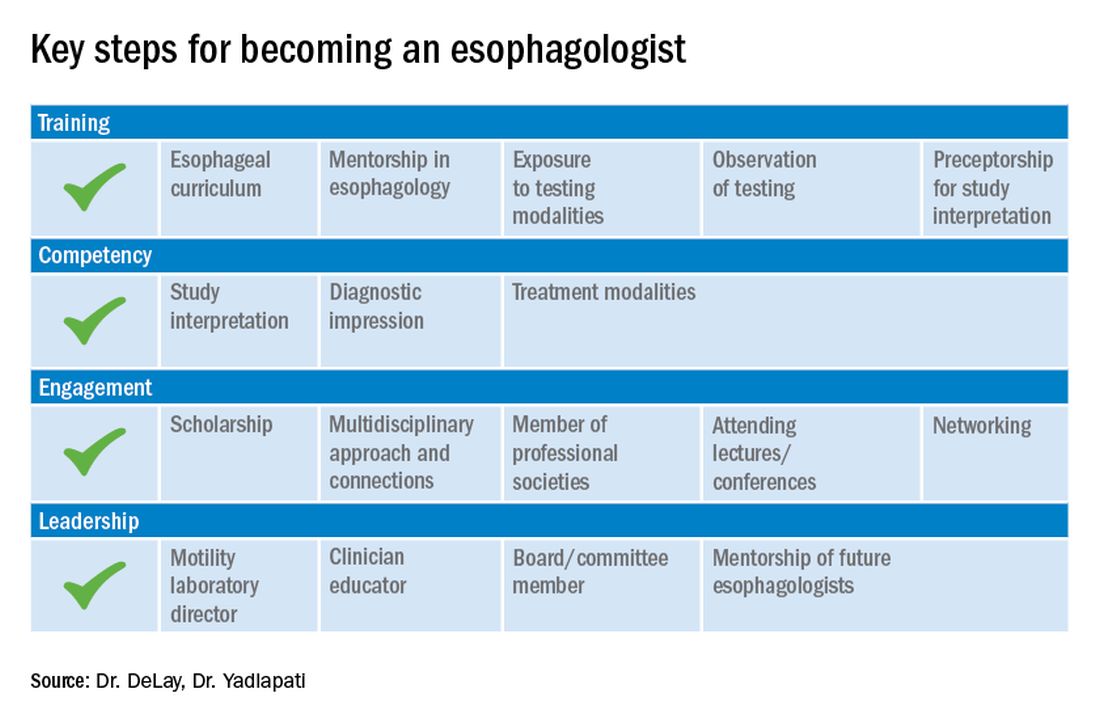
Figure 2
While esophagology is a medical specialty, it is imperative that the esophagologist has a robust understanding of therapeutic options and surgical interventions for esophageal pathology. Scrubbing into the operating room during foregut surgeries is an eye-opening experience. This includes thoracic and abdominal approaches, robotic, laparoscopic, and open techniques, and interventions for GERD, achalasia, diverticular disease, and bariatric management. Equally important is working alongside advanced endoscopy faculty to understand utilities of endoscopic ultrasound, ablative methods for Barrett’s esophagus, and advanced techniques such as peroral endoscopic myotomy and transoral incisionless fundoplication. This exposure is critical as the role of the esophagologist is to speak knowledgably of therapeutic options and the risks and benefits of alternative approaches. Further, the patient’s journey rarely ends with the intervention, and an esophagologist must understand how to evaluate symptoms and manage complications following therapy.
As with broader digestive health, the management of esophageal disorders is becoming increasingly integrated with psychological, lifestyle, and dietary interventions. Observing and understanding how other health care members interact with the patient and relay concepts of brain-gut interaction is helpful in one’s own practice and ability to speak to the value of focused interventions.
These key training aspects in esophagology can be acquired through different avenues (see Figure 3). Formal 1-year advanced esophageal or motility focused fellowships are available at leading esophageal centers. The American Neurogastroenterology and Motility Society (ANMS) offers a clinical training program for selected fellows to pursue apprenticeship-based training in gastrointestinal motility. A review of the benefits of additional training, available programs, and how to apply, can be found at The New Gastroenterologist. It may be possible to customize parts of the general clinical fellowship with a strong focus on esophagology. All budding esophagologists are strongly encouraged to attend and participate in subspecialty national meetings such as through the ANMS or the American Foregut Society.
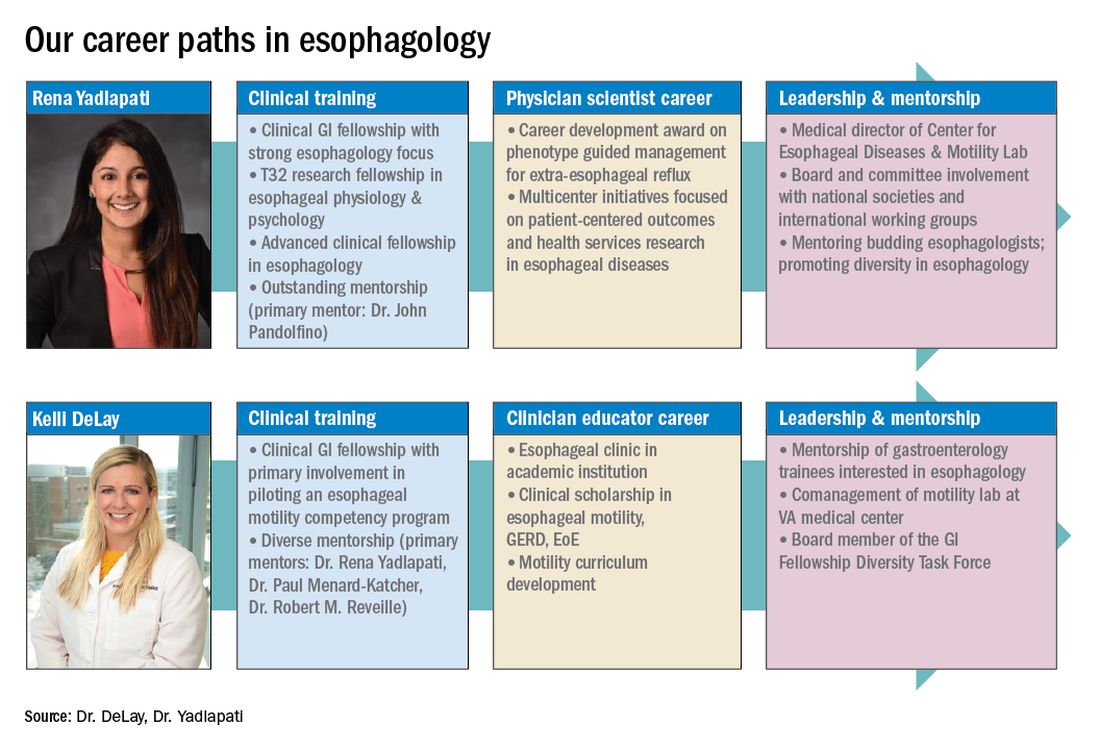
Figure 3
Steep learning curve post fellowship
Regardless of the robust nature of clinical esophagology training, early career esophagologists will face challenges and learn on the job.
Many esophagologists are directors of a motility lab early in their careers. This is often uncharted territory in terms of managing a team of nurses, technicians, and other providers. The director of a motility lab will be called upon to troubleshoot various arenas of diagnostic workup, from study acquisition and interpretation to technical barriers with equipment or software. Keys to maintaining a successful motility lab further include optimizing schedules and protocols, delineating roles and responsibilities of team members, ensuring adequate training across staff and providers, communicating expectations, and cultivating an open relationship with the motility lab supervisor. Crucial, yet often neglected during fellowship training, are the economic considerations of operating and expanding the motility lab, and the financial implications for one’s own practice.6 Participating in professional development workshops can be especially valuable in cultivating leadership skills.
The care an esophagologist provides relies heavily on collaborative relationships within the organization and peer mentorship, cooperation, and feedback. It is essential to cultivate multidisciplinary relationships with surgical (e.g., foregut surgery, laryngology), medical (e.g., pulmonology, allergy), radiology, and pathology colleagues, as well as with integrated health specialists including psychologists, dietitians, and speech language pathologists. It is also important to have open industry partnerships to ensure appropriate technical support and access to advancements.
Often organizations will have only one esophageal specialist within the group. Fortunately, the national and global community of esophagologists is highly collaborative and collegial. All esophagologists should have a network of mentors and colleagues within and outside of their organization to review complex cases, discuss challenges in the workplace, and foster research and innovation. Along these lines, both aspiring and practicing esophagologists should engage with professional societies as opportunities are abundant. Esophageal-focused societies include the ANMS, American Foregut Society, and International Society of Diseases of Esophagus, and the overarching GI societies also have a strong esophageal focus.
The path to becoming an esophagologist does not mirror the structure of the organ itself. Development is neither confined, unidirectional, nor set in length, but gradual, each step thoughtfully built on the last. Esophageal pathology is diverse, complex, and fascinating. With the appropriate training, mentorship, engagement, and leadership, esophagologists have the privilege of making a great impact on the lives of patients we meet, a fulfilling journey worth the time and effort it takes.
Dr. Delay is in the division of gastroenterology & hepatology, University of Colorado Anschutz Medical Campus, Aurora. Dr. Yadlapati is at the Center for Esophageal Diseases, division of gastroenterology, University of California San Diego, La Jolla. She is a consultant through institutional agreement to Medtronic, Ironwood Pharmaceuticals, and Diversatek; she has received research support from Ironwood Pharmaceuticals; and is on the advisory board of Phathom Pharmaceuticals.
References
1. Holinger PH. Arch Otolaryngol. 1948;47:119-26.
2. Yadlapati R et al. Clin Gastroenterol Hepatol. 2017;15:1708-14.e3.
3. Oversight Working Network et al. Gastrointest Endosc. 2014;80:16-27.
4. DeLay K et al. Am J Gastroenterol. 2020;115:1453-9.
5. Gyawali CP et al. Neurogastroenterol Motil. 2018;30(9):e13341.
6. Yadlapati R et al. Gastroenterology. 2020;158:1202-10.
Esophagology was a term coined in 1948 to describe a medical specialty devoted to the study of the anatomy, physiology, and pathology of the esophagus. The term was born out of increased interest and evolution in esophagology and supported by development in esophagoscopy.1 While still rooted in these basic tenets, the landscape of esophagology is dramatically different in 2020. The last decade alone has seen unprecedented technological advances in esophagology, from the transformation of line tracings to high-resolution esophageal pressure topography to more recent innovations such as the functional lumen imaging probe. Successful therapeutic developments have increased opportunities for effective and less invasive treatment approaches for achalasia and gastroesophageal reflux disease (GERD). With changing concepts in esophageal diseases such as eosinophilic esophagitis, successful management now incorporates findings from recent discoveries that have revolutionized care pathways. (see Figure 1).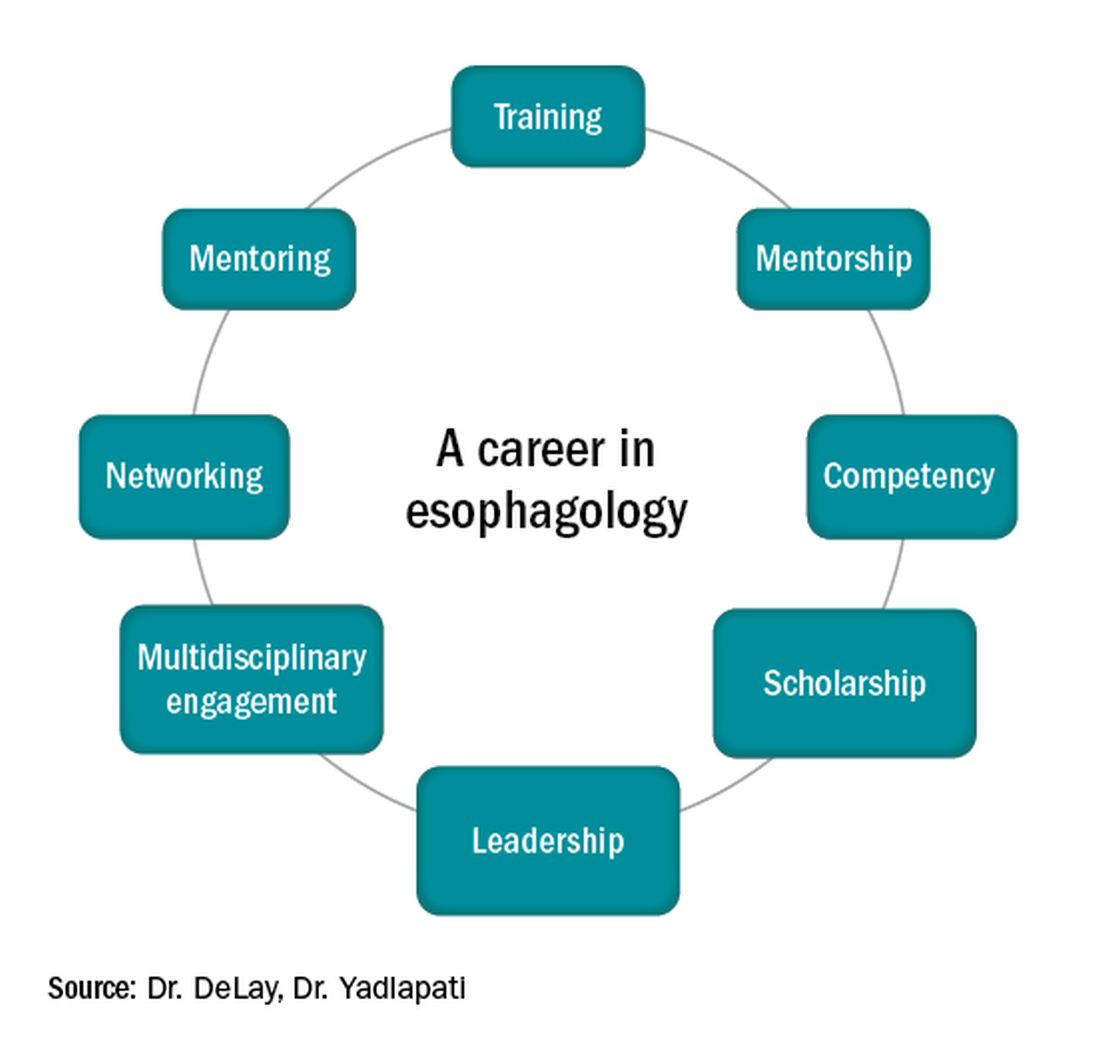
Figure 1
Optimizing esophagology training during fellowship
First, and most importantly, an esophagologist must have a foundation in the basic principles of esophageal anatomy, physiology, and pathology (see Figure 2). While newer digital learning resources exist, tried and true book-based resources – text books, chapters, and reviews – related to esophageal mechanics, the interplay between muscle function and neurogenics, and factors associated with nociception, remain the optimal learning strategy.
