User login
-
The enemy of carcinogenic fumes is my friendly begonia
Sowing the seeds of cancer prevention
Are you looking to add to your quality of life, even though pets are not your speed? Might we suggest something with lower maintenance? Something a little greener?
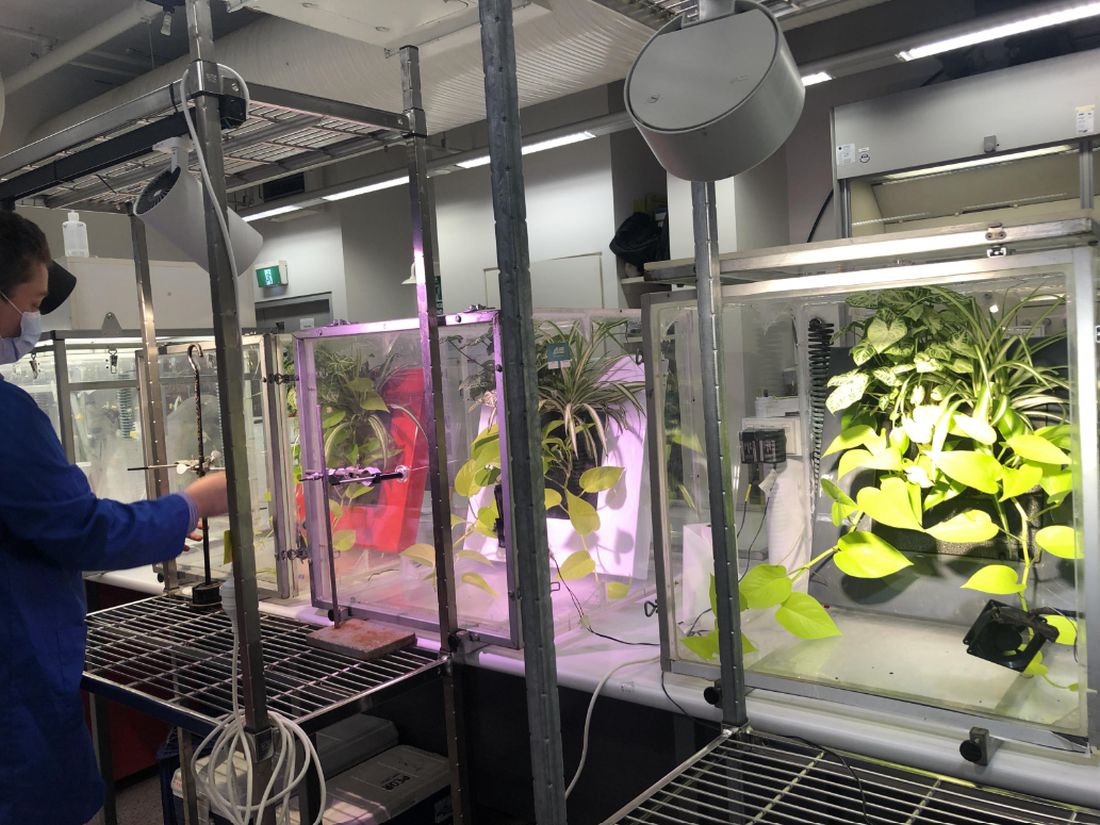
Indoor plants can purify the air that comes from outside. Researchers at the University of Technology Sydney, in partnership with the plantscaping company Ambius, showed that a “green wall” made up of mixed indoor plants was able to suck up 97% of “the most toxic compounds” from the air in just 8 hours. We’re talking about lung-irritating, headache-inducing, cancer risk–boosting compounds from gasoline fumes, including benzene.
Public health initiatives often strive to reduce cardiovascular and obesity risks, but breathing seems pretty important too. According to the World Health Organization, household air pollution is responsible for about 2.5 million global premature deaths each year. And since 2020 we’ve become accustomed to spending more time inside and at home.
“This new research proves that plants should not just be seen as ‘nice to have,’ but rather a crucial part of every workplace wellness plan,” Ambius General Manager Johan Hodgson said in statement released by the university.
So don’t spend hundreds of dollars on a fancy air filtration system when a wall of plants can do that for next to nothing. Find what works for you and your space and become a plant parent today! Your lungs will thank you.
But officer, I had to swerve to miss the duodenal ampulla
Tiny video capsule endoscopes have been around for many years, but they have one big weakness: The ingestible cameras’ journey through the GI tract is passively driven by gravity and the natural movement of the body, so they often miss potential problem areas.
Not anymore. That flaw has been addressed by medical technology company AnX Robotica, which has taken endoscopy to the next level by adding that wondrous directional control device of the modern electronic age, a joystick.
The new system “uses an external magnet and hand-held video game style joysticks to move the capsule in three dimensions,” which allows physicians to “remotely drive a miniature video capsule to all regions of the stomach to visualize and photograph potential problem areas,” according to Andrew C. Meltzer, MD, of George Washington University and associates, who conducted a pilot study funded by AnX Robotica.
The video capsule provided a 95% rate of visualization in the stomachs of 40 patients who were examined at a medical office building by an emergency medicine physician who had no previous specialty training in endoscopy. “Capsules were driven by the ER physician and then the study reports were reviewed by an attending gastroenterologist who was physically off site,” the investigators said in a written statement.
The capsule operator did receive some additional training, and development of artificial intelligence to self-drive the capsule is in the works, but for now, we’re talking about a device controlled by a human using a joystick. And we all know that 50-year-olds are not especially known for their joystick skills. For that we need real experts. Yup, we need to put those joystick-controlled capsule endoscopes in the hands of teenage gamers. Who wants to go first?
Maybe AI isn’t ready for the big time after all
“How long before some intrepid stockholder says: ‘Hey, instead of paying doctors, why don’t we just use the free robot instead?’ ” Those words appeared on LOTME but a month ago. After all, the AI is supposed to be smarter and more empathetic than a doctor. And did we mention it’s free? Or at least extremely cheap. Cheaper than, say, a group of recently unionized health care workers.
In early May, the paid employees manning the National Eating Disorders Association emergency hotline voted to unionize, as they felt overwhelmed and underpaid. Apparently, paying six people an extra few thousand a year was too much for NEDA’s leadership, as they decided a few weeks later to fire those workers, fully closing down the hotline. Instead of talking to a real person, people “calling in” for support would be met with Tessa, a wellness chatbot that would hopefully guide them through their crisis. Key word, hopefully.
In perhaps the least surprising twist of the year, NEDA was forced to walk back its decision about a week after its initial announcement. It all started with a viral Instagram post from a woman who called in and received the following advice from Tessa: Lose 1-2 pounds a week, count calories and work for a 500- to 1,000-calorie deficit, weigh herself weekly, and restrict her diet. Unfortunately, all of these suggestions were things that led to the development of the woman’s eating disorder.
Naturally, NEDA responded in good grace, accusing the woman of lying. A NEDA vice president even left some nasty comments on the post, but hastily deleted them a day later when NEDA announced it was shutting down Tessa “until further notice for a complete investigation.” NEDA’s CEO insisted they hadn’t seen that behavior from Tessa before, calling it a “bug” and insisting the bot would only be down temporarily until the triggers causing the bug were fixed.
In the aftermath, several doctors and psychologists chimed in, terming the rush to automate human roles dangerous and risky. After all, much of what makes these hotlines effective is the volunteers speaking from their own experience. An unsupervised bot doesn’t seem to have what it takes to deal with a mental health crisis, but we’re betting that Tessa will be back. As a wise cephalopod once said: Nobody gives a care about the fate of labor as long as they can get their instant gratification.
You can’t spell existential without s-t-e-n-t
This week, we’re including a special “bonus” item that, to be honest, has nothing to do with stents. That’s why our editor is making us call this a “bonus” (and making us use quote marks, too): It doesn’t really have anything to do with stents or health care or those who practice health care. Actually, his exact words were, “You can’t just give the readers someone else’s ****ing list and expect to get paid for it.” Did we mention that he looks like Jack Nicklaus but acts like BoJack Horseman?
Anywaaay, we’re pretty sure that the list in question – “America’s Top 10 Most Googled Existential Questions” – says something about the human condition, just not about stents:
1. Why is the sky blue?
2. What do dreams mean?
3. What is the meaning of life?
4. Why am I so tired?
5. Who am I?
6. What is love?
7. Is a hot dog a sandwich?
8. What came first, the chicken or the egg?
9. What should I do?
10. Do animals have souls?
Sowing the seeds of cancer prevention
Are you looking to add to your quality of life, even though pets are not your speed? Might we suggest something with lower maintenance? Something a little greener?
Indoor plants can purify the air that comes from outside. Researchers at the University of Technology Sydney, in partnership with the plantscaping company Ambius, showed that a “green wall” made up of mixed indoor plants was able to suck up 97% of “the most toxic compounds” from the air in just 8 hours. We’re talking about lung-irritating, headache-inducing, cancer risk–boosting compounds from gasoline fumes, including benzene.
Public health initiatives often strive to reduce cardiovascular and obesity risks, but breathing seems pretty important too. According to the World Health Organization, household air pollution is responsible for about 2.5 million global premature deaths each year. And since 2020 we’ve become accustomed to spending more time inside and at home.
“This new research proves that plants should not just be seen as ‘nice to have,’ but rather a crucial part of every workplace wellness plan,” Ambius General Manager Johan Hodgson said in statement released by the university.
So don’t spend hundreds of dollars on a fancy air filtration system when a wall of plants can do that for next to nothing. Find what works for you and your space and become a plant parent today! Your lungs will thank you.
But officer, I had to swerve to miss the duodenal ampulla
Tiny video capsule endoscopes have been around for many years, but they have one big weakness: The ingestible cameras’ journey through the GI tract is passively driven by gravity and the natural movement of the body, so they often miss potential problem areas.
Not anymore. That flaw has been addressed by medical technology company AnX Robotica, which has taken endoscopy to the next level by adding that wondrous directional control device of the modern electronic age, a joystick.
The new system “uses an external magnet and hand-held video game style joysticks to move the capsule in three dimensions,” which allows physicians to “remotely drive a miniature video capsule to all regions of the stomach to visualize and photograph potential problem areas,” according to Andrew C. Meltzer, MD, of George Washington University and associates, who conducted a pilot study funded by AnX Robotica.
The video capsule provided a 95% rate of visualization in the stomachs of 40 patients who were examined at a medical office building by an emergency medicine physician who had no previous specialty training in endoscopy. “Capsules were driven by the ER physician and then the study reports were reviewed by an attending gastroenterologist who was physically off site,” the investigators said in a written statement.
The capsule operator did receive some additional training, and development of artificial intelligence to self-drive the capsule is in the works, but for now, we’re talking about a device controlled by a human using a joystick. And we all know that 50-year-olds are not especially known for their joystick skills. For that we need real experts. Yup, we need to put those joystick-controlled capsule endoscopes in the hands of teenage gamers. Who wants to go first?
Maybe AI isn’t ready for the big time after all
“How long before some intrepid stockholder says: ‘Hey, instead of paying doctors, why don’t we just use the free robot instead?’ ” Those words appeared on LOTME but a month ago. After all, the AI is supposed to be smarter and more empathetic than a doctor. And did we mention it’s free? Or at least extremely cheap. Cheaper than, say, a group of recently unionized health care workers.
In early May, the paid employees manning the National Eating Disorders Association emergency hotline voted to unionize, as they felt overwhelmed and underpaid. Apparently, paying six people an extra few thousand a year was too much for NEDA’s leadership, as they decided a few weeks later to fire those workers, fully closing down the hotline. Instead of talking to a real person, people “calling in” for support would be met with Tessa, a wellness chatbot that would hopefully guide them through their crisis. Key word, hopefully.
In perhaps the least surprising twist of the year, NEDA was forced to walk back its decision about a week after its initial announcement. It all started with a viral Instagram post from a woman who called in and received the following advice from Tessa: Lose 1-2 pounds a week, count calories and work for a 500- to 1,000-calorie deficit, weigh herself weekly, and restrict her diet. Unfortunately, all of these suggestions were things that led to the development of the woman’s eating disorder.
Naturally, NEDA responded in good grace, accusing the woman of lying. A NEDA vice president even left some nasty comments on the post, but hastily deleted them a day later when NEDA announced it was shutting down Tessa “until further notice for a complete investigation.” NEDA’s CEO insisted they hadn’t seen that behavior from Tessa before, calling it a “bug” and insisting the bot would only be down temporarily until the triggers causing the bug were fixed.
In the aftermath, several doctors and psychologists chimed in, terming the rush to automate human roles dangerous and risky. After all, much of what makes these hotlines effective is the volunteers speaking from their own experience. An unsupervised bot doesn’t seem to have what it takes to deal with a mental health crisis, but we’re betting that Tessa will be back. As a wise cephalopod once said: Nobody gives a care about the fate of labor as long as they can get their instant gratification.
You can’t spell existential without s-t-e-n-t
This week, we’re including a special “bonus” item that, to be honest, has nothing to do with stents. That’s why our editor is making us call this a “bonus” (and making us use quote marks, too): It doesn’t really have anything to do with stents or health care or those who practice health care. Actually, his exact words were, “You can’t just give the readers someone else’s ****ing list and expect to get paid for it.” Did we mention that he looks like Jack Nicklaus but acts like BoJack Horseman?
Anywaaay, we’re pretty sure that the list in question – “America’s Top 10 Most Googled Existential Questions” – says something about the human condition, just not about stents:
1. Why is the sky blue?
2. What do dreams mean?
3. What is the meaning of life?
4. Why am I so tired?
5. Who am I?
6. What is love?
7. Is a hot dog a sandwich?
8. What came first, the chicken or the egg?
9. What should I do?
10. Do animals have souls?
Sowing the seeds of cancer prevention
Are you looking to add to your quality of life, even though pets are not your speed? Might we suggest something with lower maintenance? Something a little greener?
Indoor plants can purify the air that comes from outside. Researchers at the University of Technology Sydney, in partnership with the plantscaping company Ambius, showed that a “green wall” made up of mixed indoor plants was able to suck up 97% of “the most toxic compounds” from the air in just 8 hours. We’re talking about lung-irritating, headache-inducing, cancer risk–boosting compounds from gasoline fumes, including benzene.
Public health initiatives often strive to reduce cardiovascular and obesity risks, but breathing seems pretty important too. According to the World Health Organization, household air pollution is responsible for about 2.5 million global premature deaths each year. And since 2020 we’ve become accustomed to spending more time inside and at home.
“This new research proves that plants should not just be seen as ‘nice to have,’ but rather a crucial part of every workplace wellness plan,” Ambius General Manager Johan Hodgson said in statement released by the university.
So don’t spend hundreds of dollars on a fancy air filtration system when a wall of plants can do that for next to nothing. Find what works for you and your space and become a plant parent today! Your lungs will thank you.
But officer, I had to swerve to miss the duodenal ampulla
Tiny video capsule endoscopes have been around for many years, but they have one big weakness: The ingestible cameras’ journey through the GI tract is passively driven by gravity and the natural movement of the body, so they often miss potential problem areas.
Not anymore. That flaw has been addressed by medical technology company AnX Robotica, which has taken endoscopy to the next level by adding that wondrous directional control device of the modern electronic age, a joystick.
The new system “uses an external magnet and hand-held video game style joysticks to move the capsule in three dimensions,” which allows physicians to “remotely drive a miniature video capsule to all regions of the stomach to visualize and photograph potential problem areas,” according to Andrew C. Meltzer, MD, of George Washington University and associates, who conducted a pilot study funded by AnX Robotica.
The video capsule provided a 95% rate of visualization in the stomachs of 40 patients who were examined at a medical office building by an emergency medicine physician who had no previous specialty training in endoscopy. “Capsules were driven by the ER physician and then the study reports were reviewed by an attending gastroenterologist who was physically off site,” the investigators said in a written statement.
The capsule operator did receive some additional training, and development of artificial intelligence to self-drive the capsule is in the works, but for now, we’re talking about a device controlled by a human using a joystick. And we all know that 50-year-olds are not especially known for their joystick skills. For that we need real experts. Yup, we need to put those joystick-controlled capsule endoscopes in the hands of teenage gamers. Who wants to go first?
Maybe AI isn’t ready for the big time after all
“How long before some intrepid stockholder says: ‘Hey, instead of paying doctors, why don’t we just use the free robot instead?’ ” Those words appeared on LOTME but a month ago. After all, the AI is supposed to be smarter and more empathetic than a doctor. And did we mention it’s free? Or at least extremely cheap. Cheaper than, say, a group of recently unionized health care workers.
In early May, the paid employees manning the National Eating Disorders Association emergency hotline voted to unionize, as they felt overwhelmed and underpaid. Apparently, paying six people an extra few thousand a year was too much for NEDA’s leadership, as they decided a few weeks later to fire those workers, fully closing down the hotline. Instead of talking to a real person, people “calling in” for support would be met with Tessa, a wellness chatbot that would hopefully guide them through their crisis. Key word, hopefully.
In perhaps the least surprising twist of the year, NEDA was forced to walk back its decision about a week after its initial announcement. It all started with a viral Instagram post from a woman who called in and received the following advice from Tessa: Lose 1-2 pounds a week, count calories and work for a 500- to 1,000-calorie deficit, weigh herself weekly, and restrict her diet. Unfortunately, all of these suggestions were things that led to the development of the woman’s eating disorder.
Naturally, NEDA responded in good grace, accusing the woman of lying. A NEDA vice president even left some nasty comments on the post, but hastily deleted them a day later when NEDA announced it was shutting down Tessa “until further notice for a complete investigation.” NEDA’s CEO insisted they hadn’t seen that behavior from Tessa before, calling it a “bug” and insisting the bot would only be down temporarily until the triggers causing the bug were fixed.
In the aftermath, several doctors and psychologists chimed in, terming the rush to automate human roles dangerous and risky. After all, much of what makes these hotlines effective is the volunteers speaking from their own experience. An unsupervised bot doesn’t seem to have what it takes to deal with a mental health crisis, but we’re betting that Tessa will be back. As a wise cephalopod once said: Nobody gives a care about the fate of labor as long as they can get their instant gratification.
You can’t spell existential without s-t-e-n-t
This week, we’re including a special “bonus” item that, to be honest, has nothing to do with stents. That’s why our editor is making us call this a “bonus” (and making us use quote marks, too): It doesn’t really have anything to do with stents or health care or those who practice health care. Actually, his exact words were, “You can’t just give the readers someone else’s ****ing list and expect to get paid for it.” Did we mention that he looks like Jack Nicklaus but acts like BoJack Horseman?
Anywaaay, we’re pretty sure that the list in question – “America’s Top 10 Most Googled Existential Questions” – says something about the human condition, just not about stents:
1. Why is the sky blue?
2. What do dreams mean?
3. What is the meaning of life?
4. Why am I so tired?
5. Who am I?
6. What is love?
7. Is a hot dog a sandwich?
8. What came first, the chicken or the egg?
9. What should I do?
10. Do animals have souls?
PMBCL: Postremission, patients may safely skip radiation
“This study is the largest prospective study of PMBCL ever conducted,” said first author Emanuele Zucca, MD, consultant and head of the lymphoma unit at the Oncology Institute of Southern Switzerland in Bellinzona. Dr. Zucca presented the findings at the annual meeting of the American Society of Clinical Oncology (ASCO).
The results of the research underscore that “mediastinal radiation therapy in patients with complete remission after frontline immunochemotherapy can be safely omitted,” he said.
While PMBCL has a relatively low incidence, representing fewer than 5% of cases of non-Hodgkin lymphoma, the cancer is over-represented in young White women between approximately 30 and 40 years of age, and is a notably aggressive form of diffuse large B-cell lymphoma.
