User login
Large, intermittent vitamin D doses may increase fracture, fall risk in elderly
ORLANDO – The vitamin that keeps bones strong and protects against colon cancer also can, in large doses, increase the risk of falls and fractures.
Studies of high-dose vitamin D keep turning up the same concerns, Dr. Martin Weinstock said at the annual meeting of the American Academy of Dermatology. The most striking of these findings are the significantly increased risks of falls and fractures associated with vitamin D megadoses, said Dr. Weinstock of Brown University, Providence, R.I. These trials examined very-large intermittent doses of the vitamin given to elderly patients.
That amount of vitamin D, taken all at once, may seem like a therapeutic outlier to clinicians who are used to giving 2,000-4,000 IU/day, as recommended by the 2011 Institute of Medicine report.
Not so fast, said Dr. Weinstock.
“If you do the math, if you’re taking 2,000 IU every day, that’s 60,000 IU per month. That’s a high dose,” he said. However, he noted, daily supplements in that range appear safe. “It seems that this intermittent dosing in these studies might be the problem.”
The IOM report, an exhaustive, 1,000-page article summarizing the extant data on vitamin D – is considered the optimal dosing guide. For healthy patients, it recommends the following as minimum effective and maximum safe doses:
- 400-1,000 IU/day for infants younger than 6 month.
- 400-1,500 IU/day for infants aged 6-12 months.
- 600-2,000 IU/day for children aged 1-3 years.
- 600-3,000 IU/day for children aged 4-8 years.
- 600-4,000 IU/day for everyone aged 9 years and older.
But dosing of this fat-soluble vitamin should, in some cases, be individualized. For example, obese patients may have persistently low levels despite supplementation, as fat can sequester the vitamin. Patients with fat-metabolizing disorders may not absorb it well. And patients who have had gastric bypass may face the same issues of malabsorption, but from a mechanical, not a metabolic, standpoint.
Elderly people are particularly susceptible to vitamin D deficiency for a couple of reasons, Dr. Weinstock said. They may be less mobile, so lack exposure to sunlight. Age also can decrease the ability to convert 25-hydroxyvitamin D to the biologically active vitamin.
Mega-dosing has been an attractive method of raising and maintaining levels in this population. But several studies illustrate the risks that come along with this strategy, he noted.
A 2007 study randomized 9,440 men and women 75 years or older to placebo or to a single, 300,000 IU vitamin D intramuscular injection for 3 years. At the end of that time, the rate of falls had not significantly changed, but the rate of hip fractures had increased by 49% (Rheumatology [Oxford] 2007;46:1852-7).
Fractures occurred in 585 subjects, including 110 hip fractures, 116 wrist fractures, and 37 ankle fractures. This represented a 49% increase in any hip fracture and a 22% increase in wrist fracture over the placebo group.
A similar study, published in 2010, randomized 2,225 elderly women to placebo or a single 500,000 oral dose of vitamin D for 4 years. There were 171 fractures in the active group and 135 in the placebo group – a 26% increased risk (JAMA. 2010;303[18]:1815-22).
The fall rate in the active group was 83.4/100 person-years, compared with 72.7/100 person-years in the placebo group. This represented a significant 26% increased fracture risk and 15% increased fall risk.
Interestingly, most of these incidents occurred within the first 3 months after each dose,” Dr. Weinstock said. Those taking vitamin D were 31% more likely to fall in that time period, but no more likely to fall in the subsequent 9 months after each dose.
In 2016, a third study looked at functional status among 200 elderly men and women in a three-armed randomization: a low-dose control group receiving 24,000 IU of vitamin D; 60,000 IU vitamin D3; or 24,000 IU of vitamin plus 300 mcg calcifediol.
Functional status didn’t differ between the groups at the end of 1 year. But the incidence of falls did differ, with falls occurring in 67% of the 60,000 IU group, 54% of the 24,000 IU/calcifediol group, and 48% of the 24,000 IU control group (JAMA Intern Med. 2016;176[2]:175-83).
This represented a 47% increased fall risk in the high dose group, compared with the two low-dose groups.
Dr. Weinstein had no financial disclosures relevant to his lecture.
msullivan@frontlinemedcom.com
On Twitter @Alz_Gal
ORLANDO – The vitamin that keeps bones strong and protects against colon cancer also can, in large doses, increase the risk of falls and fractures.
Studies of high-dose vitamin D keep turning up the same concerns, Dr. Martin Weinstock said at the annual meeting of the American Academy of Dermatology. The most striking of these findings are the significantly increased risks of falls and fractures associated with vitamin D megadoses, said Dr. Weinstock of Brown University, Providence, R.I. These trials examined very-large intermittent doses of the vitamin given to elderly patients.
That amount of vitamin D, taken all at once, may seem like a therapeutic outlier to clinicians who are used to giving 2,000-4,000 IU/day, as recommended by the 2011 Institute of Medicine report.
Not so fast, said Dr. Weinstock.
“If you do the math, if you’re taking 2,000 IU every day, that’s 60,000 IU per month. That’s a high dose,” he said. However, he noted, daily supplements in that range appear safe. “It seems that this intermittent dosing in these studies might be the problem.”
The IOM report, an exhaustive, 1,000-page article summarizing the extant data on vitamin D – is considered the optimal dosing guide. For healthy patients, it recommends the following as minimum effective and maximum safe doses:
- 400-1,000 IU/day for infants younger than 6 month.
- 400-1,500 IU/day for infants aged 6-12 months.
- 600-2,000 IU/day for children aged 1-3 years.
- 600-3,000 IU/day for children aged 4-8 years.
- 600-4,000 IU/day for everyone aged 9 years and older.
But dosing of this fat-soluble vitamin should, in some cases, be individualized. For example, obese patients may have persistently low levels despite supplementation, as fat can sequester the vitamin. Patients with fat-metabolizing disorders may not absorb it well. And patients who have had gastric bypass may face the same issues of malabsorption, but from a mechanical, not a metabolic, standpoint.
Elderly people are particularly susceptible to vitamin D deficiency for a couple of reasons, Dr. Weinstock said. They may be less mobile, so lack exposure to sunlight. Age also can decrease the ability to convert 25-hydroxyvitamin D to the biologically active vitamin.
Mega-dosing has been an attractive method of raising and maintaining levels in this population. But several studies illustrate the risks that come along with this strategy, he noted.
A 2007 study randomized 9,440 men and women 75 years or older to placebo or to a single, 300,000 IU vitamin D intramuscular injection for 3 years. At the end of that time, the rate of falls had not significantly changed, but the rate of hip fractures had increased by 49% (Rheumatology [Oxford] 2007;46:1852-7).
Fractures occurred in 585 subjects, including 110 hip fractures, 116 wrist fractures, and 37 ankle fractures. This represented a 49% increase in any hip fracture and a 22% increase in wrist fracture over the placebo group.
A similar study, published in 2010, randomized 2,225 elderly women to placebo or a single 500,000 oral dose of vitamin D for 4 years. There were 171 fractures in the active group and 135 in the placebo group – a 26% increased risk (JAMA. 2010;303[18]:1815-22).
The fall rate in the active group was 83.4/100 person-years, compared with 72.7/100 person-years in the placebo group. This represented a significant 26% increased fracture risk and 15% increased fall risk.
Interestingly, most of these incidents occurred within the first 3 months after each dose,” Dr. Weinstock said. Those taking vitamin D were 31% more likely to fall in that time period, but no more likely to fall in the subsequent 9 months after each dose.
