User login
Involving experts in S. aureus bacteremia treatment reduces mortality
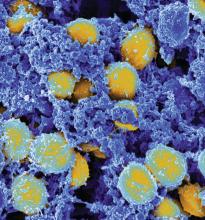
SAN DIEGO – Thirty-day mortality associated with Staphylococcus aureus bacteremia is reduced if there is guidance from either an antimicrobial stewardship team (AST) or an infectious disease consultant (IDC), according to a multivariate experience at Yale New Haven Hospital presented at an annual scientific meeting on infectious diseases.
“This has been a hot area, because there have been a lot of recent studies suggesting that expert infectious disease advice improves care, but not every study has associated expert advice with a mortality benefit,” said Jacqueline Sherbuk, MD, a fellow in the division of infectious diseases and international health at the University of Virginia, Charlottesville. She was a resident at Yale University when this study was conducted.
In this study, the impact of an IDC on outcome in patients with S. aureus bacteremia was evaluated relative to no expert advice. By itself, an IDC was associated with improved adherence to standards of care for S. aureus bacteremia management, but the reduction in mortality was not statistically significant for those who received IDC guidance relative to those who did not.
“Given that patient care may be guided by consultations from the AST independent of IDC, we looked at the overall impact of expert opinion versus no expert involvement, and this achieved significance on multivariate analysis,” Dr. Sherbuk reported.
For adherence to guidelines, IDC guidance was better than no expert advice on multiple measures, including proportion obtaining an echocardiogram (89% vs. 67%; P less than .001), appropriate definitive antibiotics (98% vs. 80%; P less than .001), and appropriate treatment duration (92% vs. 35%; P less than .001). However, the advantage for 30-day mortality rates was only a trend (11% vs. 21%, P = .07). It was only when patients who received IDC guidance or a consultation from the AST were combined that the difference climbed to significance (11% vs. 23%; P = .04).
“On multivariate analysis, the OR [odds ratio] was substantial, predicting a 60% reduction [OR 0.40; P = .03) in 30-day mortality for expert advice vs. no expert advice,” Dr. Sherbuk reported.
In this retrospective observational study, 261 unique cases of S. aureus bacteremia cases in adult patients established with positive blood cultures were evaluated. The cases were collected over a 1-year period at Yale New Haven Hospital. After exclusion of those who died within 3 days of the initial positive culture or who were transferred to other facilities, 236 were included in this analysis.
IDC guidance, which is not required for S. aureus bacteremia at Yale New Haven Hospital, was provided for 74.5% of the patients. Another 4% of patients received guidance from the AST, which is an independent service often provided prior to IDC guidance, according to Dr. Sherbuk.
Relapse (3% vs. 5%) and reinfection (6% vs. 4%) rates were low in both those who did and did not receive expert advice, respectively. These rates were not significantly different. On multivariate analysis, the two factors associated with increased 30-day mortality were patient age greater than 60 years and sepsis based on sequential organ failure assessment.
Several previous studies have associated IDC advice with improved outcomes in S. aureus bacteremia, according to Dr. Sherbuk, but this study suggests that the AST “can be a meaningful adjunct” to IDC guidance to improve outcomes. She noted that several other sets of data presented at this year’s ID Week also associated AST with improved infection management.
SAN DIEGO – Thirty-day mortality associated with Staphylococcus aureus bacteremia is reduced if there is guidance from either an antimicrobial stewardship team (AST) or an infectious disease consultant (IDC), according to a multivariate experience at Yale New Haven Hospital presented at an annual scientific meeting on infectious diseases.
“This has been a hot area, because there have been a lot of recent studies suggesting that expert infectious disease advice improves care, but not every study has associated expert advice with a mortality benefit,” said Jacqueline Sherbuk, MD, a fellow in the division of infectious diseases and international health at the University of Virginia, Charlottesville. She was a resident at Yale University when this study was conducted.
In this study, the impact of an IDC on outcome in patients with S. aureus bacteremia was evaluated relative to no expert advice. By itself, an IDC was associated with improved adherence to standards of care for S. aureus bacteremia management, but the reduction in mortality was not statistically significant for those who received IDC guidance relative to those who did not.
“Given that patient care may be guided by consultations from the AST independent of IDC, we looked at the overall impact of expert opinion versus no expert involvement, and this achieved significance on multivariate analysis,” Dr. Sherbuk reported.
For adherence to guidelines, IDC guidance was better than no expert advice on multiple measures, including proportion obtaining an echocardiogram (89% vs. 67%; P less than .001), appropriate definitive antibiotics (98% vs. 80%; P less than .001), and appropriate treatment duration (92% vs. 35%; P less than .001). However, the advantage for 30-day mortality rates was only a trend (11% vs. 21%, P = .07). It was only when patients who received IDC guidance or a consultation from the AST were combined that the difference climbed to significance (11% vs. 23%; P = .04).
“On multivariate analysis, the OR [odds ratio] was substantial, predicting a 60% reduction [OR 0.40; P = .03) in 30-day mortality for expert advice vs. no expert advice,” Dr. Sherbuk reported.
In this retrospective observational study, 261 unique cases of S. aureus bacteremia cases in adult patients established with positive blood cultures were evaluated. The cases were collected over a 1-year period at Yale New Haven Hospital. After exclusion of those who died within 3 days of the initial positive culture or who were transferred to other facilities, 236 were included in this analysis.
IDC guidance, which is not required for S. aureus bacteremia at Yale New Haven Hospital, was provided for 74.5% of the patients. Another 4% of patients received guidance from the AST, which is an independent service often provided prior to IDC guidance, according to Dr. Sherbuk.
Relapse (3% vs. 5%) and reinfection (6% vs. 4%) rates were low in both those who did and did not receive expert advice, respectively. These rates were not significantly different. On multivariate analysis, the two factors associated with increased 30-day mortality were patient age greater than 60 years and sepsis based on sequential organ failure assessment.
Several previous studies have associated IDC advice with improved outcomes in S. aureus bacteremia, according to Dr. Sherbuk, but this study suggests that the AST “can be a meaningful adjunct” to IDC guidance to improve outcomes. She noted that several other sets of data presented at this year’s ID Week also associated AST with improved infection management.
SAN DIEGO – Thirty-day mortality associated with Staphylococcus aureus bacteremia is reduced if there is guidance from either an antimicrobial stewardship team (AST) or an infectious disease consultant (IDC), according to a multivariate experience at Yale New Haven Hospital presented at an annual scientific meeting on infectious diseases.
“This has been a hot area, because there have been a lot of recent studies suggesting that expert infectious disease advice improves care, but not every study has associated expert advice with a mortality benefit,” said Jacqueline Sherbuk, MD, a fellow in the division of infectious diseases and international health at the University of Virginia, Charlottesville. She was a resident at Yale University when this study was conducted.
In this study, the impact of an IDC on outcome in patients with S. aureus bacteremia was evaluated relative to no expert advice. By itself, an IDC was associated with improved adherence to standards of care for S. aureus bacteremia management, but the reduction in mortality was not statistically significant for those who received IDC guidance relative to those who did not.
“Given that patient care may be guided by consultations from the AST independent of IDC, we looked at the overall impact of expert opinion versus no expert involvement, and this achieved significance on multivariate analysis,” Dr. Sherbuk reported.
For adherence to guidelines, IDC guidance was better than no expert advice on multiple measures, including proportion obtaining an echocardiogram (89% vs. 67%; P less than .001), appropriate definitive antibiotics (98% vs. 80%; P less than .001), and appropriate treatment duration (92% vs. 35%; P less than .001). However, the advantage for 30-day mortality rates was only a trend (11% vs. 21%, P = .07). It was only when patients who received IDC guidance or a consultation from the AST were combined that the difference climbed to significance (11% vs. 23%; P = .04).
“On multivariate analysis, the OR [odds ratio] was substantial, predicting a 60% reduction [OR 0.40; P = .03) in 30-day mortality for expert advice vs. no expert advice,” Dr. Sherbuk reported.
In this retrospective observational study, 261 unique cases of S. aureus bacteremia cases in adult patients established with positive blood cultures were evaluated. The cases were collected over a 1-year period at Yale New Haven Hospital. After exclusion of those who died within 3 days of the initial positive culture or who were transferred to other facilities, 236 were included in this analysis.
IDC guidance, which is not required for S. aureus bacteremia at Yale New Haven Hospital, was provided for 74.5% of the patients. Another 4% of patients received guidance from the AST, which is an independent service often provided prior to IDC guidance, according to Dr. Sherbuk.
Relapse (3% vs. 5%) and reinfection (6% vs. 4%) rates were low in both those who did and did not receive expert advice, respectively. These rates were not significantly different. On multivariate analysis, the two factors associated with increased 30-day mortality were patient age greater than 60 years and sepsis based on sequential organ failure assessment.
Several previous studies have associated IDC advice with improved outcomes in S. aureus bacteremia, according to Dr. Sherbuk, but this study suggests that the AST “can be a meaningful adjunct” to IDC guidance to improve outcomes. She noted that several other sets of data presented at this year’s ID Week also associated AST with improved infection management.
AT ID WEEK 2017
Key clinical point:
Major finding: For those receiving expert involvement in S. aureus bacteremia management, the odds ratio for 30-day mortality was reduced 60% (OR 0.40; P = .03) on multivariate analysis.
Data source: Retrospective, single-center study exploring the management of 236 S. aureus bacteremia cases in adult patients.
Disclosures: Dr. Sherbuk reported no financial relationships relevant to this study.
Cases of Legionnaires’ continue to rise in the United States
SAN DIEGO –
“Improved testing and surveillance are needed to improve understanding of disease and outbreak burden,” Laura A. Cooley, MD, said at an annual scientific meeting on infectious diseases. “There is more to learn about environmental sources of Legionella for cases not associated with known outbreaks and about the distribution of Legionella in the environment.”
