User login
Working adeptly to diagnose and treat adult ADHD
THE CASE
Ms. L’s family physician interviewed her and, aided by parental input, was able to identify a pattern of disorganized and impulsive behavior that was present even in grade school. Mood disorders and substance abuse were ruled out from the interview and lab testing, and cognitive ability was confirmed through a review of school testing.
●
* The patient’s name has been changed to protect her identity.
Attention-deficit/hyperactivity disorder (ADHD) is classified as a neurodevelopmental disorder in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), its hallmarks being inattentive, hyperactive, or impulsive behaviors that affect functioning or development.1 Historically, it was thought that ADHD was a disorder of children and adolescents, and that patients “grew out” of their behaviors once adulthood was reached. It is now estimated that 50% of children with ADHD will carry the diagnosis into adulthood,2 resulting in a prevalence of 5.9% to 7.1% for children3 and 3.4% for adults.4 There are 3 presentations of ADHD, known as ADHD-I (inattentive), ADHD-HI (hyperactive-impulsive), and ADHD-C (combined). The inattentive type accounts for 47% of adult cases, and adult ADHD disproportionately affects males compared with females.2
An overall pattern of underachievement and variable performance is common throughout life in patients with ADHD. Adults are much more likely to report subtle impairments in higher executive functions such as organization, time management, and modulating emotions. Consequences include poor performance at work, attendance issues, difficulty with social interactions, and an increased likelihood of unemployment.5 Among those employed, there is a large disparity in income compared with counterparts without ADHD.6 Increased risk of substance use, injury, and traffic accidents also has been reported.1
Disorders that can mimic or coexist with ADHD
The differential diagnosis for ADHD is wide, and comorbidity with other disorders is common.
Continue to: Bipolar disorder
Bipolar disorder shares with ADHD the core symptoms of hyperactivity, impulsive behavior, and difficulty completing tasks. Mania and ADHD can look very similar if symptoms are observed at a single point in time. Bipolar illness is, by definition, episodic and fluctuating, while ADHD is much more constant. In addition, bipolar illness exhibits significant variation in mood, while ADHD may or may not be associated with impaired mood regulation. Up to 20% of patients with bipolar illness also have ADHD.7
