User login
VANCOUVER – An investigational antibody that targets the calcitonin gene-related peptide (CGRP) receptor may be efficacious and safe in the longer term for preventing episodic migraine, data from an ongoing extension of a phase II trial showed.
Among the 483 adults studied, the benefit seen with Amgen’s 334 antibody (AMG 334) at the highest dose at 12 weeks persisted out to a year, according to interim results reported at the annual meeting of the American Academy of Neurology.
At that time, patients on average were having roughly 5 fewer migraine days each month. Nearly two-thirds had experienced at least a halving of monthly migraine days, and nearly one-fifth had become totally migraine free. In addition, the antibody’s good safety profile also held up.
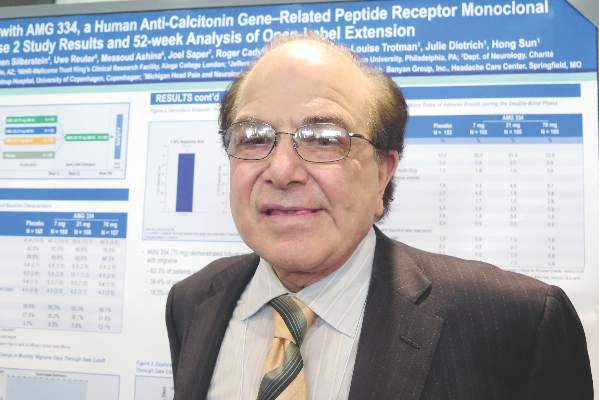
“These data strongly support the further investigation of AMG 334 as a potential preventive medication,” commented presenting author Dr. Stephen Silberstein, professor and director of the headache center at Thomas Jefferson University, Philadelphia.
“If you give a monoclonal antibody to someone with migraine and it takes away the associated features, then you just wind up with a headache day,” Dr. Silberstein noted. “But analysis clearly shows the reduction in migraine days with a concomitant reduction in headache days, showing you are not just removing the associated symptoms.”
It is too early to say whether the antibody is actually modifying the underlying disease, according to Dr. Silberstein. That will require a randomized withdrawal trial, assessing whether patients who stop treatment have a recurrence.
In any event, on the basis of the favorable findings from the phase II trial and its extension, a phase III trial, the Study to Evaluate the Efficacy and Safety of AMG 334 in Migraine Prevention (STRIVE), is now underway.
Four antibodies targeting CGRP signaling are now being investigated for migraine prevention, but AMG 334 is the only one targeting the receptor, noted session attendee Dr. Denise E. Chou of the department of neurology at Columbia University and director of the Columbia University headache center, New York.
“Particularly striking is the almost 20% rate of 100% remission. That’s remarkable, because it’s unheard of for any of the current existing migraine therapies,” she noted. The antibody’s longer half-life (translating to greater convenience for patients) and good safety profile are also pluses.
“With the four different antibodies out there, it’s kind of a race,” Dr. Chou commented. “We’ll have to see which have the best efficacy rates and side effect profiles, and which are going to be the best in terms of patient compliance and dosing scheme.”
Compared with some other trials, the AMG 334 trial enrolled a population that had episodic migraine, which is relatively easier to treat, Dr. Chou noted.
“We know, in general, that chronic refractory patients tend to have lower response rates to therapies,” she said. “But it is nice that there are different studies looking at different populations, because that’s what we see, a very heterogeneous clinic population. To be able to reflect the real-world setting is important.”
Patients were eligible for the Amgen-sponsored trial if they had 4-14 migraine days and fewer than 15 headache days per month. They could have experienced failure of up to two previous prophylactic therapies. Rescue medications were allowed, but medication overuse was not.
The patients were randomized 2:2:2:3 to monthly subcutaneous injections of AMG 334 at doses of 7 mg, 21 mg, or 70 mg, or to placebo, on a double-blind basis.
At baseline, the patients had about 9 migraine days and 10 headache days each month so that migraine accounted for most of the total, Dr. Silberstein noted.
At 12 weeks, the change in monthly migraine days – the trial’s primary outcome – was greater with the 70-mg dose than with placebo, with a reduction of 3.40 days vs. 2.28 days each month (P = .021) (Lancet Neurol. 2016 Apr.;15[4]:382-90).
