User login
Some biologics may be better than others for averting anterior uveitis
Among patients with ankylosing spondylitis or undifferentiated spondyloarthritis, risk for anterior uveitis may hinge on the choice of biologic disease-modifying antirheumatic drug (bDMARD), a large Swedish cohort study suggests.
Study results were reported in the opening plenary abstract session at the annual European Congress of Rheumatology, held online this year due to COVID-19.
“Randomized, controlled trials indicate that compared to tumor necrosis factor (TNF) inhibitors, secukinumab has similar efficacy regarding axial inflammation in spondyloarthritis and better efficacy regarding cutaneous psoriasis, but is inferior in inflammatory bowel disease,” noted lead investigator Ulf Lindström, MD, PhD, of the department of rheumatology and inflammation research in the Institute of Medicine at the University of Gothenburg (Sweden). “However, the efficacy of secukinumab, compared to TNF inhibitors, in anterior uveitis has not been extensively studied.”
The investigators used national registry data to study 3,568 patients with ankylosing spondylitis or undifferentiated spondyloarthritis who started bDMARDs in 2005-2018. They considered four agents: the anti–interleukin-17A antibody secukinumab (Cosentyx) and the TNF inhibitors etanercept (Enbrel), adalimumab (Humira), and infliximab (Remicade).
Analyses based on 4,523 treatment episodes showed that after excluding the 23% of patients who had previously experienced anterior uveitis, merely 0.9% of patients experienced new-onset anterior uveitis while on their bDMARD, Dr. Lindström reported.
There was confounding by indication, whereby patients with previous anterior uveitis were channeled toward adalimumab and infliximab, and away from secukinumab and etanercept. In addition, there was confounding by line of treatment, with secukinumab usually used in the third line.
After excluding patients who had experienced anterior uveitis in the past year to partly address confounding, the adjusted risk for first on-treatment anterior uveitis was about twice as high with secukinumab and with etanercept as compared with adalimumab. After additionally excluding all biologic treatment episodes beyond the third line, elevation of risk remained significant only for etanercept.
“There is probably a higher occurrence of anterior uveitis on treatment with secukinumab, compared to adalimumab, but there may still be residual confounding and bias that we need to consider,” Dr. Lindström concluded. “As seen previously, there is a higher occurrence of anterior uveitis on etanercept compared to adalimumab or infliximab.”
Findings in context
“These results are not surprising as we have known that secukinumab and etanercept are not good for controlling recurrent and chronic uveitis,” Nigil Haroon MD, PhD, DM, commented in an interview. However, “a single episode of uveitis or infrequent episodes are not usually considered a contraindication to starting these drugs.”
Study caveats included lack of adjustment for uveitis severity and potentially missed uveitis episodes in patients who treated it themselves with steroid eyedrops, he said. “Standard practice is to keep drops with them to start at the earliest possible time point.”
“It would be useful to know the number of patients who stopped medications as a result of uveitis,” added Dr. Haroon, who is codirector of the spondylitis program at the University Health Network and associate professor of medicine and rheumatology at the University of Toronto. “Time-to-event analysis may also be interesting.”
“The study raises an important point regarding channeling bias, and this is important to consider when interpreting clinical trial data as well. Investigators are unlikely to include patients with history of uveitis (or strong family history of inflammatory bowel disease or personal history of gut symptoms) in studies with IL-17 inhibitors and etanercept. Hence, the results have to be interpreted with caution.”
Study details
Dr. Lindström and coinvestigators assessed incidences of any anterior uveitis (ascertained from outpatient ophthalmology visits having this diagnostic code) and of anterior uveitis flares (the subset occurring after a gap of at least 90 days without the diagnosis).
When they excluded patients who had experienced anterior uveitis in the year before starting therapy, secukinumab and etanercept carried the highest incidences of anterior uveitis (6.8 and 7.5 per 100 patient-years, respectively) and anterior uveitis flares (2.8 per 100 patient-years for each), he reported.
With adalimumab as the comparator, adjusted risk for first on-treatment anterior uveitis in this population was significantly higher with secukinumab (hazard ratio, 2.23) and etanercept (hazard ratio, 1.80).
When the investigators additionally excluded episodes of therapy beyond the third line, only etanercept carried notably higher incidences of anterior uveitis (7.0 per 100 patient-years) and anterior uveitis flares (2.6 per 100 patient-years). “This could imply that some of the higher incidence rate seen for secukinumab could be due to the fact that these patients are harder to treat and have received more biologics before,” Dr. Lindström proposed.
With adalimumab again as the comparator, the adjusted risk for first on-treatment anterior uveitis in this population was significantly higher only with etanercept (hazard ratio, 1.85).
A final analysis included all patients who started adalimumab in 2004-2018 and then switched to one of the other agents, dramatically reducing confounding by indication. In this population, the incidence rate ratio of anterior uveitis flares was 3.05 for secukinumab, 1.79 for etanercept, and 0.53 for infliximab, compared with adalimumab.
Dr. Lindström disclosed that he had no relevant conflicts of interest. The study did not receive any specific funding. Dr. Haroon disclosed consulting for Amgen, Abbvie, Eli Lilly, Janssen, Novartis, and UCB.
SOURCE: Lindström U et al. Ann Rheum Dis. 2020;79[suppl 1]:9, Abstract OP0014.
Among patients with ankylosing spondylitis or undifferentiated spondyloarthritis, risk for anterior uveitis may hinge on the choice of biologic disease-modifying antirheumatic drug (bDMARD), a large Swedish cohort study suggests.
Study results were reported in the opening plenary abstract session at the annual European Congress of Rheumatology, held online this year due to COVID-19.
“Randomized, controlled trials indicate that compared to tumor necrosis factor (TNF) inhibitors, secukinumab has similar efficacy regarding axial inflammation in spondyloarthritis and better efficacy regarding cutaneous psoriasis, but is inferior in inflammatory bowel disease,” noted lead investigator Ulf Lindström, MD, PhD, of the department of rheumatology and inflammation research in the Institute of Medicine at the University of Gothenburg (Sweden). “However, the efficacy of secukinumab, compared to TNF inhibitors, in anterior uveitis has not been extensively studied.”
The investigators used national registry data to study 3,568 patients with ankylosing spondylitis or undifferentiated spondyloarthritis who started bDMARDs in 2005-2018. They considered four agents: the anti–interleukin-17A antibody secukinumab (Cosentyx) and the TNF inhibitors etanercept (Enbrel), adalimumab (Humira), and infliximab (Remicade).
Analyses based on 4,523 treatment episodes showed that after excluding the 23% of patients who had previously experienced anterior uveitis, merely 0.9% of patients experienced new-onset anterior uveitis while on their bDMARD, Dr. Lindström reported.
There was confounding by indication, whereby patients with previous anterior uveitis were channeled toward adalimumab and infliximab, and away from secukinumab and etanercept. In addition, there was confounding by line of treatment, with secukinumab usually used in the third line.
After excluding patients who had experienced anterior uveitis in the past year to partly address confounding, the adjusted risk for first on-treatment anterior uveitis was about twice as high with secukinumab and with etanercept as compared with adalimumab. After additionally excluding all biologic treatment episodes beyond the third line, elevation of risk remained significant only for etanercept.
“There is probably a higher occurrence of anterior uveitis on treatment with secukinumab, compared to adalimumab, but there may still be residual confounding and bias that we need to consider,” Dr. Lindström concluded. “As seen previously, there is a higher occurrence of anterior uveitis on etanercept compared to adalimumab or infliximab.”
Findings in context
“These results are not surprising as we have known that secukinumab and etanercept are not good for controlling recurrent and chronic uveitis,” Nigil Haroon MD, PhD, DM, commented in an interview. However, “a single episode of uveitis or infrequent episodes are not usually considered a contraindication to starting these drugs.”
Study caveats included lack of adjustment for uveitis severity and potentially missed uveitis episodes in patients who treated it themselves with steroid eyedrops, he said. “Standard practice is to keep drops with them to start at the earliest possible time point.”
“It would be useful to know the number of patients who stopped medications as a result of uveitis,” added Dr. Haroon, who is codirector of the spondylitis program at the University Health Network and associate professor of medicine and rheumatology at the University of Toronto. “Time-to-event analysis may also be interesting.”
“The study raises an important point regarding channeling bias, and this is important to consider when interpreting clinical trial data as well. Investigators are unlikely to include patients with history of uveitis (or strong family history of inflammatory bowel disease or personal history of gut symptoms) in studies with IL-17 inhibitors and etanercept. Hence, the results have to be interpreted with caution.”
Study details
Dr. Lindström and coinvestigators assessed incidences of any anterior uveitis (ascertained from outpatient ophthalmology visits having this diagnostic code) and of anterior uveitis flares (the subset occurring after a gap of at least 90 days without the diagnosis).
When they excluded patients who had experienced anterior uveitis in the year before starting therapy, secukinumab and etanercept carried the highest incidences of anterior uveitis (6.8 and 7.5 per 100 patient-years, respectively) and anterior uveitis flares (2.8 per 100 patient-years for each), he reported.
With adalimumab as the comparator, adjusted risk for first on-treatment anterior uveitis in this population was significantly higher with secukinumab (hazard ratio, 2.23) and etanercept (hazard ratio, 1.80).
When the investigators additionally excluded episodes of therapy beyond the third line, only etanercept carried notably higher incidences of anterior uveitis (7.0 per 100 patient-years) and anterior uveitis flares (2.6 per 100 patient-years). “This could imply that some of the higher incidence rate seen for secukinumab could be due to the fact that these patients are harder to treat and have received more biologics before,” Dr. Lindström proposed.
With adalimumab again as the comparator, the adjusted risk for first on-treatment anterior uveitis in this population was significantly higher only with etanercept (hazard ratio, 1.85).
A final analysis included all patients who started adalimumab in 2004-2018 and then switched to one of the other agents, dramatically reducing confounding by indication. In this population, the incidence rate ratio of anterior uveitis flares was 3.05 for secukinumab, 1.79 for etanercept, and 0.53 for infliximab, compared with adalimumab.
Dr. Lindström disclosed that he had no relevant conflicts of interest. The study did not receive any specific funding. Dr. Haroon disclosed consulting for Amgen, Abbvie, Eli Lilly, Janssen, Novartis, and UCB.
SOURCE: Lindström U et al. Ann Rheum Dis. 2020;79[suppl 1]:9, Abstract OP0014.
Among patients with ankylosing spondylitis or undifferentiated spondyloarthritis, risk for anterior uveitis may hinge on the choice of biologic disease-modifying antirheumatic drug (bDMARD), a large Swedish cohort study suggests.
Study results were reported in the opening plenary abstract session at the annual European Congress of Rheumatology, held online this year due to COVID-19.
“Randomized, controlled trials indicate that compared to tumor necrosis factor (TNF) inhibitors, secukinumab has similar efficacy regarding axial inflammation in spondyloarthritis and better efficacy regarding cutaneous psoriasis, but is inferior in inflammatory bowel disease,” noted lead investigator Ulf Lindström, MD, PhD, of the department of rheumatology and inflammation research in the Institute of Medicine at the University of Gothenburg (Sweden). “However, the efficacy of secukinumab, compared to TNF inhibitors, in anterior uveitis has not been extensively studied.”
The investigators used national registry data to study 3,568 patients with ankylosing spondylitis or undifferentiated spondyloarthritis who started bDMARDs in 2005-2018. They considered four agents: the anti–interleukin-17A antibody secukinumab (Cosentyx) and the TNF inhibitors etanercept (Enbrel), adalimumab (Humira), and infliximab (Remicade).
Analyses based on 4,523 treatment episodes showed that after excluding the 23% of patients who had previously experienced anterior uveitis, merely 0.9% of patients experienced new-onset anterior uveitis while on their bDMARD, Dr. Lindström reported.
There was confounding by indication, whereby patients with previous anterior uveitis were channeled toward adalimumab and infliximab, and away from secukinumab and etanercept. In addition, there was confounding by line of treatment, with secukinumab usually used in the third line.