Anxiety and depressive disorders can also share symptoms with ADHD-I. These include distractibility, poor concentration, and, in the case of anxiety, rapid changes in train of thought. Sleep disturbance, past trauma, and current acute stressors may manifest as clinical anxiety or depression, or may interfere with concentration and attention independently. As with bipolar illness, clinicians must look carefully at the time course of symptoms, including the age of onset. Classically, mood disorders develop in adolescence or early adulthood, while ADHD always has manifestations in childhood. Inattention and distractibility will track with mood if they are caused by an affective illness, but will remain in ADHD even when the patient is euthymic. On the other hand, patients with ADHD frequently become frustrated or overwhelmed as a result of their difficulties with task completion and social function, a presentation which can mimic anxiety or depression.8
Substance use disorder and ADHD interact in multiple ways and can present one of the more challenging diagnostic tasks when assessing a patient with impaired attention or concentration. ADHD is a powerful risk factor for future substance use,9 while substance use can impair attention, induce impulsivity, and alter concentration. Further, the treatment of choice for ADHD (stimulant medication) has the potential for misuse. The presence of continuous symptoms across settings is crucial in determining the proper diagnosis of ADHD.
Other conditions. Patients with a learning disability can be inattentive due to their cognitive limitations, or it may be comorbid with ADHD. If an intellectual deficit is suspected, referral for cognitive testing can help clarify the diagnosis. Autism also may cause significant alterations in attention with both hyper-focus and distractibility being common, as they are in ADHD. Intermittent explosive disorder shares the core symptom of impulsivity, but includes aggression, which is not always seen in ADHD. Personality disorders (eg, borderline, narcissistic) may also be difficult to distinguish from ADHD. The key to differentiation is the identification of behavior patterns outside the realms of concentration and attention.7
KEY DIAGNOSTIC CRITERIA
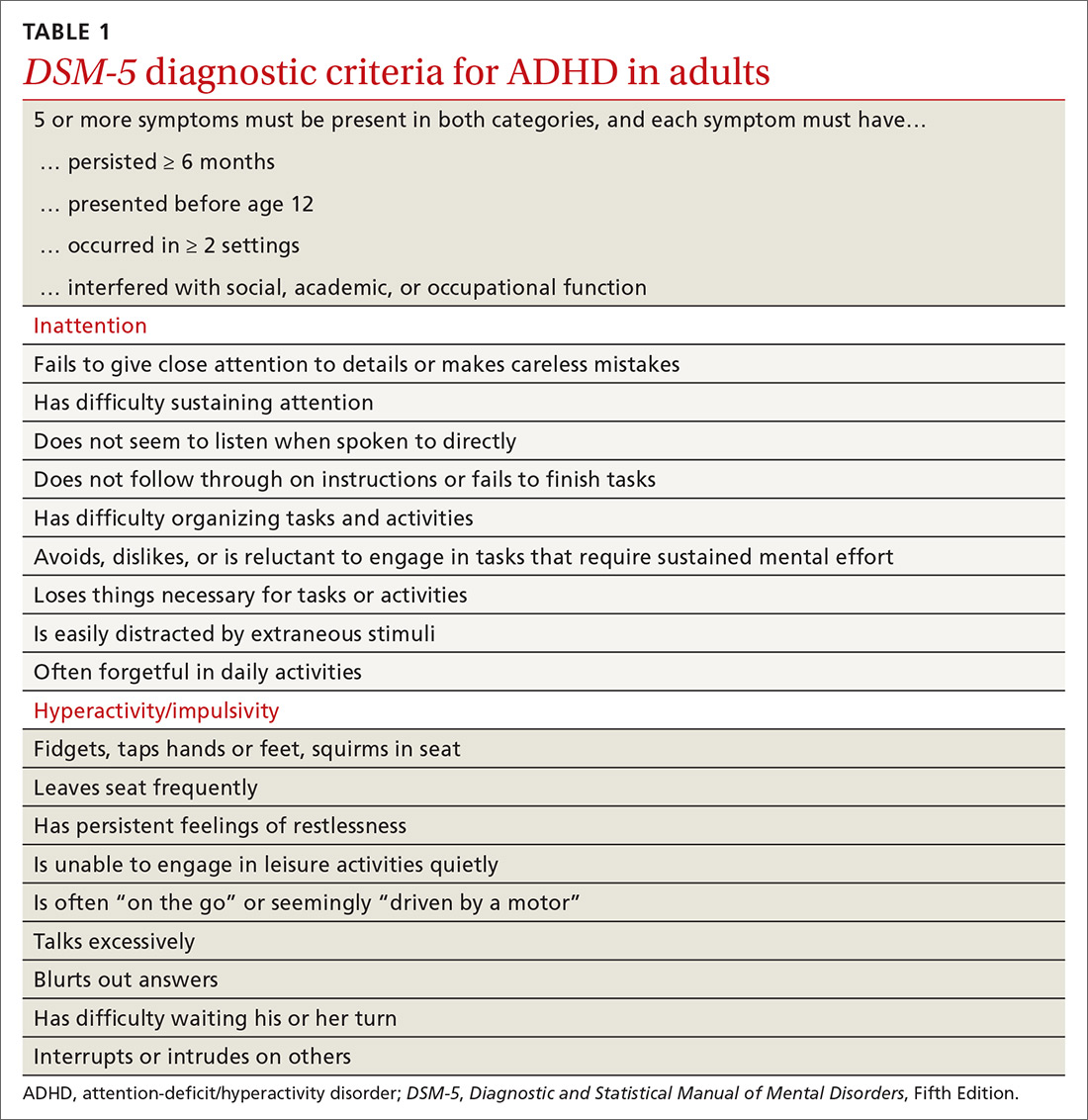
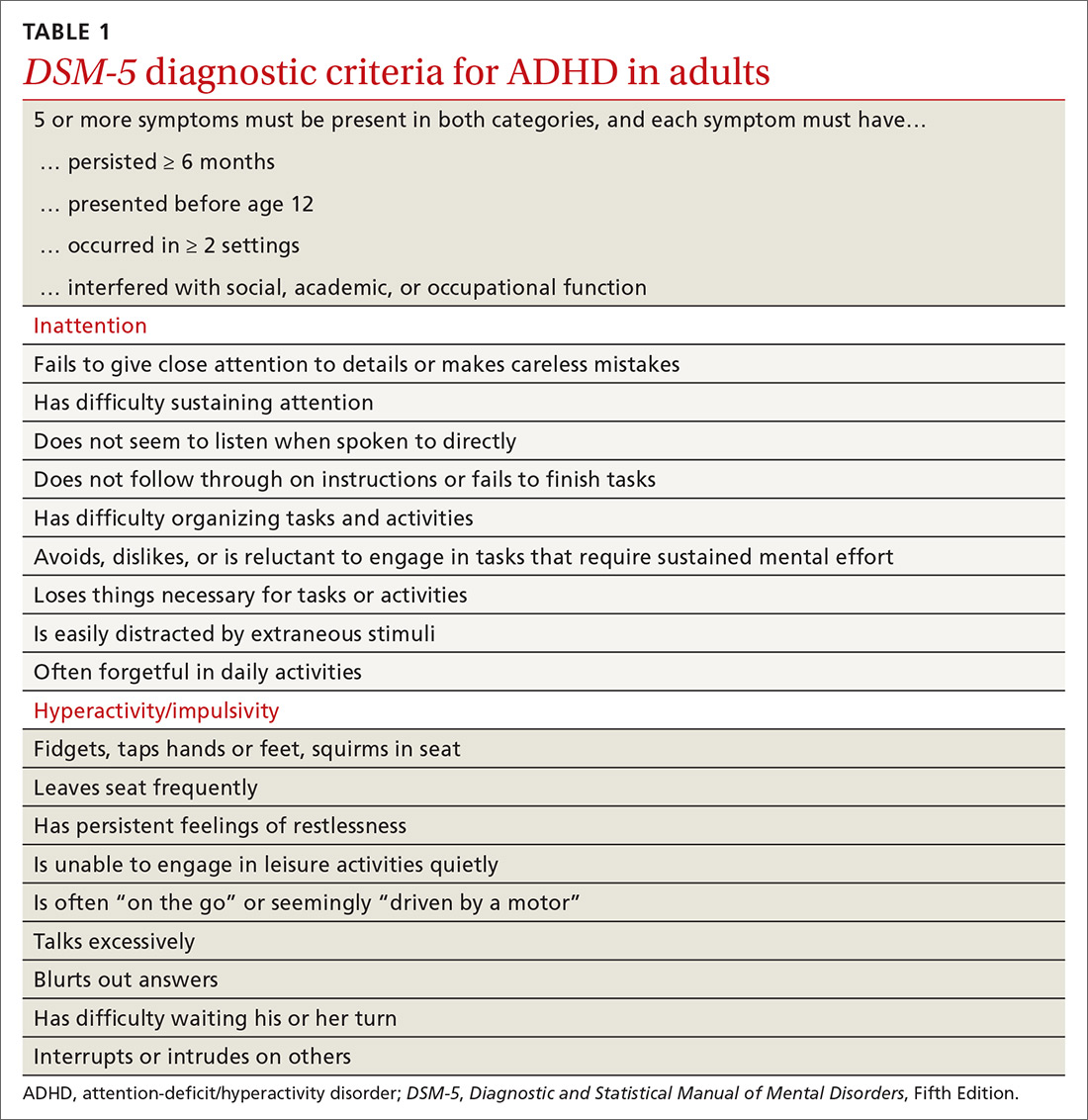
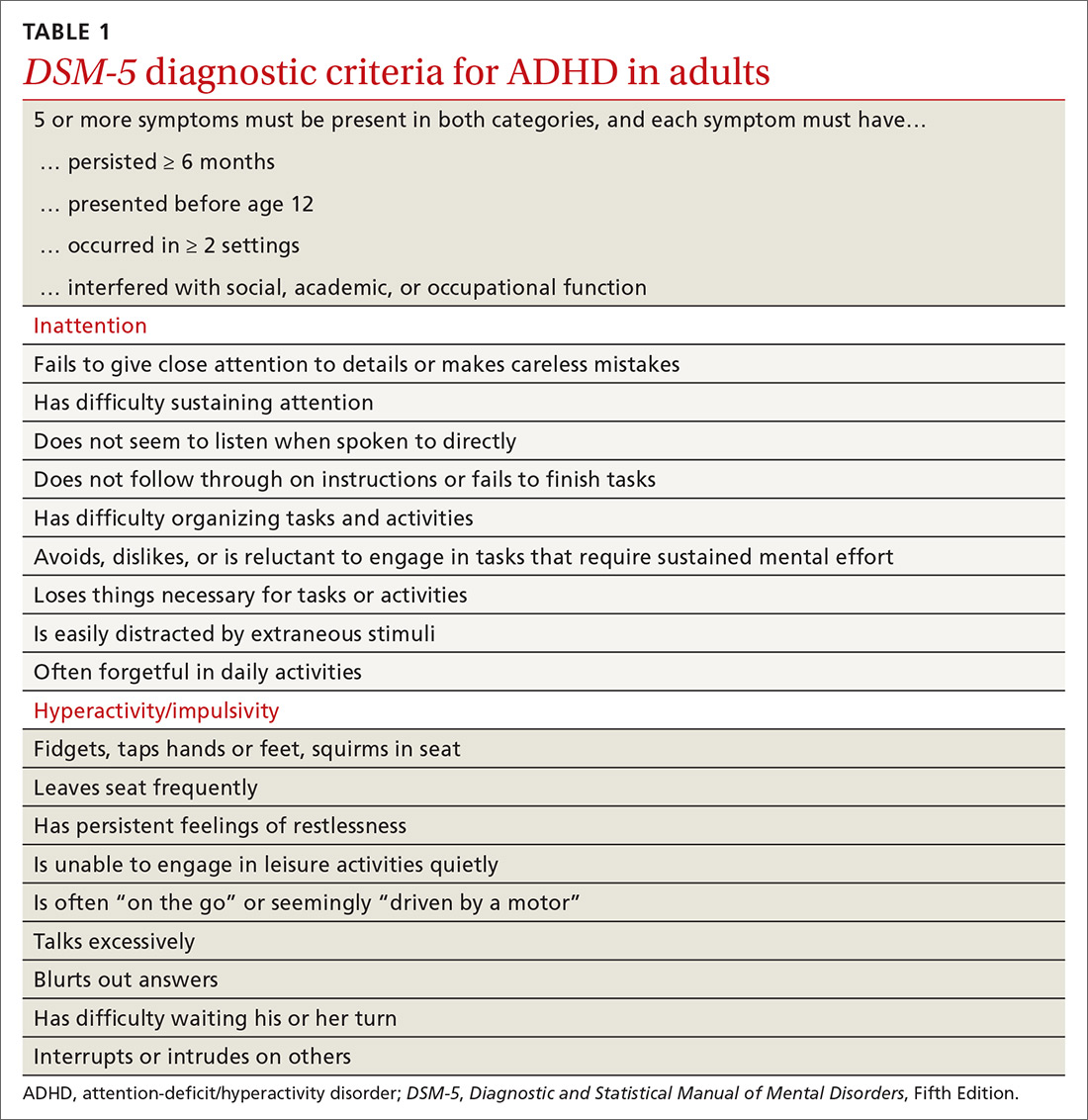