A post hoc analysis suggested that this difference was already significant merely 2 weeks into treatment, Dr. Silberstein reported. The reductions seen with the lower doses were not significant.
All patients were then switched to the 70-mg dose of AMG 334 on the open-label extension, which is planned to continue for up to 5 years. The results showed that both lower-dose groups and the placebo group quickly caught up to their peers on the higher dose when it came to the reduction in monthly migraine days.
“In contrast to both the topiramate and botulinum [toxin] studies, at 16 weeks, there was no difference between patients who had started on the higher dose of [AMG 334] or who were transferred over,” Dr. Silberstein commented. “If one does an individual analysis of patients who were before on placebo or the lower doses, each of them caught up, which suggests a difference in the [mechanism of] … botulinum toxin or topiramate – because with those drugs, they never caught up at the end of 6 months.”
At 52 weeks, the patients as a whole were having about 5 fewer migraine days each month, compared with baseline. Overall, 62.3% of patients had achieved a reduction of at least 50% in monthly migraine days; 38.4%, a reduction of at least 75%; and 18.5%, a reduction of 100%.
The pattern was similar when it came to monthly migraine-specific medication days, monthly headache days, and monthly migraine attacks, according to Dr. Silberstein.
“The safety and tolerability during the open-label phase were similar to that in the double-blind phase,” he noted. “One of the reasons this is important is that, unlike small molecules, the monoclonal antibodies are not metabolized in the liver, but are metabolized in the reticuloendothelial system. So, the concept of small-molecule toxicity does not exist.”
Amgen sponsored the trial. Dr. Silberstein disclosed that he receives consulting fees from Amgen.
VANCOUVER – An investigational antibody that targets the calcitonin gene-related peptide (CGRP) receptor may be efficacious and safe in the longer term for preventing episodic migraine, data from an ongoing extension of a phase II trial showed.
Among the 483 adults studied, the benefit seen with Amgen’s 334 antibody (AMG 334) at the highest dose at 12 weeks persisted out to a year, according to interim results reported at the annual meeting of the American Academy of Neurology.
At that time, patients on average were having roughly 5 fewer migraine days each month. Nearly two-thirds had experienced at least a halving of monthly migraine days, and nearly one-fifth had become totally migraine free. In addition, the antibody’s good safety profile also held up.
“These data strongly support the further investigation of AMG 334 as a potential preventive medication,” commented presenting author Dr. Stephen Silberstein, professor and director of the headache center at Thomas Jefferson University, Philadelphia.
“If you give a monoclonal antibody to someone with migraine and it takes away the associated features, then you just wind up with a headache day,” Dr. Silberstein noted. “But analysis clearly shows the reduction in migraine days with a concomitant reduction in headache days, showing you are not just removing the associated symptoms.”
It is too early to say whether the antibody is actually modifying the underlying disease, according to Dr. Silberstein. That will require a randomized withdrawal trial, assessing whether patients who stop treatment have a recurrence.
In any event, on the basis of the favorable findings from the phase II trial and its extension, a phase III trial, the Study to Evaluate the Efficacy and Safety of AMG 334 in Migraine Prevention (STRIVE), is now underway.
Four antibodies targeting CGRP signaling are now being investigated for migraine prevention, but AMG 334 is the only one targeting the receptor, noted session attendee Dr. Denise E. Chou of the department of neurology at Columbia University and director of the Columbia University headache center, New York.
“Particularly striking is the almost 20% rate of 100% remission. That’s remarkable, because it’s unheard of for any of the current existing migraine therapies,” she noted. The antibody’s longer half-life (translating to greater convenience for patients) and good safety profile are also pluses.
“With the four different antibodies out there, it’s kind of a race,” Dr. Chou commented. “We’ll have to see which have the best efficacy rates and side effect profiles, and which are going to be the best in terms of patient compliance and dosing scheme.”
Compared with some other trials, the AMG 334 trial enrolled a population that had episodic migraine, which is relatively easier to treat, Dr. Chou noted.
