User login
Is azithromycin prophylaxis appropriate for vaginal delivery in low- and middle-resource populations?

Tita ATN, Carlo WA, McClure EM, et al; for the A-PLUS Trial Group. Azithromycin to prevent sepsis or death in women planning a vaginal birth. N Engl J Med. 2023;388:1161-1170. doi:10:1056/NEJMoa2212111.
EXPERT COMMENTARY
Maternal peripartum infection is 1 of the top 5 causes of maternal death, accounting for about 10% of cases of maternal mortality. Cesarean delivery (CD), of course, is the most important risk factor for puerperal infection. However, even vaginal delivery, particularly in low- to middle-resource countries, where deliveries often occur under less-than-optimal conditions, may be associated with a surprisingly high frequency of both maternal and neonatal infections. The beneficial effect of prophylactic antibiotics for CD is well established. An important remaining question is whether similar benefit can be achieved with prophylaxis for women planning to have a vaginal birth.
In 2017, Oluwalana and colleagues conducted a prospective, randomized, double-blind, placebo-controlled trial of a single 2-g oral dose of azithromycin in Gambian women undergoing labor.1 During the 8 weeks after delivery, maternal infections were lower in the azithromycin group, 3.6% versus 9.2% (relative risk [RR], 0.40; 95% confidence interval [CI], 0.22–0.71; P=.002). Infections also were lower in the newborns, 18.1% versus 23.8% (RR, 0.76; 95% CI, 0.58–0.99; P=.052), delivered to mothers who received azithromycin. The greatest impact on neonatal infections was the reduced frequency of skin infections.
In 2021, Subramaniam and colleagues evaluated the effect of a single dose of oral azithromycin with, or without, amoxicillin on the prevalence of peripartum infection in laboring women in Cameroon.2 Patients and their newborns were followed for 6 weeks after delivery. Unlike the previous investigation, the authors were unable to show a protective effect of prophylaxis on either maternal or neonatal infection.
Against this backdrop, Tita and colleagues conducted a remarkably large, well-designed, randomized, placebo-controlled study of azithromycin prophylaxis in women at 8 different sites in 7 low- or middle-income countries (the A-PLUS investigation).3
Details of the study
The investigators randomly assigned 29,278 patients at or beyond 28 weeks’ gestation to receive either a 2-g oral dose of azithromycin or placebo during labor. This particular drug was chosen because it is readily available, inexpensive, well tolerated, and has a broad range of activity against many important pelvic pathogens, including genital mycoplasmas. Some patients also received other antibiotics, for example, for group B streptococcal (GBS) prophylaxis or for CD prophylaxis if abdominal delivery was indicated.
The 2 primary outcomes were a composite of maternal sepsis or death and a composite of stillbirth or neonatal death or sepsis within 4 weeks of delivery. Secondary outcomes included individual components of the primary outcomes.
Results. The results of the investigation were compelling, and the data safety monitoring committee recommended stopping the trial early because of clear maternal benefit. The groups were well balanced with respect to important characteristics, such as incidence of CD, receipt of other prophylactic antibiotics, and median time between randomization and delivery.
The incidence of maternal sepsis or death was lower in the azithromycin group (1.6% vs 2.4%; RR, 0.67; 95% CI, 0.56–0.79; P<.001). The key effect was on the frequency of maternal sepsis because the incidence of maternal death was very low in both groups, 0.1%. With respect to secondary outcomes, prophylaxis was effective in reducing the frequency of endometritis (RR, 0.66; 95% CI, 0.55–0.79) and perineal and incisional infection (RR, 0.71; 95% CI, 0.56–0.85).
There was no difference in the frequency of neonatal sepsis or death. There also was no difference in the frequency of adverse drug effects in either group. Of note, more cases of neonatal pyloric stenosis were observed in the azithromycin group, but the overall incidence was lower than the expected background rate. This possible “signal” is important because this effect has been noted with increased frequency in neonates who received this antibiotic. ●
I believe that Tita and colleagues are quite correct in concluding that the simple, inexpensive intervention of azithromycin prophylaxis should be used routinely in patient populations similar to those included in this investigation and that the intervention can be invaluable in advancing the World Health Organization’s campaign to reduce the rate of maternal mortality in low- and middleresource nations.
What is not clear, however, is whether this same intervention would be effective in high-resource countries in which the level of skill of the obstetric providers is higher and more uniform; deliveries occur under more optimal sanitary conditions; treatment and prophylaxis for infections such as gonorrhea, chlamydia, chorioamnionitis, and GBS is more consistent; and early neonatal care is more robust. A similar large trial in wellresourced nations would indeed be welcome, particularly if the trial also addressed the possibility of an adverse effect on the neonatal microbiome if a policy of nearly universal antibiotic prophylaxis was adopted.
In the interim, we should focus our attention on the key interventions that are of proven value in decreasing the risk of peripartum maternal and neonatal infection:
- consistently screening for GBS colonization and administering intrapartum antibiotic prophylaxis to patients who test positive
- consistently screening for gonococcal and chlamydia infection in the antepartum period and treating infected patients with appropriate antibiotics
- minimizing the number of internal vaginal examinations during labor, particularly following rupture of membranes
- promptly identifying patients with chorioamnionitis and treating with antibiotics that specifically target GBS and Escherichia coli, the 2 most likely causes of neonatal sepsis, pneumonia, and meningitis
- administering preoperative prophylactic antibiotics (cefazolin plus azithromycin) to women who require CD.
PATRICK DUFF, MD
- Oluwalana C, Camara B, Bottomley C, et al. Azithromycin in labor lowers clinical infections in mothers and newborns: a double-blind trial. Pediatrics. 2017;139:e20162281. doi:10.1542/peds.2016-2281.
- Subramaniam A, Ye Y, Mbah R, et al. Single dose of oral azithromycin with or without amoxicillin to prevent peripartum infection in laboring, high-risk women in Cameroon: a randomized controlled trial. Obstet Gynecol. 2021;138:703-713. doi:10.1097/AOG.0000000000004565.
- Tita ATN, Carlo WA, McClure EM, et al; for the A-PLUS Trial Group. Azithromycin to prevent sepsis or death in women planning a vaginal birth. N Engl J Med. 2023;388:1161-1170. doi:10:1056/NEJMoa2212111.

Tita ATN, Carlo WA, McClure EM, et al; for the A-PLUS Trial Group. Azithromycin to prevent sepsis or death in women planning a vaginal birth. N Engl J Med. 2023;388:1161-1170. doi:10:1056/NEJMoa2212111.
EXPERT COMMENTARY
Maternal peripartum infection is 1 of the top 5 causes of maternal death, accounting for about 10% of cases of maternal mortality. Cesarean delivery (CD), of course, is the most important risk factor for puerperal infection. However, even vaginal delivery, particularly in low- to middle-resource countries, where deliveries often occur under less-than-optimal conditions, may be associated with a surprisingly high frequency of both maternal and neonatal infections. The beneficial effect of prophylactic antibiotics for CD is well established. An important remaining question is whether similar benefit can be achieved with prophylaxis for women planning to have a vaginal birth.
In 2017, Oluwalana and colleagues conducted a prospective, randomized, double-blind, placebo-controlled trial of a single 2-g oral dose of azithromycin in Gambian women undergoing labor.1 During the 8 weeks after delivery, maternal infections were lower in the azithromycin group, 3.6% versus 9.2% (relative risk [RR], 0.40; 95% confidence interval [CI], 0.22–0.71; P=.002). Infections also were lower in the newborns, 18.1% versus 23.8% (RR, 0.76; 95% CI, 0.58–0.99; P=.052), delivered to mothers who received azithromycin. The greatest impact on neonatal infections was the reduced frequency of skin infections.
In 2021, Subramaniam and colleagues evaluated the effect of a single dose of oral azithromycin with, or without, amoxicillin on the prevalence of peripartum infection in laboring women in Cameroon.2 Patients and their newborns were followed for 6 weeks after delivery. Unlike the previous investigation, the authors were unable to show a protective effect of prophylaxis on either maternal or neonatal infection.
Against this backdrop, Tita and colleagues conducted a remarkably large, well-designed, randomized, placebo-controlled study of azithromycin prophylaxis in women at 8 different sites in 7 low- or middle-income countries (the A-PLUS investigation).3
Details of the study
The investigators randomly assigned 29,278 patients at or beyond 28 weeks’ gestation to receive either a 2-g oral dose of azithromycin or placebo during labor. This particular drug was chosen because it is readily available, inexpensive, well tolerated, and has a broad range of activity against many important pelvic pathogens, including genital mycoplasmas. Some patients also received other antibiotics, for example, for group B streptococcal (GBS) prophylaxis or for CD prophylaxis if abdominal delivery was indicated.
The 2 primary outcomes were a composite of maternal sepsis or death and a composite of stillbirth or neonatal death or sepsis within 4 weeks of delivery. Secondary outcomes included individual components of the primary outcomes.
Results. The results of the investigation were compelling, and the data safety monitoring committee recommended stopping the trial early because of clear maternal benefit. The groups were well balanced with respect to important characteristics, such as incidence of CD, receipt of other prophylactic antibiotics, and median time between randomization and delivery.
The incidence of maternal sepsis or death was lower in the azithromycin group (1.6% vs 2.4%; RR, 0.67; 95% CI, 0.56–0.79; P<.001). The key effect was on the frequency of maternal sepsis because the incidence of maternal death was very low in both groups, 0.1%. With respect to secondary outcomes, prophylaxis was effective in reducing the frequency of endometritis (RR, 0.66; 95% CI, 0.55–0.79) and perineal and incisional infection (RR, 0.71; 95% CI, 0.56–0.85).
There was no difference in the frequency of neonatal sepsis or death. There also was no difference in the frequency of adverse drug effects in either group. Of note, more cases of neonatal pyloric stenosis were observed in the azithromycin group, but the overall incidence was lower than the expected background rate. This possible “signal” is important because this effect has been noted with increased frequency in neonates who received this antibiotic. ●
I believe that Tita and colleagues are quite correct in concluding that the simple, inexpensive intervention of azithromycin prophylaxis should be used routinely in patient populations similar to those included in this investigation and that the intervention can be invaluable in advancing the World Health Organization’s campaign to reduce the rate of maternal mortality in low- and middleresource nations.
What is not clear, however, is whether this same intervention would be effective in high-resource countries in which the level of skill of the obstetric providers is higher and more uniform; deliveries occur under more optimal sanitary conditions; treatment and prophylaxis for infections such as gonorrhea, chlamydia, chorioamnionitis, and GBS is more consistent; and early neonatal care is more robust. A similar large trial in wellresourced nations would indeed be welcome, particularly if the trial also addressed the possibility of an adverse effect on the neonatal microbiome if a policy of nearly universal antibiotic prophylaxis was adopted.
In the interim, we should focus our attention on the key interventions that are of proven value in decreasing the risk of peripartum maternal and neonatal infection:
- consistently screening for GBS colonization and administering intrapartum antibiotic prophylaxis to patients who test positive
- consistently screening for gonococcal and chlamydia infection in the antepartum period and treating infected patients with appropriate antibiotics
- minimizing the number of internal vaginal examinations during labor, particularly following rupture of membranes
- promptly identifying patients with chorioamnionitis and treating with antibiotics that specifically target GBS and Escherichia coli, the 2 most likely causes of neonatal sepsis, pneumonia, and meningitis
- administering preoperative prophylactic antibiotics (cefazolin plus azithromycin) to women who require CD.
PATRICK DUFF, MD

Tita ATN, Carlo WA, McClure EM, et al; for the A-PLUS Trial Group. Azithromycin to prevent sepsis or death in women planning a vaginal birth. N Engl J Med. 2023;388:1161-1170. doi:10:1056/NEJMoa2212111.
EXPERT COMMENTARY
Maternal peripartum infection is 1 of the top 5 causes of maternal death, accounting for about 10% of cases of maternal mortality. Cesarean delivery (CD), of course, is the most important risk factor for puerperal infection. However, even vaginal delivery, particularly in low- to middle-resource countries, where deliveries often occur under less-than-optimal conditions, may be associated with a surprisingly high frequency of both maternal and neonatal infections. The beneficial effect of prophylactic antibiotics for CD is well established. An important remaining question is whether similar benefit can be achieved with prophylaxis for women planning to have a vaginal birth.
In 2017, Oluwalana and colleagues conducted a prospective, randomized, double-blind, placebo-controlled trial of a single 2-g oral dose of azithromycin in Gambian women undergoing labor.1 During the 8 weeks after delivery, maternal infections were lower in the azithromycin group, 3.6% versus 9.2% (relative risk [RR], 0.40; 95% confidence interval [CI], 0.22–0.71; P=.002). Infections also were lower in the newborns, 18.1% versus 23.8% (RR, 0.76; 95% CI, 0.58–0.99; P=.052), delivered to mothers who received azithromycin. The greatest impact on neonatal infections was the reduced frequency of skin infections.
In 2021, Subramaniam and colleagues evaluated the effect of a single dose of oral azithromycin with, or without, amoxicillin on the prevalence of peripartum infection in laboring women in Cameroon.2 Patients and their newborns were followed for 6 weeks after delivery. Unlike the previous investigation, the authors were unable to show a protective effect of prophylaxis on either maternal or neonatal infection.
Against this backdrop, Tita and colleagues conducted a remarkably large, well-designed, randomized, placebo-controlled study of azithromycin prophylaxis in women at 8 different sites in 7 low- or middle-income countries (the A-PLUS investigation).3
Details of the study
The investigators randomly assigned 29,278 patients at or beyond 28 weeks’ gestation to receive either a 2-g oral dose of azithromycin or placebo during labor. This particular drug was chosen because it is readily available, inexpensive, well tolerated, and has a broad range of activity against many important pelvic pathogens, including genital mycoplasmas. Some patients also received other antibiotics, for example, for group B streptococcal (GBS) prophylaxis or for CD prophylaxis if abdominal delivery was indicated.
The 2 primary outcomes were a composite of maternal sepsis or death and a composite of stillbirth or neonatal death or sepsis within 4 weeks of delivery. Secondary outcomes included individual components of the primary outcomes.
Results. The results of the investigation were compelling, and the data safety monitoring committee recommended stopping the trial early because of clear maternal benefit. The groups were well balanced with respect to important characteristics, such as incidence of CD, receipt of other prophylactic antibiotics, and median time between randomization and delivery.
The incidence of maternal sepsis or death was lower in the azithromycin group (1.6% vs 2.4%; RR, 0.67; 95% CI, 0.56–0.79; P<.001). The key effect was on the frequency of maternal sepsis because the incidence of maternal death was very low in both groups, 0.1%. With respect to secondary outcomes, prophylaxis was effective in reducing the frequency of endometritis (RR, 0.66; 95% CI, 0.55–0.79) and perineal and incisional infection (RR, 0.71; 95% CI, 0.56–0.85).
There was no difference in the frequency of neonatal sepsis or death. There also was no difference in the frequency of adverse drug effects in either group. Of note, more cases of neonatal pyloric stenosis were observed in the azithromycin group, but the overall incidence was lower than the expected background rate. This possible “signal” is important because this effect has been noted with increased frequency in neonates who received this antibiotic. ●
I believe that Tita and colleagues are quite correct in concluding that the simple, inexpensive intervention of azithromycin prophylaxis should be used routinely in patient populations similar to those included in this investigation and that the intervention can be invaluable in advancing the World Health Organization’s campaign to reduce the rate of maternal mortality in low- and middleresource nations.
What is not clear, however, is whether this same intervention would be effective in high-resource countries in which the level of skill of the obstetric providers is higher and more uniform; deliveries occur under more optimal sanitary conditions; treatment and prophylaxis for infections such as gonorrhea, chlamydia, chorioamnionitis, and GBS is more consistent; and early neonatal care is more robust. A similar large trial in wellresourced nations would indeed be welcome, particularly if the trial also addressed the possibility of an adverse effect on the neonatal microbiome if a policy of nearly universal antibiotic prophylaxis was adopted.
In the interim, we should focus our attention on the key interventions that are of proven value in decreasing the risk of peripartum maternal and neonatal infection:
- consistently screening for GBS colonization and administering intrapartum antibiotic prophylaxis to patients who test positive
- consistently screening for gonococcal and chlamydia infection in the antepartum period and treating infected patients with appropriate antibiotics
- minimizing the number of internal vaginal examinations during labor, particularly following rupture of membranes
- promptly identifying patients with chorioamnionitis and treating with antibiotics that specifically target GBS and Escherichia coli, the 2 most likely causes of neonatal sepsis, pneumonia, and meningitis
- administering preoperative prophylactic antibiotics (cefazolin plus azithromycin) to women who require CD.
PATRICK DUFF, MD
- Oluwalana C, Camara B, Bottomley C, et al. Azithromycin in labor lowers clinical infections in mothers and newborns: a double-blind trial. Pediatrics. 2017;139:e20162281. doi:10.1542/peds.2016-2281.
- Subramaniam A, Ye Y, Mbah R, et al. Single dose of oral azithromycin with or without amoxicillin to prevent peripartum infection in laboring, high-risk women in Cameroon: a randomized controlled trial. Obstet Gynecol. 2021;138:703-713. doi:10.1097/AOG.0000000000004565.
- Tita ATN, Carlo WA, McClure EM, et al; for the A-PLUS Trial Group. Azithromycin to prevent sepsis or death in women planning a vaginal birth. N Engl J Med. 2023;388:1161-1170. doi:10:1056/NEJMoa2212111.
