User login
-
Suits or joggers? A doctor’s dress code
Look at this guy – NFL Chargers jersey and shorts with a RVCA hat on backward. And next to him, a woman wearing her spin-class-Lulu gear. There’s also a guy sporting a 2016 San Diego Rock ‘n Roll Marathon Tee. And that young woman is actually wearing slippers. A visitor from the 1950s would be thunderstruck to see such casual wear on people waiting to board a plane. Photos from that era show men buttoned up in white shirt and tie and women wearing Chanel with hats and white gloves. This dramatic transformation from formal to unfussy wear cuts through all social situations, including in my office. As a new doc out of residency, I used to wear a tie and shoes that could hold a shine. Now I wear jogger scrubs and sneakers. Rather than be offended by the lack of formality though, patients seem to appreciate it. Should they?
At first glance this seems to be a modern phenomenon. The reasons for casual wear today are manifold: about one-third of people work from home, Millennials are taking over with their TikTok values and general irreverence, COVID made us all fat and lazy. Heck, even the U.S. Senate briefly abolished the requirement to wear suits on the Senate floor. But getting dressed up was never to signal that you are elite or superior to others. It’s the opposite. To get dressed is a signal that you are serving others, a tradition that is as old as society.
Think of Downton Abbey as an example. The servants were always required to be smartly dressed when working, whereas members of the family could be dressed up or not. It’s clear who is serving whom. This tradition lives today in the hospitality industry. When you mosey into the lobby of a luxury hotel in your Rainbow sandals you can expect everyone who greets you will be in finery, signaling that they put in effort to serve you. You’ll find the same for all staff at the Mayo Clinic in Rochester, Minn., which is no coincidence.
Suits used to be standard in medicine. In the 19th century, physicians wore formal black-tie when seeing patients. Unlike hospitality however, we had good reason to eschew the tradition: germs. Once we figured out that our pus-stained ties and jackets were doing harm, we switched to wearing sanitized uniforms. Casual wear for doctors isn’t a modern phenomenon after all, then. For proof, compare Thomas Eakins painting “The Gross Clinic” (1875) with his later “The Agnew Clinic” (1889). In the former, Dr. Gross is portrayed in formal black wear, bloody hand and all. In the latter, Dr. Agnew is wearing white FIGS (or the 1890’s equivalent anyway). Similarly, nurses uniforms traditionally resembled kitchen servants, with criss-cross aprons and floor length skirts. It wasn’t until the 1980’s that nurses stopped wearing dresses and white caps.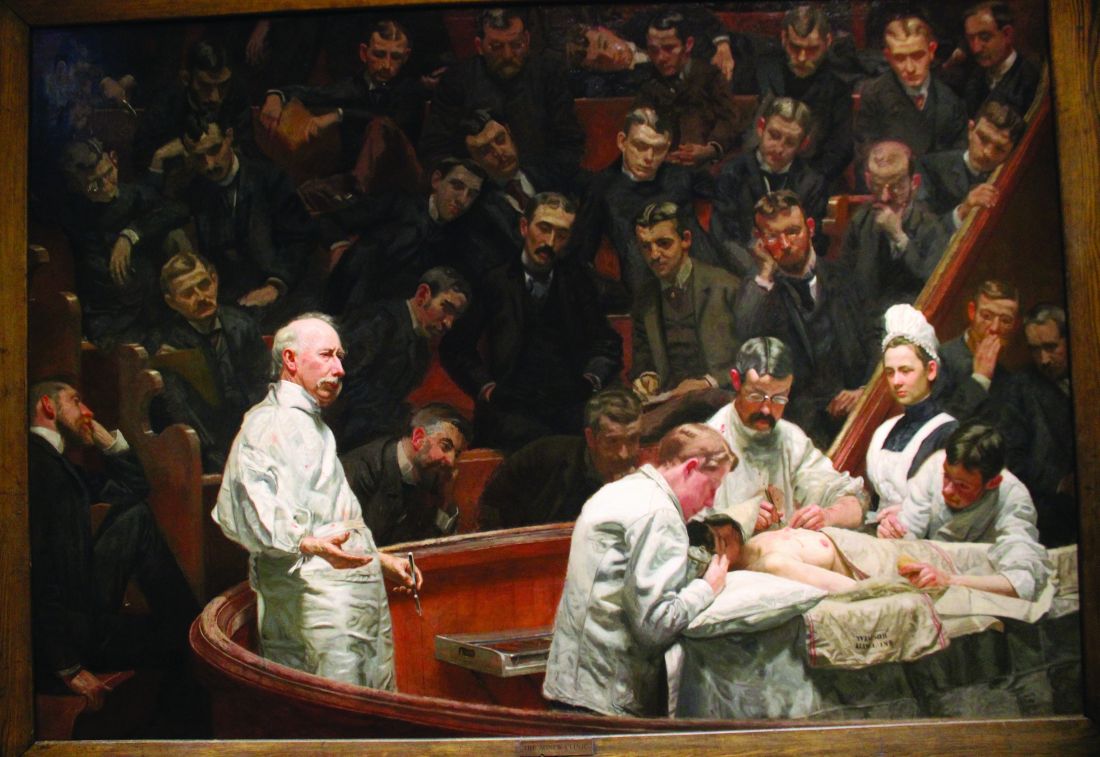
In the operating theater it’s obviously critical that we wear sanitized scrubs to mitigate the risk of infection. Originally white to signal cleanliness, scrubs were changed to blue-green because surgeons were blinded by the lights bouncing off the uniforms. (Green is also opposite red on the color wheel, supposedly enhancing the ability to distinguish shades of red).
But Over time we’ve lost significant autonomy in our practice and lost a little respect from our patients. Payers tell us what to do. Patients question our expertise. Choosing what we wear is one of the few bits of medicine we still have agency. Pewter or pink, joggers or cargo pants, we get to choose.
The last time I flew British Airways everyone was in lounge wear, except the flight crew, of course. They were all smartly dressed. Recently British Airways rolled out updated, slightly more relaxed dress codes. Very modern, but I wonder if in a way we’re not all just a bit worse off.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com
Look at this guy – NFL Chargers jersey and shorts with a RVCA hat on backward. And next to him, a woman wearing her spin-class-Lulu gear. There’s also a guy sporting a 2016 San Diego Rock ‘n Roll Marathon Tee. And that young woman is actually wearing slippers. A visitor from the 1950s would be thunderstruck to see such casual wear on people waiting to board a plane. Photos from that era show men buttoned up in white shirt and tie and women wearing Chanel with hats and white gloves. This dramatic transformation from formal to unfussy wear cuts through all social situations, including in my office. As a new doc out of residency, I used to wear a tie and shoes that could hold a shine. Now I wear jogger scrubs and sneakers. Rather than be offended by the lack of formality though, patients seem to appreciate it. Should they?
At first glance this seems to be a modern phenomenon. The reasons for casual wear today are manifold: about one-third of people work from home, Millennials are taking over with their TikTok values and general irreverence, COVID made us all fat and lazy. Heck, even the U.S. Senate briefly abolished the requirement to wear suits on the Senate floor. But getting dressed up was never to signal that you are elite or superior to others. It’s the opposite. To get dressed is a signal that you are serving others, a tradition that is as old as society.
Think of Downton Abbey as an example. The servants were always required to be smartly dressed when working, whereas members of the family could be dressed up or not. It’s clear who is serving whom. This tradition lives today in the hospitality industry. When you mosey into the lobby of a luxury hotel in your Rainbow sandals you can expect everyone who greets you will be in finery, signaling that they put in effort to serve you. You’ll find the same for all staff at the Mayo Clinic in Rochester, Minn., which is no coincidence.
Suits used to be standard in medicine. In the 19th century, physicians wore formal black-tie when seeing patients. Unlike hospitality however, we had good reason to eschew the tradition: germs. Once we figured out that our pus-stained ties and jackets were doing harm, we switched to wearing sanitized uniforms. Casual wear for doctors isn’t a modern phenomenon after all, then. For proof, compare Thomas Eakins painting “The Gross Clinic” (1875) with his later “The Agnew Clinic” (1889). In the former, Dr. Gross is portrayed in formal black wear, bloody hand and all. In the latter, Dr. Agnew is wearing white FIGS (or the 1890’s equivalent anyway). Similarly, nurses uniforms traditionally resembled kitchen servants, with criss-cross aprons and floor length skirts. It wasn’t until the 1980’s that nurses stopped wearing dresses and white caps.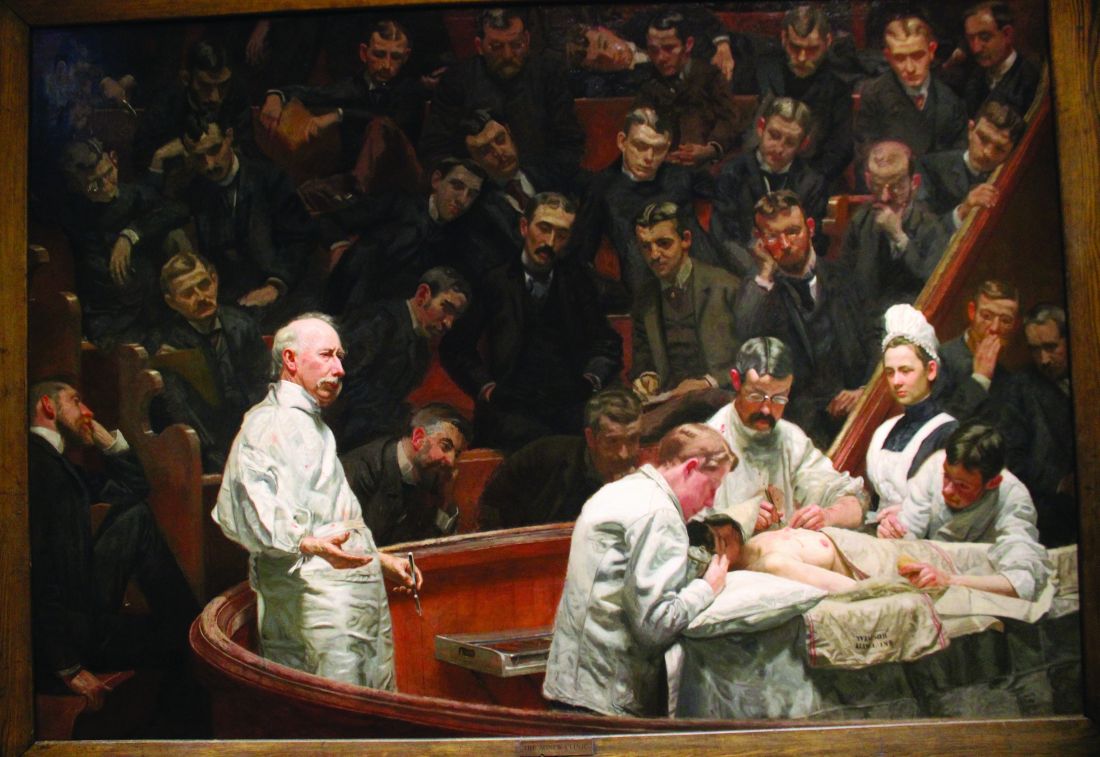
In the operating theater it’s obviously critical that we wear sanitized scrubs to mitigate the risk of infection. Originally white to signal cleanliness, scrubs were changed to blue-green because surgeons were blinded by the lights bouncing off the uniforms. (Green is also opposite red on the color wheel, supposedly enhancing the ability to distinguish shades of red).
But Over time we’ve lost significant autonomy in our practice and lost a little respect from our patients. Payers tell us what to do. Patients question our expertise. Choosing what we wear is one of the few bits of medicine we still have agency. Pewter or pink, joggers or cargo pants, we get to choose.
The last time I flew British Airways everyone was in lounge wear, except the flight crew, of course. They were all smartly dressed. Recently British Airways rolled out updated, slightly more relaxed dress codes. Very modern, but I wonder if in a way we’re not all just a bit worse off.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com
Look at this guy – NFL Chargers jersey and shorts with a RVCA hat on backward. And next to him, a woman wearing her spin-class-Lulu gear. There’s also a guy sporting a 2016 San Diego Rock ‘n Roll Marathon Tee. And that young woman is actually wearing slippers. A visitor from the 1950s would be thunderstruck to see such casual wear on people waiting to board a plane. Photos from that era show men buttoned up in white shirt and tie and women wearing Chanel with hats and white gloves. This dramatic transformation from formal to unfussy wear cuts through all social situations, including in my office. As a new doc out of residency, I used to wear a tie and shoes that could hold a shine. Now I wear jogger scrubs and sneakers. Rather than be offended by the lack of formality though, patients seem to appreciate it. Should they?
At first glance this seems to be a modern phenomenon. The reasons for casual wear today are manifold: about one-third of people work from home, Millennials are taking over with their TikTok values and general irreverence, COVID made us all fat and lazy. Heck, even the U.S. Senate briefly abolished the requirement to wear suits on the Senate floor. But getting dressed up was never to signal that you are elite or superior to others. It’s the opposite. To get dressed is a signal that you are serving others, a tradition that is as old as society.
Think of Downton Abbey as an example. The servants were always required to be smartly dressed when working, whereas members of the family could be dressed up or not. It’s clear who is serving whom. This tradition lives today in the hospitality industry. When you mosey into the lobby of a luxury hotel in your Rainbow sandals you can expect everyone who greets you will be in finery, signaling that they put in effort to serve you. You’ll find the same for all staff at the Mayo Clinic in Rochester, Minn., which is no coincidence.
Suits used to be standard in medicine. In the 19th century, physicians wore formal black-tie when seeing patients. Unlike hospitality however, we had good reason to eschew the tradition: germs. Once we figured out that our pus-stained ties and jackets were doing harm, we switched to wearing sanitized uniforms. Casual wear for doctors isn’t a modern phenomenon after all, then. For proof, compare Thomas Eakins painting “The Gross Clinic” (1875) with his later “The Agnew Clinic” (1889). In the former, Dr. Gross is portrayed in formal black wear, bloody hand and all. In the latter, Dr. Agnew is wearing white FIGS (or the 1890’s equivalent anyway). Similarly, nurses uniforms traditionally resembled kitchen servants, with criss-cross aprons and floor length skirts. It wasn’t until the 1980’s that nurses stopped wearing dresses and white caps.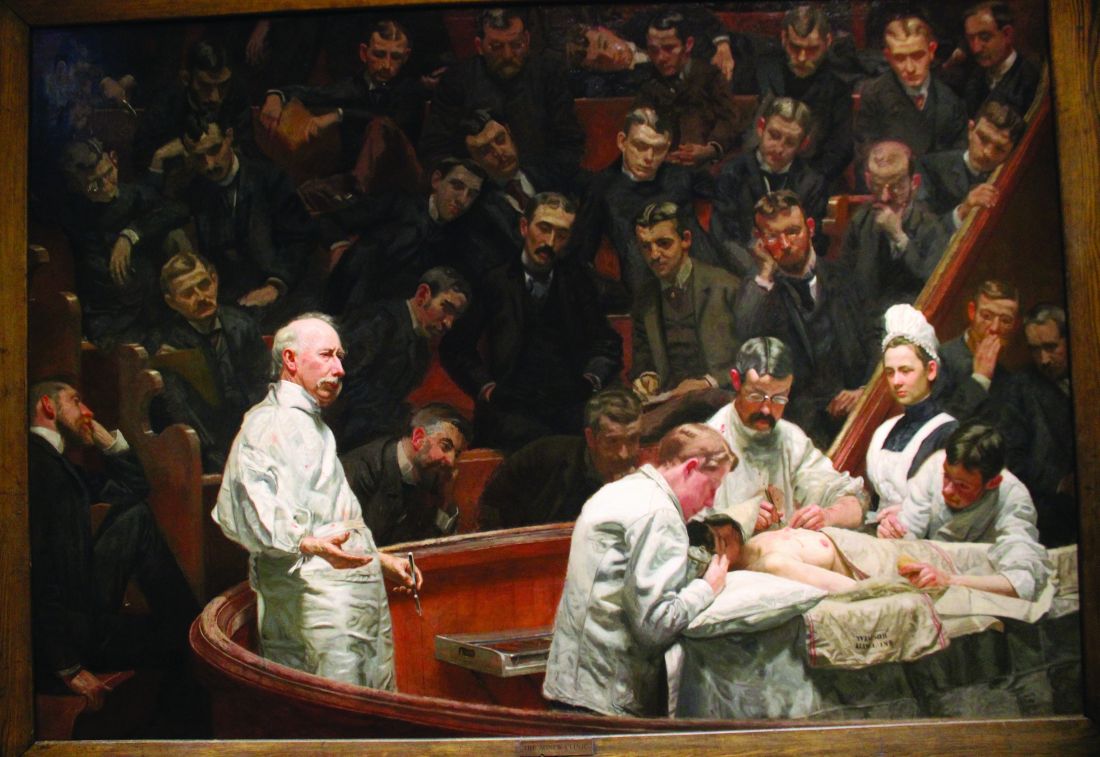
In the operating theater it’s obviously critical that we wear sanitized scrubs to mitigate the risk of infection. Originally white to signal cleanliness, scrubs were changed to blue-green because surgeons were blinded by the lights bouncing off the uniforms. (Green is also opposite red on the color wheel, supposedly enhancing the ability to distinguish shades of red).
But Over time we’ve lost significant autonomy in our practice and lost a little respect from our patients. Payers tell us what to do. Patients question our expertise. Choosing what we wear is one of the few bits of medicine we still have agency. Pewter or pink, joggers or cargo pants, we get to choose.
The last time I flew British Airways everyone was in lounge wear, except the flight crew, of course. They were all smartly dressed. Recently British Airways rolled out updated, slightly more relaxed dress codes. Very modern, but I wonder if in a way we’re not all just a bit worse off.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@mdedge.com
When to treat DLBCL with radiotherapy?
SAN DIEGO –
For example, radiation may not be needed for advanced-stage patients who’ve received at least four cycles of R-CHOP chemotherapy (cyclophosphamide, doxorubicin, vincristine, and prednisolone plus rituximab), and whose PET scans show no sign of disease at interim or end-of treatment phases, said Joanna Yang, MD, MPH, of Washington University in St. Louis, in a presentation at the annual meeting of the American Society for Radiation Oncology.
These patients “may be able to omit radiotherapy without sacrificing good outcomes,” Dr. Yang said. In contrast, those whose PET scans show signs of disease at interim and end-of-treatment points may benefit from radiotherapy to selected sites, she said.
Dr. Yang highlighted a 2021 study in Blood that tracked 723 patients with advanced-stage DLBCL who were diagnosed from 2005 to 2017. All were treated with R-CHOP, and some of those who were PET-positive – that is, showing signs of malignant disease – were treated with radiotherapy.
Over a mean follow-up of 4.3 years, the study reported “time to progression and overall survival at 3 years were 83% vs. 56% and 87% vs. 64% in patients with PET-NEG and PET-POS scans, respectively.”
These findings aren’t surprising, Dr. Yang said. But “the PET-positive patients who got radiation actually had outcomes that came close to the outcomes that the PET-negative patients were able to achieve.” Their 3-year overall survival was 80% vs. 87% in the PET-negative, no-radiation group vs. 44% in the PET-positive, no-radiation group.