After excluding patients who had experienced anterior uveitis in the past year to partly address confounding, the adjusted risk for first on-treatment anterior uveitis was about twice as high with secukinumab and with etanercept as compared with adalimumab. After additionally excluding all biologic treatment episodes beyond the third line, elevation of risk remained significant only for etanercept.
“There is probably a higher occurrence of anterior uveitis on treatment with secukinumab, compared to adalimumab, but there may still be residual confounding and bias that we need to consider,” Dr. Lindström concluded. “As seen previously, there is a higher occurrence of anterior uveitis on etanercept compared to adalimumab or infliximab.”
Findings in context
“These results are not surprising as we have known that secukinumab and etanercept are not good for controlling recurrent and chronic uveitis,” Nigil Haroon MD, PhD, DM, commented in an interview. However, “a single episode of uveitis or infrequent episodes are not usually considered a contraindication to starting these drugs.”
Study caveats included lack of adjustment for uveitis severity and potentially missed uveitis episodes in patients who treated it themselves with steroid eyedrops, he said. “Standard practice is to keep drops with them to start at the earliest possible time point.”
“It would be useful to know the number of patients who stopped medications as a result of uveitis,” added Dr. Haroon, who is codirector of the spondylitis program at the University Health Network and associate professor of medicine and rheumatology at the University of Toronto. “Time-to-event analysis may also be interesting.”
“The study raises an important point regarding channeling bias, and this is important to consider when interpreting clinical trial data as well. Investigators are unlikely to include patients with history of uveitis (or strong family history of inflammatory bowel disease or personal history of gut symptoms) in studies with IL-17 inhibitors and etanercept. Hence, the results have to be interpreted with caution.”
Study details
Dr. Lindström and coinvestigators assessed incidences of any anterior uveitis (ascertained from outpatient ophthalmology visits having this diagnostic code) and of anterior uveitis flares (the subset occurring after a gap of at least 90 days without the diagnosis).
When they excluded patients who had experienced anterior uveitis in the year before starting therapy, secukinumab and etanercept carried the highest incidences of anterior uveitis (6.8 and 7.5 per 100 patient-years, respectively) and anterior uveitis flares (2.8 per 100 patient-years for each), he reported.
With adalimumab as the comparator, adjusted risk for first on-treatment anterior uveitis in this population was significantly higher with secukinumab (hazard ratio, 2.23) and etanercept (hazard ratio, 1.80).
When the investigators additionally excluded episodes of therapy beyond the third line, only etanercept carried notably higher incidences of anterior uveitis (7.0 per 100 patient-years) and anterior uveitis flares (2.6 per 100 patient-years). “This could imply that some of the higher incidence rate seen for secukinumab could be due to the fact that these patients are harder to treat and have received more biologics before,” Dr. Lindström proposed.
With adalimumab again as the comparator, the adjusted risk for first on-treatment anterior uveitis in this population was significantly higher only with etanercept (hazard ratio, 1.85).
A final analysis included all patients who started adalimumab in 2004-2018 and then switched to one of the other agents, dramatically reducing confounding by indication. In this population, the incidence rate ratio of anterior uveitis flares was 3.05 for secukinumab, 1.79 for etanercept, and 0.53 for infliximab, compared with adalimumab.
Dr. Lindström disclosed that he had no relevant conflicts of interest. The study did not receive any specific funding. Dr. Haroon disclosed consulting for Amgen, Abbvie, Eli Lilly, Janssen, Novartis, and UCB.
SOURCE: Lindström U et al. Ann Rheum Dis. 2020;79[suppl 1]:9, Abstract OP0014.
FROM EULAR 2020 E-CONGRESS
Tramadol mortality risk in osteoarthritis could outweigh benefits
Patients with OA treated with tramadol had a 20%-50% higher risk of dying during the first year of treatment than did patients who were treated with NSAIDs, according to the results of a large, population-based study performed in British Columbia.
Within 1 year of starting treatment, 296 of 13,798 patients treated with tramadol had died, compared with 246 of 13,798 treated with naproxen, giving a death rate of 21.5 versus 17.8 per 1,000 person-years, and representing a 20% increase in all-cause mortality versus the NSAID (hazard ratio, 1.2).
Similar results were seen comparing tramadol with diclofenac and tramadol with cyclooxygenase (COX)-2 inhibitors, but with increasing death rates of 24.8 versus 19.5 per 1,000 person-years (HR, 1.3) and 23.6 versus 15.7 per 1,000 person-years (HR, 1.5), respectively.
However, all-cause mortality was lower with tramadol than with the opiate painkiller, codeine (21.5 vs. 25.5 per 1,000 person-years; HR, 0.8), reported Ms. Lingyi Li, a PhD student from the University of British Columbia, Vancouver, at the annual European Congress of Rheumatology, held online this year due to COVID-19.
This is not the first time that tramadol’s excess mortality risk has been highlighted. Indeed, just last year (JAMA. 2019;321[10]:969-82), researchers using The Health Improvement Network database reported found that tramadol was associated with higher all-cause mortality than two COX-2 inhibitors, celecoxib (31.2 versus 18.4 per 1,000 person-years) and etoricoxib (25.7 versus 12.8 per 1,000 person-years).
Ms. Li and associates’ data not only now add further weight to those findings, but also go a step further by also looking at other serious risks associated with tramadol’s use among patients with OA. “The objective of this study is to compare tramadol with other commonly prescribed pain relief medications on the risk of several severe outcomes, including mortality, cardiovascular diseases [CVD], venous thromboembolism [VTE], and hip fracture,” Ms. Li said during her virtual presentation.
Using sequential propensity score matching, the researchers compared data on patients in British Columbia during 2005-2014 with a first prescription of tramadol (56,325), the NSAIDs naproxen (n = 13,798) or diclofenac (n = 17,675), COX-2 inhibitors (17,039), or codeine (n = 7,813).
“For CVD, we found that there is a higher risk among tramadol users, compared with diclofenac [HR, 1.2] and COX-2 inhibitors [HR, 1.2], but not with naproxen [HR, 1.0] and codeine [HR, 0.9] users,” Ms. Li reported.
Similarly, the 1-year risk of VTE was significantly higher among tramadol users only when compared with diclofenac (HR, 1.5) and COX-2 inhibitors (HR, 1.7).
“For hip fractures, tramadol initiation was associated with an increased risk of hip fractures, compared with all NSAIDs, but not with codeine,” Ms. Li said. The risk of hip fractures was 40%-50% higher with tramadol versus naproxen (HR, 1.4), diclofenac and COX-2 inhibitors (both HR, 1.5).
“Our results suggest an unfavorable safety profile of tramadol use,” Ms. Li said, suggesting that “several guidelines on tramadol use in clinical practice might need to be revisited.”
According to a recent Cochrane review there is “moderate-quality evidence” that tramadol “has no important benefit on mean pain or function in people with osteoarthritis.” The authors of the review wrote that, while some patients might glean a benefit from treatment, the evidence suggests that “adverse events probably cause substantially more participants to stop taking tramadol.”
Current guidance on the use of tramadol varies. The American Academy of Orthopaedic Surgeons guidelines recommend its use in patients with symptomatic knee OA on a par with NSAIDs while the American College of Rheumatology guidance (Arthritis Care Res. 2020;72[2]:149-62) conditionally recommends that it be used only if there is no real alternative, such as a contraindication to NSAIDs or pain relief is ineffective.
Patients with rheumatic disease are increasingly taking opioid painkillers such as tramadol, with other data reported at the EULAR 2020 E-Congress showing a rise from 15% in 2007 to 25% in 2016 in the Catalonia region of Spain alone. A rise from 5% to 10% has previously been reported in the United States from 2003 to 2009.
With increasing rates of tramadol prescribing, the worry is that perhaps tramadol is not as safe a people think it is, as Thomas Schwenk, MD, pointed out when he reviewed the previous research showing excess mortality with tramadol (NEJM Journal Watch, March 2019).
“The opioid agonist tramadol often is prescribed for patients with osteoarthritis pain because it is thought to be safer than opioids or nonsteroidal anti-inflammatory drugs,” he observed. Dr. Schwenk, who is dean of the University of Nevada, Reno, added that the “results [of that study] suggest that tramadol is not as safe as some people believe.”
He suggested cautious prescribing: “Tramadol might be an option for patients in whom NSAIDs are contraindicated, but it should be prescribed as judiciously as traditional opioids.”
Responsible prescribing to avoid opioid misuse in patients with rheumatic diseases was also advocated in a EULAR press release from the congress. A study from Iceland was highlighted that found patients with inflammatory arthritis frequently did not stop taking opioids after the source of their pain had gone; in fact, their use went up despite being treated with tumor necrosis factor inhibitors.
“We would like to raise awareness of a responsible approach both by the prescribers and also the patients,” said John Isaacs, PhD, of the University of Newcastle (England). “In order to alleviate chronic pain, medications should in any case only be part of a comprehensive therapy program, in which doctors, psychologists, and physiotherapists work together.”
The study authors had no conflicts of interest.
SOURCE: Li L et al. Ann Rheum Dis. 2020;79[suppl 1]:118, Abstract OP0191.
Patients with OA treated with tramadol had a 20%-50% higher risk of dying during the first year of treatment than did patients who were treated with NSAIDs, according to the results of a large, population-based study performed in British Columbia.
Within 1 year of starting treatment, 296 of 13,798 patients treated with tramadol had died, compared with 246 of 13,798 treated with naproxen, giving a death rate of 21.5 versus 17.8 per 1,000 person-years, and representing a 20% increase in all-cause mortality versus the NSAID (hazard ratio, 1.2).
Similar results were seen comparing tramadol with diclofenac and tramadol with cyclooxygenase (COX)-2 inhibitors, but with increasing death rates of 24.8 versus 19.5 per 1,000 person-years (HR, 1.3) and 23.6 versus 15.7 per 1,000 person-years (HR, 1.5), respectively.
However, all-cause mortality was lower with tramadol than with the opiate painkiller, codeine (21.5 vs. 25.5 per 1,000 person-years; HR, 0.8), reported Ms. Lingyi Li, a PhD student from the University of British Columbia, Vancouver, at the annual European Congress of Rheumatology, held online this year due to COVID-19.
This is not the first time that tramadol’s excess mortality risk has been highlighted. Indeed, just last year (JAMA. 2019;321[10]:969-82), researchers using The Health Improvement Network database reported found that tramadol was associated with higher all-cause mortality than two COX-2 inhibitors, celecoxib (31.2 versus 18.4 per 1,000 person-years) and etoricoxib (25.7 versus 12.8 per 1,000 person-years).
Ms. Li and associates’ data not only now add further weight to those findings, but also go a step further by also looking at other serious risks associated with tramadol’s use among patients with OA. “The objective of this study is to compare tramadol with other commonly prescribed pain relief medications on the risk of several severe outcomes, including mortality, cardiovascular diseases [CVD], venous thromboembolism [VTE], and hip fracture,” Ms. Li said during her virtual presentation.
Using sequential propensity score matching, the researchers compared data on patients in British Columbia during 2005-2014 with a first prescription of tramadol (56,325), the NSAIDs naproxen (n = 13,798) or diclofenac (n = 17,675), COX-2 inhibitors (17,039), or codeine (n = 7,813).
“For CVD, we found that there is a higher risk among tramadol users, compared with diclofenac [HR, 1.2] and COX-2 inhibitors [HR, 1.2], but not with naproxen [HR, 1.0] and codeine [HR, 0.9] users,” Ms. Li reported.
Similarly, the 1-year risk of VTE was significantly higher among tramadol users only when compared with diclofenac (HR, 1.5) and COX-2 inhibitors (HR, 1.7).
“For hip fractures, tramadol initiation was associated with an increased risk of hip fractures, compared with all NSAIDs, but not with codeine,” Ms. Li said. The risk of hip fractures was 40%-50% higher with tramadol versus naproxen (HR, 1.4), diclofenac and COX-2 inhibitors (both HR, 1.5).
“Our results suggest an unfavorable safety profile of tramadol use,” Ms. Li said, suggesting that “several guidelines on tramadol use in clinical practice might need to be revisited.”
