User login
When worry is excessive: Easing the burden of GAD
THE CASE
Sandra H,* a 24-year-old single woman with a history of asthma, presented to our family medicine clinic as a new patient. Ms. H said she lived at home with her mother. She completed high school but never attended college due to anxiety. She had held several jobs since high school and recently decided to apply to a local college, which prompted a desire to gain control over the anxiety that had been present since middle school. She reported feeling anxious, having difficulty breathing, shaking all over, having difficulty concentrating, and experiencing numbness and tingling in her fingers. She was often irritable at home, which she attributed partly to anxiety but mostly to disrupted sleep. We administered the 7-question Generalized Anxiety Disorder (GAD-7) questionnaire and she scored 15 (of a possible 21) points, indicative of severe anxiety.
●
* The patient’s name has been changed to protect her identity.
Approximately 1 in 5 patients presenting to primary care clinics have at least 1 anxiety disorder and 7.6% have generalized anxiety disorder (GAD).1 Yet many go untreated. The lifetime prevalence of GAD is 3.7% worldwide and 7.8% in the United States.2 Only 5% of cases emerge by age 13,2 but incidence increases through adolescence and young adulthood, with a quarter of all cases occurring by age 25.2 GAD occurs about twice as often in women as it does in men. It is typically recurrent, and many patients require ongoing treatment.2
GAD diagnostic criteria and differential considerations
Diagnosis of GAD requires at least 6 months of excessive worry or anxiety about a variety of circumstances, occurring on most days and for more than half the day.3 The worry or anxiety in GAD is difficult to control, disrupts meaningful areas of life, and surrounds everyday concerns, such as finances, health, or family-related issues. Among adolescents with GAD, worries typically include school performance and may often present as perfectionism.4 At least 3 of the following 6 symptoms result from chronic anxiety: restlessness, fatigue, poor concentration, irritability, muscle tension, and sleep disturbance.2
Rule out other conditions. Make sure symptoms of GAD are not better explained by another medical problem, including other mental disorders or substance use disorders.3 Complaints of anxiety in the context of mania, hypomania, or withdrawal from alcohol or a sedative hypnotic suggest a different underlying cause, thereby requiring a complete history with symptom chronology and collateral information. The pattern of anxiety seen in GAD also differs from the focused sources of anxiety found in disorders such as social anxiety disorder (SAD) and post-traumatic stress disorder. For example, SAD might center on embarrassment in a social setting rather than reflect a pattern of general worry.5
Consider comorbidities. Further complicating diagnosis and treatment, GAD has been linked to higher rates of comorbidity and higher health care utilization. About 90% of GAD patients experience psychiatric comorbidity, with major depressive disorder co-occurring about 60% of the time.6 Substance use disorders co-occur with GAD more than 20% of the time.2 Despite comorbidities, it is the somatic complaints in GAD that often drive patient requests for medical care.7,8 GAD itself is an independent predictor of heart disease9 and is linked to increased risk of chronic or severe headaches10 and suicide.11,12
Continue to: Work with patients and family toward a diagnosis
Work with patients and family toward a diagnosis
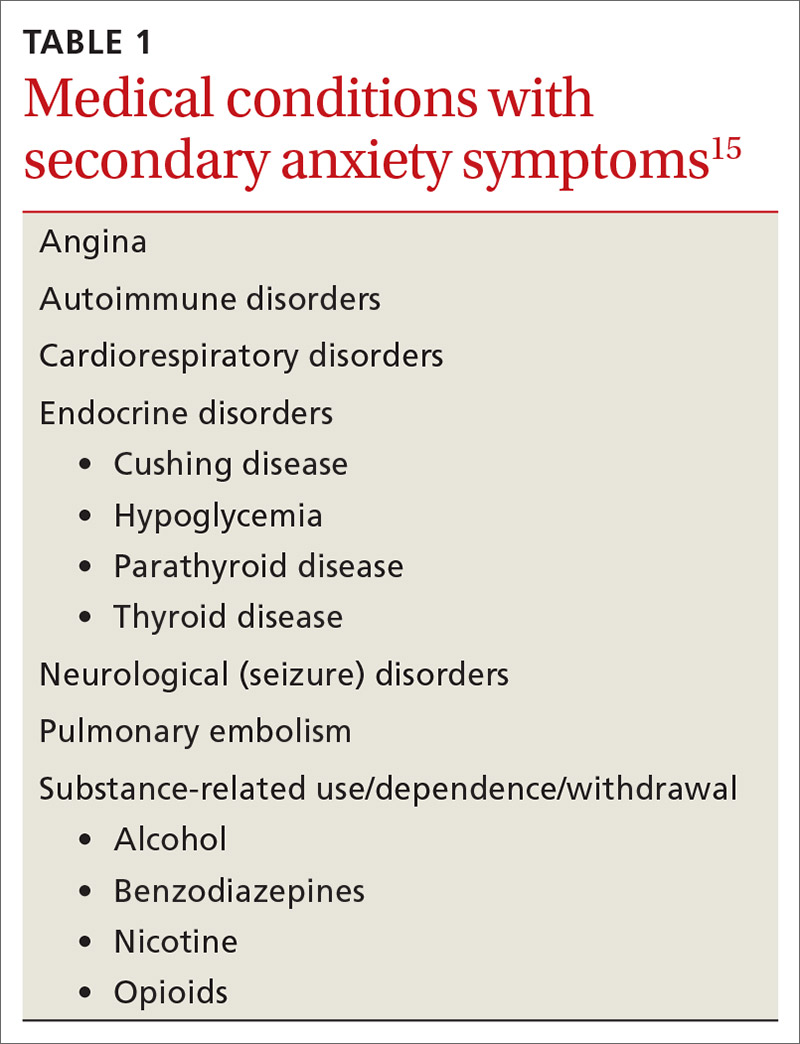
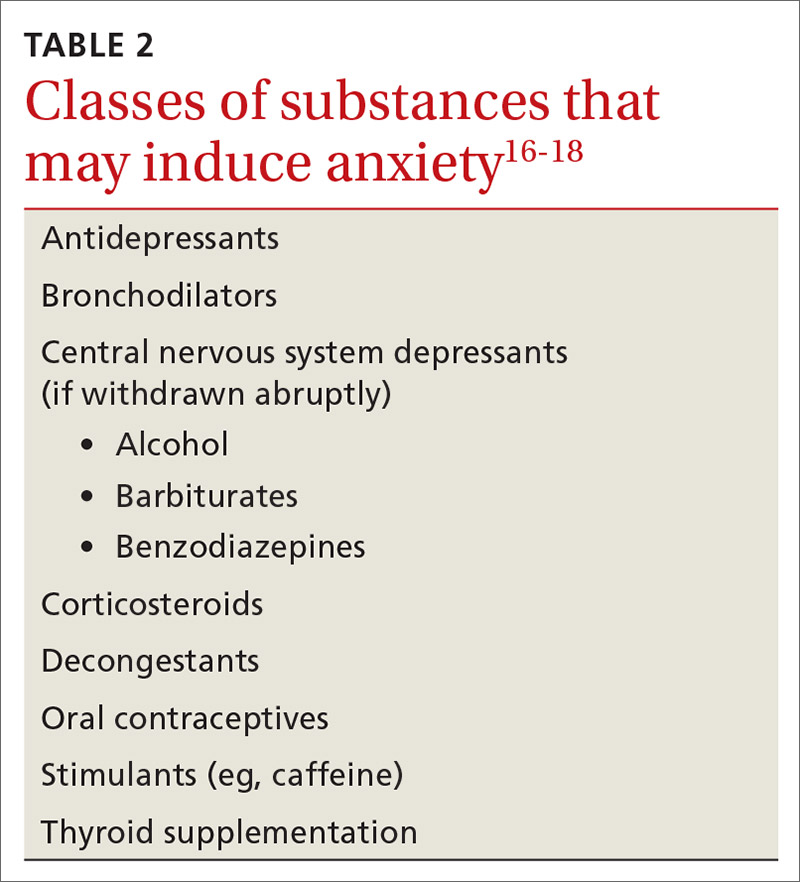
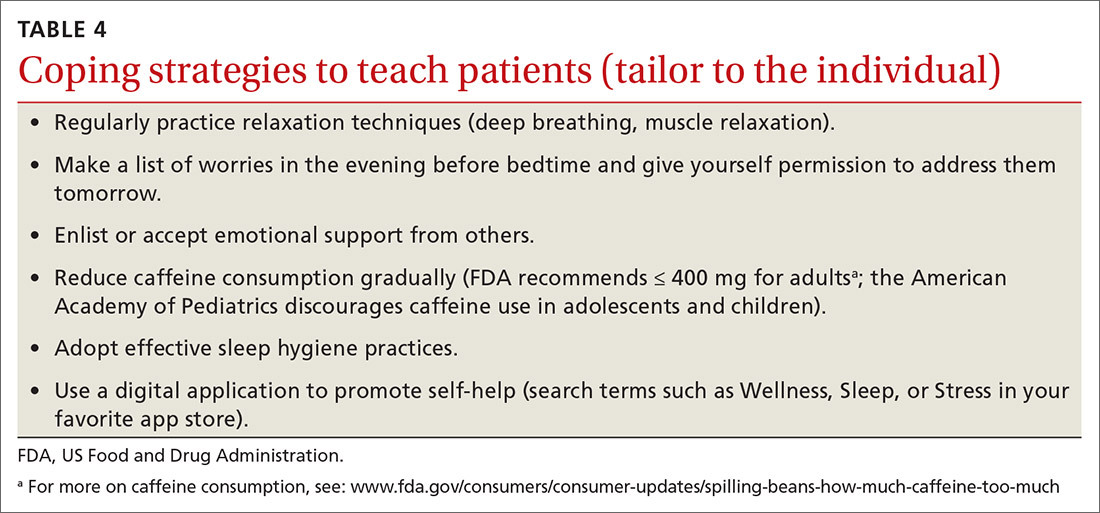
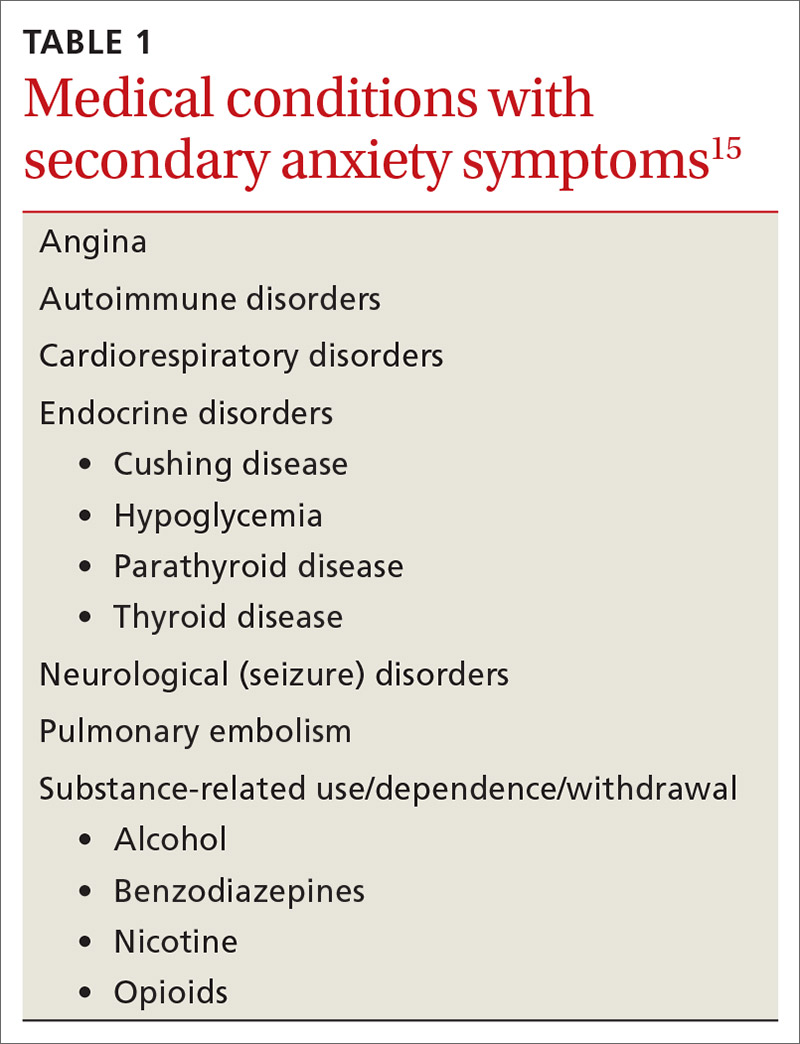
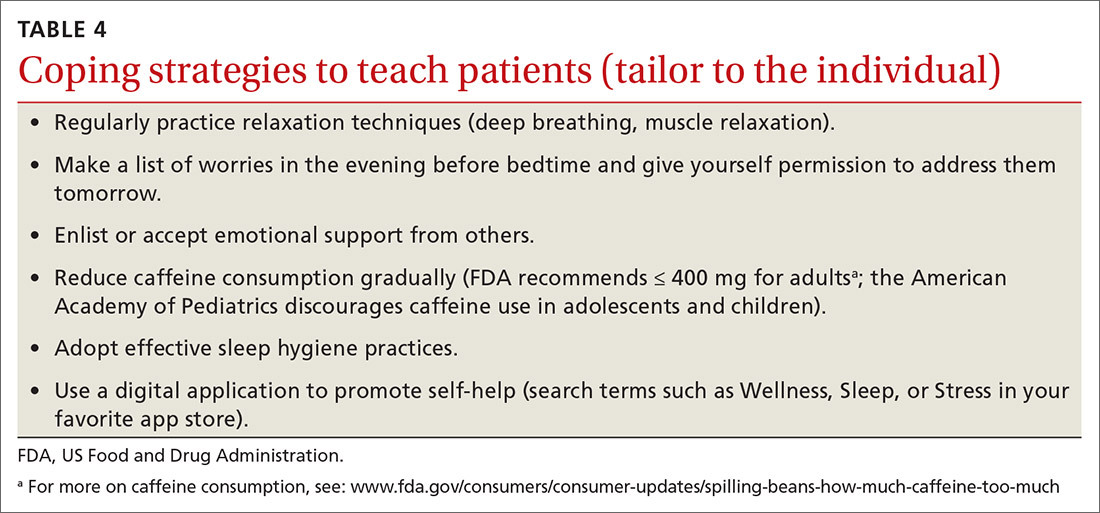
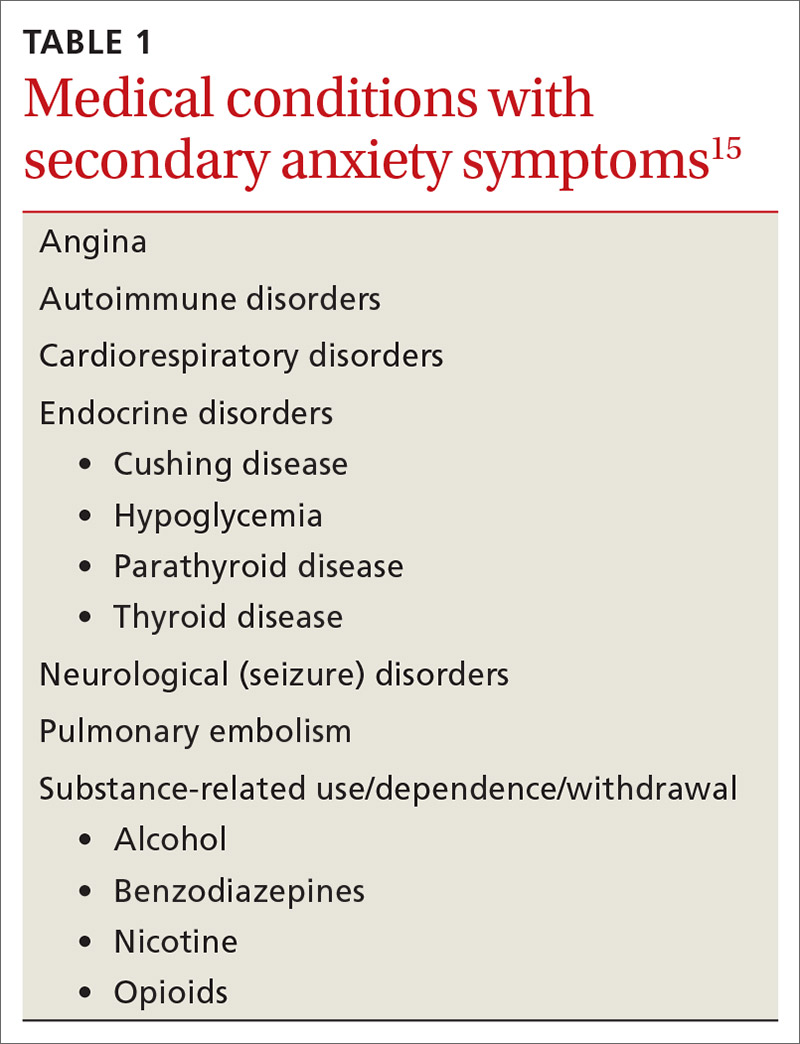
Despite the potential benefits of early identification and treatment of GAD,13 the average elapsed time from symptom onset to initial medication treatment is 7 years.14 Multiple factors likely account for this delay. Clinical presentations can be highly variable,6 with 1 patient presenting primarily with sleep complaints and another with gastrointestinal symptoms. Some medical conditions (TABLE 1)15 and substances (TABLE 2)16-18 can cause secondary anxiety symptoms, and their presence should prompt a thorough evaluation.
Address the mind-body connection. Because uncertainty and ambiguity surrounding a diagnosis often drive worry,19 anxious patients or their family members commonly seek additional medical visits and tests in search of answers. In such instances, it helps to explain the physiologic connection between somatic complaints and anxiety.8 Describe how areas of the brain that manage fear and stress can also cause muscle tension, gastrointestinal complaints, hyperarousal, or sleep disturbance.
Empathy and early psychoeducation on the reason anxiety is being considered can decrease stigma and enable appropriate follow-up and treatment. You might introduce the connection between health complaints and GAD specifically by exploring the amount of worry surrounding the presenting symptoms, followed by a question such as, “Sometimes your worry will fit the situation and sometimes it’ll be too much. Has anyone ever told you that you worry too much?” The patient’s response to such a question could signal a need to use the GAD-7 screening tool1 as an aid to diagnosis and as a baseline measure for monitoring subsequent treatment progress.
Psycho- and pharmacotherapy aspects of management
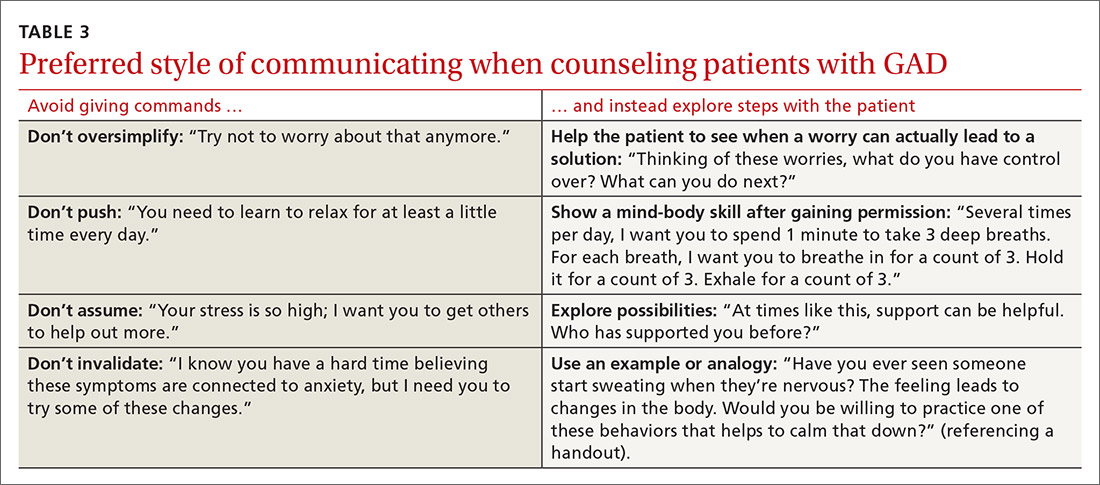
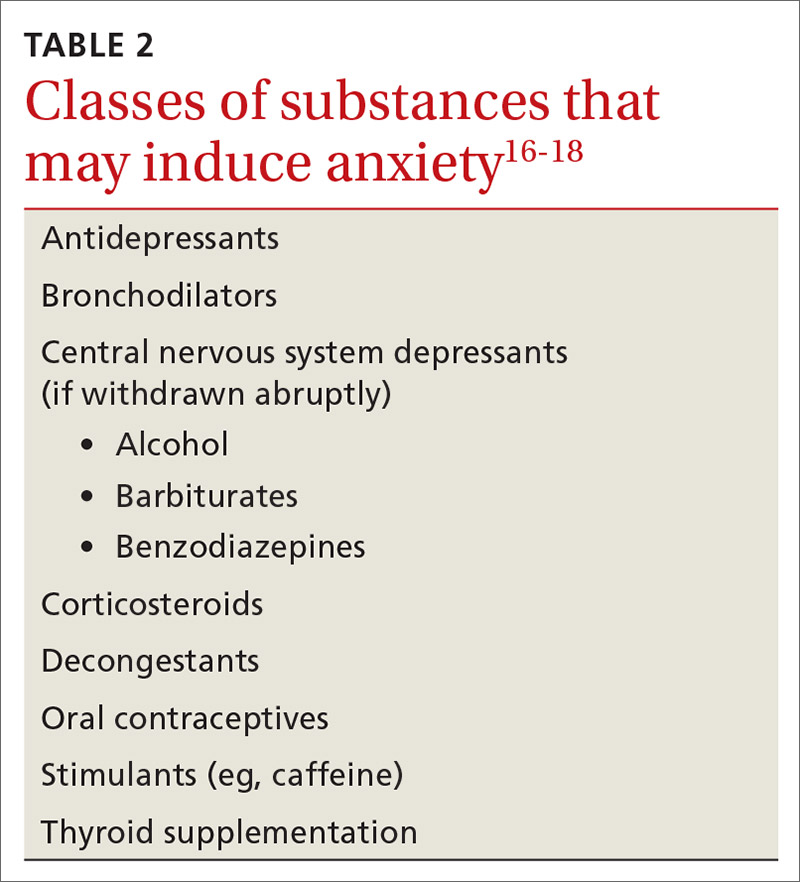
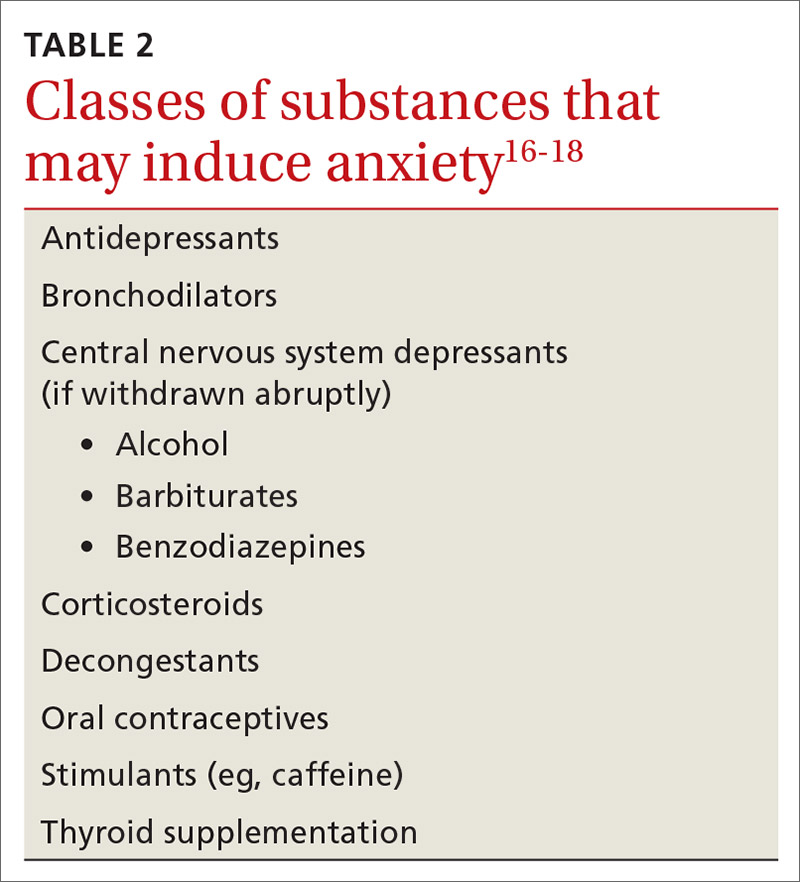
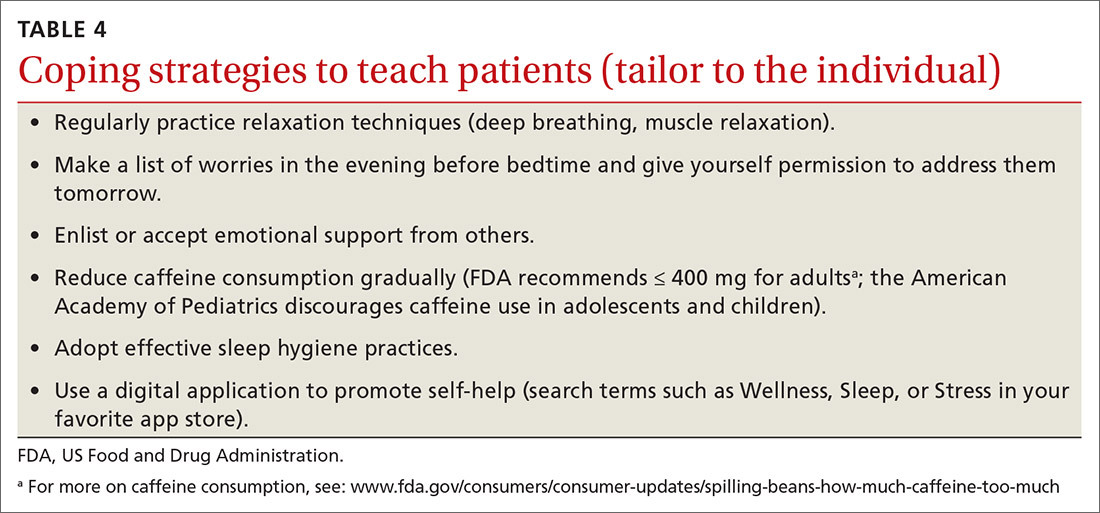
Let patients choose from among various coping strategies. Be prepared to offer patients user-friendly handouts, reading material, or links to educational Web sites. Many patients are interested in using smartphone applications to learn and practice coping strategies. Although these apps can encourage the regular practice of coping skills, caution teens and parents about privacy issues and the lack of evidence supporting this approach as stand-alone therapy.21 Offering several choices (TABLE 4)
Continue to: For patients who remain focused...
For patients who remain focused on somatic complaints and resist adopting coping skills or treatment, pushing certain recommendations can actually increase resistance to proper treatment.22 Instead, explore their ambivalence, offer facts, express concern about the current course of the illness, and emphasize the need to revisit the discussion at a future appointment. Offer follow-up monitoring to assess the course of the illness and readiness for GAD treatment.
Initiate treatment in a stepwise manner13 for the patient who is ready for GAD treatment. This approach includes education and monitoring; low-intensity interventions (eg, treatment workbooks or group sessions); medication and/or referral for psychotherapy; referral for outpatient psychiatric care; and hospitalization for patients who pose a danger to self or others.13 Studies suggest that patients receiving both psychotherapy and pharmacotherapy benefit from the complementary targeting of symptoms, exhibit increased adherence, and report fewer adverse effects.23
Patients are most likely to benefit from therapy when they have the capacity for introspection and forming friendships (ie, can form a therapeutic alliance). With such patients who have mild or moderate symptoms of GAD, offer cognitive behavioral therapy (CBT) or applied relaxation training. Consider a trial of medication when symptoms are severe, when psychotherapy is not a good option, or when response to psychotherapy is inadequate.13 Medications work by targeting primitive parts of the brain such as the amygdala (bottom up), while psychotherapy targets the cortex or more evolved part of the brain, teaching it to modulate the lower or more primitive structures (top down).24
Medication considerations. Selective serotonin reuptake inhibitors (SSRIs) are considered first-line pharmacotherapy for adult and adolescent patients with GAD.20 However, in adolescents, no SSRIs are approved by the US Food and Drug Administration (FDA) to treat anxiety disorders unassociated with obsessive-compulsive disorder. Use caution if prescribing an SSRI for off-label treatment in an adolescent; talk with the patient and family about the FDA’s black-box warning regarding the potential for suicidality in adolescents.
For adults, selective norepinephrine reuptake inhibitors (SNRIs) are also considered a first-line treatment option.23 SSRIs and SNRIs are well-studied, effective, safe, and better tolerated than earlier antidepressants. However, be aware that both SSRIs and SNRIs are often associated with headache, nausea, and sexual dysfunction. They are dosed once daily and have not been shown to cause dependence. Inform patients that onset of action is often delayed 4 to 8 weeks23 and that there is a risk for anxiety-producing effects early in treatment. To minimize these effects, consider starting treatment at a lower dose and titrate upward more gradually than when treating depression.
Continue to: Continue treatment for 12 months...
Continue treatment for 12 months to reduce the risk of recurrence.23 If response to treatment is insufficient after 2 adequate trials of an SSRI or SNRI, consider second-line agents such as azapirones or benzodiazepines for adults, keeping in mind the risk for dependence with benzodiazepines.13
Evidence supports GABAergic drugs such as gabapentin and pregabalin as off-label treatments for GAD in refractory adult cases.25 In the European Union, pregabalin is approved for use in GAD. Caution is recommended with both drugs due to abuse potential. Next steps for an inadequate response should include referral to Psychiatry or for inpatient care when risk of harm to self or others is high.
CASE
Considering Ms. H’s ability to work and complete daily activities, we talked to her about CBT as a first step and referred her to a therapist in the community. One month after her initial visit with us, Ms. H returned for a follow-up visit and scored a 17 on her GAD-7, still in the severe range. After one CBT session, she had cancelled her second and third appointments due to work conflicts. She had missed some work from oversleeping after worried sleepless nights. Her worries concerned friendships, paying bills, physical appearance, not being able to exercise and therefore gaining weight, and troubles at work and with her mother. She also described several episodes of nightmares after breaking up with a boyfriend.
She agreed to try an SSRI, and we started her on fluoxetine 10 mg/d. We counseled her on SSRI risks and benefits, including the potential for increased suicidal ideation and how to respond if such thoughts developed. Three weeks after starting fluoxetine, Ms. H reported improvement with no adverse effects from the medication, except for decreased appetite and some weight loss, which she welcomed. She had registered for college courses, and her third score on the GAD-7 was an 8.
We increased her fluoxetine dose to 20 mg/d for maintenance. We encouraged her to return to her therapist for CBT and she scheduled that appointment. Therapy records noted a GAD-7 score of 5 at follow-up 8 weeks later. Ms. H reported improved sleep, reduced irritability at home, and better relationships with her mother and friends. She had begun college classes and was writing about her thoughts and worries as part of her CBT homework. She continued follow-up appointments with both her family physician and her therapist.
CORRESPONDENCE
Christopher A. Ebberwein, PhD, Wesley Family Medicine Residency, 850 North Hillside, Wichita, KS 67214; chris. ebberwein@wesleymc.com.
1. Kroenke K, Spitzer RL, Williams JBW, et al. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med. 2007;146:317-325.
2. Ruscio AM, Hallion LS, Lim CCW, et al. Cross-sectional comparison of the epidemiology of DSM-5 generalized anxiety disorder across the globe. JAMA Psychiatry. 2017;74:465-475.
3. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5). Washington, DC: American Psychiatric Publishing; 2013.
4. Fernandez S. Anxiety disorders in childhood and adolescence: a primary care approach. Pediatr Ann. 2017;46:e213-e216.
5. Connolly SD, Bernstein GA. Practice parameter for the assessment and treatment of children and adolescents with anxiety disorders. J Am Acad Child Adolesc Psychiatry. 2007;46:267-283.
6. Reinhold JA, Rickels K. Pharmacological treatments for generalized anxiety disorder in adults: an update. Expert Opin Pharmacother. 2015;16:1669-1681.
7. Kujanpää TS, Jokelainen J, Auvinen JP, et al. The association of generalized anxiety disorder and somatic symptoms with frequent attendance to healthcare services: a cross-sectional study from the Northern Finland Birth Cohort 1966. Int J Psychiatry Med. 2017:52:147-159.
8. Ramsawh HJ, Chavira DA, Stein MB. Burden of anxiety disorders in pediatric medical settings: prevalence, phenomenology, and a research agenda. Arch Pediatr Adolesc Med. 2010;164:965-972. doi:10.1001/archpediatrics.2010.170.
9. Barger SD, Sydeman SJ. Does generalized anxiety disorder predict coronary heart disease risk factors independently of major depressive disorder? J Affect Disord. 2005;88:87-91.
10. Bruffaerts R, Demyttenaere K, Kessler RC, et al. The associations between preexisting mental disorders and subsequent onset of chronic headaches: a worldwide epidemiologic perspective. J Pain. 2015;16:42-52.
11. Husky MM, Olfson M, He J, et al. Twelve-month suicidal symptoms and use of services among adolescents: results from the National Comorbidity Survey. Psychiatr Serv. 2012;63:989-996.
12. Nepon J, Belik S, Bolton J, et al. The relationship between anxiety disorders and suicide attempts: findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Depress Anxiety. 2010;27:791–798.
13. National Institute for Health and Care Excellence (NICE). Generalised anxiety disorder and panic disorder adults: management. nice.org.uk/guidance/cg113. Accessed August 20, 2020.
14. Dell’Osso B, Camuri G, Benatti B, et al. Differences in latency to first pharmacological treatment (duration of untreated illness) in anxiety disorders: a study on patients with panic disorder, generalized anxiety disorder and obsessive-compulsive disorder. Early Interv Psychiatry. 2013;7:374-380.
15. Hales RE, Yudofsky SC, Roberts LW, eds. Textbook of Psychiatry, 6th ed. Arlington, VA: American Psychiatric Publishing: 2014:391-430.
16. Fernandez F, Levy JK, Lachar BL, et al. The management of depression and anxiety in the elderly. J Clin Psychiatry. 1995;56(suppl 2):20-29.
17. Kirkwood CK, Hayes PE. Anxiety disorders. In: DiPiro JT, Talbert RL, Yee GC, et al, eds. Pharmacotherapy: A Pathophysiologic Approach, 3rd ed. Stamford, Conn: Appleton & Lange;1997:1443-1462.
18. Culpepper L. Generalized anxiety disorder and medical illness. J Clin Psychiatry. 2009;70(suppl 2):20-24.
19. Anderson KG, Dugas MJ, Koerner N, et al. Interpretive style and intolerance of uncertainty in individuals with anxiety disorders: a focus on generalized anxiety disorder. J Anxiety Disord. 2012;26:823-832.
20. Satterfield JM, Feldman MD. Anxiety. In Feldman MD, Christensen JF, Satterfield JM, eds. Behavioral Medicine: A Guide for Clinical Practice. New York: McGraw Hill; 2014:271-282.
21. Grist R, Porter J, Stallard P. Mental health mobile apps for preadolescents and adolescents: A systematic review. J Med Internet Res. 2017;19:e176.
22. Rollnick S, Miller W, Butler C. Motivational Interviewing in Health Care: Helping Patients Change Behavior. 1st ed. New York: The Guilford Press; 2008:34-35.
23. Strawn JR, Geriacioti L, Rajdev N, et al. Pharmacotherapy for generalized anxiety disorder in adult and pediatric patients: an evidence-based review. Expert Opin Pharmacother. 2018;19:1057-1070.
24. Ehmke CJ, Nemeroff CB. Paroxetine. In Schatzberg AF, Nemeroff CB, eds. Textbook of Psychopharmacology, 4th ed. Washington, D.C.: American Psychiatric Publishing, Inc.; 2009:321-352.