“We know, in general, that chronic refractory patients tend to have lower response rates to therapies,” she said. “But it is nice that there are different studies looking at different populations, because that’s what we see, a very heterogeneous clinic population. To be able to reflect the real-world setting is important.”
Patients were eligible for the Amgen-sponsored trial if they had 4-14 migraine days and fewer than 15 headache days per month. They could have experienced failure of up to two previous prophylactic therapies. Rescue medications were allowed, but medication overuse was not.
The patients were randomized 2:2:2:3 to monthly subcutaneous injections of AMG 334 at doses of 7 mg, 21 mg, or 70 mg, or to placebo, on a double-blind basis.
At baseline, the patients had about 9 migraine days and 10 headache days each month so that migraine accounted for most of the total, Dr. Silberstein noted.
At 12 weeks, the change in monthly migraine days – the trial’s primary outcome – was greater with the 70-mg dose than with placebo, with a reduction of 3.40 days vs. 2.28 days each month (P = .021) (Lancet Neurol. 2016 Apr.;15[4]:382-90).
A post hoc analysis suggested that this difference was already significant merely 2 weeks into treatment, Dr. Silberstein reported. The reductions seen with the lower doses were not significant.
All patients were then switched to the 70-mg dose of AMG 334 on the open-label extension, which is planned to continue for up to 5 years. The results showed that both lower-dose groups and the placebo group quickly caught up to their peers on the higher dose when it came to the reduction in monthly migraine days.
“In contrast to both the topiramate and botulinum [toxin] studies, at 16 weeks, there was no difference between patients who had started on the higher dose of [AMG 334] or who were transferred over,” Dr. Silberstein commented. “If one does an individual analysis of patients who were before on placebo or the lower doses, each of them caught up, which suggests a difference in the [mechanism of] … botulinum toxin or topiramate – because with those drugs, they never caught up at the end of 6 months.”
At 52 weeks, the patients as a whole were having about 5 fewer migraine days each month, compared with baseline. Overall, 62.3% of patients had achieved a reduction of at least 50% in monthly migraine days; 38.4%, a reduction of at least 75%; and 18.5%, a reduction of 100%.
The pattern was similar when it came to monthly migraine-specific medication days, monthly headache days, and monthly migraine attacks, according to Dr. Silberstein.
“The safety and tolerability during the open-label phase were similar to that in the double-blind phase,” he noted. “One of the reasons this is important is that, unlike small molecules, the monoclonal antibodies are not metabolized in the liver, but are metabolized in the reticuloendothelial system. So, the concept of small-molecule toxicity does not exist.”
Amgen sponsored the trial. Dr. Silberstein disclosed that he receives consulting fees from Amgen.
VANCOUVER – An investigational antibody that targets the calcitonin gene-related peptide (CGRP) receptor may be efficacious and safe in the longer term for preventing episodic migraine, data from an ongoing extension of a phase II trial showed.
Among the 483 adults studied, the benefit seen with Amgen’s 334 antibody (AMG 334) at the highest dose at 12 weeks persisted out to a year, according to interim results reported at the annual meeting of the American Academy of Neurology.
At that time, patients on average were having roughly 5 fewer migraine days each month. Nearly two-thirds had experienced at least a halving of monthly migraine days, and nearly one-fifth had become totally migraine free. In addition, the antibody’s good safety profile also held up.
“These data strongly support the further investigation of AMG 334 as a potential preventive medication,” commented presenting author Dr. Stephen Silberstein, professor and director of the headache center at Thomas Jefferson University, Philadelphia.
“If you give a monoclonal antibody to someone with migraine and it takes away the associated features, then you just wind up with a headache day,” Dr. Silberstein noted. “But analysis clearly shows the reduction in migraine days with a concomitant reduction in headache days, showing you are not just removing the associated symptoms.”
It is too early to say whether the antibody is actually modifying the underlying disease, according to Dr. Silberstein. That will require a randomized withdrawal trial, assessing whether patients who stop treatment have a recurrence.
In any event, on the basis of the favorable findings from the phase II trial and its extension, a phase III trial, the Study to Evaluate the Efficacy and Safety of AMG 334 in Migraine Prevention (STRIVE), is now underway.
