User login
The Journal of Clinical Outcomes Management® is an independent, peer-reviewed journal offering evidence-based, practical information for improving the quality, safety, and value of health care.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
What’s next for COVID? Here’s what to know
As holiday celebrations wind down in the United States, COVID is on the rise.
Will there be another winter surge? If so, can we minimize it? How big a role might the boosters play in that? Are more mandates coming, along with a return to closed offices and businesses? Read on for a look at the latest info.
Cases, hospitalizations, deaths
As of Dec. 27, the latest statistics, the Centers for Disease Control and Prevention reports more than 487,000 weekly cases, compared to about 265,000 for the week ending Oct. 12. On average, 4,938 people were admitted to the hospital daily from Dec. 19 to 25, down about 6% from the 5,257 admitted daily the week before.
Deaths totaled 2,952 weekly as of Dec. 21, up from 2,699 on Dec. 14.
“What’s sobering overall is still seeing about 400 deaths a day in the U.S.,” said Peter Chin-Hong, MD, professor of medicine and infectious disease specialist at the University of California, San Francisco. “It’s still very high.”
As of Dec. 17, the variants predominating are BQ.1, BQ.1.1, and XBB. Experts said they are paying close attention to XBB, which is increasing quickly in the Northeast.
Predicting a winter surge
Experts tracking the pandemic agree there will be a surge.
“We are in the midst of it now,” said Eric Topol, MD, founder and director of the Scripps Research Translational Institute, La Jolla, Calif., and editor-in-chief of Medscape (MDedge’s sister site). “It’s not nearly like what we’ve had in Omicron or other waves; it’s not as severe. But it’s being particularly felt by seniors.”
One bit of good news: “Outside of that group it doesn’t look like – so far – it is going to be as bad a wave [as in the past],” Dr. Topol said.
Predicting the extent of the post-holiday surge “is the billion-dollar question right now,” said Katelyn Jetelina, PhD, a San Diego epidemiologist and author of the newsletter Your Local Epidemiologist.
“Much of these waves are not being driven by subvariants of concern but rather behavior,” she said.
People are opening up their social networks to gather for celebrations and family time. That’s unique to this winter, she said.
“I think our numbers will continue to go up, but certainly not like 2021 or 2020,” Dr. Chin-Hong said.
Others point out that the surge doesn’t involve just COVID.
“We are expecting a Christmas surge and we are concerned it might be a triple surge,” said William Schaffner, MD, professor of infectious diseases at Vanderbilt University, Nashville, Tenn., referring to the rising cases of flu and RSV (respiratory syncytial virus).
Dr. Jetelina shares that concern, worrying that those illnesses may be what overwhelms hospital capacity.
Another wild card is the situation in China. With the easing of China’s “zero COVID” policies, cases there are rising dramatically. Some models are predicting up to 1 million COVID deaths could occur in China in 2023. (The United States is now requiring travelers from China to show a negative COVID test before entering. Italy and Japan have taken similar measures.)
“The suffering that is going to occur in China is not good news at all,” Dr. Topol said. “We are going to be seeing that for many weeks if not months ahead.”
Theoretically, uncontained spread such as what is expected there could generate a whole new family of variants, he said. But “the main hit is going to be in China,” he predicted. “But it’s hard to project with accuracy.”
“China is 20% of the global population, so we can’t ignore it,” Dr. Jetelina said. “The question is, what’s the probability of a subvariant of concern coming from China? I think the probability is pretty low, but the possibility is there.”
What happens with cases in China may “throw a wrench” in the transition from pandemic to endemic, Dr. Chin-Hong said. But even if the rising cases in China do result in a new variant, “there’s so much T cell and B cell immunity [here], your average person is still not going to get seriously ill, even if the variant looks really scary.”
Minimizing the damage
Experts echo the same advice on stemming the surge, especially for adults who are 65 or older: Get the bivalent booster, and get it now.
“The same with the influenza vaccine,” Dr. Schaffner said.
Both the booster vaccine and the flu vaccine have been underused this year, he said. “It’s part of the general vaccine fatigue.”
The low uptake of the booster vaccine is concerning, Dr. Topol said, especially among adults aged 65 and older, the age group most vulnerable to severe disease. Just 35.7% of U.S. adults 65 and older have gotten the booster, according to the CDC. Dr. Topol calls that a tragedy.
Younger people have not taken to the booster, either. Overall, only 14.1% of people aged 5 and up have gotten an updated booster dose, according to the CDC.
Recent studies find value in the boosters. One study looked only at adults age 65 or older, finding that the bivalent booster reduced the risk of hospitalization by 84% compared to someone not vaccinated, and 73% compared to someone who had received only the monovalent vaccine. Another study of adults found those who had gotten the bivalent were less likely to need COVID-related emergency room care or urgent care.
In a Dec. 21 report in the New England Journal of Medicine, researchers took plasma samples from people who had gotten either one or two monovalent boosters or the bivalent to determine how well they worked against the circulating Omicron subvariants BA.1, BA.5, BA.2.75.2, BQ.1.1, and XBB. The bivalent worked better than the monovalent against all the Omicron subvariants, but especially against BA.2.75.2, BQ.1.1, and XBB.
Rapid testing can help minimize transmission. On Dec. 15, the Biden administration announced its Winter Preparedness Plan, urging Americans to test before and after travel as well as indoor visiting with vulnerable individuals, providing another round of free at-home tests, continuing to make community testing available and continuing to provide vaccines.
Besides the general precautions, Dr. Schaffner suggested: “Look at yourself. Who are you? If you are older than 65, or have underlying illness or are immunocompromised, or are pregnant, please put your mask back on. And think about social distancing. It might be time to worship at home and stream a movie,” instead of going to the theaters, he said.
Back to mandates?
On Dec. 9, the New York City Commissioner of Health and Mental Hygiene urged a return to masking indoors, saying people “should” mask up, including in schools, stores, offices, and when in crowded outdoor settings.
On the same date, the County of Los Angeles Public Health urged a return to masking for everyone aged 2 and older when indoors, including at schools, in transit, or in work sites when around others.
While the CDC order requiring masks on public transportation is no longer in effect, the agency continues to recommend that those using public transportation do so.
But some are taking that further. In Philadelphia, for example, School Superintendent Tony B. Watlington Sr., EdD, announced before the winter break that indoor masking would be required for all students and staff for the first 2 weeks of school return, through Jan. 13, citing guidance from the Philadelphia Department of Public Health.
Universal masking in schools does reduce COVID transmission, as a study published in late November suggests. After Massachusetts dropped the statewide universal masking policy in public schools in February 2022, researchers compared the incidence of COVID in 70 school districts there that dropped the mandate with two school districts that kept it. In the 15 weeks after the policy was rescinded, the lifting of the mandate was linked with an additional 44.9 cases of COVID per 1,000 students and staff. That corresponded to an estimated 11,901 cases and to nearly 30% of the cases in all districts during that time.
That said, experts see mandates as the exception rather than the rule, at least for now, citing public backlash against mandates to mask or follow other restrictions.
“Mandating, we know, it shuts people off,” Dr. Topol said. “It’s unenforceable. If you have a very strong recommendation, that’s probably as good as you’re going to be able to do right now.”
There may be communities where mandates go over better than others, Dr. Schaffner said, such as communities where people have confidence in their public health authorities.
Glimmers of hope
Despite uncertainties, experts offered some not-so-dismal perspectives as well.
“I think our numbers will continue to go up, but certainly not like 2021 or 2020,” Dr. Chin-Hong said.
A version of this article first appeared on WebMD.com.
As holiday celebrations wind down in the United States, COVID is on the rise.
Will there be another winter surge? If so, can we minimize it? How big a role might the boosters play in that? Are more mandates coming, along with a return to closed offices and businesses? Read on for a look at the latest info.
Cases, hospitalizations, deaths
As of Dec. 27, the latest statistics, the Centers for Disease Control and Prevention reports more than 487,000 weekly cases, compared to about 265,000 for the week ending Oct. 12. On average, 4,938 people were admitted to the hospital daily from Dec. 19 to 25, down about 6% from the 5,257 admitted daily the week before.
Deaths totaled 2,952 weekly as of Dec. 21, up from 2,699 on Dec. 14.
“What’s sobering overall is still seeing about 400 deaths a day in the U.S.,” said Peter Chin-Hong, MD, professor of medicine and infectious disease specialist at the University of California, San Francisco. “It’s still very high.”
As of Dec. 17, the variants predominating are BQ.1, BQ.1.1, and XBB. Experts said they are paying close attention to XBB, which is increasing quickly in the Northeast.
Predicting a winter surge
Experts tracking the pandemic agree there will be a surge.
“We are in the midst of it now,” said Eric Topol, MD, founder and director of the Scripps Research Translational Institute, La Jolla, Calif., and editor-in-chief of Medscape (MDedge’s sister site). “It’s not nearly like what we’ve had in Omicron or other waves; it’s not as severe. But it’s being particularly felt by seniors.”
One bit of good news: “Outside of that group it doesn’t look like – so far – it is going to be as bad a wave [as in the past],” Dr. Topol said.
Predicting the extent of the post-holiday surge “is the billion-dollar question right now,” said Katelyn Jetelina, PhD, a San Diego epidemiologist and author of the newsletter Your Local Epidemiologist.
“Much of these waves are not being driven by subvariants of concern but rather behavior,” she said.
People are opening up their social networks to gather for celebrations and family time. That’s unique to this winter, she said.
“I think our numbers will continue to go up, but certainly not like 2021 or 2020,” Dr. Chin-Hong said.
Others point out that the surge doesn’t involve just COVID.
“We are expecting a Christmas surge and we are concerned it might be a triple surge,” said William Schaffner, MD, professor of infectious diseases at Vanderbilt University, Nashville, Tenn., referring to the rising cases of flu and RSV (respiratory syncytial virus).
Dr. Jetelina shares that concern, worrying that those illnesses may be what overwhelms hospital capacity.
Another wild card is the situation in China. With the easing of China’s “zero COVID” policies, cases there are rising dramatically. Some models are predicting up to 1 million COVID deaths could occur in China in 2023. (The United States is now requiring travelers from China to show a negative COVID test before entering. Italy and Japan have taken similar measures.)
“The suffering that is going to occur in China is not good news at all,” Dr. Topol said. “We are going to be seeing that for many weeks if not months ahead.”
Theoretically, uncontained spread such as what is expected there could generate a whole new family of variants, he said. But “the main hit is going to be in China,” he predicted. “But it’s hard to project with accuracy.”
“China is 20% of the global population, so we can’t ignore it,” Dr. Jetelina said. “The question is, what’s the probability of a subvariant of concern coming from China? I think the probability is pretty low, but the possibility is there.”
What happens with cases in China may “throw a wrench” in the transition from pandemic to endemic, Dr. Chin-Hong said. But even if the rising cases in China do result in a new variant, “there’s so much T cell and B cell immunity [here], your average person is still not going to get seriously ill, even if the variant looks really scary.”
Minimizing the damage
Experts echo the same advice on stemming the surge, especially for adults who are 65 or older: Get the bivalent booster, and get it now.
“The same with the influenza vaccine,” Dr. Schaffner said.
Both the booster vaccine and the flu vaccine have been underused this year, he said. “It’s part of the general vaccine fatigue.”
The low uptake of the booster vaccine is concerning, Dr. Topol said, especially among adults aged 65 and older, the age group most vulnerable to severe disease. Just 35.7% of U.S. adults 65 and older have gotten the booster, according to the CDC. Dr. Topol calls that a tragedy.
Younger people have not taken to the booster, either. Overall, only 14.1% of people aged 5 and up have gotten an updated booster dose, according to the CDC.
Recent studies find value in the boosters. One study looked only at adults age 65 or older, finding that the bivalent booster reduced the risk of hospitalization by 84% compared to someone not vaccinated, and 73% compared to someone who had received only the monovalent vaccine. Another study of adults found those who had gotten the bivalent were less likely to need COVID-related emergency room care or urgent care.
In a Dec. 21 report in the New England Journal of Medicine, researchers took plasma samples from people who had gotten either one or two monovalent boosters or the bivalent to determine how well they worked against the circulating Omicron subvariants BA.1, BA.5, BA.2.75.2, BQ.1.1, and XBB. The bivalent worked better than the monovalent against all the Omicron subvariants, but especially against BA.2.75.2, BQ.1.1, and XBB.
Rapid testing can help minimize transmission. On Dec. 15, the Biden administration announced its Winter Preparedness Plan, urging Americans to test before and after travel as well as indoor visiting with vulnerable individuals, providing another round of free at-home tests, continuing to make community testing available and continuing to provide vaccines.
Besides the general precautions, Dr. Schaffner suggested: “Look at yourself. Who are you? If you are older than 65, or have underlying illness or are immunocompromised, or are pregnant, please put your mask back on. And think about social distancing. It might be time to worship at home and stream a movie,” instead of going to the theaters, he said.
Back to mandates?
On Dec. 9, the New York City Commissioner of Health and Mental Hygiene urged a return to masking indoors, saying people “should” mask up, including in schools, stores, offices, and when in crowded outdoor settings.
On the same date, the County of Los Angeles Public Health urged a return to masking for everyone aged 2 and older when indoors, including at schools, in transit, or in work sites when around others.
While the CDC order requiring masks on public transportation is no longer in effect, the agency continues to recommend that those using public transportation do so.
But some are taking that further. In Philadelphia, for example, School Superintendent Tony B. Watlington Sr., EdD, announced before the winter break that indoor masking would be required for all students and staff for the first 2 weeks of school return, through Jan. 13, citing guidance from the Philadelphia Department of Public Health.
Universal masking in schools does reduce COVID transmission, as a study published in late November suggests. After Massachusetts dropped the statewide universal masking policy in public schools in February 2022, researchers compared the incidence of COVID in 70 school districts there that dropped the mandate with two school districts that kept it. In the 15 weeks after the policy was rescinded, the lifting of the mandate was linked with an additional 44.9 cases of COVID per 1,000 students and staff. That corresponded to an estimated 11,901 cases and to nearly 30% of the cases in all districts during that time.
That said, experts see mandates as the exception rather than the rule, at least for now, citing public backlash against mandates to mask or follow other restrictions.
“Mandating, we know, it shuts people off,” Dr. Topol said. “It’s unenforceable. If you have a very strong recommendation, that’s probably as good as you’re going to be able to do right now.”
There may be communities where mandates go over better than others, Dr. Schaffner said, such as communities where people have confidence in their public health authorities.
Glimmers of hope
Despite uncertainties, experts offered some not-so-dismal perspectives as well.
“I think our numbers will continue to go up, but certainly not like 2021 or 2020,” Dr. Chin-Hong said.
A version of this article first appeared on WebMD.com.
As holiday celebrations wind down in the United States, COVID is on the rise.
Will there be another winter surge? If so, can we minimize it? How big a role might the boosters play in that? Are more mandates coming, along with a return to closed offices and businesses? Read on for a look at the latest info.
Cases, hospitalizations, deaths
As of Dec. 27, the latest statistics, the Centers for Disease Control and Prevention reports more than 487,000 weekly cases, compared to about 265,000 for the week ending Oct. 12. On average, 4,938 people were admitted to the hospital daily from Dec. 19 to 25, down about 6% from the 5,257 admitted daily the week before.
Deaths totaled 2,952 weekly as of Dec. 21, up from 2,699 on Dec. 14.
“What’s sobering overall is still seeing about 400 deaths a day in the U.S.,” said Peter Chin-Hong, MD, professor of medicine and infectious disease specialist at the University of California, San Francisco. “It’s still very high.”
As of Dec. 17, the variants predominating are BQ.1, BQ.1.1, and XBB. Experts said they are paying close attention to XBB, which is increasing quickly in the Northeast.
Predicting a winter surge
Experts tracking the pandemic agree there will be a surge.
“We are in the midst of it now,” said Eric Topol, MD, founder and director of the Scripps Research Translational Institute, La Jolla, Calif., and editor-in-chief of Medscape (MDedge’s sister site). “It’s not nearly like what we’ve had in Omicron or other waves; it’s not as severe. But it’s being particularly felt by seniors.”
One bit of good news: “Outside of that group it doesn’t look like – so far – it is going to be as bad a wave [as in the past],” Dr. Topol said.
Predicting the extent of the post-holiday surge “is the billion-dollar question right now,” said Katelyn Jetelina, PhD, a San Diego epidemiologist and author of the newsletter Your Local Epidemiologist.
“Much of these waves are not being driven by subvariants of concern but rather behavior,” she said.
People are opening up their social networks to gather for celebrations and family time. That’s unique to this winter, she said.
“I think our numbers will continue to go up, but certainly not like 2021 or 2020,” Dr. Chin-Hong said.
Others point out that the surge doesn’t involve just COVID.
“We are expecting a Christmas surge and we are concerned it might be a triple surge,” said William Schaffner, MD, professor of infectious diseases at Vanderbilt University, Nashville, Tenn., referring to the rising cases of flu and RSV (respiratory syncytial virus).
Dr. Jetelina shares that concern, worrying that those illnesses may be what overwhelms hospital capacity.
Another wild card is the situation in China. With the easing of China’s “zero COVID” policies, cases there are rising dramatically. Some models are predicting up to 1 million COVID deaths could occur in China in 2023. (The United States is now requiring travelers from China to show a negative COVID test before entering. Italy and Japan have taken similar measures.)
“The suffering that is going to occur in China is not good news at all,” Dr. Topol said. “We are going to be seeing that for many weeks if not months ahead.”
Theoretically, uncontained spread such as what is expected there could generate a whole new family of variants, he said. But “the main hit is going to be in China,” he predicted. “But it’s hard to project with accuracy.”
“China is 20% of the global population, so we can’t ignore it,” Dr. Jetelina said. “The question is, what’s the probability of a subvariant of concern coming from China? I think the probability is pretty low, but the possibility is there.”
What happens with cases in China may “throw a wrench” in the transition from pandemic to endemic, Dr. Chin-Hong said. But even if the rising cases in China do result in a new variant, “there’s so much T cell and B cell immunity [here], your average person is still not going to get seriously ill, even if the variant looks really scary.”
Minimizing the damage
Experts echo the same advice on stemming the surge, especially for adults who are 65 or older: Get the bivalent booster, and get it now.
“The same with the influenza vaccine,” Dr. Schaffner said.
Both the booster vaccine and the flu vaccine have been underused this year, he said. “It’s part of the general vaccine fatigue.”
The low uptake of the booster vaccine is concerning, Dr. Topol said, especially among adults aged 65 and older, the age group most vulnerable to severe disease. Just 35.7% of U.S. adults 65 and older have gotten the booster, according to the CDC. Dr. Topol calls that a tragedy.
Younger people have not taken to the booster, either. Overall, only 14.1% of people aged 5 and up have gotten an updated booster dose, according to the CDC.
Recent studies find value in the boosters. One study looked only at adults age 65 or older, finding that the bivalent booster reduced the risk of hospitalization by 84% compared to someone not vaccinated, and 73% compared to someone who had received only the monovalent vaccine. Another study of adults found those who had gotten the bivalent were less likely to need COVID-related emergency room care or urgent care.
In a Dec. 21 report in the New England Journal of Medicine, researchers took plasma samples from people who had gotten either one or two monovalent boosters or the bivalent to determine how well they worked against the circulating Omicron subvariants BA.1, BA.5, BA.2.75.2, BQ.1.1, and XBB. The bivalent worked better than the monovalent against all the Omicron subvariants, but especially against BA.2.75.2, BQ.1.1, and XBB.
Rapid testing can help minimize transmission. On Dec. 15, the Biden administration announced its Winter Preparedness Plan, urging Americans to test before and after travel as well as indoor visiting with vulnerable individuals, providing another round of free at-home tests, continuing to make community testing available and continuing to provide vaccines.
Besides the general precautions, Dr. Schaffner suggested: “Look at yourself. Who are you? If you are older than 65, or have underlying illness or are immunocompromised, or are pregnant, please put your mask back on. And think about social distancing. It might be time to worship at home and stream a movie,” instead of going to the theaters, he said.
