User login
Editor’s note on 50th Anniversary series
While this is the last piece in a series, my intention is for it to read more like the opening of a new book on family medicine, rather than an ending to a story about the specialty.
April Lockley, DO, represents a new generation of family physicians who began their careers in the 21st century, and she is hopeful that the experiences of practicing family medicine and being the patient of a family physician will change in several ways.
Among her desires for the future, is to be able to write a prescription for a medication or physical therapy to a patient who is able “to fill the prescription without having to worry about the financial implications of paying for it,” she writes. She also hopes “patients can seek out care without the fear of discrimination or racism through an increasingly diverse work force.”
In her article, Dr. Lockley both expresses how she wants family medicine to change and what she already finds satisfying about being a family physician.
I hope you enjoyed reading about the professional journeys of Dr. Lockley and other family physicians who have written commentaries or interviewed for articles in Family Practice News’ 50th Anniversary series this year.
To revisit any of these articles, go to the 50th Anniversary bucket on mdedge.com/familymedicine.
Thank you for continuing to read Family Practice News, and I hope to celebrate more milestones with you in the future.
klennon@mdedge.com
While this is the last piece in a series, my intention is for it to read more like the opening of a new book on family medicine, rather than an ending to a story about the specialty.
April Lockley, DO, represents a new generation of family physicians who began their careers in the 21st century, and she is hopeful that the experiences of practicing family medicine and being the patient of a family physician will change in several ways.
Among her desires for the future, is to be able to write a prescription for a medication or physical therapy to a patient who is able “to fill the prescription without having to worry about the financial implications of paying for it,” she writes. She also hopes “patients can seek out care without the fear of discrimination or racism through an increasingly diverse work force.”
In her article, Dr. Lockley both expresses how she wants family medicine to change and what she already finds satisfying about being a family physician.
I hope you enjoyed reading about the professional journeys of Dr. Lockley and other family physicians who have written commentaries or interviewed for articles in Family Practice News’ 50th Anniversary series this year.
To revisit any of these articles, go to the 50th Anniversary bucket on mdedge.com/familymedicine.
Thank you for continuing to read Family Practice News, and I hope to celebrate more milestones with you in the future.
klennon@mdedge.com
While this is the last piece in a series, my intention is for it to read more like the opening of a new book on family medicine, rather than an ending to a story about the specialty.
April Lockley, DO, represents a new generation of family physicians who began their careers in the 21st century, and she is hopeful that the experiences of practicing family medicine and being the patient of a family physician will change in several ways.
Among her desires for the future, is to be able to write a prescription for a medication or physical therapy to a patient who is able “to fill the prescription without having to worry about the financial implications of paying for it,” she writes. She also hopes “patients can seek out care without the fear of discrimination or racism through an increasingly diverse work force.”
In her article, Dr. Lockley both expresses how she wants family medicine to change and what she already finds satisfying about being a family physician.
I hope you enjoyed reading about the professional journeys of Dr. Lockley and other family physicians who have written commentaries or interviewed for articles in Family Practice News’ 50th Anniversary series this year.
To revisit any of these articles, go to the 50th Anniversary bucket on mdedge.com/familymedicine.
Thank you for continuing to read Family Practice News, and I hope to celebrate more milestones with you in the future.
klennon@mdedge.com
Early-in-career family physician shares hopes for future of specialty
I became interested in becoming a physician during my very last semester of college. I volunteered in a hospital psychiatric department in the unit that provided electroconvulsive therapy to patients with severe mental health diagnoses. Although this was about 15 years ago, I still vividly remember the curiosity I had walking around the hospital looking around at all the doctors and nurses and wanting to understand what their day-to-day life was like helping people to optimize their health.
Up until that time, thankfully my family and I had been relatively healthy, and, outside of routine checkups, my time spent in a hospital or clinic was limited. Therefore, those months of volunteering at the hospital were the longest periods of time I’d spent around physicians and other health care professionals really witnessing firsthand the science and the art of medicine.
During my time volunteering I saw one patient over the course of several weeks who was catatonic when I first met her, but by the end of several electroconvulsive therapy treatments she had a subtle smile on her face and we were able to have a conversation. She was a younger Black woman like myself and at that moment I knew that I wanted to become a physician and be involved in people’s lives in such a unique manner.
I worked for several years before applying to medical school. During that time two of my jobs involved doing home visits with children, young adults, and their families. I once again experienced the connection that one can make with someone and their family over a short period of time when you actively listen, understand what is important to them, and work together.
After several years of this work I got accepted into medical school and excitedly started the path to becoming a physician. While the learning curve was difficult, I genuinely enjoyed every block of medical school, including learning the anatomy, pathophysiology, and pharmacology. I could not wait to be in front of patients to use this newfound knowledge to help solve their health problems.
‘There is no such thing as a single issue-struggle’
As I started the third year of medical school and clinical rotations, I found joy in being in hospitals and clinics. I also came to recognize that understanding the pharmacology of why metformin helps improve the hemoglobin A1c in people with diabetes is not necessarily one of the keys to helping people optimize their health. I started to talk with patients and all sorts of questions would come to mind. Where did they grow up? What did they identify as their culture? What did they do in their day to day? Did they have a home and support at that home? Are they someone’s caretaker? What are their hopes for the future? And the list goes on.
I ultimately chose family medicine as a specialty because, as Audre Lorde said, “there is no such thing as a single-issue struggle because we do not live single-issue lives,” and family medicine allows one to look at the intersections of people’s lives and how they affect their health and well-being.
I currently practice as a family medicine physician in a setting in which I provide a lot of sexual and reproductive health care. I welcome patients of all ages and genders, and this care includes preconception counseling, contraceptive counseling, prenatal and postpartum care, STI testing and treatment, abortion care, and routine preventive care – just to name a few.
I decided to specialize in sexual and reproductive health care within family medicine because of the historic discrimination and inequitable treatment that is often experienced by young Black persons when they seek care for their sexual health and/or reproductive choices. In addition, there is often stigma within communities when it comes to talking about sex, bodies, and pleasure.
Recently, after a few minutes with a patient, she shared with me that she just completed nursing school and was studying for her exams. We talked about what type of jobs she was looking to apply for and where she wanted to work. I expressed to her that I was proud of the hard work she put in to complete nursing school and commiserated with her about the challenges in schooling and studying that it takes to start in the health care field. The conversation eventually found its way to talking about her sexual and reproductive health care. She shared with me that she was interested in having a child; however, at this time she put those plans on hold because she was scared about the racism within health care and the unacceptable high rates of maternal mortality among Black women in this country.
I listened and shared that as someone who also identifies as a Black woman, I have similar fears and anxieties surrounding my own reproductive health future. During the visit with this patient, I used my training in family medicine to better understand her physical and mental health needs and reassured her that I was going to partner with her through her health care journey.
Hope for the future of family medicine
As I work on a day-to-day basis I often think about my hopes for patients, as well as my hopes for medicine and the field of family medicine. My hope for the future of family medicine is that we can continue to make meaningful connections with patients to help them optimize their health and well-being.
I imagine a system in which we have the time and support to do this for all of our patients regardless of their immigration status, socioeconomic status, or any other historically excluded status. My hope for the future of family medicine is that I can write a prescription for a medication or physical therapy, and the patient is able to fill the prescription without having to worry about the financial implications of paying for it. My hope for the future of family medicine is that patients can seek out care without the fear of discrimination or racism through an increasingly diverse work force. My hope for the future of family medicine is that these improvements become a reality and that as physicians we can appreciate the connections we make with patients and the impact this has on their overall health and well-being.
Dr. Lockley is a family medicine physician currently living in Harlem, N.Y., and a member of the editorial advisory board of Family Practice News. She currently works for Public Health Solutions’ Sexual and Reproductive Health Centers in Brooklyn, providing primary care and reproductive health care services there, and as an abortion provider throughout the New York region. She completed both medical school and residency in Philadelphia and then did a fellowship in reproductive health care and advocacy through the Family Health Center of Harlem and the Reproductive Health Access Project. She can be reached at fpnews@mdedge.com.
I became interested in becoming a physician during my very last semester of college. I volunteered in a hospital psychiatric department in the unit that provided electroconvulsive therapy to patients with severe mental health diagnoses. Although this was about 15 years ago, I still vividly remember the curiosity I had walking around the hospital looking around at all the doctors and nurses and wanting to understand what their day-to-day life was like helping people to optimize their health.
Up until that time, thankfully my family and I had been relatively healthy, and, outside of routine checkups, my time spent in a hospital or clinic was limited. Therefore, those months of volunteering at the hospital were the longest periods of time I’d spent around physicians and other health care professionals really witnessing firsthand the science and the art of medicine.
During my time volunteering I saw one patient over the course of several weeks who was catatonic when I first met her, but by the end of several electroconvulsive therapy treatments she had a subtle smile on her face and we were able to have a conversation. She was a younger Black woman like myself and at that moment I knew that I wanted to become a physician and be involved in people’s lives in such a unique manner.
I worked for several years before applying to medical school. During that time two of my jobs involved doing home visits with children, young adults, and their families. I once again experienced the connection that one can make with someone and their family over a short period of time when you actively listen, understand what is important to them, and work together.
After several years of this work I got accepted into medical school and excitedly started the path to becoming a physician. While the learning curve was difficult, I genuinely enjoyed every block of medical school, including learning the anatomy, pathophysiology, and pharmacology. I could not wait to be in front of patients to use this newfound knowledge to help solve their health problems.
‘There is no such thing as a single issue-struggle’
As I started the third year of medical school and clinical rotations, I found joy in being in hospitals and clinics. I also came to recognize that understanding the pharmacology of why metformin helps improve the hemoglobin A1c in people with diabetes is not necessarily one of the keys to helping people optimize their health. I started to talk with patients and all sorts of questions would come to mind. Where did they grow up? What did they identify as their culture? What did they do in their day to day? Did they have a home and support at that home? Are they someone’s caretaker? What are their hopes for the future? And the list goes on.
I ultimately chose family medicine as a specialty because, as Audre Lorde said, “there is no such thing as a single-issue struggle because we do not live single-issue lives,” and family medicine allows one to look at the intersections of people’s lives and how they affect their health and well-being.
I currently practice as a family medicine physician in a setting in which I provide a lot of sexual and reproductive health care. I welcome patients of all ages and genders, and this care includes preconception counseling, contraceptive counseling, prenatal and postpartum care, STI testing and treatment, abortion care, and routine preventive care – just to name a few.
I decided to specialize in sexual and reproductive health care within family medicine because of the historic discrimination and inequitable treatment that is often experienced by young Black persons when they seek care for their sexual health and/or reproductive choices. In addition, there is often stigma within communities when it comes to talking about sex, bodies, and pleasure.
Recently, after a few minutes with a patient, she shared with me that she just completed nursing school and was studying for her exams. We talked about what type of jobs she was looking to apply for and where she wanted to work. I expressed to her that I was proud of the hard work she put in to complete nursing school and commiserated with her about the challenges in schooling and studying that it takes to start in the health care field. The conversation eventually found its way to talking about her sexual and reproductive health care. She shared with me that she was interested in having a child; however, at this time she put those plans on hold because she was scared about the racism within health care and the unacceptable high rates of maternal mortality among Black women in this country.
I listened and shared that as someone who also identifies as a Black woman, I have similar fears and anxieties surrounding my own reproductive health future. During the visit with this patient, I used my training in family medicine to better understand her physical and mental health needs and reassured her that I was going to partner with her through her health care journey.
Hope for the future of family medicine
As I work on a day-to-day basis I often think about my hopes for patients, as well as my hopes for medicine and the field of family medicine. My hope for the future of family medicine is that we can continue to make meaningful connections with patients to help them optimize their health and well-being.
I imagine a system in which we have the time and support to do this for all of our patients regardless of their immigration status, socioeconomic status, or any other historically excluded status. My hope for the future of family medicine is that I can write a prescription for a medication or physical therapy, and the patient is able to fill the prescription without having to worry about the financial implications of paying for it. My hope for the future of family medicine is that patients can seek out care without the fear of discrimination or racism through an increasingly diverse work force. My hope for the future of family medicine is that these improvements become a reality and that as physicians we can appreciate the connections we make with patients and the impact this has on their overall health and well-being.
Dr. Lockley is a family medicine physician currently living in Harlem, N.Y., and a member of the editorial advisory board of Family Practice News. She currently works for Public Health Solutions’ Sexual and Reproductive Health Centers in Brooklyn, providing primary care and reproductive health care services there, and as an abortion provider throughout the New York region. She completed both medical school and residency in Philadelphia and then did a fellowship in reproductive health care and advocacy through the Family Health Center of Harlem and the Reproductive Health Access Project. She can be reached at fpnews@mdedge.com.
I became interested in becoming a physician during my very last semester of college. I volunteered in a hospital psychiatric department in the unit that provided electroconvulsive therapy to patients with severe mental health diagnoses. Although this was about 15 years ago, I still vividly remember the curiosity I had walking around the hospital looking around at all the doctors and nurses and wanting to understand what their day-to-day life was like helping people to optimize their health.
Up until that time, thankfully my family and I had been relatively healthy, and, outside of routine checkups, my time spent in a hospital or clinic was limited. Therefore, those months of volunteering at the hospital were the longest periods of time I’d spent around physicians and other health care professionals really witnessing firsthand the science and the art of medicine.
During my time volunteering I saw one patient over the course of several weeks who was catatonic when I first met her, but by the end of several electroconvulsive therapy treatments she had a subtle smile on her face and we were able to have a conversation. She was a younger Black woman like myself and at that moment I knew that I wanted to become a physician and be involved in people’s lives in such a unique manner.
I worked for several years before applying to medical school. During that time two of my jobs involved doing home visits with children, young adults, and their families. I once again experienced the connection that one can make with someone and their family over a short period of time when you actively listen, understand what is important to them, and work together.
After several years of this work I got accepted into medical school and excitedly started the path to becoming a physician. While the learning curve was difficult, I genuinely enjoyed every block of medical school, including learning the anatomy, pathophysiology, and pharmacology. I could not wait to be in front of patients to use this newfound knowledge to help solve their health problems.
‘There is no such thing as a single issue-struggle’
As I started the third year of medical school and clinical rotations, I found joy in being in hospitals and clinics. I also came to recognize that understanding the pharmacology of why metformin helps improve the hemoglobin A1c in people with diabetes is not necessarily one of the keys to helping people optimize their health. I started to talk with patients and all sorts of questions would come to mind. Where did they grow up? What did they identify as their culture? What did they do in their day to day? Did they have a home and support at that home? Are they someone’s caretaker? What are their hopes for the future? And the list goes on.
I ultimately chose family medicine as a specialty because, as Audre Lorde said, “there is no such thing as a single-issue struggle because we do not live single-issue lives,” and family medicine allows one to look at the intersections of people’s lives and how they affect their health and well-being.
I currently practice as a family medicine physician in a setting in which I provide a lot of sexual and reproductive health care. I welcome patients of all ages and genders, and this care includes preconception counseling, contraceptive counseling, prenatal and postpartum care, STI testing and treatment, abortion care, and routine preventive care – just to name a few.
I decided to specialize in sexual and reproductive health care within family medicine because of the historic discrimination and inequitable treatment that is often experienced by young Black persons when they seek care for their sexual health and/or reproductive choices. In addition, there is often stigma within communities when it comes to talking about sex, bodies, and pleasure.
Recently, after a few minutes with a patient, she shared with me that she just completed nursing school and was studying for her exams. We talked about what type of jobs she was looking to apply for and where she wanted to work. I expressed to her that I was proud of the hard work she put in to complete nursing school and commiserated with her about the challenges in schooling and studying that it takes to start in the health care field. The conversation eventually found its way to talking about her sexual and reproductive health care. She shared with me that she was interested in having a child; however, at this time she put those plans on hold because she was scared about the racism within health care and the unacceptable high rates of maternal mortality among Black women in this country.
I listened and shared that as someone who also identifies as a Black woman, I have similar fears and anxieties surrounding my own reproductive health future. During the visit with this patient, I used my training in family medicine to better understand her physical and mental health needs and reassured her that I was going to partner with her through her health care journey.
Hope for the future of family medicine
As I work on a day-to-day basis I often think about my hopes for patients, as well as my hopes for medicine and the field of family medicine. My hope for the future of family medicine is that we can continue to make meaningful connections with patients to help them optimize their health and well-being.
I imagine a system in which we have the time and support to do this for all of our patients regardless of their immigration status, socioeconomic status, or any other historically excluded status. My hope for the future of family medicine is that I can write a prescription for a medication or physical therapy, and the patient is able to fill the prescription without having to worry about the financial implications of paying for it. My hope for the future of family medicine is that patients can seek out care without the fear of discrimination or racism through an increasingly diverse work force. My hope for the future of family medicine is that these improvements become a reality and that as physicians we can appreciate the connections we make with patients and the impact this has on their overall health and well-being.
Dr. Lockley is a family medicine physician currently living in Harlem, N.Y., and a member of the editorial advisory board of Family Practice News. She currently works for Public Health Solutions’ Sexual and Reproductive Health Centers in Brooklyn, providing primary care and reproductive health care services there, and as an abortion provider throughout the New York region. She completed both medical school and residency in Philadelphia and then did a fellowship in reproductive health care and advocacy through the Family Health Center of Harlem and the Reproductive Health Access Project. She can be reached at fpnews@mdedge.com.
‘Residents’ Viewpoint’ revisited
We are currently republishing an installment of this column as part of our continuing celebration of Family Practice News’s 50th anniversary.
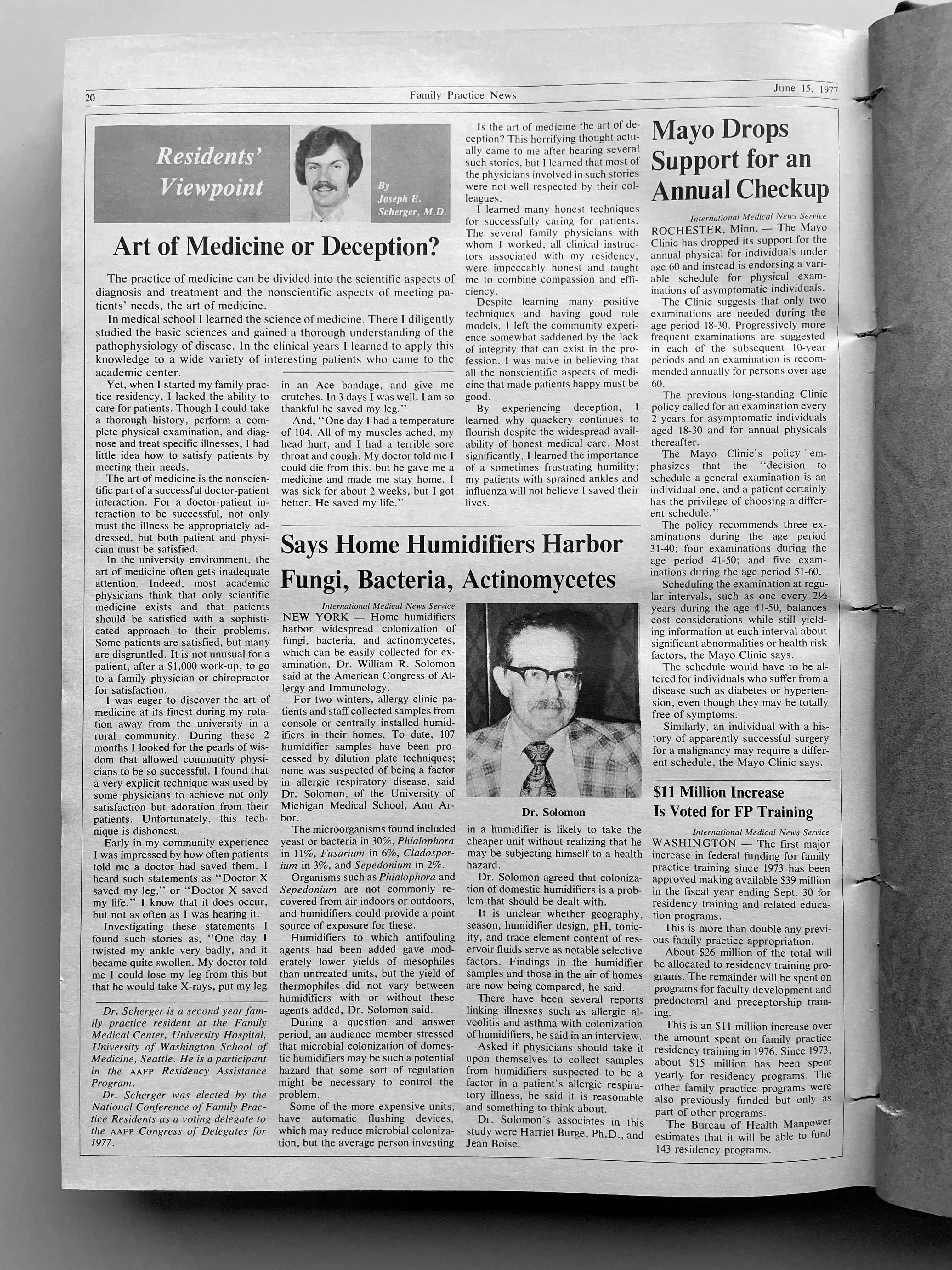
Bruce A. Bagley, MD, wrote the first batch of these columns, when he was chief resident in family medicine at St. Joseph’s Hospital, Syracuse, N.Y. Joseph E. Scherger, MD, was the second writer for Family Practice News’s monthly “Residents’ Viewpoint.” At the time Dr. Scherger became a columnist, he was a 26-year-old, 2nd-year family practice resident at the Family Medical Center, University Hospital, University of Washington, Seattle.
Dr. Scherger’s first column was published on Feb. 5, 1977. We are republishing his “Residents’ Viewpoint” from June 15, 1977 (see below) and a new column by Victoria Persampiere, DO, who is currently a 2nd-year resident in the family medicine program at Abington Jefferson Health. (See “My experience as a family medicine resident in 2021” after Dr. Scherger’s column.).
We hope you will enjoy comparing and contrasting the experiences of a resident practicing family medicine today to those of a resident practicing family medicine nearly 4½ decades ago.To learn about Dr. Scherger’s current practice and long career, you can read his profile on the cover of the September 2021 issue of Family Practice News or on MDedge.com/FamilyMedicine in our “Family Practice News 50th Anniversary” section.