Dr. Yang cautioned, however, that withholding radiation in PET-negative patients isn’t right for everyone: “This doesn’t mean this should be the approach for every single patient.”
What about early-stage DLBCL? In patients without risk factors, Dr. Yang recommends PET scans after four treatments with R-CHOP. “Getting that end-of-treatment PET is going to be super-critical because that’s going to help guide you in terms of the patients who you may feel comfortable omitting radiation versus the patients who remain PET-positive at the end of chemotherapy. Many places will also add an interim PET as well.”
According to her, radiotherapy is appropriate in patients who are PET-positive, based on the findings of the FLYER and LYSA-GOELAMS 02-03 trials.
In early-stage patients who have risk factors such as advanced age or bulky or extra-nodal disease, Dr. Yang suggests examining interim PET scans after three treatments with R-CHOP. If they are negative, another R-CHOP treatment is appropriate – with or without radiotherapy.
“There’s a lot that goes into that decision. The first thing I think about in patients who have risk factors is: What salvage options are available for my patient? Can they tolerate these salvage option? If they’re older, they might not be eligible for auto [autologous hematopoietic cell transplantation]. If they’re frail, they might not be eligible for auto or CAR T cells. If they have bulk, it’s certainly an area of concern. It seems like radiation does help control disease in areas of bulk for patients with DLBCL.”
If these patients are PET-positive, go directly to radiotherapy, Dr. Yang advised. Trials that support this approach include S1001, LYSA-GOELAMS 02-03, and RICOVER-noRTH, she said.
What about double-hit and triple-hit lymphomas, which are especially aggressive due to genetic variations? Research suggests that “even if double hit/triple hit is not responding to chemo, it still responds to radiation,” Dr. Yang said.
In regard to advanced-stage disease, “if patients are receiving full-dose chemo for least six cycles, I use that end-of-treatment PET to help guide me. And then I make an individualized decision based on how bulky that disease is, where the location is, how morbid a relapse would be. If they’re older or receiving reduced-dose chemotherapy, then I’ll more seriously consider radiation just because there are limited options for these patients. And we know that DLCBL is most commonly a disease of the elderly.”
In an adjoining presentation at ASTRO, Andrea Ng, MD, MPH, of Harvard Medical School/Dana-Farber Brigham Cancer Center, Boston, discussed which patients with incomplete response or refractory/relapsed DLCBL can benefit from radiotherapy.
She highlighted patients with good partial response and end-of-treatment PET-positive with evidence of residual 18F-fluorodeoxyglucose activity via PET scan (Deauville 4/5) – a group that “we’re increasingly seeing.” In these patients, “radiation can be quite effective” at doses of 36-45 Gy. She highlighted a study from 2011 that linked consolidation radiotherapy to 5-year event-free survival in 65% of patients.
As for relapsed/refractory disease in patients who aren’t candidates for further systemic therapy – the “frail without good options” – Dr. Ng said data about salvage radiotherapy is limited. However, a 2015 study tracked 65 patients who were treated with a median dose of 40 Gy with “curative” intent. Local control was “not great” at 72% at 2 years, Dr. Ng said, while overall survival was 60% and progress-free survival was 46%.
Dr. Ng, who was one of this study’s authors, said several groups did better: Those with refractory vs. relapsed disease and those who were responsive to chemotherapy vs. those who were not.
She also highlighted a similar 2019 study of 32 patients with refractory/relapsed disease treated with salvage radiotherapy (median dose of 42.7 Gy) found that 61.8% reached progress-free survival at 5 years – a better outcome.
Dr. Yang has no disclosures. Dr. Ng discloses royalties from UpToDate and Elsevier.
SAN DIEGO –
For example, radiation may not be needed for advanced-stage patients who’ve received at least four cycles of R-CHOP chemotherapy (cyclophosphamide, doxorubicin, vincristine, and prednisolone plus rituximab), and whose PET scans show no sign of disease at interim or end-of treatment phases, said Joanna Yang, MD, MPH, of Washington University in St. Louis, in a presentation at the annual meeting of the American Society for Radiation Oncology.
These patients “may be able to omit radiotherapy without sacrificing good outcomes,” Dr. Yang said. In contrast, those whose PET scans show signs of disease at interim and end-of-treatment points may benefit from radiotherapy to selected sites, she said.
Dr. Yang highlighted a 2021 study in Blood that tracked 723 patients with advanced-stage DLBCL who were diagnosed from 2005 to 2017. All were treated with R-CHOP, and some of those who were PET-positive – that is, showing signs of malignant disease – were treated with radiotherapy.
Over a mean follow-up of 4.3 years, the study reported “time to progression and overall survival at 3 years were 83% vs. 56% and 87% vs. 64% in patients with PET-NEG and PET-POS scans, respectively.”
These findings aren’t surprising, Dr. Yang said. But “the PET-positive patients who got radiation actually had outcomes that came close to the outcomes that the PET-negative patients were able to achieve.” Their 3-year overall survival was 80% vs. 87% in the PET-negative, no-radiation group vs. 44% in the PET-positive, no-radiation group.
Dr. Yang cautioned, however, that withholding radiation in PET-negative patients isn’t right for everyone: “This doesn’t mean this should be the approach for every single patient.”
What about early-stage DLBCL? In patients without risk factors, Dr. Yang recommends PET scans after four treatments with R-CHOP. “Getting that end-of-treatment PET is going to be super-critical because that’s going to help guide you in terms of the patients who you may feel comfortable omitting radiation versus the patients who remain PET-positive at the end of chemotherapy. Many places will also add an interim PET as well.”
According to her, radiotherapy is appropriate in patients who are PET-positive, based on the findings of the FLYER and LYSA-GOELAMS 02-03 trials.
In early-stage patients who have risk factors such as advanced age or bulky or extra-nodal disease, Dr. Yang suggests examining interim PET scans after three treatments with R-CHOP. If they are negative, another R-CHOP treatment is appropriate – with or without radiotherapy.
“There’s a lot that goes into that decision. The first thing I think about in patients who have risk factors is: What salvage options are available for my patient? Can they tolerate these salvage option? If they’re older, they might not be eligible for auto [autologous hematopoietic cell transplantation]. If they’re frail, they might not be eligible for auto or CAR T cells. If they have bulk, it’s certainly an area of concern. It seems like radiation does help control disease in areas of bulk for patients with DLBCL.”
If these patients are PET-positive, go directly to radiotherapy, Dr. Yang advised. Trials that support this approach include S1001, LYSA-GOELAMS 02-03, and RICOVER-noRTH, she said.
What about double-hit and triple-hit lymphomas, which are especially aggressive due to genetic variations? Research suggests that “even if double hit/triple hit is not responding to chemo, it still responds to radiation,” Dr. Yang said.
In regard to advanced-stage disease, “if patients are receiving full-dose chemo for least six cycles, I use that end-of-treatment PET to help guide me. And then I make an individualized decision based on how bulky that disease is, where the location is, how morbid a relapse would be. If they’re older or receiving reduced-dose chemotherapy, then I’ll more seriously consider radiation just because there are limited options for these patients. And we know that DLCBL is most commonly a disease of the elderly.”
In an adjoining presentation at ASTRO, Andrea Ng, MD, MPH, of Harvard Medical School/Dana-Farber Brigham Cancer Center, Boston, discussed which patients with incomplete response or refractory/relapsed DLCBL can benefit from radiotherapy.
She highlighted patients with good partial response and end-of-treatment PET-positive with evidence of residual 18F-fluorodeoxyglucose activity via PET scan (Deauville 4/5) – a group that “we’re increasingly seeing.” In these patients, “radiation can be quite effective” at doses of 36-45 Gy. She highlighted a study from 2011 that linked consolidation radiotherapy to 5-year event-free survival in 65% of patients.
As for relapsed/refractory disease in patients who aren’t candidates for further systemic therapy – the “frail without good options” – Dr. Ng said data about salvage radiotherapy is limited. However, a 2015 study tracked 65 patients who were treated with a median dose of 40 Gy with “curative” intent. Local control was “not great” at 72% at 2 years, Dr. Ng said, while overall survival was 60% and progress-free survival was 46%.
Dr. Ng, who was one of this study’s authors, said several groups did better: Those with refractory vs. relapsed disease and those who were responsive to chemotherapy vs. those who were not.
She also highlighted a similar 2019 study of 32 patients with refractory/relapsed disease treated with salvage radiotherapy (median dose of 42.7 Gy) found that 61.8% reached progress-free survival at 5 years – a better outcome.
Dr. Yang has no disclosures. Dr. Ng discloses royalties from UpToDate and Elsevier.
SAN DIEGO –
For example, radiation may not be needed for advanced-stage patients who’ve received at least four cycles of R-CHOP chemotherapy (cyclophosphamide, doxorubicin, vincristine, and prednisolone plus rituximab), and whose PET scans show no sign of disease at interim or end-of treatment phases, said Joanna Yang, MD, MPH, of Washington University in St. Louis, in a presentation at the annual meeting of the American Society for Radiation Oncology.
These patients “may be able to omit radiotherapy without sacrificing good outcomes,” Dr. Yang said. In contrast, those whose PET scans show signs of disease at interim and end-of-treatment points may benefit from radiotherapy to selected sites, she said.
Dr. Yang highlighted a 2021 study in Blood that tracked 723 patients with advanced-stage DLBCL who were diagnosed from 2005 to 2017. All were treated with R-CHOP, and some of those who were PET-positive – that is, showing signs of malignant disease – were treated with radiotherapy.
Over a mean follow-up of 4.3 years, the study reported “time to progression and overall survival at 3 years were 83% vs. 56% and 87% vs. 64% in patients with PET-NEG and PET-POS scans, respectively.”
These findings aren’t surprising, Dr. Yang said. But “the PET-positive patients who got radiation actually had outcomes that came close to the outcomes that the PET-negative patients were able to achieve.” Their 3-year overall survival was 80% vs. 87% in the PET-negative, no-radiation group vs. 44% in the PET-positive, no-radiation group.
Dr. Yang cautioned, however, that withholding radiation in PET-negative patients isn’t right for everyone: “This doesn’t mean this should be the approach for every single patient.”
What about early-stage DLBCL? In patients without risk factors, Dr. Yang recommends PET scans after four treatments with R-CHOP. “Getting that end-of-treatment PET is going to be super-critical because that’s going to help guide you in terms of the patients who you may feel comfortable omitting radiation versus the patients who remain PET-positive at the end of chemotherapy. Many places will also add an interim PET as well.”
According to her, radiotherapy is appropriate in patients who are PET-positive, based on the findings of the FLYER and LYSA-GOELAMS 02-03 trials.
In early-stage patients who have risk factors such as advanced age or bulky or extra-nodal disease, Dr. Yang suggests examining interim PET scans after three treatments with R-CHOP. If they are negative, another R-CHOP treatment is appropriate – with or without radiotherapy.
“There’s a lot that goes into that decision. The first thing I think about in patients who have risk factors is: What salvage options are available for my patient? Can they tolerate these salvage option? If they’re older, they might not be eligible for auto [autologous hematopoietic cell transplantation]. If they’re frail, they might not be eligible for auto or CAR T cells. If they have bulk, it’s certainly an area of concern. It seems like radiation does help control disease in areas of bulk for patients with DLBCL.”
If these patients are PET-positive, go directly to radiotherapy, Dr. Yang advised. Trials that support this approach include S1001, LYSA-GOELAMS 02-03, and RICOVER-noRTH, she said.
What about double-hit and triple-hit lymphomas, which are especially aggressive due to genetic variations? Research suggests that “even if double hit/triple hit is not responding to chemo, it still responds to radiation,” Dr. Yang said.
In regard to advanced-stage disease, “if patients are receiving full-dose chemo for least six cycles, I use that end-of-treatment PET to help guide me. And then I make an individualized decision based on how bulky that disease is, where the location is, how morbid a relapse would be. If they’re older or receiving reduced-dose chemotherapy, then I’ll more seriously consider radiation just because there are limited options for these patients. And we know that DLCBL is most commonly a disease of the elderly.”
In an adjoining presentation at ASTRO, Andrea Ng, MD, MPH, of Harvard Medical School/Dana-Farber Brigham Cancer Center, Boston, discussed which patients with incomplete response or refractory/relapsed DLCBL can benefit from radiotherapy.
She highlighted patients with good partial response and end-of-treatment PET-positive with evidence of residual 18F-fluorodeoxyglucose activity via PET scan (Deauville 4/5) – a group that “we’re increasingly seeing.” In these patients, “radiation can be quite effective” at doses of 36-45 Gy. She highlighted a study from 2011 that linked consolidation radiotherapy to 5-year event-free survival in 65% of patients.
As for relapsed/refractory disease in patients who aren’t candidates for further systemic therapy – the “frail without good options” – Dr. Ng said data about salvage radiotherapy is limited. However, a 2015 study tracked 65 patients who were treated with a median dose of 40 Gy with “curative” intent. Local control was “not great” at 72% at 2 years, Dr. Ng said, while overall survival was 60% and progress-free survival was 46%.
Dr. Ng, who was one of this study’s authors, said several groups did better: Those with refractory vs. relapsed disease and those who were responsive to chemotherapy vs. those who were not.
She also highlighted a similar 2019 study of 32 patients with refractory/relapsed disease treated with salvage radiotherapy (median dose of 42.7 Gy) found that 61.8% reached progress-free survival at 5 years – a better outcome.
Dr. Yang has no disclosures. Dr. Ng discloses royalties from UpToDate and Elsevier.
FROM ASTRO 2023
Survival on the upswing in myeloma
Back then, the treatments for MM were chemotherapy and steroids. Stem-cell transplants were on the horizon, as was a most unexpected therapy: the infamous drug thalidomide.
But in the wake of the rib facture, the health of Stanley Katz, MD, worsened and he died after 25 weeks, Dr. Berenson recalled in an interview. At that time, Dr. Katz’s horrifically shortened lifespan following diagnosis was not unusual.
About 4 decades later, hematologists like Dr. Berenson are heralding a new era in MM, a sharp reversal of the previous eras of grim prognoses.
In a new study, Dr. Berenson tracked 161 patients with MM treated at his West Hollywood, Calif., private clinic from 2006 to 2023 and found that their median survival was 136.2 months – more than 11 years. “The OS reported in this study ... is the longest reported to date in an unselected, newly diagnosed MM population,” the study authors write.
Dr. Berenson’s patients are unique: They’re largely White, and they didn’t undergo stem-cell transplants. But other recent studies also suggest that lifespans of more than 10 years are increasingly possible after MM diagnosis. Former TV news anchor Tom Brokaw, for one, has reached that point.
In fact, a pair of other hematologists say the overall survival in Dr. Berenson’s report is hardly out of the question. And, they say, patients diagnosed today could potentially live even longer, because treatments continue to improve.
“With data that’s 10 years old, we expect the median overall survival to be 10 years,” hematologist Sagar Lonial, MD, who’s been tracking survival data in MM, said in an interview. “When patients ask about my outlook, I say it’s a constantly evolving field. Things are changing fast enough that I use 10 years as a floor.”
Dr. Lonial is chair of the department of hematology and medical oncology and chief medical officer at Emory University, Atlanta, Winship Cancer Institute.
Hematologist Rafael Fonseca, MD, chief innovation officer at Mayo Clinic–Arizona, put it this way in an interview: Dr. Berenson’s results “are probably in sync with what we would anticipate with similar cohorts of patients. The reality is that we’ve seen a huge improvement in the life expectancy of patients who were diagnosed with multiple myeloma. It’s not unusual to see patients in the clinic now that are 15 or 20 years out from their diagnosis.”
According to Yale Medicine, MM accounts for 10% of blood cancers and 1%-2% of all cancers and is more common in men vs. women and Blacks vs. Whites. It’s most frequently diagnosed between the ages of 65 and 74, according to the National Cancer Institute, and the median age at diagnosis is 69.
Among the most famous American people currently battling MM are newsman Mr. Brokaw, the former NBC News anchor, and Republican Congressman Steve Scalise, majority leader of the U.S. House of Representatives and a candidate for House speaker.
Mr. Brokaw was diagnosed in 2013 while in his early 70s and has talked about his intense struggle with the disease: the infections, operations, infusions, and daily regimens of 24 pills.
“I didn’t want to be Tom Brokaw, cancer victim,” he said in 2018 at the annual meeting of the American Society of Hematology. But he opened up about his illness, and became “the multiple myeloma poster boy.”
Rep. Scalise, who’s in his late 50s, is undergoing chemotherapy. He survived being gravely wounded in an assassination attempt in 2017.
Dr. Berenson’s new study, published in Targeted Oncology, tracked 161 patients (89 women, 72 men; median age, 65.4; 125 White, 3 Black, 10 Hispanic, 15 Asian, and 8 multi-ethnic).
All started frontline treatment at Dr. Berenson’s clinic and were included if they could read consent forms and gave permission for blood draws. None underwent stem-cell transplants as part of initial therapy. Another 1,036 patients had been treated elsewhere and were not included in the study.
Over a median of 42.7 months (range, 1.9-195.1), the 1-, 3-, and 5-year survival rates were 97.5%, 85.3%, and 76.2%, respectively.
The study claims “these results are considerably better than those reported from patients enrolled in clinical trials and those from countries with national registries.”
In the interview, Dr. Berenson said the study is unique because it’s not limited like many studies to younger, healthier patients. Nor does it include those treated at other facilities, he said.
The study is unusual in other ways. Dr. Berenson said his drug regimens aren’t necessarily standard, and he doesn’t treat patients with stem-cell transplants. “I stopped transplanting in about 2000 because clearly it was not improving the length of life,” he said.
Dr. Berenson said colleagues can learn from his insistence on sensitively treating the quality of life of patients, his embrace of clinical trials with novel combinations, and his close monitoring of myeloma proteins to gauge whether patients need to rapidly switch therapies.
He noted that his drug regimens are typically off-label and vary by patient. “We’re not using as high doses of drugs like Velcade [bortezomib] or Revlimid [lenalidomide] as my colleagues. We’re not necessarily giving as many doses. Also, we’re not adding as many drugs in many cases as they are. We’re taking it slower.”
The National Comprehensive Cancer Network recommends bortezomib and lenalidomide as standard induction treatments in patients with MM who are candidates for stem-cell transplantation, a procedure it considers the “preferred approach in transplant-eligible patients.”
There are limitations to Dr. Berenson’s new study. The patients aren’t representative of people with MM as a whole: His cohort is overwhelmingly White (78%) and just 2% Black, while an estimated one-fifth of patients with MM in the United States are Black and have poorer outcomes.
Dr. Berenson also acknowledged that his patients are most likely a wealthier group, although he said it’s not feasible to ask them about income. The study provides no information about socioeconomics.
Dr. Lonial said survival of 10-11 years is fairly typical in MM, with standard-risk patients reaching 14 years.
He highlighted a 2021 Canadian study that tracked 3,030 patients with newly diagnosed MM from 2007 to 2018 (average age, 64; 58.6% men). Those who received an upfront autologous stem-cell transplant had a median overall survival of 122.0 months (95% confidence interval, 115.0-135.0 months) vs. 54.3 months (95% CI, 50.8-58.8 months) for those who didn’t get the transplants. Not surprisingly, survival dipped with each subsequent treatment regimen.
