User login
New fellowship, no problem
Using growth mindset to tackle fellowship in a new program
Growth mindset is a well-established phenomenon in childhood education that is now starting to appear in health care education literature.1 This concept emphasizes the capacity of individuals to change and grow through experience and that an individual’s basic qualities can be cultivated through hard work, open-mindedness, and help from others.2
Growth mindset opposes the concept of fixed mindset, which implies intelligence or other personal traits are set in stone, unable to be fundamentally changed.2 Individuals with fixed mindsets are less adept at coping with perceived failures and critical feedback because they view these as attacks on their own abilities.2 This oftentimes leads these individuals to avoid potential challenges and feedback because of fear of being exposed as incompetent or feeling inadequate. Conversely, individuals with a growth mindset embrace challenges and failures as learning opportunities and identify feedback as a critical element of growth.2 These individuals maintain a sense of resilience in the face of adversity and strive to become lifelong learners.
As the field of pediatric hospital medicine (PHM) continues to rapidly evolve, so too does the landscape of PHM fellowships. New programs are opening at a torrid pace to accommodate the increasing demand of residents looking to enter the field with new subspecialty accreditation. Most first-year PHM fellows in established programs enter with a clear precedent to follow, set forth by fellows who have come before them. For PHM fellows in new programs, however, there is often no beaten path to follow.
Entering fellowship as a first-year PHM fellow in a new program and blazing one’s own trail can be intriguing and exhilarating given the unique opportunities available. However, the potential challenges for both fellows and program directors during this transition cannot be understated. The role of new PHM fellows within the institutional framework may initially be unclear to others, which can lead to ambiguous expectations and disruptions to normal workflows. Furthermore, assessing and evaluating new fellows may prove difficult as a result of these unclear expectations and general uncertainties. Using the growth mindset can help both PHM fellows and program directors take a deliberate approach to the challenges and uncertainty that may accompany the creation of a new fellowship program.
One of the challenges new PHM fellows may encounter lies within the structure of the care team. Resident and medical student learners may express consternation that the new fellow role may limit their own autonomy. In addition, finding the right balance of autonomy and supervision between the attending-fellow dyad may prove to be difficult. However, using the growth mindset may allow fellows to see the inherent benefits of this new role.
Fellows should seize the opportunity to discuss the nuances and differing approaches to difficult clinical questions, managing a team and interpersonal dynamics, and balancing clinical and nonclinical responsibilities with an experienced supervising clinician; issues that are often less pressing as a resident. The fellow role also affords the opportunity to more carefully observe different clinical styles of practice to subsequently shape one’s own preferred style.
Finally, fellows should employ a growth mindset to optimize clinical time by discussing expectations with involved stakeholders prior to rotations and explicitly identifying goals for feedback and improvement. Program directors can also help stakeholders including faculty, residency programs, medical schools, and other health care professionals on the clinical teams prepare for this transition by providing expectations for the fellow role and by soliciting questions and feedback before and after fellows begin.
One of the key tenets of the growth mindset is actively seeking out constructive feedback and learning from failures to grow and improve. This can be a particularly useful practice for fellows during the course of their scholarly pursuits in clinical research, quality improvement, and medical education. From initial stages of idea development through the final steps of manuscript submission and peer review, fellows will undoubtedly navigate a plethora of challenges and setbacks along the way. Program directors and other core faculty members can promote a growth mindset culture by honestly discussing their own challenges and failures in career endeavors in addition to giving thoughtful constructive feedback.
Fellows should routinely practice explicitly identifying knowledge and skills gaps that represent areas for potential improvement. But perhaps most importantly, fellows must strive to see all feedback and perceived failures not as personal affronts or as commentaries on personal abilities, but rather as opportunities to strengthen their scholarly products and gain valuable experience for future endeavors.
Not all learners will come equipped with a growth mindset. So, what can fellows and program directors in new programs do to develop this practice and mitigate some of the inevitable uncertainty? To begin, program directors should think about how to create cultures of growth and development as the fixed and growth mindsets are not just limited to individuals.3 Program directors can strive to augment this process by committing to solicit feedback for themselves and acknowledging their own vulnerabilities and perceived weaknesses.
Fellows must have early, honest discussions with program directors and other stakeholders about expectations and goals. Program directors should consider creating lists of “must meet” individuals within the institution that can help fellows begin to carve out their roles in the clinical, educational, and research realms. Deliberately crafting a mentorship team that will encourage a commitment to growth and improvement is critical. Seeking out growth feedback, particularly in areas that prove challenging, should become common practice for fellows from the onset.
Most importantly, fellows should reframe uncertainty as opportunity for growth and progression. Seeing oneself as a work in progress provides a new perspective that prioritizes learning and emphasizes improvement potential.
Embodying this approach requires patience and practice. Being part of a newly created fellowship represents an opportunity to learn from personal challenges rather than leaning on the precedent set by previous fellows. And although fellows will often face uncertainty as a part of the novelty within a new program, they can ultimately succeed by practicing the principles of Dweck’s Growth Mindset: embracing challenges and failure as learning experiences, seeking out feedback, and pursuing the opportunities among ambiguity.
Dr. Herchline is a pediatric hospitalist at Cincinnati Children’s Hospital Medical Center and recent fellow graduate of the Children’s Hospital of Philadelphia. During fellowship, he completed a master’s degree in medical education at the University of Pennsylvania. His academic interests include graduate medical education, interprofessional collaboration and teamwork, and quality improvement.
References
1. Klein J et al. A growth mindset approach to preparing trainees for medical error. BMJ Qual Saf. 2017 Sep;26(9):771-4. doi: 10.1136/bmjqs-2016-006416.
2. Dweck C. Mindset: The new psychology of success. New York: Ballantine Books; 2006.
3. Murphy MC, Dweck CS. A culture of genius: How an organization’s lay theory shapes people’s cognition, affect, and behavior. Pers Soc Psychol Bull. 2010 Mar;36(3):283-96. doi: 10.1177/0146167209347380.
Using growth mindset to tackle fellowship in a new program
Using growth mindset to tackle fellowship in a new program
Growth mindset is a well-established phenomenon in childhood education that is now starting to appear in health care education literature.1 This concept emphasizes the capacity of individuals to change and grow through experience and that an individual’s basic qualities can be cultivated through hard work, open-mindedness, and help from others.2
Growth mindset opposes the concept of fixed mindset, which implies intelligence or other personal traits are set in stone, unable to be fundamentally changed.2 Individuals with fixed mindsets are less adept at coping with perceived failures and critical feedback because they view these as attacks on their own abilities.2 This oftentimes leads these individuals to avoid potential challenges and feedback because of fear of being exposed as incompetent or feeling inadequate. Conversely, individuals with a growth mindset embrace challenges and failures as learning opportunities and identify feedback as a critical element of growth.2 These individuals maintain a sense of resilience in the face of adversity and strive to become lifelong learners.
As the field of pediatric hospital medicine (PHM) continues to rapidly evolve, so too does the landscape of PHM fellowships. New programs are opening at a torrid pace to accommodate the increasing demand of residents looking to enter the field with new subspecialty accreditation. Most first-year PHM fellows in established programs enter with a clear precedent to follow, set forth by fellows who have come before them. For PHM fellows in new programs, however, there is often no beaten path to follow.
Entering fellowship as a first-year PHM fellow in a new program and blazing one’s own trail can be intriguing and exhilarating given the unique opportunities available. However, the potential challenges for both fellows and program directors during this transition cannot be understated. The role of new PHM fellows within the institutional framework may initially be unclear to others, which can lead to ambiguous expectations and disruptions to normal workflows. Furthermore, assessing and evaluating new fellows may prove difficult as a result of these unclear expectations and general uncertainties. Using the growth mindset can help both PHM fellows and program directors take a deliberate approach to the challenges and uncertainty that may accompany the creation of a new fellowship program.
One of the challenges new PHM fellows may encounter lies within the structure of the care team. Resident and medical student learners may express consternation that the new fellow role may limit their own autonomy. In addition, finding the right balance of autonomy and supervision between the attending-fellow dyad may prove to be difficult. However, using the growth mindset may allow fellows to see the inherent benefits of this new role.
Fellows should seize the opportunity to discuss the nuances and differing approaches to difficult clinical questions, managing a team and interpersonal dynamics, and balancing clinical and nonclinical responsibilities with an experienced supervising clinician; issues that are often less pressing as a resident. The fellow role also affords the opportunity to more carefully observe different clinical styles of practice to subsequently shape one’s own preferred style.
Finally, fellows should employ a growth mindset to optimize clinical time by discussing expectations with involved stakeholders prior to rotations and explicitly identifying goals for feedback and improvement. Program directors can also help stakeholders including faculty, residency programs, medical schools, and other health care professionals on the clinical teams prepare for this transition by providing expectations for the fellow role and by soliciting questions and feedback before and after fellows begin.
One of the key tenets of the growth mindset is actively seeking out constructive feedback and learning from failures to grow and improve. This can be a particularly useful practice for fellows during the course of their scholarly pursuits in clinical research, quality improvement, and medical education. From initial stages of idea development through the final steps of manuscript submission and peer review, fellows will undoubtedly navigate a plethora of challenges and setbacks along the way. Program directors and other core faculty members can promote a growth mindset culture by honestly discussing their own challenges and failures in career endeavors in addition to giving thoughtful constructive feedback.
Fellows should routinely practice explicitly identifying knowledge and skills gaps that represent areas for potential improvement. But perhaps most importantly, fellows must strive to see all feedback and perceived failures not as personal affronts or as commentaries on personal abilities, but rather as opportunities to strengthen their scholarly products and gain valuable experience for future endeavors.
Not all learners will come equipped with a growth mindset. So, what can fellows and program directors in new programs do to develop this practice and mitigate some of the inevitable uncertainty? To begin, program directors should think about how to create cultures of growth and development as the fixed and growth mindsets are not just limited to individuals.3 Program directors can strive to augment this process by committing to solicit feedback for themselves and acknowledging their own vulnerabilities and perceived weaknesses.
Fellows must have early, honest discussions with program directors and other stakeholders about expectations and goals. Program directors should consider creating lists of “must meet” individuals within the institution that can help fellows begin to carve out their roles in the clinical, educational, and research realms. Deliberately crafting a mentorship team that will encourage a commitment to growth and improvement is critical. Seeking out growth feedback, particularly in areas that prove challenging, should become common practice for fellows from the onset.
Most importantly, fellows should reframe uncertainty as opportunity for growth and progression. Seeing oneself as a work in progress provides a new perspective that prioritizes learning and emphasizes improvement potential.
Embodying this approach requires patience and practice. Being part of a newly created fellowship represents an opportunity to learn from personal challenges rather than leaning on the precedent set by previous fellows. And although fellows will often face uncertainty as a part of the novelty within a new program, they can ultimately succeed by practicing the principles of Dweck’s Growth Mindset: embracing challenges and failure as learning experiences, seeking out feedback, and pursuing the opportunities among ambiguity.
Dr. Herchline is a pediatric hospitalist at Cincinnati Children’s Hospital Medical Center and recent fellow graduate of the Children’s Hospital of Philadelphia. During fellowship, he completed a master’s degree in medical education at the University of Pennsylvania. His academic interests include graduate medical education, interprofessional collaboration and teamwork, and quality improvement.
References
1. Klein J et al. A growth mindset approach to preparing trainees for medical error. BMJ Qual Saf. 2017 Sep;26(9):771-4. doi: 10.1136/bmjqs-2016-006416.
2. Dweck C. Mindset: The new psychology of success. New York: Ballantine Books; 2006.
3. Murphy MC, Dweck CS. A culture of genius: How an organization’s lay theory shapes people’s cognition, affect, and behavior. Pers Soc Psychol Bull. 2010 Mar;36(3):283-96. doi: 10.1177/0146167209347380.
Growth mindset is a well-established phenomenon in childhood education that is now starting to appear in health care education literature.1 This concept emphasizes the capacity of individuals to change and grow through experience and that an individual’s basic qualities can be cultivated through hard work, open-mindedness, and help from others.2
Growth mindset opposes the concept of fixed mindset, which implies intelligence or other personal traits are set in stone, unable to be fundamentally changed.2 Individuals with fixed mindsets are less adept at coping with perceived failures and critical feedback because they view these as attacks on their own abilities.2 This oftentimes leads these individuals to avoid potential challenges and feedback because of fear of being exposed as incompetent or feeling inadequate. Conversely, individuals with a growth mindset embrace challenges and failures as learning opportunities and identify feedback as a critical element of growth.2 These individuals maintain a sense of resilience in the face of adversity and strive to become lifelong learners.
As the field of pediatric hospital medicine (PHM) continues to rapidly evolve, so too does the landscape of PHM fellowships. New programs are opening at a torrid pace to accommodate the increasing demand of residents looking to enter the field with new subspecialty accreditation. Most first-year PHM fellows in established programs enter with a clear precedent to follow, set forth by fellows who have come before them. For PHM fellows in new programs, however, there is often no beaten path to follow.
Entering fellowship as a first-year PHM fellow in a new program and blazing one’s own trail can be intriguing and exhilarating given the unique opportunities available. However, the potential challenges for both fellows and program directors during this transition cannot be understated. The role of new PHM fellows within the institutional framework may initially be unclear to others, which can lead to ambiguous expectations and disruptions to normal workflows. Furthermore, assessing and evaluating new fellows may prove difficult as a result of these unclear expectations and general uncertainties. Using the growth mindset can help both PHM fellows and program directors take a deliberate approach to the challenges and uncertainty that may accompany the creation of a new fellowship program.
One of the challenges new PHM fellows may encounter lies within the structure of the care team. Resident and medical student learners may express consternation that the new fellow role may limit their own autonomy. In addition, finding the right balance of autonomy and supervision between the attending-fellow dyad may prove to be difficult. However, using the growth mindset may allow fellows to see the inherent benefits of this new role.
Fellows should seize the opportunity to discuss the nuances and differing approaches to difficult clinical questions, managing a team and interpersonal dynamics, and balancing clinical and nonclinical responsibilities with an experienced supervising clinician; issues that are often less pressing as a resident. The fellow role also affords the opportunity to more carefully observe different clinical styles of practice to subsequently shape one’s own preferred style.
Finally, fellows should employ a growth mindset to optimize clinical time by discussing expectations with involved stakeholders prior to rotations and explicitly identifying goals for feedback and improvement. Program directors can also help stakeholders including faculty, residency programs, medical schools, and other health care professionals on the clinical teams prepare for this transition by providing expectations for the fellow role and by soliciting questions and feedback before and after fellows begin.
One of the key tenets of the growth mindset is actively seeking out constructive feedback and learning from failures to grow and improve. This can be a particularly useful practice for fellows during the course of their scholarly pursuits in clinical research, quality improvement, and medical education. From initial stages of idea development through the final steps of manuscript submission and peer review, fellows will undoubtedly navigate a plethora of challenges and setbacks along the way. Program directors and other core faculty members can promote a growth mindset culture by honestly discussing their own challenges and failures in career endeavors in addition to giving thoughtful constructive feedback.
Fellows should routinely practice explicitly identifying knowledge and skills gaps that represent areas for potential improvement. But perhaps most importantly, fellows must strive to see all feedback and perceived failures not as personal affronts or as commentaries on personal abilities, but rather as opportunities to strengthen their scholarly products and gain valuable experience for future endeavors.
Not all learners will come equipped with a growth mindset. So, what can fellows and program directors in new programs do to develop this practice and mitigate some of the inevitable uncertainty? To begin, program directors should think about how to create cultures of growth and development as the fixed and growth mindsets are not just limited to individuals.3 Program directors can strive to augment this process by committing to solicit feedback for themselves and acknowledging their own vulnerabilities and perceived weaknesses.
Fellows must have early, honest discussions with program directors and other stakeholders about expectations and goals. Program directors should consider creating lists of “must meet” individuals within the institution that can help fellows begin to carve out their roles in the clinical, educational, and research realms. Deliberately crafting a mentorship team that will encourage a commitment to growth and improvement is critical. Seeking out growth feedback, particularly in areas that prove challenging, should become common practice for fellows from the onset.
Most importantly, fellows should reframe uncertainty as opportunity for growth and progression. Seeing oneself as a work in progress provides a new perspective that prioritizes learning and emphasizes improvement potential.
Embodying this approach requires patience and practice. Being part of a newly created fellowship represents an opportunity to learn from personal challenges rather than leaning on the precedent set by previous fellows. And although fellows will often face uncertainty as a part of the novelty within a new program, they can ultimately succeed by practicing the principles of Dweck’s Growth Mindset: embracing challenges and failure as learning experiences, seeking out feedback, and pursuing the opportunities among ambiguity.
Dr. Herchline is a pediatric hospitalist at Cincinnati Children’s Hospital Medical Center and recent fellow graduate of the Children’s Hospital of Philadelphia. During fellowship, he completed a master’s degree in medical education at the University of Pennsylvania. His academic interests include graduate medical education, interprofessional collaboration and teamwork, and quality improvement.
References
1. Klein J et al. A growth mindset approach to preparing trainees for medical error. BMJ Qual Saf. 2017 Sep;26(9):771-4. doi: 10.1136/bmjqs-2016-006416.
2. Dweck C. Mindset: The new psychology of success. New York: Ballantine Books; 2006.
3. Murphy MC, Dweck CS. A culture of genius: How an organization’s lay theory shapes people’s cognition, affect, and behavior. Pers Soc Psychol Bull. 2010 Mar;36(3):283-96. doi: 10.1177/0146167209347380.
Embedding diversity, equity, inclusion, and justice in hospital medicine
A road map for success
The language of equality in America’s founding was never truly embraced, resulting in a painful legacy of slavery, racial injustice, and gender inequality inherited by all generations. However, for as long as America has fallen short of this unfulfilled promise, individuals have dedicated their lives to the tireless work of correcting injustice. Although the process has been painstakingly slow, our nation has incrementally inched toward the promised vision of equality, and these efforts continue today. With increased attention to social justice movements such as #MeToo and Black Lives Matter, our collective social consciousness may be finally waking up to the systemic injustices embedded into our fundamental institutions.
Medicine is not immune to these injustices. Persistent underrepresentation of women and minorities remains in medical school faculty and the broader physician workforce, and the same inequities exist in hospital medicine.1-6 The report by the Association of American Medical Colleges (AAMC) on diversity in medicine highlights the impact widespread implicit and explicit bias has on creating exclusionary environments, exemplified by research demonstrating lower promotion rates in non-White faculty.7-8 The report calls us, as physicians, to a broader mission: “Focusing solely on increasing compositional diversity along the academic continuum is insufficient. To effectively enact institutional change at academic medical centers ... leaders must focus their efforts on developing inclusive, equity-minded environments.”7
We have a clear moral imperative to correct these shortcomings for our profession and our patients. It is incumbent on our institutions and hospital medicine groups (HMGs) to embark on the necessary process of systemic institutional change to address inequality and justice within our field.
A road map for DEI and justice in hospital medicine
The policies and biases allowing these inequities to persist have existed for decades, and superficial efforts will not bring sufficient change. Our institutions require new building blocks from which the foundation of a wholly inclusive and equal system of practice can be constructed. Encouragingly, some institutions and HMGs have taken steps to modernize their practices. We offer examples and suggestions of concrete practices to begin this journey, organizing these efforts into three broad categories:
1. Recruitment and retention
2. Scholarship, mentorship, and sponsorship
3. Community engagement and partnership.
Recruitment and retention
Improving equity and inclusion begins with recruitment. Search and hiring committees should be assembled intentionally, with gender balance, and ideally with diversity or equity experts invited to join. All members should receive unconscious bias training. For example, the University of Colorado utilizes a toolkit to ensure appropriate steps are followed in the recruitment process, including predetermined candidate selection criteria that are ranked in advance.
Job descriptions should be reviewed by a diversity expert, ensuring unbiased and ungendered language within written text. Advertisements should be wide-reaching, and the committee should consider asking applicants for a diversity statement. Interviews should include a variety of interviewers and interview types (e.g., 1:1, group, etc.). Letters of recommendation deserve special scrutiny; letters for women and minorities may be at risk of being shorter and less record focused, and may be subject to less professional respect, such as use of first names over honorifics or titles.
Once candidates are hired, institutions and HMGs should prioritize developing strategies to improve retention of a diverse workforce. This includes special attention to workplace culture, and thoughtfully striving for cultural intelligence within the group. Some examples may include developing affinity groups, such as underrepresented in medicine (UIM), women in medicine (WIM), or LGBTQ+ groups. Affinity groups provide a safe space for members and allies to support and uplift each other. Institutional and HMG leaders must educate themselves and their members on the importance of language (see table), and the more insidious forms of bias and discrimination that adversely affect workplace culture. Microinsults and microinvalidations, for example, can hurt and result in failure to recruit or turnover. 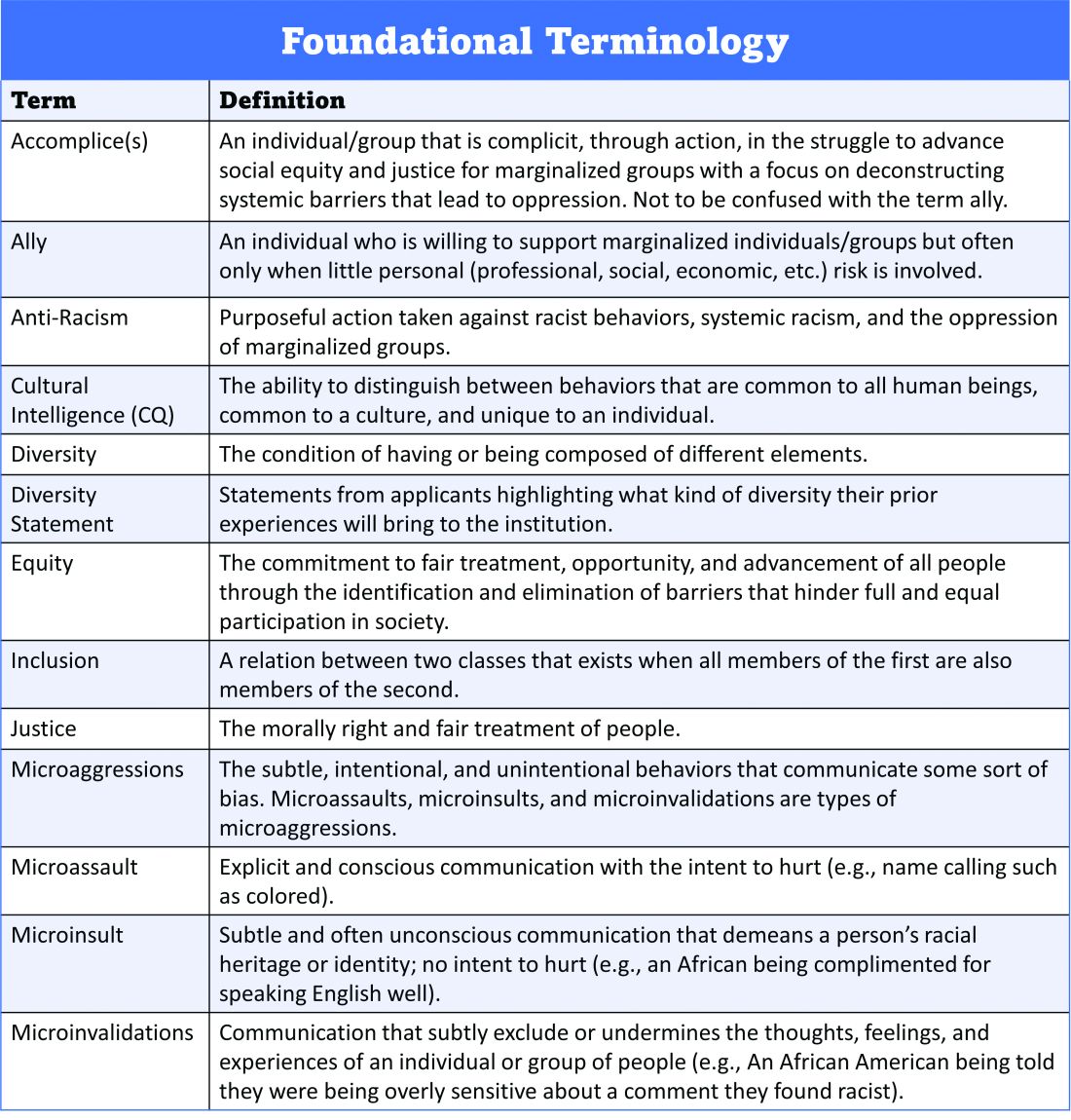
Conducting exit interviews when any hospitalist leaves is important to learn how to improve, but holding ‘stay’ interviews is mission critical. Stay interviews are an opportunity for HMG leaders to proactively understand why hospitalists stay, and what can be done to create more inclusive and equitable environments to retain them. This process creates psychological safety that brings challenges to the fore to be addressed, and spotlights best practices to be maintained and scaled.
Scholarship, mentorship, and sponsorship
Women and minorities are known to be over-mentored and under-sponsored. Sponsorship is defined by Ayyala et al. as “active support by someone appropriately placed in the organization who has significant influence on decision making processes or structures and who is advocating for the career advancement of an individual and recommends them for leadership roles, awards, or high-profile speaking opportunities.”9 While the goal of mentorship is professional development, sponsorship emphasizes professional advancement. Deliberate steps to both mentor and then sponsor diverse hospitalists and future hospitalists (including trainees) are important to ensure equity.
More inclusive HMGs can be bolstered by prioritizing peer education on the professional imperative that we have a diverse workforce and equitable, just workplaces. Academic institutions may use existing structures such as grand rounds to provide education on these crucial topics, and all HMGs can host journal clubs and professional development sessions on leadership competencies that foster inclusion and equity. Sessions coordinated by women and minorities are also a form of justice, by helping overcome barriers to career advancement. Diverse faculty presenting in educational venues will result in content that is relevant to more audience members and will exemplify that leaders and experts are of all races, ethnicities, genders, ages, and abilities.
Groups should prioritize mentoring trainees and early-career hospitalists on scholarly projects that examine equity in opportunities of care, which signals that this science is valued as much as basic research. When used to demonstrate areas needing improvement, these projects can drive meaningful change. Even projects as straightforward as studying diversity in conference presenters, disparities in adherence to guidelines, or QI projects on how race is portrayed in the medical record can be powerful tools in advancing equity.
