User login
Clinical Endocrinology News is an independent news source that provides endocrinologists with timely and relevant news and commentary about clinical developments and the impact of health care policy on the endocrinologist's practice. Specialty topics include Diabetes, Lipid & Metabolic Disorders Menopause, Obesity, Osteoporosis, Pediatric Endocrinology, Pituitary, Thyroid & Adrenal Disorders, and Reproductive Endocrinology. Featured content includes Commentaries, Implementin Health Reform, Law & Medicine, and In the Loop, the blog of Clinical Endocrinology News. Clinical Endocrinology News is owned by Frontline Medical Communications.
addict
addicted
addicting
addiction
adult sites
alcohol
antibody
ass
attorney
audit
auditor
babies
babpa
baby
ban
banned
banning
best
bisexual
bitch
bleach
blog
blow job
bondage
boobs
booty
buy
cannabis
certificate
certification
certified
cheap
cheapest
class action
cocaine
cock
counterfeit drug
crack
crap
crime
criminal
cunt
curable
cure
dangerous
dangers
dead
deadly
death
defend
defended
depedent
dependence
dependent
detergent
dick
die
dildo
drug abuse
drug recall
dying
fag
fake
fatal
fatalities
fatality
free
fuck
gangs
gingivitis
guns
hardcore
herbal
herbs
heroin
herpes
home remedies
homo
horny
hypersensitivity
hypoglycemia treatment
illegal drug use
illegal use of prescription
incest
infant
infants
job
ketoacidosis
kill
killer
killing
kinky
law suit
lawsuit
lawyer
lesbian
marijuana
medicine for hypoglycemia
murder
naked
natural
newborn
nigger
noise
nude
nudity
orgy
over the counter
overdosage
overdose
overdosed
overdosing
penis
pimp
pistol
porn
porno
pornographic
pornography
prison
profanity
purchase
purchasing
pussy
queer
rape
rapist
recall
recreational drug
rob
robberies
sale
sales
sex
sexual
shit
shoot
slut
slutty
stole
stolen
store
sue
suicidal
suicide
supplements
supply company
theft
thief
thieves
tit
toddler
toddlers
toxic
toxin
tragedy
treating dka
treating hypoglycemia
treatment for hypoglycemia
vagina
violence
whore
withdrawal
without prescription
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-imn')]
div[contains(@class, 'pane-pub-home-imn')]
div[contains(@class, 'pane-pub-topic-imn')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
In-hospital glucose management program gives dramatic savings
Initiatives targeting hypoglycemia and insulin pen wastage could lead to dramatic cost savings in small community hospitals, new data suggest.
The two projects are part of a dedicated inpatient glucose management service led by Mihail (“Misha”) Zilbermint, MD, one of the few full-time endocrine hospitalists in the United States and one of even fewer who work at a small community hospital.
In 2019, Dr. Zilbermint and colleagues reported that their inpatient glucose management program resulted in a 27% reduction in length of stay and a 10.7% lower 30-day readmission rate. The projected cost savings for the period January 2016 to May 2017 was $953,578.
Dr. Zilbermint’s team has written two new articles that document cost savings for specific elements of the program; namely, a set of hospital-wide hypoglycemia prevention measures, and an initiative that reduced duplicate inpatient insulin pen dispensing.
About 1 in 4 people in U.S. hospitals have diabetes or hyperglycemia. Large academic hospitals have endocrine divisions and training programs, but 85% of people receive care at small community hospitals.
“There are management guidelines, but they’re not always followed ... That’s why I’ve been advocating for endocrine hospitalists to be deployed nationally,” Dr. Zilbermint said. He is chief and director of endocrinology, diabetes, and metabolism at Johns Hopkins Community Physicians at Suburban Hospital, Bethesda, Maryland.
Asked to comment on behalf of the Society of Hospital Medicine (SHM), Greg Maynard, MD, program lead for SHM’s Electronic Quality Improvement Programs, said that Suburban’s overall program goals align with those of the SHM.
“Dedicated inpatient glycemic control teams are very important and desirable to improve the quality and safety of care for inpatients with hyperglycemia and diabetes,” he said.
Regarding specific initiatives, such as those aimed at reducing hypoglycemia and insulin pen wastage, Dr. Maynard said, “All of these are feasible in a wide variety of institutions. The main barrier is getting the institutional support for people to work on these interventions. This series of studies can help spread the word about the positive return on investment.”
Another barrier – the current lack of publicly reported measures or pay-for-performance programs for hypoglycemia prevention and glycemic control – may soon change, added Dr. Maynard, who is also chief quality officer at the University of California, Davis, Medical Center.
“The National Quality Forum has endorsed new measures, and the CDC’s National Healthcare Safety Network is working on ways to augment those measures and embed them into their infrastructure,” he said.
Although SHM doesn’t specifically endorse full-time glycemic control hospitalists over endocrinology-trained glycemic control experts, “certainly hospitalists who accrue added training are very well positioned to be an important part of these interdisciplinary teams,” Dr. Maynard said.
‘The nurses were so afraid of hypoglycemia’
Tackling hypoglycemia was Dr. Zilbermint’s first priority when he started the glycemic management program at Suburban in late 2015.
“One of the most common complaints from the nurses was that a lot of their patients had hypoglycemia, especially in the ICU, when patients were placed on insulin infusion protocols ... Every time, the nurse would have to call the attending and ask what to do,” he explains.
In addition, Dr. Zilbermint says, there was no standard for treating hypoglycemia. A nurse in one unit would give two cups of juice, another a 50% dextrose infusion, or another, milk. Even more concerning, “the nurses were so afraid of hypoglycemia they would reflexively discontinue all insulin, including basal.”
So one of the new initiatives, led by Carter Shelton, MSHCM, an administrative fellow at the Medical University of South Carolina, Charleston, was to implement a set of hospital-wide hypoglycemia prevention measures, as described in an article published online April 21 in the Journal of Diabetes Science and Technology.
Inpatient hypoglycemia rate was cut nearly in half
This began in 2016, when the multidisciplinary Suburban Hospital Glucose Steering Committee identified four main causes of insulin-induced hypoglycemia (defined as a blood glucose level of ≤70 mg/dL in a patient who had received at least one dose of insulin in the past 24 hours) and devised solutions for each:
1. Lack of a unified hypoglycemia protocol. A formal, evidence-based, nurse-driven treatment protocol with clinical decision support in the electronic medical record was developed. The Suburban team adapted much of the protocol from one that had been recently implemented at the flagship Johns Hopkins Hospital, in Baltimore, Maryland.
According to that protocol, if patients are able to swallow, they are given 15 g or 30 g of carbohydrates in order to achieve a blood glucose level of 50 to 70 mg/dL and <50 mg/dL, respectively. Levels are checked 15 minutes later. Intravenous D50 or glucagon is reserved for patients who can’t swallow.
2. For patients in critical care, the insulin infusion protocol that had been in use set blood glucose targets of 80 to 110 mg/dL, which resulted in hypoglycemia in nearly every patient who received an insulin infusion. This protocol was changed to the currently recommended 140 to 180 mg/dL.
3. Most patients were managed with sliding-scale insulin, an outdated yet still widely used regimen whereby insulin is given based only on current blood glucose without accounting for carbohydrates consumed with meals and not corrected until the subsequent meal. This was changed so that nurses give insulin after the patient has consumed at least 50% of their meal carbohydrates.
4. Lack of hypoglycemia reporting. A glucometrics dashboard – now used throughout the Johns Hopkins system – was adopted to produce daily hypoglycemia reports in the EMR system that could be reviewed by the inpatient glucose management service to track quality metrics and plan further interventions.
Between Jan. 1, 2016, and Sept. 30, 2019, out of a total 49,315 patient-days, there were 2,682 days on which any hypoglycemia occurred and 874 days on which moderate hypoglycemia occurred (≤54 mg/dL). Type 2 diabetes accounted for 84.4% of the total patient-days; type 1 accounted for 4.4%.
The overall frequency of any hypoglycemia patient-days per month decreased from 7.5% to 3.9% during the study period (P = .001). This was significant for the patients with type 2 diabetes (7.4% to 3.8%; P < .0001) but not for those with type 1 diabetes (18.5% to 18.0%; P = .08).
Rates of moderate hypoglycemia also decreased significantly among the patients with type 2 diabetes (1.9% to 1.0%; P = .03) but not for those with type 1 diabetes (7.4% to 6.0%; P = .14).
On the basis of these rates in reducing hypoglycemia, in which the inpatient hypoglycemia rate was cut nearly in half, the estimated savings in cost of care to the hospital was $98,635 during the period of January 2016 to September 2019.
Reducing insulin pen waste by minimizing duplicate prescriptions
Suburban Hospital had been using insulin vials and syringes when Dr. Zilbermint first arrived there. He lobbied the administration to allow use of pens, because they’re easier to use and they reduce the risk for needlestick injuries. Nurses were educated and retrained monthly in their use.
The switch to pens – aspart (Novolog Flexpen) for bolus insulin and glargine (Lantus SoloSTAR) – took place in 2018. The cost of the aspart pen was $16.19, and the cost of glargine was $25.08. Each holds 300 units of insulin.
After the first month, the team noticed a large increase in expenses. A quality improvement project was devised to address the issue.
“We were dispensing sometimes three or four pens per person. That’s a lot. Each pen holds 300 units, so one pen should last the entire hospital stay of an average 4- or 5-day stay,” Dr. Zilbermint explained. “We had to figure out where we were bleeding the money and where the pens were going.”
When pens disappeared, the pharmacy would have to dispense new ones. One problem was that when patients were transferred from one unit to another, the pen would be left behind and the room would be cleaned. Sometimes the pens weren’t stored properly or were misplaced. Often, they’d end up in a nurse’s pocket.
The second intervention was led by Urooj Najmi, MD, of the American International School of Medicine, Atlanta, Georgia. A program was instituted to reduce duplicate inpatient insulin pen dispensing, as detailed in an article published in the same issue of the Journal of Diabetes Science and Technology.
Solutions to reduce duplicate pen dispensing included having pharmacy track daily insulin pen reports and monitor duplicate orders, with “do not dispense” instructions conveyed via the EMR system. All multidose medications, including insulin pens, were to be placed in patients’ bins at the nursing station, and nurses were instructed to look for patients’ insulin pens prior to their being transferred to another unit, rather than ask for a replacement pen.
From July 2018 to July 2019, 3,121 patients received insulin, of whom 95% received aspart and 47% received glargine. Of the 9,516 pens dispensed, 68% were for aspart and 32% were for glargine. During the study period, the number of pens dispensed per patient dropped from 2.2 to 1.2 for aspart and from 2.1 to 1.3 for glargine; differences were highly significant (P = .0002 and P = .0005, respectively).
The total amount of unnecessary dispensing during the first 4 months after initiating the pen implementation program was 58%. The average monthly cost was $11,820.68; the projected cost per year was $141,848.
Six months after the waste reduction strategies were implemented, monthly waste had dropped to 42%, translating to an estimated potential cost savings of $66,261 over 12 months.
Because Suburban Hospital doesn’t have an outpatient dispensing license, there is still wastage when patients are discharged, because they can’t take their pens home with them. That remains a challenge, Dr. Zilbermint noted.
The team is working on implementing automatic A1c testing for patients admitted with hyperglycemia who either have a history of diabetes or whose blood glucose level is >140 mg/dL. Dr. Zilbermint said, “it’s in the guidelines, but it’s not always done.”
Dr. Zilbermint is a consultant for Guidepoint. Dr. Maynard, Mr. Shelton, and Dr. Najmi have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Initiatives targeting hypoglycemia and insulin pen wastage could lead to dramatic cost savings in small community hospitals, new data suggest.
The two projects are part of a dedicated inpatient glucose management service led by Mihail (“Misha”) Zilbermint, MD, one of the few full-time endocrine hospitalists in the United States and one of even fewer who work at a small community hospital.
In 2019, Dr. Zilbermint and colleagues reported that their inpatient glucose management program resulted in a 27% reduction in length of stay and a 10.7% lower 30-day readmission rate. The projected cost savings for the period January 2016 to May 2017 was $953,578.
Dr. Zilbermint’s team has written two new articles that document cost savings for specific elements of the program; namely, a set of hospital-wide hypoglycemia prevention measures, and an initiative that reduced duplicate inpatient insulin pen dispensing.
About 1 in 4 people in U.S. hospitals have diabetes or hyperglycemia. Large academic hospitals have endocrine divisions and training programs, but 85% of people receive care at small community hospitals.
“There are management guidelines, but they’re not always followed ... That’s why I’ve been advocating for endocrine hospitalists to be deployed nationally,” Dr. Zilbermint said. He is chief and director of endocrinology, diabetes, and metabolism at Johns Hopkins Community Physicians at Suburban Hospital, Bethesda, Maryland.
Asked to comment on behalf of the Society of Hospital Medicine (SHM), Greg Maynard, MD, program lead for SHM’s Electronic Quality Improvement Programs, said that Suburban’s overall program goals align with those of the SHM.
“Dedicated inpatient glycemic control teams are very important and desirable to improve the quality and safety of care for inpatients with hyperglycemia and diabetes,” he said.
Regarding specific initiatives, such as those aimed at reducing hypoglycemia and insulin pen wastage, Dr. Maynard said, “All of these are feasible in a wide variety of institutions. The main barrier is getting the institutional support for people to work on these interventions. This series of studies can help spread the word about the positive return on investment.”
Another barrier – the current lack of publicly reported measures or pay-for-performance programs for hypoglycemia prevention and glycemic control – may soon change, added Dr. Maynard, who is also chief quality officer at the University of California, Davis, Medical Center.
“The National Quality Forum has endorsed new measures, and the CDC’s National Healthcare Safety Network is working on ways to augment those measures and embed them into their infrastructure,” he said.
Although SHM doesn’t specifically endorse full-time glycemic control hospitalists over endocrinology-trained glycemic control experts, “certainly hospitalists who accrue added training are very well positioned to be an important part of these interdisciplinary teams,” Dr. Maynard said.
‘The nurses were so afraid of hypoglycemia’
Tackling hypoglycemia was Dr. Zilbermint’s first priority when he started the glycemic management program at Suburban in late 2015.
“One of the most common complaints from the nurses was that a lot of their patients had hypoglycemia, especially in the ICU, when patients were placed on insulin infusion protocols ... Every time, the nurse would have to call the attending and ask what to do,” he explains.
In addition, Dr. Zilbermint says, there was no standard for treating hypoglycemia. A nurse in one unit would give two cups of juice, another a 50% dextrose infusion, or another, milk. Even more concerning, “the nurses were so afraid of hypoglycemia they would reflexively discontinue all insulin, including basal.”
So one of the new initiatives, led by Carter Shelton, MSHCM, an administrative fellow at the Medical University of South Carolina, Charleston, was to implement a set of hospital-wide hypoglycemia prevention measures, as described in an article published online April 21 in the Journal of Diabetes Science and Technology.
Inpatient hypoglycemia rate was cut nearly in half
This began in 2016, when the multidisciplinary Suburban Hospital Glucose Steering Committee identified four main causes of insulin-induced hypoglycemia (defined as a blood glucose level of ≤70 mg/dL in a patient who had received at least one dose of insulin in the past 24 hours) and devised solutions for each:
1. Lack of a unified hypoglycemia protocol. A formal, evidence-based, nurse-driven treatment protocol with clinical decision support in the electronic medical record was developed. The Suburban team adapted much of the protocol from one that had been recently implemented at the flagship Johns Hopkins Hospital, in Baltimore, Maryland.
According to that protocol, if patients are able to swallow, they are given 15 g or 30 g of carbohydrates in order to achieve a blood glucose level of 50 to 70 mg/dL and <50 mg/dL, respectively. Levels are checked 15 minutes later. Intravenous D50 or glucagon is reserved for patients who can’t swallow.
2. For patients in critical care, the insulin infusion protocol that had been in use set blood glucose targets of 80 to 110 mg/dL, which resulted in hypoglycemia in nearly every patient who received an insulin infusion. This protocol was changed to the currently recommended 140 to 180 mg/dL.
3. Most patients were managed with sliding-scale insulin, an outdated yet still widely used regimen whereby insulin is given based only on current blood glucose without accounting for carbohydrates consumed with meals and not corrected until the subsequent meal. This was changed so that nurses give insulin after the patient has consumed at least 50% of their meal carbohydrates.
4. Lack of hypoglycemia reporting. A glucometrics dashboard – now used throughout the Johns Hopkins system – was adopted to produce daily hypoglycemia reports in the EMR system that could be reviewed by the inpatient glucose management service to track quality metrics and plan further interventions.
Between Jan. 1, 2016, and Sept. 30, 2019, out of a total 49,315 patient-days, there were 2,682 days on which any hypoglycemia occurred and 874 days on which moderate hypoglycemia occurred (≤54 mg/dL). Type 2 diabetes accounted for 84.4% of the total patient-days; type 1 accounted for 4.4%.
The overall frequency of any hypoglycemia patient-days per month decreased from 7.5% to 3.9% during the study period (P = .001). This was significant for the patients with type 2 diabetes (7.4% to 3.8%; P < .0001) but not for those with type 1 diabetes (18.5% to 18.0%; P = .08).
Rates of moderate hypoglycemia also decreased significantly among the patients with type 2 diabetes (1.9% to 1.0%; P = .03) but not for those with type 1 diabetes (7.4% to 6.0%; P = .14).
On the basis of these rates in reducing hypoglycemia, in which the inpatient hypoglycemia rate was cut nearly in half, the estimated savings in cost of care to the hospital was $98,635 during the period of January 2016 to September 2019.
Reducing insulin pen waste by minimizing duplicate prescriptions
Suburban Hospital had been using insulin vials and syringes when Dr. Zilbermint first arrived there. He lobbied the administration to allow use of pens, because they’re easier to use and they reduce the risk for needlestick injuries. Nurses were educated and retrained monthly in their use.
The switch to pens – aspart (Novolog Flexpen) for bolus insulin and glargine (Lantus SoloSTAR) – took place in 2018. The cost of the aspart pen was $16.19, and the cost of glargine was $25.08. Each holds 300 units of insulin.
After the first month, the team noticed a large increase in expenses. A quality improvement project was devised to address the issue.
“We were dispensing sometimes three or four pens per person. That’s a lot. Each pen holds 300 units, so one pen should last the entire hospital stay of an average 4- or 5-day stay,” Dr. Zilbermint explained. “We had to figure out where we were bleeding the money and where the pens were going.”
When pens disappeared, the pharmacy would have to dispense new ones. One problem was that when patients were transferred from one unit to another, the pen would be left behind and the room would be cleaned. Sometimes the pens weren’t stored properly or were misplaced. Often, they’d end up in a nurse’s pocket.
The second intervention was led by Urooj Najmi, MD, of the American International School of Medicine, Atlanta, Georgia. A program was instituted to reduce duplicate inpatient insulin pen dispensing, as detailed in an article published in the same issue of the Journal of Diabetes Science and Technology.
Solutions to reduce duplicate pen dispensing included having pharmacy track daily insulin pen reports and monitor duplicate orders, with “do not dispense” instructions conveyed via the EMR system. All multidose medications, including insulin pens, were to be placed in patients’ bins at the nursing station, and nurses were instructed to look for patients’ insulin pens prior to their being transferred to another unit, rather than ask for a replacement pen.
From July 2018 to July 2019, 3,121 patients received insulin, of whom 95% received aspart and 47% received glargine. Of the 9,516 pens dispensed, 68% were for aspart and 32% were for glargine. During the study period, the number of pens dispensed per patient dropped from 2.2 to 1.2 for aspart and from 2.1 to 1.3 for glargine; differences were highly significant (P = .0002 and P = .0005, respectively).
The total amount of unnecessary dispensing during the first 4 months after initiating the pen implementation program was 58%. The average monthly cost was $11,820.68; the projected cost per year was $141,848.
Six months after the waste reduction strategies were implemented, monthly waste had dropped to 42%, translating to an estimated potential cost savings of $66,261 over 12 months.
Because Suburban Hospital doesn’t have an outpatient dispensing license, there is still wastage when patients are discharged, because they can’t take their pens home with them. That remains a challenge, Dr. Zilbermint noted.
The team is working on implementing automatic A1c testing for patients admitted with hyperglycemia who either have a history of diabetes or whose blood glucose level is >140 mg/dL. Dr. Zilbermint said, “it’s in the guidelines, but it’s not always done.”
Dr. Zilbermint is a consultant for Guidepoint. Dr. Maynard, Mr. Shelton, and Dr. Najmi have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Initiatives targeting hypoglycemia and insulin pen wastage could lead to dramatic cost savings in small community hospitals, new data suggest.
The two projects are part of a dedicated inpatient glucose management service led by Mihail (“Misha”) Zilbermint, MD, one of the few full-time endocrine hospitalists in the United States and one of even fewer who work at a small community hospital.
In 2019, Dr. Zilbermint and colleagues reported that their inpatient glucose management program resulted in a 27% reduction in length of stay and a 10.7% lower 30-day readmission rate. The projected cost savings for the period January 2016 to May 2017 was $953,578.
Dr. Zilbermint’s team has written two new articles that document cost savings for specific elements of the program; namely, a set of hospital-wide hypoglycemia prevention measures, and an initiative that reduced duplicate inpatient insulin pen dispensing.
About 1 in 4 people in U.S. hospitals have diabetes or hyperglycemia. Large academic hospitals have endocrine divisions and training programs, but 85% of people receive care at small community hospitals.
“There are management guidelines, but they’re not always followed ... That’s why I’ve been advocating for endocrine hospitalists to be deployed nationally,” Dr. Zilbermint said. He is chief and director of endocrinology, diabetes, and metabolism at Johns Hopkins Community Physicians at Suburban Hospital, Bethesda, Maryland.
Asked to comment on behalf of the Society of Hospital Medicine (SHM), Greg Maynard, MD, program lead for SHM’s Electronic Quality Improvement Programs, said that Suburban’s overall program goals align with those of the SHM.
“Dedicated inpatient glycemic control teams are very important and desirable to improve the quality and safety of care for inpatients with hyperglycemia and diabetes,” he said.
Regarding specific initiatives, such as those aimed at reducing hypoglycemia and insulin pen wastage, Dr. Maynard said, “All of these are feasible in a wide variety of institutions. The main barrier is getting the institutional support for people to work on these interventions. This series of studies can help spread the word about the positive return on investment.”
Another barrier – the current lack of publicly reported measures or pay-for-performance programs for hypoglycemia prevention and glycemic control – may soon change, added Dr. Maynard, who is also chief quality officer at the University of California, Davis, Medical Center.
“The National Quality Forum has endorsed new measures, and the CDC’s National Healthcare Safety Network is working on ways to augment those measures and embed them into their infrastructure,” he said.
Although SHM doesn’t specifically endorse full-time glycemic control hospitalists over endocrinology-trained glycemic control experts, “certainly hospitalists who accrue added training are very well positioned to be an important part of these interdisciplinary teams,” Dr. Maynard said.
‘The nurses were so afraid of hypoglycemia’
Tackling hypoglycemia was Dr. Zilbermint’s first priority when he started the glycemic management program at Suburban in late 2015.
“One of the most common complaints from the nurses was that a lot of their patients had hypoglycemia, especially in the ICU, when patients were placed on insulin infusion protocols ... Every time, the nurse would have to call the attending and ask what to do,” he explains.
In addition, Dr. Zilbermint says, there was no standard for treating hypoglycemia. A nurse in one unit would give two cups of juice, another a 50% dextrose infusion, or another, milk. Even more concerning, “the nurses were so afraid of hypoglycemia they would reflexively discontinue all insulin, including basal.”