Dr. Lonial is coauthor of a 2020 study that tracked 1,000 consecutive patients (mean age, 61; 35.2% Black) with newly diagnosed myeloma who were treated with RVD (lenalidomide, bortezomib, and dexamethasone) induction therapy from 2007 to 2016. The median overall survival was 126.6 months (95% CI, 113.3-139.8 months).
Dr. Fonseca noted that the news about MM survival rates is not entirely positive. Patients with high-risk disease often die early on in their disease course, he said.
Research suggests even the youngest patients with MM may die within years of diagnosis. A 2021 French study tracked 214 patients in the 18-40 age group for 15 years (2000-2015). At 5 years, “relative survival compared with same age- and sex-matched individuals was 83.5%,” and estimated overall survival was 14.5 years.
Still, a “very, very fertile environment for the development of drugs” has made a huge difference, Dr. Fonseca said. “We’ve had about 19 FDA approvals in the last 15 or 20 years.”
He urged colleagues to keep in mind that survival drops as patients decline in a line of therapy and need to switch to another one. “It might make intuitive sense to say ‘I’m gonna save something for later. I want to keep my powder dry.’ But put your best foot forward. Always go with your best treatments first.”
This approach can play out in a decision, say, to start with a four-drug initial regimen instead of a weaker two-drug regimen, he said. “Be mindful of managing toxicities, but hit harder.”
As he noted, side effects were worse with older generations of drugs. In regard to cost, multidrug treatments can cost hundreds of thousands of dollars. Dr. Fonseca said insurance tends to cover drugs that are approved by guidelines.
Dr. Fonseca discloses relationships with AbbVie, Adaptive Biotechnologies, Amgen, AstraZeneca, Bayer, Binding Site, BMS (Celgene), Millennium Takeda, Janssen, Juno, Kite, Merck, Pfizer, Pharmacyclics, Regeneron, Sanofi, Adaptive Biotechnologies, Caris Life Sciences, Oncotracker, Antegene, and AZBio, and a patent in MM. Dr. Berenson discloses ties with Janssen, Amgen, Sanofi, BMS, Karyopharm, and Incyte. Dr. Lonial reports ties with TG Therapeutics, Celgene, BMS, Janssen, Novartis, GlaxoSmithKline, AbbVie, Takeda, Merck, Sanofi, Pfizer, Regeneron, and Novartis.
Back then, the treatments for MM were chemotherapy and steroids. Stem-cell transplants were on the horizon, as was a most unexpected therapy: the infamous drug thalidomide.
But in the wake of the rib facture, the health of Stanley Katz, MD, worsened and he died after 25 weeks, Dr. Berenson recalled in an interview. At that time, Dr. Katz’s horrifically shortened lifespan following diagnosis was not unusual.
About 4 decades later, hematologists like Dr. Berenson are heralding a new era in MM, a sharp reversal of the previous eras of grim prognoses.
In a new study, Dr. Berenson tracked 161 patients with MM treated at his West Hollywood, Calif., private clinic from 2006 to 2023 and found that their median survival was 136.2 months – more than 11 years. “The OS reported in this study ... is the longest reported to date in an unselected, newly diagnosed MM population,” the study authors write.
Dr. Berenson’s patients are unique: They’re largely White, and they didn’t undergo stem-cell transplants. But other recent studies also suggest that lifespans of more than 10 years are increasingly possible after MM diagnosis. Former TV news anchor Tom Brokaw, for one, has reached that point.
In fact, a pair of other hematologists say the overall survival in Dr. Berenson’s report is hardly out of the question. And, they say, patients diagnosed today could potentially live even longer, because treatments continue to improve.
“With data that’s 10 years old, we expect the median overall survival to be 10 years,” hematologist Sagar Lonial, MD, who’s been tracking survival data in MM, said in an interview. “When patients ask about my outlook, I say it’s a constantly evolving field. Things are changing fast enough that I use 10 years as a floor.”
Dr. Lonial is chair of the department of hematology and medical oncology and chief medical officer at Emory University, Atlanta, Winship Cancer Institute.
Hematologist Rafael Fonseca, MD, chief innovation officer at Mayo Clinic–Arizona, put it this way in an interview: Dr. Berenson’s results “are probably in sync with what we would anticipate with similar cohorts of patients. The reality is that we’ve seen a huge improvement in the life expectancy of patients who were diagnosed with multiple myeloma. It’s not unusual to see patients in the clinic now that are 15 or 20 years out from their diagnosis.”
According to Yale Medicine, MM accounts for 10% of blood cancers and 1%-2% of all cancers and is more common in men vs. women and Blacks vs. Whites. It’s most frequently diagnosed between the ages of 65 and 74, according to the National Cancer Institute, and the median age at diagnosis is 69.
Among the most famous American people currently battling MM are newsman Mr. Brokaw, the former NBC News anchor, and Republican Congressman Steve Scalise, majority leader of the U.S. House of Representatives and a candidate for House speaker.
Mr. Brokaw was diagnosed in 2013 while in his early 70s and has talked about his intense struggle with the disease: the infections, operations, infusions, and daily regimens of 24 pills.
“I didn’t want to be Tom Brokaw, cancer victim,” he said in 2018 at the annual meeting of the American Society of Hematology. But he opened up about his illness, and became “the multiple myeloma poster boy.”
Rep. Scalise, who’s in his late 50s, is undergoing chemotherapy. He survived being gravely wounded in an assassination attempt in 2017.
Dr. Berenson’s new study, published in Targeted Oncology, tracked 161 patients (89 women, 72 men; median age, 65.4; 125 White, 3 Black, 10 Hispanic, 15 Asian, and 8 multi-ethnic).
All started frontline treatment at Dr. Berenson’s clinic and were included if they could read consent forms and gave permission for blood draws. None underwent stem-cell transplants as part of initial therapy. Another 1,036 patients had been treated elsewhere and were not included in the study.
Over a median of 42.7 months (range, 1.9-195.1), the 1-, 3-, and 5-year survival rates were 97.5%, 85.3%, and 76.2%, respectively.
The study claims “these results are considerably better than those reported from patients enrolled in clinical trials and those from countries with national registries.”
In the interview, Dr. Berenson said the study is unique because it’s not limited like many studies to younger, healthier patients. Nor does it include those treated at other facilities, he said.
The study is unusual in other ways. Dr. Berenson said his drug regimens aren’t necessarily standard, and he doesn’t treat patients with stem-cell transplants. “I stopped transplanting in about 2000 because clearly it was not improving the length of life,” he said.
Dr. Berenson said colleagues can learn from his insistence on sensitively treating the quality of life of patients, his embrace of clinical trials with novel combinations, and his close monitoring of myeloma proteins to gauge whether patients need to rapidly switch therapies.
He noted that his drug regimens are typically off-label and vary by patient. “We’re not using as high doses of drugs like Velcade [bortezomib] or Revlimid [lenalidomide] as my colleagues. We’re not necessarily giving as many doses. Also, we’re not adding as many drugs in many cases as they are. We’re taking it slower.”
The National Comprehensive Cancer Network recommends bortezomib and lenalidomide as standard induction treatments in patients with MM who are candidates for stem-cell transplantation, a procedure it considers the “preferred approach in transplant-eligible patients.”
There are limitations to Dr. Berenson’s new study. The patients aren’t representative of people with MM as a whole: His cohort is overwhelmingly White (78%) and just 2% Black, while an estimated one-fifth of patients with MM in the United States are Black and have poorer outcomes.
Dr. Berenson also acknowledged that his patients are most likely a wealthier group, although he said it’s not feasible to ask them about income. The study provides no information about socioeconomics.
Dr. Lonial said survival of 10-11 years is fairly typical in MM, with standard-risk patients reaching 14 years.
He highlighted a 2021 Canadian study that tracked 3,030 patients with newly diagnosed MM from 2007 to 2018 (average age, 64; 58.6% men). Those who received an upfront autologous stem-cell transplant had a median overall survival of 122.0 months (95% confidence interval, 115.0-135.0 months) vs. 54.3 months (95% CI, 50.8-58.8 months) for those who didn’t get the transplants. Not surprisingly, survival dipped with each subsequent treatment regimen.
Dr. Lonial is coauthor of a 2020 study that tracked 1,000 consecutive patients (mean age, 61; 35.2% Black) with newly diagnosed myeloma who were treated with RVD (lenalidomide, bortezomib, and dexamethasone) induction therapy from 2007 to 2016. The median overall survival was 126.6 months (95% CI, 113.3-139.8 months).
Dr. Fonseca noted that the news about MM survival rates is not entirely positive. Patients with high-risk disease often die early on in their disease course, he said.
Research suggests even the youngest patients with MM may die within years of diagnosis. A 2021 French study tracked 214 patients in the 18-40 age group for 15 years (2000-2015). At 5 years, “relative survival compared with same age- and sex-matched individuals was 83.5%,” and estimated overall survival was 14.5 years.
Still, a “very, very fertile environment for the development of drugs” has made a huge difference, Dr. Fonseca said. “We’ve had about 19 FDA approvals in the last 15 or 20 years.”
He urged colleagues to keep in mind that survival drops as patients decline in a line of therapy and need to switch to another one. “It might make intuitive sense to say ‘I’m gonna save something for later. I want to keep my powder dry.’ But put your best foot forward. Always go with your best treatments first.”
This approach can play out in a decision, say, to start with a four-drug initial regimen instead of a weaker two-drug regimen, he said. “Be mindful of managing toxicities, but hit harder.”
As he noted, side effects were worse with older generations of drugs. In regard to cost, multidrug treatments can cost hundreds of thousands of dollars. Dr. Fonseca said insurance tends to cover drugs that are approved by guidelines.
Dr. Fonseca discloses relationships with AbbVie, Adaptive Biotechnologies, Amgen, AstraZeneca, Bayer, Binding Site, BMS (Celgene), Millennium Takeda, Janssen, Juno, Kite, Merck, Pfizer, Pharmacyclics, Regeneron, Sanofi, Adaptive Biotechnologies, Caris Life Sciences, Oncotracker, Antegene, and AZBio, and a patent in MM. Dr. Berenson discloses ties with Janssen, Amgen, Sanofi, BMS, Karyopharm, and Incyte. Dr. Lonial reports ties with TG Therapeutics, Celgene, BMS, Janssen, Novartis, GlaxoSmithKline, AbbVie, Takeda, Merck, Sanofi, Pfizer, Regeneron, and Novartis.
Back then, the treatments for MM were chemotherapy and steroids. Stem-cell transplants were on the horizon, as was a most unexpected therapy: the infamous drug thalidomide.
But in the wake of the rib facture, the health of Stanley Katz, MD, worsened and he died after 25 weeks, Dr. Berenson recalled in an interview. At that time, Dr. Katz’s horrifically shortened lifespan following diagnosis was not unusual.
About 4 decades later, hematologists like Dr. Berenson are heralding a new era in MM, a sharp reversal of the previous eras of grim prognoses.
In a new study, Dr. Berenson tracked 161 patients with MM treated at his West Hollywood, Calif., private clinic from 2006 to 2023 and found that their median survival was 136.2 months – more than 11 years. “The OS reported in this study ... is the longest reported to date in an unselected, newly diagnosed MM population,” the study authors write.
Dr. Berenson’s patients are unique: They’re largely White, and they didn’t undergo stem-cell transplants. But other recent studies also suggest that lifespans of more than 10 years are increasingly possible after MM diagnosis. Former TV news anchor Tom Brokaw, for one, has reached that point.
In fact, a pair of other hematologists say the overall survival in Dr. Berenson’s report is hardly out of the question. And, they say, patients diagnosed today could potentially live even longer, because treatments continue to improve.
“With data that’s 10 years old, we expect the median overall survival to be 10 years,” hematologist Sagar Lonial, MD, who’s been tracking survival data in MM, said in an interview. “When patients ask about my outlook, I say it’s a constantly evolving field. Things are changing fast enough that I use 10 years as a floor.”
Dr. Lonial is chair of the department of hematology and medical oncology and chief medical officer at Emory University, Atlanta, Winship Cancer Institute.
Hematologist Rafael Fonseca, MD, chief innovation officer at Mayo Clinic–Arizona, put it this way in an interview: Dr. Berenson’s results “are probably in sync with what we would anticipate with similar cohorts of patients. The reality is that we’ve seen a huge improvement in the life expectancy of patients who were diagnosed with multiple myeloma. It’s not unusual to see patients in the clinic now that are 15 or 20 years out from their diagnosis.”
According to Yale Medicine, MM accounts for 10% of blood cancers and 1%-2% of all cancers and is more common in men vs. women and Blacks vs. Whites. It’s most frequently diagnosed between the ages of 65 and 74, according to the National Cancer Institute, and the median age at diagnosis is 69.
Among the most famous American people currently battling MM are newsman Mr. Brokaw, the former NBC News anchor, and Republican Congressman Steve Scalise, majority leader of the U.S. House of Representatives and a candidate for House speaker.
Mr. Brokaw was diagnosed in 2013 while in his early 70s and has talked about his intense struggle with the disease: the infections, operations, infusions, and daily regimens of 24 pills.
“I didn’t want to be Tom Brokaw, cancer victim,” he said in 2018 at the annual meeting of the American Society of Hematology. But he opened up about his illness, and became “the multiple myeloma poster boy.”
Rep. Scalise, who’s in his late 50s, is undergoing chemotherapy. He survived being gravely wounded in an assassination attempt in 2017.
Dr. Berenson’s new study, published in Targeted Oncology, tracked 161 patients (89 women, 72 men; median age, 65.4; 125 White, 3 Black, 10 Hispanic, 15 Asian, and 8 multi-ethnic).
All started frontline treatment at Dr. Berenson’s clinic and were included if they could read consent forms and gave permission for blood draws. None underwent stem-cell transplants as part of initial therapy. Another 1,036 patients had been treated elsewhere and were not included in the study.
Over a median of 42.7 months (range, 1.9-195.1), the 1-, 3-, and 5-year survival rates were 97.5%, 85.3%, and 76.2%, respectively.
The study claims “these results are considerably better than those reported from patients enrolled in clinical trials and those from countries with national registries.”
In the interview, Dr. Berenson said the study is unique because it’s not limited like many studies to younger, healthier patients. Nor does it include those treated at other facilities, he said.
The study is unusual in other ways. Dr. Berenson said his drug regimens aren’t necessarily standard, and he doesn’t treat patients with stem-cell transplants. “I stopped transplanting in about 2000 because clearly it was not improving the length of life,” he said.
Dr. Berenson said colleagues can learn from his insistence on sensitively treating the quality of life of patients, his embrace of clinical trials with novel combinations, and his close monitoring of myeloma proteins to gauge whether patients need to rapidly switch therapies.
He noted that his drug regimens are typically off-label and vary by patient. “We’re not using as high doses of drugs like Velcade [bortezomib] or Revlimid [lenalidomide] as my colleagues. We’re not necessarily giving as many doses. Also, we’re not adding as many drugs in many cases as they are. We’re taking it slower.”
The National Comprehensive Cancer Network recommends bortezomib and lenalidomide as standard induction treatments in patients with MM who are candidates for stem-cell transplantation, a procedure it considers the “preferred approach in transplant-eligible patients.”
There are limitations to Dr. Berenson’s new study. The patients aren’t representative of people with MM as a whole: His cohort is overwhelmingly White (78%) and just 2% Black, while an estimated one-fifth of patients with MM in the United States are Black and have poorer outcomes.
Dr. Berenson also acknowledged that his patients are most likely a wealthier group, although he said it’s not feasible to ask them about income. The study provides no information about socioeconomics.
Dr. Lonial said survival of 10-11 years is fairly typical in MM, with standard-risk patients reaching 14 years.
He highlighted a 2021 Canadian study that tracked 3,030 patients with newly diagnosed MM from 2007 to 2018 (average age, 64; 58.6% men). Those who received an upfront autologous stem-cell transplant had a median overall survival of 122.0 months (95% confidence interval, 115.0-135.0 months) vs. 54.3 months (95% CI, 50.8-58.8 months) for those who didn’t get the transplants. Not surprisingly, survival dipped with each subsequent treatment regimen.
Dr. Lonial is coauthor of a 2020 study that tracked 1,000 consecutive patients (mean age, 61; 35.2% Black) with newly diagnosed myeloma who were treated with RVD (lenalidomide, bortezomib, and dexamethasone) induction therapy from 2007 to 2016. The median overall survival was 126.6 months (95% CI, 113.3-139.8 months).
Dr. Fonseca noted that the news about MM survival rates is not entirely positive. Patients with high-risk disease often die early on in their disease course, he said.
Research suggests even the youngest patients with MM may die within years of diagnosis. A 2021 French study tracked 214 patients in the 18-40 age group for 15 years (2000-2015). At 5 years, “relative survival compared with same age- and sex-matched individuals was 83.5%,” and estimated overall survival was 14.5 years.
Still, a “very, very fertile environment for the development of drugs” has made a huge difference, Dr. Fonseca said. “We’ve had about 19 FDA approvals in the last 15 or 20 years.”
He urged colleagues to keep in mind that survival drops as patients decline in a line of therapy and need to switch to another one. “It might make intuitive sense to say ‘I’m gonna save something for later. I want to keep my powder dry.’ But put your best foot forward. Always go with your best treatments first.”
This approach can play out in a decision, say, to start with a four-drug initial regimen instead of a weaker two-drug regimen, he said. “Be mindful of managing toxicities, but hit harder.”
As he noted, side effects were worse with older generations of drugs. In regard to cost, multidrug treatments can cost hundreds of thousands of dollars. Dr. Fonseca said insurance tends to cover drugs that are approved by guidelines.
Dr. Fonseca discloses relationships with AbbVie, Adaptive Biotechnologies, Amgen, AstraZeneca, Bayer, Binding Site, BMS (Celgene), Millennium Takeda, Janssen, Juno, Kite, Merck, Pfizer, Pharmacyclics, Regeneron, Sanofi, Adaptive Biotechnologies, Caris Life Sciences, Oncotracker, Antegene, and AZBio, and a patent in MM. Dr. Berenson discloses ties with Janssen, Amgen, Sanofi, BMS, Karyopharm, and Incyte. Dr. Lonial reports ties with TG Therapeutics, Celgene, BMS, Janssen, Novartis, GlaxoSmithKline, AbbVie, Takeda, Merck, Sanofi, Pfizer, Regeneron, and Novartis.
MOC opposition continues to gain momentum as ASH weighs in
ASH president Robert A. Brodsky, MD, sent a letter to ABIM’s President and Chief Executive Officer Richard Baron, MD, highlighting hematologists’ concerns about the MOC process and outlining immediate actions ABIM should take.
“ASH continues to support the importance of lifelong learning for hematologists via a program that is evidence-based, relevant to one’s practice, and transparent; however, these three basic requirements are not met by the current ABIM MOC program,” Dr. Brodsky stated in the Sept. 27 letter to Baron.