Art of medicine or deception?
Originally published in Family Practice News on June 15, 1977.
In medical school I learned the science of medicine. There I diligently studied the basic sciences and gained a thorough understanding of the pathophysiology of disease. In the clinical years I learned to apply this knowledge to a wide variety of interesting patients who came to the academic center.
Yet, when I started my family practice residency, I lacked the ability to care for patients. Though I could take a thorough history, perform a complete physical examination, and diagnose and treat specific illnesses, I had little idea how to satisfy patients by meeting their needs.
The art of medicine is the nonscientific part of a successful doctor-patient interaction. For a doctor-patient interaction to be successful, not only must the illness be appropriately addressed, but both patient and physician must be satisfied.
In the university environment, the art of medicine often gets inadequate attention. Indeed, most academic physicians think that only scientific medicine exists and that patients should be satisfied with a sophisticated approach to their problems. Some patients are satisfied, but many are disgruntled. It is not unusual for a patient, after a $1,000 work-up, to go to a family physician or chiropractor for satisfaction.
I was eager to discover the art of medicine at its finest during my rotation away from the university in a rural community. During these 2 months I looked for the pearls of wisdom that allowed community physicians to be so successful. I found that a very explicit technique was used by some physicians to achieve not only satisfaction but adoration from their patients. Unfortunately, this technique is dishonest.
Early in my community experience I was impressed by how often patients told me a doctor had saved them. I heard such statements as “Dr. X saved my leg,” or “Dr. X saved my life.” I know that it does occur, but not as often as I was hearing it.
Investigating these statements I found such stories as, “One day l twisted my ankle very badly, and it became quite swollen. My doctor told me 1 could lose my leg from this but that he would take x-rays, put my leg in an Ace bandage, and give me crutches. In 3 days I was well. I am so thankful he saved my leg.”
And, “One day I had a temperature of 104. All of my muscles ached, my head hurt, and I had a terrible sore throat and cough. My doctor told me l could die from this, but he gave me a medicine and made me stay home. I was sick for about 2 weeks, but I got better. He saved my life.”
Is the art of medicine the art of deception? This horrifying thought actually came to me after hearing several such stories, but I learned that most of the physicians involved in such stories were not well respected by their colleagues.
I learned many honest techniques for successfully caring for patients. The several family physicians with whom I worked, all clinical instructors associated with my residency, were impeccably honest and taught me to combine compassion and efficiency.
Despite learning many positive techniques and having good role models, I left the community experience somewhat saddened by the lack of integrity that can exist in the profession. I was naive in believing that all the nonscientific aspects of medicine that made patients happy must be good.
By experiencing deception, I learned why quackery continues to flourish despite the widespread availability of honest medical care. Most significantly, I learned the importance of a sometimes frustrating humility; my patients with sprained ankles and influenza will not believe I saved their lives.
My experience as a family medicine resident in 2021
I did not get a medical school graduation; I was one of the many thousands of newly graduated students who simply left their 4th-year rotation sites one chilly day in March 2020 and just never went back. My medical school education didn’t end with me walking triumphantly across the stage – a first-generation college student finally achieving the greatest dream in her life. Instead, it ended with a Zoom “graduation” and a cross-country move from Georgia to Pennsylvania amidst the greatest pandemic in recent memory. To say my impostor syndrome was bad would be an understatement.
Residency in the COVID-19 era
The joy and the draw to family medicine for me has always been the broad scope of conditions that we see and treat. From day 1, however, much of my residency has been devoted to one very small subset of patients – those with COVID-19. At one point, our hospital was so strained that our family medicine program had to run a second inpatient service alongside our usual five-resident service team just to provide care to everybody. Patients were in the hallways. The ER was packed to the gills. We were sleepless, terrified, unvaccinated, and desperate to help our patients survive a disease that was incompletely understood, with very few tools in our toolbox to combat it.
I distinctly remember sitting in the workroom with a coresident of mine, our faces seemingly permanently lined from wearing N95s all shift, and saying to him, “I worry I will be a bad family medicine physician. I worry I haven’t seen enough, other than COVID.” It was midway through my intern year; the days were short, so I was driving to and from the hospital in chilly darkness. My patients, like many around the country, were doing poorly. Vaccines seemed like a promise too good to be true. Worst of all: Those of us who were interns, who had no triumphant podium moment to end our medical school education, were suffering with an intense sense of impostor syndrome, which was strengthened by every “there is nothing else we can offer your loved one at this time” conversation we had. My apprehension about not having seen a wider breadth of medicine during my training is a sentiment still widely shared by COVID-era residents.
Luckily, my coresident was supportive.
“We’re going to be great family medicine physicians,” he said. “We’re learning the hard stuff – the bread and butter of FM – up-front. You’ll see.”
In some ways, I think he was right. Clinical skills, empathy, humility, and forging strong relationships are at the center of every family medicine physician’s heart; my generation has had to learn these skills early and under pressure. Sometimes, there are no answers. Sometimes, the best thing a family doctor can do for a patient is to hear them, understand them, and hold their hand.
‘We watched Cinderella together’
Shortly after that conversation with my coresident, I had a particular case which moved me. This gentleman with intellectual disability and COVID had been declining steadily since his admission to the hospital. He was isolated from everybody he knew and loved, but it did not dampen his spirits. He was cheerful to every person who entered his room, clad in their shrouds of PPE, which more often than not felt more like mourning garb than protective wear. I remember very little about this patient’s clinical picture – the COVID, the superimposed pneumonia, the repeated intubations. What I do remember is he loved the Disney classic Cinderella. I knew this because I developed a very close relationship with his family during the course of his hospitalization. Amidst the torrential onslaught of patients, I made sure to call families every day – not because I wanted to, but because my mentors and attendings and coresidents had all drilled into me from day 1 that we are family medicine, and a large part of our role is to advocate for our patients, and to communicate with their loved ones. So I called. I learned a lot about him; his likes, his dislikes, his close bond with his siblings, and of course his lifelong love for Cinderella. On the last week of my ICU rotation, my patient passed peacefully. His nurse and I were bedside. We held his hand. We told him his family loved him. We watched Cinderella together on an iPad encased in protective plastic.
My next rotation was an outpatient one and it looked more like the “bread and butter” of family medicine. But as I whisked in and out of patient rooms, attending to patients with diabetes, with depression, with pain, I could not stop thinking about my hospitalized patients who my coresidents had assumed care of. Each exam room I entered, I rather morbidly thought “this patient could be next on our hospital service.” Without realizing it, I made more of an effort to get to know each patient holistically. I learned who they were as people. I found myself writing small, medically low-yield details in the chart: “Margaret loves to sing in her church choir;” “Katherine is a self-published author.”
I learned from my attendings. As I sat at the precepting table with them, observing their conversations about patients, their collective decades of experience were apparent.
“I’ve been seeing this patient every few weeks since I was a resident,” said one of my attendings.
“I don’t even see my parents that often,” I thought.
The depth of her relationship with, understanding of, and compassion for this patient struck me deeply. This was why I went into family medicine. My attending knew her patients; they were not faceless unknowns in a hospital gown to her. She would have known to play Cinderella for them in the end.
This is a unique time for trainees. We have been challenged, terrified, overwhelmed, and heartbroken. But at no point have we been isolated. We’ve had the generations of doctors before us to lead the way, to teach us the “hard stuff.” We’ve had senior residents to lean on, who have taken us aside and told us, “I can do the goals-of-care talk today; you need a break.” While the plague seems to have passed over our hospital for now, it has left behind a class of family medicine residents who are proud to carry on our specialty’s long tradition of compassionate, empathetic, lifelong care. “We care for all life stages, from cradle to grave,” says every family medicine physician.
My class, for better or for worse, has cared more often for patients in the twilight of their lives, and while it has been hard, I believe it has made us all better doctors. Now, when I hold a newborn in my arms for a well-child check, I am exceptionally grateful – for the opportunities I have been given, for new beginnings amidst so much sadness, and for the great privilege of being a family medicine physician. ■
Dr. Persampiere is a second-year resident in the family medicine residency program at Abington (Pa.) Jefferson Health. You can contact her directly at victoria.persampiere@jefferson.edu or via fpnews@mdedge.com.
klennon@mdedge.com
We are currently republishing an installment of this column as part of our continuing celebration of Family Practice News’s 50th anniversary.
Bruce A. Bagley, MD, wrote the first batch of these columns, when he was chief resident in family medicine at St. Joseph’s Hospital, Syracuse, N.Y. Joseph E. Scherger, MD, was the second writer for Family Practice News’s monthly “Residents’ Viewpoint.” At the time Dr. Scherger became a columnist, he was a 26-year-old, 2nd-year family practice resident at the Family Medical Center, University Hospital, University of Washington, Seattle.
Dr. Scherger’s first column was published on Feb. 5, 1977. We are republishing his “Residents’ Viewpoint” from June 15, 1977 (see below) and a new column by Victoria Persampiere, DO, who is currently a 2nd-year resident in the family medicine program at Abington Jefferson Health. (See “My experience as a family medicine resident in 2021” after Dr. Scherger’s column.).
We hope you will enjoy comparing and contrasting the experiences of a resident practicing family medicine today to those of a resident practicing family medicine nearly 4½ decades ago.To learn about Dr. Scherger’s current practice and long career, you can read his profile on the cover of the September 2021 issue of Family Practice News or on MDedge.com/FamilyMedicine in our “Family Practice News 50th Anniversary” section.
Art of medicine or deception?
Originally published in Family Practice News on June 15, 1977.
In medical school I learned the science of medicine. There I diligently studied the basic sciences and gained a thorough understanding of the pathophysiology of disease. In the clinical years I learned to apply this knowledge to a wide variety of interesting patients who came to the academic center.
Yet, when I started my family practice residency, I lacked the ability to care for patients. Though I could take a thorough history, perform a complete physical examination, and diagnose and treat specific illnesses, I had little idea how to satisfy patients by meeting their needs.
The art of medicine is the nonscientific part of a successful doctor-patient interaction. For a doctor-patient interaction to be successful, not only must the illness be appropriately addressed, but both patient and physician must be satisfied.
In the university environment, the art of medicine often gets inadequate attention. Indeed, most academic physicians think that only scientific medicine exists and that patients should be satisfied with a sophisticated approach to their problems. Some patients are satisfied, but many are disgruntled. It is not unusual for a patient, after a $1,000 work-up, to go to a family physician or chiropractor for satisfaction.
I was eager to discover the art of medicine at its finest during my rotation away from the university in a rural community. During these 2 months I looked for the pearls of wisdom that allowed community physicians to be so successful. I found that a very explicit technique was used by some physicians to achieve not only satisfaction but adoration from their patients. Unfortunately, this technique is dishonest.
Early in my community experience I was impressed by how often patients told me a doctor had saved them. I heard such statements as “Dr. X saved my leg,” or “Dr. X saved my life.” I know that it does occur, but not as often as I was hearing it.
Investigating these statements I found such stories as, “One day l twisted my ankle very badly, and it became quite swollen. My doctor told me 1 could lose my leg from this but that he would take x-rays, put my leg in an Ace bandage, and give me crutches. In 3 days I was well. I am so thankful he saved my leg.”
And, “One day I had a temperature of 104. All of my muscles ached, my head hurt, and I had a terrible sore throat and cough. My doctor told me l could die from this, but he gave me a medicine and made me stay home. I was sick for about 2 weeks, but I got better. He saved my life.”
Is the art of medicine the art of deception? This horrifying thought actually came to me after hearing several such stories, but I learned that most of the physicians involved in such stories were not well respected by their colleagues.
I learned many honest techniques for successfully caring for patients. The several family physicians with whom I worked, all clinical instructors associated with my residency, were impeccably honest and taught me to combine compassion and efficiency.
Despite learning many positive techniques and having good role models, I left the community experience somewhat saddened by the lack of integrity that can exist in the profession. I was naive in believing that all the nonscientific aspects of medicine that made patients happy must be good.
By experiencing deception, I learned why quackery continues to flourish despite the widespread availability of honest medical care. Most significantly, I learned the importance of a sometimes frustrating humility; my patients with sprained ankles and influenza will not believe I saved their lives.
My experience as a family medicine resident in 2021
I did not get a medical school graduation; I was one of the many thousands of newly graduated students who simply left their 4th-year rotation sites one chilly day in March 2020 and just never went back. My medical school education didn’t end with me walking triumphantly across the stage – a first-generation college student finally achieving the greatest dream in her life. Instead, it ended with a Zoom “graduation” and a cross-country move from Georgia to Pennsylvania amidst the greatest pandemic in recent memory. To say my impostor syndrome was bad would be an understatement.
Residency in the COVID-19 era
The joy and the draw to family medicine for me has always been the broad scope of conditions that we see and treat. From day 1, however, much of my residency has been devoted to one very small subset of patients – those with COVID-19. At one point, our hospital was so strained that our family medicine program had to run a second inpatient service alongside our usual five-resident service team just to provide care to everybody. Patients were in the hallways. The ER was packed to the gills. We were sleepless, terrified, unvaccinated, and desperate to help our patients survive a disease that was incompletely understood, with very few tools in our toolbox to combat it.
I distinctly remember sitting in the workroom with a coresident of mine, our faces seemingly permanently lined from wearing N95s all shift, and saying to him, “I worry I will be a bad family medicine physician. I worry I haven’t seen enough, other than COVID.” It was midway through my intern year; the days were short, so I was driving to and from the hospital in chilly darkness. My patients, like many around the country, were doing poorly. Vaccines seemed like a promise too good to be true. Worst of all: Those of us who were interns, who had no triumphant podium moment to end our medical school education, were suffering with an intense sense of impostor syndrome, which was strengthened by every “there is nothing else we can offer your loved one at this time” conversation we had. My apprehension about not having seen a wider breadth of medicine during my training is a sentiment still widely shared by COVID-era residents.
Luckily, my coresident was supportive.
“We’re going to be great family medicine physicians,” he said. “We’re learning the hard stuff – the bread and butter of FM – up-front. You’ll see.”
In some ways, I think he was right. Clinical skills, empathy, humility, and forging strong relationships are at the center of every family medicine physician’s heart; my generation has had to learn these skills early and under pressure. Sometimes, there are no answers. Sometimes, the best thing a family doctor can do for a patient is to hear them, understand them, and hold their hand.
‘We watched Cinderella together’
Shortly after that conversation with my coresident, I had a particular case which moved me. This gentleman with intellectual disability and COVID had been declining steadily since his admission to the hospital. He was isolated from everybody he knew and loved, but it did not dampen his spirits. He was cheerful to every person who entered his room, clad in their shrouds of PPE, which more often than not felt more like mourning garb than protective wear. I remember very little about this patient’s clinical picture – the COVID, the superimposed pneumonia, the repeated intubations. What I do remember is he loved the Disney classic Cinderella. I knew this because I developed a very close relationship with his family during the course of his hospitalization. Amidst the torrential onslaught of patients, I made sure to call families every day – not because I wanted to, but because my mentors and attendings and coresidents had all drilled into me from day 1 that we are family medicine, and a large part of our role is to advocate for our patients, and to communicate with their loved ones. So I called. I learned a lot about him; his likes, his dislikes, his close bond with his siblings, and of course his lifelong love for Cinderella. On the last week of my ICU rotation, my patient passed peacefully. His nurse and I were bedside. We held his hand. We told him his family loved him. We watched Cinderella together on an iPad encased in protective plastic.
My next rotation was an outpatient one and it looked more like the “bread and butter” of family medicine. But as I whisked in and out of patient rooms, attending to patients with diabetes, with depression, with pain, I could not stop thinking about my hospitalized patients who my coresidents had assumed care of. Each exam room I entered, I rather morbidly thought “this patient could be next on our hospital service.” Without realizing it, I made more of an effort to get to know each patient holistically. I learned who they were as people. I found myself writing small, medically low-yield details in the chart: “Margaret loves to sing in her church choir;” “Katherine is a self-published author.”
I learned from my attendings. As I sat at the precepting table with them, observing their conversations about patients, their collective decades of experience were apparent.
“I’ve been seeing this patient every few weeks since I was a resident,” said one of my attendings.
“I don’t even see my parents that often,” I thought.
The depth of her relationship with, understanding of, and compassion for this patient struck me deeply. This was why I went into family medicine. My attending knew her patients; they were not faceless unknowns in a hospital gown to her. She would have known to play Cinderella for them in the end.
This is a unique time for trainees. We have been challenged, terrified, overwhelmed, and heartbroken. But at no point have we been isolated. We’ve had the generations of doctors before us to lead the way, to teach us the “hard stuff.” We’ve had senior residents to lean on, who have taken us aside and told us, “I can do the goals-of-care talk today; you need a break.” While the plague seems to have passed over our hospital for now, it has left behind a class of family medicine residents who are proud to carry on our specialty’s long tradition of compassionate, empathetic, lifelong care. “We care for all life stages, from cradle to grave,” says every family medicine physician.
My class, for better or for worse, has cared more often for patients in the twilight of their lives, and while it has been hard, I believe it has made us all better doctors. Now, when I hold a newborn in my arms for a well-child check, I am exceptionally grateful – for the opportunities I have been given, for new beginnings amidst so much sadness, and for the great privilege of being a family medicine physician. ■
Dr. Persampiere is a second-year resident in the family medicine residency program at Abington (Pa.) Jefferson Health. You can contact her directly at victoria.persampiere@jefferson.edu or via fpnews@mdedge.com.
klennon@mdedge.com
We are currently republishing an installment of this column as part of our continuing celebration of Family Practice News’s 50th anniversary.
Bruce A. Bagley, MD, wrote the first batch of these columns, when he was chief resident in family medicine at St. Joseph’s Hospital, Syracuse, N.Y. Joseph E. Scherger, MD, was the second writer for Family Practice News’s monthly “Residents’ Viewpoint.” At the time Dr. Scherger became a columnist, he was a 26-year-old, 2nd-year family practice resident at the Family Medical Center, University Hospital, University of Washington, Seattle.
Dr. Scherger’s first column was published on Feb. 5, 1977. We are republishing his “Residents’ Viewpoint” from June 15, 1977 (see below) and a new column by Victoria Persampiere, DO, who is currently a 2nd-year resident in the family medicine program at Abington Jefferson Health. (See “My experience as a family medicine resident in 2021” after Dr. Scherger’s column.).
We hope you will enjoy comparing and contrasting the experiences of a resident practicing family medicine today to those of a resident practicing family medicine nearly 4½ decades ago.To learn about Dr. Scherger’s current practice and long career, you can read his profile on the cover of the September 2021 issue of Family Practice News or on MDedge.com/FamilyMedicine in our “Family Practice News 50th Anniversary” section.
Art of medicine or deception?
Originally published in Family Practice News on June 15, 1977.
In medical school I learned the science of medicine. There I diligently studied the basic sciences and gained a thorough understanding of the pathophysiology of disease. In the clinical years I learned to apply this knowledge to a wide variety of interesting patients who came to the academic center.
Yet, when I started my family practice residency, I lacked the ability to care for patients. Though I could take a thorough history, perform a complete physical examination, and diagnose and treat specific illnesses, I had little idea how to satisfy patients by meeting their needs.
The art of medicine is the nonscientific part of a successful doctor-patient interaction. For a doctor-patient interaction to be successful, not only must the illness be appropriately addressed, but both patient and physician must be satisfied.
In the university environment, the art of medicine often gets inadequate attention. Indeed, most academic physicians think that only scientific medicine exists and that patients should be satisfied with a sophisticated approach to their problems. Some patients are satisfied, but many are disgruntled. It is not unusual for a patient, after a $1,000 work-up, to go to a family physician or chiropractor for satisfaction.
I was eager to discover the art of medicine at its finest during my rotation away from the university in a rural community. During these 2 months I looked for the pearls of wisdom that allowed community physicians to be so successful. I found that a very explicit technique was used by some physicians to achieve not only satisfaction but adoration from their patients. Unfortunately, this technique is dishonest.
Early in my community experience I was impressed by how often patients told me a doctor had saved them. I heard such statements as “Dr. X saved my leg,” or “Dr. X saved my life.” I know that it does occur, but not as often as I was hearing it.
Investigating these statements I found such stories as, “One day l twisted my ankle very badly, and it became quite swollen. My doctor told me 1 could lose my leg from this but that he would take x-rays, put my leg in an Ace bandage, and give me crutches. In 3 days I was well. I am so thankful he saved my leg.”
And, “One day I had a temperature of 104. All of my muscles ached, my head hurt, and I had a terrible sore throat and cough. My doctor told me l could die from this, but he gave me a medicine and made me stay home. I was sick for about 2 weeks, but I got better. He saved my life.”
Is the art of medicine the art of deception? This horrifying thought actually came to me after hearing several such stories, but I learned that most of the physicians involved in such stories were not well respected by their colleagues.
I learned many honest techniques for successfully caring for patients. The several family physicians with whom I worked, all clinical instructors associated with my residency, were impeccably honest and taught me to combine compassion and efficiency.
Despite learning many positive techniques and having good role models, I left the community experience somewhat saddened by the lack of integrity that can exist in the profession. I was naive in believing that all the nonscientific aspects of medicine that made patients happy must be good.
By experiencing deception, I learned why quackery continues to flourish despite the widespread availability of honest medical care. Most significantly, I learned the importance of a sometimes frustrating humility; my patients with sprained ankles and influenza will not believe I saved their lives.
My experience as a family medicine resident in 2021
I did not get a medical school graduation; I was one of the many thousands of newly graduated students who simply left their 4th-year rotation sites one chilly day in March 2020 and just never went back. My medical school education didn’t end with me walking triumphantly across the stage – a first-generation college student finally achieving the greatest dream in her life. Instead, it ended with a Zoom “graduation” and a cross-country move from Georgia to Pennsylvania amidst the greatest pandemic in recent memory. To say my impostor syndrome was bad would be an understatement.
Residency in the COVID-19 era
The joy and the draw to family medicine for me has always been the broad scope of conditions that we see and treat. From day 1, however, much of my residency has been devoted to one very small subset of patients – those with COVID-19. At one point, our hospital was so strained that our family medicine program had to run a second inpatient service alongside our usual five-resident service team just to provide care to everybody. Patients were in the hallways. The ER was packed to the gills. We were sleepless, terrified, unvaccinated, and desperate to help our patients survive a disease that was incompletely understood, with very few tools in our toolbox to combat it.
