User login
News and Views that Matter to Pediatricians
The leading independent newspaper covering news and commentary in pediatrics.
PCPs Play a Key Role in Managing and Preventing the Atopic March in Children
Primary care physicians (PCPs) play a key role in treating young patients as they progress through the “atopic march” from atopic dermatitis through food allergy, asthma, and allergic rhinitis. They can also help prevent the process from starting.
“The PCP is usually the first clinician a family with concerns about atopic conditions sees, unless they first visit urgent care or an emergency department after an allergic reaction to food. Either way, families rely on their PCP for ongoing guidance,” said Terri F. Brown-Whitehorn, MD, attending physician in the Division of Allergy and Immunology at the Center for Pediatric Eosinophilic Disorders and the Integrative Health Program at Children’s Hospital of Philadelphia.
“The most important thing PCPs can do is know that the atopic march exists, how it progresses over time, and what signs and symptoms to look for,” she told this news organization.
The Atopic March
The atopic march describes the progression of allergic diseases in a child over time, with atopic dermatitis and food allergy in infancy tending to be followed by allergic rhinitis and asthma into later childhood and adulthood.
Although the pathophysiology of the inflammation that precedes atopic dermatitis is unclear, two main hypotheses have been proposed. The first suggests a primary immune dysfunction leads to immunoglobulin E (IgE) sensitization, allergic inflammation, and a secondary disturbance of the epithelial barrier; the second starts with a primary defect in the epithelial barrier that leads to secondary immunologic dysregulation and results in inflammation.
Genetics, infection, hygiene, extreme climate, food allergens, probiotics, aeroallergens, and tobacco smoke are thought to play roles in atopic dermatitis. An estimated 10%-12% of children and 1% of adults in the United States have been reported to have the condition, and the prevalence appears to be increasing. An estimated 85% of cases occur during the first year of life and 95% before the age of 5 years.
“Atopy often, though not always, runs in families, so PCPs should inquire about the history of atopic dermatitis, IgE-mediated food allergies, allergic rhinitis, and asthma in the patient’s siblings, parents, and grandparents,” Brown-Whitehorn said.
Key Educators
PCPs treat the full gamut of atopic conditions and are key educators on ways families can help mitigate their children’s atopic march or stop it before it begins, said Gerald Bell Lee, MD, an allergist and immunologist at Children’s Healthcare of Atlanta and an associate professor in the Division of Allergy and Immunology at Emory University School of Medicine, Atlanta.
“Most parents who bring their infants with eczema to the PCP assume their child ate something that caused their rash. But the relationship between atopic dermatitis, a type of eczema, and food allergy is more complicated,” he added.
Lee said PCPs should explain to their patients what atopic dermatitis is, how it starts and progresses, and how families can help prevent the condition by, for example, introducing allergenic foods to infants at around 4-6 months of age.
Atopic Dermatitis
PCPs should inform parents and other caregivers to wash their hands before moisturizing their child, take care not to contaminate the moisturizer, and bathe their child only when the child is dirty.
“Soap removes protective natural skin oils and increases moisture loss, and exposure to soap and bathing is a main contributor to eczema,” said Lee. “Dry skin loses its protective barrier, allowing outside agents to penetrate and be identified by the immune system.”
“According to one hypothesis, parents may eat food, not wash their hands afterwards, then moisturize their baby. This unhygienic practice spreads food proteins from the adult’s meal, and possibly from contaminants present in the moisturizer, all over the baby’s body,” he added.
Lee said he and his colleagues discourage overbathing babies to minimize the risk for skin injury that begins the atopic march: “New parents are inundated with infant skincare messaging and products. But we need to weigh societal pressures against practicality and ask, ‘Is the child’s skin actually dirty?’ ”
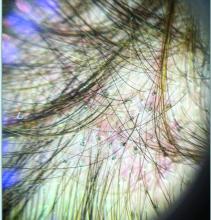
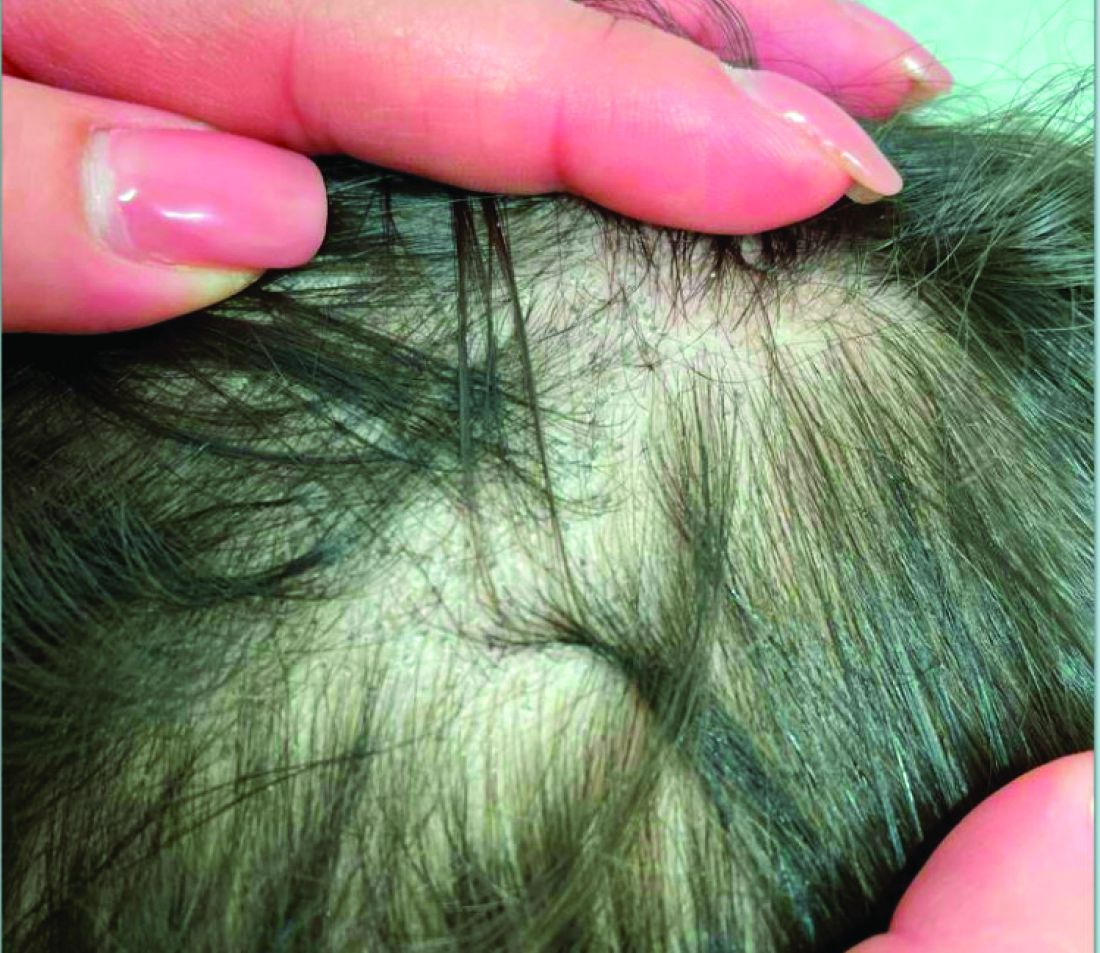
Atopic dermatitis tends to appear on the extensor surfaces, face, and scalp in infants and around arm and leg creases in toddlers and older children. Severe forms of the condition can be more widely distributed on the body, said Aarti P. Pandya, MD, medical director of the Food Allergy Center at Children’s Mercy Kansas City and clinical assistant professor of pediatrics at the University of Missouri-Kansas City School of Medicine, Kansas City, Missouri.
Avoid Triggers, Minimize Flares
Triggers of eczema are varied and common. To help minimize flares, PCPs can encourage caregivers to avoid products with fragrances or dyes, minimize the use of soaps, and completely rinse laundry detergent from clothing and household items. “Advise them to keep fingernails short and control dander, pollen, mold, household chemicals, and tobacco smoke, as well as the child’s stress and anxiety, which can also be a trigger,” Lee said.
“Skin infections from organisms such as staph, herpes, or coxsackie can also exacerbate symptoms,” Brown-Whitehorn added. “PCPs can educate caregivers to avoid all known triggers and give them an ‘action plan’ to carry out when skin flares.”
Food Allergies
Parents may be unaware food allergens can travel far beyond the plate, Lee said. Researchers vacuuming household bedding, carpets, furniture, and other surfaces have detected unnoticeably tiny quantities of allergenic food proteins in ordinary house dust. Touching this dust appears to provide the main exposure to those allergens.
“According to the dual exposure to allergen hypothesis, an infant’s tolerance to antigens occurs through high-dose exposure by mouth, and allergic sensitization occurs through low-dose exposure through the skin,” he said. “As young as four to six months of age, even before eating solid food, a child develops eczema, has a leaky skin barrier, comes in contact with food, and develops a food allergy.”
IgE-mediated food allergies can begin at any age. “Symptoms occur when a food is ingested and the patient develops symptoms including but not limited to urticaria, angioedema, pruritus, flushing, vomiting, diarrhea, coughing, wheezing, difficulty breathing, presyncope, or syncope,” Pandya noted.
In the case of eosinophilic esophagitis, which may also be part of the atopic march, infants and toddlers often have challenging-to-treat symptoms of reflux, while school-age children have reflux and abdominal pain, and adolescents and adults may experience difficulty swallowing and impactions of food or pills, Brown-Whitehorn said.
To differentiate between food allergy and contact dermatitis, Lee suggested providers ask, “ ’Is the rash hives? If yes, is the rash generalized or in a limited area?’ Then consider the statistical probabilities. Skin problems after milk, egg, wheat, soy, peanut, tree nut, fish, shellfish, or sesame are likely due to IgE-mediated food allergy, but after ketchup or strawberry are probably from skin contact.”
Allergic Rhinitis and Asthma
“For asthma, ask about frequency of night cough and symptoms with exercise, laughing, or crying. For allergic rhinitis, look for runny nose, itchy eyes, or sneezing,” Brown-Whitehorn said.
Testing and Monitoring
Assessing the extent of eczema with the Eczema Area and Severity Index or the SCORing Atopic Dermatitis index takes time but may be necessary to obtain insurance coverage for treatments such as biologics.
Avoid ordering IgE food panels, which can result in false positives that can lead to loss of tolerance and nutritional deficiencies; psychological harm from bullying, anxiety, and decreased quality of life; and higher food and healthcare costs, Pandya said.
Treatments
Caregivers may be wary about treatments, and all the three experts this news organization spoke with stressed the importance of educating caregivers about how treatments work and what to expect from them.
“Early and aggressive atopic dermatitis treatment could prevent sensitization to food or aeroallergens, which could help prevent additional atopic diseases, including those on the atopic march,” Pandya said. “Topical steroids are considered first line at any age. Topical phosphodiesterase inhibitors are approved at 3 months of age and above. Topical calcineurin inhibitors are approved at 2 years of age and above. Wet wrap therapy and bleach baths can be effective. Other options include biologic therapy, allergen immunotherapy, and UV therapy.”
“Epinephrine auto-injectors can counteract food reactions. For allergic rhinitis, non-sedating antihistamines, steroidal nasal sprays, and nasal antihistamines help. Asthma treatments include various inhaled medications,” Brown-Whitehorn added.
When to Refer to Specialists
Involving an allergist, dermatologist, pulmonologist, or ear nose throat specialist to the patient’s care team is advisable in more challenging cases.
If a child is younger than 3 months and has moderate to severe atopic dermatitis, an underlying immune defect may be to blame, so an allergy and immunology assessment is warranted, Brown-Whitehorn said. “An allergist can help any child who has recurrent coughing or wheezing avoid the emergency room or hospitalization.”
“In pediatrics, we always try to find the medication, regimen, and avoidance strategies that use the least treatment to provide the best care for each patient,” Brown-Whitehorn added. “Children eat, play, learn, and sleep, and every stage of the atopic march affects each of these activities. As clinicians, we need to be sure that we are helping children make the best of all these activities.”
Brown-Whitehorn reported financial relationships with DBV Technologies and Regeneron Pharmaceuticals. Lee reported financial relationships with Novartis. Pandya reported financial relationships with DBV Technologies, Thermo Fisher Scientific, and Sanofi.
A version of this article first appeared on Medscape.com.
Primary care physicians (PCPs) play a key role in treating young patients as they progress through the “atopic march” from atopic dermatitis through food allergy, asthma, and allergic rhinitis. They can also help prevent the process from starting.
“The PCP is usually the first clinician a family with concerns about atopic conditions sees, unless they first visit urgent care or an emergency department after an allergic reaction to food. Either way, families rely on their PCP for ongoing guidance,” said Terri F. Brown-Whitehorn, MD, attending physician in the Division of Allergy and Immunology at the Center for Pediatric Eosinophilic Disorders and the Integrative Health Program at Children’s Hospital of Philadelphia.
“The most important thing PCPs can do is know that the atopic march exists, how it progresses over time, and what signs and symptoms to look for,” she told this news organization.
The Atopic March
The atopic march describes the progression of allergic diseases in a child over time, with atopic dermatitis and food allergy in infancy tending to be followed by allergic rhinitis and asthma into later childhood and adulthood.
Although the pathophysiology of the inflammation that precedes atopic dermatitis is unclear, two main hypotheses have been proposed. The first suggests a primary immune dysfunction leads to immunoglobulin E (IgE) sensitization, allergic inflammation, and a secondary disturbance of the epithelial barrier; the second starts with a primary defect in the epithelial barrier that leads to secondary immunologic dysregulation and results in inflammation.
Genetics, infection, hygiene, extreme climate, food allergens, probiotics, aeroallergens, and tobacco smoke are thought to play roles in atopic dermatitis. An estimated 10%-12% of children and 1% of adults in the United States have been reported to have the condition, and the prevalence appears to be increasing. An estimated 85% of cases occur during the first year of life and 95% before the age of 5 years.
“Atopy often, though not always, runs in families, so PCPs should inquire about the history of atopic dermatitis, IgE-mediated food allergies, allergic rhinitis, and asthma in the patient’s siblings, parents, and grandparents,” Brown-Whitehorn said.
Key Educators
PCPs treat the full gamut of atopic conditions and are key educators on ways families can help mitigate their children’s atopic march or stop it before it begins, said Gerald Bell Lee, MD, an allergist and immunologist at Children’s Healthcare of Atlanta and an associate professor in the Division of Allergy and Immunology at Emory University School of Medicine, Atlanta.
“Most parents who bring their infants with eczema to the PCP assume their child ate something that caused their rash. But the relationship between atopic dermatitis, a type of eczema, and food allergy is more complicated,” he added.
Lee said PCPs should explain to their patients what atopic dermatitis is, how it starts and progresses, and how families can help prevent the condition by, for example, introducing allergenic foods to infants at around 4-6 months of age.
Atopic Dermatitis
PCPs should inform parents and other caregivers to wash their hands before moisturizing their child, take care not to contaminate the moisturizer, and bathe their child only when the child is dirty.
“Soap removes protective natural skin oils and increases moisture loss, and exposure to soap and bathing is a main contributor to eczema,” said Lee. “Dry skin loses its protective barrier, allowing outside agents to penetrate and be identified by the immune system.”
“According to one hypothesis, parents may eat food, not wash their hands afterwards, then moisturize their baby. This unhygienic practice spreads food proteins from the adult’s meal, and possibly from contaminants present in the moisturizer, all over the baby’s body,” he added.
Lee said he and his colleagues discourage overbathing babies to minimize the risk for skin injury that begins the atopic march: “New parents are inundated with infant skincare messaging and products. But we need to weigh societal pressures against practicality and ask, ‘Is the child’s skin actually dirty?’ ”
Atopic dermatitis tends to appear on the extensor surfaces, face, and scalp in infants and around arm and leg creases in toddlers and older children. Severe forms of the condition can be more widely distributed on the body, said Aarti P. Pandya, MD, medical director of the Food Allergy Center at Children’s Mercy Kansas City and clinical assistant professor of pediatrics at the University of Missouri-Kansas City School of Medicine, Kansas City, Missouri.
Avoid Triggers, Minimize Flares
Triggers of eczema are varied and common. To help minimize flares, PCPs can encourage caregivers to avoid products with fragrances or dyes, minimize the use of soaps, and completely rinse laundry detergent from clothing and household items. “Advise them to keep fingernails short and control dander, pollen, mold, household chemicals, and tobacco smoke, as well as the child’s stress and anxiety, which can also be a trigger,” Lee said.
“Skin infections from organisms such as staph, herpes, or coxsackie can also exacerbate symptoms,” Brown-Whitehorn added. “PCPs can educate caregivers to avoid all known triggers and give them an ‘action plan’ to carry out when skin flares.”
Food Allergies
Parents may be unaware food allergens can travel far beyond the plate, Lee said. Researchers vacuuming household bedding, carpets, furniture, and other surfaces have detected unnoticeably tiny quantities of allergenic food proteins in ordinary house dust. Touching this dust appears to provide the main exposure to those allergens.
“According to the dual exposure to allergen hypothesis, an infant’s tolerance to antigens occurs through high-dose exposure by mouth, and allergic sensitization occurs through low-dose exposure through the skin,” he said. “As young as four to six months of age, even before eating solid food, a child develops eczema, has a leaky skin barrier, comes in contact with food, and develops a food allergy.”
IgE-mediated food allergies can begin at any age. “Symptoms occur when a food is ingested and the patient develops symptoms including but not limited to urticaria, angioedema, pruritus, flushing, vomiting, diarrhea, coughing, wheezing, difficulty breathing, presyncope, or syncope,” Pandya noted.
In the case of eosinophilic esophagitis, which may also be part of the atopic march, infants and toddlers often have challenging-to-treat symptoms of reflux, while school-age children have reflux and abdominal pain, and adolescents and adults may experience difficulty swallowing and impactions of food or pills, Brown-Whitehorn said.
To differentiate between food allergy and contact dermatitis, Lee suggested providers ask, “ ’Is the rash hives? If yes, is the rash generalized or in a limited area?’ Then consider the statistical probabilities. Skin problems after milk, egg, wheat, soy, peanut, tree nut, fish, shellfish, or sesame are likely due to IgE-mediated food allergy, but after ketchup or strawberry are probably from skin contact.”
Allergic Rhinitis and Asthma
“For asthma, ask about frequency of night cough and symptoms with exercise, laughing, or crying. For allergic rhinitis, look for runny nose, itchy eyes, or sneezing,” Brown-Whitehorn said.
Testing and Monitoring
Assessing the extent of eczema with the Eczema Area and Severity Index or the SCORing Atopic Dermatitis index takes time but may be necessary to obtain insurance coverage for treatments such as biologics.
Avoid ordering IgE food panels, which can result in false positives that can lead to loss of tolerance and nutritional deficiencies; psychological harm from bullying, anxiety, and decreased quality of life; and higher food and healthcare costs, Pandya said.
Treatments
Caregivers may be wary about treatments, and all the three experts this news organization spoke with stressed the importance of educating caregivers about how treatments work and what to expect from them.
“Early and aggressive atopic dermatitis treatment could prevent sensitization to food or aeroallergens, which could help prevent additional atopic diseases, including those on the atopic march,” Pandya said. “Topical steroids are considered first line at any age. Topical phosphodiesterase inhibitors are approved at 3 months of age and above. Topical calcineurin inhibitors are approved at 2 years of age and above. Wet wrap therapy and bleach baths can be effective. Other options include biologic therapy, allergen immunotherapy, and UV therapy.”
“Epinephrine auto-injectors can counteract food reactions. For allergic rhinitis, non-sedating antihistamines, steroidal nasal sprays, and nasal antihistamines help. Asthma treatments include various inhaled medications,” Brown-Whitehorn added.
When to Refer to Specialists
Involving an allergist, dermatologist, pulmonologist, or ear nose throat specialist to the patient’s care team is advisable in more challenging cases.
If a child is younger than 3 months and has moderate to severe atopic dermatitis, an underlying immune defect may be to blame, so an allergy and immunology assessment is warranted, Brown-Whitehorn said. “An allergist can help any child who has recurrent coughing or wheezing avoid the emergency room or hospitalization.”
“In pediatrics, we always try to find the medication, regimen, and avoidance strategies that use the least treatment to provide the best care for each patient,” Brown-Whitehorn added. “Children eat, play, learn, and sleep, and every stage of the atopic march affects each of these activities. As clinicians, we need to be sure that we are helping children make the best of all these activities.”
Brown-Whitehorn reported financial relationships with DBV Technologies and Regeneron Pharmaceuticals. Lee reported financial relationships with Novartis. Pandya reported financial relationships with DBV Technologies, Thermo Fisher Scientific, and Sanofi.