In 2016, a third study looked at functional status among 200 elderly men and women in a three-armed randomization: a low-dose control group receiving 24,000 IU of vitamin D; 60,000 IU vitamin D3; or 24,000 IU of vitamin plus 300 mcg calcifediol.
Functional status didn’t differ between the groups at the end of 1 year. But the incidence of falls did differ, with falls occurring in 67% of the 60,000 IU group, 54% of the 24,000 IU/calcifediol group, and 48% of the 24,000 IU control group (JAMA Intern Med. 2016;176[2]:175-83).
This represented a 47% increased fall risk in the high dose group, compared with the two low-dose groups.
Dr. Weinstein had no financial disclosures relevant to his lecture.
msullivan@frontlinemedcom.com
On Twitter @Alz_Gal
ORLANDO – The vitamin that keeps bones strong and protects against colon cancer also can, in large doses, increase the risk of falls and fractures.
Studies of high-dose vitamin D keep turning up the same concerns, Dr. Martin Weinstock said at the annual meeting of the American Academy of Dermatology. The most striking of these findings are the significantly increased risks of falls and fractures associated with vitamin D megadoses, said Dr. Weinstock of Brown University, Providence, R.I. These trials examined very-large intermittent doses of the vitamin given to elderly patients.
That amount of vitamin D, taken all at once, may seem like a therapeutic outlier to clinicians who are used to giving 2,000-4,000 IU/day, as recommended by the 2011 Institute of Medicine report.
Not so fast, said Dr. Weinstock.
“If you do the math, if you’re taking 2,000 IU every day, that’s 60,000 IU per month. That’s a high dose,” he said. However, he noted, daily supplements in that range appear safe. “It seems that this intermittent dosing in these studies might be the problem.”
The IOM report, an exhaustive, 1,000-page article summarizing the extant data on vitamin D – is considered the optimal dosing guide. For healthy patients, it recommends the following as minimum effective and maximum safe doses:
- 400-1,000 IU/day for infants younger than 6 month.
- 400-1,500 IU/day for infants aged 6-12 months.
- 600-2,000 IU/day for children aged 1-3 years.
- 600-3,000 IU/day for children aged 4-8 years.
- 600-4,000 IU/day for everyone aged 9 years and older.
But dosing of this fat-soluble vitamin should, in some cases, be individualized. For example, obese patients may have persistently low levels despite supplementation, as fat can sequester the vitamin. Patients with fat-metabolizing disorders may not absorb it well. And patients who have had gastric bypass may face the same issues of malabsorption, but from a mechanical, not a metabolic, standpoint.
Elderly people are particularly susceptible to vitamin D deficiency for a couple of reasons, Dr. Weinstock said. They may be less mobile, so lack exposure to sunlight. Age also can decrease the ability to convert 25-hydroxyvitamin D to the biologically active vitamin.
Mega-dosing has been an attractive method of raising and maintaining levels in this population. But several studies illustrate the risks that come along with this strategy, he noted.
A 2007 study randomized 9,440 men and women 75 years or older to placebo or to a single, 300,000 IU vitamin D intramuscular injection for 3 years. At the end of that time, the rate of falls had not significantly changed, but the rate of hip fractures had increased by 49% (Rheumatology [Oxford] 2007;46:1852-7).
Fractures occurred in 585 subjects, including 110 hip fractures, 116 wrist fractures, and 37 ankle fractures. This represented a 49% increase in any hip fracture and a 22% increase in wrist fracture over the placebo group.
A similar study, published in 2010, randomized 2,225 elderly women to placebo or a single 500,000 oral dose of vitamin D for 4 years. There were 171 fractures in the active group and 135 in the placebo group – a 26% increased risk (JAMA. 2010;303[18]:1815-22).
The fall rate in the active group was 83.4/100 person-years, compared with 72.7/100 person-years in the placebo group. This represented a significant 26% increased fracture risk and 15% increased fall risk.
Interestingly, most of these incidents occurred within the first 3 months after each dose,” Dr. Weinstock said. Those taking vitamin D were 31% more likely to fall in that time period, but no more likely to fall in the subsequent 9 months after each dose.
In 2016, a third study looked at functional status among 200 elderly men and women in a three-armed randomization: a low-dose control group receiving 24,000 IU of vitamin D; 60,000 IU vitamin D3; or 24,000 IU of vitamin plus 300 mcg calcifediol.
Functional status didn’t differ between the groups at the end of 1 year. But the incidence of falls did differ, with falls occurring in 67% of the 60,000 IU group, 54% of the 24,000 IU/calcifediol group, and 48% of the 24,000 IU control group (JAMA Intern Med. 2016;176[2]:175-83).
This represented a 47% increased fall risk in the high dose group, compared with the two low-dose groups.
Dr. Weinstein had no financial disclosures relevant to his lecture.
msullivan@frontlinemedcom.com
On Twitter @Alz_Gal
Skin disease costs $75 billion a year
The direct cost of treating skin diseases in the United States was almost $75 billion in 2013, according to a report on the burden of skin disease from the American Academy of Dermatology.
For the nearly 85 million Americans who were seen by a physician for a skin disease in 2013, about $45.9 billion was spent on medical costs such as office visits, procedures, and tests; $15 billion was spent on prescription drugs; and $4.1 billion went for vaccines and skin cancer screening. Another $10 billion was spent on OTC products, the AAD’s Burden of Skin Disease Work Group reported (J Am Acad Dermatol. 2017 Feb 24. doi: 10.1016/j.jaad.2016.12.043).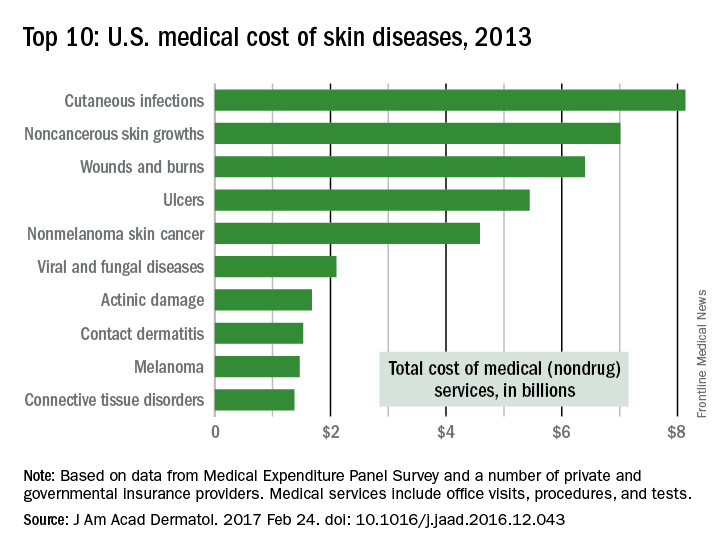
The per-capita cost of skin disease in 2013 was $213, compared with $950 per person for cardiovascular disease, $785 for diabetes, and $147 for end-stage renal disease, they noted.
In discussing the future burden of skin disease, the work group noted that the aging U.S. population and “the increased costs of currently in-use and newly developed dermatologic treatment options [need] to be addressed by an appropriate increase in dermatologic care providers.”
The direct cost of treating skin diseases in the United States was almost $75 billion in 2013, according to a report on the burden of skin disease from the American Academy of Dermatology.