Once equipped with a foundation in esophageal physiology, one can readily engage with esophageal technologies, as there exists a vast array of testing to assess esophageal function. A comprehensive understanding of each, including device configuration, clinical protocol, and data storage, promotes a depth of knowledge every esophagologist should develop. Aspiring esophagologists should take time to observe and perform procedures in their motility labs, particularly esophageal high-resolution manometry and ambulatory reflux monitoring studies. If afforded the opportunity through a research study or a clinical indication, esophagologists should also undergo the tests themselves. Empathy regarding the discomfort and tolerability of motility tests, which are notoriously challenging for patients, can promote rapport and trust with patients, increase patient satisfaction, and enhance one’s own understanding of resource utilization and safety.
Perhaps most critical to becoming an esophagologist, is acquiring sufficient competency in interpretation of esophageal studies. Prior research highlights the limitations in achieving competency when trainees adhere to the minimum case volume of studies recommended by the GI core curriculum.2,3 With the bar set higher for the burgeoning esophagologist, one must not only practice with a higher case volume, but also engage in competency-based assessments and performance feedback.4 Trainees should start by reviewing tracings for their own patients. Preliminary interpretation of pending studies and review with a mentor before the final sign-off, participation in research that requires study, or even teaching co-trainees basic tenets of motility are other creative approaches to learning. Esophagologists will be expected to know how to navigate the software to access studies, manually review tracings, and generate reports. Trainees should refer to the multitude of societal guidelines and classification scheme recommendations available when developing competency in diagnostic impression.5
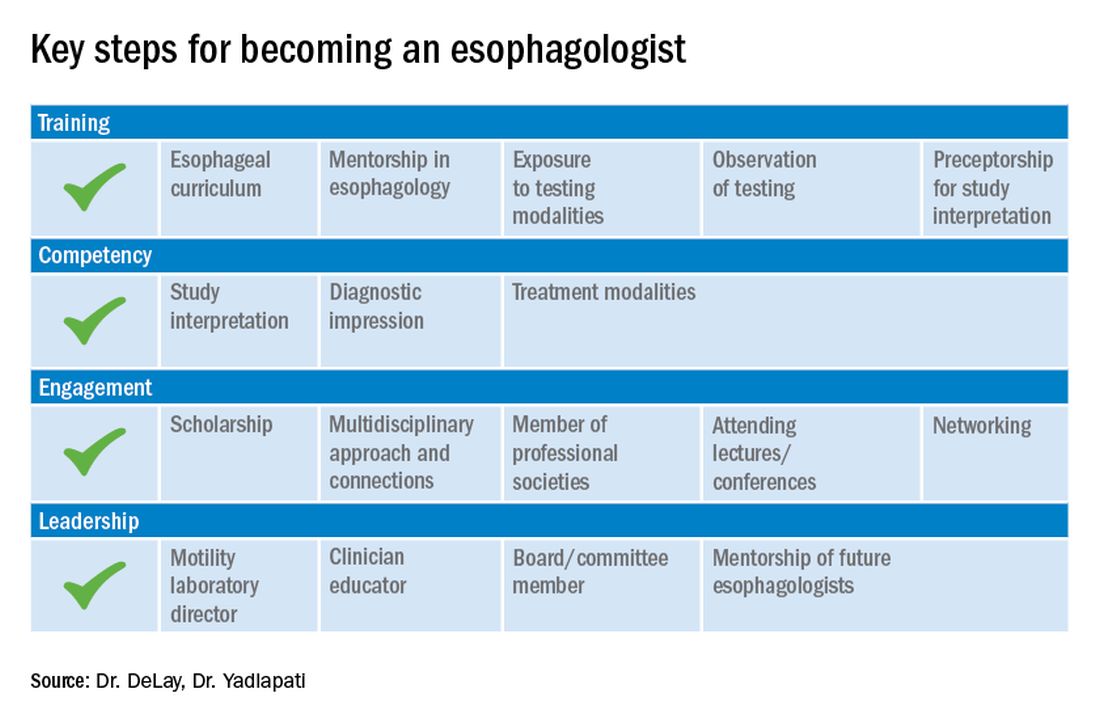
Figure 2
While esophagology is a medical specialty, it is imperative that the esophagologist has a robust understanding of therapeutic options and surgical interventions for esophageal pathology. Scrubbing into the operating room during foregut surgeries is an eye-opening experience. This includes thoracic and abdominal approaches, robotic, laparoscopic, and open techniques, and interventions for GERD, achalasia, diverticular disease, and bariatric management. Equally important is working alongside advanced endoscopy faculty to understand utilities of endoscopic ultrasound, ablative methods for Barrett’s esophagus, and advanced techniques such as peroral endoscopic myotomy and transoral incisionless fundoplication. This exposure is critical as the role of the esophagologist is to speak knowledgably of therapeutic options and the risks and benefits of alternative approaches. Further, the patient’s journey rarely ends with the intervention, and an esophagologist must understand how to evaluate symptoms and manage complications following therapy.
As with broader digestive health, the management of esophageal disorders is becoming increasingly integrated with psychological, lifestyle, and dietary interventions. Observing and understanding how other health care members interact with the patient and relay concepts of brain-gut interaction is helpful in one’s own practice and ability to speak to the value of focused interventions.
These key training aspects in esophagology can be acquired through different avenues (see Figure 3). Formal 1-year advanced esophageal or motility focused fellowships are available at leading esophageal centers. The American Neurogastroenterology and Motility Society (ANMS) offers a clinical training program for selected fellows to pursue apprenticeship-based training in gastrointestinal motility. A review of the benefits of additional training, available programs, and how to apply, can be found at The New Gastroenterologist. It may be possible to customize parts of the general clinical fellowship with a strong focus on esophagology. All budding esophagologists are strongly encouraged to attend and participate in subspecialty national meetings such as through the ANMS or the American Foregut Society.
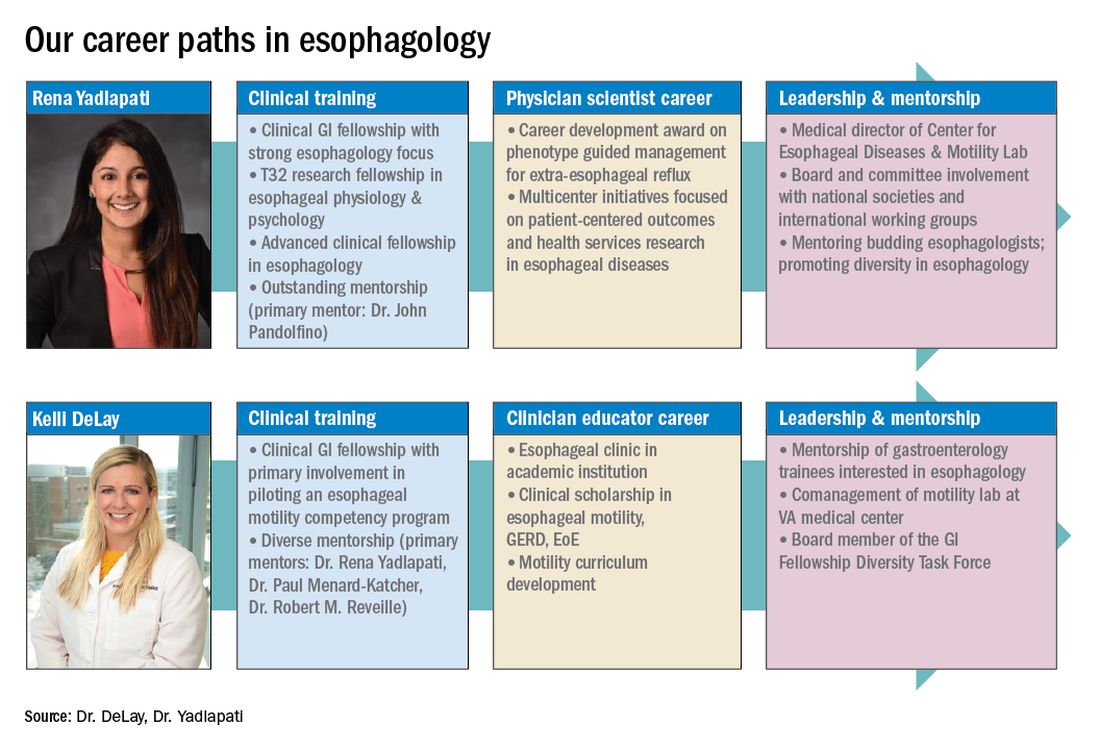
Figure 3
Steep learning curve post fellowship
Regardless of the robust nature of clinical esophagology training, early career esophagologists will face challenges and learn on the job.
Many esophagologists are directors of a motility lab early in their careers. This is often uncharted territory in terms of managing a team of nurses, technicians, and other providers. The director of a motility lab will be called upon to troubleshoot various arenas of diagnostic workup, from study acquisition and interpretation to technical barriers with equipment or software. Keys to maintaining a successful motility lab further include optimizing schedules and protocols, delineating roles and responsibilities of team members, ensuring adequate training across staff and providers, communicating expectations, and cultivating an open relationship with the motility lab supervisor. Crucial, yet often neglected during fellowship training, are the economic considerations of operating and expanding the motility lab, and the financial implications for one’s own practice.6 Participating in professional development workshops can be especially valuable in cultivating leadership skills.
The care an esophagologist provides relies heavily on collaborative relationships within the organization and peer mentorship, cooperation, and feedback. It is essential to cultivate multidisciplinary relationships with surgical (e.g., foregut surgery, laryngology), medical (e.g., pulmonology, allergy), radiology, and pathology colleagues, as well as with integrated health specialists including psychologists, dietitians, and speech language pathologists. It is also important to have open industry partnerships to ensure appropriate technical support and access to advancements.
Often organizations will have only one esophageal specialist within the group. Fortunately, the national and global community of esophagologists is highly collaborative and collegial. All esophagologists should have a network of mentors and colleagues within and outside of their organization to review complex cases, discuss challenges in the workplace, and foster research and innovation. Along these lines, both aspiring and practicing esophagologists should engage with professional societies as opportunities are abundant. Esophageal-focused societies include the ANMS, American Foregut Society, and International Society of Diseases of Esophagus, and the overarching GI societies also have a strong esophageal focus.
The path to becoming an esophagologist does not mirror the structure of the organ itself. Development is neither confined, unidirectional, nor set in length, but gradual, each step thoughtfully built on the last. Esophageal pathology is diverse, complex, and fascinating. With the appropriate training, mentorship, engagement, and leadership, esophagologists have the privilege of making a great impact on the lives of patients we meet, a fulfilling journey worth the time and effort it takes.
Dr. Delay is in the division of gastroenterology & hepatology, University of Colorado Anschutz Medical Campus, Aurora. Dr. Yadlapati is at the Center for Esophageal Diseases, division of gastroenterology, University of California San Diego, La Jolla. She is a consultant through institutional agreement to Medtronic, Ironwood Pharmaceuticals, and Diversatek; she has received research support from Ironwood Pharmaceuticals; and is on the advisory board of Phathom Pharmaceuticals.