So one of the new initiatives, led by Carter Shelton, MSHCM, an administrative fellow at the Medical University of South Carolina, Charleston, was to implement a set of hospital-wide hypoglycemia prevention measures, as described in an article published online April 21 in the Journal of Diabetes Science and Technology.
Inpatient hypoglycemia rate was cut nearly in half
This began in 2016, when the multidisciplinary Suburban Hospital Glucose Steering Committee identified four main causes of insulin-induced hypoglycemia (defined as a blood glucose level of ≤70 mg/dL in a patient who had received at least one dose of insulin in the past 24 hours) and devised solutions for each:
1. Lack of a unified hypoglycemia protocol. A formal, evidence-based, nurse-driven treatment protocol with clinical decision support in the electronic medical record was developed. The Suburban team adapted much of the protocol from one that had been recently implemented at the flagship Johns Hopkins Hospital, in Baltimore, Maryland.
According to that protocol, if patients are able to swallow, they are given 15 g or 30 g of carbohydrates in order to achieve a blood glucose level of 50 to 70 mg/dL and <50 mg/dL, respectively. Levels are checked 15 minutes later. Intravenous D50 or glucagon is reserved for patients who can’t swallow.
2. For patients in critical care, the insulin infusion protocol that had been in use set blood glucose targets of 80 to 110 mg/dL, which resulted in hypoglycemia in nearly every patient who received an insulin infusion. This protocol was changed to the currently recommended 140 to 180 mg/dL.
3. Most patients were managed with sliding-scale insulin, an outdated yet still widely used regimen whereby insulin is given based only on current blood glucose without accounting for carbohydrates consumed with meals and not corrected until the subsequent meal. This was changed so that nurses give insulin after the patient has consumed at least 50% of their meal carbohydrates.
4. Lack of hypoglycemia reporting. A glucometrics dashboard – now used throughout the Johns Hopkins system – was adopted to produce daily hypoglycemia reports in the EMR system that could be reviewed by the inpatient glucose management service to track quality metrics and plan further interventions.
Between Jan. 1, 2016, and Sept. 30, 2019, out of a total 49,315 patient-days, there were 2,682 days on which any hypoglycemia occurred and 874 days on which moderate hypoglycemia occurred (≤54 mg/dL). Type 2 diabetes accounted for 84.4% of the total patient-days; type 1 accounted for 4.4%.
The overall frequency of any hypoglycemia patient-days per month decreased from 7.5% to 3.9% during the study period (P = .001). This was significant for the patients with type 2 diabetes (7.4% to 3.8%; P < .0001) but not for those with type 1 diabetes (18.5% to 18.0%; P = .08).
Rates of moderate hypoglycemia also decreased significantly among the patients with type 2 diabetes (1.9% to 1.0%; P = .03) but not for those with type 1 diabetes (7.4% to 6.0%; P = .14).
On the basis of these rates in reducing hypoglycemia, in which the inpatient hypoglycemia rate was cut nearly in half, the estimated savings in cost of care to the hospital was $98,635 during the period of January 2016 to September 2019.
Reducing insulin pen waste by minimizing duplicate prescriptions
Suburban Hospital had been using insulin vials and syringes when Dr. Zilbermint first arrived there. He lobbied the administration to allow use of pens, because they’re easier to use and they reduce the risk for needlestick injuries. Nurses were educated and retrained monthly in their use.
The switch to pens – aspart (Novolog Flexpen) for bolus insulin and glargine (Lantus SoloSTAR) – took place in 2018. The cost of the aspart pen was $16.19, and the cost of glargine was $25.08. Each holds 300 units of insulin.
After the first month, the team noticed a large increase in expenses. A quality improvement project was devised to address the issue.
“We were dispensing sometimes three or four pens per person. That’s a lot. Each pen holds 300 units, so one pen should last the entire hospital stay of an average 4- or 5-day stay,” Dr. Zilbermint explained. “We had to figure out where we were bleeding the money and where the pens were going.”
When pens disappeared, the pharmacy would have to dispense new ones. One problem was that when patients were transferred from one unit to another, the pen would be left behind and the room would be cleaned. Sometimes the pens weren’t stored properly or were misplaced. Often, they’d end up in a nurse’s pocket.
The second intervention was led by Urooj Najmi, MD, of the American International School of Medicine, Atlanta, Georgia. A program was instituted to reduce duplicate inpatient insulin pen dispensing, as detailed in an article published in the same issue of the Journal of Diabetes Science and Technology.
Solutions to reduce duplicate pen dispensing included having pharmacy track daily insulin pen reports and monitor duplicate orders, with “do not dispense” instructions conveyed via the EMR system. All multidose medications, including insulin pens, were to be placed in patients’ bins at the nursing station, and nurses were instructed to look for patients’ insulin pens prior to their being transferred to another unit, rather than ask for a replacement pen.
From July 2018 to July 2019, 3,121 patients received insulin, of whom 95% received aspart and 47% received glargine. Of the 9,516 pens dispensed, 68% were for aspart and 32% were for glargine. During the study period, the number of pens dispensed per patient dropped from 2.2 to 1.2 for aspart and from 2.1 to 1.3 for glargine; differences were highly significant (P = .0002 and P = .0005, respectively).
The total amount of unnecessary dispensing during the first 4 months after initiating the pen implementation program was 58%. The average monthly cost was $11,820.68; the projected cost per year was $141,848.
Six months after the waste reduction strategies were implemented, monthly waste had dropped to 42%, translating to an estimated potential cost savings of $66,261 over 12 months.
Because Suburban Hospital doesn’t have an outpatient dispensing license, there is still wastage when patients are discharged, because they can’t take their pens home with them. That remains a challenge, Dr. Zilbermint noted.
The team is working on implementing automatic A1c testing for patients admitted with hyperglycemia who either have a history of diabetes or whose blood glucose level is >140 mg/dL. Dr. Zilbermint said, “it’s in the guidelines, but it’s not always done.”
Dr. Zilbermint is a consultant for Guidepoint. Dr. Maynard, Mr. Shelton, and Dr. Najmi have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Two treatments show early promise for hypothalamic obesity
Two different agents showed potential for safely treating patients with hypothalamic obesity in two pilot studies with small numbers of patients.
One study prospectively randomized 21 adults with acquired hypothalamic obesity to treatment with placebo or Tesomet, a compound that combines the novel monoamine reuptake inhibitor tesofensine with metoprolol, a beta-blocker added to protect against adverse effects from tesofensine on heart rate and cardiac contractility. After 24 weeks of treatment, people on tesofensine/metoprolol had significant weight loss, compared with controls, while showing good tolerance with no significant effects on heart rate, blood pressure, or heart rhythm, Ulla Feldt-Rasmussen, MD, DMSc, reported at the annual meeting of the Endocrine Society.
The second report reviewed 18 children and adolescents with either acquired or genetic hypothalamic obesity who received open-label treatment with dextroamphetamine for an average of 20 months, and overall patients safely lost an average of 0.43 in their body mass index (BMI) standard deviation score, reported Jiska van Schaik, MD, in a separate talk at the meeting.
‘A supplement for lost satiety’
Patients with hypothalamic obesity face a dual problem from hypothalamic dysfunction that’s addressed by tesofensine, the weight-loss agent in Tesomet that increases hypothalamic levels of dopamine, serotonin, and noradrenaline by blocking reuptake, and thereby dulls appetite and food craving while also increasing fat metabolism, explained Dr. Feldt-Rasmussen, a professor of medical endocrinology at the University of Denmark and Rigshospitalet in Copenhagen. No treatment currently has regulatory approval for treating any form of hypothalamic obesity.
Tesofensine works as “a supplement for lost satiety, and satiety is what is lost” in patients with hypothalamic obesity as well in patients as Prader-Willi syndrome, the two disorders for which tesofensine/metoprolol is currently undergoing testing. “That’s the rationale, and it seems to work,” she declared during her talk. The formulation contains 0.5 mg tesofensine and 50 mg metoprolol administered orally once daily.
The study, run at Rigshospitalet, randomized 21 patients aged 18-75 years and with a BMI of at least 27 kg/m2who all had acquired hypothalamic obesity secondary to hypothalamic damage following cancer treatment. Patients averaged about 45 years of age, three-quarters were women, and their average BMI was about 37, with 90% having a BMI of at least 30.
The study’s design calls for 48-week follow-up; Dr. Feldt-Rasmussen presented the interim results after 24 weeks, with 18 of the 21 enrolled patients remaining in the study through 24 weeks. Three patients dropped out because of adverse events: one in the placebo arm, and two who received tesofensine/metoprolol.
Weight dropped by an average of 6.6 kg from baseline among the 11 patients who completed 24 weeks on tesofensine/metoprolol treatment, compared with no average change from baseline among the seven patients who completed the study on placebo, a significant difference. The researchers measured a validated, composite satiety score every 4 weeks, and found significantly more improvement among patients on tesofensine/metoprolol than in those on placebo during the study’s first half, but subsequently average scores among the actively treated patients fell to the same level of modest improvement as in the placebo patients.
Despite this, average weight loss in the patients on tesofensine/metoprolol steadily increased throughout the full 24 weeks.
Safety measures of diastolic blood pressure, heart rate, and corrected QT interval showed no significant between-group difference. Systolic pressure showed a transient average rise of 4 mm Hg above baseline in the tesofensine/metoprolol group, compared with a small dip in the control patients, but by 24 weeks average systolic blood pressure had reverted closer to baseline levels in both subgroups and showed no significant between-group difference. Two patients on tesofensine/metoprolol developed serious adverse events. In one patient these were not treatment related. The other patient developed anxiety after 8 weeks that was possibly treatment related but remained on treatment. Other adverse effects on tesofensine/metoprolol included dizziness, sleep disorder, and dry mouth, but all of these were mild and patients were willing to tolerate them to achieve their weight loss, Dr. Feldt-Rasmussen said.
Repurposing an ADHD treatment
Dextroamphetamine increases satiety and boosts resting energy expenditure, and is a common treatment for attention deficit hyperactivity disorder. Dr. van Schaik and coauthors reviewed 13 children and adolescents with acquired hypothalamic obesity and 5 with genetic hypothalamic obesity who received the treatment at either of two Dutch hospitals during 2014-2020. All 18 patients went on dextroamphetamine after other interventions had failed to produce improvement, said Dr. van Schaik, a researcher at University Medical Center and Wilhelmina Children’s Hospital in Utrecht, the Netherlands. The patients averaged about 13 years of age.
In addition to an overall effect on weight across all 18 subjects, the researchers found they could subdivide the full cohort into 10 responders (56%), 4 (22%) with weight stabilization on treatment, and 4 nonresponders (22%) who continued to gain weight despite treatment. The 10 responding patients had an average drop in their BMI standard deviation score of 0.91. All 10 responders had acquired hypothalamic obesity, and they averaged a 12.5 percentage point rise in their resting energy expenditure level, compared with baseline, while on treatment. The four whose weight stabilized on treatment included three patients with genetic hypothalamic obesity. The four nonresponders split into two with acquired hypothalamic obesity and two with the genetic form.
Thirteen patients (72%) had improvements in hyperphagia, energy, and behavior, and no patient had a serious adverse effect. One patient stopped treatment after 1 month because of elevated blood pressure.
“Dextroamphetamine may be promising, especially for acquired hypothalamic obesity,” Dr. van Schaik concluded, adding that prospective, controlled assessments are needed, and that a healthy lifestyle is the foundation of hypothalamic obesity treatment.
The Tesomet study was sponsored by Saniona, the company developing Tesomet. Dr Feldt-Rasmussen is an advisor to Saniona, and some of the coauthors on the study are Saniona employees. Dr. van Schaik had no disclosures.
Two different agents showed potential for safely treating patients with hypothalamic obesity in two pilot studies with small numbers of patients.
One study prospectively randomized 21 adults with acquired hypothalamic obesity to treatment with placebo or Tesomet, a compound that combines the novel monoamine reuptake inhibitor tesofensine with metoprolol, a beta-blocker added to protect against adverse effects from tesofensine on heart rate and cardiac contractility. After 24 weeks of treatment, people on tesofensine/metoprolol had significant weight loss, compared with controls, while showing good tolerance with no significant effects on heart rate, blood pressure, or heart rhythm, Ulla Feldt-Rasmussen, MD, DMSc, reported at the annual meeting of the Endocrine Society.
The second report reviewed 18 children and adolescents with either acquired or genetic hypothalamic obesity who received open-label treatment with dextroamphetamine for an average of 20 months, and overall patients safely lost an average of 0.43 in their body mass index (BMI) standard deviation score, reported Jiska van Schaik, MD, in a separate talk at the meeting.
‘A supplement for lost satiety’
Patients with hypothalamic obesity face a dual problem from hypothalamic dysfunction that’s addressed by tesofensine, the weight-loss agent in Tesomet that increases hypothalamic levels of dopamine, serotonin, and noradrenaline by blocking reuptake, and thereby dulls appetite and food craving while also increasing fat metabolism, explained Dr. Feldt-Rasmussen, a professor of medical endocrinology at the University of Denmark and Rigshospitalet in Copenhagen. No treatment currently has regulatory approval for treating any form of hypothalamic obesity.
Tesofensine works as “a supplement for lost satiety, and satiety is what is lost” in patients with hypothalamic obesity as well in patients as Prader-Willi syndrome, the two disorders for which tesofensine/metoprolol is currently undergoing testing. “That’s the rationale, and it seems to work,” she declared during her talk. The formulation contains 0.5 mg tesofensine and 50 mg metoprolol administered orally once daily.
The study, run at Rigshospitalet, randomized 21 patients aged 18-75 years and with a BMI of at least 27 kg/m2who all had acquired hypothalamic obesity secondary to hypothalamic damage following cancer treatment. Patients averaged about 45 years of age, three-quarters were women, and their average BMI was about 37, with 90% having a BMI of at least 30.
The study’s design calls for 48-week follow-up; Dr. Feldt-Rasmussen presented the interim results after 24 weeks, with 18 of the 21 enrolled patients remaining in the study through 24 weeks. Three patients dropped out because of adverse events: one in the placebo arm, and two who received tesofensine/metoprolol.
Weight dropped by an average of 6.6 kg from baseline among the 11 patients who completed 24 weeks on tesofensine/metoprolol treatment, compared with no average change from baseline among the seven patients who completed the study on placebo, a significant difference. The researchers measured a validated, composite satiety score every 4 weeks, and found significantly more improvement among patients on tesofensine/metoprolol than in those on placebo during the study’s first half, but subsequently average scores among the actively treated patients fell to the same level of modest improvement as in the placebo patients.
Despite this, average weight loss in the patients on tesofensine/metoprolol steadily increased throughout the full 24 weeks.
Safety measures of diastolic blood pressure, heart rate, and corrected QT interval showed no significant between-group difference. Systolic pressure showed a transient average rise of 4 mm Hg above baseline in the tesofensine/metoprolol group, compared with a small dip in the control patients, but by 24 weeks average systolic blood pressure had reverted closer to baseline levels in both subgroups and showed no significant between-group difference. Two patients on tesofensine/metoprolol developed serious adverse events. In one patient these were not treatment related. The other patient developed anxiety after 8 weeks that was possibly treatment related but remained on treatment. Other adverse effects on tesofensine/metoprolol included dizziness, sleep disorder, and dry mouth, but all of these were mild and patients were willing to tolerate them to achieve their weight loss, Dr. Feldt-Rasmussen said.
Repurposing an ADHD treatment
Dextroamphetamine increases satiety and boosts resting energy expenditure, and is a common treatment for attention deficit hyperactivity disorder. Dr. van Schaik and coauthors reviewed 13 children and adolescents with acquired hypothalamic obesity and 5 with genetic hypothalamic obesity who received the treatment at either of two Dutch hospitals during 2014-2020. All 18 patients went on dextroamphetamine after other interventions had failed to produce improvement, said Dr. van Schaik, a researcher at University Medical Center and Wilhelmina Children’s Hospital in Utrecht, the Netherlands. The patients averaged about 13 years of age.
In addition to an overall effect on weight across all 18 subjects, the researchers found they could subdivide the full cohort into 10 responders (56%), 4 (22%) with weight stabilization on treatment, and 4 nonresponders (22%) who continued to gain weight despite treatment. The 10 responding patients had an average drop in their BMI standard deviation score of 0.91. All 10 responders had acquired hypothalamic obesity, and they averaged a 12.5 percentage point rise in their resting energy expenditure level, compared with baseline, while on treatment. The four whose weight stabilized on treatment included three patients with genetic hypothalamic obesity. The four nonresponders split into two with acquired hypothalamic obesity and two with the genetic form.
Thirteen patients (72%) had improvements in hyperphagia, energy, and behavior, and no patient had a serious adverse effect. One patient stopped treatment after 1 month because of elevated blood pressure.
“Dextroamphetamine may be promising, especially for acquired hypothalamic obesity,” Dr. van Schaik concluded, adding that prospective, controlled assessments are needed, and that a healthy lifestyle is the foundation of hypothalamic obesity treatment.
The Tesomet study was sponsored by Saniona, the company developing Tesomet. Dr Feldt-Rasmussen is an advisor to Saniona, and some of the coauthors on the study are Saniona employees. Dr. van Schaik had no disclosures.
Two different agents showed potential for safely treating patients with hypothalamic obesity in two pilot studies with small numbers of patients.
One study prospectively randomized 21 adults with acquired hypothalamic obesity to treatment with placebo or Tesomet, a compound that combines the novel monoamine reuptake inhibitor tesofensine with metoprolol, a beta-blocker added to protect against adverse effects from tesofensine on heart rate and cardiac contractility. After 24 weeks of treatment, people on tesofensine/metoprolol had significant weight loss, compared with controls, while showing good tolerance with no significant effects on heart rate, blood pressure, or heart rhythm, Ulla Feldt-Rasmussen, MD, DMSc, reported at the annual meeting of the Endocrine Society.
The second report reviewed 18 children and adolescents with either acquired or genetic hypothalamic obesity who received open-label treatment with dextroamphetamine for an average of 20 months, and overall patients safely lost an average of 0.43 in their body mass index (BMI) standard deviation score, reported Jiska van Schaik, MD, in a separate talk at the meeting.
‘A supplement for lost satiety’
Patients with hypothalamic obesity face a dual problem from hypothalamic dysfunction that’s addressed by tesofensine, the weight-loss agent in Tesomet that increases hypothalamic levels of dopamine, serotonin, and noradrenaline by blocking reuptake, and thereby dulls appetite and food craving while also increasing fat metabolism, explained Dr. Feldt-Rasmussen, a professor of medical endocrinology at the University of Denmark and Rigshospitalet in Copenhagen. No treatment currently has regulatory approval for treating any form of hypothalamic obesity.
Tesofensine works as “a supplement for lost satiety, and satiety is what is lost” in patients with hypothalamic obesity as well in patients as Prader-Willi syndrome, the two disorders for which tesofensine/metoprolol is currently undergoing testing. “That’s the rationale, and it seems to work,” she declared during her talk. The formulation contains 0.5 mg tesofensine and 50 mg metoprolol administered orally once daily.
The study, run at Rigshospitalet, randomized 21 patients aged 18-75 years and with a BMI of at least 27 kg/m2who all had acquired hypothalamic obesity secondary to hypothalamic damage following cancer treatment. Patients averaged about 45 years of age, three-quarters were women, and their average BMI was about 37, with 90% having a BMI of at least 30.
The study’s design calls for 48-week follow-up; Dr. Feldt-Rasmussen presented the interim results after 24 weeks, with 18 of the 21 enrolled patients remaining in the study through 24 weeks. Three patients dropped out because of adverse events: one in the placebo arm, and two who received tesofensine/metoprolol.
Weight dropped by an average of 6.6 kg from baseline among the 11 patients who completed 24 weeks on tesofensine/metoprolol treatment, compared with no average change from baseline among the seven patients who completed the study on placebo, a significant difference. The researchers measured a validated, composite satiety score every 4 weeks, and found significantly more improvement among patients on tesofensine/metoprolol than in those on placebo during the study’s first half, but subsequently average scores among the actively treated patients fell to the same level of modest improvement as in the placebo patients.
Despite this, average weight loss in the patients on tesofensine/metoprolol steadily increased throughout the full 24 weeks.
Safety measures of diastolic blood pressure, heart rate, and corrected QT interval showed no significant between-group difference. Systolic pressure showed a transient average rise of 4 mm Hg above baseline in the tesofensine/metoprolol group, compared with a small dip in the control patients, but by 24 weeks average systolic blood pressure had reverted closer to baseline levels in both subgroups and showed no significant between-group difference. Two patients on tesofensine/metoprolol developed serious adverse events. In one patient these were not treatment related. The other patient developed anxiety after 8 weeks that was possibly treatment related but remained on treatment. Other adverse effects on tesofensine/metoprolol included dizziness, sleep disorder, and dry mouth, but all of these were mild and patients were willing to tolerate them to achieve their weight loss, Dr. Feldt-Rasmussen said.
Repurposing an ADHD treatment
Dextroamphetamine increases satiety and boosts resting energy expenditure, and is a common treatment for attention deficit hyperactivity disorder. Dr. van Schaik and coauthors reviewed 13 children and adolescents with acquired hypothalamic obesity and 5 with genetic hypothalamic obesity who received the treatment at either of two Dutch hospitals during 2014-2020. All 18 patients went on dextroamphetamine after other interventions had failed to produce improvement, said Dr. van Schaik, a researcher at University Medical Center and Wilhelmina Children’s Hospital in Utrecht, the Netherlands. The patients averaged about 13 years of age.
In addition to an overall effect on weight across all 18 subjects, the researchers found they could subdivide the full cohort into 10 responders (56%), 4 (22%) with weight stabilization on treatment, and 4 nonresponders (22%) who continued to gain weight despite treatment. The 10 responding patients had an average drop in their BMI standard deviation score of 0.91. All 10 responders had acquired hypothalamic obesity, and they averaged a 12.5 percentage point rise in their resting energy expenditure level, compared with baseline, while on treatment. The four whose weight stabilized on treatment included three patients with genetic hypothalamic obesity. The four nonresponders split into two with acquired hypothalamic obesity and two with the genetic form.
Thirteen patients (72%) had improvements in hyperphagia, energy, and behavior, and no patient had a serious adverse effect. One patient stopped treatment after 1 month because of elevated blood pressure.
“Dextroamphetamine may be promising, especially for acquired hypothalamic obesity,” Dr. van Schaik concluded, adding that prospective, controlled assessments are needed, and that a healthy lifestyle is the foundation of hypothalamic obesity treatment.
The Tesomet study was sponsored by Saniona, the company developing Tesomet. Dr Feldt-Rasmussen is an advisor to Saniona, and some of the coauthors on the study are Saniona employees. Dr. van Schaik had no disclosures.
FROM ENDO 2021
‘Malicious peer review’ destroyed doc’s career, he says
Cardiothoracic surgeon J. Marvin Smith III, MD, had always thrived on a busy practice schedule, often performing 20-30 surgeries a week. A practicing surgeon for more than 40 years, Dr. Smith said he had no plans to slow down anytime soon.
But Dr. Smith said his career was derailed when leaders at Methodist Healthcare System of San Antonio initiated a sudden peer review proceeding against him. The hospital system alleged certain surgeries performed by Dr. Smith had excessive mortality rates. When he proved the data inaccurate, Dr. Smith said administrators next claimed he was cognitively impaired and wasn’t safe to practice.
Dr. Smith has now been embroiled in a peer review dispute with the hospital system for more than 2 years and says the conflict has essentially forced him out of surgical practice. He believes the peer review was “malicious” and was really launched because of complaints he made about nurse staffing and other issues at the hospital.