I distinctly remember sitting in the workroom with a coresident of mine, our faces seemingly permanently lined from wearing N95s all shift, and saying to him, “I worry I will be a bad family medicine physician. I worry I haven’t seen enough, other than COVID.” It was midway through my intern year; the days were short, so I was driving to and from the hospital in chilly darkness. My patients, like many around the country, were doing poorly. Vaccines seemed like a promise too good to be true. Worst of all: Those of us who were interns, who had no triumphant podium moment to end our medical school education, were suffering with an intense sense of impostor syndrome, which was strengthened by every “there is nothing else we can offer your loved one at this time” conversation we had. My apprehension about not having seen a wider breadth of medicine during my training is a sentiment still widely shared by COVID-era residents.
Luckily, my coresident was supportive.
“We’re going to be great family medicine physicians,” he said. “We’re learning the hard stuff – the bread and butter of FM – up-front. You’ll see.”
In some ways, I think he was right. Clinical skills, empathy, humility, and forging strong relationships are at the center of every family medicine physician’s heart; my generation has had to learn these skills early and under pressure. Sometimes, there are no answers. Sometimes, the best thing a family doctor can do for a patient is to hear them, understand them, and hold their hand.
‘We watched Cinderella together’
Shortly after that conversation with my coresident, I had a particular case which moved me. This gentleman with intellectual disability and COVID had been declining steadily since his admission to the hospital. He was isolated from everybody he knew and loved, but it did not dampen his spirits. He was cheerful to every person who entered his room, clad in their shrouds of PPE, which more often than not felt more like mourning garb than protective wear. I remember very little about this patient’s clinical picture – the COVID, the superimposed pneumonia, the repeated intubations. What I do remember is he loved the Disney classic Cinderella. I knew this because I developed a very close relationship with his family during the course of his hospitalization. Amidst the torrential onslaught of patients, I made sure to call families every day – not because I wanted to, but because my mentors and attendings and coresidents had all drilled into me from day 1 that we are family medicine, and a large part of our role is to advocate for our patients, and to communicate with their loved ones. So I called. I learned a lot about him; his likes, his dislikes, his close bond with his siblings, and of course his lifelong love for Cinderella. On the last week of my ICU rotation, my patient passed peacefully. His nurse and I were bedside. We held his hand. We told him his family loved him. We watched Cinderella together on an iPad encased in protective plastic.
My next rotation was an outpatient one and it looked more like the “bread and butter” of family medicine. But as I whisked in and out of patient rooms, attending to patients with diabetes, with depression, with pain, I could not stop thinking about my hospitalized patients who my coresidents had assumed care of. Each exam room I entered, I rather morbidly thought “this patient could be next on our hospital service.” Without realizing it, I made more of an effort to get to know each patient holistically. I learned who they were as people. I found myself writing small, medically low-yield details in the chart: “Margaret loves to sing in her church choir;” “Katherine is a self-published author.”
I learned from my attendings. As I sat at the precepting table with them, observing their conversations about patients, their collective decades of experience were apparent.
“I’ve been seeing this patient every few weeks since I was a resident,” said one of my attendings.
“I don’t even see my parents that often,” I thought.
The depth of her relationship with, understanding of, and compassion for this patient struck me deeply. This was why I went into family medicine. My attending knew her patients; they were not faceless unknowns in a hospital gown to her. She would have known to play Cinderella for them in the end.
This is a unique time for trainees. We have been challenged, terrified, overwhelmed, and heartbroken. But at no point have we been isolated. We’ve had the generations of doctors before us to lead the way, to teach us the “hard stuff.” We’ve had senior residents to lean on, who have taken us aside and told us, “I can do the goals-of-care talk today; you need a break.” While the plague seems to have passed over our hospital for now, it has left behind a class of family medicine residents who are proud to carry on our specialty’s long tradition of compassionate, empathetic, lifelong care. “We care for all life stages, from cradle to grave,” says every family medicine physician.
My class, for better or for worse, has cared more often for patients in the twilight of their lives, and while it has been hard, I believe it has made us all better doctors. Now, when I hold a newborn in my arms for a well-child check, I am exceptionally grateful – for the opportunities I have been given, for new beginnings amidst so much sadness, and for the great privilege of being a family medicine physician. ■
Dr. Persampiere is a second-year resident in the family medicine residency program at Abington (Pa.) Jefferson Health. You can contact her directly at victoria.persampiere@jefferson.edu or via fpnews@mdedge.com.
klennon@mdedge.com
My experience as a family medicine resident in 2021
I did not get a medical school graduation; I was one of the many thousands of newly graduated students who simply left their 4th-year rotation sites one chilly day in March 2020 and just never went back. My medical school education didn’t end with me walking triumphantly across the stage – a first-generation college student finally achieving the greatest dream in her life. Instead, it ended with a Zoom “graduation” and a cross-country move from Georgia to Pennsylvania amidst the greatest pandemic in recent memory. To say my impostor syndrome was bad would be an understatement.
Residency in the COVID-19-era
The joy and the draw to family medicine for me has always been the broad scope of conditions that we see and treat. From day 1, however, much of my residency has been devoted to one very small subset of patients – those with COVID-19. At one point, our hospital was so strained that our family medicine program had to run a second inpatient service alongside our usual five-resident service team just to provide care to everybody. Patients were in the hallways. The ER was packed to the gills. We were sleepless, terrified, unvaccinated, and desperate to help our patients survive a disease that was incompletely understood, with very few tools in our toolbox to combat it.
I distinctly remember sitting in the workroom with a coresident of mine, our faces seemingly permanently lined from wearing N95s all shift, and saying to him, “I worry I will be a bad family medicine physician. I worry I haven’t seen enough, other than COVID.” It was midway through my intern year; the days were short, so I was driving to and from the hospital in chilly darkness. My patients, like many around the country, were doing poorly. Vaccines seemed like a promise too good to be true. Worst of all: Those of us who were interns, who had no triumphant podium moment to end our medical school education, were suffering with an intense sense of impostor syndrome which was strengthened by every “there is nothing else we can offer your loved one at this time,” conversation we had. My apprehension about not having seen a wider breadth of medicine during my training is a sentiment still widely shared by COVID-era residents.
Luckily, my coresident was supportive.
“We’re going to be great family medicine physicians,” he said. “We’re learning the hard stuff – the bread and butter of FM – up-front. You’ll see.”
In some ways, I think he was right. Clinical skills, empathy, humility, and forging strong relationships are at the center of every family medicine physician’s heart; my generation has had to learn these skills early and under pressure. Sometimes, there are no answers. Sometimes, the best thing a family doctor can do for a patient is to hear them, understand them, and hold their hand.
‘We watched Cinderella together’
Shortly after that conversation with my coresident, I had a particular case which moved me. This gentleman with intellectual disability and COVID had been declining steadily since his admission to the hospital. He was isolated from everybody he knew and loved, but it did not dampen his spirits. He was cheerful to every person who entered his room, clad in their shrouds of PPE, which more often than not felt more like mourning garb than protective wear. I remember very little about this patient’s clinical picture – the COVID, the superimposed pneumonia, the repeated intubations. What I do remember is he loved the Disney classic, Cinderella. I knew this because I developed a very close relationship with his family during the course of his hospitalization. Amidst the torrential onslaught of patients, I made sure to call families every day – not because I wanted to, but because my mentors and attendings and coresidents had all drilled into me from day 1 that we are family medicine, and a large part of our role is to advocate for our patients, and to communicate with their loved ones. So I called. I learned a lot about him; his likes, his dislikes, his close bond with his siblings, and of course his lifelong love for Cinderella. On the last week of my ICU rotation, my patient passed peacefully. His nurse and I were bedside. We held his hand. We told him his family loved him. We watched Cinderella together on an iPad encased in protective plastic.
My next rotation was an outpatient one and it looked more like the “bread and butter” of family medicine. But as I whisked in and out of patient rooms, attending to patients with diabetes, with depression, with pain, I could not stop thinking about my hospitalized patients who my coresidents had assumed care of. Each exam room I entered, I rather morbidly thought “this patient could be next on our hospital service.” Without realizing it, I made more of an effort to get to know each patient holistically. I learned who they were as people. I found myself writing small, medically low-yield details in the chart: “Margaret loves to sing in her church choir;” “Katherine is a self-published author.”
I learned from my attendings. As I sat at the precepting table with them, observing their conversations about patients, their collective decades of experience were apparent.
“I’ve been seeing this patient every few weeks since I was a resident,” said one of my attendings.
“I don’t even see my parents that often,” I thought.
The depth of her relationship with, understanding of, and compassion for this patient struck me deeply. This was why I went into family medicine. My attending knew her patients; they were not faceless unknowns in a hospital gown to her. She would have known to play Cinderella for them in the end.
This is a unique time for trainees. We have been challenged, terrified, overwhelmed, and heartbroken. But at no point have we been isolated. We’ve had the generations of doctors before us to lead the way, to teach us the “hard stuff.” We’ve had senior residents to lean on, who have taken us aside and told us, “I can do the goals-of-care talk today, you need a break.” While the plague seems to have passed over our hospital for now, it has left behind a class of family medicine residents who are proud to carry on our specialty’s long tradition of compassionate, empathetic, lifelong care. “We care for all life stages, from cradle to grave,” says every family medicine physician.
My class, for better or for worse, has cared more often for patients in the twilight of their lives, and while it has been hard, I believe it has made us all better doctors. Now, when I hold a newborn in my arms for a well-child check, I am exceptionally grateful – for the opportunities I have been given, for new beginnings amidst so much sadness, and for the great privilege of being a family medicine physician.
Dr. Persampiere is a 2nd-year resident in the family medicine residency program at Abington (Pa.) Jefferson Health. You can contact her directly at victoria.persampiere@jefferson.edu or via fpnews@mdedge.com.
I did not get a medical school graduation; I was one of the many thousands of newly graduated students who simply left their 4th-year rotation sites one chilly day in March 2020 and just never went back. My medical school education didn’t end with me walking triumphantly across the stage – a first-generation college student finally achieving the greatest dream in her life. Instead, it ended with a Zoom “graduation” and a cross-country move from Georgia to Pennsylvania amidst the greatest pandemic in recent memory. To say my impostor syndrome was bad would be an understatement.
Residency in the COVID-19-era
The joy and the draw to family medicine for me has always been the broad scope of conditions that we see and treat. From day 1, however, much of my residency has been devoted to one very small subset of patients – those with COVID-19. At one point, our hospital was so strained that our family medicine program had to run a second inpatient service alongside our usual five-resident service team just to provide care to everybody. Patients were in the hallways. The ER was packed to the gills. We were sleepless, terrified, unvaccinated, and desperate to help our patients survive a disease that was incompletely understood, with very few tools in our toolbox to combat it.
I distinctly remember sitting in the workroom with a coresident of mine, our faces seemingly permanently lined from wearing N95s all shift, and saying to him, “I worry I will be a bad family medicine physician. I worry I haven’t seen enough, other than COVID.” It was midway through my intern year; the days were short, so I was driving to and from the hospital in chilly darkness. My patients, like many around the country, were doing poorly. Vaccines seemed like a promise too good to be true. Worst of all: Those of us who were interns, who had no triumphant podium moment to end our medical school education, were suffering with an intense sense of impostor syndrome which was strengthened by every “there is nothing else we can offer your loved one at this time,” conversation we had. My apprehension about not having seen a wider breadth of medicine during my training is a sentiment still widely shared by COVID-era residents.
Luckily, my coresident was supportive.
“We’re going to be great family medicine physicians,” he said. “We’re learning the hard stuff – the bread and butter of FM – up-front. You’ll see.”
In some ways, I think he was right. Clinical skills, empathy, humility, and forging strong relationships are at the center of every family medicine physician’s heart; my generation has had to learn these skills early and under pressure. Sometimes, there are no answers. Sometimes, the best thing a family doctor can do for a patient is to hear them, understand them, and hold their hand.
‘We watched Cinderella together’
Shortly after that conversation with my coresident, I had a particular case which moved me. This gentleman with intellectual disability and COVID had been declining steadily since his admission to the hospital. He was isolated from everybody he knew and loved, but it did not dampen his spirits. He was cheerful to every person who entered his room, clad in their shrouds of PPE, which more often than not felt more like mourning garb than protective wear. I remember very little about this patient’s clinical picture – the COVID, the superimposed pneumonia, the repeated intubations. What I do remember is he loved the Disney classic, Cinderella. I knew this because I developed a very close relationship with his family during the course of his hospitalization. Amidst the torrential onslaught of patients, I made sure to call families every day – not because I wanted to, but because my mentors and attendings and coresidents had all drilled into me from day 1 that we are family medicine, and a large part of our role is to advocate for our patients, and to communicate with their loved ones. So I called. I learned a lot about him; his likes, his dislikes, his close bond with his siblings, and of course his lifelong love for Cinderella. On the last week of my ICU rotation, my patient passed peacefully. His nurse and I were bedside. We held his hand. We told him his family loved him. We watched Cinderella together on an iPad encased in protective plastic.
My next rotation was an outpatient one and it looked more like the “bread and butter” of family medicine. But as I whisked in and out of patient rooms, attending to patients with diabetes, with depression, with pain, I could not stop thinking about my hospitalized patients who my coresidents had assumed care of. Each exam room I entered, I rather morbidly thought “this patient could be next on our hospital service.” Without realizing it, I made more of an effort to get to know each patient holistically. I learned who they were as people. I found myself writing small, medically low-yield details in the chart: “Margaret loves to sing in her church choir;” “Katherine is a self-published author.”
I learned from my attendings. As I sat at the precepting table with them, observing their conversations about patients, their collective decades of experience were apparent.
“I’ve been seeing this patient every few weeks since I was a resident,” said one of my attendings.
“I don’t even see my parents that often,” I thought.
The depth of her relationship with, understanding of, and compassion for this patient struck me deeply. This was why I went into family medicine. My attending knew her patients; they were not faceless unknowns in a hospital gown to her. She would have known to play Cinderella for them in the end.
This is a unique time for trainees. We have been challenged, terrified, overwhelmed, and heartbroken. But at no point have we been isolated. We’ve had the generations of doctors before us to lead the way, to teach us the “hard stuff.” We’ve had senior residents to lean on, who have taken us aside and told us, “I can do the goals-of-care talk today, you need a break.” While the plague seems to have passed over our hospital for now, it has left behind a class of family medicine residents who are proud to carry on our specialty’s long tradition of compassionate, empathetic, lifelong care. “We care for all life stages, from cradle to grave,” says every family medicine physician.
My class, for better or for worse, has cared more often for patients in the twilight of their lives, and while it has been hard, I believe it has made us all better doctors. Now, when I hold a newborn in my arms for a well-child check, I am exceptionally grateful – for the opportunities I have been given, for new beginnings amidst so much sadness, and for the great privilege of being a family medicine physician.
Dr. Persampiere is a 2nd-year resident in the family medicine residency program at Abington (Pa.) Jefferson Health. You can contact her directly at victoria.persampiere@jefferson.edu or via fpnews@mdedge.com.
I did not get a medical school graduation; I was one of the many thousands of newly graduated students who simply left their 4th-year rotation sites one chilly day in March 2020 and just never went back. My medical school education didn’t end with me walking triumphantly across the stage – a first-generation college student finally achieving the greatest dream in her life. Instead, it ended with a Zoom “graduation” and a cross-country move from Georgia to Pennsylvania amidst the greatest pandemic in recent memory. To say my impostor syndrome was bad would be an understatement.
Residency in the COVID-19-era
The joy and the draw to family medicine for me has always been the broad scope of conditions that we see and treat. From day 1, however, much of my residency has been devoted to one very small subset of patients – those with COVID-19. At one point, our hospital was so strained that our family medicine program had to run a second inpatient service alongside our usual five-resident service team just to provide care to everybody. Patients were in the hallways. The ER was packed to the gills. We were sleepless, terrified, unvaccinated, and desperate to help our patients survive a disease that was incompletely understood, with very few tools in our toolbox to combat it.
I distinctly remember sitting in the workroom with a coresident of mine, our faces seemingly permanently lined from wearing N95s all shift, and saying to him, “I worry I will be a bad family medicine physician. I worry I haven’t seen enough, other than COVID.” It was midway through my intern year; the days were short, so I was driving to and from the hospital in chilly darkness. My patients, like many around the country, were doing poorly. Vaccines seemed like a promise too good to be true. Worst of all: Those of us who were interns, who had no triumphant podium moment to end our medical school education, were suffering with an intense sense of impostor syndrome which was strengthened by every “there is nothing else we can offer your loved one at this time,” conversation we had. My apprehension about not having seen a wider breadth of medicine during my training is a sentiment still widely shared by COVID-era residents.
Luckily, my coresident was supportive.
“We’re going to be great family medicine physicians,” he said. “We’re learning the hard stuff – the bread and butter of FM – up-front. You’ll see.”
In some ways, I think he was right. Clinical skills, empathy, humility, and forging strong relationships are at the center of every family medicine physician’s heart; my generation has had to learn these skills early and under pressure. Sometimes, there are no answers. Sometimes, the best thing a family doctor can do for a patient is to hear them, understand them, and hold their hand.
‘We watched Cinderella together’
Shortly after that conversation with my coresident, I had a particular case which moved me. This gentleman with intellectual disability and COVID had been declining steadily since his admission to the hospital. He was isolated from everybody he knew and loved, but it did not dampen his spirits. He was cheerful to every person who entered his room, clad in their shrouds of PPE, which more often than not felt more like mourning garb than protective wear. I remember very little about this patient’s clinical picture – the COVID, the superimposed pneumonia, the repeated intubations. What I do remember is he loved the Disney classic, Cinderella. I knew this because I developed a very close relationship with his family during the course of his hospitalization. Amidst the torrential onslaught of patients, I made sure to call families every day – not because I wanted to, but because my mentors and attendings and coresidents had all drilled into me from day 1 that we are family medicine, and a large part of our role is to advocate for our patients, and to communicate with their loved ones. So I called. I learned a lot about him; his likes, his dislikes, his close bond with his siblings, and of course his lifelong love for Cinderella. On the last week of my ICU rotation, my patient passed peacefully. His nurse and I were bedside. We held his hand. We told him his family loved him. We watched Cinderella together on an iPad encased in protective plastic.
My next rotation was an outpatient one and it looked more like the “bread and butter” of family medicine. But as I whisked in and out of patient rooms, attending to patients with diabetes, with depression, with pain, I could not stop thinking about my hospitalized patients who my coresidents had assumed care of. Each exam room I entered, I rather morbidly thought “this patient could be next on our hospital service.” Without realizing it, I made more of an effort to get to know each patient holistically. I learned who they were as people. I found myself writing small, medically low-yield details in the chart: “Margaret loves to sing in her church choir;” “Katherine is a self-published author.”
I learned from my attendings. As I sat at the precepting table with them, observing their conversations about patients, their collective decades of experience were apparent.
“I’ve been seeing this patient every few weeks since I was a resident,” said one of my attendings.
“I don’t even see my parents that often,” I thought.
The depth of her relationship with, understanding of, and compassion for this patient struck me deeply. This was why I went into family medicine. My attending knew her patients; they were not faceless unknowns in a hospital gown to her. She would have known to play Cinderella for them in the end.
This is a unique time for trainees. We have been challenged, terrified, overwhelmed, and heartbroken. But at no point have we been isolated. We’ve had the generations of doctors before us to lead the way, to teach us the “hard stuff.” We’ve had senior residents to lean on, who have taken us aside and told us, “I can do the goals-of-care talk today, you need a break.” While the plague seems to have passed over our hospital for now, it has left behind a class of family medicine residents who are proud to carry on our specialty’s long tradition of compassionate, empathetic, lifelong care. “We care for all life stages, from cradle to grave,” says every family medicine physician.
My class, for better or for worse, has cared more often for patients in the twilight of their lives, and while it has been hard, I believe it has made us all better doctors. Now, when I hold a newborn in my arms for a well-child check, I am exceptionally grateful – for the opportunities I have been given, for new beginnings amidst so much sadness, and for the great privilege of being a family medicine physician.
Dr. Persampiere is a 2nd-year resident in the family medicine residency program at Abington (Pa.) Jefferson Health. You can contact her directly at victoria.persampiere@jefferson.edu or via fpnews@mdedge.com.
Dr. Judy C. Washington shows URM physicians how to lead
For URM physicians, she also imparts a shared experience of being a minority in the field and helps prepare them for the challenges of facing racism or feeling marginalized or not equitably supported in academic life – and for making change.
While family medicine’s demographics have become more diverse over time, and more so than other specialties, they are not yet representative of the U.S. population. Within academia, male physicians who are Black or African American, or Hispanic or Latino, comprised about 4% and 5% of family medicine faculty, respectively, at the end of 2019, according to data from the Association of American Medical Colleges. For women, these numbers were about 9% and 4%, respectively. (Only those with an MD degree exclusively were included in the report.)
“When you have the privilege to serve in leadership, you have the responsibility to reach back and identify and help others who would not otherwise have the opportunity to be recognized,” Dr. Washington said.
Her mentorship work stems in large part from her long-time involvement and leadership roles in the Society of Teachers of Family Medicine (STFM) – roles she considers a pillar of her professional life. She currently serves as president of the STFM Foundation and is associate chief medical officer of the Atlantic Medical Group, a large multisite physician-led organization. She is also coordinator of women’s health for the Overlook Family Medicine Residency Program, which is affiliated with Atlantic Medical Group.
In Dr. Washington’s role as associate chief medical officer of Atlantic Medical Group in Summit, N.J., she focuses on physician engagement, satisfaction, and diversity. She also assists in areas such as population health. For the Overlook Family Medicine Residency Program also in Summit, she precepts residents in the obstetrics clinic and in the family medicine outpatient clinic.
Diana N. Carvajal, MD, MPH, one of Dr. Washington’s mentees, called her an “inspirational leader” for young academic faculty and said she is a familiar speaker at STFM meetings on topics of workforce diversity, equity, and leadership. She is “passionate” about mentorship, Dr. Carvajal said, and has understood “that URMs and women of color were not always getting [the mentorship they need to be successful].”
Guiding future leaders
Ivonne McLean, MD, assistant professor of family and community medicine at Icahn School of Medicine at Mount Sinai, New York, and an attending at a community health center in the Bronx, called Dr. Washington for advice a couple of years ago when she was considering her next career move.