Dr. Brodsky highlighted, for instance, the fact that the Longitudinal Knowledge Assessment – the alternative to the 10-year exam – “does not reflect real life practice, nor does it target each individual’s scope of practice.” Dr. Brodsky added that, according to members of ASH, the assessment is also “creating high levels of stress and contributing to burnout.”
The letter from Dr. Brodsky urged ABIM to “establish a new MOC program” that does not involve high-stakes assessments, reduces the number of Longitudinal Knowledge Assessment questions physicians receive, and eliminates redundancy between the MOC requirement to have a current license and the requirement to report continued medical education to ABIM.
The ABIM shared a copy of the letter in a Sept. 28 blog post defending the MOC process, highlighting past collaboration with ASH that “has led to meaningful enhancements to the [MOC] program” and committing to “continue to listen to and learn from the physician community going forward.”
The recent backlash against the MOC process stemmed from a petition demanding an end to the MOC. The petition was launched in July by hematologist-oncologist Aaron Goodman, MD, from the University of California, San Diego, who has been a vocal critic of the MOC process.
The criticism largely centered around the high costs and the “complex and time-consuming process that poses significant challenges to practicing physicians,” Dr. Goodman wrote in the petition, which has garnered more than 20,700 signatures.
In August, the Society for Cardiovascular Angiography and Interventions (SCAI) published “SCAI Position on ABIM Revocation of Certification for Not Participating in MOC.” The Electrophysiology Advocacy Foundation and the Heart Rhythm Society (HRS) issued statements pushing back on the MOC as well.
On Sept. 21, the SCAI, HRS, American College of Cardiology, and the Heart Failure Society of America went a step further and announced plans to create a new certification process that is independent of the ABIM MOC system.
The American Society of Clinical Oncology (ASCO) is now also surveying members about their MOC experience. A Sept. 26 announcement encouraged recipients to check their inboxes for a link to an anonymous MOC Experience Questionnaire before Oct. 12 and thanked respondents for their “engagement as ASCO works to address this critical issue for the oncology community.”
After ASH sent its letter to ABIM, Dr. Goodman applauded the society’s stance in a post on his X (formerly Twitter) account. Vincent Rajkumar, MD, a hematologist at the Mayo Clinic in Rochester, Minn., commented on ABIM’s response to ASH’s letter via X, noting, “If I were @ASH_hematology leadership, I would take ABIM response as disrespectful. A hasty response within a day is not a sign of good faith.”
A version of this article first appeared on Medscape.com.
ASH president Robert A. Brodsky, MD, sent a letter to ABIM’s President and Chief Executive Officer Richard Baron, MD, highlighting hematologists’ concerns about the MOC process and outlining immediate actions ABIM should take.
“ASH continues to support the importance of lifelong learning for hematologists via a program that is evidence-based, relevant to one’s practice, and transparent; however, these three basic requirements are not met by the current ABIM MOC program,” Dr. Brodsky stated in the Sept. 27 letter to Baron.
Dr. Brodsky highlighted, for instance, the fact that the Longitudinal Knowledge Assessment – the alternative to the 10-year exam – “does not reflect real life practice, nor does it target each individual’s scope of practice.” Dr. Brodsky added that, according to members of ASH, the assessment is also “creating high levels of stress and contributing to burnout.”
The letter from Dr. Brodsky urged ABIM to “establish a new MOC program” that does not involve high-stakes assessments, reduces the number of Longitudinal Knowledge Assessment questions physicians receive, and eliminates redundancy between the MOC requirement to have a current license and the requirement to report continued medical education to ABIM.
The ABIM shared a copy of the letter in a Sept. 28 blog post defending the MOC process, highlighting past collaboration with ASH that “has led to meaningful enhancements to the [MOC] program” and committing to “continue to listen to and learn from the physician community going forward.”
The recent backlash against the MOC process stemmed from a petition demanding an end to the MOC. The petition was launched in July by hematologist-oncologist Aaron Goodman, MD, from the University of California, San Diego, who has been a vocal critic of the MOC process.
The criticism largely centered around the high costs and the “complex and time-consuming process that poses significant challenges to practicing physicians,” Dr. Goodman wrote in the petition, which has garnered more than 20,700 signatures.
In August, the Society for Cardiovascular Angiography and Interventions (SCAI) published “SCAI Position on ABIM Revocation of Certification for Not Participating in MOC.” The Electrophysiology Advocacy Foundation and the Heart Rhythm Society (HRS) issued statements pushing back on the MOC as well.
On Sept. 21, the SCAI, HRS, American College of Cardiology, and the Heart Failure Society of America went a step further and announced plans to create a new certification process that is independent of the ABIM MOC system.
The American Society of Clinical Oncology (ASCO) is now also surveying members about their MOC experience. A Sept. 26 announcement encouraged recipients to check their inboxes for a link to an anonymous MOC Experience Questionnaire before Oct. 12 and thanked respondents for their “engagement as ASCO works to address this critical issue for the oncology community.”
After ASH sent its letter to ABIM, Dr. Goodman applauded the society’s stance in a post on his X (formerly Twitter) account. Vincent Rajkumar, MD, a hematologist at the Mayo Clinic in Rochester, Minn., commented on ABIM’s response to ASH’s letter via X, noting, “If I were @ASH_hematology leadership, I would take ABIM response as disrespectful. A hasty response within a day is not a sign of good faith.”
A version of this article first appeared on Medscape.com.
ASH president Robert A. Brodsky, MD, sent a letter to ABIM’s President and Chief Executive Officer Richard Baron, MD, highlighting hematologists’ concerns about the MOC process and outlining immediate actions ABIM should take.
“ASH continues to support the importance of lifelong learning for hematologists via a program that is evidence-based, relevant to one’s practice, and transparent; however, these three basic requirements are not met by the current ABIM MOC program,” Dr. Brodsky stated in the Sept. 27 letter to Baron.
Dr. Brodsky highlighted, for instance, the fact that the Longitudinal Knowledge Assessment – the alternative to the 10-year exam – “does not reflect real life practice, nor does it target each individual’s scope of practice.” Dr. Brodsky added that, according to members of ASH, the assessment is also “creating high levels of stress and contributing to burnout.”
The letter from Dr. Brodsky urged ABIM to “establish a new MOC program” that does not involve high-stakes assessments, reduces the number of Longitudinal Knowledge Assessment questions physicians receive, and eliminates redundancy between the MOC requirement to have a current license and the requirement to report continued medical education to ABIM.
The ABIM shared a copy of the letter in a Sept. 28 blog post defending the MOC process, highlighting past collaboration with ASH that “has led to meaningful enhancements to the [MOC] program” and committing to “continue to listen to and learn from the physician community going forward.”
The recent backlash against the MOC process stemmed from a petition demanding an end to the MOC. The petition was launched in July by hematologist-oncologist Aaron Goodman, MD, from the University of California, San Diego, who has been a vocal critic of the MOC process.
The criticism largely centered around the high costs and the “complex and time-consuming process that poses significant challenges to practicing physicians,” Dr. Goodman wrote in the petition, which has garnered more than 20,700 signatures.
In August, the Society for Cardiovascular Angiography and Interventions (SCAI) published “SCAI Position on ABIM Revocation of Certification for Not Participating in MOC.” The Electrophysiology Advocacy Foundation and the Heart Rhythm Society (HRS) issued statements pushing back on the MOC as well.
On Sept. 21, the SCAI, HRS, American College of Cardiology, and the Heart Failure Society of America went a step further and announced plans to create a new certification process that is independent of the ABIM MOC system.
The American Society of Clinical Oncology (ASCO) is now also surveying members about their MOC experience. A Sept. 26 announcement encouraged recipients to check their inboxes for a link to an anonymous MOC Experience Questionnaire before Oct. 12 and thanked respondents for their “engagement as ASCO works to address this critical issue for the oncology community.”
After ASH sent its letter to ABIM, Dr. Goodman applauded the society’s stance in a post on his X (formerly Twitter) account. Vincent Rajkumar, MD, a hematologist at the Mayo Clinic in Rochester, Minn., commented on ABIM’s response to ASH’s letter via X, noting, “If I were @ASH_hematology leadership, I would take ABIM response as disrespectful. A hasty response within a day is not a sign of good faith.”
A version of this article first appeared on Medscape.com.
These adverse events linked to improved cancer prognosis
TOPLINE:
.
METHODOLOGY:
- Emerging evidence suggests that the presence of cutaneous immune-related adverse events may be linked with favorable outcomes among patients with cancer who receive ICIs.
- Researchers conducted a systematic review and meta-analysis that included 23 studies and a total of 22,749 patients with cancer who received ICI treatment; studies compared outcomes among patients with and those without cutaneous immune-related adverse events.
- The major outcomes evaluated in the analysis were overall survival and progression-free survival (PFS); subgroup analyses assessed cutaneous immune-related adverse event type, cancer type, and other factors.
TAKEAWAY:
- The occurrence of cutaneous immune-related adverse events was associated with improved PFS (hazard ratio, 0.52; P < .001) and overall survival (HR, 0.61; P < .001).
- In the subgroup analysis, patients with eczematous (HR, 0.69), lichenoid or lichen planus–like skin lesions (HR, 0.51), pruritus without rash (HR, 0.70), psoriasis (HR, 0.63), or vitiligo (HR, 0.30) demonstrated a significant overall survival advantage. Vitiligo was the only adverse event associated with a PFS advantage (HR, 0.28).
- Among patients with melanoma, analyses revealed a significant association between the incidence of cutaneous immune-related adverse events and improved overall survival (HR, 0.51) and PFS (HR, 0.45). The authors highlighted similar findings among patients with non–small cell lung cancer (HR, 0.50 for overall survival and 0.61 for PFS).
IN PRACTICE:
“These data suggest that [cutaneous immune-related adverse events] may have useful prognostic value in ICI treatment,” the authors concluded.
SOURCE:
The analysis, led by Fei Wang, MD, Zhong Da Hospital, School of Medicine, Southeast University, Nanjing, China, was published online in JAMA Dermatology.
LIMITATIONS:
Most of the data came from retrospective studies, and there were limited data on specific patient subgroups. The Egger tests, used to assess potential publication bias in meta-analyses, revealed publication bias.
DISCLOSURES:
No disclosures were reported. The study was supported by a grant from the Postgraduate Research and Practice Innovation Program of Jiangsu Province.
A version of this article first appeared on Medscape.com.
TOPLINE:
.
METHODOLOGY:
- Emerging evidence suggests that the presence of cutaneous immune-related adverse events may be linked with favorable outcomes among patients with cancer who receive ICIs.
- Researchers conducted a systematic review and meta-analysis that included 23 studies and a total of 22,749 patients with cancer who received ICI treatment; studies compared outcomes among patients with and those without cutaneous immune-related adverse events.
- The major outcomes evaluated in the analysis were overall survival and progression-free survival (PFS); subgroup analyses assessed cutaneous immune-related adverse event type, cancer type, and other factors.
TAKEAWAY:
- The occurrence of cutaneous immune-related adverse events was associated with improved PFS (hazard ratio, 0.52; P < .001) and overall survival (HR, 0.61; P < .001).
- In the subgroup analysis, patients with eczematous (HR, 0.69), lichenoid or lichen planus–like skin lesions (HR, 0.51), pruritus without rash (HR, 0.70), psoriasis (HR, 0.63), or vitiligo (HR, 0.30) demonstrated a significant overall survival advantage. Vitiligo was the only adverse event associated with a PFS advantage (HR, 0.28).
- Among patients with melanoma, analyses revealed a significant association between the incidence of cutaneous immune-related adverse events and improved overall survival (HR, 0.51) and PFS (HR, 0.45). The authors highlighted similar findings among patients with non–small cell lung cancer (HR, 0.50 for overall survival and 0.61 for PFS).
IN PRACTICE:
“These data suggest that [cutaneous immune-related adverse events] may have useful prognostic value in ICI treatment,” the authors concluded.
SOURCE:
The analysis, led by Fei Wang, MD, Zhong Da Hospital, School of Medicine, Southeast University, Nanjing, China, was published online in JAMA Dermatology.
LIMITATIONS:
Most of the data came from retrospective studies, and there were limited data on specific patient subgroups. The Egger tests, used to assess potential publication bias in meta-analyses, revealed publication bias.
DISCLOSURES:
No disclosures were reported. The study was supported by a grant from the Postgraduate Research and Practice Innovation Program of Jiangsu Province.
A version of this article first appeared on Medscape.com.
TOPLINE:
.
METHODOLOGY:
- Emerging evidence suggests that the presence of cutaneous immune-related adverse events may be linked with favorable outcomes among patients with cancer who receive ICIs.
- Researchers conducted a systematic review and meta-analysis that included 23 studies and a total of 22,749 patients with cancer who received ICI treatment; studies compared outcomes among patients with and those without cutaneous immune-related adverse events.
- The major outcomes evaluated in the analysis were overall survival and progression-free survival (PFS); subgroup analyses assessed cutaneous immune-related adverse event type, cancer type, and other factors.
TAKEAWAY:
- The occurrence of cutaneous immune-related adverse events was associated with improved PFS (hazard ratio, 0.52; P < .001) and overall survival (HR, 0.61; P < .001).
- In the subgroup analysis, patients with eczematous (HR, 0.69), lichenoid or lichen planus–like skin lesions (HR, 0.51), pruritus without rash (HR, 0.70), psoriasis (HR, 0.63), or vitiligo (HR, 0.30) demonstrated a significant overall survival advantage. Vitiligo was the only adverse event associated with a PFS advantage (HR, 0.28).
- Among patients with melanoma, analyses revealed a significant association between the incidence of cutaneous immune-related adverse events and improved overall survival (HR, 0.51) and PFS (HR, 0.45). The authors highlighted similar findings among patients with non–small cell lung cancer (HR, 0.50 for overall survival and 0.61 for PFS).
IN PRACTICE:
“These data suggest that [cutaneous immune-related adverse events] may have useful prognostic value in ICI treatment,” the authors concluded.
SOURCE:
The analysis, led by Fei Wang, MD, Zhong Da Hospital, School of Medicine, Southeast University, Nanjing, China, was published online in JAMA Dermatology.
LIMITATIONS:
Most of the data came from retrospective studies, and there were limited data on specific patient subgroups. The Egger tests, used to assess potential publication bias in meta-analyses, revealed publication bias.
DISCLOSURES:
No disclosures were reported. The study was supported by a grant from the Postgraduate Research and Practice Innovation Program of Jiangsu Province.
A version of this article first appeared on Medscape.com.
FDA approves bosutinib for children with CML
The agency also approved new 50-mg and 100-mg capsules to help treat children.
For newly diagnosed disease, the dose is 300 mg/m2 once daily with food. For resistant/intolerant disease, the dose is 400 mg/m2 once daily. For children who cannot swallow capsules, the contents can be mixed into applesauce or yogurt, the FDA said in a press release announcing the approval.
The tyrosine kinase inhibitor (TKI) was previously approved for adults. Three other TKIs were previously approved for pediatric CML.
The approval was based on the BCHILD trial, a pediatric dose-finding study involving patients aged 1 year or older. Among the 21 children with newly diagnosed chronic phase, Ph+ CML treated with 300 mg/m2, the rate of major cytogenetic response was 76.2%, the rate of complete cytogenetic response was 71.4%, and the rate of major molecular response rate was 28.6% over a median duration of 14.2 months.
Among the 28 children with relapsed/intolerant disease treated with up to 400 mg/m2, the rate of major cytogenetic response was 82.1%, the rate of complete cytogenetic response was 78.6%, and the rate of major molecular response was 50% over a median duration of 23.2 months. Among the 14 patients who had a major molecular response, two lost it – one after 13.6 months of treatment, and the other after 24.7 months of treatment.
Adverse events that occurred in 20% or more of children included diarrhea, abdominal pain, vomiting, nausea, rash, fatigue, hepatic dysfunction, headache, pyrexia, decreased appetite, and constipation. Overall, 45% or more of patients experienced an increase in creatinine, alanine aminotransferase, or aspartate aminotransferase levels, or a decrease in white blood cell count or platelet count.
The full labeling information is available online.
A version of this article first appeared on Medscape.com.
The agency also approved new 50-mg and 100-mg capsules to help treat children.
For newly diagnosed disease, the dose is 300 mg/m2 once daily with food. For resistant/intolerant disease, the dose is 400 mg/m2 once daily. For children who cannot swallow capsules, the contents can be mixed into applesauce or yogurt, the FDA said in a press release announcing the approval.
The tyrosine kinase inhibitor (TKI) was previously approved for adults. Three other TKIs were previously approved for pediatric CML.
The approval was based on the BCHILD trial, a pediatric dose-finding study involving patients aged 1 year or older. Among the 21 children with newly diagnosed chronic phase, Ph+ CML treated with 300 mg/m2, the rate of major cytogenetic response was 76.2%, the rate of complete cytogenetic response was 71.4%, and the rate of major molecular response rate was 28.6% over a median duration of 14.2 months.
Among the 28 children with relapsed/intolerant disease treated with up to 400 mg/m2, the rate of major cytogenetic response was 82.1%, the rate of complete cytogenetic response was 78.6%, and the rate of major molecular response was 50% over a median duration of 23.2 months. Among the 14 patients who had a major molecular response, two lost it – one after 13.6 months of treatment, and the other after 24.7 months of treatment.
Adverse events that occurred in 20% or more of children included diarrhea, abdominal pain, vomiting, nausea, rash, fatigue, hepatic dysfunction, headache, pyrexia, decreased appetite, and constipation. Overall, 45% or more of patients experienced an increase in creatinine, alanine aminotransferase, or aspartate aminotransferase levels, or a decrease in white blood cell count or platelet count.
The full labeling information is available online.
A version of this article first appeared on Medscape.com.
The agency also approved new 50-mg and 100-mg capsules to help treat children.
For newly diagnosed disease, the dose is 300 mg/m2 once daily with food. For resistant/intolerant disease, the dose is 400 mg/m2 once daily. For children who cannot swallow capsules, the contents can be mixed into applesauce or yogurt, the FDA said in a press release announcing the approval.
The tyrosine kinase inhibitor (TKI) was previously approved for adults. Three other TKIs were previously approved for pediatric CML.
The approval was based on the BCHILD trial, a pediatric dose-finding study involving patients aged 1 year or older. Among the 21 children with newly diagnosed chronic phase, Ph+ CML treated with 300 mg/m2, the rate of major cytogenetic response was 76.2%, the rate of complete cytogenetic response was 71.4%, and the rate of major molecular response rate was 28.6% over a median duration of 14.2 months.
Among the 28 children with relapsed/intolerant disease treated with up to 400 mg/m2, the rate of major cytogenetic response was 82.1%, the rate of complete cytogenetic response was 78.6%, and the rate of major molecular response was 50% over a median duration of 23.2 months. Among the 14 patients who had a major molecular response, two lost it – one after 13.6 months of treatment, and the other after 24.7 months of treatment.
Adverse events that occurred in 20% or more of children included diarrhea, abdominal pain, vomiting, nausea, rash, fatigue, hepatic dysfunction, headache, pyrexia, decreased appetite, and constipation. Overall, 45% or more of patients experienced an increase in creatinine, alanine aminotransferase, or aspartate aminotransferase levels, or a decrease in white blood cell count or platelet count.