- Oluwalana C, Camara B, Bottomley C, et al. Azithromycin in labor lowers clinical infections in mothers and newborns: a double-blind trial. Pediatrics. 2017;139:e20162281. doi:10.1542/peds.2016-2281.
- Subramaniam A, Ye Y, Mbah R, et al. Single dose of oral azithromycin with or without amoxicillin to prevent peripartum infection in laboring, high-risk women in Cameroon: a randomized controlled trial. Obstet Gynecol. 2021;138:703-713. doi:10.1097/AOG.0000000000004565.
- Tita ATN, Carlo WA, McClure EM, et al; for the A-PLUS Trial Group. Azithromycin to prevent sepsis or death in women planning a vaginal birth. N Engl J Med. 2023;388:1161-1170. doi:10:1056/NEJMoa2212111.
Headache before the revolution: A clinician looks back
Headache treatment before the early 1990s was marked by decades of improvisation with mostly unapproved agents, followed by an explosion of scientific interest and new treatments developed specifically for migraine.
But this is largely thanks to the sea change that occurred 30 years ago.
In an interview, Alan M. Rapoport, MD, editor-in-chief of Neurology Reviews, past president of the International Headache Society and clinical professor of neurology at UCLA’s David Geffen School of Medicine in Los Angeles, recalled what it was like to treat patients before and after triptan medications came onto the market.
After the first of these anti-migraine agents, sumatriptan, was approved by the Food and Drug Administration in late December 1992, headache specialists found themselves with a powerful, approved treatment that validated their commitment to solving the disorder, and helped put to rest a persistent but mistaken notion that migraine was a psychiatric condition affecting young women.
But in the 1970s and 1980s, “there wasn’t great science explaining the pathophysiology of common primary headaches like tension-type headache, cluster headache, and migraine,” Dr. Rapoport recalled. “There is often comorbid depression and anxiety with migraine, and sometimes more serious psychiatric disease, but it doesn’t mean migraine is caused by psychological issues. Now we see it clearly as a disease of the brain, but it took years of investigation to prove that.”
The early years
Dr. Rapoport’s journey with headache began in 1972, when he joined a private neurology practice in Stamford and Greenwich, Conn. Neurologists were frowned upon then for having too much interest in headache, he said. There was poor remuneration for doctors treating headache patients, who were hard to properly diagnose and effectively care for. Few medications could effectively stop a migraine attack or reliably reduce the frequency of headaches or the disability they caused.
On weekends Dr. Rapoport covered emergency departments and ICUs at three hospitals, where standard treatment for a migraine attack was injectable opiates. Not only did this treatment aggravate nausea, a common migraine symptom, “but it did not stop the migraine process.” Once the pain relief wore off, patients woke up with the same headache, Dr. Rapoport recalled. “The other drug that was available was ergotamine tartrate” – a fungal alkaloid used since medieval times to treat headache – “given sublingually. It helped the headache slightly but increased the nausea. DHE, or dihydroergotamine, was available only by injection and not used very much.”
DHE, a semi-synthetic molecule based on ergotamine, had FDA approval for migraine, but was complicated to administer. Like the opioids, it provoked vomiting when given intravenously, in patients already suffering migraine-induced nausea. But Dr. Rapoport, along with some of his colleagues, felt that there was a role for DHE for the most severe subtypes of patients, those with long histories of frequent migraines.
“We put people in the hospital and we gave them intravenous DHE. Eventually I got the idea to give it intramuscularly or subcutaneously in the emergency room or my office. When you give it that way, it doesn’t work as quickly but has fewer side effects.” Dr. Rapoport designed a cocktail by coadministering promethazine for nausea, and eventually added a steroid, dexamethasone. The triple shots worked on most patients experiencing severe daily or near-daily migraine attacks, Dr. Rapoport saw, and he began administering the drug combination at The New England Center for Headache in Stamford and Greenwich, Conn., which he opened with Dr. Fred D. Sheftell in 1979.
“The triple shots really worked,” Dr. Rapoport recalled. “There was no need to keep patients in the office or emergency room for intravenous therapy. The patients never called to complain or came back the next day,” he said, as often occurred with opioid treatment.
Dr. Rapoport had learned early in his residency, in the late 1960s, from Dr. David R. Coddon, a neurologist at Mount Sinai hospital in New York, that a tricyclic antidepressant, imipramine, could be helpful in some patients with frequent migraine attacks. As evidence trickled in that other antidepressants, beta-blockers, and antiepileptic drugs might have preventive properties, Dr. Rapoport and others prescribed them for certain patients. But of all the drugs in the headache specialists’ repertoire, few were approved for either treatment or prevention. “And this continued until the triptans,” Dr. Rapoport said.
The triptan era
Sumatriptan was developed by Glaxo for the acute treatment of migraine. The medication, first available only as self-administered subcutaneous injections, was originally designed to bind to vascular serotonin receptors to allow selective constriction of cranial vessels that dilate, causing pain, during a migraine attack. (Years later it was discovered that triptans also worked as anti-inflammatory agents that decreased the release of the neurotransmitter calcitonin gene-related peptide, or CGRP.)
Triptans “changed the world for migraine patients and for me,” Dr. Rapoport said. “I could now prescribe a medication that people could take at home to decrease or stop the migraine process in an hour or two.” The success of the triptans prompted pharmaceutical companies to search for new, more effective ways to treat migraine attacks, with better tolerability.
Seven different triptans were developed, some as injections or tablets and others as nasal sprays. “If one triptan didn’t work, we’d give a second and rarely a third,” Dr. Rapoport said. “We learned that if oral triptans did not work, the most likely issue was that it was not rapidly absorbed from the small intestine, as migraine patients have nausea, poor GI absorption, and slow transit times. This prompted the greater use of injections and nasal sprays.” Headache specialists began combining triptan treatment with nonsteroidal anti-inflammatory drugs, offering further relief for the acute care of migraine.
Medication overuse headache
The years between 1993 and 2000, which saw all the current triptan drugs come onto the market, was an exhilarating one for headache specialists. But even those who were thrilled by the possibilities of the triptans, like Dr. Rapoport, soon came to recognize their limitations, in terms of side effects and poor tolerability for some patients.
Specialists also noticed something unsettling about the triptans: that patients’ headaches seemed to recur within a day, or occur more frequently over time, with higher medication use.
Medication overuse headache (MOH) was known to occur when patients treated migraine too often with acute care medications, especially over-the-counter analgesics and prescription opioids and barbiturates. Dr. Rapoport began warning at conferences and in seminars that MOH seemed to occur with the triptans as well. “In the beginning other doctors didn’t think the triptans could cause MOH, but I observed that patients who were taking triptans daily or almost daily were having increased headache frequency and the triptans stopped being effective. If they didn’t take the drug they were overusing, they were going to get much worse, almost like a withdrawal.”
Today, all seven triptans are now generic, and they remain a mainstay of migraine treatment: “Almost all of my patients are using, or have used a triptan,” Dr. Rapoport said. Yet researchers came to recognize the need for treatments targeting different pathways, both for prevention and acute care.
The next revolution: CGRP and gepants
Studies in the early 2000s began to show a link between the release of one ubiquitous nervous system neurotransmitter, calcitonin gene-related peptide, or CGRP, and migraine. They also noticed that blocking meningeal inflammation could lead to improvement in headache. Two new drug classes emerged from this science: monoclonal antibodies against CGRP or its receptor that had to be given by injection, and oral CGRP receptor blockers that could be used both as a preventive or as an acute care medication.
In 2018 the first monoclonal antibody against the CGRP receptor, erenumab (Aimovig, marketed by Amgen), delivered by injection, was approved for migraine prevention. Three others followed, most given by autoinjector, and one by IV infusion in office or hospital settings. “Those drugs are great,” Dr. Rapoport said. “You take one shot a month or every 3 months, and your headaches drop by 50% or more with very few side effects. Some patients actually see their migraines disappear.”
The following year ubrogepant (Ubrelvy, marketed by AbbVie), the first of a novel class of oral CGRP receptor blockers known as “gepants,” was approved to treat acute migraine. The FDA soon approved another gepant, rimegepant (Nurtec, marketed by Pfizer), which received indications both for prevention and for stopping a migraine attack acutely.
Both classes of therapies – the antibodies and the gepants – are far costlier than the triptans, which are all generic, and may not be needed for every migraine patient. With the gepants, for example, insurers may restrict use to people who have not responded to triptans or for whom triptans are contraindicated or cause too many adverse events. But the CGRP-targeted therapies as a whole “have been every bit as revolutionary” as the triptans, Dr. Rapoport said. The treatments work quickly to resolve headache and disability and get the patient functioning within an hour or two, and there are fewer side effects.
In a review article published in CNS Drugs in 2021, Dr. Rapoport and his colleagues reported that the anti-CGRP treatment with gepants did not appear linked to medication overuse headache, as virtually all previous acute care medication classes did, and could be used in patients who had previously reported MOH. “I am confident that over the next few years, more people will be using them as insurance coverage will improve for patients living with migraine,” he said.
Headache treatment today
Migraine specialists and patients now have a staggering range of therapeutic options. Approved treatments now include prevention of migraine with onabotulinumtoxinA (Botox, marketed by the Allergan division of AbbVie) injections, which work alone and with other medicines; acute care treatment with ditans like lasmiditan (Reyvow, marketed by Lilly*), a category of acute care medicines that work like triptans but target different serotonin receptors. Five devices have been cleared for migraine and other types of headache by the FDA. These work alone or along with medication and can be used acutely or preventively. The devices “should be used more,” Dr. Rapoport said, but are not yet well covered by insurance.
Thirty years after the triptans, scientists and researchers continue to explore the pathophysiology of headache disorders, finding new pathways and identifying new potential targets.
“There are many parts of the brain and brain stem that are involved, as well as the thalamus and hypothalamus,” Dr. Rapoport said. “It’s interesting that the newer medications, and some of the older ones, work in the peripheral nervous system, outside the brain stem in the trigeminovascular system, to modulate the central nervous system. We also know that the CGRP system is involved with cellular second-order messengers. Stimulating and blocking this chain of reactions with newer drugs may become treatments in the future.”
Recent research has focused on a blood vessel dilating neurotransmitter, pituitary adenylate-cyclase-activating polypeptide, or PACAP-38, as a potential therapeutic target. Psychedelic medications such as psilocybin, strong pain medications such as ketamine, and even cannabinoids such as marijuana have all been investigated in migraine. Biofeedback therapies, mindfulness, and other behavioral interventions also have proved effective.
“I expect the next 2-5 years to bring us many important clinical trials on new types of pharmacological treatments,” Dr. Rapoport said. “This is a wonderful time to be a doctor or nurse treating patients living with migraine. When I started out treating headache, 51 years ago, we had only ergotamine tartrate. Today we have so many therapies and combinations of therapies that I hardly know where to start.”
Dr. Rapoport has served as a consultant to or speaker for AbbVie, Amgen, Biohaven, Cala Health, Lundbeck, Satsuma, and Teva, among others.
*Correction, 3/30/23: An earlier version of this article misstated the name of the company that markets Reyvow.
Headache treatment before the early 1990s was marked by decades of improvisation with mostly unapproved agents, followed by an explosion of scientific interest and new treatments developed specifically for migraine.
But this is largely thanks to the sea change that occurred 30 years ago.
In an interview, Alan M. Rapoport, MD, editor-in-chief of Neurology Reviews, past president of the International Headache Society and clinical professor of neurology at UCLA’s David Geffen School of Medicine in Los Angeles, recalled what it was like to treat patients before and after triptan medications came onto the market.
After the first of these anti-migraine agents, sumatriptan, was approved by the Food and Drug Administration in late December 1992, headache specialists found themselves with a powerful, approved treatment that validated their commitment to solving the disorder, and helped put to rest a persistent but mistaken notion that migraine was a psychiatric condition affecting young women.
But in the 1970s and 1980s, “there wasn’t great science explaining the pathophysiology of common primary headaches like tension-type headache, cluster headache, and migraine,” Dr. Rapoport recalled. “There is often comorbid depression and anxiety with migraine, and sometimes more serious psychiatric disease, but it doesn’t mean migraine is caused by psychological issues. Now we see it clearly as a disease of the brain, but it took years of investigation to prove that.”
The early years
Dr. Rapoport’s journey with headache began in 1972, when he joined a private neurology practice in Stamford and Greenwich, Conn. Neurologists were frowned upon then for having too much interest in headache, he said. There was poor remuneration for doctors treating headache patients, who were hard to properly diagnose and effectively care for. Few medications could effectively stop a migraine attack or reliably reduce the frequency of headaches or the disability they caused.
On weekends Dr. Rapoport covered emergency departments and ICUs at three hospitals, where standard treatment for a migraine attack was injectable opiates. Not only did this treatment aggravate nausea, a common migraine symptom, “but it did not stop the migraine process.” Once the pain relief wore off, patients woke up with the same headache, Dr. Rapoport recalled. “The other drug that was available was ergotamine tartrate” – a fungal alkaloid used since medieval times to treat headache – “given sublingually. It helped the headache slightly but increased the nausea. DHE, or dihydroergotamine, was available only by injection and not used very much.”
DHE, a semi-synthetic molecule based on ergotamine, had FDA approval for migraine, but was complicated to administer. Like the opioids, it provoked vomiting when given intravenously, in patients already suffering migraine-induced nausea. But Dr. Rapoport, along with some of his colleagues, felt that there was a role for DHE for the most severe subtypes of patients, those with long histories of frequent migraines.
“We put people in the hospital and we gave them intravenous DHE. Eventually I got the idea to give it intramuscularly or subcutaneously in the emergency room or my office. When you give it that way, it doesn’t work as quickly but has fewer side effects.” Dr. Rapoport designed a cocktail by coadministering promethazine for nausea, and eventually added a steroid, dexamethasone. The triple shots worked on most patients experiencing severe daily or near-daily migraine attacks, Dr. Rapoport saw, and he began administering the drug combination at The New England Center for Headache in Stamford and Greenwich, Conn., which he opened with Dr. Fred D. Sheftell in 1979.
“The triple shots really worked,” Dr. Rapoport recalled. “There was no need to keep patients in the office or emergency room for intravenous therapy. The patients never called to complain or came back the next day,” he said, as often occurred with opioid treatment.
Dr. Rapoport had learned early in his residency, in the late 1960s, from Dr. David R. Coddon, a neurologist at Mount Sinai hospital in New York, that a tricyclic antidepressant, imipramine, could be helpful in some patients with frequent migraine attacks. As evidence trickled in that other antidepressants, beta-blockers, and antiepileptic drugs might have preventive properties, Dr. Rapoport and others prescribed them for certain patients. But of all the drugs in the headache specialists’ repertoire, few were approved for either treatment or prevention. “And this continued until the triptans,” Dr. Rapoport said.
The triptan era
Sumatriptan was developed by Glaxo for the acute treatment of migraine. The medication, first available only as self-administered subcutaneous injections, was originally designed to bind to vascular serotonin receptors to allow selective constriction of cranial vessels that dilate, causing pain, during a migraine attack. (Years later it was discovered that triptans also worked as anti-inflammatory agents that decreased the release of the neurotransmitter calcitonin gene-related peptide, or CGRP.)
Triptans “changed the world for migraine patients and for me,” Dr. Rapoport said. “I could now prescribe a medication that people could take at home to decrease or stop the migraine process in an hour or two.” The success of the triptans prompted pharmaceutical companies to search for new, more effective ways to treat migraine attacks, with better tolerability.
Seven different triptans were developed, some as injections or tablets and others as nasal sprays. “If one triptan didn’t work, we’d give a second and rarely a third,” Dr. Rapoport said. “We learned that if oral triptans did not work, the most likely issue was that it was not rapidly absorbed from the small intestine, as migraine patients have nausea, poor GI absorption, and slow transit times. This prompted the greater use of injections and nasal sprays.” Headache specialists began combining triptan treatment with nonsteroidal anti-inflammatory drugs, offering further relief for the acute care of migraine.
Medication overuse headache
The years between 1993 and 2000, which saw all the current triptan drugs come onto the market, was an exhilarating one for headache specialists. But even those who were thrilled by the possibilities of the triptans, like Dr. Rapoport, soon came to recognize their limitations, in terms of side effects and poor tolerability for some patients.
Specialists also noticed something unsettling about the triptans: that patients’ headaches seemed to recur within a day, or occur more frequently over time, with higher medication use.
Medication overuse headache (MOH) was known to occur when patients treated migraine too often with acute care medications, especially over-the-counter analgesics and prescription opioids and barbiturates. Dr. Rapoport began warning at conferences and in seminars that MOH seemed to occur with the triptans as well. “In the beginning other doctors didn’t think the triptans could cause MOH, but I observed that patients who were taking triptans daily or almost daily were having increased headache frequency and the triptans stopped being effective. If they didn’t take the drug they were overusing, they were going to get much worse, almost like a withdrawal.”
Today, all seven triptans are now generic, and they remain a mainstay of migraine treatment: “Almost all of my patients are using, or have used a triptan,” Dr. Rapoport said. Yet researchers came to recognize the need for treatments targeting different pathways, both for prevention and acute care.
The next revolution: CGRP and gepants
Studies in the early 2000s began to show a link between the release of one ubiquitous nervous system neurotransmitter, calcitonin gene-related peptide, or CGRP, and migraine. They also noticed that blocking meningeal inflammation could lead to improvement in headache. Two new drug classes emerged from this science: monoclonal antibodies against CGRP or its receptor that had to be given by injection, and oral CGRP receptor blockers that could be used both as a preventive or as an acute care medication.