The diagnostic criteria for ADHD defined in DSM-5 are found in TABLE 1.1 Individuals ≥ 17 years old must meet 5 of 9 characteristics of inattention or 5 of 9 characteristics of hyperactivity/impulsivity (criterion A).1 Some symptoms must have been present prior to age 12 (criterion B). This cutoff is an increase from age 7 advised in DSM-IV.10 Symptoms must occur across at least 2 settings (criterion C) and significantly interfere with social, academic, or occupational functioning (criterion D). Exclusions include symptoms that occur exclusively in the context of a psychotic disorder or symptoms that are better explained in the context of other mental disorders (criterion E).1
Continue to: In the primary care setting
In the primary care setting, an assessment for ADHD should, at minimum, involve a review of the patient’s academic and work history, assessment of psychiatric comorbidities and substance use history, and administration of appropriate rating scales. When evaluating adults, these tools include the Adult ADHD Self-Report Scale (ASRS)11,12 screening tool and the Diagnostic Interview for ADHD in adults (DIVA-5).13,14 If possible, obtain scale assessments not only from the patient but from family members or other observers who can provide information about the patient in childhood/adolescence and present day.
In an integrated care setting, consider involving a behavioral health consultant for a more comprehensive evaluation of educational, employment, driving, and relationship histories. Historical record review may include report cards from elementary school through high school, standardized test scores, psycho-educational and individual education plan reports, and medical records. Having a snapshot of the patient as a younger child, adolescent, and young adult can help to identify overall patterns of academic underachievement and reveal gaps between potential and overall achievement and performance. Pursue a more thorough evaluation in cases where other comorbid psychiatric disorders are present or when the patient is unfamiliar to you.
TWO GROUPS OF TREATMENT OPTIONS
The treatment of ADHD in adults (and children) can be broadly divided into pharmacologic and nonpharmacologic modalities.
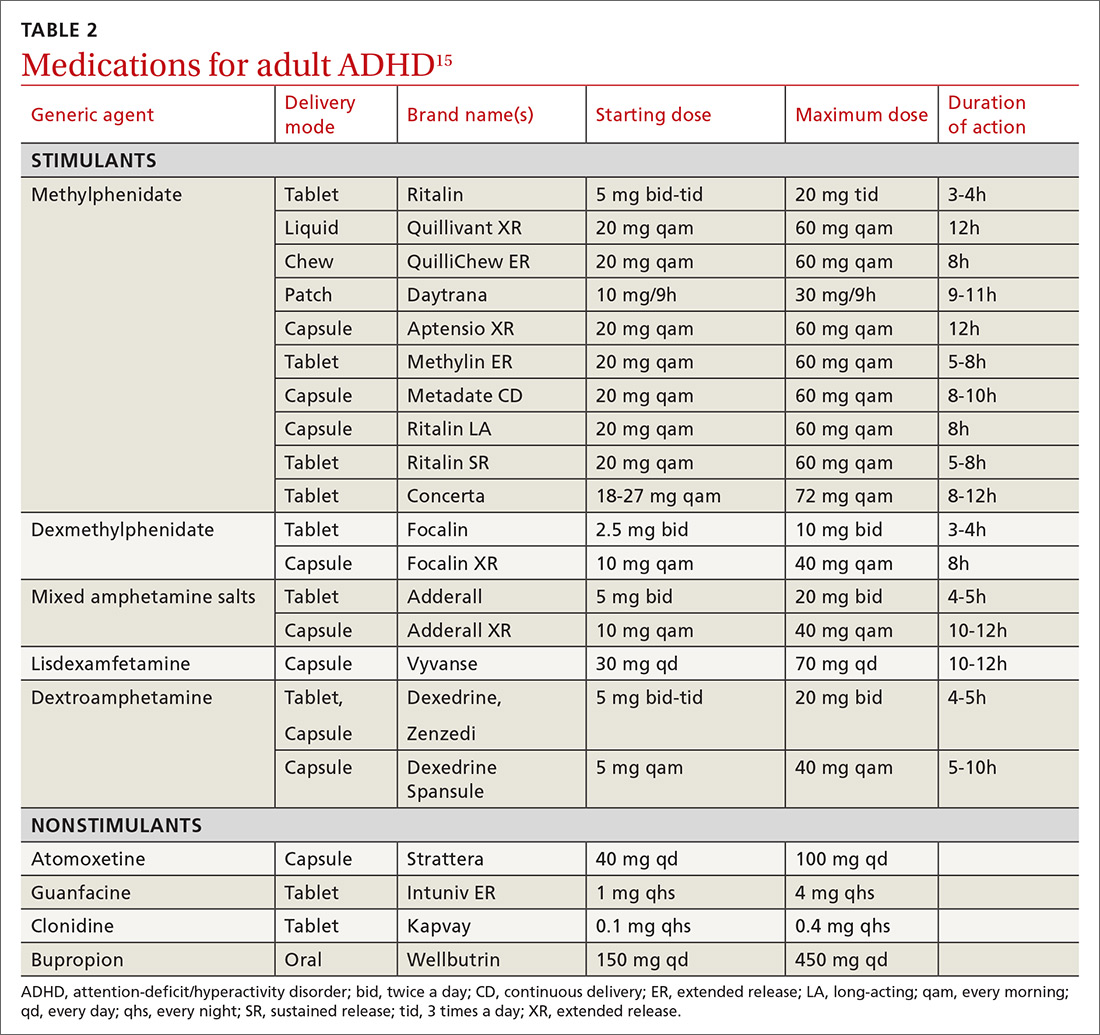
Stimulants are first-line pharmacologic treatment for ADHD in patients with low risk for misuse. Stimulants improve cognitive function, decrease impulsivity, and increase alertness.15 However, these effects are not exclusive to those with ADHD, and response does not aid in diagnosis. No stimulant is preferred over another, although individuals may respond better to 1 specific agent than to others. Be aware that stimulants may be diverted; patients at increased risk include those with comorbid substance use or mood disorders. Misuse may be especially common on college campuses, where nonprescribed stimulants may be used as study aids or recreationally.
