User login
Cardiovascular consequences of extreme prematurity persist into late adolescence
CHICAGO – The abnormal arterial hemodynamics identified in 11-year-olds with an extremely preterm birth persist at age 19, according to an update from the landmark longitudinal EPICure study.
“Given the implications of these significant findings, cardiovascular monitoring and risk prevention would be highly recommended for all individuals born extremely preterm,” Dr. Joanne Beckmann said in presenting the EPICure results on the long-term consequences of extreme prematurity at the annual meeting of the American College of Cardiology.
EPICure is a longitudinal study investigating health outcomes in a national cohort of babies born extremely preterm at 22-25 weeks’ gestation in the United Kingdom during 1995-1996. It is the longest such study conducted anywhere.
“Neonatal survival at the lowest gestations has improved significantly since the 1990s with the advancement in neonatal care treatments and the implementation of evidence-based practices. Therefore, long-term health outcomes following extremely preterm birth will have increasing relevance to adult physicians,” observed Dr. Beckmann of University College London.
She reported on the results of detailed cardiovascular assessments conducted in 130 extremely premature EPICure participants and 64 matched controls who made it to London for 2 days of health testing when they turned 19 years of age. The findings update the results of similar comprehensive examinations done at age 11 years.
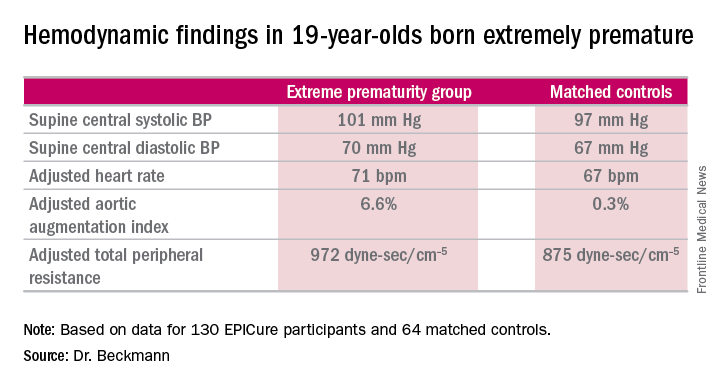
The extremely premature birth (EP) subjects were shorter and weighed less than did the controls. The two groups had similar seated systolic and diastolic blood pressure, and cardiac index didn’t differ between the two groups. However, the EP group had significantly higher supine central systolic and diastolic blood pressure and a higher heart rate.
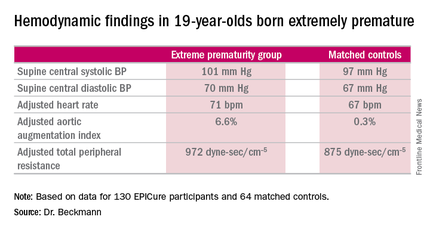
Moreover, the increases in aortic augmentation index – a composite of arterial stiffness and global wave reflections – and total peripheral resistance seen in the EP group at age 11 years persisted at the 19-year mark. It’s unclear whether the abnormal peripheral resistance in the EP group is structural or functional in nature. All hemodynamic differences between the two groups remained significant after adjustment for potential confounders.
Aortic pulse wave velocity was not significantly different between the two groups of 19-year-olds.
Data pertaining to other aspects of health in the 19-year-olds are now being analyzed. At the age-11 assessment, the EP group was found to have significantly impaired lung function (J Pediatr. 2012 Oct;161[4]:595-601.e2), high risk for neurodevelopmental disability (Pediatrics. 2009 Aug;124[2]:3249-57), a high rate of learning impairments, and an 18-fold increased risk of poor academic attainment compared to their matched peers (Arch Dis Child Fetal Neonatal Ed. 2009 Jul;94[4]:F283-9).
EPICure is funded by the Medical Research Council. Dr. Beckmann reported having no financial conflicts of interest.
CHICAGO – The abnormal arterial hemodynamics identified in 11-year-olds with an extremely preterm birth persist at age 19, according to an update from the landmark longitudinal EPICure study.
“Given the implications of these significant findings, cardiovascular monitoring and risk prevention would be highly recommended for all individuals born extremely preterm,” Dr. Joanne Beckmann said in presenting the EPICure results on the long-term consequences of extreme prematurity at the annual meeting of the American College of Cardiology.
EPICure is a longitudinal study investigating health outcomes in a national cohort of babies born extremely preterm at 22-25 weeks’ gestation in the United Kingdom during 1995-1996. It is the longest such study conducted anywhere.
“Neonatal survival at the lowest gestations has improved significantly since the 1990s with the advancement in neonatal care treatments and the implementation of evidence-based practices. Therefore, long-term health outcomes following extremely preterm birth will have increasing relevance to adult physicians,” observed Dr. Beckmann of University College London.
She reported on the results of detailed cardiovascular assessments conducted in 130 extremely premature EPICure participants and 64 matched controls who made it to London for 2 days of health testing when they turned 19 years of age. The findings update the results of similar comprehensive examinations done at age 11 years.
The extremely premature birth (EP) subjects were shorter and weighed less than did the controls. The two groups had similar seated systolic and diastolic blood pressure, and cardiac index didn’t differ between the two groups. However, the EP group had significantly higher supine central systolic and diastolic blood pressure and a higher heart rate.
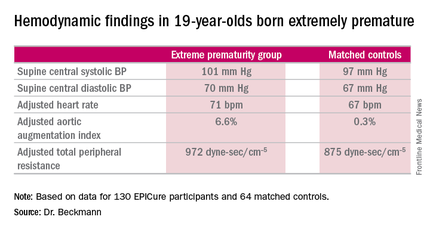
Moreover, the increases in aortic augmentation index – a composite of arterial stiffness and global wave reflections – and total peripheral resistance seen in the EP group at age 11 years persisted at the 19-year mark. It’s unclear whether the abnormal peripheral resistance in the EP group is structural or functional in nature. All hemodynamic differences between the two groups remained significant after adjustment for potential confounders.
Aortic pulse wave velocity was not significantly different between the two groups of 19-year-olds.
Data pertaining to other aspects of health in the 19-year-olds are now being analyzed. At the age-11 assessment, the EP group was found to have significantly impaired lung function (J Pediatr. 2012 Oct;161[4]:595-601.e2), high risk for neurodevelopmental disability (Pediatrics. 2009 Aug;124[2]:3249-57), a high rate of learning impairments, and an 18-fold increased risk of poor academic attainment compared to their matched peers (Arch Dis Child Fetal Neonatal Ed. 2009 Jul;94[4]:F283-9).
EPICure is funded by the Medical Research Council. Dr. Beckmann reported having no financial conflicts of interest.
CHICAGO – The abnormal arterial hemodynamics identified in 11-year-olds with an extremely preterm birth persist at age 19, according to an update from the landmark longitudinal EPICure study.
“Given the implications of these significant findings, cardiovascular monitoring and risk prevention would be highly recommended for all individuals born extremely preterm,” Dr. Joanne Beckmann said in presenting the EPICure results on the long-term consequences of extreme prematurity at the annual meeting of the American College of Cardiology.
EPICure is a longitudinal study investigating health outcomes in a national cohort of babies born extremely preterm at 22-25 weeks’ gestation in the United Kingdom during 1995-1996. It is the longest such study conducted anywhere.
“Neonatal survival at the lowest gestations has improved significantly since the 1990s with the advancement in neonatal care treatments and the implementation of evidence-based practices. Therefore, long-term health outcomes following extremely preterm birth will have increasing relevance to adult physicians,” observed Dr. Beckmann of University College London.
She reported on the results of detailed cardiovascular assessments conducted in 130 extremely premature EPICure participants and 64 matched controls who made it to London for 2 days of health testing when they turned 19 years of age. The findings update the results of similar comprehensive examinations done at age 11 years.
The extremely premature birth (EP) subjects were shorter and weighed less than did the controls. The two groups had similar seated systolic and diastolic blood pressure, and cardiac index didn’t differ between the two groups. However, the EP group had significantly higher supine central systolic and diastolic blood pressure and a higher heart rate.
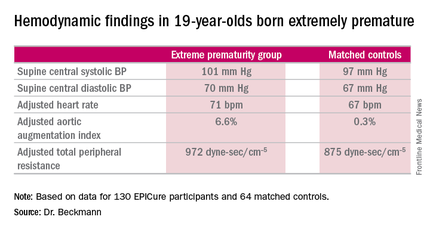
Moreover, the increases in aortic augmentation index – a composite of arterial stiffness and global wave reflections – and total peripheral resistance seen in the EP group at age 11 years persisted at the 19-year mark. It’s unclear whether the abnormal peripheral resistance in the EP group is structural or functional in nature. All hemodynamic differences between the two groups remained significant after adjustment for potential confounders.
Aortic pulse wave velocity was not significantly different between the two groups of 19-year-olds.
Data pertaining to other aspects of health in the 19-year-olds are now being analyzed. At the age-11 assessment, the EP group was found to have significantly impaired lung function (J Pediatr. 2012 Oct;161[4]:595-601.e2), high risk for neurodevelopmental disability (Pediatrics. 2009 Aug;124[2]:3249-57), a high rate of learning impairments, and an 18-fold increased risk of poor academic attainment compared to their matched peers (Arch Dis Child Fetal Neonatal Ed. 2009 Jul;94[4]:F283-9).
EPICure is funded by the Medical Research Council. Dr. Beckmann reported having no financial conflicts of interest.
AT ACC 16
Key clinical point: At age 19 years, persons born extremely premature still show significant abnormalities in arterial hemodynamics and peripheral resistance.
Major finding: The adjusted aortic augmentation index was 6.6% in 19-year-olds born at 22-25 weeks gestation compared with 0.3% in matched controls.
Data source: EPICure, a longitudinal study of health outcomes in a national cohort of babies born extremely preterm at 22-25 weeks gestation in the United Kingdom during 1995-1996.
Disclosures: EPICure is funded by the Medical Research Council. The presenter reported having no financial conflicts of interest.
Seven highly effective hospital strategies for reducing PCI mortality
CHICAGO – Researchers have identified seven specific hospital practices and procedures that are independently associated with very low 30-day risk-standardized mortality rates for percutaneous coronary interventions.
“Hospitals seeking to improve their outcomes may consider adopting one or more of these strategies if they haven’t done so already,” Dr. Jeptha P. Curtis said at the annual meeting of the American College of Cardiology.
He presented highlights of the Translating Outstanding Performance in Percutaneous Coronary Intervention (TOP PCI) study, a 5-year examination of hospital organizational strategies and enabling structures associated with lower 30-day risk-standardized rates for Medicare fee-for-service patients who underwent PCI in 2010-2012. The study included 398 randomly selected hospitals participating in the ACC’s National Cardiovascular Data Registry. The effort involved site visits and completion of a detailed 76-question survey by hospital officials.
The TOP PCI results have important practice implications.
“Despite improved technology and expansion of our evidence base, PCI carries a significant risk of adverse outcomes, including mortality. PCI outcomes are being considered for inclusion in public reporting and value-based purchasing programs, which reinforces the importance of trying to reduce mortality rates for hospitals,” observed Dr. Curtis of Yale University in New Haven, Conn.
Top among the findings that came as a surprise to him was that officials at 26% of hospitals reported that, at their institution, revenue and profits drove most decisions by senior management.
Another unexpected finding: “We asked if this hospital used data from the ACC CathPCI Registry or other sources to support specific quality improvement initiatives. I’m proud to say 84% did. I’m ashamed to say that 16% of hospitals that are making the investment to participate in this registry had not identified a single quality improvement project that was based off the data they were getting back,” Dr. Curtis said.
Many different hospital strategies and practices were looked at in TOP PCI, but in multivariate analysis, these seven stood out as having a significant association with lower 30-day risk-standardized mortality rates in PCI:
• Conducting regular reviews of PCI appropriateness by an interdisciplinary team including noninterventional cardiologists: 37% of hospitals reported doing so.
• Retaining and rewarding high-quality staff. Eight percent of hospitals were unable to do so, and they were at the high end of the 30-day mortality range.
• Using the radial approach to perform most or all PCIs. This was the practice at 22% of hospitals.
• Clinicians holding regular meetings with home health agencies to review the postdischarge care of cardiac patients. This was the practice at 24% of hospitals.
• Having PCI patients cared for by hospitalists only rarely or sometimes. At 22% of hospitals, hospitalists always cared for the PCI patients, and that practice was associated with higher 30-day mortality.
• Implementing hospital-initiated quality improvements aimed at reducing postdischarge mortality. Thirty percent of hospitals engaged in this approach.
• Use of the Plan-Do-Study-Act method of quality of improvement. This approach, widely accepted within the quality improvement field, was practiced routinely at 30% of hospitals.
Dr. Curtis noted that the nearly 400 hospitals participating in TOP PCI followed a bell-shaped curve in terms of the number of these successful strategies utilized. Some hospitals used none or one, a fewer number used five or six. None used all seven.
Discussant Spencer B. King III voiced skepticism about the TOP PCI effort.
“I know mortality is easy to measure, but in my view it does not assure quality of a PCI program by itself. I think one of the problems is that quality is kind of like pornography: Everybody knows it when they see it, but it’s hard to define. You’ve got to realize that the major mortality from interventions is patient related,” said Dr. King, who is president of the Heart and Vascular Institute at Saint Joseph’s Health System in Atlanta.
“This is a first step, it’s not the end of the story,” Dr. Curtis replied. “What this data set really represents is a unique snapshot of how at a very granular level hospitals are caring for their patients. That’s information we’ve really never had before. We can use it to look at differences in appropriateness, differences in discharge medications – any quality outcome you can come up with we can probably assess what strategies may or not be effective for those outcomes.”
Another audience critique was that, while each of the seven hospital strategies was associated with a statistically significant improvement in 30-day risk-stratified mortality, the absolute differences were quite small.
“Changing mortality is challenging. You’re really trying to change the direction of the Titanic,” Dr. Curtis responded. “It takes a long time, and it’s a matter of doing a bunch of small, subtle things. The issue is that we’ve never had any evidence to say what specific care and practices are effective. This is really the first toe in the water to say there are things you can do that actually make a difference at the end of the day.”
TOP PCI was funded by the National Heart, Lung, and Blood Institute. Dr. Curtis reported receiving salary support from the ACC’s National Cardiovascular Data Registry and the Centers for Medicare & Medicaid Services.
CHICAGO – Researchers have identified seven specific hospital practices and procedures that are independently associated with very low 30-day risk-standardized mortality rates for percutaneous coronary interventions.
“Hospitals seeking to improve their outcomes may consider adopting one or more of these strategies if they haven’t done so already,” Dr. Jeptha P. Curtis said at the annual meeting of the American College of Cardiology.
He presented highlights of the Translating Outstanding Performance in Percutaneous Coronary Intervention (TOP PCI) study, a 5-year examination of hospital organizational strategies and enabling structures associated with lower 30-day risk-standardized rates for Medicare fee-for-service patients who underwent PCI in 2010-2012. The study included 398 randomly selected hospitals participating in the ACC’s National Cardiovascular Data Registry. The effort involved site visits and completion of a detailed 76-question survey by hospital officials.