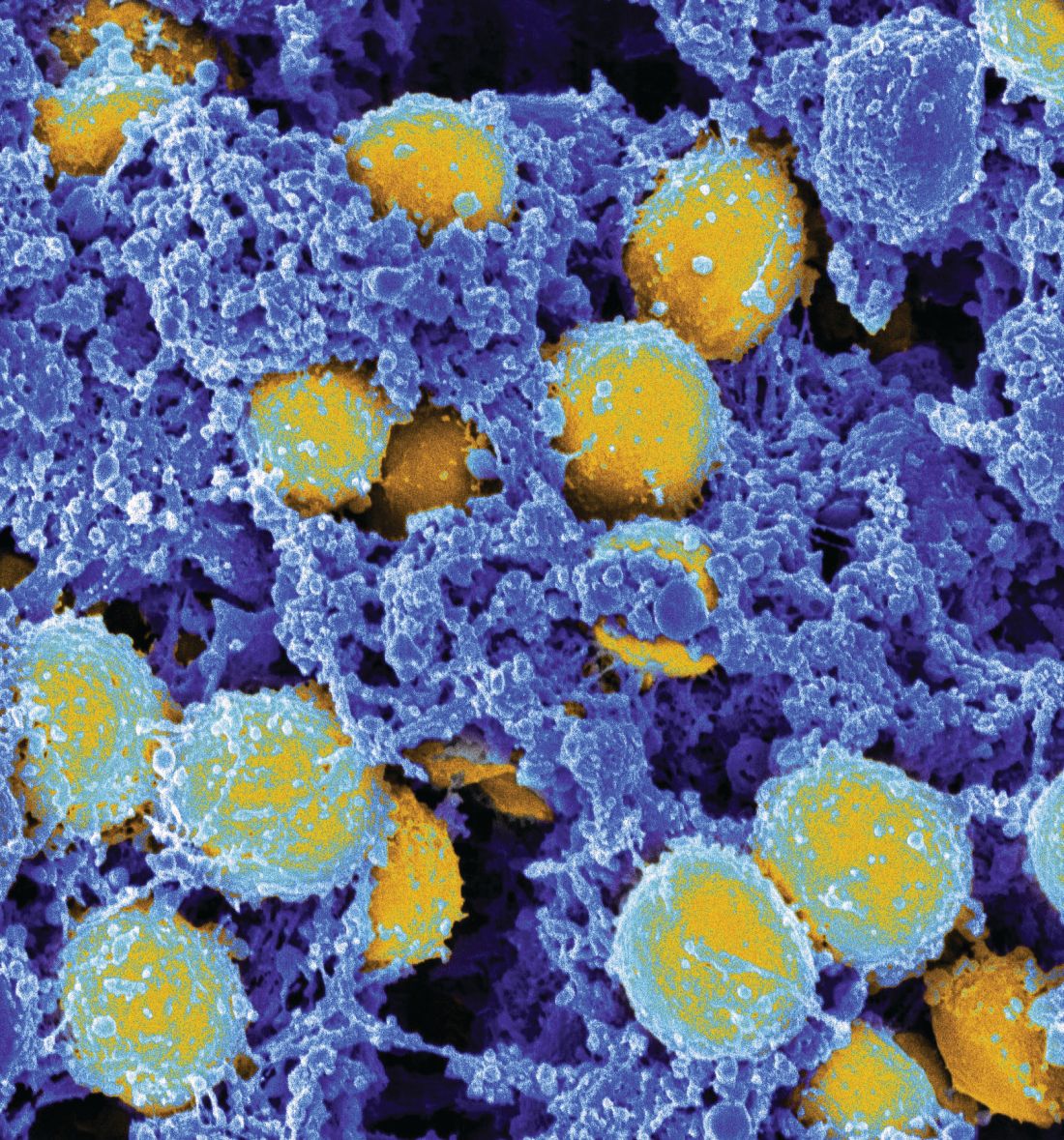
A Gram-negative bacillus, Legionella is an intracellular parasite of free-living protozoa primarily found in freshwater. “It can live and grow in biofilm, and there are more than 60 species of the bacterium,” she said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Cases are higher in the warmer months, and the rates are highest among the elderly, men, and those of black race. Currently, L. pneumophila accounts for about 90% of cases in the United States. “Once it’s transmitted, it has to hit a susceptible population to cause disease, generally older individuals and people with underlying conditions,” Dr. Cooley said.
A separate analysis evaluated Legionella cases reported among U.S. residents between 2005 and 2009 (MMWR. 2011;60[32]:1083-6). It found that only 4% were associated with outbreaks, and 96% were sporadic. “That doesn’t mean that [the cases] weren’t associated with the same kind of source, they just weren’t identified as an outbreak,” Dr. Cooley said. “It shows that there is a lot to learn about transmission of Legionella.”
Data from the National Notifiable Diseases Surveillance System indicate that rates of Legionella continue to rise nationwide, especially in the Midwest and Northeast. “Why? It’s possible that there are differences in testing preferences and reporting preferences in this region of the country,” Dr. Cooley noted. “Maybe people are more tuned in to the potential for outbreaks, but there are reasons why there could be differences in disease, like differences in infrastructure, climate, population density, and cooling tower density.” CDC data from 2015 indicate that most cases are not associated with a known exposure, and that the case fatality rate differs by exposure type: 12% for cases reporting health care exposure during the 10 days before symptom onset (25% for definite cases), 9% for cases reporting assisted or senior living exposure, 7% when no specific exposure is reported, and 4% for cases reporting travel exposure (MMWR. 2017;66[22]:584-9).
The U.S. case definition of Legionnaires’ disease consists of clinical or radiologic pneumonia plus confirmatory laboratory testing, either by urinary antigen test (UAT), lower respiratory culture, or appropriate serological testing. Polymerase chain reaction can be used as a presumptive test for a suspect case. “UAT is easy and it detects L. pneumophila serogroup 1 (Lp1), but it has some gaps,” Dr. Cooley said. “It isn’t completely sensitive for Lp1, and it doesn’t detect any other species or serogroups. That’s why we also recommend that a culture of respiratory secretions on selective media be performed at the same time. That being said, in the U.S., nearly all reported cases of Legionella are diagnosed by UAT only.”
A 2016 CDC MMWR and Vital Signs report found that almost all Legionella outbreaks could be prevented with effective water management, and the CDC has published a step-by-step guide to creating a water management program to reduce Legionella growth and spread in buildings. The 2017 MMWR Report found that definite health care–associated Legionnaires’ disease is deadly for one in four people who get it. The report also found that this issue is widespread; 76% of complete reporting jurisdictions reported at least one definite case of health care–associated Legionella disease in 2015. More recently, the Centers for Medicare & Medicaid Services issued a requirement to reduce risk in health care facility water systems to prevent cases and outbreaks. It applies to hospitals, skilled nursing facilities, and critical access hospitals.
Dr. Cooley reported having no financial disclosures.
SAN DIEGO –
“Improved testing and surveillance are needed to improve understanding of disease and outbreak burden,” Laura A. Cooley, MD, said at an annual scientific meeting on infectious diseases. “There is more to learn about environmental sources of Legionella for cases not associated with known outbreaks and about the distribution of Legionella in the environment.”
A Gram-negative bacillus, Legionella is an intracellular parasite of free-living protozoa primarily found in freshwater. “It can live and grow in biofilm, and there are more than 60 species of the bacterium,” she said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Cases are higher in the warmer months, and the rates are highest among the elderly, men, and those of black race. Currently, L. pneumophila accounts for about 90% of cases in the United States. “Once it’s transmitted, it has to hit a susceptible population to cause disease, generally older individuals and people with underlying conditions,” Dr. Cooley said.
A separate analysis evaluated Legionella cases reported among U.S. residents between 2005 and 2009 (MMWR. 2011;60[32]:1083-6). It found that only 4% were associated with outbreaks, and 96% were sporadic. “That doesn’t mean that [the cases] weren’t associated with the same kind of source, they just weren’t identified as an outbreak,” Dr. Cooley said. “It shows that there is a lot to learn about transmission of Legionella.”
Data from the National Notifiable Diseases Surveillance System indicate that rates of Legionella continue to rise nationwide, especially in the Midwest and Northeast. “Why? It’s possible that there are differences in testing preferences and reporting preferences in this region of the country,” Dr. Cooley noted. “Maybe people are more tuned in to the potential for outbreaks, but there are reasons why there could be differences in disease, like differences in infrastructure, climate, population density, and cooling tower density.” CDC data from 2015 indicate that most cases are not associated with a known exposure, and that the case fatality rate differs by exposure type: 12% for cases reporting health care exposure during the 10 days before symptom onset (25% for definite cases), 9% for cases reporting assisted or senior living exposure, 7% when no specific exposure is reported, and 4% for cases reporting travel exposure (MMWR. 2017;66[22]:584-9).
The U.S. case definition of Legionnaires’ disease consists of clinical or radiologic pneumonia plus confirmatory laboratory testing, either by urinary antigen test (UAT), lower respiratory culture, or appropriate serological testing. Polymerase chain reaction can be used as a presumptive test for a suspect case. “UAT is easy and it detects L. pneumophila serogroup 1 (Lp1), but it has some gaps,” Dr. Cooley said. “It isn’t completely sensitive for Lp1, and it doesn’t detect any other species or serogroups. That’s why we also recommend that a culture of respiratory secretions on selective media be performed at the same time. That being said, in the U.S., nearly all reported cases of Legionella are diagnosed by UAT only.”
A 2016 CDC MMWR and Vital Signs report found that almost all Legionella outbreaks could be prevented with effective water management, and the CDC has published a step-by-step guide to creating a water management program to reduce Legionella growth and spread in buildings. The 2017 MMWR Report found that definite health care–associated Legionnaires’ disease is deadly for one in four people who get it. The report also found that this issue is widespread; 76% of complete reporting jurisdictions reported at least one definite case of health care–associated Legionella disease in 2015. More recently, the Centers for Medicare & Medicaid Services issued a requirement to reduce risk in health care facility water systems to prevent cases and outbreaks. It applies to hospitals, skilled nursing facilities, and critical access hospitals.
Dr. Cooley reported having no financial disclosures.
SAN DIEGO –
“Improved testing and surveillance are needed to improve understanding of disease and outbreak burden,” Laura A. Cooley, MD, said at an annual scientific meeting on infectious diseases. “There is more to learn about environmental sources of Legionella for cases not associated with known outbreaks and about the distribution of Legionella in the environment.”
A Gram-negative bacillus, Legionella is an intracellular parasite of free-living protozoa primarily found in freshwater. “It can live and grow in biofilm, and there are more than 60 species of the bacterium,” she said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Cases are higher in the warmer months, and the rates are highest among the elderly, men, and those of black race. Currently, L. pneumophila accounts for about 90% of cases in the United States. “Once it’s transmitted, it has to hit a susceptible population to cause disease, generally older individuals and people with underlying conditions,” Dr. Cooley said.
A separate analysis evaluated Legionella cases reported among U.S. residents between 2005 and 2009 (MMWR. 2011;60[32]:1083-6). It found that only 4% were associated with outbreaks, and 96% were sporadic. “That doesn’t mean that [the cases] weren’t associated with the same kind of source, they just weren’t identified as an outbreak,” Dr. Cooley said. “It shows that there is a lot to learn about transmission of Legionella.”
Data from the National Notifiable Diseases Surveillance System indicate that rates of Legionella continue to rise nationwide, especially in the Midwest and Northeast. “Why? It’s possible that there are differences in testing preferences and reporting preferences in this region of the country,” Dr. Cooley noted. “Maybe people are more tuned in to the potential for outbreaks, but there are reasons why there could be differences in disease, like differences in infrastructure, climate, population density, and cooling tower density.” CDC data from 2015 indicate that most cases are not associated with a known exposure, and that the case fatality rate differs by exposure type: 12% for cases reporting health care exposure during the 10 days before symptom onset (25% for definite cases), 9% for cases reporting assisted or senior living exposure, 7% when no specific exposure is reported, and 4% for cases reporting travel exposure (MMWR. 2017;66[22]:584-9).
The U.S. case definition of Legionnaires’ disease consists of clinical or radiologic pneumonia plus confirmatory laboratory testing, either by urinary antigen test (UAT), lower respiratory culture, or appropriate serological testing. Polymerase chain reaction can be used as a presumptive test for a suspect case. “UAT is easy and it detects L. pneumophila serogroup 1 (Lp1), but it has some gaps,” Dr. Cooley said. “It isn’t completely sensitive for Lp1, and it doesn’t detect any other species or serogroups. That’s why we also recommend that a culture of respiratory secretions on selective media be performed at the same time. That being said, in the U.S., nearly all reported cases of Legionella are diagnosed by UAT only.”
A 2016 CDC MMWR and Vital Signs report found that almost all Legionella outbreaks could be prevented with effective water management, and the CDC has published a step-by-step guide to creating a water management program to reduce Legionella growth and spread in buildings. The 2017 MMWR Report found that definite health care–associated Legionnaires’ disease is deadly for one in four people who get it. The report also found that this issue is widespread; 76% of complete reporting jurisdictions reported at least one definite case of health care–associated Legionella disease in 2015. More recently, the Centers for Medicare & Medicaid Services issued a requirement to reduce risk in health care facility water systems to prevent cases and outbreaks. It applies to hospitals, skilled nursing facilities, and critical access hospitals.
Dr. Cooley reported having no financial disclosures.