“I think it is absolutely in bad faith and is disingenuous what they’ve told me along the way,” said Dr. Smith, 73. “It’s because I pointed out deficiencies in nursing care, and they want to get rid of me. It would be a lot easier for them if I had a contract and they could control me better. But the fact that I was independent, meant they had to resort to a malicious peer review to try and push me out.”
Dr. Smith had a peer review hearing with Methodist in March 2021, and in April, a panel found in Dr. Smith’s favor, according to Dr. Smith. The findings were sent to the hospital’s medical board for review, which issued a decision in early May.
Eric A. Pullen, an attorney for Dr. Smith, said he could not go into detail about the board’s decision for legal reasons, but that “the medical board’s decision did not completely resolve the matter, and Dr. Smith intends to exercise his procedural rights, which could include an appeal.”
Methodist Hospital Texsan and its parent company, Methodist Health System of San Antonio, did not respond to messages seeking comment about the case. Without hearing from the hospital system, its side is unknown and it is unclear if there is more to the story from Methodist’s view.
The problem is not new, but some experts, such as Lawrence Huntoon, MD, PhD, say the practice has become more common in recent years, particularly against independent doctors.
Dr. Huntoon believes there is a nationwide trend at many hospitals to get rid of independent physicians and replace them with employed doctors, he said.
However, because most sham peer reviews go on behind closed doors, there are no data to pinpoint its prevalence or measure its growth.
“Independent physicians are basically being purged from medical staffs across the United States,” said Dr. Huntoon, who is chair of the Association of American Physicians and Surgeons’ Committee to Combat Sham Peer Review. “The hospitals want more control over how physicians practice and who they refer to, and they do that by having employees.”
Anthony P. Weiss, MD, MBA, chief medical officer for Beth Israel Deaconess Medical Center said it has not been his experience that independent physicians are being targeted in such a way. Dr. Weiss responded to an inquiry sent to the American Hospital Association for this story.
“As the authority for peer review rests with the organized medical staff (i.e., physicians), and not formally with the hospital per se, the peer review lever is not typically available as a management tool for hospital administration,” said Dr. Weiss, who is a former member of the AHA’s Committee on Clinical Leadership, but who was speaking on behalf of himself.
A spokesman for the AHA said the organization stands behinds Dr. Weiss’ comments.
Peer review remains a foundational aspect of overseeing the safety and appropriateness of healthcare provided by physicians, Dr. Weiss said. Peer review likely varies from hospital to hospital, he added, although the Healthcare Quality Improvement Act provides some level of guidance as does the American Medical Association Code of Medical Ethics (section 9.4.1).
“In essence, both require that the evaluation be conducted in good faith with the intention to improve care, by physicians with adequate training and knowledge, using a process that is fair and inclusive of the physician under review,” he said. “I believe that most medical staffs abide by these ethical principles, but we have little data to confirm this supposition.”
Did hospital target doc for being vocal?
When members of Methodist’s medical staff first approached Dr. Smith with concerns about his surgery outcomes in November 2018, the physician says he was surprised, but that he was open to an assessment.
“They came to me and said they thought my numbers were bad, and I said: ‘Well my gosh, I certainly don’t want that to be the case. I need to see what numbers you are talking about,’ ” Dr. Smith recalled. “I’ve been president of the Bexar County Medical Society; I’ve been involved with standards and ethics for the Society of Thoracic Surgeons. Quality health care means a whole lot to me.”
The statistical information provided by hospital administrators indicated that Dr. Smith’s mortality rates for coronary artery surgery in 2018 were “excessive” and that his rates for aortic surgery were “unacceptable,” according to a lawsuit Dr. Smith filed against the hospital system. Dr. Smith, who is double boarded with the American Board of Surgery and the American Board of Thoracic Surgery, said his outcomes had never come into question in the past. Dr. Smith said the timing was suspicious to him, however, considering he had recently raised concerns with the hospital through letters about nursing performance, staffing, and compensation.
A peer review investigation was initiated. In the meantime, Dr. Smith agreed to intensivist consults on his postoperative patients and consults with the hospital’s “Heart Team” on all preoperative cardiac, valve, and aortic cases. A vocal critic of the Heart Team, Dr. Smith had long contended the entity provided no meaningful benefit to his patients in most cases and, rather, increased hospital stays and raised medical expenses. Despite his agreement, Dr. Smith was later asked to voluntarily stop performing surgeries at the hospital.
“I agreed, convinced that we’d get this all settled,” he said.
Another report issued by the hospital in 2019 also indicated elevated mortality rates associated with some of Smith’s surgeries, although the document differed from the first report, according to the lawsuit. Dr. Smith says he was ignored when he pointed out problems with the data, including a lack of appropriate risk stratification in the report, departure from Society of Thoracic Surgeons data rules, and improper inclusion of his cases in the denominator of the ratio when a comparison was made of his outcomes with those hospitalwide. A subsequent report from Methodist in March 2019 indicated Dr. Smith’s surgery outcomes were “within the expected parameters of performance,” according to court documents.
The surgery accusations were dropped, but the peer review proceeding against Dr. Smith wasn’t over. The hospital next requested that Dr. Smith undergo a competency evaluation.
“When they realized the data was bad, they then changed their argument in the peer review proceeding and essentially started to argue that Dr. Smith had some sort of cognitive disability that prevented him from continuing to practice,” said Mr. Pullen. “The way I look at it, when the initial basis for the peer review was proven false, the hospital found something else and some other reason to try to keep Dr. Smith from practicing.”
Thus began a lengthy disagreement about which entity would conduct the evaluation, who would pay, and the type of acceptable assessment. An evaluation by the hospital’s preferred organization resulted in a finding of mild cognitive impairment, Dr. Smith said. He hired his own experts who conducted separate evaluations, finding no impairment and no basis for the former evaluation’s conclusion.
“Literally, the determinant as to whether I was normal or below normal on their test was one point, which was associated with a finding that I didn’t draw a clock correctly,” Dr. Smith claimed. “The reviewer said my minute hand was a little too short and docked me a point. It was purely subjective. To me, the gold standard of whether you are learned in thoracic surgery is the American Board of Thoracic Surgery’s test. The board’s test shows my cognitive ability is entirely in keeping with my practice. That contrasts with the one point off I got for drawing a clock wrong in somebody’s estimation.”
Conflict leads to legal case
In September 2020, Dr. Smith filed a lawsuit against Methodist Healthcare System of San Antonio, alleging business disparagement by Methodist for allegedly publishing false and disparaging information about Dr. Smith and tortious interference with business relations. The latter claim stems from Methodist refusing to provide documents to other hospitals about the status of Dr. Smith’s privileges at Methodist, Mr. Pullen said.
Because Methodist refused to confirm his status, the renewal process for Baptist Health System could not be completed and Dr. Smith lost his privileges at Baptist Health System facilities, according to the lawsuit.
Notably, Dr. Smith’s legal challenge also asks the court to take a stance against alleged amendments by Methodist to its Unified Medical Staff Bylaws. The hospital allegedly proposed changes that would prevent physicians from seeking legal action against the hospital for malicious peer review, according to Dr. Smith’s lawsuit.
The amendments would make the peer review process itself the “sole and exclusive remedy with respect to any action or recommendation taken at the hospital affecting medical staff appointment and/or clinical privileges,” according to an excerpt of the proposed amendments included in Dr. Smith’s lawsuit. In addition, the changes would hold practitioners liable for lost revenues if the doctor initiates “any type of legal action challenging credentialing, privileging, or other medical peer review or professional review activity,” according to the lawsuit.
Dr. Smith’s lawsuit seeks a declaration that the proposed amendments to the bylaws are “void as against public policy,” and a declaration that the proposed amendments to the bylaws cannot take away physicians’ statutory right to bring litigation against Methodist for malicious peer review.
“The proposed amendments have a tendency to and will injure the public good,” Dr. Smith argued in the lawsuit. “The proposed amendments allow Methodist to act with malice and in bad faith in conducting peer review proceedings and face no legal repercussions.”
Regardless of the final outcome of the peer review proceeding, Mr. Pullen said the harm Dr. Smith has already endured cannot be reversed.
“Even if comes out in his favor, the damage is already done,” he said. “It will not remedy the damage Dr. Smith has incurred.”
Fighting sham peer review is difficult
Battling a malicious peer review has long been an uphill battle for physicians, according to Dr. Huntoon. That’s because the Health Care Quality Improvement Act (HCQIA), a federal law passed in 1986, provides near absolute immunity to hospitals and peer reviewers in legal disputes.
The HCQIA was created by Congress to extend immunity to good-faith peer review of doctors and to increase overall participation in peer review by removing fear of litigation. However, the act has also enabled abuse of peer review by shielding bad-faith reviewers from accountability, said Dr. Huntoon.
“The Health Care Quality Improvement Act presumes that what the hospital did was warranted and reasonable and shifts the burden to the physician to prove his innocence by a preponderance of evidence,” he said. “That’s an entirely foreign concept to most people who think a person should be considered innocent until proven guilty. Here, it’s the exact opposite.”
The HCQIA has been challenged numerous times over the years and tested at the appellate level, but continues to survive and remain settled law, added Richard B. Willner, DPM, founder and director of the Center for Peer Review Justice, which assists and counsels physicians about sham peer review.
In 2011, former Rep. Joe Heck, DO, (R-Nev.) introduced a bill that would have amended the HCQIA to prohibit a professional review entity from submitting a report to the National Practitioner Data Bank (NPDB) while the doctor was still under investigation and before the doctor was afforded adequate notice and a hearing. Although the measure had 16 cosponsors and plenty of support from the physician community, it failed.
In addition to a heavy legal burden, physicians who experience malicious peer reviews also face ramifications from being reported to the NPDB. Peer review organizations are required to report certain negative actions or findings to the NPDB.
“A databank entry is a scarlet letter on your forehead,” Dr. Willner said. “The rules at a lot of institutions are not to take anyone who has been databanked, rightfully or wrongfully. And what is the evidence necessary to databank you? None. There’s no evidence needed to databank somebody.”
Despite the bleak landscape, experts say progress has been made on a case-by-case basis by physicians who have succeeded in fighting back against questionable peer reviews in recent years.
In January 2020, Indiana ob.gyn. Rebecca Denman, MD, prevailed in her defamation lawsuit against St Vincent Carmel Hospital and St Vincent Carmel Medical Group, winning $4.75 million in damages. Dr. Denman alleged administrators failed to conduct a proper peer review investigation after a false allegation by a nurse that she was under the influence while on the job.
Indianapolis attorney Kathleen A. DeLaney, who represented Dr. Denman, said hospital leaders misled Dr. Denman into believing a peer review had occurred when no formal peer review hearing or proceeding took place.
“The CMO of the medical group claimed that he performed a peer review ‘screening,’ but he never informed the other members of the peer review executive committee of the matter until after he had placed Dr. Denman on administrative leave,” Ms. DeLaney said. “He also neglected to tell the peer review executive committee that the substance abuse policy had not been followed, or that Dr. Denman had not been tested for alcohol use – due to the 12-hour delay in report.”
Dr. Denman was ultimately required to undergo an alcohol abuse evaluation, enter a treatment program, and sign a 5-year monitoring contract with the Indiana State Medical Association as a condition of her employment, according to the lawsuit. She claimed repercussions from the false allegation resulted in lost compensation, out-of-pocket expenses, emotional distress, and damage to her professional reputation.
She sued the hospital in July 2018, alleging fraud, defamation, tortious interference with an employment relationship, and negligent misrepresentation. After a 4-day trial, jurors found in her favor, awarding Dr. Denman $2 million for her defamation claims, $2 million for her claims of fraud and constructive fraud, $500,000 for her claim of tortious interference with an employment relationship, and $250,000 for her claim of negligent misrepresentation.
A hospital spokesperson said Ascension St Vincent is pursuing an appeal, and that it looks “forward to the opportunity to bring this matter before the Indiana Court of Appeals in June.”
In another case, South Dakota surgeon Linda Miller, MD, was awarded $1.1 million in 2017 after a federal jury found Huron Regional Medical Center breached her contract and violated her due process rights. Dr. Miller became the subject of a peer review at Huron Regional Medical Center when the hospital began analyzing some of her surgery outcomes.
Ken Barker, an attorney for Dr. Miller, said he feels it became evident at trial that the campaign to force Dr. Miller to either resign or lose her privileges was led by the lay board of directors of the hospital and upper-level administration at the hospital.
“They began the process by ordering an unprecedented 90-day review of her medical charts, looking for errors in the medical care she provided patients,” he said. “They could find nothing, so they did a second 90-day review, waiting for a patient’s ‘bad outcome.’ As any general surgeon will say, a ‘bad outcome’ is inevitable. And so it was. Upon that occurrence, they had a medical review committee review the patient’s chart and use it as an excuse to force her to reduce her privileges. Unbeknown to Dr. Miller, an external review had been conducted on another patient’s chart, in which the external review found her care above the standards and, in some measure, ‘exemplary.’ ”
Dr. Miller was eventually pressured to resign, according to her claim. Because of reports made to the NPDB by the medical center, including a patient complication that was allegedly falsified by the hospital, Dr. Miller said she was unable to find work as a general surgeon and went to work as a wound care doctor. At trial, jurors awarded Dr. Miller $586,617 in lost wages, $343,640 for lost future earning capacity, and $250,000 for mental anguish. (The mental anguish award was subsequently struck by a district court.)
Attorneys for Huron Regional Medical Center argued the jury improperly awarded damages and requested a new trial, which was denied by an appeals court.
In the end, the evidence came to light and the jury’s verdict spoke loudly that the hospital had taken unfair advantage of Dr. Miller, Mr. Barker said. But he emphasized that such cases often end differently.
“There are a handful of cases in which physicians like Dr. Miller have challenged the system and won,” he said. “In most cases, however, it is a ‘David vs. Goliath’ scenario where the giant prevails.”
What to do if faced with malicious peer review
An important step when doctors encounter a peer review that they believe is malicious is to consult with an experienced attorney as early as possible, Dr. Huntoon said. “Not all attorneys who set themselves out to be health law attorneys necessarily have knowledge and expertise in sham peer review. And before such a thing happens, I always encourage physicians to read their medical staff bylaws. That’s where everything is set forth, [such as] the corrective action section that tells how peer review is to take place.”
Mr. Barker added that documentation is also key in the event of a potential malicious peer review.
“When a physician senses [the] administration has targeted them, they should start documenting their conversations and actions very carefully, and if possible, recruit another ‘observer’ who can provide a third-party perspective, if necessary,” Mr. Barker said.
Dr. Huntoon recently wrote an article with advice about preparedness and defense of sham peer reviews. The guidance includes that physicians educate themselves about the tactics used by some hospitals to conduct sham peer reviews and the factors that place doctors more at risk. Factors that may raise a doctor’s danger of being targeted include being in solo practice or a small group, being new on staff, or being an older physician approaching retirement as some bad-actor hospitals may view older physicians as being less likely to fight back, said Dr. Huntoon.
Doctors should also keep detailed records and a timeline in the event of a malicious peer review and insist that an independent court reporter record all peer review hearings, even if that means the physician has to pay for the reporter him or herself, according to the guidance. An independent record is invaluable should the physician ultimately issue a future legal challenge against the hospital.
Mr. Willner encourages physicians to call the Center for Peer Review Justice hotline at (504) 621-1670 or visit the website for help with peer review and NPDB issues.
As for Dr. Smith, his days are much quieter and slower today, compared with the active practice he was accustomed to for more than half his life. He misses the fast pace, the patients, and the work that always brought him great joy.
“I hope to get back to doing surgeries eventually,” he said. “I graduated medical school in 1972. Practicing surgery has been my whole life and my career. They have taken my identity and my livelihood away from me based on false numbers and false premises. I want it back.”
A version of this article first appeared on Medscape.com.
Cardiothoracic surgeon J. Marvin Smith III, MD, had always thrived on a busy practice schedule, often performing 20-30 surgeries a week. A practicing surgeon for more than 40 years, Dr. Smith said he had no plans to slow down anytime soon.
But Dr. Smith said his career was derailed when leaders at Methodist Healthcare System of San Antonio initiated a sudden peer review proceeding against him. The hospital system alleged certain surgeries performed by Dr. Smith had excessive mortality rates. When he proved the data inaccurate, Dr. Smith said administrators next claimed he was cognitively impaired and wasn’t safe to practice.
Dr. Smith has now been embroiled in a peer review dispute with the hospital system for more than 2 years and says the conflict has essentially forced him out of surgical practice. He believes the peer review was “malicious” and was really launched because of complaints he made about nurse staffing and other issues at the hospital.
“I think it is absolutely in bad faith and is disingenuous what they’ve told me along the way,” said Dr. Smith, 73. “It’s because I pointed out deficiencies in nursing care, and they want to get rid of me. It would be a lot easier for them if I had a contract and they could control me better. But the fact that I was independent, meant they had to resort to a malicious peer review to try and push me out.”
Dr. Smith had a peer review hearing with Methodist in March 2021, and in April, a panel found in Dr. Smith’s favor, according to Dr. Smith. The findings were sent to the hospital’s medical board for review, which issued a decision in early May.
Eric A. Pullen, an attorney for Dr. Smith, said he could not go into detail about the board’s decision for legal reasons, but that “the medical board’s decision did not completely resolve the matter, and Dr. Smith intends to exercise his procedural rights, which could include an appeal.”
Methodist Hospital Texsan and its parent company, Methodist Health System of San Antonio, did not respond to messages seeking comment about the case. Without hearing from the hospital system, its side is unknown and it is unclear if there is more to the story from Methodist’s view.
The problem is not new, but some experts, such as Lawrence Huntoon, MD, PhD, say the practice has become more common in recent years, particularly against independent doctors.
Dr. Huntoon believes there is a nationwide trend at many hospitals to get rid of independent physicians and replace them with employed doctors, he said.
However, because most sham peer reviews go on behind closed doors, there are no data to pinpoint its prevalence or measure its growth.
“Independent physicians are basically being purged from medical staffs across the United States,” said Dr. Huntoon, who is chair of the Association of American Physicians and Surgeons’ Committee to Combat Sham Peer Review. “The hospitals want more control over how physicians practice and who they refer to, and they do that by having employees.”
Anthony P. Weiss, MD, MBA, chief medical officer for Beth Israel Deaconess Medical Center said it has not been his experience that independent physicians are being targeted in such a way. Dr. Weiss responded to an inquiry sent to the American Hospital Association for this story.
“As the authority for peer review rests with the organized medical staff (i.e., physicians), and not formally with the hospital per se, the peer review lever is not typically available as a management tool for hospital administration,” said Dr. Weiss, who is a former member of the AHA’s Committee on Clinical Leadership, but who was speaking on behalf of himself.
A spokesman for the AHA said the organization stands behinds Dr. Weiss’ comments.
Peer review remains a foundational aspect of overseeing the safety and appropriateness of healthcare provided by physicians, Dr. Weiss said. Peer review likely varies from hospital to hospital, he added, although the Healthcare Quality Improvement Act provides some level of guidance as does the American Medical Association Code of Medical Ethics (section 9.4.1).
“In essence, both require that the evaluation be conducted in good faith with the intention to improve care, by physicians with adequate training and knowledge, using a process that is fair and inclusive of the physician under review,” he said. “I believe that most medical staffs abide by these ethical principles, but we have little data to confirm this supposition.”
Did hospital target doc for being vocal?
When members of Methodist’s medical staff first approached Dr. Smith with concerns about his surgery outcomes in November 2018, the physician says he was surprised, but that he was open to an assessment.
“They came to me and said they thought my numbers were bad, and I said: ‘Well my gosh, I certainly don’t want that to be the case. I need to see what numbers you are talking about,’ ” Dr. Smith recalled. “I’ve been president of the Bexar County Medical Society; I’ve been involved with standards and ethics for the Society of Thoracic Surgeons. Quality health care means a whole lot to me.”
The statistical information provided by hospital administrators indicated that Dr. Smith’s mortality rates for coronary artery surgery in 2018 were “excessive” and that his rates for aortic surgery were “unacceptable,” according to a lawsuit Dr. Smith filed against the hospital system. Dr. Smith, who is double boarded with the American Board of Surgery and the American Board of Thoracic Surgery, said his outcomes had never come into question in the past. Dr. Smith said the timing was suspicious to him, however, considering he had recently raised concerns with the hospital through letters about nursing performance, staffing, and compensation.
A peer review investigation was initiated. In the meantime, Dr. Smith agreed to intensivist consults on his postoperative patients and consults with the hospital’s “Heart Team” on all preoperative cardiac, valve, and aortic cases. A vocal critic of the Heart Team, Dr. Smith had long contended the entity provided no meaningful benefit to his patients in most cases and, rather, increased hospital stays and raised medical expenses. Despite his agreement, Dr. Smith was later asked to voluntarily stop performing surgeries at the hospital.
“I agreed, convinced that we’d get this all settled,” he said.
Another report issued by the hospital in 2019 also indicated elevated mortality rates associated with some of Smith’s surgeries, although the document differed from the first report, according to the lawsuit. Dr. Smith says he was ignored when he pointed out problems with the data, including a lack of appropriate risk stratification in the report, departure from Society of Thoracic Surgeons data rules, and improper inclusion of his cases in the denominator of the ratio when a comparison was made of his outcomes with those hospitalwide. A subsequent report from Methodist in March 2019 indicated Dr. Smith’s surgery outcomes were “within the expected parameters of performance,” according to court documents.
The surgery accusations were dropped, but the peer review proceeding against Dr. Smith wasn’t over. The hospital next requested that Dr. Smith undergo a competency evaluation.
“When they realized the data was bad, they then changed their argument in the peer review proceeding and essentially started to argue that Dr. Smith had some sort of cognitive disability that prevented him from continuing to practice,” said Mr. Pullen. “The way I look at it, when the initial basis for the peer review was proven false, the hospital found something else and some other reason to try to keep Dr. Smith from practicing.”
Thus began a lengthy disagreement about which entity would conduct the evaluation, who would pay, and the type of acceptable assessment. An evaluation by the hospital’s preferred organization resulted in a finding of mild cognitive impairment, Dr. Smith said. He hired his own experts who conducted separate evaluations, finding no impairment and no basis for the former evaluation’s conclusion.
“Literally, the determinant as to whether I was normal or below normal on their test was one point, which was associated with a finding that I didn’t draw a clock correctly,” Dr. Smith claimed. “The reviewer said my minute hand was a little too short and docked me a point. It was purely subjective. To me, the gold standard of whether you are learned in thoracic surgery is the American Board of Thoracic Surgery’s test. The board’s test shows my cognitive ability is entirely in keeping with my practice. That contrasts with the one point off I got for drawing a clock wrong in somebody’s estimation.”
Conflict leads to legal case
In September 2020, Dr. Smith filed a lawsuit against Methodist Healthcare System of San Antonio, alleging business disparagement by Methodist for allegedly publishing false and disparaging information about Dr. Smith and tortious interference with business relations. The latter claim stems from Methodist refusing to provide documents to other hospitals about the status of Dr. Smith’s privileges at Methodist, Mr. Pullen said.
Because Methodist refused to confirm his status, the renewal process for Baptist Health System could not be completed and Dr. Smith lost his privileges at Baptist Health System facilities, according to the lawsuit.
Notably, Dr. Smith’s legal challenge also asks the court to take a stance against alleged amendments by Methodist to its Unified Medical Staff Bylaws. The hospital allegedly proposed changes that would prevent physicians from seeking legal action against the hospital for malicious peer review, according to Dr. Smith’s lawsuit.