25. Huh J, Goebert D, Takeshita J, et al. Treatment of generalized anxiety disorder: a comprehensive review of the literature for psychopharmacologic alternatives to newer antidepressants and benzodiazepines. Prim Care Companion CNS Disord. 2011;13: doi:10.4088/PCC.08r00709blu.
THE CASE
Sandra H,* a 24-year-old single woman with a history of asthma, presented to our family medicine clinic as a new patient. Ms. H said she lived at home with her mother. She completed high school but never attended college due to anxiety. She had held several jobs since high school and recently decided to apply to a local college, which prompted a desire to gain control over the anxiety that had been present since middle school. She reported feeling anxious, having difficulty breathing, shaking all over, having difficulty concentrating, and experiencing numbness and tingling in her fingers. She was often irritable at home, which she attributed partly to anxiety but mostly to disrupted sleep. We administered the 7-question Generalized Anxiety Disorder (GAD-7) questionnaire and she scored 15 (of a possible 21) points, indicative of severe anxiety.
●
* The patient’s name has been changed to protect her identity.
Approximately 1 in 5 patients presenting to primary care clinics have at least 1 anxiety disorder and 7.6% have generalized anxiety disorder (GAD).1 Yet many go untreated. The lifetime prevalence of GAD is 3.7% worldwide and 7.8% in the United States.2 Only 5% of cases emerge by age 13,2 but incidence increases through adolescence and young adulthood, with a quarter of all cases occurring by age 25.2 GAD occurs about twice as often in women as it does in men. It is typically recurrent, and many patients require ongoing treatment.2
GAD diagnostic criteria and differential considerations
Diagnosis of GAD requires at least 6 months of excessive worry or anxiety about a variety of circumstances, occurring on most days and for more than half the day.3 The worry or anxiety in GAD is difficult to control, disrupts meaningful areas of life, and surrounds everyday concerns, such as finances, health, or family-related issues. Among adolescents with GAD, worries typically include school performance and may often present as perfectionism.4 At least 3 of the following 6 symptoms result from chronic anxiety: restlessness, fatigue, poor concentration, irritability, muscle tension, and sleep disturbance.2
Rule out other conditions. Make sure symptoms of GAD are not better explained by another medical problem, including other mental disorders or substance use disorders.3 Complaints of anxiety in the context of mania, hypomania, or withdrawal from alcohol or a sedative hypnotic suggest a different underlying cause, thereby requiring a complete history with symptom chronology and collateral information. The pattern of anxiety seen in GAD also differs from the focused sources of anxiety found in disorders such as social anxiety disorder (SAD) and post-traumatic stress disorder. For example, SAD might center on embarrassment in a social setting rather than reflect a pattern of general worry.5
Consider comorbidities. Further complicating diagnosis and treatment, GAD has been linked to higher rates of comorbidity and higher health care utilization. About 90% of GAD patients experience psychiatric comorbidity, with major depressive disorder co-occurring about 60% of the time.6 Substance use disorders co-occur with GAD more than 20% of the time.2 Despite comorbidities, it is the somatic complaints in GAD that often drive patient requests for medical care.7,8 GAD itself is an independent predictor of heart disease9 and is linked to increased risk of chronic or severe headaches10 and suicide.11,12
Continue to: Work with patients and family toward a diagnosis
Work with patients and family toward a diagnosis
Despite the potential benefits of early identification and treatment of GAD,13 the average elapsed time from symptom onset to initial medication treatment is 7 years.14 Multiple factors likely account for this delay. Clinical presentations can be highly variable,6 with 1 patient presenting primarily with sleep complaints and another with gastrointestinal symptoms. Some medical conditions (TABLE 1)15 and substances (TABLE 2)16-18 can cause secondary anxiety symptoms, and their presence should prompt a thorough evaluation.
Address the mind-body connection. Because uncertainty and ambiguity surrounding a diagnosis often drive worry,19 anxious patients or their family members commonly seek additional medical visits and tests in search of answers. In such instances, it helps to explain the physiologic connection between somatic complaints and anxiety.8 Describe how areas of the brain that manage fear and stress can also cause muscle tension, gastrointestinal complaints, hyperarousal, or sleep disturbance.
Empathy and early psychoeducation on the reason anxiety is being considered can decrease stigma and enable appropriate follow-up and treatment. You might introduce the connection between health complaints and GAD specifically by exploring the amount of worry surrounding the presenting symptoms, followed by a question such as, “Sometimes your worry will fit the situation and sometimes it’ll be too much. Has anyone ever told you that you worry too much?” The patient’s response to such a question could signal a need to use the GAD-7 screening tool1 as an aid to diagnosis and as a baseline measure for monitoring subsequent treatment progress.
Psycho- and pharmacotherapy aspects of management
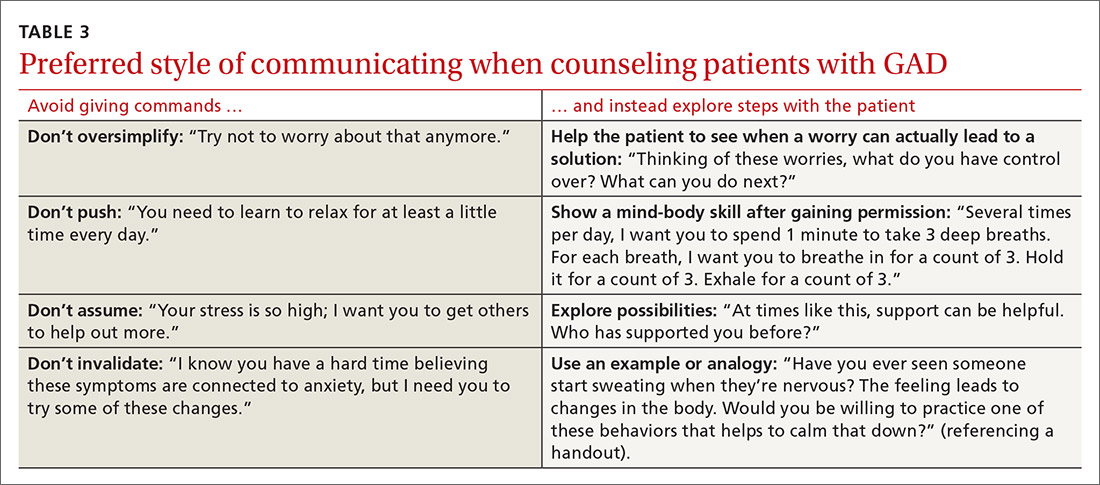
Let patients choose from among various coping strategies. Be prepared to offer patients user-friendly handouts, reading material, or links to educational Web sites. Many patients are interested in using smartphone applications to learn and practice coping strategies. Although these apps can encourage the regular practice of coping skills, caution teens and parents about privacy issues and the lack of evidence supporting this approach as stand-alone therapy.21 Offering several choices (TABLE 4)
Continue to: For patients who remain focused...
For patients who remain focused on somatic complaints and resist adopting coping skills or treatment, pushing certain recommendations can actually increase resistance to proper treatment.22 Instead, explore their ambivalence, offer facts, express concern about the current course of the illness, and emphasize the need to revisit the discussion at a future appointment. Offer follow-up monitoring to assess the course of the illness and readiness for GAD treatment.
Initiate treatment in a stepwise manner13 for the patient who is ready for GAD treatment. This approach includes education and monitoring; low-intensity interventions (eg, treatment workbooks or group sessions); medication and/or referral for psychotherapy; referral for outpatient psychiatric care; and hospitalization for patients who pose a danger to self or others.13 Studies suggest that patients receiving both psychotherapy and pharmacotherapy benefit from the complementary targeting of symptoms, exhibit increased adherence, and report fewer adverse effects.23
Patients are most likely to benefit from therapy when they have the capacity for introspection and forming friendships (ie, can form a therapeutic alliance). With such patients who have mild or moderate symptoms of GAD, offer cognitive behavioral therapy (CBT) or applied relaxation training. Consider a trial of medication when symptoms are severe, when psychotherapy is not a good option, or when response to psychotherapy is inadequate.13 Medications work by targeting primitive parts of the brain such as the amygdala (bottom up), while psychotherapy targets the cortex or more evolved part of the brain, teaching it to modulate the lower or more primitive structures (top down).24
Medication considerations. Selective serotonin reuptake inhibitors (SSRIs) are considered first-line pharmacotherapy for adult and adolescent patients with GAD.20 However, in adolescents, no SSRIs are approved by the US Food and Drug Administration (FDA) to treat anxiety disorders unassociated with obsessive-compulsive disorder. Use caution if prescribing an SSRI for off-label treatment in an adolescent; talk with the patient and family about the FDA’s black-box warning regarding the potential for suicidality in adolescents.
For adults, selective norepinephrine reuptake inhibitors (SNRIs) are also considered a first-line treatment option.23 SSRIs and SNRIs are well-studied, effective, safe, and better tolerated than earlier antidepressants. However, be aware that both SSRIs and SNRIs are often associated with headache, nausea, and sexual dysfunction. They are dosed once daily and have not been shown to cause dependence. Inform patients that onset of action is often delayed 4 to 8 weeks23 and that there is a risk for anxiety-producing effects early in treatment. To minimize these effects, consider starting treatment at a lower dose and titrate upward more gradually than when treating depression.
Continue to: Continue treatment for 12 months...
Continue treatment for 12 months to reduce the risk of recurrence.23 If response to treatment is insufficient after 2 adequate trials of an SSRI or SNRI, consider second-line agents such as azapirones or benzodiazepines for adults, keeping in mind the risk for dependence with benzodiazepines.13
Evidence supports GABAergic drugs such as gabapentin and pregabalin as off-label treatments for GAD in refractory adult cases.25 In the European Union, pregabalin is approved for use in GAD. Caution is recommended with both drugs due to abuse potential. Next steps for an inadequate response should include referral to Psychiatry or for inpatient care when risk of harm to self or others is high.
CASE
Considering Ms. H’s ability to work and complete daily activities, we talked to her about CBT as a first step and referred her to a therapist in the community. One month after her initial visit with us, Ms. H returned for a follow-up visit and scored a 17 on her GAD-7, still in the severe range. After one CBT session, she had cancelled her second and third appointments due to work conflicts. She had missed some work from oversleeping after worried sleepless nights. Her worries concerned friendships, paying bills, physical appearance, not being able to exercise and therefore gaining weight, and troubles at work and with her mother. She also described several episodes of nightmares after breaking up with a boyfriend.
She agreed to try an SSRI, and we started her on fluoxetine 10 mg/d. We counseled her on SSRI risks and benefits, including the potential for increased suicidal ideation and how to respond if such thoughts developed. Three weeks after starting fluoxetine, Ms. H reported improvement with no adverse effects from the medication, except for decreased appetite and some weight loss, which she welcomed. She had registered for college courses, and her third score on the GAD-7 was an 8.
We increased her fluoxetine dose to 20 mg/d for maintenance. We encouraged her to return to her therapist for CBT and she scheduled that appointment. Therapy records noted a GAD-7 score of 5 at follow-up 8 weeks later. Ms. H reported improved sleep, reduced irritability at home, and better relationships with her mother and friends. She had begun college classes and was writing about her thoughts and worries as part of her CBT homework. She continued follow-up appointments with both her family physician and her therapist.
CORRESPONDENCE
Christopher A. Ebberwein, PhD, Wesley Family Medicine Residency, 850 North Hillside, Wichita, KS 67214; chris. ebberwein@wesleymc.com.
THE CASE
Sandra H,* a 24-year-old single woman with a history of asthma, presented to our family medicine clinic as a new patient. Ms. H said she lived at home with her mother. She completed high school but never attended college due to anxiety. She had held several jobs since high school and recently decided to apply to a local college, which prompted a desire to gain control over the anxiety that had been present since middle school. She reported feeling anxious, having difficulty breathing, shaking all over, having difficulty concentrating, and experiencing numbness and tingling in her fingers. She was often irritable at home, which she attributed partly to anxiety but mostly to disrupted sleep. We administered the 7-question Generalized Anxiety Disorder (GAD-7) questionnaire and she scored 15 (of a possible 21) points, indicative of severe anxiety.
●
* The patient’s name has been changed to protect her identity.
Approximately 1 in 5 patients presenting to primary care clinics have at least 1 anxiety disorder and 7.6% have generalized anxiety disorder (GAD).1 Yet many go untreated. The lifetime prevalence of GAD is 3.7% worldwide and 7.8% in the United States.2 Only 5% of cases emerge by age 13,2 but incidence increases through adolescence and young adulthood, with a quarter of all cases occurring by age 25.2 GAD occurs about twice as often in women as it does in men. It is typically recurrent, and many patients require ongoing treatment.2
GAD diagnostic criteria and differential considerations
Diagnosis of GAD requires at least 6 months of excessive worry or anxiety about a variety of circumstances, occurring on most days and for more than half the day.3 The worry or anxiety in GAD is difficult to control, disrupts meaningful areas of life, and surrounds everyday concerns, such as finances, health, or family-related issues. Among adolescents with GAD, worries typically include school performance and may often present as perfectionism.4 At least 3 of the following 6 symptoms result from chronic anxiety: restlessness, fatigue, poor concentration, irritability, muscle tension, and sleep disturbance.2
Rule out other conditions. Make sure symptoms of GAD are not better explained by another medical problem, including other mental disorders or substance use disorders.3 Complaints of anxiety in the context of mania, hypomania, or withdrawal from alcohol or a sedative hypnotic suggest a different underlying cause, thereby requiring a complete history with symptom chronology and collateral information. The pattern of anxiety seen in GAD also differs from the focused sources of anxiety found in disorders such as social anxiety disorder (SAD) and post-traumatic stress disorder. For example, SAD might center on embarrassment in a social setting rather than reflect a pattern of general worry.5
Consider comorbidities. Further complicating diagnosis and treatment, GAD has been linked to higher rates of comorbidity and higher health care utilization. About 90% of GAD patients experience psychiatric comorbidity, with major depressive disorder co-occurring about 60% of the time.6 Substance use disorders co-occur with GAD more than 20% of the time.2 Despite comorbidities, it is the somatic complaints in GAD that often drive patient requests for medical care.7,8 GAD itself is an independent predictor of heart disease9 and is linked to increased risk of chronic or severe headaches10 and suicide.11,12
Continue to: Work with patients and family toward a diagnosis
Work with patients and family toward a diagnosis
Despite the potential benefits of early identification and treatment of GAD,13 the average elapsed time from symptom onset to initial medication treatment is 7 years.14 Multiple factors likely account for this delay. Clinical presentations can be highly variable,6 with 1 patient presenting primarily with sleep complaints and another with gastrointestinal symptoms. Some medical conditions (TABLE 1)15 and substances (TABLE 2)16-18 can cause secondary anxiety symptoms, and their presence should prompt a thorough evaluation.
Address the mind-body connection. Because uncertainty and ambiguity surrounding a diagnosis often drive worry,19 anxious patients or their family members commonly seek additional medical visits and tests in search of answers. In such instances, it helps to explain the physiologic connection between somatic complaints and anxiety.8 Describe how areas of the brain that manage fear and stress can also cause muscle tension, gastrointestinal complaints, hyperarousal, or sleep disturbance.
Empathy and early psychoeducation on the reason anxiety is being considered can decrease stigma and enable appropriate follow-up and treatment. You might introduce the connection between health complaints and GAD specifically by exploring the amount of worry surrounding the presenting symptoms, followed by a question such as, “Sometimes your worry will fit the situation and sometimes it’ll be too much. Has anyone ever told you that you worry too much?” The patient’s response to such a question could signal a need to use the GAD-7 screening tool1 as an aid to diagnosis and as a baseline measure for monitoring subsequent treatment progress.
Psycho- and pharmacotherapy aspects of management
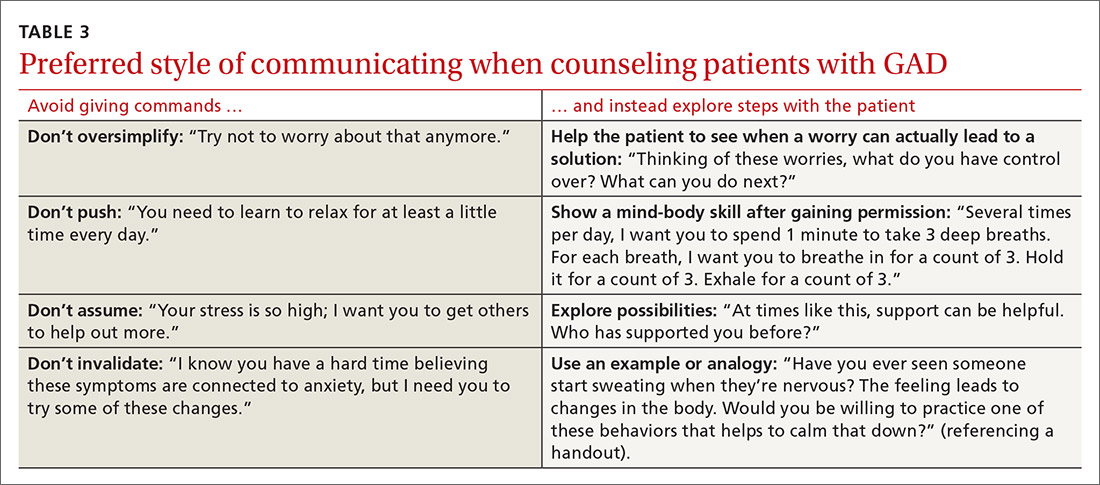
Let patients choose from among various coping strategies. Be prepared to offer patients user-friendly handouts, reading material, or links to educational Web sites. Many patients are interested in using smartphone applications to learn and practice coping strategies. Although these apps can encourage the regular practice of coping skills, caution teens and parents about privacy issues and the lack of evidence supporting this approach as stand-alone therapy.21 Offering several choices (TABLE 4)
Continue to: For patients who remain focused...
For patients who remain focused on somatic complaints and resist adopting coping skills or treatment, pushing certain recommendations can actually increase resistance to proper treatment.22 Instead, explore their ambivalence, offer facts, express concern about the current course of the illness, and emphasize the need to revisit the discussion at a future appointment. Offer follow-up monitoring to assess the course of the illness and readiness for GAD treatment.
Initiate treatment in a stepwise manner13 for the patient who is ready for GAD treatment. This approach includes education and monitoring; low-intensity interventions (eg, treatment workbooks or group sessions); medication and/or referral for psychotherapy; referral for outpatient psychiatric care; and hospitalization for patients who pose a danger to self or others.13 Studies suggest that patients receiving both psychotherapy and pharmacotherapy benefit from the complementary targeting of symptoms, exhibit increased adherence, and report fewer adverse effects.23
Patients are most likely to benefit from therapy when they have the capacity for introspection and forming friendships (ie, can form a therapeutic alliance). With such patients who have mild or moderate symptoms of GAD, offer cognitive behavioral therapy (CBT) or applied relaxation training. Consider a trial of medication when symptoms are severe, when psychotherapy is not a good option, or when response to psychotherapy is inadequate.13 Medications work by targeting primitive parts of the brain such as the amygdala (bottom up), while psychotherapy targets the cortex or more evolved part of the brain, teaching it to modulate the lower or more primitive structures (top down).24
Medication considerations. Selective serotonin reuptake inhibitors (SSRIs) are considered first-line pharmacotherapy for adult and adolescent patients with GAD.20 However, in adolescents, no SSRIs are approved by the US Food and Drug Administration (FDA) to treat anxiety disorders unassociated with obsessive-compulsive disorder. Use caution if prescribing an SSRI for off-label treatment in an adolescent; talk with the patient and family about the FDA’s black-box warning regarding the potential for suicidality in adolescents.
For adults, selective norepinephrine reuptake inhibitors (SNRIs) are also considered a first-line treatment option.23 SSRIs and SNRIs are well-studied, effective, safe, and better tolerated than earlier antidepressants. However, be aware that both SSRIs and SNRIs are often associated with headache, nausea, and sexual dysfunction. They are dosed once daily and have not been shown to cause dependence. Inform patients that onset of action is often delayed 4 to 8 weeks23 and that there is a risk for anxiety-producing effects early in treatment. To minimize these effects, consider starting treatment at a lower dose and titrate upward more gradually than when treating depression.
Continue to: Continue treatment for 12 months...
Continue treatment for 12 months to reduce the risk of recurrence.23 If response to treatment is insufficient after 2 adequate trials of an SSRI or SNRI, consider second-line agents such as azapirones or benzodiazepines for adults, keeping in mind the risk for dependence with benzodiazepines.13
Evidence supports GABAergic drugs such as gabapentin and pregabalin as off-label treatments for GAD in refractory adult cases.25 In the European Union, pregabalin is approved for use in GAD. Caution is recommended with both drugs due to abuse potential. Next steps for an inadequate response should include referral to Psychiatry or for inpatient care when risk of harm to self or others is high.
CASE
Considering Ms. H’s ability to work and complete daily activities, we talked to her about CBT as a first step and referred her to a therapist in the community. One month after her initial visit with us, Ms. H returned for a follow-up visit and scored a 17 on her GAD-7, still in the severe range. After one CBT session, she had cancelled her second and third appointments due to work conflicts. She had missed some work from oversleeping after worried sleepless nights. Her worries concerned friendships, paying bills, physical appearance, not being able to exercise and therefore gaining weight, and troubles at work and with her mother. She also described several episodes of nightmares after breaking up with a boyfriend.
She agreed to try an SSRI, and we started her on fluoxetine 10 mg/d. We counseled her on SSRI risks and benefits, including the potential for increased suicidal ideation and how to respond if such thoughts developed. Three weeks after starting fluoxetine, Ms. H reported improvement with no adverse effects from the medication, except for decreased appetite and some weight loss, which she welcomed. She had registered for college courses, and her third score on the GAD-7 was an 8.
We increased her fluoxetine dose to 20 mg/d for maintenance. We encouraged her to return to her therapist for CBT and she scheduled that appointment. Therapy records noted a GAD-7 score of 5 at follow-up 8 weeks later. Ms. H reported improved sleep, reduced irritability at home, and better relationships with her mother and friends. She had begun college classes and was writing about her thoughts and worries as part of her CBT homework. She continued follow-up appointments with both her family physician and her therapist.
CORRESPONDENCE
Christopher A. Ebberwein, PhD, Wesley Family Medicine Residency, 850 North Hillside, Wichita, KS 67214; chris. ebberwein@wesleymc.com.
1. Kroenke K, Spitzer RL, Williams JBW, et al. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med. 2007;146:317-325.
2. Ruscio AM, Hallion LS, Lim CCW, et al. Cross-sectional comparison of the epidemiology of DSM-5 generalized anxiety disorder across the globe. JAMA Psychiatry. 2017;74:465-475.
3. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5). Washington, DC: American Psychiatric Publishing; 2013.
4. Fernandez S. Anxiety disorders in childhood and adolescence: a primary care approach. Pediatr Ann. 2017;46:e213-e216.
5. Connolly SD, Bernstein GA. Practice parameter for the assessment and treatment of children and adolescents with anxiety disorders. J Am Acad Child Adolesc Psychiatry. 2007;46:267-283.
6. Reinhold JA, Rickels K. Pharmacological treatments for generalized anxiety disorder in adults: an update. Expert Opin Pharmacother. 2015;16:1669-1681.
7. Kujanpää TS, Jokelainen J, Auvinen JP, et al. The association of generalized anxiety disorder and somatic symptoms with frequent attendance to healthcare services: a cross-sectional study from the Northern Finland Birth Cohort 1966. Int J Psychiatry Med. 2017:52:147-159.
8. Ramsawh HJ, Chavira DA, Stein MB. Burden of anxiety disorders in pediatric medical settings: prevalence, phenomenology, and a research agenda. Arch Pediatr Adolesc Med. 2010;164:965-972. doi:10.1001/archpediatrics.2010.170.
9. Barger SD, Sydeman SJ. Does generalized anxiety disorder predict coronary heart disease risk factors independently of major depressive disorder? J Affect Disord. 2005;88:87-91.
10. Bruffaerts R, Demyttenaere K, Kessler RC, et al. The associations between preexisting mental disorders and subsequent onset of chronic headaches: a worldwide epidemiologic perspective. J Pain. 2015;16:42-52.
11. Husky MM, Olfson M, He J, et al. Twelve-month suicidal symptoms and use of services among adolescents: results from the National Comorbidity Survey. Psychiatr Serv. 2012;63:989-996.
12. Nepon J, Belik S, Bolton J, et al. The relationship between anxiety disorders and suicide attempts: findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Depress Anxiety. 2010;27:791–798.
13. National Institute for Health and Care Excellence (NICE). Generalised anxiety disorder and panic disorder adults: management. nice.org.uk/guidance/cg113. Accessed August 20, 2020.
14. Dell’Osso B, Camuri G, Benatti B, et al. Differences in latency to first pharmacological treatment (duration of untreated illness) in anxiety disorders: a study on patients with panic disorder, generalized anxiety disorder and obsessive-compulsive disorder. Early Interv Psychiatry. 2013;7:374-380.
15. Hales RE, Yudofsky SC, Roberts LW, eds. Textbook of Psychiatry, 6th ed. Arlington, VA: American Psychiatric Publishing: 2014:391-430.
16. Fernandez F, Levy JK, Lachar BL, et al. The management of depression and anxiety in the elderly. J Clin Psychiatry. 1995;56(suppl 2):20-29.
17. Kirkwood CK, Hayes PE. Anxiety disorders. In: DiPiro JT, Talbert RL, Yee GC, et al, eds. Pharmacotherapy: A Pathophysiologic Approach, 3rd ed. Stamford, Conn: Appleton & Lange;1997:1443-1462.
18. Culpepper L. Generalized anxiety disorder and medical illness. J Clin Psychiatry. 2009;70(suppl 2):20-24.
19. Anderson KG, Dugas MJ, Koerner N, et al. Interpretive style and intolerance of uncertainty in individuals with anxiety disorders: a focus on generalized anxiety disorder. J Anxiety Disord. 2012;26:823-832.
20. Satterfield JM, Feldman MD. Anxiety. In Feldman MD, Christensen JF, Satterfield JM, eds. Behavioral Medicine: A Guide for Clinical Practice. New York: McGraw Hill; 2014:271-282.
21. Grist R, Porter J, Stallard P. Mental health mobile apps for preadolescents and adolescents: A systematic review. J Med Internet Res. 2017;19:e176.
22. Rollnick S, Miller W, Butler C. Motivational Interviewing in Health Care: Helping Patients Change Behavior. 1st ed. New York: The Guilford Press; 2008:34-35.
23. Strawn JR, Geriacioti L, Rajdev N, et al. Pharmacotherapy for generalized anxiety disorder in adult and pediatric patients: an evidence-based review. Expert Opin Pharmacother. 2018;19:1057-1070.
24. Ehmke CJ, Nemeroff CB. Paroxetine. In Schatzberg AF, Nemeroff CB, eds. Textbook of Psychopharmacology, 4th ed. Washington, D.C.: American Psychiatric Publishing, Inc.; 2009:321-352.
25. Huh J, Goebert D, Takeshita J, et al. Treatment of generalized anxiety disorder: a comprehensive review of the literature for psychopharmacologic alternatives to newer antidepressants and benzodiazepines. Prim Care Companion CNS Disord. 2011;13: doi:10.4088/PCC.08r00709blu.
1. Kroenke K, Spitzer RL, Williams JBW, et al. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med. 2007;146:317-325.
2. Ruscio AM, Hallion LS, Lim CCW, et al. Cross-sectional comparison of the epidemiology of DSM-5 generalized anxiety disorder across the globe. JAMA Psychiatry. 2017;74:465-475.
3. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5). Washington, DC: American Psychiatric Publishing; 2013.
4. Fernandez S. Anxiety disorders in childhood and adolescence: a primary care approach. Pediatr Ann. 2017;46:e213-e216.
5. Connolly SD, Bernstein GA. Practice parameter for the assessment and treatment of children and adolescents with anxiety disorders. J Am Acad Child Adolesc Psychiatry. 2007;46:267-283.
6. Reinhold JA, Rickels K. Pharmacological treatments for generalized anxiety disorder in adults: an update. Expert Opin Pharmacother. 2015;16:1669-1681.
7. Kujanpää TS, Jokelainen J, Auvinen JP, et al. The association of generalized anxiety disorder and somatic symptoms with frequent attendance to healthcare services: a cross-sectional study from the Northern Finland Birth Cohort 1966. Int J Psychiatry Med. 2017:52:147-159.
8. Ramsawh HJ, Chavira DA, Stein MB. Burden of anxiety disorders in pediatric medical settings: prevalence, phenomenology, and a research agenda. Arch Pediatr Adolesc Med. 2010;164:965-972. doi:10.1001/archpediatrics.2010.170.
9. Barger SD, Sydeman SJ. Does generalized anxiety disorder predict coronary heart disease risk factors independently of major depressive disorder? J Affect Disord. 2005;88:87-91.
10. Bruffaerts R, Demyttenaere K, Kessler RC, et al. The associations between preexisting mental disorders and subsequent onset of chronic headaches: a worldwide epidemiologic perspective. J Pain. 2015;16:42-52.
11. Husky MM, Olfson M, He J, et al. Twelve-month suicidal symptoms and use of services among adolescents: results from the National Comorbidity Survey. Psychiatr Serv. 2012;63:989-996.
12. Nepon J, Belik S, Bolton J, et al. The relationship between anxiety disorders and suicide attempts: findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Depress Anxiety. 2010;27:791–798.
13. National Institute for Health and Care Excellence (NICE). Generalised anxiety disorder and panic disorder adults: management. nice.org.uk/guidance/cg113. Accessed August 20, 2020.
14. Dell’Osso B, Camuri G, Benatti B, et al. Differences in latency to first pharmacological treatment (duration of untreated illness) in anxiety disorders: a study on patients with panic disorder, generalized anxiety disorder and obsessive-compulsive disorder. Early Interv Psychiatry. 2013;7:374-380.
15. Hales RE, Yudofsky SC, Roberts LW, eds. Textbook of Psychiatry, 6th ed. Arlington, VA: American Psychiatric Publishing: 2014:391-430.
16. Fernandez F, Levy JK, Lachar BL, et al. The management of depression and anxiety in the elderly. J Clin Psychiatry. 1995;56(suppl 2):20-29.
17. Kirkwood CK, Hayes PE. Anxiety disorders. In: DiPiro JT, Talbert RL, Yee GC, et al, eds. Pharmacotherapy: A Pathophysiologic Approach, 3rd ed. Stamford, Conn: Appleton & Lange;1997:1443-1462.
18. Culpepper L. Generalized anxiety disorder and medical illness. J Clin Psychiatry. 2009;70(suppl 2):20-24.
19. Anderson KG, Dugas MJ, Koerner N, et al. Interpretive style and intolerance of uncertainty in individuals with anxiety disorders: a focus on generalized anxiety disorder. J Anxiety Disord. 2012;26:823-832.
20. Satterfield JM, Feldman MD. Anxiety. In Feldman MD, Christensen JF, Satterfield JM, eds. Behavioral Medicine: A Guide for Clinical Practice. New York: McGraw Hill; 2014:271-282.
21. Grist R, Porter J, Stallard P. Mental health mobile apps for preadolescents and adolescents: A systematic review. J Med Internet Res. 2017;19:e176.
22. Rollnick S, Miller W, Butler C. Motivational Interviewing in Health Care: Helping Patients Change Behavior. 1st ed. New York: The Guilford Press; 2008:34-35.
23. Strawn JR, Geriacioti L, Rajdev N, et al. Pharmacotherapy for generalized anxiety disorder in adult and pediatric patients: an evidence-based review. Expert Opin Pharmacother. 2018;19:1057-1070.
24. Ehmke CJ, Nemeroff CB. Paroxetine. In Schatzberg AF, Nemeroff CB, eds. Textbook of Psychopharmacology, 4th ed. Washington, D.C.: American Psychiatric Publishing, Inc.; 2009:321-352.
25. Huh J, Goebert D, Takeshita J, et al. Treatment of generalized anxiety disorder: a comprehensive review of the literature for psychopharmacologic alternatives to newer antidepressants and benzodiazepines. Prim Care Companion CNS Disord. 2011;13: doi:10.4088/PCC.08r00709blu.
Erectile dysfunction: How to help patients & partners
THE CASE
Eric M,* a 36-year-old new patient, visits a primary care clinic for a check-up accompanied by his wife. A thorough history and physical exam reveal no concerns. He is active and a nonsmoker, drinks only socially, takes no medications, and reports no concerning symptoms. At the end of the visit, though, he says he has been experiencing erectile dysfunction for the past 6 months. What began as intermittent difficulty maintaining erections now “happens a lot.” He is distressed and says, “It just came out of the blue.” The patient’s wife then says she believes men cannot achieve erections if they are having an affair. When the chagrined patient simply asks for “those pills,” his wife says in a raised voice, “He’s a liar!”
●
*The patient’s name has been changed to protect his identity.