According to a recent Cochrane review there is “moderate-quality evidence” that tramadol “has no important benefit on mean pain or function in people with osteoarthritis.” The authors of the review wrote that, while some patients might glean a benefit from treatment, the evidence suggests that “adverse events probably cause substantially more participants to stop taking tramadol.”
Current guidance on the use of tramadol varies. The American Academy of Orthopaedic Surgeons guidelines recommend its use in patients with symptomatic knee OA on a par with NSAIDs while the American College of Rheumatology guidance (Arthritis Care Res. 2020;72[2]:149-62) conditionally recommends that it be used only if there is no real alternative, such as a contraindication to NSAIDs or pain relief is ineffective.
Patients with rheumatic disease are increasingly taking opioid painkillers such as tramadol, with other data reported at the EULAR 2020 E-Congress showing a rise from 15% in 2007 to 25% in 2016 in the Catalonia region of Spain alone. A rise from 5% to 10% has previously been reported in the United States from 2003 to 2009.
With increasing rates of tramadol prescribing, the worry is that perhaps tramadol is not as safe a people think it is, as Thomas Schwenk, MD, pointed out when he reviewed the previous research showing excess mortality with tramadol (NEJM Journal Watch, March 2019).
“The opioid agonist tramadol often is prescribed for patients with osteoarthritis pain because it is thought to be safer than opioids or nonsteroidal anti-inflammatory drugs,” he observed. Dr. Schwenk, who is dean of the University of Nevada, Reno, added that the “results [of that study] suggest that tramadol is not as safe as some people believe.”
He suggested cautious prescribing: “Tramadol might be an option for patients in whom NSAIDs are contraindicated, but it should be prescribed as judiciously as traditional opioids.”
Responsible prescribing to avoid opioid misuse in patients with rheumatic diseases was also advocated in a EULAR press release from the congress. A study from Iceland was highlighted that found patients with inflammatory arthritis frequently did not stop taking opioids after the source of their pain had gone; in fact, their use went up despite being treated with tumor necrosis factor inhibitors.
“We would like to raise awareness of a responsible approach both by the prescribers and also the patients,” said John Isaacs, PhD, of the University of Newcastle (England). “In order to alleviate chronic pain, medications should in any case only be part of a comprehensive therapy program, in which doctors, psychologists, and physiotherapists work together.”
The study authors had no conflicts of interest.
SOURCE: Li L et al. Ann Rheum Dis. 2020;79[suppl 1]:118, Abstract OP0191.
Patients with OA treated with tramadol had a 20%-50% higher risk of dying during the first year of treatment than did patients who were treated with NSAIDs, according to the results of a large, population-based study performed in British Columbia.
Within 1 year of starting treatment, 296 of 13,798 patients treated with tramadol had died, compared with 246 of 13,798 treated with naproxen, giving a death rate of 21.5 versus 17.8 per 1,000 person-years, and representing a 20% increase in all-cause mortality versus the NSAID (hazard ratio, 1.2).
Similar results were seen comparing tramadol with diclofenac and tramadol with cyclooxygenase (COX)-2 inhibitors, but with increasing death rates of 24.8 versus 19.5 per 1,000 person-years (HR, 1.3) and 23.6 versus 15.7 per 1,000 person-years (HR, 1.5), respectively.
However, all-cause mortality was lower with tramadol than with the opiate painkiller, codeine (21.5 vs. 25.5 per 1,000 person-years; HR, 0.8), reported Ms. Lingyi Li, a PhD student from the University of British Columbia, Vancouver, at the annual European Congress of Rheumatology, held online this year due to COVID-19.
This is not the first time that tramadol’s excess mortality risk has been highlighted. Indeed, just last year (JAMA. 2019;321[10]:969-82), researchers using The Health Improvement Network database reported found that tramadol was associated with higher all-cause mortality than two COX-2 inhibitors, celecoxib (31.2 versus 18.4 per 1,000 person-years) and etoricoxib (25.7 versus 12.8 per 1,000 person-years).
Ms. Li and associates’ data not only now add further weight to those findings, but also go a step further by also looking at other serious risks associated with tramadol’s use among patients with OA. “The objective of this study is to compare tramadol with other commonly prescribed pain relief medications on the risk of several severe outcomes, including mortality, cardiovascular diseases [CVD], venous thromboembolism [VTE], and hip fracture,” Ms. Li said during her virtual presentation.
Using sequential propensity score matching, the researchers compared data on patients in British Columbia during 2005-2014 with a first prescription of tramadol (56,325), the NSAIDs naproxen (n = 13,798) or diclofenac (n = 17,675), COX-2 inhibitors (17,039), or codeine (n = 7,813).
“For CVD, we found that there is a higher risk among tramadol users, compared with diclofenac [HR, 1.2] and COX-2 inhibitors [HR, 1.2], but not with naproxen [HR, 1.0] and codeine [HR, 0.9] users,” Ms. Li reported.
Similarly, the 1-year risk of VTE was significantly higher among tramadol users only when compared with diclofenac (HR, 1.5) and COX-2 inhibitors (HR, 1.7).
“For hip fractures, tramadol initiation was associated with an increased risk of hip fractures, compared with all NSAIDs, but not with codeine,” Ms. Li said. The risk of hip fractures was 40%-50% higher with tramadol versus naproxen (HR, 1.4), diclofenac and COX-2 inhibitors (both HR, 1.5).
“Our results suggest an unfavorable safety profile of tramadol use,” Ms. Li said, suggesting that “several guidelines on tramadol use in clinical practice might need to be revisited.”
According to a recent Cochrane review there is “moderate-quality evidence” that tramadol “has no important benefit on mean pain or function in people with osteoarthritis.” The authors of the review wrote that, while some patients might glean a benefit from treatment, the evidence suggests that “adverse events probably cause substantially more participants to stop taking tramadol.”
Current guidance on the use of tramadol varies. The American Academy of Orthopaedic Surgeons guidelines recommend its use in patients with symptomatic knee OA on a par with NSAIDs while the American College of Rheumatology guidance (Arthritis Care Res. 2020;72[2]:149-62) conditionally recommends that it be used only if there is no real alternative, such as a contraindication to NSAIDs or pain relief is ineffective.
Patients with rheumatic disease are increasingly taking opioid painkillers such as tramadol, with other data reported at the EULAR 2020 E-Congress showing a rise from 15% in 2007 to 25% in 2016 in the Catalonia region of Spain alone. A rise from 5% to 10% has previously been reported in the United States from 2003 to 2009.
With increasing rates of tramadol prescribing, the worry is that perhaps tramadol is not as safe a people think it is, as Thomas Schwenk, MD, pointed out when he reviewed the previous research showing excess mortality with tramadol (NEJM Journal Watch, March 2019).
“The opioid agonist tramadol often is prescribed for patients with osteoarthritis pain because it is thought to be safer than opioids or nonsteroidal anti-inflammatory drugs,” he observed. Dr. Schwenk, who is dean of the University of Nevada, Reno, added that the “results [of that study] suggest that tramadol is not as safe as some people believe.”
He suggested cautious prescribing: “Tramadol might be an option for patients in whom NSAIDs are contraindicated, but it should be prescribed as judiciously as traditional opioids.”
Responsible prescribing to avoid opioid misuse in patients with rheumatic diseases was also advocated in a EULAR press release from the congress. A study from Iceland was highlighted that found patients with inflammatory arthritis frequently did not stop taking opioids after the source of their pain had gone; in fact, their use went up despite being treated with tumor necrosis factor inhibitors.
“We would like to raise awareness of a responsible approach both by the prescribers and also the patients,” said John Isaacs, PhD, of the University of Newcastle (England). “In order to alleviate chronic pain, medications should in any case only be part of a comprehensive therapy program, in which doctors, psychologists, and physiotherapists work together.”
The study authors had no conflicts of interest.
SOURCE: Li L et al. Ann Rheum Dis. 2020;79[suppl 1]:118, Abstract OP0191.
FROM EULAR 2020 E-CONGRESS
Most rheumatology drugs don’t increase COVID-19 hospitalization risk
The vast majority of patients with rheumatic and musculoskeletal diseases who contract COVID-19 recover from the virus, regardless of which medication they receive for their rheumatic condition, new international research suggests.
“These results provide, for the first time, information about the outcome of COVID-19 in patients with rheumatic and musculoskeletal diseases,” said study investigator Pedro Machado, MD, PhD, from University College London. “They should provide some reassurance to patients and healthcare providers.”
Machado and his colleagues looked at 600 COVID-19 patients from 40 countries, and found that those taking TNF inhibitors for their rheumatic disease were less likely to be hospitalized for COVID-19. However, treatment with more than 10 mg of prednisone daily — considered a moderate to high dose — was associated with a higher probability of hospitalization.
In addition, hospitalization was not associated with biologics; JAK inhibitors; conventional disease-modifying antirheumatic drugs (DMARDs), such as methotrexate; antimalarials, such as hydroxychloroquine; or nonsteroidal anti-inflammatory drugs (NSAIDs) — either alone or in combination with other biologics, such as TNF-alpha inhibitors.
The findings were presented at the virtual European League Against Rheumatism (EULAR) 2020 Congress and were published online in Annals of the Rheumatic Diseases.
“Initially, there was a huge concern that these drugs could affect the outcome of patients getting COVID-19, but what this is showing is that probably these drugs do not increase their risk of severe outcome,” Machado, who is chair of the EULAR standing committee on epidemiology and health services research, told Medscape Medical News.
As of June 1, 1061 patients from 28 participating countries had been entered into the EULAR COVID-19 database, which was launched as part of the international Global Rheumatology Alliance registry. Patient data are categorized by factors such as top rheumatology diagnosis, comorbidities, top-five COVID-19 symptoms, and DMARD therapy at the time of virus infection. Anonymized data will be shared with an international register based in the United States.
Machado’s team combined data from the EULAR and Global Rheumatology Alliance COVID-19 registries from March 24 to April 20. They looked at patient factors — such as age, sex, smoking status, rheumatic diagnosis, comorbidities, and rheumatic therapies — to examine the association of rheumatic therapies with hospitalization rates and COVID-19 disease course.
Of the 277 patients (46%) in the study cohort who required hospitalization, 55 (9%) died. But this finding shouldn’t be viewed as the true rate of hospitalization or death in patients with rheumatic disease and COVID-19, said Gerd Burmester, MD, from Charité–University Medicine Berlin.
“There’s tremendous bias in terms of more serious cases of COVID-19 being reported to the registries,” he explained, “because the mild cases won’t even show up at their rheumatologist’s office.”
“This can skew the idea that COVID-19 is much more dangerous to rheumatic patients than to the regular population,” Burmester told Medscape Medical News. “It scares the patients, obviously, but we believe this is not justified.”
It’s still unclear whether rituximab use raises the risk for severe COVID-19, he said. “It appears to be the only biologic for which the jury is still out,” he said.
“Anti-TNFs and anti-IL-6 drugs may even be beneficial, although we don’t have robust data,” he added.
The study can only highlight associations between rheumatic drugs and COVID-19 outcomes. “We cannot say there is a causal relationship between the findings,” Machado said.
Longer-term data, when available, should illuminate “more granular” aspects of COVID-19 outcomes in rheumatic patients, including their risks of requiring ventilation or developing a cytokine storm, he noted.
Burmester and Machado agree that research needs to continue as the pandemic rages on. But so far, “there are no data suggesting that, if you’re on a targeted, dedicated immunomodulator, your risk is higher to have a worse course of COVID-19 than the general population,” Burmester said.
“We simply didn’t know that when the pandemic started, and some patients even discontinued their drugs out of this fear,” he added. “It’s more reassuring than we originally thought.”
This article first appeared on Medscape.com.
The vast majority of patients with rheumatic and musculoskeletal diseases who contract COVID-19 recover from the virus, regardless of which medication they receive for their rheumatic condition, new international research suggests.
“These results provide, for the first time, information about the outcome of COVID-19 in patients with rheumatic and musculoskeletal diseases,” said study investigator Pedro Machado, MD, PhD, from University College London. “They should provide some reassurance to patients and healthcare providers.”
Machado and his colleagues looked at 600 COVID-19 patients from 40 countries, and found that those taking TNF inhibitors for their rheumatic disease were less likely to be hospitalized for COVID-19. However, treatment with more than 10 mg of prednisone daily — considered a moderate to high dose — was associated with a higher probability of hospitalization.
