User login
American Academy of Neurology (AAN): Annual Meeting
AAN updates botulinum toxin guidelines for most established uses
VANCOUVER – A new American Academy of Neurology practice guideline on the efficacy and safety evidence for botulinum toxin treatment of blepharospasm, cervical dystonia, spasticity, and headache has updated the last recommendations published in 2008, but leaves some relevant clinical concerns and off-label uses unaddressed.
The 2016 update, published April 18 in Neurology, adds new individual evidence for the use of the four branded formulations of the two commercially available botulinum toxin serotypes, A and B, for the aforementioned indications rather than lumping all recommendations for botulinum toxin together as in the 2008 guidelines. However, questions remain on the differences between the different products in clinical practice, especially since the formulations show little clinical difference in head-to-head comparisons for some of the indications, especially for the serotype A formulations.
In a press briefing on the new guidelines at the annual meeting of the American Academy of Neurology, guidelines coauthor Dr. Mark Hallett noted that nothing really surprised the experienced 14-member committee that put the guidelines together. “The reason that we chose these four different diseases is because we already had the sense that they were going to change in the particular ways that they did. We didn’t know exactly, of course, what was going to happen, but we had a sense that there were sufficient data that it was worth looking at them.”
For blepharospasm, the totality of evidence suggests that onabotulinumtoxinA (onaBoNT-A; Botox) and incobotulinumtoxinA (incoBoNT-A; Xeomin) injections should be considered and are probably safe and effective (level B recommendation), while abobotulinumtoxinA (aboBoNT-A; Dysport) may be considered (level C) and is possibly effective. The evidence shows that incoBoNT-A and onaBoNT-A have equivalent efficacy and aboBoNT-A and onaBoNT-A are possibly equivalent. There was not enough evidence to determine the efficacy of rimabotulinumtoxinB for blepharospasm (rimaBoNT-B; Myobloc).
The rigorousness of clinical trials in evaluating the efficacy and safety of botulinum toxin has evolved since the Food and Drug Administration approved onaBoNT-A and incoBoNT-A to treat blepharospasm, but no new trials have been conducted to give it a higher level of recommendation despite their well-known magnitude of benefit, said Dr. Hallett, chief of the National Institute of Neurological Disorders and Stroke medical neurology branch and its human motor control section.
New evidence added to the already well-established data on the effectiveness of botulinum toxin for cervical dystonia suggest that onaBoNT-A and incoBoNT-A are probably safe and effective and should be considered. In addition, aboBoNT-A and rimaBoNT-B have already proven effectiveness and safety and should be offered. The lack of class I studies for onaBoNT-A and incoBoNT-A led to the lower level of recommendation for them despite an extensive clinical history of their use in cervical dystonia, the guideline committee wrote (Neurology. 2016 Apr 18. doi: 10.1212/WNL.0000000000002560).
In adults with upper-limb spasticity, all three serotype A formulations – onaBoNT-A, aboBoNT-A, and incoBoNT-A – are effective and safe in reducing symptoms and improving passive limb function. All three achieved level A evidence to recommend that they should be offered. One comparative trial showed enough evidence to say that onaBoNT-A is probably superior to tizanidine for reducing upper-extremity tone and should be considered before it. RimaBoNT-B has level B evidence to advise that it should be considered and is probably safe and effective. None of the formulations have enough data to determine their efficacy on active limb function.
Fewer trials have examined the safety and effectiveness of botulinum toxin formulations for reducing lower leg spasticity in adults. The guidelines panel found enough evidence to recommend that aboBoNT-A and onaBoNT-A are safe and effective and should be offered (level A). There were no trials with high enough level of quality to determine whether incoBoNT-A or rimaBoNT-B were effective for lower-leg spasticity. None of the four agents had enough evidence to support their ability to improve active function associated with lower-limb spasticity.
At the press briefing, guidelines first author Dr. David M. Simpson expressed hope that a more refined methodology for evaluating spasticity might be achieved in future trials of botulinum toxin to detect the potentially subtle effects the agents may have on certain patients who are more likely to achieve benefits in active limb function. Currently, trials use a standardized set of outcomes to try to detect differences in patients with wide-ranging severity of symptoms and types of injury that led to spasticity. Dr. Simpson is professor of neurology at Mount Sinai in New York, as well as director of the neuromuscular diseases division and director of the clinical neurophysiology laboratories.
Positive results for onaBoNT-A in two pivotal trials in chronic migraine that were published since the last guidelines give the formulation the only FDA-approved indication for a botulinum toxin in chronic migraine and earned it a level A recommendation from the guidelines committee. However, in the trials it had a relatively small magnitude of efficacy in reducing the number of headache days by 15% versus placebo. The guidelines also advise not using onaBoNT-A in episodic migraine based on three negative trials. No high-quality trials have evaluated any formulation to change the overall 2008 guidelines’ advice that botulinum toxin is probably ineffective for treating chronic tension-type headaches.
Familiarity with appropriate dosing and side effects may allow clinicians to use the products off-label for indications in the guidelines for which clinical trials were not available, Dr. Richard L. Barbano of the movement disorders division at the University of Rochester noted in an editorial about the guidelines (Neurol Clin Pract. 2016 Apr 18. doi: 10.1212/CPJ.0000000000000244). “Off-label use is common in clinical practice. Little data exist to indicate that any of the different formulations, with attention to appropriate dosing and side effects, would not be effective in treating these other conditions. There are also a number of other neurologic conditions not discussed in the guideline in which botulinum toxin has shown efficacy, such as hemifacial spasm and other focal dystonias. Lack of sufficient high-level evidence to support a level A or B guideline recommendation does not negate their potential utility and likewise, there is little evidence to recommend one formulation over another.”
“In some circumstances where the drugs are relatively equivalent, some people prefer to stick with one so they get used to it more, and they can have more of a sense of what the dosing is, given that the doses may be different with the compounds and have different side effects,” Dr. Hallett said in an interview, noting that availability and price also might enter into a clinician’s decision on what to do.
Dr. Barbano also said that cost and value are becoming more important, and neurologists should consider when botulinum toxin therapy should be chosen among existing alternative treatment options, particularly for chronic migraine.
The guidelines are endorsed by the American Association of Neuromuscular & Electrodiagnostic Medicine and the American Society of Plastic Surgeons.
Dr. Hallett reported serving as chair of the Neurotoxin Institute Advisory Council and has received research grants from Allergan and Merz Pharmaceuticals. Dr. Simpson reported receiving research grants from and served as a consultant for Allergan, Ipsen, Merz Pharmaceuticals, and Acorda Therapeutics. Five other coauthors of the guidelines disclosed relationships with manufacturers of botulinum toxin formulations. Dr. Barbano reported serving on a scientific advisory board for Allergan and receiving research support from Allergan, Vaccinex, and Biotie.
VANCOUVER – A new American Academy of Neurology practice guideline on the efficacy and safety evidence for botulinum toxin treatment of blepharospasm, cervical dystonia, spasticity, and headache has updated the last recommendations published in 2008, but leaves some relevant clinical concerns and off-label uses unaddressed.
The 2016 update, published April 18 in Neurology, adds new individual evidence for the use of the four branded formulations of the two commercially available botulinum toxin serotypes, A and B, for the aforementioned indications rather than lumping all recommendations for botulinum toxin together as in the 2008 guidelines. However, questions remain on the differences between the different products in clinical practice, especially since the formulations show little clinical difference in head-to-head comparisons for some of the indications, especially for the serotype A formulations.
In a press briefing on the new guidelines at the annual meeting of the American Academy of Neurology, guidelines coauthor Dr. Mark Hallett noted that nothing really surprised the experienced 14-member committee that put the guidelines together. “The reason that we chose these four different diseases is because we already had the sense that they were going to change in the particular ways that they did. We didn’t know exactly, of course, what was going to happen, but we had a sense that there were sufficient data that it was worth looking at them.”
For blepharospasm, the totality of evidence suggests that onabotulinumtoxinA (onaBoNT-A; Botox) and incobotulinumtoxinA (incoBoNT-A; Xeomin) injections should be considered and are probably safe and effective (level B recommendation), while abobotulinumtoxinA (aboBoNT-A; Dysport) may be considered (level C) and is possibly effective. The evidence shows that incoBoNT-A and onaBoNT-A have equivalent efficacy and aboBoNT-A and onaBoNT-A are possibly equivalent. There was not enough evidence to determine the efficacy of rimabotulinumtoxinB for blepharospasm (rimaBoNT-B; Myobloc).
The rigorousness of clinical trials in evaluating the efficacy and safety of botulinum toxin has evolved since the Food and Drug Administration approved onaBoNT-A and incoBoNT-A to treat blepharospasm, but no new trials have been conducted to give it a higher level of recommendation despite their well-known magnitude of benefit, said Dr. Hallett, chief of the National Institute of Neurological Disorders and Stroke medical neurology branch and its human motor control section.
New evidence added to the already well-established data on the effectiveness of botulinum toxin for cervical dystonia suggest that onaBoNT-A and incoBoNT-A are probably safe and effective and should be considered. In addition, aboBoNT-A and rimaBoNT-B have already proven effectiveness and safety and should be offered. The lack of class I studies for onaBoNT-A and incoBoNT-A led to the lower level of recommendation for them despite an extensive clinical history of their use in cervical dystonia, the guideline committee wrote (Neurology. 2016 Apr 18. doi: 10.1212/WNL.0000000000002560).
In adults with upper-limb spasticity, all three serotype A formulations – onaBoNT-A, aboBoNT-A, and incoBoNT-A – are effective and safe in reducing symptoms and improving passive limb function. All three achieved level A evidence to recommend that they should be offered. One comparative trial showed enough evidence to say that onaBoNT-A is probably superior to tizanidine for reducing upper-extremity tone and should be considered before it. RimaBoNT-B has level B evidence to advise that it should be considered and is probably safe and effective. None of the formulations have enough data to determine their efficacy on active limb function.
Fewer trials have examined the safety and effectiveness of botulinum toxin formulations for reducing lower leg spasticity in adults. The guidelines panel found enough evidence to recommend that aboBoNT-A and onaBoNT-A are safe and effective and should be offered (level A). There were no trials with high enough level of quality to determine whether incoBoNT-A or rimaBoNT-B were effective for lower-leg spasticity. None of the four agents had enough evidence to support their ability to improve active function associated with lower-limb spasticity.
