User login
Timing of Blood Pressure Dosing Doesn’t Matter (Again): BedMed and BedMed-Frail
This transcript has been edited for clarity.
Tricia Ward: I’m joined today by Dr. Scott R. Garrison, MD, PhD. He is a professor in the Department of Family Medicine at the University of Alberta in Edmonton, Alberta, Canada, and director of the Pragmatic Trials Collaborative.
You presented two studies at ESC. One is the BedMed study, comparing day vs nighttime dosing of blood pressure therapy. Can you tell us the top-line findings?
BedMed and BedMed-Frail
Dr. Garrison: We were looking to validate an earlier study that suggested a large benefit of taking blood pressure medication at bedtime, as far as reducing major adverse cardiovascular events (MACEs). That was the MAPEC study. They suggested a 60% reduction. The BedMed trial was in hypertensive primary care patients in five Canadian provinces. We randomized well over 3000 patients to bedtime or morning medications. We looked at MACEs — so all-cause death or hospitalizations for acute coronary syndrome, stroke, or heart failure, and a bunch of safety outcomes.
Essentially, . It was safe to take it at bedtime. But it did not convey any extra cardiovascular benefit.
Ms. Ward: And then you did a second study, called BedMed-Frail. Do you want to tell us the reason you did that?
Dr. Garrison: BedMed-Frail took place in a nursing home population. We believed that it was possible that frail, older adults might have very different risks and benefits, and that they would probably be underrepresented, as they normally are in the main trial.
We thought that because bedtime blood pressure medications would be theoretically preferentially lowering night pressure, which is already the lowest pressure of the day, that if you were at risk for hypotensive or ischemic adverse events, that might make it worse. We looked at falls and fractures; worsening cognition in case they had vascular dementia; and whether they developed decubitus ulcers (pressure sores) because you need a certain amount of pressure to get past any obstruction — in this case, it’s the weight of your body if you’re lying in bed all the time.
We also looked at problem behaviors. People who have dementia have what’s called “sundowning,” where agitation and confusion are worse as the evening is going on. We looked at that on the off chance that it had anything to do with blood pressures being lower. And the BedMed-Frail results mirror those of BedMed exactly. So there was no cardiovascular benefit, and in this population, that was largely driven by mortality; one third of these people died every year.
Ms. Ward: The median age was about 88?
Dr. Garrison: Yes, the median age was 88. There was no cardiovascular mortality advantage to bedtime dosing, but neither was there any signal of safety concerns.
Other Complementary and Conflicting Studies
Ms. Ward: These two studies mirror the TIME study from the United Kingdom.
Dr. Garrison: Yes. We found exactly what TIME found. Our point estimate was pretty much the same. The hazard ratio in the main trial was 0.96. Theirs, I believe, was 0.95. Our findings agree completely with those of TIME and differ substantially from the previous trials that suggested a large benefit.
Ms. Ward: Those previous trials were MAPEC and the Hygia Chronotherapy Trial.
Dr. Garrison: MAPEC was the first one. While we were doing our trial, and while the TIME investigators were doing their trial, both of us trying to validate MAPEC, the same group published another study called Hygia, which also reported a large reduction: a 45% reduction in MACE with bedtime dosing.
Ms. Ward: You didn’t present it, but there was also a meta-analysis presented here by somebody independent.
Dr. Garrison: Yes, Ricky Turgeon. I know Ricky. We gave him patient-level data for his meta-analysis, but I was not otherwise involved.
Ms. Ward: And the conclusion is the same.
Dr. Garrison: It’s the same. He only found the same five trials: MAPEC, Hygia, TIME, BedMed, and BedMed-Frail. Combining them all together, the CIs still span 1.0, so it didn’t end up being significant. But he also analyzed TIME and the BedMed trials separately — again suggesting that those trials showed no benefit.
Ms. Ward: There was a TIME substudy of night owls vs early risers or morning people, and there was a hint (or whatever you should say for a subanalysis of a neutral trial) that timing might make a difference there.
Dr. Garrison: They recently published, I guess it is a substudy, where they looked at people’s chronotype according to whether you consider yourself an early bird or a night owl. Their assessment was more detailed. They reported that if people were tending toward being early birds and they took their blood pressure medicine in the morning, or if they were night owls and they took it in the evening, that they tended to have statistically significantly better outcomes than the opposite timing. In that analysis, they were only looking at nonfatal myocardial infarction and nonfatal stroke.
We did ask something that was related. We asked people: “Do we consider yourself more of an early bird or a night owl?” So we do have those data. For what I presented at ESC, we just looked at the primary outcome; we did subgroups according to early bird, night owl, and neither, and that was not statistically significant. It didn’t rule it out. There were some trends in the direction that the TIME group were suggesting. We do intend to do a closer look at that.
But, you know, they call these “late-breaking trials,” and it really was in our case. We didn’t get the last of our data from the last province until the end of June, so we still are finishing up the analysis of the chronotype portion — so more to come in another month or so.
Do What You Like, or Stick to Morning Dosing?
Ms. Ward: For the purposes of people’s take-home message, does this mostly apply to once-daily–dosed antihypertensives?
Dr. Garrison: It was essentially once-daily medicines that were changed. The docs did have the opportunity to consolidate twice-daily meds into once-daily or switch to a different medication. That’s probably the area where adherence was the biggest issue, because it’s largely beta-blockers that were given twice daily at baseline, and they were less likely to want to change.
At 6 months, 83% of once-daily medications were taken per allocation in the bedtime group and 95% per allocation in the morning group, which was actually pretty good. For angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, and calcium-channel blockers, the adherence was excellent. Again, it was beta-blockers taken twice a day where it fell down, and then also diuretics. But if you combine all diuretic medications (ie, pure diuretics and combo agents), still, 75% of them were successful at taking them at bedtime. Only 15% of people switching a diuretic to bedtime dosing actually had problems with nocturia. Most physicians think that they can’t get their patients to take those meds at bedtime, but you can. There’s probably no reason to take it at bedtime, but most people do tolerate it.
Ms. Ward: Is your advice to take it whenever you feel like? I know when TIME came out, Professor George Stergiou, who’s the incoming president of the International Society of Hypertension, said, well, maybe we should stick with the morning, because that’s what most of the trials did.
Dr. Garrison: I think that›s a perfectly valid point of view, and maybe for a lot of people, that could be the default. There are some people, though, who will have a particular reason why one time is better. For instance, most people have no problems with calcium-channel blockers, but some get ankle swelling and you’re more likely to have that happen if you take them in the morning. Or lots of people want to take all their pills at the same time; blood pressure pills are easy ones to switch the timing of if you’re trying to accomplish that, and if that will help adherence. Basically, whatever time of day you can remember to take it the best is probably the right time.
Ms. Ward: Given where we are today, with your trials and TIME, do you think this is now settled science that it doesn’t make a difference?
Dr. Garrison: I’m probably the wrong person to ask, because I clearly have a bias. I think the methods in the TIME trial are really transparent and solid. I hope that when our papers come out, people will feel the same. You just have to look at the different trials. You need people like Dr. Stergiou to wade through the trials to help you with that.
Ms. Ward: Thank you very much for joining me today and discussing this trial.
Scott R. Garrison, MD, PhD, is Professor, Department of Family Medicine, University of Alberta in Edmonton, Alberta, Canada, and Staff Physician, Department of Family Medicine, Kaye Edmonton Clinic, and he has disclosed receiving research grants from Alberta Innovates (the Alberta Provincial Government) and the Canadian Institutes of Health Research (the Canadian Federal Government).
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Tricia Ward: I’m joined today by Dr. Scott R. Garrison, MD, PhD. He is a professor in the Department of Family Medicine at the University of Alberta in Edmonton, Alberta, Canada, and director of the Pragmatic Trials Collaborative.
You presented two studies at ESC. One is the BedMed study, comparing day vs nighttime dosing of blood pressure therapy. Can you tell us the top-line findings?
BedMed and BedMed-Frail
Dr. Garrison: We were looking to validate an earlier study that suggested a large benefit of taking blood pressure medication at bedtime, as far as reducing major adverse cardiovascular events (MACEs). That was the MAPEC study. They suggested a 60% reduction. The BedMed trial was in hypertensive primary care patients in five Canadian provinces. We randomized well over 3000 patients to bedtime or morning medications. We looked at MACEs — so all-cause death or hospitalizations for acute coronary syndrome, stroke, or heart failure, and a bunch of safety outcomes.
Essentially, . It was safe to take it at bedtime. But it did not convey any extra cardiovascular benefit.
Ms. Ward: And then you did a second study, called BedMed-Frail. Do you want to tell us the reason you did that?
Dr. Garrison: BedMed-Frail took place in a nursing home population. We believed that it was possible that frail, older adults might have very different risks and benefits, and that they would probably be underrepresented, as they normally are in the main trial.
We thought that because bedtime blood pressure medications would be theoretically preferentially lowering night pressure, which is already the lowest pressure of the day, that if you were at risk for hypotensive or ischemic adverse events, that might make it worse. We looked at falls and fractures; worsening cognition in case they had vascular dementia; and whether they developed decubitus ulcers (pressure sores) because you need a certain amount of pressure to get past any obstruction — in this case, it’s the weight of your body if you’re lying in bed all the time.
We also looked at problem behaviors. People who have dementia have what’s called “sundowning,” where agitation and confusion are worse as the evening is going on. We looked at that on the off chance that it had anything to do with blood pressures being lower. And the BedMed-Frail results mirror those of BedMed exactly. So there was no cardiovascular benefit, and in this population, that was largely driven by mortality; one third of these people died every year.
Ms. Ward: The median age was about 88?
Dr. Garrison: Yes, the median age was 88. There was no cardiovascular mortality advantage to bedtime dosing, but neither was there any signal of safety concerns.
Other Complementary and Conflicting Studies
Ms. Ward: These two studies mirror the TIME study from the United Kingdom.
Dr. Garrison: Yes. We found exactly what TIME found. Our point estimate was pretty much the same. The hazard ratio in the main trial was 0.96. Theirs, I believe, was 0.95. Our findings agree completely with those of TIME and differ substantially from the previous trials that suggested a large benefit.
Ms. Ward: Those previous trials were MAPEC and the Hygia Chronotherapy Trial.
Dr. Garrison: MAPEC was the first one. While we were doing our trial, and while the TIME investigators were doing their trial, both of us trying to validate MAPEC, the same group published another study called Hygia, which also reported a large reduction: a 45% reduction in MACE with bedtime dosing.
Ms. Ward: You didn’t present it, but there was also a meta-analysis presented here by somebody independent.
Dr. Garrison: Yes, Ricky Turgeon. I know Ricky. We gave him patient-level data for his meta-analysis, but I was not otherwise involved.
Ms. Ward: And the conclusion is the same.
Dr. Garrison: It’s the same. He only found the same five trials: MAPEC, Hygia, TIME, BedMed, and BedMed-Frail. Combining them all together, the CIs still span 1.0, so it didn’t end up being significant. But he also analyzed TIME and the BedMed trials separately — again suggesting that those trials showed no benefit.
Ms. Ward: There was a TIME substudy of night owls vs early risers or morning people, and there was a hint (or whatever you should say for a subanalysis of a neutral trial) that timing might make a difference there.
Dr. Garrison: They recently published, I guess it is a substudy, where they looked at people’s chronotype according to whether you consider yourself an early bird or a night owl. Their assessment was more detailed. They reported that if people were tending toward being early birds and they took their blood pressure medicine in the morning, or if they were night owls and they took it in the evening, that they tended to have statistically significantly better outcomes than the opposite timing. In that analysis, they were only looking at nonfatal myocardial infarction and nonfatal stroke.
We did ask something that was related. We asked people: “Do we consider yourself more of an early bird or a night owl?” So we do have those data. For what I presented at ESC, we just looked at the primary outcome; we did subgroups according to early bird, night owl, and neither, and that was not statistically significant. It didn’t rule it out. There were some trends in the direction that the TIME group were suggesting. We do intend to do a closer look at that.
But, you know, they call these “late-breaking trials,” and it really was in our case. We didn’t get the last of our data from the last province until the end of June, so we still are finishing up the analysis of the chronotype portion — so more to come in another month or so.
Do What You Like, or Stick to Morning Dosing?
Ms. Ward: For the purposes of people’s take-home message, does this mostly apply to once-daily–dosed antihypertensives?
Dr. Garrison: It was essentially once-daily medicines that were changed. The docs did have the opportunity to consolidate twice-daily meds into once-daily or switch to a different medication. That’s probably the area where adherence was the biggest issue, because it’s largely beta-blockers that were given twice daily at baseline, and they were less likely to want to change.
At 6 months, 83% of once-daily medications were taken per allocation in the bedtime group and 95% per allocation in the morning group, which was actually pretty good. For angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, and calcium-channel blockers, the adherence was excellent. Again, it was beta-blockers taken twice a day where it fell down, and then also diuretics. But if you combine all diuretic medications (ie, pure diuretics and combo agents), still, 75% of them were successful at taking them at bedtime. Only 15% of people switching a diuretic to bedtime dosing actually had problems with nocturia. Most physicians think that they can’t get their patients to take those meds at bedtime, but you can. There’s probably no reason to take it at bedtime, but most people do tolerate it.
Ms. Ward: Is your advice to take it whenever you feel like? I know when TIME came out, Professor George Stergiou, who’s the incoming president of the International Society of Hypertension, said, well, maybe we should stick with the morning, because that’s what most of the trials did.
Dr. Garrison: I think that›s a perfectly valid point of view, and maybe for a lot of people, that could be the default. There are some people, though, who will have a particular reason why one time is better. For instance, most people have no problems with calcium-channel blockers, but some get ankle swelling and you’re more likely to have that happen if you take them in the morning. Or lots of people want to take all their pills at the same time; blood pressure pills are easy ones to switch the timing of if you’re trying to accomplish that, and if that will help adherence. Basically, whatever time of day you can remember to take it the best is probably the right time.
Ms. Ward: Given where we are today, with your trials and TIME, do you think this is now settled science that it doesn’t make a difference?
Dr. Garrison: I’m probably the wrong person to ask, because I clearly have a bias. I think the methods in the TIME trial are really transparent and solid. I hope that when our papers come out, people will feel the same. You just have to look at the different trials. You need people like Dr. Stergiou to wade through the trials to help you with that.
Ms. Ward: Thank you very much for joining me today and discussing this trial.
Scott R. Garrison, MD, PhD, is Professor, Department of Family Medicine, University of Alberta in Edmonton, Alberta, Canada, and Staff Physician, Department of Family Medicine, Kaye Edmonton Clinic, and he has disclosed receiving research grants from Alberta Innovates (the Alberta Provincial Government) and the Canadian Institutes of Health Research (the Canadian Federal Government).
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Tricia Ward: I’m joined today by Dr. Scott R. Garrison, MD, PhD. He is a professor in the Department of Family Medicine at the University of Alberta in Edmonton, Alberta, Canada, and director of the Pragmatic Trials Collaborative.
You presented two studies at ESC. One is the BedMed study, comparing day vs nighttime dosing of blood pressure therapy. Can you tell us the top-line findings?
BedMed and BedMed-Frail
Dr. Garrison: We were looking to validate an earlier study that suggested a large benefit of taking blood pressure medication at bedtime, as far as reducing major adverse cardiovascular events (MACEs). That was the MAPEC study. They suggested a 60% reduction. The BedMed trial was in hypertensive primary care patients in five Canadian provinces. We randomized well over 3000 patients to bedtime or morning medications. We looked at MACEs — so all-cause death or hospitalizations for acute coronary syndrome, stroke, or heart failure, and a bunch of safety outcomes.
Essentially, . It was safe to take it at bedtime. But it did not convey any extra cardiovascular benefit.
Ms. Ward: And then you did a second study, called BedMed-Frail. Do you want to tell us the reason you did that?
Dr. Garrison: BedMed-Frail took place in a nursing home population. We believed that it was possible that frail, older adults might have very different risks and benefits, and that they would probably be underrepresented, as they normally are in the main trial.
We thought that because bedtime blood pressure medications would be theoretically preferentially lowering night pressure, which is already the lowest pressure of the day, that if you were at risk for hypotensive or ischemic adverse events, that might make it worse. We looked at falls and fractures; worsening cognition in case they had vascular dementia; and whether they developed decubitus ulcers (pressure sores) because you need a certain amount of pressure to get past any obstruction — in this case, it’s the weight of your body if you’re lying in bed all the time.
We also looked at problem behaviors. People who have dementia have what’s called “sundowning,” where agitation and confusion are worse as the evening is going on. We looked at that on the off chance that it had anything to do with blood pressures being lower. And the BedMed-Frail results mirror those of BedMed exactly. So there was no cardiovascular benefit, and in this population, that was largely driven by mortality; one third of these people died every year.
Ms. Ward: The median age was about 88?
Dr. Garrison: Yes, the median age was 88. There was no cardiovascular mortality advantage to bedtime dosing, but neither was there any signal of safety concerns.
Other Complementary and Conflicting Studies
Ms. Ward: These two studies mirror the TIME study from the United Kingdom.
Dr. Garrison: Yes. We found exactly what TIME found. Our point estimate was pretty much the same. The hazard ratio in the main trial was 0.96. Theirs, I believe, was 0.95. Our findings agree completely with those of TIME and differ substantially from the previous trials that suggested a large benefit.
Ms. Ward: Those previous trials were MAPEC and the Hygia Chronotherapy Trial.
Dr. Garrison: MAPEC was the first one. While we were doing our trial, and while the TIME investigators were doing their trial, both of us trying to validate MAPEC, the same group published another study called Hygia, which also reported a large reduction: a 45% reduction in MACE with bedtime dosing.
Ms. Ward: You didn’t present it, but there was also a meta-analysis presented here by somebody independent.
Dr. Garrison: Yes, Ricky Turgeon. I know Ricky. We gave him patient-level data for his meta-analysis, but I was not otherwise involved.
Ms. Ward: And the conclusion is the same.
Dr. Garrison: It’s the same. He only found the same five trials: MAPEC, Hygia, TIME, BedMed, and BedMed-Frail. Combining them all together, the CIs still span 1.0, so it didn’t end up being significant. But he also analyzed TIME and the BedMed trials separately — again suggesting that those trials showed no benefit.
Ms. Ward: There was a TIME substudy of night owls vs early risers or morning people, and there was a hint (or whatever you should say for a subanalysis of a neutral trial) that timing might make a difference there.
Dr. Garrison: They recently published, I guess it is a substudy, where they looked at people’s chronotype according to whether you consider yourself an early bird or a night owl. Their assessment was more detailed. They reported that if people were tending toward being early birds and they took their blood pressure medicine in the morning, or if they were night owls and they took it in the evening, that they tended to have statistically significantly better outcomes than the opposite timing. In that analysis, they were only looking at nonfatal myocardial infarction and nonfatal stroke.
We did ask something that was related. We asked people: “Do we consider yourself more of an early bird or a night owl?” So we do have those data. For what I presented at ESC, we just looked at the primary outcome; we did subgroups according to early bird, night owl, and neither, and that was not statistically significant. It didn’t rule it out. There were some trends in the direction that the TIME group were suggesting. We do intend to do a closer look at that.
But, you know, they call these “late-breaking trials,” and it really was in our case. We didn’t get the last of our data from the last province until the end of June, so we still are finishing up the analysis of the chronotype portion — so more to come in another month or so.
Do What You Like, or Stick to Morning Dosing?
Ms. Ward: For the purposes of people’s take-home message, does this mostly apply to once-daily–dosed antihypertensives?