Some family physicians may feel ill-equipped to talk about sexual and relational problems and lack the skills to effectively counsel on these matters.1 Despite the fact that more than 70% of adult patients want to discuss sexual topics with their family physician, sexual problems are documented in as few as 2% of patient notes.2 One of the most commonly noted sexual health concerns is erectile dysfunction (ED), estimated to occur in 35% of men ages 40 to 70.3 Many ED cases have psychological antecedents including stress, depression, performance anxiety, pornography addiction, and relationship concerns.4,5
Assessing ED. The inability to achieve or maintain an erection needed for satisfactory sexual activity is typically diagnosed through symptom self-report and with thorough history taking and physical examination.6 However, more objective scales can be used. In particular, the International Index of Erectile Function, a 15-question scale, is useful for both diagnosis and treatment monitoring (www.baus.org.uk/_userfiles/pages/files/Patients/Leaflets/iief.pdf).7 Common contributors to ED can be vascular (eg, hypertension), neurologic (eg, multiple sclerosis), psychological (noted earlier), or hormonal (eg, thyroid imbalances).6 In this article, we focus on the relationship context in which ED exists. A review of medical evaluation and management can be found elsewhere.8
Key relational questions
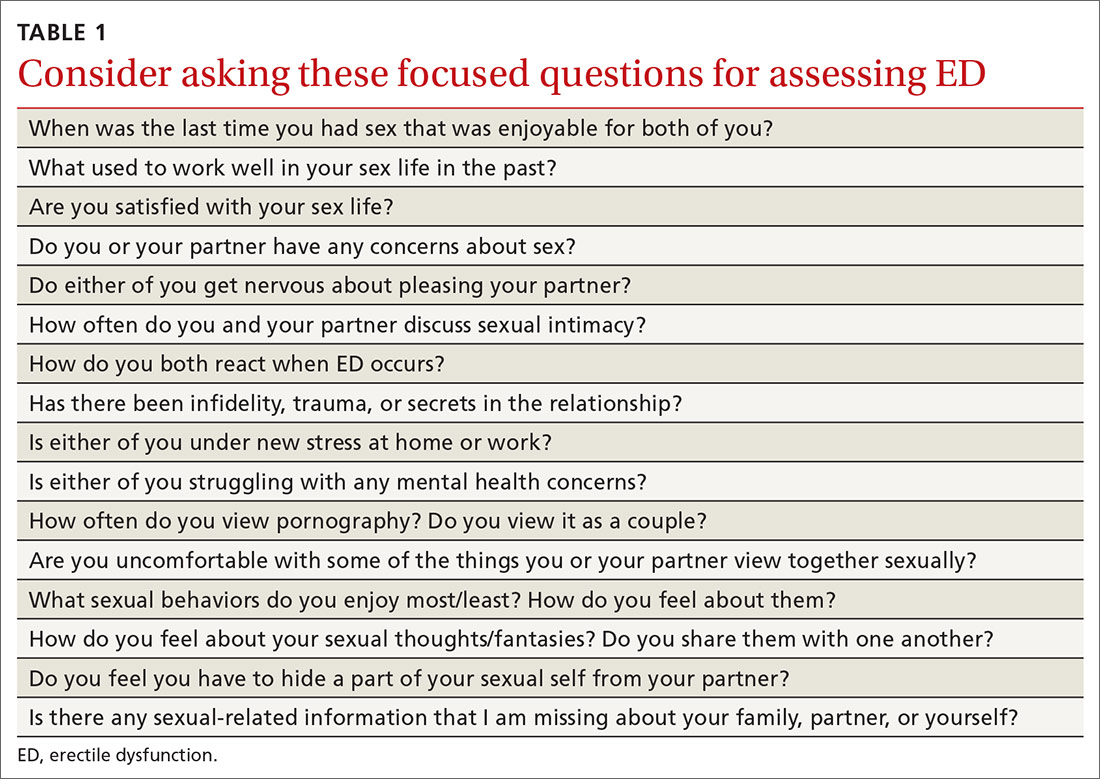
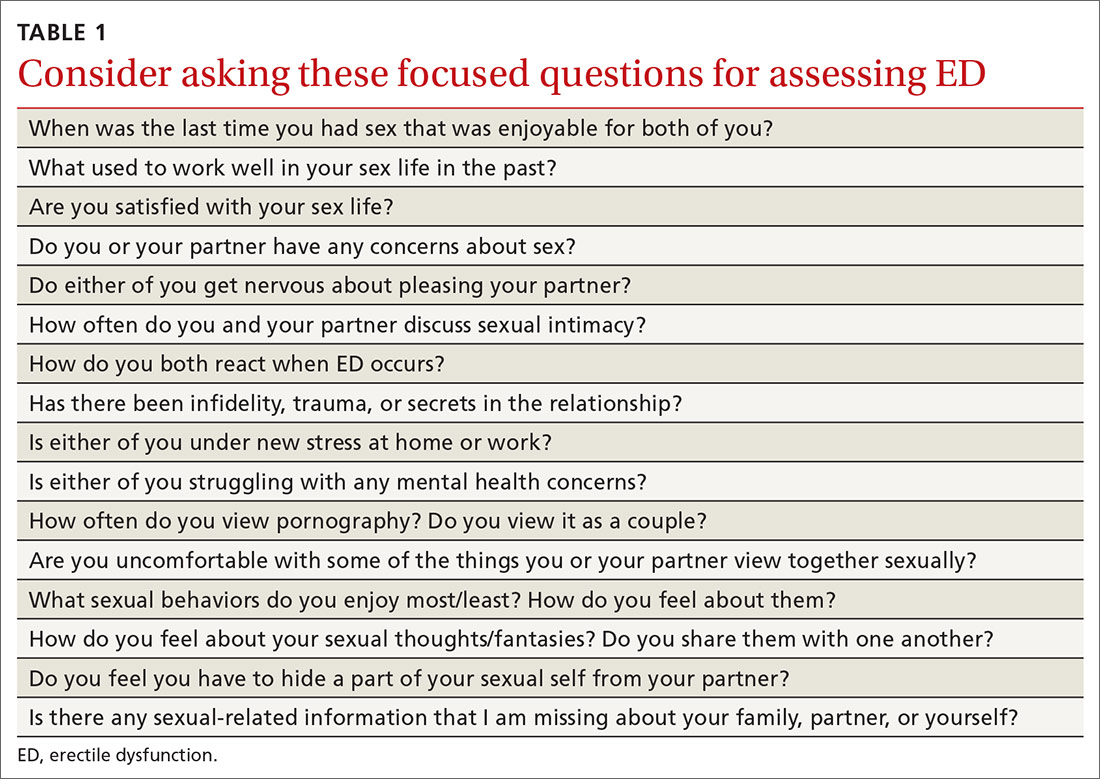
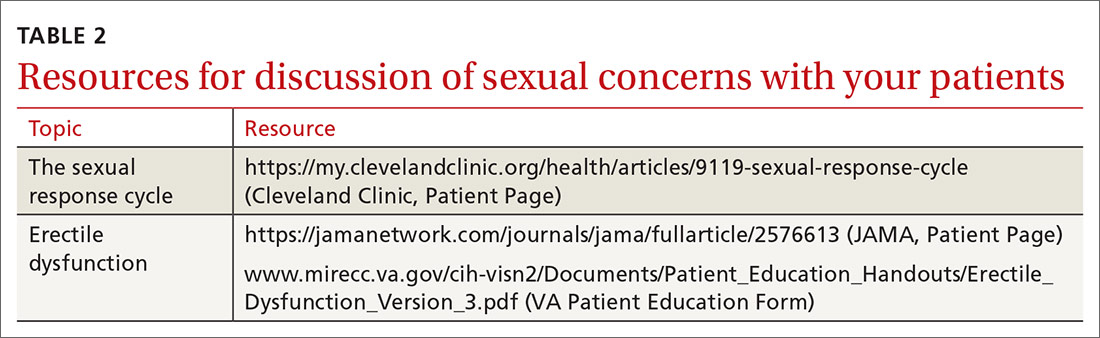
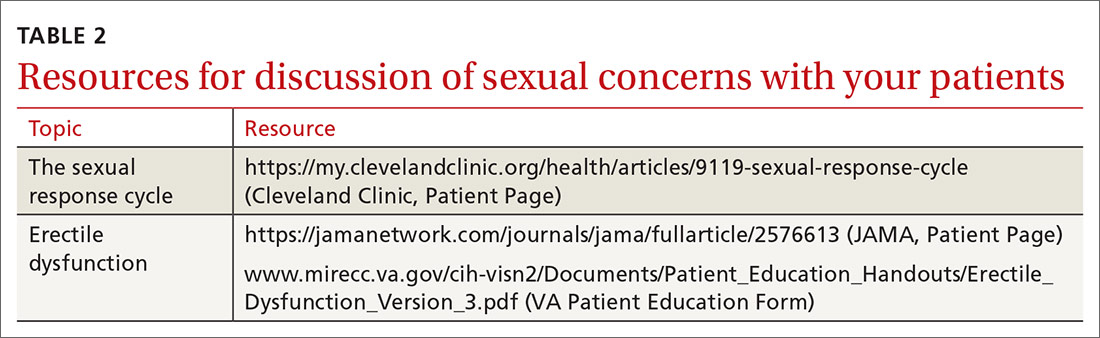
Identify norms that are specific to the couple. Patients from a variety of cultures prefer that their clinicians initiate the conversation about ED.11,12 We specifically recommend that clinicians, using relationally focused questions, inquire about sexual norms and desires that may be situated in culture, family of origin, or gender (TABLE 1).
Continue to: Treating ED within a relationship
Treating ED within a relationship
Once a couple’s sexual relationship has been fully assessed, you may confidently develop a treatment plan for managing sexual dysfunction relationally as well as medically, an approach to ED advised by the American Urological Association.13 We propose that primary care treatment for ED involve collaboration between the physician, the patient/couple (if the patient is partnered), and, as needed, a behavioral health specialist.
The physician’s role ...
Managing ED relationally is important on many fronts. If, for instance, a type-5 phosphodiesterase (PDE-5) inhibitor is needed, both the patient and partner should learn about best practices for optimizing success, such as avoiding excessive alcohol intake or high-fat meals immediately before and after taking a PDE-5.14
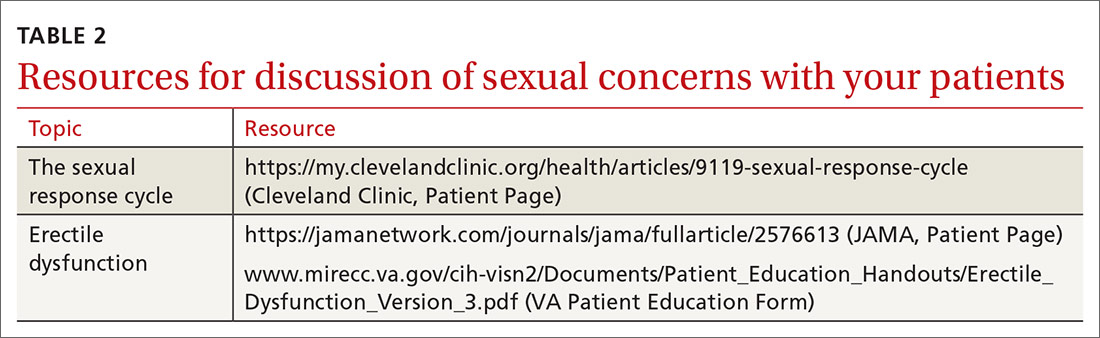
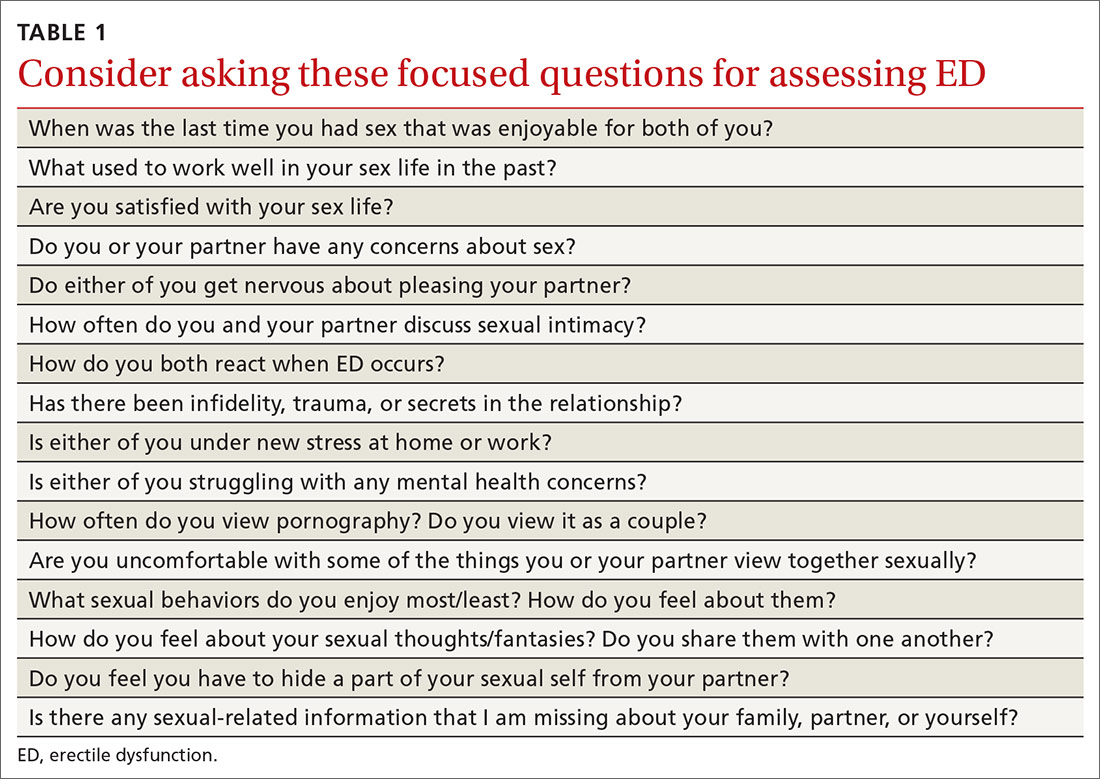
Sex ed. Regardless of the couple’s age, be prepared to offer high-quality sexual education. Either partner may have faulty knowledge (or even a lack of knowledge) of basic sexual functioning. Physicians have an opportunity to explain healthy erectile functioning, the sexual response cycle, and ways in which PDE-5 medications work (and do not work). (For a list of resources to facilitate these discussions, see TABLE 2.)
Avoid avoidance. Physicians can intervene on patterns of shame that may surround ED simply by discussing sexual functioning openly and honestly. ED often persists due to avoidance—ie, anxiety about sexual performance can lead couples to avoid sex, which perpetuates more anxiety and avoidance. Normalizing typical sexual functioning, encouraging couples to “avoid avoidance,” and providing referrals as needed are core elements of relational intervention for ED.
Setting the tone. Family physicians are not routinely trained in couples therapy. However, you can employ communication skills that allow each partner to be heard by using empathic/reflective listening, de-escalation, and reframing. Asking “What effect are the sexual concerns having on both of you?” and “What were the circumstances of the last sexual encounter that were pleasing to both of you?” can help promote intimacy and mutual satisfaction.
Continue to: The behavioral specialist's role
The behavioral specialist’s role
Behavioral health specialists may treat ED using methods such as cognitive behavioral therapy or evidence-based couple interventions.4 Cognitive methods for the treatment of ED include examination of maladaptive thoughts around pressure to perform and achieving sexual pleasure. Behavioral methods for treatment of ED are typically aimed at the de-coupling of anxiety and sexual activity. These treatments can include relaxation and desensitization, specifically sensate focus therapy.15
Sensate focus therapy involves a specific set of prescriptive rules for sexual activity, initially restricting touch to non-demand pleasurable touch (eg, holding hands) that allows couples to connect in a low-anxiety context focused on relaxation and connection. As couples are able to control anxiety while engaging in these activities, they engage in increasingly more intimate activities. Additionally, behavioral health specialists trained in couples therapy are vital to helping increase communication regarding sexual activity, sexual scripts, and the relationship in general.4
Identifying a treatment team
In coordinating couples care in the treatment of ED, enlist the help of a therapist who has specific knowledge and skills in the treatment of sexual disorders. While the number of qualified or certified sex therapists is limited, referring providers can visit the American Association of Sexuality Educators, Counselors, and Therapists Web site (www.aasect.org) for possible referral sources. Another option is the American Association for Marriage and Family Therapy Web site (www.aamft.org) under “Find a therapist.” Lastly, the Society for Sex Therapy and Research (www.sstarnet.org) is another professional association that provides information and local referral sources. For patients and partners located in rural areas where access is limited, telehealth options may need to be explored.
THE CASE
Mr. M and his wife were seen for a follow-up appointment by his primary care provider, who ruled out any additional causes of ED (eg, hormonal, vascular), discussed with both the patient and his wife basic sexual health and sexual functioning, dispelled several commonly held myths (ie, individuals cannot obtain an erection because of infidelity or lying), validated sexual concerns as a significant health issue, and prescribed a PDE-5 inhibitor.
Mr. M and his wife were referred to a behavioral health specialist in the clinic who had expertise in couples therapy. At several subsequent visits, the patient and his wife worked on improving the quality and quantity of communication regarding their sexual goals, mutual de-escalation of anxiety, increased emotional intimacy, and sensate focus techniques.
Continue to: As the result of the interventions...
As the result of these interventions, both the patient and his wife were able to engage in sex with less anxiety, and the patient increasingly was able to achieve more satisfactory erections without the use of the PDE-5 inhibitor. At the conclusion of therapy, the patient and his wife reported an increase in sexual satisfaction.
CORRESPONDENCE
Katherine Buck, PhD, Family Health Center, John Peter Smith Health Network, 1500 S. Main Street, Fort Worth, TX 76104; kbuck@jpshealth.org.
1. Macdowall W, Parker R, Nanchahal K, et al. ‘Talking of Sex’: developing and piloting a sexual health communication tool for use in primary care. Patient Educ Couns. 2010;81:332-337.
2. Sadovsky R. Asking the questions and offering solutions: the ongoing dialogue between the primary care physician and the patient with erectile dysfunction. Rev Urol. 2003;5(suppl 7):S35-S48.
3. Boston University School of Medicine. Sexual Medicine. Epidemiology of ED. 2019. www.bumc.bu.edu/sexualmedicine/physicianinformation/epidemiology-of-ed/. Accessed May 27, 2020.
4. Weeks GR, Gambescia N, Hertlein KM, eds. A Clinician’s Guide to Systemic Sex Therapy. 2nd ed. London, England: Routledge; 2016.
5. Colson MH, Cuzin A, Faix A, et al. Current epidemiology of erectile dysfunction, an update. Sexologies. 2018;27:e7-e13.
6. Rew KT, Heidelbaugh JJ. Erectile dysfunction. Am Fam Physician. 2016;94820-94827.
7. Rosen RC, Cappelleri JC, Smith MD, et al. Development and evaluation of an abridged, 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction. Int J Impot Res. 1999;11:319-326.
8. Rew KT, Heidelbaugh JJ. Erectile dysfunction. Am Fam Physician. 2016;94:820-827.
9. Dean J, Rubio-Aurioles E, McCabe M, et al. Integrating partners into erectile dysfunction treatment: improving the sexual experience for the couple. Int J Clin Pract. 2008;62:127-133.
10. Shamloul R, Ghanem H. Erectile dysfunction. Lancet. 2013; 381:153-165.
11. Lo WH, Fu SN, Wong SN, et al. Prevalence, correlates, attitude and treatment seeking of erectile dysfunction among type 2 diabetic Chinese men attending primary care outpatient clinics. Asian J Androl. 2014;16:755-760.
12. Zweifler J, Padilla A, Schafer S. Barriers to recognition of erectile dysfunction among diabetic Mexican-American men. J Am Board Fam Pract. 1998;11:259-263.
13. American Urological Society. Erectile dysfunction: AUA guideline (2018). www.auanet.org/guidelines/erectile-dysfunction-(ed)-guideline. Accessed May 27, 2020.
14. Huang S, Lie J. Phosphodiesterase-5 (PDE5) inhibitors in the management of erectile dysfunction. P T. 2013;38;414-419.
15. Masters WH, Johnson VE. Human Sexual Inadequacy. Boston: Little Brown; 1970.
THE CASE
Eric M,* a 36-year-old new patient, visits a primary care clinic for a check-up accompanied by his wife. A thorough history and physical exam reveal no concerns. He is active and a nonsmoker, drinks only socially, takes no medications, and reports no concerning symptoms. At the end of the visit, though, he says he has been experiencing erectile dysfunction for the past 6 months. What began as intermittent difficulty maintaining erections now “happens a lot.” He is distressed and says, “It just came out of the blue.” The patient’s wife then says she believes men cannot achieve erections if they are having an affair. When the chagrined patient simply asks for “those pills,” his wife says in a raised voice, “He’s a liar!”
●
*The patient’s name has been changed to protect his identity.
Some family physicians may feel ill-equipped to talk about sexual and relational problems and lack the skills to effectively counsel on these matters.1 Despite the fact that more than 70% of adult patients want to discuss sexual topics with their family physician, sexual problems are documented in as few as 2% of patient notes.2 One of the most commonly noted sexual health concerns is erectile dysfunction (ED), estimated to occur in 35% of men ages 40 to 70.3 Many ED cases have psychological antecedents including stress, depression, performance anxiety, pornography addiction, and relationship concerns.4,5
Assessing ED. The inability to achieve or maintain an erection needed for satisfactory sexual activity is typically diagnosed through symptom self-report and with thorough history taking and physical examination.6 However, more objective scales can be used. In particular, the International Index of Erectile Function, a 15-question scale, is useful for both diagnosis and treatment monitoring (www.baus.org.uk/_userfiles/pages/files/Patients/Leaflets/iief.pdf).7 Common contributors to ED can be vascular (eg, hypertension), neurologic (eg, multiple sclerosis), psychological (noted earlier), or hormonal (eg, thyroid imbalances).6 In this article, we focus on the relationship context in which ED exists. A review of medical evaluation and management can be found elsewhere.8
Key relational questions
Identify norms that are specific to the couple. Patients from a variety of cultures prefer that their clinicians initiate the conversation about ED.11,12 We specifically recommend that clinicians, using relationally focused questions, inquire about sexual norms and desires that may be situated in culture, family of origin, or gender (TABLE 1).
Continue to: Treating ED within a relationship
Treating ED within a relationship
Once a couple’s sexual relationship has been fully assessed, you may confidently develop a treatment plan for managing sexual dysfunction relationally as well as medically, an approach to ED advised by the American Urological Association.13 We propose that primary care treatment for ED involve collaboration between the physician, the patient/couple (if the patient is partnered), and, as needed, a behavioral health specialist.
The physician’s role ...
Managing ED relationally is important on many fronts. If, for instance, a type-5 phosphodiesterase (PDE-5) inhibitor is needed, both the patient and partner should learn about best practices for optimizing success, such as avoiding excessive alcohol intake or high-fat meals immediately before and after taking a PDE-5.14
Sex ed. Regardless of the couple’s age, be prepared to offer high-quality sexual education. Either partner may have faulty knowledge (or even a lack of knowledge) of basic sexual functioning. Physicians have an opportunity to explain healthy erectile functioning, the sexual response cycle, and ways in which PDE-5 medications work (and do not work). (For a list of resources to facilitate these discussions, see TABLE 2.)
Avoid avoidance. Physicians can intervene on patterns of shame that may surround ED simply by discussing sexual functioning openly and honestly. ED often persists due to avoidance—ie, anxiety about sexual performance can lead couples to avoid sex, which perpetuates more anxiety and avoidance. Normalizing typical sexual functioning, encouraging couples to “avoid avoidance,” and providing referrals as needed are core elements of relational intervention for ED.
Setting the tone. Family physicians are not routinely trained in couples therapy. However, you can employ communication skills that allow each partner to be heard by using empathic/reflective listening, de-escalation, and reframing. Asking “What effect are the sexual concerns having on both of you?” and “What were the circumstances of the last sexual encounter that were pleasing to both of you?” can help promote intimacy and mutual satisfaction.
Continue to: The behavioral specialist's role
The behavioral specialist’s role
Behavioral health specialists may treat ED using methods such as cognitive behavioral therapy or evidence-based couple interventions.4 Cognitive methods for the treatment of ED include examination of maladaptive thoughts around pressure to perform and achieving sexual pleasure. Behavioral methods for treatment of ED are typically aimed at the de-coupling of anxiety and sexual activity. These treatments can include relaxation and desensitization, specifically sensate focus therapy.15
Sensate focus therapy involves a specific set of prescriptive rules for sexual activity, initially restricting touch to non-demand pleasurable touch (eg, holding hands) that allows couples to connect in a low-anxiety context focused on relaxation and connection. As couples are able to control anxiety while engaging in these activities, they engage in increasingly more intimate activities. Additionally, behavioral health specialists trained in couples therapy are vital to helping increase communication regarding sexual activity, sexual scripts, and the relationship in general.4
Identifying a treatment team
In coordinating couples care in the treatment of ED, enlist the help of a therapist who has specific knowledge and skills in the treatment of sexual disorders. While the number of qualified or certified sex therapists is limited, referring providers can visit the American Association of Sexuality Educators, Counselors, and Therapists Web site (www.aasect.org) for possible referral sources. Another option is the American Association for Marriage and Family Therapy Web site (www.aamft.org) under “Find a therapist.” Lastly, the Society for Sex Therapy and Research (www.sstarnet.org) is another professional association that provides information and local referral sources. For patients and partners located in rural areas where access is limited, telehealth options may need to be explored.
THE CASE
Mr. M and his wife were seen for a follow-up appointment by his primary care provider, who ruled out any additional causes of ED (eg, hormonal, vascular), discussed with both the patient and his wife basic sexual health and sexual functioning, dispelled several commonly held myths (ie, individuals cannot obtain an erection because of infidelity or lying), validated sexual concerns as a significant health issue, and prescribed a PDE-5 inhibitor.
Mr. M and his wife were referred to a behavioral health specialist in the clinic who had expertise in couples therapy. At several subsequent visits, the patient and his wife worked on improving the quality and quantity of communication regarding their sexual goals, mutual de-escalation of anxiety, increased emotional intimacy, and sensate focus techniques.
Continue to: As the result of the interventions...
As the result of these interventions, both the patient and his wife were able to engage in sex with less anxiety, and the patient increasingly was able to achieve more satisfactory erections without the use of the PDE-5 inhibitor. At the conclusion of therapy, the patient and his wife reported an increase in sexual satisfaction.
CORRESPONDENCE
Katherine Buck, PhD, Family Health Center, John Peter Smith Health Network, 1500 S. Main Street, Fort Worth, TX 76104; kbuck@jpshealth.org.
THE CASE
Eric M,* a 36-year-old new patient, visits a primary care clinic for a check-up accompanied by his wife. A thorough history and physical exam reveal no concerns. He is active and a nonsmoker, drinks only socially, takes no medications, and reports no concerning symptoms. At the end of the visit, though, he says he has been experiencing erectile dysfunction for the past 6 months. What began as intermittent difficulty maintaining erections now “happens a lot.” He is distressed and says, “It just came out of the blue.” The patient’s wife then says she believes men cannot achieve erections if they are having an affair. When the chagrined patient simply asks for “those pills,” his wife says in a raised voice, “He’s a liar!”
●
*The patient’s name has been changed to protect his identity.
Some family physicians may feel ill-equipped to talk about sexual and relational problems and lack the skills to effectively counsel on these matters.1 Despite the fact that more than 70% of adult patients want to discuss sexual topics with their family physician, sexual problems are documented in as few as 2% of patient notes.2 One of the most commonly noted sexual health concerns is erectile dysfunction (ED), estimated to occur in 35% of men ages 40 to 70.3 Many ED cases have psychological antecedents including stress, depression, performance anxiety, pornography addiction, and relationship concerns.4,5
Assessing ED. The inability to achieve or maintain an erection needed for satisfactory sexual activity is typically diagnosed through symptom self-report and with thorough history taking and physical examination.6 However, more objective scales can be used. In particular, the International Index of Erectile Function, a 15-question scale, is useful for both diagnosis and treatment monitoring (www.baus.org.uk/_userfiles/pages/files/Patients/Leaflets/iief.pdf).7 Common contributors to ED can be vascular (eg, hypertension), neurologic (eg, multiple sclerosis), psychological (noted earlier), or hormonal (eg, thyroid imbalances).6 In this article, we focus on the relationship context in which ED exists. A review of medical evaluation and management can be found elsewhere.8
Key relational questions
Identify norms that are specific to the couple. Patients from a variety of cultures prefer that their clinicians initiate the conversation about ED.11,12 We specifically recommend that clinicians, using relationally focused questions, inquire about sexual norms and desires that may be situated in culture, family of origin, or gender (TABLE 1).
Continue to: Treating ED within a relationship
Treating ED within a relationship
Once a couple’s sexual relationship has been fully assessed, you may confidently develop a treatment plan for managing sexual dysfunction relationally as well as medically, an approach to ED advised by the American Urological Association.13 We propose that primary care treatment for ED involve collaboration between the physician, the patient/couple (if the patient is partnered), and, as needed, a behavioral health specialist.
The physician’s role ...
Managing ED relationally is important on many fronts. If, for instance, a type-5 phosphodiesterase (PDE-5) inhibitor is needed, both the patient and partner should learn about best practices for optimizing success, such as avoiding excessive alcohol intake or high-fat meals immediately before and after taking a PDE-5.14
Sex ed. Regardless of the couple’s age, be prepared to offer high-quality sexual education. Either partner may have faulty knowledge (or even a lack of knowledge) of basic sexual functioning. Physicians have an opportunity to explain healthy erectile functioning, the sexual response cycle, and ways in which PDE-5 medications work (and do not work). (For a list of resources to facilitate these discussions, see TABLE 2.)
Avoid avoidance. Physicians can intervene on patterns of shame that may surround ED simply by discussing sexual functioning openly and honestly. ED often persists due to avoidance—ie, anxiety about sexual performance can lead couples to avoid sex, which perpetuates more anxiety and avoidance. Normalizing typical sexual functioning, encouraging couples to “avoid avoidance,” and providing referrals as needed are core elements of relational intervention for ED.
Setting the tone. Family physicians are not routinely trained in couples therapy. However, you can employ communication skills that allow each partner to be heard by using empathic/reflective listening, de-escalation, and reframing. Asking “What effect are the sexual concerns having on both of you?” and “What were the circumstances of the last sexual encounter that were pleasing to both of you?” can help promote intimacy and mutual satisfaction.
Continue to: The behavioral specialist's role
The behavioral specialist’s role
Behavioral health specialists may treat ED using methods such as cognitive behavioral therapy or evidence-based couple interventions.4 Cognitive methods for the treatment of ED include examination of maladaptive thoughts around pressure to perform and achieving sexual pleasure. Behavioral methods for treatment of ED are typically aimed at the de-coupling of anxiety and sexual activity. These treatments can include relaxation and desensitization, specifically sensate focus therapy.15
Sensate focus therapy involves a specific set of prescriptive rules for sexual activity, initially restricting touch to non-demand pleasurable touch (eg, holding hands) that allows couples to connect in a low-anxiety context focused on relaxation and connection. As couples are able to control anxiety while engaging in these activities, they engage in increasingly more intimate activities. Additionally, behavioral health specialists trained in couples therapy are vital to helping increase communication regarding sexual activity, sexual scripts, and the relationship in general.4
Identifying a treatment team
In coordinating couples care in the treatment of ED, enlist the help of a therapist who has specific knowledge and skills in the treatment of sexual disorders. While the number of qualified or certified sex therapists is limited, referring providers can visit the American Association of Sexuality Educators, Counselors, and Therapists Web site (www.aasect.org) for possible referral sources. Another option is the American Association for Marriage and Family Therapy Web site (www.aamft.org) under “Find a therapist.” Lastly, the Society for Sex Therapy and Research (www.sstarnet.org) is another professional association that provides information and local referral sources. For patients and partners located in rural areas where access is limited, telehealth options may need to be explored.
THE CASE
Mr. M and his wife were seen for a follow-up appointment by his primary care provider, who ruled out any additional causes of ED (eg, hormonal, vascular), discussed with both the patient and his wife basic sexual health and sexual functioning, dispelled several commonly held myths (ie, individuals cannot obtain an erection because of infidelity or lying), validated sexual concerns as a significant health issue, and prescribed a PDE-5 inhibitor.
Mr. M and his wife were referred to a behavioral health specialist in the clinic who had expertise in couples therapy. At several subsequent visits, the patient and his wife worked on improving the quality and quantity of communication regarding their sexual goals, mutual de-escalation of anxiety, increased emotional intimacy, and sensate focus techniques.
Continue to: As the result of the interventions...
As the result of these interventions, both the patient and his wife were able to engage in sex with less anxiety, and the patient increasingly was able to achieve more satisfactory erections without the use of the PDE-5 inhibitor. At the conclusion of therapy, the patient and his wife reported an increase in sexual satisfaction.
CORRESPONDENCE
Katherine Buck, PhD, Family Health Center, John Peter Smith Health Network, 1500 S. Main Street, Fort Worth, TX 76104; kbuck@jpshealth.org.
1. Macdowall W, Parker R, Nanchahal K, et al. ‘Talking of Sex’: developing and piloting a sexual health communication tool for use in primary care. Patient Educ Couns. 2010;81:332-337.
2. Sadovsky R. Asking the questions and offering solutions: the ongoing dialogue between the primary care physician and the patient with erectile dysfunction. Rev Urol. 2003;5(suppl 7):S35-S48.
3. Boston University School of Medicine. Sexual Medicine. Epidemiology of ED. 2019. www.bumc.bu.edu/sexualmedicine/physicianinformation/epidemiology-of-ed/. Accessed May 27, 2020.
4. Weeks GR, Gambescia N, Hertlein KM, eds. A Clinician’s Guide to Systemic Sex Therapy. 2nd ed. London, England: Routledge; 2016.
5. Colson MH, Cuzin A, Faix A, et al. Current epidemiology of erectile dysfunction, an update. Sexologies. 2018;27:e7-e13.
6. Rew KT, Heidelbaugh JJ. Erectile dysfunction. Am Fam Physician. 2016;94820-94827.
7. Rosen RC, Cappelleri JC, Smith MD, et al. Development and evaluation of an abridged, 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction. Int J Impot Res. 1999;11:319-326.
8. Rew KT, Heidelbaugh JJ. Erectile dysfunction. Am Fam Physician. 2016;94:820-827.
9. Dean J, Rubio-Aurioles E, McCabe M, et al. Integrating partners into erectile dysfunction treatment: improving the sexual experience for the couple. Int J Clin Pract. 2008;62:127-133.
10. Shamloul R, Ghanem H. Erectile dysfunction. Lancet. 2013; 381:153-165.
11. Lo WH, Fu SN, Wong SN, et al. Prevalence, correlates, attitude and treatment seeking of erectile dysfunction among type 2 diabetic Chinese men attending primary care outpatient clinics. Asian J Androl. 2014;16:755-760.
12. Zweifler J, Padilla A, Schafer S. Barriers to recognition of erectile dysfunction among diabetic Mexican-American men. J Am Board Fam Pract. 1998;11:259-263.
13. American Urological Society. Erectile dysfunction: AUA guideline (2018). www.auanet.org/guidelines/erectile-dysfunction-(ed)-guideline. Accessed May 27, 2020.
14. Huang S, Lie J. Phosphodiesterase-5 (PDE5) inhibitors in the management of erectile dysfunction. P T. 2013;38;414-419.
15. Masters WH, Johnson VE. Human Sexual Inadequacy. Boston: Little Brown; 1970.
1. Macdowall W, Parker R, Nanchahal K, et al. ‘Talking of Sex’: developing and piloting a sexual health communication tool for use in primary care. Patient Educ Couns. 2010;81:332-337.
2. Sadovsky R. Asking the questions and offering solutions: the ongoing dialogue between the primary care physician and the patient with erectile dysfunction. Rev Urol. 2003;5(suppl 7):S35-S48.
3. Boston University School of Medicine. Sexual Medicine. Epidemiology of ED. 2019. www.bumc.bu.edu/sexualmedicine/physicianinformation/epidemiology-of-ed/. Accessed May 27, 2020.
4. Weeks GR, Gambescia N, Hertlein KM, eds. A Clinician’s Guide to Systemic Sex Therapy. 2nd ed. London, England: Routledge; 2016.
5. Colson MH, Cuzin A, Faix A, et al. Current epidemiology of erectile dysfunction, an update. Sexologies. 2018;27:e7-e13.
6. Rew KT, Heidelbaugh JJ. Erectile dysfunction. Am Fam Physician. 2016;94820-94827.
7. Rosen RC, Cappelleri JC, Smith MD, et al. Development and evaluation of an abridged, 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction. Int J Impot Res. 1999;11:319-326.
8. Rew KT, Heidelbaugh JJ. Erectile dysfunction. Am Fam Physician. 2016;94:820-827.
9. Dean J, Rubio-Aurioles E, McCabe M, et al. Integrating partners into erectile dysfunction treatment: improving the sexual experience for the couple. Int J Clin Pract. 2008;62:127-133.
10. Shamloul R, Ghanem H. Erectile dysfunction. Lancet. 2013; 381:153-165.
11. Lo WH, Fu SN, Wong SN, et al. Prevalence, correlates, attitude and treatment seeking of erectile dysfunction among type 2 diabetic Chinese men attending primary care outpatient clinics. Asian J Androl. 2014;16:755-760.
12. Zweifler J, Padilla A, Schafer S. Barriers to recognition of erectile dysfunction among diabetic Mexican-American men. J Am Board Fam Pract. 1998;11:259-263.
13. American Urological Society. Erectile dysfunction: AUA guideline (2018). www.auanet.org/guidelines/erectile-dysfunction-(ed)-guideline. Accessed May 27, 2020.
14. Huang S, Lie J. Phosphodiesterase-5 (PDE5) inhibitors in the management of erectile dysfunction. P T. 2013;38;414-419.
15. Masters WH, Johnson VE. Human Sexual Inadequacy. Boston: Little Brown; 1970.
Working adeptly to diagnose and treat adult ADHD
THE CASE
Ms. L’s family physician interviewed her and, aided by parental input, was able to identify a pattern of disorganized and impulsive behavior that was present even in grade school. Mood disorders and substance abuse were ruled out from the interview and lab testing, and cognitive ability was confirmed through a review of school testing.
●
* The patient’s name has been changed to protect her identity.