Back to mandates?
On Dec. 9, the New York City Commissioner of Health and Mental Hygiene urged a return to masking indoors, saying people “should” mask up, including in schools, stores, offices, and when in crowded outdoor settings.
On the same date, the County of Los Angeles Public Health urged a return to masking for everyone aged 2 and older when indoors, including at schools, in transit, or in work sites when around others.
While the CDC order requiring masks on public transportation is no longer in effect, the agency continues to recommend that those using public transportation do so.
But some are taking that further. In Philadelphia, for example, School Superintendent Tony B. Watlington Sr., EdD, announced before the winter break that indoor masking would be required for all students and staff for the first 2 weeks of school return, through Jan. 13, citing guidance from the Philadelphia Department of Public Health.
Universal masking in schools does reduce COVID transmission, as a study published in late November suggests. After Massachusetts dropped the statewide universal masking policy in public schools in February 2022, researchers compared the incidence of COVID in 70 school districts there that dropped the mandate with two school districts that kept it. In the 15 weeks after the policy was rescinded, the lifting of the mandate was linked with an additional 44.9 cases of COVID per 1,000 students and staff. That corresponded to an estimated 11,901 cases and to nearly 30% of the cases in all districts during that time.
That said, experts see mandates as the exception rather than the rule, at least for now, citing public backlash against mandates to mask or follow other restrictions.
“Mandating, we know, it shuts people off,” Dr. Topol said. “It’s unenforceable. If you have a very strong recommendation, that’s probably as good as you’re going to be able to do right now.”
There may be communities where mandates go over better than others, Dr. Schaffner said, such as communities where people have confidence in their public health authorities.
Glimmers of hope
Despite uncertainties, experts offered some not-so-dismal perspectives as well.
“I think our numbers will continue to go up, but certainly not like 2021 or 2020,” Dr. Chin-Hong said.
A version of this article first appeared on WebMD.com.
Medical practice gave 8,000 patients cancer for Christmas
We wish you a merry Christmas and a happy heart failure
Does anyone really like it when places of business send out cards or messages for the holidays? A card from a truly small family business is one thing, but when you start getting emails from multibillion dollar corporations, it feels a bit dishonest. And that’s not even mentioning the potential blowback when things go wrong.
Now, you may wonder how a company could possibly mess up something so simple. “We wish you a merry Christmas and a happy New Year.” Not that difficult. Unless you’re Askern Medical Practice in Doncaster, England. Instead of expressing a simple expression of joy for the holiday season, Askern informed all 8,000 of its patients that they had aggressive lung cancer with metastases and they needed to fill out a DS1500 form, which entitles terminal patients to certain benefits.
It only took an hour for Askern to recognize its mistake and send a second text apologizing and adding in the appropriate season’s greetings, but obviously the damage was done. Presumably patients who were last at the doctor to have their cold treated were able to shrug off the text, or simply didn’t see it before the correction came through, but obviously many patients had concerns directly related to cancer and panicked. They called in but were by and large unable to reach anyone at the practice. Some patients close by even went to center itself to clear things up.
One patient, Mr. Carl Chegwin, raised an excellent point about the debacle: “What if that message was meant for someone, and then they are told it’s a Christmas message, then again told, ‘Oh no, that was actually meant for you?’ ” The old double backtrack into yes, you actually do have cancer has got to be a candidate for worst Christmas gift of all. Yes, even worse than socks.
Genes know it: You are when you eat
There’s been a lot of recent research on intermittent fasting and what it can and can’t do for one’s health. Much of it has focused on participants’ metabolic rates, but a study just published in Cell Metabolism shows how time-restricted feeding (TRF) has an impact on gene expression, the process through which genes are activated and respond to their environment by creating proteins.
The research conducted by Satchidananda Panda, PhD, of the Salk Institute and his team involved two groups of mice, one with free access to food and the other with a daily 9-hour feeding window. Analysis of tissue samples collected from 22 organ groups revealed that nearly 80% of mouse genes responded to TRF. Interestingly, 40% of the genes in the hypothalamus, adrenal gland, and pancreas, which handle hormone regulation, were affected, suggesting that TRF could potentially aid in diabetes and stress disorder management, the investigators said in a written statement.
The researchers also found that TRF aligned the circadian rhythms of multiple organs of the body, which brings sleep into the picture. “Time-restricted eating synchronized the circadian rhythms to have two major waves: one during fasting, and another just after eating. We suspect this allows the body to coordinate different processes,” said Dr. Panda, whose previous research looked at TRF in firefighters, who typically work on shift schedules.
Time-restricted eating, it appears, affects gene expression throughout the body and allows interconnected organ systems to work smoothly. It’s not just about eating. Go figure.
This group practice reduced stress for everyone
It’s been awhile since we checked in on the good folks at Maharishi International University in Fairfield, Iowa – fictional home of the Fighting Transcendentalists [MAHARISHI RULES!] – but we just have to mention their long-term effort to reduce the national stress.
Way back in the year 2000, a group from MIU began practicing transcendental meditation. The size of the group increased over the next few years and eventually reached 1,725 in 2006. That number is important because it represents the square root of 1% of the U.S. population. When that “transition threshold was achieved,” the university explained in a written statement, “all stress indicators immediately started decreasing.”
By stress indicators they mean the U.S. stress index, the mean of eight variables – murder, rape, assault, robbery, infant mortality, drug deaths, vehicle fatalities, and child deaths by injuries – that the study investigators used to track the effectiveness of the meditation program, they said in the World Journal of Social Science.
After 2011, “when the size of the group size began to decline the rate of decrease in stress slowed and then it reversed and began to increase,” MIU reported.
Coauthor Dr. Kenneth Cavanaugh of MIU explained the process: “This study used state-of-the-art methods of time series regression analysis for eliminating potential alternative explanations due to intrinsic preexisting trends and fluctuations in the data. We carefully studied potential alternative explanations in terms of changes in economic conditions, political leadership, population demographics, and policing strategies. None of these factors could account for the results.”
Since we here at LOTME are serious professional journalists, the use of quotes means we are not making this up. Here’s one more thing in quotes: “A grant for 75 million dollars from the Howard and Alice Settle Foundation provided stipends for participants to be in the group and provided funding to bring several hundred visiting [meditation] experts from India to further augment the MIU group.”
Who needs to make up stuff? Not us.
We wish you a merry Christmas and a happy heart failure
Does anyone really like it when places of business send out cards or messages for the holidays? A card from a truly small family business is one thing, but when you start getting emails from multibillion dollar corporations, it feels a bit dishonest. And that’s not even mentioning the potential blowback when things go wrong.
Now, you may wonder how a company could possibly mess up something so simple. “We wish you a merry Christmas and a happy New Year.” Not that difficult. Unless you’re Askern Medical Practice in Doncaster, England. Instead of expressing a simple expression of joy for the holiday season, Askern informed all 8,000 of its patients that they had aggressive lung cancer with metastases and they needed to fill out a DS1500 form, which entitles terminal patients to certain benefits.
It only took an hour for Askern to recognize its mistake and send a second text apologizing and adding in the appropriate season’s greetings, but obviously the damage was done. Presumably patients who were last at the doctor to have their cold treated were able to shrug off the text, or simply didn’t see it before the correction came through, but obviously many patients had concerns directly related to cancer and panicked. They called in but were by and large unable to reach anyone at the practice. Some patients close by even went to center itself to clear things up.
One patient, Mr. Carl Chegwin, raised an excellent point about the debacle: “What if that message was meant for someone, and then they are told it’s a Christmas message, then again told, ‘Oh no, that was actually meant for you?’ ” The old double backtrack into yes, you actually do have cancer has got to be a candidate for worst Christmas gift of all. Yes, even worse than socks.
Genes know it: You are when you eat
There’s been a lot of recent research on intermittent fasting and what it can and can’t do for one’s health. Much of it has focused on participants’ metabolic rates, but a study just published in Cell Metabolism shows how time-restricted feeding (TRF) has an impact on gene expression, the process through which genes are activated and respond to their environment by creating proteins.
The research conducted by Satchidananda Panda, PhD, of the Salk Institute and his team involved two groups of mice, one with free access to food and the other with a daily 9-hour feeding window. Analysis of tissue samples collected from 22 organ groups revealed that nearly 80% of mouse genes responded to TRF. Interestingly, 40% of the genes in the hypothalamus, adrenal gland, and pancreas, which handle hormone regulation, were affected, suggesting that TRF could potentially aid in diabetes and stress disorder management, the investigators said in a written statement.
The researchers also found that TRF aligned the circadian rhythms of multiple organs of the body, which brings sleep into the picture. “Time-restricted eating synchronized the circadian rhythms to have two major waves: one during fasting, and another just after eating. We suspect this allows the body to coordinate different processes,” said Dr. Panda, whose previous research looked at TRF in firefighters, who typically work on shift schedules.
Time-restricted eating, it appears, affects gene expression throughout the body and allows interconnected organ systems to work smoothly. It’s not just about eating. Go figure.
This group practice reduced stress for everyone
It’s been awhile since we checked in on the good folks at Maharishi International University in Fairfield, Iowa – fictional home of the Fighting Transcendentalists [MAHARISHI RULES!] – but we just have to mention their long-term effort to reduce the national stress.
Way back in the year 2000, a group from MIU began practicing transcendental meditation. The size of the group increased over the next few years and eventually reached 1,725 in 2006. That number is important because it represents the square root of 1% of the U.S. population. When that “transition threshold was achieved,” the university explained in a written statement, “all stress indicators immediately started decreasing.”
By stress indicators they mean the U.S. stress index, the mean of eight variables – murder, rape, assault, robbery, infant mortality, drug deaths, vehicle fatalities, and child deaths by injuries – that the study investigators used to track the effectiveness of the meditation program, they said in the World Journal of Social Science.
After 2011, “when the size of the group size began to decline the rate of decrease in stress slowed and then it reversed and began to increase,” MIU reported.
Coauthor Dr. Kenneth Cavanaugh of MIU explained the process: “This study used state-of-the-art methods of time series regression analysis for eliminating potential alternative explanations due to intrinsic preexisting trends and fluctuations in the data. We carefully studied potential alternative explanations in terms of changes in economic conditions, political leadership, population demographics, and policing strategies. None of these factors could account for the results.”
Since we here at LOTME are serious professional journalists, the use of quotes means we are not making this up. Here’s one more thing in quotes: “A grant for 75 million dollars from the Howard and Alice Settle Foundation provided stipends for participants to be in the group and provided funding to bring several hundred visiting [meditation] experts from India to further augment the MIU group.”
Who needs to make up stuff? Not us.
We wish you a merry Christmas and a happy heart failure
Does anyone really like it when places of business send out cards or messages for the holidays? A card from a truly small family business is one thing, but when you start getting emails from multibillion dollar corporations, it feels a bit dishonest. And that’s not even mentioning the potential blowback when things go wrong.
Now, you may wonder how a company could possibly mess up something so simple. “We wish you a merry Christmas and a happy New Year.” Not that difficult. Unless you’re Askern Medical Practice in Doncaster, England. Instead of expressing a simple expression of joy for the holiday season, Askern informed all 8,000 of its patients that they had aggressive lung cancer with metastases and they needed to fill out a DS1500 form, which entitles terminal patients to certain benefits.
It only took an hour for Askern to recognize its mistake and send a second text apologizing and adding in the appropriate season’s greetings, but obviously the damage was done. Presumably patients who were last at the doctor to have their cold treated were able to shrug off the text, or simply didn’t see it before the correction came through, but obviously many patients had concerns directly related to cancer and panicked. They called in but were by and large unable to reach anyone at the practice. Some patients close by even went to center itself to clear things up.
One patient, Mr. Carl Chegwin, raised an excellent point about the debacle: “What if that message was meant for someone, and then they are told it’s a Christmas message, then again told, ‘Oh no, that was actually meant for you?’ ” The old double backtrack into yes, you actually do have cancer has got to be a candidate for worst Christmas gift of all. Yes, even worse than socks.
Genes know it: You are when you eat
There’s been a lot of recent research on intermittent fasting and what it can and can’t do for one’s health. Much of it has focused on participants’ metabolic rates, but a study just published in Cell Metabolism shows how time-restricted feeding (TRF) has an impact on gene expression, the process through which genes are activated and respond to their environment by creating proteins.
The research conducted by Satchidananda Panda, PhD, of the Salk Institute and his team involved two groups of mice, one with free access to food and the other with a daily 9-hour feeding window. Analysis of tissue samples collected from 22 organ groups revealed that nearly 80% of mouse genes responded to TRF. Interestingly, 40% of the genes in the hypothalamus, adrenal gland, and pancreas, which handle hormone regulation, were affected, suggesting that TRF could potentially aid in diabetes and stress disorder management, the investigators said in a written statement.
The researchers also found that TRF aligned the circadian rhythms of multiple organs of the body, which brings sleep into the picture. “Time-restricted eating synchronized the circadian rhythms to have two major waves: one during fasting, and another just after eating. We suspect this allows the body to coordinate different processes,” said Dr. Panda, whose previous research looked at TRF in firefighters, who typically work on shift schedules.
Time-restricted eating, it appears, affects gene expression throughout the body and allows interconnected organ systems to work smoothly. It’s not just about eating. Go figure.
This group practice reduced stress for everyone
It’s been awhile since we checked in on the good folks at Maharishi International University in Fairfield, Iowa – fictional home of the Fighting Transcendentalists [MAHARISHI RULES!] – but we just have to mention their long-term effort to reduce the national stress.
Way back in the year 2000, a group from MIU began practicing transcendental meditation. The size of the group increased over the next few years and eventually reached 1,725 in 2006. That number is important because it represents the square root of 1% of the U.S. population. When that “transition threshold was achieved,” the university explained in a written statement, “all stress indicators immediately started decreasing.”
By stress indicators they mean the U.S. stress index, the mean of eight variables – murder, rape, assault, robbery, infant mortality, drug deaths, vehicle fatalities, and child deaths by injuries – that the study investigators used to track the effectiveness of the meditation program, they said in the World Journal of Social Science.
After 2011, “when the size of the group size began to decline the rate of decrease in stress slowed and then it reversed and began to increase,” MIU reported.
Coauthor Dr. Kenneth Cavanaugh of MIU explained the process: “This study used state-of-the-art methods of time series regression analysis for eliminating potential alternative explanations due to intrinsic preexisting trends and fluctuations in the data. We carefully studied potential alternative explanations in terms of changes in economic conditions, political leadership, population demographics, and policing strategies. None of these factors could account for the results.”
Since we here at LOTME are serious professional journalists, the use of quotes means we are not making this up. Here’s one more thing in quotes: “A grant for 75 million dollars from the Howard and Alice Settle Foundation provided stipends for participants to be in the group and provided funding to bring several hundred visiting [meditation] experts from India to further augment the MIU group.”
Who needs to make up stuff? Not us.
New osteoporosis guideline says start with a bisphosphonate
This is the first update for 5 years since the previous guidance was published in 2017.
It strongly recommends initial therapy with bisphosphonates for postmenopausal women with osteoporosis, as well as men with osteoporosis, among other recommendations.
However, the author of an accompanying editorial, Susan M. Ott, MD, says: “The decision to start a bisphosphonate is actually not that easy.”
She also queries some of the other recommendations in the guidance.
Her editorial, along with the guideline by Amir Qaseem, MD, PhD, MPH, and colleagues, and systematic review by Chelsea Ayers, MPH, and colleagues, were published in the Annals of Internal Medicine.
Ryan D. Mire, MD, MACP, president of the ACP, gave a brief overview of the new guidance in a video.
Systematic review
The ACP commissioned a review of the evidence because it says new data have emerged on the efficacy of newer medications for osteoporosis and low bone mass, as well as treatment comparisons, and treatment in men.
The review authors identified 34 randomized controlled trials (in 100 publications) and 36 observational studies, which evaluated the following pharmacologic interventions:
- Antiresorptive drugs: four bisphosphonates (alendronate, ibandronate, risedronate, zoledronate) and a RANK ligand inhibitor (denosumab).
- Anabolic drugs: an analog of human parathyroid hormone (PTH)–related protein (abaloparatide), recombinant human PTH (teriparatide), and a sclerostin inhibitor (romosozumab).
- Estrogen agonists: selective estrogen receptor modulators (bazedoxifene, raloxifene).
The authors focused on effectiveness and harms of active drugs compared with placebo or bisphosphonates.
Major changes from 2017 guidelines, some questions
“Though there are many nuanced changes in this [2023 guideline] version, perhaps the major change is the explicit hierarchy of pharmacologic recommendations: bisphosphonates first, then denosumab,” Thomas G. Cooney, MD, senior author of the clinical guideline, explained in an interview.
“Bisphosphonates had the most favorable balance among benefits, harms, patient values and preferences, and cost among the examined drugs in postmenopausal females with primary osteoporosis,” Dr. Cooney, professor of medicine, Oregon Health & Science University, Portland, noted, as is stated in the guideline.
“Denosumab also had a favorable long-term net benefit, but bisphosphonates are much cheaper than other pharmacologic treatments and available in generic formulations,” the document states.
The new guideline suggests use of denosumab as second-line pharmacotherapy in adults who have contraindications to or experience adverse effects with bisphosphonates.
The choice among bisphosphonates (alendronate, risedronate, zoledronic acid) would be based on a patient-centered discussion between physician and patient, addressing costs (often related to insurance), delivery-mode preferences (oral versus intravenous), and “values,” which includes the patient’s priorities, concerns, and expectations regarding their health care, Dr. Cooney explained.
Another update in the new guideline is, “We also clarify the specific, albeit more limited, role of sclerostin inhibitors and recombinant PTH ‘to reduce the risk of fractures only in females with primary osteoporosis with very high-risk of fracture’,” Dr. Cooney noted.
In addition, the guideline now states, “treatment to reduce the risk of fractures in males rather than limiting it to ‘vertebral fracture’ in men,” as in the 2017 guideline.
It also explicitly includes denosumab as second-line therapy for men, Dr. Cooney noted, but as in 2017, the strength of evidence in men remains low.
“Finally, we also clarified that in females over the age of 65 with low bone mass or osteopenia that an individualized approach be taken to treatment (similar to last guideline), but if treatment is initiated, that a bisphosphonate be used (new content),” he said.
The use of estrogen, treatment duration, drug discontinuation, and serial bone mineral density monitoring were not addressed in this guideline, but will likely be evaluated within 2 to 3 years.
‘Osteoporosis treatment: Not easy’ – editorial
In her editorial, Dr. Ott writes: “The data about bisphosphonates may seem overwhelmingly positive, leading to strong recommendations for their use to treat osteoporosis, but the decision to start a bisphosphonate is actually not that easy.”
“A strong recommendation should be given only when future studies are unlikely to change it,” continues Dr. Ott, professor of medicine, University of Washington, Seattle.
“Yet, data already suggest that, in patients with serious osteoporosis, treatment should start with anabolic medications because previous treatment with either bisphosphonates or denosumab will prevent the anabolic response of newer medications.”
“Starting with bisphosphonate will change the bone so it will not respond to the newer medicines, and then a patient will lose the chance for getting the best improvement,” Dr. Ott clarified in an email to this news organization.
But, in fact, the new guidance does suggest that, to reduce the risk of fractures in females with primary osteoporosis at very high risk of fracture, one should consider use of the sclerostin inhibitor romosozumab (moderate-certainty evidence) or recombinant human parathyroid hormone (teriparatide) (low-certainty evidence) followed by a bisphosphonate (conditional recommendation).
Dr. Ott said: “If the [fracture] risk is high, then we should start with an anabolic medication for 1-2 years. If the risk is medium, then use a bisphosphonate for up to 5 years, and then stop and monitor the patient for signs that the medicine is wearing off,” based on blood and urine tests.
‘We need medicines that will stop bone aging’
Osteopenia is defined by an arbitrary bone density measurement, Dr. Ott explained. “About half of women over 65 will have osteopenia, and by age 85 there are hardly any ‘normal’ women left.”
“We need medicines that will stop bone aging, which might sound impossible, but we should still try,” she continued.