In 2018 the first monoclonal antibody against the CGRP receptor, erenumab (Aimovig, marketed by Amgen), delivered by injection, was approved for migraine prevention. Three others followed, most given by autoinjector, and one by IV infusion in office or hospital settings. “Those drugs are great,” Dr. Rapoport said. “You take one shot a month or every 3 months, and your headaches drop by 50% or more with very few side effects. Some patients actually see their migraines disappear.”
The following year ubrogepant (Ubrelvy, marketed by AbbVie), the first of a novel class of oral CGRP receptor blockers known as “gepants,” was approved to treat acute migraine. The FDA soon approved another gepant, rimegepant (Nurtec, marketed by Pfizer), which received indications both for prevention and for stopping a migraine attack acutely.
Both classes of therapies – the antibodies and the gepants – are far costlier than the triptans, which are all generic, and may not be needed for every migraine patient. With the gepants, for example, insurers may restrict use to people who have not responded to triptans or for whom triptans are contraindicated or cause too many adverse events. But the CGRP-targeted therapies as a whole “have been every bit as revolutionary” as the triptans, Dr. Rapoport said. The treatments work quickly to resolve headache and disability and get the patient functioning within an hour or two, and there are fewer side effects.
In a review article published in CNS Drugs in 2021, Dr. Rapoport and his colleagues reported that the anti-CGRP treatment with gepants did not appear linked to medication overuse headache, as virtually all previous acute care medication classes did, and could be used in patients who had previously reported MOH. “I am confident that over the next few years, more people will be using them as insurance coverage will improve for patients living with migraine,” he said.
Headache treatment today
Migraine specialists and patients now have a staggering range of therapeutic options. Approved treatments now include prevention of migraine with onabotulinumtoxinA (Botox, marketed by the Allergan division of AbbVie) injections, which work alone and with other medicines; acute care treatment with ditans like lasmiditan (Reyvow, marketed by Lilly*), a category of acute care medicines that work like triptans but target different serotonin receptors. Five devices have been cleared for migraine and other types of headache by the FDA. These work alone or along with medication and can be used acutely or preventively. The devices “should be used more,” Dr. Rapoport said, but are not yet well covered by insurance.
Thirty years after the triptans, scientists and researchers continue to explore the pathophysiology of headache disorders, finding new pathways and identifying new potential targets.
“There are many parts of the brain and brain stem that are involved, as well as the thalamus and hypothalamus,” Dr. Rapoport said. “It’s interesting that the newer medications, and some of the older ones, work in the peripheral nervous system, outside the brain stem in the trigeminovascular system, to modulate the central nervous system. We also know that the CGRP system is involved with cellular second-order messengers. Stimulating and blocking this chain of reactions with newer drugs may become treatments in the future.”
Recent research has focused on a blood vessel dilating neurotransmitter, pituitary adenylate-cyclase-activating polypeptide, or PACAP-38, as a potential therapeutic target. Psychedelic medications such as psilocybin, strong pain medications such as ketamine, and even cannabinoids such as marijuana have all been investigated in migraine. Biofeedback therapies, mindfulness, and other behavioral interventions also have proved effective.
“I expect the next 2-5 years to bring us many important clinical trials on new types of pharmacological treatments,” Dr. Rapoport said. “This is a wonderful time to be a doctor or nurse treating patients living with migraine. When I started out treating headache, 51 years ago, we had only ergotamine tartrate. Today we have so many therapies and combinations of therapies that I hardly know where to start.”
Dr. Rapoport has served as a consultant to or speaker for AbbVie, Amgen, Biohaven, Cala Health, Lundbeck, Satsuma, and Teva, among others.
*Correction, 3/30/23: An earlier version of this article misstated the name of the company that markets Reyvow.
Headache treatment before the early 1990s was marked by decades of improvisation with mostly unapproved agents, followed by an explosion of scientific interest and new treatments developed specifically for migraine.
But this is largely thanks to the sea change that occurred 30 years ago.
In an interview, Alan M. Rapoport, MD, editor-in-chief of Neurology Reviews, past president of the International Headache Society and clinical professor of neurology at UCLA’s David Geffen School of Medicine in Los Angeles, recalled what it was like to treat patients before and after triptan medications came onto the market.
After the first of these anti-migraine agents, sumatriptan, was approved by the Food and Drug Administration in late December 1992, headache specialists found themselves with a powerful, approved treatment that validated their commitment to solving the disorder, and helped put to rest a persistent but mistaken notion that migraine was a psychiatric condition affecting young women.
But in the 1970s and 1980s, “there wasn’t great science explaining the pathophysiology of common primary headaches like tension-type headache, cluster headache, and migraine,” Dr. Rapoport recalled. “There is often comorbid depression and anxiety with migraine, and sometimes more serious psychiatric disease, but it doesn’t mean migraine is caused by psychological issues. Now we see it clearly as a disease of the brain, but it took years of investigation to prove that.”
The early years
Dr. Rapoport’s journey with headache began in 1972, when he joined a private neurology practice in Stamford and Greenwich, Conn. Neurologists were frowned upon then for having too much interest in headache, he said. There was poor remuneration for doctors treating headache patients, who were hard to properly diagnose and effectively care for. Few medications could effectively stop a migraine attack or reliably reduce the frequency of headaches or the disability they caused.
On weekends Dr. Rapoport covered emergency departments and ICUs at three hospitals, where standard treatment for a migraine attack was injectable opiates. Not only did this treatment aggravate nausea, a common migraine symptom, “but it did not stop the migraine process.” Once the pain relief wore off, patients woke up with the same headache, Dr. Rapoport recalled. “The other drug that was available was ergotamine tartrate” – a fungal alkaloid used since medieval times to treat headache – “given sublingually. It helped the headache slightly but increased the nausea. DHE, or dihydroergotamine, was available only by injection and not used very much.”
DHE, a semi-synthetic molecule based on ergotamine, had FDA approval for migraine, but was complicated to administer. Like the opioids, it provoked vomiting when given intravenously, in patients already suffering migraine-induced nausea. But Dr. Rapoport, along with some of his colleagues, felt that there was a role for DHE for the most severe subtypes of patients, those with long histories of frequent migraines.
“We put people in the hospital and we gave them intravenous DHE. Eventually I got the idea to give it intramuscularly or subcutaneously in the emergency room or my office. When you give it that way, it doesn’t work as quickly but has fewer side effects.” Dr. Rapoport designed a cocktail by coadministering promethazine for nausea, and eventually added a steroid, dexamethasone. The triple shots worked on most patients experiencing severe daily or near-daily migraine attacks, Dr. Rapoport saw, and he began administering the drug combination at The New England Center for Headache in Stamford and Greenwich, Conn., which he opened with Dr. Fred D. Sheftell in 1979.
“The triple shots really worked,” Dr. Rapoport recalled. “There was no need to keep patients in the office or emergency room for intravenous therapy. The patients never called to complain or came back the next day,” he said, as often occurred with opioid treatment.
Dr. Rapoport had learned early in his residency, in the late 1960s, from Dr. David R. Coddon, a neurologist at Mount Sinai hospital in New York, that a tricyclic antidepressant, imipramine, could be helpful in some patients with frequent migraine attacks. As evidence trickled in that other antidepressants, beta-blockers, and antiepileptic drugs might have preventive properties, Dr. Rapoport and others prescribed them for certain patients. But of all the drugs in the headache specialists’ repertoire, few were approved for either treatment or prevention. “And this continued until the triptans,” Dr. Rapoport said.
The triptan era
Sumatriptan was developed by Glaxo for the acute treatment of migraine. The medication, first available only as self-administered subcutaneous injections, was originally designed to bind to vascular serotonin receptors to allow selective constriction of cranial vessels that dilate, causing pain, during a migraine attack. (Years later it was discovered that triptans also worked as anti-inflammatory agents that decreased the release of the neurotransmitter calcitonin gene-related peptide, or CGRP.)
Triptans “changed the world for migraine patients and for me,” Dr. Rapoport said. “I could now prescribe a medication that people could take at home to decrease or stop the migraine process in an hour or two.” The success of the triptans prompted pharmaceutical companies to search for new, more effective ways to treat migraine attacks, with better tolerability.
Seven different triptans were developed, some as injections or tablets and others as nasal sprays. “If one triptan didn’t work, we’d give a second and rarely a third,” Dr. Rapoport said. “We learned that if oral triptans did not work, the most likely issue was that it was not rapidly absorbed from the small intestine, as migraine patients have nausea, poor GI absorption, and slow transit times. This prompted the greater use of injections and nasal sprays.” Headache specialists began combining triptan treatment with nonsteroidal anti-inflammatory drugs, offering further relief for the acute care of migraine.
Medication overuse headache
The years between 1993 and 2000, which saw all the current triptan drugs come onto the market, was an exhilarating one for headache specialists. But even those who were thrilled by the possibilities of the triptans, like Dr. Rapoport, soon came to recognize their limitations, in terms of side effects and poor tolerability for some patients.
Specialists also noticed something unsettling about the triptans: that patients’ headaches seemed to recur within a day, or occur more frequently over time, with higher medication use.
Medication overuse headache (MOH) was known to occur when patients treated migraine too often with acute care medications, especially over-the-counter analgesics and prescription opioids and barbiturates. Dr. Rapoport began warning at conferences and in seminars that MOH seemed to occur with the triptans as well. “In the beginning other doctors didn’t think the triptans could cause MOH, but I observed that patients who were taking triptans daily or almost daily were having increased headache frequency and the triptans stopped being effective. If they didn’t take the drug they were overusing, they were going to get much worse, almost like a withdrawal.”
Today, all seven triptans are now generic, and they remain a mainstay of migraine treatment: “Almost all of my patients are using, or have used a triptan,” Dr. Rapoport said. Yet researchers came to recognize the need for treatments targeting different pathways, both for prevention and acute care.
The next revolution: CGRP and gepants
Studies in the early 2000s began to show a link between the release of one ubiquitous nervous system neurotransmitter, calcitonin gene-related peptide, or CGRP, and migraine. They also noticed that blocking meningeal inflammation could lead to improvement in headache. Two new drug classes emerged from this science: monoclonal antibodies against CGRP or its receptor that had to be given by injection, and oral CGRP receptor blockers that could be used both as a preventive or as an acute care medication.
In 2018 the first monoclonal antibody against the CGRP receptor, erenumab (Aimovig, marketed by Amgen), delivered by injection, was approved for migraine prevention. Three others followed, most given by autoinjector, and one by IV infusion in office or hospital settings. “Those drugs are great,” Dr. Rapoport said. “You take one shot a month or every 3 months, and your headaches drop by 50% or more with very few side effects. Some patients actually see their migraines disappear.”
The following year ubrogepant (Ubrelvy, marketed by AbbVie), the first of a novel class of oral CGRP receptor blockers known as “gepants,” was approved to treat acute migraine. The FDA soon approved another gepant, rimegepant (Nurtec, marketed by Pfizer), which received indications both for prevention and for stopping a migraine attack acutely.
Both classes of therapies – the antibodies and the gepants – are far costlier than the triptans, which are all generic, and may not be needed for every migraine patient. With the gepants, for example, insurers may restrict use to people who have not responded to triptans or for whom triptans are contraindicated or cause too many adverse events. But the CGRP-targeted therapies as a whole “have been every bit as revolutionary” as the triptans, Dr. Rapoport said. The treatments work quickly to resolve headache and disability and get the patient functioning within an hour or two, and there are fewer side effects.
In a review article published in CNS Drugs in 2021, Dr. Rapoport and his colleagues reported that the anti-CGRP treatment with gepants did not appear linked to medication overuse headache, as virtually all previous acute care medication classes did, and could be used in patients who had previously reported MOH. “I am confident that over the next few years, more people will be using them as insurance coverage will improve for patients living with migraine,” he said.
Headache treatment today
Migraine specialists and patients now have a staggering range of therapeutic options. Approved treatments now include prevention of migraine with onabotulinumtoxinA (Botox, marketed by the Allergan division of AbbVie) injections, which work alone and with other medicines; acute care treatment with ditans like lasmiditan (Reyvow, marketed by Lilly*), a category of acute care medicines that work like triptans but target different serotonin receptors. Five devices have been cleared for migraine and other types of headache by the FDA. These work alone or along with medication and can be used acutely or preventively. The devices “should be used more,” Dr. Rapoport said, but are not yet well covered by insurance.
Thirty years after the triptans, scientists and researchers continue to explore the pathophysiology of headache disorders, finding new pathways and identifying new potential targets.
“There are many parts of the brain and brain stem that are involved, as well as the thalamus and hypothalamus,” Dr. Rapoport said. “It’s interesting that the newer medications, and some of the older ones, work in the peripheral nervous system, outside the brain stem in the trigeminovascular system, to modulate the central nervous system. We also know that the CGRP system is involved with cellular second-order messengers. Stimulating and blocking this chain of reactions with newer drugs may become treatments in the future.”
Recent research has focused on a blood vessel dilating neurotransmitter, pituitary adenylate-cyclase-activating polypeptide, or PACAP-38, as a potential therapeutic target. Psychedelic medications such as psilocybin, strong pain medications such as ketamine, and even cannabinoids such as marijuana have all been investigated in migraine. Biofeedback therapies, mindfulness, and other behavioral interventions also have proved effective.
“I expect the next 2-5 years to bring us many important clinical trials on new types of pharmacological treatments,” Dr. Rapoport said. “This is a wonderful time to be a doctor or nurse treating patients living with migraine. When I started out treating headache, 51 years ago, we had only ergotamine tartrate. Today we have so many therapies and combinations of therapies that I hardly know where to start.”
Dr. Rapoport has served as a consultant to or speaker for AbbVie, Amgen, Biohaven, Cala Health, Lundbeck, Satsuma, and Teva, among others.
*Correction, 3/30/23: An earlier version of this article misstated the name of the company that markets Reyvow.
Are there long-term benefits to infants born to patients after bariatric surgery?
Rives-Lange C, Poghosyan T, Phan A, et al. Risk-benefit balance associated with obstetric, neonatal, and child outcomes after metabolic and bariatric surgery. JAMA Surg. 2023;158:36-44. doi:10.1001/jamasurg.2022.5450.
EXPERT COMMENTARY
Prepregnancy obesity continues to rise, with approximately 40% of reproductive-aged patients having a body mass index greater than 30 kg/m2.1 Several adverse perinatal outcomes are more common in pregnant patients with obesity.2 In addition, their infants have a higher risk of obesity, insulin resistance, hypertension, and neurodevelopmental disorders in the long term.
Bariatric surgery is an effective procedure for weight loss and has been shown to lower adverse pregnancy outcomes, such as hypertensive disorders of pregnancy and gestational diabetes.5,6 Benefits to newborns, however, have been debated.5 In addition, long-term benefits to infants were unknown until a recent study evaluated neonatal and child outcomes up to 2 years after pregnancy among patients who had undergone bariatric surgery.
Details of the study
Using the French nationwide database, Rives-Lange and colleagues performed a population-based study that included patients who had at least 1 pregnancy before and 1 pregnancy after bariatric surgery. Their objective was to compare pregnancy, neonatal, and child outcomes between pregnancies pre- and post-bariatric surgery.
Results. Among 3,686 patients who had at least 1 pregnancy before and after bariatric surgery, the authors found that pregnancies after bariatric surgery had lower rates of several adverse pregnancy outcomes, including preeclampsia (OR, 0.19), gestational hypertension (OR, 0.16), and gestational diabetes (OR, 0.39), compared with pregnancies before bariatric surgery. Regarding neonatal and child outcomes up to 2 years after pregnancy, there were lower rates of birth injuries (OR, 0.27), convulsions (OR, 0.43), newborn carbohydrate metabolism disorders (OR, 0.54),and viral intestinal infections (OR, 0.56) in pregnancies after bariatric surgery compared with those before surgery.
Notably, respiratory failure rates associated with bronchiolitis increased in pregnancies after bariatric surgery (OR, 2.42). This finding remained associated after adjusting for prematurity and small for gestational age as well as including 2 successive pregnancies before bariatric surgery (OR, 1.37).
Study strengths and limitations
A limitation of this study is the use of an administrative database, which may be biased and missing relevant variables. However, the study’s major strength was the large sample of patients serving as their own control to compare outcomes from pre-bariatric surgery with those of post-bariatric surgery. In addition, to account for confounders such as age and parity, the authors also evaluated for associations between 2 consecutive pregnancies among patients before bariatric surgery. They did not consider diagnoses found to be associated with bariatric surgery if they were also significant in the analysis between 2 consecutive pregnancies before bariatric surgery.
The finding of increased risk of respiratory failure from bronchiolitis after bariatric surgery is surprising given that obesity is a risk factor for the severity of bronchiolitis.7 Although this risk remained significant after including the analysis that used 2 consecutive pregnancies pre-bariatric surgery, the risk was lower (from an OR of 2.42 to an OR of 1.37). Thus, more data are required to confirm this potential risk. Despite this concerning finding, the overwhelming pregnancy, neonatal, and child benefits found and confirmed in this large, well-designed study support the continued practice of counseling on the benefits of bariatric surgery to our obese patients. ●
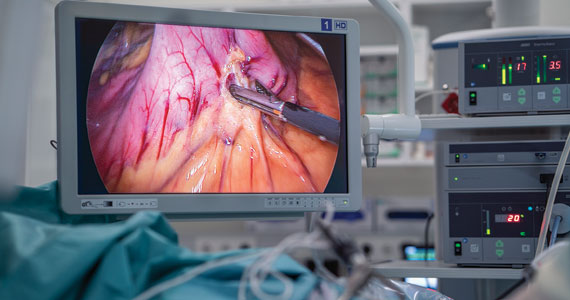
Bariatric surgery remains an effective procedure for weight loss, and it lowers the risks of several important perinatal, neonatal, and child outcomes, including hypertensive disorders, birth injuries, convulsions, and viral intestinal infections. Clinicians should include the benefits of neonatal and child outcomes in their counseling of bariatric surgery for their obese patients who are planning pregnancy.