For the nearly 85 million Americans who were seen by a physician for a skin disease in 2013, about $45.9 billion was spent on medical costs such as office visits, procedures, and tests; $15 billion was spent on prescription drugs; and $4.1 billion went for vaccines and skin cancer screening. Another $10 billion was spent on OTC products, the AAD’s Burden of Skin Disease Work Group reported (J Am Acad Dermatol. 2017 Feb 24. doi: 10.1016/j.jaad.2016.12.043).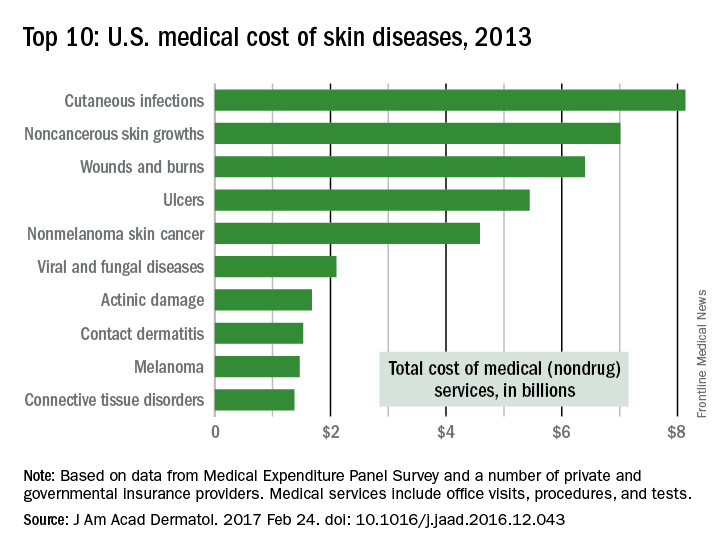
The per-capita cost of skin disease in 2013 was $213, compared with $950 per person for cardiovascular disease, $785 for diabetes, and $147 for end-stage renal disease, they noted.
In discussing the future burden of skin disease, the work group noted that the aging U.S. population and “the increased costs of currently in-use and newly developed dermatologic treatment options [need] to be addressed by an appropriate increase in dermatologic care providers.”
The direct cost of treating skin diseases in the United States was almost $75 billion in 2013, according to a report on the burden of skin disease from the American Academy of Dermatology.
For the nearly 85 million Americans who were seen by a physician for a skin disease in 2013, about $45.9 billion was spent on medical costs such as office visits, procedures, and tests; $15 billion was spent on prescription drugs; and $4.1 billion went for vaccines and skin cancer screening. Another $10 billion was spent on OTC products, the AAD’s Burden of Skin Disease Work Group reported (J Am Acad Dermatol. 2017 Feb 24. doi: 10.1016/j.jaad.2016.12.043).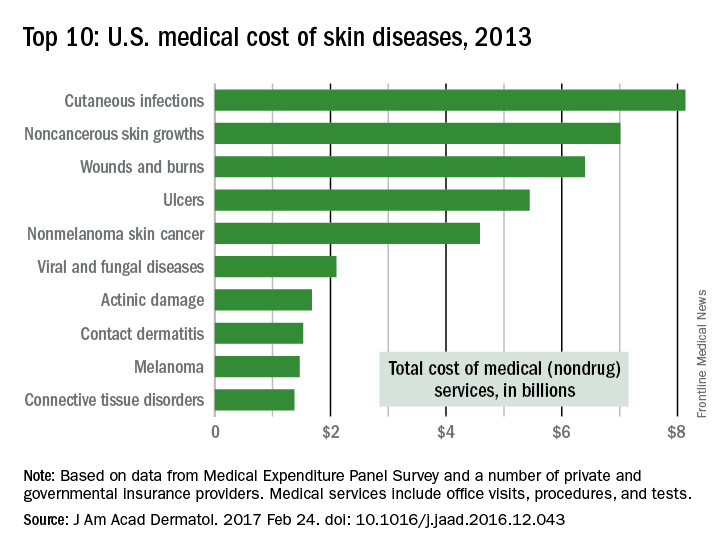
The per-capita cost of skin disease in 2013 was $213, compared with $950 per person for cardiovascular disease, $785 for diabetes, and $147 for end-stage renal disease, they noted.
In discussing the future burden of skin disease, the work group noted that the aging U.S. population and “the increased costs of currently in-use and newly developed dermatologic treatment options [need] to be addressed by an appropriate increase in dermatologic care providers.”
Teen indoor tanning drops, but schools fall short on sun safety
Indoor tanning among adolescents in the United States has dropped significantly, but fewer than half of schools in the United States reported sun safety practices to help minimize students’ UV exposure in the school setting, based on data from two studies presented at the annual meeting of the American Academy of Dermatology and published simultaneously in JAMA Dermatology.
“Data suggest that intermittent, recreational exposure (vs. chronic exposure, as with outdoor workers) more often leads to sunburn,” wrote Sherry Everett Jones, PhD, MPH, and Gery P. Guy Jr, PhD, MPH, of the Centers for Disease Control and Prevention. “Although a small proportion of school districts and schools have adopted policies to address sun safety, most have not, even though it is common for students to be outside during the midday hours or after school when the sun is still at peak intensity.”
To characterize sun safety practices at schools, the researchers reviewed data from the 2014 School Health Policies and Practices Study Healthy and Safe School Environment questionnaire including 577 elementary, middle, and high schools (JAMA Dermatol. 2017. doi: 10.1001/jamadermatol.2016.6274).
Overall, 48% of schools reported that teachers allowed students time to apply sunscreen at school (the most frequent sun safety practice). However, only 13% made sunscreen available, 16% asked parents to ensure sunscreen application before school, and 15% made an effort to avoid scheduling outdoor activities during times of peak sun intensity. High schools were less likely than elementary or middle schools to follow sun safety practices.
“None of the sun safety policies or practices were statistically significantly associated with metropolitan status,” the researchers noted. However, the findings were limited by the cross-sectional nature of the study and lack of data about natural shade and man made shade structures in outdoor areas of the schools.
“Interventions driven by the public health and medical community educating school leadership and policy makers about the importance of sun safety are needed regardless of level, location, size, and poverty concentration of the school. These efforts could be instrumental in increasing the adoption of sun safety practices among schools,” Dr. Jones and Dr. Guy emphasized.
However, data from another study showed a significant reduction in the prevalence of indoor tanning among adolescents.
In particular, indoor tanning among non-Hispanic white females (the group at highest risk for skin cancer) dropped from 37% in 2009 to 15% in 2015. CDC researchers led by Dr. Guy pooled data from the 2009, 2011, 2013, and 2015 national Youth Risk Behavior Surveillance System Surveys (JAMA Dermatol. 2017. doi:10.1001/jamadermatol.2016.6273). Overall, the prevalence of indoor tanning among U.S. high school students decreased from 16% in 2009 to 7% in 2015.
“Despite declines in indoor tanning, continued efforts are needed,” the researchers wrote. “Public health efforts could help address the misconception that indoor tanning protects against sunburn. The medical community also can play a key role in counseling adolescents and young adults in accordance with the U.S. Preventive Services Task Force guidelines.”
The findings were limited by several factors including the use of self-reports and the inability to control for skin type, the researchers wrote. However, “Reducing the proportion of youth who engage in indoor tanning and experience sunburns presents an important cancer prevention opportunity.”
None of the researchers on either study had relevant financial conflicts to disclose.