REPORTING FROM ID WEEK 2017
Nearly 10% of patients with candidemia had CDI
SAN DIEGO – Nearly one in ten adults hospitalized with candidemia had Clostridium difficile coinfections in a large multistate study.
“,” Sharon Tsay, MD, said at an annual scientific meeting on infectious diseases. “In patients with CDI, one in 100 developed candidemia, but in patients with candidemia, nearly one in 10 had CDI,” she said. Patients with diabetes, hemodialysis, solid organ transplantation, or a prior recent hospital stay were significantly more likely to have a CDI coinfection even after the researchers controlled for potential confounders, she reported.
Both candidemia and CDI are serious health care–associated infections that disproportionately affect older, severely ill, and immunosuppressed patients, noted Dr. Tsay, an Epidemic Intelligence Service officer in the mycotic diseases branch at the Centers for Disease Control and Prevention, Atlanta. Every year in the United States, about 50,000 individuals are hospitalized with candidemia, and about 30% die within 30 days of diagnosis. The prevalence of CDI is about tenfold higher, and 30-day mortality rates range between about 1% and 9%.
To understand why candidemia and CDI occur together, consider the effects of oral vancomycin therapy, Dr. Tsay said. Antibiotic pressure disrupts normal gut flora, leading to decreased immunity and Candida colonization. Disrupting the gut microbiome also increases the risk of CDI, which can damage gut mucosa, especially in hypervirulent cases such as C. difficile ribotype 027. Vancomycin can also directly damage the gut mucosa, after which Candida can translocate into the bloodstream.
To better characterize CDI and candidemia coinfections in the United States, Dr. Tsay and her associates analyzed data from CDC’s Emerging Infections Program, which tracks infections of high public health significance in 10 states across the country. Among 2,129 patients with a positive blood culture for Candida from 2014 through 2016, 193 (9%) had a diagnosis of CDI within 90 days. Two-thirds of CDI cases preceded candidemia (median, 10 days) and one-third occurred afterward (median, 7 days). Rates of 30-day mortality rates were 25% in patients with and without CDI. For both groups, Candida albicans was the most commonly identified species, followed by C. glabrata and C. parapsilosis.
A multivariate model identified four risk factors for CDI in patients with candidemia – solid organ transplantation (odds ratio, 3.0), hemodialysis (OR, 1.8), prior hospital stay (OR, 1.7), and diabetes (OR, 1.4). Data were limited to case report forms and did not include information about CDI severity or treatment, Dr. Tsay said.
Dr. Tsay and her associates reported having no conflicts of interest.
SAN DIEGO – Nearly one in ten adults hospitalized with candidemia had Clostridium difficile coinfections in a large multistate study.
“,” Sharon Tsay, MD, said at an annual scientific meeting on infectious diseases. “In patients with CDI, one in 100 developed candidemia, but in patients with candidemia, nearly one in 10 had CDI,” she said. Patients with diabetes, hemodialysis, solid organ transplantation, or a prior recent hospital stay were significantly more likely to have a CDI coinfection even after the researchers controlled for potential confounders, she reported.
Both candidemia and CDI are serious health care–associated infections that disproportionately affect older, severely ill, and immunosuppressed patients, noted Dr. Tsay, an Epidemic Intelligence Service officer in the mycotic diseases branch at the Centers for Disease Control and Prevention, Atlanta. Every year in the United States, about 50,000 individuals are hospitalized with candidemia, and about 30% die within 30 days of diagnosis. The prevalence of CDI is about tenfold higher, and 30-day mortality rates range between about 1% and 9%.
To understand why candidemia and CDI occur together, consider the effects of oral vancomycin therapy, Dr. Tsay said. Antibiotic pressure disrupts normal gut flora, leading to decreased immunity and Candida colonization. Disrupting the gut microbiome also increases the risk of CDI, which can damage gut mucosa, especially in hypervirulent cases such as C. difficile ribotype 027. Vancomycin can also directly damage the gut mucosa, after which Candida can translocate into the bloodstream.
To better characterize CDI and candidemia coinfections in the United States, Dr. Tsay and her associates analyzed data from CDC’s Emerging Infections Program, which tracks infections of high public health significance in 10 states across the country. Among 2,129 patients with a positive blood culture for Candida from 2014 through 2016, 193 (9%) had a diagnosis of CDI within 90 days. Two-thirds of CDI cases preceded candidemia (median, 10 days) and one-third occurred afterward (median, 7 days). Rates of 30-day mortality rates were 25% in patients with and without CDI. For both groups, Candida albicans was the most commonly identified species, followed by C. glabrata and C. parapsilosis.
A multivariate model identified four risk factors for CDI in patients with candidemia – solid organ transplantation (odds ratio, 3.0), hemodialysis (OR, 1.8), prior hospital stay (OR, 1.7), and diabetes (OR, 1.4). Data were limited to case report forms and did not include information about CDI severity or treatment, Dr. Tsay said.
Dr. Tsay and her associates reported having no conflicts of interest.
SAN DIEGO – Nearly one in ten adults hospitalized with candidemia had Clostridium difficile coinfections in a large multistate study.
“,” Sharon Tsay, MD, said at an annual scientific meeting on infectious diseases. “In patients with CDI, one in 100 developed candidemia, but in patients with candidemia, nearly one in 10 had CDI,” she said. Patients with diabetes, hemodialysis, solid organ transplantation, or a prior recent hospital stay were significantly more likely to have a CDI coinfection even after the researchers controlled for potential confounders, she reported.
Both candidemia and CDI are serious health care–associated infections that disproportionately affect older, severely ill, and immunosuppressed patients, noted Dr. Tsay, an Epidemic Intelligence Service officer in the mycotic diseases branch at the Centers for Disease Control and Prevention, Atlanta. Every year in the United States, about 50,000 individuals are hospitalized with candidemia, and about 30% die within 30 days of diagnosis. The prevalence of CDI is about tenfold higher, and 30-day mortality rates range between about 1% and 9%.
To understand why candidemia and CDI occur together, consider the effects of oral vancomycin therapy, Dr. Tsay said. Antibiotic pressure disrupts normal gut flora, leading to decreased immunity and Candida colonization. Disrupting the gut microbiome also increases the risk of CDI, which can damage gut mucosa, especially in hypervirulent cases such as C. difficile ribotype 027. Vancomycin can also directly damage the gut mucosa, after which Candida can translocate into the bloodstream.
To better characterize CDI and candidemia coinfections in the United States, Dr. Tsay and her associates analyzed data from CDC’s Emerging Infections Program, which tracks infections of high public health significance in 10 states across the country. Among 2,129 patients with a positive blood culture for Candida from 2014 through 2016, 193 (9%) had a diagnosis of CDI within 90 days. Two-thirds of CDI cases preceded candidemia (median, 10 days) and one-third occurred afterward (median, 7 days). Rates of 30-day mortality rates were 25% in patients with and without CDI. For both groups, Candida albicans was the most commonly identified species, followed by C. glabrata and C. parapsilosis.
A multivariate model identified four risk factors for CDI in patients with candidemia – solid organ transplantation (odds ratio, 3.0), hemodialysis (OR, 1.8), prior hospital stay (OR, 1.7), and diabetes (OR, 1.4). Data were limited to case report forms and did not include information about CDI severity or treatment, Dr. Tsay said.
Dr. Tsay and her associates reported having no conflicts of interest.
AT IDWEEK 2017
Key clinical point: Look for candidemia and Clostridium difficile infection occurring together.
Major finding: Among 2,129 patients with a positive blood culture for Candida, 193 (9%) had a diagnosis of CDI within 90 days. Risk factors for coinfection included solid organ transplant, hemodialysis, recent hospital stay, and diabetes.
Data source: A multistate analysis of data from the Centers for Disease Control’s Emerging Infections Program.
Disclosures: Dr. Tsay and her associates reported having no conflicts of interest.
Thirty-one percent of multidrug-resistant infections were community acquired
SAN DIEGO – Thirty-one percent of multidrug-resistant infections were acquired from the community in a prospective single-center study of a regional hospital.
“Multidrug-resistant organisms have escaped the hospital,” Nicholas A. Turner, MD, of Duke University Medical Center, Durham, N.C., and his associates wrote in a poster presented at an annual scientific meeting on infectious diseases. “Community acquisition of multidrug-resistant organisms [MDROs] is increasing, not just within referral centers but also community hospitals. Providers will need to be increasingly aware of this trend.”
Infections of MDROs cause about 2,000,000 illnesses and 23,000 deaths annually in the United States, according to the Centers for Disease Control and Prevention. Until recently, MDROs were considered a plague of hospitals. Amid reports of increasing levels of community acquisition, the researchers studied adults admitted to a 202-bed regional hospital between 2013 and 2016. They defined MDROs as infections of methicillin-resistant Staphylococcus aureus (MRSA), gram-negative bacteria resistant to more than three antimicrobial classes, vancomycin-resistant Enterococcus (VRE), or diarrhea with a positive stool culture for Clostridium difficile.
A total of 285 patients had MDROs. Clostridium difficile (45%) and MRSA (35%) were most common. In all, 88 (31%) MDROs were community-acquired – that is, diagnosed within 48 hours of admission in patients who were not on dialysis, did not live in a long-term care facility, and had not been hospitalized for more than 48 hours in the past 90 days. A total of 36% of MRSA and multidrug-resistant gram-negative infections were community acquired, as were 25% of Clostridium difficile infections. There were only 10 VRE infections, of which none were community-acquired.
After the researchers controlled for clinical and demographic variables, the only significant predictor of community-acquired MDRO was cancer (odds ratio [OR], 2.3; 95% confidence interval [CI], 1.02-5.2). Surgery within the previous 12 months was significantly associated with hospital-acquired MDRO (OR, 0.16; 95% CI, 0.05-0.5).
Traditional risk factors for community-acquired MRSA or C. difficile infection did not achieve statistical significance in the multivariable analysis, the researchers noted. “Similar to data from large tertiary care centers, our findings suggest that MDROs are increasingly acquired in the community setting, even at smaller regional hospitals,” they concluded. “Further study is needed to track the expansion of MDROs in the community setting.”
Dr. Turner reported having no conflicts of interest.
SAN DIEGO – Thirty-one percent of multidrug-resistant infections were acquired from the community in a prospective single-center study of a regional hospital.
“Multidrug-resistant organisms have escaped the hospital,” Nicholas A. Turner, MD, of Duke University Medical Center, Durham, N.C., and his associates wrote in a poster presented at an annual scientific meeting on infectious diseases. “Community acquisition of multidrug-resistant organisms [MDROs] is increasing, not just within referral centers but also community hospitals. Providers will need to be increasingly aware of this trend.”
Infections of MDROs cause about 2,000,000 illnesses and 23,000 deaths annually in the United States, according to the Centers for Disease Control and Prevention. Until recently, MDROs were considered a plague of hospitals. Amid reports of increasing levels of community acquisition, the researchers studied adults admitted to a 202-bed regional hospital between 2013 and 2016. They defined MDROs as infections of methicillin-resistant Staphylococcus aureus (MRSA), gram-negative bacteria resistant to more than three antimicrobial classes, vancomycin-resistant Enterococcus (VRE), or diarrhea with a positive stool culture for Clostridium difficile.
A total of 285 patients had MDROs. Clostridium difficile (45%) and MRSA (35%) were most common. In all, 88 (31%) MDROs were community-acquired – that is, diagnosed within 48 hours of admission in patients who were not on dialysis, did not live in a long-term care facility, and had not been hospitalized for more than 48 hours in the past 90 days. A total of 36% of MRSA and multidrug-resistant gram-negative infections were community acquired, as were 25% of Clostridium difficile infections. There were only 10 VRE infections, of which none were community-acquired.