A version of this article first appeared on Medscape.com.
Primary care physicians (PCPs) play a key role in treating young patients as they progress through the “atopic march” from atopic dermatitis through food allergy, asthma, and allergic rhinitis. They can also help prevent the process from starting.
“The PCP is usually the first clinician a family with concerns about atopic conditions sees, unless they first visit urgent care or an emergency department after an allergic reaction to food. Either way, families rely on their PCP for ongoing guidance,” said Terri F. Brown-Whitehorn, MD, attending physician in the Division of Allergy and Immunology at the Center for Pediatric Eosinophilic Disorders and the Integrative Health Program at Children’s Hospital of Philadelphia.
“The most important thing PCPs can do is know that the atopic march exists, how it progresses over time, and what signs and symptoms to look for,” she told this news organization.
The Atopic March
The atopic march describes the progression of allergic diseases in a child over time, with atopic dermatitis and food allergy in infancy tending to be followed by allergic rhinitis and asthma into later childhood and adulthood.
Although the pathophysiology of the inflammation that precedes atopic dermatitis is unclear, two main hypotheses have been proposed. The first suggests a primary immune dysfunction leads to immunoglobulin E (IgE) sensitization, allergic inflammation, and a secondary disturbance of the epithelial barrier; the second starts with a primary defect in the epithelial barrier that leads to secondary immunologic dysregulation and results in inflammation.
Genetics, infection, hygiene, extreme climate, food allergens, probiotics, aeroallergens, and tobacco smoke are thought to play roles in atopic dermatitis. An estimated 10%-12% of children and 1% of adults in the United States have been reported to have the condition, and the prevalence appears to be increasing. An estimated 85% of cases occur during the first year of life and 95% before the age of 5 years.
“Atopy often, though not always, runs in families, so PCPs should inquire about the history of atopic dermatitis, IgE-mediated food allergies, allergic rhinitis, and asthma in the patient’s siblings, parents, and grandparents,” Brown-Whitehorn said.
Key Educators
PCPs treat the full gamut of atopic conditions and are key educators on ways families can help mitigate their children’s atopic march or stop it before it begins, said Gerald Bell Lee, MD, an allergist and immunologist at Children’s Healthcare of Atlanta and an associate professor in the Division of Allergy and Immunology at Emory University School of Medicine, Atlanta.
“Most parents who bring their infants with eczema to the PCP assume their child ate something that caused their rash. But the relationship between atopic dermatitis, a type of eczema, and food allergy is more complicated,” he added.
Lee said PCPs should explain to their patients what atopic dermatitis is, how it starts and progresses, and how families can help prevent the condition by, for example, introducing allergenic foods to infants at around 4-6 months of age.
Atopic Dermatitis
PCPs should inform parents and other caregivers to wash their hands before moisturizing their child, take care not to contaminate the moisturizer, and bathe their child only when the child is dirty.
“Soap removes protective natural skin oils and increases moisture loss, and exposure to soap and bathing is a main contributor to eczema,” said Lee. “Dry skin loses its protective barrier, allowing outside agents to penetrate and be identified by the immune system.”
“According to one hypothesis, parents may eat food, not wash their hands afterwards, then moisturize their baby. This unhygienic practice spreads food proteins from the adult’s meal, and possibly from contaminants present in the moisturizer, all over the baby’s body,” he added.
Lee said he and his colleagues discourage overbathing babies to minimize the risk for skin injury that begins the atopic march: “New parents are inundated with infant skincare messaging and products. But we need to weigh societal pressures against practicality and ask, ‘Is the child’s skin actually dirty?’ ”
Atopic dermatitis tends to appear on the extensor surfaces, face, and scalp in infants and around arm and leg creases in toddlers and older children. Severe forms of the condition can be more widely distributed on the body, said Aarti P. Pandya, MD, medical director of the Food Allergy Center at Children’s Mercy Kansas City and clinical assistant professor of pediatrics at the University of Missouri-Kansas City School of Medicine, Kansas City, Missouri.
Avoid Triggers, Minimize Flares
Triggers of eczema are varied and common. To help minimize flares, PCPs can encourage caregivers to avoid products with fragrances or dyes, minimize the use of soaps, and completely rinse laundry detergent from clothing and household items. “Advise them to keep fingernails short and control dander, pollen, mold, household chemicals, and tobacco smoke, as well as the child’s stress and anxiety, which can also be a trigger,” Lee said.
“Skin infections from organisms such as staph, herpes, or coxsackie can also exacerbate symptoms,” Brown-Whitehorn added. “PCPs can educate caregivers to avoid all known triggers and give them an ‘action plan’ to carry out when skin flares.”
Food Allergies
Parents may be unaware food allergens can travel far beyond the plate, Lee said. Researchers vacuuming household bedding, carpets, furniture, and other surfaces have detected unnoticeably tiny quantities of allergenic food proteins in ordinary house dust. Touching this dust appears to provide the main exposure to those allergens.
“According to the dual exposure to allergen hypothesis, an infant’s tolerance to antigens occurs through high-dose exposure by mouth, and allergic sensitization occurs through low-dose exposure through the skin,” he said. “As young as four to six months of age, even before eating solid food, a child develops eczema, has a leaky skin barrier, comes in contact with food, and develops a food allergy.”
IgE-mediated food allergies can begin at any age. “Symptoms occur when a food is ingested and the patient develops symptoms including but not limited to urticaria, angioedema, pruritus, flushing, vomiting, diarrhea, coughing, wheezing, difficulty breathing, presyncope, or syncope,” Pandya noted.
In the case of eosinophilic esophagitis, which may also be part of the atopic march, infants and toddlers often have challenging-to-treat symptoms of reflux, while school-age children have reflux and abdominal pain, and adolescents and adults may experience difficulty swallowing and impactions of food or pills, Brown-Whitehorn said.
To differentiate between food allergy and contact dermatitis, Lee suggested providers ask, “ ’Is the rash hives? If yes, is the rash generalized or in a limited area?’ Then consider the statistical probabilities. Skin problems after milk, egg, wheat, soy, peanut, tree nut, fish, shellfish, or sesame are likely due to IgE-mediated food allergy, but after ketchup or strawberry are probably from skin contact.”
Allergic Rhinitis and Asthma
“For asthma, ask about frequency of night cough and symptoms with exercise, laughing, or crying. For allergic rhinitis, look for runny nose, itchy eyes, or sneezing,” Brown-Whitehorn said.
Testing and Monitoring
Assessing the extent of eczema with the Eczema Area and Severity Index or the SCORing Atopic Dermatitis index takes time but may be necessary to obtain insurance coverage for treatments such as biologics.
Avoid ordering IgE food panels, which can result in false positives that can lead to loss of tolerance and nutritional deficiencies; psychological harm from bullying, anxiety, and decreased quality of life; and higher food and healthcare costs, Pandya said.
Treatments
Caregivers may be wary about treatments, and all the three experts this news organization spoke with stressed the importance of educating caregivers about how treatments work and what to expect from them.
“Early and aggressive atopic dermatitis treatment could prevent sensitization to food or aeroallergens, which could help prevent additional atopic diseases, including those on the atopic march,” Pandya said. “Topical steroids are considered first line at any age. Topical phosphodiesterase inhibitors are approved at 3 months of age and above. Topical calcineurin inhibitors are approved at 2 years of age and above. Wet wrap therapy and bleach baths can be effective. Other options include biologic therapy, allergen immunotherapy, and UV therapy.”
“Epinephrine auto-injectors can counteract food reactions. For allergic rhinitis, non-sedating antihistamines, steroidal nasal sprays, and nasal antihistamines help. Asthma treatments include various inhaled medications,” Brown-Whitehorn added.
When to Refer to Specialists
Involving an allergist, dermatologist, pulmonologist, or ear nose throat specialist to the patient’s care team is advisable in more challenging cases.
If a child is younger than 3 months and has moderate to severe atopic dermatitis, an underlying immune defect may be to blame, so an allergy and immunology assessment is warranted, Brown-Whitehorn said. “An allergist can help any child who has recurrent coughing or wheezing avoid the emergency room or hospitalization.”
“In pediatrics, we always try to find the medication, regimen, and avoidance strategies that use the least treatment to provide the best care for each patient,” Brown-Whitehorn added. “Children eat, play, learn, and sleep, and every stage of the atopic march affects each of these activities. As clinicians, we need to be sure that we are helping children make the best of all these activities.”
Brown-Whitehorn reported financial relationships with DBV Technologies and Regeneron Pharmaceuticals. Lee reported financial relationships with Novartis. Pandya reported financial relationships with DBV Technologies, Thermo Fisher Scientific, and Sanofi.
A version of this article first appeared on Medscape.com.
One-Dose HPV Vaccine Program Would Be Efficient in Canada
In Canada, switching to a one-dose, gender-neutral vaccination program for human papillomavirus (HPV) could use vaccine doses more efficiently and prevent a similar number of cervical cancer cases, compared with a two-dose program, according to a new modeling analysis.
If vaccine protection remains high during the ages of peak sexual activity, all one-dose vaccination options are projected to be “substantially more efficient” than two-dose programs, even in the most pessimistic scenarios, the study authors wrote.
In addition, the scenarios projected the elimination of cervical cancer in Canada between 2032 and 2040. HPV can also lead to oral, throat, and penile cancers, and most are preventable through vaccination.
“The COVID-19 pandemic has impacted HPV vaccination in Canada, particularly among vulnerable population subgroups,” said study author Chantal Sauvageau, MD, a consultant in infectious diseases at the National Institute of Public Health of Quebec and associate professor of social and preventive medicine at the University of Laval, Quebec City, Canada.
Switching to one-dose vaccination would offer potential economic savings and programmatic flexibility, she added. The change also could enable investments aimed at increasing vaccination rates in regions where coverage is suboptimal, as well as in subgroups with a high HPV burden. Such initiatives could mitigate the pandemic’s impact on health programs and reduce inequalities.
The study was published online in CMAJ.
Vaccination Program Changes
Globally, countries have been investigating whether to shift from a two-dose to a one-dose HPV vaccine strategy since the World Health Organization’s Strategic Advisory Group of Experts on Immunization issued a single-dose recommendation in 2022.
In July, Canada’s National Advisory Committee on Immunization (NACI) updated its guidelines to recommend the single-dose approach for ages 9-20 years. The change aligns Canada with 35 other countries, including Australia and the United Kingdom. Canada›s vaccine advisory group still recommends two doses for ages 21-26 years and three doses for patients who are immunocompromised or have HIV.
To help inform new NACI policies, Sauvageau and colleagues modeled several one-dose and two-dose strategies using HPV-ADVISE, an individual-based transmission-dynamic model of HPV infections and diseases. They looked at vaccination programs in Quebec, which has a high HPV vaccine coverage rate of around 85%, and Ontario, which has lower coverage of around 65%.
For one-dose programs, the researchers analyzed noninferior (98% efficacy) and pessimistic (90% efficacy) scenarios and different average vaccine duration periods, including lifelong, 30-year, and 25-year coverage. They compared the scenarios with a two-dose program with 98% efficacy and lifelong duration, estimating the relative reduction in HPV-16 infection and cervical cancer incidence and the number of doses needed to prevent one cervical cancer case.
Overall, the model projected that gender-neutral HPV vaccine programs with either two doses or a noninferior one dose would nearly eliminate HPV-16 infection by 2040-2045 in Quebec and reduce infection by more than 90% in Ontario. Under a one-dose strategy with 90% vaccine efficacy, rebounds in HPV-16 infection would start more than 25-30 years after a switch to a lower-dose strategy, thus providing time for officials to detect any signs of waning efficacy and change policies, if needed, the authors wrote.
In addition, the model projected that a noninferior one-dose, gender-neutral HPV vaccination program would avert a similar number of cervical cancer cases, compared with a two-dose program. The reduction would be about 60% in Quebec and 55% in Ontario, compared with no vaccination. Under the most pessimistic scenario with 25-year vaccine duration, a one-dose program would be slightly less effective in averting cancer: about 3% lower than a two-dose program over 100 years.
All one-dose scenarios were projected to lead to the elimination of cervical cancer in 8-16 years — at fewer than four cervical cancer cases per 100,000 female-years.
One-dose programs would also lead to more efficient use of vaccine doses, with about 800-1000 doses needed to prevent one cervical cancer case in a one-dose program and more than 10,000 incremental doses needed to prevent one additional cervical cancer case in a two-dose program.
What Next?
In Canada, the HPV vaccine is authorized for patients aged 9-45 years. Current immunization coverage among adolescents and young adults varies across provinces and falls below the national target of 90%. In its July 2024 update, NACI estimated that 76% of 14-year-olds of both genders received at least one vaccine dose and that 67% received two doses in 2023. Vaccine uptake was slightly higher among girls than boys.
To boost the coverage rate, shifting to a one-dose schedule could appeal to young people, as well as maintain vaccination efficacy.
“When you look at the studies that have been published worldwide, the effectiveness of one dose of the HPV vaccine is actually quite high,” said Caroline Quach-Thanh, MD, professor of microbiology, infectious diseases, immunology, and pediatrics at the University of Montreal, Quebec, Canada.
Quach-Thanh, who wasn’t involved with this study, previously served as NACI chair and now serves as chair of the Quebec Immunization Committee.
“In terms of prevention of HPV infections that may lead to cancer, whether you give one dose or two doses basically gives you the same amount of protection,” she said.
However, not all physicians agree about the switch in vaccination approaches. In early October, the Federation of Medical Women of Canada released a report with 12 recommendations to increase HPV vaccination rates, including a call for healthcare providers to continue with multidose immunization schedules for now.
“Vaccination is the most powerful action we can take in preventing HPV-related cancers. Canada is falling behind, but we can get back on track if we act quickly,” said Vivien Brown, MD, chair of the group’s HPV Immunization Task Force, chair and cofounder of HPV Prevention Week in Canada, and a past president of the federation.
After the NACI update in July, the task force evaluated the risks and benefits of a single-dose vaccine regimen, she said. They concluded that a multidose schedule should continue at this time because of its proven effectiveness.
“Until more research on the efficacy of a single-dose schedule becomes available, healthcare providers and public health agencies should continue to offer patients a multidose schedule,” said Brown. “This is the only way to ensure individuals are protected against HPV infection and cancer over the long term.”
The study was supported by the Public Health Agency of Canada, the Canadian Institutes of Health Research, the Bill & Melinda Gates Foundation, and Canadian Immunization Research Network. Sauvageau, Quach-Thanh, and Brown declared no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
In Canada, switching to a one-dose, gender-neutral vaccination program for human papillomavirus (HPV) could use vaccine doses more efficiently and prevent a similar number of cervical cancer cases, compared with a two-dose program, according to a new modeling analysis.
If vaccine protection remains high during the ages of peak sexual activity, all one-dose vaccination options are projected to be “substantially more efficient” than two-dose programs, even in the most pessimistic scenarios, the study authors wrote.
In addition, the scenarios projected the elimination of cervical cancer in Canada between 2032 and 2040. HPV can also lead to oral, throat, and penile cancers, and most are preventable through vaccination.
“The COVID-19 pandemic has impacted HPV vaccination in Canada, particularly among vulnerable population subgroups,” said study author Chantal Sauvageau, MD, a consultant in infectious diseases at the National Institute of Public Health of Quebec and associate professor of social and preventive medicine at the University of Laval, Quebec City, Canada.
Switching to one-dose vaccination would offer potential economic savings and programmatic flexibility, she added. The change also could enable investments aimed at increasing vaccination rates in regions where coverage is suboptimal, as well as in subgroups with a high HPV burden. Such initiatives could mitigate the pandemic’s impact on health programs and reduce inequalities.
The study was published online in CMAJ.
Vaccination Program Changes
Globally, countries have been investigating whether to shift from a two-dose to a one-dose HPV vaccine strategy since the World Health Organization’s Strategic Advisory Group of Experts on Immunization issued a single-dose recommendation in 2022.
In July, Canada’s National Advisory Committee on Immunization (NACI) updated its guidelines to recommend the single-dose approach for ages 9-20 years. The change aligns Canada with 35 other countries, including Australia and the United Kingdom. Canada›s vaccine advisory group still recommends two doses for ages 21-26 years and three doses for patients who are immunocompromised or have HIV.
To help inform new NACI policies, Sauvageau and colleagues modeled several one-dose and two-dose strategies using HPV-ADVISE, an individual-based transmission-dynamic model of HPV infections and diseases. They looked at vaccination programs in Quebec, which has a high HPV vaccine coverage rate of around 85%, and Ontario, which has lower coverage of around 65%.
For one-dose programs, the researchers analyzed noninferior (98% efficacy) and pessimistic (90% efficacy) scenarios and different average vaccine duration periods, including lifelong, 30-year, and 25-year coverage. They compared the scenarios with a two-dose program with 98% efficacy and lifelong duration, estimating the relative reduction in HPV-16 infection and cervical cancer incidence and the number of doses needed to prevent one cervical cancer case.
Overall, the model projected that gender-neutral HPV vaccine programs with either two doses or a noninferior one dose would nearly eliminate HPV-16 infection by 2040-2045 in Quebec and reduce infection by more than 90% in Ontario. Under a one-dose strategy with 90% vaccine efficacy, rebounds in HPV-16 infection would start more than 25-30 years after a switch to a lower-dose strategy, thus providing time for officials to detect any signs of waning efficacy and change policies, if needed, the authors wrote.
In addition, the model projected that a noninferior one-dose, gender-neutral HPV vaccination program would avert a similar number of cervical cancer cases, compared with a two-dose program. The reduction would be about 60% in Quebec and 55% in Ontario, compared with no vaccination. Under the most pessimistic scenario with 25-year vaccine duration, a one-dose program would be slightly less effective in averting cancer: about 3% lower than a two-dose program over 100 years.
All one-dose scenarios were projected to lead to the elimination of cervical cancer in 8-16 years — at fewer than four cervical cancer cases per 100,000 female-years.
One-dose programs would also lead to more efficient use of vaccine doses, with about 800-1000 doses needed to prevent one cervical cancer case in a one-dose program and more than 10,000 incremental doses needed to prevent one additional cervical cancer case in a two-dose program.
What Next?
In Canada, the HPV vaccine is authorized for patients aged 9-45 years. Current immunization coverage among adolescents and young adults varies across provinces and falls below the national target of 90%. In its July 2024 update, NACI estimated that 76% of 14-year-olds of both genders received at least one vaccine dose and that 67% received two doses in 2023. Vaccine uptake was slightly higher among girls than boys.
To boost the coverage rate, shifting to a one-dose schedule could appeal to young people, as well as maintain vaccination efficacy.
“When you look at the studies that have been published worldwide, the effectiveness of one dose of the HPV vaccine is actually quite high,” said Caroline Quach-Thanh, MD, professor of microbiology, infectious diseases, immunology, and pediatrics at the University of Montreal, Quebec, Canada.
Quach-Thanh, who wasn’t involved with this study, previously served as NACI chair and now serves as chair of the Quebec Immunization Committee.
“In terms of prevention of HPV infections that may lead to cancer, whether you give one dose or two doses basically gives you the same amount of protection,” she said.
However, not all physicians agree about the switch in vaccination approaches. In early October, the Federation of Medical Women of Canada released a report with 12 recommendations to increase HPV vaccination rates, including a call for healthcare providers to continue with multidose immunization schedules for now.
“Vaccination is the most powerful action we can take in preventing HPV-related cancers. Canada is falling behind, but we can get back on track if we act quickly,” said Vivien Brown, MD, chair of the group’s HPV Immunization Task Force, chair and cofounder of HPV Prevention Week in Canada, and a past president of the federation.
After the NACI update in July, the task force evaluated the risks and benefits of a single-dose vaccine regimen, she said. They concluded that a multidose schedule should continue at this time because of its proven effectiveness.
“Until more research on the efficacy of a single-dose schedule becomes available, healthcare providers and public health agencies should continue to offer patients a multidose schedule,” said Brown. “This is the only way to ensure individuals are protected against HPV infection and cancer over the long term.”
The study was supported by the Public Health Agency of Canada, the Canadian Institutes of Health Research, the Bill & Melinda Gates Foundation, and Canadian Immunization Research Network. Sauvageau, Quach-Thanh, and Brown declared no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
In Canada, switching to a one-dose, gender-neutral vaccination program for human papillomavirus (HPV) could use vaccine doses more efficiently and prevent a similar number of cervical cancer cases, compared with a two-dose program, according to a new modeling analysis.
If vaccine protection remains high during the ages of peak sexual activity, all one-dose vaccination options are projected to be “substantially more efficient” than two-dose programs, even in the most pessimistic scenarios, the study authors wrote.