Dr. Garrison: It was essentially once-daily medicines that were changed. The docs did have the opportunity to consolidate twice-daily meds into once-daily or switch to a different medication. That’s probably the area where adherence was the biggest issue, because it’s largely beta-blockers that were given twice daily at baseline, and they were less likely to want to change.
At 6 months, 83% of once-daily medications were taken per allocation in the bedtime group and 95% per allocation in the morning group, which was actually pretty good. For angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, and calcium-channel blockers, the adherence was excellent. Again, it was beta-blockers taken twice a day where it fell down, and then also diuretics. But if you combine all diuretic medications (ie, pure diuretics and combo agents), still, 75% of them were successful at taking them at bedtime. Only 15% of people switching a diuretic to bedtime dosing actually had problems with nocturia. Most physicians think that they can’t get their patients to take those meds at bedtime, but you can. There’s probably no reason to take it at bedtime, but most people do tolerate it.
Ms. Ward: Is your advice to take it whenever you feel like? I know when TIME came out, Professor George Stergiou, who’s the incoming president of the International Society of Hypertension, said, well, maybe we should stick with the morning, because that’s what most of the trials did.
Dr. Garrison: I think that›s a perfectly valid point of view, and maybe for a lot of people, that could be the default. There are some people, though, who will have a particular reason why one time is better. For instance, most people have no problems with calcium-channel blockers, but some get ankle swelling and you’re more likely to have that happen if you take them in the morning. Or lots of people want to take all their pills at the same time; blood pressure pills are easy ones to switch the timing of if you’re trying to accomplish that, and if that will help adherence. Basically, whatever time of day you can remember to take it the best is probably the right time.
Ms. Ward: Given where we are today, with your trials and TIME, do you think this is now settled science that it doesn’t make a difference?
Dr. Garrison: I’m probably the wrong person to ask, because I clearly have a bias. I think the methods in the TIME trial are really transparent and solid. I hope that when our papers come out, people will feel the same. You just have to look at the different trials. You need people like Dr. Stergiou to wade through the trials to help you with that.
Ms. Ward: Thank you very much for joining me today and discussing this trial.
Scott R. Garrison, MD, PhD, is Professor, Department of Family Medicine, University of Alberta in Edmonton, Alberta, Canada, and Staff Physician, Department of Family Medicine, Kaye Edmonton Clinic, and he has disclosed receiving research grants from Alberta Innovates (the Alberta Provincial Government) and the Canadian Institutes of Health Research (the Canadian Federal Government).
A version of this article first appeared on Medscape.com.
FROM ESC 2024
Calcium and CV Risk: Are Supplements and Vitamin D to Blame?
This transcript has been edited for clarity.
Tricia Ward: Hi. I’m Tricia Ward, from theheart.org/Medscape Cardiology. I’m joined today by Dr Matthew Budoff. He is professor of medicine at UCLA and the endowed chair of preventive cardiology at the Lundquist Institute. Welcome, Dr Budoff.
Matthew J. Budoff, MD: Thank you.
Dietary Calcium vs Coronary Calcium
Ms. Ward: The reason I wanted to talk to you today is because there have been some recent studies linking calcium supplements to an increased risk for cardiovascular disease. I’m old enough to remember when we used to tell people that dietary calcium and coronary calcium weren’t connected and weren’t the same. Were we wrong?
Dr. Budoff: I think there’s a large amount of mixed data out there still. The US Preventive Services Task Force looked into this a number of years ago and said there’s no association between calcium supplementation and increased risk for cardiovascular disease.
As you mentioned, there are a couple of newer studies that point us toward a relationship. I think that we still have a little bit of a mixed bag, but we need to dive a little deeper into that to figure out what’s going on.
Ms. Ward: Does it appear to be connected to calcium in the form of supplements vs calcium from foods?
Dr. Budoff: We looked very carefully at dietary calcium in the MESA study, the multiethnic study of atherosclerosis. There is no relationship between dietary calcium intake and coronary calcium or cardiovascular events. We’re talking mostly about supplements now when we talk about this increased risk that we’re seeing.
Does Vitamin D Exacerbate Risk?
Ms. Ward: Because it’s seen with supplements, is that likely because that’s a much higher concentration of calcium coming in or do you think it’s something inherent in its being in the form of a supplement?
Dr. Budoff: I think there are two things. One, it’s definitely a higher concentration all at once. You get many more milligrams at a time when you take a supplement than if you had a high-calcium food or drink.
Also, most supplements have vitamin D as well. I think vitamin D and calcium work synergistically. When you give them both together simultaneously, I think that may have more of a potentiating effect that might exacerbate any potential risk.
Ms. Ward: Is there any reason to think there might be a difference in type of calcium supplement? I always think of the chalky tablet form vs calcium chews.
Dr. Budoff: I’m not aware of a difference in the supplement type. I think the vitamin D issue is a big problem because we all have patients who take thousands of units of vitamin D — just crazy numbers. People advocate really high numbers and that stays in the system.
Personally, I think part of the explanation is that with very high levels of vitamin D on top of calcium supplementation, you now absorb it better. You now get it into the bone, but maybe also into the coronary arteries. If you’re very high in vitamin D and then are taking a large calcium supplement, it might be the calcium/vitamin D combination that’s giving us some trouble. I think people on vitamin D supplements really need to watch their levels and not get supratherapeutic.
Ms. Ward: With the vitamin D?
Dr. Budoff: With the vitamin D.
Diabetes and Renal Function
Ms. Ward: In some of the studies, there seems to be a higher risk in patients with diabetes. Is there any reason why that would be?
Dr. Budoff: I can’t think of a reason exactly why with diabetes per se, except for renal disease. Patients with diabetes have more intrinsic renal disease, proteinuria, and even a reduced eGFR. We’ve seen that the kidney is very strongly tied to this. We have a very strong relationship, in work I’ve done a decade ago now, showing that calcium supplementation (in the form of phosphate binders) in patients on dialysis or with advanced renal disease is linked to much higher coronary calcium progression.
We did prospective, randomized trials showing that calcium intake as binders to reduce phosphorus led to more coronary calcium. We always thought that was just relegated to the renal population, and there might be an overlap here with the diabetes and more renal disease. I have a feeling that it has to do with more of that. It might be regulation of parathyroid hormone as well, which might be more abnormal in patients with diabetes.
Avoid Supratherapeutic Vitamin D Levels
Ms. Ward:: What are you telling your patients?
Dr. Budoff: I tell patients with normal kidney function that the bone will modulate 99.9% of the calcium uptake. If they have osteopenia or osteoporosis, regardless of their calcium score, I’m very comfortable putting them on supplements.
I’m a little more cautious with the vitamin D levels, and I keep an eye on that and regulate how much vitamin D they get based on their levels. I get them into the normal range, but I don’t want them supratherapeutic. You can even follow their calcium score. Again, we’ve shown that if you’re taking too much calcium, your calcium score will go up. I can just check it again in a couple of years to make sure that it’s safe.
Ms. Ward:: In terms of vitamin D levels, when you’re saying “supratherapeutic,” what levels do you consider a safe amount to take?
Dr. Budoff: I’d like them under 100 ng/mL as far as their upper level. Normal is around 70 ng/mL at most labs. I try to keep them in the normal range. I don’t even want them to be high-normal if I’m going to be concomitantly giving them calcium supplements. Of course, if they have renal insufficiency, then I’m much more cautious. We’ve even seen calcium supplements raise the serum calcium, which you never see with dietary calcium. That’s another potential proof that it might be too much too fast.
For renal patients, even in mild renal insufficiency, maybe even in diabetes where we’ve seen a signal, maybe aim lower in the amount of calcium supplementation if diet is insufficient, and aim a little lower in vitamin D targets, and I think you’ll be in a safer place.
Ms. Ward: Is there anything else you want to add?
Dr. Budoff: The evidence is still evolving. I’d say that it’s interesting and maybe a little frustrating that we don’t have a final answer on all of this. I would stay tuned for more data because we’re looking at many of the epidemiologic studies to try to see what happens in the real world, with both dietary intake of calcium and calcium supplementation.
Ms. Ward: Thank you very much for joining me today.
Dr. Budoff: It’s a pleasure. Thanks for having me.
Dr. Budoff disclosed being a speaker for Amarin Pharma.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
Tricia Ward: Hi. I’m Tricia Ward, from theheart.org/Medscape Cardiology. I’m joined today by Dr Matthew Budoff. He is professor of medicine at UCLA and the endowed chair of preventive cardiology at the Lundquist Institute. Welcome, Dr Budoff.
Matthew J. Budoff, MD: Thank you.
Dietary Calcium vs Coronary Calcium
Ms. Ward: The reason I wanted to talk to you today is because there have been some recent studies linking calcium supplements to an increased risk for cardiovascular disease. I’m old enough to remember when we used to tell people that dietary calcium and coronary calcium weren’t connected and weren’t the same. Were we wrong?
Dr. Budoff: I think there’s a large amount of mixed data out there still. The US Preventive Services Task Force looked into this a number of years ago and said there’s no association between calcium supplementation and increased risk for cardiovascular disease.
As you mentioned, there are a couple of newer studies that point us toward a relationship. I think that we still have a little bit of a mixed bag, but we need to dive a little deeper into that to figure out what’s going on.
Ms. Ward: Does it appear to be connected to calcium in the form of supplements vs calcium from foods?
Dr. Budoff: We looked very carefully at dietary calcium in the MESA study, the multiethnic study of atherosclerosis. There is no relationship between dietary calcium intake and coronary calcium or cardiovascular events. We’re talking mostly about supplements now when we talk about this increased risk that we’re seeing.
Does Vitamin D Exacerbate Risk?
Ms. Ward: Because it’s seen with supplements, is that likely because that’s a much higher concentration of calcium coming in or do you think it’s something inherent in its being in the form of a supplement?
Dr. Budoff: I think there are two things. One, it’s definitely a higher concentration all at once. You get many more milligrams at a time when you take a supplement than if you had a high-calcium food or drink.
Also, most supplements have vitamin D as well. I think vitamin D and calcium work synergistically. When you give them both together simultaneously, I think that may have more of a potentiating effect that might exacerbate any potential risk.
Ms. Ward: Is there any reason to think there might be a difference in type of calcium supplement? I always think of the chalky tablet form vs calcium chews.
Dr. Budoff: I’m not aware of a difference in the supplement type. I think the vitamin D issue is a big problem because we all have patients who take thousands of units of vitamin D — just crazy numbers. People advocate really high numbers and that stays in the system.
Personally, I think part of the explanation is that with very high levels of vitamin D on top of calcium supplementation, you now absorb it better. You now get it into the bone, but maybe also into the coronary arteries. If you’re very high in vitamin D and then are taking a large calcium supplement, it might be the calcium/vitamin D combination that’s giving us some trouble. I think people on vitamin D supplements really need to watch their levels and not get supratherapeutic.
Ms. Ward: With the vitamin D?
Dr. Budoff: With the vitamin D.
Diabetes and Renal Function
Ms. Ward: In some of the studies, there seems to be a higher risk in patients with diabetes. Is there any reason why that would be?
Dr. Budoff: I can’t think of a reason exactly why with diabetes per se, except for renal disease. Patients with diabetes have more intrinsic renal disease, proteinuria, and even a reduced eGFR. We’ve seen that the kidney is very strongly tied to this. We have a very strong relationship, in work I’ve done a decade ago now, showing that calcium supplementation (in the form of phosphate binders) in patients on dialysis or with advanced renal disease is linked to much higher coronary calcium progression.
We did prospective, randomized trials showing that calcium intake as binders to reduce phosphorus led to more coronary calcium. We always thought that was just relegated to the renal population, and there might be an overlap here with the diabetes and more renal disease. I have a feeling that it has to do with more of that. It might be regulation of parathyroid hormone as well, which might be more abnormal in patients with diabetes.
Avoid Supratherapeutic Vitamin D Levels
Ms. Ward:: What are you telling your patients?
Dr. Budoff: I tell patients with normal kidney function that the bone will modulate 99.9% of the calcium uptake. If they have osteopenia or osteoporosis, regardless of their calcium score, I’m very comfortable putting them on supplements.
I’m a little more cautious with the vitamin D levels, and I keep an eye on that and regulate how much vitamin D they get based on their levels. I get them into the normal range, but I don’t want them supratherapeutic. You can even follow their calcium score. Again, we’ve shown that if you’re taking too much calcium, your calcium score will go up. I can just check it again in a couple of years to make sure that it’s safe.
Ms. Ward:: In terms of vitamin D levels, when you’re saying “supratherapeutic,” what levels do you consider a safe amount to take?
Dr. Budoff: I’d like them under 100 ng/mL as far as their upper level. Normal is around 70 ng/mL at most labs. I try to keep them in the normal range. I don’t even want them to be high-normal if I’m going to be concomitantly giving them calcium supplements. Of course, if they have renal insufficiency, then I’m much more cautious. We’ve even seen calcium supplements raise the serum calcium, which you never see with dietary calcium. That’s another potential proof that it might be too much too fast.
For renal patients, even in mild renal insufficiency, maybe even in diabetes where we’ve seen a signal, maybe aim lower in the amount of calcium supplementation if diet is insufficient, and aim a little lower in vitamin D targets, and I think you’ll be in a safer place.
Ms. Ward: Is there anything else you want to add?
Dr. Budoff: The evidence is still evolving. I’d say that it’s interesting and maybe a little frustrating that we don’t have a final answer on all of this. I would stay tuned for more data because we’re looking at many of the epidemiologic studies to try to see what happens in the real world, with both dietary intake of calcium and calcium supplementation.
Ms. Ward: Thank you very much for joining me today.
Dr. Budoff: It’s a pleasure. Thanks for having me.
Dr. Budoff disclosed being a speaker for Amarin Pharma.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
Tricia Ward: Hi. I’m Tricia Ward, from theheart.org/Medscape Cardiology. I’m joined today by Dr Matthew Budoff. He is professor of medicine at UCLA and the endowed chair of preventive cardiology at the Lundquist Institute. Welcome, Dr Budoff.
Matthew J. Budoff, MD: Thank you.
Dietary Calcium vs Coronary Calcium
Ms. Ward: The reason I wanted to talk to you today is because there have been some recent studies linking calcium supplements to an increased risk for cardiovascular disease. I’m old enough to remember when we used to tell people that dietary calcium and coronary calcium weren’t connected and weren’t the same. Were we wrong?
Dr. Budoff: I think there’s a large amount of mixed data out there still. The US Preventive Services Task Force looked into this a number of years ago and said there’s no association between calcium supplementation and increased risk for cardiovascular disease.
As you mentioned, there are a couple of newer studies that point us toward a relationship. I think that we still have a little bit of a mixed bag, but we need to dive a little deeper into that to figure out what’s going on.
Ms. Ward: Does it appear to be connected to calcium in the form of supplements vs calcium from foods?
Dr. Budoff: We looked very carefully at dietary calcium in the MESA study, the multiethnic study of atherosclerosis. There is no relationship between dietary calcium intake and coronary calcium or cardiovascular events. We’re talking mostly about supplements now when we talk about this increased risk that we’re seeing.
Does Vitamin D Exacerbate Risk?
Ms. Ward: Because it’s seen with supplements, is that likely because that’s a much higher concentration of calcium coming in or do you think it’s something inherent in its being in the form of a supplement?
Dr. Budoff: I think there are two things. One, it’s definitely a higher concentration all at once. You get many more milligrams at a time when you take a supplement than if you had a high-calcium food or drink.
Also, most supplements have vitamin D as well. I think vitamin D and calcium work synergistically. When you give them both together simultaneously, I think that may have more of a potentiating effect that might exacerbate any potential risk.
Ms. Ward: Is there any reason to think there might be a difference in type of calcium supplement? I always think of the chalky tablet form vs calcium chews.
Dr. Budoff: I’m not aware of a difference in the supplement type. I think the vitamin D issue is a big problem because we all have patients who take thousands of units of vitamin D — just crazy numbers. People advocate really high numbers and that stays in the system.
Personally, I think part of the explanation is that with very high levels of vitamin D on top of calcium supplementation, you now absorb it better. You now get it into the bone, but maybe also into the coronary arteries. If you’re very high in vitamin D and then are taking a large calcium supplement, it might be the calcium/vitamin D combination that’s giving us some trouble. I think people on vitamin D supplements really need to watch their levels and not get supratherapeutic.
Ms. Ward: With the vitamin D?
Dr. Budoff: With the vitamin D.
Diabetes and Renal Function
Ms. Ward: In some of the studies, there seems to be a higher risk in patients with diabetes. Is there any reason why that would be?
Dr. Budoff: I can’t think of a reason exactly why with diabetes per se, except for renal disease. Patients with diabetes have more intrinsic renal disease, proteinuria, and even a reduced eGFR. We’ve seen that the kidney is very strongly tied to this. We have a very strong relationship, in work I’ve done a decade ago now, showing that calcium supplementation (in the form of phosphate binders) in patients on dialysis or with advanced renal disease is linked to much higher coronary calcium progression.
We did prospective, randomized trials showing that calcium intake as binders to reduce phosphorus led to more coronary calcium. We always thought that was just relegated to the renal population, and there might be an overlap here with the diabetes and more renal disease. I have a feeling that it has to do with more of that. It might be regulation of parathyroid hormone as well, which might be more abnormal in patients with diabetes.
Avoid Supratherapeutic Vitamin D Levels
Ms. Ward:: What are you telling your patients?
Dr. Budoff: I tell patients with normal kidney function that the bone will modulate 99.9% of the calcium uptake. If they have osteopenia or osteoporosis, regardless of their calcium score, I’m very comfortable putting them on supplements.
I’m a little more cautious with the vitamin D levels, and I keep an eye on that and regulate how much vitamin D they get based on their levels. I get them into the normal range, but I don’t want them supratherapeutic. You can even follow their calcium score. Again, we’ve shown that if you’re taking too much calcium, your calcium score will go up. I can just check it again in a couple of years to make sure that it’s safe.
Ms. Ward:: In terms of vitamin D levels, when you’re saying “supratherapeutic,” what levels do you consider a safe amount to take?
Dr. Budoff: I’d like them under 100 ng/mL as far as their upper level. Normal is around 70 ng/mL at most labs. I try to keep them in the normal range. I don’t even want them to be high-normal if I’m going to be concomitantly giving them calcium supplements. Of course, if they have renal insufficiency, then I’m much more cautious. We’ve even seen calcium supplements raise the serum calcium, which you never see with dietary calcium. That’s another potential proof that it might be too much too fast.
For renal patients, even in mild renal insufficiency, maybe even in diabetes where we’ve seen a signal, maybe aim lower in the amount of calcium supplementation if diet is insufficient, and aim a little lower in vitamin D targets, and I think you’ll be in a safer place.
Ms. Ward: Is there anything else you want to add?
Dr. Budoff: The evidence is still evolving. I’d say that it’s interesting and maybe a little frustrating that we don’t have a final answer on all of this. I would stay tuned for more data because we’re looking at many of the epidemiologic studies to try to see what happens in the real world, with both dietary intake of calcium and calcium supplementation.
Ms. Ward: Thank you very much for joining me today.
Dr. Budoff: It’s a pleasure. Thanks for having me.
Dr. Budoff disclosed being a speaker for Amarin Pharma.
A version of this article appeared on Medscape.com.
Doc releases song after racist massacre in Buffalo
Physician-musician Cleveland Francis, MD, responded to the recent mass shooting in Buffalo, New York, which left 10 dead, in the only way he knew how. He wrote and recorded a song to honor the victims as “a plea to the other side to recognize us as people,” the Black cardiologist told this news organization.