RODNEY A. MCLAREN JR, MD
- Hales CM, Carroll MD, Fryar CD, et al. Prevalence of obesity and severe obesity among adults: United States, 2017-2018. NCHS Data Brief. 2020;(360):1-8.
- Sagi-Dain L. Obesity in pregnancy: ACOG practice bulletin, number 230. Obstet Gynecol. 2021;138:489. doi:10.1097 /AOG.0000000000004527.
- O’Reilly JR, Reynolds RM. The risk of maternal obesity to the long-term health of the offspring. Clin Endocrinol (Oxf). 2013;78:9-16. doi:10.1111/cen.12055.
- Edlow AG. Maternal obesity and neurodevelopmental and psychiatric disorders in offspring. Prenat Diagn. 2017;37:95-110. doi:10.1002/pd.4932.
- Johansson K, Cnattinguius S, Näslund I, et al. Outcomes of pregnancy after bariatric surgery. N Engl J Med. 2015;372:814-824. doi:10.1056/NEJMoa1405789.
- Getahun D, Fassett MJ, Jacobsen SJ, et al. Perinatal outcomes after bariatric surgery. Am J Obstet Gynecol. 2022;226:121.e1-121.e16. doi:10.1016/j.ajog.2021.06.087.
- James T, Samakar K, Martin MJ. Special delivery—metabolic bariatric surgery as a key component of maternal-fetal health care. JAMA Surg. 2023;158:44-45. doi:10.1001 /jamasurg.2022.5458.
Rives-Lange C, Poghosyan T, Phan A, et al. Risk-benefit balance associated with obstetric, neonatal, and child outcomes after metabolic and bariatric surgery. JAMA Surg. 2023;158:36-44. doi:10.1001/jamasurg.2022.5450.
EXPERT COMMENTARY
Prepregnancy obesity continues to rise, with approximately 40% of reproductive-aged patients having a body mass index greater than 30 kg/m2.1 Several adverse perinatal outcomes are more common in pregnant patients with obesity.2 In addition, their infants have a higher risk of obesity, insulin resistance, hypertension, and neurodevelopmental disorders in the long term.
Bariatric surgery is an effective procedure for weight loss and has been shown to lower adverse pregnancy outcomes, such as hypertensive disorders of pregnancy and gestational diabetes.5,6 Benefits to newborns, however, have been debated.5 In addition, long-term benefits to infants were unknown until a recent study evaluated neonatal and child outcomes up to 2 years after pregnancy among patients who had undergone bariatric surgery.
Details of the study
Using the French nationwide database, Rives-Lange and colleagues performed a population-based study that included patients who had at least 1 pregnancy before and 1 pregnancy after bariatric surgery. Their objective was to compare pregnancy, neonatal, and child outcomes between pregnancies pre- and post-bariatric surgery.
Results. Among 3,686 patients who had at least 1 pregnancy before and after bariatric surgery, the authors found that pregnancies after bariatric surgery had lower rates of several adverse pregnancy outcomes, including preeclampsia (OR, 0.19), gestational hypertension (OR, 0.16), and gestational diabetes (OR, 0.39), compared with pregnancies before bariatric surgery. Regarding neonatal and child outcomes up to 2 years after pregnancy, there were lower rates of birth injuries (OR, 0.27), convulsions (OR, 0.43), newborn carbohydrate metabolism disorders (OR, 0.54),and viral intestinal infections (OR, 0.56) in pregnancies after bariatric surgery compared with those before surgery.
Notably, respiratory failure rates associated with bronchiolitis increased in pregnancies after bariatric surgery (OR, 2.42). This finding remained associated after adjusting for prematurity and small for gestational age as well as including 2 successive pregnancies before bariatric surgery (OR, 1.37).
Study strengths and limitations
A limitation of this study is the use of an administrative database, which may be biased and missing relevant variables. However, the study’s major strength was the large sample of patients serving as their own control to compare outcomes from pre-bariatric surgery with those of post-bariatric surgery. In addition, to account for confounders such as age and parity, the authors also evaluated for associations between 2 consecutive pregnancies among patients before bariatric surgery. They did not consider diagnoses found to be associated with bariatric surgery if they were also significant in the analysis between 2 consecutive pregnancies before bariatric surgery.
The finding of increased risk of respiratory failure from bronchiolitis after bariatric surgery is surprising given that obesity is a risk factor for the severity of bronchiolitis.7 Although this risk remained significant after including the analysis that used 2 consecutive pregnancies pre-bariatric surgery, the risk was lower (from an OR of 2.42 to an OR of 1.37). Thus, more data are required to confirm this potential risk. Despite this concerning finding, the overwhelming pregnancy, neonatal, and child benefits found and confirmed in this large, well-designed study support the continued practice of counseling on the benefits of bariatric surgery to our obese patients. ●
Bariatric surgery remains an effective procedure for weight loss, and it lowers the risks of several important perinatal, neonatal, and child outcomes, including hypertensive disorders, birth injuries, convulsions, and viral intestinal infections. Clinicians should include the benefits of neonatal and child outcomes in their counseling of bariatric surgery for their obese patients who are planning pregnancy.
RODNEY A. MCLAREN JR, MD
Rives-Lange C, Poghosyan T, Phan A, et al. Risk-benefit balance associated with obstetric, neonatal, and child outcomes after metabolic and bariatric surgery. JAMA Surg. 2023;158:36-44. doi:10.1001/jamasurg.2022.5450.
EXPERT COMMENTARY
Prepregnancy obesity continues to rise, with approximately 40% of reproductive-aged patients having a body mass index greater than 30 kg/m2.1 Several adverse perinatal outcomes are more common in pregnant patients with obesity.2 In addition, their infants have a higher risk of obesity, insulin resistance, hypertension, and neurodevelopmental disorders in the long term.
Bariatric surgery is an effective procedure for weight loss and has been shown to lower adverse pregnancy outcomes, such as hypertensive disorders of pregnancy and gestational diabetes.5,6 Benefits to newborns, however, have been debated.5 In addition, long-term benefits to infants were unknown until a recent study evaluated neonatal and child outcomes up to 2 years after pregnancy among patients who had undergone bariatric surgery.
Details of the study
Using the French nationwide database, Rives-Lange and colleagues performed a population-based study that included patients who had at least 1 pregnancy before and 1 pregnancy after bariatric surgery. Their objective was to compare pregnancy, neonatal, and child outcomes between pregnancies pre- and post-bariatric surgery.
Results. Among 3,686 patients who had at least 1 pregnancy before and after bariatric surgery, the authors found that pregnancies after bariatric surgery had lower rates of several adverse pregnancy outcomes, including preeclampsia (OR, 0.19), gestational hypertension (OR, 0.16), and gestational diabetes (OR, 0.39), compared with pregnancies before bariatric surgery. Regarding neonatal and child outcomes up to 2 years after pregnancy, there were lower rates of birth injuries (OR, 0.27), convulsions (OR, 0.43), newborn carbohydrate metabolism disorders (OR, 0.54),and viral intestinal infections (OR, 0.56) in pregnancies after bariatric surgery compared with those before surgery.
Notably, respiratory failure rates associated with bronchiolitis increased in pregnancies after bariatric surgery (OR, 2.42). This finding remained associated after adjusting for prematurity and small for gestational age as well as including 2 successive pregnancies before bariatric surgery (OR, 1.37).
Study strengths and limitations
A limitation of this study is the use of an administrative database, which may be biased and missing relevant variables. However, the study’s major strength was the large sample of patients serving as their own control to compare outcomes from pre-bariatric surgery with those of post-bariatric surgery. In addition, to account for confounders such as age and parity, the authors also evaluated for associations between 2 consecutive pregnancies among patients before bariatric surgery. They did not consider diagnoses found to be associated with bariatric surgery if they were also significant in the analysis between 2 consecutive pregnancies before bariatric surgery.
The finding of increased risk of respiratory failure from bronchiolitis after bariatric surgery is surprising given that obesity is a risk factor for the severity of bronchiolitis.7 Although this risk remained significant after including the analysis that used 2 consecutive pregnancies pre-bariatric surgery, the risk was lower (from an OR of 2.42 to an OR of 1.37). Thus, more data are required to confirm this potential risk. Despite this concerning finding, the overwhelming pregnancy, neonatal, and child benefits found and confirmed in this large, well-designed study support the continued practice of counseling on the benefits of bariatric surgery to our obese patients. ●
Bariatric surgery remains an effective procedure for weight loss, and it lowers the risks of several important perinatal, neonatal, and child outcomes, including hypertensive disorders, birth injuries, convulsions, and viral intestinal infections. Clinicians should include the benefits of neonatal and child outcomes in their counseling of bariatric surgery for their obese patients who are planning pregnancy.
RODNEY A. MCLAREN JR, MD
- Hales CM, Carroll MD, Fryar CD, et al. Prevalence of obesity and severe obesity among adults: United States, 2017-2018. NCHS Data Brief. 2020;(360):1-8.
- Sagi-Dain L. Obesity in pregnancy: ACOG practice bulletin, number 230. Obstet Gynecol. 2021;138:489. doi:10.1097 /AOG.0000000000004527.
- O’Reilly JR, Reynolds RM. The risk of maternal obesity to the long-term health of the offspring. Clin Endocrinol (Oxf). 2013;78:9-16. doi:10.1111/cen.12055.
- Edlow AG. Maternal obesity and neurodevelopmental and psychiatric disorders in offspring. Prenat Diagn. 2017;37:95-110. doi:10.1002/pd.4932.
- Johansson K, Cnattinguius S, Näslund I, et al. Outcomes of pregnancy after bariatric surgery. N Engl J Med. 2015;372:814-824. doi:10.1056/NEJMoa1405789.
- Getahun D, Fassett MJ, Jacobsen SJ, et al. Perinatal outcomes after bariatric surgery. Am J Obstet Gynecol. 2022;226:121.e1-121.e16. doi:10.1016/j.ajog.2021.06.087.
- James T, Samakar K, Martin MJ. Special delivery—metabolic bariatric surgery as a key component of maternal-fetal health care. JAMA Surg. 2023;158:44-45. doi:10.1001 /jamasurg.2022.5458.
- Hales CM, Carroll MD, Fryar CD, et al. Prevalence of obesity and severe obesity among adults: United States, 2017-2018. NCHS Data Brief. 2020;(360):1-8.
- Sagi-Dain L. Obesity in pregnancy: ACOG practice bulletin, number 230. Obstet Gynecol. 2021;138:489. doi:10.1097 /AOG.0000000000004527.
- O’Reilly JR, Reynolds RM. The risk of maternal obesity to the long-term health of the offspring. Clin Endocrinol (Oxf). 2013;78:9-16. doi:10.1111/cen.12055.
- Edlow AG. Maternal obesity and neurodevelopmental and psychiatric disorders in offspring. Prenat Diagn. 2017;37:95-110. doi:10.1002/pd.4932.
- Johansson K, Cnattinguius S, Näslund I, et al. Outcomes of pregnancy after bariatric surgery. N Engl J Med. 2015;372:814-824. doi:10.1056/NEJMoa1405789.
- Getahun D, Fassett MJ, Jacobsen SJ, et al. Perinatal outcomes after bariatric surgery. Am J Obstet Gynecol. 2022;226:121.e1-121.e16. doi:10.1016/j.ajog.2021.06.087.
- James T, Samakar K, Martin MJ. Special delivery—metabolic bariatric surgery as a key component of maternal-fetal health care. JAMA Surg. 2023;158:44-45. doi:10.1001 /jamasurg.2022.5458.
Despite ongoing challenges, experts are optimistic about the future of MS therapy
Prior to 1993, a multiple sclerosis (MS) diagnosis could often mean an abbreviated lifespan marked by progressive disability and loss of function. That changed when the Food and Drug Administration approved interferon beta-1b (Betaseron) in 1993, which revolutionized MS therapy and gave hope to the entire MS community.
"The most surprising thing about MS management over the last 30 years is that we’ve been able to treat MS – especially relapsing MS,” said Fred D. Lublin, MD, professor of neurology and director of the Corinne Goldsmith Dickinson Center for Multiple Sclerosis in Mount Sinai in New York. “The approval of interferon was a major therapeutic advancement because it was the first treatment for what was an untreatable disease.”
Mark Gudesblatt, MD, medical director of the Comprehensive MS Care Center of South Shore Neurologic Associates in Patchogue, N.Y., agrees.
“For people with MS, it’s an extraordinarily lucky and amazingly optimistic time,” he said. “Before interferon beta-1b, MS was called ‘the crippler of young adults’ because more than 50% of these people would require a walker 10 years after diagnosis, and a large number of young and middle-age patients with MS were residing in nursing homes.”
According to Dr. Lublin, the emergence of the immunomodulating therapies placed MS at the leading edge of neurotherapeutics. Interferon beta-1b laid the foundation for new therapies such as another interferon (interferon beta-1a; Avonex), glatiramer acetate (Copaxone), and many other effective therapies with different mechanisms of action. Since the emergence of the first therapy, more than 20 oral and infusion agents with moderate to high efficacy have come to market for relapsing MS.
Treatment options, treatment challenges
Dr. Gudesblatt points out that having numerous therapies from which to choose is both a blessing and a problem.
“The good news is that there are so many options for treating relapsing MS today,” he said. “The bad news is there are so many options. Like doctors who are treating high blood pressure, doctors managing patients with MS often struggle to determine which medication is best for individual patients.”
Despite the promise of vastly better outcomes and prolonged lifespan, MS therapy still faces its share of challenges, including effective therapies for progressive MS and reparative-restorative therapies.
“Choice in route of administration and timing of administration allow for larger and broader discussions to try to meet patients’ needs,” Dr. Lublin said. “We’ve been extremely successful at treating relapses, but not as successful in treating progressive disease.”
The unclear mechanism of pathogenesis amplifies the challenges clinicians face in successful management of patients with MS. For example, experts agree that the therapies for progressive MS have only proven moderately effective at best. The paucity of therapies available for progressive MS and the limitations of the current therapies further limit the outcomes.
Looking ahead
Experts expressed optimistic views about the future of MS therapy as a whole. From Dr. Lublin’s perspective, the MS community stands to gain valuable insights from emerging research focused on treating progressive disease along with new testing to understand the underlying mechanism of progressive disease. Enhanced understanding of the underlying pathogenesis of progressive MS coupled with the ability to diagnose MS – such as improved MRI techniques – have facilitated this process.
Among the therapies with novel mechanisms of action in the pipeline include agents that generate myelin sheath repair. Another potential therapeutic class on the horizon, known as TPK inhibitors, addresses the smoldering of the disease. With these and other therapeutic advances, Dr. Lublin hopes to see better control of progressive disease.
An agenda for the future
In addition, barriers such as access to care, cost, insurance coverage, and tolerance remain ongoing stressors that will likely continue weighing on the MS community and its stakeholders into the future.
Dr. Gudesblatt concluded that advancing MS outcomes in the future hinges on several additional factors.
“We need medicines that are better for relapse and progression; medicines that are better tolerated and safer; and better medicine to address the underlying disease as well as its symptoms. But we also need to appreciate, recognize, and address cognitive impairment along the MS continuum and develop effective reparative options,” he said.
Regardless, he emphasized that these “amazing advancements” in MS therapy have renewed hope that research may identify and expand effective treatments for multiple other neurologic conditions such as muscular dystrophies, neurodegenerative and genetic disorders, movement disorders, and dysautonomia-related diseases. Like MS, all of these conditions have limited therapies, some of which have minimal efficacy. But none of these other disorders has disease-modifying therapies currently available.
‘A beacon of hope’
“MS is the beacon of hope for multiple disease states because it’s cracked the door wide open,” Dr. Gudesblatt said. Relapse no longer gauges the prognosis of today’s MS patient – a prognosis both experts think will only continue to improve with forthcoming innovations.
While the challenges for MS still exist, the bright future that lies ahead may eventually eclipse them.
Prior to 1993, a multiple sclerosis (MS) diagnosis could often mean an abbreviated lifespan marked by progressive disability and loss of function. That changed when the Food and Drug Administration approved interferon beta-1b (Betaseron) in 1993, which revolutionized MS therapy and gave hope to the entire MS community.
"The most surprising thing about MS management over the last 30 years is that we’ve been able to treat MS – especially relapsing MS,” said Fred D. Lublin, MD, professor of neurology and director of the Corinne Goldsmith Dickinson Center for Multiple Sclerosis in Mount Sinai in New York. “The approval of interferon was a major therapeutic advancement because it was the first treatment for what was an untreatable disease.”
Mark Gudesblatt, MD, medical director of the Comprehensive MS Care Center of South Shore Neurologic Associates in Patchogue, N.Y., agrees.
“For people with MS, it’s an extraordinarily lucky and amazingly optimistic time,” he said. “Before interferon beta-1b, MS was called ‘the crippler of young adults’ because more than 50% of these people would require a walker 10 years after diagnosis, and a large number of young and middle-age patients with MS were residing in nursing homes.”