References
1. Holinger PH. Arch Otolaryngol. 1948;47:119-26.
2. Yadlapati R et al. Clin Gastroenterol Hepatol. 2017;15:1708-14.e3.
3. Oversight Working Network et al. Gastrointest Endosc. 2014;80:16-27.
4. DeLay K et al. Am J Gastroenterol. 2020;115:1453-9.
5. Gyawali CP et al. Neurogastroenterol Motil. 2018;30(9):e13341.
6. Yadlapati R et al. Gastroenterology. 2020;158:1202-10.
Esophagology was a term coined in 1948 to describe a medical specialty devoted to the study of the anatomy, physiology, and pathology of the esophagus. The term was born out of increased interest and evolution in esophagology and supported by development in esophagoscopy.1 While still rooted in these basic tenets, the landscape of esophagology is dramatically different in 2020. The last decade alone has seen unprecedented technological advances in esophagology, from the transformation of line tracings to high-resolution esophageal pressure topography to more recent innovations such as the functional lumen imaging probe. Successful therapeutic developments have increased opportunities for effective and less invasive treatment approaches for achalasia and gastroesophageal reflux disease (GERD). With changing concepts in esophageal diseases such as eosinophilic esophagitis, successful management now incorporates findings from recent discoveries that have revolutionized care pathways. (see Figure 1).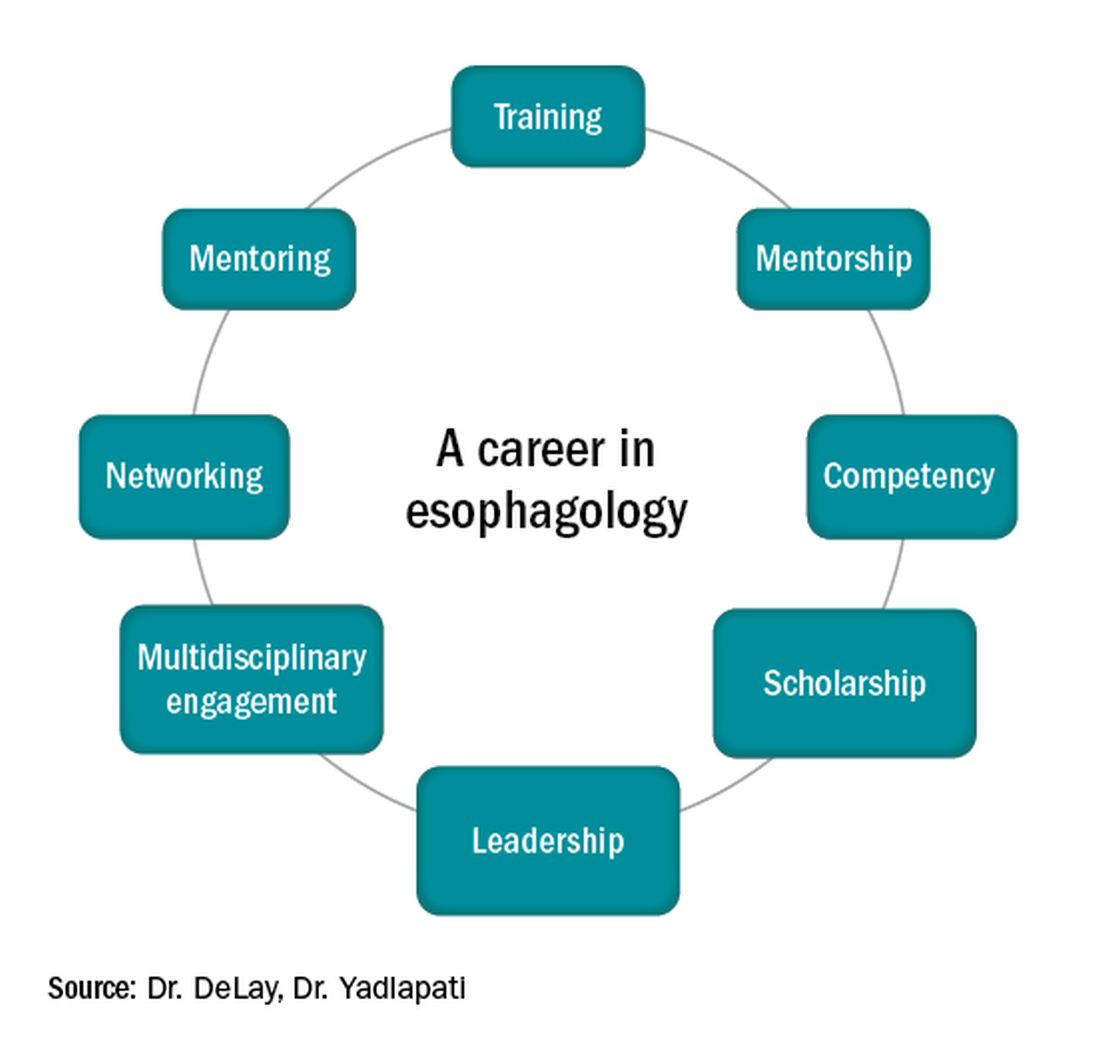
Figure 1
Optimizing esophagology training during fellowship
First, and most importantly, an esophagologist must have a foundation in the basic principles of esophageal anatomy, physiology, and pathology (see Figure 2). While newer digital learning resources exist, tried and true book-based resources – text books, chapters, and reviews – related to esophageal mechanics, the interplay between muscle function and neurogenics, and factors associated with nociception, remain the optimal learning strategy.
Once equipped with a foundation in esophageal physiology, one can readily engage with esophageal technologies, as there exists a vast array of testing to assess esophageal function. A comprehensive understanding of each, including device configuration, clinical protocol, and data storage, promotes a depth of knowledge every esophagologist should develop. Aspiring esophagologists should take time to observe and perform procedures in their motility labs, particularly esophageal high-resolution manometry and ambulatory reflux monitoring studies. If afforded the opportunity through a research study or a clinical indication, esophagologists should also undergo the tests themselves. Empathy regarding the discomfort and tolerability of motility tests, which are notoriously challenging for patients, can promote rapport and trust with patients, increase patient satisfaction, and enhance one’s own understanding of resource utilization and safety.
Perhaps most critical to becoming an esophagologist, is acquiring sufficient competency in interpretation of esophageal studies. Prior research highlights the limitations in achieving competency when trainees adhere to the minimum case volume of studies recommended by the GI core curriculum.2,3 With the bar set higher for the burgeoning esophagologist, one must not only practice with a higher case volume, but also engage in competency-based assessments and performance feedback.4 Trainees should start by reviewing tracings for their own patients. Preliminary interpretation of pending studies and review with a mentor before the final sign-off, participation in research that requires study, or even teaching co-trainees basic tenets of motility are other creative approaches to learning. Esophagologists will be expected to know how to navigate the software to access studies, manually review tracings, and generate reports. Trainees should refer to the multitude of societal guidelines and classification scheme recommendations available when developing competency in diagnostic impression.5
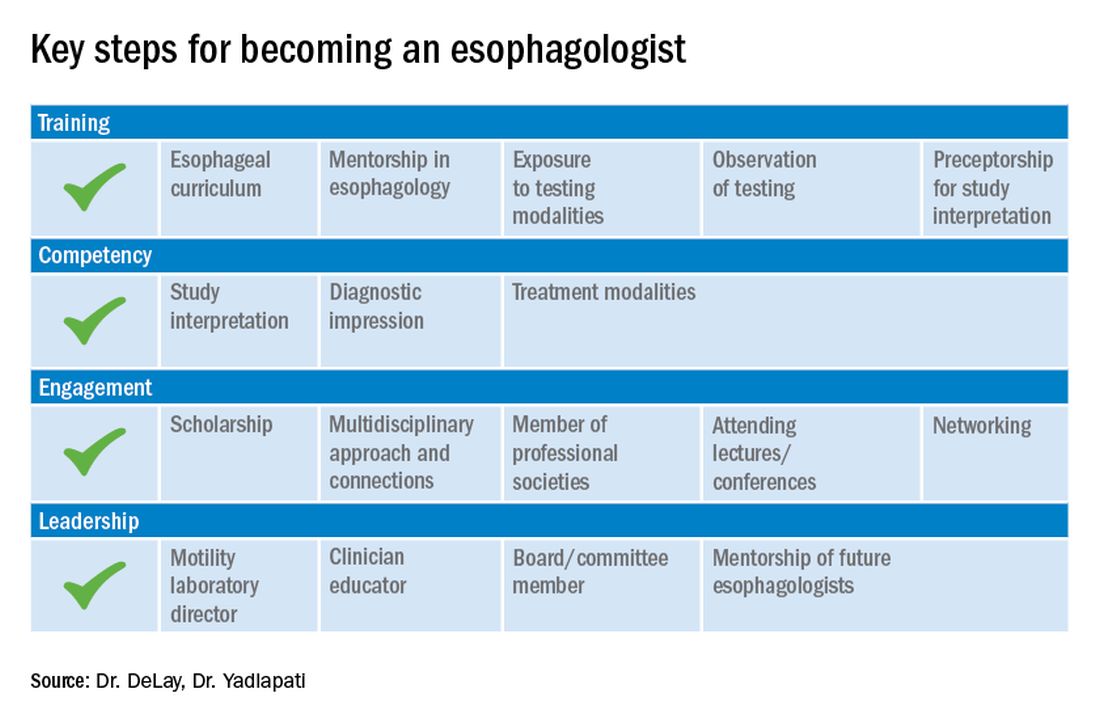
Figure 2
While esophagology is a medical specialty, it is imperative that the esophagologist has a robust understanding of therapeutic options and surgical interventions for esophageal pathology. Scrubbing into the operating room during foregut surgeries is an eye-opening experience. This includes thoracic and abdominal approaches, robotic, laparoscopic, and open techniques, and interventions for GERD, achalasia, diverticular disease, and bariatric management. Equally important is working alongside advanced endoscopy faculty to understand utilities of endoscopic ultrasound, ablative methods for Barrett’s esophagus, and advanced techniques such as peroral endoscopic myotomy and transoral incisionless fundoplication. This exposure is critical as the role of the esophagologist is to speak knowledgably of therapeutic options and the risks and benefits of alternative approaches. Further, the patient’s journey rarely ends with the intervention, and an esophagologist must understand how to evaluate symptoms and manage complications following therapy.
As with broader digestive health, the management of esophageal disorders is becoming increasingly integrated with psychological, lifestyle, and dietary interventions. Observing and understanding how other health care members interact with the patient and relay concepts of brain-gut interaction is helpful in one’s own practice and ability to speak to the value of focused interventions.
These key training aspects in esophagology can be acquired through different avenues (see Figure 3). Formal 1-year advanced esophageal or motility focused fellowships are available at leading esophageal centers. The American Neurogastroenterology and Motility Society (ANMS) offers a clinical training program for selected fellows to pursue apprenticeship-based training in gastrointestinal motility. A review of the benefits of additional training, available programs, and how to apply, can be found at The New Gastroenterologist. It may be possible to customize parts of the general clinical fellowship with a strong focus on esophagology. All budding esophagologists are strongly encouraged to attend and participate in subspecialty national meetings such as through the ANMS or the American Foregut Society.
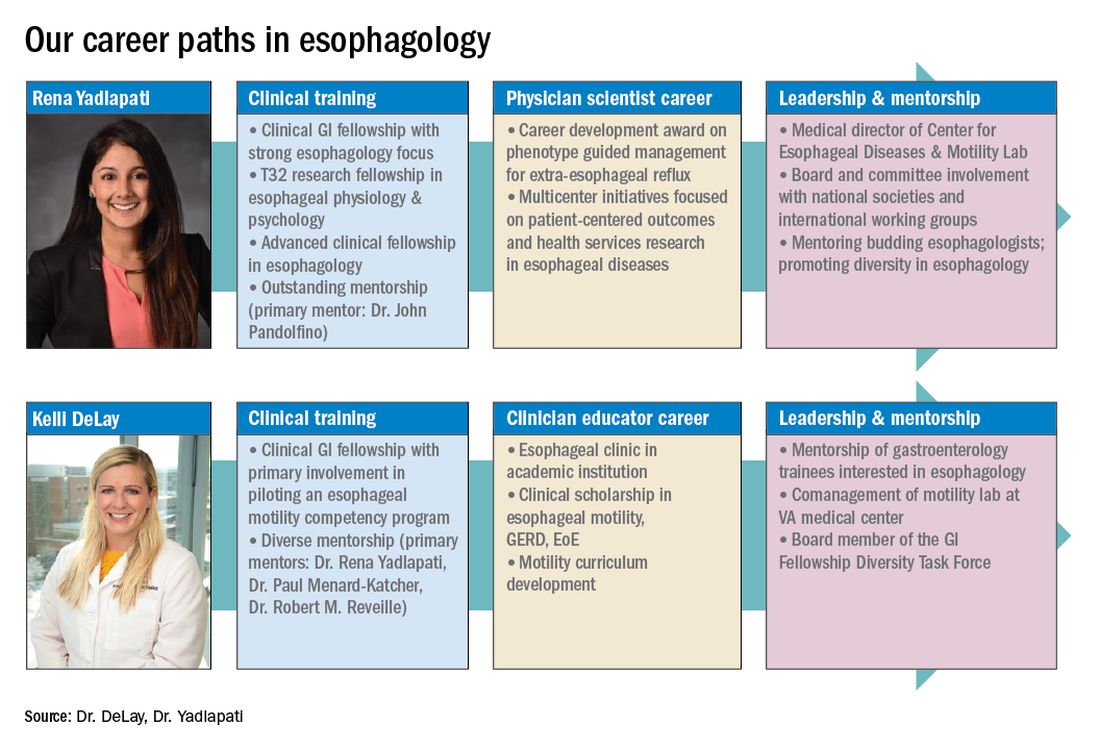
Figure 3
Steep learning curve post fellowship
Regardless of the robust nature of clinical esophagology training, early career esophagologists will face challenges and learn on the job.
Many esophagologists are directors of a motility lab early in their careers. This is often uncharted territory in terms of managing a team of nurses, technicians, and other providers. The director of a motility lab will be called upon to troubleshoot various arenas of diagnostic workup, from study acquisition and interpretation to technical barriers with equipment or software. Keys to maintaining a successful motility lab further include optimizing schedules and protocols, delineating roles and responsibilities of team members, ensuring adequate training across staff and providers, communicating expectations, and cultivating an open relationship with the motility lab supervisor. Crucial, yet often neglected during fellowship training, are the economic considerations of operating and expanding the motility lab, and the financial implications for one’s own practice.6 Participating in professional development workshops can be especially valuable in cultivating leadership skills.
The care an esophagologist provides relies heavily on collaborative relationships within the organization and peer mentorship, cooperation, and feedback. It is essential to cultivate multidisciplinary relationships with surgical (e.g., foregut surgery, laryngology), medical (e.g., pulmonology, allergy), radiology, and pathology colleagues, as well as with integrated health specialists including psychologists, dietitians, and speech language pathologists. It is also important to have open industry partnerships to ensure appropriate technical support and access to advancements.
Often organizations will have only one esophageal specialist within the group. Fortunately, the national and global community of esophagologists is highly collaborative and collegial. All esophagologists should have a network of mentors and colleagues within and outside of their organization to review complex cases, discuss challenges in the workplace, and foster research and innovation. Along these lines, both aspiring and practicing esophagologists should engage with professional societies as opportunities are abundant. Esophageal-focused societies include the ANMS, American Foregut Society, and International Society of Diseases of Esophagus, and the overarching GI societies also have a strong esophageal focus.
The path to becoming an esophagologist does not mirror the structure of the organ itself. Development is neither confined, unidirectional, nor set in length, but gradual, each step thoughtfully built on the last. Esophageal pathology is diverse, complex, and fascinating. With the appropriate training, mentorship, engagement, and leadership, esophagologists have the privilege of making a great impact on the lives of patients we meet, a fulfilling journey worth the time and effort it takes.
Dr. Delay is in the division of gastroenterology & hepatology, University of Colorado Anschutz Medical Campus, Aurora. Dr. Yadlapati is at the Center for Esophageal Diseases, division of gastroenterology, University of California San Diego, La Jolla. She is a consultant through institutional agreement to Medtronic, Ironwood Pharmaceuticals, and Diversatek; she has received research support from Ironwood Pharmaceuticals; and is on the advisory board of Phathom Pharmaceuticals.