After the researchers controlled for clinical and demographic variables, the only significant predictor of community-acquired MDRO was cancer (odds ratio [OR], 2.3; 95% confidence interval [CI], 1.02-5.2). Surgery within the previous 12 months was significantly associated with hospital-acquired MDRO (OR, 0.16; 95% CI, 0.05-0.5).
Traditional risk factors for community-acquired MRSA or C. difficile infection did not achieve statistical significance in the multivariable analysis, the researchers noted. “Similar to data from large tertiary care centers, our findings suggest that MDROs are increasingly acquired in the community setting, even at smaller regional hospitals,” they concluded. “Further study is needed to track the expansion of MDROs in the community setting.”
Dr. Turner reported having no conflicts of interest.
SAN DIEGO – Thirty-one percent of multidrug-resistant infections were acquired from the community in a prospective single-center study of a regional hospital.
“Multidrug-resistant organisms have escaped the hospital,” Nicholas A. Turner, MD, of Duke University Medical Center, Durham, N.C., and his associates wrote in a poster presented at an annual scientific meeting on infectious diseases. “Community acquisition of multidrug-resistant organisms [MDROs] is increasing, not just within referral centers but also community hospitals. Providers will need to be increasingly aware of this trend.”
Infections of MDROs cause about 2,000,000 illnesses and 23,000 deaths annually in the United States, according to the Centers for Disease Control and Prevention. Until recently, MDROs were considered a plague of hospitals. Amid reports of increasing levels of community acquisition, the researchers studied adults admitted to a 202-bed regional hospital between 2013 and 2016. They defined MDROs as infections of methicillin-resistant Staphylococcus aureus (MRSA), gram-negative bacteria resistant to more than three antimicrobial classes, vancomycin-resistant Enterococcus (VRE), or diarrhea with a positive stool culture for Clostridium difficile.
A total of 285 patients had MDROs. Clostridium difficile (45%) and MRSA (35%) were most common. In all, 88 (31%) MDROs were community-acquired – that is, diagnosed within 48 hours of admission in patients who were not on dialysis, did not live in a long-term care facility, and had not been hospitalized for more than 48 hours in the past 90 days. A total of 36% of MRSA and multidrug-resistant gram-negative infections were community acquired, as were 25% of Clostridium difficile infections. There were only 10 VRE infections, of which none were community-acquired.
After the researchers controlled for clinical and demographic variables, the only significant predictor of community-acquired MDRO was cancer (odds ratio [OR], 2.3; 95% confidence interval [CI], 1.02-5.2). Surgery within the previous 12 months was significantly associated with hospital-acquired MDRO (OR, 0.16; 95% CI, 0.05-0.5).
Traditional risk factors for community-acquired MRSA or C. difficile infection did not achieve statistical significance in the multivariable analysis, the researchers noted. “Similar to data from large tertiary care centers, our findings suggest that MDROs are increasingly acquired in the community setting, even at smaller regional hospitals,” they concluded. “Further study is needed to track the expansion of MDROs in the community setting.”
Dr. Turner reported having no conflicts of interest.
AT IDWEEK 2017
Key clinical point: Multidrug resistant infections are increasingly being acquired in communities.
Major finding:
Data source: A prospective study of 285 patients with multidrug-resistant infections at a 202-bed hospital.
Disclosures: Dr. Turner reported having no conflicts of interest.
Simple rule boosted yield of molecular tests for enteric pathogens
SAN DIEGO – For adult outpatients with diarrhea, consider limiting molecular testing for enteric pathogens to cases in which patients are immunocompromised or have abdominal pain or fever without vomiting, said Stephen Clark, MD.
“This simple clinical decision rule would reduce testing by 43% while retaining a high sensitivity for clinically relevant infections,” Dr. Clark said at an annual meeting on infectious diseases. In a single-center retrospective cohort study, the decision rule covered 96% of patients with molecular evidence of clinically relevant pathogens.
Several Food and Drug and Administration–approved molecular diagnostic panels for enteric pathogens have become available in the United States during the past 4 years. These panels are fast and sensitive, but costly and not clinically relevant unless they detect a pathogen that merits a change in treatment, such as titrating immunosuppressive drugs or prescribing a course of antimicrobial therapy, said Dr. Clark, a third-year resident at the department of medicine at the University of Virginia in Charlottesville.
Physicians at the University of Virginia often order the FilmArray Gastrointestinal Panel (Biofire Diagnostics) for adult outpatients, especially if they have persistent diarrhea, Dr. Clark said. However, medical records from 452 tested patients showed that only 88 (20%) tested positive for an enteric pathogen and only 4% had an infection clearly meriting antimicrobial therapy. Therefore, the researchers sought predictors of clinically relevant FilmArray results.
Among 376 immunocompetent patients in this cohort, only 12 (3%) had a treatable pathogen detected. None of these 12 patients reported vomiting, while 11 (92%) reported fever or abdominal pain without vomiting, compared with only 47% of immunocompetent patients with no treatable pathogen (P = .002). For immunocompetent patients, the combination of subjective fever or abdominal pain without vomiting was the only demographic or clinical predictor of a clinically relevant positive test result, Dr. Clark said.
Importantly, the FilmArray GI panel showed a much higher clinical yield (about 20%) in immunocompromised patients, who often lacked clinical signs of gastrointestinal infection. “Thinking about this overall, we would recommend testing if patients are either immunocompromised, or if they have abdominal pain or fever in the absence of vomiting,” Dr. Clark said. For this cohort, this decision rule had a sensitivity of 96% (95% confidence interval [CI], 81%-100%) and a negative predictive value of 99% (95% CI, 97%-100%). Specificity was only 45% (95% CI, 41%-51%), but “the aim of this rule was more to help clinicians think about whether it’s possible that there could be a detection, instead of pinpointing what it might be,” Dr. Clark said.
Applying guidelines from the American College of Gastroenterology did not increase testing efficiency, Dr. Clark said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. The researchers are now reviewing another 6 months of medical records to create a validation cohort for the decision rule.
Dr. Clark and his associates reported having no conflicts of interest.
SAN DIEGO – For adult outpatients with diarrhea, consider limiting molecular testing for enteric pathogens to cases in which patients are immunocompromised or have abdominal pain or fever without vomiting, said Stephen Clark, MD.
“This simple clinical decision rule would reduce testing by 43% while retaining a high sensitivity for clinically relevant infections,” Dr. Clark said at an annual meeting on infectious diseases. In a single-center retrospective cohort study, the decision rule covered 96% of patients with molecular evidence of clinically relevant pathogens.
Several Food and Drug and Administration–approved molecular diagnostic panels for enteric pathogens have become available in the United States during the past 4 years. These panels are fast and sensitive, but costly and not clinically relevant unless they detect a pathogen that merits a change in treatment, such as titrating immunosuppressive drugs or prescribing a course of antimicrobial therapy, said Dr. Clark, a third-year resident at the department of medicine at the University of Virginia in Charlottesville.
Physicians at the University of Virginia often order the FilmArray Gastrointestinal Panel (Biofire Diagnostics) for adult outpatients, especially if they have persistent diarrhea, Dr. Clark said. However, medical records from 452 tested patients showed that only 88 (20%) tested positive for an enteric pathogen and only 4% had an infection clearly meriting antimicrobial therapy. Therefore, the researchers sought predictors of clinically relevant FilmArray results.
Among 376 immunocompetent patients in this cohort, only 12 (3%) had a treatable pathogen detected. None of these 12 patients reported vomiting, while 11 (92%) reported fever or abdominal pain without vomiting, compared with only 47% of immunocompetent patients with no treatable pathogen (P = .002). For immunocompetent patients, the combination of subjective fever or abdominal pain without vomiting was the only demographic or clinical predictor of a clinically relevant positive test result, Dr. Clark said.
Importantly, the FilmArray GI panel showed a much higher clinical yield (about 20%) in immunocompromised patients, who often lacked clinical signs of gastrointestinal infection. “Thinking about this overall, we would recommend testing if patients are either immunocompromised, or if they have abdominal pain or fever in the absence of vomiting,” Dr. Clark said. For this cohort, this decision rule had a sensitivity of 96% (95% confidence interval [CI], 81%-100%) and a negative predictive value of 99% (95% CI, 97%-100%). Specificity was only 45% (95% CI, 41%-51%), but “the aim of this rule was more to help clinicians think about whether it’s possible that there could be a detection, instead of pinpointing what it might be,” Dr. Clark said.
Applying guidelines from the American College of Gastroenterology did not increase testing efficiency, Dr. Clark said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. The researchers are now reviewing another 6 months of medical records to create a validation cohort for the decision rule.
Dr. Clark and his associates reported having no conflicts of interest.
SAN DIEGO – For adult outpatients with diarrhea, consider limiting molecular testing for enteric pathogens to cases in which patients are immunocompromised or have abdominal pain or fever without vomiting, said Stephen Clark, MD.
“This simple clinical decision rule would reduce testing by 43% while retaining a high sensitivity for clinically relevant infections,” Dr. Clark said at an annual meeting on infectious diseases. In a single-center retrospective cohort study, the decision rule covered 96% of patients with molecular evidence of clinically relevant pathogens.
Several Food and Drug and Administration–approved molecular diagnostic panels for enteric pathogens have become available in the United States during the past 4 years. These panels are fast and sensitive, but costly and not clinically relevant unless they detect a pathogen that merits a change in treatment, such as titrating immunosuppressive drugs or prescribing a course of antimicrobial therapy, said Dr. Clark, a third-year resident at the department of medicine at the University of Virginia in Charlottesville.
Physicians at the University of Virginia often order the FilmArray Gastrointestinal Panel (Biofire Diagnostics) for adult outpatients, especially if they have persistent diarrhea, Dr. Clark said. However, medical records from 452 tested patients showed that only 88 (20%) tested positive for an enteric pathogen and only 4% had an infection clearly meriting antimicrobial therapy. Therefore, the researchers sought predictors of clinically relevant FilmArray results.
Among 376 immunocompetent patients in this cohort, only 12 (3%) had a treatable pathogen detected. None of these 12 patients reported vomiting, while 11 (92%) reported fever or abdominal pain without vomiting, compared with only 47% of immunocompetent patients with no treatable pathogen (P = .002). For immunocompetent patients, the combination of subjective fever or abdominal pain without vomiting was the only demographic or clinical predictor of a clinically relevant positive test result, Dr. Clark said.
Importantly, the FilmArray GI panel showed a much higher clinical yield (about 20%) in immunocompromised patients, who often lacked clinical signs of gastrointestinal infection. “Thinking about this overall, we would recommend testing if patients are either immunocompromised, or if they have abdominal pain or fever in the absence of vomiting,” Dr. Clark said. For this cohort, this decision rule had a sensitivity of 96% (95% confidence interval [CI], 81%-100%) and a negative predictive value of 99% (95% CI, 97%-100%). Specificity was only 45% (95% CI, 41%-51%), but “the aim of this rule was more to help clinicians think about whether it’s possible that there could be a detection, instead of pinpointing what it might be,” Dr. Clark said.
Applying guidelines from the American College of Gastroenterology did not increase testing efficiency, Dr. Clark said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. The researchers are now reviewing another 6 months of medical records to create a validation cohort for the decision rule.
Dr. Clark and his associates reported having no conflicts of interest.
AT IDWEEK 2017
Key clinical point:
Major finding: This approach would have identified 26 of 27 (96%) infections of clinically relevant pathogens, while cutting testing by 43%.
Data source: A single-center retrospective study of 452 adult outpatients with diarrhea.
