User login
TriHealth of Cincinnati is testing the waters of value-based payment for maternity care.
The impetus came from a Cincinnati-based employer that contracts with TriHealth under its self-insured health care plan, according to Jennifer Pavelka, project lead for the health system’s Maternity Bundling Care Select Program.
“Employers are looking at the value proposition and are having keen interest in the achievement of the triple aim of optimal outcomes, optimal experience, both with a mindfulness on value, Ms. Pavelka said in an interview. “An employer that had extensive experience with other episodes of care [payments], particularly in the space of knee and hip replacements in the orthopedic world, wanted to dip their toe into a value-based program for maternity.”
“Many forays into value-based payments are very much code driven, saying this code, this service is included in the bundle and this is not,” Ms. Pavelka said. “Part of what makes our work really challenging and exciting is the fact that we have taken in the realm of the methodology and philosophy of bundles, we are implementing a prospective bundled payment model.”
Their engaged physician community has been a key factor in early successes, she added. “What heartens me the most is the degree to which the physicians have really led and informed that evolution of the program and the commitment on the partner side to say first and foremost what does the evidence say, what is clinically appropriate. That has always been our North Star.”
Even with the guidelines of eligibility, patient selection is at the physician’s discretion.
And doctors are helping to shape how women are included in the process.
“We actually have two tiers,” Dr. Marcotte said. “Tier one is the uncomplicated pregnancy and our first project was really to get consensus [around those patients]. There was quite a bit of engagement. We had several meetings at the beginning of our project to help build consensus and we continue to look at that as new evidence comes out to make sure that we are staying consistent with best practice.”
The second tier focuses on more complicated pregnancies.
“There was a reengagement with providers, both our subspecialists in maternal fetal medicine and our generalists [ob.gyns.], to rethink what are the essential elements of best practice care for a patient that has certain complications like hypertension or twins or some of the other things that we included in the tier two clinical care pathways.”
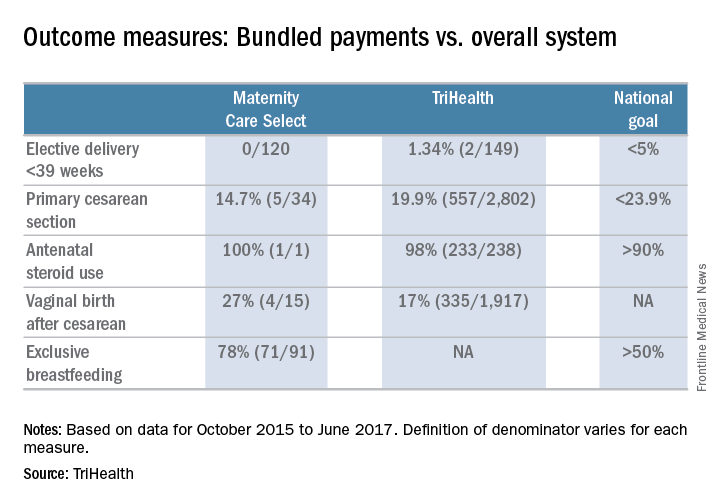
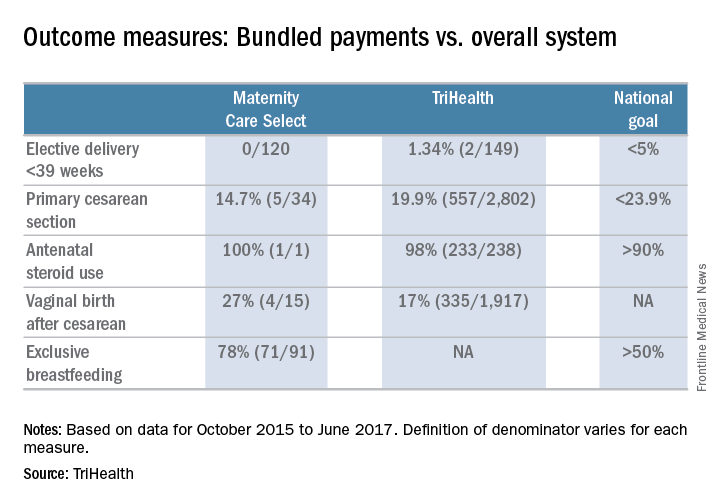
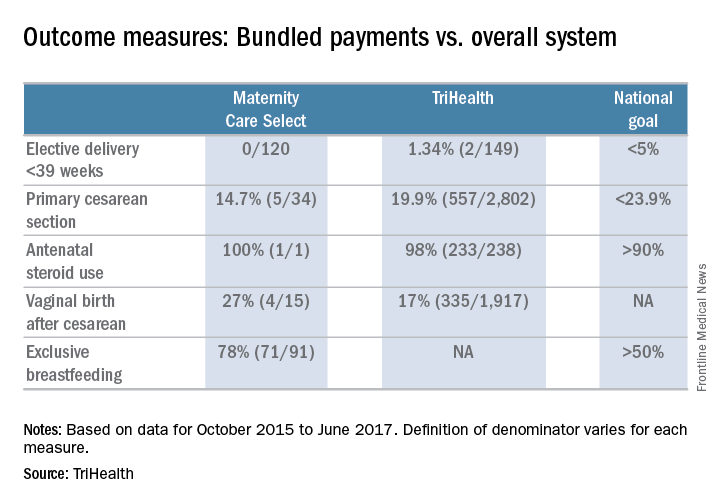
So far, very early results show that those in the bundle are in fact seeing better outcomes, something that in general is expected of a value-based payment model.