According to Dr. Lublin, the emergence of the immunomodulating therapies placed MS at the leading edge of neurotherapeutics. Interferon beta-1b laid the foundation for new therapies such as another interferon (interferon beta-1a; Avonex), glatiramer acetate (Copaxone), and many other effective therapies with different mechanisms of action. Since the emergence of the first therapy, more than 20 oral and infusion agents with moderate to high efficacy have come to market for relapsing MS.
Treatment options, treatment challenges
Dr. Gudesblatt points out that having numerous therapies from which to choose is both a blessing and a problem.
“The good news is that there are so many options for treating relapsing MS today,” he said. “The bad news is there are so many options. Like doctors who are treating high blood pressure, doctors managing patients with MS often struggle to determine which medication is best for individual patients.”
Despite the promise of vastly better outcomes and prolonged lifespan, MS therapy still faces its share of challenges, including effective therapies for progressive MS and reparative-restorative therapies.
“Choice in route of administration and timing of administration allow for larger and broader discussions to try to meet patients’ needs,” Dr. Lublin said. “We’ve been extremely successful at treating relapses, but not as successful in treating progressive disease.”
The unclear mechanism of pathogenesis amplifies the challenges clinicians face in successful management of patients with MS. For example, experts agree that the therapies for progressive MS have only proven moderately effective at best. The paucity of therapies available for progressive MS and the limitations of the current therapies further limit the outcomes.
Looking ahead
Experts expressed optimistic views about the future of MS therapy as a whole. From Dr. Lublin’s perspective, the MS community stands to gain valuable insights from emerging research focused on treating progressive disease along with new testing to understand the underlying mechanism of progressive disease. Enhanced understanding of the underlying pathogenesis of progressive MS coupled with the ability to diagnose MS – such as improved MRI techniques – have facilitated this process.
Among the therapies with novel mechanisms of action in the pipeline include agents that generate myelin sheath repair. Another potential therapeutic class on the horizon, known as TPK inhibitors, addresses the smoldering of the disease. With these and other therapeutic advances, Dr. Lublin hopes to see better control of progressive disease.
An agenda for the future
In addition, barriers such as access to care, cost, insurance coverage, and tolerance remain ongoing stressors that will likely continue weighing on the MS community and its stakeholders into the future.
Dr. Gudesblatt concluded that advancing MS outcomes in the future hinges on several additional factors.
“We need medicines that are better for relapse and progression; medicines that are better tolerated and safer; and better medicine to address the underlying disease as well as its symptoms. But we also need to appreciate, recognize, and address cognitive impairment along the MS continuum and develop effective reparative options,” he said.
Regardless, he emphasized that these “amazing advancements” in MS therapy have renewed hope that research may identify and expand effective treatments for multiple other neurologic conditions such as muscular dystrophies, neurodegenerative and genetic disorders, movement disorders, and dysautonomia-related diseases. Like MS, all of these conditions have limited therapies, some of which have minimal efficacy. But none of these other disorders has disease-modifying therapies currently available.
‘A beacon of hope’
“MS is the beacon of hope for multiple disease states because it’s cracked the door wide open,” Dr. Gudesblatt said. Relapse no longer gauges the prognosis of today’s MS patient – a prognosis both experts think will only continue to improve with forthcoming innovations.
While the challenges for MS still exist, the bright future that lies ahead may eventually eclipse them.
Prior to 1993, a multiple sclerosis (MS) diagnosis could often mean an abbreviated lifespan marked by progressive disability and loss of function. That changed when the Food and Drug Administration approved interferon beta-1b (Betaseron) in 1993, which revolutionized MS therapy and gave hope to the entire MS community.
"The most surprising thing about MS management over the last 30 years is that we’ve been able to treat MS – especially relapsing MS,” said Fred D. Lublin, MD, professor of neurology and director of the Corinne Goldsmith Dickinson Center for Multiple Sclerosis in Mount Sinai in New York. “The approval of interferon was a major therapeutic advancement because it was the first treatment for what was an untreatable disease.”
Mark Gudesblatt, MD, medical director of the Comprehensive MS Care Center of South Shore Neurologic Associates in Patchogue, N.Y., agrees.
“For people with MS, it’s an extraordinarily lucky and amazingly optimistic time,” he said. “Before interferon beta-1b, MS was called ‘the crippler of young adults’ because more than 50% of these people would require a walker 10 years after diagnosis, and a large number of young and middle-age patients with MS were residing in nursing homes.”
According to Dr. Lublin, the emergence of the immunomodulating therapies placed MS at the leading edge of neurotherapeutics. Interferon beta-1b laid the foundation for new therapies such as another interferon (interferon beta-1a; Avonex), glatiramer acetate (Copaxone), and many other effective therapies with different mechanisms of action. Since the emergence of the first therapy, more than 20 oral and infusion agents with moderate to high efficacy have come to market for relapsing MS.
Treatment options, treatment challenges
Dr. Gudesblatt points out that having numerous therapies from which to choose is both a blessing and a problem.
“The good news is that there are so many options for treating relapsing MS today,” he said. “The bad news is there are so many options. Like doctors who are treating high blood pressure, doctors managing patients with MS often struggle to determine which medication is best for individual patients.”
Despite the promise of vastly better outcomes and prolonged lifespan, MS therapy still faces its share of challenges, including effective therapies for progressive MS and reparative-restorative therapies.
“Choice in route of administration and timing of administration allow for larger and broader discussions to try to meet patients’ needs,” Dr. Lublin said. “We’ve been extremely successful at treating relapses, but not as successful in treating progressive disease.”
The unclear mechanism of pathogenesis amplifies the challenges clinicians face in successful management of patients with MS. For example, experts agree that the therapies for progressive MS have only proven moderately effective at best. The paucity of therapies available for progressive MS and the limitations of the current therapies further limit the outcomes.
Looking ahead
Experts expressed optimistic views about the future of MS therapy as a whole. From Dr. Lublin’s perspective, the MS community stands to gain valuable insights from emerging research focused on treating progressive disease along with new testing to understand the underlying mechanism of progressive disease. Enhanced understanding of the underlying pathogenesis of progressive MS coupled with the ability to diagnose MS – such as improved MRI techniques – have facilitated this process.
Among the therapies with novel mechanisms of action in the pipeline include agents that generate myelin sheath repair. Another potential therapeutic class on the horizon, known as TPK inhibitors, addresses the smoldering of the disease. With these and other therapeutic advances, Dr. Lublin hopes to see better control of progressive disease.
An agenda for the future
In addition, barriers such as access to care, cost, insurance coverage, and tolerance remain ongoing stressors that will likely continue weighing on the MS community and its stakeholders into the future.
Dr. Gudesblatt concluded that advancing MS outcomes in the future hinges on several additional factors.
“We need medicines that are better for relapse and progression; medicines that are better tolerated and safer; and better medicine to address the underlying disease as well as its symptoms. But we also need to appreciate, recognize, and address cognitive impairment along the MS continuum and develop effective reparative options,” he said.
Regardless, he emphasized that these “amazing advancements” in MS therapy have renewed hope that research may identify and expand effective treatments for multiple other neurologic conditions such as muscular dystrophies, neurodegenerative and genetic disorders, movement disorders, and dysautonomia-related diseases. Like MS, all of these conditions have limited therapies, some of which have minimal efficacy. But none of these other disorders has disease-modifying therapies currently available.
‘A beacon of hope’
“MS is the beacon of hope for multiple disease states because it’s cracked the door wide open,” Dr. Gudesblatt said. Relapse no longer gauges the prognosis of today’s MS patient – a prognosis both experts think will only continue to improve with forthcoming innovations.
While the challenges for MS still exist, the bright future that lies ahead may eventually eclipse them.
Have investigators reached the first steps for redefining a diagnostic definition of preeclampsia that includes morbidity?
Thadhani R, Lemoine E, Rana S, et al. Circulating angiogenic factor levels in hypertensive disorders of pregnancy. N Engl J Med. 2022;1. DOI: 10.1056/EVIDoa2200161
EXPERT COMMENTARY
The standard core lecture on preeclampsia given to all medical students frequently begins with an epic, if not potentially apocryphal, statement regarding how this disease has been noted in the annals of medical history since the time of the Ancients. Although contemporary diagnostic criteria for preeclampsia are not that far out of date, they are close. The increased urinary protein loss and hypertension preceding eclamptic seizures was first noted at the end of the 19th century. The blood pressure and proteinuria criteria used for diagnosis was codified in its contemporary form in the late 1940s. Since then, “tweak” rather than “overhaul” probably best describes the updates of the obstetrical community to the definition of preeclampsia. This has just changed.
Details of the study
Thadhani and colleagues prospectively recruited a nationally representative observational cohort of patients hospitalized for hypertension during pregnancy, then followed the patients until either the diagnosis of preeclampsia with severe features or for 2 weeks, whichever came first. At enrollment, circulating levels of the soluble fms-like tyrosine kinase 1 (sFlt-1) and placental growth factor (PlGF) were measured. In a 2-phased design, the first 219 participants were used to define a sFlt-1/PlGF ratio that would predict progression to severe preeclampsia within 2 weeks. The next 556 enrollees served to validate the predictive properties of the ratio. The authors found that a sFlt-1/PlGF ratio of ≥40 predicted progression to preeclampsia with severe features with an area under the curve (AUC) of 0.92.

As products of the trophoblasts, both sFlt-1 and PlGF have been mooted for almost 2 decades as potential predictive, if not diagnostic, aids with respect to preeclampsia. Indeed, both analytes are commercially available in Europe for specifically this purpose and many maternal-fetal medicine practitioners working in the European equivalent American tertiary referral centers use an sFlt-1/PlGF ratio as their primary criteria for a diagnosis of preeclampsia. Within the United States, there was an initial flurry of interest in and an infusion of corporate and federal research support for sFlt-1 and PlGF as diagnostic aids for preeclampsia in the mid-2000s. However, at present, the US Food and Drug Administration (FDA) has not sanctioned these (or any) biomarkers to aid in the diagnosis of preeclampsia. As Thermo-Fisher Scientific (Waltham, Massachusetts) is a supporting partner in this study, it is almost certain that these data will be submitted for review by the FDA as part of an application for a preeclampsia diagnostic. At some point in the near future, American practitioners will potentially be able to join their European colleagues in utilizing these biomarkers in the diagnosis of preeclampsia with severe features. ●
Thadhani and colleagues observed that the majority of both maternal and neonatal morbidity in their study, including 8 of the 9 neonatal deaths and both cases of eclampsia, occurred among patients with a ratio ≥40 at admission. There was an inverse relation between the sFlt-1/PlGF ratio and the admission to delivery interval. Where only 17% of patients in the highest quartile of ratios remained pregnant at 14 days post-enrollment, more than 79% of the lowest quartile were still pregnant. If not a causal relationship, sFlt-1 and PlGF are clearly associated with not only the occurrence of preeclampsia with severe features but also the degree of morbidity.
The implication for the disposition of patient care resources is clear. Patients at higher risk for preeclampsia could be seen in specialty high-risk clinics with an emphasis on increased monitoring. In situations where tertiary care is more remote, plans could be developed should they need to be transported to centers able to provide the appropriate level of care. Conversely, patients screening at lower ratios may be more appropriately managed as outpatients, or at least in less clinically involved accommodations.
Thadhani et al do note that there were false negative cases in which the sFlt-1/PlGF ratio at admission was <40 but patients nonetheless progressed to preeclampsia with severe features. The majority of these cases had concurrent pre-pregnancy, chronic hypertension. This observation suggests not only the potential for insights into the pathophysiology of the hypertensive diseases in pregnancy but also that the interpretation of the sFlt/PlGF ratio may eventually need to be stratified by preexisting conditions.
The final implications for the observations of this study are perhaps the most tantalizing. If there is a causal relation between the level of the sFlt-1/PlGF ratio and the morbidity of preeclampsia with severe features, then lowering the circulating concentration of sFlt-1 would ameliorate not only the morbidity but also the risk of preeclampsia. Work with plasma phoresies has suggested that this might be possible, albeit via a clinical intervention demanding more intensive resources. The potential for a targeted pharmacologic moderation of sFlt-1 levels would hold great promise in that those identified as at increased risk could be offered an intervention widely available to all.
Thadhani R, Lemoine E, Rana S, et al. Circulating angiogenic factor levels in hypertensive disorders of pregnancy. N Engl J Med. 2022;1. DOI: 10.1056/EVIDoa2200161
EXPERT COMMENTARY
The standard core lecture on preeclampsia given to all medical students frequently begins with an epic, if not potentially apocryphal, statement regarding how this disease has been noted in the annals of medical history since the time of the Ancients. Although contemporary diagnostic criteria for preeclampsia are not that far out of date, they are close. The increased urinary protein loss and hypertension preceding eclamptic seizures was first noted at the end of the 19th century. The blood pressure and proteinuria criteria used for diagnosis was codified in its contemporary form in the late 1940s. Since then, “tweak” rather than “overhaul” probably best describes the updates of the obstetrical community to the definition of preeclampsia. This has just changed.
Details of the study
Thadhani and colleagues prospectively recruited a nationally representative observational cohort of patients hospitalized for hypertension during pregnancy, then followed the patients until either the diagnosis of preeclampsia with severe features or for 2 weeks, whichever came first. At enrollment, circulating levels of the soluble fms-like tyrosine kinase 1 (sFlt-1) and placental growth factor (PlGF) were measured. In a 2-phased design, the first 219 participants were used to define a sFlt-1/PlGF ratio that would predict progression to severe preeclampsia within 2 weeks. The next 556 enrollees served to validate the predictive properties of the ratio. The authors found that a sFlt-1/PlGF ratio of ≥40 predicted progression to preeclampsia with severe features with an area under the curve (AUC) of 0.92.

As products of the trophoblasts, both sFlt-1 and PlGF have been mooted for almost 2 decades as potential predictive, if not diagnostic, aids with respect to preeclampsia. Indeed, both analytes are commercially available in Europe for specifically this purpose and many maternal-fetal medicine practitioners working in the European equivalent American tertiary referral centers use an sFlt-1/PlGF ratio as their primary criteria for a diagnosis of preeclampsia. Within the United States, there was an initial flurry of interest in and an infusion of corporate and federal research support for sFlt-1 and PlGF as diagnostic aids for preeclampsia in the mid-2000s. However, at present, the US Food and Drug Administration (FDA) has not sanctioned these (or any) biomarkers to aid in the diagnosis of preeclampsia. As Thermo-Fisher Scientific (Waltham, Massachusetts) is a supporting partner in this study, it is almost certain that these data will be submitted for review by the FDA as part of an application for a preeclampsia diagnostic. At some point in the near future, American practitioners will potentially be able to join their European colleagues in utilizing these biomarkers in the diagnosis of preeclampsia with severe features. ●
Thadhani and colleagues observed that the majority of both maternal and neonatal morbidity in their study, including 8 of the 9 neonatal deaths and both cases of eclampsia, occurred among patients with a ratio ≥40 at admission. There was an inverse relation between the sFlt-1/PlGF ratio and the admission to delivery interval. Where only 17% of patients in the highest quartile of ratios remained pregnant at 14 days post-enrollment, more than 79% of the lowest quartile were still pregnant. If not a causal relationship, sFlt-1 and PlGF are clearly associated with not only the occurrence of preeclampsia with severe features but also the degree of morbidity.
The implication for the disposition of patient care resources is clear. Patients at higher risk for preeclampsia could be seen in specialty high-risk clinics with an emphasis on increased monitoring. In situations where tertiary care is more remote, plans could be developed should they need to be transported to centers able to provide the appropriate level of care. Conversely, patients screening at lower ratios may be more appropriately managed as outpatients, or at least in less clinically involved accommodations.
Thadhani et al do note that there were false negative cases in which the sFlt-1/PlGF ratio at admission was <40 but patients nonetheless progressed to preeclampsia with severe features. The majority of these cases had concurrent pre-pregnancy, chronic hypertension. This observation suggests not only the potential for insights into the pathophysiology of the hypertensive diseases in pregnancy but also that the interpretation of the sFlt/PlGF ratio may eventually need to be stratified by preexisting conditions.
The final implications for the observations of this study are perhaps the most tantalizing. If there is a causal relation between the level of the sFlt-1/PlGF ratio and the morbidity of preeclampsia with severe features, then lowering the circulating concentration of sFlt-1 would ameliorate not only the morbidity but also the risk of preeclampsia. Work with plasma phoresies has suggested that this might be possible, albeit via a clinical intervention demanding more intensive resources. The potential for a targeted pharmacologic moderation of sFlt-1 levels would hold great promise in that those identified as at increased risk could be offered an intervention widely available to all.
Thadhani R, Lemoine E, Rana S, et al. Circulating angiogenic factor levels in hypertensive disorders of pregnancy. N Engl J Med. 2022;1. DOI: 10.1056/EVIDoa2200161
EXPERT COMMENTARY
The standard core lecture on preeclampsia given to all medical students frequently begins with an epic, if not potentially apocryphal, statement regarding how this disease has been noted in the annals of medical history since the time of the Ancients. Although contemporary diagnostic criteria for preeclampsia are not that far out of date, they are close. The increased urinary protein loss and hypertension preceding eclamptic seizures was first noted at the end of the 19th century. The blood pressure and proteinuria criteria used for diagnosis was codified in its contemporary form in the late 1940s. Since then, “tweak” rather than “overhaul” probably best describes the updates of the obstetrical community to the definition of preeclampsia. This has just changed.