However, in patients who rapidly achieve remission with dose-intensive immunochemotherapy, the prognosis is good.
In such cases, the use of mediastinal radiation therapy has been seen as a measure to further consolidate the immunochemotherapy response, but the additional treatment comes at the cost of an increased risk of second malignancies, as well as coronary or valvular heart disease.
Meanwhile, in recent decades promising data has shown that aggressive chemoimmunotherapy regimens alone, such as DA-EPOCH-R (dose-adjusted etoposide, prednisone, vincristine, cyclophosphamide, doxorubicin, and rituximab) can be enough for patients achieving a complete remission, while novel approaches such as checkpoint inhibitors and CAR T-cell therapy further show benefits in patients with lymphoma that relapses after treatment.
With ongoing controversy over whether to include the added radiation therapy among patients with a complete metabolic response, Dr. Zucca and his colleagues conducted the IELSG37 international study, enrolling 545 patients from 74 centers in 13 countries, including 336 women, with newly diagnosed PMBCL.
The patients were treated with induction chemoimmunotherapy with rituximab and anthracycline-based therapy based on local practice, and response assessed among of 530 of the 545 patients showed that 268 (50.6%) achieved a complete metabolic response.
Those patients were then randomized to either observation (n = 132) or consolidation radiation therapy (30 Gy; n = 136). The characteristics between the two groups were similar, with a mean age of 35.5, and about 65% female.
With a median follow-up of 63 months (range, 48-60 months), the primary endpoint of progression-free survival at 30 months was not significantly different between the observation arm (98.5%) and radiation therapy arm (96.2%; P = .278).
After adjustment for factors including sex, chemotherapy, country, and positron emission tomography (PET) response score, the estimated relative effect of radiotherapy versus observation was a hazard ratio of 0.68, and the absolute risk reduction associated with radiotherapy at 30 months was 1.2% after adjustment.
The number needed to treat is high, at 126.3 after stratification, and the 5-year overall survival was excellent in both arms, at 99%.
“What this tells us is that treatment with radiation therapy in well over 100 patients is needed just to avoid a single recurrence,” Dr. Zucca explained.
Overall survival after 3 years was excellent and identical in both arms, at about 99%.
To date, three severe cardiac events and three second cancers have been recorded in the study, all occurring among patients randomized to receive radiation therapy.
Dr. Zucca noted that longer follow-up is needed to better examine late toxicities.
“The long-term toxicities of mediastinal radiotherapy are well documented, particularly second breast, thyroid, and lung cancers and increased risk of coronary or valvular heart disease, in a patient group dominated by young adults,” Dr. Zucca said in a press statement.
“This study shows chemoimmunotherapy alone is an effective treatment for primary mediastinal B-cell lymphoma and strongly supports omitting radiotherapy without impacting chances of cure.”
Commenting on the study, Corey W. Speers, MD, PhD, assistant professor, radiation oncology, department of surgery, University of Michigan Hospital, Ann Arbor, said the findings have important clinical implications.
“We all should be encouraged by the low rates in this trial, which are lower than expected,” Dr. Speers said in a press briefing.
In further comments, he added that “these results will inform and likely change clinical practice.”
Dr. Speers said the study is notable for being the first of its kind.
“This clinical question has not previously been directly addressed, and this is the first study to do so,” he said.
“With more effective systemic therapies, many patients have their lymphoma disappear with early aggressive treatment, and although radiation is very effective at treating lymphoma, it has not been clear if it is needed in these patients that have an early rapid response to systemic therapy before starting radiation,” Dr. Speers explained.
“We have struggled as oncologists to know whether omitting this effective radiotherapy would compromise outcomes, and thus many were inclined to continue offering it to patients, even with the great early response. This study helps answer this critical question,” he said.
The results add reassuring evidence, buttressing efforts to avoid unnecessary interventions that may provide little or no benefit, Dr. Speers added.
“We are now in an era of ‘less being more’ as we seek ways to provide optimal quality and quantity of life to patients with cancer and their families, and this is just another example of the tremendous progress being made.”
Further commenting on the study at the press briefing, Julie R. Gralow, MD, ASCO chief medical officer and executive vice president, said the research supports ASCO’s ongoing efforts to reduce the toxicities of cancer treatment.
“Our ASCO vision is a world where cancer is either prevented or cured, and every patient is cured – and every survivor is healthy, and that part about every survivor being healthy is what we’re working on here [in this study],” Dr. Gralow said.
The study was funded by the Swiss Cancer League and Cancer Research UK, with partial support from the Swiss National Science Foundation. Dr. Zucca reported relationships with AstraZeneca, Beigene, Celgene, Incyte, Janssen, Merck, Roche, Celltrion Healthcare, Kite, and Abbvie. Dr. Speers disclosed his coinvention of technology that assesses radiosensitivity and predicts benefits from adjutant radiotherapy.
“This study is the largest prospective study of PMBCL ever conducted,” said first author Emanuele Zucca, MD, consultant and head of the lymphoma unit at the Oncology Institute of Southern Switzerland in Bellinzona. Dr. Zucca presented the findings at the annual meeting of the American Society of Clinical Oncology (ASCO).
The results of the research underscore that “mediastinal radiation therapy in patients with complete remission after frontline immunochemotherapy can be safely omitted,” he said.
While PMBCL has a relatively low incidence, representing fewer than 5% of cases of non-Hodgkin lymphoma, the cancer is over-represented in young White women between approximately 30 and 40 years of age, and is a notably aggressive form of diffuse large B-cell lymphoma.
However, in patients who rapidly achieve remission with dose-intensive immunochemotherapy, the prognosis is good.
In such cases, the use of mediastinal radiation therapy has been seen as a measure to further consolidate the immunochemotherapy response, but the additional treatment comes at the cost of an increased risk of second malignancies, as well as coronary or valvular heart disease.
Meanwhile, in recent decades promising data has shown that aggressive chemoimmunotherapy regimens alone, such as DA-EPOCH-R (dose-adjusted etoposide, prednisone, vincristine, cyclophosphamide, doxorubicin, and rituximab) can be enough for patients achieving a complete remission, while novel approaches such as checkpoint inhibitors and CAR T-cell therapy further show benefits in patients with lymphoma that relapses after treatment.
With ongoing controversy over whether to include the added radiation therapy among patients with a complete metabolic response, Dr. Zucca and his colleagues conducted the IELSG37 international study, enrolling 545 patients from 74 centers in 13 countries, including 336 women, with newly diagnosed PMBCL.
The patients were treated with induction chemoimmunotherapy with rituximab and anthracycline-based therapy based on local practice, and response assessed among of 530 of the 545 patients showed that 268 (50.6%) achieved a complete metabolic response.
Those patients were then randomized to either observation (n = 132) or consolidation radiation therapy (30 Gy; n = 136). The characteristics between the two groups were similar, with a mean age of 35.5, and about 65% female.
With a median follow-up of 63 months (range, 48-60 months), the primary endpoint of progression-free survival at 30 months was not significantly different between the observation arm (98.5%) and radiation therapy arm (96.2%; P = .278).
After adjustment for factors including sex, chemotherapy, country, and positron emission tomography (PET) response score, the estimated relative effect of radiotherapy versus observation was a hazard ratio of 0.68, and the absolute risk reduction associated with radiotherapy at 30 months was 1.2% after adjustment.
The number needed to treat is high, at 126.3 after stratification, and the 5-year overall survival was excellent in both arms, at 99%.
“What this tells us is that treatment with radiation therapy in well over 100 patients is needed just to avoid a single recurrence,” Dr. Zucca explained.
Overall survival after 3 years was excellent and identical in both arms, at about 99%.
To date, three severe cardiac events and three second cancers have been recorded in the study, all occurring among patients randomized to receive radiation therapy.
Dr. Zucca noted that longer follow-up is needed to better examine late toxicities.
“The long-term toxicities of mediastinal radiotherapy are well documented, particularly second breast, thyroid, and lung cancers and increased risk of coronary or valvular heart disease, in a patient group dominated by young adults,” Dr. Zucca said in a press statement.
“This study shows chemoimmunotherapy alone is an effective treatment for primary mediastinal B-cell lymphoma and strongly supports omitting radiotherapy without impacting chances of cure.”
Commenting on the study, Corey W. Speers, MD, PhD, assistant professor, radiation oncology, department of surgery, University of Michigan Hospital, Ann Arbor, said the findings have important clinical implications.
“We all should be encouraged by the low rates in this trial, which are lower than expected,” Dr. Speers said in a press briefing.
In further comments, he added that “these results will inform and likely change clinical practice.”
Dr. Speers said the study is notable for being the first of its kind.
“This clinical question has not previously been directly addressed, and this is the first study to do so,” he said.
“With more effective systemic therapies, many patients have their lymphoma disappear with early aggressive treatment, and although radiation is very effective at treating lymphoma, it has not been clear if it is needed in these patients that have an early rapid response to systemic therapy before starting radiation,” Dr. Speers explained.
“We have struggled as oncologists to know whether omitting this effective radiotherapy would compromise outcomes, and thus many were inclined to continue offering it to patients, even with the great early response. This study helps answer this critical question,” he said.
The results add reassuring evidence, buttressing efforts to avoid unnecessary interventions that may provide little or no benefit, Dr. Speers added.
“We are now in an era of ‘less being more’ as we seek ways to provide optimal quality and quantity of life to patients with cancer and their families, and this is just another example of the tremendous progress being made.”
Further commenting on the study at the press briefing, Julie R. Gralow, MD, ASCO chief medical officer and executive vice president, said the research supports ASCO’s ongoing efforts to reduce the toxicities of cancer treatment.
“Our ASCO vision is a world where cancer is either prevented or cured, and every patient is cured – and every survivor is healthy, and that part about every survivor being healthy is what we’re working on here [in this study],” Dr. Gralow said.
The study was funded by the Swiss Cancer League and Cancer Research UK, with partial support from the Swiss National Science Foundation. Dr. Zucca reported relationships with AstraZeneca, Beigene, Celgene, Incyte, Janssen, Merck, Roche, Celltrion Healthcare, Kite, and Abbvie. Dr. Speers disclosed his coinvention of technology that assesses radiosensitivity and predicts benefits from adjutant radiotherapy.
“This study is the largest prospective study of PMBCL ever conducted,” said first author Emanuele Zucca, MD, consultant and head of the lymphoma unit at the Oncology Institute of Southern Switzerland in Bellinzona. Dr. Zucca presented the findings at the annual meeting of the American Society of Clinical Oncology (ASCO).
The results of the research underscore that “mediastinal radiation therapy in patients with complete remission after frontline immunochemotherapy can be safely omitted,” he said.
While PMBCL has a relatively low incidence, representing fewer than 5% of cases of non-Hodgkin lymphoma, the cancer is over-represented in young White women between approximately 30 and 40 years of age, and is a notably aggressive form of diffuse large B-cell lymphoma.
However, in patients who rapidly achieve remission with dose-intensive immunochemotherapy, the prognosis is good.
In such cases, the use of mediastinal radiation therapy has been seen as a measure to further consolidate the immunochemotherapy response, but the additional treatment comes at the cost of an increased risk of second malignancies, as well as coronary or valvular heart disease.
Meanwhile, in recent decades promising data has shown that aggressive chemoimmunotherapy regimens alone, such as DA-EPOCH-R (dose-adjusted etoposide, prednisone, vincristine, cyclophosphamide, doxorubicin, and rituximab) can be enough for patients achieving a complete remission, while novel approaches such as checkpoint inhibitors and CAR T-cell therapy further show benefits in patients with lymphoma that relapses after treatment.
With ongoing controversy over whether to include the added radiation therapy among patients with a complete metabolic response, Dr. Zucca and his colleagues conducted the IELSG37 international study, enrolling 545 patients from 74 centers in 13 countries, including 336 women, with newly diagnosed PMBCL.
The patients were treated with induction chemoimmunotherapy with rituximab and anthracycline-based therapy based on local practice, and response assessed among of 530 of the 545 patients showed that 268 (50.6%) achieved a complete metabolic response.
Those patients were then randomized to either observation (n = 132) or consolidation radiation therapy (30 Gy; n = 136). The characteristics between the two groups were similar, with a mean age of 35.5, and about 65% female.
With a median follow-up of 63 months (range, 48-60 months), the primary endpoint of progression-free survival at 30 months was not significantly different between the observation arm (98.5%) and radiation therapy arm (96.2%; P = .278).
After adjustment for factors including sex, chemotherapy, country, and positron emission tomography (PET) response score, the estimated relative effect of radiotherapy versus observation was a hazard ratio of 0.68, and the absolute risk reduction associated with radiotherapy at 30 months was 1.2% after adjustment.
The number needed to treat is high, at 126.3 after stratification, and the 5-year overall survival was excellent in both arms, at 99%.
“What this tells us is that treatment with radiation therapy in well over 100 patients is needed just to avoid a single recurrence,” Dr. Zucca explained.
Overall survival after 3 years was excellent and identical in both arms, at about 99%.
To date, three severe cardiac events and three second cancers have been recorded in the study, all occurring among patients randomized to receive radiation therapy.
Dr. Zucca noted that longer follow-up is needed to better examine late toxicities.
“The long-term toxicities of mediastinal radiotherapy are well documented, particularly second breast, thyroid, and lung cancers and increased risk of coronary or valvular heart disease, in a patient group dominated by young adults,” Dr. Zucca said in a press statement.
“This study shows chemoimmunotherapy alone is an effective treatment for primary mediastinal B-cell lymphoma and strongly supports omitting radiotherapy without impacting chances of cure.”
Commenting on the study, Corey W. Speers, MD, PhD, assistant professor, radiation oncology, department of surgery, University of Michigan Hospital, Ann Arbor, said the findings have important clinical implications.
“We all should be encouraged by the low rates in this trial, which are lower than expected,” Dr. Speers said in a press briefing.
In further comments, he added that “these results will inform and likely change clinical practice.”
Dr. Speers said the study is notable for being the first of its kind.
“This clinical question has not previously been directly addressed, and this is the first study to do so,” he said.
“With more effective systemic therapies, many patients have their lymphoma disappear with early aggressive treatment, and although radiation is very effective at treating lymphoma, it has not been clear if it is needed in these patients that have an early rapid response to systemic therapy before starting radiation,” Dr. Speers explained.
“We have struggled as oncologists to know whether omitting this effective radiotherapy would compromise outcomes, and thus many were inclined to continue offering it to patients, even with the great early response. This study helps answer this critical question,” he said.
The results add reassuring evidence, buttressing efforts to avoid unnecessary interventions that may provide little or no benefit, Dr. Speers added.
“We are now in an era of ‘less being more’ as we seek ways to provide optimal quality and quantity of life to patients with cancer and their families, and this is just another example of the tremendous progress being made.”
Further commenting on the study at the press briefing, Julie R. Gralow, MD, ASCO chief medical officer and executive vice president, said the research supports ASCO’s ongoing efforts to reduce the toxicities of cancer treatment.
“Our ASCO vision is a world where cancer is either prevented or cured, and every patient is cured – and every survivor is healthy, and that part about every survivor being healthy is what we’re working on here [in this study],” Dr. Gralow said.
The study was funded by the Swiss Cancer League and Cancer Research UK, with partial support from the Swiss National Science Foundation. Dr. Zucca reported relationships with AstraZeneca, Beigene, Celgene, Incyte, Janssen, Merck, Roche, Celltrion Healthcare, Kite, and Abbvie. Dr. Speers disclosed his coinvention of technology that assesses radiosensitivity and predicts benefits from adjutant radiotherapy.
FROM ASCO 2023
New CLL meds: Improved survival rates, 1990-2018
“The clinical take-away from our study is that population-based statistics show a decline in mortality and an increase in survival that is concurrent with the introduction of new therapies for treating CLL,” said lead study author Nadia Howlader, PhD, of the Surveillance Research Program, Division of Cancer Control and Population Sciences, National Cancer Institute, Bethesda, Md. This research was published in Cancer Epidemiology, Biomarkers & Prevention.
From 1992 to 2011, CLL mortality decreased 1.1% annually, then the pace of the decline hastened to 3.6% per year from 2011 to 2021 among adults aged ≥ 20 years. Furthermore, 5-year survival rates among patients with CLL increased 0.7% per year on average from 1992 to 2016. To account for yearly random fluctuations in the number of cases detected, incidence data was fit to a model to determine the trend.
Although the study was not designed to specify which treatments were disseminated among patients or to estimate the impact of a specific drug, there were only six new drugs approved for CLL from 1991 to 2010. In contrast, between 2011 and 2018, 11 new CLL drugs (in particular the approval of new tyrosine kinase inhibitors (TKIs)) ushered in a period of more rapid annual decreases in mortality.
“The approval of ibrutinib [2014] was a sea change in decreasing CLL mortality. Earlier therapies like chemoimmunotherapies were not as effective in patients with TP53 mutation and/or 17P deletions,” said Binsah George, MD, of McGovern Medical School at UTHealth, Houston, who was not associated with the study.
New TKIs not only decrease mortality, but also have fewer side effects than earlier cytotoxic therapies, do not require inpatient treatment, and are available to all patients on Medicare and Medicaid.
Although patients with relapsed CLL may benefit from bone marrow transplants or CAR T-cell therapy, these treatments are not available at many community oncology practices. Furthermore, some patients are too sick to receive them or don’t have the economic and social resources to get them.
Even though TKIs increase overall survival in patients with CLL, they are not curative and require lifelong treatment.
“The estimated cost for CLL treatment is around $600,000 in a lifetime per patient, possibly placing significant burden on patients and the health care system,” said Dr. George.
“Certain trials are looking at stopping TKI treatment after a fixed period of time. This will let us learn more about the disease and could possibly lead to a decrease in cost and side effects of therapy,” concluded Dr. George.
Due to the study’s retrospective nature and data being sourced from state cancer registries and federal statistics, authors posited that rates of CLL could be underestimated, due to miscoding and missing information, particularly from those who get treatment outside of hospital settings. Additionally, some of the improvement in mortality could be attributed to better supportive care and less toxicity in medications, rather than then efficacy of novel agents.
Dr. Howlader and Dr. Binsah reported no conflicts of interest.
“The clinical take-away from our study is that population-based statistics show a decline in mortality and an increase in survival that is concurrent with the introduction of new therapies for treating CLL,” said lead study author Nadia Howlader, PhD, of the Surveillance Research Program, Division of Cancer Control and Population Sciences, National Cancer Institute, Bethesda, Md. This research was published in Cancer Epidemiology, Biomarkers & Prevention.
From 1992 to 2011, CLL mortality decreased 1.1% annually, then the pace of the decline hastened to 3.6% per year from 2011 to 2021 among adults aged ≥ 20 years. Furthermore, 5-year survival rates among patients with CLL increased 0.7% per year on average from 1992 to 2016. To account for yearly random fluctuations in the number of cases detected, incidence data was fit to a model to determine the trend.
Although the study was not designed to specify which treatments were disseminated among patients or to estimate the impact of a specific drug, there were only six new drugs approved for CLL from 1991 to 2010. In contrast, between 2011 and 2018, 11 new CLL drugs (in particular the approval of new tyrosine kinase inhibitors (TKIs)) ushered in a period of more rapid annual decreases in mortality.
“The approval of ibrutinib [2014] was a sea change in decreasing CLL mortality. Earlier therapies like chemoimmunotherapies were not as effective in patients with TP53 mutation and/or 17P deletions,” said Binsah George, MD, of McGovern Medical School at UTHealth, Houston, who was not associated with the study.
New TKIs not only decrease mortality, but also have fewer side effects than earlier cytotoxic therapies, do not require inpatient treatment, and are available to all patients on Medicare and Medicaid.