References
1. Holinger PH. Arch Otolaryngol. 1948;47:119-26.
2. Yadlapati R et al. Clin Gastroenterol Hepatol. 2017;15:1708-14.e3.
3. Oversight Working Network et al. Gastrointest Endosc. 2014;80:16-27.
4. DeLay K et al. Am J Gastroenterol. 2020;115:1453-9.
5. Gyawali CP et al. Neurogastroenterol Motil. 2018;30(9):e13341.
6. Yadlapati R et al. Gastroenterology. 2020;158:1202-10.
Choosing a career in health equity and health care policy
Dr. Anyane-Yeboa is a Commonwealth Fund Fellow in Minority Health Policy at Harvard University and a recent graduate of the Harvard T.H. Chan School of Public Health. She previously completed her gastroenterology fellowship at the University of Chicago. She will be an academic gastroenterologist at Massachusetts General Hospital starting in the fall of 2020.
How did your career pathway lead you to a career in health equity and policy?
I have been passionate about issues related to health equity, workforce diversity, and care of vulnerable populations since the early years of my career. For instance, as undergraduates my friends and I received a grant to start a program to provide mentorship for endangered youth in Boston. During my residency and chief residency, I advocated for increased resident diversity and created programs for underrepresented minority medical students to increase minority representation in medicine. During my gastroenterology fellowship, I remained passionate about the care of minority and underserved populations. During my second year of fellowship, I looked for advanced training opportunities where I could learn the skills to tackle health disparities in minority communities, and almost serendipitously came across the Commonwealth Fund Fellowship in Minority Health Policy. When I decided to apply for the fellowship, I knew that this would be a nontraditional path for most gastroenterology fellows, but the right path for me.
About the Commonwealth Fund Fellowship
The purpose of the Commonwealth Fund Fellowship in Minority Health Policy at Harvard University is to train the next generation of leaders in health care. The program is based at Harvard Medical School and supported by the Commonwealth Fund whose mission is to “provide affordable quality health care for all.” To date, the fellowship has trained more than 130 physicians who are advancing health care across the nation as leaders in public health, academic medicine, and health policy.
The fellowship is a year-long, full-time, degree-granting program. Fellows are eligible for a master’s in public health with a concentration in health management or health policy from the Harvard T.H. Chan School of Public Health or a master’s in public administration from the Harvard Kennedy School.
The fellowship program and experiences have been transformative for me. The structure of the program consists of visits to the Massachusetts Department of Public Health, the Boston Public Health Commission, and the Commonwealth Fund, as well as lectures, seminars, and journal club sessions with national leaders in public health, health policy, and health care delivery reform. Additional opportunities include one-on-one shadowing experiences with leaders in hospital administration at academic institutions in Boston and private meetings with leaders and staff at several government agencies in Washington, including the Centers for Medicaid & Medicare Services, the Office of Minority Health, the Food and Drug Administration, the Health Resources & Services Administration, and the National Institutes of Health.
The program has given me an opportunity to meet and learn from physicians who have chosen a variety of different career paths. Through the program I have had exposure to physicians in academic medicine, health care administration, health policy, and public service as well as those who have chosen a combination of clinical practice with any of the above. This experience has opened my eyes to the different possibilities for physician careers and has encouraged me to be open if new opportunities should arise.
As part of the fellowship, we also have regular meetings with Joan Reede, MD, MPH, who is the director of the fellowship and has been with the program since its inception; she is also the Dean of Diversity and Inclusion at Harvard Medical School. Dr. Reede is an incredibly wise, insightful, and caring mentor, but also a powerhouse in issues surrounding workforce diversity, mentorship, policy, care of underserved communities, and being an advocate for change. To have access to such a powerful individual who has dedicated her career to the mentorship of individuals like myself, who cares deeply about the impact of our careers, and who genuinely values each fellow almost as her own child is a unique gift that is hard to describe in words.
The Commonwealth Fund Fellowship also provides a large network of mentors and advisers. My direct mentor for the program is Monica Bharel, MD, MPH, who is a former Commonwealth Fund fellow and the current Commissioner of the Massachusetts Department of Public Health. However, I also have a wealth of other mentors and advisers in the alumni fellows, including Darrell Gray II, MD, MPH, a former fellow and gastroenterologist at the Ohio State University College of Medicine, as well as the other faculty associated with the program. I never imagined that I would have access to leaders in so many different sectors of health care and policy who are genuinely and passionately rooting for my success. In addition, my cofellows and I have created a uniquely special bond, and they will likely continue as my close network of peer advisers as I move forward throughout my career.
After the fellowship
I have no doubt that the Commonwealth Fund Fellowship will alter the trajectory of my career. It has already affected my career path in ways that I could not have anticipated years ago. The knowledge that I have gained in health care policy, innovation, and equity, as well as the networks that I have access to as a fellow, will be invaluable as I move forward. In terms of next steps, I will be working as an academic gastroenterologist; I will continue to lead initiatives, perform research, and participate in projects to elevate the voices of underserved communities and work toward health equity in gastroenterology. I am particularly passionate about ending disparities in colorectal cancer in minority communities and increasing awareness around minorities with inflammatory bowel disease.
I plan to work with health centers, city- and state-level organizations, and community partners to raise awareness around issues of equity in gastroenterology and develop interventions to create change. I will also work with local legislators and community-based organizations to advocate for policies that remove barriers to screening both locally and nationally. Further down the line, I am open to exploring careers in the public sector or health care administration if that is where my career takes me. The exposure that I had to these fields as part of the fellowship has shown me that it is possible to be a practicing gastroenterologist and simultaneously work in the public sector, health policy, or health care administration. If you are interested in applying to the Commonwealth Fund Fellowship in Minority Health Policy at Harvard University, please feel free to contact me at adjoa.anyaneyeboa@gmail.com. More information about the program and how to apply can be found at https://cff.hms.harvard.edu/.
Dr. Anyane-Yeboa is a Commonwealth Fund Fellow in Minority Health Policy at Harvard University and a recent graduate of the Harvard T.H. Chan School of Public Health. She previously completed her gastroenterology fellowship at the University of Chicago. She will be an academic gastroenterologist at Massachusetts General Hospital starting in the fall of 2020.
How did your career pathway lead you to a career in health equity and policy?
I have been passionate about issues related to health equity, workforce diversity, and care of vulnerable populations since the early years of my career. For instance, as undergraduates my friends and I received a grant to start a program to provide mentorship for endangered youth in Boston. During my residency and chief residency, I advocated for increased resident diversity and created programs for underrepresented minority medical students to increase minority representation in medicine. During my gastroenterology fellowship, I remained passionate about the care of minority and underserved populations. During my second year of fellowship, I looked for advanced training opportunities where I could learn the skills to tackle health disparities in minority communities, and almost serendipitously came across the Commonwealth Fund Fellowship in Minority Health Policy. When I decided to apply for the fellowship, I knew that this would be a nontraditional path for most gastroenterology fellows, but the right path for me.
About the Commonwealth Fund Fellowship
The purpose of the Commonwealth Fund Fellowship in Minority Health Policy at Harvard University is to train the next generation of leaders in health care. The program is based at Harvard Medical School and supported by the Commonwealth Fund whose mission is to “provide affordable quality health care for all.” To date, the fellowship has trained more than 130 physicians who are advancing health care across the nation as leaders in public health, academic medicine, and health policy.
The fellowship is a year-long, full-time, degree-granting program. Fellows are eligible for a master’s in public health with a concentration in health management or health policy from the Harvard T.H. Chan School of Public Health or a master’s in public administration from the Harvard Kennedy School.
The fellowship program and experiences have been transformative for me. The structure of the program consists of visits to the Massachusetts Department of Public Health, the Boston Public Health Commission, and the Commonwealth Fund, as well as lectures, seminars, and journal club sessions with national leaders in public health, health policy, and health care delivery reform. Additional opportunities include one-on-one shadowing experiences with leaders in hospital administration at academic institutions in Boston and private meetings with leaders and staff at several government agencies in Washington, including the Centers for Medicaid & Medicare Services, the Office of Minority Health, the Food and Drug Administration, the Health Resources & Services Administration, and the National Institutes of Health.
The program has given me an opportunity to meet and learn from physicians who have chosen a variety of different career paths. Through the program I have had exposure to physicians in academic medicine, health care administration, health policy, and public service as well as those who have chosen a combination of clinical practice with any of the above. This experience has opened my eyes to the different possibilities for physician careers and has encouraged me to be open if new opportunities should arise.
As part of the fellowship, we also have regular meetings with Joan Reede, MD, MPH, who is the director of the fellowship and has been with the program since its inception; she is also the Dean of Diversity and Inclusion at Harvard Medical School. Dr. Reede is an incredibly wise, insightful, and caring mentor, but also a powerhouse in issues surrounding workforce diversity, mentorship, policy, care of underserved communities, and being an advocate for change. To have access to such a powerful individual who has dedicated her career to the mentorship of individuals like myself, who cares deeply about the impact of our careers, and who genuinely values each fellow almost as her own child is a unique gift that is hard to describe in words.
The Commonwealth Fund Fellowship also provides a large network of mentors and advisers. My direct mentor for the program is Monica Bharel, MD, MPH, who is a former Commonwealth Fund fellow and the current Commissioner of the Massachusetts Department of Public Health. However, I also have a wealth of other mentors and advisers in the alumni fellows, including Darrell Gray II, MD, MPH, a former fellow and gastroenterologist at the Ohio State University College of Medicine, as well as the other faculty associated with the program. I never imagined that I would have access to leaders in so many different sectors of health care and policy who are genuinely and passionately rooting for my success. In addition, my cofellows and I have created a uniquely special bond, and they will likely continue as my close network of peer advisers as I move forward throughout my career.
After the fellowship
I have no doubt that the Commonwealth Fund Fellowship will alter the trajectory of my career. It has already affected my career path in ways that I could not have anticipated years ago. The knowledge that I have gained in health care policy, innovation, and equity, as well as the networks that I have access to as a fellow, will be invaluable as I move forward. In terms of next steps, I will be working as an academic gastroenterologist; I will continue to lead initiatives, perform research, and participate in projects to elevate the voices of underserved communities and work toward health equity in gastroenterology. I am particularly passionate about ending disparities in colorectal cancer in minority communities and increasing awareness around minorities with inflammatory bowel disease.
I plan to work with health centers, city- and state-level organizations, and community partners to raise awareness around issues of equity in gastroenterology and develop interventions to create change. I will also work with local legislators and community-based organizations to advocate for policies that remove barriers to screening both locally and nationally. Further down the line, I am open to exploring careers in the public sector or health care administration if that is where my career takes me. The exposure that I had to these fields as part of the fellowship has shown me that it is possible to be a practicing gastroenterologist and simultaneously work in the public sector, health policy, or health care administration. If you are interested in applying to the Commonwealth Fund Fellowship in Minority Health Policy at Harvard University, please feel free to contact me at adjoa.anyaneyeboa@gmail.com. More information about the program and how to apply can be found at https://cff.hms.harvard.edu/.
Dr. Anyane-Yeboa is a Commonwealth Fund Fellow in Minority Health Policy at Harvard University and a recent graduate of the Harvard T.H. Chan School of Public Health. She previously completed her gastroenterology fellowship at the University of Chicago. She will be an academic gastroenterologist at Massachusetts General Hospital starting in the fall of 2020.
How did your career pathway lead you to a career in health equity and policy?
I have been passionate about issues related to health equity, workforce diversity, and care of vulnerable populations since the early years of my career. For instance, as undergraduates my friends and I received a grant to start a program to provide mentorship for endangered youth in Boston. During my residency and chief residency, I advocated for increased resident diversity and created programs for underrepresented minority medical students to increase minority representation in medicine. During my gastroenterology fellowship, I remained passionate about the care of minority and underserved populations. During my second year of fellowship, I looked for advanced training opportunities where I could learn the skills to tackle health disparities in minority communities, and almost serendipitously came across the Commonwealth Fund Fellowship in Minority Health Policy. When I decided to apply for the fellowship, I knew that this would be a nontraditional path for most gastroenterology fellows, but the right path for me.
About the Commonwealth Fund Fellowship
The purpose of the Commonwealth Fund Fellowship in Minority Health Policy at Harvard University is to train the next generation of leaders in health care. The program is based at Harvard Medical School and supported by the Commonwealth Fund whose mission is to “provide affordable quality health care for all.” To date, the fellowship has trained more than 130 physicians who are advancing health care across the nation as leaders in public health, academic medicine, and health policy.
The fellowship is a year-long, full-time, degree-granting program. Fellows are eligible for a master’s in public health with a concentration in health management or health policy from the Harvard T.H. Chan School of Public Health or a master’s in public administration from the Harvard Kennedy School.
The fellowship program and experiences have been transformative for me. The structure of the program consists of visits to the Massachusetts Department of Public Health, the Boston Public Health Commission, and the Commonwealth Fund, as well as lectures, seminars, and journal club sessions with national leaders in public health, health policy, and health care delivery reform. Additional opportunities include one-on-one shadowing experiences with leaders in hospital administration at academic institutions in Boston and private meetings with leaders and staff at several government agencies in Washington, including the Centers for Medicaid & Medicare Services, the Office of Minority Health, the Food and Drug Administration, the Health Resources & Services Administration, and the National Institutes of Health.
The program has given me an opportunity to meet and learn from physicians who have chosen a variety of different career paths. Through the program I have had exposure to physicians in academic medicine, health care administration, health policy, and public service as well as those who have chosen a combination of clinical practice with any of the above. This experience has opened my eyes to the different possibilities for physician careers and has encouraged me to be open if new opportunities should arise.
As part of the fellowship, we also have regular meetings with Joan Reede, MD, MPH, who is the director of the fellowship and has been with the program since its inception; she is also the Dean of Diversity and Inclusion at Harvard Medical School. Dr. Reede is an incredibly wise, insightful, and caring mentor, but also a powerhouse in issues surrounding workforce diversity, mentorship, policy, care of underserved communities, and being an advocate for change. To have access to such a powerful individual who has dedicated her career to the mentorship of individuals like myself, who cares deeply about the impact of our careers, and who genuinely values each fellow almost as her own child is a unique gift that is hard to describe in words.
The Commonwealth Fund Fellowship also provides a large network of mentors and advisers. My direct mentor for the program is Monica Bharel, MD, MPH, who is a former Commonwealth Fund fellow and the current Commissioner of the Massachusetts Department of Public Health. However, I also have a wealth of other mentors and advisers in the alumni fellows, including Darrell Gray II, MD, MPH, a former fellow and gastroenterologist at the Ohio State University College of Medicine, as well as the other faculty associated with the program. I never imagined that I would have access to leaders in so many different sectors of health care and policy who are genuinely and passionately rooting for my success. In addition, my cofellows and I have created a uniquely special bond, and they will likely continue as my close network of peer advisers as I move forward throughout my career.