Attention-deficit/hyperactivity disorder (ADHD) is classified as a neurodevelopmental disorder in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), its hallmarks being inattentive, hyperactive, or impulsive behaviors that affect functioning or development.1 Historically, it was thought that ADHD was a disorder of children and adolescents, and that patients “grew out” of their behaviors once adulthood was reached. It is now estimated that 50% of children with ADHD will carry the diagnosis into adulthood,2 resulting in a prevalence of 5.9% to 7.1% for children3 and 3.4% for adults.4 There are 3 presentations of ADHD, known as ADHD-I (inattentive), ADHD-HI (hyperactive-impulsive), and ADHD-C (combined). The inattentive type accounts for 47% of adult cases, and adult ADHD disproportionately affects males compared with females.2
An overall pattern of underachievement and variable performance is common throughout life in patients with ADHD. Adults are much more likely to report subtle impairments in higher executive functions such as organization, time management, and modulating emotions. Consequences include poor performance at work, attendance issues, difficulty with social interactions, and an increased likelihood of unemployment.5 Among those employed, there is a large disparity in income compared with counterparts without ADHD.6 Increased risk of substance use, injury, and traffic accidents also has been reported.1
Disorders that can mimic or coexist with ADHD
The differential diagnosis for ADHD is wide, and comorbidity with other disorders is common.
Continue to: Bipolar disorder
Bipolar disorder shares with ADHD the core symptoms of hyperactivity, impulsive behavior, and difficulty completing tasks. Mania and ADHD can look very similar if symptoms are observed at a single point in time. Bipolar illness is, by definition, episodic and fluctuating, while ADHD is much more constant. In addition, bipolar illness exhibits significant variation in mood, while ADHD may or may not be associated with impaired mood regulation. Up to 20% of patients with bipolar illness also have ADHD.7
Anxiety and depressive disorders can also share symptoms with ADHD-I. These include distractibility, poor concentration, and, in the case of anxiety, rapid changes in train of thought. Sleep disturbance, past trauma, and current acute stressors may manifest as clinical anxiety or depression, or may interfere with concentration and attention independently. As with bipolar illness, clinicians must look carefully at the time course of symptoms, including the age of onset. Classically, mood disorders develop in adolescence or early adulthood, while ADHD always has manifestations in childhood. Inattention and distractibility will track with mood if they are caused by an affective illness, but will remain in ADHD even when the patient is euthymic. On the other hand, patients with ADHD frequently become frustrated or overwhelmed as a result of their difficulties with task completion and social function, a presentation which can mimic anxiety or depression.8
Substance use disorder and ADHD interact in multiple ways and can present one of the more challenging diagnostic tasks when assessing a patient with impaired attention or concentration. ADHD is a powerful risk factor for future substance use,9 while substance use can impair attention, induce impulsivity, and alter concentration. Further, the treatment of choice for ADHD (stimulant medication) has the potential for misuse. The presence of continuous symptoms across settings is crucial in determining the proper diagnosis of ADHD.
Other conditions. Patients with a learning disability can be inattentive due to their cognitive limitations, or it may be comorbid with ADHD. If an intellectual deficit is suspected, referral for cognitive testing can help clarify the diagnosis. Autism also may cause significant alterations in attention with both hyper-focus and distractibility being common, as they are in ADHD. Intermittent explosive disorder shares the core symptom of impulsivity, but includes aggression, which is not always seen in ADHD. Personality disorders (eg, borderline, narcissistic) may also be difficult to distinguish from ADHD. The key to differentiation is the identification of behavior patterns outside the realms of concentration and attention.7
KEY DIAGNOSTIC CRITERIA
The diagnostic criteria for ADHD defined in DSM-5 are found in TABLE 1.1 Individuals ≥ 17 years old must meet 5 of 9 characteristics of inattention or 5 of 9 characteristics of hyperactivity/impulsivity (criterion A).1 Some symptoms must have been present prior to age 12 (criterion B). This cutoff is an increase from age 7 advised in DSM-IV.10 Symptoms must occur across at least 2 settings (criterion C) and significantly interfere with social, academic, or occupational functioning (criterion D). Exclusions include symptoms that occur exclusively in the context of a psychotic disorder or symptoms that are better explained in the context of other mental disorders (criterion E).1
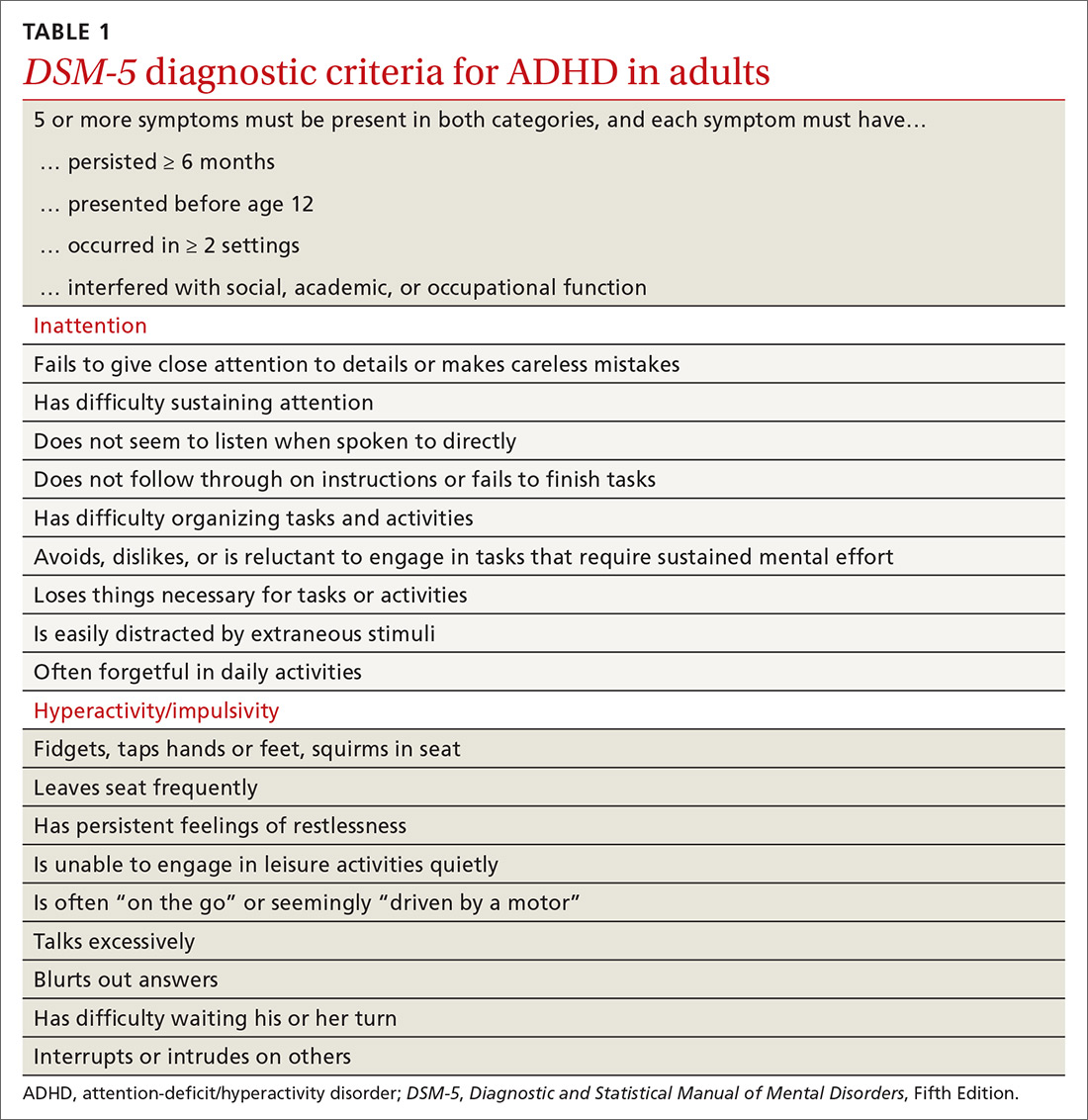
Continue to: In the primary care setting
In the primary care setting, an assessment for ADHD should, at minimum, involve a review of the patient’s academic and work history, assessment of psychiatric comorbidities and substance use history, and administration of appropriate rating scales. When evaluating adults, these tools include the Adult ADHD Self-Report Scale (ASRS)11,12 screening tool and the Diagnostic Interview for ADHD in adults (DIVA-5).13,14 If possible, obtain scale assessments not only from the patient but from family members or other observers who can provide information about the patient in childhood/adolescence and present day.
In an integrated care setting, consider involving a behavioral health consultant for a more comprehensive evaluation of educational, employment, driving, and relationship histories. Historical record review may include report cards from elementary school through high school, standardized test scores, psycho-educational and individual education plan reports, and medical records. Having a snapshot of the patient as a younger child, adolescent, and young adult can help to identify overall patterns of academic underachievement and reveal gaps between potential and overall achievement and performance. Pursue a more thorough evaluation in cases where other comorbid psychiatric disorders are present or when the patient is unfamiliar to you.
TWO GROUPS OF TREATMENT OPTIONS
The treatment of ADHD in adults (and children) can be broadly divided into pharmacologic and nonpharmacologic modalities.
Stimulants are first-line pharmacologic treatment for ADHD in patients with low risk for misuse. Stimulants improve cognitive function, decrease impulsivity, and increase alertness.15 However, these effects are not exclusive to those with ADHD, and response does not aid in diagnosis. No stimulant is preferred over another, although individuals may respond better to 1 specific agent than to others. Be aware that stimulants may be diverted; patients at increased risk include those with comorbid substance use or mood disorders. Misuse may be especially common on college campuses, where nonprescribed stimulants may be used as study aids or recreationally.
Stimulants come in a variety of formulations that differ primarily in their time profile or mode of delivery. Some preparations (eg, Ritalin LA and Adderall XR) contain a mixture of immediate-release and extended-release mechanisms and therefore have bimodal peaks. Others (eg, Concerta) use an osmotic system to approximate a steadier flow of drug delivery. However, as these drugs have entered the generic market, time response between products is much less predictable. Individual differences in metabolism may also alter duration of action.
Continue to: Lisdexamfetamine (Vyvanse)...
Lisdexamfetamine (Vyvanse) is a pro-drug that requires first-pass metabolism for conversion to an active drug. This may reduce risk of overdose or misuse. Adverse effects of stimulants include decreased appetite, irritability, tics, and cardiac toxicity.16 Proper titration of dose over successive visits is essential as providers often must balance efficacy, appetite, and sleep.
Nonstimulant therapies are options for patients who cannot tolerate stimulants or are at high risk for misuse. Atomoxetine, a norepinephrine reuptake inhibitor, has qualities that may resemble antidepressants in its 2- to 4-week time lapse before taking effect. Alpha-2 agonists clonidine and guanfacine are approved by the US Food and Drug Administration in their extended release forms for adjunct therapy with stimulants. Pharmacologic therapies are listed in TABLE 2.16
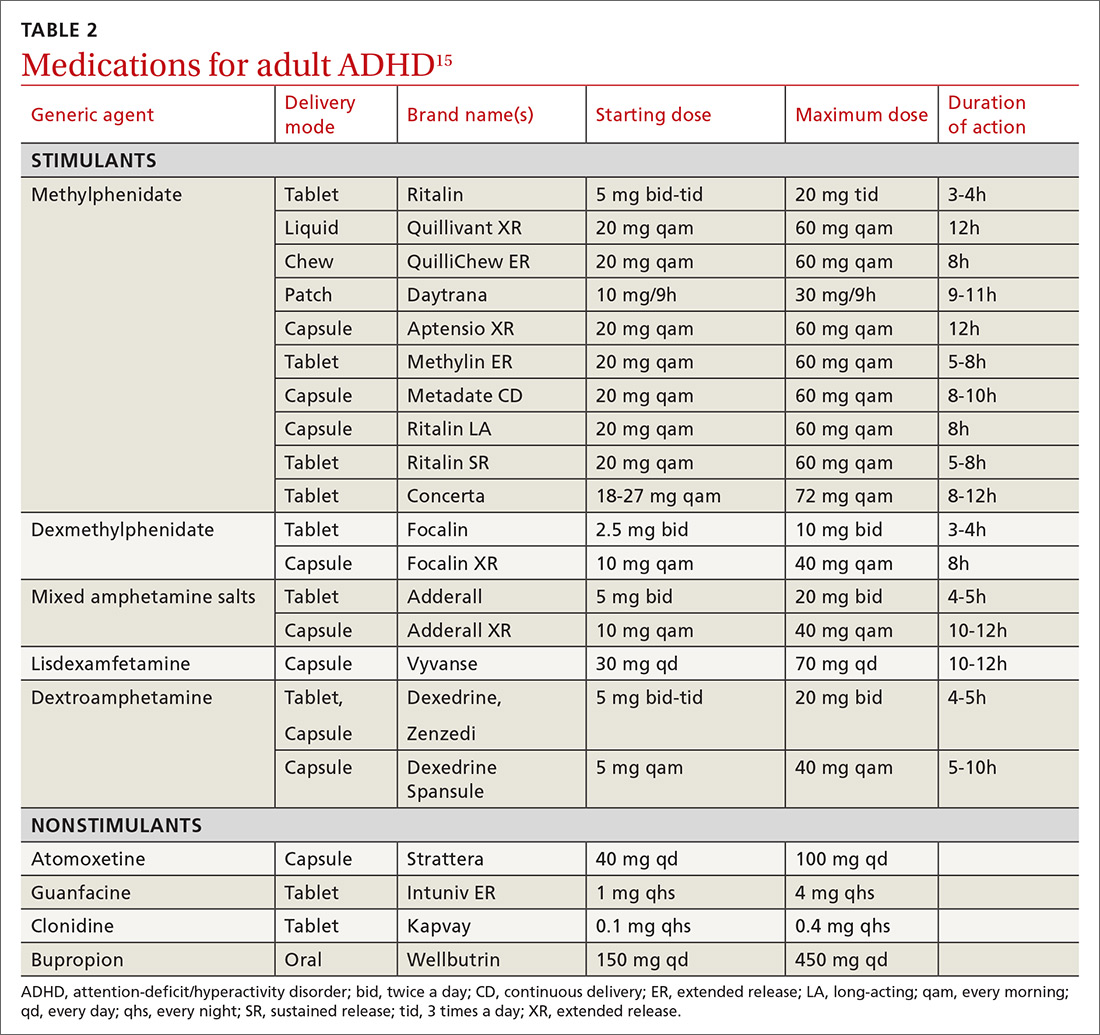
Nonpharmacologic modalities for adult ADHD include psychoeducation, cognitive behavioral therapy, and work environment modification. While coordination with schools is recognized as an essential aspect of the care of ADHD in children, team care in the treatment of adults with ADHD is often forgotten. Referral for occupational or educational support, written materials on study habits and organizational skills, and the use of memory tools can be very helpful. Modifications in physical environment and time constraints in both work and school settings can enhance productivity in adults with ADHD. Attention to sleep scheduling and sleep hygiene can also improve attention and concentration throughout the day.
CASE
She engaged with the education specialists at her school, who helped her discuss testing and assignment modifications with her professors. She began to develop a time-management strategy to complete her assignments; these included reduced evening caffeine intake and improved sleep hygiene. Over time, Ms. L was able to maintain attention for the more extended homework tasks assigned in college. She was also able to enjoy a similar level of success that she had achieved in high school.
CORRESPONDENCE
Jay Brieler, MD, Family and Community Medicine, Saint Louis University School of Medicine, 6420 Clayton Road, Room 2234, St. Louis MO 63117; jay.brieler@health.slu.edu.
1. Neurodevelopmental disorders. In: Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013:59-65.
2. Moreno-Alcázar A, Ramos-Quiroga JA, Radua J, et al. Brain abnormalities in adults with Attention Deficit Hyperactivity Disorder revealed by voxel-based morphometry. Psychiatry Res Neuroimaging. 2016;254:41-47.
3. Willcutt EG. The prevalence of DSM-IV attention-deficit/hyperactivity disorder: a meta-analytic review. Neurotherapeutics. 2012;9:490-499.
4. Fayyad J, De Graaf R, Kessler R, et al. Cross-national prevalence and correlates of adult attention-deficit hyperactivity disorder. Br J Psychiatry. 2007;190:402-409.
5. Kessler R, Adler L, Barkley R, et al. The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am J Psychiatry. 2006;163:716-723.
6. Klein RG, Mannuzza S, Olazagasti MA, et al. Clinical and functional outcome of childhood attention-deficit/hyperactivity disorder 33 years later. Arch Gen Psychiatry. 2012;69:1295-1303.
7. Asherson P, Young AH, Eich-Hochli D, et al. Differential diagnosis, comorbidity, and treatment of ADHD in relation to bipolar disorder or borderline personality disorder in adults. Curr Med Res Opin. 2014;30:1657-1672.
8. Grogan K, Gormley CI, Rooney B, et al. Differential diagnosis and co-morbidity of ADHD and anxiety in adults. Br J Clin Psychol. 2018;57:99-115.
9. Ilbegi S, Groenman AP, Schellekens A, et al. Substance use and nicotine dependence in persistent, remittent, and late-onset ADHD: a 10-year longitudinal study from childhood to young adulthood. J Neurodev Disord. 2018;10:42.
10. Attention-deficit/hyperactivity disorder. In: Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC: American Psychiatric
11. , , , et al. The World Health Organization Adult ADHD Self‐Report Scale (ASRS): a short screening scale for use in the general population. Psychol Med. 2005;35:245‐256.
12. Ustun B, Adler LA, Rudin C, et al. The World Health Organization Adult Attention-Deficit/Hyperactivity Disorder Self-Report Screening Scale for DSM-5. JAMA Psychiatry. 2017;74:520-527.
13. Ramos-Quiroga JA, Nasillo V, Richarte V, et al. Criteria and concurrent validity of DIVA 2.0: a semi-structured diagnostic interview for adult ADHD. J Atten Disord. 2019;23:1126-1135.
14. Pettersson R, Söderström S, Nilsson KW. Diagnosing ADHD in adults: an examination of the discriminative validity of neuropsychological tests and diagnostic assessment instruments. J Atten Disord. 2018;22:1019-1031.
15. Parikh AR, Baker SA. Adult ADHD: pharmacologic treatment in the DSM-5 era. Curr Psychiatry. 2016;15:18-25.
16. Searight HR, Gafford J, Evans SL. Attention Deficit Hyperactivity Disorder. In: Smith MA, Shimp LA, Schrager S, eds. Family Medicine: Ambulatory Care and Prevention. 6th ed. New York, NY: McGraw-Hill; 2014:829-846.
THE CASE
Ms. L’s family physician interviewed her and, aided by parental input, was able to identify a pattern of disorganized and impulsive behavior that was present even in grade school. Mood disorders and substance abuse were ruled out from the interview and lab testing, and cognitive ability was confirmed through a review of school testing.
●
* The patient’s name has been changed to protect her identity.
Attention-deficit/hyperactivity disorder (ADHD) is classified as a neurodevelopmental disorder in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), its hallmarks being inattentive, hyperactive, or impulsive behaviors that affect functioning or development.1 Historically, it was thought that ADHD was a disorder of children and adolescents, and that patients “grew out” of their behaviors once adulthood was reached. It is now estimated that 50% of children with ADHD will carry the diagnosis into adulthood,2 resulting in a prevalence of 5.9% to 7.1% for children3 and 3.4% for adults.4 There are 3 presentations of ADHD, known as ADHD-I (inattentive), ADHD-HI (hyperactive-impulsive), and ADHD-C (combined). The inattentive type accounts for 47% of adult cases, and adult ADHD disproportionately affects males compared with females.2
An overall pattern of underachievement and variable performance is common throughout life in patients with ADHD. Adults are much more likely to report subtle impairments in higher executive functions such as organization, time management, and modulating emotions. Consequences include poor performance at work, attendance issues, difficulty with social interactions, and an increased likelihood of unemployment.5 Among those employed, there is a large disparity in income compared with counterparts without ADHD.6 Increased risk of substance use, injury, and traffic accidents also has been reported.1
Disorders that can mimic or coexist with ADHD
The differential diagnosis for ADHD is wide, and comorbidity with other disorders is common.
Continue to: Bipolar disorder
Bipolar disorder shares with ADHD the core symptoms of hyperactivity, impulsive behavior, and difficulty completing tasks. Mania and ADHD can look very similar if symptoms are observed at a single point in time. Bipolar illness is, by definition, episodic and fluctuating, while ADHD is much more constant. In addition, bipolar illness exhibits significant variation in mood, while ADHD may or may not be associated with impaired mood regulation. Up to 20% of patients with bipolar illness also have ADHD.7
Anxiety and depressive disorders can also share symptoms with ADHD-I. These include distractibility, poor concentration, and, in the case of anxiety, rapid changes in train of thought. Sleep disturbance, past trauma, and current acute stressors may manifest as clinical anxiety or depression, or may interfere with concentration and attention independently. As with bipolar illness, clinicians must look carefully at the time course of symptoms, including the age of onset. Classically, mood disorders develop in adolescence or early adulthood, while ADHD always has manifestations in childhood. Inattention and distractibility will track with mood if they are caused by an affective illness, but will remain in ADHD even when the patient is euthymic. On the other hand, patients with ADHD frequently become frustrated or overwhelmed as a result of their difficulties with task completion and social function, a presentation which can mimic anxiety or depression.8
Substance use disorder and ADHD interact in multiple ways and can present one of the more challenging diagnostic tasks when assessing a patient with impaired attention or concentration. ADHD is a powerful risk factor for future substance use,9 while substance use can impair attention, induce impulsivity, and alter concentration. Further, the treatment of choice for ADHD (stimulant medication) has the potential for misuse. The presence of continuous symptoms across settings is crucial in determining the proper diagnosis of ADHD.
Other conditions. Patients with a learning disability can be inattentive due to their cognitive limitations, or it may be comorbid with ADHD. If an intellectual deficit is suspected, referral for cognitive testing can help clarify the diagnosis. Autism also may cause significant alterations in attention with both hyper-focus and distractibility being common, as they are in ADHD. Intermittent explosive disorder shares the core symptom of impulsivity, but includes aggression, which is not always seen in ADHD. Personality disorders (eg, borderline, narcissistic) may also be difficult to distinguish from ADHD. The key to differentiation is the identification of behavior patterns outside the realms of concentration and attention.7
KEY DIAGNOSTIC CRITERIA
The diagnostic criteria for ADHD defined in DSM-5 are found in TABLE 1.1 Individuals ≥ 17 years old must meet 5 of 9 characteristics of inattention or 5 of 9 characteristics of hyperactivity/impulsivity (criterion A).1 Some symptoms must have been present prior to age 12 (criterion B). This cutoff is an increase from age 7 advised in DSM-IV.10 Symptoms must occur across at least 2 settings (criterion C) and significantly interfere with social, academic, or occupational functioning (criterion D). Exclusions include symptoms that occur exclusively in the context of a psychotic disorder or symptoms that are better explained in the context of other mental disorders (criterion E).1
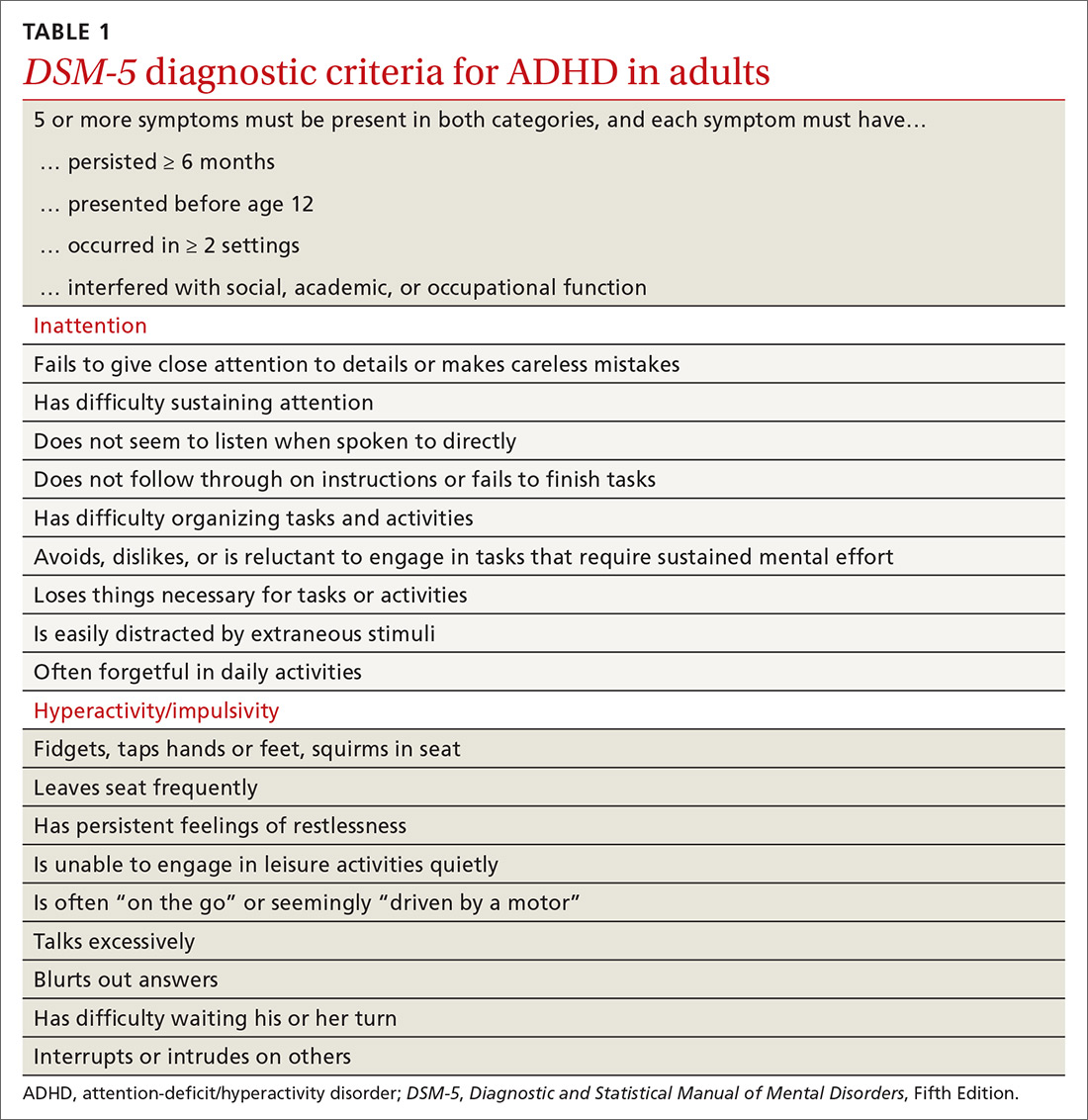
Continue to: In the primary care setting
In the primary care setting, an assessment for ADHD should, at minimum, involve a review of the patient’s academic and work history, assessment of psychiatric comorbidities and substance use history, and administration of appropriate rating scales. When evaluating adults, these tools include the Adult ADHD Self-Report Scale (ASRS)11,12 screening tool and the Diagnostic Interview for ADHD in adults (DIVA-5).13,14 If possible, obtain scale assessments not only from the patient but from family members or other observers who can provide information about the patient in childhood/adolescence and present day.
In an integrated care setting, consider involving a behavioral health consultant for a more comprehensive evaluation of educational, employment, driving, and relationship histories. Historical record review may include report cards from elementary school through high school, standardized test scores, psycho-educational and individual education plan reports, and medical records. Having a snapshot of the patient as a younger child, adolescent, and young adult can help to identify overall patterns of academic underachievement and reveal gaps between potential and overall achievement and performance. Pursue a more thorough evaluation in cases where other comorbid psychiatric disorders are present or when the patient is unfamiliar to you.
TWO GROUPS OF TREATMENT OPTIONS
The treatment of ADHD in adults (and children) can be broadly divided into pharmacologic and nonpharmacologic modalities.
Stimulants are first-line pharmacologic treatment for ADHD in patients with low risk for misuse. Stimulants improve cognitive function, decrease impulsivity, and increase alertness.15 However, these effects are not exclusive to those with ADHD, and response does not aid in diagnosis. No stimulant is preferred over another, although individuals may respond better to 1 specific agent than to others. Be aware that stimulants may be diverted; patients at increased risk include those with comorbid substance use or mood disorders. Misuse may be especially common on college campuses, where nonprescribed stimulants may be used as study aids or recreationally.
Stimulants come in a variety of formulations that differ primarily in their time profile or mode of delivery. Some preparations (eg, Ritalin LA and Adderall XR) contain a mixture of immediate-release and extended-release mechanisms and therefore have bimodal peaks. Others (eg, Concerta) use an osmotic system to approximate a steadier flow of drug delivery. However, as these drugs have entered the generic market, time response between products is much less predictable. Individual differences in metabolism may also alter duration of action.
Continue to: Lisdexamfetamine (Vyvanse)...
Lisdexamfetamine (Vyvanse) is a pro-drug that requires first-pass metabolism for conversion to an active drug. This may reduce risk of overdose or misuse. Adverse effects of stimulants include decreased appetite, irritability, tics, and cardiac toxicity.16 Proper titration of dose over successive visits is essential as providers often must balance efficacy, appetite, and sleep.
Nonstimulant therapies are options for patients who cannot tolerate stimulants or are at high risk for misuse. Atomoxetine, a norepinephrine reuptake inhibitor, has qualities that may resemble antidepressants in its 2- to 4-week time lapse before taking effect. Alpha-2 agonists clonidine and guanfacine are approved by the US Food and Drug Administration in their extended release forms for adjunct therapy with stimulants. Pharmacologic therapies are listed in TABLE 2.16
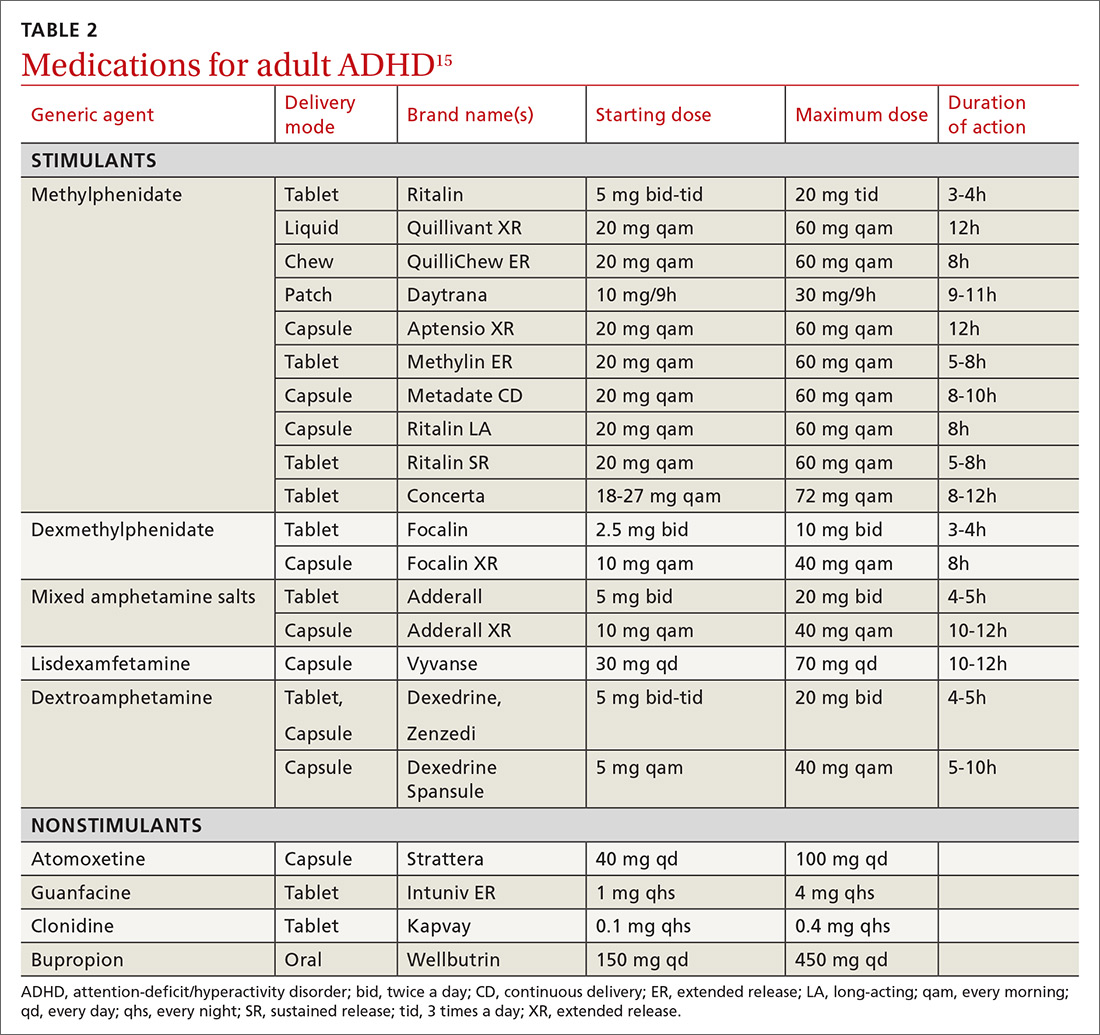
Nonpharmacologic modalities for adult ADHD include psychoeducation, cognitive behavioral therapy, and work environment modification. While coordination with schools is recognized as an essential aspect of the care of ADHD in children, team care in the treatment of adults with ADHD is often forgotten. Referral for occupational or educational support, written materials on study habits and organizational skills, and the use of memory tools can be very helpful. Modifications in physical environment and time constraints in both work and school settings can enhance productivity in adults with ADHD. Attention to sleep scheduling and sleep hygiene can also improve attention and concentration throughout the day.
CASE
She engaged with the education specialists at her school, who helped her discuss testing and assignment modifications with her professors. She began to develop a time-management strategy to complete her assignments; these included reduced evening caffeine intake and improved sleep hygiene. Over time, Ms. L was able to maintain attention for the more extended homework tasks assigned in college. She was also able to enjoy a similar level of success that she had achieved in high school.
CORRESPONDENCE
Jay Brieler, MD, Family and Community Medicine, Saint Louis University School of Medicine, 6420 Clayton Road, Room 2234, St. Louis MO 63117; jay.brieler@health.slu.edu.
THE CASE
Ms. L’s family physician interviewed her and, aided by parental input, was able to identify a pattern of disorganized and impulsive behavior that was present even in grade school. Mood disorders and substance abuse were ruled out from the interview and lab testing, and cognitive ability was confirmed through a review of school testing.
●
* The patient’s name has been changed to protect her identity.
Attention-deficit/hyperactivity disorder (ADHD) is classified as a neurodevelopmental disorder in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), its hallmarks being inattentive, hyperactive, or impulsive behaviors that affect functioning or development.1 Historically, it was thought that ADHD was a disorder of children and adolescents, and that patients “grew out” of their behaviors once adulthood was reached. It is now estimated that 50% of children with ADHD will carry the diagnosis into adulthood,2 resulting in a prevalence of 5.9% to 7.1% for children3 and 3.4% for adults.4 There are 3 presentations of ADHD, known as ADHD-I (inattentive), ADHD-HI (hyperactive-impulsive), and ADHD-C (combined). The inattentive type accounts for 47% of adult cases, and adult ADHD disproportionately affects males compared with females.2
An overall pattern of underachievement and variable performance is common throughout life in patients with ADHD. Adults are much more likely to report subtle impairments in higher executive functions such as organization, time management, and modulating emotions. Consequences include poor performance at work, attendance issues, difficulty with social interactions, and an increased likelihood of unemployment.5 Among those employed, there is a large disparity in income compared with counterparts without ADHD.6 Increased risk of substance use, injury, and traffic accidents also has been reported.1
Disorders that can mimic or coexist with ADHD
The differential diagnosis for ADHD is wide, and comorbidity with other disorders is common.
