User login
Less Invasive Screening May Identify Barrett’s Esophagus Earlier
A new combination modality demonstrated excellent sensitivity and negative predictive value compared with endoscopy in a prospective study of at-risk veterans screened for Barrett’s esophagus (BE) and esophageal adenocarcinoma (EAC), a small comparative study in US veterans found.
BE is up to three times more prevalent in veterans than in the general population.
This and other minimally invasive approaches may reduce patient anxiety and increase screening rates, according to investigators led by Katarina B. Greer, MD, MS, of the VA Northeast Ohio Healthcare System and Case Western University in Cleveland. Such screening platforms are expected to open a window on improved prognosis for EAC by offering well-tolerated, office-based testing, the authors wrote in The American Journal of Gastroenterology.
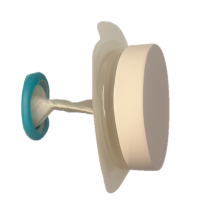
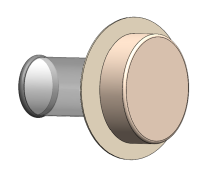
Greer and colleagues compared standard upper endoscopy with EsoCheck (EC), a nonendoscopic esophageal balloon cell-sampling device coupled with EsoGuard (EG), a DNA-based precancer screening assay, with standard upper endoscopy, an FDA-approved minimally invasive alternative.
Sensitivity and specificity of combined EC/EG for esophagogastroduodenoscopy (EGD)-detected BE/EAC were 92.9% (95% CI, 66.1-99.8) and 72.2% (95% CI, 62.1-80.8), respectively. Positive and negative predictive values were 32.5% (95% CI, 18.6-49.1) and 98.6% (95% CI, 92.4-100), respectively.
“With its strong negative predictive power, this screening modality could be a first-line tool available to a greater number of patients,” Greer and associates wrote. “Data from this test support the notion that EC could be performed as a triaging test to increase the yield of diagnostic upper endoscopy 2.5-fold.”
The US rates of EAC have increased more than six-fold in the past four decades and continue to rise. In 2023, 21,560 cases of EAC were diagnosed here. The prognosis for EAC is still poor, with fewer than 22% of patients surviving beyond 5 years.
Current guidelines recommend sedated EGD for patients with chronic gastroesophageal reflux disease (GERD) and additional BE risk factors such as smoking, obesity, and family history. This strategy, however, often fails to detect BE when symptoms are well controlled with over-the-counter or physician-prescribed therapies, Greer and colleagues noted. It also fails to detect BE in individuals without GERD, who comprise 40% of those who develop EAC.
Fewer than 5% of EACs are diagnosed as early-stage lesions caught by surveillance of patients with previously detected BE.
Study Details
The researchers recruited veterans meeting American College of Gastroenterology criteria for endoscopic BE and EAC screening at the Louis Stokes Cleveland Veterans Affairs Medical Center.
Of 782 eligible veterans, 130 (16.6%) entered the study and 124 completed screening. Common reasons for nonparticipation included completion of upper endoscopy outside of the VA healthcare system, lack of interest in joining a research study, and no recommendation for screening from referring gastroenterology or primary care providers. Eligible candidates had gastroesophageal reflux disorder plus three additional risk factors, such as smoking, higher BMI, male sex, age 50 years or older, and family history. The mean number of risk factors was 4.1.
“Available data suggest that family history is the strongest predictor of BE diagnosis, as prevalence of BE among those with family history was 23%,” Greer’s group wrote. “This points to high priority of pursuing screening in patients with family history of the condition, followed by patients who share multiple risk factors.”
All participants completed unsedated EC-guided distal esophageal sampling followed by a sedated EGD on the same day. The prevalence of BE/EAC was 12.9% (n = 14/2), based on standard EGD.
“The study was not powered to prospectively determine EC diagnostic accuracy for subgroups of nondysplastic and dysplastic BE and EAC. These data are reported for this device in development studies but not available for our study population,” the authors wrote. In comparison, they noted, the Cytosponge-TFF3, another nonendoscopic screening device for EAC and BE, exhibited lower sensitivity of 79.5%-87.2%, depending on lesion length, but higher specificity of 92.4%.
Procedural Anxiety
Baseline scores on the short-form six-item Spielberger State-Trait Anxiety Inventory-6 (STAI-6) revealed notable levels of periprocedural anxiety. STAI-6 scores range from 20 to 80, with higher scores indicating more severe anxiety. In the VA study, scores ranged from 20 to 60, and most domains constituting the scores were the same before and after the procedure. Participants did, however, report a statistically significant decrease in sense of worry after EC and reported good tolerability for both EC and EG.
Offering an outsider’s perspective on the study, Joshua Sloan, DO, an esophageal gastroenterologist at University of Minnesota Medical Center in Minneapolis, said that with the acceleration of US rates of EAC, developing a nonendoscopic screening tool to improve identification of Barrett’s and perhaps early EAC is important. “The study by Greer et al helps support the use of nonendoscopic screening with EsoCheck and EsoGuard to identify these conditions,” he told this news organization. “It will be interesting to see similar studies in the non-VA population as well. As the study notes, veterans are an enriched population with a higher prevalence of Barrett’s esophagus.”
Ultimately, Sloan added, “the hope is to increase our ability to identify and manage BE before it becomes EAC. Nonendoscopic screening tools have the potential to increase diagnosis and funnel the appropriate patients for endoscopic surveillance.”
The Bottom Line
“Calculations regarding effectiveness of the two-step screening strategy afforded by EC indicate that the burden of screening would be reduced by at least half (53%),” the authors wrote. Since the estimated size of the US screen-eligible population ranges from 19.7 million to 120.1 million, noninvasive tools could significantly decrease EGD procedures. A formal cost effectiveness analysis is being conducted and will be published separately.
This study was funded by a Department of Defense award.
Co-Author Chak reported device patents assigned to Case Western Reserve University and licensed to Lucid Diagnostics. The other authors had no competing interests to declare. Sloan disclosed speaking and/or advisory work for Sanofi-Regeneron, Phathom Pharmaceuticals, and Takeda Pharmaceuticals unrelated to his comments.
A version of this article first appeared on Medscape.com.
A new combination modality demonstrated excellent sensitivity and negative predictive value compared with endoscopy in a prospective study of at-risk veterans screened for Barrett’s esophagus (BE) and esophageal adenocarcinoma (EAC), a small comparative study in US veterans found.
BE is up to three times more prevalent in veterans than in the general population.
This and other minimally invasive approaches may reduce patient anxiety and increase screening rates, according to investigators led by Katarina B. Greer, MD, MS, of the VA Northeast Ohio Healthcare System and Case Western University in Cleveland. Such screening platforms are expected to open a window on improved prognosis for EAC by offering well-tolerated, office-based testing, the authors wrote in The American Journal of Gastroenterology.
Greer and colleagues compared standard upper endoscopy with EsoCheck (EC), a nonendoscopic esophageal balloon cell-sampling device coupled with EsoGuard (EG), a DNA-based precancer screening assay, with standard upper endoscopy, an FDA-approved minimally invasive alternative.
Sensitivity and specificity of combined EC/EG for esophagogastroduodenoscopy (EGD)-detected BE/EAC were 92.9% (95% CI, 66.1-99.8) and 72.2% (95% CI, 62.1-80.8), respectively. Positive and negative predictive values were 32.5% (95% CI, 18.6-49.1) and 98.6% (95% CI, 92.4-100), respectively.
“With its strong negative predictive power, this screening modality could be a first-line tool available to a greater number of patients,” Greer and associates wrote. “Data from this test support the notion that EC could be performed as a triaging test to increase the yield of diagnostic upper endoscopy 2.5-fold.”
The US rates of EAC have increased more than six-fold in the past four decades and continue to rise. In 2023, 21,560 cases of EAC were diagnosed here. The prognosis for EAC is still poor, with fewer than 22% of patients surviving beyond 5 years.
Current guidelines recommend sedated EGD for patients with chronic gastroesophageal reflux disease (GERD) and additional BE risk factors such as smoking, obesity, and family history. This strategy, however, often fails to detect BE when symptoms are well controlled with over-the-counter or physician-prescribed therapies, Greer and colleagues noted. It also fails to detect BE in individuals without GERD, who comprise 40% of those who develop EAC.
Fewer than 5% of EACs are diagnosed as early-stage lesions caught by surveillance of patients with previously detected BE.
Study Details
The researchers recruited veterans meeting American College of Gastroenterology criteria for endoscopic BE and EAC screening at the Louis Stokes Cleveland Veterans Affairs Medical Center.
Of 782 eligible veterans, 130 (16.6%) entered the study and 124 completed screening. Common reasons for nonparticipation included completion of upper endoscopy outside of the VA healthcare system, lack of interest in joining a research study, and no recommendation for screening from referring gastroenterology or primary care providers. Eligible candidates had gastroesophageal reflux disorder plus three additional risk factors, such as smoking, higher BMI, male sex, age 50 years or older, and family history. The mean number of risk factors was 4.1.
“Available data suggest that family history is the strongest predictor of BE diagnosis, as prevalence of BE among those with family history was 23%,” Greer’s group wrote. “This points to high priority of pursuing screening in patients with family history of the condition, followed by patients who share multiple risk factors.”
All participants completed unsedated EC-guided distal esophageal sampling followed by a sedated EGD on the same day. The prevalence of BE/EAC was 12.9% (n = 14/2), based on standard EGD.
“The study was not powered to prospectively determine EC diagnostic accuracy for subgroups of nondysplastic and dysplastic BE and EAC. These data are reported for this device in development studies but not available for our study population,” the authors wrote. In comparison, they noted, the Cytosponge-TFF3, another nonendoscopic screening device for EAC and BE, exhibited lower sensitivity of 79.5%-87.2%, depending on lesion length, but higher specificity of 92.4%.
Procedural Anxiety
Baseline scores on the short-form six-item Spielberger State-Trait Anxiety Inventory-6 (STAI-6) revealed notable levels of periprocedural anxiety. STAI-6 scores range from 20 to 80, with higher scores indicating more severe anxiety. In the VA study, scores ranged from 20 to 60, and most domains constituting the scores were the same before and after the procedure. Participants did, however, report a statistically significant decrease in sense of worry after EC and reported good tolerability for both EC and EG.
Offering an outsider’s perspective on the study, Joshua Sloan, DO, an esophageal gastroenterologist at University of Minnesota Medical Center in Minneapolis, said that with the acceleration of US rates of EAC, developing a nonendoscopic screening tool to improve identification of Barrett’s and perhaps early EAC is important. “The study by Greer et al helps support the use of nonendoscopic screening with EsoCheck and EsoGuard to identify these conditions,” he told this news organization. “It will be interesting to see similar studies in the non-VA population as well. As the study notes, veterans are an enriched population with a higher prevalence of Barrett’s esophagus.”
Ultimately, Sloan added, “the hope is to increase our ability to identify and manage BE before it becomes EAC. Nonendoscopic screening tools have the potential to increase diagnosis and funnel the appropriate patients for endoscopic surveillance.”
The Bottom Line
“Calculations regarding effectiveness of the two-step screening strategy afforded by EC indicate that the burden of screening would be reduced by at least half (53%),” the authors wrote. Since the estimated size of the US screen-eligible population ranges from 19.7 million to 120.1 million, noninvasive tools could significantly decrease EGD procedures. A formal cost effectiveness analysis is being conducted and will be published separately.
This study was funded by a Department of Defense award.
Co-Author Chak reported device patents assigned to Case Western Reserve University and licensed to Lucid Diagnostics. The other authors had no competing interests to declare. Sloan disclosed speaking and/or advisory work for Sanofi-Regeneron, Phathom Pharmaceuticals, and Takeda Pharmaceuticals unrelated to his comments.
A version of this article first appeared on Medscape.com.
A new combination modality demonstrated excellent sensitivity and negative predictive value compared with endoscopy in a prospective study of at-risk veterans screened for Barrett’s esophagus (BE) and esophageal adenocarcinoma (EAC), a small comparative study in US veterans found.
BE is up to three times more prevalent in veterans than in the general population.
This and other minimally invasive approaches may reduce patient anxiety and increase screening rates, according to investigators led by Katarina B. Greer, MD, MS, of the VA Northeast Ohio Healthcare System and Case Western University in Cleveland. Such screening platforms are expected to open a window on improved prognosis for EAC by offering well-tolerated, office-based testing, the authors wrote in The American Journal of Gastroenterology.
Greer and colleagues compared standard upper endoscopy with EsoCheck (EC), a nonendoscopic esophageal balloon cell-sampling device coupled with EsoGuard (EG), a DNA-based precancer screening assay, with standard upper endoscopy, an FDA-approved minimally invasive alternative.
Sensitivity and specificity of combined EC/EG for esophagogastroduodenoscopy (EGD)-detected BE/EAC were 92.9% (95% CI, 66.1-99.8) and 72.2% (95% CI, 62.1-80.8), respectively. Positive and negative predictive values were 32.5% (95% CI, 18.6-49.1) and 98.6% (95% CI, 92.4-100), respectively.
“With its strong negative predictive power, this screening modality could be a first-line tool available to a greater number of patients,” Greer and associates wrote. “Data from this test support the notion that EC could be performed as a triaging test to increase the yield of diagnostic upper endoscopy 2.5-fold.”
The US rates of EAC have increased more than six-fold in the past four decades and continue to rise. In 2023, 21,560 cases of EAC were diagnosed here. The prognosis for EAC is still poor, with fewer than 22% of patients surviving beyond 5 years.
Current guidelines recommend sedated EGD for patients with chronic gastroesophageal reflux disease (GERD) and additional BE risk factors such as smoking, obesity, and family history. This strategy, however, often fails to detect BE when symptoms are well controlled with over-the-counter or physician-prescribed therapies, Greer and colleagues noted. It also fails to detect BE in individuals without GERD, who comprise 40% of those who develop EAC.
Fewer than 5% of EACs are diagnosed as early-stage lesions caught by surveillance of patients with previously detected BE.
Study Details
The researchers recruited veterans meeting American College of Gastroenterology criteria for endoscopic BE and EAC screening at the Louis Stokes Cleveland Veterans Affairs Medical Center.
Of 782 eligible veterans, 130 (16.6%) entered the study and 124 completed screening. Common reasons for nonparticipation included completion of upper endoscopy outside of the VA healthcare system, lack of interest in joining a research study, and no recommendation for screening from referring gastroenterology or primary care providers. Eligible candidates had gastroesophageal reflux disorder plus three additional risk factors, such as smoking, higher BMI, male sex, age 50 years or older, and family history. The mean number of risk factors was 4.1.
“Available data suggest that family history is the strongest predictor of BE diagnosis, as prevalence of BE among those with family history was 23%,” Greer’s group wrote. “This points to high priority of pursuing screening in patients with family history of the condition, followed by patients who share multiple risk factors.”
All participants completed unsedated EC-guided distal esophageal sampling followed by a sedated EGD on the same day. The prevalence of BE/EAC was 12.9% (n = 14/2), based on standard EGD.
“The study was not powered to prospectively determine EC diagnostic accuracy for subgroups of nondysplastic and dysplastic BE and EAC. These data are reported for this device in development studies but not available for our study population,” the authors wrote. In comparison, they noted, the Cytosponge-TFF3, another nonendoscopic screening device for EAC and BE, exhibited lower sensitivity of 79.5%-87.2%, depending on lesion length, but higher specificity of 92.4%.
Procedural Anxiety
Baseline scores on the short-form six-item Spielberger State-Trait Anxiety Inventory-6 (STAI-6) revealed notable levels of periprocedural anxiety. STAI-6 scores range from 20 to 80, with higher scores indicating more severe anxiety. In the VA study, scores ranged from 20 to 60, and most domains constituting the scores were the same before and after the procedure. Participants did, however, report a statistically significant decrease in sense of worry after EC and reported good tolerability for both EC and EG.
Offering an outsider’s perspective on the study, Joshua Sloan, DO, an esophageal gastroenterologist at University of Minnesota Medical Center in Minneapolis, said that with the acceleration of US rates of EAC, developing a nonendoscopic screening tool to improve identification of Barrett’s and perhaps early EAC is important. “The study by Greer et al helps support the use of nonendoscopic screening with EsoCheck and EsoGuard to identify these conditions,” he told this news organization. “It will be interesting to see similar studies in the non-VA population as well. As the study notes, veterans are an enriched population with a higher prevalence of Barrett’s esophagus.”
Ultimately, Sloan added, “the hope is to increase our ability to identify and manage BE before it becomes EAC. Nonendoscopic screening tools have the potential to increase diagnosis and funnel the appropriate patients for endoscopic surveillance.”
The Bottom Line
“Calculations regarding effectiveness of the two-step screening strategy afforded by EC indicate that the burden of screening would be reduced by at least half (53%),” the authors wrote. Since the estimated size of the US screen-eligible population ranges from 19.7 million to 120.1 million, noninvasive tools could significantly decrease EGD procedures. A formal cost effectiveness analysis is being conducted and will be published separately.
This study was funded by a Department of Defense award.
Co-Author Chak reported device patents assigned to Case Western Reserve University and licensed to Lucid Diagnostics. The other authors had no competing interests to declare. Sloan disclosed speaking and/or advisory work for Sanofi-Regeneron, Phathom Pharmaceuticals, and Takeda Pharmaceuticals unrelated to his comments.
A version of this article first appeared on Medscape.com.
FROM AMERICAN JOURNAL OF GASTROENTEROLOGY
What About Stolen Valor is Actually Illegal?
What About Stolen Valor is Actually Illegal?
Memorial Day is the most solemn of all American military commemorations. It is the day when we honor those who sacrificed their lives so that their fellow citizens could flourish in freedom. At 3 PM, a grateful nation is called to observe 2 minutes of silence in remembrance of the heroes who died in battle or of the wounds they sustained in combat. Communities across the country will carry out ceremonies, lining national cemeteries with flags, holding patriotic parades, and conducting spiritual observances.1
Sadly, almost as long as there has been a United States, there has been a parallel practice dishonoring the uniform and deceiving veterans and the public alike known as stolen valor. Stolen valor is a persistent, yet strange, psychological behavior: individuals who never served in the US Armed Forces claim they have done heroic deeds for which they often sustained serious injuries in the line of duty and almost always won medals for their heroism.2 This editorial will trace the US legal history of stolen valor cases to provide the background for next month’s editorial examining its clinical and ethical aspects.