The TOP PCI results have important practice implications.
“Despite improved technology and expansion of our evidence base, PCI carries a significant risk of adverse outcomes, including mortality. PCI outcomes are being considered for inclusion in public reporting and value-based purchasing programs, which reinforces the importance of trying to reduce mortality rates for hospitals,” observed Dr. Curtis of Yale University in New Haven, Conn.
Top among the findings that came as a surprise to him was that officials at 26% of hospitals reported that, at their institution, revenue and profits drove most decisions by senior management.
Another unexpected finding: “We asked if this hospital used data from the ACC CathPCI Registry or other sources to support specific quality improvement initiatives. I’m proud to say 84% did. I’m ashamed to say that 16% of hospitals that are making the investment to participate in this registry had not identified a single quality improvement project that was based off the data they were getting back,” Dr. Curtis said.
Many different hospital strategies and practices were looked at in TOP PCI, but in multivariate analysis, these seven stood out as having a significant association with lower 30-day risk-standardized mortality rates in PCI:
• Conducting regular reviews of PCI appropriateness by an interdisciplinary team including noninterventional cardiologists: 37% of hospitals reported doing so.
• Retaining and rewarding high-quality staff. Eight percent of hospitals were unable to do so, and they were at the high end of the 30-day mortality range.
• Using the radial approach to perform most or all PCIs. This was the practice at 22% of hospitals.
• Clinicians holding regular meetings with home health agencies to review the postdischarge care of cardiac patients. This was the practice at 24% of hospitals.
• Having PCI patients cared for by hospitalists only rarely or sometimes. At 22% of hospitals, hospitalists always cared for the PCI patients, and that practice was associated with higher 30-day mortality.
• Implementing hospital-initiated quality improvements aimed at reducing postdischarge mortality. Thirty percent of hospitals engaged in this approach.
• Use of the Plan-Do-Study-Act method of quality of improvement. This approach, widely accepted within the quality improvement field, was practiced routinely at 30% of hospitals.
Dr. Curtis noted that the nearly 400 hospitals participating in TOP PCI followed a bell-shaped curve in terms of the number of these successful strategies utilized. Some hospitals used none or one, a fewer number used five or six. None used all seven.
Discussant Spencer B. King III voiced skepticism about the TOP PCI effort.
“I know mortality is easy to measure, but in my view it does not assure quality of a PCI program by itself. I think one of the problems is that quality is kind of like pornography: Everybody knows it when they see it, but it’s hard to define. You’ve got to realize that the major mortality from interventions is patient related,” said Dr. King, who is president of the Heart and Vascular Institute at Saint Joseph’s Health System in Atlanta.
“This is a first step, it’s not the end of the story,” Dr. Curtis replied. “What this data set really represents is a unique snapshot of how at a very granular level hospitals are caring for their patients. That’s information we’ve really never had before. We can use it to look at differences in appropriateness, differences in discharge medications – any quality outcome you can come up with we can probably assess what strategies may or not be effective for those outcomes.”
Another audience critique was that, while each of the seven hospital strategies was associated with a statistically significant improvement in 30-day risk-stratified mortality, the absolute differences were quite small.
“Changing mortality is challenging. You’re really trying to change the direction of the Titanic,” Dr. Curtis responded. “It takes a long time, and it’s a matter of doing a bunch of small, subtle things. The issue is that we’ve never had any evidence to say what specific care and practices are effective. This is really the first toe in the water to say there are things you can do that actually make a difference at the end of the day.”
TOP PCI was funded by the National Heart, Lung, and Blood Institute. Dr. Curtis reported receiving salary support from the ACC’s National Cardiovascular Data Registry and the Centers for Medicare & Medicaid Services.
CHICAGO – Researchers have identified seven specific hospital practices and procedures that are independently associated with very low 30-day risk-standardized mortality rates for percutaneous coronary interventions.
“Hospitals seeking to improve their outcomes may consider adopting one or more of these strategies if they haven’t done so already,” Dr. Jeptha P. Curtis said at the annual meeting of the American College of Cardiology.
He presented highlights of the Translating Outstanding Performance in Percutaneous Coronary Intervention (TOP PCI) study, a 5-year examination of hospital organizational strategies and enabling structures associated with lower 30-day risk-standardized rates for Medicare fee-for-service patients who underwent PCI in 2010-2012. The study included 398 randomly selected hospitals participating in the ACC’s National Cardiovascular Data Registry. The effort involved site visits and completion of a detailed 76-question survey by hospital officials.
The TOP PCI results have important practice implications.
“Despite improved technology and expansion of our evidence base, PCI carries a significant risk of adverse outcomes, including mortality. PCI outcomes are being considered for inclusion in public reporting and value-based purchasing programs, which reinforces the importance of trying to reduce mortality rates for hospitals,” observed Dr. Curtis of Yale University in New Haven, Conn.
Top among the findings that came as a surprise to him was that officials at 26% of hospitals reported that, at their institution, revenue and profits drove most decisions by senior management.
Another unexpected finding: “We asked if this hospital used data from the ACC CathPCI Registry or other sources to support specific quality improvement initiatives. I’m proud to say 84% did. I’m ashamed to say that 16% of hospitals that are making the investment to participate in this registry had not identified a single quality improvement project that was based off the data they were getting back,” Dr. Curtis said.
Many different hospital strategies and practices were looked at in TOP PCI, but in multivariate analysis, these seven stood out as having a significant association with lower 30-day risk-standardized mortality rates in PCI:
• Conducting regular reviews of PCI appropriateness by an interdisciplinary team including noninterventional cardiologists: 37% of hospitals reported doing so.
• Retaining and rewarding high-quality staff. Eight percent of hospitals were unable to do so, and they were at the high end of the 30-day mortality range.
• Using the radial approach to perform most or all PCIs. This was the practice at 22% of hospitals.
• Clinicians holding regular meetings with home health agencies to review the postdischarge care of cardiac patients. This was the practice at 24% of hospitals.
• Having PCI patients cared for by hospitalists only rarely or sometimes. At 22% of hospitals, hospitalists always cared for the PCI patients, and that practice was associated with higher 30-day mortality.
• Implementing hospital-initiated quality improvements aimed at reducing postdischarge mortality. Thirty percent of hospitals engaged in this approach.
• Use of the Plan-Do-Study-Act method of quality of improvement. This approach, widely accepted within the quality improvement field, was practiced routinely at 30% of hospitals.
Dr. Curtis noted that the nearly 400 hospitals participating in TOP PCI followed a bell-shaped curve in terms of the number of these successful strategies utilized. Some hospitals used none or one, a fewer number used five or six. None used all seven.
Discussant Spencer B. King III voiced skepticism about the TOP PCI effort.
“I know mortality is easy to measure, but in my view it does not assure quality of a PCI program by itself. I think one of the problems is that quality is kind of like pornography: Everybody knows it when they see it, but it’s hard to define. You’ve got to realize that the major mortality from interventions is patient related,” said Dr. King, who is president of the Heart and Vascular Institute at Saint Joseph’s Health System in Atlanta.
“This is a first step, it’s not the end of the story,” Dr. Curtis replied. “What this data set really represents is a unique snapshot of how at a very granular level hospitals are caring for their patients. That’s information we’ve really never had before. We can use it to look at differences in appropriateness, differences in discharge medications – any quality outcome you can come up with we can probably assess what strategies may or not be effective for those outcomes.”
Another audience critique was that, while each of the seven hospital strategies was associated with a statistically significant improvement in 30-day risk-stratified mortality, the absolute differences were quite small.
“Changing mortality is challenging. You’re really trying to change the direction of the Titanic,” Dr. Curtis responded. “It takes a long time, and it’s a matter of doing a bunch of small, subtle things. The issue is that we’ve never had any evidence to say what specific care and practices are effective. This is really the first toe in the water to say there are things you can do that actually make a difference at the end of the day.”
TOP PCI was funded by the National Heart, Lung, and Blood Institute. Dr. Curtis reported receiving salary support from the ACC’s National Cardiovascular Data Registry and the Centers for Medicare & Medicaid Services.
AT ACC 16
Key clinical point: Specific hospital strategies and practices are associated with differences in 30-day risk-standardized mortality rates in PCI.
Major finding: Seven specific strategies associated with significantly lower PCI mortality were identified.
Data source: The TOP PCI study was a detailed survey of 398 hospitals.
Disclosures: The study was funded by the National Heart, Lung, and Blood Institute. The presenter reported receiving salary support from the ACC’s National Cardiovascular Data Registry and the Centers for Medicare and Medicaid Services.
Cardioband scores hit for percutaneous direct mitral annuloplasty
CHICAGO – One-year results of a pivotal European trial of the percutaneous Cardioband mitral valve reconstruction system show a stable, consistent, and clinically meaningful reduction in mitral regurgitation coupled with significant quality of life improvements and a safety profile equivalent to that of other transcatheter valve procedures.
“The results are quite impressive. Ladies and gentlemen, I can tell you that I’ve used almost all the devices for direct and indirect annuloplasty, and this is the only device that works in a reproducible fashion,” Dr. Karl-Heinz Kuck said at the annual meeting of the American College of Cardiology.
He presented the results for the first 50 patients to reach 12 months of follow-up after undergoing the Cardioband procedure in a multicenter prospective study in which participants served as their own before-and-after controls. On the strength of these results, the Cardioband device has been approved by European Union regulatory authorities for the nonsurgical treatment of symptomatic moderate to severe secondary, or functional, mitral regurgitation. In Germany, the Cardioband procedure is now routinely reimbursed at a level similar to that of the MitraClip, according to Dr. Kuck, president of the German Cardiac Society and head of cardiology at St. Georg Hospital in Hamburg, Germany.
The Cardioband procedure essentially entails percutaneous implantation of an adjustable surgical ring designed to remodel a severely dysfunctional mitral valve by repairing the valve annulus. The implantation procedure features transfemoral venous access, which the TAVR experience has shown to be safer than transapical access. As in surgery, the percutaneous procedure utilizes supra-annular fixation. And it accomplishes a significant reduction in annular dimensions, comparable to what is achieved with a size 28 surgical ring.
“And the most important thing: Because we are not interfering with the leaflets or any other part of the mitral valve, the procedure leaves all options open for the future by preserving the native anatomy,” Dr. Kuck noted.
The procedure entails a transseptal puncture, insertion of the system, deployment of the implant, and adjustment of its size by cinching it down under echocardiographic guidance in order to reduce the septolateral valve dimension. The whole thing takes about 75 minutes.
The connection of the implant to the annulus is achieved in sutureless fashion using a series of screw-in anchors.
All 50 participants in the consecutive series were deemed by a heart team to be at unacceptably high surgical risk. They averaged 71 years of age, with an left ventricular ejection fraction of 33% and a left ventricular end diastolic diameter of 61 mm. Among them, 31 had ischemic heart disease, 11 had chronic obstructive pulmonary disease, 38 were in moderate or severe renal failure, 39 had atrial fibrillation, 12 had severe pulmonary hypertension, and 16 had previously undergone CABG surgery.
The 30-day safety adverse events consisted of one hemorrhagic stroke, a single major bleeding complication, two cases of acute renal failure, and one of cardiac tamponade. There were no MIs, and neither of the two deaths were related to the procedure.
In terms of efficacy, at baseline three-quarters of patients had grade 3-4 mitral regurgitation (MR). At discharge that was true for only 12%. At 1 year of follow-up, 90% of subjects had MR grade 2 or less, and roughly two-thirds of patients had MR grade 0-1.
The procedure did what it was designed to do: The mean valve septolateral dimension decreased by 30%, from 37 mm at baseline to 26 mm at discharge.
Dr. Kuck provided 6-month data on functional improvement. The mean 6-minute walk distance improved from 262 to 339 meters. At baseline, 87% of subjects were NYHA class III or IV; at 6 months, 77% were NYHA class I or II. Scores on the Minnesota Living with Heart Failure Questionnaire improved from a mean of 39 to 16 at follow-up.
A much larger European postmarketing commercial use study of the Cardioband system is now underway.
The Cardioband procedure addresses a major unmet need, Dr. Kuck observed. More than 4 million patients in the United States alone have mitral valve disease. When medically managed, patients with severe secondary mitral regurgitation have a poor prognosis, with 1- and 5-year mortality rates of 20% and 50%, and an extremely high rate of rehospitalization for heart failure. And yet multiple surveys have shown only a minority of these patients undergo surgery.
Discussant Dr. Spencer B. King III called the transcatheter mitral valve reconstruction system “quite fascinating.” He wondered what happens if the operator accidentally grabs the nearby circumflex artery with one of the device anchors. The answer, Dr. Kuck replied, is that the anchors can be unscrewed and repositioned at any point during the procedure.
Dr. King, president of the Heart and Vascular Institute at Saint Joseph’s Health System in Atlanta, has developed several devices widely used in interventional cardiology. He shook his head in amazement at the speed at which the European regulatory agency operated in this case, noting that EU marketing approval for the Valtech Cardioband device was granted and a payment structure was almost immediately established on the basis of a 50-patient, first-in-man study.
“The data are very consistent. I think that‘s what made the difference,” Dr. Kuck said.
The study was funded by Valtech. Dr. Kuck reported serving as a consultant to Biosense Webster, Edwards, and St. Jude, and on a speakers’ bureau for Medtronic.
CHICAGO – One-year results of a pivotal European trial of the percutaneous Cardioband mitral valve reconstruction system show a stable, consistent, and clinically meaningful reduction in mitral regurgitation coupled with significant quality of life improvements and a safety profile equivalent to that of other transcatheter valve procedures.
“The results are quite impressive. Ladies and gentlemen, I can tell you that I’ve used almost all the devices for direct and indirect annuloplasty, and this is the only device that works in a reproducible fashion,” Dr. Karl-Heinz Kuck said at the annual meeting of the American College of Cardiology.
He presented the results for the first 50 patients to reach 12 months of follow-up after undergoing the Cardioband procedure in a multicenter prospective study in which participants served as their own before-and-after controls. On the strength of these results, the Cardioband device has been approved by European Union regulatory authorities for the nonsurgical treatment of symptomatic moderate to severe secondary, or functional, mitral regurgitation. In Germany, the Cardioband procedure is now routinely reimbursed at a level similar to that of the MitraClip, according to Dr. Kuck, president of the German Cardiac Society and head of cardiology at St. Georg Hospital in Hamburg, Germany.
The Cardioband procedure essentially entails percutaneous implantation of an adjustable surgical ring designed to remodel a severely dysfunctional mitral valve by repairing the valve annulus. The implantation procedure features transfemoral venous access, which the TAVR experience has shown to be safer than transapical access. As in surgery, the percutaneous procedure utilizes supra-annular fixation. And it accomplishes a significant reduction in annular dimensions, comparable to what is achieved with a size 28 surgical ring.
“And the most important thing: Because we are not interfering with the leaflets or any other part of the mitral valve, the procedure leaves all options open for the future by preserving the native anatomy,” Dr. Kuck noted.
The procedure entails a transseptal puncture, insertion of the system, deployment of the implant, and adjustment of its size by cinching it down under echocardiographic guidance in order to reduce the septolateral valve dimension. The whole thing takes about 75 minutes.