Disclosures: Dr. Clark and his associates reported having no conflicts of interest.
Wait at least 2 days to replace central venous catheters in patients with candidemia
SAN DIEGO – Wait at least 2 days before replacing central venous catheters (CVC) in patients with catheter-associated candidemia, according to the results of a single-center retrospective cohort study of 228 patients.
Waiting less than 2 days to replace a CVC increased the odds of 30-day mortality nearly sixfold among patients with catheter-related bloodstream infections due to candidemia, even after controlling for potential confounders, Takahiro Matsuo, MD, said at an annual scientific meeting on infectious diseases. No other factor significantly predicted mortality in univariate or multivariate analyses, he said. “This is the first study to demonstrate the optimal timing of central venous catheter replacement in catheter-related [bloodstream infection] due to Candida.”
Invasive candidiasis is associated with mortality rates of up to 50%, noted Dr. Matsuo, who is a fellow in infectious diseases at St. Luke’s International Hospital, Tokyo. Antifungal therapy improves outcomes, and most physicians agree that removing a CVC does, too. To better pinpoint optimal timing of catheter replacement, Dr. Matsuo and his associates examined risk factors for 30-day mortality among patients with candidemia who were treated at St. Luke’s between 2004 and 2015.
Among 228 patients with candidemia, 166 had CVCs, and 144 had their CVC removed. Among 71 patients who needed their CVC replaced, 15 died within 30 days. Central venous catheters were replaced less than 2 days after removal in 87% of patients who died and in 54% of survivors (P = .04). The association remained statistically significant after the researchers accounted for potential confounders (adjusted odds ratio, 5.9; 95% confidence interval, 1.2-29.7; P = .03).
Patients who died within 30 days of CVC replacement also were more likely to have hematologic malignancies (20% versus 4%), diabetes (13% vs. 11%), to be on hemodialysis (27% vs. 16%), and to have a history of recent corticosteroid exposure (20% versus 11%) compared with survivors, but none of these associations reached statistical significance. Furthermore, 30-day mortality was not associated with gender, age, Candida species, endophthalmitis, or type of antifungal therapy, said Dr. Matsuo, who spoke at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
An infectious disease consultation was associated with about a 70% reduction in the odds of mortality in the multivariate analysis, but the 95% confidence interval crossed 1.0, rendering the link statistically insignificant.
Given the small sample size and single-center design of this study, its findings ideally should be confirmed in a larger randomized controlled trial, Dr. Matsuo said. The investigators also did not track whether patients were fungemic at the time of CVC replacement, he noted.
The researchers reported having no conflicts of interest.
SAN DIEGO – Wait at least 2 days before replacing central venous catheters (CVC) in patients with catheter-associated candidemia, according to the results of a single-center retrospective cohort study of 228 patients.
Waiting less than 2 days to replace a CVC increased the odds of 30-day mortality nearly sixfold among patients with catheter-related bloodstream infections due to candidemia, even after controlling for potential confounders, Takahiro Matsuo, MD, said at an annual scientific meeting on infectious diseases. No other factor significantly predicted mortality in univariate or multivariate analyses, he said. “This is the first study to demonstrate the optimal timing of central venous catheter replacement in catheter-related [bloodstream infection] due to Candida.”
Invasive candidiasis is associated with mortality rates of up to 50%, noted Dr. Matsuo, who is a fellow in infectious diseases at St. Luke’s International Hospital, Tokyo. Antifungal therapy improves outcomes, and most physicians agree that removing a CVC does, too. To better pinpoint optimal timing of catheter replacement, Dr. Matsuo and his associates examined risk factors for 30-day mortality among patients with candidemia who were treated at St. Luke’s between 2004 and 2015.
Among 228 patients with candidemia, 166 had CVCs, and 144 had their CVC removed. Among 71 patients who needed their CVC replaced, 15 died within 30 days. Central venous catheters were replaced less than 2 days after removal in 87% of patients who died and in 54% of survivors (P = .04). The association remained statistically significant after the researchers accounted for potential confounders (adjusted odds ratio, 5.9; 95% confidence interval, 1.2-29.7; P = .03).
Patients who died within 30 days of CVC replacement also were more likely to have hematologic malignancies (20% versus 4%), diabetes (13% vs. 11%), to be on hemodialysis (27% vs. 16%), and to have a history of recent corticosteroid exposure (20% versus 11%) compared with survivors, but none of these associations reached statistical significance. Furthermore, 30-day mortality was not associated with gender, age, Candida species, endophthalmitis, or type of antifungal therapy, said Dr. Matsuo, who spoke at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
An infectious disease consultation was associated with about a 70% reduction in the odds of mortality in the multivariate analysis, but the 95% confidence interval crossed 1.0, rendering the link statistically insignificant.
Given the small sample size and single-center design of this study, its findings ideally should be confirmed in a larger randomized controlled trial, Dr. Matsuo said. The investigators also did not track whether patients were fungemic at the time of CVC replacement, he noted.
The researchers reported having no conflicts of interest.
SAN DIEGO – Wait at least 2 days before replacing central venous catheters (CVC) in patients with catheter-associated candidemia, according to the results of a single-center retrospective cohort study of 228 patients.
Waiting less than 2 days to replace a CVC increased the odds of 30-day mortality nearly sixfold among patients with catheter-related bloodstream infections due to candidemia, even after controlling for potential confounders, Takahiro Matsuo, MD, said at an annual scientific meeting on infectious diseases. No other factor significantly predicted mortality in univariate or multivariate analyses, he said. “This is the first study to demonstrate the optimal timing of central venous catheter replacement in catheter-related [bloodstream infection] due to Candida.”
Invasive candidiasis is associated with mortality rates of up to 50%, noted Dr. Matsuo, who is a fellow in infectious diseases at St. Luke’s International Hospital, Tokyo. Antifungal therapy improves outcomes, and most physicians agree that removing a CVC does, too. To better pinpoint optimal timing of catheter replacement, Dr. Matsuo and his associates examined risk factors for 30-day mortality among patients with candidemia who were treated at St. Luke’s between 2004 and 2015.
Among 228 patients with candidemia, 166 had CVCs, and 144 had their CVC removed. Among 71 patients who needed their CVC replaced, 15 died within 30 days. Central venous catheters were replaced less than 2 days after removal in 87% of patients who died and in 54% of survivors (P = .04). The association remained statistically significant after the researchers accounted for potential confounders (adjusted odds ratio, 5.9; 95% confidence interval, 1.2-29.7; P = .03).
Patients who died within 30 days of CVC replacement also were more likely to have hematologic malignancies (20% versus 4%), diabetes (13% vs. 11%), to be on hemodialysis (27% vs. 16%), and to have a history of recent corticosteroid exposure (20% versus 11%) compared with survivors, but none of these associations reached statistical significance. Furthermore, 30-day mortality was not associated with gender, age, Candida species, endophthalmitis, or type of antifungal therapy, said Dr. Matsuo, who spoke at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
An infectious disease consultation was associated with about a 70% reduction in the odds of mortality in the multivariate analysis, but the 95% confidence interval crossed 1.0, rendering the link statistically insignificant.
Given the small sample size and single-center design of this study, its findings ideally should be confirmed in a larger randomized controlled trial, Dr. Matsuo said. The investigators also did not track whether patients were fungemic at the time of CVC replacement, he noted.
The researchers reported having no conflicts of interest.
AT IDWEEK 2017
Key clinical point: Consider waiting at least 2 days to replace a central venous catheter that has been removed because of candidemia.
Major finding: (odds ratio, 5.9; 95% confidence interval, 1.2-27.3).
Data source: A single-center retrospective cohort study of 228 patients with candidemia.
Disclosures: The researchers reported having no conflicts of interest.
Ciprofloxacin cured gyrA wild-type Neisseria gonorrhoeae infections
SAN DIEGO – Ciprofloxacin cured 100% of gyrase A wild-type Neisseria gonorrhoeae infections, and physicians prescribed it significantly more frequently when they received electronic reminders of test results and recommendations, in a single-center study.
“Recent reports of untreatable gonorrhea have caused great concern. Treatment with ceftriaxone may be a major driver of resistance, and reducing its use may curb the emergence of resistant infections,” Lao-Tzu Allan-Blitz, a medical student at the David Geffen School of Medicine at the University of California, Los Angeles, said at an annual scientific meeting on infectious diseases.
The Centers for Disease Control and Prevention ranks multidrug-resistant N. gonorrhoeae third among all drug-resistant threats in the United States, Mr. Allan-Blitz noted during an oral presentation at the meeting. Beginning in the late 1990s, strains of N. gonorrhoeae developed resistance to sulfanilamides, penicillin, tetracycline, and fluoroquinolones, leaving only the extended-spectrum cephalosporins for empiric treatment. Recent reports of cephalosporin-resistant N. gonorrhoeae in other countries have raised the specter of untreatable gonorrhea.
Because antimicrobial resistance can shift in response to selective pressure, experts are exploring the use of antibiotics once considered ineffective for treating N. gonorrhoeae infections. At UCLA, researchers developed a real-time reverse transcription polymerase chain reaction test for a mutation of codon 91 in the gyrase A (gyrA) gene in N. gonorrhoeae that reliably predicts resistance to ciprofloxacin.
Test results take 24-48 hours. The test is not Food and Drug Administration approved but has been validated in accordance with Clinical Laboratory Improvement Amendments, Mr. Allan-Blitz said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
In November 2015, UCLA Health began gyrA genotyping all N. gonorrhoeae positive specimens, and in May 2016, it began sending providers electronic reminders of genotype results and treatment recommendations. For gyrA wild-type infections, UCLA Health recommends 500 mg oral ciprofloxacin, Mr. Allan-Blitz said.
Initial test-of-cure data are promising. All 25 patients with wild-type infections who received ciprofloxacin and returned 7-90 days later tested negative for N. gonorrhoeae. Culture sites included the urethra (seven cases), pharynx (seven cases), rectum (seven cases), and genitals (four cases), Mr. Allan-Blitz said. “Prior studies have demonstrated that reminder notifications improve uptake of antimicrobial stewardship,” he said. “Other health centers should consider implementing the gyrA assay, and using reminder notifications may improve uptake by providers.”
The National Institutes of Health provided funding. The investigators reported having no conflicts of interest.
SAN DIEGO – Ciprofloxacin cured 100% of gyrase A wild-type Neisseria gonorrhoeae infections, and physicians prescribed it significantly more frequently when they received electronic reminders of test results and recommendations, in a single-center study.
“Recent reports of untreatable gonorrhea have caused great concern. Treatment with ceftriaxone may be a major driver of resistance, and reducing its use may curb the emergence of resistant infections,” Lao-Tzu Allan-Blitz, a medical student at the David Geffen School of Medicine at the University of California, Los Angeles, said at an annual scientific meeting on infectious diseases.
The Centers for Disease Control and Prevention ranks multidrug-resistant N. gonorrhoeae third among all drug-resistant threats in the United States, Mr. Allan-Blitz noted during an oral presentation at the meeting. Beginning in the late 1990s, strains of N. gonorrhoeae developed resistance to sulfanilamides, penicillin, tetracycline, and fluoroquinolones, leaving only the extended-spectrum cephalosporins for empiric treatment. Recent reports of cephalosporin-resistant N. gonorrhoeae in other countries have raised the specter of untreatable gonorrhea.
Because antimicrobial resistance can shift in response to selective pressure, experts are exploring the use of antibiotics once considered ineffective for treating N. gonorrhoeae infections. At UCLA, researchers developed a real-time reverse transcription polymerase chain reaction test for a mutation of codon 91 in the gyrase A (gyrA) gene in N. gonorrhoeae that reliably predicts resistance to ciprofloxacin.