In addition, the scenarios projected the elimination of cervical cancer in Canada between 2032 and 2040. HPV can also lead to oral, throat, and penile cancers, and most are preventable through vaccination.
“The COVID-19 pandemic has impacted HPV vaccination in Canada, particularly among vulnerable population subgroups,” said study author Chantal Sauvageau, MD, a consultant in infectious diseases at the National Institute of Public Health of Quebec and associate professor of social and preventive medicine at the University of Laval, Quebec City, Canada.
Switching to one-dose vaccination would offer potential economic savings and programmatic flexibility, she added. The change also could enable investments aimed at increasing vaccination rates in regions where coverage is suboptimal, as well as in subgroups with a high HPV burden. Such initiatives could mitigate the pandemic’s impact on health programs and reduce inequalities.
The study was published online in CMAJ.
Vaccination Program Changes
Globally, countries have been investigating whether to shift from a two-dose to a one-dose HPV vaccine strategy since the World Health Organization’s Strategic Advisory Group of Experts on Immunization issued a single-dose recommendation in 2022.
In July, Canada’s National Advisory Committee on Immunization (NACI) updated its guidelines to recommend the single-dose approach for ages 9-20 years. The change aligns Canada with 35 other countries, including Australia and the United Kingdom. Canada›s vaccine advisory group still recommends two doses for ages 21-26 years and three doses for patients who are immunocompromised or have HIV.
To help inform new NACI policies, Sauvageau and colleagues modeled several one-dose and two-dose strategies using HPV-ADVISE, an individual-based transmission-dynamic model of HPV infections and diseases. They looked at vaccination programs in Quebec, which has a high HPV vaccine coverage rate of around 85%, and Ontario, which has lower coverage of around 65%.
For one-dose programs, the researchers analyzed noninferior (98% efficacy) and pessimistic (90% efficacy) scenarios and different average vaccine duration periods, including lifelong, 30-year, and 25-year coverage. They compared the scenarios with a two-dose program with 98% efficacy and lifelong duration, estimating the relative reduction in HPV-16 infection and cervical cancer incidence and the number of doses needed to prevent one cervical cancer case.
Overall, the model projected that gender-neutral HPV vaccine programs with either two doses or a noninferior one dose would nearly eliminate HPV-16 infection by 2040-2045 in Quebec and reduce infection by more than 90% in Ontario. Under a one-dose strategy with 90% vaccine efficacy, rebounds in HPV-16 infection would start more than 25-30 years after a switch to a lower-dose strategy, thus providing time for officials to detect any signs of waning efficacy and change policies, if needed, the authors wrote.
In addition, the model projected that a noninferior one-dose, gender-neutral HPV vaccination program would avert a similar number of cervical cancer cases, compared with a two-dose program. The reduction would be about 60% in Quebec and 55% in Ontario, compared with no vaccination. Under the most pessimistic scenario with 25-year vaccine duration, a one-dose program would be slightly less effective in averting cancer: about 3% lower than a two-dose program over 100 years.
All one-dose scenarios were projected to lead to the elimination of cervical cancer in 8-16 years — at fewer than four cervical cancer cases per 100,000 female-years.
One-dose programs would also lead to more efficient use of vaccine doses, with about 800-1000 doses needed to prevent one cervical cancer case in a one-dose program and more than 10,000 incremental doses needed to prevent one additional cervical cancer case in a two-dose program.
What Next?
In Canada, the HPV vaccine is authorized for patients aged 9-45 years. Current immunization coverage among adolescents and young adults varies across provinces and falls below the national target of 90%. In its July 2024 update, NACI estimated that 76% of 14-year-olds of both genders received at least one vaccine dose and that 67% received two doses in 2023. Vaccine uptake was slightly higher among girls than boys.
To boost the coverage rate, shifting to a one-dose schedule could appeal to young people, as well as maintain vaccination efficacy.
“When you look at the studies that have been published worldwide, the effectiveness of one dose of the HPV vaccine is actually quite high,” said Caroline Quach-Thanh, MD, professor of microbiology, infectious diseases, immunology, and pediatrics at the University of Montreal, Quebec, Canada.
Quach-Thanh, who wasn’t involved with this study, previously served as NACI chair and now serves as chair of the Quebec Immunization Committee.
“In terms of prevention of HPV infections that may lead to cancer, whether you give one dose or two doses basically gives you the same amount of protection,” she said.
However, not all physicians agree about the switch in vaccination approaches. In early October, the Federation of Medical Women of Canada released a report with 12 recommendations to increase HPV vaccination rates, including a call for healthcare providers to continue with multidose immunization schedules for now.
“Vaccination is the most powerful action we can take in preventing HPV-related cancers. Canada is falling behind, but we can get back on track if we act quickly,” said Vivien Brown, MD, chair of the group’s HPV Immunization Task Force, chair and cofounder of HPV Prevention Week in Canada, and a past president of the federation.
After the NACI update in July, the task force evaluated the risks and benefits of a single-dose vaccine regimen, she said. They concluded that a multidose schedule should continue at this time because of its proven effectiveness.
“Until more research on the efficacy of a single-dose schedule becomes available, healthcare providers and public health agencies should continue to offer patients a multidose schedule,” said Brown. “This is the only way to ensure individuals are protected against HPV infection and cancer over the long term.”
The study was supported by the Public Health Agency of Canada, the Canadian Institutes of Health Research, the Bill & Melinda Gates Foundation, and Canadian Immunization Research Network. Sauvageau, Quach-Thanh, and Brown declared no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
FROM CMAJ
Live Rotavirus Vaccine Safe for Newborns of Biologic-Treated Moms With IBD
No adverse events or impairment of the immune system emerged in babies at 7 days, 1 month, and 9 months post vaccination, in findings from a small Canadian study published in Clinical Gastroenterology and Hepatology.
The study found normal extended immune function testing in infants despite third-trimester maternal biologic therapy and regardless of circulating drug levels. The data provide reassurance about live rotavirus vaccination in this population and may also offer insights into the safety of other live vaccines in biologic-exposed individuals, wrote investigators led by gastroenterologist Cynthia H. Seow, MD, a professor in the Cumming School of Medicine at the University of Calgary in Alberta, Canada.
“Despite the well-established safety and effectiveness of non–live vaccination in individuals with IBD, including those on immunomodulators and biologic therapy, vaccine uptake in pregnant women with IBD and their infants remains suboptimal,” Seow said in an interview. This largely arises from maternal and physician concerns regarding transplacental transfer of IBD therapies and their impact on the safety of vaccination.
“These concerns were heightened after reports emerged of five fatal outcomes following the administration of the live Bacille Calmette-Guérin [BCG] vaccine in biologic-exposed infants. However, it had already been reported that inadvertent administration of the live oral rotavirus vaccine, a very different vaccine in terms of target and mechanism of action, in biologic-exposed individuals had not been associated with significant adverse effects,” she said.
They undertook their analysis with the hypothesis that vaccination would carry low risk, although the live oral vaccine is not currently recommended in biologic-exposed infants. “Yet rotavirus is a leading cause of severe, dehydrating diarrhea in children under the age of 5 years globally, and vaccination has led to significant reductions in hospitalizations and mortality,” Seow added.
Provision of the vaccine to anti–tumor necrosis factor (TNF)–exposed infants has been incorporated into the Canadian Public Health and Immunization guidelines, as the majority of the biologic-exposed infants were exposed to anti-TNF agents. “And with collection of further data, we expect that this will be extended to other biologic agent exposure. These data are important to pregnant women with IBD as they help to normalize their care. Pregnancy is difficult enough without having to remember exceptions to care,” Seow said.
“Before some of the studies came out, broad guidelines recommended that live vaccines should not be used in biologic-exposed infants, but this had been thought to be overly zealous and too conservative, and the risk was thought to be low,” said Elizabeth Spencer, MD, an assistant professor of pediatrics in the Division of Pediatric Gastroenterology at the Icahn School of Medicine at Mount Sinai in New York City, in an interview. Spencer was not involved in the Canadian study.
“At our center, we had some moms on biologics during pregnancy who forgot and had their babies vaccinated for rotavirus, and the babies were all fine,” she said.
The safety of this vaccine has been confirmed by several small studies and recently the PIANO Helmsley Global Consensus on Pregnancy and Inflammatory Bowel Disease, which was presented at Digestive Disease Week 2024. The consensus encompasses preconception counseling and the safety of IBD medications during pregnancy and lactation.
“Another concern, however, was that giving a live GI bug like rotavirus to babies might overstimulate their immune systems and provoke IBD,” Spencer added. “While a number of population-based studies in the US and Europe showed that was not the case, at least in the general population, there was a suggestion that, down the road, vaccination might be mildly protective against IBD in some cases.”
She added the caveat that these studies were not done in mothers and their babies with IBD, who might be inherently at greater risk for IBD. “So, a question for future research would be, ‘Is immune stimulation of the gut in IBD moms and their babies a good or a bad thing for their gut?’ ”
Spencer conceded that “the data present a bit of a blurry picture, but I think it’s always better just to vaccinate according to the regular schedule. The current data say there is no added risk, but it would be nice to look specifically at risk in moms with IBD and their children.”
The Study
The prospective cohort study is a substudy of a larger 2023 one that included biologic use in a range of maternal illnesses, not just IBD.
For the current study, Seow and colleagues identified 57 infants born to 52 mothers with IBD attending a pregnancy clinic at the University of Calgary in the period 2019-2023. Almost 81% of the mothers had Crohn’s disease, and the median duration of IBD was 10 years. The median gestational age at delivery was 39 weeks, and almost 60% of deliveries were vaginal. The infants had been exposed in utero to infliximab (n = 21), adalimumab (n = 19), vedolizumab (n = 10), and ustekinumab (n = 7) in the third trimester.
The 57 biologic-exposed infants underwent standardized clinical assessments, drug concentration, and immune function testing. The live oral rotavirus vaccine series was provided to 50 infants, with the first dose at a median of 13 weeks of age. Immunologic assessments validated for age were normal in all infants despite median infliximab concentrations of 6.1 μg/mL (range, 0.4-28.8 μg/mL), adalimumab concentrations of 1.7 μg/mL (range, 0.7-7.9 μg/mL), ustekinumab concentrations of 0.6 μg/mL (range, 0-1.1), and undetectable for vedolizumab at 10.7 weeks of age.
As anticipated, infant immune function was normal regardless of circulating drug levels.
The overall message, said Seow, is “healthy mum equals healthy baby. Be more concerned regarding active inflammation than active medications. In almost all circumstances, treat to target in pregnancy as you would in the nonpregnant state.” She added, however, that further studies are needed to determine the safety and optimal timing of other live vaccines, such as the BCG, in the presence of biologic therapy.
This study was funded by the Alberta Children’s Hospital Research Institute. Seow reported advisory/speaker’s fees for Janssen, AbbVie, Takeda, Pfizer, Fresenius Kabi, Bristol-Myers Squibb, Pharmascience, and Lilly, as well as funding from Alberta Children’s Hospital Research Institute, Crohn’s and Colitis Canada, the Canadian Institutes of Health Research, and Calgary Health Trust, and data safety monitoring from New South Wales Government Health, Australia. Multiple coauthors disclosed similar consulting or speaker relationships with private industry. Spencer had no competing interests with regard to her comments.
A version of this article first appeared on Medscape.com.
No adverse events or impairment of the immune system emerged in babies at 7 days, 1 month, and 9 months post vaccination, in findings from a small Canadian study published in Clinical Gastroenterology and Hepatology.
The study found normal extended immune function testing in infants despite third-trimester maternal biologic therapy and regardless of circulating drug levels. The data provide reassurance about live rotavirus vaccination in this population and may also offer insights into the safety of other live vaccines in biologic-exposed individuals, wrote investigators led by gastroenterologist Cynthia H. Seow, MD, a professor in the Cumming School of Medicine at the University of Calgary in Alberta, Canada.
“Despite the well-established safety and effectiveness of non–live vaccination in individuals with IBD, including those on immunomodulators and biologic therapy, vaccine uptake in pregnant women with IBD and their infants remains suboptimal,” Seow said in an interview. This largely arises from maternal and physician concerns regarding transplacental transfer of IBD therapies and their impact on the safety of vaccination.
“These concerns were heightened after reports emerged of five fatal outcomes following the administration of the live Bacille Calmette-Guérin [BCG] vaccine in biologic-exposed infants. However, it had already been reported that inadvertent administration of the live oral rotavirus vaccine, a very different vaccine in terms of target and mechanism of action, in biologic-exposed individuals had not been associated with significant adverse effects,” she said.
They undertook their analysis with the hypothesis that vaccination would carry low risk, although the live oral vaccine is not currently recommended in biologic-exposed infants. “Yet rotavirus is a leading cause of severe, dehydrating diarrhea in children under the age of 5 years globally, and vaccination has led to significant reductions in hospitalizations and mortality,” Seow added.
Provision of the vaccine to anti–tumor necrosis factor (TNF)–exposed infants has been incorporated into the Canadian Public Health and Immunization guidelines, as the majority of the biologic-exposed infants were exposed to anti-TNF agents. “And with collection of further data, we expect that this will be extended to other biologic agent exposure. These data are important to pregnant women with IBD as they help to normalize their care. Pregnancy is difficult enough without having to remember exceptions to care,” Seow said.
“Before some of the studies came out, broad guidelines recommended that live vaccines should not be used in biologic-exposed infants, but this had been thought to be overly zealous and too conservative, and the risk was thought to be low,” said Elizabeth Spencer, MD, an assistant professor of pediatrics in the Division of Pediatric Gastroenterology at the Icahn School of Medicine at Mount Sinai in New York City, in an interview. Spencer was not involved in the Canadian study.
“At our center, we had some moms on biologics during pregnancy who forgot and had their babies vaccinated for rotavirus, and the babies were all fine,” she said.
The safety of this vaccine has been confirmed by several small studies and recently the PIANO Helmsley Global Consensus on Pregnancy and Inflammatory Bowel Disease, which was presented at Digestive Disease Week 2024. The consensus encompasses preconception counseling and the safety of IBD medications during pregnancy and lactation.
“Another concern, however, was that giving a live GI bug like rotavirus to babies might overstimulate their immune systems and provoke IBD,” Spencer added. “While a number of population-based studies in the US and Europe showed that was not the case, at least in the general population, there was a suggestion that, down the road, vaccination might be mildly protective against IBD in some cases.”
She added the caveat that these studies were not done in mothers and their babies with IBD, who might be inherently at greater risk for IBD. “So, a question for future research would be, ‘Is immune stimulation of the gut in IBD moms and their babies a good or a bad thing for their gut?’ ”
Spencer conceded that “the data present a bit of a blurry picture, but I think it’s always better just to vaccinate according to the regular schedule. The current data say there is no added risk, but it would be nice to look specifically at risk in moms with IBD and their children.”
The Study
The prospective cohort study is a substudy of a larger 2023 one that included biologic use in a range of maternal illnesses, not just IBD.
For the current study, Seow and colleagues identified 57 infants born to 52 mothers with IBD attending a pregnancy clinic at the University of Calgary in the period 2019-2023. Almost 81% of the mothers had Crohn’s disease, and the median duration of IBD was 10 years. The median gestational age at delivery was 39 weeks, and almost 60% of deliveries were vaginal. The infants had been exposed in utero to infliximab (n = 21), adalimumab (n = 19), vedolizumab (n = 10), and ustekinumab (n = 7) in the third trimester.
The 57 biologic-exposed infants underwent standardized clinical assessments, drug concentration, and immune function testing. The live oral rotavirus vaccine series was provided to 50 infants, with the first dose at a median of 13 weeks of age. Immunologic assessments validated for age were normal in all infants despite median infliximab concentrations of 6.1 μg/mL (range, 0.4-28.8 μg/mL), adalimumab concentrations of 1.7 μg/mL (range, 0.7-7.9 μg/mL), ustekinumab concentrations of 0.6 μg/mL (range, 0-1.1), and undetectable for vedolizumab at 10.7 weeks of age.
As anticipated, infant immune function was normal regardless of circulating drug levels.
The overall message, said Seow, is “healthy mum equals healthy baby. Be more concerned regarding active inflammation than active medications. In almost all circumstances, treat to target in pregnancy as you would in the nonpregnant state.” She added, however, that further studies are needed to determine the safety and optimal timing of other live vaccines, such as the BCG, in the presence of biologic therapy.
This study was funded by the Alberta Children’s Hospital Research Institute. Seow reported advisory/speaker’s fees for Janssen, AbbVie, Takeda, Pfizer, Fresenius Kabi, Bristol-Myers Squibb, Pharmascience, and Lilly, as well as funding from Alberta Children’s Hospital Research Institute, Crohn’s and Colitis Canada, the Canadian Institutes of Health Research, and Calgary Health Trust, and data safety monitoring from New South Wales Government Health, Australia. Multiple coauthors disclosed similar consulting or speaker relationships with private industry. Spencer had no competing interests with regard to her comments.
A version of this article first appeared on Medscape.com.
No adverse events or impairment of the immune system emerged in babies at 7 days, 1 month, and 9 months post vaccination, in findings from a small Canadian study published in Clinical Gastroenterology and Hepatology.
The study found normal extended immune function testing in infants despite third-trimester maternal biologic therapy and regardless of circulating drug levels. The data provide reassurance about live rotavirus vaccination in this population and may also offer insights into the safety of other live vaccines in biologic-exposed individuals, wrote investigators led by gastroenterologist Cynthia H. Seow, MD, a professor in the Cumming School of Medicine at the University of Calgary in Alberta, Canada.
“Despite the well-established safety and effectiveness of non–live vaccination in individuals with IBD, including those on immunomodulators and biologic therapy, vaccine uptake in pregnant women with IBD and their infants remains suboptimal,” Seow said in an interview. This largely arises from maternal and physician concerns regarding transplacental transfer of IBD therapies and their impact on the safety of vaccination.
“These concerns were heightened after reports emerged of five fatal outcomes following the administration of the live Bacille Calmette-Guérin [BCG] vaccine in biologic-exposed infants. However, it had already been reported that inadvertent administration of the live oral rotavirus vaccine, a very different vaccine in terms of target and mechanism of action, in biologic-exposed individuals had not been associated with significant adverse effects,” she said.
They undertook their analysis with the hypothesis that vaccination would carry low risk, although the live oral vaccine is not currently recommended in biologic-exposed infants. “Yet rotavirus is a leading cause of severe, dehydrating diarrhea in children under the age of 5 years globally, and vaccination has led to significant reductions in hospitalizations and mortality,” Seow added.
Provision of the vaccine to anti–tumor necrosis factor (TNF)–exposed infants has been incorporated into the Canadian Public Health and Immunization guidelines, as the majority of the biologic-exposed infants were exposed to anti-TNF agents. “And with collection of further data, we expect that this will be extended to other biologic agent exposure. These data are important to pregnant women with IBD as they help to normalize their care. Pregnancy is difficult enough without having to remember exceptions to care,” Seow said.
“Before some of the studies came out, broad guidelines recommended that live vaccines should not be used in biologic-exposed infants, but this had been thought to be overly zealous and too conservative, and the risk was thought to be low,” said Elizabeth Spencer, MD, an assistant professor of pediatrics in the Division of Pediatric Gastroenterology at the Icahn School of Medicine at Mount Sinai in New York City, in an interview. Spencer was not involved in the Canadian study.
“At our center, we had some moms on biologics during pregnancy who forgot and had their babies vaccinated for rotavirus, and the babies were all fine,” she said.
The safety of this vaccine has been confirmed by several small studies and recently the PIANO Helmsley Global Consensus on Pregnancy and Inflammatory Bowel Disease, which was presented at Digestive Disease Week 2024. The consensus encompasses preconception counseling and the safety of IBD medications during pregnancy and lactation.
“Another concern, however, was that giving a live GI bug like rotavirus to babies might overstimulate their immune systems and provoke IBD,” Spencer added. “While a number of population-based studies in the US and Europe showed that was not the case, at least in the general population, there was a suggestion that, down the road, vaccination might be mildly protective against IBD in some cases.”
She added the caveat that these studies were not done in mothers and their babies with IBD, who might be inherently at greater risk for IBD. “So, a question for future research would be, ‘Is immune stimulation of the gut in IBD moms and their babies a good or a bad thing for their gut?’ ”
Spencer conceded that “the data present a bit of a blurry picture, but I think it’s always better just to vaccinate according to the regular schedule. The current data say there is no added risk, but it would be nice to look specifically at risk in moms with IBD and their children.”
The Study
The prospective cohort study is a substudy of a larger 2023 one that included biologic use in a range of maternal illnesses, not just IBD.