Although patients with relapsed CLL may benefit from bone marrow transplants or CAR T-cell therapy, these treatments are not available at many community oncology practices. Furthermore, some patients are too sick to receive them or don’t have the economic and social resources to get them.
Even though TKIs increase overall survival in patients with CLL, they are not curative and require lifelong treatment.
“The estimated cost for CLL treatment is around $600,000 in a lifetime per patient, possibly placing significant burden on patients and the health care system,” said Dr. George.
“Certain trials are looking at stopping TKI treatment after a fixed period of time. This will let us learn more about the disease and could possibly lead to a decrease in cost and side effects of therapy,” concluded Dr. George.
Due to the study’s retrospective nature and data being sourced from state cancer registries and federal statistics, authors posited that rates of CLL could be underestimated, due to miscoding and missing information, particularly from those who get treatment outside of hospital settings. Additionally, some of the improvement in mortality could be attributed to better supportive care and less toxicity in medications, rather than then efficacy of novel agents.
Dr. Howlader and Dr. Binsah reported no conflicts of interest.
“The clinical take-away from our study is that population-based statistics show a decline in mortality and an increase in survival that is concurrent with the introduction of new therapies for treating CLL,” said lead study author Nadia Howlader, PhD, of the Surveillance Research Program, Division of Cancer Control and Population Sciences, National Cancer Institute, Bethesda, Md. This research was published in Cancer Epidemiology, Biomarkers & Prevention.
From 1992 to 2011, CLL mortality decreased 1.1% annually, then the pace of the decline hastened to 3.6% per year from 2011 to 2021 among adults aged ≥ 20 years. Furthermore, 5-year survival rates among patients with CLL increased 0.7% per year on average from 1992 to 2016. To account for yearly random fluctuations in the number of cases detected, incidence data was fit to a model to determine the trend.
Although the study was not designed to specify which treatments were disseminated among patients or to estimate the impact of a specific drug, there were only six new drugs approved for CLL from 1991 to 2010. In contrast, between 2011 and 2018, 11 new CLL drugs (in particular the approval of new tyrosine kinase inhibitors (TKIs)) ushered in a period of more rapid annual decreases in mortality.
“The approval of ibrutinib [2014] was a sea change in decreasing CLL mortality. Earlier therapies like chemoimmunotherapies were not as effective in patients with TP53 mutation and/or 17P deletions,” said Binsah George, MD, of McGovern Medical School at UTHealth, Houston, who was not associated with the study.
New TKIs not only decrease mortality, but also have fewer side effects than earlier cytotoxic therapies, do not require inpatient treatment, and are available to all patients on Medicare and Medicaid.
Although patients with relapsed CLL may benefit from bone marrow transplants or CAR T-cell therapy, these treatments are not available at many community oncology practices. Furthermore, some patients are too sick to receive them or don’t have the economic and social resources to get them.
Even though TKIs increase overall survival in patients with CLL, they are not curative and require lifelong treatment.
“The estimated cost for CLL treatment is around $600,000 in a lifetime per patient, possibly placing significant burden on patients and the health care system,” said Dr. George.
“Certain trials are looking at stopping TKI treatment after a fixed period of time. This will let us learn more about the disease and could possibly lead to a decrease in cost and side effects of therapy,” concluded Dr. George.
Due to the study’s retrospective nature and data being sourced from state cancer registries and federal statistics, authors posited that rates of CLL could be underestimated, due to miscoding and missing information, particularly from those who get treatment outside of hospital settings. Additionally, some of the improvement in mortality could be attributed to better supportive care and less toxicity in medications, rather than then efficacy of novel agents.
Dr. Howlader and Dr. Binsah reported no conflicts of interest.
FROM CANCER EPIDEMIOLOGY, BIOMARKERS & PREVENTION
Medicaid expansion closing racial gap in GI cancer deaths
Across the United States, minority patients with cancer often have worse outcomes than White patients, with Black patients more likely to die sooner.
But new data suggest that these racial disparities are lessening. They come from a cross-sectional cohort study of patients with gastrointestinal cancers and show that the gap in mortality rates was reduced in Medicaid expansion states, compared with nonexpansion states.
The results were particularly notable for Black patients, for whom there was a consistent increase in receiving therapy (chemotherapy or surgery) and a decrease in mortality from stomach, colorectal, and pancreatic cancer, the investigators commented.
The study was highlighted at a press briefing held in advance of the annual meeting of the American Society of Clinical Oncology.
“The findings of this study provide a solid step for closing the gap, showing that the Medicaid expansion opportunity offered by the Affordable Care Act, which allows participating states to improve health care access for disadvantaged populations, results in better cancer outcomes and mitigation of racial disparities in cancer survival,” commented Julie Gralow, MD, chief medical officer and executive vice president of ASCO.
The study included 86,052 patients from the National Cancer Database who, from 2009 to 2019, were diagnosed with pancreatic cancer, colorectal cancer, or stomach cancer. Just over 22,000 patients (25.7%) were Black; the remainder 63,943 (74.3%) were White.
In Medicaid expansion states, there was a greater absolute reduction in 2-year mortality among Black patients with pancreatic cancer of –11.8%, compared with nonexpansion states, at –2.4%, a difference-in-difference (DID) of –9.4%. Additionally, there was an increase in treatment with chemotherapy for patients with stage III-IV pancreatic cancer (4.5% for Black patients and 3.2% for White), compared with patients in nonexpansion states (0.8% for Black patients and 0.4% for White; DID, 3.7% for Black patients and DID, 2.7% for White).
“We found similar results in colorectal cancer, but this effect is primarily observed among the stage IV patients,” commented lead author Naveen Manisundaram, MD, a research fellow at the University of Texas MD Anderson Cancer Center, Houston. “Black patients with advanced stage disease experienced a 12.6% reduction in mortality in expansion states.”
Among Black patients with stage IV colorectal cancer, there was an increase in rates of surgery in expansion states, compared with nonexpansion states (DID, 5.7%). However, there was no increase in treatment with chemotherapy (DID, 1%; P = .66).
Mortality rates for Black patients with stomach cancer also decreased. In expansion states, there was a –13% absolute decrease in mortality, compared with a –5.2% decrease in nonexpansion states.
The investigators noted that Medicaid coverage was a key component in access to care through the Affordable Care Act. About two-thirds (66.7%) of Black patients had Medicaid; 33.3% were uninsured. Coverage was similar among White patients; 64.1% had Medicaid and 35.9% were uninsured.
“Our study provides compelling data that show Medicaid expansion was associated with improvement in survival for both Black and White patients with gastrointestinal cancers. Additionally, it suggests that Medicaid expansion is one potential avenue to mitigate existing racial survival disparities among these patients,” Dr. Manisundaram concluded.
The study was funded by the National Institutes of Health. One coauthor reported an advisory role with Medicaroid. Dr. Gralow has had a consulting or advisory role with Genentech and Roche.
A version of this article first appeared on Medscape.com.
Across the United States, minority patients with cancer often have worse outcomes than White patients, with Black patients more likely to die sooner.
But new data suggest that these racial disparities are lessening. They come from a cross-sectional cohort study of patients with gastrointestinal cancers and show that the gap in mortality rates was reduced in Medicaid expansion states, compared with nonexpansion states.
The results were particularly notable for Black patients, for whom there was a consistent increase in receiving therapy (chemotherapy or surgery) and a decrease in mortality from stomach, colorectal, and pancreatic cancer, the investigators commented.
The study was highlighted at a press briefing held in advance of the annual meeting of the American Society of Clinical Oncology.
“The findings of this study provide a solid step for closing the gap, showing that the Medicaid expansion opportunity offered by the Affordable Care Act, which allows participating states to improve health care access for disadvantaged populations, results in better cancer outcomes and mitigation of racial disparities in cancer survival,” commented Julie Gralow, MD, chief medical officer and executive vice president of ASCO.
The study included 86,052 patients from the National Cancer Database who, from 2009 to 2019, were diagnosed with pancreatic cancer, colorectal cancer, or stomach cancer. Just over 22,000 patients (25.7%) were Black; the remainder 63,943 (74.3%) were White.
In Medicaid expansion states, there was a greater absolute reduction in 2-year mortality among Black patients with pancreatic cancer of –11.8%, compared with nonexpansion states, at –2.4%, a difference-in-difference (DID) of –9.4%. Additionally, there was an increase in treatment with chemotherapy for patients with stage III-IV pancreatic cancer (4.5% for Black patients and 3.2% for White), compared with patients in nonexpansion states (0.8% for Black patients and 0.4% for White; DID, 3.7% for Black patients and DID, 2.7% for White).
“We found similar results in colorectal cancer, but this effect is primarily observed among the stage IV patients,” commented lead author Naveen Manisundaram, MD, a research fellow at the University of Texas MD Anderson Cancer Center, Houston. “Black patients with advanced stage disease experienced a 12.6% reduction in mortality in expansion states.”
Among Black patients with stage IV colorectal cancer, there was an increase in rates of surgery in expansion states, compared with nonexpansion states (DID, 5.7%). However, there was no increase in treatment with chemotherapy (DID, 1%; P = .66).
Mortality rates for Black patients with stomach cancer also decreased. In expansion states, there was a –13% absolute decrease in mortality, compared with a –5.2% decrease in nonexpansion states.
The investigators noted that Medicaid coverage was a key component in access to care through the Affordable Care Act. About two-thirds (66.7%) of Black patients had Medicaid; 33.3% were uninsured. Coverage was similar among White patients; 64.1% had Medicaid and 35.9% were uninsured.
“Our study provides compelling data that show Medicaid expansion was associated with improvement in survival for both Black and White patients with gastrointestinal cancers. Additionally, it suggests that Medicaid expansion is one potential avenue to mitigate existing racial survival disparities among these patients,” Dr. Manisundaram concluded.
The study was funded by the National Institutes of Health. One coauthor reported an advisory role with Medicaroid. Dr. Gralow has had a consulting or advisory role with Genentech and Roche.
A version of this article first appeared on Medscape.com.
Across the United States, minority patients with cancer often have worse outcomes than White patients, with Black patients more likely to die sooner.
But new data suggest that these racial disparities are lessening. They come from a cross-sectional cohort study of patients with gastrointestinal cancers and show that the gap in mortality rates was reduced in Medicaid expansion states, compared with nonexpansion states.
The results were particularly notable for Black patients, for whom there was a consistent increase in receiving therapy (chemotherapy or surgery) and a decrease in mortality from stomach, colorectal, and pancreatic cancer, the investigators commented.
The study was highlighted at a press briefing held in advance of the annual meeting of the American Society of Clinical Oncology.
“The findings of this study provide a solid step for closing the gap, showing that the Medicaid expansion opportunity offered by the Affordable Care Act, which allows participating states to improve health care access for disadvantaged populations, results in better cancer outcomes and mitigation of racial disparities in cancer survival,” commented Julie Gralow, MD, chief medical officer and executive vice president of ASCO.
The study included 86,052 patients from the National Cancer Database who, from 2009 to 2019, were diagnosed with pancreatic cancer, colorectal cancer, or stomach cancer. Just over 22,000 patients (25.7%) were Black; the remainder 63,943 (74.3%) were White.
In Medicaid expansion states, there was a greater absolute reduction in 2-year mortality among Black patients with pancreatic cancer of –11.8%, compared with nonexpansion states, at –2.4%, a difference-in-difference (DID) of –9.4%. Additionally, there was an increase in treatment with chemotherapy for patients with stage III-IV pancreatic cancer (4.5% for Black patients and 3.2% for White), compared with patients in nonexpansion states (0.8% for Black patients and 0.4% for White; DID, 3.7% for Black patients and DID, 2.7% for White).
“We found similar results in colorectal cancer, but this effect is primarily observed among the stage IV patients,” commented lead author Naveen Manisundaram, MD, a research fellow at the University of Texas MD Anderson Cancer Center, Houston. “Black patients with advanced stage disease experienced a 12.6% reduction in mortality in expansion states.”
Among Black patients with stage IV colorectal cancer, there was an increase in rates of surgery in expansion states, compared with nonexpansion states (DID, 5.7%). However, there was no increase in treatment with chemotherapy (DID, 1%; P = .66).
Mortality rates for Black patients with stomach cancer also decreased. In expansion states, there was a –13% absolute decrease in mortality, compared with a –5.2% decrease in nonexpansion states.
The investigators noted that Medicaid coverage was a key component in access to care through the Affordable Care Act. About two-thirds (66.7%) of Black patients had Medicaid; 33.3% were uninsured. Coverage was similar among White patients; 64.1% had Medicaid and 35.9% were uninsured.
“Our study provides compelling data that show Medicaid expansion was associated with improvement in survival for both Black and White patients with gastrointestinal cancers. Additionally, it suggests that Medicaid expansion is one potential avenue to mitigate existing racial survival disparities among these patients,” Dr. Manisundaram concluded.
The study was funded by the National Institutes of Health. One coauthor reported an advisory role with Medicaroid. Dr. Gralow has had a consulting or advisory role with Genentech and Roche.
A version of this article first appeared on Medscape.com.
FROM ASCO 2023
Cross-border U.S.-Mexican collaboration drives up ALL survival
A team from a hospital in San Diego combined a previously established training program from the World Health Organization with a new collaboration, which resulted in improvements in care standards and sustainability of care in a center in Tijuana, Mexico, just 23 miles away.
Implementation of the program in 2013 led to a significant 6% improvement in 5-year overall survival for children with ALL.
For patients at standard risk, 5-year overall survival increased from 73% to 100% after implementation of the program.
“This is really remarkable because this survival is the same as we have here in San Diego,” commented Paula Aristizabal, MD, MAS, a pediatric hematologist/oncologist at Rady Children’s Hospital, San Diego, at a press briefing before the annual meeting of the American Society of Clinical Oncology.
The findings show that “sustained improvements in cancer outcomes in low- and middle-income countries [LMICs] are feasible with innovative cross-border programs, particularly in borders that are shared” between a high- and low-income country, she commented. In other words, “it takes a village in both countries” to drive up standards.
Dr. Aristizabal also noted that the partnership will continue with a particularly focus on improving survival among patients with high-risk disease.
“We like to call it ‘twinning,’ because that means we are twins forever,” she said. “This is not a marriage that can be dissolved.”
‘Huge survival gap’
“The burden of childhood cancer has increased globally, but unfortunately, survival in low- and middle-income countries has not improved at the same level as in high-income countries,” Dr. Aristizabal commented.
This has resulted in a “huge survival gap” between high-income countries and the LMICs. ALL is now a leading cause of death among children in these countries, she commented.
“This study illustrates collaborative strategies that can be put into place today that could greatly improve outcomes for children with cancer globally,” commented Julie R. Gralow, MD, ASCO chief medical officer and executive vice president.
Speaking at the press conference, she added: “As I’ve heard Princess Dina Mired of Jordan say many times: ‘Your ZIP code should not determine if you survive cancer.’ ”
She said the differences in ALL survival between the United States and Mexico are an “example of children being so close in terms of proximity not having the same advantages.”
Also commenting, ASCO President Eric Winer, MD, from the Yale Cancer Center, New Haven, Conn., asked whether the proximity of the hospitals in San Diego and Tijuana “makes a difference, or do you think this is something that done ... at a distance?”
Dr. Aristizabal said that the proximity between the institutions “has been extremely helpful,” as they can go between hospitals in just 30 minutes.
However, “one of the things that we learned with COVID is that we can do a lot of things remotely,” she answered.
“Some of the projects that we started in Tijuana, through our collaboration with St. Jude Children’s Research Hospital, we have been able to implement in many other centers in Mexico,” she said.
Study details
Rady Children’s Hospital partnered with the public sector in Baja California, with the aim of improving outcomes in children’s cancer, she explained.
In 2008, the team collaborated with St. Jude Children’s Research Hospital, Memphis, to establish a training program in the Hospital General Tijuana in Tijuana that shared knowledge, technology, and organizational skills.
The team also consulted on clinical cases and set up education and research programs, all with the aim of building capacity and sustainability in Mexico.
“As the number of leukemia patients increased, we wanted to decrease depending on their international collaborators in the U.S. and ensure long-term sustainability,” Dr. Aristizabal explained.
This led in 2013 to the implementation of the WHO Framework for Action HSS training model, which has several components, including health service delivery.
Combined with the previously established model, the overall goals of the program were to improve health outcomes, systems efficiency, timely access to care, and social and financial risk protection.
Dr. Aristizabal said in an interview that this involved developing highly specific leukemia treatment guidelines, which have now gone through three iterations, as well as guidelines for supportive care.
Working with a local foundation, the team has also “focused on providing psychosocial support, nutritional support, a shelter for families that live 12-14 hours away from the pediatric cancer center, as well as food subsidies, trying to address financial toxicity and food insecurity in these families.”
Impact of the collaboration
To assess the impact of the WHO framework, the researchers conducted a study that involved 109 children with ALL who were treated at Hospital General Tijuana over the preimplementation phase in 2008-2012 and the postimplementation phase in 2013-2017.
The mean age of the patients was 7.04 years, and 50.4% were girls. The majority (67%) were classified as having high-risk disease.
Over the entire study period, the 5-year overall survival rate was 65%. Analysis revealed that between the pre- and postimplementation periods, 5-year overall survival increased from 59% to 65%, which Dr. Aristizabal described as “a significant improvement.”
Among high-risk patients, the improvement in 5-year survival between the pre- and postimplementation period went from 48% to 55%.
“This is an area for improvement,” Dr. Aristizabal said, “and we’re working on additional strategies to help improve survival for high-risk patients.
The study was funded by Rady Children’s Hospital, the Mexican Secretary of Health, and the Patronato Foundation. Dr. Aristizabal and coauthors reported no relevant financial relationships. Dr. Gralow reported relationships with Genentech and Roche. Dr. Winer reported relationships with Leap Therapeutics, Jounce Therapeutics, Carrick Therapeutics, and Genentech.
A version of this article first appeared on Medscape.com.
A team from a hospital in San Diego combined a previously established training program from the World Health Organization with a new collaboration, which resulted in improvements in care standards and sustainability of care in a center in Tijuana, Mexico, just 23 miles away.
Implementation of the program in 2013 led to a significant 6% improvement in 5-year overall survival for children with ALL.
For patients at standard risk, 5-year overall survival increased from 73% to 100% after implementation of the program.
“This is really remarkable because this survival is the same as we have here in San Diego,” commented Paula Aristizabal, MD, MAS, a pediatric hematologist/oncologist at Rady Children’s Hospital, San Diego, at a press briefing before the annual meeting of the American Society of Clinical Oncology.
The findings show that “sustained improvements in cancer outcomes in low- and middle-income countries [LMICs] are feasible with innovative cross-border programs, particularly in borders that are shared” between a high- and low-income country, she commented. In other words, “it takes a village in both countries” to drive up standards.
Dr. Aristizabal also noted that the partnership will continue with a particularly focus on improving survival among patients with high-risk disease.
“We like to call it ‘twinning,’ because that means we are twins forever,” she said. “This is not a marriage that can be dissolved.”
‘Huge survival gap’
“The burden of childhood cancer has increased globally, but unfortunately, survival in low- and middle-income countries has not improved at the same level as in high-income countries,” Dr. Aristizabal commented.
This has resulted in a “huge survival gap” between high-income countries and the LMICs. ALL is now a leading cause of death among children in these countries, she commented.
“This study illustrates collaborative strategies that can be put into place today that could greatly improve outcomes for children with cancer globally,” commented Julie R. Gralow, MD, ASCO chief medical officer and executive vice president.
Speaking at the press conference, she added: “As I’ve heard Princess Dina Mired of Jordan say many times: ‘Your ZIP code should not determine if you survive cancer.’ ”
She said the differences in ALL survival between the United States and Mexico are an “example of children being so close in terms of proximity not having the same advantages.”