Continue to: Bipolar disorder
Bipolar disorder shares with ADHD the core symptoms of hyperactivity, impulsive behavior, and difficulty completing tasks. Mania and ADHD can look very similar if symptoms are observed at a single point in time. Bipolar illness is, by definition, episodic and fluctuating, while ADHD is much more constant. In addition, bipolar illness exhibits significant variation in mood, while ADHD may or may not be associated with impaired mood regulation. Up to 20% of patients with bipolar illness also have ADHD.7
Anxiety and depressive disorders can also share symptoms with ADHD-I. These include distractibility, poor concentration, and, in the case of anxiety, rapid changes in train of thought. Sleep disturbance, past trauma, and current acute stressors may manifest as clinical anxiety or depression, or may interfere with concentration and attention independently. As with bipolar illness, clinicians must look carefully at the time course of symptoms, including the age of onset. Classically, mood disorders develop in adolescence or early adulthood, while ADHD always has manifestations in childhood. Inattention and distractibility will track with mood if they are caused by an affective illness, but will remain in ADHD even when the patient is euthymic. On the other hand, patients with ADHD frequently become frustrated or overwhelmed as a result of their difficulties with task completion and social function, a presentation which can mimic anxiety or depression.8
Substance use disorder and ADHD interact in multiple ways and can present one of the more challenging diagnostic tasks when assessing a patient with impaired attention or concentration. ADHD is a powerful risk factor for future substance use,9 while substance use can impair attention, induce impulsivity, and alter concentration. Further, the treatment of choice for ADHD (stimulant medication) has the potential for misuse. The presence of continuous symptoms across settings is crucial in determining the proper diagnosis of ADHD.
Other conditions. Patients with a learning disability can be inattentive due to their cognitive limitations, or it may be comorbid with ADHD. If an intellectual deficit is suspected, referral for cognitive testing can help clarify the diagnosis. Autism also may cause significant alterations in attention with both hyper-focus and distractibility being common, as they are in ADHD. Intermittent explosive disorder shares the core symptom of impulsivity, but includes aggression, which is not always seen in ADHD. Personality disorders (eg, borderline, narcissistic) may also be difficult to distinguish from ADHD. The key to differentiation is the identification of behavior patterns outside the realms of concentration and attention.7
KEY DIAGNOSTIC CRITERIA
The diagnostic criteria for ADHD defined in DSM-5 are found in TABLE 1.1 Individuals ≥ 17 years old must meet 5 of 9 characteristics of inattention or 5 of 9 characteristics of hyperactivity/impulsivity (criterion A).1 Some symptoms must have been present prior to age 12 (criterion B). This cutoff is an increase from age 7 advised in DSM-IV.10 Symptoms must occur across at least 2 settings (criterion C) and significantly interfere with social, academic, or occupational functioning (criterion D). Exclusions include symptoms that occur exclusively in the context of a psychotic disorder or symptoms that are better explained in the context of other mental disorders (criterion E).1
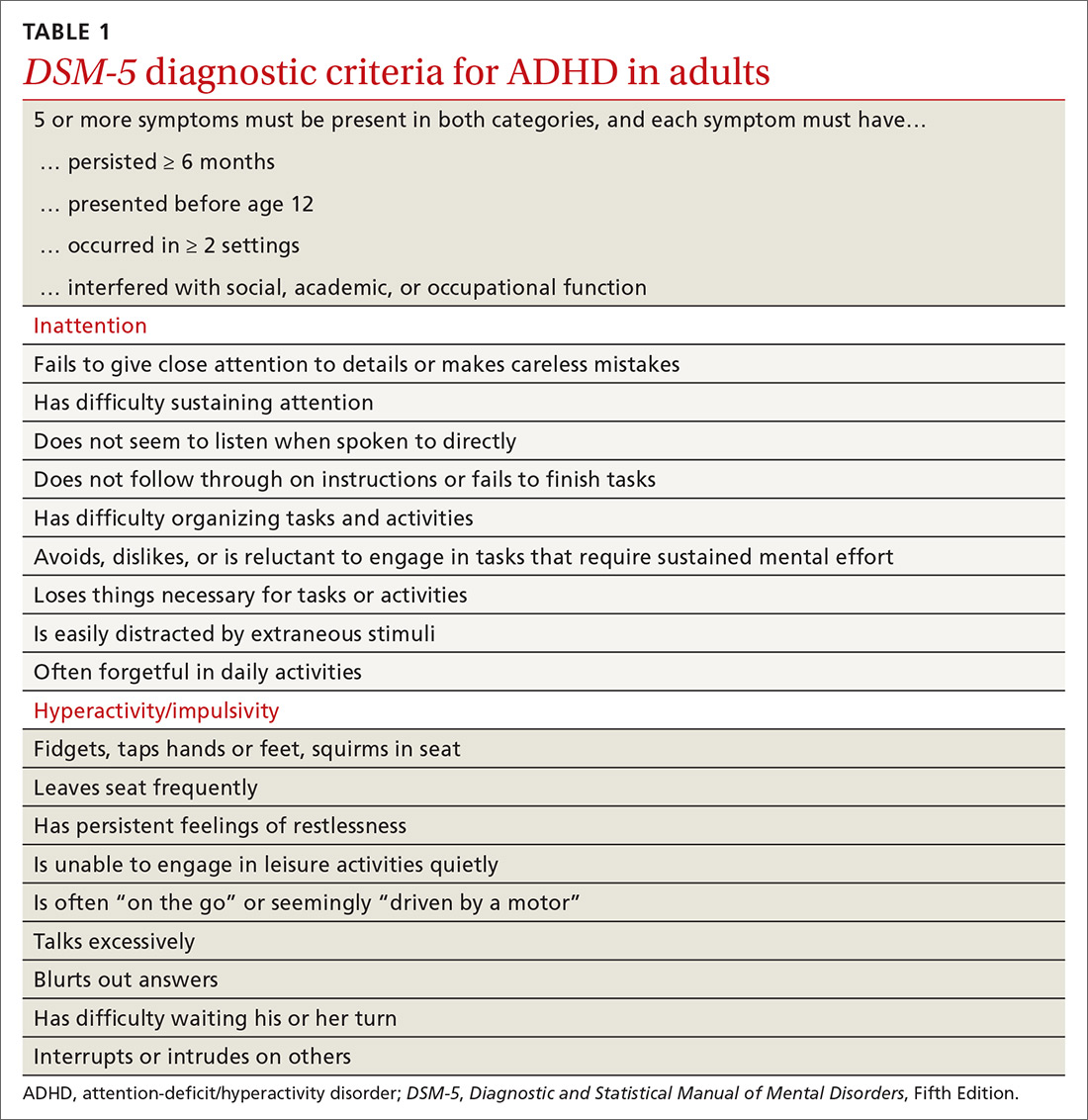
Continue to: In the primary care setting
In the primary care setting, an assessment for ADHD should, at minimum, involve a review of the patient’s academic and work history, assessment of psychiatric comorbidities and substance use history, and administration of appropriate rating scales. When evaluating adults, these tools include the Adult ADHD Self-Report Scale (ASRS)11,12 screening tool and the Diagnostic Interview for ADHD in adults (DIVA-5).13,14 If possible, obtain scale assessments not only from the patient but from family members or other observers who can provide information about the patient in childhood/adolescence and present day.
In an integrated care setting, consider involving a behavioral health consultant for a more comprehensive evaluation of educational, employment, driving, and relationship histories. Historical record review may include report cards from elementary school through high school, standardized test scores, psycho-educational and individual education plan reports, and medical records. Having a snapshot of the patient as a younger child, adolescent, and young adult can help to identify overall patterns of academic underachievement and reveal gaps between potential and overall achievement and performance. Pursue a more thorough evaluation in cases where other comorbid psychiatric disorders are present or when the patient is unfamiliar to you.
TWO GROUPS OF TREATMENT OPTIONS
The treatment of ADHD in adults (and children) can be broadly divided into pharmacologic and nonpharmacologic modalities.
Stimulants are first-line pharmacologic treatment for ADHD in patients with low risk for misuse. Stimulants improve cognitive function, decrease impulsivity, and increase alertness.15 However, these effects are not exclusive to those with ADHD, and response does not aid in diagnosis. No stimulant is preferred over another, although individuals may respond better to 1 specific agent than to others. Be aware that stimulants may be diverted; patients at increased risk include those with comorbid substance use or mood disorders. Misuse may be especially common on college campuses, where nonprescribed stimulants may be used as study aids or recreationally.
Stimulants come in a variety of formulations that differ primarily in their time profile or mode of delivery. Some preparations (eg, Ritalin LA and Adderall XR) contain a mixture of immediate-release and extended-release mechanisms and therefore have bimodal peaks. Others (eg, Concerta) use an osmotic system to approximate a steadier flow of drug delivery. However, as these drugs have entered the generic market, time response between products is much less predictable. Individual differences in metabolism may also alter duration of action.
Continue to: Lisdexamfetamine (Vyvanse)...
Lisdexamfetamine (Vyvanse) is a pro-drug that requires first-pass metabolism for conversion to an active drug. This may reduce risk of overdose or misuse. Adverse effects of stimulants include decreased appetite, irritability, tics, and cardiac toxicity.16 Proper titration of dose over successive visits is essential as providers often must balance efficacy, appetite, and sleep.
Nonstimulant therapies are options for patients who cannot tolerate stimulants or are at high risk for misuse. Atomoxetine, a norepinephrine reuptake inhibitor, has qualities that may resemble antidepressants in its 2- to 4-week time lapse before taking effect. Alpha-2 agonists clonidine and guanfacine are approved by the US Food and Drug Administration in their extended release forms for adjunct therapy with stimulants. Pharmacologic therapies are listed in TABLE 2.16
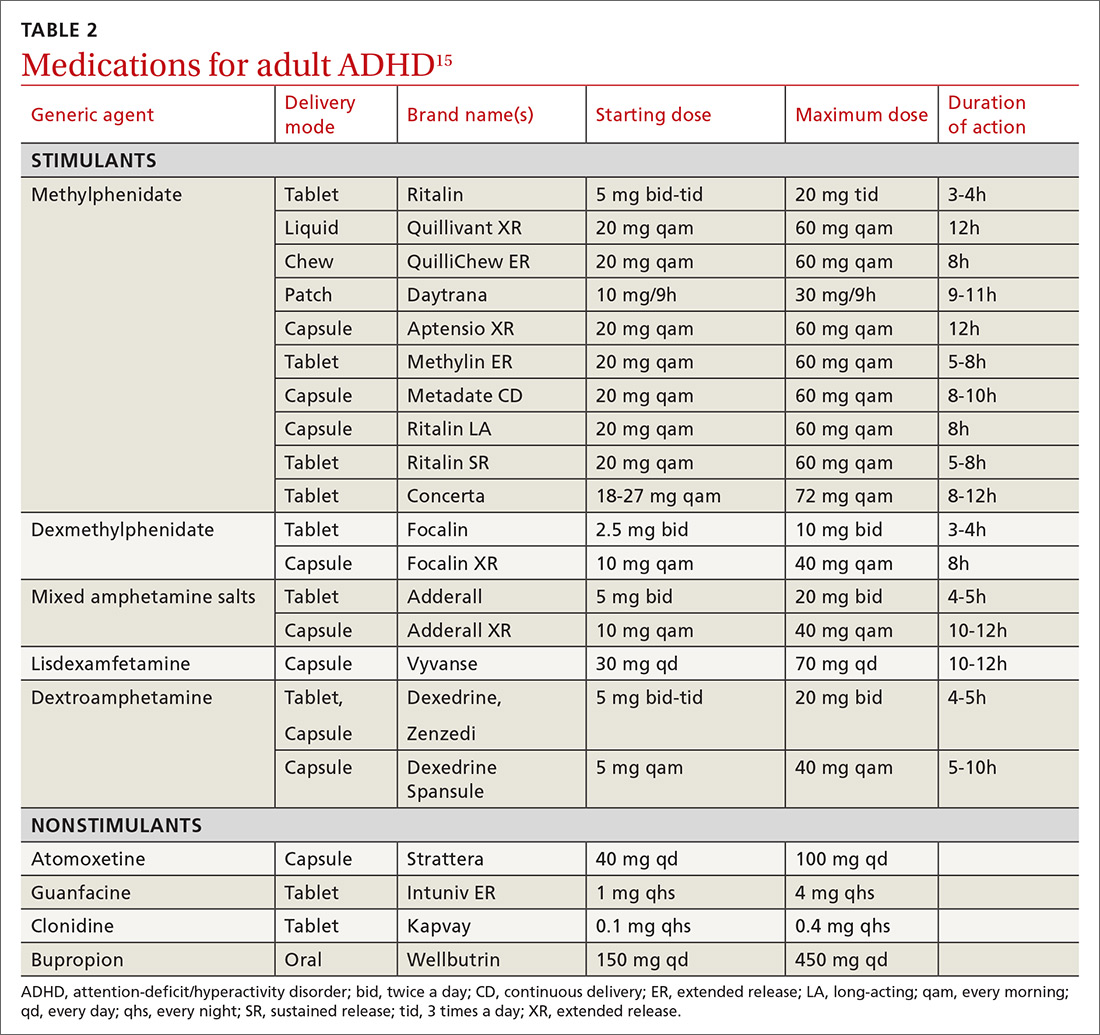
Nonpharmacologic modalities for adult ADHD include psychoeducation, cognitive behavioral therapy, and work environment modification. While coordination with schools is recognized as an essential aspect of the care of ADHD in children, team care in the treatment of adults with ADHD is often forgotten. Referral for occupational or educational support, written materials on study habits and organizational skills, and the use of memory tools can be very helpful. Modifications in physical environment and time constraints in both work and school settings can enhance productivity in adults with ADHD. Attention to sleep scheduling and sleep hygiene can also improve attention and concentration throughout the day.
CASE
She engaged with the education specialists at her school, who helped her discuss testing and assignment modifications with her professors. She began to develop a time-management strategy to complete her assignments; these included reduced evening caffeine intake and improved sleep hygiene. Over time, Ms. L was able to maintain attention for the more extended homework tasks assigned in college. She was also able to enjoy a similar level of success that she had achieved in high school.
CORRESPONDENCE
Jay Brieler, MD, Family and Community Medicine, Saint Louis University School of Medicine, 6420 Clayton Road, Room 2234, St. Louis MO 63117; jay.brieler@health.slu.edu.
1. Neurodevelopmental disorders. In: Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013:59-65.
2. Moreno-Alcázar A, Ramos-Quiroga JA, Radua J, et al. Brain abnormalities in adults with Attention Deficit Hyperactivity Disorder revealed by voxel-based morphometry. Psychiatry Res Neuroimaging. 2016;254:41-47.
3. Willcutt EG. The prevalence of DSM-IV attention-deficit/hyperactivity disorder: a meta-analytic review. Neurotherapeutics. 2012;9:490-499.
4. Fayyad J, De Graaf R, Kessler R, et al. Cross-national prevalence and correlates of adult attention-deficit hyperactivity disorder. Br J Psychiatry. 2007;190:402-409.
5. Kessler R, Adler L, Barkley R, et al. The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am J Psychiatry. 2006;163:716-723.
6. Klein RG, Mannuzza S, Olazagasti MA, et al. Clinical and functional outcome of childhood attention-deficit/hyperactivity disorder 33 years later. Arch Gen Psychiatry. 2012;69:1295-1303.
7. Asherson P, Young AH, Eich-Hochli D, et al. Differential diagnosis, comorbidity, and treatment of ADHD in relation to bipolar disorder or borderline personality disorder in adults. Curr Med Res Opin. 2014;30:1657-1672.
8. Grogan K, Gormley CI, Rooney B, et al. Differential diagnosis and co-morbidity of ADHD and anxiety in adults. Br J Clin Psychol. 2018;57:99-115.
9. Ilbegi S, Groenman AP, Schellekens A, et al. Substance use and nicotine dependence in persistent, remittent, and late-onset ADHD: a 10-year longitudinal study from childhood to young adulthood. J Neurodev Disord. 2018;10:42.
10. Attention-deficit/hyperactivity disorder. In: Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC: American Psychiatric
11. , , , et al. The World Health Organization Adult ADHD Self‐Report Scale (ASRS): a short screening scale for use in the general population. Psychol Med. 2005;35:245‐256.
12. Ustun B, Adler LA, Rudin C, et al. The World Health Organization Adult Attention-Deficit/Hyperactivity Disorder Self-Report Screening Scale for DSM-5. JAMA Psychiatry. 2017;74:520-527.
13. Ramos-Quiroga JA, Nasillo V, Richarte V, et al. Criteria and concurrent validity of DIVA 2.0: a semi-structured diagnostic interview for adult ADHD. J Atten Disord. 2019;23:1126-1135.
14. Pettersson R, Söderström S, Nilsson KW. Diagnosing ADHD in adults: an examination of the discriminative validity of neuropsychological tests and diagnostic assessment instruments. J Atten Disord. 2018;22:1019-1031.
15. Parikh AR, Baker SA. Adult ADHD: pharmacologic treatment in the DSM-5 era. Curr Psychiatry. 2016;15:18-25.
16. Searight HR, Gafford J, Evans SL. Attention Deficit Hyperactivity Disorder. In: Smith MA, Shimp LA, Schrager S, eds. Family Medicine: Ambulatory Care and Prevention. 6th ed. New York, NY: McGraw-Hill; 2014:829-846.
1. Neurodevelopmental disorders. In: Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013:59-65.
2. Moreno-Alcázar A, Ramos-Quiroga JA, Radua J, et al. Brain abnormalities in adults with Attention Deficit Hyperactivity Disorder revealed by voxel-based morphometry. Psychiatry Res Neuroimaging. 2016;254:41-47.
3. Willcutt EG. The prevalence of DSM-IV attention-deficit/hyperactivity disorder: a meta-analytic review. Neurotherapeutics. 2012;9:490-499.
4. Fayyad J, De Graaf R, Kessler R, et al. Cross-national prevalence and correlates of adult attention-deficit hyperactivity disorder. Br J Psychiatry. 2007;190:402-409.
5. Kessler R, Adler L, Barkley R, et al. The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am J Psychiatry. 2006;163:716-723.
6. Klein RG, Mannuzza S, Olazagasti MA, et al. Clinical and functional outcome of childhood attention-deficit/hyperactivity disorder 33 years later. Arch Gen Psychiatry. 2012;69:1295-1303.
7. Asherson P, Young AH, Eich-Hochli D, et al. Differential diagnosis, comorbidity, and treatment of ADHD in relation to bipolar disorder or borderline personality disorder in adults. Curr Med Res Opin. 2014;30:1657-1672.
8. Grogan K, Gormley CI, Rooney B, et al. Differential diagnosis and co-morbidity of ADHD and anxiety in adults. Br J Clin Psychol. 2018;57:99-115.
9. Ilbegi S, Groenman AP, Schellekens A, et al. Substance use and nicotine dependence in persistent, remittent, and late-onset ADHD: a 10-year longitudinal study from childhood to young adulthood. J Neurodev Disord. 2018;10:42.
10. Attention-deficit/hyperactivity disorder. In: Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC: American Psychiatric
11. , , , et al. The World Health Organization Adult ADHD Self‐Report Scale (ASRS): a short screening scale for use in the general population. Psychol Med. 2005;35:245‐256.
12. Ustun B, Adler LA, Rudin C, et al. The World Health Organization Adult Attention-Deficit/Hyperactivity Disorder Self-Report Screening Scale for DSM-5. JAMA Psychiatry. 2017;74:520-527.
13. Ramos-Quiroga JA, Nasillo V, Richarte V, et al. Criteria and concurrent validity of DIVA 2.0: a semi-structured diagnostic interview for adult ADHD. J Atten Disord. 2019;23:1126-1135.
14. Pettersson R, Söderström S, Nilsson KW. Diagnosing ADHD in adults: an examination of the discriminative validity of neuropsychological tests and diagnostic assessment instruments. J Atten Disord. 2018;22:1019-1031.
15. Parikh AR, Baker SA. Adult ADHD: pharmacologic treatment in the DSM-5 era. Curr Psychiatry. 2016;15:18-25.
16. Searight HR, Gafford J, Evans SL. Attention Deficit Hyperactivity Disorder. In: Smith MA, Shimp LA, Schrager S, eds. Family Medicine: Ambulatory Care and Prevention. 6th ed. New York, NY: McGraw-Hill; 2014:829-846.
A practical guide to the management of phobias
THE CASE
Joe S* is a 25-year-old white man who lives with his mother and has a 5-year history of worsening hypertension. He recently presented to the clinic with heart palpitations, shortness of breath, abdominal distress, and dizziness. He said that it was difficult for him to leave his home due to the intense fear he experiences. He said that these symptoms did not occur at home, nor when he visited specific “safe” locations, such as his girlfriend’s apartment. He reported that his fear had increased over the previous 2 years, and that he had progressively limited the distance he traveled from home. He also reported difficulty being in crowds and said, “The idea of going to the movies is torture.”
●
*The patient’s name has been changed to protect his identity.
The most prevalent psychiatric maladies in primary care are anxiety and mood disorders.1,2 Anxiety disorders are patterns of maladaptive behaviors in conjunction with or response to excessive fear or anxiety.3 The most prevalent anxiety disorder in the United States is specific phobia, the fear of a particular object or situation, with a 12-month prevalence rate of 12.1%.2
Other phobias diagnosed separately in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), include social phobia and agoraphobia, which are, respectively, the fear of being negatively evaluated in social situations and the fear of being trapped in public/open spaces. Social phobia and agoraphobia have diagnostic criteria nearly identical to those of simple phobias regarding the fear response, with the primary differences being the specific phobic situations or stimuli.
Unfortunately, these phobias are likely to be undiagnosed and untreated in primary care partly because patients may not seek treatment.4-6 The ease of avoiding some phobic situations contributes to a lack of treatment seeking.5 Furthermore, commonly used brief measures for psychiatric conditions generally identify depression and anxiety but not phobias. However, family physicians do have resources not only to diagnose these disorders, but also to work with patients to ameliorate them. Collaboration with behavioral health providers is key, as patients with phobias generally benefit from cognitive behavioral therapy (CBT), while those with comorbid psychiatric conditions may benefit from a combination of CBT and medication.
Phobic response vs adaptive fear and anxiety
The terms anxiety and fear often overlap when used to describe a negative emotional state of arousal. However, fear is a response to an actual (or perceived) imminent threat, whereas anxiety is the response to a perceived future threat.3 Fear, although unpleasant, serves an adaptive function in responding to immediate danger.7 Anxiety, in turn, may represent an adaptive function for future activities associated with fear. For example, a cave dweller having seen a bear enter a cave in the past (fear-evoking stimulus) may experience anxiety when exploring a different cave (anxiety that a bear may be present). In this situation, the cave dweller’s fear and anxiety responses are important for survival.
Continue to: With phobias...
With phobias, the fear and anxiety responses become maladaptive.3 Specifically, they involve inaccurate beliefs about a specific type of stimulus that could be an object (snake), environment (ocean), or situation (crowded room). Accompanying the maladaptive thoughts are correspondingly exaggerated emotions, physiologic effects, and behavioral responses in alignment with one another.8 The development of this response and the etiology of phobias is complex and is still being debated.7,9,10 Research points to 4 primary pathways: direct psychological conditioning, modeling (watching others), instruction/information, and nonassociative (innate) acquisition.7,10 While the first 3 pathways involve learned responses, the last results from biological predispositions.
DIAGNOSING PHOBIAS: WHAT TO ZERO IN ON
DSM-5 provides diagnostic criteria for specific phobia, agoraphobia, and social phobia, with each diagnosis requiring that symptoms be present for at least 6 months (TABLE 1).3 Diagnosis of phobias should include evaluation of 4 components of a patient’s functioning: subjective fears, cognitions, physiologic responses, and behaviors.8
- Subjective fears: the patient’s described level of distress/agitation to a specific stimulus.
- Cognitions: the patient’s thoughts/beliefs regarding the stimulus.
- Physiologic responses: changes in heart rate, respiration, blood pressure, and other sympathetic nervous system responses with exposure to stimuli.
- Behavioral responses: the most common response is avoidance, with displays of anger, irritability, or apprehension when avoidance of the stimulus is impossible.
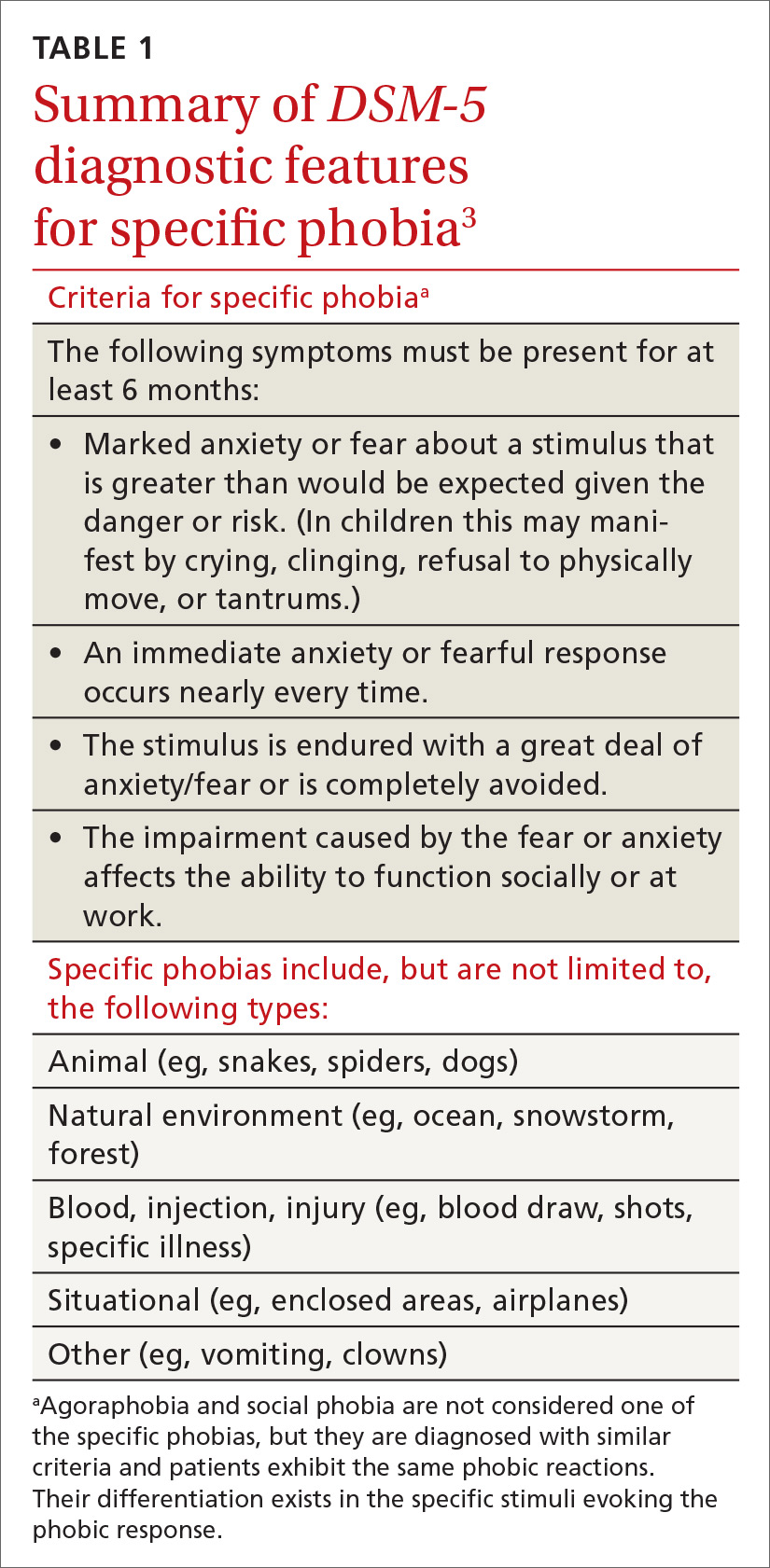
Evaluating these 4 components can be accomplished with structured interviews, behavioral observations, or collateral reports from family members or the patient’s peers.8 Thorough questioning and evaluation (TABLE 28) can enable accurate differentiation between phobias unique to specific stimuli and other DSM-5 disorders that might cause similar symptoms. For example, a patient diagnosed with post-traumatic stress disorder (PTSD) might have a fear response even when triggering stimuli are not present. Identification of a clear, life-threatening incident could help with a differential between phobias and PTSD. However, a patient could be diagnosed with both disorders, as the 2 conditions are not mutually exclusive.
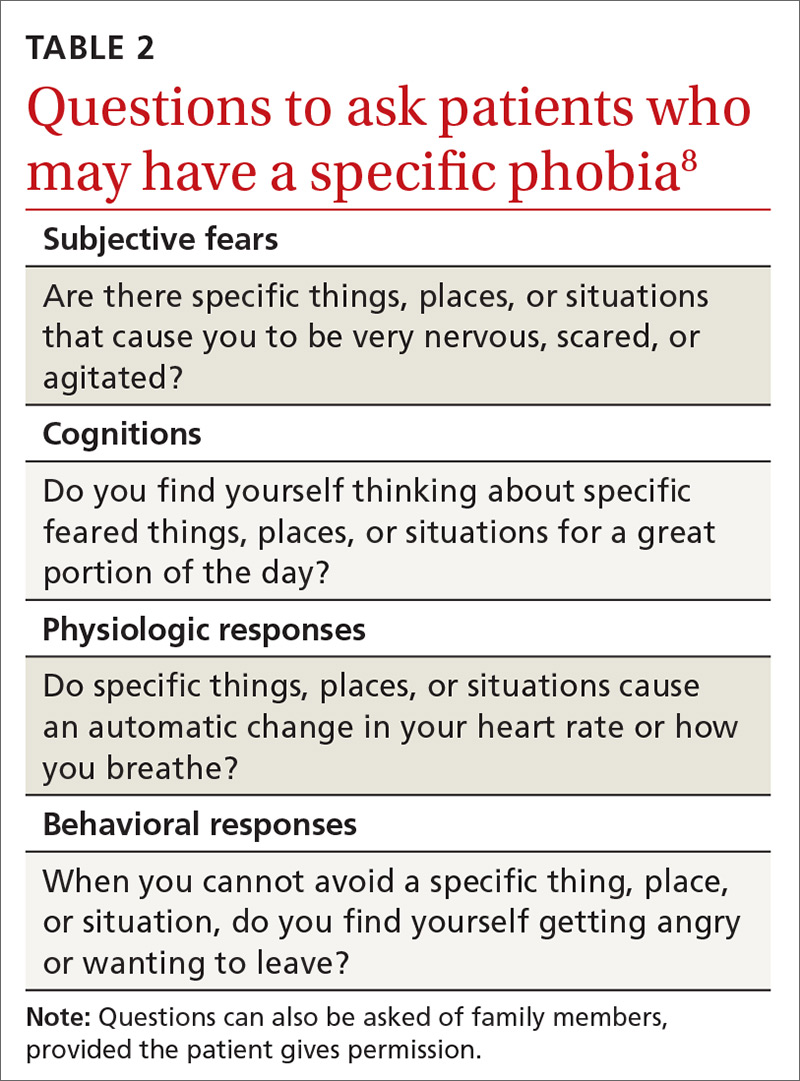
The physiologic and behavioral response symptoms of phobia can also mimic purely medical conditions. Hypertension or tachycardia observed during a medical visit could be due to the fear associated with agoraphobia or with a medically related specific phobia. Blood pressure elevated during testing at the medical appointment could be normal with at-home monitoring by the patient. Thus, blood pressure and heart rate screenings performed at home instead of in public places may help to rule out whether potentially elevated numbers are related to a fear response. Fear and avoidance-like symptoms can also be due to substance abuse, and appropriate drug screening can provide information for an accurate diagnosis.
HOW BEST TO TREAT PHOBIAS
Although research demonstrates that a variety of psychotherapeutic and pharmacologic treatments are efficacious for phobias, in some instances the true utility of an intervention to meaningfully improve a patient’s life is questionable. The issue is that the research evaluating treatment often evaluates only one component of a phobic response (eg,
Continue to: Psychotherapeutic interventions...
Psychotherapeutic interventions for phobias have shown substantial benefit. CBT is helpful, with the most efficacious technique being exposure therapy.5,6,8,11,12 CBT can begin during the initial primary care visit with the family physician educating the patient about phobias and available treatments.
With exposure therapy, patients are introduced to the source of anxiety over time, whereby they learn to manage the distress
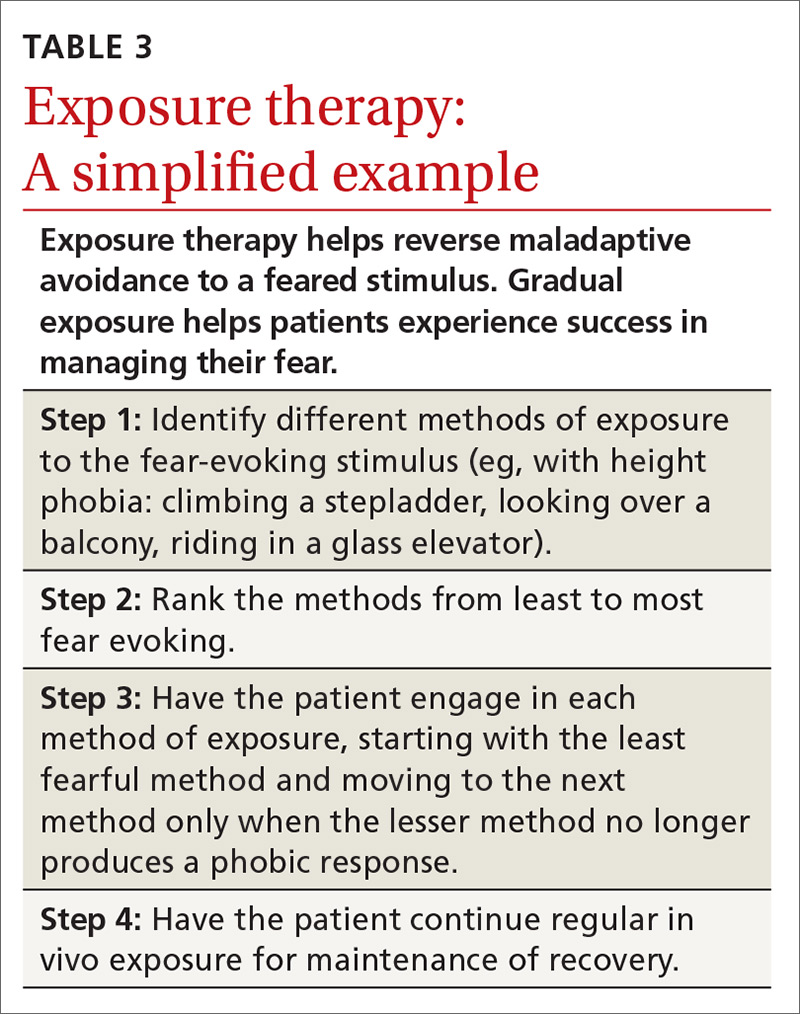
Pharmacologic interventions—specifically selective serotonin reuptake inhibitors (SSRIs) and selective serotonin norepinephrine reuptake inhibitors (SNRIs)—have been effective in treating social phobia and agoraphobia.6 However, treatment of specific phobias via pharmacologic interventions is not supported due to limited efficacy and few studies for SSRIs and SNRIs.5,6
Benzodiazepines, although effective in alleviating some phobic symptoms, are not recommended per current guidelines due to adverse effects and potential exacerbation of the phobic response once discontinued.5,6 This poor result with benzodiazepines may be due to the absence of simultaneous emotional exposure to the feared stimuli. Unfortunately, little research has been done on the long-term effects of pharmacologic intervention once the treatment has been discontinued.11 So, for medication, the question of how long treatment effect lasts after discontinuation remains unanswered.
THE CASE
Mr. S’s family physician diagnosed his condition as agoraphobia with panic attacks. He was prescribed sertraline for his panic attacks and referred for CBT with a psychologist. CBT focused on cognitive restructuring as well as gradual exposure where he would travel with increasing distances to various locations. After 10 months of treatment, Mr. S was able to overcome the agoraphobia and took an “awesome” vacation. He also reported a significant decrease in panic symptoms.
CORRESPONDENCE
Scott A. Fields, PhD, 3200 MacCorkle Avenue Southeast, 5th Floor, Robert C. Byrd Clinical Teaching Center, Department of Family Medicine, Charleston, WV 25304; sfields@hsc.wvu.edu.
1. Simon G, Ormel J, VonKorff M, et al. Health care costs associated with depressive and anxiety disorders in primary care. Am J Psychiatry. 1995; 152:352-357.