The amendments would make the peer review process itself the “sole and exclusive remedy with respect to any action or recommendation taken at the hospital affecting medical staff appointment and/or clinical privileges,” according to an excerpt of the proposed amendments included in Dr. Smith’s lawsuit. In addition, the changes would hold practitioners liable for lost revenues if the doctor initiates “any type of legal action challenging credentialing, privileging, or other medical peer review or professional review activity,” according to the lawsuit.
Dr. Smith’s lawsuit seeks a declaration that the proposed amendments to the bylaws are “void as against public policy,” and a declaration that the proposed amendments to the bylaws cannot take away physicians’ statutory right to bring litigation against Methodist for malicious peer review.
“The proposed amendments have a tendency to and will injure the public good,” Dr. Smith argued in the lawsuit. “The proposed amendments allow Methodist to act with malice and in bad faith in conducting peer review proceedings and face no legal repercussions.”
Regardless of the final outcome of the peer review proceeding, Mr. Pullen said the harm Dr. Smith has already endured cannot be reversed.
“Even if comes out in his favor, the damage is already done,” he said. “It will not remedy the damage Dr. Smith has incurred.”
Fighting sham peer review is difficult
Battling a malicious peer review has long been an uphill battle for physicians, according to Dr. Huntoon. That’s because the Health Care Quality Improvement Act (HCQIA), a federal law passed in 1986, provides near absolute immunity to hospitals and peer reviewers in legal disputes.
The HCQIA was created by Congress to extend immunity to good-faith peer review of doctors and to increase overall participation in peer review by removing fear of litigation. However, the act has also enabled abuse of peer review by shielding bad-faith reviewers from accountability, said Dr. Huntoon.
“The Health Care Quality Improvement Act presumes that what the hospital did was warranted and reasonable and shifts the burden to the physician to prove his innocence by a preponderance of evidence,” he said. “That’s an entirely foreign concept to most people who think a person should be considered innocent until proven guilty. Here, it’s the exact opposite.”
The HCQIA has been challenged numerous times over the years and tested at the appellate level, but continues to survive and remain settled law, added Richard B. Willner, DPM, founder and director of the Center for Peer Review Justice, which assists and counsels physicians about sham peer review.
In 2011, former Rep. Joe Heck, DO, (R-Nev.) introduced a bill that would have amended the HCQIA to prohibit a professional review entity from submitting a report to the National Practitioner Data Bank (NPDB) while the doctor was still under investigation and before the doctor was afforded adequate notice and a hearing. Although the measure had 16 cosponsors and plenty of support from the physician community, it failed.
In addition to a heavy legal burden, physicians who experience malicious peer reviews also face ramifications from being reported to the NPDB. Peer review organizations are required to report certain negative actions or findings to the NPDB.
“A databank entry is a scarlet letter on your forehead,” Dr. Willner said. “The rules at a lot of institutions are not to take anyone who has been databanked, rightfully or wrongfully. And what is the evidence necessary to databank you? None. There’s no evidence needed to databank somebody.”
Despite the bleak landscape, experts say progress has been made on a case-by-case basis by physicians who have succeeded in fighting back against questionable peer reviews in recent years.
In January 2020, Indiana ob.gyn. Rebecca Denman, MD, prevailed in her defamation lawsuit against St Vincent Carmel Hospital and St Vincent Carmel Medical Group, winning $4.75 million in damages. Dr. Denman alleged administrators failed to conduct a proper peer review investigation after a false allegation by a nurse that she was under the influence while on the job.
Indianapolis attorney Kathleen A. DeLaney, who represented Dr. Denman, said hospital leaders misled Dr. Denman into believing a peer review had occurred when no formal peer review hearing or proceeding took place.
“The CMO of the medical group claimed that he performed a peer review ‘screening,’ but he never informed the other members of the peer review executive committee of the matter until after he had placed Dr. Denman on administrative leave,” Ms. DeLaney said. “He also neglected to tell the peer review executive committee that the substance abuse policy had not been followed, or that Dr. Denman had not been tested for alcohol use – due to the 12-hour delay in report.”
Dr. Denman was ultimately required to undergo an alcohol abuse evaluation, enter a treatment program, and sign a 5-year monitoring contract with the Indiana State Medical Association as a condition of her employment, according to the lawsuit. She claimed repercussions from the false allegation resulted in lost compensation, out-of-pocket expenses, emotional distress, and damage to her professional reputation.
She sued the hospital in July 2018, alleging fraud, defamation, tortious interference with an employment relationship, and negligent misrepresentation. After a 4-day trial, jurors found in her favor, awarding Dr. Denman $2 million for her defamation claims, $2 million for her claims of fraud and constructive fraud, $500,000 for her claim of tortious interference with an employment relationship, and $250,000 for her claim of negligent misrepresentation.
A hospital spokesperson said Ascension St Vincent is pursuing an appeal, and that it looks “forward to the opportunity to bring this matter before the Indiana Court of Appeals in June.”
In another case, South Dakota surgeon Linda Miller, MD, was awarded $1.1 million in 2017 after a federal jury found Huron Regional Medical Center breached her contract and violated her due process rights. Dr. Miller became the subject of a peer review at Huron Regional Medical Center when the hospital began analyzing some of her surgery outcomes.
Ken Barker, an attorney for Dr. Miller, said he feels it became evident at trial that the campaign to force Dr. Miller to either resign or lose her privileges was led by the lay board of directors of the hospital and upper-level administration at the hospital.
“They began the process by ordering an unprecedented 90-day review of her medical charts, looking for errors in the medical care she provided patients,” he said. “They could find nothing, so they did a second 90-day review, waiting for a patient’s ‘bad outcome.’ As any general surgeon will say, a ‘bad outcome’ is inevitable. And so it was. Upon that occurrence, they had a medical review committee review the patient’s chart and use it as an excuse to force her to reduce her privileges. Unbeknown to Dr. Miller, an external review had been conducted on another patient’s chart, in which the external review found her care above the standards and, in some measure, ‘exemplary.’ ”
Dr. Miller was eventually pressured to resign, according to her claim. Because of reports made to the NPDB by the medical center, including a patient complication that was allegedly falsified by the hospital, Dr. Miller said she was unable to find work as a general surgeon and went to work as a wound care doctor. At trial, jurors awarded Dr. Miller $586,617 in lost wages, $343,640 for lost future earning capacity, and $250,000 for mental anguish. (The mental anguish award was subsequently struck by a district court.)
Attorneys for Huron Regional Medical Center argued the jury improperly awarded damages and requested a new trial, which was denied by an appeals court.
In the end, the evidence came to light and the jury’s verdict spoke loudly that the hospital had taken unfair advantage of Dr. Miller, Mr. Barker said. But he emphasized that such cases often end differently.
“There are a handful of cases in which physicians like Dr. Miller have challenged the system and won,” he said. “In most cases, however, it is a ‘David vs. Goliath’ scenario where the giant prevails.”
What to do if faced with malicious peer review
An important step when doctors encounter a peer review that they believe is malicious is to consult with an experienced attorney as early as possible, Dr. Huntoon said. “Not all attorneys who set themselves out to be health law attorneys necessarily have knowledge and expertise in sham peer review. And before such a thing happens, I always encourage physicians to read their medical staff bylaws. That’s where everything is set forth, [such as] the corrective action section that tells how peer review is to take place.”
Mr. Barker added that documentation is also key in the event of a potential malicious peer review.
“When a physician senses [the] administration has targeted them, they should start documenting their conversations and actions very carefully, and if possible, recruit another ‘observer’ who can provide a third-party perspective, if necessary,” Mr. Barker said.
Dr. Huntoon recently wrote an article with advice about preparedness and defense of sham peer reviews. The guidance includes that physicians educate themselves about the tactics used by some hospitals to conduct sham peer reviews and the factors that place doctors more at risk. Factors that may raise a doctor’s danger of being targeted include being in solo practice or a small group, being new on staff, or being an older physician approaching retirement as some bad-actor hospitals may view older physicians as being less likely to fight back, said Dr. Huntoon.
Doctors should also keep detailed records and a timeline in the event of a malicious peer review and insist that an independent court reporter record all peer review hearings, even if that means the physician has to pay for the reporter him or herself, according to the guidance. An independent record is invaluable should the physician ultimately issue a future legal challenge against the hospital.
Mr. Willner encourages physicians to call the Center for Peer Review Justice hotline at (504) 621-1670 or visit the website for help with peer review and NPDB issues.
As for Dr. Smith, his days are much quieter and slower today, compared with the active practice he was accustomed to for more than half his life. He misses the fast pace, the patients, and the work that always brought him great joy.
“I hope to get back to doing surgeries eventually,” he said. “I graduated medical school in 1972. Practicing surgery has been my whole life and my career. They have taken my identity and my livelihood away from me based on false numbers and false premises. I want it back.”
A version of this article first appeared on Medscape.com.
Cardiothoracic surgeon J. Marvin Smith III, MD, had always thrived on a busy practice schedule, often performing 20-30 surgeries a week. A practicing surgeon for more than 40 years, Dr. Smith said he had no plans to slow down anytime soon.
But Dr. Smith said his career was derailed when leaders at Methodist Healthcare System of San Antonio initiated a sudden peer review proceeding against him. The hospital system alleged certain surgeries performed by Dr. Smith had excessive mortality rates. When he proved the data inaccurate, Dr. Smith said administrators next claimed he was cognitively impaired and wasn’t safe to practice.
Dr. Smith has now been embroiled in a peer review dispute with the hospital system for more than 2 years and says the conflict has essentially forced him out of surgical practice. He believes the peer review was “malicious” and was really launched because of complaints he made about nurse staffing and other issues at the hospital.
“I think it is absolutely in bad faith and is disingenuous what they’ve told me along the way,” said Dr. Smith, 73. “It’s because I pointed out deficiencies in nursing care, and they want to get rid of me. It would be a lot easier for them if I had a contract and they could control me better. But the fact that I was independent, meant they had to resort to a malicious peer review to try and push me out.”
Dr. Smith had a peer review hearing with Methodist in March 2021, and in April, a panel found in Dr. Smith’s favor, according to Dr. Smith. The findings were sent to the hospital’s medical board for review, which issued a decision in early May.
Eric A. Pullen, an attorney for Dr. Smith, said he could not go into detail about the board’s decision for legal reasons, but that “the medical board’s decision did not completely resolve the matter, and Dr. Smith intends to exercise his procedural rights, which could include an appeal.”
Methodist Hospital Texsan and its parent company, Methodist Health System of San Antonio, did not respond to messages seeking comment about the case. Without hearing from the hospital system, its side is unknown and it is unclear if there is more to the story from Methodist’s view.
The problem is not new, but some experts, such as Lawrence Huntoon, MD, PhD, say the practice has become more common in recent years, particularly against independent doctors.
Dr. Huntoon believes there is a nationwide trend at many hospitals to get rid of independent physicians and replace them with employed doctors, he said.
However, because most sham peer reviews go on behind closed doors, there are no data to pinpoint its prevalence or measure its growth.
“Independent physicians are basically being purged from medical staffs across the United States,” said Dr. Huntoon, who is chair of the Association of American Physicians and Surgeons’ Committee to Combat Sham Peer Review. “The hospitals want more control over how physicians practice and who they refer to, and they do that by having employees.”
Anthony P. Weiss, MD, MBA, chief medical officer for Beth Israel Deaconess Medical Center said it has not been his experience that independent physicians are being targeted in such a way. Dr. Weiss responded to an inquiry sent to the American Hospital Association for this story.
“As the authority for peer review rests with the organized medical staff (i.e., physicians), and not formally with the hospital per se, the peer review lever is not typically available as a management tool for hospital administration,” said Dr. Weiss, who is a former member of the AHA’s Committee on Clinical Leadership, but who was speaking on behalf of himself.
A spokesman for the AHA said the organization stands behinds Dr. Weiss’ comments.
Peer review remains a foundational aspect of overseeing the safety and appropriateness of healthcare provided by physicians, Dr. Weiss said. Peer review likely varies from hospital to hospital, he added, although the Healthcare Quality Improvement Act provides some level of guidance as does the American Medical Association Code of Medical Ethics (section 9.4.1).
“In essence, both require that the evaluation be conducted in good faith with the intention to improve care, by physicians with adequate training and knowledge, using a process that is fair and inclusive of the physician under review,” he said. “I believe that most medical staffs abide by these ethical principles, but we have little data to confirm this supposition.”
Did hospital target doc for being vocal?
When members of Methodist’s medical staff first approached Dr. Smith with concerns about his surgery outcomes in November 2018, the physician says he was surprised, but that he was open to an assessment.
“They came to me and said they thought my numbers were bad, and I said: ‘Well my gosh, I certainly don’t want that to be the case. I need to see what numbers you are talking about,’ ” Dr. Smith recalled. “I’ve been president of the Bexar County Medical Society; I’ve been involved with standards and ethics for the Society of Thoracic Surgeons. Quality health care means a whole lot to me.”
The statistical information provided by hospital administrators indicated that Dr. Smith’s mortality rates for coronary artery surgery in 2018 were “excessive” and that his rates for aortic surgery were “unacceptable,” according to a lawsuit Dr. Smith filed against the hospital system. Dr. Smith, who is double boarded with the American Board of Surgery and the American Board of Thoracic Surgery, said his outcomes had never come into question in the past. Dr. Smith said the timing was suspicious to him, however, considering he had recently raised concerns with the hospital through letters about nursing performance, staffing, and compensation.
A peer review investigation was initiated. In the meantime, Dr. Smith agreed to intensivist consults on his postoperative patients and consults with the hospital’s “Heart Team” on all preoperative cardiac, valve, and aortic cases. A vocal critic of the Heart Team, Dr. Smith had long contended the entity provided no meaningful benefit to his patients in most cases and, rather, increased hospital stays and raised medical expenses. Despite his agreement, Dr. Smith was later asked to voluntarily stop performing surgeries at the hospital.
“I agreed, convinced that we’d get this all settled,” he said.
Another report issued by the hospital in 2019 also indicated elevated mortality rates associated with some of Smith’s surgeries, although the document differed from the first report, according to the lawsuit. Dr. Smith says he was ignored when he pointed out problems with the data, including a lack of appropriate risk stratification in the report, departure from Society of Thoracic Surgeons data rules, and improper inclusion of his cases in the denominator of the ratio when a comparison was made of his outcomes with those hospitalwide. A subsequent report from Methodist in March 2019 indicated Dr. Smith’s surgery outcomes were “within the expected parameters of performance,” according to court documents.
The surgery accusations were dropped, but the peer review proceeding against Dr. Smith wasn’t over. The hospital next requested that Dr. Smith undergo a competency evaluation.
“When they realized the data was bad, they then changed their argument in the peer review proceeding and essentially started to argue that Dr. Smith had some sort of cognitive disability that prevented him from continuing to practice,” said Mr. Pullen. “The way I look at it, when the initial basis for the peer review was proven false, the hospital found something else and some other reason to try to keep Dr. Smith from practicing.”
Thus began a lengthy disagreement about which entity would conduct the evaluation, who would pay, and the type of acceptable assessment. An evaluation by the hospital’s preferred organization resulted in a finding of mild cognitive impairment, Dr. Smith said. He hired his own experts who conducted separate evaluations, finding no impairment and no basis for the former evaluation’s conclusion.
“Literally, the determinant as to whether I was normal or below normal on their test was one point, which was associated with a finding that I didn’t draw a clock correctly,” Dr. Smith claimed. “The reviewer said my minute hand was a little too short and docked me a point. It was purely subjective. To me, the gold standard of whether you are learned in thoracic surgery is the American Board of Thoracic Surgery’s test. The board’s test shows my cognitive ability is entirely in keeping with my practice. That contrasts with the one point off I got for drawing a clock wrong in somebody’s estimation.”
Conflict leads to legal case
In September 2020, Dr. Smith filed a lawsuit against Methodist Healthcare System of San Antonio, alleging business disparagement by Methodist for allegedly publishing false and disparaging information about Dr. Smith and tortious interference with business relations. The latter claim stems from Methodist refusing to provide documents to other hospitals about the status of Dr. Smith’s privileges at Methodist, Mr. Pullen said.
Because Methodist refused to confirm his status, the renewal process for Baptist Health System could not be completed and Dr. Smith lost his privileges at Baptist Health System facilities, according to the lawsuit.
Notably, Dr. Smith’s legal challenge also asks the court to take a stance against alleged amendments by Methodist to its Unified Medical Staff Bylaws. The hospital allegedly proposed changes that would prevent physicians from seeking legal action against the hospital for malicious peer review, according to Dr. Smith’s lawsuit.
The amendments would make the peer review process itself the “sole and exclusive remedy with respect to any action or recommendation taken at the hospital affecting medical staff appointment and/or clinical privileges,” according to an excerpt of the proposed amendments included in Dr. Smith’s lawsuit. In addition, the changes would hold practitioners liable for lost revenues if the doctor initiates “any type of legal action challenging credentialing, privileging, or other medical peer review or professional review activity,” according to the lawsuit.
Dr. Smith’s lawsuit seeks a declaration that the proposed amendments to the bylaws are “void as against public policy,” and a declaration that the proposed amendments to the bylaws cannot take away physicians’ statutory right to bring litigation against Methodist for malicious peer review.
“The proposed amendments have a tendency to and will injure the public good,” Dr. Smith argued in the lawsuit. “The proposed amendments allow Methodist to act with malice and in bad faith in conducting peer review proceedings and face no legal repercussions.”
Regardless of the final outcome of the peer review proceeding, Mr. Pullen said the harm Dr. Smith has already endured cannot be reversed.
“Even if comes out in his favor, the damage is already done,” he said. “It will not remedy the damage Dr. Smith has incurred.”
Fighting sham peer review is difficult
Battling a malicious peer review has long been an uphill battle for physicians, according to Dr. Huntoon. That’s because the Health Care Quality Improvement Act (HCQIA), a federal law passed in 1986, provides near absolute immunity to hospitals and peer reviewers in legal disputes.
The HCQIA was created by Congress to extend immunity to good-faith peer review of doctors and to increase overall participation in peer review by removing fear of litigation. However, the act has also enabled abuse of peer review by shielding bad-faith reviewers from accountability, said Dr. Huntoon.
“The Health Care Quality Improvement Act presumes that what the hospital did was warranted and reasonable and shifts the burden to the physician to prove his innocence by a preponderance of evidence,” he said. “That’s an entirely foreign concept to most people who think a person should be considered innocent until proven guilty. Here, it’s the exact opposite.”
The HCQIA has been challenged numerous times over the years and tested at the appellate level, but continues to survive and remain settled law, added Richard B. Willner, DPM, founder and director of the Center for Peer Review Justice, which assists and counsels physicians about sham peer review.
In 2011, former Rep. Joe Heck, DO, (R-Nev.) introduced a bill that would have amended the HCQIA to prohibit a professional review entity from submitting a report to the National Practitioner Data Bank (NPDB) while the doctor was still under investigation and before the doctor was afforded adequate notice and a hearing. Although the measure had 16 cosponsors and plenty of support from the physician community, it failed.
In addition to a heavy legal burden, physicians who experience malicious peer reviews also face ramifications from being reported to the NPDB. Peer review organizations are required to report certain negative actions or findings to the NPDB.
“A databank entry is a scarlet letter on your forehead,” Dr. Willner said. “The rules at a lot of institutions are not to take anyone who has been databanked, rightfully or wrongfully. And what is the evidence necessary to databank you? None. There’s no evidence needed to databank somebody.”
Despite the bleak landscape, experts say progress has been made on a case-by-case basis by physicians who have succeeded in fighting back against questionable peer reviews in recent years.
In January 2020, Indiana ob.gyn. Rebecca Denman, MD, prevailed in her defamation lawsuit against St Vincent Carmel Hospital and St Vincent Carmel Medical Group, winning $4.75 million in damages. Dr. Denman alleged administrators failed to conduct a proper peer review investigation after a false allegation by a nurse that she was under the influence while on the job.
Indianapolis attorney Kathleen A. DeLaney, who represented Dr. Denman, said hospital leaders misled Dr. Denman into believing a peer review had occurred when no formal peer review hearing or proceeding took place.
“The CMO of the medical group claimed that he performed a peer review ‘screening,’ but he never informed the other members of the peer review executive committee of the matter until after he had placed Dr. Denman on administrative leave,” Ms. DeLaney said. “He also neglected to tell the peer review executive committee that the substance abuse policy had not been followed, or that Dr. Denman had not been tested for alcohol use – due to the 12-hour delay in report.”
Dr. Denman was ultimately required to undergo an alcohol abuse evaluation, enter a treatment program, and sign a 5-year monitoring contract with the Indiana State Medical Association as a condition of her employment, according to the lawsuit. She claimed repercussions from the false allegation resulted in lost compensation, out-of-pocket expenses, emotional distress, and damage to her professional reputation.
She sued the hospital in July 2018, alleging fraud, defamation, tortious interference with an employment relationship, and negligent misrepresentation. After a 4-day trial, jurors found in her favor, awarding Dr. Denman $2 million for her defamation claims, $2 million for her claims of fraud and constructive fraud, $500,000 for her claim of tortious interference with an employment relationship, and $250,000 for her claim of negligent misrepresentation.
A hospital spokesperson said Ascension St Vincent is pursuing an appeal, and that it looks “forward to the opportunity to bring this matter before the Indiana Court of Appeals in June.”
In another case, South Dakota surgeon Linda Miller, MD, was awarded $1.1 million in 2017 after a federal jury found Huron Regional Medical Center breached her contract and violated her due process rights. Dr. Miller became the subject of a peer review at Huron Regional Medical Center when the hospital began analyzing some of her surgery outcomes.
Ken Barker, an attorney for Dr. Miller, said he feels it became evident at trial that the campaign to force Dr. Miller to either resign or lose her privileges was led by the lay board of directors of the hospital and upper-level administration at the hospital.
“They began the process by ordering an unprecedented 90-day review of her medical charts, looking for errors in the medical care she provided patients,” he said. “They could find nothing, so they did a second 90-day review, waiting for a patient’s ‘bad outcome.’ As any general surgeon will say, a ‘bad outcome’ is inevitable. And so it was. Upon that occurrence, they had a medical review committee review the patient’s chart and use it as an excuse to force her to reduce her privileges. Unbeknown to Dr. Miller, an external review had been conducted on another patient’s chart, in which the external review found her care above the standards and, in some measure, ‘exemplary.’ ”
Dr. Miller was eventually pressured to resign, according to her claim. Because of reports made to the NPDB by the medical center, including a patient complication that was allegedly falsified by the hospital, Dr. Miller said she was unable to find work as a general surgeon and went to work as a wound care doctor. At trial, jurors awarded Dr. Miller $586,617 in lost wages, $343,640 for lost future earning capacity, and $250,000 for mental anguish. (The mental anguish award was subsequently struck by a district court.)
Attorneys for Huron Regional Medical Center argued the jury improperly awarded damages and requested a new trial, which was denied by an appeals court.
In the end, the evidence came to light and the jury’s verdict spoke loudly that the hospital had taken unfair advantage of Dr. Miller, Mr. Barker said. But he emphasized that such cases often end differently.
“There are a handful of cases in which physicians like Dr. Miller have challenged the system and won,” he said. “In most cases, however, it is a ‘David vs. Goliath’ scenario where the giant prevails.”
What to do if faced with malicious peer review
An important step when doctors encounter a peer review that they believe is malicious is to consult with an experienced attorney as early as possible, Dr. Huntoon said. “Not all attorneys who set themselves out to be health law attorneys necessarily have knowledge and expertise in sham peer review. And before such a thing happens, I always encourage physicians to read their medical staff bylaws. That’s where everything is set forth, [such as] the corrective action section that tells how peer review is to take place.”
Mr. Barker added that documentation is also key in the event of a potential malicious peer review.