“She took a genuine interest in me. She never said, this is what you should do. But the questions she asked and the examples she gave from her own life were incredibly helpful to me [in deciding to pursue a research fellowship] ... it was a pivotal conversation,” said Dr. McLean, associate director of a reproductive health fellowship and a research fellow in a New York State–funded program.
“From a lived experience angle, she also told me, here are some of the challenges you’ll have as a woman of color, and here are some of the ways you can approach that,” she said.
Dr. Carvajal, also a URM family physician, credits Dr. Washington’s mentorship with the development of a day-long workshop – held before the annual Society of Teachers of Family Medicine (STFM) meeting – on the low and declining rates of Black males in medicine. “We’d planned it as a presentation, and [she heard of it and] helped us expand it,” she said, calling Dr. Washington “warm, welcoming, and encouraging.
“That work and collaboration with her and the others she brought [into the process] have resulted in publications and more presentations and strategy building for diversifying the workforce,” said Dr. Carvajal, assistant professor, director of reproductive health education in family medicine, and codirector of the research section, all in the department of family and community medicine at the University of Maryland, Baltimore.
STFM involvement
Dr. Washington, who says that all or almost all of her mentees are now leaders in their academic institutions and communities, has been instrumental in developing STFM’s mentoring programming and in facilitating the organization’s multifaceted URM Initiative.
She has been active in STFM since the start of her academic career, and in 2009, while serving as assistant program director for the residency program in which she’d trained, she joined two other African American women, Monique Y. Davis-Smith, MD, and Joedrecka Brown-Speights, MD, in cochairing the society’s Group on Minority and Multicultural Health.
It was in this space, that Dr. Washington said she “heard people’s stories of being in major academic institutions and not feeling supported, not being given roadmaps to success, not getting assistance with publishing, or just kind of feeling like an outsider ... of not being pulled in.” Hispanic and African American females, in particular, “were feeling marginalized,” she said.
In 2018, having co-led development of the STFM Quality Mentoring Program for URM faculty, Dr. Washington was asked to join the STFM Foundation and subsequently led the STFM Foundation’s fundraising campaign for a new URM Initiative. She exceeded her goal, increasing support for URM participation in meetings and activities, and then participated in an STFM steering committee to create broader and longer-lasting support for URM faculty, community teachers, and medical students and residents going into academic family medicine.
Increasing the percentage of URM family medicine faculty in leadership positions – and raising awareness of structural barriers to achievement – is one of the current pillars of the URM Initiative.
Navigating the ‘minority tax’
As part of her mentoring, Dr. Washington helps URM physicians navigate the minority tax – a term referring to the uncompensated citizenship tasks that are more often assigned to Black and other URM physicians than to White physicians, and that take time away from scholarship, further perpetuating inequities.
“Some of our young faculty members find themselves thrust into being the diversity and inclusion leaders in their institutions at a level at which they feel little power and little buy-in from [leadership],” she noted.
A commentary written by Dr. Washington and several colleagues on the minority tax as it impacts women – and the need to build a “tax shelter” to make academic medicine a more just environment for URM women – was published earlier this year in the Journal of Women’s Health.
She also answers e-mails and fields phone calls from young URM faculty who are mulling career moves and facing other familiar challenges.
Physicians who are URM, and African American physicians in particular, tend to “get pulled into the [often underserved] communities, into the patient care and community service areas,” Dr. Washington explained. “But unless you convert these projects into scholarship and publications, and unless you serve on a national committee outside of your institution, you’re not going to be promoted.”
Dr. Washington helps junior faculty envision themselves 5-plus years down the road, find what she calls scholarly “passion projects,” and prepare themselves for their next steps.
She helps her mentees navigate other parts of the continuum of unconscious bias and racism as well, from microaggressions from colleagues to overt discrimination from patients.
“I spend countless minutes fielding texts and phone calls from those who need support,” she wrote in a blog post. “They are a constant reminder that I must continue to speak up when I get the opportunity to do so.”
A journey through family medicine, and through bias and racism
Dr. Washington’s early days in medicine included graduating from Meharry Medical College in 1983 and the Mountainside Family Practice Residency Program in 1990. Following 6 years of working in a private practice in rural Maryland, she moved to academia, spending 6 years at East Tennessee State University and 4 years at the UMDNJ–New Jersey Medical School in Newark as an assistant professor of family medicine.
As had happened in rural Maryland, bias and racism have too often lurked during her career as a physician.
“I grew up in Alabama so I was pretty much ready to deal with racism in the South,” Dr. Washington said. “What I was not ready for was coming to the Northeast and seeing that you’re marginalized because you’re not invited into the room. Or if you do go into spaces when you’re the only one, you often don’t feel as welcomed as you thought you might be.”
Her ideas and contributions were too often dismissed, she wrote in a 2020 blog entry posted on her LinkedIn page. And during contract negotiations, “I was not aware of all the information that my White colleagues had. They had the advantage of inside information.”
Dr. Washington says that “it took a village” to make her who she is today: teachers in her segregated schools in Alabama, one of her college professors, her best friend in medical school – and STFM, “where the list [of her own mentors] is long.”
For URM physicians, she also imparts a shared experience of being a minority in the field and helps prepare them for the challenges of facing racism or feeling marginalized or not equitably supported in academic life – and for making change.
While family medicine’s demographics have become more diverse over time, and more so than other specialties, they are not yet representative of the U.S. population. Within academia, male physicians who are Black or African American, or Hispanic or Latino, comprised about 4% and 5% of family medicine faculty, respectively, at the end of 2019, according to data from the Association of American Medical Colleges. For women, these numbers were about 9% and 4%, respectively. (Only those with an MD degree exclusively were included in the report.)
“When you have the privilege to serve in leadership, you have the responsibility to reach back and identify and help others who would not otherwise have the opportunity to be recognized,” Dr. Washington said.
Her mentorship work stems in large part from her long-time involvement and leadership roles in the Society of Teachers of Family Medicine (STFM) – roles she considers a pillar of her professional life. She currently serves as president of the STFM Foundation and is associate chief medical officer of the Atlantic Medical Group, a large multisite physician-led organization. She is also coordinator of women’s health for the Overlook Family Medicine Residency Program, which is affiliated with Atlantic Medical Group.
In Dr. Washington’s role as associate chief medical officer of Atlantic Medical Group in Summit, N.J., she focuses on physician engagement, satisfaction, and diversity. She also assists in areas such as population health. For the Overlook Family Medicine Residency Program also in Summit, she precepts residents in the obstetrics clinic and in the family medicine outpatient clinic.
Diana N. Carvajal, MD, MPH, one of Dr. Washington’s mentees, called her an “inspirational leader” for young academic faculty and said she is a familiar speaker at STFM meetings on topics of workforce diversity, equity, and leadership. She is “passionate” about mentorship, Dr. Carvajal said, and has understood “that URMs and women of color were not always getting [the mentorship they need to be successful].”
Guiding future leaders
Ivonne McLean, MD, assistant professor of family and community medicine at Icahn School of Medicine at Mount Sinai, New York, and an attending at a community health center in the Bronx, called Dr. Washington for advice a couple of years ago when she was considering her next career move.
“She took a genuine interest in me. She never said, this is what you should do. But the questions she asked and the examples she gave from her own life were incredibly helpful to me [in deciding to pursue a research fellowship] ... it was a pivotal conversation,” said Dr. McLean, associate director of a reproductive health fellowship and a research fellow in a New York State–funded program.
“From a lived experience angle, she also told me, here are some of the challenges you’ll have as a woman of color, and here are some of the ways you can approach that,” she said.
Dr. Carvajal, also a URM family physician, credits Dr. Washington’s mentorship with the development of a day-long workshop – held before the annual Society of Teachers of Family Medicine (STFM) meeting – on the low and declining rates of Black males in medicine. “We’d planned it as a presentation, and [she heard of it and] helped us expand it,” she said, calling Dr. Washington “warm, welcoming, and encouraging.
“That work and collaboration with her and the others she brought [into the process] have resulted in publications and more presentations and strategy building for diversifying the workforce,” said Dr. Carvajal, assistant professor, director of reproductive health education in family medicine, and codirector of the research section, all in the department of family and community medicine at the University of Maryland, Baltimore.
STFM involvement
Dr. Washington, who says that all or almost all of her mentees are now leaders in their academic institutions and communities, has been instrumental in developing STFM’s mentoring programming and in facilitating the organization’s multifaceted URM Initiative.
She has been active in STFM since the start of her academic career, and in 2009, while serving as assistant program director for the residency program in which she’d trained, she joined two other African American women, Monique Y. Davis-Smith, MD, and Joedrecka Brown-Speights, MD, in cochairing the society’s Group on Minority and Multicultural Health.
It was in this space, that Dr. Washington said she “heard people’s stories of being in major academic institutions and not feeling supported, not being given roadmaps to success, not getting assistance with publishing, or just kind of feeling like an outsider ... of not being pulled in.” Hispanic and African American females, in particular, “were feeling marginalized,” she said.
In 2018, having co-led development of the STFM Quality Mentoring Program for URM faculty, Dr. Washington was asked to join the STFM Foundation and subsequently led the STFM Foundation’s fundraising campaign for a new URM Initiative. She exceeded her goal, increasing support for URM participation in meetings and activities, and then participated in an STFM steering committee to create broader and longer-lasting support for URM faculty, community teachers, and medical students and residents going into academic family medicine.
Increasing the percentage of URM family medicine faculty in leadership positions – and raising awareness of structural barriers to achievement – is one of the current pillars of the URM Initiative.
Navigating the ‘minority tax’
As part of her mentoring, Dr. Washington helps URM physicians navigate the minority tax – a term referring to the uncompensated citizenship tasks that are more often assigned to Black and other URM physicians than to White physicians, and that take time away from scholarship, further perpetuating inequities.
“Some of our young faculty members find themselves thrust into being the diversity and inclusion leaders in their institutions at a level at which they feel little power and little buy-in from [leadership],” she noted.
A commentary written by Dr. Washington and several colleagues on the minority tax as it impacts women – and the need to build a “tax shelter” to make academic medicine a more just environment for URM women – was published earlier this year in the Journal of Women’s Health.
She also answers e-mails and fields phone calls from young URM faculty who are mulling career moves and facing other familiar challenges.
Physicians who are URM, and African American physicians in particular, tend to “get pulled into the [often underserved] communities, into the patient care and community service areas,” Dr. Washington explained. “But unless you convert these projects into scholarship and publications, and unless you serve on a national committee outside of your institution, you’re not going to be promoted.”
Dr. Washington helps junior faculty envision themselves 5-plus years down the road, find what she calls scholarly “passion projects,” and prepare themselves for their next steps.
She helps her mentees navigate other parts of the continuum of unconscious bias and racism as well, from microaggressions from colleagues to overt discrimination from patients.
“I spend countless minutes fielding texts and phone calls from those who need support,” she wrote in a blog post. “They are a constant reminder that I must continue to speak up when I get the opportunity to do so.”
A journey through family medicine, and through bias and racism
Dr. Washington’s early days in medicine included graduating from Meharry Medical College in 1983 and the Mountainside Family Practice Residency Program in 1990. Following 6 years of working in a private practice in rural Maryland, she moved to academia, spending 6 years at East Tennessee State University and 4 years at the UMDNJ–New Jersey Medical School in Newark as an assistant professor of family medicine.
As had happened in rural Maryland, bias and racism have too often lurked during her career as a physician.
“I grew up in Alabama so I was pretty much ready to deal with racism in the South,” Dr. Washington said. “What I was not ready for was coming to the Northeast and seeing that you’re marginalized because you’re not invited into the room. Or if you do go into spaces when you’re the only one, you often don’t feel as welcomed as you thought you might be.”
Her ideas and contributions were too often dismissed, she wrote in a 2020 blog entry posted on her LinkedIn page. And during contract negotiations, “I was not aware of all the information that my White colleagues had. They had the advantage of inside information.”
Dr. Washington says that “it took a village” to make her who she is today: teachers in her segregated schools in Alabama, one of her college professors, her best friend in medical school – and STFM, “where the list [of her own mentors] is long.”
For URM physicians, she also imparts a shared experience of being a minority in the field and helps prepare them for the challenges of facing racism or feeling marginalized or not equitably supported in academic life – and for making change.
While family medicine’s demographics have become more diverse over time, and more so than other specialties, they are not yet representative of the U.S. population. Within academia, male physicians who are Black or African American, or Hispanic or Latino, comprised about 4% and 5% of family medicine faculty, respectively, at the end of 2019, according to data from the Association of American Medical Colleges. For women, these numbers were about 9% and 4%, respectively. (Only those with an MD degree exclusively were included in the report.)
“When you have the privilege to serve in leadership, you have the responsibility to reach back and identify and help others who would not otherwise have the opportunity to be recognized,” Dr. Washington said.
Her mentorship work stems in large part from her long-time involvement and leadership roles in the Society of Teachers of Family Medicine (STFM) – roles she considers a pillar of her professional life. She currently serves as president of the STFM Foundation and is associate chief medical officer of the Atlantic Medical Group, a large multisite physician-led organization. She is also coordinator of women’s health for the Overlook Family Medicine Residency Program, which is affiliated with Atlantic Medical Group.
In Dr. Washington’s role as associate chief medical officer of Atlantic Medical Group in Summit, N.J., she focuses on physician engagement, satisfaction, and diversity. She also assists in areas such as population health. For the Overlook Family Medicine Residency Program also in Summit, she precepts residents in the obstetrics clinic and in the family medicine outpatient clinic.
Diana N. Carvajal, MD, MPH, one of Dr. Washington’s mentees, called her an “inspirational leader” for young academic faculty and said she is a familiar speaker at STFM meetings on topics of workforce diversity, equity, and leadership. She is “passionate” about mentorship, Dr. Carvajal said, and has understood “that URMs and women of color were not always getting [the mentorship they need to be successful].”
Guiding future leaders
Ivonne McLean, MD, assistant professor of family and community medicine at Icahn School of Medicine at Mount Sinai, New York, and an attending at a community health center in the Bronx, called Dr. Washington for advice a couple of years ago when she was considering her next career move.
“She took a genuine interest in me. She never said, this is what you should do. But the questions she asked and the examples she gave from her own life were incredibly helpful to me [in deciding to pursue a research fellowship] ... it was a pivotal conversation,” said Dr. McLean, associate director of a reproductive health fellowship and a research fellow in a New York State–funded program.
“From a lived experience angle, she also told me, here are some of the challenges you’ll have as a woman of color, and here are some of the ways you can approach that,” she said.
Dr. Carvajal, also a URM family physician, credits Dr. Washington’s mentorship with the development of a day-long workshop – held before the annual Society of Teachers of Family Medicine (STFM) meeting – on the low and declining rates of Black males in medicine. “We’d planned it as a presentation, and [she heard of it and] helped us expand it,” she said, calling Dr. Washington “warm, welcoming, and encouraging.
“That work and collaboration with her and the others she brought [into the process] have resulted in publications and more presentations and strategy building for diversifying the workforce,” said Dr. Carvajal, assistant professor, director of reproductive health education in family medicine, and codirector of the research section, all in the department of family and community medicine at the University of Maryland, Baltimore.
STFM involvement
Dr. Washington, who says that all or almost all of her mentees are now leaders in their academic institutions and communities, has been instrumental in developing STFM’s mentoring programming and in facilitating the organization’s multifaceted URM Initiative.
She has been active in STFM since the start of her academic career, and in 2009, while serving as assistant program director for the residency program in which she’d trained, she joined two other African American women, Monique Y. Davis-Smith, MD, and Joedrecka Brown-Speights, MD, in cochairing the society’s Group on Minority and Multicultural Health.
It was in this space, that Dr. Washington said she “heard people’s stories of being in major academic institutions and not feeling supported, not being given roadmaps to success, not getting assistance with publishing, or just kind of feeling like an outsider ... of not being pulled in.” Hispanic and African American females, in particular, “were feeling marginalized,” she said.
In 2018, having co-led development of the STFM Quality Mentoring Program for URM faculty, Dr. Washington was asked to join the STFM Foundation and subsequently led the STFM Foundation’s fundraising campaign for a new URM Initiative. She exceeded her goal, increasing support for URM participation in meetings and activities, and then participated in an STFM steering committee to create broader and longer-lasting support for URM faculty, community teachers, and medical students and residents going into academic family medicine.
Increasing the percentage of URM family medicine faculty in leadership positions – and raising awareness of structural barriers to achievement – is one of the current pillars of the URM Initiative.
Navigating the ‘minority tax’
As part of her mentoring, Dr. Washington helps URM physicians navigate the minority tax – a term referring to the uncompensated citizenship tasks that are more often assigned to Black and other URM physicians than to White physicians, and that take time away from scholarship, further perpetuating inequities.
“Some of our young faculty members find themselves thrust into being the diversity and inclusion leaders in their institutions at a level at which they feel little power and little buy-in from [leadership],” she noted.
A commentary written by Dr. Washington and several colleagues on the minority tax as it impacts women – and the need to build a “tax shelter” to make academic medicine a more just environment for URM women – was published earlier this year in the Journal of Women’s Health.
She also answers e-mails and fields phone calls from young URM faculty who are mulling career moves and facing other familiar challenges.
Physicians who are URM, and African American physicians in particular, tend to “get pulled into the [often underserved] communities, into the patient care and community service areas,” Dr. Washington explained. “But unless you convert these projects into scholarship and publications, and unless you serve on a national committee outside of your institution, you’re not going to be promoted.”
Dr. Washington helps junior faculty envision themselves 5-plus years down the road, find what she calls scholarly “passion projects,” and prepare themselves for their next steps.
She helps her mentees navigate other parts of the continuum of unconscious bias and racism as well, from microaggressions from colleagues to overt discrimination from patients.
“I spend countless minutes fielding texts and phone calls from those who need support,” she wrote in a blog post. “They are a constant reminder that I must continue to speak up when I get the opportunity to do so.”
A journey through family medicine, and through bias and racism
Dr. Washington’s early days in medicine included graduating from Meharry Medical College in 1983 and the Mountainside Family Practice Residency Program in 1990. Following 6 years of working in a private practice in rural Maryland, she moved to academia, spending 6 years at East Tennessee State University and 4 years at the UMDNJ–New Jersey Medical School in Newark as an assistant professor of family medicine.
As had happened in rural Maryland, bias and racism have too often lurked during her career as a physician.
“I grew up in Alabama so I was pretty much ready to deal with racism in the South,” Dr. Washington said. “What I was not ready for was coming to the Northeast and seeing that you’re marginalized because you’re not invited into the room. Or if you do go into spaces when you’re the only one, you often don’t feel as welcomed as you thought you might be.”
Her ideas and contributions were too often dismissed, she wrote in a 2020 blog entry posted on her LinkedIn page. And during contract negotiations, “I was not aware of all the information that my White colleagues had. They had the advantage of inside information.”
Dr. Washington says that “it took a village” to make her who she is today: teachers in her segregated schools in Alabama, one of her college professors, her best friend in medical school – and STFM, “where the list [of her own mentors] is long.”
Family physician Joseph E. Scherger champions lifestyle change
Joseph E. Scherger, MD, MPH, is a family physician of 40 years and an avid runner who has carried over his passion for fitness and nutrition into treating patients.
He achieved this through moving to practicing functional medicine a decade ago.
According to Dr. Scherger, functional medicine “shifts the whole approach [to family medicine], recognizing that people’s chronic diseases, like hypertension and diabetes, are completely reversible, and the reason why is because they’re caused by what we eat and how we live.”
Practicing functional medicine continues to make working exciting for Dr. Scherger, he says.
“Now that I’ve shifted into nutrition and lifestyle, I feel like I’m a healer, you know? I’m not just refilling prescriptions anymore,” he said.
The burden of disease brought about by bad nutrition and our profit-hungry food industry is staggering, explained Dr. Scherger, As such, he encourages his patients to adopt lifestyle and nutritional changes that allow the body to become healthy again.
Dr. Scherger’s shift into lifestyle-oriented medicine reflects his own experiences with healthy living, and how it has impacted his life.
“I’m 70 years old, and I’m still running, and I feel the same as when I was 40 or 50.” He has completed 40 marathons, ten 50K and five 50-mile ultramarathon trail runs, and, although retired from long-distance running, he is currently training for an upcoming 5K Thanksgiving turkey trot with his 6-year-old grandson. “He loves it. He’s faster than I am, I have trouble keeping up with him,” he confessed.
Earlier days of career
“I’ve been very blessed to have a career that kept changing every 5-10 years,” he said. “I’ve been able to evolve in a way of shifting my interests from one area to another,” he said.
Dr. Scherger has held many positions in the medical field, from serving in the National Health Service Corps in Dixon, Calif., as a migrant health physician during 1978-1980, to being chair of graduate medical education at Eisenhower Medical Center in Rancho Mirage, Calif., from 2009 to 2015. In between, he taught at the University of California, Davis, and served as founding dean of the Florida State University College of Medicine.
Originally from Ohio, Dr. Scherger was born in 1950 in the small town of Delphos. He graduated from the University of Dayton in 1971 before attending medical school at University of California, Los Angeles, for 4 years. He then completed a family medicine residency and a masters in public health at the University of Washington, Seattle, in 1978.
A resident of the Golden State for 50 years now, Dr. Scherger describes himself as a “true Californian.” Currently, he is in practice at Eisenhower Health in La Quinta, Calif., where he is a core faculty member in the family medicine residency program. He is also a physician under the health center’s Primary Care 365 program, which offers patients regular communication with and increased access to their physicians, emphasizing on telemedicine. He also founded Restore Health – Disease Reversal, a wellness center in Indian Wells, Calif., that focuses on improving patients’ health through changes in nutrition and lifestyle.
Within his medical practice, Dr. Scherger is seen by colleagues as a doctor who not only advocates for his patients, but also goes above and beyond to solve their problems.
“He’s a leader, an advocate, and he inspires others to do what they do,” said Julia L. Martin, MD, a fellow family medicine practitioner who has been working with Dr. Scherger at the Eisenhower Medical Center for the past 5 years. “Being a physician is a very challenging role. You need to be patient and understanding in trying to investigate what the patient wants and work through that to try to find the solution. Dr. Scherger is really good at that.”
Inspiration for writing
Apart from his roles as a physician and faculty member, Dr. Scherger is also an author of two books: “40 Years in Family Medicine” (Scotts Valley, Calif.: CreateSpace, 2014) and “Lean and Fit: A Doctor’s Journey to Healthy Nutrition and Greater Wellness” (Scotts Valley, Calif.: CreateSpace, 2015). He admits to not being a naturally gifted writer, and is more intrinsically skilled at speaking. When he was in medical school, however, a mentor told him that the written word is eternal, and this left a deep impression on him.