Stimulants come in a variety of formulations that differ primarily in their time profile or mode of delivery. Some preparations (eg, Ritalin LA and Adderall XR) contain a mixture of immediate-release and extended-release mechanisms and therefore have bimodal peaks. Others (eg, Concerta) use an osmotic system to approximate a steadier flow of drug delivery. However, as these drugs have entered the generic market, time response between products is much less predictable. Individual differences in metabolism may also alter duration of action.
Continue to: Lisdexamfetamine (Vyvanse)...
Lisdexamfetamine (Vyvanse) is a pro-drug that requires first-pass metabolism for conversion to an active drug. This may reduce risk of overdose or misuse. Adverse effects of stimulants include decreased appetite, irritability, tics, and cardiac toxicity.16 Proper titration of dose over successive visits is essential as providers often must balance efficacy, appetite, and sleep.
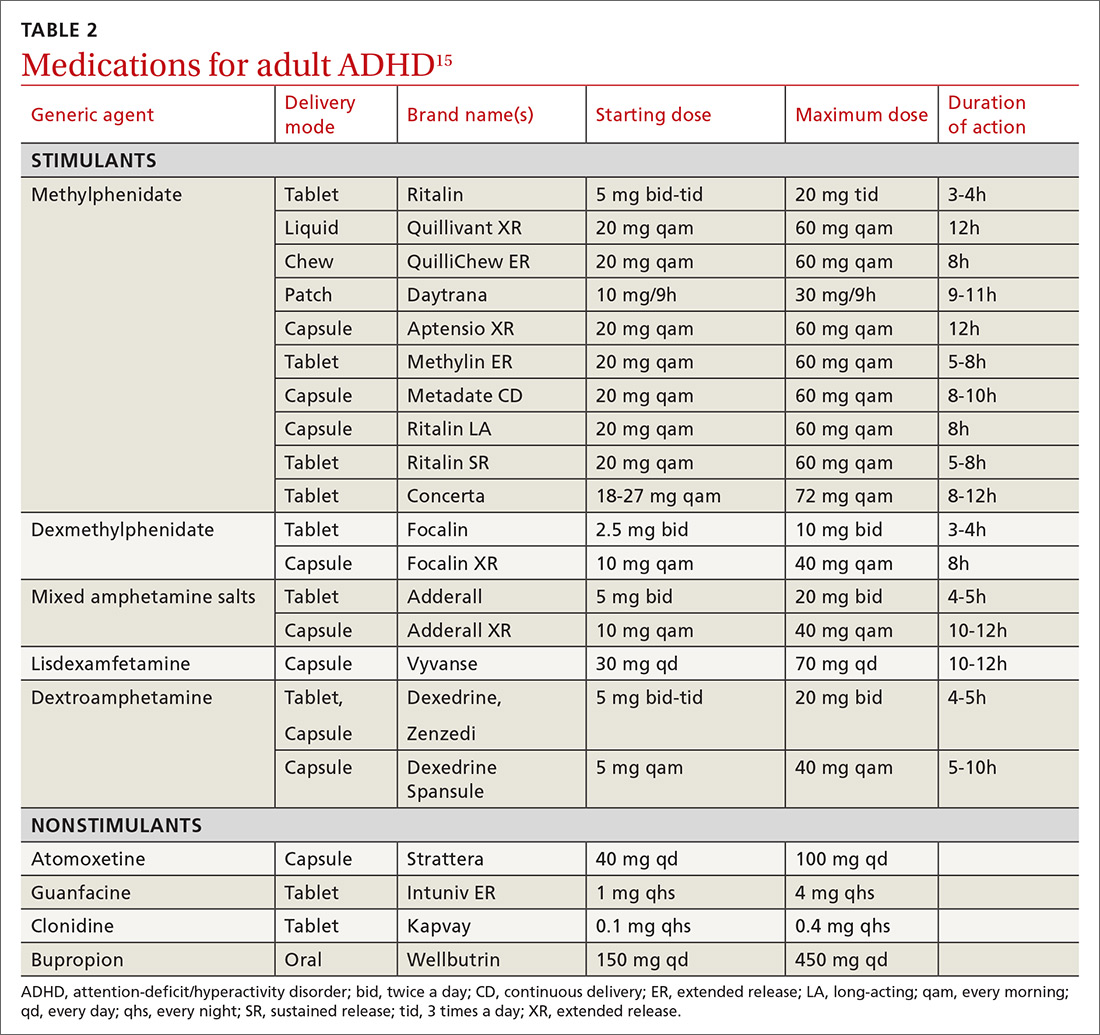
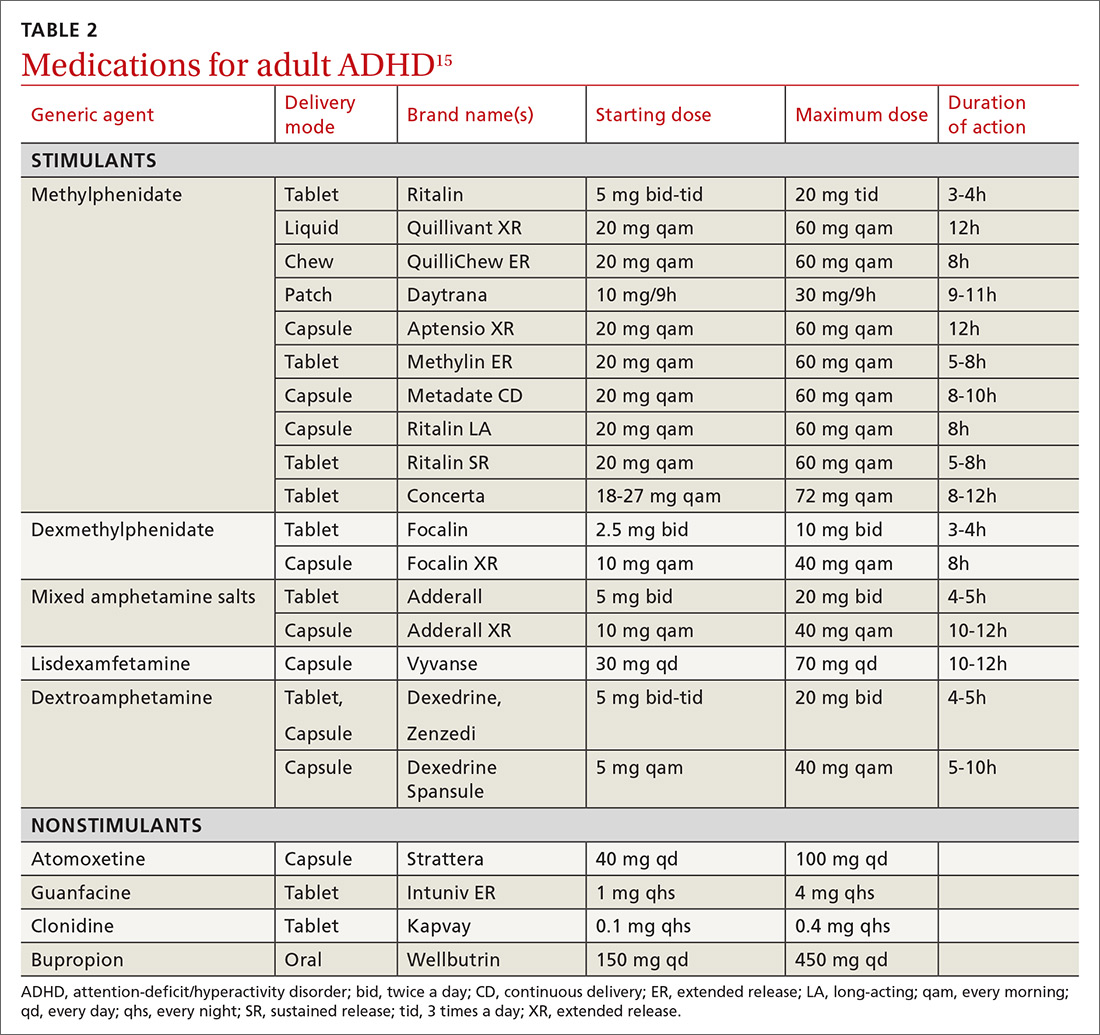
Nonstimulant therapies are options for patients who cannot tolerate stimulants or are at high risk for misuse. Atomoxetine, a norepinephrine reuptake inhibitor, has qualities that may resemble antidepressants in its 2- to 4-week time lapse before taking effect. Alpha-2 agonists clonidine and guanfacine are approved by the US Food and Drug Administration in their extended release forms for adjunct therapy with stimulants. Pharmacologic therapies are listed in TABLE 2.16
Nonpharmacologic modalities for adult ADHD include psychoeducation, cognitive behavioral therapy, and work environment modification. While coordination with schools is recognized as an essential aspect of the care of ADHD in children, team care in the treatment of adults with ADHD is often forgotten. Referral for occupational or educational support, written materials on study habits and organizational skills, and the use of memory tools can be very helpful. Modifications in physical environment and time constraints in both work and school settings can enhance productivity in adults with ADHD. Attention to sleep scheduling and sleep hygiene can also improve attention and concentration throughout the day.