For the current study, Seow and colleagues identified 57 infants born to 52 mothers with IBD attending a pregnancy clinic at the University of Calgary in the period 2019-2023. Almost 81% of the mothers had Crohn’s disease, and the median duration of IBD was 10 years. The median gestational age at delivery was 39 weeks, and almost 60% of deliveries were vaginal. The infants had been exposed in utero to infliximab (n = 21), adalimumab (n = 19), vedolizumab (n = 10), and ustekinumab (n = 7) in the third trimester.
The 57 biologic-exposed infants underwent standardized clinical assessments, drug concentration, and immune function testing. The live oral rotavirus vaccine series was provided to 50 infants, with the first dose at a median of 13 weeks of age. Immunologic assessments validated for age were normal in all infants despite median infliximab concentrations of 6.1 μg/mL (range, 0.4-28.8 μg/mL), adalimumab concentrations of 1.7 μg/mL (range, 0.7-7.9 μg/mL), ustekinumab concentrations of 0.6 μg/mL (range, 0-1.1), and undetectable for vedolizumab at 10.7 weeks of age.
As anticipated, infant immune function was normal regardless of circulating drug levels.
The overall message, said Seow, is “healthy mum equals healthy baby. Be more concerned regarding active inflammation than active medications. In almost all circumstances, treat to target in pregnancy as you would in the nonpregnant state.” She added, however, that further studies are needed to determine the safety and optimal timing of other live vaccines, such as the BCG, in the presence of biologic therapy.
This study was funded by the Alberta Children’s Hospital Research Institute. Seow reported advisory/speaker’s fees for Janssen, AbbVie, Takeda, Pfizer, Fresenius Kabi, Bristol-Myers Squibb, Pharmascience, and Lilly, as well as funding from Alberta Children’s Hospital Research Institute, Crohn’s and Colitis Canada, the Canadian Institutes of Health Research, and Calgary Health Trust, and data safety monitoring from New South Wales Government Health, Australia. Multiple coauthors disclosed similar consulting or speaker relationships with private industry. Spencer had no competing interests with regard to her comments.
A version of this article first appeared on Medscape.com.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Study Evaluates Safety of Benzoyl Peroxide Products for Acne
according to results from an analysis that used gas chromatography–mass spectrometry and other methods.
The analysis, which was published in the Journal of Investigative Dermatology and expands on a similar study released more than 6 months ago, also found that encapsulated BPO products break down into benzene at room temperature but that refrigerating them may mitigate this effect.
“Our research provides the first experimental evidence that cold storage can help reduce the rate of benzoyl peroxide breakdown into benzene,” said one of the study authors, Christopher G. Bunick, MD, PhD, associate professor of dermatology at Yale University, New Haven, Connecticut. “Therefore, cold storage throughout the entire supply chain — from manufacturing to patient use — is a reasonable and proportional measure at this time for those continuing to use benzoyl peroxide medicine.” One acne product, the newer prescription triple-combination therapy (adapalene-clindamycin-BPO) “already has a cold shipping process in place; the patient just needs to continue that at home,” he noted.
For the study — which was funded by an independent lab, Valisure — researchers led by Valisure CEO and founder David Light, used gas chromatography-mass spectrometry to detect benzene levels in 111 BPO drug products from major US retailers and selected ion flow tube mass-spectrometry to quantify the release of benzene in real time. Benzene levels ranged from 0.16 ppm to 35.30 ppm, and 38 of the products (34%) had levels above the FDA limit of 2 ppm for drug products. “The results of the products sampled in this study suggest that formulation is likely the strongest contributor to benzene concentrations in BPO drug products that are commercially available, since the magnitude of benzene detected correlates most closely with specific brands or product types within certain brands,” the study authors wrote.
When the researchers tested the stability of a prescription encapsulated BPO drug product at cold (2 °C) and elevated temperature (50 °C), no apparent benzene formation was observed at 2 °C, whereas high levels of benzene formed at 50 °C, “suggesting that encapsulation technology may not stabilize BPO drug products, but cold storage may greatly reduce benzene formation,” they wrote.
In another component of the study, researchers exposed a BP drug product to a UVA/UVB lamp for 2 hours and found detectable benzene through evaporation and substantial benzene formation when exposed to UV light at levels below peak sunlight. The experiment “strongly justifies the package label warnings to avoid sun exposure when using BPO drug products,” the authors wrote. “Further evaluation to determine the influence of sun exposure on BPO drug product degradation and benzene formation is warranted.”
In an interview, John Barbieri, MD, MBA, assistant professor of dermatology at Harvard Medical School and director of the Advanced Acne Therapeutics Clinic at Brigham and Women’s Hospital, Boston, Massachusetts characterized the findings as “an important issue that we should take seriously.” However, “we also must not overreact.”
BPO is a foundational acne treatment without any clear alternative, he said, pointing out that no evidence currently exists “to support that routine use of benzoyl peroxide–containing products for acne is associated with a meaningful risk of benzene in the blood or an increased risk of cancer.”
And although it is prudent to minimize benzene exposure as much as possible, Barbieri continued, “it is not clear that these levels are a clinically meaningful incremental risk in the setting of an acne cream or wash. There is minimal cutaneous absorption of benzene, and it is uncertain how much benzene aerosolizes with routine use, particularly for washes which are not left on the skin.”
Bunick said that the combined data from this and the study published in March 2024 affected which BPO products he recommends for patients with acne. “I am using exclusively the triple combination therapy (adapalene-clindamycin-benzoyl peroxide) because I know it has the necessary cold supply chain in place to protect the product’s stability. I further encourage patients to place all their benzoyl peroxide–containing products in the refrigerator at home to reduce benzene formation and exposure.”
Bunick reported having served as an investigator and/or a consultant/speaker for many pharmaceutical companies, including as a consultant for Ortho-Dermatologics; but none related to this study. Barbieri reported having no relevant disclosures.
A version of this article first appeared on Medscape.com.
according to results from an analysis that used gas chromatography–mass spectrometry and other methods.
The analysis, which was published in the Journal of Investigative Dermatology and expands on a similar study released more than 6 months ago, also found that encapsulated BPO products break down into benzene at room temperature but that refrigerating them may mitigate this effect.
“Our research provides the first experimental evidence that cold storage can help reduce the rate of benzoyl peroxide breakdown into benzene,” said one of the study authors, Christopher G. Bunick, MD, PhD, associate professor of dermatology at Yale University, New Haven, Connecticut. “Therefore, cold storage throughout the entire supply chain — from manufacturing to patient use — is a reasonable and proportional measure at this time for those continuing to use benzoyl peroxide medicine.” One acne product, the newer prescription triple-combination therapy (adapalene-clindamycin-BPO) “already has a cold shipping process in place; the patient just needs to continue that at home,” he noted.
For the study — which was funded by an independent lab, Valisure — researchers led by Valisure CEO and founder David Light, used gas chromatography-mass spectrometry to detect benzene levels in 111 BPO drug products from major US retailers and selected ion flow tube mass-spectrometry to quantify the release of benzene in real time. Benzene levels ranged from 0.16 ppm to 35.30 ppm, and 38 of the products (34%) had levels above the FDA limit of 2 ppm for drug products. “The results of the products sampled in this study suggest that formulation is likely the strongest contributor to benzene concentrations in BPO drug products that are commercially available, since the magnitude of benzene detected correlates most closely with specific brands or product types within certain brands,” the study authors wrote.
When the researchers tested the stability of a prescription encapsulated BPO drug product at cold (2 °C) and elevated temperature (50 °C), no apparent benzene formation was observed at 2 °C, whereas high levels of benzene formed at 50 °C, “suggesting that encapsulation technology may not stabilize BPO drug products, but cold storage may greatly reduce benzene formation,” they wrote.
In another component of the study, researchers exposed a BP drug product to a UVA/UVB lamp for 2 hours and found detectable benzene through evaporation and substantial benzene formation when exposed to UV light at levels below peak sunlight. The experiment “strongly justifies the package label warnings to avoid sun exposure when using BPO drug products,” the authors wrote. “Further evaluation to determine the influence of sun exposure on BPO drug product degradation and benzene formation is warranted.”
In an interview, John Barbieri, MD, MBA, assistant professor of dermatology at Harvard Medical School and director of the Advanced Acne Therapeutics Clinic at Brigham and Women’s Hospital, Boston, Massachusetts characterized the findings as “an important issue that we should take seriously.” However, “we also must not overreact.”
BPO is a foundational acne treatment without any clear alternative, he said, pointing out that no evidence currently exists “to support that routine use of benzoyl peroxide–containing products for acne is associated with a meaningful risk of benzene in the blood or an increased risk of cancer.”
And although it is prudent to minimize benzene exposure as much as possible, Barbieri continued, “it is not clear that these levels are a clinically meaningful incremental risk in the setting of an acne cream or wash. There is minimal cutaneous absorption of benzene, and it is uncertain how much benzene aerosolizes with routine use, particularly for washes which are not left on the skin.”
Bunick said that the combined data from this and the study published in March 2024 affected which BPO products he recommends for patients with acne. “I am using exclusively the triple combination therapy (adapalene-clindamycin-benzoyl peroxide) because I know it has the necessary cold supply chain in place to protect the product’s stability. I further encourage patients to place all their benzoyl peroxide–containing products in the refrigerator at home to reduce benzene formation and exposure.”
Bunick reported having served as an investigator and/or a consultant/speaker for many pharmaceutical companies, including as a consultant for Ortho-Dermatologics; but none related to this study. Barbieri reported having no relevant disclosures.
A version of this article first appeared on Medscape.com.
according to results from an analysis that used gas chromatography–mass spectrometry and other methods.
The analysis, which was published in the Journal of Investigative Dermatology and expands on a similar study released more than 6 months ago, also found that encapsulated BPO products break down into benzene at room temperature but that refrigerating them may mitigate this effect.
“Our research provides the first experimental evidence that cold storage can help reduce the rate of benzoyl peroxide breakdown into benzene,” said one of the study authors, Christopher G. Bunick, MD, PhD, associate professor of dermatology at Yale University, New Haven, Connecticut. “Therefore, cold storage throughout the entire supply chain — from manufacturing to patient use — is a reasonable and proportional measure at this time for those continuing to use benzoyl peroxide medicine.” One acne product, the newer prescription triple-combination therapy (adapalene-clindamycin-BPO) “already has a cold shipping process in place; the patient just needs to continue that at home,” he noted.
For the study — which was funded by an independent lab, Valisure — researchers led by Valisure CEO and founder David Light, used gas chromatography-mass spectrometry to detect benzene levels in 111 BPO drug products from major US retailers and selected ion flow tube mass-spectrometry to quantify the release of benzene in real time. Benzene levels ranged from 0.16 ppm to 35.30 ppm, and 38 of the products (34%) had levels above the FDA limit of 2 ppm for drug products. “The results of the products sampled in this study suggest that formulation is likely the strongest contributor to benzene concentrations in BPO drug products that are commercially available, since the magnitude of benzene detected correlates most closely with specific brands or product types within certain brands,” the study authors wrote.
When the researchers tested the stability of a prescription encapsulated BPO drug product at cold (2 °C) and elevated temperature (50 °C), no apparent benzene formation was observed at 2 °C, whereas high levels of benzene formed at 50 °C, “suggesting that encapsulation technology may not stabilize BPO drug products, but cold storage may greatly reduce benzene formation,” they wrote.
In another component of the study, researchers exposed a BP drug product to a UVA/UVB lamp for 2 hours and found detectable benzene through evaporation and substantial benzene formation when exposed to UV light at levels below peak sunlight. The experiment “strongly justifies the package label warnings to avoid sun exposure when using BPO drug products,” the authors wrote. “Further evaluation to determine the influence of sun exposure on BPO drug product degradation and benzene formation is warranted.”
In an interview, John Barbieri, MD, MBA, assistant professor of dermatology at Harvard Medical School and director of the Advanced Acne Therapeutics Clinic at Brigham and Women’s Hospital, Boston, Massachusetts characterized the findings as “an important issue that we should take seriously.” However, “we also must not overreact.”
BPO is a foundational acne treatment without any clear alternative, he said, pointing out that no evidence currently exists “to support that routine use of benzoyl peroxide–containing products for acne is associated with a meaningful risk of benzene in the blood or an increased risk of cancer.”
And although it is prudent to minimize benzene exposure as much as possible, Barbieri continued, “it is not clear that these levels are a clinically meaningful incremental risk in the setting of an acne cream or wash. There is minimal cutaneous absorption of benzene, and it is uncertain how much benzene aerosolizes with routine use, particularly for washes which are not left on the skin.”
Bunick said that the combined data from this and the study published in March 2024 affected which BPO products he recommends for patients with acne. “I am using exclusively the triple combination therapy (adapalene-clindamycin-benzoyl peroxide) because I know it has the necessary cold supply chain in place to protect the product’s stability. I further encourage patients to place all their benzoyl peroxide–containing products in the refrigerator at home to reduce benzene formation and exposure.”
Bunick reported having served as an investigator and/or a consultant/speaker for many pharmaceutical companies, including as a consultant for Ortho-Dermatologics; but none related to this study. Barbieri reported having no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF INVESTIGATIVE DERMATOLOGY
Room for Improvement in Screening for Sexually Transmitted Diseases
Syphilis. It is often called the “great imitator.” It is speculated that this infection led to King George III of England going mad and likely contributing to his death. In the modern era, the discovery of penicillin in 1928 was instrumental in treating this once-deadly infection. Over the ensuing decades, rates of syphilis continued to decline. However, according to the Centers for Disease Control and Prevention, from 2018-2022 reported cases of syphilis in the United States have increased by 79% and continue to increase each year. Men who have sex with men (MSM) accounted for 41.4% of infections nationwide during this time period. This extraordinary rise highlights the need for better screening in our patients.
I currently live and practice in Texas, so I will use it as a case example. In 2013, Texas reported 1,471 cases of primary or secondary syphilis. By 2022, this number had risen to 4,655, a 216% increase. CDC data shows that Texas cases among men increased from 1,917 in 2019 to 3,324 in 2022, with MSM accounting for 1,341 (40%) of those infections. Adolescents and young adults aged 15-24 accounted for the second-highest number of new infections. Interestingly, rates of syphilis in men began to rise in Texas starting in 2013, the first full year that Truvada (emtricitabine and tenofovir disoproxil fumarate) was available for HIV pre-exposure prophylaxis (PrEP). While no definitive study has proven that the availability of PrEP caused an increase in condomless sexual intercourse, the number of high school students in Texas who did not use a condom at their last intercourse increased from 47.1% in 2013 to 50% in 2021.
The data above highlights the need to increase screening, especially in primary care and emergency room settings. According to the 2021 Youth Risk Behavior Survey, 94.8% of high school students surveyed that they were not tested for STIs in the 12 months prior to the survey. This compares with 91.4% in the 2019 survey. When STI testing is done, many adolescents often choose to forgo blood testing for HIV and syphilis and decide only to do urine NAATs testing for Neisseria gonorrhoeae and Chlamydia trachomatis. Therefore, those physicians and other healthcare providers who take care of adolescents and young adults must work to improve screening for ALL STIs. According to the American Academy of Pediatrics Bright Futures Periodicity Guidelines, pediatricians should screen for HIV in all patients at least once starting at age 15 and then thereafter based on risk assessment. Adding syphilis screening at the same time as the above HIV screening is an easy way to improve testing and treatment for this potentially deadly condition. If access to phlebotomy is not available, there are rapid HIV and syphilis tests that can be done in physicians’ offices. To perform these risk assessments, pediatricians must spend time alone with their adolescent and young patients at nearly every visit to discuss behaviors. Pediatricians should also be aware to consider syphilis on their differential for patients with unexplained rashes, sores in the mouth, or flu-like symptoms if that young person is sexually active.
Compounding the issue of increasing cases of syphilis is a national shortage of intramuscular penicillin G benzathine, the preferred treatment, which began in April 2023 only recently began to improve as of August 2024. Oral doxycycline can be used as a backup for some patients. Still, IM penicillin G is the only recommended treatment available for pregnant patients or those with advanced disease. The increasing number of cases, as well as the medication shortages, remind all of us that
Dr. M. Brett Cooper, is an assistant professor of pediatrics at University of Texas Southwestern, Dallas, and an adolescent medicine specialist at Children’s Medical Center Dallas.
Syphilis. It is often called the “great imitator.” It is speculated that this infection led to King George III of England going mad and likely contributing to his death. In the modern era, the discovery of penicillin in 1928 was instrumental in treating this once-deadly infection. Over the ensuing decades, rates of syphilis continued to decline. However, according to the Centers for Disease Control and Prevention, from 2018-2022 reported cases of syphilis in the United States have increased by 79% and continue to increase each year. Men who have sex with men (MSM) accounted for 41.4% of infections nationwide during this time period. This extraordinary rise highlights the need for better screening in our patients.
I currently live and practice in Texas, so I will use it as a case example. In 2013, Texas reported 1,471 cases of primary or secondary syphilis. By 2022, this number had risen to 4,655, a 216% increase. CDC data shows that Texas cases among men increased from 1,917 in 2019 to 3,324 in 2022, with MSM accounting for 1,341 (40%) of those infections. Adolescents and young adults aged 15-24 accounted for the second-highest number of new infections. Interestingly, rates of syphilis in men began to rise in Texas starting in 2013, the first full year that Truvada (emtricitabine and tenofovir disoproxil fumarate) was available for HIV pre-exposure prophylaxis (PrEP). While no definitive study has proven that the availability of PrEP caused an increase in condomless sexual intercourse, the number of high school students in Texas who did not use a condom at their last intercourse increased from 47.1% in 2013 to 50% in 2021.
The data above highlights the need to increase screening, especially in primary care and emergency room settings. According to the 2021 Youth Risk Behavior Survey, 94.8% of high school students surveyed that they were not tested for STIs in the 12 months prior to the survey. This compares with 91.4% in the 2019 survey. When STI testing is done, many adolescents often choose to forgo blood testing for HIV and syphilis and decide only to do urine NAATs testing for Neisseria gonorrhoeae and Chlamydia trachomatis. Therefore, those physicians and other healthcare providers who take care of adolescents and young adults must work to improve screening for ALL STIs. According to the American Academy of Pediatrics Bright Futures Periodicity Guidelines, pediatricians should screen for HIV in all patients at least once starting at age 15 and then thereafter based on risk assessment. Adding syphilis screening at the same time as the above HIV screening is an easy way to improve testing and treatment for this potentially deadly condition. If access to phlebotomy is not available, there are rapid HIV and syphilis tests that can be done in physicians’ offices. To perform these risk assessments, pediatricians must spend time alone with their adolescent and young patients at nearly every visit to discuss behaviors. Pediatricians should also be aware to consider syphilis on their differential for patients with unexplained rashes, sores in the mouth, or flu-like symptoms if that young person is sexually active.
Compounding the issue of increasing cases of syphilis is a national shortage of intramuscular penicillin G benzathine, the preferred treatment, which began in April 2023 only recently began to improve as of August 2024. Oral doxycycline can be used as a backup for some patients. Still, IM penicillin G is the only recommended treatment available for pregnant patients or those with advanced disease. The increasing number of cases, as well as the medication shortages, remind all of us that
Dr. M. Brett Cooper, is an assistant professor of pediatrics at University of Texas Southwestern, Dallas, and an adolescent medicine specialist at Children’s Medical Center Dallas.
Syphilis. It is often called the “great imitator.” It is speculated that this infection led to King George III of England going mad and likely contributing to his death. In the modern era, the discovery of penicillin in 1928 was instrumental in treating this once-deadly infection. Over the ensuing decades, rates of syphilis continued to decline. However, according to the Centers for Disease Control and Prevention, from 2018-2022 reported cases of syphilis in the United States have increased by 79% and continue to increase each year. Men who have sex with men (MSM) accounted for 41.4% of infections nationwide during this time period. This extraordinary rise highlights the need for better screening in our patients.
I currently live and practice in Texas, so I will use it as a case example. In 2013, Texas reported 1,471 cases of primary or secondary syphilis. By 2022, this number had risen to 4,655, a 216% increase. CDC data shows that Texas cases among men increased from 1,917 in 2019 to 3,324 in 2022, with MSM accounting for 1,341 (40%) of those infections. Adolescents and young adults aged 15-24 accounted for the second-highest number of new infections. Interestingly, rates of syphilis in men began to rise in Texas starting in 2013, the first full year that Truvada (emtricitabine and tenofovir disoproxil fumarate) was available for HIV pre-exposure prophylaxis (PrEP). While no definitive study has proven that the availability of PrEP caused an increase in condomless sexual intercourse, the number of high school students in Texas who did not use a condom at their last intercourse increased from 47.1% in 2013 to 50% in 2021.