While many cases of stolen valor do not receive media attention, the experience of Sarah Cavanaugh, a former VA social worker who claimed to be a marine veteran who served in Iraq and Afghanistan, was the subject of the Deep Cover podcast series.3 Cavanaugh had claimed that an improvised explosive device blew up her Humvee, crushing her hip. Still she somehow was able to help her fellow Marines and earned the Bronze Star among other decorations for her heroism. That was not the only lie Cavanaugh told: she also told her friends and wife that she had advanced lung cancer due to burn pit exposure. In line with the best-worst of those who have stolen valor, her mastery of manipulation enabled her to become the commander of a local Veterans of Foreign Wars post. Using stolen identities and fraudulent documents, Cavanaugh was able to purloin veteran benefits, donated leave from other VA employees and money, and stole goods and services from various charitable organizations whose mission was to help wounded veterans and those struggling to adjust to civilian life. Before law enforcement unraveled her sordid tale, she misappropriated hundreds of thousands of dollars in VA benefits and donations and exploited dozens of generous veterans and compassionate civilians.4
Cavanaugh’s story was so sordidly compelling that I kept saying out loud to myself (and my spouse), “This has to be illegal.” The truth about stolen valor law is far more ambivalent and frustrating than I had anticipated or wanted. The first insult to my sense of justice was that lying about military service is not in itself illegal: you can pad your military resume with unearned decorations or impress a future partner or employer with your combat exploits without much fear of legal repercussions. The legal history of attempting to make stealing valor a crime has almost as many twists and turns as the fallacious narratives of military imposters and illustrates the uniquely American experiment in balancing freedom and fairness.
The Stolen Valor Act of 2005 made it a federal misdemeanor to wear, manufacture, or sell military decorations, or medals (Cavanaugh bought her medals online) without legal authorization. It also made it a crime to falsely represent oneself as having been the recipient of a decoration, medical, or service badge that Congress or the Armed Forces authorized. There were even stiffer penalties if the medal was a Silver Star, Distinguished Service Cross, US Air Force or US Navy Cross, or Purple Heart. Punishments include fines and imprisonment. The stated legislative purpose was to prohibit fraud that devalued military awards and the dignity of those who legitimately earned them.5
Next comes a distinctly American reaction to the initial Congressional attempt to protect the legacy of those who served—a lawsuit. Xavier Alvarez was an official on a California district water board claimed to be a 25-year veteran of the US Marine Corps wounded in combat and received the Congressional Medal of Honor. The Federal Bureau of Investigation exposed the lie and instead of the nation’s highest honor, Alvarez was the first to be convicted under the Stolen Valor Act of 2005. Alvarez appealed the decision, ironically claiming the law violated his free speech rights. The case landed in the Supreme Court, which ruled that the Stolen Valor Act did indeed violate the Free Speech Clause of the First Amendment. The majority opinion found the Act as passed was too encompassing of all speech and needed to target only cases in which false statements resulted in actual harm.6
The Stolen Valor Act of 2013 amends the criminal code regarding fraudulent claims about military service to include those who don’t only lie but also profit from it, as Cavanaugh did. The revised act specifically focuses on individuals who claim to have earned military honors for the intended purpose of obtaining money, property, or any other tangible benefit.7
Despite the complicated nature of Stolen Valor Law, it did prevail in Cavanaugh’s case. A US District Court Judge in Rhode Island found her guilty of stolen valor in all its permutations, along with identity theft of other veterans’ military and medical records and fraud in obtaining benefits and services intended for real veterans. Cavanaugh was sentenced to 70 months in federal prison, 3 years of supervised release, ordered to pay $284,796.82 in restitution, and to restore 261 hours of donated leave to the federal government, charitable organizations, and good Samaritans she duped and swindled.8
The revised law under which Cavanaugh was punished lasted 10 years until another classically American ethical concern—privacy—motivated additional legislative effort. A 2023/2024 US House of Representatives proposal to amend the Stolen Valor Act would have strengthened the privacy protections afforded military records. It would have required the information to only be accessed with the permission of the individual who served or their family or through a Freedom of Information Act request. This would make the kind of journalistic and law enforcement investigations that eventually caught Cavanaugh in her lies far more laborious for false valor hunters while at the same time preventing unscrupulous inquiries into service members’ personal information. Advocates for free speech and defenders of military honor are both lobbying Congress; as of this writing the legislation has not been passed.9
As we close part 1 of this review of stolen valor, we return to Memorial Day. This day provides the somber recognition that without the brave men and women of integrity who died in defense of a democracy that promotes the political activity of its citizens, we would not even be able to have this debate over justice, freedom, and truth.
- US Department of Veterans Affairs. The difference between Veterans Day and Memorial Day. October 30, 2023. Accessed May 27, 2025. https://news.va.gov/125549/difference-between-veterans-day-memorial-day/
- Home of Heroes. Stolen valor. Accessed May 27, 2025. https://homeofheroes.com/stolen-valor
- Halpern J. Deep cover: the truth about Sarah. May 2025. Accessed May 27, 2025. https://www.pushkin.fm/podcasts/deep-cover
- Stillwell B. The latest season of the ‘deep cover’ podcast dives into one of the biggest stolen valor cases ever. Military. com. May 22, 2025. Accessed May 27, 2025. https:// www.military.com/off-duty/2025/05/22/latest-season-of-deep-cover-podcast-dives-one-of-biggest-stolen-valor-cases-ever.html
- The Stolen Valor Act of 2005. Pub L No: 109-437. 120 Stat 3266
- Alvarez v United States. 567 US 2012.
- The Stolen Valor Act of 2013. 18 USC § 704(b)
- US Attorney’s Office, District of Rhode Island. Rhode Island woman sentenced to federal prison for falsifying military service; false use of military medals; identify theft, and fraudulently collecting more than $250,000, in veteran benefits and charitable contributions. March 14, 2023. Accessed May 27, 2025. https://www.justice.gov/usao-ri/pr/rhode-island-woman-sentenced-federal-prison-falsifying-military-service-false-use
- Armed Forces Benefit Association. Stolen Valor Act: all you need to know. February 21, 2024. Accessed May 27, 2025. https://www.afba.com/military-life/active-duty-and-veterans/stolen-valor-act-all-you-need-to-know/
Memorial Day is the most solemn of all American military commemorations. It is the day when we honor those who sacrificed their lives so that their fellow citizens could flourish in freedom. At 3 PM, a grateful nation is called to observe 2 minutes of silence in remembrance of the heroes who died in battle or of the wounds they sustained in combat. Communities across the country will carry out ceremonies, lining national cemeteries with flags, holding patriotic parades, and conducting spiritual observances.1
Sadly, almost as long as there has been a United States, there has been a parallel practice dishonoring the uniform and deceiving veterans and the public alike known as stolen valor. Stolen valor is a persistent, yet strange, psychological behavior: individuals who never served in the US Armed Forces claim they have done heroic deeds for which they often sustained serious injuries in the line of duty and almost always won medals for their heroism.2 This editorial will trace the US legal history of stolen valor cases to provide the background for next month’s editorial examining its clinical and ethical aspects.
While many cases of stolen valor do not receive media attention, the experience of Sarah Cavanaugh, a former VA social worker who claimed to be a marine veteran who served in Iraq and Afghanistan, was the subject of the Deep Cover podcast series.3 Cavanaugh had claimed that an improvised explosive device blew up her Humvee, crushing her hip. Still she somehow was able to help her fellow Marines and earned the Bronze Star among other decorations for her heroism. That was not the only lie Cavanaugh told: she also told her friends and wife that she had advanced lung cancer due to burn pit exposure. In line with the best-worst of those who have stolen valor, her mastery of manipulation enabled her to become the commander of a local Veterans of Foreign Wars post. Using stolen identities and fraudulent documents, Cavanaugh was able to purloin veteran benefits, donated leave from other VA employees and money, and stole goods and services from various charitable organizations whose mission was to help wounded veterans and those struggling to adjust to civilian life. Before law enforcement unraveled her sordid tale, she misappropriated hundreds of thousands of dollars in VA benefits and donations and exploited dozens of generous veterans and compassionate civilians.4
Cavanaugh’s story was so sordidly compelling that I kept saying out loud to myself (and my spouse), “This has to be illegal.” The truth about stolen valor law is far more ambivalent and frustrating than I had anticipated or wanted. The first insult to my sense of justice was that lying about military service is not in itself illegal: you can pad your military resume with unearned decorations or impress a future partner or employer with your combat exploits without much fear of legal repercussions. The legal history of attempting to make stealing valor a crime has almost as many twists and turns as the fallacious narratives of military imposters and illustrates the uniquely American experiment in balancing freedom and fairness.
The Stolen Valor Act of 2005 made it a federal misdemeanor to wear, manufacture, or sell military decorations, or medals (Cavanaugh bought her medals online) without legal authorization. It also made it a crime to falsely represent oneself as having been the recipient of a decoration, medical, or service badge that Congress or the Armed Forces authorized. There were even stiffer penalties if the medal was a Silver Star, Distinguished Service Cross, US Air Force or US Navy Cross, or Purple Heart. Punishments include fines and imprisonment. The stated legislative purpose was to prohibit fraud that devalued military awards and the dignity of those who legitimately earned them.5
Next comes a distinctly American reaction to the initial Congressional attempt to protect the legacy of those who served—a lawsuit. Xavier Alvarez was an official on a California district water board claimed to be a 25-year veteran of the US Marine Corps wounded in combat and received the Congressional Medal of Honor. The Federal Bureau of Investigation exposed the lie and instead of the nation’s highest honor, Alvarez was the first to be convicted under the Stolen Valor Act of 2005. Alvarez appealed the decision, ironically claiming the law violated his free speech rights. The case landed in the Supreme Court, which ruled that the Stolen Valor Act did indeed violate the Free Speech Clause of the First Amendment. The majority opinion found the Act as passed was too encompassing of all speech and needed to target only cases in which false statements resulted in actual harm.6
The Stolen Valor Act of 2013 amends the criminal code regarding fraudulent claims about military service to include those who don’t only lie but also profit from it, as Cavanaugh did. The revised act specifically focuses on individuals who claim to have earned military honors for the intended purpose of obtaining money, property, or any other tangible benefit.7
Despite the complicated nature of Stolen Valor Law, it did prevail in Cavanaugh’s case. A US District Court Judge in Rhode Island found her guilty of stolen valor in all its permutations, along with identity theft of other veterans’ military and medical records and fraud in obtaining benefits and services intended for real veterans. Cavanaugh was sentenced to 70 months in federal prison, 3 years of supervised release, ordered to pay $284,796.82 in restitution, and to restore 261 hours of donated leave to the federal government, charitable organizations, and good Samaritans she duped and swindled.8
The revised law under which Cavanaugh was punished lasted 10 years until another classically American ethical concern—privacy—motivated additional legislative effort. A 2023/2024 US House of Representatives proposal to amend the Stolen Valor Act would have strengthened the privacy protections afforded military records. It would have required the information to only be accessed with the permission of the individual who served or their family or through a Freedom of Information Act request. This would make the kind of journalistic and law enforcement investigations that eventually caught Cavanaugh in her lies far more laborious for false valor hunters while at the same time preventing unscrupulous inquiries into service members’ personal information. Advocates for free speech and defenders of military honor are both lobbying Congress; as of this writing the legislation has not been passed.9
As we close part 1 of this review of stolen valor, we return to Memorial Day. This day provides the somber recognition that without the brave men and women of integrity who died in defense of a democracy that promotes the political activity of its citizens, we would not even be able to have this debate over justice, freedom, and truth.
Memorial Day is the most solemn of all American military commemorations. It is the day when we honor those who sacrificed their lives so that their fellow citizens could flourish in freedom. At 3 PM, a grateful nation is called to observe 2 minutes of silence in remembrance of the heroes who died in battle or of the wounds they sustained in combat. Communities across the country will carry out ceremonies, lining national cemeteries with flags, holding patriotic parades, and conducting spiritual observances.1
Sadly, almost as long as there has been a United States, there has been a parallel practice dishonoring the uniform and deceiving veterans and the public alike known as stolen valor. Stolen valor is a persistent, yet strange, psychological behavior: individuals who never served in the US Armed Forces claim they have done heroic deeds for which they often sustained serious injuries in the line of duty and almost always won medals for their heroism.2 This editorial will trace the US legal history of stolen valor cases to provide the background for next month’s editorial examining its clinical and ethical aspects.
While many cases of stolen valor do not receive media attention, the experience of Sarah Cavanaugh, a former VA social worker who claimed to be a marine veteran who served in Iraq and Afghanistan, was the subject of the Deep Cover podcast series.3 Cavanaugh had claimed that an improvised explosive device blew up her Humvee, crushing her hip. Still she somehow was able to help her fellow Marines and earned the Bronze Star among other decorations for her heroism. That was not the only lie Cavanaugh told: she also told her friends and wife that she had advanced lung cancer due to burn pit exposure. In line with the best-worst of those who have stolen valor, her mastery of manipulation enabled her to become the commander of a local Veterans of Foreign Wars post. Using stolen identities and fraudulent documents, Cavanaugh was able to purloin veteran benefits, donated leave from other VA employees and money, and stole goods and services from various charitable organizations whose mission was to help wounded veterans and those struggling to adjust to civilian life. Before law enforcement unraveled her sordid tale, she misappropriated hundreds of thousands of dollars in VA benefits and donations and exploited dozens of generous veterans and compassionate civilians.4
Cavanaugh’s story was so sordidly compelling that I kept saying out loud to myself (and my spouse), “This has to be illegal.” The truth about stolen valor law is far more ambivalent and frustrating than I had anticipated or wanted. The first insult to my sense of justice was that lying about military service is not in itself illegal: you can pad your military resume with unearned decorations or impress a future partner or employer with your combat exploits without much fear of legal repercussions. The legal history of attempting to make stealing valor a crime has almost as many twists and turns as the fallacious narratives of military imposters and illustrates the uniquely American experiment in balancing freedom and fairness.
The Stolen Valor Act of 2005 made it a federal misdemeanor to wear, manufacture, or sell military decorations, or medals (Cavanaugh bought her medals online) without legal authorization. It also made it a crime to falsely represent oneself as having been the recipient of a decoration, medical, or service badge that Congress or the Armed Forces authorized. There were even stiffer penalties if the medal was a Silver Star, Distinguished Service Cross, US Air Force or US Navy Cross, or Purple Heart. Punishments include fines and imprisonment. The stated legislative purpose was to prohibit fraud that devalued military awards and the dignity of those who legitimately earned them.5
Next comes a distinctly American reaction to the initial Congressional attempt to protect the legacy of those who served—a lawsuit. Xavier Alvarez was an official on a California district water board claimed to be a 25-year veteran of the US Marine Corps wounded in combat and received the Congressional Medal of Honor. The Federal Bureau of Investigation exposed the lie and instead of the nation’s highest honor, Alvarez was the first to be convicted under the Stolen Valor Act of 2005. Alvarez appealed the decision, ironically claiming the law violated his free speech rights. The case landed in the Supreme Court, which ruled that the Stolen Valor Act did indeed violate the Free Speech Clause of the First Amendment. The majority opinion found the Act as passed was too encompassing of all speech and needed to target only cases in which false statements resulted in actual harm.6
The Stolen Valor Act of 2013 amends the criminal code regarding fraudulent claims about military service to include those who don’t only lie but also profit from it, as Cavanaugh did. The revised act specifically focuses on individuals who claim to have earned military honors for the intended purpose of obtaining money, property, or any other tangible benefit.7
Despite the complicated nature of Stolen Valor Law, it did prevail in Cavanaugh’s case. A US District Court Judge in Rhode Island found her guilty of stolen valor in all its permutations, along with identity theft of other veterans’ military and medical records and fraud in obtaining benefits and services intended for real veterans. Cavanaugh was sentenced to 70 months in federal prison, 3 years of supervised release, ordered to pay $284,796.82 in restitution, and to restore 261 hours of donated leave to the federal government, charitable organizations, and good Samaritans she duped and swindled.8
The revised law under which Cavanaugh was punished lasted 10 years until another classically American ethical concern—privacy—motivated additional legislative effort. A 2023/2024 US House of Representatives proposal to amend the Stolen Valor Act would have strengthened the privacy protections afforded military records. It would have required the information to only be accessed with the permission of the individual who served or their family or through a Freedom of Information Act request. This would make the kind of journalistic and law enforcement investigations that eventually caught Cavanaugh in her lies far more laborious for false valor hunters while at the same time preventing unscrupulous inquiries into service members’ personal information. Advocates for free speech and defenders of military honor are both lobbying Congress; as of this writing the legislation has not been passed.9
As we close part 1 of this review of stolen valor, we return to Memorial Day. This day provides the somber recognition that without the brave men and women of integrity who died in defense of a democracy that promotes the political activity of its citizens, we would not even be able to have this debate over justice, freedom, and truth.
- US Department of Veterans Affairs. The difference between Veterans Day and Memorial Day. October 30, 2023. Accessed May 27, 2025. https://news.va.gov/125549/difference-between-veterans-day-memorial-day/
- Home of Heroes. Stolen valor. Accessed May 27, 2025. https://homeofheroes.com/stolen-valor
- Halpern J. Deep cover: the truth about Sarah. May 2025. Accessed May 27, 2025. https://www.pushkin.fm/podcasts/deep-cover
- Stillwell B. The latest season of the ‘deep cover’ podcast dives into one of the biggest stolen valor cases ever. Military. com. May 22, 2025. Accessed May 27, 2025. https:// www.military.com/off-duty/2025/05/22/latest-season-of-deep-cover-podcast-dives-one-of-biggest-stolen-valor-cases-ever.html
- The Stolen Valor Act of 2005. Pub L No: 109-437. 120 Stat 3266
- Alvarez v United States. 567 US 2012.
- The Stolen Valor Act of 2013. 18 USC § 704(b)
- US Attorney’s Office, District of Rhode Island. Rhode Island woman sentenced to federal prison for falsifying military service; false use of military medals; identify theft, and fraudulently collecting more than $250,000, in veteran benefits and charitable contributions. March 14, 2023. Accessed May 27, 2025. https://www.justice.gov/usao-ri/pr/rhode-island-woman-sentenced-federal-prison-falsifying-military-service-false-use
- Armed Forces Benefit Association. Stolen Valor Act: all you need to know. February 21, 2024. Accessed May 27, 2025. https://www.afba.com/military-life/active-duty-and-veterans/stolen-valor-act-all-you-need-to-know/
- US Department of Veterans Affairs. The difference between Veterans Day and Memorial Day. October 30, 2023. Accessed May 27, 2025. https://news.va.gov/125549/difference-between-veterans-day-memorial-day/
- Home of Heroes. Stolen valor. Accessed May 27, 2025. https://homeofheroes.com/stolen-valor
- Halpern J. Deep cover: the truth about Sarah. May 2025. Accessed May 27, 2025. https://www.pushkin.fm/podcasts/deep-cover
- Stillwell B. The latest season of the ‘deep cover’ podcast dives into one of the biggest stolen valor cases ever. Military. com. May 22, 2025. Accessed May 27, 2025. https:// www.military.com/off-duty/2025/05/22/latest-season-of-deep-cover-podcast-dives-one-of-biggest-stolen-valor-cases-ever.html
- The Stolen Valor Act of 2005. Pub L No: 109-437. 120 Stat 3266
- Alvarez v United States. 567 US 2012.