Also commenting, ASCO President Eric Winer, MD, from the Yale Cancer Center, New Haven, Conn., asked whether the proximity of the hospitals in San Diego and Tijuana “makes a difference, or do you think this is something that done ... at a distance?”
Dr. Aristizabal said that the proximity between the institutions “has been extremely helpful,” as they can go between hospitals in just 30 minutes.
However, “one of the things that we learned with COVID is that we can do a lot of things remotely,” she answered.
“Some of the projects that we started in Tijuana, through our collaboration with St. Jude Children’s Research Hospital, we have been able to implement in many other centers in Mexico,” she said.
Study details
Rady Children’s Hospital partnered with the public sector in Baja California, with the aim of improving outcomes in children’s cancer, she explained.
In 2008, the team collaborated with St. Jude Children’s Research Hospital, Memphis, to establish a training program in the Hospital General Tijuana in Tijuana that shared knowledge, technology, and organizational skills.
The team also consulted on clinical cases and set up education and research programs, all with the aim of building capacity and sustainability in Mexico.
“As the number of leukemia patients increased, we wanted to decrease depending on their international collaborators in the U.S. and ensure long-term sustainability,” Dr. Aristizabal explained.
This led in 2013 to the implementation of the WHO Framework for Action HSS training model, which has several components, including health service delivery.
Combined with the previously established model, the overall goals of the program were to improve health outcomes, systems efficiency, timely access to care, and social and financial risk protection.
Dr. Aristizabal said in an interview that this involved developing highly specific leukemia treatment guidelines, which have now gone through three iterations, as well as guidelines for supportive care.
Working with a local foundation, the team has also “focused on providing psychosocial support, nutritional support, a shelter for families that live 12-14 hours away from the pediatric cancer center, as well as food subsidies, trying to address financial toxicity and food insecurity in these families.”
Impact of the collaboration
To assess the impact of the WHO framework, the researchers conducted a study that involved 109 children with ALL who were treated at Hospital General Tijuana over the preimplementation phase in 2008-2012 and the postimplementation phase in 2013-2017.
The mean age of the patients was 7.04 years, and 50.4% were girls. The majority (67%) were classified as having high-risk disease.
Over the entire study period, the 5-year overall survival rate was 65%. Analysis revealed that between the pre- and postimplementation periods, 5-year overall survival increased from 59% to 65%, which Dr. Aristizabal described as “a significant improvement.”
Among high-risk patients, the improvement in 5-year survival between the pre- and postimplementation period went from 48% to 55%.
“This is an area for improvement,” Dr. Aristizabal said, “and we’re working on additional strategies to help improve survival for high-risk patients.
The study was funded by Rady Children’s Hospital, the Mexican Secretary of Health, and the Patronato Foundation. Dr. Aristizabal and coauthors reported no relevant financial relationships. Dr. Gralow reported relationships with Genentech and Roche. Dr. Winer reported relationships with Leap Therapeutics, Jounce Therapeutics, Carrick Therapeutics, and Genentech.
A version of this article first appeared on Medscape.com.
A team from a hospital in San Diego combined a previously established training program from the World Health Organization with a new collaboration, which resulted in improvements in care standards and sustainability of care in a center in Tijuana, Mexico, just 23 miles away.
Implementation of the program in 2013 led to a significant 6% improvement in 5-year overall survival for children with ALL.
For patients at standard risk, 5-year overall survival increased from 73% to 100% after implementation of the program.
“This is really remarkable because this survival is the same as we have here in San Diego,” commented Paula Aristizabal, MD, MAS, a pediatric hematologist/oncologist at Rady Children’s Hospital, San Diego, at a press briefing before the annual meeting of the American Society of Clinical Oncology.
The findings show that “sustained improvements in cancer outcomes in low- and middle-income countries [LMICs] are feasible with innovative cross-border programs, particularly in borders that are shared” between a high- and low-income country, she commented. In other words, “it takes a village in both countries” to drive up standards.
Dr. Aristizabal also noted that the partnership will continue with a particularly focus on improving survival among patients with high-risk disease.
“We like to call it ‘twinning,’ because that means we are twins forever,” she said. “This is not a marriage that can be dissolved.”
‘Huge survival gap’
“The burden of childhood cancer has increased globally, but unfortunately, survival in low- and middle-income countries has not improved at the same level as in high-income countries,” Dr. Aristizabal commented.
This has resulted in a “huge survival gap” between high-income countries and the LMICs. ALL is now a leading cause of death among children in these countries, she commented.
“This study illustrates collaborative strategies that can be put into place today that could greatly improve outcomes for children with cancer globally,” commented Julie R. Gralow, MD, ASCO chief medical officer and executive vice president.
Speaking at the press conference, she added: “As I’ve heard Princess Dina Mired of Jordan say many times: ‘Your ZIP code should not determine if you survive cancer.’ ”
She said the differences in ALL survival between the United States and Mexico are an “example of children being so close in terms of proximity not having the same advantages.”
Also commenting, ASCO President Eric Winer, MD, from the Yale Cancer Center, New Haven, Conn., asked whether the proximity of the hospitals in San Diego and Tijuana “makes a difference, or do you think this is something that done ... at a distance?”
Dr. Aristizabal said that the proximity between the institutions “has been extremely helpful,” as they can go between hospitals in just 30 minutes.
However, “one of the things that we learned with COVID is that we can do a lot of things remotely,” she answered.
“Some of the projects that we started in Tijuana, through our collaboration with St. Jude Children’s Research Hospital, we have been able to implement in many other centers in Mexico,” she said.
Study details
Rady Children’s Hospital partnered with the public sector in Baja California, with the aim of improving outcomes in children’s cancer, she explained.
In 2008, the team collaborated with St. Jude Children’s Research Hospital, Memphis, to establish a training program in the Hospital General Tijuana in Tijuana that shared knowledge, technology, and organizational skills.
The team also consulted on clinical cases and set up education and research programs, all with the aim of building capacity and sustainability in Mexico.
“As the number of leukemia patients increased, we wanted to decrease depending on their international collaborators in the U.S. and ensure long-term sustainability,” Dr. Aristizabal explained.
This led in 2013 to the implementation of the WHO Framework for Action HSS training model, which has several components, including health service delivery.
Combined with the previously established model, the overall goals of the program were to improve health outcomes, systems efficiency, timely access to care, and social and financial risk protection.
Dr. Aristizabal said in an interview that this involved developing highly specific leukemia treatment guidelines, which have now gone through three iterations, as well as guidelines for supportive care.
Working with a local foundation, the team has also “focused on providing psychosocial support, nutritional support, a shelter for families that live 12-14 hours away from the pediatric cancer center, as well as food subsidies, trying to address financial toxicity and food insecurity in these families.”
Impact of the collaboration
To assess the impact of the WHO framework, the researchers conducted a study that involved 109 children with ALL who were treated at Hospital General Tijuana over the preimplementation phase in 2008-2012 and the postimplementation phase in 2013-2017.
The mean age of the patients was 7.04 years, and 50.4% were girls. The majority (67%) were classified as having high-risk disease.
Over the entire study period, the 5-year overall survival rate was 65%. Analysis revealed that between the pre- and postimplementation periods, 5-year overall survival increased from 59% to 65%, which Dr. Aristizabal described as “a significant improvement.”
Among high-risk patients, the improvement in 5-year survival between the pre- and postimplementation period went from 48% to 55%.
“This is an area for improvement,” Dr. Aristizabal said, “and we’re working on additional strategies to help improve survival for high-risk patients.
The study was funded by Rady Children’s Hospital, the Mexican Secretary of Health, and the Patronato Foundation. Dr. Aristizabal and coauthors reported no relevant financial relationships. Dr. Gralow reported relationships with Genentech and Roche. Dr. Winer reported relationships with Leap Therapeutics, Jounce Therapeutics, Carrick Therapeutics, and Genentech.
A version of this article first appeared on Medscape.com.
FROM ASCO 2023
Groundbreaking new regimen for advanced Hodgkin lymphoma
“[SWOG] S1826, the largest Hodgkin lymphoma study in National Clinical Trials Network history, is a key step toward harmonizing the pediatric and adult treatment of advanced-stage Hodgkin lymphoma,” the authors reported in late-breaking research presented at the annual meeting of the American Society of Clinical Oncology.
“Based on the magnitude of the benefit and with nivolumab being better tolerated than brentuximab, we anticipate that these results will be practice changing and nivolumab [and chemotherapy] will become a new standard of care,” lead author Alex Francisco Herrera, MD, an associate professor and chief of the division of lymphoma in the department of hematology and hematopoietic cell transplantation, City of Hope Medical Center, Duarte, Calif., said in an interview.
The randomized SWOG S1826 trial of 976 patients with newly diagnosed stage 3 or 4 Hodgkin lymphoma included patients ranging in age from as young as 12 to 83 years, and at a median follow-up of 12.1 months, the addition of nivolumab to the chemotherapy regimen of doxorubicin, vinblastine, and dacarbazine (AVD) was associated with as much as a 52% reduction in the risk of disease-related death, compared with the addition of brentuximab.
The results are especially important considering that Hodgkin lymphoma disproportionately affects younger patients, including those in their teens, 20s, and 30s, Dr. Herrera noted in an interview.
“We found that treatment with nivolumab reduced the risk of progression by half, and, importantly, the benefit was observed across subgroups,” he said.
Relapse/refractory disease common in advanced HL
In general, outcomes are relatively good even for stage III or IV Hodgkin lymphoma; however, about a quarter of patients still have relapses or refractory disease.
While the introduction of novel frontline treatment with brentuximab-AVD was important in improving overall survival, the regimen adds toxicity, particularly among older patients, and many pediatric patients receiving the therapy still require radiation therapy, with its undesirable side effects.
Meanwhile, the progressive death 1 inhibitor nivolumab, approved by the Food and Drug Administration, gained interest as a potentially ideal alternative in light of Hodgkin lymphoma’s status basically as “the poster child for PD-1 blockade,” Dr. Herrera said.
“There are genetic changes in the Hodgkin lymphoma tumor cell that lead to expression of PD-1 ligands on the surface of Hodgkin lymphoma cells, and when we use a drug like nivolumab, we see that even patients with the most treatment-resistant rates of lymphoma have as much as a 70% response rate,” he explained in a press briefing.
To further investigate, the first-of-its-kind collaboration of adult and pediatric cancer teams conducted the S1826 trial to evaluate the treatment across age groups with stage 3 and 4 Hodgkin lymphoma.
For the study, conducted between July 2019 and October 2022, 976 patients were randomized to treatment either with nivolumab (n = 489) or brentuximab (n = 487), each in combination with the AVD regimen.
Of the patients, the median age was 27, with 24% under the age of 18, 10% over 60 and 32% with IPS 4-7. Among them, 56% were male and 76% were White.
For the primary endpoint, at a median follow-up of 12.1 months, the rate of progression-free survival was significantly higher in the nivolumab arm (hazard ratio, 0.48; one-sided P = .0005), with the rate of 1-year survival at 94% in the nivolumab group versus 86% in the brentuximab group, for a 52% reduction in the risk of disease-related death with nivolumab versus brentuximab.
A total of 11 deaths occurred in the brentuximab group, 7 of which were related to adverse events, compared with 4 deaths in the nivolumab group, 3 of which were related to nivolumab.
Importantly, fewer than 1% of patients with nivolumab required radiation therapy.
“That’s a dramatic reduction of the proportion of the very youngest patients receiving radiotherapy,” Dr. Herrera noted.
Grade 3 or higher hematologic adverse events were higher in the nivolumab group, at 48.4%, including 45.1% that were grade 3 or higher neutropenia, compared with 30.5% with brentuximab, including 23.9% with grade 3 or higher neutropenia.
However, rates of any grade of febrile neutropenia were similar with nivolumab and brentuximab (5.6% vs. 6.4%, respectively), as were rates of pneumonitis (2.0% vs. 3.2%), ALT elevation (30.7% vs. 39.8%), and colitis (1% vs. 1.3%).
In addition, rates of hypo- and hyperthyroidism were more frequent after nivolumab (7% and 3% with nivolumab, respectively, vs. fewer than 1% with brentuximab).
But, of note, peripheral neuropathy of any grade was more common after brentuximab (sensory: 28.1% nivolumab vs. 54.2% brentuximab; motor: 4% nivolumab vs. 6.8% brentuximab).
“I can’t emphasize how important neuropathy is as a side effect in these young patients who have the rest of their life ahead of them,” Dr. Herrera explained. “It’s fantastic to be cured of cancer, but tough to not be able to feel your fingers and toes.”
With its broad inclusion of age groups and a diverse population, he added that the study was importantly a “representative” trial, reflecting a “real-world population.”
“Incredibly, a quarter of patients were under the age of 18; 10% were over the age of 60, a quarter of patients were Hispanic and Black, and in fact we had a quite good representation of higher-risk subgroups,” he said.
Looking forward, longer-term follow-up from this study will be important in determining if the improvement observed in disease-related deaths is maintained over time, Dr. Herrera noted.
“Additionally, it is crucial to obtain data on other key outcomes such as overall survival and quality of life from longer-term follow of this study,” he said.
‘A huge step forward’
Commenting on the study, Oreofe Odejide, MD, a medical oncologist at the Dana-Farber Cancer Institute and an assistant professor of medicine at Harvard Medical School, both in Boston, said that results were unprecedented.
“Although a majority of patients with advanced stage Hodgkin lymphoma will be cured with initial therapy, about 20% of patients still end up with relapsed or refractory disease,” she said in an interview. “Therefore, the findings from this study represent a huge step forward in the management of advanced Hodgkin lymphoma in children and adults, leading to an improved and well-tolerated standard of care.”
Dr. Odejide agreed that the findings are potentially practice changing.
“Brentuximab-AVD set a high bar for the treatment of advanced-stage Hodgkin lymphoma, as it was the first regimen to show a meaningful improvement in disease-related death compared to ABVD chemotherapy in several years,” she explained.
“The fact that the SWOG1826 trial now shows a significant benefit of nivolumab-AVD over brentuximab and included both pediatric and adult patients unlike prior studies, is highly compelling,” Dr. Odejide added. “This has strong potential to change the standard of care for patients with previously untreated, advanced-stage Hodgkin lymphoma.”
The study received funding from the National Cancer Institute and from Bristol-Myers Squibb. Dr. Herrera reported relationships with Abbvie, ADC Therapeutics, Adicet Bio, AstraZeneca/MedImmune, Bristol-Myers Squibb, Caribou Biosciences, Genentech/Roche, Genmab, Karyopharm Therapeutics, Merck, Pfizer, Regeneron, Seagen, Takeda, and Tubulis Gmbh. Dr. Odejide reported no disclosures.
“[SWOG] S1826, the largest Hodgkin lymphoma study in National Clinical Trials Network history, is a key step toward harmonizing the pediatric and adult treatment of advanced-stage Hodgkin lymphoma,” the authors reported in late-breaking research presented at the annual meeting of the American Society of Clinical Oncology.
“Based on the magnitude of the benefit and with nivolumab being better tolerated than brentuximab, we anticipate that these results will be practice changing and nivolumab [and chemotherapy] will become a new standard of care,” lead author Alex Francisco Herrera, MD, an associate professor and chief of the division of lymphoma in the department of hematology and hematopoietic cell transplantation, City of Hope Medical Center, Duarte, Calif., said in an interview.
The randomized SWOG S1826 trial of 976 patients with newly diagnosed stage 3 or 4 Hodgkin lymphoma included patients ranging in age from as young as 12 to 83 years, and at a median follow-up of 12.1 months, the addition of nivolumab to the chemotherapy regimen of doxorubicin, vinblastine, and dacarbazine (AVD) was associated with as much as a 52% reduction in the risk of disease-related death, compared with the addition of brentuximab.
The results are especially important considering that Hodgkin lymphoma disproportionately affects younger patients, including those in their teens, 20s, and 30s, Dr. Herrera noted in an interview.
“We found that treatment with nivolumab reduced the risk of progression by half, and, importantly, the benefit was observed across subgroups,” he said.
Relapse/refractory disease common in advanced HL
In general, outcomes are relatively good even for stage III or IV Hodgkin lymphoma; however, about a quarter of patients still have relapses or refractory disease.
While the introduction of novel frontline treatment with brentuximab-AVD was important in improving overall survival, the regimen adds toxicity, particularly among older patients, and many pediatric patients receiving the therapy still require radiation therapy, with its undesirable side effects.
Meanwhile, the progressive death 1 inhibitor nivolumab, approved by the Food and Drug Administration, gained interest as a potentially ideal alternative in light of Hodgkin lymphoma’s status basically as “the poster child for PD-1 blockade,” Dr. Herrera said.
“There are genetic changes in the Hodgkin lymphoma tumor cell that lead to expression of PD-1 ligands on the surface of Hodgkin lymphoma cells, and when we use a drug like nivolumab, we see that even patients with the most treatment-resistant rates of lymphoma have as much as a 70% response rate,” he explained in a press briefing.
To further investigate, the first-of-its-kind collaboration of adult and pediatric cancer teams conducted the S1826 trial to evaluate the treatment across age groups with stage 3 and 4 Hodgkin lymphoma.
For the study, conducted between July 2019 and October 2022, 976 patients were randomized to treatment either with nivolumab (n = 489) or brentuximab (n = 487), each in combination with the AVD regimen.
Of the patients, the median age was 27, with 24% under the age of 18, 10% over 60 and 32% with IPS 4-7. Among them, 56% were male and 76% were White.
For the primary endpoint, at a median follow-up of 12.1 months, the rate of progression-free survival was significantly higher in the nivolumab arm (hazard ratio, 0.48; one-sided P = .0005), with the rate of 1-year survival at 94% in the nivolumab group versus 86% in the brentuximab group, for a 52% reduction in the risk of disease-related death with nivolumab versus brentuximab.
A total of 11 deaths occurred in the brentuximab group, 7 of which were related to adverse events, compared with 4 deaths in the nivolumab group, 3 of which were related to nivolumab.
Importantly, fewer than 1% of patients with nivolumab required radiation therapy.
“That’s a dramatic reduction of the proportion of the very youngest patients receiving radiotherapy,” Dr. Herrera noted.
Grade 3 or higher hematologic adverse events were higher in the nivolumab group, at 48.4%, including 45.1% that were grade 3 or higher neutropenia, compared with 30.5% with brentuximab, including 23.9% with grade 3 or higher neutropenia.
However, rates of any grade of febrile neutropenia were similar with nivolumab and brentuximab (5.6% vs. 6.4%, respectively), as were rates of pneumonitis (2.0% vs. 3.2%), ALT elevation (30.7% vs. 39.8%), and colitis (1% vs. 1.3%).
In addition, rates of hypo- and hyperthyroidism were more frequent after nivolumab (7% and 3% with nivolumab, respectively, vs. fewer than 1% with brentuximab).
But, of note, peripheral neuropathy of any grade was more common after brentuximab (sensory: 28.1% nivolumab vs. 54.2% brentuximab; motor: 4% nivolumab vs. 6.8% brentuximab).
“I can’t emphasize how important neuropathy is as a side effect in these young patients who have the rest of their life ahead of them,” Dr. Herrera explained. “It’s fantastic to be cured of cancer, but tough to not be able to feel your fingers and toes.”
With its broad inclusion of age groups and a diverse population, he added that the study was importantly a “representative” trial, reflecting a “real-world population.”
“Incredibly, a quarter of patients were under the age of 18; 10% were over the age of 60, a quarter of patients were Hispanic and Black, and in fact we had a quite good representation of higher-risk subgroups,” he said.