He couldn’t sleep after the shooting, and “this song was just in my head.” In the 1990s, Dr. Francis took a 3-year sabbatical from medicine to perform and tour as a country singer. He leveraged his Nashville connections to get “Buffalo” produced and recorded.
Acclaimed artist James Threalkill created the accompanying art, titled “The Heavenly Escort of the Buffalo 10,” after listening to a scratch demo.
Dr. Francis doesn’t want people to overlook the massacre as just another gun violence incident because this was “overt hate-crime racism,” he said.
According to the affidavit submitted by FBI agent Christopher J. Dlugokinski, the suspect’s “motive for the mass shooting was to prevent Black people from replacing White people and eliminating the White race, and to inspire others to commit similar attacks.”
Dr. Francis views the Buffalo shooting as distinct from cases like the murder of George Floyd that involved crime or police. It immediately made him think of the Mother Emanuel Church shooting in Charleston, South Carolina. “Having a black skin is now a death warrant,” he said.
The song is also an appeal for White people to fight racism. Dr. Francis is concerned about young men caught up in white supremacy and suggests that we be more alert to children or grandchildren who disconnect from their families, spend time on the dark web, and access guns. The lyrics deliberately don’t mention guns because Dr. Francis wanted to stay out of that debate. “I just sang: ‘What else do I have to do to prove to you that I’m human too?’ ”
Despite his country credentials, Dr. Francis wrote “Buffalo” as a Gospel song because that genre “connects with Black people more and because that civil rights movement was through the church with Dr. Martin Luther King,” he explained. Although he sings all styles of music, the song is performed by Nashville-based singer Michael Lusk so that it’s not a “Cleve Francis thing,” he said, referring to his stage name.
Songwriter Norman Kerner collaborated on the song. The music was produced and recorded by David Thein and mixed by Bob Bullock of Nashville, who Dr. Francis had worked with when he was an artist on Capitol Records.
They sent the video and artwork to the Mayor of Buffalo, Byron Brown, but have yet to hear back. Dr. Francis hopes it could be part of their healing, noting that some people used the song in their Juneteenth celebrations.
The Louisiana native grew up during segregation and was one of two Black students in the Medical College of Virginia class of 1973. After completing his cardiology fellowship, no one would hire him, so Dr. Francis set up his own practice in Northern Virginia. He now works at Inova Heart and Vascular Institute in Alexandria, Va. He remains optimistic about race relations in America and would love a Black pop or Gospel star to record “Buffalo” and bring it to a wider audience.
Dr. Francis is a regular blogger for Medscape. His contribution to country music is recognized in the National Museum of African American History and Culture in Washington, DC. You can find more of his music on YouTube.
A version of this article first appeared on Medscape.com.
Physician-musician Cleveland Francis, MD, responded to the recent mass shooting in Buffalo, New York, which left 10 dead, in the only way he knew how. He wrote and recorded a song to honor the victims as “a plea to the other side to recognize us as people,” the Black cardiologist told this news organization.
He couldn’t sleep after the shooting, and “this song was just in my head.” In the 1990s, Dr. Francis took a 3-year sabbatical from medicine to perform and tour as a country singer. He leveraged his Nashville connections to get “Buffalo” produced and recorded.
Acclaimed artist James Threalkill created the accompanying art, titled “The Heavenly Escort of the Buffalo 10,” after listening to a scratch demo.
Dr. Francis doesn’t want people to overlook the massacre as just another gun violence incident because this was “overt hate-crime racism,” he said.
According to the affidavit submitted by FBI agent Christopher J. Dlugokinski, the suspect’s “motive for the mass shooting was to prevent Black people from replacing White people and eliminating the White race, and to inspire others to commit similar attacks.”
Dr. Francis views the Buffalo shooting as distinct from cases like the murder of George Floyd that involved crime or police. It immediately made him think of the Mother Emanuel Church shooting in Charleston, South Carolina. “Having a black skin is now a death warrant,” he said.
The song is also an appeal for White people to fight racism. Dr. Francis is concerned about young men caught up in white supremacy and suggests that we be more alert to children or grandchildren who disconnect from their families, spend time on the dark web, and access guns. The lyrics deliberately don’t mention guns because Dr. Francis wanted to stay out of that debate. “I just sang: ‘What else do I have to do to prove to you that I’m human too?’ ”
Despite his country credentials, Dr. Francis wrote “Buffalo” as a Gospel song because that genre “connects with Black people more and because that civil rights movement was through the church with Dr. Martin Luther King,” he explained. Although he sings all styles of music, the song is performed by Nashville-based singer Michael Lusk so that it’s not a “Cleve Francis thing,” he said, referring to his stage name.
Songwriter Norman Kerner collaborated on the song. The music was produced and recorded by David Thein and mixed by Bob Bullock of Nashville, who Dr. Francis had worked with when he was an artist on Capitol Records.
They sent the video and artwork to the Mayor of Buffalo, Byron Brown, but have yet to hear back. Dr. Francis hopes it could be part of their healing, noting that some people used the song in their Juneteenth celebrations.
The Louisiana native grew up during segregation and was one of two Black students in the Medical College of Virginia class of 1973. After completing his cardiology fellowship, no one would hire him, so Dr. Francis set up his own practice in Northern Virginia. He now works at Inova Heart and Vascular Institute in Alexandria, Va. He remains optimistic about race relations in America and would love a Black pop or Gospel star to record “Buffalo” and bring it to a wider audience.
Dr. Francis is a regular blogger for Medscape. His contribution to country music is recognized in the National Museum of African American History and Culture in Washington, DC. You can find more of his music on YouTube.
A version of this article first appeared on Medscape.com.
Physician-musician Cleveland Francis, MD, responded to the recent mass shooting in Buffalo, New York, which left 10 dead, in the only way he knew how. He wrote and recorded a song to honor the victims as “a plea to the other side to recognize us as people,” the Black cardiologist told this news organization.
He couldn’t sleep after the shooting, and “this song was just in my head.” In the 1990s, Dr. Francis took a 3-year sabbatical from medicine to perform and tour as a country singer. He leveraged his Nashville connections to get “Buffalo” produced and recorded.
Acclaimed artist James Threalkill created the accompanying art, titled “The Heavenly Escort of the Buffalo 10,” after listening to a scratch demo.
Dr. Francis doesn’t want people to overlook the massacre as just another gun violence incident because this was “overt hate-crime racism,” he said.
According to the affidavit submitted by FBI agent Christopher J. Dlugokinski, the suspect’s “motive for the mass shooting was to prevent Black people from replacing White people and eliminating the White race, and to inspire others to commit similar attacks.”
Dr. Francis views the Buffalo shooting as distinct from cases like the murder of George Floyd that involved crime or police. It immediately made him think of the Mother Emanuel Church shooting in Charleston, South Carolina. “Having a black skin is now a death warrant,” he said.
The song is also an appeal for White people to fight racism. Dr. Francis is concerned about young men caught up in white supremacy and suggests that we be more alert to children or grandchildren who disconnect from their families, spend time on the dark web, and access guns. The lyrics deliberately don’t mention guns because Dr. Francis wanted to stay out of that debate. “I just sang: ‘What else do I have to do to prove to you that I’m human too?’ ”
Despite his country credentials, Dr. Francis wrote “Buffalo” as a Gospel song because that genre “connects with Black people more and because that civil rights movement was through the church with Dr. Martin Luther King,” he explained. Although he sings all styles of music, the song is performed by Nashville-based singer Michael Lusk so that it’s not a “Cleve Francis thing,” he said, referring to his stage name.
Songwriter Norman Kerner collaborated on the song. The music was produced and recorded by David Thein and mixed by Bob Bullock of Nashville, who Dr. Francis had worked with when he was an artist on Capitol Records.
They sent the video and artwork to the Mayor of Buffalo, Byron Brown, but have yet to hear back. Dr. Francis hopes it could be part of their healing, noting that some people used the song in their Juneteenth celebrations.
The Louisiana native grew up during segregation and was one of two Black students in the Medical College of Virginia class of 1973. After completing his cardiology fellowship, no one would hire him, so Dr. Francis set up his own practice in Northern Virginia. He now works at Inova Heart and Vascular Institute in Alexandria, Va. He remains optimistic about race relations in America and would love a Black pop or Gospel star to record “Buffalo” and bring it to a wider audience.
Dr. Francis is a regular blogger for Medscape. His contribution to country music is recognized in the National Museum of African American History and Culture in Washington, DC. You can find more of his music on YouTube.
A version of this article first appeared on Medscape.com.
Trans women in female sports: A sports scientist’s take
An interview with Ross Tucker, PhD
When Lia Thomas won the women’s 500-yard freestyle at the 2022 NCAA Division 1 swimming championships, the issue of trans women’s participation in female sports ignited national headlines.
which prohibit trans women’s participation.
This interview has been edited for length and clarity.
Let’s start with the proinclusion argument that there are always advantages in sports.
That’s true. The whole point of sports is to recognize people who have advantages and reward them for it. By the time this argument comes out, people have already accepted that males have advantages, right?
Some do, some don’t.
If someone uses this argument to say that we should allow trans women, basically biological males, to compete in women’s sports, they’ve implicitly accepted that there are advantages. Otherwise, what advantage are you talking about?
They would say it’s like the advantage Michael Phelps has because of his wingspan.
To answer that, you have to start by asking why women’s sports exist.
Women’s sports exist because we recognize that male physiology has biological differences that create performance advantages. Women’s sports exist to ensure that male advantages are excluded. If you allow male advantage in, you’re allowing something to cross into a category that specifically tries to exclude it. That makes the advantage possessed by trans women conceptually and substantively different from an advantage that’s possessed by Michael Phelps because his advantage doesn’t cross a category boundary line.
If someone wants to allow natural advantages to be celebrated in sports, they’re arguing against the existence of any categories, because every single category in sports is trying to filter out certain advantages.
Weight categories in boxing exist to get rid of the advantage of being stronger, taller, with greater reach. Paralympic categories filter out the natural advantage that someone has if, for example, they are only mildly affected by cerebral palsy, compared with more severely affected.
If someone wants to allow natural advantages, they’re making an argument for all advantages to be eliminated from regulation, and we would end up with sports dominated by males between the ages of 20 and 28.
There are some people suggesting open categories by height and weight.
The problem is that for any height, males will be stronger, faster, more powerful than females. For any mass, and we know this because weightlifting has categories by mass, males lift about 30% heavier than females. They’ll be about 10%-15% faster at the same height and weight.
There’d be one or two sports where you might have some women, like gymnastics. Otherwise you would have to create categories that are so small – say, under 100 pounds. But in every other category, most sports would be completely dominated by males.
It’s not a viable solution for me unless we as a society are satisfied with filtering out women.
Another argument is that if trans women have an advantage, then they would be dominating.
That one misunderstands how you assess advantage. For a trans woman to win, she still has to be good enough at the base level without the advantage, in order to parlay that advantage into winning the women’s events.
If I was in the Tour de France and you gave me a bicycle with a 100-watt motor, I wouldn’t win the Tour de France. I’d do better than I would have done without it, but I wouldn’t win. Does my failure to win prove that motors don’t give an advantage? Of course not. My failure says more about my base level of performance than it does about the motor.
In terms of trans athletes, the retention of biological attributes creates the retention of performance advantages, which means that the person’s ranking relative to their peers’ will go up when they compare themselves to women rather than men. Someone who’s ranked 500 might improve to the 250s, but you still won’t see them on a podium.
It’s the change in performance that matters, not the final outcome.
Wasn’t Lia Thomas ranked in the 500s in the men’s division?
There’s some dispute as to whether it was 460 or 550 in the 200- and 65th in the 500-yard freestyle. But the concept is the same and we can use that case because we know the percentage performance change.
As Will Thomas, the performance was 4:18 in the 500-yard freestyle. As Lia Thomas, it’s 4:33. Ms. Thomas has slowed by 5.8% as a result of testosterone suppression. That’s fairly typical; most studies so far suggest performance impairments in that range.
The thing is that the male-female gap in swimming times is 10%-12% on average. That means that Ms. Thomas has retained about half the male advantage.
In strength events, for instance, weightlifting, where the gap is 30% or more, if you lost 10%, you’d still retain a 20% advantage and you’d jump more ranking places.
The retention of about half the male advantage is enough for No. 1 in the NCAA, but it’s not enough to move Ms. Thomas to No. 1 in the world.
The record set by Katie Ledecky in the 500 freestyle is 4:24. Thomas swam 4:18 as a man so could only afford to lose about 1% to be the record holder in women’s swimming.
When Ms. Thomas was beaten by cisgender women in other events, your point is that’s just because her baseline (pretransition) time wasn’t good enough.
Exactly. Are your performances in men’s sports close enough to the best woman such that you can turn that retained advantage into dominance, winning in women’s sports?
If the answer to that is yes, then you get Thomas in the 500. If the answer to that is not quite, then you get Thomas in the other distances.
On your podcast, you expressed frustration at having to keep debunking these arguments. Why do you think they persist?
There are a few things in play. There are nuances around the idea of advantage that people from outside sports don’t always appreciate.
But then the second thing comes into play and that’s the fact that this is an emotive issue. If you come to this debate wanting trans inclusion, then you reject the idea that it’s unfair. You will dismiss everything I’ve just said.
There’s a third thing. When people invoke the Phelps wingspan argument, they haven’t thought through the implications. If you could sit them down and say: “Okay. If you want to get rid of regulating natural advantages, then we would get rid of male and female categories,” what do you think would happen then?
They may still support inclusion because that’s their world view, but at least they’re honest now and understand the implications. But most people don’t go through that process.
I get that men are faster but I was shocked at how many are faster than elite women – for example, Allyson Felix.
There’s an amazing visual representation of that.
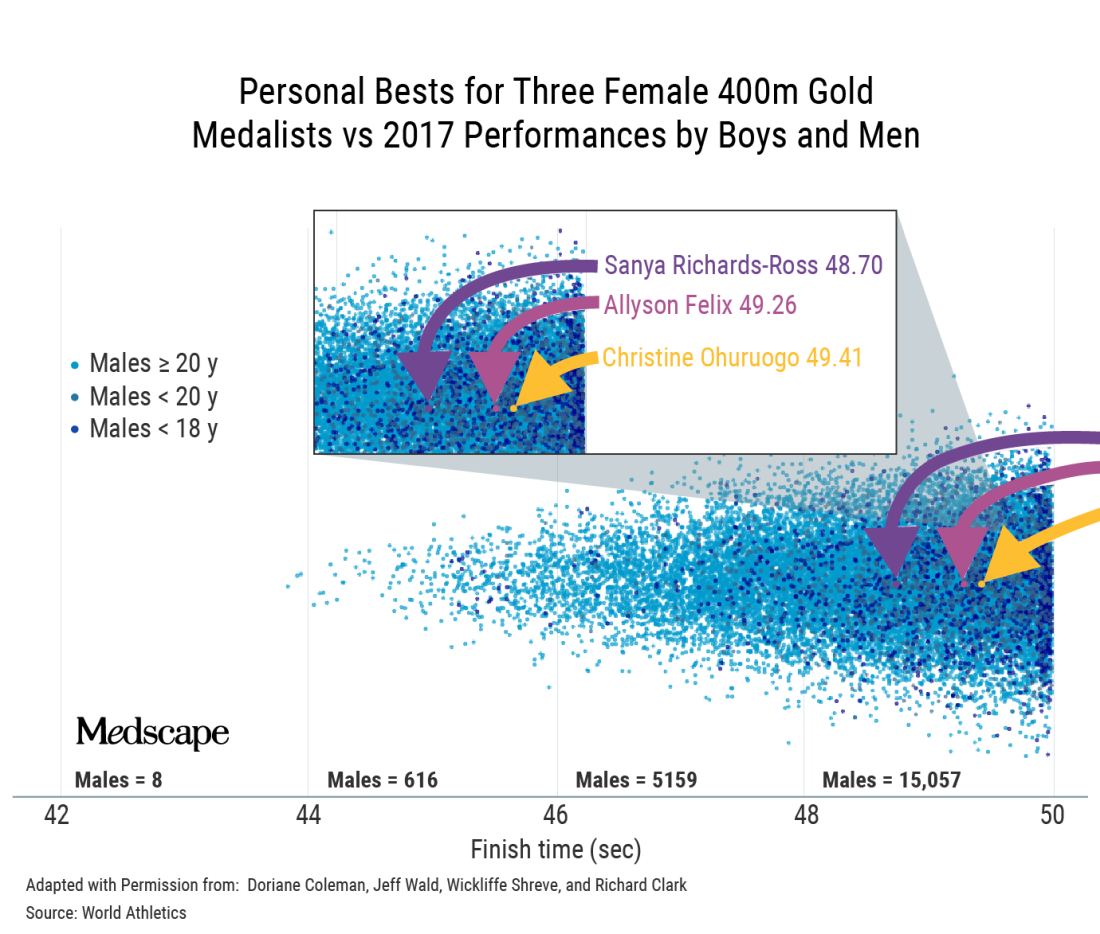
That’s a classic example where, if you’re immersed in sports, it becomes intuitive. If you’re not, you do a double-take and think, is that right? Position determines perspective.
Do you think some of it is because we’re constantly told that girls and women can do anything?
It’s a paradox that is difficult for people to get their minds around because in most walks of life, we can say that women can do anything. Of course, it’s arguably more difficult for women to become CEOs of Fortune 500 companies. This is a work in progress.
But sports are different. In sports, it’s not possible to directly compare male and female, and then tell girls they can be the best at whatever in the whole human race. That’s the uniqueness of sports and the reason categories exist in the first place. The biology does matter.
Speaking of biology, you’ve said that the focus on testosterone levels is a bit of a red herring.
Yes. The authorities were looking for a solution.
They grabbed onto the idea that lowering testosterone was the solution and perpetuated that as the mechanism by which we would ensure fairness. The problem is that my concentration of testosterone today is only a tiny part of the story.
I’ve been exposed to testosterone my whole life. My twin sister has not. There are many differences between us, but in terms of sports, the main biological difference is not that my testosterone is higher today; it’s that my testosterone has been higher my whole life. It’s the work done by that hormone over many years that makes a difference.
The key issue is, has this body, this physiology, been exposed to and benefited in the sports context, from male hormones – yes or no?
If your answer is yes, then that body belongs in male sports. With gender identity, we want to accommodate as far as possible, but we can’t take away that difference. That’s where we create this collision of rights between trans women and women.
Ultimately, your point is that we can’t have both fairness and inclusion.
When we sat down to do the World Rugby trans guidance, we had an epiphany: It doesn’t matter which way we go; we’re going to face hostility.
Once you accept that there are two parties that are affected and one of them will always be unhappy, then you start to see that fairness and inclusion can’t be balanced.
What about Joanna Harper’s proposal to make rules case by case and sport by sport?
First, it could be tricky legally because you’re effectively discriminating against some people within a subset of a subset. You’re going to end up saying to some trans women: “You can play because you don’t pose a safety or fairness issue.” But to another: “You can’t because you’re too strong.”
Then the problem is, how do you do that screening? It’s not like you can measure half a dozen variables and then have an algorithm spit out a performance level that tells you that this trans woman can compete here safely and fairly. It’s a theoretical solution that is practically impossible.
At a conference in Boston recently, Joanna said that when there are no medals, prize money, scholarships, or record times, we should allow inclusion. But just because a woman isn’t winning medals or going to the Olympics doesn’t mean there’s not considerable value for her if she were to make her school team, for instance.
There are only 11 places on the soccer field, eight lanes in a swimming pool. The moment you allow someone in, you potentially exclude someone else. And that happens everywhere, not only at the elite level.
Would you ever make a distinction between elite and subelite?