The full labeling information is available online.
A version of this article first appeared on Medscape.com.
Dispelling clinicians’ misconceptions about sickle cell disease
Affecting more than 20 million people globally and 100,000 people nationwide, SCD is the most common inherited blood disorder in the United States. It occurs largely but not exclusively among people of African descent.
Patients with SCD develop crescent-shaped or “sickled” red blood cells that, unlike normally round cells, can potentially block blood flow and thus cause a host of problems ranging from a risk of stroke or infections to sometimes severe pain crises, called vaso-occlusive episodes.
To help ward off such complications, some key preventative measures and an array of therapies have become available in recent years: Newborn screening and prophylaxis, including the introduction of pneumococcal vaccines, have substantially reduced rates of invasive pneumococcal infection, which previously accounted for 32% of all causes of death in patients with SCD under the age of 20.
And while hydroxyurea was the only medication from 1998 to 2017 to alleviate acute pain episodes in SCD, newer options have become available in recent years, with l-glutamine, voxelotor, and crizanlizumab gaining FDA approval to further help prevent the episodes.
However, studies show that many if not most patients fail to receive adequate treatment, with one recent report indicating that, between 2016 and 2020, hydroxyurea was prescribed to fewer than 25% of patients with SCD, and fewer than 4% of people with the disease who experience chronic pain episodes had prescriptions for the newer FDA-approved drugs.
Myths and truths
To help clarify some common misconceptions that contribute to the problems, Lewis Hsu, MD, PhD, chief medical officer of the Sickle Cell Disease Association of America, detailed some of the most prevalent and persistent myths among clinicians about SCD:
Pain level
Myths: Firstly, that sickle cell pain is not that bad, and patients therefore don’t really need opioid pain treatment, and secondly, that sickle cell pain is measurable by lab tests, such as the number of sickled red blood cells on a blood smear, reticulocytes, or hemoglobin level.
Truths: “Sickle cell vaso-occlusive pain can be very severe – a 10 on a scale of 10 – but the pain is usually only known by subjective report,” said Dr. Hsu, a pediatric hematologist who serves as director of the Sickle Cell Center and professor of pediatrics for the University of Illinois at Chicago.
“No lab test can be used to measure pain,” he said. “Other lab tests can be abnormal, and some have statistical correlation with lifetime severity of disease course, but the lab tests are not for determination of acute level of pain or absence of pain.”
Blacks only
Myth: SCD only affects Black people.
Truth: People who have sickle cell disease from many ethnic backgrounds and skin colors.
“Around the Mediterranean, there are sickle cell patients from Greece, Turkey, Italy, and Spain. Some are blond and blue-eyed. People in India and Pakistan have sickle cell disease,” Dr. Hsu explained.
In addition, “people from the Arabian Peninsula have sickle cell disease; some Malaysians have sickle cell disease; one child who is about third generation in Hong Kong has sickle cell disease.”
Parental link
Myth: Sickle cell disease only occurs in individuals both of whose parents have the sickle gene.
Truth: “There are types of sickle cell disease [involving] a sickle cell gene from one parent and a gene for hemoglobin C from the other parent,” Dr. Hsu noted. “Others inherited one sickle gene [from one parent] and inherited from the other parent a gene for beta thalassemia. Others involve an inherited sickle gene and hemoglobin E; others have inherited one sickle gene and inherited a gene for hemoglobin D-Punjab, while others have sickle and hemoglobin O-Arab.”
Effects beyond pain
Myth: A person who is not having sickle cell pain is otherwise not significantly affected by their disease.
Truth: “Organs can be damaged silently every day,” Dr. Hsu said. “Kidney failure, retina damage, and pulmonary hypertension are the most notable of organ systems that can suffer damage for a long time without symptoms, then develop symptoms when it is too late to intervene.”
“For this reason, individuals with sickle cell disease should have regular expert care for health maintenance that is disease specific,” Dr. Hsu added.
Consult guidelines
One final concern is a basic failure to utilize critical information sources and guidelines, especially by primary care providers and/or other nonspecialists from whom patients with SCD may often seek treatment. “Awareness of these guidelines is low,” Dr. Hsu said.
Key resources that can be helpful include evidence-based guidelines developed by an expert panel of the National Heart, Lung, and Blood Institute, and the American Society of Hematology has a Pocket Guide app on management of sickle cell disease.
Another key resource being highlighted in September, which is National Sickle Cell Disease Awareness Month, is the NHLBI’s comprehensive website, providing information ranging from fact sheets on the disease and treatments to social media resources and inspiring stories of people with SCD.
“We are trying to bring more sickle cell information and case studies into medical school curricula, nursing curricula, social workers and community health workers awareness, [and] apps and online guidelines are proliferating,” Dr. Hsu says.
He goes on to say, “We need more recognition and resources from insurance providers that quality care for sickle cell disease is measured and rewarded.”
Dr. Hsu coauthored “Hope and Destiny: The Patient and Parent’s Guide to Sickle Cell Disease and Sickle Cell Trait.” He reported relationships with Novartis, Emmaus, Forma Therapeutic, Dupont/Nemours Children’s Hospital, Hilton Publishing, Asklepion, Bayer, CRISPR/Vertex, Cyclerion, Pfizer, and Aruvant.
Affecting more than 20 million people globally and 100,000 people nationwide, SCD is the most common inherited blood disorder in the United States. It occurs largely but not exclusively among people of African descent.
Patients with SCD develop crescent-shaped or “sickled” red blood cells that, unlike normally round cells, can potentially block blood flow and thus cause a host of problems ranging from a risk of stroke or infections to sometimes severe pain crises, called vaso-occlusive episodes.
To help ward off such complications, some key preventative measures and an array of therapies have become available in recent years: Newborn screening and prophylaxis, including the introduction of pneumococcal vaccines, have substantially reduced rates of invasive pneumococcal infection, which previously accounted for 32% of all causes of death in patients with SCD under the age of 20.
And while hydroxyurea was the only medication from 1998 to 2017 to alleviate acute pain episodes in SCD, newer options have become available in recent years, with l-glutamine, voxelotor, and crizanlizumab gaining FDA approval to further help prevent the episodes.
However, studies show that many if not most patients fail to receive adequate treatment, with one recent report indicating that, between 2016 and 2020, hydroxyurea was prescribed to fewer than 25% of patients with SCD, and fewer than 4% of people with the disease who experience chronic pain episodes had prescriptions for the newer FDA-approved drugs.
Myths and truths
To help clarify some common misconceptions that contribute to the problems, Lewis Hsu, MD, PhD, chief medical officer of the Sickle Cell Disease Association of America, detailed some of the most prevalent and persistent myths among clinicians about SCD:
Pain level
Myths: Firstly, that sickle cell pain is not that bad, and patients therefore don’t really need opioid pain treatment, and secondly, that sickle cell pain is measurable by lab tests, such as the number of sickled red blood cells on a blood smear, reticulocytes, or hemoglobin level.
Truths: “Sickle cell vaso-occlusive pain can be very severe – a 10 on a scale of 10 – but the pain is usually only known by subjective report,” said Dr. Hsu, a pediatric hematologist who serves as director of the Sickle Cell Center and professor of pediatrics for the University of Illinois at Chicago.
“No lab test can be used to measure pain,” he said. “Other lab tests can be abnormal, and some have statistical correlation with lifetime severity of disease course, but the lab tests are not for determination of acute level of pain or absence of pain.”
Blacks only
Myth: SCD only affects Black people.
Truth: People who have sickle cell disease from many ethnic backgrounds and skin colors.
“Around the Mediterranean, there are sickle cell patients from Greece, Turkey, Italy, and Spain. Some are blond and blue-eyed. People in India and Pakistan have sickle cell disease,” Dr. Hsu explained.
In addition, “people from the Arabian Peninsula have sickle cell disease; some Malaysians have sickle cell disease; one child who is about third generation in Hong Kong has sickle cell disease.”
Parental link
Myth: Sickle cell disease only occurs in individuals both of whose parents have the sickle gene.
Truth: “There are types of sickle cell disease [involving] a sickle cell gene from one parent and a gene for hemoglobin C from the other parent,” Dr. Hsu noted. “Others inherited one sickle gene [from one parent] and inherited from the other parent a gene for beta thalassemia. Others involve an inherited sickle gene and hemoglobin E; others have inherited one sickle gene and inherited a gene for hemoglobin D-Punjab, while others have sickle and hemoglobin O-Arab.”
Effects beyond pain
Myth: A person who is not having sickle cell pain is otherwise not significantly affected by their disease.
Truth: “Organs can be damaged silently every day,” Dr. Hsu said. “Kidney failure, retina damage, and pulmonary hypertension are the most notable of organ systems that can suffer damage for a long time without symptoms, then develop symptoms when it is too late to intervene.”
“For this reason, individuals with sickle cell disease should have regular expert care for health maintenance that is disease specific,” Dr. Hsu added.
Consult guidelines
One final concern is a basic failure to utilize critical information sources and guidelines, especially by primary care providers and/or other nonspecialists from whom patients with SCD may often seek treatment. “Awareness of these guidelines is low,” Dr. Hsu said.
Key resources that can be helpful include evidence-based guidelines developed by an expert panel of the National Heart, Lung, and Blood Institute, and the American Society of Hematology has a Pocket Guide app on management of sickle cell disease.
Another key resource being highlighted in September, which is National Sickle Cell Disease Awareness Month, is the NHLBI’s comprehensive website, providing information ranging from fact sheets on the disease and treatments to social media resources and inspiring stories of people with SCD.
“We are trying to bring more sickle cell information and case studies into medical school curricula, nursing curricula, social workers and community health workers awareness, [and] apps and online guidelines are proliferating,” Dr. Hsu says.
He goes on to say, “We need more recognition and resources from insurance providers that quality care for sickle cell disease is measured and rewarded.”
Dr. Hsu coauthored “Hope and Destiny: The Patient and Parent’s Guide to Sickle Cell Disease and Sickle Cell Trait.” He reported relationships with Novartis, Emmaus, Forma Therapeutic, Dupont/Nemours Children’s Hospital, Hilton Publishing, Asklepion, Bayer, CRISPR/Vertex, Cyclerion, Pfizer, and Aruvant.
Affecting more than 20 million people globally and 100,000 people nationwide, SCD is the most common inherited blood disorder in the United States. It occurs largely but not exclusively among people of African descent.
Patients with SCD develop crescent-shaped or “sickled” red blood cells that, unlike normally round cells, can potentially block blood flow and thus cause a host of problems ranging from a risk of stroke or infections to sometimes severe pain crises, called vaso-occlusive episodes.
To help ward off such complications, some key preventative measures and an array of therapies have become available in recent years: Newborn screening and prophylaxis, including the introduction of pneumococcal vaccines, have substantially reduced rates of invasive pneumococcal infection, which previously accounted for 32% of all causes of death in patients with SCD under the age of 20.
And while hydroxyurea was the only medication from 1998 to 2017 to alleviate acute pain episodes in SCD, newer options have become available in recent years, with l-glutamine, voxelotor, and crizanlizumab gaining FDA approval to further help prevent the episodes.
However, studies show that many if not most patients fail to receive adequate treatment, with one recent report indicating that, between 2016 and 2020, hydroxyurea was prescribed to fewer than 25% of patients with SCD, and fewer than 4% of people with the disease who experience chronic pain episodes had prescriptions for the newer FDA-approved drugs.
Myths and truths
To help clarify some common misconceptions that contribute to the problems, Lewis Hsu, MD, PhD, chief medical officer of the Sickle Cell Disease Association of America, detailed some of the most prevalent and persistent myths among clinicians about SCD:
Pain level
Myths: Firstly, that sickle cell pain is not that bad, and patients therefore don’t really need opioid pain treatment, and secondly, that sickle cell pain is measurable by lab tests, such as the number of sickled red blood cells on a blood smear, reticulocytes, or hemoglobin level.
Truths: “Sickle cell vaso-occlusive pain can be very severe – a 10 on a scale of 10 – but the pain is usually only known by subjective report,” said Dr. Hsu, a pediatric hematologist who serves as director of the Sickle Cell Center and professor of pediatrics for the University of Illinois at Chicago.
“No lab test can be used to measure pain,” he said. “Other lab tests can be abnormal, and some have statistical correlation with lifetime severity of disease course, but the lab tests are not for determination of acute level of pain or absence of pain.”
Blacks only
Myth: SCD only affects Black people.
Truth: People who have sickle cell disease from many ethnic backgrounds and skin colors.
“Around the Mediterranean, there are sickle cell patients from Greece, Turkey, Italy, and Spain. Some are blond and blue-eyed. People in India and Pakistan have sickle cell disease,” Dr. Hsu explained.
In addition, “people from the Arabian Peninsula have sickle cell disease; some Malaysians have sickle cell disease; one child who is about third generation in Hong Kong has sickle cell disease.”
Parental link
Myth: Sickle cell disease only occurs in individuals both of whose parents have the sickle gene.
Truth: “There are types of sickle cell disease [involving] a sickle cell gene from one parent and a gene for hemoglobin C from the other parent,” Dr. Hsu noted. “Others inherited one sickle gene [from one parent] and inherited from the other parent a gene for beta thalassemia. Others involve an inherited sickle gene and hemoglobin E; others have inherited one sickle gene and inherited a gene for hemoglobin D-Punjab, while others have sickle and hemoglobin O-Arab.”
Effects beyond pain
Myth: A person who is not having sickle cell pain is otherwise not significantly affected by their disease.
Truth: “Organs can be damaged silently every day,” Dr. Hsu said. “Kidney failure, retina damage, and pulmonary hypertension are the most notable of organ systems that can suffer damage for a long time without symptoms, then develop symptoms when it is too late to intervene.”
“For this reason, individuals with sickle cell disease should have regular expert care for health maintenance that is disease specific,” Dr. Hsu added.
Consult guidelines
One final concern is a basic failure to utilize critical information sources and guidelines, especially by primary care providers and/or other nonspecialists from whom patients with SCD may often seek treatment. “Awareness of these guidelines is low,” Dr. Hsu said.
Key resources that can be helpful include evidence-based guidelines developed by an expert panel of the National Heart, Lung, and Blood Institute, and the American Society of Hematology has a Pocket Guide app on management of sickle cell disease.
Another key resource being highlighted in September, which is National Sickle Cell Disease Awareness Month, is the NHLBI’s comprehensive website, providing information ranging from fact sheets on the disease and treatments to social media resources and inspiring stories of people with SCD.
“We are trying to bring more sickle cell information and case studies into medical school curricula, nursing curricula, social workers and community health workers awareness, [and] apps and online guidelines are proliferating,” Dr. Hsu says.
He goes on to say, “We need more recognition and resources from insurance providers that quality care for sickle cell disease is measured and rewarded.”
Dr. Hsu coauthored “Hope and Destiny: The Patient and Parent’s Guide to Sickle Cell Disease and Sickle Cell Trait.” He reported relationships with Novartis, Emmaus, Forma Therapeutic, Dupont/Nemours Children’s Hospital, Hilton Publishing, Asklepion, Bayer, CRISPR/Vertex, Cyclerion, Pfizer, and Aruvant.
Pediatrician with SCD gives her young patients hope
These days, thanks to transformative advances in treating SCD that have substantially improved survival, Dr. Fasipe’s mission for a new generation of patients and their families is to replace their pain and fear with relief and hope.
“If you grow up thinking that you’re going to die when you’re 18, it changes your world and your viewpoints, and it impacts your mental health,” she told this news organization.
“We are trying to make sure our children and their families know that there is a new story for sickle cell disease, and you don’t have to use any age as your prediction marker for your lifespan,” Dr. Fasipe said.
SCD, which affects about 100,000 people nationwide, is an inherited blood disorder, with the majority of patients – but not all – being of African descent. This condition is characterized by pain crises, or vaso-occlusive episodes, triggered when cells that are sickled get stuck and impede blood flow. These crises can come on suddenly and range from mild to severe.
Dr. Fasipe was born in Nigeria, where rates of SCD are among the world’s highest. She attended elementary school in the United States, where her father was studying theology, before returning to Nigeria with her family at age 11.
Back in those days, in both nations only about 50% of children with SCD lived beyond their 18th birthday. The survival rates in Nigeria and sub-Saharan Africa countries continue to be poor. In some more developed regions elsewhere, advances such as universal newborn screening, penicillin prophylaxis, pneumococcal vaccination, stroke screening, and hydroxyurea therapy have yielded substantial improvements, with 95% or more patients with SCD reaching their 18th birthday.
“With measures such as newborn screening, we can immediately start prevention measures in sickle cell disease, such as prevention of infection, which was the number one reason why children were dying,” Dr. Fasipe explained. “With global initiatives, we want that story to be the same in sub-Saharan Africa as well.”
Cousin’s early death inspires medical studies
In an essay published by Texas Medical Center that describes her childhood experiences, Dr. Fasipe recounts a pivotal event in her life: The heartbreaking death of her beloved cousin at the age of just 17, from a complication of SCD. This bereavement fueled Dr. Fasipe’s determination to pursue a medical career, to do all that she could to prevent such losses.
“Having sickle cell disease myself wasn’t the trigger that made me become a doctor. But when Femi [her cousin] died, I thought: ‘This shouldn’t happen,’ ” Dr. Fasipe wrote.
When she applied to medical school back in the United States, she declared in her application essay: “I want to cure sickle cell.”
By the time Dr. Fasipe was ready to undertake residency and fellowship applications, her essay had shifted to focus on pediatrics “specifically because I want to reach sickle cell patients before they’ve defined how their lives are going to be,” she said. “I want to give them hope.”
Hope for a cure
Fast-forwarding to this point in Dr. Fasipe’s career, she noted that her dream of a cure for SCD is no longer a distant aspiration, thanks to the advent of stem cell transplantation and more recently, gene therapy. These advancements have elevated her hope for a cure to an entirely new level.
Each new treatment comes with caveats. Stem cell transplantation requires a matching donor, leaving the majority of patients ineligible. And while gene therapy eliminates the need for a donor, treatment can reportedly cost nearly $3 million. Nevertheless, Dr. Fasipe emphasized the promise that these new advancements represent.
“The scientists that work in these spaces do appreciate these [accessibility barriers], and the expectation is these therapies will be more accessible with time and effort,” she said. “We’ve got to start somewhere, and it’s exciting that they’re making these early successes.”
Advice for clinicians
With firsthand knowledge of how it feels to be the patient, as well as on the clinician side of SCD treatment, Dr. Fasipe advises colleagues on some ways that they can improve care while boosting their patients’ hope:
Speak with empathy
Acknowledge the ‘elephant in the room’; the pain that patients with SCD can experience is real.
“When I’m managing any patient with pain, I first acknowledge the suffering because while we may not understand what that person is going through, acknowledgment is part of showing empathy,” she explains.
Seek out resources
Patients with SCD may typically seek treatment in primary care, where expertise in the disease may be lacking, and general practitioners may feel frustrated that there are limited treatment options.
“If you do find yourself treating a sickle cell disease patient, you may not have all of the answers, but there are good resources, whether it’s a nearby sickle cell disease centers or national guidelines,” Dr. Fasipe said.