Looking forward, longer-term follow-up from this study will be important in determining if the improvement observed in disease-related deaths is maintained over time, Dr. Herrera noted.
“Additionally, it is crucial to obtain data on other key outcomes such as overall survival and quality of life from longer-term follow of this study,” he said.
‘A huge step forward’
Commenting on the study, Oreofe Odejide, MD, a medical oncologist at the Dana-Farber Cancer Institute and an assistant professor of medicine at Harvard Medical School, both in Boston, said that results were unprecedented.
“Although a majority of patients with advanced stage Hodgkin lymphoma will be cured with initial therapy, about 20% of patients still end up with relapsed or refractory disease,” she said in an interview. “Therefore, the findings from this study represent a huge step forward in the management of advanced Hodgkin lymphoma in children and adults, leading to an improved and well-tolerated standard of care.”
Dr. Odejide agreed that the findings are potentially practice changing.
“Brentuximab-AVD set a high bar for the treatment of advanced-stage Hodgkin lymphoma, as it was the first regimen to show a meaningful improvement in disease-related death compared to ABVD chemotherapy in several years,” she explained.
“The fact that the SWOG1826 trial now shows a significant benefit of nivolumab-AVD over brentuximab and included both pediatric and adult patients unlike prior studies, is highly compelling,” Dr. Odejide added. “This has strong potential to change the standard of care for patients with previously untreated, advanced-stage Hodgkin lymphoma.”
The study received funding from the National Cancer Institute and from Bristol-Myers Squibb. Dr. Herrera reported relationships with Abbvie, ADC Therapeutics, Adicet Bio, AstraZeneca/MedImmune, Bristol-Myers Squibb, Caribou Biosciences, Genentech/Roche, Genmab, Karyopharm Therapeutics, Merck, Pfizer, Regeneron, Seagen, Takeda, and Tubulis Gmbh. Dr. Odejide reported no disclosures.
“[SWOG] S1826, the largest Hodgkin lymphoma study in National Clinical Trials Network history, is a key step toward harmonizing the pediatric and adult treatment of advanced-stage Hodgkin lymphoma,” the authors reported in late-breaking research presented at the annual meeting of the American Society of Clinical Oncology.
“Based on the magnitude of the benefit and with nivolumab being better tolerated than brentuximab, we anticipate that these results will be practice changing and nivolumab [and chemotherapy] will become a new standard of care,” lead author Alex Francisco Herrera, MD, an associate professor and chief of the division of lymphoma in the department of hematology and hematopoietic cell transplantation, City of Hope Medical Center, Duarte, Calif., said in an interview.
The randomized SWOG S1826 trial of 976 patients with newly diagnosed stage 3 or 4 Hodgkin lymphoma included patients ranging in age from as young as 12 to 83 years, and at a median follow-up of 12.1 months, the addition of nivolumab to the chemotherapy regimen of doxorubicin, vinblastine, and dacarbazine (AVD) was associated with as much as a 52% reduction in the risk of disease-related death, compared with the addition of brentuximab.
The results are especially important considering that Hodgkin lymphoma disproportionately affects younger patients, including those in their teens, 20s, and 30s, Dr. Herrera noted in an interview.
“We found that treatment with nivolumab reduced the risk of progression by half, and, importantly, the benefit was observed across subgroups,” he said.
Relapse/refractory disease common in advanced HL
In general, outcomes are relatively good even for stage III or IV Hodgkin lymphoma; however, about a quarter of patients still have relapses or refractory disease.
While the introduction of novel frontline treatment with brentuximab-AVD was important in improving overall survival, the regimen adds toxicity, particularly among older patients, and many pediatric patients receiving the therapy still require radiation therapy, with its undesirable side effects.
Meanwhile, the progressive death 1 inhibitor nivolumab, approved by the Food and Drug Administration, gained interest as a potentially ideal alternative in light of Hodgkin lymphoma’s status basically as “the poster child for PD-1 blockade,” Dr. Herrera said.
“There are genetic changes in the Hodgkin lymphoma tumor cell that lead to expression of PD-1 ligands on the surface of Hodgkin lymphoma cells, and when we use a drug like nivolumab, we see that even patients with the most treatment-resistant rates of lymphoma have as much as a 70% response rate,” he explained in a press briefing.
To further investigate, the first-of-its-kind collaboration of adult and pediatric cancer teams conducted the S1826 trial to evaluate the treatment across age groups with stage 3 and 4 Hodgkin lymphoma.
For the study, conducted between July 2019 and October 2022, 976 patients were randomized to treatment either with nivolumab (n = 489) or brentuximab (n = 487), each in combination with the AVD regimen.
Of the patients, the median age was 27, with 24% under the age of 18, 10% over 60 and 32% with IPS 4-7. Among them, 56% were male and 76% were White.
For the primary endpoint, at a median follow-up of 12.1 months, the rate of progression-free survival was significantly higher in the nivolumab arm (hazard ratio, 0.48; one-sided P = .0005), with the rate of 1-year survival at 94% in the nivolumab group versus 86% in the brentuximab group, for a 52% reduction in the risk of disease-related death with nivolumab versus brentuximab.
A total of 11 deaths occurred in the brentuximab group, 7 of which were related to adverse events, compared with 4 deaths in the nivolumab group, 3 of which were related to nivolumab.
Importantly, fewer than 1% of patients with nivolumab required radiation therapy.
“That’s a dramatic reduction of the proportion of the very youngest patients receiving radiotherapy,” Dr. Herrera noted.
Grade 3 or higher hematologic adverse events were higher in the nivolumab group, at 48.4%, including 45.1% that were grade 3 or higher neutropenia, compared with 30.5% with brentuximab, including 23.9% with grade 3 or higher neutropenia.
However, rates of any grade of febrile neutropenia were similar with nivolumab and brentuximab (5.6% vs. 6.4%, respectively), as were rates of pneumonitis (2.0% vs. 3.2%), ALT elevation (30.7% vs. 39.8%), and colitis (1% vs. 1.3%).
In addition, rates of hypo- and hyperthyroidism were more frequent after nivolumab (7% and 3% with nivolumab, respectively, vs. fewer than 1% with brentuximab).
But, of note, peripheral neuropathy of any grade was more common after brentuximab (sensory: 28.1% nivolumab vs. 54.2% brentuximab; motor: 4% nivolumab vs. 6.8% brentuximab).
“I can’t emphasize how important neuropathy is as a side effect in these young patients who have the rest of their life ahead of them,” Dr. Herrera explained. “It’s fantastic to be cured of cancer, but tough to not be able to feel your fingers and toes.”
With its broad inclusion of age groups and a diverse population, he added that the study was importantly a “representative” trial, reflecting a “real-world population.”
“Incredibly, a quarter of patients were under the age of 18; 10% were over the age of 60, a quarter of patients were Hispanic and Black, and in fact we had a quite good representation of higher-risk subgroups,” he said.
Looking forward, longer-term follow-up from this study will be important in determining if the improvement observed in disease-related deaths is maintained over time, Dr. Herrera noted.
“Additionally, it is crucial to obtain data on other key outcomes such as overall survival and quality of life from longer-term follow of this study,” he said.
‘A huge step forward’
Commenting on the study, Oreofe Odejide, MD, a medical oncologist at the Dana-Farber Cancer Institute and an assistant professor of medicine at Harvard Medical School, both in Boston, said that results were unprecedented.
“Although a majority of patients with advanced stage Hodgkin lymphoma will be cured with initial therapy, about 20% of patients still end up with relapsed or refractory disease,” she said in an interview. “Therefore, the findings from this study represent a huge step forward in the management of advanced Hodgkin lymphoma in children and adults, leading to an improved and well-tolerated standard of care.”
Dr. Odejide agreed that the findings are potentially practice changing.
“Brentuximab-AVD set a high bar for the treatment of advanced-stage Hodgkin lymphoma, as it was the first regimen to show a meaningful improvement in disease-related death compared to ABVD chemotherapy in several years,” she explained.
“The fact that the SWOG1826 trial now shows a significant benefit of nivolumab-AVD over brentuximab and included both pediatric and adult patients unlike prior studies, is highly compelling,” Dr. Odejide added. “This has strong potential to change the standard of care for patients with previously untreated, advanced-stage Hodgkin lymphoma.”
The study received funding from the National Cancer Institute and from Bristol-Myers Squibb. Dr. Herrera reported relationships with Abbvie, ADC Therapeutics, Adicet Bio, AstraZeneca/MedImmune, Bristol-Myers Squibb, Caribou Biosciences, Genentech/Roche, Genmab, Karyopharm Therapeutics, Merck, Pfizer, Regeneron, Seagen, Takeda, and Tubulis Gmbh. Dr. Odejide reported no disclosures.
FROM ASCO 2023
Ancient plague, cyclical pandemics … history lesson?
Even the plague wanted to visit Stonehenge
We’re about to blow your mind: The history you learned in school was often inaccurate. Shocking, we know, so we’ll give you a minute to process this incredible news.
Better? Good. Now, let’s look back at high school European history. The Black Death, specifically. The common narrative is that the Mongols, while besieging a Crimean city belonging to the Genoese, catapulted dead bodies infected with some mystery disease that turned out to be the plague. The Genoese then brought the plague back to Italy, and from there, we all know the rest of the story.
The Black Death was certainly extremely important to the development of modern Europe as we know it, but the history books gloss over the much longer history of the plague. Yersinia pestis did not suddenly appear unbidden in a Mongol war camp in 1347. The Black Death wasn’t even the first horrific, continent-wide pandemic caused by the plague; the Plague of Justinian 800 years earlier crippled the Byzantine Empire during an expansionist phase and killed anywhere between 15 million and 100 million.
Today, though, LOTME looks even deeper into history, nearly beyond even history itself, back into the depths of early Bronze Age northern Europe. Specifically, to two ancient burial sites in England, where researchers have identified three 4,000-year-old cases of Y. pestis, the first recorded incidence of the disease in Britain.
Two of the individuals, identified through analysis of dental pulp, were young children buried at a mass grave in Somerset, while the third, a middle-aged woman, was found in a ring cairn in Cumbria. These sites are hundreds of miles apart, yet carbon dating suggests all three people lived and died at roughly the same time. The strain found is very similar to other samples of plague found across central and western Europe starting around 3,000 BCE, suggesting a single, easily spread disease affecting a large area in a relatively small period of time. In other words, a pandemic. Even in these ancient times, the world was connected. Not even the island of Britain could escape.
Beyond that though, the research helps confirm the cyclical nature of the plague; over time, it loses its effectiveness and goes into hiding, only to mutate and come roaring back. This is a story with absolutely no relevance at all to the modern world. Nope, no plagues or pandemics going around right now, no viruses fading into the background in any way. What a ridiculous inference to make.
Uncovering the invisible with artificial intelligence
This week in “What Else Can AI Do?” new research shows that a computer program can reveal brain injury that couldn’t be seen before with typical MRI.
The hot new AI, birthed by researchers at New York University, could potentially be a game changer by linking repeated head impacts with tiny, structural changes in the brains of athletes who have not been diagnosed with a concussion. By using machine learning to train the AI, the researchers were, for the first time, able to distinguish the brain of athletes who played contact sports (football, soccer, lacrosse) from those participating in noncontact sports such as baseball, basketball, and cross-country.
How did they do it? The investigators “designed statistical techniques that gave their computer program the ability to ‘learn’ how to predict exposure to repeated head impacts using mathematical models,” they explained in a written statement. Adding in data from the MRI scans of 81 male athletes with no known concussion diagnosis and the ability to identify unusual brain features between athletes with and without head trauma allowed the AI to predict results with accuracy even Miss Cleo would envy.
“This method may provide an important diagnostic tool not only for concussion, but also for detecting the damage that stems from subtler and more frequent head impacts,” said lead author Junbo Chen, an engineering doctoral candidate at NYU. That could make this new AI a valuable asset to science and medicine.
There are many things the human brain can do that AI can’t, and delegation could be one of them. Examining the data that represent the human brain in minute detail? Maybe we leave that to the machine.
Talk about your field promotions
If you’re a surgeon doing an amputation, the list of possible assistants pretty much starts and ends in only one place: Not the closest available janitor.
That may seem like an oddly obvious thing for us to say, but there’s at least one former Mainz (Germany) University Hospital physician who really needed to get this bit of advice before he attempted an unassisted toe amputation back in October of 2020. Yes, that does seem like kind of a long time ago for us to be reporting it now, but the details of the incident only just came to light a few days ago, thanks to German public broadcaster SWR.
Since it was just a toe, the surgeon thought he could perform the operation without any help. The toe, unfortunately, had other plans. The partially anesthetized patient got restless in the operating room, but with no actual trained nurse in the vicinity, the surgeon asked the closest available person – that would be the janitor – to lend a hand.
The surgical manager heard about these goings-on and got to the operating room too late to stop the procedure but soon enough to see the cleaning staffer “at the operating table with a bloody suction cup and a bloody compress in their hands,” SWR recently reported.
The incident was reported to the hospital’s medical director and the surgeon was fired, but since the patient experienced no complications not much fuss was made about it at the time.
Well, guess what? It’s toe-tally our job to make a fuss about these kinds of things. Or could it be that our job, much like the surgeon’s employment and the patient’s digit, is here toe-day and gone toe-morrow?
Even the plague wanted to visit Stonehenge
We’re about to blow your mind: The history you learned in school was often inaccurate. Shocking, we know, so we’ll give you a minute to process this incredible news.
Better? Good. Now, let’s look back at high school European history. The Black Death, specifically. The common narrative is that the Mongols, while besieging a Crimean city belonging to the Genoese, catapulted dead bodies infected with some mystery disease that turned out to be the plague. The Genoese then brought the plague back to Italy, and from there, we all know the rest of the story.
The Black Death was certainly extremely important to the development of modern Europe as we know it, but the history books gloss over the much longer history of the plague. Yersinia pestis did not suddenly appear unbidden in a Mongol war camp in 1347. The Black Death wasn’t even the first horrific, continent-wide pandemic caused by the plague; the Plague of Justinian 800 years earlier crippled the Byzantine Empire during an expansionist phase and killed anywhere between 15 million and 100 million.
Today, though, LOTME looks even deeper into history, nearly beyond even history itself, back into the depths of early Bronze Age northern Europe. Specifically, to two ancient burial sites in England, where researchers have identified three 4,000-year-old cases of Y. pestis, the first recorded incidence of the disease in Britain.
Two of the individuals, identified through analysis of dental pulp, were young children buried at a mass grave in Somerset, while the third, a middle-aged woman, was found in a ring cairn in Cumbria. These sites are hundreds of miles apart, yet carbon dating suggests all three people lived and died at roughly the same time. The strain found is very similar to other samples of plague found across central and western Europe starting around 3,000 BCE, suggesting a single, easily spread disease affecting a large area in a relatively small period of time. In other words, a pandemic. Even in these ancient times, the world was connected. Not even the island of Britain could escape.
Beyond that though, the research helps confirm the cyclical nature of the plague; over time, it loses its effectiveness and goes into hiding, only to mutate and come roaring back. This is a story with absolutely no relevance at all to the modern world. Nope, no plagues or pandemics going around right now, no viruses fading into the background in any way. What a ridiculous inference to make.
Uncovering the invisible with artificial intelligence
This week in “What Else Can AI Do?” new research shows that a computer program can reveal brain injury that couldn’t be seen before with typical MRI.
The hot new AI, birthed by researchers at New York University, could potentially be a game changer by linking repeated head impacts with tiny, structural changes in the brains of athletes who have not been diagnosed with a concussion. By using machine learning to train the AI, the researchers were, for the first time, able to distinguish the brain of athletes who played contact sports (football, soccer, lacrosse) from those participating in noncontact sports such as baseball, basketball, and cross-country.
How did they do it? The investigators “designed statistical techniques that gave their computer program the ability to ‘learn’ how to predict exposure to repeated head impacts using mathematical models,” they explained in a written statement. Adding in data from the MRI scans of 81 male athletes with no known concussion diagnosis and the ability to identify unusual brain features between athletes with and without head trauma allowed the AI to predict results with accuracy even Miss Cleo would envy.
“This method may provide an important diagnostic tool not only for concussion, but also for detecting the damage that stems from subtler and more frequent head impacts,” said lead author Junbo Chen, an engineering doctoral candidate at NYU. That could make this new AI a valuable asset to science and medicine.
There are many things the human brain can do that AI can’t, and delegation could be one of them. Examining the data that represent the human brain in minute detail? Maybe we leave that to the machine.
Talk about your field promotions
If you’re a surgeon doing an amputation, the list of possible assistants pretty much starts and ends in only one place: Not the closest available janitor.
That may seem like an oddly obvious thing for us to say, but there’s at least one former Mainz (Germany) University Hospital physician who really needed to get this bit of advice before he attempted an unassisted toe amputation back in October of 2020. Yes, that does seem like kind of a long time ago for us to be reporting it now, but the details of the incident only just came to light a few days ago, thanks to German public broadcaster SWR.
Since it was just a toe, the surgeon thought he could perform the operation without any help. The toe, unfortunately, had other plans. The partially anesthetized patient got restless in the operating room, but with no actual trained nurse in the vicinity, the surgeon asked the closest available person – that would be the janitor – to lend a hand.
The surgical manager heard about these goings-on and got to the operating room too late to stop the procedure but soon enough to see the cleaning staffer “at the operating table with a bloody suction cup and a bloody compress in their hands,” SWR recently reported.
The incident was reported to the hospital’s medical director and the surgeon was fired, but since the patient experienced no complications not much fuss was made about it at the time.
Well, guess what? It’s toe-tally our job to make a fuss about these kinds of things. Or could it be that our job, much like the surgeon’s employment and the patient’s digit, is here toe-day and gone toe-morrow?
Even the plague wanted to visit Stonehenge
We’re about to blow your mind: The history you learned in school was often inaccurate. Shocking, we know, so we’ll give you a minute to process this incredible news.
Better? Good. Now, let’s look back at high school European history. The Black Death, specifically. The common narrative is that the Mongols, while besieging a Crimean city belonging to the Genoese, catapulted dead bodies infected with some mystery disease that turned out to be the plague. The Genoese then brought the plague back to Italy, and from there, we all know the rest of the story.
The Black Death was certainly extremely important to the development of modern Europe as we know it, but the history books gloss over the much longer history of the plague. Yersinia pestis did not suddenly appear unbidden in a Mongol war camp in 1347. The Black Death wasn’t even the first horrific, continent-wide pandemic caused by the plague; the Plague of Justinian 800 years earlier crippled the Byzantine Empire during an expansionist phase and killed anywhere between 15 million and 100 million.
Today, though, LOTME looks even deeper into history, nearly beyond even history itself, back into the depths of early Bronze Age northern Europe. Specifically, to two ancient burial sites in England, where researchers have identified three 4,000-year-old cases of Y. pestis, the first recorded incidence of the disease in Britain.
Two of the individuals, identified through analysis of dental pulp, were young children buried at a mass grave in Somerset, while the third, a middle-aged woman, was found in a ring cairn in Cumbria. These sites are hundreds of miles apart, yet carbon dating suggests all three people lived and died at roughly the same time. The strain found is very similar to other samples of plague found across central and western Europe starting around 3,000 BCE, suggesting a single, easily spread disease affecting a large area in a relatively small period of time. In other words, a pandemic. Even in these ancient times, the world was connected. Not even the island of Britain could escape.
Beyond that though, the research helps confirm the cyclical nature of the plague; over time, it loses its effectiveness and goes into hiding, only to mutate and come roaring back. This is a story with absolutely no relevance at all to the modern world. Nope, no plagues or pandemics going around right now, no viruses fading into the background in any way. What a ridiculous inference to make.