- The Stolen Valor Act of 2013. 18 USC § 704(b)
- US Attorney’s Office, District of Rhode Island. Rhode Island woman sentenced to federal prison for falsifying military service; false use of military medals; identify theft, and fraudulently collecting more than $250,000, in veteran benefits and charitable contributions. March 14, 2023. Accessed May 27, 2025. https://www.justice.gov/usao-ri/pr/rhode-island-woman-sentenced-federal-prison-falsifying-military-service-false-use
- Armed Forces Benefit Association. Stolen Valor Act: all you need to know. February 21, 2024. Accessed May 27, 2025. https://www.afba.com/military-life/active-duty-and-veterans/stolen-valor-act-all-you-need-to-know/
What About Stolen Valor is Actually Illegal?
What About Stolen Valor is Actually Illegal?
Intestinal Ultrasound Shows Promise in Prognosis of Early Crohn’s Disease
, a prospective, population-based cohort of newly diagnosed patients in Denmark reported.
Adding to the growing body of evidence on the utility of this noninvasive imaging tool in monitoring disease activity in the newly diagnosed, the multicenter study published in Clinical Gastroenterology and Hepatology characterized ultrasonographic features at diagnosis and evaluated IUS’s prognostic value. Existing literature has focused on patients with long-standing disease.
Investigators led by first author Gorm R. Madsen, MD, PhD, of the Copenhagen Center for Inflammatory Bowel Disease in Children, Adolescents and Adults at Copenhagen University Hospital, observed continued improvement in most IUS parameters throughout the first year. “Our findings thereby emphasize the role of IUS in improving patient management, and its use in patient risk stratification already at diagnosis,” the investigators wrote.
Some 38% of patients reached ultrasonic transmural remission within 3 months of diagnosis, an achievement associated with higher rates of sustained steroid-free clinical remission and reduced need for treatment escalation.
“Ultrasonic transmural remission is achievable early in Crohn’s disease and is associated with favorable outcomes, underscoring the value of intestinal ultrasound in early disease management,” the researchers wrote.
Study Details
While IUS is increasingly recognized for monitoring CD, little was known about its prognostic value early in the disease course. “We aimed to determine whether sonographic inflammation at diagnosis — and particularly the achievement pftransmural remission after 3 months — could predict future outcomes,” Madsen told GI & Hepatology News. “This is important, as early identification of patients at risk of surgery or treatment escalation may help guide therapy decisions more effectively.”
From May 2021 to April 2023, 201 patients (mean age, 35 years; 54.2% men) with new adult-onset CD were followed by IUS and monitored with symptomatic, biochemical, and endoscopic evaluations.
After 3 months, transmural remission was achieved more often by patients with colonic disease, and no associations were found between sonographic inflammation at diagnosis and diagnostic delay.
“We were positively surprised. Nearly 40% of newly diagnosed Crohn’s patients achieved transmural remission within 3 months — a higher proportion than seen in earlier studies, which mostly focused on long-standing or trial-selected populations,” Madsen said. “It was also striking how strongly early IUS findings predicted the need for surgery, outperforming endoscopy and biomarkers.”
In other findings, transmural remission at 3 months was significantly associated with steroid-free clinical remission at both 3 months and all subsequent follow-ups within the first year. It was also linked to a lower risk for treatment escalation during the follow-up through to 12 months: 26% vs 53% (P =.003). At 12 months, 41% had achieved transmural remission.
Higher baseline body mass index significantly reduced the likelihood of 12-month transmural remission. For overweight, the odds ratio (OR) was 0.34 (95% CI, 0.12-0.94), while for obesity, the OR was 0.16 (95% CI, 0.04-0.73).
The International Bowel Ultrasound Segmental Activity Score in the terminal ileum at diagnosis emerged as the best predictor of ileocecal resection during the first year, with an optimal threshold of 63 (area under the curve, 0.92; sensitivity, 100%; specificity, 73%).
The use of IUS has expanded considerably in the past 3 years, and in 2024, the American Gastroenterological Association updated its clinical practice guidance on the role of this modality in inflammatory bowel disease.
IUS is noninvasive, radiation-free, inexpensive, and doable at the bedside with immediate results, Madsen said. “For patients, this means less anxiety and discomfort. For healthcare systems, it enables faster clinical decisions, reduced need for endoscopy or MRI, and closer disease monitoring, particularly valuable in treat-to-target strategies.”
In terms of limitations, however, IUS is operator-dependent and consistent training is crucial, he added. “Certain anatomical regions, particularly the proximal small bowel, can be more challenging to evaluate. Additionally, while IUS is highly effective for assessing inflammatory activity, it becomes more difficult to accurately assess disease involvement when inflammation extends beyond approximately 20 cm of the small bowel.”
Key Insights
Commenting on the Danish study from a US perspective, Anna L. Silverman, MD, a gastroenterology fellow at Icahn School of Medicine at Mount Sinai in New York City, agreed the findings in adult patients with newly diagnosed, rather than long-standing, CD contribute to the growing body of evidence supporting IUS’s applicability for both treatment monitoring and prognosis.
“By focusing on early-stage CD, the study provides clearer insights into initial disease activity and response to therapy, reinforcing the value of this noninvasive, point-of-care modality,” she told GI & Hepatology News. “These findings enhance our understanding of IUS as a tool to help guide early management decisions in CD.”
Ashwin Ananthakrishnan, MBBS, MPH, AGAF, director of the Crohn’s and Colitis Center at Massachusetts General Hospital and an associate professor at Harvard Medical School, both in Boston, concurred that this is an important study. “It includes newly diagnosed patients — so a very ‘clean’ cohort in terms of not being influenced by confounders,” he told GI & Hepatology News.
“We don’t fully know yet the best treatment target in CD, and this study highlights the importance of early transmural healing in determining outcomes at 1 year,” he noted. In addition, the study highlighted a convenient tool that can increasingly be applied at point of care in the United States. “Colonoscopy at 3 months is not practical and has low patient acceptability, so using IUS in this circumstance would have value and impact.”
Ananthakrishnan pointed to several unanswered questions, however. “Are there patients who may not have healing early but may take some extra time to achieve transmural remission, and if so, what are their outcomes? What is the best timepoint for transmural healing assessment? What is the incremental value of measuring it at 3 vs 6 months?”
In addition, he wondered, how much is the added value of IUS over clinical symptoms and/or markers such as calprotectin and C-reactive protein? “In the subset of patients with clinical and transmural remission, there was no difference in endoscopic outcomes at 1 year, so this is an unanswered question,” Ananthakrishnan said.
This study was funded by an unrestricted grant from the Novo Nordisk Foundation.
Madsen reported receiving a speaker’s fee from Tillotts. Multiple coauthors disclosed having various financial relationships with numerous private-sector companies, including Novo Nordisk. Silverman and Ananthakrishnan reported having no competing interests relevant to their comments.
A version of this article appeared on Medscape.com.
, a prospective, population-based cohort of newly diagnosed patients in Denmark reported.
Adding to the growing body of evidence on the utility of this noninvasive imaging tool in monitoring disease activity in the newly diagnosed, the multicenter study published in Clinical Gastroenterology and Hepatology characterized ultrasonographic features at diagnosis and evaluated IUS’s prognostic value. Existing literature has focused on patients with long-standing disease.
Investigators led by first author Gorm R. Madsen, MD, PhD, of the Copenhagen Center for Inflammatory Bowel Disease in Children, Adolescents and Adults at Copenhagen University Hospital, observed continued improvement in most IUS parameters throughout the first year. “Our findings thereby emphasize the role of IUS in improving patient management, and its use in patient risk stratification already at diagnosis,” the investigators wrote.
Some 38% of patients reached ultrasonic transmural remission within 3 months of diagnosis, an achievement associated with higher rates of sustained steroid-free clinical remission and reduced need for treatment escalation.
“Ultrasonic transmural remission is achievable early in Crohn’s disease and is associated with favorable outcomes, underscoring the value of intestinal ultrasound in early disease management,” the researchers wrote.
Study Details
While IUS is increasingly recognized for monitoring CD, little was known about its prognostic value early in the disease course. “We aimed to determine whether sonographic inflammation at diagnosis — and particularly the achievement pftransmural remission after 3 months — could predict future outcomes,” Madsen told GI & Hepatology News. “This is important, as early identification of patients at risk of surgery or treatment escalation may help guide therapy decisions more effectively.”
From May 2021 to April 2023, 201 patients (mean age, 35 years; 54.2% men) with new adult-onset CD were followed by IUS and monitored with symptomatic, biochemical, and endoscopic evaluations.
After 3 months, transmural remission was achieved more often by patients with colonic disease, and no associations were found between sonographic inflammation at diagnosis and diagnostic delay.
“We were positively surprised. Nearly 40% of newly diagnosed Crohn’s patients achieved transmural remission within 3 months — a higher proportion than seen in earlier studies, which mostly focused on long-standing or trial-selected populations,” Madsen said. “It was also striking how strongly early IUS findings predicted the need for surgery, outperforming endoscopy and biomarkers.”
In other findings, transmural remission at 3 months was significantly associated with steroid-free clinical remission at both 3 months and all subsequent follow-ups within the first year. It was also linked to a lower risk for treatment escalation during the follow-up through to 12 months: 26% vs 53% (P =.003). At 12 months, 41% had achieved transmural remission.
Higher baseline body mass index significantly reduced the likelihood of 12-month transmural remission. For overweight, the odds ratio (OR) was 0.34 (95% CI, 0.12-0.94), while for obesity, the OR was 0.16 (95% CI, 0.04-0.73).
The International Bowel Ultrasound Segmental Activity Score in the terminal ileum at diagnosis emerged as the best predictor of ileocecal resection during the first year, with an optimal threshold of 63 (area under the curve, 0.92; sensitivity, 100%; specificity, 73%).
The use of IUS has expanded considerably in the past 3 years, and in 2024, the American Gastroenterological Association updated its clinical practice guidance on the role of this modality in inflammatory bowel disease.
IUS is noninvasive, radiation-free, inexpensive, and doable at the bedside with immediate results, Madsen said. “For patients, this means less anxiety and discomfort. For healthcare systems, it enables faster clinical decisions, reduced need for endoscopy or MRI, and closer disease monitoring, particularly valuable in treat-to-target strategies.”
In terms of limitations, however, IUS is operator-dependent and consistent training is crucial, he added. “Certain anatomical regions, particularly the proximal small bowel, can be more challenging to evaluate. Additionally, while IUS is highly effective for assessing inflammatory activity, it becomes more difficult to accurately assess disease involvement when inflammation extends beyond approximately 20 cm of the small bowel.”
Key Insights
Commenting on the Danish study from a US perspective, Anna L. Silverman, MD, a gastroenterology fellow at Icahn School of Medicine at Mount Sinai in New York City, agreed the findings in adult patients with newly diagnosed, rather than long-standing, CD contribute to the growing body of evidence supporting IUS’s applicability for both treatment monitoring and prognosis.
“By focusing on early-stage CD, the study provides clearer insights into initial disease activity and response to therapy, reinforcing the value of this noninvasive, point-of-care modality,” she told GI & Hepatology News. “These findings enhance our understanding of IUS as a tool to help guide early management decisions in CD.”
Ashwin Ananthakrishnan, MBBS, MPH, AGAF, director of the Crohn’s and Colitis Center at Massachusetts General Hospital and an associate professor at Harvard Medical School, both in Boston, concurred that this is an important study. “It includes newly diagnosed patients — so a very ‘clean’ cohort in terms of not being influenced by confounders,” he told GI & Hepatology News.
“We don’t fully know yet the best treatment target in CD, and this study highlights the importance of early transmural healing in determining outcomes at 1 year,” he noted. In addition, the study highlighted a convenient tool that can increasingly be applied at point of care in the United States. “Colonoscopy at 3 months is not practical and has low patient acceptability, so using IUS in this circumstance would have value and impact.”
Ananthakrishnan pointed to several unanswered questions, however. “Are there patients who may not have healing early but may take some extra time to achieve transmural remission, and if so, what are their outcomes? What is the best timepoint for transmural healing assessment? What is the incremental value of measuring it at 3 vs 6 months?”
In addition, he wondered, how much is the added value of IUS over clinical symptoms and/or markers such as calprotectin and C-reactive protein? “In the subset of patients with clinical and transmural remission, there was no difference in endoscopic outcomes at 1 year, so this is an unanswered question,” Ananthakrishnan said.
This study was funded by an unrestricted grant from the Novo Nordisk Foundation.
Madsen reported receiving a speaker’s fee from Tillotts. Multiple coauthors disclosed having various financial relationships with numerous private-sector companies, including Novo Nordisk. Silverman and Ananthakrishnan reported having no competing interests relevant to their comments.
A version of this article appeared on Medscape.com.
, a prospective, population-based cohort of newly diagnosed patients in Denmark reported.
Adding to the growing body of evidence on the utility of this noninvasive imaging tool in monitoring disease activity in the newly diagnosed, the multicenter study published in Clinical Gastroenterology and Hepatology characterized ultrasonographic features at diagnosis and evaluated IUS’s prognostic value. Existing literature has focused on patients with long-standing disease.
Investigators led by first author Gorm R. Madsen, MD, PhD, of the Copenhagen Center for Inflammatory Bowel Disease in Children, Adolescents and Adults at Copenhagen University Hospital, observed continued improvement in most IUS parameters throughout the first year. “Our findings thereby emphasize the role of IUS in improving patient management, and its use in patient risk stratification already at diagnosis,” the investigators wrote.
Some 38% of patients reached ultrasonic transmural remission within 3 months of diagnosis, an achievement associated with higher rates of sustained steroid-free clinical remission and reduced need for treatment escalation.
“Ultrasonic transmural remission is achievable early in Crohn’s disease and is associated with favorable outcomes, underscoring the value of intestinal ultrasound in early disease management,” the researchers wrote.
Study Details
While IUS is increasingly recognized for monitoring CD, little was known about its prognostic value early in the disease course. “We aimed to determine whether sonographic inflammation at diagnosis — and particularly the achievement pftransmural remission after 3 months — could predict future outcomes,” Madsen told GI & Hepatology News. “This is important, as early identification of patients at risk of surgery or treatment escalation may help guide therapy decisions more effectively.”
From May 2021 to April 2023, 201 patients (mean age, 35 years; 54.2% men) with new adult-onset CD were followed by IUS and monitored with symptomatic, biochemical, and endoscopic evaluations.
After 3 months, transmural remission was achieved more often by patients with colonic disease, and no associations were found between sonographic inflammation at diagnosis and diagnostic delay.
“We were positively surprised. Nearly 40% of newly diagnosed Crohn’s patients achieved transmural remission within 3 months — a higher proportion than seen in earlier studies, which mostly focused on long-standing or trial-selected populations,” Madsen said. “It was also striking how strongly early IUS findings predicted the need for surgery, outperforming endoscopy and biomarkers.”
In other findings, transmural remission at 3 months was significantly associated with steroid-free clinical remission at both 3 months and all subsequent follow-ups within the first year. It was also linked to a lower risk for treatment escalation during the follow-up through to 12 months: 26% vs 53% (P =.003). At 12 months, 41% had achieved transmural remission.
Higher baseline body mass index significantly reduced the likelihood of 12-month transmural remission. For overweight, the odds ratio (OR) was 0.34 (95% CI, 0.12-0.94), while for obesity, the OR was 0.16 (95% CI, 0.04-0.73).
The International Bowel Ultrasound Segmental Activity Score in the terminal ileum at diagnosis emerged as the best predictor of ileocecal resection during the first year, with an optimal threshold of 63 (area under the curve, 0.92; sensitivity, 100%; specificity, 73%).
The use of IUS has expanded considerably in the past 3 years, and in 2024, the American Gastroenterological Association updated its clinical practice guidance on the role of this modality in inflammatory bowel disease.
IUS is noninvasive, radiation-free, inexpensive, and doable at the bedside with immediate results, Madsen said. “For patients, this means less anxiety and discomfort. For healthcare systems, it enables faster clinical decisions, reduced need for endoscopy or MRI, and closer disease monitoring, particularly valuable in treat-to-target strategies.”
In terms of limitations, however, IUS is operator-dependent and consistent training is crucial, he added. “Certain anatomical regions, particularly the proximal small bowel, can be more challenging to evaluate. Additionally, while IUS is highly effective for assessing inflammatory activity, it becomes more difficult to accurately assess disease involvement when inflammation extends beyond approximately 20 cm of the small bowel.”
Key Insights
Commenting on the Danish study from a US perspective, Anna L. Silverman, MD, a gastroenterology fellow at Icahn School of Medicine at Mount Sinai in New York City, agreed the findings in adult patients with newly diagnosed, rather than long-standing, CD contribute to the growing body of evidence supporting IUS’s applicability for both treatment monitoring and prognosis.
“By focusing on early-stage CD, the study provides clearer insights into initial disease activity and response to therapy, reinforcing the value of this noninvasive, point-of-care modality,” she told GI & Hepatology News. “These findings enhance our understanding of IUS as a tool to help guide early management decisions in CD.”
Ashwin Ananthakrishnan, MBBS, MPH, AGAF, director of the Crohn’s and Colitis Center at Massachusetts General Hospital and an associate professor at Harvard Medical School, both in Boston, concurred that this is an important study. “It includes newly diagnosed patients — so a very ‘clean’ cohort in terms of not being influenced by confounders,” he told GI & Hepatology News.
“We don’t fully know yet the best treatment target in CD, and this study highlights the importance of early transmural healing in determining outcomes at 1 year,” he noted. In addition, the study highlighted a convenient tool that can increasingly be applied at point of care in the United States. “Colonoscopy at 3 months is not practical and has low patient acceptability, so using IUS in this circumstance would have value and impact.”
Ananthakrishnan pointed to several unanswered questions, however. “Are there patients who may not have healing early but may take some extra time to achieve transmural remission, and if so, what are their outcomes? What is the best timepoint for transmural healing assessment? What is the incremental value of measuring it at 3 vs 6 months?”
In addition, he wondered, how much is the added value of IUS over clinical symptoms and/or markers such as calprotectin and C-reactive protein? “In the subset of patients with clinical and transmural remission, there was no difference in endoscopic outcomes at 1 year, so this is an unanswered question,” Ananthakrishnan said.
This study was funded by an unrestricted grant from the Novo Nordisk Foundation.
Madsen reported receiving a speaker’s fee from Tillotts. Multiple coauthors disclosed having various financial relationships with numerous private-sector companies, including Novo Nordisk. Silverman and Ananthakrishnan reported having no competing interests relevant to their comments.
