User login
American College of Surgeons (ACS): Annual Clinical Congress
High NLR predicts poor survival in trauma patients
CHICAGO – A high neutrophil to lymphocyte ratio on days 2 and 5 of surgical ICU hospitalization independently predicts increased mortality in critically ill trauma patients, an award-winning study showed.
The risk of death was two times higher for patients with a neutrophil to lymphocyte ratio (NLR) of at least 10.45 on day 2 (adjusted hazard ratio, 2.07; 95% confidence interval, 1.38-3.13; P = .001) and 5.7 times higher for those with an NLR of at least 7.91 on day 5 (adjusted HR, 5.79; 95% CI, 2.93-11.44; P less than .001) in a multivariate analysis, after adjustment for age 65 years or older, male sex, a systolic blood pressure of 90 mm Hg or less, a Glasgow Coma Scale (GCS) score of 8 or less, an Injury Severity Score (ISS) of at least 25, and operation on admission.
“The neutrophil to lymphocyte ratio is easily accessible, the calculation is simple, it adds no additional costs, and virtually all critically ill patients will have these labs,” study author Dr. Evren Dilektasli said at the American College of Surgeons annual clinical congress.
The simple calculation has been shown to be useful in the diagnosis of appendicitis and to be associated with overall survivalin metastatic colorectal cancer, but its association with mortality in trauma patients is not known, he said.
The retrospective cohort comprised 1,356 trauma patients, at least 16 years old, admitted to the Los Angeles County–University of Southern California Medical Center surgical ICU between January 2013 and January 2014. The median NLR was calculated for each day of the surgical ICU stay. At baseline, 16% of patients had an ISS of at least 25, 16.5% had a GCS of 8 or less, 4.5% had a systolic BP of 90 mm Hg or less, 74.3% were male, 23.7% were aged 65 or older, and 86% had a blunt injury. The most common operations on admission were laparotomy (39.6%) and craniectomy/craniotomy (20.7%).
In receiver operating characteristic (ROC) analysis for the first 10 days of hospitalization, the area under the curve (AUC) values for predicting mortality were between 0.55 on day 1 and a high of 0.79 on day 5, Dr. Dilektasli reported.
Starting from day 2 to day 10, the AUCs were statistically significant for predicting mortality.
The NLRs on day 2 (AUC, 0.73; P less than .001) and day 5 (AUC, 0.79; P less than .001) were selected in order to adjust for the clinical probability of early and late complications, he said.
Subsequent ROC curve analysis revealed an NLR cutoff of 10.45 on day 2 (AUC, 0.73; sensitivity, 73.2%; specificity, 61.8%) and a cutoff of 7.91 on day 5 (AUC, 0.79; sensitivity, 82.8%; specificity, 65.2%).
A high NLR on day 2 (at least 10.45) versus a low NLR (less than 10.45) was associated with significantly more ventilator days (5 days vs. 3 days), a longer surgical ICU length of stay (5 days vs. 3 days), a longer hospital stay (11 days vs. 8 days), and greater mortality (18.3% vs. 4.8%; all P values less than .001), reported Dr. Dilektasli, who was a research fellow at USC at the time of the study and has returned to Turkey to continue his training.
On day 5, a high NLR (at least 7.91) versus a low NLR (less than 7.91) was associated with significantly more ventilator days (7 days vs. 4 days; P less than .001), a longer surgical ICU stay (9 days vs. 5 days; P less than .001), and increased mortality (20.4% vs. 2.8%; P less than .001), but not a longer hospital stay (17 days vs. 14 days; P = .119).
In Kaplan-Meier analysis, a significant difference was observed between the high and low NLR groups on day 2 (log rank P less than .001) and day 5 (log rank P less than .001), he said.
“NLR may be a promising tool for assessing the risk of in-hospital mortality,” Dr. Dilektasli concluded. “Prospective external validation is warranted in a larger heterogeneous trauma population.”
During a discussion of the study, it was noted that the ROC curves were impressive, but that other biologic markers known to be associated with poor survival such as C-reactive protein level and class II major hepatitis C expression should have been included in the analysis.
When asked whether any patients with a low NLR on day 2 went on to have a high NLR on day 5, Dr. Dilektasli said there were such patients and that they also had an increased risk of death.
The findings of the study, which earned an excellence in research award, are only an “observation” at this point and are not being used in clinical practice, he added.
The authors reported having no relevant financial conflicts of interest.
CHICAGO – A high neutrophil to lymphocyte ratio on days 2 and 5 of surgical ICU hospitalization independently predicts increased mortality in critically ill trauma patients, an award-winning study showed.
The risk of death was two times higher for patients with a neutrophil to lymphocyte ratio (NLR) of at least 10.45 on day 2 (adjusted hazard ratio, 2.07; 95% confidence interval, 1.38-3.13; P = .001) and 5.7 times higher for those with an NLR of at least 7.91 on day 5 (adjusted HR, 5.79; 95% CI, 2.93-11.44; P less than .001) in a multivariate analysis, after adjustment for age 65 years or older, male sex, a systolic blood pressure of 90 mm Hg or less, a Glasgow Coma Scale (GCS) score of 8 or less, an Injury Severity Score (ISS) of at least 25, and operation on admission.
“The neutrophil to lymphocyte ratio is easily accessible, the calculation is simple, it adds no additional costs, and virtually all critically ill patients will have these labs,” study author Dr. Evren Dilektasli said at the American College of Surgeons annual clinical congress.
The simple calculation has been shown to be useful in the diagnosis of appendicitis and to be associated with overall survivalin metastatic colorectal cancer, but its association with mortality in trauma patients is not known, he said.
The retrospective cohort comprised 1,356 trauma patients, at least 16 years old, admitted to the Los Angeles County–University of Southern California Medical Center surgical ICU between January 2013 and January 2014. The median NLR was calculated for each day of the surgical ICU stay. At baseline, 16% of patients had an ISS of at least 25, 16.5% had a GCS of 8 or less, 4.5% had a systolic BP of 90 mm Hg or less, 74.3% were male, 23.7% were aged 65 or older, and 86% had a blunt injury. The most common operations on admission were laparotomy (39.6%) and craniectomy/craniotomy (20.7%).
In receiver operating characteristic (ROC) analysis for the first 10 days of hospitalization, the area under the curve (AUC) values for predicting mortality were between 0.55 on day 1 and a high of 0.79 on day 5, Dr. Dilektasli reported.
Starting from day 2 to day 10, the AUCs were statistically significant for predicting mortality.
The NLRs on day 2 (AUC, 0.73; P less than .001) and day 5 (AUC, 0.79; P less than .001) were selected in order to adjust for the clinical probability of early and late complications, he said.
Subsequent ROC curve analysis revealed an NLR cutoff of 10.45 on day 2 (AUC, 0.73; sensitivity, 73.2%; specificity, 61.8%) and a cutoff of 7.91 on day 5 (AUC, 0.79; sensitivity, 82.8%; specificity, 65.2%).
A high NLR on day 2 (at least 10.45) versus a low NLR (less than 10.45) was associated with significantly more ventilator days (5 days vs. 3 days), a longer surgical ICU length of stay (5 days vs. 3 days), a longer hospital stay (11 days vs. 8 days), and greater mortality (18.3% vs. 4.8%; all P values less than .001), reported Dr. Dilektasli, who was a research fellow at USC at the time of the study and has returned to Turkey to continue his training.
On day 5, a high NLR (at least 7.91) versus a low NLR (less than 7.91) was associated with significantly more ventilator days (7 days vs. 4 days; P less than .001), a longer surgical ICU stay (9 days vs. 5 days; P less than .001), and increased mortality (20.4% vs. 2.8%; P less than .001), but not a longer hospital stay (17 days vs. 14 days; P = .119).
In Kaplan-Meier analysis, a significant difference was observed between the high and low NLR groups on day 2 (log rank P less than .001) and day 5 (log rank P less than .001), he said.
“NLR may be a promising tool for assessing the risk of in-hospital mortality,” Dr. Dilektasli concluded. “Prospective external validation is warranted in a larger heterogeneous trauma population.”
During a discussion of the study, it was noted that the ROC curves were impressive, but that other biologic markers known to be associated with poor survival such as C-reactive protein level and class II major hepatitis C expression should have been included in the analysis.
When asked whether any patients with a low NLR on day 2 went on to have a high NLR on day 5, Dr. Dilektasli said there were such patients and that they also had an increased risk of death.
The findings of the study, which earned an excellence in research award, are only an “observation” at this point and are not being used in clinical practice, he added.
The authors reported having no relevant financial conflicts of interest.
CHICAGO – A high neutrophil to lymphocyte ratio on days 2 and 5 of surgical ICU hospitalization independently predicts increased mortality in critically ill trauma patients, an award-winning study showed.
The risk of death was two times higher for patients with a neutrophil to lymphocyte ratio (NLR) of at least 10.45 on day 2 (adjusted hazard ratio, 2.07; 95% confidence interval, 1.38-3.13; P = .001) and 5.7 times higher for those with an NLR of at least 7.91 on day 5 (adjusted HR, 5.79; 95% CI, 2.93-11.44; P less than .001) in a multivariate analysis, after adjustment for age 65 years or older, male sex, a systolic blood pressure of 90 mm Hg or less, a Glasgow Coma Scale (GCS) score of 8 or less, an Injury Severity Score (ISS) of at least 25, and operation on admission.
“The neutrophil to lymphocyte ratio is easily accessible, the calculation is simple, it adds no additional costs, and virtually all critically ill patients will have these labs,” study author Dr. Evren Dilektasli said at the American College of Surgeons annual clinical congress.
The simple calculation has been shown to be useful in the diagnosis of appendicitis and to be associated with overall survivalin metastatic colorectal cancer, but its association with mortality in trauma patients is not known, he said.
The retrospective cohort comprised 1,356 trauma patients, at least 16 years old, admitted to the Los Angeles County–University of Southern California Medical Center surgical ICU between January 2013 and January 2014. The median NLR was calculated for each day of the surgical ICU stay. At baseline, 16% of patients had an ISS of at least 25, 16.5% had a GCS of 8 or less, 4.5% had a systolic BP of 90 mm Hg or less, 74.3% were male, 23.7% were aged 65 or older, and 86% had a blunt injury. The most common operations on admission were laparotomy (39.6%) and craniectomy/craniotomy (20.7%).
In receiver operating characteristic (ROC) analysis for the first 10 days of hospitalization, the area under the curve (AUC) values for predicting mortality were between 0.55 on day 1 and a high of 0.79 on day 5, Dr. Dilektasli reported.
Starting from day 2 to day 10, the AUCs were statistically significant for predicting mortality.
The NLRs on day 2 (AUC, 0.73; P less than .001) and day 5 (AUC, 0.79; P less than .001) were selected in order to adjust for the clinical probability of early and late complications, he said.
Subsequent ROC curve analysis revealed an NLR cutoff of 10.45 on day 2 (AUC, 0.73; sensitivity, 73.2%; specificity, 61.8%) and a cutoff of 7.91 on day 5 (AUC, 0.79; sensitivity, 82.8%; specificity, 65.2%).
A high NLR on day 2 (at least 10.45) versus a low NLR (less than 10.45) was associated with significantly more ventilator days (5 days vs. 3 days), a longer surgical ICU length of stay (5 days vs. 3 days), a longer hospital stay (11 days vs. 8 days), and greater mortality (18.3% vs. 4.8%; all P values less than .001), reported Dr. Dilektasli, who was a research fellow at USC at the time of the study and has returned to Turkey to continue his training.
On day 5, a high NLR (at least 7.91) versus a low NLR (less than 7.91) was associated with significantly more ventilator days (7 days vs. 4 days; P less than .001), a longer surgical ICU stay (9 days vs. 5 days; P less than .001), and increased mortality (20.4% vs. 2.8%; P less than .001), but not a longer hospital stay (17 days vs. 14 days; P = .119).
In Kaplan-Meier analysis, a significant difference was observed between the high and low NLR groups on day 2 (log rank P less than .001) and day 5 (log rank P less than .001), he said.
“NLR may be a promising tool for assessing the risk of in-hospital mortality,” Dr. Dilektasli concluded. “Prospective external validation is warranted in a larger heterogeneous trauma population.”
During a discussion of the study, it was noted that the ROC curves were impressive, but that other biologic markers known to be associated with poor survival such as C-reactive protein level and class II major hepatitis C expression should have been included in the analysis.
When asked whether any patients with a low NLR on day 2 went on to have a high NLR on day 5, Dr. Dilektasli said there were such patients and that they also had an increased risk of death.
The findings of the study, which earned an excellence in research award, are only an “observation” at this point and are not being used in clinical practice, he added.
The authors reported having no relevant financial conflicts of interest.
AT THE ACS CLINICAL CONGRESS
Key clinical point: A high neutrophil to lymphocyte ratio on day 2 and day 5 of surgical ICU admission may be a useful predictor of poor survival in trauma patients.
Major finding: The adjusted hazard ratios for mortality were 2.07 with a neutrophil to lymphocyte ratio of at least 10.45 on day 2 (95% CI, 1.38-3.13; P = .001) and 5.79 with an NLR of at least 7.91 on day 5 (95% CI, 2.93-11.44; P less than .001).
Data source: A retrospective study involving 1,356 trauma patients.
Disclosures: The authors reported having no relevant financial conflicts of interest.
Die not yet cast for lymphazurin and methylene blue dye
CHICAGO – Two commonly used dyes produced mixed results in sentinel lymph node mapping of early stage breast cancer in what was described as the highest-powered study to date.
The average number of sentinel lymph nodes identified per person was significantly higher with 1% methylene blue dye than with 1% lymphazurin (2.89 vs. 2.22; P less than .001).
Although there is extensive support for methylene blue as a safe and efficacious alternative to lymphazurin, this finding on the number of sentinel nodes identified is not replicated in any other study, Dr. Vaishali Patel said at the annual clinical congress of the American College of Surgeons. The study was conducted at the McLaren Flint (Mich.) Medical Center. Dr. Sukamal Saha was principal investigator.
On the other hand, lymphazurin identified significantly more additional lymph nodes than methylene blue (mean 4.48 vs. 2.84; P less than .001).
Nodal positivity was also significantly higher with lymphazurin than methylene blue (14.93% vs. 8.85%; P less than .001), which also has not been reported in other trials.