Access to treatment
With research, including a recent study, showing that only about 25% of patients with SCD are prescribed hydroxyurea and even fewer – only about 5% – receive more recently approved SCD treatments, clinicians should be proactive by making sure that patients receive needed treatments.
“Clearly medicines like hydroxyurea are not as optimized in this community space as they should be, and then there are newer therapies that families, patients, and even providers may not be aware of, so it is important to be informed of the guidelines and provide all patients with comprehensive, high-quality care,” Dr. Fasipe said.
In the ED, patients with SCD are ‘care-seeking,’ not drug-seeking
Due to the sometimes rapid onset of severe pain symptoms, patients with SCD commonly wind up in the emergency department. In this time of an opioid epidemic, patients too often are suspected of merely seeking drugs.
“Sickle cell disease tends to get lumped into a category of a disease of pain, but pain is subjective and it is difficult to quantify, so unfortunately, patients can be labeled as potentially drug-seeking,” Dr. Fasipe explained, citing an article that detailed this problem.
Consequently, patients may have particularly negative experiences in the emergency department, but the use of resources such as a sickle cell disease point-of-care tool developed by the American College of Emergency Physicians and the American Society of Hematology can help improve care for those patients.
“One of the [point-of-care recommendations] before even managing the pain is that physicians show compassion by acknowledging the patient’s pain and that they understand why pain with sickle cell disease might look different than other types of pain,” Dr. Fasipe said.
Building trust
Encounters such as negative emergency department experiences can perpetuate a deeper issue of distrust between those with SCD and the medical community, which originated in long-held, well-documented racial disparities in health care.
“We know historically and even today that there are difficulties facing our families who are impacted by sickle cell disease, and they are related to structural racism and socioeconomic barriers,” Dr. Fasipe explained.
With these issues in mind, she said, “I refer to sickle cell disease as the medical representation of the Black experience in America.” However, she added, the good news is “we are now doing our best now to improve that.”
Among key efforts in building trust is the inclusion of patients with SCD and their families in as many aspects of research and clinical care as possible.
“In the global health care community, it is imperative to invite people with sickle cell disease and from the community to the decision-making table,” she noted.
“Now, when we’re talking about research for therapies, their expectation is that research trials and other initiatives for sickle cell disease must have input from the community; there are no initiatives for sickle cell disease that do not have input from the community.
“The patients and community members may not be experts on the science of sickle cell, but they’re experts on the lived experience and that’s very important when you’re thinking about new bringing in a new therapy.”
Forward momentum
Meanwhile, Dr. Fasipe observed, with the collective, advocacy-driven, forward momentum of the SCD community as a whole, things should only continue to improve.
“Because of the various barriers, some progress may not be immediately around the corner, but I do have confidence that this current generation of children with sickle cell will have improved health equity by the time they reach adulthood,” she said.
“I believe in this future, so I’m doing the work now, and it’s a promise I tell parents: I want your future adult child to live their best life, and we’re working hard to ensure that that becomes their future reality.”
Sickle cell disease awareness
September is National Sickle Cell Disease Awareness Month, and the National Heart, Lung, and Blood Institute offers a comprehensive website that clinicians can pass along to their patients, with information ranging from fact sheets on the disease and treatments to social media resources and inspiring stories of people with the disease.
In a comment, Lewis Hsu, MD, PhD, chief medical officer of the Sickle Cell Disease Association of America, underscored the uniquely important contributions of people like Dr. Fasipe, in providing inspiration to patients and clinicians alike.
“I have worked with several physicians, nurses, psychologists, and public health specialists who have sickle cell disease,” said Dr. Hsu, who is a pediatric hematologist who also serves as director of the Sickle Cell Center and professor of pediatrics for the University of Illinois at Chicago.
“They are ambassadors who have the trust of both patients and healthcare providers,” Dr. Hsu said.
In addition to providing inspiration of resilience, such care providers can serve as “communication bridges,” he explained.
“When they are conference speakers, everybody wants to hear them; when they sit on advisory committees or focus groups, they can help find the compromise or set the priorities.”
“Their impact on the whole sickle cell community is very large,” Dr. Hsu said.
These days, thanks to transformative advances in treating SCD that have substantially improved survival, Dr. Fasipe’s mission for a new generation of patients and their families is to replace their pain and fear with relief and hope.
“If you grow up thinking that you’re going to die when you’re 18, it changes your world and your viewpoints, and it impacts your mental health,” she told this news organization.
“We are trying to make sure our children and their families know that there is a new story for sickle cell disease, and you don’t have to use any age as your prediction marker for your lifespan,” Dr. Fasipe said.
SCD, which affects about 100,000 people nationwide, is an inherited blood disorder, with the majority of patients – but not all – being of African descent. This condition is characterized by pain crises, or vaso-occlusive episodes, triggered when cells that are sickled get stuck and impede blood flow. These crises can come on suddenly and range from mild to severe.
Dr. Fasipe was born in Nigeria, where rates of SCD are among the world’s highest. She attended elementary school in the United States, where her father was studying theology, before returning to Nigeria with her family at age 11.
Back in those days, in both nations only about 50% of children with SCD lived beyond their 18th birthday. The survival rates in Nigeria and sub-Saharan Africa countries continue to be poor. In some more developed regions elsewhere, advances such as universal newborn screening, penicillin prophylaxis, pneumococcal vaccination, stroke screening, and hydroxyurea therapy have yielded substantial improvements, with 95% or more patients with SCD reaching their 18th birthday.
“With measures such as newborn screening, we can immediately start prevention measures in sickle cell disease, such as prevention of infection, which was the number one reason why children were dying,” Dr. Fasipe explained. “With global initiatives, we want that story to be the same in sub-Saharan Africa as well.”
Cousin’s early death inspires medical studies
In an essay published by Texas Medical Center that describes her childhood experiences, Dr. Fasipe recounts a pivotal event in her life: The heartbreaking death of her beloved cousin at the age of just 17, from a complication of SCD. This bereavement fueled Dr. Fasipe’s determination to pursue a medical career, to do all that she could to prevent such losses.
“Having sickle cell disease myself wasn’t the trigger that made me become a doctor. But when Femi [her cousin] died, I thought: ‘This shouldn’t happen,’ ” Dr. Fasipe wrote.
When she applied to medical school back in the United States, she declared in her application essay: “I want to cure sickle cell.”
By the time Dr. Fasipe was ready to undertake residency and fellowship applications, her essay had shifted to focus on pediatrics “specifically because I want to reach sickle cell patients before they’ve defined how their lives are going to be,” she said. “I want to give them hope.”
Hope for a cure
Fast-forwarding to this point in Dr. Fasipe’s career, she noted that her dream of a cure for SCD is no longer a distant aspiration, thanks to the advent of stem cell transplantation and more recently, gene therapy. These advancements have elevated her hope for a cure to an entirely new level.
Each new treatment comes with caveats. Stem cell transplantation requires a matching donor, leaving the majority of patients ineligible. And while gene therapy eliminates the need for a donor, treatment can reportedly cost nearly $3 million. Nevertheless, Dr. Fasipe emphasized the promise that these new advancements represent.
“The scientists that work in these spaces do appreciate these [accessibility barriers], and the expectation is these therapies will be more accessible with time and effort,” she said. “We’ve got to start somewhere, and it’s exciting that they’re making these early successes.”
Advice for clinicians
With firsthand knowledge of how it feels to be the patient, as well as on the clinician side of SCD treatment, Dr. Fasipe advises colleagues on some ways that they can improve care while boosting their patients’ hope:
Speak with empathy
Acknowledge the ‘elephant in the room’; the pain that patients with SCD can experience is real.
“When I’m managing any patient with pain, I first acknowledge the suffering because while we may not understand what that person is going through, acknowledgment is part of showing empathy,” she explains.
Seek out resources
Patients with SCD may typically seek treatment in primary care, where expertise in the disease may be lacking, and general practitioners may feel frustrated that there are limited treatment options.
“If you do find yourself treating a sickle cell disease patient, you may not have all of the answers, but there are good resources, whether it’s a nearby sickle cell disease centers or national guidelines,” Dr. Fasipe said.
Access to treatment
With research, including a recent study, showing that only about 25% of patients with SCD are prescribed hydroxyurea and even fewer – only about 5% – receive more recently approved SCD treatments, clinicians should be proactive by making sure that patients receive needed treatments.
“Clearly medicines like hydroxyurea are not as optimized in this community space as they should be, and then there are newer therapies that families, patients, and even providers may not be aware of, so it is important to be informed of the guidelines and provide all patients with comprehensive, high-quality care,” Dr. Fasipe said.
In the ED, patients with SCD are ‘care-seeking,’ not drug-seeking
Due to the sometimes rapid onset of severe pain symptoms, patients with SCD commonly wind up in the emergency department. In this time of an opioid epidemic, patients too often are suspected of merely seeking drugs.
“Sickle cell disease tends to get lumped into a category of a disease of pain, but pain is subjective and it is difficult to quantify, so unfortunately, patients can be labeled as potentially drug-seeking,” Dr. Fasipe explained, citing an article that detailed this problem.
Consequently, patients may have particularly negative experiences in the emergency department, but the use of resources such as a sickle cell disease point-of-care tool developed by the American College of Emergency Physicians and the American Society of Hematology can help improve care for those patients.
“One of the [point-of-care recommendations] before even managing the pain is that physicians show compassion by acknowledging the patient’s pain and that they understand why pain with sickle cell disease might look different than other types of pain,” Dr. Fasipe said.
Building trust
Encounters such as negative emergency department experiences can perpetuate a deeper issue of distrust between those with SCD and the medical community, which originated in long-held, well-documented racial disparities in health care.
“We know historically and even today that there are difficulties facing our families who are impacted by sickle cell disease, and they are related to structural racism and socioeconomic barriers,” Dr. Fasipe explained.
With these issues in mind, she said, “I refer to sickle cell disease as the medical representation of the Black experience in America.” However, she added, the good news is “we are now doing our best now to improve that.”
Among key efforts in building trust is the inclusion of patients with SCD and their families in as many aspects of research and clinical care as possible.
“In the global health care community, it is imperative to invite people with sickle cell disease and from the community to the decision-making table,” she noted.
“Now, when we’re talking about research for therapies, their expectation is that research trials and other initiatives for sickle cell disease must have input from the community; there are no initiatives for sickle cell disease that do not have input from the community.
“The patients and community members may not be experts on the science of sickle cell, but they’re experts on the lived experience and that’s very important when you’re thinking about new bringing in a new therapy.”
Forward momentum
Meanwhile, Dr. Fasipe observed, with the collective, advocacy-driven, forward momentum of the SCD community as a whole, things should only continue to improve.
“Because of the various barriers, some progress may not be immediately around the corner, but I do have confidence that this current generation of children with sickle cell will have improved health equity by the time they reach adulthood,” she said.
“I believe in this future, so I’m doing the work now, and it’s a promise I tell parents: I want your future adult child to live their best life, and we’re working hard to ensure that that becomes their future reality.”
Sickle cell disease awareness
September is National Sickle Cell Disease Awareness Month, and the National Heart, Lung, and Blood Institute offers a comprehensive website that clinicians can pass along to their patients, with information ranging from fact sheets on the disease and treatments to social media resources and inspiring stories of people with the disease.
In a comment, Lewis Hsu, MD, PhD, chief medical officer of the Sickle Cell Disease Association of America, underscored the uniquely important contributions of people like Dr. Fasipe, in providing inspiration to patients and clinicians alike.
“I have worked with several physicians, nurses, psychologists, and public health specialists who have sickle cell disease,” said Dr. Hsu, who is a pediatric hematologist who also serves as director of the Sickle Cell Center and professor of pediatrics for the University of Illinois at Chicago.
“They are ambassadors who have the trust of both patients and healthcare providers,” Dr. Hsu said.
In addition to providing inspiration of resilience, such care providers can serve as “communication bridges,” he explained.
“When they are conference speakers, everybody wants to hear them; when they sit on advisory committees or focus groups, they can help find the compromise or set the priorities.”
“Their impact on the whole sickle cell community is very large,” Dr. Hsu said.
These days, thanks to transformative advances in treating SCD that have substantially improved survival, Dr. Fasipe’s mission for a new generation of patients and their families is to replace their pain and fear with relief and hope.
“If you grow up thinking that you’re going to die when you’re 18, it changes your world and your viewpoints, and it impacts your mental health,” she told this news organization.
“We are trying to make sure our children and their families know that there is a new story for sickle cell disease, and you don’t have to use any age as your prediction marker for your lifespan,” Dr. Fasipe said.
SCD, which affects about 100,000 people nationwide, is an inherited blood disorder, with the majority of patients – but not all – being of African descent. This condition is characterized by pain crises, or vaso-occlusive episodes, triggered when cells that are sickled get stuck and impede blood flow. These crises can come on suddenly and range from mild to severe.
Dr. Fasipe was born in Nigeria, where rates of SCD are among the world’s highest. She attended elementary school in the United States, where her father was studying theology, before returning to Nigeria with her family at age 11.
Back in those days, in both nations only about 50% of children with SCD lived beyond their 18th birthday. The survival rates in Nigeria and sub-Saharan Africa countries continue to be poor. In some more developed regions elsewhere, advances such as universal newborn screening, penicillin prophylaxis, pneumococcal vaccination, stroke screening, and hydroxyurea therapy have yielded substantial improvements, with 95% or more patients with SCD reaching their 18th birthday.
“With measures such as newborn screening, we can immediately start prevention measures in sickle cell disease, such as prevention of infection, which was the number one reason why children were dying,” Dr. Fasipe explained. “With global initiatives, we want that story to be the same in sub-Saharan Africa as well.”
Cousin’s early death inspires medical studies
In an essay published by Texas Medical Center that describes her childhood experiences, Dr. Fasipe recounts a pivotal event in her life: The heartbreaking death of her beloved cousin at the age of just 17, from a complication of SCD. This bereavement fueled Dr. Fasipe’s determination to pursue a medical career, to do all that she could to prevent such losses.
“Having sickle cell disease myself wasn’t the trigger that made me become a doctor. But when Femi [her cousin] died, I thought: ‘This shouldn’t happen,’ ” Dr. Fasipe wrote.
When she applied to medical school back in the United States, she declared in her application essay: “I want to cure sickle cell.”
By the time Dr. Fasipe was ready to undertake residency and fellowship applications, her essay had shifted to focus on pediatrics “specifically because I want to reach sickle cell patients before they’ve defined how their lives are going to be,” she said. “I want to give them hope.”
Hope for a cure
Fast-forwarding to this point in Dr. Fasipe’s career, she noted that her dream of a cure for SCD is no longer a distant aspiration, thanks to the advent of stem cell transplantation and more recently, gene therapy. These advancements have elevated her hope for a cure to an entirely new level.
Each new treatment comes with caveats. Stem cell transplantation requires a matching donor, leaving the majority of patients ineligible. And while gene therapy eliminates the need for a donor, treatment can reportedly cost nearly $3 million. Nevertheless, Dr. Fasipe emphasized the promise that these new advancements represent.
“The scientists that work in these spaces do appreciate these [accessibility barriers], and the expectation is these therapies will be more accessible with time and effort,” she said. “We’ve got to start somewhere, and it’s exciting that they’re making these early successes.”
Advice for clinicians
With firsthand knowledge of how it feels to be the patient, as well as on the clinician side of SCD treatment, Dr. Fasipe advises colleagues on some ways that they can improve care while boosting their patients’ hope:
Speak with empathy
Acknowledge the ‘elephant in the room’; the pain that patients with SCD can experience is real.
“When I’m managing any patient with pain, I first acknowledge the suffering because while we may not understand what that person is going through, acknowledgment is part of showing empathy,” she explains.
Seek out resources
Patients with SCD may typically seek treatment in primary care, where expertise in the disease may be lacking, and general practitioners may feel frustrated that there are limited treatment options.
“If you do find yourself treating a sickle cell disease patient, you may not have all of the answers, but there are good resources, whether it’s a nearby sickle cell disease centers or national guidelines,” Dr. Fasipe said.
Access to treatment
With research, including a recent study, showing that only about 25% of patients with SCD are prescribed hydroxyurea and even fewer – only about 5% – receive more recently approved SCD treatments, clinicians should be proactive by making sure that patients receive needed treatments.
“Clearly medicines like hydroxyurea are not as optimized in this community space as they should be, and then there are newer therapies that families, patients, and even providers may not be aware of, so it is important to be informed of the guidelines and provide all patients with comprehensive, high-quality care,” Dr. Fasipe said.
In the ED, patients with SCD are ‘care-seeking,’ not drug-seeking
Due to the sometimes rapid onset of severe pain symptoms, patients with SCD commonly wind up in the emergency department. In this time of an opioid epidemic, patients too often are suspected of merely seeking drugs.
“Sickle cell disease tends to get lumped into a category of a disease of pain, but pain is subjective and it is difficult to quantify, so unfortunately, patients can be labeled as potentially drug-seeking,” Dr. Fasipe explained, citing an article that detailed this problem.
Consequently, patients may have particularly negative experiences in the emergency department, but the use of resources such as a sickle cell disease point-of-care tool developed by the American College of Emergency Physicians and the American Society of Hematology can help improve care for those patients.
“One of the [point-of-care recommendations] before even managing the pain is that physicians show compassion by acknowledging the patient’s pain and that they understand why pain with sickle cell disease might look different than other types of pain,” Dr. Fasipe said.
Building trust
Encounters such as negative emergency department experiences can perpetuate a deeper issue of distrust between those with SCD and the medical community, which originated in long-held, well-documented racial disparities in health care.
“We know historically and even today that there are difficulties facing our families who are impacted by sickle cell disease, and they are related to structural racism and socioeconomic barriers,” Dr. Fasipe explained.
With these issues in mind, she said, “I refer to sickle cell disease as the medical representation of the Black experience in America.” However, she added, the good news is “we are now doing our best now to improve that.”
Among key efforts in building trust is the inclusion of patients with SCD and their families in as many aspects of research and clinical care as possible.
“In the global health care community, it is imperative to invite people with sickle cell disease and from the community to the decision-making table,” she noted.
“Now, when we’re talking about research for therapies, their expectation is that research trials and other initiatives for sickle cell disease must have input from the community; there are no initiatives for sickle cell disease that do not have input from the community.
“The patients and community members may not be experts on the science of sickle cell, but they’re experts on the lived experience and that’s very important when you’re thinking about new bringing in a new therapy.”
Forward momentum
Meanwhile, Dr. Fasipe observed, with the collective, advocacy-driven, forward momentum of the SCD community as a whole, things should only continue to improve.
“Because of the various barriers, some progress may not be immediately around the corner, but I do have confidence that this current generation of children with sickle cell will have improved health equity by the time they reach adulthood,” she said.
“I believe in this future, so I’m doing the work now, and it’s a promise I tell parents: I want your future adult child to live their best life, and we’re working hard to ensure that that becomes their future reality.”
Sickle cell disease awareness
September is National Sickle Cell Disease Awareness Month, and the National Heart, Lung, and Blood Institute offers a comprehensive website that clinicians can pass along to their patients, with information ranging from fact sheets on the disease and treatments to social media resources and inspiring stories of people with the disease.