At the press briefing, guidelines first author Dr. David M. Simpson expressed hope that a more refined methodology for evaluating spasticity might be achieved in future trials of botulinum toxin to detect the potentially subtle effects the agents may have on certain patients who are more likely to achieve benefits in active limb function. Currently, trials use a standardized set of outcomes to try to detect differences in patients with wide-ranging severity of symptoms and types of injury that led to spasticity. Dr. Simpson is professor of neurology at Mount Sinai in New York, as well as director of the neuromuscular diseases division and director of the clinical neurophysiology laboratories.
Positive results for onaBoNT-A in two pivotal trials in chronic migraine that were published since the last guidelines give the formulation the only FDA-approved indication for a botulinum toxin in chronic migraine and earned it a level A recommendation from the guidelines committee. However, in the trials it had a relatively small magnitude of efficacy in reducing the number of headache days by 15% versus placebo. The guidelines also advise not using onaBoNT-A in episodic migraine based on three negative trials. No high-quality trials have evaluated any formulation to change the overall 2008 guidelines’ advice that botulinum toxin is probably ineffective for treating chronic tension-type headaches.
Familiarity with appropriate dosing and side effects may allow clinicians to use the products off-label for indications in the guidelines for which clinical trials were not available, Dr. Richard L. Barbano of the movement disorders division at the University of Rochester noted in an editorial about the guidelines (Neurol Clin Pract. 2016 Apr 18. doi: 10.1212/CPJ.0000000000000244). “Off-label use is common in clinical practice. Little data exist to indicate that any of the different formulations, with attention to appropriate dosing and side effects, would not be effective in treating these other conditions. There are also a number of other neurologic conditions not discussed in the guideline in which botulinum toxin has shown efficacy, such as hemifacial spasm and other focal dystonias. Lack of sufficient high-level evidence to support a level A or B guideline recommendation does not negate their potential utility and likewise, there is little evidence to recommend one formulation over another.”
“In some circumstances where the drugs are relatively equivalent, some people prefer to stick with one so they get used to it more, and they can have more of a sense of what the dosing is, given that the doses may be different with the compounds and have different side effects,” Dr. Hallett said in an interview, noting that availability and price also might enter into a clinician’s decision on what to do.
Dr. Barbano also said that cost and value are becoming more important, and neurologists should consider when botulinum toxin therapy should be chosen among existing alternative treatment options, particularly for chronic migraine.
The guidelines are endorsed by the American Association of Neuromuscular & Electrodiagnostic Medicine and the American Society of Plastic Surgeons.
Dr. Hallett reported serving as chair of the Neurotoxin Institute Advisory Council and has received research grants from Allergan and Merz Pharmaceuticals. Dr. Simpson reported receiving research grants from and served as a consultant for Allergan, Ipsen, Merz Pharmaceuticals, and Acorda Therapeutics. Five other coauthors of the guidelines disclosed relationships with manufacturers of botulinum toxin formulations. Dr. Barbano reported serving on a scientific advisory board for Allergan and receiving research support from Allergan, Vaccinex, and Biotie.
VANCOUVER – A new American Academy of Neurology practice guideline on the efficacy and safety evidence for botulinum toxin treatment of blepharospasm, cervical dystonia, spasticity, and headache has updated the last recommendations published in 2008, but leaves some relevant clinical concerns and off-label uses unaddressed.
The 2016 update, published April 18 in Neurology, adds new individual evidence for the use of the four branded formulations of the two commercially available botulinum toxin serotypes, A and B, for the aforementioned indications rather than lumping all recommendations for botulinum toxin together as in the 2008 guidelines. However, questions remain on the differences between the different products in clinical practice, especially since the formulations show little clinical difference in head-to-head comparisons for some of the indications, especially for the serotype A formulations.
In a press briefing on the new guidelines at the annual meeting of the American Academy of Neurology, guidelines coauthor Dr. Mark Hallett noted that nothing really surprised the experienced 14-member committee that put the guidelines together. “The reason that we chose these four different diseases is because we already had the sense that they were going to change in the particular ways that they did. We didn’t know exactly, of course, what was going to happen, but we had a sense that there were sufficient data that it was worth looking at them.”
For blepharospasm, the totality of evidence suggests that onabotulinumtoxinA (onaBoNT-A; Botox) and incobotulinumtoxinA (incoBoNT-A; Xeomin) injections should be considered and are probably safe and effective (level B recommendation), while abobotulinumtoxinA (aboBoNT-A; Dysport) may be considered (level C) and is possibly effective. The evidence shows that incoBoNT-A and onaBoNT-A have equivalent efficacy and aboBoNT-A and onaBoNT-A are possibly equivalent. There was not enough evidence to determine the efficacy of rimabotulinumtoxinB for blepharospasm (rimaBoNT-B; Myobloc).
The rigorousness of clinical trials in evaluating the efficacy and safety of botulinum toxin has evolved since the Food and Drug Administration approved onaBoNT-A and incoBoNT-A to treat blepharospasm, but no new trials have been conducted to give it a higher level of recommendation despite their well-known magnitude of benefit, said Dr. Hallett, chief of the National Institute of Neurological Disorders and Stroke medical neurology branch and its human motor control section.
New evidence added to the already well-established data on the effectiveness of botulinum toxin for cervical dystonia suggest that onaBoNT-A and incoBoNT-A are probably safe and effective and should be considered. In addition, aboBoNT-A and rimaBoNT-B have already proven effectiveness and safety and should be offered. The lack of class I studies for onaBoNT-A and incoBoNT-A led to the lower level of recommendation for them despite an extensive clinical history of their use in cervical dystonia, the guideline committee wrote (Neurology. 2016 Apr 18. doi: 10.1212/WNL.0000000000002560).
In adults with upper-limb spasticity, all three serotype A formulations – onaBoNT-A, aboBoNT-A, and incoBoNT-A – are effective and safe in reducing symptoms and improving passive limb function. All three achieved level A evidence to recommend that they should be offered. One comparative trial showed enough evidence to say that onaBoNT-A is probably superior to tizanidine for reducing upper-extremity tone and should be considered before it. RimaBoNT-B has level B evidence to advise that it should be considered and is probably safe and effective. None of the formulations have enough data to determine their efficacy on active limb function.
Fewer trials have examined the safety and effectiveness of botulinum toxin formulations for reducing lower leg spasticity in adults. The guidelines panel found enough evidence to recommend that aboBoNT-A and onaBoNT-A are safe and effective and should be offered (level A). There were no trials with high enough level of quality to determine whether incoBoNT-A or rimaBoNT-B were effective for lower-leg spasticity. None of the four agents had enough evidence to support their ability to improve active function associated with lower-limb spasticity.
At the press briefing, guidelines first author Dr. David M. Simpson expressed hope that a more refined methodology for evaluating spasticity might be achieved in future trials of botulinum toxin to detect the potentially subtle effects the agents may have on certain patients who are more likely to achieve benefits in active limb function. Currently, trials use a standardized set of outcomes to try to detect differences in patients with wide-ranging severity of symptoms and types of injury that led to spasticity. Dr. Simpson is professor of neurology at Mount Sinai in New York, as well as director of the neuromuscular diseases division and director of the clinical neurophysiology laboratories.
Positive results for onaBoNT-A in two pivotal trials in chronic migraine that were published since the last guidelines give the formulation the only FDA-approved indication for a botulinum toxin in chronic migraine and earned it a level A recommendation from the guidelines committee. However, in the trials it had a relatively small magnitude of efficacy in reducing the number of headache days by 15% versus placebo. The guidelines also advise not using onaBoNT-A in episodic migraine based on three negative trials. No high-quality trials have evaluated any formulation to change the overall 2008 guidelines’ advice that botulinum toxin is probably ineffective for treating chronic tension-type headaches.
Familiarity with appropriate dosing and side effects may allow clinicians to use the products off-label for indications in the guidelines for which clinical trials were not available, Dr. Richard L. Barbano of the movement disorders division at the University of Rochester noted in an editorial about the guidelines (Neurol Clin Pract. 2016 Apr 18. doi: 10.1212/CPJ.0000000000000244). “Off-label use is common in clinical practice. Little data exist to indicate that any of the different formulations, with attention to appropriate dosing and side effects, would not be effective in treating these other conditions. There are also a number of other neurologic conditions not discussed in the guideline in which botulinum toxin has shown efficacy, such as hemifacial spasm and other focal dystonias. Lack of sufficient high-level evidence to support a level A or B guideline recommendation does not negate their potential utility and likewise, there is little evidence to recommend one formulation over another.”
“In some circumstances where the drugs are relatively equivalent, some people prefer to stick with one so they get used to it more, and they can have more of a sense of what the dosing is, given that the doses may be different with the compounds and have different side effects,” Dr. Hallett said in an interview, noting that availability and price also might enter into a clinician’s decision on what to do.
Dr. Barbano also said that cost and value are becoming more important, and neurologists should consider when botulinum toxin therapy should be chosen among existing alternative treatment options, particularly for chronic migraine.
The guidelines are endorsed by the American Association of Neuromuscular & Electrodiagnostic Medicine and the American Society of Plastic Surgeons.
Dr. Hallett reported serving as chair of the Neurotoxin Institute Advisory Council and has received research grants from Allergan and Merz Pharmaceuticals. Dr. Simpson reported receiving research grants from and served as a consultant for Allergan, Ipsen, Merz Pharmaceuticals, and Acorda Therapeutics. Five other coauthors of the guidelines disclosed relationships with manufacturers of botulinum toxin formulations. Dr. Barbano reported serving on a scientific advisory board for Allergan and receiving research support from Allergan, Vaccinex, and Biotie.
AT THE AAN 2016 ANNUAL MEETING
Anti-CGRP agent delivered durable episodic migraine prevention
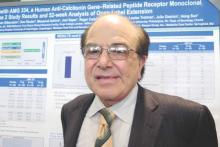
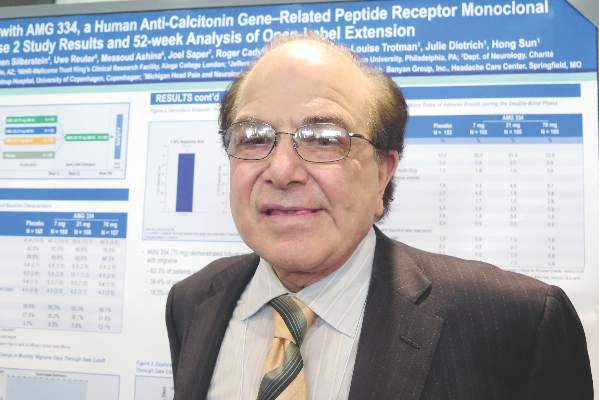
VANCOUVER – An investigational antibody that targets the calcitonin gene-related peptide (CGRP) receptor may be efficacious and safe in the longer term for preventing episodic migraine, data from an ongoing extension of a phase II trial showed.