The bundled payment program also is opening the door to new service that can be provided to maternity patients.
“We are still relatively early in that journey,” Dr. Marcotte said. “We have a full-time concierge navigator who really works with this population, and we are beginning to make plans to expand that service to more patients beyond just our one population that are in the bundled care package. That’s one concrete area.”
He continued: “I think there is recognition of the need to provide more [patient] education and resources for our entire population that we are working with. Lastly, I think some of our specialized obstetric services for women with complicated pregnancies have gotten a boost. We can additionally provide those kind of services that might be extended beyond just our local community and provide attractive things that can be best in class for even those complicated pregnancies.”
TriHealth really found the key with its early and robust physician involvement, according to Malini Nijagal, MD, associate professor of ob.gyn. and reproductive sciences at the University of California, San Francisco.
“The strong sense that I have is that there is a bit of a disconnect, where it feels on the ground like people believe that value-based payment models may be good for finance and health care expenditures but they are not going to be good for patients and providers,” Dr. Nijagal said in an interview. “I totally disagree.”
Rather, value-based payment models are a way to increase provider autonomy.
“Specific to maternity care and across health care, at this point, insurers are the ones who decide what services we can provide,” she said. “They have their fee schedules and that limits what we can do. What value-based payments and episode payments allow us to do is that, as providers, if we end up saving money from avoiding unnecessary interventions and diagnostics, we then get some of that money back to provide services that may not be covered.”
Dr. Nijagal and her colleagues looked at maternity care bundles and episode payment models in state Medicaid programs, managed care plans, and self-insured employers and found that physicians and other providers can benefit from participation in four ways, by:
- Finding opportunities to improve outcomes and patient experience.
- Developing better quality metrics.
- Reducing waste in the system.
- Creating stronger health care teams.
Value-based payments can “actually bring together hospitals and health care providers onto the same team and the way they do that is by tying the payment together,” Dr. Nijagal said.
The biggest challenge, according to Dr. Nijagal, is that the conversion takes time and the patience to realize that benefits will likely not be fully realized until the system is able to get to a prospective payment model, in which the real innovation can take place (Am J Obstet Gynecol. 2018 Jan 12. doi. org/10.1016/j.ajog.2018.01.014).
“We are having to prioritize just getting providers to agree to doing them and because of that, we are not actually seeing the improvements in quality and cost that we would expect,” Dr. Nijagal said. “For example, a number of the programs that have been rolled out have been the upside risk only, which is superimportant because that is the way you are going to get people to feel more comfortable. It’s a stepping-stone, but you are not going to see the benefits.” And if you can’t prove benefit, it will be harder to get people to move to a two-sided risk model where the real innovation can take place.
To that end, TriHealth provides full transparency with the program so physicians can see how patients in the bundle are doing compared to the overall TriHealth patient population.
“We provide those to them in a dashboard on a monthly basis with transparency so they can see how the other providers in other practices are doing within the system,” Dr, Marcotte said.
TriHealth of Cincinnati is testing the waters of value-based payment for maternity care.
The impetus came from a Cincinnati-based employer that contracts with TriHealth under its self-insured health care plan, according to Jennifer Pavelka, project lead for the health system’s Maternity Bundling Care Select Program.
“Employers are looking at the value proposition and are having keen interest in the achievement of the triple aim of optimal outcomes, optimal experience, both with a mindfulness on value, Ms. Pavelka said in an interview. “An employer that had extensive experience with other episodes of care [payments], particularly in the space of knee and hip replacements in the orthopedic world, wanted to dip their toe into a value-based program for maternity.”