Details of the study
Thadhani and colleagues prospectively recruited a nationally representative observational cohort of patients hospitalized for hypertension during pregnancy, then followed the patients until either the diagnosis of preeclampsia with severe features or for 2 weeks, whichever came first. At enrollment, circulating levels of the soluble fms-like tyrosine kinase 1 (sFlt-1) and placental growth factor (PlGF) were measured. In a 2-phased design, the first 219 participants were used to define a sFlt-1/PlGF ratio that would predict progression to severe preeclampsia within 2 weeks. The next 556 enrollees served to validate the predictive properties of the ratio. The authors found that a sFlt-1/PlGF ratio of ≥40 predicted progression to preeclampsia with severe features with an area under the curve (AUC) of 0.92.

As products of the trophoblasts, both sFlt-1 and PlGF have been mooted for almost 2 decades as potential predictive, if not diagnostic, aids with respect to preeclampsia. Indeed, both analytes are commercially available in Europe for specifically this purpose and many maternal-fetal medicine practitioners working in the European equivalent American tertiary referral centers use an sFlt-1/PlGF ratio as their primary criteria for a diagnosis of preeclampsia. Within the United States, there was an initial flurry of interest in and an infusion of corporate and federal research support for sFlt-1 and PlGF as diagnostic aids for preeclampsia in the mid-2000s. However, at present, the US Food and Drug Administration (FDA) has not sanctioned these (or any) biomarkers to aid in the diagnosis of preeclampsia. As Thermo-Fisher Scientific (Waltham, Massachusetts) is a supporting partner in this study, it is almost certain that these data will be submitted for review by the FDA as part of an application for a preeclampsia diagnostic. At some point in the near future, American practitioners will potentially be able to join their European colleagues in utilizing these biomarkers in the diagnosis of preeclampsia with severe features. ●
Thadhani and colleagues observed that the majority of both maternal and neonatal morbidity in their study, including 8 of the 9 neonatal deaths and both cases of eclampsia, occurred among patients with a ratio ≥40 at admission. There was an inverse relation between the sFlt-1/PlGF ratio and the admission to delivery interval. Where only 17% of patients in the highest quartile of ratios remained pregnant at 14 days post-enrollment, more than 79% of the lowest quartile were still pregnant. If not a causal relationship, sFlt-1 and PlGF are clearly associated with not only the occurrence of preeclampsia with severe features but also the degree of morbidity.
The implication for the disposition of patient care resources is clear. Patients at higher risk for preeclampsia could be seen in specialty high-risk clinics with an emphasis on increased monitoring. In situations where tertiary care is more remote, plans could be developed should they need to be transported to centers able to provide the appropriate level of care. Conversely, patients screening at lower ratios may be more appropriately managed as outpatients, or at least in less clinically involved accommodations.
Thadhani et al do note that there were false negative cases in which the sFlt-1/PlGF ratio at admission was <40 but patients nonetheless progressed to preeclampsia with severe features. The majority of these cases had concurrent pre-pregnancy, chronic hypertension. This observation suggests not only the potential for insights into the pathophysiology of the hypertensive diseases in pregnancy but also that the interpretation of the sFlt/PlGF ratio may eventually need to be stratified by preexisting conditions.
The final implications for the observations of this study are perhaps the most tantalizing. If there is a causal relation between the level of the sFlt-1/PlGF ratio and the morbidity of preeclampsia with severe features, then lowering the circulating concentration of sFlt-1 would ameliorate not only the morbidity but also the risk of preeclampsia. Work with plasma phoresies has suggested that this might be possible, albeit via a clinical intervention demanding more intensive resources. The potential for a targeted pharmacologic moderation of sFlt-1 levels would hold great promise in that those identified as at increased risk could be offered an intervention widely available to all.
Is the limit of viability shifting again?
Chawla S, Wyckoff MH, Rysavy MA, et al; Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Association of antenatal steroid exposure at 21 to 22 weeks of gestation with neonatal survival and survival without morbidities. JAMA Netw Open. 2022;5:e2233331. doi:10.1001/jamanet workopen.2022.33331.
EXPERT COMMENTARY
The single most important intervention available in obstetrics to improve the health outcomes of preterm newborns is the maternal administration of corticosteroids. The 27 randomized controlled trials that formed the basis for this knowledge1 did not include infants delivered at 24 weeks’ gestation or less. This has not dissuaded us, over the last several decades, from using corticosteroids for impending delivery at 24 weeks’ gestation; in the absence of randomized data, this has been based on observational evidence of benefit.
Following the 2011 publication of a retrospective cohort study that analyzed data collected by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) Neonatal Research Network between 1993 and 2009 (the Carlo study),2 ACS started to be used widely even for impending delivery at 23 weeks’ gestation. That study had found that the odds of death and neurodevelopmental impairment at 18 to 22 months of age were significantly lower in cases that received ACS and were born at 23 weeks (n = 1,978). The same benefit could not be verified for infants born at 22 weeks’ gestational age (n = 402).
In a recent study conducted by the same NICHD Neonatal Research Network, antenatal steroid exposure at 21 to 22 weeks of gestation was examined.

Details of the study
Using prospectively collected data from 2016 to 2019, Chawla and colleagues conducted a retrospective cohort study that analyzed data from 431 infants who were born between 22 0/7 and 23 6/7 weeks’ gestation and received neonatal intensive care (179 infants born at 22 weeks’ gestation).3 The infants not exposed to ACS were compared with those who had partial exposure (only 1 dose) and those with complete ACS exposure (2 doses).
Complete ACS exposure proved to be beneficial, increasing survival to discharge from 35.5% in the no-exposure group to 53.9% (adjusted odds ratio [aOR], 1.95; 95% confidence interval [CI], 1.07–3.56). Of the survivors, 26.9% in the complete-exposure group had no major morbidities compared with 10% in the no-exposure group (aOR, 2.74; 95% CI, 1.19–6.30).
Study strengths and limitations
The strengths of this study include the use of a diverse, multicenter cohort, with contemporary delivery data, which increases the generalizability of the findings. The analysis included aspects often overlooked in other similar studies, such as the dose of ACS exposure and the gestational age at the time of exposure.
The observational study design, however, can suggest only associations rather than causal relationships. Observational studies also are apt to be affected by residual confounding. Such limitations can only be overcome by a randomized controlled trial, but such a trial of ACS at periviable gestational ages seems unfeasible due to limited ethical justification.
Another limitation is the reporting on outcomes as a collective group (22–23 weeks’ gestation). It is important to consider each gestational age week separately due to differences in physiology and potential biological limitations. It cannot be assumed that 22 weeks behaves like 23 weeks, just as 21 weeks is not equivalent to 22 weeks.
The study results suggest that the protective effect of ACS was dose dependent. However, the interpretation that only a complete ACS exposure was beneficial should be viewed cautiously because the study had no power to assess the impact of a partial exposure.
A further limitation is the lack of consideration in analysis for maternal comorbidities and fetal growth restriction. In the Carlo study, the beneficial effect of corticosteroids in 23-week gestational age deliveries was not demonstrable in pregnancies affected by fetal growth restriction or maternal hypertension.
Other studies considered
Given all its limitations, can we assume that the study by Chawla and colleagues has reliably refuted the Carlo study’s suggestion of lack of ACS efficacy in infants born at 22 weeks’ gestation? Taken by itself, probably not. In the context of other recent investigations, yes.
A retrospective registry study that used data from the Vermont Oxford Network for the period 2012–2016 on 1,058 infants born at 22 weeks’ gestation found that infants who were exposed to ACS and received postnatal life support were more likely to survive to hospital discharge without major morbidity compared with infants who received postnatal life support alone.4 Overall survival was 38.5% versus 17.7% (adjusted risk ratio [aRR], 2.11; 95% CI, 1.68–2.65), and survival without major morbidity was 4.4% versus 1.0% (aRR, 4.35; 95% CI, 1.84–10.28).
An even larger cohort study that used data from the National Center for Health Statistics concluded that survival at age 1 year for infants born at 22 weeks (n = 2,635) during 2009–2014 was improved in those exposed to ACS followed by postnatal life support compared with postnatal life support alone (45.2% vs 27.8%; aRR, 1.6; 95% CI, 1.2–2.1).5
A meta-analysis of observational studies that reported on infants born between 22 0/7 and 22 6/7 weeks’ gestation (n = 2,226) who received proactive neonatal treatment found that administration of ACS doubled the rate of survival when compared with no ACS administration (39% vs 19.5%; P<.01).6
In September 2021, the recommendations from the American College of Obstetricians and Gynecologists changed, stating that ACS can be considered at 22 weeks’ gestation when active postnatal management is desired.7 This recommendation is largely congruent with those from several other national and international medical organizations, including the World Association of Perinatal Medicine, the Royal Collegeof Obstetricians and Gynaecologists, and the German, Austrian and Swiss societies of gynecology and obstetrics. The implication is that the limit of viability may have shifted again, from 23 to 22 weeks’ gestation, and considering the importance of adequate timing in ACS administration (within 1 week from delivery), Chawla and colleagues posited that ACS administration can be considered as early as 21 weeks’ gestation when birth is anticipated at 22 weeks and active postnatal management is planned (notably, this should be the correct interpretation of the article title, not that ACS may be beneficial in 21-weeks’ gestational age births). ●
In 2001, the Institute of Medicine of the National Academies introduced the concept of shared decision-making as a key component of quality care. In very few other clinical situations is shared decision-making as critical as in the context of planning intervention when delivery is anticipated at 22 weeks’ gestation. The truth remains that even with the coordinated provision of ACS and active postnatal care, survival at this gestational age is still a toss-up, and survivors face a high probability of neurodevelopmental impairment and other long-term adverse health outcomes. In this setting, decision-making is complex, with the need to balance patient autonomy and nonmaleficence. On the other hand, the concept of patient autonomy is blurred because the patient (fetus) is incompetent and the negotiation is conducted between physicians and parents. However, no intervention should be undertaken unless the parents so desire. Since parental wishes are frequently emotional, overwhelmingly driving intervention, thorough and timely interdisciplinary counseling is needed. Evidence indicates that both obstetricians and neonatologists may, at times, underestimate the chance of a favorable health outcome for infants born extremely preterm.8,9 Early involvement of the neonatal and obstetric team is pivotal to put forward a coherent, nonconfusing, nonpaternalistic, balanced message. When outcomes information is shared during prenatal counseling, it should be based on local, not only national, data. Following appropriate consultation with the parents, the physicians will adjust the expectations to the local standards, outcomes data, and availability regarding periviable neonatal support.
Recent data suggest that the rate of cesarean delivery (CD) in the periviable period is increasing.10 There is no clear evidence in favor of CD to improve neonatal outcomes, whereas there is concern that periviable CD is associated with significantly increased maternal risks. Regardless of uterine incision type, periviable CD results in an increased risk of uterine rupture in a subsequent pregnancy.11 Consistent with the principle of nonmaleficence, a discussion of these risks should be included in shared decision-making.
ALEX C. VIDAEFF, MD, MPH, AND NATHAN C. SUNDGREN, MD, PHD
- McGoldrick E, Stewart F, Parker R, et al. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev. 2020;12(12):CD004454.
- Carlo WA, McDonald SA, Fanaroff AA, et al; Eunice Kennedy Schriver National Institute for Child Health and Human Development Neonatal Research Network. Association of antenatal corticosteroids with mortality and neurodevelopmental outcomes among infants born at 22-25 weeks gestation. JAMA. 2011;306:2348-2358.
- Chawla S, Wyckoff MH, Rysavy MA, et al; Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Association of antenatal steroid exposure at 21 to 22 weeks of gestation with neonatal survival and survival without morbidities. JAMA Netw Open. 2022;5(9):e2233331. doi:10.1001/ jamanetworkopen.2022.33331.
- Ehret DEY, Edwards EM, Greenberg LT, et al. Association of antenatal steroid exposure with survival among infants receiving postnatal life support at 22 to 25 weeks’ gestation. JAMA Netw Open. 2018;1(6):e183235. doi:10.1001/ jamanetworkopen.2018.3235.
- Rossi RM, DeFranco EA, Hall ES. Association of antenatal corticosteroid exposure and infant survival at 22 and 23 weeks. Am J Perinatol. November 28, 2021. doi:10.1055/s-0041-1740062.
- Backes CH, Rivera BK, Pavlek L, et al. Proactive neonatal treatment at 22 weeks of gestation: a systematic review and meta-analysis. Am J Obstet Gynecol. 2021;224:158-174.
- Cahill AG, Kaimal AJ, Kuller JA, et al; American College of Obstetricians and Gynecologists and Society for Maternal-Fetal Medicine. Practice advisory: Use of antenatal corticosteroids at 22 weeks of gestation. Accessed December 7, 2022. https://www.acog.org/clinical/clinical-guidance /practice-advisory/articles/2021/09/use-of-antenatal -corticosteroids-at-22-weeks-of-gestation#
- Boland RA, Davis PG, Dawson JA, et al. What are we telling the parents of extremely preterm babies? Aust N Z J Obstet Gynaecol. 2016;56:274-281.
- Blanco F, Suresh G, Howard D, et al. Ensuring accurate knowledge of prematurity outcomes for prenatal counseling. Pediatrics. 2005;115:e478-e487.
- Rossi RM, Hall E, DeFranco EA. Contemporary trends in cesarean delivery utilization for live births between 22 0/7 and 23 6/7 weeks of gestation. Obstet Gynecol. 2019;133:451-458.
- Lannon SMR, Guthrie KA, Vanderhoeven JP, et al. Uterine rupture risk after periviable cesarean delivery. Obstet Gynecol. 2015;125:1095-1100.
Chawla S, Wyckoff MH, Rysavy MA, et al; Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Association of antenatal steroid exposure at 21 to 22 weeks of gestation with neonatal survival and survival without morbidities. JAMA Netw Open. 2022;5:e2233331. doi:10.1001/jamanet workopen.2022.33331.
EXPERT COMMENTARY
The single most important intervention available in obstetrics to improve the health outcomes of preterm newborns is the maternal administration of corticosteroids. The 27 randomized controlled trials that formed the basis for this knowledge1 did not include infants delivered at 24 weeks’ gestation or less. This has not dissuaded us, over the last several decades, from using corticosteroids for impending delivery at 24 weeks’ gestation; in the absence of randomized data, this has been based on observational evidence of benefit.
Following the 2011 publication of a retrospective cohort study that analyzed data collected by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) Neonatal Research Network between 1993 and 2009 (the Carlo study),2 ACS started to be used widely even for impending delivery at 23 weeks’ gestation. That study had found that the odds of death and neurodevelopmental impairment at 18 to 22 months of age were significantly lower in cases that received ACS and were born at 23 weeks (n = 1,978). The same benefit could not be verified for infants born at 22 weeks’ gestational age (n = 402).
In a recent study conducted by the same NICHD Neonatal Research Network, antenatal steroid exposure at 21 to 22 weeks of gestation was examined.

Details of the study
Using prospectively collected data from 2016 to 2019, Chawla and colleagues conducted a retrospective cohort study that analyzed data from 431 infants who were born between 22 0/7 and 23 6/7 weeks’ gestation and received neonatal intensive care (179 infants born at 22 weeks’ gestation).3 The infants not exposed to ACS were compared with those who had partial exposure (only 1 dose) and those with complete ACS exposure (2 doses).
Complete ACS exposure proved to be beneficial, increasing survival to discharge from 35.5% in the no-exposure group to 53.9% (adjusted odds ratio [aOR], 1.95; 95% confidence interval [CI], 1.07–3.56). Of the survivors, 26.9% in the complete-exposure group had no major morbidities compared with 10% in the no-exposure group (aOR, 2.74; 95% CI, 1.19–6.30).
Study strengths and limitations
The strengths of this study include the use of a diverse, multicenter cohort, with contemporary delivery data, which increases the generalizability of the findings. The analysis included aspects often overlooked in other similar studies, such as the dose of ACS exposure and the gestational age at the time of exposure.
The observational study design, however, can suggest only associations rather than causal relationships. Observational studies also are apt to be affected by residual confounding. Such limitations can only be overcome by a randomized controlled trial, but such a trial of ACS at periviable gestational ages seems unfeasible due to limited ethical justification.
Another limitation is the reporting on outcomes as a collective group (22–23 weeks’ gestation). It is important to consider each gestational age week separately due to differences in physiology and potential biological limitations. It cannot be assumed that 22 weeks behaves like 23 weeks, just as 21 weeks is not equivalent to 22 weeks.
The study results suggest that the protective effect of ACS was dose dependent. However, the interpretation that only a complete ACS exposure was beneficial should be viewed cautiously because the study had no power to assess the impact of a partial exposure.
A further limitation is the lack of consideration in analysis for maternal comorbidities and fetal growth restriction. In the Carlo study, the beneficial effect of corticosteroids in 23-week gestational age deliveries was not demonstrable in pregnancies affected by fetal growth restriction or maternal hypertension.
Other studies considered
Given all its limitations, can we assume that the study by Chawla and colleagues has reliably refuted the Carlo study’s suggestion of lack of ACS efficacy in infants born at 22 weeks’ gestation? Taken by itself, probably not. In the context of other recent investigations, yes.
A retrospective registry study that used data from the Vermont Oxford Network for the period 2012–2016 on 1,058 infants born at 22 weeks’ gestation found that infants who were exposed to ACS and received postnatal life support were more likely to survive to hospital discharge without major morbidity compared with infants who received postnatal life support alone.4 Overall survival was 38.5% versus 17.7% (adjusted risk ratio [aRR], 2.11; 95% CI, 1.68–2.65), and survival without major morbidity was 4.4% versus 1.0% (aRR, 4.35; 95% CI, 1.84–10.28).