In a comment, Lewis Hsu, MD, PhD, chief medical officer of the Sickle Cell Disease Association of America, underscored the uniquely important contributions of people like Dr. Fasipe, in providing inspiration to patients and clinicians alike.
“I have worked with several physicians, nurses, psychologists, and public health specialists who have sickle cell disease,” said Dr. Hsu, who is a pediatric hematologist who also serves as director of the Sickle Cell Center and professor of pediatrics for the University of Illinois at Chicago.
“They are ambassadors who have the trust of both patients and healthcare providers,” Dr. Hsu said.
In addition to providing inspiration of resilience, such care providers can serve as “communication bridges,” he explained.
“When they are conference speakers, everybody wants to hear them; when they sit on advisory committees or focus groups, they can help find the compromise or set the priorities.”
“Their impact on the whole sickle cell community is very large,” Dr. Hsu said.
How targeted drugs can vanquish a virulent leukemia
“We went almost 3 decades with nothing, then all of a sudden we’ve had nine approvals in 5 or 6 years,” said Harvard Medical School, Boston, leukemia specialist Amir Fathi, MD, in an interview. “We’ve had a lot of advancement and a number of good options emerge.”
However, Dr. Fathi and other hematologists cautioned that the treatment landscape is becoming more complex to navigate. And they noted that prognoses for many older patients with AML remain grim. The expensive new treatments may only extend their lifespans by a matter of months, although some are surviving for years.
As the specialists explained, there are a variety of reasons why AML is especially difficult to treat.
“AML is one of the fastest growing human cancers, with tumor cell doubling times measured in mere hours in some patients. Therefore patients can present critically ill with white blood cell counts in the [hundreds of thousands of white blood cells per microliter instead of the normal range of 4,000-11,000]," said leukemia specialist Eunice S. Wang, MD, of Roswell Park Comprehensive Cancer Center in Buffalo, N.Y. “Because blood cells are found in every organ of the body, the sheer volume of rapidly growing cancer cells can overwhelm multiple organ systems in a very short amount of time. These rapid growing cells and the fact that the median age of diagnosis with AML is 67-70 years old makes this a clinically challenging cancer to treat. Chemotherapy strong enough to kill cancer cells run the risk of also harming the patient as well.”
Also, older patients often have comorbidities, and they face risks of infection from both the disease and its treatments, said AML specialist Nicole R. Grieselhuber, MD, PhD, of the Ohio State University, Columbus, in an interview.
Enter targeted therapy, which “has allowed individuals who previously were not candidates for cytotoxic chemotherapy because of their age or possible toxicities to receive effective therapy for AML,” Dr. Wang said. “Therapy directed at specific biological features of AML cells such as mutations (FLT3, IDH1, IDH2) or surface proteins (CD33) can augment the efficacy of conventional chemotherapy or in some cases (i.e., FLT3 inhibitors) be more effective than chemotherapy in controlling AML.”
Targeted therapy drugs “are expected to more selectively kill cancer cells and spare normal counterparts,” she added.
The FDA has approved nine targeted therapy drugs for AML in the last few years.
Retinoic acid and arsenic trioxide therapy for acute promyelocytic leukemia “has transformed this AML subtype into one of the most curable AML diseases,” Dr. Wang said. A 2017 long-term analysis of the drug combination found that complete remission was reached in 96% of 54 high-risk patients and 133 low-risk patients; the 5-year survival rate was 88%. (Some patients also received gemtuzumab ozogamicin, a CD33 antibody-drug conjugate.)
According to Dr. Wang, three FLT3 inhibitors have been approved for AML with the FLT3 mutation: midostaurin and quizartinib in the frontline setting in conjunction with intensive chemotherapy and gilteritinib for relapsed/refractory FLT3-mutant AML.
A 2017 study linked midostaurin plus chemotherapy to longer survival (hazard ratio for death = 0.78; P = .009), versus placebo plus chemotherapy, in patients aged 18-59. This year, a phase 3 randomized trial of quizartinib versus placebo linked the drug to longer survival median overall (31.9 months versus 15.1 months; P = .032) In a 2019 trial, patients who took gilteritinib had longer median overall survival (9.3 months versus 5.6 months; HR for death = 0.64; P < .001).
The success of these treatments “has led FLT3 mutant AML to be reclassified from a poor risk AML subtype to intermediate risk AML,” Dr. Wang said.
A 2022 report about FLT3 inhibitors cautioned, however, that “several drug resistance mechanisms have been identified” and added that “the benefit of FLT3 inhibitor maintenance therapy, either post chemotherapy or post transplant, remains controversial, although several studies are ongoing.”
Gemtuzumab ozogamicin is a monoclonal antibody connected to a chemotherapy drug, according to the American Cancer Society. “The addition of gemtuzumab ozogamicin to intensive chemotherapy has enhanced outcomes of favorable and intermediate risk disease,” Dr. Wang said.
Ivosidenib, olutasidenib, and enasidenib target the IDH1 or IDH2 genes in ADL. “These drugs seem to work by helping the leukemia cells mature (differentiate) into more normal cells,” according to the American Cancer Society. “Because of this, they are sometimes referred to as differentiation agents.”
In older adults, a combination treatment with venetoclax, a BCL-2 inhibitor, and a hypomethylating agent has become standard, Ohio State’s Dr. Grieselhuber said. The treatment is FDA approved.
There are caveats to targeted therapy in AML. The treatments can be enormously expensive, “and even patients with insurance are often shocked by the copay,” Dr. Grieselhuber said. It helps to work with pharmacists, social workers, or nurse navigators to help patients afford the treatments, she said.
Side effects vary by therapy and can include QT elongation and differentiation syndrome.
Most challenging of all, many AML patients still face shortened lifespans even if new treatments are available for them.
“Typically for older patients with AML, the lifespan of patients with therapy was 5-7 months and without therapy was 2-3 months,” Dr. Wang said. “Now, with regimens specifically designed for elderly and/or unfit subjects, many individuals are now routinely living more than a year: 14-18 months to 3-4 years.”
But “the vast majority of AML patients will still die of their disease with overall 5-year outcomes still less than 30% in all age categories,” she said. In addition, “fewer than 50% of AML patients are eligible for treatment with FDA-approved targeted therapies, as their disease biology does not express the mutation or protein needed for efficacy.”
Still, she said, “this represents a vast improvement.” And, she added, “in younger individuals, the combination of chemotherapy followed by allogeneic transplant has now permitted more of these individuals to be cured of their disease.” Dr. Grieselhuber noted that transplants are now considered appropriate even for patients in their 60s or early 70s, and they can be combined with targeted therapy.
Dr. Grieselhuber urged colleagues to keep in mind that quality-of-life preferences will play a role in some patient choices. For example, a elderly patient may reject burdensome infusion therapy and choose a pill instead, even if it has less efficacy. “There’s really no one-size-fits-all,” she said.
And, she added, it can be difficult to make choices about treatment because of the lack of randomized, head-to-head data regarding new therapies.
What’s on the horizon? Dr. Wang highlighted a novel class of targeted therapies called menin inhibitors for patients with NPM1-mutated AML, which she said accounts for one-third of patients with the disease. A treatment targeting disease in the 5%-10% patients with the KMT2A gene is also in the works, she said.
For now, Dr. Wang said it’s essential for clinicians “to perform timely comprehensive molecular and genomic tests on all AML patients at diagnosis and relapse to determine which individuals would benefit from targeted therapy versus cytotoxic chemotherapy. And participation in clinical trials at every stage of AML therapy can help accelerate clinical development of new agents for this disease.”
Dr. Fathi discloses relationships with Daiichi Sankyo, Pfizer, Rigel, Autolus, Amgen, Servier, Takeda, Orum, Menarini, Remix, AbbVie, Astellas, BMS, Ibsen, Gilead, Genentech, and AstraZeneca. Dr. Wang discloses ties with AbbVie, Astellas, BMS, CTI Biopharma, Daiichi Sankyo, Gilead, GSK, Johnson & Johnson, Kite, Kura, Novartis, Pfizer, Rigel, Sellas, and Sumitomo Pharma. Dr. Grieselhuber has no disclosures.
“We went almost 3 decades with nothing, then all of a sudden we’ve had nine approvals in 5 or 6 years,” said Harvard Medical School, Boston, leukemia specialist Amir Fathi, MD, in an interview. “We’ve had a lot of advancement and a number of good options emerge.”
However, Dr. Fathi and other hematologists cautioned that the treatment landscape is becoming more complex to navigate. And they noted that prognoses for many older patients with AML remain grim. The expensive new treatments may only extend their lifespans by a matter of months, although some are surviving for years.
As the specialists explained, there are a variety of reasons why AML is especially difficult to treat.
“AML is one of the fastest growing human cancers, with tumor cell doubling times measured in mere hours in some patients. Therefore patients can present critically ill with white blood cell counts in the [hundreds of thousands of white blood cells per microliter instead of the normal range of 4,000-11,000]," said leukemia specialist Eunice S. Wang, MD, of Roswell Park Comprehensive Cancer Center in Buffalo, N.Y. “Because blood cells are found in every organ of the body, the sheer volume of rapidly growing cancer cells can overwhelm multiple organ systems in a very short amount of time. These rapid growing cells and the fact that the median age of diagnosis with AML is 67-70 years old makes this a clinically challenging cancer to treat. Chemotherapy strong enough to kill cancer cells run the risk of also harming the patient as well.”
Also, older patients often have comorbidities, and they face risks of infection from both the disease and its treatments, said AML specialist Nicole R. Grieselhuber, MD, PhD, of the Ohio State University, Columbus, in an interview.
Enter targeted therapy, which “has allowed individuals who previously were not candidates for cytotoxic chemotherapy because of their age or possible toxicities to receive effective therapy for AML,” Dr. Wang said. “Therapy directed at specific biological features of AML cells such as mutations (FLT3, IDH1, IDH2) or surface proteins (CD33) can augment the efficacy of conventional chemotherapy or in some cases (i.e., FLT3 inhibitors) be more effective than chemotherapy in controlling AML.”
Targeted therapy drugs “are expected to more selectively kill cancer cells and spare normal counterparts,” she added.
The FDA has approved nine targeted therapy drugs for AML in the last few years.
Retinoic acid and arsenic trioxide therapy for acute promyelocytic leukemia “has transformed this AML subtype into one of the most curable AML diseases,” Dr. Wang said. A 2017 long-term analysis of the drug combination found that complete remission was reached in 96% of 54 high-risk patients and 133 low-risk patients; the 5-year survival rate was 88%. (Some patients also received gemtuzumab ozogamicin, a CD33 antibody-drug conjugate.)
According to Dr. Wang, three FLT3 inhibitors have been approved for AML with the FLT3 mutation: midostaurin and quizartinib in the frontline setting in conjunction with intensive chemotherapy and gilteritinib for relapsed/refractory FLT3-mutant AML.
A 2017 study linked midostaurin plus chemotherapy to longer survival (hazard ratio for death = 0.78; P = .009), versus placebo plus chemotherapy, in patients aged 18-59. This year, a phase 3 randomized trial of quizartinib versus placebo linked the drug to longer survival median overall (31.9 months versus 15.1 months; P = .032) In a 2019 trial, patients who took gilteritinib had longer median overall survival (9.3 months versus 5.6 months; HR for death = 0.64; P < .001).
The success of these treatments “has led FLT3 mutant AML to be reclassified from a poor risk AML subtype to intermediate risk AML,” Dr. Wang said.
A 2022 report about FLT3 inhibitors cautioned, however, that “several drug resistance mechanisms have been identified” and added that “the benefit of FLT3 inhibitor maintenance therapy, either post chemotherapy or post transplant, remains controversial, although several studies are ongoing.”
Gemtuzumab ozogamicin is a monoclonal antibody connected to a chemotherapy drug, according to the American Cancer Society. “The addition of gemtuzumab ozogamicin to intensive chemotherapy has enhanced outcomes of favorable and intermediate risk disease,” Dr. Wang said.
Ivosidenib, olutasidenib, and enasidenib target the IDH1 or IDH2 genes in ADL. “These drugs seem to work by helping the leukemia cells mature (differentiate) into more normal cells,” according to the American Cancer Society. “Because of this, they are sometimes referred to as differentiation agents.”
In older adults, a combination treatment with venetoclax, a BCL-2 inhibitor, and a hypomethylating agent has become standard, Ohio State’s Dr. Grieselhuber said. The treatment is FDA approved.
There are caveats to targeted therapy in AML. The treatments can be enormously expensive, “and even patients with insurance are often shocked by the copay,” Dr. Grieselhuber said. It helps to work with pharmacists, social workers, or nurse navigators to help patients afford the treatments, she said.
Side effects vary by therapy and can include QT elongation and differentiation syndrome.
Most challenging of all, many AML patients still face shortened lifespans even if new treatments are available for them.
“Typically for older patients with AML, the lifespan of patients with therapy was 5-7 months and without therapy was 2-3 months,” Dr. Wang said. “Now, with regimens specifically designed for elderly and/or unfit subjects, many individuals are now routinely living more than a year: 14-18 months to 3-4 years.”
But “the vast majority of AML patients will still die of their disease with overall 5-year outcomes still less than 30% in all age categories,” she said. In addition, “fewer than 50% of AML patients are eligible for treatment with FDA-approved targeted therapies, as their disease biology does not express the mutation or protein needed for efficacy.”
Still, she said, “this represents a vast improvement.” And, she added, “in younger individuals, the combination of chemotherapy followed by allogeneic transplant has now permitted more of these individuals to be cured of their disease.” Dr. Grieselhuber noted that transplants are now considered appropriate even for patients in their 60s or early 70s, and they can be combined with targeted therapy.
Dr. Grieselhuber urged colleagues to keep in mind that quality-of-life preferences will play a role in some patient choices. For example, a elderly patient may reject burdensome infusion therapy and choose a pill instead, even if it has less efficacy. “There’s really no one-size-fits-all,” she said.
And, she added, it can be difficult to make choices about treatment because of the lack of randomized, head-to-head data regarding new therapies.
What’s on the horizon? Dr. Wang highlighted a novel class of targeted therapies called menin inhibitors for patients with NPM1-mutated AML, which she said accounts for one-third of patients with the disease. A treatment targeting disease in the 5%-10% patients with the KMT2A gene is also in the works, she said.
For now, Dr. Wang said it’s essential for clinicians “to perform timely comprehensive molecular and genomic tests on all AML patients at diagnosis and relapse to determine which individuals would benefit from targeted therapy versus cytotoxic chemotherapy. And participation in clinical trials at every stage of AML therapy can help accelerate clinical development of new agents for this disease.”
Dr. Fathi discloses relationships with Daiichi Sankyo, Pfizer, Rigel, Autolus, Amgen, Servier, Takeda, Orum, Menarini, Remix, AbbVie, Astellas, BMS, Ibsen, Gilead, Genentech, and AstraZeneca. Dr. Wang discloses ties with AbbVie, Astellas, BMS, CTI Biopharma, Daiichi Sankyo, Gilead, GSK, Johnson & Johnson, Kite, Kura, Novartis, Pfizer, Rigel, Sellas, and Sumitomo Pharma. Dr. Grieselhuber has no disclosures.
“We went almost 3 decades with nothing, then all of a sudden we’ve had nine approvals in 5 or 6 years,” said Harvard Medical School, Boston, leukemia specialist Amir Fathi, MD, in an interview. “We’ve had a lot of advancement and a number of good options emerge.”
However, Dr. Fathi and other hematologists cautioned that the treatment landscape is becoming more complex to navigate. And they noted that prognoses for many older patients with AML remain grim. The expensive new treatments may only extend their lifespans by a matter of months, although some are surviving for years.
As the specialists explained, there are a variety of reasons why AML is especially difficult to treat.
“AML is one of the fastest growing human cancers, with tumor cell doubling times measured in mere hours in some patients. Therefore patients can present critically ill with white blood cell counts in the [hundreds of thousands of white blood cells per microliter instead of the normal range of 4,000-11,000]," said leukemia specialist Eunice S. Wang, MD, of Roswell Park Comprehensive Cancer Center in Buffalo, N.Y. “Because blood cells are found in every organ of the body, the sheer volume of rapidly growing cancer cells can overwhelm multiple organ systems in a very short amount of time. These rapid growing cells and the fact that the median age of diagnosis with AML is 67-70 years old makes this a clinically challenging cancer to treat. Chemotherapy strong enough to kill cancer cells run the risk of also harming the patient as well.”
Also, older patients often have comorbidities, and they face risks of infection from both the disease and its treatments, said AML specialist Nicole R. Grieselhuber, MD, PhD, of the Ohio State University, Columbus, in an interview.
Enter targeted therapy, which “has allowed individuals who previously were not candidates for cytotoxic chemotherapy because of their age or possible toxicities to receive effective therapy for AML,” Dr. Wang said. “Therapy directed at specific biological features of AML cells such as mutations (FLT3, IDH1, IDH2) or surface proteins (CD33) can augment the efficacy of conventional chemotherapy or in some cases (i.e., FLT3 inhibitors) be more effective than chemotherapy in controlling AML.”
Targeted therapy drugs “are expected to more selectively kill cancer cells and spare normal counterparts,” she added.
The FDA has approved nine targeted therapy drugs for AML in the last few years.
Retinoic acid and arsenic trioxide therapy for acute promyelocytic leukemia “has transformed this AML subtype into one of the most curable AML diseases,” Dr. Wang said. A 2017 long-term analysis of the drug combination found that complete remission was reached in 96% of 54 high-risk patients and 133 low-risk patients; the 5-year survival rate was 88%. (Some patients also received gemtuzumab ozogamicin, a CD33 antibody-drug conjugate.)
According to Dr. Wang, three FLT3 inhibitors have been approved for AML with the FLT3 mutation: midostaurin and quizartinib in the frontline setting in conjunction with intensive chemotherapy and gilteritinib for relapsed/refractory FLT3-mutant AML.
A 2017 study linked midostaurin plus chemotherapy to longer survival (hazard ratio for death = 0.78; P = .009), versus placebo plus chemotherapy, in patients aged 18-59. This year, a phase 3 randomized trial of quizartinib versus placebo linked the drug to longer survival median overall (31.9 months versus 15.1 months; P = .032) In a 2019 trial, patients who took gilteritinib had longer median overall survival (9.3 months versus 5.6 months; HR for death = 0.64; P < .001).
The success of these treatments “has led FLT3 mutant AML to be reclassified from a poor risk AML subtype to intermediate risk AML,” Dr. Wang said.
A 2022 report about FLT3 inhibitors cautioned, however, that “several drug resistance mechanisms have been identified” and added that “the benefit of FLT3 inhibitor maintenance therapy, either post chemotherapy or post transplant, remains controversial, although several studies are ongoing.”
Gemtuzumab ozogamicin is a monoclonal antibody connected to a chemotherapy drug, according to the American Cancer Society. “The addition of gemtuzumab ozogamicin to intensive chemotherapy has enhanced outcomes of favorable and intermediate risk disease,” Dr. Wang said.