Among the 483 adults studied, the benefit seen with Amgen’s 334 antibody (AMG 334) at the highest dose at 12 weeks persisted out to a year, according to interim results reported at the annual meeting of the American Academy of Neurology.
At that time, patients on average were having roughly 5 fewer migraine days each month. Nearly two-thirds had experienced at least a halving of monthly migraine days, and nearly one-fifth had become totally migraine free. In addition, the antibody’s good safety profile also held up.
“These data strongly support the further investigation of AMG 334 as a potential preventive medication,” commented presenting author Dr. Stephen Silberstein, professor and director of the headache center at Thomas Jefferson University, Philadelphia.
“If you give a monoclonal antibody to someone with migraine and it takes away the associated features, then you just wind up with a headache day,” Dr. Silberstein noted. “But analysis clearly shows the reduction in migraine days with a concomitant reduction in headache days, showing you are not just removing the associated symptoms.”
It is too early to say whether the antibody is actually modifying the underlying disease, according to Dr. Silberstein. That will require a randomized withdrawal trial, assessing whether patients who stop treatment have a recurrence.
In any event, on the basis of the favorable findings from the phase II trial and its extension, a phase III trial, the Study to Evaluate the Efficacy and Safety of AMG 334 in Migraine Prevention (STRIVE), is now underway.
Four antibodies targeting CGRP signaling are now being investigated for migraine prevention, but AMG 334 is the only one targeting the receptor, noted session attendee Dr. Denise E. Chou of the department of neurology at Columbia University and director of the Columbia University headache center, New York.
“Particularly striking is the almost 20% rate of 100% remission. That’s remarkable, because it’s unheard of for any of the current existing migraine therapies,” she noted. The antibody’s longer half-life (translating to greater convenience for patients) and good safety profile are also pluses.
“With the four different antibodies out there, it’s kind of a race,” Dr. Chou commented. “We’ll have to see which have the best efficacy rates and side effect profiles, and which are going to be the best in terms of patient compliance and dosing scheme.”
Compared with some other trials, the AMG 334 trial enrolled a population that had episodic migraine, which is relatively easier to treat, Dr. Chou noted.
“We know, in general, that chronic refractory patients tend to have lower response rates to therapies,” she said. “But it is nice that there are different studies looking at different populations, because that’s what we see, a very heterogeneous clinic population. To be able to reflect the real-world setting is important.”
Patients were eligible for the Amgen-sponsored trial if they had 4-14 migraine days and fewer than 15 headache days per month. They could have experienced failure of up to two previous prophylactic therapies. Rescue medications were allowed, but medication overuse was not.
The patients were randomized 2:2:2:3 to monthly subcutaneous injections of AMG 334 at doses of 7 mg, 21 mg, or 70 mg, or to placebo, on a double-blind basis.
At baseline, the patients had about 9 migraine days and 10 headache days each month so that migraine accounted for most of the total, Dr. Silberstein noted.
At 12 weeks, the change in monthly migraine days – the trial’s primary outcome – was greater with the 70-mg dose than with placebo, with a reduction of 3.40 days vs. 2.28 days each month (P = .021) (Lancet Neurol. 2016 Apr.;15[4]:382-90).
A post hoc analysis suggested that this difference was already significant merely 2 weeks into treatment, Dr. Silberstein reported. The reductions seen with the lower doses were not significant.
All patients were then switched to the 70-mg dose of AMG 334 on the open-label extension, which is planned to continue for up to 5 years. The results showed that both lower-dose groups and the placebo group quickly caught up to their peers on the higher dose when it came to the reduction in monthly migraine days.
“In contrast to both the topiramate and botulinum [toxin] studies, at 16 weeks, there was no difference between patients who had started on the higher dose of [AMG 334] or who were transferred over,” Dr. Silberstein commented. “If one does an individual analysis of patients who were before on placebo or the lower doses, each of them caught up, which suggests a difference in the [mechanism of] … botulinum toxin or topiramate – because with those drugs, they never caught up at the end of 6 months.”
At 52 weeks, the patients as a whole were having about 5 fewer migraine days each month, compared with baseline. Overall, 62.3% of patients had achieved a reduction of at least 50% in monthly migraine days; 38.4%, a reduction of at least 75%; and 18.5%, a reduction of 100%.
The pattern was similar when it came to monthly migraine-specific medication days, monthly headache days, and monthly migraine attacks, according to Dr. Silberstein.
“The safety and tolerability during the open-label phase were similar to that in the double-blind phase,” he noted. “One of the reasons this is important is that, unlike small molecules, the monoclonal antibodies are not metabolized in the liver, but are metabolized in the reticuloendothelial system. So, the concept of small-molecule toxicity does not exist.”
Amgen sponsored the trial. Dr. Silberstein disclosed that he receives consulting fees from Amgen.
VANCOUVER – An investigational antibody that targets the calcitonin gene-related peptide (CGRP) receptor may be efficacious and safe in the longer term for preventing episodic migraine, data from an ongoing extension of a phase II trial showed.
Among the 483 adults studied, the benefit seen with Amgen’s 334 antibody (AMG 334) at the highest dose at 12 weeks persisted out to a year, according to interim results reported at the annual meeting of the American Academy of Neurology.
At that time, patients on average were having roughly 5 fewer migraine days each month. Nearly two-thirds had experienced at least a halving of monthly migraine days, and nearly one-fifth had become totally migraine free. In addition, the antibody’s good safety profile also held up.
“These data strongly support the further investigation of AMG 334 as a potential preventive medication,” commented presenting author Dr. Stephen Silberstein, professor and director of the headache center at Thomas Jefferson University, Philadelphia.
“If you give a monoclonal antibody to someone with migraine and it takes away the associated features, then you just wind up with a headache day,” Dr. Silberstein noted. “But analysis clearly shows the reduction in migraine days with a concomitant reduction in headache days, showing you are not just removing the associated symptoms.”
It is too early to say whether the antibody is actually modifying the underlying disease, according to Dr. Silberstein. That will require a randomized withdrawal trial, assessing whether patients who stop treatment have a recurrence.
In any event, on the basis of the favorable findings from the phase II trial and its extension, a phase III trial, the Study to Evaluate the Efficacy and Safety of AMG 334 in Migraine Prevention (STRIVE), is now underway.
Four antibodies targeting CGRP signaling are now being investigated for migraine prevention, but AMG 334 is the only one targeting the receptor, noted session attendee Dr. Denise E. Chou of the department of neurology at Columbia University and director of the Columbia University headache center, New York.
“Particularly striking is the almost 20% rate of 100% remission. That’s remarkable, because it’s unheard of for any of the current existing migraine therapies,” she noted. The antibody’s longer half-life (translating to greater convenience for patients) and good safety profile are also pluses.
“With the four different antibodies out there, it’s kind of a race,” Dr. Chou commented. “We’ll have to see which have the best efficacy rates and side effect profiles, and which are going to be the best in terms of patient compliance and dosing scheme.”
Compared with some other trials, the AMG 334 trial enrolled a population that had episodic migraine, which is relatively easier to treat, Dr. Chou noted.
“We know, in general, that chronic refractory patients tend to have lower response rates to therapies,” she said. “But it is nice that there are different studies looking at different populations, because that’s what we see, a very heterogeneous clinic population. To be able to reflect the real-world setting is important.”
Patients were eligible for the Amgen-sponsored trial if they had 4-14 migraine days and fewer than 15 headache days per month. They could have experienced failure of up to two previous prophylactic therapies. Rescue medications were allowed, but medication overuse was not.
The patients were randomized 2:2:2:3 to monthly subcutaneous injections of AMG 334 at doses of 7 mg, 21 mg, or 70 mg, or to placebo, on a double-blind basis.
At baseline, the patients had about 9 migraine days and 10 headache days each month so that migraine accounted for most of the total, Dr. Silberstein noted.
At 12 weeks, the change in monthly migraine days – the trial’s primary outcome – was greater with the 70-mg dose than with placebo, with a reduction of 3.40 days vs. 2.28 days each month (P = .021) (Lancet Neurol. 2016 Apr.;15[4]:382-90).
A post hoc analysis suggested that this difference was already significant merely 2 weeks into treatment, Dr. Silberstein reported. The reductions seen with the lower doses were not significant.
All patients were then switched to the 70-mg dose of AMG 334 on the open-label extension, which is planned to continue for up to 5 years. The results showed that both lower-dose groups and the placebo group quickly caught up to their peers on the higher dose when it came to the reduction in monthly migraine days.
“In contrast to both the topiramate and botulinum [toxin] studies, at 16 weeks, there was no difference between patients who had started on the higher dose of [AMG 334] or who were transferred over,” Dr. Silberstein commented. “If one does an individual analysis of patients who were before on placebo or the lower doses, each of them caught up, which suggests a difference in the [mechanism of] … botulinum toxin or topiramate – because with those drugs, they never caught up at the end of 6 months.”
At 52 weeks, the patients as a whole were having about 5 fewer migraine days each month, compared with baseline. Overall, 62.3% of patients had achieved a reduction of at least 50% in monthly migraine days; 38.4%, a reduction of at least 75%; and 18.5%, a reduction of 100%.
The pattern was similar when it came to monthly migraine-specific medication days, monthly headache days, and monthly migraine attacks, according to Dr. Silberstein.
“The safety and tolerability during the open-label phase were similar to that in the double-blind phase,” he noted. “One of the reasons this is important is that, unlike small molecules, the monoclonal antibodies are not metabolized in the liver, but are metabolized in the reticuloendothelial system. So, the concept of small-molecule toxicity does not exist.”
Amgen sponsored the trial. Dr. Silberstein disclosed that he receives consulting fees from Amgen.