CASE
She engaged with the education specialists at her school, who helped her discuss testing and assignment modifications with her professors. She began to develop a time-management strategy to complete her assignments; these included reduced evening caffeine intake and improved sleep hygiene. Over time, Ms. L was able to maintain attention for the more extended homework tasks assigned in college. She was also able to enjoy a similar level of success that she had achieved in high school.
CORRESPONDENCE
Jay Brieler, MD, Family and Community Medicine, Saint Louis University School of Medicine, 6420 Clayton Road, Room 2234, St. Louis MO 63117; jay.brieler@health.slu.edu.
1. Neurodevelopmental disorders. In: Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013:59-65.
2. Moreno-Alcázar A, Ramos-Quiroga JA, Radua J, et al. Brain abnormalities in adults with Attention Deficit Hyperactivity Disorder revealed by voxel-based morphometry. Psychiatry Res Neuroimaging. 2016;254:41-47.
3. Willcutt EG. The prevalence of DSM-IV attention-deficit/hyperactivity disorder: a meta-analytic review. Neurotherapeutics. 2012;9:490-499.
4. Fayyad J, De Graaf R, Kessler R, et al. Cross-national prevalence and correlates of adult attention-deficit hyperactivity disorder. Br J Psychiatry. 2007;190:402-409.
5. Kessler R, Adler L, Barkley R, et al. The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am J Psychiatry. 2006;163:716-723.
6. Klein RG, Mannuzza S, Olazagasti MA, et al. Clinical and functional outcome of childhood attention-deficit/hyperactivity disorder 33 years later. Arch Gen Psychiatry. 2012;69:1295-1303.
7. Asherson P, Young AH, Eich-Hochli D, et al. Differential diagnosis, comorbidity, and treatment of ADHD in relation to bipolar disorder or borderline personality disorder in adults. Curr Med Res Opin. 2014;30:1657-1672.
8. Grogan K, Gormley CI, Rooney B, et al. Differential diagnosis and co-morbidity of ADHD and anxiety in adults. Br J Clin Psychol. 2018;57:99-115.
9. Ilbegi S, Groenman AP, Schellekens A, et al. Substance use and nicotine dependence in persistent, remittent, and late-onset ADHD: a 10-year longitudinal study from childhood to young adulthood. J Neurodev Disord. 2018;10:42.
10. Attention-deficit/hyperactivity disorder. In: Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC: American Psychiatric
11. , , , et al. The World Health Organization Adult ADHD Self‐Report Scale (ASRS): a short screening scale for use in the general population. Psychol Med. 2005;35:245‐256.
12. Ustun B, Adler LA, Rudin C, et al. The World Health Organization Adult Attention-Deficit/Hyperactivity Disorder Self-Report Screening Scale for DSM-5. JAMA Psychiatry. 2017;74:520-527.
13. Ramos-Quiroga JA, Nasillo V, Richarte V, et al. Criteria and concurrent validity of DIVA 2.0: a semi-structured diagnostic interview for adult ADHD. J Atten Disord. 2019;23:1126-1135.
14. Pettersson R, Söderström S, Nilsson KW. Diagnosing ADHD in adults: an examination of the discriminative validity of neuropsychological tests and diagnostic assessment instruments. J Atten Disord. 2018;22:1019-1031.
15. Parikh AR, Baker SA. Adult ADHD: pharmacologic treatment in the DSM-5 era. Curr Psychiatry. 2016;15:18-25.
16. Searight HR, Gafford J, Evans SL. Attention Deficit Hyperactivity Disorder. In: Smith MA, Shimp LA, Schrager S, eds. Family Medicine: Ambulatory Care and Prevention. 6th ed. New York, NY: McGraw-Hill; 2014:829-846.
THE CASE
Ms. L’s family physician interviewed her and, aided by parental input, was able to identify a pattern of disorganized and impulsive behavior that was present even in grade school. Mood disorders and substance abuse were ruled out from the interview and lab testing, and cognitive ability was confirmed through a review of school testing.
●
* The patient’s name has been changed to protect her identity.
Attention-deficit/hyperactivity disorder (ADHD) is classified as a neurodevelopmental disorder in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), its hallmarks being inattentive, hyperactive, or impulsive behaviors that affect functioning or development.1 Historically, it was thought that ADHD was a disorder of children and adolescents, and that patients “grew out” of their behaviors once adulthood was reached. It is now estimated that 50% of children with ADHD will carry the diagnosis into adulthood,2 resulting in a prevalence of 5.9% to 7.1% for children3 and 3.4% for adults.4 There are 3 presentations of ADHD, known as ADHD-I (inattentive), ADHD-HI (hyperactive-impulsive), and ADHD-C (combined). The inattentive type accounts for 47% of adult cases, and adult ADHD disproportionately affects males compared with females.2
An overall pattern of underachievement and variable performance is common throughout life in patients with ADHD. Adults are much more likely to report subtle impairments in higher executive functions such as organization, time management, and modulating emotions. Consequences include poor performance at work, attendance issues, difficulty with social interactions, and an increased likelihood of unemployment.5 Among those employed, there is a large disparity in income compared with counterparts without ADHD.6 Increased risk of substance use, injury, and traffic accidents also has been reported.1
Disorders that can mimic or coexist with ADHD
The differential diagnosis for ADHD is wide, and comorbidity with other disorders is common.