Ivosidenib, olutasidenib, and enasidenib target the IDH1 or IDH2 genes in ADL. “These drugs seem to work by helping the leukemia cells mature (differentiate) into more normal cells,” according to the American Cancer Society. “Because of this, they are sometimes referred to as differentiation agents.”
In older adults, a combination treatment with venetoclax, a BCL-2 inhibitor, and a hypomethylating agent has become standard, Ohio State’s Dr. Grieselhuber said. The treatment is FDA approved.
There are caveats to targeted therapy in AML. The treatments can be enormously expensive, “and even patients with insurance are often shocked by the copay,” Dr. Grieselhuber said. It helps to work with pharmacists, social workers, or nurse navigators to help patients afford the treatments, she said.
Side effects vary by therapy and can include QT elongation and differentiation syndrome.
Most challenging of all, many AML patients still face shortened lifespans even if new treatments are available for them.
“Typically for older patients with AML, the lifespan of patients with therapy was 5-7 months and without therapy was 2-3 months,” Dr. Wang said. “Now, with regimens specifically designed for elderly and/or unfit subjects, many individuals are now routinely living more than a year: 14-18 months to 3-4 years.”
But “the vast majority of AML patients will still die of their disease with overall 5-year outcomes still less than 30% in all age categories,” she said. In addition, “fewer than 50% of AML patients are eligible for treatment with FDA-approved targeted therapies, as their disease biology does not express the mutation or protein needed for efficacy.”
Still, she said, “this represents a vast improvement.” And, she added, “in younger individuals, the combination of chemotherapy followed by allogeneic transplant has now permitted more of these individuals to be cured of their disease.” Dr. Grieselhuber noted that transplants are now considered appropriate even for patients in their 60s or early 70s, and they can be combined with targeted therapy.
Dr. Grieselhuber urged colleagues to keep in mind that quality-of-life preferences will play a role in some patient choices. For example, a elderly patient may reject burdensome infusion therapy and choose a pill instead, even if it has less efficacy. “There’s really no one-size-fits-all,” she said.
And, she added, it can be difficult to make choices about treatment because of the lack of randomized, head-to-head data regarding new therapies.
What’s on the horizon? Dr. Wang highlighted a novel class of targeted therapies called menin inhibitors for patients with NPM1-mutated AML, which she said accounts for one-third of patients with the disease. A treatment targeting disease in the 5%-10% patients with the KMT2A gene is also in the works, she said.
For now, Dr. Wang said it’s essential for clinicians “to perform timely comprehensive molecular and genomic tests on all AML patients at diagnosis and relapse to determine which individuals would benefit from targeted therapy versus cytotoxic chemotherapy. And participation in clinical trials at every stage of AML therapy can help accelerate clinical development of new agents for this disease.”
Dr. Fathi discloses relationships with Daiichi Sankyo, Pfizer, Rigel, Autolus, Amgen, Servier, Takeda, Orum, Menarini, Remix, AbbVie, Astellas, BMS, Ibsen, Gilead, Genentech, and AstraZeneca. Dr. Wang discloses ties with AbbVie, Astellas, BMS, CTI Biopharma, Daiichi Sankyo, Gilead, GSK, Johnson & Johnson, Kite, Kura, Novartis, Pfizer, Rigel, Sellas, and Sumitomo Pharma. Dr. Grieselhuber has no disclosures.
Nationwide hematologists shortage: What’s being done?
Over decades, the shrinking pool of CHs – who are compensated far less than hematologist-oncologists – has put patients at risk without access to adequate and timely care. To alleviate this crisis, individual doctors and national organizations are taking action and making more resources available to CHs and their patients.
`Vicious cycle’
The root cause of the CH shortage can be traced to a dramatic reduction in the number of physicians trained in this field, as Leonard Valentino, MD, President of the National Bleeding Disorders Foundation in New York, explained in an interview.
“There is a vicious cycle where there’s not enough classical hematologists to be program directors, and therefore trainees are often steered to fellowships in oncology,” said Dr. Valentino.
According to data published in JAMA, in 1995 there were 74 classical hematology programs in the United States; by 2018, there were only 2, During this same time period, the number of combined hematology/oncology training programs (HOPs) nearly doubled, from 75 to 146. However, it is estimated that less than 5% of graduates of adult HOPs pursued a career in classical hematology, as reported in Blood Advances. This low percentage can be attributed, at least in part, to the emphasis that most HOPs place on oncology.
Dr. Valentino noted that financial pressures are also diverting medical students from becoming CHs, adding that a hematologist-oncologist can make three times the annual salary of a CH.
Furthermore, when CHs treat bleeding and clotting disorders, they often need to meet with a patient for a 60- to 90-minute initial consultation, then they go on to provide a lifetime of labor-intensive care.
“This work is neither verticalized [that is, supported by radiologists, surgeons, and a cadre of nurses], nor is it billable per hour on a scale comparable to what oncologists can charge,” Dr. Valentino explained.
The survey published in Blood Advances illustrates the consequences of such a disparity in income potential: 34% of hematology/oncology fellows surveyed were likely to enter solid tumor oncology, while 20% and 4.6% would proceed to malignant hematology and CH, respectively.
Toll on patients
Primary care doctors treat some common blood disorders, but they almost always refer more difficult or complicated cases to a shrinking population of CHs.
“For many Americans, it is getting more difficult to find providers who subspecialize in hemostasis and thrombosis disorders. Patients can expect prolonged waiting times to get evaluated after a referral” said Mukul Singal, MD, of the Indiana Hemophilia and Thrombosis Center in Indianapolis.
Dr. Singal said the shortage is so acute that “at many institutions, malignant hematologists or oncologists are having to staff in-patient hematology consult services and see outpatient classical hematology patients. General hematologist/oncologists or medical oncologists are often not as comfortable or experienced with dealing with some of the complex CH conditions.”
A working care model, without enough doctors
In 1975, responding to patient advocacy groups, the federal government began funding hemophilia treatment centers (HTCs). Such centers offer a comprehensive care model that gives patients access to practitioners and administrative staff with the expertise to help them stay as healthy as possible. According to the Centers for Disease Control and Prevention, people with hemophilia who used an HTC were 40% less likely to die of a hemophilia-related complication and 40% less likely to be hospitalized for bleeding complications, compared to those who did not receive such specialized care.
“HTCs are effective at keeping patients out of the hospital and engaged in their lives. Between 80% and 95% of hemophilia patients get their care from an HTC and more patients want more services from them,” said Joe Pugliese, president of the Hemophilia Alliance in Lansdale, Pa.
Expanding care to meet patient demand is challenged by the restrictions on doctors’ salaries. All 140 U.S.-based HTCs share a $4.9 million federal grant but, by law, they can’t pay any provider more than $211,000 a year. “These restrictions push many people to industry, leaving too few doctors to meet patient demand,” Mr. Pugliese explained.
The fact that most HTCs are located in or near major cities also presents patients with the challenge of commuting, sometimes across state lines, to see a specialist. However, an uptick in telemedicine has provided one bright spot for many patients, allowing care to be brought to them.
The Hemophilia Alliance is also working on a multifaceted approach to change the rules, so that CHs are offered better compensation. “We have lobbyists in Washington, as well as an advocacy committee and a payer committee working to better support the HTC model,” Mr. Pugliese said.
Beyond the paycheck: Supporting CHs and patients
As market and regulatory restrictions make it difficult to boost the pay of CHs, doctors and nonprofit organizations are collaborating to support young CHs and bring more into the field. The American Society of Hematology has started and fully funded the Hematology Focused Fellowship Training Program (HFFTP). This program pairs comprehensive classical hematology training with education in transfusion medicine, sickle cell disease, hemostasis/thrombosis, systems-based hematology, health equity research, and global health. According to the program’s website, HFFTP’s goal is to add 50 new academic hematologists nationwide by 2030, in an effort to “improve the lives of patients with blood and bone marrow disorders.”
Additionally, classic hematologists are aiming to attract younger physicians and trainees to their field by introducing them to the various rewarding aspects of dealing with patients with inherited, chronic blood diseases. Programs like the Partners Physicians Academy (PPA), a 5-day training course that is specifically designed to encourage and retain young hematology students as classical hematologists, are essential to this effort.
“Along with preparing physicians to work in an HTC, programs like the Hematology Focused Fellowship Training Program and the Partners Physicians Academy are so important because they might convince young doctors to stick with non–oncology-based hematology careers, through the right mix of knowing about exciting research like gene therapy, financial and mentorship support, and a desire to meet unmet medical need,” explained Dr. Valentino.
The next PPA is taking place Sept. 18-22 in Indianapolis.
Dr. Singal, Dr. Valentino, and Mr. Pugliese had no financial disclosures to report.
Over decades, the shrinking pool of CHs – who are compensated far less than hematologist-oncologists – has put patients at risk without access to adequate and timely care. To alleviate this crisis, individual doctors and national organizations are taking action and making more resources available to CHs and their patients.
`Vicious cycle’
The root cause of the CH shortage can be traced to a dramatic reduction in the number of physicians trained in this field, as Leonard Valentino, MD, President of the National Bleeding Disorders Foundation in New York, explained in an interview.
“There is a vicious cycle where there’s not enough classical hematologists to be program directors, and therefore trainees are often steered to fellowships in oncology,” said Dr. Valentino.
According to data published in JAMA, in 1995 there were 74 classical hematology programs in the United States; by 2018, there were only 2, During this same time period, the number of combined hematology/oncology training programs (HOPs) nearly doubled, from 75 to 146. However, it is estimated that less than 5% of graduates of adult HOPs pursued a career in classical hematology, as reported in Blood Advances. This low percentage can be attributed, at least in part, to the emphasis that most HOPs place on oncology.
Dr. Valentino noted that financial pressures are also diverting medical students from becoming CHs, adding that a hematologist-oncologist can make three times the annual salary of a CH.
Furthermore, when CHs treat bleeding and clotting disorders, they often need to meet with a patient for a 60- to 90-minute initial consultation, then they go on to provide a lifetime of labor-intensive care.
“This work is neither verticalized [that is, supported by radiologists, surgeons, and a cadre of nurses], nor is it billable per hour on a scale comparable to what oncologists can charge,” Dr. Valentino explained.
The survey published in Blood Advances illustrates the consequences of such a disparity in income potential: 34% of hematology/oncology fellows surveyed were likely to enter solid tumor oncology, while 20% and 4.6% would proceed to malignant hematology and CH, respectively.
Toll on patients
Primary care doctors treat some common blood disorders, but they almost always refer more difficult or complicated cases to a shrinking population of CHs.
“For many Americans, it is getting more difficult to find providers who subspecialize in hemostasis and thrombosis disorders. Patients can expect prolonged waiting times to get evaluated after a referral” said Mukul Singal, MD, of the Indiana Hemophilia and Thrombosis Center in Indianapolis.
Dr. Singal said the shortage is so acute that “at many institutions, malignant hematologists or oncologists are having to staff in-patient hematology consult services and see outpatient classical hematology patients. General hematologist/oncologists or medical oncologists are often not as comfortable or experienced with dealing with some of the complex CH conditions.”
A working care model, without enough doctors
In 1975, responding to patient advocacy groups, the federal government began funding hemophilia treatment centers (HTCs). Such centers offer a comprehensive care model that gives patients access to practitioners and administrative staff with the expertise to help them stay as healthy as possible. According to the Centers for Disease Control and Prevention, people with hemophilia who used an HTC were 40% less likely to die of a hemophilia-related complication and 40% less likely to be hospitalized for bleeding complications, compared to those who did not receive such specialized care.
“HTCs are effective at keeping patients out of the hospital and engaged in their lives. Between 80% and 95% of hemophilia patients get their care from an HTC and more patients want more services from them,” said Joe Pugliese, president of the Hemophilia Alliance in Lansdale, Pa.
Expanding care to meet patient demand is challenged by the restrictions on doctors’ salaries. All 140 U.S.-based HTCs share a $4.9 million federal grant but, by law, they can’t pay any provider more than $211,000 a year. “These restrictions push many people to industry, leaving too few doctors to meet patient demand,” Mr. Pugliese explained.
The fact that most HTCs are located in or near major cities also presents patients with the challenge of commuting, sometimes across state lines, to see a specialist. However, an uptick in telemedicine has provided one bright spot for many patients, allowing care to be brought to them.
The Hemophilia Alliance is also working on a multifaceted approach to change the rules, so that CHs are offered better compensation. “We have lobbyists in Washington, as well as an advocacy committee and a payer committee working to better support the HTC model,” Mr. Pugliese said.
Beyond the paycheck: Supporting CHs and patients
As market and regulatory restrictions make it difficult to boost the pay of CHs, doctors and nonprofit organizations are collaborating to support young CHs and bring more into the field. The American Society of Hematology has started and fully funded the Hematology Focused Fellowship Training Program (HFFTP). This program pairs comprehensive classical hematology training with education in transfusion medicine, sickle cell disease, hemostasis/thrombosis, systems-based hematology, health equity research, and global health. According to the program’s website, HFFTP’s goal is to add 50 new academic hematologists nationwide by 2030, in an effort to “improve the lives of patients with blood and bone marrow disorders.”
Additionally, classic hematologists are aiming to attract younger physicians and trainees to their field by introducing them to the various rewarding aspects of dealing with patients with inherited, chronic blood diseases. Programs like the Partners Physicians Academy (PPA), a 5-day training course that is specifically designed to encourage and retain young hematology students as classical hematologists, are essential to this effort.
“Along with preparing physicians to work in an HTC, programs like the Hematology Focused Fellowship Training Program and the Partners Physicians Academy are so important because they might convince young doctors to stick with non–oncology-based hematology careers, through the right mix of knowing about exciting research like gene therapy, financial and mentorship support, and a desire to meet unmet medical need,” explained Dr. Valentino.
The next PPA is taking place Sept. 18-22 in Indianapolis.
Dr. Singal, Dr. Valentino, and Mr. Pugliese had no financial disclosures to report.
Over decades, the shrinking pool of CHs – who are compensated far less than hematologist-oncologists – has put patients at risk without access to adequate and timely care. To alleviate this crisis, individual doctors and national organizations are taking action and making more resources available to CHs and their patients.
`Vicious cycle’
The root cause of the CH shortage can be traced to a dramatic reduction in the number of physicians trained in this field, as Leonard Valentino, MD, President of the National Bleeding Disorders Foundation in New York, explained in an interview.
“There is a vicious cycle where there’s not enough classical hematologists to be program directors, and therefore trainees are often steered to fellowships in oncology,” said Dr. Valentino.
According to data published in JAMA, in 1995 there were 74 classical hematology programs in the United States; by 2018, there were only 2, During this same time period, the number of combined hematology/oncology training programs (HOPs) nearly doubled, from 75 to 146. However, it is estimated that less than 5% of graduates of adult HOPs pursued a career in classical hematology, as reported in Blood Advances. This low percentage can be attributed, at least in part, to the emphasis that most HOPs place on oncology.
Dr. Valentino noted that financial pressures are also diverting medical students from becoming CHs, adding that a hematologist-oncologist can make three times the annual salary of a CH.
Furthermore, when CHs treat bleeding and clotting disorders, they often need to meet with a patient for a 60- to 90-minute initial consultation, then they go on to provide a lifetime of labor-intensive care.
“This work is neither verticalized [that is, supported by radiologists, surgeons, and a cadre of nurses], nor is it billable per hour on a scale comparable to what oncologists can charge,” Dr. Valentino explained.
The survey published in Blood Advances illustrates the consequences of such a disparity in income potential: 34% of hematology/oncology fellows surveyed were likely to enter solid tumor oncology, while 20% and 4.6% would proceed to malignant hematology and CH, respectively.
Toll on patients
Primary care doctors treat some common blood disorders, but they almost always refer more difficult or complicated cases to a shrinking population of CHs.
“For many Americans, it is getting more difficult to find providers who subspecialize in hemostasis and thrombosis disorders. Patients can expect prolonged waiting times to get evaluated after a referral” said Mukul Singal, MD, of the Indiana Hemophilia and Thrombosis Center in Indianapolis.
Dr. Singal said the shortage is so acute that “at many institutions, malignant hematologists or oncologists are having to staff in-patient hematology consult services and see outpatient classical hematology patients. General hematologist/oncologists or medical oncologists are often not as comfortable or experienced with dealing with some of the complex CH conditions.”
A working care model, without enough doctors
In 1975, responding to patient advocacy groups, the federal government began funding hemophilia treatment centers (HTCs). Such centers offer a comprehensive care model that gives patients access to practitioners and administrative staff with the expertise to help them stay as healthy as possible. According to the Centers for Disease Control and Prevention, people with hemophilia who used an HTC were 40% less likely to die of a hemophilia-related complication and 40% less likely to be hospitalized for bleeding complications, compared to those who did not receive such specialized care.
“HTCs are effective at keeping patients out of the hospital and engaged in their lives. Between 80% and 95% of hemophilia patients get their care from an HTC and more patients want more services from them,” said Joe Pugliese, president of the Hemophilia Alliance in Lansdale, Pa.
Expanding care to meet patient demand is challenged by the restrictions on doctors’ salaries. All 140 U.S.-based HTCs share a $4.9 million federal grant but, by law, they can’t pay any provider more than $211,000 a year. “These restrictions push many people to industry, leaving too few doctors to meet patient demand,” Mr. Pugliese explained.
The fact that most HTCs are located in or near major cities also presents patients with the challenge of commuting, sometimes across state lines, to see a specialist. However, an uptick in telemedicine has provided one bright spot for many patients, allowing care to be brought to them.
The Hemophilia Alliance is also working on a multifaceted approach to change the rules, so that CHs are offered better compensation. “We have lobbyists in Washington, as well as an advocacy committee and a payer committee working to better support the HTC model,” Mr. Pugliese said.
Beyond the paycheck: Supporting CHs and patients
As market and regulatory restrictions make it difficult to boost the pay of CHs, doctors and nonprofit organizations are collaborating to support young CHs and bring more into the field. The American Society of Hematology has started and fully funded the Hematology Focused Fellowship Training Program (HFFTP). This program pairs comprehensive classical hematology training with education in transfusion medicine, sickle cell disease, hemostasis/thrombosis, systems-based hematology, health equity research, and global health. According to the program’s website, HFFTP’s goal is to add 50 new academic hematologists nationwide by 2030, in an effort to “improve the lives of patients with blood and bone marrow disorders.”
Additionally, classic hematologists are aiming to attract younger physicians and trainees to their field by introducing them to the various rewarding aspects of dealing with patients with inherited, chronic blood diseases. Programs like the Partners Physicians Academy (PPA), a 5-day training course that is specifically designed to encourage and retain young hematology students as classical hematologists, are essential to this effort.
“Along with preparing physicians to work in an HTC, programs like the Hematology Focused Fellowship Training Program and the Partners Physicians Academy are so important because they might convince young doctors to stick with non–oncology-based hematology careers, through the right mix of knowing about exciting research like gene therapy, financial and mentorship support, and a desire to meet unmet medical need,” explained Dr. Valentino.
The next PPA is taking place Sept. 18-22 in Indianapolis.
Dr. Singal, Dr. Valentino, and Mr. Pugliese had no financial disclosures to report.