A key part of mentoring is training hospitalists and future hospitalists in how to be an upstander, as in how to intervene when a peer or patient is affected by bias, harassment, or discrimination. Receiving such training can prepare hospitalists for these nearly inevitable experiences and receiving training during usual work hours communicates that this is a valuable and necessary professional competency.
Community engagement and partnership
Institutions and HMGs should deliberately work to promote community engagement and partnership within their groups. Beyond promoting health equity, community engagement also fosters inclusivity by allowing community members to share their ideas and give recommendations to the institutions that serve them.
There is a growing body of literature that demonstrates how disadvantages by individual and neighborhood-level socioeconomic status (SES) contribute to disparities in specific disease conditions.10-11 Strategies to narrow the gap in SES disadvantages may help reduce race-related health disparities. Institutions that engage the community and develop programs to promote health equity can do so through bidirectional exchange of knowledge and mutual benefit.
An institution-specific example is Medicine for the Greater Good at Johns Hopkins. The founders of this program wrote, “health is not synonymous with medicine. To truly care for our patients and their communities, health care professionals must understand how to deliver equitable health care that meets the needs of the diverse populations we care for. The mission of Medicine for the Greater Good is to promote health and wellness beyond the confines of the hospital through an interactive and engaging partnership with the community ...” Community engagement also provides an opportunity for growing the cultural intelligence of institutions and HMGs.
Tools for advancing comprehensive change – Repurposing PDSA cycles
Whether institutions and HMGs are at the beginning of their journey or further along in the work of reducing disparities, having a systematic approach for implementing and refining policies and procedures can cultivate more inclusive and equitable environments. Thankfully, hospitalists are already equipped with the fundamental tools needed to advance change across their institutions – QI processes in the form of Plan-Do-Study-Act (PDSA) cycles.
They allow a continuous cycle of successful incremental change based on direct evidence and experience. Any efforts to deconstruct systematic bias within our organizations must also be a continual process. Our female colleagues and colleagues of color need our institutions to engage unceasingly to bring about the equality they deserve. To that end, PDSA cycles are an apt tool to utilize in this work as they can naturally function in a never-ending process of improvement.
With PDSA as a model, we envision a cycle with steps that are intentionally purposed to fit the needs of equitable institutional change: Target-Engage-Assess-Modify. As highlighted (see graphic), these modifications ensure that stakeholders (i.e., those that unequal practices and policies affect the most) are engaged early and remain involved throughout the cycle. 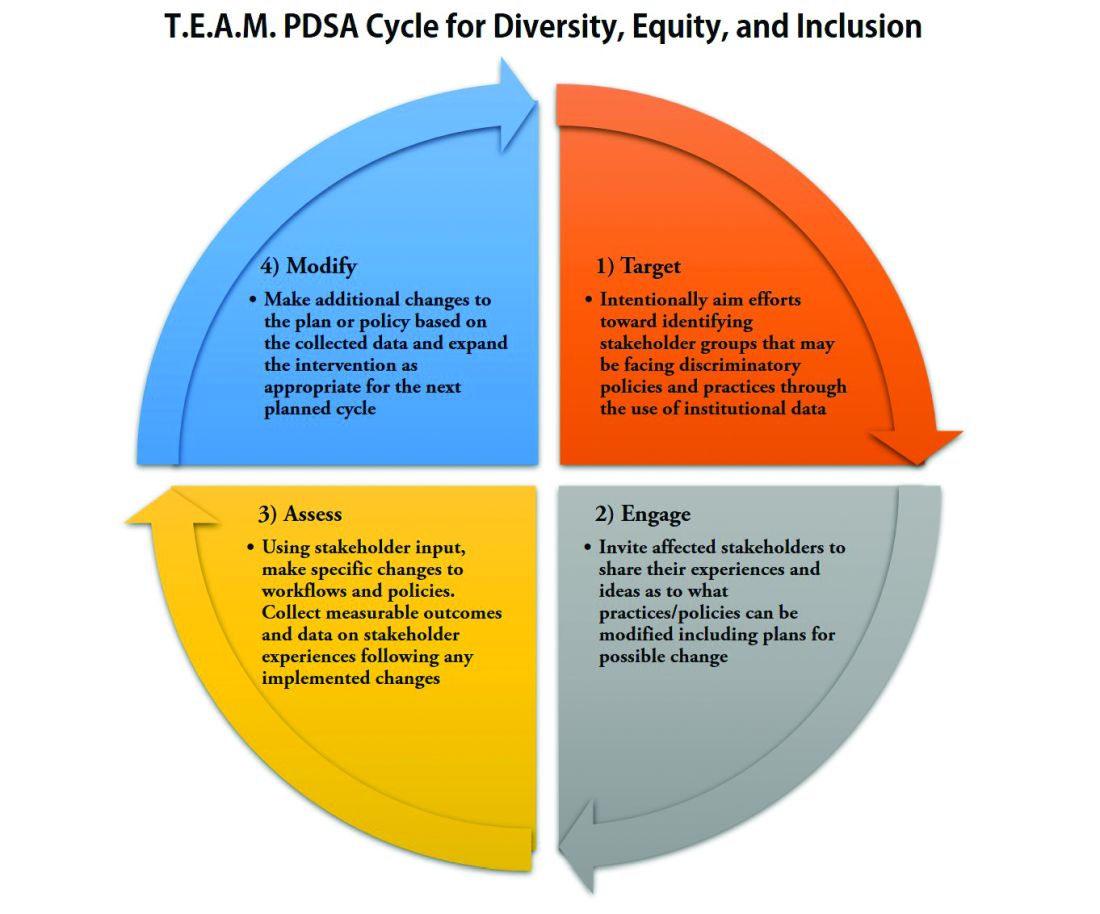
As hospitalists, we have significant work ahead to ensure that we develop and maintain a diverse, equitable and inclusive workforce. This work to bring change will not be easy and will require a considerable investment of time and resources. However, with the strategies and tools that we have outlined, our institutions and HMGs can start the change needed in our profession for our patients and the workforce. In doing so, we can all be accomplices in the fight to achieve racial and gender equity, and social justice.
Dr. Delapenha and Dr. Kisuule are based in the department of internal medicine, division of hospital medicine, at the Johns Hopkins University, Baltimore. Dr. Martin is based in the department of medicine, section of hospital medicine at the University of Chicago. Dr. Barrett is a hospitalist in the department of internal medicine, University of New Mexico, Albuquerque.
References
1. Diversity in Medicine: Facts and Figures 2019: Figure 19. Percentage of physicians by sex, 2018. AAMC website.
2. Diversity in Medicine: Facts and Figures 2019. Figure 16. Percentage of full-time U.S. medical school faculty by sex and race/ethnicity, 2018. AAMC website.
3. Diversity in Medicine: Facts and Figures 2019. Figure 15. Percentage of full-time U.S. medical school faculty by race/ethnicity, 2018. AAMC website.
4. Diversity in Medicine: Facts and Figures 2019. Figure 6. Percentage of acceptees to U.S. medical schools by race/ethnicity (alone), academic year 2018-2019. AAMC website.
5. Diversity in Medicine: Facts and Figures 2019 Figure 18. Percentage of all active physicians by race/ethnicity, 2018. AAMC website.
6. Herzke C et al. Gender issues in academic hospital medicine: A national survey of hospitalist leaders. J Gen Intern Med. 2020;35(6):1641-6.
7. Diversity in Medicine: Facts and Figures 2019. Fostering diversity and inclusion. AAMC website.
8. Diversity in Medicine: Facts and Figures 2019. Executive summary. AAMC website.
9. Ayyala MS et al. Mentorship is not enough: Exploring sponsorship and its role in career advancement in academic medicine. Acad Med. 2019;94(1):94-100.
10. Ejike OC et al. Contribution of individual and neighborhood factors to racial disparities in respiratory outcomes. Am J Respir Crit Care Med. 2021 Apr 15;203(8):987-97.
11. Galiatsatos P et al. The effect of community socioeconomic status on sepsis-attributable mortality. J Crit Care. 2018 Aug;46:129-33.
A road map for success
A road map for success
The language of equality in America’s founding was never truly embraced, resulting in a painful legacy of slavery, racial injustice, and gender inequality inherited by all generations. However, for as long as America has fallen short of this unfulfilled promise, individuals have dedicated their lives to the tireless work of correcting injustice. Although the process has been painstakingly slow, our nation has incrementally inched toward the promised vision of equality, and these efforts continue today. With increased attention to social justice movements such as #MeToo and Black Lives Matter, our collective social consciousness may be finally waking up to the systemic injustices embedded into our fundamental institutions.
Medicine is not immune to these injustices. Persistent underrepresentation of women and minorities remains in medical school faculty and the broader physician workforce, and the same inequities exist in hospital medicine.1-6 The report by the Association of American Medical Colleges (AAMC) on diversity in medicine highlights the impact widespread implicit and explicit bias has on creating exclusionary environments, exemplified by research demonstrating lower promotion rates in non-White faculty.7-8 The report calls us, as physicians, to a broader mission: “Focusing solely on increasing compositional diversity along the academic continuum is insufficient. To effectively enact institutional change at academic medical centers ... leaders must focus their efforts on developing inclusive, equity-minded environments.”7
We have a clear moral imperative to correct these shortcomings for our profession and our patients. It is incumbent on our institutions and hospital medicine groups (HMGs) to embark on the necessary process of systemic institutional change to address inequality and justice within our field.
A road map for DEI and justice in hospital medicine
The policies and biases allowing these inequities to persist have existed for decades, and superficial efforts will not bring sufficient change. Our institutions require new building blocks from which the foundation of a wholly inclusive and equal system of practice can be constructed. Encouragingly, some institutions and HMGs have taken steps to modernize their practices. We offer examples and suggestions of concrete practices to begin this journey, organizing these efforts into three broad categories:
1. Recruitment and retention
2. Scholarship, mentorship, and sponsorship
3. Community engagement and partnership.
Recruitment and retention
Improving equity and inclusion begins with recruitment. Search and hiring committees should be assembled intentionally, with gender balance, and ideally with diversity or equity experts invited to join. All members should receive unconscious bias training. For example, the University of Colorado utilizes a toolkit to ensure appropriate steps are followed in the recruitment process, including predetermined candidate selection criteria that are ranked in advance.
Job descriptions should be reviewed by a diversity expert, ensuring unbiased and ungendered language within written text. Advertisements should be wide-reaching, and the committee should consider asking applicants for a diversity statement. Interviews should include a variety of interviewers and interview types (e.g., 1:1, group, etc.). Letters of recommendation deserve special scrutiny; letters for women and minorities may be at risk of being shorter and less record focused, and may be subject to less professional respect, such as use of first names over honorifics or titles.
Once candidates are hired, institutions and HMGs should prioritize developing strategies to improve retention of a diverse workforce. This includes special attention to workplace culture, and thoughtfully striving for cultural intelligence within the group. Some examples may include developing affinity groups, such as underrepresented in medicine (UIM), women in medicine (WIM), or LGBTQ+ groups. Affinity groups provide a safe space for members and allies to support and uplift each other. Institutional and HMG leaders must educate themselves and their members on the importance of language (see table), and the more insidious forms of bias and discrimination that adversely affect workplace culture. Microinsults and microinvalidations, for example, can hurt and result in failure to recruit or turnover. 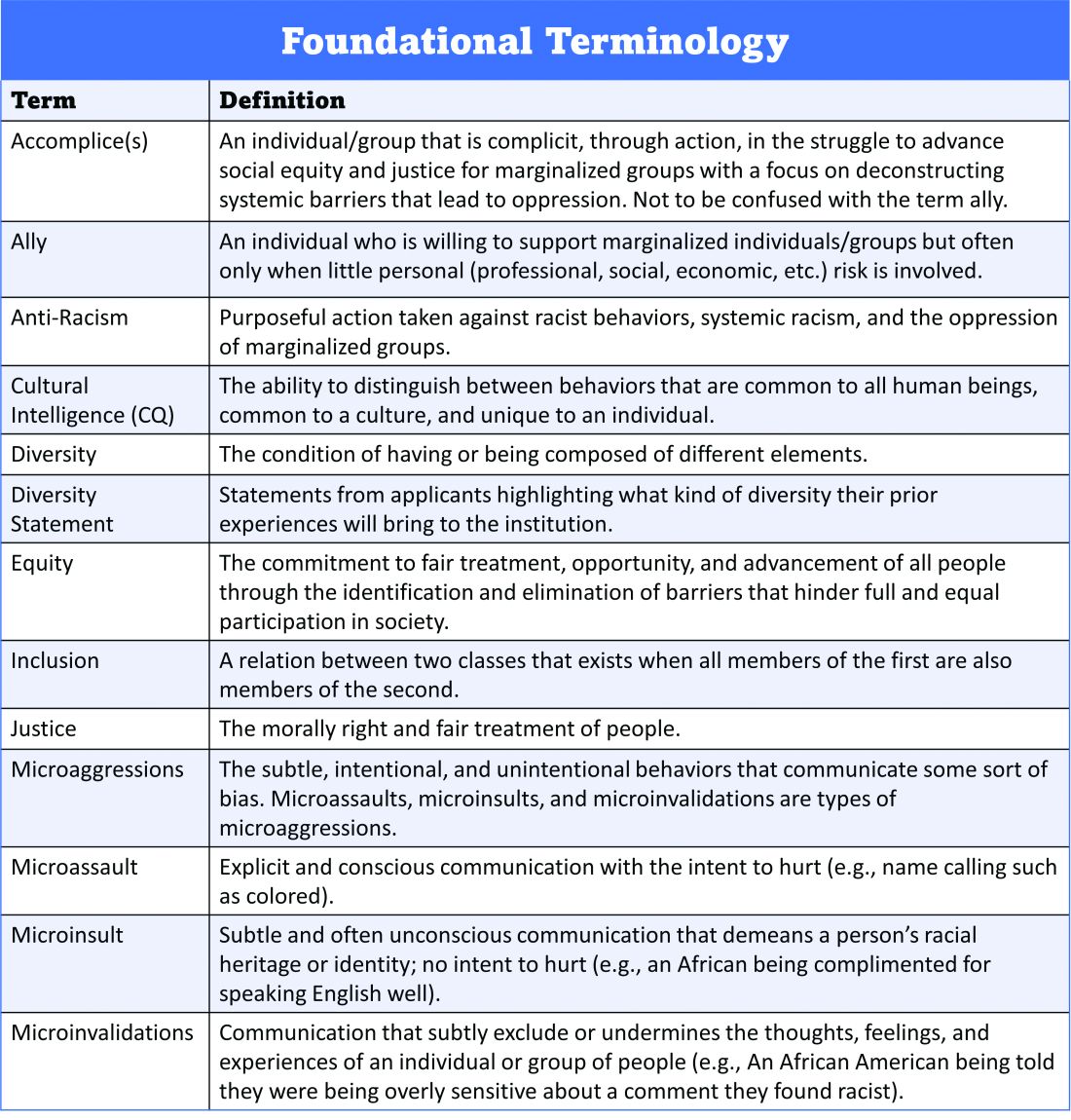
Conducting exit interviews when any hospitalist leaves is important to learn how to improve, but holding ‘stay’ interviews is mission critical. Stay interviews are an opportunity for HMG leaders to proactively understand why hospitalists stay, and what can be done to create more inclusive and equitable environments to retain them. This process creates psychological safety that brings challenges to the fore to be addressed, and spotlights best practices to be maintained and scaled.
Scholarship, mentorship, and sponsorship
Women and minorities are known to be over-mentored and under-sponsored. Sponsorship is defined by Ayyala et al. as “active support by someone appropriately placed in the organization who has significant influence on decision making processes or structures and who is advocating for the career advancement of an individual and recommends them for leadership roles, awards, or high-profile speaking opportunities.”9 While the goal of mentorship is professional development, sponsorship emphasizes professional advancement. Deliberate steps to both mentor and then sponsor diverse hospitalists and future hospitalists (including trainees) are important to ensure equity.
More inclusive HMGs can be bolstered by prioritizing peer education on the professional imperative that we have a diverse workforce and equitable, just workplaces. Academic institutions may use existing structures such as grand rounds to provide education on these crucial topics, and all HMGs can host journal clubs and professional development sessions on leadership competencies that foster inclusion and equity. Sessions coordinated by women and minorities are also a form of justice, by helping overcome barriers to career advancement. Diverse faculty presenting in educational venues will result in content that is relevant to more audience members and will exemplify that leaders and experts are of all races, ethnicities, genders, ages, and abilities.
Groups should prioritize mentoring trainees and early-career hospitalists on scholarly projects that examine equity in opportunities of care, which signals that this science is valued as much as basic research. When used to demonstrate areas needing improvement, these projects can drive meaningful change. Even projects as straightforward as studying diversity in conference presenters, disparities in adherence to guidelines, or QI projects on how race is portrayed in the medical record can be powerful tools in advancing equity.
A key part of mentoring is training hospitalists and future hospitalists in how to be an upstander, as in how to intervene when a peer or patient is affected by bias, harassment, or discrimination. Receiving such training can prepare hospitalists for these nearly inevitable experiences and receiving training during usual work hours communicates that this is a valuable and necessary professional competency.
Community engagement and partnership
Institutions and HMGs should deliberately work to promote community engagement and partnership within their groups. Beyond promoting health equity, community engagement also fosters inclusivity by allowing community members to share their ideas and give recommendations to the institutions that serve them.
There is a growing body of literature that demonstrates how disadvantages by individual and neighborhood-level socioeconomic status (SES) contribute to disparities in specific disease conditions.10-11 Strategies to narrow the gap in SES disadvantages may help reduce race-related health disparities. Institutions that engage the community and develop programs to promote health equity can do so through bidirectional exchange of knowledge and mutual benefit.
An institution-specific example is Medicine for the Greater Good at Johns Hopkins. The founders of this program wrote, “health is not synonymous with medicine. To truly care for our patients and their communities, health care professionals must understand how to deliver equitable health care that meets the needs of the diverse populations we care for. The mission of Medicine for the Greater Good is to promote health and wellness beyond the confines of the hospital through an interactive and engaging partnership with the community ...” Community engagement also provides an opportunity for growing the cultural intelligence of institutions and HMGs.
Tools for advancing comprehensive change – Repurposing PDSA cycles
Whether institutions and HMGs are at the beginning of their journey or further along in the work of reducing disparities, having a systematic approach for implementing and refining policies and procedures can cultivate more inclusive and equitable environments. Thankfully, hospitalists are already equipped with the fundamental tools needed to advance change across their institutions – QI processes in the form of Plan-Do-Study-Act (PDSA) cycles.
They allow a continuous cycle of successful incremental change based on direct evidence and experience. Any efforts to deconstruct systematic bias within our organizations must also be a continual process. Our female colleagues and colleagues of color need our institutions to engage unceasingly to bring about the equality they deserve. To that end, PDSA cycles are an apt tool to utilize in this work as they can naturally function in a never-ending process of improvement.
With PDSA as a model, we envision a cycle with steps that are intentionally purposed to fit the needs of equitable institutional change: Target-Engage-Assess-Modify. As highlighted (see graphic), these modifications ensure that stakeholders (i.e., those that unequal practices and policies affect the most) are engaged early and remain involved throughout the cycle. 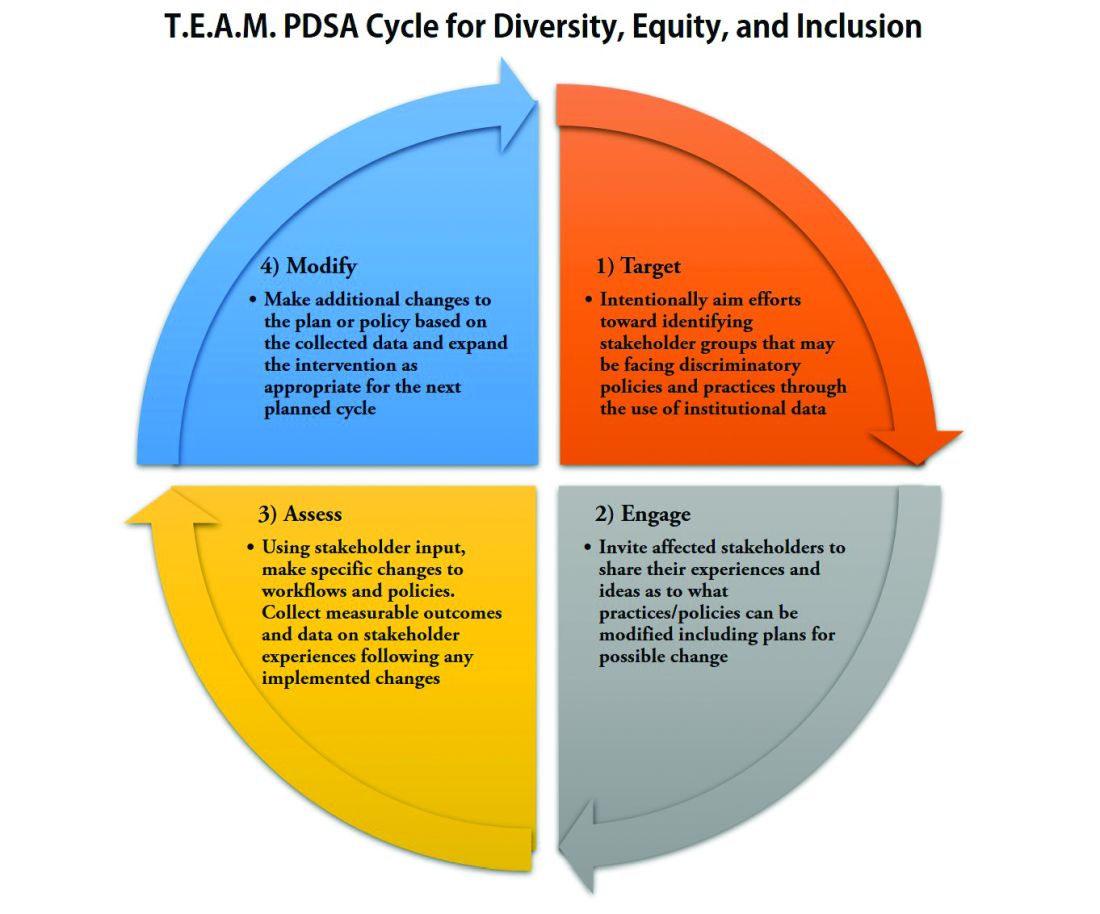
As hospitalists, we have significant work ahead to ensure that we develop and maintain a diverse, equitable and inclusive workforce. This work to bring change will not be easy and will require a considerable investment of time and resources. However, with the strategies and tools that we have outlined, our institutions and HMGs can start the change needed in our profession for our patients and the workforce. In doing so, we can all be accomplices in the fight to achieve racial and gender equity, and social justice.
Dr. Delapenha and Dr. Kisuule are based in the department of internal medicine, division of hospital medicine, at the Johns Hopkins University, Baltimore. Dr. Martin is based in the department of medicine, section of hospital medicine at the University of Chicago. Dr. Barrett is a hospitalist in the department of internal medicine, University of New Mexico, Albuquerque.
References
1. Diversity in Medicine: Facts and Figures 2019: Figure 19. Percentage of physicians by sex, 2018. AAMC website.
2. Diversity in Medicine: Facts and Figures 2019. Figure 16. Percentage of full-time U.S. medical school faculty by sex and race/ethnicity, 2018. AAMC website.
3. Diversity in Medicine: Facts and Figures 2019. Figure 15. Percentage of full-time U.S. medical school faculty by race/ethnicity, 2018. AAMC website.
4. Diversity in Medicine: Facts and Figures 2019. Figure 6. Percentage of acceptees to U.S. medical schools by race/ethnicity (alone), academic year 2018-2019. AAMC website.
5. Diversity in Medicine: Facts and Figures 2019 Figure 18. Percentage of all active physicians by race/ethnicity, 2018. AAMC website.
6. Herzke C et al. Gender issues in academic hospital medicine: A national survey of hospitalist leaders. J Gen Intern Med. 2020;35(6):1641-6.
7. Diversity in Medicine: Facts and Figures 2019. Fostering diversity and inclusion. AAMC website.
8. Diversity in Medicine: Facts and Figures 2019. Executive summary. AAMC website.
9. Ayyala MS et al. Mentorship is not enough: Exploring sponsorship and its role in career advancement in academic medicine. Acad Med. 2019;94(1):94-100.
10. Ejike OC et al. Contribution of individual and neighborhood factors to racial disparities in respiratory outcomes. Am J Respir Crit Care Med. 2021 Apr 15;203(8):987-97.
11. Galiatsatos P et al. The effect of community socioeconomic status on sepsis-attributable mortality. J Crit Care. 2018 Aug;46:129-33.
The language of equality in America’s founding was never truly embraced, resulting in a painful legacy of slavery, racial injustice, and gender inequality inherited by all generations. However, for as long as America has fallen short of this unfulfilled promise, individuals have dedicated their lives to the tireless work of correcting injustice. Although the process has been painstakingly slow, our nation has incrementally inched toward the promised vision of equality, and these efforts continue today. With increased attention to social justice movements such as #MeToo and Black Lives Matter, our collective social consciousness may be finally waking up to the systemic injustices embedded into our fundamental institutions.
Medicine is not immune to these injustices. Persistent underrepresentation of women and minorities remains in medical school faculty and the broader physician workforce, and the same inequities exist in hospital medicine.1-6 The report by the Association of American Medical Colleges (AAMC) on diversity in medicine highlights the impact widespread implicit and explicit bias has on creating exclusionary environments, exemplified by research demonstrating lower promotion rates in non-White faculty.7-8 The report calls us, as physicians, to a broader mission: “Focusing solely on increasing compositional diversity along the academic continuum is insufficient. To effectively enact institutional change at academic medical centers ... leaders must focus their efforts on developing inclusive, equity-minded environments.”7
We have a clear moral imperative to correct these shortcomings for our profession and our patients. It is incumbent on our institutions and hospital medicine groups (HMGs) to embark on the necessary process of systemic institutional change to address inequality and justice within our field.