“When a physician senses [the] administration has targeted them, they should start documenting their conversations and actions very carefully, and if possible, recruit another ‘observer’ who can provide a third-party perspective, if necessary,” Mr. Barker said.
Dr. Huntoon recently wrote an article with advice about preparedness and defense of sham peer reviews. The guidance includes that physicians educate themselves about the tactics used by some hospitals to conduct sham peer reviews and the factors that place doctors more at risk. Factors that may raise a doctor’s danger of being targeted include being in solo practice or a small group, being new on staff, or being an older physician approaching retirement as some bad-actor hospitals may view older physicians as being less likely to fight back, said Dr. Huntoon.
Doctors should also keep detailed records and a timeline in the event of a malicious peer review and insist that an independent court reporter record all peer review hearings, even if that means the physician has to pay for the reporter him or herself, according to the guidance. An independent record is invaluable should the physician ultimately issue a future legal challenge against the hospital.
Mr. Willner encourages physicians to call the Center for Peer Review Justice hotline at (504) 621-1670 or visit the website for help with peer review and NPDB issues.
As for Dr. Smith, his days are much quieter and slower today, compared with the active practice he was accustomed to for more than half his life. He misses the fast pace, the patients, and the work that always brought him great joy.
“I hope to get back to doing surgeries eventually,” he said. “I graduated medical school in 1972. Practicing surgery has been my whole life and my career. They have taken my identity and my livelihood away from me based on false numbers and false premises. I want it back.”
A version of this article first appeared on Medscape.com.
Possible obesity effect detected in cancer death rates
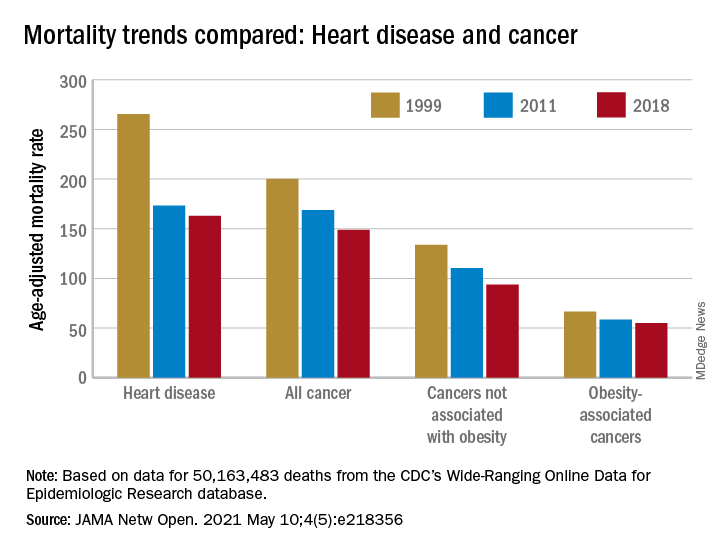
“By integrating 20 years of cancer mortality data, we demonstrated that trends in obesity-associated cancer mortality showed signs of recent deceleration, consistent with recent findings for heart disease mortality,” Christy L. Avery, PhD, and associates wrote in JAMA Network Open.
Improvements in mortality related to heart disease slowed after 2011, a phenomenon that has been associated with rising obesity rates. The age-adjusted mortality rate (AAMR) declined at an average of 3.8 deaths per 100,000 persons from 1999 to 2011 but only 0.7 deaths per 100,000 from 2011 to 2018, based on data from the Centers for Disease Control and Prevention’s Wide-Ranging Online Data for Epidemiologic Research (WONDER).
To understand trends in cancer mortality and their possible connection with obesity, data for 1999-2018 from the WONDER database were divided into obesity-associated and non–obesity-associated categories and compared with heart disease mortality, they explained. The database included more than 50 million deaths that matched inclusion criteria.
The analysis showed there was difference between obesity-associated and non–obesity-associated cancers that was obscured when all cancer deaths were considered together. The average annual change in AAMR for obesity-associated cancers slowed from –1.19 deaths per 100,000 in 1999-2011 to –0.83 in 2011-2018, Dr. Avery and associates reported.
For non–obesity-associated cancers, the annual change in AAMR increased from –1.62 per 100,000 for 1999-2011 to –2.29 for 2011-2018, following the trend for all cancers: –1.48 per 100,000 during 1999-2011 and –1.77 in 2011-2018, they said.
“The largest mortality decreases were observed for melanoma of the skin and lung cancer, two cancers not associated with obesity. For obesity-associated cancers, stable or increasing mortality rates have been observed for liver and pancreatic cancer among both men and women as well as for uterine cancer among women,” the investigators wrote.
Demographically, however, the slowing improvement in mortality for obesity-associated cancers did not follow the trend for heart disease. The deceleration for cancer was more pronounced for women and for non-Hispanic Whites and not seen at all in non-Hispanic Asian/Pacific Islander individuals. “For heart disease, evidence of a deceleration was consistent across sex, race, and ethnicity,” they said.
There are “longstanding disparities in obesity” among various populations in the United States, and the recent trend of obesity occurring earlier in life may be having an effect. “Whether the findings of decelerating mortality rates potentially signal a changing profile of cancer and heart disease mortality as the consequences of the obesity epidemic are realized remains to be seen,” they concluded.
The investigators reported receiving grants from the National Institutes of Health during the conduct of the study, but no other disclosures were reported.
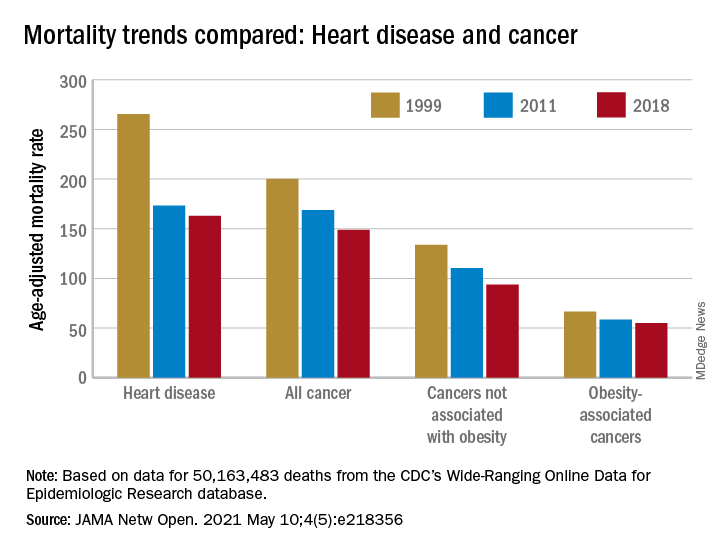
“By integrating 20 years of cancer mortality data, we demonstrated that trends in obesity-associated cancer mortality showed signs of recent deceleration, consistent with recent findings for heart disease mortality,” Christy L. Avery, PhD, and associates wrote in JAMA Network Open.
Improvements in mortality related to heart disease slowed after 2011, a phenomenon that has been associated with rising obesity rates. The age-adjusted mortality rate (AAMR) declined at an average of 3.8 deaths per 100,000 persons from 1999 to 2011 but only 0.7 deaths per 100,000 from 2011 to 2018, based on data from the Centers for Disease Control and Prevention’s Wide-Ranging Online Data for Epidemiologic Research (WONDER).
To understand trends in cancer mortality and their possible connection with obesity, data for 1999-2018 from the WONDER database were divided into obesity-associated and non–obesity-associated categories and compared with heart disease mortality, they explained. The database included more than 50 million deaths that matched inclusion criteria.
The analysis showed there was difference between obesity-associated and non–obesity-associated cancers that was obscured when all cancer deaths were considered together. The average annual change in AAMR for obesity-associated cancers slowed from –1.19 deaths per 100,000 in 1999-2011 to –0.83 in 2011-2018, Dr. Avery and associates reported.
For non–obesity-associated cancers, the annual change in AAMR increased from –1.62 per 100,000 for 1999-2011 to –2.29 for 2011-2018, following the trend for all cancers: –1.48 per 100,000 during 1999-2011 and –1.77 in 2011-2018, they said.
“The largest mortality decreases were observed for melanoma of the skin and lung cancer, two cancers not associated with obesity. For obesity-associated cancers, stable or increasing mortality rates have been observed for liver and pancreatic cancer among both men and women as well as for uterine cancer among women,” the investigators wrote.
Demographically, however, the slowing improvement in mortality for obesity-associated cancers did not follow the trend for heart disease. The deceleration for cancer was more pronounced for women and for non-Hispanic Whites and not seen at all in non-Hispanic Asian/Pacific Islander individuals. “For heart disease, evidence of a deceleration was consistent across sex, race, and ethnicity,” they said.
There are “longstanding disparities in obesity” among various populations in the United States, and the recent trend of obesity occurring earlier in life may be having an effect. “Whether the findings of decelerating mortality rates potentially signal a changing profile of cancer and heart disease mortality as the consequences of the obesity epidemic are realized remains to be seen,” they concluded.
The investigators reported receiving grants from the National Institutes of Health during the conduct of the study, but no other disclosures were reported.
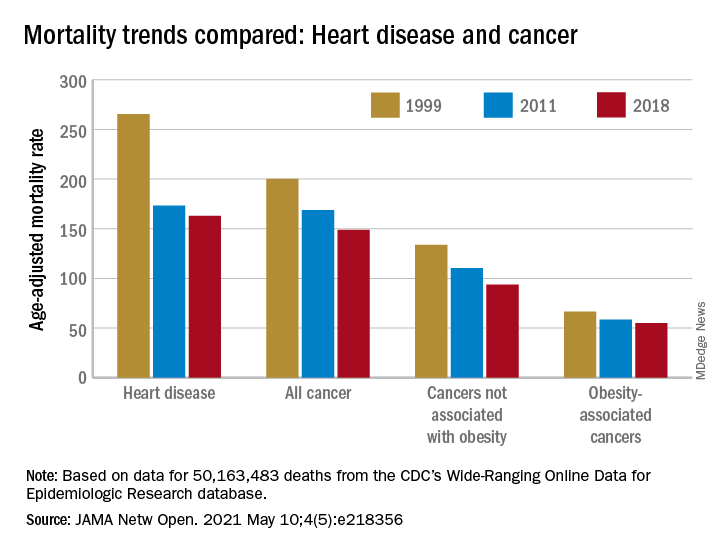
“By integrating 20 years of cancer mortality data, we demonstrated that trends in obesity-associated cancer mortality showed signs of recent deceleration, consistent with recent findings for heart disease mortality,” Christy L. Avery, PhD, and associates wrote in JAMA Network Open.
Improvements in mortality related to heart disease slowed after 2011, a phenomenon that has been associated with rising obesity rates. The age-adjusted mortality rate (AAMR) declined at an average of 3.8 deaths per 100,000 persons from 1999 to 2011 but only 0.7 deaths per 100,000 from 2011 to 2018, based on data from the Centers for Disease Control and Prevention’s Wide-Ranging Online Data for Epidemiologic Research (WONDER).
To understand trends in cancer mortality and their possible connection with obesity, data for 1999-2018 from the WONDER database were divided into obesity-associated and non–obesity-associated categories and compared with heart disease mortality, they explained. The database included more than 50 million deaths that matched inclusion criteria.
The analysis showed there was difference between obesity-associated and non–obesity-associated cancers that was obscured when all cancer deaths were considered together. The average annual change in AAMR for obesity-associated cancers slowed from –1.19 deaths per 100,000 in 1999-2011 to –0.83 in 2011-2018, Dr. Avery and associates reported.
For non–obesity-associated cancers, the annual change in AAMR increased from –1.62 per 100,000 for 1999-2011 to –2.29 for 2011-2018, following the trend for all cancers: –1.48 per 100,000 during 1999-2011 and –1.77 in 2011-2018, they said.
“The largest mortality decreases were observed for melanoma of the skin and lung cancer, two cancers not associated with obesity. For obesity-associated cancers, stable or increasing mortality rates have been observed for liver and pancreatic cancer among both men and women as well as for uterine cancer among women,” the investigators wrote.
Demographically, however, the slowing improvement in mortality for obesity-associated cancers did not follow the trend for heart disease. The deceleration for cancer was more pronounced for women and for non-Hispanic Whites and not seen at all in non-Hispanic Asian/Pacific Islander individuals. “For heart disease, evidence of a deceleration was consistent across sex, race, and ethnicity,” they said.
There are “longstanding disparities in obesity” among various populations in the United States, and the recent trend of obesity occurring earlier in life may be having an effect. “Whether the findings of decelerating mortality rates potentially signal a changing profile of cancer and heart disease mortality as the consequences of the obesity epidemic are realized remains to be seen,” they concluded.
The investigators reported receiving grants from the National Institutes of Health during the conduct of the study, but no other disclosures were reported.
FROM JAMA NETWORK OPEN
A simple new definition for ‘metabolically healthy obesity’?
Scientists have proposed a simple new definition for “metabolically healthy obesity” to identify individuals who do not have an increased risk of cardiovascular disease (CVD) death and total mortality.
The team – led by Anika Zembic, MPH, German Institute of Human Nutrition Potsdam-Rehbruecke, Nuthetal, Germany – performed an assessment of anthropometric and metabolic risk factors as well as mortality data from two cohorts that “yielded a simple definition to categorize participants with obesity as metabolically healthy or unhealthy.”
They defined “metabolically healthy” as systolic blood pressure <130 mm Hg and no use of blood pressure-lowering medication; waist-to-hip ratio <0.95 (in women) and <1.03 (in men); and no prevalent type 2 diabetes.
Based on this new definition, 42% of participants in the third U.S. National Health and Nutrition Examination Survey (NHANES-III) and 19% of participants in the UK Biobank study had metabolically healthy obesity and did not have an increased risk for CVD mortality and total mortality compared with individuals with metabolically healthy normal weight.
“People with a phenotype defined as metabolically unhealthy using this definition had significantly higher hazard ratios for [CVD] mortality and total mortality irrespective of body mass index category, and people with phenotypes defined as having metabolically healthy obesity displayed no increased risk,” the researchers noted in their article, published May 7 in JAMA Network Open.
“Our new definition may be important not only to stratify risk of mortality in people with obesity, but also in people with overweight and normal weight,” they concluded.
Thirty different definitions of ‘metabolically healthy obesity’
“To date, there is no universally accepted standard for defining [metabolically healthy obesity] and more than 30 different definitions have been used to operationalize the phenotypes in studies,” which may explain the “continued unresolved debate” about outcomes in patients with metabolically unhealthy obesity, Ayana K. April-Sanders, PhD, and Carlos J. Rodriguez, MD, MPH, from Albert Einstein College of Medicine, New York, wrote in an accompanying commentary.
The current study, they noted, suggests that waist-to-hip ratio is a better measure of central adiposity than waist circumference, and that the effect of dyslipidemia on CVD mortality may be weaker among individuals with obesity.
However, the findings may not be generalizable to other CVD outcomes, they cautioned.
And importantly, some individuals with metabolically healthy obesity will likely transition to unhealthy obesity over time due to weight gain, aging, and lack of physical activity.
Therefore, “the present study provides a prototype of how that definition can be derived, but more rigorous tests and evidence using similar techniques are needed, particularly in prospective studies,” according to Dr. April-Sanders and Dr. Rodriguez.
They call for more research to establish a standardized definition of metabolically healthy obesity and then, using that definition, to determine the prevalence of healthy and unhealthy obesity and identify factors that preserve healthy obesity.
Definition developed from NHANES cohort, validated in UK biobank
Ms. Zembic and colleagues explained that previous definitions for metabolically healthy obesity were mainly based on the absence of either metabolic syndrome or insulin resistance, but some individuals with obesity but without metabolic disease still have increased risks of CVD mortality and total mortality.
To develop a more precise definition of metabolically healthy obesity, the researchers analyzed data from 12,341 individuals in the United States who participated in NHANES-III, conducted between 1988 and 1994. The individuals were a mean age of 42 and 51% were women, and they were followed for an average of 14.5 years.
The researchers validated this definition using data from 374,079 individuals in the population-based UK Biobank cohort who were assessed in 2006 to 2010. Those individuals were a mean age of 56 and 55% were women, and they were followed for a mean of 7.8 years.
The combination of systolic blood pressure and waist-to-hip ratio had the strongest association with CVD mortality and total mortality, and the prevalence of type 2 diabetes was also associated with greater risk.
Regardless of BMI, all groups of metabolically unhealthy individuals had increased risks of CVD mortality and total mortality.
The study and some of the researchers were supported by grants from the German Federal Ministry of Education and Research.
A version of this article first appeared on Medscape.com.
Scientists have proposed a simple new definition for “metabolically healthy obesity” to identify individuals who do not have an increased risk of cardiovascular disease (CVD) death and total mortality.
The team – led by Anika Zembic, MPH, German Institute of Human Nutrition Potsdam-Rehbruecke, Nuthetal, Germany – performed an assessment of anthropometric and metabolic risk factors as well as mortality data from two cohorts that “yielded a simple definition to categorize participants with obesity as metabolically healthy or unhealthy.”
They defined “metabolically healthy” as systolic blood pressure <130 mm Hg and no use of blood pressure-lowering medication; waist-to-hip ratio <0.95 (in women) and <1.03 (in men); and no prevalent type 2 diabetes.
Based on this new definition, 42% of participants in the third U.S. National Health and Nutrition Examination Survey (NHANES-III) and 19% of participants in the UK Biobank study had metabolically healthy obesity and did not have an increased risk for CVD mortality and total mortality compared with individuals with metabolically healthy normal weight.
“People with a phenotype defined as metabolically unhealthy using this definition had significantly higher hazard ratios for [CVD] mortality and total mortality irrespective of body mass index category, and people with phenotypes defined as having metabolically healthy obesity displayed no increased risk,” the researchers noted in their article, published May 7 in JAMA Network Open.
“Our new definition may be important not only to stratify risk of mortality in people with obesity, but also in people with overweight and normal weight,” they concluded.
Thirty different definitions of ‘metabolically healthy obesity’
“To date, there is no universally accepted standard for defining [metabolically healthy obesity] and more than 30 different definitions have been used to operationalize the phenotypes in studies,” which may explain the “continued unresolved debate” about outcomes in patients with metabolically unhealthy obesity, Ayana K. April-Sanders, PhD, and Carlos J. Rodriguez, MD, MPH, from Albert Einstein College of Medicine, New York, wrote in an accompanying commentary.
The current study, they noted, suggests that waist-to-hip ratio is a better measure of central adiposity than waist circumference, and that the effect of dyslipidemia on CVD mortality may be weaker among individuals with obesity.
However, the findings may not be generalizable to other CVD outcomes, they cautioned.
And importantly, some individuals with metabolically healthy obesity will likely transition to unhealthy obesity over time due to weight gain, aging, and lack of physical activity.
Therefore, “the present study provides a prototype of how that definition can be derived, but more rigorous tests and evidence using similar techniques are needed, particularly in prospective studies,” according to Dr. April-Sanders and Dr. Rodriguez.
They call for more research to establish a standardized definition of metabolically healthy obesity and then, using that definition, to determine the prevalence of healthy and unhealthy obesity and identify factors that preserve healthy obesity.
Definition developed from NHANES cohort, validated in UK biobank
Ms. Zembic and colleagues explained that previous definitions for metabolically healthy obesity were mainly based on the absence of either metabolic syndrome or insulin resistance, but some individuals with obesity but without metabolic disease still have increased risks of CVD mortality and total mortality.
To develop a more precise definition of metabolically healthy obesity, the researchers analyzed data from 12,341 individuals in the United States who participated in NHANES-III, conducted between 1988 and 1994. The individuals were a mean age of 42 and 51% were women, and they were followed for an average of 14.5 years.
The researchers validated this definition using data from 374,079 individuals in the population-based UK Biobank cohort who were assessed in 2006 to 2010. Those individuals were a mean age of 56 and 55% were women, and they were followed for a mean of 7.8 years.
The combination of systolic blood pressure and waist-to-hip ratio had the strongest association with CVD mortality and total mortality, and the prevalence of type 2 diabetes was also associated with greater risk.
Regardless of BMI, all groups of metabolically unhealthy individuals had increased risks of CVD mortality and total mortality.
The study and some of the researchers were supported by grants from the German Federal Ministry of Education and Research.
A version of this article first appeared on Medscape.com.
Scientists have proposed a simple new definition for “metabolically healthy obesity” to identify individuals who do not have an increased risk of cardiovascular disease (CVD) death and total mortality.
The team – led by Anika Zembic, MPH, German Institute of Human Nutrition Potsdam-Rehbruecke, Nuthetal, Germany – performed an assessment of anthropometric and metabolic risk factors as well as mortality data from two cohorts that “yielded a simple definition to categorize participants with obesity as metabolically healthy or unhealthy.”
They defined “metabolically healthy” as systolic blood pressure <130 mm Hg and no use of blood pressure-lowering medication; waist-to-hip ratio <0.95 (in women) and <1.03 (in men); and no prevalent type 2 diabetes.
Based on this new definition, 42% of participants in the third U.S. National Health and Nutrition Examination Survey (NHANES-III) and 19% of participants in the UK Biobank study had metabolically healthy obesity and did not have an increased risk for CVD mortality and total mortality compared with individuals with metabolically healthy normal weight.
“People with a phenotype defined as metabolically unhealthy using this definition had significantly higher hazard ratios for [CVD] mortality and total mortality irrespective of body mass index category, and people with phenotypes defined as having metabolically healthy obesity displayed no increased risk,” the researchers noted in their article, published May 7 in JAMA Network Open.
“Our new definition may be important not only to stratify risk of mortality in people with obesity, but also in people with overweight and normal weight,” they concluded.
Thirty different definitions of ‘metabolically healthy obesity’
“To date, there is no universally accepted standard for defining [metabolically healthy obesity] and more than 30 different definitions have been used to operationalize the phenotypes in studies,” which may explain the “continued unresolved debate” about outcomes in patients with metabolically unhealthy obesity, Ayana K. April-Sanders, PhD, and Carlos J. Rodriguez, MD, MPH, from Albert Einstein College of Medicine, New York, wrote in an accompanying commentary.
The current study, they noted, suggests that waist-to-hip ratio is a better measure of central adiposity than waist circumference, and that the effect of dyslipidemia on CVD mortality may be weaker among individuals with obesity.
However, the findings may not be generalizable to other CVD outcomes, they cautioned.
And importantly, some individuals with metabolically healthy obesity will likely transition to unhealthy obesity over time due to weight gain, aging, and lack of physical activity.
Therefore, “the present study provides a prototype of how that definition can be derived, but more rigorous tests and evidence using similar techniques are needed, particularly in prospective studies,” according to Dr. April-Sanders and Dr. Rodriguez.
They call for more research to establish a standardized definition of metabolically healthy obesity and then, using that definition, to determine the prevalence of healthy and unhealthy obesity and identify factors that preserve healthy obesity.
Definition developed from NHANES cohort, validated in UK biobank
Ms. Zembic and colleagues explained that previous definitions for metabolically healthy obesity were mainly based on the absence of either metabolic syndrome or insulin resistance, but some individuals with obesity but without metabolic disease still have increased risks of CVD mortality and total mortality.
To develop a more precise definition of metabolically healthy obesity, the researchers analyzed data from 12,341 individuals in the United States who participated in NHANES-III, conducted between 1988 and 1994. The individuals were a mean age of 42 and 51% were women, and they were followed for an average of 14.5 years.
The researchers validated this definition using data from 374,079 individuals in the population-based UK Biobank cohort who were assessed in 2006 to 2010. Those individuals were a mean age of 56 and 55% were women, and they were followed for a mean of 7.8 years.
The combination of systolic blood pressure and waist-to-hip ratio had the strongest association with CVD mortality and total mortality, and the prevalence of type 2 diabetes was also associated with greater risk.