“We think this does offer a true comparison between the two dyes,” Dr. Patel of Detroit Medical Center Sinai-Grace Hospital said. “The volume of dye and technique were consistent for all 651 patients. … with one surgeon performing the injections and one surgeon performing the procedures.” The 651 consecutive patients were randomly assigned based on agent availability to a preoperative injection of lymphazurin (half intraparenchymal and half subareolar in the upper outer quadrant) or an intraoperative injection of methylene blue over 5 minutes (3 ccs intraparenchymal, 1 cc subareolar, and 1 cc intradermal).
The lymphazurin and methylene blue groups were also similar in number (298 patients vs. 353 patients), age (mean 61.6 years vs. 63.5 years), and T stage (in situ 12% vs. 17.8%; T1 64% vs. 65%; T2 23% vs. 17.5%).
In contrast, three smaller, well-established studies that came to different conclusions used four different surgeons and novel techniques to inject their radiocolloid and supervised residents for lymphatic mapping, she noted.
The radiocolloid lymphazurin first demonstrated superiority over methylene blue in 1990, but alternatives continue to be investigated due to frequent nonavailability and a host of adverse events including blue hives, blue discoloration or tattooing, and anaphylaxis.
Lymphazurin also costs 10-12 times more than methylene blue, which was reflected in the study in an average per patient cost of $815 vs. $75 for methylene blue, Dr. Patel said.
The American Society of Breast Surgeons, however, recommends dual-agent mapping using blue dye and a radioisotope in breast cancer to further improve the success in identifying the sentinel lymph nodes. The improvement is likely because of the dual mechanism at play: radiocolloids become entrapped within the lymph node, whereas certain blue dyes bind to interstitial albumin and are taken up by lymphatics, she explained.
The higher number of sentinel lymph nodes in the methylene blue group may be due to its particle size, which is smaller, weighs less, and diffused faster, Dr. Patel suggested.
The higher number of additional lymph nodes captured with lymphazurin may be because of the higher frequency of nodal dissection in this group than in the methylene blue group (25% vs. 16%).
The finding of greater nodal positivity in the lymphazurin group may be related to mechanism of action or the high percentage of patients with T1 disease enrolled in the study. Still, nodal positivity was higher with lymphazurin than methylene blue regardless of T stage, she said.
The lymphazurin group had higher rates than the methylene blue group of pseudohypoxemia (10% vs. 0%; P less than .0001), but blue hives (1.34% vs. 0%; P = .043) and anaphylaxis (.67% vs. 0%; P = .20) were kept in check. Patients were premedicated and early in the series, the surgeon began excising the area of injected blue skin during the primary surgery, Dr. Patel observed.
Despite being diluted, methylene blue was associated with higher rates of seroma (3.4% vs. 1.7%; P = .005) and skin necrosis (2.55% vs. 9%; P = .005).
Discussant Dr. Alyssa Throckmorton of Baptist Memorial Health Care in Memphis pointed out that more recent data show radiocolloid mapping alone is comparable to dual-agent mapping, suggesting that blue dye may not be needed. That said, there have been national shortages of methylene blue as well as lymphazurin.
“I think in surgeons who are going to use blue dye, with the way drug shortages have become in the last few years, you are going to have to be facile and familiar with both types of dye if you are going to use that as part of your clinical practice,” she said.
CHICAGO – Two commonly used dyes produced mixed results in sentinel lymph node mapping of early stage breast cancer in what was described as the highest-powered study to date.
The average number of sentinel lymph nodes identified per person was significantly higher with 1% methylene blue dye than with 1% lymphazurin (2.89 vs. 2.22; P less than .001).
Although there is extensive support for methylene blue as a safe and efficacious alternative to lymphazurin, this finding on the number of sentinel nodes identified is not replicated in any other study, Dr. Vaishali Patel said at the annual clinical congress of the American College of Surgeons. The study was conducted at the McLaren Flint (Mich.) Medical Center. Dr. Sukamal Saha was principal investigator.
On the other hand, lymphazurin identified significantly more additional lymph nodes than methylene blue (mean 4.48 vs. 2.84; P less than .001).
Nodal positivity was also significantly higher with lymphazurin than methylene blue (14.93% vs. 8.85%; P less than .001), which also has not been reported in other trials.
“We think this does offer a true comparison between the two dyes,” Dr. Patel of Detroit Medical Center Sinai-Grace Hospital said. “The volume of dye and technique were consistent for all 651 patients. … with one surgeon performing the injections and one surgeon performing the procedures.” The 651 consecutive patients were randomly assigned based on agent availability to a preoperative injection of lymphazurin (half intraparenchymal and half subareolar in the upper outer quadrant) or an intraoperative injection of methylene blue over 5 minutes (3 ccs intraparenchymal, 1 cc subareolar, and 1 cc intradermal).
The lymphazurin and methylene blue groups were also similar in number (298 patients vs. 353 patients), age (mean 61.6 years vs. 63.5 years), and T stage (in situ 12% vs. 17.8%; T1 64% vs. 65%; T2 23% vs. 17.5%).
In contrast, three smaller, well-established studies that came to different conclusions used four different surgeons and novel techniques to inject their radiocolloid and supervised residents for lymphatic mapping, she noted.
The radiocolloid lymphazurin first demonstrated superiority over methylene blue in 1990, but alternatives continue to be investigated due to frequent nonavailability and a host of adverse events including blue hives, blue discoloration or tattooing, and anaphylaxis.
Lymphazurin also costs 10-12 times more than methylene blue, which was reflected in the study in an average per patient cost of $815 vs. $75 for methylene blue, Dr. Patel said.
The American Society of Breast Surgeons, however, recommends dual-agent mapping using blue dye and a radioisotope in breast cancer to further improve the success in identifying the sentinel lymph nodes. The improvement is likely because of the dual mechanism at play: radiocolloids become entrapped within the lymph node, whereas certain blue dyes bind to interstitial albumin and are taken up by lymphatics, she explained.
The higher number of sentinel lymph nodes in the methylene blue group may be due to its particle size, which is smaller, weighs less, and diffused faster, Dr. Patel suggested.
The higher number of additional lymph nodes captured with lymphazurin may be because of the higher frequency of nodal dissection in this group than in the methylene blue group (25% vs. 16%).
The finding of greater nodal positivity in the lymphazurin group may be related to mechanism of action or the high percentage of patients with T1 disease enrolled in the study. Still, nodal positivity was higher with lymphazurin than methylene blue regardless of T stage, she said.
The lymphazurin group had higher rates than the methylene blue group of pseudohypoxemia (10% vs. 0%; P less than .0001), but blue hives (1.34% vs. 0%; P = .043) and anaphylaxis (.67% vs. 0%; P = .20) were kept in check. Patients were premedicated and early in the series, the surgeon began excising the area of injected blue skin during the primary surgery, Dr. Patel observed.
Despite being diluted, methylene blue was associated with higher rates of seroma (3.4% vs. 1.7%; P = .005) and skin necrosis (2.55% vs. 9%; P = .005).
Discussant Dr. Alyssa Throckmorton of Baptist Memorial Health Care in Memphis pointed out that more recent data show radiocolloid mapping alone is comparable to dual-agent mapping, suggesting that blue dye may not be needed. That said, there have been national shortages of methylene blue as well as lymphazurin.
“I think in surgeons who are going to use blue dye, with the way drug shortages have become in the last few years, you are going to have to be facile and familiar with both types of dye if you are going to use that as part of your clinical practice,” she said.
CHICAGO – Two commonly used dyes produced mixed results in sentinel lymph node mapping of early stage breast cancer in what was described as the highest-powered study to date.
The average number of sentinel lymph nodes identified per person was significantly higher with 1% methylene blue dye than with 1% lymphazurin (2.89 vs. 2.22; P less than .001).
Although there is extensive support for methylene blue as a safe and efficacious alternative to lymphazurin, this finding on the number of sentinel nodes identified is not replicated in any other study, Dr. Vaishali Patel said at the annual clinical congress of the American College of Surgeons. The study was conducted at the McLaren Flint (Mich.) Medical Center. Dr. Sukamal Saha was principal investigator.
On the other hand, lymphazurin identified significantly more additional lymph nodes than methylene blue (mean 4.48 vs. 2.84; P less than .001).
Nodal positivity was also significantly higher with lymphazurin than methylene blue (14.93% vs. 8.85%; P less than .001), which also has not been reported in other trials.
“We think this does offer a true comparison between the two dyes,” Dr. Patel of Detroit Medical Center Sinai-Grace Hospital said. “The volume of dye and technique were consistent for all 651 patients. … with one surgeon performing the injections and one surgeon performing the procedures.” The 651 consecutive patients were randomly assigned based on agent availability to a preoperative injection of lymphazurin (half intraparenchymal and half subareolar in the upper outer quadrant) or an intraoperative injection of methylene blue over 5 minutes (3 ccs intraparenchymal, 1 cc subareolar, and 1 cc intradermal).
The lymphazurin and methylene blue groups were also similar in number (298 patients vs. 353 patients), age (mean 61.6 years vs. 63.5 years), and T stage (in situ 12% vs. 17.8%; T1 64% vs. 65%; T2 23% vs. 17.5%).
In contrast, three smaller, well-established studies that came to different conclusions used four different surgeons and novel techniques to inject their radiocolloid and supervised residents for lymphatic mapping, she noted.
The radiocolloid lymphazurin first demonstrated superiority over methylene blue in 1990, but alternatives continue to be investigated due to frequent nonavailability and a host of adverse events including blue hives, blue discoloration or tattooing, and anaphylaxis.
Lymphazurin also costs 10-12 times more than methylene blue, which was reflected in the study in an average per patient cost of $815 vs. $75 for methylene blue, Dr. Patel said.
The American Society of Breast Surgeons, however, recommends dual-agent mapping using blue dye and a radioisotope in breast cancer to further improve the success in identifying the sentinel lymph nodes. The improvement is likely because of the dual mechanism at play: radiocolloids become entrapped within the lymph node, whereas certain blue dyes bind to interstitial albumin and are taken up by lymphatics, she explained.
The higher number of sentinel lymph nodes in the methylene blue group may be due to its particle size, which is smaller, weighs less, and diffused faster, Dr. Patel suggested.
The higher number of additional lymph nodes captured with lymphazurin may be because of the higher frequency of nodal dissection in this group than in the methylene blue group (25% vs. 16%).
The finding of greater nodal positivity in the lymphazurin group may be related to mechanism of action or the high percentage of patients with T1 disease enrolled in the study. Still, nodal positivity was higher with lymphazurin than methylene blue regardless of T stage, she said.
The lymphazurin group had higher rates than the methylene blue group of pseudohypoxemia (10% vs. 0%; P less than .0001), but blue hives (1.34% vs. 0%; P = .043) and anaphylaxis (.67% vs. 0%; P = .20) were kept in check. Patients were premedicated and early in the series, the surgeon began excising the area of injected blue skin during the primary surgery, Dr. Patel observed.
Despite being diluted, methylene blue was associated with higher rates of seroma (3.4% vs. 1.7%; P = .005) and skin necrosis (2.55% vs. 9%; P = .005).
Discussant Dr. Alyssa Throckmorton of Baptist Memorial Health Care in Memphis pointed out that more recent data show radiocolloid mapping alone is comparable to dual-agent mapping, suggesting that blue dye may not be needed. That said, there have been national shortages of methylene blue as well as lymphazurin.
“I think in surgeons who are going to use blue dye, with the way drug shortages have become in the last few years, you are going to have to be facile and familiar with both types of dye if you are going to use that as part of your clinical practice,” she said.
AT THE ACS CLINICAL CONGRESS
Key clinical point: Contrary to prior studies, lymph node positivity was higher with lymphazurin than methylene blue in patients with early breast cancer.
Major finding: Nodal positivity was 14.93% with lymphazurin vs. 8.85% with methylene blue (P less than .001).
Data source: Prospective study in 651 patients undergoing lymphatic mapping for breast cancer.
Disclosures: Dr. Patel and Dr. Throckmorton reported having no relevant conflicts.
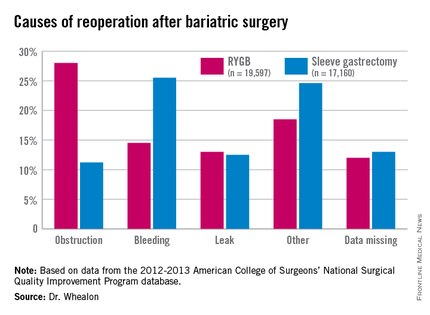
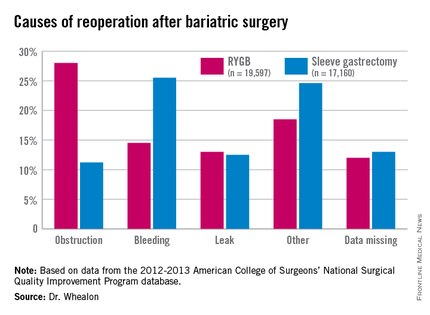
Reoperation risk doubled in Roux-en-Y over sleeve gastrectomy
CHICAGO – Patients undergoing Roux-en-Y gastric bypass are twice as likely to need a reoperation as those having sleeve gastrectomy, according to ACS NSQIP data.
Reoperation among Roux-en-Y patients was associated with a 10-fold increase in mortality over sleeve gastrectomy (1.2% vs. 0.1%; P less than .01) and a 3-fold increase in length of stay (6 days vs. 2 days; P less than .01), Dr. Matthew Whealon reported at the American College of Surgeons Clinical Congress
The results are consistent with prior contemporary analyses using ACS National Surgical Quality Improvement Program (NSQIP) data reporting reoperation rates of 2.5%-5.1% for Roux-en-Y gastric bypass (RYGB) and 1.6%-3% for sleeve gastrectomy. Those analyses, however, did not include the reasons for reoperation, as these data were not available until the 2012 database release, he said.
With these data now in hand, lead author Dr. Mark Hanna and his fellow investigators at the University of California, Irvine, identified 36,757 adults in the 2012-2013 database who underwent RYGB (n = 19,597) or sleeve gastrectomy (n = 17,160) for morbid obesity and performed multivariate regression analyses to identify risk factors associated with reoperation.
In all, 518 RYGB patients and 231 sleeve gastrectomy patients required an unplanned return to the operating room (2.6% vs. 1.3%), Dr. Whealon said. The mean time from the index procedure to reoperation was 7.6 days and 7.1 days, respectively.