“In the meantime, while waiting on new discoveries,” Dr. Ott said, “I would not use bisphosphonates in patients who did not already have a fracture or whose bone density T-score was better than –2.5 because, in the major study, alendronate did not prevent fractures in this group.”
Many people are worried about bisphosphonates because of problems with the jaw or femur. These are real, but they are very rare during the first 5 years of treatment, Dr. Ott noted. Then the risk starts to rise, up to more than 1 in 1,000 after 8 years. So people can get the benefits of these drugs with very low risk for 5 years.
“An immediate [guideline] update is necessary to address the severity of bone loss and the high risk for vertebral fractures after discontinuation of denosumab,” Dr. Ott urged.
“I don’t agree with using denosumab for osteoporosis as a second-line treatment,” she said. “I would use it only in patients who have cancer or unusually high bone resorption. You have to get a dose strictly every 6 months, and if you need to stop, it is recommended to treat with bisphosphonates. Denosumab is a poor choice for somebody who does not want to take a bisphosphonate. Many patients and even too many doctors do not realize how serious it can be to skip a dose.”
“I also think that men could be treated with anabolic medications,” Dr. Ott said. “Clinical trials show they respond the same as women. Many men have osteoporosis as a consequence of low testosterone, and then they can usually be treated with testosterone. Osteoporosis in men is a serious problem that is too often ignored – almost reverse discrimination.”
It is also unfortunate that the review and recommendations do not address estrogen, one of the most effective medications to prevent osteoporotic fractures, according to Dr. Ott.
Clinical considerations in addition to drug types
The new guideline also advises:
- Clinicians treating adults with osteoporosis should encourage adherence to recommended treatments and healthy lifestyle habits, including exercise, and counseling to evaluate and prevent falls.
- All adults with osteopenia or osteoporosis should have adequate calcium and vitamin D intake, as part of fracture prevention.
- Clinicians should assess baseline fracture risk based on bone density, fracture history, fracture risk factors, and response to prior osteoporosis treatments.
- Current evidence suggests that more than 3-5 years of bisphosphonate therapy reduces risk for new vertebral but not other fractures; however, it also increases risk for long-term harms. Therefore, clinicians should consider stopping bisphosphonate treatment after 5 years unless the patient has a strong indication for treatment continuation.
- The decision for a bisphosphonate holiday (temporary discontinuation) and its duration should be based on baseline fracture risk, medication half-life in bone, and benefits and harms.
- Women treated with an anabolic agent who discontinue it should be offered an antiresorptive agent to preserve gains and because of serious risk for rebound and multiple vertebral fractures.
- Adults older than 65 years with osteoporosis may be at increased risk for falls or other adverse events because of drug interactions.
- Transgender persons have variable risk for low bone mass.
The review and guideline were funded by the ACP. Dr. Ott has reported no relevant disclosures. Relevant financial disclosures for other authors are listed with the guideline and review.
A version of this article first appeared on Medscape.com.
This is the first update for 5 years since the previous guidance was published in 2017.
It strongly recommends initial therapy with bisphosphonates for postmenopausal women with osteoporosis, as well as men with osteoporosis, among other recommendations.
However, the author of an accompanying editorial, Susan M. Ott, MD, says: “The decision to start a bisphosphonate is actually not that easy.”
She also queries some of the other recommendations in the guidance.
Her editorial, along with the guideline by Amir Qaseem, MD, PhD, MPH, and colleagues, and systematic review by Chelsea Ayers, MPH, and colleagues, were published in the Annals of Internal Medicine.
Ryan D. Mire, MD, MACP, president of the ACP, gave a brief overview of the new guidance in a video.
Systematic review
The ACP commissioned a review of the evidence because it says new data have emerged on the efficacy of newer medications for osteoporosis and low bone mass, as well as treatment comparisons, and treatment in men.
The review authors identified 34 randomized controlled trials (in 100 publications) and 36 observational studies, which evaluated the following pharmacologic interventions:
- Antiresorptive drugs: four bisphosphonates (alendronate, ibandronate, risedronate, zoledronate) and a RANK ligand inhibitor (denosumab).
- Anabolic drugs: an analog of human parathyroid hormone (PTH)–related protein (abaloparatide), recombinant human PTH (teriparatide), and a sclerostin inhibitor (romosozumab).
- Estrogen agonists: selective estrogen receptor modulators (bazedoxifene, raloxifene).
The authors focused on effectiveness and harms of active drugs compared with placebo or bisphosphonates.
Major changes from 2017 guidelines, some questions
“Though there are many nuanced changes in this [2023 guideline] version, perhaps the major change is the explicit hierarchy of pharmacologic recommendations: bisphosphonates first, then denosumab,” Thomas G. Cooney, MD, senior author of the clinical guideline, explained in an interview.
“Bisphosphonates had the most favorable balance among benefits, harms, patient values and preferences, and cost among the examined drugs in postmenopausal females with primary osteoporosis,” Dr. Cooney, professor of medicine, Oregon Health & Science University, Portland, noted, as is stated in the guideline.
“Denosumab also had a favorable long-term net benefit, but bisphosphonates are much cheaper than other pharmacologic treatments and available in generic formulations,” the document states.
The new guideline suggests use of denosumab as second-line pharmacotherapy in adults who have contraindications to or experience adverse effects with bisphosphonates.
The choice among bisphosphonates (alendronate, risedronate, zoledronic acid) would be based on a patient-centered discussion between physician and patient, addressing costs (often related to insurance), delivery-mode preferences (oral versus intravenous), and “values,” which includes the patient’s priorities, concerns, and expectations regarding their health care, Dr. Cooney explained.
Another update in the new guideline is, “We also clarify the specific, albeit more limited, role of sclerostin inhibitors and recombinant PTH ‘to reduce the risk of fractures only in females with primary osteoporosis with very high-risk of fracture’,” Dr. Cooney noted.
In addition, the guideline now states, “treatment to reduce the risk of fractures in males rather than limiting it to ‘vertebral fracture’ in men,” as in the 2017 guideline.
It also explicitly includes denosumab as second-line therapy for men, Dr. Cooney noted, but as in 2017, the strength of evidence in men remains low.
“Finally, we also clarified that in females over the age of 65 with low bone mass or osteopenia that an individualized approach be taken to treatment (similar to last guideline), but if treatment is initiated, that a bisphosphonate be used (new content),” he said.
The use of estrogen, treatment duration, drug discontinuation, and serial bone mineral density monitoring were not addressed in this guideline, but will likely be evaluated within 2 to 3 years.
‘Osteoporosis treatment: Not easy’ – editorial
In her editorial, Dr. Ott writes: “The data about bisphosphonates may seem overwhelmingly positive, leading to strong recommendations for their use to treat osteoporosis, but the decision to start a bisphosphonate is actually not that easy.”
“A strong recommendation should be given only when future studies are unlikely to change it,” continues Dr. Ott, professor of medicine, University of Washington, Seattle.
“Yet, data already suggest that, in patients with serious osteoporosis, treatment should start with anabolic medications because previous treatment with either bisphosphonates or denosumab will prevent the anabolic response of newer medications.”
“Starting with bisphosphonate will change the bone so it will not respond to the newer medicines, and then a patient will lose the chance for getting the best improvement,” Dr. Ott clarified in an email to this news organization.
But, in fact, the new guidance does suggest that, to reduce the risk of fractures in females with primary osteoporosis at very high risk of fracture, one should consider use of the sclerostin inhibitor romosozumab (moderate-certainty evidence) or recombinant human parathyroid hormone (teriparatide) (low-certainty evidence) followed by a bisphosphonate (conditional recommendation).
Dr. Ott said: “If the [fracture] risk is high, then we should start with an anabolic medication for 1-2 years. If the risk is medium, then use a bisphosphonate for up to 5 years, and then stop and monitor the patient for signs that the medicine is wearing off,” based on blood and urine tests.
‘We need medicines that will stop bone aging’
Osteopenia is defined by an arbitrary bone density measurement, Dr. Ott explained. “About half of women over 65 will have osteopenia, and by age 85 there are hardly any ‘normal’ women left.”
“We need medicines that will stop bone aging, which might sound impossible, but we should still try,” she continued.
“In the meantime, while waiting on new discoveries,” Dr. Ott said, “I would not use bisphosphonates in patients who did not already have a fracture or whose bone density T-score was better than –2.5 because, in the major study, alendronate did not prevent fractures in this group.”
Many people are worried about bisphosphonates because of problems with the jaw or femur. These are real, but they are very rare during the first 5 years of treatment, Dr. Ott noted. Then the risk starts to rise, up to more than 1 in 1,000 after 8 years. So people can get the benefits of these drugs with very low risk for 5 years.
“An immediate [guideline] update is necessary to address the severity of bone loss and the high risk for vertebral fractures after discontinuation of denosumab,” Dr. Ott urged.
“I don’t agree with using denosumab for osteoporosis as a second-line treatment,” she said. “I would use it only in patients who have cancer or unusually high bone resorption. You have to get a dose strictly every 6 months, and if you need to stop, it is recommended to treat with bisphosphonates. Denosumab is a poor choice for somebody who does not want to take a bisphosphonate. Many patients and even too many doctors do not realize how serious it can be to skip a dose.”
“I also think that men could be treated with anabolic medications,” Dr. Ott said. “Clinical trials show they respond the same as women. Many men have osteoporosis as a consequence of low testosterone, and then they can usually be treated with testosterone. Osteoporosis in men is a serious problem that is too often ignored – almost reverse discrimination.”
It is also unfortunate that the review and recommendations do not address estrogen, one of the most effective medications to prevent osteoporotic fractures, according to Dr. Ott.
Clinical considerations in addition to drug types
The new guideline also advises:
- Clinicians treating adults with osteoporosis should encourage adherence to recommended treatments and healthy lifestyle habits, including exercise, and counseling to evaluate and prevent falls.
- All adults with osteopenia or osteoporosis should have adequate calcium and vitamin D intake, as part of fracture prevention.
- Clinicians should assess baseline fracture risk based on bone density, fracture history, fracture risk factors, and response to prior osteoporosis treatments.
- Current evidence suggests that more than 3-5 years of bisphosphonate therapy reduces risk for new vertebral but not other fractures; however, it also increases risk for long-term harms. Therefore, clinicians should consider stopping bisphosphonate treatment after 5 years unless the patient has a strong indication for treatment continuation.
- The decision for a bisphosphonate holiday (temporary discontinuation) and its duration should be based on baseline fracture risk, medication half-life in bone, and benefits and harms.
- Women treated with an anabolic agent who discontinue it should be offered an antiresorptive agent to preserve gains and because of serious risk for rebound and multiple vertebral fractures.
- Adults older than 65 years with osteoporosis may be at increased risk for falls or other adverse events because of drug interactions.
- Transgender persons have variable risk for low bone mass.
The review and guideline were funded by the ACP. Dr. Ott has reported no relevant disclosures. Relevant financial disclosures for other authors are listed with the guideline and review.
A version of this article first appeared on Medscape.com.
This is the first update for 5 years since the previous guidance was published in 2017.
It strongly recommends initial therapy with bisphosphonates for postmenopausal women with osteoporosis, as well as men with osteoporosis, among other recommendations.
However, the author of an accompanying editorial, Susan M. Ott, MD, says: “The decision to start a bisphosphonate is actually not that easy.”
She also queries some of the other recommendations in the guidance.
Her editorial, along with the guideline by Amir Qaseem, MD, PhD, MPH, and colleagues, and systematic review by Chelsea Ayers, MPH, and colleagues, were published in the Annals of Internal Medicine.
Ryan D. Mire, MD, MACP, president of the ACP, gave a brief overview of the new guidance in a video.
Systematic review
The ACP commissioned a review of the evidence because it says new data have emerged on the efficacy of newer medications for osteoporosis and low bone mass, as well as treatment comparisons, and treatment in men.
The review authors identified 34 randomized controlled trials (in 100 publications) and 36 observational studies, which evaluated the following pharmacologic interventions:
- Antiresorptive drugs: four bisphosphonates (alendronate, ibandronate, risedronate, zoledronate) and a RANK ligand inhibitor (denosumab).
- Anabolic drugs: an analog of human parathyroid hormone (PTH)–related protein (abaloparatide), recombinant human PTH (teriparatide), and a sclerostin inhibitor (romosozumab).
- Estrogen agonists: selective estrogen receptor modulators (bazedoxifene, raloxifene).
The authors focused on effectiveness and harms of active drugs compared with placebo or bisphosphonates.
Major changes from 2017 guidelines, some questions
“Though there are many nuanced changes in this [2023 guideline] version, perhaps the major change is the explicit hierarchy of pharmacologic recommendations: bisphosphonates first, then denosumab,” Thomas G. Cooney, MD, senior author of the clinical guideline, explained in an interview.
“Bisphosphonates had the most favorable balance among benefits, harms, patient values and preferences, and cost among the examined drugs in postmenopausal females with primary osteoporosis,” Dr. Cooney, professor of medicine, Oregon Health & Science University, Portland, noted, as is stated in the guideline.
“Denosumab also had a favorable long-term net benefit, but bisphosphonates are much cheaper than other pharmacologic treatments and available in generic formulations,” the document states.
The new guideline suggests use of denosumab as second-line pharmacotherapy in adults who have contraindications to or experience adverse effects with bisphosphonates.
The choice among bisphosphonates (alendronate, risedronate, zoledronic acid) would be based on a patient-centered discussion between physician and patient, addressing costs (often related to insurance), delivery-mode preferences (oral versus intravenous), and “values,” which includes the patient’s priorities, concerns, and expectations regarding their health care, Dr. Cooney explained.
Another update in the new guideline is, “We also clarify the specific, albeit more limited, role of sclerostin inhibitors and recombinant PTH ‘to reduce the risk of fractures only in females with primary osteoporosis with very high-risk of fracture’,” Dr. Cooney noted.
In addition, the guideline now states, “treatment to reduce the risk of fractures in males rather than limiting it to ‘vertebral fracture’ in men,” as in the 2017 guideline.
It also explicitly includes denosumab as second-line therapy for men, Dr. Cooney noted, but as in 2017, the strength of evidence in men remains low.
“Finally, we also clarified that in females over the age of 65 with low bone mass or osteopenia that an individualized approach be taken to treatment (similar to last guideline), but if treatment is initiated, that a bisphosphonate be used (new content),” he said.
The use of estrogen, treatment duration, drug discontinuation, and serial bone mineral density monitoring were not addressed in this guideline, but will likely be evaluated within 2 to 3 years.
‘Osteoporosis treatment: Not easy’ – editorial
In her editorial, Dr. Ott writes: “The data about bisphosphonates may seem overwhelmingly positive, leading to strong recommendations for their use to treat osteoporosis, but the decision to start a bisphosphonate is actually not that easy.”
“A strong recommendation should be given only when future studies are unlikely to change it,” continues Dr. Ott, professor of medicine, University of Washington, Seattle.
“Yet, data already suggest that, in patients with serious osteoporosis, treatment should start with anabolic medications because previous treatment with either bisphosphonates or denosumab will prevent the anabolic response of newer medications.”
“Starting with bisphosphonate will change the bone so it will not respond to the newer medicines, and then a patient will lose the chance for getting the best improvement,” Dr. Ott clarified in an email to this news organization.
But, in fact, the new guidance does suggest that, to reduce the risk of fractures in females with primary osteoporosis at very high risk of fracture, one should consider use of the sclerostin inhibitor romosozumab (moderate-certainty evidence) or recombinant human parathyroid hormone (teriparatide) (low-certainty evidence) followed by a bisphosphonate (conditional recommendation).
Dr. Ott said: “If the [fracture] risk is high, then we should start with an anabolic medication for 1-2 years. If the risk is medium, then use a bisphosphonate for up to 5 years, and then stop and monitor the patient for signs that the medicine is wearing off,” based on blood and urine tests.
‘We need medicines that will stop bone aging’
Osteopenia is defined by an arbitrary bone density measurement, Dr. Ott explained. “About half of women over 65 will have osteopenia, and by age 85 there are hardly any ‘normal’ women left.”
“We need medicines that will stop bone aging, which might sound impossible, but we should still try,” she continued.
“In the meantime, while waiting on new discoveries,” Dr. Ott said, “I would not use bisphosphonates in patients who did not already have a fracture or whose bone density T-score was better than –2.5 because, in the major study, alendronate did not prevent fractures in this group.”
Many people are worried about bisphosphonates because of problems with the jaw or femur. These are real, but they are very rare during the first 5 years of treatment, Dr. Ott noted. Then the risk starts to rise, up to more than 1 in 1,000 after 8 years. So people can get the benefits of these drugs with very low risk for 5 years.
“An immediate [guideline] update is necessary to address the severity of bone loss and the high risk for vertebral fractures after discontinuation of denosumab,” Dr. Ott urged.
“I don’t agree with using denosumab for osteoporosis as a second-line treatment,” she said. “I would use it only in patients who have cancer or unusually high bone resorption. You have to get a dose strictly every 6 months, and if you need to stop, it is recommended to treat with bisphosphonates. Denosumab is a poor choice for somebody who does not want to take a bisphosphonate. Many patients and even too many doctors do not realize how serious it can be to skip a dose.”
“I also think that men could be treated with anabolic medications,” Dr. Ott said. “Clinical trials show they respond the same as women. Many men have osteoporosis as a consequence of low testosterone, and then they can usually be treated with testosterone. Osteoporosis in men is a serious problem that is too often ignored – almost reverse discrimination.”
It is also unfortunate that the review and recommendations do not address estrogen, one of the most effective medications to prevent osteoporotic fractures, according to Dr. Ott.
Clinical considerations in addition to drug types
The new guideline also advises:
- Clinicians treating adults with osteoporosis should encourage adherence to recommended treatments and healthy lifestyle habits, including exercise, and counseling to evaluate and prevent falls.
- All adults with osteopenia or osteoporosis should have adequate calcium and vitamin D intake, as part of fracture prevention.
- Clinicians should assess baseline fracture risk based on bone density, fracture history, fracture risk factors, and response to prior osteoporosis treatments.
- Current evidence suggests that more than 3-5 years of bisphosphonate therapy reduces risk for new vertebral but not other fractures; however, it also increases risk for long-term harms. Therefore, clinicians should consider stopping bisphosphonate treatment after 5 years unless the patient has a strong indication for treatment continuation.
- The decision for a bisphosphonate holiday (temporary discontinuation) and its duration should be based on baseline fracture risk, medication half-life in bone, and benefits and harms.
- Women treated with an anabolic agent who discontinue it should be offered an antiresorptive agent to preserve gains and because of serious risk for rebound and multiple vertebral fractures.
- Adults older than 65 years with osteoporosis may be at increased risk for falls or other adverse events because of drug interactions.
- Transgender persons have variable risk for low bone mass.
The review and guideline were funded by the ACP. Dr. Ott has reported no relevant disclosures. Relevant financial disclosures for other authors are listed with the guideline and review.
A version of this article first appeared on Medscape.com.
FROM THE ANNALS OF INTERNAL MEDICINE
Best diets in 2023: Mediterranean diet wins again
After all, weight loss usually lands one of the top spots on New Year’s resolution surveys.
And just in time, there’s guidance to pick the best plan, as U.S. News & World Report’s annual rankings of the best diet plans were released on Jan. 3.
Once again, the Mediterranean diet, which emphasizes fruits, vegetables, olive oil, and fish, got the top spot, as best diet overall. It’s the sixth consecutive year for that win. But many other diets got top marks as well.
In 2023, U.S. News, with the help of more than 30 nutritionists, doctors, and epidemiologists, ranked 24 diets in several categories to help people find a plan that meets their goals, whether it’s finding the best weight loss diet, easiest one to follow, or plans for other goals, such as managing diabetes or heart disease. Two new categories were added: Best Diets for Bone & Joint Health and Best Family-Friendly Diets.
In previous years, the publication ranked 40 diets. Even if a diet is no longer ranked, its profile with detailed information remains on the site.