A version of this article appeared on Medscape.com.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Can Lifestyle Changes Save Lives in Colon Cancer?
Can Lifestyle Changes Save Lives in Colon Cancer?
Can exercise “therapy” and diet improve survival in patients with colon cancer? It appears so, according to two pivotal studies presented at American Society of Clinical Oncology (ASCO) 2025 annual meeting.
In the CHALLENGE trial, a structured exercise program after surgery and adjuvant chemotherapy cut the risk for colon cancer recurrence in patients with stage III and high-risk stage II disease by more than one quarter and the risk for death by more than one third.
“The magnitude of benefit with exercise is substantial. In fact, it is comparable, and in some cases exceeds the magnitude of benefit of many of our very good standard medical therapies in oncology,” study presenter Christopher Booth, MD, with Queen’s University, Kingston, Ontario, Canada, told attendees.
Results of the study were published online in The New England Journal of Medicine to coincide with the presentation at the meeting.
The findings are “nothing short of a major milestone,” said study discussant Peter Campbell, PhD, with Montefiore Einstein Comprehensive Cancer Center, Bronx, New York.
The other study showed that eating a less inflammatory diet may reduce the risk for death in patients with colon cancer, with the greatest benefits seen in those who embraced anti-inflammatory foods and exercised regularly.
“Putting these two abstracts into perspective, we as physicians need to be essentially prescribing healthy diet and exercise. The combination of the two are synergistic,” Julie Gralow, MD, ASCO chief medical officer and executive vice president, told attendees.
Despite the benefits of these lifestyle changes, exercise and diet are meant to supplement, not replace, established colon cancer treatments.
It would be a false binary to frame this as lifestyle vs cancer treatment, explained Mark Lewis, MD, director of Gastrointestinal Oncology at Intermountain Healthcare in Salt Lake City, Utah. With exercise, for instance, “the key is giving enough chemo to protect against recurrence and eliminate micrometastases but not so much that we cause neuropathy and reduce function and ability to follow the CHALLENGE structured program,” Lewis said.
Exercise and Survival
Colon cancer remains the second-leading cause of cancer death worldwide. Even with surgery and chemotherapy, roughly 30% of patients with stage III and high-risk stage II colon cancer will experience disease recurrence.
“As oncologists, one of the most common questions we get asked by patients is — what else can I do to improve my outcome?” Booth said.
Observational studies published nearly two decades ago hinted that physically active cancer survivors fare better, but no randomized trial has definitively tested whether exercise could alter disease course. That knowledge gap prompted the Canadian Cancer Trials Group to launch the CHALLENGE trial.
Between 2009 and 2023, the phase 3 study enrolled 889 adults (median age, 61 years; 51% women) who had completed surgery and adjuvant chemotherapy for stage III (90%) or high-risk stage II (10%) colon cancer. Most patients were from Canada and Australia and were enrolled 2-6 months after completing chemotherapy.
Half of study participants were randomly allocated to a structured exercise program (n = 445) and half to receive standard health education materials promoting physical activity and healthy eating (control individuals, n = 444).
As part of the structured exercise intervention, patients met with a physical activity consultant twice a month for the first 6 months. These sessions included exercise coaching and supervised exercise. Patients could choose their preferred aerobic exercise and most picked brisk walking.
The consultants gave each patient an “exercise prescription” to hit a specific amount of exercise. The target was an additional 10 metabolic equivalent (MET)–hours of aerobic activity per week — about three to four brisk walks each lasting 45-60 minutes. After 6 months, patients met with their consultants once a month, with additional sessions available for extra support if needed.
Structured exercise led to “substantial and sustained” increases in the amount of exercise participants did, as well as physiologic measures of their fitness, with “highly relevant” improvements in VO2 max, 6-minute walk test, and patient-reported physical function, underscoring that participants were not only exercising more but also getting fitter, Booth said.
Exercise was associated with a clinically meaningful and statistically significant 28% reduction in the risk for recurrent or new cancer (hazard ratio [HR], 0.72; P = .017), with a 5-year disease free survival rate of 80% in the exercise group and 74% in the control group.
In other words, “for every 16 patients that went on the exercise program, exercise prevented 1 person from recurrent or new cancer” at 5 years, Booth reported.
Overall survival results were “even more impressive,” he said.
At 8 years, 90% of patients in the exercise program were alive vs 83% of those in the control group, which translated to a 37% lower risk for death (HR, 0.63; P = .022).
“For every 14 patients who went on the exercise program, exercise prevented 1 person from dying” at the 8-year mark, Booth noted.
“Notably, this difference in survival was not driven by difference in cardiovascular deaths but by a reduction in the risk of death from colon cancer,” he said.
Besides a slight uptick in musculoskeletal aches, no major safety signals emerged in the exercise group.
It’s important to note that the survival benefit associated with exercise came after patients had received surgery followed by chemotherapy — in other words, exercise did not replace established cancer treatments. It’s also unclear whether initiating an exercise intervention earlier in the treatment trajectory — before surgery or during chemotherapy, instead of after chemotherapy — could further improve cancer outcomes, the authors noted.
Still, “exercise as an intervention is a no brainer and should be implemented broadly,” said ASCO expert Pamela Kunz, MD, with Yale School of Medicine, New Haven, Connecticut.
Marco Gerlinger, MD, with Barts Cancer Institute, London, England, agreed.
“Oncologists can now make a very clear evidence-based recommendation for patients who just completed their chemotherapy for bowel cancer and are fit enough for such an exercise program,” Gerlinger said in a statement from the nonprofit UK Science Media Centre.
Booth noted that knowledge alone will not be sufficient to allow most patients to change their lifestyle and realize the health benefits.
“The policy implementation piece of this is really key, and we need health systems, hospitals, and payers to invest in these behavior support programs so that patients have access to a physical activity consultant and can realize the health benefits,” he said.
“This intervention is empowering and achievable for patients and with much, much lower cost than many of our therapies. It is also sustainable for health systems,” he concluded.
Diet and Survival
Diet can also affect outcomes in patients with colon cancer.
In the same session describing the CHALLENGE results, Sara Char, MD, with Dana-Farber Cancer Institute in Boston, reported findings showing that consuming a diet high in proinflammatory foods was associated with worse overall survival in patients with stage III colon cancer. A proinflammatory diet includes red and processed meats, sugary drinks, and refined grains, while an anti-inflammatory diet focuses on fruits, vegetables, whole grains, fish, and olive oil.
Chronic systemic inflammation has been implicated in both colon cancer development and in its progression, and elevated levels of inflammatory markers in the blood have previously been associated with worse survival outcomes in patients with stage III colon cancer.
Char and colleagues analyzed dietary patterns of a subset of 1625 patients (mean age, 61 years) with resected stage III colon cancer enrolled in the phase 3 CALGB/SWOG 80702 (Alliance) clinical trial, which compared 3 months of adjuvant chemotherapy with 6 months of adjuvant chemotherapy, with or without the anti-inflammatory medication celecoxib.
As part of the trial, participants reported their diet and exercise habits at various timepoints. Their diets were scored using the validated empirical dietary inflammatory pattern (EDIP) tool, which is a weighted sum of 18 food groups — nine proinflammatory and nine anti-inflammatory. A high EDIP score marks a proinflammatory diet, and a low EDIP score indicates a less inflammatory diet.
During median follow-up of nearly 4 years, researchers noted a trend toward worse disease-free survival in patients with high proinflammatory diets (HR, 1.46), but this association was not significant in the multivariable adjusted model (HR, 1.36; P = .22), Char reported.
However, higher intake of proinflammatory foods was associated with significantly worse overall survival.
Patients who consumed the most proinflammatory foods (top 20%) had an 87% higher risk for death compared with those who consumed the least (bottom 20%; HR, 1.87). The median overall survival in the highest quintile was 7.7 years and was not reached in the lowest quintile.
Combine Exercise and Diet for Best Results
To examine the joint effect of physical activity and diet on overall survival, patients were divided into higher and lower levels of physical activity using a cut-off of 9 MET hours per week, which roughly correlates to 30 minutes of vigorous walking five days a week with a little bit of light yoga, Char explained.
In this analysis, patients with less proinflammatory diets and higher physical activity levels had the best overall survival outcomes, with a 63% lower risk for death compared with peers who consumed more pro-inflammatory diets and exercised less (HR, 0.37; P < .0001).
Daily celecoxib use and low-dose aspirin use (< 100 mg/d) did not affect the association between inflammatory diet and survival.
Char cautioned, that while the EDIP tool is useful to measure the inflammatory potential of a diet, “this is not a dietary recommendation, and we need further studies to be able to tailor our findings into dietary recommendations that can be provided to patients at the bedside.”
Gralow said this “early but promising observational study suggests a powerful synergy: Patients with stage III colon cancer who embraced anti-inflammatory foods and exercised regularly showed the best overall survival compared to those with inflammatory diets and limited exercise.”
The CHALLENGE trial was funded by the Canadian Cancer Society, the National Health and Medical Research Council, Cancer Research UK, and the University of Sydney Cancer Research Fund. Booth had no disclosures. The diet study was funded by the National Institutes of Health, Pfizer, and the Project P Fund. Char disclosed an advisory/consultant role with Goodpath. Kunz, Gralow and Campbell had no relevant disclosures.
A version of this article first appeared on Medscape.com.
Can exercise “therapy” and diet improve survival in patients with colon cancer? It appears so, according to two pivotal studies presented at American Society of Clinical Oncology (ASCO) 2025 annual meeting.
In the CHALLENGE trial, a structured exercise program after surgery and adjuvant chemotherapy cut the risk for colon cancer recurrence in patients with stage III and high-risk stage II disease by more than one quarter and the risk for death by more than one third.
“The magnitude of benefit with exercise is substantial. In fact, it is comparable, and in some cases exceeds the magnitude of benefit of many of our very good standard medical therapies in oncology,” study presenter Christopher Booth, MD, with Queen’s University, Kingston, Ontario, Canada, told attendees.
Results of the study were published online in The New England Journal of Medicine to coincide with the presentation at the meeting.
The findings are “nothing short of a major milestone,” said study discussant Peter Campbell, PhD, with Montefiore Einstein Comprehensive Cancer Center, Bronx, New York.
The other study showed that eating a less inflammatory diet may reduce the risk for death in patients with colon cancer, with the greatest benefits seen in those who embraced anti-inflammatory foods and exercised regularly.
“Putting these two abstracts into perspective, we as physicians need to be essentially prescribing healthy diet and exercise. The combination of the two are synergistic,” Julie Gralow, MD, ASCO chief medical officer and executive vice president, told attendees.
Despite the benefits of these lifestyle changes, exercise and diet are meant to supplement, not replace, established colon cancer treatments.
It would be a false binary to frame this as lifestyle vs cancer treatment, explained Mark Lewis, MD, director of Gastrointestinal Oncology at Intermountain Healthcare in Salt Lake City, Utah. With exercise, for instance, “the key is giving enough chemo to protect against recurrence and eliminate micrometastases but not so much that we cause neuropathy and reduce function and ability to follow the CHALLENGE structured program,” Lewis said.
Exercise and Survival
Colon cancer remains the second-leading cause of cancer death worldwide. Even with surgery and chemotherapy, roughly 30% of patients with stage III and high-risk stage II colon cancer will experience disease recurrence.
“As oncologists, one of the most common questions we get asked by patients is — what else can I do to improve my outcome?” Booth said.
Observational studies published nearly two decades ago hinted that physically active cancer survivors fare better, but no randomized trial has definitively tested whether exercise could alter disease course. That knowledge gap prompted the Canadian Cancer Trials Group to launch the CHALLENGE trial.
Between 2009 and 2023, the phase 3 study enrolled 889 adults (median age, 61 years; 51% women) who had completed surgery and adjuvant chemotherapy for stage III (90%) or high-risk stage II (10%) colon cancer. Most patients were from Canada and Australia and were enrolled 2-6 months after completing chemotherapy.
Half of study participants were randomly allocated to a structured exercise program (n = 445) and half to receive standard health education materials promoting physical activity and healthy eating (control individuals, n = 444).
As part of the structured exercise intervention, patients met with a physical activity consultant twice a month for the first 6 months. These sessions included exercise coaching and supervised exercise. Patients could choose their preferred aerobic exercise and most picked brisk walking.
The consultants gave each patient an “exercise prescription” to hit a specific amount of exercise. The target was an additional 10 metabolic equivalent (MET)–hours of aerobic activity per week — about three to four brisk walks each lasting 45-60 minutes. After 6 months, patients met with their consultants once a month, with additional sessions available for extra support if needed.
Structured exercise led to “substantial and sustained” increases in the amount of exercise participants did, as well as physiologic measures of their fitness, with “highly relevant” improvements in VO2 max, 6-minute walk test, and patient-reported physical function, underscoring that participants were not only exercising more but also getting fitter, Booth said.
Exercise was associated with a clinically meaningful and statistically significant 28% reduction in the risk for recurrent or new cancer (hazard ratio [HR], 0.72; P = .017), with a 5-year disease free survival rate of 80% in the exercise group and 74% in the control group.
In other words, “for every 16 patients that went on the exercise program, exercise prevented 1 person from recurrent or new cancer” at 5 years, Booth reported.
Overall survival results were “even more impressive,” he said.
At 8 years, 90% of patients in the exercise program were alive vs 83% of those in the control group, which translated to a 37% lower risk for death (HR, 0.63; P = .022).
“For every 14 patients who went on the exercise program, exercise prevented 1 person from dying” at the 8-year mark, Booth noted.
“Notably, this difference in survival was not driven by difference in cardiovascular deaths but by a reduction in the risk of death from colon cancer,” he said.
Besides a slight uptick in musculoskeletal aches, no major safety signals emerged in the exercise group.
It’s important to note that the survival benefit associated with exercise came after patients had received surgery followed by chemotherapy — in other words, exercise did not replace established cancer treatments. It’s also unclear whether initiating an exercise intervention earlier in the treatment trajectory — before surgery or during chemotherapy, instead of after chemotherapy — could further improve cancer outcomes, the authors noted.
Still, “exercise as an intervention is a no brainer and should be implemented broadly,” said ASCO expert Pamela Kunz, MD, with Yale School of Medicine, New Haven, Connecticut.
Marco Gerlinger, MD, with Barts Cancer Institute, London, England, agreed.
“Oncologists can now make a very clear evidence-based recommendation for patients who just completed their chemotherapy for bowel cancer and are fit enough for such an exercise program,” Gerlinger said in a statement from the nonprofit UK Science Media Centre.
Booth noted that knowledge alone will not be sufficient to allow most patients to change their lifestyle and realize the health benefits.
“The policy implementation piece of this is really key, and we need health systems, hospitals, and payers to invest in these behavior support programs so that patients have access to a physical activity consultant and can realize the health benefits,” he said.
“This intervention is empowering and achievable for patients and with much, much lower cost than many of our therapies. It is also sustainable for health systems,” he concluded.
Diet and Survival
Diet can also affect outcomes in patients with colon cancer.
In the same session describing the CHALLENGE results, Sara Char, MD, with Dana-Farber Cancer Institute in Boston, reported findings showing that consuming a diet high in proinflammatory foods was associated with worse overall survival in patients with stage III colon cancer. A proinflammatory diet includes red and processed meats, sugary drinks, and refined grains, while an anti-inflammatory diet focuses on fruits, vegetables, whole grains, fish, and olive oil.
Chronic systemic inflammation has been implicated in both colon cancer development and in its progression, and elevated levels of inflammatory markers in the blood have previously been associated with worse survival outcomes in patients with stage III colon cancer.
Char and colleagues analyzed dietary patterns of a subset of 1625 patients (mean age, 61 years) with resected stage III colon cancer enrolled in the phase 3 CALGB/SWOG 80702 (Alliance) clinical trial, which compared 3 months of adjuvant chemotherapy with 6 months of adjuvant chemotherapy, with or without the anti-inflammatory medication celecoxib.
As part of the trial, participants reported their diet and exercise habits at various timepoints. Their diets were scored using the validated empirical dietary inflammatory pattern (EDIP) tool, which is a weighted sum of 18 food groups — nine proinflammatory and nine anti-inflammatory. A high EDIP score marks a proinflammatory diet, and a low EDIP score indicates a less inflammatory diet.
During median follow-up of nearly 4 years, researchers noted a trend toward worse disease-free survival in patients with high proinflammatory diets (HR, 1.46), but this association was not significant in the multivariable adjusted model (HR, 1.36; P = .22), Char reported.
However, higher intake of proinflammatory foods was associated with significantly worse overall survival.
Patients who consumed the most proinflammatory foods (top 20%) had an 87% higher risk for death compared with those who consumed the least (bottom 20%; HR, 1.87). The median overall survival in the highest quintile was 7.7 years and was not reached in the lowest quintile.
Combine Exercise and Diet for Best Results
To examine the joint effect of physical activity and diet on overall survival, patients were divided into higher and lower levels of physical activity using a cut-off of 9 MET hours per week, which roughly correlates to 30 minutes of vigorous walking five days a week with a little bit of light yoga, Char explained.
In this analysis, patients with less proinflammatory diets and higher physical activity levels had the best overall survival outcomes, with a 63% lower risk for death compared with peers who consumed more pro-inflammatory diets and exercised less (HR, 0.37; P < .0001).
Daily celecoxib use and low-dose aspirin use (< 100 mg/d) did not affect the association between inflammatory diet and survival.
Char cautioned, that while the EDIP tool is useful to measure the inflammatory potential of a diet, “this is not a dietary recommendation, and we need further studies to be able to tailor our findings into dietary recommendations that can be provided to patients at the bedside.”
Gralow said this “early but promising observational study suggests a powerful synergy: Patients with stage III colon cancer who embraced anti-inflammatory foods and exercised regularly showed the best overall survival compared to those with inflammatory diets and limited exercise.”
The CHALLENGE trial was funded by the Canadian Cancer Society, the National Health and Medical Research Council, Cancer Research UK, and the University of Sydney Cancer Research Fund. Booth had no disclosures. The diet study was funded by the National Institutes of Health, Pfizer, and the Project P Fund. Char disclosed an advisory/consultant role with Goodpath. Kunz, Gralow and Campbell had no relevant disclosures.
A version of this article first appeared on Medscape.com.
Can exercise “therapy” and diet improve survival in patients with colon cancer? It appears so, according to two pivotal studies presented at American Society of Clinical Oncology (ASCO) 2025 annual meeting.
In the CHALLENGE trial, a structured exercise program after surgery and adjuvant chemotherapy cut the risk for colon cancer recurrence in patients with stage III and high-risk stage II disease by more than one quarter and the risk for death by more than one third.
“The magnitude of benefit with exercise is substantial. In fact, it is comparable, and in some cases exceeds the magnitude of benefit of many of our very good standard medical therapies in oncology,” study presenter Christopher Booth, MD, with Queen’s University, Kingston, Ontario, Canada, told attendees.