VANCOUVER – An investigational antibody that targets the calcitonin gene-related peptide (CGRP) receptor may be efficacious and safe in the longer term for preventing episodic migraine, data from an ongoing extension of a phase II trial showed.
Among the 483 adults studied, the benefit seen with Amgen’s 334 antibody (AMG 334) at the highest dose at 12 weeks persisted out to a year, according to interim results reported at the annual meeting of the American Academy of Neurology.
At that time, patients on average were having roughly 5 fewer migraine days each month. Nearly two-thirds had experienced at least a halving of monthly migraine days, and nearly one-fifth had become totally migraine free. In addition, the antibody’s good safety profile also held up.
“These data strongly support the further investigation of AMG 334 as a potential preventive medication,” commented presenting author Dr. Stephen Silberstein, professor and director of the headache center at Thomas Jefferson University, Philadelphia.
“If you give a monoclonal antibody to someone with migraine and it takes away the associated features, then you just wind up with a headache day,” Dr. Silberstein noted. “But analysis clearly shows the reduction in migraine days with a concomitant reduction in headache days, showing you are not just removing the associated symptoms.”
It is too early to say whether the antibody is actually modifying the underlying disease, according to Dr. Silberstein. That will require a randomized withdrawal trial, assessing whether patients who stop treatment have a recurrence.
In any event, on the basis of the favorable findings from the phase II trial and its extension, a phase III trial, the Study to Evaluate the Efficacy and Safety of AMG 334 in Migraine Prevention (STRIVE), is now underway.
Four antibodies targeting CGRP signaling are now being investigated for migraine prevention, but AMG 334 is the only one targeting the receptor, noted session attendee Dr. Denise E. Chou of the department of neurology at Columbia University and director of the Columbia University headache center, New York.
“Particularly striking is the almost 20% rate of 100% remission. That’s remarkable, because it’s unheard of for any of the current existing migraine therapies,” she noted. The antibody’s longer half-life (translating to greater convenience for patients) and good safety profile are also pluses.
“With the four different antibodies out there, it’s kind of a race,” Dr. Chou commented. “We’ll have to see which have the best efficacy rates and side effect profiles, and which are going to be the best in terms of patient compliance and dosing scheme.”
Compared with some other trials, the AMG 334 trial enrolled a population that had episodic migraine, which is relatively easier to treat, Dr. Chou noted.
“We know, in general, that chronic refractory patients tend to have lower response rates to therapies,” she said. “But it is nice that there are different studies looking at different populations, because that’s what we see, a very heterogeneous clinic population. To be able to reflect the real-world setting is important.”
Patients were eligible for the Amgen-sponsored trial if they had 4-14 migraine days and fewer than 15 headache days per month. They could have experienced failure of up to two previous prophylactic therapies. Rescue medications were allowed, but medication overuse was not.
The patients were randomized 2:2:2:3 to monthly subcutaneous injections of AMG 334 at doses of 7 mg, 21 mg, or 70 mg, or to placebo, on a double-blind basis.
At baseline, the patients had about 9 migraine days and 10 headache days each month so that migraine accounted for most of the total, Dr. Silberstein noted.
At 12 weeks, the change in monthly migraine days – the trial’s primary outcome – was greater with the 70-mg dose than with placebo, with a reduction of 3.40 days vs. 2.28 days each month (P = .021) (Lancet Neurol. 2016 Apr.;15[4]:382-90).
A post hoc analysis suggested that this difference was already significant merely 2 weeks into treatment, Dr. Silberstein reported. The reductions seen with the lower doses were not significant.
All patients were then switched to the 70-mg dose of AMG 334 on the open-label extension, which is planned to continue for up to 5 years. The results showed that both lower-dose groups and the placebo group quickly caught up to their peers on the higher dose when it came to the reduction in monthly migraine days.
“In contrast to both the topiramate and botulinum [toxin] studies, at 16 weeks, there was no difference between patients who had started on the higher dose of [AMG 334] or who were transferred over,” Dr. Silberstein commented. “If one does an individual analysis of patients who were before on placebo or the lower doses, each of them caught up, which suggests a difference in the [mechanism of] … botulinum toxin or topiramate – because with those drugs, they never caught up at the end of 6 months.”
At 52 weeks, the patients as a whole were having about 5 fewer migraine days each month, compared with baseline. Overall, 62.3% of patients had achieved a reduction of at least 50% in monthly migraine days; 38.4%, a reduction of at least 75%; and 18.5%, a reduction of 100%.
The pattern was similar when it came to monthly migraine-specific medication days, monthly headache days, and monthly migraine attacks, according to Dr. Silberstein.
“The safety and tolerability during the open-label phase were similar to that in the double-blind phase,” he noted. “One of the reasons this is important is that, unlike small molecules, the monoclonal antibodies are not metabolized in the liver, but are metabolized in the reticuloendothelial system. So, the concept of small-molecule toxicity does not exist.”
Amgen sponsored the trial. Dr. Silberstein disclosed that he receives consulting fees from Amgen.
AT THE AAN 2016 ANNUAL MEETING
Key clinical point: AMG 334 has durable efficacy and safety in reducing episodic migraine.
Major finding: At 1 year, patients were experiencing about 5 fewer migraine days each month on average, and 62.3% had achieved at least a 50% reduction in monthly migraine days.
Data source: An interim analysis of an open-label extension of a phase II trial in 483 adults with episodic migraine.
Disclosures: Amgen sponsored the trial. Dr. Silberstein disclosed that he receives consulting fees from Amgen.
Patients suffer morbidity due to MS misdiagnosis
VANCOUVER – More than two-thirds of patients with definite or probable misdiagnosis of multiple sclerosis took unnecessary disease-modifying therapy and nearly one-third experienced unnecessary morbidity in a prospective pilot study.
The findings highlight a problem that has been noted before in the medical literature, but since many instances are case reports of unusual cases or were published about 20 or more years ago, they may not reflect the current spectrum of misdiagnosis, Dr. Andrew J. Solomon said at the annual meeting of the American Academy of Neurology.
During a 13-month period, neurologists at four U.S. academic multiple sclerosis centers reported that 51 (46%) of 110 misdiagnosed patients had “definite” misdiagnosis because an alternate diagnosis was identified after assessing clinical, laboratory, and neuroimaging data, while 59 had “probable” misdiagnoses.
Participating neurologists felt that the misdiagnoses were based in part on inappropriately attributing symptoms to demyelinating disease in 65% of cases. MS diagnostic criteria were not rigorously validated for use in patients with atypical presentations, suggesting that the misuse of the criteria could represent a misunderstanding of what constitutes a typical demyelinating attack, said Dr. Solomon of the department of neurological sciences at the University of Vermont, Burlington.
In 48% of cases, the participating neurologists said that objective evidence of a lesion was not used to corroborate historical symptoms.
Many instances also were seen in which the neurologists felt magnetic resonance imaging criteria were misinterpreted or misapplied. In 60%, the MS misdiagnosis relied too heavily on MRI abnormalities to meet the MS diagnostic criteria for dissemination in space when the patient had nonspecific neurologic symptoms, and in another 33% there was an incorrect determination of juxtacortical or periventricular lesion location to fulfill the diagnostic criteria for dissemination in space. Dr. Solomon said that the MRI criteria for MS were not developed to differentiate MS from other conditions, but instead to identify patients at high risk for MS after initial typical presentations of demyelination.
“Overreliance on MRI abnormalities in the setting of atypical symptoms and unverified prior symptoms may be a major cause of misdiagnosis,” he said.
Many earlier patient visits contained red flags that could have led to a correct diagnosis, according to the neurologists who participated in the study. There was evidence for this opportunity being missed in 79 (72%) patients.
“We don’t know how frequent this problem is in practice. I think it’s pretty frequent just based on my own clinical experience, but no one’s done a population-based study, as you can imagine that would be kind of difficult to do,” said Dr. Jonathan Carter, an MS specialist at the Mayo Clinic in Scottsdale, Ariz., who was part of the study.
Study patients were previously diagnosed with MS; none were allowed to have MS as one of several potential diagnoses. Patients were mostly female (85%) and had a mean age of 49 years. They were referred to the Mayo Clinic (55%), the University of Vermont (25%), Washington University (11%), and Oregon Health and Science University (9%). The high highest percentage of misdiagnoses were from physicians with an unknown level of specific training in neurology or (42%), followed by neurologists without MS fellowship training (34%), neurologists with MS fellowship training or a practice focus on MS (24%), and nonneurologists (3%).
It was no surprise to see MS fellowship–trained neurologists among those making misdiagnoses, Dr. Carter said in an interview. “The criteria are somewhat subjective and interpretation of test results are somewhat subjective, then it’s quite possible to have another MS specialist diagnose somebody and then have them come to a different center and have that diagnosis questioned. I think it happens probably less frequently with MS fellowship–trained physicians than with general neurologists, but it still happens.”
All but three patients were informed that their MS diagnosis was incorrect: one who had died and was determined on autopsy to have neuromyelitis optica spectrum disorder, one who had been informed already of a possible alternate diagnosis, and one who had an upcoming follow-up visit.
Many of the patients had a longstanding MS misdiagnosis. A total of 29% had been misdiagnosed for 3-9 years, and 33% for 10 or more years.
The patients received a variety of primary diagnoses following reevaluation at the centers. The most common, accounting for two-thirds of all diagnoses, were migraine alone or in combination with other diagnoses in 24 (22%), fibromyalgia in 16 (15%), nonspecific or nonlocalizing neurological symptoms with abnormal MRI in 13 (12%), conversion or psychogenic disorder in 12 (11%), and neuromyelitis optica spectrum disorder in 7 (6%). Twenty six additional diagnoses were made.
The most common primary diagnoses, except for neuromyelitis spectrum disorder, all share the lack a specific biomarker, Dr. Solomon noted. Most of them require clinical skills and critical thinking to make the diagnosis, he said.
Most (70%) patients had received immunomodulatory treatment for MS, including 36% with more than one disease-modifying therapy. The treatments included natalizumab (Tysabri) in 13%, dimethyl fumarate (Tecfidera) in 6%, and fingolimod (Gilenya) in 5% – all of which have known risk for progressive multifocal leukoencephalopathy – as well as mitoxantrone in two patients and cyclophosphamide in one. Overall, 29% of those who received immunomodulatory therapy used it for 3-9 years, and another 29% used it for 10 or more years.