“Each year we ask ourselves what we can do better or differently next time,” said Gretel Schueller, managing editor of health for U.S. News. When the publication got feedback from their experts this year, they had requests to consider sustainability of diets and whether they meet a busy family’s needs, in addition to considering many other factors.
This year’s report ranks plans in 11 categories.
The winners and the categories:
Best diets overall
After the Mediterranean diet, two others tied for second place:
- DASH (Dietary Approaches to Stop Hypertension) diet, which fights high blood pressure and emphasizes fruits, vegetables, whole grains, lean protein, and low-fat dairy.
- Flexitarian diet, which focuses on fruits, vegetables, and other healthy foods but also allows occasional meat.
Best weight-loss diets
WW, formerly known as Weight Watchers, got first place. The plan emphasizes not only weight loss but healthier eating and regular activity. The Points program, which assigns specific points to foods, with a daily Points budget, is more personalized than in the past.
- DASH got second place.
- Mayo Clinic Diet and TLC diet tied for third place. The Mayo Clinic Diet focuses on fruits, vegetables, and whole grains. It helps people improve their eating habits. The TLC diet (Therapeutic Lifestyle Changes) focuses on vegetables, fruit, lean protein, and reducing cholesterol levels.
Best fast weight-loss diets
The keto diet got first place. It’s a high-fat, low-carb diet that aims to achieve weight loss through fat burning. Four others tied for second place:
- Atkins, a diet created by the cardiologist Robert Atkins, which begins with very few carbs and then recommends progressively eating more until the weight loss goal is achieved
- Nutrisystem, a commercial program that includes prepackaged meals and focuses on high-protein, lower-glycemic foods to stabilize blood sugar levels
- Optavia, a plan focused on low-carb, low-calorie foods and including fortified meal replacements
- SlimFast Diet, a plan of shakes, smoothies, and meal bars to replace two of three meals a day
Best diets for healthy eating
- Mediterranean
- DASH
- Flexitarian
Best heart-healthy diets
- DASH
- Mediterranean
- Flexitarian and Ornish tied for third. The Ornish Diet focuses on plant-based and whole foods and limiting animal products. It recommends daily exercise and stress reduction.
Best diets for diabetes
- DASH
- Mediterranean
- Flexitarian
Best diets for bone and joint health
DASH and Mediterranean are in a first-place tie, followed by the flexitarian diet.
Best family-friendly diets
This category has a three-way tie: the flexitarian, Mediterranean, and TLC diets.
Best plant-based diets
Mediterranean was first, then flexitarian and the MIND diet. The MIND diet combines the DASH and Mediterranean diets and focuses on “brain-healthy” foods.
Easiest diets to follow
Flexitarian and TLC tied for first, followed by a tie between DASH and Mediterranean.
Best diet programs (formerly called commercial plans)
- WW
- There was a tie for second place between Jenny Craig and Noom, the latter of which focuses on low-calorie foods, with personalized calorie ranges and coaching to help meet goals.
Methodology
A variety of factors were considered, such as whether a diet includes all food groups, how easy it is to follow, whether it can be customized to meet cultural and personal preferences, and if it has a realistic timeline for weight loss.
Response from diet plans
Representatives from two plans that received mixed reviews in the rankings responded.
Jenny Craig was ranked second for best diet program but much lower for family friendly, landing at 22nd place of 24.
“Our program is designed to address the needs of the individual through personalized experiences,” Jenny Craig CEO Mandy Dowson said. “We have many families that participate in our program together but are still evaluated separately to determine appropriate individual goals.”
Its high ranking for best diet program reflects feedback from satisfied members, she said. Among advances will be the new Jenny Fresh program, a line of entrées prepared fresh and delivered to customers’ doors.
Atkins got second place for best fast weight loss but ranked near the bottom for best overall, best weight loss, diabetes, healthy eating, and heart health. In response, Colette Heimowitz, vice president of nutrition and education for Simply Good Foods, which makes Atkins’s food products, said that low-carb eating approaches are a viable option for anyone today.
“There are more than 130 independent, peer-reviewed published studies that show the efficacy and safety of low-carb eating,” she said. “The studies have been conducted for several decades and counting.”
Expert perspective
Samantha Cassetty, a registered dietitian, nutritionist, and wellness expert in New York and author of Sugar Shock, reviewed the report for this news organization. She was not involved in the rankings.
“I think what this shows you is, the best diet overall is also the best for various conditions,” she said. For instance, the Mediterranean, the No. 1 overall, also got high ranking for diabetes, heart health, and bone and joint health.
For consumers trying to lose weight: “If you see fast weight loss, that should be a red flag. A healthy diet for weight loss is one you can sustain,” she said.
She’s not a fan of the programs with prepackaged foods. “It takes the guesswork out, but the portion sizes tend to be unsatisfying. They don’t teach you how to deal with some of the challenges [such as realizing an ‘ideal’ portion size].”
How to use the report
Ms. Schueller’s advice: “Recognize that no diet fits everyone.” When considering which plan to choose, she suggests thinking long-term.
“Whatever we choose has to work in the long run,” she said.
Consumers should consider expenses, meal prep time, and whether the diet fits their lifestyle.
Ideally, she said, the best diet “teaches you smart food preparation and how to make healthy choices, allows the flexibility to be social and eat with groups, whether family or friends.”
Before choosing a diet to follow, consult a medical professional for input on the decision, U.S. News cautioned.
A version of this article first appeared on Medscape.com.
After all, weight loss usually lands one of the top spots on New Year’s resolution surveys.
And just in time, there’s guidance to pick the best plan, as U.S. News & World Report’s annual rankings of the best diet plans were released on Jan. 3.
Once again, the Mediterranean diet, which emphasizes fruits, vegetables, olive oil, and fish, got the top spot, as best diet overall. It’s the sixth consecutive year for that win. But many other diets got top marks as well.
In 2023, U.S. News, with the help of more than 30 nutritionists, doctors, and epidemiologists, ranked 24 diets in several categories to help people find a plan that meets their goals, whether it’s finding the best weight loss diet, easiest one to follow, or plans for other goals, such as managing diabetes or heart disease. Two new categories were added: Best Diets for Bone & Joint Health and Best Family-Friendly Diets.
In previous years, the publication ranked 40 diets. Even if a diet is no longer ranked, its profile with detailed information remains on the site.
“Each year we ask ourselves what we can do better or differently next time,” said Gretel Schueller, managing editor of health for U.S. News. When the publication got feedback from their experts this year, they had requests to consider sustainability of diets and whether they meet a busy family’s needs, in addition to considering many other factors.
This year’s report ranks plans in 11 categories.
The winners and the categories:
Best diets overall
After the Mediterranean diet, two others tied for second place:
- DASH (Dietary Approaches to Stop Hypertension) diet, which fights high blood pressure and emphasizes fruits, vegetables, whole grains, lean protein, and low-fat dairy.
- Flexitarian diet, which focuses on fruits, vegetables, and other healthy foods but also allows occasional meat.
Best weight-loss diets
WW, formerly known as Weight Watchers, got first place. The plan emphasizes not only weight loss but healthier eating and regular activity. The Points program, which assigns specific points to foods, with a daily Points budget, is more personalized than in the past.
- DASH got second place.
- Mayo Clinic Diet and TLC diet tied for third place. The Mayo Clinic Diet focuses on fruits, vegetables, and whole grains. It helps people improve their eating habits. The TLC diet (Therapeutic Lifestyle Changes) focuses on vegetables, fruit, lean protein, and reducing cholesterol levels.
Best fast weight-loss diets
The keto diet got first place. It’s a high-fat, low-carb diet that aims to achieve weight loss through fat burning. Four others tied for second place:
- Atkins, a diet created by the cardiologist Robert Atkins, which begins with very few carbs and then recommends progressively eating more until the weight loss goal is achieved
- Nutrisystem, a commercial program that includes prepackaged meals and focuses on high-protein, lower-glycemic foods to stabilize blood sugar levels
- Optavia, a plan focused on low-carb, low-calorie foods and including fortified meal replacements
- SlimFast Diet, a plan of shakes, smoothies, and meal bars to replace two of three meals a day
Best diets for healthy eating
- Mediterranean
- DASH
- Flexitarian
Best heart-healthy diets
- DASH
- Mediterranean
- Flexitarian and Ornish tied for third. The Ornish Diet focuses on plant-based and whole foods and limiting animal products. It recommends daily exercise and stress reduction.
Best diets for diabetes
- DASH
- Mediterranean
- Flexitarian
Best diets for bone and joint health
DASH and Mediterranean are in a first-place tie, followed by the flexitarian diet.
Best family-friendly diets
This category has a three-way tie: the flexitarian, Mediterranean, and TLC diets.
Best plant-based diets
Mediterranean was first, then flexitarian and the MIND diet. The MIND diet combines the DASH and Mediterranean diets and focuses on “brain-healthy” foods.
Easiest diets to follow
Flexitarian and TLC tied for first, followed by a tie between DASH and Mediterranean.
Best diet programs (formerly called commercial plans)
- WW
- There was a tie for second place between Jenny Craig and Noom, the latter of which focuses on low-calorie foods, with personalized calorie ranges and coaching to help meet goals.
Methodology
A variety of factors were considered, such as whether a diet includes all food groups, how easy it is to follow, whether it can be customized to meet cultural and personal preferences, and if it has a realistic timeline for weight loss.
Response from diet plans
Representatives from two plans that received mixed reviews in the rankings responded.
Jenny Craig was ranked second for best diet program but much lower for family friendly, landing at 22nd place of 24.
“Our program is designed to address the needs of the individual through personalized experiences,” Jenny Craig CEO Mandy Dowson said. “We have many families that participate in our program together but are still evaluated separately to determine appropriate individual goals.”
Its high ranking for best diet program reflects feedback from satisfied members, she said. Among advances will be the new Jenny Fresh program, a line of entrées prepared fresh and delivered to customers’ doors.
Atkins got second place for best fast weight loss but ranked near the bottom for best overall, best weight loss, diabetes, healthy eating, and heart health. In response, Colette Heimowitz, vice president of nutrition and education for Simply Good Foods, which makes Atkins’s food products, said that low-carb eating approaches are a viable option for anyone today.
“There are more than 130 independent, peer-reviewed published studies that show the efficacy and safety of low-carb eating,” she said. “The studies have been conducted for several decades and counting.”
Expert perspective
Samantha Cassetty, a registered dietitian, nutritionist, and wellness expert in New York and author of Sugar Shock, reviewed the report for this news organization. She was not involved in the rankings.
“I think what this shows you is, the best diet overall is also the best for various conditions,” she said. For instance, the Mediterranean, the No. 1 overall, also got high ranking for diabetes, heart health, and bone and joint health.
For consumers trying to lose weight: “If you see fast weight loss, that should be a red flag. A healthy diet for weight loss is one you can sustain,” she said.
She’s not a fan of the programs with prepackaged foods. “It takes the guesswork out, but the portion sizes tend to be unsatisfying. They don’t teach you how to deal with some of the challenges [such as realizing an ‘ideal’ portion size].”
How to use the report
Ms. Schueller’s advice: “Recognize that no diet fits everyone.” When considering which plan to choose, she suggests thinking long-term.
“Whatever we choose has to work in the long run,” she said.
Consumers should consider expenses, meal prep time, and whether the diet fits their lifestyle.
Ideally, she said, the best diet “teaches you smart food preparation and how to make healthy choices, allows the flexibility to be social and eat with groups, whether family or friends.”
Before choosing a diet to follow, consult a medical professional for input on the decision, U.S. News cautioned.
A version of this article first appeared on Medscape.com.
After all, weight loss usually lands one of the top spots on New Year’s resolution surveys.
And just in time, there’s guidance to pick the best plan, as U.S. News & World Report’s annual rankings of the best diet plans were released on Jan. 3.
Once again, the Mediterranean diet, which emphasizes fruits, vegetables, olive oil, and fish, got the top spot, as best diet overall. It’s the sixth consecutive year for that win. But many other diets got top marks as well.
In 2023, U.S. News, with the help of more than 30 nutritionists, doctors, and epidemiologists, ranked 24 diets in several categories to help people find a plan that meets their goals, whether it’s finding the best weight loss diet, easiest one to follow, or plans for other goals, such as managing diabetes or heart disease. Two new categories were added: Best Diets for Bone & Joint Health and Best Family-Friendly Diets.
In previous years, the publication ranked 40 diets. Even if a diet is no longer ranked, its profile with detailed information remains on the site.
“Each year we ask ourselves what we can do better or differently next time,” said Gretel Schueller, managing editor of health for U.S. News. When the publication got feedback from their experts this year, they had requests to consider sustainability of diets and whether they meet a busy family’s needs, in addition to considering many other factors.
This year’s report ranks plans in 11 categories.
The winners and the categories:
Best diets overall
After the Mediterranean diet, two others tied for second place:
- DASH (Dietary Approaches to Stop Hypertension) diet, which fights high blood pressure and emphasizes fruits, vegetables, whole grains, lean protein, and low-fat dairy.
- Flexitarian diet, which focuses on fruits, vegetables, and other healthy foods but also allows occasional meat.
Best weight-loss diets
WW, formerly known as Weight Watchers, got first place. The plan emphasizes not only weight loss but healthier eating and regular activity. The Points program, which assigns specific points to foods, with a daily Points budget, is more personalized than in the past.
- DASH got second place.
- Mayo Clinic Diet and TLC diet tied for third place. The Mayo Clinic Diet focuses on fruits, vegetables, and whole grains. It helps people improve their eating habits. The TLC diet (Therapeutic Lifestyle Changes) focuses on vegetables, fruit, lean protein, and reducing cholesterol levels.
Best fast weight-loss diets
The keto diet got first place. It’s a high-fat, low-carb diet that aims to achieve weight loss through fat burning. Four others tied for second place:
- Atkins, a diet created by the cardiologist Robert Atkins, which begins with very few carbs and then recommends progressively eating more until the weight loss goal is achieved
- Nutrisystem, a commercial program that includes prepackaged meals and focuses on high-protein, lower-glycemic foods to stabilize blood sugar levels
- Optavia, a plan focused on low-carb, low-calorie foods and including fortified meal replacements
- SlimFast Diet, a plan of shakes, smoothies, and meal bars to replace two of three meals a day
Best diets for healthy eating
- Mediterranean
- DASH
- Flexitarian
Best heart-healthy diets
- DASH
- Mediterranean
- Flexitarian and Ornish tied for third. The Ornish Diet focuses on plant-based and whole foods and limiting animal products. It recommends daily exercise and stress reduction.
Best diets for diabetes
- DASH
- Mediterranean
- Flexitarian
Best diets for bone and joint health
DASH and Mediterranean are in a first-place tie, followed by the flexitarian diet.
Best family-friendly diets
This category has a three-way tie: the flexitarian, Mediterranean, and TLC diets.
Best plant-based diets
Mediterranean was first, then flexitarian and the MIND diet. The MIND diet combines the DASH and Mediterranean diets and focuses on “brain-healthy” foods.
Easiest diets to follow
Flexitarian and TLC tied for first, followed by a tie between DASH and Mediterranean.
Best diet programs (formerly called commercial plans)
- WW
- There was a tie for second place between Jenny Craig and Noom, the latter of which focuses on low-calorie foods, with personalized calorie ranges and coaching to help meet goals.
Methodology
A variety of factors were considered, such as whether a diet includes all food groups, how easy it is to follow, whether it can be customized to meet cultural and personal preferences, and if it has a realistic timeline for weight loss.
Response from diet plans
Representatives from two plans that received mixed reviews in the rankings responded.
Jenny Craig was ranked second for best diet program but much lower for family friendly, landing at 22nd place of 24.
“Our program is designed to address the needs of the individual through personalized experiences,” Jenny Craig CEO Mandy Dowson said. “We have many families that participate in our program together but are still evaluated separately to determine appropriate individual goals.”
Its high ranking for best diet program reflects feedback from satisfied members, she said. Among advances will be the new Jenny Fresh program, a line of entrées prepared fresh and delivered to customers’ doors.
Atkins got second place for best fast weight loss but ranked near the bottom for best overall, best weight loss, diabetes, healthy eating, and heart health. In response, Colette Heimowitz, vice president of nutrition and education for Simply Good Foods, which makes Atkins’s food products, said that low-carb eating approaches are a viable option for anyone today.
“There are more than 130 independent, peer-reviewed published studies that show the efficacy and safety of low-carb eating,” she said. “The studies have been conducted for several decades and counting.”
Expert perspective
Samantha Cassetty, a registered dietitian, nutritionist, and wellness expert in New York and author of Sugar Shock, reviewed the report for this news organization. She was not involved in the rankings.
“I think what this shows you is, the best diet overall is also the best for various conditions,” she said. For instance, the Mediterranean, the No. 1 overall, also got high ranking for diabetes, heart health, and bone and joint health.
For consumers trying to lose weight: “If you see fast weight loss, that should be a red flag. A healthy diet for weight loss is one you can sustain,” she said.
She’s not a fan of the programs with prepackaged foods. “It takes the guesswork out, but the portion sizes tend to be unsatisfying. They don’t teach you how to deal with some of the challenges [such as realizing an ‘ideal’ portion size].”
How to use the report
Ms. Schueller’s advice: “Recognize that no diet fits everyone.” When considering which plan to choose, she suggests thinking long-term.
“Whatever we choose has to work in the long run,” she said.
Consumers should consider expenses, meal prep time, and whether the diet fits their lifestyle.
Ideally, she said, the best diet “teaches you smart food preparation and how to make healthy choices, allows the flexibility to be social and eat with groups, whether family or friends.”
Before choosing a diet to follow, consult a medical professional for input on the decision, U.S. News cautioned.
A version of this article first appeared on Medscape.com.
Proximal ADR could become important new quality metric
Measurement of the proximal adenoma detection rate may be an important new quality metric for screening colonoscopy, propose researchers in a study that found proportionately more adenomas detected in the right colon with increasing patient age.
As patients age, in fact, the rate of increase of proximal adenomas is far greater than for distal adenomas in both men and women and in all races, wrote Lawrence Kosinski, MD, founder and chief medical officer of Sonar MD in Chicago, and colleagues.
Adenoma detection rate (ADR), the proportion of screening colonoscopies performed by a physician that detect at least one histologically confirmed colorectal adenoma or adenocarcinoma, has become an accepted quality metric because of the association of high ADR with lower rates of postcolonoscopy colorectal cancer (CRC). ADR varies widely among endoscopists, however, which could be related to differences in adenoma detection in different parts of the colon.
the authors wrote. “These differences could be clinically important if CRC occurs after colonoscopy.” The study was published in Techniques and Innovations in Gastrointestinal Endoscopy .
Dr. Kosinski and colleagues analyzed retrospective claims data from all colonoscopies performed between 2016-2018 submitted to the Health Care Service Corporation, which is the exclusive Blue Cross Blue Shield licensee for Illinois, Texas, Oklahoma, New Mexico, and Montana. All 50 states were represented in the patient population, though Illinois and Texas accounted for 66% of the cases.
The research team limited the study group to include patients who underwent a screening colonoscopy, representing 30.9% of the total population. They further refined the data to include only screening colonoscopies performed by the 710 endoscopists with at least 100 screenings during the study period, representing 34.5% of the total patients. They also excluded 10,685 cases with family history because the high-risk patients could alter the results.
Using ICD-10 codes, the researchers identified the polyp detection locations and then calculated the ADR for the entire colon (T-ADR) and both the proximal (P-ADR) and distal (D-ADR) colon to determine differences in the ratio of P-ADR versus D-ADR by age, sex, and race. They were unable to determine whether the polyps were adenomas or sessile serrated lesions, so the ADR calculations include both.
The 182,296 screening colonoscopies included 93,164 women (51%) and 89,132 men (49%). About 79% of patients were aged 50-64 years, and 5.8% were under age 50. The dataset preceded the U.S. Preventive Services Task Force recommendation to initiate screening at age 45.
Overall, T-ADR was consistent with accepted norms in both men (25.99%) and women (19.72%). Compared with women, men had a 4.5% higher prevalence of proximal adenomas and a 2.5% higher prevalence of distal adenomas at any age. The small cohort of Native Americans (296 patients) had a numerically higher T-ADR, P-ADR, and D-ADR than other groups.