After the fellowship
I have no doubt that the Commonwealth Fund Fellowship will alter the trajectory of my career. It has already affected my career path in ways that I could not have anticipated years ago. The knowledge that I have gained in health care policy, innovation, and equity, as well as the networks that I have access to as a fellow, will be invaluable as I move forward. In terms of next steps, I will be working as an academic gastroenterologist; I will continue to lead initiatives, perform research, and participate in projects to elevate the voices of underserved communities and work toward health equity in gastroenterology. I am particularly passionate about ending disparities in colorectal cancer in minority communities and increasing awareness around minorities with inflammatory bowel disease.
I plan to work with health centers, city- and state-level organizations, and community partners to raise awareness around issues of equity in gastroenterology and develop interventions to create change. I will also work with local legislators and community-based organizations to advocate for policies that remove barriers to screening both locally and nationally. Further down the line, I am open to exploring careers in the public sector or health care administration if that is where my career takes me. The exposure that I had to these fields as part of the fellowship has shown me that it is possible to be a practicing gastroenterologist and simultaneously work in the public sector, health policy, or health care administration. If you are interested in applying to the Commonwealth Fund Fellowship in Minority Health Policy at Harvard University, please feel free to contact me at adjoa.anyaneyeboa@gmail.com. More information about the program and how to apply can be found at https://cff.hms.harvard.edu/.
Developing a career in nutrition support and small-bowel disorders
The role of diet and nutrition is becoming increasingly recognized in the cause, management, and prevention of disease. Despite the clear importance of the role of nutrition in the field of medicine, among health professionals, formal training in nutrition support is lacking. A lack of nutrition training has been recognized in multiple subspecialty fields1 and is highlighted by a shortage of physicians trained to manage disease-related malnutrition.2 Gastroenterologists, in particular, have a special responsibility related to nutrition in disorders of the gastrointestinal tract and are in a unique position to recognize and manage disorders of maldigestion and malabsorption. Unfortunately, surveys of both U.S. and Canadian fellows have demonstrated deficiencies in the training of nutrition support and management of enteral and parenteral nutrition (PN).3,4
Current status of nutrition training
The impact of diet and nutrition on health and disease is universally recognized but unfortunately lagging with respect to formal training at all levels of medical education. A survey of program directors from primary care, surgery, and anesthesia showed only 26% of respondent programs had a formal curriculum in nutrition education.1 Specific to gastroenterology, a majority of trainees and recent graduates perceived that nutrition education was an important aspect of their training; however, only 50% of respondents had training in nutrition support with 36% reporting mandatory training.3
The Gastroenterology Core Curriculum, most recently updated in 2007 – and sponsored by the American Association for the Study of Liver Diseases, American College of Gastroenterology, the American Society for Gastrointestinal Endoscopy, and the American Gastroenterological Association – includes six domains of nutrition training within the training track: nutrition assessment, basic nutrition requirements, specific gastrointestinal disorders and other allied diseases, enteral nutrition, PN, and diet therapy. Level 1 training is expected for all gastroenterology fellows. Level 2 is comprised, on average, of an additional 12 months with described objectives, either occurring outside of a standard gastroenterology fellowship or coinciding with a dedicated third year of training. Although training durations for level 1 are not defined, level 2 recommends at least 6 months of experience working with an inpatient nutrition support team (NST) and the management of outpatients in nutrition and weight management clinics.5
Role of a nutrition support team
Training in nutrition is a heterogeneous field, with a wide range that covers understanding metabolism in health and disease, micronutrient and macronutrient requirements, nutrient digestion and absorption, and the best route and provision of nutrition support. Therefore, a critical aspect of education includes access to a dedicated NST. Such teams were common and necessary in the late 1900s with the inception of specialized nutrition therapy. However, with an increase in the use of home infusion therapies, NSTs were dismantled in favor of shifting responsibility to decentralized home infusion companies. A dedicated NST often will include some combination of pharmacists with an interest in the safe compounding of parenteral formulas, nurses with experience in the home management of intravenous therapies and catheters, and dietitians with dedicated interests in intestinal failure, recognition of malnutrition, and provision of calories. Collectively, a highly functioning NST also provides dedicated multidisciplinary training to health professionals of varying backgrounds.
My entry into the field of nutrition support
Entering a fellowship in gastroenterology should be pursued with an open mind. We all have varying experiences in the management of patients with gastrointestinal conditions, both in the inpatient and outpatient arenas through residency training. My early experiences in fellowship at the University of Chicago centered on the management of patients with inflammatory bowel disease (IBD) and with research interests related to the clinical course of IBD. I was also fortunate to be part of a fellowship program offering both level 1 and level 2 training with a longstanding track record of graduating fellows responsible for the running of NSTs at their local institutions. Categorical fellows spend 3 months of training on a rotation with combined inpatient and outpatient responsibilities focusing on the management of patients with intestinal failure, inpatient management of complications from PN support, and an outpatient clinic focused on small-bowel disorders (celiac disease, small-bowel bleeding, and intestinal malabsorption). This experience led me to pursue level 2 training at Northwestern University with a combined focus on small-bowel diseases and enteroscopy.
These collective experiences in fellowship and postfellowship training grounded my ideas on the role of nutrition pervading many gastrointestinal conditions from acute and chronic pancreatitis and IBD to rare conditions such as enteropathy associated with immune deficiencies and autoimmune enteropathy. Now, as a junior faculty member with a focus in nutrition support and small-bowel disorders, my clinical responsibilities include a dedicated half-day in the management of outpatients (parenteral and enteral nutrition), inpatient rounding with our dedicated NST focusing on the initiation of PN, management of home PN complications, and dedicated procedural time focusing on enteral access techniques (percutaneous gastrostomy/jejunostomy tubes) and small-bowel enteroscopy. To my surprise, entry into the field of nutrition support and small-bowel disorders has been filled with excitement and a growing list of collaborations and opportunities. While initial work in the management of PN has been in existence since the 1970s and earlier with respect to the development of safe administration techniques, most of my current work transcends specialties as we develop appropriateness criteria related to PN support in collaboration with a wide range of specialties that include surgery, oncology, and palliative care.
Seeking opportunities for additional training
As the field of gastroenterology grows outward in various directions, mastery of subjects has led to subspecialization in specific areas including interventional gastroenterology, pancreatology, IBD, and motility disorders. The field is primed for broader access to specialty training in nutrition support and small-bowel disorders. Exposure to dedicated training in nutrition and nutrition-related disorders is vital as part of a categorical fellowship, but can also be complemented via visiting observerships, access to formal level 2 training programs, and external programs related to promoting nutrition education.
Since 2001, formal nutrition fellowship programs offering level 2 training have been compiled by the National Board of Physician Nutrition Specialists, although attraction of interested fellows has been lacking.2 The Nestlé Nutrition Institute Clinical Nutrition Fellowship, endorsed by the American Society for Parenteral and Enteral Nutrition and the AGA, is an ongoing program that pairs interested trainees with expert program faculty through onsite clinical rotations lasting a total of 4 weeks.2 Attendance at national and international conferences can supplement a fellows training in nutrition, and an increased focus on nutrition lectures should be a priority of meeting education committees to increase the exposure of trainees to leaders in the field.
Conclusion
A career in nutrition support and small-bowel disorders is incredibly rewarding as it incorporates the basic physiologic processes of digestion and absorption with a wide array of pathologic conditions. Incorporation of the basic principles of intestinal absorption allows for a greater understanding of the role of the low–fermentable oligo-, di-, monosaccharides and polyols (FODMAP) diet in the management of irritable bowel syndrome to the varying principles of diets currently under study for the management of IBD. Outside of this spectrum, working with an NST allows for the management of complex cases of malnutrition resulting from disorders ranging from cancer to various postsurgical intestinal alterations. Although observerships and external training programs allow for an introduction into the field, formal level 2 training, combining both work with a NST and small-bowel enteroscopy, allows for exposure to the full range of disorders of the small bowel. As patients continue to seek disease management options rooted in diet, the demand for gastroenterologists with subspecialty training in nutritional disorders will continue to grow and will require further support across training programs to incorporate additional training into categorical fellowships.
References
1. Daley BJ et al. JPEN J Paren Enteral Nutr. 2016;40(1):95-9. doi: 10.1177/0148607115571155.
2. Kiraly LN et al. Nutr Clin Pract. 2014;29(3):332-7. doi: 10.1177/0884533614525212.
3. Hu J et al. Nutr Clin Pract. 2018 Apr;33(2):191-7. doi: 10.1177/0884533617700852.
4. Scolapio JS et al. J Clin Gastroenterol. 2008 Feb;42(2):122-7. doi: 10.1097/MCG.0b013e3181595b6a.
5. American Association for the Study of Liver Diseases et al. The Gastroenterology Core Curriculum, 3rd ed. Gastroenterology. 2007;132(5):2012-8. doi: 10.1053/j.gastro.2007.03.079.
Dr. Micic is assistant professor of medicine, department of internal medicine, section of gastroenterology, hepatology, and nutrition, University of Chicago.
The role of diet and nutrition is becoming increasingly recognized in the cause, management, and prevention of disease. Despite the clear importance of the role of nutrition in the field of medicine, among health professionals, formal training in nutrition support is lacking. A lack of nutrition training has been recognized in multiple subspecialty fields1 and is highlighted by a shortage of physicians trained to manage disease-related malnutrition.2 Gastroenterologists, in particular, have a special responsibility related to nutrition in disorders of the gastrointestinal tract and are in a unique position to recognize and manage disorders of maldigestion and malabsorption. Unfortunately, surveys of both U.S. and Canadian fellows have demonstrated deficiencies in the training of nutrition support and management of enteral and parenteral nutrition (PN).3,4
Current status of nutrition training
The impact of diet and nutrition on health and disease is universally recognized but unfortunately lagging with respect to formal training at all levels of medical education. A survey of program directors from primary care, surgery, and anesthesia showed only 26% of respondent programs had a formal curriculum in nutrition education.1 Specific to gastroenterology, a majority of trainees and recent graduates perceived that nutrition education was an important aspect of their training; however, only 50% of respondents had training in nutrition support with 36% reporting mandatory training.3
The Gastroenterology Core Curriculum, most recently updated in 2007 – and sponsored by the American Association for the Study of Liver Diseases, American College of Gastroenterology, the American Society for Gastrointestinal Endoscopy, and the American Gastroenterological Association – includes six domains of nutrition training within the training track: nutrition assessment, basic nutrition requirements, specific gastrointestinal disorders and other allied diseases, enteral nutrition, PN, and diet therapy. Level 1 training is expected for all gastroenterology fellows. Level 2 is comprised, on average, of an additional 12 months with described objectives, either occurring outside of a standard gastroenterology fellowship or coinciding with a dedicated third year of training. Although training durations for level 1 are not defined, level 2 recommends at least 6 months of experience working with an inpatient nutrition support team (NST) and the management of outpatients in nutrition and weight management clinics.5
Role of a nutrition support team
Training in nutrition is a heterogeneous field, with a wide range that covers understanding metabolism in health and disease, micronutrient and macronutrient requirements, nutrient digestion and absorption, and the best route and provision of nutrition support. Therefore, a critical aspect of education includes access to a dedicated NST. Such teams were common and necessary in the late 1900s with the inception of specialized nutrition therapy. However, with an increase in the use of home infusion therapies, NSTs were dismantled in favor of shifting responsibility to decentralized home infusion companies. A dedicated NST often will include some combination of pharmacists with an interest in the safe compounding of parenteral formulas, nurses with experience in the home management of intravenous therapies and catheters, and dietitians with dedicated interests in intestinal failure, recognition of malnutrition, and provision of calories. Collectively, a highly functioning NST also provides dedicated multidisciplinary training to health professionals of varying backgrounds.
My entry into the field of nutrition support
Entering a fellowship in gastroenterology should be pursued with an open mind. We all have varying experiences in the management of patients with gastrointestinal conditions, both in the inpatient and outpatient arenas through residency training. My early experiences in fellowship at the University of Chicago centered on the management of patients with inflammatory bowel disease (IBD) and with research interests related to the clinical course of IBD. I was also fortunate to be part of a fellowship program offering both level 1 and level 2 training with a longstanding track record of graduating fellows responsible for the running of NSTs at their local institutions. Categorical fellows spend 3 months of training on a rotation with combined inpatient and outpatient responsibilities focusing on the management of patients with intestinal failure, inpatient management of complications from PN support, and an outpatient clinic focused on small-bowel disorders (celiac disease, small-bowel bleeding, and intestinal malabsorption). This experience led me to pursue level 2 training at Northwestern University with a combined focus on small-bowel diseases and enteroscopy.
These collective experiences in fellowship and postfellowship training grounded my ideas on the role of nutrition pervading many gastrointestinal conditions from acute and chronic pancreatitis and IBD to rare conditions such as enteropathy associated with immune deficiencies and autoimmune enteropathy. Now, as a junior faculty member with a focus in nutrition support and small-bowel disorders, my clinical responsibilities include a dedicated half-day in the management of outpatients (parenteral and enteral nutrition), inpatient rounding with our dedicated NST focusing on the initiation of PN, management of home PN complications, and dedicated procedural time focusing on enteral access techniques (percutaneous gastrostomy/jejunostomy tubes) and small-bowel enteroscopy. To my surprise, entry into the field of nutrition support and small-bowel disorders has been filled with excitement and a growing list of collaborations and opportunities. While initial work in the management of PN has been in existence since the 1970s and earlier with respect to the development of safe administration techniques, most of my current work transcends specialties as we develop appropriateness criteria related to PN support in collaboration with a wide range of specialties that include surgery, oncology, and palliative care.
Seeking opportunities for additional training
As the field of gastroenterology grows outward in various directions, mastery of subjects has led to subspecialization in specific areas including interventional gastroenterology, pancreatology, IBD, and motility disorders. The field is primed for broader access to specialty training in nutrition support and small-bowel disorders. Exposure to dedicated training in nutrition and nutrition-related disorders is vital as part of a categorical fellowship, but can also be complemented via visiting observerships, access to formal level 2 training programs, and external programs related to promoting nutrition education.