A road map for DEI and justice in hospital medicine
The policies and biases allowing these inequities to persist have existed for decades, and superficial efforts will not bring sufficient change. Our institutions require new building blocks from which the foundation of a wholly inclusive and equal system of practice can be constructed. Encouragingly, some institutions and HMGs have taken steps to modernize their practices. We offer examples and suggestions of concrete practices to begin this journey, organizing these efforts into three broad categories:
1. Recruitment and retention
2. Scholarship, mentorship, and sponsorship
3. Community engagement and partnership.
Recruitment and retention
Improving equity and inclusion begins with recruitment. Search and hiring committees should be assembled intentionally, with gender balance, and ideally with diversity or equity experts invited to join. All members should receive unconscious bias training. For example, the University of Colorado utilizes a toolkit to ensure appropriate steps are followed in the recruitment process, including predetermined candidate selection criteria that are ranked in advance.
Job descriptions should be reviewed by a diversity expert, ensuring unbiased and ungendered language within written text. Advertisements should be wide-reaching, and the committee should consider asking applicants for a diversity statement. Interviews should include a variety of interviewers and interview types (e.g., 1:1, group, etc.). Letters of recommendation deserve special scrutiny; letters for women and minorities may be at risk of being shorter and less record focused, and may be subject to less professional respect, such as use of first names over honorifics or titles.
Once candidates are hired, institutions and HMGs should prioritize developing strategies to improve retention of a diverse workforce. This includes special attention to workplace culture, and thoughtfully striving for cultural intelligence within the group. Some examples may include developing affinity groups, such as underrepresented in medicine (UIM), women in medicine (WIM), or LGBTQ+ groups. Affinity groups provide a safe space for members and allies to support and uplift each other. Institutional and HMG leaders must educate themselves and their members on the importance of language (see table), and the more insidious forms of bias and discrimination that adversely affect workplace culture. Microinsults and microinvalidations, for example, can hurt and result in failure to recruit or turnover. 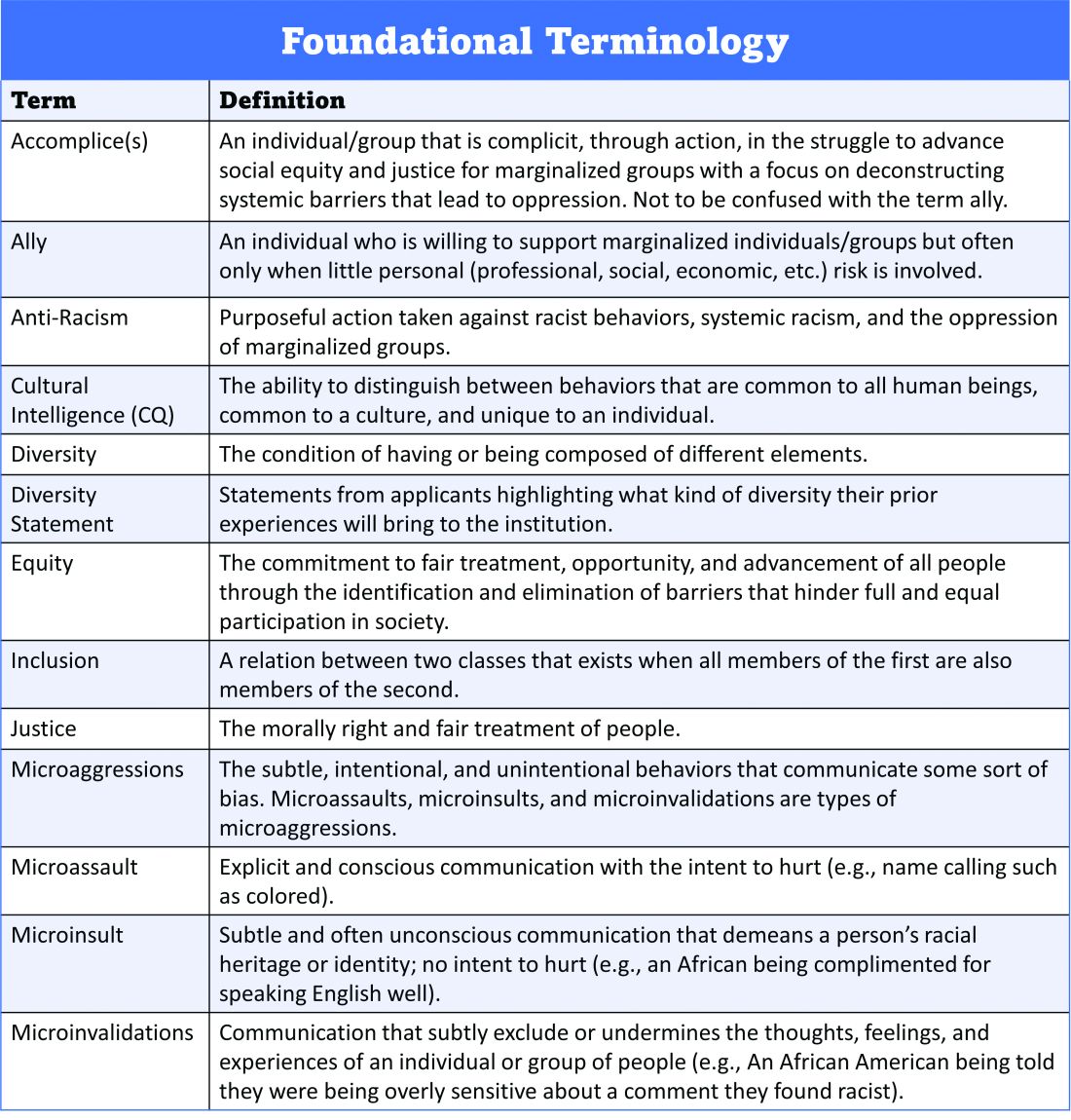
Conducting exit interviews when any hospitalist leaves is important to learn how to improve, but holding ‘stay’ interviews is mission critical. Stay interviews are an opportunity for HMG leaders to proactively understand why hospitalists stay, and what can be done to create more inclusive and equitable environments to retain them. This process creates psychological safety that brings challenges to the fore to be addressed, and spotlights best practices to be maintained and scaled.
Scholarship, mentorship, and sponsorship
Women and minorities are known to be over-mentored and under-sponsored. Sponsorship is defined by Ayyala et al. as “active support by someone appropriately placed in the organization who has significant influence on decision making processes or structures and who is advocating for the career advancement of an individual and recommends them for leadership roles, awards, or high-profile speaking opportunities.”9 While the goal of mentorship is professional development, sponsorship emphasizes professional advancement. Deliberate steps to both mentor and then sponsor diverse hospitalists and future hospitalists (including trainees) are important to ensure equity.
More inclusive HMGs can be bolstered by prioritizing peer education on the professional imperative that we have a diverse workforce and equitable, just workplaces. Academic institutions may use existing structures such as grand rounds to provide education on these crucial topics, and all HMGs can host journal clubs and professional development sessions on leadership competencies that foster inclusion and equity. Sessions coordinated by women and minorities are also a form of justice, by helping overcome barriers to career advancement. Diverse faculty presenting in educational venues will result in content that is relevant to more audience members and will exemplify that leaders and experts are of all races, ethnicities, genders, ages, and abilities.
Groups should prioritize mentoring trainees and early-career hospitalists on scholarly projects that examine equity in opportunities of care, which signals that this science is valued as much as basic research. When used to demonstrate areas needing improvement, these projects can drive meaningful change. Even projects as straightforward as studying diversity in conference presenters, disparities in adherence to guidelines, or QI projects on how race is portrayed in the medical record can be powerful tools in advancing equity.
A key part of mentoring is training hospitalists and future hospitalists in how to be an upstander, as in how to intervene when a peer or patient is affected by bias, harassment, or discrimination. Receiving such training can prepare hospitalists for these nearly inevitable experiences and receiving training during usual work hours communicates that this is a valuable and necessary professional competency.
Community engagement and partnership
Institutions and HMGs should deliberately work to promote community engagement and partnership within their groups. Beyond promoting health equity, community engagement also fosters inclusivity by allowing community members to share their ideas and give recommendations to the institutions that serve them.
There is a growing body of literature that demonstrates how disadvantages by individual and neighborhood-level socioeconomic status (SES) contribute to disparities in specific disease conditions.10-11 Strategies to narrow the gap in SES disadvantages may help reduce race-related health disparities. Institutions that engage the community and develop programs to promote health equity can do so through bidirectional exchange of knowledge and mutual benefit.
An institution-specific example is Medicine for the Greater Good at Johns Hopkins. The founders of this program wrote, “health is not synonymous with medicine. To truly care for our patients and their communities, health care professionals must understand how to deliver equitable health care that meets the needs of the diverse populations we care for. The mission of Medicine for the Greater Good is to promote health and wellness beyond the confines of the hospital through an interactive and engaging partnership with the community ...” Community engagement also provides an opportunity for growing the cultural intelligence of institutions and HMGs.
Tools for advancing comprehensive change – Repurposing PDSA cycles
Whether institutions and HMGs are at the beginning of their journey or further along in the work of reducing disparities, having a systematic approach for implementing and refining policies and procedures can cultivate more inclusive and equitable environments. Thankfully, hospitalists are already equipped with the fundamental tools needed to advance change across their institutions – QI processes in the form of Plan-Do-Study-Act (PDSA) cycles.
They allow a continuous cycle of successful incremental change based on direct evidence and experience. Any efforts to deconstruct systematic bias within our organizations must also be a continual process. Our female colleagues and colleagues of color need our institutions to engage unceasingly to bring about the equality they deserve. To that end, PDSA cycles are an apt tool to utilize in this work as they can naturally function in a never-ending process of improvement.
With PDSA as a model, we envision a cycle with steps that are intentionally purposed to fit the needs of equitable institutional change: Target-Engage-Assess-Modify. As highlighted (see graphic), these modifications ensure that stakeholders (i.e., those that unequal practices and policies affect the most) are engaged early and remain involved throughout the cycle. 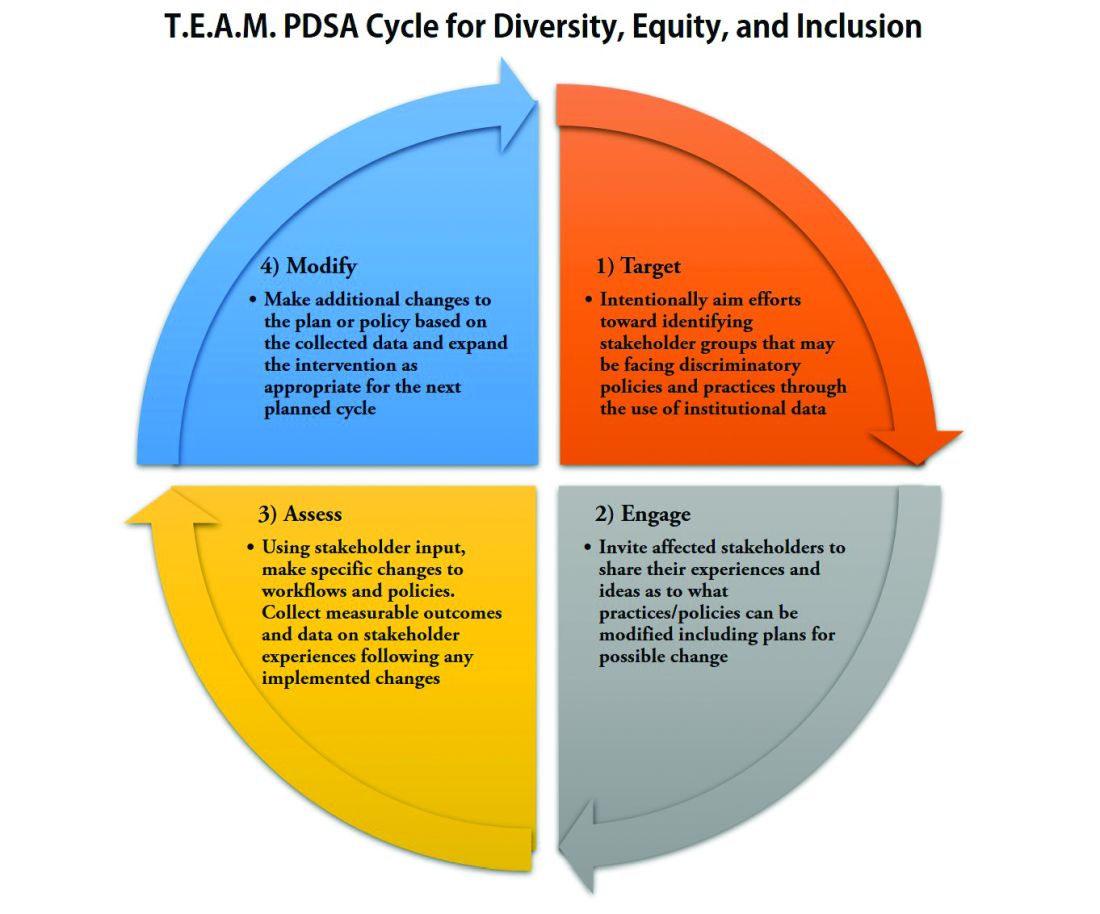
As hospitalists, we have significant work ahead to ensure that we develop and maintain a diverse, equitable and inclusive workforce. This work to bring change will not be easy and will require a considerable investment of time and resources. However, with the strategies and tools that we have outlined, our institutions and HMGs can start the change needed in our profession for our patients and the workforce. In doing so, we can all be accomplices in the fight to achieve racial and gender equity, and social justice.
Dr. Delapenha and Dr. Kisuule are based in the department of internal medicine, division of hospital medicine, at the Johns Hopkins University, Baltimore. Dr. Martin is based in the department of medicine, section of hospital medicine at the University of Chicago. Dr. Barrett is a hospitalist in the department of internal medicine, University of New Mexico, Albuquerque.
References
1. Diversity in Medicine: Facts and Figures 2019: Figure 19. Percentage of physicians by sex, 2018. AAMC website.
2. Diversity in Medicine: Facts and Figures 2019. Figure 16. Percentage of full-time U.S. medical school faculty by sex and race/ethnicity, 2018. AAMC website.
3. Diversity in Medicine: Facts and Figures 2019. Figure 15. Percentage of full-time U.S. medical school faculty by race/ethnicity, 2018. AAMC website.
4. Diversity in Medicine: Facts and Figures 2019. Figure 6. Percentage of acceptees to U.S. medical schools by race/ethnicity (alone), academic year 2018-2019. AAMC website.
5. Diversity in Medicine: Facts and Figures 2019 Figure 18. Percentage of all active physicians by race/ethnicity, 2018. AAMC website.
6. Herzke C et al. Gender issues in academic hospital medicine: A national survey of hospitalist leaders. J Gen Intern Med. 2020;35(6):1641-6.
7. Diversity in Medicine: Facts and Figures 2019. Fostering diversity and inclusion. AAMC website.
8. Diversity in Medicine: Facts and Figures 2019. Executive summary. AAMC website.
9. Ayyala MS et al. Mentorship is not enough: Exploring sponsorship and its role in career advancement in academic medicine. Acad Med. 2019;94(1):94-100.
10. Ejike OC et al. Contribution of individual and neighborhood factors to racial disparities in respiratory outcomes. Am J Respir Crit Care Med. 2021 Apr 15;203(8):987-97.
11. Galiatsatos P et al. The effect of community socioeconomic status on sepsis-attributable mortality. J Crit Care. 2018 Aug;46:129-33.
Navigating parenthood as pediatricians
PHM 2021 session
The Baby at Work or the Baby at Home: Navigating Parenthood as Pediatricians
Presenters
Jessica Gold, MD; Dana Foradori, MD, MEd; Nivedita Srinivas, MD; Honora Burnett, MD; Julie Pantaleoni, MD; and Barrett Fromme, MD, MHPE
Session summary
A group of physician-mothers from multiple academic children’s hospitals came together in a storytelling format to discuss topics relating to being a parent and pediatric hospitalist. Through short and poignant stories, the presenters shared their experiences and reviewed recent literature and policy changes relating to the topic. This mini-plenary focused on three themes:
1. Easing the transition back to work after the birth of a child.
2. Coping with the tension between being a parent and pediatrician.
3. The role that divisions, departments, and institutions can play in supporting parents and promoting workplace engagement.
The session concluded with a robust question-and-answer portion where participants built upon the themes above and shared their own experiences as pediatric hospitalist parents.
Key takeaways
- “Use your voice.” Physicians who are parents must continue having conversations about the challenging aspects of being a parent and hospitalist and advocate for the changes they would like to see.
- There will always be tension as a physician parent, but we can learn to embrace it while also learning how to ask for help, set boundaries, and share when we are struggling.
- There are numerous challenges for hospitalists who are parents because of poor parental leave policies in the United States, but this is slowly changing. For example, starting in July 2021, the ACGME mandated 6 weeks of parental leave during training without having to extend training.
- “You are not alone.” The presenters emphasized that their reason for hosting this session was to shed light on this topic and let all pediatric hospitalist parents know that they are not alone in this experience.
Dr. Scott is a second-year pediatric hospital medicine fellow at New York–Presbyterian Columbia/Cornell. Her academic interests are in curriculum development and evaluation in medical education with a focus on telemedicine.
PHM 2021 session
The Baby at Work or the Baby at Home: Navigating Parenthood as Pediatricians
Presenters
Jessica Gold, MD; Dana Foradori, MD, MEd; Nivedita Srinivas, MD; Honora Burnett, MD; Julie Pantaleoni, MD; and Barrett Fromme, MD, MHPE
Session summary
A group of physician-mothers from multiple academic children’s hospitals came together in a storytelling format to discuss topics relating to being a parent and pediatric hospitalist. Through short and poignant stories, the presenters shared their experiences and reviewed recent literature and policy changes relating to the topic. This mini-plenary focused on three themes:
1. Easing the transition back to work after the birth of a child.
2. Coping with the tension between being a parent and pediatrician.
3. The role that divisions, departments, and institutions can play in supporting parents and promoting workplace engagement.
The session concluded with a robust question-and-answer portion where participants built upon the themes above and shared their own experiences as pediatric hospitalist parents.
Key takeaways
- “Use your voice.” Physicians who are parents must continue having conversations about the challenging aspects of being a parent and hospitalist and advocate for the changes they would like to see.
- There will always be tension as a physician parent, but we can learn to embrace it while also learning how to ask for help, set boundaries, and share when we are struggling.
- There are numerous challenges for hospitalists who are parents because of poor parental leave policies in the United States, but this is slowly changing. For example, starting in July 2021, the ACGME mandated 6 weeks of parental leave during training without having to extend training.
- “You are not alone.” The presenters emphasized that their reason for hosting this session was to shed light on this topic and let all pediatric hospitalist parents know that they are not alone in this experience.
Dr. Scott is a second-year pediatric hospital medicine fellow at New York–Presbyterian Columbia/Cornell. Her academic interests are in curriculum development and evaluation in medical education with a focus on telemedicine.
PHM 2021 session
The Baby at Work or the Baby at Home: Navigating Parenthood as Pediatricians
Presenters
Jessica Gold, MD; Dana Foradori, MD, MEd; Nivedita Srinivas, MD; Honora Burnett, MD; Julie Pantaleoni, MD; and Barrett Fromme, MD, MHPE
Session summary
A group of physician-mothers from multiple academic children’s hospitals came together in a storytelling format to discuss topics relating to being a parent and pediatric hospitalist. Through short and poignant stories, the presenters shared their experiences and reviewed recent literature and policy changes relating to the topic. This mini-plenary focused on three themes:
1. Easing the transition back to work after the birth of a child.
2. Coping with the tension between being a parent and pediatrician.
3. The role that divisions, departments, and institutions can play in supporting parents and promoting workplace engagement.
The session concluded with a robust question-and-answer portion where participants built upon the themes above and shared their own experiences as pediatric hospitalist parents.
Key takeaways
- “Use your voice.” Physicians who are parents must continue having conversations about the challenging aspects of being a parent and hospitalist and advocate for the changes they would like to see.
- There will always be tension as a physician parent, but we can learn to embrace it while also learning how to ask for help, set boundaries, and share when we are struggling.
- There are numerous challenges for hospitalists who are parents because of poor parental leave policies in the United States, but this is slowly changing. For example, starting in July 2021, the ACGME mandated 6 weeks of parental leave during training without having to extend training.
- “You are not alone.” The presenters emphasized that their reason for hosting this session was to shed light on this topic and let all pediatric hospitalist parents know that they are not alone in this experience.
Dr. Scott is a second-year pediatric hospital medicine fellow at New York–Presbyterian Columbia/Cornell. Her academic interests are in curriculum development and evaluation in medical education with a focus on telemedicine.
Trio of awardees illustrate excellence in SHM chapters
2020 required resiliency, innovation
The Society of Hospital Medicine’s annual Chapter Excellence Exemplary Awards have additional meaning this year, in the wake of the persistent challenges faced by the medical profession as a result of the COVID-19 pandemic.

“The Chapter Excellence Award program is an annual rewards program to recognize outstanding work conducted by chapters to carry out the SHM mission locally,” Lisa Kroll, associate director of membership at SHM, said in an interview.
The Chapter Excellence Award program is composed of Status Awards (Platinum, Gold, Silver, and Bronze) and Exemplary Awards. “Chapters that receive these awards have demonstrated growth, sustenance, and innovation within their chapter activities,” Ms. Kroll said.
For 2020, the Houston Chapter received the Outstanding Chapter of the Year Award, the Hampton Roads (Va.) Chapter received the Resiliency Award, and Amith Skandhan, MD, SFHM, of the Wiregrass Chapter in Alabama, received the Most Engaged Chapter Leader Award.
“SHM members are assigned to a chapter based on their geographical location and are provided opportunities for education and networking through in-person and virtual events, volunteering in a chapter leadership position, and connecting with local hospitalists through the chapter’s community in HMX, SHM’s online engagement platform,” Ms. Kroll said.
The Houston Chapter received the Outstanding Chapter of the Year Award because it “exemplified high performance during 2020,” Ms. Kroll said. “During a particularly challenging year for everyone, the chapter was able to rethink how they could make the largest impact for members and expand their audience with the use of virtual meetings, provide incentives for participants, and expand their leadership team.”
“The Houston Chapter has been successful in establishing a Houston-wide Resident Interest Group to better involve and provide SHM resources to the residents within the four local internal medicine residency programs who are interested in hospital medicine,” Ms. Kroll said. “Additionally, the chapter created its first curriculum to assist residents in knowing more about hospital medicine and how to approach the job search. The Houston Chapter has provided sources of support, both emotionally and professionally, and incorporated comedians and musicians into their web meetings to provide a much-needed break from medical content.”
The Resiliency Award is a new SHM award category that goes to one chapter that has gone “above and beyond” to showcase their ability to withstand and rise above hardships, as well as to successfully adapt and position the chapter for long term sustainability and success, according to Ms. Kroll. “The Hampton Roads Chapter received this award for the 2020 year. Some of the chapter’s accomplishments included initiating a provider well-being series.”
Ms. Kroll noted that the Hampton Roads Chapter thrived by trying new approaches and ideas to bring hospitalists together across a wide region, such as by utilizing the virtual format to provide more specialized outreach to providers and recognize hospitalists’ contributions to the broader community.
The Most Engaged Chapter Leader Award was given to Alabama-based hospitalist Dr. Skandhan, who “has demonstrated how he goes above and beyond to grow and sustain the Wiregrass Chapter of SHM and continues to carry out the SHM mission,” Ms. Kroll said.
Dr. Skandhan’s accomplishments in 2020 include inviting four Alabama state representatives and three Alabama state senators to participate in a case discussion with Wiregrass Chapter leaders; creating and moderating a weekly check-in platform for the Alabama state hospital-medicine program directors’ forum through the Wiregrass Chapter – a project that enabled him to encourage the sharing of information between hospital medicine program directors; and working with the other Wiregrass Chapter leaders to launch a poster competition on Twitter with more than 80 posters presented.
Hampton Roads Chapter embraces virtual connections
“I believe chapters are one of the best answers to the question: ‘What’s the value of joining SHM?’” Thomas Miller, MD, FHM, leader of the Hampton Roads Chapter, said in an interview.
“Sharing ideas and experiences with other hospitalist teams in a region, coordinating efforts to improve care, and the personal connection with others in your field are very important for hospitalists,” he emphasized. “Chapters are uniquely positioned to do just that. Recognizing individual chapters is a great way to highlight these benefits and to promote new ideas – which other chapters can incorporate into their future plans.”
The Hampton Roads Chapter demonstrated its resilience in many ways during the challenging year of 2020, Dr. Miller said.
“We love our in-person meetings,” he emphasized. “When 2020 took that away from us, we tried to make the most of the situation by embracing the reduced overhead of the virtual format to offer more specialized outreach programs, such as ‘Cultural Context Matters: How Race and Culture Impact Health Outcomes’ and ‘Critical Care: Impact of Immigration Policy on U.S. Healthcare.’ ” The critical care and immigration program “was a great outreach to our many international physicians who have faced special struggles during COVID; it not only highlighted these issues to other hospitalists, but to the broader community, since it was a joint meeting with our local World Affairs Council,” he added.
Dr. Miller also was impressed with the resilience of other chapter members, “such as our vice president, Dr. Gwen Williams, who put together a provider well-being series, ‘Hospitalist Well Being & Support in Times of Crisis.’ ” He expressed further appreciation for the multiple chapter members who supported the chapter’s virtual resident abstract/poster competition.
“Despite the limitations imposed by 2020, we have used unique approaches that have held together a strong core group while broadening outreach to new providers in our region through programs like those described,” said Dr. Miller. “At the same time, we have promoted hospital medicine to the broader community through a joint program, increased social media presence, and achieved cover articles in Hampton Roads Physician about hospital medicine and a ‘Heroes of COVID’ story featuring chapter members. We also continued our effort to add value by providing ready access to the newly state-mandated CME with ‘Opiate Prescribing in the 21st Century.’
“In a time when even family and close friends struggled to maintain connection, we found ways to offer that to our hospitalist teams, at the same time experimenting with new tools that we can put to use long after COVID is gone,” Dr. Miller added.