Uncovering the invisible with artificial intelligence
This week in “What Else Can AI Do?” new research shows that a computer program can reveal brain injury that couldn’t be seen before with typical MRI.
The hot new AI, birthed by researchers at New York University, could potentially be a game changer by linking repeated head impacts with tiny, structural changes in the brains of athletes who have not been diagnosed with a concussion. By using machine learning to train the AI, the researchers were, for the first time, able to distinguish the brain of athletes who played contact sports (football, soccer, lacrosse) from those participating in noncontact sports such as baseball, basketball, and cross-country.
How did they do it? The investigators “designed statistical techniques that gave their computer program the ability to ‘learn’ how to predict exposure to repeated head impacts using mathematical models,” they explained in a written statement. Adding in data from the MRI scans of 81 male athletes with no known concussion diagnosis and the ability to identify unusual brain features between athletes with and without head trauma allowed the AI to predict results with accuracy even Miss Cleo would envy.
“This method may provide an important diagnostic tool not only for concussion, but also for detecting the damage that stems from subtler and more frequent head impacts,” said lead author Junbo Chen, an engineering doctoral candidate at NYU. That could make this new AI a valuable asset to science and medicine.
There are many things the human brain can do that AI can’t, and delegation could be one of them. Examining the data that represent the human brain in minute detail? Maybe we leave that to the machine.
Talk about your field promotions
If you’re a surgeon doing an amputation, the list of possible assistants pretty much starts and ends in only one place: Not the closest available janitor.
That may seem like an oddly obvious thing for us to say, but there’s at least one former Mainz (Germany) University Hospital physician who really needed to get this bit of advice before he attempted an unassisted toe amputation back in October of 2020. Yes, that does seem like kind of a long time ago for us to be reporting it now, but the details of the incident only just came to light a few days ago, thanks to German public broadcaster SWR.
Since it was just a toe, the surgeon thought he could perform the operation without any help. The toe, unfortunately, had other plans. The partially anesthetized patient got restless in the operating room, but with no actual trained nurse in the vicinity, the surgeon asked the closest available person – that would be the janitor – to lend a hand.
The surgical manager heard about these goings-on and got to the operating room too late to stop the procedure but soon enough to see the cleaning staffer “at the operating table with a bloody suction cup and a bloody compress in their hands,” SWR recently reported.
The incident was reported to the hospital’s medical director and the surgeon was fired, but since the patient experienced no complications not much fuss was made about it at the time.
Well, guess what? It’s toe-tally our job to make a fuss about these kinds of things. Or could it be that our job, much like the surgeon’s employment and the patient’s digit, is here toe-day and gone toe-morrow?
Blood cancer patient takes on bias and ‘gaslighting’
Diagnosed with Hodgkin lymphoma in 2021, Ms. Ngon underwent port surgery to allow chemotherapy to be administered. Her right arm lost circulation and went numb, so she sought guidance from her blood cancer specialist. He dismissed her worries, saying that her tumors were pinching a nerve. She’d get better, he predicted, after more chemo.
“I knew in my body that something was wrong,” Ms. Ngon recalled. When the oncologist continued to downplay her concerns, she and a fellow communications specialist sat down together in the hospital lobby to draft an email to her physician. “We were trying to articulate the urgency in an email that expresses that I’m not being dramatic. We had to do it in a way that didn’t insult his intelligence: ‘Respectfully, you’re the doctor, but I know something is wrong.’ ”
In essence, Ms. Ngon was trying to be diplomatic and not trigger her oncologist’s defenses, while still convincing him to take action. Her approach to getting her doctor’s attention worked. He referred Ms. Ngon to a radiologist, who discovered that she had blood clots in her arm. Ms. Ngon then landed in the ICU for a week, as clinicians tried to break up the clots.
“I was the perfect person for this to happen to, because of my job and education. But it makes me sad because I understand I was in a fortunate position, with a background in communication. Most people don’t have that,” Ms. Ngon said.
This and other negative experiences during her medical saga inspired Ms. Ngon to partner with the Lymphoma Research Foundation in order to spread the word about unique challenges facing patients like her: people of color.
Ms. Ngon, who is Black, said her goal as a patient advocate is to “empower communities of color to speak up for themselves and hold oncologists responsible for listening and understanding differences across cultures.” And she wants to take a stand against the “gaslighting” of patients.
African Americans with hematologic disease like Ms. Ngon face a higher risk of poor outcomes than Whites, even as they are less likely than Whites to develop certain blood cancers. The reasons for this disparity aren’t clear, but researchers suspect they’re related to factors such as poverty, lack of insurance, genetics, and limited access to high-quality care.
Some researchers have blamed another factor: racism. A 2022 study sought to explain why Black and Hispanic patients with acute myeloid leukemia in urban areas have higher mortality rates than Whites, “despite more favorable genetics and younger age” (hazard ratio, 1.59, 95% confidence interval, 1.15-2.22 and HR, 1.25; 95% CI, 0.88-1.79). The study authors determined that “structural racism” – which they measured by examining segregation and “disadvantage” in neighborhoods where patients lived – accounted for nearly all of the disparities.
Ms. Ngon said her experiences and her awareness about poorer outcomes in medicine for African Americans – such as higher death rates for Black women during pregnancy – affect how she interacts with clinicians. “I automatically assume a barrier between me and my doctors, and it’s their responsibility to dismantle it.”
Making an connection with a physician can make a huge difference, she said. “I walked into my primary care doctor’s office and saw that she was a Latino woman. My guard went down, and I could feel her care for me as a human being. Whether that was because she was also a woman of color or not, I don’t know. But I did feel more cared for.”
However, Ms. Ngon could not find a Black oncologist to care for her in New York City, and that’s no surprise.
Ethnic and gender diversity remains an immense challenge in the hematology/oncology field. According to the American Society of Clinical Oncology, only about a third of oncologists are women, and the percentages identifying themselves as Black/African American and Hispanic are just 2.3% and 5.8%, respectively.
These numbers don’t seem likely to budge much any time soon. An analysis of medical students in U.S. oncology training programs from 2015-2020 found that just 3.8% identified themselves as Black/African American and 5.1% as Hispanic/Latino versus 52.15% as White and 31% as Asian/Pacific Islander/Native Hawaiian.
Ms. Ngon encountered challenges on other fronts during her cancer care. When she needed a wig during chemotherapy, a list of insurer-approved shops didn’t include any that catered to African Americans. Essentially, she said, she was being told that she couldn’t “purchase a wig from a place that makes you feel comfortable and from a woman who understand your needs as a Black woman. It needs to be from these specific shops that really don’t cater to my community.”
She also found it difficult to find fellow patients who shared her unique challenges. “I remember when I was diagnosed, I was looking through the support groups on Facebook, trying to find someone Black to ask about whether braiding my hair might stop it from falling out.”
Now, Ms. Ngon is in remission. And she’s happy with her oncologist, who’s White. “He listened to me, and he promised me that I would have the most boring recovery process ever, after everything I’d experienced. That explains a lot of why I felt so comfortable with him.”
She hopes to use her partnership with the Lymphoma Research Foundation to be a resource for people of color and alert them to the support that’s available for them. “I would love to let them know how to advocate for themselves as patients, how to trust their bodies, how to push back if they feel like they’re not getting the care that they deserve.”
Ms. Ngon would also like to see more support for medical students of color. “I hope to exist in a world one day where it wouldn’t be so hard to find an oncologist who looks like me in a city as large as this one,” she said.
As for oncologists, she urged them to “go the extra mile and really, really listen to what patients are saying. It’s easier said than done because there are natural biases in this world, and it’s hard to overcome those obstacles. But to not be heard and have to push every time. It was just exhausting to do that on top of trying to beat cancer.”
Diagnosed with Hodgkin lymphoma in 2021, Ms. Ngon underwent port surgery to allow chemotherapy to be administered. Her right arm lost circulation and went numb, so she sought guidance from her blood cancer specialist. He dismissed her worries, saying that her tumors were pinching a nerve. She’d get better, he predicted, after more chemo.
“I knew in my body that something was wrong,” Ms. Ngon recalled. When the oncologist continued to downplay her concerns, she and a fellow communications specialist sat down together in the hospital lobby to draft an email to her physician. “We were trying to articulate the urgency in an email that expresses that I’m not being dramatic. We had to do it in a way that didn’t insult his intelligence: ‘Respectfully, you’re the doctor, but I know something is wrong.’ ”
In essence, Ms. Ngon was trying to be diplomatic and not trigger her oncologist’s defenses, while still convincing him to take action. Her approach to getting her doctor’s attention worked. He referred Ms. Ngon to a radiologist, who discovered that she had blood clots in her arm. Ms. Ngon then landed in the ICU for a week, as clinicians tried to break up the clots.
“I was the perfect person for this to happen to, because of my job and education. But it makes me sad because I understand I was in a fortunate position, with a background in communication. Most people don’t have that,” Ms. Ngon said.
This and other negative experiences during her medical saga inspired Ms. Ngon to partner with the Lymphoma Research Foundation in order to spread the word about unique challenges facing patients like her: people of color.
Ms. Ngon, who is Black, said her goal as a patient advocate is to “empower communities of color to speak up for themselves and hold oncologists responsible for listening and understanding differences across cultures.” And she wants to take a stand against the “gaslighting” of patients.
African Americans with hematologic disease like Ms. Ngon face a higher risk of poor outcomes than Whites, even as they are less likely than Whites to develop certain blood cancers. The reasons for this disparity aren’t clear, but researchers suspect they’re related to factors such as poverty, lack of insurance, genetics, and limited access to high-quality care.
Some researchers have blamed another factor: racism. A 2022 study sought to explain why Black and Hispanic patients with acute myeloid leukemia in urban areas have higher mortality rates than Whites, “despite more favorable genetics and younger age” (hazard ratio, 1.59, 95% confidence interval, 1.15-2.22 and HR, 1.25; 95% CI, 0.88-1.79). The study authors determined that “structural racism” – which they measured by examining segregation and “disadvantage” in neighborhoods where patients lived – accounted for nearly all of the disparities.
Ms. Ngon said her experiences and her awareness about poorer outcomes in medicine for African Americans – such as higher death rates for Black women during pregnancy – affect how she interacts with clinicians. “I automatically assume a barrier between me and my doctors, and it’s their responsibility to dismantle it.”
Making an connection with a physician can make a huge difference, she said. “I walked into my primary care doctor’s office and saw that she was a Latino woman. My guard went down, and I could feel her care for me as a human being. Whether that was because she was also a woman of color or not, I don’t know. But I did feel more cared for.”
However, Ms. Ngon could not find a Black oncologist to care for her in New York City, and that’s no surprise.
Ethnic and gender diversity remains an immense challenge in the hematology/oncology field. According to the American Society of Clinical Oncology, only about a third of oncologists are women, and the percentages identifying themselves as Black/African American and Hispanic are just 2.3% and 5.8%, respectively.
These numbers don’t seem likely to budge much any time soon. An analysis of medical students in U.S. oncology training programs from 2015-2020 found that just 3.8% identified themselves as Black/African American and 5.1% as Hispanic/Latino versus 52.15% as White and 31% as Asian/Pacific Islander/Native Hawaiian.
Ms. Ngon encountered challenges on other fronts during her cancer care. When she needed a wig during chemotherapy, a list of insurer-approved shops didn’t include any that catered to African Americans. Essentially, she said, she was being told that she couldn’t “purchase a wig from a place that makes you feel comfortable and from a woman who understand your needs as a Black woman. It needs to be from these specific shops that really don’t cater to my community.”
She also found it difficult to find fellow patients who shared her unique challenges. “I remember when I was diagnosed, I was looking through the support groups on Facebook, trying to find someone Black to ask about whether braiding my hair might stop it from falling out.”
Now, Ms. Ngon is in remission. And she’s happy with her oncologist, who’s White. “He listened to me, and he promised me that I would have the most boring recovery process ever, after everything I’d experienced. That explains a lot of why I felt so comfortable with him.”
She hopes to use her partnership with the Lymphoma Research Foundation to be a resource for people of color and alert them to the support that’s available for them. “I would love to let them know how to advocate for themselves as patients, how to trust their bodies, how to push back if they feel like they’re not getting the care that they deserve.”
Ms. Ngon would also like to see more support for medical students of color. “I hope to exist in a world one day where it wouldn’t be so hard to find an oncologist who looks like me in a city as large as this one,” she said.
As for oncologists, she urged them to “go the extra mile and really, really listen to what patients are saying. It’s easier said than done because there are natural biases in this world, and it’s hard to overcome those obstacles. But to not be heard and have to push every time. It was just exhausting to do that on top of trying to beat cancer.”
Diagnosed with Hodgkin lymphoma in 2021, Ms. Ngon underwent port surgery to allow chemotherapy to be administered. Her right arm lost circulation and went numb, so she sought guidance from her blood cancer specialist. He dismissed her worries, saying that her tumors were pinching a nerve. She’d get better, he predicted, after more chemo.
“I knew in my body that something was wrong,” Ms. Ngon recalled. When the oncologist continued to downplay her concerns, she and a fellow communications specialist sat down together in the hospital lobby to draft an email to her physician. “We were trying to articulate the urgency in an email that expresses that I’m not being dramatic. We had to do it in a way that didn’t insult his intelligence: ‘Respectfully, you’re the doctor, but I know something is wrong.’ ”
In essence, Ms. Ngon was trying to be diplomatic and not trigger her oncologist’s defenses, while still convincing him to take action. Her approach to getting her doctor’s attention worked. He referred Ms. Ngon to a radiologist, who discovered that she had blood clots in her arm. Ms. Ngon then landed in the ICU for a week, as clinicians tried to break up the clots.
“I was the perfect person for this to happen to, because of my job and education. But it makes me sad because I understand I was in a fortunate position, with a background in communication. Most people don’t have that,” Ms. Ngon said.
This and other negative experiences during her medical saga inspired Ms. Ngon to partner with the Lymphoma Research Foundation in order to spread the word about unique challenges facing patients like her: people of color.
Ms. Ngon, who is Black, said her goal as a patient advocate is to “empower communities of color to speak up for themselves and hold oncologists responsible for listening and understanding differences across cultures.” And she wants to take a stand against the “gaslighting” of patients.
African Americans with hematologic disease like Ms. Ngon face a higher risk of poor outcomes than Whites, even as they are less likely than Whites to develop certain blood cancers. The reasons for this disparity aren’t clear, but researchers suspect they’re related to factors such as poverty, lack of insurance, genetics, and limited access to high-quality care.
Some researchers have blamed another factor: racism. A 2022 study sought to explain why Black and Hispanic patients with acute myeloid leukemia in urban areas have higher mortality rates than Whites, “despite more favorable genetics and younger age” (hazard ratio, 1.59, 95% confidence interval, 1.15-2.22 and HR, 1.25; 95% CI, 0.88-1.79). The study authors determined that “structural racism” – which they measured by examining segregation and “disadvantage” in neighborhoods where patients lived – accounted for nearly all of the disparities.
Ms. Ngon said her experiences and her awareness about poorer outcomes in medicine for African Americans – such as higher death rates for Black women during pregnancy – affect how she interacts with clinicians. “I automatically assume a barrier between me and my doctors, and it’s their responsibility to dismantle it.”
Making an connection with a physician can make a huge difference, she said. “I walked into my primary care doctor’s office and saw that she was a Latino woman. My guard went down, and I could feel her care for me as a human being. Whether that was because she was also a woman of color or not, I don’t know. But I did feel more cared for.”
However, Ms. Ngon could not find a Black oncologist to care for her in New York City, and that’s no surprise.
Ethnic and gender diversity remains an immense challenge in the hematology/oncology field. According to the American Society of Clinical Oncology, only about a third of oncologists are women, and the percentages identifying themselves as Black/African American and Hispanic are just 2.3% and 5.8%, respectively.
These numbers don’t seem likely to budge much any time soon. An analysis of medical students in U.S. oncology training programs from 2015-2020 found that just 3.8% identified themselves as Black/African American and 5.1% as Hispanic/Latino versus 52.15% as White and 31% as Asian/Pacific Islander/Native Hawaiian.
Ms. Ngon encountered challenges on other fronts during her cancer care. When she needed a wig during chemotherapy, a list of insurer-approved shops didn’t include any that catered to African Americans. Essentially, she said, she was being told that she couldn’t “purchase a wig from a place that makes you feel comfortable and from a woman who understand your needs as a Black woman. It needs to be from these specific shops that really don’t cater to my community.”
She also found it difficult to find fellow patients who shared her unique challenges. “I remember when I was diagnosed, I was looking through the support groups on Facebook, trying to find someone Black to ask about whether braiding my hair might stop it from falling out.”
Now, Ms. Ngon is in remission. And she’s happy with her oncologist, who’s White. “He listened to me, and he promised me that I would have the most boring recovery process ever, after everything I’d experienced. That explains a lot of why I felt so comfortable with him.”
She hopes to use her partnership with the Lymphoma Research Foundation to be a resource for people of color and alert them to the support that’s available for them. “I would love to let them know how to advocate for themselves as patients, how to trust their bodies, how to push back if they feel like they’re not getting the care that they deserve.”
Ms. Ngon would also like to see more support for medical students of color. “I hope to exist in a world one day where it wouldn’t be so hard to find an oncologist who looks like me in a city as large as this one,” she said.
As for oncologists, she urged them to “go the extra mile and really, really listen to what patients are saying. It’s easier said than done because there are natural biases in this world, and it’s hard to overcome those obstacles. But to not be heard and have to push every time. It was just exhausting to do that on top of trying to beat cancer.”
States move to curb insurers’ prior authorization requirements as federal reforms lag
Amid growing criticism of health insurers’ onerous prior authorization practices, lawmakers in 30 states have introduced bills this year that aim to rein in insurer gatekeeping and improve patient care.
“This is something that goes on in every doctor’s office every day; the frustrations, the delays, and the use of office staff time are just unbelievable,” said Steven Orland, MD, a board-certified urologist and president of the Medical Society of New Jersey.
The bills, which cover private health plans and insurers that states regulate, may provide some relief for physicians as federal efforts to streamline prior authorization for some Medicare patients have lagged.
Last year, Congress failed to pass the Improving Seniors’ Timely Access to Care Act of 2021, despite 326 co-sponsors. The bill would have compelled insurers covering Medicare Advantage enrollees to speed up prior authorizations, make the process more transparent, and remove obstacles such as requiring fax machine submissions.
Last month, however, the Centers for Medicare & Medicaid Services issued a final rule that will improve some aspects of prior authorizations in Medicare Advantage insurance plans and ensure that enrollees have the same access to necessary care as traditional Medicare enrollees.
The insurance industry has long defended prior authorization requirements and opposed legislation that would limit them.
America’s Health Insurance Plans (AHIP) and the Blue Cross Blue Shield Association said in a 2019 letter to a congressional committee when the federal legislation was first introduced, “Prior authorizations enforce best practices and guidelines for care management and help physicians identify and avoid care techniques that would harm patient outcomes, such as designating prescriptions that could feed into an opioid addiction.” AHIP didn’t respond to repeated requests for comment.
But some major insurers now appear willing to compromise and voluntarily reduce the volume of prior authorizations they require. Days before the federal final rule was released, three major insurers – United HealthCare, Cigna, and Aetna CVS Health – announced they plan to drop some prior authorization requirements and automate processes.
United HealthCare said it will eliminate almost 20% of its prior authorizations for some nonurgent surgeries and procedures starting this summer. It also will create a national Gold Card program in 2024 for physicians who meet its eligibility requirements, which would eliminate prior authorization requirements for most procedures. Both initiatives will apply to commercial, Medicare Advantage, and Medicaid businesses, said the insurer in a statement.