2. Kessler RC, Petukhova M, Sampson NA, et al. Twelve‐month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. Int J Methods Psychiatr Res. 2012; 21:169-184.
3. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth edition (DSM-5). Arlington, VA: American Psychiatric Association; 2013:189-233.
4. Bandelow B, Michaelis S. Epidemiology of anxiety disorders in the 21st century. Dialogues Clin Neurosci. 2015; 17:327-335.
5. Choy Y, Fyer AJ, Lipsitz JD. Treatment of specific phobia in adults. Clin Psychol Rev. 2007; 27:266-286.
6. Bandelow B, Michaelis S, Wedekind D. Treatment of anxiety disorders. Dialogues Clin Neurosci. 2017; 19:93-107.
7. Poulton R, Menzies RG. Non-associative fear acquisition: a review of the evidence from retrospective and longitudinal research. Behav Res Ther. 2002; 40:127-149.
8. Davis III TE, Ollendick TH. Empirically supported treatments for specific phobia in children: Do efficacious treatments address the components of a phobic response? Clin Psychol Sci Pract. 2005; 12:144-160.
9. Field AP. Is conditioning a useful framework for understanding the development and treatment of phobias? Clin Psychol Rev. 2006; 26:857-875.
10. King NJ, Eleonora G, Ollendick TH. Etiology of childhood phobias: current status of Rachman’s three pathways theory. Behav Res Ther. 1998; 36:297-309.
11. Fedoroff IC, Taylor S. Psychological and pharmacological treatments of social phobia: a meta-analysis. J Clin Psychopharmacol. 2001; 21:311-324.
12. Wolitzky-Taylor KB, Horowitz JD, Powers MB, et al. Psychological approaches in the treatment of specific phobias: a meta-analysis. Clin Psychol Rev. 2008; 28:1021-1037.
13. Zlomke K, Davis III TE. One-session treatment of specific phobias: a detailed description and review of treatment efficacy. Behav Ther. 2008; 39:207-223.
THE CASE
Joe S* is a 25-year-old white man who lives with his mother and has a 5-year history of worsening hypertension. He recently presented to the clinic with heart palpitations, shortness of breath, abdominal distress, and dizziness. He said that it was difficult for him to leave his home due to the intense fear he experiences. He said that these symptoms did not occur at home, nor when he visited specific “safe” locations, such as his girlfriend’s apartment. He reported that his fear had increased over the previous 2 years, and that he had progressively limited the distance he traveled from home. He also reported difficulty being in crowds and said, “The idea of going to the movies is torture.”
●
*The patient’s name has been changed to protect his identity.
The most prevalent psychiatric maladies in primary care are anxiety and mood disorders.1,2 Anxiety disorders are patterns of maladaptive behaviors in conjunction with or response to excessive fear or anxiety.3 The most prevalent anxiety disorder in the United States is specific phobia, the fear of a particular object or situation, with a 12-month prevalence rate of 12.1%.2
Other phobias diagnosed separately in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), include social phobia and agoraphobia, which are, respectively, the fear of being negatively evaluated in social situations and the fear of being trapped in public/open spaces. Social phobia and agoraphobia have diagnostic criteria nearly identical to those of simple phobias regarding the fear response, with the primary differences being the specific phobic situations or stimuli.
Unfortunately, these phobias are likely to be undiagnosed and untreated in primary care partly because patients may not seek treatment.4-6 The ease of avoiding some phobic situations contributes to a lack of treatment seeking.5 Furthermore, commonly used brief measures for psychiatric conditions generally identify depression and anxiety but not phobias. However, family physicians do have resources not only to diagnose these disorders, but also to work with patients to ameliorate them. Collaboration with behavioral health providers is key, as patients with phobias generally benefit from cognitive behavioral therapy (CBT), while those with comorbid psychiatric conditions may benefit from a combination of CBT and medication.
Phobic response vs adaptive fear and anxiety
The terms anxiety and fear often overlap when used to describe a negative emotional state of arousal. However, fear is a response to an actual (or perceived) imminent threat, whereas anxiety is the response to a perceived future threat.3 Fear, although unpleasant, serves an adaptive function in responding to immediate danger.7 Anxiety, in turn, may represent an adaptive function for future activities associated with fear. For example, a cave dweller having seen a bear enter a cave in the past (fear-evoking stimulus) may experience anxiety when exploring a different cave (anxiety that a bear may be present). In this situation, the cave dweller’s fear and anxiety responses are important for survival.
Continue to: With phobias...
With phobias, the fear and anxiety responses become maladaptive.3 Specifically, they involve inaccurate beliefs about a specific type of stimulus that could be an object (snake), environment (ocean), or situation (crowded room). Accompanying the maladaptive thoughts are correspondingly exaggerated emotions, physiologic effects, and behavioral responses in alignment with one another.8 The development of this response and the etiology of phobias is complex and is still being debated.7,9,10 Research points to 4 primary pathways: direct psychological conditioning, modeling (watching others), instruction/information, and nonassociative (innate) acquisition.7,10 While the first 3 pathways involve learned responses, the last results from biological predispositions.
DIAGNOSING PHOBIAS: WHAT TO ZERO IN ON
DSM-5 provides diagnostic criteria for specific phobia, agoraphobia, and social phobia, with each diagnosis requiring that symptoms be present for at least 6 months (TABLE 1).3 Diagnosis of phobias should include evaluation of 4 components of a patient’s functioning: subjective fears, cognitions, physiologic responses, and behaviors.8
- Subjective fears: the patient’s described level of distress/agitation to a specific stimulus.
- Cognitions: the patient’s thoughts/beliefs regarding the stimulus.
- Physiologic responses: changes in heart rate, respiration, blood pressure, and other sympathetic nervous system responses with exposure to stimuli.
- Behavioral responses: the most common response is avoidance, with displays of anger, irritability, or apprehension when avoidance of the stimulus is impossible.
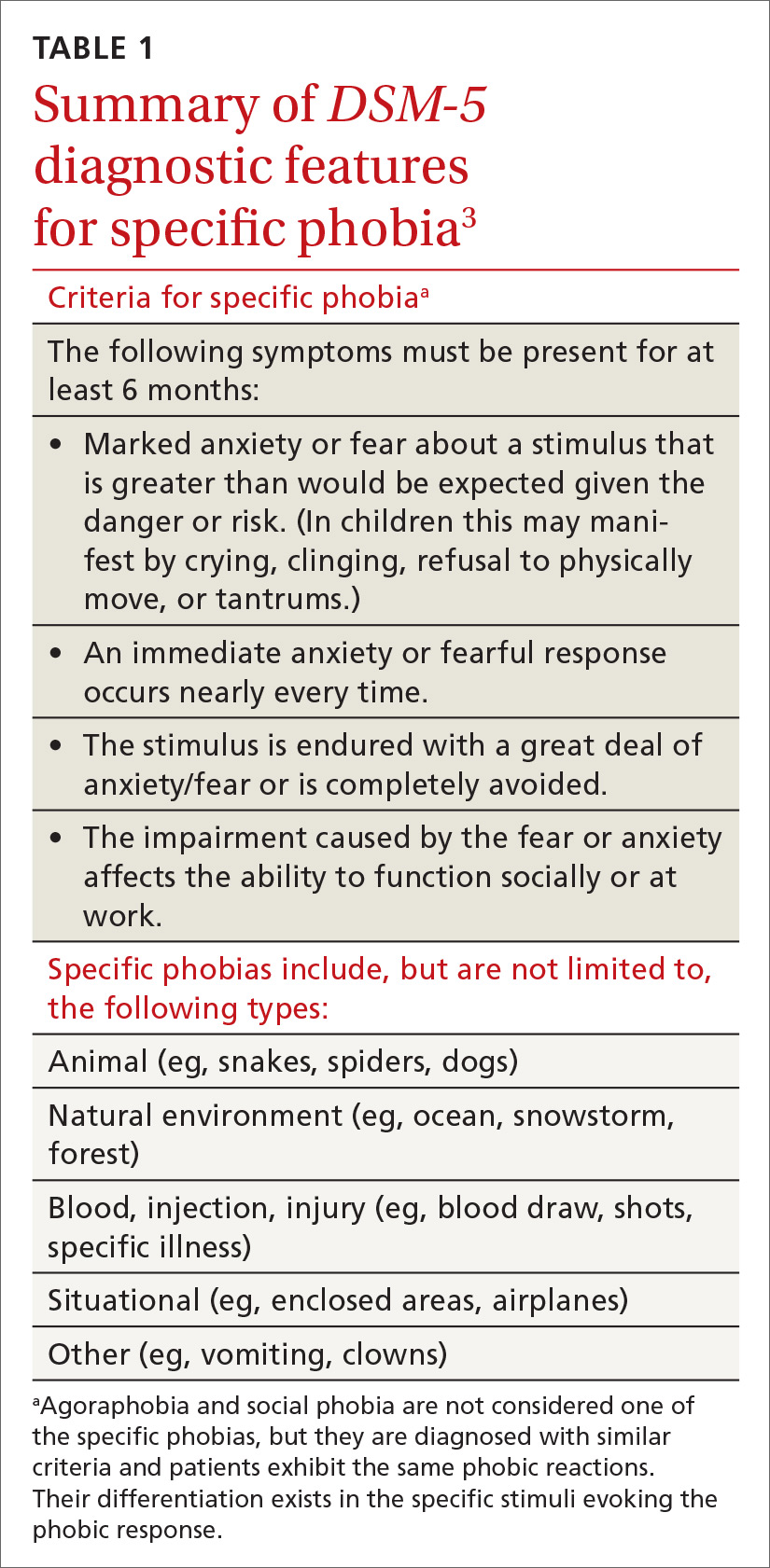
Evaluating these 4 components can be accomplished with structured interviews, behavioral observations, or collateral reports from family members or the patient’s peers.8 Thorough questioning and evaluation (TABLE 28) can enable accurate differentiation between phobias unique to specific stimuli and other DSM-5 disorders that might cause similar symptoms. For example, a patient diagnosed with post-traumatic stress disorder (PTSD) might have a fear response even when triggering stimuli are not present. Identification of a clear, life-threatening incident could help with a differential between phobias and PTSD. However, a patient could be diagnosed with both disorders, as the 2 conditions are not mutually exclusive.
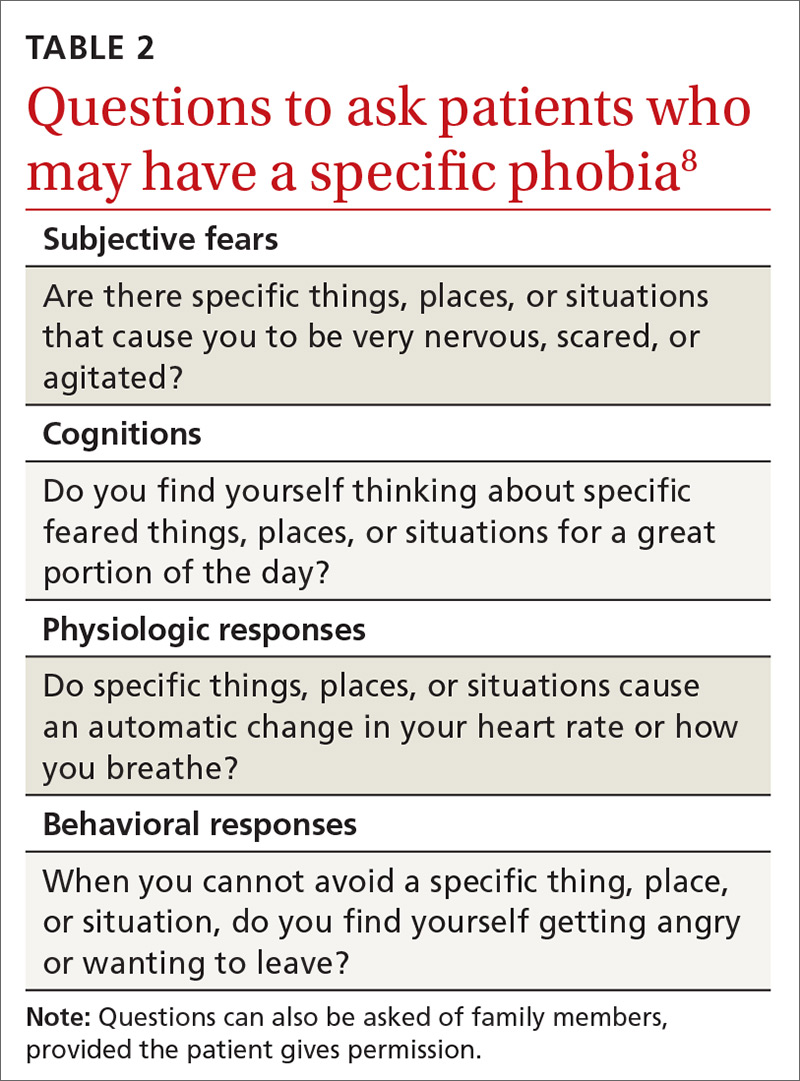
The physiologic and behavioral response symptoms of phobia can also mimic purely medical conditions. Hypertension or tachycardia observed during a medical visit could be due to the fear associated with agoraphobia or with a medically related specific phobia. Blood pressure elevated during testing at the medical appointment could be normal with at-home monitoring by the patient. Thus, blood pressure and heart rate screenings performed at home instead of in public places may help to rule out whether potentially elevated numbers are related to a fear response. Fear and avoidance-like symptoms can also be due to substance abuse, and appropriate drug screening can provide information for an accurate diagnosis.
HOW BEST TO TREAT PHOBIAS
Although research demonstrates that a variety of psychotherapeutic and pharmacologic treatments are efficacious for phobias, in some instances the true utility of an intervention to meaningfully improve a patient’s life is questionable. The issue is that the research evaluating treatment often evaluates only one component of a phobic response (eg,
Continue to: Psychotherapeutic interventions...
Psychotherapeutic interventions for phobias have shown substantial benefit. CBT is helpful, with the most efficacious technique being exposure therapy.5,6,8,11,12 CBT can begin during the initial primary care visit with the family physician educating the patient about phobias and available treatments.
With exposure therapy, patients are introduced to the source of anxiety over time, whereby they learn to manage the distress
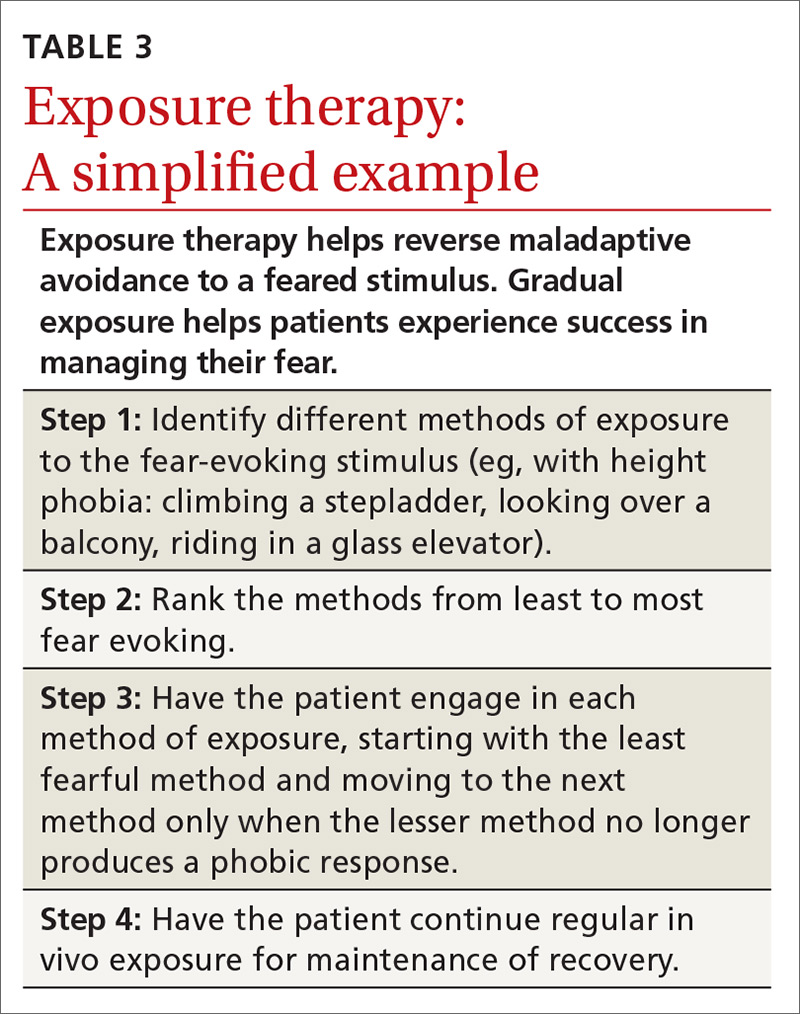
Pharmacologic interventions—specifically selective serotonin reuptake inhibitors (SSRIs) and selective serotonin norepinephrine reuptake inhibitors (SNRIs)—have been effective in treating social phobia and agoraphobia.6 However, treatment of specific phobias via pharmacologic interventions is not supported due to limited efficacy and few studies for SSRIs and SNRIs.5,6
Benzodiazepines, although effective in alleviating some phobic symptoms, are not recommended per current guidelines due to adverse effects and potential exacerbation of the phobic response once discontinued.5,6 This poor result with benzodiazepines may be due to the absence of simultaneous emotional exposure to the feared stimuli. Unfortunately, little research has been done on the long-term effects of pharmacologic intervention once the treatment has been discontinued.11 So, for medication, the question of how long treatment effect lasts after discontinuation remains unanswered.
THE CASE
Mr. S’s family physician diagnosed his condition as agoraphobia with panic attacks. He was prescribed sertraline for his panic attacks and referred for CBT with a psychologist. CBT focused on cognitive restructuring as well as gradual exposure where he would travel with increasing distances to various locations. After 10 months of treatment, Mr. S was able to overcome the agoraphobia and took an “awesome” vacation. He also reported a significant decrease in panic symptoms.
CORRESPONDENCE
Scott A. Fields, PhD, 3200 MacCorkle Avenue Southeast, 5th Floor, Robert C. Byrd Clinical Teaching Center, Department of Family Medicine, Charleston, WV 25304; sfields@hsc.wvu.edu.
THE CASE
Joe S* is a 25-year-old white man who lives with his mother and has a 5-year history of worsening hypertension. He recently presented to the clinic with heart palpitations, shortness of breath, abdominal distress, and dizziness. He said that it was difficult for him to leave his home due to the intense fear he experiences. He said that these symptoms did not occur at home, nor when he visited specific “safe” locations, such as his girlfriend’s apartment. He reported that his fear had increased over the previous 2 years, and that he had progressively limited the distance he traveled from home. He also reported difficulty being in crowds and said, “The idea of going to the movies is torture.”
●
*The patient’s name has been changed to protect his identity.
The most prevalent psychiatric maladies in primary care are anxiety and mood disorders.1,2 Anxiety disorders are patterns of maladaptive behaviors in conjunction with or response to excessive fear or anxiety.3 The most prevalent anxiety disorder in the United States is specific phobia, the fear of a particular object or situation, with a 12-month prevalence rate of 12.1%.2
Other phobias diagnosed separately in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), include social phobia and agoraphobia, which are, respectively, the fear of being negatively evaluated in social situations and the fear of being trapped in public/open spaces. Social phobia and agoraphobia have diagnostic criteria nearly identical to those of simple phobias regarding the fear response, with the primary differences being the specific phobic situations or stimuli.
Unfortunately, these phobias are likely to be undiagnosed and untreated in primary care partly because patients may not seek treatment.4-6 The ease of avoiding some phobic situations contributes to a lack of treatment seeking.5 Furthermore, commonly used brief measures for psychiatric conditions generally identify depression and anxiety but not phobias. However, family physicians do have resources not only to diagnose these disorders, but also to work with patients to ameliorate them. Collaboration with behavioral health providers is key, as patients with phobias generally benefit from cognitive behavioral therapy (CBT), while those with comorbid psychiatric conditions may benefit from a combination of CBT and medication.
Phobic response vs adaptive fear and anxiety
The terms anxiety and fear often overlap when used to describe a negative emotional state of arousal. However, fear is a response to an actual (or perceived) imminent threat, whereas anxiety is the response to a perceived future threat.3 Fear, although unpleasant, serves an adaptive function in responding to immediate danger.7 Anxiety, in turn, may represent an adaptive function for future activities associated with fear. For example, a cave dweller having seen a bear enter a cave in the past (fear-evoking stimulus) may experience anxiety when exploring a different cave (anxiety that a bear may be present). In this situation, the cave dweller’s fear and anxiety responses are important for survival.
Continue to: With phobias...
With phobias, the fear and anxiety responses become maladaptive.3 Specifically, they involve inaccurate beliefs about a specific type of stimulus that could be an object (snake), environment (ocean), or situation (crowded room). Accompanying the maladaptive thoughts are correspondingly exaggerated emotions, physiologic effects, and behavioral responses in alignment with one another.8 The development of this response and the etiology of phobias is complex and is still being debated.7,9,10 Research points to 4 primary pathways: direct psychological conditioning, modeling (watching others), instruction/information, and nonassociative (innate) acquisition.7,10 While the first 3 pathways involve learned responses, the last results from biological predispositions.
DIAGNOSING PHOBIAS: WHAT TO ZERO IN ON
DSM-5 provides diagnostic criteria for specific phobia, agoraphobia, and social phobia, with each diagnosis requiring that symptoms be present for at least 6 months (TABLE 1).3 Diagnosis of phobias should include evaluation of 4 components of a patient’s functioning: subjective fears, cognitions, physiologic responses, and behaviors.8
- Subjective fears: the patient’s described level of distress/agitation to a specific stimulus.
- Cognitions: the patient’s thoughts/beliefs regarding the stimulus.
- Physiologic responses: changes in heart rate, respiration, blood pressure, and other sympathetic nervous system responses with exposure to stimuli.
- Behavioral responses: the most common response is avoidance, with displays of anger, irritability, or apprehension when avoidance of the stimulus is impossible.
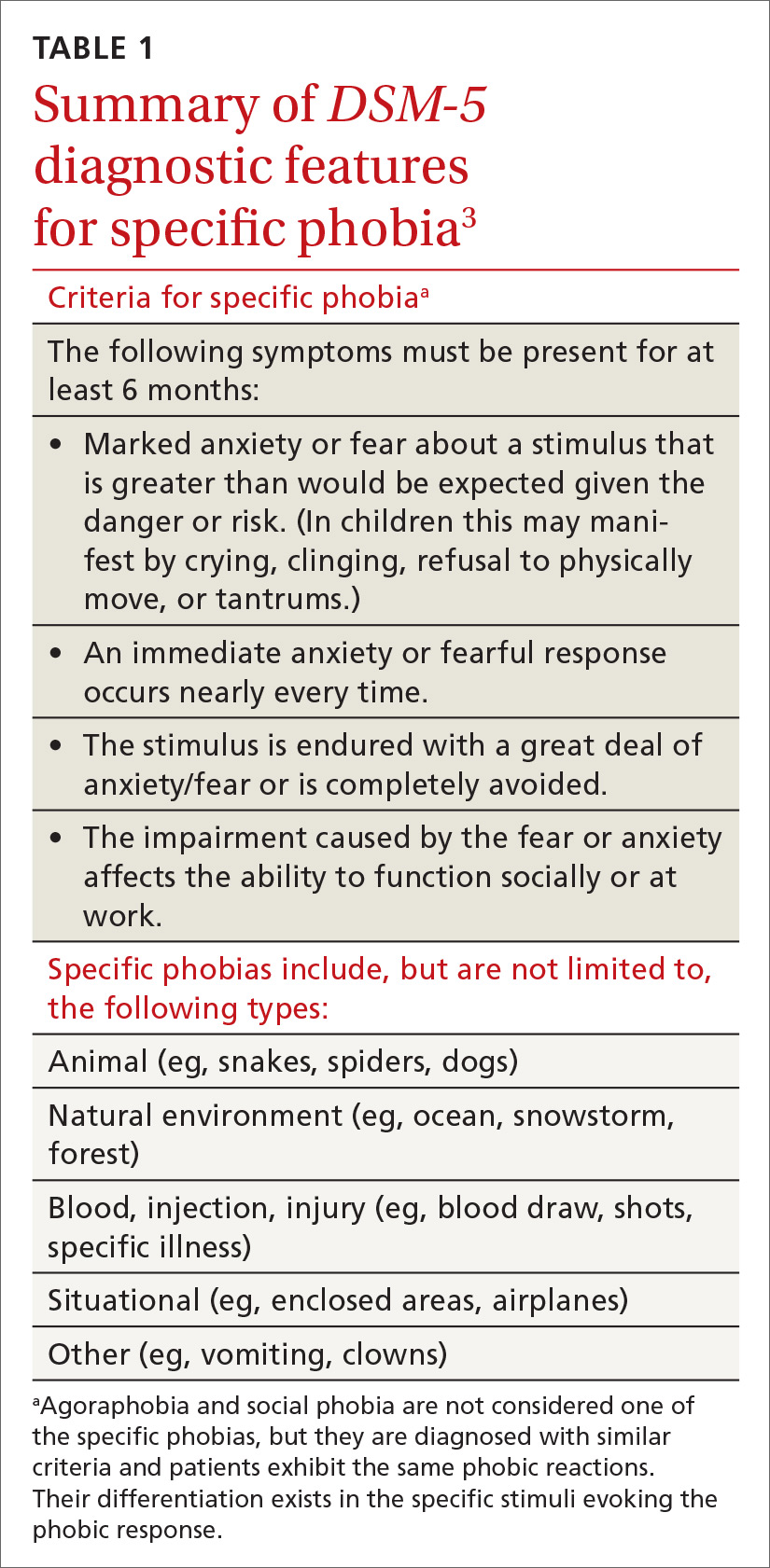
Evaluating these 4 components can be accomplished with structured interviews, behavioral observations, or collateral reports from family members or the patient’s peers.8 Thorough questioning and evaluation (TABLE 28) can enable accurate differentiation between phobias unique to specific stimuli and other DSM-5 disorders that might cause similar symptoms. For example, a patient diagnosed with post-traumatic stress disorder (PTSD) might have a fear response even when triggering stimuli are not present. Identification of a clear, life-threatening incident could help with a differential between phobias and PTSD. However, a patient could be diagnosed with both disorders, as the 2 conditions are not mutually exclusive.
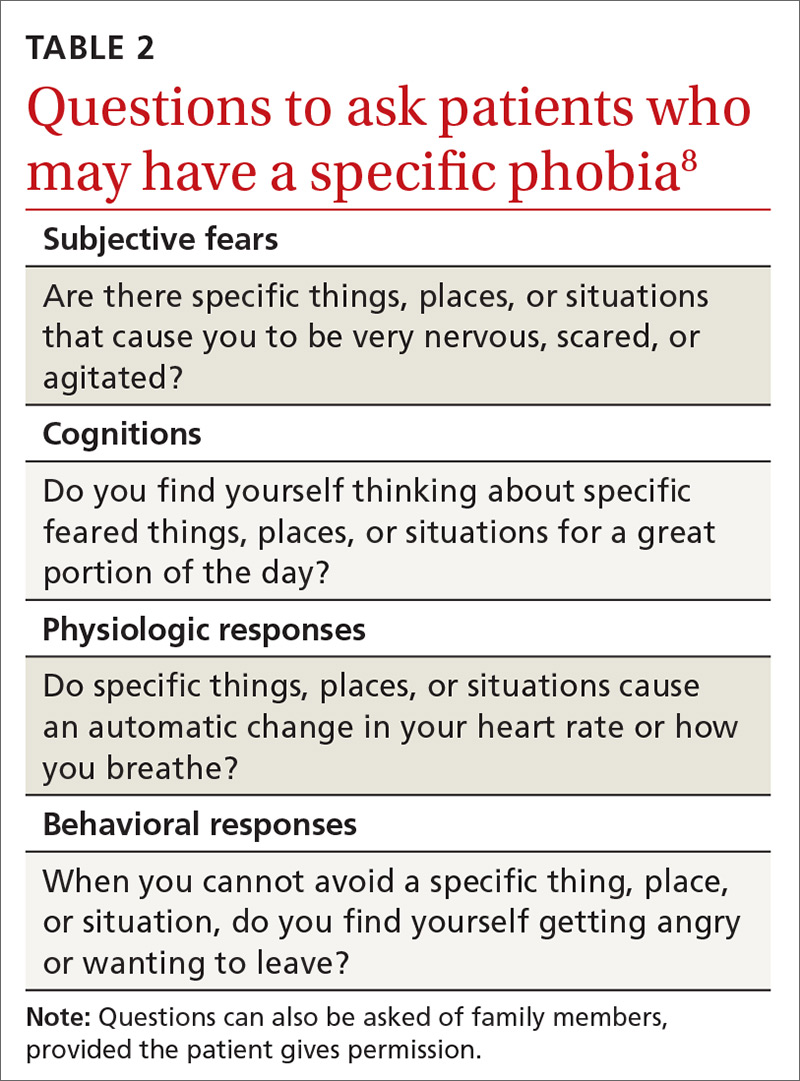
The physiologic and behavioral response symptoms of phobia can also mimic purely medical conditions. Hypertension or tachycardia observed during a medical visit could be due to the fear associated with agoraphobia or with a medically related specific phobia. Blood pressure elevated during testing at the medical appointment could be normal with at-home monitoring by the patient. Thus, blood pressure and heart rate screenings performed at home instead of in public places may help to rule out whether potentially elevated numbers are related to a fear response. Fear and avoidance-like symptoms can also be due to substance abuse, and appropriate drug screening can provide information for an accurate diagnosis.
HOW BEST TO TREAT PHOBIAS
Although research demonstrates that a variety of psychotherapeutic and pharmacologic treatments are efficacious for phobias, in some instances the true utility of an intervention to meaningfully improve a patient’s life is questionable. The issue is that the research evaluating treatment often evaluates only one component of a phobic response (eg,
Continue to: Psychotherapeutic interventions...
Psychotherapeutic interventions for phobias have shown substantial benefit. CBT is helpful, with the most efficacious technique being exposure therapy.5,6,8,11,12 CBT can begin during the initial primary care visit with the family physician educating the patient about phobias and available treatments.
With exposure therapy, patients are introduced to the source of anxiety over time, whereby they learn to manage the distress
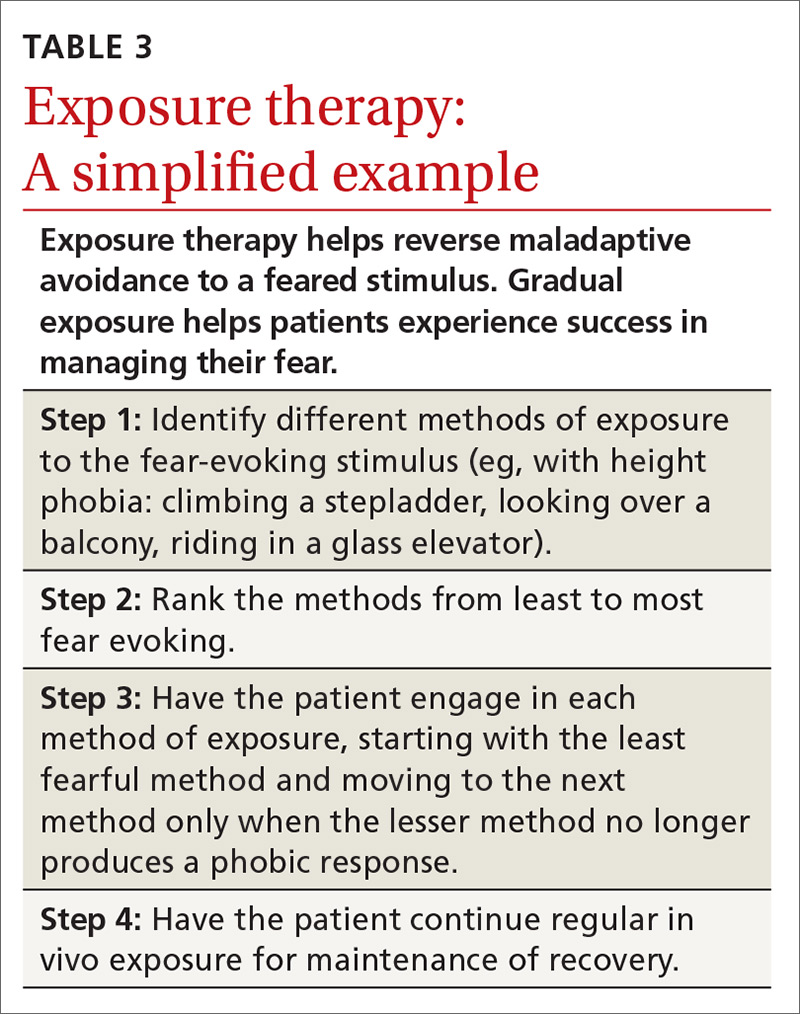
Pharmacologic interventions—specifically selective serotonin reuptake inhibitors (SSRIs) and selective serotonin norepinephrine reuptake inhibitors (SNRIs)—have been effective in treating social phobia and agoraphobia.6 However, treatment of specific phobias via pharmacologic interventions is not supported due to limited efficacy and few studies for SSRIs and SNRIs.5,6
Benzodiazepines, although effective in alleviating some phobic symptoms, are not recommended per current guidelines due to adverse effects and potential exacerbation of the phobic response once discontinued.5,6 This poor result with benzodiazepines may be due to the absence of simultaneous emotional exposure to the feared stimuli. Unfortunately, little research has been done on the long-term effects of pharmacologic intervention once the treatment has been discontinued.11 So, for medication, the question of how long treatment effect lasts after discontinuation remains unanswered.
THE CASE
Mr. S’s family physician diagnosed his condition as agoraphobia with panic attacks. He was prescribed sertraline for his panic attacks and referred for CBT with a psychologist. CBT focused on cognitive restructuring as well as gradual exposure where he would travel with increasing distances to various locations. After 10 months of treatment, Mr. S was able to overcome the agoraphobia and took an “awesome” vacation. He also reported a significant decrease in panic symptoms.
CORRESPONDENCE
Scott A. Fields, PhD, 3200 MacCorkle Avenue Southeast, 5th Floor, Robert C. Byrd Clinical Teaching Center, Department of Family Medicine, Charleston, WV 25304; sfields@hsc.wvu.edu.
1. Simon G, Ormel J, VonKorff M, et al. Health care costs associated with depressive and anxiety disorders in primary care. Am J Psychiatry. 1995; 152:352-357.
2. Kessler RC, Petukhova M, Sampson NA, et al. Twelve‐month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. Int J Methods Psychiatr Res. 2012; 21:169-184.
3. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth edition (DSM-5). Arlington, VA: American Psychiatric Association; 2013:189-233.
4. Bandelow B, Michaelis S. Epidemiology of anxiety disorders in the 21st century. Dialogues Clin Neurosci. 2015; 17:327-335.
5. Choy Y, Fyer AJ, Lipsitz JD. Treatment of specific phobia in adults. Clin Psychol Rev. 2007; 27:266-286.
6. Bandelow B, Michaelis S, Wedekind D. Treatment of anxiety disorders. Dialogues Clin Neurosci. 2017; 19:93-107.
7. Poulton R, Menzies RG. Non-associative fear acquisition: a review of the evidence from retrospective and longitudinal research. Behav Res Ther. 2002; 40:127-149.
8. Davis III TE, Ollendick TH. Empirically supported treatments for specific phobia in children: Do efficacious treatments address the components of a phobic response? Clin Psychol Sci Pract. 2005; 12:144-160.
9. Field AP. Is conditioning a useful framework for understanding the development and treatment of phobias? Clin Psychol Rev. 2006; 26:857-875.
10. King NJ, Eleonora G, Ollendick TH. Etiology of childhood phobias: current status of Rachman’s three pathways theory. Behav Res Ther. 1998; 36:297-309.
11. Fedoroff IC, Taylor S. Psychological and pharmacological treatments of social phobia: a meta-analysis. J Clin Psychopharmacol. 2001; 21:311-324.