Houston Chapter supports residents, provides levity
“As a medical community, we hope that the award recognition brings more attention to the issues for which our chapter advocates,” Jeffrey W. Chen, MD, of the Houston Chapter and a hospitalist at Memorial Hermann Hospital Texas Medical Center, said in an interview.
“We hope that it encourages more residents to pursue hospital medicine, and encourages early career hospitalists to get plugged in to the incredible opportunities our chapter offers,” he said. “We are so incredibly honored that the Society of Hospital Medicine has recognized the decade of work that has gone on to get to where we are now. We started with one officer, and we have worked so hard to grow and expand over the years so we can help support our fellow hospitalists across the city and state.
“We are excited about what our chapter has been able to achieve,” said Dr. Chen. “We united the four internal medicine residencies around Houston and created a Houston-wide Hospitalist Interest Group to support residents, providing them the resources they need to be successful in pursuing a career in hospital medicine. We also are proud of the support we provided this year to our early career hospitalists, helping them navigate the transitions and stay up to date in topics relevant to hospital medicine. We held our biggest abstract competition yet, and held a virtual research showcase to celebrate the incredible clinical advancements still happening during the midst of the pandemic.
“It was certainly a tough and challenging year for all chapters, but despite us not being able to hold the in-person dinners that our members love so much, we were proud that we were able to have such a big year,” said Dr. Chen. “We were thankful for the physicians who led our COVID-19 talks, which provided an opportunity for hospitalists across Houston to collaborate and share ideas on which treatments and therapies were working well for their patients. During such a difficult year, we also hosted our first wellness events, including a comedian and band to bring some light during tough times.”
Strong leader propels team efforts
“The Chapter Exemplary Awards Program is important because it encourages higher performance while increasing membership engagement and retaining talent,” said Dr. Skandhan, of Southeast Health Medical Center in Dothan, Ala., and winner of the Most Engaged Chapter Leader award. “Being recognized as the most engaged chapter leader is an honor, especially given the national and international presence of SHM.
“Success is achieved through the help and support of your peers and mentors, and I am fortunate to have found them through this organization,” said Dr. Skandhan. “This award brings attention to the fantastic work done by the engaged membership and leadership of the Wiregrass Chapter. This recognition makes me proud to be part of a team that prides itself on improving the quality health and wellbeing of the patients, providers, and public through innovation and collaboration; this is a testament to their work.”
Dr. Skandhan’s activities as a chapter leader included visiting health care facilities in the rural Southeastern United States. “I slowly began to learn how small towns and their economies tied into a health system, how invested the health care providers were towards their communities, and how health care disparities existed between the rural and urban populations,” he explained. “When the COVID-19 pandemic hit, I worried about these hospitals and their providers. COVID-19 was a new disease with limited understanding of the virus, treatment options, and prevention protocols.” To help smaller hospitals, the Wiregrass Chapter created a weekly check-in for hospital medicine program directors in the state of Alabama, he said.
“We would start the meeting with each participant reporting the total number of cases, ventilator usage, COVID-19 deaths, and one policy change they did that week to address a pressing issue,” Dr. Skandhan said. “Over time the meetings helped address common challenges and were a source of physician well-being.”
In addition, Dr. Skandhan and his chapter colleagues were concerned that academics were taking a back seat to the pandemic, so they rose to the challenge by designing a Twitter-based poster competition using judges from across the country. “This project was led by one of our chapter leaders, Dr. Arash Velayati of Southeast Health Medical Center,” said Dr. Skandhan. The contest included 82 posters, and the participants were able to showcase their work to a large, virtual audience.
Dr. Skandhan and colleagues also decided to partner with religious leaders in their community to help combat the spread of misinformation about COVID-19. “We teamed with the Southern Alabama Baptist Association and Interfaith Council to educate these religious leaders on the issues around COVID-19,” and addressed topics including masking and social distancing, and provided resources for religious leaders to tackle misinformation in their communities, he said.
“As chapter leaders, we need to learn to think outside the box,” Dr. Skandhan emphasized. “We can affect health care quality when we strive to solve more significant problems by bringing people together, brainstorming, and collaborating. SHM and chapter-level engagement provide us with that opportunity.“Hospitalists are often affected by the downstream effects of limited preventive care addressing chronic illnesses. Therefore, we have to strive to see the bigger picture. As we make changes at our local institutions and chapter levels, we will start seeing the improvement we hope to see in the care of our patients and our communities.”
2020 required resiliency, innovation
2020 required resiliency, innovation
The Society of Hospital Medicine’s annual Chapter Excellence Exemplary Awards have additional meaning this year, in the wake of the persistent challenges faced by the medical profession as a result of the COVID-19 pandemic.

“The Chapter Excellence Award program is an annual rewards program to recognize outstanding work conducted by chapters to carry out the SHM mission locally,” Lisa Kroll, associate director of membership at SHM, said in an interview.
The Chapter Excellence Award program is composed of Status Awards (Platinum, Gold, Silver, and Bronze) and Exemplary Awards. “Chapters that receive these awards have demonstrated growth, sustenance, and innovation within their chapter activities,” Ms. Kroll said.
For 2020, the Houston Chapter received the Outstanding Chapter of the Year Award, the Hampton Roads (Va.) Chapter received the Resiliency Award, and Amith Skandhan, MD, SFHM, of the Wiregrass Chapter in Alabama, received the Most Engaged Chapter Leader Award.
“SHM members are assigned to a chapter based on their geographical location and are provided opportunities for education and networking through in-person and virtual events, volunteering in a chapter leadership position, and connecting with local hospitalists through the chapter’s community in HMX, SHM’s online engagement platform,” Ms. Kroll said.
The Houston Chapter received the Outstanding Chapter of the Year Award because it “exemplified high performance during 2020,” Ms. Kroll said. “During a particularly challenging year for everyone, the chapter was able to rethink how they could make the largest impact for members and expand their audience with the use of virtual meetings, provide incentives for participants, and expand their leadership team.”
“The Houston Chapter has been successful in establishing a Houston-wide Resident Interest Group to better involve and provide SHM resources to the residents within the four local internal medicine residency programs who are interested in hospital medicine,” Ms. Kroll said. “Additionally, the chapter created its first curriculum to assist residents in knowing more about hospital medicine and how to approach the job search. The Houston Chapter has provided sources of support, both emotionally and professionally, and incorporated comedians and musicians into their web meetings to provide a much-needed break from medical content.”
The Resiliency Award is a new SHM award category that goes to one chapter that has gone “above and beyond” to showcase their ability to withstand and rise above hardships, as well as to successfully adapt and position the chapter for long term sustainability and success, according to Ms. Kroll. “The Hampton Roads Chapter received this award for the 2020 year. Some of the chapter’s accomplishments included initiating a provider well-being series.”
Ms. Kroll noted that the Hampton Roads Chapter thrived by trying new approaches and ideas to bring hospitalists together across a wide region, such as by utilizing the virtual format to provide more specialized outreach to providers and recognize hospitalists’ contributions to the broader community.
The Most Engaged Chapter Leader Award was given to Alabama-based hospitalist Dr. Skandhan, who “has demonstrated how he goes above and beyond to grow and sustain the Wiregrass Chapter of SHM and continues to carry out the SHM mission,” Ms. Kroll said.
Dr. Skandhan’s accomplishments in 2020 include inviting four Alabama state representatives and three Alabama state senators to participate in a case discussion with Wiregrass Chapter leaders; creating and moderating a weekly check-in platform for the Alabama state hospital-medicine program directors’ forum through the Wiregrass Chapter – a project that enabled him to encourage the sharing of information between hospital medicine program directors; and working with the other Wiregrass Chapter leaders to launch a poster competition on Twitter with more than 80 posters presented.
Hampton Roads Chapter embraces virtual connections
“I believe chapters are one of the best answers to the question: ‘What’s the value of joining SHM?’” Thomas Miller, MD, FHM, leader of the Hampton Roads Chapter, said in an interview.
“Sharing ideas and experiences with other hospitalist teams in a region, coordinating efforts to improve care, and the personal connection with others in your field are very important for hospitalists,” he emphasized. “Chapters are uniquely positioned to do just that. Recognizing individual chapters is a great way to highlight these benefits and to promote new ideas – which other chapters can incorporate into their future plans.”
The Hampton Roads Chapter demonstrated its resilience in many ways during the challenging year of 2020, Dr. Miller said.
“We love our in-person meetings,” he emphasized. “When 2020 took that away from us, we tried to make the most of the situation by embracing the reduced overhead of the virtual format to offer more specialized outreach programs, such as ‘Cultural Context Matters: How Race and Culture Impact Health Outcomes’ and ‘Critical Care: Impact of Immigration Policy on U.S. Healthcare.’ ” The critical care and immigration program “was a great outreach to our many international physicians who have faced special struggles during COVID; it not only highlighted these issues to other hospitalists, but to the broader community, since it was a joint meeting with our local World Affairs Council,” he added.
Dr. Miller also was impressed with the resilience of other chapter members, “such as our vice president, Dr. Gwen Williams, who put together a provider well-being series, ‘Hospitalist Well Being & Support in Times of Crisis.’ ” He expressed further appreciation for the multiple chapter members who supported the chapter’s virtual resident abstract/poster competition.
“Despite the limitations imposed by 2020, we have used unique approaches that have held together a strong core group while broadening outreach to new providers in our region through programs like those described,” said Dr. Miller. “At the same time, we have promoted hospital medicine to the broader community through a joint program, increased social media presence, and achieved cover articles in Hampton Roads Physician about hospital medicine and a ‘Heroes of COVID’ story featuring chapter members. We also continued our effort to add value by providing ready access to the newly state-mandated CME with ‘Opiate Prescribing in the 21st Century.’
“In a time when even family and close friends struggled to maintain connection, we found ways to offer that to our hospitalist teams, at the same time experimenting with new tools that we can put to use long after COVID is gone,” Dr. Miller added.
Houston Chapter supports residents, provides levity
“As a medical community, we hope that the award recognition brings more attention to the issues for which our chapter advocates,” Jeffrey W. Chen, MD, of the Houston Chapter and a hospitalist at Memorial Hermann Hospital Texas Medical Center, said in an interview.
“We hope that it encourages more residents to pursue hospital medicine, and encourages early career hospitalists to get plugged in to the incredible opportunities our chapter offers,” he said. “We are so incredibly honored that the Society of Hospital Medicine has recognized the decade of work that has gone on to get to where we are now. We started with one officer, and we have worked so hard to grow and expand over the years so we can help support our fellow hospitalists across the city and state.
“We are excited about what our chapter has been able to achieve,” said Dr. Chen. “We united the four internal medicine residencies around Houston and created a Houston-wide Hospitalist Interest Group to support residents, providing them the resources they need to be successful in pursuing a career in hospital medicine. We also are proud of the support we provided this year to our early career hospitalists, helping them navigate the transitions and stay up to date in topics relevant to hospital medicine. We held our biggest abstract competition yet, and held a virtual research showcase to celebrate the incredible clinical advancements still happening during the midst of the pandemic.
“It was certainly a tough and challenging year for all chapters, but despite us not being able to hold the in-person dinners that our members love so much, we were proud that we were able to have such a big year,” said Dr. Chen. “We were thankful for the physicians who led our COVID-19 talks, which provided an opportunity for hospitalists across Houston to collaborate and share ideas on which treatments and therapies were working well for their patients. During such a difficult year, we also hosted our first wellness events, including a comedian and band to bring some light during tough times.”
Strong leader propels team efforts
“The Chapter Exemplary Awards Program is important because it encourages higher performance while increasing membership engagement and retaining talent,” said Dr. Skandhan, of Southeast Health Medical Center in Dothan, Ala., and winner of the Most Engaged Chapter Leader award. “Being recognized as the most engaged chapter leader is an honor, especially given the national and international presence of SHM.
“Success is achieved through the help and support of your peers and mentors, and I am fortunate to have found them through this organization,” said Dr. Skandhan. “This award brings attention to the fantastic work done by the engaged membership and leadership of the Wiregrass Chapter. This recognition makes me proud to be part of a team that prides itself on improving the quality health and wellbeing of the patients, providers, and public through innovation and collaboration; this is a testament to their work.”
Dr. Skandhan’s activities as a chapter leader included visiting health care facilities in the rural Southeastern United States. “I slowly began to learn how small towns and their economies tied into a health system, how invested the health care providers were towards their communities, and how health care disparities existed between the rural and urban populations,” he explained. “When the COVID-19 pandemic hit, I worried about these hospitals and their providers. COVID-19 was a new disease with limited understanding of the virus, treatment options, and prevention protocols.” To help smaller hospitals, the Wiregrass Chapter created a weekly check-in for hospital medicine program directors in the state of Alabama, he said.
“We would start the meeting with each participant reporting the total number of cases, ventilator usage, COVID-19 deaths, and one policy change they did that week to address a pressing issue,” Dr. Skandhan said. “Over time the meetings helped address common challenges and were a source of physician well-being.”
In addition, Dr. Skandhan and his chapter colleagues were concerned that academics were taking a back seat to the pandemic, so they rose to the challenge by designing a Twitter-based poster competition using judges from across the country. “This project was led by one of our chapter leaders, Dr. Arash Velayati of Southeast Health Medical Center,” said Dr. Skandhan. The contest included 82 posters, and the participants were able to showcase their work to a large, virtual audience.
Dr. Skandhan and colleagues also decided to partner with religious leaders in their community to help combat the spread of misinformation about COVID-19. “We teamed with the Southern Alabama Baptist Association and Interfaith Council to educate these religious leaders on the issues around COVID-19,” and addressed topics including masking and social distancing, and provided resources for religious leaders to tackle misinformation in their communities, he said.
“As chapter leaders, we need to learn to think outside the box,” Dr. Skandhan emphasized. “We can affect health care quality when we strive to solve more significant problems by bringing people together, brainstorming, and collaborating. SHM and chapter-level engagement provide us with that opportunity.“Hospitalists are often affected by the downstream effects of limited preventive care addressing chronic illnesses. Therefore, we have to strive to see the bigger picture. As we make changes at our local institutions and chapter levels, we will start seeing the improvement we hope to see in the care of our patients and our communities.”
The Society of Hospital Medicine’s annual Chapter Excellence Exemplary Awards have additional meaning this year, in the wake of the persistent challenges faced by the medical profession as a result of the COVID-19 pandemic.

“The Chapter Excellence Award program is an annual rewards program to recognize outstanding work conducted by chapters to carry out the SHM mission locally,” Lisa Kroll, associate director of membership at SHM, said in an interview.
The Chapter Excellence Award program is composed of Status Awards (Platinum, Gold, Silver, and Bronze) and Exemplary Awards. “Chapters that receive these awards have demonstrated growth, sustenance, and innovation within their chapter activities,” Ms. Kroll said.
For 2020, the Houston Chapter received the Outstanding Chapter of the Year Award, the Hampton Roads (Va.) Chapter received the Resiliency Award, and Amith Skandhan, MD, SFHM, of the Wiregrass Chapter in Alabama, received the Most Engaged Chapter Leader Award.
“SHM members are assigned to a chapter based on their geographical location and are provided opportunities for education and networking through in-person and virtual events, volunteering in a chapter leadership position, and connecting with local hospitalists through the chapter’s community in HMX, SHM’s online engagement platform,” Ms. Kroll said.
The Houston Chapter received the Outstanding Chapter of the Year Award because it “exemplified high performance during 2020,” Ms. Kroll said. “During a particularly challenging year for everyone, the chapter was able to rethink how they could make the largest impact for members and expand their audience with the use of virtual meetings, provide incentives for participants, and expand their leadership team.”
“The Houston Chapter has been successful in establishing a Houston-wide Resident Interest Group to better involve and provide SHM resources to the residents within the four local internal medicine residency programs who are interested in hospital medicine,” Ms. Kroll said. “Additionally, the chapter created its first curriculum to assist residents in knowing more about hospital medicine and how to approach the job search. The Houston Chapter has provided sources of support, both emotionally and professionally, and incorporated comedians and musicians into their web meetings to provide a much-needed break from medical content.”
The Resiliency Award is a new SHM award category that goes to one chapter that has gone “above and beyond” to showcase their ability to withstand and rise above hardships, as well as to successfully adapt and position the chapter for long term sustainability and success, according to Ms. Kroll. “The Hampton Roads Chapter received this award for the 2020 year. Some of the chapter’s accomplishments included initiating a provider well-being series.”
Ms. Kroll noted that the Hampton Roads Chapter thrived by trying new approaches and ideas to bring hospitalists together across a wide region, such as by utilizing the virtual format to provide more specialized outreach to providers and recognize hospitalists’ contributions to the broader community.
The Most Engaged Chapter Leader Award was given to Alabama-based hospitalist Dr. Skandhan, who “has demonstrated how he goes above and beyond to grow and sustain the Wiregrass Chapter of SHM and continues to carry out the SHM mission,” Ms. Kroll said.
Dr. Skandhan’s accomplishments in 2020 include inviting four Alabama state representatives and three Alabama state senators to participate in a case discussion with Wiregrass Chapter leaders; creating and moderating a weekly check-in platform for the Alabama state hospital-medicine program directors’ forum through the Wiregrass Chapter – a project that enabled him to encourage the sharing of information between hospital medicine program directors; and working with the other Wiregrass Chapter leaders to launch a poster competition on Twitter with more than 80 posters presented.
Hampton Roads Chapter embraces virtual connections
“I believe chapters are one of the best answers to the question: ‘What’s the value of joining SHM?’” Thomas Miller, MD, FHM, leader of the Hampton Roads Chapter, said in an interview.
“Sharing ideas and experiences with other hospitalist teams in a region, coordinating efforts to improve care, and the personal connection with others in your field are very important for hospitalists,” he emphasized. “Chapters are uniquely positioned to do just that. Recognizing individual chapters is a great way to highlight these benefits and to promote new ideas – which other chapters can incorporate into their future plans.”
The Hampton Roads Chapter demonstrated its resilience in many ways during the challenging year of 2020, Dr. Miller said.
“We love our in-person meetings,” he emphasized. “When 2020 took that away from us, we tried to make the most of the situation by embracing the reduced overhead of the virtual format to offer more specialized outreach programs, such as ‘Cultural Context Matters: How Race and Culture Impact Health Outcomes’ and ‘Critical Care: Impact of Immigration Policy on U.S. Healthcare.’ ” The critical care and immigration program “was a great outreach to our many international physicians who have faced special struggles during COVID; it not only highlighted these issues to other hospitalists, but to the broader community, since it was a joint meeting with our local World Affairs Council,” he added.
Dr. Miller also was impressed with the resilience of other chapter members, “such as our vice president, Dr. Gwen Williams, who put together a provider well-being series, ‘Hospitalist Well Being & Support in Times of Crisis.’ ” He expressed further appreciation for the multiple chapter members who supported the chapter’s virtual resident abstract/poster competition.
“Despite the limitations imposed by 2020, we have used unique approaches that have held together a strong core group while broadening outreach to new providers in our region through programs like those described,” said Dr. Miller. “At the same time, we have promoted hospital medicine to the broader community through a joint program, increased social media presence, and achieved cover articles in Hampton Roads Physician about hospital medicine and a ‘Heroes of COVID’ story featuring chapter members. We also continued our effort to add value by providing ready access to the newly state-mandated CME with ‘Opiate Prescribing in the 21st Century.’
“In a time when even family and close friends struggled to maintain connection, we found ways to offer that to our hospitalist teams, at the same time experimenting with new tools that we can put to use long after COVID is gone,” Dr. Miller added.
Houston Chapter supports residents, provides levity
“As a medical community, we hope that the award recognition brings more attention to the issues for which our chapter advocates,” Jeffrey W. Chen, MD, of the Houston Chapter and a hospitalist at Memorial Hermann Hospital Texas Medical Center, said in an interview.
“We hope that it encourages more residents to pursue hospital medicine, and encourages early career hospitalists to get plugged in to the incredible opportunities our chapter offers,” he said. “We are so incredibly honored that the Society of Hospital Medicine has recognized the decade of work that has gone on to get to where we are now. We started with one officer, and we have worked so hard to grow and expand over the years so we can help support our fellow hospitalists across the city and state.
“We are excited about what our chapter has been able to achieve,” said Dr. Chen. “We united the four internal medicine residencies around Houston and created a Houston-wide Hospitalist Interest Group to support residents, providing them the resources they need to be successful in pursuing a career in hospital medicine. We also are proud of the support we provided this year to our early career hospitalists, helping them navigate the transitions and stay up to date in topics relevant to hospital medicine. We held our biggest abstract competition yet, and held a virtual research showcase to celebrate the incredible clinical advancements still happening during the midst of the pandemic.
“It was certainly a tough and challenging year for all chapters, but despite us not being able to hold the in-person dinners that our members love so much, we were proud that we were able to have such a big year,” said Dr. Chen. “We were thankful for the physicians who led our COVID-19 talks, which provided an opportunity for hospitalists across Houston to collaborate and share ideas on which treatments and therapies were working well for their patients. During such a difficult year, we also hosted our first wellness events, including a comedian and band to bring some light during tough times.”
Strong leader propels team efforts
“The Chapter Exemplary Awards Program is important because it encourages higher performance while increasing membership engagement and retaining talent,” said Dr. Skandhan, of Southeast Health Medical Center in Dothan, Ala., and winner of the Most Engaged Chapter Leader award. “Being recognized as the most engaged chapter leader is an honor, especially given the national and international presence of SHM.
“Success is achieved through the help and support of your peers and mentors, and I am fortunate to have found them through this organization,” said Dr. Skandhan. “This award brings attention to the fantastic work done by the engaged membership and leadership of the Wiregrass Chapter. This recognition makes me proud to be part of a team that prides itself on improving the quality health and wellbeing of the patients, providers, and public through innovation and collaboration; this is a testament to their work.”
Dr. Skandhan’s activities as a chapter leader included visiting health care facilities in the rural Southeastern United States. “I slowly began to learn how small towns and their economies tied into a health system, how invested the health care providers were towards their communities, and how health care disparities existed between the rural and urban populations,” he explained. “When the COVID-19 pandemic hit, I worried about these hospitals and their providers. COVID-19 was a new disease with limited understanding of the virus, treatment options, and prevention protocols.” To help smaller hospitals, the Wiregrass Chapter created a weekly check-in for hospital medicine program directors in the state of Alabama, he said.
“We would start the meeting with each participant reporting the total number of cases, ventilator usage, COVID-19 deaths, and one policy change they did that week to address a pressing issue,” Dr. Skandhan said. “Over time the meetings helped address common challenges and were a source of physician well-being.”
In addition, Dr. Skandhan and his chapter colleagues were concerned that academics were taking a back seat to the pandemic, so they rose to the challenge by designing a Twitter-based poster competition using judges from across the country. “This project was led by one of our chapter leaders, Dr. Arash Velayati of Southeast Health Medical Center,” said Dr. Skandhan. The contest included 82 posters, and the participants were able to showcase their work to a large, virtual audience.
Dr. Skandhan and colleagues also decided to partner with religious leaders in their community to help combat the spread of misinformation about COVID-19. “We teamed with the Southern Alabama Baptist Association and Interfaith Council to educate these religious leaders on the issues around COVID-19,” and addressed topics including masking and social distancing, and provided resources for religious leaders to tackle misinformation in their communities, he said.
“As chapter leaders, we need to learn to think outside the box,” Dr. Skandhan emphasized. “We can affect health care quality when we strive to solve more significant problems by bringing people together, brainstorming, and collaborating. SHM and chapter-level engagement provide us with that opportunity.“Hospitalists are often affected by the downstream effects of limited preventive care addressing chronic illnesses. Therefore, we have to strive to see the bigger picture. As we make changes at our local institutions and chapter levels, we will start seeing the improvement we hope to see in the care of our patients and our communities.”
PHM 2021: Leading through adversity
PHM 2021 session
Leading through adversity
Presenter
Ilan Alhadeff, MD, MBA, SFHM, CLHM
Session summary
As the VP of hospitalist services and a practicing hospitalist in Boca Raton, Fla., Dr. Alhadeff shared an emotional journey where the impact of lives lost has led to organizational innovation and advocacy. He started this journey on the date of the Parkland High School shooting, Feb. 14, 2018. On this day, he lost his 14 year-old daughter Alyssa and described subsequent emotions of anger, sadness, hopelessness, and feeling the pressure to be the protector of his family. Despite receiving an outpouring of support through memorials, texts, letters, and social media posts, he was immersed in “survival mode.” He likens this to the experience many of us may be having during the pandemic. He described caring for patients with limited empathy and the impact this likely had on patient care. During this challenging time, the strongest supports became those that stated they couldn’t imagine how this event could have impacted Dr. Alhadeff’s life but offered support in any way needed – true empathic communication.
“It ain’t about how hard you hit. It’s about how hard you can get hit and keep moving forward.” – Rocky Balboa (2006)
Despite the above, he and his wife founded Make Our Schools Safe (MOSS), a student-forward organization that promotes a culture of safety where all involved are counseled, “If you see something, say something.” Students are encouraged to use social media as an anonymous reporting tool. Likewise, this organization supports efforts for silent safety alerts in schools and fencing around schools to allow for 1-point entry. Lessons Dr. Alhadeff learned that might impact any pediatric hospitalist include the knowledge that mental health concerns aren’t going away; for example, after a school shooting any student affected should be provided counseling services as needed, the need to prevent triggering events, and turning grief into action can help.
“Life is like riding a bicycle. To keep your balance, you must keep moving.” – Albert Einstein (1930)
Dr. Alhadeff then described the process of “moving on” for him and his family. For his children, this initially meant “busying” their lives. They then gradually eased into therapy, and ultimately adopted a support dog. He experienced recurrent loss with his father passing away in March 2019, and he persevered in legislative advocacy in New Jersey and Florida and personal/professional development with work toward his MBA degree. Through this work, he collaborated with many legislators and two presidents. He describes resiliency as the ability to bounce back from adversity, with components including self-awareness, mindfulness, self-care, positive relationships, and purpose. While many of us have not had the great personal losses and challenge experienced by Dr. Alhadeff, we all are experiencing an once-in-a-lifetime transformation of health care with political and social interference. It is up to each of us to determine our role and how we can use our influence for positive change.
As noted by Dr. Alhadeff, “We are not all in the same boat. We ARE in the same storm.”