However, United HealthCare also announced that in June it will start requiring prior authorization for diagnostic (not screening) gastrointestinal endoscopies for its nearly 27 million privately insured patients, citing data it says shows potentially harmful overuse of scopes. Physician groups have publicly criticized the move, saying it could delay lifesaving treatment, and have asked the insurer to reconsider.
Cigna and Aetna also have moved to pare back prior authorization processes. Scott Josephs, national medical officer for Cigna, told Healthcare Dive that Cigna has removed prior authorization reviews from nearly 500 services since 2020.
An Aetna spokesperson told Healthcare Dive that the CVS-owned payer has implemented a gold card program and rolled back prior authorization requirements on cataract surgeries, video EEGs, and home infusion for some drugs, according to Healthcare Dive.
Cigna has faced increased scrutiny from some state regulators since a ProPublica/The Capitol Forum article revealed in March that its doctors were denying claims without opening patients’ files, contrary to what insurance laws and regulations require in many states.
Over a period of 2 months last year, Cigna doctors denied over 300,000 requests for payments using this method, spending an average of 1.2 seconds on each case, the investigation found. In a written response, Cigna said the reporting by ProPublica and The Capitol Forum was “biased and incomplete.”
States aim to reduce prior authorization volume
The American Medical Association said it has been tracking nearly 90 prior authorization reform bills in 30 states. More than a dozen bills are still being considered in this legislative session, including in Arkansas, California, New Jersey, North Carolina, Maryland, and Washington, D.C.
“The groundswell of activity in the states reflects how big a problem this is,” said an AMA legislative expert. “The issue used to be ‘how can we automate and streamline processes’; now the issue is focused on reducing the volume of prior authorizations and the harm that can cause patients.”
The state bills use different strategies to reduce excessive prior authorization requirements. Maryland’s proposed bill, for example, would require just one prior authorization to stay on a prescription drug, if the insurer has previously approved the drug and the patient continues to successfully be treated by the drug.
Washington, D.C. and New Jersey have introduced comprehensive reform bills that include a “grace period” of 60 days, to ensure continuity of care when a patient switches health plans. They also would eliminate repeat authorizations for chronic and long-term conditions, set explicit timelines for insurers to respond to prior authorization requests and appeals, and require that practicing physicians review denials that are appealed.
Many state bills also would require insurers to be more transparent by posting information on their websites about which services and drugs require prior authorization and what their approval rates are for them, said AMA’s legislative expert.
“There’s a black hole of information that insurers have access to. We would really like to know how many prior authorization requests are denied, the time it takes to deny them, and the reasons for denial,” said Josh Bengal, JD, the director of government relations for the Medical Society of New Jersey.
The legislation in New Jersey and other states faces stiff opposition from the insurance lobby, especially state associations of health plans affiliated with AHIP. The California Association of Health Plans, for example, opposes a “gold card” bill (SB 598), introduced in February, that would allow a select group of high-performing doctors to skip prior authorizations for 1 year.
The CAHP states, “Californians deserve safe, high quality, high-value health care. Yet SB 598 will derail the progress we have made in our health care system by lowering the value and safety that Californians should expect from their health care providers,” according to a fact sheet.
The fact-sheet defines “low-value care” as medical services for which there is little to no benefit and poses potential physical or financial harm to patients, such as unnecessary CT scans or MRIs for uncomplicated conditions.
California is one of about a dozen states that have introduced gold card legislation this year. If enacted, they would join five states with gold card laws: West Virginia, Texas, Vermont, Michigan, and Louisiana.
How do gold cards work?
Physicians who achieve a high approval rate of prior authorizations from insurers for 1 year are eligible to be exempted from obtaining prior authorizations the following year.
The approval rate is at least 90% for a certain number of eligible health services, but the number of prior authorizations required to qualify can range from 5 to 30, depending on the state law.
Gold card legislation typically also gives the treating physician the right to have an appeal of a prior authorization denial by a physician peer of the same or similar specialty.
California’s bill would also apply to all covered health services, which is broader than what United HealthCare has proposed for its gold card exemption. The bill would also require a plan or insurer to annually monitor rates of prior authorization approval, modification, appeal, and denial, and to discontinue services, items, and supplies that are approved 95% of the time.
“These are important reforms that will help ensure that patients can receive the care they need, when they need it,” said CMA president Donaldo Hernandez, MD.
However, it’s not clear how many physicians will meet “gold card” status based on Texas’ recent experience with its own “gold card” law.
The Texas Department of Insurance estimated that only 3.3% of licensed physicians in the state have met “gold card” status since the bill became law in 2021, said Zeke Silva, MD, an interventional radiologist who serves on the Council of Legislation for the Texas Medical Association.
He noted that the legislation has had a limited effect for several reasons. Commercial health plans only make up only about 20% of all health plans in Texas. Also, the final regulations didn’t go into effect until last May and physicians are evaluated by health plans for “gold card” status every 6 months, said Dr. Silva.
In addition, physicians must have at least five prior authorizations approved for the same health service, which the law left up to the health plans to define, said Dr. Silva.
Now, the Texas Medical Association is lobbying for legislative improvements. “We want to reduce the number of eligible services that health plans require for prior authorizations and have more oversight of prior authorization denials by the Texas Department of Insurance and the Texas Medical Board,” said Dr. Silva.
He’s optimistic that if the bill becomes law, the number of physicians eligible for gold cards may increase.
Meanwhile, the AMA’s legislative expert, who declined to be identified because of organization policy, acknowledged the possibility that some prior authorization bills will die in state legislatures this year.
“We remain hopeful, but it’s an uphill battle. The state medical associations face a lot of opposition from health plans who don’t want to see these reforms become law.”
A version of this article originally appeared on Medscape.com.
Amid growing criticism of health insurers’ onerous prior authorization practices, lawmakers in 30 states have introduced bills this year that aim to rein in insurer gatekeeping and improve patient care.
“This is something that goes on in every doctor’s office every day; the frustrations, the delays, and the use of office staff time are just unbelievable,” said Steven Orland, MD, a board-certified urologist and president of the Medical Society of New Jersey.
The bills, which cover private health plans and insurers that states regulate, may provide some relief for physicians as federal efforts to streamline prior authorization for some Medicare patients have lagged.
Last year, Congress failed to pass the Improving Seniors’ Timely Access to Care Act of 2021, despite 326 co-sponsors. The bill would have compelled insurers covering Medicare Advantage enrollees to speed up prior authorizations, make the process more transparent, and remove obstacles such as requiring fax machine submissions.
Last month, however, the Centers for Medicare & Medicaid Services issued a final rule that will improve some aspects of prior authorizations in Medicare Advantage insurance plans and ensure that enrollees have the same access to necessary care as traditional Medicare enrollees.
The insurance industry has long defended prior authorization requirements and opposed legislation that would limit them.
America’s Health Insurance Plans (AHIP) and the Blue Cross Blue Shield Association said in a 2019 letter to a congressional committee when the federal legislation was first introduced, “Prior authorizations enforce best practices and guidelines for care management and help physicians identify and avoid care techniques that would harm patient outcomes, such as designating prescriptions that could feed into an opioid addiction.” AHIP didn’t respond to repeated requests for comment.
But some major insurers now appear willing to compromise and voluntarily reduce the volume of prior authorizations they require. Days before the federal final rule was released, three major insurers – United HealthCare, Cigna, and Aetna CVS Health – announced they plan to drop some prior authorization requirements and automate processes.
United HealthCare said it will eliminate almost 20% of its prior authorizations for some nonurgent surgeries and procedures starting this summer. It also will create a national Gold Card program in 2024 for physicians who meet its eligibility requirements, which would eliminate prior authorization requirements for most procedures. Both initiatives will apply to commercial, Medicare Advantage, and Medicaid businesses, said the insurer in a statement.
However, United HealthCare also announced that in June it will start requiring prior authorization for diagnostic (not screening) gastrointestinal endoscopies for its nearly 27 million privately insured patients, citing data it says shows potentially harmful overuse of scopes. Physician groups have publicly criticized the move, saying it could delay lifesaving treatment, and have asked the insurer to reconsider.
Cigna and Aetna also have moved to pare back prior authorization processes. Scott Josephs, national medical officer for Cigna, told Healthcare Dive that Cigna has removed prior authorization reviews from nearly 500 services since 2020.
An Aetna spokesperson told Healthcare Dive that the CVS-owned payer has implemented a gold card program and rolled back prior authorization requirements on cataract surgeries, video EEGs, and home infusion for some drugs, according to Healthcare Dive.
Cigna has faced increased scrutiny from some state regulators since a ProPublica/The Capitol Forum article revealed in March that its doctors were denying claims without opening patients’ files, contrary to what insurance laws and regulations require in many states.
Over a period of 2 months last year, Cigna doctors denied over 300,000 requests for payments using this method, spending an average of 1.2 seconds on each case, the investigation found. In a written response, Cigna said the reporting by ProPublica and The Capitol Forum was “biased and incomplete.”
States aim to reduce prior authorization volume
The American Medical Association said it has been tracking nearly 90 prior authorization reform bills in 30 states. More than a dozen bills are still being considered in this legislative session, including in Arkansas, California, New Jersey, North Carolina, Maryland, and Washington, D.C.
“The groundswell of activity in the states reflects how big a problem this is,” said an AMA legislative expert. “The issue used to be ‘how can we automate and streamline processes’; now the issue is focused on reducing the volume of prior authorizations and the harm that can cause patients.”
The state bills use different strategies to reduce excessive prior authorization requirements. Maryland’s proposed bill, for example, would require just one prior authorization to stay on a prescription drug, if the insurer has previously approved the drug and the patient continues to successfully be treated by the drug.
Washington, D.C. and New Jersey have introduced comprehensive reform bills that include a “grace period” of 60 days, to ensure continuity of care when a patient switches health plans. They also would eliminate repeat authorizations for chronic and long-term conditions, set explicit timelines for insurers to respond to prior authorization requests and appeals, and require that practicing physicians review denials that are appealed.
Many state bills also would require insurers to be more transparent by posting information on their websites about which services and drugs require prior authorization and what their approval rates are for them, said AMA’s legislative expert.
“There’s a black hole of information that insurers have access to. We would really like to know how many prior authorization requests are denied, the time it takes to deny them, and the reasons for denial,” said Josh Bengal, JD, the director of government relations for the Medical Society of New Jersey.
The legislation in New Jersey and other states faces stiff opposition from the insurance lobby, especially state associations of health plans affiliated with AHIP. The California Association of Health Plans, for example, opposes a “gold card” bill (SB 598), introduced in February, that would allow a select group of high-performing doctors to skip prior authorizations for 1 year.
The CAHP states, “Californians deserve safe, high quality, high-value health care. Yet SB 598 will derail the progress we have made in our health care system by lowering the value and safety that Californians should expect from their health care providers,” according to a fact sheet.
The fact-sheet defines “low-value care” as medical services for which there is little to no benefit and poses potential physical or financial harm to patients, such as unnecessary CT scans or MRIs for uncomplicated conditions.
California is one of about a dozen states that have introduced gold card legislation this year. If enacted, they would join five states with gold card laws: West Virginia, Texas, Vermont, Michigan, and Louisiana.
How do gold cards work?
Physicians who achieve a high approval rate of prior authorizations from insurers for 1 year are eligible to be exempted from obtaining prior authorizations the following year.
The approval rate is at least 90% for a certain number of eligible health services, but the number of prior authorizations required to qualify can range from 5 to 30, depending on the state law.
Gold card legislation typically also gives the treating physician the right to have an appeal of a prior authorization denial by a physician peer of the same or similar specialty.
California’s bill would also apply to all covered health services, which is broader than what United HealthCare has proposed for its gold card exemption. The bill would also require a plan or insurer to annually monitor rates of prior authorization approval, modification, appeal, and denial, and to discontinue services, items, and supplies that are approved 95% of the time.
“These are important reforms that will help ensure that patients can receive the care they need, when they need it,” said CMA president Donaldo Hernandez, MD.
However, it’s not clear how many physicians will meet “gold card” status based on Texas’ recent experience with its own “gold card” law.
The Texas Department of Insurance estimated that only 3.3% of licensed physicians in the state have met “gold card” status since the bill became law in 2021, said Zeke Silva, MD, an interventional radiologist who serves on the Council of Legislation for the Texas Medical Association.
He noted that the legislation has had a limited effect for several reasons. Commercial health plans only make up only about 20% of all health plans in Texas. Also, the final regulations didn’t go into effect until last May and physicians are evaluated by health plans for “gold card” status every 6 months, said Dr. Silva.
In addition, physicians must have at least five prior authorizations approved for the same health service, which the law left up to the health plans to define, said Dr. Silva.
Now, the Texas Medical Association is lobbying for legislative improvements. “We want to reduce the number of eligible services that health plans require for prior authorizations and have more oversight of prior authorization denials by the Texas Department of Insurance and the Texas Medical Board,” said Dr. Silva.
He’s optimistic that if the bill becomes law, the number of physicians eligible for gold cards may increase.
Meanwhile, the AMA’s legislative expert, who declined to be identified because of organization policy, acknowledged the possibility that some prior authorization bills will die in state legislatures this year.
“We remain hopeful, but it’s an uphill battle. The state medical associations face a lot of opposition from health plans who don’t want to see these reforms become law.”
A version of this article originally appeared on Medscape.com.
Amid growing criticism of health insurers’ onerous prior authorization practices, lawmakers in 30 states have introduced bills this year that aim to rein in insurer gatekeeping and improve patient care.
“This is something that goes on in every doctor’s office every day; the frustrations, the delays, and the use of office staff time are just unbelievable,” said Steven Orland, MD, a board-certified urologist and president of the Medical Society of New Jersey.
The bills, which cover private health plans and insurers that states regulate, may provide some relief for physicians as federal efforts to streamline prior authorization for some Medicare patients have lagged.
Last year, Congress failed to pass the Improving Seniors’ Timely Access to Care Act of 2021, despite 326 co-sponsors. The bill would have compelled insurers covering Medicare Advantage enrollees to speed up prior authorizations, make the process more transparent, and remove obstacles such as requiring fax machine submissions.
Last month, however, the Centers for Medicare & Medicaid Services issued a final rule that will improve some aspects of prior authorizations in Medicare Advantage insurance plans and ensure that enrollees have the same access to necessary care as traditional Medicare enrollees.
The insurance industry has long defended prior authorization requirements and opposed legislation that would limit them.
America’s Health Insurance Plans (AHIP) and the Blue Cross Blue Shield Association said in a 2019 letter to a congressional committee when the federal legislation was first introduced, “Prior authorizations enforce best practices and guidelines for care management and help physicians identify and avoid care techniques that would harm patient outcomes, such as designating prescriptions that could feed into an opioid addiction.” AHIP didn’t respond to repeated requests for comment.
But some major insurers now appear willing to compromise and voluntarily reduce the volume of prior authorizations they require. Days before the federal final rule was released, three major insurers – United HealthCare, Cigna, and Aetna CVS Health – announced they plan to drop some prior authorization requirements and automate processes.
United HealthCare said it will eliminate almost 20% of its prior authorizations for some nonurgent surgeries and procedures starting this summer. It also will create a national Gold Card program in 2024 for physicians who meet its eligibility requirements, which would eliminate prior authorization requirements for most procedures. Both initiatives will apply to commercial, Medicare Advantage, and Medicaid businesses, said the insurer in a statement.
However, United HealthCare also announced that in June it will start requiring prior authorization for diagnostic (not screening) gastrointestinal endoscopies for its nearly 27 million privately insured patients, citing data it says shows potentially harmful overuse of scopes. Physician groups have publicly criticized the move, saying it could delay lifesaving treatment, and have asked the insurer to reconsider.
Cigna and Aetna also have moved to pare back prior authorization processes. Scott Josephs, national medical officer for Cigna, told Healthcare Dive that Cigna has removed prior authorization reviews from nearly 500 services since 2020.
An Aetna spokesperson told Healthcare Dive that the CVS-owned payer has implemented a gold card program and rolled back prior authorization requirements on cataract surgeries, video EEGs, and home infusion for some drugs, according to Healthcare Dive.
Cigna has faced increased scrutiny from some state regulators since a ProPublica/The Capitol Forum article revealed in March that its doctors were denying claims without opening patients’ files, contrary to what insurance laws and regulations require in many states.
Over a period of 2 months last year, Cigna doctors denied over 300,000 requests for payments using this method, spending an average of 1.2 seconds on each case, the investigation found. In a written response, Cigna said the reporting by ProPublica and The Capitol Forum was “biased and incomplete.”
States aim to reduce prior authorization volume
The American Medical Association said it has been tracking nearly 90 prior authorization reform bills in 30 states. More than a dozen bills are still being considered in this legislative session, including in Arkansas, California, New Jersey, North Carolina, Maryland, and Washington, D.C.
“The groundswell of activity in the states reflects how big a problem this is,” said an AMA legislative expert. “The issue used to be ‘how can we automate and streamline processes’; now the issue is focused on reducing the volume of prior authorizations and the harm that can cause patients.”
The state bills use different strategies to reduce excessive prior authorization requirements. Maryland’s proposed bill, for example, would require just one prior authorization to stay on a prescription drug, if the insurer has previously approved the drug and the patient continues to successfully be treated by the drug.
Washington, D.C. and New Jersey have introduced comprehensive reform bills that include a “grace period” of 60 days, to ensure continuity of care when a patient switches health plans. They also would eliminate repeat authorizations for chronic and long-term conditions, set explicit timelines for insurers to respond to prior authorization requests and appeals, and require that practicing physicians review denials that are appealed.
Many state bills also would require insurers to be more transparent by posting information on their websites about which services and drugs require prior authorization and what their approval rates are for them, said AMA’s legislative expert.
“There’s a black hole of information that insurers have access to. We would really like to know how many prior authorization requests are denied, the time it takes to deny them, and the reasons for denial,” said Josh Bengal, JD, the director of government relations for the Medical Society of New Jersey.
The legislation in New Jersey and other states faces stiff opposition from the insurance lobby, especially state associations of health plans affiliated with AHIP. The California Association of Health Plans, for example, opposes a “gold card” bill (SB 598), introduced in February, that would allow a select group of high-performing doctors to skip prior authorizations for 1 year.
The CAHP states, “Californians deserve safe, high quality, high-value health care. Yet SB 598 will derail the progress we have made in our health care system by lowering the value and safety that Californians should expect from their health care providers,” according to a fact sheet.
The fact-sheet defines “low-value care” as medical services for which there is little to no benefit and poses potential physical or financial harm to patients, such as unnecessary CT scans or MRIs for uncomplicated conditions.
California is one of about a dozen states that have introduced gold card legislation this year. If enacted, they would join five states with gold card laws: West Virginia, Texas, Vermont, Michigan, and Louisiana.
How do gold cards work?
Physicians who achieve a high approval rate of prior authorizations from insurers for 1 year are eligible to be exempted from obtaining prior authorizations the following year.
The approval rate is at least 90% for a certain number of eligible health services, but the number of prior authorizations required to qualify can range from 5 to 30, depending on the state law.
Gold card legislation typically also gives the treating physician the right to have an appeal of a prior authorization denial by a physician peer of the same or similar specialty.
California’s bill would also apply to all covered health services, which is broader than what United HealthCare has proposed for its gold card exemption. The bill would also require a plan or insurer to annually monitor rates of prior authorization approval, modification, appeal, and denial, and to discontinue services, items, and supplies that are approved 95% of the time.
“These are important reforms that will help ensure that patients can receive the care they need, when they need it,” said CMA president Donaldo Hernandez, MD.
However, it’s not clear how many physicians will meet “gold card” status based on Texas’ recent experience with its own “gold card” law.