Results of the study were published online in The New England Journal of Medicine to coincide with the presentation at the meeting.
The findings are “nothing short of a major milestone,” said study discussant Peter Campbell, PhD, with Montefiore Einstein Comprehensive Cancer Center, Bronx, New York.
The other study showed that eating a less inflammatory diet may reduce the risk for death in patients with colon cancer, with the greatest benefits seen in those who embraced anti-inflammatory foods and exercised regularly.
“Putting these two abstracts into perspective, we as physicians need to be essentially prescribing healthy diet and exercise. The combination of the two are synergistic,” Julie Gralow, MD, ASCO chief medical officer and executive vice president, told attendees.
Despite the benefits of these lifestyle changes, exercise and diet are meant to supplement, not replace, established colon cancer treatments.
It would be a false binary to frame this as lifestyle vs cancer treatment, explained Mark Lewis, MD, director of Gastrointestinal Oncology at Intermountain Healthcare in Salt Lake City, Utah. With exercise, for instance, “the key is giving enough chemo to protect against recurrence and eliminate micrometastases but not so much that we cause neuropathy and reduce function and ability to follow the CHALLENGE structured program,” Lewis said.
Exercise and Survival
Colon cancer remains the second-leading cause of cancer death worldwide. Even with surgery and chemotherapy, roughly 30% of patients with stage III and high-risk stage II colon cancer will experience disease recurrence.
“As oncologists, one of the most common questions we get asked by patients is — what else can I do to improve my outcome?” Booth said.
Observational studies published nearly two decades ago hinted that physically active cancer survivors fare better, but no randomized trial has definitively tested whether exercise could alter disease course. That knowledge gap prompted the Canadian Cancer Trials Group to launch the CHALLENGE trial.
Between 2009 and 2023, the phase 3 study enrolled 889 adults (median age, 61 years; 51% women) who had completed surgery and adjuvant chemotherapy for stage III (90%) or high-risk stage II (10%) colon cancer. Most patients were from Canada and Australia and were enrolled 2-6 months after completing chemotherapy.
Half of study participants were randomly allocated to a structured exercise program (n = 445) and half to receive standard health education materials promoting physical activity and healthy eating (control individuals, n = 444).
As part of the structured exercise intervention, patients met with a physical activity consultant twice a month for the first 6 months. These sessions included exercise coaching and supervised exercise. Patients could choose their preferred aerobic exercise and most picked brisk walking.
The consultants gave each patient an “exercise prescription” to hit a specific amount of exercise. The target was an additional 10 metabolic equivalent (MET)–hours of aerobic activity per week — about three to four brisk walks each lasting 45-60 minutes. After 6 months, patients met with their consultants once a month, with additional sessions available for extra support if needed.
Structured exercise led to “substantial and sustained” increases in the amount of exercise participants did, as well as physiologic measures of their fitness, with “highly relevant” improvements in VO2 max, 6-minute walk test, and patient-reported physical function, underscoring that participants were not only exercising more but also getting fitter, Booth said.
Exercise was associated with a clinically meaningful and statistically significant 28% reduction in the risk for recurrent or new cancer (hazard ratio [HR], 0.72; P = .017), with a 5-year disease free survival rate of 80% in the exercise group and 74% in the control group.
In other words, “for every 16 patients that went on the exercise program, exercise prevented 1 person from recurrent or new cancer” at 5 years, Booth reported.
Overall survival results were “even more impressive,” he said.
At 8 years, 90% of patients in the exercise program were alive vs 83% of those in the control group, which translated to a 37% lower risk for death (HR, 0.63; P = .022).
“For every 14 patients who went on the exercise program, exercise prevented 1 person from dying” at the 8-year mark, Booth noted.
“Notably, this difference in survival was not driven by difference in cardiovascular deaths but by a reduction in the risk of death from colon cancer,” he said.
Besides a slight uptick in musculoskeletal aches, no major safety signals emerged in the exercise group.
It’s important to note that the survival benefit associated with exercise came after patients had received surgery followed by chemotherapy — in other words, exercise did not replace established cancer treatments. It’s also unclear whether initiating an exercise intervention earlier in the treatment trajectory — before surgery or during chemotherapy, instead of after chemotherapy — could further improve cancer outcomes, the authors noted.
Still, “exercise as an intervention is a no brainer and should be implemented broadly,” said ASCO expert Pamela Kunz, MD, with Yale School of Medicine, New Haven, Connecticut.
Marco Gerlinger, MD, with Barts Cancer Institute, London, England, agreed.
“Oncologists can now make a very clear evidence-based recommendation for patients who just completed their chemotherapy for bowel cancer and are fit enough for such an exercise program,” Gerlinger said in a statement from the nonprofit UK Science Media Centre.
Booth noted that knowledge alone will not be sufficient to allow most patients to change their lifestyle and realize the health benefits.
“The policy implementation piece of this is really key, and we need health systems, hospitals, and payers to invest in these behavior support programs so that patients have access to a physical activity consultant and can realize the health benefits,” he said.
“This intervention is empowering and achievable for patients and with much, much lower cost than many of our therapies. It is also sustainable for health systems,” he concluded.
Diet and Survival
Diet can also affect outcomes in patients with colon cancer.
In the same session describing the CHALLENGE results, Sara Char, MD, with Dana-Farber Cancer Institute in Boston, reported findings showing that consuming a diet high in proinflammatory foods was associated with worse overall survival in patients with stage III colon cancer. A proinflammatory diet includes red and processed meats, sugary drinks, and refined grains, while an anti-inflammatory diet focuses on fruits, vegetables, whole grains, fish, and olive oil.
Chronic systemic inflammation has been implicated in both colon cancer development and in its progression, and elevated levels of inflammatory markers in the blood have previously been associated with worse survival outcomes in patients with stage III colon cancer.
Char and colleagues analyzed dietary patterns of a subset of 1625 patients (mean age, 61 years) with resected stage III colon cancer enrolled in the phase 3 CALGB/SWOG 80702 (Alliance) clinical trial, which compared 3 months of adjuvant chemotherapy with 6 months of adjuvant chemotherapy, with or without the anti-inflammatory medication celecoxib.
As part of the trial, participants reported their diet and exercise habits at various timepoints. Their diets were scored using the validated empirical dietary inflammatory pattern (EDIP) tool, which is a weighted sum of 18 food groups — nine proinflammatory and nine anti-inflammatory. A high EDIP score marks a proinflammatory diet, and a low EDIP score indicates a less inflammatory diet.
During median follow-up of nearly 4 years, researchers noted a trend toward worse disease-free survival in patients with high proinflammatory diets (HR, 1.46), but this association was not significant in the multivariable adjusted model (HR, 1.36; P = .22), Char reported.
However, higher intake of proinflammatory foods was associated with significantly worse overall survival.
Patients who consumed the most proinflammatory foods (top 20%) had an 87% higher risk for death compared with those who consumed the least (bottom 20%; HR, 1.87). The median overall survival in the highest quintile was 7.7 years and was not reached in the lowest quintile.
Combine Exercise and Diet for Best Results
To examine the joint effect of physical activity and diet on overall survival, patients were divided into higher and lower levels of physical activity using a cut-off of 9 MET hours per week, which roughly correlates to 30 minutes of vigorous walking five days a week with a little bit of light yoga, Char explained.
In this analysis, patients with less proinflammatory diets and higher physical activity levels had the best overall survival outcomes, with a 63% lower risk for death compared with peers who consumed more pro-inflammatory diets and exercised less (HR, 0.37; P < .0001).
Daily celecoxib use and low-dose aspirin use (< 100 mg/d) did not affect the association between inflammatory diet and survival.
Char cautioned, that while the EDIP tool is useful to measure the inflammatory potential of a diet, “this is not a dietary recommendation, and we need further studies to be able to tailor our findings into dietary recommendations that can be provided to patients at the bedside.”
Gralow said this “early but promising observational study suggests a powerful synergy: Patients with stage III colon cancer who embraced anti-inflammatory foods and exercised regularly showed the best overall survival compared to those with inflammatory diets and limited exercise.”
The CHALLENGE trial was funded by the Canadian Cancer Society, the National Health and Medical Research Council, Cancer Research UK, and the University of Sydney Cancer Research Fund. Booth had no disclosures. The diet study was funded by the National Institutes of Health, Pfizer, and the Project P Fund. Char disclosed an advisory/consultant role with Goodpath. Kunz, Gralow and Campbell had no relevant disclosures.
A version of this article first appeared on Medscape.com.
Can Lifestyle Changes Save Lives in Colon Cancer?
Can Lifestyle Changes Save Lives in Colon Cancer?
EoE Prevalence in US Reaches 1 in 700, Costs $1B Annually
, according to recent research.
Although EoE has been considered a rare disease, the chronic condition is becoming more common, and healthcare providers should expect to encounter EoE in clinical settings, the study authors wrote.
“Our last assessment of the prevalence and burden of EoE was more than 10 years ago, and we had a strong suspicion we would continue to see increased numbers of patients with EoE and an increasing cost burden related to the condition in the United States,” said senior author Evan S. Dellon, MD, MPH, AGAF, professor of gastroenterology and hepatology and director of the Center for Esophageal Diseases and Swallowing at the University of North Carolina School of Medicine, Chapel Hill, North Carolina.
“EoE is becoming more common,” Dellon said. “Healthcare providers should expect to see EoE in their practices, including in the primary care setting, emergency departments, allergy practices, GI [gastrointestinal] practices, ENT clinics, and endoscopy suites.”
The study was published in Clinical Gastroenterology and Hepatology.
Estimating EoE Prevalence
Dellon and colleagues analyzed the Merative MarketScan Commercial Claims and Encounters and Medicare Fee-for-Service databases to calculate the annual prevalence of EoE, as well as age- and sex-stratified estimates standardized to the US population. They also calculated healthcare utilization, including medications and endoscopic procedures, to estimate annual EoE-associated costs. Since the EoE billing code was introduced in 2008, the analysis included 2009-2022 MarketScan and 2009-2017 Medicare data.
In the MarketScan database, the research team identified 20,435 EoE cases in 2022, with a mean age of 38 years, 16% younger than 18 years, 62% men, and 41% with a comorbid allergic disease code. The most common symptoms and diagnoses were dysphagia (39%), abdominal pain or dyspepsia (24%), and esophageal stricture (19%). Over time, patients also had previous codes for comorbid allergic diseases (64%), dysphagia (62%), or esophageal stricture (32%).
In the Medicare database, the research team identified 1913 EoE cases in 2017, with a mean age of 73 years, 47% men, 90% non-Hispanic White, and 36% with a comorbid allergic disease. The most common symptoms and diagnoses were dysphagia (49%), abdominal pain or dyspepsia (35%), and esophageal stricture (30%). Over time, patients also had codes for comorbid allergic diseases (64%), dysphagia (65%), or esophageal stricture (42%).
The database numbers translated to EoE prevalences of about 163 cases per 100,000 people in MarketScan in 2022 and 64 cases per 100,000 people in Medicare in 2017. Since 2009, there has been a fivefold increase in prevalence in both databases.
In MarketScan, the prevalence was higher among men than among women, at 204 vs 122 cases per 100,000 people. For both sexes, peak prevalence occurred between ages 40 and 44.
In Medicare, prevalence was also higher among men than among women, at 79 vs 55 cases per 100,000 people. Peak prevalence occurred between ages 65 and 69.
Standardized to the US population, EoE prevalence was 142.5 cases per 100,000 people, extrapolating to 472,380 cases. The overall prevalence was approximately 1 in 700, with rates of 1 in 617 for those younger than 65 years and 1 in 1562 for those aged ≥ 65 years.
“The rapidly increasing prevalence year over year for the entire timeframe of the study was surprising, as were our estimates of the total number of EoE patients in the US, which suggests that EoE is no longer a rare disease and is now seen in about 1 in 700 people,” Dellon said. “This almost triples our prior estimates of 1 in 2000 from 10 years ago, with all trends suggesting that the prevalence will continue to increase.”
Calculating EoE Costs
In terms of procedures, endoscopy with dilation or biopsy was used in about 60%-70% of patients with EoE in both MarketScan and Medicare during the years analyzed. In addition, upper endoscopy with biopsy was coded in 80%-90% of patients, guidewire-based dilation in 11%-17% of patients, and balloon-based dilation in 13%-20% of patients.
In terms of prescription medications, proton pump inhibitors (41%) and topical steroids (26%) were the most common in MarketScan in 2022, as well as in Medicare in 2017, at 32% and 9%, respectively.
When looking at costs by age and sex, the male cohort with the highest costs was aged 10-14 years, estimated at $106.7 million. Among the female cohort, the highest costs were associated with ages 15-19, estimated at $46.5 million.
Overall, total EoE-associated healthcare costs were estimated to be $1.04 billion in 2017, and when adjusted for inflation, the costs were estimated at $1.32 billion in 2024. This is likely an underestimate, the authors wrote, given that EoE prevalence has likely increased for ages 65 or older since 2017 and for all ages since 2022.
“Researching the prevalence and costs is essential to improving patient care by highlighting the growing burden of this recently recognized and growing chronic disease, guiding policy and insurer decisions, and advocating for better access to effective treatments and support for patients,” said Joy Chang, MD, assistant professor of medicine in the Division of Gastroenterology, University of Michigan, Ann Arbor, Michigan.Chang, who wasn’t involved with this study, specializes in eosinophilic GI diseases and researches patient-physician preferences and decision-making in EoE care.
“Clinicians should remain vigilant for symptoms, utilize guideline-based diagnostic approaches, and consider both medical and dietary treatment strategies to optimize patient outcomes and reduce long-term costs,” she said. “Increased awareness and timely intervention can help mitigate the growing impact of this chronic condition.”
The study was supported by a National Institutes of Health grant and used resources from the University of North Carolina Center for Gastrointestinal Biology and Disease. Dellon reported receiving research funding from and having consultant roles with numerous pharmaceutical companies and organizations. Chang reported having no relevant disclosures.
A version of this article appeared on Medscape.com.
, according to recent research.
Although EoE has been considered a rare disease, the chronic condition is becoming more common, and healthcare providers should expect to encounter EoE in clinical settings, the study authors wrote.
“Our last assessment of the prevalence and burden of EoE was more than 10 years ago, and we had a strong suspicion we would continue to see increased numbers of patients with EoE and an increasing cost burden related to the condition in the United States,” said senior author Evan S. Dellon, MD, MPH, AGAF, professor of gastroenterology and hepatology and director of the Center for Esophageal Diseases and Swallowing at the University of North Carolina School of Medicine, Chapel Hill, North Carolina.
“EoE is becoming more common,” Dellon said. “Healthcare providers should expect to see EoE in their practices, including in the primary care setting, emergency departments, allergy practices, GI [gastrointestinal] practices, ENT clinics, and endoscopy suites.”
The study was published in Clinical Gastroenterology and Hepatology.
Estimating EoE Prevalence
Dellon and colleagues analyzed the Merative MarketScan Commercial Claims and Encounters and Medicare Fee-for-Service databases to calculate the annual prevalence of EoE, as well as age- and sex-stratified estimates standardized to the US population. They also calculated healthcare utilization, including medications and endoscopic procedures, to estimate annual EoE-associated costs. Since the EoE billing code was introduced in 2008, the analysis included 2009-2022 MarketScan and 2009-2017 Medicare data.
In the MarketScan database, the research team identified 20,435 EoE cases in 2022, with a mean age of 38 years, 16% younger than 18 years, 62% men, and 41% with a comorbid allergic disease code. The most common symptoms and diagnoses were dysphagia (39%), abdominal pain or dyspepsia (24%), and esophageal stricture (19%). Over time, patients also had previous codes for comorbid allergic diseases (64%), dysphagia (62%), or esophageal stricture (32%).
In the Medicare database, the research team identified 1913 EoE cases in 2017, with a mean age of 73 years, 47% men, 90% non-Hispanic White, and 36% with a comorbid allergic disease. The most common symptoms and diagnoses were dysphagia (49%), abdominal pain or dyspepsia (35%), and esophageal stricture (30%). Over time, patients also had codes for comorbid allergic diseases (64%), dysphagia (65%), or esophageal stricture (42%).
The database numbers translated to EoE prevalences of about 163 cases per 100,000 people in MarketScan in 2022 and 64 cases per 100,000 people in Medicare in 2017. Since 2009, there has been a fivefold increase in prevalence in both databases.
In MarketScan, the prevalence was higher among men than among women, at 204 vs 122 cases per 100,000 people. For both sexes, peak prevalence occurred between ages 40 and 44.
In Medicare, prevalence was also higher among men than among women, at 79 vs 55 cases per 100,000 people. Peak prevalence occurred between ages 65 and 69.
Standardized to the US population, EoE prevalence was 142.5 cases per 100,000 people, extrapolating to 472,380 cases. The overall prevalence was approximately 1 in 700, with rates of 1 in 617 for those younger than 65 years and 1 in 1562 for those aged ≥ 65 years.
“The rapidly increasing prevalence year over year for the entire timeframe of the study was surprising, as were our estimates of the total number of EoE patients in the US, which suggests that EoE is no longer a rare disease and is now seen in about 1 in 700 people,” Dellon said. “This almost triples our prior estimates of 1 in 2000 from 10 years ago, with all trends suggesting that the prevalence will continue to increase.”
Calculating EoE Costs
In terms of procedures, endoscopy with dilation or biopsy was used in about 60%-70% of patients with EoE in both MarketScan and Medicare during the years analyzed. In addition, upper endoscopy with biopsy was coded in 80%-90% of patients, guidewire-based dilation in 11%-17% of patients, and balloon-based dilation in 13%-20% of patients.
In terms of prescription medications, proton pump inhibitors (41%) and topical steroids (26%) were the most common in MarketScan in 2022, as well as in Medicare in 2017, at 32% and 9%, respectively.
When looking at costs by age and sex, the male cohort with the highest costs was aged 10-14 years, estimated at $106.7 million. Among the female cohort, the highest costs were associated with ages 15-19, estimated at $46.5 million.
Overall, total EoE-associated healthcare costs were estimated to be $1.04 billion in 2017, and when adjusted for inflation, the costs were estimated at $1.32 billion in 2024. This is likely an underestimate, the authors wrote, given that EoE prevalence has likely increased for ages 65 or older since 2017 and for all ages since 2022.
“Researching the prevalence and costs is essential to improving patient care by highlighting the growing burden of this recently recognized and growing chronic disease, guiding policy and insurer decisions, and advocating for better access to effective treatments and support for patients,” said Joy Chang, MD, assistant professor of medicine in the Division of Gastroenterology, University of Michigan, Ann Arbor, Michigan.Chang, who wasn’t involved with this study, specializes in eosinophilic GI diseases and researches patient-physician preferences and decision-making in EoE care.