Explore best practices for public education campaigns “For more than 10 years, much effort has been made to educate the public on sun-safety practices, including warnings about the harmful effects of indoor tanning on those at higher risk, such as young adults and children. In this issue of JAMA Dermatology, 2 important articles describe the progress made toward sun safety,” wrote Henry W. Lim, MD, and Samantha L. Schneider, MD, in the accompanying editorial.
Data from a study of indoor tanning showed a significant decrease in prevalence of indoor tanning among adolescents, from 16% in 2009 to 7% in 2015. Although these results are encouraging, public education is needed for further improvement, they said. “One myth is that UV radiation prevents vitamin D deficiency; however, oral vitamin D supplementation is known to be a safer alternative. Another myth is that obtaining a baseline tan before the summer or a vacation reduces the risk of sunburn. However, as Guy and colleagues observed, those who tanned indoors were more likely to develop sunburn than students who did not engage in indoor tanning.”
“Clearly, both the dermatology and medical communities need to continue public awareness campaigns regarding photoprotection, including sun-safety practices such as seeking shade when outdoors and wearing photoprotective clothing, wide-brimmed hats, and sunglasses,” they emphasized.
In addition, “A highly effective means of public education may be to identify a campaign, such as Portugal’s sugar packet initiative, that makes sun-safety awareness and practice a part of everyone’s daily routine,” they said (JAMA Dermatol. 2017. doi: 10.1001/jamadermatol.2016.6272).
Dr. Lim and Dr. Schneider are affiliated with the department of dermatology at Henry Ford Hospital in Detroit. Dr Lim disclosed serving as an investigator or coinvestigator on clinical research projects for Ferndale Pharma, Estée Lauder, and Allergan. Dr. Schneider had no relevant conflicts to disclose.
Explore best practices for public education campaigns “For more than 10 years, much effort has been made to educate the public on sun-safety practices, including warnings about the harmful effects of indoor tanning on those at higher risk, such as young adults and children. In this issue of JAMA Dermatology, 2 important articles describe the progress made toward sun safety,” wrote Henry W. Lim, MD, and Samantha L. Schneider, MD, in the accompanying editorial.
Data from a study of indoor tanning showed a significant decrease in prevalence of indoor tanning among adolescents, from 16% in 2009 to 7% in 2015. Although these results are encouraging, public education is needed for further improvement, they said. “One myth is that UV radiation prevents vitamin D deficiency; however, oral vitamin D supplementation is known to be a safer alternative. Another myth is that obtaining a baseline tan before the summer or a vacation reduces the risk of sunburn. However, as Guy and colleagues observed, those who tanned indoors were more likely to develop sunburn than students who did not engage in indoor tanning.”
“Clearly, both the dermatology and medical communities need to continue public awareness campaigns regarding photoprotection, including sun-safety practices such as seeking shade when outdoors and wearing photoprotective clothing, wide-brimmed hats, and sunglasses,” they emphasized.
In addition, “A highly effective means of public education may be to identify a campaign, such as Portugal’s sugar packet initiative, that makes sun-safety awareness and practice a part of everyone’s daily routine,” they said (JAMA Dermatol. 2017. doi: 10.1001/jamadermatol.2016.6272).
Dr. Lim and Dr. Schneider are affiliated with the department of dermatology at Henry Ford Hospital in Detroit. Dr Lim disclosed serving as an investigator or coinvestigator on clinical research projects for Ferndale Pharma, Estée Lauder, and Allergan. Dr. Schneider had no relevant conflicts to disclose.
Explore best practices for public education campaigns “For more than 10 years, much effort has been made to educate the public on sun-safety practices, including warnings about the harmful effects of indoor tanning on those at higher risk, such as young adults and children. In this issue of JAMA Dermatology, 2 important articles describe the progress made toward sun safety,” wrote Henry W. Lim, MD, and Samantha L. Schneider, MD, in the accompanying editorial.
Data from a study of indoor tanning showed a significant decrease in prevalence of indoor tanning among adolescents, from 16% in 2009 to 7% in 2015. Although these results are encouraging, public education is needed for further improvement, they said. “One myth is that UV radiation prevents vitamin D deficiency; however, oral vitamin D supplementation is known to be a safer alternative. Another myth is that obtaining a baseline tan before the summer or a vacation reduces the risk of sunburn. However, as Guy and colleagues observed, those who tanned indoors were more likely to develop sunburn than students who did not engage in indoor tanning.”
“Clearly, both the dermatology and medical communities need to continue public awareness campaigns regarding photoprotection, including sun-safety practices such as seeking shade when outdoors and wearing photoprotective clothing, wide-brimmed hats, and sunglasses,” they emphasized.
In addition, “A highly effective means of public education may be to identify a campaign, such as Portugal’s sugar packet initiative, that makes sun-safety awareness and practice a part of everyone’s daily routine,” they said (JAMA Dermatol. 2017. doi: 10.1001/jamadermatol.2016.6272).
Dr. Lim and Dr. Schneider are affiliated with the department of dermatology at Henry Ford Hospital in Detroit. Dr Lim disclosed serving as an investigator or coinvestigator on clinical research projects for Ferndale Pharma, Estée Lauder, and Allergan. Dr. Schneider had no relevant conflicts to disclose.
Indoor tanning among adolescents in the United States has dropped significantly, but fewer than half of schools in the United States reported sun safety practices to help minimize students’ UV exposure in the school setting, based on data from two studies presented at the annual meeting of the American Academy of Dermatology and published simultaneously in JAMA Dermatology.
“Data suggest that intermittent, recreational exposure (vs. chronic exposure, as with outdoor workers) more often leads to sunburn,” wrote Sherry Everett Jones, PhD, MPH, and Gery P. Guy Jr, PhD, MPH, of the Centers for Disease Control and Prevention. “Although a small proportion of school districts and schools have adopted policies to address sun safety, most have not, even though it is common for students to be outside during the midday hours or after school when the sun is still at peak intensity.”
To characterize sun safety practices at schools, the researchers reviewed data from the 2014 School Health Policies and Practices Study Healthy and Safe School Environment questionnaire including 577 elementary, middle, and high schools (JAMA Dermatol. 2017. doi: 10.1001/jamadermatol.2016.6274).
Overall, 48% of schools reported that teachers allowed students time to apply sunscreen at school (the most frequent sun safety practice). However, only 13% made sunscreen available, 16% asked parents to ensure sunscreen application before school, and 15% made an effort to avoid scheduling outdoor activities during times of peak sun intensity. High schools were less likely than elementary or middle schools to follow sun safety practices.
“None of the sun safety policies or practices were statistically significantly associated with metropolitan status,” the researchers noted. However, the findings were limited by the cross-sectional nature of the study and lack of data about natural shade and man made shade structures in outdoor areas of the schools.
“Interventions driven by the public health and medical community educating school leadership and policy makers about the importance of sun safety are needed regardless of level, location, size, and poverty concentration of the school. These efforts could be instrumental in increasing the adoption of sun safety practices among schools,” Dr. Jones and Dr. Guy emphasized.
However, data from another study showed a significant reduction in the prevalence of indoor tanning among adolescents.
In particular, indoor tanning among non-Hispanic white females (the group at highest risk for skin cancer) dropped from 37% in 2009 to 15% in 2015. CDC researchers led by Dr. Guy pooled data from the 2009, 2011, 2013, and 2015 national Youth Risk Behavior Surveillance System Surveys (JAMA Dermatol. 2017. doi:10.1001/jamadermatol.2016.6273). Overall, the prevalence of indoor tanning among U.S. high school students decreased from 16% in 2009 to 7% in 2015.