The connection of the implant to the annulus is achieved in sutureless fashion using a series of screw-in anchors.
All 50 participants in the consecutive series were deemed by a heart team to be at unacceptably high surgical risk. They averaged 71 years of age, with an left ventricular ejection fraction of 33% and a left ventricular end diastolic diameter of 61 mm. Among them, 31 had ischemic heart disease, 11 had chronic obstructive pulmonary disease, 38 were in moderate or severe renal failure, 39 had atrial fibrillation, 12 had severe pulmonary hypertension, and 16 had previously undergone CABG surgery.
The 30-day safety adverse events consisted of one hemorrhagic stroke, a single major bleeding complication, two cases of acute renal failure, and one of cardiac tamponade. There were no MIs, and neither of the two deaths were related to the procedure.
In terms of efficacy, at baseline three-quarters of patients had grade 3-4 mitral regurgitation (MR). At discharge that was true for only 12%. At 1 year of follow-up, 90% of subjects had MR grade 2 or less, and roughly two-thirds of patients had MR grade 0-1.
The procedure did what it was designed to do: The mean valve septolateral dimension decreased by 30%, from 37 mm at baseline to 26 mm at discharge.
Dr. Kuck provided 6-month data on functional improvement. The mean 6-minute walk distance improved from 262 to 339 meters. At baseline, 87% of subjects were NYHA class III or IV; at 6 months, 77% were NYHA class I or II. Scores on the Minnesota Living with Heart Failure Questionnaire improved from a mean of 39 to 16 at follow-up.
A much larger European postmarketing commercial use study of the Cardioband system is now underway.
The Cardioband procedure addresses a major unmet need, Dr. Kuck observed. More than 4 million patients in the United States alone have mitral valve disease. When medically managed, patients with severe secondary mitral regurgitation have a poor prognosis, with 1- and 5-year mortality rates of 20% and 50%, and an extremely high rate of rehospitalization for heart failure. And yet multiple surveys have shown only a minority of these patients undergo surgery.
Discussant Dr. Spencer B. King III called the transcatheter mitral valve reconstruction system “quite fascinating.” He wondered what happens if the operator accidentally grabs the nearby circumflex artery with one of the device anchors. The answer, Dr. Kuck replied, is that the anchors can be unscrewed and repositioned at any point during the procedure.
Dr. King, president of the Heart and Vascular Institute at Saint Joseph’s Health System in Atlanta, has developed several devices widely used in interventional cardiology. He shook his head in amazement at the speed at which the European regulatory agency operated in this case, noting that EU marketing approval for the Valtech Cardioband device was granted and a payment structure was almost immediately established on the basis of a 50-patient, first-in-man study.
“The data are very consistent. I think that‘s what made the difference,” Dr. Kuck said.
The study was funded by Valtech. Dr. Kuck reported serving as a consultant to Biosense Webster, Edwards, and St. Jude, and on a speakers’ bureau for Medtronic.
CHICAGO – One-year results of a pivotal European trial of the percutaneous Cardioband mitral valve reconstruction system show a stable, consistent, and clinically meaningful reduction in mitral regurgitation coupled with significant quality of life improvements and a safety profile equivalent to that of other transcatheter valve procedures.
“The results are quite impressive. Ladies and gentlemen, I can tell you that I’ve used almost all the devices for direct and indirect annuloplasty, and this is the only device that works in a reproducible fashion,” Dr. Karl-Heinz Kuck said at the annual meeting of the American College of Cardiology.
He presented the results for the first 50 patients to reach 12 months of follow-up after undergoing the Cardioband procedure in a multicenter prospective study in which participants served as their own before-and-after controls. On the strength of these results, the Cardioband device has been approved by European Union regulatory authorities for the nonsurgical treatment of symptomatic moderate to severe secondary, or functional, mitral regurgitation. In Germany, the Cardioband procedure is now routinely reimbursed at a level similar to that of the MitraClip, according to Dr. Kuck, president of the German Cardiac Society and head of cardiology at St. Georg Hospital in Hamburg, Germany.
The Cardioband procedure essentially entails percutaneous implantation of an adjustable surgical ring designed to remodel a severely dysfunctional mitral valve by repairing the valve annulus. The implantation procedure features transfemoral venous access, which the TAVR experience has shown to be safer than transapical access. As in surgery, the percutaneous procedure utilizes supra-annular fixation. And it accomplishes a significant reduction in annular dimensions, comparable to what is achieved with a size 28 surgical ring.
“And the most important thing: Because we are not interfering with the leaflets or any other part of the mitral valve, the procedure leaves all options open for the future by preserving the native anatomy,” Dr. Kuck noted.
The procedure entails a transseptal puncture, insertion of the system, deployment of the implant, and adjustment of its size by cinching it down under echocardiographic guidance in order to reduce the septolateral valve dimension. The whole thing takes about 75 minutes.
The connection of the implant to the annulus is achieved in sutureless fashion using a series of screw-in anchors.
All 50 participants in the consecutive series were deemed by a heart team to be at unacceptably high surgical risk. They averaged 71 years of age, with an left ventricular ejection fraction of 33% and a left ventricular end diastolic diameter of 61 mm. Among them, 31 had ischemic heart disease, 11 had chronic obstructive pulmonary disease, 38 were in moderate or severe renal failure, 39 had atrial fibrillation, 12 had severe pulmonary hypertension, and 16 had previously undergone CABG surgery.
The 30-day safety adverse events consisted of one hemorrhagic stroke, a single major bleeding complication, two cases of acute renal failure, and one of cardiac tamponade. There were no MIs, and neither of the two deaths were related to the procedure.
In terms of efficacy, at baseline three-quarters of patients had grade 3-4 mitral regurgitation (MR). At discharge that was true for only 12%. At 1 year of follow-up, 90% of subjects had MR grade 2 or less, and roughly two-thirds of patients had MR grade 0-1.
The procedure did what it was designed to do: The mean valve septolateral dimension decreased by 30%, from 37 mm at baseline to 26 mm at discharge.
Dr. Kuck provided 6-month data on functional improvement. The mean 6-minute walk distance improved from 262 to 339 meters. At baseline, 87% of subjects were NYHA class III or IV; at 6 months, 77% were NYHA class I or II. Scores on the Minnesota Living with Heart Failure Questionnaire improved from a mean of 39 to 16 at follow-up.
A much larger European postmarketing commercial use study of the Cardioband system is now underway.
The Cardioband procedure addresses a major unmet need, Dr. Kuck observed. More than 4 million patients in the United States alone have mitral valve disease. When medically managed, patients with severe secondary mitral regurgitation have a poor prognosis, with 1- and 5-year mortality rates of 20% and 50%, and an extremely high rate of rehospitalization for heart failure. And yet multiple surveys have shown only a minority of these patients undergo surgery.
Discussant Dr. Spencer B. King III called the transcatheter mitral valve reconstruction system “quite fascinating.” He wondered what happens if the operator accidentally grabs the nearby circumflex artery with one of the device anchors. The answer, Dr. Kuck replied, is that the anchors can be unscrewed and repositioned at any point during the procedure.
Dr. King, president of the Heart and Vascular Institute at Saint Joseph’s Health System in Atlanta, has developed several devices widely used in interventional cardiology. He shook his head in amazement at the speed at which the European regulatory agency operated in this case, noting that EU marketing approval for the Valtech Cardioband device was granted and a payment structure was almost immediately established on the basis of a 50-patient, first-in-man study.
“The data are very consistent. I think that‘s what made the difference,” Dr. Kuck said.
The study was funded by Valtech. Dr. Kuck reported serving as a consultant to Biosense Webster, Edwards, and St. Jude, and on a speakers’ bureau for Medtronic.
AT ACC 16
Key clinical point: A new percutaneous repair option has been developed for patients with secondary mitral regurgitation.
Major finding: At 1 year of follow-up after receiving the Cardioband mitral reconstruction system, 90% of treated subjects with baseline severe mitral valve disease had mitral regurgitation of grade 2 or less.
Data source: A prospective, multicenter clinical trial featuring 12 months of follow-up of 50 treated patients with severe secondary mitral regurgitation.
Disclosures: The study was sponsored by Valtech, maker of the Cardioband system. The presenter reported serving as a consultant to Biosense Webster, Edwards, and St. Jude, and on a speakers bureau for Medtronic.
ACC survey: Women remain underrepresented in cardiology
CHICAGO – The latest American College of Cardiology Professional Life Survey paints a picture of a medical specialty with an aging workforce, low numbers of women, a growing preoccupation with career burnout, and large changes in practice settings in recent years.
“I’m very concerned that we haven’t seen much growth in the number of women in adult cardiology. Twenty years ago we acknowledged a need to increase the number of women in cardiology, and 10 years ago we saw an increase, but we’ve hit a wall,” Dr. Sandra J. Lewis said in presenting the survey results at the annual meeting of the American College of Cardiology.
Women comprise 50% of all medical school graduates, 47% of internal medicine residents, but only 11% of adult cardiologists, noted Dr. Lewis, chair of the ACC Women in Cardiology section, which conducted the survey in the fall of 2015.
It was completed by 1,349 male and 964 female cardiologists. This was the third such ACC survey; the others were done in 1996 and 2006.
The 2015 survey was the first to incorporate a section on burnout. Only 20% of female cardiologists and 26% of male cardiologists reported having no symptoms of burnout; the sex difference was statistically significant. Twenty-two percent of women and 17% of men characterized themselves as having “definite burnout,” noted Dr. Lewis, a cardiologist in group practice in Portland, Ore.
Recurring major sources of concern among both men and women were hassles related to electronic medical records, issues pertaining to Maintenance of Certification and the American Board of Internal Medicine, and the challenge of finding a suitable work-life balance.
On the other hand, 88% of female and 90% of male cardiologists pronounced themselves moderately or very satisfied with their work, and 63% of women and 65% of men indicated they were moderately or very satisfied with their compensation. In addition, 72% of women and 74% of men said they would recommend cardiology as a career.
About 65% of women reported experiencing past career discrimination, such as being passed over for a promotion, compared with just 23% of men. Furthermore, 26% of female cardiologists indicated their level of career advancement was slower than their peers, as did 8% of male cardiologists.
Other areas where significant sex-related differences were identified included subspecialty choice and practice pattern.
The shrinkage of private practice cardiology during the past 2 decades was impressive, Dr. Lewis said. In the 1996 survey, 53% of female cardiologists were in private practice. In 2006, it was down to 35%. And in the 2015 survey, only 17% of female cardiologists were in private practice. Similarly, 73% of male cardiologists were in private practice in 1996, 56% in 2006, and 23% in 2015.
In the latest survey, 18% of female and 17% of male respondents were aged 60 or older. In the 1996 survey, that was the case for 6% of women and 11% of men.
Dr. Lewis reported having no relevant financial conflicts.
CHICAGO – The latest American College of Cardiology Professional Life Survey paints a picture of a medical specialty with an aging workforce, low numbers of women, a growing preoccupation with career burnout, and large changes in practice settings in recent years.
“I’m very concerned that we haven’t seen much growth in the number of women in adult cardiology. Twenty years ago we acknowledged a need to increase the number of women in cardiology, and 10 years ago we saw an increase, but we’ve hit a wall,” Dr. Sandra J. Lewis said in presenting the survey results at the annual meeting of the American College of Cardiology.
Women comprise 50% of all medical school graduates, 47% of internal medicine residents, but only 11% of adult cardiologists, noted Dr. Lewis, chair of the ACC Women in Cardiology section, which conducted the survey in the fall of 2015.
It was completed by 1,349 male and 964 female cardiologists. This was the third such ACC survey; the others were done in 1996 and 2006.
The 2015 survey was the first to incorporate a section on burnout. Only 20% of female cardiologists and 26% of male cardiologists reported having no symptoms of burnout; the sex difference was statistically significant. Twenty-two percent of women and 17% of men characterized themselves as having “definite burnout,” noted Dr. Lewis, a cardiologist in group practice in Portland, Ore.
Recurring major sources of concern among both men and women were hassles related to electronic medical records, issues pertaining to Maintenance of Certification and the American Board of Internal Medicine, and the challenge of finding a suitable work-life balance.
On the other hand, 88% of female and 90% of male cardiologists pronounced themselves moderately or very satisfied with their work, and 63% of women and 65% of men indicated they were moderately or very satisfied with their compensation. In addition, 72% of women and 74% of men said they would recommend cardiology as a career.
About 65% of women reported experiencing past career discrimination, such as being passed over for a promotion, compared with just 23% of men. Furthermore, 26% of female cardiologists indicated their level of career advancement was slower than their peers, as did 8% of male cardiologists.
Other areas where significant sex-related differences were identified included subspecialty choice and practice pattern.
The shrinkage of private practice cardiology during the past 2 decades was impressive, Dr. Lewis said. In the 1996 survey, 53% of female cardiologists were in private practice. In 2006, it was down to 35%. And in the 2015 survey, only 17% of female cardiologists were in private practice. Similarly, 73% of male cardiologists were in private practice in 1996, 56% in 2006, and 23% in 2015.
In the latest survey, 18% of female and 17% of male respondents were aged 60 or older. In the 1996 survey, that was the case for 6% of women and 11% of men.
Dr. Lewis reported having no relevant financial conflicts.
CHICAGO – The latest American College of Cardiology Professional Life Survey paints a picture of a medical specialty with an aging workforce, low numbers of women, a growing preoccupation with career burnout, and large changes in practice settings in recent years.
“I’m very concerned that we haven’t seen much growth in the number of women in adult cardiology. Twenty years ago we acknowledged a need to increase the number of women in cardiology, and 10 years ago we saw an increase, but we’ve hit a wall,” Dr. Sandra J. Lewis said in presenting the survey results at the annual meeting of the American College of Cardiology.
Women comprise 50% of all medical school graduates, 47% of internal medicine residents, but only 11% of adult cardiologists, noted Dr. Lewis, chair of the ACC Women in Cardiology section, which conducted the survey in the fall of 2015.
It was completed by 1,349 male and 964 female cardiologists. This was the third such ACC survey; the others were done in 1996 and 2006.
The 2015 survey was the first to incorporate a section on burnout. Only 20% of female cardiologists and 26% of male cardiologists reported having no symptoms of burnout; the sex difference was statistically significant. Twenty-two percent of women and 17% of men characterized themselves as having “definite burnout,” noted Dr. Lewis, a cardiologist in group practice in Portland, Ore.
Recurring major sources of concern among both men and women were hassles related to electronic medical records, issues pertaining to Maintenance of Certification and the American Board of Internal Medicine, and the challenge of finding a suitable work-life balance.
On the other hand, 88% of female and 90% of male cardiologists pronounced themselves moderately or very satisfied with their work, and 63% of women and 65% of men indicated they were moderately or very satisfied with their compensation. In addition, 72% of women and 74% of men said they would recommend cardiology as a career.
About 65% of women reported experiencing past career discrimination, such as being passed over for a promotion, compared with just 23% of men. Furthermore, 26% of female cardiologists indicated their level of career advancement was slower than their peers, as did 8% of male cardiologists.
Other areas where significant sex-related differences were identified included subspecialty choice and practice pattern.