Continue to: Bipolar disorder
Bipolar disorder shares with ADHD the core symptoms of hyperactivity, impulsive behavior, and difficulty completing tasks. Mania and ADHD can look very similar if symptoms are observed at a single point in time. Bipolar illness is, by definition, episodic and fluctuating, while ADHD is much more constant. In addition, bipolar illness exhibits significant variation in mood, while ADHD may or may not be associated with impaired mood regulation. Up to 20% of patients with bipolar illness also have ADHD.7
Anxiety and depressive disorders can also share symptoms with ADHD-I. These include distractibility, poor concentration, and, in the case of anxiety, rapid changes in train of thought. Sleep disturbance, past trauma, and current acute stressors may manifest as clinical anxiety or depression, or may interfere with concentration and attention independently. As with bipolar illness, clinicians must look carefully at the time course of symptoms, including the age of onset. Classically, mood disorders develop in adolescence or early adulthood, while ADHD always has manifestations in childhood. Inattention and distractibility will track with mood if they are caused by an affective illness, but will remain in ADHD even when the patient is euthymic. On the other hand, patients with ADHD frequently become frustrated or overwhelmed as a result of their difficulties with task completion and social function, a presentation which can mimic anxiety or depression.8
Substance use disorder and ADHD interact in multiple ways and can present one of the more challenging diagnostic tasks when assessing a patient with impaired attention or concentration. ADHD is a powerful risk factor for future substance use,9 while substance use can impair attention, induce impulsivity, and alter concentration. Further, the treatment of choice for ADHD (stimulant medication) has the potential for misuse. The presence of continuous symptoms across settings is crucial in determining the proper diagnosis of ADHD.
Other conditions. Patients with a learning disability can be inattentive due to their cognitive limitations, or it may be comorbid with ADHD. If an intellectual deficit is suspected, referral for cognitive testing can help clarify the diagnosis. Autism also may cause significant alterations in attention with both hyper-focus and distractibility being common, as they are in ADHD. Intermittent explosive disorder shares the core symptom of impulsivity, but includes aggression, which is not always seen in ADHD. Personality disorders (eg, borderline, narcissistic) may also be difficult to distinguish from ADHD. The key to differentiation is the identification of behavior patterns outside the realms of concentration and attention.7
KEY DIAGNOSTIC CRITERIA
The diagnostic criteria for ADHD defined in DSM-5 are found in TABLE 1.1 Individuals ≥ 17 years old must meet 5 of 9 characteristics of inattention or 5 of 9 characteristics of hyperactivity/impulsivity (criterion A).1 Some symptoms must have been present prior to age 12 (criterion B). This cutoff is an increase from age 7 advised in DSM-IV.10 Symptoms must occur across at least 2 settings (criterion C) and significantly interfere with social, academic, or occupational functioning (criterion D). Exclusions include symptoms that occur exclusively in the context of a psychotic disorder or symptoms that are better explained in the context of other mental disorders (criterion E).1
Continue to: In the primary care setting
In the primary care setting, an assessment for ADHD should, at minimum, involve a review of the patient’s academic and work history, assessment of psychiatric comorbidities and substance use history, and administration of appropriate rating scales. When evaluating adults, these tools include the Adult ADHD Self-Report Scale (ASRS)11,12 screening tool and the Diagnostic Interview for ADHD in adults (DIVA-5).13,14 If possible, obtain scale assessments not only from the patient but from family members or other observers who can provide information about the patient in childhood/adolescence and present day.
In an integrated care setting, consider involving a behavioral health consultant for a more comprehensive evaluation of educational, employment, driving, and relationship histories. Historical record review may include report cards from elementary school through high school, standardized test scores, psycho-educational and individual education plan reports, and medical records. Having a snapshot of the patient as a younger child, adolescent, and young adult can help to identify overall patterns of academic underachievement and reveal gaps between potential and overall achievement and performance. Pursue a more thorough evaluation in cases where other comorbid psychiatric disorders are present or when the patient is unfamiliar to you.
TWO GROUPS OF TREATMENT OPTIONS
The treatment of ADHD in adults (and children) can be broadly divided into pharmacologic and nonpharmacologic modalities.
Stimulants are first-line pharmacologic treatment for ADHD in patients with low risk for misuse. Stimulants improve cognitive function, decrease impulsivity, and increase alertness.15 However, these effects are not exclusive to those with ADHD, and response does not aid in diagnosis. No stimulant is preferred over another, although individuals may respond better to 1 specific agent than to others. Be aware that stimulants may be diverted; patients at increased risk include those with comorbid substance use or mood disorders. Misuse may be especially common on college campuses, where nonprescribed stimulants may be used as study aids or recreationally.
Stimulants come in a variety of formulations that differ primarily in their time profile or mode of delivery. Some preparations (eg, Ritalin LA and Adderall XR) contain a mixture of immediate-release and extended-release mechanisms and therefore have bimodal peaks. Others (eg, Concerta) use an osmotic system to approximate a steadier flow of drug delivery. However, as these drugs have entered the generic market, time response between products is much less predictable. Individual differences in metabolism may also alter duration of action.
Continue to: Lisdexamfetamine (Vyvanse)...
Lisdexamfetamine (Vyvanse) is a pro-drug that requires first-pass metabolism for conversion to an active drug. This may reduce risk of overdose or misuse. Adverse effects of stimulants include decreased appetite, irritability, tics, and cardiac toxicity.16 Proper titration of dose over successive visits is essential as providers often must balance efficacy, appetite, and sleep.
Nonstimulant therapies are options for patients who cannot tolerate stimulants or are at high risk for misuse. Atomoxetine, a norepinephrine reuptake inhibitor, has qualities that may resemble antidepressants in its 2- to 4-week time lapse before taking effect. Alpha-2 agonists clonidine and guanfacine are approved by the US Food and Drug Administration in their extended release forms for adjunct therapy with stimulants. Pharmacologic therapies are listed in TABLE 2.16
Nonpharmacologic modalities for adult ADHD include psychoeducation, cognitive behavioral therapy, and work environment modification. While coordination with schools is recognized as an essential aspect of the care of ADHD in children, team care in the treatment of adults with ADHD is often forgotten. Referral for occupational or educational support, written materials on study habits and organizational skills, and the use of memory tools can be very helpful. Modifications in physical environment and time constraints in both work and school settings can enhance productivity in adults with ADHD. Attention to sleep scheduling and sleep hygiene can also improve attention and concentration throughout the day.
CASE
She engaged with the education specialists at her school, who helped her discuss testing and assignment modifications with her professors. She began to develop a time-management strategy to complete her assignments; these included reduced evening caffeine intake and improved sleep hygiene. Over time, Ms. L was able to maintain attention for the more extended homework tasks assigned in college. She was also able to enjoy a similar level of success that she had achieved in high school.
CORRESPONDENCE
Jay Brieler, MD, Family and Community Medicine, Saint Louis University School of Medicine, 6420 Clayton Road, Room 2234, St. Louis MO 63117; jay.brieler@health.slu.edu.
THE CASE
Ms. L’s family physician interviewed her and, aided by parental input, was able to identify a pattern of disorganized and impulsive behavior that was present even in grade school. Mood disorders and substance abuse were ruled out from the interview and lab testing, and cognitive ability was confirmed through a review of school testing.
●
* The patient’s name has been changed to protect her identity.