“Clinicians should remain vigilant for symptoms, utilize guideline-based diagnostic approaches, and consider both medical and dietary treatment strategies to optimize patient outcomes and reduce long-term costs,” she said. “Increased awareness and timely intervention can help mitigate the growing impact of this chronic condition.”
The study was supported by a National Institutes of Health grant and used resources from the University of North Carolina Center for Gastrointestinal Biology and Disease. Dellon reported receiving research funding from and having consultant roles with numerous pharmaceutical companies and organizations. Chang reported having no relevant disclosures.
A version of this article appeared on Medscape.com.
, according to recent research.
Although EoE has been considered a rare disease, the chronic condition is becoming more common, and healthcare providers should expect to encounter EoE in clinical settings, the study authors wrote.
“Our last assessment of the prevalence and burden of EoE was more than 10 years ago, and we had a strong suspicion we would continue to see increased numbers of patients with EoE and an increasing cost burden related to the condition in the United States,” said senior author Evan S. Dellon, MD, MPH, AGAF, professor of gastroenterology and hepatology and director of the Center for Esophageal Diseases and Swallowing at the University of North Carolina School of Medicine, Chapel Hill, North Carolina.
“EoE is becoming more common,” Dellon said. “Healthcare providers should expect to see EoE in their practices, including in the primary care setting, emergency departments, allergy practices, GI [gastrointestinal] practices, ENT clinics, and endoscopy suites.”
The study was published in Clinical Gastroenterology and Hepatology.
Estimating EoE Prevalence
Dellon and colleagues analyzed the Merative MarketScan Commercial Claims and Encounters and Medicare Fee-for-Service databases to calculate the annual prevalence of EoE, as well as age- and sex-stratified estimates standardized to the US population. They also calculated healthcare utilization, including medications and endoscopic procedures, to estimate annual EoE-associated costs. Since the EoE billing code was introduced in 2008, the analysis included 2009-2022 MarketScan and 2009-2017 Medicare data.
In the MarketScan database, the research team identified 20,435 EoE cases in 2022, with a mean age of 38 years, 16% younger than 18 years, 62% men, and 41% with a comorbid allergic disease code. The most common symptoms and diagnoses were dysphagia (39%), abdominal pain or dyspepsia (24%), and esophageal stricture (19%). Over time, patients also had previous codes for comorbid allergic diseases (64%), dysphagia (62%), or esophageal stricture (32%).
In the Medicare database, the research team identified 1913 EoE cases in 2017, with a mean age of 73 years, 47% men, 90% non-Hispanic White, and 36% with a comorbid allergic disease. The most common symptoms and diagnoses were dysphagia (49%), abdominal pain or dyspepsia (35%), and esophageal stricture (30%). Over time, patients also had codes for comorbid allergic diseases (64%), dysphagia (65%), or esophageal stricture (42%).
The database numbers translated to EoE prevalences of about 163 cases per 100,000 people in MarketScan in 2022 and 64 cases per 100,000 people in Medicare in 2017. Since 2009, there has been a fivefold increase in prevalence in both databases.
In MarketScan, the prevalence was higher among men than among women, at 204 vs 122 cases per 100,000 people. For both sexes, peak prevalence occurred between ages 40 and 44.
In Medicare, prevalence was also higher among men than among women, at 79 vs 55 cases per 100,000 people. Peak prevalence occurred between ages 65 and 69.
Standardized to the US population, EoE prevalence was 142.5 cases per 100,000 people, extrapolating to 472,380 cases. The overall prevalence was approximately 1 in 700, with rates of 1 in 617 for those younger than 65 years and 1 in 1562 for those aged ≥ 65 years.
“The rapidly increasing prevalence year over year for the entire timeframe of the study was surprising, as were our estimates of the total number of EoE patients in the US, which suggests that EoE is no longer a rare disease and is now seen in about 1 in 700 people,” Dellon said. “This almost triples our prior estimates of 1 in 2000 from 10 years ago, with all trends suggesting that the prevalence will continue to increase.”
Calculating EoE Costs
In terms of procedures, endoscopy with dilation or biopsy was used in about 60%-70% of patients with EoE in both MarketScan and Medicare during the years analyzed. In addition, upper endoscopy with biopsy was coded in 80%-90% of patients, guidewire-based dilation in 11%-17% of patients, and balloon-based dilation in 13%-20% of patients.
In terms of prescription medications, proton pump inhibitors (41%) and topical steroids (26%) were the most common in MarketScan in 2022, as well as in Medicare in 2017, at 32% and 9%, respectively.
When looking at costs by age and sex, the male cohort with the highest costs was aged 10-14 years, estimated at $106.7 million. Among the female cohort, the highest costs were associated with ages 15-19, estimated at $46.5 million.
Overall, total EoE-associated healthcare costs were estimated to be $1.04 billion in 2017, and when adjusted for inflation, the costs were estimated at $1.32 billion in 2024. This is likely an underestimate, the authors wrote, given that EoE prevalence has likely increased for ages 65 or older since 2017 and for all ages since 2022.
“Researching the prevalence and costs is essential to improving patient care by highlighting the growing burden of this recently recognized and growing chronic disease, guiding policy and insurer decisions, and advocating for better access to effective treatments and support for patients,” said Joy Chang, MD, assistant professor of medicine in the Division of Gastroenterology, University of Michigan, Ann Arbor, Michigan.Chang, who wasn’t involved with this study, specializes in eosinophilic GI diseases and researches patient-physician preferences and decision-making in EoE care.
“Clinicians should remain vigilant for symptoms, utilize guideline-based diagnostic approaches, and consider both medical and dietary treatment strategies to optimize patient outcomes and reduce long-term costs,” she said. “Increased awareness and timely intervention can help mitigate the growing impact of this chronic condition.”
The study was supported by a National Institutes of Health grant and used resources from the University of North Carolina Center for Gastrointestinal Biology and Disease. Dellon reported receiving research funding from and having consultant roles with numerous pharmaceutical companies and organizations. Chang reported having no relevant disclosures.
A version of this article appeared on Medscape.com.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
AI Algorithm Predicts Transfusion Need, Mortality Risk in Acute GI Bleeds
SAN DIEGO — , researchers reported at Digestive Disease Week® (DDW) 2025.
Acute GI bleeding is the most common cause of digestive disease–related hospitalization, with an estimated 500,000 hospital admissions annually. It’s known that predicting the need for red blood cell transfusion in the first 24 hours may improve resuscitation and decrease both morbidity and mortality.
However, an existing clinical score known as the Rockall Score does not perform well for predicting mortality, Xi (Nicole) Zhang, an MD-PhD student at McGill University, Montreal, Quebec, Canada, told attendees at DDW. With an area under the curve of 0.65-0.75, better prediction is needed, said Zhang, whose coresearchers included Dennis Shung, MD, MHS, PhD, director of Applied Artificial Intelligence at Yale University School of Medicine, New Haven, Connecticut.
“We’d like to predict multiple outcomes in addition to mortality,” said Zhang, who is also a student at the Mila-Quebec Artificial Intelligence Institute.
As a result, the researchers turned to the TFM approach, applying it to ICU patients with acute GI bleeding to predict both the need for transfusion and in-hospital mortality risk. The all-cause mortality rate is up to 11%, according to a 2020 study by James Y. W. Lau, MD, and colleagues. The rebleeding rate of nonvariceal upper GI bleeds is up to 10.4%. Zhang said the rebleeding rate for variceal upper gastrointestinal bleeding is up to 65%.
The AI method the researchers used outperformed a standard deep learning model at predicting the need for transfusion and estimating mortality risk.
Defining the AI Framework
“Probabilistic flow matching is a class of generative artificial intelligence that learns how a simple distribution becomes a more complex distribution with ordinary differential equations,” Zhang told GI & Hepatology News. “For example, if you had a few lines and shapes you could learn how it could become a detailed portrait of a face. In our case, we start with a few blood pressure and heart rate measurements and learn the pattern of blood pressures and heart rates over time, particularly if they reflect clinical deterioration with hemodynamic instability.”
Another way to think about the underlying algorithm, Zhang said, is to think about a river with boats where the river flow determines where the boats end up. “We are trying to direct the boat to the correct dock by adjusting the flow of water in the canal. In this case we are mapping the distribution with the first few data points to the distribution with the entire patient trajectory.”
The information gained, she said, could be helpful in timing endoscopic evaluation or allocating red blood cell products for emergent transfusion.
Study Details
The researchers evaluated a cohort of 2602 patients admitted to the ICU, identified from the publicly available MIMIC-III database. They divided the patients into a training set of 2342 patients and an internal validation set of 260 patients. Input variables were severe liver disease comorbidity, administration of vasopressor medications, mean arterial blood pressure, and heart rate over the first 24 hours.
Excluded was hemoglobin, since the point was to test the trajectory of hemodynamic parameters independent of hemoglobin thresholds used to guide red blood cell transfusion.
The outcome measures were administration of packed red blood cell transfusion within 24 hours and all-cause hospital mortality.
The TFM was more accurate than a standard deep learning model in predicting red blood cell transfusion, with an accuracy of 93.6% vs 43.2%; P ≤ .001. It was also more accurate at predicting all-cause in-hospital mortality, with an accuracy of 89.5% vs 42.5%, P = .01.
The researchers concluded that the TFM approach was able to predict the hemodynamic trajectories of patients with acute GI bleeding defined as deviation and outperformed the baseline from the measured mean arterial pressure and heart rate.
Expert Perspective
“This is an exciting proof-of-concept study that shows generative AI methods may be applied to complex datasets in order to improve on our current predictive models and improve patient care,” said Jeremy Glissen Brown, MD, MSc, an assistant professor of medicine and a practicing gastroenterologist at Duke University who has published research on the use of AI in clinical practice. He reviewed the study for GI & Hepatology News but was not involved in the research.
“Future work will likely look into the implementation of a version of this model on real-time data.” he said. “We are at an exciting inflection point in predictive models within GI and clinical medicine. Predictive models based on deep learning and generative AI hold the promise of improving how we predict and treat disease states, but the excitement being generated with studies such as this needs to be balanced with the trade-offs inherent to the current paradigm of deep learning and generative models compared to more traditional regression-based models. These include many of the same ‘black box’ explainability questions that have risen in the age of convolutional neural networks as well as some method-specific questions due to the continuous and implicit nature of TFM.”
Elaborating on that, Glissen Brown said: “TFM, like many deep learning techniques, raises concerns about explainability that we’ve long seen with convolutional neural networks — the ‘black box’ problem, where it’s difficult to interpret exactly how and why the model arrives at a particular decision. But TFM also introduces unique challenges due to its continuous and implicit formulation. Since it often learns flows without explicitly defining intermediate representations or steps, it can be harder to trace the logic or pathways it uses to connect inputs to outputs. This makes standard interpretability tools less effective and calls for new techniques tailored to these continuous architectures.”
“This approach could have a real clinical impact,” said Robert Hirten, MD, associate professor of medicine and artificial intelligence, Icahn School of Medicine at Mount Sinai, New York City, who also reviewed the study. “Accurately predicting transfusion needs and mortality risk in real time could support earlier, more targeted interventions for high-risk patients. While these findings still need to be validated in prospective studies, it could enhance ICU decision-making and resource allocation.”
“For the practicing gastroenterologist, we envision this system could help them figure out when to perform endoscopy in a patient admitted with acute gastrointestinal bleeding in the ICU at very high risk of exsanguination,” Zhang told GI & Hepatology News.
The approach, the researchers said, will be useful in identifying unique patient characteristics, make possible the identification of high-risk patients and lead to more personalized medicine.
Hirten, Zhang, and Shung had no disclosures. Glissen Brown reported consulting relationships with Medtronic, OdinVision, Doximity, and Olympus. The National Institutes of Health funded this study.
A version of this article appeared on Medscape.com.
SAN DIEGO — , researchers reported at Digestive Disease Week® (DDW) 2025.
Acute GI bleeding is the most common cause of digestive disease–related hospitalization, with an estimated 500,000 hospital admissions annually. It’s known that predicting the need for red blood cell transfusion in the first 24 hours may improve resuscitation and decrease both morbidity and mortality.
However, an existing clinical score known as the Rockall Score does not perform well for predicting mortality, Xi (Nicole) Zhang, an MD-PhD student at McGill University, Montreal, Quebec, Canada, told attendees at DDW. With an area under the curve of 0.65-0.75, better prediction is needed, said Zhang, whose coresearchers included Dennis Shung, MD, MHS, PhD, director of Applied Artificial Intelligence at Yale University School of Medicine, New Haven, Connecticut.
“We’d like to predict multiple outcomes in addition to mortality,” said Zhang, who is also a student at the Mila-Quebec Artificial Intelligence Institute.
As a result, the researchers turned to the TFM approach, applying it to ICU patients with acute GI bleeding to predict both the need for transfusion and in-hospital mortality risk. The all-cause mortality rate is up to 11%, according to a 2020 study by James Y. W. Lau, MD, and colleagues. The rebleeding rate of nonvariceal upper GI bleeds is up to 10.4%. Zhang said the rebleeding rate for variceal upper gastrointestinal bleeding is up to 65%.
The AI method the researchers used outperformed a standard deep learning model at predicting the need for transfusion and estimating mortality risk.
Defining the AI Framework
“Probabilistic flow matching is a class of generative artificial intelligence that learns how a simple distribution becomes a more complex distribution with ordinary differential equations,” Zhang told GI & Hepatology News. “For example, if you had a few lines and shapes you could learn how it could become a detailed portrait of a face. In our case, we start with a few blood pressure and heart rate measurements and learn the pattern of blood pressures and heart rates over time, particularly if they reflect clinical deterioration with hemodynamic instability.”
Another way to think about the underlying algorithm, Zhang said, is to think about a river with boats where the river flow determines where the boats end up. “We are trying to direct the boat to the correct dock by adjusting the flow of water in the canal. In this case we are mapping the distribution with the first few data points to the distribution with the entire patient trajectory.”
The information gained, she said, could be helpful in timing endoscopic evaluation or allocating red blood cell products for emergent transfusion.
Study Details
The researchers evaluated a cohort of 2602 patients admitted to the ICU, identified from the publicly available MIMIC-III database. They divided the patients into a training set of 2342 patients and an internal validation set of 260 patients. Input variables were severe liver disease comorbidity, administration of vasopressor medications, mean arterial blood pressure, and heart rate over the first 24 hours.
Excluded was hemoglobin, since the point was to test the trajectory of hemodynamic parameters independent of hemoglobin thresholds used to guide red blood cell transfusion.
The outcome measures were administration of packed red blood cell transfusion within 24 hours and all-cause hospital mortality.
The TFM was more accurate than a standard deep learning model in predicting red blood cell transfusion, with an accuracy of 93.6% vs 43.2%; P ≤ .001. It was also more accurate at predicting all-cause in-hospital mortality, with an accuracy of 89.5% vs 42.5%, P = .01.
The researchers concluded that the TFM approach was able to predict the hemodynamic trajectories of patients with acute GI bleeding defined as deviation and outperformed the baseline from the measured mean arterial pressure and heart rate.
Expert Perspective
“This is an exciting proof-of-concept study that shows generative AI methods may be applied to complex datasets in order to improve on our current predictive models and improve patient care,” said Jeremy Glissen Brown, MD, MSc, an assistant professor of medicine and a practicing gastroenterologist at Duke University who has published research on the use of AI in clinical practice. He reviewed the study for GI & Hepatology News but was not involved in the research.
“Future work will likely look into the implementation of a version of this model on real-time data.” he said. “We are at an exciting inflection point in predictive models within GI and clinical medicine. Predictive models based on deep learning and generative AI hold the promise of improving how we predict and treat disease states, but the excitement being generated with studies such as this needs to be balanced with the trade-offs inherent to the current paradigm of deep learning and generative models compared to more traditional regression-based models. These include many of the same ‘black box’ explainability questions that have risen in the age of convolutional neural networks as well as some method-specific questions due to the continuous and implicit nature of TFM.”
Elaborating on that, Glissen Brown said: “TFM, like many deep learning techniques, raises concerns about explainability that we’ve long seen with convolutional neural networks — the ‘black box’ problem, where it’s difficult to interpret exactly how and why the model arrives at a particular decision. But TFM also introduces unique challenges due to its continuous and implicit formulation. Since it often learns flows without explicitly defining intermediate representations or steps, it can be harder to trace the logic or pathways it uses to connect inputs to outputs. This makes standard interpretability tools less effective and calls for new techniques tailored to these continuous architectures.”
“This approach could have a real clinical impact,” said Robert Hirten, MD, associate professor of medicine and artificial intelligence, Icahn School of Medicine at Mount Sinai, New York City, who also reviewed the study. “Accurately predicting transfusion needs and mortality risk in real time could support earlier, more targeted interventions for high-risk patients. While these findings still need to be validated in prospective studies, it could enhance ICU decision-making and resource allocation.”
“For the practicing gastroenterologist, we envision this system could help them figure out when to perform endoscopy in a patient admitted with acute gastrointestinal bleeding in the ICU at very high risk of exsanguination,” Zhang told GI & Hepatology News.
The approach, the researchers said, will be useful in identifying unique patient characteristics, make possible the identification of high-risk patients and lead to more personalized medicine.
Hirten, Zhang, and Shung had no disclosures. Glissen Brown reported consulting relationships with Medtronic, OdinVision, Doximity, and Olympus. The National Institutes of Health funded this study.
A version of this article appeared on Medscape.com.
SAN DIEGO — , researchers reported at Digestive Disease Week® (DDW) 2025.
Acute GI bleeding is the most common cause of digestive disease–related hospitalization, with an estimated 500,000 hospital admissions annually. It’s known that predicting the need for red blood cell transfusion in the first 24 hours may improve resuscitation and decrease both morbidity and mortality.
However, an existing clinical score known as the Rockall Score does not perform well for predicting mortality, Xi (Nicole) Zhang, an MD-PhD student at McGill University, Montreal, Quebec, Canada, told attendees at DDW. With an area under the curve of 0.65-0.75, better prediction is needed, said Zhang, whose coresearchers included Dennis Shung, MD, MHS, PhD, director of Applied Artificial Intelligence at Yale University School of Medicine, New Haven, Connecticut.
“We’d like to predict multiple outcomes in addition to mortality,” said Zhang, who is also a student at the Mila-Quebec Artificial Intelligence Institute.
As a result, the researchers turned to the TFM approach, applying it to ICU patients with acute GI bleeding to predict both the need for transfusion and in-hospital mortality risk. The all-cause mortality rate is up to 11%, according to a 2020 study by James Y. W. Lau, MD, and colleagues. The rebleeding rate of nonvariceal upper GI bleeds is up to 10.4%. Zhang said the rebleeding rate for variceal upper gastrointestinal bleeding is up to 65%.