An even larger cohort study that used data from the National Center for Health Statistics concluded that survival at age 1 year for infants born at 22 weeks (n = 2,635) during 2009–2014 was improved in those exposed to ACS followed by postnatal life support compared with postnatal life support alone (45.2% vs 27.8%; aRR, 1.6; 95% CI, 1.2–2.1).5
A meta-analysis of observational studies that reported on infants born between 22 0/7 and 22 6/7 weeks’ gestation (n = 2,226) who received proactive neonatal treatment found that administration of ACS doubled the rate of survival when compared with no ACS administration (39% vs 19.5%; P<.01).6
In September 2021, the recommendations from the American College of Obstetricians and Gynecologists changed, stating that ACS can be considered at 22 weeks’ gestation when active postnatal management is desired.7 This recommendation is largely congruent with those from several other national and international medical organizations, including the World Association of Perinatal Medicine, the Royal Collegeof Obstetricians and Gynaecologists, and the German, Austrian and Swiss societies of gynecology and obstetrics. The implication is that the limit of viability may have shifted again, from 23 to 22 weeks’ gestation, and considering the importance of adequate timing in ACS administration (within 1 week from delivery), Chawla and colleagues posited that ACS administration can be considered as early as 21 weeks’ gestation when birth is anticipated at 22 weeks and active postnatal management is planned (notably, this should be the correct interpretation of the article title, not that ACS may be beneficial in 21-weeks’ gestational age births). ●
In 2001, the Institute of Medicine of the National Academies introduced the concept of shared decision-making as a key component of quality care. In very few other clinical situations is shared decision-making as critical as in the context of planning intervention when delivery is anticipated at 22 weeks’ gestation. The truth remains that even with the coordinated provision of ACS and active postnatal care, survival at this gestational age is still a toss-up, and survivors face a high probability of neurodevelopmental impairment and other long-term adverse health outcomes. In this setting, decision-making is complex, with the need to balance patient autonomy and nonmaleficence. On the other hand, the concept of patient autonomy is blurred because the patient (fetus) is incompetent and the negotiation is conducted between physicians and parents. However, no intervention should be undertaken unless the parents so desire. Since parental wishes are frequently emotional, overwhelmingly driving intervention, thorough and timely interdisciplinary counseling is needed. Evidence indicates that both obstetricians and neonatologists may, at times, underestimate the chance of a favorable health outcome for infants born extremely preterm.8,9 Early involvement of the neonatal and obstetric team is pivotal to put forward a coherent, nonconfusing, nonpaternalistic, balanced message. When outcomes information is shared during prenatal counseling, it should be based on local, not only national, data. Following appropriate consultation with the parents, the physicians will adjust the expectations to the local standards, outcomes data, and availability regarding periviable neonatal support.
Recent data suggest that the rate of cesarean delivery (CD) in the periviable period is increasing.10 There is no clear evidence in favor of CD to improve neonatal outcomes, whereas there is concern that periviable CD is associated with significantly increased maternal risks. Regardless of uterine incision type, periviable CD results in an increased risk of uterine rupture in a subsequent pregnancy.11 Consistent with the principle of nonmaleficence, a discussion of these risks should be included in shared decision-making.
ALEX C. VIDAEFF, MD, MPH, AND NATHAN C. SUNDGREN, MD, PHD
Chawla S, Wyckoff MH, Rysavy MA, et al; Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Association of antenatal steroid exposure at 21 to 22 weeks of gestation with neonatal survival and survival without morbidities. JAMA Netw Open. 2022;5:e2233331. doi:10.1001/jamanet workopen.2022.33331.
EXPERT COMMENTARY
The single most important intervention available in obstetrics to improve the health outcomes of preterm newborns is the maternal administration of corticosteroids. The 27 randomized controlled trials that formed the basis for this knowledge1 did not include infants delivered at 24 weeks’ gestation or less. This has not dissuaded us, over the last several decades, from using corticosteroids for impending delivery at 24 weeks’ gestation; in the absence of randomized data, this has been based on observational evidence of benefit.
Following the 2011 publication of a retrospective cohort study that analyzed data collected by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) Neonatal Research Network between 1993 and 2009 (the Carlo study),2 ACS started to be used widely even for impending delivery at 23 weeks’ gestation. That study had found that the odds of death and neurodevelopmental impairment at 18 to 22 months of age were significantly lower in cases that received ACS and were born at 23 weeks (n = 1,978). The same benefit could not be verified for infants born at 22 weeks’ gestational age (n = 402).
In a recent study conducted by the same NICHD Neonatal Research Network, antenatal steroid exposure at 21 to 22 weeks of gestation was examined.

Details of the study
Using prospectively collected data from 2016 to 2019, Chawla and colleagues conducted a retrospective cohort study that analyzed data from 431 infants who were born between 22 0/7 and 23 6/7 weeks’ gestation and received neonatal intensive care (179 infants born at 22 weeks’ gestation).3 The infants not exposed to ACS were compared with those who had partial exposure (only 1 dose) and those with complete ACS exposure (2 doses).
Complete ACS exposure proved to be beneficial, increasing survival to discharge from 35.5% in the no-exposure group to 53.9% (adjusted odds ratio [aOR], 1.95; 95% confidence interval [CI], 1.07–3.56). Of the survivors, 26.9% in the complete-exposure group had no major morbidities compared with 10% in the no-exposure group (aOR, 2.74; 95% CI, 1.19–6.30).
Study strengths and limitations
The strengths of this study include the use of a diverse, multicenter cohort, with contemporary delivery data, which increases the generalizability of the findings. The analysis included aspects often overlooked in other similar studies, such as the dose of ACS exposure and the gestational age at the time of exposure.
The observational study design, however, can suggest only associations rather than causal relationships. Observational studies also are apt to be affected by residual confounding. Such limitations can only be overcome by a randomized controlled trial, but such a trial of ACS at periviable gestational ages seems unfeasible due to limited ethical justification.
Another limitation is the reporting on outcomes as a collective group (22–23 weeks’ gestation). It is important to consider each gestational age week separately due to differences in physiology and potential biological limitations. It cannot be assumed that 22 weeks behaves like 23 weeks, just as 21 weeks is not equivalent to 22 weeks.
The study results suggest that the protective effect of ACS was dose dependent. However, the interpretation that only a complete ACS exposure was beneficial should be viewed cautiously because the study had no power to assess the impact of a partial exposure.
A further limitation is the lack of consideration in analysis for maternal comorbidities and fetal growth restriction. In the Carlo study, the beneficial effect of corticosteroids in 23-week gestational age deliveries was not demonstrable in pregnancies affected by fetal growth restriction or maternal hypertension.
Other studies considered
Given all its limitations, can we assume that the study by Chawla and colleagues has reliably refuted the Carlo study’s suggestion of lack of ACS efficacy in infants born at 22 weeks’ gestation? Taken by itself, probably not. In the context of other recent investigations, yes.
A retrospective registry study that used data from the Vermont Oxford Network for the period 2012–2016 on 1,058 infants born at 22 weeks’ gestation found that infants who were exposed to ACS and received postnatal life support were more likely to survive to hospital discharge without major morbidity compared with infants who received postnatal life support alone.4 Overall survival was 38.5% versus 17.7% (adjusted risk ratio [aRR], 2.11; 95% CI, 1.68–2.65), and survival without major morbidity was 4.4% versus 1.0% (aRR, 4.35; 95% CI, 1.84–10.28).
An even larger cohort study that used data from the National Center for Health Statistics concluded that survival at age 1 year for infants born at 22 weeks (n = 2,635) during 2009–2014 was improved in those exposed to ACS followed by postnatal life support compared with postnatal life support alone (45.2% vs 27.8%; aRR, 1.6; 95% CI, 1.2–2.1).5
A meta-analysis of observational studies that reported on infants born between 22 0/7 and 22 6/7 weeks’ gestation (n = 2,226) who received proactive neonatal treatment found that administration of ACS doubled the rate of survival when compared with no ACS administration (39% vs 19.5%; P<.01).6
In September 2021, the recommendations from the American College of Obstetricians and Gynecologists changed, stating that ACS can be considered at 22 weeks’ gestation when active postnatal management is desired.7 This recommendation is largely congruent with those from several other national and international medical organizations, including the World Association of Perinatal Medicine, the Royal Collegeof Obstetricians and Gynaecologists, and the German, Austrian and Swiss societies of gynecology and obstetrics. The implication is that the limit of viability may have shifted again, from 23 to 22 weeks’ gestation, and considering the importance of adequate timing in ACS administration (within 1 week from delivery), Chawla and colleagues posited that ACS administration can be considered as early as 21 weeks’ gestation when birth is anticipated at 22 weeks and active postnatal management is planned (notably, this should be the correct interpretation of the article title, not that ACS may be beneficial in 21-weeks’ gestational age births). ●
In 2001, the Institute of Medicine of the National Academies introduced the concept of shared decision-making as a key component of quality care. In very few other clinical situations is shared decision-making as critical as in the context of planning intervention when delivery is anticipated at 22 weeks’ gestation. The truth remains that even with the coordinated provision of ACS and active postnatal care, survival at this gestational age is still a toss-up, and survivors face a high probability of neurodevelopmental impairment and other long-term adverse health outcomes. In this setting, decision-making is complex, with the need to balance patient autonomy and nonmaleficence. On the other hand, the concept of patient autonomy is blurred because the patient (fetus) is incompetent and the negotiation is conducted between physicians and parents. However, no intervention should be undertaken unless the parents so desire. Since parental wishes are frequently emotional, overwhelmingly driving intervention, thorough and timely interdisciplinary counseling is needed. Evidence indicates that both obstetricians and neonatologists may, at times, underestimate the chance of a favorable health outcome for infants born extremely preterm.8,9 Early involvement of the neonatal and obstetric team is pivotal to put forward a coherent, nonconfusing, nonpaternalistic, balanced message. When outcomes information is shared during prenatal counseling, it should be based on local, not only national, data. Following appropriate consultation with the parents, the physicians will adjust the expectations to the local standards, outcomes data, and availability regarding periviable neonatal support.
Recent data suggest that the rate of cesarean delivery (CD) in the periviable period is increasing.10 There is no clear evidence in favor of CD to improve neonatal outcomes, whereas there is concern that periviable CD is associated with significantly increased maternal risks. Regardless of uterine incision type, periviable CD results in an increased risk of uterine rupture in a subsequent pregnancy.11 Consistent with the principle of nonmaleficence, a discussion of these risks should be included in shared decision-making.
ALEX C. VIDAEFF, MD, MPH, AND NATHAN C. SUNDGREN, MD, PHD
- McGoldrick E, Stewart F, Parker R, et al. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev. 2020;12(12):CD004454.
- Carlo WA, McDonald SA, Fanaroff AA, et al; Eunice Kennedy Schriver National Institute for Child Health and Human Development Neonatal Research Network. Association of antenatal corticosteroids with mortality and neurodevelopmental outcomes among infants born at 22-25 weeks gestation. JAMA. 2011;306:2348-2358.
- Chawla S, Wyckoff MH, Rysavy MA, et al; Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Association of antenatal steroid exposure at 21 to 22 weeks of gestation with neonatal survival and survival without morbidities. JAMA Netw Open. 2022;5(9):e2233331. doi:10.1001/ jamanetworkopen.2022.33331.
- Ehret DEY, Edwards EM, Greenberg LT, et al. Association of antenatal steroid exposure with survival among infants receiving postnatal life support at 22 to 25 weeks’ gestation. JAMA Netw Open. 2018;1(6):e183235. doi:10.1001/ jamanetworkopen.2018.3235.
- Rossi RM, DeFranco EA, Hall ES. Association of antenatal corticosteroid exposure and infant survival at 22 and 23 weeks. Am J Perinatol. November 28, 2021. doi:10.1055/s-0041-1740062.
- Backes CH, Rivera BK, Pavlek L, et al. Proactive neonatal treatment at 22 weeks of gestation: a systematic review and meta-analysis. Am J Obstet Gynecol. 2021;224:158-174.
- Cahill AG, Kaimal AJ, Kuller JA, et al; American College of Obstetricians and Gynecologists and Society for Maternal-Fetal Medicine. Practice advisory: Use of antenatal corticosteroids at 22 weeks of gestation. Accessed December 7, 2022. https://www.acog.org/clinical/clinical-guidance /practice-advisory/articles/2021/09/use-of-antenatal -corticosteroids-at-22-weeks-of-gestation#
- Boland RA, Davis PG, Dawson JA, et al. What are we telling the parents of extremely preterm babies? Aust N Z J Obstet Gynaecol. 2016;56:274-281.
- Blanco F, Suresh G, Howard D, et al. Ensuring accurate knowledge of prematurity outcomes for prenatal counseling. Pediatrics. 2005;115:e478-e487.
- Rossi RM, Hall E, DeFranco EA. Contemporary trends in cesarean delivery utilization for live births between 22 0/7 and 23 6/7 weeks of gestation. Obstet Gynecol. 2019;133:451-458.
- Lannon SMR, Guthrie KA, Vanderhoeven JP, et al. Uterine rupture risk after periviable cesarean delivery. Obstet Gynecol. 2015;125:1095-1100.
- McGoldrick E, Stewart F, Parker R, et al. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev. 2020;12(12):CD004454.
- Carlo WA, McDonald SA, Fanaroff AA, et al; Eunice Kennedy Schriver National Institute for Child Health and Human Development Neonatal Research Network. Association of antenatal corticosteroids with mortality and neurodevelopmental outcomes among infants born at 22-25 weeks gestation. JAMA. 2011;306:2348-2358.
- Chawla S, Wyckoff MH, Rysavy MA, et al; Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Association of antenatal steroid exposure at 21 to 22 weeks of gestation with neonatal survival and survival without morbidities. JAMA Netw Open. 2022;5(9):e2233331. doi:10.1001/ jamanetworkopen.2022.33331.
- Ehret DEY, Edwards EM, Greenberg LT, et al. Association of antenatal steroid exposure with survival among infants receiving postnatal life support at 22 to 25 weeks’ gestation. JAMA Netw Open. 2018;1(6):e183235. doi:10.1001/ jamanetworkopen.2018.3235.
- Rossi RM, DeFranco EA, Hall ES. Association of antenatal corticosteroid exposure and infant survival at 22 and 23 weeks. Am J Perinatol. November 28, 2021. doi:10.1055/s-0041-1740062.
- Backes CH, Rivera BK, Pavlek L, et al. Proactive neonatal treatment at 22 weeks of gestation: a systematic review and meta-analysis. Am J Obstet Gynecol. 2021;224:158-174.
- Cahill AG, Kaimal AJ, Kuller JA, et al; American College of Obstetricians and Gynecologists and Society for Maternal-Fetal Medicine. Practice advisory: Use of antenatal corticosteroids at 22 weeks of gestation. Accessed December 7, 2022. https://www.acog.org/clinical/clinical-guidance /practice-advisory/articles/2021/09/use-of-antenatal -corticosteroids-at-22-weeks-of-gestation#
- Boland RA, Davis PG, Dawson JA, et al. What are we telling the parents of extremely preterm babies? Aust N Z J Obstet Gynaecol. 2016;56:274-281.
- Blanco F, Suresh G, Howard D, et al. Ensuring accurate knowledge of prematurity outcomes for prenatal counseling. Pediatrics. 2005;115:e478-e487.
- Rossi RM, Hall E, DeFranco EA. Contemporary trends in cesarean delivery utilization for live births between 22 0/7 and 23 6/7 weeks of gestation. Obstet Gynecol. 2019;133:451-458.
- Lannon SMR, Guthrie KA, Vanderhoeven JP, et al. Uterine rupture risk after periviable cesarean delivery. Obstet Gynecol. 2015;125:1095-1100.
Does fertility preservation in patients with breast cancer impact relapse rates and disease-specific mortality?
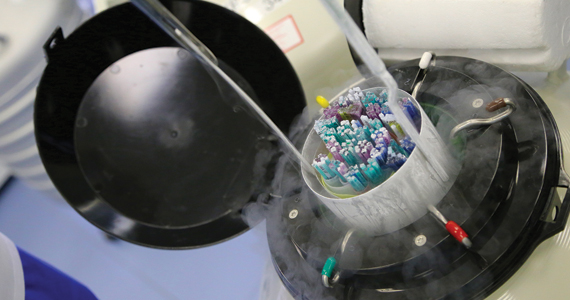
Marklund A, Lekberg T, Hedayati E, et al. Relapse rates and disease-specific mortality following procedures for fertility preservation at time of breast cancer diagnosis. JAMA Oncol. 2022;8:1438-1446. doi:10.1001/jamaoncol.2022.3677.
EXPERT COMMENTARY
Breast cancer is the most diagnosed cancer among US women after skin cancer.1 As of the end of 2020, 7.8 million women were alive who were diagnosed with breast cancer in the past 5 years, making it the world’s most prevalent cancer. Given the wide reach of breast cancer and the increase in its distant stage by more than 4% per year in women of reproductive age (20–39 years), clinicians are urged to address fertility preservation due to reproductive compromise of gonadotoxic therapies and gonadectomy.2 To predict the risk of infertility following chemotherapy, a Cyclophosphamide Equivalent Dose (CED) calculator can be used. A CED of 4,000 mg/m2 has been associated with a significant risk of infertility.3
In 2012, the American Society for Reproductive Medicine removed the experimental label of oocyte cryopreservation then recently endorsed ovarian cryopreservation, thereby providing acceptable procedures for fertility preservation.4 Gonadotropin-releasing hormone agonist use during chemotherapy, which is used to protect the ovary in premenopausal women against the effects of chemotherapy, has been shown to have inconsistent findings and should not replace the established modalities of oocyte/embryo/ovarian tissue cryopreservation.2,5
Details of the study
While studies have been reassuring that ovarian stimulation for fertility preservation in women with breast cancer does not worsen the prognosis, findings are limited by short-term follow-up.6
The recent study by Marklund and colleagues presented an analysis of breast cancer relapse and mortality following fertility preservation with and without hormonal stimulation. In their prospective cohort study of 425 Swedish women who underwent fertility preservation, the authors categorized patients into 2 groups: oocyte and embryo cryopreservation by ovarian hormonal stimulation and ovarian tissue cryopreservation without hormonal stimulation. The control group included 850 women with breast cancer who did not undergo fertility preservation. The cohort and the control groups were matched on age, calendar period of diagnosis, and region. Three Swedish registers for breast cancer were used to obtain the study cohort, and for each participant, 2 breast cancer patients who were unexposed to fertility preservation were used for comparison. The primary outcome was mortality while the secondary outcome was any event of death due to breast cancer or relapse.