Obstruction was the biggest driver of reoperation following RYGB, accounting for 28% of reoperations. Other causes were bleeding (14.5%), leak (13%), and other unspecified reasons (18.5%), with data missing in 12%.
Bleeding was the most common indication for reoperation after sleeve gastrectomy (25.5%), followed by other unspecified reasons(24.6%), missing data (13%), leak (12.55%), and obstruction (11.2%), he said.
In adjusted multivariate analyses, factors that significantly increased the risk for reoperation were heart failure (adjusted odds ratio, 2.3), dependent functional status (aOR, 2.1), RYGB (aOR, 1.94), chronic obstructive pulmonary disease (aOR, 1.7), open operation (aOR, 1.6), and male sex (aOR, 1.1). The P values were less than .05 for all comparisons.
Factors not significant for reoperation included body mass index, age, smoking status, bleeding disorder, steroid use, dialysis, hypertension, diabetes, preoperative sepsis, emergent admission, elective operation, and preoperative weight loss.
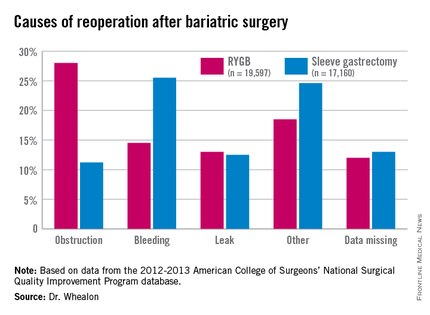
While bariatric surgery remains a safe operation with low mortality and reoperation rates, additional studies are needed, because of the increased mortality associated with reoperation, to identify ways to mitigate these complications, Dr. Whealon said.
Limitations of the study were that ICD-9 codes for postoperative hemorrhage could not differentiate between intra-abdominal and gastrointestinal bleeding, the database is subject to coding errors, and missing data may have introduced bias into the study, he noted.
Discussant Dr. Matthew Goldblatt of the Medical College of Wisconsin in Milwaukee commented that use of the ACS MBSAQIP (Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program) database would have avoided some of the coding errors for reoperation.
He also questioned whether the average 7-day return to surgery interval reflects the use of endoscopy, as few surgeons would wait that long if, as the analysis suggests, a primary reason for reoperation was postoperative bleeding.
Endoscopy was included in the reoperations, Dr. Whealon said, but he could not speak to the exact percentage it comprised.
Finally, Dr. Goldblatt said, “the patients that you identified as being the highest risk for complication, as is often the case in these reviews, are really the ones most likely to gain the most from the procedure. … So how can people avoid operating on these patients when they are the ones that can get the most out of it?”
Dr. Whealon agreed that high-risk patients have the most to gain and suggested that “optimizing their comorbid conditions before operation will help reduce their risk.”
The authors reported having no conflicts of interest.
CHICAGO – Patients undergoing Roux-en-Y gastric bypass are twice as likely to need a reoperation as those having sleeve gastrectomy, according to ACS NSQIP data.
Reoperation among Roux-en-Y patients was associated with a 10-fold increase in mortality over sleeve gastrectomy (1.2% vs. 0.1%; P less than .01) and a 3-fold increase in length of stay (6 days vs. 2 days; P less than .01), Dr. Matthew Whealon reported at the American College of Surgeons Clinical Congress
The results are consistent with prior contemporary analyses using ACS National Surgical Quality Improvement Program (NSQIP) data reporting reoperation rates of 2.5%-5.1% for Roux-en-Y gastric bypass (RYGB) and 1.6%-3% for sleeve gastrectomy. Those analyses, however, did not include the reasons for reoperation, as these data were not available until the 2012 database release, he said.
With these data now in hand, lead author Dr. Mark Hanna and his fellow investigators at the University of California, Irvine, identified 36,757 adults in the 2012-2013 database who underwent RYGB (n = 19,597) or sleeve gastrectomy (n = 17,160) for morbid obesity and performed multivariate regression analyses to identify risk factors associated with reoperation.
In all, 518 RYGB patients and 231 sleeve gastrectomy patients required an unplanned return to the operating room (2.6% vs. 1.3%), Dr. Whealon said. The mean time from the index procedure to reoperation was 7.6 days and 7.1 days, respectively.
Obstruction was the biggest driver of reoperation following RYGB, accounting for 28% of reoperations. Other causes were bleeding (14.5%), leak (13%), and other unspecified reasons (18.5%), with data missing in 12%.
Bleeding was the most common indication for reoperation after sleeve gastrectomy (25.5%), followed by other unspecified reasons(24.6%), missing data (13%), leak (12.55%), and obstruction (11.2%), he said.
In adjusted multivariate analyses, factors that significantly increased the risk for reoperation were heart failure (adjusted odds ratio, 2.3), dependent functional status (aOR, 2.1), RYGB (aOR, 1.94), chronic obstructive pulmonary disease (aOR, 1.7), open operation (aOR, 1.6), and male sex (aOR, 1.1). The P values were less than .05 for all comparisons.
Factors not significant for reoperation included body mass index, age, smoking status, bleeding disorder, steroid use, dialysis, hypertension, diabetes, preoperative sepsis, emergent admission, elective operation, and preoperative weight loss.
While bariatric surgery remains a safe operation with low mortality and reoperation rates, additional studies are needed, because of the increased mortality associated with reoperation, to identify ways to mitigate these complications, Dr. Whealon said.
Limitations of the study were that ICD-9 codes for postoperative hemorrhage could not differentiate between intra-abdominal and gastrointestinal bleeding, the database is subject to coding errors, and missing data may have introduced bias into the study, he noted.
Discussant Dr. Matthew Goldblatt of the Medical College of Wisconsin in Milwaukee commented that use of the ACS MBSAQIP (Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program) database would have avoided some of the coding errors for reoperation.
He also questioned whether the average 7-day return to surgery interval reflects the use of endoscopy, as few surgeons would wait that long if, as the analysis suggests, a primary reason for reoperation was postoperative bleeding.
Endoscopy was included in the reoperations, Dr. Whealon said, but he could not speak to the exact percentage it comprised.
Finally, Dr. Goldblatt said, “the patients that you identified as being the highest risk for complication, as is often the case in these reviews, are really the ones most likely to gain the most from the procedure. … So how can people avoid operating on these patients when they are the ones that can get the most out of it?”
Dr. Whealon agreed that high-risk patients have the most to gain and suggested that “optimizing their comorbid conditions before operation will help reduce their risk.”
The authors reported having no conflicts of interest.
CHICAGO – Patients undergoing Roux-en-Y gastric bypass are twice as likely to need a reoperation as those having sleeve gastrectomy, according to ACS NSQIP data.
Reoperation among Roux-en-Y patients was associated with a 10-fold increase in mortality over sleeve gastrectomy (1.2% vs. 0.1%; P less than .01) and a 3-fold increase in length of stay (6 days vs. 2 days; P less than .01), Dr. Matthew Whealon reported at the American College of Surgeons Clinical Congress
The results are consistent with prior contemporary analyses using ACS National Surgical Quality Improvement Program (NSQIP) data reporting reoperation rates of 2.5%-5.1% for Roux-en-Y gastric bypass (RYGB) and 1.6%-3% for sleeve gastrectomy. Those analyses, however, did not include the reasons for reoperation, as these data were not available until the 2012 database release, he said.
With these data now in hand, lead author Dr. Mark Hanna and his fellow investigators at the University of California, Irvine, identified 36,757 adults in the 2012-2013 database who underwent RYGB (n = 19,597) or sleeve gastrectomy (n = 17,160) for morbid obesity and performed multivariate regression analyses to identify risk factors associated with reoperation.
In all, 518 RYGB patients and 231 sleeve gastrectomy patients required an unplanned return to the operating room (2.6% vs. 1.3%), Dr. Whealon said. The mean time from the index procedure to reoperation was 7.6 days and 7.1 days, respectively.
Obstruction was the biggest driver of reoperation following RYGB, accounting for 28% of reoperations. Other causes were bleeding (14.5%), leak (13%), and other unspecified reasons (18.5%), with data missing in 12%.
Bleeding was the most common indication for reoperation after sleeve gastrectomy (25.5%), followed by other unspecified reasons(24.6%), missing data (13%), leak (12.55%), and obstruction (11.2%), he said.
In adjusted multivariate analyses, factors that significantly increased the risk for reoperation were heart failure (adjusted odds ratio, 2.3), dependent functional status (aOR, 2.1), RYGB (aOR, 1.94), chronic obstructive pulmonary disease (aOR, 1.7), open operation (aOR, 1.6), and male sex (aOR, 1.1). The P values were less than .05 for all comparisons.
Factors not significant for reoperation included body mass index, age, smoking status, bleeding disorder, steroid use, dialysis, hypertension, diabetes, preoperative sepsis, emergent admission, elective operation, and preoperative weight loss.
While bariatric surgery remains a safe operation with low mortality and reoperation rates, additional studies are needed, because of the increased mortality associated with reoperation, to identify ways to mitigate these complications, Dr. Whealon said.
Limitations of the study were that ICD-9 codes for postoperative hemorrhage could not differentiate between intra-abdominal and gastrointestinal bleeding, the database is subject to coding errors, and missing data may have introduced bias into the study, he noted.
Discussant Dr. Matthew Goldblatt of the Medical College of Wisconsin in Milwaukee commented that use of the ACS MBSAQIP (Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program) database would have avoided some of the coding errors for reoperation.
He also questioned whether the average 7-day return to surgery interval reflects the use of endoscopy, as few surgeons would wait that long if, as the analysis suggests, a primary reason for reoperation was postoperative bleeding.
Endoscopy was included in the reoperations, Dr. Whealon said, but he could not speak to the exact percentage it comprised.
Finally, Dr. Goldblatt said, “the patients that you identified as being the highest risk for complication, as is often the case in these reviews, are really the ones most likely to gain the most from the procedure. … So how can people avoid operating on these patients when they are the ones that can get the most out of it?”
Dr. Whealon agreed that high-risk patients have the most to gain and suggested that “optimizing their comorbid conditions before operation will help reduce their risk.”
The authors reported having no conflicts of interest.
AT THE ACS CLINICAL CONGRESS
Key clinical point: Patients undergoing Roux-en-Y gastric bypass were twice as likely to need a reoperation as with sleeve gastrectomy, and reoperation increased morbidity 10-fold.
Major finding: The reoperation rate for Roux-en-Y gastric bypass was 2.6% vs. 1.3% for sleeve gastrectomy.
Data source: An ACS NSQIP database analysis of 36,757 patients undergoing bariatric surgery.
Disclosures: The authors reported having no conflicts of interest.
ACS: Infected hernia salvage success most likely with lightweight polypropylene
CHICAGO – Infected ventral hernia mesh is most likely to be salvaged if it’s made from lightweight polypropylene, according to data from a series of 161 mesh infection cases at Carolinas Medical Center in Charlotte, N.C.
Investigators there were able to salvage 33% of lightweight polypropylene and 8% of polytetrafluoroethylene mesh patients, but salvage failed in patients with composite, polyester, or heavyweight polypropylene meshes. The overall salvage rate was less than 10%.
“We sometimes think that we’ve salvaged the mesh, but if we follow these patients long enough” – follow-up was an average of 37 months in the series – “the majority of them will need to be excised,” said investigator Dr. Vedra Augenstein of the department of surgery at the medical center.
Wound complications are common in ventral hernia repairs, and mesh infections, said Dr. Augenstein, are among “the most dreaded.” The North Carolina findings help define the small pool of patients in whom salvage might work.
The average body mass index in the series was 36 kg/m2, and patients had an average of 2.6 previous ventral hernia repairs. The majority had a polypropylene mesh. Most of the cases were referred to the medical center from elsewhere, so mesh excision came an average of 10 months after the diagnosis of infection.
Almost a third of patients had their infections diagnosed a year or more after mesh implant, which goes against the common notion that mesh patients are out of the woods after a year. “It took a very long time for some of these infections to present. This was a big surprise for us,” Dr. Augenstein said.
The team tried to salvage all of their patients, using antibiotics in 90%, vacuum-assisted closure and/or debridement in 57%, and percutaneous drainage in 17%.
No patient presented with an obvious fistula, but the investigators found fistulas during surgery in about 16% of patients. Meanwhile, salvage failed in every patient who continued to smoke despite being diagnosed with a mesh infection.
The team assembled their findings into an informal algorithm for considering mesh salvage.
“Think about what you need to ask yourself. First, does the patient have a fistula or do you suspect one” from, for instance, gut bacteria in the wound or oral contrast above the mesh on CT? If so, “they are going to need an operation,” Dr. Augenstein said.
Smoking is the next stop point; salvage is likely to fail in smokers.
Mesh type is the third consideration; lightweight polypropylene is a good sign. “If they have heavyweight polypropylene, composite, or polyester mesh, they were not salvageable in our series,” she said.
For patients still in the running, Methicillin-resistant Staphylococcus aureus (MRSA) is the next concern. If it’s in the wound, mesh is going to be harder to salvage, said Dr. Augenstein. Most of the infections in the series were caused by Staphylococcus, with MRSA present in 45% of patients.
Infection recurrence is common even when salvage seems to work, so “we need to follow these patients for a very, very long time,” Dr. Augenstein said.
Along with clinical exams, the North Carolina team follows C-reactive protein and erythrocyte sedimentation rate. “If the abdomen gets red or if, for example, the C-reactive protein goes up, we’ll do a CT scan or ultrasound to make sure they are not brewing an infection,” she said.
Dr. Augenstein has received research and educational grants from Gore, Ethicon, Novadaq, Bard, and LifeCell.
CHICAGO – Infected ventral hernia mesh is most likely to be salvaged if it’s made from lightweight polypropylene, according to data from a series of 161 mesh infection cases at Carolinas Medical Center in Charlotte, N.C.
Investigators there were able to salvage 33% of lightweight polypropylene and 8% of polytetrafluoroethylene mesh patients, but salvage failed in patients with composite, polyester, or heavyweight polypropylene meshes. The overall salvage rate was less than 10%.
“We sometimes think that we’ve salvaged the mesh, but if we follow these patients long enough” – follow-up was an average of 37 months in the series – “the majority of them will need to be excised,” said investigator Dr. Vedra Augenstein of the department of surgery at the medical center.