Attention-deficit/hyperactivity disorder (ADHD) is classified as a neurodevelopmental disorder in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), its hallmarks being inattentive, hyperactive, or impulsive behaviors that affect functioning or development.1 Historically, it was thought that ADHD was a disorder of children and adolescents, and that patients “grew out” of their behaviors once adulthood was reached. It is now estimated that 50% of children with ADHD will carry the diagnosis into adulthood,2 resulting in a prevalence of 5.9% to 7.1% for children3 and 3.4% for adults.4 There are 3 presentations of ADHD, known as ADHD-I (inattentive), ADHD-HI (hyperactive-impulsive), and ADHD-C (combined). The inattentive type accounts for 47% of adult cases, and adult ADHD disproportionately affects males compared with females.2
An overall pattern of underachievement and variable performance is common throughout life in patients with ADHD. Adults are much more likely to report subtle impairments in higher executive functions such as organization, time management, and modulating emotions. Consequences include poor performance at work, attendance issues, difficulty with social interactions, and an increased likelihood of unemployment.5 Among those employed, there is a large disparity in income compared with counterparts without ADHD.6 Increased risk of substance use, injury, and traffic accidents also has been reported.1
Disorders that can mimic or coexist with ADHD
The differential diagnosis for ADHD is wide, and comorbidity with other disorders is common.
Continue to: Bipolar disorder
Bipolar disorder shares with ADHD the core symptoms of hyperactivity, impulsive behavior, and difficulty completing tasks. Mania and ADHD can look very similar if symptoms are observed at a single point in time. Bipolar illness is, by definition, episodic and fluctuating, while ADHD is much more constant. In addition, bipolar illness exhibits significant variation in mood, while ADHD may or may not be associated with impaired mood regulation. Up to 20% of patients with bipolar illness also have ADHD.7
Anxiety and depressive disorders can also share symptoms with ADHD-I. These include distractibility, poor concentration, and, in the case of anxiety, rapid changes in train of thought. Sleep disturbance, past trauma, and current acute stressors may manifest as clinical anxiety or depression, or may interfere with concentration and attention independently. As with bipolar illness, clinicians must look carefully at the time course of symptoms, including the age of onset. Classically, mood disorders develop in adolescence or early adulthood, while ADHD always has manifestations in childhood. Inattention and distractibility will track with mood if they are caused by an affective illness, but will remain in ADHD even when the patient is euthymic. On the other hand, patients with ADHD frequently become frustrated or overwhelmed as a result of their difficulties with task completion and social function, a presentation which can mimic anxiety or depression.8
Substance use disorder and ADHD interact in multiple ways and can present one of the more challenging diagnostic tasks when assessing a patient with impaired attention or concentration. ADHD is a powerful risk factor for future substance use,9 while substance use can impair attention, induce impulsivity, and alter concentration. Further, the treatment of choice for ADHD (stimulant medication) has the potential for misuse. The presence of continuous symptoms across settings is crucial in determining the proper diagnosis of ADHD.
Other conditions. Patients with a learning disability can be inattentive due to their cognitive limitations, or it may be comorbid with ADHD. If an intellectual deficit is suspected, referral for cognitive testing can help clarify the diagnosis. Autism also may cause significant alterations in attention with both hyper-focus and distractibility being common, as they are in ADHD. Intermittent explosive disorder shares the core symptom of impulsivity, but includes aggression, which is not always seen in ADHD. Personality disorders (eg, borderline, narcissistic) may also be difficult to distinguish from ADHD. The key to differentiation is the identification of behavior patterns outside the realms of concentration and attention.7
KEY DIAGNOSTIC CRITERIA
The diagnostic criteria for ADHD defined in DSM-5 are found in TABLE 1.1 Individuals ≥ 17 years old must meet 5 of 9 characteristics of inattention or 5 of 9 characteristics of hyperactivity/impulsivity (criterion A).1 Some symptoms must have been present prior to age 12 (criterion B). This cutoff is an increase from age 7 advised in DSM-IV.10 Symptoms must occur across at least 2 settings (criterion C) and significantly interfere with social, academic, or occupational functioning (criterion D). Exclusions include symptoms that occur exclusively in the context of a psychotic disorder or symptoms that are better explained in the context of other mental disorders (criterion E).1
Continue to: In the primary care setting
In the primary care setting, an assessment for ADHD should, at minimum, involve a review of the patient’s academic and work history, assessment of psychiatric comorbidities and substance use history, and administration of appropriate rating scales. When evaluating adults, these tools include the Adult ADHD Self-Report Scale (ASRS)11,12 screening tool and the Diagnostic Interview for ADHD in adults (DIVA-5).13,14 If possible, obtain scale assessments not only from the patient but from family members or other observers who can provide information about the patient in childhood/adolescence and present day.
In an integrated care setting, consider involving a behavioral health consultant for a more comprehensive evaluation of educational, employment, driving, and relationship histories. Historical record review may include report cards from elementary school through high school, standardized test scores, psycho-educational and individual education plan reports, and medical records. Having a snapshot of the patient as a younger child, adolescent, and young adult can help to identify overall patterns of academic underachievement and reveal gaps between potential and overall achievement and performance. Pursue a more thorough evaluation in cases where other comorbid psychiatric disorders are present or when the patient is unfamiliar to you.
TWO GROUPS OF TREATMENT OPTIONS
The treatment of ADHD in adults (and children) can be broadly divided into pharmacologic and nonpharmacologic modalities.
Stimulants are first-line pharmacologic treatment for ADHD in patients with low risk for misuse. Stimulants improve cognitive function, decrease impulsivity, and increase alertness.15 However, these effects are not exclusive to those with ADHD, and response does not aid in diagnosis. No stimulant is preferred over another, although individuals may respond better to 1 specific agent than to others. Be aware that stimulants may be diverted; patients at increased risk include those with comorbid substance use or mood disorders. Misuse may be especially common on college campuses, where nonprescribed stimulants may be used as study aids or recreationally.
Stimulants come in a variety of formulations that differ primarily in their time profile or mode of delivery. Some preparations (eg, Ritalin LA and Adderall XR) contain a mixture of immediate-release and extended-release mechanisms and therefore have bimodal peaks. Others (eg, Concerta) use an osmotic system to approximate a steadier flow of drug delivery. However, as these drugs have entered the generic market, time response between products is much less predictable. Individual differences in metabolism may also alter duration of action.
Continue to: Lisdexamfetamine (Vyvanse)...
Lisdexamfetamine (Vyvanse) is a pro-drug that requires first-pass metabolism for conversion to an active drug. This may reduce risk of overdose or misuse. Adverse effects of stimulants include decreased appetite, irritability, tics, and cardiac toxicity.16 Proper titration of dose over successive visits is essential as providers often must balance efficacy, appetite, and sleep.