One of the beauties of sports is that it’s a meritocracy; it functions on a pathway system. I don’t think the level matters if you can track that this person’s presence denied a place on the team or a place at the competition to someone else.
With Lia Thomas, it’s not only denying the silver medalist gold or fourth place a bronze; it’s also the fact that there are only so many places at that meet. For some, that was their ambition and they weren’t able to realize it.
Now, a lot of sports are played outside that pathway. Say your local tennis club has a social league. There is little there to stand in the way of inclusion. Although I’m mindful that there may be a women’s league where it does matter to them.
We can try to accommodate trans women when the stakes are not high, provided that two requirements are met: One is that there’s no disruption to the selection/meritocracy pathway; and the second key point is that women must be okay with that inclusion, particularly if there are safety considerations, but even if it’s just a fairness consideration.
That’s where it gets tricky, because there are bigoted people in the world. Unfortunately, sometimes it’s difficult to tell whether people are using scientific arguments to prop up bigotry or whether they are genuine.
Joanna Harper has said that if you support inclusion, you have to be okay with trans women winning.
Winning the summer tennis league is not winning in the same sense as winning at the NCAA.
But the moment winning means selection and performance pathways, then I think we have to draw a line. The moment participation disrupts the natural order in sports, then it’s a problem.
In World Rugby, we proposed open competitions lower in contact to deal with the safety concerns. That was rejected by the trans community because they felt it was othering – that we were trying to squeeze them off to the side.
If you offered me one of two choices: no participation, or inclusion and they have to be able to win, I’d go for the former.
How did you get involved in this topic?
I got involved because I testified in the Caster Semenya case at the Court of Arbitration for Sport.
That is not a transgender issue; it’s a difference of sex development issue. What it has in common is the question of what to do with male-bodied biological advantage in sports.
When World Rugby joined the Olympic Games, we followed the IOC transgender policy. In 2019, it became apparent from the latest research that male advantage isn’t removed by testosterone suppression. We decided to delete the previous policy and make a new one.
The latest IOC policy is kind of no policy; it leaves it up to the governing bodies for each sport.
The one element of progress in what the IOC released, and it really is the only one, is that they’ve recognized that sports have to manage three imperatives: fairness, inclusion, and safety.
The 2015 IOC document says something like “sports should strive to be as inclusive as possible, but the overriding objective remains to guarantee a fair competition.” Basically, fair competition was nonnegotiable and must be guaranteed.
Of course, that policy allowed for testosterone suppression, and you’d have a difficult time convincing a physiologist that lowering testosterone guarantees fair competition.
Where there is merit in the current policy is that it’s clear that sports like rugby, boxing, taekwondo, and judo have a different equation with respect to safety, fairness, and inclusion than sports like equestrian, shooting, and archery. I think that’s wise to acknowledge.
However, the IOC policy doesn’t do anything to lead. In fact, what they said was extraordinary: There should be no presumption of advantage. If there’s no presumption of advantage for male-bodied athletes, then why do they persist with two categories? If there’s no presumption of advantage for trans women, are they saying that gender identity removes the advantage? We know that’s not true. We know that at the very least, you should presume that there is some advantage. How you manage it is up to you, but you can’t say that it’s not there.
This is a hostile debate. Have you ever thought: Maybe I’ll just shut up and stick to other sports topics?
Big time. The Lia Thomas case brought out a lot of vitriol. From about 2017, the situation we had with Ms. Thomas was predictable. The problem is that 95% of the world didn’t know this was happening and were taken by surprise.
The number of people who have opinions has exploded. A lot wade in without much thought. I’ve seen people question Lia Thomas’s motives. Presumably, Lia Thomas is trans, identifies as a woman, and therefore thinks she belongs in women’s sports. But I’ve seen people saying she only wants to swim in women’s sports because she knows she’ll win. And that’s not the worst of it. I’ve seen people saying Lia Thomas is only identifying as a woman so she can get into women’s changing rooms.
I don’t see how that helps the conversation. It just polarizes to the point that neither side is listening to the other. Before it was the trans community that wasn’t interested in talking about the idea of advantage, fairness, and safety. Their position is that trans women are women; how do you even have a discussion when they’ve got that dogma as their foundation?
Now, unfortunately, on the other side, we’re seeing unnecessary offensive tactics. For example, I’ve referred to Lia Thomas as “she.” I’ll have people shouting at me for using “she.” You’ve got to pick your battles, and that’s not the one you want to be fighting, in my opinion.
A version of this article first appeared on Medscape.com.
An interview with Ross Tucker, PhD
An interview with Ross Tucker, PhD
When Lia Thomas won the women’s 500-yard freestyle at the 2022 NCAA Division 1 swimming championships, the issue of trans women’s participation in female sports ignited national headlines.
which prohibit trans women’s participation.
This interview has been edited for length and clarity.
Let’s start with the proinclusion argument that there are always advantages in sports.
That’s true. The whole point of sports is to recognize people who have advantages and reward them for it. By the time this argument comes out, people have already accepted that males have advantages, right?
Some do, some don’t.
If someone uses this argument to say that we should allow trans women, basically biological males, to compete in women’s sports, they’ve implicitly accepted that there are advantages. Otherwise, what advantage are you talking about?
They would say it’s like the advantage Michael Phelps has because of his wingspan.
To answer that, you have to start by asking why women’s sports exist.
Women’s sports exist because we recognize that male physiology has biological differences that create performance advantages. Women’s sports exist to ensure that male advantages are excluded. If you allow male advantage in, you’re allowing something to cross into a category that specifically tries to exclude it. That makes the advantage possessed by trans women conceptually and substantively different from an advantage that’s possessed by Michael Phelps because his advantage doesn’t cross a category boundary line.
If someone wants to allow natural advantages to be celebrated in sports, they’re arguing against the existence of any categories, because every single category in sports is trying to filter out certain advantages.
Weight categories in boxing exist to get rid of the advantage of being stronger, taller, with greater reach. Paralympic categories filter out the natural advantage that someone has if, for example, they are only mildly affected by cerebral palsy, compared with more severely affected.
If someone wants to allow natural advantages, they’re making an argument for all advantages to be eliminated from regulation, and we would end up with sports dominated by males between the ages of 20 and 28.
There are some people suggesting open categories by height and weight.
The problem is that for any height, males will be stronger, faster, more powerful than females. For any mass, and we know this because weightlifting has categories by mass, males lift about 30% heavier than females. They’ll be about 10%-15% faster at the same height and weight.
There’d be one or two sports where you might have some women, like gymnastics. Otherwise you would have to create categories that are so small – say, under 100 pounds. But in every other category, most sports would be completely dominated by males.
It’s not a viable solution for me unless we as a society are satisfied with filtering out women.
Another argument is that if trans women have an advantage, then they would be dominating.
That one misunderstands how you assess advantage. For a trans woman to win, she still has to be good enough at the base level without the advantage, in order to parlay that advantage into winning the women’s events.
If I was in the Tour de France and you gave me a bicycle with a 100-watt motor, I wouldn’t win the Tour de France. I’d do better than I would have done without it, but I wouldn’t win. Does my failure to win prove that motors don’t give an advantage? Of course not. My failure says more about my base level of performance than it does about the motor.
In terms of trans athletes, the retention of biological attributes creates the retention of performance advantages, which means that the person’s ranking relative to their peers’ will go up when they compare themselves to women rather than men. Someone who’s ranked 500 might improve to the 250s, but you still won’t see them on a podium.
It’s the change in performance that matters, not the final outcome.
Wasn’t Lia Thomas ranked in the 500s in the men’s division?
There’s some dispute as to whether it was 460 or 550 in the 200- and 65th in the 500-yard freestyle. But the concept is the same and we can use that case because we know the percentage performance change.
As Will Thomas, the performance was 4:18 in the 500-yard freestyle. As Lia Thomas, it’s 4:33. Ms. Thomas has slowed by 5.8% as a result of testosterone suppression. That’s fairly typical; most studies so far suggest performance impairments in that range.
The thing is that the male-female gap in swimming times is 10%-12% on average. That means that Ms. Thomas has retained about half the male advantage.
In strength events, for instance, weightlifting, where the gap is 30% or more, if you lost 10%, you’d still retain a 20% advantage and you’d jump more ranking places.
The retention of about half the male advantage is enough for No. 1 in the NCAA, but it’s not enough to move Ms. Thomas to No. 1 in the world.
The record set by Katie Ledecky in the 500 freestyle is 4:24. Thomas swam 4:18 as a man so could only afford to lose about 1% to be the record holder in women’s swimming.
When Ms. Thomas was beaten by cisgender women in other events, your point is that’s just because her baseline (pretransition) time wasn’t good enough.
Exactly. Are your performances in men’s sports close enough to the best woman such that you can turn that retained advantage into dominance, winning in women’s sports?
If the answer to that is yes, then you get Thomas in the 500. If the answer to that is not quite, then you get Thomas in the other distances.
On your podcast, you expressed frustration at having to keep debunking these arguments. Why do you think they persist?
There are a few things in play. There are nuances around the idea of advantage that people from outside sports don’t always appreciate.
But then the second thing comes into play and that’s the fact that this is an emotive issue. If you come to this debate wanting trans inclusion, then you reject the idea that it’s unfair. You will dismiss everything I’ve just said.
There’s a third thing. When people invoke the Phelps wingspan argument, they haven’t thought through the implications. If you could sit them down and say: “Okay. If you want to get rid of regulating natural advantages, then we would get rid of male and female categories,” what do you think would happen then?
They may still support inclusion because that’s their world view, but at least they’re honest now and understand the implications. But most people don’t go through that process.
I get that men are faster but I was shocked at how many are faster than elite women – for example, Allyson Felix.
There’s an amazing visual representation of that.
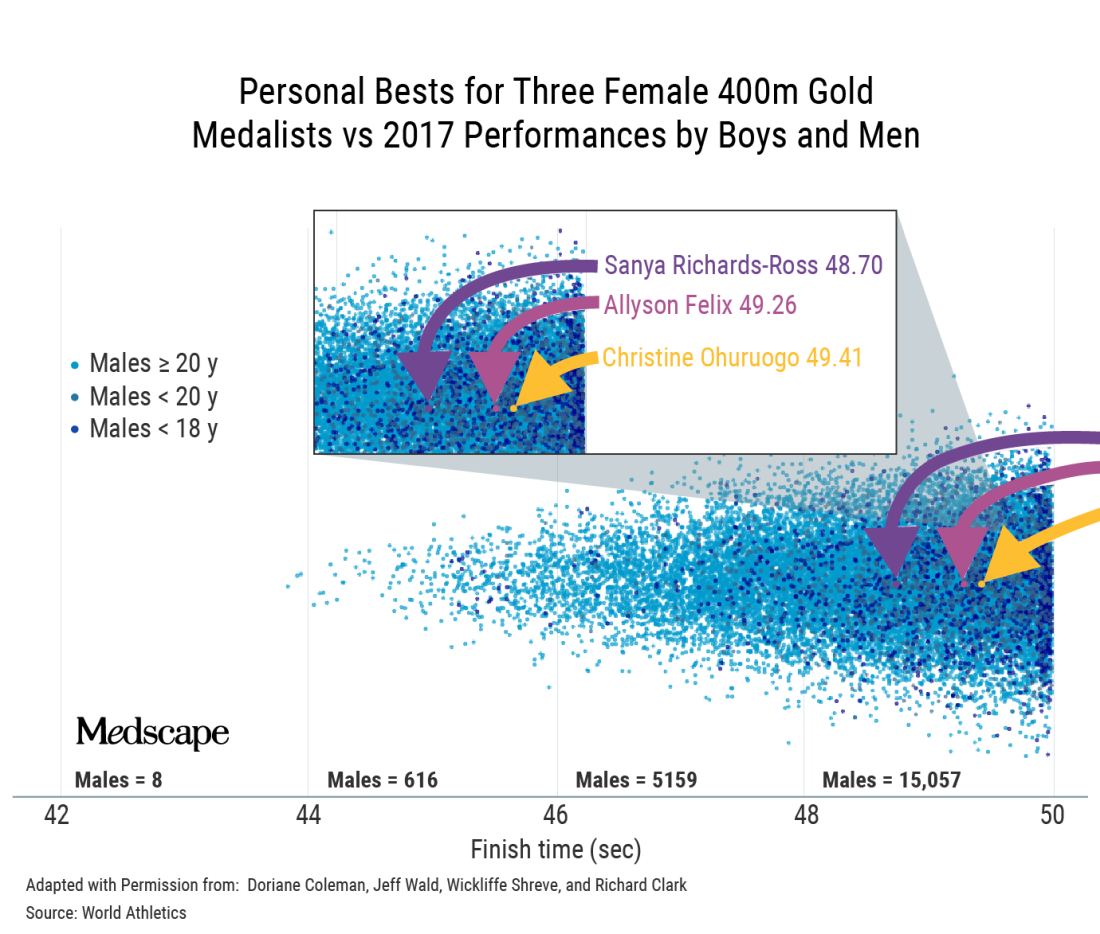
That’s a classic example where, if you’re immersed in sports, it becomes intuitive. If you’re not, you do a double-take and think, is that right? Position determines perspective.
Do you think some of it is because we’re constantly told that girls and women can do anything?
It’s a paradox that is difficult for people to get their minds around because in most walks of life, we can say that women can do anything. Of course, it’s arguably more difficult for women to become CEOs of Fortune 500 companies. This is a work in progress.
But sports are different. In sports, it’s not possible to directly compare male and female, and then tell girls they can be the best at whatever in the whole human race. That’s the uniqueness of sports and the reason categories exist in the first place. The biology does matter.
Speaking of biology, you’ve said that the focus on testosterone levels is a bit of a red herring.
Yes. The authorities were looking for a solution.
They grabbed onto the idea that lowering testosterone was the solution and perpetuated that as the mechanism by which we would ensure fairness. The problem is that my concentration of testosterone today is only a tiny part of the story.
I’ve been exposed to testosterone my whole life. My twin sister has not. There are many differences between us, but in terms of sports, the main biological difference is not that my testosterone is higher today; it’s that my testosterone has been higher my whole life. It’s the work done by that hormone over many years that makes a difference.
The key issue is, has this body, this physiology, been exposed to and benefited in the sports context, from male hormones – yes or no?
If your answer is yes, then that body belongs in male sports. With gender identity, we want to accommodate as far as possible, but we can’t take away that difference. That’s where we create this collision of rights between trans women and women.
Ultimately, your point is that we can’t have both fairness and inclusion.
When we sat down to do the World Rugby trans guidance, we had an epiphany: It doesn’t matter which way we go; we’re going to face hostility.
Once you accept that there are two parties that are affected and one of them will always be unhappy, then you start to see that fairness and inclusion can’t be balanced.
What about Joanna Harper’s proposal to make rules case by case and sport by sport?
First, it could be tricky legally because you’re effectively discriminating against some people within a subset of a subset. You’re going to end up saying to some trans women: “You can play because you don’t pose a safety or fairness issue.” But to another: “You can’t because you’re too strong.”
Then the problem is, how do you do that screening? It’s not like you can measure half a dozen variables and then have an algorithm spit out a performance level that tells you that this trans woman can compete here safely and fairly. It’s a theoretical solution that is practically impossible.
At a conference in Boston recently, Joanna said that when there are no medals, prize money, scholarships, or record times, we should allow inclusion. But just because a woman isn’t winning medals or going to the Olympics doesn’t mean there’s not considerable value for her if she were to make her school team, for instance.
There are only 11 places on the soccer field, eight lanes in a swimming pool. The moment you allow someone in, you potentially exclude someone else. And that happens everywhere, not only at the elite level.
Would you ever make a distinction between elite and subelite?
One of the beauties of sports is that it’s a meritocracy; it functions on a pathway system. I don’t think the level matters if you can track that this person’s presence denied a place on the team or a place at the competition to someone else.
With Lia Thomas, it’s not only denying the silver medalist gold or fourth place a bronze; it’s also the fact that there are only so many places at that meet. For some, that was their ambition and they weren’t able to realize it.
Now, a lot of sports are played outside that pathway. Say your local tennis club has a social league. There is little there to stand in the way of inclusion. Although I’m mindful that there may be a women’s league where it does matter to them.
We can try to accommodate trans women when the stakes are not high, provided that two requirements are met: One is that there’s no disruption to the selection/meritocracy pathway; and the second key point is that women must be okay with that inclusion, particularly if there are safety considerations, but even if it’s just a fairness consideration.
That’s where it gets tricky, because there are bigoted people in the world. Unfortunately, sometimes it’s difficult to tell whether people are using scientific arguments to prop up bigotry or whether they are genuine.
Joanna Harper has said that if you support inclusion, you have to be okay with trans women winning.
Winning the summer tennis league is not winning in the same sense as winning at the NCAA.
But the moment winning means selection and performance pathways, then I think we have to draw a line. The moment participation disrupts the natural order in sports, then it’s a problem.
In World Rugby, we proposed open competitions lower in contact to deal with the safety concerns. That was rejected by the trans community because they felt it was othering – that we were trying to squeeze them off to the side.
If you offered me one of two choices: no participation, or inclusion and they have to be able to win, I’d go for the former.
How did you get involved in this topic?
I got involved because I testified in the Caster Semenya case at the Court of Arbitration for Sport.
That is not a transgender issue; it’s a difference of sex development issue. What it has in common is the question of what to do with male-bodied biological advantage in sports.
When World Rugby joined the Olympic Games, we followed the IOC transgender policy. In 2019, it became apparent from the latest research that male advantage isn’t removed by testosterone suppression. We decided to delete the previous policy and make a new one.
The latest IOC policy is kind of no policy; it leaves it up to the governing bodies for each sport.
The one element of progress in what the IOC released, and it really is the only one, is that they’ve recognized that sports have to manage three imperatives: fairness, inclusion, and safety.
The 2015 IOC document says something like “sports should strive to be as inclusive as possible, but the overriding objective remains to guarantee a fair competition.” Basically, fair competition was nonnegotiable and must be guaranteed.
Of course, that policy allowed for testosterone suppression, and you’d have a difficult time convincing a physiologist that lowering testosterone guarantees fair competition.
Where there is merit in the current policy is that it’s clear that sports like rugby, boxing, taekwondo, and judo have a different equation with respect to safety, fairness, and inclusion than sports like equestrian, shooting, and archery. I think that’s wise to acknowledge.
However, the IOC policy doesn’t do anything to lead. In fact, what they said was extraordinary: There should be no presumption of advantage. If there’s no presumption of advantage for male-bodied athletes, then why do they persist with two categories? If there’s no presumption of advantage for trans women, are they saying that gender identity removes the advantage? We know that’s not true. We know that at the very least, you should presume that there is some advantage. How you manage it is up to you, but you can’t say that it’s not there.
This is a hostile debate. Have you ever thought: Maybe I’ll just shut up and stick to other sports topics?
Big time. The Lia Thomas case brought out a lot of vitriol. From about 2017, the situation we had with Ms. Thomas was predictable. The problem is that 95% of the world didn’t know this was happening and were taken by surprise.
The number of people who have opinions has exploded. A lot wade in without much thought. I’ve seen people question Lia Thomas’s motives. Presumably, Lia Thomas is trans, identifies as a woman, and therefore thinks she belongs in women’s sports. But I’ve seen people saying she only wants to swim in women’s sports because she knows she’ll win. And that’s not the worst of it. I’ve seen people saying Lia Thomas is only identifying as a woman so she can get into women’s changing rooms.
I don’t see how that helps the conversation. It just polarizes to the point that neither side is listening to the other. Before it was the trans community that wasn’t interested in talking about the idea of advantage, fairness, and safety. Their position is that trans women are women; how do you even have a discussion when they’ve got that dogma as their foundation?