By age, T-ADR increased significantly with advancing age, from 0.13 in patients under age 40 to 0.39 in ages 70 and older. The increase was driven by a sharp rise in P-ADR, particularly after age 60. There was a relatively small increase in D-ADR after ages 45-49.
Notably, the P-ADR/D-ADR ratio increased from 1.2 in patients under age 40 to 2.65 in ages 75 and older in both men and women.
Since the experience of the endoscopist affects ADR, the research team also calculated the ADR data by the number of total colonoscopies by endoscopist per decile. T-ADR, P-ADR, and D-ADR were associated directly in a linear relationship with the number of total colonoscopies performed. The slope of the P-ADR trendline was 2.3 times higher than the slope of the D-ADR trendline, indicating a higher volume of procedures directly related to higher polyp detection – specifically the P-ADR.
“Our data demonstrate that it is feasible to measure P-ADR in clinical practice,” the authors wrote. “We propose that P-ADR be considered a quality metric for colonoscopy.”
In addition, because of considerable variation in ADR based on age and sex, calculated ADR should be normalized by the age and sex of the specific patient profile of each endoscopist so relevant benchmarks can be established based on practice demographics, they wrote. For example, an endoscopist with a practice that includes predominantly younger women would have a different benchmark than a colleague with an older male population.
“With appropriate use of gender and age adjustments to ADR, endoscopists in need of further education and mentoring can be identified,” they wrote.
The authors declared no funding for the study. One author reported advisory roles for several medical companies, and the remaining authors disclosed no conflicts.
“What gets measured gets managed” is a common mantra in quality improvement. Adenoma detection rate (ADR) is currently one measure of a “quality” colonoscopy and a metric that is studied to determine means for improvement. ADR is an imperfect measure as it does not necessarily reflect true risk of a postcolonoscopy cancer in all parts of the colon since many post colonoscopy cancers are found in the proximal colon. To try to better understand potential differences in polyps found in different segments of the colon, and to determine if this was a metric that could be measured, Kosinski and colleagues studied a large claims database to understand the potential difference in ADR in the proximal versus distal colon.
Sunanda Kane, MD, MSPH, is professor of medicine in the division of gastroenterology and hepatology at the Mayo Clinic, Rochester, Minn. Dr. Kane has no relevant conflicts of interest.
“What gets measured gets managed” is a common mantra in quality improvement. Adenoma detection rate (ADR) is currently one measure of a “quality” colonoscopy and a metric that is studied to determine means for improvement. ADR is an imperfect measure as it does not necessarily reflect true risk of a postcolonoscopy cancer in all parts of the colon since many post colonoscopy cancers are found in the proximal colon. To try to better understand potential differences in polyps found in different segments of the colon, and to determine if this was a metric that could be measured, Kosinski and colleagues studied a large claims database to understand the potential difference in ADR in the proximal versus distal colon.
Sunanda Kane, MD, MSPH, is professor of medicine in the division of gastroenterology and hepatology at the Mayo Clinic, Rochester, Minn. Dr. Kane has no relevant conflicts of interest.
“What gets measured gets managed” is a common mantra in quality improvement. Adenoma detection rate (ADR) is currently one measure of a “quality” colonoscopy and a metric that is studied to determine means for improvement. ADR is an imperfect measure as it does not necessarily reflect true risk of a postcolonoscopy cancer in all parts of the colon since many post colonoscopy cancers are found in the proximal colon. To try to better understand potential differences in polyps found in different segments of the colon, and to determine if this was a metric that could be measured, Kosinski and colleagues studied a large claims database to understand the potential difference in ADR in the proximal versus distal colon.
Sunanda Kane, MD, MSPH, is professor of medicine in the division of gastroenterology and hepatology at the Mayo Clinic, Rochester, Minn. Dr. Kane has no relevant conflicts of interest.
Measurement of the proximal adenoma detection rate may be an important new quality metric for screening colonoscopy, propose researchers in a study that found proportionately more adenomas detected in the right colon with increasing patient age.
As patients age, in fact, the rate of increase of proximal adenomas is far greater than for distal adenomas in both men and women and in all races, wrote Lawrence Kosinski, MD, founder and chief medical officer of Sonar MD in Chicago, and colleagues.
Adenoma detection rate (ADR), the proportion of screening colonoscopies performed by a physician that detect at least one histologically confirmed colorectal adenoma or adenocarcinoma, has become an accepted quality metric because of the association of high ADR with lower rates of postcolonoscopy colorectal cancer (CRC). ADR varies widely among endoscopists, however, which could be related to differences in adenoma detection in different parts of the colon.
the authors wrote. “These differences could be clinically important if CRC occurs after colonoscopy.” The study was published in Techniques and Innovations in Gastrointestinal Endoscopy .
Dr. Kosinski and colleagues analyzed retrospective claims data from all colonoscopies performed between 2016-2018 submitted to the Health Care Service Corporation, which is the exclusive Blue Cross Blue Shield licensee for Illinois, Texas, Oklahoma, New Mexico, and Montana. All 50 states were represented in the patient population, though Illinois and Texas accounted for 66% of the cases.
The research team limited the study group to include patients who underwent a screening colonoscopy, representing 30.9% of the total population. They further refined the data to include only screening colonoscopies performed by the 710 endoscopists with at least 100 screenings during the study period, representing 34.5% of the total patients. They also excluded 10,685 cases with family history because the high-risk patients could alter the results.
Using ICD-10 codes, the researchers identified the polyp detection locations and then calculated the ADR for the entire colon (T-ADR) and both the proximal (P-ADR) and distal (D-ADR) colon to determine differences in the ratio of P-ADR versus D-ADR by age, sex, and race. They were unable to determine whether the polyps were adenomas or sessile serrated lesions, so the ADR calculations include both.
The 182,296 screening colonoscopies included 93,164 women (51%) and 89,132 men (49%). About 79% of patients were aged 50-64 years, and 5.8% were under age 50. The dataset preceded the U.S. Preventive Services Task Force recommendation to initiate screening at age 45.
Overall, T-ADR was consistent with accepted norms in both men (25.99%) and women (19.72%). Compared with women, men had a 4.5% higher prevalence of proximal adenomas and a 2.5% higher prevalence of distal adenomas at any age. The small cohort of Native Americans (296 patients) had a numerically higher T-ADR, P-ADR, and D-ADR than other groups.
By age, T-ADR increased significantly with advancing age, from 0.13 in patients under age 40 to 0.39 in ages 70 and older. The increase was driven by a sharp rise in P-ADR, particularly after age 60. There was a relatively small increase in D-ADR after ages 45-49.
Notably, the P-ADR/D-ADR ratio increased from 1.2 in patients under age 40 to 2.65 in ages 75 and older in both men and women.
Since the experience of the endoscopist affects ADR, the research team also calculated the ADR data by the number of total colonoscopies by endoscopist per decile. T-ADR, P-ADR, and D-ADR were associated directly in a linear relationship with the number of total colonoscopies performed. The slope of the P-ADR trendline was 2.3 times higher than the slope of the D-ADR trendline, indicating a higher volume of procedures directly related to higher polyp detection – specifically the P-ADR.
“Our data demonstrate that it is feasible to measure P-ADR in clinical practice,” the authors wrote. “We propose that P-ADR be considered a quality metric for colonoscopy.”
In addition, because of considerable variation in ADR based on age and sex, calculated ADR should be normalized by the age and sex of the specific patient profile of each endoscopist so relevant benchmarks can be established based on practice demographics, they wrote. For example, an endoscopist with a practice that includes predominantly younger women would have a different benchmark than a colleague with an older male population.
“With appropriate use of gender and age adjustments to ADR, endoscopists in need of further education and mentoring can be identified,” they wrote.
The authors declared no funding for the study. One author reported advisory roles for several medical companies, and the remaining authors disclosed no conflicts.
Measurement of the proximal adenoma detection rate may be an important new quality metric for screening colonoscopy, propose researchers in a study that found proportionately more adenomas detected in the right colon with increasing patient age.
As patients age, in fact, the rate of increase of proximal adenomas is far greater than for distal adenomas in both men and women and in all races, wrote Lawrence Kosinski, MD, founder and chief medical officer of Sonar MD in Chicago, and colleagues.
Adenoma detection rate (ADR), the proportion of screening colonoscopies performed by a physician that detect at least one histologically confirmed colorectal adenoma or adenocarcinoma, has become an accepted quality metric because of the association of high ADR with lower rates of postcolonoscopy colorectal cancer (CRC). ADR varies widely among endoscopists, however, which could be related to differences in adenoma detection in different parts of the colon.
the authors wrote. “These differences could be clinically important if CRC occurs after colonoscopy.” The study was published in Techniques and Innovations in Gastrointestinal Endoscopy .
Dr. Kosinski and colleagues analyzed retrospective claims data from all colonoscopies performed between 2016-2018 submitted to the Health Care Service Corporation, which is the exclusive Blue Cross Blue Shield licensee for Illinois, Texas, Oklahoma, New Mexico, and Montana. All 50 states were represented in the patient population, though Illinois and Texas accounted for 66% of the cases.
The research team limited the study group to include patients who underwent a screening colonoscopy, representing 30.9% of the total population. They further refined the data to include only screening colonoscopies performed by the 710 endoscopists with at least 100 screenings during the study period, representing 34.5% of the total patients. They also excluded 10,685 cases with family history because the high-risk patients could alter the results.
Using ICD-10 codes, the researchers identified the polyp detection locations and then calculated the ADR for the entire colon (T-ADR) and both the proximal (P-ADR) and distal (D-ADR) colon to determine differences in the ratio of P-ADR versus D-ADR by age, sex, and race. They were unable to determine whether the polyps were adenomas or sessile serrated lesions, so the ADR calculations include both.
The 182,296 screening colonoscopies included 93,164 women (51%) and 89,132 men (49%). About 79% of patients were aged 50-64 years, and 5.8% were under age 50. The dataset preceded the U.S. Preventive Services Task Force recommendation to initiate screening at age 45.
Overall, T-ADR was consistent with accepted norms in both men (25.99%) and women (19.72%). Compared with women, men had a 4.5% higher prevalence of proximal adenomas and a 2.5% higher prevalence of distal adenomas at any age. The small cohort of Native Americans (296 patients) had a numerically higher T-ADR, P-ADR, and D-ADR than other groups.
By age, T-ADR increased significantly with advancing age, from 0.13 in patients under age 40 to 0.39 in ages 70 and older. The increase was driven by a sharp rise in P-ADR, particularly after age 60. There was a relatively small increase in D-ADR after ages 45-49.
Notably, the P-ADR/D-ADR ratio increased from 1.2 in patients under age 40 to 2.65 in ages 75 and older in both men and women.
Since the experience of the endoscopist affects ADR, the research team also calculated the ADR data by the number of total colonoscopies by endoscopist per decile. T-ADR, P-ADR, and D-ADR were associated directly in a linear relationship with the number of total colonoscopies performed. The slope of the P-ADR trendline was 2.3 times higher than the slope of the D-ADR trendline, indicating a higher volume of procedures directly related to higher polyp detection – specifically the P-ADR.
“Our data demonstrate that it is feasible to measure P-ADR in clinical practice,” the authors wrote. “We propose that P-ADR be considered a quality metric for colonoscopy.”
In addition, because of considerable variation in ADR based on age and sex, calculated ADR should be normalized by the age and sex of the specific patient profile of each endoscopist so relevant benchmarks can be established based on practice demographics, they wrote. For example, an endoscopist with a practice that includes predominantly younger women would have a different benchmark than a colleague with an older male population.
“With appropriate use of gender and age adjustments to ADR, endoscopists in need of further education and mentoring can be identified,” they wrote.
The authors declared no funding for the study. One author reported advisory roles for several medical companies, and the remaining authors disclosed no conflicts.
FROM TECHNIQUES AND INNOVATIONS IN GASTROINTESTINAL ENDOSCOPY
Children and COVID: New cases fell as the old year ended
The end of 2022 saw a drop in new COVID-19 cases in children, even as rates of emergency department visits continued upward trends that began in late October.
New cases for the week of Dec. 23-29 fell for the first time since late November, according to the American Academy of Pediatrics and the Children’s Hospital Association.
The AAP/CHA analysis of publicly available state data differs somewhat from figures reported by the Centers for Disease Control and Prevention, which has new cases for the latest available week, Dec.18-24, at just over 27,000 after 3 straight weeks of declines from a count of almost 63,000 for the week ending Nov. 26. The CDC, however, updates previously reported data on a regular basis, so that 27,000 is likely to increase in the coming weeks.
The CDC line on the graph also shows a peak for the week of Oct. 30 to Nov. 5 when new cases reached almost 50,000, compared with almost 30,000 reported for the week of Oct. 28 to Nov. 3 by the AAP and CHA in their report of state-level data. The AAP and CHA put the total number of child COVID cases since the start of the pandemic at 15.2 million as of Dec. 29, while the CDC reports 16.2 million cases as of Dec. 28.
There have been 1,975 deaths from COVID-19 in children aged 0-17 years, according to the CDC, which amounts to just over 0.2% of all COVID deaths for which age group data were available.
CDC data on emergency department visits involving diagnosed COVID-19 have been rising since late October. In children aged 0-11 years, for example, COVID was involved in 1.0% of ED visits (7-day average) as late as Nov. 4, but by Dec. 27 that rate was 2.6%. Children aged 12-15 years went from 0.6% on Oct. 28 to 1.5% on Dec. 27, while 16- to 17-year-olds had ED visit rates of 0.6% on Oct. 19 and 1.7% on Dec. 27, the CDC said on its COVID Data Tracker.
New hospital admissions with diagnosed COVID, which had been following the same upward trend as ED visits since late October, halted that rise in children aged 0-17 years and have gone no higher than 0.29 per 100,000 population since Dec. 9, the CDC data show.
The end of 2022 saw a drop in new COVID-19 cases in children, even as rates of emergency department visits continued upward trends that began in late October.
New cases for the week of Dec. 23-29 fell for the first time since late November, according to the American Academy of Pediatrics and the Children’s Hospital Association.
The AAP/CHA analysis of publicly available state data differs somewhat from figures reported by the Centers for Disease Control and Prevention, which has new cases for the latest available week, Dec.18-24, at just over 27,000 after 3 straight weeks of declines from a count of almost 63,000 for the week ending Nov. 26. The CDC, however, updates previously reported data on a regular basis, so that 27,000 is likely to increase in the coming weeks.
The CDC line on the graph also shows a peak for the week of Oct. 30 to Nov. 5 when new cases reached almost 50,000, compared with almost 30,000 reported for the week of Oct. 28 to Nov. 3 by the AAP and CHA in their report of state-level data. The AAP and CHA put the total number of child COVID cases since the start of the pandemic at 15.2 million as of Dec. 29, while the CDC reports 16.2 million cases as of Dec. 28.
There have been 1,975 deaths from COVID-19 in children aged 0-17 years, according to the CDC, which amounts to just over 0.2% of all COVID deaths for which age group data were available.
CDC data on emergency department visits involving diagnosed COVID-19 have been rising since late October. In children aged 0-11 years, for example, COVID was involved in 1.0% of ED visits (7-day average) as late as Nov. 4, but by Dec. 27 that rate was 2.6%. Children aged 12-15 years went from 0.6% on Oct. 28 to 1.5% on Dec. 27, while 16- to 17-year-olds had ED visit rates of 0.6% on Oct. 19 and 1.7% on Dec. 27, the CDC said on its COVID Data Tracker.
New hospital admissions with diagnosed COVID, which had been following the same upward trend as ED visits since late October, halted that rise in children aged 0-17 years and have gone no higher than 0.29 per 100,000 population since Dec. 9, the CDC data show.
The end of 2022 saw a drop in new COVID-19 cases in children, even as rates of emergency department visits continued upward trends that began in late October.
New cases for the week of Dec. 23-29 fell for the first time since late November, according to the American Academy of Pediatrics and the Children’s Hospital Association.
The AAP/CHA analysis of publicly available state data differs somewhat from figures reported by the Centers for Disease Control and Prevention, which has new cases for the latest available week, Dec.18-24, at just over 27,000 after 3 straight weeks of declines from a count of almost 63,000 for the week ending Nov. 26. The CDC, however, updates previously reported data on a regular basis, so that 27,000 is likely to increase in the coming weeks.
The CDC line on the graph also shows a peak for the week of Oct. 30 to Nov. 5 when new cases reached almost 50,000, compared with almost 30,000 reported for the week of Oct. 28 to Nov. 3 by the AAP and CHA in their report of state-level data. The AAP and CHA put the total number of child COVID cases since the start of the pandemic at 15.2 million as of Dec. 29, while the CDC reports 16.2 million cases as of Dec. 28.
There have been 1,975 deaths from COVID-19 in children aged 0-17 years, according to the CDC, which amounts to just over 0.2% of all COVID deaths for which age group data were available.
CDC data on emergency department visits involving diagnosed COVID-19 have been rising since late October. In children aged 0-11 years, for example, COVID was involved in 1.0% of ED visits (7-day average) as late as Nov. 4, but by Dec. 27 that rate was 2.6%. Children aged 12-15 years went from 0.6% on Oct. 28 to 1.5% on Dec. 27, while 16- to 17-year-olds had ED visit rates of 0.6% on Oct. 19 and 1.7% on Dec. 27, the CDC said on its COVID Data Tracker.
New hospital admissions with diagnosed COVID, which had been following the same upward trend as ED visits since late October, halted that rise in children aged 0-17 years and have gone no higher than 0.29 per 100,000 population since Dec. 9, the CDC data show.
Antiepileptic drugs tied to increased Parkinson’s disease risk
, new research suggests.
Drawing on data from the UK Biobank, investigators compared more than 1,400 individuals diagnosed with Parkinson’s disease with matched control persons and found a considerably higher risk of developing Parkinson’s disease among those who had taken AEDs in comparison with those who had not. There was a trend linking a greater number of AED prescriptions and multiple AEDs associated with a greater risk for Parkinson’s disease.
“We observed an association between the most commonly prescribed antiepileptic drugs in the U.K. and Parkinson’s disease using data from UK Biobank,” said senior author Alastair Noyce, PhD, professor of neurology and neuroepidemiology and honorary consultant neurologist, Queen Mary University of London.
“This is the first time that a comprehensive study of the link between AEDs and Parkinson’s disease has been undertaken,” said Dr. Noyce.
He added that the findings have no immediate clinical implications, “but further research is definitely needed, [as] this is an interesting observation made in a research setting.”
The study was published online in JAMA Neurology.
Plausible, but unclear link
Recent observational studies have found a “temporal association” between epilepsy and incident Parkinson’s disease, but the mechanism underlying this association is “unclear,” the authors wrote.
It is “plausible” that AEDs “may account for some or all of the apparent association between epilepsy and Parkinson’s disease” and that movement disorders are potential side effects of AEDs, but the association between AEDs and Parkinson’s disease has “not been well studied,” so it remains “unclear” whether AEDs play a role in the association.
“We have previously reported an association between epilepsy and Parkinson’s disease in several different datasets. Here, we wanted to see if it could be explained by an association with the drugs used to treat epilepsy rather than epilepsy per se,” Dr. Noyce explained.
Are AEDs the culprit?
The researchers used data from the UK Biobank, a longitudinal cohort study with more than 500,000 participants, as well as linked primary care medication data to conduct a nested case-control study to investigate this potential association. Participants ranged in age from 40 to 69 years and were recruited between 2006 and 2010.
The researchers compared 1,433 individuals diagnosed with Parkinson’s disease with 8,598 control persons who were matched in a 6:1 ratio for age, sex, race, ethnicity, and socioeconomic status (median [interquartile range] age, 71 [65-75] years; 60.9% men; 97.5% White).
Of those with Parkinson’s disease, 4.3% had been prescribed an AED prior to the date of their being diagnosed with Parkinson’s disease, compared with 2.5% in the control group; 4.4% had been diagnosed with epilepsy, compared with 1% of the control persons.