Wound complications are common in ventral hernia repairs, and mesh infections, said Dr. Augenstein, are among “the most dreaded.” The North Carolina findings help define the small pool of patients in whom salvage might work.
The average body mass index in the series was 36 kg/m2, and patients had an average of 2.6 previous ventral hernia repairs. The majority had a polypropylene mesh. Most of the cases were referred to the medical center from elsewhere, so mesh excision came an average of 10 months after the diagnosis of infection.
Almost a third of patients had their infections diagnosed a year or more after mesh implant, which goes against the common notion that mesh patients are out of the woods after a year. “It took a very long time for some of these infections to present. This was a big surprise for us,” Dr. Augenstein said.
The team tried to salvage all of their patients, using antibiotics in 90%, vacuum-assisted closure and/or debridement in 57%, and percutaneous drainage in 17%.
No patient presented with an obvious fistula, but the investigators found fistulas during surgery in about 16% of patients. Meanwhile, salvage failed in every patient who continued to smoke despite being diagnosed with a mesh infection.
The team assembled their findings into an informal algorithm for considering mesh salvage.
“Think about what you need to ask yourself. First, does the patient have a fistula or do you suspect one” from, for instance, gut bacteria in the wound or oral contrast above the mesh on CT? If so, “they are going to need an operation,” Dr. Augenstein said.
Smoking is the next stop point; salvage is likely to fail in smokers.
Mesh type is the third consideration; lightweight polypropylene is a good sign. “If they have heavyweight polypropylene, composite, or polyester mesh, they were not salvageable in our series,” she said.
For patients still in the running, Methicillin-resistant Staphylococcus aureus (MRSA) is the next concern. If it’s in the wound, mesh is going to be harder to salvage, said Dr. Augenstein. Most of the infections in the series were caused by Staphylococcus, with MRSA present in 45% of patients.
Infection recurrence is common even when salvage seems to work, so “we need to follow these patients for a very, very long time,” Dr. Augenstein said.
Along with clinical exams, the North Carolina team follows C-reactive protein and erythrocyte sedimentation rate. “If the abdomen gets red or if, for example, the C-reactive protein goes up, we’ll do a CT scan or ultrasound to make sure they are not brewing an infection,” she said.
Dr. Augenstein has received research and educational grants from Gore, Ethicon, Novadaq, Bard, and LifeCell.
CHICAGO – Infected ventral hernia mesh is most likely to be salvaged if it’s made from lightweight polypropylene, according to data from a series of 161 mesh infection cases at Carolinas Medical Center in Charlotte, N.C.
Investigators there were able to salvage 33% of lightweight polypropylene and 8% of polytetrafluoroethylene mesh patients, but salvage failed in patients with composite, polyester, or heavyweight polypropylene meshes. The overall salvage rate was less than 10%.
“We sometimes think that we’ve salvaged the mesh, but if we follow these patients long enough” – follow-up was an average of 37 months in the series – “the majority of them will need to be excised,” said investigator Dr. Vedra Augenstein of the department of surgery at the medical center.
Wound complications are common in ventral hernia repairs, and mesh infections, said Dr. Augenstein, are among “the most dreaded.” The North Carolina findings help define the small pool of patients in whom salvage might work.
The average body mass index in the series was 36 kg/m2, and patients had an average of 2.6 previous ventral hernia repairs. The majority had a polypropylene mesh. Most of the cases were referred to the medical center from elsewhere, so mesh excision came an average of 10 months after the diagnosis of infection.
Almost a third of patients had their infections diagnosed a year or more after mesh implant, which goes against the common notion that mesh patients are out of the woods after a year. “It took a very long time for some of these infections to present. This was a big surprise for us,” Dr. Augenstein said.
The team tried to salvage all of their patients, using antibiotics in 90%, vacuum-assisted closure and/or debridement in 57%, and percutaneous drainage in 17%.
No patient presented with an obvious fistula, but the investigators found fistulas during surgery in about 16% of patients. Meanwhile, salvage failed in every patient who continued to smoke despite being diagnosed with a mesh infection.
The team assembled their findings into an informal algorithm for considering mesh salvage.
“Think about what you need to ask yourself. First, does the patient have a fistula or do you suspect one” from, for instance, gut bacteria in the wound or oral contrast above the mesh on CT? If so, “they are going to need an operation,” Dr. Augenstein said.
Smoking is the next stop point; salvage is likely to fail in smokers.
Mesh type is the third consideration; lightweight polypropylene is a good sign. “If they have heavyweight polypropylene, composite, or polyester mesh, they were not salvageable in our series,” she said.
For patients still in the running, Methicillin-resistant Staphylococcus aureus (MRSA) is the next concern. If it’s in the wound, mesh is going to be harder to salvage, said Dr. Augenstein. Most of the infections in the series were caused by Staphylococcus, with MRSA present in 45% of patients.
Infection recurrence is common even when salvage seems to work, so “we need to follow these patients for a very, very long time,” Dr. Augenstein said.
Along with clinical exams, the North Carolina team follows C-reactive protein and erythrocyte sedimentation rate. “If the abdomen gets red or if, for example, the C-reactive protein goes up, we’ll do a CT scan or ultrasound to make sure they are not brewing an infection,” she said.
Dr. Augenstein has received research and educational grants from Gore, Ethicon, Novadaq, Bard, and LifeCell.
AT THE ACS CLINICAL CONGRESS
Key clinical point: The ideal infected mesh salvage candidate is a MRSA-free nonsmoker with a lightweight polypropylene implant and no fistulas.
Major finding: Mesh salvage worked in about a third of lightweight polypropylene patients and 8% of polytetrafluoroethylene mesh patients but failed in patients with composite, polyester, or heavyweight polypropylene meshes.
Data source: Series of 161 infected ventral hernia mesh patients.
Disclosures: The presenting investigator has received research and educational grants from Gore, Ethicon, Novadaq, Bard, and LifeCell.
ACS: Watchful waiting for some rectal cancers almost ready for ‘prime time’
CHICAGO – Watchful waiting with careful surveillance may become an option for the majority of locally advanced rectal cancer patients who have a complete clinical response to neoadjuvant therapy, according to a review of 442 rectal cancer patients at Memorial Sloan Kettering Cancer Center in New York.
Seventy-three of those patients had a complete clinical response to neoadjuvant therapy and opted for watchful waiting instead of surgery after weighing the risks and benefits – including about a 25% chance of local recurrence – with their doctors.
At 4 years’ follow-up, 54 (74%) remained cancer free. Nineteen patients had local tumor recurrence, generally within 13 months. Two of those patients had successful local excisions, and the remaining 17 had salvage total mesorectal excisions (TME).
There were no statistically significant differences in 4-year disease-specific and overall survival among the 73 patients and 72 other patients who opted for TME after neoadjuvant chemotherapy and were found to have had pathologic complete responses.
“In our cohort, watch and wait was safe. It’s an effective treatment strategy achieving a high rate of rectal preservation in tumors that respond to neoadjuvant therapy. I don’t think the rectum needs to come out in everybody,” said investigator Dr. J. Joshua Smith, a surgical oncologist at Sloan Kettering.
Several studies have reported similar results similar to the Sloan Kettering study, but other investigations have been retrospective, so optimal patient selection, assessment of response, surveillance protocols, and other matters remain uncertain. Sloan Kettering and about 20 other cancer centers in United States – all members of the Rectal Cancer Consortium – recently launched a randomized clinical trial to get a better handle on those issues.
Locally advanced rectal cancer patients will be randomized to either chemoradiation for 5.5 weeks followed by folinic acid, fluorouracil, and oxaliplatin (FOLFOX) or capecitabine and oxaliplatin (CapeOX) over about 16 weeks, or FOLFOX/CapeOX first and chemoradiation second. Those who have a significant clinical response will then undergo watchful waiting; those who do not will have TME.
About 50 patients have enrolled in the phase II trial so far; the investigators are looking for more than 200.
“I think ‘prime time for watchful waiting’ is around the corner, but not yet here. It must be preceded by a prospective trial.” Meanwhile, “how we define complete clinical response is important” when considering watchful waiting, Dr. Smith said at the annual clinical congress of the American College of Surgeons..
At Sloan Kettering, where watchful waiting has become more popular in recent years, complete clinical response means no tumor or lymph nodes on imaging, and, on digital rectal exam (DRE) and proctoscopy, normal flat mucosa, smooth induration, no mass, no nodules, no ulcerations, and no luminal narrowing; a pale scar and telangiectasias are okay.
In the first year, surveillance includes DRE and endoscopy every 3 months and imaging every 6 months. In the second year, DRE and endoscopy come every 4 months, and imaging again every 6 months. From years 3 to 5, DRE and endoscopy are done every 6 months, and imaging every 6-12 months. After 5 years, surveillance is by yearly DRE and endoscopy.
When discussing the option with patients, they need to know – besides the risk of recurrence – that watchful waiting is currently not standard medical management; surveillance must be frequent; they are at risk for a more extensive salvage TME than they might have had otherwise; and the approach might compromise the chance of a cure, Dr. Smith said.
Dr. Smith said he has no relevant disclosures.
CHICAGO – Watchful waiting with careful surveillance may become an option for the majority of locally advanced rectal cancer patients who have a complete clinical response to neoadjuvant therapy, according to a review of 442 rectal cancer patients at Memorial Sloan Kettering Cancer Center in New York.
Seventy-three of those patients had a complete clinical response to neoadjuvant therapy and opted for watchful waiting instead of surgery after weighing the risks and benefits – including about a 25% chance of local recurrence – with their doctors.
At 4 years’ follow-up, 54 (74%) remained cancer free. Nineteen patients had local tumor recurrence, generally within 13 months. Two of those patients had successful local excisions, and the remaining 17 had salvage total mesorectal excisions (TME).
There were no statistically significant differences in 4-year disease-specific and overall survival among the 73 patients and 72 other patients who opted for TME after neoadjuvant chemotherapy and were found to have had pathologic complete responses.
“In our cohort, watch and wait was safe. It’s an effective treatment strategy achieving a high rate of rectal preservation in tumors that respond to neoadjuvant therapy. I don’t think the rectum needs to come out in everybody,” said investigator Dr. J. Joshua Smith, a surgical oncologist at Sloan Kettering.
Several studies have reported similar results similar to the Sloan Kettering study, but other investigations have been retrospective, so optimal patient selection, assessment of response, surveillance protocols, and other matters remain uncertain. Sloan Kettering and about 20 other cancer centers in United States – all members of the Rectal Cancer Consortium – recently launched a randomized clinical trial to get a better handle on those issues.
Locally advanced rectal cancer patients will be randomized to either chemoradiation for 5.5 weeks followed by folinic acid, fluorouracil, and oxaliplatin (FOLFOX) or capecitabine and oxaliplatin (CapeOX) over about 16 weeks, or FOLFOX/CapeOX first and chemoradiation second. Those who have a significant clinical response will then undergo watchful waiting; those who do not will have TME.
About 50 patients have enrolled in the phase II trial so far; the investigators are looking for more than 200.
“I think ‘prime time for watchful waiting’ is around the corner, but not yet here. It must be preceded by a prospective trial.” Meanwhile, “how we define complete clinical response is important” when considering watchful waiting, Dr. Smith said at the annual clinical congress of the American College of Surgeons..
At Sloan Kettering, where watchful waiting has become more popular in recent years, complete clinical response means no tumor or lymph nodes on imaging, and, on digital rectal exam (DRE) and proctoscopy, normal flat mucosa, smooth induration, no mass, no nodules, no ulcerations, and no luminal narrowing; a pale scar and telangiectasias are okay.
In the first year, surveillance includes DRE and endoscopy every 3 months and imaging every 6 months. In the second year, DRE and endoscopy come every 4 months, and imaging again every 6 months. From years 3 to 5, DRE and endoscopy are done every 6 months, and imaging every 6-12 months. After 5 years, surveillance is by yearly DRE and endoscopy.
When discussing the option with patients, they need to know – besides the risk of recurrence – that watchful waiting is currently not standard medical management; surveillance must be frequent; they are at risk for a more extensive salvage TME than they might have had otherwise; and the approach might compromise the chance of a cure, Dr. Smith said.
Dr. Smith said he has no relevant disclosures.
CHICAGO – Watchful waiting with careful surveillance may become an option for the majority of locally advanced rectal cancer patients who have a complete clinical response to neoadjuvant therapy, according to a review of 442 rectal cancer patients at Memorial Sloan Kettering Cancer Center in New York.
Seventy-three of those patients had a complete clinical response to neoadjuvant therapy and opted for watchful waiting instead of surgery after weighing the risks and benefits – including about a 25% chance of local recurrence – with their doctors.
At 4 years’ follow-up, 54 (74%) remained cancer free. Nineteen patients had local tumor recurrence, generally within 13 months. Two of those patients had successful local excisions, and the remaining 17 had salvage total mesorectal excisions (TME).
There were no statistically significant differences in 4-year disease-specific and overall survival among the 73 patients and 72 other patients who opted for TME after neoadjuvant chemotherapy and were found to have had pathologic complete responses.
“In our cohort, watch and wait was safe. It’s an effective treatment strategy achieving a high rate of rectal preservation in tumors that respond to neoadjuvant therapy. I don’t think the rectum needs to come out in everybody,” said investigator Dr. J. Joshua Smith, a surgical oncologist at Sloan Kettering.
Several studies have reported similar results similar to the Sloan Kettering study, but other investigations have been retrospective, so optimal patient selection, assessment of response, surveillance protocols, and other matters remain uncertain. Sloan Kettering and about 20 other cancer centers in United States – all members of the Rectal Cancer Consortium – recently launched a randomized clinical trial to get a better handle on those issues.
Locally advanced rectal cancer patients will be randomized to either chemoradiation for 5.5 weeks followed by folinic acid, fluorouracil, and oxaliplatin (FOLFOX) or capecitabine and oxaliplatin (CapeOX) over about 16 weeks, or FOLFOX/CapeOX first and chemoradiation second. Those who have a significant clinical response will then undergo watchful waiting; those who do not will have TME.
About 50 patients have enrolled in the phase II trial so far; the investigators are looking for more than 200.
“I think ‘prime time for watchful waiting’ is around the corner, but not yet here. It must be preceded by a prospective trial.” Meanwhile, “how we define complete clinical response is important” when considering watchful waiting, Dr. Smith said at the annual clinical congress of the American College of Surgeons..