The data above highlights the need to increase screening, especially in primary care and emergency room settings. According to the 2021 Youth Risk Behavior Survey, 94.8% of high school students surveyed that they were not tested for STIs in the 12 months prior to the survey. This compares with 91.4% in the 2019 survey. When STI testing is done, many adolescents often choose to forgo blood testing for HIV and syphilis and decide only to do urine NAATs testing for Neisseria gonorrhoeae and Chlamydia trachomatis. Therefore, those physicians and other healthcare providers who take care of adolescents and young adults must work to improve screening for ALL STIs. According to the American Academy of Pediatrics Bright Futures Periodicity Guidelines, pediatricians should screen for HIV in all patients at least once starting at age 15 and then thereafter based on risk assessment. Adding syphilis screening at the same time as the above HIV screening is an easy way to improve testing and treatment for this potentially deadly condition. If access to phlebotomy is not available, there are rapid HIV and syphilis tests that can be done in physicians’ offices. To perform these risk assessments, pediatricians must spend time alone with their adolescent and young patients at nearly every visit to discuss behaviors. Pediatricians should also be aware to consider syphilis on their differential for patients with unexplained rashes, sores in the mouth, or flu-like symptoms if that young person is sexually active.
Compounding the issue of increasing cases of syphilis is a national shortage of intramuscular penicillin G benzathine, the preferred treatment, which began in April 2023 only recently began to improve as of August 2024. Oral doxycycline can be used as a backup for some patients. Still, IM penicillin G is the only recommended treatment available for pregnant patients or those with advanced disease. The increasing number of cases, as well as the medication shortages, remind all of us that
Dr. M. Brett Cooper, is an assistant professor of pediatrics at University of Texas Southwestern, Dallas, and an adolescent medicine specialist at Children’s Medical Center Dallas.
A 7-Year-Old Boy Presents With Dark Spots on His Scalp and Areas of Poor Hair Growth
Given the trichoscopic findings, scrapings from the scaly areas were taken and revealed hyphae, confirming the diagnosis of tinea capitis. A fungal culture identified Trichophyton tonsurans as the causative organism.
Tinea capitis is the most common dermatophyte infection in children. Risk factors include participation in close-contact sports like wrestling or jiu-jitsu, attendance at daycare for younger children, African American hair care practices, pet ownership (particularly cats and rodents), and living in overcrowded conditions.
Diagnosis of tinea capitis requires a thorough clinical history to identify potential risk factors. On physical examination, patchy hair loss with associated scaling should raise suspicion for tinea capitis. Inflammatory signs, such as pustules and swelling, may suggest the presence of a kerion, further supporting the diagnosis. Although some practitioners use Wood’s lamp to help with diagnosis, its utility is limited. It detects fluorescence in Microsporum species (exothrix infections) but not in Trichophyton species (endothrix infections).
Trichoscopy can be a valuable tool when inflammation is minimal, and only hair loss and scaling are observed. Trichoscopic findings suggestive of tinea capitis include comma hairs, corkscrew hairs (as seen in this patient), Morse code-like hairs, zigzag hairs, bent hairs, block hairs, and i-hairs. Other common, though not characteristic, findings include broken hairs, black dots, perifollicular scaling, and diffuse scaling.
KOH (potassium hydroxide) analysis is another useful method for detecting fungal elements, though it does not identify the specific fungus and may not be available in all clinical settings. Mycologic culture remains the gold standard for diagnosing tinea capitis, though results can take 3-4 weeks. Newer diagnostic techniques, such as PCR analysis and MALDI-TOF/MS, offer more rapid identification of the causative organism.
The differential diagnosis includes:
- Seborrheic dermatitis, which presents with greasy, yellowish scales and itching, with trichoscopy showing twisted, coiled hairs and yellowish scaling.
- Psoriasis, which can mimic tinea capitis but presents with well-demarcated red plaques and silvery-white scales. Trichoscopy shows red dots and uniform scaling.
- Alopecia areata, which causes patchy hair loss without inflammation or scaling, with trichoscopic findings of exclamation mark hairs, black dots, and yellow dots.
- Trichotillomania, a hair-pulling disorder, which results in irregular patches of hair loss. Trichoscopy shows broken hairs of varying lengths, V-sign hairs, and flame-shaped residues at follicular openings.
Treatment of tinea capitis requires systemic antifungals and topical agents to prevent fungal spore spread. Several treatment guidelines are available from different institutions. Griseofulvin (FDA-approved for patients > 2 years of age) has been widely used, particularly for Microsporum canis infections. However, due to limited availability in many countries, terbinafine (FDA-approved for patients > 4 years of age) is now commonly used as first-line therapy, especially for Trichophyton species. Treatment typically lasts 4-6 weeks, and post-treatment cultures may be recommended to confirm mycologic cure.
Concerns about drug resistance have emerged, particularly for terbinafine-resistant dermatophytes linked to mutations in the squalene epoxidase enzyme. Resistance may be driven by limited antifungal availability and poor adherence to prolonged treatment regimens. While fluconazole and itraconazole are used off-label, growing evidence supports their effectiveness, although one large trial showed suboptimal cure rates with fluconazole.
Though systemic antifungals are generally safe, hepatotoxicity remains a concern, especially in patients with hepatic conditions or other comorbidities. Lab monitoring is advised for patients on prolonged or multiple therapies, or for those with coexisting conditions. The decision to conduct lab monitoring should be discussed with parents, balancing the very low risk of hepatotoxicity in healthy children against their comfort level.
An alternative to systemic therapy is photodynamic therapy (PDT), which has been reported as successful in treating tinea capitis infections, particularly in cases of T. mentagrophytes and M. canis. However, large-scale trials are needed to confirm PDT’s efficacy and safety.
In conclusion, children presenting with hair loss, scaling, and associated dark spots on the scalp should be evaluated for fungal infection. While trichoscopy can aid in diagnosis, fungal culture remains the gold standard for confirmation.
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego.
References
Rudnicka L et al. Hair shafts in trichoscopy: clues for diagnosis of hair and scalp diseases. Dermatol Clin. 2013 Oct;31(4):695-708, x. doi: 10.1016/j.det.2013.06.007.
Gupta AK et al. An update on tinea capitis in children. Pediatr Dermatol. 2024 Aug 7. doi: 10.1111/pde.15708.
Anna Waskiel-Burnat et al. Trichoscopy of tinea capitis: A systematic review. Dermatol Ther (Heidelb). 2020 Feb;10(1):43-52. doi: 10.1007/s13555-019-00350-1.
Given the trichoscopic findings, scrapings from the scaly areas were taken and revealed hyphae, confirming the diagnosis of tinea capitis. A fungal culture identified Trichophyton tonsurans as the causative organism.
Tinea capitis is the most common dermatophyte infection in children. Risk factors include participation in close-contact sports like wrestling or jiu-jitsu, attendance at daycare for younger children, African American hair care practices, pet ownership (particularly cats and rodents), and living in overcrowded conditions.
Diagnosis of tinea capitis requires a thorough clinical history to identify potential risk factors. On physical examination, patchy hair loss with associated scaling should raise suspicion for tinea capitis. Inflammatory signs, such as pustules and swelling, may suggest the presence of a kerion, further supporting the diagnosis. Although some practitioners use Wood’s lamp to help with diagnosis, its utility is limited. It detects fluorescence in Microsporum species (exothrix infections) but not in Trichophyton species (endothrix infections).
Trichoscopy can be a valuable tool when inflammation is minimal, and only hair loss and scaling are observed. Trichoscopic findings suggestive of tinea capitis include comma hairs, corkscrew hairs (as seen in this patient), Morse code-like hairs, zigzag hairs, bent hairs, block hairs, and i-hairs. Other common, though not characteristic, findings include broken hairs, black dots, perifollicular scaling, and diffuse scaling.
KOH (potassium hydroxide) analysis is another useful method for detecting fungal elements, though it does not identify the specific fungus and may not be available in all clinical settings. Mycologic culture remains the gold standard for diagnosing tinea capitis, though results can take 3-4 weeks. Newer diagnostic techniques, such as PCR analysis and MALDI-TOF/MS, offer more rapid identification of the causative organism.
The differential diagnosis includes:
- Seborrheic dermatitis, which presents with greasy, yellowish scales and itching, with trichoscopy showing twisted, coiled hairs and yellowish scaling.
- Psoriasis, which can mimic tinea capitis but presents with well-demarcated red plaques and silvery-white scales. Trichoscopy shows red dots and uniform scaling.
- Alopecia areata, which causes patchy hair loss without inflammation or scaling, with trichoscopic findings of exclamation mark hairs, black dots, and yellow dots.
- Trichotillomania, a hair-pulling disorder, which results in irregular patches of hair loss. Trichoscopy shows broken hairs of varying lengths, V-sign hairs, and flame-shaped residues at follicular openings.
Treatment of tinea capitis requires systemic antifungals and topical agents to prevent fungal spore spread. Several treatment guidelines are available from different institutions. Griseofulvin (FDA-approved for patients > 2 years of age) has been widely used, particularly for Microsporum canis infections. However, due to limited availability in many countries, terbinafine (FDA-approved for patients > 4 years of age) is now commonly used as first-line therapy, especially for Trichophyton species. Treatment typically lasts 4-6 weeks, and post-treatment cultures may be recommended to confirm mycologic cure.
Concerns about drug resistance have emerged, particularly for terbinafine-resistant dermatophytes linked to mutations in the squalene epoxidase enzyme. Resistance may be driven by limited antifungal availability and poor adherence to prolonged treatment regimens. While fluconazole and itraconazole are used off-label, growing evidence supports their effectiveness, although one large trial showed suboptimal cure rates with fluconazole.
Though systemic antifungals are generally safe, hepatotoxicity remains a concern, especially in patients with hepatic conditions or other comorbidities. Lab monitoring is advised for patients on prolonged or multiple therapies, or for those with coexisting conditions. The decision to conduct lab monitoring should be discussed with parents, balancing the very low risk of hepatotoxicity in healthy children against their comfort level.
An alternative to systemic therapy is photodynamic therapy (PDT), which has been reported as successful in treating tinea capitis infections, particularly in cases of T. mentagrophytes and M. canis. However, large-scale trials are needed to confirm PDT’s efficacy and safety.
In conclusion, children presenting with hair loss, scaling, and associated dark spots on the scalp should be evaluated for fungal infection. While trichoscopy can aid in diagnosis, fungal culture remains the gold standard for confirmation.
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego.
References
Rudnicka L et al. Hair shafts in trichoscopy: clues for diagnosis of hair and scalp diseases. Dermatol Clin. 2013 Oct;31(4):695-708, x. doi: 10.1016/j.det.2013.06.007.
Gupta AK et al. An update on tinea capitis in children. Pediatr Dermatol. 2024 Aug 7. doi: 10.1111/pde.15708.
Anna Waskiel-Burnat et al. Trichoscopy of tinea capitis: A systematic review. Dermatol Ther (Heidelb). 2020 Feb;10(1):43-52. doi: 10.1007/s13555-019-00350-1.
Given the trichoscopic findings, scrapings from the scaly areas were taken and revealed hyphae, confirming the diagnosis of tinea capitis. A fungal culture identified Trichophyton tonsurans as the causative organism.
Tinea capitis is the most common dermatophyte infection in children. Risk factors include participation in close-contact sports like wrestling or jiu-jitsu, attendance at daycare for younger children, African American hair care practices, pet ownership (particularly cats and rodents), and living in overcrowded conditions.
Diagnosis of tinea capitis requires a thorough clinical history to identify potential risk factors. On physical examination, patchy hair loss with associated scaling should raise suspicion for tinea capitis. Inflammatory signs, such as pustules and swelling, may suggest the presence of a kerion, further supporting the diagnosis. Although some practitioners use Wood’s lamp to help with diagnosis, its utility is limited. It detects fluorescence in Microsporum species (exothrix infections) but not in Trichophyton species (endothrix infections).
Trichoscopy can be a valuable tool when inflammation is minimal, and only hair loss and scaling are observed. Trichoscopic findings suggestive of tinea capitis include comma hairs, corkscrew hairs (as seen in this patient), Morse code-like hairs, zigzag hairs, bent hairs, block hairs, and i-hairs. Other common, though not characteristic, findings include broken hairs, black dots, perifollicular scaling, and diffuse scaling.
KOH (potassium hydroxide) analysis is another useful method for detecting fungal elements, though it does not identify the specific fungus and may not be available in all clinical settings. Mycologic culture remains the gold standard for diagnosing tinea capitis, though results can take 3-4 weeks. Newer diagnostic techniques, such as PCR analysis and MALDI-TOF/MS, offer more rapid identification of the causative organism.
The differential diagnosis includes:
- Seborrheic dermatitis, which presents with greasy, yellowish scales and itching, with trichoscopy showing twisted, coiled hairs and yellowish scaling.
- Psoriasis, which can mimic tinea capitis but presents with well-demarcated red plaques and silvery-white scales. Trichoscopy shows red dots and uniform scaling.
- Alopecia areata, which causes patchy hair loss without inflammation or scaling, with trichoscopic findings of exclamation mark hairs, black dots, and yellow dots.
- Trichotillomania, a hair-pulling disorder, which results in irregular patches of hair loss. Trichoscopy shows broken hairs of varying lengths, V-sign hairs, and flame-shaped residues at follicular openings.
Treatment of tinea capitis requires systemic antifungals and topical agents to prevent fungal spore spread. Several treatment guidelines are available from different institutions. Griseofulvin (FDA-approved for patients > 2 years of age) has been widely used, particularly for Microsporum canis infections. However, due to limited availability in many countries, terbinafine (FDA-approved for patients > 4 years of age) is now commonly used as first-line therapy, especially for Trichophyton species. Treatment typically lasts 4-6 weeks, and post-treatment cultures may be recommended to confirm mycologic cure.
Concerns about drug resistance have emerged, particularly for terbinafine-resistant dermatophytes linked to mutations in the squalene epoxidase enzyme. Resistance may be driven by limited antifungal availability and poor adherence to prolonged treatment regimens. While fluconazole and itraconazole are used off-label, growing evidence supports their effectiveness, although one large trial showed suboptimal cure rates with fluconazole.
Though systemic antifungals are generally safe, hepatotoxicity remains a concern, especially in patients with hepatic conditions or other comorbidities. Lab monitoring is advised for patients on prolonged or multiple therapies, or for those with coexisting conditions. The decision to conduct lab monitoring should be discussed with parents, balancing the very low risk of hepatotoxicity in healthy children against their comfort level.
An alternative to systemic therapy is photodynamic therapy (PDT), which has been reported as successful in treating tinea capitis infections, particularly in cases of T. mentagrophytes and M. canis. However, large-scale trials are needed to confirm PDT’s efficacy and safety.
In conclusion, children presenting with hair loss, scaling, and associated dark spots on the scalp should be evaluated for fungal infection. While trichoscopy can aid in diagnosis, fungal culture remains the gold standard for confirmation.
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego.
References
Rudnicka L et al. Hair shafts in trichoscopy: clues for diagnosis of hair and scalp diseases. Dermatol Clin. 2013 Oct;31(4):695-708, x. doi: 10.1016/j.det.2013.06.007.
Gupta AK et al. An update on tinea capitis in children. Pediatr Dermatol. 2024 Aug 7. doi: 10.1111/pde.15708.
Anna Waskiel-Burnat et al. Trichoscopy of tinea capitis: A systematic review. Dermatol Ther (Heidelb). 2020 Feb;10(1):43-52. doi: 10.1007/s13555-019-00350-1.
What Are the Best Tools for Early Childhood Developmental Concerns?
Early recognition of neurodevelopmental concerns and timely access to services have been shown to result in better outcomes for young children. But not all instruments are of equal value, and new research has sought to identify the most useful among them.
For their research, published online in Developmental Medicine & Child Neurology, Andrea Burgess, PhD, of the University of Queensland in Brisbane, Australia, and her colleagues looked at two decades’ worth of systematic reviews of screening, assessment, and diagnostic tools used in children younger than 6 years.
Eighty-six clinical reviews and six practice guidelines, all published between 2000 and 2023, were included in the scoping review, which covered nearly 250 different multi-domain and domain- and disorder-specific tools.
The diagnostic instruments were those used to diagnose the most common early childhood disorders, including intellectual disability, global developmental delay, communication disorders, autism spectrum disorder, attention-deficit/hyperactivity disorder, cerebral palsy, movement disorders, and fetal alcohol spectrum disorder. Burgess and her colleagues sought to determine which tools had the strongest evidence behind them, noting that comparisons were inherently limited by differences in the tested populations, cutoff values, and other factors.
Burgess and her colleagues identified 67 instruments — about a third of those analyzed in the study — “with good discriminative or predictive validity for the screening and assessment of developmental concerns or disability.” Recommended tools were classified by tool type and by patient age groups.
The reason a tool might not be recommended, Burgess said in an email, was for lack of psychometric testing or published evidence, or because the tool was very narrow in scope (eg, covering only a single aspect of a domain), had a small time window for use, or was too new to have been captured in published systematic reviews.
Top Recommendations
Among multi-domain assessment tools, the Bayley Scales of Infant and Toddler Development, the Battelle Developmental Inventory, and the Mullen Scales of Early Learning all emerged as highly recommended. The top diagnostic screening tool for autism was the revised version of Social Attention and Communication Surveillance. For cerebral palsy, the top-rated diagnostic assessment tools were Prechtl’s Qualitative Assessment of General Movements and the Hammersmith Infant Neurological Examination.
Ratifying findings by other groups, the researchers determined the Ages & Stages Questionnaires, Third Edition (ASQ-3) to be the best overall multi-domain screening instrument for early childhood development, thanks to its simplicity and ease of use by a wide range of practitioner types. Burgess and her colleagues noted, however, that the ASQ-3 “will not identify all children with developmental concerns and may incorrectly identify others,” and that it may be more accurate in children 2 years or older.
Patient Care Setting and Cultural, Socioeconomic Factors Are Key
This news organization spoke to two clinicians working with these and similar tools in the United States. Both said that the care setting can also influence the utility of tools, with cultural and socioeconomic factors playing important roles.
Liz Schwandt, PsyD, an early intervention specialist in Los Angeles, said in an interview that children living in high-risk communities in the United States have a larger burden of developmental delays. But for many families in these communities, accessing care can be complex, which is why well-designed, efficient screening tools like ASQ-3 are especially valuable in practice.
“The reality is you have 10 minutes with a lot of families, and if it’s an emergency, you need to know,” she said. “The ASQ-3 has a very broad age range for this type of instrument and can be used by different practitioner types. The reason it’s successful lies in its parent-centric approach and inherent ease of use. It’s quick, and you can score it using pencil and paper while chatting with the parent, and you can use it for multiple siblings in the space of one appointment.”
With very young children, in whom neurodevelopmental concerns often overlap domains, Schwandt said it can be more important to flag a potential problem early and initiate a nonspecific developmental intervention than wait for results from more precise assessments using more specialized tools. These often require multiple, multi-hour appointments, which can be difficult to attain in lower-resource settings in the United States and can delay care, she said.
Liza Mackintosh, MD, a pediatrician at a federally funded healthcare center in Los Angeles that serves mostly publicly insured families, called validated first-line screening tools “incredibly important.” While rates of developmental screenings in pediatric clinics are increasing, there is still room for improvement, she said.
Mackintosh’s institution does not currently use the ASQ-3 but a different screening tool, called the Survey of Well-Being of Young Children (SWYC), that is embedded into the electronic health record. (The SWYC was not among the tools highlighted in Burgess and colleagues’ review.) Like the ASQ-3, it is short and efficient, she said, and it is used in all children in the recommended age ranges.
“Our visits are on average only 20 minutes,” Mackintosh said. “There’s not enough time for an in-depth developmental assessment. We will flag things such as a speech delay, gross motor delay, or fine motor delay” and refer to early intervention centers for more in-depth developmental assessments as needed, she said.
“The biggest job of pediatricians working in communities that are under-resourced is advocating for those early intervention services,” Mackintosh added. “We really see our job as doing the recommended screening, putting that together with what we’re seeing clinically and on history, and then advocating for the right next step or early intervention. Because sometimes the diagnosis is — I don’t want to say irrelevant, but your treatment plan is still going to be the same. So while I don’t have a formal diagnosis yet, the child definitely needs therapies and we’re still going to get those therapies.”
Burgess and her colleagues stressed in their paper the importance of selecting tools that are culturally appropriate for Indigenous communities in Australia, noting that “inappropriate tools may lead to over- or under-recognition of children with developmental concerns.”
Schwandt and Mackintosh said that the same applies in US settings.