Dr. Solomon acknowledged selection and referral bias as limitations to the study, as well as possibly incorrect alternate diagnoses. The disease duration and hindshight bias also may have allowed a correct diagnosis to come to light. The study could not provide information on the frequency of misdiagnosis but “provides rationale for such data in the future,” he said.
It’s hard to know how big of a problem the misdiagnosis of MS is in clinical practice. There are numerous reasons, including limitations in how it has been reported in the literature, a lack of knowledge of how many patients are evaluated for MS overall, lack of knowledge on whether it is widespread or confined to a small number of bad diagnosers, and the need for human interpretation of clinical, imaging, and laboratory evidence.
Revisions to MS diagnostic criteria over time have made it easier to diagnose the disease earlier with less clinical history but without any pathologic standard. Even though MRI is the best biomarker for MS, its specificity reaches only 87% under various criteria among experienced researchers. The full criteria also are not generally used in real-world practice.
Regardless of the extent of misdiagnosis, the limited extent of our ability to identify MS through exclusively objective methods means that we must adhere to diagnostic criteria; keep an open mind for alternative diagnoses; know MRI features that give greatest specificity; assess both brain and spine MRI; read MRIs ourselves; get help if needed; improve the education of neurologists, primary care physicians, and radiologists; make MS an affirmative diagnosis, not a default one; and develop better biomarkers in blood, cerebrospinal fluid, or MRI.
Dr. John Corboy is professor of neurology and codirector of the Rocky Mountain MS Center at the University of Colorado-Denver in Aurora. In the past 2 years he has served as a consultant to Novartis, Teva Neurosciences, and Biogen; been a primary investigator in trials for Novartis, Sun Pharma, and the National Multiple Sclerosis Society; and received research grants from the National Multiple Sclerosis Society, Diogenix, and the Patient-Centered Outcomes Research Institute. He made these comments as the discussant for the study presented by Dr. Solomon.
It’s hard to know how big of a problem the misdiagnosis of MS is in clinical practice. There are numerous reasons, including limitations in how it has been reported in the literature, a lack of knowledge of how many patients are evaluated for MS overall, lack of knowledge on whether it is widespread or confined to a small number of bad diagnosers, and the need for human interpretation of clinical, imaging, and laboratory evidence.
Revisions to MS diagnostic criteria over time have made it easier to diagnose the disease earlier with less clinical history but without any pathologic standard. Even though MRI is the best biomarker for MS, its specificity reaches only 87% under various criteria among experienced researchers. The full criteria also are not generally used in real-world practice.
Regardless of the extent of misdiagnosis, the limited extent of our ability to identify MS through exclusively objective methods means that we must adhere to diagnostic criteria; keep an open mind for alternative diagnoses; know MRI features that give greatest specificity; assess both brain and spine MRI; read MRIs ourselves; get help if needed; improve the education of neurologists, primary care physicians, and radiologists; make MS an affirmative diagnosis, not a default one; and develop better biomarkers in blood, cerebrospinal fluid, or MRI.
Dr. John Corboy is professor of neurology and codirector of the Rocky Mountain MS Center at the University of Colorado-Denver in Aurora. In the past 2 years he has served as a consultant to Novartis, Teva Neurosciences, and Biogen; been a primary investigator in trials for Novartis, Sun Pharma, and the National Multiple Sclerosis Society; and received research grants from the National Multiple Sclerosis Society, Diogenix, and the Patient-Centered Outcomes Research Institute. He made these comments as the discussant for the study presented by Dr. Solomon.
It’s hard to know how big of a problem the misdiagnosis of MS is in clinical practice. There are numerous reasons, including limitations in how it has been reported in the literature, a lack of knowledge of how many patients are evaluated for MS overall, lack of knowledge on whether it is widespread or confined to a small number of bad diagnosers, and the need for human interpretation of clinical, imaging, and laboratory evidence.
Revisions to MS diagnostic criteria over time have made it easier to diagnose the disease earlier with less clinical history but without any pathologic standard. Even though MRI is the best biomarker for MS, its specificity reaches only 87% under various criteria among experienced researchers. The full criteria also are not generally used in real-world practice.
Regardless of the extent of misdiagnosis, the limited extent of our ability to identify MS through exclusively objective methods means that we must adhere to diagnostic criteria; keep an open mind for alternative diagnoses; know MRI features that give greatest specificity; assess both brain and spine MRI; read MRIs ourselves; get help if needed; improve the education of neurologists, primary care physicians, and radiologists; make MS an affirmative diagnosis, not a default one; and develop better biomarkers in blood, cerebrospinal fluid, or MRI.
Dr. John Corboy is professor of neurology and codirector of the Rocky Mountain MS Center at the University of Colorado-Denver in Aurora. In the past 2 years he has served as a consultant to Novartis, Teva Neurosciences, and Biogen; been a primary investigator in trials for Novartis, Sun Pharma, and the National Multiple Sclerosis Society; and received research grants from the National Multiple Sclerosis Society, Diogenix, and the Patient-Centered Outcomes Research Institute. He made these comments as the discussant for the study presented by Dr. Solomon.
VANCOUVER – More than two-thirds of patients with definite or probable misdiagnosis of multiple sclerosis took unnecessary disease-modifying therapy and nearly one-third experienced unnecessary morbidity in a prospective pilot study.
The findings highlight a problem that has been noted before in the medical literature, but since many instances are case reports of unusual cases or were published about 20 or more years ago, they may not reflect the current spectrum of misdiagnosis, Dr. Andrew J. Solomon said at the annual meeting of the American Academy of Neurology.
During a 13-month period, neurologists at four U.S. academic multiple sclerosis centers reported that 51 (46%) of 110 misdiagnosed patients had “definite” misdiagnosis because an alternate diagnosis was identified after assessing clinical, laboratory, and neuroimaging data, while 59 had “probable” misdiagnoses.
Participating neurologists felt that the misdiagnoses were based in part on inappropriately attributing symptoms to demyelinating disease in 65% of cases. MS diagnostic criteria were not rigorously validated for use in patients with atypical presentations, suggesting that the misuse of the criteria could represent a misunderstanding of what constitutes a typical demyelinating attack, said Dr. Solomon of the department of neurological sciences at the University of Vermont, Burlington.
In 48% of cases, the participating neurologists said that objective evidence of a lesion was not used to corroborate historical symptoms.
Many instances also were seen in which the neurologists felt magnetic resonance imaging criteria were misinterpreted or misapplied. In 60%, the MS misdiagnosis relied too heavily on MRI abnormalities to meet the MS diagnostic criteria for dissemination in space when the patient had nonspecific neurologic symptoms, and in another 33% there was an incorrect determination of juxtacortical or periventricular lesion location to fulfill the diagnostic criteria for dissemination in space. Dr. Solomon said that the MRI criteria for MS were not developed to differentiate MS from other conditions, but instead to identify patients at high risk for MS after initial typical presentations of demyelination.
“Overreliance on MRI abnormalities in the setting of atypical symptoms and unverified prior symptoms may be a major cause of misdiagnosis,” he said.
Many earlier patient visits contained red flags that could have led to a correct diagnosis, according to the neurologists who participated in the study. There was evidence for this opportunity being missed in 79 (72%) patients.
“We don’t know how frequent this problem is in practice. I think it’s pretty frequent just based on my own clinical experience, but no one’s done a population-based study, as you can imagine that would be kind of difficult to do,” said Dr. Jonathan Carter, an MS specialist at the Mayo Clinic in Scottsdale, Ariz., who was part of the study.
Study patients were previously diagnosed with MS; none were allowed to have MS as one of several potential diagnoses. Patients were mostly female (85%) and had a mean age of 49 years. They were referred to the Mayo Clinic (55%), the University of Vermont (25%), Washington University (11%), and Oregon Health and Science University (9%). The high highest percentage of misdiagnoses were from physicians with an unknown level of specific training in neurology or (42%), followed by neurologists without MS fellowship training (34%), neurologists with MS fellowship training or a practice focus on MS (24%), and nonneurologists (3%).
It was no surprise to see MS fellowship–trained neurologists among those making misdiagnoses, Dr. Carter said in an interview. “The criteria are somewhat subjective and interpretation of test results are somewhat subjective, then it’s quite possible to have another MS specialist diagnose somebody and then have them come to a different center and have that diagnosis questioned. I think it happens probably less frequently with MS fellowship–trained physicians than with general neurologists, but it still happens.”
All but three patients were informed that their MS diagnosis was incorrect: one who had died and was determined on autopsy to have neuromyelitis optica spectrum disorder, one who had been informed already of a possible alternate diagnosis, and one who had an upcoming follow-up visit.
Many of the patients had a longstanding MS misdiagnosis. A total of 29% had been misdiagnosed for 3-9 years, and 33% for 10 or more years.
The patients received a variety of primary diagnoses following reevaluation at the centers. The most common, accounting for two-thirds of all diagnoses, were migraine alone or in combination with other diagnoses in 24 (22%), fibromyalgia in 16 (15%), nonspecific or nonlocalizing neurological symptoms with abnormal MRI in 13 (12%), conversion or psychogenic disorder in 12 (11%), and neuromyelitis optica spectrum disorder in 7 (6%). Twenty six additional diagnoses were made.
The most common primary diagnoses, except for neuromyelitis spectrum disorder, all share the lack a specific biomarker, Dr. Solomon noted. Most of them require clinical skills and critical thinking to make the diagnosis, he said.
Most (70%) patients had received immunomodulatory treatment for MS, including 36% with more than one disease-modifying therapy. The treatments included natalizumab (Tysabri) in 13%, dimethyl fumarate (Tecfidera) in 6%, and fingolimod (Gilenya) in 5% – all of which have known risk for progressive multifocal leukoencephalopathy – as well as mitoxantrone in two patients and cyclophosphamide in one. Overall, 29% of those who received immunomodulatory therapy used it for 3-9 years, and another 29% used it for 10 or more years.
Dr. Solomon acknowledged selection and referral bias as limitations to the study, as well as possibly incorrect alternate diagnoses. The disease duration and hindshight bias also may have allowed a correct diagnosis to come to light. The study could not provide information on the frequency of misdiagnosis but “provides rationale for such data in the future,” he said.
VANCOUVER – More than two-thirds of patients with definite or probable misdiagnosis of multiple sclerosis took unnecessary disease-modifying therapy and nearly one-third experienced unnecessary morbidity in a prospective pilot study.