The strongest evidence was for the association between lamotrigine, levetiracetam, and sodium valproate and Parkinson’s disease. There was “weaker evidence” for carbamazepine, although all the AEDs were associated with a higher risk of Parkinson’s disease.
The odds of incident Parkinson’s disease were higher among those who were prescribed one or more AEDs and among individuals who were issued a higher number of prescriptions, the authors reported.
It is possible that it is the epilepsy itself that is associated with the risk of Parkinson’s disease, rather than the drugs, and that “likely explains part of the association we are seeing,” said Dr. Noyce.
“The bottom line is that more research into the links between epilepsy – and drugs used to treat epilepsy – and Parkinson’s disease is needed,” he said.
Moreover, “only with time will we work out whether the findings hold any real clinical relevance,” he added.
Alternative explanations
Commenting on the research, Rebecca Gilbert, MD, PhD, chief scientific officer, American Parkinson Disease Association, said, “It has been established in prior research that there is an association between epilepsy and Parkinson’s disease.” The current study “shows that having had a prescription written for one of four antiepileptic medications was associated with subsequently receiving a diagnosis of Parkinson’s disease.”
Although one possible conclusion is that the AEDs themselves increase the risk of developing Parkinson’s disease, “there seem to be other alternative explanations as to why a person who had been prescribed AEDs has an increased risk of receiving a diagnosis of Parkinson’s disease,” said Dr. Gilbert, an associate professor of neurology at Bellevue Hospital Center, New York, who was not involved with the current study.
For example, pre-motor changes in the brain of persons with Parkinson’s disease “may increase the risk of requiring an AED by potentially increasing the risk of having a seizure,” and “changes in the brain caused by the seizures for which AEDs are prescribed may increase the risk of Parkinson’s disease.”
Moreover, psychiatric changes related to Parkinson’s disease may have led to the prescription for AEDs, because at least two of the AEDs are also prescribed for mood stabilization, Dr. Gilbert suggested.
“An unanswered question that the paper acknowledges is, what about people who receive AEDs for reasons other than seizures? Do they also have an increased risk of Parkinson’s disease? This would be an interesting population to focus on because it would remove the link between AEDs and seizure and focus on the association between AEDs and Parkinson’s disease,” Dr. Gilbert said.
She emphasized that people who take AEDs for seizures “should not jump to the conclusion that they must come off these medications so as not to increase their risk of developing Parkinson’s disease.” She noted that having seizures “can be dangerous – injuries can occur during a seizure, and if a seizure can’t be stopped or a number occur in rapid succession, brain injury may result.”
For these reasons, people with “a tendency to have seizures need to protect themselves with AEDs” and “should certainly reach out to their neurologists with any questions,” Dr. Gilbert said.
The Preventive Neurology Unit is funded by Barts Charity. The Apocrita High Performance Cluster facility, supported by Queen Mary University London Research–IT Services, was used for this research. Dr. Noyce has received grants from Barts Charity, Parkinson’s UK, Cure Parkinson’s, the Michael J. Fox Foundation, Innovate UK, Solvemed, and Alchemab and personal fees from AstraZeneca, AbbVie, Zambon, BIAL, uMedeor, Alchemab, Britannia, and Charco Neurotech outside the submitted work. The other authors’ disclosures are listed on the original article. Dr. Gilbert reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new research suggests.
Drawing on data from the UK Biobank, investigators compared more than 1,400 individuals diagnosed with Parkinson’s disease with matched control persons and found a considerably higher risk of developing Parkinson’s disease among those who had taken AEDs in comparison with those who had not. There was a trend linking a greater number of AED prescriptions and multiple AEDs associated with a greater risk for Parkinson’s disease.
“We observed an association between the most commonly prescribed antiepileptic drugs in the U.K. and Parkinson’s disease using data from UK Biobank,” said senior author Alastair Noyce, PhD, professor of neurology and neuroepidemiology and honorary consultant neurologist, Queen Mary University of London.
“This is the first time that a comprehensive study of the link between AEDs and Parkinson’s disease has been undertaken,” said Dr. Noyce.
He added that the findings have no immediate clinical implications, “but further research is definitely needed, [as] this is an interesting observation made in a research setting.”
The study was published online in JAMA Neurology.
Plausible, but unclear link
Recent observational studies have found a “temporal association” between epilepsy and incident Parkinson’s disease, but the mechanism underlying this association is “unclear,” the authors wrote.
It is “plausible” that AEDs “may account for some or all of the apparent association between epilepsy and Parkinson’s disease” and that movement disorders are potential side effects of AEDs, but the association between AEDs and Parkinson’s disease has “not been well studied,” so it remains “unclear” whether AEDs play a role in the association.
“We have previously reported an association between epilepsy and Parkinson’s disease in several different datasets. Here, we wanted to see if it could be explained by an association with the drugs used to treat epilepsy rather than epilepsy per se,” Dr. Noyce explained.
Are AEDs the culprit?
The researchers used data from the UK Biobank, a longitudinal cohort study with more than 500,000 participants, as well as linked primary care medication data to conduct a nested case-control study to investigate this potential association. Participants ranged in age from 40 to 69 years and were recruited between 2006 and 2010.
The researchers compared 1,433 individuals diagnosed with Parkinson’s disease with 8,598 control persons who were matched in a 6:1 ratio for age, sex, race, ethnicity, and socioeconomic status (median [interquartile range] age, 71 [65-75] years; 60.9% men; 97.5% White).
Of those with Parkinson’s disease, 4.3% had been prescribed an AED prior to the date of their being diagnosed with Parkinson’s disease, compared with 2.5% in the control group; 4.4% had been diagnosed with epilepsy, compared with 1% of the control persons.
The strongest evidence was for the association between lamotrigine, levetiracetam, and sodium valproate and Parkinson’s disease. There was “weaker evidence” for carbamazepine, although all the AEDs were associated with a higher risk of Parkinson’s disease.
The odds of incident Parkinson’s disease were higher among those who were prescribed one or more AEDs and among individuals who were issued a higher number of prescriptions, the authors reported.
It is possible that it is the epilepsy itself that is associated with the risk of Parkinson’s disease, rather than the drugs, and that “likely explains part of the association we are seeing,” said Dr. Noyce.
“The bottom line is that more research into the links between epilepsy – and drugs used to treat epilepsy – and Parkinson’s disease is needed,” he said.
Moreover, “only with time will we work out whether the findings hold any real clinical relevance,” he added.
Alternative explanations
Commenting on the research, Rebecca Gilbert, MD, PhD, chief scientific officer, American Parkinson Disease Association, said, “It has been established in prior research that there is an association between epilepsy and Parkinson’s disease.” The current study “shows that having had a prescription written for one of four antiepileptic medications was associated with subsequently receiving a diagnosis of Parkinson’s disease.”
Although one possible conclusion is that the AEDs themselves increase the risk of developing Parkinson’s disease, “there seem to be other alternative explanations as to why a person who had been prescribed AEDs has an increased risk of receiving a diagnosis of Parkinson’s disease,” said Dr. Gilbert, an associate professor of neurology at Bellevue Hospital Center, New York, who was not involved with the current study.
For example, pre-motor changes in the brain of persons with Parkinson’s disease “may increase the risk of requiring an AED by potentially increasing the risk of having a seizure,” and “changes in the brain caused by the seizures for which AEDs are prescribed may increase the risk of Parkinson’s disease.”
Moreover, psychiatric changes related to Parkinson’s disease may have led to the prescription for AEDs, because at least two of the AEDs are also prescribed for mood stabilization, Dr. Gilbert suggested.
“An unanswered question that the paper acknowledges is, what about people who receive AEDs for reasons other than seizures? Do they also have an increased risk of Parkinson’s disease? This would be an interesting population to focus on because it would remove the link between AEDs and seizure and focus on the association between AEDs and Parkinson’s disease,” Dr. Gilbert said.
She emphasized that people who take AEDs for seizures “should not jump to the conclusion that they must come off these medications so as not to increase their risk of developing Parkinson’s disease.” She noted that having seizures “can be dangerous – injuries can occur during a seizure, and if a seizure can’t be stopped or a number occur in rapid succession, brain injury may result.”
For these reasons, people with “a tendency to have seizures need to protect themselves with AEDs” and “should certainly reach out to their neurologists with any questions,” Dr. Gilbert said.
The Preventive Neurology Unit is funded by Barts Charity. The Apocrita High Performance Cluster facility, supported by Queen Mary University London Research–IT Services, was used for this research. Dr. Noyce has received grants from Barts Charity, Parkinson’s UK, Cure Parkinson’s, the Michael J. Fox Foundation, Innovate UK, Solvemed, and Alchemab and personal fees from AstraZeneca, AbbVie, Zambon, BIAL, uMedeor, Alchemab, Britannia, and Charco Neurotech outside the submitted work. The other authors’ disclosures are listed on the original article. Dr. Gilbert reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new research suggests.
Drawing on data from the UK Biobank, investigators compared more than 1,400 individuals diagnosed with Parkinson’s disease with matched control persons and found a considerably higher risk of developing Parkinson’s disease among those who had taken AEDs in comparison with those who had not. There was a trend linking a greater number of AED prescriptions and multiple AEDs associated with a greater risk for Parkinson’s disease.
“We observed an association between the most commonly prescribed antiepileptic drugs in the U.K. and Parkinson’s disease using data from UK Biobank,” said senior author Alastair Noyce, PhD, professor of neurology and neuroepidemiology and honorary consultant neurologist, Queen Mary University of London.
“This is the first time that a comprehensive study of the link between AEDs and Parkinson’s disease has been undertaken,” said Dr. Noyce.
He added that the findings have no immediate clinical implications, “but further research is definitely needed, [as] this is an interesting observation made in a research setting.”
The study was published online in JAMA Neurology.
Plausible, but unclear link
Recent observational studies have found a “temporal association” between epilepsy and incident Parkinson’s disease, but the mechanism underlying this association is “unclear,” the authors wrote.
It is “plausible” that AEDs “may account for some or all of the apparent association between epilepsy and Parkinson’s disease” and that movement disorders are potential side effects of AEDs, but the association between AEDs and Parkinson’s disease has “not been well studied,” so it remains “unclear” whether AEDs play a role in the association.
“We have previously reported an association between epilepsy and Parkinson’s disease in several different datasets. Here, we wanted to see if it could be explained by an association with the drugs used to treat epilepsy rather than epilepsy per se,” Dr. Noyce explained.
Are AEDs the culprit?
The researchers used data from the UK Biobank, a longitudinal cohort study with more than 500,000 participants, as well as linked primary care medication data to conduct a nested case-control study to investigate this potential association. Participants ranged in age from 40 to 69 years and were recruited between 2006 and 2010.
The researchers compared 1,433 individuals diagnosed with Parkinson’s disease with 8,598 control persons who were matched in a 6:1 ratio for age, sex, race, ethnicity, and socioeconomic status (median [interquartile range] age, 71 [65-75] years; 60.9% men; 97.5% White).
Of those with Parkinson’s disease, 4.3% had been prescribed an AED prior to the date of their being diagnosed with Parkinson’s disease, compared with 2.5% in the control group; 4.4% had been diagnosed with epilepsy, compared with 1% of the control persons.
The strongest evidence was for the association between lamotrigine, levetiracetam, and sodium valproate and Parkinson’s disease. There was “weaker evidence” for carbamazepine, although all the AEDs were associated with a higher risk of Parkinson’s disease.
The odds of incident Parkinson’s disease were higher among those who were prescribed one or more AEDs and among individuals who were issued a higher number of prescriptions, the authors reported.
It is possible that it is the epilepsy itself that is associated with the risk of Parkinson’s disease, rather than the drugs, and that “likely explains part of the association we are seeing,” said Dr. Noyce.
“The bottom line is that more research into the links between epilepsy – and drugs used to treat epilepsy – and Parkinson’s disease is needed,” he said.
Moreover, “only with time will we work out whether the findings hold any real clinical relevance,” he added.
Alternative explanations
Commenting on the research, Rebecca Gilbert, MD, PhD, chief scientific officer, American Parkinson Disease Association, said, “It has been established in prior research that there is an association between epilepsy and Parkinson’s disease.” The current study “shows that having had a prescription written for one of four antiepileptic medications was associated with subsequently receiving a diagnosis of Parkinson’s disease.”
Although one possible conclusion is that the AEDs themselves increase the risk of developing Parkinson’s disease, “there seem to be other alternative explanations as to why a person who had been prescribed AEDs has an increased risk of receiving a diagnosis of Parkinson’s disease,” said Dr. Gilbert, an associate professor of neurology at Bellevue Hospital Center, New York, who was not involved with the current study.
For example, pre-motor changes in the brain of persons with Parkinson’s disease “may increase the risk of requiring an AED by potentially increasing the risk of having a seizure,” and “changes in the brain caused by the seizures for which AEDs are prescribed may increase the risk of Parkinson’s disease.”
Moreover, psychiatric changes related to Parkinson’s disease may have led to the prescription for AEDs, because at least two of the AEDs are also prescribed for mood stabilization, Dr. Gilbert suggested.
“An unanswered question that the paper acknowledges is, what about people who receive AEDs for reasons other than seizures? Do they also have an increased risk of Parkinson’s disease? This would be an interesting population to focus on because it would remove the link between AEDs and seizure and focus on the association between AEDs and Parkinson’s disease,” Dr. Gilbert said.
She emphasized that people who take AEDs for seizures “should not jump to the conclusion that they must come off these medications so as not to increase their risk of developing Parkinson’s disease.” She noted that having seizures “can be dangerous – injuries can occur during a seizure, and if a seizure can’t be stopped or a number occur in rapid succession, brain injury may result.”
For these reasons, people with “a tendency to have seizures need to protect themselves with AEDs” and “should certainly reach out to their neurologists with any questions,” Dr. Gilbert said.
The Preventive Neurology Unit is funded by Barts Charity. The Apocrita High Performance Cluster facility, supported by Queen Mary University London Research–IT Services, was used for this research. Dr. Noyce has received grants from Barts Charity, Parkinson’s UK, Cure Parkinson’s, the Michael J. Fox Foundation, Innovate UK, Solvemed, and Alchemab and personal fees from AstraZeneca, AbbVie, Zambon, BIAL, uMedeor, Alchemab, Britannia, and Charco Neurotech outside the submitted work. The other authors’ disclosures are listed on the original article. Dr. Gilbert reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA NEUROLOGY
STEMI times to treatment usually miss established goals
Therapy initiated within national treatment-time goals set a decade ago for patients with ST-segment elevation myocardial infarction (STEMI) remains associated with improved survival in recent years. But for many such patients, time from first symptoms to initiation of reperfusion therapy still fails to meet those goals, suggests a cross-sectional registry analysis.
For example, patients initially transported to centers with percutaneous coronary intervention (PCI) capability had a median treatment time of 148 minutes, in the analysis spanning the second quarter (Q2) of 2018 to the third quarter (Q3) of 2021. But the goal for centers called for treatment initiation within 90 minutes for at least 75% of such STEMI patients.
Moreover, overall STEMI treatment times and in-hospital mortality rose in tandem significantly from Q2 2018 through the first quarter (Q1) of 2021, which included the first year of the COVID-19 pandemic. Median time to treatment went from 86 minutes to 91 minutes during that period. Meanwhile, in-hospital mortality went from 5.6% to 8.7%, report the study authors led by James G. Jollis, MD, Duke University, Durham, N.C.
Their report, based on 114,871 STEMI patients at 601 US hospitals contributing to the Get With The Guidelines – Coronary Artery Disease registry, was published online in JAMA.
Of those patients, 25,085 had been transferred from non-PCI hospitals, 32,483 were walk-ins, and 57,303 arrived via emergency medical services (EMS). Their median times from symptom onset to PCI were 240, 195, and 148 minutes, respectively.
In-hospital mortality was significantly reduced in an adjusted analysis for patients treated within target times, compared with those whose treatment missed the time goals, regardless of whether they were transported by EMS, walked into a hospital with on-site PCI, or were transferred from a non-PCI center (Table 1).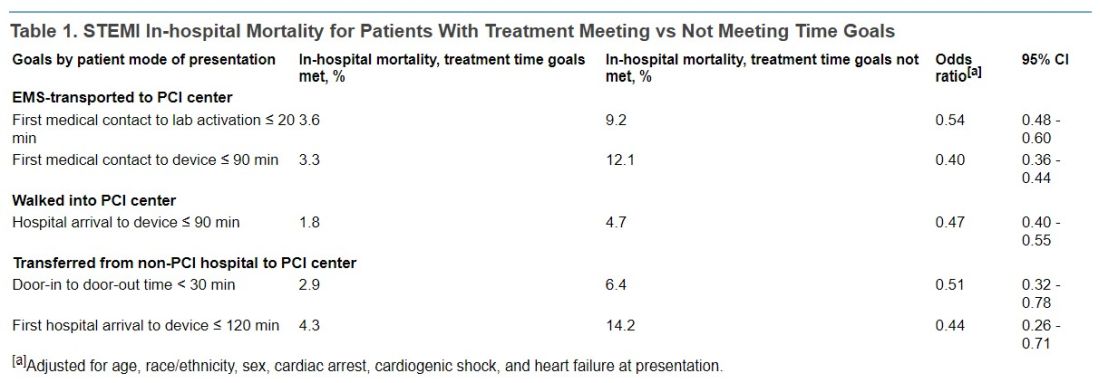
Regardless of mode of patient presentation, treatment time goals were not met most of the time, the group reports. Patients who required interhospital transfer experienced the longest system delays; only 17% were treated within 120 minutes.
Among patients who received primary PCI, 20% had a registry-defined hospital-specified reason for delay, including cardiac arrest and/or need for intubation in 6.8%, “difficulty crossing the culprit lesion” in 3.8%, and “other reasons” in 5.8%, the group reports.
“In 2020, a new reason for delay was added to the registry, ‘need for additional personal protective equipment for suspected/confirmed infectious disease.’ This reason was most commonly used in the second quarter of 2020 (6%) and then declined over time to 1% in the final 2 quarters,” they write.
“Thus, active SARS-CoV-2 infection appeared to have a smaller direct role in longer treatment times or worse outcomes.” Rather, they continue, “the pandemic potentially had a significant indirect role as hospitals were overwhelmed with patients, EMS and hospitals were challenged in maintaining paramedic and nurse staffing and intensive care bed availability, and patients experienced delayed care due to barriers to access or perceived fear of becoming entangled in an overwhelmed medical system.”
Still an important quality metric
STEMI treatment times remain an important quality metric to which hospitals should continue to pay attention because shorter times improve patient care, Deepak Bhatt, MD, MPH, told this news organization.
“Having said that, as with all metrics, one needs to be thoughtful and realize that a difference of a couple of minutes is probably not a crucial thing,” said Dr. Bhatt, Brigham and Women’s Hospital and Harvard Medical School, Boston, who was not involved with the current study.
Interhospital transfers indeed involve longer delays, he observed, suggesting that regional integrated health systems should develop methods for optimizing STEMI care – even, for example, if they involve bypassing non-PCI centers or stopping patients briefly for stabilization followed by rapid transport to a PCI-capable facility.
“That, of course, requires cooperation among hospitals. Sometimes that requires hospitals putting aside economic considerations and just focusing on doing the right thing for that individual patient,” Dr. Bhatt said.
Transfer delays are common for patients presenting with STEMI at hospitals without PCI capability, he noted. “Having clear protocols in place that expedite that type of transfer, I think, could go a long way in reducing the time to treatment in patients that are presenting to the hospital without cath labs. That’s an important message that these data provide.”
The onset of COVID-19 led to widespread delays in STEMI time to treatment early in the pandemic. There were concerns about exposing cath lab personnel to SARS-CoV-2 and potential adverse consequences of sick personnel being unable to provide patient care in the subsequent weeks and months, Dr. Bhatt observed.
However, “All of that seems to have quieted down, and I don’t think COVID is impacting time to treatment right now.”