At Sloan Kettering, where watchful waiting has become more popular in recent years, complete clinical response means no tumor or lymph nodes on imaging, and, on digital rectal exam (DRE) and proctoscopy, normal flat mucosa, smooth induration, no mass, no nodules, no ulcerations, and no luminal narrowing; a pale scar and telangiectasias are okay.
In the first year, surveillance includes DRE and endoscopy every 3 months and imaging every 6 months. In the second year, DRE and endoscopy come every 4 months, and imaging again every 6 months. From years 3 to 5, DRE and endoscopy are done every 6 months, and imaging every 6-12 months. After 5 years, surveillance is by yearly DRE and endoscopy.
When discussing the option with patients, they need to know – besides the risk of recurrence – that watchful waiting is currently not standard medical management; surveillance must be frequent; they are at risk for a more extensive salvage TME than they might have had otherwise; and the approach might compromise the chance of a cure, Dr. Smith said.
Dr. Smith said he has no relevant disclosures.
AT THE ACS CLINICAL CONGRESS
Key clinical point: Organ preservation seems to be a valid option when locally advanced rectal cancers respond completely to neoadjuvant therapy.
Major finding: Almost three-quarters of 73 patients who opted for watchful waiting after complete clinical responses to neodjuvant therapy remained cancer free at 4 years.
Data source: Review of 442 patients at Memorial Sloan Kettering Cancer Center.
Disclosures: The presenting investigator has no relevant financial disclosures.
ACS: Health, weight benefits of gastric bypass durable at 10 years
CHICAGO – Weight loss and comorbidity reduction from Roux-en-Y gastric bypass remain durable at 10 years, according to a reviewof 651 patients at the University of Virginia in Charlottesville.
Investigators checked up on their patients after a decade because “the long-term durability of this operation remains ill-defined in the American population.” Their study, likely the largest American series with 10-year follow-up, helps “to more clearly define long-term outcomes that may be achieved following performance of Roux-en-Y gastric bypass and establish a benchmark for future clinical investigation,” they said.
The study included 335 open and 316 laparoscopic Roux-en-Y gastric bypass (RYGB) patients. Although gastric bypass is preformed laparoscopically at the university now, the team felt comfortable including open cases in the analysis because patients and outcomes were similar in both groups. The mean preoperative body mass index, for instance, was about 53 kg/m2 and the mean operative time about 230 minutes. Postoperative incisional hernia and anastomotic stenosis were more likely with open surgery.
As in other studies, weight loss peaked at 24 months, with patients shedding a mean of 74% of their excess weight. Although that had fallen to a mean of 52% at 10 years, “they still kept off half of their excess weight, which is outstanding,” investigator and general surgery resident Dr. Hunter Mehaffey said at the annual clinical congress of the American College of Surgeons.
Surgery also led to persistent reductions in obesity-related comorbidities. Before RYGB, for instance, 38% of patients had gastroesophageal reflux disease, versus 29% after 10 years. Similarly, the prevalence of degenerative joint disease fell from 61% to 32%, diabetes from 41% to 18%, obstructive sleep apnea from 36% to 16%, hypertension from 59% to 47%, pulmonary problems from 28% to 13%, and psychiatric issues from 39% to 29%. About a quarter of patients had cardiac comorbidities before RYGB, versus 16% at 10 years after surgery. The data came from chart reviews and patient interviews, and the findings were statistically significant.
Overall, patients seemed glad to have had the operation, reporting an average satisfaction score of 8.7 out of 10 points, he said, adding, “I would expect these findings to be generalizable to other institutions. This is a good, durable operation.”
Given the scope of the comorbidity reductions, “the savings in health care costs” from RYGB “are likely underestimated,” Dr. Mehaffey said.
There was another lesson from the study, as well. It took a while to track down patients for 10-year follow-up because they were no longer seeing their surgeons. “If we are not going to see these patients much after 2 years, we really have to make sure that their primary care physician knows” how to recognize and manage possible complications, such as nutritional deficiency or hypoglycemia, he said.
Dr. Mehaffey had no disclosures, and there was no outside funding for the work.
CHICAGO – Weight loss and comorbidity reduction from Roux-en-Y gastric bypass remain durable at 10 years, according to a reviewof 651 patients at the University of Virginia in Charlottesville.
Investigators checked up on their patients after a decade because “the long-term durability of this operation remains ill-defined in the American population.” Their study, likely the largest American series with 10-year follow-up, helps “to more clearly define long-term outcomes that may be achieved following performance of Roux-en-Y gastric bypass and establish a benchmark for future clinical investigation,” they said.
The study included 335 open and 316 laparoscopic Roux-en-Y gastric bypass (RYGB) patients. Although gastric bypass is preformed laparoscopically at the university now, the team felt comfortable including open cases in the analysis because patients and outcomes were similar in both groups. The mean preoperative body mass index, for instance, was about 53 kg/m2 and the mean operative time about 230 minutes. Postoperative incisional hernia and anastomotic stenosis were more likely with open surgery.
As in other studies, weight loss peaked at 24 months, with patients shedding a mean of 74% of their excess weight. Although that had fallen to a mean of 52% at 10 years, “they still kept off half of their excess weight, which is outstanding,” investigator and general surgery resident Dr. Hunter Mehaffey said at the annual clinical congress of the American College of Surgeons.
Surgery also led to persistent reductions in obesity-related comorbidities. Before RYGB, for instance, 38% of patients had gastroesophageal reflux disease, versus 29% after 10 years. Similarly, the prevalence of degenerative joint disease fell from 61% to 32%, diabetes from 41% to 18%, obstructive sleep apnea from 36% to 16%, hypertension from 59% to 47%, pulmonary problems from 28% to 13%, and psychiatric issues from 39% to 29%. About a quarter of patients had cardiac comorbidities before RYGB, versus 16% at 10 years after surgery. The data came from chart reviews and patient interviews, and the findings were statistically significant.
Overall, patients seemed glad to have had the operation, reporting an average satisfaction score of 8.7 out of 10 points, he said, adding, “I would expect these findings to be generalizable to other institutions. This is a good, durable operation.”
Given the scope of the comorbidity reductions, “the savings in health care costs” from RYGB “are likely underestimated,” Dr. Mehaffey said.
There was another lesson from the study, as well. It took a while to track down patients for 10-year follow-up because they were no longer seeing their surgeons. “If we are not going to see these patients much after 2 years, we really have to make sure that their primary care physician knows” how to recognize and manage possible complications, such as nutritional deficiency or hypoglycemia, he said.
Dr. Mehaffey had no disclosures, and there was no outside funding for the work.
CHICAGO – Weight loss and comorbidity reduction from Roux-en-Y gastric bypass remain durable at 10 years, according to a reviewof 651 patients at the University of Virginia in Charlottesville.
Investigators checked up on their patients after a decade because “the long-term durability of this operation remains ill-defined in the American population.” Their study, likely the largest American series with 10-year follow-up, helps “to more clearly define long-term outcomes that may be achieved following performance of Roux-en-Y gastric bypass and establish a benchmark for future clinical investigation,” they said.
The study included 335 open and 316 laparoscopic Roux-en-Y gastric bypass (RYGB) patients. Although gastric bypass is preformed laparoscopically at the university now, the team felt comfortable including open cases in the analysis because patients and outcomes were similar in both groups. The mean preoperative body mass index, for instance, was about 53 kg/m2 and the mean operative time about 230 minutes. Postoperative incisional hernia and anastomotic stenosis were more likely with open surgery.
As in other studies, weight loss peaked at 24 months, with patients shedding a mean of 74% of their excess weight. Although that had fallen to a mean of 52% at 10 years, “they still kept off half of their excess weight, which is outstanding,” investigator and general surgery resident Dr. Hunter Mehaffey said at the annual clinical congress of the American College of Surgeons.
Surgery also led to persistent reductions in obesity-related comorbidities. Before RYGB, for instance, 38% of patients had gastroesophageal reflux disease, versus 29% after 10 years. Similarly, the prevalence of degenerative joint disease fell from 61% to 32%, diabetes from 41% to 18%, obstructive sleep apnea from 36% to 16%, hypertension from 59% to 47%, pulmonary problems from 28% to 13%, and psychiatric issues from 39% to 29%. About a quarter of patients had cardiac comorbidities before RYGB, versus 16% at 10 years after surgery. The data came from chart reviews and patient interviews, and the findings were statistically significant.
Overall, patients seemed glad to have had the operation, reporting an average satisfaction score of 8.7 out of 10 points, he said, adding, “I would expect these findings to be generalizable to other institutions. This is a good, durable operation.”
Given the scope of the comorbidity reductions, “the savings in health care costs” from RYGB “are likely underestimated,” Dr. Mehaffey said.
There was another lesson from the study, as well. It took a while to track down patients for 10-year follow-up because they were no longer seeing their surgeons. “If we are not going to see these patients much after 2 years, we really have to make sure that their primary care physician knows” how to recognize and manage possible complications, such as nutritional deficiency or hypoglycemia, he said.
Dr. Mehaffey had no disclosures, and there was no outside funding for the work.
AT THE ACS CLINICAL CONGRESS
Key clinical point: Patients considering bariatric surgery can be reassured that many of the benefits are long lasting.
Major finding: At 10 years, patients had kept off a mean of 52% of their excess preoperative weight.
Data source: Follow-up of 651 Roux-en-Y gastric bypass patients 10 years after their surgery.
Disclosures: The lead investigator had no disclosures, and there was no outside funding.
Decision model shows prophylactic double mastectomy more costly to patients
CHICAGO – Contralateral prophylactic mastectomy is more expensive and provides a lower quality of life than unilateral mastectomy in younger women with sporadic breast cancer, a cost-effectiveness analysis shows.
“Unilateral mastectomy dominated contralateral prophylactic mastectomy in the treatment of unilateral, sporadic breast cancer,” Robert C. Keskey said at the annual clinical congress of the American College of Surgeons.
Among these women without a family history of breast cancer, unilateral mastectomy (UM) with 20 years of routine surveillance cost an average of $5,583 less than contralateral prophylactic mastectomy (CPM) ($13,703 vs. $19,286).
Women who chose UM also gained 0.21 quality adjusted life-years (QALYs), or about 2-3 months in perfect health (21.75 vs. 21.54).
Despite a decline in contralateral breast cancers, the national rate of CPM has risen from 9.7% to 24% in women 45 years of age or younger, due in part to the Angelina Jolie effect.
CPM reduces the risk of contralateral breast cancer by up to 95%, but has not been proven to provide a survival advantage and increases complications, Mr. Keskey of the University of Louisville (Ky.) said.
Discussant Dr. Judy Boughey of the Mayo Clinic in Rochester, Minn., observed that this is the third model to tackle this important issue and that all three came up with different results and conclusions.
“This probably highlights that our models are highly dependent on the assumptions made and the costs that are involved in building the model,” she said.
The first model developed at the Mayo Clinic by Dr. Boughey and others, reported that CPM is cost effective for women younger than 70 years. However, it did not take into account reconstruction and complications (J Clin Oncol. 2011;29:2993-3000), Mr. Keskey said during his talk.
The second model showed that CPM is cost saving, but provides a lower quality of life than UM in women younger than 50 years (Ann Surg Oncol. 2014 Jul;21:2209-17). This study only provided 10-year follow-up and overestimated reconstruction and complication rates, he said.
Dr. Boughey observed that the new model did not include symmetry, which was shown to be a big driver of CPM in a separate University of Michigan survey presented during the same session.
In addition, the quality-of-life assumptions used are the same as those in the second model, but significantly different from those in the Mayo model. In that analysis, if a patient felt that their quality of life was improved by a CPM, then the CPM was clearly cost effective, Dr. Boughey noted.
“So for a patient you see in the clinic who feels their quality of life is better with a CPM than without a CPM, does this model really apply?” she asked.
Mr. Keskey replied, “I think it still does in terms of the patient understanding what they’re going to face financially. It’s an important component of the puzzle. If they’re okay spending that money because they feel that either psychologically they are going to have a better quality of life or they feel their outcomes will be positive no matter what, then I think it’s important to understand this difference in cost and use that to make their decision.”
Study details
The investigators, led by Dr. Nicolas Ajkay, also of Louisville, created a decision tree using TreeAge Pro 2015 software to analyze the long-term costs of CPM vs. UM with routine surveillance in women aged 45 years and younger with sporadic breast cancer. The model included 16 event probabilities taken from the recent literature including complications with and without reconstruction, 5- and 10-year contralateral breast cancer risk, cancer stage, and hormone-receptor status.
Effectiveness was measured by QALYs taken from surveyed breast cancer patients. Medical costs were obtained from the 2014 Medicare physician fee schedule.
Because the physician fee schedule is not all inclusive, the investigators compared CPM and UM using costs from the Healthcare Cost and Utilization Project (HCUP), which contain total costs on hospital discharge after a procedure. When this was done, CPM cost an average of $15,425 more than UM and provided a lower quality of life, Mr. Keskey said.
The investigators also replaced yearly mammography in the unilateral mastectomy group with more expensive surveillance using breast magnetic resonance imaging. In this model, CPM actually saved about $300 ($19,286 vs. $19,560), but again provided a lower quality of life (21.54 vs. 21.75), he said. It resulted in a savings of $1,300 per QALY lost, which is not enough to be deemed cost effective.
“So even using a more expensive surveillance method, contralateral prophylactic mastectomy was still not cost effective,” Mr. Keskey said.
Finally, reconstruction rates were varied to see whether this would impact outcomes. The national reconstruction rate following unilateral mastectomy is about 28%, which resulted in a lifetime cost in the initial analysis model of about $13,703.
In order to make CPM less expensive than UM, the reconstruction rate following CPM would have to be dropped to 0% ($12,580) from the national rate of 75% ($19,286), he said. Further, even if the UM reconstruction rate was hiked to 100%, the lifetime costs associated with a unilateral mastectomy were cheaper at $19,275.
Limitations of the model include the subjective nature of QALYs, the cost-effectiveness analysis is a theoretical model, and its costs need to be validated against real-world numbers, Mr. Keskey said.
During a discussion of the study, however, an attendee expressed concern that the data will be used to deny insurance coverage for women seeking a prophylactic contralateral mastectomy.