The shrinkage of private practice cardiology during the past 2 decades was impressive, Dr. Lewis said. In the 1996 survey, 53% of female cardiologists were in private practice. In 2006, it was down to 35%. And in the 2015 survey, only 17% of female cardiologists were in private practice. Similarly, 73% of male cardiologists were in private practice in 1996, 56% in 2006, and 23% in 2015.
In the latest survey, 18% of female and 17% of male respondents were aged 60 or older. In the 1996 survey, that was the case for 6% of women and 11% of men.
Dr. Lewis reported having no relevant financial conflicts.
AT ACC 16
ACCELERATE: Evacetrapib’s clinical failure sinks lipid-drug class
CHICAGO – A class of cholesterol drugs once considered a potentially very promising approach to beneficially reset lipid levels instead produced its third flameout in a pivotal clinical endpoints trial with more than 12,000 patients.
The failure of evacetrapib treatment to produce any clinical benefit despite dramatically elevating serum levels of high-density lipoprotein cholesterol by an average 130% and substantially dropping levels of low-density lipoprotein cholesterol by a mean 37% pretty much spells the end of the cholesterol ester transfer protein (CETP) inhibitors as drug candidates, agreed many experts who heard the disappointing results. The findings also added to existing questions about the reliability of elevated HDL cholesterol levels as a marker for better clinical outcomes, and raised new concerns that a similar limitation might also apply to LDL cholesterol.
“The findings continue to challenge the hope that CETP inhibition might successfully address residual cardiovascular risk,” Dr. Stephen J. Nicholls said at the annual meeting of the American College of Cardiology.
In past reports, the only other CETP inhibitors to complete phase III trials either showed no incremental benefit like evacetrapib, which happened with dalcetrapib (N Engl J Med. 2012 Nov 29;367[22]:2089-99), or clinical harm, which occurred with torcetrapib (N Engl J Med. 2007 Nov 22;357[21]:2109-22).
“Three strikes and you’re out,” declared Dr. Steven E. Nissen, a coinvestigator on the evacetrapib trial, encapsulating his read on where the CETP class now stands.
In addition, “the failure of decreases in LDL-cholesterol to result in an overall morbidity and mortality benefit emphasizes the limitations of surrogate endpoints,” said Dr. Nicholls, the study’s lead investigator and professor of cardiology at the University of Adelaide, Australia.
“We were astonished by the LDL effects in our study. Conventional wisdom says that a 37% drop in LDL cholesterol should translate into a benefit in high-risk patients,” he noted. “This reinforces the concept that mechanism matters. Surrogate endpoints are not a replacement for clinical endpoints. We need to understand more about LDL cholesterol. We thought that [lowering LDL cholesterol] was straightforward, but it’s not.”
“The most important lesson from this study is the hazard of making [efficacy] assumptions based on surrogate endpoints,” said Dr. Frederick Masoudi, a professor of medicine at the University of Colorado in Aurora. “The way you get to a lower LDL cholesterol level is important.”
“There are two hypotheses to explain the results: Either lowering LDL cholesterol was beneficial but something else evacetrapib did caused toxicity” and counterbalanced the benefit of LDL cholesterol lowering, “or it matters how you lower LDL cholesterol,” said Dr. Nissen, chairman of the department of cardiovascular medicine at the Cleveland Clinic. “I personally think it’s the latter, that mechanism [of LDL cholesterol lowering] counts,” he said in an interview.
ACCELERATE (A Study of Evacetrapib in High-Risk Vascular Disease) enrolled 12,092 patients at more than 400 centers worldwide, about half in U.S. locations. The trial identified high-risk patients based on a history of acute coronary syndrome 30-365 days before enrollment, diabetes plus known coronary artery disease, peripheral artery disease, or cerebrovascular disease. The most common risk factor was diabetes plus coronary disease, in nearly two-thirds. The average age was 65 years, three-quarters were men, and the average body mass index was 30 kg/m2. Average LDL cholesterol at baseline was 81 mg/dL, and the average HDL cholesterol level was 45 mg/dL. About 98% of enrolled patients were on a statin at baseline, with 46% on a “high intensity” statin regimen.
The 6,038 patients randomized to receive evacetrapib took 130 mg orally daily; the remaining 6,054 were randomized to receive placebo.
The trial protocol called for treatment of up to 4 years, but the data monitoring committee stopped the study prematurely in October of 2015 after an average treatment period of 25 months because of “clinical futility” for the primary endpoint, a composite of cardiovascular death, MI, stroke, coronary revascularization, or hospitalization for unstable angina. At the time the trial halted, the primary endpoint had occurred in 13% of patients in both arms of the study. The results showed trends toward a somewhat reduced rate of all-cause death and cardiovascular death in the evacetrapib-treated patients, but the between-group differences for these two endpoints did not reach statistical significance.
The results showed two significant between-group differences for possible adverse effects from treatment that may possibly partially explain why the positive lipid changes produced by evacetrapib did not produce positive clinical outcomes: Patients on evacetrapib had a median 5% increase in their serum level of C-reactive protein, a marker of systemic inflammation, compared with a median 8% decrease in the placebo group. And on average, systolic blood pressure was 0.9 mm Hg higher in patients taking evacetrapib compared with those on placebo. Investigator reports of hypertension occurred 1.3% more often in the evacetrapib patients, a statistically significant difference. But in other respects, evacetrapib was safe, leading to no excess in overall adverse effects producing discontinuations, and resulting in significantly fewer patients with substantial elevations of creatine kinase compared with placebo. The evacetrapib patients also showed strong trends toward fewer episodes of new-onset diabetes and fewer patients with substantial increases in bilirubin, compared with placebo-treated patients.
A pivotal trial for a fourth new drug from the class of cholesterol ester transfer protein inhibitors is in progress, the REVEAL study, using the drug anacetrapib. More than 30,000 patients have been enrolled, and a report on the results should be available in 2017.
Dr. Nicholls and Dr. Nissen disclosed ties with several drug companies including Eli Lilly, which sponsored the trial and is developing evacetrapib. Dr. Masoudi had no disclosures.
On Twitter @mitchelzoler
The ACCELERATE results reaffirm the lack of accuracy for high-density lipoprotein cholesterol as a surrogate biomarker for therapeutic interventions. We’re beginning to learn that HDL cholesterol is not such a good cholesterol; it’s a difficult lipoprotein.
The results also raise questions about low-density lipoprotein cholesterol. We had believed that it was good for patients to lower their LDL cholesterol level regardless of how that was accomplished. The 37% lowering we saw in ACCELERATE should have translated into about a 15% drop in cardiovascular disease events. One possible reason why this reduction wasn’t seen is that the HDL-cholesterol increase was not neutral in its effect but harmful.
Other potentially harmful effects from evacetrapib might explain its lack of incremental clinical benefit despite lowering LDL cholesterol. Patients who received the drug had on average about a 1-mm Hg increase in their systolic blood pressure, which suggests a potentially meaningful difference in blood pressure among at least some patients on the drug. Evacetrapib treatment also raised serum levels of C-reactive protein by an average of almost 5%, suggesting that the drug might be proinflammatory.
Evacetrapib led to a lipidologist’s dream effect on plasma lipids without producing clinical benefit. I think this finding, following the failures with dalcetrapib and torcetrapib, is the last nail into the coffin of the cholesterol ester transfer protein inhibitor drug class. A pivotal trial is ongoing for a fourth drug in this class, anacetrapib, but I will be surprised if those results show a clinical benefit.
Dr. Prediman K. Shah, professor of medicine and director of the Atherosclerosis Prevention and Management Center at Cedars-Sinai Medical Center in Los Angeles, made these comments as a designated discussant of ACCELERATE. He has received research support from Aegerion, Amgen, Sanofi, and Cardiovax.
The ACCELERATE results reaffirm the lack of accuracy for high-density lipoprotein cholesterol as a surrogate biomarker for therapeutic interventions. We’re beginning to learn that HDL cholesterol is not such a good cholesterol; it’s a difficult lipoprotein.
The results also raise questions about low-density lipoprotein cholesterol. We had believed that it was good for patients to lower their LDL cholesterol level regardless of how that was accomplished. The 37% lowering we saw in ACCELERATE should have translated into about a 15% drop in cardiovascular disease events. One possible reason why this reduction wasn’t seen is that the HDL-cholesterol increase was not neutral in its effect but harmful.
Other potentially harmful effects from evacetrapib might explain its lack of incremental clinical benefit despite lowering LDL cholesterol. Patients who received the drug had on average about a 1-mm Hg increase in their systolic blood pressure, which suggests a potentially meaningful difference in blood pressure among at least some patients on the drug. Evacetrapib treatment also raised serum levels of C-reactive protein by an average of almost 5%, suggesting that the drug might be proinflammatory.
Evacetrapib led to a lipidologist’s dream effect on plasma lipids without producing clinical benefit. I think this finding, following the failures with dalcetrapib and torcetrapib, is the last nail into the coffin of the cholesterol ester transfer protein inhibitor drug class. A pivotal trial is ongoing for a fourth drug in this class, anacetrapib, but I will be surprised if those results show a clinical benefit.
Dr. Prediman K. Shah, professor of medicine and director of the Atherosclerosis Prevention and Management Center at Cedars-Sinai Medical Center in Los Angeles, made these comments as a designated discussant of ACCELERATE. He has received research support from Aegerion, Amgen, Sanofi, and Cardiovax.
The ACCELERATE results reaffirm the lack of accuracy for high-density lipoprotein cholesterol as a surrogate biomarker for therapeutic interventions. We’re beginning to learn that HDL cholesterol is not such a good cholesterol; it’s a difficult lipoprotein.
The results also raise questions about low-density lipoprotein cholesterol. We had believed that it was good for patients to lower their LDL cholesterol level regardless of how that was accomplished. The 37% lowering we saw in ACCELERATE should have translated into about a 15% drop in cardiovascular disease events. One possible reason why this reduction wasn’t seen is that the HDL-cholesterol increase was not neutral in its effect but harmful.
Other potentially harmful effects from evacetrapib might explain its lack of incremental clinical benefit despite lowering LDL cholesterol. Patients who received the drug had on average about a 1-mm Hg increase in their systolic blood pressure, which suggests a potentially meaningful difference in blood pressure among at least some patients on the drug. Evacetrapib treatment also raised serum levels of C-reactive protein by an average of almost 5%, suggesting that the drug might be proinflammatory.
Evacetrapib led to a lipidologist’s dream effect on plasma lipids without producing clinical benefit. I think this finding, following the failures with dalcetrapib and torcetrapib, is the last nail into the coffin of the cholesterol ester transfer protein inhibitor drug class. A pivotal trial is ongoing for a fourth drug in this class, anacetrapib, but I will be surprised if those results show a clinical benefit.
Dr. Prediman K. Shah, professor of medicine and director of the Atherosclerosis Prevention and Management Center at Cedars-Sinai Medical Center in Los Angeles, made these comments as a designated discussant of ACCELERATE. He has received research support from Aegerion, Amgen, Sanofi, and Cardiovax.
CHICAGO – A class of cholesterol drugs once considered a potentially very promising approach to beneficially reset lipid levels instead produced its third flameout in a pivotal clinical endpoints trial with more than 12,000 patients.
The failure of evacetrapib treatment to produce any clinical benefit despite dramatically elevating serum levels of high-density lipoprotein cholesterol by an average 130% and substantially dropping levels of low-density lipoprotein cholesterol by a mean 37% pretty much spells the end of the cholesterol ester transfer protein (CETP) inhibitors as drug candidates, agreed many experts who heard the disappointing results. The findings also added to existing questions about the reliability of elevated HDL cholesterol levels as a marker for better clinical outcomes, and raised new concerns that a similar limitation might also apply to LDL cholesterol.
“The findings continue to challenge the hope that CETP inhibition might successfully address residual cardiovascular risk,” Dr. Stephen J. Nicholls said at the annual meeting of the American College of Cardiology.
In past reports, the only other CETP inhibitors to complete phase III trials either showed no incremental benefit like evacetrapib, which happened with dalcetrapib (N Engl J Med. 2012 Nov 29;367[22]:2089-99), or clinical harm, which occurred with torcetrapib (N Engl J Med. 2007 Nov 22;357[21]:2109-22).
“Three strikes and you’re out,” declared Dr. Steven E. Nissen, a coinvestigator on the evacetrapib trial, encapsulating his read on where the CETP class now stands.
In addition, “the failure of decreases in LDL-cholesterol to result in an overall morbidity and mortality benefit emphasizes the limitations of surrogate endpoints,” said Dr. Nicholls, the study’s lead investigator and professor of cardiology at the University of Adelaide, Australia.
“We were astonished by the LDL effects in our study. Conventional wisdom says that a 37% drop in LDL cholesterol should translate into a benefit in high-risk patients,” he noted. “This reinforces the concept that mechanism matters. Surrogate endpoints are not a replacement for clinical endpoints. We need to understand more about LDL cholesterol. We thought that [lowering LDL cholesterol] was straightforward, but it’s not.”
“The most important lesson from this study is the hazard of making [efficacy] assumptions based on surrogate endpoints,” said Dr. Frederick Masoudi, a professor of medicine at the University of Colorado in Aurora. “The way you get to a lower LDL cholesterol level is important.”
“There are two hypotheses to explain the results: Either lowering LDL cholesterol was beneficial but something else evacetrapib did caused toxicity” and counterbalanced the benefit of LDL cholesterol lowering, “or it matters how you lower LDL cholesterol,” said Dr. Nissen, chairman of the department of cardiovascular medicine at the Cleveland Clinic. “I personally think it’s the latter, that mechanism [of LDL cholesterol lowering] counts,” he said in an interview.
ACCELERATE (A Study of Evacetrapib in High-Risk Vascular Disease) enrolled 12,092 patients at more than 400 centers worldwide, about half in U.S. locations. The trial identified high-risk patients based on a history of acute coronary syndrome 30-365 days before enrollment, diabetes plus known coronary artery disease, peripheral artery disease, or cerebrovascular disease. The most common risk factor was diabetes plus coronary disease, in nearly two-thirds. The average age was 65 years, three-quarters were men, and the average body mass index was 30 kg/m2. Average LDL cholesterol at baseline was 81 mg/dL, and the average HDL cholesterol level was 45 mg/dL. About 98% of enrolled patients were on a statin at baseline, with 46% on a “high intensity” statin regimen.
The 6,038 patients randomized to receive evacetrapib took 130 mg orally daily; the remaining 6,054 were randomized to receive placebo.
The trial protocol called for treatment of up to 4 years, but the data monitoring committee stopped the study prematurely in October of 2015 after an average treatment period of 25 months because of “clinical futility” for the primary endpoint, a composite of cardiovascular death, MI, stroke, coronary revascularization, or hospitalization for unstable angina. At the time the trial halted, the primary endpoint had occurred in 13% of patients in both arms of the study. The results showed trends toward a somewhat reduced rate of all-cause death and cardiovascular death in the evacetrapib-treated patients, but the between-group differences for these two endpoints did not reach statistical significance.