“We’ve done a good job translating screening tools into Chinese, Spanish, Vietnamese, and Russian,” Schwandt said. “But some of them assume a way of taking care of children that is not always shared across cultures. The expectations of how children should play and interact with adults can be very different, and there needs to be an understanding of that. Just putting something in Vietnamese doesn’t mean that there are obvious analogues to understanding what the questionnaire is asking.”
Mackintosh concurred. “A lot of times our patients will not do well on screening, even though they’re fine, because they don’t have the exposure to that activity that’s being asked about. So — is the child scribbling with crayons? Is she climbing up a ladder at a playground? In order to be able to do that, you need to have an environment that you are doing it in. The screeners have to really be appropriate for what the child is exposed to. And sometimes our patients just don’t have that exposure.”
Burgess and colleagues’ study was funded by the Australian government and the Merchant Charitable Foundation. The authors disclosed no financial conflicts of interest. Schwandt and Mackintosh disclosed no conflicts of interest related to their comments.
A version of this article appeared on Medscape.com.
Early recognition of neurodevelopmental concerns and timely access to services have been shown to result in better outcomes for young children. But not all instruments are of equal value, and new research has sought to identify the most useful among them.
For their research, published online in Developmental Medicine & Child Neurology, Andrea Burgess, PhD, of the University of Queensland in Brisbane, Australia, and her colleagues looked at two decades’ worth of systematic reviews of screening, assessment, and diagnostic tools used in children younger than 6 years.
Eighty-six clinical reviews and six practice guidelines, all published between 2000 and 2023, were included in the scoping review, which covered nearly 250 different multi-domain and domain- and disorder-specific tools.
The diagnostic instruments were those used to diagnose the most common early childhood disorders, including intellectual disability, global developmental delay, communication disorders, autism spectrum disorder, attention-deficit/hyperactivity disorder, cerebral palsy, movement disorders, and fetal alcohol spectrum disorder. Burgess and her colleagues sought to determine which tools had the strongest evidence behind them, noting that comparisons were inherently limited by differences in the tested populations, cutoff values, and other factors.
Burgess and her colleagues identified 67 instruments — about a third of those analyzed in the study — “with good discriminative or predictive validity for the screening and assessment of developmental concerns or disability.” Recommended tools were classified by tool type and by patient age groups.
The reason a tool might not be recommended, Burgess said in an email, was for lack of psychometric testing or published evidence, or because the tool was very narrow in scope (eg, covering only a single aspect of a domain), had a small time window for use, or was too new to have been captured in published systematic reviews.
Top Recommendations
Among multi-domain assessment tools, the Bayley Scales of Infant and Toddler Development, the Battelle Developmental Inventory, and the Mullen Scales of Early Learning all emerged as highly recommended. The top diagnostic screening tool for autism was the revised version of Social Attention and Communication Surveillance. For cerebral palsy, the top-rated diagnostic assessment tools were Prechtl’s Qualitative Assessment of General Movements and the Hammersmith Infant Neurological Examination.
Ratifying findings by other groups, the researchers determined the Ages & Stages Questionnaires, Third Edition (ASQ-3) to be the best overall multi-domain screening instrument for early childhood development, thanks to its simplicity and ease of use by a wide range of practitioner types. Burgess and her colleagues noted, however, that the ASQ-3 “will not identify all children with developmental concerns and may incorrectly identify others,” and that it may be more accurate in children 2 years or older.
Patient Care Setting and Cultural, Socioeconomic Factors Are Key
This news organization spoke to two clinicians working with these and similar tools in the United States. Both said that the care setting can also influence the utility of tools, with cultural and socioeconomic factors playing important roles.
Liz Schwandt, PsyD, an early intervention specialist in Los Angeles, said in an interview that children living in high-risk communities in the United States have a larger burden of developmental delays. But for many families in these communities, accessing care can be complex, which is why well-designed, efficient screening tools like ASQ-3 are especially valuable in practice.
“The reality is you have 10 minutes with a lot of families, and if it’s an emergency, you need to know,” she said. “The ASQ-3 has a very broad age range for this type of instrument and can be used by different practitioner types. The reason it’s successful lies in its parent-centric approach and inherent ease of use. It’s quick, and you can score it using pencil and paper while chatting with the parent, and you can use it for multiple siblings in the space of one appointment.”
With very young children, in whom neurodevelopmental concerns often overlap domains, Schwandt said it can be more important to flag a potential problem early and initiate a nonspecific developmental intervention than wait for results from more precise assessments using more specialized tools. These often require multiple, multi-hour appointments, which can be difficult to attain in lower-resource settings in the United States and can delay care, she said.
Liza Mackintosh, MD, a pediatrician at a federally funded healthcare center in Los Angeles that serves mostly publicly insured families, called validated first-line screening tools “incredibly important.” While rates of developmental screenings in pediatric clinics are increasing, there is still room for improvement, she said.
Mackintosh’s institution does not currently use the ASQ-3 but a different screening tool, called the Survey of Well-Being of Young Children (SWYC), that is embedded into the electronic health record. (The SWYC was not among the tools highlighted in Burgess and colleagues’ review.) Like the ASQ-3, it is short and efficient, she said, and it is used in all children in the recommended age ranges.
“Our visits are on average only 20 minutes,” Mackintosh said. “There’s not enough time for an in-depth developmental assessment. We will flag things such as a speech delay, gross motor delay, or fine motor delay” and refer to early intervention centers for more in-depth developmental assessments as needed, she said.
“The biggest job of pediatricians working in communities that are under-resourced is advocating for those early intervention services,” Mackintosh added. “We really see our job as doing the recommended screening, putting that together with what we’re seeing clinically and on history, and then advocating for the right next step or early intervention. Because sometimes the diagnosis is — I don’t want to say irrelevant, but your treatment plan is still going to be the same. So while I don’t have a formal diagnosis yet, the child definitely needs therapies and we’re still going to get those therapies.”
Burgess and her colleagues stressed in their paper the importance of selecting tools that are culturally appropriate for Indigenous communities in Australia, noting that “inappropriate tools may lead to over- or under-recognition of children with developmental concerns.”
Schwandt and Mackintosh said that the same applies in US settings.
“We’ve done a good job translating screening tools into Chinese, Spanish, Vietnamese, and Russian,” Schwandt said. “But some of them assume a way of taking care of children that is not always shared across cultures. The expectations of how children should play and interact with adults can be very different, and there needs to be an understanding of that. Just putting something in Vietnamese doesn’t mean that there are obvious analogues to understanding what the questionnaire is asking.”
Mackintosh concurred. “A lot of times our patients will not do well on screening, even though they’re fine, because they don’t have the exposure to that activity that’s being asked about. So — is the child scribbling with crayons? Is she climbing up a ladder at a playground? In order to be able to do that, you need to have an environment that you are doing it in. The screeners have to really be appropriate for what the child is exposed to. And sometimes our patients just don’t have that exposure.”
Burgess and colleagues’ study was funded by the Australian government and the Merchant Charitable Foundation. The authors disclosed no financial conflicts of interest. Schwandt and Mackintosh disclosed no conflicts of interest related to their comments.
A version of this article appeared on Medscape.com.
Early recognition of neurodevelopmental concerns and timely access to services have been shown to result in better outcomes for young children. But not all instruments are of equal value, and new research has sought to identify the most useful among them.
For their research, published online in Developmental Medicine & Child Neurology, Andrea Burgess, PhD, of the University of Queensland in Brisbane, Australia, and her colleagues looked at two decades’ worth of systematic reviews of screening, assessment, and diagnostic tools used in children younger than 6 years.
Eighty-six clinical reviews and six practice guidelines, all published between 2000 and 2023, were included in the scoping review, which covered nearly 250 different multi-domain and domain- and disorder-specific tools.
The diagnostic instruments were those used to diagnose the most common early childhood disorders, including intellectual disability, global developmental delay, communication disorders, autism spectrum disorder, attention-deficit/hyperactivity disorder, cerebral palsy, movement disorders, and fetal alcohol spectrum disorder. Burgess and her colleagues sought to determine which tools had the strongest evidence behind them, noting that comparisons were inherently limited by differences in the tested populations, cutoff values, and other factors.
Burgess and her colleagues identified 67 instruments — about a third of those analyzed in the study — “with good discriminative or predictive validity for the screening and assessment of developmental concerns or disability.” Recommended tools were classified by tool type and by patient age groups.
The reason a tool might not be recommended, Burgess said in an email, was for lack of psychometric testing or published evidence, or because the tool was very narrow in scope (eg, covering only a single aspect of a domain), had a small time window for use, or was too new to have been captured in published systematic reviews.
Top Recommendations
Among multi-domain assessment tools, the Bayley Scales of Infant and Toddler Development, the Battelle Developmental Inventory, and the Mullen Scales of Early Learning all emerged as highly recommended. The top diagnostic screening tool for autism was the revised version of Social Attention and Communication Surveillance. For cerebral palsy, the top-rated diagnostic assessment tools were Prechtl’s Qualitative Assessment of General Movements and the Hammersmith Infant Neurological Examination.
Ratifying findings by other groups, the researchers determined the Ages & Stages Questionnaires, Third Edition (ASQ-3) to be the best overall multi-domain screening instrument for early childhood development, thanks to its simplicity and ease of use by a wide range of practitioner types. Burgess and her colleagues noted, however, that the ASQ-3 “will not identify all children with developmental concerns and may incorrectly identify others,” and that it may be more accurate in children 2 years or older.
Patient Care Setting and Cultural, Socioeconomic Factors Are Key
This news organization spoke to two clinicians working with these and similar tools in the United States. Both said that the care setting can also influence the utility of tools, with cultural and socioeconomic factors playing important roles.
Liz Schwandt, PsyD, an early intervention specialist in Los Angeles, said in an interview that children living in high-risk communities in the United States have a larger burden of developmental delays. But for many families in these communities, accessing care can be complex, which is why well-designed, efficient screening tools like ASQ-3 are especially valuable in practice.
“The reality is you have 10 minutes with a lot of families, and if it’s an emergency, you need to know,” she said. “The ASQ-3 has a very broad age range for this type of instrument and can be used by different practitioner types. The reason it’s successful lies in its parent-centric approach and inherent ease of use. It’s quick, and you can score it using pencil and paper while chatting with the parent, and you can use it for multiple siblings in the space of one appointment.”
With very young children, in whom neurodevelopmental concerns often overlap domains, Schwandt said it can be more important to flag a potential problem early and initiate a nonspecific developmental intervention than wait for results from more precise assessments using more specialized tools. These often require multiple, multi-hour appointments, which can be difficult to attain in lower-resource settings in the United States and can delay care, she said.
Liza Mackintosh, MD, a pediatrician at a federally funded healthcare center in Los Angeles that serves mostly publicly insured families, called validated first-line screening tools “incredibly important.” While rates of developmental screenings in pediatric clinics are increasing, there is still room for improvement, she said.
Mackintosh’s institution does not currently use the ASQ-3 but a different screening tool, called the Survey of Well-Being of Young Children (SWYC), that is embedded into the electronic health record. (The SWYC was not among the tools highlighted in Burgess and colleagues’ review.) Like the ASQ-3, it is short and efficient, she said, and it is used in all children in the recommended age ranges.
“Our visits are on average only 20 minutes,” Mackintosh said. “There’s not enough time for an in-depth developmental assessment. We will flag things such as a speech delay, gross motor delay, or fine motor delay” and refer to early intervention centers for more in-depth developmental assessments as needed, she said.
“The biggest job of pediatricians working in communities that are under-resourced is advocating for those early intervention services,” Mackintosh added. “We really see our job as doing the recommended screening, putting that together with what we’re seeing clinically and on history, and then advocating for the right next step or early intervention. Because sometimes the diagnosis is — I don’t want to say irrelevant, but your treatment plan is still going to be the same. So while I don’t have a formal diagnosis yet, the child definitely needs therapies and we’re still going to get those therapies.”
Burgess and her colleagues stressed in their paper the importance of selecting tools that are culturally appropriate for Indigenous communities in Australia, noting that “inappropriate tools may lead to over- or under-recognition of children with developmental concerns.”
Schwandt and Mackintosh said that the same applies in US settings.
“We’ve done a good job translating screening tools into Chinese, Spanish, Vietnamese, and Russian,” Schwandt said. “But some of them assume a way of taking care of children that is not always shared across cultures. The expectations of how children should play and interact with adults can be very different, and there needs to be an understanding of that. Just putting something in Vietnamese doesn’t mean that there are obvious analogues to understanding what the questionnaire is asking.”
Mackintosh concurred. “A lot of times our patients will not do well on screening, even though they’re fine, because they don’t have the exposure to that activity that’s being asked about. So — is the child scribbling with crayons? Is she climbing up a ladder at a playground? In order to be able to do that, you need to have an environment that you are doing it in. The screeners have to really be appropriate for what the child is exposed to. And sometimes our patients just don’t have that exposure.”
Burgess and colleagues’ study was funded by the Australian government and the Merchant Charitable Foundation. The authors disclosed no financial conflicts of interest. Schwandt and Mackintosh disclosed no conflicts of interest related to their comments.
A version of this article appeared on Medscape.com.
A Hard Look at Toxic Workplace Culture in Medicine
While Kellie Lease Stecher, MD, was working as an ob.gyn. in Minneapolis, Minnesota, a patient confided in her a sexual assault allegation about one of Stecher’s male colleagues. Stecher shared the allegation with her supervisor, who told Stecher not to file a report and chose not to address the issue with the patient. Stecher weighed how to do the right thing: Should she speak up? What were the ethical and legal implications of speaking up vs staying silent?
After seeking advice from her mentors, Stecher felt it was her moral and legal duty to report the allegation to the Minnesota Medical Board. Once she did, her supervisor chastised her repeatedly for reporting the allegation. Stecher soon found herself in a hostile work environment where she was regularly singled out and silenced by her supervisor and colleagues.
“I got to a point where I felt like I couldn’t say anything at any meetings without somehow being targeted after the meeting. There was an individual who was even allowed to fat-shame me with no consequences,” Stecher said. “[Being bullied at work is] a struggle because you have no voice, you have no opportunities, and there’s someone who is intentionally making your life uncomfortable.”
Stecher’s experience is not unusual. Mistreatment is a common issue among healthcare workers, ranging from rudeness to bullying and harassment and permeating every level and specialty of the medical profession. A 2019 research review estimated that 26.3% of healthcare workers had experienced bullying and found bullying in healthcare to be associated with mental health problems such as burnout and depression, physical health problems such as insomnia and headaches, and physicians taking more sick leave.
The Medscape Physician Workplace Culture Report 2024 found similarly bleak results:
- 38% said workplace culture is declining.
- 70% don’t see a big commitment from employers for positive culture.
- 48% said staff isn’t committed to positive culture.
The irony, of course, is that most physicians enter the field to care for people. As individuals go from medical school to residency and on with the rest of their careers, they often experience a rude awakening.
It’s Everywhere
Noticing the prevalence of workplace bullying in the medical field, endocrinologist Farah Khan, MD, at UW Medicine in Seattle, Washington, decided to conduct a survey on the issue.
Khan collected 122 responses from colleagues, friends, and acquaintances in the field. When asked if they had ever been bullied in medicine, 68% of respondents said yes. But here’s the fascinating part: She tried to pinpoint one particular area or source of toxicity in the progression of a physician’s career — and couldn’t because it existed at all levels.
More than one third of respondents said their worst bullying experiences occurred in residency, while 30% said mistreatment was worst in medical school, and 24% indicated their worst experience had occurred once they became an attending.
The litany of experiences included being belittled, excluded, yelled at, criticized, shamed, unfairly blamed, threatened, sexually harassed, subjected to bigotry and slurs, and humiliated.
“What surprised me the most was how widespread this problem is and the many different layers of healthcare it permeates through, from operating room staff to medical students to hospital HR to residents and attendings,” Khan said of her findings.
Who Cares for the Caregivers?
When hematologist Mikkael Sekeres, MD, was in medical school, he seriously considered a career as a surgeon. Following success in his surgical rotations, he scrubbed in with a cardiothoracic surgeon who was well known for both his status as a surgeon and his fiery temper. Sekeres witnessed the surgeon yelling at whoever was nearby: Medical students, fellows, residents, operating room nurses.
“At the end of that experience, any passing thoughts I had of going into cardiothoracic surgery were gone,” Sekeres said. “Some of the people I met in surgery were truly wonderful. Some were unhappy people.”
He has clear ideas why. Mental health struggles that are all too common among physicians can be caused or exacerbated by mistreatment and can also lead a physician to mistreat others.
“People bully when they themselves are hurting,” Sekeres said. “It begs the question, why are people hurting? What’s driving them to be bullies? I think part of the reason is that they’re working really hard and they’re tired, and nobody’s caring for them. It’s hard to care for others when you feel as if you’re hurting more than they are.”
Gail Gazelle, MD, experienced something like this. In her case, the pressure to please and to be a perfect professional and mother affected how she interacted with those around her. While working as a hospice medical director and an academician and clinician at Harvard Medical School, Boston, Massachusetts, she found herself feeling exhausted and burnt out but simultaneously guilty for not doing enough at work or at home.
Guess what happened? She became irritable, lashing out at her son and not putting her best foot forward with coworkers or patients.
After trying traditional therapy and self-help through books and podcasts, Gazelle found her solution in life coaching. “I realized just how harsh I was being on myself and found ways to reverse that pattern,” she said. “I learned ways of regulating myself emotionally that I definitely didn’t learn in my training.”
Today, Gazelle works as a life coach herself, guiding physicians through common challenges of the profession — particularly bullying, which she sees often. She remembers one client, an oncologist, who was being targeted by a nurse practitioner she was training. The nurse practitioner began talking back to the oncologist, as well as gossiping and bad-mouthing her to the nurses in the practice. The nurses then began excluding the oncologist from their cafeteria table at lunchtime, which felt blatant in such a small practice.
A core component of Gazelle’s coaching strategy was helping the client reclaim her self-esteem by focusing on her strengths. She instructed the client to write down what went well that day each night rather than lying in bed ruminating. Such self-care strategies can not only help bullied physicians but also prevent some of the challenges that might cause a physician to bully or lash out at another in the first place.
Such strategies, along with the recent influx of wellness programs available in healthcare facilities, can help physicians cope with the mental health impacts of bullying and the job in general. But even life coaches like Gazelle acknowledge that they are often band-aids on the system’s deeper wounds. Bullying in healthcare is not an individual issue; at its core, it’s an institutional one.
Negative Hierarchies in Healthcare
When Stecher’s contract expired, she was fired by the supervisor who had been bullying her. Stecher has since filed a lawsuit, claiming sexual discrimination, defamation, and wrongful termination.
The medical field has a long history of hierarchy, and while this rigidity has softened over time, negative hierarchical dynamics are often perpetuated by leaders. Phenomena like cronyism and cliques and behaviors like petty gossip, lunchroom exclusion (which in the worst cases can mimic high school dynamics), and targeting can be at play in the healthcare workplace.
The classic examples, Stecher said, can usually be spotted: “If you threaten the status quo or offer different ideas, you are seen as a threat. Cronyism ... strict hierarchies ... people who elevate individuals in their social arena into leadership positions. Physicians don’t get the leadership training that they really need; they are often just dumped into roles with no previous experience because they’re someone’s golfing buddy.”
The question is how to get workplace culture momentum moving in a positive direction. When Gazelle’s clients are hesitant to voice concerns, she emphasizes doing so can and should benefit leadership, as well as patients and the wider healthcare system.
“The win-win is that you have a healthy culture of respect and dignity and civility rather than the opposite,” she said. “The leader will actually have more staff retention, which everybody’s concerned about, given the shortage of healthcare workers.”
And that’s a key incentive that may not be discussed as much: Talent drain from toxicity. The Medscape Workplace Culture Report asked about culture as it applies to physicians looking to join up. Notably, 93% of doctors say culture is important when mulling a job offer, 70% said culture is equal to money, and 18% ranked it as more important than money, and 46% say a positive atmosphere is the top priority.
Ultimately, it comes down to who is willing to step in and stand up. Respondents to Khan’s survey counted anonymous reporting systems, more supportive administration teams, and zero-tolerance policies as potential remedies. Gazelle, Sekeres, and Stecher all emphasize the need for zero-tolerance policies for bullying and mistreatment.
“We can’t afford to have things going on like this that just destroy the fabric of the healthcare endeavor,” Gazelle said. “They come out sideways eventually. They come out in terms of poor patient care because there are greater errors. There’s a lack of respect for patients. There’s anger and irritability and so much spillover. We have to have zero-tolerance policies from the top down.”
A version of this article appeared on Medscape.com.
While Kellie Lease Stecher, MD, was working as an ob.gyn. in Minneapolis, Minnesota, a patient confided in her a sexual assault allegation about one of Stecher’s male colleagues. Stecher shared the allegation with her supervisor, who told Stecher not to file a report and chose not to address the issue with the patient. Stecher weighed how to do the right thing: Should she speak up? What were the ethical and legal implications of speaking up vs staying silent?