Since 2001, formal nutrition fellowship programs offering level 2 training have been compiled by the National Board of Physician Nutrition Specialists, although attraction of interested fellows has been lacking.2 The Nestlé Nutrition Institute Clinical Nutrition Fellowship, endorsed by the American Society for Parenteral and Enteral Nutrition and the AGA, is an ongoing program that pairs interested trainees with expert program faculty through onsite clinical rotations lasting a total of 4 weeks.2 Attendance at national and international conferences can supplement a fellows training in nutrition, and an increased focus on nutrition lectures should be a priority of meeting education committees to increase the exposure of trainees to leaders in the field.
Conclusion
A career in nutrition support and small-bowel disorders is incredibly rewarding as it incorporates the basic physiologic processes of digestion and absorption with a wide array of pathologic conditions. Incorporation of the basic principles of intestinal absorption allows for a greater understanding of the role of the low–fermentable oligo-, di-, monosaccharides and polyols (FODMAP) diet in the management of irritable bowel syndrome to the varying principles of diets currently under study for the management of IBD. Outside of this spectrum, working with an NST allows for the management of complex cases of malnutrition resulting from disorders ranging from cancer to various postsurgical intestinal alterations. Although observerships and external training programs allow for an introduction into the field, formal level 2 training, combining both work with a NST and small-bowel enteroscopy, allows for exposure to the full range of disorders of the small bowel. As patients continue to seek disease management options rooted in diet, the demand for gastroenterologists with subspecialty training in nutritional disorders will continue to grow and will require further support across training programs to incorporate additional training into categorical fellowships.
References
1. Daley BJ et al. JPEN J Paren Enteral Nutr. 2016;40(1):95-9. doi: 10.1177/0148607115571155.
2. Kiraly LN et al. Nutr Clin Pract. 2014;29(3):332-7. doi: 10.1177/0884533614525212.
3. Hu J et al. Nutr Clin Pract. 2018 Apr;33(2):191-7. doi: 10.1177/0884533617700852.
4. Scolapio JS et al. J Clin Gastroenterol. 2008 Feb;42(2):122-7. doi: 10.1097/MCG.0b013e3181595b6a.
5. American Association for the Study of Liver Diseases et al. The Gastroenterology Core Curriculum, 3rd ed. Gastroenterology. 2007;132(5):2012-8. doi: 10.1053/j.gastro.2007.03.079.
Dr. Micic is assistant professor of medicine, department of internal medicine, section of gastroenterology, hepatology, and nutrition, University of Chicago.
The role of diet and nutrition is becoming increasingly recognized in the cause, management, and prevention of disease. Despite the clear importance of the role of nutrition in the field of medicine, among health professionals, formal training in nutrition support is lacking. A lack of nutrition training has been recognized in multiple subspecialty fields1 and is highlighted by a shortage of physicians trained to manage disease-related malnutrition.2 Gastroenterologists, in particular, have a special responsibility related to nutrition in disorders of the gastrointestinal tract and are in a unique position to recognize and manage disorders of maldigestion and malabsorption. Unfortunately, surveys of both U.S. and Canadian fellows have demonstrated deficiencies in the training of nutrition support and management of enteral and parenteral nutrition (PN).3,4
Current status of nutrition training
The impact of diet and nutrition on health and disease is universally recognized but unfortunately lagging with respect to formal training at all levels of medical education. A survey of program directors from primary care, surgery, and anesthesia showed only 26% of respondent programs had a formal curriculum in nutrition education.1 Specific to gastroenterology, a majority of trainees and recent graduates perceived that nutrition education was an important aspect of their training; however, only 50% of respondents had training in nutrition support with 36% reporting mandatory training.3
The Gastroenterology Core Curriculum, most recently updated in 2007 – and sponsored by the American Association for the Study of Liver Diseases, American College of Gastroenterology, the American Society for Gastrointestinal Endoscopy, and the American Gastroenterological Association – includes six domains of nutrition training within the training track: nutrition assessment, basic nutrition requirements, specific gastrointestinal disorders and other allied diseases, enteral nutrition, PN, and diet therapy. Level 1 training is expected for all gastroenterology fellows. Level 2 is comprised, on average, of an additional 12 months with described objectives, either occurring outside of a standard gastroenterology fellowship or coinciding with a dedicated third year of training. Although training durations for level 1 are not defined, level 2 recommends at least 6 months of experience working with an inpatient nutrition support team (NST) and the management of outpatients in nutrition and weight management clinics.5
Role of a nutrition support team
Training in nutrition is a heterogeneous field, with a wide range that covers understanding metabolism in health and disease, micronutrient and macronutrient requirements, nutrient digestion and absorption, and the best route and provision of nutrition support. Therefore, a critical aspect of education includes access to a dedicated NST. Such teams were common and necessary in the late 1900s with the inception of specialized nutrition therapy. However, with an increase in the use of home infusion therapies, NSTs were dismantled in favor of shifting responsibility to decentralized home infusion companies. A dedicated NST often will include some combination of pharmacists with an interest in the safe compounding of parenteral formulas, nurses with experience in the home management of intravenous therapies and catheters, and dietitians with dedicated interests in intestinal failure, recognition of malnutrition, and provision of calories. Collectively, a highly functioning NST also provides dedicated multidisciplinary training to health professionals of varying backgrounds.
My entry into the field of nutrition support
Entering a fellowship in gastroenterology should be pursued with an open mind. We all have varying experiences in the management of patients with gastrointestinal conditions, both in the inpatient and outpatient arenas through residency training. My early experiences in fellowship at the University of Chicago centered on the management of patients with inflammatory bowel disease (IBD) and with research interests related to the clinical course of IBD. I was also fortunate to be part of a fellowship program offering both level 1 and level 2 training with a longstanding track record of graduating fellows responsible for the running of NSTs at their local institutions. Categorical fellows spend 3 months of training on a rotation with combined inpatient and outpatient responsibilities focusing on the management of patients with intestinal failure, inpatient management of complications from PN support, and an outpatient clinic focused on small-bowel disorders (celiac disease, small-bowel bleeding, and intestinal malabsorption). This experience led me to pursue level 2 training at Northwestern University with a combined focus on small-bowel diseases and enteroscopy.
These collective experiences in fellowship and postfellowship training grounded my ideas on the role of nutrition pervading many gastrointestinal conditions from acute and chronic pancreatitis and IBD to rare conditions such as enteropathy associated with immune deficiencies and autoimmune enteropathy. Now, as a junior faculty member with a focus in nutrition support and small-bowel disorders, my clinical responsibilities include a dedicated half-day in the management of outpatients (parenteral and enteral nutrition), inpatient rounding with our dedicated NST focusing on the initiation of PN, management of home PN complications, and dedicated procedural time focusing on enteral access techniques (percutaneous gastrostomy/jejunostomy tubes) and small-bowel enteroscopy. To my surprise, entry into the field of nutrition support and small-bowel disorders has been filled with excitement and a growing list of collaborations and opportunities. While initial work in the management of PN has been in existence since the 1970s and earlier with respect to the development of safe administration techniques, most of my current work transcends specialties as we develop appropriateness criteria related to PN support in collaboration with a wide range of specialties that include surgery, oncology, and palliative care.
Seeking opportunities for additional training
As the field of gastroenterology grows outward in various directions, mastery of subjects has led to subspecialization in specific areas including interventional gastroenterology, pancreatology, IBD, and motility disorders. The field is primed for broader access to specialty training in nutrition support and small-bowel disorders. Exposure to dedicated training in nutrition and nutrition-related disorders is vital as part of a categorical fellowship, but can also be complemented via visiting observerships, access to formal level 2 training programs, and external programs related to promoting nutrition education.
Since 2001, formal nutrition fellowship programs offering level 2 training have been compiled by the National Board of Physician Nutrition Specialists, although attraction of interested fellows has been lacking.2 The Nestlé Nutrition Institute Clinical Nutrition Fellowship, endorsed by the American Society for Parenteral and Enteral Nutrition and the AGA, is an ongoing program that pairs interested trainees with expert program faculty through onsite clinical rotations lasting a total of 4 weeks.2 Attendance at national and international conferences can supplement a fellows training in nutrition, and an increased focus on nutrition lectures should be a priority of meeting education committees to increase the exposure of trainees to leaders in the field.
Conclusion
A career in nutrition support and small-bowel disorders is incredibly rewarding as it incorporates the basic physiologic processes of digestion and absorption with a wide array of pathologic conditions. Incorporation of the basic principles of intestinal absorption allows for a greater understanding of the role of the low–fermentable oligo-, di-, monosaccharides and polyols (FODMAP) diet in the management of irritable bowel syndrome to the varying principles of diets currently under study for the management of IBD. Outside of this spectrum, working with an NST allows for the management of complex cases of malnutrition resulting from disorders ranging from cancer to various postsurgical intestinal alterations. Although observerships and external training programs allow for an introduction into the field, formal level 2 training, combining both work with a NST and small-bowel enteroscopy, allows for exposure to the full range of disorders of the small bowel. As patients continue to seek disease management options rooted in diet, the demand for gastroenterologists with subspecialty training in nutritional disorders will continue to grow and will require further support across training programs to incorporate additional training into categorical fellowships.
References
1. Daley BJ et al. JPEN J Paren Enteral Nutr. 2016;40(1):95-9. doi: 10.1177/0148607115571155.
2. Kiraly LN et al. Nutr Clin Pract. 2014;29(3):332-7. doi: 10.1177/0884533614525212.
3. Hu J et al. Nutr Clin Pract. 2018 Apr;33(2):191-7. doi: 10.1177/0884533617700852.
4. Scolapio JS et al. J Clin Gastroenterol. 2008 Feb;42(2):122-7. doi: 10.1097/MCG.0b013e3181595b6a.
5. American Association for the Study of Liver Diseases et al. The Gastroenterology Core Curriculum, 3rd ed. Gastroenterology. 2007;132(5):2012-8. doi: 10.1053/j.gastro.2007.03.079.
Dr. Micic is assistant professor of medicine, department of internal medicine, section of gastroenterology, hepatology, and nutrition, University of Chicago.
Advanced endoscopy training in the United States
Introduction
Comprehensive training in endoscopic retrograde cholangioscopy (ERCP) and endoscopic ultrasound (EUS) is difficult to achieve within the curriculum of a standard 3-year Accreditation Council for Graduate Medical Education (ACGME)–accredited gastroenterology fellowship. ERCP and EUS are technically challenging, operator-dependent procedures that require specialized cognitive, technical, and integrative skills.1-4 A survey of physicians performing ERCP found that only 60% felt “very comfortable” performing the procedure after completion of a standard gastroenterology fellowship.5 Procedural volumes in ERCP and EUS tend to be low among general gastroenterology fellows; in a survey, only 9% and 4.5% of trainees in standard gastrointestinal fellowships had anticipated volumes of more than 200 ERCP and EUS procedures, respectively.6 The unique skills required to safely and effectively perform ERCP and EUS, along with the growing portfolio of therapeutic procedures such as endoscopic mucosal resection (EMR), endoluminal stent placement, deep enteroscopy, advanced closure techniques, bariatric endoscopy, therapeutic EUS, and submucosal endoscopy (including endoscopic submucosal dissection and peroral endoscopic myotomy), has led to the development of dedicated postgraduate advanced endoscopy training programs.7-9
Status of advanced endoscopy training in the United States
Advanced endoscopy fellowships are typically year-long training programs completed at tertiary care centers. Over the last 2 decades, there has been a dramatic increase in the number of advanced endoscopy training positions.9 In 2012, the American Society for Gastrointestinal Endoscopy established a match program to standardize the application process (www.asgematch.com).10 Since its inception, there have been approximately 100 applicants per year and 60 participating programs. In the 2018 match, there were 90 advanced endoscopy applicants for 69 positions. Each year, about 20% of graduating gastroenterology fellows apply for advanced endoscopy fellowship, and applicant match rates are approximately 60%.
The goal of advanced endoscopy fellowship is to teach trainees to safely and effectively perform high-risk endoscopic procedures.1,11,12 Without ACGME oversight, no defined curricular requirements exist, and programs can be quite variable. Stronger programs offer close mentorship, conferences, comprehensive didactics, research support, and regular feedback. All programs participating in this year’s match offered training in both ERCP and EUS with most offering training in EMR, ablation, and deep enteroscopy.10 Many programs also offered training in endoluminal stenting and advanced closure techniques, such as suturing. More than half offered training in endoscopic submucosal dissection, peroral endoscopic myotomy, and bariatric endoscopy, but trainee hands-on time is usually limited, and competence is not guaranteed. A recent, large, multicenter, prospective study found that the median number of ERCPs and EUSs performed by trainees during advancing endoscopy training was 350 (range 125-500) and 300 (range 155-650), respectively.2 Median number of ERCPs performed in patients with native papilla was 51 (range 32-79). Most ERCPs were performed for biliary indications, and most EUSs were performed for pancreaticobiliary indications. The study found that most advanced endoscopy trainees have limited exposure to interventional EUS procedures, ERCPs for pancreatic indications, and ERCPs requiring advanced cannulation techniques.