“Despite declines in indoor tanning, continued efforts are needed,” the researchers wrote. “Public health efforts could help address the misconception that indoor tanning protects against sunburn. The medical community also can play a key role in counseling adolescents and young adults in accordance with the U.S. Preventive Services Task Force guidelines.”
The findings were limited by several factors including the use of self-reports and the inability to control for skin type, the researchers wrote. However, “Reducing the proportion of youth who engage in indoor tanning and experience sunburns presents an important cancer prevention opportunity.”
None of the researchers on either study had relevant financial conflicts to disclose.
Indoor tanning among adolescents in the United States has dropped significantly, but fewer than half of schools in the United States reported sun safety practices to help minimize students’ UV exposure in the school setting, based on data from two studies presented at the annual meeting of the American Academy of Dermatology and published simultaneously in JAMA Dermatology.
“Data suggest that intermittent, recreational exposure (vs. chronic exposure, as with outdoor workers) more often leads to sunburn,” wrote Sherry Everett Jones, PhD, MPH, and Gery P. Guy Jr, PhD, MPH, of the Centers for Disease Control and Prevention. “Although a small proportion of school districts and schools have adopted policies to address sun safety, most have not, even though it is common for students to be outside during the midday hours or after school when the sun is still at peak intensity.”
To characterize sun safety practices at schools, the researchers reviewed data from the 2014 School Health Policies and Practices Study Healthy and Safe School Environment questionnaire including 577 elementary, middle, and high schools (JAMA Dermatol. 2017. doi: 10.1001/jamadermatol.2016.6274).
Overall, 48% of schools reported that teachers allowed students time to apply sunscreen at school (the most frequent sun safety practice). However, only 13% made sunscreen available, 16% asked parents to ensure sunscreen application before school, and 15% made an effort to avoid scheduling outdoor activities during times of peak sun intensity. High schools were less likely than elementary or middle schools to follow sun safety practices.
“None of the sun safety policies or practices were statistically significantly associated with metropolitan status,” the researchers noted. However, the findings were limited by the cross-sectional nature of the study and lack of data about natural shade and man made shade structures in outdoor areas of the schools.
“Interventions driven by the public health and medical community educating school leadership and policy makers about the importance of sun safety are needed regardless of level, location, size, and poverty concentration of the school. These efforts could be instrumental in increasing the adoption of sun safety practices among schools,” Dr. Jones and Dr. Guy emphasized.
However, data from another study showed a significant reduction in the prevalence of indoor tanning among adolescents.
In particular, indoor tanning among non-Hispanic white females (the group at highest risk for skin cancer) dropped from 37% in 2009 to 15% in 2015. CDC researchers led by Dr. Guy pooled data from the 2009, 2011, 2013, and 2015 national Youth Risk Behavior Surveillance System Surveys (JAMA Dermatol. 2017. doi:10.1001/jamadermatol.2016.6273). Overall, the prevalence of indoor tanning among U.S. high school students decreased from 16% in 2009 to 7% in 2015.
“Despite declines in indoor tanning, continued efforts are needed,” the researchers wrote. “Public health efforts could help address the misconception that indoor tanning protects against sunburn. The medical community also can play a key role in counseling adolescents and young adults in accordance with the U.S. Preventive Services Task Force guidelines.”
The findings were limited by several factors including the use of self-reports and the inability to control for skin type, the researchers wrote. However, “Reducing the proportion of youth who engage in indoor tanning and experience sunburns presents an important cancer prevention opportunity.”
None of the researchers on either study had relevant financial conflicts to disclose.
FROM AAD 2017
Key clinical point:
Major finding: Fewer than half (48%) of schools in the United States allowed time for sunscreen application, and fewer than 15% provided sunscreen. However, overall prevalence of indoor tanning among U.S. adolescents dropped from 16% in 2009 to 7% in 2015.
Data source: Data were taken from the 2014 School Health Policies and Practices Study in the first study and from the 2009, 2011, 2013, and 2015 national Youth Risk Behavior Surveys in the second.
Disclosures: The researchers had no financial conflicts to disclose.
Ecofriendly surfactant is allergen of the year
ORLANDO – Alkyl glucosides, mild surfactants derived from natural, sustainable sources, have been named allergen of the year by the American Contact Dermatitis Society.
The ecofriendly nature of these compounds has led to their inclusion in more personal care products in the last decade and a half. Alkyl glucosides are derived from coconut, palm, or rapeseed oil with glucose supplied by corn, wheat starch, or potatoes. They can be found in rinse-off products such as shampoos, shower gels, and liquid cleansers but also in leave-on products such as deodorants, sunscreens, and moisturizers, investigators said at the annual meeting of the American Contact Dermatitis Society, held just prior to the start of the American Academy of Dermatology’s annual meeting.
Camille Loranger, MD, of the department of dermatology, McGill University Health Center, Montreal, presented her institution’s experience with allergic contact dermatitis caused by alkyl glucosides. A total of 3,095 patients were patch tested at the clinic between January 2009 and June 2016. Researchers used the North American Contact Dermatitis Group 65-allergen series, which includes decyl glucoside (5% in petrolatum). Slightly more than half of patients (1,628) also were tested for reactions to lauryl glucoside (3% in petrolatum) as part of an additional cosmetic series. Twenty patients in the larger series reacted to decyl glucoside, while 15 of those who tested for lauryl glucoside reacted. Of those 15 patients, 6 were found to be allergic to decyl glucoside as well (Dermatitis. 2017 Jan/Feb;28[1]:5-13).
Allergy to alkyl glucosides became more common over time in the McGill series. The rate of positivity was low in the early years of the series, but increased from 1.37% of 437 patients in 2014 to 2.2% of 227 patients tested in the first half of 2016, Dr. Loranger said.
“Most of our patients were women with an average age of 48 years,” she added. “Body sites most commonly affected were the head and the hands. Only one case could be attributed to occupational exposure.”
Most patients – 86% – also were atopic (asthma, eczema, and rhinitis).
Products identified as most commonly causing a positive reaction were leave-on moisturizers and hand creams.
Donald V. Belsito, MD, professor of dermatology at Columbia University, N.Y., introduced the allergen of the year, pointing out that the compounds selected are not necessarily “bad actors.”
“The allergen of the year is really chosen to educate dermatologists about allergens that may be of low prevalence but a high relevance,” Dr. Belsito said. The allergens selected “are difficult to test for because they are tested for at irritant concentrations. It doesn’t mean they are these horrible substances that are damaging the world necessarily.”
The ACDS has been naming an allergen of the year since 2004.
dfulton@frontlinemedcom.com
On Twitter @denisefulton
ORLANDO – Alkyl glucosides, mild surfactants derived from natural, sustainable sources, have been named allergen of the year by the American Contact Dermatitis Society.
The ecofriendly nature of these compounds has led to their inclusion in more personal care products in the last decade and a half. Alkyl glucosides are derived from coconut, palm, or rapeseed oil with glucose supplied by corn, wheat starch, or potatoes. They can be found in rinse-off products such as shampoos, shower gels, and liquid cleansers but also in leave-on products such as deodorants, sunscreens, and moisturizers, investigators said at the annual meeting of the American Contact Dermatitis Society, held just prior to the start of the American Academy of Dermatology’s annual meeting.