Now, unfortunately, on the other side, we’re seeing unnecessary offensive tactics. For example, I’ve referred to Lia Thomas as “she.” I’ll have people shouting at me for using “she.” You’ve got to pick your battles, and that’s not the one you want to be fighting, in my opinion.
A version of this article first appeared on Medscape.com.
When Lia Thomas won the women’s 500-yard freestyle at the 2022 NCAA Division 1 swimming championships, the issue of trans women’s participation in female sports ignited national headlines.
which prohibit trans women’s participation.
This interview has been edited for length and clarity.
Let’s start with the proinclusion argument that there are always advantages in sports.
That’s true. The whole point of sports is to recognize people who have advantages and reward them for it. By the time this argument comes out, people have already accepted that males have advantages, right?
Some do, some don’t.
If someone uses this argument to say that we should allow trans women, basically biological males, to compete in women’s sports, they’ve implicitly accepted that there are advantages. Otherwise, what advantage are you talking about?
They would say it’s like the advantage Michael Phelps has because of his wingspan.
To answer that, you have to start by asking why women’s sports exist.
Women’s sports exist because we recognize that male physiology has biological differences that create performance advantages. Women’s sports exist to ensure that male advantages are excluded. If you allow male advantage in, you’re allowing something to cross into a category that specifically tries to exclude it. That makes the advantage possessed by trans women conceptually and substantively different from an advantage that’s possessed by Michael Phelps because his advantage doesn’t cross a category boundary line.
If someone wants to allow natural advantages to be celebrated in sports, they’re arguing against the existence of any categories, because every single category in sports is trying to filter out certain advantages.
Weight categories in boxing exist to get rid of the advantage of being stronger, taller, with greater reach. Paralympic categories filter out the natural advantage that someone has if, for example, they are only mildly affected by cerebral palsy, compared with more severely affected.
If someone wants to allow natural advantages, they’re making an argument for all advantages to be eliminated from regulation, and we would end up with sports dominated by males between the ages of 20 and 28.
There are some people suggesting open categories by height and weight.
The problem is that for any height, males will be stronger, faster, more powerful than females. For any mass, and we know this because weightlifting has categories by mass, males lift about 30% heavier than females. They’ll be about 10%-15% faster at the same height and weight.
There’d be one or two sports where you might have some women, like gymnastics. Otherwise you would have to create categories that are so small – say, under 100 pounds. But in every other category, most sports would be completely dominated by males.
It’s not a viable solution for me unless we as a society are satisfied with filtering out women.
Another argument is that if trans women have an advantage, then they would be dominating.
That one misunderstands how you assess advantage. For a trans woman to win, she still has to be good enough at the base level without the advantage, in order to parlay that advantage into winning the women’s events.
If I was in the Tour de France and you gave me a bicycle with a 100-watt motor, I wouldn’t win the Tour de France. I’d do better than I would have done without it, but I wouldn’t win. Does my failure to win prove that motors don’t give an advantage? Of course not. My failure says more about my base level of performance than it does about the motor.
In terms of trans athletes, the retention of biological attributes creates the retention of performance advantages, which means that the person’s ranking relative to their peers’ will go up when they compare themselves to women rather than men. Someone who’s ranked 500 might improve to the 250s, but you still won’t see them on a podium.
It’s the change in performance that matters, not the final outcome.
Wasn’t Lia Thomas ranked in the 500s in the men’s division?
There’s some dispute as to whether it was 460 or 550 in the 200- and 65th in the 500-yard freestyle. But the concept is the same and we can use that case because we know the percentage performance change.
As Will Thomas, the performance was 4:18 in the 500-yard freestyle. As Lia Thomas, it’s 4:33. Ms. Thomas has slowed by 5.8% as a result of testosterone suppression. That’s fairly typical; most studies so far suggest performance impairments in that range.
The thing is that the male-female gap in swimming times is 10%-12% on average. That means that Ms. Thomas has retained about half the male advantage.
In strength events, for instance, weightlifting, where the gap is 30% or more, if you lost 10%, you’d still retain a 20% advantage and you’d jump more ranking places.
The retention of about half the male advantage is enough for No. 1 in the NCAA, but it’s not enough to move Ms. Thomas to No. 1 in the world.
The record set by Katie Ledecky in the 500 freestyle is 4:24. Thomas swam 4:18 as a man so could only afford to lose about 1% to be the record holder in women’s swimming.
When Ms. Thomas was beaten by cisgender women in other events, your point is that’s just because her baseline (pretransition) time wasn’t good enough.
Exactly. Are your performances in men’s sports close enough to the best woman such that you can turn that retained advantage into dominance, winning in women’s sports?
If the answer to that is yes, then you get Thomas in the 500. If the answer to that is not quite, then you get Thomas in the other distances.
On your podcast, you expressed frustration at having to keep debunking these arguments. Why do you think they persist?
There are a few things in play. There are nuances around the idea of advantage that people from outside sports don’t always appreciate.
But then the second thing comes into play and that’s the fact that this is an emotive issue. If you come to this debate wanting trans inclusion, then you reject the idea that it’s unfair. You will dismiss everything I’ve just said.
There’s a third thing. When people invoke the Phelps wingspan argument, they haven’t thought through the implications. If you could sit them down and say: “Okay. If you want to get rid of regulating natural advantages, then we would get rid of male and female categories,” what do you think would happen then?
They may still support inclusion because that’s their world view, but at least they’re honest now and understand the implications. But most people don’t go through that process.
I get that men are faster but I was shocked at how many are faster than elite women – for example, Allyson Felix.
There’s an amazing visual representation of that.
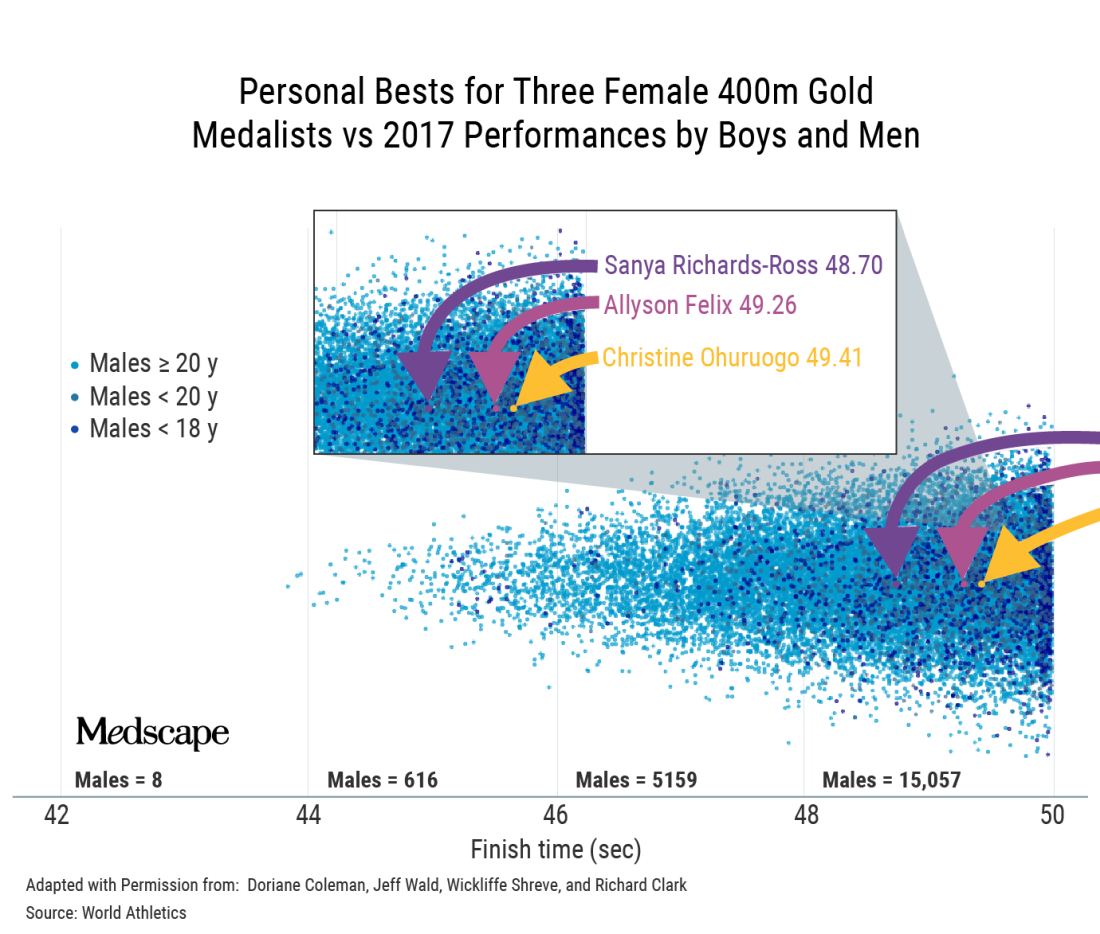
That’s a classic example where, if you’re immersed in sports, it becomes intuitive. If you’re not, you do a double-take and think, is that right? Position determines perspective.
Do you think some of it is because we’re constantly told that girls and women can do anything?
It’s a paradox that is difficult for people to get their minds around because in most walks of life, we can say that women can do anything. Of course, it’s arguably more difficult for women to become CEOs of Fortune 500 companies. This is a work in progress.
But sports are different. In sports, it’s not possible to directly compare male and female, and then tell girls they can be the best at whatever in the whole human race. That’s the uniqueness of sports and the reason categories exist in the first place. The biology does matter.
Speaking of biology, you’ve said that the focus on testosterone levels is a bit of a red herring.
Yes. The authorities were looking for a solution.
They grabbed onto the idea that lowering testosterone was the solution and perpetuated that as the mechanism by which we would ensure fairness. The problem is that my concentration of testosterone today is only a tiny part of the story.
I’ve been exposed to testosterone my whole life. My twin sister has not. There are many differences between us, but in terms of sports, the main biological difference is not that my testosterone is higher today; it’s that my testosterone has been higher my whole life. It’s the work done by that hormone over many years that makes a difference.
The key issue is, has this body, this physiology, been exposed to and benefited in the sports context, from male hormones – yes or no?
If your answer is yes, then that body belongs in male sports. With gender identity, we want to accommodate as far as possible, but we can’t take away that difference. That’s where we create this collision of rights between trans women and women.
Ultimately, your point is that we can’t have both fairness and inclusion.
When we sat down to do the World Rugby trans guidance, we had an epiphany: It doesn’t matter which way we go; we’re going to face hostility.
Once you accept that there are two parties that are affected and one of them will always be unhappy, then you start to see that fairness and inclusion can’t be balanced.
What about Joanna Harper’s proposal to make rules case by case and sport by sport?
First, it could be tricky legally because you’re effectively discriminating against some people within a subset of a subset. You’re going to end up saying to some trans women: “You can play because you don’t pose a safety or fairness issue.” But to another: “You can’t because you’re too strong.”
Then the problem is, how do you do that screening? It’s not like you can measure half a dozen variables and then have an algorithm spit out a performance level that tells you that this trans woman can compete here safely and fairly. It’s a theoretical solution that is practically impossible.
At a conference in Boston recently, Joanna said that when there are no medals, prize money, scholarships, or record times, we should allow inclusion. But just because a woman isn’t winning medals or going to the Olympics doesn’t mean there’s not considerable value for her if she were to make her school team, for instance.
There are only 11 places on the soccer field, eight lanes in a swimming pool. The moment you allow someone in, you potentially exclude someone else. And that happens everywhere, not only at the elite level.
Would you ever make a distinction between elite and subelite?
One of the beauties of sports is that it’s a meritocracy; it functions on a pathway system. I don’t think the level matters if you can track that this person’s presence denied a place on the team or a place at the competition to someone else.
With Lia Thomas, it’s not only denying the silver medalist gold or fourth place a bronze; it’s also the fact that there are only so many places at that meet. For some, that was their ambition and they weren’t able to realize it.
Now, a lot of sports are played outside that pathway. Say your local tennis club has a social league. There is little there to stand in the way of inclusion. Although I’m mindful that there may be a women’s league where it does matter to them.
We can try to accommodate trans women when the stakes are not high, provided that two requirements are met: One is that there’s no disruption to the selection/meritocracy pathway; and the second key point is that women must be okay with that inclusion, particularly if there are safety considerations, but even if it’s just a fairness consideration.
That’s where it gets tricky, because there are bigoted people in the world. Unfortunately, sometimes it’s difficult to tell whether people are using scientific arguments to prop up bigotry or whether they are genuine.
Joanna Harper has said that if you support inclusion, you have to be okay with trans women winning.
Winning the summer tennis league is not winning in the same sense as winning at the NCAA.
But the moment winning means selection and performance pathways, then I think we have to draw a line. The moment participation disrupts the natural order in sports, then it’s a problem.
In World Rugby, we proposed open competitions lower in contact to deal with the safety concerns. That was rejected by the trans community because they felt it was othering – that we were trying to squeeze them off to the side.
If you offered me one of two choices: no participation, or inclusion and they have to be able to win, I’d go for the former.
How did you get involved in this topic?
I got involved because I testified in the Caster Semenya case at the Court of Arbitration for Sport.
That is not a transgender issue; it’s a difference of sex development issue. What it has in common is the question of what to do with male-bodied biological advantage in sports.
When World Rugby joined the Olympic Games, we followed the IOC transgender policy. In 2019, it became apparent from the latest research that male advantage isn’t removed by testosterone suppression. We decided to delete the previous policy and make a new one.
The latest IOC policy is kind of no policy; it leaves it up to the governing bodies for each sport.
The one element of progress in what the IOC released, and it really is the only one, is that they’ve recognized that sports have to manage three imperatives: fairness, inclusion, and safety.
The 2015 IOC document says something like “sports should strive to be as inclusive as possible, but the overriding objective remains to guarantee a fair competition.” Basically, fair competition was nonnegotiable and must be guaranteed.
Of course, that policy allowed for testosterone suppression, and you’d have a difficult time convincing a physiologist that lowering testosterone guarantees fair competition.
Where there is merit in the current policy is that it’s clear that sports like rugby, boxing, taekwondo, and judo have a different equation with respect to safety, fairness, and inclusion than sports like equestrian, shooting, and archery. I think that’s wise to acknowledge.
However, the IOC policy doesn’t do anything to lead. In fact, what they said was extraordinary: There should be no presumption of advantage. If there’s no presumption of advantage for male-bodied athletes, then why do they persist with two categories? If there’s no presumption of advantage for trans women, are they saying that gender identity removes the advantage? We know that’s not true. We know that at the very least, you should presume that there is some advantage. How you manage it is up to you, but you can’t say that it’s not there.
This is a hostile debate. Have you ever thought: Maybe I’ll just shut up and stick to other sports topics?
Big time. The Lia Thomas case brought out a lot of vitriol. From about 2017, the situation we had with Ms. Thomas was predictable. The problem is that 95% of the world didn’t know this was happening and were taken by surprise.
The number of people who have opinions has exploded. A lot wade in without much thought. I’ve seen people question Lia Thomas’s motives. Presumably, Lia Thomas is trans, identifies as a woman, and therefore thinks she belongs in women’s sports. But I’ve seen people saying she only wants to swim in women’s sports because she knows she’ll win. And that’s not the worst of it. I’ve seen people saying Lia Thomas is only identifying as a woman so she can get into women’s changing rooms.
I don’t see how that helps the conversation. It just polarizes to the point that neither side is listening to the other. Before it was the trans community that wasn’t interested in talking about the idea of advantage, fairness, and safety. Their position is that trans women are women; how do you even have a discussion when they’ve got that dogma as their foundation?
Now, unfortunately, on the other side, we’re seeing unnecessary offensive tactics. For example, I’ve referred to Lia Thomas as “she.” I’ll have people shouting at me for using “she.” You’ve got to pick your battles, and that’s not the one you want to be fighting, in my opinion.
A version of this article first appeared on Medscape.com.
What a sleep expert thinks of sleep trackers
The pandemic not only disrupted sleep but may have also triggered an uptick in the use of wearable tech. Sleep tracking was featured at the Cardiovascular Health Tech virtual conference 2022, sponsored by the Institute of Electrical and Electronics Engineers Engineering in Medicine & Biology Society technical committee on Cardiopulmonary Systems and Physiology-Based Engineering.
This news organization interviewed presenter Kelly Glazer Baron, PhD, MPH, DBSM, an associate professor at the University of Utah, Salt Lake City, and a clinical psychologist specializing in behavioral sleep medicine.
The interview has been edited for length and clarity.
Question: Are consumer sleep trackers mainly divided into “nearables” – things that you put at the side of the bed or under the pillow – vs. wearables?
Dr. Baron: There are so many different devices these days. There are things that you put under your mattress or pillow; there are bedside recording devices; then there are headbands, rings, wrist-worn, all kinds of things.
Q: At the conference, Philip de Chazal, PhD, (University of Sydney) described the evidence on sleep tracking smartphone apps as woeful. Would you agree with that?
A: Yes. I would agree if you’re looking at how accurate they are at recording sleep, particularly compared with what we would define as the gold standard, which is a sleep study wherein you have electrodes on the scalp and you’re measuring the electrical activity directly.
They are best at detecting when you get into the bed and when you get out. But even then, there isn’t good evidence that they do that accurately when there are two people in the bed.
Overall, they may give you a general gist of what’s happening in terms of time in and out of bed, but we’re doubtful on their recording ability to tell sleep from wake time.
Q: Are the wrist-worn devices better for sleep tracking?
A: They’re getting better. We’ve used wrist activity monitors in research for years. They use an accelerometer to measure movement, and then an algorithm determines whether an interval of time is called sleep or wake.
Recently, they’ve incorporated more sensors, such as heart rate, and they can more accurately decipher rapid eye movement (REM) sleep from non-REM. They’re still not as good as doing a full sleep study. But they’re getting closer.
Q: If asked how you slept, most of us think we can answer without needing to look at a smartphone, but maybe not. Can you explain “paradoxical insomnia”?
A: You can’t really know if you’re sleeping because if you know you’re asleep, then you can’t be asleep because it’s a state of unconsciousness. How people decide whether they had a good night’s sleep probably depends on a lot of things about how they feel when they wake up in the morning or if they remember being up in the night.
Quality of sleep is not really something that people can directly ascertain. There is a selection of people who feel awake all night but they actually are sleeping. They feel that their sleep quality is poor: They’re suffering; they have insomnia, but from the objective data, they are sleeping fine.
Q: Is this related to non-REM stage 1 sleep, when you may not be aware that you’re asleep?
A: No. I’m talking about people who come into the sleep lab for an overnight study and get hooked up. And in the morning, they’ll tell the tech I was awake all night, but the tech will see that their sleep was just fine.
There is a disconnect between how people perceive their sleep and how they actually sleep. For most people it’s impossible to be completely accurate to know how much you’re sleeping. Then there are some people who perceive it very differently.
Sleep trackers don’t have the level of detail of sleep studies that use scalp electrodes. When we get into the details of sleep measurement, we’re measuring 30-second epochs (sampling periods), where we look at broad measures of electrical activity. There is even more detail there that can be pulled out using other techniques, such as analyzing the spectrum of the EEG. For example, some studies have found a beta frequency in the EEG of people with insomnia, so even though they are sleeping, they often feel awake.
Basically, the subjective experience of sleep somewhat overlaps with the objective recording of what’s happening on a sleep study, but not completely.
Q: You said that first thing in the morning might not be the best time to assess your sleep – if you wake up groggy and are already thinking, “The day is shot.”