Four antibodies targeting CGRP signaling are now being investigated for migraine prevention, but AMG 334 is the only one targeting the receptor, noted session attendee Dr. Denise E. Chou of the department of neurology at Columbia University and director of the Columbia University headache center, New York.
“Particularly striking is the almost 20% rate of 100% remission. That’s remarkable, because it’s unheard of for any of the current existing migraine therapies,” she noted. The antibody’s longer half-life (translating to greater convenience for patients) and good safety profile are also pluses.
“With the four different antibodies out there, it’s kind of a race,” Dr. Chou commented. “We’ll have to see which have the best efficacy rates and side effect profiles, and which are going to be the best in terms of patient compliance and dosing scheme.”
Compared with some other trials, the AMG 334 trial enrolled a population that had episodic migraine, which is relatively easier to treat, Dr. Chou noted.
“We know, in general, that chronic refractory patients tend to have lower response rates to therapies,” she said. “But it is nice that there are different studies looking at different populations, because that’s what we see, a very heterogeneous clinic population. To be able to reflect the real-world setting is important.”
Patients were eligible for the Amgen-sponsored trial if they had 4-14 migraine days and fewer than 15 headache days per month. They could have experienced failure of up to two previous prophylactic therapies. Rescue medications were allowed, but medication overuse was not.
The patients were randomized 2:2:2:3 to monthly subcutaneous injections of AMG 334 at doses of 7 mg, 21 mg, or 70 mg, or to placebo, on a double-blind basis.
At baseline, the patients had about 9 migraine days and 10 headache days each month so that migraine accounted for most of the total, Dr. Silberstein noted.
At 12 weeks, the change in monthly migraine days – the trial’s primary outcome – was greater with the 70-mg dose than with placebo, with a reduction of 3.40 days vs. 2.28 days each month (P = .021) (Lancet Neurol. 2016 Apr.;15[4]:382-90).
A post hoc analysis suggested that this difference was already significant merely 2 weeks into treatment, Dr. Silberstein reported. The reductions seen with the lower doses were not significant.
All patients were then switched to the 70-mg dose of AMG 334 on the open-label extension, which is planned to continue for up to 5 years. The results showed that both lower-dose groups and the placebo group quickly caught up to their peers on the higher dose when it came to the reduction in monthly migraine days.
“In contrast to both the topiramate and botulinum [toxin] studies, at 16 weeks, there was no difference between patients who had started on the higher dose of [AMG 334] or who were transferred over,” Dr. Silberstein commented. “If one does an individual analysis of patients who were before on placebo or the lower doses, each of them caught up, which suggests a difference in the [mechanism of] … botulinum toxin or topiramate – because with those drugs, they never caught up at the end of 6 months.”
At 52 weeks, the patients as a whole were having about 5 fewer migraine days each month, compared with baseline. Overall, 62.3% of patients had achieved a reduction of at least 50% in monthly migraine days; 38.4%, a reduction of at least 75%; and 18.5%, a reduction of 100%.
The pattern was similar when it came to monthly migraine-specific medication days, monthly headache days, and monthly migraine attacks, according to Dr. Silberstein.
“The safety and tolerability during the open-label phase were similar to that in the double-blind phase,” he noted. “One of the reasons this is important is that, unlike small molecules, the monoclonal antibodies are not metabolized in the liver, but are metabolized in the reticuloendothelial system. So, the concept of small-molecule toxicity does not exist.”
Amgen sponsored the trial. Dr. Silberstein disclosed that he receives consulting fees from Amgen.
AT THE AAN 2016 ANNUAL MEETING
Key clinical point: AMG 334 has durable efficacy and safety in reducing episodic migraine.
Major finding: At 1 year, patients were experiencing about 5 fewer migraine days each month on average, and 62.3% had achieved at least a 50% reduction in monthly migraine days.
Data source: An interim analysis of an open-label extension of a phase II trial in 483 adults with episodic migraine.
Disclosures: Amgen sponsored the trial. Dr. Silberstein disclosed that he receives consulting fees from Amgen.