In addition, hospitalization was not associated with biologics; JAK inhibitors; conventional disease-modifying antirheumatic drugs (DMARDs), such as methotrexate; antimalarials, such as hydroxychloroquine; or nonsteroidal anti-inflammatory drugs (NSAIDs) — either alone or in combination with other biologics, such as TNF-alpha inhibitors.
The findings were presented at the virtual European League Against Rheumatism (EULAR) 2020 Congress and were published online in Annals of the Rheumatic Diseases.
“Initially, there was a huge concern that these drugs could affect the outcome of patients getting COVID-19, but what this is showing is that probably these drugs do not increase their risk of severe outcome,” Machado, who is chair of the EULAR standing committee on epidemiology and health services research, told Medscape Medical News.
As of June 1, 1061 patients from 28 participating countries had been entered into the EULAR COVID-19 database, which was launched as part of the international Global Rheumatology Alliance registry. Patient data are categorized by factors such as top rheumatology diagnosis, comorbidities, top-five COVID-19 symptoms, and DMARD therapy at the time of virus infection. Anonymized data will be shared with an international register based in the United States.
Machado’s team combined data from the EULAR and Global Rheumatology Alliance COVID-19 registries from March 24 to April 20. They looked at patient factors — such as age, sex, smoking status, rheumatic diagnosis, comorbidities, and rheumatic therapies — to examine the association of rheumatic therapies with hospitalization rates and COVID-19 disease course.
Of the 277 patients (46%) in the study cohort who required hospitalization, 55 (9%) died. But this finding shouldn’t be viewed as the true rate of hospitalization or death in patients with rheumatic disease and COVID-19, said Gerd Burmester, MD, from Charité–University Medicine Berlin.
“There’s tremendous bias in terms of more serious cases of COVID-19 being reported to the registries,” he explained, “because the mild cases won’t even show up at their rheumatologist’s office.”
“This can skew the idea that COVID-19 is much more dangerous to rheumatic patients than to the regular population,” Burmester told Medscape Medical News. “It scares the patients, obviously, but we believe this is not justified.”
It’s still unclear whether rituximab use raises the risk for severe COVID-19, he said. “It appears to be the only biologic for which the jury is still out,” he said.
“Anti-TNFs and anti-IL-6 drugs may even be beneficial, although we don’t have robust data,” he added.
The study can only highlight associations between rheumatic drugs and COVID-19 outcomes. “We cannot say there is a causal relationship between the findings,” Machado said.
Longer-term data, when available, should illuminate “more granular” aspects of COVID-19 outcomes in rheumatic patients, including their risks of requiring ventilation or developing a cytokine storm, he noted.
Burmester and Machado agree that research needs to continue as the pandemic rages on. But so far, “there are no data suggesting that, if you’re on a targeted, dedicated immunomodulator, your risk is higher to have a worse course of COVID-19 than the general population,” Burmester said.
“We simply didn’t know that when the pandemic started, and some patients even discontinued their drugs out of this fear,” he added. “It’s more reassuring than we originally thought.”
This article first appeared on Medscape.com.
The vast majority of patients with rheumatic and musculoskeletal diseases who contract COVID-19 recover from the virus, regardless of which medication they receive for their rheumatic condition, new international research suggests.
“These results provide, for the first time, information about the outcome of COVID-19 in patients with rheumatic and musculoskeletal diseases,” said study investigator Pedro Machado, MD, PhD, from University College London. “They should provide some reassurance to patients and healthcare providers.”
Machado and his colleagues looked at 600 COVID-19 patients from 40 countries, and found that those taking TNF inhibitors for their rheumatic disease were less likely to be hospitalized for COVID-19. However, treatment with more than 10 mg of prednisone daily — considered a moderate to high dose — was associated with a higher probability of hospitalization.
In addition, hospitalization was not associated with biologics; JAK inhibitors; conventional disease-modifying antirheumatic drugs (DMARDs), such as methotrexate; antimalarials, such as hydroxychloroquine; or nonsteroidal anti-inflammatory drugs (NSAIDs) — either alone or in combination with other biologics, such as TNF-alpha inhibitors.
The findings were presented at the virtual European League Against Rheumatism (EULAR) 2020 Congress and were published online in Annals of the Rheumatic Diseases.
“Initially, there was a huge concern that these drugs could affect the outcome of patients getting COVID-19, but what this is showing is that probably these drugs do not increase their risk of severe outcome,” Machado, who is chair of the EULAR standing committee on epidemiology and health services research, told Medscape Medical News.
As of June 1, 1061 patients from 28 participating countries had been entered into the EULAR COVID-19 database, which was launched as part of the international Global Rheumatology Alliance registry. Patient data are categorized by factors such as top rheumatology diagnosis, comorbidities, top-five COVID-19 symptoms, and DMARD therapy at the time of virus infection. Anonymized data will be shared with an international register based in the United States.
Machado’s team combined data from the EULAR and Global Rheumatology Alliance COVID-19 registries from March 24 to April 20. They looked at patient factors — such as age, sex, smoking status, rheumatic diagnosis, comorbidities, and rheumatic therapies — to examine the association of rheumatic therapies with hospitalization rates and COVID-19 disease course.
Of the 277 patients (46%) in the study cohort who required hospitalization, 55 (9%) died. But this finding shouldn’t be viewed as the true rate of hospitalization or death in patients with rheumatic disease and COVID-19, said Gerd Burmester, MD, from Charité–University Medicine Berlin.
“There’s tremendous bias in terms of more serious cases of COVID-19 being reported to the registries,” he explained, “because the mild cases won’t even show up at their rheumatologist’s office.”
“This can skew the idea that COVID-19 is much more dangerous to rheumatic patients than to the regular population,” Burmester told Medscape Medical News. “It scares the patients, obviously, but we believe this is not justified.”
It’s still unclear whether rituximab use raises the risk for severe COVID-19, he said. “It appears to be the only biologic for which the jury is still out,” he said.
“Anti-TNFs and anti-IL-6 drugs may even be beneficial, although we don’t have robust data,” he added.
The study can only highlight associations between rheumatic drugs and COVID-19 outcomes. “We cannot say there is a causal relationship between the findings,” Machado said.
Longer-term data, when available, should illuminate “more granular” aspects of COVID-19 outcomes in rheumatic patients, including their risks of requiring ventilation or developing a cytokine storm, he noted.
Burmester and Machado agree that research needs to continue as the pandemic rages on. But so far, “there are no data suggesting that, if you’re on a targeted, dedicated immunomodulator, your risk is higher to have a worse course of COVID-19 than the general population,” Burmester said.
“We simply didn’t know that when the pandemic started, and some patients even discontinued their drugs out of this fear,” he added. “It’s more reassuring than we originally thought.”
This article first appeared on Medscape.com.
Avacopan notches a win in ANCA-associated vasculitis
Avacopan, an investigational oral inhibitor of complement activation, is efficacious and safe for treating antineutrophil cytoplasmic antibody (ANCA)–associated vasculitis, based on the results of the pivotal phase 3 ADVOCATE trial.
The trial results were reported in the opening plenary abstract session at the annual European Congress of Rheumatology, held online this year because of COVID-19.
“Standard of care for induction of remission includes high-dose glucocorticoids with either cyclophosphamide or rituximab. However, glucocorticoids are the major cause of treatment-related harm,” noted lead investigator Peter A. Merkel, MD, MPH, chief of the division of rheumatology at the University of Pennsylvania, Philadelphia.
The 331 patients in the trial had active ANCA-associated vasculitis (granulomatosis with polyangiitis or microscopic polyangiitis), either new onset or relapsed, with positivity for either proteinase 3 or myeloperoxidase antibodies and moderate to high disease activity.
They were randomized evenly to double-blind avacopan 30 mg or tapering prednisone from 60 mg/day to zero over 20 weeks, each combined either with rituximab (Rituxan) or with cyclophosphamide followed by azathioprine. Avacopan (formerly called CCX168) is a selective antagonist of the complement C5a receptor that has orphan-drug designation from the Food and Drug Administration for this disease.
Trial results showed that avacopan was noninferior to prednisone with respect to the week 26 rate of remission on the Birmingham Vasculitis Activity Score, with an estimate of common difference of 3.4%. And it was superior to prednisone with respect to the week 52 rate of sustained remission, which required remission from week 26 onward, with an estimate of common difference of 12.5%.
The avacopan group also had less glucocorticoid-related toxicity and, among patients with preexisting renal disease, greater improvement in renal function.
“This large, randomized trial met both of its primary endpoints. Important secondary endpoints were also achieved, with a very acceptable safety profile,” Dr. Merkel summarized.
Making sense of the results
The optimal duration of avacopan therapy is unclear, he noted. “We are still going to be learning how to use this drug, if it’s approved, in routine practice. But the data from the second 6 months – from week 26 to week 52 – implies that there is ongoing benefit to being on avacopan after remission is achieved.”
Avacopan worked similarly well regardless of disease status in ADVOCATE, according to Dr. Merkel. “We have not seen significant differences in efficacy of other drugs in our trials [by disease status], in the trials of ANCA-associated vasculitis. So I think we would treat moderate to serious disease similarly, whether it is new onset or recurrence, in terms of efficacy of the drug.”
“The topline phase 3 data from ADVOCATE sort of even exceeded my expectations in terms of the ability to show not just noninferiority, but superiority of avacopan at week 52 in maintaining sustained remission,” Lindsay S. Lally, MD, assistant professor of medicine at the Hospital for Special Surgery in New York, commented in an interview. “It’s spectacular to treat patients with this serious vasculitis without any steroids or with very minimal steroids, and see superiority at a year. That is really game changing.”
The ADVOCATE findings will likely pass muster with the FDA, according to Dr. Lally. “The bar that was set in terms of the coprimary endpoints was very stringent and in line with other registration trials, particularly the RAVE trial that led to the approval of rituximab,” she elaborated. “I don’t think there is any significant safety signal in the data related to avacopan.
“This study is going to move forward our ability to treat this disease effectively, as we have been able to do in some of our other vasculitis syndromes, by finding drugs that have significant steroid-sparing effects,” Dr. Lally predicted.
Study details
ADVOCATE results reported at the congress showed that the week 26 rate of disease remission was 72.3% with avacopan versus 70.1% with prednisone, with the difference falling within the 20% boundary for noninferiority (P < .0001) but missing the mark for superiority (P = .2387).
However, the week 52 rate of sustained disease remission was 65.7% versus 54.9%, respectively, yielding a difference in favor of avacopan that was statistically both noninferior (P < .0001) and superior (P = .0066).
At week 26, patients in the avacopan group had more favorable Glucocorticoid Toxicity Index scores for cumulative worsening (39.7 vs. 56.6; P = .0002) and for aggregate improvement (11.2 vs. 23.4; P = .008).
Among patients who had renal disease at baseline, those in the avacopan group had a greater increase in estimated glomerular filtration rate at week 52 (7.3 vs. 4.1 mL/min per 1.73 m2; P = .029).
“Particularly interesting is the fact that, even after week 26, when the patients were in remission, there was continued improvement in renal function,” Dr. Merkel noted.
Overall, avacopan had a good safety profile. “This was a sick population with many complications, but there were no important safety signals of the study medication,” he reported.
The avacopan and prednisone groups had a similar rate of severe adverse events (23.5% vs. 25.0%). But the former had lower rates of life-threatening adverse events (4.8% vs. 8.5%), adverse events potentially related to glucocorticoids (66.3% vs. 80.5%), deaths (1.2% vs. 2.4%), and deaths specifically caused by infection (0.6% vs. 1.2%).
The trial was sponsored by ChemoCentryx. Dr. Merkel disclosed receiving grant/research support from and consulting fees from ChemoCentryx, among other disclosures. Dr. Lally disclosed that she was an investigator in the trial.
SOURCE: Merkel PA et al. Ann Rheum Dis. 2020;79[suppl 1]:8, Abstract OP0011.