Regardless of BMI, all groups of metabolically unhealthy individuals had increased risks of CVD mortality and total mortality.
The study and some of the researchers were supported by grants from the German Federal Ministry of Education and Research.
A version of this article first appeared on Medscape.com.
Dr. Topol talks: COVID-19 variants are innocent until proven guilty
Editor in Chief of this news organization Eric Topol, MD, founder and director of the Scripps Research Translational Institute in La Jolla, Calif., and professor of molecular medicine, has been closely following COVID-19 data since the pandemic began. He spoke with writer Miriam E. Tucker about the latest on SARS-CoV-2 variants and their impact on vaccine efficacy. The conversation serves as a follow-up to his April 13, 2021, New York Times opinion piece, in which he advised readers that “all variants are innocent until proven guilty.”
You have expressed overall confidence in the efficacy of the vaccines thus far despite the emergence of variants, with some caveats. How do you see the current situation?
The Centers for Disease Control and Prevention has designated five “variants of concern,” but only three of them are real concerns – B.1.1.7, first detected in the United Kingdom; P.1, in Brazil and Japan; and B.1.351, in South Africa. Yet, all three are susceptible to our current vaccines.
The U.K. B.1.1.7 is the worst variant of all because it’s hypertransmissible, so I call it a “superspreader strain.” It also causes more severe illness independent of the spread, so it’s a double whammy. It’s clear that it also causes more deaths. The only arguable point is whether it’s 30% or 50% more deaths, but regardless, it’s more lethal and more transmissible.
The B.1.1.7 is going to be the dominant strain worldwide. It could develop new mutations within it that could come back to haunt us. We must keep watch.
But for now, it’s fully responsive to all the vaccines, which is great because if we didn’t have them, we wouldn’t have gotten through this U.S. pandemic like we have, and neither would Israel and the United Kingdom and other countries that have been able to get out of the crisis. We met the enemy and put it in check.
As for the South Africa variant of concern, B.1.351, we just got some encouraging news showing that it›s very responsive to the Pfizer/BioNTech mRNA vaccine in large numbers of people. The study was conducted in Qatar following that country’s mass immunization campaign in which a total of 385,853 people had received at least one vaccine dose and 265,410 had completed the two doses as of March 31, 2021.
At 2 weeks past the second dose, the vaccine was 75% effective at preventing any documented infection with the B.1.351 variant and 89.5% effective against B.1.1.7. The vaccine’s effectiveness against severe, critical, or fatal COVID-19 was greater than 97.4% for all circulating strains in Qatar, where B.1.1.7 and B.1.351 are most prominent.
We also know that B.1.351 is very responsive to the Johnson & Johnson vaccine and the Novavax [vaccine in development] to a lesser degree. It is the most immune-evading variant we’ve seen thus far, with the highest likelihood of providing some vaccine resistance, yet not enough to interfere with vaccination campaigns. So that’s great news.
The caveats here are that you definitely need two doses of the mRNA vaccines to combat the B.1.351 variant. Also, the AstraZeneca vaccine failed to prevent it in South Africa. However, that study was hard to judge because it was underpowered for number of people with mild infections. So, it didn’t look as if it had any efficacy, but maybe it would if tested in a real trial.
The P.1 (Brazil) variant is the second-highest concern after B.1.1.7 because it’s the only one in the United States that’s still headed up. It seems to be competing a bit with B.1.1.7 here. We know it was associated with the crisis in Brazil, in Chile, and some other South American countries. It has some immune escape, but not as bad as B.1.351. It also appears to have somewhat greater transmissibility but not as much as B.1.1.7.
With P.1, we just don’t know enough yet. It was difficult to assess in Brazil because they were in the midst of a catastrophe – like India is now – and you don’t know how much of it is dragged by the catastrophe vs driving it.
We have to respond to P.1 carefully. There are some good data that it does respond to the Chinese vaccine Sinovac and the AstraZeneca vaccine, and it appears to respond to the others as well, based on serum studies. So it doesn’t look like vaccines will be the worry with this variant. Rather, it could be competing with B.1.1.7 and could lead to breakthrough infections in vaccinated people or reinfections in unvaccinated people who had COVID-19. We need several more weeks to sort it out.
Although the B.1.427 and B.1.429 variants initially seen in California remain on the CDC’s concern list, I’m not worried about them.
You mentioned the current COVID-19 crisis in India, where a new variant has been described as a “double mutant,” but on Twitter you called it a “scariant.” Why?
First of all, the B.1.617 variant isn’t a double mutant. It has 15 mutations. It’s a stupid term, focusing on two mutations which largely have been put aside as to concern. One of them is the L452R, which is the same as one of the California variants, and that hasn’t proved to be particularly serious or concerning. The other is the 484Q, and it’s not clear whether that has any function.
The B.1.617 is not the driver of the catastrophe in India. It may be contributing a small amount, but it has been overhyped as the double mutant that’s causing it all. Adding to that are what I call “scariant” headlines here in the United States when a few cases of that variant have been seen.
I coined the term scariant in early February because it was a pretty clear trend. People don’t know what variants are. They know a little bit about mutations but not variants, and they’re scared. A few variants are concerning, but we keep learning more and more things to decrease the concern. That’s why I wrote the New York Times op-ed, to try to provide some reassurance, since there’s such paranoia.
Do you think booster vaccinations will be necessary? If so, will those be of the original vaccines or new ones that incorporate the variants?
As we go forward, there’s still potential for new variants that we haven’t seen yet that combine the worst of all features – transmissibility and immune evasion – especially since we have a world where COVID-19 is unchecked. So, we’re not out of it yet, but at least for the moment, we have vaccines that are capable of protecting against all variants.
In most people, the immune response against SARS-CoV-2 is very durable and strong and may well last for years. With the most closely related SARS-CoV-1, people still had immune responses up to 18 years later. However, some people will have less robust vaccine responses, including the elderly and the immunocompromised. If they don’t have great responses to the vaccine to start with, over time they’re likely to become more vulnerable, especially if they’re exposed to the variants with some degree of immune evasion.
I think we need to study these individuals post vaccination. A lot of people fit into those categories, including seniors, people being treated for cancer or autoimmune conditions, or post organ transplant. We could set up a prospective study to see whether they develop symptomatic COVID-19 and if so, from what – the original strain, B.1.1.7, or the newer variants.
That’s where I think booster shots may be needed. They may not be necessary across the board, but perhaps just in these special subgroups.
All of the current vaccines can be tweaked to include new variants, but the need for that is uncertain as of now. Moderna is working on a so-called bivalent vaccine that includes the original SARS-CoV-2 strain plus the B.1.351 variant, but it isn’t clear that that’s going to be necessary.
Currently, at least 200 COVID-19 vaccines are in development. There will be vaccines you can inhale, room temperature mRNA vaccines, and potentially even oral vaccines.
In the near future, Novavax is close, and there will likely be a two-dose Johnson & Johnson version that has the same potency as the mRNA vaccines. There are a lot of moving parts here.
There may be a step down in efficacy from mRNA to the others, though, and that shouldn’t be discounted. All of the available vaccines so far protect very well against severe disease and death, but some are less effective against mild to moderate infections, which may then lead to long COVID. We don’t yet know whether those who get mild infection post vaccination can still get long COVID.
What do you think it will take to achieve herd immunity?
I prefer the term “containment.” It’s quantitative. If you get to an infection rate of less than 1 in 100,000 people, as they’ve done in Israel, with 0.8 per 100,000, then you have the virus in check, and there will be very little spread when it’s at that controlled rate, with no outbreaks. The United States is currently at about 15 per 100,000. California is at 4. That still has to get lower.
It will be a challenge to get to President Biden’s goal of having 70% of U.S. adults given at least one dose by July 4. We’re now at about 57%. To get that next 13% of adults is going to take an all-out effort: mobile units, going to homes, making it ultraconvenient, education for people with safety concerns, incentivization, and days off.
We also need to get employers, universities, and health systems to get to the mandatory level. We haven’t done that yet. Some universities have mandated it for students, faculty, and staff. We need it in more health care systems. Right now, we only have a couple. We mandate flu shots, and flu is nothing, compared with COVID-19. And the COVID-19 vaccine is far more efficacious – flu shots are 40% efficacious, while these are 95%. COVID-19 is a tenfold more lethal and serious disease, and much more spreadable.
People are using the lack of full licensure by the Food and Drug Administration – as opposed to emergency use authorization – as an excuse not to get vaccinated. A biologics license application takes time to approve. Meanwhile, we have hundreds of millions of doses that have been well tolerated and incredibly effective.
Another aspect to consider regarding containment is that about 110 million Americans have already had COVID-19, even though only about 30 million cases have been confirmed. Most of these people have immune protection, although it’s not as good as if they have one vaccine dose. But they have enough protection to be part of the story here of the wall against COVID-19 and will help us get through this.
That’s a silver lining of having an unchecked epidemic for the entire year of 2020. The good part is that’s helping to get us to achieve an incredible level of containment when we haven’t even been close. Right now, we’re as good as the country has been in the pandemic, but we still have a long gap to get down to that 1 per 100,000. That’s what we should be working toward, and we can get there.
A version of this article first appeared on Medscape.com.
Editor in Chief of this news organization Eric Topol, MD, founder and director of the Scripps Research Translational Institute in La Jolla, Calif., and professor of molecular medicine, has been closely following COVID-19 data since the pandemic began. He spoke with writer Miriam E. Tucker about the latest on SARS-CoV-2 variants and their impact on vaccine efficacy. The conversation serves as a follow-up to his April 13, 2021, New York Times opinion piece, in which he advised readers that “all variants are innocent until proven guilty.”
You have expressed overall confidence in the efficacy of the vaccines thus far despite the emergence of variants, with some caveats. How do you see the current situation?
The Centers for Disease Control and Prevention has designated five “variants of concern,” but only three of them are real concerns – B.1.1.7, first detected in the United Kingdom; P.1, in Brazil and Japan; and B.1.351, in South Africa. Yet, all three are susceptible to our current vaccines.
The U.K. B.1.1.7 is the worst variant of all because it’s hypertransmissible, so I call it a “superspreader strain.” It also causes more severe illness independent of the spread, so it’s a double whammy. It’s clear that it also causes more deaths. The only arguable point is whether it’s 30% or 50% more deaths, but regardless, it’s more lethal and more transmissible.
The B.1.1.7 is going to be the dominant strain worldwide. It could develop new mutations within it that could come back to haunt us. We must keep watch.
But for now, it’s fully responsive to all the vaccines, which is great because if we didn’t have them, we wouldn’t have gotten through this U.S. pandemic like we have, and neither would Israel and the United Kingdom and other countries that have been able to get out of the crisis. We met the enemy and put it in check.
As for the South Africa variant of concern, B.1.351, we just got some encouraging news showing that it›s very responsive to the Pfizer/BioNTech mRNA vaccine in large numbers of people. The study was conducted in Qatar following that country’s mass immunization campaign in which a total of 385,853 people had received at least one vaccine dose and 265,410 had completed the two doses as of March 31, 2021.
At 2 weeks past the second dose, the vaccine was 75% effective at preventing any documented infection with the B.1.351 variant and 89.5% effective against B.1.1.7. The vaccine’s effectiveness against severe, critical, or fatal COVID-19 was greater than 97.4% for all circulating strains in Qatar, where B.1.1.7 and B.1.351 are most prominent.
We also know that B.1.351 is very responsive to the Johnson & Johnson vaccine and the Novavax [vaccine in development] to a lesser degree. It is the most immune-evading variant we’ve seen thus far, with the highest likelihood of providing some vaccine resistance, yet not enough to interfere with vaccination campaigns. So that’s great news.
The caveats here are that you definitely need two doses of the mRNA vaccines to combat the B.1.351 variant. Also, the AstraZeneca vaccine failed to prevent it in South Africa. However, that study was hard to judge because it was underpowered for number of people with mild infections. So, it didn’t look as if it had any efficacy, but maybe it would if tested in a real trial.
The P.1 (Brazil) variant is the second-highest concern after B.1.1.7 because it’s the only one in the United States that’s still headed up. It seems to be competing a bit with B.1.1.7 here. We know it was associated with the crisis in Brazil, in Chile, and some other South American countries. It has some immune escape, but not as bad as B.1.351. It also appears to have somewhat greater transmissibility but not as much as B.1.1.7.
With P.1, we just don’t know enough yet. It was difficult to assess in Brazil because they were in the midst of a catastrophe – like India is now – and you don’t know how much of it is dragged by the catastrophe vs driving it.
We have to respond to P.1 carefully. There are some good data that it does respond to the Chinese vaccine Sinovac and the AstraZeneca vaccine, and it appears to respond to the others as well, based on serum studies. So it doesn’t look like vaccines will be the worry with this variant. Rather, it could be competing with B.1.1.7 and could lead to breakthrough infections in vaccinated people or reinfections in unvaccinated people who had COVID-19. We need several more weeks to sort it out.
Although the B.1.427 and B.1.429 variants initially seen in California remain on the CDC’s concern list, I’m not worried about them.
You mentioned the current COVID-19 crisis in India, where a new variant has been described as a “double mutant,” but on Twitter you called it a “scariant.” Why?
First of all, the B.1.617 variant isn’t a double mutant. It has 15 mutations. It’s a stupid term, focusing on two mutations which largely have been put aside as to concern. One of them is the L452R, which is the same as one of the California variants, and that hasn’t proved to be particularly serious or concerning. The other is the 484Q, and it’s not clear whether that has any function.
The B.1.617 is not the driver of the catastrophe in India. It may be contributing a small amount, but it has been overhyped as the double mutant that’s causing it all. Adding to that are what I call “scariant” headlines here in the United States when a few cases of that variant have been seen.
I coined the term scariant in early February because it was a pretty clear trend. People don’t know what variants are. They know a little bit about mutations but not variants, and they’re scared. A few variants are concerning, but we keep learning more and more things to decrease the concern. That’s why I wrote the New York Times op-ed, to try to provide some reassurance, since there’s such paranoia.
Do you think booster vaccinations will be necessary? If so, will those be of the original vaccines or new ones that incorporate the variants?
As we go forward, there’s still potential for new variants that we haven’t seen yet that combine the worst of all features – transmissibility and immune evasion – especially since we have a world where COVID-19 is unchecked. So, we’re not out of it yet, but at least for the moment, we have vaccines that are capable of protecting against all variants.
In most people, the immune response against SARS-CoV-2 is very durable and strong and may well last for years. With the most closely related SARS-CoV-1, people still had immune responses up to 18 years later. However, some people will have less robust vaccine responses, including the elderly and the immunocompromised. If they don’t have great responses to the vaccine to start with, over time they’re likely to become more vulnerable, especially if they’re exposed to the variants with some degree of immune evasion.
I think we need to study these individuals post vaccination. A lot of people fit into those categories, including seniors, people being treated for cancer or autoimmune conditions, or post organ transplant. We could set up a prospective study to see whether they develop symptomatic COVID-19 and if so, from what – the original strain, B.1.1.7, or the newer variants.
That’s where I think booster shots may be needed. They may not be necessary across the board, but perhaps just in these special subgroups.
All of the current vaccines can be tweaked to include new variants, but the need for that is uncertain as of now. Moderna is working on a so-called bivalent vaccine that includes the original SARS-CoV-2 strain plus the B.1.351 variant, but it isn’t clear that that’s going to be necessary.
Currently, at least 200 COVID-19 vaccines are in development. There will be vaccines you can inhale, room temperature mRNA vaccines, and potentially even oral vaccines.
In the near future, Novavax is close, and there will likely be a two-dose Johnson & Johnson version that has the same potency as the mRNA vaccines. There are a lot of moving parts here.
There may be a step down in efficacy from mRNA to the others, though, and that shouldn’t be discounted. All of the available vaccines so far protect very well against severe disease and death, but some are less effective against mild to moderate infections, which may then lead to long COVID. We don’t yet know whether those who get mild infection post vaccination can still get long COVID.
What do you think it will take to achieve herd immunity?
I prefer the term “containment.” It’s quantitative. If you get to an infection rate of less than 1 in 100,000 people, as they’ve done in Israel, with 0.8 per 100,000, then you have the virus in check, and there will be very little spread when it’s at that controlled rate, with no outbreaks. The United States is currently at about 15 per 100,000. California is at 4. That still has to get lower.
It will be a challenge to get to President Biden’s goal of having 70% of U.S. adults given at least one dose by July 4. We’re now at about 57%. To get that next 13% of adults is going to take an all-out effort: mobile units, going to homes, making it ultraconvenient, education for people with safety concerns, incentivization, and days off.
We also need to get employers, universities, and health systems to get to the mandatory level. We haven’t done that yet. Some universities have mandated it for students, faculty, and staff. We need it in more health care systems. Right now, we only have a couple. We mandate flu shots, and flu is nothing, compared with COVID-19. And the COVID-19 vaccine is far more efficacious – flu shots are 40% efficacious, while these are 95%. COVID-19 is a tenfold more lethal and serious disease, and much more spreadable.
People are using the lack of full licensure by the Food and Drug Administration – as opposed to emergency use authorization – as an excuse not to get vaccinated. A biologics license application takes time to approve. Meanwhile, we have hundreds of millions of doses that have been well tolerated and incredibly effective.
Another aspect to consider regarding containment is that about 110 million Americans have already had COVID-19, even though only about 30 million cases have been confirmed. Most of these people have immune protection, although it’s not as good as if they have one vaccine dose. But they have enough protection to be part of the story here of the wall against COVID-19 and will help us get through this.
That’s a silver lining of having an unchecked epidemic for the entire year of 2020. The good part is that’s helping to get us to achieve an incredible level of containment when we haven’t even been close. Right now, we’re as good as the country has been in the pandemic, but we still have a long gap to get down to that 1 per 100,000. That’s what we should be working toward, and we can get there.
A version of this article first appeared on Medscape.com.
Editor in Chief of this news organization Eric Topol, MD, founder and director of the Scripps Research Translational Institute in La Jolla, Calif., and professor of molecular medicine, has been closely following COVID-19 data since the pandemic began. He spoke with writer Miriam E. Tucker about the latest on SARS-CoV-2 variants and their impact on vaccine efficacy. The conversation serves as a follow-up to his April 13, 2021, New York Times opinion piece, in which he advised readers that “all variants are innocent until proven guilty.”
You have expressed overall confidence in the efficacy of the vaccines thus far despite the emergence of variants, with some caveats. How do you see the current situation?
The Centers for Disease Control and Prevention has designated five “variants of concern,” but only three of them are real concerns – B.1.1.7, first detected in the United Kingdom; P.1, in Brazil and Japan; and B.1.351, in South Africa. Yet, all three are susceptible to our current vaccines.
The U.K. B.1.1.7 is the worst variant of all because it’s hypertransmissible, so I call it a “superspreader strain.” It also causes more severe illness independent of the spread, so it’s a double whammy. It’s clear that it also causes more deaths. The only arguable point is whether it’s 30% or 50% more deaths, but regardless, it’s more lethal and more transmissible.
The B.1.1.7 is going to be the dominant strain worldwide. It could develop new mutations within it that could come back to haunt us. We must keep watch.
But for now, it’s fully responsive to all the vaccines, which is great because if we didn’t have them, we wouldn’t have gotten through this U.S. pandemic like we have, and neither would Israel and the United Kingdom and other countries that have been able to get out of the crisis. We met the enemy and put it in check.
As for the South Africa variant of concern, B.1.351, we just got some encouraging news showing that it›s very responsive to the Pfizer/BioNTech mRNA vaccine in large numbers of people. The study was conducted in Qatar following that country’s mass immunization campaign in which a total of 385,853 people had received at least one vaccine dose and 265,410 had completed the two doses as of March 31, 2021.
At 2 weeks past the second dose, the vaccine was 75% effective at preventing any documented infection with the B.1.351 variant and 89.5% effective against B.1.1.7. The vaccine’s effectiveness against severe, critical, or fatal COVID-19 was greater than 97.4% for all circulating strains in Qatar, where B.1.1.7 and B.1.351 are most prominent.
We also know that B.1.351 is very responsive to the Johnson & Johnson vaccine and the Novavax [vaccine in development] to a lesser degree. It is the most immune-evading variant we’ve seen thus far, with the highest likelihood of providing some vaccine resistance, yet not enough to interfere with vaccination campaigns. So that’s great news.
The caveats here are that you definitely need two doses of the mRNA vaccines to combat the B.1.351 variant. Also, the AstraZeneca vaccine failed to prevent it in South Africa. However, that study was hard to judge because it was underpowered for number of people with mild infections. So, it didn’t look as if it had any efficacy, but maybe it would if tested in a real trial.
The P.1 (Brazil) variant is the second-highest concern after B.1.1.7 because it’s the only one in the United States that’s still headed up. It seems to be competing a bit with B.1.1.7 here. We know it was associated with the crisis in Brazil, in Chile, and some other South American countries. It has some immune escape, but not as bad as B.1.351. It also appears to have somewhat greater transmissibility but not as much as B.1.1.7.
With P.1, we just don’t know enough yet. It was difficult to assess in Brazil because they were in the midst of a catastrophe – like India is now – and you don’t know how much of it is dragged by the catastrophe vs driving it.
We have to respond to P.1 carefully. There are some good data that it does respond to the Chinese vaccine Sinovac and the AstraZeneca vaccine, and it appears to respond to the others as well, based on serum studies. So it doesn’t look like vaccines will be the worry with this variant. Rather, it could be competing with B.1.1.7 and could lead to breakthrough infections in vaccinated people or reinfections in unvaccinated people who had COVID-19. We need several more weeks to sort it out.
Although the B.1.427 and B.1.429 variants initially seen in California remain on the CDC’s concern list, I’m not worried about them.
You mentioned the current COVID-19 crisis in India, where a new variant has been described as a “double mutant,” but on Twitter you called it a “scariant.” Why?
First of all, the B.1.617 variant isn’t a double mutant. It has 15 mutations. It’s a stupid term, focusing on two mutations which largely have been put aside as to concern. One of them is the L452R, which is the same as one of the California variants, and that hasn’t proved to be particularly serious or concerning. The other is the 484Q, and it’s not clear whether that has any function.
The B.1.617 is not the driver of the catastrophe in India. It may be contributing a small amount, but it has been overhyped as the double mutant that’s causing it all. Adding to that are what I call “scariant” headlines here in the United States when a few cases of that variant have been seen.
I coined the term scariant in early February because it was a pretty clear trend. People don’t know what variants are. They know a little bit about mutations but not variants, and they’re scared. A few variants are concerning, but we keep learning more and more things to decrease the concern. That’s why I wrote the New York Times op-ed, to try to provide some reassurance, since there’s such paranoia.
Do you think booster vaccinations will be necessary? If so, will those be of the original vaccines or new ones that incorporate the variants?
As we go forward, there’s still potential for new variants that we haven’t seen yet that combine the worst of all features – transmissibility and immune evasion – especially since we have a world where COVID-19 is unchecked. So, we’re not out of it yet, but at least for the moment, we have vaccines that are capable of protecting against all variants.
In most people, the immune response against SARS-CoV-2 is very durable and strong and may well last for years. With the most closely related SARS-CoV-1, people still had immune responses up to 18 years later. However, some people will have less robust vaccine responses, including the elderly and the immunocompromised. If they don’t have great responses to the vaccine to start with, over time they’re likely to become more vulnerable, especially if they’re exposed to the variants with some degree of immune evasion.
I think we need to study these individuals post vaccination. A lot of people fit into those categories, including seniors, people being treated for cancer or autoimmune conditions, or post organ transplant. We could set up a prospective study to see whether they develop symptomatic COVID-19 and if so, from what – the original strain, B.1.1.7, or the newer variants.