Competency assessment
Advanced endoscopy fellowship programs must ensure trainees have achieved technical and cognitive competence and are safe for independent practice. Methods to assess trainee competence in advanced procedures have changed significantly over the last several years.1 Historically, endoscopic training was based on an apprenticeship model. Procedural volume and subjective assessments from trainers were used as surrogates for competence. Most current societal guidelines now recommend competency thresholds – a minimum number of supervised procedures that a trainee should complete before competency can be assessed – instead of absolute procedure volume requirements.4,13,14 The ASGE recommends that at least 200 supervised independent ERCPs, including 80 independent sphincterotomies and 60 biliary stent placements, should be performed before assessing competence.4 Similarly, 225 supervised independent EUS cases are recommended before assessing competence. Importantly, these guidelines are not validated and do not account for the inherent variability in which different trainees acquire endoscopic skills.15-18
Because of the limitations of volume-based assessments of competence, a greater emphasis has been placed on developing comprehensive, standardized competency assessments. With the ACGME’s adoption of the Next Accreditation System (NAS), a greater emphasis has been placed on competency-based medical education throughout the United States. The goal of the Next Accreditation System is to ensure that specific milestones are achieved by trainees and that trainee progress is clearly reported. Similarly, within advanced endoscopic training, it is now accepted that a minimum procedural volume is a necessary, but insufficient, marker of competence.1 Therefore, recent work has focused on defining milestones, developing assessment tools with strong validity, establishing trainee learning curves, and providing trainees with continuous feedback that allows for targeted improvement. Although the data are limited, a few studies have assessed learning curves among trainees. A prospective study of 15 trainees from the Netherlands found that trainees acquire competence in ERCP skills at variable rates; specifically, trainees achieved competence in native papilla cannulation later than other ERCP skills.18 Similarly, a recent prospective multicenter study of advanced endoscopy trainees using a standardized assessment tool and cumulative sum analysis found significant variability in the learning curves for cognitive and technical aspects of ERCP.15
The EUS and ERCP Skills Assessment Tool (TEESAT) is a competence assessment tool for EUS and ERCP with strong validity evidence.2,15,19-21 The tool assesses several individual technical and cognitive skills, in addition to a global assessment of competence, and should be used in a continuous fashion throughout fellowship training. A prospective, multicenter study using the TEESAT showed substantial variability in EUS and ERCP learning curves among trainees and demonstrated the feasibility of creating a national, centralized database that allows for continuous monitoring and reporting of individualized learning curves for EUS and ERCP among advanced endoscopy trainees.2 Such a database is an important step in evolving with the ACGME/NAS reporting requirement and would allow for fellowship program directors and trainers to identify specific trainee deficiencies in order to deliver targeted remediation.
The impact of individualized feedback on trainee learning curves and EUS and ERCP quality indicators was addressed in a recently published prospective multicenter cohort study.22 In phase 1 of the study, 24 advanced endoscopy trainees from 20 programs were assessed using the TEESAT and given quarterly feedback. By the end of training, 92% and 74% of fellows had achieved overall technical competence in EUS and ERCP, respectively. In phase 2, trainees were assessed in their first year of independent practice to determine whether participation in competency-based fellowship programs results in high-quality care in independent practice. The study found that most trainees met performance thresholds for quality indicators in EUS (94% diagnostic rate of adequate samples and 84% diagnostic yield of malignancy in pancreatic masses) and ERCP (95% overall cannulation rate). While competence could not be confirmed for all trainees after fellowship completion, most met quality indicator thresholds for EUS and ERCP during the first year of independent practice. These data provide construct validity evidence for TEESAT and the data collection and reporting system that provides periodic feedback using learning curves and ultimately affirm the effectiveness of current training programs.
Establishing minimal standards for training programs
Although the ASGE offers rudimentary metrics to characterize fellowships through the match program, a more comprehensive evaluation of advanced endoscopy training programs would be of value to potential trainees. It is in this context that we offered the minimum ERCP (~250 cases for Grade 1 ERCP and ~300 cases for Grade 2 ERCP) and EUS (~225 cases) volumes that should serve as a basis for a more rigorous assessment of advanced endoscopy training programs. We also recently proposed structure, process, and outcomes measures that should be defined along with associated benchmarks (Table 1). These quality metrics could then be utilized to guide trainees in the selection of a program.
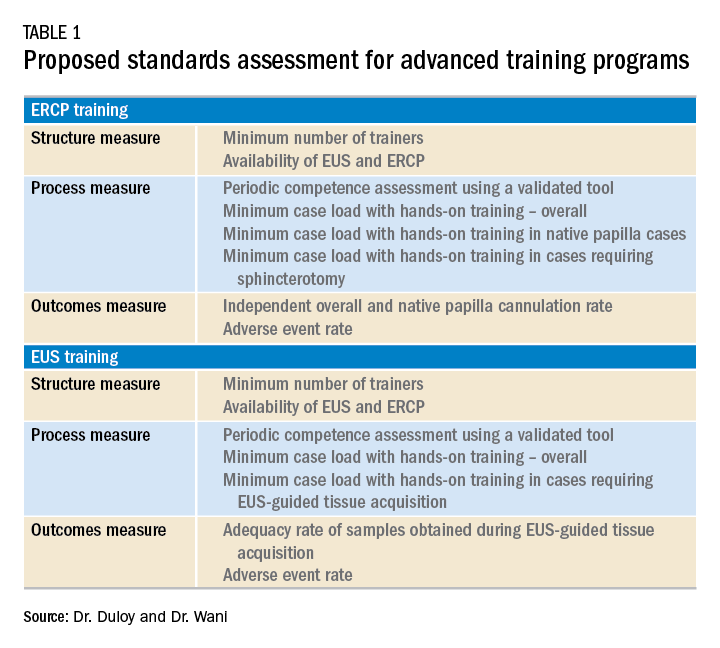
Conclusion
Advanced endoscopy training is a critical first step to ensuring endoscopists have the procedural and cognitive skills necessary to safely and effectively perform these high-risk procedures. As the portfolio of new procedures grows longer and more complex, it will become even more important for training programs to establish a standardized curriculum, adopt universal competency assessment tools, and provide continuous and targeted feedback to their trainees.
References
1. Wani S et al. Gastrointest Endosc. 2018;87:1371-82.
2. Wani S et al. Clin Gastroenterol Hepatol. 2017;15:1758-67 e11.
3. Patel SG et al. Am J Gastroenterol. 2015;110:956-62.
4. Committee ASoP et al. Gastrointest Endosc. 2017;85:273-81.
5. Cote GA et al. Gastrointest Endosc. 2011;74:65-73 e12.
6. Cotton PB et al. Gastrointest Endosc 2017;86:866-9.
7. Moffatt DC et al. Gastrointest Endosc. 2014;79:615-22.
8. Training and Education Committee of the American Gastroenterological Association. Gastroenterology 1988;94:1083-6.
9. Elta GH et al. Gastroenterology 2015;148:488-90.
10. www.asgematch.com. (Accessed June 21, 2018)
11. Jowell PS et al. Ann Intern Med 1996;125:983-9.
12. Eisen GM et al. Gastrointest Endosc 2002;55:780-3.
13. Polkowski M et al. Endoscopy 2012;44:190-206.
14. Committee AT et al. Gastrointest Endosc 2016;83:279-89.
15. Wani S et al. Gastrointest Endosc 2016;83:711-9 e11.
16. Northup PG et al. Gastroenterology 2013;144:677-80.
17. Eisen GM et al. Gastrointest Endosc 2001;53:846-8.
18. Ekkelenkamp VE et al. Endoscopy 2014;46:949-55.
19. Wani S et al. Clin Gastroenterol Hepatol 2015;13:1318-25 e2.
20. Wani S et al. Gastrointest Endosc 2013;77:558-65.
Dr. Duloy is a therapeutic gastroenterology fellow; Dr. Wani is an associate professor of medicine, University of Colorado Anschutz Medical Campus, Aurora, Colo.
Introduction
Comprehensive training in endoscopic retrograde cholangioscopy (ERCP) and endoscopic ultrasound (EUS) is difficult to achieve within the curriculum of a standard 3-year Accreditation Council for Graduate Medical Education (ACGME)–accredited gastroenterology fellowship. ERCP and EUS are technically challenging, operator-dependent procedures that require specialized cognitive, technical, and integrative skills.1-4 A survey of physicians performing ERCP found that only 60% felt “very comfortable” performing the procedure after completion of a standard gastroenterology fellowship.5 Procedural volumes in ERCP and EUS tend to be low among general gastroenterology fellows; in a survey, only 9% and 4.5% of trainees in standard gastrointestinal fellowships had anticipated volumes of more than 200 ERCP and EUS procedures, respectively.6 The unique skills required to safely and effectively perform ERCP and EUS, along with the growing portfolio of therapeutic procedures such as endoscopic mucosal resection (EMR), endoluminal stent placement, deep enteroscopy, advanced closure techniques, bariatric endoscopy, therapeutic EUS, and submucosal endoscopy (including endoscopic submucosal dissection and peroral endoscopic myotomy), has led to the development of dedicated postgraduate advanced endoscopy training programs.7-9
Status of advanced endoscopy training in the United States
Advanced endoscopy fellowships are typically year-long training programs completed at tertiary care centers. Over the last 2 decades, there has been a dramatic increase in the number of advanced endoscopy training positions.9 In 2012, the American Society for Gastrointestinal Endoscopy established a match program to standardize the application process (www.asgematch.com).10 Since its inception, there have been approximately 100 applicants per year and 60 participating programs. In the 2018 match, there were 90 advanced endoscopy applicants for 69 positions. Each year, about 20% of graduating gastroenterology fellows apply for advanced endoscopy fellowship, and applicant match rates are approximately 60%.
The goal of advanced endoscopy fellowship is to teach trainees to safely and effectively perform high-risk endoscopic procedures.1,11,12 Without ACGME oversight, no defined curricular requirements exist, and programs can be quite variable. Stronger programs offer close mentorship, conferences, comprehensive didactics, research support, and regular feedback. All programs participating in this year’s match offered training in both ERCP and EUS with most offering training in EMR, ablation, and deep enteroscopy.10 Many programs also offered training in endoluminal stenting and advanced closure techniques, such as suturing. More than half offered training in endoscopic submucosal dissection, peroral endoscopic myotomy, and bariatric endoscopy, but trainee hands-on time is usually limited, and competence is not guaranteed. A recent, large, multicenter, prospective study found that the median number of ERCPs and EUSs performed by trainees during advancing endoscopy training was 350 (range 125-500) and 300 (range 155-650), respectively.2 Median number of ERCPs performed in patients with native papilla was 51 (range 32-79). Most ERCPs were performed for biliary indications, and most EUSs were performed for pancreaticobiliary indications. The study found that most advanced endoscopy trainees have limited exposure to interventional EUS procedures, ERCPs for pancreatic indications, and ERCPs requiring advanced cannulation techniques.
Competency assessment
Advanced endoscopy fellowship programs must ensure trainees have achieved technical and cognitive competence and are safe for independent practice. Methods to assess trainee competence in advanced procedures have changed significantly over the last several years.1 Historically, endoscopic training was based on an apprenticeship model. Procedural volume and subjective assessments from trainers were used as surrogates for competence. Most current societal guidelines now recommend competency thresholds – a minimum number of supervised procedures that a trainee should complete before competency can be assessed – instead of absolute procedure volume requirements.4,13,14 The ASGE recommends that at least 200 supervised independent ERCPs, including 80 independent sphincterotomies and 60 biliary stent placements, should be performed before assessing competence.4 Similarly, 225 supervised independent EUS cases are recommended before assessing competence. Importantly, these guidelines are not validated and do not account for the inherent variability in which different trainees acquire endoscopic skills.15-18
Because of the limitations of volume-based assessments of competence, a greater emphasis has been placed on developing comprehensive, standardized competency assessments. With the ACGME’s adoption of the Next Accreditation System (NAS), a greater emphasis has been placed on competency-based medical education throughout the United States. The goal of the Next Accreditation System is to ensure that specific milestones are achieved by trainees and that trainee progress is clearly reported. Similarly, within advanced endoscopic training, it is now accepted that a minimum procedural volume is a necessary, but insufficient, marker of competence.1 Therefore, recent work has focused on defining milestones, developing assessment tools with strong validity, establishing trainee learning curves, and providing trainees with continuous feedback that allows for targeted improvement. Although the data are limited, a few studies have assessed learning curves among trainees. A prospective study of 15 trainees from the Netherlands found that trainees acquire competence in ERCP skills at variable rates; specifically, trainees achieved competence in native papilla cannulation later than other ERCP skills.18 Similarly, a recent prospective multicenter study of advanced endoscopy trainees using a standardized assessment tool and cumulative sum analysis found significant variability in the learning curves for cognitive and technical aspects of ERCP.15
The EUS and ERCP Skills Assessment Tool (TEESAT) is a competence assessment tool for EUS and ERCP with strong validity evidence.2,15,19-21 The tool assesses several individual technical and cognitive skills, in addition to a global assessment of competence, and should be used in a continuous fashion throughout fellowship training. A prospective, multicenter study using the TEESAT showed substantial variability in EUS and ERCP learning curves among trainees and demonstrated the feasibility of creating a national, centralized database that allows for continuous monitoring and reporting of individualized learning curves for EUS and ERCP among advanced endoscopy trainees.2 Such a database is an important step in evolving with the ACGME/NAS reporting requirement and would allow for fellowship program directors and trainers to identify specific trainee deficiencies in order to deliver targeted remediation.
The impact of individualized feedback on trainee learning curves and EUS and ERCP quality indicators was addressed in a recently published prospective multicenter cohort study.22 In phase 1 of the study, 24 advanced endoscopy trainees from 20 programs were assessed using the TEESAT and given quarterly feedback. By the end of training, 92% and 74% of fellows had achieved overall technical competence in EUS and ERCP, respectively. In phase 2, trainees were assessed in their first year of independent practice to determine whether participation in competency-based fellowship programs results in high-quality care in independent practice. The study found that most trainees met performance thresholds for quality indicators in EUS (94% diagnostic rate of adequate samples and 84% diagnostic yield of malignancy in pancreatic masses) and ERCP (95% overall cannulation rate). While competence could not be confirmed for all trainees after fellowship completion, most met quality indicator thresholds for EUS and ERCP during the first year of independent practice. These data provide construct validity evidence for TEESAT and the data collection and reporting system that provides periodic feedback using learning curves and ultimately affirm the effectiveness of current training programs.
Establishing minimal standards for training programs
Although the ASGE offers rudimentary metrics to characterize fellowships through the match program, a more comprehensive evaluation of advanced endoscopy training programs would be of value to potential trainees. It is in this context that we offered the minimum ERCP (~250 cases for Grade 1 ERCP and ~300 cases for Grade 2 ERCP) and EUS (~225 cases) volumes that should serve as a basis for a more rigorous assessment of advanced endoscopy training programs. We also recently proposed structure, process, and outcomes measures that should be defined along with associated benchmarks (Table 1). These quality metrics could then be utilized to guide trainees in the selection of a program.