Avacopan, an investigational oral inhibitor of complement activation, is efficacious and safe for treating antineutrophil cytoplasmic antibody (ANCA)–associated vasculitis, based on the results of the pivotal phase 3 ADVOCATE trial.
The trial results were reported in the opening plenary abstract session at the annual European Congress of Rheumatology, held online this year because of COVID-19.
“Standard of care for induction of remission includes high-dose glucocorticoids with either cyclophosphamide or rituximab. However, glucocorticoids are the major cause of treatment-related harm,” noted lead investigator Peter A. Merkel, MD, MPH, chief of the division of rheumatology at the University of Pennsylvania, Philadelphia.
The 331 patients in the trial had active ANCA-associated vasculitis (granulomatosis with polyangiitis or microscopic polyangiitis), either new onset or relapsed, with positivity for either proteinase 3 or myeloperoxidase antibodies and moderate to high disease activity.
They were randomized evenly to double-blind avacopan 30 mg or tapering prednisone from 60 mg/day to zero over 20 weeks, each combined either with rituximab (Rituxan) or with cyclophosphamide followed by azathioprine. Avacopan (formerly called CCX168) is a selective antagonist of the complement C5a receptor that has orphan-drug designation from the Food and Drug Administration for this disease.
Trial results showed that avacopan was noninferior to prednisone with respect to the week 26 rate of remission on the Birmingham Vasculitis Activity Score, with an estimate of common difference of 3.4%. And it was superior to prednisone with respect to the week 52 rate of sustained remission, which required remission from week 26 onward, with an estimate of common difference of 12.5%.
The avacopan group also had less glucocorticoid-related toxicity and, among patients with preexisting renal disease, greater improvement in renal function.
“This large, randomized trial met both of its primary endpoints. Important secondary endpoints were also achieved, with a very acceptable safety profile,” Dr. Merkel summarized.
Making sense of the results
The optimal duration of avacopan therapy is unclear, he noted. “We are still going to be learning how to use this drug, if it’s approved, in routine practice. But the data from the second 6 months – from week 26 to week 52 – implies that there is ongoing benefit to being on avacopan after remission is achieved.”
Avacopan worked similarly well regardless of disease status in ADVOCATE, according to Dr. Merkel. “We have not seen significant differences in efficacy of other drugs in our trials [by disease status], in the trials of ANCA-associated vasculitis. So I think we would treat moderate to serious disease similarly, whether it is new onset or recurrence, in terms of efficacy of the drug.”
“The topline phase 3 data from ADVOCATE sort of even exceeded my expectations in terms of the ability to show not just noninferiority, but superiority of avacopan at week 52 in maintaining sustained remission,” Lindsay S. Lally, MD, assistant professor of medicine at the Hospital for Special Surgery in New York, commented in an interview. “It’s spectacular to treat patients with this serious vasculitis without any steroids or with very minimal steroids, and see superiority at a year. That is really game changing.”
The ADVOCATE findings will likely pass muster with the FDA, according to Dr. Lally. “The bar that was set in terms of the coprimary endpoints was very stringent and in line with other registration trials, particularly the RAVE trial that led to the approval of rituximab,” she elaborated. “I don’t think there is any significant safety signal in the data related to avacopan.
“This study is going to move forward our ability to treat this disease effectively, as we have been able to do in some of our other vasculitis syndromes, by finding drugs that have significant steroid-sparing effects,” Dr. Lally predicted.
Study details
ADVOCATE results reported at the congress showed that the week 26 rate of disease remission was 72.3% with avacopan versus 70.1% with prednisone, with the difference falling within the 20% boundary for noninferiority (P < .0001) but missing the mark for superiority (P = .2387).
However, the week 52 rate of sustained disease remission was 65.7% versus 54.9%, respectively, yielding a difference in favor of avacopan that was statistically both noninferior (P < .0001) and superior (P = .0066).
At week 26, patients in the avacopan group had more favorable Glucocorticoid Toxicity Index scores for cumulative worsening (39.7 vs. 56.6; P = .0002) and for aggregate improvement (11.2 vs. 23.4; P = .008).
Among patients who had renal disease at baseline, those in the avacopan group had a greater increase in estimated glomerular filtration rate at week 52 (7.3 vs. 4.1 mL/min per 1.73 m2; P = .029).
“Particularly interesting is the fact that, even after week 26, when the patients were in remission, there was continued improvement in renal function,” Dr. Merkel noted.
Overall, avacopan had a good safety profile. “This was a sick population with many complications, but there were no important safety signals of the study medication,” he reported.
The avacopan and prednisone groups had a similar rate of severe adverse events (23.5% vs. 25.0%). But the former had lower rates of life-threatening adverse events (4.8% vs. 8.5%), adverse events potentially related to glucocorticoids (66.3% vs. 80.5%), deaths (1.2% vs. 2.4%), and deaths specifically caused by infection (0.6% vs. 1.2%).
The trial was sponsored by ChemoCentryx. Dr. Merkel disclosed receiving grant/research support from and consulting fees from ChemoCentryx, among other disclosures. Dr. Lally disclosed that she was an investigator in the trial.
SOURCE: Merkel PA et al. Ann Rheum Dis. 2020;79[suppl 1]:8, Abstract OP0011.
Avacopan, an investigational oral inhibitor of complement activation, is efficacious and safe for treating antineutrophil cytoplasmic antibody (ANCA)–associated vasculitis, based on the results of the pivotal phase 3 ADVOCATE trial.
The trial results were reported in the opening plenary abstract session at the annual European Congress of Rheumatology, held online this year because of COVID-19.
“Standard of care for induction of remission includes high-dose glucocorticoids with either cyclophosphamide or rituximab. However, glucocorticoids are the major cause of treatment-related harm,” noted lead investigator Peter A. Merkel, MD, MPH, chief of the division of rheumatology at the University of Pennsylvania, Philadelphia.
The 331 patients in the trial had active ANCA-associated vasculitis (granulomatosis with polyangiitis or microscopic polyangiitis), either new onset or relapsed, with positivity for either proteinase 3 or myeloperoxidase antibodies and moderate to high disease activity.
They were randomized evenly to double-blind avacopan 30 mg or tapering prednisone from 60 mg/day to zero over 20 weeks, each combined either with rituximab (Rituxan) or with cyclophosphamide followed by azathioprine. Avacopan (formerly called CCX168) is a selective antagonist of the complement C5a receptor that has orphan-drug designation from the Food and Drug Administration for this disease.
Trial results showed that avacopan was noninferior to prednisone with respect to the week 26 rate of remission on the Birmingham Vasculitis Activity Score, with an estimate of common difference of 3.4%. And it was superior to prednisone with respect to the week 52 rate of sustained remission, which required remission from week 26 onward, with an estimate of common difference of 12.5%.
The avacopan group also had less glucocorticoid-related toxicity and, among patients with preexisting renal disease, greater improvement in renal function.
“This large, randomized trial met both of its primary endpoints. Important secondary endpoints were also achieved, with a very acceptable safety profile,” Dr. Merkel summarized.
Making sense of the results
The optimal duration of avacopan therapy is unclear, he noted. “We are still going to be learning how to use this drug, if it’s approved, in routine practice. But the data from the second 6 months – from week 26 to week 52 – implies that there is ongoing benefit to being on avacopan after remission is achieved.”
Avacopan worked similarly well regardless of disease status in ADVOCATE, according to Dr. Merkel. “We have not seen significant differences in efficacy of other drugs in our trials [by disease status], in the trials of ANCA-associated vasculitis. So I think we would treat moderate to serious disease similarly, whether it is new onset or recurrence, in terms of efficacy of the drug.”
“The topline phase 3 data from ADVOCATE sort of even exceeded my expectations in terms of the ability to show not just noninferiority, but superiority of avacopan at week 52 in maintaining sustained remission,” Lindsay S. Lally, MD, assistant professor of medicine at the Hospital for Special Surgery in New York, commented in an interview. “It’s spectacular to treat patients with this serious vasculitis without any steroids or with very minimal steroids, and see superiority at a year. That is really game changing.”
The ADVOCATE findings will likely pass muster with the FDA, according to Dr. Lally. “The bar that was set in terms of the coprimary endpoints was very stringent and in line with other registration trials, particularly the RAVE trial that led to the approval of rituximab,” she elaborated. “I don’t think there is any significant safety signal in the data related to avacopan.
“This study is going to move forward our ability to treat this disease effectively, as we have been able to do in some of our other vasculitis syndromes, by finding drugs that have significant steroid-sparing effects,” Dr. Lally predicted.
Study details
ADVOCATE results reported at the congress showed that the week 26 rate of disease remission was 72.3% with avacopan versus 70.1% with prednisone, with the difference falling within the 20% boundary for noninferiority (P < .0001) but missing the mark for superiority (P = .2387).
However, the week 52 rate of sustained disease remission was 65.7% versus 54.9%, respectively, yielding a difference in favor of avacopan that was statistically both noninferior (P < .0001) and superior (P = .0066).
At week 26, patients in the avacopan group had more favorable Glucocorticoid Toxicity Index scores for cumulative worsening (39.7 vs. 56.6; P = .0002) and for aggregate improvement (11.2 vs. 23.4; P = .008).
Among patients who had renal disease at baseline, those in the avacopan group had a greater increase in estimated glomerular filtration rate at week 52 (7.3 vs. 4.1 mL/min per 1.73 m2; P = .029).
“Particularly interesting is the fact that, even after week 26, when the patients were in remission, there was continued improvement in renal function,” Dr. Merkel noted.
Overall, avacopan had a good safety profile. “This was a sick population with many complications, but there were no important safety signals of the study medication,” he reported.
The avacopan and prednisone groups had a similar rate of severe adverse events (23.5% vs. 25.0%). But the former had lower rates of life-threatening adverse events (4.8% vs. 8.5%), adverse events potentially related to glucocorticoids (66.3% vs. 80.5%), deaths (1.2% vs. 2.4%), and deaths specifically caused by infection (0.6% vs. 1.2%).
The trial was sponsored by ChemoCentryx. Dr. Merkel disclosed receiving grant/research support from and consulting fees from ChemoCentryx, among other disclosures. Dr. Lally disclosed that she was an investigator in the trial.
SOURCE: Merkel PA et al. Ann Rheum Dis. 2020;79[suppl 1]:8, Abstract OP0011.
FROM EULAR 2020 E-CONGRESS
Study tests a simpler low disease activity measure for lupus
An alternative disease activity index for patients with systemic lupus erythematosus called the SLE-DAS (Disease Activity Score) has shown similar results to the Lupus Low Disease Activity State (LLDAS) in classifying low disease activity but may be easier to potentially apply in daily clinical practice in treat-to-target strategies, according to research presented at the annual European Congress of Rheumatology, held online this year because of COVID-19.
A treat-to-target approach, in which therapies are adjusted and the patient monitored to achieve the desired endpoint, has been proposed for patients with SLE. Clinical remission is the ideal goal, followed by achieving low disease activity (LDA) when clinical remission is unattainable, the first author of the SLE-DAS study, Helena Assunção, MD, of the department of rheumatology at Centro Hospitalar e Universitário de Coimbra (Portugal), said in an interview prior to the presentation of the study at the e-congress.
But to conduct a treat-to-target approach in the clinical setting, clinicians must have reliable, user-friendly targets to assess a patient’s progress, she said. But that’s not available right now. Proposed definitions of LDA, such as the LLDAS, are based on the Systemic Lupus Erythematosus Disease Activity Index 2000 (SLEDAI-2K). This index doesn’t address some important manifestations of SLE and it is scored dichotomously – for example, giving a similar score for thrombocytopenia when platelet count is reduced to 100,000 or to 10,000.
To compensate for these limitations, the current LLDAS definition also requires the Physician Global Assessment and other steps, including a review of medication and changes to treatment or clinical status since the previous visit.
“It is not easy to apply,” Dr. Assunção said.
The SLE-DAS is a continuous index involving 17 parameters (4 continuous: arthritis, proteinuria, thrombocytopenia, and leukopenia), assigning higher scores when a manifestation is more severe, and has manifestation information that SLEDAI-2K lacks (cardiopulmonary involvement, lupus enteritis, and hemolytic anemia).