The results showed two significant between-group differences for possible adverse effects from treatment that may possibly partially explain why the positive lipid changes produced by evacetrapib did not produce positive clinical outcomes: Patients on evacetrapib had a median 5% increase in their serum level of C-reactive protein, a marker of systemic inflammation, compared with a median 8% decrease in the placebo group. And on average, systolic blood pressure was 0.9 mm Hg higher in patients taking evacetrapib compared with those on placebo. Investigator reports of hypertension occurred 1.3% more often in the evacetrapib patients, a statistically significant difference. But in other respects, evacetrapib was safe, leading to no excess in overall adverse effects producing discontinuations, and resulting in significantly fewer patients with substantial elevations of creatine kinase compared with placebo. The evacetrapib patients also showed strong trends toward fewer episodes of new-onset diabetes and fewer patients with substantial increases in bilirubin, compared with placebo-treated patients.
A pivotal trial for a fourth new drug from the class of cholesterol ester transfer protein inhibitors is in progress, the REVEAL study, using the drug anacetrapib. More than 30,000 patients have been enrolled, and a report on the results should be available in 2017.
Dr. Nicholls and Dr. Nissen disclosed ties with several drug companies including Eli Lilly, which sponsored the trial and is developing evacetrapib. Dr. Masoudi had no disclosures.
On Twitter @mitchelzoler
CHICAGO – A class of cholesterol drugs once considered a potentially very promising approach to beneficially reset lipid levels instead produced its third flameout in a pivotal clinical endpoints trial with more than 12,000 patients.
The failure of evacetrapib treatment to produce any clinical benefit despite dramatically elevating serum levels of high-density lipoprotein cholesterol by an average 130% and substantially dropping levels of low-density lipoprotein cholesterol by a mean 37% pretty much spells the end of the cholesterol ester transfer protein (CETP) inhibitors as drug candidates, agreed many experts who heard the disappointing results. The findings also added to existing questions about the reliability of elevated HDL cholesterol levels as a marker for better clinical outcomes, and raised new concerns that a similar limitation might also apply to LDL cholesterol.
“The findings continue to challenge the hope that CETP inhibition might successfully address residual cardiovascular risk,” Dr. Stephen J. Nicholls said at the annual meeting of the American College of Cardiology.
In past reports, the only other CETP inhibitors to complete phase III trials either showed no incremental benefit like evacetrapib, which happened with dalcetrapib (N Engl J Med. 2012 Nov 29;367[22]:2089-99), or clinical harm, which occurred with torcetrapib (N Engl J Med. 2007 Nov 22;357[21]:2109-22).
“Three strikes and you’re out,” declared Dr. Steven E. Nissen, a coinvestigator on the evacetrapib trial, encapsulating his read on where the CETP class now stands.
In addition, “the failure of decreases in LDL-cholesterol to result in an overall morbidity and mortality benefit emphasizes the limitations of surrogate endpoints,” said Dr. Nicholls, the study’s lead investigator and professor of cardiology at the University of Adelaide, Australia.
“We were astonished by the LDL effects in our study. Conventional wisdom says that a 37% drop in LDL cholesterol should translate into a benefit in high-risk patients,” he noted. “This reinforces the concept that mechanism matters. Surrogate endpoints are not a replacement for clinical endpoints. We need to understand more about LDL cholesterol. We thought that [lowering LDL cholesterol] was straightforward, but it’s not.”
“The most important lesson from this study is the hazard of making [efficacy] assumptions based on surrogate endpoints,” said Dr. Frederick Masoudi, a professor of medicine at the University of Colorado in Aurora. “The way you get to a lower LDL cholesterol level is important.”
“There are two hypotheses to explain the results: Either lowering LDL cholesterol was beneficial but something else evacetrapib did caused toxicity” and counterbalanced the benefit of LDL cholesterol lowering, “or it matters how you lower LDL cholesterol,” said Dr. Nissen, chairman of the department of cardiovascular medicine at the Cleveland Clinic. “I personally think it’s the latter, that mechanism [of LDL cholesterol lowering] counts,” he said in an interview.
ACCELERATE (A Study of Evacetrapib in High-Risk Vascular Disease) enrolled 12,092 patients at more than 400 centers worldwide, about half in U.S. locations. The trial identified high-risk patients based on a history of acute coronary syndrome 30-365 days before enrollment, diabetes plus known coronary artery disease, peripheral artery disease, or cerebrovascular disease. The most common risk factor was diabetes plus coronary disease, in nearly two-thirds. The average age was 65 years, three-quarters were men, and the average body mass index was 30 kg/m2. Average LDL cholesterol at baseline was 81 mg/dL, and the average HDL cholesterol level was 45 mg/dL. About 98% of enrolled patients were on a statin at baseline, with 46% on a “high intensity” statin regimen.
The 6,038 patients randomized to receive evacetrapib took 130 mg orally daily; the remaining 6,054 were randomized to receive placebo.
The trial protocol called for treatment of up to 4 years, but the data monitoring committee stopped the study prematurely in October of 2015 after an average treatment period of 25 months because of “clinical futility” for the primary endpoint, a composite of cardiovascular death, MI, stroke, coronary revascularization, or hospitalization for unstable angina. At the time the trial halted, the primary endpoint had occurred in 13% of patients in both arms of the study. The results showed trends toward a somewhat reduced rate of all-cause death and cardiovascular death in the evacetrapib-treated patients, but the between-group differences for these two endpoints did not reach statistical significance.
The results showed two significant between-group differences for possible adverse effects from treatment that may possibly partially explain why the positive lipid changes produced by evacetrapib did not produce positive clinical outcomes: Patients on evacetrapib had a median 5% increase in their serum level of C-reactive protein, a marker of systemic inflammation, compared with a median 8% decrease in the placebo group. And on average, systolic blood pressure was 0.9 mm Hg higher in patients taking evacetrapib compared with those on placebo. Investigator reports of hypertension occurred 1.3% more often in the evacetrapib patients, a statistically significant difference. But in other respects, evacetrapib was safe, leading to no excess in overall adverse effects producing discontinuations, and resulting in significantly fewer patients with substantial elevations of creatine kinase compared with placebo. The evacetrapib patients also showed strong trends toward fewer episodes of new-onset diabetes and fewer patients with substantial increases in bilirubin, compared with placebo-treated patients.
A pivotal trial for a fourth new drug from the class of cholesterol ester transfer protein inhibitors is in progress, the REVEAL study, using the drug anacetrapib. More than 30,000 patients have been enrolled, and a report on the results should be available in 2017.
Dr. Nicholls and Dr. Nissen disclosed ties with several drug companies including Eli Lilly, which sponsored the trial and is developing evacetrapib. Dr. Masoudi had no disclosures.
On Twitter @mitchelzoler
AT ACC 2016
Key clinical point: Despite producing dramatically beneficially changes in lipid levels, treatment with evacetrapib failed to produce clinical benefit in its pivotal trial, adding to questions about benefits from the entire cholesterol ester transfer protein inhibitor class of drugs for cardiovascular disease prevention.
Major finding: During 25-month follow-up, cardiovascular disease events occurred in 13% of patients on evacetrapib and 13% of those on placebo.
Data source: ACCELERATE, a multicenter, international pivotal trial with 12,092 high-risk patients.
Disclosures: Dr. Nicholls and Dr. Nissen disclosed ties with several drug companies including Eli Lilly, which sponsored the trial and is developing evacetrapib. Dr. Masoudi had no disclosures.
STAMPEDE: Metabolic Surgery Bests Medical Therapy Long Term
CHICAGO – The superiority of metabolic surgery over intensive medical therapy for achieving glycemic control in patients with type 2 diabetes was largely maintained at the final 5-year follow-up evaluation in the randomized, controlled STAMPEDE trial.
The 150 subjects, who had “fairly severe diabetes” with an average disease duration of 8 years, were randomized to receive intensive medical therapy alone, or intensive medical therapy with Roux-en-Y gastric bypass surgery or sleeve gastrectomy surgery. The primary endpoint of hemoglobin A1c less than 6% was achieved in 5%, 29%, and 23% of patients in the groups, respectively. The difference was statistically significant in favor of both types of surgery, Dr. Philip Raymond Schauer reported at the annual meeting of the American College of Cardiology.
Furthermore, patients in the surgery groups fared better than those in the intensive medical therapy group on several other measures, including disease remission (defied as HbA1c less than 6% without diabetes medication), HbA1c less than 7% (the American Diabetes Association target for therapy), change in fasting plasma glucose from baseline, and changes in high- and low-density lipoprotein cholesterol levels, said Dr. Schauer, director of the Cleveland Clinic Bariatric and Metabolic Institute.
Patients in the surgery groups also experienced a significantly greater reduction in the use of antihypertensive medications and lipid-lowering agents, he added.
The “very dramatic drop” in HbA1c seen early on in the surgical patients was, for the most part, sustained out to 5 years, he said.
The results for both surgeries were significantly better than those for intensive medical therapy, but the results with gastric bypass were more effective at 5 years than were those for sleeve gastrectomy, he added, noting that the surgery patients had better quality of life, compared with the intensive medical therapy patients.
As for adverse events in the surgery groups, no perioperative deaths occurred, and while there were some surgical complications, none resulted in long-term disability, Dr. Schauer said.
Anemia was more common in the surgery patients, but was fairly mild. The most common complication was weight gain in 20% of patients, and the overall reoperation rate was 7%.
Of note, patients in the study had body mass index ranging from 27 to 43 kg/m2, and those with BMI less than 35 had similar benefits as those with more severe obesity. This is important, as many insurance companies won’t cover metabolic surgery for patients with BMI less than 35, he explained.
These findings represent the longest follow-up to date comparing the efficacy of the two most common metabolic surgery procedures with medical treatment of type 2 diabetes for maintaining glycemic control or reducing end-organ complications. Three-year outcomes of STAMPEDE (Surgical Treatment and Medications Potentially Eradicate Diabetes Efficiently) were reported in 2014 (N Engl J Med. 2014;370:2002-13).
The participants ranged in age from 20 to 60 years. The average HbA1c was about 9%, the average BMI was 36, and most were on at least three antidiabetic medications at baseline. Half were on insulin.
The findings are important, because of the roughly 25 million Americans with type 2 diabetes, only about half have good glycemic control on their current medical treatment strategies, Dr. Schauer said.
Though limited by the single-center study design, the STAMPEDE findings show that metabolic surgery is more effective long term than intensive medical therapy in patients with uncontrolled type 2 diabetes and should be considered a treatment option in this population, he concluded, adding that multicenter studies would be helpful for determining the generalizability of the findings.
Dr. Schauer reported receiving consulting fees/honoraria from Ethicon Endosurgery and The Medicines Company, and having ownership interest in Surgical Excellence.
CHICAGO – The superiority of metabolic surgery over intensive medical therapy for achieving glycemic control in patients with type 2 diabetes was largely maintained at the final 5-year follow-up evaluation in the randomized, controlled STAMPEDE trial.
The 150 subjects, who had “fairly severe diabetes” with an average disease duration of 8 years, were randomized to receive intensive medical therapy alone, or intensive medical therapy with Roux-en-Y gastric bypass surgery or sleeve gastrectomy surgery. The primary endpoint of hemoglobin A1c less than 6% was achieved in 5%, 29%, and 23% of patients in the groups, respectively. The difference was statistically significant in favor of both types of surgery, Dr. Philip Raymond Schauer reported at the annual meeting of the American College of Cardiology.
Furthermore, patients in the surgery groups fared better than those in the intensive medical therapy group on several other measures, including disease remission (defied as HbA1c less than 6% without diabetes medication), HbA1c less than 7% (the American Diabetes Association target for therapy), change in fasting plasma glucose from baseline, and changes in high- and low-density lipoprotein cholesterol levels, said Dr. Schauer, director of the Cleveland Clinic Bariatric and Metabolic Institute.
Patients in the surgery groups also experienced a significantly greater reduction in the use of antihypertensive medications and lipid-lowering agents, he added.
The “very dramatic drop” in HbA1c seen early on in the surgical patients was, for the most part, sustained out to 5 years, he said.
The results for both surgeries were significantly better than those for intensive medical therapy, but the results with gastric bypass were more effective at 5 years than were those for sleeve gastrectomy, he added, noting that the surgery patients had better quality of life, compared with the intensive medical therapy patients.
As for adverse events in the surgery groups, no perioperative deaths occurred, and while there were some surgical complications, none resulted in long-term disability, Dr. Schauer said.
Anemia was more common in the surgery patients, but was fairly mild. The most common complication was weight gain in 20% of patients, and the overall reoperation rate was 7%.
Of note, patients in the study had body mass index ranging from 27 to 43 kg/m2, and those with BMI less than 35 had similar benefits as those with more severe obesity. This is important, as many insurance companies won’t cover metabolic surgery for patients with BMI less than 35, he explained.
These findings represent the longest follow-up to date comparing the efficacy of the two most common metabolic surgery procedures with medical treatment of type 2 diabetes for maintaining glycemic control or reducing end-organ complications. Three-year outcomes of STAMPEDE (Surgical Treatment and Medications Potentially Eradicate Diabetes Efficiently) were reported in 2014 (N Engl J Med. 2014;370:2002-13).
The participants ranged in age from 20 to 60 years. The average HbA1c was about 9%, the average BMI was 36, and most were on at least three antidiabetic medications at baseline. Half were on insulin.
The findings are important, because of the roughly 25 million Americans with type 2 diabetes, only about half have good glycemic control on their current medical treatment strategies, Dr. Schauer said.
Though limited by the single-center study design, the STAMPEDE findings show that metabolic surgery is more effective long term than intensive medical therapy in patients with uncontrolled type 2 diabetes and should be considered a treatment option in this population, he concluded, adding that multicenter studies would be helpful for determining the generalizability of the findings.
Dr. Schauer reported receiving consulting fees/honoraria from Ethicon Endosurgery and The Medicines Company, and having ownership interest in Surgical Excellence.
CHICAGO – The superiority of metabolic surgery over intensive medical therapy for achieving glycemic control in patients with type 2 diabetes was largely maintained at the final 5-year follow-up evaluation in the randomized, controlled STAMPEDE trial.
The 150 subjects, who had “fairly severe diabetes” with an average disease duration of 8 years, were randomized to receive intensive medical therapy alone, or intensive medical therapy with Roux-en-Y gastric bypass surgery or sleeve gastrectomy surgery. The primary endpoint of hemoglobin A1c less than 6% was achieved in 5%, 29%, and 23% of patients in the groups, respectively. The difference was statistically significant in favor of both types of surgery, Dr. Philip Raymond Schauer reported at the annual meeting of the American College of Cardiology.
Furthermore, patients in the surgery groups fared better than those in the intensive medical therapy group on several other measures, including disease remission (defied as HbA1c less than 6% without diabetes medication), HbA1c less than 7% (the American Diabetes Association target for therapy), change in fasting plasma glucose from baseline, and changes in high- and low-density lipoprotein cholesterol levels, said Dr. Schauer, director of the Cleveland Clinic Bariatric and Metabolic Institute.
Patients in the surgery groups also experienced a significantly greater reduction in the use of antihypertensive medications and lipid-lowering agents, he added.
The “very dramatic drop” in HbA1c seen early on in the surgical patients was, for the most part, sustained out to 5 years, he said.