The AI method the researchers used outperformed a standard deep learning model at predicting the need for transfusion and estimating mortality risk.
Defining the AI Framework
“Probabilistic flow matching is a class of generative artificial intelligence that learns how a simple distribution becomes a more complex distribution with ordinary differential equations,” Zhang told GI & Hepatology News. “For example, if you had a few lines and shapes you could learn how it could become a detailed portrait of a face. In our case, we start with a few blood pressure and heart rate measurements and learn the pattern of blood pressures and heart rates over time, particularly if they reflect clinical deterioration with hemodynamic instability.”
Another way to think about the underlying algorithm, Zhang said, is to think about a river with boats where the river flow determines where the boats end up. “We are trying to direct the boat to the correct dock by adjusting the flow of water in the canal. In this case we are mapping the distribution with the first few data points to the distribution with the entire patient trajectory.”
The information gained, she said, could be helpful in timing endoscopic evaluation or allocating red blood cell products for emergent transfusion.
Study Details
The researchers evaluated a cohort of 2602 patients admitted to the ICU, identified from the publicly available MIMIC-III database. They divided the patients into a training set of 2342 patients and an internal validation set of 260 patients. Input variables were severe liver disease comorbidity, administration of vasopressor medications, mean arterial blood pressure, and heart rate over the first 24 hours.
Excluded was hemoglobin, since the point was to test the trajectory of hemodynamic parameters independent of hemoglobin thresholds used to guide red blood cell transfusion.
The outcome measures were administration of packed red blood cell transfusion within 24 hours and all-cause hospital mortality.
The TFM was more accurate than a standard deep learning model in predicting red blood cell transfusion, with an accuracy of 93.6% vs 43.2%; P ≤ .001. It was also more accurate at predicting all-cause in-hospital mortality, with an accuracy of 89.5% vs 42.5%, P = .01.
The researchers concluded that the TFM approach was able to predict the hemodynamic trajectories of patients with acute GI bleeding defined as deviation and outperformed the baseline from the measured mean arterial pressure and heart rate.
Expert Perspective
“This is an exciting proof-of-concept study that shows generative AI methods may be applied to complex datasets in order to improve on our current predictive models and improve patient care,” said Jeremy Glissen Brown, MD, MSc, an assistant professor of medicine and a practicing gastroenterologist at Duke University who has published research on the use of AI in clinical practice. He reviewed the study for GI & Hepatology News but was not involved in the research.
“Future work will likely look into the implementation of a version of this model on real-time data.” he said. “We are at an exciting inflection point in predictive models within GI and clinical medicine. Predictive models based on deep learning and generative AI hold the promise of improving how we predict and treat disease states, but the excitement being generated with studies such as this needs to be balanced with the trade-offs inherent to the current paradigm of deep learning and generative models compared to more traditional regression-based models. These include many of the same ‘black box’ explainability questions that have risen in the age of convolutional neural networks as well as some method-specific questions due to the continuous and implicit nature of TFM.”
Elaborating on that, Glissen Brown said: “TFM, like many deep learning techniques, raises concerns about explainability that we’ve long seen with convolutional neural networks — the ‘black box’ problem, where it’s difficult to interpret exactly how and why the model arrives at a particular decision. But TFM also introduces unique challenges due to its continuous and implicit formulation. Since it often learns flows without explicitly defining intermediate representations or steps, it can be harder to trace the logic or pathways it uses to connect inputs to outputs. This makes standard interpretability tools less effective and calls for new techniques tailored to these continuous architectures.”
“This approach could have a real clinical impact,” said Robert Hirten, MD, associate professor of medicine and artificial intelligence, Icahn School of Medicine at Mount Sinai, New York City, who also reviewed the study. “Accurately predicting transfusion needs and mortality risk in real time could support earlier, more targeted interventions for high-risk patients. While these findings still need to be validated in prospective studies, it could enhance ICU decision-making and resource allocation.”
“For the practicing gastroenterologist, we envision this system could help them figure out when to perform endoscopy in a patient admitted with acute gastrointestinal bleeding in the ICU at very high risk of exsanguination,” Zhang told GI & Hepatology News.
The approach, the researchers said, will be useful in identifying unique patient characteristics, make possible the identification of high-risk patients and lead to more personalized medicine.
Hirten, Zhang, and Shung had no disclosures. Glissen Brown reported consulting relationships with Medtronic, OdinVision, Doximity, and Olympus. The National Institutes of Health funded this study.
A version of this article appeared on Medscape.com.
FROM DDW 2025
Ostomy Innovation Grabs ‘Shark Tank’ Win
The “Shark Tank” winning innovation at the American Gastroenterological Association (AGA) Tech Summit in Chicago this April has “life-altering” potential for ostomy patients, according to one of the judges, and eliminates the need for constant pouch wear.
The innovation is called Twistomy and it is designed to replace current ostomy-pouch systems that can cause leaks, odor, skin irritation, embarrassment, and social and emotional distress. The AGA Committee for GI Innovation and Technology (CGIT) organizes the annual Tech Summit.
Twistomy’s winning design includes a flexible ring and sleeve, which are inserted into the stoma and secured on the outside with a set of rings that make up the housing unit attached to a standard wafer. The housing unit twists the sleeve closed, allowing the user to control fecal output. For evacuation, the user attaches a pouch, untwists the sleeve, evacuates cleanly and effectively, and then discards the pouch.
Twistomy cofounders Devon Horton, BS, senior bioengineer, and Lily Williams, BS, biomedical researcher and engineer, both work for the department of surgery at University of Colorado, Denver.
Horton said in an interview that when he was approached with the idea to create a better ostomy solution for a senior-year capstone project he was intrigued because the traditional ostomy system “has not changed in more than 70 years. It was crazy that no one had done anything to change that.”
The Twistomy team also won the Grand Prize this spring at the Emerging Medical Innovation Valuation Competition at the Design of Medical Devices Conference held at the University of Minnesota, Minneapolis.
Witnessing the Struggle as a CNA
Horton also works as a certified nursing assistant at an inpatient unit at University of Colorado Hospital and the ostomy patients he sees there every shift help drive his passion to find a better solution.
He hears the emotional stories of people who manage their ostomy daily.
“Many express feelings of depression and anxiety, feeling isolated with their severe inability to go out and do things because of the fear of the noise the stoma makes, or the crinkling of the plastic bag in a yoga class,” he said. “We want to help them regain that control of quality of life.”
They also hope to cut down on the ostomy management time. “Initial user testing [for Twistomy] was less than 75 seconds to insert and assemble,” he said. “I did an interview with a patient yesterday who said they probably spend an hour a day managing their ostomy,” including cleaning and replacing.
Horton and Williams have a patent on the device and currently use three-dimensional printing for the prototypes.
Williams said they are now conducting consumer discovery studies through the National Science Foundation and are interviewing 30 stakeholders — “anyone who has a relationship with an ostomy,” whether a colorectal surgeon, a gastrointestinal nurse, ostomy patients, or insurers.
Those interviews will help in refining the device so they can start consulting with manufacturers and work toward approval as a Class II medical device from the US Food and Drug Administration (FDA), Williams said.
Saving Healthcare Costs
Another potential benefit for Twistomy is its ability to cut healthcare costs, Horton said. Traditional ostomies are prone to leakage, which can lead to peristomal skin complications.
He pointed to a National Institutes of Health analysis that found that on average peristomal skin complications caused upwards of $80,000 more per ostomy patient in increased healthcare costs over a 3-month period than for those without the complications.
“With Twistomy, we are reducing leakage most likely to zero,” Horton said. “We set out to say if we could reduce [infections] by half or a little less than half, we can cut out those tens of thousands of dollars that insurance companies and payers are spending.”
Permanent and Temporary Ostomy Markets
He pointed out that not all ostomies are permanent ostomies, adding that the reversal rate “is about 65%.” Often those reversal surgeries cannot take place until peristomal skin complications have been healed.
“We’re not only hoping to market to the permanent stoma patients, but the patients with temporary stomas as well,” he said.
The team estimates it will need $4 million–$6 million in funding for manufacturing and consultation costs as well as costs involved in seeking FDA approval.
Horton and Williams project the housing unit cost will be $399 based on known out-of-pocket expenses for patients with ostomy care products and the unit would be replaced annually. Disposable elements would be an additional cost.
Assuming insurance acceptance of the product, he said, “With about an 80/20 insurance coverage, typical for many patients, it would be about $100 in out-of-pocket expenses per month to use our device, which is around the lower end of what a lot of patients are spending out of pocket.”
One of the Tech Summit judges, Somaya Albhaisi, MD, a gastroenterology/hepatology fellow at University of Southern California, Los Angeles, said in an interview that the Shark Tank results were unanimous among the five judges and Twistomy also took the fan favorite vote.
She said the teams were judged on quality of pitch, potential clinical impact, and feasibility of business plan. Teams got 5-7 minutes to pitch and answered questions afterward.
“Deep Understanding” of Patient Need
“They combined smart engineering with deep understanding of patient need, which is restoring control, dignity, and quality of life for ostomy users while also reducing healthcare costs. It is rare to see a solution this scalable and impactful. It was a deeply empathetic solution overall.” She noted that nearly 1 million people in the United States currently use an ostomy.
Ostomy users’ quality of life is compromised, and they often have mental health challenges, Albhaisi said. This innovation appears to offer easy use, more dignity and control.
The other four Shark Tank finalists were:
- AI Lumen, which developed a retroview camera system, which attaches to the colonoscope and enhances imaging to detect hidden polyps that may evade conventional endoscopes.
- Amplified Sciences, which developed an ultrasensitive diagnostic platform that detects biomarker activities in minute volumes of fluid from pancreatic cystic lesions, helping to stratify patients into low risk or potential malignancy, reducing unneeded surgeries, costs, and comorbidities.
- KITE Endoscopic Innovations, which designed the Dynaflex TruCut needle to offer a simpler endoscopic ultrasound (EUS)–guided biopsy procedure with fewer needle passes, deeper insights into tumor pathology, and more tissue for geonomic analysis.
- MicroSteer, which designed a device to facilitate semiautomated endoscopic submucosal dissection (ESD) by decoupling the dissecting knife from the endoscope, enhancing safety and effectiveness during the procedure.
The Twistomy Team “Surprised Everyone”
The competitors’ scores were “very close,” one of the judges, Kevin Berliner, said in an interview. “The Twistomy team surprised everyone — the judges and the crowd — with their succinct, informative, and impactful pitch. That presentation disparity was the tiebreaker for me,” said Berliner, who works for Medtronic, a sponsor of the competition, in Chicago.
He said Horton and Williams were the youngest presenters and had the earliest stage pitch they judged, but they “outpresented other competitors in clarity, simplification, and storytelling.”
Also impressive was their description of their “commercially viable path to success” and their plan for the challenges ahead, he said.
Those challenges to get Twistomy to market center “on the ongoing changing climate we have with research funds lately,” Horton said. “We’re giving it an estimate of 3-5 years.”
Horton, Williams, Albhaisi, and Berliner reported no relevant financial relationships.
The “Shark Tank” winning innovation at the American Gastroenterological Association (AGA) Tech Summit in Chicago this April has “life-altering” potential for ostomy patients, according to one of the judges, and eliminates the need for constant pouch wear.
The innovation is called Twistomy and it is designed to replace current ostomy-pouch systems that can cause leaks, odor, skin irritation, embarrassment, and social and emotional distress. The AGA Committee for GI Innovation and Technology (CGIT) organizes the annual Tech Summit.
Twistomy’s winning design includes a flexible ring and sleeve, which are inserted into the stoma and secured on the outside with a set of rings that make up the housing unit attached to a standard wafer. The housing unit twists the sleeve closed, allowing the user to control fecal output. For evacuation, the user attaches a pouch, untwists the sleeve, evacuates cleanly and effectively, and then discards the pouch.
Twistomy cofounders Devon Horton, BS, senior bioengineer, and Lily Williams, BS, biomedical researcher and engineer, both work for the department of surgery at University of Colorado, Denver.
Horton said in an interview that when he was approached with the idea to create a better ostomy solution for a senior-year capstone project he was intrigued because the traditional ostomy system “has not changed in more than 70 years. It was crazy that no one had done anything to change that.”
The Twistomy team also won the Grand Prize this spring at the Emerging Medical Innovation Valuation Competition at the Design of Medical Devices Conference held at the University of Minnesota, Minneapolis.
Witnessing the Struggle as a CNA
Horton also works as a certified nursing assistant at an inpatient unit at University of Colorado Hospital and the ostomy patients he sees there every shift help drive his passion to find a better solution.
He hears the emotional stories of people who manage their ostomy daily.
“Many express feelings of depression and anxiety, feeling isolated with their severe inability to go out and do things because of the fear of the noise the stoma makes, or the crinkling of the plastic bag in a yoga class,” he said. “We want to help them regain that control of quality of life.”
They also hope to cut down on the ostomy management time. “Initial user testing [for Twistomy] was less than 75 seconds to insert and assemble,” he said. “I did an interview with a patient yesterday who said they probably spend an hour a day managing their ostomy,” including cleaning and replacing.
Horton and Williams have a patent on the device and currently use three-dimensional printing for the prototypes.
Williams said they are now conducting consumer discovery studies through the National Science Foundation and are interviewing 30 stakeholders — “anyone who has a relationship with an ostomy,” whether a colorectal surgeon, a gastrointestinal nurse, ostomy patients, or insurers.
Those interviews will help in refining the device so they can start consulting with manufacturers and work toward approval as a Class II medical device from the US Food and Drug Administration (FDA), Williams said.
Saving Healthcare Costs
Another potential benefit for Twistomy is its ability to cut healthcare costs, Horton said. Traditional ostomies are prone to leakage, which can lead to peristomal skin complications.
He pointed to a National Institutes of Health analysis that found that on average peristomal skin complications caused upwards of $80,000 more per ostomy patient in increased healthcare costs over a 3-month period than for those without the complications.
“With Twistomy, we are reducing leakage most likely to zero,” Horton said. “We set out to say if we could reduce [infections] by half or a little less than half, we can cut out those tens of thousands of dollars that insurance companies and payers are spending.”
Permanent and Temporary Ostomy Markets
He pointed out that not all ostomies are permanent ostomies, adding that the reversal rate “is about 65%.” Often those reversal surgeries cannot take place until peristomal skin complications have been healed.
“We’re not only hoping to market to the permanent stoma patients, but the patients with temporary stomas as well,” he said.
The team estimates it will need $4 million–$6 million in funding for manufacturing and consultation costs as well as costs involved in seeking FDA approval.
Horton and Williams project the housing unit cost will be $399 based on known out-of-pocket expenses for patients with ostomy care products and the unit would be replaced annually. Disposable elements would be an additional cost.
Assuming insurance acceptance of the product, he said, “With about an 80/20 insurance coverage, typical for many patients, it would be about $100 in out-of-pocket expenses per month to use our device, which is around the lower end of what a lot of patients are spending out of pocket.”
One of the Tech Summit judges, Somaya Albhaisi, MD, a gastroenterology/hepatology fellow at University of Southern California, Los Angeles, said in an interview that the Shark Tank results were unanimous among the five judges and Twistomy also took the fan favorite vote.
She said the teams were judged on quality of pitch, potential clinical impact, and feasibility of business plan. Teams got 5-7 minutes to pitch and answered questions afterward.
“Deep Understanding” of Patient Need
“They combined smart engineering with deep understanding of patient need, which is restoring control, dignity, and quality of life for ostomy users while also reducing healthcare costs. It is rare to see a solution this scalable and impactful. It was a deeply empathetic solution overall.” She noted that nearly 1 million people in the United States currently use an ostomy.
Ostomy users’ quality of life is compromised, and they often have mental health challenges, Albhaisi said. This innovation appears to offer easy use, more dignity and control.
The other four Shark Tank finalists were:
- AI Lumen, which developed a retroview camera system, which attaches to the colonoscope and enhances imaging to detect hidden polyps that may evade conventional endoscopes.
- Amplified Sciences, which developed an ultrasensitive diagnostic platform that detects biomarker activities in minute volumes of fluid from pancreatic cystic lesions, helping to stratify patients into low risk or potential malignancy, reducing unneeded surgeries, costs, and comorbidities.
- KITE Endoscopic Innovations, which designed the Dynaflex TruCut needle to offer a simpler endoscopic ultrasound (EUS)–guided biopsy procedure with fewer needle passes, deeper insights into tumor pathology, and more tissue for geonomic analysis.
- MicroSteer, which designed a device to facilitate semiautomated endoscopic submucosal dissection (ESD) by decoupling the dissecting knife from the endoscope, enhancing safety and effectiveness during the procedure.
The Twistomy Team “Surprised Everyone”
The competitors’ scores were “very close,” one of the judges, Kevin Berliner, said in an interview. “The Twistomy team surprised everyone — the judges and the crowd — with their succinct, informative, and impactful pitch. That presentation disparity was the tiebreaker for me,” said Berliner, who works for Medtronic, a sponsor of the competition, in Chicago.
He said Horton and Williams were the youngest presenters and had the earliest stage pitch they judged, but they “outpresented other competitors in clarity, simplification, and storytelling.”
Also impressive was their description of their “commercially viable path to success” and their plan for the challenges ahead, he said.
Those challenges to get Twistomy to market center “on the ongoing changing climate we have with research funds lately,” Horton said. “We’re giving it an estimate of 3-5 years.”
Horton, Williams, Albhaisi, and Berliner reported no relevant financial relationships.
The “Shark Tank” winning innovation at the American Gastroenterological Association (AGA) Tech Summit in Chicago this April has “life-altering” potential for ostomy patients, according to one of the judges, and eliminates the need for constant pouch wear.
The innovation is called Twistomy and it is designed to replace current ostomy-pouch systems that can cause leaks, odor, skin irritation, embarrassment, and social and emotional distress. The AGA Committee for GI Innovation and Technology (CGIT) organizes the annual Tech Summit.
Twistomy’s winning design includes a flexible ring and sleeve, which are inserted into the stoma and secured on the outside with a set of rings that make up the housing unit attached to a standard wafer. The housing unit twists the sleeve closed, allowing the user to control fecal output. For evacuation, the user attaches a pouch, untwists the sleeve, evacuates cleanly and effectively, and then discards the pouch.
Twistomy cofounders Devon Horton, BS, senior bioengineer, and Lily Williams, BS, biomedical researcher and engineer, both work for the department of surgery at University of Colorado, Denver.
Horton said in an interview that when he was approached with the idea to create a better ostomy solution for a senior-year capstone project he was intrigued because the traditional ostomy system “has not changed in more than 70 years. It was crazy that no one had done anything to change that.”
The Twistomy team also won the Grand Prize this spring at the Emerging Medical Innovation Valuation Competition at the Design of Medical Devices Conference held at the University of Minnesota, Minneapolis.