In contrast, the LLDAS is defined as:
- A SLEDAI-2k score of 4 or less with no major organ involvement
- No new disease activity
- A physician global assessment of the patient of 1 or less on a 0-3 scale
- Maintenance on a prednisolone dosage of 7.5 mg/day or less
- Maintenance on a standard immunosuppressive regimen
A previous study validated the SLE-DAS (Ann Rheum Dis. 2019 Mar;78[3]:365-71), and another exploratory study identified a cutoff SLE-DAS value of 3.77 or lower for LDA with SLE-DAS (Ann Rheum Dis. 2019;78:411-2).
Her group compared LDA status as measured with LLDAS versus the SLE-DAS in a cross-sectional study of 292 consecutive patients at their hospital. LDA on the SLE-DAS was defined as a score 3.77 or lower and a prednisolone dose of 7.5 mg/day or less. A total of 85% of patients were in LDA with SLE-DAS and 83.9% with LLDAS, and the agreement between LLDAS and SLE-DAS LDA was very high (Cohen’s kappa coefficient test; kappa = 0.831; P < .01). Out of 292 patients, only 13 were classified differently by the two definitions, 8 of which were classified as LDA by SLE-DAS, and 5 by LLDAS. Overall, 87% of patients were women and had a mean age of nearly 49 years, with a mean disease duration of about 14 years.
Dr. Assunção feels that the SLE-DAS LDA should be sufficient to monitor disease activity without adding the Physician Global Assessment and other steps, which would make it easier to apply than LLDAS. The fact that it is based on a continuous index is also an important difference. “Especially for low disease activity, it’s very good to be able to define it with a continuous index, because you are not that bad, but not that good, you’re in the middle,” she said.
The study should be regarded as exploratory, she said, but the results were encouraging. “We got similar results, and it’s definitely easier to apply.” She can also personally attest that the new model is easier to use, since she personally collected data for LLDAS assignment. “I had to check this, and this, and this … [SLE-DAS] is easier.”
Future work from her group will aim at deriving and validating a more robust definition of LDA, which will again be compared with the current LLDAS definition.
Her colleagues have already developed and validated a definition for clinical remission using SLE-DAS, although those results have not yet been published. They hope to define activity states using SLE-DAS, including mild, moderate, and high disease activity.
The team has produced an online SLE-DAS calculator (http://sle-das.eu/) where clinicians can score the 17 parameters. “You just input the values and it gives a number reflecting disease activity. Using this definition of SLE-DAS LDA you only need that number and to verify that the prednisolone dose is equal to or inferior to 7.5 mg/day,” said Dr. Assunção.
The study received no funding. Dr. Assunção has no financial disclosures, but one coauthor reported receiving grant/research support from Pfizer and AbbVie and serving as a consultant to Pfizer, AbbVie, Roche, Lilly, and Novartis.
SOURCE: Assunção H et al. Ann Rheum Dis 2020;79[suppl 1]:60, Abstract OP0092.
An alternative disease activity index for patients with systemic lupus erythematosus called the SLE-DAS (Disease Activity Score) has shown similar results to the Lupus Low Disease Activity State (LLDAS) in classifying low disease activity but may be easier to potentially apply in daily clinical practice in treat-to-target strategies, according to research presented at the annual European Congress of Rheumatology, held online this year because of COVID-19.
A treat-to-target approach, in which therapies are adjusted and the patient monitored to achieve the desired endpoint, has been proposed for patients with SLE. Clinical remission is the ideal goal, followed by achieving low disease activity (LDA) when clinical remission is unattainable, the first author of the SLE-DAS study, Helena Assunção, MD, of the department of rheumatology at Centro Hospitalar e Universitário de Coimbra (Portugal), said in an interview prior to the presentation of the study at the e-congress.
But to conduct a treat-to-target approach in the clinical setting, clinicians must have reliable, user-friendly targets to assess a patient’s progress, she said. But that’s not available right now. Proposed definitions of LDA, such as the LLDAS, are based on the Systemic Lupus Erythematosus Disease Activity Index 2000 (SLEDAI-2K). This index doesn’t address some important manifestations of SLE and it is scored dichotomously – for example, giving a similar score for thrombocytopenia when platelet count is reduced to 100,000 or to 10,000.
To compensate for these limitations, the current LLDAS definition also requires the Physician Global Assessment and other steps, including a review of medication and changes to treatment or clinical status since the previous visit.
“It is not easy to apply,” Dr. Assunção said.
The SLE-DAS is a continuous index involving 17 parameters (4 continuous: arthritis, proteinuria, thrombocytopenia, and leukopenia), assigning higher scores when a manifestation is more severe, and has manifestation information that SLEDAI-2K lacks (cardiopulmonary involvement, lupus enteritis, and hemolytic anemia).
In contrast, the LLDAS is defined as:
- A SLEDAI-2k score of 4 or less with no major organ involvement
- No new disease activity
- A physician global assessment of the patient of 1 or less on a 0-3 scale
- Maintenance on a prednisolone dosage of 7.5 mg/day or less
- Maintenance on a standard immunosuppressive regimen
A previous study validated the SLE-DAS (Ann Rheum Dis. 2019 Mar;78[3]:365-71), and another exploratory study identified a cutoff SLE-DAS value of 3.77 or lower for LDA with SLE-DAS (Ann Rheum Dis. 2019;78:411-2).
Her group compared LDA status as measured with LLDAS versus the SLE-DAS in a cross-sectional study of 292 consecutive patients at their hospital. LDA on the SLE-DAS was defined as a score 3.77 or lower and a prednisolone dose of 7.5 mg/day or less. A total of 85% of patients were in LDA with SLE-DAS and 83.9% with LLDAS, and the agreement between LLDAS and SLE-DAS LDA was very high (Cohen’s kappa coefficient test; kappa = 0.831; P < .01). Out of 292 patients, only 13 were classified differently by the two definitions, 8 of which were classified as LDA by SLE-DAS, and 5 by LLDAS. Overall, 87% of patients were women and had a mean age of nearly 49 years, with a mean disease duration of about 14 years.
Dr. Assunção feels that the SLE-DAS LDA should be sufficient to monitor disease activity without adding the Physician Global Assessment and other steps, which would make it easier to apply than LLDAS. The fact that it is based on a continuous index is also an important difference. “Especially for low disease activity, it’s very good to be able to define it with a continuous index, because you are not that bad, but not that good, you’re in the middle,” she said.
The study should be regarded as exploratory, she said, but the results were encouraging. “We got similar results, and it’s definitely easier to apply.” She can also personally attest that the new model is easier to use, since she personally collected data for LLDAS assignment. “I had to check this, and this, and this … [SLE-DAS] is easier.”
Future work from her group will aim at deriving and validating a more robust definition of LDA, which will again be compared with the current LLDAS definition.
Her colleagues have already developed and validated a definition for clinical remission using SLE-DAS, although those results have not yet been published. They hope to define activity states using SLE-DAS, including mild, moderate, and high disease activity.
The team has produced an online SLE-DAS calculator (http://sle-das.eu/) where clinicians can score the 17 parameters. “You just input the values and it gives a number reflecting disease activity. Using this definition of SLE-DAS LDA you only need that number and to verify that the prednisolone dose is equal to or inferior to 7.5 mg/day,” said Dr. Assunção.
The study received no funding. Dr. Assunção has no financial disclosures, but one coauthor reported receiving grant/research support from Pfizer and AbbVie and serving as a consultant to Pfizer, AbbVie, Roche, Lilly, and Novartis.
SOURCE: Assunção H et al. Ann Rheum Dis 2020;79[suppl 1]:60, Abstract OP0092.
An alternative disease activity index for patients with systemic lupus erythematosus called the SLE-DAS (Disease Activity Score) has shown similar results to the Lupus Low Disease Activity State (LLDAS) in classifying low disease activity but may be easier to potentially apply in daily clinical practice in treat-to-target strategies, according to research presented at the annual European Congress of Rheumatology, held online this year because of COVID-19.
A treat-to-target approach, in which therapies are adjusted and the patient monitored to achieve the desired endpoint, has been proposed for patients with SLE. Clinical remission is the ideal goal, followed by achieving low disease activity (LDA) when clinical remission is unattainable, the first author of the SLE-DAS study, Helena Assunção, MD, of the department of rheumatology at Centro Hospitalar e Universitário de Coimbra (Portugal), said in an interview prior to the presentation of the study at the e-congress.
But to conduct a treat-to-target approach in the clinical setting, clinicians must have reliable, user-friendly targets to assess a patient’s progress, she said. But that’s not available right now. Proposed definitions of LDA, such as the LLDAS, are based on the Systemic Lupus Erythematosus Disease Activity Index 2000 (SLEDAI-2K). This index doesn’t address some important manifestations of SLE and it is scored dichotomously – for example, giving a similar score for thrombocytopenia when platelet count is reduced to 100,000 or to 10,000.
To compensate for these limitations, the current LLDAS definition also requires the Physician Global Assessment and other steps, including a review of medication and changes to treatment or clinical status since the previous visit.
“It is not easy to apply,” Dr. Assunção said.
The SLE-DAS is a continuous index involving 17 parameters (4 continuous: arthritis, proteinuria, thrombocytopenia, and leukopenia), assigning higher scores when a manifestation is more severe, and has manifestation information that SLEDAI-2K lacks (cardiopulmonary involvement, lupus enteritis, and hemolytic anemia).
In contrast, the LLDAS is defined as:
- A SLEDAI-2k score of 4 or less with no major organ involvement
- No new disease activity
- A physician global assessment of the patient of 1 or less on a 0-3 scale
- Maintenance on a prednisolone dosage of 7.5 mg/day or less
- Maintenance on a standard immunosuppressive regimen
A previous study validated the SLE-DAS (Ann Rheum Dis. 2019 Mar;78[3]:365-71), and another exploratory study identified a cutoff SLE-DAS value of 3.77 or lower for LDA with SLE-DAS (Ann Rheum Dis. 2019;78:411-2).
Her group compared LDA status as measured with LLDAS versus the SLE-DAS in a cross-sectional study of 292 consecutive patients at their hospital. LDA on the SLE-DAS was defined as a score 3.77 or lower and a prednisolone dose of 7.5 mg/day or less. A total of 85% of patients were in LDA with SLE-DAS and 83.9% with LLDAS, and the agreement between LLDAS and SLE-DAS LDA was very high (Cohen’s kappa coefficient test; kappa = 0.831; P < .01). Out of 292 patients, only 13 were classified differently by the two definitions, 8 of which were classified as LDA by SLE-DAS, and 5 by LLDAS. Overall, 87% of patients were women and had a mean age of nearly 49 years, with a mean disease duration of about 14 years.
Dr. Assunção feels that the SLE-DAS LDA should be sufficient to monitor disease activity without adding the Physician Global Assessment and other steps, which would make it easier to apply than LLDAS. The fact that it is based on a continuous index is also an important difference. “Especially for low disease activity, it’s very good to be able to define it with a continuous index, because you are not that bad, but not that good, you’re in the middle,” she said.
The study should be regarded as exploratory, she said, but the results were encouraging. “We got similar results, and it’s definitely easier to apply.” She can also personally attest that the new model is easier to use, since she personally collected data for LLDAS assignment. “I had to check this, and this, and this … [SLE-DAS] is easier.”
Future work from her group will aim at deriving and validating a more robust definition of LDA, which will again be compared with the current LLDAS definition.
Her colleagues have already developed and validated a definition for clinical remission using SLE-DAS, although those results have not yet been published. They hope to define activity states using SLE-DAS, including mild, moderate, and high disease activity.
The team has produced an online SLE-DAS calculator (http://sle-das.eu/) where clinicians can score the 17 parameters. “You just input the values and it gives a number reflecting disease activity. Using this definition of SLE-DAS LDA you only need that number and to verify that the prednisolone dose is equal to or inferior to 7.5 mg/day,” said Dr. Assunção.
The study received no funding. Dr. Assunção has no financial disclosures, but one coauthor reported receiving grant/research support from Pfizer and AbbVie and serving as a consultant to Pfizer, AbbVie, Roche, Lilly, and Novartis.