Camille Loranger, MD, of the department of dermatology, McGill University Health Center, Montreal, presented her institution’s experience with allergic contact dermatitis caused by alkyl glucosides. A total of 3,095 patients were patch tested at the clinic between January 2009 and June 2016. Researchers used the North American Contact Dermatitis Group 65-allergen series, which includes decyl glucoside (5% in petrolatum). Slightly more than half of patients (1,628) also were tested for reactions to lauryl glucoside (3% in petrolatum) as part of an additional cosmetic series. Twenty patients in the larger series reacted to decyl glucoside, while 15 of those who tested for lauryl glucoside reacted. Of those 15 patients, 6 were found to be allergic to decyl glucoside as well (Dermatitis. 2017 Jan/Feb;28[1]:5-13).
Allergy to alkyl glucosides became more common over time in the McGill series. The rate of positivity was low in the early years of the series, but increased from 1.37% of 437 patients in 2014 to 2.2% of 227 patients tested in the first half of 2016, Dr. Loranger said.
“Most of our patients were women with an average age of 48 years,” she added. “Body sites most commonly affected were the head and the hands. Only one case could be attributed to occupational exposure.”
Most patients – 86% – also were atopic (asthma, eczema, and rhinitis).
Products identified as most commonly causing a positive reaction were leave-on moisturizers and hand creams.
Donald V. Belsito, MD, professor of dermatology at Columbia University, N.Y., introduced the allergen of the year, pointing out that the compounds selected are not necessarily “bad actors.”
“The allergen of the year is really chosen to educate dermatologists about allergens that may be of low prevalence but a high relevance,” Dr. Belsito said. The allergens selected “are difficult to test for because they are tested for at irritant concentrations. It doesn’t mean they are these horrible substances that are damaging the world necessarily.”
The ACDS has been naming an allergen of the year since 2004.
dfulton@frontlinemedcom.com
On Twitter @denisefulton
ORLANDO – Alkyl glucosides, mild surfactants derived from natural, sustainable sources, have been named allergen of the year by the American Contact Dermatitis Society.
The ecofriendly nature of these compounds has led to their inclusion in more personal care products in the last decade and a half. Alkyl glucosides are derived from coconut, palm, or rapeseed oil with glucose supplied by corn, wheat starch, or potatoes. They can be found in rinse-off products such as shampoos, shower gels, and liquid cleansers but also in leave-on products such as deodorants, sunscreens, and moisturizers, investigators said at the annual meeting of the American Contact Dermatitis Society, held just prior to the start of the American Academy of Dermatology’s annual meeting.
Camille Loranger, MD, of the department of dermatology, McGill University Health Center, Montreal, presented her institution’s experience with allergic contact dermatitis caused by alkyl glucosides. A total of 3,095 patients were patch tested at the clinic between January 2009 and June 2016. Researchers used the North American Contact Dermatitis Group 65-allergen series, which includes decyl glucoside (5% in petrolatum). Slightly more than half of patients (1,628) also were tested for reactions to lauryl glucoside (3% in petrolatum) as part of an additional cosmetic series. Twenty patients in the larger series reacted to decyl glucoside, while 15 of those who tested for lauryl glucoside reacted. Of those 15 patients, 6 were found to be allergic to decyl glucoside as well (Dermatitis. 2017 Jan/Feb;28[1]:5-13).
Allergy to alkyl glucosides became more common over time in the McGill series. The rate of positivity was low in the early years of the series, but increased from 1.37% of 437 patients in 2014 to 2.2% of 227 patients tested in the first half of 2016, Dr. Loranger said.
“Most of our patients were women with an average age of 48 years,” she added. “Body sites most commonly affected were the head and the hands. Only one case could be attributed to occupational exposure.”
Most patients – 86% – also were atopic (asthma, eczema, and rhinitis).
Products identified as most commonly causing a positive reaction were leave-on moisturizers and hand creams.
Donald V. Belsito, MD, professor of dermatology at Columbia University, N.Y., introduced the allergen of the year, pointing out that the compounds selected are not necessarily “bad actors.”
“The allergen of the year is really chosen to educate dermatologists about allergens that may be of low prevalence but a high relevance,” Dr. Belsito said. The allergens selected “are difficult to test for because they are tested for at irritant concentrations. It doesn’t mean they are these horrible substances that are damaging the world necessarily.”
The ACDS has been naming an allergen of the year since 2004.
dfulton@frontlinemedcom.com
On Twitter @denisefulton
AAD Plenary session topics range from telemedicine to Ebola
Features of the plenary session (P151) at this year’s American Academy of Dermatology annual meeting include the Clarence S. Livingood, MD Memorial Award and Lectureship, on “Telemedicine and the Future of Medicine,” presented by Carrie L. Kovarik, MD, of the department of dermatology at the University of Pennsylvania, Philadelphia.
Dr. Kovarik’s presentation will be followed by the AAD president’s address, by outgoing president Abel Torres, MD, JD, professor and chairman of the department of dermatology at Case Western Reserve University MetroHealth Systems, Cleveland; and professor and chairman of the department of dermatology at Loma Linda University Medical Center, Loma Linda, California.
Christine Léauté-Labrèze, MD, of the Hôpital Pellegrin–Enfants, Centre Hospitalier Universitaire, Bordeaux, France, will then present the Eugene J. Van Scott Award for Innovative Therapy of the Skin and Phillip Frost Leadership Lecture: “Propranolol in Infantile Hemangiomas: A Successful Drug Repurposing.” Dr. Léauté-Labrèze was the lead author of the multicenter, randomized controlled study that evaluated the efficacy and safety of oral propranolol for treating infantile hemangiomas (N Engl J Med. 2015;372:735-46).
Incoming AAD president Henry W. Lim, MD, will follow, with the president-elect’s address. Dr. Lim is the chairman of the department of dermatology and Clarence S. Livingood Chair in Dermatology at Henry Ford Health System in Detroit.
Boris C. Bastian, MD, professor of dermatology and pathology, University of California, San Francisco, will give the Lila and Murray Gruber Memorial Cancer Research Award and Lectureship, on “How Moles Become Cancer.” Dr. Bastian is also the director of the Clinical Cancer Genomics Laboratory at UCSF.
This year, the Marion B. Sulzberger, MD, Memorial Award and Lectureship – titled “Getting to the Heart (and other Comorbidities) of Psoriasis” – will be given by Joel M. Gelfand, MD, professor of dermatology, University of Pennsylvania.
Finally, this year’s guest speaker is the Center for Disease Control and Prevention’s Jordan W. Tappero, MD, whose lecture is titled: “The West African Ebola Epidemic and the Global Health Security Agenda.” Dr. Tappero is director of the Division of Global Health Protection, in the CDC’s Center for Global Health.
The plenary session is scheduled for Sunday March 5, 8 AM to 11:30 AM, in the Chapin Theater at the Orange County Convention Center, Orlando.
Features of the plenary session (P151) at this year’s American Academy of Dermatology annual meeting include the Clarence S. Livingood, MD Memorial Award and Lectureship, on “Telemedicine and the Future of Medicine,” presented by Carrie L. Kovarik, MD, of the department of dermatology at the University of Pennsylvania, Philadelphia.