Nonstimulant therapies are options for patients who cannot tolerate stimulants or are at high risk for misuse. Atomoxetine, a norepinephrine reuptake inhibitor, has qualities that may resemble antidepressants in its 2- to 4-week time lapse before taking effect. Alpha-2 agonists clonidine and guanfacine are approved by the US Food and Drug Administration in their extended release forms for adjunct therapy with stimulants. Pharmacologic therapies are listed in TABLE 2.16
Nonpharmacologic modalities for adult ADHD include psychoeducation, cognitive behavioral therapy, and work environment modification. While coordination with schools is recognized as an essential aspect of the care of ADHD in children, team care in the treatment of adults with ADHD is often forgotten. Referral for occupational or educational support, written materials on study habits and organizational skills, and the use of memory tools can be very helpful. Modifications in physical environment and time constraints in both work and school settings can enhance productivity in adults with ADHD. Attention to sleep scheduling and sleep hygiene can also improve attention and concentration throughout the day.
CASE
She engaged with the education specialists at her school, who helped her discuss testing and assignment modifications with her professors. She began to develop a time-management strategy to complete her assignments; these included reduced evening caffeine intake and improved sleep hygiene. Over time, Ms. L was able to maintain attention for the more extended homework tasks assigned in college. She was also able to enjoy a similar level of success that she had achieved in high school.
CORRESPONDENCE
Jay Brieler, MD, Family and Community Medicine, Saint Louis University School of Medicine, 6420 Clayton Road, Room 2234, St. Louis MO 63117; jay.brieler@health.slu.edu.
1. Neurodevelopmental disorders. In: Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013:59-65.
2. Moreno-Alcázar A, Ramos-Quiroga JA, Radua J, et al. Brain abnormalities in adults with Attention Deficit Hyperactivity Disorder revealed by voxel-based morphometry. Psychiatry Res Neuroimaging. 2016;254:41-47.
3. Willcutt EG. The prevalence of DSM-IV attention-deficit/hyperactivity disorder: a meta-analytic review. Neurotherapeutics. 2012;9:490-499.
4. Fayyad J, De Graaf R, Kessler R, et al. Cross-national prevalence and correlates of adult attention-deficit hyperactivity disorder. Br J Psychiatry. 2007;190:402-409.
5. Kessler R, Adler L, Barkley R, et al. The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am J Psychiatry. 2006;163:716-723.
6. Klein RG, Mannuzza S, Olazagasti MA, et al. Clinical and functional outcome of childhood attention-deficit/hyperactivity disorder 33 years later. Arch Gen Psychiatry. 2012;69:1295-1303.
7. Asherson P, Young AH, Eich-Hochli D, et al. Differential diagnosis, comorbidity, and treatment of ADHD in relation to bipolar disorder or borderline personality disorder in adults. Curr Med Res Opin. 2014;30:1657-1672.
8. Grogan K, Gormley CI, Rooney B, et al. Differential diagnosis and co-morbidity of ADHD and anxiety in adults. Br J Clin Psychol. 2018;57:99-115.
9. Ilbegi S, Groenman AP, Schellekens A, et al. Substance use and nicotine dependence in persistent, remittent, and late-onset ADHD: a 10-year longitudinal study from childhood to young adulthood. J Neurodev Disord. 2018;10:42.
10. Attention-deficit/hyperactivity disorder. In: Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC: American Psychiatric
11. , , , et al. The World Health Organization Adult ADHD Self‐Report Scale (ASRS): a short screening scale for use in the general population. Psychol Med. 2005;35:245‐256.
12. Ustun B, Adler LA, Rudin C, et al. The World Health Organization Adult Attention-Deficit/Hyperactivity Disorder Self-Report Screening Scale for DSM-5. JAMA Psychiatry. 2017;74:520-527.
13. Ramos-Quiroga JA, Nasillo V, Richarte V, et al. Criteria and concurrent validity of DIVA 2.0: a semi-structured diagnostic interview for adult ADHD. J Atten Disord. 2019;23:1126-1135.
14. Pettersson R, Söderström S, Nilsson KW. Diagnosing ADHD in adults: an examination of the discriminative validity of neuropsychological tests and diagnostic assessment instruments. J Atten Disord. 2018;22:1019-1031.
15. Parikh AR, Baker SA. Adult ADHD: pharmacologic treatment in the DSM-5 era. Curr Psychiatry. 2016;15:18-25.
16. Searight HR, Gafford J, Evans SL. Attention Deficit Hyperactivity Disorder. In: Smith MA, Shimp LA, Schrager S, eds. Family Medicine: Ambulatory Care and Prevention. 6th ed. New York, NY: McGraw-Hill; 2014:829-846.
1. Neurodevelopmental disorders. In: Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013:59-65.
2. Moreno-Alcázar A, Ramos-Quiroga JA, Radua J, et al. Brain abnormalities in adults with Attention Deficit Hyperactivity Disorder revealed by voxel-based morphometry. Psychiatry Res Neuroimaging. 2016;254:41-47.
3. Willcutt EG. The prevalence of DSM-IV attention-deficit/hyperactivity disorder: a meta-analytic review. Neurotherapeutics. 2012;9:490-499.
4. Fayyad J, De Graaf R, Kessler R, et al. Cross-national prevalence and correlates of adult attention-deficit hyperactivity disorder. Br J Psychiatry. 2007;190:402-409.
5. Kessler R, Adler L, Barkley R, et al. The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am J Psychiatry. 2006;163:716-723.
6. Klein RG, Mannuzza S, Olazagasti MA, et al. Clinical and functional outcome of childhood attention-deficit/hyperactivity disorder 33 years later. Arch Gen Psychiatry. 2012;69:1295-1303.
7. Asherson P, Young AH, Eich-Hochli D, et al. Differential diagnosis, comorbidity, and treatment of ADHD in relation to bipolar disorder or borderline personality disorder in adults. Curr Med Res Opin. 2014;30:1657-1672.
8. Grogan K, Gormley CI, Rooney B, et al. Differential diagnosis and co-morbidity of ADHD and anxiety in adults. Br J Clin Psychol. 2018;57:99-115.
9. Ilbegi S, Groenman AP, Schellekens A, et al. Substance use and nicotine dependence in persistent, remittent, and late-onset ADHD: a 10-year longitudinal study from childhood to young adulthood. J Neurodev Disord. 2018;10:42.
10. Attention-deficit/hyperactivity disorder. In: Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC: American Psychiatric
11. , , , et al. The World Health Organization Adult ADHD Self‐Report Scale (ASRS): a short screening scale for use in the general population. Psychol Med. 2005;35:245‐256.
12. Ustun B, Adler LA, Rudin C, et al. The World Health Organization Adult Attention-Deficit/Hyperactivity Disorder Self-Report Screening Scale for DSM-5. JAMA Psychiatry. 2017;74:520-527.
13. Ramos-Quiroga JA, Nasillo V, Richarte V, et al. Criteria and concurrent validity of DIVA 2.0: a semi-structured diagnostic interview for adult ADHD. J Atten Disord. 2019;23:1126-1135.
14. Pettersson R, Söderström S, Nilsson KW. Diagnosing ADHD in adults: an examination of the discriminative validity of neuropsychological tests and diagnostic assessment instruments. J Atten Disord. 2018;22:1019-1031.
15. Parikh AR, Baker SA. Adult ADHD: pharmacologic treatment in the DSM-5 era. Curr Psychiatry. 2016;15:18-25.
16. Searight HR, Gafford J, Evans SL. Attention Deficit Hyperactivity Disorder. In: Smith MA, Shimp LA, Schrager S, eds. Family Medicine: Ambulatory Care and Prevention. 6th ed. New York, NY: McGraw-Hill; 2014:829-846.