The results for both surgeries were significantly better than those for intensive medical therapy, but the results with gastric bypass were more effective at 5 years than were those for sleeve gastrectomy, he added, noting that the surgery patients had better quality of life, compared with the intensive medical therapy patients.
As for adverse events in the surgery groups, no perioperative deaths occurred, and while there were some surgical complications, none resulted in long-term disability, Dr. Schauer said.
Anemia was more common in the surgery patients, but was fairly mild. The most common complication was weight gain in 20% of patients, and the overall reoperation rate was 7%.
Of note, patients in the study had body mass index ranging from 27 to 43 kg/m2, and those with BMI less than 35 had similar benefits as those with more severe obesity. This is important, as many insurance companies won’t cover metabolic surgery for patients with BMI less than 35, he explained.
These findings represent the longest follow-up to date comparing the efficacy of the two most common metabolic surgery procedures with medical treatment of type 2 diabetes for maintaining glycemic control or reducing end-organ complications. Three-year outcomes of STAMPEDE (Surgical Treatment and Medications Potentially Eradicate Diabetes Efficiently) were reported in 2014 (N Engl J Med. 2014;370:2002-13).
The participants ranged in age from 20 to 60 years. The average HbA1c was about 9%, the average BMI was 36, and most were on at least three antidiabetic medications at baseline. Half were on insulin.
The findings are important, because of the roughly 25 million Americans with type 2 diabetes, only about half have good glycemic control on their current medical treatment strategies, Dr. Schauer said.
Though limited by the single-center study design, the STAMPEDE findings show that metabolic surgery is more effective long term than intensive medical therapy in patients with uncontrolled type 2 diabetes and should be considered a treatment option in this population, he concluded, adding that multicenter studies would be helpful for determining the generalizability of the findings.
Dr. Schauer reported receiving consulting fees/honoraria from Ethicon Endosurgery and The Medicines Company, and having ownership interest in Surgical Excellence.
AT ACC 16
STAMPEDE: Metabolic surgery bests medical therapy long term
CHICAGO – The superiority of metabolic surgery over intensive medical therapy for achieving glycemic control in patients with type 2 diabetes was largely maintained at the final 5-year follow-up evaluation in the randomized, controlled STAMPEDE trial.
The 150 subjects, who had “fairly severe diabetes” with an average disease duration of 8 years, were randomized to receive intensive medical therapy alone, or intensive medical therapy with Roux-en-Y gastric bypass surgery or sleeve gastrectomy surgery. The primary endpoint of hemoglobin A1c less than 6% was achieved in 5%, 29%, and 23% of patients in the groups, respectively. The difference was statistically significant in favor of both types of surgery, Dr. Philip Raymond Schauer reported at the annual meeting of the American College of Cardiology.
Furthermore, patients in the surgery groups fared better than those in the intensive medical therapy group on several other measures, including disease remission (defied as HbA1c less than 6% without diabetes medication), HbA1c less than 7% (the American Diabetes Association target for therapy), change in fasting plasma glucose from baseline, and changes in high- and low-density lipoprotein cholesterol levels, said Dr. Schauer, director of the Cleveland Clinic Bariatric and Metabolic Institute.
Patients in the surgery groups also experienced a significantly greater reduction in the use of antihypertensive medications and lipid-lowering agents, he added.
The “very dramatic drop” in HbA1c seen early on in the surgical patients was, for the most part, sustained out to 5 years, he said.
The results for both surgeries were significantly better than those for intensive medical therapy, but the results with gastric bypass were more effective at 5 years than were those for sleeve gastrectomy, he added, noting that the surgery patients had better quality of life, compared with the intensive medical therapy patients.
As for adverse events in the surgery groups, no perioperative deaths occurred, and while there were some surgical complications, none resulted in long-term disability, Dr. Schauer said.
Anemia was more common in the surgery patients, but was fairly mild. The most common complication was weight gain in 20% of patients, and the overall reoperation rate was 7%.
Of note, patients in the study had body mass index ranging from 27 to 43 kg/m2, and those with BMI less than 35 had similar benefits as those with more severe obesity. This is important, as many insurance companies won’t cover metabolic surgery for patients with BMI less than 35, he explained.
These findings represent the longest follow-up to date comparing the efficacy of the two most common metabolic surgery procedures with medical treatment of type 2 diabetes for maintaining glycemic control or reducing end-organ complications. Three-year outcomes of STAMPEDE (Surgical Treatment and Medications Potentially Eradicate Diabetes Efficiently) were reported in 2014 (N Engl J Med. 2014;370:2002-13).
The participants ranged in age from 20 to 60 years. The average HbA1c was about 9%, the average BMI was 36, and most were on at least three antidiabetic medications at baseline. Half were on insulin.
The findings are important, because of the roughly 25 million Americans with type 2 diabetes, only about half have good glycemic control on their current medical treatment strategies, Dr. Schauer said.
Though limited by the single-center study design, the STAMPEDE findings show that metabolic surgery is more effective long term than intensive medical therapy in patients with uncontrolled type 2 diabetes and should be considered a treatment option in this population, he concluded, adding that multicenter studies would be helpful for determining the generalizability of the findings.
Dr. Schauer reported receiving consulting fees/honoraria from Ethicon Endosurgery and The Medicines Company, and having ownership interest in Surgical Excellence.
CHICAGO – The superiority of metabolic surgery over intensive medical therapy for achieving glycemic control in patients with type 2 diabetes was largely maintained at the final 5-year follow-up evaluation in the randomized, controlled STAMPEDE trial.
The 150 subjects, who had “fairly severe diabetes” with an average disease duration of 8 years, were randomized to receive intensive medical therapy alone, or intensive medical therapy with Roux-en-Y gastric bypass surgery or sleeve gastrectomy surgery. The primary endpoint of hemoglobin A1c less than 6% was achieved in 5%, 29%, and 23% of patients in the groups, respectively. The difference was statistically significant in favor of both types of surgery, Dr. Philip Raymond Schauer reported at the annual meeting of the American College of Cardiology.
Furthermore, patients in the surgery groups fared better than those in the intensive medical therapy group on several other measures, including disease remission (defied as HbA1c less than 6% without diabetes medication), HbA1c less than 7% (the American Diabetes Association target for therapy), change in fasting plasma glucose from baseline, and changes in high- and low-density lipoprotein cholesterol levels, said Dr. Schauer, director of the Cleveland Clinic Bariatric and Metabolic Institute.
Patients in the surgery groups also experienced a significantly greater reduction in the use of antihypertensive medications and lipid-lowering agents, he added.
The “very dramatic drop” in HbA1c seen early on in the surgical patients was, for the most part, sustained out to 5 years, he said.
The results for both surgeries were significantly better than those for intensive medical therapy, but the results with gastric bypass were more effective at 5 years than were those for sleeve gastrectomy, he added, noting that the surgery patients had better quality of life, compared with the intensive medical therapy patients.
As for adverse events in the surgery groups, no perioperative deaths occurred, and while there were some surgical complications, none resulted in long-term disability, Dr. Schauer said.
Anemia was more common in the surgery patients, but was fairly mild. The most common complication was weight gain in 20% of patients, and the overall reoperation rate was 7%.
Of note, patients in the study had body mass index ranging from 27 to 43 kg/m2, and those with BMI less than 35 had similar benefits as those with more severe obesity. This is important, as many insurance companies won’t cover metabolic surgery for patients with BMI less than 35, he explained.
These findings represent the longest follow-up to date comparing the efficacy of the two most common metabolic surgery procedures with medical treatment of type 2 diabetes for maintaining glycemic control or reducing end-organ complications. Three-year outcomes of STAMPEDE (Surgical Treatment and Medications Potentially Eradicate Diabetes Efficiently) were reported in 2014 (N Engl J Med. 2014;370:2002-13).
The participants ranged in age from 20 to 60 years. The average HbA1c was about 9%, the average BMI was 36, and most were on at least three antidiabetic medications at baseline. Half were on insulin.
The findings are important, because of the roughly 25 million Americans with type 2 diabetes, only about half have good glycemic control on their current medical treatment strategies, Dr. Schauer said.
Though limited by the single-center study design, the STAMPEDE findings show that metabolic surgery is more effective long term than intensive medical therapy in patients with uncontrolled type 2 diabetes and should be considered a treatment option in this population, he concluded, adding that multicenter studies would be helpful for determining the generalizability of the findings.
Dr. Schauer reported receiving consulting fees/honoraria from Ethicon Endosurgery and The Medicines Company, and having ownership interest in Surgical Excellence.
CHICAGO – The superiority of metabolic surgery over intensive medical therapy for achieving glycemic control in patients with type 2 diabetes was largely maintained at the final 5-year follow-up evaluation in the randomized, controlled STAMPEDE trial.
The 150 subjects, who had “fairly severe diabetes” with an average disease duration of 8 years, were randomized to receive intensive medical therapy alone, or intensive medical therapy with Roux-en-Y gastric bypass surgery or sleeve gastrectomy surgery. The primary endpoint of hemoglobin A1c less than 6% was achieved in 5%, 29%, and 23% of patients in the groups, respectively. The difference was statistically significant in favor of both types of surgery, Dr. Philip Raymond Schauer reported at the annual meeting of the American College of Cardiology.
Furthermore, patients in the surgery groups fared better than those in the intensive medical therapy group on several other measures, including disease remission (defied as HbA1c less than 6% without diabetes medication), HbA1c less than 7% (the American Diabetes Association target for therapy), change in fasting plasma glucose from baseline, and changes in high- and low-density lipoprotein cholesterol levels, said Dr. Schauer, director of the Cleveland Clinic Bariatric and Metabolic Institute.
Patients in the surgery groups also experienced a significantly greater reduction in the use of antihypertensive medications and lipid-lowering agents, he added.
The “very dramatic drop” in HbA1c seen early on in the surgical patients was, for the most part, sustained out to 5 years, he said.
The results for both surgeries were significantly better than those for intensive medical therapy, but the results with gastric bypass were more effective at 5 years than were those for sleeve gastrectomy, he added, noting that the surgery patients had better quality of life, compared with the intensive medical therapy patients.
As for adverse events in the surgery groups, no perioperative deaths occurred, and while there were some surgical complications, none resulted in long-term disability, Dr. Schauer said.
Anemia was more common in the surgery patients, but was fairly mild. The most common complication was weight gain in 20% of patients, and the overall reoperation rate was 7%.
Of note, patients in the study had body mass index ranging from 27 to 43 kg/m2, and those with BMI less than 35 had similar benefits as those with more severe obesity. This is important, as many insurance companies won’t cover metabolic surgery for patients with BMI less than 35, he explained.
These findings represent the longest follow-up to date comparing the efficacy of the two most common metabolic surgery procedures with medical treatment of type 2 diabetes for maintaining glycemic control or reducing end-organ complications. Three-year outcomes of STAMPEDE (Surgical Treatment and Medications Potentially Eradicate Diabetes Efficiently) were reported in 2014 (N Engl J Med. 2014;370:2002-13).
The participants ranged in age from 20 to 60 years. The average HbA1c was about 9%, the average BMI was 36, and most were on at least three antidiabetic medications at baseline. Half were on insulin.
The findings are important, because of the roughly 25 million Americans with type 2 diabetes, only about half have good glycemic control on their current medical treatment strategies, Dr. Schauer said.
Though limited by the single-center study design, the STAMPEDE findings show that metabolic surgery is more effective long term than intensive medical therapy in patients with uncontrolled type 2 diabetes and should be considered a treatment option in this population, he concluded, adding that multicenter studies would be helpful for determining the generalizability of the findings.
Dr. Schauer reported receiving consulting fees/honoraria from Ethicon Endosurgery and The Medicines Company, and having ownership interest in Surgical Excellence.
AT ACC 16
Key clinical point: The superiority of metabolic surgery over intensive medical therapy for achieving glycemic control among patients with type 2 diabetes in the randomized, controlled STAMPEDE persisted at the final 5-year follow-up evaluation.
Major finding: The primary endpoint of HbA1c less than 6% was achieved in 5%, 29%, and 23% of patients in the medication and medication plus Roux-en-Y or sleeve gastrectomy groups, respectively.
Data source: The randomized, controlled STAMPEDE trial in 150 subjects.
Disclosures: Dr. Schauer reported receiving consulting fees/honoraria from Ethicon Endosurgery and The Medicines Company, and having ownership interest in Surgical Excellence.
Earlier Bariatric Surgery May Improve Cardiovascular Outcomes
CHICAGO – Sooner may be better than later when it comes to the timing of bariatric surgery in patients with morbid obesity.
Of 828 patients with body mass index of at least 35 kg/m2 who underwent laparoscopic adjustable gastric banding performed by a single surgeon and were followed for up to 11 years (mean of 10 years), 423 were aged 45 years or younger, and 405 were over age 45 years at the time of surgery. A comparison of outcomes between the two age groups showed that older age at the time of surgery was an independent predictor of cardiovascular events (hazard ratio, 1.8), Maharaj Singh, Ph.D., a biostatistician at the Aurora Research Institute, Milwaukee, reported in a poster at the annual meeting of the American College of Cardiology.
Despite a similar reduction in body weight after gastric banding surgery, the older patients experienced more cardiovascular events: myocardial infarction occurred in 0.2% and 1.7% of patients in the younger and older age groups, respectively, pulmonary embolism occurred in 0.7% and 4.3%, congestive heart failure occurred in 2.8% and 7.8%, and stroke occurred in 3.7% and 7.6%, Dr. Singh said.
“Although the older group had more comorbidities, these were accounted for by multivariate analysis and age over 45 years remained an independent predictor of poor cardiovascular outcomes,” senior coauthor Dr. Arshad Jahangir, professor of medicine at the University of Wisconsin–Madison, said in an interview.
Other independent predictors of adverse cardiovascular outcomes in the study were sleep apnea (hazard ratio, 4), history of hypertension (HR, 1.9), and depression, (HR, 1.8), Dr. Jahangir said.
“Gender, race, and diabetes mellitus did not independently predict cardiovascular events,” he said.
Weight loss after bariatric surgery has been shown to reduce the risk of adverse cardiovascular events, but it has remained unclear whether the reduction in risk varies based on age at the time of surgery, he said.
The current findings suggest that the effects of laparoscopic adjustable gastric banding–induced weight loss on cardiovascular outcomes are greater in patients who undergo the surgery at a younger age, he said, adding that the findings also “raise important questions about whether better control of sleep apnea, hypertension, and depression could help further reduce cardiovascular events in morbidly obese individuals undergoing bariatric surgery and should be addressed in a prospective study of these patients.”
The authors reported having no disclosures.
CHICAGO – Sooner may be better than later when it comes to the timing of bariatric surgery in patients with morbid obesity.
Of 828 patients with body mass index of at least 35 kg/m2 who underwent laparoscopic adjustable gastric banding performed by a single surgeon and were followed for up to 11 years (mean of 10 years), 423 were aged 45 years or younger, and 405 were over age 45 years at the time of surgery. A comparison of outcomes between the two age groups showed that older age at the time of surgery was an independent predictor of cardiovascular events (hazard ratio, 1.8), Maharaj Singh, Ph.D., a biostatistician at the Aurora Research Institute, Milwaukee, reported in a poster at the annual meeting of the American College of Cardiology.