‘Suboptimal compliance’ with standards
The current findings of “suboptimal compliance with national targets underscore why reassessing quality metrics, in light of changing practice patterns and other secular trends, is critical,” write Andrew S. Oseran, MD, MBA, and Robert W. Yeh, MD, both of Harvard Medical School, in an accompanying editorial.
“While the importance of coordinated and expeditious care for this high-risk patient population is undeniable, the specific actions that hospitals can – or should – take to further improve overall STEMI outcomes are less clear,” they say.
“As physicians contemplate the optimal path forward in managing the care of STEMI patients, they must recognize the clinical and operational nuance that exists in caring for this diverse population and acknowledge the trade-offs associated with uniform quality metrics,” write the editorialists.
“Global reductions in time to treatment for STEMI patients has been one of health care’s great success stories. As we move forward, it may be time to consider whether efforts to achieve additional improvement in target treatment times will result in substantive benefits, or whether we have reached the point of diminishing returns.”
A version of this article first appeared on Medscape.com.
Therapy initiated within national treatment-time goals set a decade ago for patients with ST-segment elevation myocardial infarction (STEMI) remains associated with improved survival in recent years. But for many such patients, time from first symptoms to initiation of reperfusion therapy still fails to meet those goals, suggests a cross-sectional registry analysis.
For example, patients initially transported to centers with percutaneous coronary intervention (PCI) capability had a median treatment time of 148 minutes, in the analysis spanning the second quarter (Q2) of 2018 to the third quarter (Q3) of 2021. But the goal for centers called for treatment initiation within 90 minutes for at least 75% of such STEMI patients.
Moreover, overall STEMI treatment times and in-hospital mortality rose in tandem significantly from Q2 2018 through the first quarter (Q1) of 2021, which included the first year of the COVID-19 pandemic. Median time to treatment went from 86 minutes to 91 minutes during that period. Meanwhile, in-hospital mortality went from 5.6% to 8.7%, report the study authors led by James G. Jollis, MD, Duke University, Durham, N.C.
Their report, based on 114,871 STEMI patients at 601 US hospitals contributing to the Get With The Guidelines – Coronary Artery Disease registry, was published online in JAMA.
Of those patients, 25,085 had been transferred from non-PCI hospitals, 32,483 were walk-ins, and 57,303 arrived via emergency medical services (EMS). Their median times from symptom onset to PCI were 240, 195, and 148 minutes, respectively.
In-hospital mortality was significantly reduced in an adjusted analysis for patients treated within target times, compared with those whose treatment missed the time goals, regardless of whether they were transported by EMS, walked into a hospital with on-site PCI, or were transferred from a non-PCI center (Table 1).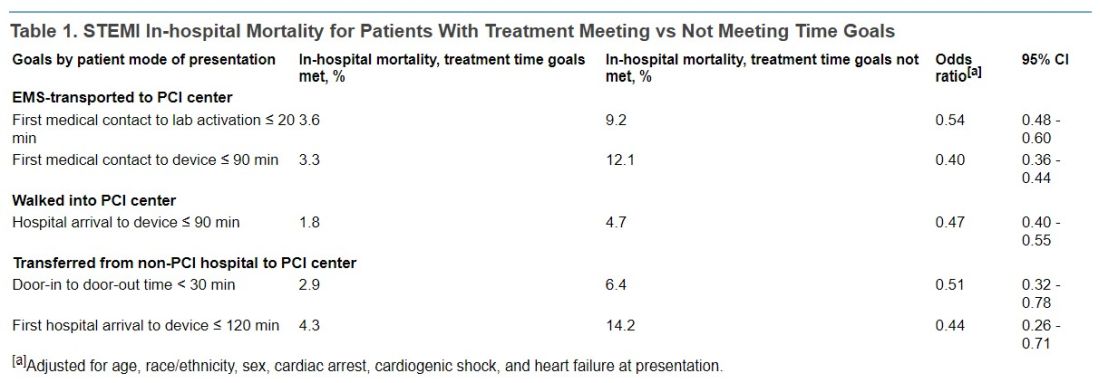
Regardless of mode of patient presentation, treatment time goals were not met most of the time, the group reports. Patients who required interhospital transfer experienced the longest system delays; only 17% were treated within 120 minutes.
Among patients who received primary PCI, 20% had a registry-defined hospital-specified reason for delay, including cardiac arrest and/or need for intubation in 6.8%, “difficulty crossing the culprit lesion” in 3.8%, and “other reasons” in 5.8%, the group reports.
“In 2020, a new reason for delay was added to the registry, ‘need for additional personal protective equipment for suspected/confirmed infectious disease.’ This reason was most commonly used in the second quarter of 2020 (6%) and then declined over time to 1% in the final 2 quarters,” they write.
“Thus, active SARS-CoV-2 infection appeared to have a smaller direct role in longer treatment times or worse outcomes.” Rather, they continue, “the pandemic potentially had a significant indirect role as hospitals were overwhelmed with patients, EMS and hospitals were challenged in maintaining paramedic and nurse staffing and intensive care bed availability, and patients experienced delayed care due to barriers to access or perceived fear of becoming entangled in an overwhelmed medical system.”
Still an important quality metric
STEMI treatment times remain an important quality metric to which hospitals should continue to pay attention because shorter times improve patient care, Deepak Bhatt, MD, MPH, told this news organization.
“Having said that, as with all metrics, one needs to be thoughtful and realize that a difference of a couple of minutes is probably not a crucial thing,” said Dr. Bhatt, Brigham and Women’s Hospital and Harvard Medical School, Boston, who was not involved with the current study.
Interhospital transfers indeed involve longer delays, he observed, suggesting that regional integrated health systems should develop methods for optimizing STEMI care – even, for example, if they involve bypassing non-PCI centers or stopping patients briefly for stabilization followed by rapid transport to a PCI-capable facility.
“That, of course, requires cooperation among hospitals. Sometimes that requires hospitals putting aside economic considerations and just focusing on doing the right thing for that individual patient,” Dr. Bhatt said.
Transfer delays are common for patients presenting with STEMI at hospitals without PCI capability, he noted. “Having clear protocols in place that expedite that type of transfer, I think, could go a long way in reducing the time to treatment in patients that are presenting to the hospital without cath labs. That’s an important message that these data provide.”
The onset of COVID-19 led to widespread delays in STEMI time to treatment early in the pandemic. There were concerns about exposing cath lab personnel to SARS-CoV-2 and potential adverse consequences of sick personnel being unable to provide patient care in the subsequent weeks and months, Dr. Bhatt observed.
However, “All of that seems to have quieted down, and I don’t think COVID is impacting time to treatment right now.”
‘Suboptimal compliance’ with standards
The current findings of “suboptimal compliance with national targets underscore why reassessing quality metrics, in light of changing practice patterns and other secular trends, is critical,” write Andrew S. Oseran, MD, MBA, and Robert W. Yeh, MD, both of Harvard Medical School, in an accompanying editorial.
“While the importance of coordinated and expeditious care for this high-risk patient population is undeniable, the specific actions that hospitals can – or should – take to further improve overall STEMI outcomes are less clear,” they say.
“As physicians contemplate the optimal path forward in managing the care of STEMI patients, they must recognize the clinical and operational nuance that exists in caring for this diverse population and acknowledge the trade-offs associated with uniform quality metrics,” write the editorialists.
“Global reductions in time to treatment for STEMI patients has been one of health care’s great success stories. As we move forward, it may be time to consider whether efforts to achieve additional improvement in target treatment times will result in substantive benefits, or whether we have reached the point of diminishing returns.”
A version of this article first appeared on Medscape.com.
Therapy initiated within national treatment-time goals set a decade ago for patients with ST-segment elevation myocardial infarction (STEMI) remains associated with improved survival in recent years. But for many such patients, time from first symptoms to initiation of reperfusion therapy still fails to meet those goals, suggests a cross-sectional registry analysis.
For example, patients initially transported to centers with percutaneous coronary intervention (PCI) capability had a median treatment time of 148 minutes, in the analysis spanning the second quarter (Q2) of 2018 to the third quarter (Q3) of 2021. But the goal for centers called for treatment initiation within 90 minutes for at least 75% of such STEMI patients.
Moreover, overall STEMI treatment times and in-hospital mortality rose in tandem significantly from Q2 2018 through the first quarter (Q1) of 2021, which included the first year of the COVID-19 pandemic. Median time to treatment went from 86 minutes to 91 minutes during that period. Meanwhile, in-hospital mortality went from 5.6% to 8.7%, report the study authors led by James G. Jollis, MD, Duke University, Durham, N.C.
Their report, based on 114,871 STEMI patients at 601 US hospitals contributing to the Get With The Guidelines – Coronary Artery Disease registry, was published online in JAMA.
Of those patients, 25,085 had been transferred from non-PCI hospitals, 32,483 were walk-ins, and 57,303 arrived via emergency medical services (EMS). Their median times from symptom onset to PCI were 240, 195, and 148 minutes, respectively.
In-hospital mortality was significantly reduced in an adjusted analysis for patients treated within target times, compared with those whose treatment missed the time goals, regardless of whether they were transported by EMS, walked into a hospital with on-site PCI, or were transferred from a non-PCI center (Table 1).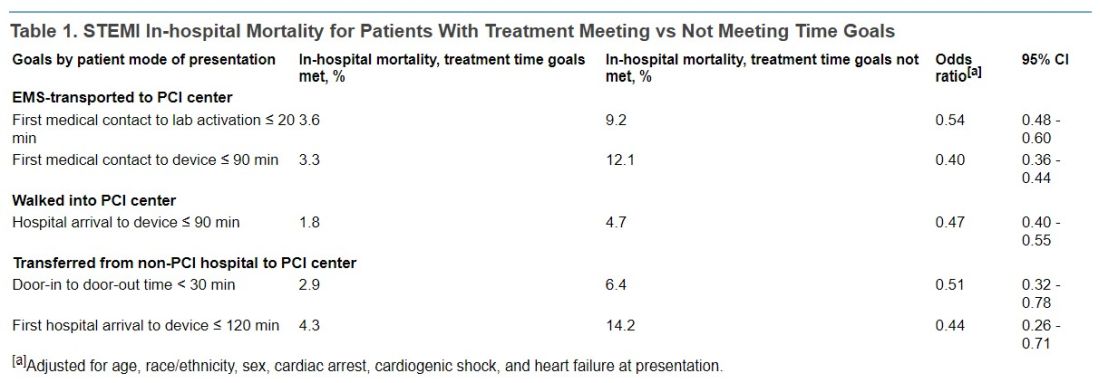
Regardless of mode of patient presentation, treatment time goals were not met most of the time, the group reports. Patients who required interhospital transfer experienced the longest system delays; only 17% were treated within 120 minutes.
Among patients who received primary PCI, 20% had a registry-defined hospital-specified reason for delay, including cardiac arrest and/or need for intubation in 6.8%, “difficulty crossing the culprit lesion” in 3.8%, and “other reasons” in 5.8%, the group reports.
“In 2020, a new reason for delay was added to the registry, ‘need for additional personal protective equipment for suspected/confirmed infectious disease.’ This reason was most commonly used in the second quarter of 2020 (6%) and then declined over time to 1% in the final 2 quarters,” they write.
“Thus, active SARS-CoV-2 infection appeared to have a smaller direct role in longer treatment times or worse outcomes.” Rather, they continue, “the pandemic potentially had a significant indirect role as hospitals were overwhelmed with patients, EMS and hospitals were challenged in maintaining paramedic and nurse staffing and intensive care bed availability, and patients experienced delayed care due to barriers to access or perceived fear of becoming entangled in an overwhelmed medical system.”
Still an important quality metric
STEMI treatment times remain an important quality metric to which hospitals should continue to pay attention because shorter times improve patient care, Deepak Bhatt, MD, MPH, told this news organization.
“Having said that, as with all metrics, one needs to be thoughtful and realize that a difference of a couple of minutes is probably not a crucial thing,” said Dr. Bhatt, Brigham and Women’s Hospital and Harvard Medical School, Boston, who was not involved with the current study.
Interhospital transfers indeed involve longer delays, he observed, suggesting that regional integrated health systems should develop methods for optimizing STEMI care – even, for example, if they involve bypassing non-PCI centers or stopping patients briefly for stabilization followed by rapid transport to a PCI-capable facility.
“That, of course, requires cooperation among hospitals. Sometimes that requires hospitals putting aside economic considerations and just focusing on doing the right thing for that individual patient,” Dr. Bhatt said.
Transfer delays are common for patients presenting with STEMI at hospitals without PCI capability, he noted. “Having clear protocols in place that expedite that type of transfer, I think, could go a long way in reducing the time to treatment in patients that are presenting to the hospital without cath labs. That’s an important message that these data provide.”
The onset of COVID-19 led to widespread delays in STEMI time to treatment early in the pandemic. There were concerns about exposing cath lab personnel to SARS-CoV-2 and potential adverse consequences of sick personnel being unable to provide patient care in the subsequent weeks and months, Dr. Bhatt observed.
However, “All of that seems to have quieted down, and I don’t think COVID is impacting time to treatment right now.”
‘Suboptimal compliance’ with standards
The current findings of “suboptimal compliance with national targets underscore why reassessing quality metrics, in light of changing practice patterns and other secular trends, is critical,” write Andrew S. Oseran, MD, MBA, and Robert W. Yeh, MD, both of Harvard Medical School, in an accompanying editorial.
“While the importance of coordinated and expeditious care for this high-risk patient population is undeniable, the specific actions that hospitals can – or should – take to further improve overall STEMI outcomes are less clear,” they say.
“As physicians contemplate the optimal path forward in managing the care of STEMI patients, they must recognize the clinical and operational nuance that exists in caring for this diverse population and acknowledge the trade-offs associated with uniform quality metrics,” write the editorialists.
“Global reductions in time to treatment for STEMI patients has been one of health care’s great success stories. As we move forward, it may be time to consider whether efforts to achieve additional improvement in target treatment times will result in substantive benefits, or whether we have reached the point of diminishing returns.”
A version of this article first appeared on Medscape.com.
FROM JAMA
SARS-CoV-2 seroprevalence grew rapidly in pandemic’s early waves
By August 2022, two-and-a-half years into the COVID-19 pandemic, most children as well as most adults under age 60 years had evidence of SARS-CoV-2 vaccination and/or infection, a Canadian seroprevalence study of almost 14,000 people over the first seven waves of the pandemic reports.
However, fewer than 50% people older than age 60, the age group most vulnerable to severe outcomes, showed evidence of immunity from infection or vaccination. The authors noted that older adults – who have the lowest infection rates but highest risk of severe outcomes – continue to warrant prioritized vaccination, writing online in the Canadian Medical Association Journal.
Previous evidence suggests that a combination of both infection and vaccination exposure may induce more robust and durable hybrid immunity than either exposure alone, according to lead author Danuta M. Skowronski, MD, MHSc, an epidemiologist at the British Columbia Centre for Disease Control in Vancouver.
“Our main objective was to chronicle the changing proportion of the population considered immunologically naive and therefore susceptible to SARS-CoV-2,” Dr. Skowronski said in an interview. “It’s relevant for risk assessment to know what proportion have acquired some priming for more efficient immune memory response to the virus because that reduces the likelihood of severe outcomes.” Standardized seroprevalence studies are essential to inform COVID-19 response, particularly in resource-limited regions.
The study
Conducted in British Columbia’s Greater Vancouver and Fraser Valley, the analysis found that in the first year of the pandemic, when extraordinary measures were in place to curtail transmission, virtually everyone remained immunologically naive. Thereafter, however, age-based vaccine rollouts dramatically changed the immuno-epidemiological landscape so that by September 2021, more than 80% of the study population had antibody evidence of immunological priming, while more than 85% remained uninfected.
By August 2022, after the Omicron-variant waves, overall vaccine- and infection-induced seroprevalence exceeded 95%, with 60% having been actually infected, including at least three-quarters of children. Fewer than 50% of older adults, however, showed immunological evidence of exposure.
The study results were based on anonymized residual sera from children and adults in an outpatient laboratory network. At least three immunoassays per serosurvey were used to detect antibodies to SARS-CoV-2 spike (from vaccine) and to nucleocapsid antibodies (from infection).
The researchers assessed any seroprevalence – vaccine-, infection-induced, or both – as defined by positivity on any two assays. Infection-induced seroprevalence was also defined by dual-assay positivity but required both antinucleocapsid and antispike detection. Their estimates of infection-induced seroprevalence indicated considerable under-ascertainment of infections by standard surveillance case reports.
Results
During the first year of the pandemic, fewer than 1% manifested seroprevalence during the first three snapshots and fewer than 5% by January 2021. With vaccine rollout, however, seroprevalence increased dramatically during the first half of 2021 to 56% by May/June 2021 and to 83% by September/October 2021.
In addition, infection-induced seroprevalence was low at less than 15% in September/October 2021 until the arrival of the Omicron waves, after which it rose to 42% by March 2022 and 61% by July/August 2022. Combined seroprevalence for vaccination or infection was more than 95% by the summer, with most children but less than half of adults older than 60 years showing evidence of having been infected.
“We found the highest infection rates among children, closely followed by young adults, which may reflect their greater interconnectedness, including between siblings and parents in the household, as well as with peers in schools and the community,” the authors wrote, adding that the low cumulative infection rates among older adults may reflect their higher vaccination rates and greater social isolation.
U.S. data show similar age-related infection rates, but data among children from other Canadian provinces are limited, the authors said.
Commenting on the survey but not involved in it, infectious diseases expert Marc Germain, MD, PhD, a vice president at Héma-Québec in Quebec City, believes the pattern observed in British Columbia is fairly representative of what happened across Canada and the United States, including the sweeping effect of the Omicron variant and the differential impact according to age.
“But regional differences might very well exist – for example, due to differential vaccine uptake – and are also probably related in part to the different testing platforms being used,” Dr. Germain told this news organization.
Caroline Quach-Tanh, MD, PhD, a pediatrician and epidemiologist/infectologist at the University of Montreal, pointed out that Quebec seroprevalence surveys using residual blood samples from children and adults visiting emergency departments for any reason showed higher rates of prior infection than did the BC surveys. “But Dr. Skowronski’s findings are likely applicable to settings where some nonpharmacological interventions were put in place, but without strict confinement – and thus are likely applicable to most settings in the U.S. and Canada.”
Dr. Quach-Tanh added that there is always a risk of bias with the use of residual blood samples, “but the fact that the study method was stable should have captured a similar population from time to time. It would be unlikely to result in a major overestimation in the proportion of individuals positive for SARS-CoV-2 antibodies.”
A recent global meta-analysis found that while global seroprevalence has risen considerably, albeit variably by region, more than a third of the world’s population is still seronegative to the SARS-CoV-2 virus.
Dr. Skowronski reported institutional grants from the Canadian Institutes of Health Research and the British Columbia Centre for Disease Control Foundation for Public Health for other SARSCoV-2 work. Coauthor Romina C. Reyes, MD, chairs the BC Diagnostic Accreditation Program committee. Coauthor Mel Krajden, MD, reported institutional grants from Roche, Hologic, and Siemens. Dr. Germain and Dr. Quach-Tanh disclosed no competing interests relevant to their comments.
By August 2022, two-and-a-half years into the COVID-19 pandemic, most children as well as most adults under age 60 years had evidence of SARS-CoV-2 vaccination and/or infection, a Canadian seroprevalence study of almost 14,000 people over the first seven waves of the pandemic reports.
However, fewer than 50% people older than age 60, the age group most vulnerable to severe outcomes, showed evidence of immunity from infection or vaccination. The authors noted that older adults – who have the lowest infection rates but highest risk of severe outcomes – continue to warrant prioritized vaccination, writing online in the Canadian Medical Association Journal.
Previous evidence suggests that a combination of both infection and vaccination exposure may induce more robust and durable hybrid immunity than either exposure alone, according to lead author Danuta M. Skowronski, MD, MHSc, an epidemiologist at the British Columbia Centre for Disease Control in Vancouver.