12. Wolitzky-Taylor KB, Horowitz JD, Powers MB, et al. Psychological approaches in the treatment of specific phobias: a meta-analysis. Clin Psychol Rev. 2008; 28:1021-1037.
13. Zlomke K, Davis III TE. One-session treatment of specific phobias: a detailed description and review of treatment efficacy. Behav Ther. 2008; 39:207-223.
1. Simon G, Ormel J, VonKorff M, et al. Health care costs associated with depressive and anxiety disorders in primary care. Am J Psychiatry. 1995; 152:352-357.
2. Kessler RC, Petukhova M, Sampson NA, et al. Twelve‐month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. Int J Methods Psychiatr Res. 2012; 21:169-184.
3. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth edition (DSM-5). Arlington, VA: American Psychiatric Association; 2013:189-233.
4. Bandelow B, Michaelis S. Epidemiology of anxiety disorders in the 21st century. Dialogues Clin Neurosci. 2015; 17:327-335.
5. Choy Y, Fyer AJ, Lipsitz JD. Treatment of specific phobia in adults. Clin Psychol Rev. 2007; 27:266-286.
6. Bandelow B, Michaelis S, Wedekind D. Treatment of anxiety disorders. Dialogues Clin Neurosci. 2017; 19:93-107.
7. Poulton R, Menzies RG. Non-associative fear acquisition: a review of the evidence from retrospective and longitudinal research. Behav Res Ther. 2002; 40:127-149.
8. Davis III TE, Ollendick TH. Empirically supported treatments for specific phobia in children: Do efficacious treatments address the components of a phobic response? Clin Psychol Sci Pract. 2005; 12:144-160.
9. Field AP. Is conditioning a useful framework for understanding the development and treatment of phobias? Clin Psychol Rev. 2006; 26:857-875.
10. King NJ, Eleonora G, Ollendick TH. Etiology of childhood phobias: current status of Rachman’s three pathways theory. Behav Res Ther. 1998; 36:297-309.
11. Fedoroff IC, Taylor S. Psychological and pharmacological treatments of social phobia: a meta-analysis. J Clin Psychopharmacol. 2001; 21:311-324.
12. Wolitzky-Taylor KB, Horowitz JD, Powers MB, et al. Psychological approaches in the treatment of specific phobias: a meta-analysis. Clin Psychol Rev. 2008; 28:1021-1037.
13. Zlomke K, Davis III TE. One-session treatment of specific phobias: a detailed description and review of treatment efficacy. Behav Ther. 2008; 39:207-223.
Suicide screening: How to recognize and treat at-risk adults
THE CASE
Emily T,* a 30-year-old woman, visited her primary care physician as follow-up to reassess her grief over the loss of her father a year earlier. Emily was her father’s primary caretaker and still lived alone in his home. Emily had a history of chronic pain and major depressive disorder and had expressed feelings of worthlessness and hopelessness about her future since her father’s passing. In addition to her continuing grief response, she reported feeling worse on most days. She completed the Patient Health Questionnaire-9, and results indicated anhedonia, depressed mood, psychomotor retardation, hypersomnia, decreased appetite, decreased concentration, and thoughts that she would be better off dead.
- HOW WOULD YOU PROCEED WITH THIS PATIENT?
* The patient’s name has been changed to protect her identity.
In the United States, 1 suicide occurs on average every 12 minutes; lifetime prevalence of suicide attempts ranges from 1.9% to 8.7%.1 Suicide is the 10th overall cause of death in the United States, and it is the second leading cause of death for adults 18 to 34 years of age.2 In one study, nearly half of suicide victims had contact with primary care providers within 1 month of their suicide.3 Unfortunately, additional research suggests that primary care physicians appropriately screen for suicide in fewer than 40% of patient encounters.4,5
Suicide is defined as “death caused by self-directed injurious behavior with any intent to die as a result of the behavior.”6 When screening for suicide, be aware of the many terms related to suicide evaluation (TABLE 16). Be mindful, too, of the differences between suicidal and nonsuicidal ideation (death wish); the continuum of such thoughts ranges from those that lead to suicide to those that do not.
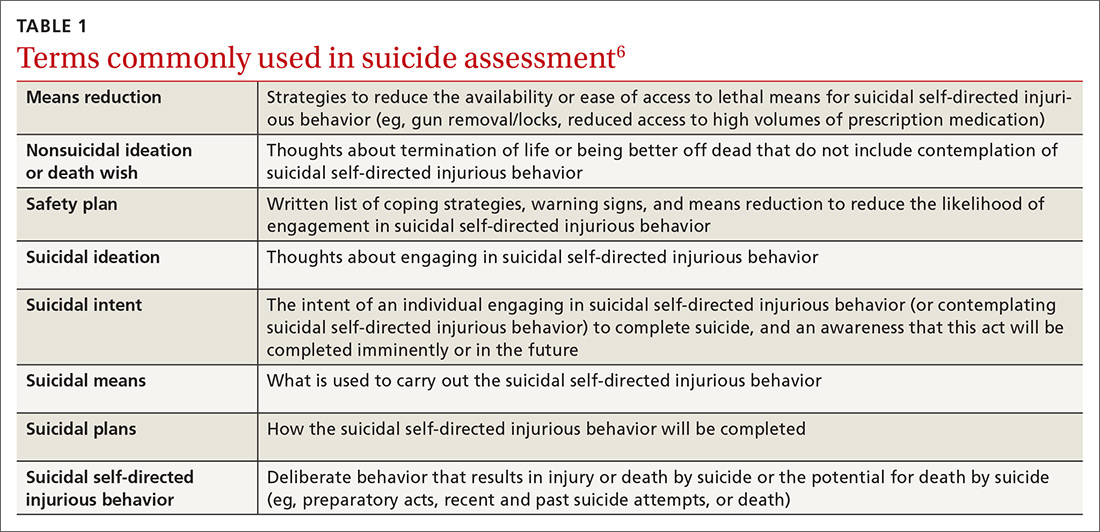
SUICIDE SCREENING RECOMMENDATIONS VARY
Although most health care providers would agree that intervening with a suicidal patient first requires competence in assessing suicide risk, regulating bodies differ on the use of routine screening and on appropriate screening tools for primary care. The Joint Commission recommends assessing suicide risk with all primary care patients,7 while the US Preventive Services Tasks Force (USPSTF) advises against universal suicide screening in primary care8 due to insufficient evidence that its benefit outweighs potential harm (TABLE 27-12). Instead, the USPSTF recommends screening primary care patients with known mental health disorders, recent inpatient psychiatric hospitalization, prior suicide or self-harm attempts, or increased emotional distress.8 USPSTF does support screening for depression with routine mental health measures that include items assessing suicidality.8,13,14 The American Academy of Family Physicians supports the recommendations by USPSTF.13
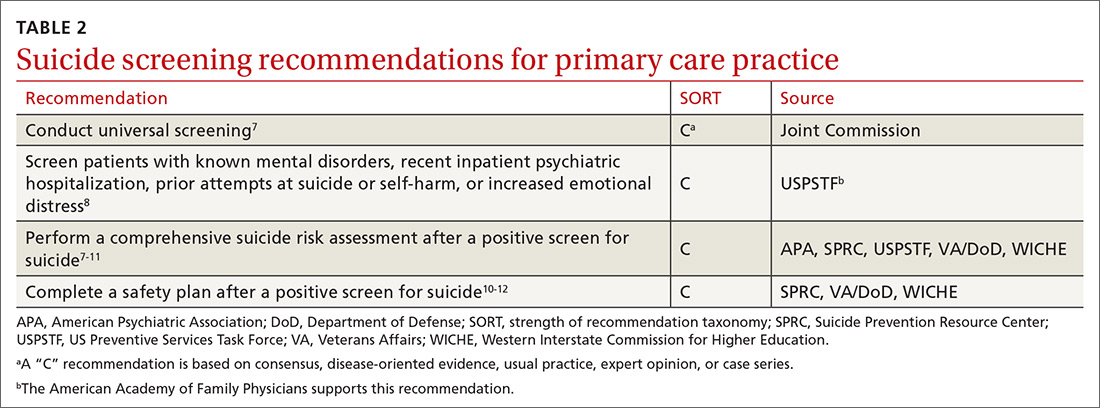
When screening for suicide, a comprehensive suicide risk assessment is recommended by both the Joint Commission and USPSTF.7,8 A comprehensive suicide risk assessment has 4 components: (1) identification of current suicide risk factors, (2) identification of protective factors, (3) inquiry about suicidal ideation, intent, and plan, and (4) primary care practitioner judgment of risk level and plan for clinical intervention.9-11
Take into account both risks and protective factors
Unfortunately, there is no “typical” description of a patient at risk for suicide and no validated models to predict suicide risk.8,10 A multitude of factors, both individual and societal, can increase or reduce risk of suicide.11,15 Each patient’s unique history includes risk factors for suicide including precipitating events (eg, job loss, termination of a relationship, death of a loved one) and protective factors that may be evaluated to determine overall risk for suicide (TABLE 38,10,11,15). According to the Centers for Disease Control and Prevention (CDC), there are several warning signs for patients who may be at greater risk for suicide: isolation, increased anxiety or anger, obtaining lethal means (eg, guns, knives, ropes), frequent mood swings, sleep changes, feeling trapped or in pain, increased substance use, discussing plans for death or wishes of death, and feeling like a burden.16
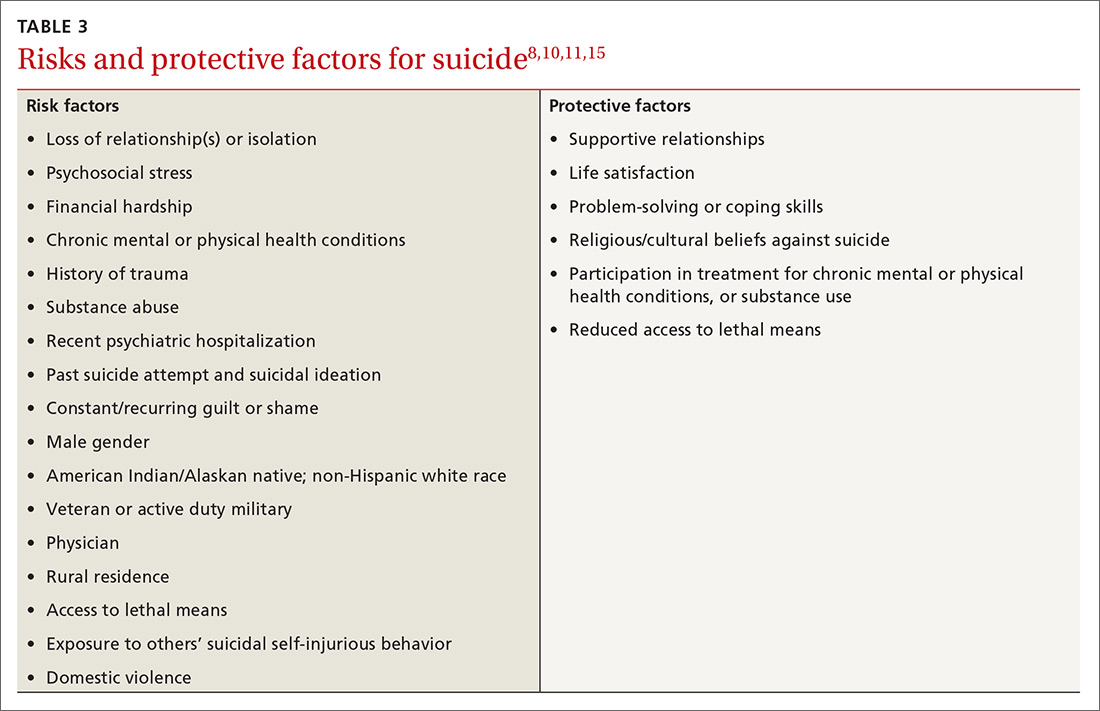
CHOOSING FROM AMONG SUICIDE SCREENING TOOLS
Brief mental health screening tools such as the Patient Health Questionnaire-9 (PHQ-9) are commonly used as primary screening tools for suicidal ideation.17 However, to attain a fuller understanding of a patient’s suicidality, select a screening tool that specifically
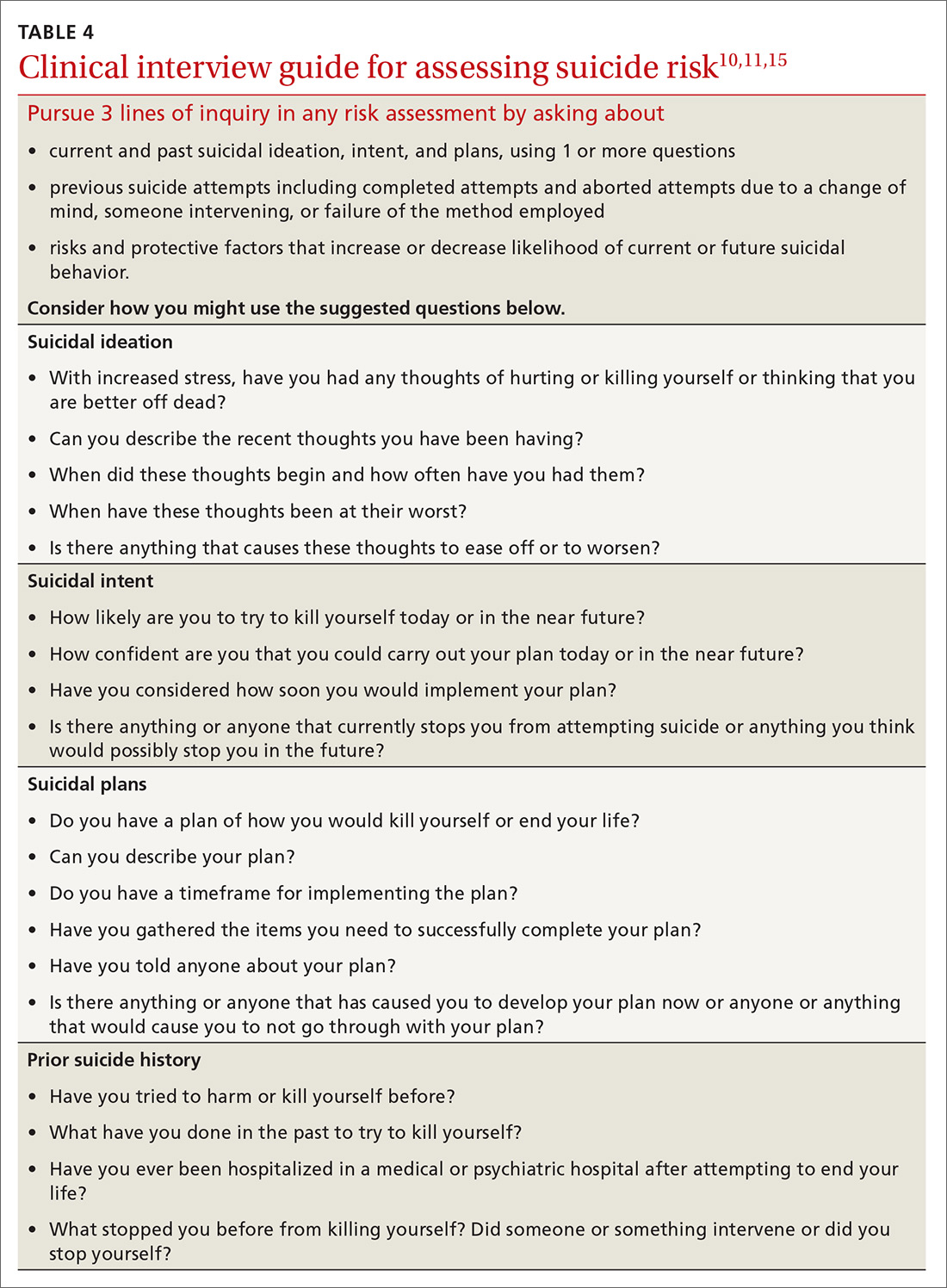
Continue to: Several screening tools...
Several screening tools are available for exploring a patient’s suicidality. Unfortunately, most of them are supported by limited evidence of effectiveness in identifying suicide risk.8-10 An exception is the well-researched and commonly used Columbia-Suicide Severity Rating Scale (C-SSRS).18,19 In a comparative study conducted at 2 primary care clinics, researchers found that the suicide item included in the PHQ-9 provided poor sensitivity but moderate specificity (60% and 84%, respectively),20 while the C-SSRS showed high sensitivity (100%) and specificity (96%-100%) in accurately identifying various suicidal self-injurious behaviors above and beyond what was identified through a structured clinical interview.20 Free copies of the C-SSRS, training materials, and follow-up assessments in multiple languages can be obtained on The Columbia Lighthouse Project Web site (http://cssrs.columbia.edu/).19
RECOMMENDATIONS FOR INTERVENTION
While there is debate regarding whom to screen for suicide, the importance of intervention when a patient is revealed to be at risk is clear. After completing a
When a patient is at high risk for suicide and reports an imminent plan or intent, ensure their safety through inpatient psychiatric hospitalization and then close follow-up upon hospital discharge. First encourage voluntary hospitalization in a collaborative discussion with the patient; resort to involuntary hospitalization only if the patient resists.
What not to do. When the patient does not require immediate hospitalization, evidence recommends against contracting for patient safety via a written contract or requiring patients to verbally guarantee that they will not commit suicide upon leaving a provider’s office.21 Concerns about such contracts include a lack of evidence supporting their use, decreased vigilance by health care workers when such contracts are in place, and questions regarding informed consent and competence.21 Instead, engage a patient who is at moderate or low risk in safety planning, and meet with the patient frequently to discuss continued safety planning through close follow-up (or with a behavioral health provider if available).10-12,22 With patients previously identified as at high risk for suicide who return from inpatient psychiatric hospitalization, continue to screen them for suicide at subsequent visits and engage them in collaborative safety planning.
Safety planning (TABLE 512), also known as crisis response planning, is considered a best practice and effective suicide prevention intervention by the Suicide Prevention Resource Center and the American Foundation for Suicide Prevention Best Practices Registry for Suicide Prevention.23 Safety planning involves a collaboration between patient and physician to identify risk factors and protective factors along with crisis resources and strategies to reduce
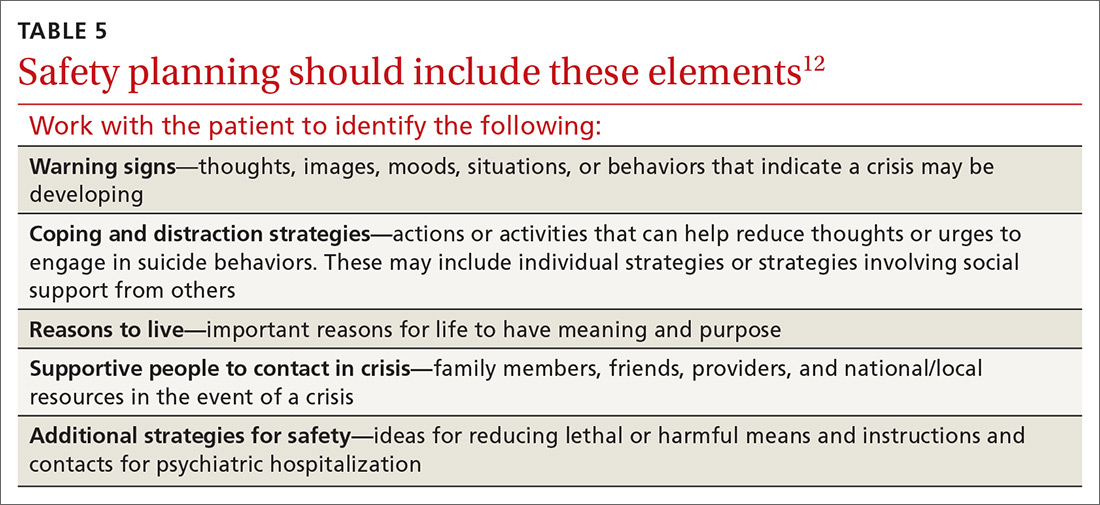
Continue to: THE CASE
THE CASE
Based on the concerning results from the PHQ-9 suicide item, Emily’s physician conducted a comprehensive suicide risk assessment using both clinical interview and the C-SSRS. Emily reported that she was experiencing daily suicidal ideations due to a lack of social support and longing to be with her deceased father. She had not previously attempted suicide and had no imminent intent to commit suicide. Emily did, however, have a plan to overdose on opioid medications she had been collecting for many months. Her physician determined that Emily was at moderate risk for suicide and consulted with the clinic’s behavioral health consultant, a psychologist, to confirm a treatment plan.
Emily and her physician collaboratively developed a safety plan including means reduction. Emily agreed to have her physician contact a friend to assist with safety planning, and she brought her opioid medications to the primary care clinic for disposal. Follow-up appointments were scheduled with the physician for every other week. The psychologist was available at the time of the first biweekly appointment to consult with the physician if needed. This initial appointment was focused on Emily’s suicide risk and her ability to engage in safety planning. In addition, the physician recommended that Emily schedule time with the psychologist so that she could work on her grief and depressive symptoms.
After several weeks of the biweekly appointments with both the primary care provider and the psychologist, Emily was no longer reporting suicidal ideation and she was ready to engage in coping strategies to deal with her grief and depressive symptoms.
CORRESPONDENCE
Meredith L.C. Williamson, PhD, 2900 E. 29th Street, Suite 100, Bryan, TX 77802; meredith.williamson@tamu.edu.
1. Nock MK, Borges G, Bromet EJ, et al. Suicide and suicidal behavior. Epidemiol Rev. 2008;30:133-154.
2. National Institute of Mental Health. Suicide. https://www.nimh.nih.gov/health/statistics/suicide.shtml#part_154968. Accessed October 18, 2019.
3. Luoma JB, Martin CE, Pearson JL. Contact with mental health and primary care providers before suicide: a review of the evidence. Am J Psychiatry. 2002;159:909-916.
4. Vannoy SD, Robins LS. Suicide-related discussions with depressed primary care patients in the USA: gender and quality gaps. A mixed methods analysis. BMJ Open. 2011;1:e000198.
5. Feldman MD, Franks P, Duberstein PR, et al. Let’s not talk about it: suicide inquiry in primary care. Ann Fam Med. 2007;5:412-418.
6. U.S. Department of Health and Human Services (HHS) Office of the Surgeon General and National Action Alliance for Suicide Prevention. 2012 National strategy for suicide prevention: goals and objectives for action. https://mnprc.org/wp-content/uploads/2019/01/2012-National-Strategy-for-suicide-prevention-goals-and-objectives-for-action.pdf. Accessed October 18, 2019.
7. The Joint Commission. Detecting and treating suicide ideation in all settings. Sentinel Event Alert. 2016;(56):1-7.
8. LeFevre ML, U.S. Preventive Services Task Force. Screening for suicide risk in adolescents, adults, and older adults in primary care: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2014;160:719-726.
9. American Psychiatric Association. Practice guidelines for the assessment and treatment of patients with suicidal behaviors. 2010. http://psychiatryonline.org/pb/assets/raw/sitewide/practice_guidelines/guidelines/suicide.pdf. Accessed October 18, 2019.
10. Department of Veterans Affairs & Department of Defense. VA/DoD clinical practice guideline for assessment and management of patients at risk for suicide. 2013. https://www.healthquality.va.gov/guidelines/MH/srb/VADODCP_SuicideRisk_Full.pdf. Accessed October 18, 2019.
11. Western Interstate Commission for Higher Education. Suicide prevention toolkit for primary care practices. 2017. https://www.sprc.org/sites/default/files/Final%20National%20Suicide%20Prevention%20Toolkit%202.15.18%20FINAL.pdf. Accessed October 18, 2019.
12. Stanley B, Brown GK. Safety planning intervention: a brief intervention to mitigate suicide risk. Cogn Behav Pract. 2012;19:256-264.
13. Screening for suicide risk in adolescents, adults, and older adults in primary care: recommendation statement. Am Fam Physician. 2015;91:190F-190I.
14. O’Connor E, Gaynes B, Burda BU, et al. Screening for suicide risk in primary care: a systematic evidence review for the U.S. Preventive Services Task Force. Evidence synthesis no. 103. https://www.ncbi.nlm.nih.gov/books/NBK137737/. Accessed October 25, 2019.
15. Suicide Prevention Resource Center. Risk and protective factors. https://www.sprc.org/about-suicide/risk-protective-factors. Accessed October 18, 2019.
16. CDC. Suicide rising across the US: more than a mental health concern. https://www.cdc.gov/vitalsigns/suicide/index.html. Accessed October 18, 2019.
17. Martin A, Rief W, Klaiberg A, et al. Validity of the Brief Patient Health Questionnaire Mood Scale (PHQ-9) in the general population. Gen Hosp Psychiatry. 2006;28:71-77.
18. Posner K, Brown GK, Stanley B, et al. The Columbia-Suicide Severity Rating Scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatry. 2011;168:1266-1277.
19. The Columbia Lighthouse Project. Identify risk. Prevent suicide. http://cssrs.columbia.edu. Accessed October 25, 2019.
20. Uebelacker LA, German NM, Gaudiano BA, et al. Patient health questionnaire depression scale as a suicide screening instrument in depressed primary care patients: a cross-sectional study. Prim Care Companion CNS Disord. 2011;13:pii: PCC.10m01027.
21. Hoffman RM. Contracting for safety: a misused tool. Pa Patient Saf Advis. 2013;10:82-84.
22. Stanley B, Brown GK, Brenner LA, et al. Comparison of the safety planning intervention with follow-up vs usual care of suicidal patients treated in the emergency department. JAMA Psychiatry. 2018;75:894-900.
23. Suicide Prevention Resource Center. Safety planning in emergency settings. http://www.sprc.org/news/safety-planning-emergency-settings. Accessed October 25, 2019.
THE CASE
Emily T,* a 30-year-old woman, visited her primary care physician as follow-up to reassess her grief over the loss of her father a year earlier. Emily was her father’s primary caretaker and still lived alone in his home. Emily had a history of chronic pain and major depressive disorder and had expressed feelings of worthlessness and hopelessness about her future since her father’s passing. In addition to her continuing grief response, she reported feeling worse on most days. She completed the Patient Health Questionnaire-9, and results indicated anhedonia, depressed mood, psychomotor retardation, hypersomnia, decreased appetite, decreased concentration, and thoughts that she would be better off dead.
- HOW WOULD YOU PROCEED WITH THIS PATIENT?
* The patient’s name has been changed to protect her identity.
In the United States, 1 suicide occurs on average every 12 minutes; lifetime prevalence of suicide attempts ranges from 1.9% to 8.7%.1 Suicide is the 10th overall cause of death in the United States, and it is the second leading cause of death for adults 18 to 34 years of age.2 In one study, nearly half of suicide victims had contact with primary care providers within 1 month of their suicide.3 Unfortunately, additional research suggests that primary care physicians appropriately screen for suicide in fewer than 40% of patient encounters.4,5
Suicide is defined as “death caused by self-directed injurious behavior with any intent to die as a result of the behavior.”6 When screening for suicide, be aware of the many terms related to suicide evaluation (TABLE 16). Be mindful, too, of the differences between suicidal and nonsuicidal ideation (death wish); the continuum of such thoughts ranges from those that lead to suicide to those that do not.
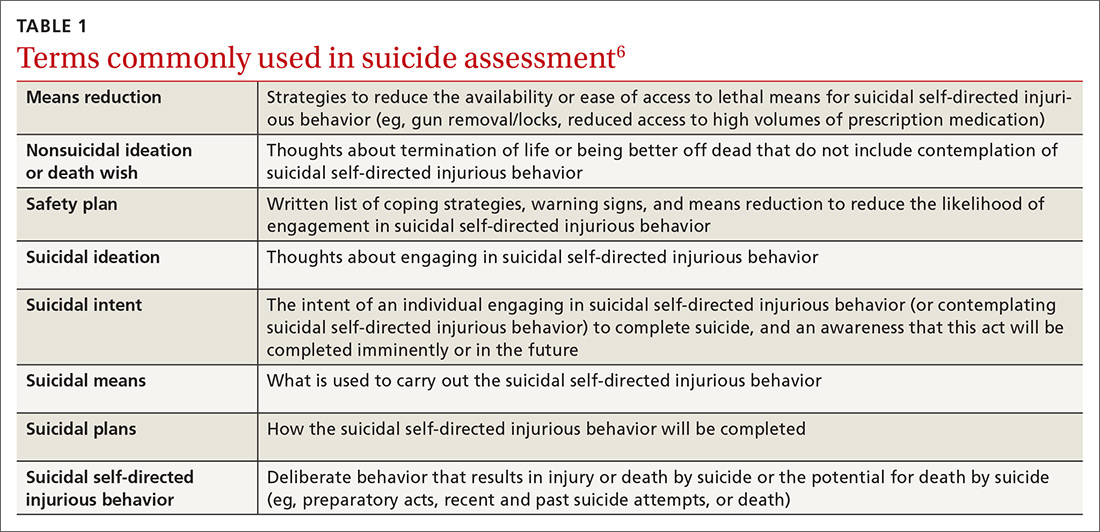
SUICIDE SCREENING RECOMMENDATIONS VARY
Although most health care providers would agree that intervening with a suicidal patient first requires competence in assessing suicide risk, regulating bodies differ on the use of routine screening and on appropriate screening tools for primary care. The Joint Commission recommends assessing suicide risk with all primary care patients,7 while the US Preventive Services Tasks Force (USPSTF) advises against universal suicide screening in primary care8 due to insufficient evidence that its benefit outweighs potential harm (TABLE 27-12). Instead, the USPSTF recommends screening primary care patients with known mental health disorders, recent inpatient psychiatric hospitalization, prior suicide or self-harm attempts, or increased emotional distress.8 USPSTF does support screening for depression with routine mental health measures that include items assessing suicidality.8,13,14 The American Academy of Family Physicians supports the recommendations by USPSTF.13
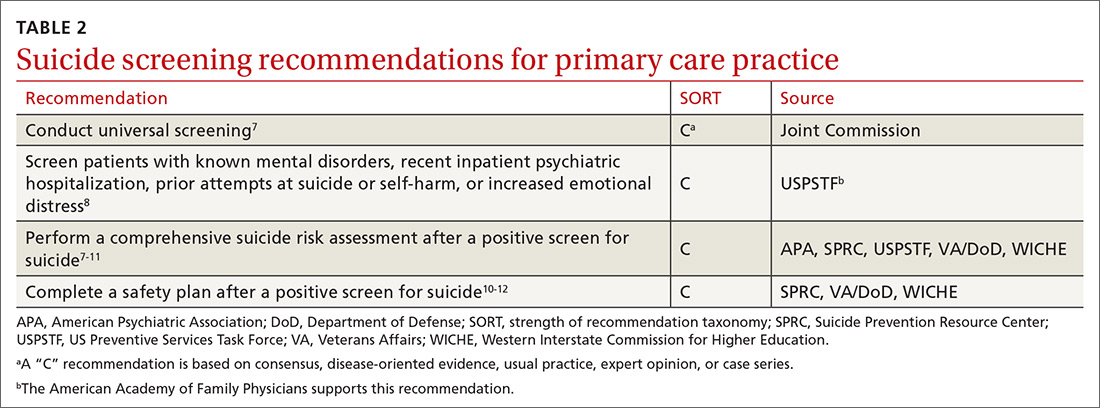
When screening for suicide, a comprehensive suicide risk assessment is recommended by both the Joint Commission and USPSTF.7,8 A comprehensive suicide risk assessment has 4 components: (1) identification of current suicide risk factors, (2) identification of protective factors, (3) inquiry about suicidal ideation, intent, and plan, and (4) primary care practitioner judgment of risk level and plan for clinical intervention.9-11
Take into account both risks and protective factors
Unfortunately, there is no “typical” description of a patient at risk for suicide and no validated models to predict suicide risk.8,10 A multitude of factors, both individual and societal, can increase or reduce risk of suicide.11,15 Each patient’s unique history includes risk factors for suicide including precipitating events (eg, job loss, termination of a relationship, death of a loved one) and protective factors that may be evaluated to determine overall risk for suicide (TABLE 38,10,11,15). According to the Centers for Disease Control and Prevention (CDC), there are several warning signs for patients who may be at greater risk for suicide: isolation, increased anxiety or anger, obtaining lethal means (eg, guns, knives, ropes), frequent mood swings, sleep changes, feeling trapped or in pain, increased substance use, discussing plans for death or wishes of death, and feeling like a burden.16
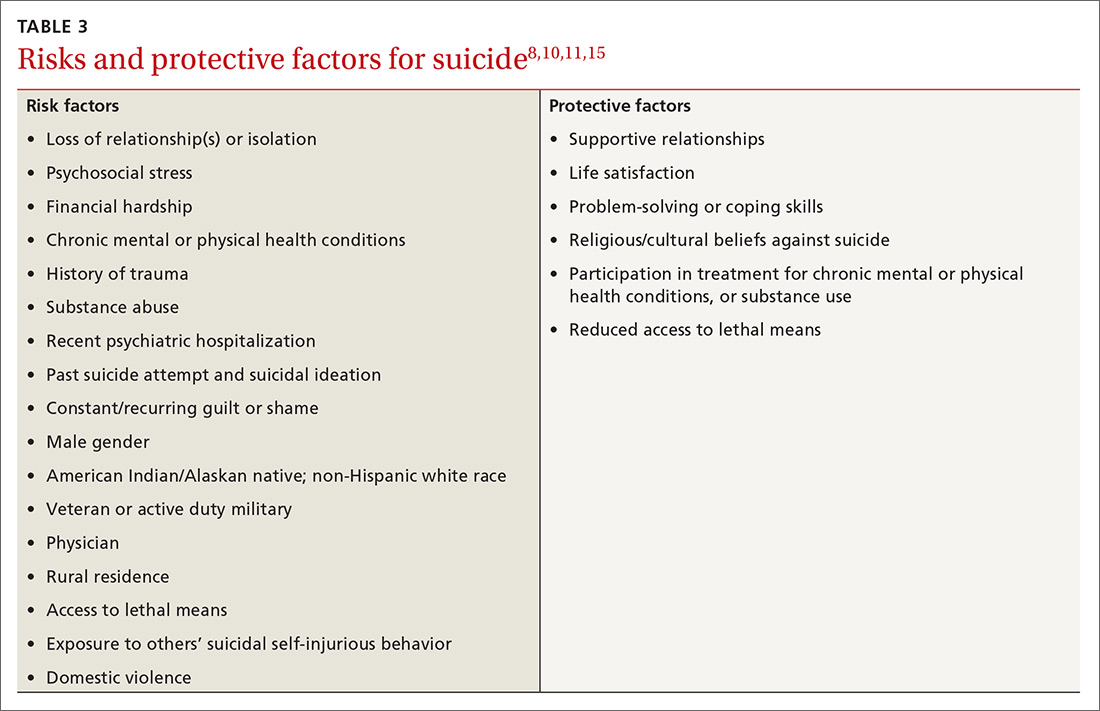
CHOOSING FROM AMONG SUICIDE SCREENING TOOLS
Brief mental health screening tools such as the Patient Health Questionnaire-9 (PHQ-9) are commonly used as primary screening tools for suicidal ideation.17 However, to attain a fuller understanding of a patient’s suicidality, select a screening tool that specifically
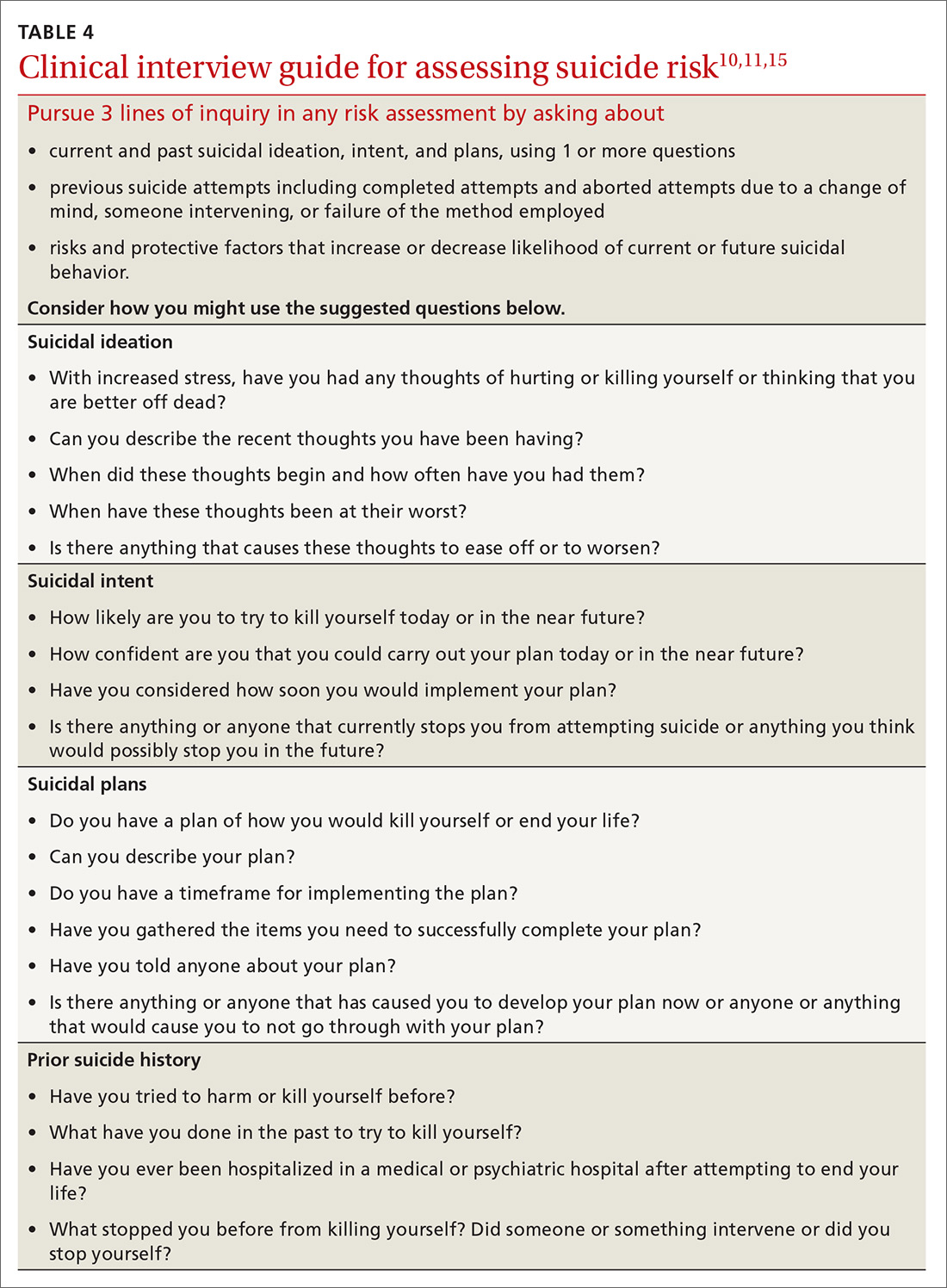
Continue to: Several screening tools...