Key takeaways
- How PHM can promote MOSS: Allow children to be part of the work to keep schools safe. Advocate for local MOSS chapters. Support legislative advocacy for school safety.
- Despite adversity, we have the ability to demonstrate resilience. We do so through development of self-awareness, mindfulness, engagement in self-care, nurturing positive relationships, and continuing to pursue our greater purpose.
Dr. King is a pediatric hospitalist at Children’s MN and the director of medical education, an associate program director for the Pediatrics Residency program at the University of Minnesota. She received her medical degree from Wright State University Boonshoft School of Medicine and completed pediatric residency and chief residency at the University of Minnesota.
PHM 2021 session
Leading through adversity
Presenter
Ilan Alhadeff, MD, MBA, SFHM, CLHM
Session summary
As the VP of hospitalist services and a practicing hospitalist in Boca Raton, Fla., Dr. Alhadeff shared an emotional journey where the impact of lives lost has led to organizational innovation and advocacy. He started this journey on the date of the Parkland High School shooting, Feb. 14, 2018. On this day, he lost his 14 year-old daughter Alyssa and described subsequent emotions of anger, sadness, hopelessness, and feeling the pressure to be the protector of his family. Despite receiving an outpouring of support through memorials, texts, letters, and social media posts, he was immersed in “survival mode.” He likens this to the experience many of us may be having during the pandemic. He described caring for patients with limited empathy and the impact this likely had on patient care. During this challenging time, the strongest supports became those that stated they couldn’t imagine how this event could have impacted Dr. Alhadeff’s life but offered support in any way needed – true empathic communication.
“It ain’t about how hard you hit. It’s about how hard you can get hit and keep moving forward.” – Rocky Balboa (2006)
Despite the above, he and his wife founded Make Our Schools Safe (MOSS), a student-forward organization that promotes a culture of safety where all involved are counseled, “If you see something, say something.” Students are encouraged to use social media as an anonymous reporting tool. Likewise, this organization supports efforts for silent safety alerts in schools and fencing around schools to allow for 1-point entry. Lessons Dr. Alhadeff learned that might impact any pediatric hospitalist include the knowledge that mental health concerns aren’t going away; for example, after a school shooting any student affected should be provided counseling services as needed, the need to prevent triggering events, and turning grief into action can help.
“Life is like riding a bicycle. To keep your balance, you must keep moving.” – Albert Einstein (1930)
Dr. Alhadeff then described the process of “moving on” for him and his family. For his children, this initially meant “busying” their lives. They then gradually eased into therapy, and ultimately adopted a support dog. He experienced recurrent loss with his father passing away in March 2019, and he persevered in legislative advocacy in New Jersey and Florida and personal/professional development with work toward his MBA degree. Through this work, he collaborated with many legislators and two presidents. He describes resiliency as the ability to bounce back from adversity, with components including self-awareness, mindfulness, self-care, positive relationships, and purpose. While many of us have not had the great personal losses and challenge experienced by Dr. Alhadeff, we all are experiencing an once-in-a-lifetime transformation of health care with political and social interference. It is up to each of us to determine our role and how we can use our influence for positive change.
As noted by Dr. Alhadeff, “We are not all in the same boat. We ARE in the same storm.”
Key takeaways
- How PHM can promote MOSS: Allow children to be part of the work to keep schools safe. Advocate for local MOSS chapters. Support legislative advocacy for school safety.
- Despite adversity, we have the ability to demonstrate resilience. We do so through development of self-awareness, mindfulness, engagement in self-care, nurturing positive relationships, and continuing to pursue our greater purpose.
Dr. King is a pediatric hospitalist at Children’s MN and the director of medical education, an associate program director for the Pediatrics Residency program at the University of Minnesota. She received her medical degree from Wright State University Boonshoft School of Medicine and completed pediatric residency and chief residency at the University of Minnesota.
PHM 2021 session
Leading through adversity
Presenter
Ilan Alhadeff, MD, MBA, SFHM, CLHM
Session summary
As the VP of hospitalist services and a practicing hospitalist in Boca Raton, Fla., Dr. Alhadeff shared an emotional journey where the impact of lives lost has led to organizational innovation and advocacy. He started this journey on the date of the Parkland High School shooting, Feb. 14, 2018. On this day, he lost his 14 year-old daughter Alyssa and described subsequent emotions of anger, sadness, hopelessness, and feeling the pressure to be the protector of his family. Despite receiving an outpouring of support through memorials, texts, letters, and social media posts, he was immersed in “survival mode.” He likens this to the experience many of us may be having during the pandemic. He described caring for patients with limited empathy and the impact this likely had on patient care. During this challenging time, the strongest supports became those that stated they couldn’t imagine how this event could have impacted Dr. Alhadeff’s life but offered support in any way needed – true empathic communication.
“It ain’t about how hard you hit. It’s about how hard you can get hit and keep moving forward.” – Rocky Balboa (2006)
Despite the above, he and his wife founded Make Our Schools Safe (MOSS), a student-forward organization that promotes a culture of safety where all involved are counseled, “If you see something, say something.” Students are encouraged to use social media as an anonymous reporting tool. Likewise, this organization supports efforts for silent safety alerts in schools and fencing around schools to allow for 1-point entry. Lessons Dr. Alhadeff learned that might impact any pediatric hospitalist include the knowledge that mental health concerns aren’t going away; for example, after a school shooting any student affected should be provided counseling services as needed, the need to prevent triggering events, and turning grief into action can help.
“Life is like riding a bicycle. To keep your balance, you must keep moving.” – Albert Einstein (1930)
Dr. Alhadeff then described the process of “moving on” for him and his family. For his children, this initially meant “busying” their lives. They then gradually eased into therapy, and ultimately adopted a support dog. He experienced recurrent loss with his father passing away in March 2019, and he persevered in legislative advocacy in New Jersey and Florida and personal/professional development with work toward his MBA degree. Through this work, he collaborated with many legislators and two presidents. He describes resiliency as the ability to bounce back from adversity, with components including self-awareness, mindfulness, self-care, positive relationships, and purpose. While many of us have not had the great personal losses and challenge experienced by Dr. Alhadeff, we all are experiencing an once-in-a-lifetime transformation of health care with political and social interference. It is up to each of us to determine our role and how we can use our influence for positive change.
As noted by Dr. Alhadeff, “We are not all in the same boat. We ARE in the same storm.”
Key takeaways
- How PHM can promote MOSS: Allow children to be part of the work to keep schools safe. Advocate for local MOSS chapters. Support legislative advocacy for school safety.
- Despite adversity, we have the ability to demonstrate resilience. We do so through development of self-awareness, mindfulness, engagement in self-care, nurturing positive relationships, and continuing to pursue our greater purpose.
Dr. King is a pediatric hospitalist at Children’s MN and the director of medical education, an associate program director for the Pediatrics Residency program at the University of Minnesota. She received her medical degree from Wright State University Boonshoft School of Medicine and completed pediatric residency and chief residency at the University of Minnesota.
PHM 2021: Achieving gender equity in medicine
PHM 2021 session
Accelerating Patient Care and Healthcare Workforce Diversity and Inclusion
Presenter
Julie Silver, MD
Session summary
Gender inequity in medicine has been well documented and further highlighted by the tremendous impact of the COVID-19 pandemic on women in medicine. While more women than men are entering medical schools across the U.S., women still struggle to reach the highest levels of academic rank, achieve leadership positions of power and influence, receive fair equitable pay, attain leadership roles in national societies, and receive funding from national agencies. They also continue to face discrimination and implicit and explicit biases. Women of color or from other minority backgrounds face even greater barriers and biases. Despite being a specialty in which women represent almost 70% of the workforce, pediatrics is not immune to these disparities.
In her PHM21 plenary on Aug. 3, 2021, Dr. Julie Silver, a national expert in gender equity disparities, detailed the landscape for women in medicine and proposed some solutions to accelerate systemic change for gender equity. In order to understand and mitigate gender inequity, Dr. Silver encouraged the PHM community to identify influential “gatekeepers” of promotion, advancement, and salary compensation. In academic medicine medical schools, funding agencies, professional societies, and journals are the gatekeepers to advancement and compensation for women. Women are traditionally underrepresented as members and influential leaders of these gatekeeping organizations and in their recognition structures, therefore their advancement, compensation, and wellbeing are hindered.
Key takeaways
- Critical mass theory will not help alleviate gender inequity in medicine, as women make up a critical mass in pediatrics and are still experiencing stark inequities. Critical actor leaders are needed to highlight disparities and drive change even once a critical mass is reached.
- Our current diversity, equity, and inclusion (DEI) efforts are ineffective and are creating an “illusion of fairness that causes majority group members to become less sensitive to recognizing discrimination against minorities.” Many of the activities that are considered citizenship, including committees focused on DEI efforts, should be counted as scholarship, and appropriately compensated to ensure promotion of our women and minority colleagues.
- Male allies are critical to documenting, disseminating, and addressing gender inequality. Without the support of men in the field, we will see little progress.
- While there are numerous advocacy angles we can take when advocating for gender equity, the most effective will be the financial angle. Gender pay gaps at the start of a career can lead to roughly 2 million dollars of salary loss for a woman over the course of her career. In order to alleviate those salary pay gaps our institutions must not expect women to negotiate for fair pay, make salary benchmarks transparent, continue to monitor and conduct research on compensation disparities, and attempt to alleviate the weight of educational debt.
- COVID-19 is causing immense stress on women in medicine, and the impact could be disastrous. We must recognize and reward the “4th shift” women are working for COVID-19–related activities at home and at work, and put measures in place to #GiveHerAReasonToStay in health care.
- Men and other women leaders have a responsibility to sponsor the many and well-qualified women in medicine for awards, committees, and speaking engagements. These opportunities are key markers of success in academic medicine and are critical to advancement and salary compensation.
Dr. Casillas is the internal medicine-pediatric chief resident for the University of Cincinnati/Cincinnati Children’s Internal Medicine-Pediatric program. His career goal is to serve as a hospitalist for children and adults, and he is interested in health equity and Latinx health. Dr. O’Toole is a pediatric and adult hospitalist at Cincinnati Children’s Hospital Medical Center and University of Cincinnati Medical Center, and a professor of pediatrics and internal medicine at the University of Cincinnati College of Medicine. She serves as program director of Cincinnati’s Combined Internal Medicine and Pediatrics Residency Program.
PHM 2021 session
Accelerating Patient Care and Healthcare Workforce Diversity and Inclusion
Presenter
Julie Silver, MD
Session summary
Gender inequity in medicine has been well documented and further highlighted by the tremendous impact of the COVID-19 pandemic on women in medicine. While more women than men are entering medical schools across the U.S., women still struggle to reach the highest levels of academic rank, achieve leadership positions of power and influence, receive fair equitable pay, attain leadership roles in national societies, and receive funding from national agencies. They also continue to face discrimination and implicit and explicit biases. Women of color or from other minority backgrounds face even greater barriers and biases. Despite being a specialty in which women represent almost 70% of the workforce, pediatrics is not immune to these disparities.
In her PHM21 plenary on Aug. 3, 2021, Dr. Julie Silver, a national expert in gender equity disparities, detailed the landscape for women in medicine and proposed some solutions to accelerate systemic change for gender equity. In order to understand and mitigate gender inequity, Dr. Silver encouraged the PHM community to identify influential “gatekeepers” of promotion, advancement, and salary compensation. In academic medicine medical schools, funding agencies, professional societies, and journals are the gatekeepers to advancement and compensation for women. Women are traditionally underrepresented as members and influential leaders of these gatekeeping organizations and in their recognition structures, therefore their advancement, compensation, and wellbeing are hindered.
Key takeaways
- Critical mass theory will not help alleviate gender inequity in medicine, as women make up a critical mass in pediatrics and are still experiencing stark inequities. Critical actor leaders are needed to highlight disparities and drive change even once a critical mass is reached.
- Our current diversity, equity, and inclusion (DEI) efforts are ineffective and are creating an “illusion of fairness that causes majority group members to become less sensitive to recognizing discrimination against minorities.” Many of the activities that are considered citizenship, including committees focused on DEI efforts, should be counted as scholarship, and appropriately compensated to ensure promotion of our women and minority colleagues.
- Male allies are critical to documenting, disseminating, and addressing gender inequality. Without the support of men in the field, we will see little progress.
- While there are numerous advocacy angles we can take when advocating for gender equity, the most effective will be the financial angle. Gender pay gaps at the start of a career can lead to roughly 2 million dollars of salary loss for a woman over the course of her career. In order to alleviate those salary pay gaps our institutions must not expect women to negotiate for fair pay, make salary benchmarks transparent, continue to monitor and conduct research on compensation disparities, and attempt to alleviate the weight of educational debt.
- COVID-19 is causing immense stress on women in medicine, and the impact could be disastrous. We must recognize and reward the “4th shift” women are working for COVID-19–related activities at home and at work, and put measures in place to #GiveHerAReasonToStay in health care.
- Men and other women leaders have a responsibility to sponsor the many and well-qualified women in medicine for awards, committees, and speaking engagements. These opportunities are key markers of success in academic medicine and are critical to advancement and salary compensation.
Dr. Casillas is the internal medicine-pediatric chief resident for the University of Cincinnati/Cincinnati Children’s Internal Medicine-Pediatric program. His career goal is to serve as a hospitalist for children and adults, and he is interested in health equity and Latinx health. Dr. O’Toole is a pediatric and adult hospitalist at Cincinnati Children’s Hospital Medical Center and University of Cincinnati Medical Center, and a professor of pediatrics and internal medicine at the University of Cincinnati College of Medicine. She serves as program director of Cincinnati’s Combined Internal Medicine and Pediatrics Residency Program.
PHM 2021 session
Accelerating Patient Care and Healthcare Workforce Diversity and Inclusion
Presenter
Julie Silver, MD
Session summary
Gender inequity in medicine has been well documented and further highlighted by the tremendous impact of the COVID-19 pandemic on women in medicine. While more women than men are entering medical schools across the U.S., women still struggle to reach the highest levels of academic rank, achieve leadership positions of power and influence, receive fair equitable pay, attain leadership roles in national societies, and receive funding from national agencies. They also continue to face discrimination and implicit and explicit biases. Women of color or from other minority backgrounds face even greater barriers and biases. Despite being a specialty in which women represent almost 70% of the workforce, pediatrics is not immune to these disparities.
In her PHM21 plenary on Aug. 3, 2021, Dr. Julie Silver, a national expert in gender equity disparities, detailed the landscape for women in medicine and proposed some solutions to accelerate systemic change for gender equity. In order to understand and mitigate gender inequity, Dr. Silver encouraged the PHM community to identify influential “gatekeepers” of promotion, advancement, and salary compensation. In academic medicine medical schools, funding agencies, professional societies, and journals are the gatekeepers to advancement and compensation for women. Women are traditionally underrepresented as members and influential leaders of these gatekeeping organizations and in their recognition structures, therefore their advancement, compensation, and wellbeing are hindered.
Key takeaways
- Critical mass theory will not help alleviate gender inequity in medicine, as women make up a critical mass in pediatrics and are still experiencing stark inequities. Critical actor leaders are needed to highlight disparities and drive change even once a critical mass is reached.
- Our current diversity, equity, and inclusion (DEI) efforts are ineffective and are creating an “illusion of fairness that causes majority group members to become less sensitive to recognizing discrimination against minorities.” Many of the activities that are considered citizenship, including committees focused on DEI efforts, should be counted as scholarship, and appropriately compensated to ensure promotion of our women and minority colleagues.
- Male allies are critical to documenting, disseminating, and addressing gender inequality. Without the support of men in the field, we will see little progress.
- While there are numerous advocacy angles we can take when advocating for gender equity, the most effective will be the financial angle. Gender pay gaps at the start of a career can lead to roughly 2 million dollars of salary loss for a woman over the course of her career. In order to alleviate those salary pay gaps our institutions must not expect women to negotiate for fair pay, make salary benchmarks transparent, continue to monitor and conduct research on compensation disparities, and attempt to alleviate the weight of educational debt.
- COVID-19 is causing immense stress on women in medicine, and the impact could be disastrous. We must recognize and reward the “4th shift” women are working for COVID-19–related activities at home and at work, and put measures in place to #GiveHerAReasonToStay in health care.
- Men and other women leaders have a responsibility to sponsor the many and well-qualified women in medicine for awards, committees, and speaking engagements. These opportunities are key markers of success in academic medicine and are critical to advancement and salary compensation.
Dr. Casillas is the internal medicine-pediatric chief resident for the University of Cincinnati/Cincinnati Children’s Internal Medicine-Pediatric program. His career goal is to serve as a hospitalist for children and adults, and he is interested in health equity and Latinx health. Dr. O’Toole is a pediatric and adult hospitalist at Cincinnati Children’s Hospital Medical Center and University of Cincinnati Medical Center, and a professor of pediatrics and internal medicine at the University of Cincinnati College of Medicine. She serves as program director of Cincinnati’s Combined Internal Medicine and Pediatrics Residency Program.
Report urges complete residency overhaul
from the Graduate Medical Education Review Committee (UGRC) of the Coalition for Physician Accountability.
The 275-page report presents preliminary findings that were released in April 2021 and a long list of stakeholder comments. According to the report, the coalition will meet soon to discuss the final recommendations and consider next steps toward implementation.
The UGRC includes representatives of national medical organizations, medical schools, and residency programs. Among the organizations that participated in the report’s creation are the American Medical Association, the National Board of Medical Examiners, the American Osteopathic Association, the National Board of Osteopathic Medical Examiners, the Educational Commission for Foreign Medical Graduates, and the Association of American Medical Colleges.
The report identifies a list of challenges that affect the transition of medical students into residency programs and beyond. They include:
- Too much focus on finding and filling residency positions instead of “assuring learner competence and readiness for residency training”
- Inattention to assuring congruence between applicant goals and program missions
- Overreliance on licensure exam scores rather than “valid, trustworthy measures of students’ competence and clinical abilities”
- Increasing financial costs to students
- Individual and systemic biases in the UME-GME transition, as well as inequities related to international medical graduates
Seeking a common framework for competence
Overall, the report calls for increased standardization of how students are evaluated in medical school and how residency programs evaluate students. Less reliance should be placed on the numerical scores of the U.S. Medical Licensing Examination (USMLE), the report says, and more attention should be paid to the direct observation of student performance in clinical situations. In addition, the various organizations involved in the UME-GME transition process are asked to work better together.
To develop better methods of evaluating medical students and residents, UME and GME educators should jointly define and implement a common framework and set of competencies to apply to learners across the UME-GME transition, the report suggests.
While emphasizing the need for a broader student assessment framework, the report says, USMLE scores should also continue to be used in judging residency applicants. “Assessment information should be shared in residency applications and a postmatch learner handover. Licensing examinations should be used for their intended purpose to ensure requisite competence.”
Among the committee’s three dozen recommendations are the following:
- The Centers for Medicare & Medicaid Services should change the GME funding structure so that the initial residency period is calculated starting with the second year of postgraduate training. This change would allow residents to reconsider their career choices. Currently, if a resident decides to switch to another program or specialty after beginning training, the hospital may not receive full GME funding, so may be less likely to approve the change.
- Residency programs should improve recruitment practices to increase specialty-specific diversity of residents. Medical educators should also receive additional training regarding antiracism, avoiding bias, and ensuring equity.
- The self-reported demographic information of applicants to residency programs should be measured and shared with stakeholders, including the programs and medical schools, to promote equity. “A residency program that finds bias in its selection process could go back in real time to find qualified applicants who may have been missed, potentially improving outcomes,” the report notes.
- An interactive database of GME program and specialty track information should be created and made available to all applicants, medical schools, and residency programs at no cost to applicants. “Applicants and their advisors should be able to sort the information according to demographic and educational features that may significantly impact the likelihood of matching at a program.”
Less than half of applicants get in-depth reviews
The 2020 National Resident Matching Program Program Director Survey found that only 49% of applications received in-depth review. In light of this, the report suggests that the application system be updated to use modern information technology, including discrete fields for key data to expedite application reviews.
Many applications have been discarded because of various filters used to block consideration of certain applications. The report suggests that new filters be designed to ensure that each detects meaningful differences among applicants and promotes review based on mission alignment and likelihood of success in a program. Filters should be improved to decrease the likelihood of random exclusions of qualified applicants.
Specialty-specific, just-in-time training for all incoming first-year residents is also suggested to support the transition from the role of student to a physician ready to assume increased responsibility for patient care. In addition, the report urges adequate time be allowed between medical school graduation and residency to enable new residents to relocate and find homes.
The report also calls for a standardized process in the United States for initial licensing of doctors at entrance to residency in order to streamline the process of credentialing for both residency training and continuing practice.
Osteopathic students’ dilemma
To promote equitable treatment of applicants regardless of licensure examination requirements, comparable exams with different scales (COMLEX-USA and USMLE) should be reported within the electronic application system in a single field, the report said.
Osteopathic students, who make up 25% of U.S. medical students, must take the COMLEX-USA exam, but residency programs may filter them out if they don’t also take the USMLE exam. Thus, many osteopathic students take both exams, incurring extra time, cost, and stress.
The UGRC recommends creating a combined field in the electronic residency application service that normalizes the scores between the two exams. Residency programs could then filter applications based only on the single normalized score.
This approach makes sense from the viewpoint that it would reduce the pressure on osteopathic students to take the USMLE, Bryan Carmody, MD, an outspoken critic of various current training policies, said in an interview. But it could also have serious disadvantages.
For one thing, only osteopathic students can take the COMLEX-USA exam, he noted. If they don’t like their score, they can then take the USMLE test to get a higher score – an option that allopathic students don’t have. It’s not clear that they’d be prevented from doing this under the UGRC recommendation.
Second, he said, osteopathic students, on average, don’t do as well as allopathic students on the UMSLE exam. If they only take the COMLEX-USA test, they’re competing against other students who don’t do as well on tests as allopathic students do. If their scores were normalized with those of the USMLE test takers, they’d gain an unfair advantage against students who can only take the USMLE, including international medical graduates.
Although Dr. Carmody admitted that osteopathic students face a harder challenge than allopathic students in matching to residency programs, he said that the UGRC approach to the licensing exams might actually penalize them further. As a result of the scores of the two exams being averaged, residency program directors might discount the scores of all osteopathic students.
A version of this article first appeared on Medscape.com.
from the Graduate Medical Education Review Committee (UGRC) of the Coalition for Physician Accountability.
The 275-page report presents preliminary findings that were released in April 2021 and a long list of stakeholder comments. According to the report, the coalition will meet soon to discuss the final recommendations and consider next steps toward implementation.
The UGRC includes representatives of national medical organizations, medical schools, and residency programs. Among the organizations that participated in the report’s creation are the American Medical Association, the National Board of Medical Examiners, the American Osteopathic Association, the National Board of Osteopathic Medical Examiners, the Educational Commission for Foreign Medical Graduates, and the Association of American Medical Colleges.
The report identifies a list of challenges that affect the transition of medical students into residency programs and beyond. They include:
- Too much focus on finding and filling residency positions instead of “assuring learner competence and readiness for residency training”
- Inattention to assuring congruence between applicant goals and program missions
- Overreliance on licensure exam scores rather than “valid, trustworthy measures of students’ competence and clinical abilities”
- Increasing financial costs to students
- Individual and systemic biases in the UME-GME transition, as well as inequities related to international medical graduates
Seeking a common framework for competence
Overall, the report calls for increased standardization of how students are evaluated in medical school and how residency programs evaluate students. Less reliance should be placed on the numerical scores of the U.S. Medical Licensing Examination (USMLE), the report says, and more attention should be paid to the direct observation of student performance in clinical situations. In addition, the various organizations involved in the UME-GME transition process are asked to work better together.
To develop better methods of evaluating medical students and residents, UME and GME educators should jointly define and implement a common framework and set of competencies to apply to learners across the UME-GME transition, the report suggests.
While emphasizing the need for a broader student assessment framework, the report says, USMLE scores should also continue to be used in judging residency applicants. “Assessment information should be shared in residency applications and a postmatch learner handover. Licensing examinations should be used for their intended purpose to ensure requisite competence.”
Among the committee’s three dozen recommendations are the following:
- The Centers for Medicare & Medicaid Services should change the GME funding structure so that the initial residency period is calculated starting with the second year of postgraduate training. This change would allow residents to reconsider their career choices. Currently, if a resident decides to switch to another program or specialty after beginning training, the hospital may not receive full GME funding, so may be less likely to approve the change.
- Residency programs should improve recruitment practices to increase specialty-specific diversity of residents. Medical educators should also receive additional training regarding antiracism, avoiding bias, and ensuring equity.
- The self-reported demographic information of applicants to residency programs should be measured and shared with stakeholders, including the programs and medical schools, to promote equity. “A residency program that finds bias in its selection process could go back in real time to find qualified applicants who may have been missed, potentially improving outcomes,” the report notes.
- An interactive database of GME program and specialty track information should be created and made available to all applicants, medical schools, and residency programs at no cost to applicants. “Applicants and their advisors should be able to sort the information according to demographic and educational features that may significantly impact the likelihood of matching at a program.”
Less than half of applicants get in-depth reviews
The 2020 National Resident Matching Program Program Director Survey found that only 49% of applications received in-depth review. In light of this, the report suggests that the application system be updated to use modern information technology, including discrete fields for key data to expedite application reviews.
Many applications have been discarded because of various filters used to block consideration of certain applications. The report suggests that new filters be designed to ensure that each detects meaningful differences among applicants and promotes review based on mission alignment and likelihood of success in a program. Filters should be improved to decrease the likelihood of random exclusions of qualified applicants.
Specialty-specific, just-in-time training for all incoming first-year residents is also suggested to support the transition from the role of student to a physician ready to assume increased responsibility for patient care. In addition, the report urges adequate time be allowed between medical school graduation and residency to enable new residents to relocate and find homes.
The report also calls for a standardized process in the United States for initial licensing of doctors at entrance to residency in order to streamline the process of credentialing for both residency training and continuing practice.
Osteopathic students’ dilemma
To promote equitable treatment of applicants regardless of licensure examination requirements, comparable exams with different scales (COMLEX-USA and USMLE) should be reported within the electronic application system in a single field, the report said.