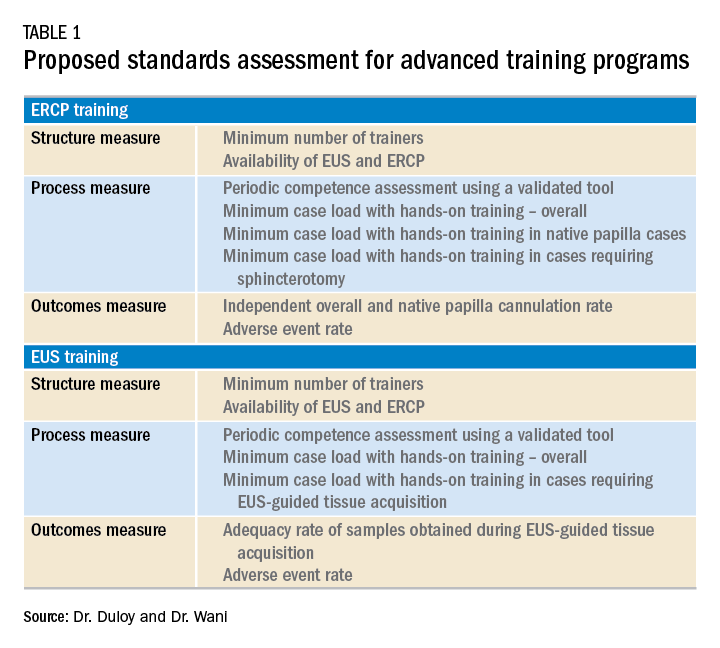
Conclusion
Advanced endoscopy training is a critical first step to ensuring endoscopists have the procedural and cognitive skills necessary to safely and effectively perform these high-risk procedures. As the portfolio of new procedures grows longer and more complex, it will become even more important for training programs to establish a standardized curriculum, adopt universal competency assessment tools, and provide continuous and targeted feedback to their trainees.
References
1. Wani S et al. Gastrointest Endosc. 2018;87:1371-82.
2. Wani S et al. Clin Gastroenterol Hepatol. 2017;15:1758-67 e11.
3. Patel SG et al. Am J Gastroenterol. 2015;110:956-62.
4. Committee ASoP et al. Gastrointest Endosc. 2017;85:273-81.
5. Cote GA et al. Gastrointest Endosc. 2011;74:65-73 e12.
6. Cotton PB et al. Gastrointest Endosc 2017;86:866-9.
7. Moffatt DC et al. Gastrointest Endosc. 2014;79:615-22.
8. Training and Education Committee of the American Gastroenterological Association. Gastroenterology 1988;94:1083-6.
9. Elta GH et al. Gastroenterology 2015;148:488-90.
10. www.asgematch.com. (Accessed June 21, 2018)
11. Jowell PS et al. Ann Intern Med 1996;125:983-9.
12. Eisen GM et al. Gastrointest Endosc 2002;55:780-3.
13. Polkowski M et al. Endoscopy 2012;44:190-206.
14. Committee AT et al. Gastrointest Endosc 2016;83:279-89.
15. Wani S et al. Gastrointest Endosc 2016;83:711-9 e11.
16. Northup PG et al. Gastroenterology 2013;144:677-80.
17. Eisen GM et al. Gastrointest Endosc 2001;53:846-8.
18. Ekkelenkamp VE et al. Endoscopy 2014;46:949-55.
19. Wani S et al. Clin Gastroenterol Hepatol 2015;13:1318-25 e2.
20. Wani S et al. Gastrointest Endosc 2013;77:558-65.
Dr. Duloy is a therapeutic gastroenterology fellow; Dr. Wani is an associate professor of medicine, University of Colorado Anschutz Medical Campus, Aurora, Colo.
Introduction
Comprehensive training in endoscopic retrograde cholangioscopy (ERCP) and endoscopic ultrasound (EUS) is difficult to achieve within the curriculum of a standard 3-year Accreditation Council for Graduate Medical Education (ACGME)–accredited gastroenterology fellowship. ERCP and EUS are technically challenging, operator-dependent procedures that require specialized cognitive, technical, and integrative skills.1-4 A survey of physicians performing ERCP found that only 60% felt “very comfortable” performing the procedure after completion of a standard gastroenterology fellowship.5 Procedural volumes in ERCP and EUS tend to be low among general gastroenterology fellows; in a survey, only 9% and 4.5% of trainees in standard gastrointestinal fellowships had anticipated volumes of more than 200 ERCP and EUS procedures, respectively.6 The unique skills required to safely and effectively perform ERCP and EUS, along with the growing portfolio of therapeutic procedures such as endoscopic mucosal resection (EMR), endoluminal stent placement, deep enteroscopy, advanced closure techniques, bariatric endoscopy, therapeutic EUS, and submucosal endoscopy (including endoscopic submucosal dissection and peroral endoscopic myotomy), has led to the development of dedicated postgraduate advanced endoscopy training programs.7-9
Status of advanced endoscopy training in the United States
Advanced endoscopy fellowships are typically year-long training programs completed at tertiary care centers. Over the last 2 decades, there has been a dramatic increase in the number of advanced endoscopy training positions.9 In 2012, the American Society for Gastrointestinal Endoscopy established a match program to standardize the application process (www.asgematch.com).10 Since its inception, there have been approximately 100 applicants per year and 60 participating programs. In the 2018 match, there were 90 advanced endoscopy applicants for 69 positions. Each year, about 20% of graduating gastroenterology fellows apply for advanced endoscopy fellowship, and applicant match rates are approximately 60%.
The goal of advanced endoscopy fellowship is to teach trainees to safely and effectively perform high-risk endoscopic procedures.1,11,12 Without ACGME oversight, no defined curricular requirements exist, and programs can be quite variable. Stronger programs offer close mentorship, conferences, comprehensive didactics, research support, and regular feedback. All programs participating in this year’s match offered training in both ERCP and EUS with most offering training in EMR, ablation, and deep enteroscopy.10 Many programs also offered training in endoluminal stenting and advanced closure techniques, such as suturing. More than half offered training in endoscopic submucosal dissection, peroral endoscopic myotomy, and bariatric endoscopy, but trainee hands-on time is usually limited, and competence is not guaranteed. A recent, large, multicenter, prospective study found that the median number of ERCPs and EUSs performed by trainees during advancing endoscopy training was 350 (range 125-500) and 300 (range 155-650), respectively.2 Median number of ERCPs performed in patients with native papilla was 51 (range 32-79). Most ERCPs were performed for biliary indications, and most EUSs were performed for pancreaticobiliary indications. The study found that most advanced endoscopy trainees have limited exposure to interventional EUS procedures, ERCPs for pancreatic indications, and ERCPs requiring advanced cannulation techniques.
Competency assessment
Advanced endoscopy fellowship programs must ensure trainees have achieved technical and cognitive competence and are safe for independent practice. Methods to assess trainee competence in advanced procedures have changed significantly over the last several years.1 Historically, endoscopic training was based on an apprenticeship model. Procedural volume and subjective assessments from trainers were used as surrogates for competence. Most current societal guidelines now recommend competency thresholds – a minimum number of supervised procedures that a trainee should complete before competency can be assessed – instead of absolute procedure volume requirements.4,13,14 The ASGE recommends that at least 200 supervised independent ERCPs, including 80 independent sphincterotomies and 60 biliary stent placements, should be performed before assessing competence.4 Similarly, 225 supervised independent EUS cases are recommended before assessing competence. Importantly, these guidelines are not validated and do not account for the inherent variability in which different trainees acquire endoscopic skills.15-18
Because of the limitations of volume-based assessments of competence, a greater emphasis has been placed on developing comprehensive, standardized competency assessments. With the ACGME’s adoption of the Next Accreditation System (NAS), a greater emphasis has been placed on competency-based medical education throughout the United States. The goal of the Next Accreditation System is to ensure that specific milestones are achieved by trainees and that trainee progress is clearly reported. Similarly, within advanced endoscopic training, it is now accepted that a minimum procedural volume is a necessary, but insufficient, marker of competence.1 Therefore, recent work has focused on defining milestones, developing assessment tools with strong validity, establishing trainee learning curves, and providing trainees with continuous feedback that allows for targeted improvement. Although the data are limited, a few studies have assessed learning curves among trainees. A prospective study of 15 trainees from the Netherlands found that trainees acquire competence in ERCP skills at variable rates; specifically, trainees achieved competence in native papilla cannulation later than other ERCP skills.18 Similarly, a recent prospective multicenter study of advanced endoscopy trainees using a standardized assessment tool and cumulative sum analysis found significant variability in the learning curves for cognitive and technical aspects of ERCP.15
The EUS and ERCP Skills Assessment Tool (TEESAT) is a competence assessment tool for EUS and ERCP with strong validity evidence.2,15,19-21 The tool assesses several individual technical and cognitive skills, in addition to a global assessment of competence, and should be used in a continuous fashion throughout fellowship training. A prospective, multicenter study using the TEESAT showed substantial variability in EUS and ERCP learning curves among trainees and demonstrated the feasibility of creating a national, centralized database that allows for continuous monitoring and reporting of individualized learning curves for EUS and ERCP among advanced endoscopy trainees.2 Such a database is an important step in evolving with the ACGME/NAS reporting requirement and would allow for fellowship program directors and trainers to identify specific trainee deficiencies in order to deliver targeted remediation.
The impact of individualized feedback on trainee learning curves and EUS and ERCP quality indicators was addressed in a recently published prospective multicenter cohort study.22 In phase 1 of the study, 24 advanced endoscopy trainees from 20 programs were assessed using the TEESAT and given quarterly feedback. By the end of training, 92% and 74% of fellows had achieved overall technical competence in EUS and ERCP, respectively. In phase 2, trainees were assessed in their first year of independent practice to determine whether participation in competency-based fellowship programs results in high-quality care in independent practice. The study found that most trainees met performance thresholds for quality indicators in EUS (94% diagnostic rate of adequate samples and 84% diagnostic yield of malignancy in pancreatic masses) and ERCP (95% overall cannulation rate). While competence could not be confirmed for all trainees after fellowship completion, most met quality indicator thresholds for EUS and ERCP during the first year of independent practice. These data provide construct validity evidence for TEESAT and the data collection and reporting system that provides periodic feedback using learning curves and ultimately affirm the effectiveness of current training programs.
Establishing minimal standards for training programs
Although the ASGE offers rudimentary metrics to characterize fellowships through the match program, a more comprehensive evaluation of advanced endoscopy training programs would be of value to potential trainees. It is in this context that we offered the minimum ERCP (~250 cases for Grade 1 ERCP and ~300 cases for Grade 2 ERCP) and EUS (~225 cases) volumes that should serve as a basis for a more rigorous assessment of advanced endoscopy training programs. We also recently proposed structure, process, and outcomes measures that should be defined along with associated benchmarks (Table 1). These quality metrics could then be utilized to guide trainees in the selection of a program.
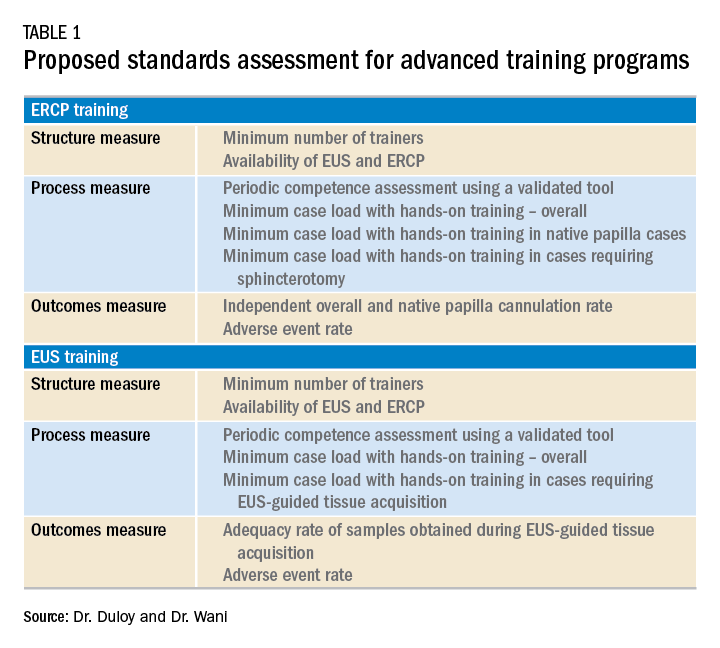
Conclusion
Advanced endoscopy training is a critical first step to ensuring endoscopists have the procedural and cognitive skills necessary to safely and effectively perform these high-risk procedures. As the portfolio of new procedures grows longer and more complex, it will become even more important for training programs to establish a standardized curriculum, adopt universal competency assessment tools, and provide continuous and targeted feedback to their trainees.
References
1. Wani S et al. Gastrointest Endosc. 2018;87:1371-82.
2. Wani S et al. Clin Gastroenterol Hepatol. 2017;15:1758-67 e11.
3. Patel SG et al. Am J Gastroenterol. 2015;110:956-62.
4. Committee ASoP et al. Gastrointest Endosc. 2017;85:273-81.
5. Cote GA et al. Gastrointest Endosc. 2011;74:65-73 e12.
6. Cotton PB et al. Gastrointest Endosc 2017;86:866-9.
7. Moffatt DC et al. Gastrointest Endosc. 2014;79:615-22.
8. Training and Education Committee of the American Gastroenterological Association. Gastroenterology 1988;94:1083-6.
9. Elta GH et al. Gastroenterology 2015;148:488-90.
10. www.asgematch.com. (Accessed June 21, 2018)
11. Jowell PS et al. Ann Intern Med 1996;125:983-9.
12. Eisen GM et al. Gastrointest Endosc 2002;55:780-3.
13. Polkowski M et al. Endoscopy 2012;44:190-206.
14. Committee AT et al. Gastrointest Endosc 2016;83:279-89.
15. Wani S et al. Gastrointest Endosc 2016;83:711-9 e11.
16. Northup PG et al. Gastroenterology 2013;144:677-80.
17. Eisen GM et al. Gastrointest Endosc 2001;53:846-8.
18. Ekkelenkamp VE et al. Endoscopy 2014;46:949-55.
19. Wani S et al. Clin Gastroenterol Hepatol 2015;13:1318-25 e2.
20. Wani S et al. Gastrointest Endosc 2013;77:558-65.
Dr. Duloy is a therapeutic gastroenterology fellow; Dr. Wani is an associate professor of medicine, University of Colorado Anschutz Medical Campus, Aurora, Colo.