Test results take 24-48 hours. The test is not Food and Drug Administration approved but has been validated in accordance with Clinical Laboratory Improvement Amendments, Mr. Allan-Blitz said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
In November 2015, UCLA Health began gyrA genotyping all N. gonorrhoeae positive specimens, and in May 2016, it began sending providers electronic reminders of genotype results and treatment recommendations. For gyrA wild-type infections, UCLA Health recommends 500 mg oral ciprofloxacin, Mr. Allan-Blitz said.
Initial test-of-cure data are promising. All 25 patients with wild-type infections who received ciprofloxacin and returned 7-90 days later tested negative for N. gonorrhoeae. Culture sites included the urethra (seven cases), pharynx (seven cases), rectum (seven cases), and genitals (four cases), Mr. Allan-Blitz said. “Prior studies have demonstrated that reminder notifications improve uptake of antimicrobial stewardship,” he said. “Other health centers should consider implementing the gyrA assay, and using reminder notifications may improve uptake by providers.”
The National Institutes of Health provided funding. The investigators reported having no conflicts of interest.
SAN DIEGO – Ciprofloxacin cured 100% of gyrase A wild-type Neisseria gonorrhoeae infections, and physicians prescribed it significantly more frequently when they received electronic reminders of test results and recommendations, in a single-center study.
“Recent reports of untreatable gonorrhea have caused great concern. Treatment with ceftriaxone may be a major driver of resistance, and reducing its use may curb the emergence of resistant infections,” Lao-Tzu Allan-Blitz, a medical student at the David Geffen School of Medicine at the University of California, Los Angeles, said at an annual scientific meeting on infectious diseases.
The Centers for Disease Control and Prevention ranks multidrug-resistant N. gonorrhoeae third among all drug-resistant threats in the United States, Mr. Allan-Blitz noted during an oral presentation at the meeting. Beginning in the late 1990s, strains of N. gonorrhoeae developed resistance to sulfanilamides, penicillin, tetracycline, and fluoroquinolones, leaving only the extended-spectrum cephalosporins for empiric treatment. Recent reports of cephalosporin-resistant N. gonorrhoeae in other countries have raised the specter of untreatable gonorrhea.
Because antimicrobial resistance can shift in response to selective pressure, experts are exploring the use of antibiotics once considered ineffective for treating N. gonorrhoeae infections. At UCLA, researchers developed a real-time reverse transcription polymerase chain reaction test for a mutation of codon 91 in the gyrase A (gyrA) gene in N. gonorrhoeae that reliably predicts resistance to ciprofloxacin.
Test results take 24-48 hours. The test is not Food and Drug Administration approved but has been validated in accordance with Clinical Laboratory Improvement Amendments, Mr. Allan-Blitz said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
In November 2015, UCLA Health began gyrA genotyping all N. gonorrhoeae positive specimens, and in May 2016, it began sending providers electronic reminders of genotype results and treatment recommendations. For gyrA wild-type infections, UCLA Health recommends 500 mg oral ciprofloxacin, Mr. Allan-Blitz said.
Initial test-of-cure data are promising. All 25 patients with wild-type infections who received ciprofloxacin and returned 7-90 days later tested negative for N. gonorrhoeae. Culture sites included the urethra (seven cases), pharynx (seven cases), rectum (seven cases), and genitals (four cases), Mr. Allan-Blitz said. “Prior studies have demonstrated that reminder notifications improve uptake of antimicrobial stewardship,” he said. “Other health centers should consider implementing the gyrA assay, and using reminder notifications may improve uptake by providers.”
The National Institutes of Health provided funding. The investigators reported having no conflicts of interest.
AT IDWEEK 2017
Key clinical point:
Major finding: The cure rate was 100% among 25 patients who received ciprofloxacin for wild-type gyrA gonorrhea.
Data source: A single-center study of 582 patients with gonorrhea.
Disclosures: The National Institutes of Health provided funding. The investigators reported having no conflicts of interest.
Rectal swabs concurred with stool tests in children with GI illness
SAN DIEGO – Clinicians who treat children with acute gastrointestinal illness should consider testing rectal swabs when they need to rapidly identify enteropathogens and cannot immediately obtain a bulk stool sample, Stephen Freedman, MD, said at an annual scientific meeting on infectious diseases.
Among 1,519 children and adolescents with diarrhea, vomiting, or both symptoms, diagnostic yields of paired stool and rectal swab specimens were 76% and 68%, respectively, Dr. Freedman reported on behalf of the Alberta Provincial Pediatric Enteric Infection Team.
Kappa values for concordance were 0.76 overall (95% confidence interval [CI], 0.71-0.80), .82 for viruses (0.79-0.86), and .74 for bacteria (0.68-0.80). A kappa value between 0.61 and 0.80 indicates “substantial” concordance between two results, while a value between 0.81 and 1.0 suggests “near perfect” concordance, explained Dr. Freedman of the University of Calgary (Alta.). In addition, 95% of health care providers and 82% of home caregivers considered rectal swabs easy to use, while 10% considered them unacceptable. “Recommendations against rectal swab use should be reconsidered,” he said.
Traditional testing of diarrheal bulk stool is highly specific, but burdensome and subject to various handling issues that can substantially delay diagnosis and outbreak detection, Dr. Freedman said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
“Flocked rectal swabs are used at the point of care and are quick and acceptable, but there are few precedents in the literature for their use in children or in patients with vomiting without diarrhea,” he said.
To help fill that gap, the researchers collected 1,147 stool specimens and 1,468 rectal swabs from patients under age 18 years who were seen at emergency departments in Calgary and Edmonton for diarrhea, vomiting, or both, with at least three episodes in the previous 24 hours. All of the patients had been ill for less than 7 days and had no detected psychiatric illness or neutropenia. Stool and rectal samples were evaluated three ways – by routine enteric bacterial culture, an in-house gastroenteric viral panel, and with the polymerase chain reaction-based Luminex xTAG Gastrointestinal Pathogen Panel. Swabs were taken by rotating them 360 degrees one time within the anus. Stool and swab specimens collected at home were stored at room temperature for less than 12 hours.
Among all paired specimens, 76% of stool samples and 68% of rectal swabs tested positive for at least one pathogen (P less than .0001). Thus, stool testing had about a 30% higher odds of detection than did swab testing in the same patient (OR, 1.3; 95% CI, 1.3-1.5). Odds ratios also favored stool testing in subgroups of patients with diarrhea (OR, 1.2; 95% CI, 1.1-1.4) or isolated vomiting (OR, 1.8; 95% CI, 1.5-2.1).
However, many stool specimens were never submitted, Dr. Freedman said. When the researchers assumed that these unsubmitted samples all tested negative, the diagnostic yield of stool samples fell to 57% and several odds ratios inverted in favor of rectal swabs. The study findings did not change when the researchers excluded positive results for Clostridium difficile in children younger than 2 years or when they restricted the analysis to paired specimens obtained within 24 hours.
The researchers are continuing to explore the diagnostic yield of rectal swab tests for multidrug-resistant pathogens, including those that are notifiable to public health departments, Dr. Freedman said.
Dr. Freedman disclosed ties to Copan Diagnostics, Luminex, and Alere.
SAN DIEGO – Clinicians who treat children with acute gastrointestinal illness should consider testing rectal swabs when they need to rapidly identify enteropathogens and cannot immediately obtain a bulk stool sample, Stephen Freedman, MD, said at an annual scientific meeting on infectious diseases.
Among 1,519 children and adolescents with diarrhea, vomiting, or both symptoms, diagnostic yields of paired stool and rectal swab specimens were 76% and 68%, respectively, Dr. Freedman reported on behalf of the Alberta Provincial Pediatric Enteric Infection Team.
Kappa values for concordance were 0.76 overall (95% confidence interval [CI], 0.71-0.80), .82 for viruses (0.79-0.86), and .74 for bacteria (0.68-0.80). A kappa value between 0.61 and 0.80 indicates “substantial” concordance between two results, while a value between 0.81 and 1.0 suggests “near perfect” concordance, explained Dr. Freedman of the University of Calgary (Alta.). In addition, 95% of health care providers and 82% of home caregivers considered rectal swabs easy to use, while 10% considered them unacceptable. “Recommendations against rectal swab use should be reconsidered,” he said.
Traditional testing of diarrheal bulk stool is highly specific, but burdensome and subject to various handling issues that can substantially delay diagnosis and outbreak detection, Dr. Freedman said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
“Flocked rectal swabs are used at the point of care and are quick and acceptable, but there are few precedents in the literature for their use in children or in patients with vomiting without diarrhea,” he said.
To help fill that gap, the researchers collected 1,147 stool specimens and 1,468 rectal swabs from patients under age 18 years who were seen at emergency departments in Calgary and Edmonton for diarrhea, vomiting, or both, with at least three episodes in the previous 24 hours. All of the patients had been ill for less than 7 days and had no detected psychiatric illness or neutropenia. Stool and rectal samples were evaluated three ways – by routine enteric bacterial culture, an in-house gastroenteric viral panel, and with the polymerase chain reaction-based Luminex xTAG Gastrointestinal Pathogen Panel. Swabs were taken by rotating them 360 degrees one time within the anus. Stool and swab specimens collected at home were stored at room temperature for less than 12 hours.
Among all paired specimens, 76% of stool samples and 68% of rectal swabs tested positive for at least one pathogen (P less than .0001). Thus, stool testing had about a 30% higher odds of detection than did swab testing in the same patient (OR, 1.3; 95% CI, 1.3-1.5). Odds ratios also favored stool testing in subgroups of patients with diarrhea (OR, 1.2; 95% CI, 1.1-1.4) or isolated vomiting (OR, 1.8; 95% CI, 1.5-2.1).
However, many stool specimens were never submitted, Dr. Freedman said. When the researchers assumed that these unsubmitted samples all tested negative, the diagnostic yield of stool samples fell to 57% and several odds ratios inverted in favor of rectal swabs. The study findings did not change when the researchers excluded positive results for Clostridium difficile in children younger than 2 years or when they restricted the analysis to paired specimens obtained within 24 hours.
The researchers are continuing to explore the diagnostic yield of rectal swab tests for multidrug-resistant pathogens, including those that are notifiable to public health departments, Dr. Freedman said.
Dr. Freedman disclosed ties to Copan Diagnostics, Luminex, and Alere.
SAN DIEGO – Clinicians who treat children with acute gastrointestinal illness should consider testing rectal swabs when they need to rapidly identify enteropathogens and cannot immediately obtain a bulk stool sample, Stephen Freedman, MD, said at an annual scientific meeting on infectious diseases.
Among 1,519 children and adolescents with diarrhea, vomiting, or both symptoms, diagnostic yields of paired stool and rectal swab specimens were 76% and 68%, respectively, Dr. Freedman reported on behalf of the Alberta Provincial Pediatric Enteric Infection Team.
Kappa values for concordance were 0.76 overall (95% confidence interval [CI], 0.71-0.80), .82 for viruses (0.79-0.86), and .74 for bacteria (0.68-0.80). A kappa value between 0.61 and 0.80 indicates “substantial” concordance between two results, while a value between 0.81 and 1.0 suggests “near perfect” concordance, explained Dr. Freedman of the University of Calgary (Alta.). In addition, 95% of health care providers and 82% of home caregivers considered rectal swabs easy to use, while 10% considered them unacceptable. “Recommendations against rectal swab use should be reconsidered,” he said.
Traditional testing of diarrheal bulk stool is highly specific, but burdensome and subject to various handling issues that can substantially delay diagnosis and outbreak detection, Dr. Freedman said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
“Flocked rectal swabs are used at the point of care and are quick and acceptable, but there are few precedents in the literature for their use in children or in patients with vomiting without diarrhea,” he said.