Osteopathic students, who make up 25% of U.S. medical students, must take the COMLEX-USA exam, but residency programs may filter them out if they don’t also take the USMLE exam. Thus, many osteopathic students take both exams, incurring extra time, cost, and stress.
The UGRC recommends creating a combined field in the electronic residency application service that normalizes the scores between the two exams. Residency programs could then filter applications based only on the single normalized score.
This approach makes sense from the viewpoint that it would reduce the pressure on osteopathic students to take the USMLE, Bryan Carmody, MD, an outspoken critic of various current training policies, said in an interview. But it could also have serious disadvantages.
For one thing, only osteopathic students can take the COMLEX-USA exam, he noted. If they don’t like their score, they can then take the USMLE test to get a higher score – an option that allopathic students don’t have. It’s not clear that they’d be prevented from doing this under the UGRC recommendation.
Second, he said, osteopathic students, on average, don’t do as well as allopathic students on the UMSLE exam. If they only take the COMLEX-USA test, they’re competing against other students who don’t do as well on tests as allopathic students do. If their scores were normalized with those of the USMLE test takers, they’d gain an unfair advantage against students who can only take the USMLE, including international medical graduates.
Although Dr. Carmody admitted that osteopathic students face a harder challenge than allopathic students in matching to residency programs, he said that the UGRC approach to the licensing exams might actually penalize them further. As a result of the scores of the two exams being averaged, residency program directors might discount the scores of all osteopathic students.
A version of this article first appeared on Medscape.com.
from the Graduate Medical Education Review Committee (UGRC) of the Coalition for Physician Accountability.
The 275-page report presents preliminary findings that were released in April 2021 and a long list of stakeholder comments. According to the report, the coalition will meet soon to discuss the final recommendations and consider next steps toward implementation.
The UGRC includes representatives of national medical organizations, medical schools, and residency programs. Among the organizations that participated in the report’s creation are the American Medical Association, the National Board of Medical Examiners, the American Osteopathic Association, the National Board of Osteopathic Medical Examiners, the Educational Commission for Foreign Medical Graduates, and the Association of American Medical Colleges.
The report identifies a list of challenges that affect the transition of medical students into residency programs and beyond. They include:
- Too much focus on finding and filling residency positions instead of “assuring learner competence and readiness for residency training”
- Inattention to assuring congruence between applicant goals and program missions
- Overreliance on licensure exam scores rather than “valid, trustworthy measures of students’ competence and clinical abilities”
- Increasing financial costs to students
- Individual and systemic biases in the UME-GME transition, as well as inequities related to international medical graduates
Seeking a common framework for competence
Overall, the report calls for increased standardization of how students are evaluated in medical school and how residency programs evaluate students. Less reliance should be placed on the numerical scores of the U.S. Medical Licensing Examination (USMLE), the report says, and more attention should be paid to the direct observation of student performance in clinical situations. In addition, the various organizations involved in the UME-GME transition process are asked to work better together.
To develop better methods of evaluating medical students and residents, UME and GME educators should jointly define and implement a common framework and set of competencies to apply to learners across the UME-GME transition, the report suggests.
While emphasizing the need for a broader student assessment framework, the report says, USMLE scores should also continue to be used in judging residency applicants. “Assessment information should be shared in residency applications and a postmatch learner handover. Licensing examinations should be used for their intended purpose to ensure requisite competence.”
Among the committee’s three dozen recommendations are the following:
- The Centers for Medicare & Medicaid Services should change the GME funding structure so that the initial residency period is calculated starting with the second year of postgraduate training. This change would allow residents to reconsider their career choices. Currently, if a resident decides to switch to another program or specialty after beginning training, the hospital may not receive full GME funding, so may be less likely to approve the change.
- Residency programs should improve recruitment practices to increase specialty-specific diversity of residents. Medical educators should also receive additional training regarding antiracism, avoiding bias, and ensuring equity.
- The self-reported demographic information of applicants to residency programs should be measured and shared with stakeholders, including the programs and medical schools, to promote equity. “A residency program that finds bias in its selection process could go back in real time to find qualified applicants who may have been missed, potentially improving outcomes,” the report notes.
- An interactive database of GME program and specialty track information should be created and made available to all applicants, medical schools, and residency programs at no cost to applicants. “Applicants and their advisors should be able to sort the information according to demographic and educational features that may significantly impact the likelihood of matching at a program.”
Less than half of applicants get in-depth reviews
The 2020 National Resident Matching Program Program Director Survey found that only 49% of applications received in-depth review. In light of this, the report suggests that the application system be updated to use modern information technology, including discrete fields for key data to expedite application reviews.
Many applications have been discarded because of various filters used to block consideration of certain applications. The report suggests that new filters be designed to ensure that each detects meaningful differences among applicants and promotes review based on mission alignment and likelihood of success in a program. Filters should be improved to decrease the likelihood of random exclusions of qualified applicants.
Specialty-specific, just-in-time training for all incoming first-year residents is also suggested to support the transition from the role of student to a physician ready to assume increased responsibility for patient care. In addition, the report urges adequate time be allowed between medical school graduation and residency to enable new residents to relocate and find homes.
The report also calls for a standardized process in the United States for initial licensing of doctors at entrance to residency in order to streamline the process of credentialing for both residency training and continuing practice.
Osteopathic students’ dilemma
To promote equitable treatment of applicants regardless of licensure examination requirements, comparable exams with different scales (COMLEX-USA and USMLE) should be reported within the electronic application system in a single field, the report said.
Osteopathic students, who make up 25% of U.S. medical students, must take the COMLEX-USA exam, but residency programs may filter them out if they don’t also take the USMLE exam. Thus, many osteopathic students take both exams, incurring extra time, cost, and stress.
The UGRC recommends creating a combined field in the electronic residency application service that normalizes the scores between the two exams. Residency programs could then filter applications based only on the single normalized score.
This approach makes sense from the viewpoint that it would reduce the pressure on osteopathic students to take the USMLE, Bryan Carmody, MD, an outspoken critic of various current training policies, said in an interview. But it could also have serious disadvantages.
For one thing, only osteopathic students can take the COMLEX-USA exam, he noted. If they don’t like their score, they can then take the USMLE test to get a higher score – an option that allopathic students don’t have. It’s not clear that they’d be prevented from doing this under the UGRC recommendation.
Second, he said, osteopathic students, on average, don’t do as well as allopathic students on the UMSLE exam. If they only take the COMLEX-USA test, they’re competing against other students who don’t do as well on tests as allopathic students do. If their scores were normalized with those of the USMLE test takers, they’d gain an unfair advantage against students who can only take the USMLE, including international medical graduates.
Although Dr. Carmody admitted that osteopathic students face a harder challenge than allopathic students in matching to residency programs, he said that the UGRC approach to the licensing exams might actually penalize them further. As a result of the scores of the two exams being averaged, residency program directors might discount the scores of all osteopathic students.
A version of this article first appeared on Medscape.com.
Microlearning during the pandemic
How to become a hospitalist
The vast amounts of information generated this past year related to the COVID-19 pandemic was a feat of wonder – recommendations and guidelines on the hospital level and on the national level came in a flurry, more often overwhelming and confusing than clarifying for the frontline provider. In addition, “routine” hospital care for non-infected patients and improvement processes had to continue as we all dealt with the whirlwind of increasing COVID cases, torrents of new guidelines, and educating our trainees.
Thus, the individual-level question: how does a clinician stay engaged and distill the relentless stream of new information?
In Spring 2020, when the first patients with COVID were admitted, our hospital medicine section was tasked to create a surge plan. This included organizing, orienting, and educating off-service providers on how to become hospitalists. Undoubtedly, the call to arms for our center was heard, and many responded. However, backgrounds were diverse in specialty – clinicians and trainees from psychiatry, general surgery, and various fellowships all answered. It was an exhausting and inefficient effort to produce the material, hold webinars, and schedule training, especially for those who were more removed from a hospital medicine experience. We knew we had to come up with an alternative plan moving forward.
Thus, the systems-level question: how does a health care system educate its clinicians, or any other health care providers, when reallocation of their talents and skills is both necessary, time-sensitive, and occuring during a period where new information is constantly being produced and changing?
To reach the most clinicians as possible, with the most succinct and distilled information, we had to come up with a method to do so. Ultimately, in considering the situation at hand, we had to understand who we were as the provider of the information, and who the recipient would be. We would like to share the initiatives and processes by which we constructed our solution to the two questions – microlearning through hospital podcasting.
Learning from our health care colleagues
With the initial webinars and training sessions for our staff, we assessed our learners’ motivations and background in managing in a hospital medicine capacity. Overall, we discovered that our trainees and clinicians have an innate drive to learn; all of them recognized the importance of keeping up with evidence-based information. However, the difficulty highlighted was the individual time available to dedicate to acquiring new information and awareness of new information being available to the health care sector during the chaotic times of the pandemic.
From our section’s perspective, we had a difficulty with coordinating among multiple professional development groups within our hospital, cost, and resources to execute training. These difficulties between providing knowledge and receiving knowledge have already been expertly analyzed.1
Parallel to this, the pedagogic paradigm shifts as we progress through our careers – the methods and skills we used in school contrast in many ways with those we use on a daily basis when it comes to learning. Instead of dedicating hours at a time to new challenges in our workflow or our interests, we watch videos, search retailers for product solutions, check our email correspondence, and peruse social media accounts several times a day. Information comes at us very quickly, but in small pieces.
One such innovation in pedagogy is the practice of microlearning. This refers to the use of small lesson modules and short-term activities intended to teach and reinforce concepts.2 It is the opposite of “macrolearning,” which is the principle of dedicating reading material, structured coursework, and traditional knowledge evaluation in the form of exams to reinforce learning. Certainly, microlearning has other names as well – “just-in-time,” “just-enough,” and “micro-courses” are a few synonyms seen in the current literature. Though a highly relevant concept for our situation, translating it to an endproduct for our trainees and clinicians required more thought.
From theory to application
Microlearning allows for faster delivery of information – fewer things to write means shorter course distribution times, allowing the learner to respond faster to changing educational goals and training demands. Microlearning is flexible – “micro-courses” can give a broad overview of a subject or cover complex topics broken down into simple parts. In addition, micro-learning promotes retention of key concepts – given the length of each lesson, repetition of the topic by the learner is possible at any point in time. The whole experience is similar to checking your favorite social media application on your smartphone.
Certainly, many examples of the application of microlearning are available in the health care sector – pharmaceutical and nursing training both have utilized the theory extensively.3-4 However, in many instances, individuals were still required to sit at a workstation to complete modules and lessons. We envisioned our application of microlearning to be “on-the-go,” without necessarily requiring a computer workstation or laptop to complete.
In thinking about how social media attracts and influences clinicians, many content creators on social media come to mind. In addition, most, if not all, have branched into various social media platforms – podcasting, blogging, YouTube, for example. In thinking about our colleagues and trainees, we wanted a platform that they could take on the go, without the need to focus their visual attention (such as while driving or running). Ultimately, we believe the podcast would be the best platform to disseminate our information.
Podcasting is not foreign to medicine. A variety of medical podcasts exist, whether produced by major medical journals or by various independent health care practitioners. Both, however, have their drawbacks – the podcasts created by major medical journals are typically a summary of the publication’s content and are less engaging. Alternatively, podcasts produced by independent creators are certainly engaging and entertaining, and have a wealth of information, but the line is often blurred between just that: education and entertainment. In both instances, there is no follow-up or feedback offered to the learner in the form of surveys, or other types of feedback, which is arguably an important piece in any form of pedagogy. Thus, we sought to strike a balance between the two forms for our purposes.
Process of two podcasts
Our section was aware of the two aims during the pandemic – (1) disseminate new information regarding COVID-19 to the rest of our staff members and trainees as quickly as possible, and (2) maintain and improve the current quality of care of our patients. Thus, we sought to apply the reach and efficiency of the podcasting medium to provide ongoing education and feedback with respect to these two aims.
“The Cure” podcast. We recognized the constant flow of new COVID-19 information and updates and we wanted to find a readily accessible platform to reach staff with timely updates. Our marketing & communications team later helped us realize that the content we wanted to share was relevant to our patients and the community, so we formatted the material to be practical and easily digestible- something that may help an individual make decisions at the bedside as well as have conversations at the dinner table. Most recently, we engaged with our human resources department to use our platform in orienting new hires with the goal of helping staff familiarize with the institutions policies, procedures, and job aids that keep staff and patients safe.
“Antibiotry” podcast. Prior to the COVID-19 pandemic, our antibiotic stewardship group noticed an increase in antibiotic use on our medical floors. This is monitored not only through internal metrics by our pharmacy department, but also via the SAAR (standardized antibiotic administration ratio). Both sources demonstrated an increase in antibiotic use, greater than expected. An initiative was formed between our hospital medicine and infectious disease sections, and our pharmacy department to raise awareness of this increase in use, provide education to our trainees, and to create systems solutions for clinicians.
Initially, we sought to hold in-person sessions once a month for our trainees. This was led by a senior resident at the time. Topics of discussion were geared towards clinical decision making regarding empiric antibiotic use on the hospital medicine service. At the same time, our team published empiric antibiotic use guidelines, accessible through our electronic medical record. In addition, the resident leader gave a voluntary survey at the end of the session to assess not only confidence of antibiotic use, but also baseline knowledge regarding antibiotics in various clinical scenarios. This survey was repeated at the end of the resident group’s month-long rotation. Altogether, each in-person session was no longer than 10 minutes.
Unfortunately, the initiative was just gaining momentum when the COVID-19 pandemic was declared. However, we sought to take this challenge and translate it into an opportunity.
We directed our focus towards stewardship during pandemic times. Initially, our resident leader sent out email primers, approximately 3-5 minute reads, as a substitute for the in-person sessions. Our primers’ uniqueness was in its incorporation of prescription pattern data that was developed by our resident leader and our initiative’s data analyst. In doing so, we provided professional feedback regarding our antibiotic use based on the clinical indication. This was a powerful tool to not only engage our learners and staff clinicians, but also as a benchmarking tool for continued quality improvement.
But email primers are not engaging, and despite the ubiquity of teleconferencing, it was difficult to ask our housestaff to break from their morning rounds for a 10 minute tele-meeting. Thus, we devised a podcast method of education – 5-10 minute audio clips with conversation regarding a topic of discussion. This way, our trainees and learners can access episodes of education on their own time throughout the pandemic without disrupting their workflow. Given the brevity of, but high-yield content in, each episode, it would not only be convenient for listeners to access and repeat, but also for the podcaster (our resident leader) to create, as recording of the audio portion takes anywhere between 10-20 minutes for each episode, with postprocessing similarly fast.
The interdisciplinary nature of continued medical education cannot be stressed enough. With the help of our professional development team and their educators, we were able to centralize our podcast and attach surveys and additional graphics for each episode, if appropriate. This additional detail allowed for feedback, engagement with our learners, and the chance to provide additional educational points, if the learner was interested. Given the integrated nature of this platform, quality metrics could easily be recorded in the form of “click” data and various other more conventional metrics, such as listener counts and the duration of each podcast played.
Future applications and initiatives
Thus far, we have had great success in the reception and use of both podcasts within our institution as an application of microlearning. “The Cure” has been widely listened to by all hospital staff from various services; it has caught the attention of state-wide radio programs, and plans to expand it into the community are being discussed.
As for “Antibiotry” podcast, the concept has been lauded by our medical educators. Given its centralization within our institution, we are able to publish institution-based data as a form of professional and educational feedback to our trainees and staff physicians. This is currently coupled with the development of a provider dashboard, visualizing antibiotic prescriptions and narrowing patterns of practice within our medicine department. We plan to expand “Antibiotry” to other services at the hospital.
For both podcasts, the steps it took to achieve the final product from the microlearning concept were possible through a combination of institutional need and a motivated team. We are fortunate to have highly energetic individuals, making the coordination and planning with our hospitalists, various sub-specialists, and professional development teams straightforward. As the team grows with more individuals interested in the initiatives, keen insight into interests, individual clinical expertise, presentation skills, and technical skills ought to be carefully weighed to sustain our podcasts most efficiently, and perhaps expand them through different social media platforms.
Our objective for sustainability is through the continued outreach to and recruitment of residents and medical students, who can play key roles in the development of future projects related to these educational innovations. Both microlearning podcasts were developed through the initial planning, trial and error, and execution by two resident leaders. Their initiative and motivation to educate our institution through these platforms were highly unique; their pathfinding set the foundation for sustainability and expansion to other services.
Of course, one of the key measures we would like to investigate is whether our microlearning platform translates to improved patient outcomes. Regarding “Antibiotry,” we hope to see a decrease in unnecessary broad-spectrum antibiotic use by drawing attention to clinician practice patterns. Quality and outcome metrics will continue to be developed and measured. In addition to patient care metrics, further investigation of pedagogical metrics will be conducted, especially in the evolving realm of graduate and continuing medical education.
Measuring educational quality is neither a new ethical nor philosophical debate – neither does it carry a definitive answer. Further help from education experts may be needed to assess the quality of the information provided and its impact on our learners.
Conclusion
Medicine is ever-changing – the guidelines and criteria for patient care and pathology that we learned in medical school have likely changed. There is no single “best” method of learning new information in medicine, simply due to the breadth and volume of such information generated on a daily basis. This poses both a challenge for present-day clinicians and trainees, and a stimulus for change in the methods of acquiring, absorbing, and applying new information to clinical decision making and practice.
We have found that podcasting is a well-received medium of information transfer that is convenient for both the learner and the content creator. Through the podcast format, we were able to distill non-engaging pieces of education and information and transform them into short-duration lessons that the learner can listen to at their own convenience. This proved to be especially handy during the chaos of the pandemic, not only for dissemination of information regarding the management of COVID-19, but also for sustaining quality improvement goals within our institution.
Further investigation on patient outcomes and information quality are the planned next steps. In addition, expansion of other microlearning media, such as group SMS texting, YouTube videos, and Twitter, ought to be considered. Though many publications discuss the theory, potential benefits, and predicted pitfalls of microlearning, few assess the real-world application of microlearning to the clinical setting for medical education.
So what did we learn? We should think of microlearning as moments when you turn to your smartphone or tablet in order to discover something, answer a question, or complete a task. These are moments when decisions are made and knowledge is reinforced. The goal is to capture these moments and fill them with essential pieces of information.
We offer these suggestions as a place to start. The microlearning platform allows for the collection of data on the interaction between user and course content. The data collected can be used for continuous quality improvement of the curriculum. Microlearning is a dynamic platform where creative ideas are encouraged and a multi-disciplinary approach is valuable to keeping an audience engaged. In the future, we hope to be able to correlate microlearning courses to provider performance and measurable patient outcomes.
Dr. Mercado is medical director at Alice Peck Day Memorial Hospital, and associate hospital epidemiologist, Dartmouth-Hitchcock Medical Center, both in Lebanon, N.H., and assistant professor at the Geisel School of Medicine at Dartmouth, Hanover, N.H. Dr. Feng is a Fellow in the Leadership/Preventive Medicine Program in the Department of Internal Medicine at Dartmouth-Hitchcock Medical Center.
References
1. Duggan F and Banwell L. Constructing a model of effective information dissemination in a crisis. Information Research. 2004;9(3). Paper 178 [Available at http://InformationR.net/ir/9-3/paper178.html].
2. Filipe HP, et al. Microlearning to improve CPD learning objectives. Clin Teach. 2020 Dec;17(6):695-699. doi: 10.1111/tct.13208.
3. Hegerius A, et al. E-Learning in Pharmacovigilance: An Evaluation of Microlearning-Based Modules Developed by Uppsala Monitoring Centre. Drug Saf. 2020 Nov;43(11):1171-1180. doi: 10.1007/s40264-020-00981-w.
4. Orwoll B, et al. Gamification and Microlearning for Engagement With Quality Improvement (GAMEQI): A Bundled Digital Intervention for the Prevention of Central Line-Associated Bloodstream Infection. Am J Med Qual. Jan/Feb 2018;33(1):21-29. doi: 10.1177/1062860617706542.
How to become a hospitalist
How to become a hospitalist
The vast amounts of information generated this past year related to the COVID-19 pandemic was a feat of wonder – recommendations and guidelines on the hospital level and on the national level came in a flurry, more often overwhelming and confusing than clarifying for the frontline provider. In addition, “routine” hospital care for non-infected patients and improvement processes had to continue as we all dealt with the whirlwind of increasing COVID cases, torrents of new guidelines, and educating our trainees.
Thus, the individual-level question: how does a clinician stay engaged and distill the relentless stream of new information?
In Spring 2020, when the first patients with COVID were admitted, our hospital medicine section was tasked to create a surge plan. This included organizing, orienting, and educating off-service providers on how to become hospitalists. Undoubtedly, the call to arms for our center was heard, and many responded. However, backgrounds were diverse in specialty – clinicians and trainees from psychiatry, general surgery, and various fellowships all answered. It was an exhausting and inefficient effort to produce the material, hold webinars, and schedule training, especially for those who were more removed from a hospital medicine experience. We knew we had to come up with an alternative plan moving forward.
Thus, the systems-level question: how does a health care system educate its clinicians, or any other health care providers, when reallocation of their talents and skills is both necessary, time-sensitive, and occuring during a period where new information is constantly being produced and changing?
To reach the most clinicians as possible, with the most succinct and distilled information, we had to come up with a method to do so. Ultimately, in considering the situation at hand, we had to understand who we were as the provider of the information, and who the recipient would be. We would like to share the initiatives and processes by which we constructed our solution to the two questions – microlearning through hospital podcasting.
Learning from our health care colleagues
With the initial webinars and training sessions for our staff, we assessed our learners’ motivations and background in managing in a hospital medicine capacity. Overall, we discovered that our trainees and clinicians have an innate drive to learn; all of them recognized the importance of keeping up with evidence-based information. However, the difficulty highlighted was the individual time available to dedicate to acquiring new information and awareness of new information being available to the health care sector during the chaotic times of the pandemic.
From our section’s perspective, we had a difficulty with coordinating among multiple professional development groups within our hospital, cost, and resources to execute training. These difficulties between providing knowledge and receiving knowledge have already been expertly analyzed.1
Parallel to this, the pedagogic paradigm shifts as we progress through our careers – the methods and skills we used in school contrast in many ways with those we use on a daily basis when it comes to learning. Instead of dedicating hours at a time to new challenges in our workflow or our interests, we watch videos, search retailers for product solutions, check our email correspondence, and peruse social media accounts several times a day. Information comes at us very quickly, but in small pieces.
One such innovation in pedagogy is the practice of microlearning. This refers to the use of small lesson modules and short-term activities intended to teach and reinforce concepts.2 It is the opposite of “macrolearning,” which is the principle of dedicating reading material, structured coursework, and traditional knowledge evaluation in the form of exams to reinforce learning. Certainly, microlearning has other names as well – “just-in-time,” “just-enough,” and “micro-courses” are a few synonyms seen in the current literature. Though a highly relevant concept for our situation, translating it to an endproduct for our trainees and clinicians required more thought.
From theory to application
Microlearning allows for faster delivery of information – fewer things to write means shorter course distribution times, allowing the learner to respond faster to changing educational goals and training demands. Microlearning is flexible – “micro-courses” can give a broad overview of a subject or cover complex topics broken down into simple parts. In addition, micro-learning promotes retention of key concepts – given the length of each lesson, repetition of the topic by the learner is possible at any point in time. The whole experience is similar to checking your favorite social media application on your smartphone.
Certainly, many examples of the application of microlearning are available in the health care sector – pharmaceutical and nursing training both have utilized the theory extensively.3-4 However, in many instances, individuals were still required to sit at a workstation to complete modules and lessons. We envisioned our application of microlearning to be “on-the-go,” without necessarily requiring a computer workstation or laptop to complete.
In thinking about how social media attracts and influences clinicians, many content creators on social media come to mind. In addition, most, if not all, have branched into various social media platforms – podcasting, blogging, YouTube, for example. In thinking about our colleagues and trainees, we wanted a platform that they could take on the go, without the need to focus their visual attention (such as while driving or running). Ultimately, we believe the podcast would be the best platform to disseminate our information.
Podcasting is not foreign to medicine. A variety of medical podcasts exist, whether produced by major medical journals or by various independent health care practitioners. Both, however, have their drawbacks – the podcasts created by major medical journals are typically a summary of the publication’s content and are less engaging. Alternatively, podcasts produced by independent creators are certainly engaging and entertaining, and have a wealth of information, but the line is often blurred between just that: education and entertainment. In both instances, there is no follow-up or feedback offered to the learner in the form of surveys, or other types of feedback, which is arguably an important piece in any form of pedagogy. Thus, we sought to strike a balance between the two forms for our purposes.
Process of two podcasts
Our section was aware of the two aims during the pandemic – (1) disseminate new information regarding COVID-19 to the rest of our staff members and trainees as quickly as possible, and (2) maintain and improve the current quality of care of our patients. Thus, we sought to apply the reach and efficiency of the podcasting medium to provide ongoing education and feedback with respect to these two aims.
“The Cure” podcast. We recognized the constant flow of new COVID-19 information and updates and we wanted to find a readily accessible platform to reach staff with timely updates. Our marketing & communications team later helped us realize that the content we wanted to share was relevant to our patients and the community, so we formatted the material to be practical and easily digestible- something that may help an individual make decisions at the bedside as well as have conversations at the dinner table. Most recently, we engaged with our human resources department to use our platform in orienting new hires with the goal of helping staff familiarize with the institutions policies, procedures, and job aids that keep staff and patients safe.
“Antibiotry” podcast. Prior to the COVID-19 pandemic, our antibiotic stewardship group noticed an increase in antibiotic use on our medical floors. This is monitored not only through internal metrics by our pharmacy department, but also via the SAAR (standardized antibiotic administration ratio). Both sources demonstrated an increase in antibiotic use, greater than expected. An initiative was formed between our hospital medicine and infectious disease sections, and our pharmacy department to raise awareness of this increase in use, provide education to our trainees, and to create systems solutions for clinicians.