After seeking advice from her mentors, Stecher felt it was her moral and legal duty to report the allegation to the Minnesota Medical Board. Once she did, her supervisor chastised her repeatedly for reporting the allegation. Stecher soon found herself in a hostile work environment where she was regularly singled out and silenced by her supervisor and colleagues.
“I got to a point where I felt like I couldn’t say anything at any meetings without somehow being targeted after the meeting. There was an individual who was even allowed to fat-shame me with no consequences,” Stecher said. “[Being bullied at work is] a struggle because you have no voice, you have no opportunities, and there’s someone who is intentionally making your life uncomfortable.”
Stecher’s experience is not unusual. Mistreatment is a common issue among healthcare workers, ranging from rudeness to bullying and harassment and permeating every level and specialty of the medical profession. A 2019 research review estimated that 26.3% of healthcare workers had experienced bullying and found bullying in healthcare to be associated with mental health problems such as burnout and depression, physical health problems such as insomnia and headaches, and physicians taking more sick leave.
The Medscape Physician Workplace Culture Report 2024 found similarly bleak results:
- 38% said workplace culture is declining.
- 70% don’t see a big commitment from employers for positive culture.
- 48% said staff isn’t committed to positive culture.
The irony, of course, is that most physicians enter the field to care for people. As individuals go from medical school to residency and on with the rest of their careers, they often experience a rude awakening.
It’s Everywhere
Noticing the prevalence of workplace bullying in the medical field, endocrinologist Farah Khan, MD, at UW Medicine in Seattle, Washington, decided to conduct a survey on the issue.
Khan collected 122 responses from colleagues, friends, and acquaintances in the field. When asked if they had ever been bullied in medicine, 68% of respondents said yes. But here’s the fascinating part: She tried to pinpoint one particular area or source of toxicity in the progression of a physician’s career — and couldn’t because it existed at all levels.
More than one third of respondents said their worst bullying experiences occurred in residency, while 30% said mistreatment was worst in medical school, and 24% indicated their worst experience had occurred once they became an attending.
The litany of experiences included being belittled, excluded, yelled at, criticized, shamed, unfairly blamed, threatened, sexually harassed, subjected to bigotry and slurs, and humiliated.
“What surprised me the most was how widespread this problem is and the many different layers of healthcare it permeates through, from operating room staff to medical students to hospital HR to residents and attendings,” Khan said of her findings.
Who Cares for the Caregivers?
When hematologist Mikkael Sekeres, MD, was in medical school, he seriously considered a career as a surgeon. Following success in his surgical rotations, he scrubbed in with a cardiothoracic surgeon who was well known for both his status as a surgeon and his fiery temper. Sekeres witnessed the surgeon yelling at whoever was nearby: Medical students, fellows, residents, operating room nurses.
“At the end of that experience, any passing thoughts I had of going into cardiothoracic surgery were gone,” Sekeres said. “Some of the people I met in surgery were truly wonderful. Some were unhappy people.”
He has clear ideas why. Mental health struggles that are all too common among physicians can be caused or exacerbated by mistreatment and can also lead a physician to mistreat others.
“People bully when they themselves are hurting,” Sekeres said. “It begs the question, why are people hurting? What’s driving them to be bullies? I think part of the reason is that they’re working really hard and they’re tired, and nobody’s caring for them. It’s hard to care for others when you feel as if you’re hurting more than they are.”
Gail Gazelle, MD, experienced something like this. In her case, the pressure to please and to be a perfect professional and mother affected how she interacted with those around her. While working as a hospice medical director and an academician and clinician at Harvard Medical School, Boston, Massachusetts, she found herself feeling exhausted and burnt out but simultaneously guilty for not doing enough at work or at home.
Guess what happened? She became irritable, lashing out at her son and not putting her best foot forward with coworkers or patients.
After trying traditional therapy and self-help through books and podcasts, Gazelle found her solution in life coaching. “I realized just how harsh I was being on myself and found ways to reverse that pattern,” she said. “I learned ways of regulating myself emotionally that I definitely didn’t learn in my training.”
Today, Gazelle works as a life coach herself, guiding physicians through common challenges of the profession — particularly bullying, which she sees often. She remembers one client, an oncologist, who was being targeted by a nurse practitioner she was training. The nurse practitioner began talking back to the oncologist, as well as gossiping and bad-mouthing her to the nurses in the practice. The nurses then began excluding the oncologist from their cafeteria table at lunchtime, which felt blatant in such a small practice.
A core component of Gazelle’s coaching strategy was helping the client reclaim her self-esteem by focusing on her strengths. She instructed the client to write down what went well that day each night rather than lying in bed ruminating. Such self-care strategies can not only help bullied physicians but also prevent some of the challenges that might cause a physician to bully or lash out at another in the first place.
Such strategies, along with the recent influx of wellness programs available in healthcare facilities, can help physicians cope with the mental health impacts of bullying and the job in general. But even life coaches like Gazelle acknowledge that they are often band-aids on the system’s deeper wounds. Bullying in healthcare is not an individual issue; at its core, it’s an institutional one.
Negative Hierarchies in Healthcare
When Stecher’s contract expired, she was fired by the supervisor who had been bullying her. Stecher has since filed a lawsuit, claiming sexual discrimination, defamation, and wrongful termination.
The medical field has a long history of hierarchy, and while this rigidity has softened over time, negative hierarchical dynamics are often perpetuated by leaders. Phenomena like cronyism and cliques and behaviors like petty gossip, lunchroom exclusion (which in the worst cases can mimic high school dynamics), and targeting can be at play in the healthcare workplace.
The classic examples, Stecher said, can usually be spotted: “If you threaten the status quo or offer different ideas, you are seen as a threat. Cronyism ... strict hierarchies ... people who elevate individuals in their social arena into leadership positions. Physicians don’t get the leadership training that they really need; they are often just dumped into roles with no previous experience because they’re someone’s golfing buddy.”
The question is how to get workplace culture momentum moving in a positive direction. When Gazelle’s clients are hesitant to voice concerns, she emphasizes doing so can and should benefit leadership, as well as patients and the wider healthcare system.
“The win-win is that you have a healthy culture of respect and dignity and civility rather than the opposite,” she said. “The leader will actually have more staff retention, which everybody’s concerned about, given the shortage of healthcare workers.”
And that’s a key incentive that may not be discussed as much: Talent drain from toxicity. The Medscape Workplace Culture Report asked about culture as it applies to physicians looking to join up. Notably, 93% of doctors say culture is important when mulling a job offer, 70% said culture is equal to money, and 18% ranked it as more important than money, and 46% say a positive atmosphere is the top priority.
Ultimately, it comes down to who is willing to step in and stand up. Respondents to Khan’s survey counted anonymous reporting systems, more supportive administration teams, and zero-tolerance policies as potential remedies. Gazelle, Sekeres, and Stecher all emphasize the need for zero-tolerance policies for bullying and mistreatment.
“We can’t afford to have things going on like this that just destroy the fabric of the healthcare endeavor,” Gazelle said. “They come out sideways eventually. They come out in terms of poor patient care because there are greater errors. There’s a lack of respect for patients. There’s anger and irritability and so much spillover. We have to have zero-tolerance policies from the top down.”
A version of this article appeared on Medscape.com.
While Kellie Lease Stecher, MD, was working as an ob.gyn. in Minneapolis, Minnesota, a patient confided in her a sexual assault allegation about one of Stecher’s male colleagues. Stecher shared the allegation with her supervisor, who told Stecher not to file a report and chose not to address the issue with the patient. Stecher weighed how to do the right thing: Should she speak up? What were the ethical and legal implications of speaking up vs staying silent?
After seeking advice from her mentors, Stecher felt it was her moral and legal duty to report the allegation to the Minnesota Medical Board. Once she did, her supervisor chastised her repeatedly for reporting the allegation. Stecher soon found herself in a hostile work environment where she was regularly singled out and silenced by her supervisor and colleagues.
“I got to a point where I felt like I couldn’t say anything at any meetings without somehow being targeted after the meeting. There was an individual who was even allowed to fat-shame me with no consequences,” Stecher said. “[Being bullied at work is] a struggle because you have no voice, you have no opportunities, and there’s someone who is intentionally making your life uncomfortable.”
Stecher’s experience is not unusual. Mistreatment is a common issue among healthcare workers, ranging from rudeness to bullying and harassment and permeating every level and specialty of the medical profession. A 2019 research review estimated that 26.3% of healthcare workers had experienced bullying and found bullying in healthcare to be associated with mental health problems such as burnout and depression, physical health problems such as insomnia and headaches, and physicians taking more sick leave.
The Medscape Physician Workplace Culture Report 2024 found similarly bleak results:
- 38% said workplace culture is declining.
- 70% don’t see a big commitment from employers for positive culture.
- 48% said staff isn’t committed to positive culture.
The irony, of course, is that most physicians enter the field to care for people. As individuals go from medical school to residency and on with the rest of their careers, they often experience a rude awakening.
It’s Everywhere
Noticing the prevalence of workplace bullying in the medical field, endocrinologist Farah Khan, MD, at UW Medicine in Seattle, Washington, decided to conduct a survey on the issue.
Khan collected 122 responses from colleagues, friends, and acquaintances in the field. When asked if they had ever been bullied in medicine, 68% of respondents said yes. But here’s the fascinating part: She tried to pinpoint one particular area or source of toxicity in the progression of a physician’s career — and couldn’t because it existed at all levels.
More than one third of respondents said their worst bullying experiences occurred in residency, while 30% said mistreatment was worst in medical school, and 24% indicated their worst experience had occurred once they became an attending.
The litany of experiences included being belittled, excluded, yelled at, criticized, shamed, unfairly blamed, threatened, sexually harassed, subjected to bigotry and slurs, and humiliated.
“What surprised me the most was how widespread this problem is and the many different layers of healthcare it permeates through, from operating room staff to medical students to hospital HR to residents and attendings,” Khan said of her findings.
Who Cares for the Caregivers?
When hematologist Mikkael Sekeres, MD, was in medical school, he seriously considered a career as a surgeon. Following success in his surgical rotations, he scrubbed in with a cardiothoracic surgeon who was well known for both his status as a surgeon and his fiery temper. Sekeres witnessed the surgeon yelling at whoever was nearby: Medical students, fellows, residents, operating room nurses.
“At the end of that experience, any passing thoughts I had of going into cardiothoracic surgery were gone,” Sekeres said. “Some of the people I met in surgery were truly wonderful. Some were unhappy people.”
He has clear ideas why. Mental health struggles that are all too common among physicians can be caused or exacerbated by mistreatment and can also lead a physician to mistreat others.
“People bully when they themselves are hurting,” Sekeres said. “It begs the question, why are people hurting? What’s driving them to be bullies? I think part of the reason is that they’re working really hard and they’re tired, and nobody’s caring for them. It’s hard to care for others when you feel as if you’re hurting more than they are.”
Gail Gazelle, MD, experienced something like this. In her case, the pressure to please and to be a perfect professional and mother affected how she interacted with those around her. While working as a hospice medical director and an academician and clinician at Harvard Medical School, Boston, Massachusetts, she found herself feeling exhausted and burnt out but simultaneously guilty for not doing enough at work or at home.
Guess what happened? She became irritable, lashing out at her son and not putting her best foot forward with coworkers or patients.
After trying traditional therapy and self-help through books and podcasts, Gazelle found her solution in life coaching. “I realized just how harsh I was being on myself and found ways to reverse that pattern,” she said. “I learned ways of regulating myself emotionally that I definitely didn’t learn in my training.”
Today, Gazelle works as a life coach herself, guiding physicians through common challenges of the profession — particularly bullying, which she sees often. She remembers one client, an oncologist, who was being targeted by a nurse practitioner she was training. The nurse practitioner began talking back to the oncologist, as well as gossiping and bad-mouthing her to the nurses in the practice. The nurses then began excluding the oncologist from their cafeteria table at lunchtime, which felt blatant in such a small practice.
A core component of Gazelle’s coaching strategy was helping the client reclaim her self-esteem by focusing on her strengths. She instructed the client to write down what went well that day each night rather than lying in bed ruminating. Such self-care strategies can not only help bullied physicians but also prevent some of the challenges that might cause a physician to bully or lash out at another in the first place.
Such strategies, along with the recent influx of wellness programs available in healthcare facilities, can help physicians cope with the mental health impacts of bullying and the job in general. But even life coaches like Gazelle acknowledge that they are often band-aids on the system’s deeper wounds. Bullying in healthcare is not an individual issue; at its core, it’s an institutional one.
Negative Hierarchies in Healthcare
When Stecher’s contract expired, she was fired by the supervisor who had been bullying her. Stecher has since filed a lawsuit, claiming sexual discrimination, defamation, and wrongful termination.
The medical field has a long history of hierarchy, and while this rigidity has softened over time, negative hierarchical dynamics are often perpetuated by leaders. Phenomena like cronyism and cliques and behaviors like petty gossip, lunchroom exclusion (which in the worst cases can mimic high school dynamics), and targeting can be at play in the healthcare workplace.
The classic examples, Stecher said, can usually be spotted: “If you threaten the status quo or offer different ideas, you are seen as a threat. Cronyism ... strict hierarchies ... people who elevate individuals in their social arena into leadership positions. Physicians don’t get the leadership training that they really need; they are often just dumped into roles with no previous experience because they’re someone’s golfing buddy.”
The question is how to get workplace culture momentum moving in a positive direction. When Gazelle’s clients are hesitant to voice concerns, she emphasizes doing so can and should benefit leadership, as well as patients and the wider healthcare system.
“The win-win is that you have a healthy culture of respect and dignity and civility rather than the opposite,” she said. “The leader will actually have more staff retention, which everybody’s concerned about, given the shortage of healthcare workers.”
And that’s a key incentive that may not be discussed as much: Talent drain from toxicity. The Medscape Workplace Culture Report asked about culture as it applies to physicians looking to join up. Notably, 93% of doctors say culture is important when mulling a job offer, 70% said culture is equal to money, and 18% ranked it as more important than money, and 46% say a positive atmosphere is the top priority.
Ultimately, it comes down to who is willing to step in and stand up. Respondents to Khan’s survey counted anonymous reporting systems, more supportive administration teams, and zero-tolerance policies as potential remedies. Gazelle, Sekeres, and Stecher all emphasize the need for zero-tolerance policies for bullying and mistreatment.
“We can’t afford to have things going on like this that just destroy the fabric of the healthcare endeavor,” Gazelle said. “They come out sideways eventually. They come out in terms of poor patient care because there are greater errors. There’s a lack of respect for patients. There’s anger and irritability and so much spillover. We have to have zero-tolerance policies from the top down.”
A version of this article appeared on Medscape.com.
NY Nurse Practitioners Sue State Over Pay Equity, Alleged Gender Inequality
A
The New York State Civil Service Commission understates the job function of NPs, overstates their dependence on physicians, and inadequately pays them for their work, according to the complaint filed in the US District Court for the Northern District of New York.
The nurses claim the mistreatment is a consequence of the fact that “at least 80% of the state’s employed NPs are women.”
Michael H. Sussman, a Goshen, New York–based attorney for the nurses, said in an interview that New York NPs are increasingly being used essentially as doctors at state-run facilities, including prisons, yet the state has failed to adequately pay them.
The lawsuit comes after a decade-long attempt by NPs to attain equitable pay and the ability to advance their civil service careers, he said.
“New York state has not addressed the heart of the issue, which is that the classification of this position is much lower than other positions in the state which are not so female-dominated and which engage in very similar activities,” Sussman said.
The lawsuit claims that “the work of NPs is complex, equaling that of a medical specialist, psychiatrist, or clinical physician.”
A spokesman for the New York State Civil Service Commission declined comment, saying the department does not comment on pending litigation.
Novel Gender Discrimination Argument
Gender discrimination is a relatively new argument avenue in the larger equal work, equal pay debate, said Joanne Spetz, PhD, director of the Institute for Health Policy Studies at the University of California, San Francisco.
“This is the first time I’ve heard of [such] a case being really gender discrimination focused,” she said in an interview. “On one level, I think it’s groundbreaking as a legal approach, but it’s also limited because it’s focused on public, state employees.”
Spetz noted that New York has significantly expanded NPs’ scope of practice, enacting in 2022 legislation that granted NPs full practice authority. The law means NPs can evaluate, order, diagnose, manage treatments, and prescribe medications for patients without physician supervision.
“They are in a role where they are stepping back and saying, ‘Wait, why are [we] not receiving equal pay for equal work?’ ” Spetz said. “It’s a totally fair area for debate, especially because they are now authorized to do essentially equal work with a high degree of autonomy.”
Debate Over Pay Grade
The nurses’ complaint centers on the New York State Civil Service Commission’s classification for NPs, which hasn’t changed since 2006. NPs are classified at grade 24, and they have no possibility of internal advancement associated with their title, according to the legal complaint filed on September 17.
To comply with a state legislative directive, the commission in 2018 conducted a study of the NP classification but recommended against reclassification or implementing a career ladder. The study noted the subordinate role of NPs to physicians and the substantial difference between physician classification (entry at grade 34) and that of NPs, psychologists (grade 25), and pharmacists (grade 25).
The study concluded that higher classified positions have higher levels of educational attainment and licensure requirements and no supervision or collaboration requirements, according to the complaint.
At the time, groups such as the Nurse Practitioner Association and the Public Employees Federation (PEF) criticized the findings, but the commission stuck to its classification.
Following the NP Modernization Act that allowed NPs to practice independently, PEF sought an increase for NPs to grade 28 with a progression to grade 34 depending on experience.
“But to this date, despite altering the starting salaries of NPs, defendants have failed and refused to alter the compensation offered to the substantial majority of NPs, and each plaintiff remains cabined in a grade 24 with a discriminatorily low salary when compared with males in other job classifications doing highly similar functions,” the lawsuit contended.
Six plaintiffs are named in the lawsuit, all of whom are women and work for state agencies. Plaintiff Rachel Burns, for instance, works as a psychiatric mental health NP in West Seneca and is responsible for performing psychiatric evaluations for patients, diagnosis, prescribing medication, ordering labs, and determining risks. The evaluations are identical for a psychiatrist and require her to complete the same forms, according to the suit.
Another plaintiff, Amber Hawthorne Lashway, works at a correctional facility in Altona, where for many years she was the sole medical provider, according to the lawsuit. Lashway’s duties, which include diagnoses and treatment of inmates’ medical conditions, mirror those performed by clinical physicians, the suit stated.
The plaintiffs are requesting the court accept jurisdiction of the matter and certify the class they seek to represent. They are also demanding prospective pay equity and compensatory damages for the distress caused by “the long-standing discriminatory” treatment by the state.
The Civil Service Commission and state of New York have not yet responded to the complaint. Their responses are due on November 12.
Attorney: Case Impact Limited
Benjamin McMichael, PhD, JD, said the New York case is not surprising as more states across the country are granting nurses more practice autonomy. The current landscape tends to favor the nurses, he said, with about half of states now allowing NPs full practice authority.
“I think the [New York] NPs are correct that they are underpaid,” said McMichael, an associate professor of law and director of the Interdisciplinary Legal Studies Initiative at The University of Alabama in Tuscaloosa. “With that said, the nature of the case does not clearly lend itself to national change.”
The fact that the NP plaintiffs are employed by the state means they are using a specific set of laws to advance their cause, he said. Other NPs in other employment situations may not have access to the same laws.
A version of this article first appeared on Medscape.com.
A
The New York State Civil Service Commission understates the job function of NPs, overstates their dependence on physicians, and inadequately pays them for their work, according to the complaint filed in the US District Court for the Northern District of New York.
The nurses claim the mistreatment is a consequence of the fact that “at least 80% of the state’s employed NPs are women.”
Michael H. Sussman, a Goshen, New York–based attorney for the nurses, said in an interview that New York NPs are increasingly being used essentially as doctors at state-run facilities, including prisons, yet the state has failed to adequately pay them.
The lawsuit comes after a decade-long attempt by NPs to attain equitable pay and the ability to advance their civil service careers, he said.
“New York state has not addressed the heart of the issue, which is that the classification of this position is much lower than other positions in the state which are not so female-dominated and which engage in very similar activities,” Sussman said.
The lawsuit claims that “the work of NPs is complex, equaling that of a medical specialist, psychiatrist, or clinical physician.”
A spokesman for the New York State Civil Service Commission declined comment, saying the department does not comment on pending litigation.
Novel Gender Discrimination Argument
Gender discrimination is a relatively new argument avenue in the larger equal work, equal pay debate, said Joanne Spetz, PhD, director of the Institute for Health Policy Studies at the University of California, San Francisco.