Dr. Kovarik’s presentation will be followed by the AAD president’s address, by outgoing president Abel Torres, MD, JD, professor and chairman of the department of dermatology at Case Western Reserve University MetroHealth Systems, Cleveland; and professor and chairman of the department of dermatology at Loma Linda University Medical Center, Loma Linda, California.
Christine Léauté-Labrèze, MD, of the Hôpital Pellegrin–Enfants, Centre Hospitalier Universitaire, Bordeaux, France, will then present the Eugene J. Van Scott Award for Innovative Therapy of the Skin and Phillip Frost Leadership Lecture: “Propranolol in Infantile Hemangiomas: A Successful Drug Repurposing.” Dr. Léauté-Labrèze was the lead author of the multicenter, randomized controlled study that evaluated the efficacy and safety of oral propranolol for treating infantile hemangiomas (N Engl J Med. 2015;372:735-46).
Incoming AAD president Henry W. Lim, MD, will follow, with the president-elect’s address. Dr. Lim is the chairman of the department of dermatology and Clarence S. Livingood Chair in Dermatology at Henry Ford Health System in Detroit.
Boris C. Bastian, MD, professor of dermatology and pathology, University of California, San Francisco, will give the Lila and Murray Gruber Memorial Cancer Research Award and Lectureship, on “How Moles Become Cancer.” Dr. Bastian is also the director of the Clinical Cancer Genomics Laboratory at UCSF.
This year, the Marion B. Sulzberger, MD, Memorial Award and Lectureship – titled “Getting to the Heart (and other Comorbidities) of Psoriasis” – will be given by Joel M. Gelfand, MD, professor of dermatology, University of Pennsylvania.
Finally, this year’s guest speaker is the Center for Disease Control and Prevention’s Jordan W. Tappero, MD, whose lecture is titled: “The West African Ebola Epidemic and the Global Health Security Agenda.” Dr. Tappero is director of the Division of Global Health Protection, in the CDC’s Center for Global Health.
The plenary session is scheduled for Sunday March 5, 8 AM to 11:30 AM, in the Chapin Theater at the Orange County Convention Center, Orlando.
Features of the plenary session (P151) at this year’s American Academy of Dermatology annual meeting include the Clarence S. Livingood, MD Memorial Award and Lectureship, on “Telemedicine and the Future of Medicine,” presented by Carrie L. Kovarik, MD, of the department of dermatology at the University of Pennsylvania, Philadelphia.
Dr. Kovarik’s presentation will be followed by the AAD president’s address, by outgoing president Abel Torres, MD, JD, professor and chairman of the department of dermatology at Case Western Reserve University MetroHealth Systems, Cleveland; and professor and chairman of the department of dermatology at Loma Linda University Medical Center, Loma Linda, California.
Christine Léauté-Labrèze, MD, of the Hôpital Pellegrin–Enfants, Centre Hospitalier Universitaire, Bordeaux, France, will then present the Eugene J. Van Scott Award for Innovative Therapy of the Skin and Phillip Frost Leadership Lecture: “Propranolol in Infantile Hemangiomas: A Successful Drug Repurposing.” Dr. Léauté-Labrèze was the lead author of the multicenter, randomized controlled study that evaluated the efficacy and safety of oral propranolol for treating infantile hemangiomas (N Engl J Med. 2015;372:735-46).
Incoming AAD president Henry W. Lim, MD, will follow, with the president-elect’s address. Dr. Lim is the chairman of the department of dermatology and Clarence S. Livingood Chair in Dermatology at Henry Ford Health System in Detroit.
Boris C. Bastian, MD, professor of dermatology and pathology, University of California, San Francisco, will give the Lila and Murray Gruber Memorial Cancer Research Award and Lectureship, on “How Moles Become Cancer.” Dr. Bastian is also the director of the Clinical Cancer Genomics Laboratory at UCSF.
This year, the Marion B. Sulzberger, MD, Memorial Award and Lectureship – titled “Getting to the Heart (and other Comorbidities) of Psoriasis” – will be given by Joel M. Gelfand, MD, professor of dermatology, University of Pennsylvania.
Finally, this year’s guest speaker is the Center for Disease Control and Prevention’s Jordan W. Tappero, MD, whose lecture is titled: “The West African Ebola Epidemic and the Global Health Security Agenda.” Dr. Tappero is director of the Division of Global Health Protection, in the CDC’s Center for Global Health.
The plenary session is scheduled for Sunday March 5, 8 AM to 11:30 AM, in the Chapin Theater at the Orange County Convention Center, Orlando.
Late-breaking research presented March 4-5 at AAD meeting
Dermatology News will be on site later this week at the annual meeting of the American Academy of Dermatology in Orlando. Look for the latest news in medical, surgical, and aesthetic dermatology starting Friday, March 3. The late-breaker sessions are on Saturday and Sunday March 4 and 5.
The late-breaking research session on clinical trials on March 4 will highlight:
- 16-week results from two phase III studies of certolizumab for chronic plaque psoriasis.
- Phase III results on the long-term management of moderate to severe atopic dermatitis (AD) with dupilumab plus topical corticosteroids.
Additional late breakers focus on pediatric, procedural, and pathology studies:
- Data from the Pediatric Eczema Elective Registry, on racial/ethnic disparities in health care utilization and school attendance among children with AD.
- Results of a prospective study evaluating the efficacy and systemic absorption of topical timolol for infantile hemangioma.
- Results of a randomized, placebo-controlled, double-blind study of oral tranexamic acid for treating moderate to severe melasma.
- The efficacy of adjuvant treatment with the long-pulsed 1064nm Nd:YAG Laser for toe onychomycosis.
- Risk factors associated with a recent change in the size, shape or color of moles among participants in the AAD SPOTme® Program (2009-2010).
- A survey-based study on the management of longitudinal melanonychia among attending and resident dermatologists.
Dermatology News will be on site later this week at the annual meeting of the American Academy of Dermatology in Orlando. Look for the latest news in medical, surgical, and aesthetic dermatology starting Friday, March 3. The late-breaker sessions are on Saturday and Sunday March 4 and 5.
The late-breaking research session on clinical trials on March 4 will highlight:
- 16-week results from two phase III studies of certolizumab for chronic plaque psoriasis.
- Phase III results on the long-term management of moderate to severe atopic dermatitis (AD) with dupilumab plus topical corticosteroids.
Additional late breakers focus on pediatric, procedural, and pathology studies:
- Data from the Pediatric Eczema Elective Registry, on racial/ethnic disparities in health care utilization and school attendance among children with AD.
- Results of a prospective study evaluating the efficacy and systemic absorption of topical timolol for infantile hemangioma.
- Results of a randomized, placebo-controlled, double-blind study of oral tranexamic acid for treating moderate to severe melasma.
- The efficacy of adjuvant treatment with the long-pulsed 1064nm Nd:YAG Laser for toe onychomycosis.
- Risk factors associated with a recent change in the size, shape or color of moles among participants in the AAD SPOTme® Program (2009-2010).
- A survey-based study on the management of longitudinal melanonychia among attending and resident dermatologists.
Dermatology News will be on site later this week at the annual meeting of the American Academy of Dermatology in Orlando. Look for the latest news in medical, surgical, and aesthetic dermatology starting Friday, March 3. The late-breaker sessions are on Saturday and Sunday March 4 and 5.
The late-breaking research session on clinical trials on March 4 will highlight:
- 16-week results from two phase III studies of certolizumab for chronic plaque psoriasis.
- Phase III results on the long-term management of moderate to severe atopic dermatitis (AD) with dupilumab plus topical corticosteroids.