Results. A total of 1,275 women were studied at the time of breast cancer diagnosis. After stratification, which included age, parity at diagnosis, tumor size, number of lymph node metastases, and estrogen receptor status, disease-specific mortality was similar in all categories of women, that is, hormonal fertility preservation, nonhormonal fertility preservation, and controls. In the subcohort of 723 women, the adjusted rate of relapse and disease-specific mortality remained the same among all groups.
Study strengths and limitations
This study prompts several areas of criticism. The follow-up of breast cancer patients was only 5 years, adding to the limitations of short-term monitoring seen in prior studies. The authors also considered a delay in pregnancy attempts following breast cancer treatment of hormonally sensitive cancers of 5 to 10 years. However, the long-term safety of pregnancy following breast cancer has shown a statistically significantly superior disease-free survival (DFS) in patients who became pregnant less than 2 years from diagnosis and no difference in those who became pregnant 2 or more years from diagnosis.7
Only 58 women in the nonhormonal fertility preservation group (ovarian tissue cryopreservation) were studied, which may limit an adequate evaluation although it is not expected to negatively impact breast cancer prognosis. Another area of potential bias was the use of only a subcohort to assess relapse-free survival as opposed to the entire cohort that was used to assess mortality.
Strengths of this study include obligatory reporting to the registry and equal access to anticancer treatment and fertility preservation in Sweden. Ovarian stimulating drugs were examined, as letrozole is often used in breast cancer patients to maintain lower estradiol levels due to aromatase inhibition. Nevertheless, this study did not demonstrate a difference in mortality with or without letrozole use. ●
Marklund and colleagues’ findings revealed no increase of breast cancer relapse and mortality following fertility preservation with or without hormonal stimulation. They also propose a “healthy user effect” whereby a woman who feels healthy may choose to undergo fertility preservation, thereby biasing the outcome by having a better survival.8
Future studies with longer follow-up are needed to address the hormonal impact of fertility preservation, if any, on breast cancer DFS and mortality, as well as to evaluate subsequent pregnancy outcomes, stratified for medication treatment type via the CED calculator. To date, evidence continues to support fertility preservation options that use hormonal ovarian stimulation in breast cancer patients as apparently safe for, at least, up to 5 years of follow-up.
MARK P. TROLICE, MD
- Giaquinto AN, Sung H, Miller KD, et al. Breast cancer statistics, 2022. CA Cancer J Clin. 2022;72:524-541. doi:10.3322/caac.21754.
- Oktay K, Harvey BE, Partridge AH, et al. Fertility preservation in patients with cancer: ASCO clinical practice guideline update. J Clin Oncol. 2018;1;36:1994-2001. doi:10.1200/JCO.2018.78.1914.
- Fertility Preservation in Pittsburgh. CED calculator. Accessed November 14, 2022. https://fertilitypreservationpittsburgh.org/fertility-resources/fertility-risk-calculator/
- Practice Committee of the American Society for Reproductive Medicine. Fertility preservation in patients undergoing gonadotoxic therapy or gonadectomy: a committee opinion. Fertil Steril. 2019;112:1022-1033. doi:10.1016/j.fertnstert.2019.09.013.
- Blumenfeld Z. Fertility preservation using GnRH agonists: rationale, possible mechanisms, and explanation of controversy. Clin Med Insights Reprod Health. 2019;13: 1179558119870163. doi:10.1177/1179558119870163.
- Beebeejaun Y, Athithan A, Copeland TP, et al. Risk of breast cancer in women treated with ovarian stimulation drugs for infertility: a systematic review and meta-analysis. Fertil Steril. 2021;116:198-207. doi:10.1016/j.fertnstert.2021.01.044.
- Lambertini M, Kroman N, Ameye L, et al. Long-term safety of pregnancy following breast cancer according to estrogen receptor status. J Natl Cancer Inst. 2018;110:426-429. doi:10.1093/jnci/djx206.
- Marklund A, Lundberg FE, Eloranta S, et al. Reproductive outcomes after breast cancer in women with vs without fertility preservation. JAMA Oncol. 2021;7:86-91. doi:10.1001/ jamaoncol.2020.5957.
Marklund A, Lekberg T, Hedayati E, et al. Relapse rates and disease-specific mortality following procedures for fertility preservation at time of breast cancer diagnosis. JAMA Oncol. 2022;8:1438-1446. doi:10.1001/jamaoncol.2022.3677.
EXPERT COMMENTARY
Breast cancer is the most diagnosed cancer among US women after skin cancer.1 As of the end of 2020, 7.8 million women were alive who were diagnosed with breast cancer in the past 5 years, making it the world’s most prevalent cancer. Given the wide reach of breast cancer and the increase in its distant stage by more than 4% per year in women of reproductive age (20–39 years), clinicians are urged to address fertility preservation due to reproductive compromise of gonadotoxic therapies and gonadectomy.2 To predict the risk of infertility following chemotherapy, a Cyclophosphamide Equivalent Dose (CED) calculator can be used. A CED of 4,000 mg/m2 has been associated with a significant risk of infertility.3
In 2012, the American Society for Reproductive Medicine removed the experimental label of oocyte cryopreservation then recently endorsed ovarian cryopreservation, thereby providing acceptable procedures for fertility preservation.4 Gonadotropin-releasing hormone agonist use during chemotherapy, which is used to protect the ovary in premenopausal women against the effects of chemotherapy, has been shown to have inconsistent findings and should not replace the established modalities of oocyte/embryo/ovarian tissue cryopreservation.2,5
Details of the study
While studies have been reassuring that ovarian stimulation for fertility preservation in women with breast cancer does not worsen the prognosis, findings are limited by short-term follow-up.6
The recent study by Marklund and colleagues presented an analysis of breast cancer relapse and mortality following fertility preservation with and without hormonal stimulation. In their prospective cohort study of 425 Swedish women who underwent fertility preservation, the authors categorized patients into 2 groups: oocyte and embryo cryopreservation by ovarian hormonal stimulation and ovarian tissue cryopreservation without hormonal stimulation. The control group included 850 women with breast cancer who did not undergo fertility preservation. The cohort and the control groups were matched on age, calendar period of diagnosis, and region. Three Swedish registers for breast cancer were used to obtain the study cohort, and for each participant, 2 breast cancer patients who were unexposed to fertility preservation were used for comparison. The primary outcome was mortality while the secondary outcome was any event of death due to breast cancer or relapse.
Results. A total of 1,275 women were studied at the time of breast cancer diagnosis. After stratification, which included age, parity at diagnosis, tumor size, number of lymph node metastases, and estrogen receptor status, disease-specific mortality was similar in all categories of women, that is, hormonal fertility preservation, nonhormonal fertility preservation, and controls. In the subcohort of 723 women, the adjusted rate of relapse and disease-specific mortality remained the same among all groups.
Study strengths and limitations
This study prompts several areas of criticism. The follow-up of breast cancer patients was only 5 years, adding to the limitations of short-term monitoring seen in prior studies. The authors also considered a delay in pregnancy attempts following breast cancer treatment of hormonally sensitive cancers of 5 to 10 years. However, the long-term safety of pregnancy following breast cancer has shown a statistically significantly superior disease-free survival (DFS) in patients who became pregnant less than 2 years from diagnosis and no difference in those who became pregnant 2 or more years from diagnosis.7
Only 58 women in the nonhormonal fertility preservation group (ovarian tissue cryopreservation) were studied, which may limit an adequate evaluation although it is not expected to negatively impact breast cancer prognosis. Another area of potential bias was the use of only a subcohort to assess relapse-free survival as opposed to the entire cohort that was used to assess mortality.
Strengths of this study include obligatory reporting to the registry and equal access to anticancer treatment and fertility preservation in Sweden. Ovarian stimulating drugs were examined, as letrozole is often used in breast cancer patients to maintain lower estradiol levels due to aromatase inhibition. Nevertheless, this study did not demonstrate a difference in mortality with or without letrozole use. ●
Marklund and colleagues’ findings revealed no increase of breast cancer relapse and mortality following fertility preservation with or without hormonal stimulation. They also propose a “healthy user effect” whereby a woman who feels healthy may choose to undergo fertility preservation, thereby biasing the outcome by having a better survival.8
Future studies with longer follow-up are needed to address the hormonal impact of fertility preservation, if any, on breast cancer DFS and mortality, as well as to evaluate subsequent pregnancy outcomes, stratified for medication treatment type via the CED calculator. To date, evidence continues to support fertility preservation options that use hormonal ovarian stimulation in breast cancer patients as apparently safe for, at least, up to 5 years of follow-up.
MARK P. TROLICE, MD
Marklund A, Lekberg T, Hedayati E, et al. Relapse rates and disease-specific mortality following procedures for fertility preservation at time of breast cancer diagnosis. JAMA Oncol. 2022;8:1438-1446. doi:10.1001/jamaoncol.2022.3677.
EXPERT COMMENTARY
Breast cancer is the most diagnosed cancer among US women after skin cancer.1 As of the end of 2020, 7.8 million women were alive who were diagnosed with breast cancer in the past 5 years, making it the world’s most prevalent cancer. Given the wide reach of breast cancer and the increase in its distant stage by more than 4% per year in women of reproductive age (20–39 years), clinicians are urged to address fertility preservation due to reproductive compromise of gonadotoxic therapies and gonadectomy.2 To predict the risk of infertility following chemotherapy, a Cyclophosphamide Equivalent Dose (CED) calculator can be used. A CED of 4,000 mg/m2 has been associated with a significant risk of infertility.3
In 2012, the American Society for Reproductive Medicine removed the experimental label of oocyte cryopreservation then recently endorsed ovarian cryopreservation, thereby providing acceptable procedures for fertility preservation.4 Gonadotropin-releasing hormone agonist use during chemotherapy, which is used to protect the ovary in premenopausal women against the effects of chemotherapy, has been shown to have inconsistent findings and should not replace the established modalities of oocyte/embryo/ovarian tissue cryopreservation.2,5
Details of the study
While studies have been reassuring that ovarian stimulation for fertility preservation in women with breast cancer does not worsen the prognosis, findings are limited by short-term follow-up.6
The recent study by Marklund and colleagues presented an analysis of breast cancer relapse and mortality following fertility preservation with and without hormonal stimulation. In their prospective cohort study of 425 Swedish women who underwent fertility preservation, the authors categorized patients into 2 groups: oocyte and embryo cryopreservation by ovarian hormonal stimulation and ovarian tissue cryopreservation without hormonal stimulation. The control group included 850 women with breast cancer who did not undergo fertility preservation. The cohort and the control groups were matched on age, calendar period of diagnosis, and region. Three Swedish registers for breast cancer were used to obtain the study cohort, and for each participant, 2 breast cancer patients who were unexposed to fertility preservation were used for comparison. The primary outcome was mortality while the secondary outcome was any event of death due to breast cancer or relapse.
Results. A total of 1,275 women were studied at the time of breast cancer diagnosis. After stratification, which included age, parity at diagnosis, tumor size, number of lymph node metastases, and estrogen receptor status, disease-specific mortality was similar in all categories of women, that is, hormonal fertility preservation, nonhormonal fertility preservation, and controls. In the subcohort of 723 women, the adjusted rate of relapse and disease-specific mortality remained the same among all groups.
Study strengths and limitations
This study prompts several areas of criticism. The follow-up of breast cancer patients was only 5 years, adding to the limitations of short-term monitoring seen in prior studies. The authors also considered a delay in pregnancy attempts following breast cancer treatment of hormonally sensitive cancers of 5 to 10 years. However, the long-term safety of pregnancy following breast cancer has shown a statistically significantly superior disease-free survival (DFS) in patients who became pregnant less than 2 years from diagnosis and no difference in those who became pregnant 2 or more years from diagnosis.7
Only 58 women in the nonhormonal fertility preservation group (ovarian tissue cryopreservation) were studied, which may limit an adequate evaluation although it is not expected to negatively impact breast cancer prognosis. Another area of potential bias was the use of only a subcohort to assess relapse-free survival as opposed to the entire cohort that was used to assess mortality.
Strengths of this study include obligatory reporting to the registry and equal access to anticancer treatment and fertility preservation in Sweden. Ovarian stimulating drugs were examined, as letrozole is often used in breast cancer patients to maintain lower estradiol levels due to aromatase inhibition. Nevertheless, this study did not demonstrate a difference in mortality with or without letrozole use. ●
Marklund and colleagues’ findings revealed no increase of breast cancer relapse and mortality following fertility preservation with or without hormonal stimulation. They also propose a “healthy user effect” whereby a woman who feels healthy may choose to undergo fertility preservation, thereby biasing the outcome by having a better survival.8
Future studies with longer follow-up are needed to address the hormonal impact of fertility preservation, if any, on breast cancer DFS and mortality, as well as to evaluate subsequent pregnancy outcomes, stratified for medication treatment type via the CED calculator. To date, evidence continues to support fertility preservation options that use hormonal ovarian stimulation in breast cancer patients as apparently safe for, at least, up to 5 years of follow-up.
MARK P. TROLICE, MD
- Giaquinto AN, Sung H, Miller KD, et al. Breast cancer statistics, 2022. CA Cancer J Clin. 2022;72:524-541. doi:10.3322/caac.21754.
- Oktay K, Harvey BE, Partridge AH, et al. Fertility preservation in patients with cancer: ASCO clinical practice guideline update. J Clin Oncol. 2018;1;36:1994-2001. doi:10.1200/JCO.2018.78.1914.
- Fertility Preservation in Pittsburgh. CED calculator. Accessed November 14, 2022. https://fertilitypreservationpittsburgh.org/fertility-resources/fertility-risk-calculator/
- Practice Committee of the American Society for Reproductive Medicine. Fertility preservation in patients undergoing gonadotoxic therapy or gonadectomy: a committee opinion. Fertil Steril. 2019;112:1022-1033. doi:10.1016/j.fertnstert.2019.09.013.
- Blumenfeld Z. Fertility preservation using GnRH agonists: rationale, possible mechanisms, and explanation of controversy. Clin Med Insights Reprod Health. 2019;13: 1179558119870163. doi:10.1177/1179558119870163.
- Beebeejaun Y, Athithan A, Copeland TP, et al. Risk of breast cancer in women treated with ovarian stimulation drugs for infertility: a systematic review and meta-analysis. Fertil Steril. 2021;116:198-207. doi:10.1016/j.fertnstert.2021.01.044.
- Lambertini M, Kroman N, Ameye L, et al. Long-term safety of pregnancy following breast cancer according to estrogen receptor status. J Natl Cancer Inst. 2018;110:426-429. doi:10.1093/jnci/djx206.
- Marklund A, Lundberg FE, Eloranta S, et al. Reproductive outcomes after breast cancer in women with vs without fertility preservation. JAMA Oncol. 2021;7:86-91. doi:10.1001/ jamaoncol.2020.5957.
- Giaquinto AN, Sung H, Miller KD, et al. Breast cancer statistics, 2022. CA Cancer J Clin. 2022;72:524-541. doi:10.3322/caac.21754.
- Oktay K, Harvey BE, Partridge AH, et al. Fertility preservation in patients with cancer: ASCO clinical practice guideline update. J Clin Oncol. 2018;1;36:1994-2001. doi:10.1200/JCO.2018.78.1914.
- Fertility Preservation in Pittsburgh. CED calculator. Accessed November 14, 2022. https://fertilitypreservationpittsburgh.org/fertility-resources/fertility-risk-calculator/
- Practice Committee of the American Society for Reproductive Medicine. Fertility preservation in patients undergoing gonadotoxic therapy or gonadectomy: a committee opinion. Fertil Steril. 2019;112:1022-1033. doi:10.1016/j.fertnstert.2019.09.013.
- Blumenfeld Z. Fertility preservation using GnRH agonists: rationale, possible mechanisms, and explanation of controversy. Clin Med Insights Reprod Health. 2019;13: 1179558119870163. doi:10.1177/1179558119870163.
- Beebeejaun Y, Athithan A, Copeland TP, et al. Risk of breast cancer in women treated with ovarian stimulation drugs for infertility: a systematic review and meta-analysis. Fertil Steril. 2021;116:198-207. doi:10.1016/j.fertnstert.2021.01.044.
- Lambertini M, Kroman N, Ameye L, et al. Long-term safety of pregnancy following breast cancer according to estrogen receptor status. J Natl Cancer Inst. 2018;110:426-429. doi:10.1093/jnci/djx206.
- Marklund A, Lundberg FE, Eloranta S, et al. Reproductive outcomes after breast cancer in women with vs without fertility preservation. JAMA Oncol. 2021;7:86-91. doi:10.1001/ jamaoncol.2020.5957.