“This is the first time I’ve heard of [such] a case being really gender discrimination focused,” she said in an interview. “On one level, I think it’s groundbreaking as a legal approach, but it’s also limited because it’s focused on public, state employees.”
Spetz noted that New York has significantly expanded NPs’ scope of practice, enacting in 2022 legislation that granted NPs full practice authority. The law means NPs can evaluate, order, diagnose, manage treatments, and prescribe medications for patients without physician supervision.
“They are in a role where they are stepping back and saying, ‘Wait, why are [we] not receiving equal pay for equal work?’ ” Spetz said. “It’s a totally fair area for debate, especially because they are now authorized to do essentially equal work with a high degree of autonomy.”
Debate Over Pay Grade
The nurses’ complaint centers on the New York State Civil Service Commission’s classification for NPs, which hasn’t changed since 2006. NPs are classified at grade 24, and they have no possibility of internal advancement associated with their title, according to the legal complaint filed on September 17.
To comply with a state legislative directive, the commission in 2018 conducted a study of the NP classification but recommended against reclassification or implementing a career ladder. The study noted the subordinate role of NPs to physicians and the substantial difference between physician classification (entry at grade 34) and that of NPs, psychologists (grade 25), and pharmacists (grade 25).
The study concluded that higher classified positions have higher levels of educational attainment and licensure requirements and no supervision or collaboration requirements, according to the complaint.
At the time, groups such as the Nurse Practitioner Association and the Public Employees Federation (PEF) criticized the findings, but the commission stuck to its classification.
Following the NP Modernization Act that allowed NPs to practice independently, PEF sought an increase for NPs to grade 28 with a progression to grade 34 depending on experience.
“But to this date, despite altering the starting salaries of NPs, defendants have failed and refused to alter the compensation offered to the substantial majority of NPs, and each plaintiff remains cabined in a grade 24 with a discriminatorily low salary when compared with males in other job classifications doing highly similar functions,” the lawsuit contended.
Six plaintiffs are named in the lawsuit, all of whom are women and work for state agencies. Plaintiff Rachel Burns, for instance, works as a psychiatric mental health NP in West Seneca and is responsible for performing psychiatric evaluations for patients, diagnosis, prescribing medication, ordering labs, and determining risks. The evaluations are identical for a psychiatrist and require her to complete the same forms, according to the suit.
Another plaintiff, Amber Hawthorne Lashway, works at a correctional facility in Altona, where for many years she was the sole medical provider, according to the lawsuit. Lashway’s duties, which include diagnoses and treatment of inmates’ medical conditions, mirror those performed by clinical physicians, the suit stated.
The plaintiffs are requesting the court accept jurisdiction of the matter and certify the class they seek to represent. They are also demanding prospective pay equity and compensatory damages for the distress caused by “the long-standing discriminatory” treatment by the state.
The Civil Service Commission and state of New York have not yet responded to the complaint. Their responses are due on November 12.
Attorney: Case Impact Limited
Benjamin McMichael, PhD, JD, said the New York case is not surprising as more states across the country are granting nurses more practice autonomy. The current landscape tends to favor the nurses, he said, with about half of states now allowing NPs full practice authority.
“I think the [New York] NPs are correct that they are underpaid,” said McMichael, an associate professor of law and director of the Interdisciplinary Legal Studies Initiative at The University of Alabama in Tuscaloosa. “With that said, the nature of the case does not clearly lend itself to national change.”
The fact that the NP plaintiffs are employed by the state means they are using a specific set of laws to advance their cause, he said. Other NPs in other employment situations may not have access to the same laws.
A version of this article first appeared on Medscape.com.
A
The New York State Civil Service Commission understates the job function of NPs, overstates their dependence on physicians, and inadequately pays them for their work, according to the complaint filed in the US District Court for the Northern District of New York.
The nurses claim the mistreatment is a consequence of the fact that “at least 80% of the state’s employed NPs are women.”
Michael H. Sussman, a Goshen, New York–based attorney for the nurses, said in an interview that New York NPs are increasingly being used essentially as doctors at state-run facilities, including prisons, yet the state has failed to adequately pay them.
The lawsuit comes after a decade-long attempt by NPs to attain equitable pay and the ability to advance their civil service careers, he said.
“New York state has not addressed the heart of the issue, which is that the classification of this position is much lower than other positions in the state which are not so female-dominated and which engage in very similar activities,” Sussman said.
The lawsuit claims that “the work of NPs is complex, equaling that of a medical specialist, psychiatrist, or clinical physician.”
A spokesman for the New York State Civil Service Commission declined comment, saying the department does not comment on pending litigation.
Novel Gender Discrimination Argument
Gender discrimination is a relatively new argument avenue in the larger equal work, equal pay debate, said Joanne Spetz, PhD, director of the Institute for Health Policy Studies at the University of California, San Francisco.
“This is the first time I’ve heard of [such] a case being really gender discrimination focused,” she said in an interview. “On one level, I think it’s groundbreaking as a legal approach, but it’s also limited because it’s focused on public, state employees.”
Spetz noted that New York has significantly expanded NPs’ scope of practice, enacting in 2022 legislation that granted NPs full practice authority. The law means NPs can evaluate, order, diagnose, manage treatments, and prescribe medications for patients without physician supervision.
“They are in a role where they are stepping back and saying, ‘Wait, why are [we] not receiving equal pay for equal work?’ ” Spetz said. “It’s a totally fair area for debate, especially because they are now authorized to do essentially equal work with a high degree of autonomy.”
Debate Over Pay Grade
The nurses’ complaint centers on the New York State Civil Service Commission’s classification for NPs, which hasn’t changed since 2006. NPs are classified at grade 24, and they have no possibility of internal advancement associated with their title, according to the legal complaint filed on September 17.
To comply with a state legislative directive, the commission in 2018 conducted a study of the NP classification but recommended against reclassification or implementing a career ladder. The study noted the subordinate role of NPs to physicians and the substantial difference between physician classification (entry at grade 34) and that of NPs, psychologists (grade 25), and pharmacists (grade 25).
The study concluded that higher classified positions have higher levels of educational attainment and licensure requirements and no supervision or collaboration requirements, according to the complaint.
At the time, groups such as the Nurse Practitioner Association and the Public Employees Federation (PEF) criticized the findings, but the commission stuck to its classification.
Following the NP Modernization Act that allowed NPs to practice independently, PEF sought an increase for NPs to grade 28 with a progression to grade 34 depending on experience.
“But to this date, despite altering the starting salaries of NPs, defendants have failed and refused to alter the compensation offered to the substantial majority of NPs, and each plaintiff remains cabined in a grade 24 with a discriminatorily low salary when compared with males in other job classifications doing highly similar functions,” the lawsuit contended.
Six plaintiffs are named in the lawsuit, all of whom are women and work for state agencies. Plaintiff Rachel Burns, for instance, works as a psychiatric mental health NP in West Seneca and is responsible for performing psychiatric evaluations for patients, diagnosis, prescribing medication, ordering labs, and determining risks. The evaluations are identical for a psychiatrist and require her to complete the same forms, according to the suit.
Another plaintiff, Amber Hawthorne Lashway, works at a correctional facility in Altona, where for many years she was the sole medical provider, according to the lawsuit. Lashway’s duties, which include diagnoses and treatment of inmates’ medical conditions, mirror those performed by clinical physicians, the suit stated.
The plaintiffs are requesting the court accept jurisdiction of the matter and certify the class they seek to represent. They are also demanding prospective pay equity and compensatory damages for the distress caused by “the long-standing discriminatory” treatment by the state.
The Civil Service Commission and state of New York have not yet responded to the complaint. Their responses are due on November 12.
Attorney: Case Impact Limited
Benjamin McMichael, PhD, JD, said the New York case is not surprising as more states across the country are granting nurses more practice autonomy. The current landscape tends to favor the nurses, he said, with about half of states now allowing NPs full practice authority.
“I think the [New York] NPs are correct that they are underpaid,” said McMichael, an associate professor of law and director of the Interdisciplinary Legal Studies Initiative at The University of Alabama in Tuscaloosa. “With that said, the nature of the case does not clearly lend itself to national change.”
The fact that the NP plaintiffs are employed by the state means they are using a specific set of laws to advance their cause, he said. Other NPs in other employment situations may not have access to the same laws.
A version of this article first appeared on Medscape.com.
Beyond Scope Creep: Why Physicians and PAs Should Come Together for Patients
Over the past few years, many states have attempted to address the ongoing shortage of healthcare workers by introducing new bills to increase the scope of practice for nurse practitioners (NPs) and physician assistants (PAs). The goal of each bill was to improve access to care, particularly for patients who may live in areas where it’s difficult to find a doctor.
In response, the American Medical Association (AMA) launched a targeted campaign to fight “scope creep.” Their goal was to gain the momentum necessary to block proposed legislation to modify or expand the practice authority of nonphysicians, including PAs. A spokesperson for the organization told this news organization that the AMA “greatly values and respects the contributions of PAs as important members of the healthcare team” but emphasized that they do not have the same “skill set or breadth of experience of physicians.”
As such, the AMA argued that expanded practice authority would not only dismantle physician-led care teams but also ultimately lead to higher costs and lower-quality patient care.
The AMA has since launched a large-scale advocacy effort to fight practice expansion legislation — and has a specific page on its website to highlight those efforts. In addition, they have authored model legislation, talking points for AMA members, and a widely read article in AMA News to help them in what they call a “fight for physicians.”
These resources have also been disseminated to the greater healthcare stakeholder community.
Marilyn Suri, PA-C, chief operating officer and senior executive for Advanced Practice Professional Affairs at Vincenzo Novara MDPA and Associates, a critical care pulmonary medicine practice in Miami, Florida, said she found the AMA’s campaign to be “very misleading.”
“PAs are created in the image of physicians to help manage the physician shortage. We are trained very rigorously — to diagnose illness, develop treatment plans, and prescribe medications,” she said. “We’re not trying to expand our scope. We are trying to eliminate or lessen barriers that prevent patients from getting access to care.”
Suri is not alone. Last summer, the American Academy of Physician Associates (AAPA) requested a meeting with the AMA to find ways for the two organizations to collaborate to improve care delivery — as well as find common ground to address issues regarding patient access to care. When the AMA did not respond, the AAPA sent a second letter in September 2024, reiterating their request for a meeting.
That correspondence also included a letter, signed by more than 8000 PAs from across the country, calling for an end to what the AAPA refers to as “damaging rhetoric,” as well as data from a recent survey of PAs regarding the fallout of AMA’s scope creep messaging.
Those survey results highlighted that the vast majority of PAs surveyed feel that the AMA is doing more than just attacking proposed legislation: They believe the association is negatively influencing patients’ understanding of PA qualifications, ultimately affecting their ability to provide care.
“The campaign is unintentionally harming patients by suggesting we are doing more than what we are trained to do,” said Elisa Hock, PA-C, a behavioral health PA in Texas. “And when you work in a place with limited resources, medically speaking — including limited access to providers — this kind of campaign is really detrimental to helping patients.”
Lisa M. Gables, CEO of the AAPA, said the organization is “deeply disappointed” in the AMA’s lack of response to their letters thus far — but remains committed to working with the organization to bring forward new solutions to address healthcare’s most pressing challenges.
“AAPA remains committed to pushing for modernization of practice laws to ensure all providers can practice medicine to the fullest extent of their training, education, and experience,” she said. “That is what patients deserve and want.”
Hock agreed. She told this news organization that the public is not always aware of what PAs can offer in terms of patient care. That said, she believes newer generations of physicians understand the value of PAs and the many skills they bring to the table.
“I’ve been doing this for 17 years, and it’s been an uphill battle, at times, to educate the public about what PAs can and can’t do,” she explained. “To throw more mud in the mix that will confuse patients more about what we do doesn’t help. Healthcare works best with a team-based approach. And that team has been and always will be led by the physician. We are aware of our role and our limitations. But we also know what we can offer patients, especially in areas like El Paso, where there is a real shortage of providers.”
With a growing aging population — and the physician shortage expected to increase in the coming decade — Suri hopes that the AMA will accept AAPA’s invitation to meet — because no one wins with this kind of healthcare infighting. In fact, she said patients will suffer because of it. She hopes that future discussions and collaborations can show providers and patients what team-based healthcare can offer.
“I think it’s important for those in healthcare to be aware that none of us work alone. Even physicians collaborate with other subspecialties, as well as nurses and other healthcare professionals,” said Suri.
A version of this article appeared on Medscape.com.
Over the past few years, many states have attempted to address the ongoing shortage of healthcare workers by introducing new bills to increase the scope of practice for nurse practitioners (NPs) and physician assistants (PAs). The goal of each bill was to improve access to care, particularly for patients who may live in areas where it’s difficult to find a doctor.
In response, the American Medical Association (AMA) launched a targeted campaign to fight “scope creep.” Their goal was to gain the momentum necessary to block proposed legislation to modify or expand the practice authority of nonphysicians, including PAs. A spokesperson for the organization told this news organization that the AMA “greatly values and respects the contributions of PAs as important members of the healthcare team” but emphasized that they do not have the same “skill set or breadth of experience of physicians.”
As such, the AMA argued that expanded practice authority would not only dismantle physician-led care teams but also ultimately lead to higher costs and lower-quality patient care.
The AMA has since launched a large-scale advocacy effort to fight practice expansion legislation — and has a specific page on its website to highlight those efforts. In addition, they have authored model legislation, talking points for AMA members, and a widely read article in AMA News to help them in what they call a “fight for physicians.”
These resources have also been disseminated to the greater healthcare stakeholder community.
Marilyn Suri, PA-C, chief operating officer and senior executive for Advanced Practice Professional Affairs at Vincenzo Novara MDPA and Associates, a critical care pulmonary medicine practice in Miami, Florida, said she found the AMA’s campaign to be “very misleading.”
“PAs are created in the image of physicians to help manage the physician shortage. We are trained very rigorously — to diagnose illness, develop treatment plans, and prescribe medications,” she said. “We’re not trying to expand our scope. We are trying to eliminate or lessen barriers that prevent patients from getting access to care.”
Suri is not alone. Last summer, the American Academy of Physician Associates (AAPA) requested a meeting with the AMA to find ways for the two organizations to collaborate to improve care delivery — as well as find common ground to address issues regarding patient access to care. When the AMA did not respond, the AAPA sent a second letter in September 2024, reiterating their request for a meeting.
That correspondence also included a letter, signed by more than 8000 PAs from across the country, calling for an end to what the AAPA refers to as “damaging rhetoric,” as well as data from a recent survey of PAs regarding the fallout of AMA’s scope creep messaging.
Those survey results highlighted that the vast majority of PAs surveyed feel that the AMA is doing more than just attacking proposed legislation: They believe the association is negatively influencing patients’ understanding of PA qualifications, ultimately affecting their ability to provide care.
“The campaign is unintentionally harming patients by suggesting we are doing more than what we are trained to do,” said Elisa Hock, PA-C, a behavioral health PA in Texas. “And when you work in a place with limited resources, medically speaking — including limited access to providers — this kind of campaign is really detrimental to helping patients.”
Lisa M. Gables, CEO of the AAPA, said the organization is “deeply disappointed” in the AMA’s lack of response to their letters thus far — but remains committed to working with the organization to bring forward new solutions to address healthcare’s most pressing challenges.
“AAPA remains committed to pushing for modernization of practice laws to ensure all providers can practice medicine to the fullest extent of their training, education, and experience,” she said. “That is what patients deserve and want.”
Hock agreed. She told this news organization that the public is not always aware of what PAs can offer in terms of patient care. That said, she believes newer generations of physicians understand the value of PAs and the many skills they bring to the table.
“I’ve been doing this for 17 years, and it’s been an uphill battle, at times, to educate the public about what PAs can and can’t do,” she explained. “To throw more mud in the mix that will confuse patients more about what we do doesn’t help. Healthcare works best with a team-based approach. And that team has been and always will be led by the physician. We are aware of our role and our limitations. But we also know what we can offer patients, especially in areas like El Paso, where there is a real shortage of providers.”
With a growing aging population — and the physician shortage expected to increase in the coming decade — Suri hopes that the AMA will accept AAPA’s invitation to meet — because no one wins with this kind of healthcare infighting. In fact, she said patients will suffer because of it. She hopes that future discussions and collaborations can show providers and patients what team-based healthcare can offer.
“I think it’s important for those in healthcare to be aware that none of us work alone. Even physicians collaborate with other subspecialties, as well as nurses and other healthcare professionals,” said Suri.
A version of this article appeared on Medscape.com.
Over the past few years, many states have attempted to address the ongoing shortage of healthcare workers by introducing new bills to increase the scope of practice for nurse practitioners (NPs) and physician assistants (PAs). The goal of each bill was to improve access to care, particularly for patients who may live in areas where it’s difficult to find a doctor.
In response, the American Medical Association (AMA) launched a targeted campaign to fight “scope creep.” Their goal was to gain the momentum necessary to block proposed legislation to modify or expand the practice authority of nonphysicians, including PAs. A spokesperson for the organization told this news organization that the AMA “greatly values and respects the contributions of PAs as important members of the healthcare team” but emphasized that they do not have the same “skill set or breadth of experience of physicians.”
As such, the AMA argued that expanded practice authority would not only dismantle physician-led care teams but also ultimately lead to higher costs and lower-quality patient care.
The AMA has since launched a large-scale advocacy effort to fight practice expansion legislation — and has a specific page on its website to highlight those efforts. In addition, they have authored model legislation, talking points for AMA members, and a widely read article in AMA News to help them in what they call a “fight for physicians.”
These resources have also been disseminated to the greater healthcare stakeholder community.
Marilyn Suri, PA-C, chief operating officer and senior executive for Advanced Practice Professional Affairs at Vincenzo Novara MDPA and Associates, a critical care pulmonary medicine practice in Miami, Florida, said she found the AMA’s campaign to be “very misleading.”
“PAs are created in the image of physicians to help manage the physician shortage. We are trained very rigorously — to diagnose illness, develop treatment plans, and prescribe medications,” she said. “We’re not trying to expand our scope. We are trying to eliminate or lessen barriers that prevent patients from getting access to care.”
Suri is not alone. Last summer, the American Academy of Physician Associates (AAPA) requested a meeting with the AMA to find ways for the two organizations to collaborate to improve care delivery — as well as find common ground to address issues regarding patient access to care. When the AMA did not respond, the AAPA sent a second letter in September 2024, reiterating their request for a meeting.
That correspondence also included a letter, signed by more than 8000 PAs from across the country, calling for an end to what the AAPA refers to as “damaging rhetoric,” as well as data from a recent survey of PAs regarding the fallout of AMA’s scope creep messaging.
Those survey results highlighted that the vast majority of PAs surveyed feel that the AMA is doing more than just attacking proposed legislation: They believe the association is negatively influencing patients’ understanding of PA qualifications, ultimately affecting their ability to provide care.
“The campaign is unintentionally harming patients by suggesting we are doing more than what we are trained to do,” said Elisa Hock, PA-C, a behavioral health PA in Texas. “And when you work in a place with limited resources, medically speaking — including limited access to providers — this kind of campaign is really detrimental to helping patients.”
Lisa M. Gables, CEO of the AAPA, said the organization is “deeply disappointed” in the AMA’s lack of response to their letters thus far — but remains committed to working with the organization to bring forward new solutions to address healthcare’s most pressing challenges.
“AAPA remains committed to pushing for modernization of practice laws to ensure all providers can practice medicine to the fullest extent of their training, education, and experience,” she said. “That is what patients deserve and want.”
Hock agreed. She told this news organization that the public is not always aware of what PAs can offer in terms of patient care. That said, she believes newer generations of physicians understand the value of PAs and the many skills they bring to the table.
“I’ve been doing this for 17 years, and it’s been an uphill battle, at times, to educate the public about what PAs can and can’t do,” she explained. “To throw more mud in the mix that will confuse patients more about what we do doesn’t help. Healthcare works best with a team-based approach. And that team has been and always will be led by the physician. We are aware of our role and our limitations. But we also know what we can offer patients, especially in areas like El Paso, where there is a real shortage of providers.”
With a growing aging population — and the physician shortage expected to increase in the coming decade — Suri hopes that the AMA will accept AAPA’s invitation to meet — because no one wins with this kind of healthcare infighting. In fact, she said patients will suffer because of it. She hopes that future discussions and collaborations can show providers and patients what team-based healthcare can offer.
“I think it’s important for those in healthcare to be aware that none of us work alone. Even physicians collaborate with other subspecialties, as well as nurses and other healthcare professionals,” said Suri.
A version of this article appeared on Medscape.com.