“When I think of something that’s worth writing about, that I think will be a contribution to my field, I don’t hesitate to begin to write and develop,” said Dr. Scherger. “ I’ve done some research that I’m proud of, but most of [my writings] are hopefully thoughtful essays to help move my field along, and it’s enormously satisfying to make these contributions.”
Awards and other contributions to family medicine
Dr. Scherger’s contributions to the field of family medicine have been recognized continuously over his career.
He has served on the board of directors of the American Academy of Family Physicians and the American Board of Family Medicine. He is also the recipient of numerous awards, such as being chosen as Family Physician of the Year by the American Academy of Family Physicians and the California Academy of Family Physicians in 1989. From 1988 to 1991, he was a fellow in the Kellogg National Fellowship Program.
While he has managed to reinvent his own practice and medical focus, Dr. Scherger is also concerned with the need to remodel the current state of primary care and family medicine. Regarding challenges facing the field, he mentions the burnout faced by many doctors.
Nowadays, the work of family medicine includes much more than those common acute illnesses – it includes preventive medicine, chronic illness management and mental health counseling. “Yet, somehow, the whole economic and schedule model is based on brief visits,” said Dr. Scherger. “I think the most common reason that a lot of family doctors are burned out is that they’re expected to see so many people a day, and they know they don’t have enough time to do a really good job.”
He elaborated: “The real challenge now for family practice is to be re-engineered to be for the modern age, and not be still stuck in a ‘make an appointment, come and get it’ model of care, which is outdated. So I’ve been working a long time in trying to reinvent primary care. And, you know, it’s hard to make those changes, and it’s still a work in progress.”
One of the ways Dr. Scherger has been working on the primary care model is to help redesign it for the computer age. He started doing telemedicine and online care in 1997, even though other doctors gave him pushback for doing so at the time. Today, in his practice, half of his patients are remote, and under Eisenhower’s Primary Care 365 service, he uses telemedicine to its fullest potential.
Dr. Martin calls Dr. Scherger an “innovator,” adding: “He really tries to find what works for a solution, in different ways – not just one cookie cutter way.”
Despite nearly 50 years of being a doctor, the profession has not gotten any less rewarding for Dr. Scherger, who says he does not intend to retire as long as he is any good at it.
“My mother always said, ‘Joe, your life should be dedicated to making the world a better place.’ I really took that to heart and realized that my greatest joy is to help other people.”
Joseph E. Scherger, MD, MPH, is a family physician of 40 years and an avid runner who has carried over his passion for fitness and nutrition into treating patients.
He achieved this through moving to practicing functional medicine a decade ago.
According to Dr. Scherger, functional medicine “shifts the whole approach [to family medicine], recognizing that people’s chronic diseases, like hypertension and diabetes, are completely reversible, and the reason why is because they’re caused by what we eat and how we live.”
Practicing functional medicine continues to make working exciting for Dr. Scherger, he says.
“Now that I’ve shifted into nutrition and lifestyle, I feel like I’m a healer, you know? I’m not just refilling prescriptions anymore,” he said.
The burden of disease brought about by bad nutrition and our profit-hungry food industry is staggering, explained Dr. Scherger, As such, he encourages his patients to adopt lifestyle and nutritional changes that allow the body to become healthy again.
Dr. Scherger’s shift into lifestyle-oriented medicine reflects his own experiences with healthy living, and how it has impacted his life.
“I’m 70 years old, and I’m still running, and I feel the same as when I was 40 or 50.” He has completed 40 marathons, ten 50K and five 50-mile ultramarathon trail runs, and, although retired from long-distance running, he is currently training for an upcoming 5K Thanksgiving turkey trot with his 6-year-old grandson. “He loves it. He’s faster than I am, I have trouble keeping up with him,” he confessed.
Earlier days of career
“I’ve been very blessed to have a career that kept changing every 5-10 years,” he said. “I’ve been able to evolve in a way of shifting my interests from one area to another,” he said.
Dr. Scherger has held many positions in the medical field, from serving in the National Health Service Corps in Dixon, Calif., as a migrant health physician during 1978-1980, to being chair of graduate medical education at Eisenhower Medical Center in Rancho Mirage, Calif., from 2009 to 2015. In between, he taught at the University of California, Davis, and served as founding dean of the Florida State University College of Medicine.
Originally from Ohio, Dr. Scherger was born in 1950 in the small town of Delphos. He graduated from the University of Dayton in 1971 before attending medical school at University of California, Los Angeles, for 4 years. He then completed a family medicine residency and a masters in public health at the University of Washington, Seattle, in 1978.
A resident of the Golden State for 50 years now, Dr. Scherger describes himself as a “true Californian.” Currently, he is in practice at Eisenhower Health in La Quinta, Calif., where he is a core faculty member in the family medicine residency program. He is also a physician under the health center’s Primary Care 365 program, which offers patients regular communication with and increased access to their physicians, emphasizing on telemedicine. He also founded Restore Health – Disease Reversal, a wellness center in Indian Wells, Calif., that focuses on improving patients’ health through changes in nutrition and lifestyle.
Within his medical practice, Dr. Scherger is seen by colleagues as a doctor who not only advocates for his patients, but also goes above and beyond to solve their problems.
“He’s a leader, an advocate, and he inspires others to do what they do,” said Julia L. Martin, MD, a fellow family medicine practitioner who has been working with Dr. Scherger at the Eisenhower Medical Center for the past 5 years. “Being a physician is a very challenging role. You need to be patient and understanding in trying to investigate what the patient wants and work through that to try to find the solution. Dr. Scherger is really good at that.”
Inspiration for writing
Apart from his roles as a physician and faculty member, Dr. Scherger is also an author of two books: “40 Years in Family Medicine” (Scotts Valley, Calif.: CreateSpace, 2014) and “Lean and Fit: A Doctor’s Journey to Healthy Nutrition and Greater Wellness” (Scotts Valley, Calif.: CreateSpace, 2015). He admits to not being a naturally gifted writer, and is more intrinsically skilled at speaking. When he was in medical school, however, a mentor told him that the written word is eternal, and this left a deep impression on him.
“When I think of something that’s worth writing about, that I think will be a contribution to my field, I don’t hesitate to begin to write and develop,” said Dr. Scherger. “ I’ve done some research that I’m proud of, but most of [my writings] are hopefully thoughtful essays to help move my field along, and it’s enormously satisfying to make these contributions.”
Awards and other contributions to family medicine
Dr. Scherger’s contributions to the field of family medicine have been recognized continuously over his career.
He has served on the board of directors of the American Academy of Family Physicians and the American Board of Family Medicine. He is also the recipient of numerous awards, such as being chosen as Family Physician of the Year by the American Academy of Family Physicians and the California Academy of Family Physicians in 1989. From 1988 to 1991, he was a fellow in the Kellogg National Fellowship Program.
While he has managed to reinvent his own practice and medical focus, Dr. Scherger is also concerned with the need to remodel the current state of primary care and family medicine. Regarding challenges facing the field, he mentions the burnout faced by many doctors.
Nowadays, the work of family medicine includes much more than those common acute illnesses – it includes preventive medicine, chronic illness management and mental health counseling. “Yet, somehow, the whole economic and schedule model is based on brief visits,” said Dr. Scherger. “I think the most common reason that a lot of family doctors are burned out is that they’re expected to see so many people a day, and they know they don’t have enough time to do a really good job.”
He elaborated: “The real challenge now for family practice is to be re-engineered to be for the modern age, and not be still stuck in a ‘make an appointment, come and get it’ model of care, which is outdated. So I’ve been working a long time in trying to reinvent primary care. And, you know, it’s hard to make those changes, and it’s still a work in progress.”
One of the ways Dr. Scherger has been working on the primary care model is to help redesign it for the computer age. He started doing telemedicine and online care in 1997, even though other doctors gave him pushback for doing so at the time. Today, in his practice, half of his patients are remote, and under Eisenhower’s Primary Care 365 service, he uses telemedicine to its fullest potential.
Dr. Martin calls Dr. Scherger an “innovator,” adding: “He really tries to find what works for a solution, in different ways – not just one cookie cutter way.”
Despite nearly 50 years of being a doctor, the profession has not gotten any less rewarding for Dr. Scherger, who says he does not intend to retire as long as he is any good at it.
“My mother always said, ‘Joe, your life should be dedicated to making the world a better place.’ I really took that to heart and realized that my greatest joy is to help other people.”
Joseph E. Scherger, MD, MPH, is a family physician of 40 years and an avid runner who has carried over his passion for fitness and nutrition into treating patients.
He achieved this through moving to practicing functional medicine a decade ago.
According to Dr. Scherger, functional medicine “shifts the whole approach [to family medicine], recognizing that people’s chronic diseases, like hypertension and diabetes, are completely reversible, and the reason why is because they’re caused by what we eat and how we live.”
Practicing functional medicine continues to make working exciting for Dr. Scherger, he says.
“Now that I’ve shifted into nutrition and lifestyle, I feel like I’m a healer, you know? I’m not just refilling prescriptions anymore,” he said.
The burden of disease brought about by bad nutrition and our profit-hungry food industry is staggering, explained Dr. Scherger, As such, he encourages his patients to adopt lifestyle and nutritional changes that allow the body to become healthy again.
Dr. Scherger’s shift into lifestyle-oriented medicine reflects his own experiences with healthy living, and how it has impacted his life.
“I’m 70 years old, and I’m still running, and I feel the same as when I was 40 or 50.” He has completed 40 marathons, ten 50K and five 50-mile ultramarathon trail runs, and, although retired from long-distance running, he is currently training for an upcoming 5K Thanksgiving turkey trot with his 6-year-old grandson. “He loves it. He’s faster than I am, I have trouble keeping up with him,” he confessed.
Earlier days of career
“I’ve been very blessed to have a career that kept changing every 5-10 years,” he said. “I’ve been able to evolve in a way of shifting my interests from one area to another,” he said.
Dr. Scherger has held many positions in the medical field, from serving in the National Health Service Corps in Dixon, Calif., as a migrant health physician during 1978-1980, to being chair of graduate medical education at Eisenhower Medical Center in Rancho Mirage, Calif., from 2009 to 2015. In between, he taught at the University of California, Davis, and served as founding dean of the Florida State University College of Medicine.
Originally from Ohio, Dr. Scherger was born in 1950 in the small town of Delphos. He graduated from the University of Dayton in 1971 before attending medical school at University of California, Los Angeles, for 4 years. He then completed a family medicine residency and a masters in public health at the University of Washington, Seattle, in 1978.
A resident of the Golden State for 50 years now, Dr. Scherger describes himself as a “true Californian.” Currently, he is in practice at Eisenhower Health in La Quinta, Calif., where he is a core faculty member in the family medicine residency program. He is also a physician under the health center’s Primary Care 365 program, which offers patients regular communication with and increased access to their physicians, emphasizing on telemedicine. He also founded Restore Health – Disease Reversal, a wellness center in Indian Wells, Calif., that focuses on improving patients’ health through changes in nutrition and lifestyle.
Within his medical practice, Dr. Scherger is seen by colleagues as a doctor who not only advocates for his patients, but also goes above and beyond to solve their problems.
“He’s a leader, an advocate, and he inspires others to do what they do,” said Julia L. Martin, MD, a fellow family medicine practitioner who has been working with Dr. Scherger at the Eisenhower Medical Center for the past 5 years. “Being a physician is a very challenging role. You need to be patient and understanding in trying to investigate what the patient wants and work through that to try to find the solution. Dr. Scherger is really good at that.”
Inspiration for writing
Apart from his roles as a physician and faculty member, Dr. Scherger is also an author of two books: “40 Years in Family Medicine” (Scotts Valley, Calif.: CreateSpace, 2014) and “Lean and Fit: A Doctor’s Journey to Healthy Nutrition and Greater Wellness” (Scotts Valley, Calif.: CreateSpace, 2015). He admits to not being a naturally gifted writer, and is more intrinsically skilled at speaking. When he was in medical school, however, a mentor told him that the written word is eternal, and this left a deep impression on him.
“When I think of something that’s worth writing about, that I think will be a contribution to my field, I don’t hesitate to begin to write and develop,” said Dr. Scherger. “ I’ve done some research that I’m proud of, but most of [my writings] are hopefully thoughtful essays to help move my field along, and it’s enormously satisfying to make these contributions.”
Awards and other contributions to family medicine
Dr. Scherger’s contributions to the field of family medicine have been recognized continuously over his career.
He has served on the board of directors of the American Academy of Family Physicians and the American Board of Family Medicine. He is also the recipient of numerous awards, such as being chosen as Family Physician of the Year by the American Academy of Family Physicians and the California Academy of Family Physicians in 1989. From 1988 to 1991, he was a fellow in the Kellogg National Fellowship Program.
While he has managed to reinvent his own practice and medical focus, Dr. Scherger is also concerned with the need to remodel the current state of primary care and family medicine. Regarding challenges facing the field, he mentions the burnout faced by many doctors.
Nowadays, the work of family medicine includes much more than those common acute illnesses – it includes preventive medicine, chronic illness management and mental health counseling. “Yet, somehow, the whole economic and schedule model is based on brief visits,” said Dr. Scherger. “I think the most common reason that a lot of family doctors are burned out is that they’re expected to see so many people a day, and they know they don’t have enough time to do a really good job.”
He elaborated: “The real challenge now for family practice is to be re-engineered to be for the modern age, and not be still stuck in a ‘make an appointment, come and get it’ model of care, which is outdated. So I’ve been working a long time in trying to reinvent primary care. And, you know, it’s hard to make those changes, and it’s still a work in progress.”
One of the ways Dr. Scherger has been working on the primary care model is to help redesign it for the computer age. He started doing telemedicine and online care in 1997, even though other doctors gave him pushback for doing so at the time. Today, in his practice, half of his patients are remote, and under Eisenhower’s Primary Care 365 service, he uses telemedicine to its fullest potential.
Dr. Martin calls Dr. Scherger an “innovator,” adding: “He really tries to find what works for a solution, in different ways – not just one cookie cutter way.”
Despite nearly 50 years of being a doctor, the profession has not gotten any less rewarding for Dr. Scherger, who says he does not intend to retire as long as he is any good at it.
“My mother always said, ‘Joe, your life should be dedicated to making the world a better place.’ I really took that to heart and realized that my greatest joy is to help other people.”
FM diversity has increased, but more physicians of color needed
The specialty has been on the path to a racially diverse workforce over the past few decades. Since family medicine is a discipline where doctors look not just at individual patients, but also at the health of the community, some family physicians see working in their specialty as a way to integrate public health with medicine to curb health inequities.
Maria Harsha Wusu, MD, MSEd, is an example of such a family physician.
Dr. Wusu, who is Black and of Japanese descent, chose to practice family medicine to address health in communities of color “which we know in the United States experience health inequities due to structural racism,” she said in an interview.
“It’s a discipline where you look at the health of the entire family and the community and you really look at the environmental, the political, the historical factors that are influencing the health of the community,” explained Dr. Wusu, who is currently the director of health equity at Morehouse School of Medicine, Atlanta. Family physicians are not just asking: “Does a patient have hypertension?” but also whether a patient has access to healthy food, green space and other things.
While the field of family medicine is more diverse in the 21st century than it was at its beginning, Dr. Wusu, who completed her residency in 2016, still faced challenges to achieving her goal of helping communities of color. These specifically stemmed from a lack of diversity among the people in the places where she studied to become a doctor and family physician.
There were moments when Dr. Wusu felt isolated while in medical school and residency, because so few students and faculty members she saw looked like her.
Plus, studies have shown that a racially and ethnically diverse physician workforce is necessary to address health inequities. Research published in 2018 in the Journal of Health Care for the Poor and Underserved, for example, found that underrepresented physicians are more likely to practice in underserved areas than their White peers.
“I went to medical school at a historically White institution, and so there were very few people who identified as what we would say are underrepresented minorities in medicine,” Dr. Wusu explained. “There are issues with both implicit and explicit racism, which I think could be echoed by colleagues across the country that are additional challenges that I think medical students, particularly students of color, experience during what is an already kind of challenging time of medical school and the rigorous training of residency.”
Ada Stewart, MD, FAAFP, president of the American Academy of Family Physicians, echoed Dr. Wusu’s medical school experience. Dr. Stewart, who finished her residency in 2003, said that, out of the 120 students in her graduating medical class, only 10 were Black.
Marginalized groups are still underrepresented in residences. According to data compiled by the Association of American Medical Colleges, only 9.3% of Black people, 10% of Latino, and 0.3% of Native Hawaiian or other Pacific Islanders are residents in family medicine residency programs in 2019-2020. Meanwhile, White residents make up 50.8% of the residency program.
“We really need to do all that we can to increase diversity within our medical schools and residencies,” Dr. Stewart said.
In regards to gender, there has been an increasing number of women in the family medicine specialty. A 2021 study found that the proportion of female physicians in family medicine has grown from 33.9% 2010 to 41.9% in 2020.
“There’s still room for growth and we have to change the system and those structures that created these problems,” noted Dr. Stewart.
The social responsibility of family medicine
The family medicine specialty was born during an era of protest of social change, alongside the Civil Rights Movement, the peace movement, and counterculture protests. In April 1966, 3 years before American Boards approved family practice as a new specialty; the National Commission on Community Health stated that every person should have a personal physician who is the “central point for the integration and continuity of all medical services to his patient.” They also said such physicians should be aware of the “many and varied social, emotional and environmental factors that influence the health of his patient and family.”
While the diversity of family medicine specialty has significantly increased since its beginnings, it continues to lag behind the general U.S. population. A 2018 study published in the Journal of the American Board of Family Medicine, which aggregated data from 1987 to 2017, found that the proportion of Black and Latino board certified family physicians increased from 1.3% to 7.8% and 2.3% to 9.1%, respectively, in 30 years.
A 2014 study included 2 decades worth of data from the U.S. Census and the Association of American Medical Colleges to examine trends in racial and ethnic composition among family medicine residents. The U.S. population increased from 9% to 17% for Latinos, 11.7% to 12.2% for Blacks/African Americans, and 0.87% to 0.89% for Native Americans from 1990 to 2012. Meanwhile, minority representation in family residencies increased 4.9% to 9.4% for Hispanics/Latinos, from 4.2% to 7.9% for Blacks/African Americans, and from 0.7% to 0.9% for Native Americans.
Furthermore, 13.4% of the U.S. population is Black and 18.5% of the population is Latino, while only 7.8% of family medicine residents in 2019 were Black and 9.1% of family medicine residents were Latino, according to a recent study published in Family Medicine.
Recruiting a diverse physician workforce
The AAFP has launched a few initiatives to increase diversity within the specialty. In 2017, the AAFP established the Center for Diversity and Health Equity, a center to address social determinants of health. The EveryONE Project, an initiative that’s part of the AAFP’s center, offers members education and resources to promote workforce diversity. Some of those resources include “The Ladder Program,” an initiative founded by an AAFP member which involves monthly meetings and events for students as young as 9 years old to introduce them to medicine at a young age.
“You can’t see what you don’t see,” noted Dr. Stewart, who is the first Black, female president of the AAFP, and the fourth woman in the role. “I really have seen how important it is to be a mentor and to be out there so that individuals who look like me can see that they too can become a family physician and be that member of their community.”
In addition to The Ladder Program, some other resources aimed at increasing diversity among family physicians include Tour for Diversity in Medicine and the Doctors Back to School Program.
The Tour for Diversity in Medicine involves a team of physicians, other clinicians and students hosting events nationwide for minority students to help them see a path to medicine and other health professions. Meanwhile, the AAFP’s Doctors Back to School Program involves family physicians visiting children at schools, clubs, community organizations, and other places to raise childhood awareness of family medicine and help them see their own potential in health care careers.
Dr. Stewart said these programs have been successful in increasing underrepresented groups.
“We are trying to see how best to measure their success,” the AAFP president said. “Looking at the high numbers of individuals who chose the specialty of family medicine last year is what I would deem a success.”
Dr. Wusu also believes outreach to children in elementary schools is important when it comes to increasing diversity in the family medicine specialty.
One organization that’s proving such outreach is the Student National Medical Association, a branch of the National Medical Association, which is a professional organization of Black physicians. This group’s initiative, the Health Professions Recruitment Exposure Programs, exposes teens to science-related activities while introducing them to careers in health professions. Another SMNA program, called Youth Science Enrichment Program, targets elementary and junior high school students.
Dr. Wusu led a 2019 project that focused on creating a more diverse family medicine residency program by developing and implementing a strategic plan for diversity recruitment, which involved increasing outreach to marginalized groups and revising interviews to minimize bias. In a paper published on the results of the initiative, Dr. Wusu and coauthors noted that, between 2014 and 2017, the total number of underrepresented minority applicants to the Boston Medical Center Family Medicine Residency Program increased by 80%. Before the intervention, the percentage of applicants who were part of an underrepresented group ranged from 0% to 20%. During the intervention, that range jumped to 25% to 50%, according to the paper.
While Dr. Wusu considers these programs to be beneficial for the specialty, she doesn’t believe they should be done in isolation. There should also be efforts to tackle lack of opportunities and structural racism.
“With any inequity, you have to address it on multiple levels,” Dr. Wusu explained. “It’s great that there has been recognition for a need for diversity in family medicine, but my hope is that the call for equity would reach beyond that.”
Fostering an inclusive environment
While family medicine has come a long way with regards to increasing the amount of underrepresented groups in its specialty, Stephen Richmond, MD, MPH, believes there also needs to be a focus on the infrastructure of support to help retain these physicians.
“The problem of diversity within family medicine and largely in other specialties cannot be summed up simply as a matter of poor representation. We must do be better to understand the lived experience of physicians of color, in particular Black physicians, once they arrive in the medical professional environment. Doing so will help institutions to provide that infrastructure of support – including antiracism policies and practices – that will enhance wellness and representation,” said Dr. Richmond, clinical assistant professor of medicine in the division of primary care and population health at Stanford (Calif.) University.
Dr. Wusu also suggested establishing an explicitly antiracist environment. This can be done in multiple ways, including by holding programs that acknowledge the impact of structural racism on both the patients, medical students and faculty, and by educating staff about the history of racism, she said.