That’s where I think booster shots may be needed. They may not be necessary across the board, but perhaps just in these special subgroups.
All of the current vaccines can be tweaked to include new variants, but the need for that is uncertain as of now. Moderna is working on a so-called bivalent vaccine that includes the original SARS-CoV-2 strain plus the B.1.351 variant, but it isn’t clear that that’s going to be necessary.
Currently, at least 200 COVID-19 vaccines are in development. There will be vaccines you can inhale, room temperature mRNA vaccines, and potentially even oral vaccines.
In the near future, Novavax is close, and there will likely be a two-dose Johnson & Johnson version that has the same potency as the mRNA vaccines. There are a lot of moving parts here.
There may be a step down in efficacy from mRNA to the others, though, and that shouldn’t be discounted. All of the available vaccines so far protect very well against severe disease and death, but some are less effective against mild to moderate infections, which may then lead to long COVID. We don’t yet know whether those who get mild infection post vaccination can still get long COVID.
What do you think it will take to achieve herd immunity?
I prefer the term “containment.” It’s quantitative. If you get to an infection rate of less than 1 in 100,000 people, as they’ve done in Israel, with 0.8 per 100,000, then you have the virus in check, and there will be very little spread when it’s at that controlled rate, with no outbreaks. The United States is currently at about 15 per 100,000. California is at 4. That still has to get lower.
It will be a challenge to get to President Biden’s goal of having 70% of U.S. adults given at least one dose by July 4. We’re now at about 57%. To get that next 13% of adults is going to take an all-out effort: mobile units, going to homes, making it ultraconvenient, education for people with safety concerns, incentivization, and days off.
We also need to get employers, universities, and health systems to get to the mandatory level. We haven’t done that yet. Some universities have mandated it for students, faculty, and staff. We need it in more health care systems. Right now, we only have a couple. We mandate flu shots, and flu is nothing, compared with COVID-19. And the COVID-19 vaccine is far more efficacious – flu shots are 40% efficacious, while these are 95%. COVID-19 is a tenfold more lethal and serious disease, and much more spreadable.
People are using the lack of full licensure by the Food and Drug Administration – as opposed to emergency use authorization – as an excuse not to get vaccinated. A biologics license application takes time to approve. Meanwhile, we have hundreds of millions of doses that have been well tolerated and incredibly effective.
Another aspect to consider regarding containment is that about 110 million Americans have already had COVID-19, even though only about 30 million cases have been confirmed. Most of these people have immune protection, although it’s not as good as if they have one vaccine dose. But they have enough protection to be part of the story here of the wall against COVID-19 and will help us get through this.
That’s a silver lining of having an unchecked epidemic for the entire year of 2020. The good part is that’s helping to get us to achieve an incredible level of containment when we haven’t even been close. Right now, we’re as good as the country has been in the pandemic, but we still have a long gap to get down to that 1 per 100,000. That’s what we should be working toward, and we can get there.
A version of this article first appeared on Medscape.com.
High body fat tied to slowed breast maturation in girls with obesity
Girls in late stages of puberty who had elevated levels of body fat showed unusually high levels of several hormones that could contribute to an earlier age of menarche and also slow breast development, according to data from 90 girls who spanned a wide range of body fat in the first longitudinal study to examine links between fat volume, levels of reproductive hormones, and clinical manifestations of hormone action during puberty.
The results showed that girls with greater body fat had higher levels of follicle stimulating hormone, inhibin B, estrone, and certain male-like reproductive hormones, and that this pattern “is specifically tied to body fat,” said Natalie D. Shaw, MD, senior investigator for the study, reported at the annual meeting of the Endocrine Society.
“We found that total body fat is associated with the timing of menarche, as others have reported for body weight,” she noted. The new findings showed that every 1% rise in percent total body fat linked with a significant 3% rise in the likelihood of menarche, menstrual onset. In the new study the average age of menarche was 11.7 years among the overweight or obese girls and 12.8 years among those with normal weights.
But the study’s unique use of an average of about three serial ultrasound breast examinations of each subject during an average 4 years of follow-up also showed that higher levels of body fat linked with slowed breast development in later stages, specifically maturation from stage D to stages D/E and E.
For example, girls with 33% body fat spent an average of 8.2 months in stage D, which stretched to an average of 11.2 months among girls with 38% body fat, reported Madison T. Ortega, a researcher with the Pediatric Endocrinology Group of the National Institute of Environmental Health Sciences in Research Triangle Park, N.C., who presented the report at the meeting.
Ultrasound shows what inspection can’t
Results from “several studies have shown earlier breast development in overweight and obese girls by inspection and palpation,” but the new findings from ultrasound examination provide more nuance about the structural breast changes actually occurring in these adolescents, said Dr. Shaw, who heads the Pediatric Endocrinology Group. The current study “was not designed to capture the onset of breast development,” and “it is possible that increased androgens or insulin resistance in girls with higher body fat interferes with normal breast development,” she explained in an interview.
“The authors showed that the timing and progress of early stages of puberty were not earlier in overweight or obese girls. Luteinizing hormone, the indicator of neuroendocrine pubertal onset, and timing of early stages of breast development were the same in all weight groups. The authors also discovered falsely advanced Turner breast stage designations with ultrasonography in some girls with obesity. This might suggest that prior findings in epidemiologic studies of an earlier start to puberty based mostly on breast development stages identified by self-reported inspection and, rarely, palpation, may have been biased by breast adipose tissue,” said Christine M. Burt Solorzano, MD, a pediatric endocrinologist at the University of Virginia in Charlottesville, who was not involved in the study.
“Development of increased follicle-stimulating hormone in late puberty suggests that pubertal tempo, not onset, may be increased in girls with obesity, and goes along with earlier menarche. Their finding of increased androgen levels during mid to late puberty with obesity are consistent with prior findings,” including work published Dr. Burt Solorzano and her associates, she noted. “Delayed timing of advanced breast morphology was unexpected and may reflect relatively lower levels of progesterone in girls with obesity,” a hormone necessary for later stages of breast maturation.
The findings “reinforce that early breast development in the setting of obesity may in fact reflect adipose tissue and not be a true representation of neuroendocrine precocious puberty,” Dr. Burt Solorzano said in an interview. The findings “also suggest that pubertal initiation may not happen earlier in girls with obesity, as has been thought, but rather the tempo of puberty may be more rapid, leading to earlier menarche.”
A possible step toward PCOS
The long-term clinical consequences of the hormonal state linked with overweight and obesity “are unknown,” said Dr. Shaw. However, she and her coworkers followed a few of their subjects with elevated testosterone levels during midpuberty, and several developed signs of early polycystic ovarian syndrome (PCOS) such as irregular menstrual cycles, acne, and hirsutism. “It may be possible to identify girls at high risk for PCOS before menarche,” she suggested.
Dr. Burt Solorzano agreed that delayed breast development in girls with high levels of body fat may reflect inadequate progesterone production, which when coupled with an obesity-related excess level of androgens could put girls at risk for chronic anovulation and later PCOS.
“Weight management during childhood and early puberty may mitigate the adverse effects of obesity on pubertal progression and avoid some of the lifetime complications related to early menarche,” Dr. Burt Solorzano said.
The Body Weight and Puberty Study enrolled 36 girls who were overweight or obese and 54 girls with normal weight. They averaged 11 years of age, with a range of 8.2-14.7 years. Average percent body fat was 41% among the overweight or obese girls and 27% among those with normal weight. The results reported by Ms. Ortega also appeared in a report published Feb 22, 2021 (J Clin Endocrinol Metab. doi: 10.1210/clinem/dgab092).
Dr. Shaw, Ms. Ortega, and Dr. Burt Solorzano had no disclosures.
Girls in late stages of puberty who had elevated levels of body fat showed unusually high levels of several hormones that could contribute to an earlier age of menarche and also slow breast development, according to data from 90 girls who spanned a wide range of body fat in the first longitudinal study to examine links between fat volume, levels of reproductive hormones, and clinical manifestations of hormone action during puberty.
The results showed that girls with greater body fat had higher levels of follicle stimulating hormone, inhibin B, estrone, and certain male-like reproductive hormones, and that this pattern “is specifically tied to body fat,” said Natalie D. Shaw, MD, senior investigator for the study, reported at the annual meeting of the Endocrine Society.
“We found that total body fat is associated with the timing of menarche, as others have reported for body weight,” she noted. The new findings showed that every 1% rise in percent total body fat linked with a significant 3% rise in the likelihood of menarche, menstrual onset. In the new study the average age of menarche was 11.7 years among the overweight or obese girls and 12.8 years among those with normal weights.
But the study’s unique use of an average of about three serial ultrasound breast examinations of each subject during an average 4 years of follow-up also showed that higher levels of body fat linked with slowed breast development in later stages, specifically maturation from stage D to stages D/E and E.
For example, girls with 33% body fat spent an average of 8.2 months in stage D, which stretched to an average of 11.2 months among girls with 38% body fat, reported Madison T. Ortega, a researcher with the Pediatric Endocrinology Group of the National Institute of Environmental Health Sciences in Research Triangle Park, N.C., who presented the report at the meeting.
Ultrasound shows what inspection can’t
Results from “several studies have shown earlier breast development in overweight and obese girls by inspection and palpation,” but the new findings from ultrasound examination provide more nuance about the structural breast changes actually occurring in these adolescents, said Dr. Shaw, who heads the Pediatric Endocrinology Group. The current study “was not designed to capture the onset of breast development,” and “it is possible that increased androgens or insulin resistance in girls with higher body fat interferes with normal breast development,” she explained in an interview.
“The authors showed that the timing and progress of early stages of puberty were not earlier in overweight or obese girls. Luteinizing hormone, the indicator of neuroendocrine pubertal onset, and timing of early stages of breast development were the same in all weight groups. The authors also discovered falsely advanced Turner breast stage designations with ultrasonography in some girls with obesity. This might suggest that prior findings in epidemiologic studies of an earlier start to puberty based mostly on breast development stages identified by self-reported inspection and, rarely, palpation, may have been biased by breast adipose tissue,” said Christine M. Burt Solorzano, MD, a pediatric endocrinologist at the University of Virginia in Charlottesville, who was not involved in the study.
“Development of increased follicle-stimulating hormone in late puberty suggests that pubertal tempo, not onset, may be increased in girls with obesity, and goes along with earlier menarche. Their finding of increased androgen levels during mid to late puberty with obesity are consistent with prior findings,” including work published Dr. Burt Solorzano and her associates, she noted. “Delayed timing of advanced breast morphology was unexpected and may reflect relatively lower levels of progesterone in girls with obesity,” a hormone necessary for later stages of breast maturation.
The findings “reinforce that early breast development in the setting of obesity may in fact reflect adipose tissue and not be a true representation of neuroendocrine precocious puberty,” Dr. Burt Solorzano said in an interview. The findings “also suggest that pubertal initiation may not happen earlier in girls with obesity, as has been thought, but rather the tempo of puberty may be more rapid, leading to earlier menarche.”
A possible step toward PCOS
The long-term clinical consequences of the hormonal state linked with overweight and obesity “are unknown,” said Dr. Shaw. However, she and her coworkers followed a few of their subjects with elevated testosterone levels during midpuberty, and several developed signs of early polycystic ovarian syndrome (PCOS) such as irregular menstrual cycles, acne, and hirsutism. “It may be possible to identify girls at high risk for PCOS before menarche,” she suggested.
Dr. Burt Solorzano agreed that delayed breast development in girls with high levels of body fat may reflect inadequate progesterone production, which when coupled with an obesity-related excess level of androgens could put girls at risk for chronic anovulation and later PCOS.
“Weight management during childhood and early puberty may mitigate the adverse effects of obesity on pubertal progression and avoid some of the lifetime complications related to early menarche,” Dr. Burt Solorzano said.
The Body Weight and Puberty Study enrolled 36 girls who were overweight or obese and 54 girls with normal weight. They averaged 11 years of age, with a range of 8.2-14.7 years. Average percent body fat was 41% among the overweight or obese girls and 27% among those with normal weight. The results reported by Ms. Ortega also appeared in a report published Feb 22, 2021 (J Clin Endocrinol Metab. doi: 10.1210/clinem/dgab092).
Dr. Shaw, Ms. Ortega, and Dr. Burt Solorzano had no disclosures.
Girls in late stages of puberty who had elevated levels of body fat showed unusually high levels of several hormones that could contribute to an earlier age of menarche and also slow breast development, according to data from 90 girls who spanned a wide range of body fat in the first longitudinal study to examine links between fat volume, levels of reproductive hormones, and clinical manifestations of hormone action during puberty.
The results showed that girls with greater body fat had higher levels of follicle stimulating hormone, inhibin B, estrone, and certain male-like reproductive hormones, and that this pattern “is specifically tied to body fat,” said Natalie D. Shaw, MD, senior investigator for the study, reported at the annual meeting of the Endocrine Society.
“We found that total body fat is associated with the timing of menarche, as others have reported for body weight,” she noted. The new findings showed that every 1% rise in percent total body fat linked with a significant 3% rise in the likelihood of menarche, menstrual onset. In the new study the average age of menarche was 11.7 years among the overweight or obese girls and 12.8 years among those with normal weights.
But the study’s unique use of an average of about three serial ultrasound breast examinations of each subject during an average 4 years of follow-up also showed that higher levels of body fat linked with slowed breast development in later stages, specifically maturation from stage D to stages D/E and E.
For example, girls with 33% body fat spent an average of 8.2 months in stage D, which stretched to an average of 11.2 months among girls with 38% body fat, reported Madison T. Ortega, a researcher with the Pediatric Endocrinology Group of the National Institute of Environmental Health Sciences in Research Triangle Park, N.C., who presented the report at the meeting.
Ultrasound shows what inspection can’t
Results from “several studies have shown earlier breast development in overweight and obese girls by inspection and palpation,” but the new findings from ultrasound examination provide more nuance about the structural breast changes actually occurring in these adolescents, said Dr. Shaw, who heads the Pediatric Endocrinology Group. The current study “was not designed to capture the onset of breast development,” and “it is possible that increased androgens or insulin resistance in girls with higher body fat interferes with normal breast development,” she explained in an interview.
“The authors showed that the timing and progress of early stages of puberty were not earlier in overweight or obese girls. Luteinizing hormone, the indicator of neuroendocrine pubertal onset, and timing of early stages of breast development were the same in all weight groups. The authors also discovered falsely advanced Turner breast stage designations with ultrasonography in some girls with obesity. This might suggest that prior findings in epidemiologic studies of an earlier start to puberty based mostly on breast development stages identified by self-reported inspection and, rarely, palpation, may have been biased by breast adipose tissue,” said Christine M. Burt Solorzano, MD, a pediatric endocrinologist at the University of Virginia in Charlottesville, who was not involved in the study.
“Development of increased follicle-stimulating hormone in late puberty suggests that pubertal tempo, not onset, may be increased in girls with obesity, and goes along with earlier menarche. Their finding of increased androgen levels during mid to late puberty with obesity are consistent with prior findings,” including work published Dr. Burt Solorzano and her associates, she noted. “Delayed timing of advanced breast morphology was unexpected and may reflect relatively lower levels of progesterone in girls with obesity,” a hormone necessary for later stages of breast maturation.
The findings “reinforce that early breast development in the setting of obesity may in fact reflect adipose tissue and not be a true representation of neuroendocrine precocious puberty,” Dr. Burt Solorzano said in an interview. The findings “also suggest that pubertal initiation may not happen earlier in girls with obesity, as has been thought, but rather the tempo of puberty may be more rapid, leading to earlier menarche.”
A possible step toward PCOS
The long-term clinical consequences of the hormonal state linked with overweight and obesity “are unknown,” said Dr. Shaw. However, she and her coworkers followed a few of their subjects with elevated testosterone levels during midpuberty, and several developed signs of early polycystic ovarian syndrome (PCOS) such as irregular menstrual cycles, acne, and hirsutism. “It may be possible to identify girls at high risk for PCOS before menarche,” she suggested.
Dr. Burt Solorzano agreed that delayed breast development in girls with high levels of body fat may reflect inadequate progesterone production, which when coupled with an obesity-related excess level of androgens could put girls at risk for chronic anovulation and later PCOS.
“Weight management during childhood and early puberty may mitigate the adverse effects of obesity on pubertal progression and avoid some of the lifetime complications related to early menarche,” Dr. Burt Solorzano said.
The Body Weight and Puberty Study enrolled 36 girls who were overweight or obese and 54 girls with normal weight. They averaged 11 years of age, with a range of 8.2-14.7 years. Average percent body fat was 41% among the overweight or obese girls and 27% among those with normal weight. The results reported by Ms. Ortega also appeared in a report published Feb 22, 2021 (J Clin Endocrinol Metab. doi: 10.1210/clinem/dgab092).
Dr. Shaw, Ms. Ortega, and Dr. Burt Solorzano had no disclosures.
FROM ENDO 2021
Nutritional support may be lifesaving in heart failure
Personalized nutritional support for adults hospitalized with chronic heart failure and deemed to be at high nutritional risk reduced the risk of death or adverse cardiovascular events, compared with standard hospital food, new research indicates.
The Swiss EFFORT trial focused on patients with chronic heart failure and high risk of malnutrition defined by low body mass index, weight loss, and low food intake upon hospital admission.
“This high-risk group of chronic heart failure patients showed a significant improvement in mortality over 30 and 180 days, as well as other clinical outcomes, when individualized nutritional support interventions were offered to patients,” Philipp Schuetz, MD, MPH, Kantonsspital Aarau, Switzerland, said in an interview.
“While monitoring the nutritional status should be done also in outpatient settings by [general practitioners], malnutrition screening upon hospital admission may help to identify high-risk patients with high risk for nutritional status deterioration during the hospital stay who will benefit from nutritional assessment and treatment,” said Dr. Schuetz.
The study was published online May 3 in the Journal of the American College of Cardiology.
It’s not all about salt
The findings are based on a prespecified secondary analysis of outcomes in 645 patients (median age, 78.8 years, 52% men) hospitalized with chronic heart failure who participated in the open-label EFFORT study.
One-third of patients were hospitalized for acute decompensated heart failure and two-thirds had chronic heart failure and other acute medical illnesses requiring hospitalization.
All patients were at risk of malnutrition based on a Nutritional Risk Screening (NRS) score of 3 points or higher. They were randomly allocated 1:1 to individualized nutritional support to reach energy, protein, and micronutrient goals or usual hospital food (control group).
By 30 days, 27 of 321 patients (8.4%) receiving nutritional support had died compared with 48 of 324 patients (14.8%) in the control group (adjusted odds ratio [OR]: 0.44; 95% confidence interval, 0.26-0.75; P = .002)
Patients with high nutritional risk (NRS >4 points) showed the most benefit from nutritional support.
Compared with patients with moderate nutritional risk scores (NRS score 3-4), those with high nutritional risk (NRS >4) had a highly significant 65% increased mortality risk over 180 days.
The individual component of the NRS with the strongest association with mortality was low food intake in the week before hospitalization.
Patients who received nutritional support in the hospital also had a lower risk for major cardiovascular events at 30 days (17.4% vs. 26.9%; OR, 0.50; 95% CI, 0.34-0.75; P = .001).
“Historically, cardiologists and internists caring for patients with heart failure have mainly focused on salt-restrictive diets to reduce blood volume and thus optimize heart function. Yet, reduction of salt intake has not been shown to effectively improve clinical outcome but may, on the contrary, increase the risk of malnutrition as low-salt diets are often not tasty,” Dr. Schuetz said.
“Our data suggest that we should move our focus away from salt-restrictive diets to high-protein diets to cover individual nutritional goals in this high-risk group of patients, which includes screening, assessment, and nutritional support by dietitians,” Dr. Schuetz said.
In a linked editorial, Sheldon Gottlieb, MD, Johns Hopkins University, Baltimore, said there has been “relatively little attention” paid to the role of diet in heart failure other than recommending reduced salt intake.
In fact, in the 2021 American College of Cardiology expert consensus recommendations for optimizing heart failure treatment, roughly five words are devoted to diet and exercise and there is no mention of nutrition assessment by a dietitian, he points out.
“This study adds another tile to the still-fragmentary mosaic picture of the patient with heart failure at nutritional risk who might benefit from nutritional support,” Dr. Dr. Gottlieb wrote.
“ ‘Good medical care’ dictates that all hospitalized patients deserve to have a standardized nutritional assessment; the challenge remains: how to determine which patient with heart failure at nutritional risk will benefit by medical nutrition therapy,” Dr. Gottlieb said.
The Swiss National Science Foundation and the Research Council of the Kantonsspital Aarau provided funding for the trial. Dr. Schuetz’s institution has previously received unrestricted grant money unrelated to this project from Nestle Health Science and Abbott Nutrition. Dr. Gottlieb owns a federal trademark for the “Greens, Beans, and Leans” diet, and has a pending federal trademark for “FLOATS”: flax + oats cereal.
A version of this article first appeared on Medscape.com.
Personalized nutritional support for adults hospitalized with chronic heart failure and deemed to be at high nutritional risk reduced the risk of death or adverse cardiovascular events, compared with standard hospital food, new research indicates.
The Swiss EFFORT trial focused on patients with chronic heart failure and high risk of malnutrition defined by low body mass index, weight loss, and low food intake upon hospital admission.
“This high-risk group of chronic heart failure patients showed a significant improvement in mortality over 30 and 180 days, as well as other clinical outcomes, when individualized nutritional support interventions were offered to patients,” Philipp Schuetz, MD, MPH, Kantonsspital Aarau, Switzerland, said in an interview.
“While monitoring the nutritional status should be done also in outpatient settings by [general practitioners], malnutrition screening upon hospital admission may help to identify high-risk patients with high risk for nutritional status deterioration during the hospital stay who will benefit from nutritional assessment and treatment,” said Dr. Schuetz.
The study was published online May 3 in the Journal of the American College of Cardiology.
It’s not all about salt
The findings are based on a prespecified secondary analysis of outcomes in 645 patients (median age, 78.8 years, 52% men) hospitalized with chronic heart failure who participated in the open-label EFFORT study.
One-third of patients were hospitalized for acute decompensated heart failure and two-thirds had chronic heart failure and other acute medical illnesses requiring hospitalization.
All patients were at risk of malnutrition based on a Nutritional Risk Screening (NRS) score of 3 points or higher. They were randomly allocated 1:1 to individualized nutritional support to reach energy, protein, and micronutrient goals or usual hospital food (control group).
By 30 days, 27 of 321 patients (8.4%) receiving nutritional support had died compared with 48 of 324 patients (14.8%) in the control group (adjusted odds ratio [OR]: 0.44; 95% confidence interval, 0.26-0.75; P = .002)
Patients with high nutritional risk (NRS >4 points) showed the most benefit from nutritional support.
Compared with patients with moderate nutritional risk scores (NRS score 3-4), those with high nutritional risk (NRS >4) had a highly significant 65% increased mortality risk over 180 days.
The individual component of the NRS with the strongest association with mortality was low food intake in the week before hospitalization.
Patients who received nutritional support in the hospital also had a lower risk for major cardiovascular events at 30 days (17.4% vs. 26.9%; OR, 0.50; 95% CI, 0.34-0.75; P = .001).
“Historically, cardiologists and internists caring for patients with heart failure have mainly focused on salt-restrictive diets to reduce blood volume and thus optimize heart function. Yet, reduction of salt intake has not been shown to effectively improve clinical outcome but may, on the contrary, increase the risk of malnutrition as low-salt diets are often not tasty,” Dr. Schuetz said.
“Our data suggest that we should move our focus away from salt-restrictive diets to high-protein diets to cover individual nutritional goals in this high-risk group of patients, which includes screening, assessment, and nutritional support by dietitians,” Dr. Schuetz said.