The Texas Department of Insurance estimated that only 3.3% of licensed physicians in the state have met “gold card” status since the bill became law in 2021, said Zeke Silva, MD, an interventional radiologist who serves on the Council of Legislation for the Texas Medical Association.
He noted that the legislation has had a limited effect for several reasons. Commercial health plans only make up only about 20% of all health plans in Texas. Also, the final regulations didn’t go into effect until last May and physicians are evaluated by health plans for “gold card” status every 6 months, said Dr. Silva.
In addition, physicians must have at least five prior authorizations approved for the same health service, which the law left up to the health plans to define, said Dr. Silva.
Now, the Texas Medical Association is lobbying for legislative improvements. “We want to reduce the number of eligible services that health plans require for prior authorizations and have more oversight of prior authorization denials by the Texas Department of Insurance and the Texas Medical Board,” said Dr. Silva.
He’s optimistic that if the bill becomes law, the number of physicians eligible for gold cards may increase.
Meanwhile, the AMA’s legislative expert, who declined to be identified because of organization policy, acknowledged the possibility that some prior authorization bills will die in state legislatures this year.
“We remain hopeful, but it’s an uphill battle. The state medical associations face a lot of opposition from health plans who don’t want to see these reforms become law.”
A version of this article originally appeared on Medscape.com.
'Paradigm shift’: Luspatercept for MDS
“Luspatercept is the first and only therapy to demonstrate superiority in a head-to-head study against ESAs in [transfusion-dependent] LR-MDS,” first author Guillermo Garcia-Manero, MD, chief of the MDS section, department of leukemia, at the University of Texas MD Anderson Cancer Center, Houston, said in a premeeting press briefing in advance of the annual meeting of the American Society of Clinical Oncology.
“It should be considered a paradigm shift in the treatment of LR-MDS–associated anemia,” Dr. Garcia-Manero said.
Commenting on the study, Andrew Artz, MD, a professor at the Hematologic Malignancies Research Institute, City of Hope National Medical Center, Duarte, Calif., agreed that the results could be practice changing.
“We biologically expected luspatercept to best ESA [in ring sideroblast transfusion–dependent MDS], based on luspatercept often rescuing ESA failures in this setting,” Dr. Artz said in an interview.
“The results have the potential to change initial therapy for patients with low-risk red blood cell transfusion-dependent MDS,” he said.
In LR-MDS, which encompasses a variety of bone marrow disorders, chronic anemia is very common, and patients, who are typically elderly, can become burdened by developing dependencies on RBC transfusions.
Transfusion dependency, in addition to creating a host of challenges, can increase the risk of death by as much as 50%, compared with patients who are not transfusion dependent, Dr. Garcia-Manero noted.
While ESAs such as epoetin alfa are the first-line treatment for LR-MDS, patients who are dependent on transfusions are less likely to respond to the agents, hence “there is an unmet need for effective and durable options other than ESAs for treating anemia in patients with LR-MDS,” Dr. Garcia-Manero said.
Luspatercept, a first-in-class monoclonal antibody, has a mechanism of action that is distinct from ESAs, modulating the transforming growth factor–beta pathway and increasing erythrocytosis.
In the previous phase 3 MEDALIST trial, the drug was shown to have efficacy over placebo in reducing the severity of anemia in LR-MDS. In 2020, in what was deemed the first advance in MDS treatment in more than a decade, those results led to approval by the Food and Drug Administration for patients with LR-MDS with ring sideroblasts who are transfusion dependent and are refractory, intolerant, or ineligible to receive ESAs.
To further investigate luspatercept’s efficacy in a head-to-head comparison with an ESA in LR-MDS patients who are ESA naive, Dr. Garcia-Manero and colleagues conducted the phase 3 COMMANDS trial.
For the global, open-label study, patients with LR-MDS who were dependent on RBC transfusions and had no prior use of ESAs were randomized 1:1 to treatment either with subcutaneous luspatercept (starting dose, 1.0 mg/kg with titration up to 1.75 mg/kg; n = 178) once every 3 weeks or subcutaneous epoetin alfa (starting dose, 450 IU/kg with titration up to 1,050 IU/kg; n = 176) once every week, for a minimum of 24 weeks.
Patients in each arm were also able to receive best supportive care, including blood transfusions. Their baseline characteristics were similar in each arm.
For the primary endpoint, patients receiving luspatercept in the intent-to-treat population were nearly twice as likely as those treated with epoetin alfa to become independent of RBC transfusions, with a concurrent mean hemoglobin increase of 1.5 g/dL or more, for at least 12 weeks in the first 24 weeks on study, at a rate of 58.5% with luspatercept versus 31.2% with epoetin alfa (P < .0001).
In addition, patients treated with luspatercept had a longer median duration of transfusion independence, at 126.6 weeks versus 77 weeks in the epoetin alfa group (hazard ratio, 0.456).
Importantly, the statistically significant improvement with luspatercept was consistent among patients with ring sideroblasts (HR, 0.626) as well as without them (HR, 0.492). Dr. Garcia-Manero noted that about 70% of patients in the study had ring sideroblasts, consistent with their common occurrence in LR-MDS.
Luspatercept was also superior in secondary endpoints, including in achieving hematologic improvement, with an erythroid response of at least 8 weeks, per International Working Group 2006 criteria, which was achieved by 74.1% with luspatercept versus 51.3% with epoetin alfa (P < .0001).
The greater improvement with luspatercept was also observed in other subgroups, including based on baseline serum erythropoietin or levels of transfusion dependence, as well as SF381 mutation status.
In terms of safety, treatment emergent adverse events (TEAEs) of any grade were reported among 92.1% of luspatercept and 85.2% of epoetin alfa patients. Longer-term posttreatment safety analyses showed no significant differences between the groups in terms of progression to high-risk MDS, in five (2.8%) with luspatercept and seven(4.0%) epoetin alfa, and progression to acute myeloid leukemia, occurring in four (2.2%) luspatercept and five (2.8%) epoetin alfa patients.
Overall rates of death between the groups were also similar during the treatment and posttreatment periods (32 [18.0%] luspatercept; 32 [18.2%] epoetin alfa patients).
“The toxicity profile was consistent with previous clinical experience,” Dr. Garcia-Manero said.
Dr. Garcia-Manero underscored that “the results of the COMMANDS trial are very important.”
“ESAs are really not optimal agents [for LR-MDS], and these results indicate that luspatercept almost doubles response rates in this patient population, therefore becoming potentially the standard of care for patients with transfusion-dependent LR-MDS who have not received prior ESA treatment,” he said.
Further commenting, Dr. Artz added that the effects in patient subgroups will be of great interest as further data on luspatercept emerges.
“Of highest interest will be the differential responses among patients with and without ring sideroblasts, as well as by SF3B1 mutational status,” he said. Furthermore, “patient-centric data emerge as even more relevant when considering the quantitatively higher rates of treatment-emergent adverse effects in the luspatercept arm.”
“We need to understand how to best sequence anemia therapies in low-risk MDS when we have two active agents, or even if [there is] a role for combined ESA/luspatercept therapy,” he noted.
“The results are exciting, but we need the final data including relevant subsets before declaring luspatercept the winner,” Dr. Artz concluded.
The study was sponsored by Celgene/Bristol-Myers Squibb. Dr. Garcia-Manero reported relationships with Abbvie, Acceleron Pharma, Aprea Therapeutics, Astex Pharmaceuticals, Bristol-Myers Squibb, Genentech, Gilead Sciences, and Novartis. Dr. Artz disclosed previous consulting relationships with Abbvie and Magenta Therapeutics.
“Luspatercept is the first and only therapy to demonstrate superiority in a head-to-head study against ESAs in [transfusion-dependent] LR-MDS,” first author Guillermo Garcia-Manero, MD, chief of the MDS section, department of leukemia, at the University of Texas MD Anderson Cancer Center, Houston, said in a premeeting press briefing in advance of the annual meeting of the American Society of Clinical Oncology.
“It should be considered a paradigm shift in the treatment of LR-MDS–associated anemia,” Dr. Garcia-Manero said.
Commenting on the study, Andrew Artz, MD, a professor at the Hematologic Malignancies Research Institute, City of Hope National Medical Center, Duarte, Calif., agreed that the results could be practice changing.
“We biologically expected luspatercept to best ESA [in ring sideroblast transfusion–dependent MDS], based on luspatercept often rescuing ESA failures in this setting,” Dr. Artz said in an interview.
“The results have the potential to change initial therapy for patients with low-risk red blood cell transfusion-dependent MDS,” he said.
In LR-MDS, which encompasses a variety of bone marrow disorders, chronic anemia is very common, and patients, who are typically elderly, can become burdened by developing dependencies on RBC transfusions.
Transfusion dependency, in addition to creating a host of challenges, can increase the risk of death by as much as 50%, compared with patients who are not transfusion dependent, Dr. Garcia-Manero noted.
While ESAs such as epoetin alfa are the first-line treatment for LR-MDS, patients who are dependent on transfusions are less likely to respond to the agents, hence “there is an unmet need for effective and durable options other than ESAs for treating anemia in patients with LR-MDS,” Dr. Garcia-Manero said.
Luspatercept, a first-in-class monoclonal antibody, has a mechanism of action that is distinct from ESAs, modulating the transforming growth factor–beta pathway and increasing erythrocytosis.
In the previous phase 3 MEDALIST trial, the drug was shown to have efficacy over placebo in reducing the severity of anemia in LR-MDS. In 2020, in what was deemed the first advance in MDS treatment in more than a decade, those results led to approval by the Food and Drug Administration for patients with LR-MDS with ring sideroblasts who are transfusion dependent and are refractory, intolerant, or ineligible to receive ESAs.
To further investigate luspatercept’s efficacy in a head-to-head comparison with an ESA in LR-MDS patients who are ESA naive, Dr. Garcia-Manero and colleagues conducted the phase 3 COMMANDS trial.
For the global, open-label study, patients with LR-MDS who were dependent on RBC transfusions and had no prior use of ESAs were randomized 1:1 to treatment either with subcutaneous luspatercept (starting dose, 1.0 mg/kg with titration up to 1.75 mg/kg; n = 178) once every 3 weeks or subcutaneous epoetin alfa (starting dose, 450 IU/kg with titration up to 1,050 IU/kg; n = 176) once every week, for a minimum of 24 weeks.
Patients in each arm were also able to receive best supportive care, including blood transfusions. Their baseline characteristics were similar in each arm.
For the primary endpoint, patients receiving luspatercept in the intent-to-treat population were nearly twice as likely as those treated with epoetin alfa to become independent of RBC transfusions, with a concurrent mean hemoglobin increase of 1.5 g/dL or more, for at least 12 weeks in the first 24 weeks on study, at a rate of 58.5% with luspatercept versus 31.2% with epoetin alfa (P < .0001).
In addition, patients treated with luspatercept had a longer median duration of transfusion independence, at 126.6 weeks versus 77 weeks in the epoetin alfa group (hazard ratio, 0.456).
Importantly, the statistically significant improvement with luspatercept was consistent among patients with ring sideroblasts (HR, 0.626) as well as without them (HR, 0.492). Dr. Garcia-Manero noted that about 70% of patients in the study had ring sideroblasts, consistent with their common occurrence in LR-MDS.
Luspatercept was also superior in secondary endpoints, including in achieving hematologic improvement, with an erythroid response of at least 8 weeks, per International Working Group 2006 criteria, which was achieved by 74.1% with luspatercept versus 51.3% with epoetin alfa (P < .0001).
The greater improvement with luspatercept was also observed in other subgroups, including based on baseline serum erythropoietin or levels of transfusion dependence, as well as SF381 mutation status.
In terms of safety, treatment emergent adverse events (TEAEs) of any grade were reported among 92.1% of luspatercept and 85.2% of epoetin alfa patients. Longer-term posttreatment safety analyses showed no significant differences between the groups in terms of progression to high-risk MDS, in five (2.8%) with luspatercept and seven(4.0%) epoetin alfa, and progression to acute myeloid leukemia, occurring in four (2.2%) luspatercept and five (2.8%) epoetin alfa patients.
Overall rates of death between the groups were also similar during the treatment and posttreatment periods (32 [18.0%] luspatercept; 32 [18.2%] epoetin alfa patients).
“The toxicity profile was consistent with previous clinical experience,” Dr. Garcia-Manero said.
Dr. Garcia-Manero underscored that “the results of the COMMANDS trial are very important.”
“ESAs are really not optimal agents [for LR-MDS], and these results indicate that luspatercept almost doubles response rates in this patient population, therefore becoming potentially the standard of care for patients with transfusion-dependent LR-MDS who have not received prior ESA treatment,” he said.
Further commenting, Dr. Artz added that the effects in patient subgroups will be of great interest as further data on luspatercept emerges.
“Of highest interest will be the differential responses among patients with and without ring sideroblasts, as well as by SF3B1 mutational status,” he said. Furthermore, “patient-centric data emerge as even more relevant when considering the quantitatively higher rates of treatment-emergent adverse effects in the luspatercept arm.”
“We need to understand how to best sequence anemia therapies in low-risk MDS when we have two active agents, or even if [there is] a role for combined ESA/luspatercept therapy,” he noted.
“The results are exciting, but we need the final data including relevant subsets before declaring luspatercept the winner,” Dr. Artz concluded.
The study was sponsored by Celgene/Bristol-Myers Squibb. Dr. Garcia-Manero reported relationships with Abbvie, Acceleron Pharma, Aprea Therapeutics, Astex Pharmaceuticals, Bristol-Myers Squibb, Genentech, Gilead Sciences, and Novartis. Dr. Artz disclosed previous consulting relationships with Abbvie and Magenta Therapeutics.
“Luspatercept is the first and only therapy to demonstrate superiority in a head-to-head study against ESAs in [transfusion-dependent] LR-MDS,” first author Guillermo Garcia-Manero, MD, chief of the MDS section, department of leukemia, at the University of Texas MD Anderson Cancer Center, Houston, said in a premeeting press briefing in advance of the annual meeting of the American Society of Clinical Oncology.
“It should be considered a paradigm shift in the treatment of LR-MDS–associated anemia,” Dr. Garcia-Manero said.
Commenting on the study, Andrew Artz, MD, a professor at the Hematologic Malignancies Research Institute, City of Hope National Medical Center, Duarte, Calif., agreed that the results could be practice changing.
“We biologically expected luspatercept to best ESA [in ring sideroblast transfusion–dependent MDS], based on luspatercept often rescuing ESA failures in this setting,” Dr. Artz said in an interview.
“The results have the potential to change initial therapy for patients with low-risk red blood cell transfusion-dependent MDS,” he said.
In LR-MDS, which encompasses a variety of bone marrow disorders, chronic anemia is very common, and patients, who are typically elderly, can become burdened by developing dependencies on RBC transfusions.
Transfusion dependency, in addition to creating a host of challenges, can increase the risk of death by as much as 50%, compared with patients who are not transfusion dependent, Dr. Garcia-Manero noted.
While ESAs such as epoetin alfa are the first-line treatment for LR-MDS, patients who are dependent on transfusions are less likely to respond to the agents, hence “there is an unmet need for effective and durable options other than ESAs for treating anemia in patients with LR-MDS,” Dr. Garcia-Manero said.
Luspatercept, a first-in-class monoclonal antibody, has a mechanism of action that is distinct from ESAs, modulating the transforming growth factor–beta pathway and increasing erythrocytosis.
In the previous phase 3 MEDALIST trial, the drug was shown to have efficacy over placebo in reducing the severity of anemia in LR-MDS. In 2020, in what was deemed the first advance in MDS treatment in more than a decade, those results led to approval by the Food and Drug Administration for patients with LR-MDS with ring sideroblasts who are transfusion dependent and are refractory, intolerant, or ineligible to receive ESAs.
To further investigate luspatercept’s efficacy in a head-to-head comparison with an ESA in LR-MDS patients who are ESA naive, Dr. Garcia-Manero and colleagues conducted the phase 3 COMMANDS trial.
For the global, open-label study, patients with LR-MDS who were dependent on RBC transfusions and had no prior use of ESAs were randomized 1:1 to treatment either with subcutaneous luspatercept (starting dose, 1.0 mg/kg with titration up to 1.75 mg/kg; n = 178) once every 3 weeks or subcutaneous epoetin alfa (starting dose, 450 IU/kg with titration up to 1,050 IU/kg; n = 176) once every week, for a minimum of 24 weeks.
Patients in each arm were also able to receive best supportive care, including blood transfusions. Their baseline characteristics were similar in each arm.
For the primary endpoint, patients receiving luspatercept in the intent-to-treat population were nearly twice as likely as those treated with epoetin alfa to become independent of RBC transfusions, with a concurrent mean hemoglobin increase of 1.5 g/dL or more, for at least 12 weeks in the first 24 weeks on study, at a rate of 58.5% with luspatercept versus 31.2% with epoetin alfa (P < .0001).
In addition, patients treated with luspatercept had a longer median duration of transfusion independence, at 126.6 weeks versus 77 weeks in the epoetin alfa group (hazard ratio, 0.456).
Importantly, the statistically significant improvement with luspatercept was consistent among patients with ring sideroblasts (HR, 0.626) as well as without them (HR, 0.492). Dr. Garcia-Manero noted that about 70% of patients in the study had ring sideroblasts, consistent with their common occurrence in LR-MDS.
Luspatercept was also superior in secondary endpoints, including in achieving hematologic improvement, with an erythroid response of at least 8 weeks, per International Working Group 2006 criteria, which was achieved by 74.1% with luspatercept versus 51.3% with epoetin alfa (P < .0001).
The greater improvement with luspatercept was also observed in other subgroups, including based on baseline serum erythropoietin or levels of transfusion dependence, as well as SF381 mutation status.
In terms of safety, treatment emergent adverse events (TEAEs) of any grade were reported among 92.1% of luspatercept and 85.2% of epoetin alfa patients. Longer-term posttreatment safety analyses showed no significant differences between the groups in terms of progression to high-risk MDS, in five (2.8%) with luspatercept and seven(4.0%) epoetin alfa, and progression to acute myeloid leukemia, occurring in four (2.2%) luspatercept and five (2.8%) epoetin alfa patients.
Overall rates of death between the groups were also similar during the treatment and posttreatment periods (32 [18.0%] luspatercept; 32 [18.2%] epoetin alfa patients).
“The toxicity profile was consistent with previous clinical experience,” Dr. Garcia-Manero said.
Dr. Garcia-Manero underscored that “the results of the COMMANDS trial are very important.”
“ESAs are really not optimal agents [for LR-MDS], and these results indicate that luspatercept almost doubles response rates in this patient population, therefore becoming potentially the standard of care for patients with transfusion-dependent LR-MDS who have not received prior ESA treatment,” he said.
Further commenting, Dr. Artz added that the effects in patient subgroups will be of great interest as further data on luspatercept emerges.
“Of highest interest will be the differential responses among patients with and without ring sideroblasts, as well as by SF3B1 mutational status,” he said. Furthermore, “patient-centric data emerge as even more relevant when considering the quantitatively higher rates of treatment-emergent adverse effects in the luspatercept arm.”
“We need to understand how to best sequence anemia therapies in low-risk MDS when we have two active agents, or even if [there is] a role for combined ESA/luspatercept therapy,” he noted.
“The results are exciting, but we need the final data including relevant subsets before declaring luspatercept the winner,” Dr. Artz concluded.
The study was sponsored by Celgene/Bristol-Myers Squibb. Dr. Garcia-Manero reported relationships with Abbvie, Acceleron Pharma, Aprea Therapeutics, Astex Pharmaceuticals, Bristol-Myers Squibb, Genentech, Gilead Sciences, and Novartis. Dr. Artz disclosed previous consulting relationships with Abbvie and Magenta Therapeutics.
FROM ASCO 2023