Dr. Stewart and Dr. Wusu think the specialty has improved in its representation of minorities, but that it has a “long way to go.”
“I think family medicine is really one of the more inclusive specialties. I mean, it has higher numbers of Black and Brown residents and physicians than other specialties,” Dr. Wusu said. “We still have a very long way to go to be at numbers that match the general population. But I think, in that way, family medicine is a place where a lot of Black and Brown physicians can find a home.”
The specialty has been on the path to a racially diverse workforce over the past few decades. Since family medicine is a discipline where doctors look not just at individual patients, but also at the health of the community, some family physicians see working in their specialty as a way to integrate public health with medicine to curb health inequities.
Maria Harsha Wusu, MD, MSEd, is an example of such a family physician.
Dr. Wusu, who is Black and of Japanese descent, chose to practice family medicine to address health in communities of color “which we know in the United States experience health inequities due to structural racism,” she said in an interview.
“It’s a discipline where you look at the health of the entire family and the community and you really look at the environmental, the political, the historical factors that are influencing the health of the community,” explained Dr. Wusu, who is currently the director of health equity at Morehouse School of Medicine, Atlanta. Family physicians are not just asking: “Does a patient have hypertension?” but also whether a patient has access to healthy food, green space and other things.
While the field of family medicine is more diverse in the 21st century than it was at its beginning, Dr. Wusu, who completed her residency in 2016, still faced challenges to achieving her goal of helping communities of color. These specifically stemmed from a lack of diversity among the people in the places where she studied to become a doctor and family physician.
There were moments when Dr. Wusu felt isolated while in medical school and residency, because so few students and faculty members she saw looked like her.
Plus, studies have shown that a racially and ethnically diverse physician workforce is necessary to address health inequities. Research published in 2018 in the Journal of Health Care for the Poor and Underserved, for example, found that underrepresented physicians are more likely to practice in underserved areas than their White peers.
“I went to medical school at a historically White institution, and so there were very few people who identified as what we would say are underrepresented minorities in medicine,” Dr. Wusu explained. “There are issues with both implicit and explicit racism, which I think could be echoed by colleagues across the country that are additional challenges that I think medical students, particularly students of color, experience during what is an already kind of challenging time of medical school and the rigorous training of residency.”
Ada Stewart, MD, FAAFP, president of the American Academy of Family Physicians, echoed Dr. Wusu’s medical school experience. Dr. Stewart, who finished her residency in 2003, said that, out of the 120 students in her graduating medical class, only 10 were Black.
Marginalized groups are still underrepresented in residences. According to data compiled by the Association of American Medical Colleges, only 9.3% of Black people, 10% of Latino, and 0.3% of Native Hawaiian or other Pacific Islanders are residents in family medicine residency programs in 2019-2020. Meanwhile, White residents make up 50.8% of the residency program.
“We really need to do all that we can to increase diversity within our medical schools and residencies,” Dr. Stewart said.
In regards to gender, there has been an increasing number of women in the family medicine specialty. A 2021 study found that the proportion of female physicians in family medicine has grown from 33.9% 2010 to 41.9% in 2020.
“There’s still room for growth and we have to change the system and those structures that created these problems,” noted Dr. Stewart.
The social responsibility of family medicine
The family medicine specialty was born during an era of protest of social change, alongside the Civil Rights Movement, the peace movement, and counterculture protests. In April 1966, 3 years before American Boards approved family practice as a new specialty; the National Commission on Community Health stated that every person should have a personal physician who is the “central point for the integration and continuity of all medical services to his patient.” They also said such physicians should be aware of the “many and varied social, emotional and environmental factors that influence the health of his patient and family.”
While the diversity of family medicine specialty has significantly increased since its beginnings, it continues to lag behind the general U.S. population. A 2018 study published in the Journal of the American Board of Family Medicine, which aggregated data from 1987 to 2017, found that the proportion of Black and Latino board certified family physicians increased from 1.3% to 7.8% and 2.3% to 9.1%, respectively, in 30 years.
A 2014 study included 2 decades worth of data from the U.S. Census and the Association of American Medical Colleges to examine trends in racial and ethnic composition among family medicine residents. The U.S. population increased from 9% to 17% for Latinos, 11.7% to 12.2% for Blacks/African Americans, and 0.87% to 0.89% for Native Americans from 1990 to 2012. Meanwhile, minority representation in family residencies increased 4.9% to 9.4% for Hispanics/Latinos, from 4.2% to 7.9% for Blacks/African Americans, and from 0.7% to 0.9% for Native Americans.
Furthermore, 13.4% of the U.S. population is Black and 18.5% of the population is Latino, while only 7.8% of family medicine residents in 2019 were Black and 9.1% of family medicine residents were Latino, according to a recent study published in Family Medicine.
Recruiting a diverse physician workforce
The AAFP has launched a few initiatives to increase diversity within the specialty. In 2017, the AAFP established the Center for Diversity and Health Equity, a center to address social determinants of health. The EveryONE Project, an initiative that’s part of the AAFP’s center, offers members education and resources to promote workforce diversity. Some of those resources include “The Ladder Program,” an initiative founded by an AAFP member which involves monthly meetings and events for students as young as 9 years old to introduce them to medicine at a young age.
“You can’t see what you don’t see,” noted Dr. Stewart, who is the first Black, female president of the AAFP, and the fourth woman in the role. “I really have seen how important it is to be a mentor and to be out there so that individuals who look like me can see that they too can become a family physician and be that member of their community.”
In addition to The Ladder Program, some other resources aimed at increasing diversity among family physicians include Tour for Diversity in Medicine and the Doctors Back to School Program.
The Tour for Diversity in Medicine involves a team of physicians, other clinicians and students hosting events nationwide for minority students to help them see a path to medicine and other health professions. Meanwhile, the AAFP’s Doctors Back to School Program involves family physicians visiting children at schools, clubs, community organizations, and other places to raise childhood awareness of family medicine and help them see their own potential in health care careers.
Dr. Stewart said these programs have been successful in increasing underrepresented groups.
“We are trying to see how best to measure their success,” the AAFP president said. “Looking at the high numbers of individuals who chose the specialty of family medicine last year is what I would deem a success.”
Dr. Wusu also believes outreach to children in elementary schools is important when it comes to increasing diversity in the family medicine specialty.
One organization that’s proving such outreach is the Student National Medical Association, a branch of the National Medical Association, which is a professional organization of Black physicians. This group’s initiative, the Health Professions Recruitment Exposure Programs, exposes teens to science-related activities while introducing them to careers in health professions. Another SMNA program, called Youth Science Enrichment Program, targets elementary and junior high school students.
Dr. Wusu led a 2019 project that focused on creating a more diverse family medicine residency program by developing and implementing a strategic plan for diversity recruitment, which involved increasing outreach to marginalized groups and revising interviews to minimize bias. In a paper published on the results of the initiative, Dr. Wusu and coauthors noted that, between 2014 and 2017, the total number of underrepresented minority applicants to the Boston Medical Center Family Medicine Residency Program increased by 80%. Before the intervention, the percentage of applicants who were part of an underrepresented group ranged from 0% to 20%. During the intervention, that range jumped to 25% to 50%, according to the paper.
While Dr. Wusu considers these programs to be beneficial for the specialty, she doesn’t believe they should be done in isolation. There should also be efforts to tackle lack of opportunities and structural racism.
“With any inequity, you have to address it on multiple levels,” Dr. Wusu explained. “It’s great that there has been recognition for a need for diversity in family medicine, but my hope is that the call for equity would reach beyond that.”
Fostering an inclusive environment
While family medicine has come a long way with regards to increasing the amount of underrepresented groups in its specialty, Stephen Richmond, MD, MPH, believes there also needs to be a focus on the infrastructure of support to help retain these physicians.
“The problem of diversity within family medicine and largely in other specialties cannot be summed up simply as a matter of poor representation. We must do be better to understand the lived experience of physicians of color, in particular Black physicians, once they arrive in the medical professional environment. Doing so will help institutions to provide that infrastructure of support – including antiracism policies and practices – that will enhance wellness and representation,” said Dr. Richmond, clinical assistant professor of medicine in the division of primary care and population health at Stanford (Calif.) University.
Dr. Wusu also suggested establishing an explicitly antiracist environment. This can be done in multiple ways, including by holding programs that acknowledge the impact of structural racism on both the patients, medical students and faculty, and by educating staff about the history of racism, she said.
Dr. Stewart and Dr. Wusu think the specialty has improved in its representation of minorities, but that it has a “long way to go.”
“I think family medicine is really one of the more inclusive specialties. I mean, it has higher numbers of Black and Brown residents and physicians than other specialties,” Dr. Wusu said. “We still have a very long way to go to be at numbers that match the general population. But I think, in that way, family medicine is a place where a lot of Black and Brown physicians can find a home.”
The specialty has been on the path to a racially diverse workforce over the past few decades. Since family medicine is a discipline where doctors look not just at individual patients, but also at the health of the community, some family physicians see working in their specialty as a way to integrate public health with medicine to curb health inequities.
Maria Harsha Wusu, MD, MSEd, is an example of such a family physician.
Dr. Wusu, who is Black and of Japanese descent, chose to practice family medicine to address health in communities of color “which we know in the United States experience health inequities due to structural racism,” she said in an interview.
“It’s a discipline where you look at the health of the entire family and the community and you really look at the environmental, the political, the historical factors that are influencing the health of the community,” explained Dr. Wusu, who is currently the director of health equity at Morehouse School of Medicine, Atlanta. Family physicians are not just asking: “Does a patient have hypertension?” but also whether a patient has access to healthy food, green space and other things.
While the field of family medicine is more diverse in the 21st century than it was at its beginning, Dr. Wusu, who completed her residency in 2016, still faced challenges to achieving her goal of helping communities of color. These specifically stemmed from a lack of diversity among the people in the places where she studied to become a doctor and family physician.
There were moments when Dr. Wusu felt isolated while in medical school and residency, because so few students and faculty members she saw looked like her.
Plus, studies have shown that a racially and ethnically diverse physician workforce is necessary to address health inequities. Research published in 2018 in the Journal of Health Care for the Poor and Underserved, for example, found that underrepresented physicians are more likely to practice in underserved areas than their White peers.
“I went to medical school at a historically White institution, and so there were very few people who identified as what we would say are underrepresented minorities in medicine,” Dr. Wusu explained. “There are issues with both implicit and explicit racism, which I think could be echoed by colleagues across the country that are additional challenges that I think medical students, particularly students of color, experience during what is an already kind of challenging time of medical school and the rigorous training of residency.”
Ada Stewart, MD, FAAFP, president of the American Academy of Family Physicians, echoed Dr. Wusu’s medical school experience. Dr. Stewart, who finished her residency in 2003, said that, out of the 120 students in her graduating medical class, only 10 were Black.
Marginalized groups are still underrepresented in residences. According to data compiled by the Association of American Medical Colleges, only 9.3% of Black people, 10% of Latino, and 0.3% of Native Hawaiian or other Pacific Islanders are residents in family medicine residency programs in 2019-2020. Meanwhile, White residents make up 50.8% of the residency program.
“We really need to do all that we can to increase diversity within our medical schools and residencies,” Dr. Stewart said.
In regards to gender, there has been an increasing number of women in the family medicine specialty. A 2021 study found that the proportion of female physicians in family medicine has grown from 33.9% 2010 to 41.9% in 2020.
“There’s still room for growth and we have to change the system and those structures that created these problems,” noted Dr. Stewart.
The social responsibility of family medicine
The family medicine specialty was born during an era of protest of social change, alongside the Civil Rights Movement, the peace movement, and counterculture protests. In April 1966, 3 years before American Boards approved family practice as a new specialty; the National Commission on Community Health stated that every person should have a personal physician who is the “central point for the integration and continuity of all medical services to his patient.” They also said such physicians should be aware of the “many and varied social, emotional and environmental factors that influence the health of his patient and family.”
While the diversity of family medicine specialty has significantly increased since its beginnings, it continues to lag behind the general U.S. population. A 2018 study published in the Journal of the American Board of Family Medicine, which aggregated data from 1987 to 2017, found that the proportion of Black and Latino board certified family physicians increased from 1.3% to 7.8% and 2.3% to 9.1%, respectively, in 30 years.
A 2014 study included 2 decades worth of data from the U.S. Census and the Association of American Medical Colleges to examine trends in racial and ethnic composition among family medicine residents. The U.S. population increased from 9% to 17% for Latinos, 11.7% to 12.2% for Blacks/African Americans, and 0.87% to 0.89% for Native Americans from 1990 to 2012. Meanwhile, minority representation in family residencies increased 4.9% to 9.4% for Hispanics/Latinos, from 4.2% to 7.9% for Blacks/African Americans, and from 0.7% to 0.9% for Native Americans.
Furthermore, 13.4% of the U.S. population is Black and 18.5% of the population is Latino, while only 7.8% of family medicine residents in 2019 were Black and 9.1% of family medicine residents were Latino, according to a recent study published in Family Medicine.
Recruiting a diverse physician workforce
The AAFP has launched a few initiatives to increase diversity within the specialty. In 2017, the AAFP established the Center for Diversity and Health Equity, a center to address social determinants of health. The EveryONE Project, an initiative that’s part of the AAFP’s center, offers members education and resources to promote workforce diversity. Some of those resources include “The Ladder Program,” an initiative founded by an AAFP member which involves monthly meetings and events for students as young as 9 years old to introduce them to medicine at a young age.
“You can’t see what you don’t see,” noted Dr. Stewart, who is the first Black, female president of the AAFP, and the fourth woman in the role. “I really have seen how important it is to be a mentor and to be out there so that individuals who look like me can see that they too can become a family physician and be that member of their community.”
In addition to The Ladder Program, some other resources aimed at increasing diversity among family physicians include Tour for Diversity in Medicine and the Doctors Back to School Program.
The Tour for Diversity in Medicine involves a team of physicians, other clinicians and students hosting events nationwide for minority students to help them see a path to medicine and other health professions. Meanwhile, the AAFP’s Doctors Back to School Program involves family physicians visiting children at schools, clubs, community organizations, and other places to raise childhood awareness of family medicine and help them see their own potential in health care careers.
Dr. Stewart said these programs have been successful in increasing underrepresented groups.
“We are trying to see how best to measure their success,” the AAFP president said. “Looking at the high numbers of individuals who chose the specialty of family medicine last year is what I would deem a success.”
Dr. Wusu also believes outreach to children in elementary schools is important when it comes to increasing diversity in the family medicine specialty.
One organization that’s proving such outreach is the Student National Medical Association, a branch of the National Medical Association, which is a professional organization of Black physicians. This group’s initiative, the Health Professions Recruitment Exposure Programs, exposes teens to science-related activities while introducing them to careers in health professions. Another SMNA program, called Youth Science Enrichment Program, targets elementary and junior high school students.
Dr. Wusu led a 2019 project that focused on creating a more diverse family medicine residency program by developing and implementing a strategic plan for diversity recruitment, which involved increasing outreach to marginalized groups and revising interviews to minimize bias. In a paper published on the results of the initiative, Dr. Wusu and coauthors noted that, between 2014 and 2017, the total number of underrepresented minority applicants to the Boston Medical Center Family Medicine Residency Program increased by 80%. Before the intervention, the percentage of applicants who were part of an underrepresented group ranged from 0% to 20%. During the intervention, that range jumped to 25% to 50%, according to the paper.
While Dr. Wusu considers these programs to be beneficial for the specialty, she doesn’t believe they should be done in isolation. There should also be efforts to tackle lack of opportunities and structural racism.
“With any inequity, you have to address it on multiple levels,” Dr. Wusu explained. “It’s great that there has been recognition for a need for diversity in family medicine, but my hope is that the call for equity would reach beyond that.”
Fostering an inclusive environment
While family medicine has come a long way with regards to increasing the amount of underrepresented groups in its specialty, Stephen Richmond, MD, MPH, believes there also needs to be a focus on the infrastructure of support to help retain these physicians.
“The problem of diversity within family medicine and largely in other specialties cannot be summed up simply as a matter of poor representation. We must do be better to understand the lived experience of physicians of color, in particular Black physicians, once they arrive in the medical professional environment. Doing so will help institutions to provide that infrastructure of support – including antiracism policies and practices – that will enhance wellness and representation,” said Dr. Richmond, clinical assistant professor of medicine in the division of primary care and population health at Stanford (Calif.) University.
Dr. Wusu also suggested establishing an explicitly antiracist environment. This can be done in multiple ways, including by holding programs that acknowledge the impact of structural racism on both the patients, medical students and faculty, and by educating staff about the history of racism, she said.
Dr. Stewart and Dr. Wusu think the specialty has improved in its representation of minorities, but that it has a “long way to go.”
“I think family medicine is really one of the more inclusive specialties. I mean, it has higher numbers of Black and Brown residents and physicians than other specialties,” Dr. Wusu said. “We still have a very long way to go to be at numbers that match the general population. But I think, in that way, family medicine is a place where a lot of Black and Brown physicians can find a home.”
First issue vs. April 2021 issue: Much has changed since 1971
For the first readers of Family Practice News, it started with this: “How safe is the pill? An extensive epidemiologic study being carried out in the United Kingdom by the Royal College of General Practitioners is expected to provide definitive answers to this question within the next few years.”
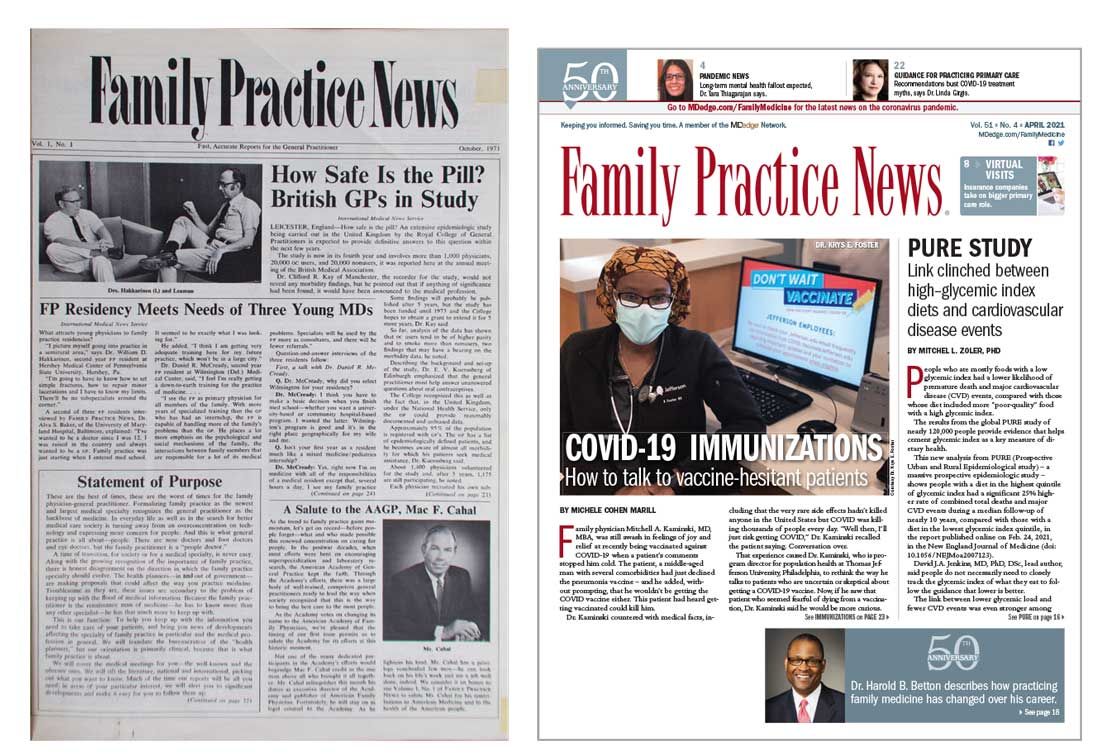
That was the first paragraph of the lead article on the front page of our very first issue, published in October 1971. The report on oral contraceptives, coming from the annual meeting of the British Medical Association in Leicester, largely focused on recruiting – noting that “all women in the study are married” – and data-gathering methods.
That first issue also covered such topics as the effect of “early and frequent coitus” on cervical dysplasia incidence (p. 4), breast cancer in men (p. 13), and treatment of prostate inflammation in patients with impotence (p. 34).
Our April 2021 issue included five articles related to the COVID-19 pandemic, starting on the front page and featuring a photo – a physician sitting at a computer, wearing a mask – and a topic – vaccine-hesitant patients.
Business of medicine today vs. in 1971
At the time of publication of our first issue the United States was in the midst of a 90-day freeze on wages and prices ordered by President Richard Nixon. Two articles in that first issue discussed the subject: “Freeze clouds future of health insurance plans” and “Freeze lets physicians ‘stabilize’ office fees.”
Besides COVID-19, here are some other topics covered in April 2021 but not in 1971: lessons learned from an electronic health records conversion, competition for physicians in the form of a “virtual primary care service” offered by United Healthcare, and the sleep effects of smartphone “addiction.”
Technology, clearly, plays a much larger role in physicians’ lives these days.
Similarities between issues
Not everything has changed, of course. We were informing physicians about heart disease in 1971 with “Primary MD can treat most vascular cases” and “Job satisfaction can help prevent heart disease.”
A look at the latest issue uncovered “Link clinched between high-glycemic index diets and cardiovascular disease events” and “Ultraprocessed ‘healthy’ foods raise cardiovascular disease events risk.” Diabetes is another topic that we have began covering since day one and continue to consider to be relevant to practicing family medicine. “Family attitude key to diabetic’s state” was published in our first issue and “Type 1 diabetes prevention moves toward reality as studies published” ran in our April 2021 issue.
The photos in that first issue, however, present a somewhat jarring counterpoint to our latest issue. The faces that look back from 50 years ago are men’s faces: 29 men, to be exact. There were no photos of women physicians in that issue.
That was not the case in April of 2021. Of the 26 physicians or research scientists who appeared in photos in that issue, 8 were women. Plus, three of those women appeared on the cover.
Among the photos from 1971 were 6 of the 14 founding members of our editorial advisory board, who were, again, all men. Our current board consists of 13 men and 8 women.
Times have changed.
This article was updated 5/27/21.
For the first readers of Family Practice News, it started with this: “How safe is the pill? An extensive epidemiologic study being carried out in the United Kingdom by the Royal College of General Practitioners is expected to provide definitive answers to this question within the next few years.”