“Many forays into value-based payments are very much code driven, saying this code, this service is included in the bundle and this is not,” Ms. Pavelka said. “Part of what makes our work really challenging and exciting is the fact that we have taken in the realm of the methodology and philosophy of bundles, we are implementing a prospective bundled payment model.”
Their engaged physician community has been a key factor in early successes, she added. “What heartens me the most is the degree to which the physicians have really led and informed that evolution of the program and the commitment on the partner side to say first and foremost what does the evidence say, what is clinically appropriate. That has always been our North Star.”
Even with the guidelines of eligibility, patient selection is at the physician’s discretion.
And doctors are helping to shape how women are included in the process.
“We actually have two tiers,” Dr. Marcotte said. “Tier one is the uncomplicated pregnancy and our first project was really to get consensus [around those patients]. There was quite a bit of engagement. We had several meetings at the beginning of our project to help build consensus and we continue to look at that as new evidence comes out to make sure that we are staying consistent with best practice.”
The second tier focuses on more complicated pregnancies.
“There was a reengagement with providers, both our subspecialists in maternal fetal medicine and our generalists [ob.gyns.], to rethink what are the essential elements of best practice care for a patient that has certain complications like hypertension or twins or some of the other things that we included in the tier two clinical care pathways.”
So far, very early results show that those in the bundle are in fact seeing better outcomes, something that in general is expected of a value-based payment model.
The bundled payment program also is opening the door to new service that can be provided to maternity patients.
“We are still relatively early in that journey,” Dr. Marcotte said. “We have a full-time concierge navigator who really works with this population, and we are beginning to make plans to expand that service to more patients beyond just our one population that are in the bundled care package. That’s one concrete area.”
He continued: “I think there is recognition of the need to provide more [patient] education and resources for our entire population that we are working with. Lastly, I think some of our specialized obstetric services for women with complicated pregnancies have gotten a boost. We can additionally provide those kind of services that might be extended beyond just our local community and provide attractive things that can be best in class for even those complicated pregnancies.”
TriHealth really found the key with its early and robust physician involvement, according to Malini Nijagal, MD, associate professor of ob.gyn. and reproductive sciences at the University of California, San Francisco.
“The strong sense that I have is that there is a bit of a disconnect, where it feels on the ground like people believe that value-based payment models may be good for finance and health care expenditures but they are not going to be good for patients and providers,” Dr. Nijagal said in an interview. “I totally disagree.”
Rather, value-based payment models are a way to increase provider autonomy.
“Specific to maternity care and across health care, at this point, insurers are the ones who decide what services we can provide,” she said. “They have their fee schedules and that limits what we can do. What value-based payments and episode payments allow us to do is that, as providers, if we end up saving money from avoiding unnecessary interventions and diagnostics, we then get some of that money back to provide services that may not be covered.”
Dr. Nijagal and her colleagues looked at maternity care bundles and episode payment models in state Medicaid programs, managed care plans, and self-insured employers and found that physicians and other providers can benefit from participation in four ways, by:
- Finding opportunities to improve outcomes and patient experience.
- Developing better quality metrics.
- Reducing waste in the system.
- Creating stronger health care teams.
Value-based payments can “actually bring together hospitals and health care providers onto the same team and the way they do that is by tying the payment together,” Dr. Nijagal said.
The biggest challenge, according to Dr. Nijagal, is that the conversion takes time and the patience to realize that benefits will likely not be fully realized until the system is able to get to a prospective payment model, in which the real innovation can take place (Am J Obstet Gynecol. 2018 Jan 12. doi. org/10.1016/j.ajog.2018.01.014).
“We are having to prioritize just getting providers to agree to doing them and because of that, we are not actually seeing the improvements in quality and cost that we would expect,” Dr. Nijagal said. “For example, a number of the programs that have been rolled out have been the upside risk only, which is superimportant because that is the way you are going to get people to feel more comfortable. It’s a stepping-stone, but you are not going to see the benefits.” And if you can’t prove benefit, it will be harder to get people to move to a two-sided risk model where the real innovation can take place.
To that end, TriHealth provides full transparency with the program so physicians can see how patients in the bundle are doing compared to the overall TriHealth patient population.
“We provide those to them in a dashboard on a monthly basis with transparency so they can see how the other providers in other practices are doing within the system,” Dr, Marcotte said.
TriHealth of Cincinnati is testing the waters of value-based payment for maternity care.
The impetus came from a Cincinnati-based employer that contracts with TriHealth under its self-insured health care plan, according to Jennifer Pavelka, project lead for the health system’s Maternity Bundling Care Select Program.