Despite a similar reduction in body weight after gastric banding surgery, the older patients experienced more cardiovascular events: myocardial infarction occurred in 0.2% and 1.7% of patients in the younger and older age groups, respectively, pulmonary embolism occurred in 0.7% and 4.3%, congestive heart failure occurred in 2.8% and 7.8%, and stroke occurred in 3.7% and 7.6%, Dr. Singh said.
“Although the older group had more comorbidities, these were accounted for by multivariate analysis and age over 45 years remained an independent predictor of poor cardiovascular outcomes,” senior coauthor Dr. Arshad Jahangir, professor of medicine at the University of Wisconsin–Madison, said in an interview.
Other independent predictors of adverse cardiovascular outcomes in the study were sleep apnea (hazard ratio, 4), history of hypertension (HR, 1.9), and depression, (HR, 1.8), Dr. Jahangir said.
“Gender, race, and diabetes mellitus did not independently predict cardiovascular events,” he said.
Weight loss after bariatric surgery has been shown to reduce the risk of adverse cardiovascular events, but it has remained unclear whether the reduction in risk varies based on age at the time of surgery, he said.
The current findings suggest that the effects of laparoscopic adjustable gastric banding–induced weight loss on cardiovascular outcomes are greater in patients who undergo the surgery at a younger age, he said, adding that the findings also “raise important questions about whether better control of sleep apnea, hypertension, and depression could help further reduce cardiovascular events in morbidly obese individuals undergoing bariatric surgery and should be addressed in a prospective study of these patients.”
The authors reported having no disclosures.
CHICAGO – Sooner may be better than later when it comes to the timing of bariatric surgery in patients with morbid obesity.
Of 828 patients with body mass index of at least 35 kg/m2 who underwent laparoscopic adjustable gastric banding performed by a single surgeon and were followed for up to 11 years (mean of 10 years), 423 were aged 45 years or younger, and 405 were over age 45 years at the time of surgery. A comparison of outcomes between the two age groups showed that older age at the time of surgery was an independent predictor of cardiovascular events (hazard ratio, 1.8), Maharaj Singh, Ph.D., a biostatistician at the Aurora Research Institute, Milwaukee, reported in a poster at the annual meeting of the American College of Cardiology.
Despite a similar reduction in body weight after gastric banding surgery, the older patients experienced more cardiovascular events: myocardial infarction occurred in 0.2% and 1.7% of patients in the younger and older age groups, respectively, pulmonary embolism occurred in 0.7% and 4.3%, congestive heart failure occurred in 2.8% and 7.8%, and stroke occurred in 3.7% and 7.6%, Dr. Singh said.
“Although the older group had more comorbidities, these were accounted for by multivariate analysis and age over 45 years remained an independent predictor of poor cardiovascular outcomes,” senior coauthor Dr. Arshad Jahangir, professor of medicine at the University of Wisconsin–Madison, said in an interview.
Other independent predictors of adverse cardiovascular outcomes in the study were sleep apnea (hazard ratio, 4), history of hypertension (HR, 1.9), and depression, (HR, 1.8), Dr. Jahangir said.
“Gender, race, and diabetes mellitus did not independently predict cardiovascular events,” he said.
Weight loss after bariatric surgery has been shown to reduce the risk of adverse cardiovascular events, but it has remained unclear whether the reduction in risk varies based on age at the time of surgery, he said.
The current findings suggest that the effects of laparoscopic adjustable gastric banding–induced weight loss on cardiovascular outcomes are greater in patients who undergo the surgery at a younger age, he said, adding that the findings also “raise important questions about whether better control of sleep apnea, hypertension, and depression could help further reduce cardiovascular events in morbidly obese individuals undergoing bariatric surgery and should be addressed in a prospective study of these patients.”
The authors reported having no disclosures.
AT ACC 16
Earlier bariatric surgery may improve cardiovascular outcomes
CHICAGO – Sooner may be better than later when it comes to the timing of bariatric surgery in patients with morbid obesity.
Of 828 patients with body mass index of at least 35 kg/m2 who underwent laparoscopic adjustable gastric banding performed by a single surgeon and were followed for up to 11 years (mean of 10 years), 423 were aged 45 years or younger, and 405 were over age 45 years at the time of surgery. A comparison of outcomes between the two age groups showed that older age at the time of surgery was an independent predictor of cardiovascular events (hazard ratio, 1.8), Maharaj Singh, Ph.D., a biostatistician at the Aurora Research Institute, Milwaukee, reported in a poster at the annual meeting of the American College of Cardiology.
Despite a similar reduction in body weight after gastric banding surgery, the older patients experienced more cardiovascular events: myocardial infarction occurred in 0.2% and 1.7% of patients in the younger and older age groups, respectively, pulmonary embolism occurred in 0.7% and 4.3%, congestive heart failure occurred in 2.8% and 7.8%, and stroke occurred in 3.7% and 7.6%, Dr. Singh said.
“Although the older group had more comorbidities, these were accounted for by multivariate analysis and age over 45 years remained an independent predictor of poor cardiovascular outcomes,” senior coauthor Dr. Arshad Jahangir, professor of medicine at the University of Wisconsin–Madison, said in an interview.
Other independent predictors of adverse cardiovascular outcomes in the study were sleep apnea (hazard ratio, 4), history of hypertension (HR, 1.9), and depression, (HR, 1.8), Dr. Jahangir said.
“Gender, race, and diabetes mellitus did not independently predict cardiovascular events,” he said.
Weight loss after bariatric surgery has been shown to reduce the risk of adverse cardiovascular events, but it has remained unclear whether the reduction in risk varies based on age at the time of surgery, he said.
The current findings suggest that the effects of laparoscopic adjustable gastric banding–induced weight loss on cardiovascular outcomes are greater in patients who undergo the surgery at a younger age, he said, adding that the findings also “raise important questions about whether better control of sleep apnea, hypertension, and depression could help further reduce cardiovascular events in morbidly obese individuals undergoing bariatric surgery and should be addressed in a prospective study of these patients.”
The authors reported having no disclosures.
CHICAGO – Sooner may be better than later when it comes to the timing of bariatric surgery in patients with morbid obesity.
Of 828 patients with body mass index of at least 35 kg/m2 who underwent laparoscopic adjustable gastric banding performed by a single surgeon and were followed for up to 11 years (mean of 10 years), 423 were aged 45 years or younger, and 405 were over age 45 years at the time of surgery. A comparison of outcomes between the two age groups showed that older age at the time of surgery was an independent predictor of cardiovascular events (hazard ratio, 1.8), Maharaj Singh, Ph.D., a biostatistician at the Aurora Research Institute, Milwaukee, reported in a poster at the annual meeting of the American College of Cardiology.
Despite a similar reduction in body weight after gastric banding surgery, the older patients experienced more cardiovascular events: myocardial infarction occurred in 0.2% and 1.7% of patients in the younger and older age groups, respectively, pulmonary embolism occurred in 0.7% and 4.3%, congestive heart failure occurred in 2.8% and 7.8%, and stroke occurred in 3.7% and 7.6%, Dr. Singh said.
“Although the older group had more comorbidities, these were accounted for by multivariate analysis and age over 45 years remained an independent predictor of poor cardiovascular outcomes,” senior coauthor Dr. Arshad Jahangir, professor of medicine at the University of Wisconsin–Madison, said in an interview.
Other independent predictors of adverse cardiovascular outcomes in the study were sleep apnea (hazard ratio, 4), history of hypertension (HR, 1.9), and depression, (HR, 1.8), Dr. Jahangir said.
“Gender, race, and diabetes mellitus did not independently predict cardiovascular events,” he said.
Weight loss after bariatric surgery has been shown to reduce the risk of adverse cardiovascular events, but it has remained unclear whether the reduction in risk varies based on age at the time of surgery, he said.
The current findings suggest that the effects of laparoscopic adjustable gastric banding–induced weight loss on cardiovascular outcomes are greater in patients who undergo the surgery at a younger age, he said, adding that the findings also “raise important questions about whether better control of sleep apnea, hypertension, and depression could help further reduce cardiovascular events in morbidly obese individuals undergoing bariatric surgery and should be addressed in a prospective study of these patients.”
The authors reported having no disclosures.
CHICAGO – Sooner may be better than later when it comes to the timing of bariatric surgery in patients with morbid obesity.
Of 828 patients with body mass index of at least 35 kg/m2 who underwent laparoscopic adjustable gastric banding performed by a single surgeon and were followed for up to 11 years (mean of 10 years), 423 were aged 45 years or younger, and 405 were over age 45 years at the time of surgery. A comparison of outcomes between the two age groups showed that older age at the time of surgery was an independent predictor of cardiovascular events (hazard ratio, 1.8), Maharaj Singh, Ph.D., a biostatistician at the Aurora Research Institute, Milwaukee, reported in a poster at the annual meeting of the American College of Cardiology.
Despite a similar reduction in body weight after gastric banding surgery, the older patients experienced more cardiovascular events: myocardial infarction occurred in 0.2% and 1.7% of patients in the younger and older age groups, respectively, pulmonary embolism occurred in 0.7% and 4.3%, congestive heart failure occurred in 2.8% and 7.8%, and stroke occurred in 3.7% and 7.6%, Dr. Singh said.
“Although the older group had more comorbidities, these were accounted for by multivariate analysis and age over 45 years remained an independent predictor of poor cardiovascular outcomes,” senior coauthor Dr. Arshad Jahangir, professor of medicine at the University of Wisconsin–Madison, said in an interview.
Other independent predictors of adverse cardiovascular outcomes in the study were sleep apnea (hazard ratio, 4), history of hypertension (HR, 1.9), and depression, (HR, 1.8), Dr. Jahangir said.
“Gender, race, and diabetes mellitus did not independently predict cardiovascular events,” he said.
Weight loss after bariatric surgery has been shown to reduce the risk of adverse cardiovascular events, but it has remained unclear whether the reduction in risk varies based on age at the time of surgery, he said.
The current findings suggest that the effects of laparoscopic adjustable gastric banding–induced weight loss on cardiovascular outcomes are greater in patients who undergo the surgery at a younger age, he said, adding that the findings also “raise important questions about whether better control of sleep apnea, hypertension, and depression could help further reduce cardiovascular events in morbidly obese individuals undergoing bariatric surgery and should be addressed in a prospective study of these patients.”
The authors reported having no disclosures.
AT ACC 16
Key clinical point: Morbidly obese patients who underwent bariatric surgery before age 45 years had a reduced risk of adverse cardiovascular outcomes vs. those aged 45 or older at the time of surgery, despite similar weight loss.
Major finding: Older vs. younger age at the time of surgery was an independent predictor of cardiovascular events (hazard ratio, 1.8).
Data source: A review of outcomes in 828 laparoscopic adjustable gastric banding patients.
Disclosures: The authors reported having no disclosures.
PPI Cuts GI Events From Low- and High-dose Aspirin
CHICAGO – Six months of treatment with a proton pump inhibitor (PPI) is a safe way to cut the incidence of major gastrointestinal events in cardiovascular disease patients on dual-antiplatelet therapy regardless of whether they receive low-dose or high-dose aspirin, according to a post-hoc analysis of data from more than 3,700 patients enrolled in the multicenter, randomized COGENT trial.
“Short-term, prophylactic PPI therapy consistently reduced rates of adjudicated upper-gastrointestinal events without increasing cardiovascular events, regardless of the aspirin dose,” Dr. Muthiah Vaduganathan said while presenting his study at the annual meeting of the American College of Cardiology. “Gastroprotection with PPI therapy should be used in appropriately selected patients with coronary artery disease who require dual-antiplatelet therapy even if they are on low-dose aspirin.”
In addition to documenting the safety and efficacy of 6 months of PPI treatment for patients at high risk for cardiovascular disease events and low or moderate risk for a GI event, the results from the analysis also documented how common GI events are in this population, even when patients receive low-dose aspirin. Nearly two-thirds of the 3,752 patients included in the analysis took low-dose aspirin, either 75 mg or 81 mg per day. Their incidence of an adjudicated upper GI bleed, the study’s primary GI endpoint, occurred in 3.1% of patients on placebo, and in 1.2% of patients taking a prophylactic PPI. Among the other 34% of patients on high-dose aspirin – a daily dosage of at least 150 mg – the rate of adjudicated upper-GI bleeds was 2.6% without a PPI and 0.9% in those on a PPI.
In other words, even among patients deemed to have a relatively low risk for GI complications from aspirin because their entry into this study required no history of major GI bleeds or recent treatment with a gastroprotection agent, treatment with low-dose aspirin resulted in upper-GI bleeds at the same rate, about 3%, as a high-dose aspirin regimen. And in both of these aspirin subgroups 6 months of concurrent treatment with a PPI cut the incidence of major GI bleeds by more than half.
The findings are especially notable because the enrollment criteria stacked the deck toward patients with high cardiovascular disease risk and relatively low GI risk. The study enrolled “a unique population at high risk for cardiovascular disease – 71% had previously undergone a percutaneous coronary intervention, and 42% had a history of an acute coronary syndrome – and low GI risk, but even in this population enriched for cardiovascular disease risk, there was no increased rate of cardiovascular disease events” during a median follow-up while on PPI treatment of 110 days, Dr. Vaduganathan said.
Among patients on low-dose aspirin, the rate of cardiovascular disease death, MI, stroke, or coronary revascularization was 5.6% with PPI treatment and 5.5% without, and in the high-dose aspirin patients the rates were 4.2% with PPI treatment and 5.5% without. Neither of these differences between the subgroups on or off a PPI were statistically significant.
Concurrent with Dr. Vaduganathan’s report at the meeting the results also appeared online (J Am Coll Cardiol. 2016 April 12;67[14]:661-71).
“There appeared to be no adverse clinical effect from PPI treatment. When used short-term, for up to 6 months, PPI treatment appears to be safe in patients with cardiovascular disease,” Dr. Vaduganathan concluded.
The analysis used data collected in COGENT (Clopidogrel and the Optimization of Gastrointestinal Events Trial), a phase 3 study designed to compare a single-pill formulation of 20 mg omeprazole and 75 mg clopidogrel taken orally once daily with 75 mg clopidogrel against a background of all patients taking aspirin. COGENT stopped prematurely in late 2008 as the company developing this formulation and sponsoring the trial, Cogentus Pharmaceuticals, filed for bankruptcy. Despite its abrupt conclusion, the trial had enrolled and followed enough patients to show that treatment with omeprazole plus clopidogrel and aspirin led to a significant reduction in upper GI bleeding without increasing the rate of cardiovascular disease events, compared with clopidogrel plus aspirin (N Engl J Med. 2010 Nov 11;363[20]:1909-17).
The new analysis focused on the greater than 99% of patients in the total COGENT cohort for whom information was available on whether they received high- or low-dose aspirin.