That was the first paragraph of the lead article on the front page of our very first issue, published in October 1971. The report on oral contraceptives, coming from the annual meeting of the British Medical Association in Leicester, largely focused on recruiting – noting that “all women in the study are married” – and data-gathering methods.
That first issue also covered such topics as the effect of “early and frequent coitus” on cervical dysplasia incidence (p. 4), breast cancer in men (p. 13), and treatment of prostate inflammation in patients with impotence (p. 34).
Our April 2021 issue included five articles related to the COVID-19 pandemic, starting on the front page and featuring a photo – a physician sitting at a computer, wearing a mask – and a topic – vaccine-hesitant patients.
Business of medicine today vs. in 1971
At the time of publication of our first issue the United States was in the midst of a 90-day freeze on wages and prices ordered by President Richard Nixon. Two articles in that first issue discussed the subject: “Freeze clouds future of health insurance plans” and “Freeze lets physicians ‘stabilize’ office fees.”
Besides COVID-19, here are some other topics covered in April 2021 but not in 1971: lessons learned from an electronic health records conversion, competition for physicians in the form of a “virtual primary care service” offered by United Healthcare, and the sleep effects of smartphone “addiction.”
Technology, clearly, plays a much larger role in physicians’ lives these days.
Similarities between issues
Not everything has changed, of course. We were informing physicians about heart disease in 1971 with “Primary MD can treat most vascular cases” and “Job satisfaction can help prevent heart disease.”
A look at the latest issue uncovered “Link clinched between high-glycemic index diets and cardiovascular disease events” and “Ultraprocessed ‘healthy’ foods raise cardiovascular disease events risk.” Diabetes is another topic that we have began covering since day one and continue to consider to be relevant to practicing family medicine. “Family attitude key to diabetic’s state” was published in our first issue and “Type 1 diabetes prevention moves toward reality as studies published” ran in our April 2021 issue.
The photos in that first issue, however, present a somewhat jarring counterpoint to our latest issue. The faces that look back from 50 years ago are men’s faces: 29 men, to be exact. There were no photos of women physicians in that issue.
That was not the case in April of 2021. Of the 26 physicians or research scientists who appeared in photos in that issue, 8 were women. Plus, three of those women appeared on the cover.
Among the photos from 1971 were 6 of the 14 founding members of our editorial advisory board, who were, again, all men. Our current board consists of 13 men and 8 women.
Times have changed.
This article was updated 5/27/21.
For the first readers of Family Practice News, it started with this: “How safe is the pill? An extensive epidemiologic study being carried out in the United Kingdom by the Royal College of General Practitioners is expected to provide definitive answers to this question within the next few years.”
That was the first paragraph of the lead article on the front page of our very first issue, published in October 1971. The report on oral contraceptives, coming from the annual meeting of the British Medical Association in Leicester, largely focused on recruiting – noting that “all women in the study are married” – and data-gathering methods.
That first issue also covered such topics as the effect of “early and frequent coitus” on cervical dysplasia incidence (p. 4), breast cancer in men (p. 13), and treatment of prostate inflammation in patients with impotence (p. 34).
Our April 2021 issue included five articles related to the COVID-19 pandemic, starting on the front page and featuring a photo – a physician sitting at a computer, wearing a mask – and a topic – vaccine-hesitant patients.
Business of medicine today vs. in 1971
At the time of publication of our first issue the United States was in the midst of a 90-day freeze on wages and prices ordered by President Richard Nixon. Two articles in that first issue discussed the subject: “Freeze clouds future of health insurance plans” and “Freeze lets physicians ‘stabilize’ office fees.”
Besides COVID-19, here are some other topics covered in April 2021 but not in 1971: lessons learned from an electronic health records conversion, competition for physicians in the form of a “virtual primary care service” offered by United Healthcare, and the sleep effects of smartphone “addiction.”
Technology, clearly, plays a much larger role in physicians’ lives these days.
Similarities between issues
Not everything has changed, of course. We were informing physicians about heart disease in 1971 with “Primary MD can treat most vascular cases” and “Job satisfaction can help prevent heart disease.”
A look at the latest issue uncovered “Link clinched between high-glycemic index diets and cardiovascular disease events” and “Ultraprocessed ‘healthy’ foods raise cardiovascular disease events risk.” Diabetes is another topic that we have began covering since day one and continue to consider to be relevant to practicing family medicine. “Family attitude key to diabetic’s state” was published in our first issue and “Type 1 diabetes prevention moves toward reality as studies published” ran in our April 2021 issue.
The photos in that first issue, however, present a somewhat jarring counterpoint to our latest issue. The faces that look back from 50 years ago are men’s faces: 29 men, to be exact. There were no photos of women physicians in that issue.
That was not the case in April of 2021. Of the 26 physicians or research scientists who appeared in photos in that issue, 8 were women. Plus, three of those women appeared on the cover.
Among the photos from 1971 were 6 of the 14 founding members of our editorial advisory board, who were, again, all men. Our current board consists of 13 men and 8 women.
Times have changed.
This article was updated 5/27/21.
Dr. G. Gayle Stephens was a teacher, progressive force, and ‘poet laureate of family medicine’
G. Gayle Stephens, MD, who is roundly regarded as one of the founders of family medicine, gave his talk “Family Medicine as Counterculture” at the Society of Teachers of Family Medicine annual conference in 1979, 10 years after the specialty’s establishment.
The speech was then published, republished 10 years later, and, like many of Dr. Stephen’s other essays and articles, remains very much alive in the minds of practicing family physicians, in the teachings of FP academicians, and in the Google searches of budding FPs.
The late Dr. Stephens saw family medicine as a counterculture within medicine, rooted in social change. In his speech he examined these roots – in reform initiatives in the 1960s, and in certain philosophies and “minority” movements such as agrarianism and the preservation of rural life, utopianism, humanism, consumerism, and feminism.
He also looked forward, challenging the specialty to remain true to itself and its roots – to its belief in “uninhibited access” to medical care for everyone, for instance, and to continual whole-person and family-oriented care – and cautioned against moving to resemble the “rest of the medical bureaucracy.”
“Clearly we have been on the side of change in American life. We have identified ourselves with certain minorities and minority positions ... [and] been counter to many of the dominant forces in society,” Dr. Stephens said in his talk. Family practice “succeeded in the decade just past because we were identified with reforms that are more pervasive and powerful than ourselves.”
The family practice movement has “more in common with [the] counterculture than it does with the dominant scientific medical establishment,” he said.
A teacher and founder of medical education programs
Larry A. Green, MD, who was pursuing his own residency training as Dr. Stephens was leading a department of family practice, said
“It was from this philosophical position that he became a synthesizer and observer and interpreter of what was going on in the development of family medicine,” said Dr. Green, Distinguished Professor and Epperson Zorn Chair for Innovation in Family Medicine and Primary Care at the University of Colorado at Denver, Aurora.
Dr. Stephens, who died at home in 2014 at the age of 85, was “probably the most important person in exposing what I now consider to be a fact – that family medicine was the product of social changes ... of social movements related to women’s rights, civil rights, and social responsibility,” Dr. Green said. “He could recall lessons from the past and forecast the challenges of the future. And there was no one more effective in clarifying the importance of personal [doctor-patient] relationships in family medicine.”
After years of general practice in rural Wichita, Kan., his wife Eula Jean’s hometown, Dr. Stephens founded and led one of the first family medicine residencies at Wesley Hospital in Wichita in 1967. His core principles, as described on today’s Wesley Family Medicine Residency website, included that a family physician consider the whole person, be honest, have a full scope of training including behavioral and mental health, and be “reflective about him/herself ... [learning about] his/her assets, liabilities, foibles, and idiosyncrasies.” Dr. Stephens, who had grown up in rural Ashburn, Mo., later became the founding dean of the School of Primary Medical Care at the University of Alabama in Huntsville and then chaired the department of family practice at the University of Alabama at Birmingham.
A thought leader for family medicine
He held numerous state and national leadership positions, and initiated what became the Keystone Conference Series – an invitational gathering of leaders in family medicine that examined and discuss the specialty’s ongoing development. In 2006, he was elected to the Institute of Medicine of the National Academies of Science.
Dr. Stephens authored a textbook, The Intellectual Basis of Family Medicine (Tucson, Ariz.: Winter Publishing Company, 1982), and authored essays, which Dr. Green said will stand the test of time.
“Some of us refer to him as the poet laureate of family medicine,” Dr. Green noted.
In a 1974 article on clinical wisdom, Dr. Stephens wrote that “it is not enough to determine what condition the patient has, but also what patient has the condition.” In another of these essays, which was published in 1979, Dr. Stephens wrote that “physicians need to keep in touch with their own tradition and with public welfare if they are to be considered moral by the society that sponsors them, and from which they take their strength and privilege.”
These excerpts are featured in an article by John P. Geyman, MD, published in 2011 in Family Medicine, called “G. Gayle Stephens Festschrift”.
A ‘progressive force’
Linda Prine, MD, professor of family and community medicine at the Icahn School of Medicine at Mount Sinai, New York, knows of Dr. Stephens from her teachers. “The people I looked up to when I was a younger physician were quoting his Counterculture article,” she said.
“It’s not that I studied him. But whenever I heard someone speak about the values of family medicine, his name would come up [and] the values of universal health care and community care and putting the patients’ interests first ahead of the insurance companies and being a doctor for the whole family,” Dr. Prine said. Dr. Stephens was a “progressive force that our specialty has not always lived up to.”
Dr. Stephens voiced serious concerns about the impact of managed care in the 1980s and of “gatekeeping,” a practice intended to control access to specialists and reduce costs.
“He was many times not welcomed by family medicine [for his warnings] against the temptations that managed care presented,” said Dr. Green, the founding director of the Robert Graham Center, Washington. “He saw the conflict of interest of being a gatekeeper, how that would erode trust in a personal relationship with your personal doctor.”
“Gayle thought it was a disaster waiting to happen, and it was,” he said, referring to the eventual rejection by the public of barriers to direct access to specialists.
Through the 1990s and more recently, Dr. Stephens expressed frustration with the “medical-industrial complex” and the decline of family medicine after its surge in the 1970s and 1980s, Dr. Green said. “But in my opinion, near the end of his life, he was encouraged by young leaders who he saw grasped the important ideas from the ages.”
Dr. Stephens’ interest in medical education extended to nurses and nurse practitioners (the latter of whom had begun their discipline in the mid-1960s), and to optometrists, for whom he taught a recurring course in “physical diagnosis.”
A listener and proponent of listening
Linda Tompkins, RN, FNP, of Newton, Kan., trained with Dr. Stephens at part of a year-long nurse education program in the early 1970s at Wichita (Kan.) State University, where he was leading the department of family practice (prior to moving to Alabama). “You couldn’t ask too many questions,” she said. “And he never talked down to us, he wasn’t condescending. There were not a lot of doctors like that.”
Dr. Stephens spoke and wrote often about the importance of listening –about how it was vital to the “durable clinical relationship.” It was also vital to his writing and to his impact on the teachers of family medicine, said Dan Ostergaard, MD, who served as a residency director and in various staff leadership positions at the American Academy of Family Physicians, including in its division of education.
“He created a lot of aha moments for me, about where we came from and what we really need to be [as a specialty] and where we need to go,” said Dr. Ostergaard. “To be such a great thinker and a great writer, you have to be a great listener.”
“I can just visualize him,” he said, “leaning back in his chair while we were talking about residency criteria [or other issues], with a half-smile on his face and his reading glasses down his note, smoking his pipe and just looking at all of us, listening.”
Dr. Stephens’ papers are housed in the Center for the History of Family Medicine, a project of the AAFP Foundation.
G. Gayle Stephens, MD, who is roundly regarded as one of the founders of family medicine, gave his talk “Family Medicine as Counterculture” at the Society of Teachers of Family Medicine annual conference in 1979, 10 years after the specialty’s establishment.
The speech was then published, republished 10 years later, and, like many of Dr. Stephen’s other essays and articles, remains very much alive in the minds of practicing family physicians, in the teachings of FP academicians, and in the Google searches of budding FPs.
The late Dr. Stephens saw family medicine as a counterculture within medicine, rooted in social change. In his speech he examined these roots – in reform initiatives in the 1960s, and in certain philosophies and “minority” movements such as agrarianism and the preservation of rural life, utopianism, humanism, consumerism, and feminism.
He also looked forward, challenging the specialty to remain true to itself and its roots – to its belief in “uninhibited access” to medical care for everyone, for instance, and to continual whole-person and family-oriented care – and cautioned against moving to resemble the “rest of the medical bureaucracy.”
“Clearly we have been on the side of change in American life. We have identified ourselves with certain minorities and minority positions ... [and] been counter to many of the dominant forces in society,” Dr. Stephens said in his talk. Family practice “succeeded in the decade just past because we were identified with reforms that are more pervasive and powerful than ourselves.”
The family practice movement has “more in common with [the] counterculture than it does with the dominant scientific medical establishment,” he said.
A teacher and founder of medical education programs
Larry A. Green, MD, who was pursuing his own residency training as Dr. Stephens was leading a department of family practice, said
“It was from this philosophical position that he became a synthesizer and observer and interpreter of what was going on in the development of family medicine,” said Dr. Green, Distinguished Professor and Epperson Zorn Chair for Innovation in Family Medicine and Primary Care at the University of Colorado at Denver, Aurora.
Dr. Stephens, who died at home in 2014 at the age of 85, was “probably the most important person in exposing what I now consider to be a fact – that family medicine was the product of social changes ... of social movements related to women’s rights, civil rights, and social responsibility,” Dr. Green said. “He could recall lessons from the past and forecast the challenges of the future. And there was no one more effective in clarifying the importance of personal [doctor-patient] relationships in family medicine.”
After years of general practice in rural Wichita, Kan., his wife Eula Jean’s hometown, Dr. Stephens founded and led one of the first family medicine residencies at Wesley Hospital in Wichita in 1967. His core principles, as described on today’s Wesley Family Medicine Residency website, included that a family physician consider the whole person, be honest, have a full scope of training including behavioral and mental health, and be “reflective about him/herself ... [learning about] his/her assets, liabilities, foibles, and idiosyncrasies.” Dr. Stephens, who had grown up in rural Ashburn, Mo., later became the founding dean of the School of Primary Medical Care at the University of Alabama in Huntsville and then chaired the department of family practice at the University of Alabama at Birmingham.
A thought leader for family medicine
He held numerous state and national leadership positions, and initiated what became the Keystone Conference Series – an invitational gathering of leaders in family medicine that examined and discuss the specialty’s ongoing development. In 2006, he was elected to the Institute of Medicine of the National Academies of Science.
Dr. Stephens authored a textbook, The Intellectual Basis of Family Medicine (Tucson, Ariz.: Winter Publishing Company, 1982), and authored essays, which Dr. Green said will stand the test of time.
“Some of us refer to him as the poet laureate of family medicine,” Dr. Green noted.
In a 1974 article on clinical wisdom, Dr. Stephens wrote that “it is not enough to determine what condition the patient has, but also what patient has the condition.” In another of these essays, which was published in 1979, Dr. Stephens wrote that “physicians need to keep in touch with their own tradition and with public welfare if they are to be considered moral by the society that sponsors them, and from which they take their strength and privilege.”
These excerpts are featured in an article by John P. Geyman, MD, published in 2011 in Family Medicine, called “G. Gayle Stephens Festschrift”.
A ‘progressive force’
Linda Prine, MD, professor of family and community medicine at the Icahn School of Medicine at Mount Sinai, New York, knows of Dr. Stephens from her teachers. “The people I looked up to when I was a younger physician were quoting his Counterculture article,” she said.
“It’s not that I studied him. But whenever I heard someone speak about the values of family medicine, his name would come up [and] the values of universal health care and community care and putting the patients’ interests first ahead of the insurance companies and being a doctor for the whole family,” Dr. Prine said. Dr. Stephens was a “progressive force that our specialty has not always lived up to.”
Dr. Stephens voiced serious concerns about the impact of managed care in the 1980s and of “gatekeeping,” a practice intended to control access to specialists and reduce costs.
“He was many times not welcomed by family medicine [for his warnings] against the temptations that managed care presented,” said Dr. Green, the founding director of the Robert Graham Center, Washington. “He saw the conflict of interest of being a gatekeeper, how that would erode trust in a personal relationship with your personal doctor.”
“Gayle thought it was a disaster waiting to happen, and it was,” he said, referring to the eventual rejection by the public of barriers to direct access to specialists.
Through the 1990s and more recently, Dr. Stephens expressed frustration with the “medical-industrial complex” and the decline of family medicine after its surge in the 1970s and 1980s, Dr. Green said. “But in my opinion, near the end of his life, he was encouraged by young leaders who he saw grasped the important ideas from the ages.”
Dr. Stephens’ interest in medical education extended to nurses and nurse practitioners (the latter of whom had begun their discipline in the mid-1960s), and to optometrists, for whom he taught a recurring course in “physical diagnosis.”
A listener and proponent of listening
Linda Tompkins, RN, FNP, of Newton, Kan., trained with Dr. Stephens at part of a year-long nurse education program in the early 1970s at Wichita (Kan.) State University, where he was leading the department of family practice (prior to moving to Alabama). “You couldn’t ask too many questions,” she said. “And he never talked down to us, he wasn’t condescending. There were not a lot of doctors like that.”
Dr. Stephens spoke and wrote often about the importance of listening –about how it was vital to the “durable clinical relationship.” It was also vital to his writing and to his impact on the teachers of family medicine, said Dan Ostergaard, MD, who served as a residency director and in various staff leadership positions at the American Academy of Family Physicians, including in its division of education.
“He created a lot of aha moments for me, about where we came from and what we really need to be [as a specialty] and where we need to go,” said Dr. Ostergaard. “To be such a great thinker and a great writer, you have to be a great listener.”
“I can just visualize him,” he said, “leaning back in his chair while we were talking about residency criteria [or other issues], with a half-smile on his face and his reading glasses down his note, smoking his pipe and just looking at all of us, listening.”
Dr. Stephens’ papers are housed in the Center for the History of Family Medicine, a project of the AAFP Foundation.
G. Gayle Stephens, MD, who is roundly regarded as one of the founders of family medicine, gave his talk “Family Medicine as Counterculture” at the Society of Teachers of Family Medicine annual conference in 1979, 10 years after the specialty’s establishment.
The speech was then published, republished 10 years later, and, like many of Dr. Stephen’s other essays and articles, remains very much alive in the minds of practicing family physicians, in the teachings of FP academicians, and in the Google searches of budding FPs.
The late Dr. Stephens saw family medicine as a counterculture within medicine, rooted in social change. In his speech he examined these roots – in reform initiatives in the 1960s, and in certain philosophies and “minority” movements such as agrarianism and the preservation of rural life, utopianism, humanism, consumerism, and feminism.
He also looked forward, challenging the specialty to remain true to itself and its roots – to its belief in “uninhibited access” to medical care for everyone, for instance, and to continual whole-person and family-oriented care – and cautioned against moving to resemble the “rest of the medical bureaucracy.”
“Clearly we have been on the side of change in American life. We have identified ourselves with certain minorities and minority positions ... [and] been counter to many of the dominant forces in society,” Dr. Stephens said in his talk. Family practice “succeeded in the decade just past because we were identified with reforms that are more pervasive and powerful than ourselves.”
The family practice movement has “more in common with [the] counterculture than it does with the dominant scientific medical establishment,” he said.
A teacher and founder of medical education programs
Larry A. Green, MD, who was pursuing his own residency training as Dr. Stephens was leading a department of family practice, said
“It was from this philosophical position that he became a synthesizer and observer and interpreter of what was going on in the development of family medicine,” said Dr. Green, Distinguished Professor and Epperson Zorn Chair for Innovation in Family Medicine and Primary Care at the University of Colorado at Denver, Aurora.
Dr. Stephens, who died at home in 2014 at the age of 85, was “probably the most important person in exposing what I now consider to be a fact – that family medicine was the product of social changes ... of social movements related to women’s rights, civil rights, and social responsibility,” Dr. Green said. “He could recall lessons from the past and forecast the challenges of the future. And there was no one more effective in clarifying the importance of personal [doctor-patient] relationships in family medicine.”
After years of general practice in rural Wichita, Kan., his wife Eula Jean’s hometown, Dr. Stephens founded and led one of the first family medicine residencies at Wesley Hospital in Wichita in 1967. His core principles, as described on today’s Wesley Family Medicine Residency website, included that a family physician consider the whole person, be honest, have a full scope of training including behavioral and mental health, and be “reflective about him/herself ... [learning about] his/her assets, liabilities, foibles, and idiosyncrasies.” Dr. Stephens, who had grown up in rural Ashburn, Mo., later became the founding dean of the School of Primary Medical Care at the University of Alabama in Huntsville and then chaired the department of family practice at the University of Alabama at Birmingham.
A thought leader for family medicine
He held numerous state and national leadership positions, and initiated what became the Keystone Conference Series – an invitational gathering of leaders in family medicine that examined and discuss the specialty’s ongoing development. In 2006, he was elected to the Institute of Medicine of the National Academies of Science.
Dr. Stephens authored a textbook, The Intellectual Basis of Family Medicine (Tucson, Ariz.: Winter Publishing Company, 1982), and authored essays, which Dr. Green said will stand the test of time.
“Some of us refer to him as the poet laureate of family medicine,” Dr. Green noted.
In a 1974 article on clinical wisdom, Dr. Stephens wrote that “it is not enough to determine what condition the patient has, but also what patient has the condition.” In another of these essays, which was published in 1979, Dr. Stephens wrote that “physicians need to keep in touch with their own tradition and with public welfare if they are to be considered moral by the society that sponsors them, and from which they take their strength and privilege.”
These excerpts are featured in an article by John P. Geyman, MD, published in 2011 in Family Medicine, called “G. Gayle Stephens Festschrift”.
A ‘progressive force’
Linda Prine, MD, professor of family and community medicine at the Icahn School of Medicine at Mount Sinai, New York, knows of Dr. Stephens from her teachers. “The people I looked up to when I was a younger physician were quoting his Counterculture article,” she said.
“It’s not that I studied him. But whenever I heard someone speak about the values of family medicine, his name would come up [and] the values of universal health care and community care and putting the patients’ interests first ahead of the insurance companies and being a doctor for the whole family,” Dr. Prine said. Dr. Stephens was a “progressive force that our specialty has not always lived up to.”