A: In general, people really feel worst in the morning. Their circadian drive is low, especially if they’re a little sleep deprived. You shouldn’t judge the day on the first hour after waking – most people are pretty cognitively impaired. I tell people they need some boot-up time.
You feel differently as the day goes on and even at different points of the day. There’s a lull in the early afternoon because of your circadian dip and then we get a second wind in the evening. How you feel isn’t one flat line; it’s really a rhythm throughout the day
Q: Would you say that consumer sleep trackers are okay for individuals to use to see a pattern but are maybe not accurate enough to use more globally in research?
A: I think there is a huge opportunity to understand sleep at a population level. For example, if there’s been a hurricane or an earthquake or Superbowl Sunday, companies have an opportunity to look at the impact – say, daylight saving time and how it affects sleep across different countries, or men vs. women, or different age groups.
There was a paper about sleep among hospital workers in Wuhan during the outbreak of the pandemic. That was a creative use of wearable devices to look at sleep in a large population.
Now, of course, the devices are not given out randomly; the people who buy them are probably a little bit healthier, maybe a little bit younger – that sort of thing. It is a biased sample.
Q: As you note, mobile health trackers tend to be used by the “worried well.” Can you tell us about your paper that introduced the term “orthosomnia,” or “a perfectionistic quest for the ideal sleep in order to optimize daytime function”?
A: As these devices came out, more people were coming into the clinic and shoving their data in front of us saying, “I don’t feel well, and I don’t sleep 7 hours.” They were focused on this specific number. Back when we wrote this paper, the devices were primarily movement based (now the devices are a bit more accurate). Some would say, “My sleep is light, and it’s not deep.” We’d do a sleep study that showed that they have deep sleep, but they would still believe their device even though the device really wasn’t able to classify sleep accurately.
We even found people making their sleep worse because of the device. For example, trying to get the number higher by spending more time lying in bed trying to sleep which is the opposite of what you want someone with insomnia to do. These people held the data so tight and really felt that it characterized their experience, even though we sleep medicine practitioners didn’t find it very accurate and felt that it was somewhat unhelpful to their treatment.
Q: What advice would you give the harried primary care physician presented with a patient’s hypnogram or sleep pattern?
A: As someone once pointed out to me, it’s a conversation opener about their sleep. Did they buy the device because they’re worried about their sleep? It’s unlikely that you can glean anything clinically useful from the data.
I briefly look at it to see the duration of their sleep, the regularity in their sleep pattern – the pattern of awakenings during the night might suggest that they have some insomnia. But it doesn’t take the place of clinical assessment for conditions like sleep apnea: Are they snoring? Are they unrefreshed?
I had a patient in the orthosomnia study who was given a sleep tracker by a family member. He brought the data to his doctor who ordered a sleep study that found he had sleep apnea. He would say, “The device diagnosed my sleep apnea.” But that wasn’t actually the case; it just opened the conversation and the clinician said, “Well, let’s order a sleep study.”
Q: The device told him he wasn’t getting much sleep and then the sleep study told him it was apnea.
A: Right. It’s impossible to pick up sleep apnea. Some of the latest devices have some oximetry reading but it is not a clinically validated oximetry that could diagnose sleep apnea.
When these first came out I thought I’d get more referrals. So far, I haven’t had a single person come in and ask if they have sleep apnea. If you have a patient saying, “Hey, I’m worried about my oxygen level and here’s my data,” then the clinician should consider whether they need a sleep study for sleep apnea.
Q: You did a survey that suggests that clinicians are less keen on these devices than consumers. Conor Heneghan of Fitbit/Google also mentioned a study using the Fitbit Charge and a SleepLife portal. The patients were very engaged but only one physician (out of 49) logged into the portal to look at the data.
A: Our survey of sleep professionals (which we need to publish) showed that they were wary of the data. They found it frustrating in some ways because it took time out of the clinical encounter.
Some of them said that parents are putting trackers on their children and then catastrophizing their children’s sleep.
Q: Is there such a thing as an ideal hypnogram or does it vary by individual?
A: I would say that it depends on a lot of things. If you think about a hypnogram from a sleep study, the patient is not sleeping in their home environment, and it’s only one night. There’s a range of what would be considered normal, and it’s related to your sex and your age.
One night is not going to be sufficient to characterize your percentage in this or that sleep stage. Our patients come in saying, “I’m not getting enough REM.” But there isn’t a sleep disorder called lack of REM; there’s no treatment for that. It’s probably pretty normal for them or maybe they’re taking medications that suppress their REM, such as antidepressants.
The tech world is very interested to sense REM properly and to display it. But on the treatment side of things, there’s not much that we do with that data. We’re more interested in the consolidation of their sleep, the duration of their sleep, breathing-related sleep disorders, those sorts of things.
Q: Is there any reason to be concerned about the amount of REM sleep in terms of outcomes? We know that poor sleep can lead to bad cardiovascular outcomes, but has any of that correlated to sleep stage?
A: There are studies where they’ve experimentally deprived people of certain stages of sleep, but they’re not very useful in the real world. We’re looking at sleep holistically: Do you have a good sleep pattern? Any breathing-related sleep disorders? Insomnia? We don’t treat sleep by the stage.
Q: Any concern that people who are focused on a device may be ignoring the basic tenets of good sleep hygiene?
A: If people are doing things that are obviously bad for their sleep, like working too late, not exercising enough, sleeping in on weekends to compensate for being up late during the week, or probably the biggest thing contributing to insomnia – stress. A device itself won’t fix those things but it could show you the evidence.
If somebody really has a sleep disorder, then sleep hygiene alone is probably not going to be enough. They’re going to need to engage in a more extensive program to improve their sleep, such as cognitive-behavioral therapy for insomnia.
Q: Is there anything else you want to mention?
A: I don’t want to leave with a reputation of being against sleep trackers. I think they are a great opportunity for people to get excited about and learn about their sleep and try to improve it. We have a lot to learn about what people want from their data and how we can use that data to improve people’s sleep.
As providers, we can engage with our patients – sleep is an automatic process, but improving sleep takes some effort. Buying a device is not going to automatically make you sleep better. It takes work to establish a better sleep pattern; it may require some cognitive-behavioral therapy or treating a sleep disorder. That takes some work.
Dr. Baron reported no conflicts of interest.A version of this article first appeared on Medscape.com.
The pandemic not only disrupted sleep but may have also triggered an uptick in the use of wearable tech. Sleep tracking was featured at the Cardiovascular Health Tech virtual conference 2022, sponsored by the Institute of Electrical and Electronics Engineers Engineering in Medicine & Biology Society technical committee on Cardiopulmonary Systems and Physiology-Based Engineering.
This news organization interviewed presenter Kelly Glazer Baron, PhD, MPH, DBSM, an associate professor at the University of Utah, Salt Lake City, and a clinical psychologist specializing in behavioral sleep medicine.
The interview has been edited for length and clarity.
Question: Are consumer sleep trackers mainly divided into “nearables” – things that you put at the side of the bed or under the pillow – vs. wearables?
Dr. Baron: There are so many different devices these days. There are things that you put under your mattress or pillow; there are bedside recording devices; then there are headbands, rings, wrist-worn, all kinds of things.
Q: At the conference, Philip de Chazal, PhD, (University of Sydney) described the evidence on sleep tracking smartphone apps as woeful. Would you agree with that?
A: Yes. I would agree if you’re looking at how accurate they are at recording sleep, particularly compared with what we would define as the gold standard, which is a sleep study wherein you have electrodes on the scalp and you’re measuring the electrical activity directly.
They are best at detecting when you get into the bed and when you get out. But even then, there isn’t good evidence that they do that accurately when there are two people in the bed.
Overall, they may give you a general gist of what’s happening in terms of time in and out of bed, but we’re doubtful on their recording ability to tell sleep from wake time.
Q: Are the wrist-worn devices better for sleep tracking?
A: They’re getting better. We’ve used wrist activity monitors in research for years. They use an accelerometer to measure movement, and then an algorithm determines whether an interval of time is called sleep or wake.
Recently, they’ve incorporated more sensors, such as heart rate, and they can more accurately decipher rapid eye movement (REM) sleep from non-REM. They’re still not as good as doing a full sleep study. But they’re getting closer.
Q: If asked how you slept, most of us think we can answer without needing to look at a smartphone, but maybe not. Can you explain “paradoxical insomnia”?
A: You can’t really know if you’re sleeping because if you know you’re asleep, then you can’t be asleep because it’s a state of unconsciousness. How people decide whether they had a good night’s sleep probably depends on a lot of things about how they feel when they wake up in the morning or if they remember being up in the night.
Quality of sleep is not really something that people can directly ascertain. There is a selection of people who feel awake all night but they actually are sleeping. They feel that their sleep quality is poor: They’re suffering; they have insomnia, but from the objective data, they are sleeping fine.
Q: Is this related to non-REM stage 1 sleep, when you may not be aware that you’re asleep?
A: No. I’m talking about people who come into the sleep lab for an overnight study and get hooked up. And in the morning, they’ll tell the tech I was awake all night, but the tech will see that their sleep was just fine.
There is a disconnect between how people perceive their sleep and how they actually sleep. For most people it’s impossible to be completely accurate to know how much you’re sleeping. Then there are some people who perceive it very differently.
Sleep trackers don’t have the level of detail of sleep studies that use scalp electrodes. When we get into the details of sleep measurement, we’re measuring 30-second epochs (sampling periods), where we look at broad measures of electrical activity. There is even more detail there that can be pulled out using other techniques, such as analyzing the spectrum of the EEG. For example, some studies have found a beta frequency in the EEG of people with insomnia, so even though they are sleeping, they often feel awake.
Basically, the subjective experience of sleep somewhat overlaps with the objective recording of what’s happening on a sleep study, but not completely.
Q: You said that first thing in the morning might not be the best time to assess your sleep – if you wake up groggy and are already thinking, “The day is shot.”
A: In general, people really feel worst in the morning. Their circadian drive is low, especially if they’re a little sleep deprived. You shouldn’t judge the day on the first hour after waking – most people are pretty cognitively impaired. I tell people they need some boot-up time.
You feel differently as the day goes on and even at different points of the day. There’s a lull in the early afternoon because of your circadian dip and then we get a second wind in the evening. How you feel isn’t one flat line; it’s really a rhythm throughout the day
Q: Would you say that consumer sleep trackers are okay for individuals to use to see a pattern but are maybe not accurate enough to use more globally in research?
A: I think there is a huge opportunity to understand sleep at a population level. For example, if there’s been a hurricane or an earthquake or Superbowl Sunday, companies have an opportunity to look at the impact – say, daylight saving time and how it affects sleep across different countries, or men vs. women, or different age groups.
There was a paper about sleep among hospital workers in Wuhan during the outbreak of the pandemic. That was a creative use of wearable devices to look at sleep in a large population.
Now, of course, the devices are not given out randomly; the people who buy them are probably a little bit healthier, maybe a little bit younger – that sort of thing. It is a biased sample.
Q: As you note, mobile health trackers tend to be used by the “worried well.” Can you tell us about your paper that introduced the term “orthosomnia,” or “a perfectionistic quest for the ideal sleep in order to optimize daytime function”?
A: As these devices came out, more people were coming into the clinic and shoving their data in front of us saying, “I don’t feel well, and I don’t sleep 7 hours.” They were focused on this specific number. Back when we wrote this paper, the devices were primarily movement based (now the devices are a bit more accurate). Some would say, “My sleep is light, and it’s not deep.” We’d do a sleep study that showed that they have deep sleep, but they would still believe their device even though the device really wasn’t able to classify sleep accurately.
We even found people making their sleep worse because of the device. For example, trying to get the number higher by spending more time lying in bed trying to sleep which is the opposite of what you want someone with insomnia to do. These people held the data so tight and really felt that it characterized their experience, even though we sleep medicine practitioners didn’t find it very accurate and felt that it was somewhat unhelpful to their treatment.
Q: What advice would you give the harried primary care physician presented with a patient’s hypnogram or sleep pattern?
A: As someone once pointed out to me, it’s a conversation opener about their sleep. Did they buy the device because they’re worried about their sleep? It’s unlikely that you can glean anything clinically useful from the data.
I briefly look at it to see the duration of their sleep, the regularity in their sleep pattern – the pattern of awakenings during the night might suggest that they have some insomnia. But it doesn’t take the place of clinical assessment for conditions like sleep apnea: Are they snoring? Are they unrefreshed?
I had a patient in the orthosomnia study who was given a sleep tracker by a family member. He brought the data to his doctor who ordered a sleep study that found he had sleep apnea. He would say, “The device diagnosed my sleep apnea.” But that wasn’t actually the case; it just opened the conversation and the clinician said, “Well, let’s order a sleep study.”
Q: The device told him he wasn’t getting much sleep and then the sleep study told him it was apnea.
A: Right. It’s impossible to pick up sleep apnea. Some of the latest devices have some oximetry reading but it is not a clinically validated oximetry that could diagnose sleep apnea.
When these first came out I thought I’d get more referrals. So far, I haven’t had a single person come in and ask if they have sleep apnea. If you have a patient saying, “Hey, I’m worried about my oxygen level and here’s my data,” then the clinician should consider whether they need a sleep study for sleep apnea.
Q: You did a survey that suggests that clinicians are less keen on these devices than consumers. Conor Heneghan of Fitbit/Google also mentioned a study using the Fitbit Charge and a SleepLife portal. The patients were very engaged but only one physician (out of 49) logged into the portal to look at the data.
A: Our survey of sleep professionals (which we need to publish) showed that they were wary of the data. They found it frustrating in some ways because it took time out of the clinical encounter.
Some of them said that parents are putting trackers on their children and then catastrophizing their children’s sleep.
Q: Is there such a thing as an ideal hypnogram or does it vary by individual?
A: I would say that it depends on a lot of things. If you think about a hypnogram from a sleep study, the patient is not sleeping in their home environment, and it’s only one night. There’s a range of what would be considered normal, and it’s related to your sex and your age.
One night is not going to be sufficient to characterize your percentage in this or that sleep stage. Our patients come in saying, “I’m not getting enough REM.” But there isn’t a sleep disorder called lack of REM; there’s no treatment for that. It’s probably pretty normal for them or maybe they’re taking medications that suppress their REM, such as antidepressants.
The tech world is very interested to sense REM properly and to display it. But on the treatment side of things, there’s not much that we do with that data. We’re more interested in the consolidation of their sleep, the duration of their sleep, breathing-related sleep disorders, those sorts of things.
Q: Is there any reason to be concerned about the amount of REM sleep in terms of outcomes? We know that poor sleep can lead to bad cardiovascular outcomes, but has any of that correlated to sleep stage?
A: There are studies where they’ve experimentally deprived people of certain stages of sleep, but they’re not very useful in the real world. We’re looking at sleep holistically: Do you have a good sleep pattern? Any breathing-related sleep disorders? Insomnia? We don’t treat sleep by the stage.
Q: Any concern that people who are focused on a device may be ignoring the basic tenets of good sleep hygiene?
A: If people are doing things that are obviously bad for their sleep, like working too late, not exercising enough, sleeping in on weekends to compensate for being up late during the week, or probably the biggest thing contributing to insomnia – stress. A device itself won’t fix those things but it could show you the evidence.
If somebody really has a sleep disorder, then sleep hygiene alone is probably not going to be enough. They’re going to need to engage in a more extensive program to improve their sleep, such as cognitive-behavioral therapy for insomnia.
Q: Is there anything else you want to mention?
A: I don’t want to leave with a reputation of being against sleep trackers. I think they are a great opportunity for people to get excited about and learn about their sleep and try to improve it. We have a lot to learn about what people want from their data and how we can use that data to improve people’s sleep.
As providers, we can engage with our patients – sleep is an automatic process, but improving sleep takes some effort. Buying a device is not going to automatically make you sleep better. It takes work to establish a better sleep pattern; it may require some cognitive-behavioral therapy or treating a sleep disorder. That takes some work.
Dr. Baron reported no conflicts of interest.A version of this article first appeared on Medscape.com.
The pandemic not only disrupted sleep but may have also triggered an uptick in the use of wearable tech. Sleep tracking was featured at the Cardiovascular Health Tech virtual conference 2022, sponsored by the Institute of Electrical and Electronics Engineers Engineering in Medicine & Biology Society technical committee on Cardiopulmonary Systems and Physiology-Based Engineering.
This news organization interviewed presenter Kelly Glazer Baron, PhD, MPH, DBSM, an associate professor at the University of Utah, Salt Lake City, and a clinical psychologist specializing in behavioral sleep medicine.
The interview has been edited for length and clarity.
Question: Are consumer sleep trackers mainly divided into “nearables” – things that you put at the side of the bed or under the pillow – vs. wearables?
Dr. Baron: There are so many different devices these days. There are things that you put under your mattress or pillow; there are bedside recording devices; then there are headbands, rings, wrist-worn, all kinds of things.
Q: At the conference, Philip de Chazal, PhD, (University of Sydney) described the evidence on sleep tracking smartphone apps as woeful. Would you agree with that?
A: Yes. I would agree if you’re looking at how accurate they are at recording sleep, particularly compared with what we would define as the gold standard, which is a sleep study wherein you have electrodes on the scalp and you’re measuring the electrical activity directly.
They are best at detecting when you get into the bed and when you get out. But even then, there isn’t good evidence that they do that accurately when there are two people in the bed.
Overall, they may give you a general gist of what’s happening in terms of time in and out of bed, but we’re doubtful on their recording ability to tell sleep from wake time.
Q: Are the wrist-worn devices better for sleep tracking?
A: They’re getting better. We’ve used wrist activity monitors in research for years. They use an accelerometer to measure movement, and then an algorithm determines whether an interval of time is called sleep or wake.
Recently, they’ve incorporated more sensors, such as heart rate, and they can more accurately decipher rapid eye movement (REM) sleep from non-REM. They’re still not as good as doing a full sleep study. But they’re getting closer.
Q: If asked how you slept, most of us think we can answer without needing to look at a smartphone, but maybe not. Can you explain “paradoxical insomnia”?
A: You can’t really know if you’re sleeping because if you know you’re asleep, then you can’t be asleep because it’s a state of unconsciousness. How people decide whether they had a good night’s sleep probably depends on a lot of things about how they feel when they wake up in the morning or if they remember being up in the night.
Quality of sleep is not really something that people can directly ascertain. There is a selection of people who feel awake all night but they actually are sleeping. They feel that their sleep quality is poor: They’re suffering; they have insomnia, but from the objective data, they are sleeping fine.
Q: Is this related to non-REM stage 1 sleep, when you may not be aware that you’re asleep?
A: No. I’m talking about people who come into the sleep lab for an overnight study and get hooked up. And in the morning, they’ll tell the tech I was awake all night, but the tech will see that their sleep was just fine.
There is a disconnect between how people perceive their sleep and how they actually sleep. For most people it’s impossible to be completely accurate to know how much you’re sleeping. Then there are some people who perceive it very differently.
Sleep trackers don’t have the level of detail of sleep studies that use scalp electrodes. When we get into the details of sleep measurement, we’re measuring 30-second epochs (sampling periods), where we look at broad measures of electrical activity. There is even more detail there that can be pulled out using other techniques, such as analyzing the spectrum of the EEG. For example, some studies have found a beta frequency in the EEG of people with insomnia, so even though they are sleeping, they often feel awake.
Basically, the subjective experience of sleep somewhat overlaps with the objective recording of what’s happening on a sleep study, but not completely.
Q: You said that first thing in the morning might not be the best time to assess your sleep – if you wake up groggy and are already thinking, “The day is shot.”
A: In general, people really feel worst in the morning. Their circadian drive is low, especially if they’re a little sleep deprived. You shouldn’t judge the day on the first hour after waking – most people are pretty cognitively impaired. I tell people they need some boot-up time.