“Employers are looking at the value proposition and are having keen interest in the achievement of the triple aim of optimal outcomes, optimal experience, both with a mindfulness on value, Ms. Pavelka said in an interview. “An employer that had extensive experience with other episodes of care [payments], particularly in the space of knee and hip replacements in the orthopedic world, wanted to dip their toe into a value-based program for maternity.”
“Many forays into value-based payments are very much code driven, saying this code, this service is included in the bundle and this is not,” Ms. Pavelka said. “Part of what makes our work really challenging and exciting is the fact that we have taken in the realm of the methodology and philosophy of bundles, we are implementing a prospective bundled payment model.”
Their engaged physician community has been a key factor in early successes, she added. “What heartens me the most is the degree to which the physicians have really led and informed that evolution of the program and the commitment on the partner side to say first and foremost what does the evidence say, what is clinically appropriate. That has always been our North Star.”
Even with the guidelines of eligibility, patient selection is at the physician’s discretion.
And doctors are helping to shape how women are included in the process.
“We actually have two tiers,” Dr. Marcotte said. “Tier one is the uncomplicated pregnancy and our first project was really to get consensus [around those patients]. There was quite a bit of engagement. We had several meetings at the beginning of our project to help build consensus and we continue to look at that as new evidence comes out to make sure that we are staying consistent with best practice.”
The second tier focuses on more complicated pregnancies.
“There was a reengagement with providers, both our subspecialists in maternal fetal medicine and our generalists [ob.gyns.], to rethink what are the essential elements of best practice care for a patient that has certain complications like hypertension or twins or some of the other things that we included in the tier two clinical care pathways.”
So far, very early results show that those in the bundle are in fact seeing better outcomes, something that in general is expected of a value-based payment model.
The bundled payment program also is opening the door to new service that can be provided to maternity patients.
“We are still relatively early in that journey,” Dr. Marcotte said. “We have a full-time concierge navigator who really works with this population, and we are beginning to make plans to expand that service to more patients beyond just our one population that are in the bundled care package. That’s one concrete area.”
He continued: “I think there is recognition of the need to provide more [patient] education and resources for our entire population that we are working with. Lastly, I think some of our specialized obstetric services for women with complicated pregnancies have gotten a boost. We can additionally provide those kind of services that might be extended beyond just our local community and provide attractive things that can be best in class for even those complicated pregnancies.”
TriHealth really found the key with its early and robust physician involvement, according to Malini Nijagal, MD, associate professor of ob.gyn. and reproductive sciences at the University of California, San Francisco.
“The strong sense that I have is that there is a bit of a disconnect, where it feels on the ground like people believe that value-based payment models may be good for finance and health care expenditures but they are not going to be good for patients and providers,” Dr. Nijagal said in an interview. “I totally disagree.”
Rather, value-based payment models are a way to increase provider autonomy.
“Specific to maternity care and across health care, at this point, insurers are the ones who decide what services we can provide,” she said. “They have their fee schedules and that limits what we can do. What value-based payments and episode payments allow us to do is that, as providers, if we end up saving money from avoiding unnecessary interventions and diagnostics, we then get some of that money back to provide services that may not be covered.”
Dr. Nijagal and her colleagues looked at maternity care bundles and episode payment models in state Medicaid programs, managed care plans, and self-insured employers and found that physicians and other providers can benefit from participation in four ways, by:
- Finding opportunities to improve outcomes and patient experience.
- Developing better quality metrics.
- Reducing waste in the system.
- Creating stronger health care teams.
Value-based payments can “actually bring together hospitals and health care providers onto the same team and the way they do that is by tying the payment together,” Dr. Nijagal said.
The biggest challenge, according to Dr. Nijagal, is that the conversion takes time and the patience to realize that benefits will likely not be fully realized until the system is able to get to a prospective payment model, in which the real innovation can take place (Am J Obstet Gynecol. 2018 Jan 12. doi. org/10.1016/j.ajog.2018.01.014).
“We are having to prioritize just getting providers to agree to doing them and because of that, we are not actually seeing the improvements in quality and cost that we would expect,” Dr. Nijagal said. “For example, a number of the programs that have been rolled out have been the upside risk only, which is superimportant because that is the way you are going to get people to feel more comfortable. It’s a stepping-stone, but you are not going to see the benefits.” And if you can’t prove benefit, it will be harder to get people to move to a two-sided risk model where the real innovation can take place.
To that end, TriHealth provides full transparency with the program so physicians can see how patients in the bundle are doing compared to the overall TriHealth patient population.
“We provide those to them in a dashboard on a monthly basis with transparency so they can see how the other providers in other practices are doing within the system,” Dr, Marcotte said.