Dr. Stephens voiced serious concerns about the impact of managed care in the 1980s and of “gatekeeping,” a practice intended to control access to specialists and reduce costs.
“He was many times not welcomed by family medicine [for his warnings] against the temptations that managed care presented,” said Dr. Green, the founding director of the Robert Graham Center, Washington. “He saw the conflict of interest of being a gatekeeper, how that would erode trust in a personal relationship with your personal doctor.”
“Gayle thought it was a disaster waiting to happen, and it was,” he said, referring to the eventual rejection by the public of barriers to direct access to specialists.
Through the 1990s and more recently, Dr. Stephens expressed frustration with the “medical-industrial complex” and the decline of family medicine after its surge in the 1970s and 1980s, Dr. Green said. “But in my opinion, near the end of his life, he was encouraged by young leaders who he saw grasped the important ideas from the ages.”
Dr. Stephens’ interest in medical education extended to nurses and nurse practitioners (the latter of whom had begun their discipline in the mid-1960s), and to optometrists, for whom he taught a recurring course in “physical diagnosis.”
A listener and proponent of listening
Linda Tompkins, RN, FNP, of Newton, Kan., trained with Dr. Stephens at part of a year-long nurse education program in the early 1970s at Wichita (Kan.) State University, where he was leading the department of family practice (prior to moving to Alabama). “You couldn’t ask too many questions,” she said. “And he never talked down to us, he wasn’t condescending. There were not a lot of doctors like that.”
Dr. Stephens spoke and wrote often about the importance of listening –about how it was vital to the “durable clinical relationship.” It was also vital to his writing and to his impact on the teachers of family medicine, said Dan Ostergaard, MD, who served as a residency director and in various staff leadership positions at the American Academy of Family Physicians, including in its division of education.
“He created a lot of aha moments for me, about where we came from and what we really need to be [as a specialty] and where we need to go,” said Dr. Ostergaard. “To be such a great thinker and a great writer, you have to be a great listener.”
“I can just visualize him,” he said, “leaning back in his chair while we were talking about residency criteria [or other issues], with a half-smile on his face and his reading glasses down his note, smoking his pipe and just looking at all of us, listening.”
Dr. Stephens’ papers are housed in the Center for the History of Family Medicine, a project of the AAFP Foundation.
How family medicine has changed over the past half century
From my residency training graduation date, June 1978, many changes to the family medicine specialty have occurred. These are not due to certification requirements but to the dilution of physician control in health care.
The need to provide more affordable health care by insurance companies while maintaining quality prompted more changes. Additionally, employer-based decisions to change insurance plans, since they were the payer for employer-based health insurance, sometimes yearly, prompted mandatory changes in health insurance.
To achieve hospital-based goals and cost containment the advent and use of hospitalists and the expanded use of physician extenders emerged. While I have some support for these changes, they have redefined elements of the Folsom report, which concluded that every American should have a personal physician to care for them and help integrate them into the health care system.
Changes in the health care delivery system and insurance companies’ need to contain costs, while expanding preventative medicine, coupled with a decreasing number of trained family medicine physicians, represents the background of some of the changes in family medicine over the past 50 years. Managed health care, I believe, was certainly part of the answer to implementing the following recommendation of the Folsom report: every American should have a physician-manager for their health care.
Despite the continual output of new family physicians, a shortage of physicians trained in this specialty remained. Advances in health care, which lengthened life expectancy and the fact that most health insurance companies required its members to name a primary care physician expanded the population requiring primary health care services. This only exacerbated the shortage of family physicians and lowered earning power for doctors practicing family medicine, and it created greater professional demands on family physicians, compared with those in other, more limited-scope specialties. The primary care physician shortage needed to be addressed, prompting a redefinition in the traditional nurse practitioner role.
The expansion of nurse practitioners and physician assistants’ roles
The nursing profession began training advanced-placement nurses and instituted a Doctor of Nurse Practitioner degree. At the same time physician assistants, a program that began while I was a resident, had a further role expansion, including training confined to a single specialty area of medicine. These roles were expanded by state legislators who added them to the list of primary care providers, in some locations, permitting independent practice and placing the physician assistant under the state medical boards and the nurse practitioner and Doctor of Nurse Practitioners under the nursing boards, for expanded regulations and the implementation of the new provider requirements for licensure.
The effects of insurance companies on primary care physicians and patients
When I started practicing medicine the physician was truly the manager of a person’s health care. With the advent of managed health care, that has changed. Physicians are no longer the managers; an uninvited marriage between physician, physician extender, insurance company, employer, and patient jointly controls health care.
Patients are opting for less care at the cheapest price based on incentives driven by cost and abetted by insurance companies and employers. The cost of medications has increased and provider services, coupled with medication and specialty costs have nearly priced many beyond their economic limits to pay. As a result, the patient is not always as committed as their provider to meeting the metrics of their insurance company, especially if that is increasing their out-of-pocket cost.
In addition to usual services, the primary care physician is required to demonstrate the adequacy of services provided through meeting certain practice quality metrics for nearly all insurance carriers, including Medicare and Medicaid. Because meeting these metrics carries a significant economic incentive many practices are retaining fewer noncompliant patients and have opted to bolster their bottom line with the more complaint. This adversely impacts the delivery of primary care to a significant portion of the population.
Patients that reside in poorer neighborhoods, rural areas, as well the marginalized compose a significant portion of many primary care provider’s practices and make up a significant percentage of noncompliant patients. Recognizing that the primary care physician’s overhead is high, coupled with the amount of financial and personal resources put into place to meet metrics, it costs much more to care for the marginalized, poor, and rural populations than easier-to-care for patient groups. This creates a disparity in health care.
A study that revisited the Folsom report concluded that “the 21st century primary care physician must be a true public health professional, forming partnerships and assisting data sharing with community organizations to facilitate healthy changes.” These observations have redefined primary care. This type of medicine is no longer tied to a physician; it is tied to a fairly expensive team of providers, which includes a nurse manager, physician, physician extender, social worker, and in some cases, a pharmacist. The days of mostly solo practitioners are waning and the days of the traditional family medicine residency training requires continuous nuancing, to accommodate the expanded list of practice-related responsibilities assigned to the family doctor.
Low reimbursements rates and high office overhead
The last change I have observed in the practice of family medicine over the past 50 years is a decline in the ratio of reimbursement rate for services to practice expenses. Many practitioners opt out of Medicaid or have certainly curtailed the number of Medicaid recipients on their panel because of its unacceptably low reimbursement rates combined with their high office overhead. The requirements for organizing community resources, including nursing agencies and church and community groups, carry no reimbursement for time invested. The primary care provider is responsible and evaluated on patient outcomes despite the noncompliant behavior of the patient.
What is the future of the primary care physician or provider?
The factors that determine this answer lie in what will be required of the provider and the role of the insurance company in assisting the provider of services. Insurance companies have a responsibility because they receive money to pay for metrics while remaining profitable. They must be brought into the success formula and assist the provider in order for the latter to survive. Currently the primary care provider, in an abundance of caution, is required to seek more specialty services, which drives up the cost of health care. Instead, the insurance company should allow the primary care provider to direct the health care and stop being the manager, approving or disapproving services. In summary, much has happened in family medicine over the past 50 years. The ongoing personal doctor-patient relationship has turned into a doctor-patient-insurance company relationship. The introduction of the third party has created an economic incentive for the physician to meet practice metrics, which sometimes, from the patient’s economic perspective, creates economic hardship.
Some patients enlist a primary care physician in name only but continue to drive their health care by the older model, thanks to the advent of the urgent care centers. These patients see participating in the crisis-care model as resulting in lower out-of-pocket costs. Insurance companies should enlist patient support by expanding their patient education to include the benefits of health, the benefits of meeting quality metrics by their physician, and the necessity of maintaining a compliant doctor-patient relationship. Just as they offer incentives to the primary care practitioner for meeting quality metrics incentives should be offered to those patients that meet quality metrics as well.
In the 21st century, a new model of health care emerged, which includes a primary care practitioner, nurse manager-educator, social worker, and a pharmacist. To deliver quality health care one person can’t be responsible for this burden and do it effectively. Many family practice residencies already use this model and most likely advise their graduates to seek employment where this model exists. Additionally, I am sure that family practice residencies are continually nuanced to achieve the teaching mantra required for successful postgraduate employment and good patient outcomes.
What is the future of family medicine?
The family medicine specialty is represented by a practice that looks at outcome metrics primarily without an incentive for helping the marginalized, poor, homeless, and displaced members of our society.
Urban family medicine, much like what I have practiced in this my 43rd year, is different. My practice community includes every segment of society and my approach lies in the improvement of outcomes from all that I serve. It is my impression that the future of family medicine education must include all members of our society and train residents to effectively care for all, irrespective of economic status, and evolve ways to improve the health outcomes for all.
The federal government, through reimbursement and incentive programs, needs to include such efforts in the model of care for these individuals to reduce the expense burden on the practitioner achieving better practice success and less burnout.
Dr. Betton practices family medicine in Little Rock, Ark. He also serves on the editorial advisory board of Family Practice News.
From my residency training graduation date, June 1978, many changes to the family medicine specialty have occurred. These are not due to certification requirements but to the dilution of physician control in health care.
The need to provide more affordable health care by insurance companies while maintaining quality prompted more changes. Additionally, employer-based decisions to change insurance plans, since they were the payer for employer-based health insurance, sometimes yearly, prompted mandatory changes in health insurance.
To achieve hospital-based goals and cost containment the advent and use of hospitalists and the expanded use of physician extenders emerged. While I have some support for these changes, they have redefined elements of the Folsom report, which concluded that every American should have a personal physician to care for them and help integrate them into the health care system.
Changes in the health care delivery system and insurance companies’ need to contain costs, while expanding preventative medicine, coupled with a decreasing number of trained family medicine physicians, represents the background of some of the changes in family medicine over the past 50 years. Managed health care, I believe, was certainly part of the answer to implementing the following recommendation of the Folsom report: every American should have a physician-manager for their health care.
Despite the continual output of new family physicians, a shortage of physicians trained in this specialty remained. Advances in health care, which lengthened life expectancy and the fact that most health insurance companies required its members to name a primary care physician expanded the population requiring primary health care services. This only exacerbated the shortage of family physicians and lowered earning power for doctors practicing family medicine, and it created greater professional demands on family physicians, compared with those in other, more limited-scope specialties. The primary care physician shortage needed to be addressed, prompting a redefinition in the traditional nurse practitioner role.
The expansion of nurse practitioners and physician assistants’ roles
The nursing profession began training advanced-placement nurses and instituted a Doctor of Nurse Practitioner degree. At the same time physician assistants, a program that began while I was a resident, had a further role expansion, including training confined to a single specialty area of medicine. These roles were expanded by state legislators who added them to the list of primary care providers, in some locations, permitting independent practice and placing the physician assistant under the state medical boards and the nurse practitioner and Doctor of Nurse Practitioners under the nursing boards, for expanded regulations and the implementation of the new provider requirements for licensure.
The effects of insurance companies on primary care physicians and patients
When I started practicing medicine the physician was truly the manager of a person’s health care. With the advent of managed health care, that has changed. Physicians are no longer the managers; an uninvited marriage between physician, physician extender, insurance company, employer, and patient jointly controls health care.
Patients are opting for less care at the cheapest price based on incentives driven by cost and abetted by insurance companies and employers. The cost of medications has increased and provider services, coupled with medication and specialty costs have nearly priced many beyond their economic limits to pay. As a result, the patient is not always as committed as their provider to meeting the metrics of their insurance company, especially if that is increasing their out-of-pocket cost.
In addition to usual services, the primary care physician is required to demonstrate the adequacy of services provided through meeting certain practice quality metrics for nearly all insurance carriers, including Medicare and Medicaid. Because meeting these metrics carries a significant economic incentive many practices are retaining fewer noncompliant patients and have opted to bolster their bottom line with the more complaint. This adversely impacts the delivery of primary care to a significant portion of the population.
Patients that reside in poorer neighborhoods, rural areas, as well the marginalized compose a significant portion of many primary care provider’s practices and make up a significant percentage of noncompliant patients. Recognizing that the primary care physician’s overhead is high, coupled with the amount of financial and personal resources put into place to meet metrics, it costs much more to care for the marginalized, poor, and rural populations than easier-to-care for patient groups. This creates a disparity in health care.
A study that revisited the Folsom report concluded that “the 21st century primary care physician must be a true public health professional, forming partnerships and assisting data sharing with community organizations to facilitate healthy changes.” These observations have redefined primary care. This type of medicine is no longer tied to a physician; it is tied to a fairly expensive team of providers, which includes a nurse manager, physician, physician extender, social worker, and in some cases, a pharmacist. The days of mostly solo practitioners are waning and the days of the traditional family medicine residency training requires continuous nuancing, to accommodate the expanded list of practice-related responsibilities assigned to the family doctor.
Low reimbursements rates and high office overhead
The last change I have observed in the practice of family medicine over the past 50 years is a decline in the ratio of reimbursement rate for services to practice expenses. Many practitioners opt out of Medicaid or have certainly curtailed the number of Medicaid recipients on their panel because of its unacceptably low reimbursement rates combined with their high office overhead. The requirements for organizing community resources, including nursing agencies and church and community groups, carry no reimbursement for time invested. The primary care provider is responsible and evaluated on patient outcomes despite the noncompliant behavior of the patient.
What is the future of the primary care physician or provider?
The factors that determine this answer lie in what will be required of the provider and the role of the insurance company in assisting the provider of services. Insurance companies have a responsibility because they receive money to pay for metrics while remaining profitable. They must be brought into the success formula and assist the provider in order for the latter to survive. Currently the primary care provider, in an abundance of caution, is required to seek more specialty services, which drives up the cost of health care. Instead, the insurance company should allow the primary care provider to direct the health care and stop being the manager, approving or disapproving services. In summary, much has happened in family medicine over the past 50 years. The ongoing personal doctor-patient relationship has turned into a doctor-patient-insurance company relationship. The introduction of the third party has created an economic incentive for the physician to meet practice metrics, which sometimes, from the patient’s economic perspective, creates economic hardship.
Some patients enlist a primary care physician in name only but continue to drive their health care by the older model, thanks to the advent of the urgent care centers. These patients see participating in the crisis-care model as resulting in lower out-of-pocket costs. Insurance companies should enlist patient support by expanding their patient education to include the benefits of health, the benefits of meeting quality metrics by their physician, and the necessity of maintaining a compliant doctor-patient relationship. Just as they offer incentives to the primary care practitioner for meeting quality metrics incentives should be offered to those patients that meet quality metrics as well.
In the 21st century, a new model of health care emerged, which includes a primary care practitioner, nurse manager-educator, social worker, and a pharmacist. To deliver quality health care one person can’t be responsible for this burden and do it effectively. Many family practice residencies already use this model and most likely advise their graduates to seek employment where this model exists. Additionally, I am sure that family practice residencies are continually nuanced to achieve the teaching mantra required for successful postgraduate employment and good patient outcomes.
What is the future of family medicine?
The family medicine specialty is represented by a practice that looks at outcome metrics primarily without an incentive for helping the marginalized, poor, homeless, and displaced members of our society.
Urban family medicine, much like what I have practiced in this my 43rd year, is different. My practice community includes every segment of society and my approach lies in the improvement of outcomes from all that I serve. It is my impression that the future of family medicine education must include all members of our society and train residents to effectively care for all, irrespective of economic status, and evolve ways to improve the health outcomes for all.
The federal government, through reimbursement and incentive programs, needs to include such efforts in the model of care for these individuals to reduce the expense burden on the practitioner achieving better practice success and less burnout.
Dr. Betton practices family medicine in Little Rock, Ark. He also serves on the editorial advisory board of Family Practice News.
From my residency training graduation date, June 1978, many changes to the family medicine specialty have occurred. These are not due to certification requirements but to the dilution of physician control in health care.
The need to provide more affordable health care by insurance companies while maintaining quality prompted more changes. Additionally, employer-based decisions to change insurance plans, since they were the payer for employer-based health insurance, sometimes yearly, prompted mandatory changes in health insurance.
To achieve hospital-based goals and cost containment the advent and use of hospitalists and the expanded use of physician extenders emerged. While I have some support for these changes, they have redefined elements of the Folsom report, which concluded that every American should have a personal physician to care for them and help integrate them into the health care system.
Changes in the health care delivery system and insurance companies’ need to contain costs, while expanding preventative medicine, coupled with a decreasing number of trained family medicine physicians, represents the background of some of the changes in family medicine over the past 50 years. Managed health care, I believe, was certainly part of the answer to implementing the following recommendation of the Folsom report: every American should have a physician-manager for their health care.
Despite the continual output of new family physicians, a shortage of physicians trained in this specialty remained. Advances in health care, which lengthened life expectancy and the fact that most health insurance companies required its members to name a primary care physician expanded the population requiring primary health care services. This only exacerbated the shortage of family physicians and lowered earning power for doctors practicing family medicine, and it created greater professional demands on family physicians, compared with those in other, more limited-scope specialties. The primary care physician shortage needed to be addressed, prompting a redefinition in the traditional nurse practitioner role.
The expansion of nurse practitioners and physician assistants’ roles
The nursing profession began training advanced-placement nurses and instituted a Doctor of Nurse Practitioner degree. At the same time physician assistants, a program that began while I was a resident, had a further role expansion, including training confined to a single specialty area of medicine. These roles were expanded by state legislators who added them to the list of primary care providers, in some locations, permitting independent practice and placing the physician assistant under the state medical boards and the nurse practitioner and Doctor of Nurse Practitioners under the nursing boards, for expanded regulations and the implementation of the new provider requirements for licensure.
The effects of insurance companies on primary care physicians and patients
When I started practicing medicine the physician was truly the manager of a person’s health care. With the advent of managed health care, that has changed. Physicians are no longer the managers; an uninvited marriage between physician, physician extender, insurance company, employer, and patient jointly controls health care.
Patients are opting for less care at the cheapest price based on incentives driven by cost and abetted by insurance companies and employers. The cost of medications has increased and provider services, coupled with medication and specialty costs have nearly priced many beyond their economic limits to pay. As a result, the patient is not always as committed as their provider to meeting the metrics of their insurance company, especially if that is increasing their out-of-pocket cost.
In addition to usual services, the primary care physician is required to demonstrate the adequacy of services provided through meeting certain practice quality metrics for nearly all insurance carriers, including Medicare and Medicaid. Because meeting these metrics carries a significant economic incentive many practices are retaining fewer noncompliant patients and have opted to bolster their bottom line with the more complaint. This adversely impacts the delivery of primary care to a significant portion of the population.
Patients that reside in poorer neighborhoods, rural areas, as well the marginalized compose a significant portion of many primary care provider’s practices and make up a significant percentage of noncompliant patients. Recognizing that the primary care physician’s overhead is high, coupled with the amount of financial and personal resources put into place to meet metrics, it costs much more to care for the marginalized, poor, and rural populations than easier-to-care for patient groups. This creates a disparity in health care.
A study that revisited the Folsom report concluded that “the 21st century primary care physician must be a true public health professional, forming partnerships and assisting data sharing with community organizations to facilitate healthy changes.” These observations have redefined primary care. This type of medicine is no longer tied to a physician; it is tied to a fairly expensive team of providers, which includes a nurse manager, physician, physician extender, social worker, and in some cases, a pharmacist. The days of mostly solo practitioners are waning and the days of the traditional family medicine residency training requires continuous nuancing, to accommodate the expanded list of practice-related responsibilities assigned to the family doctor.
Low reimbursements rates and high office overhead
The last change I have observed in the practice of family medicine over the past 50 years is a decline in the ratio of reimbursement rate for services to practice expenses. Many practitioners opt out of Medicaid or have certainly curtailed the number of Medicaid recipients on their panel because of its unacceptably low reimbursement rates combined with their high office overhead. The requirements for organizing community resources, including nursing agencies and church and community groups, carry no reimbursement for time invested. The primary care provider is responsible and evaluated on patient outcomes despite the noncompliant behavior of the patient.
What is the future of the primary care physician or provider?
The factors that determine this answer lie in what will be required of the provider and the role of the insurance company in assisting the provider of services. Insurance companies have a responsibility because they receive money to pay for metrics while remaining profitable. They must be brought into the success formula and assist the provider in order for the latter to survive. Currently the primary care provider, in an abundance of caution, is required to seek more specialty services, which drives up the cost of health care. Instead, the insurance company should allow the primary care provider to direct the health care and stop being the manager, approving or disapproving services. In summary, much has happened in family medicine over the past 50 years. The ongoing personal doctor-patient relationship has turned into a doctor-patient-insurance company relationship. The introduction of the third party has created an economic incentive for the physician to meet practice metrics, which sometimes, from the patient’s economic perspective, creates economic hardship.
Some patients enlist a primary care physician in name only but continue to drive their health care by the older model, thanks to the advent of the urgent care centers. These patients see participating in the crisis-care model as resulting in lower out-of-pocket costs. Insurance companies should enlist patient support by expanding their patient education to include the benefits of health, the benefits of meeting quality metrics by their physician, and the necessity of maintaining a compliant doctor-patient relationship. Just as they offer incentives to the primary care practitioner for meeting quality metrics incentives should be offered to those patients that meet quality metrics as well.
In the 21st century, a new model of health care emerged, which includes a primary care practitioner, nurse manager-educator, social worker, and a pharmacist. To deliver quality health care one person can’t be responsible for this burden and do it effectively. Many family practice residencies already use this model and most likely advise their graduates to seek employment where this model exists. Additionally, I am sure that family practice residencies are continually nuanced to achieve the teaching mantra required for successful postgraduate employment and good patient outcomes.
What is the future of family medicine?
The family medicine specialty is represented by a practice that looks at outcome metrics primarily without an incentive for helping the marginalized, poor, homeless, and displaced members of our society.
Urban family medicine, much like what I have practiced in this my 43rd year, is different. My practice community includes every segment of society and my approach lies in the improvement of outcomes from all that I serve. It is my impression that the future of family medicine education must include all members of our society and train residents to effectively care for all, irrespective of economic status, and evolve ways to improve the health outcomes for all.
The federal government, through reimbursement and incentive programs, needs to include such efforts in the model of care for these individuals to reduce the expense burden on the practitioner achieving better practice success and less burnout.
Dr. Betton practices family medicine in Little Rock, Ark. He also serves on the editorial advisory board of Family Practice News.