In a linked editorial, Sheldon Gottlieb, MD, Johns Hopkins University, Baltimore, said there has been “relatively little attention” paid to the role of diet in heart failure other than recommending reduced salt intake.
In fact, in the 2021 American College of Cardiology expert consensus recommendations for optimizing heart failure treatment, roughly five words are devoted to diet and exercise and there is no mention of nutrition assessment by a dietitian, he points out.
“This study adds another tile to the still-fragmentary mosaic picture of the patient with heart failure at nutritional risk who might benefit from nutritional support,” Dr. Dr. Gottlieb wrote.
“ ‘Good medical care’ dictates that all hospitalized patients deserve to have a standardized nutritional assessment; the challenge remains: how to determine which patient with heart failure at nutritional risk will benefit by medical nutrition therapy,” Dr. Gottlieb said.
The Swiss National Science Foundation and the Research Council of the Kantonsspital Aarau provided funding for the trial. Dr. Schuetz’s institution has previously received unrestricted grant money unrelated to this project from Nestle Health Science and Abbott Nutrition. Dr. Gottlieb owns a federal trademark for the “Greens, Beans, and Leans” diet, and has a pending federal trademark for “FLOATS”: flax + oats cereal.
A version of this article first appeared on Medscape.com.
Personalized nutritional support for adults hospitalized with chronic heart failure and deemed to be at high nutritional risk reduced the risk of death or adverse cardiovascular events, compared with standard hospital food, new research indicates.
The Swiss EFFORT trial focused on patients with chronic heart failure and high risk of malnutrition defined by low body mass index, weight loss, and low food intake upon hospital admission.
“This high-risk group of chronic heart failure patients showed a significant improvement in mortality over 30 and 180 days, as well as other clinical outcomes, when individualized nutritional support interventions were offered to patients,” Philipp Schuetz, MD, MPH, Kantonsspital Aarau, Switzerland, said in an interview.
“While monitoring the nutritional status should be done also in outpatient settings by [general practitioners], malnutrition screening upon hospital admission may help to identify high-risk patients with high risk for nutritional status deterioration during the hospital stay who will benefit from nutritional assessment and treatment,” said Dr. Schuetz.
The study was published online May 3 in the Journal of the American College of Cardiology.
It’s not all about salt
The findings are based on a prespecified secondary analysis of outcomes in 645 patients (median age, 78.8 years, 52% men) hospitalized with chronic heart failure who participated in the open-label EFFORT study.
One-third of patients were hospitalized for acute decompensated heart failure and two-thirds had chronic heart failure and other acute medical illnesses requiring hospitalization.
All patients were at risk of malnutrition based on a Nutritional Risk Screening (NRS) score of 3 points or higher. They were randomly allocated 1:1 to individualized nutritional support to reach energy, protein, and micronutrient goals or usual hospital food (control group).
By 30 days, 27 of 321 patients (8.4%) receiving nutritional support had died compared with 48 of 324 patients (14.8%) in the control group (adjusted odds ratio [OR]: 0.44; 95% confidence interval, 0.26-0.75; P = .002)
Patients with high nutritional risk (NRS >4 points) showed the most benefit from nutritional support.
Compared with patients with moderate nutritional risk scores (NRS score 3-4), those with high nutritional risk (NRS >4) had a highly significant 65% increased mortality risk over 180 days.
The individual component of the NRS with the strongest association with mortality was low food intake in the week before hospitalization.
Patients who received nutritional support in the hospital also had a lower risk for major cardiovascular events at 30 days (17.4% vs. 26.9%; OR, 0.50; 95% CI, 0.34-0.75; P = .001).
“Historically, cardiologists and internists caring for patients with heart failure have mainly focused on salt-restrictive diets to reduce blood volume and thus optimize heart function. Yet, reduction of salt intake has not been shown to effectively improve clinical outcome but may, on the contrary, increase the risk of malnutrition as low-salt diets are often not tasty,” Dr. Schuetz said.
“Our data suggest that we should move our focus away from salt-restrictive diets to high-protein diets to cover individual nutritional goals in this high-risk group of patients, which includes screening, assessment, and nutritional support by dietitians,” Dr. Schuetz said.
In a linked editorial, Sheldon Gottlieb, MD, Johns Hopkins University, Baltimore, said there has been “relatively little attention” paid to the role of diet in heart failure other than recommending reduced salt intake.
In fact, in the 2021 American College of Cardiology expert consensus recommendations for optimizing heart failure treatment, roughly five words are devoted to diet and exercise and there is no mention of nutrition assessment by a dietitian, he points out.
“This study adds another tile to the still-fragmentary mosaic picture of the patient with heart failure at nutritional risk who might benefit from nutritional support,” Dr. Dr. Gottlieb wrote.
“ ‘Good medical care’ dictates that all hospitalized patients deserve to have a standardized nutritional assessment; the challenge remains: how to determine which patient with heart failure at nutritional risk will benefit by medical nutrition therapy,” Dr. Gottlieb said.
The Swiss National Science Foundation and the Research Council of the Kantonsspital Aarau provided funding for the trial. Dr. Schuetz’s institution has previously received unrestricted grant money unrelated to this project from Nestle Health Science and Abbott Nutrition. Dr. Gottlieb owns a federal trademark for the “Greens, Beans, and Leans” diet, and has a pending federal trademark for “FLOATS”: flax + oats cereal.
A version of this article first appeared on Medscape.com.
Who can call themselves ‘doctor’? The debate heats up
Who Should Get to Be Called ‘Doctor’? shows. The topic has clearly struck a nerve, since a record number of respondents – over 12,000 – voted in the poll.
Most physicians think it’s appropriate for people with other doctorate degrees such as a PhD or EdD to call themselves ‘doctor,’ although slightly more than half said it depends on the context.
The controversy over who gets to be called a doctor was reignited when a Wall Street Journal opinion piece criticized First Lady Jill Biden, EdD, for wanting to be called “Dr Biden.” The piece also challenged the idea that having a PhD is worth the honorific of ‘doctor.’
Medical ethicist Arthur Caplan, PhD, disagreed with that viewpoint, saying the context matters. For example, he prefers to be called “professor” when he’s introduced to the public rather than “doctor” to avoid any confusion about his professional status.
More than 12,000 clinicians including physicians, medical students, nurses, pharmacists, and other health care professionals responded to the poll. The non-MD clinicians were the most likely to say it was always appropriate to be called “doctor” while physicians were the least likely.
Context matters
Large percentages of clinicians – 54% of doctors, 62% of medical students, and 41% of nurses – said that the context matters for being called “doctor.’’
“I earned my PhD in 1995 and my MD in 2000. I think it is contextual. In a research or University setting, “Dr.” seems appropriate for a PhD. That same person in public should probably not hold themselves out as “Dr.” So, maybe MDs and DOs can choose, while others maintain the title in their specific setting.”
Some readers proposed that people with MDs call themselves physicians rather than doctors. Said one: “Anyone with a terminal doctorate degree has the right to use the word doctor. As a physician when someone asks what I do, I say: ‘I am a physician.’ Problem solved. There can only be one physician but there are many types of doctors.”
Physicians and nurses differed most in their views. Just 24% of physicians said it was always appropriate for people with other doctorate degrees to call themselves doctor whereas about an equal number (22%) thought it was never appropriate.
In contrast, 43% of nurses (including advance practice nurses) said it was always appropriate for people with non-MD doctorates to be called doctor. Only 16% said it’s never appropriate.
This difference may reflect the growing number of nurses with doctorate degrees, either a DNP or PhD, who want to be called doctor in clinical settings.
Age made a difference too. Only 16% of physicians younger than age 45 said it was always appropriate for people with non-MD doctorate degrees to be called doctor, compared with 27% of physicians aged 45 and up.
Medical students (31%) were also more likely than physicians to say it was always appropriate for non-MD doctorates to use the title “doctor” and 64% said it depends on the context. This was noteworthy because twice as many medical students as physicians (16% vs. 8%) said they work in academia, research, or military government settings.
Too many ‘doctors’ confuse the public
Physicians (70%) were also more likely to say it was always or often confusing for the public to hear someone without a medical degree addressed as “doctor.” Only 6% of physicians thought it was never or rarely confusing.
Nurses disagreed. Just 45% said that it was always or often confusing while 16% said it was never or rarely confusing.
Medical students were more aligned with physicians on this issue – 60% said it was always or often confusing to the public and just 10% said it was never or rarely confusing.
One reader commented, “The problem is the confusion the ‘doctor’ title causes for patients, especially in a hospital setting. Is the ‘doctor’ a physician, a pharmacist, a psychologist, a nurse, etc., etc.? We need to think not of our own egos but if and how the confusion about this plethora of titles may be hindering good patient care.”
These concerns are not unfounded. The American Medical Association reported in its Truth in Advertising campaign that “patients mistake physicians with nonphysician providers” based on an online survey of 802 adults in 2018. The participants thought these specialists were MDs: dentists (61%), podiatrists (67%), optometrists (47%), psychologists (43%), doctors of nursing (39%), and chiropractors (27%).
The AMA has advocated that states pass the “Health Care Professional Transparency Act,” which New Jersey has enacted. The law requires all health care professionals dealing with patients to wear a name tag that clearly identifies their licensure. Health care professionals must also display their education, training, and licensure in their office.
A version of this article first appeared on Medscape.com.
Who Should Get to Be Called ‘Doctor’? shows. The topic has clearly struck a nerve, since a record number of respondents – over 12,000 – voted in the poll.
Most physicians think it’s appropriate for people with other doctorate degrees such as a PhD or EdD to call themselves ‘doctor,’ although slightly more than half said it depends on the context.
The controversy over who gets to be called a doctor was reignited when a Wall Street Journal opinion piece criticized First Lady Jill Biden, EdD, for wanting to be called “Dr Biden.” The piece also challenged the idea that having a PhD is worth the honorific of ‘doctor.’
Medical ethicist Arthur Caplan, PhD, disagreed with that viewpoint, saying the context matters. For example, he prefers to be called “professor” when he’s introduced to the public rather than “doctor” to avoid any confusion about his professional status.
More than 12,000 clinicians including physicians, medical students, nurses, pharmacists, and other health care professionals responded to the poll. The non-MD clinicians were the most likely to say it was always appropriate to be called “doctor” while physicians were the least likely.
Context matters
Large percentages of clinicians – 54% of doctors, 62% of medical students, and 41% of nurses – said that the context matters for being called “doctor.’’
“I earned my PhD in 1995 and my MD in 2000. I think it is contextual. In a research or University setting, “Dr.” seems appropriate for a PhD. That same person in public should probably not hold themselves out as “Dr.” So, maybe MDs and DOs can choose, while others maintain the title in their specific setting.”
Some readers proposed that people with MDs call themselves physicians rather than doctors. Said one: “Anyone with a terminal doctorate degree has the right to use the word doctor. As a physician when someone asks what I do, I say: ‘I am a physician.’ Problem solved. There can only be one physician but there are many types of doctors.”
Physicians and nurses differed most in their views. Just 24% of physicians said it was always appropriate for people with other doctorate degrees to call themselves doctor whereas about an equal number (22%) thought it was never appropriate.
In contrast, 43% of nurses (including advance practice nurses) said it was always appropriate for people with non-MD doctorates to be called doctor. Only 16% said it’s never appropriate.
This difference may reflect the growing number of nurses with doctorate degrees, either a DNP or PhD, who want to be called doctor in clinical settings.
Age made a difference too. Only 16% of physicians younger than age 45 said it was always appropriate for people with non-MD doctorate degrees to be called doctor, compared with 27% of physicians aged 45 and up.
Medical students (31%) were also more likely than physicians to say it was always appropriate for non-MD doctorates to use the title “doctor” and 64% said it depends on the context. This was noteworthy because twice as many medical students as physicians (16% vs. 8%) said they work in academia, research, or military government settings.
Too many ‘doctors’ confuse the public
Physicians (70%) were also more likely to say it was always or often confusing for the public to hear someone without a medical degree addressed as “doctor.” Only 6% of physicians thought it was never or rarely confusing.
Nurses disagreed. Just 45% said that it was always or often confusing while 16% said it was never or rarely confusing.
Medical students were more aligned with physicians on this issue – 60% said it was always or often confusing to the public and just 10% said it was never or rarely confusing.
One reader commented, “The problem is the confusion the ‘doctor’ title causes for patients, especially in a hospital setting. Is the ‘doctor’ a physician, a pharmacist, a psychologist, a nurse, etc., etc.? We need to think not of our own egos but if and how the confusion about this plethora of titles may be hindering good patient care.”
These concerns are not unfounded. The American Medical Association reported in its Truth in Advertising campaign that “patients mistake physicians with nonphysician providers” based on an online survey of 802 adults in 2018. The participants thought these specialists were MDs: dentists (61%), podiatrists (67%), optometrists (47%), psychologists (43%), doctors of nursing (39%), and chiropractors (27%).
The AMA has advocated that states pass the “Health Care Professional Transparency Act,” which New Jersey has enacted. The law requires all health care professionals dealing with patients to wear a name tag that clearly identifies their licensure. Health care professionals must also display their education, training, and licensure in their office.
A version of this article first appeared on Medscape.com.
Who Should Get to Be Called ‘Doctor’? shows. The topic has clearly struck a nerve, since a record number of respondents – over 12,000 – voted in the poll.
Most physicians think it’s appropriate for people with other doctorate degrees such as a PhD or EdD to call themselves ‘doctor,’ although slightly more than half said it depends on the context.
The controversy over who gets to be called a doctor was reignited when a Wall Street Journal opinion piece criticized First Lady Jill Biden, EdD, for wanting to be called “Dr Biden.” The piece also challenged the idea that having a PhD is worth the honorific of ‘doctor.’
Medical ethicist Arthur Caplan, PhD, disagreed with that viewpoint, saying the context matters. For example, he prefers to be called “professor” when he’s introduced to the public rather than “doctor” to avoid any confusion about his professional status.
More than 12,000 clinicians including physicians, medical students, nurses, pharmacists, and other health care professionals responded to the poll. The non-MD clinicians were the most likely to say it was always appropriate to be called “doctor” while physicians were the least likely.
Context matters
Large percentages of clinicians – 54% of doctors, 62% of medical students, and 41% of nurses – said that the context matters for being called “doctor.’’
“I earned my PhD in 1995 and my MD in 2000. I think it is contextual. In a research or University setting, “Dr.” seems appropriate for a PhD. That same person in public should probably not hold themselves out as “Dr.” So, maybe MDs and DOs can choose, while others maintain the title in their specific setting.”
Some readers proposed that people with MDs call themselves physicians rather than doctors. Said one: “Anyone with a terminal doctorate degree has the right to use the word doctor. As a physician when someone asks what I do, I say: ‘I am a physician.’ Problem solved. There can only be one physician but there are many types of doctors.”
Physicians and nurses differed most in their views. Just 24% of physicians said it was always appropriate for people with other doctorate degrees to call themselves doctor whereas about an equal number (22%) thought it was never appropriate.
In contrast, 43% of nurses (including advance practice nurses) said it was always appropriate for people with non-MD doctorates to be called doctor. Only 16% said it’s never appropriate.
This difference may reflect the growing number of nurses with doctorate degrees, either a DNP or PhD, who want to be called doctor in clinical settings.
Age made a difference too. Only 16% of physicians younger than age 45 said it was always appropriate for people with non-MD doctorate degrees to be called doctor, compared with 27% of physicians aged 45 and up.
Medical students (31%) were also more likely than physicians to say it was always appropriate for non-MD doctorates to use the title “doctor” and 64% said it depends on the context. This was noteworthy because twice as many medical students as physicians (16% vs. 8%) said they work in academia, research, or military government settings.
Too many ‘doctors’ confuse the public
Physicians (70%) were also more likely to say it was always or often confusing for the public to hear someone without a medical degree addressed as “doctor.” Only 6% of physicians thought it was never or rarely confusing.
Nurses disagreed. Just 45% said that it was always or often confusing while 16% said it was never or rarely confusing.
Medical students were more aligned with physicians on this issue – 60% said it was always or often confusing to the public and just 10% said it was never or rarely confusing.
One reader commented, “The problem is the confusion the ‘doctor’ title causes for patients, especially in a hospital setting. Is the ‘doctor’ a physician, a pharmacist, a psychologist, a nurse, etc., etc.? We need to think not of our own egos but if and how the confusion about this plethora of titles may be hindering good patient care.”
These concerns are not unfounded. The American Medical Association reported in its Truth in Advertising campaign that “patients mistake physicians with nonphysician providers” based on an online survey of 802 adults in 2018. The participants thought these specialists were MDs: dentists (61%), podiatrists (67%), optometrists (47%), psychologists (43%), doctors of nursing (39%), and chiropractors (27%).
The AMA has advocated that states pass the “Health Care Professional Transparency Act,” which New Jersey has enacted. The law requires all health care professionals dealing with patients to wear a name tag that clearly identifies their licensure. Health care professionals must also display their education, training, and licensure in their office.
A version of this article first appeared on Medscape.com.
Moderna announces first data showing efficacy of COVID-19 vaccine booster in development
among people already vaccinated for COVID-19, according to first results released May 5.
Furthermore, data from the company’s ongoing phase 2 study show the variant-specific booster, known as mRNA-1273.351, achieved higher antibody titers against the B.1.351 variant than did a booster with the original Moderna vaccine.
“We are encouraged by these new data, which reinforce our confidence that our booster strategy should be protective against these newly detected variants. The strong and rapid boost in titers to levels above primary vaccination also clearly demonstrates the ability of mRNA-1273 to induce immune memory,” Stéphane Bancel, chief executive officer of Moderna, said in a statement.
The phase 2 study researchers also are evaluating a multivariant booster that is a 50/50 mix of mRNA-1273.351 and mRNA-1273, the initial vaccine given Food and Drug Administration emergency use authorization, in a single vial.
Unlike the two-dose regimen with the original vaccine, the boosters are administered as a single dose immunization.
The trial participants received a booster 6-8 months after primary vaccination. Titers to the wild-type SARS-CoV-2 virus remained high and detectable in 37 out of 40 participants. However, prior to the booster, titers against the two variants of concern, B.1.351 and P.1, were lower, with about half of participants showing undetectable levels.
In contrast, 2 weeks after a booster with the original vaccine or the B.1.351 strain-specific product, pseudovirus neutralizing titers were boosted in all participants and all variants tested.
“Following [the] boost, geometric mean titers against the wild-type, B.1.351, and P.1 variants increased to levels similar to or higher than the previously reported peak titers against the ancestral (D614G) strain following primary vaccination,” the company stated.
Both mRNA-1273.351 and mRNA-1273 booster doses were generally well tolerated, the company reported. Safety and tolerability were generally comparable to those reported after the second dose of the original vaccine. Most adverse events were mild to moderate, with injection site pain most common in both groups. Participants also reported fatigue, headache, myalgia, and arthralgia.
The company plans to release data shortly on the booster efficacy at additional time points beyond 2 weeks for mRNA-1273.351, a lower-dose booster with mRNA-1272/351, as well as data on the multivariant mRNA vaccine booster.
In addition to the company’s phase 2 study, the National Institute of Allergy and Infectious Diseases is conducting a separate phase 1 study of mRNA-1273.351.
A version of this article first appeared on Medscape.com.
among people already vaccinated for COVID-19, according to first results released May 5.
Furthermore, data from the company’s ongoing phase 2 study show the variant-specific booster, known as mRNA-1273.351, achieved higher antibody titers against the B.1.351 variant than did a booster with the original Moderna vaccine.
“We are encouraged by these new data, which reinforce our confidence that our booster strategy should be protective against these newly detected variants. The strong and rapid boost in titers to levels above primary vaccination also clearly demonstrates the ability of mRNA-1273 to induce immune memory,” Stéphane Bancel, chief executive officer of Moderna, said in a statement.
The phase 2 study researchers also are evaluating a multivariant booster that is a 50/50 mix of mRNA-1273.351 and mRNA-1273, the initial vaccine given Food and Drug Administration emergency use authorization, in a single vial.
Unlike the two-dose regimen with the original vaccine, the boosters are administered as a single dose immunization.
The trial participants received a booster 6-8 months after primary vaccination. Titers to the wild-type SARS-CoV-2 virus remained high and detectable in 37 out of 40 participants. However, prior to the booster, titers against the two variants of concern, B.1.351 and P.1, were lower, with about half of participants showing undetectable levels.
In contrast, 2 weeks after a booster with the original vaccine or the B.1.351 strain-specific product, pseudovirus neutralizing titers were boosted in all participants and all variants tested.
“Following [the] boost, geometric mean titers against the wild-type, B.1.351, and P.1 variants increased to levels similar to or higher than the previously reported peak titers against the ancestral (D614G) strain following primary vaccination,” the company stated.
Both mRNA-1273.351 and mRNA-1273 booster doses were generally well tolerated, the company reported. Safety and tolerability were generally comparable to those reported after the second dose of the original vaccine. Most adverse events were mild to moderate, with injection site pain most common in both groups. Participants also reported fatigue, headache, myalgia, and arthralgia.
The company plans to release data shortly on the booster efficacy at additional time points beyond 2 weeks for mRNA-1273.351, a lower-dose booster with mRNA-1272/351, as well as data on the multivariant mRNA vaccine booster.
In addition to the company’s phase 2 study, the National Institute of Allergy and Infectious Diseases is conducting a separate phase 1 study of mRNA-1273.351.
A version of this article first appeared on Medscape.com.
among people already vaccinated for COVID-19, according to first results released May 5.
Furthermore, data from the company’s ongoing phase 2 study show the variant-specific booster, known as mRNA-1273.351, achieved higher antibody titers against the B.1.351 variant than did a booster with the original Moderna vaccine.
“We are encouraged by these new data, which reinforce our confidence that our booster strategy should be protective against these newly detected variants. The strong and rapid boost in titers to levels above primary vaccination also clearly demonstrates the ability of mRNA-1273 to induce immune memory,” Stéphane Bancel, chief executive officer of Moderna, said in a statement.
The phase 2 study researchers also are evaluating a multivariant booster that is a 50/50 mix of mRNA-1273.351 and mRNA-1273, the initial vaccine given Food and Drug Administration emergency use authorization, in a single vial.
Unlike the two-dose regimen with the original vaccine, the boosters are administered as a single dose immunization.
The trial participants received a booster 6-8 months after primary vaccination. Titers to the wild-type SARS-CoV-2 virus remained high and detectable in 37 out of 40 participants. However, prior to the booster, titers against the two variants of concern, B.1.351 and P.1, were lower, with about half of participants showing undetectable levels.
In contrast, 2 weeks after a booster with the original vaccine or the B.1.351 strain-specific product, pseudovirus neutralizing titers were boosted in all participants and all variants tested.
“Following [the] boost, geometric mean titers against the wild-type, B.1.351, and P.1 variants increased to levels similar to or higher than the previously reported peak titers against the ancestral (D614G) strain following primary vaccination,” the company stated.
Both mRNA-1273.351 and mRNA-1273 booster doses were generally well tolerated, the company reported. Safety and tolerability were generally comparable to those reported after the second dose of the original vaccine. Most adverse events were mild to moderate, with injection site pain most common in both groups. Participants also reported fatigue, headache, myalgia, and arthralgia.
The company plans to release data shortly on the booster efficacy at additional time points beyond 2 weeks for mRNA-1273.351, a lower-dose booster with mRNA-1272/351, as well as data on the multivariant mRNA vaccine booster.
In addition to the company’s phase 2 study, the National Institute of Allergy and Infectious Diseases is conducting a separate phase 1 study of mRNA-1273.351.
A version of this article first appeared on Medscape.com.