Witnessing the Struggle as a CNA
Horton also works as a certified nursing assistant at an inpatient unit at University of Colorado Hospital and the ostomy patients he sees there every shift help drive his passion to find a better solution.
He hears the emotional stories of people who manage their ostomy daily.
“Many express feelings of depression and anxiety, feeling isolated with their severe inability to go out and do things because of the fear of the noise the stoma makes, or the crinkling of the plastic bag in a yoga class,” he said. “We want to help them regain that control of quality of life.”
They also hope to cut down on the ostomy management time. “Initial user testing [for Twistomy] was less than 75 seconds to insert and assemble,” he said. “I did an interview with a patient yesterday who said they probably spend an hour a day managing their ostomy,” including cleaning and replacing.
Horton and Williams have a patent on the device and currently use three-dimensional printing for the prototypes.
Williams said they are now conducting consumer discovery studies through the National Science Foundation and are interviewing 30 stakeholders — “anyone who has a relationship with an ostomy,” whether a colorectal surgeon, a gastrointestinal nurse, ostomy patients, or insurers.
Those interviews will help in refining the device so they can start consulting with manufacturers and work toward approval as a Class II medical device from the US Food and Drug Administration (FDA), Williams said.
Saving Healthcare Costs
Another potential benefit for Twistomy is its ability to cut healthcare costs, Horton said. Traditional ostomies are prone to leakage, which can lead to peristomal skin complications.
He pointed to a National Institutes of Health analysis that found that on average peristomal skin complications caused upwards of $80,000 more per ostomy patient in increased healthcare costs over a 3-month period than for those without the complications.
“With Twistomy, we are reducing leakage most likely to zero,” Horton said. “We set out to say if we could reduce [infections] by half or a little less than half, we can cut out those tens of thousands of dollars that insurance companies and payers are spending.”
Permanent and Temporary Ostomy Markets
He pointed out that not all ostomies are permanent ostomies, adding that the reversal rate “is about 65%.” Often those reversal surgeries cannot take place until peristomal skin complications have been healed.
“We’re not only hoping to market to the permanent stoma patients, but the patients with temporary stomas as well,” he said.
The team estimates it will need $4 million–$6 million in funding for manufacturing and consultation costs as well as costs involved in seeking FDA approval.
Horton and Williams project the housing unit cost will be $399 based on known out-of-pocket expenses for patients with ostomy care products and the unit would be replaced annually. Disposable elements would be an additional cost.
Assuming insurance acceptance of the product, he said, “With about an 80/20 insurance coverage, typical for many patients, it would be about $100 in out-of-pocket expenses per month to use our device, which is around the lower end of what a lot of patients are spending out of pocket.”
One of the Tech Summit judges, Somaya Albhaisi, MD, a gastroenterology/hepatology fellow at University of Southern California, Los Angeles, said in an interview that the Shark Tank results were unanimous among the five judges and Twistomy also took the fan favorite vote.
She said the teams were judged on quality of pitch, potential clinical impact, and feasibility of business plan. Teams got 5-7 minutes to pitch and answered questions afterward.
“Deep Understanding” of Patient Need
“They combined smart engineering with deep understanding of patient need, which is restoring control, dignity, and quality of life for ostomy users while also reducing healthcare costs. It is rare to see a solution this scalable and impactful. It was a deeply empathetic solution overall.” She noted that nearly 1 million people in the United States currently use an ostomy.
Ostomy users’ quality of life is compromised, and they often have mental health challenges, Albhaisi said. This innovation appears to offer easy use, more dignity and control.
The other four Shark Tank finalists were:
- AI Lumen, which developed a retroview camera system, which attaches to the colonoscope and enhances imaging to detect hidden polyps that may evade conventional endoscopes.
- Amplified Sciences, which developed an ultrasensitive diagnostic platform that detects biomarker activities in minute volumes of fluid from pancreatic cystic lesions, helping to stratify patients into low risk or potential malignancy, reducing unneeded surgeries, costs, and comorbidities.
- KITE Endoscopic Innovations, which designed the Dynaflex TruCut needle to offer a simpler endoscopic ultrasound (EUS)–guided biopsy procedure with fewer needle passes, deeper insights into tumor pathology, and more tissue for geonomic analysis.
- MicroSteer, which designed a device to facilitate semiautomated endoscopic submucosal dissection (ESD) by decoupling the dissecting knife from the endoscope, enhancing safety and effectiveness during the procedure.
The Twistomy Team “Surprised Everyone”
The competitors’ scores were “very close,” one of the judges, Kevin Berliner, said in an interview. “The Twistomy team surprised everyone — the judges and the crowd — with their succinct, informative, and impactful pitch. That presentation disparity was the tiebreaker for me,” said Berliner, who works for Medtronic, a sponsor of the competition, in Chicago.
He said Horton and Williams were the youngest presenters and had the earliest stage pitch they judged, but they “outpresented other competitors in clarity, simplification, and storytelling.”
Also impressive was their description of their “commercially viable path to success” and their plan for the challenges ahead, he said.
Those challenges to get Twistomy to market center “on the ongoing changing climate we have with research funds lately,” Horton said. “We’re giving it an estimate of 3-5 years.”
Horton, Williams, Albhaisi, and Berliner reported no relevant financial relationships.
Chatbot Helps Users Adopt a Low FODMAP Diet
SAN DIEGO — Low fermentable oligo-, di-, and monosaccharides and polyols (FODMAPs) dietary advice has been shown to be effective in easing bloating and abdominal pain, especially in patients with irritable bowel syndrome (IBS), but limited availability of dietitians makes delivering this advice challenging. Researchers from Thailand have successfully enlisted a chatbot to help.
In a randomized controlled trial, they found that chatbot-assisted dietary advice with brief guidance effectively reduced high FODMAP intake, bloating severity, and improved dietary knowledge, particularly in patients with bothersome bloating.
“Chatbot-assisted dietary advice for FODMAPs restriction was feasible and applicable in patients with bloating symptoms that had baseline symptoms of moderate severity,” study chief Pochara Somvanapanich, with the Division of Gastroenterology, Chulalongkorn University and King Chulalongkorn Memorial Hospital, Bangkok, Thailand, told GI & Hepatology News.
Somvanapanich, who developed the chatbot algorithm, presented the study results at Digestive Disease Week (DDW) 2025.
More Knowledge, Less Bloating
The trial enrolled 86 adults with disorders of gut-brain interaction experiencing bloating symptoms for more than 6 months and consuming more than seven high-FODMAPs items per week. Half of them had IBS.
At baseline, gastrointestinal (GI) symptoms and the ability to identify FODMAPs were assessed. All participants received a 5-minute consultation on FODMAPs avoidance from a GI fellow and were randomly allocated (stratified by IBS diagnosis and education) into two groups.
The chatbot-assisted group received real-time dietary advice via a chatbot which helped them identify high, low, and non-FODMAP foods from a list of more than 300 ingredients/dishes of Thai and western cuisines.
The control group received only brief advice on high FODMAPs restriction. Both groups used a diary app to log food intake and postprandial symptoms. Baseline bloating, abdominal pain and global symptoms severity were similar between the two groups. Data on 64 participants (32 in each group) were analyzed.
After 4 weeks, significantly more people in the chatbot group than the control group responded — achieving a 30% or greater reduction in daily worst bloating, abdominal pain or global symptoms (19 [59%] vs 10 [31%], P < .05). Responder rates were similar in the IBS and non-IBS subgroups.
Subgroup analysis revealed significant differences between groups only for participants with bothersome bloating, not those with mild bloating severity.
In those with bothersome bloating severity, the chatbot group had a higher response rate (69.5% vs 36.3%) and fewer bloating symptoms (P < .05). They also had a greater reduction in high FODMAPs intake (10 vs 23 items/week) and demonstrated improved knowledge in identifying FODMAPs (P < .05).
“Responders in a chatbot group consistently engaged more with the app, performing significantly more weekly item searches than nonresponders (P < .05),” the authors noted in their conference abstract.
“Our next step is to develop the chatbot-assisted approach for the reintroduction and personalization phase based on messenger applications (including Facebook Messenger and other messaging platforms),” Somvanapanich told GI & Hepatology News.
“Once we’ve gathered enough data to confirm these are working effectively, we definitely plan to create a one-stop service application for FODMAPs dietary advice,” Somvanapanich added.
Lack of Robust Data on Digital GI Health Apps
Commenting on this research for GI & Hepatology News, Sidhartha R. Sinha, MD, Director of Digital Health and Innovation, Division of Gastroenterology and Hepatology, Stanford University in Stanford, California, noted that there is a “notable lack of robust data supporting digital health tools in gastroenterology. Despite hundreds of apps available, very few are supported by well-designed trials.”
“The study demonstrated that chatbot-assisted dietary advice significantly improved bloating symptoms, reduced intake of high-FODMAP foods, and enhanced patients’ dietary knowledge compared to brief dietary counseling alone, especially in those with bothersome symptoms,” said Sinha, who wasn’t involved in the study.
“Patients actively used the chatbot to manage their symptoms, achieving a higher response rate than those in the control arm who received brief counseling on avoiding high-FODMAP food,” he noted.
Sinha said in his practice at Stanford, “in the heart of Silicon Valley,” patients do use digital resources to manage their GI symptoms, including diseases like IBS and inflammatory bowel disease (IBD) — and he believes this is “increasingly common nationally.”
“However, the need for evidence-based tools is critical and the lack here often prevents many practitioners from regularly recommending them to patients. This study aligns well with clinical practice, and supports the use of this particular app to improve IBS symptoms, particularly when access to dietitians is limited. These results support chatbot-assisted dietary management as a feasible, effective, and scalable approach to patient care,” Sinha told GI & Hepatology News.
The study received no commercial funding. Somvanapanich and Sinha had no relevant disclosures.
A version of this article appeared on Medscape.com.
SAN DIEGO — Low fermentable oligo-, di-, and monosaccharides and polyols (FODMAPs) dietary advice has been shown to be effective in easing bloating and abdominal pain, especially in patients with irritable bowel syndrome (IBS), but limited availability of dietitians makes delivering this advice challenging. Researchers from Thailand have successfully enlisted a chatbot to help.
In a randomized controlled trial, they found that chatbot-assisted dietary advice with brief guidance effectively reduced high FODMAP intake, bloating severity, and improved dietary knowledge, particularly in patients with bothersome bloating.
“Chatbot-assisted dietary advice for FODMAPs restriction was feasible and applicable in patients with bloating symptoms that had baseline symptoms of moderate severity,” study chief Pochara Somvanapanich, with the Division of Gastroenterology, Chulalongkorn University and King Chulalongkorn Memorial Hospital, Bangkok, Thailand, told GI & Hepatology News.
Somvanapanich, who developed the chatbot algorithm, presented the study results at Digestive Disease Week (DDW) 2025.
More Knowledge, Less Bloating
The trial enrolled 86 adults with disorders of gut-brain interaction experiencing bloating symptoms for more than 6 months and consuming more than seven high-FODMAPs items per week. Half of them had IBS.
At baseline, gastrointestinal (GI) symptoms and the ability to identify FODMAPs were assessed. All participants received a 5-minute consultation on FODMAPs avoidance from a GI fellow and were randomly allocated (stratified by IBS diagnosis and education) into two groups.
The chatbot-assisted group received real-time dietary advice via a chatbot which helped them identify high, low, and non-FODMAP foods from a list of more than 300 ingredients/dishes of Thai and western cuisines.
The control group received only brief advice on high FODMAPs restriction. Both groups used a diary app to log food intake and postprandial symptoms. Baseline bloating, abdominal pain and global symptoms severity were similar between the two groups. Data on 64 participants (32 in each group) were analyzed.
After 4 weeks, significantly more people in the chatbot group than the control group responded — achieving a 30% or greater reduction in daily worst bloating, abdominal pain or global symptoms (19 [59%] vs 10 [31%], P < .05). Responder rates were similar in the IBS and non-IBS subgroups.
Subgroup analysis revealed significant differences between groups only for participants with bothersome bloating, not those with mild bloating severity.
In those with bothersome bloating severity, the chatbot group had a higher response rate (69.5% vs 36.3%) and fewer bloating symptoms (P < .05). They also had a greater reduction in high FODMAPs intake (10 vs 23 items/week) and demonstrated improved knowledge in identifying FODMAPs (P < .05).
“Responders in a chatbot group consistently engaged more with the app, performing significantly more weekly item searches than nonresponders (P < .05),” the authors noted in their conference abstract.
“Our next step is to develop the chatbot-assisted approach for the reintroduction and personalization phase based on messenger applications (including Facebook Messenger and other messaging platforms),” Somvanapanich told GI & Hepatology News.
“Once we’ve gathered enough data to confirm these are working effectively, we definitely plan to create a one-stop service application for FODMAPs dietary advice,” Somvanapanich added.
Lack of Robust Data on Digital GI Health Apps
Commenting on this research for GI & Hepatology News, Sidhartha R. Sinha, MD, Director of Digital Health and Innovation, Division of Gastroenterology and Hepatology, Stanford University in Stanford, California, noted that there is a “notable lack of robust data supporting digital health tools in gastroenterology. Despite hundreds of apps available, very few are supported by well-designed trials.”
“The study demonstrated that chatbot-assisted dietary advice significantly improved bloating symptoms, reduced intake of high-FODMAP foods, and enhanced patients’ dietary knowledge compared to brief dietary counseling alone, especially in those with bothersome symptoms,” said Sinha, who wasn’t involved in the study.
“Patients actively used the chatbot to manage their symptoms, achieving a higher response rate than those in the control arm who received brief counseling on avoiding high-FODMAP food,” he noted.
Sinha said in his practice at Stanford, “in the heart of Silicon Valley,” patients do use digital resources to manage their GI symptoms, including diseases like IBS and inflammatory bowel disease (IBD) — and he believes this is “increasingly common nationally.”
“However, the need for evidence-based tools is critical and the lack here often prevents many practitioners from regularly recommending them to patients. This study aligns well with clinical practice, and supports the use of this particular app to improve IBS symptoms, particularly when access to dietitians is limited. These results support chatbot-assisted dietary management as a feasible, effective, and scalable approach to patient care,” Sinha told GI & Hepatology News.
The study received no commercial funding. Somvanapanich and Sinha had no relevant disclosures.
A version of this article appeared on Medscape.com.
SAN DIEGO — Low fermentable oligo-, di-, and monosaccharides and polyols (FODMAPs) dietary advice has been shown to be effective in easing bloating and abdominal pain, especially in patients with irritable bowel syndrome (IBS), but limited availability of dietitians makes delivering this advice challenging. Researchers from Thailand have successfully enlisted a chatbot to help.
In a randomized controlled trial, they found that chatbot-assisted dietary advice with brief guidance effectively reduced high FODMAP intake, bloating severity, and improved dietary knowledge, particularly in patients with bothersome bloating.
“Chatbot-assisted dietary advice for FODMAPs restriction was feasible and applicable in patients with bloating symptoms that had baseline symptoms of moderate severity,” study chief Pochara Somvanapanich, with the Division of Gastroenterology, Chulalongkorn University and King Chulalongkorn Memorial Hospital, Bangkok, Thailand, told GI & Hepatology News.
Somvanapanich, who developed the chatbot algorithm, presented the study results at Digestive Disease Week (DDW) 2025.
More Knowledge, Less Bloating
The trial enrolled 86 adults with disorders of gut-brain interaction experiencing bloating symptoms for more than 6 months and consuming more than seven high-FODMAPs items per week. Half of them had IBS.
At baseline, gastrointestinal (GI) symptoms and the ability to identify FODMAPs were assessed. All participants received a 5-minute consultation on FODMAPs avoidance from a GI fellow and were randomly allocated (stratified by IBS diagnosis and education) into two groups.
The chatbot-assisted group received real-time dietary advice via a chatbot which helped them identify high, low, and non-FODMAP foods from a list of more than 300 ingredients/dishes of Thai and western cuisines.
The control group received only brief advice on high FODMAPs restriction. Both groups used a diary app to log food intake and postprandial symptoms. Baseline bloating, abdominal pain and global symptoms severity were similar between the two groups. Data on 64 participants (32 in each group) were analyzed.
After 4 weeks, significantly more people in the chatbot group than the control group responded — achieving a 30% or greater reduction in daily worst bloating, abdominal pain or global symptoms (19 [59%] vs 10 [31%], P < .05). Responder rates were similar in the IBS and non-IBS subgroups.
Subgroup analysis revealed significant differences between groups only for participants with bothersome bloating, not those with mild bloating severity.
In those with bothersome bloating severity, the chatbot group had a higher response rate (69.5% vs 36.3%) and fewer bloating symptoms (P < .05). They also had a greater reduction in high FODMAPs intake (10 vs 23 items/week) and demonstrated improved knowledge in identifying FODMAPs (P < .05).
“Responders in a chatbot group consistently engaged more with the app, performing significantly more weekly item searches than nonresponders (P < .05),” the authors noted in their conference abstract.
“Our next step is to develop the chatbot-assisted approach for the reintroduction and personalization phase based on messenger applications (including Facebook Messenger and other messaging platforms),” Somvanapanich told GI & Hepatology News.
“Once we’ve gathered enough data to confirm these are working effectively, we definitely plan to create a one-stop service application for FODMAPs dietary advice,” Somvanapanich added.
Lack of Robust Data on Digital GI Health Apps
Commenting on this research for GI & Hepatology News, Sidhartha R. Sinha, MD, Director of Digital Health and Innovation, Division of Gastroenterology and Hepatology, Stanford University in Stanford, California, noted that there is a “notable lack of robust data supporting digital health tools in gastroenterology. Despite hundreds of apps available, very few are supported by well-designed trials.”
“The study demonstrated that chatbot-assisted dietary advice significantly improved bloating symptoms, reduced intake of high-FODMAP foods, and enhanced patients’ dietary knowledge compared to brief dietary counseling alone, especially in those with bothersome symptoms,” said Sinha, who wasn’t involved in the study.
“Patients actively used the chatbot to manage their symptoms, achieving a higher response rate than those in the control arm who received brief counseling on avoiding high-FODMAP food,” he noted.
Sinha said in his practice at Stanford, “in the heart of Silicon Valley,” patients do use digital resources to manage their GI symptoms, including diseases like IBS and inflammatory bowel disease (IBD) — and he believes this is “increasingly common nationally.”
“However, the need for evidence-based tools is critical and the lack here often prevents many practitioners from regularly recommending them to patients. This study aligns well with clinical practice, and supports the use of this particular app to improve IBS symptoms, particularly when access to dietitians is limited. These results support chatbot-assisted dietary management as a feasible, effective, and scalable approach to patient care,” Sinha told GI & Hepatology News.
The study received no commercial funding. Somvanapanich and Sinha had no relevant disclosures.
A version of this article appeared on Medscape.com.
FROM DDW 2025