The findings highlight a problem that has been noted before in the medical literature, but since many instances are case reports of unusual cases or were published about 20 or more years ago, they may not reflect the current spectrum of misdiagnosis, Dr. Andrew J. Solomon said at the annual meeting of the American Academy of Neurology.
During a 13-month period, neurologists at four U.S. academic multiple sclerosis centers reported that 51 (46%) of 110 misdiagnosed patients had “definite” misdiagnosis because an alternate diagnosis was identified after assessing clinical, laboratory, and neuroimaging data, while 59 had “probable” misdiagnoses.
Participating neurologists felt that the misdiagnoses were based in part on inappropriately attributing symptoms to demyelinating disease in 65% of cases. MS diagnostic criteria were not rigorously validated for use in patients with atypical presentations, suggesting that the misuse of the criteria could represent a misunderstanding of what constitutes a typical demyelinating attack, said Dr. Solomon of the department of neurological sciences at the University of Vermont, Burlington.
In 48% of cases, the participating neurologists said that objective evidence of a lesion was not used to corroborate historical symptoms.
Many instances also were seen in which the neurologists felt magnetic resonance imaging criteria were misinterpreted or misapplied. In 60%, the MS misdiagnosis relied too heavily on MRI abnormalities to meet the MS diagnostic criteria for dissemination in space when the patient had nonspecific neurologic symptoms, and in another 33% there was an incorrect determination of juxtacortical or periventricular lesion location to fulfill the diagnostic criteria for dissemination in space. Dr. Solomon said that the MRI criteria for MS were not developed to differentiate MS from other conditions, but instead to identify patients at high risk for MS after initial typical presentations of demyelination.
“Overreliance on MRI abnormalities in the setting of atypical symptoms and unverified prior symptoms may be a major cause of misdiagnosis,” he said.
Many earlier patient visits contained red flags that could have led to a correct diagnosis, according to the neurologists who participated in the study. There was evidence for this opportunity being missed in 79 (72%) patients.
“We don’t know how frequent this problem is in practice. I think it’s pretty frequent just based on my own clinical experience, but no one’s done a population-based study, as you can imagine that would be kind of difficult to do,” said Dr. Jonathan Carter, an MS specialist at the Mayo Clinic in Scottsdale, Ariz., who was part of the study.
Study patients were previously diagnosed with MS; none were allowed to have MS as one of several potential diagnoses. Patients were mostly female (85%) and had a mean age of 49 years. They were referred to the Mayo Clinic (55%), the University of Vermont (25%), Washington University (11%), and Oregon Health and Science University (9%). The high highest percentage of misdiagnoses were from physicians with an unknown level of specific training in neurology or (42%), followed by neurologists without MS fellowship training (34%), neurologists with MS fellowship training or a practice focus on MS (24%), and nonneurologists (3%).
It was no surprise to see MS fellowship–trained neurologists among those making misdiagnoses, Dr. Carter said in an interview. “The criteria are somewhat subjective and interpretation of test results are somewhat subjective, then it’s quite possible to have another MS specialist diagnose somebody and then have them come to a different center and have that diagnosis questioned. I think it happens probably less frequently with MS fellowship–trained physicians than with general neurologists, but it still happens.”
All but three patients were informed that their MS diagnosis was incorrect: one who had died and was determined on autopsy to have neuromyelitis optica spectrum disorder, one who had been informed already of a possible alternate diagnosis, and one who had an upcoming follow-up visit.
Many of the patients had a longstanding MS misdiagnosis. A total of 29% had been misdiagnosed for 3-9 years, and 33% for 10 or more years.
The patients received a variety of primary diagnoses following reevaluation at the centers. The most common, accounting for two-thirds of all diagnoses, were migraine alone or in combination with other diagnoses in 24 (22%), fibromyalgia in 16 (15%), nonspecific or nonlocalizing neurological symptoms with abnormal MRI in 13 (12%), conversion or psychogenic disorder in 12 (11%), and neuromyelitis optica spectrum disorder in 7 (6%). Twenty six additional diagnoses were made.
The most common primary diagnoses, except for neuromyelitis spectrum disorder, all share the lack a specific biomarker, Dr. Solomon noted. Most of them require clinical skills and critical thinking to make the diagnosis, he said.
Most (70%) patients had received immunomodulatory treatment for MS, including 36% with more than one disease-modifying therapy. The treatments included natalizumab (Tysabri) in 13%, dimethyl fumarate (Tecfidera) in 6%, and fingolimod (Gilenya) in 5% – all of which have known risk for progressive multifocal leukoencephalopathy – as well as mitoxantrone in two patients and cyclophosphamide in one. Overall, 29% of those who received immunomodulatory therapy used it for 3-9 years, and another 29% used it for 10 or more years.
Dr. Solomon acknowledged selection and referral bias as limitations to the study, as well as possibly incorrect alternate diagnoses. The disease duration and hindshight bias also may have allowed a correct diagnosis to come to light. The study could not provide information on the frequency of misdiagnosis but “provides rationale for such data in the future,” he said.
AT THE AAN 2016 ANNUAL MEETING
Key clinical point: Misapplication or misinterpretation of diagnostic criteria for multiple sclerosis can lead to misdiagnosis and potential morbidity as a result of inappropriate treatment.
Major finding: Most (70%) of the patients had received immunomodulatory treatment for MS, including 36% with more than one disease-modifying therapy.
Data source: A prospective pilot study of 110 patients misdiagnosed with MS who were referred to four U.S. academic medical centers.
Disclosures: The study was funded by the National Multiple Sclerosis Society. Half of the study’s investigators disclosed consulting, serving on data safety monitoring committees, receiving personal compensation from, or other activities for manufacturers of MS drugs. Dr. Carter reported serving on a data safety monitoring committee for Merck-Serono and receiving research support from Roche, Sanofi, and Genzyme through funding paid to the Mayo Clinic.
Childhood Emotional Abuse Fuels Odds for Migraine in Adulthood
Emotionally abused children are 52% more likely to develop migraine in young adulthood than are those who were never abused, based on longitudinal survey data from nearly 15,000 individuals.
“Childhood maltreatment, and especially emotional abuse, is a common, likely under-recognized occurrence, which has enduring consequences for health throughout life. The association of emotional abuse with migraine has not heretofore been well studied, being the subject of only population-based study,” lead author Dr. Gretchen E. Tietjen of the University of Toledo (Ohio) said in an interview in advance of the presentation of the study at the annual meeting of the American Academy of Neurology in Vancouver in April.
Dr. Tietjen and her colleagues assessed data from 14,484 adults aged 24-32 years who took part in wave four of the National Longitudinal Study of Adolescent to Adult Health. Of these, 2,061 (14%) reported a migraine diagnosis, and 1,246 (60%) of those diagnosed with migraines reported some type of childhood abuse. A total of 6,088 (49%) individuals without migraine reported some type of childhood abuse.
Overall, the odds of migraine in adulthood was 55% higher in children who reported emotional abuse, physical abuse, or sexual abuse, compared with those who reported no childhood abuse, after controlling for age, race, sex, and income (odds ratio, 1.55; 95% confidence interval, 1.35-1.77). However, only emotional abuse remained significantly associated with increased odds for migraine after controlling for other types of abuse (OR, 1.52; 95% CI, 1.34-1.73).
Emotional abuse was assessed by asking, “How often did a parent or other adult caregiver say things that really hurt your feelings or made you feel like you were not wanted or loved?” Physical abuse was defined as being hit with a fist, kicked, or thrown down on the floor, into a wall, or down stairs. Sexual abuse included forced sexual touching or sexual relations.
Controlling for depression and anxiety weakened the associations between childhood abuse overall and likelihood of migraine in young adulthood, as well as for emotional abuse in particular, but the relationships remained statistically significant (OR, 1.32 and 1.33, respectively).
Dr. Tietjen said she was surprised by the absence of an association between migraine and physical and sexual abuse after controlling for other types of abuse.
“Sexual and physical abuse may be less frequent, occur over a briefer duration, and if limited, lead in some cases to resilience,” Dr. Tietjen noted. “Emotional abuse is likely more insidious, being ingrained in the fabric of the family dynamic. It may occur over years without recognition or intervention,” she said. “This type of abuse may cause more cumulative stress, with subsequent dysregulation of the HPA axis, immune, autonomic, and metabolic systems,” she added.
The study does not show cause and effect, the researchers noted, and more research is needed. But the findings suggest that clinicians might consider childhood abuse when counseling adult migraine patients.
“In migraineurs, childhood abuse, particularly emotional abuse, is common and possibly causally related,” Dr. Tietjen said. “Knowledge of adverse childhood experiences allows physicians to identify migraineurs at higher risk for psychiatric disease, pain comorbidities, and conditions associated with inflammation. These patients would likely benefit from exposure to cognitive behavioral therapy strategies, in order to decrease neurophysiological responses to stress,” she noted.
“There are currently therapies which reverse stress-induced epigenetic changes, which might be particularly useful in the subset of migraineurs who have been abused,” said Dr. Tietjen. Her next steps for research involve studying the effect of early life stress on factors such as pain sensitivity, anxiety, and depression.
The University of Toledo and the Clair Martig Endowment funded the study.
Emotionally abused children are 52% more likely to develop migraine in young adulthood than are those who were never abused, based on longitudinal survey data from nearly 15,000 individuals.
“Childhood maltreatment, and especially emotional abuse, is a common, likely under-recognized occurrence, which has enduring consequences for health throughout life. The association of emotional abuse with migraine has not heretofore been well studied, being the subject of only population-based study,” lead author Dr. Gretchen E. Tietjen of the University of Toledo (Ohio) said in an interview in advance of the presentation of the study at the annual meeting of the American Academy of Neurology in Vancouver in April.
Dr. Tietjen and her colleagues assessed data from 14,484 adults aged 24-32 years who took part in wave four of the National Longitudinal Study of Adolescent to Adult Health. Of these, 2,061 (14%) reported a migraine diagnosis, and 1,246 (60%) of those diagnosed with migraines reported some type of childhood abuse. A total of 6,088 (49%) individuals without migraine reported some type of childhood abuse.
Overall, the odds of migraine in adulthood was 55% higher in children who reported emotional abuse, physical abuse, or sexual abuse, compared with those who reported no childhood abuse, after controlling for age, race, sex, and income (odds ratio, 1.55; 95% confidence interval, 1.35-1.77). However, only emotional abuse remained significantly associated with increased odds for migraine after controlling for other types of abuse (OR, 1.52; 95% CI, 1.34-1.73).