Several screening tools are available for exploring a patient’s suicidality. Unfortunately, most of them are supported by limited evidence of effectiveness in identifying suicide risk.8-10 An exception is the well-researched and commonly used Columbia-Suicide Severity Rating Scale (C-SSRS).18,19 In a comparative study conducted at 2 primary care clinics, researchers found that the suicide item included in the PHQ-9 provided poor sensitivity but moderate specificity (60% and 84%, respectively),20 while the C-SSRS showed high sensitivity (100%) and specificity (96%-100%) in accurately identifying various suicidal self-injurious behaviors above and beyond what was identified through a structured clinical interview.20 Free copies of the C-SSRS, training materials, and follow-up assessments in multiple languages can be obtained on The Columbia Lighthouse Project Web site (http://cssrs.columbia.edu/).19
RECOMMENDATIONS FOR INTERVENTION
While there is debate regarding whom to screen for suicide, the importance of intervention when a patient is revealed to be at risk is clear. After completing a
When a patient is at high risk for suicide and reports an imminent plan or intent, ensure their safety through inpatient psychiatric hospitalization and then close follow-up upon hospital discharge. First encourage voluntary hospitalization in a collaborative discussion with the patient; resort to involuntary hospitalization only if the patient resists.
What not to do. When the patient does not require immediate hospitalization, evidence recommends against contracting for patient safety via a written contract or requiring patients to verbally guarantee that they will not commit suicide upon leaving a provider’s office.21 Concerns about such contracts include a lack of evidence supporting their use, decreased vigilance by health care workers when such contracts are in place, and questions regarding informed consent and competence.21 Instead, engage a patient who is at moderate or low risk in safety planning, and meet with the patient frequently to discuss continued safety planning through close follow-up (or with a behavioral health provider if available).10-12,22 With patients previously identified as at high risk for suicide who return from inpatient psychiatric hospitalization, continue to screen them for suicide at subsequent visits and engage them in collaborative safety planning.
Safety planning (TABLE 512), also known as crisis response planning, is considered a best practice and effective suicide prevention intervention by the Suicide Prevention Resource Center and the American Foundation for Suicide Prevention Best Practices Registry for Suicide Prevention.23 Safety planning involves a collaboration between patient and physician to identify risk factors and protective factors along with crisis resources and strategies to reduce
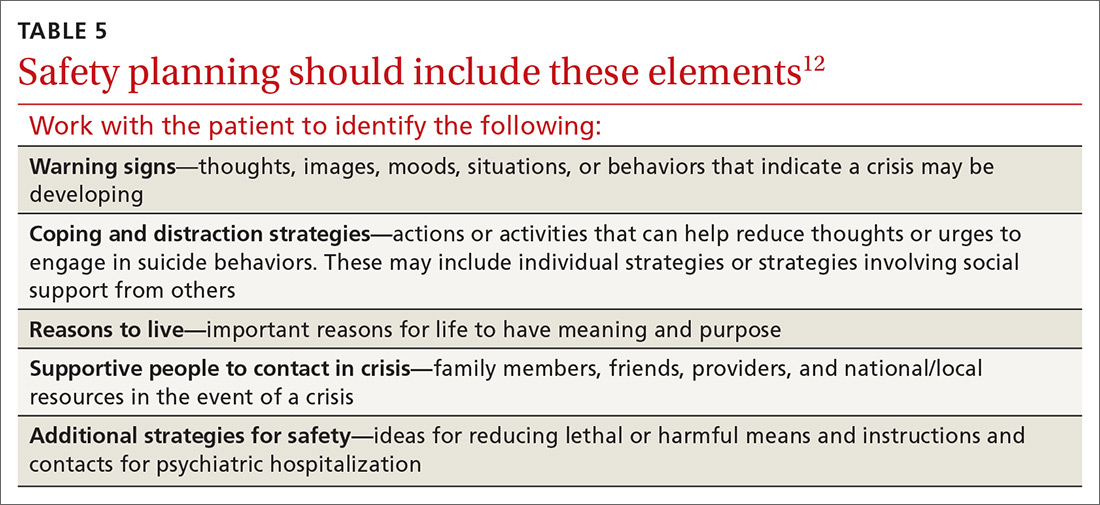
Continue to: THE CASE
THE CASE
Based on the concerning results from the PHQ-9 suicide item, Emily’s physician conducted a comprehensive suicide risk assessment using both clinical interview and the C-SSRS. Emily reported that she was experiencing daily suicidal ideations due to a lack of social support and longing to be with her deceased father. She had not previously attempted suicide and had no imminent intent to commit suicide. Emily did, however, have a plan to overdose on opioid medications she had been collecting for many months. Her physician determined that Emily was at moderate risk for suicide and consulted with the clinic’s behavioral health consultant, a psychologist, to confirm a treatment plan.
Emily and her physician collaboratively developed a safety plan including means reduction. Emily agreed to have her physician contact a friend to assist with safety planning, and she brought her opioid medications to the primary care clinic for disposal. Follow-up appointments were scheduled with the physician for every other week. The psychologist was available at the time of the first biweekly appointment to consult with the physician if needed. This initial appointment was focused on Emily’s suicide risk and her ability to engage in safety planning. In addition, the physician recommended that Emily schedule time with the psychologist so that she could work on her grief and depressive symptoms.
After several weeks of the biweekly appointments with both the primary care provider and the psychologist, Emily was no longer reporting suicidal ideation and she was ready to engage in coping strategies to deal with her grief and depressive symptoms.
CORRESPONDENCE
Meredith L.C. Williamson, PhD, 2900 E. 29th Street, Suite 100, Bryan, TX 77802; meredith.williamson@tamu.edu.
THE CASE
Emily T,* a 30-year-old woman, visited her primary care physician as follow-up to reassess her grief over the loss of her father a year earlier. Emily was her father’s primary caretaker and still lived alone in his home. Emily had a history of chronic pain and major depressive disorder and had expressed feelings of worthlessness and hopelessness about her future since her father’s passing. In addition to her continuing grief response, she reported feeling worse on most days. She completed the Patient Health Questionnaire-9, and results indicated anhedonia, depressed mood, psychomotor retardation, hypersomnia, decreased appetite, decreased concentration, and thoughts that she would be better off dead.
- HOW WOULD YOU PROCEED WITH THIS PATIENT?
* The patient’s name has been changed to protect her identity.
In the United States, 1 suicide occurs on average every 12 minutes; lifetime prevalence of suicide attempts ranges from 1.9% to 8.7%.1 Suicide is the 10th overall cause of death in the United States, and it is the second leading cause of death for adults 18 to 34 years of age.2 In one study, nearly half of suicide victims had contact with primary care providers within 1 month of their suicide.3 Unfortunately, additional research suggests that primary care physicians appropriately screen for suicide in fewer than 40% of patient encounters.4,5
Suicide is defined as “death caused by self-directed injurious behavior with any intent to die as a result of the behavior.”6 When screening for suicide, be aware of the many terms related to suicide evaluation (TABLE 16). Be mindful, too, of the differences between suicidal and nonsuicidal ideation (death wish); the continuum of such thoughts ranges from those that lead to suicide to those that do not.
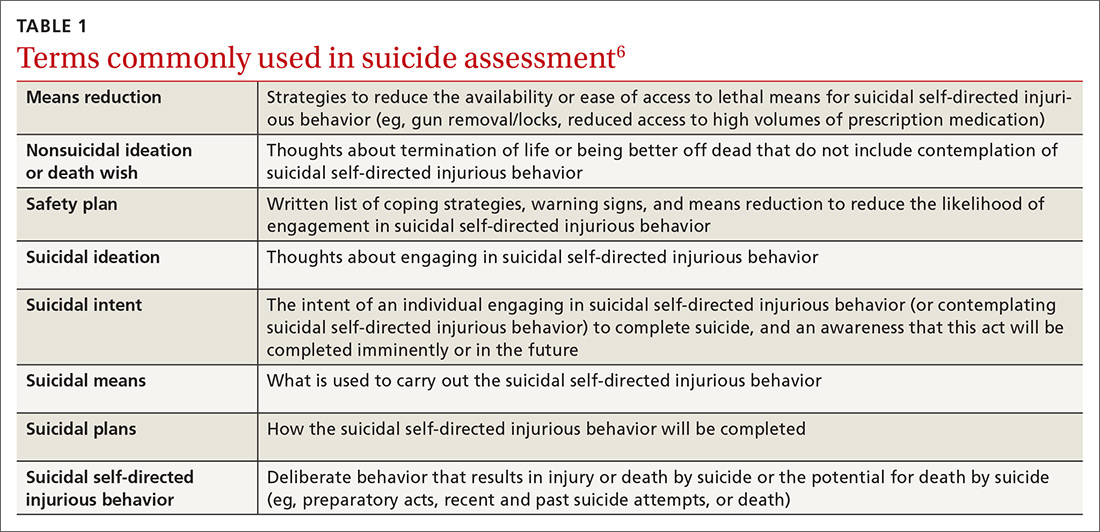
SUICIDE SCREENING RECOMMENDATIONS VARY
Although most health care providers would agree that intervening with a suicidal patient first requires competence in assessing suicide risk, regulating bodies differ on the use of routine screening and on appropriate screening tools for primary care. The Joint Commission recommends assessing suicide risk with all primary care patients,7 while the US Preventive Services Tasks Force (USPSTF) advises against universal suicide screening in primary care8 due to insufficient evidence that its benefit outweighs potential harm (TABLE 27-12). Instead, the USPSTF recommends screening primary care patients with known mental health disorders, recent inpatient psychiatric hospitalization, prior suicide or self-harm attempts, or increased emotional distress.8 USPSTF does support screening for depression with routine mental health measures that include items assessing suicidality.8,13,14 The American Academy of Family Physicians supports the recommendations by USPSTF.13
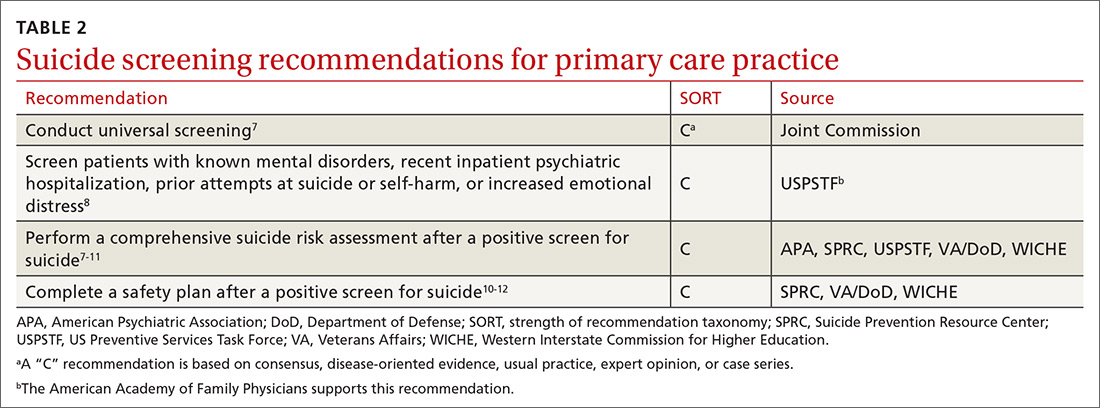
When screening for suicide, a comprehensive suicide risk assessment is recommended by both the Joint Commission and USPSTF.7,8 A comprehensive suicide risk assessment has 4 components: (1) identification of current suicide risk factors, (2) identification of protective factors, (3) inquiry about suicidal ideation, intent, and plan, and (4) primary care practitioner judgment of risk level and plan for clinical intervention.9-11
Take into account both risks and protective factors
Unfortunately, there is no “typical” description of a patient at risk for suicide and no validated models to predict suicide risk.8,10 A multitude of factors, both individual and societal, can increase or reduce risk of suicide.11,15 Each patient’s unique history includes risk factors for suicide including precipitating events (eg, job loss, termination of a relationship, death of a loved one) and protective factors that may be evaluated to determine overall risk for suicide (TABLE 38,10,11,15). According to the Centers for Disease Control and Prevention (CDC), there are several warning signs for patients who may be at greater risk for suicide: isolation, increased anxiety or anger, obtaining lethal means (eg, guns, knives, ropes), frequent mood swings, sleep changes, feeling trapped or in pain, increased substance use, discussing plans for death or wishes of death, and feeling like a burden.16
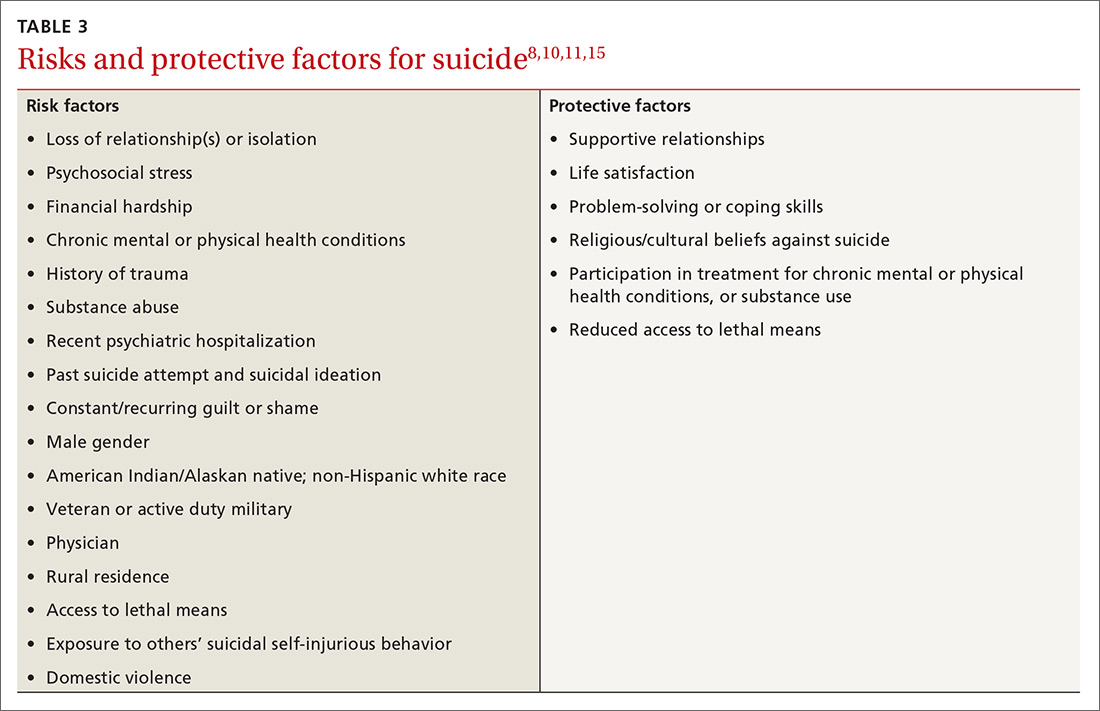
CHOOSING FROM AMONG SUICIDE SCREENING TOOLS
Brief mental health screening tools such as the Patient Health Questionnaire-9 (PHQ-9) are commonly used as primary screening tools for suicidal ideation.17 However, to attain a fuller understanding of a patient’s suicidality, select a screening tool that specifically
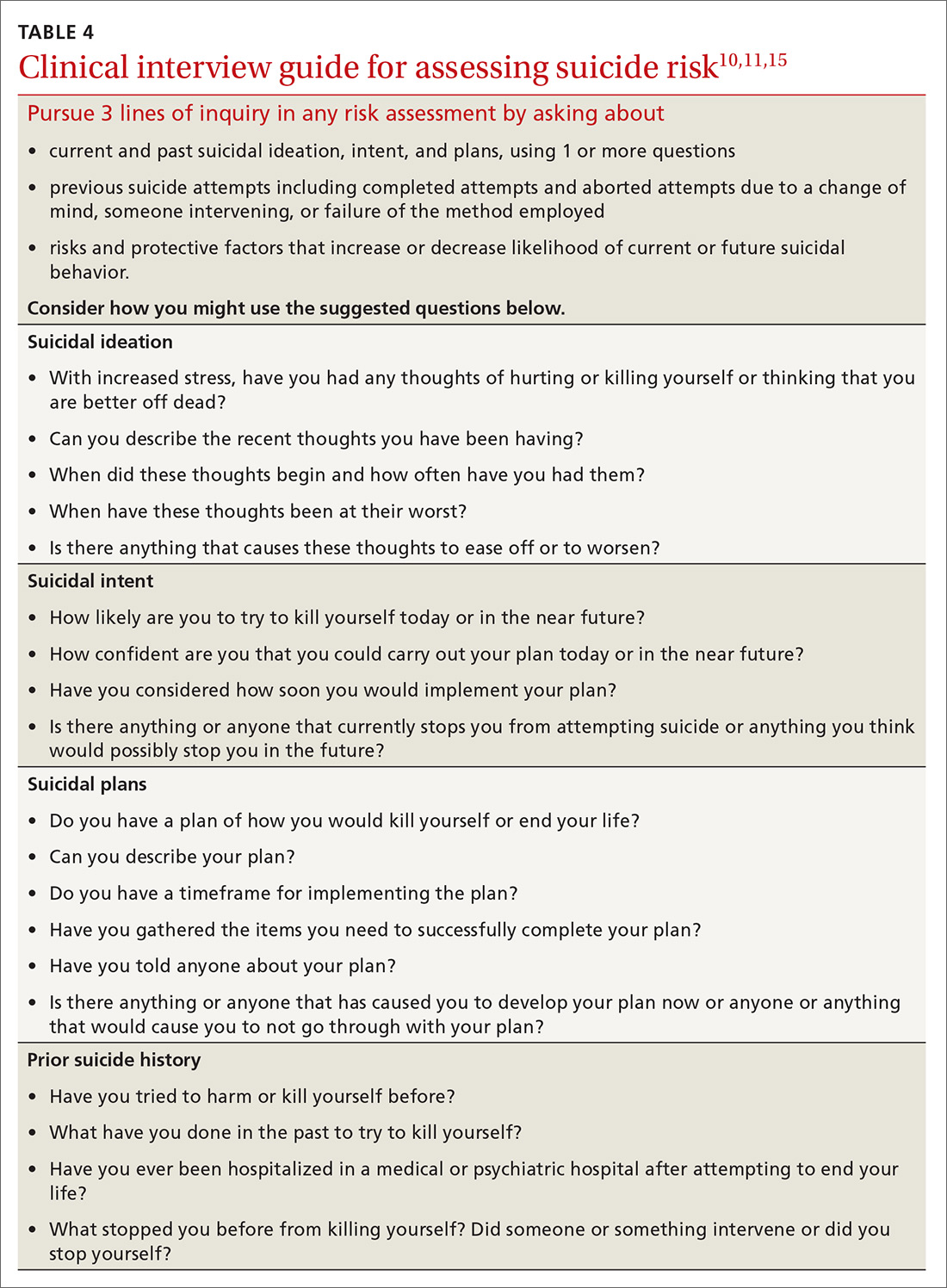
Continue to: Several screening tools...
Several screening tools are available for exploring a patient’s suicidality. Unfortunately, most of them are supported by limited evidence of effectiveness in identifying suicide risk.8-10 An exception is the well-researched and commonly used Columbia-Suicide Severity Rating Scale (C-SSRS).18,19 In a comparative study conducted at 2 primary care clinics, researchers found that the suicide item included in the PHQ-9 provided poor sensitivity but moderate specificity (60% and 84%, respectively),20 while the C-SSRS showed high sensitivity (100%) and specificity (96%-100%) in accurately identifying various suicidal self-injurious behaviors above and beyond what was identified through a structured clinical interview.20 Free copies of the C-SSRS, training materials, and follow-up assessments in multiple languages can be obtained on The Columbia Lighthouse Project Web site (http://cssrs.columbia.edu/).19
RECOMMENDATIONS FOR INTERVENTION
While there is debate regarding whom to screen for suicide, the importance of intervention when a patient is revealed to be at risk is clear. After completing a
When a patient is at high risk for suicide and reports an imminent plan or intent, ensure their safety through inpatient psychiatric hospitalization and then close follow-up upon hospital discharge. First encourage voluntary hospitalization in a collaborative discussion with the patient; resort to involuntary hospitalization only if the patient resists.
What not to do. When the patient does not require immediate hospitalization, evidence recommends against contracting for patient safety via a written contract or requiring patients to verbally guarantee that they will not commit suicide upon leaving a provider’s office.21 Concerns about such contracts include a lack of evidence supporting their use, decreased vigilance by health care workers when such contracts are in place, and questions regarding informed consent and competence.21 Instead, engage a patient who is at moderate or low risk in safety planning, and meet with the patient frequently to discuss continued safety planning through close follow-up (or with a behavioral health provider if available).10-12,22 With patients previously identified as at high risk for suicide who return from inpatient psychiatric hospitalization, continue to screen them for suicide at subsequent visits and engage them in collaborative safety planning.
Safety planning (TABLE 512), also known as crisis response planning, is considered a best practice and effective suicide prevention intervention by the Suicide Prevention Resource Center and the American Foundation for Suicide Prevention Best Practices Registry for Suicide Prevention.23 Safety planning involves a collaboration between patient and physician to identify risk factors and protective factors along with crisis resources and strategies to reduce
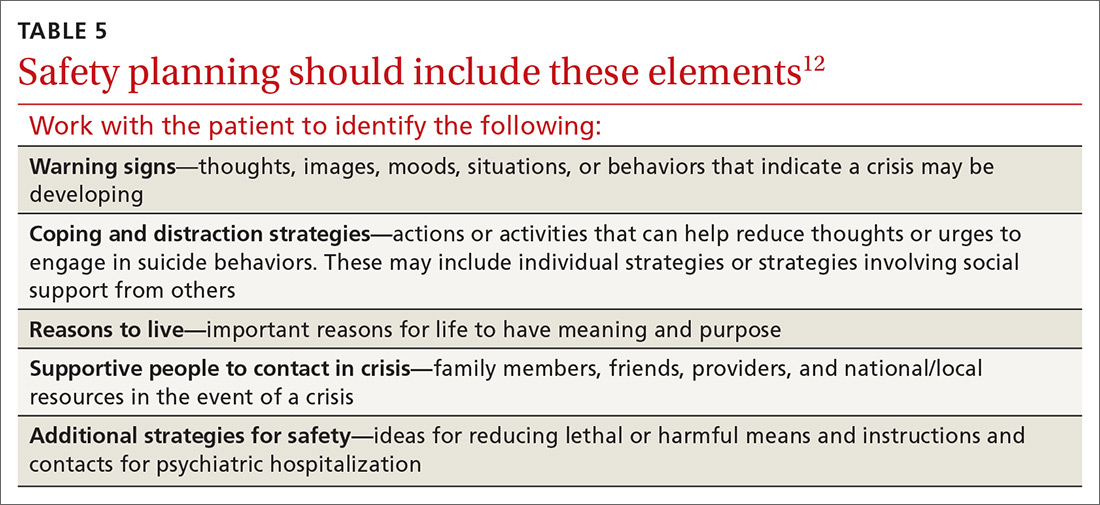
Continue to: THE CASE
THE CASE
Based on the concerning results from the PHQ-9 suicide item, Emily’s physician conducted a comprehensive suicide risk assessment using both clinical interview and the C-SSRS. Emily reported that she was experiencing daily suicidal ideations due to a lack of social support and longing to be with her deceased father. She had not previously attempted suicide and had no imminent intent to commit suicide. Emily did, however, have a plan to overdose on opioid medications she had been collecting for many months. Her physician determined that Emily was at moderate risk for suicide and consulted with the clinic’s behavioral health consultant, a psychologist, to confirm a treatment plan.
Emily and her physician collaboratively developed a safety plan including means reduction. Emily agreed to have her physician contact a friend to assist with safety planning, and she brought her opioid medications to the primary care clinic for disposal. Follow-up appointments were scheduled with the physician for every other week. The psychologist was available at the time of the first biweekly appointment to consult with the physician if needed. This initial appointment was focused on Emily’s suicide risk and her ability to engage in safety planning. In addition, the physician recommended that Emily schedule time with the psychologist so that she could work on her grief and depressive symptoms.
After several weeks of the biweekly appointments with both the primary care provider and the psychologist, Emily was no longer reporting suicidal ideation and she was ready to engage in coping strategies to deal with her grief and depressive symptoms.
CORRESPONDENCE
Meredith L.C. Williamson, PhD, 2900 E. 29th Street, Suite 100, Bryan, TX 77802; meredith.williamson@tamu.edu.
1. Nock MK, Borges G, Bromet EJ, et al. Suicide and suicidal behavior. Epidemiol Rev. 2008;30:133-154.
2. National Institute of Mental Health. Suicide. https://www.nimh.nih.gov/health/statistics/suicide.shtml#part_154968. Accessed October 18, 2019.
3. Luoma JB, Martin CE, Pearson JL. Contact with mental health and primary care providers before suicide: a review of the evidence. Am J Psychiatry. 2002;159:909-916.
4. Vannoy SD, Robins LS. Suicide-related discussions with depressed primary care patients in the USA: gender and quality gaps. A mixed methods analysis. BMJ Open. 2011;1:e000198.
5. Feldman MD, Franks P, Duberstein PR, et al. Let’s not talk about it: suicide inquiry in primary care. Ann Fam Med. 2007;5:412-418.
6. U.S. Department of Health and Human Services (HHS) Office of the Surgeon General and National Action Alliance for Suicide Prevention. 2012 National strategy for suicide prevention: goals and objectives for action. https://mnprc.org/wp-content/uploads/2019/01/2012-National-Strategy-for-suicide-prevention-goals-and-objectives-for-action.pdf. Accessed October 18, 2019.
7. The Joint Commission. Detecting and treating suicide ideation in all settings. Sentinel Event Alert. 2016;(56):1-7.
8. LeFevre ML, U.S. Preventive Services Task Force. Screening for suicide risk in adolescents, adults, and older adults in primary care: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2014;160:719-726.
9. American Psychiatric Association. Practice guidelines for the assessment and treatment of patients with suicidal behaviors. 2010. http://psychiatryonline.org/pb/assets/raw/sitewide/practice_guidelines/guidelines/suicide.pdf. Accessed October 18, 2019.
10. Department of Veterans Affairs & Department of Defense. VA/DoD clinical practice guideline for assessment and management of patients at risk for suicide. 2013. https://www.healthquality.va.gov/guidelines/MH/srb/VADODCP_SuicideRisk_Full.pdf. Accessed October 18, 2019.
11. Western Interstate Commission for Higher Education. Suicide prevention toolkit for primary care practices. 2017. https://www.sprc.org/sites/default/files/Final%20National%20Suicide%20Prevention%20Toolkit%202.15.18%20FINAL.pdf. Accessed October 18, 2019.
12. Stanley B, Brown GK. Safety planning intervention: a brief intervention to mitigate suicide risk. Cogn Behav Pract. 2012;19:256-264.
13. Screening for suicide risk in adolescents, adults, and older adults in primary care: recommendation statement. Am Fam Physician. 2015;91:190F-190I.
14. O’Connor E, Gaynes B, Burda BU, et al. Screening for suicide risk in primary care: a systematic evidence review for the U.S. Preventive Services Task Force. Evidence synthesis no. 103. https://www.ncbi.nlm.nih.gov/books/NBK137737/. Accessed October 25, 2019.
15. Suicide Prevention Resource Center. Risk and protective factors. https://www.sprc.org/about-suicide/risk-protective-factors. Accessed October 18, 2019.
16. CDC. Suicide rising across the US: more than a mental health concern. https://www.cdc.gov/vitalsigns/suicide/index.html. Accessed October 18, 2019.
17. Martin A, Rief W, Klaiberg A, et al. Validity of the Brief Patient Health Questionnaire Mood Scale (PHQ-9) in the general population. Gen Hosp Psychiatry. 2006;28:71-77.
18. Posner K, Brown GK, Stanley B, et al. The Columbia-Suicide Severity Rating Scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatry. 2011;168:1266-1277.
19. The Columbia Lighthouse Project. Identify risk. Prevent suicide. http://cssrs.columbia.edu. Accessed October 25, 2019.
20. Uebelacker LA, German NM, Gaudiano BA, et al. Patient health questionnaire depression scale as a suicide screening instrument in depressed primary care patients: a cross-sectional study. Prim Care Companion CNS Disord. 2011;13:pii: PCC.10m01027.
21. Hoffman RM. Contracting for safety: a misused tool. Pa Patient Saf Advis. 2013;10:82-84.
22. Stanley B, Brown GK, Brenner LA, et al. Comparison of the safety planning intervention with follow-up vs usual care of suicidal patients treated in the emergency department. JAMA Psychiatry. 2018;75:894-900.
23. Suicide Prevention Resource Center. Safety planning in emergency settings. http://www.sprc.org/news/safety-planning-emergency-settings. Accessed October 25, 2019.
1. Nock MK, Borges G, Bromet EJ, et al. Suicide and suicidal behavior. Epidemiol Rev. 2008;30:133-154.
2. National Institute of Mental Health. Suicide. https://www.nimh.nih.gov/health/statistics/suicide.shtml#part_154968. Accessed October 18, 2019.
3. Luoma JB, Martin CE, Pearson JL. Contact with mental health and primary care providers before suicide: a review of the evidence. Am J Psychiatry. 2002;159:909-916.
4. Vannoy SD, Robins LS. Suicide-related discussions with depressed primary care patients in the USA: gender and quality gaps. A mixed methods analysis. BMJ Open. 2011;1:e000198.
5. Feldman MD, Franks P, Duberstein PR, et al. Let’s not talk about it: suicide inquiry in primary care. Ann Fam Med. 2007;5:412-418.
6. U.S. Department of Health and Human Services (HHS) Office of the Surgeon General and National Action Alliance for Suicide Prevention. 2012 National strategy for suicide prevention: goals and objectives for action. https://mnprc.org/wp-content/uploads/2019/01/2012-National-Strategy-for-suicide-prevention-goals-and-objectives-for-action.pdf. Accessed October 18, 2019.
7. The Joint Commission. Detecting and treating suicide ideation in all settings. Sentinel Event Alert. 2016;(56):1-7.
8. LeFevre ML, U.S. Preventive Services Task Force. Screening for suicide risk in adolescents, adults, and older adults in primary care: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2014;160:719-726.
9. American Psychiatric Association. Practice guidelines for the assessment and treatment of patients with suicidal behaviors. 2010. http://psychiatryonline.org/pb/assets/raw/sitewide/practice_guidelines/guidelines/suicide.pdf. Accessed October 18, 2019.
10. Department of Veterans Affairs & Department of Defense. VA/DoD clinical practice guideline for assessment and management of patients at risk for suicide. 2013. https://www.healthquality.va.gov/guidelines/MH/srb/VADODCP_SuicideRisk_Full.pdf. Accessed October 18, 2019.
11. Western Interstate Commission for Higher Education. Suicide prevention toolkit for primary care practices. 2017. https://www.sprc.org/sites/default/files/Final%20National%20Suicide%20Prevention%20Toolkit%202.15.18%20FINAL.pdf. Accessed October 18, 2019.
12. Stanley B, Brown GK. Safety planning intervention: a brief intervention to mitigate suicide risk. Cogn Behav Pract. 2012;19:256-264.
13. Screening for suicide risk in adolescents, adults, and older adults in primary care: recommendation statement. Am Fam Physician. 2015;91:190F-190I.
14. O’Connor E, Gaynes B, Burda BU, et al. Screening for suicide risk in primary care: a systematic evidence review for the U.S. Preventive Services Task Force. Evidence synthesis no. 103. https://www.ncbi.nlm.nih.gov/books/NBK137737/. Accessed October 25, 2019.
15. Suicide Prevention Resource Center. Risk and protective factors. https://www.sprc.org/about-suicide/risk-protective-factors. Accessed October 18, 2019.
16. CDC. Suicide rising across the US: more than a mental health concern. https://www.cdc.gov/vitalsigns/suicide/index.html. Accessed October 18, 2019.
17. Martin A, Rief W, Klaiberg A, et al. Validity of the Brief Patient Health Questionnaire Mood Scale (PHQ-9) in the general population. Gen Hosp Psychiatry. 2006;28:71-77.
18. Posner K, Brown GK, Stanley B, et al. The Columbia-Suicide Severity Rating Scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatry. 2011;168:1266-1277.
19. The Columbia Lighthouse Project. Identify risk. Prevent suicide. http://cssrs.columbia.edu. Accessed October 25, 2019.
20. Uebelacker LA, German NM, Gaudiano BA, et al. Patient health questionnaire depression scale as a suicide screening instrument in depressed primary care patients: a cross-sectional study. Prim Care Companion CNS Disord. 2011;13:pii: PCC.10m01027.
21. Hoffman RM. Contracting for safety: a misused tool. Pa Patient Saf Advis. 2013;10:82-84.
22. Stanley B, Brown GK, Brenner LA, et al. Comparison of the safety planning intervention with follow-up vs usual care of suicidal patients treated in the emergency department. JAMA Psychiatry. 2018;75:894-900.
23. Suicide Prevention Resource Center. Safety planning in emergency settings. http://www.sprc.org/news/safety-planning-emergency-settings. Accessed October 25, 2019.