SOURCE: Assunção H et al. Ann Rheum Dis 2020;79[suppl 1]:60, Abstract OP0092.
FROM EULAR 2020 E-CONGRESS
Working group proposes MRI definitions of structural lesions indicative of axial spondyloarthritis
What constitutes a structural lesion of the sacroiliac joints on MRI that’s indicative of axial spondyloarthritis (axSpA) has long been a matter of conjecture, but the Assessment of SpondyloArthritis International Society (ASAS) MRI Working Group has developed new definitions that showed a high degree of specificity in identifying such lesions in the disease.
“There is a lack of consensus as to what defines a structural lesion on MRI of the sacroiliac joint [SIJ] typical of axial spondyloarthritis. Previous studies have described structural lesions in different ways, precluding meaningful comparisons between studies. The ASAS MRI group has generated updated consensus lesion definitions that describe each of the MRI lesions in the sacroiliac joint. These definitions have been validated by seven expert readers from the ASAS MRI group on MRI images from the ASAS classification cohort,” Walter P. Maksymowych, MD, said at the annual European Congress of Rheumatology, held online this year due to COVID-19.
Making a definitive diagnosis of axSpA can be difficult because MRI can show a variety of SIJ abnormalities in healthy people as well as those with axSpA, said Dr. Maksymowych, chief medical officer of CARE Arthritis and professor in rheumatology at the University of Alberta in Edmonton, said in an interview prior to his presentation at the e-congress. “People who evaluate MRI scans are looking for clues as to what types of lesions they can be confident are indicative of axSpA.”
That started a process by the ASAS MRI group to evaluate scans from the landmark ASAS Classification Cohort study (Ann Rheum Dis. 2019;78:1550-8). “But,” said Dr. Maksymowych, “the MRI scans from that study were never evaluated.” So that work was handed off to the working group, whose 25 members included 7 expert image readers who evaluated the MRI scans.
The group adopted a standardized approach for evaluating MRIs of the SIJ in 148 cases, dividing each SIJ into quadrants and then evaluating consecutive MRI slices. The readers first documented whether they observed a definite structural lesion on the scan, which they then used as an external reference standard. They then analyzed which lesion, and in how many SIJ quadrants or slices, best reflected this external standard.
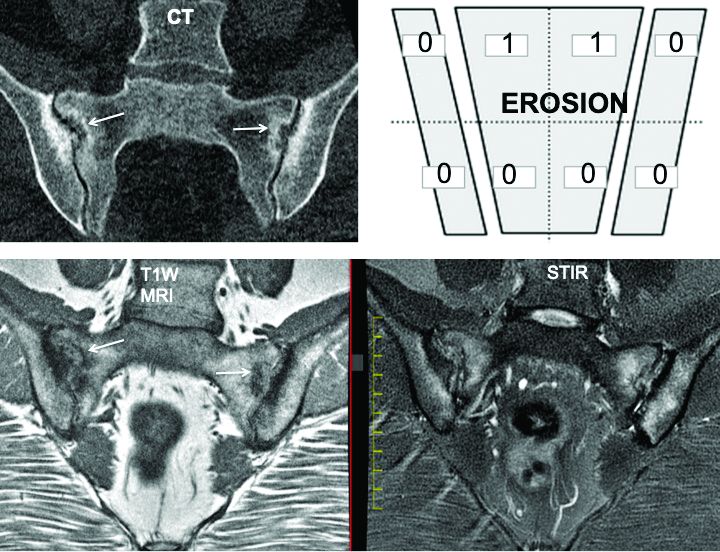
The investigators defined an erosion as “a defect in subchondral bone associated with full-thickness loss of a dark appearance of the subchondral cortex at its expected location, with loss of signal on a T1-weighted, non–fat-suppressed sequence, compared with the normal bright appearance of adjacent bone marrow.” They defined a fat lesion or fat metaplasia as a “bright signal seen on a T1-weighted, non–fat-suppressed sequence that is brighter than normal bone marrow which meets the following requirements: It is homogeneously bright, located in a typical anatomical area (specifically subchondral bone), and has a sharply defined border along its nonarticular border with normal bone marrow.”
An erosion in one quadrant isn’t sufficient to define a scan as positive for a definite structural lesion, said Dr. Maksymowych; but an erosion in three quadrants or in two or more consecutive slices meets the group’s designation of a definite structural lesion. “This showed over a 95% specificity for being associated with a definite structural lesion as defined by a majority of the seven experts,” he said.
The group also determined that a fat lesion typical of axSpA has a homogeneous white appearance on T1-weighted scans with a sharply defined border. The group also determined that such a fat lesion with at least 1-cm horizontal depth from the joint margin in at least one SIJ quadrant is strongly indicative of axSpA.
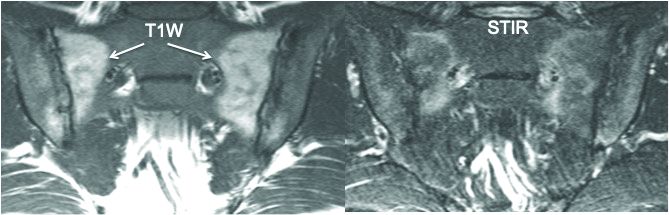
“So we now have definitions for two structural lesions, erosion and fat lesions, that reflect what a majority of experts consider to be a definite structural lesion according to at least 95% specificity,” he said. Sensitivity values were 90% for erosion in three quadrants and 83% for erosions in two or more consecutive slices. and 59% for a fat lesion with at least 1-cm horizontal depth from the joint margin in at least one SIJ quadrant.
The second part of the analysis evaluated the predictive capacity of these lesion definitions for a rheumatologic diagnosis of axSpA at 4.4 years of follow-up. “These lesions predicted SpA with over 95% positive predictive value,” he said. “In other words, if you see them at baseline they’re going to predict SpA with high certainty at follow-up after 4.4 years.”
Three aspects of this study design are unique, Dr. Maksymowych noted. First is the high number of expert MRI readers who evaluated the scans. “There aren’t really too many studies I can think of that used more than two or three expert MRI readers,” he said.
Second is the way in which the study “very precisely and in a very standardized way” applied all the consensus-based ASAS definitions of structural SIJ lesions. “In the past, a variety of ways were used to define these lesions,” he said. “A good example would be the different ways in which erosions have been defined.”
The third novel aspect of the study is that the expert readers’ assessment of what constitutes a definite structural lesion was used as an external reference standard. For example, the study calculated sensitivity and specificity for numbers of SIJ quadrants and consecutive slices with erosion, sclerosis, and fat lesions where a majority of readers agreed on the presence of a structural lesion typical of axSpA with high confidence (3 or greater on a scale of 1-4). “The reason this was put in place is because we recognize sometimes lesions are very subtle and you can’t be certain that they’re reflecting SpA,” he said.
The investigators disclosed relationships with AbbVie, Amgen, Astellas, AstraZeneca, Bristol-Myers Squibb, Boehringer Ingelheim, Celgene, Eli Lilly, Galapagos, Janssen, Merck, Novo Nordisk, Novartis, Orion, Pfizer, Regeneron, Roche, Sandoz, Sanofi, and UCB.
Maksymowych WP et al. Ann Rheum Dis, 2020;79[suppl 1]:53. Abstract OP0079.
What constitutes a structural lesion of the sacroiliac joints on MRI that’s indicative of axial spondyloarthritis (axSpA) has long been a matter of conjecture, but the Assessment of SpondyloArthritis International Society (ASAS) MRI Working Group has developed new definitions that showed a high degree of specificity in identifying such lesions in the disease.
“There is a lack of consensus as to what defines a structural lesion on MRI of the sacroiliac joint [SIJ] typical of axial spondyloarthritis. Previous studies have described structural lesions in different ways, precluding meaningful comparisons between studies. The ASAS MRI group has generated updated consensus lesion definitions that describe each of the MRI lesions in the sacroiliac joint. These definitions have been validated by seven expert readers from the ASAS MRI group on MRI images from the ASAS classification cohort,” Walter P. Maksymowych, MD, said at the annual European Congress of Rheumatology, held online this year due to COVID-19.
Making a definitive diagnosis of axSpA can be difficult because MRI can show a variety of SIJ abnormalities in healthy people as well as those with axSpA, said Dr. Maksymowych, chief medical officer of CARE Arthritis and professor in rheumatology at the University of Alberta in Edmonton, said in an interview prior to his presentation at the e-congress. “People who evaluate MRI scans are looking for clues as to what types of lesions they can be confident are indicative of axSpA.”
That started a process by the ASAS MRI group to evaluate scans from the landmark ASAS Classification Cohort study (Ann Rheum Dis. 2019;78:1550-8). “But,” said Dr. Maksymowych, “the MRI scans from that study were never evaluated.” So that work was handed off to the working group, whose 25 members included 7 expert image readers who evaluated the MRI scans.
The group adopted a standardized approach for evaluating MRIs of the SIJ in 148 cases, dividing each SIJ into quadrants and then evaluating consecutive MRI slices. The readers first documented whether they observed a definite structural lesion on the scan, which they then used as an external reference standard. They then analyzed which lesion, and in how many SIJ quadrants or slices, best reflected this external standard.
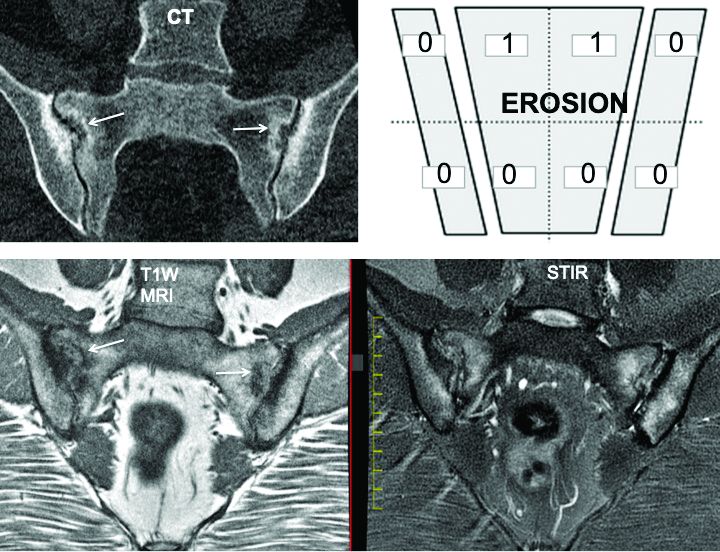
The investigators defined an erosion as “a defect in subchondral bone associated with full-thickness loss of a dark appearance of the subchondral cortex at its expected location, with loss of signal on a T1-weighted, non–fat-suppressed sequence, compared with the normal bright appearance of adjacent bone marrow.” They defined a fat lesion or fat metaplasia as a “bright signal seen on a T1-weighted, non–fat-suppressed sequence that is brighter than normal bone marrow which meets the following requirements: It is homogeneously bright, located in a typical anatomical area (specifically subchondral bone), and has a sharply defined border along its nonarticular border with normal bone marrow.”
An erosion in one quadrant isn’t sufficient to define a scan as positive for a definite structural lesion, said Dr. Maksymowych; but an erosion in three quadrants or in two or more consecutive slices meets the group’s designation of a definite structural lesion. “This showed over a 95% specificity for being associated with a definite structural lesion as defined by a majority of the seven experts,” he said.
The group also determined that a fat lesion typical of axSpA has a homogeneous white appearance on T1-weighted scans with a sharply defined border. The group also determined that such a fat lesion with at least 1-cm horizontal depth from the joint margin in at least one SIJ quadrant is strongly indicative of axSpA.
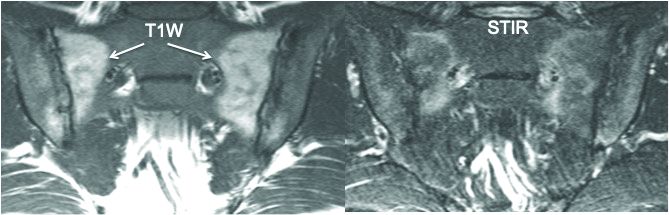
“So we now have definitions for two structural lesions, erosion and fat lesions, that reflect what a majority of experts consider to be a definite structural lesion according to at least 95% specificity,” he said. Sensitivity values were 90% for erosion in three quadrants and 83% for erosions in two or more consecutive slices. and 59% for a fat lesion with at least 1-cm horizontal depth from the joint margin in at least one SIJ quadrant.