Emotional abuse was assessed by asking, “How often did a parent or other adult caregiver say things that really hurt your feelings or made you feel like you were not wanted or loved?” Physical abuse was defined as being hit with a fist, kicked, or thrown down on the floor, into a wall, or down stairs. Sexual abuse included forced sexual touching or sexual relations.
Controlling for depression and anxiety weakened the associations between childhood abuse overall and likelihood of migraine in young adulthood, as well as for emotional abuse in particular, but the relationships remained statistically significant (OR, 1.32 and 1.33, respectively).
Dr. Tietjen said she was surprised by the absence of an association between migraine and physical and sexual abuse after controlling for other types of abuse.
“Sexual and physical abuse may be less frequent, occur over a briefer duration, and if limited, lead in some cases to resilience,” Dr. Tietjen noted. “Emotional abuse is likely more insidious, being ingrained in the fabric of the family dynamic. It may occur over years without recognition or intervention,” she said. “This type of abuse may cause more cumulative stress, with subsequent dysregulation of the HPA axis, immune, autonomic, and metabolic systems,” she added.
The study does not show cause and effect, the researchers noted, and more research is needed. But the findings suggest that clinicians might consider childhood abuse when counseling adult migraine patients.
“In migraineurs, childhood abuse, particularly emotional abuse, is common and possibly causally related,” Dr. Tietjen said. “Knowledge of adverse childhood experiences allows physicians to identify migraineurs at higher risk for psychiatric disease, pain comorbidities, and conditions associated with inflammation. These patients would likely benefit from exposure to cognitive behavioral therapy strategies, in order to decrease neurophysiological responses to stress,” she noted.
“There are currently therapies which reverse stress-induced epigenetic changes, which might be particularly useful in the subset of migraineurs who have been abused,” said Dr. Tietjen. Her next steps for research involve studying the effect of early life stress on factors such as pain sensitivity, anxiety, and depression.
The University of Toledo and the Clair Martig Endowment funded the study.
Emotionally abused children are 52% more likely to develop migraine in young adulthood than are those who were never abused, based on longitudinal survey data from nearly 15,000 individuals.
“Childhood maltreatment, and especially emotional abuse, is a common, likely under-recognized occurrence, which has enduring consequences for health throughout life. The association of emotional abuse with migraine has not heretofore been well studied, being the subject of only population-based study,” lead author Dr. Gretchen E. Tietjen of the University of Toledo (Ohio) said in an interview in advance of the presentation of the study at the annual meeting of the American Academy of Neurology in Vancouver in April.
Dr. Tietjen and her colleagues assessed data from 14,484 adults aged 24-32 years who took part in wave four of the National Longitudinal Study of Adolescent to Adult Health. Of these, 2,061 (14%) reported a migraine diagnosis, and 1,246 (60%) of those diagnosed with migraines reported some type of childhood abuse. A total of 6,088 (49%) individuals without migraine reported some type of childhood abuse.
Overall, the odds of migraine in adulthood was 55% higher in children who reported emotional abuse, physical abuse, or sexual abuse, compared with those who reported no childhood abuse, after controlling for age, race, sex, and income (odds ratio, 1.55; 95% confidence interval, 1.35-1.77). However, only emotional abuse remained significantly associated with increased odds for migraine after controlling for other types of abuse (OR, 1.52; 95% CI, 1.34-1.73).
Emotional abuse was assessed by asking, “How often did a parent or other adult caregiver say things that really hurt your feelings or made you feel like you were not wanted or loved?” Physical abuse was defined as being hit with a fist, kicked, or thrown down on the floor, into a wall, or down stairs. Sexual abuse included forced sexual touching or sexual relations.
Controlling for depression and anxiety weakened the associations between childhood abuse overall and likelihood of migraine in young adulthood, as well as for emotional abuse in particular, but the relationships remained statistically significant (OR, 1.32 and 1.33, respectively).
Dr. Tietjen said she was surprised by the absence of an association between migraine and physical and sexual abuse after controlling for other types of abuse.
“Sexual and physical abuse may be less frequent, occur over a briefer duration, and if limited, lead in some cases to resilience,” Dr. Tietjen noted. “Emotional abuse is likely more insidious, being ingrained in the fabric of the family dynamic. It may occur over years without recognition or intervention,” she said. “This type of abuse may cause more cumulative stress, with subsequent dysregulation of the HPA axis, immune, autonomic, and metabolic systems,” she added.
The study does not show cause and effect, the researchers noted, and more research is needed. But the findings suggest that clinicians might consider childhood abuse when counseling adult migraine patients.
“In migraineurs, childhood abuse, particularly emotional abuse, is common and possibly causally related,” Dr. Tietjen said. “Knowledge of adverse childhood experiences allows physicians to identify migraineurs at higher risk for psychiatric disease, pain comorbidities, and conditions associated with inflammation. These patients would likely benefit from exposure to cognitive behavioral therapy strategies, in order to decrease neurophysiological responses to stress,” she noted.
“There are currently therapies which reverse stress-induced epigenetic changes, which might be particularly useful in the subset of migraineurs who have been abused,” said Dr. Tietjen. Her next steps for research involve studying the effect of early life stress on factors such as pain sensitivity, anxiety, and depression.
The University of Toledo and the Clair Martig Endowment funded the study.
FROM THE AAN 2016 ANNUAL MEETING
Childhood emotional abuse fuels odds for migraine in adulthood
Emotionally abused children are 52% more likely to develop migraine in young adulthood than are those who were never abused, based on longitudinal survey data from nearly 15,000 individuals.
“Childhood maltreatment, and especially emotional abuse, is a common, likely under-recognized occurrence, which has enduring consequences for health throughout life. The association of emotional abuse with migraine has not heretofore been well studied, being the subject of only population-based study,” lead author Dr. Gretchen E. Tietjen of the University of Toledo (Ohio) said in an interview in advance of the presentation of the study at the annual meeting of the American Academy of Neurology in Vancouver in April.
Dr. Tietjen and her colleagues assessed data from 14,484 adults aged 24-32 years who took part in wave four of the National Longitudinal Study of Adolescent to Adult Health. Of these, 2,061 (14%) reported a migraine diagnosis, and 1,246 (60%) of those diagnosed with migraines reported some type of childhood abuse. A total of 6,088 (49%) individuals without migraine reported some type of childhood abuse.
Overall, the odds of migraine in adulthood was 55% higher in children who reported emotional abuse, physical abuse, or sexual abuse, compared with those who reported no childhood abuse, after controlling for age, race, sex, and income (odds ratio, 1.55; 95% confidence interval, 1.35-1.77). However, only emotional abuse remained significantly associated with increased odds for migraine after controlling for other types of abuse (OR, 1.52; 95% CI, 1.34-1.73).
Emotional abuse was assessed by asking, “How often did a parent or other adult caregiver say things that really hurt your feelings or made you feel like you were not wanted or loved?” Physical abuse was defined as being hit with a fist, kicked, or thrown down on the floor, into a wall, or down stairs. Sexual abuse included forced sexual touching or sexual relations.
Controlling for depression and anxiety weakened the associations between childhood abuse overall and likelihood of migraine in young adulthood, as well as for emotional abuse in particular, but the relationships remained statistically significant (OR, 1.32 and 1.33, respectively).
Dr. Tietjen said she was surprised by the absence of an association between migraine and physical and sexual abuse after controlling for other types of abuse.
“Sexual and physical abuse may be less frequent, occur over a briefer duration, and if limited, lead in some cases to resilience,” Dr. Tietjen noted. “Emotional abuse is likely more insidious, being ingrained in the fabric of the family dynamic. It may occur over years without recognition or intervention,” she said. “This type of abuse may cause more cumulative stress, with subsequent dysregulation of the HPA axis, immune, autonomic, and metabolic systems,” she added.
The study does not show cause and effect, the researchers noted, and more research is needed. But the findings suggest that clinicians might consider childhood abuse when counseling adult migraine patients.
“In migraineurs, childhood abuse, particularly emotional abuse, is common and possibly causally related,” Dr. Tietjen said. “Knowledge of adverse childhood experiences allows physicians to identify migraineurs at higher risk for psychiatric disease, pain comorbidities, and conditions associated with inflammation. These patients would likely benefit from exposure to cognitive behavioral therapy strategies, in order to decrease neurophysiological responses to stress,” she noted.
“There are currently therapies which reverse stress-induced epigenetic changes, which might be particularly useful in the subset of migraineurs who have been abused,” said Dr. Tietjen. Her next steps for research involve studying the effect of early life stress on factors such as pain sensitivity, anxiety, and depression.
The University of Toledo and the Clair Martig Endowment funded the study.
Emotionally abused children are 52% more likely to develop migraine in young adulthood than are those who were never abused, based on longitudinal survey data from nearly 15,000 individuals.
“Childhood maltreatment, and especially emotional abuse, is a common, likely under-recognized occurrence, which has enduring consequences for health throughout life. The association of emotional abuse with migraine has not heretofore been well studied, being the subject of only population-based study,” lead author Dr. Gretchen E. Tietjen of the University of Toledo (Ohio) said in an interview in advance of the presentation of the study at the annual meeting of the American Academy of Neurology in Vancouver in April.
Dr. Tietjen and her colleagues assessed data from 14,484 adults aged 24-32 years who took part in wave four of the National Longitudinal Study of Adolescent to Adult Health. Of these, 2,061 (14%) reported a migraine diagnosis, and 1,246 (60%) of those diagnosed with migraines reported some type of childhood abuse. A total of 6,088 (49%) individuals without migraine reported some type of childhood abuse.
Overall, the odds of migraine in adulthood was 55% higher in children who reported emotional abuse, physical abuse, or sexual abuse, compared with those who reported no childhood abuse, after controlling for age, race, sex, and income (odds ratio, 1.55; 95% confidence interval, 1.35-1.77). However, only emotional abuse remained significantly associated with increased odds for migraine after controlling for other types of abuse (OR, 1.52; 95% CI, 1.34-1.73).
Emotional abuse was assessed by asking, “How often did a parent or other adult caregiver say things that really hurt your feelings or made you feel like you were not wanted or loved?” Physical abuse was defined as being hit with a fist, kicked, or thrown down on the floor, into a wall, or down stairs. Sexual abuse included forced sexual touching or sexual relations.