The decision to undergo prophylactic mastectomy is very personal and needs to be individualized, despite the suggestion of increased cost and less quality of life in the study, according to senior author and colleague Dr. Nicolas Ajkay.
“For some patients, the thought of repeating breast cancer treatment, though a low probability, may be unacceptable; for others, imaging surveillance may not be a reasonable option; and a patient with preexisting breast asymmetry may consider bilateral mastectomy as a way to achieve symmetry and better cosmesis,” he said in an interview. “Our objective from the inception of the study, even before analyzing the results, was that this information could be part of a patient-physician discussion, never the main factor in the decision-making process.”
The authors and Dr. Boughey reported no conflicts of interest.
CHICAGO – Contralateral prophylactic mastectomy is more expensive and provides a lower quality of life than unilateral mastectomy in younger women with sporadic breast cancer, a cost-effectiveness analysis shows.
“Unilateral mastectomy dominated contralateral prophylactic mastectomy in the treatment of unilateral, sporadic breast cancer,” Robert C. Keskey said at the annual clinical congress of the American College of Surgeons.
Among these women without a family history of breast cancer, unilateral mastectomy (UM) with 20 years of routine surveillance cost an average of $5,583 less than contralateral prophylactic mastectomy (CPM) ($13,703 vs. $19,286).
Women who chose UM also gained 0.21 quality adjusted life-years (QALYs), or about 2-3 months in perfect health (21.75 vs. 21.54).
Despite a decline in contralateral breast cancers, the national rate of CPM has risen from 9.7% to 24% in women 45 years of age or younger, due in part to the Angelina Jolie effect.
CPM reduces the risk of contralateral breast cancer by up to 95%, but has not been proven to provide a survival advantage and increases complications, Mr. Keskey of the University of Louisville (Ky.) said.
Discussant Dr. Judy Boughey of the Mayo Clinic in Rochester, Minn., observed that this is the third model to tackle this important issue and that all three came up with different results and conclusions.
“This probably highlights that our models are highly dependent on the assumptions made and the costs that are involved in building the model,” she said.
The first model developed at the Mayo Clinic by Dr. Boughey and others, reported that CPM is cost effective for women younger than 70 years. However, it did not take into account reconstruction and complications (J Clin Oncol. 2011;29:2993-3000), Mr. Keskey said during his talk.
The second model showed that CPM is cost saving, but provides a lower quality of life than UM in women younger than 50 years (Ann Surg Oncol. 2014 Jul;21:2209-17). This study only provided 10-year follow-up and overestimated reconstruction and complication rates, he said.
Dr. Boughey observed that the new model did not include symmetry, which was shown to be a big driver of CPM in a separate University of Michigan survey presented during the same session.
In addition, the quality-of-life assumptions used are the same as those in the second model, but significantly different from those in the Mayo model. In that analysis, if a patient felt that their quality of life was improved by a CPM, then the CPM was clearly cost effective, Dr. Boughey noted.
“So for a patient you see in the clinic who feels their quality of life is better with a CPM than without a CPM, does this model really apply?” she asked.
Mr. Keskey replied, “I think it still does in terms of the patient understanding what they’re going to face financially. It’s an important component of the puzzle. If they’re okay spending that money because they feel that either psychologically they are going to have a better quality of life or they feel their outcomes will be positive no matter what, then I think it’s important to understand this difference in cost and use that to make their decision.”
Study details
The investigators, led by Dr. Nicolas Ajkay, also of Louisville, created a decision tree using TreeAge Pro 2015 software to analyze the long-term costs of CPM vs. UM with routine surveillance in women aged 45 years and younger with sporadic breast cancer. The model included 16 event probabilities taken from the recent literature including complications with and without reconstruction, 5- and 10-year contralateral breast cancer risk, cancer stage, and hormone-receptor status.
Effectiveness was measured by QALYs taken from surveyed breast cancer patients. Medical costs were obtained from the 2014 Medicare physician fee schedule.
Because the physician fee schedule is not all inclusive, the investigators compared CPM and UM using costs from the Healthcare Cost and Utilization Project (HCUP), which contain total costs on hospital discharge after a procedure. When this was done, CPM cost an average of $15,425 more than UM and provided a lower quality of life, Mr. Keskey said.
The investigators also replaced yearly mammography in the unilateral mastectomy group with more expensive surveillance using breast magnetic resonance imaging. In this model, CPM actually saved about $300 ($19,286 vs. $19,560), but again provided a lower quality of life (21.54 vs. 21.75), he said. It resulted in a savings of $1,300 per QALY lost, which is not enough to be deemed cost effective.
“So even using a more expensive surveillance method, contralateral prophylactic mastectomy was still not cost effective,” Mr. Keskey said.
Finally, reconstruction rates were varied to see whether this would impact outcomes. The national reconstruction rate following unilateral mastectomy is about 28%, which resulted in a lifetime cost in the initial analysis model of about $13,703.
In order to make CPM less expensive than UM, the reconstruction rate following CPM would have to be dropped to 0% ($12,580) from the national rate of 75% ($19,286), he said. Further, even if the UM reconstruction rate was hiked to 100%, the lifetime costs associated with a unilateral mastectomy were cheaper at $19,275.
Limitations of the model include the subjective nature of QALYs, the cost-effectiveness analysis is a theoretical model, and its costs need to be validated against real-world numbers, Mr. Keskey said.
During a discussion of the study, however, an attendee expressed concern that the data will be used to deny insurance coverage for women seeking a prophylactic contralateral mastectomy.
The decision to undergo prophylactic mastectomy is very personal and needs to be individualized, despite the suggestion of increased cost and less quality of life in the study, according to senior author and colleague Dr. Nicolas Ajkay.
“For some patients, the thought of repeating breast cancer treatment, though a low probability, may be unacceptable; for others, imaging surveillance may not be a reasonable option; and a patient with preexisting breast asymmetry may consider bilateral mastectomy as a way to achieve symmetry and better cosmesis,” he said in an interview. “Our objective from the inception of the study, even before analyzing the results, was that this information could be part of a patient-physician discussion, never the main factor in the decision-making process.”
The authors and Dr. Boughey reported no conflicts of interest.
CHICAGO – Contralateral prophylactic mastectomy is more expensive and provides a lower quality of life than unilateral mastectomy in younger women with sporadic breast cancer, a cost-effectiveness analysis shows.
“Unilateral mastectomy dominated contralateral prophylactic mastectomy in the treatment of unilateral, sporadic breast cancer,” Robert C. Keskey said at the annual clinical congress of the American College of Surgeons.
Among these women without a family history of breast cancer, unilateral mastectomy (UM) with 20 years of routine surveillance cost an average of $5,583 less than contralateral prophylactic mastectomy (CPM) ($13,703 vs. $19,286).
Women who chose UM also gained 0.21 quality adjusted life-years (QALYs), or about 2-3 months in perfect health (21.75 vs. 21.54).
Despite a decline in contralateral breast cancers, the national rate of CPM has risen from 9.7% to 24% in women 45 years of age or younger, due in part to the Angelina Jolie effect.
CPM reduces the risk of contralateral breast cancer by up to 95%, but has not been proven to provide a survival advantage and increases complications, Mr. Keskey of the University of Louisville (Ky.) said.
Discussant Dr. Judy Boughey of the Mayo Clinic in Rochester, Minn., observed that this is the third model to tackle this important issue and that all three came up with different results and conclusions.
“This probably highlights that our models are highly dependent on the assumptions made and the costs that are involved in building the model,” she said.
The first model developed at the Mayo Clinic by Dr. Boughey and others, reported that CPM is cost effective for women younger than 70 years. However, it did not take into account reconstruction and complications (J Clin Oncol. 2011;29:2993-3000), Mr. Keskey said during his talk.
The second model showed that CPM is cost saving, but provides a lower quality of life than UM in women younger than 50 years (Ann Surg Oncol. 2014 Jul;21:2209-17). This study only provided 10-year follow-up and overestimated reconstruction and complication rates, he said.
Dr. Boughey observed that the new model did not include symmetry, which was shown to be a big driver of CPM in a separate University of Michigan survey presented during the same session.
In addition, the quality-of-life assumptions used are the same as those in the second model, but significantly different from those in the Mayo model. In that analysis, if a patient felt that their quality of life was improved by a CPM, then the CPM was clearly cost effective, Dr. Boughey noted.
“So for a patient you see in the clinic who feels their quality of life is better with a CPM than without a CPM, does this model really apply?” she asked.
Mr. Keskey replied, “I think it still does in terms of the patient understanding what they’re going to face financially. It’s an important component of the puzzle. If they’re okay spending that money because they feel that either psychologically they are going to have a better quality of life or they feel their outcomes will be positive no matter what, then I think it’s important to understand this difference in cost and use that to make their decision.”
Study details
The investigators, led by Dr. Nicolas Ajkay, also of Louisville, created a decision tree using TreeAge Pro 2015 software to analyze the long-term costs of CPM vs. UM with routine surveillance in women aged 45 years and younger with sporadic breast cancer. The model included 16 event probabilities taken from the recent literature including complications with and without reconstruction, 5- and 10-year contralateral breast cancer risk, cancer stage, and hormone-receptor status.
Effectiveness was measured by QALYs taken from surveyed breast cancer patients. Medical costs were obtained from the 2014 Medicare physician fee schedule.
Because the physician fee schedule is not all inclusive, the investigators compared CPM and UM using costs from the Healthcare Cost and Utilization Project (HCUP), which contain total costs on hospital discharge after a procedure. When this was done, CPM cost an average of $15,425 more than UM and provided a lower quality of life, Mr. Keskey said.
The investigators also replaced yearly mammography in the unilateral mastectomy group with more expensive surveillance using breast magnetic resonance imaging. In this model, CPM actually saved about $300 ($19,286 vs. $19,560), but again provided a lower quality of life (21.54 vs. 21.75), he said. It resulted in a savings of $1,300 per QALY lost, which is not enough to be deemed cost effective.
“So even using a more expensive surveillance method, contralateral prophylactic mastectomy was still not cost effective,” Mr. Keskey said.
Finally, reconstruction rates were varied to see whether this would impact outcomes. The national reconstruction rate following unilateral mastectomy is about 28%, which resulted in a lifetime cost in the initial analysis model of about $13,703.
In order to make CPM less expensive than UM, the reconstruction rate following CPM would have to be dropped to 0% ($12,580) from the national rate of 75% ($19,286), he said. Further, even if the UM reconstruction rate was hiked to 100%, the lifetime costs associated with a unilateral mastectomy were cheaper at $19,275.
Limitations of the model include the subjective nature of QALYs, the cost-effectiveness analysis is a theoretical model, and its costs need to be validated against real-world numbers, Mr. Keskey said.
During a discussion of the study, however, an attendee expressed concern that the data will be used to deny insurance coverage for women seeking a prophylactic contralateral mastectomy.
The decision to undergo prophylactic mastectomy is very personal and needs to be individualized, despite the suggestion of increased cost and less quality of life in the study, according to senior author and colleague Dr. Nicolas Ajkay.
“For some patients, the thought of repeating breast cancer treatment, though a low probability, may be unacceptable; for others, imaging surveillance may not be a reasonable option; and a patient with preexisting breast asymmetry may consider bilateral mastectomy as a way to achieve symmetry and better cosmesis,” he said in an interview. “Our objective from the inception of the study, even before analyzing the results, was that this information could be part of a patient-physician discussion, never the main factor in the decision-making process.”
The authors and Dr. Boughey reported no conflicts of interest.
AT THE ACS CLINICAL CONGRESS
Key clinical point: Unilateral mastectomy costs less and provides better quality of life than contralateral prophylactic mastectomy in younger women with sporadic breast cancer.
Major finding: Unilateral mastectomy with routine surveillance cost on average $5,583 less than prophylactic contralateral mastectomy.
Data source: Cost-effectiveness analysis of contralateral prophylactic mastectomy.
Disclosures: The authors and Dr. Boughey reported no conflicts of interest.
ACS: No clear answers to black patients’ worse rectal cancer outcomes
CHICAGO – Access to equal care decreases but does not eliminate the survival disparities between black and white patients with rectal cancer, according to investigators from the University of Cincinnati, Ohio.
After rigorous propensity score matching of thousands of black and white patients for patient, disease, and treatment characteristics, median survival was 109.6 months among white patients and 85.8 months among black patients (J Am Coll Surg. 2015 Nov [doi: 10.1016/j.jamcollsurg.2015.07.056]).
“Blacks have worse outcomes, but we don’t have a clear explanation,” explained investigator and surgery resident Dr. Meghan Nolan. For now, the findings suggest that it might be a good idea to start screening black patients before age 50 years, perhaps even as early as age 40 years.
“We are urging people to screen at a lower age in black patients,” Dr. Nolan said at the annual clinical congress of the American College of Surgeons.
Racial disparities in rectal cancer are well known. The investigators wanted to see if they simply are because of unequal access to care, so they analyzed 178,414 white and 18,385 black patients in the National Cancer Data Base from 1998 to 2006.
Mean 5-year survival for blacks was 50.7%, compared with 56.2% for whites, and black patients were more likely to present with stage IV disease. Such findings aren’t new, the investigators noted.
To account for the difference in late-stage presentation, the investigators limited their analysis to patients with stage I-III rectal cancer. But even then, 5-year survival was 66.7% among whites and 58.7% among blacks.
That might have had something to do with the fact 85% of white patients, but only 78% of black patients, had surgery for those potentially curable lower-stage tumors. Among those who didn’t undergo surgery, patient refusal was slightly more common among black patients than white patients, which suggests that “cultural factors may be playing a role” in the surgery disparity, Dr. Nolan said.
The investigators controlled for the different surgery rates by limiting their analysis to stage I-III patients who had appropriate operations. The survival gap narrowed but did not disappear: 65.8% of white patients were alive at 5 years, compared with 61% of black patients. Blacks were also more likely to have positive margins on pathology. “I’m not sure why. That was a surprise,” Dr. Nolan said.
The propensity score matching led the team to conclude that there’s more at work than differences in access to care. A total of 7,569 pairs of black and white patients were matched for age at diagnosis, gender, insurance coverage, income, education, facility type, tumor stage, Charlson-Deyo score, surgical management, margin status, and other potential confounders.
Every matched patient completed their recommended therapy, and there was no statistical difference between matched black and white patients who received appropriate, stage-specific chemoradiation. Still, the survival differences persisted.