The second part of the analysis evaluated the predictive capacity of these lesion definitions for a rheumatologic diagnosis of axSpA at 4.4 years of follow-up. “These lesions predicted SpA with over 95% positive predictive value,” he said. “In other words, if you see them at baseline they’re going to predict SpA with high certainty at follow-up after 4.4 years.”
Three aspects of this study design are unique, Dr. Maksymowych noted. First is the high number of expert MRI readers who evaluated the scans. “There aren’t really too many studies I can think of that used more than two or three expert MRI readers,” he said.
Second is the way in which the study “very precisely and in a very standardized way” applied all the consensus-based ASAS definitions of structural SIJ lesions. “In the past, a variety of ways were used to define these lesions,” he said. “A good example would be the different ways in which erosions have been defined.”
The third novel aspect of the study is that the expert readers’ assessment of what constitutes a definite structural lesion was used as an external reference standard. For example, the study calculated sensitivity and specificity for numbers of SIJ quadrants and consecutive slices with erosion, sclerosis, and fat lesions where a majority of readers agreed on the presence of a structural lesion typical of axSpA with high confidence (3 or greater on a scale of 1-4). “The reason this was put in place is because we recognize sometimes lesions are very subtle and you can’t be certain that they’re reflecting SpA,” he said.
The investigators disclosed relationships with AbbVie, Amgen, Astellas, AstraZeneca, Bristol-Myers Squibb, Boehringer Ingelheim, Celgene, Eli Lilly, Galapagos, Janssen, Merck, Novo Nordisk, Novartis, Orion, Pfizer, Regeneron, Roche, Sandoz, Sanofi, and UCB.
Maksymowych WP et al. Ann Rheum Dis, 2020;79[suppl 1]:53. Abstract OP0079.
What constitutes a structural lesion of the sacroiliac joints on MRI that’s indicative of axial spondyloarthritis (axSpA) has long been a matter of conjecture, but the Assessment of SpondyloArthritis International Society (ASAS) MRI Working Group has developed new definitions that showed a high degree of specificity in identifying such lesions in the disease.
“There is a lack of consensus as to what defines a structural lesion on MRI of the sacroiliac joint [SIJ] typical of axial spondyloarthritis. Previous studies have described structural lesions in different ways, precluding meaningful comparisons between studies. The ASAS MRI group has generated updated consensus lesion definitions that describe each of the MRI lesions in the sacroiliac joint. These definitions have been validated by seven expert readers from the ASAS MRI group on MRI images from the ASAS classification cohort,” Walter P. Maksymowych, MD, said at the annual European Congress of Rheumatology, held online this year due to COVID-19.
Making a definitive diagnosis of axSpA can be difficult because MRI can show a variety of SIJ abnormalities in healthy people as well as those with axSpA, said Dr. Maksymowych, chief medical officer of CARE Arthritis and professor in rheumatology at the University of Alberta in Edmonton, said in an interview prior to his presentation at the e-congress. “People who evaluate MRI scans are looking for clues as to what types of lesions they can be confident are indicative of axSpA.”
That started a process by the ASAS MRI group to evaluate scans from the landmark ASAS Classification Cohort study (Ann Rheum Dis. 2019;78:1550-8). “But,” said Dr. Maksymowych, “the MRI scans from that study were never evaluated.” So that work was handed off to the working group, whose 25 members included 7 expert image readers who evaluated the MRI scans.
The group adopted a standardized approach for evaluating MRIs of the SIJ in 148 cases, dividing each SIJ into quadrants and then evaluating consecutive MRI slices. The readers first documented whether they observed a definite structural lesion on the scan, which they then used as an external reference standard. They then analyzed which lesion, and in how many SIJ quadrants or slices, best reflected this external standard.
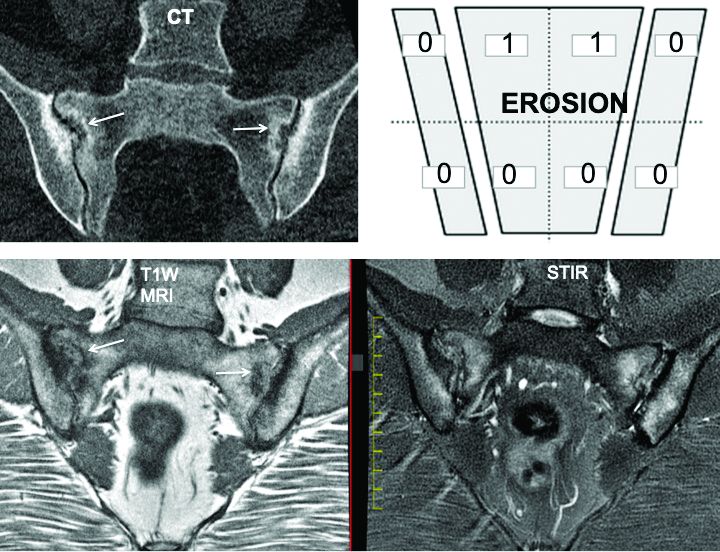
The investigators defined an erosion as “a defect in subchondral bone associated with full-thickness loss of a dark appearance of the subchondral cortex at its expected location, with loss of signal on a T1-weighted, non–fat-suppressed sequence, compared with the normal bright appearance of adjacent bone marrow.” They defined a fat lesion or fat metaplasia as a “bright signal seen on a T1-weighted, non–fat-suppressed sequence that is brighter than normal bone marrow which meets the following requirements: It is homogeneously bright, located in a typical anatomical area (specifically subchondral bone), and has a sharply defined border along its nonarticular border with normal bone marrow.”
An erosion in one quadrant isn’t sufficient to define a scan as positive for a definite structural lesion, said Dr. Maksymowych; but an erosion in three quadrants or in two or more consecutive slices meets the group’s designation of a definite structural lesion. “This showed over a 95% specificity for being associated with a definite structural lesion as defined by a majority of the seven experts,” he said.
The group also determined that a fat lesion typical of axSpA has a homogeneous white appearance on T1-weighted scans with a sharply defined border. The group also determined that such a fat lesion with at least 1-cm horizontal depth from the joint margin in at least one SIJ quadrant is strongly indicative of axSpA.
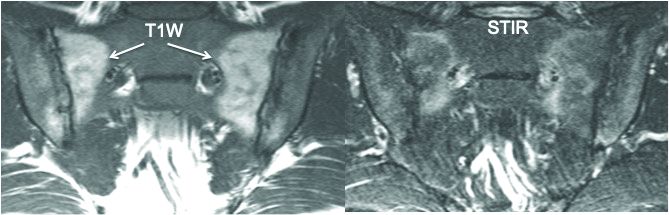
“So we now have definitions for two structural lesions, erosion and fat lesions, that reflect what a majority of experts consider to be a definite structural lesion according to at least 95% specificity,” he said. Sensitivity values were 90% for erosion in three quadrants and 83% for erosions in two or more consecutive slices. and 59% for a fat lesion with at least 1-cm horizontal depth from the joint margin in at least one SIJ quadrant.
The second part of the analysis evaluated the predictive capacity of these lesion definitions for a rheumatologic diagnosis of axSpA at 4.4 years of follow-up. “These lesions predicted SpA with over 95% positive predictive value,” he said. “In other words, if you see them at baseline they’re going to predict SpA with high certainty at follow-up after 4.4 years.”
Three aspects of this study design are unique, Dr. Maksymowych noted. First is the high number of expert MRI readers who evaluated the scans. “There aren’t really too many studies I can think of that used more than two or three expert MRI readers,” he said.
Second is the way in which the study “very precisely and in a very standardized way” applied all the consensus-based ASAS definitions of structural SIJ lesions. “In the past, a variety of ways were used to define these lesions,” he said. “A good example would be the different ways in which erosions have been defined.”
The third novel aspect of the study is that the expert readers’ assessment of what constitutes a definite structural lesion was used as an external reference standard. For example, the study calculated sensitivity and specificity for numbers of SIJ quadrants and consecutive slices with erosion, sclerosis, and fat lesions where a majority of readers agreed on the presence of a structural lesion typical of axSpA with high confidence (3 or greater on a scale of 1-4). “The reason this was put in place is because we recognize sometimes lesions are very subtle and you can’t be certain that they’re reflecting SpA,” he said.
The investigators disclosed relationships with AbbVie, Amgen, Astellas, AstraZeneca, Bristol-Myers Squibb, Boehringer Ingelheim, Celgene, Eli Lilly, Galapagos, Janssen, Merck, Novo Nordisk, Novartis, Orion, Pfizer, Regeneron, Roche, Sandoz, Sanofi, and UCB.
Maksymowych WP et al. Ann Rheum Dis, 2020;79[suppl 1]:53. Abstract OP0079.
FROM EULAR 2020 E-CONGRESS
EULAR cancels June congress, will hold virtual meeting instead
The European League Against Rheumatism has canceled its annual congress scheduled for June 3-6, 2020, in Frankfurt, Germany, and will instead hold a virtual meeting around the same time frame, according to a message from the organization’s president, Iain McInnes, MD, PhD.
“As a scientific medical society, it is our duty to ensure that our medical and health professional participants are available at the forefront of patient care. We are also concerned that bringing our RMD [rheumatic and musculoskeletal disease] patient delegates into a large meeting venue would be extremely unwise at this time,” Dr. McInnes wrote.
While the details of the virtual congress experience have yet to be worked out, Dr. McInnes said that its offerings “will be accessible on demand over a timeframe of several months,” and they “will also publish abstracts/posters online and provide registered delegates with the 1-year access to our journal, the Annals of Rheumatic Diseases.”
The EULAR president also asked for patience as the details of the virtual congress are determined. “We ask you to be patient for a little while longer to give us the time to develop clear answers to all your questions. Our volunteers and staff in the EULAR Office are currently working hard to develop the best possible solutions for this new scenario.”
The European League Against Rheumatism has canceled its annual congress scheduled for June 3-6, 2020, in Frankfurt, Germany, and will instead hold a virtual meeting around the same time frame, according to a message from the organization’s president, Iain McInnes, MD, PhD.
“As a scientific medical society, it is our duty to ensure that our medical and health professional participants are available at the forefront of patient care. We are also concerned that bringing our RMD [rheumatic and musculoskeletal disease] patient delegates into a large meeting venue would be extremely unwise at this time,” Dr. McInnes wrote.
While the details of the virtual congress experience have yet to be worked out, Dr. McInnes said that its offerings “will be accessible on demand over a timeframe of several months,” and they “will also publish abstracts/posters online and provide registered delegates with the 1-year access to our journal, the Annals of Rheumatic Diseases.”
The EULAR president also asked for patience as the details of the virtual congress are determined. “We ask you to be patient for a little while longer to give us the time to develop clear answers to all your questions. Our volunteers and staff in the EULAR Office are currently working hard to develop the best possible solutions for this new scenario.”
The European League Against Rheumatism has canceled its annual congress scheduled for June 3-6, 2020, in Frankfurt, Germany, and will instead hold a virtual meeting around the same time frame, according to a message from the organization’s president, Iain McInnes, MD, PhD.
“As a scientific medical society, it is our duty to ensure that our medical and health professional participants are available at the forefront of patient care. We are also concerned that bringing our RMD [rheumatic and musculoskeletal disease] patient delegates into a large meeting venue would be extremely unwise at this time,” Dr. McInnes wrote.
While the details of the virtual congress experience have yet to be worked out, Dr. McInnes said that its offerings “will be accessible on demand over a timeframe of several months,” and they “will also publish abstracts/posters online and provide registered delegates with the 1-year access to our journal, the Annals of Rheumatic Diseases.”
The EULAR president also asked for patience as the details of the virtual congress are determined. “We ask you to be patient for a little while longer to give us the time to develop clear answers to all your questions. Our volunteers and staff in the EULAR Office are currently working hard to develop the best possible solutions for this new scenario.”