Controlling for depression and anxiety weakened the associations between childhood abuse overall and likelihood of migraine in young adulthood, as well as for emotional abuse in particular, but the relationships remained statistically significant (OR, 1.32 and 1.33, respectively).
Dr. Tietjen said she was surprised by the absence of an association between migraine and physical and sexual abuse after controlling for other types of abuse.
“Sexual and physical abuse may be less frequent, occur over a briefer duration, and if limited, lead in some cases to resilience,” Dr. Tietjen noted. “Emotional abuse is likely more insidious, being ingrained in the fabric of the family dynamic. It may occur over years without recognition or intervention,” she said. “This type of abuse may cause more cumulative stress, with subsequent dysregulation of the HPA axis, immune, autonomic, and metabolic systems,” she added.
The study does not show cause and effect, the researchers noted, and more research is needed. But the findings suggest that clinicians might consider childhood abuse when counseling adult migraine patients.
“In migraineurs, childhood abuse, particularly emotional abuse, is common and possibly causally related,” Dr. Tietjen said. “Knowledge of adverse childhood experiences allows physicians to identify migraineurs at higher risk for psychiatric disease, pain comorbidities, and conditions associated with inflammation. These patients would likely benefit from exposure to cognitive behavioral therapy strategies, in order to decrease neurophysiological responses to stress,” she noted.
“There are currently therapies which reverse stress-induced epigenetic changes, which might be particularly useful in the subset of migraineurs who have been abused,” said Dr. Tietjen. Her next steps for research involve studying the effect of early life stress on factors such as pain sensitivity, anxiety, and depression.
The University of Toledo and the Clair Martig Endowment funded the study.
Emotionally abused children are 52% more likely to develop migraine in young adulthood than are those who were never abused, based on longitudinal survey data from nearly 15,000 individuals.
“Childhood maltreatment, and especially emotional abuse, is a common, likely under-recognized occurrence, which has enduring consequences for health throughout life. The association of emotional abuse with migraine has not heretofore been well studied, being the subject of only population-based study,” lead author Dr. Gretchen E. Tietjen of the University of Toledo (Ohio) said in an interview in advance of the presentation of the study at the annual meeting of the American Academy of Neurology in Vancouver in April.
Dr. Tietjen and her colleagues assessed data from 14,484 adults aged 24-32 years who took part in wave four of the National Longitudinal Study of Adolescent to Adult Health. Of these, 2,061 (14%) reported a migraine diagnosis, and 1,246 (60%) of those diagnosed with migraines reported some type of childhood abuse. A total of 6,088 (49%) individuals without migraine reported some type of childhood abuse.
Overall, the odds of migraine in adulthood was 55% higher in children who reported emotional abuse, physical abuse, or sexual abuse, compared with those who reported no childhood abuse, after controlling for age, race, sex, and income (odds ratio, 1.55; 95% confidence interval, 1.35-1.77). However, only emotional abuse remained significantly associated with increased odds for migraine after controlling for other types of abuse (OR, 1.52; 95% CI, 1.34-1.73).
Emotional abuse was assessed by asking, “How often did a parent or other adult caregiver say things that really hurt your feelings or made you feel like you were not wanted or loved?” Physical abuse was defined as being hit with a fist, kicked, or thrown down on the floor, into a wall, or down stairs. Sexual abuse included forced sexual touching or sexual relations.
Controlling for depression and anxiety weakened the associations between childhood abuse overall and likelihood of migraine in young adulthood, as well as for emotional abuse in particular, but the relationships remained statistically significant (OR, 1.32 and 1.33, respectively).
Dr. Tietjen said she was surprised by the absence of an association between migraine and physical and sexual abuse after controlling for other types of abuse.
“Sexual and physical abuse may be less frequent, occur over a briefer duration, and if limited, lead in some cases to resilience,” Dr. Tietjen noted. “Emotional abuse is likely more insidious, being ingrained in the fabric of the family dynamic. It may occur over years without recognition or intervention,” she said. “This type of abuse may cause more cumulative stress, with subsequent dysregulation of the HPA axis, immune, autonomic, and metabolic systems,” she added.
The study does not show cause and effect, the researchers noted, and more research is needed. But the findings suggest that clinicians might consider childhood abuse when counseling adult migraine patients.
“In migraineurs, childhood abuse, particularly emotional abuse, is common and possibly causally related,” Dr. Tietjen said. “Knowledge of adverse childhood experiences allows physicians to identify migraineurs at higher risk for psychiatric disease, pain comorbidities, and conditions associated with inflammation. These patients would likely benefit from exposure to cognitive behavioral therapy strategies, in order to decrease neurophysiological responses to stress,” she noted.
“There are currently therapies which reverse stress-induced epigenetic changes, which might be particularly useful in the subset of migraineurs who have been abused,” said Dr. Tietjen. Her next steps for research involve studying the effect of early life stress on factors such as pain sensitivity, anxiety, and depression.
The University of Toledo and the Clair Martig Endowment funded the study.
FROM THE AAN 2016 ANNUAL MEETING
Key clinical point: Childhood abuse had a significant effect on the likelihood of developing migraine in young adulthood, and emotional abuse was a stronger factor than physical or sexual abuse.
Major finding: Childhood abuse increased the odds of a migraine diagnosis in young adulthood by 55%; emotional abuse was associated with a 52% increased likelihood of migraine.
Data source: The data were taken from 14,484 adults aged 24-32 years in wave four of the National Longitudinal Study of Adolescent to Adult Health.
Disclosures: The University of Toledo and the Clair Martig Endowment funded the study.
Drug targeting Huntington’s disease–causing protein undergoing clinical trial
A drug that was found to have no dose-limiting side effects in nonhuman primates is being evaluated in a clinical trial for its ability to reduce production of the protein that causes Huntington’s disease (HD).
The new drug, which is an antisense oligonucleotide, was formerly known as ISIS-HTTRx and was renamed IONIS-HTTRx, because its developer changed its name in December 2015 to Ionis Pharmaceuticals from Isis Pharmaceuticals. IONIS-HTTRx acts as a gene silencer to inhibit the production of huntington protein in people with HD. The clinical trial now underway is a randomized, double-blind, placebo-controlled study aimed at evaluating the safety, tolerability, pharmacokinetics, and pharmacodynamics of multiple ascending doses of IONIS-HTTRx in up to 36 patients with early manifest HD. If the trial is successful, IONIS-HTTRx would be the first drug to modify HD progression in patients, according to an abstract to be presented at the annual meeting of the American Academy of Neurology in Vancouver in April.
Ionis found the drug to be well tolerated in rodents and nonhuman primates in investigational new drug-enabling toxicology studies, with nonhuman primates having received doses up to 20 mg of the drug intrathecally, according to the trial’s principal investigator Dr. Blair R. Leavitt of the University of British Columbia, Vancouver, and colleagues.
“It is very exciting to have the possibility of a treatment that could alter the course of this devastating disease. Right now we only have treatments that work on the symptoms of the disease.” Dr. Leavitt said in a written statement.
The study is supported by Ionis Pharmaceuticals and is part of Ionis’ collaboration with Roche to develop antisense drugs to treat HD, according to the investigators.
A drug that was found to have no dose-limiting side effects in nonhuman primates is being evaluated in a clinical trial for its ability to reduce production of the protein that causes Huntington’s disease (HD).
The new drug, which is an antisense oligonucleotide, was formerly known as ISIS-HTTRx and was renamed IONIS-HTTRx, because its developer changed its name in December 2015 to Ionis Pharmaceuticals from Isis Pharmaceuticals. IONIS-HTTRx acts as a gene silencer to inhibit the production of huntington protein in people with HD. The clinical trial now underway is a randomized, double-blind, placebo-controlled study aimed at evaluating the safety, tolerability, pharmacokinetics, and pharmacodynamics of multiple ascending doses of IONIS-HTTRx in up to 36 patients with early manifest HD. If the trial is successful, IONIS-HTTRx would be the first drug to modify HD progression in patients, according to an abstract to be presented at the annual meeting of the American Academy of Neurology in Vancouver in April.
Ionis found the drug to be well tolerated in rodents and nonhuman primates in investigational new drug-enabling toxicology studies, with nonhuman primates having received doses up to 20 mg of the drug intrathecally, according to the trial’s principal investigator Dr. Blair R. Leavitt of the University of British Columbia, Vancouver, and colleagues.
“It is very exciting to have the possibility of a treatment that could alter the course of this devastating disease. Right now we only have treatments that work on the symptoms of the disease.” Dr. Leavitt said in a written statement.
The study is supported by Ionis Pharmaceuticals and is part of Ionis’ collaboration with Roche to develop antisense drugs to treat HD, according to the investigators.
A drug that was found to have no dose-limiting side effects in nonhuman primates is being evaluated in a clinical trial for its ability to reduce production of the protein that causes Huntington’s disease (HD).
The new drug, which is an antisense oligonucleotide, was formerly known as ISIS-HTTRx and was renamed IONIS-HTTRx, because its developer changed its name in December 2015 to Ionis Pharmaceuticals from Isis Pharmaceuticals. IONIS-HTTRx acts as a gene silencer to inhibit the production of huntington protein in people with HD. The clinical trial now underway is a randomized, double-blind, placebo-controlled study aimed at evaluating the safety, tolerability, pharmacokinetics, and pharmacodynamics of multiple ascending doses of IONIS-HTTRx in up to 36 patients with early manifest HD. If the trial is successful, IONIS-HTTRx would be the first drug to modify HD progression in patients, according to an abstract to be presented at the annual meeting of the American Academy of Neurology in Vancouver in April.
Ionis found the drug to be well tolerated in rodents and nonhuman primates in investigational new drug-enabling toxicology studies, with nonhuman primates having received doses up to 20 mg of the drug intrathecally, according to the trial’s principal investigator Dr. Blair R. Leavitt of the University of British Columbia, Vancouver, and colleagues.
“It is very exciting to have the possibility of a treatment that could alter the course of this devastating disease. Right now we only have treatments that work on the symptoms of the disease.” Dr. Leavitt said in a written statement.
The study is supported by Ionis Pharmaceuticals and is part of Ionis’ collaboration with Roche to develop antisense drugs to treat HD, according to the investigators.