To help fill that gap, the researchers collected 1,147 stool specimens and 1,468 rectal swabs from patients under age 18 years who were seen at emergency departments in Calgary and Edmonton for diarrhea, vomiting, or both, with at least three episodes in the previous 24 hours. All of the patients had been ill for less than 7 days and had no detected psychiatric illness or neutropenia. Stool and rectal samples were evaluated three ways – by routine enteric bacterial culture, an in-house gastroenteric viral panel, and with the polymerase chain reaction-based Luminex xTAG Gastrointestinal Pathogen Panel. Swabs were taken by rotating them 360 degrees one time within the anus. Stool and swab specimens collected at home were stored at room temperature for less than 12 hours.
Among all paired specimens, 76% of stool samples and 68% of rectal swabs tested positive for at least one pathogen (P less than .0001). Thus, stool testing had about a 30% higher odds of detection than did swab testing in the same patient (OR, 1.3; 95% CI, 1.3-1.5). Odds ratios also favored stool testing in subgroups of patients with diarrhea (OR, 1.2; 95% CI, 1.1-1.4) or isolated vomiting (OR, 1.8; 95% CI, 1.5-2.1).
However, many stool specimens were never submitted, Dr. Freedman said. When the researchers assumed that these unsubmitted samples all tested negative, the diagnostic yield of stool samples fell to 57% and several odds ratios inverted in favor of rectal swabs. The study findings did not change when the researchers excluded positive results for Clostridium difficile in children younger than 2 years or when they restricted the analysis to paired specimens obtained within 24 hours.
The researchers are continuing to explore the diagnostic yield of rectal swab tests for multidrug-resistant pathogens, including those that are notifiable to public health departments, Dr. Freedman said.
Dr. Freedman disclosed ties to Copan Diagnostics, Luminex, and Alere.
AT IDWEEK 2017
Key clinical point: and cannot immediately obtain a bulk stool sample.
Major finding: Diagnostic yields of paired stool and rectal swab specimens were 76% and 68%, respectively.
Data source: A multicenter retrospective cohort study of 1,519 children and adolescents with acute-onset diarrhea, vomiting, or both.
Disclosures: Dr. Freedman disclosed ties to Copan Diagnostics, Luminex, and Alere.
Steroids underused in bacterial meningitis despite low risk
SAN DIEGO – Physicians often skipped out on using steroids when treating bacterial meningitis even though the benefits clearly outweigh the risks, Cinthia Gallegos, MD, reported during an oral presentation at an annual meeting on infectious diseases.
In a recent multicenter retrospective cohort study, only 40% of adults with bacterial meningitis received steroids within 4 hours of hospital admission, as recommended by the European Society of Clinical Microbiology and Infectious Diseases (ESCMID), and only 14% received steroids concomitantly or 10-20 minutes prior to antibiotic initiation, as recommended by the Infectious Diseases Society of America (IDSA), said Dr. Gallegos, an infectious disease fellow at University of Texas, Houston.
“Steroids are being underutilized in our patient population,” she said. “And when steroids are used, they are being used later than is recommended.”
To evaluate the prevalence of guideline-concordant steroid use, Dr. Gallegos and her associates analyzed the medical records of 120 adults with culture-confirmed, community-acquired bacterial meningitis treated at 10 Houston-area hospitals between 2008 and 2016.
Median duration of steroid therapy was 4 hours, which is consistent with IDSA guidelines, she noted.
Among the five patients (4%) who developed delayed cerebral thrombosis, three had Streptococcus pneumoniae meningitis, one had methicillin-resistant Staphylococcus aureus meningitis, and one had Listeria meningitis. All had received either dexamethasone monotherapy or dexamethasone and methylprednisolone within 4 hours of antibiotic initiation. They showed an initial improvement in clinical course, including normal CT and MRI, but their clinical condition deteriorated between 5 and 12 days later. “Repeat imaging showed thrombosis of different areas of the brain,” Dr. Gallegos said. Two patients died, two developed moderate or severe disability, and one fully recovered. The patients ranged in age from 26 to 69; three were male, and two were female.
The 4% rate closely resembles what is seen in the Netherlands, said Diederik van de Beek, MD, PhD, of the Academic Medical Center in Amsterdam, who comoderated the session at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. “We have some recent data where we did autopsies of cases and we saw a huge amount of bacterial fragments around the blood vessels,” he said. “We have seen this in previous autopsy studies, but here it was a massive amount of bacterial fragments.”
Researchers have suggested that delayed cerebral thrombosis in bacterial meningitis results from increases in C5a and C5b-9 levels in the cerebrospinal fluid and from an increase in the tissue factor VII pathway, Dr. Gallegos said.
Researchers think that these patients historically developed vasculitis, but that this complication “has disappeared somewhat in the dexamethasone era,” said Dr. van de Beek, lead author of the 2016 ESCMID guidelines on bacterial meningitis. “It appears that some patients are ‘pro-inflammatory’ and still react 7-9 days after treatment,” he said. “The difficult question is whether we give 4 days of steroids or longer. A clinical trial is not feasible, so we [recommend] 4 days.”
Left untreated, bacterial meningitis is fatal in up to 70% of cases, and about one in five survivors faces limb loss or neurologic disability, according to the Centers for Disease Control and Prevention. The advent of penicillin and other antibiotics dramatically improved survival, but death rates remained around 10% for meningitis associated with Neisseria meningitides and Haemophilus influenza infection, and often exceeded 30% for S. pneumoniae meningitis. “That’s important because besides antibiotics, the only treatment that decreases mortality has been shown to be steroids,” Dr. Gallegos said.
High-quality evidence supports their use. In a double-blind, randomized, multicenter trial of 301 adults with bacterial meningitis, adjunctive dexamethasone was associated with a 50% improvement in mortality, compared with adjunctive placebo (N Engl J Med. 2002 Nov 14;347[20]:1549-56). Other data confirm that steroids do not prevent vancomycin from concentrating in CSF or increase the risk of hippocampal apoptosis. But although both IDSA and ESCMID endorse steroids as adjunctive therapy to help control intracranial pressure in patients with bacterial meningitis, studies have shown much higher rates of steroid use in the Netherlands, Sweden, and Denmark than in the United States.
The Grant A. Starr Foundation provided funding. The investigators had no conflicts of interest.
SAN DIEGO – Physicians often skipped out on using steroids when treating bacterial meningitis even though the benefits clearly outweigh the risks, Cinthia Gallegos, MD, reported during an oral presentation at an annual meeting on infectious diseases.
In a recent multicenter retrospective cohort study, only 40% of adults with bacterial meningitis received steroids within 4 hours of hospital admission, as recommended by the European Society of Clinical Microbiology and Infectious Diseases (ESCMID), and only 14% received steroids concomitantly or 10-20 minutes prior to antibiotic initiation, as recommended by the Infectious Diseases Society of America (IDSA), said Dr. Gallegos, an infectious disease fellow at University of Texas, Houston.
“Steroids are being underutilized in our patient population,” she said. “And when steroids are used, they are being used later than is recommended.”
To evaluate the prevalence of guideline-concordant steroid use, Dr. Gallegos and her associates analyzed the medical records of 120 adults with culture-confirmed, community-acquired bacterial meningitis treated at 10 Houston-area hospitals between 2008 and 2016.
Median duration of steroid therapy was 4 hours, which is consistent with IDSA guidelines, she noted.
Among the five patients (4%) who developed delayed cerebral thrombosis, three had Streptococcus pneumoniae meningitis, one had methicillin-resistant Staphylococcus aureus meningitis, and one had Listeria meningitis. All had received either dexamethasone monotherapy or dexamethasone and methylprednisolone within 4 hours of antibiotic initiation. They showed an initial improvement in clinical course, including normal CT and MRI, but their clinical condition deteriorated between 5 and 12 days later. “Repeat imaging showed thrombosis of different areas of the brain,” Dr. Gallegos said. Two patients died, two developed moderate or severe disability, and one fully recovered. The patients ranged in age from 26 to 69; three were male, and two were female.
The 4% rate closely resembles what is seen in the Netherlands, said Diederik van de Beek, MD, PhD, of the Academic Medical Center in Amsterdam, who comoderated the session at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. “We have some recent data where we did autopsies of cases and we saw a huge amount of bacterial fragments around the blood vessels,” he said. “We have seen this in previous autopsy studies, but here it was a massive amount of bacterial fragments.”
Researchers have suggested that delayed cerebral thrombosis in bacterial meningitis results from increases in C5a and C5b-9 levels in the cerebrospinal fluid and from an increase in the tissue factor VII pathway, Dr. Gallegos said.
Researchers think that these patients historically developed vasculitis, but that this complication “has disappeared somewhat in the dexamethasone era,” said Dr. van de Beek, lead author of the 2016 ESCMID guidelines on bacterial meningitis. “It appears that some patients are ‘pro-inflammatory’ and still react 7-9 days after treatment,” he said. “The difficult question is whether we give 4 days of steroids or longer. A clinical trial is not feasible, so we [recommend] 4 days.”
Left untreated, bacterial meningitis is fatal in up to 70% of cases, and about one in five survivors faces limb loss or neurologic disability, according to the Centers for Disease Control and Prevention. The advent of penicillin and other antibiotics dramatically improved survival, but death rates remained around 10% for meningitis associated with Neisseria meningitides and Haemophilus influenza infection, and often exceeded 30% for S. pneumoniae meningitis. “That’s important because besides antibiotics, the only treatment that decreases mortality has been shown to be steroids,” Dr. Gallegos said.
High-quality evidence supports their use. In a double-blind, randomized, multicenter trial of 301 adults with bacterial meningitis, adjunctive dexamethasone was associated with a 50% improvement in mortality, compared with adjunctive placebo (N Engl J Med. 2002 Nov 14;347[20]:1549-56). Other data confirm that steroids do not prevent vancomycin from concentrating in CSF or increase the risk of hippocampal apoptosis. But although both IDSA and ESCMID endorse steroids as adjunctive therapy to help control intracranial pressure in patients with bacterial meningitis, studies have shown much higher rates of steroid use in the Netherlands, Sweden, and Denmark than in the United States.
The Grant A. Starr Foundation provided funding. The investigators had no conflicts of interest.
SAN DIEGO – Physicians often skipped out on using steroids when treating bacterial meningitis even though the benefits clearly outweigh the risks, Cinthia Gallegos, MD, reported during an oral presentation at an annual meeting on infectious diseases.
In a recent multicenter retrospective cohort study, only 40% of adults with bacterial meningitis received steroids within 4 hours of hospital admission, as recommended by the European Society of Clinical Microbiology and Infectious Diseases (ESCMID), and only 14% received steroids concomitantly or 10-20 minutes prior to antibiotic initiation, as recommended by the Infectious Diseases Society of America (IDSA), said Dr. Gallegos, an infectious disease fellow at University of Texas, Houston.
“Steroids are being underutilized in our patient population,” she said. “And when steroids are used, they are being used later than is recommended.”
To evaluate the prevalence of guideline-concordant steroid use, Dr. Gallegos and her associates analyzed the medical records of 120 adults with culture-confirmed, community-acquired bacterial meningitis treated at 10 Houston-area hospitals between 2008 and 2016.
Median duration of steroid therapy was 4 hours, which is consistent with IDSA guidelines, she noted.