Initially, we sought to hold in-person sessions once a month for our trainees. This was led by a senior resident at the time. Topics of discussion were geared towards clinical decision making regarding empiric antibiotic use on the hospital medicine service. At the same time, our team published empiric antibiotic use guidelines, accessible through our electronic medical record. In addition, the resident leader gave a voluntary survey at the end of the session to assess not only confidence of antibiotic use, but also baseline knowledge regarding antibiotics in various clinical scenarios. This survey was repeated at the end of the resident group’s month-long rotation. Altogether, each in-person session was no longer than 10 minutes.
Unfortunately, the initiative was just gaining momentum when the COVID-19 pandemic was declared. However, we sought to take this challenge and translate it into an opportunity.
We directed our focus towards stewardship during pandemic times. Initially, our resident leader sent out email primers, approximately 3-5 minute reads, as a substitute for the in-person sessions. Our primers’ uniqueness was in its incorporation of prescription pattern data that was developed by our resident leader and our initiative’s data analyst. In doing so, we provided professional feedback regarding our antibiotic use based on the clinical indication. This was a powerful tool to not only engage our learners and staff clinicians, but also as a benchmarking tool for continued quality improvement.
But email primers are not engaging, and despite the ubiquity of teleconferencing, it was difficult to ask our housestaff to break from their morning rounds for a 10 minute tele-meeting. Thus, we devised a podcast method of education – 5-10 minute audio clips with conversation regarding a topic of discussion. This way, our trainees and learners can access episodes of education on their own time throughout the pandemic without disrupting their workflow. Given the brevity of, but high-yield content in, each episode, it would not only be convenient for listeners to access and repeat, but also for the podcaster (our resident leader) to create, as recording of the audio portion takes anywhere between 10-20 minutes for each episode, with postprocessing similarly fast.
The interdisciplinary nature of continued medical education cannot be stressed enough. With the help of our professional development team and their educators, we were able to centralize our podcast and attach surveys and additional graphics for each episode, if appropriate. This additional detail allowed for feedback, engagement with our learners, and the chance to provide additional educational points, if the learner was interested. Given the integrated nature of this platform, quality metrics could easily be recorded in the form of “click” data and various other more conventional metrics, such as listener counts and the duration of each podcast played.
Future applications and initiatives
Thus far, we have had great success in the reception and use of both podcasts within our institution as an application of microlearning. “The Cure” has been widely listened to by all hospital staff from various services; it has caught the attention of state-wide radio programs, and plans to expand it into the community are being discussed.
As for “Antibiotry” podcast, the concept has been lauded by our medical educators. Given its centralization within our institution, we are able to publish institution-based data as a form of professional and educational feedback to our trainees and staff physicians. This is currently coupled with the development of a provider dashboard, visualizing antibiotic prescriptions and narrowing patterns of practice within our medicine department. We plan to expand “Antibiotry” to other services at the hospital.
For both podcasts, the steps it took to achieve the final product from the microlearning concept were possible through a combination of institutional need and a motivated team. We are fortunate to have highly energetic individuals, making the coordination and planning with our hospitalists, various sub-specialists, and professional development teams straightforward. As the team grows with more individuals interested in the initiatives, keen insight into interests, individual clinical expertise, presentation skills, and technical skills ought to be carefully weighed to sustain our podcasts most efficiently, and perhaps expand them through different social media platforms.
Our objective for sustainability is through the continued outreach to and recruitment of residents and medical students, who can play key roles in the development of future projects related to these educational innovations. Both microlearning podcasts were developed through the initial planning, trial and error, and execution by two resident leaders. Their initiative and motivation to educate our institution through these platforms were highly unique; their pathfinding set the foundation for sustainability and expansion to other services.
Of course, one of the key measures we would like to investigate is whether our microlearning platform translates to improved patient outcomes. Regarding “Antibiotry,” we hope to see a decrease in unnecessary broad-spectrum antibiotic use by drawing attention to clinician practice patterns. Quality and outcome metrics will continue to be developed and measured. In addition to patient care metrics, further investigation of pedagogical metrics will be conducted, especially in the evolving realm of graduate and continuing medical education.
Measuring educational quality is neither a new ethical nor philosophical debate – neither does it carry a definitive answer. Further help from education experts may be needed to assess the quality of the information provided and its impact on our learners.
Conclusion
Medicine is ever-changing – the guidelines and criteria for patient care and pathology that we learned in medical school have likely changed. There is no single “best” method of learning new information in medicine, simply due to the breadth and volume of such information generated on a daily basis. This poses both a challenge for present-day clinicians and trainees, and a stimulus for change in the methods of acquiring, absorbing, and applying new information to clinical decision making and practice.
We have found that podcasting is a well-received medium of information transfer that is convenient for both the learner and the content creator. Through the podcast format, we were able to distill non-engaging pieces of education and information and transform them into short-duration lessons that the learner can listen to at their own convenience. This proved to be especially handy during the chaos of the pandemic, not only for dissemination of information regarding the management of COVID-19, but also for sustaining quality improvement goals within our institution.
Further investigation on patient outcomes and information quality are the planned next steps. In addition, expansion of other microlearning media, such as group SMS texting, YouTube videos, and Twitter, ought to be considered. Though many publications discuss the theory, potential benefits, and predicted pitfalls of microlearning, few assess the real-world application of microlearning to the clinical setting for medical education.
So what did we learn? We should think of microlearning as moments when you turn to your smartphone or tablet in order to discover something, answer a question, or complete a task. These are moments when decisions are made and knowledge is reinforced. The goal is to capture these moments and fill them with essential pieces of information.
We offer these suggestions as a place to start. The microlearning platform allows for the collection of data on the interaction between user and course content. The data collected can be used for continuous quality improvement of the curriculum. Microlearning is a dynamic platform where creative ideas are encouraged and a multi-disciplinary approach is valuable to keeping an audience engaged. In the future, we hope to be able to correlate microlearning courses to provider performance and measurable patient outcomes.
Dr. Mercado is medical director at Alice Peck Day Memorial Hospital, and associate hospital epidemiologist, Dartmouth-Hitchcock Medical Center, both in Lebanon, N.H., and assistant professor at the Geisel School of Medicine at Dartmouth, Hanover, N.H. Dr. Feng is a Fellow in the Leadership/Preventive Medicine Program in the Department of Internal Medicine at Dartmouth-Hitchcock Medical Center.
References
1. Duggan F and Banwell L. Constructing a model of effective information dissemination in a crisis. Information Research. 2004;9(3). Paper 178 [Available at http://InformationR.net/ir/9-3/paper178.html].
2. Filipe HP, et al. Microlearning to improve CPD learning objectives. Clin Teach. 2020 Dec;17(6):695-699. doi: 10.1111/tct.13208.
3. Hegerius A, et al. E-Learning in Pharmacovigilance: An Evaluation of Microlearning-Based Modules Developed by Uppsala Monitoring Centre. Drug Saf. 2020 Nov;43(11):1171-1180. doi: 10.1007/s40264-020-00981-w.
4. Orwoll B, et al. Gamification and Microlearning for Engagement With Quality Improvement (GAMEQI): A Bundled Digital Intervention for the Prevention of Central Line-Associated Bloodstream Infection. Am J Med Qual. Jan/Feb 2018;33(1):21-29. doi: 10.1177/1062860617706542.
The vast amounts of information generated this past year related to the COVID-19 pandemic was a feat of wonder – recommendations and guidelines on the hospital level and on the national level came in a flurry, more often overwhelming and confusing than clarifying for the frontline provider. In addition, “routine” hospital care for non-infected patients and improvement processes had to continue as we all dealt with the whirlwind of increasing COVID cases, torrents of new guidelines, and educating our trainees.
Thus, the individual-level question: how does a clinician stay engaged and distill the relentless stream of new information?
In Spring 2020, when the first patients with COVID were admitted, our hospital medicine section was tasked to create a surge plan. This included organizing, orienting, and educating off-service providers on how to become hospitalists. Undoubtedly, the call to arms for our center was heard, and many responded. However, backgrounds were diverse in specialty – clinicians and trainees from psychiatry, general surgery, and various fellowships all answered. It was an exhausting and inefficient effort to produce the material, hold webinars, and schedule training, especially for those who were more removed from a hospital medicine experience. We knew we had to come up with an alternative plan moving forward.
Thus, the systems-level question: how does a health care system educate its clinicians, or any other health care providers, when reallocation of their talents and skills is both necessary, time-sensitive, and occuring during a period where new information is constantly being produced and changing?
To reach the most clinicians as possible, with the most succinct and distilled information, we had to come up with a method to do so. Ultimately, in considering the situation at hand, we had to understand who we were as the provider of the information, and who the recipient would be. We would like to share the initiatives and processes by which we constructed our solution to the two questions – microlearning through hospital podcasting.
Learning from our health care colleagues
With the initial webinars and training sessions for our staff, we assessed our learners’ motivations and background in managing in a hospital medicine capacity. Overall, we discovered that our trainees and clinicians have an innate drive to learn; all of them recognized the importance of keeping up with evidence-based information. However, the difficulty highlighted was the individual time available to dedicate to acquiring new information and awareness of new information being available to the health care sector during the chaotic times of the pandemic.
From our section’s perspective, we had a difficulty with coordinating among multiple professional development groups within our hospital, cost, and resources to execute training. These difficulties between providing knowledge and receiving knowledge have already been expertly analyzed.1
Parallel to this, the pedagogic paradigm shifts as we progress through our careers – the methods and skills we used in school contrast in many ways with those we use on a daily basis when it comes to learning. Instead of dedicating hours at a time to new challenges in our workflow or our interests, we watch videos, search retailers for product solutions, check our email correspondence, and peruse social media accounts several times a day. Information comes at us very quickly, but in small pieces.
One such innovation in pedagogy is the practice of microlearning. This refers to the use of small lesson modules and short-term activities intended to teach and reinforce concepts.2 It is the opposite of “macrolearning,” which is the principle of dedicating reading material, structured coursework, and traditional knowledge evaluation in the form of exams to reinforce learning. Certainly, microlearning has other names as well – “just-in-time,” “just-enough,” and “micro-courses” are a few synonyms seen in the current literature. Though a highly relevant concept for our situation, translating it to an endproduct for our trainees and clinicians required more thought.
From theory to application
Microlearning allows for faster delivery of information – fewer things to write means shorter course distribution times, allowing the learner to respond faster to changing educational goals and training demands. Microlearning is flexible – “micro-courses” can give a broad overview of a subject or cover complex topics broken down into simple parts. In addition, micro-learning promotes retention of key concepts – given the length of each lesson, repetition of the topic by the learner is possible at any point in time. The whole experience is similar to checking your favorite social media application on your smartphone.
Certainly, many examples of the application of microlearning are available in the health care sector – pharmaceutical and nursing training both have utilized the theory extensively.3-4 However, in many instances, individuals were still required to sit at a workstation to complete modules and lessons. We envisioned our application of microlearning to be “on-the-go,” without necessarily requiring a computer workstation or laptop to complete.
In thinking about how social media attracts and influences clinicians, many content creators on social media come to mind. In addition, most, if not all, have branched into various social media platforms – podcasting, blogging, YouTube, for example. In thinking about our colleagues and trainees, we wanted a platform that they could take on the go, without the need to focus their visual attention (such as while driving or running). Ultimately, we believe the podcast would be the best platform to disseminate our information.
Podcasting is not foreign to medicine. A variety of medical podcasts exist, whether produced by major medical journals or by various independent health care practitioners. Both, however, have their drawbacks – the podcasts created by major medical journals are typically a summary of the publication’s content and are less engaging. Alternatively, podcasts produced by independent creators are certainly engaging and entertaining, and have a wealth of information, but the line is often blurred between just that: education and entertainment. In both instances, there is no follow-up or feedback offered to the learner in the form of surveys, or other types of feedback, which is arguably an important piece in any form of pedagogy. Thus, we sought to strike a balance between the two forms for our purposes.
Process of two podcasts
Our section was aware of the two aims during the pandemic – (1) disseminate new information regarding COVID-19 to the rest of our staff members and trainees as quickly as possible, and (2) maintain and improve the current quality of care of our patients. Thus, we sought to apply the reach and efficiency of the podcasting medium to provide ongoing education and feedback with respect to these two aims.
“The Cure” podcast. We recognized the constant flow of new COVID-19 information and updates and we wanted to find a readily accessible platform to reach staff with timely updates. Our marketing & communications team later helped us realize that the content we wanted to share was relevant to our patients and the community, so we formatted the material to be practical and easily digestible- something that may help an individual make decisions at the bedside as well as have conversations at the dinner table. Most recently, we engaged with our human resources department to use our platform in orienting new hires with the goal of helping staff familiarize with the institutions policies, procedures, and job aids that keep staff and patients safe.
“Antibiotry” podcast. Prior to the COVID-19 pandemic, our antibiotic stewardship group noticed an increase in antibiotic use on our medical floors. This is monitored not only through internal metrics by our pharmacy department, but also via the SAAR (standardized antibiotic administration ratio). Both sources demonstrated an increase in antibiotic use, greater than expected. An initiative was formed between our hospital medicine and infectious disease sections, and our pharmacy department to raise awareness of this increase in use, provide education to our trainees, and to create systems solutions for clinicians.
Initially, we sought to hold in-person sessions once a month for our trainees. This was led by a senior resident at the time. Topics of discussion were geared towards clinical decision making regarding empiric antibiotic use on the hospital medicine service. At the same time, our team published empiric antibiotic use guidelines, accessible through our electronic medical record. In addition, the resident leader gave a voluntary survey at the end of the session to assess not only confidence of antibiotic use, but also baseline knowledge regarding antibiotics in various clinical scenarios. This survey was repeated at the end of the resident group’s month-long rotation. Altogether, each in-person session was no longer than 10 minutes.
Unfortunately, the initiative was just gaining momentum when the COVID-19 pandemic was declared. However, we sought to take this challenge and translate it into an opportunity.
We directed our focus towards stewardship during pandemic times. Initially, our resident leader sent out email primers, approximately 3-5 minute reads, as a substitute for the in-person sessions. Our primers’ uniqueness was in its incorporation of prescription pattern data that was developed by our resident leader and our initiative’s data analyst. In doing so, we provided professional feedback regarding our antibiotic use based on the clinical indication. This was a powerful tool to not only engage our learners and staff clinicians, but also as a benchmarking tool for continued quality improvement.
But email primers are not engaging, and despite the ubiquity of teleconferencing, it was difficult to ask our housestaff to break from their morning rounds for a 10 minute tele-meeting. Thus, we devised a podcast method of education – 5-10 minute audio clips with conversation regarding a topic of discussion. This way, our trainees and learners can access episodes of education on their own time throughout the pandemic without disrupting their workflow. Given the brevity of, but high-yield content in, each episode, it would not only be convenient for listeners to access and repeat, but also for the podcaster (our resident leader) to create, as recording of the audio portion takes anywhere between 10-20 minutes for each episode, with postprocessing similarly fast.
The interdisciplinary nature of continued medical education cannot be stressed enough. With the help of our professional development team and their educators, we were able to centralize our podcast and attach surveys and additional graphics for each episode, if appropriate. This additional detail allowed for feedback, engagement with our learners, and the chance to provide additional educational points, if the learner was interested. Given the integrated nature of this platform, quality metrics could easily be recorded in the form of “click” data and various other more conventional metrics, such as listener counts and the duration of each podcast played.
Future applications and initiatives
Thus far, we have had great success in the reception and use of both podcasts within our institution as an application of microlearning. “The Cure” has been widely listened to by all hospital staff from various services; it has caught the attention of state-wide radio programs, and plans to expand it into the community are being discussed.
As for “Antibiotry” podcast, the concept has been lauded by our medical educators. Given its centralization within our institution, we are able to publish institution-based data as a form of professional and educational feedback to our trainees and staff physicians. This is currently coupled with the development of a provider dashboard, visualizing antibiotic prescriptions and narrowing patterns of practice within our medicine department. We plan to expand “Antibiotry” to other services at the hospital.
For both podcasts, the steps it took to achieve the final product from the microlearning concept were possible through a combination of institutional need and a motivated team. We are fortunate to have highly energetic individuals, making the coordination and planning with our hospitalists, various sub-specialists, and professional development teams straightforward. As the team grows with more individuals interested in the initiatives, keen insight into interests, individual clinical expertise, presentation skills, and technical skills ought to be carefully weighed to sustain our podcasts most efficiently, and perhaps expand them through different social media platforms.
Our objective for sustainability is through the continued outreach to and recruitment of residents and medical students, who can play key roles in the development of future projects related to these educational innovations. Both microlearning podcasts were developed through the initial planning, trial and error, and execution by two resident leaders. Their initiative and motivation to educate our institution through these platforms were highly unique; their pathfinding set the foundation for sustainability and expansion to other services.
Of course, one of the key measures we would like to investigate is whether our microlearning platform translates to improved patient outcomes. Regarding “Antibiotry,” we hope to see a decrease in unnecessary broad-spectrum antibiotic use by drawing attention to clinician practice patterns. Quality and outcome metrics will continue to be developed and measured. In addition to patient care metrics, further investigation of pedagogical metrics will be conducted, especially in the evolving realm of graduate and continuing medical education.
Measuring educational quality is neither a new ethical nor philosophical debate – neither does it carry a definitive answer. Further help from education experts may be needed to assess the quality of the information provided and its impact on our learners.
Conclusion
Medicine is ever-changing – the guidelines and criteria for patient care and pathology that we learned in medical school have likely changed. There is no single “best” method of learning new information in medicine, simply due to the breadth and volume of such information generated on a daily basis. This poses both a challenge for present-day clinicians and trainees, and a stimulus for change in the methods of acquiring, absorbing, and applying new information to clinical decision making and practice.
We have found that podcasting is a well-received medium of information transfer that is convenient for both the learner and the content creator. Through the podcast format, we were able to distill non-engaging pieces of education and information and transform them into short-duration lessons that the learner can listen to at their own convenience. This proved to be especially handy during the chaos of the pandemic, not only for dissemination of information regarding the management of COVID-19, but also for sustaining quality improvement goals within our institution.
Further investigation on patient outcomes and information quality are the planned next steps. In addition, expansion of other microlearning media, such as group SMS texting, YouTube videos, and Twitter, ought to be considered. Though many publications discuss the theory, potential benefits, and predicted pitfalls of microlearning, few assess the real-world application of microlearning to the clinical setting for medical education.
So what did we learn? We should think of microlearning as moments when you turn to your smartphone or tablet in order to discover something, answer a question, or complete a task. These are moments when decisions are made and knowledge is reinforced. The goal is to capture these moments and fill them with essential pieces of information.
We offer these suggestions as a place to start. The microlearning platform allows for the collection of data on the interaction between user and course content. The data collected can be used for continuous quality improvement of the curriculum. Microlearning is a dynamic platform where creative ideas are encouraged and a multi-disciplinary approach is valuable to keeping an audience engaged. In the future, we hope to be able to correlate microlearning courses to provider performance and measurable patient outcomes.
Dr. Mercado is medical director at Alice Peck Day Memorial Hospital, and associate hospital epidemiologist, Dartmouth-Hitchcock Medical Center, both in Lebanon, N.H., and assistant professor at the Geisel School of Medicine at Dartmouth, Hanover, N.H. Dr. Feng is a Fellow in the Leadership/Preventive Medicine Program in the Department of Internal Medicine at Dartmouth-Hitchcock Medical Center.
References
1. Duggan F and Banwell L. Constructing a model of effective information dissemination in a crisis. Information Research. 2004;9(3). Paper 178 [Available at http://InformationR.net/ir/9-3/paper178.html].
2. Filipe HP, et al. Microlearning to improve CPD learning objectives. Clin Teach. 2020 Dec;17(6):695-699. doi: 10.1111/tct.13208.
3. Hegerius A, et al. E-Learning in Pharmacovigilance: An Evaluation of Microlearning-Based Modules Developed by Uppsala Monitoring Centre. Drug Saf. 2020 Nov;43(11):1171-1180. doi: 10.1007/s40264-020-00981-w.
4. Orwoll B, et al. Gamification and Microlearning for Engagement With Quality Improvement (GAMEQI): A Bundled Digital Intervention for the Prevention of Central Line-Associated Bloodstream Infection. Am J Med Qual. Jan/Feb 2018;33(1):21-29. doi: 10.1177/1062860617706542.
PHM virtual conference promises practical pearls, plus Dr. Fauci
The Pediatric Hospital Medicine annual conference, though virtual in 2021, promises to retain its role as the premier educational event for pediatric hospitalists and other clinicians involved in treating pediatric patients.
The “can’t-miss” session, on August 5, at 6:30 p.m. ET, is a one-on-one discussion between Anthony S. Fauci, MD, and Lee Savio Beers, MD, president of the American Academic of Pediatrics, according to members of the meeting planning committee.
In addition to the conversation between Dr. Beers and Dr. Fauci, this year’s meeting offers a mix of workshops with pointers and pearls to improve practice, keynote and plenary sessions to inform and inspire, and abstract presentations of new research. Three members of the PHM Planning Committee shared their insights on the hot topics, advice for new clinicians, and tips for making the most of this year’s meeting.
Workshops worth watching
“The keynote plenary sessions by Julie Silver, MD, on ‘Accelerating Patient Care and Healthcare Workforce Diversity and Inclusion,’ and by Ilan Alhadeff, MD, on ‘Leading through Adversity’ should inspire even the least enthusiastic among us,” Mirna Giordano, MD, FHM, of Columbia University Medical Center, New York, said in an interview. A talk by Nathan T. Chomilo, MD, “will likely prompt reflection on how George Floyd’s death changed us, and how we practice medicine forever.” In addition, “PHM Stories are not to be missed, they are voices that speak loud and move mountains.”
The PHM Stories are concise, narrative talks with minimal use of slides; each PHM Stories session includes three distinct talks and a 15-minute question and answer session. PHM Stories sessions are scheduled for each day of the conference, and topics include “Practicing Medicine While Human: The Secrets Physicians Keep,” by Uchenna Ewulonu, MD; “Finding the Power of the Imposter: How I Learned to Be Exactly the Color I Am, Everywhere I Go,” by Alexandra Coria, MD; and “Purple Butterflies: A Reflection on Why I’m a Pediatric Hospitalist,” by Joanne Mendoza, MD.
“The PHM community has been through a lot in the aftermath of the pandemic,” said Dr. Giordano. “The mini-plenary session on the mental health needs of our patients, and clinical quick-hit sessions on verbal deescalation of the agitated patients and cardiac effects of COVID-19 will likely be not only very popular, but also useful in clinical endeavors. The workshop on how to navigate the adult issues in hospitalized patients will provide the Med-Peds pearls we all wish we heard earlier.”
Although a 75-minute workshop session may seem long, “the workshop choices will offer something for everyone’s taste: education, research, clinical topics, diversity, and advocacy,” Dr. Giordano said. “I suggest that attendees check in advance which sessions will be available after the meeting, so that they prioritize highly interactive sessions like workshops, and that they experience, even if virtual, small group/room gatherings and networking.” There will be time for fun, too, she emphasized, with social sessions “that we hope will break the screen monotony and bring smiles to everyone’s faces.”
For younger clinicians relatively new to practice, Dr. Giordano recommended several workshops for a wealth of advice and guidance, including “New Kids on the Block: Thriving in your First Faculty Position,” “Channeling Your Inner Coach: Techniques to Enhance Clinical Teaching & Feedback,” “Palliative Care Pearls for the Pediatric Hospitalist,” “Perioperative Medicine for Medically Complex Children: Case Studies in Programmatic Approaches,” “The Bare Necessities: Social Determinant of Health Screening for the Hospitalist,” and “Mentorship, Autonomy, and Supervising a PHM Fellow.”
Classic topics and new concepts
“We are so excited to be able to offer a full spectrum of offerings at this year’s virtual meeting,” Yemisi Jones, MD, FHM, of Cincinnati Children’s Hospital, said in an interview. “We are covering some classic topics that we can’t do without at PHM, such as clinical updates in the management of sick and well newborns; workshops on best practices for educators; as well as the latest in PHM scholarship.” Sessions include “timely topics such as equity for women in medicine with one of our plenary speakers, Julie Silver, MD, and new febrile infant guidelines,” she added.
In particular, the COVID-19 and mental health session will help address clinicians’ evolving understanding of the COVID-19 pandemic and its effects on hospitalized children, said Dr. Jones. “Attendees can expect practical, timely updates on the current state of the science and ways to improve their practice to provide the best care for our patients.”
Attendees will be able to maximize the virtual conference format by accessing archived recordings, including clinical quick hits, mini-plenaries, and PHM Stories, which can be viewed during the scheduled meeting time or after, Dr. Jones said. “Workshops and abstract presentations will involve real-time interaction with presenters, so would be highest yield to attend during the live meeting. We also encourage all participants to take full advantage of the platform and the various networking opportunities to engage with others in our PHM community.”
For residents and new fellows, Dr. Jones advised making the workshop, “A Whole New World: Tips and Tools to Soar Into Your First Year of Fellowship,” a priority. “For early-career faculty, the ‘New Kids on the Block: Thriving in your First Faculty Position workshop will be a valuable resource.”
Make the meeting content a priority
This year’s conference has an exceptional slate of plenary speakers, Michelle Marks, DO, SFHM, of the Cleveland Clinic said in an interview. In addition to the much-anticipated session on vaccinations, school guidelines, and other topics with Dr. Fauci and Dr. Beers, the sessions on leading through adversity and workforce diversity and inclusion are “important topics to the PHM community and to our greater communities as a whole.”
Dr. Marks also highlighted the value of the COVID-19 and mental health session, as the long-term impact of COVID-19 on mental health of children and adults continues to grab headlines. “From this session specifically, I hope the attendees will gain awareness of the special mental health needs for child during a global disaster like a pandemic, which can be generalized to other situations and gain skills and resources to help meet and advocate for children’s mental health needs.”
For clinicians attending the virtual conference, “The most important strategy is to schedule time off of clinical work for the virtual meeting if you can so you can focus on the content,” said Dr. Marks. “For the longer sessions, it would be very important to block time in your day to fully attend the session, attend in a private space if possible since there will be breakouts with discussion, have your camera on, and engage with the workshop group as much as possible. The virtual format can be challenging because of all the external distractions, so intentional focus is necessary,” to get the most out of the experience.