“Our main objective was to chronicle the changing proportion of the population considered immunologically naive and therefore susceptible to SARS-CoV-2,” Dr. Skowronski said in an interview. “It’s relevant for risk assessment to know what proportion have acquired some priming for more efficient immune memory response to the virus because that reduces the likelihood of severe outcomes.” Standardized seroprevalence studies are essential to inform COVID-19 response, particularly in resource-limited regions.
The study
Conducted in British Columbia’s Greater Vancouver and Fraser Valley, the analysis found that in the first year of the pandemic, when extraordinary measures were in place to curtail transmission, virtually everyone remained immunologically naive. Thereafter, however, age-based vaccine rollouts dramatically changed the immuno-epidemiological landscape so that by September 2021, more than 80% of the study population had antibody evidence of immunological priming, while more than 85% remained uninfected.
By August 2022, after the Omicron-variant waves, overall vaccine- and infection-induced seroprevalence exceeded 95%, with 60% having been actually infected, including at least three-quarters of children. Fewer than 50% of older adults, however, showed immunological evidence of exposure.
The study results were based on anonymized residual sera from children and adults in an outpatient laboratory network. At least three immunoassays per serosurvey were used to detect antibodies to SARS-CoV-2 spike (from vaccine) and to nucleocapsid antibodies (from infection).
The researchers assessed any seroprevalence – vaccine-, infection-induced, or both – as defined by positivity on any two assays. Infection-induced seroprevalence was also defined by dual-assay positivity but required both antinucleocapsid and antispike detection. Their estimates of infection-induced seroprevalence indicated considerable under-ascertainment of infections by standard surveillance case reports.
Results
During the first year of the pandemic, fewer than 1% manifested seroprevalence during the first three snapshots and fewer than 5% by January 2021. With vaccine rollout, however, seroprevalence increased dramatically during the first half of 2021 to 56% by May/June 2021 and to 83% by September/October 2021.
In addition, infection-induced seroprevalence was low at less than 15% in September/October 2021 until the arrival of the Omicron waves, after which it rose to 42% by March 2022 and 61% by July/August 2022. Combined seroprevalence for vaccination or infection was more than 95% by the summer, with most children but less than half of adults older than 60 years showing evidence of having been infected.
“We found the highest infection rates among children, closely followed by young adults, which may reflect their greater interconnectedness, including between siblings and parents in the household, as well as with peers in schools and the community,” the authors wrote, adding that the low cumulative infection rates among older adults may reflect their higher vaccination rates and greater social isolation.
U.S. data show similar age-related infection rates, but data among children from other Canadian provinces are limited, the authors said.
Commenting on the survey but not involved in it, infectious diseases expert Marc Germain, MD, PhD, a vice president at Héma-Québec in Quebec City, believes the pattern observed in British Columbia is fairly representative of what happened across Canada and the United States, including the sweeping effect of the Omicron variant and the differential impact according to age.
“But regional differences might very well exist – for example, due to differential vaccine uptake – and are also probably related in part to the different testing platforms being used,” Dr. Germain told this news organization.
Caroline Quach-Tanh, MD, PhD, a pediatrician and epidemiologist/infectologist at the University of Montreal, pointed out that Quebec seroprevalence surveys using residual blood samples from children and adults visiting emergency departments for any reason showed higher rates of prior infection than did the BC surveys. “But Dr. Skowronski’s findings are likely applicable to settings where some nonpharmacological interventions were put in place, but without strict confinement – and thus are likely applicable to most settings in the U.S. and Canada.”
Dr. Quach-Tanh added that there is always a risk of bias with the use of residual blood samples, “but the fact that the study method was stable should have captured a similar population from time to time. It would be unlikely to result in a major overestimation in the proportion of individuals positive for SARS-CoV-2 antibodies.”
A recent global meta-analysis found that while global seroprevalence has risen considerably, albeit variably by region, more than a third of the world’s population is still seronegative to the SARS-CoV-2 virus.
Dr. Skowronski reported institutional grants from the Canadian Institutes of Health Research and the British Columbia Centre for Disease Control Foundation for Public Health for other SARSCoV-2 work. Coauthor Romina C. Reyes, MD, chairs the BC Diagnostic Accreditation Program committee. Coauthor Mel Krajden, MD, reported institutional grants from Roche, Hologic, and Siemens. Dr. Germain and Dr. Quach-Tanh disclosed no competing interests relevant to their comments.
By August 2022, two-and-a-half years into the COVID-19 pandemic, most children as well as most adults under age 60 years had evidence of SARS-CoV-2 vaccination and/or infection, a Canadian seroprevalence study of almost 14,000 people over the first seven waves of the pandemic reports.
However, fewer than 50% people older than age 60, the age group most vulnerable to severe outcomes, showed evidence of immunity from infection or vaccination. The authors noted that older adults – who have the lowest infection rates but highest risk of severe outcomes – continue to warrant prioritized vaccination, writing online in the Canadian Medical Association Journal.
Previous evidence suggests that a combination of both infection and vaccination exposure may induce more robust and durable hybrid immunity than either exposure alone, according to lead author Danuta M. Skowronski, MD, MHSc, an epidemiologist at the British Columbia Centre for Disease Control in Vancouver.
“Our main objective was to chronicle the changing proportion of the population considered immunologically naive and therefore susceptible to SARS-CoV-2,” Dr. Skowronski said in an interview. “It’s relevant for risk assessment to know what proportion have acquired some priming for more efficient immune memory response to the virus because that reduces the likelihood of severe outcomes.” Standardized seroprevalence studies are essential to inform COVID-19 response, particularly in resource-limited regions.
The study
Conducted in British Columbia’s Greater Vancouver and Fraser Valley, the analysis found that in the first year of the pandemic, when extraordinary measures were in place to curtail transmission, virtually everyone remained immunologically naive. Thereafter, however, age-based vaccine rollouts dramatically changed the immuno-epidemiological landscape so that by September 2021, more than 80% of the study population had antibody evidence of immunological priming, while more than 85% remained uninfected.
By August 2022, after the Omicron-variant waves, overall vaccine- and infection-induced seroprevalence exceeded 95%, with 60% having been actually infected, including at least three-quarters of children. Fewer than 50% of older adults, however, showed immunological evidence of exposure.
The study results were based on anonymized residual sera from children and adults in an outpatient laboratory network. At least three immunoassays per serosurvey were used to detect antibodies to SARS-CoV-2 spike (from vaccine) and to nucleocapsid antibodies (from infection).
The researchers assessed any seroprevalence – vaccine-, infection-induced, or both – as defined by positivity on any two assays. Infection-induced seroprevalence was also defined by dual-assay positivity but required both antinucleocapsid and antispike detection. Their estimates of infection-induced seroprevalence indicated considerable under-ascertainment of infections by standard surveillance case reports.
Results
During the first year of the pandemic, fewer than 1% manifested seroprevalence during the first three snapshots and fewer than 5% by January 2021. With vaccine rollout, however, seroprevalence increased dramatically during the first half of 2021 to 56% by May/June 2021 and to 83% by September/October 2021.
In addition, infection-induced seroprevalence was low at less than 15% in September/October 2021 until the arrival of the Omicron waves, after which it rose to 42% by March 2022 and 61% by July/August 2022. Combined seroprevalence for vaccination or infection was more than 95% by the summer, with most children but less than half of adults older than 60 years showing evidence of having been infected.
“We found the highest infection rates among children, closely followed by young adults, which may reflect their greater interconnectedness, including between siblings and parents in the household, as well as with peers in schools and the community,” the authors wrote, adding that the low cumulative infection rates among older adults may reflect their higher vaccination rates and greater social isolation.
U.S. data show similar age-related infection rates, but data among children from other Canadian provinces are limited, the authors said.
Commenting on the survey but not involved in it, infectious diseases expert Marc Germain, MD, PhD, a vice president at Héma-Québec in Quebec City, believes the pattern observed in British Columbia is fairly representative of what happened across Canada and the United States, including the sweeping effect of the Omicron variant and the differential impact according to age.
“But regional differences might very well exist – for example, due to differential vaccine uptake – and are also probably related in part to the different testing platforms being used,” Dr. Germain told this news organization.
Caroline Quach-Tanh, MD, PhD, a pediatrician and epidemiologist/infectologist at the University of Montreal, pointed out that Quebec seroprevalence surveys using residual blood samples from children and adults visiting emergency departments for any reason showed higher rates of prior infection than did the BC surveys. “But Dr. Skowronski’s findings are likely applicable to settings where some nonpharmacological interventions were put in place, but without strict confinement – and thus are likely applicable to most settings in the U.S. and Canada.”
Dr. Quach-Tanh added that there is always a risk of bias with the use of residual blood samples, “but the fact that the study method was stable should have captured a similar population from time to time. It would be unlikely to result in a major overestimation in the proportion of individuals positive for SARS-CoV-2 antibodies.”
A recent global meta-analysis found that while global seroprevalence has risen considerably, albeit variably by region, more than a third of the world’s population is still seronegative to the SARS-CoV-2 virus.
Dr. Skowronski reported institutional grants from the Canadian Institutes of Health Research and the British Columbia Centre for Disease Control Foundation for Public Health for other SARSCoV-2 work. Coauthor Romina C. Reyes, MD, chairs the BC Diagnostic Accreditation Program committee. Coauthor Mel Krajden, MD, reported institutional grants from Roche, Hologic, and Siemens. Dr. Germain and Dr. Quach-Tanh disclosed no competing interests relevant to their comments.
FROM THE CANADIAN MEDICAL ASSOCIATION JOURNAL
Heart benefits begin at well under 10,000 daily steps
– and the benefits accrue at well below the widely promoted threshold of 10,000 steps per day, new research shows.
Among adults aged 60 and older, those who took roughly 6,000 to 9,000 steps per day had a 40% to 50% lower risk of CVD, compared with peers logging just 2,000 steps per day.
“We hope this study will contribute evidence to future public health and clinical guidance on how many steps we need for health,” Amanda Paluch, PhD, with University of Massachusetts Amherst, told this news organization.
Getting in more steps per day can lower an individual’s risk for heart disease – but it’s not an “all or nothing” situation, Dr. Paluch said.
“The heart health benefits begin at lower than 10,000 steps per day. So, for the many adults that may find 10,000 steps a bit out of reach, it is important to promote that even small increases in steps can be beneficial for health,” Dr. Paluch said.
The study was published online in Circulation.
Attainable step goals
As part of the Steps for Health Collaborative, Dr. Paluch and colleagues examined the dose-response relationship between steps per day and CVD in a meta-analysis of eight prospective studies involving 20,152 adults (mean age 63, 52% women).
Steps were measured in each study using one of five different commercially available step-measuring devices. Adults aged 60 years and older took a median of 4,323 steps per day (interquartile range, 2,760-6,924), while younger adults walked a bit more (median 6,911 daily steps; IQR, 4,783-9,794).
During follow-up lasting an average of 6.2 years, a total of 1,523 CVD events were reported.
In the final adjusted model, for older adults, compared with those in quartile 1 who got the fewest steps per day (median 1,811), the risk of CVD was 20% lower in those in quartile 2, who got a median of 3,823 steps per day (hazard ratio, 0.80; 95% confidence interval, 0.69-0.93).
CVD risk was 38% lower in older adults in quartile 3 who got a median of 5,520 steps per day (HR, 0.62; 95% CI, 0.52-0.74) and 49% lower in those in quartile 4 who walked the most (a median of 9,259 steps per day; HR, 0.51; 95% CI, 0.41-0.63).
Restricting the analysis to individuals without known CVD at baseline showed similar results.
Among six studies that excluded adults with a history of CVD at baseline, compared with the lowest quartile, the HR for incident CVD events was 0.74 (95% CI, 0.60-0.91) in the second quartile, 0.60 (95% CI, 0.47-0.77) in the third quartile, and 0.55 (95% CI, 0.40-0.76) in the fourth quartile.
Despite the inverse association of steps with CVD in older adults, there was no association in younger adults. The researchers caution, however, that CVD is a disease of aging, and the follow-up period in these studies may not have been long enough to capture CVD incidence in younger adults.
Stepping rate (pace or cadence) was not associated with CVD risk beyond that of total steps per day. However, only four of the eight studies reported data on stepping rate, so this finding should be viewed as preliminary, Dr. Paluch and colleagues say.
Start small and go from there
Dr. Paluch said the take-home message from this study and numerous others is simple.
“Move more and sit less! Being physically active, by getting in your steps, is an important part of keeping your heart healthy,” she said in an interview.
For adults who are currently inactive, Dr. Paluch suggests finding small ways to get in a few more steps per day. “It does not need to be drastic changes. Consider a brief 5- to 10-minute walking break at lunch, taking the stairs, or playing a game of hide and seek with the grandchildren,” Dr. Paluch advised.
“For adults starting at 3,000 steps a day, set a goal of 4,000, and then 5,000. Each improvement can lead to better heart health,” Dr. Paluch said. “And for those who are already active, keep it up, as there are benefits with higher volumes of steps per day as well.”
Support for this research was provided by the Intergovernmental Personnel Act Agreement through the Centers for Disease Control and Prevention. The authors have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
– and the benefits accrue at well below the widely promoted threshold of 10,000 steps per day, new research shows.
Among adults aged 60 and older, those who took roughly 6,000 to 9,000 steps per day had a 40% to 50% lower risk of CVD, compared with peers logging just 2,000 steps per day.
“We hope this study will contribute evidence to future public health and clinical guidance on how many steps we need for health,” Amanda Paluch, PhD, with University of Massachusetts Amherst, told this news organization.
Getting in more steps per day can lower an individual’s risk for heart disease – but it’s not an “all or nothing” situation, Dr. Paluch said.
“The heart health benefits begin at lower than 10,000 steps per day. So, for the many adults that may find 10,000 steps a bit out of reach, it is important to promote that even small increases in steps can be beneficial for health,” Dr. Paluch said.
The study was published online in Circulation.
Attainable step goals
As part of the Steps for Health Collaborative, Dr. Paluch and colleagues examined the dose-response relationship between steps per day and CVD in a meta-analysis of eight prospective studies involving 20,152 adults (mean age 63, 52% women).
Steps were measured in each study using one of five different commercially available step-measuring devices. Adults aged 60 years and older took a median of 4,323 steps per day (interquartile range, 2,760-6,924), while younger adults walked a bit more (median 6,911 daily steps; IQR, 4,783-9,794).
During follow-up lasting an average of 6.2 years, a total of 1,523 CVD events were reported.
In the final adjusted model, for older adults, compared with those in quartile 1 who got the fewest steps per day (median 1,811), the risk of CVD was 20% lower in those in quartile 2, who got a median of 3,823 steps per day (hazard ratio, 0.80; 95% confidence interval, 0.69-0.93).
CVD risk was 38% lower in older adults in quartile 3 who got a median of 5,520 steps per day (HR, 0.62; 95% CI, 0.52-0.74) and 49% lower in those in quartile 4 who walked the most (a median of 9,259 steps per day; HR, 0.51; 95% CI, 0.41-0.63).
Restricting the analysis to individuals without known CVD at baseline showed similar results.
Among six studies that excluded adults with a history of CVD at baseline, compared with the lowest quartile, the HR for incident CVD events was 0.74 (95% CI, 0.60-0.91) in the second quartile, 0.60 (95% CI, 0.47-0.77) in the third quartile, and 0.55 (95% CI, 0.40-0.76) in the fourth quartile.
Despite the inverse association of steps with CVD in older adults, there was no association in younger adults. The researchers caution, however, that CVD is a disease of aging, and the follow-up period in these studies may not have been long enough to capture CVD incidence in younger adults.
Stepping rate (pace or cadence) was not associated with CVD risk beyond that of total steps per day. However, only four of the eight studies reported data on stepping rate, so this finding should be viewed as preliminary, Dr. Paluch and colleagues say.
Start small and go from there
Dr. Paluch said the take-home message from this study and numerous others is simple.
“Move more and sit less! Being physically active, by getting in your steps, is an important part of keeping your heart healthy,” she said in an interview.
For adults who are currently inactive, Dr. Paluch suggests finding small ways to get in a few more steps per day. “It does not need to be drastic changes. Consider a brief 5- to 10-minute walking break at lunch, taking the stairs, or playing a game of hide and seek with the grandchildren,” Dr. Paluch advised.
“For adults starting at 3,000 steps a day, set a goal of 4,000, and then 5,000. Each improvement can lead to better heart health,” Dr. Paluch said. “And for those who are already active, keep it up, as there are benefits with higher volumes of steps per day as well.”
Support for this research was provided by the Intergovernmental Personnel Act Agreement through the Centers for Disease Control and Prevention. The authors have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
– and the benefits accrue at well below the widely promoted threshold of 10,000 steps per day, new research shows.
Among adults aged 60 and older, those who took roughly 6,000 to 9,000 steps per day had a 40% to 50% lower risk of CVD, compared with peers logging just 2,000 steps per day.
“We hope this study will contribute evidence to future public health and clinical guidance on how many steps we need for health,” Amanda Paluch, PhD, with University of Massachusetts Amherst, told this news organization.
Getting in more steps per day can lower an individual’s risk for heart disease – but it’s not an “all or nothing” situation, Dr. Paluch said.
“The heart health benefits begin at lower than 10,000 steps per day. So, for the many adults that may find 10,000 steps a bit out of reach, it is important to promote that even small increases in steps can be beneficial for health,” Dr. Paluch said.
The study was published online in Circulation.
Attainable step goals
As part of the Steps for Health Collaborative, Dr. Paluch and colleagues examined the dose-response relationship between steps per day and CVD in a meta-analysis of eight prospective studies involving 20,152 adults (mean age 63, 52% women).
Steps were measured in each study using one of five different commercially available step-measuring devices. Adults aged 60 years and older took a median of 4,323 steps per day (interquartile range, 2,760-6,924), while younger adults walked a bit more (median 6,911 daily steps; IQR, 4,783-9,794).
During follow-up lasting an average of 6.2 years, a total of 1,523 CVD events were reported.
In the final adjusted model, for older adults, compared with those in quartile 1 who got the fewest steps per day (median 1,811), the risk of CVD was 20% lower in those in quartile 2, who got a median of 3,823 steps per day (hazard ratio, 0.80; 95% confidence interval, 0.69-0.93).
CVD risk was 38% lower in older adults in quartile 3 who got a median of 5,520 steps per day (HR, 0.62; 95% CI, 0.52-0.74) and 49% lower in those in quartile 4 who walked the most (a median of 9,259 steps per day; HR, 0.51; 95% CI, 0.41-0.63).
Restricting the analysis to individuals without known CVD at baseline showed similar results.
Among six studies that excluded adults with a history of CVD at baseline, compared with the lowest quartile, the HR for incident CVD events was 0.74 (95% CI, 0.60-0.91) in the second quartile, 0.60 (95% CI, 0.47-0.77) in the third quartile, and 0.55 (95% CI, 0.40-0.76) in the fourth quartile.
Despite the inverse association of steps with CVD in older adults, there was no association in younger adults. The researchers caution, however, that CVD is a disease of aging, and the follow-up period in these studies may not have been long enough to capture CVD incidence in younger adults.
Stepping rate (pace or cadence) was not associated with CVD risk beyond that of total steps per day. However, only four of the eight studies reported data on stepping rate, so this finding should be viewed as preliminary, Dr. Paluch and colleagues say.
Start small and go from there
Dr. Paluch said the take-home message from this study and numerous others is simple.
“Move more and sit less! Being physically active, by getting in your steps, is an important part of keeping your heart healthy,” she said in an interview.
For adults who are currently inactive, Dr. Paluch suggests finding small ways to get in a few more steps per day. “It does not need to be drastic changes. Consider a brief 5- to 10-minute walking break at lunch, taking the stairs, or playing a game of hide and seek with the grandchildren,” Dr. Paluch advised.
“For adults starting at 3,000 steps a day, set a goal of 4,000, and then 5,000. Each improvement can lead to better heart health,” Dr. Paluch said. “And for those who are already active, keep it up, as there are benefits with higher volumes of steps per day as well.”
Support for this research was provided by the Intergovernmental Personnel Act Agreement through the Centers for Disease Control and Prevention. The authors have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM CIRCULATION