Among the five patients (4%) who developed delayed cerebral thrombosis, three had Streptococcus pneumoniae meningitis, one had methicillin-resistant Staphylococcus aureus meningitis, and one had Listeria meningitis. All had received either dexamethasone monotherapy or dexamethasone and methylprednisolone within 4 hours of antibiotic initiation. They showed an initial improvement in clinical course, including normal CT and MRI, but their clinical condition deteriorated between 5 and 12 days later. “Repeat imaging showed thrombosis of different areas of the brain,” Dr. Gallegos said. Two patients died, two developed moderate or severe disability, and one fully recovered. The patients ranged in age from 26 to 69; three were male, and two were female.
The 4% rate closely resembles what is seen in the Netherlands, said Diederik van de Beek, MD, PhD, of the Academic Medical Center in Amsterdam, who comoderated the session at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. “We have some recent data where we did autopsies of cases and we saw a huge amount of bacterial fragments around the blood vessels,” he said. “We have seen this in previous autopsy studies, but here it was a massive amount of bacterial fragments.”
Researchers have suggested that delayed cerebral thrombosis in bacterial meningitis results from increases in C5a and C5b-9 levels in the cerebrospinal fluid and from an increase in the tissue factor VII pathway, Dr. Gallegos said.
Researchers think that these patients historically developed vasculitis, but that this complication “has disappeared somewhat in the dexamethasone era,” said Dr. van de Beek, lead author of the 2016 ESCMID guidelines on bacterial meningitis. “It appears that some patients are ‘pro-inflammatory’ and still react 7-9 days after treatment,” he said. “The difficult question is whether we give 4 days of steroids or longer. A clinical trial is not feasible, so we [recommend] 4 days.”
Left untreated, bacterial meningitis is fatal in up to 70% of cases, and about one in five survivors faces limb loss or neurologic disability, according to the Centers for Disease Control and Prevention. The advent of penicillin and other antibiotics dramatically improved survival, but death rates remained around 10% for meningitis associated with Neisseria meningitides and Haemophilus influenza infection, and often exceeded 30% for S. pneumoniae meningitis. “That’s important because besides antibiotics, the only treatment that decreases mortality has been shown to be steroids,” Dr. Gallegos said.
High-quality evidence supports their use. In a double-blind, randomized, multicenter trial of 301 adults with bacterial meningitis, adjunctive dexamethasone was associated with a 50% improvement in mortality, compared with adjunctive placebo (N Engl J Med. 2002 Nov 14;347[20]:1549-56). Other data confirm that steroids do not prevent vancomycin from concentrating in CSF or increase the risk of hippocampal apoptosis. But although both IDSA and ESCMID endorse steroids as adjunctive therapy to help control intracranial pressure in patients with bacterial meningitis, studies have shown much higher rates of steroid use in the Netherlands, Sweden, and Denmark than in the United States.
The Grant A. Starr Foundation provided funding. The investigators had no conflicts of interest.
AT IDWEEK 2017
Key clinical point:
Major finding: Five of 120 (4%) of patients developed delayed cerebral thrombosis. Only 40% received steroids within the maximum recommended time frame.
Data source: A retrospective multicenter study of 120 adults with culture-confirmed bacterial meningitis.
Disclosures: The Grant A. Starr Foundation provided funding. The investigators had no conflicts of interest.
C. auris: ‘A yeast that acts like a bacteria’
SAN DIEGO – The rise of Candida auris as a superbug represents a paradigm shift, because, in the words of Dr. Tom M. Chiller, it’s a yeast that acts like a bacteria.
“Treatment resistance is now the norm,” Dr. Chiller, chief of the mycotic diseases branch at the Centers for Disease Control and Prevention, Atlanta, said an annual scientific meeting on infectious diseases. “It thrives on skin, it contaminates patient rooms, and it spreads readily in health care settings.”
Since it was first described in Japan in 2009, C. auris has been identified in multiple countries in four continents, including the United States, prompting the CDC to issue a clinical alert to health care facilities in June of 2016. To date, more than 130 cases have been reported in 10 states, mostly in New York and New Jersey. At the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society, Dr. Chiller said that C. auris is a challenging superbug for four main reasons:
It’s not easily identified
Matrix assisted laser desorption ionization–time of flight (MALDI-TOF) or DNA sequencing are required to make the diagnosis. “It turns out that only about 25% of clinical labs have MALDI-TOF available, so we’re still lacking in our ability to identify it,” he said.
It’s easily transmitted
C. auris “is really happy in a hospital room,” Dr. Chiller said. “You can grow it from the floor, on the bottom of shoes, and on hand alcohol dispensers. It also likes the skin, and it also likes to grow in slightly higher temperatures. You find it readily in the axilla and groin. Those are the main locations we’re using for developing screening culture techniques.”
It’s difficult to treat
Treatment, if clinically indicated, includes an echinocandin such as micafungin, anidulafungin, and caspofungin at standard dosing. However, there have been cases of development of resistance to echinocandins while on therapy. “That bothers me,” Dr. Chiller said. “We don’t like to see that happen, and I am concerned. These bugs are really happy to be resistant, but based on the epidemiology, we remain convinced that it’s important to treat with an echinocandin.”
It can cause severe invasive disease and death
Global epidemiologic evaluation of the first 50 or so cases found that some patients were on antifungal treatment when C. auris was isolated. The mortality was greater than 60%, and there was a clustering in some hospitals. “Some hospitals reported that up to 40% of candidemia cases were from C. auris,” he said.
Among cases in the United States to date, the median age of affected patients is 70 years and patients’ 30-day mortality is about 30%. “They were quite ill, with multiple underlying conditions and indwelling devices,” Dr. Chiller said. They had “extensive health care exposure” with stays in acute care hospitals and nursing homes with ventilator units, and several recent cases with travel and health care exposures abroad, mainly to India, Pakistan, Venezuela, and South Africa.
Clinicians should report suspected cases to their local health department or to the CDC at candidaauris@cdc.gov.
“We also want them to implement and reinforce infection control measures,” Dr. Chiller advised. “Get the lab to review other potential Candida cases or Candida species you might have. Conduct contact tracing to identify other colonized patients, and consider point-prevalence surveys.”
He reported having no financial disclosures.
SAN DIEGO – The rise of Candida auris as a superbug represents a paradigm shift, because, in the words of Dr. Tom M. Chiller, it’s a yeast that acts like a bacteria.
“Treatment resistance is now the norm,” Dr. Chiller, chief of the mycotic diseases branch at the Centers for Disease Control and Prevention, Atlanta, said an annual scientific meeting on infectious diseases. “It thrives on skin, it contaminates patient rooms, and it spreads readily in health care settings.”
Since it was first described in Japan in 2009, C. auris has been identified in multiple countries in four continents, including the United States, prompting the CDC to issue a clinical alert to health care facilities in June of 2016. To date, more than 130 cases have been reported in 10 states, mostly in New York and New Jersey. At the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society, Dr. Chiller said that C. auris is a challenging superbug for four main reasons:
It’s not easily identified
Matrix assisted laser desorption ionization–time of flight (MALDI-TOF) or DNA sequencing are required to make the diagnosis. “It turns out that only about 25% of clinical labs have MALDI-TOF available, so we’re still lacking in our ability to identify it,” he said.
It’s easily transmitted
C. auris “is really happy in a hospital room,” Dr. Chiller said. “You can grow it from the floor, on the bottom of shoes, and on hand alcohol dispensers. It also likes the skin, and it also likes to grow in slightly higher temperatures. You find it readily in the axilla and groin. Those are the main locations we’re using for developing screening culture techniques.”
It’s difficult to treat
Treatment, if clinically indicated, includes an echinocandin such as micafungin, anidulafungin, and caspofungin at standard dosing. However, there have been cases of development of resistance to echinocandins while on therapy. “That bothers me,” Dr. Chiller said. “We don’t like to see that happen, and I am concerned. These bugs are really happy to be resistant, but based on the epidemiology, we remain convinced that it’s important to treat with an echinocandin.”
It can cause severe invasive disease and death
Global epidemiologic evaluation of the first 50 or so cases found that some patients were on antifungal treatment when C. auris was isolated. The mortality was greater than 60%, and there was a clustering in some hospitals. “Some hospitals reported that up to 40% of candidemia cases were from C. auris,” he said.
Among cases in the United States to date, the median age of affected patients is 70 years and patients’ 30-day mortality is about 30%. “They were quite ill, with multiple underlying conditions and indwelling devices,” Dr. Chiller said. They had “extensive health care exposure” with stays in acute care hospitals and nursing homes with ventilator units, and several recent cases with travel and health care exposures abroad, mainly to India, Pakistan, Venezuela, and South Africa.
Clinicians should report suspected cases to their local health department or to the CDC at candidaauris@cdc.gov.
“We also want them to implement and reinforce infection control measures,” Dr. Chiller advised. “Get the lab to review other potential Candida cases or Candida species you might have. Conduct contact tracing to identify other colonized patients, and consider point-prevalence surveys.”
He reported having no financial disclosures.
SAN DIEGO – The rise of Candida auris as a superbug represents a paradigm shift, because, in the words of Dr. Tom M. Chiller, it’s a yeast that acts like a bacteria.
“Treatment resistance is now the norm,” Dr. Chiller, chief of the mycotic diseases branch at the Centers for Disease Control and Prevention, Atlanta, said an annual scientific meeting on infectious diseases. “It thrives on skin, it contaminates patient rooms, and it spreads readily in health care settings.”
Since it was first described in Japan in 2009, C. auris has been identified in multiple countries in four continents, including the United States, prompting the CDC to issue a clinical alert to health care facilities in June of 2016. To date, more than 130 cases have been reported in 10 states, mostly in New York and New Jersey. At the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society, Dr. Chiller said that C. auris is a challenging superbug for four main reasons:
It’s not easily identified
Matrix assisted laser desorption ionization–time of flight (MALDI-TOF) or DNA sequencing are required to make the diagnosis. “It turns out that only about 25% of clinical labs have MALDI-TOF available, so we’re still lacking in our ability to identify it,” he said.
It’s easily transmitted
C. auris “is really happy in a hospital room,” Dr. Chiller said. “You can grow it from the floor, on the bottom of shoes, and on hand alcohol dispensers. It also likes the skin, and it also likes to grow in slightly higher temperatures. You find it readily in the axilla and groin. Those are the main locations we’re using for developing screening culture techniques.”
It’s difficult to treat
Treatment, if clinically indicated, includes an echinocandin such as micafungin, anidulafungin, and caspofungin at standard dosing. However, there have been cases of development of resistance to echinocandins while on therapy. “That bothers me,” Dr. Chiller said. “We don’t like to see that happen, and I am concerned. These bugs are really happy to be resistant, but based on the epidemiology, we remain convinced that it’s important to treat with an echinocandin.”
It can cause severe invasive disease and death
Global epidemiologic evaluation of the first 50 or so cases found that some patients were on antifungal treatment when C. auris was isolated. The mortality was greater than 60%, and there was a clustering in some hospitals. “Some hospitals reported that up to 40% of candidemia cases were from C. auris,” he said.
Among cases in the United States to date, the median age of affected patients is 70 years and patients’ 30-day mortality is about 30%. “They were quite ill, with multiple underlying conditions and indwelling devices,” Dr. Chiller said. They had “extensive health care exposure” with stays in acute care hospitals and nursing homes with ventilator units, and several recent cases with travel and health care exposures abroad, mainly to India, Pakistan, Venezuela, and South Africa.
Clinicians should report suspected cases to their local health department or to the CDC at candidaauris@cdc.gov.
“We also want them to implement and reinforce infection control measures,” Dr. Chiller advised. “Get the lab to review other potential Candida cases or Candida species you might have. Conduct contact tracing to identify other colonized patients, and consider point-prevalence surveys.”
He reported having no financial disclosures.
REPORTING FROM ID WEEK 2017