You feel differently as the day goes on and even at different points of the day. There’s a lull in the early afternoon because of your circadian dip and then we get a second wind in the evening. How you feel isn’t one flat line; it’s really a rhythm throughout the day
Q: Would you say that consumer sleep trackers are okay for individuals to use to see a pattern but are maybe not accurate enough to use more globally in research?
A: I think there is a huge opportunity to understand sleep at a population level. For example, if there’s been a hurricane or an earthquake or Superbowl Sunday, companies have an opportunity to look at the impact – say, daylight saving time and how it affects sleep across different countries, or men vs. women, or different age groups.
There was a paper about sleep among hospital workers in Wuhan during the outbreak of the pandemic. That was a creative use of wearable devices to look at sleep in a large population.
Now, of course, the devices are not given out randomly; the people who buy them are probably a little bit healthier, maybe a little bit younger – that sort of thing. It is a biased sample.
Q: As you note, mobile health trackers tend to be used by the “worried well.” Can you tell us about your paper that introduced the term “orthosomnia,” or “a perfectionistic quest for the ideal sleep in order to optimize daytime function”?
A: As these devices came out, more people were coming into the clinic and shoving their data in front of us saying, “I don’t feel well, and I don’t sleep 7 hours.” They were focused on this specific number. Back when we wrote this paper, the devices were primarily movement based (now the devices are a bit more accurate). Some would say, “My sleep is light, and it’s not deep.” We’d do a sleep study that showed that they have deep sleep, but they would still believe their device even though the device really wasn’t able to classify sleep accurately.
We even found people making their sleep worse because of the device. For example, trying to get the number higher by spending more time lying in bed trying to sleep which is the opposite of what you want someone with insomnia to do. These people held the data so tight and really felt that it characterized their experience, even though we sleep medicine practitioners didn’t find it very accurate and felt that it was somewhat unhelpful to their treatment.
Q: What advice would you give the harried primary care physician presented with a patient’s hypnogram or sleep pattern?
A: As someone once pointed out to me, it’s a conversation opener about their sleep. Did they buy the device because they’re worried about their sleep? It’s unlikely that you can glean anything clinically useful from the data.
I briefly look at it to see the duration of their sleep, the regularity in their sleep pattern – the pattern of awakenings during the night might suggest that they have some insomnia. But it doesn’t take the place of clinical assessment for conditions like sleep apnea: Are they snoring? Are they unrefreshed?
I had a patient in the orthosomnia study who was given a sleep tracker by a family member. He brought the data to his doctor who ordered a sleep study that found he had sleep apnea. He would say, “The device diagnosed my sleep apnea.” But that wasn’t actually the case; it just opened the conversation and the clinician said, “Well, let’s order a sleep study.”
Q: The device told him he wasn’t getting much sleep and then the sleep study told him it was apnea.
A: Right. It’s impossible to pick up sleep apnea. Some of the latest devices have some oximetry reading but it is not a clinically validated oximetry that could diagnose sleep apnea.
When these first came out I thought I’d get more referrals. So far, I haven’t had a single person come in and ask if they have sleep apnea. If you have a patient saying, “Hey, I’m worried about my oxygen level and here’s my data,” then the clinician should consider whether they need a sleep study for sleep apnea.
Q: You did a survey that suggests that clinicians are less keen on these devices than consumers. Conor Heneghan of Fitbit/Google also mentioned a study using the Fitbit Charge and a SleepLife portal. The patients were very engaged but only one physician (out of 49) logged into the portal to look at the data.
A: Our survey of sleep professionals (which we need to publish) showed that they were wary of the data. They found it frustrating in some ways because it took time out of the clinical encounter.
Some of them said that parents are putting trackers on their children and then catastrophizing their children’s sleep.
Q: Is there such a thing as an ideal hypnogram or does it vary by individual?
A: I would say that it depends on a lot of things. If you think about a hypnogram from a sleep study, the patient is not sleeping in their home environment, and it’s only one night. There’s a range of what would be considered normal, and it’s related to your sex and your age.
One night is not going to be sufficient to characterize your percentage in this or that sleep stage. Our patients come in saying, “I’m not getting enough REM.” But there isn’t a sleep disorder called lack of REM; there’s no treatment for that. It’s probably pretty normal for them or maybe they’re taking medications that suppress their REM, such as antidepressants.
The tech world is very interested to sense REM properly and to display it. But on the treatment side of things, there’s not much that we do with that data. We’re more interested in the consolidation of their sleep, the duration of their sleep, breathing-related sleep disorders, those sorts of things.
Q: Is there any reason to be concerned about the amount of REM sleep in terms of outcomes? We know that poor sleep can lead to bad cardiovascular outcomes, but has any of that correlated to sleep stage?
A: There are studies where they’ve experimentally deprived people of certain stages of sleep, but they’re not very useful in the real world. We’re looking at sleep holistically: Do you have a good sleep pattern? Any breathing-related sleep disorders? Insomnia? We don’t treat sleep by the stage.
Q: Any concern that people who are focused on a device may be ignoring the basic tenets of good sleep hygiene?
A: If people are doing things that are obviously bad for their sleep, like working too late, not exercising enough, sleeping in on weekends to compensate for being up late during the week, or probably the biggest thing contributing to insomnia – stress. A device itself won’t fix those things but it could show you the evidence.
If somebody really has a sleep disorder, then sleep hygiene alone is probably not going to be enough. They’re going to need to engage in a more extensive program to improve their sleep, such as cognitive-behavioral therapy for insomnia.
Q: Is there anything else you want to mention?
A: I don’t want to leave with a reputation of being against sleep trackers. I think they are a great opportunity for people to get excited about and learn about their sleep and try to improve it. We have a lot to learn about what people want from their data and how we can use that data to improve people’s sleep.
As providers, we can engage with our patients – sleep is an automatic process, but improving sleep takes some effort. Buying a device is not going to automatically make you sleep better. It takes work to establish a better sleep pattern; it may require some cognitive-behavioral therapy or treating a sleep disorder. That takes some work.
Dr. Baron reported no conflicts of interest.A version of this article first appeared on Medscape.com.
Long-haul COVID-19 brings welcome attention to POTS
Before COVID-19, postural orthostatic tachycardia syndrome (POTS) was one of those diseases that many people, including physicians, dismissed.
“They thought it was just anxious, crazy young women,” said Pam R. Taub, MD, who runs the cardiac rehabilitation program at the University of California, San Diego.
The cryptic autonomic condition was estimated to affect 1-3 million Americans before the pandemic hit. Now case reports confirm that it is a manifestation of postacute sequelae of SARS-CoV-2 infection (PASC), or so-called long-haul COVID-19.
“I’m excited that this condition that has been so often the ugly stepchild of both cardiology and neurology is getting some attention,” said Dr. Taub. She said she is hopeful that the National Institutes of Health’s commitment to PASC research will benefit patients affected by the cardiovascular dysautonomia characterized by orthostatic intolerance in the absence of orthostatic hypotension.
Postinfection POTS is not exclusive to SARS-CoV-2. It has been reported after Lyme disease and Epstein-Barr virus infections, for example. One theory is that some of the antibodies generated against the virus cross react and damage the autonomic nervous system, which regulates heart rate and blood pressure, Dr. Taub explained.
It is not known whether COVID-19 is more likely to trigger POTS than are other infections or whether the rise in cases merely reflects the fact that more than 115 million people worldwide have been infected with the novel coronavirus.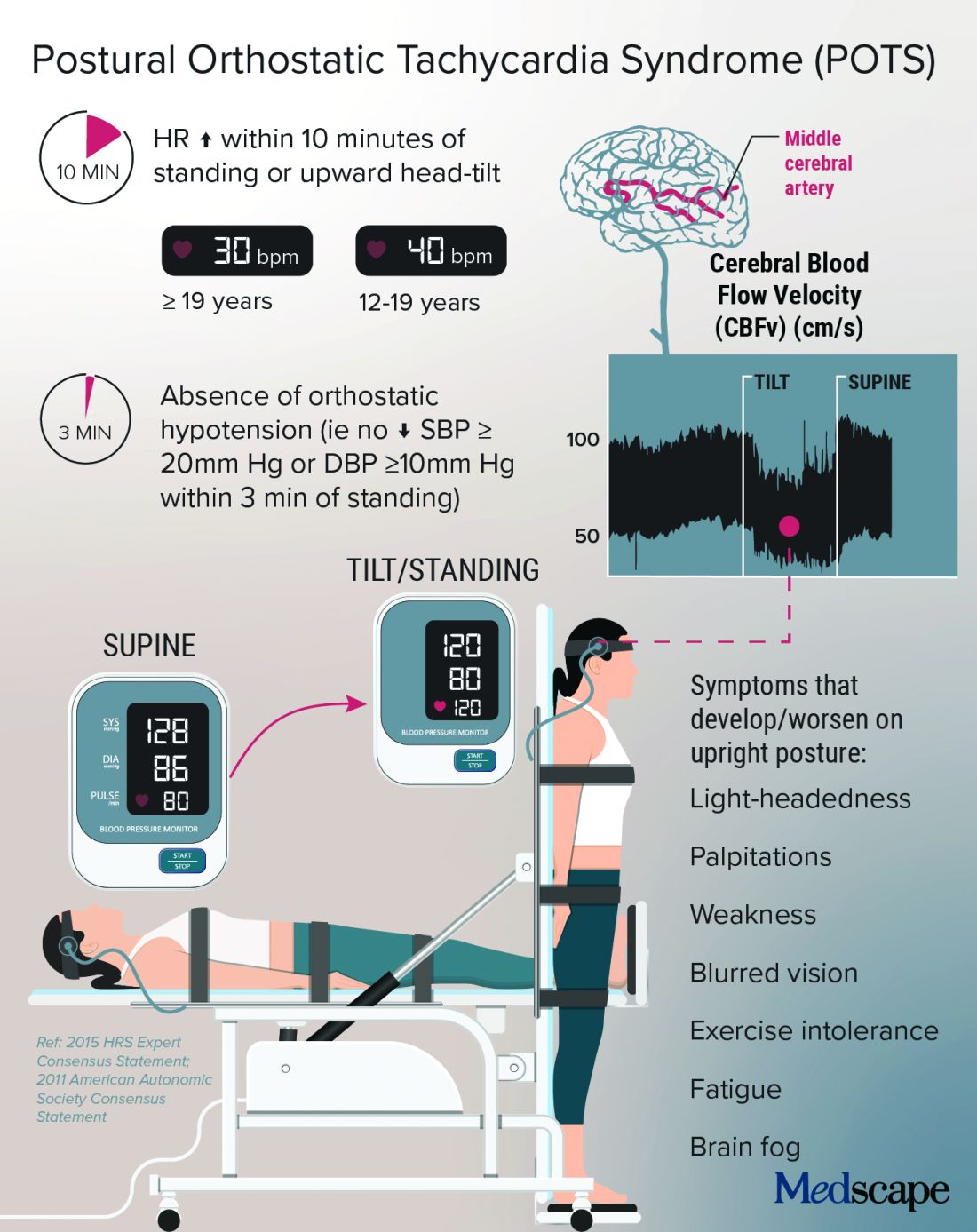
Low blood volume, dysregulation of the autonomic nervous system, and autoimmunity may all play a role in POTS, perhaps leading to distinct subtypes, according to a State of the Science document from the NIH; the National Heart, Lung, and Blood Institute; and the National Institute of Neurological Disorders and Stroke.
In Dr. Taub’s experience, “The truth is that patients actually have a mix of the subtypes.”
Kamal Shouman, MD, an autonomic neurologist at Mayo Clinic, Rochester, Minn., said in an interview that he has seen patients present with post–COVID-19 POTS in “all flavors,” including “neuropathic POTS, which is thought of as the classic postinfectious phenomenon.”
Why does it mostly affect athletic women?
The condition, which can be the result of dehydration or prolonged bed rest, leading to deconditioning, affects women disproportionately.
According to Manesh Patel, MD, if a patient with POTS who is not a young woman is presented on medical rounds, the response is, “Tell me again why you think this patient has POTS.”
Dr. Patel, chief of the division of cardiology at Duke University, Durham, N.C., has a theory for why many of the women who have POTS are athletes or are highly active: They likely have an underlying predisposition, compounded by a smaller body volume, leaving less margin for error. “If they decondition and lose 500 cc’s, it makes a bigger difference to them than, say, a 300-pound offensive lineman,” Dr. Patel explained.
That hypothesis makes sense to Dr. Taub, who added, “There are just some people metabolically that are more hyperadrenergic,” and it may be that “all their activity really helps tone down that sympathetic output,” but the infection affects these regulatory processes, and deconditioning disrupts things further.
Women also have more autoimmune disorders than do men. The driving force of the dysregulation of the autonomic nervous system is thought to be “immune mediated; we think it’s triggered by a response to a virus,” she said.
Dr. Shouman said the underlying susceptibility may predispose toward orthostatic intolerance. For example, patients will tell him, “Well, many years ago, I was prone to fainting.” He emphasized that POTS is not exclusive to women – he sees men with POTS, and one of the three recent case reports of post–COVID-19 POTS involved a 37-year-old man. So far, the male POTS patients that Dr. Patel has encountered have been deconditioned athletes.
Poor (wo)man’s tilt test and treatment options
POTS is typically diagnosed with a tilt test and transcranial Doppler. Dr. Taub described her “poor man’s tilt test” of asking the patient to lie down for 5-10 minutes and then having the patient stand up.
She likes the fact that transcranial Doppler helps validate the brain fog that patients report, which can be dismissed as “just your excuse for not wanting to work.” If blood perfusion to the brain is cut by 40%-50%, “how are you going to think clearly?” she said.
Dr. Shouman noted that overall volume expansion with salt water, compression garments, and a graduated exercise program play a major role in the rehabilitation of all POTS patients.
He likes to tailor treatments to the most likely underlying cause. But patients should first undergo a medical assessment by their internists to make sure there isn’t a primary lung or heart problem.
“Once the decision is made for them to be evaluated in the autonomic practice and [a] POTS diagnosis is made, I think it is very useful to determine what type of POTS,” he said.
With hyperadrenergic POTS, “you are looking at a standing norepinephrine level of over 600 pg/mL or so.” For these patients, drugs such as ivabradine or beta-blockers can help, he noted.
Dr. Taub recently conducted a small study that showed a benefit with the selective If channel blocker ivabradine for patients with hyperadrenergic POTS unrelated to COVID-19. She tends to favor ivabradine over beta-blockers because it lowers heart rate but not blood pressure. In addition, beta-blockers can exacerbate fatigue and brain fog.
A small crossover study will compare propranolol and ivabradine in POTS. For someone who is very hypovolemic, “you might try a salt tablet or a prescription drug like fludrocortisone,” Dr. Taub explained.
Another problem that patients with POTS experience is an inability to exercise because of orthostatic intolerance. Recumbent exercise targets deconditioning and can tamp down the hyperadrenergic effect. Dr. Shouman’s approach is to start gradually with swimming or the use of a recumbent bike or a rowing machine.
Dr. Taub recommends wearables to patients because POTS is “a very dynamic condition” that is easy to overmedicate or undermedicate. If it’s a good day, the patients are well hydrated, and the standing heart rate is only 80 bpm, she tells them they could titrate down their second dose of ivabradine, for example. The feedback from wearables also helps patients manage their exercise response.
For Dr. Shouman, wearables are not always as accurate as he would like. He tells his patients that it’s okay to use one as long as it doesn’t become a source of anxiety such that they’re constantly checking it.
POTS hope: A COVID-19 silver lining?
With increasing attention being paid to long-haul COVID-19, are there any concerns that POTS will get lost among the myriad symptoms connected to PASC?
Dr. Shouman cautioned, “Not all long COVID is POTS,” and said that clinicians at long-haul clinics should be able to recognize the different conditions “when POTS is suspected. I think it is useful for those providers to make the appropriate referral for POTS clinic autonomic assessment.”
He and his colleagues at Mayo have seen quite a few patients who have post–COVID-19 autonomic dysfunction, such as vasodepressor syncope, not just POTS. They plan to write about this soon.
“Of all the things I treat in cardiology, this is the most complex, because there’s so many different systems involved,” said Dr. Taub, who has seen patients recover fully from POTS. “There’s a spectrum, and there’s people that are definitely on one end of the spectrum where they have very severe diseases.”
For her, the important message is, “No matter where you are on the spectrum, there are things we can do to make your symptoms better.” And with grant funding for PASC research, “hopefully we will address the mechanisms of disease, and we’ll be able to cure this,” she said.
Dr. Patel has served as a consultant for Bayer, Janssen, AstraZeneca, and Heartflow and has received research grants from Bayer, Janssen, AstraZeneca, and the National Heart, Lung, and Blood Institute. Dr. Shouman reports no relevant financial relationships. Dr. Taub has served as a consultant for Amgen, Bayer, Esperion, Boehringer Ingelheim, Novo Nordisk, and Sanofi; is a shareholder in Epirium Bio; and has received research grants from the National Institutes of Health, the American Heart Association, and the Department of Homeland Security/FEMA.
A version of this article first appeared on Medscape.com.
Before COVID-19, postural orthostatic tachycardia syndrome (POTS) was one of those diseases that many people, including physicians, dismissed.
“They thought it was just anxious, crazy young women,” said Pam R. Taub, MD, who runs the cardiac rehabilitation program at the University of California, San Diego.
The cryptic autonomic condition was estimated to affect 1-3 million Americans before the pandemic hit. Now case reports confirm that it is a manifestation of postacute sequelae of SARS-CoV-2 infection (PASC), or so-called long-haul COVID-19.
“I’m excited that this condition that has been so often the ugly stepchild of both cardiology and neurology is getting some attention,” said Dr. Taub. She said she is hopeful that the National Institutes of Health’s commitment to PASC research will benefit patients affected by the cardiovascular dysautonomia characterized by orthostatic intolerance in the absence of orthostatic hypotension.
Postinfection POTS is not exclusive to SARS-CoV-2. It has been reported after Lyme disease and Epstein-Barr virus infections, for example. One theory is that some of the antibodies generated against the virus cross react and damage the autonomic nervous system, which regulates heart rate and blood pressure, Dr. Taub explained.