Dr. Nolan had no relevant disclosures.
CHICAGO – Access to equal care decreases but does not eliminate the survival disparities between black and white patients with rectal cancer, according to investigators from the University of Cincinnati, Ohio.
After rigorous propensity score matching of thousands of black and white patients for patient, disease, and treatment characteristics, median survival was 109.6 months among white patients and 85.8 months among black patients (J Am Coll Surg. 2015 Nov [doi: 10.1016/j.jamcollsurg.2015.07.056]).
“Blacks have worse outcomes, but we don’t have a clear explanation,” explained investigator and surgery resident Dr. Meghan Nolan. For now, the findings suggest that it might be a good idea to start screening black patients before age 50 years, perhaps even as early as age 40 years.
“We are urging people to screen at a lower age in black patients,” Dr. Nolan said at the annual clinical congress of the American College of Surgeons.
Racial disparities in rectal cancer are well known. The investigators wanted to see if they simply are because of unequal access to care, so they analyzed 178,414 white and 18,385 black patients in the National Cancer Data Base from 1998 to 2006.
Mean 5-year survival for blacks was 50.7%, compared with 56.2% for whites, and black patients were more likely to present with stage IV disease. Such findings aren’t new, the investigators noted.
To account for the difference in late-stage presentation, the investigators limited their analysis to patients with stage I-III rectal cancer. But even then, 5-year survival was 66.7% among whites and 58.7% among blacks.
That might have had something to do with the fact 85% of white patients, but only 78% of black patients, had surgery for those potentially curable lower-stage tumors. Among those who didn’t undergo surgery, patient refusal was slightly more common among black patients than white patients, which suggests that “cultural factors may be playing a role” in the surgery disparity, Dr. Nolan said.
The investigators controlled for the different surgery rates by limiting their analysis to stage I-III patients who had appropriate operations. The survival gap narrowed but did not disappear: 65.8% of white patients were alive at 5 years, compared with 61% of black patients. Blacks were also more likely to have positive margins on pathology. “I’m not sure why. That was a surprise,” Dr. Nolan said.
The propensity score matching led the team to conclude that there’s more at work than differences in access to care. A total of 7,569 pairs of black and white patients were matched for age at diagnosis, gender, insurance coverage, income, education, facility type, tumor stage, Charlson-Deyo score, surgical management, margin status, and other potential confounders.
Every matched patient completed their recommended therapy, and there was no statistical difference between matched black and white patients who received appropriate, stage-specific chemoradiation. Still, the survival differences persisted.
Dr. Nolan had no relevant disclosures.
CHICAGO – Access to equal care decreases but does not eliminate the survival disparities between black and white patients with rectal cancer, according to investigators from the University of Cincinnati, Ohio.
After rigorous propensity score matching of thousands of black and white patients for patient, disease, and treatment characteristics, median survival was 109.6 months among white patients and 85.8 months among black patients (J Am Coll Surg. 2015 Nov [doi: 10.1016/j.jamcollsurg.2015.07.056]).
“Blacks have worse outcomes, but we don’t have a clear explanation,” explained investigator and surgery resident Dr. Meghan Nolan. For now, the findings suggest that it might be a good idea to start screening black patients before age 50 years, perhaps even as early as age 40 years.
“We are urging people to screen at a lower age in black patients,” Dr. Nolan said at the annual clinical congress of the American College of Surgeons.
Racial disparities in rectal cancer are well known. The investigators wanted to see if they simply are because of unequal access to care, so they analyzed 178,414 white and 18,385 black patients in the National Cancer Data Base from 1998 to 2006.
Mean 5-year survival for blacks was 50.7%, compared with 56.2% for whites, and black patients were more likely to present with stage IV disease. Such findings aren’t new, the investigators noted.
To account for the difference in late-stage presentation, the investigators limited their analysis to patients with stage I-III rectal cancer. But even then, 5-year survival was 66.7% among whites and 58.7% among blacks.
That might have had something to do with the fact 85% of white patients, but only 78% of black patients, had surgery for those potentially curable lower-stage tumors. Among those who didn’t undergo surgery, patient refusal was slightly more common among black patients than white patients, which suggests that “cultural factors may be playing a role” in the surgery disparity, Dr. Nolan said.
The investigators controlled for the different surgery rates by limiting their analysis to stage I-III patients who had appropriate operations. The survival gap narrowed but did not disappear: 65.8% of white patients were alive at 5 years, compared with 61% of black patients. Blacks were also more likely to have positive margins on pathology. “I’m not sure why. That was a surprise,” Dr. Nolan said.
The propensity score matching led the team to conclude that there’s more at work than differences in access to care. A total of 7,569 pairs of black and white patients were matched for age at diagnosis, gender, insurance coverage, income, education, facility type, tumor stage, Charlson-Deyo score, surgical management, margin status, and other potential confounders.
Every matched patient completed their recommended therapy, and there was no statistical difference between matched black and white patients who received appropriate, stage-specific chemoradiation. Still, the survival differences persisted.
Dr. Nolan had no relevant disclosures.
AT THE ACS CLINICAL CONGRESS
Key clinical point: Screen black patients for rectal cancer before the age of 50.
Major finding: Even with rigorous propensity score matching, median survival was 109.6 months among white patients and 85.8 months among black patients with rectal cancer.
Data source: Review of almost 200,000 rectal cancer patients in the National Cancer Data Base.
Disclosures: Dr. Nolan had no relevant disclosures.
Magnetic sphincter device clicks in real-world GERD patients
CHICAGO – Patients receiving the LINX magnetic sphincter device for gastroesophageal reflux disease (GERD) at a community hospital have outcomes comparable with those achieved at the best academic centers, a study suggests.
“This is a safe and effective operation that, importantly, is very reproducible in the community setting,” Dr. F. Paul “Tripp” Buckley III said at the annual clinical congress of the American College of Surgeons. “Unlike a Nissen [fundoplication] where you have to have 50 [surgeries completed] to be considered an expert and then do over 35 a year to continue to have great outcomes, this is a highly teachable event and can be employed out in the community with little hesitation.”
The magnetic sphincter augmentation device (LINX, Torax Medical) was approved in the United States in 2012 for the treatment of GERD and consists of a series of interlinked titanium-encased magnets implanted laparoscopically around the esophagus. The magnets augment a weak lower esophageal sphincter and avoid some of the complications of fundoplication, said Dr. Buckley, who disclosed serving as a proctor and speaker for Torax.
In the 5-year study leading to its approval, 64% of patients achieved the primary outcome of normalization of esophageal acid exposure or at least a 50% reduction in exposure at 1 year after sphincter augmentation and 93% of patients cut their use of proton-pump inhibitors (PPIs) by at least 50%. Six serious adverse events occurred (N Engl J Med. 2013;368:719-27).
Dr. Buckley, of Scott & White Health in Round Rock, Tex., and his associates evaluated their first 102 patients undergoing magnetic sphincter augmentation under general anesthesia at two community hospitals. GERD health-related quality of life (GERD-HRQL) scores were compared before and after surgery and overall results were compared with the clinical trial data. The highest possible total GERD-HRQL score is 75 (worst symptoms) and lowest score 0 (no symptoms).
The community and clinical trial cohorts were similar in age (median, 54 vs. 53 years), sex (both 52% male), median body mass index (both 28 kg/m2), and PPI use (98% vs. 100%), which was a requirement for trial entry.
After patients in the community underwent magnetic sphincter augmentation, PPI use decreased from 98% to 8%, median GERD-HRQL scores declined from 27 to 5, and patient satisfaction with GERD rose from 8% to 84%, which fell short of the satisfaction rate in the clinical trial (84% vs. 94%; P = .05), Dr. Buckley said.
The reduction in PPI use, however, was similar with that reported in the clinical trial, as was the percentage achieving at least 50% improvement in GERD-HRQL scores (86% vs. 92%), and operative times (median 49 vs. 36 minutes), he noted.
Device removal was rare at 1% in the community vs. 6% in the trial (P = .06).
Lower rates of dilation were noted in the community (9% vs. 19%; P = .04), perhaps because of refinements in technique and postoperative management, Dr. Buckley said.
“We know with this device you have to eat normally after implantation so that it will open and close within the scar capsule that’s naturally going to form,” he noted. “You have some patients that scar very tightly and you’ve got other patients that have a little bit of pain with eating and then suddenly they’re back on a liquid diet, which is a death knell for the success of this operation. So you really have to talk with these patients. I tell folks, ‘This is not a fix-it-and-forget-it type of operation.’ You’re going to get to know these patients pretty well, particularly in the early postoperative period.”
Final results recently reported with 5 years of follow-up in the clinical trial showed that 85% of patients were free from daily dependence on PPIs, heartburn was reduced from 89% to 12%, and moderate or severe regurgitation declined from 57% to 1.2%. No migrations or malfunctions occurred (J Laparoendosc Adv Surg Tech A. 2015 Oct;25[10]:787-92).
“One key aspect of this operation, and we think one of the reasons for its success and lack of migrations of the device, is that we keep the phrenoesophogeal ligament intact, so you are never in the mediastinum,” Dr. Buckley said. “For those of us who do a lot of Nissens, you end up blowing through it every time. But here when you keep it intact, you can roll it up on the distal esophagus and you can really reduce the hiatal hernia pretty significantly, even pretty large ones.”
A 3-cm cutoff was used for hiatal hernias in the trial and is recommended for early adoption in the community. A study is planned looking at hernias greater than 3 cm with no upper limit, where the minimal dissection method cannot reduce the hernia and full dissection is required, and the only requirement is that the patient have normal esophageal motility, he said.
Discussant Dr. Douglas Smink from Brigham and Women’s Hospital in Boston, said, “[There is a] lot of interest in this procedure obviously and it’s really nice to see what it’s like outside of the trials and to see your data is very similar.”
He went on to ask whether Dr. Buckley is still recommending fundoplication and, if so, in whom.
The LINX device has supplanted a classic Nissen fundoplication as the first-line operation in patients with good esophageal motility, although the device is not entirely covered by insurance, Dr. Buckley said.
“Basically, I tell patients I think it’s a marginally better operation. It’s not leaps and bounds, but it’s a marginally better operation,” he said, adding that though there has been concern about erosions, their erosion rate is zero and thus far, only seven erosions out of nearly 4,000 devices placed.
CHICAGO – Patients receiving the LINX magnetic sphincter device for gastroesophageal reflux disease (GERD) at a community hospital have outcomes comparable with those achieved at the best academic centers, a study suggests.
“This is a safe and effective operation that, importantly, is very reproducible in the community setting,” Dr. F. Paul “Tripp” Buckley III said at the annual clinical congress of the American College of Surgeons. “Unlike a Nissen [fundoplication] where you have to have 50 [surgeries completed] to be considered an expert and then do over 35 a year to continue to have great outcomes, this is a highly teachable event and can be employed out in the community with little hesitation.”
The magnetic sphincter augmentation device (LINX, Torax Medical) was approved in the United States in 2012 for the treatment of GERD and consists of a series of interlinked titanium-encased magnets implanted laparoscopically around the esophagus. The magnets augment a weak lower esophageal sphincter and avoid some of the complications of fundoplication, said Dr. Buckley, who disclosed serving as a proctor and speaker for Torax.
In the 5-year study leading to its approval, 64% of patients achieved the primary outcome of normalization of esophageal acid exposure or at least a 50% reduction in exposure at 1 year after sphincter augmentation and 93% of patients cut their use of proton-pump inhibitors (PPIs) by at least 50%. Six serious adverse events occurred (N Engl J Med. 2013;368:719-27).
Dr. Buckley, of Scott & White Health in Round Rock, Tex., and his associates evaluated their first 102 patients undergoing magnetic sphincter augmentation under general anesthesia at two community hospitals. GERD health-related quality of life (GERD-HRQL) scores were compared before and after surgery and overall results were compared with the clinical trial data. The highest possible total GERD-HRQL score is 75 (worst symptoms) and lowest score 0 (no symptoms).
The community and clinical trial cohorts were similar in age (median, 54 vs. 53 years), sex (both 52% male), median body mass index (both 28 kg/m2), and PPI use (98% vs. 100%), which was a requirement for trial entry.
After patients in the community underwent magnetic sphincter augmentation, PPI use decreased from 98% to 8%, median GERD-HRQL scores declined from 27 to 5, and patient satisfaction with GERD rose from 8% to 84%, which fell short of the satisfaction rate in the clinical trial (84% vs. 94%; P = .05), Dr. Buckley said.
The reduction in PPI use, however, was similar with that reported in the clinical trial, as was the percentage achieving at least 50% improvement in GERD-HRQL scores (86% vs. 92%), and operative times (median 49 vs. 36 minutes), he noted.
Device removal was rare at 1% in the community vs. 6% in the trial (P = .06).
Lower rates of dilation were noted in the community (9% vs. 19%; P = .04), perhaps because of refinements in technique and postoperative management, Dr. Buckley said.
“We know with this device you have to eat normally after implantation so that it will open and close within the scar capsule that’s naturally going to form,” he noted. “You have some patients that scar very tightly and you’ve got other patients that have a little bit of pain with eating and then suddenly they’re back on a liquid diet, which is a death knell for the success of this operation. So you really have to talk with these patients. I tell folks, ‘This is not a fix-it-and-forget-it type of operation.’ You’re going to get to know these patients pretty well, particularly in the early postoperative period.”
Final results recently reported with 5 years of follow-up in the clinical trial showed that 85% of patients were free from daily dependence on PPIs, heartburn was reduced from 89% to 12%, and moderate or severe regurgitation declined from 57% to 1.2%. No migrations or malfunctions occurred (J Laparoendosc Adv Surg Tech A. 2015 Oct;25[10]:787-92).
“One key aspect of this operation, and we think one of the reasons for its success and lack of migrations of the device, is that we keep the phrenoesophogeal ligament intact, so you are never in the mediastinum,” Dr. Buckley said. “For those of us who do a lot of Nissens, you end up blowing through it every time. But here when you keep it intact, you can roll it up on the distal esophagus and you can really reduce the hiatal hernia pretty significantly, even pretty large ones.”
A 3-cm cutoff was used for hiatal hernias in the trial and is recommended for early adoption in the community. A study is planned looking at hernias greater than 3 cm with no upper limit, where the minimal dissection method cannot reduce the hernia and full dissection is required, and the only requirement is that the patient have normal esophageal motility, he said.