The mini-plenary session on “The New AAP Clinical Practice Guideline on the Evaluation and Management of Febrile Infants 8-60 Days Old,” is an important session for all attendees, Dr. Marks said. She also recommended the Clinical Quick Hits sessions for anyone seeking “a diverse array of practical knowledge which can be easily applied to everyday practice.” The Clinical Quick Hits are designed as 35-minute, rapid-fire presentations focused on clinical knowledge. Each of these presentations will focus on the latest updates or evolutions in clinical practice in one area. Some key topics include counseling parents when a child has an abnormal exam finding, assessing pelvic pain in adolescent girls, and preventing venous thromboembolism in the inpatient setting.
“I would also recommend that younger clinicians take in at least one or two workshops or sessions on nonclinical topics to see the breath of content at the meeting and to develop a niche interest for themselves outside of clinical work,” Dr. Marks noted.
Nonclinical sessions at PHM 2021 include workshops on a pilot for a comprehensive LGBTQ+ curriculum, using media tools for public health messaging, and practicing health literacy.
To register for the Pediatric Hospital Medicine 2021 virtual conference, visit https://apaevents.regfox.com/phm21-virtual-conference.
Dr. Giordano, Dr. Jones, and Dr. Marks are members of the PHM conference planning committee and had no relevant financial conflicts to disclose.
The Pediatric Hospital Medicine annual conference, though virtual in 2021, promises to retain its role as the premier educational event for pediatric hospitalists and other clinicians involved in treating pediatric patients.
The “can’t-miss” session, on August 5, at 6:30 p.m. ET, is a one-on-one discussion between Anthony S. Fauci, MD, and Lee Savio Beers, MD, president of the American Academic of Pediatrics, according to members of the meeting planning committee.
In addition to the conversation between Dr. Beers and Dr. Fauci, this year’s meeting offers a mix of workshops with pointers and pearls to improve practice, keynote and plenary sessions to inform and inspire, and abstract presentations of new research. Three members of the PHM Planning Committee shared their insights on the hot topics, advice for new clinicians, and tips for making the most of this year’s meeting.
Workshops worth watching
“The keynote plenary sessions by Julie Silver, MD, on ‘Accelerating Patient Care and Healthcare Workforce Diversity and Inclusion,’ and by Ilan Alhadeff, MD, on ‘Leading through Adversity’ should inspire even the least enthusiastic among us,” Mirna Giordano, MD, FHM, of Columbia University Medical Center, New York, said in an interview. A talk by Nathan T. Chomilo, MD, “will likely prompt reflection on how George Floyd’s death changed us, and how we practice medicine forever.” In addition, “PHM Stories are not to be missed, they are voices that speak loud and move mountains.”
The PHM Stories are concise, narrative talks with minimal use of slides; each PHM Stories session includes three distinct talks and a 15-minute question and answer session. PHM Stories sessions are scheduled for each day of the conference, and topics include “Practicing Medicine While Human: The Secrets Physicians Keep,” by Uchenna Ewulonu, MD; “Finding the Power of the Imposter: How I Learned to Be Exactly the Color I Am, Everywhere I Go,” by Alexandra Coria, MD; and “Purple Butterflies: A Reflection on Why I’m a Pediatric Hospitalist,” by Joanne Mendoza, MD.
“The PHM community has been through a lot in the aftermath of the pandemic,” said Dr. Giordano. “The mini-plenary session on the mental health needs of our patients, and clinical quick-hit sessions on verbal deescalation of the agitated patients and cardiac effects of COVID-19 will likely be not only very popular, but also useful in clinical endeavors. The workshop on how to navigate the adult issues in hospitalized patients will provide the Med-Peds pearls we all wish we heard earlier.”
Although a 75-minute workshop session may seem long, “the workshop choices will offer something for everyone’s taste: education, research, clinical topics, diversity, and advocacy,” Dr. Giordano said. “I suggest that attendees check in advance which sessions will be available after the meeting, so that they prioritize highly interactive sessions like workshops, and that they experience, even if virtual, small group/room gatherings and networking.” There will be time for fun, too, she emphasized, with social sessions “that we hope will break the screen monotony and bring smiles to everyone’s faces.”
For younger clinicians relatively new to practice, Dr. Giordano recommended several workshops for a wealth of advice and guidance, including “New Kids on the Block: Thriving in your First Faculty Position,” “Channeling Your Inner Coach: Techniques to Enhance Clinical Teaching & Feedback,” “Palliative Care Pearls for the Pediatric Hospitalist,” “Perioperative Medicine for Medically Complex Children: Case Studies in Programmatic Approaches,” “The Bare Necessities: Social Determinant of Health Screening for the Hospitalist,” and “Mentorship, Autonomy, and Supervising a PHM Fellow.”
Classic topics and new concepts
“We are so excited to be able to offer a full spectrum of offerings at this year’s virtual meeting,” Yemisi Jones, MD, FHM, of Cincinnati Children’s Hospital, said in an interview. “We are covering some classic topics that we can’t do without at PHM, such as clinical updates in the management of sick and well newborns; workshops on best practices for educators; as well as the latest in PHM scholarship.” Sessions include “timely topics such as equity for women in medicine with one of our plenary speakers, Julie Silver, MD, and new febrile infant guidelines,” she added.
In particular, the COVID-19 and mental health session will help address clinicians’ evolving understanding of the COVID-19 pandemic and its effects on hospitalized children, said Dr. Jones. “Attendees can expect practical, timely updates on the current state of the science and ways to improve their practice to provide the best care for our patients.”
Attendees will be able to maximize the virtual conference format by accessing archived recordings, including clinical quick hits, mini-plenaries, and PHM Stories, which can be viewed during the scheduled meeting time or after, Dr. Jones said. “Workshops and abstract presentations will involve real-time interaction with presenters, so would be highest yield to attend during the live meeting. We also encourage all participants to take full advantage of the platform and the various networking opportunities to engage with others in our PHM community.”
For residents and new fellows, Dr. Jones advised making the workshop, “A Whole New World: Tips and Tools to Soar Into Your First Year of Fellowship,” a priority. “For early-career faculty, the ‘New Kids on the Block: Thriving in your First Faculty Position workshop will be a valuable resource.”
Make the meeting content a priority
This year’s conference has an exceptional slate of plenary speakers, Michelle Marks, DO, SFHM, of the Cleveland Clinic said in an interview. In addition to the much-anticipated session on vaccinations, school guidelines, and other topics with Dr. Fauci and Dr. Beers, the sessions on leading through adversity and workforce diversity and inclusion are “important topics to the PHM community and to our greater communities as a whole.”
Dr. Marks also highlighted the value of the COVID-19 and mental health session, as the long-term impact of COVID-19 on mental health of children and adults continues to grab headlines. “From this session specifically, I hope the attendees will gain awareness of the special mental health needs for child during a global disaster like a pandemic, which can be generalized to other situations and gain skills and resources to help meet and advocate for children’s mental health needs.”
For clinicians attending the virtual conference, “The most important strategy is to schedule time off of clinical work for the virtual meeting if you can so you can focus on the content,” said Dr. Marks. “For the longer sessions, it would be very important to block time in your day to fully attend the session, attend in a private space if possible since there will be breakouts with discussion, have your camera on, and engage with the workshop group as much as possible. The virtual format can be challenging because of all the external distractions, so intentional focus is necessary,” to get the most out of the experience.
The mini-plenary session on “The New AAP Clinical Practice Guideline on the Evaluation and Management of Febrile Infants 8-60 Days Old,” is an important session for all attendees, Dr. Marks said. She also recommended the Clinical Quick Hits sessions for anyone seeking “a diverse array of practical knowledge which can be easily applied to everyday practice.” The Clinical Quick Hits are designed as 35-minute, rapid-fire presentations focused on clinical knowledge. Each of these presentations will focus on the latest updates or evolutions in clinical practice in one area. Some key topics include counseling parents when a child has an abnormal exam finding, assessing pelvic pain in adolescent girls, and preventing venous thromboembolism in the inpatient setting.
“I would also recommend that younger clinicians take in at least one or two workshops or sessions on nonclinical topics to see the breath of content at the meeting and to develop a niche interest for themselves outside of clinical work,” Dr. Marks noted.
Nonclinical sessions at PHM 2021 include workshops on a pilot for a comprehensive LGBTQ+ curriculum, using media tools for public health messaging, and practicing health literacy.
To register for the Pediatric Hospital Medicine 2021 virtual conference, visit https://apaevents.regfox.com/phm21-virtual-conference.
Dr. Giordano, Dr. Jones, and Dr. Marks are members of the PHM conference planning committee and had no relevant financial conflicts to disclose.
The Pediatric Hospital Medicine annual conference, though virtual in 2021, promises to retain its role as the premier educational event for pediatric hospitalists and other clinicians involved in treating pediatric patients.
The “can’t-miss” session, on August 5, at 6:30 p.m. ET, is a one-on-one discussion between Anthony S. Fauci, MD, and Lee Savio Beers, MD, president of the American Academic of Pediatrics, according to members of the meeting planning committee.
In addition to the conversation between Dr. Beers and Dr. Fauci, this year’s meeting offers a mix of workshops with pointers and pearls to improve practice, keynote and plenary sessions to inform and inspire, and abstract presentations of new research. Three members of the PHM Planning Committee shared their insights on the hot topics, advice for new clinicians, and tips for making the most of this year’s meeting.
Workshops worth watching
“The keynote plenary sessions by Julie Silver, MD, on ‘Accelerating Patient Care and Healthcare Workforce Diversity and Inclusion,’ and by Ilan Alhadeff, MD, on ‘Leading through Adversity’ should inspire even the least enthusiastic among us,” Mirna Giordano, MD, FHM, of Columbia University Medical Center, New York, said in an interview. A talk by Nathan T. Chomilo, MD, “will likely prompt reflection on how George Floyd’s death changed us, and how we practice medicine forever.” In addition, “PHM Stories are not to be missed, they are voices that speak loud and move mountains.”
The PHM Stories are concise, narrative talks with minimal use of slides; each PHM Stories session includes three distinct talks and a 15-minute question and answer session. PHM Stories sessions are scheduled for each day of the conference, and topics include “Practicing Medicine While Human: The Secrets Physicians Keep,” by Uchenna Ewulonu, MD; “Finding the Power of the Imposter: How I Learned to Be Exactly the Color I Am, Everywhere I Go,” by Alexandra Coria, MD; and “Purple Butterflies: A Reflection on Why I’m a Pediatric Hospitalist,” by Joanne Mendoza, MD.
“The PHM community has been through a lot in the aftermath of the pandemic,” said Dr. Giordano. “The mini-plenary session on the mental health needs of our patients, and clinical quick-hit sessions on verbal deescalation of the agitated patients and cardiac effects of COVID-19 will likely be not only very popular, but also useful in clinical endeavors. The workshop on how to navigate the adult issues in hospitalized patients will provide the Med-Peds pearls we all wish we heard earlier.”
Although a 75-minute workshop session may seem long, “the workshop choices will offer something for everyone’s taste: education, research, clinical topics, diversity, and advocacy,” Dr. Giordano said. “I suggest that attendees check in advance which sessions will be available after the meeting, so that they prioritize highly interactive sessions like workshops, and that they experience, even if virtual, small group/room gatherings and networking.” There will be time for fun, too, she emphasized, with social sessions “that we hope will break the screen monotony and bring smiles to everyone’s faces.”
For younger clinicians relatively new to practice, Dr. Giordano recommended several workshops for a wealth of advice and guidance, including “New Kids on the Block: Thriving in your First Faculty Position,” “Channeling Your Inner Coach: Techniques to Enhance Clinical Teaching & Feedback,” “Palliative Care Pearls for the Pediatric Hospitalist,” “Perioperative Medicine for Medically Complex Children: Case Studies in Programmatic Approaches,” “The Bare Necessities: Social Determinant of Health Screening for the Hospitalist,” and “Mentorship, Autonomy, and Supervising a PHM Fellow.”
Classic topics and new concepts
“We are so excited to be able to offer a full spectrum of offerings at this year’s virtual meeting,” Yemisi Jones, MD, FHM, of Cincinnati Children’s Hospital, said in an interview. “We are covering some classic topics that we can’t do without at PHM, such as clinical updates in the management of sick and well newborns; workshops on best practices for educators; as well as the latest in PHM scholarship.” Sessions include “timely topics such as equity for women in medicine with one of our plenary speakers, Julie Silver, MD, and new febrile infant guidelines,” she added.
In particular, the COVID-19 and mental health session will help address clinicians’ evolving understanding of the COVID-19 pandemic and its effects on hospitalized children, said Dr. Jones. “Attendees can expect practical, timely updates on the current state of the science and ways to improve their practice to provide the best care for our patients.”
Attendees will be able to maximize the virtual conference format by accessing archived recordings, including clinical quick hits, mini-plenaries, and PHM Stories, which can be viewed during the scheduled meeting time or after, Dr. Jones said. “Workshops and abstract presentations will involve real-time interaction with presenters, so would be highest yield to attend during the live meeting. We also encourage all participants to take full advantage of the platform and the various networking opportunities to engage with others in our PHM community.”
For residents and new fellows, Dr. Jones advised making the workshop, “A Whole New World: Tips and Tools to Soar Into Your First Year of Fellowship,” a priority. “For early-career faculty, the ‘New Kids on the Block: Thriving in your First Faculty Position workshop will be a valuable resource.”
Make the meeting content a priority
This year’s conference has an exceptional slate of plenary speakers, Michelle Marks, DO, SFHM, of the Cleveland Clinic said in an interview. In addition to the much-anticipated session on vaccinations, school guidelines, and other topics with Dr. Fauci and Dr. Beers, the sessions on leading through adversity and workforce diversity and inclusion are “important topics to the PHM community and to our greater communities as a whole.”
Dr. Marks also highlighted the value of the COVID-19 and mental health session, as the long-term impact of COVID-19 on mental health of children and adults continues to grab headlines. “From this session specifically, I hope the attendees will gain awareness of the special mental health needs for child during a global disaster like a pandemic, which can be generalized to other situations and gain skills and resources to help meet and advocate for children’s mental health needs.”
For clinicians attending the virtual conference, “The most important strategy is to schedule time off of clinical work for the virtual meeting if you can so you can focus on the content,” said Dr. Marks. “For the longer sessions, it would be very important to block time in your day to fully attend the session, attend in a private space if possible since there will be breakouts with discussion, have your camera on, and engage with the workshop group as much as possible. The virtual format can be challenging because of all the external distractions, so intentional focus is necessary,” to get the most out of the experience.
The mini-plenary session on “The New AAP Clinical Practice Guideline on the Evaluation and Management of Febrile Infants 8-60 Days Old,” is an important session for all attendees, Dr. Marks said. She also recommended the Clinical Quick Hits sessions for anyone seeking “a diverse array of practical knowledge which can be easily applied to everyday practice.” The Clinical Quick Hits are designed as 35-minute, rapid-fire presentations focused on clinical knowledge. Each of these presentations will focus on the latest updates or evolutions in clinical practice in one area. Some key topics include counseling parents when a child has an abnormal exam finding, assessing pelvic pain in adolescent girls, and preventing venous thromboembolism in the inpatient setting.
“I would also recommend that younger clinicians take in at least one or two workshops or sessions on nonclinical topics to see the breath of content at the meeting and to develop a niche interest for themselves outside of clinical work,” Dr. Marks noted.
Nonclinical sessions at PHM 2021 include workshops on a pilot for a comprehensive LGBTQ+ curriculum, using media tools for public health messaging, and practicing health literacy.
To register for the Pediatric Hospital Medicine 2021 virtual conference, visit https://apaevents.regfox.com/phm21-virtual-conference.
Dr. Giordano, Dr. Jones, and Dr. Marks are members of the PHM conference planning committee and had no relevant financial conflicts to disclose.
Hospitalist movers and shakers – July 2021
Vineet Arora, MD, MHM, has been appointed dean of medical education for the University of Chicago’s biological sciences division. She began her assignment on July 1, 2021, taking over for the retiring Halina Brukner, MD, a 36-year veteran in medicine.
Dr. Arora will take charge of undergraduate, graduate, and continuing education for the University of Chicago’s medical education program, with a focus on simulation-based training. She also will represent the medical school within the university proper, as well as with outside organizations such as the Association of American Colleges, the Liaison Committee on Medical Education, and the Accreditation Council for Graduate Medical Education.
Dr. Arora has been a faculty member at Chicago Medicine since 2005. She is a professor of medicine, assistant dean for scholarship and discovery, associate chief medical officer for clinical learning, and Master of the Academy of Distinguished Medical Educators. Dr. Arora is a member of the National Academy of Medicine and is on the board of directors for the American Board of Internal Medicine.
Zeshan Anwar, MD, SFHM, was named new chief of the section of inpatient internal medicine and director of hospitalist services at Reading Hospital–Tower Health (West Reading, Pa.) in January 2021. He provides support to hospitalists, nurses, pharmacists, care managers, support service professionals and others.
Previously, Dr. Anwar worked as vice chair of the department of medicine and medical director of the hospitalist program at Evangelical Community Hospital (Lewisburg, Pa.). He has a background in education, having taught as an assistant professor of clinical medicine at Geisinger Commonwealth School of Medicine (Scranton, Pa.) since 2014.
Katherine Hochman, MD, FHM, has been appointed the first director of the newly established division of hospital medicine at NYU Langone Health in New York. Dr. Hochman is the founder of NYU Langone’s hospitalist program (2004), and the new division was established this year in the wake of the COVID-19 pandemic.
Dr. Hochman will be charged with expanding on the hospitalist program, analyzing best practices, and educating residents, clinicians, and other health care professionals. She plans to emphasize mentorship and creating career pathways for the program’s students.
Dr. Hochman was NYU Langone’s first hospitalist and later became associate program director of medicine at Langone’s Tisch Hospital. She helped grow the hospitalist program to 40 professionals in 2020.
Daniel Asher, MD, recently was named a Top Hospitalist by Continental Who’s Who. Dr. Asher is a night hospitalist at Piedmont Columbus Regional (Columbus, Ga.), where he works with residents and consults with other physicians regarding patients at the facility.
Dr. Asher has spent his entire post–medical school career at Piedmont, serving as a family medicine resident from 2018 to 2020. He was named chief resident in 2019-20, and has continued his efforts at the hospital since then, including front-line work with COVID-19 patients.
Nicholas O’Dell, MD, has been selected as medical director of the Murray Medical Associates hospitalist program at Murray-Calloway County Hospital (Murray, Ky.). Dr. O’Dell, who has been a hospitalist at the facility since 2014, has served as chief medical officer at the hospital since February 2020. He will continue in his role as CMO, but will no longer see clinical patients.
Brad Tate, MD, has been elevated to associate chief medical officer at Children’s Medical Center Plano (Texas), starting in the new leadership role in June 2021.
Dr. Tate has been affiliated with Children’s Health since 2010, when he was a hospitalist in Plano, as well as medical director of the Children’s Health Medical Group Hospitalist Group. He advanced that program from Plano to the network’s Dallas campus.
Touchette Regional Hospital (Centreville, Ill.) has contracted with MEDS Emergency Physician Staffing and Management (O’Fallon, Ill.) to provide inpatient physician and nurse practitioner staffing. The move is an extension of the existing relationship between the two entities, as MEDS has provided emergency room staffing services at Touchette since 2019.
Vineet Arora, MD, MHM, has been appointed dean of medical education for the University of Chicago’s biological sciences division. She began her assignment on July 1, 2021, taking over for the retiring Halina Brukner, MD, a 36-year veteran in medicine.
Dr. Arora will take charge of undergraduate, graduate, and continuing education for the University of Chicago’s medical education program, with a focus on simulation-based training. She also will represent the medical school within the university proper, as well as with outside organizations such as the Association of American Colleges, the Liaison Committee on Medical Education, and the Accreditation Council for Graduate Medical Education.
Dr. Arora has been a faculty member at Chicago Medicine since 2005. She is a professor of medicine, assistant dean for scholarship and discovery, associate chief medical officer for clinical learning, and Master of the Academy of Distinguished Medical Educators. Dr. Arora is a member of the National Academy of Medicine and is on the board of directors for the American Board of Internal Medicine.
Zeshan Anwar, MD, SFHM, was named new chief of the section of inpatient internal medicine and director of hospitalist services at Reading Hospital–Tower Health (West Reading, Pa.) in January 2021. He provides support to hospitalists, nurses, pharmacists, care managers, support service professionals and others.
Previously, Dr. Anwar worked as vice chair of the department of medicine and medical director of the hospitalist program at Evangelical Community Hospital (Lewisburg, Pa.). He has a background in education, having taught as an assistant professor of clinical medicine at Geisinger Commonwealth School of Medicine (Scranton, Pa.) since 2014.
Katherine Hochman, MD, FHM, has been appointed the first director of the newly established division of hospital medicine at NYU Langone Health in New York. Dr. Hochman is the founder of NYU Langone’s hospitalist program (2004), and the new division was established this year in the wake of the COVID-19 pandemic.
Dr. Hochman will be charged with expanding on the hospitalist program, analyzing best practices, and educating residents, clinicians, and other health care professionals. She plans to emphasize mentorship and creating career pathways for the program’s students.
Dr. Hochman was NYU Langone’s first hospitalist and later became associate program director of medicine at Langone’s Tisch Hospital. She helped grow the hospitalist program to 40 professionals in 2020.
Daniel Asher, MD, recently was named a Top Hospitalist by Continental Who’s Who. Dr. Asher is a night hospitalist at Piedmont Columbus Regional (Columbus, Ga.), where he works with residents and consults with other physicians regarding patients at the facility.
Dr. Asher has spent his entire post–medical school career at Piedmont, serving as a family medicine resident from 2018 to 2020. He was named chief resident in 2019-20, and has continued his efforts at the hospital since then, including front-line work with COVID-19 patients.
Nicholas O’Dell, MD, has been selected as medical director of the Murray Medical Associates hospitalist program at Murray-Calloway County Hospital (Murray, Ky.). Dr. O’Dell, who has been a hospitalist at the facility since 2014, has served as chief medical officer at the hospital since February 2020. He will continue in his role as CMO, but will no longer see clinical patients.
Brad Tate, MD, has been elevated to associate chief medical officer at Children’s Medical Center Plano (Texas), starting in the new leadership role in June 2021.
Dr. Tate has been affiliated with Children’s Health since 2010, when he was a hospitalist in Plano, as well as medical director of the Children’s Health Medical Group Hospitalist Group. He advanced that program from Plano to the network’s Dallas campus.
Touchette Regional Hospital (Centreville, Ill.) has contracted with MEDS Emergency Physician Staffing and Management (O’Fallon, Ill.) to provide inpatient physician and nurse practitioner staffing. The move is an extension of the existing relationship between the two entities, as MEDS has provided emergency room staffing services at Touchette since 2019.
Vineet Arora, MD, MHM, has been appointed dean of medical education for the University of Chicago’s biological sciences division. She began her assignment on July 1, 2021, taking over for the retiring Halina Brukner, MD, a 36-year veteran in medicine.
Dr. Arora will take charge of undergraduate, graduate, and continuing education for the University of Chicago’s medical education program, with a focus on simulation-based training. She also will represent the medical school within the university proper, as well as with outside organizations such as the Association of American Colleges, the Liaison Committee on Medical Education, and the Accreditation Council for Graduate Medical Education.
Dr. Arora has been a faculty member at Chicago Medicine since 2005. She is a professor of medicine, assistant dean for scholarship and discovery, associate chief medical officer for clinical learning, and Master of the Academy of Distinguished Medical Educators. Dr. Arora is a member of the National Academy of Medicine and is on the board of directors for the American Board of Internal Medicine.
Zeshan Anwar, MD, SFHM, was named new chief of the section of inpatient internal medicine and director of hospitalist services at Reading Hospital–Tower Health (West Reading, Pa.) in January 2021. He provides support to hospitalists, nurses, pharmacists, care managers, support service professionals and others.
Previously, Dr. Anwar worked as vice chair of the department of medicine and medical director of the hospitalist program at Evangelical Community Hospital (Lewisburg, Pa.). He has a background in education, having taught as an assistant professor of clinical medicine at Geisinger Commonwealth School of Medicine (Scranton, Pa.) since 2014.
Katherine Hochman, MD, FHM, has been appointed the first director of the newly established division of hospital medicine at NYU Langone Health in New York. Dr. Hochman is the founder of NYU Langone’s hospitalist program (2004), and the new division was established this year in the wake of the COVID-19 pandemic.
Dr. Hochman will be charged with expanding on the hospitalist program, analyzing best practices, and educating residents, clinicians, and other health care professionals. She plans to emphasize mentorship and creating career pathways for the program’s students.
Dr. Hochman was NYU Langone’s first hospitalist and later became associate program director of medicine at Langone’s Tisch Hospital. She helped grow the hospitalist program to 40 professionals in 2020.
Daniel Asher, MD, recently was named a Top Hospitalist by Continental Who’s Who. Dr. Asher is a night hospitalist at Piedmont Columbus Regional (Columbus, Ga.), where he works with residents and consults with other physicians regarding patients at the facility.
Dr. Asher has spent his entire post–medical school career at Piedmont, serving as a family medicine resident from 2018 to 2020. He was named chief resident in 2019-20, and has continued his efforts at the hospital since then, including front-line work with COVID-19 patients.
Nicholas O’Dell, MD, has been selected as medical director of the Murray Medical Associates hospitalist program at Murray-Calloway County Hospital (Murray, Ky.). Dr. O’Dell, who has been a hospitalist at the facility since 2014, has served as chief medical officer at the hospital since February 2020. He will continue in his role as CMO, but will no longer see clinical patients.
Brad Tate, MD, has been elevated to associate chief medical officer at Children’s Medical Center Plano (Texas), starting in the new leadership role in June 2021.
Dr. Tate has been affiliated with Children’s Health since 2010, when he was a hospitalist in Plano, as well as medical director of the Children’s Health Medical Group Hospitalist Group. He advanced that program from Plano to the network’s Dallas campus.
Touchette Regional Hospital (Centreville, Ill.) has contracted with MEDS Emergency Physician Staffing and Management (O’Fallon, Ill.) to provide inpatient physician and nurse practitioner staffing. The move is an extension of the existing relationship between the two entities, as MEDS has provided emergency room staffing services at Touchette since 2019.