Although the primary findings from COGENT, reported in 2010, documented the safety and efficacy of concomitant PPI treatment during dual-antiplatelet therapy, and despite guidelines revised in 2010 that called for PPI treatment when appropriate, this strategy for preventing GI complications remains underused, Dr. Vaduganathan said. The most recent U.S. recommendations that address this issue called for assessing the potential risk and benefit from PPI treatment in patients receiving dual-antiplatelet therapy: “The risk reduction with PPIs is substantial in patients with risk factors for GI bleeding and may outweigh any potential reduction in the CV efficacy of antiplatelet treatment because of a drug-drug interaction (J Am Coll Cardiol. 2010 Dec;56[24]:2051-66).”
The only caveat Dr. Vaduganathan placed on PPI use was that the COGENT data addressed only 6 months of PPI use; the safety of longer-term use has not been studied. But “the trend is to use PPIs for as short a period as possible,” and the risk for adverse effects from PPI treatment on cardiovascular disease events is likely greatest during the first 6 months of PPI treatment, he noted. If PPI treatment needs to continue beyond 6 months, he suggested systematically reassessing the risk-benefit balance for individual patients from continued PPI treatment every 3 months.
The new analysis of COGENT provides important insights into patients treated with clopidogrel and aspirin. The data show that patients on low-dose aspirin do not have an increased risk of cardiovascular events, and that patients who take low-dose aspirin still face a significant risk for upper-gastrointestinal events. Patients taking low-dose aspirin have about the same rate of upper-GI events as patients on high-dose aspirin.
The issue of GI safety for patients on low-dose aspirin as part of dual-antiplatelet therapy has been long overshadowed by concern over a hypothetical interaction between clopidogrel and proton pump inhibitors. The issue has also been distorted by a false sense of security that when patients receive low-dose aspirin they do not require protection against GI events.
Treatment of patients taking low-dose aspirin with a PPI is underutilized. The confirmation this analysis provides, that PPI treatment gives GI protection without causing an excess of cardiovascular events, calls for a change in current practice when clinicians prescribe low-dose aspirin. I’m concerned by the apparent lack of enthusiasm by clinicians to prescribe PPIs to their patients on low-dose aspirin despite their significant risk for GI events. The real question is whether all patients on low-dose aspirin should receive a PPI long term or only the subgroup of patients with high risk for an upper-GI bleed.
Dr. Michael E. Farkouh is a cardiologist at Mount Sinai Hospital in Toronto. He has no disclosures. He made these comments in an editorial that accompanied the published report (J Am Coll Cardiol. 2016 April 12;67[14]:1672-3).
The new analysis of COGENT provides important insights into patients treated with clopidogrel and aspirin. The data show that patients on low-dose aspirin do not have an increased risk of cardiovascular events, and that patients who take low-dose aspirin still face a significant risk for upper-gastrointestinal events. Patients taking low-dose aspirin have about the same rate of upper-GI events as patients on high-dose aspirin.
The issue of GI safety for patients on low-dose aspirin as part of dual-antiplatelet therapy has been long overshadowed by concern over a hypothetical interaction between clopidogrel and proton pump inhibitors. The issue has also been distorted by a false sense of security that when patients receive low-dose aspirin they do not require protection against GI events.
Treatment of patients taking low-dose aspirin with a PPI is underutilized. The confirmation this analysis provides, that PPI treatment gives GI protection without causing an excess of cardiovascular events, calls for a change in current practice when clinicians prescribe low-dose aspirin. I’m concerned by the apparent lack of enthusiasm by clinicians to prescribe PPIs to their patients on low-dose aspirin despite their significant risk for GI events. The real question is whether all patients on low-dose aspirin should receive a PPI long term or only the subgroup of patients with high risk for an upper-GI bleed.
Dr. Michael E. Farkouh is a cardiologist at Mount Sinai Hospital in Toronto. He has no disclosures. He made these comments in an editorial that accompanied the published report (J Am Coll Cardiol. 2016 April 12;67[14]:1672-3).
The new analysis of COGENT provides important insights into patients treated with clopidogrel and aspirin. The data show that patients on low-dose aspirin do not have an increased risk of cardiovascular events, and that patients who take low-dose aspirin still face a significant risk for upper-gastrointestinal events. Patients taking low-dose aspirin have about the same rate of upper-GI events as patients on high-dose aspirin.
The issue of GI safety for patients on low-dose aspirin as part of dual-antiplatelet therapy has been long overshadowed by concern over a hypothetical interaction between clopidogrel and proton pump inhibitors. The issue has also been distorted by a false sense of security that when patients receive low-dose aspirin they do not require protection against GI events.
Treatment of patients taking low-dose aspirin with a PPI is underutilized. The confirmation this analysis provides, that PPI treatment gives GI protection without causing an excess of cardiovascular events, calls for a change in current practice when clinicians prescribe low-dose aspirin. I’m concerned by the apparent lack of enthusiasm by clinicians to prescribe PPIs to their patients on low-dose aspirin despite their significant risk for GI events. The real question is whether all patients on low-dose aspirin should receive a PPI long term or only the subgroup of patients with high risk for an upper-GI bleed.
Dr. Michael E. Farkouh is a cardiologist at Mount Sinai Hospital in Toronto. He has no disclosures. He made these comments in an editorial that accompanied the published report (J Am Coll Cardiol. 2016 April 12;67[14]:1672-3).
CHICAGO – Six months of treatment with a proton pump inhibitor (PPI) is a safe way to cut the incidence of major gastrointestinal events in cardiovascular disease patients on dual-antiplatelet therapy regardless of whether they receive low-dose or high-dose aspirin, according to a post-hoc analysis of data from more than 3,700 patients enrolled in the multicenter, randomized COGENT trial.
“Short-term, prophylactic PPI therapy consistently reduced rates of adjudicated upper-gastrointestinal events without increasing cardiovascular events, regardless of the aspirin dose,” Dr. Muthiah Vaduganathan said while presenting his study at the annual meeting of the American College of Cardiology. “Gastroprotection with PPI therapy should be used in appropriately selected patients with coronary artery disease who require dual-antiplatelet therapy even if they are on low-dose aspirin.”
In addition to documenting the safety and efficacy of 6 months of PPI treatment for patients at high risk for cardiovascular disease events and low or moderate risk for a GI event, the results from the analysis also documented how common GI events are in this population, even when patients receive low-dose aspirin. Nearly two-thirds of the 3,752 patients included in the analysis took low-dose aspirin, either 75 mg or 81 mg per day. Their incidence of an adjudicated upper GI bleed, the study’s primary GI endpoint, occurred in 3.1% of patients on placebo, and in 1.2% of patients taking a prophylactic PPI. Among the other 34% of patients on high-dose aspirin – a daily dosage of at least 150 mg – the rate of adjudicated upper-GI bleeds was 2.6% without a PPI and 0.9% in those on a PPI.
In other words, even among patients deemed to have a relatively low risk for GI complications from aspirin because their entry into this study required no history of major GI bleeds or recent treatment with a gastroprotection agent, treatment with low-dose aspirin resulted in upper-GI bleeds at the same rate, about 3%, as a high-dose aspirin regimen. And in both of these aspirin subgroups 6 months of concurrent treatment with a PPI cut the incidence of major GI bleeds by more than half.
The findings are especially notable because the enrollment criteria stacked the deck toward patients with high cardiovascular disease risk and relatively low GI risk. The study enrolled “a unique population at high risk for cardiovascular disease – 71% had previously undergone a percutaneous coronary intervention, and 42% had a history of an acute coronary syndrome – and low GI risk, but even in this population enriched for cardiovascular disease risk, there was no increased rate of cardiovascular disease events” during a median follow-up while on PPI treatment of 110 days, Dr. Vaduganathan said.
Among patients on low-dose aspirin, the rate of cardiovascular disease death, MI, stroke, or coronary revascularization was 5.6% with PPI treatment and 5.5% without, and in the high-dose aspirin patients the rates were 4.2% with PPI treatment and 5.5% without. Neither of these differences between the subgroups on or off a PPI were statistically significant.
Concurrent with Dr. Vaduganathan’s report at the meeting the results also appeared online (J Am Coll Cardiol. 2016 April 12;67[14]:661-71).
“There appeared to be no adverse clinical effect from PPI treatment. When used short-term, for up to 6 months, PPI treatment appears to be safe in patients with cardiovascular disease,” Dr. Vaduganathan concluded.
The analysis used data collected in COGENT (Clopidogrel and the Optimization of Gastrointestinal Events Trial), a phase 3 study designed to compare a single-pill formulation of 20 mg omeprazole and 75 mg clopidogrel taken orally once daily with 75 mg clopidogrel against a background of all patients taking aspirin. COGENT stopped prematurely in late 2008 as the company developing this formulation and sponsoring the trial, Cogentus Pharmaceuticals, filed for bankruptcy. Despite its abrupt conclusion, the trial had enrolled and followed enough patients to show that treatment with omeprazole plus clopidogrel and aspirin led to a significant reduction in upper GI bleeding without increasing the rate of cardiovascular disease events, compared with clopidogrel plus aspirin (N Engl J Med. 2010 Nov 11;363[20]:1909-17).
The new analysis focused on the greater than 99% of patients in the total COGENT cohort for whom information was available on whether they received high- or low-dose aspirin.
Although the primary findings from COGENT, reported in 2010, documented the safety and efficacy of concomitant PPI treatment during dual-antiplatelet therapy, and despite guidelines revised in 2010 that called for PPI treatment when appropriate, this strategy for preventing GI complications remains underused, Dr. Vaduganathan said. The most recent U.S. recommendations that address this issue called for assessing the potential risk and benefit from PPI treatment in patients receiving dual-antiplatelet therapy: “The risk reduction with PPIs is substantial in patients with risk factors for GI bleeding and may outweigh any potential reduction in the CV efficacy of antiplatelet treatment because of a drug-drug interaction (J Am Coll Cardiol. 2010 Dec;56[24]:2051-66).”
The only caveat Dr. Vaduganathan placed on PPI use was that the COGENT data addressed only 6 months of PPI use; the safety of longer-term use has not been studied. But “the trend is to use PPIs for as short a period as possible,” and the risk for adverse effects from PPI treatment on cardiovascular disease events is likely greatest during the first 6 months of PPI treatment, he noted. If PPI treatment needs to continue beyond 6 months, he suggested systematically reassessing the risk-benefit balance for individual patients from continued PPI treatment every 3 months.
CHICAGO – Six months of treatment with a proton pump inhibitor (PPI) is a safe way to cut the incidence of major gastrointestinal events in cardiovascular disease patients on dual-antiplatelet therapy regardless of whether they receive low-dose or high-dose aspirin, according to a post-hoc analysis of data from more than 3,700 patients enrolled in the multicenter, randomized COGENT trial.
“Short-term, prophylactic PPI therapy consistently reduced rates of adjudicated upper-gastrointestinal events without increasing cardiovascular events, regardless of the aspirin dose,” Dr. Muthiah Vaduganathan said while presenting his study at the annual meeting of the American College of Cardiology. “Gastroprotection with PPI therapy should be used in appropriately selected patients with coronary artery disease who require dual-antiplatelet therapy even if they are on low-dose aspirin.”
In addition to documenting the safety and efficacy of 6 months of PPI treatment for patients at high risk for cardiovascular disease events and low or moderate risk for a GI event, the results from the analysis also documented how common GI events are in this population, even when patients receive low-dose aspirin. Nearly two-thirds of the 3,752 patients included in the analysis took low-dose aspirin, either 75 mg or 81 mg per day. Their incidence of an adjudicated upper GI bleed, the study’s primary GI endpoint, occurred in 3.1% of patients on placebo, and in 1.2% of patients taking a prophylactic PPI. Among the other 34% of patients on high-dose aspirin – a daily dosage of at least 150 mg – the rate of adjudicated upper-GI bleeds was 2.6% without a PPI and 0.9% in those on a PPI.
In other words, even among patients deemed to have a relatively low risk for GI complications from aspirin because their entry into this study required no history of major GI bleeds or recent treatment with a gastroprotection agent, treatment with low-dose aspirin resulted in upper-GI bleeds at the same rate, about 3%, as a high-dose aspirin regimen. And in both of these aspirin subgroups 6 months of concurrent treatment with a PPI cut the incidence of major GI bleeds by more than half.
The findings are especially notable because the enrollment criteria stacked the deck toward patients with high cardiovascular disease risk and relatively low GI risk. The study enrolled “a unique population at high risk for cardiovascular disease – 71% had previously undergone a percutaneous coronary intervention, and 42% had a history of an acute coronary syndrome – and low GI risk, but even in this population enriched for cardiovascular disease risk, there was no increased rate of cardiovascular disease events” during a median follow-up while on PPI treatment of 110 days, Dr. Vaduganathan said.
Among patients on low-dose aspirin, the rate of cardiovascular disease death, MI, stroke, or coronary revascularization was 5.6% with PPI treatment and 5.5% without, and in the high-dose aspirin patients the rates were 4.2% with PPI treatment and 5.5% without. Neither of these differences between the subgroups on or off a PPI were statistically significant.
Concurrent with Dr. Vaduganathan’s report at the meeting the results also appeared online (J Am Coll Cardiol. 2016 April 12;67[14]:661-71).
“There appeared to be no adverse clinical effect from PPI treatment. When used short-term, for up to 6 months, PPI treatment appears to be safe in patients with cardiovascular disease,” Dr. Vaduganathan concluded.
The analysis used data collected in COGENT (Clopidogrel and the Optimization of Gastrointestinal Events Trial), a phase 3 study designed to compare a single-pill formulation of 20 mg omeprazole and 75 mg clopidogrel taken orally once daily with 75 mg clopidogrel against a background of all patients taking aspirin. COGENT stopped prematurely in late 2008 as the company developing this formulation and sponsoring the trial, Cogentus Pharmaceuticals, filed for bankruptcy. Despite its abrupt conclusion, the trial had enrolled and followed enough patients to show that treatment with omeprazole plus clopidogrel and aspirin led to a significant reduction in upper GI bleeding without increasing the rate of cardiovascular disease events, compared with clopidogrel plus aspirin (N Engl J Med. 2010 Nov 11;363[20]:1909-17).
The new analysis focused on the greater than 99% of patients in the total COGENT cohort for whom information was available on whether they received high- or low-dose aspirin.
Although the primary findings from COGENT, reported in 2010, documented the safety and efficacy of concomitant PPI treatment during dual-antiplatelet therapy, and despite guidelines revised in 2010 that called for PPI treatment when appropriate, this strategy for preventing GI complications remains underused, Dr. Vaduganathan said. The most recent U.S. recommendations that address this issue called for assessing the potential risk and benefit from PPI treatment in patients receiving dual-antiplatelet therapy: “The risk reduction with PPIs is substantial in patients with risk factors for GI bleeding and may outweigh any potential reduction in the CV efficacy of antiplatelet treatment because of a drug-drug interaction (J Am Coll Cardiol. 2010 Dec;56[24]:2051-66).”
The only caveat Dr. Vaduganathan placed on PPI use was that the COGENT data addressed only 6 months of PPI use; the safety of longer-term use has not been studied. But “the trend is to use PPIs for as short a period as possible,” and the risk for adverse effects from PPI treatment on cardiovascular disease events is likely greatest during the first 6 months of PPI treatment, he noted. If PPI treatment needs to continue beyond 6 months, he suggested systematically reassessing the risk-benefit balance for individual patients from continued PPI treatment every 3 months.
AT ACC 2016