It is not known whether COVID-19 is more likely to trigger POTS than are other infections or whether the rise in cases merely reflects the fact that more than 115 million people worldwide have been infected with the novel coronavirus.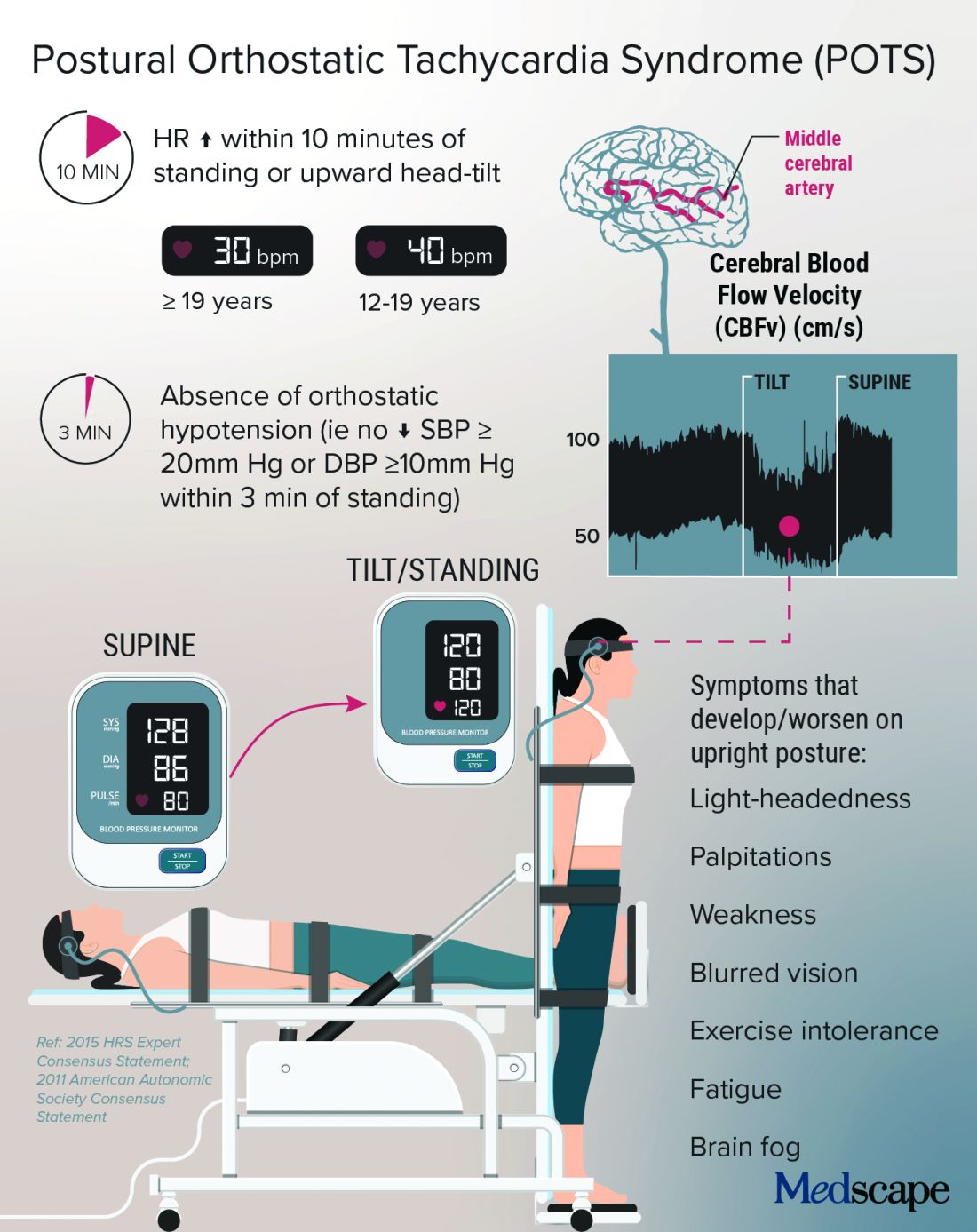
Low blood volume, dysregulation of the autonomic nervous system, and autoimmunity may all play a role in POTS, perhaps leading to distinct subtypes, according to a State of the Science document from the NIH; the National Heart, Lung, and Blood Institute; and the National Institute of Neurological Disorders and Stroke.
In Dr. Taub’s experience, “The truth is that patients actually have a mix of the subtypes.”
Kamal Shouman, MD, an autonomic neurologist at Mayo Clinic, Rochester, Minn., said in an interview that he has seen patients present with post–COVID-19 POTS in “all flavors,” including “neuropathic POTS, which is thought of as the classic postinfectious phenomenon.”
Why does it mostly affect athletic women?
The condition, which can be the result of dehydration or prolonged bed rest, leading to deconditioning, affects women disproportionately.
According to Manesh Patel, MD, if a patient with POTS who is not a young woman is presented on medical rounds, the response is, “Tell me again why you think this patient has POTS.”
Dr. Patel, chief of the division of cardiology at Duke University, Durham, N.C., has a theory for why many of the women who have POTS are athletes or are highly active: They likely have an underlying predisposition, compounded by a smaller body volume, leaving less margin for error. “If they decondition and lose 500 cc’s, it makes a bigger difference to them than, say, a 300-pound offensive lineman,” Dr. Patel explained.
That hypothesis makes sense to Dr. Taub, who added, “There are just some people metabolically that are more hyperadrenergic,” and it may be that “all their activity really helps tone down that sympathetic output,” but the infection affects these regulatory processes, and deconditioning disrupts things further.
Women also have more autoimmune disorders than do men. The driving force of the dysregulation of the autonomic nervous system is thought to be “immune mediated; we think it’s triggered by a response to a virus,” she said.
Dr. Shouman said the underlying susceptibility may predispose toward orthostatic intolerance. For example, patients will tell him, “Well, many years ago, I was prone to fainting.” He emphasized that POTS is not exclusive to women – he sees men with POTS, and one of the three recent case reports of post–COVID-19 POTS involved a 37-year-old man. So far, the male POTS patients that Dr. Patel has encountered have been deconditioned athletes.
Poor (wo)man’s tilt test and treatment options
POTS is typically diagnosed with a tilt test and transcranial Doppler. Dr. Taub described her “poor man’s tilt test” of asking the patient to lie down for 5-10 minutes and then having the patient stand up.
She likes the fact that transcranial Doppler helps validate the brain fog that patients report, which can be dismissed as “just your excuse for not wanting to work.” If blood perfusion to the brain is cut by 40%-50%, “how are you going to think clearly?” she said.
Dr. Shouman noted that overall volume expansion with salt water, compression garments, and a graduated exercise program play a major role in the rehabilitation of all POTS patients.
He likes to tailor treatments to the most likely underlying cause. But patients should first undergo a medical assessment by their internists to make sure there isn’t a primary lung or heart problem.
“Once the decision is made for them to be evaluated in the autonomic practice and [a] POTS diagnosis is made, I think it is very useful to determine what type of POTS,” he said.
With hyperadrenergic POTS, “you are looking at a standing norepinephrine level of over 600 pg/mL or so.” For these patients, drugs such as ivabradine or beta-blockers can help, he noted.
Dr. Taub recently conducted a small study that showed a benefit with the selective If channel blocker ivabradine for patients with hyperadrenergic POTS unrelated to COVID-19. She tends to favor ivabradine over beta-blockers because it lowers heart rate but not blood pressure. In addition, beta-blockers can exacerbate fatigue and brain fog.
A small crossover study will compare propranolol and ivabradine in POTS. For someone who is very hypovolemic, “you might try a salt tablet or a prescription drug like fludrocortisone,” Dr. Taub explained.
Another problem that patients with POTS experience is an inability to exercise because of orthostatic intolerance. Recumbent exercise targets deconditioning and can tamp down the hyperadrenergic effect. Dr. Shouman’s approach is to start gradually with swimming or the use of a recumbent bike or a rowing machine.
Dr. Taub recommends wearables to patients because POTS is “a very dynamic condition” that is easy to overmedicate or undermedicate. If it’s a good day, the patients are well hydrated, and the standing heart rate is only 80 bpm, she tells them they could titrate down their second dose of ivabradine, for example. The feedback from wearables also helps patients manage their exercise response.
For Dr. Shouman, wearables are not always as accurate as he would like. He tells his patients that it’s okay to use one as long as it doesn’t become a source of anxiety such that they’re constantly checking it.
POTS hope: A COVID-19 silver lining?
With increasing attention being paid to long-haul COVID-19, are there any concerns that POTS will get lost among the myriad symptoms connected to PASC?
Dr. Shouman cautioned, “Not all long COVID is POTS,” and said that clinicians at long-haul clinics should be able to recognize the different conditions “when POTS is suspected. I think it is useful for those providers to make the appropriate referral for POTS clinic autonomic assessment.”
He and his colleagues at Mayo have seen quite a few patients who have post–COVID-19 autonomic dysfunction, such as vasodepressor syncope, not just POTS. They plan to write about this soon.
“Of all the things I treat in cardiology, this is the most complex, because there’s so many different systems involved,” said Dr. Taub, who has seen patients recover fully from POTS. “There’s a spectrum, and there’s people that are definitely on one end of the spectrum where they have very severe diseases.”
For her, the important message is, “No matter where you are on the spectrum, there are things we can do to make your symptoms better.” And with grant funding for PASC research, “hopefully we will address the mechanisms of disease, and we’ll be able to cure this,” she said.
Dr. Patel has served as a consultant for Bayer, Janssen, AstraZeneca, and Heartflow and has received research grants from Bayer, Janssen, AstraZeneca, and the National Heart, Lung, and Blood Institute. Dr. Shouman reports no relevant financial relationships. Dr. Taub has served as a consultant for Amgen, Bayer, Esperion, Boehringer Ingelheim, Novo Nordisk, and Sanofi; is a shareholder in Epirium Bio; and has received research grants from the National Institutes of Health, the American Heart Association, and the Department of Homeland Security/FEMA.
A version of this article first appeared on Medscape.com.
Before COVID-19, postural orthostatic tachycardia syndrome (POTS) was one of those diseases that many people, including physicians, dismissed.
“They thought it was just anxious, crazy young women,” said Pam R. Taub, MD, who runs the cardiac rehabilitation program at the University of California, San Diego.
The cryptic autonomic condition was estimated to affect 1-3 million Americans before the pandemic hit. Now case reports confirm that it is a manifestation of postacute sequelae of SARS-CoV-2 infection (PASC), or so-called long-haul COVID-19.
“I’m excited that this condition that has been so often the ugly stepchild of both cardiology and neurology is getting some attention,” said Dr. Taub. She said she is hopeful that the National Institutes of Health’s commitment to PASC research will benefit patients affected by the cardiovascular dysautonomia characterized by orthostatic intolerance in the absence of orthostatic hypotension.
Postinfection POTS is not exclusive to SARS-CoV-2. It has been reported after Lyme disease and Epstein-Barr virus infections, for example. One theory is that some of the antibodies generated against the virus cross react and damage the autonomic nervous system, which regulates heart rate and blood pressure, Dr. Taub explained.
It is not known whether COVID-19 is more likely to trigger POTS than are other infections or whether the rise in cases merely reflects the fact that more than 115 million people worldwide have been infected with the novel coronavirus.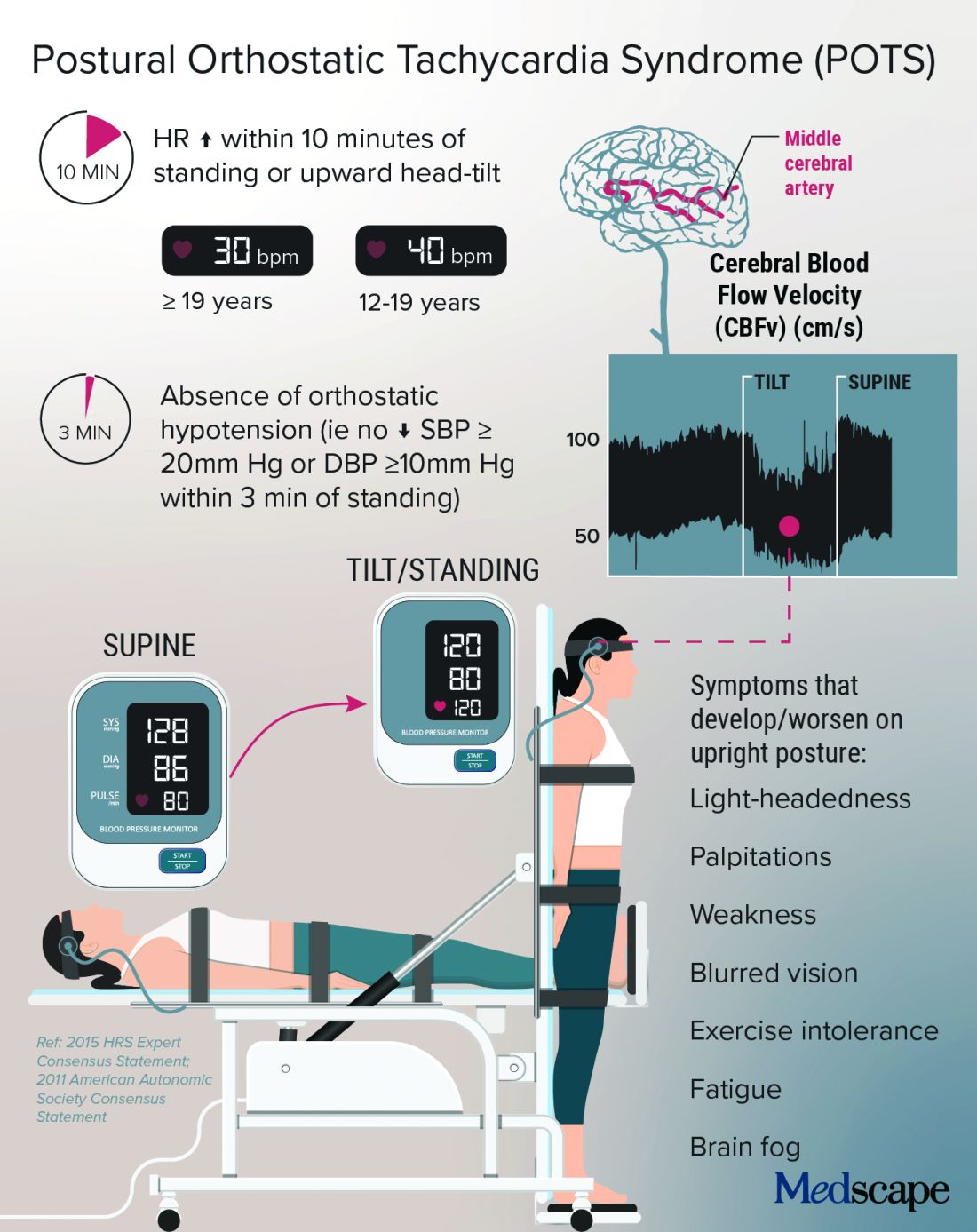
Low blood volume, dysregulation of the autonomic nervous system, and autoimmunity may all play a role in POTS, perhaps leading to distinct subtypes, according to a State of the Science document from the NIH; the National Heart, Lung, and Blood Institute; and the National Institute of Neurological Disorders and Stroke.
In Dr. Taub’s experience, “The truth is that patients actually have a mix of the subtypes.”
Kamal Shouman, MD, an autonomic neurologist at Mayo Clinic, Rochester, Minn., said in an interview that he has seen patients present with post–COVID-19 POTS in “all flavors,” including “neuropathic POTS, which is thought of as the classic postinfectious phenomenon.”
Why does it mostly affect athletic women?
The condition, which can be the result of dehydration or prolonged bed rest, leading to deconditioning, affects women disproportionately.
According to Manesh Patel, MD, if a patient with POTS who is not a young woman is presented on medical rounds, the response is, “Tell me again why you think this patient has POTS.”
Dr. Patel, chief of the division of cardiology at Duke University, Durham, N.C., has a theory for why many of the women who have POTS are athletes or are highly active: They likely have an underlying predisposition, compounded by a smaller body volume, leaving less margin for error. “If they decondition and lose 500 cc’s, it makes a bigger difference to them than, say, a 300-pound offensive lineman,” Dr. Patel explained.
That hypothesis makes sense to Dr. Taub, who added, “There are just some people metabolically that are more hyperadrenergic,” and it may be that “all their activity really helps tone down that sympathetic output,” but the infection affects these regulatory processes, and deconditioning disrupts things further.
Women also have more autoimmune disorders than do men. The driving force of the dysregulation of the autonomic nervous system is thought to be “immune mediated; we think it’s triggered by a response to a virus,” she said.
Dr. Shouman said the underlying susceptibility may predispose toward orthostatic intolerance. For example, patients will tell him, “Well, many years ago, I was prone to fainting.” He emphasized that POTS is not exclusive to women – he sees men with POTS, and one of the three recent case reports of post–COVID-19 POTS involved a 37-year-old man. So far, the male POTS patients that Dr. Patel has encountered have been deconditioned athletes.
Poor (wo)man’s tilt test and treatment options
POTS is typically diagnosed with a tilt test and transcranial Doppler. Dr. Taub described her “poor man’s tilt test” of asking the patient to lie down for 5-10 minutes and then having the patient stand up.
She likes the fact that transcranial Doppler helps validate the brain fog that patients report, which can be dismissed as “just your excuse for not wanting to work.” If blood perfusion to the brain is cut by 40%-50%, “how are you going to think clearly?” she said.
Dr. Shouman noted that overall volume expansion with salt water, compression garments, and a graduated exercise program play a major role in the rehabilitation of all POTS patients.
He likes to tailor treatments to the most likely underlying cause. But patients should first undergo a medical assessment by their internists to make sure there isn’t a primary lung or heart problem.
“Once the decision is made for them to be evaluated in the autonomic practice and [a] POTS diagnosis is made, I think it is very useful to determine what type of POTS,” he said.
With hyperadrenergic POTS, “you are looking at a standing norepinephrine level of over 600 pg/mL or so.” For these patients, drugs such as ivabradine or beta-blockers can help, he noted.
Dr. Taub recently conducted a small study that showed a benefit with the selective If channel blocker ivabradine for patients with hyperadrenergic POTS unrelated to COVID-19. She tends to favor ivabradine over beta-blockers because it lowers heart rate but not blood pressure. In addition, beta-blockers can exacerbate fatigue and brain fog.
A small crossover study will compare propranolol and ivabradine in POTS. For someone who is very hypovolemic, “you might try a salt tablet or a prescription drug like fludrocortisone,” Dr. Taub explained.
Another problem that patients with POTS experience is an inability to exercise because of orthostatic intolerance. Recumbent exercise targets deconditioning and can tamp down the hyperadrenergic effect. Dr. Shouman’s approach is to start gradually with swimming or the use of a recumbent bike or a rowing machine.
Dr. Taub recommends wearables to patients because POTS is “a very dynamic condition” that is easy to overmedicate or undermedicate. If it’s a good day, the patients are well hydrated, and the standing heart rate is only 80 bpm, she tells them they could titrate down their second dose of ivabradine, for example. The feedback from wearables also helps patients manage their exercise response.
For Dr. Shouman, wearables are not always as accurate as he would like. He tells his patients that it’s okay to use one as long as it doesn’t become a source of anxiety such that they’re constantly checking it.
POTS hope: A COVID-19 silver lining?
With increasing attention being paid to long-haul COVID-19, are there any concerns that POTS will get lost among the myriad symptoms connected to PASC?
Dr. Shouman cautioned, “Not all long COVID is POTS,” and said that clinicians at long-haul clinics should be able to recognize the different conditions “when POTS is suspected. I think it is useful for those providers to make the appropriate referral for POTS clinic autonomic assessment.”
He and his colleagues at Mayo have seen quite a few patients who have post–COVID-19 autonomic dysfunction, such as vasodepressor syncope, not just POTS. They plan to write about this soon.
“Of all the things I treat in cardiology, this is the most complex, because there’s so many different systems involved,” said Dr. Taub, who has seen patients recover fully from POTS. “There’s a spectrum, and there’s people that are definitely on one end of the spectrum where they have very severe diseases.”
For her, the important message is, “No matter where you are on the spectrum, there are things we can do to make your symptoms better.” And with grant funding for PASC research, “hopefully we will address the mechanisms of disease, and we’ll be able to cure this,” she said.
Dr. Patel has served as a consultant for Bayer, Janssen, AstraZeneca, and Heartflow and has received research grants from Bayer, Janssen, AstraZeneca, and the National Heart, Lung, and Blood Institute. Dr. Shouman reports no relevant financial relationships. Dr. Taub has served as a consultant for Amgen, Bayer, Esperion, Boehringer Ingelheim, Novo Nordisk, and Sanofi; is a shareholder in Epirium Bio; and has received research grants from the National Institutes of Health, the American Heart Association, and the Department of Homeland Security/FEMA.
A version of this article first appeared on Medscape.com.