Additional late breakers focus on pediatric, procedural, and pathology studies:
- Data from the Pediatric Eczema Elective Registry, on racial/ethnic disparities in health care utilization and school attendance among children with AD.
- Results of a prospective study evaluating the efficacy and systemic absorption of topical timolol for infantile hemangioma.
- Results of a randomized, placebo-controlled, double-blind study of oral tranexamic acid for treating moderate to severe melasma.
- The efficacy of adjuvant treatment with the long-pulsed 1064nm Nd:YAG Laser for toe onychomycosis.
- Risk factors associated with a recent change in the size, shape or color of moles among participants in the AAD SPOTme® Program (2009-2010).
- A survey-based study on the management of longitudinal melanonychia among attending and resident dermatologists.
AAD 2017: Top tips to managing your time at the annual meeting
Dermatology News editorial advisor Adam Friedman, MD, provided the following recommendations for navigating the upcoming American Academy of Dermatology annual meeting, at the Orange County Convention Center in Orlando, March 3-6:
Don’t spread yourself too thin
Who’s ready to be overwhelmed by the almost 500 session options at the annual AAD meeting? It’s that time again, so here is my advice on how to stay on track during this circus. First, download the AAD mobile app. This makes life a lot easier when trying to find your room or search for an ongoing session. The paper program is so 2008. The AAD has created various tracks to enable dermatologists of varying stages in career or clinical foci to easily go after their interests. Follow those bread crumbs.
My general advice when deciding what to attend at this meeting is pick two or three specific topics or skills you want to expand upon or develop and go after sessions pertaining to them. Don’t spread yourself too thin as learning a little about a lot won’t strengthen your knowledge base.
Residents: Look at practice-based sessions
For residents, there are multiple professional development and board prep courses available. At this stage in your career, it’s important to acquire practical tips on topics from contract negotiation to speaker training as many of these skills are beyond the scope of residency training. Whether you are preparing for the in-training exam or the boards, programs such as “Boards Blitz” (S049) and “Conquer the Boards: An Experiential Review” (C006) will help you along the way. If you want practical career-building advice, hit up “Boards and Beyond” (F116) and “Careers in Academic Dermatology” (D004).
Get scorched in Orlando
Interested in what’s hot right now in dermatology? Look no further. There are multiple “Hot Topics” sessions scheduled throughout the meeting, with the main event on Saturday from 1 p.m. to 4 p.m. (S024) led by none other than AAD presidential candidate Kenneth J. Tomecki, MD. Other Hot Topic sessions include: “Hot Topics in Acute and Inpatient Pediatric Dermatology” (F007), “Hot Topics in Translational Dermatology” (U065), and “FDA Hot Topics: The Evolving Regulatory Landscape” (F005).
What about playing catch up on this year’s hottest publications? Check out “New Medical Dermatology Literature that Changed my Approach to Practice” (U025) with legendary academician Warren Heymann, MD. Not to be missed!
Dr. Friedman is director of the residency program and director of translational research in the department of dermatology, George Washington University, Washington.
Dermatology News editorial advisor Adam Friedman, MD, provided the following recommendations for navigating the upcoming American Academy of Dermatology annual meeting, at the Orange County Convention Center in Orlando, March 3-6:
Don’t spread yourself too thin
Who’s ready to be overwhelmed by the almost 500 session options at the annual AAD meeting? It’s that time again, so here is my advice on how to stay on track during this circus. First, download the AAD mobile app. This makes life a lot easier when trying to find your room or search for an ongoing session. The paper program is so 2008. The AAD has created various tracks to enable dermatologists of varying stages in career or clinical foci to easily go after their interests. Follow those bread crumbs.
My general advice when deciding what to attend at this meeting is pick two or three specific topics or skills you want to expand upon or develop and go after sessions pertaining to them. Don’t spread yourself too thin as learning a little about a lot won’t strengthen your knowledge base.
Residents: Look at practice-based sessions
For residents, there are multiple professional development and board prep courses available. At this stage in your career, it’s important to acquire practical tips on topics from contract negotiation to speaker training as many of these skills are beyond the scope of residency training. Whether you are preparing for the in-training exam or the boards, programs such as “Boards Blitz” (S049) and “Conquer the Boards: An Experiential Review” (C006) will help you along the way. If you want practical career-building advice, hit up “Boards and Beyond” (F116) and “Careers in Academic Dermatology” (D004).
Get scorched in Orlando
Interested in what’s hot right now in dermatology? Look no further. There are multiple “Hot Topics” sessions scheduled throughout the meeting, with the main event on Saturday from 1 p.m. to 4 p.m. (S024) led by none other than AAD presidential candidate Kenneth J. Tomecki, MD. Other Hot Topic sessions include: “Hot Topics in Acute and Inpatient Pediatric Dermatology” (F007), “Hot Topics in Translational Dermatology” (U065), and “FDA Hot Topics: The Evolving Regulatory Landscape” (F005).
What about playing catch up on this year’s hottest publications? Check out “New Medical Dermatology Literature that Changed my Approach to Practice” (U025) with legendary academician Warren Heymann, MD. Not to be missed!
Dr. Friedman is director of the residency program and director of translational research in the department of dermatology, George Washington University, Washington.
Dermatology News editorial advisor Adam Friedman, MD, provided the following recommendations for navigating the upcoming American Academy of Dermatology annual meeting, at the Orange County Convention Center in Orlando, March 3-6:
Don’t spread yourself too thin
Who’s ready to be overwhelmed by the almost 500 session options at the annual AAD meeting? It’s that time again, so here is my advice on how to stay on track during this circus. First, download the AAD mobile app. This makes life a lot easier when trying to find your room or search for an ongoing session. The paper program is so 2008. The AAD has created various tracks to enable dermatologists of varying stages in career or clinical foci to easily go after their interests. Follow those bread crumbs.
My general advice when deciding what to attend at this meeting is pick two or three specific topics or skills you want to expand upon or develop and go after sessions pertaining to them. Don’t spread yourself too thin as learning a little about a lot won’t strengthen your knowledge base.
Residents: Look at practice-based sessions
For residents, there are multiple professional development and board prep courses available. At this stage in your career, it’s important to acquire practical tips on topics from contract negotiation to speaker training as many of these skills are beyond the scope of residency training. Whether you are preparing for the in-training exam or the boards, programs such as “Boards Blitz” (S049) and “Conquer the Boards: An Experiential Review” (C006) will help you along the way. If you want practical career-building advice, hit up “Boards and Beyond” (F116) and “Careers in Academic Dermatology” (D004).
Get scorched in Orlando
Interested in what’s hot right now in dermatology? Look no further. There are multiple “Hot Topics” sessions scheduled throughout the meeting, with the main event on Saturday from 1 p.m. to 4 p.m. (S024) led by none other than AAD presidential candidate Kenneth J. Tomecki, MD. Other Hot Topic sessions include: “Hot Topics in Acute and Inpatient Pediatric Dermatology” (F007), “Hot Topics in Translational Dermatology” (U065), and “FDA Hot Topics: The Evolving Regulatory Landscape” (F005).
What about playing catch up on this year’s hottest publications? Check out “New Medical Dermatology Literature that Changed my Approach to Practice” (U025) with legendary academician Warren Heymann, MD. Not to be missed!
Dr. Friedman is director of the residency program and director of translational research in the department of dermatology, George Washington University, Washington.