Discussant Dr. Douglas Smink from Brigham and Women’s Hospital in Boston, said, “[There is a] lot of interest in this procedure obviously and it’s really nice to see what it’s like outside of the trials and to see your data is very similar.”
He went on to ask whether Dr. Buckley is still recommending fundoplication and, if so, in whom.
The LINX device has supplanted a classic Nissen fundoplication as the first-line operation in patients with good esophageal motility, although the device is not entirely covered by insurance, Dr. Buckley said.
“Basically, I tell patients I think it’s a marginally better operation. It’s not leaps and bounds, but it’s a marginally better operation,” he said, adding that though there has been concern about erosions, their erosion rate is zero and thus far, only seven erosions out of nearly 4,000 devices placed.
CHICAGO – Patients receiving the LINX magnetic sphincter device for gastroesophageal reflux disease (GERD) at a community hospital have outcomes comparable with those achieved at the best academic centers, a study suggests.
“This is a safe and effective operation that, importantly, is very reproducible in the community setting,” Dr. F. Paul “Tripp” Buckley III said at the annual clinical congress of the American College of Surgeons. “Unlike a Nissen [fundoplication] where you have to have 50 [surgeries completed] to be considered an expert and then do over 35 a year to continue to have great outcomes, this is a highly teachable event and can be employed out in the community with little hesitation.”
The magnetic sphincter augmentation device (LINX, Torax Medical) was approved in the United States in 2012 for the treatment of GERD and consists of a series of interlinked titanium-encased magnets implanted laparoscopically around the esophagus. The magnets augment a weak lower esophageal sphincter and avoid some of the complications of fundoplication, said Dr. Buckley, who disclosed serving as a proctor and speaker for Torax.
In the 5-year study leading to its approval, 64% of patients achieved the primary outcome of normalization of esophageal acid exposure or at least a 50% reduction in exposure at 1 year after sphincter augmentation and 93% of patients cut their use of proton-pump inhibitors (PPIs) by at least 50%. Six serious adverse events occurred (N Engl J Med. 2013;368:719-27).
Dr. Buckley, of Scott & White Health in Round Rock, Tex., and his associates evaluated their first 102 patients undergoing magnetic sphincter augmentation under general anesthesia at two community hospitals. GERD health-related quality of life (GERD-HRQL) scores were compared before and after surgery and overall results were compared with the clinical trial data. The highest possible total GERD-HRQL score is 75 (worst symptoms) and lowest score 0 (no symptoms).
The community and clinical trial cohorts were similar in age (median, 54 vs. 53 years), sex (both 52% male), median body mass index (both 28 kg/m2), and PPI use (98% vs. 100%), which was a requirement for trial entry.
After patients in the community underwent magnetic sphincter augmentation, PPI use decreased from 98% to 8%, median GERD-HRQL scores declined from 27 to 5, and patient satisfaction with GERD rose from 8% to 84%, which fell short of the satisfaction rate in the clinical trial (84% vs. 94%; P = .05), Dr. Buckley said.
The reduction in PPI use, however, was similar with that reported in the clinical trial, as was the percentage achieving at least 50% improvement in GERD-HRQL scores (86% vs. 92%), and operative times (median 49 vs. 36 minutes), he noted.
Device removal was rare at 1% in the community vs. 6% in the trial (P = .06).
Lower rates of dilation were noted in the community (9% vs. 19%; P = .04), perhaps because of refinements in technique and postoperative management, Dr. Buckley said.
“We know with this device you have to eat normally after implantation so that it will open and close within the scar capsule that’s naturally going to form,” he noted. “You have some patients that scar very tightly and you’ve got other patients that have a little bit of pain with eating and then suddenly they’re back on a liquid diet, which is a death knell for the success of this operation. So you really have to talk with these patients. I tell folks, ‘This is not a fix-it-and-forget-it type of operation.’ You’re going to get to know these patients pretty well, particularly in the early postoperative period.”
Final results recently reported with 5 years of follow-up in the clinical trial showed that 85% of patients were free from daily dependence on PPIs, heartburn was reduced from 89% to 12%, and moderate or severe regurgitation declined from 57% to 1.2%. No migrations or malfunctions occurred (J Laparoendosc Adv Surg Tech A. 2015 Oct;25[10]:787-92).
“One key aspect of this operation, and we think one of the reasons for its success and lack of migrations of the device, is that we keep the phrenoesophogeal ligament intact, so you are never in the mediastinum,” Dr. Buckley said. “For those of us who do a lot of Nissens, you end up blowing through it every time. But here when you keep it intact, you can roll it up on the distal esophagus and you can really reduce the hiatal hernia pretty significantly, even pretty large ones.”
A 3-cm cutoff was used for hiatal hernias in the trial and is recommended for early adoption in the community. A study is planned looking at hernias greater than 3 cm with no upper limit, where the minimal dissection method cannot reduce the hernia and full dissection is required, and the only requirement is that the patient have normal esophageal motility, he said.
Discussant Dr. Douglas Smink from Brigham and Women’s Hospital in Boston, said, “[There is a] lot of interest in this procedure obviously and it’s really nice to see what it’s like outside of the trials and to see your data is very similar.”
He went on to ask whether Dr. Buckley is still recommending fundoplication and, if so, in whom.
The LINX device has supplanted a classic Nissen fundoplication as the first-line operation in patients with good esophageal motility, although the device is not entirely covered by insurance, Dr. Buckley said.
“Basically, I tell patients I think it’s a marginally better operation. It’s not leaps and bounds, but it’s a marginally better operation,” he said, adding that though there has been concern about erosions, their erosion rate is zero and thus far, only seven erosions out of nearly 4,000 devices placed.
AT THE ACS CLINICAL CONGRESS
Key clinical point: Magnetic sphincter augmentation in the community setting provides results comparable with those seen in clinical trials.
Major finding: PPI use decreased from 98% to 8% after magnetic sphincter augmentation.
Data source: Prospective study in 102 patients with gastroesophageal reflux disease.
Disclosures: Dr. Buckley reported serving as a proctor and speaker for Torax Medical, which markets the Linx system.
ACS: No pull-out pneumothorax with ‘party balloon Valsalva’
CHICAGO – Investigators have come up with a simple way to reduce and maybe even eliminate pull-out pneumothoraces during chest tube removal.
Instead of standard inhale or exhale Valsalva maneuvers, they have their patients blow up a party balloon as the tube is pulled.
That produces the same Valsalva effects as the standard maneuvers, but with two significant advantages. First, it’s easy to explain and for patients to understand and do – not much more instruction is required than “blow up the balloon” – and, secondly, the inflating balloon is a visual check to make sure patients are doing the maneuver correctly. “It’s easy. Everyone can do it,” said lead investigator Dr. Puwadon Thitivaraporn, who developed the technique with Dr. Kritaya Kritayakirana and colleagues at King Chulalongkorn Memorial Hospital in Bangkok, Thailand.
To see how well it works, the team randomized 10 women and 38 men about equally to four removal techniques: the standard expire Valsalva, the standard inspire Valsalva, and two balloon maneuvers – blowing the balloon up after a deep breath and blowing it up with residual lung volume after an initial exhalation.
The subjects were trauma patients 15-64 years old, with a mean age of 38 years. Lung injuries, rib fractures, and tube suction were a bit more common in the standard maneuver groups. Patients with tracheotomies, chronic lung disease, and Glasgow Coma Scores below 13 were excluded from the study. Hemopneumothorax was the most common indication for tube placement.
Two patients in each of the standard groups (16%) developed a pull-out pneumothorax within 24 hours of tube removal, confirmed by x-ray. One required chest tube reinsertion, and all four ended up spending extra time in the hospital. Similar problems have been reported in American medicine (J Trauma. 2001 Apr;50[4]:674-7).
Meanwhile, not a single balloon patient had a lung collapse when their tube was pulled.
Because of the small number of subjects, the differences weren’t statistically significant, but they came close in a group comparison of standard patients with balloon patients (P = .11). The investigators estimated they would need almost 600 hundred subjects to reach statistical significance.
Even so, the party balloon technique appears to be “easier and safer” than standard maneuvers, as well as “reproducible and cheap, and it can prevent recurrent pneumothorax. It can be used as an alternative to the classic Valsalva,” said Dr. Thitivaraporn, a cardiothoracic surgery resident at the Bangkok hospital.
The balloon method is being used there now in nontrauma patients, as well, but the standard maneuvers are also being used until the balloon technique shows statistically significant benefits, he said.
With manometry, the team found that a party balloon’s internal pressure builds quickly as it’s inflated from a starting diameter of about 4.5 cm to about 9 cm, peaking at about 60 mm Hg; pressure trails off to about 40 mm Hg as inflation continues past 9 cm.
The investigators have no relevant disclosures.
CHICAGO – Investigators have come up with a simple way to reduce and maybe even eliminate pull-out pneumothoraces during chest tube removal.
Instead of standard inhale or exhale Valsalva maneuvers, they have their patients blow up a party balloon as the tube is pulled.
That produces the same Valsalva effects as the standard maneuvers, but with two significant advantages. First, it’s easy to explain and for patients to understand and do – not much more instruction is required than “blow up the balloon” – and, secondly, the inflating balloon is a visual check to make sure patients are doing the maneuver correctly. “It’s easy. Everyone can do it,” said lead investigator Dr. Puwadon Thitivaraporn, who developed the technique with Dr. Kritaya Kritayakirana and colleagues at King Chulalongkorn Memorial Hospital in Bangkok, Thailand.
To see how well it works, the team randomized 10 women and 38 men about equally to four removal techniques: the standard expire Valsalva, the standard inspire Valsalva, and two balloon maneuvers – blowing the balloon up after a deep breath and blowing it up with residual lung volume after an initial exhalation.
The subjects were trauma patients 15-64 years old, with a mean age of 38 years. Lung injuries, rib fractures, and tube suction were a bit more common in the standard maneuver groups. Patients with tracheotomies, chronic lung disease, and Glasgow Coma Scores below 13 were excluded from the study. Hemopneumothorax was the most common indication for tube placement.
Two patients in each of the standard groups (16%) developed a pull-out pneumothorax within 24 hours of tube removal, confirmed by x-ray. One required chest tube reinsertion, and all four ended up spending extra time in the hospital. Similar problems have been reported in American medicine (J Trauma. 2001 Apr;50[4]:674-7).
Meanwhile, not a single balloon patient had a lung collapse when their tube was pulled.
Because of the small number of subjects, the differences weren’t statistically significant, but they came close in a group comparison of standard patients with balloon patients (P = .11). The investigators estimated they would need almost 600 hundred subjects to reach statistical significance.
Even so, the party balloon technique appears to be “easier and safer” than standard maneuvers, as well as “reproducible and cheap, and it can prevent recurrent pneumothorax. It can be used as an alternative to the classic Valsalva,” said Dr. Thitivaraporn, a cardiothoracic surgery resident at the Bangkok hospital.
The balloon method is being used there now in nontrauma patients, as well, but the standard maneuvers are also being used until the balloon technique shows statistically significant benefits, he said.
With manometry, the team found that a party balloon’s internal pressure builds quickly as it’s inflated from a starting diameter of about 4.5 cm to about 9 cm, peaking at about 60 mm Hg; pressure trails off to about 40 mm Hg as inflation continues past 9 cm.
The investigators have no relevant disclosures.
CHICAGO – Investigators have come up with a simple way to reduce and maybe even eliminate pull-out pneumothoraces during chest tube removal.
Instead of standard inhale or exhale Valsalva maneuvers, they have their patients blow up a party balloon as the tube is pulled.
That produces the same Valsalva effects as the standard maneuvers, but with two significant advantages. First, it’s easy to explain and for patients to understand and do – not much more instruction is required than “blow up the balloon” – and, secondly, the inflating balloon is a visual check to make sure patients are doing the maneuver correctly. “It’s easy. Everyone can do it,” said lead investigator Dr. Puwadon Thitivaraporn, who developed the technique with Dr. Kritaya Kritayakirana and colleagues at King Chulalongkorn Memorial Hospital in Bangkok, Thailand.
To see how well it works, the team randomized 10 women and 38 men about equally to four removal techniques: the standard expire Valsalva, the standard inspire Valsalva, and two balloon maneuvers – blowing the balloon up after a deep breath and blowing it up with residual lung volume after an initial exhalation.
The subjects were trauma patients 15-64 years old, with a mean age of 38 years. Lung injuries, rib fractures, and tube suction were a bit more common in the standard maneuver groups. Patients with tracheotomies, chronic lung disease, and Glasgow Coma Scores below 13 were excluded from the study. Hemopneumothorax was the most common indication for tube placement.
Two patients in each of the standard groups (16%) developed a pull-out pneumothorax within 24 hours of tube removal, confirmed by x-ray. One required chest tube reinsertion, and all four ended up spending extra time in the hospital. Similar problems have been reported in American medicine (J Trauma. 2001 Apr;50[4]:674-7).
Meanwhile, not a single balloon patient had a lung collapse when their tube was pulled.
Because of the small number of subjects, the differences weren’t statistically significant, but they came close in a group comparison of standard patients with balloon patients (P = .11). The investigators estimated they would need almost 600 hundred subjects to reach statistical significance.
Even so, the party balloon technique appears to be “easier and safer” than standard maneuvers, as well as “reproducible and cheap, and it can prevent recurrent pneumothorax. It can be used as an alternative to the classic Valsalva,” said Dr. Thitivaraporn, a cardiothoracic surgery resident at the Bangkok hospital.
The balloon method is being used there now in nontrauma patients, as well, but the standard maneuvers are also being used until the balloon technique shows statistically significant benefits, he said.
With manometry, the team found that a party balloon’s internal pressure builds quickly as it’s inflated from a starting diameter of about 4.5 cm to about 9 cm, peaking at about 60 mm Hg; pressure trails off to about 40 mm Hg as inflation continues past 9 cm.
The investigators have no relevant disclosures.
AT THE ACS CLINICAL CONGRESS
Key clinical point: The next time you pull a chest tube, you might want to ask your patient to blow up a balloon.
Major finding: Sixteen percent of patients collapsed a lung with classic inhale/exhale Valsalva maneuvers during chest tube removal, but none did with the balloon technique.
Data source: Randomized, controlled trial of 48 chest tube patients.
Disclosures: The investigators have no relevant disclosures.